User login
COVID-19 and the myth of the super doctor
Let us begin with a thought exercise. Close your eyes and picture the word, “hero.” What comes to mind? A relative, a teacher, a fictional character wielding a hammer or flying gracefully through the air?
Several months ago, our country was introduced to a foe that brought us to our knees. Before that time, the idea of a hero had fluctuated with circumstance and had been guided by aging and maturity; however, since the moment COVID-19 struck, a new image has emerged. Not all heroes wear capes, but some wield stethoscopes.
Over these past months the phrase, “Health Care Heroes” has spread throughout our collective consciousness, highlighted everywhere from talk shows and news media to billboards and journals. Doctors, nurses, and other health care professionals are lauded for their strength, dedication, resilience, and compassion. Citizens line up to clap, honk horns, and shower praise in recognition of those who have risked their health, sacrificed their personal lives, and committed themselves to the greater good. Yet, what does it mean to be a hero, and what is the cost of hero worship?
The focus of medical training has gradually shifted to include the physical as well as mental well-being of future physicians, but the remnants of traditional doctrine linger. Hours of focused training through study and direct clinical interaction reinforce dedication to patient care. Rewards are given for time spent and compassion lent, and research is lauded, but family time is rarely applauded. We are encouraged to do our greatest, work our hardest, be the best, rise and defeat every test. Failure (or the perception thereof) is not an option.
According to Rikinkumar S. Patel, MD, MPH, and associates, physicians have nearly twice the burnout rate of other professionals (Behav Sci. [Basel]. 2018 Nov;8[11]:98). The dedication to our craft propels excellence as well as sacrifice. When COVID-19 entered our lives, many of my colleagues did not hesitate to heed to the call for action. They immersed themselves in the ICU, led triage units, and extended work hours in the service of the sick and dying. Several were years removed from emergency/intensive care, while others were allocated from their chosen residency programs and voluntarily thrust into an environment they had never before traversed.
These individuals are praised as “brave,” “dedicated,” “selfless.” A few even provided insight into their experiences through various publications highlighting their appreciation and gratitude toward such a treacherous, albeit, tremendous experience. Even though their words are an honest perspective of life through one of the worst health care crises in 100 years, in effect, they perpetuate the noble hero; the myth of the super doctor.
In a profession that has borne witness to multiple suicides over the past few months, why do we not encourage open dialogue of our victories as well as our defeats? Our wins as much as our losses? Why does an esteemed veteran physician feel guilt over declining to provide emergency services to patients whom they have long forgotten how to manage? What drives the guilt and the self-doubt? Are we ashamed of what others will think? Is it that the fear of not living up to our cherished medical oath outweighs our own boundaries and acknowledgment of our limitations?
A hero is an entity, a person encompassing a state of being, yet health care professionals are bestowed this title and this burden on a near-daily basis. We are perfectly imperfect. The more in tune we are to vulnerability, the more honest we can become with ourselves and one another.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
Let us begin with a thought exercise. Close your eyes and picture the word, “hero.” What comes to mind? A relative, a teacher, a fictional character wielding a hammer or flying gracefully through the air?
Several months ago, our country was introduced to a foe that brought us to our knees. Before that time, the idea of a hero had fluctuated with circumstance and had been guided by aging and maturity; however, since the moment COVID-19 struck, a new image has emerged. Not all heroes wear capes, but some wield stethoscopes.
Over these past months the phrase, “Health Care Heroes” has spread throughout our collective consciousness, highlighted everywhere from talk shows and news media to billboards and journals. Doctors, nurses, and other health care professionals are lauded for their strength, dedication, resilience, and compassion. Citizens line up to clap, honk horns, and shower praise in recognition of those who have risked their health, sacrificed their personal lives, and committed themselves to the greater good. Yet, what does it mean to be a hero, and what is the cost of hero worship?
The focus of medical training has gradually shifted to include the physical as well as mental well-being of future physicians, but the remnants of traditional doctrine linger. Hours of focused training through study and direct clinical interaction reinforce dedication to patient care. Rewards are given for time spent and compassion lent, and research is lauded, but family time is rarely applauded. We are encouraged to do our greatest, work our hardest, be the best, rise and defeat every test. Failure (or the perception thereof) is not an option.
According to Rikinkumar S. Patel, MD, MPH, and associates, physicians have nearly twice the burnout rate of other professionals (Behav Sci. [Basel]. 2018 Nov;8[11]:98). The dedication to our craft propels excellence as well as sacrifice. When COVID-19 entered our lives, many of my colleagues did not hesitate to heed to the call for action. They immersed themselves in the ICU, led triage units, and extended work hours in the service of the sick and dying. Several were years removed from emergency/intensive care, while others were allocated from their chosen residency programs and voluntarily thrