User login
Addressing Maternal Mortality Through Education: The Mommies Methadone Program
From the UT Health Long School of Medicine San Antonio, Texas.
Abstract
Objective: To educate pregnant patients with opioid use disorder (OUD) about the effects of opioids in order to improve understanding and help achieve sustained abstinence.
Methods: The Center for Health Care Services and University Hospital System (UHS) in San Antonio, TX, jointly o
Results: Of 68 women enrolled in the program, 33 completed both the pre-survey and the post-survey (48.5%). Nearly half (48%) were very motivated to quit before pregnancy, but 85% were very motivated to quit once pregnant. All participants said learning more about the effects of opiates would increase motivation for sobriety. Prior to the educational intervention, 39% of participants knew it was safe to breastfeed on methadone, which improved to 97% in the post-survey, and 76% incorrectly thought they would be reported to authorities by their health care providers if they used illegal drugs during pregnancy, while in the post-survey, 100% knew they would not be reported for doing so.
Conclusion: Pregnancy and education about opioids increased patients’ motivation to quit. Patients also advanced their breastfeeding knowledge and learned about patient-provider confidentiality. Our greatest challenge was participant follow-up; however, this improved with the help of a full-time Mommies Program nurse. Our future aim is to increase project awareness and extend the educational research.
Keywords: pregnancy; addiction; opioids; OUD; counseling.
In 2012 more than 259 million prescriptions for opioids were written in the United States, which was a 200% increase since 1998.1 Since the early 2000s, admissions to opioid substance abuse programs and the death rate from opioids have quadrupled.2-4 Specifically, the rate of heroin use increased more than 300% from 2010 to 2014.5 Opioid use in pregnancy has also escalated in recent years, with a 3- to 4-fold increase from 2000 to 2009 and with 4 in 1000 deliveries being complicated by opioid use disorder (OUD) in 2011.6-8
Between 2000 and 2014, the maternal mortality rate in the United States increased 24%, making it the only industrialized nation with a maternal mortality rate that is rising rather than falling.9 The Texas Maternal Mortality and Morbidity Task Force found that between 2012 and 2015 drug overdose was the leading cause of maternal death in the period from delivery to 365 days postpartum, and it has increased dramatically since 2010.10,11
In addition, maternal mortality reviews in several states have identified substance use as a major risk factor for pregnancy-associated deaths.12,13 In Texas between 2012 and 2015, opioids were found in 58% of maternal drug overdoses.10 In 2007, 22.8% of women who were enrolled in Medicaid programs in 46 states filled an opioid prescription during pregnancy.14 Additionally, the rising prevalence of opioid use in pregnancy has led to a sharp increase in neonatal abstinence syndrome (NAS), rising from 1.5 cases per 1000 hospital births in 1999 to 6.0 per 1000 hospital births in 2013.15 Unsurprisingly, states with the highest rates of opioid prescribing also have the highest rates of NAS.16
Methadone combined with counseling and behavioral therapy has been the standard of care for the treatment of OUD in pregnancy since the 1970s. Methadone treatment prevents opioid withdrawal symptoms and increases adherence to prenatal care.17 One of the largest methadone treatment clinics in the San Antonio, TX, area is the Center for Health Care Services (CHCS). University Health System in San Antonio (UHS) has established a clinic called The Mommies Program, where mothers addicted to opioids can receive prenatal care by a dedicated physician, registered nurse, and a certified nurse midwife, who work in collaboration with the CHCS methadone clinic. Pregnant patients with OUD in pregnancy are concurrently enrolled in the Mommies Program and receive prenatal care through UHS and methadone treatment and counseling through CHCS. The continuity effort aims to increase prenatal care rates and adherence to methadone treatment.
Once mothers are off illicit opioids and on methadone, it is essential to discuss breastfeeding with them, as many mothers addicted to illicit opioids may have been told that they should not be breastfeeding. However, breastfeeding should be encouraged in women who are stable on methadone if they are not using illicit drugs and do not have other contraindications, regardless of maternal methadone dose, since the transfer of methadone into breast milk is minimal.18-20 Breastfeeding is beneficial in women taking methadone and has been associated with decreased severity of NAS symptoms, decreased need for pharmacotherapy, and a shorter hospital stay for the baby.21 In addition, breastfeeding contributes to the development of an attachment between mother and infant, while also providing the infant with natural immunity. Women should be counseled about the need to stop breastfeeding in the event of a relapse.22
Finally, the postpartum period represents a time of increased stressors, such as loss of sleep, child protective services involvement, and frustration with constant demands from new baby. For mothers with addiction, this is an especially sensitive time, as the stressors may be exacerbated by their new sobriety and a sudden end to the motivation they experienced from pregnancy.23 Therefore, early and frequent postpartum care with methadone dose evaluation is essential in order to decrease drug relapse and screen for postpartum depression in detail, since patients with a history of drug use are at increased risk of postpartum depression.
In 2017 medical students at UT Health Long School of Medicine in San Antonio created a project to educate women about OUD in pregnancy and provide motivational incentives for sustained abstinence; this project has continued each year since. Students provide education about methadone treatment and the dangers of using illicit opioids during and after pregnancy. Students especially focus on educating patients on the key problem areas in the literature, such as overdose, NAS, breastfeeding, postpartum substance use, and postpartum depression.
Methods
From October 2018 to February 2020, a total of 15 medical students volunteered between 1 and 20 times at the Mommies Program clinic, which was held once or twice per week from 8
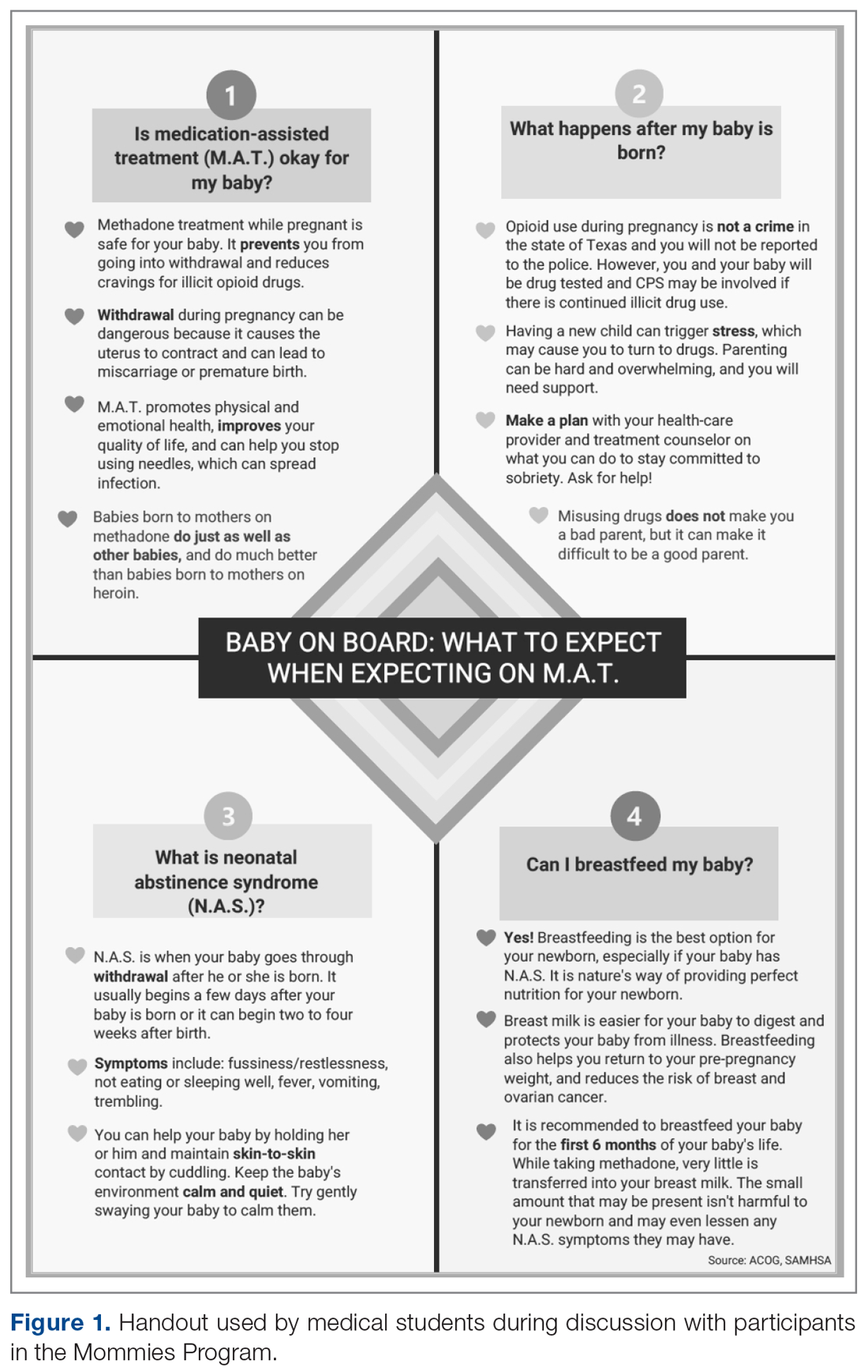
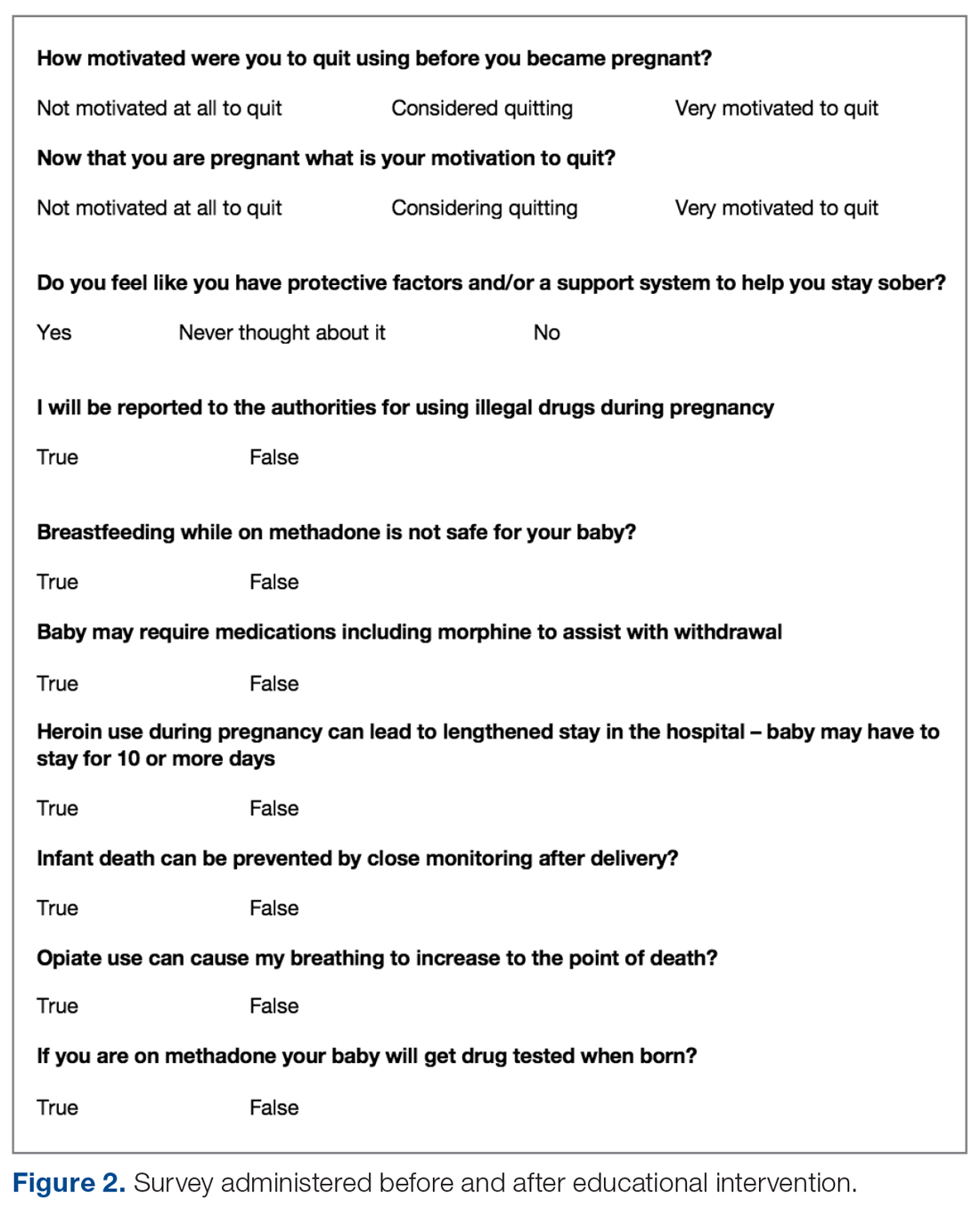
The only inclusion criteria for participating in the educational intervention and survey was participants had to be 18 years of age or older and enrolled in the Mommies Program. Patients who met the inclusion criteria and agreed to participate completed a pre-survey administered by the students during the patient’s initial prenatal visit (Figure 2). This survey collected baseline information about the patient’s history with opioid use and their current knowledge of methadone treatment, NAS, legal aspects of drug use disclosure, and drug testing prior to the education portion of the encounter. After the pre-survey was administered, students spent 30 minutes reviewing the correct answers of the survey with the patients by utilizing the standardized handout to help patients understand details of methadone and opioid use in pregnancy (Figure 1). The post-survey was administered by a student once patients entered the third trimester to assess whether the education session increased patients’ knowledge of these topics.
At the time patients completed the post-survey, they received a Baby Bag as well as education regarding each item in the bag. The aim of distributing Baby Bags was to relieve some possible postnatal stressors and educate the patients about infant care. Items included in the bag were diapers, wipes, bottles, clothes, and swaddles. Prenatal vitamins were added in January 2020, as many patients struggle to afford vitamins if they are not currently covered by Medicaid or have other barriers. The Baby Bag items were purchased through a Community Service Learning grant through UT Health San Antonio.
Results
Of 68 women enrolled in the Mommies Program during the intervention period, 33 completed the pre-survey and the post-survey (48.5%). Even though all patients enrolled in the program met the inclusion criteria, patients were not included in the educational program for multiple reasons, including refusal to participate, poor clinic follow-up, or lack of students to collect surveys. However, all patients who completed the pre-survey did complete the post-survey. In the pre-survey, only 39% of participants knew it was safe to breastfeed while on methadone. In the post-survey, 97% knew it safe to breastfeed. Nearly half (48%) reported being very motivated to quit opioids before pregnancy, but 85% were very motivated to quit once pregnant. In the pre-survey, 76% incorrectly thought they would be reported to authorities by their health providers if they used illegal drugs during pregnancy, while in the post-survey, 100% knew they would not be reported for doing so. Also, all participants said learning more about the effects of opiates would increase motivation for sobriety.
Discussion
Questions assessed during the educational surveys revolved around patients’ knowledge of the intricacies, legally and physiologically, of methadone treatment for OUD, as well as beneficial aspects for patients and future child health, such as breastfeeding and motivation to quit and stay sober.
It was clear that there was a lack of knowledge and education about breastfeeding, as only 39% of the participants thought that it was safe to breastfeed while on methadone in the pre-survey; in the post survey, this improved to 97%. Students spent a large portion of the educational time going over the safety of breastfeeding for patients on methadone and the many benefits to mother and baby. Students also reviewed breastfeeding with patients every time patients came in for a visit and debunked any falsehoods about the negatives of breastfeeding while on methadone. This is another testament to the benefits of reinforcement around patient education.
The area of trust between provider and patient is essential in all provider-patient relationships. However, in the area of addiction, a trusting bond is especially important, as patients must feel confident and comfortable to disclose every aspect of their lives so the provider can give the best care. It was clear from our initial data that many patients did not feel this trust or understand the legal aspects regarding the provider-patient relationship in the terms of drug use, as the pre-survey shows 76% of patients originally thought they would be reported to authorities if they told their provider they used illegal drugs during pregnancy. This was an enormous issue in the clinic and something that needed to be addressed because, based on these data, we feared many patients would not be honest about using illegal drugs to supplement their methadone if they believed they would be reported to the authorities or even jailed. The medical student education team continually assured patients that their honesty about illegal drug use during pregnancy would not be revealed to the authorities, and also made it clear to patients that it was essential they were honest about illegal drug use so the optimal care could be provided by the team. These discussions were successful, as the post-survey showed that 100% of patients knew they would not be reported to the authorities if they used illegal drugs during the pregnancy. This showed an increase in knowledge, but also suggested an increase in confidence in the provider-patient relationship by patients, which we speculate allowed for a better patient experience, better patient outcomes, and less emotional stress for the patient and provider.
Last, we wanted to study and address the motivation to quit using drugs and stay sober through learning about the effects of opiates and how this motivation was related to pregnancy. A study by Mitchell et al makes clear that pregnancy is a motivation to seek treatment for drug use and to quit,24 and our survey data support these findings, with 48% of patients motivated to quit before they were pregnant and 85% motivated to quit once they knew they were pregnant. In addition, all patients attested on the pre- and post-survey that learning more about opioids would increase their motivation for sobriety. Therefore, we believe education about the use of opioids and other drugs is a strong motivation towards sobriety and should be further studied in methadone treatment and other drugs as well.
We will continue to focus on sobriety postpartum by using the education in pregnancy as a springboard to further postpartum education, as education seems to be very beneficial to future sobriety. In the future, we believe extending the educational program past pregnancy and discussing opioid use and addiction with patients at multiple follow-up visits will be beneficial to patients’ sobriety.
We faced 2 main challenges in implementing this intervention and survey: patients would often miss multiple appointments during their third trimester or would not attend their postpartum visit if they only had 1 prenatal visit; and many clinic sessions had low student attendance because students often had many other responsibilities in medical school and there were only 15 volunteers over the study time. These challenges decreased our post-survey completion rate. However, there has been improvement in follow-up as the project has continued. The Mommies Program now has a full-time registered nurse, and a larger number of medical student teachers have volunteered to attend the clinic. In the future, we aim to increase awareness of our project and the benefits of participation, expand advertising at our medical school to increase student participation, and increase follow-up education in the postpartum period.
Another future direction is to include local, free doula services, which are offered through Catholic Charities in San Antonio. Doulas provide antepartum, intrapartum, and postpartum services, which we believe will help our patients through advocacy and support for sobriety during this emotional and stressful time.
Conclusion
Counseled participants were receptive to learning about the effects of OUD and methadone on themselves and their newborn. Participants unanimously stated that learning more about OUD increased their motivation for sobriety. It was also clear that the increased motivation to be sober during pregnancy, as compared to before pregnancy, is an opportunity to help these women take steps to get sober. Patients also advanced their breastfeeding knowledge, as we helped debunk falsehoods surrounding breastfeeding while on methadone, and we anticipate this will lead to greater breastfeeding rates for our patients on methadone, although this was not specifically studied. Finally, patients learned about patient-provider confidentiality, which allowed for more open and clear communication with patients so they could be cared for to the greatest degree and trust could remain paramount.
Drug use is a common problem in the health care system, and exposure to patients with addiction is important for medical students in training. We believe that attending the Mommies Program allowed medical students to gain exposure and skills to better help patients with OUD.
Corresponding author: Nicholas Stansbury, MD, Nmstansbury85@gmail.com.
Financial disclosures: None.
1. Centers for Disease Control and Prevention. Opioid painkiller prescribing: where you live makes a difference. CDC website. www.cdc.gov/vitalsigns/opioid-prescribing. Accessed October 28, 2020.
2. Substance Abuse and Mental Health Services Administration. Drug Abuse Warning Network, 2011: national estimates of drug-related emergency department visits. HHS Publication No. (SMA) 13-4760, DAWN Series D-39. Rockville (MD): SAMHSA; 2013. www.samhsa.gov/data/sites/default/files/DAWN2k11ED/DAWN2k11ED/DAWN2k11ED.pdf. Accessed October 28, 2020.
3. Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374:154-63.
4. National Center for Health Statistics. NCHS data on drug-poisoning deaths. NCHS Factsheet. https://www.cdc.gov/nchs/data/factsheets/factsheet-drug-poisoning-H.pdf. Accessed October 28, 2020.
5. National Institute on Drug Abuse. America’s addiction to opioids: heroin and prescription drug abuse. Bethesda (MD): NIDA; 2014. www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2016/americas-addiction-to-opioids-heroin-prescription-drug-abuse. Accessed October 28, 2020.
6. Substance Abuse and Mental Health Services Administration (SAMHSA). Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: SAMHSA, 2011 Contract No.: HHS Publication no. (SMA) 11–4658.
7. Maeda A, Bateman BT, Clancy CR, et al. Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology. 2014;121:1158-1165.
8. Whiteman VE, Salemi JL, Mogos MF, et al. Maternal opioid drug use during pregnancy and its impact on perinatal morbidity, mortality, and the costs of medical care in the United States. J Pregnancy. 2014;2014:1-8
9. Pregnancy Mortality Surveillance System. www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm#trends. Accessed February 4, 2020.
10. Macdorman MF, Declercq E, Cabral H, Morton C. Recent increases in the U.S. maternal mortality rate. Obstet Gynecol. 2016;128:447-455.
11. Texas Health and Human Services. Maternal Mortality and Morbidity Task Force and Department of State Health Services Joint Biennial Report, September 2018. www.dshs.texas.gov/legislative/2018-Reports/MMMTFJointReport2018.pdf
12. Virginia Department of Health. Pregnancy-associated deaths from drug overdose in Virginia, 1999-2007: a report from the Virginia Maternal Mortality Review Team. Richmond, VA: VDH; 2015. www.vdh.virginia.gov/content/uploads/sites/18/2016/04/Final-Pregnancy-Associated-Deaths-Due-to-Drug-Overdose.pdf. Accessed October 28, 2020.
13. Maryland Department of Health and Mental Hygiene. Maryland maternal mortality review 2016 annual report. Baltimore: DHMH; 2016. https://phpa.health.maryland.gov/Documents/Maryland-Maternal-Mortality-Review-2016-Report.pdf. Accessed October 28, 2020.
14. Desai RJ, Hernandez-Diaz S, Bateman BT, Huybrechts KF. Increase in prescription opioid use during pregnancy among Medicaid-enrolled women. Obstet Gynecol. 2014;123:997-1002.
15. Reddy UM, Davis JM, Ren Z, et al. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes. Obstet Gynecol Survey. 2017;72:703-705.
16. Patrick SW, Davis MM, Lehmann CU, Cooper WO. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J Perinatol. 2015;35:650-655.
17. Center for Substance Abuse Treatment. Medication-assisted treatment for opioid addiction during pregnancy. In: Medication-assisted treatment for opioid addiction in opioid treatment programs. Treatment Improvement Protocol (TIP) Series, No. 43. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2005:211-224.
18. Wojnar-Horton RE, Kristensen JH, Yapp P, et al. Methadone distribution and excretion into breast milk of clients in a methadone maintenance programme. Br J Clin Pharmacol. 1997;44:543-547.
19. Reece-Stremtan S, Marinelli KA. ABM clinical protocol #21: guidelines for breastfeeding and substance use or substance use disorder, revised 2015. Breastfeed Med. 2015;10:135-141.
20. Sachs HC. The transfer of drugs and therapeutics into human breast milk: an update on selected topics. Committee on Drugs. Pediatrics. 2013;132:e796-809.
21. Bagley SM, Wachman EM, Holland E, Brogly SB. Review of the assessment and management of neonatal abstinence syndrome. Addict Sci Clin Pract. 2014;9:19.
22. Opioid use and opioid use disorder in pregnancy. Committee Opinion No. 711. Obstet Gynecol. 2017;130:488-489.
23. Gopman S. Prenatal and postpartum care of women with substance use disorders. Obstet Gynecol Clin North Am. 2014;41:213-228.
24. Mitchell M, Severtson S, Latimer W. Pregnancy and race/ethnicity as predictors of motivation for drug treatment. Am J Drug Alcohol Abuse. 2008;34:397-404.
From the UT Health Long School of Medicine San Antonio, Texas.
Abstract
Objective: To educate pregnant patients with opioid use disorder (OUD) about the effects of opioids in order to improve understanding and help achieve sustained abstinence.
Methods: The Center for Health Care Services and University Hospital System (UHS) in San Antonio, TX, jointly o
Results: Of 68 women enrolled in the program, 33 completed both the pre-survey and the post-survey (48.5%). Nearly half (48%) were very motivated to quit before pregnancy, but 85% were very motivated to quit once pregnant. All participants said learning more about the effects of opiates would increase motivation for sobriety. Prior to the educational intervention, 39% of participants knew it was safe to breastfeed on methadone, which improved to 97% in the post-survey, and 76% incorrectly thought they would be reported to authorities by their health care providers if they used illegal drugs during pregnancy, while in the post-survey, 100% knew they would not be reported for doing so.
Conclusion: Pregnancy and education about opioids increased patients’ motivation to quit. Patients also advanced their breastfeeding knowledge and learned about patient-provider confidentiality. Our greatest challenge was participant follow-up; however, this improved with the help of a full-time Mommies Program nurse. Our future aim is to increase project awareness and extend the educational research.
Keywords: pregnancy; addiction; opioids; OUD; counseling.
In 2012 more than 259 million prescriptions for opioids were written in the United States, which was a 200% increase since 1998.1 Since the early 2000s, admissions to opioid substance abuse programs and the death rate from opioids have quadrupled.2-4 Specifically, the rate of heroin use increased more than 300% from 2010 to 2014.5 Opioid use in pregnancy has also escalated in recent years, with a 3- to 4-fold increase from 2000 to 2009 and with 4 in 1000 deliveries being complicated by opioid use disorder (OUD) in 2011.6-8
Between 2000 and 2014, the maternal mortality rate in the United States increased 24%, making it the only industrialized nation with a maternal mortality rate that is rising rather than falling.9 The Texas Maternal Mortality and Morbidity Task Force found that between 2012 and 2015 drug overdose was the leading cause of maternal death in the period from delivery to 365 days postpartum, and it has increased dramatically since 2010.10,11
In addition, maternal mortality reviews in several states have identified substance use as a major risk factor for pregnancy-associated deaths.12,13 In Texas between 2012 and 2015, opioids were found in 58% of maternal drug overdoses.10 In 2007, 22.8% of women who were enrolled in Medicaid programs in 46 states filled an opioid prescription during pregnancy.14 Additionally, the rising prevalence of opioid use in pregnancy has led to a sharp increase in neonatal abstinence syndrome (NAS), rising from 1.5 cases per 1000 hospital births in 1999 to 6.0 per 1000 hospital births in 2013.15 Unsurprisingly, states with the highest rates of opioid prescribing also have the highest rates of NAS.16
Methadone combined with counseling and behavioral therapy has been the standard of care for the treatment of OUD in pregnancy since the 1970s. Methadone treatment prevents opioid withdrawal symptoms and increases adherence to prenatal care.17 One of the largest methadone treatment clinics in the San Antonio, TX, area is the Center for Health Care Services (CHCS). University Health System in San Antonio (UHS) has established a clinic called The Mommies Program, where mothers addicted to opioids can receive prenatal care by a dedicated physician, registered nurse, and a certified nurse midwife, who work in collaboration with the CHCS methadone clinic. Pregnant patients with OUD in pregnancy are concurrently enrolled in the Mommies Program and receive prenatal care through UHS and methadone treatment and counseling through CHCS. The continuity effort aims to increase prenatal care rates and adherence to methadone treatment.
Once mothers are off illicit opioids and on methadone, it is essential to discuss breastfeeding with them, as many mothers addicted to illicit opioids may have been told that they should not be breastfeeding. However, breastfeeding should be encouraged in women who are stable on methadone if they are not using illicit drugs and do not have other contraindications, regardless of maternal methadone dose, since the transfer of methadone into breast milk is minimal.18-20 Breastfeeding is beneficial in women taking methadone and has been associated with decreased severity of NAS symptoms, decreased need for pharmacotherapy, and a shorter hospital stay for the baby.21 In addition, breastfeeding contributes to the development of an attachment between mother and infant, while also providing the infant with natural immunity. Women should be counseled about the need to stop breastfeeding in the event of a relapse.22
Finally, the postpartum period represents a time of increased stressors, such as loss of sleep, child protective services involvement, and frustration with constant demands from new baby. For mothers with addiction, this is an especially sensitive time, as the stressors may be exacerbated by their new sobriety and a sudden end to the motivation they experienced from pregnancy.23 Therefore, early and frequent postpartum care with methadone dose evaluation is essential in order to decrease drug relapse and screen for postpartum depression in detail, since patients with a history of drug use are at increased risk of postpartum depression.
In 2017 medical students at UT Health Long School of Medicine in San Antonio created a project to educate women about OUD in pregnancy and provide motivational incentives for sustained abstinence; this project has continued each year since. Students provide education about methadone treatment and the dangers of using illicit opioids during and after pregnancy. Students especially focus on educating patients on the key problem areas in the literature, such as overdose, NAS, breastfeeding, postpartum substance use, and postpartum depression.
Methods
From October 2018 to February 2020, a total of 15 medical students volunteered between 1 and 20 times at the Mommies Program clinic, which was held once or twice per week from 8
The only inclusion criteria for participating in the educational intervention and survey was participants had to be 18 years of age or older and enrolled in the Mommies Program. Patients who met the inclusion criteria and agreed to participate completed a pre-survey administered by the students during the patient’s initial prenatal visit (Figure 2). This survey collected baseline information about the patient’s history with opioid use and their current knowledge of methadone treatment, NAS, legal aspects of drug use disclosure, and drug testing prior to the education portion of the encounter. After the pre-survey was administered, students spent 30 minutes reviewing the correct answers of the survey with the patients by utilizing the standardized handout to help patients understand details of methadone and opioid use in pregnancy (Figure 1). The post-survey was administered by a student once patients entered the third trimester to assess whether the education session increased patients’ knowledge of these topics.
At the time patients completed the post-survey, they received a Baby Bag as well as education regarding each item in the bag. The aim of distributing Baby Bags was to relieve some possible postnatal stressors and educate the patients about infant care. Items included in the bag were diapers, wipes, bottles, clothes, and swaddles. Prenatal vitamins were added in January 2020, as many patients struggle to afford vitamins if they are not currently covered by Medicaid or have other barriers. The Baby Bag items were purchased through a Community Service Learning grant through UT Health San Antonio.
Results
Of 68 women enrolled in the Mommies Program during the intervention period, 33 completed the pre-survey and the post-survey (48.5%). Even though all patients enrolled in the program met the inclusion criteria, patients were not included in the educational program for multiple reasons, including refusal to participate, poor clinic follow-up, or lack of students to collect surveys. However, all patients who completed the pre-survey did complete the post-survey. In the pre-survey, only 39% of participants knew it was safe to breastfeed while on methadone. In the post-survey, 97% knew it safe to breastfeed. Nearly half (48%) reported being very motivated to quit opioids before pregnancy, but 85% were very motivated to quit once pregnant. In the pre-survey, 76% incorrectly thought they would be reported to authorities by their health providers if they used illegal drugs during pregnancy, while in the post-survey, 100% knew they would not be reported for doing so. Also, all participants said learning more about the effects of opiates would increase motivation for sobriety.
Discussion
Questions assessed during the educational surveys revolved around patients’ knowledge of the intricacies, legally and physiologically, of methadone treatment for OUD, as well as beneficial aspects for patients and future child health, such as breastfeeding and motivation to quit and stay sober.
It was clear that there was a lack of knowledge and education about breastfeeding, as only 39% of the participants thought that it was safe to breastfeed while on methadone in the pre-survey; in the post survey, this improved to 97%. Students spent a large portion of the educational time going over the safety of breastfeeding for patients on methadone and the many benefits to mother and baby. Students also reviewed breastfeeding with patients every time patients came in for a visit and debunked any falsehoods about the negatives of breastfeeding while on methadone. This is another testament to the benefits of reinforcement around patient education.
The area of trust between provider and patient is essential in all provider-patient relationships. However, in the area of addiction, a trusting bond is especially important, as patients must feel confident and comfortable to disclose every aspect of their lives so the provider can give the best care. It was clear from our initial data that many patients did not feel this trust or understand the legal aspects regarding the provider-patient relationship in the terms of drug use, as the pre-survey shows 76% of patients originally thought they would be reported to authorities if they told their provider they used illegal drugs during pregnancy. This was an enormous issue in the clinic and something that needed to be addressed because, based on these data, we feared many patients would not be honest about using illegal drugs to supplement their methadone if they believed they would be reported to the authorities or even jailed. The medical student education team continually assured patients that their honesty about illegal drug use during pregnancy would not be revealed to the authorities, and also made it clear to patients that it was essential they were honest about illegal drug use so the optimal care could be provided by the team. These discussions were successful, as the post-survey showed that 100% of patients knew they would not be reported to the authorities if they used illegal drugs during the pregnancy. This showed an increase in knowledge, but also suggested an increase in confidence in the provider-patient relationship by patients, which we speculate allowed for a better patient experience, better patient outcomes, and less emotional stress for the patient and provider.
Last, we wanted to study and address the motivation to quit using drugs and stay sober through learning about the effects of opiates and how this motivation was related to pregnancy. A study by Mitchell et al makes clear that pregnancy is a motivation to seek treatment for drug use and to quit,24 and our survey data support these findings, with 48% of patients motivated to quit before they were pregnant and 85% motivated to quit once they knew they were pregnant. In addition, all patients attested on the pre- and post-survey that learning more about opioids would increase their motivation for sobriety. Therefore, we believe education about the use of opioids and other drugs is a strong motivation towards sobriety and should be further studied in methadone treatment and other drugs as well.
We will continue to focus on sobriety postpartum by using the education in pregnancy as a springboard to further postpartum education, as education seems to be very beneficial to future sobriety. In the future, we believe extending the educational program past pregnancy and discussing opioid use and addiction with patients at multiple follow-up visits will be beneficial to patients’ sobriety.
We faced 2 main challenges in implementing this intervention and survey: patients would often miss multiple appointments during their third trimester or would not attend their postpartum visit if they only had 1 prenatal visit; and many clinic sessions had low student attendance because students often had many other responsibilities in medical school and there were only 15 volunteers over the study time. These challenges decreased our post-survey completion rate. However, there has been improvement in follow-up as the project has continued. The Mommies Program now has a full-time registered nurse, and a larger number of medical student teachers have volunteered to attend the clinic. In the future, we aim to increase awareness of our project and the benefits of participation, expand advertising at our medical school to increase student participation, and increase follow-up education in the postpartum period.
Another future direction is to include local, free doula services, which are offered through Catholic Charities in San Antonio. Doulas provide antepartum, intrapartum, and postpartum services, which we believe will help our patients through advocacy and support for sobriety during this emotional and stressful time.
Conclusion
Counseled participants were receptive to learning about the effects of OUD and methadone on themselves and their newborn. Participants unanimously stated that learning more about OUD increased their motivation for sobriety. It was also clear that the increased motivation to be sober during pregnancy, as compared to before pregnancy, is an opportunity to help these women take steps to get sober. Patients also advanced their breastfeeding knowledge, as we helped debunk falsehoods surrounding breastfeeding while on methadone, and we anticipate this will lead to greater breastfeeding rates for our patients on methadone, although this was not specifically studied. Finally, patients learned about patient-provider confidentiality, which allowed for more open and clear communication with patients so they could be cared for to the greatest degree and trust could remain paramount.
Drug use is a common problem in the health care system, and exposure to patients with addiction is important for medical students in training. We believe that attending the Mommies Program allowed medical students to gain exposure and skills to better help patients with OUD.
Corresponding author: Nicholas Stansbury, MD, Nmstansbury85@gmail.com.
Financial disclosures: None.
From the UT Health Long School of Medicine San Antonio, Texas.
Abstract
Objective: To educate pregnant patients with opioid use disorder (OUD) about the effects of opioids in order to improve understanding and help achieve sustained abstinence.
Methods: The Center for Health Care Services and University Hospital System (UHS) in San Antonio, TX, jointly o
Results: Of 68 women enrolled in the program, 33 completed both the pre-survey and the post-survey (48.5%). Nearly half (48%) were very motivated to quit before pregnancy, but 85% were very motivated to quit once pregnant. All participants said learning more about the effects of opiates would increase motivation for sobriety. Prior to the educational intervention, 39% of participants knew it was safe to breastfeed on methadone, which improved to 97% in the post-survey, and 76% incorrectly thought they would be reported to authorities by their health care providers if they used illegal drugs during pregnancy, while in the post-survey, 100% knew they would not be reported for doing so.
Conclusion: Pregnancy and education about opioids increased patients’ motivation to quit. Patients also advanced their breastfeeding knowledge and learned about patient-provider confidentiality. Our greatest challenge was participant follow-up; however, this improved with the help of a full-time Mommies Program nurse. Our future aim is to increase project awareness and extend the educational research.
Keywords: pregnancy; addiction; opioids; OUD; counseling.
In 2012 more than 259 million prescriptions for opioids were written in the United States, which was a 200% increase since 1998.1 Since the early 2000s, admissions to opioid substance abuse programs and the death rate from opioids have quadrupled.2-4 Specifically, the rate of heroin use increased more than 300% from 2010 to 2014.5 Opioid use in pregnancy has also escalated in recent years, with a 3- to 4-fold increase from 2000 to 2009 and with 4 in 1000 deliveries being complicated by opioid use disorder (OUD) in 2011.6-8
Between 2000 and 2014, the maternal mortality rate in the United States increased 24%, making it the only industrialized nation with a maternal mortality rate that is rising rather than falling.9 The Texas Maternal Mortality and Morbidity Task Force found that between 2012 and 2015 drug overdose was the leading cause of maternal death in the period from delivery to 365 days postpartum, and it has increased dramatically since 2010.10,11
In addition, maternal mortality reviews in several states have identified substance use as a major risk factor for pregnancy-associated deaths.12,13 In Texas between 2012 and 2015, opioids were found in 58% of maternal drug overdoses.10 In 2007, 22.8% of women who were enrolled in Medicaid programs in 46 states filled an opioid prescription during pregnancy.14 Additionally, the rising prevalence of opioid use in pregnancy has led to a sharp increase in neonatal abstinence syndrome (NAS), rising from 1.5 cases per 1000 hospital births in 1999 to 6.0 per 1000 hospital births in 2013.15 Unsurprisingly, states with the highest rates of opioid prescribing also have the highest rates of NAS.16
Methadone combined with counseling and behavioral therapy has been the standard of care for the treatment of OUD in pregnancy since the 1970s. Methadone treatment prevents opioid withdrawal symptoms and increases adherence to prenatal care.17 One of the largest methadone treatment clinics in the San Antonio, TX, area is the Center for Health Care Services (CHCS). University Health System in San Antonio (UHS) has established a clinic called The Mommies Program, where mothers addicted to opioids can receive prenatal care by a dedicated physician, registered nurse, and a certified nurse midwife, who work in collaboration with the CHCS methadone clinic. Pregnant patients with OUD in pregnancy are concurrently enrolled in the Mommies Program and receive prenatal care through UHS and methadone treatment and counseling through CHCS. The continuity effort aims to increase prenatal care rates and adherence to methadone treatment.
Once mothers are off illicit opioids and on methadone, it is essential to discuss breastfeeding with them, as many mothers addicted to illicit opioids may have been told that they should not be breastfeeding. However, breastfeeding should be encouraged in women who are stable on methadone if they are not using illicit drugs and do not have other contraindications, regardless of maternal methadone dose, since the transfer of methadone into breast milk is minimal.18-20 Breastfeeding is beneficial in women taking methadone and has been associated with decreased severity of NAS symptoms, decreased need for pharmacotherapy, and a shorter hospital stay for the baby.21 In addition, breastfeeding contributes to the development of an attachment between mother and infant, while also providing the infant with natural immunity. Women should be counseled about the need to stop breastfeeding in the event of a relapse.22
Finally, the postpartum period represents a time of increased stressors, such as loss of sleep, child protective services involvement, and frustration with constant demands from new baby. For mothers with addiction, this is an especially sensitive time, as the stressors may be exacerbated by their new sobriety and a sudden end to the motivation they experienced from pregnancy.23 Therefore, early and frequent postpartum care with methadone dose evaluation is essential in order to decrease drug relapse and screen for postpartum depression in detail, since patients with a history of drug use are at increased risk of postpartum depression.
In 2017 medical students at UT Health Long School of Medicine in San Antonio created a project to educate women about OUD in pregnancy and provide motivational incentives for sustained abstinence; this project has continued each year since. Students provide education about methadone treatment and the dangers of using illicit opioids during and after pregnancy. Students especially focus on educating patients on the key problem areas in the literature, such as overdose, NAS, breastfeeding, postpartum substance use, and postpartum depression.
Methods
From October 2018 to February 2020, a total of 15 medical students volunteered between 1 and 20 times at the Mommies Program clinic, which was held once or twice per week from 8
The only inclusion criteria for participating in the educational intervention and survey was participants had to be 18 years of age or older and enrolled in the Mommies Program. Patients who met the inclusion criteria and agreed to participate completed a pre-survey administered by the students during the patient’s initial prenatal visit (Figure 2). This survey collected baseline information about the patient’s history with opioid use and their current knowledge of methadone treatment, NAS, legal aspects of drug use disclosure, and drug testing prior to the education portion of the encounter. After the pre-survey was administered, students spent 30 minutes reviewing the correct answers of the survey with the patients by utilizing the standardized handout to help patients understand details of methadone and opioid use in pregnancy (Figure 1). The post-survey was administered by a student once patients entered the third trimester to assess whether the education session increased patients’ knowledge of these topics.
At the time patients completed the post-survey, they received a Baby Bag as well as education regarding each item in the bag. The aim of distributing Baby Bags was to relieve some possible postnatal stressors and educate the patients about infant care. Items included in the bag were diapers, wipes, bottles, clothes, and swaddles. Prenatal vitamins were added in January 2020, as many patients struggle to afford vitamins if they are not currently covered by Medicaid or have other barriers. The Baby Bag items were purchased through a Community Service Learning grant through UT Health San Antonio.
Results
Of 68 women enrolled in the Mommies Program during the intervention period, 33 completed the pre-survey and the post-survey (48.5%). Even though all patients enrolled in the program met the inclusion criteria, patients were not included in the educational program for multiple reasons, including refusal to participate, poor clinic follow-up, or lack of students to collect surveys. However, all patients who completed the pre-survey did complete the post-survey. In the pre-survey, only 39% of participants knew it was safe to breastfeed while on methadone. In the post-survey, 97% knew it safe to breastfeed. Nearly half (48%) reported being very motivated to quit opioids before pregnancy, but 85% were very motivated to quit once pregnant. In the pre-survey, 76% incorrectly thought they would be reported to authorities by their health providers if they used illegal drugs during pregnancy, while in the post-survey, 100% knew they would not be reported for doing so. Also, all participants said learning more about the effects of opiates would increase motivation for sobriety.
Discussion
Questions assessed during the educational surveys revolved around patients’ knowledge of the intricacies, legally and physiologically, of methadone treatment for OUD, as well as beneficial aspects for patients and future child health, such as breastfeeding and motivation to quit and stay sober.
It was clear that there was a lack of knowledge and education about breastfeeding, as only 39% of the participants thought that it was safe to breastfeed while on methadone in the pre-survey; in the post survey, this improved to 97%. Students spent a large portion of the educational time going over the safety of breastfeeding for patients on methadone and the many benefits to mother and baby. Students also reviewed breastfeeding with patients every time patients came in for a visit and debunked any falsehoods about the negatives of breastfeeding while on methadone. This is another testament to the benefits of reinforcement around patient education.
The area of trust between provider and patient is essential in all provider-patient relationships. However, in the area of addiction, a trusting bond is especially important, as patients must feel confident and comfortable to disclose every aspect of their lives so the provider can give the best care. It was clear from our initial data that many patients did not feel this trust or understand the legal aspects regarding the provider-patient relationship in the terms of drug use, as the pre-survey shows 76% of patients originally thought they would be reported to authorities if they told their provider they used illegal drugs during pregnancy. This was an enormous issue in the clinic and something that needed to be addressed because, based on these data, we feared many patients would not be honest about using illegal drugs to supplement their methadone if they believed they would be reported to the authorities or even jailed. The medical student education team continually assured patients that their honesty about illegal drug use during pregnancy would not be revealed to the authorities, and also made it clear to patients that it was essential they were honest about illegal drug use so the optimal care could be provided by the team. These discussions were successful, as the post-survey showed that 100% of patients knew they would not be reported to the authorities if they used illegal drugs during the pregnancy. This showed an increase in knowledge, but also suggested an increase in confidence in the provider-patient relationship by patients, which we speculate allowed for a better patient experience, better patient outcomes, and less emotional stress for the patient and provider.
Last, we wanted to study and address the motivation to quit using drugs and stay sober through learning about the effects of opiates and how this motivation was related to pregnancy. A study by Mitchell et al makes clear that pregnancy is a motivation to seek treatment for drug use and to quit,24 and our survey data support these findings, with 48% of patients motivated to quit before they were pregnant and 85% motivated to quit once they knew they were pregnant. In addition, all patients attested on the pre- and post-survey that learning more about opioids would increase their motivation for sobriety. Therefore, we believe education about the use of opioids and other drugs is a strong motivation towards sobriety and should be further studied in methadone treatment and other drugs as well.
We will continue to focus on sobriety postpartum by using the education in pregnancy as a springboard to further postpartum education, as education seems to be very beneficial to future sobriety. In the future, we believe extending the educational program past pregnancy and discussing opioid use and addiction with patients at multiple follow-up visits will be beneficial to patients’ sobriety.
We faced 2 main challenges in implementing this intervention and survey: patients would often miss multiple appointments during their third trimester or would not attend their postpartum visit if they only had 1 prenatal visit; and many clinic sessions had low student attendance because students often had many other responsibilities in medical school and there were only 15 volunteers over the study time. These challenges decreased our post-survey completion rate. However, there has been improvement in follow-up as the project has continued. The Mommies Program now has a full-time registered nurse, and a larger number of medical student teachers have volunteered to attend the clinic. In the future, we aim to increase awareness of our project and the benefits of participation, expand advertising at our medical school to increase student participation, and increase follow-up education in the postpartum period.
Another future direction is to include local, free doula services, which are offered through Catholic Charities in San Antonio. Doulas provide antepartum, intrapartum, and postpartum services, which we believe will help our patients through advocacy and support for sobriety during this emotional and stressful time.
Conclusion
Counseled participants were receptive to learning about the effects of OUD and methadone on themselves and their newborn. Participants unanimously stated that learning more about OUD increased their motivation for sobriety. It was also clear that the increased motivation to be sober during pregnancy, as compared to before pregnancy, is an opportunity to help these women take steps to get sober. Patients also advanced their breastfeeding knowledge, as we helped debunk falsehoods surrounding breastfeeding while on methadone, and we anticipate this will lead to greater breastfeeding rates for our patients on methadone, although this was not specifically studied. Finally, patients learned about patient-provider confidentiality, which allowed for more open and clear communication with patients so they could be cared for to the greatest degree and trust could remain paramount.
Drug use is a common problem in the health care system, and exposure to patients with addiction is important for medical students in training. We believe that attending the Mommies Program allowed medical students to gain exposure and skills to better help patients with OUD.
Corresponding author: Nicholas Stansbury, MD, Nmstansbury85@gmail.com.
Financial disclosures: None.
1. Centers for Disease Control and Prevention. Opioid painkiller prescribing: where you live makes a difference. CDC website. www.cdc.gov/vitalsigns/opioid-prescribing. Accessed October 28, 2020.
2. Substance Abuse and Mental Health Services Administration. Drug Abuse Warning Network, 2011: national estimates of drug-related emergency department visits. HHS Publication No. (SMA) 13-4760, DAWN Series D-39. Rockville (MD): SAMHSA; 2013. www.samhsa.gov/data/sites/default/files/DAWN2k11ED/DAWN2k11ED/DAWN2k11ED.pdf. Accessed October 28, 2020.
3. Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374:154-63.
4. National Center for Health Statistics. NCHS data on drug-poisoning deaths. NCHS Factsheet. https://www.cdc.gov/nchs/data/factsheets/factsheet-drug-poisoning-H.pdf. Accessed October 28, 2020.
5. National Institute on Drug Abuse. America’s addiction to opioids: heroin and prescription drug abuse. Bethesda (MD): NIDA; 2014. www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2016/americas-addiction-to-opioids-heroin-prescription-drug-abuse. Accessed October 28, 2020.
6. Substance Abuse and Mental Health Services Administration (SAMHSA). Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: SAMHSA, 2011 Contract No.: HHS Publication no. (SMA) 11–4658.
7. Maeda A, Bateman BT, Clancy CR, et al. Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology. 2014;121:1158-1165.
8. Whiteman VE, Salemi JL, Mogos MF, et al. Maternal opioid drug use during pregnancy and its impact on perinatal morbidity, mortality, and the costs of medical care in the United States. J Pregnancy. 2014;2014:1-8
9. Pregnancy Mortality Surveillance System. www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm#trends. Accessed February 4, 2020.
10. Macdorman MF, Declercq E, Cabral H, Morton C. Recent increases in the U.S. maternal mortality rate. Obstet Gynecol. 2016;128:447-455.
11. Texas Health and Human Services. Maternal Mortality and Morbidity Task Force and Department of State Health Services Joint Biennial Report, September 2018. www.dshs.texas.gov/legislative/2018-Reports/MMMTFJointReport2018.pdf
12. Virginia Department of Health. Pregnancy-associated deaths from drug overdose in Virginia, 1999-2007: a report from the Virginia Maternal Mortality Review Team. Richmond, VA: VDH; 2015. www.vdh.virginia.gov/content/uploads/sites/18/2016/04/Final-Pregnancy-Associated-Deaths-Due-to-Drug-Overdose.pdf. Accessed October 28, 2020.
13. Maryland Department of Health and Mental Hygiene. Maryland maternal mortality review 2016 annual report. Baltimore: DHMH; 2016. https://phpa.health.maryland.gov/Documents/Maryland-Maternal-Mortality-Review-2016-Report.pdf. Accessed October 28, 2020.
14. Desai RJ, Hernandez-Diaz S, Bateman BT, Huybrechts KF. Increase in prescription opioid use during pregnancy among Medicaid-enrolled women. Obstet Gynecol. 2014;123:997-1002.
15. Reddy UM, Davis JM, Ren Z, et al. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes. Obstet Gynecol Survey. 2017;72:703-705.
16. Patrick SW, Davis MM, Lehmann CU, Cooper WO. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J Perinatol. 2015;35:650-655.
17. Center for Substance Abuse Treatment. Medication-assisted treatment for opioid addiction during pregnancy. In: Medication-assisted treatment for opioid addiction in opioid treatment programs. Treatment Improvement Protocol (TIP) Series, No. 43. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2005:211-224.
18. Wojnar-Horton RE, Kristensen JH, Yapp P, et al. Methadone distribution and excretion into breast milk of clients in a methadone maintenance programme. Br J Clin Pharmacol. 1997;44:543-547.
19. Reece-Stremtan S, Marinelli KA. ABM clinical protocol #21: guidelines for breastfeeding and substance use or substance use disorder, revised 2015. Breastfeed Med. 2015;10:135-141.
20. Sachs HC. The transfer of drugs and therapeutics into human breast milk: an update on selected topics. Committee on Drugs. Pediatrics. 2013;132:e796-809.
21. Bagley SM, Wachman EM, Holland E, Brogly SB. Review of the assessment and management of neonatal abstinence syndrome. Addict Sci Clin Pract. 2014;9:19.
22. Opioid use and opioid use disorder in pregnancy. Committee Opinion No. 711. Obstet Gynecol. 2017;130:488-489.
23. Gopman S. Prenatal and postpartum care of women with substance use disorders. Obstet Gynecol Clin North Am. 2014;41:213-228.
24. Mitchell M, Severtson S, Latimer W. Pregnancy and race/ethnicity as predictors of motivation for drug treatment. Am J Drug Alcohol Abuse. 2008;34:397-404.
1. Centers for Disease Control and Prevention. Opioid painkiller prescribing: where you live makes a difference. CDC website. www.cdc.gov/vitalsigns/opioid-prescribing. Accessed October 28, 2020.
2. Substance Abuse and Mental Health Services Administration. Drug Abuse Warning Network, 2011: national estimates of drug-related emergency department visits. HHS Publication No. (SMA) 13-4760, DAWN Series D-39. Rockville (MD): SAMHSA; 2013. www.samhsa.gov/data/sites/default/files/DAWN2k11ED/DAWN2k11ED/DAWN2k11ED.pdf. Accessed October 28, 2020.
3. Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374:154-63.
4. National Center for Health Statistics. NCHS data on drug-poisoning deaths. NCHS Factsheet. https://www.cdc.gov/nchs/data/factsheets/factsheet-drug-poisoning-H.pdf. Accessed October 28, 2020.
5. National Institute on Drug Abuse. America’s addiction to opioids: heroin and prescription drug abuse. Bethesda (MD): NIDA; 2014. www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2016/americas-addiction-to-opioids-heroin-prescription-drug-abuse. Accessed October 28, 2020.
6. Substance Abuse and Mental Health Services Administration (SAMHSA). Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: SAMHSA, 2011 Contract No.: HHS Publication no. (SMA) 11–4658.
7. Maeda A, Bateman BT, Clancy CR, et al. Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology. 2014;121:1158-1165.
8. Whiteman VE, Salemi JL, Mogos MF, et al. Maternal opioid drug use during pregnancy and its impact on perinatal morbidity, mortality, and the costs of medical care in the United States. J Pregnancy. 2014;2014:1-8
9. Pregnancy Mortality Surveillance System. www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm#trends. Accessed February 4, 2020.
10. Macdorman MF, Declercq E, Cabral H, Morton C. Recent increases in the U.S. maternal mortality rate. Obstet Gynecol. 2016;128:447-455.
11. Texas Health and Human Services. Maternal Mortality and Morbidity Task Force and Department of State Health Services Joint Biennial Report, September 2018. www.dshs.texas.gov/legislative/2018-Reports/MMMTFJointReport2018.pdf
12. Virginia Department of Health. Pregnancy-associated deaths from drug overdose in Virginia, 1999-2007: a report from the Virginia Maternal Mortality Review Team. Richmond, VA: VDH; 2015. www.vdh.virginia.gov/content/uploads/sites/18/2016/04/Final-Pregnancy-Associated-Deaths-Due-to-Drug-Overdose.pdf. Accessed October 28, 2020.
13. Maryland Department of Health and Mental Hygiene. Maryland maternal mortality review 2016 annual report. Baltimore: DHMH; 2016. https://phpa.health.maryland.gov/Documents/Maryland-Maternal-Mortality-Review-2016-Report.pdf. Accessed October 28, 2020.
14. Desai RJ, Hernandez-Diaz S, Bateman BT, Huybrechts KF. Increase in prescription opioid use during pregnancy among Medicaid-enrolled women. Obstet Gynecol. 2014;123:997-1002.
15. Reddy UM, Davis JM, Ren Z, et al. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes. Obstet Gynecol Survey. 2017;72:703-705.
16. Patrick SW, Davis MM, Lehmann CU, Cooper WO. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J Perinatol. 2015;35:650-655.
17. Center for Substance Abuse Treatment. Medication-assisted treatment for opioid addiction during pregnancy. In: Medication-assisted treatment for opioid addiction in opioid treatment programs. Treatment Improvement Protocol (TIP) Series, No. 43. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2005:211-224.
18. Wojnar-Horton RE, Kristensen JH, Yapp P, et al. Methadone distribution and excretion into breast milk of clients in a methadone maintenance programme. Br J Clin Pharmacol. 1997;44:543-547.
19. Reece-Stremtan S, Marinelli KA. ABM clinical protocol #21: guidelines for breastfeeding and substance use or substance use disorder, revised 2015. Breastfeed Med. 2015;10:135-141.
20. Sachs HC. The transfer of drugs and therapeutics into human breast milk: an update on selected topics. Committee on Drugs. Pediatrics. 2013;132:e796-809.
21. Bagley SM, Wachman EM, Holland E, Brogly SB. Review of the assessment and management of neonatal abstinence syndrome. Addict Sci Clin Pract. 2014;9:19.
22. Opioid use and opioid use disorder in pregnancy. Committee Opinion No. 711. Obstet Gynecol. 2017;130:488-489.
23. Gopman S. Prenatal and postpartum care of women with substance use disorders. Obstet Gynecol Clin North Am. 2014;41:213-228.
24. Mitchell M, Severtson S, Latimer W. Pregnancy and race/ethnicity as predictors of motivation for drug treatment. Am J Drug Alcohol Abuse. 2008;34:397-404.
SABCS 2020: What’s hot, including a major chemotherapy trial
That’s the word from Virginia Kaklamani, MD, from the University of Texas Health Sciences Center San Antonio. Dr. Kaklamani, a professor of medicine in the division of hematology/oncology, is codirector of the meeting that runs online Dec. 8-11.
If the new trial sounds familiar, that’s because it’s a lot like the TAILORx trial, the results of which were first presented in 2018 and have changed practice in women with early-stage disease and no lymph node involvement.
“This is the lymph-node positive TAILORx. It’s extremely important,” Dr. Kaklamani said in an interview, adding that both trials involved women with hormone receptor (HR)–positive, HER2-negative disease.
If the RxPONDER trial shows similar outcomes between women randomized to adjuvant endocrine therapy alone versus endocrine therapy plus chemotherapy, then clinicians “can potentially avoid giving chemotherapy to a large number of women who are currently receiving it,” she explained.
Because women with nodal involvement (one to three positive axillary nodes) are at a higher risk of recurrence, RxPONDER may provide needed insight on the management of these types of breast cancers, Dr. Kaklamani suggested.
Both trials have used the 21-tumor gene expression assay (Oncotype Dx) to determine recurrence-risk status.
Dr. Kaklamani also spotlighted the phase 3 CONTESSA trial (abstract GS4-01) in 600+ patients with locally advanced or metastatic breast cancer that is HR positive and HER2 negative and has been previously treated with a taxane.
The trial features an experimental oral taxane, tesetaxel. The primary objective is to compare the efficacy of tesetaxel plus a reduced dose of capecitabine (Xeloda) versus the approved dose of capecitabine alone. Presented data will include progression-free survival results, indicating about a 3-month PFS advantage with tesetaxel, which is taken once every 3 weeks.
“Oral drugs are convenient for patients and, despite limitations, they are, all in all, a revolution in cancer treatment,” noted Dr. Kaklamani, adding that they beneficially eliminate the need for time-consuming infusions and related clinic visits as well as drug ports.
It will be interesting to see what Steven Vogl, MD, a private practitioner in New Yorky, has to say about CONTESSA and the rest of the SABCS.
He is usually a commentator from the meeting floor, whose self-introduction, “Vogl, New York,” is well known to perennial meeting attendees, according to a profile piece published some years ago.
This year the medical oncologist will also serve as the chair of the “View from the Trenches” session, which is devoted to summarizing the meeting’s most important findings for everyday practitioners.
A number of years ago, Dr. Vogl proposed the idea of this where-the-rubber-meets-the-road session to SABCS meeting planners, which they then adopted. This year, Dr. Kaklamani invited Dr. Vogl to run the session and he accepted.
Dr. Vogl is a “really smart guy who is always right on” with his comments and questions, and he will be the first-ever independent, community-based oncologist to chair a meeting session, said Dr. Kaklamani.
Other hot topics
Another hot topic featured at the meeting will be the use of CDK4/6 inhibitors in the adjuvant treatment of HR-positive and HER2-negative disease that has a high risk of recurrence, Dr. Kaklamani said. New data from two trials, monarchE and PENELOPE-B, will be presented.
First, there will be an update from the monarchE trial (abstract GS1-01). The first results from this trial were reported in September at the European Society for Medical Oncology Virtual Congress 2020. They showed that adding abemaciclib (Verzenio) to endocrine therapy reduced the risk of early recurrence. The positive outcome represented the first treatment improvement in this high-risk setting in more than 20 years, according to experts.
A similar trial, PENELOPE-B (abstract GS1-02), looks at palbociclib (Ibrance) in a somewhat different population – those patients with high relapse risk after neoadjuvant chemotherapy. “These are even higher risk ER+ patients [than those in monarchE], which is why they received chemotherapy before surgery,” commented Dr. Kaklamani.
In triple-negative disease, there will be overall survival (OS) results from the phase 3 KEYNOTE-355 study (abstract GS3-01) of pembrolizumab (Keytruda) versus placebo (plus chemotherapy for all patients) as first-line therapy for locally recurrent inoperable or metastatic triple-negative breast cancer. “It’s potentially a huge deal,” said Dr. Kaklamani about the OS data, if they are statistically significant.
A meta-analysis (abstract GS4-08) of data on circulating tumor cells (CTCs), which are shed from the primary tumor into the bloodstream, may point to their value as a tool to determine whether or not a breast cancer treatment is effective. “CTCs allow you to assess how a treatment is doing before you do scans, which typically occur 3 months or so later,” explained Dr. Kaklamani.
CTC results can be assessed in 3-4 weeks and allow clinicians to change treatments if CTC volume increases. However, a previous study of CTCs did not show a clinical benefit with the tool among patients treated mainly with chemotherapies. What’s different about the new study, which is from an international group of investigators, is in the treatments patients with metastatic breast cancer received. “This study is from a different era – with targeted therapies,” said Dr. Kaklamani.
In the new study, changes in CTC levels (with a reduction being a good result) between baseline (pretreatment) and follow-up were analyzed to determine whether they were associated with overall survival.
COVID sessions
On the meeting’s first day, SABCS will feature a special session on COVID-19 and breast cancer. The meeting organizers sought to separate the wheat from the chaff in this subject, as much has already been written, published, or presented.
“We received a lot of abstracts on COVID that were studies that were poorly done. We tried to tease through them and select the well-researched ones,” acknowledged Dr. Kaklamani.
The organizers included two patient advocates who have had COVID-19, including during treatment for breast cancer, as participants in the meeting session. The session will also feature global perspectives, with presenters from Brazil, Italy, and the Netherlands.
Plenary lectures
The meeting’s two plenary lectures will focus, respectively, on the increasingly used clinical approach of neoadjuvant therapy in breast cancer, and research in the time of a pandemic.
Elizabeth Mittendorf, MD, PhD, a surgical oncologist and director of the Breast lmmuno-Oncology program and co-director of the Breast Cancer Clinical Research Program at the Dana-Farber/Brigham and Women’s Cancer Center, Boston, will present “Local regional management following neoadjuvant therapy: Minding the knowledge gaps.”
Ned Sharpless, MD, director of the National Cancer Institute, will present “Advancing cancer research during challenging times.”
Dr. Kaklamani disclosed recieving consulting fees with Amgen, Eisai, Puma, Celldex, AstraZeneca, and Athenex; receiving fees for non-CME services received directly from commercial interest or their agents from Pfizer, Celgene, Genentech, Genomic Health, Puma, Eisai, and Novartis; and contracted research with Eisai.
This article first appeared on Medscape.com.
That’s the word from Virginia Kaklamani, MD, from the University of Texas Health Sciences Center San Antonio. Dr. Kaklamani, a professor of medicine in the division of hematology/oncology, is codirector of the meeting that runs online Dec. 8-11.
If the new trial sounds familiar, that’s because it’s a lot like the TAILORx trial, the results of which were first presented in 2018 and have changed practice in women with early-stage disease and no lymph node involvement.
“This is the lymph-node positive TAILORx. It’s extremely important,” Dr. Kaklamani said in an interview, adding that both trials involved women with hormone receptor (HR)–positive, HER2-negative disease.
If the RxPONDER trial shows similar outcomes between women randomized to adjuvant endocrine therapy alone versus endocrine therapy plus chemotherapy, then clinicians “can potentially avoid giving chemotherapy to a large number of women who are currently receiving it,” she explained.
Because women with nodal involvement (one to three positive axillary nodes) are at a higher risk of recurrence, RxPONDER may provide needed insight on the management of these types of breast cancers, Dr. Kaklamani suggested.
Both trials have used the 21-tumor gene expression assay (Oncotype Dx) to determine recurrence-risk status.
Dr. Kaklamani also spotlighted the phase 3 CONTESSA trial (abstract GS4-01) in 600+ patients with locally advanced or metastatic breast cancer that is HR positive and HER2 negative and has been previously treated with a taxane.
The trial features an experimental oral taxane, tesetaxel. The primary objective is to compare the efficacy of tesetaxel plus a reduced dose of capecitabine (Xeloda) versus the approved dose of capecitabine alone. Presented data will include progression-free survival results, indicating about a 3-month PFS advantage with tesetaxel, which is taken once every 3 weeks.
“Oral drugs are convenient for patients and, despite limitations, they are, all in all, a revolution in cancer treatment,” noted Dr. Kaklamani, adding that they beneficially eliminate the need for time-consuming infusions and related clinic visits as well as drug ports.
It will be interesting to see what Steven Vogl, MD, a private practitioner in New Yorky, has to say about CONTESSA and the rest of the SABCS.
He is usually a commentator from the meeting floor, whose self-introduction, “Vogl, New York,” is well known to perennial meeting attendees, according to a profile piece published some years ago.
This year the medical oncologist will also serve as the chair of the “View from the Trenches” session, which is devoted to summarizing the meeting’s most important findings for everyday practitioners.
A number of years ago, Dr. Vogl proposed the idea of this where-the-rubber-meets-the-road session to SABCS meeting planners, which they then adopted. This year, Dr. Kaklamani invited Dr. Vogl to run the session and he accepted.
Dr. Vogl is a “really smart guy who is always right on” with his comments and questions, and he will be the first-ever independent, community-based oncologist to chair a meeting session, said Dr. Kaklamani.
Other hot topics
Another hot topic featured at the meeting will be the use of CDK4/6 inhibitors in the adjuvant treatment of HR-positive and HER2-negative disease that has a high risk of recurrence, Dr. Kaklamani said. New data from two trials, monarchE and PENELOPE-B, will be presented.
First, there will be an update from the monarchE trial (abstract GS1-01). The first results from this trial were reported in September at the European Society for Medical Oncology Virtual Congress 2020. They showed that adding abemaciclib (Verzenio) to endocrine therapy reduced the risk of early recurrence. The positive outcome represented the first treatment improvement in this high-risk setting in more than 20 years, according to experts.
A similar trial, PENELOPE-B (abstract GS1-02), looks at palbociclib (Ibrance) in a somewhat different population – those patients with high relapse risk after neoadjuvant chemotherapy. “These are even higher risk ER+ patients [than those in monarchE], which is why they received chemotherapy before surgery,” commented Dr. Kaklamani.
In triple-negative disease, there will be overall survival (OS) results from the phase 3 KEYNOTE-355 study (abstract GS3-01) of pembrolizumab (Keytruda) versus placebo (plus chemotherapy for all patients) as first-line therapy for locally recurrent inoperable or metastatic triple-negative breast cancer. “It’s potentially a huge deal,” said Dr. Kaklamani about the OS data, if they are statistically significant.
A meta-analysis (abstract GS4-08) of data on circulating tumor cells (CTCs), which are shed from the primary tumor into the bloodstream, may point to their value as a tool to determine whether or not a breast cancer treatment is effective. “CTCs allow you to assess how a treatment is doing before you do scans, which typically occur 3 months or so later,” explained Dr. Kaklamani.
CTC results can be assessed in 3-4 weeks and allow clinicians to change treatments if CTC volume increases. However, a previous study of CTCs did not show a clinical benefit with the tool among patients treated mainly with chemotherapies. What’s different about the new study, which is from an international group of investigators, is in the treatments patients with metastatic breast cancer received. “This study is from a different era – with targeted therapies,” said Dr. Kaklamani.
In the new study, changes in CTC levels (with a reduction being a good result) between baseline (pretreatment) and follow-up were analyzed to determine whether they were associated with overall survival.
COVID sessions
On the meeting’s first day, SABCS will feature a special session on COVID-19 and breast cancer. The meeting organizers sought to separate the wheat from the chaff in this subject, as much has already been written, published, or presented.
“We received a lot of abstracts on COVID that were studies that were poorly done. We tried to tease through them and select the well-researched ones,” acknowledged Dr. Kaklamani.
The organizers included two patient advocates who have had COVID-19, including during treatment for breast cancer, as participants in the meeting session. The session will also feature global perspectives, with presenters from Brazil, Italy, and the Netherlands.
Plenary lectures
The meeting’s two plenary lectures will focus, respectively, on the increasingly used clinical approach of neoadjuvant therapy in breast cancer, and research in the time of a pandemic.
Elizabeth Mittendorf, MD, PhD, a surgical oncologist and director of the Breast lmmuno-Oncology program and co-director of the Breast Cancer Clinical Research Program at the Dana-Farber/Brigham and Women’s Cancer Center, Boston, will present “Local regional management following neoadjuvant therapy: Minding the knowledge gaps.”
Ned Sharpless, MD, director of the National Cancer Institute, will present “Advancing cancer research during challenging times.”
Dr. Kaklamani disclosed recieving consulting fees with Amgen, Eisai, Puma, Celldex, AstraZeneca, and Athenex; receiving fees for non-CME services received directly from commercial interest or their agents from Pfizer, Celgene, Genentech, Genomic Health, Puma, Eisai, and Novartis; and contracted research with Eisai.
This article first appeared on Medscape.com.
That’s the word from Virginia Kaklamani, MD, from the University of Texas Health Sciences Center San Antonio. Dr. Kaklamani, a professor of medicine in the division of hematology/oncology, is codirector of the meeting that runs online Dec. 8-11.
If the new trial sounds familiar, that’s because it’s a lot like the TAILORx trial, the results of which were first presented in 2018 and have changed practice in women with early-stage disease and no lymph node involvement.
“This is the lymph-node positive TAILORx. It’s extremely important,” Dr. Kaklamani said in an interview, adding that both trials involved women with hormone receptor (HR)–positive, HER2-negative disease.
If the RxPONDER trial shows similar outcomes between women randomized to adjuvant endocrine therapy alone versus endocrine therapy plus chemotherapy, then clinicians “can potentially avoid giving chemotherapy to a large number of women who are currently receiving it,” she explained.
Because women with nodal involvement (one to three positive axillary nodes) are at a higher risk of recurrence, RxPONDER may provide needed insight on the management of these types of breast cancers, Dr. Kaklamani suggested.
Both trials have used the 21-tumor gene expression assay (Oncotype Dx) to determine recurrence-risk status.
Dr. Kaklamani also spotlighted the phase 3 CONTESSA trial (abstract GS4-01) in 600+ patients with locally advanced or metastatic breast cancer that is HR positive and HER2 negative and has been previously treated with a taxane.
The trial features an experimental oral taxane, tesetaxel. The primary objective is to compare the efficacy of tesetaxel plus a reduced dose of capecitabine (Xeloda) versus the approved dose of capecitabine alone. Presented data will include progression-free survival results, indicating about a 3-month PFS advantage with tesetaxel, which is taken once every 3 weeks.
“Oral drugs are convenient for patients and, despite limitations, they are, all in all, a revolution in cancer treatment,” noted Dr. Kaklamani, adding that they beneficially eliminate the need for time-consuming infusions and related clinic visits as well as drug ports.
It will be interesting to see what Steven Vogl, MD, a private practitioner in New Yorky, has to say about CONTESSA and the rest of the SABCS.
He is usually a commentator from the meeting floor, whose self-introduction, “Vogl, New York,” is well known to perennial meeting attendees, according to a profile piece published some years ago.
This year the medical oncologist will also serve as the chair of the “View from the Trenches” session, which is devoted to summarizing the meeting’s most important findings for everyday practitioners.
A number of years ago, Dr. Vogl proposed the idea of this where-the-rubber-meets-the-road session to SABCS meeting planners, which they then adopted. This year, Dr. Kaklamani invited Dr. Vogl to run the session and he accepted.
Dr. Vogl is a “really smart guy who is always right on” with his comments and questions, and he will be the first-ever independent, community-based oncologist to chair a meeting session, said Dr. Kaklamani.
Other hot topics
Another hot topic featured at the meeting will be the use of CDK4/6 inhibitors in the adjuvant treatment of HR-positive and HER2-negative disease that has a high risk of recurrence, Dr. Kaklamani said. New data from two trials, monarchE and PENELOPE-B, will be presented.
First, there will be an update from the monarchE trial (abstract GS1-01). The first results from this trial were reported in September at the European Society for Medical Oncology Virtual Congress 2020. They showed that adding abemaciclib (Verzenio) to endocrine therapy reduced the risk of early recurrence. The positive outcome represented the first treatment improvement in this high-risk setting in more than 20 years, according to experts.
A similar trial, PENELOPE-B (abstract GS1-02), looks at palbociclib (Ibrance) in a somewhat different population – those patients with high relapse risk after neoadjuvant chemotherapy. “These are even higher risk ER+ patients [than those in monarchE], which is why they received chemotherapy before surgery,” commented Dr. Kaklamani.
In triple-negative disease, there will be overall survival (OS) results from the phase 3 KEYNOTE-355 study (abstract GS3-01) of pembrolizumab (Keytruda) versus placebo (plus chemotherapy for all patients) as first-line therapy for locally recurrent inoperable or metastatic triple-negative breast cancer. “It’s potentially a huge deal,” said Dr. Kaklamani about the OS data, if they are statistically significant.
A meta-analysis (abstract GS4-08) of data on circulating tumor cells (CTCs), which are shed from the primary tumor into the bloodstream, may point to their value as a tool to determine whether or not a breast cancer treatment is effective. “CTCs allow you to assess how a treatment is doing before you do scans, which typically occur 3 months or so later,” explained Dr. Kaklamani.
CTC results can be assessed in 3-4 weeks and allow clinicians to change treatments if CTC volume increases. However, a previous study of CTCs did not show a clinical benefit with the tool among patients treated mainly with chemotherapies. What’s different about the new study, which is from an international group of investigators, is in the treatments patients with metastatic breast cancer received. “This study is from a different era – with targeted therapies,” said Dr. Kaklamani.
In the new study, changes in CTC levels (with a reduction being a good result) between baseline (pretreatment) and follow-up were analyzed to determine whether they were associated with overall survival.
COVID sessions
On the meeting’s first day, SABCS will feature a special session on COVID-19 and breast cancer. The meeting organizers sought to separate the wheat from the chaff in this subject, as much has already been written, published, or presented.
“We received a lot of abstracts on COVID that were studies that were poorly done. We tried to tease through them and select the well-researched ones,” acknowledged Dr. Kaklamani.
The organizers included two patient advocates who have had COVID-19, including during treatment for breast cancer, as participants in the meeting session. The session will also feature global perspectives, with presenters from Brazil, Italy, and the Netherlands.
Plenary lectures
The meeting’s two plenary lectures will focus, respectively, on the increasingly used clinical approach of neoadjuvant therapy in breast cancer, and research in the time of a pandemic.
Elizabeth Mittendorf, MD, PhD, a surgical oncologist and director of the Breast lmmuno-Oncology program and co-director of the Breast Cancer Clinical Research Program at the Dana-Farber/Brigham and Women’s Cancer Center, Boston, will present “Local regional management following neoadjuvant therapy: Minding the knowledge gaps.”
Ned Sharpless, MD, director of the National Cancer Institute, will present “Advancing cancer research during challenging times.”
Dr. Kaklamani disclosed recieving consulting fees with Amgen, Eisai, Puma, Celldex, AstraZeneca, and Athenex; receiving fees for non-CME services received directly from commercial interest or their agents from Pfizer, Celgene, Genentech, Genomic Health, Puma, Eisai, and Novartis; and contracted research with Eisai.
This article first appeared on Medscape.com.
FROM SABCS 2020
Vaginal cleansing protocol curbs deep SSIs after cesarean
reported Johanna Quist-Nelson, MD, of the University of North Carolina, Chapel Hill.
“Surgical site infections after a cesarean delivery are more common if the patient is in labor or has ruptured membranes,” she said at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists..
Two options to decrease the risk of SSIs after cesarean for those patients in labor or with ruptured membranes are vaginal cleansing and azithromycin, given in addition to preoperative antibiotics, Dr. Quist-Nelson said. She and her colleagues conducted a quality improvement study of the effects of a stepwise implementation of vaginal cleansing and azithromycin to reduce SSIs at cesarean delivery in this high-risk population. The data were collected from 2016 to 2019 at Thomas Jefferson University, Philadelphia.
“We aimed to decrease our SSI rate by 30% by adopting an intervention of cleansing followed by azithromycin,” she said.
The researchers added vaginal cleansing to the SSI prevention protocol in January 2017, with the addition of azithromycin in March 2018. Vaginal cleansing involved 30 seconds of anterior to posterior cleaning prior to urinary catheter placement. Azithromycin was given at a dose of 500 mg intravenously in addition to preoperative antibiotics and within an hour of cesarean delivery.
A total of 1,033 deliveries qualified for the study by being in labor or with ruptured membranes; of these 291 were performed prior to the interventions, 335 received vaginal cleansing only, and 407 received vaginal cleansing and azithromycin. The average age of the participants was 30 years; approximately 42% were Black, and 32% were White.
Cleansing protocol reduces SSIs
Overall, the rate of SSIs was 22% in the standard care group, 17% in the vaginal cleansing group, and 15% in the vaginal cleansing plus azithromycin group. When broken down by infection type, no deep SSI occurred in the vaginal cleansing or cleansing plus azithromycin group, compared with 2% of the standard care group (P = .009). In addition, endometritis, which is an organ-space SSI, was significantly lower in the cleansing group (10%) and the cleansing plus azithromycin group (11%), compared with the standard care group (16%).
The study findings were limited by factors including the use of EMRs for collection of data, and given that it is a quality improvement study, there is a potential lack of generalizability to other institutions. The study focused on patients at high risk for SSI and the use of the Plan-Do-Study-Act (PDSA) method of conducting the research, Dr. Quist-Nelson said. Compared with standard care, the implementation of vaginal cleansing reduced the SSI rate by 33%, with no significantly further change in SSI after the addition of azithromycin, she concluded.
Data sharing boosts compliance
In a question-and-answer session, Dr. Quist-Nelson noted that povidone iodine (Betadine) was chosen for vaginal cleansing because it was easily accessible at her institution, but that patients with allergies were given chlorhexidine. The cleansing itself was “primarily vaginal, not a full vulvar cleansing,” she clarified. The cleansing was performed immediately before catheter placement and included the urethra.
When asked about strategies to increase compliance, Dr. Quist-Nelson noted that sharing data was valuable, namely “reporting to our group the current compliance,” as well as sharing information by email and discussing it during multidisciplinary rounds.
The study was a quality improvement project and not a randomized trial, so the researchers were not able to tease out the impact of vaginal cleansing from the impact of azithromycin, Dr. Quist-Nelson said.
Based on her results, Dr. Quist-Nelson said she would recommend the protocol for use in patients who require cesarean delivery after being in labor or having ruptured membranes, and that “there are trials to support the use of both interventions.”
The results suggest opportunities for further randomized trials, including examination of the use of oral versus IV azithromycin, she added.
The study received no outside funding. Dr. Quist-Nelson had no financial conflicts to disclose.
reported Johanna Quist-Nelson, MD, of the University of North Carolina, Chapel Hill.
“Surgical site infections after a cesarean delivery are more common if the patient is in labor or has ruptured membranes,” she said at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists..
Two options to decrease the risk of SSIs after cesarean for those patients in labor or with ruptured membranes are vaginal cleansing and azithromycin, given in addition to preoperative antibiotics, Dr. Quist-Nelson said. She and her colleagues conducted a quality improvement study of the effects of a stepwise implementation of vaginal cleansing and azithromycin to reduce SSIs at cesarean delivery in this high-risk population. The data were collected from 2016 to 2019 at Thomas Jefferson University, Philadelphia.
“We aimed to decrease our SSI rate by 30% by adopting an intervention of cleansing followed by azithromycin,” she said.
The researchers added vaginal cleansing to the SSI prevention protocol in January 2017, with the addition of azithromycin in March 2018. Vaginal cleansing involved 30 seconds of anterior to posterior cleaning prior to urinary catheter placement. Azithromycin was given at a dose of 500 mg intravenously in addition to preoperative antibiotics and within an hour of cesarean delivery.
A total of 1,033 deliveries qualified for the study by being in labor or with ruptured membranes; of these 291 were performed prior to the interventions, 335 received vaginal cleansing only, and 407 received vaginal cleansing and azithromycin. The average age of the participants was 30 years; approximately 42% were Black, and 32% were White.
Cleansing protocol reduces SSIs
Overall, the rate of SSIs was 22% in the standard care group, 17% in the vaginal cleansing group, and 15% in the vaginal cleansing plus azithromycin group. When broken down by infection type, no deep SSI occurred in the vaginal cleansing or cleansing plus azithromycin group, compared with 2% of the standard care group (P = .009). In addition, endometritis, which is an organ-space SSI, was significantly lower in the cleansing group (10%) and the cleansing plus azithromycin group (11%), compared with the standard care group (16%).
The study findings were limited by factors including the use of EMRs for collection of data, and given that it is a quality improvement study, there is a potential lack of generalizability to other institutions. The study focused on patients at high risk for SSI and the use of the Plan-Do-Study-Act (PDSA) method of conducting the research, Dr. Quist-Nelson said. Compared with standard care, the implementation of vaginal cleansing reduced the SSI rate by 33%, with no significantly further change in SSI after the addition of azithromycin, she concluded.
Data sharing boosts compliance
In a question-and-answer session, Dr. Quist-Nelson noted that povidone iodine (Betadine) was chosen for vaginal cleansing because it was easily accessible at her institution, but that patients with allergies were given chlorhexidine. The cleansing itself was “primarily vaginal, not a full vulvar cleansing,” she clarified. The cleansing was performed immediately before catheter placement and included the urethra.
When asked about strategies to increase compliance, Dr. Quist-Nelson noted that sharing data was valuable, namely “reporting to our group the current compliance,” as well as sharing information by email and discussing it during multidisciplinary rounds.
The study was a quality improvement project and not a randomized trial, so the researchers were not able to tease out the impact of vaginal cleansing from the impact of azithromycin, Dr. Quist-Nelson said.
Based on her results, Dr. Quist-Nelson said she would recommend the protocol for use in patients who require cesarean delivery after being in labor or having ruptured membranes, and that “there are trials to support the use of both interventions.”
The results suggest opportunities for further randomized trials, including examination of the use of oral versus IV azithromycin, she added.
The study received no outside funding. Dr. Quist-Nelson had no financial conflicts to disclose.
reported Johanna Quist-Nelson, MD, of the University of North Carolina, Chapel Hill.
“Surgical site infections after a cesarean delivery are more common if the patient is in labor or has ruptured membranes,” she said at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists..
Two options to decrease the risk of SSIs after cesarean for those patients in labor or with ruptured membranes are vaginal cleansing and azithromycin, given in addition to preoperative antibiotics, Dr. Quist-Nelson said. She and her colleagues conducted a quality improvement study of the effects of a stepwise implementation of vaginal cleansing and azithromycin to reduce SSIs at cesarean delivery in this high-risk population. The data were collected from 2016 to 2019 at Thomas Jefferson University, Philadelphia.
“We aimed to decrease our SSI rate by 30% by adopting an intervention of cleansing followed by azithromycin,” she said.
The researchers added vaginal cleansing to the SSI prevention protocol in January 2017, with the addition of azithromycin in March 2018. Vaginal cleansing involved 30 seconds of anterior to posterior cleaning prior to urinary catheter placement. Azithromycin was given at a dose of 500 mg intravenously in addition to preoperative antibiotics and within an hour of cesarean delivery.
A total of 1,033 deliveries qualified for the study by being in labor or with ruptured membranes; of these 291 were performed prior to the interventions, 335 received vaginal cleansing only, and 407 received vaginal cleansing and azithromycin. The average age of the participants was 30 years; approximately 42% were Black, and 32% were White.
Cleansing protocol reduces SSIs
Overall, the rate of SSIs was 22% in the standard care group, 17% in the vaginal cleansing group, and 15% in the vaginal cleansing plus azithromycin group. When broken down by infection type, no deep SSI occurred in the vaginal cleansing or cleansing plus azithromycin group, compared with 2% of the standard care group (P = .009). In addition, endometritis, which is an organ-space SSI, was significantly lower in the cleansing group (10%) and the cleansing plus azithromycin group (11%), compared with the standard care group (16%).
The study findings were limited by factors including the use of EMRs for collection of data, and given that it is a quality improvement study, there is a potential lack of generalizability to other institutions. The study focused on patients at high risk for SSI and the use of the Plan-Do-Study-Act (PDSA) method of conducting the research, Dr. Quist-Nelson said. Compared with standard care, the implementation of vaginal cleansing reduced the SSI rate by 33%, with no significantly further change in SSI after the addition of azithromycin, she concluded.
Data sharing boosts compliance
In a question-and-answer session, Dr. Quist-Nelson noted that povidone iodine (Betadine) was chosen for vaginal cleansing because it was easily accessible at her institution, but that patients with allergies were given chlorhexidine. The cleansing itself was “primarily vaginal, not a full vulvar cleansing,” she clarified. The cleansing was performed immediately before catheter placement and included the urethra.
When asked about strategies to increase compliance, Dr. Quist-Nelson noted that sharing data was valuable, namely “reporting to our group the current compliance,” as well as sharing information by email and discussing it during multidisciplinary rounds.
The study was a quality improvement project and not a randomized trial, so the researchers were not able to tease out the impact of vaginal cleansing from the impact of azithromycin, Dr. Quist-Nelson said.
Based on her results, Dr. Quist-Nelson said she would recommend the protocol for use in patients who require cesarean delivery after being in labor or having ruptured membranes, and that “there are trials to support the use of both interventions.”
The results suggest opportunities for further randomized trials, including examination of the use of oral versus IV azithromycin, she added.
The study received no outside funding. Dr. Quist-Nelson had no financial conflicts to disclose.
FROM ACOG 2020
COVID-19 impacts women’s contraception choices
The rate of unintended pregnancies in the United States has decreased to approximately 45%, based on data published in 2016, and “for the first time in many years, this decrease affected women of all race/ethnicity, income levels, and education levels,” Eve Espey, MD, said at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists.
Changes in contraceptive choices drove much of this decrease, said Dr. Espey, professor of obstetrics and gynecology at the University of New Mexico, Albuquerque.
“What is really striking is the very large increase in use of the IUD,” she noted. However, the increased use of IUDs has raised concerns about coercive tactics being used to push for IUD use in communities of color.
“The focus we should have is on reproductive autonomy and not on unintended pregnancy, a metric that is classist and racist and may value the reproduction of some groups over others,” Dr. Espey said. Previous studies have suggested that providers are biased in how they promote long-acting reversible contraception (LARC), and reports from patients suggest that women and people of color particularly may feel marginalized, not heard, and coerced, she noted.
Help patients feel empowered
Overall, the goal of contraception should be to empower women and people to make the reproductive decisions that are best for them. “My own approach to contraceptive counseling has changed over the years; I currently start by asking if the patient wants to talk about contraception,” Dr. Espey said.
The COVID-19 pandemic has impacted many women’s reproductive options and plans, she said.
A survey showed that after COVID-19, more than 40% of women reported changing their plans about childbearing, 34% wanted to get pregnant later, and 33% reported trouble getting birth control or getting an appointment with a health care provider, she said.
ACOG issued a statement in March 2020 about the provision of contraception and how contraception is an essential component of comprehensive health care. The COVID-19 ACOG guidance on contraception includes use of telehealth for services including screening new patients, offering prescriptions and refills as appropriate, and managing side effects. Providers can counsel patients on the use of emergency contraception and provide advance prescriptions for ulipristal acetate, and ideally provide a year’s worth of prescription refills to reduce pharmacy visits, although not all insurance companies allow this, Dr. Espey noted.
ACOG’s COVID-19 guidance on the use of LARCs includes preserving access when possible, and focusing on postpartum contraception as a key access point.
“The postpartum period is a very convenient time for patients who want contraceptives, including LARC,” especially since they are already in the hospital setting, Dr. Espey said. However, it is important to preserve patients’ reproductive autonomy and avoid placing barriers to LARC removal for those who request it, she emphasized.
Consider MEC categories for contraception
When advising patients about contraception, Dr. Espey noted the development of a simple app with the U.S. Medical Eligibility Criteria (MEC) as a useful tool. The app includes the four MEC categories based on the latest evidence-based guidance from the Centers for Disease Control and Prevention on contraceptive practice.
Patients in category 1 have no restriction on the use of a particular contraceptive method; category 2 means that “advantages generally outweigh the theoretical or proven risks”; in category 3, these risks usually outweigh the advantages; and category 4 indicates “unacceptable health risk if the contraceptive method is used,” according to the MEC.
“What complicates category 3 is that many patients have a condition that is associated with adverse outcomes in pregnancy,” Dr. Espey noted, “So it is even more important that category 3 options only be considered if other options are not available or not acceptable to the patient,”
For example, a patient with complicated diabetes who wants depot medroxyprogesterone acetate (DMPA) for contraception for a year must weigh the benefits with the theoretical risk of thromboembolic disease related to a higher dose progestin, and the fact that the injection is not reversible in the case of an adverse event. “Close follow-up is recommended for patients using contraception with category 3 recommendations,” Dr. Espey emphasized.
Some new elements of contraception that are ongoing in the pandemic health care setting include increased pharmacist prescribing of hormonal contraception, Dr. Espey said. Over-the-counter access to contraception is not yet an option, but a progestin-only pill will likely be the first, she added.
Although the Essure birth control implant is no longer available in the United States, new options for a contraceptive patch (Twirla [ethinyl estradiol and levonorgestrel] and Xulane [ethinyl estradiol and norelgestromin]) offer weekly contraceptive options for women with a body mass index less than 30 kg/m2.
Annovera offers more options
The newest choice on the market is Annovera, a flexible ring that delivers 150 mcg/day of segesterone acetate and 13 mcg/day of ethinyl estradiol. The ring is meant to remain in place for 21 days, with 7 days out, to repeat for a year.
During the question-and-answer session, Dr. Espey was asked whether it would be an off-label use to leave Annovera in continuously. Although this has not been studied, there is no biologically plausible reason not to leave it in for a year without taking it out. In either case, this is a patient-controlled LARC, she said.
Overall, “it remains to be seen how Annovera will do, as a potentially exciting, new, long-acting option” she said. “A major advantage is that it is controlled by the user,” she noted. However, “the price point will be very important as well.”
As for the off-label use by women with a BMI greater than 29 kg/m2, it is complicated. Two women with higher BMIs enrolled in clinical trials developed venous thromboembolisms, so an increased risk can’t be ruled out, although the good news is that BMI has not been shown to impact effectiveness of the product, she added.
IUDs appropriate for younger women
When asked for her guidelines about IUD options in the absence of head-to-head trials, Dr. Espey said that she often recommends either Mirena and Liletta. These levonorgestrel-releasing IUDS are essentially the same, can be used off label for 7 years (both are currently Food and Drug Administration approved for 6 years), and have a favorable bleeding profile. Other IUDs are marketed as having a smaller diameter designed for increased patient comfort with insertion, but she views this as less important than bleeding profile and duration given the length of time the device is in place.
Dr. Espey added that she doesn’t see age as a barrier to IUD use, and that the evidence does not support an increased risk of infertility. In fact, “we are seeing a higher demand among younger and nulliparous women.”
“We should respect the reproductive autonomy and the choices that our patients make,” Dr. Espey concluded.
Dr. Espey had no relevant financial disclosures. She is a member of the Ob.Gyn. News editorial advisory board.
The rate of unintended pregnancies in the United States has decreased to approximately 45%, based on data published in 2016, and “for the first time in many years, this decrease affected women of all race/ethnicity, income levels, and education levels,” Eve Espey, MD, said at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists.
Changes in contraceptive choices drove much of this decrease, said Dr. Espey, professor of obstetrics and gynecology at the University of New Mexico, Albuquerque.
“What is really striking is the very large increase in use of the IUD,” she noted. However, the increased use of IUDs has raised concerns about coercive tactics being used to push for IUD use in communities of color.
“The focus we should have is on reproductive autonomy and not on unintended pregnancy, a metric that is classist and racist and may value the reproduction of some groups over others,” Dr. Espey said. Previous studies have suggested that providers are biased in how they promote long-acting reversible contraception (LARC), and reports from patients suggest that women and people of color particularly may feel marginalized, not heard, and coerced, she noted.
Help patients feel empowered
Overall, the goal of contraception should be to empower women and people to make the reproductive decisions that are best for them. “My own approach to contraceptive counseling has changed over the years; I currently start by asking if the patient wants to talk about contraception,” Dr. Espey said.
The COVID-19 pandemic has impacted many women’s reproductive options and plans, she said.
A survey showed that after COVID-19, more than 40% of women reported changing their plans about childbearing, 34% wanted to get pregnant later, and 33% reported trouble getting birth control or getting an appointment with a health care provider, she said.
ACOG issued a statement in March 2020 about the provision of contraception and how contraception is an essential component of comprehensive health care. The COVID-19 ACOG guidance on contraception includes use of telehealth for services including screening new patients, offering prescriptions and refills as appropriate, and managing side effects. Providers can counsel patients on the use of emergency contraception and provide advance prescriptions for ulipristal acetate, and ideally provide a year’s worth of prescription refills to reduce pharmacy visits, although not all insurance companies allow this, Dr. Espey noted.
ACOG’s COVID-19 guidance on the use of LARCs includes preserving access when possible, and focusing on postpartum contraception as a key access point.
“The postpartum period is a very convenient time for patients who want contraceptives, including LARC,” especially since they are already in the hospital setting, Dr. Espey said. However, it is important to preserve patients’ reproductive autonomy and avoid placing barriers to LARC removal for those who request it, she emphasized.
Consider MEC categories for contraception
When advising patients about contraception, Dr. Espey noted the development of a simple app with the U.S. Medical Eligibility Criteria (MEC) as a useful tool. The app includes the four MEC categories based on the latest evidence-based guidance from the Centers for Disease Control and Prevention on contraceptive practice.
Patients in category 1 have no restriction on the use of a particular contraceptive method; category 2 means that “advantages generally outweigh the theoretical or proven risks”; in category 3, these risks usually outweigh the advantages; and category 4 indicates “unacceptable health risk if the contraceptive method is used,” according to the MEC.
“What complicates category 3 is that many patients have a condition that is associated with adverse outcomes in pregnancy,” Dr. Espey noted, “So it is even more important that category 3 options only be considered if other options are not available or not acceptable to the patient,”
For example, a patient with complicated diabetes who wants depot medroxyprogesterone acetate (DMPA) for contraception for a year must weigh the benefits with the theoretical risk of thromboembolic disease related to a higher dose progestin, and the fact that the injection is not reversible in the case of an adverse event. “Close follow-up is recommended for patients using contraception with category 3 recommendations,” Dr. Espey emphasized.
Some new elements of contraception that are ongoing in the pandemic health care setting include increased pharmacist prescribing of hormonal contraception, Dr. Espey said. Over-the-counter access to contraception is not yet an option, but a progestin-only pill will likely be the first, she added.
Although the Essure birth control implant is no longer available in the United States, new options for a contraceptive patch (Twirla [ethinyl estradiol and levonorgestrel] and Xulane [ethinyl estradiol and norelgestromin]) offer weekly contraceptive options for women with a body mass index less than 30 kg/m2.
Annovera offers more options
The newest choice on the market is Annovera, a flexible ring that delivers 150 mcg/day of segesterone acetate and 13 mcg/day of ethinyl estradiol. The ring is meant to remain in place for 21 days, with 7 days out, to repeat for a year.
During the question-and-answer session, Dr. Espey was asked whether it would be an off-label use to leave Annovera in continuously. Although this has not been studied, there is no biologically plausible reason not to leave it in for a year without taking it out. In either case, this is a patient-controlled LARC, she said.
Overall, “it remains to be seen how Annovera will do, as a potentially exciting, new, long-acting option” she said. “A major advantage is that it is controlled by the user,” she noted. However, “the price point will be very important as well.”
As for the off-label use by women with a BMI greater than 29 kg/m2, it is complicated. Two women with higher BMIs enrolled in clinical trials developed venous thromboembolisms, so an increased risk can’t be ruled out, although the good news is that BMI has not been shown to impact effectiveness of the product, she added.
IUDs appropriate for younger women
When asked for her guidelines about IUD options in the absence of head-to-head trials, Dr. Espey said that she often recommends either Mirena and Liletta. These levonorgestrel-releasing IUDS are essentially the same, can be used off label for 7 years (both are currently Food and Drug Administration approved for 6 years), and have a favorable bleeding profile. Other IUDs are marketed as having a smaller diameter designed for increased patient comfort with insertion, but she views this as less important than bleeding profile and duration given the length of time the device is in place.
Dr. Espey added that she doesn’t see age as a barrier to IUD use, and that the evidence does not support an increased risk of infertility. In fact, “we are seeing a higher demand among younger and nulliparous women.”
“We should respect the reproductive autonomy and the choices that our patients make,” Dr. Espey concluded.
Dr. Espey had no relevant financial disclosures. She is a member of the Ob.Gyn. News editorial advisory board.
The rate of unintended pregnancies in the United States has decreased to approximately 45%, based on data published in 2016, and “for the first time in many years, this decrease affected women of all race/ethnicity, income levels, and education levels,” Eve Espey, MD, said at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists.
Changes in contraceptive choices drove much of this decrease, said Dr. Espey, professor of obstetrics and gynecology at the University of New Mexico, Albuquerque.
“What is really striking is the very large increase in use of the IUD,” she noted. However, the increased use of IUDs has raised concerns about coercive tactics being used to push for IUD use in communities of color.
“The focus we should have is on reproductive autonomy and not on unintended pregnancy, a metric that is classist and racist and may value the reproduction of some groups over others,” Dr. Espey said. Previous studies have suggested that providers are biased in how they promote long-acting reversible contraception (LARC), and reports from patients suggest that women and people of color particularly may feel marginalized, not heard, and coerced, she noted.
Help patients feel empowered
Overall, the goal of contraception should be to empower women and people to make the reproductive decisions that are best for them. “My own approach to contraceptive counseling has changed over the years; I currently start by asking if the patient wants to talk about contraception,” Dr. Espey said.
The COVID-19 pandemic has impacted many women’s reproductive options and plans, she said.
A survey showed that after COVID-19, more than 40% of women reported changing their plans about childbearing, 34% wanted to get pregnant later, and 33% reported trouble getting birth control or getting an appointment with a health care provider, she said.
ACOG issued a statement in March 2020 about the provision of contraception and how contraception is an essential component of comprehensive health care. The COVID-19 ACOG guidance on contraception includes use of telehealth for services including screening new patients, offering prescriptions and refills as appropriate, and managing side effects. Providers can counsel patients on the use of emergency contraception and provide advance prescriptions for ulipristal acetate, and ideally provide a year’s worth of prescription refills to reduce pharmacy visits, although not all insurance companies allow this, Dr. Espey noted.
ACOG’s COVID-19 guidance on the use of LARCs includes preserving access when possible, and focusing on postpartum contraception as a key access point.
“The postpartum period is a very convenient time for patients who want contraceptives, including LARC,” especially since they are already in the hospital setting, Dr. Espey said. However, it is important to preserve patients’ reproductive autonomy and avoid placing barriers to LARC removal for those who request it, she emphasized.
Consider MEC categories for contraception
When advising patients about contraception, Dr. Espey noted the development of a simple app with the U.S. Medical Eligibility Criteria (MEC) as a useful tool. The app includes the four MEC categories based on the latest evidence-based guidance from the Centers for Disease Control and Prevention on contraceptive practice.
Patients in category 1 have no restriction on the use of a particular contraceptive method; category 2 means that “advantages generally outweigh the theoretical or proven risks”; in category 3, these risks usually outweigh the advantages; and category 4 indicates “unacceptable health risk if the contraceptive method is used,” according to the MEC.
“What complicates category 3 is that many patients have a condition that is associated with adverse outcomes in pregnancy,” Dr. Espey noted, “So it is even more important that category 3 options only be considered if other options are not available or not acceptable to the patient,”
For example, a patient with complicated diabetes who wants depot medroxyprogesterone acetate (DMPA) for contraception for a year must weigh the benefits with the theoretical risk of thromboembolic disease related to a higher dose progestin, and the fact that the injection is not reversible in the case of an adverse event. “Close follow-up is recommended for patients using contraception with category 3 recommendations,” Dr. Espey emphasized.
Some new elements of contraception that are ongoing in the pandemic health care setting include increased pharmacist prescribing of hormonal contraception, Dr. Espey said. Over-the-counter access to contraception is not yet an option, but a progestin-only pill will likely be the first, she added.
Although the Essure birth control implant is no longer available in the United States, new options for a contraceptive patch (Twirla [ethinyl estradiol and levonorgestrel] and Xulane [ethinyl estradiol and norelgestromin]) offer weekly contraceptive options for women with a body mass index less than 30 kg/m2.
Annovera offers more options
The newest choice on the market is Annovera, a flexible ring that delivers 150 mcg/day of segesterone acetate and 13 mcg/day of ethinyl estradiol. The ring is meant to remain in place for 21 days, with 7 days out, to repeat for a year.
During the question-and-answer session, Dr. Espey was asked whether it would be an off-label use to leave Annovera in continuously. Although this has not been studied, there is no biologically plausible reason not to leave it in for a year without taking it out. In either case, this is a patient-controlled LARC, she said.
Overall, “it remains to be seen how Annovera will do, as a potentially exciting, new, long-acting option” she said. “A major advantage is that it is controlled by the user,” she noted. However, “the price point will be very important as well.”
As for the off-label use by women with a BMI greater than 29 kg/m2, it is complicated. Two women with higher BMIs enrolled in clinical trials developed venous thromboembolisms, so an increased risk can’t be ruled out, although the good news is that BMI has not been shown to impact effectiveness of the product, she added.
IUDs appropriate for younger women
When asked for her guidelines about IUD options in the absence of head-to-head trials, Dr. Espey said that she often recommends either Mirena and Liletta. These levonorgestrel-releasing IUDS are essentially the same, can be used off label for 7 years (both are currently Food and Drug Administration approved for 6 years), and have a favorable bleeding profile. Other IUDs are marketed as having a smaller diameter designed for increased patient comfort with insertion, but she views this as less important than bleeding profile and duration given the length of time the device is in place.
Dr. Espey added that she doesn’t see age as a barrier to IUD use, and that the evidence does not support an increased risk of infertility. In fact, “we are seeing a higher demand among younger and nulliparous women.”
“We should respect the reproductive autonomy and the choices that our patients make,” Dr. Espey concluded.
Dr. Espey had no relevant financial disclosures. She is a member of the Ob.Gyn. News editorial advisory board.
EXPERT ANALYSIS FROM ACOG 2020
Menstrual cup use increases risk of IUD expulsion
Menstrual cup use is becoming increasingly popular as an option for menstrual hygiene among women in the United States, but little is known about the potential for IUD expulsion with menstrual cup use, Jill Long, MD, said at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists.
Dr. Long cited a 2019 Internet survey of IUD users in which 11% reported menstrual cup use; reports of IUD expulsion were approximately three times higher among menstrual cup users. The results of the survey were limited by the self-reported responses and lack of data on when the expulsions occurred related to menstrual cup use.
Similar concerns about expulsion surfaced in an ongoing phase 3, randomized trial designed to support the marketing application of the Mona Lisa NT Cu380 Mini IUD, which is not currently approved in the United States.
“Nine months into the study, more expulsions were observed than expected, particularly among menstrual cup users,” said Dr. Long, medical officer and project officer for the Contraceptive Clinical Trials Network at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The researchers then began to advise study participants to avoid menstrual cup use, and to collect data on use of menstrual hygiene products.
The preliminary study results reported by Dr. Long included 1,092 women assigned in a 4:1 ratio to receive the Mona Lisa NT Cu380 Mini and ParaGard, an IUD approved in the United States. Participants had follow-up visits at 6 weeks and at 3, 6, 12, 24, and 36 months after placement to verify the IUD position.
At 34 months, the overall rate of IUD expulsion was 9%. Of 277 women who reported menstrual cup use, the expulsion rate was 18%, compared with a 6% expulsion rates among the 704 women who reported tampon use.
Patient behavior persists despite advisory
Overall IUD expulsion was not significantly different among patients enrolled before and after the advisory against menstrual cup use (9.8% vs. 8.8%, respectively). In addition, menstrual cup use did not decrease after the implementation of the advisory (24% preadvisory vs. 28% post advisory).
The expulsion rates between menstrual cup users and nonusers were significantly different at both 12 months (14% vs. 5%) and 24 months (21% vs. 6%).
In addition, the researchers created a category of accidental self-removal, defined as the percent of expulsions occurring at the time the menstrual hygiene product was removed. Accidental self-removal was significantly higher among menstrual cup users, compared with tampon users (43% vs. 10%).
Study limitations included study blinding with regard to IUD type, parity, and age, so the impact of these factors on expulsion remains unclear, Dr. Long said. In addition, data on menstrual hygiene product use was collected retrospectively for the first 9 months, and no data were available on the impact on expulsion of combined use of menstrual cups and tampons.
Despite the apparent lack of impact of counseling, “women should be informed of the increased risk of expulsion if they choose to use menstrual cups concurrently with copper IUDs,” Dr. Long concluded.
More data to come from further analysis
During a question-and-answer session following the presentation, Dr. Long was asked whether suction might contribute to expulsion. “We advised subjects to break the seal on the menstrual cup prior to removal, but we did not see a decrease in expulsion rates with menstrual cup use after this advisory,” she said.
“The type of menstrual cup may be a factor,” she added. “We still need to analyze the data by the type of menstrual cup used as different cups have different degrees of suction.”
When asked about the potential role of coital activity on expulsion, Dr. Long said that the researchers had not yet reviewed coital activity logs to compare expulsion data with the timing of sexual activity.
Any increased pregnancy rates among menstrual cup users are “unlikely, but we don’t know for sure,” she added.
The current study also did not evaluate quantitative differences in bleeding, and participants are using bleeding diaries, Dr. Long noted. She added that participants are able to report problems with bleeding to the study sites, and that these are captured as adverse events.
The study was supported by a partnership between NICHD and FHI 360, a nonprofit human development organization based in North Carolina, with FHI 360 funding from the Bill and Melinda Gates Foundation. Dr. Long had no financial conflicts to disclose.
Menstrual cup use is becoming increasingly popular as an option for menstrual hygiene among women in the United States, but little is known about the potential for IUD expulsion with menstrual cup use, Jill Long, MD, said at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists.
Dr. Long cited a 2019 Internet survey of IUD users in which 11% reported menstrual cup use; reports of IUD expulsion were approximately three times higher among menstrual cup users. The results of the survey were limited by the self-reported responses and lack of data on when the expulsions occurred related to menstrual cup use.
Similar concerns about expulsion surfaced in an ongoing phase 3, randomized trial designed to support the marketing application of the Mona Lisa NT Cu380 Mini IUD, which is not currently approved in the United States.
“Nine months into the study, more expulsions were observed than expected, particularly among menstrual cup users,” said Dr. Long, medical officer and project officer for the Contraceptive Clinical Trials Network at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The researchers then began to advise study participants to avoid menstrual cup use, and to collect data on use of menstrual hygiene products.
The preliminary study results reported by Dr. Long included 1,092 women assigned in a 4:1 ratio to receive the Mona Lisa NT Cu380 Mini and ParaGard, an IUD approved in the United States. Participants had follow-up visits at 6 weeks and at 3, 6, 12, 24, and 36 months after placement to verify the IUD position.
At 34 months, the overall rate of IUD expulsion was 9%. Of 277 women who reported menstrual cup use, the expulsion rate was 18%, compared with a 6% expulsion rates among the 704 women who reported tampon use.
Patient behavior persists despite advisory
Overall IUD expulsion was not significantly different among patients enrolled before and after the advisory against menstrual cup use (9.8% vs. 8.8%, respectively). In addition, menstrual cup use did not decrease after the implementation of the advisory (24% preadvisory vs. 28% post advisory).
The expulsion rates between menstrual cup users and nonusers were significantly different at both 12 months (14% vs. 5%) and 24 months (21% vs. 6%).
In addition, the researchers created a category of accidental self-removal, defined as the percent of expulsions occurring at the time the menstrual hygiene product was removed. Accidental self-removal was significantly higher among menstrual cup users, compared with tampon users (43% vs. 10%).
Study limitations included study blinding with regard to IUD type, parity, and age, so the impact of these factors on expulsion remains unclear, Dr. Long said. In addition, data on menstrual hygiene product use was collected retrospectively for the first 9 months, and no data were available on the impact on expulsion of combined use of menstrual cups and tampons.
Despite the apparent lack of impact of counseling, “women should be informed of the increased risk of expulsion if they choose to use menstrual cups concurrently with copper IUDs,” Dr. Long concluded.
More data to come from further analysis
During a question-and-answer session following the presentation, Dr. Long was asked whether suction might contribute to expulsion. “We advised subjects to break the seal on the menstrual cup prior to removal, but we did not see a decrease in expulsion rates with menstrual cup use after this advisory,” she said.
“The type of menstrual cup may be a factor,” she added. “We still need to analyze the data by the type of menstrual cup used as different cups have different degrees of suction.”
When asked about the potential role of coital activity on expulsion, Dr. Long said that the researchers had not yet reviewed coital activity logs to compare expulsion data with the timing of sexual activity.
Any increased pregnancy rates among menstrual cup users are “unlikely, but we don’t know for sure,” she added.
The current study also did not evaluate quantitative differences in bleeding, and participants are using bleeding diaries, Dr. Long noted. She added that participants are able to report problems with bleeding to the study sites, and that these are captured as adverse events.
The study was supported by a partnership between NICHD and FHI 360, a nonprofit human development organization based in North Carolina, with FHI 360 funding from the Bill and Melinda Gates Foundation. Dr. Long had no financial conflicts to disclose.
Menstrual cup use is becoming increasingly popular as an option for menstrual hygiene among women in the United States, but little is known about the potential for IUD expulsion with menstrual cup use, Jill Long, MD, said at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists.
Dr. Long cited a 2019 Internet survey of IUD users in which 11% reported menstrual cup use; reports of IUD expulsion were approximately three times higher among menstrual cup users. The results of the survey were limited by the self-reported responses and lack of data on when the expulsions occurred related to menstrual cup use.
Similar concerns about expulsion surfaced in an ongoing phase 3, randomized trial designed to support the marketing application of the Mona Lisa NT Cu380 Mini IUD, which is not currently approved in the United States.
“Nine months into the study, more expulsions were observed than expected, particularly among menstrual cup users,” said Dr. Long, medical officer and project officer for the Contraceptive Clinical Trials Network at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The researchers then began to advise study participants to avoid menstrual cup use, and to collect data on use of menstrual hygiene products.
The preliminary study results reported by Dr. Long included 1,092 women assigned in a 4:1 ratio to receive the Mona Lisa NT Cu380 Mini and ParaGard, an IUD approved in the United States. Participants had follow-up visits at 6 weeks and at 3, 6, 12, 24, and 36 months after placement to verify the IUD position.
At 34 months, the overall rate of IUD expulsion was 9%. Of 277 women who reported menstrual cup use, the expulsion rate was 18%, compared with a 6% expulsion rates among the 704 women who reported tampon use.
Patient behavior persists despite advisory
Overall IUD expulsion was not significantly different among patients enrolled before and after the advisory against menstrual cup use (9.8% vs. 8.8%, respectively). In addition, menstrual cup use did not decrease after the implementation of the advisory (24% preadvisory vs. 28% post advisory).
The expulsion rates between menstrual cup users and nonusers were significantly different at both 12 months (14% vs. 5%) and 24 months (21% vs. 6%).
In addition, the researchers created a category of accidental self-removal, defined as the percent of expulsions occurring at the time the menstrual hygiene product was removed. Accidental self-removal was significantly higher among menstrual cup users, compared with tampon users (43% vs. 10%).
Study limitations included study blinding with regard to IUD type, parity, and age, so the impact of these factors on expulsion remains unclear, Dr. Long said. In addition, data on menstrual hygiene product use was collected retrospectively for the first 9 months, and no data were available on the impact on expulsion of combined use of menstrual cups and tampons.
Despite the apparent lack of impact of counseling, “women should be informed of the increased risk of expulsion if they choose to use menstrual cups concurrently with copper IUDs,” Dr. Long concluded.
More data to come from further analysis
During a question-and-answer session following the presentation, Dr. Long was asked whether suction might contribute to expulsion. “We advised subjects to break the seal on the menstrual cup prior to removal, but we did not see a decrease in expulsion rates with menstrual cup use after this advisory,” she said.
“The type of menstrual cup may be a factor,” she added. “We still need to analyze the data by the type of menstrual cup used as different cups have different degrees of suction.”
When asked about the potential role of coital activity on expulsion, Dr. Long said that the researchers had not yet reviewed coital activity logs to compare expulsion data with the timing of sexual activity.
Any increased pregnancy rates among menstrual cup users are “unlikely, but we don’t know for sure,” she added.
The current study also did not evaluate quantitative differences in bleeding, and participants are using bleeding diaries, Dr. Long noted. She added that participants are able to report problems with bleeding to the study sites, and that these are captured as adverse events.
The study was supported by a partnership between NICHD and FHI 360, a nonprofit human development organization based in North Carolina, with FHI 360 funding from the Bill and Melinda Gates Foundation. Dr. Long had no financial conflicts to disclose.
FROM ACOG 2020
New AHA scientific statement on menopause and CVD risk
Changes in hormones, body composition, lipids, and vascular health during the menopause transition can increase a woman’s chance of developing cardiovascular disease (CVD) after menopause, the American Heart Association said in a scientific statement.
“This statement aims to raise awareness of both healthcare providers and women about the menopause transition as a time of increasing heart disease risk,” Samar R. El Khoudary, PhD, MPH, who chaired the writing group, said in an interview.
“As such, it emphasizes the importance of monitoring women’s health during midlife and targeting this stage as a critical window for applying early intervention strategies that aim to maintain a healthy heart and reduce the risk of heart disease,” said Dr. El Khoudary, of the University of Pittsburgh.
The statement was published online Nov. 30 in Circulation.
Evolution in knowledge
During the past 20 years, knowledge of how menopause might contribute to CVD has evolved “dramatically,” Dr. El Khoudary noted. The accumulated data consistently point to the menopause transition as a time of change in heart health.
“Importantly,” she said, the latest AHA guidelines for CVD prevention in women, published in 2011, do not include data now available on the menopause transition as a time of increased CVD risk.
“As such, there is a compelling need to discuss the implications of the accumulating body of literature on this topic,” said Dr. El Khoudary.
The statement provides a contemporary synthesis of the existing data on menopause and how it relates to CVD, the leading cause of death of U.S. women.
Earlier age at natural menopause has generally been found to be a marker of greater CVD risk. Iatrogenically induced menopause (bilateral oophorectomy) during the premenopausal period is also associated with higher CVD risk, the data suggest.
Vasomotor symptoms are associated with worse levels of CVD risk factors and measures of subclinical atherosclerosis. Sleep disturbance has also been linked to greater risk for subclinical CVD and worse CV health indexes in women during midlife.
Increases in central/visceral fat and decreases in lean muscle mass are more pronounced during the menopause transition. This increased central adiposity is associated with increased risk for mortality, even among those with normal body mass index, the writing group found.
Increases in lipid levels (LDL cholesterol and apolipoprotein B), metabolic syndrome risk, and vascular remodeling at midlife are driven by the menopause transition more than aging, whereas increases in blood pressure, insulin level, and glucose level are likely more influenced by chronological aging, they reported.
Lifestyle interventions
The writing group noted that, because of the increase in overall life expectancy in the United States, a significant proportion of women will spend up to 40% of their lives after menopause.
Yet data suggest that only 7.2% of women transitioning to menopause are meeting physical activity guidelines and that fewer than 20% of those women are consistently maintaining a healthy diet.
Limited data from randomized, controlled trials suggest that a multidimensional lifestyle intervention during the menopause transition can prevent weight gain and reduce blood pressure and levels of triglycerides, blood glucose, and insulin and reduce the incidence of subclinical carotid atherosclerosis, they pointed out.
“Novel data” indicate a reversal in the associations of HDL cholesterol with CVD risk over the menopause transition, suggesting that higher HDL cholesterol levels may not consistently reflect good cardiovascular health in middle-aged women, the group noted.
There are also data suggesting that starting menopause hormone therapy when younger than 60 years or within 10 years of menopause is associated with reduced CVD risk.
The group said further research is needed into the cardiometabolic effects of menopause hormone therapy, including effects associated with form, route, and duration of administration, in women traversing menopause.
They also noted that data for the primary and secondary prevention of atherosclerotic CVD and improved survival with lipid-lowering interventions “remain elusive” for women and that further study is needed to develop evidence-based recommendations tailored specifically to women.
The research had no commercial funding. Dr. El Khoudary has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Changes in hormones, body composition, lipids, and vascular health during the menopause transition can increase a woman’s chance of developing cardiovascular disease (CVD) after menopause, the American Heart Association said in a scientific statement.
“This statement aims to raise awareness of both healthcare providers and women about the menopause transition as a time of increasing heart disease risk,” Samar R. El Khoudary, PhD, MPH, who chaired the writing group, said in an interview.
“As such, it emphasizes the importance of monitoring women’s health during midlife and targeting this stage as a critical window for applying early intervention strategies that aim to maintain a healthy heart and reduce the risk of heart disease,” said Dr. El Khoudary, of the University of Pittsburgh.
The statement was published online Nov. 30 in Circulation.
Evolution in knowledge
During the past 20 years, knowledge of how menopause might contribute to CVD has evolved “dramatically,” Dr. El Khoudary noted. The accumulated data consistently point to the menopause transition as a time of change in heart health.
“Importantly,” she said, the latest AHA guidelines for CVD prevention in women, published in 2011, do not include data now available on the menopause transition as a time of increased CVD risk.
“As such, there is a compelling need to discuss the implications of the accumulating body of literature on this topic,” said Dr. El Khoudary.
The statement provides a contemporary synthesis of the existing data on menopause and how it relates to CVD, the leading cause of death of U.S. women.
Earlier age at natural menopause has generally been found to be a marker of greater CVD risk. Iatrogenically induced menopause (bilateral oophorectomy) during the premenopausal period is also associated with higher CVD risk, the data suggest.
Vasomotor symptoms are associated with worse levels of CVD risk factors and measures of subclinical atherosclerosis. Sleep disturbance has also been linked to greater risk for subclinical CVD and worse CV health indexes in women during midlife.
Increases in central/visceral fat and decreases in lean muscle mass are more pronounced during the menopause transition. This increased central adiposity is associated with increased risk for mortality, even among those with normal body mass index, the writing group found.
Increases in lipid levels (LDL cholesterol and apolipoprotein B), metabolic syndrome risk, and vascular remodeling at midlife are driven by the menopause transition more than aging, whereas increases in blood pressure, insulin level, and glucose level are likely more influenced by chronological aging, they reported.
Lifestyle interventions
The writing group noted that, because of the increase in overall life expectancy in the United States, a significant proportion of women will spend up to 40% of their lives after menopause.
Yet data suggest that only 7.2% of women transitioning to menopause are meeting physical activity guidelines and that fewer than 20% of those women are consistently maintaining a healthy diet.
Limited data from randomized, controlled trials suggest that a multidimensional lifestyle intervention during the menopause transition can prevent weight gain and reduce blood pressure and levels of triglycerides, blood glucose, and insulin and reduce the incidence of subclinical carotid atherosclerosis, they pointed out.
“Novel data” indicate a reversal in the associations of HDL cholesterol with CVD risk over the menopause transition, suggesting that higher HDL cholesterol levels may not consistently reflect good cardiovascular health in middle-aged women, the group noted.
There are also data suggesting that starting menopause hormone therapy when younger than 60 years or within 10 years of menopause is associated with reduced CVD risk.
The group said further research is needed into the cardiometabolic effects of menopause hormone therapy, including effects associated with form, route, and duration of administration, in women traversing menopause.
They also noted that data for the primary and secondary prevention of atherosclerotic CVD and improved survival with lipid-lowering interventions “remain elusive” for women and that further study is needed to develop evidence-based recommendations tailored specifically to women.
The research had no commercial funding. Dr. El Khoudary has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Changes in hormones, body composition, lipids, and vascular health during the menopause transition can increase a woman’s chance of developing cardiovascular disease (CVD) after menopause, the American Heart Association said in a scientific statement.
“This statement aims to raise awareness of both healthcare providers and women about the menopause transition as a time of increasing heart disease risk,” Samar R. El Khoudary, PhD, MPH, who chaired the writing group, said in an interview.
“As such, it emphasizes the importance of monitoring women’s health during midlife and targeting this stage as a critical window for applying early intervention strategies that aim to maintain a healthy heart and reduce the risk of heart disease,” said Dr. El Khoudary, of the University of Pittsburgh.
The statement was published online Nov. 30 in Circulation.
Evolution in knowledge
During the past 20 years, knowledge of how menopause might contribute to CVD has evolved “dramatically,” Dr. El Khoudary noted. The accumulated data consistently point to the menopause transition as a time of change in heart health.
“Importantly,” she said, the latest AHA guidelines for CVD prevention in women, published in 2011, do not include data now available on the menopause transition as a time of increased CVD risk.
“As such, there is a compelling need to discuss the implications of the accumulating body of literature on this topic,” said Dr. El Khoudary.
The statement provides a contemporary synthesis of the existing data on menopause and how it relates to CVD, the leading cause of death of U.S. women.
Earlier age at natural menopause has generally been found to be a marker of greater CVD risk. Iatrogenically induced menopause (bilateral oophorectomy) during the premenopausal period is also associated with higher CVD risk, the data suggest.
Vasomotor symptoms are associated with worse levels of CVD risk factors and measures of subclinical atherosclerosis. Sleep disturbance has also been linked to greater risk for subclinical CVD and worse CV health indexes in women during midlife.
Increases in central/visceral fat and decreases in lean muscle mass are more pronounced during the menopause transition. This increased central adiposity is associated with increased risk for mortality, even among those with normal body mass index, the writing group found.
Increases in lipid levels (LDL cholesterol and apolipoprotein B), metabolic syndrome risk, and vascular remodeling at midlife are driven by the menopause transition more than aging, whereas increases in blood pressure, insulin level, and glucose level are likely more influenced by chronological aging, they reported.
Lifestyle interventions
The writing group noted that, because of the increase in overall life expectancy in the United States, a significant proportion of women will spend up to 40% of their lives after menopause.
Yet data suggest that only 7.2% of women transitioning to menopause are meeting physical activity guidelines and that fewer than 20% of those women are consistently maintaining a healthy diet.
Limited data from randomized, controlled trials suggest that a multidimensional lifestyle intervention during the menopause transition can prevent weight gain and reduce blood pressure and levels of triglycerides, blood glucose, and insulin and reduce the incidence of subclinical carotid atherosclerosis, they pointed out.
“Novel data” indicate a reversal in the associations of HDL cholesterol with CVD risk over the menopause transition, suggesting that higher HDL cholesterol levels may not consistently reflect good cardiovascular health in middle-aged women, the group noted.
There are also data suggesting that starting menopause hormone therapy when younger than 60 years or within 10 years of menopause is associated with reduced CVD risk.
The group said further research is needed into the cardiometabolic effects of menopause hormone therapy, including effects associated with form, route, and duration of administration, in women traversing menopause.
They also noted that data for the primary and secondary prevention of atherosclerotic CVD and improved survival with lipid-lowering interventions “remain elusive” for women and that further study is needed to develop evidence-based recommendations tailored specifically to women.
The research had no commercial funding. Dr. El Khoudary has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Treating insomnia, anxiety in a pandemic
Since the start of the pandemic, we have been conducting an extra hour of Virtual Rounds at the Center for Women’s Mental Health. Virtual Rounds has been an opportunity to discuss cases around a spectrum of clinical management issues with respect to depression, bipolar disorder, and a spectrum of anxiety disorders like obsessive-compulsive disorder (OCD), posttraumatic stress disorder (PTSD), and generalized anxiety disorder. How to apply the calculus of risk-benefit decision-making around management of psychiatric disorder during pregnancy and the postpartum period has been the cornerstone of the work at our center for over 2 decades.
When we went virtual at our center in the early Spring, we decided to keep the format of our faculty rounds the way they have been for years and to sustain cohesiveness of our program during the pandemic. But we thought the needs of pregnant and postpartum women warranted being addressed in a context more specific to COVID-19, and also that reproductive psychiatrists and other clinicians could learn from each other about novel issues coming up for this group of patients during the pandemic. With that backdrop, Marlene Freeman, MD, and I founded “Virtual Rounds at the Center” to respond to queries from our colleagues across the country; we do this just after our own rounds on Wednesdays at 2:00 p.m.
As the pandemic has progressed, Virtual Rounds has blossomed into a virtual community on the Zoom platform, where social workers, psychologists, nurse prescribers, psychiatrists, and obstetricians discuss the needs of pregnant and postpartum women specific to COVID-19. Frequently, our discussions involve a review of the risks and benefits of treatment before, during, and after pregnancy.
Seemingly, week to week, more and more colleagues raise questions about the treatment of anxiety and insomnia during pregnancy and the postpartum period. I’ve spoken in previous columns about the enhanced use of telemedicine. Telemedicine not only facilitates efforts like Virtual Rounds and our ability to reach out to colleagues across the country and share cases, but also has allowed us to keep even closer tabs on the emotional well-being of our pregnant and postpartum women during COVID-19.
The question is not just about the effects of a medicine that a woman might take to treat anxiety or insomnia during pregnancy, but the experience of the pandemic per se, which we are measuring in multiple studies now using a variety of psychological instruments that patients complete. The pandemic is unequivocally taking a still unquantified toll on the mental health of Americans and potentially on the next generation to come.
Midcycle awakening during pregnancy
Complaints of insomnia and midcycle awakening during pregnancy are not new – it is the rule, rather than the exception for many pregnant women, particularly later in pregnancy. We have unequivocally seen a worsening of complaints of sleep disruption including insomnia and midcycle awakening during the pandemic that is greater than what we have seen previously. Both patients and colleagues have asked us the safest ways to manage it. One of the first things we consider when we hear about insomnia is whether it is part of an underlying mood disorder. While we see primary insomnia clinically, it really is important to remember that insomnia can be part and parcel of an underlying mood disorder.
With that in mind, what are the options? During the pandemic, we’ve seen an increased use of digital cognitive behavioral therapy for insomnia (CBT-I) for patients who cannot initiate sleep, which has a very strong evidence base for effectiveness as a first-line intervention for many.
If a patient has an incomplete response to CBT-I, what might be pursued next? In our center, we have a low threshold for using low doses of benzodiazepines, such as lorazepam or clonazepam, because the majority of data do not support an increased risk of major congenital malformations even when used in the first trimester. It is quite common to see medicines such as newer nonbenzodiazepine sedative hypnotics such as Ambien CR (zolpidem) or Lunesta (eszopiclone) used by our colleagues in ob.gyn. The reproductive safety data on those medicines are particularly sparse, and they may have greater risk of cognitive side effects the next day, so we tend to avoid them.
Another sometimes-forgotten option to consider is using low doses of tricyclic antidepressants (i.e., 10-25 mg of nortriptyline at bedtime), with tricyclics having a 40-year history and at least one pooled analysis showing the absence of increased risk for major congenital malformations when used. This may be a very easy way of managing insomnia, with low-dose tricyclics having an anxiolytic effect as well.
Anxiety during pregnancy
The most common rise in symptoms during COVID-19 for women who are pregnant or post partum has been an increase in anxiety. Women present with a spectrum of concerns leading to anxiety symptoms in the context of the pandemic. Earlier on in the pandemic, concerns focused mostly on how to stay healthy, and how to mitigate risk and not catch SARS-CoV-2 during pregnancy, as well as the very complex issues that were playing out in real time as hospital systems were figuring out how to manage pregnant women in labor and to keep both them and staff safe. Over time, anxiety has shifted to still staying safe during the pandemic and the potential impact of SARS-CoV-2 infection on pregnancy outcomes. The No. 1 concern is what the implications of COVID-19 disease are on mother and child. New mothers also are anxious about how they will practically navigate life with a newborn in the postpartum setting.
Early on in the pandemic, some hospital systems severely limited who was in the room with a woman during labor, potentially impeding the wishes of women during delivery who would have wanted their loved ones and/or a doula present, as an example. With enhanced testing available now, protocols have since relaxed in many hospitals to allow partners – but not a team – to remain in the hospital during the labor process. Still, the prospect of delivering during a pandemic is undoubtedly a source of anxiety for some women.
This sort of anxiety, particularly in patients with preexisting anxiety disorders, can be particularly challenging. Fortunately, there has been a rapid increase over the last several years of digital apps to mitigate anxiety. While many of them have not been systematically studied, the data on biobehavioral intervention for anxiety is enormous, and this should be used as first-line treatment for patients with mild to moderate symptoms; so many women would prefer to avoid pharmacological intervention during pregnancy, if possible, to avoid fetal drug exposure. For patients who meet criteria for frank anxiety disorder, other nonpharmacologic interventions such as CBT have been shown to be effective.
Frequently, we see women who are experiencing levels of anxiety where nonpharmacological interventions have an incomplete response, and colleagues have asked about the safest way to treat these patients. As has been discussed in multiple previous columns, selective serotonin reuptake inhibitors (SSRIs) should be thought of sooner rather than later, particularly with medicines with good reproductive safety data such as sertraline, citalopram, or fluoxetine.
We also reported over 15 years ago that at least 30%-40% of women presenting with histories of recurrent major depression at the beginning of pregnancy had comorbid anxiety disorders, and that the use of benzodiazepines in that population in addition to SSRIs was exceedingly common, with doses of approximately 0.5-1.5 mg of clonazepam or lorazepam being standard fare. Again, this is very appropriate treatment to mitigate anxiety symptoms because now have enough data as a field that support the existence of adverse outcomes associated with untreated anxiety during pregnancy in terms of both adverse obstetric and neonatal outcomes, higher rates of preterm birth, and other obstetric complications. Hence, managing anxiety during pregnancy should be considered like managing a toxic exposure – the same way that one would be concerned about anything else that a pregnant woman could be exposed to.
Lastly, although no atypical antipsychotic has been approved for the treatment of anxiety, its use off label is extremely common. More and more data support the absence of a signal of teratogenicity across the family of molecules including atypical antipsychotics. Beyond potential use of atypical antipsychotics, at Virtual Rounds last week, a colleague asked about the use of gabapentin in a patient who was diagnosed with substance use disorder and who had inadvertently conceived on gabapentin, which was being used to treat both anxiety and insomnia. We have typically avoided the use of gabapentin during pregnancy because prospective data have been limited to relatively small case series and one report, with a total of exposures in roughly the 300 range.
However, our colleagues at the Harvard School of Public Health have recently published an article that looked at the United States Medicaid Analytic eXtract (MAX) dataset, which has been used to publish other articles addressing atypical antipsychotics, SSRIs, lithium, and pharmacovigilance investigations among other important topics. In this study, the database was used to look specifically at 4,642 pregnancies with gabapentin exposure relative to 1,744,447 unexposed pregnancies, without a significant finding for increased risk for major congenital malformations.
The question of an increased risk of cardiac malformations and of increased risk for obstetric complications are difficult to untangle from anxiety and depression, as they also are associated with those same outcomes. With that said, the analysis is a welcome addition to our knowledge base for a medicine used more widely to treat symptoms such as anxiety and insomnia in the general population, with a question mark around where it may fit into the algorithm during pregnancy.
In our center, gabapentin still would not be used as a first-line treatment for the management of anxiety or insomnia during pregnancy. But these new data still are reassuring for patients who come in, frequently with unplanned pregnancies. It is an important reminder to those of us taking care of patients during the pandemic to review use of contraception, because although data are unavailable specific to the period of the pandemic, what is clear is that, even prior to COVID-19, 50% of pregnancies in America were unplanned. Addressing issues of reliable use of contraception, particularly during the pandemic, is that much more important.
In this particular case, our clinician colleague in Virtual Rounds decided to continue gabapentin across pregnancy in the context of these reassuring data, but others may choose to discontinue or pursue some of the other treatment options noted above.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at obnews@mdedge.com.
Since the start of the pandemic, we have been conducting an extra hour of Virtual Rounds at the Center for Women’s Mental Health. Virtual Rounds has been an opportunity to discuss cases around a spectrum of clinical management issues with respect to depression, bipolar disorder, and a spectrum of anxiety disorders like obsessive-compulsive disorder (OCD), posttraumatic stress disorder (PTSD), and generalized anxiety disorder. How to apply the calculus of risk-benefit decision-making around management of psychiatric disorder during pregnancy and the postpartum period has been the cornerstone of the work at our center for over 2 decades.
When we went virtual at our center in the early Spring, we decided to keep the format of our faculty rounds the way they have been for years and to sustain cohesiveness of our program during the pandemic. But we thought the needs of pregnant and postpartum women warranted being addressed in a context more specific to COVID-19, and also that reproductive psychiatrists and other clinicians could learn from each other about novel issues coming up for this group of patients during the pandemic. With that backdrop, Marlene Freeman, MD, and I founded “Virtual Rounds at the Center” to respond to queries from our colleagues across the country; we do this just after our own rounds on Wednesdays at 2:00 p.m.
As the pandemic has progressed, Virtual Rounds has blossomed into a virtual community on the Zoom platform, where social workers, psychologists, nurse prescribers, psychiatrists, and obstetricians discuss the needs of pregnant and postpartum women specific to COVID-19. Frequently, our discussions involve a review of the risks and benefits of treatment before, during, and after pregnancy.
Seemingly, week to week, more and more colleagues raise questions about the treatment of anxiety and insomnia during pregnancy and the postpartum period. I’ve spoken in previous columns about the enhanced use of telemedicine. Telemedicine not only facilitates efforts like Virtual Rounds and our ability to reach out to colleagues across the country and share cases, but also has allowed us to keep even closer tabs on the emotional well-being of our pregnant and postpartum women during COVID-19.
The question is not just about the effects of a medicine that a woman might take to treat anxiety or insomnia during pregnancy, but the experience of the pandemic per se, which we are measuring in multiple studies now using a variety of psychological instruments that patients complete. The pandemic is unequivocally taking a still unquantified toll on the mental health of Americans and potentially on the next generation to come.
Midcycle awakening during pregnancy
Complaints of insomnia and midcycle awakening during pregnancy are not new – it is the rule, rather than the exception for many pregnant women, particularly later in pregnancy. We have unequivocally seen a worsening of complaints of sleep disruption including insomnia and midcycle awakening during the pandemic that is greater than what we have seen previously. Both patients and colleagues have asked us the safest ways to manage it. One of the first things we consider when we hear about insomnia is whether it is part of an underlying mood disorder. While we see primary insomnia clinically, it really is important to remember that insomnia can be part and parcel of an underlying mood disorder.
With that in mind, what are the options? During the pandemic, we’ve seen an increased use of digital cognitive behavioral therapy for insomnia (CBT-I) for patients who cannot initiate sleep, which has a very strong evidence base for effectiveness as a first-line intervention for many.
If a patient has an incomplete response to CBT-I, what might be pursued next? In our center, we have a low threshold for using low doses of benzodiazepines, such as lorazepam or clonazepam, because the majority of data do not support an increased risk of major congenital malformations even when used in the first trimester. It is quite common to see medicines such as newer nonbenzodiazepine sedative hypnotics such as Ambien CR (zolpidem) or Lunesta (eszopiclone) used by our colleagues in ob.gyn. The reproductive safety data on those medicines are particularly sparse, and they may have greater risk of cognitive side effects the next day, so we tend to avoid them.
Another sometimes-forgotten option to consider is using low doses of tricyclic antidepressants (i.e., 10-25 mg of nortriptyline at bedtime), with tricyclics having a 40-year history and at least one pooled analysis showing the absence of increased risk for major congenital malformations when used. This may be a very easy way of managing insomnia, with low-dose tricyclics having an anxiolytic effect as well.
Anxiety during pregnancy
The most common rise in symptoms during COVID-19 for women who are pregnant or post partum has been an increase in anxiety. Women present with a spectrum of concerns leading to anxiety symptoms in the context of the pandemic. Earlier on in the pandemic, concerns focused mostly on how to stay healthy, and how to mitigate risk and not catch SARS-CoV-2 during pregnancy, as well as the very complex issues that were playing out in real time as hospital systems were figuring out how to manage pregnant women in labor and to keep both them and staff safe. Over time, anxiety has shifted to still staying safe during the pandemic and the potential impact of SARS-CoV-2 infection on pregnancy outcomes. The No. 1 concern is what the implications of COVID-19 disease are on mother and child. New mothers also are anxious about how they will practically navigate life with a newborn in the postpartum setting.
Early on in the pandemic, some hospital systems severely limited who was in the room with a woman during labor, potentially impeding the wishes of women during delivery who would have wanted their loved ones and/or a doula present, as an example. With enhanced testing available now, protocols have since relaxed in many hospitals to allow partners – but not a team – to remain in the hospital during the labor process. Still, the prospect of delivering during a pandemic is undoubtedly a source of anxiety for some women.
This sort of anxiety, particularly in patients with preexisting anxiety disorders, can be particularly challenging. Fortunately, there has been a rapid increase over the last several years of digital apps to mitigate anxiety. While many of them have not been systematically studied, the data on biobehavioral intervention for anxiety is enormous, and this should be used as first-line treatment for patients with mild to moderate symptoms; so many women would prefer to avoid pharmacological intervention during pregnancy, if possible, to avoid fetal drug exposure. For patients who meet criteria for frank anxiety disorder, other nonpharmacologic interventions such as CBT have been shown to be effective.
Frequently, we see women who are experiencing levels of anxiety where nonpharmacological interventions have an incomplete response, and colleagues have asked about the safest way to treat these patients. As has been discussed in multiple previous columns, selective serotonin reuptake inhibitors (SSRIs) should be thought of sooner rather than later, particularly with medicines with good reproductive safety data such as sertraline, citalopram, or fluoxetine.
We also reported over 15 years ago that at least 30%-40% of women presenting with histories of recurrent major depression at the beginning of pregnancy had comorbid anxiety disorders, and that the use of benzodiazepines in that population in addition to SSRIs was exceedingly common, with doses of approximately 0.5-1.5 mg of clonazepam or lorazepam being standard fare. Again, this is very appropriate treatment to mitigate anxiety symptoms because now have enough data as a field that support the existence of adverse outcomes associated with untreated anxiety during pregnancy in terms of both adverse obstetric and neonatal outcomes, higher rates of preterm birth, and other obstetric complications. Hence, managing anxiety during pregnancy should be considered like managing a toxic exposure – the same way that one would be concerned about anything else that a pregnant woman could be exposed to.
Lastly, although no atypical antipsychotic has been approved for the treatment of anxiety, its use off label is extremely common. More and more data support the absence of a signal of teratogenicity across the family of molecules including atypical antipsychotics. Beyond potential use of atypical antipsychotics, at Virtual Rounds last week, a colleague asked about the use of gabapentin in a patient who was diagnosed with substance use disorder and who had inadvertently conceived on gabapentin, which was being used to treat both anxiety and insomnia. We have typically avoided the use of gabapentin during pregnancy because prospective data have been limited to relatively small case series and one report, with a total of exposures in roughly the 300 range.
However, our colleagues at the Harvard School of Public Health have recently published an article that looked at the United States Medicaid Analytic eXtract (MAX) dataset, which has been used to publish other articles addressing atypical antipsychotics, SSRIs, lithium, and pharmacovigilance investigations among other important topics. In this study, the database was used to look specifically at 4,642 pregnancies with gabapentin exposure relative to 1,744,447 unexposed pregnancies, without a significant finding for increased risk for major congenital malformations.
The question of an increased risk of cardiac malformations and of increased risk for obstetric complications are difficult to untangle from anxiety and depression, as they also are associated with those same outcomes. With that said, the analysis is a welcome addition to our knowledge base for a medicine used more widely to treat symptoms such as anxiety and insomnia in the general population, with a question mark around where it may fit into the algorithm during pregnancy.
In our center, gabapentin still would not be used as a first-line treatment for the management of anxiety or insomnia during pregnancy. But these new data still are reassuring for patients who come in, frequently with unplanned pregnancies. It is an important reminder to those of us taking care of patients during the pandemic to review use of contraception, because although data are unavailable specific to the period of the pandemic, what is clear is that, even prior to COVID-19, 50% of pregnancies in America were unplanned. Addressing issues of reliable use of contraception, particularly during the pandemic, is that much more important.
In this particular case, our clinician colleague in Virtual Rounds decided to continue gabapentin across pregnancy in the context of these reassuring data, but others may choose to discontinue or pursue some of the other treatment options noted above.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at obnews@mdedge.com.
Since the start of the pandemic, we have been conducting an extra hour of Virtual Rounds at the Center for Women’s Mental Health. Virtual Rounds has been an opportunity to discuss cases around a spectrum of clinical management issues with respect to depression, bipolar disorder, and a spectrum of anxiety disorders like obsessive-compulsive disorder (OCD), posttraumatic stress disorder (PTSD), and generalized anxiety disorder. How to apply the calculus of risk-benefit decision-making around management of psychiatric disorder during pregnancy and the postpartum period has been the cornerstone of the work at our center for over 2 decades.
When we went virtual at our center in the early Spring, we decided to keep the format of our faculty rounds the way they have been for years and to sustain cohesiveness of our program during the pandemic. But we thought the needs of pregnant and postpartum women warranted being addressed in a context more specific to COVID-19, and also that reproductive psychiatrists and other clinicians could learn from each other about novel issues coming up for this group of patients during the pandemic. With that backdrop, Marlene Freeman, MD, and I founded “Virtual Rounds at the Center” to respond to queries from our colleagues across the country; we do this just after our own rounds on Wednesdays at 2:00 p.m.
As the pandemic has progressed, Virtual Rounds has blossomed into a virtual community on the Zoom platform, where social workers, psychologists, nurse prescribers, psychiatrists, and obstetricians discuss the needs of pregnant and postpartum women specific to COVID-19. Frequently, our discussions involve a review of the risks and benefits of treatment before, during, and after pregnancy.
Seemingly, week to week, more and more colleagues raise questions about the treatment of anxiety and insomnia during pregnancy and the postpartum period. I’ve spoken in previous columns about the enhanced use of telemedicine. Telemedicine not only facilitates efforts like Virtual Rounds and our ability to reach out to colleagues across the country and share cases, but also has allowed us to keep even closer tabs on the emotional well-being of our pregnant and postpartum women during COVID-19.
The question is not just about the effects of a medicine that a woman might take to treat anxiety or insomnia during pregnancy, but the experience of the pandemic per se, which we are measuring in multiple studies now using a variety of psychological instruments that patients complete. The pandemic is unequivocally taking a still unquantified toll on the mental health of Americans and potentially on the next generation to come.
Midcycle awakening during pregnancy
Complaints of insomnia and midcycle awakening during pregnancy are not new – it is the rule, rather than the exception for many pregnant women, particularly later in pregnancy. We have unequivocally seen a worsening of complaints of sleep disruption including insomnia and midcycle awakening during the pandemic that is greater than what we have seen previously. Both patients and colleagues have asked us the safest ways to manage it. One of the first things we consider when we hear about insomnia is whether it is part of an underlying mood disorder. While we see primary insomnia clinically, it really is important to remember that insomnia can be part and parcel of an underlying mood disorder.
With that in mind, what are the options? During the pandemic, we’ve seen an increased use of digital cognitive behavioral therapy for insomnia (CBT-I) for patients who cannot initiate sleep, which has a very strong evidence base for effectiveness as a first-line intervention for many.
If a patient has an incomplete response to CBT-I, what might be pursued next? In our center, we have a low threshold for using low doses of benzodiazepines, such as lorazepam or clonazepam, because the majority of data do not support an increased risk of major congenital malformations even when used in the first trimester. It is quite common to see medicines such as newer nonbenzodiazepine sedative hypnotics such as Ambien CR (zolpidem) or Lunesta (eszopiclone) used by our colleagues in ob.gyn. The reproductive safety data on those medicines are particularly sparse, and they may have greater risk of cognitive side effects the next day, so we tend to avoid them.
Another sometimes-forgotten option to consider is using low doses of tricyclic antidepressants (i.e., 10-25 mg of nortriptyline at bedtime), with tricyclics having a 40-year history and at least one pooled analysis showing the absence of increased risk for major congenital malformations when used. This may be a very easy way of managing insomnia, with low-dose tricyclics having an anxiolytic effect as well.
Anxiety during pregnancy
The most common rise in symptoms during COVID-19 for women who are pregnant or post partum has been an increase in anxiety. Women present with a spectrum of concerns leading to anxiety symptoms in the context of the pandemic. Earlier on in the pandemic, concerns focused mostly on how to stay healthy, and how to mitigate risk and not catch SARS-CoV-2 during pregnancy, as well as the very complex issues that were playing out in real time as hospital systems were figuring out how to manage pregnant women in labor and to keep both them and staff safe. Over time, anxiety has shifted to still staying safe during the pandemic and the potential impact of SARS-CoV-2 infection on pregnancy outcomes. The No. 1 concern is what the implications of COVID-19 disease are on mother and child. New mothers also are anxious about how they will practically navigate life with a newborn in the postpartum setting.
Early on in the pandemic, some hospital systems severely limited who was in the room with a woman during labor, potentially impeding the wishes of women during delivery who would have wanted their loved ones and/or a doula present, as an example. With enhanced testing available now, protocols have since relaxed in many hospitals to allow partners – but not a team – to remain in the hospital during the labor process. Still, the prospect of delivering during a pandemic is undoubtedly a source of anxiety for some women.
This sort of anxiety, particularly in patients with preexisting anxiety disorders, can be particularly challenging. Fortunately, there has been a rapid increase over the last several years of digital apps to mitigate anxiety. While many of them have not been systematically studied, the data on biobehavioral intervention for anxiety is enormous, and this should be used as first-line treatment for patients with mild to moderate symptoms; so many women would prefer to avoid pharmacological intervention during pregnancy, if possible, to avoid fetal drug exposure. For patients who meet criteria for frank anxiety disorder, other nonpharmacologic interventions such as CBT have been shown to be effective.
Frequently, we see women who are experiencing levels of anxiety where nonpharmacological interventions have an incomplete response, and colleagues have asked about the safest way to treat these patients. As has been discussed in multiple previous columns, selective serotonin reuptake inhibitors (SSRIs) should be thought of sooner rather than later, particularly with medicines with good reproductive safety data such as sertraline, citalopram, or fluoxetine.
We also reported over 15 years ago that at least 30%-40% of women presenting with histories of recurrent major depression at the beginning of pregnancy had comorbid anxiety disorders, and that the use of benzodiazepines in that population in addition to SSRIs was exceedingly common, with doses of approximately 0.5-1.5 mg of clonazepam or lorazepam being standard fare. Again, this is very appropriate treatment to mitigate anxiety symptoms because now have enough data as a field that support the existence of adverse outcomes associated with untreated anxiety during pregnancy in terms of both adverse obstetric and neonatal outcomes, higher rates of preterm birth, and other obstetric complications. Hence, managing anxiety during pregnancy should be considered like managing a toxic exposure – the same way that one would be concerned about anything else that a pregnant woman could be exposed to.
Lastly, although no atypical antipsychotic has been approved for the treatment of anxiety, its use off label is extremely common. More and more data support the absence of a signal of teratogenicity across the family of molecules including atypical antipsychotics. Beyond potential use of atypical antipsychotics, at Virtual Rounds last week, a colleague asked about the use of gabapentin in a patient who was diagnosed with substance use disorder and who had inadvertently conceived on gabapentin, which was being used to treat both anxiety and insomnia. We have typically avoided the use of gabapentin during pregnancy because prospective data have been limited to relatively small case series and one report, with a total of exposures in roughly the 300 range.
However, our colleagues at the Harvard School of Public Health have recently published an article that looked at the United States Medicaid Analytic eXtract (MAX) dataset, which has been used to publish other articles addressing atypical antipsychotics, SSRIs, lithium, and pharmacovigilance investigations among other important topics. In this study, the database was used to look specifically at 4,642 pregnancies with gabapentin exposure relative to 1,744,447 unexposed pregnancies, without a significant finding for increased risk for major congenital malformations.
The question of an increased risk of cardiac malformations and of increased risk for obstetric complications are difficult to untangle from anxiety and depression, as they also are associated with those same outcomes. With that said, the analysis is a welcome addition to our knowledge base for a medicine used more widely to treat symptoms such as anxiety and insomnia in the general population, with a question mark around where it may fit into the algorithm during pregnancy.
In our center, gabapentin still would not be used as a first-line treatment for the management of anxiety or insomnia during pregnancy. But these new data still are reassuring for patients who come in, frequently with unplanned pregnancies. It is an important reminder to those of us taking care of patients during the pandemic to review use of contraception, because although data are unavailable specific to the period of the pandemic, what is clear is that, even prior to COVID-19, 50% of pregnancies in America were unplanned. Addressing issues of reliable use of contraception, particularly during the pandemic, is that much more important.
In this particular case, our clinician colleague in Virtual Rounds decided to continue gabapentin across pregnancy in the context of these reassuring data, but others may choose to discontinue or pursue some of the other treatment options noted above.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at obnews@mdedge.com.
The fourth trimester: Achieving improved postpartum care
The field of ob.gyn. has long focused significantly more attention on the prenatal period – on determining the optimal frequency of ultrasound examinations, for instance, and on screening for diabetes and other conditions – than on women’s health and well-being after delivery.
The traditional 6-week postpartum visit has too often been a quick and cursory visit, with new mothers typically navigating the preceding postpartum transitions on their own.
The need to redefine postpartum care was a central message of Haywood Brown, MD, who in 2017 served as the president of the America College of Obstetricians and Gynecologists. Dr. Brown established a task force whose work resulted in important guidance for taking a more comprehensive and patient-centered approach to postpartum care.1
Improved care in the “fourth trimester,” as it has come to be known, is comprehensive and includes ensuring that our patients have a solid transition to health care beyond the pregnancy. We also hope that it will help us to reduce maternal mortality, given that more than half of pregnancy-related deaths occur after delivery.
Timing and frequency of contact
Historically, we’ve had a single 6-week postpartum visit, with little or no maternal support or patient contact before this visit unless the patient reported a complication. In the new paradigm, as described in the ACOG committee opinion on optimizing postpartum care, maternal care should be an ongoing process.1
so that any questions or concerns may be addressed and support can be provided.
This should be followed by individualized, ongoing care until a comprehensive postpartum visit covering physical, social, and psychological well-being is conducted by 12 weeks after birth – anytime between 4 and 12 weeks.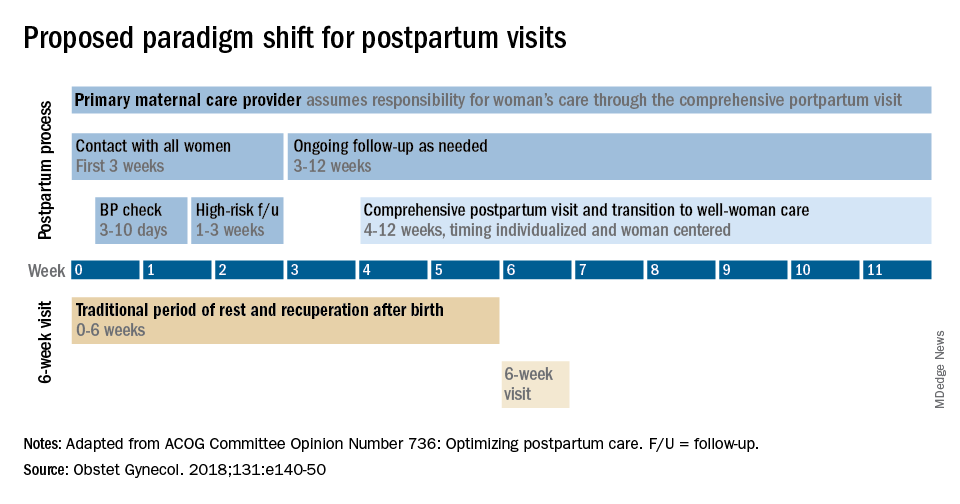
By stressing the importance of postpartum care during prenatal visits – and by talking about some of its key elements such as mental health, breastfeeding, and chronic disease management – we can let our patients know that postpartum care is not just an afterthought, but that it involves planning backed by evidence and expert opinion. Currently, as many as 40% of women do not attend a postpartum visit; early discussion, it is hoped, will increase attendance.
Certain high-risk groups should be seen or screened earlier than 3 weeks post partum. For instance, women who have hypertensive disorders of pregnancy should be evaluated no later than 7-10 days post partum, and women with severe hypertension should be seen within 72 hours, according to ACOG.
Early blood pressure checks – and follow-up as necessary – are critical for reducing the risk of postpartum stroke and other complications. I advocate uniformly checking blood pressure within several days after hospital discharge for all women who have hypertension at the end of their pregnancy.
Other high-risk conditions requiring early follow-up include diabetes and autoimmune conditions such as lupus, multiple sclerosis, and psoriasis that may flare in the postpartum period. Women with a history of postpartum depression similarly may benefit from early contact; they are at higher risk of having depression again, and there are clearly effective treatments, both medication and psychotherapy based.
In between the initial early contact (by 7-10 days post partum or by 3 weeks post partum) and the comprehensive visit between 4 and 12 weeks, the need for and timing of patient contact can be individualized. Some women will need only a brief contact and a visit at 8-10 weeks, while others will need much more. Our goal, as in all of medicine, is to provide individualized, patient-centered care.
Methods of contact
With the exception of the final comprehensive visit, postpartum care need not occur in person. Some conditions require an early office visit, but in general, as ACOG states, the usefulness of an in-person visit should be weighed against the burden of traveling to and attending that visit.
For many women, in-person visits are difficult, and we must be creative in utilizing telemedicine and phone support, text messaging, and app-based support. Having practiced during this pandemic, we are better positioned than ever before to make it relatively easy for new mothers to obtain ongoing postpartum care.
Notably, research is demonstrating that the use of technology may allow us to provide improved care and monitoring of hypertension in the postpartum period. For example, a randomized trial published in 2018 of over 200 women with a hypertensive disorder of pregnancy found that text-based surveillance with home blood pressure monitoring was more effective than usual in-person blood pressure checks in meeting clinical guidelines for postpartum monitoring.2
Women in the texting group were significantly more likely to have a single blood pressure obtained in the first 10 days post partum than women in the office group.
Postpartum care is also not a completely physician-driven endeavor. Much of what is needed to help women successfully navigate the fourth trimester can be provided by certified nurse midwives, advanced practice nurses, and other members of our maternal care teams.
Components of postpartum care
The postpartum care plan should be comprehensive, and having a checklist to guide one through initial and comprehensive visits may be helpful. The ACOG committee opinion categorizes the components of postpartum care into seven domains: mood and emotional well-being; infant care and feeding; sexuality, contraception, and birth spacing; sleep and fatigue; physical recovery from birth; chronic disease management; and health maintenance.1
The importance of screening for depression and anxiety cannot be emphasized enough. Perinatal depression is highly prevalent: It affects as many as one in seven women and can result in adverse short- and long-term effects on both the mother and child.
The U.S. Preventive Services Task Force has offered guidance for years, most recently in 2019 with its recommendations that clinicians refer pregnant and postpartum women who are at increased risk for depression to counseling interventions such as cognitive behavioral therapy and interpersonal therapy.3 There is evidence that some form of treatment for women who screen positive reduces the risk of perinatal depression.
Additionally, there is emerging evidence that postpartum PTSD may be as prevalent as postpartum depression.4 As ACOG points out, trauma is “in the eye of the beholder,” and an estimated 3%-16% of women have PTSD related to a traumatic birth experience. Complications like shoulder dystocia or postpartum hemorrhage, in which delivery processes rapidly change course, can be experienced as traumatic by women even though they and their infants are healthy. The risk of posttraumatic stress should be on our radar screen.
Interpregnancy intervals similarly are not discussed enough. We do not commonly talk to patients about how pregnancy and breastfeeding are nutritionally depleting and how it takes time to replenish these stores – yet birth spacing is so important.
Compared with interpregnancy intervals of at least 18 months, intervals shorter than 6 months were associated in a meta-analysis with increased risks of preterm birth, low birth weight, and small for gestational age.5 Optimal birth spacing is one of the few low-cost interventions available for reducing pregnancy complications in the future.
Finally, that chronic disease management is a domain of postpartum care warrants emphasis. We must work to ensure that patients have a solid plan of care in place for their diabetes, hypertension, lupus, or other chronic conditions. This includes who will provide that ongoing care, as well as when medical management should be restarted.
Some women are aware of the importance of timely care – of not waiting for 12 months, for instance, to see an internist or specialist – but others are not.
Again, certain health conditions such as multiple sclerosis and RA necessitate follow-up within a couple weeks after delivery so that medications can be restarted or dose adjustments made. The need for early postpartum follow-up can be discussed during prenatal visits, along with anticipatory guidance about breastfeeding, the signs and symptoms of perinatal depression and anxiety, and other components of the fourth trimester.
Dr. Macones has no relevant financial disclosures.
References
1. Obstet Gynecol. 2018 May;131(5):e140-50.
2. BMJ Qual Saf. 2018 Apr 27;27(11):871-7.
3. JAMA. 2019 Feb 12;321(6):580-7.
4. Clin Psychol Rev. 2014 Jul;34:389-401.JAMA. 2006 Apr 19;295(15):1809-23.
The field of ob.gyn. has long focused significantly more attention on the prenatal period – on determining the optimal frequency of ultrasound examinations, for instance, and on screening for diabetes and other conditions – than on women’s health and well-being after delivery.
The traditional 6-week postpartum visit has too often been a quick and cursory visit, with new mothers typically navigating the preceding postpartum transitions on their own.
The need to redefine postpartum care was a central message of Haywood Brown, MD, who in 2017 served as the president of the America College of Obstetricians and Gynecologists. Dr. Brown established a task force whose work resulted in important guidance for taking a more comprehensive and patient-centered approach to postpartum care.1
Improved care in the “fourth trimester,” as it has come to be known, is comprehensive and includes ensuring that our patients have a solid transition to health care beyond the pregnancy. We also hope that it will help us to reduce maternal mortality, given that more than half of pregnancy-related deaths occur after delivery.
Timing and frequency of contact
Historically, we’ve had a single 6-week postpartum visit, with little or no maternal support or patient contact before this visit unless the patient reported a complication. In the new paradigm, as described in the ACOG committee opinion on optimizing postpartum care, maternal care should be an ongoing process.1
so that any questions or concerns may be addressed and support can be provided.
This should be followed by individualized, ongoing care until a comprehensive postpartum visit covering physical, social, and psychological well-being is conducted by 12 weeks after birth – anytime between 4 and 12 weeks.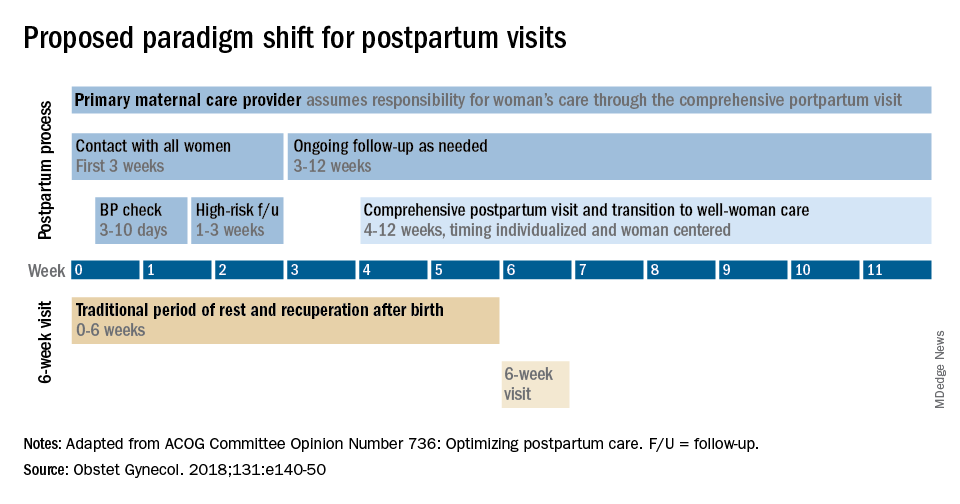
By stressing the importance of postpartum care during prenatal visits – and by talking about some of its key elements such as mental health, breastfeeding, and chronic disease management – we can let our patients know that postpartum care is not just an afterthought, but that it involves planning backed by evidence and expert opinion. Currently, as many as 40% of women do not attend a postpartum visit; early discussion, it is hoped, will increase attendance.
Certain high-risk groups should be seen or screened earlier than 3 weeks post partum. For instance, women who have hypertensive disorders of pregnancy should be evaluated no later than 7-10 days post partum, and women with severe hypertension should be seen within 72 hours, according to ACOG.
Early blood pressure checks – and follow-up as necessary – are critical for reducing the risk of postpartum stroke and other complications. I advocate uniformly checking blood pressure within several days after hospital discharge for all women who have hypertension at the end of their pregnancy.
Other high-risk conditions requiring early follow-up include diabetes and autoimmune conditions such as lupus, multiple sclerosis, and psoriasis that may flare in the postpartum period. Women with a history of postpartum depression similarly may benefit from early contact; they are at higher risk of having depression again, and there are clearly effective treatments, both medication and psychotherapy based.
In between the initial early contact (by 7-10 days post partum or by 3 weeks post partum) and the comprehensive visit between 4 and 12 weeks, the need for and timing of patient contact can be individualized. Some women will need only a brief contact and a visit at 8-10 weeks, while others will need much more. Our goal, as in all of medicine, is to provide individualized, patient-centered care.
Methods of contact
With the exception of the final comprehensive visit, postpartum care need not occur in person. Some conditions require an early office visit, but in general, as ACOG states, the usefulness of an in-person visit should be weighed against the burden of traveling to and attending that visit.
For many women, in-person visits are difficult, and we must be creative in utilizing telemedicine and phone support, text messaging, and app-based support. Having practiced during this pandemic, we are better positioned than ever before to make it relatively easy for new mothers to obtain ongoing postpartum care.
Notably, research is demonstrating that the use of technology may allow us to provide improved care and monitoring of hypertension in the postpartum period. For example, a randomized trial published in 2018 of over 200 women with a hypertensive disorder of pregnancy found that text-based surveillance with home blood pressure monitoring was more effective than usual in-person blood pressure checks in meeting clinical guidelines for postpartum monitoring.2
Women in the texting group were significantly more likely to have a single blood pressure obtained in the first 10 days post partum than women in the office group.
Postpartum care is also not a completely physician-driven endeavor. Much of what is needed to help women successfully navigate the fourth trimester can be provided by certified nurse midwives, advanced practice nurses, and other members of our maternal care teams.
Components of postpartum care
The postpartum care plan should be comprehensive, and having a checklist to guide one through initial and comprehensive visits may be helpful. The ACOG committee opinion categorizes the components of postpartum care into seven domains: mood and emotional well-being; infant care and feeding; sexuality, contraception, and birth spacing; sleep and fatigue; physical recovery from birth; chronic disease management; and health maintenance.1
The importance of screening for depression and anxiety cannot be emphasized enough. Perinatal depression is highly prevalent: It affects as many as one in seven women and can result in adverse short- and long-term effects on both the mother and child.
The U.S. Preventive Services Task Force has offered guidance for years, most recently in 2019 with its recommendations that clinicians refer pregnant and postpartum women who are at increased risk for depression to counseling interventions such as cognitive behavioral therapy and interpersonal therapy.3 There is evidence that some form of treatment for women who screen positive reduces the risk of perinatal depression.
Additionally, there is emerging evidence that postpartum PTSD may be as prevalent as postpartum depression.4 As ACOG points out, trauma is “in the eye of the beholder,” and an estimated 3%-16% of women have PTSD related to a traumatic birth experience. Complications like shoulder dystocia or postpartum hemorrhage, in which delivery processes rapidly change course, can be experienced as traumatic by women even though they and their infants are healthy. The risk of posttraumatic stress should be on our radar screen.
Interpregnancy intervals similarly are not discussed enough. We do not commonly talk to patients about how pregnancy and breastfeeding are nutritionally depleting and how it takes time to replenish these stores – yet birth spacing is so important.
Compared with interpregnancy intervals of at least 18 months, intervals shorter than 6 months were associated in a meta-analysis with increased risks of preterm birth, low birth weight, and small for gestational age.5 Optimal birth spacing is one of the few low-cost interventions available for reducing pregnancy complications in the future.
Finally, that chronic disease management is a domain of postpartum care warrants emphasis. We must work to ensure that patients have a solid plan of care in place for their diabetes, hypertension, lupus, or other chronic conditions. This includes who will provide that ongoing care, as well as when medical management should be restarted.
Some women are aware of the importance of timely care – of not waiting for 12 months, for instance, to see an internist or specialist – but others are not.
Again, certain health conditions such as multiple sclerosis and RA necessitate follow-up within a couple weeks after delivery so that medications can be restarted or dose adjustments made. The need for early postpartum follow-up can be discussed during prenatal visits, along with anticipatory guidance about breastfeeding, the signs and symptoms of perinatal depression and anxiety, and other components of the fourth trimester.
Dr. Macones has no relevant financial disclosures.
References
1. Obstet Gynecol. 2018 May;131(5):e140-50.
2. BMJ Qual Saf. 2018 Apr 27;27(11):871-7.
3. JAMA. 2019 Feb 12;321(6):580-7.
4. Clin Psychol Rev. 2014 Jul;34:389-401.JAMA. 2006 Apr 19;295(15):1809-23.
The field of ob.gyn. has long focused significantly more attention on the prenatal period – on determining the optimal frequency of ultrasound examinations, for instance, and on screening for diabetes and other conditions – than on women’s health and well-being after delivery.
The traditional 6-week postpartum visit has too often been a quick and cursory visit, with new mothers typically navigating the preceding postpartum transitions on their own.
The need to redefine postpartum care was a central message of Haywood Brown, MD, who in 2017 served as the president of the America College of Obstetricians and Gynecologists. Dr. Brown established a task force whose work resulted in important guidance for taking a more comprehensive and patient-centered approach to postpartum care.1
Improved care in the “fourth trimester,” as it has come to be known, is comprehensive and includes ensuring that our patients have a solid transition to health care beyond the pregnancy. We also hope that it will help us to reduce maternal mortality, given that more than half of pregnancy-related deaths occur after delivery.
Timing and frequency of contact
Historically, we’ve had a single 6-week postpartum visit, with little or no maternal support or patient contact before this visit unless the patient reported a complication. In the new paradigm, as described in the ACOG committee opinion on optimizing postpartum care, maternal care should be an ongoing process.1
so that any questions or concerns may be addressed and support can be provided.
This should be followed by individualized, ongoing care until a comprehensive postpartum visit covering physical, social, and psychological well-being is conducted by 12 weeks after birth – anytime between 4 and 12 weeks.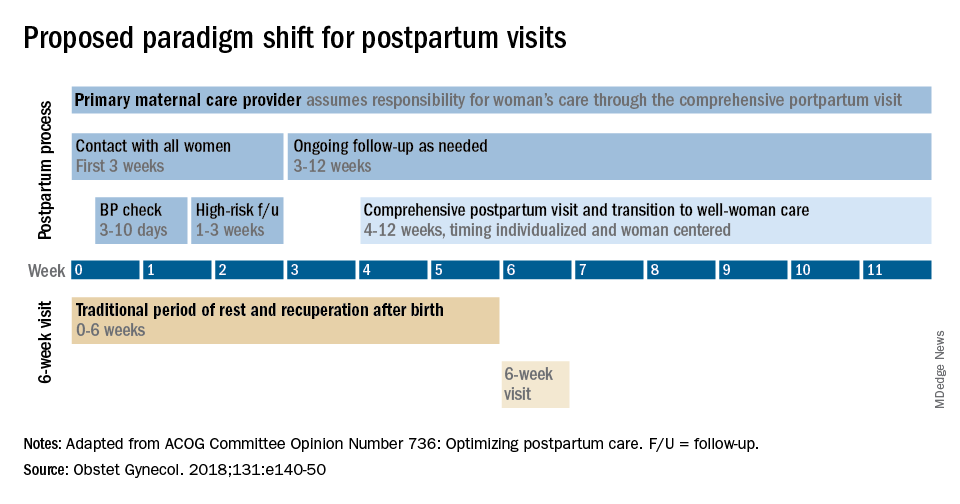
By stressing the importance of postpartum care during prenatal visits – and by talking about some of its key elements such as mental health, breastfeeding, and chronic disease management – we can let our patients know that postpartum care is not just an afterthought, but that it involves planning backed by evidence and expert opinion. Currently, as many as 40% of women do not attend a postpartum visit; early discussion, it is hoped, will increase attendance.
Certain high-risk groups should be seen or screened earlier than 3 weeks post partum. For instance, women who have hypertensive disorders of pregnancy should be evaluated no later than 7-10 days post partum, and women with severe hypertension should be seen within 72 hours, according to ACOG.
Early blood pressure checks – and follow-up as necessary – are critical for reducing the risk of postpartum stroke and other complications. I advocate uniformly checking blood pressure within several days after hospital discharge for all women who have hypertension at the end of their pregnancy.
Other high-risk conditions requiring early follow-up include diabetes and autoimmune conditions such as lupus, multiple sclerosis, and psoriasis that may flare in the postpartum period. Women with a history of postpartum depression similarly may benefit from early contact; they are at higher risk of having depression again, and there are clearly effective treatments, both medication and psychotherapy based.
In between the initial early contact (by 7-10 days post partum or by 3 weeks post partum) and the comprehensive visit between 4 and 12 weeks, the need for and timing of patient contact can be individualized. Some women will need only a brief contact and a visit at 8-10 weeks, while others will need much more. Our goal, as in all of medicine, is to provide individualized, patient-centered care.
Methods of contact
With the exception of the final comprehensive visit, postpartum care need not occur in person. Some conditions require an early office visit, but in general, as ACOG states, the usefulness of an in-person visit should be weighed against the burden of traveling to and attending that visit.
For many women, in-person visits are difficult, and we must be creative in utilizing telemedicine and phone support, text messaging, and app-based support. Having practiced during this pandemic, we are better positioned than ever before to make it relatively easy for new mothers to obtain ongoing postpartum care.
Notably, research is demonstrating that the use of technology may allow us to provide improved care and monitoring of hypertension in the postpartum period. For example, a randomized trial published in 2018 of over 200 women with a hypertensive disorder of pregnancy found that text-based surveillance with home blood pressure monitoring was more effective than usual in-person blood pressure checks in meeting clinical guidelines for postpartum monitoring.2
Women in the texting group were significantly more likely to have a single blood pressure obtained in the first 10 days post partum than women in the office group.
Postpartum care is also not a completely physician-driven endeavor. Much of what is needed to help women successfully navigate the fourth trimester can be provided by certified nurse midwives, advanced practice nurses, and other members of our maternal care teams.
Components of postpartum care
The postpartum care plan should be comprehensive, and having a checklist to guide one through initial and comprehensive visits may be helpful. The ACOG committee opinion categorizes the components of postpartum care into seven domains: mood and emotional well-being; infant care and feeding; sexuality, contraception, and birth spacing; sleep and fatigue; physical recovery from birth; chronic disease management; and health maintenance.1
The importance of screening for depression and anxiety cannot be emphasized enough. Perinatal depression is highly prevalent: It affects as many as one in seven women and can result in adverse short- and long-term effects on both the mother and child.
The U.S. Preventive Services Task Force has offered guidance for years, most recently in 2019 with its recommendations that clinicians refer pregnant and postpartum women who are at increased risk for depression to counseling interventions such as cognitive behavioral therapy and interpersonal therapy.3 There is evidence that some form of treatment for women who screen positive reduces the risk of perinatal depression.
Additionally, there is emerging evidence that postpartum PTSD may be as prevalent as postpartum depression.4 As ACOG points out, trauma is “in the eye of the beholder,” and an estimated 3%-16% of women have PTSD related to a traumatic birth experience. Complications like shoulder dystocia or postpartum hemorrhage, in which delivery processes rapidly change course, can be experienced as traumatic by women even though they and their infants are healthy. The risk of posttraumatic stress should be on our radar screen.
Interpregnancy intervals similarly are not discussed enough. We do not commonly talk to patients about how pregnancy and breastfeeding are nutritionally depleting and how it takes time to replenish these stores – yet birth spacing is so important.
Compared with interpregnancy intervals of at least 18 months, intervals shorter than 6 months were associated in a meta-analysis with increased risks of preterm birth, low birth weight, and small for gestational age.5 Optimal birth spacing is one of the few low-cost interventions available for reducing pregnancy complications in the future.
Finally, that chronic disease management is a domain of postpartum care warrants emphasis. We must work to ensure that patients have a solid plan of care in place for their diabetes, hypertension, lupus, or other chronic conditions. This includes who will provide that ongoing care, as well as when medical management should be restarted.
Some women are aware of the importance of timely care – of not waiting for 12 months, for instance, to see an internist or specialist – but others are not.
Again, certain health conditions such as multiple sclerosis and RA necessitate follow-up within a couple weeks after delivery so that medications can be restarted or dose adjustments made. The need for early postpartum follow-up can be discussed during prenatal visits, along with anticipatory guidance about breastfeeding, the signs and symptoms of perinatal depression and anxiety, and other components of the fourth trimester.
Dr. Macones has no relevant financial disclosures.
References
1. Obstet Gynecol. 2018 May;131(5):e140-50.
2. BMJ Qual Saf. 2018 Apr 27;27(11):871-7.
3. JAMA. 2019 Feb 12;321(6):580-7.
4. Clin Psychol Rev. 2014 Jul;34:389-401.JAMA. 2006 Apr 19;295(15):1809-23.
The fourth trimester
As we approach the end of this year, one of the most surreal times in human history, we will look back on the many things we taught ourselves, the many things we took for granted, the many things we were grateful for, the many things we missed, and the many things we plan to do once we can do things again. Among the many things 2020 taught us to appreciate was the very real manifestation of the old adage, “prevention is the best medicine.” To prevent transmission of SARS-CoV-2, we wore masks, we sanitized everything, we avoided crowds, we traded in-person meetings for virtual meetings, we learned how to homeschool our children, and we delayed seeing relatives and friends.
Ob.gyns. in small and large practices around the world had the tremendous challenge of balancing necessary in-person prenatal care services with keeping their patients and babies safe. Labor and delivery units had even greater demands to keep women and neonates free of SARS-CoV-2 infection. Practices quickly put into place new treatment protocols and new management strategies to maintain the health of their staff while ensuring a high quality of care.
While we have focused much of our attention on greater precautions during pregnancy and childbirth, an important component of care is the immediate postpartum period – colloquially referred to as the “fourth trimester” – which remains critical to maintaining physical and mental health and well-being.
Despite concerns regarding COVID-19 safety, we should continue monitoring our patients during these crucial first weeks after childbirth. This year of social isolation, financial strain, and incredible uncertainty has created additional stress in many women’s lives. The usual support that some women would receive from family members, friends, and other mothers in the early days post partum may not be available. The pandemic also has further highlighted inequities in access to health care for vulnerable groups. In addition, restrictions have increased the incidence of intimate partner violence as many women and children have needed to shelter with their abusers. Perhaps now more than any time previously, ob.gyns. must be attuned to their patients’ needs and be ready to provide compassionate and sensitive care.
In this final month of the year, we have invited George A. Macones, MD, professor and chair of the department of women’s health at the University of Texas, Austin, to address the importance of care in the final “trimester” of pregnancy – the first 3 months post partum.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at obnews@mdedge.com.
*This version has been updated to correct an erroneous byline, photo, and bio.
As we approach the end of this year, one of the most surreal times in human history, we will look back on the many things we taught ourselves, the many things we took for granted, the many things we were grateful for, the many things we missed, and the many things we plan to do once we can do things again. Among the many things 2020 taught us to appreciate was the very real manifestation of the old adage, “prevention is the best medicine.” To prevent transmission of SARS-CoV-2, we wore masks, we sanitized everything, we avoided crowds, we traded in-person meetings for virtual meetings, we learned how to homeschool our children, and we delayed seeing relatives and friends.
Ob.gyns. in small and large practices around the world had the tremendous challenge of balancing necessary in-person prenatal care services with keeping their patients and babies safe. Labor and delivery units had even greater demands to keep women and neonates free of SARS-CoV-2 infection. Practices quickly put into place new treatment protocols and new management strategies to maintain the health of their staff while ensuring a high quality of care.
While we have focused much of our attention on greater precautions during pregnancy and childbirth, an important component of care is the immediate postpartum period – colloquially referred to as the “fourth trimester” – which remains critical to maintaining physical and mental health and well-being.
Despite concerns regarding COVID-19 safety, we should continue monitoring our patients during these crucial first weeks after childbirth. This year of social isolation, financial strain, and incredible uncertainty has created additional stress in many women’s lives. The usual support that some women would receive from family members, friends, and other mothers in the early days post partum may not be available. The pandemic also has further highlighted inequities in access to health care for vulnerable groups. In addition, restrictions have increased the incidence of intimate partner violence as many women and children have needed to shelter with their abusers. Perhaps now more than any time previously, ob.gyns. must be attuned to their patients’ needs and be ready to provide compassionate and sensitive care.
In this final month of the year, we have invited George A. Macones, MD, professor and chair of the department of women’s health at the University of Texas, Austin, to address the importance of care in the final “trimester” of pregnancy – the first 3 months post partum.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at obnews@mdedge.com.
*This version has been updated to correct an erroneous byline, photo, and bio.
As we approach the end of this year, one of the most surreal times in human history, we will look back on the many things we taught ourselves, the many things we took for granted, the many things we were grateful for, the many things we missed, and the many things we plan to do once we can do things again. Among the many things 2020 taught us to appreciate was the very real manifestation of the old adage, “prevention is the best medicine.” To prevent transmission of SARS-CoV-2, we wore masks, we sanitized everything, we avoided crowds, we traded in-person meetings for virtual meetings, we learned how to homeschool our children, and we delayed seeing relatives and friends.
Ob.gyns. in small and large practices around the world had the tremendous challenge of balancing necessary in-person prenatal care services with keeping their patients and babies safe. Labor and delivery units had even greater demands to keep women and neonates free of SARS-CoV-2 infection. Practices quickly put into place new treatment protocols and new management strategies to maintain the health of their staff while ensuring a high quality of care.
While we have focused much of our attention on greater precautions during pregnancy and childbirth, an important component of care is the immediate postpartum period – colloquially referred to as the “fourth trimester” – which remains critical to maintaining physical and mental health and well-being.
Despite concerns regarding COVID-19 safety, we should continue monitoring our patients during these crucial first weeks after childbirth. This year of social isolation, financial strain, and incredible uncertainty has created additional stress in many women’s lives. The usual support that some women would receive from family members, friends, and other mothers in the early days post partum may not be available. The pandemic also has further highlighted inequities in access to health care for vulnerable groups. In addition, restrictions have increased the incidence of intimate partner violence as many women and children have needed to shelter with their abusers. Perhaps now more than any time previously, ob.gyns. must be attuned to their patients’ needs and be ready to provide compassionate and sensitive care.
In this final month of the year, we have invited George A. Macones, MD, professor and chair of the department of women’s health at the University of Texas, Austin, to address the importance of care in the final “trimester” of pregnancy – the first 3 months post partum.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at obnews@mdedge.com.
*This version has been updated to correct an erroneous byline, photo, and bio.
Prophylactic HIV treatment in female STI patients is rare
reported Kirk D. Henny, PhD, and colleagues of the Centers for Disease Control and Prevention.
In an effort to quantify HIV testing rates as well as the rate of pre-exposure prophylaxis (PrEP) among women with gonorrhea or syphilis, Dr. Henny and his colleagues performed a multivariate logistic regression analysis of 13,074 female patients aged 15-64 diagnosed with a STI in the absence of HIV. Data was pulled in 2017 from the IBM MarketScan commercial and Medicaid insurance databases, and the research was published in Obstetrics & Gynecology.
Medicaid patients were more likely to be tested for HIV
A total of 3,709 patients with commercial insurance were diagnosed with gonorrhea and 1,696 with syphilis. Among those with Medicaid, 6,172 were diagnosed with gonorrhea and 1,497 with syphilis. Medicaid patients diagnosed with either STI were more likely to be tested for HIV than the commercially insured patients. With an adjusted prevalence ratio, patients commercially insured with had either STI were more likely to be tested for HIV than patients who had no STI. Prophylactic treatment rates were similar in both insurance groups: 0.15% in the commercial insurance group and 0.26% in the Medicaid group. No patient from either group who was diagnosed with gonorrhea or syphilis and subsequently tested for HIV received pre-exposure prophylactic (PrEP) treatment.
STI diagnosis is a significant indicator of future HIV
Female patients diagnosed with either STI are more likely to contract HIV, the researchers noted. They cautioned that their findings of low HIV testing rates and the absence of prophylactic treatment means that “these missed opportunities for health care professionals to intervene with female patients diagnosed with gonorrhea or syphilis might have contributed to HIV infections that could have been averted.”
The researchers also pointed out that, in a recent analysis of pharmacy data, prophylactic prescribing for female patients with clinical indications for PrEP was 6.6%, less than one-third the coverage provided to male patients.
Future research should target understanding “individual and contextual factors associated with low HIV testing” and PrEP treatment in female patients, especially those with STIs, Dr. Henny and his colleagues advised.
In a separate interview, Constance Bohon, MD FACOG, observed: “The authors present data to document the low incidence of pre-exposure prophylaxis in women who are at substantial risk of acquiring HIV and possible causes for the low utilization of this treatment.” It is important to identify barriers to diagnosis, counseling, and treatment, she advised.
“Multicenter studies to determine the best methodologies to improve the identification, management, and treatment of these at-risk women need to be done, and the conclusions disseminated to health care providers caring for women,” Dr. Bohon said.
PrEP is an important, simple strategy for reducing HIV transmission
“Pre-exposure prophylaxis has been demonstrated to decrease HIV acquisition in those at risk by up to 90% when taken appropriately,” and yet prescribing rates are extremely low (2%-6%) in at-risk women and especially women of color. These disparities have only grown over time, with prophylactic prescriptions for women at 5% between 2012 and 2017, compared with 68% for men, Catherine S. Eppes, MD, MPH, and Jennifer McKinney, MD, MPH, said in a related editorial commenting on the Research Letter by Dr. Henny and colleagues in Obstetrics & Gynecology (2020 Dec;136[6]:1080-2).
Given the abundant research demonstrating the importance and ease of prescribing PrEP, the question remains: “why does preexposure prophylaxis uptake remain so low, especially for women and women of color? There are three important issues about preexposure prophylaxis raised by this study: the research gap, the implementation gap, and the effect of systemic racism and bias,” noted Dr. Eppes and Dr. McKinney.
Women constitute a significant portion of the population that would benefit from HIV-prevention strategies, yet they continue to be excluded from research, they noted. “Much focus on research into barriers and implementation interventions for preexposure prophylaxis have focused on men who have sex with men and transgender women,” the authors of the editorial wrote.
Most women eligible for treatment would be willing to consider it if they were aware of the option, but numerous studies have cited a lack of awareness, especially among high-risk women of color in the United States, Dr. Eppes and Dr. McKinney noted.
Clinicians also need to add it to their growing checklist of mandatory appointment discussion topics, the editorialists said. “We propose standardized inclusion of preexposure prophylaxis counseling during reproductive healthcare visits. This could be aided through an electronic medical record-based best practice advisory alert. … Standardized order sets with the medication and laboratory studies necessary for safe monitoring could facilitate ease of incorporating into routine visits,” they suggested.
“Preexposure prophylaxis is extremely effective in preventing HIV, is safe, and is the only prevention method that leaves control entirely in the hands of the female partner. As a specialty, we have a responsibility to make sure our patients know about this option,” the editorialists concluded.
The authors had no financial disclosures to report. Dr. Bohon had no conflicts of interest to report.
SOURCE: Henny KD et al. Obstet Gynecol. 2020 Dec;136(6):1083-5.
reported Kirk D. Henny, PhD, and colleagues of the Centers for Disease Control and Prevention.
In an effort to quantify HIV testing rates as well as the rate of pre-exposure prophylaxis (PrEP) among women with gonorrhea or syphilis, Dr. Henny and his colleagues performed a multivariate logistic regression analysis of 13,074 female patients aged 15-64 diagnosed with a STI in the absence of HIV. Data was pulled in 2017 from the IBM MarketScan commercial and Medicaid insurance databases, and the research was published in Obstetrics & Gynecology.
Medicaid patients were more likely to be tested for HIV
A total of 3,709 patients with commercial insurance were diagnosed with gonorrhea and 1,696 with syphilis. Among those with Medicaid, 6,172 were diagnosed with gonorrhea and 1,497 with syphilis. Medicaid patients diagnosed with either STI were more likely to be tested for HIV than the commercially insured patients. With an adjusted prevalence ratio, patients commercially insured with had either STI were more likely to be tested for HIV than patients who had no STI. Prophylactic treatment rates were similar in both insurance groups: 0.15% in the commercial insurance group and 0.26% in the Medicaid group. No patient from either group who was diagnosed with gonorrhea or syphilis and subsequently tested for HIV received pre-exposure prophylactic (PrEP) treatment.
STI diagnosis is a significant indicator of future HIV
Female patients diagnosed with either STI are more likely to contract HIV, the researchers noted. They cautioned that their findings of low HIV testing rates and the absence of prophylactic treatment means that “these missed opportunities for health care professionals to intervene with female patients diagnosed with gonorrhea or syphilis might have contributed to HIV infections that could have been averted.”
The researchers also pointed out that, in a recent analysis of pharmacy data, prophylactic prescribing for female patients with clinical indications for PrEP was 6.6%, less than one-third the coverage provided to male patients.
Future research should target understanding “individual and contextual factors associated with low HIV testing” and PrEP treatment in female patients, especially those with STIs, Dr. Henny and his colleagues advised.
In a separate interview, Constance Bohon, MD FACOG, observed: “The authors present data to document the low incidence of pre-exposure prophylaxis in women who are at substantial risk of acquiring HIV and possible causes for the low utilization of this treatment.” It is important to identify barriers to diagnosis, counseling, and treatment, she advised.
“Multicenter studies to determine the best methodologies to improve the identification, management, and treatment of these at-risk women need to be done, and the conclusions disseminated to health care providers caring for women,” Dr. Bohon said.
PrEP is an important, simple strategy for reducing HIV transmission
“Pre-exposure prophylaxis has been demonstrated to decrease HIV acquisition in those at risk by up to 90% when taken appropriately,” and yet prescribing rates are extremely low (2%-6%) in at-risk women and especially women of color. These disparities have only grown over time, with prophylactic prescriptions for women at 5% between 2012 and 2017, compared with 68% for men, Catherine S. Eppes, MD, MPH, and Jennifer McKinney, MD, MPH, said in a related editorial commenting on the Research Letter by Dr. Henny and colleagues in Obstetrics & Gynecology (2020 Dec;136[6]:1080-2).
Given the abundant research demonstrating the importance and ease of prescribing PrEP, the question remains: “why does preexposure prophylaxis uptake remain so low, especially for women and women of color? There are three important issues about preexposure prophylaxis raised by this study: the research gap, the implementation gap, and the effect of systemic racism and bias,” noted Dr. Eppes and Dr. McKinney.
Women constitute a significant portion of the population that would benefit from HIV-prevention strategies, yet they continue to be excluded from research, they noted. “Much focus on research into barriers and implementation interventions for preexposure prophylaxis have focused on men who have sex with men and transgender women,” the authors of the editorial wrote.
Most women eligible for treatment would be willing to consider it if they were aware of the option, but numerous studies have cited a lack of awareness, especially among high-risk women of color in the United States, Dr. Eppes and Dr. McKinney noted.
Clinicians also need to add it to their growing checklist of mandatory appointment discussion topics, the editorialists said. “We propose standardized inclusion of preexposure prophylaxis counseling during reproductive healthcare visits. This could be aided through an electronic medical record-based best practice advisory alert. … Standardized order sets with the medication and laboratory studies necessary for safe monitoring could facilitate ease of incorporating into routine visits,” they suggested.
“Preexposure prophylaxis is extremely effective in preventing HIV, is safe, and is the only prevention method that leaves control entirely in the hands of the female partner. As a specialty, we have a responsibility to make sure our patients know about this option,” the editorialists concluded.
The authors had no financial disclosures to report. Dr. Bohon had no conflicts of interest to report.
SOURCE: Henny KD et al. Obstet Gynecol. 2020 Dec;136(6):1083-5.
reported Kirk D. Henny, PhD, and colleagues of the Centers for Disease Control and Prevention.
In an effort to quantify HIV testing rates as well as the rate of pre-exposure prophylaxis (PrEP) among women with gonorrhea or syphilis, Dr. Henny and his colleagues performed a multivariate logistic regression analysis of 13,074 female patients aged 15-64 diagnosed with a STI in the absence of HIV. Data was pulled in 2017 from the IBM MarketScan commercial and Medicaid insurance databases, and the research was published in Obstetrics & Gynecology.
Medicaid patients were more likely to be tested for HIV
A total of 3,709 patients with commercial insurance were diagnosed with gonorrhea and 1,696 with syphilis. Among those with Medicaid, 6,172 were diagnosed with gonorrhea and 1,497 with syphilis. Medicaid patients diagnosed with either STI were more likely to be tested for HIV than the commercially insured patients. With an adjusted prevalence ratio, patients commercially insured with had either STI were more likely to be tested for HIV than patients who had no STI. Prophylactic treatment rates were similar in both insurance groups: 0.15% in the commercial insurance group and 0.26% in the Medicaid group. No patient from either group who was diagnosed with gonorrhea or syphilis and subsequently tested for HIV received pre-exposure prophylactic (PrEP) treatment.
STI diagnosis is a significant indicator of future HIV
Female patients diagnosed with either STI are more likely to contract HIV, the researchers noted. They cautioned that their findings of low HIV testing rates and the absence of prophylactic treatment means that “these missed opportunities for health care professionals to intervene with female patients diagnosed with gonorrhea or syphilis might have contributed to HIV infections that could have been averted.”
The researchers also pointed out that, in a recent analysis of pharmacy data, prophylactic prescribing for female patients with clinical indications for PrEP was 6.6%, less than one-third the coverage provided to male patients.
Future research should target understanding “individual and contextual factors associated with low HIV testing” and PrEP treatment in female patients, especially those with STIs, Dr. Henny and his colleagues advised.
In a separate interview, Constance Bohon, MD FACOG, observed: “The authors present data to document the low incidence of pre-exposure prophylaxis in women who are at substantial risk of acquiring HIV and possible causes for the low utilization of this treatment.” It is important to identify barriers to diagnosis, counseling, and treatment, she advised.
“Multicenter studies to determine the best methodologies to improve the identification, management, and treatment of these at-risk women need to be done, and the conclusions disseminated to health care providers caring for women,” Dr. Bohon said.
PrEP is an important, simple strategy for reducing HIV transmission
“Pre-exposure prophylaxis has been demonstrated to decrease HIV acquisition in those at risk by up to 90% when taken appropriately,” and yet prescribing rates are extremely low (2%-6%) in at-risk women and especially women of color. These disparities have only grown over time, with prophylactic prescriptions for women at 5% between 2012 and 2017, compared with 68% for men, Catherine S. Eppes, MD, MPH, and Jennifer McKinney, MD, MPH, said in a related editorial commenting on the Research Letter by Dr. Henny and colleagues in Obstetrics & Gynecology (2020 Dec;136[6]:1080-2).
Given the abundant research demonstrating the importance and ease of prescribing PrEP, the question remains: “why does preexposure prophylaxis uptake remain so low, especially for women and women of color? There are three important issues about preexposure prophylaxis raised by this study: the research gap, the implementation gap, and the effect of systemic racism and bias,” noted Dr. Eppes and Dr. McKinney.
Women constitute a significant portion of the population that would benefit from HIV-prevention strategies, yet they continue to be excluded from research, they noted. “Much focus on research into barriers and implementation interventions for preexposure prophylaxis have focused on men who have sex with men and transgender women,” the authors of the editorial wrote.
Most women eligible for treatment would be willing to consider it if they were aware of the option, but numerous studies have cited a lack of awareness, especially among high-risk women of color in the United States, Dr. Eppes and Dr. McKinney noted.
Clinicians also need to add it to their growing checklist of mandatory appointment discussion topics, the editorialists said. “We propose standardized inclusion of preexposure prophylaxis counseling during reproductive healthcare visits. This could be aided through an electronic medical record-based best practice advisory alert. … Standardized order sets with the medication and laboratory studies necessary for safe monitoring could facilitate ease of incorporating into routine visits,” they suggested.
“Preexposure prophylaxis is extremely effective in preventing HIV, is safe, and is the only prevention method that leaves control entirely in the hands of the female partner. As a specialty, we have a responsibility to make sure our patients know about this option,” the editorialists concluded.
The authors had no financial disclosures to report. Dr. Bohon had no conflicts of interest to report.
SOURCE: Henny KD et al. Obstet Gynecol. 2020 Dec;136(6):1083-5.
FROM OBSTETRICS & GYNECOLOGY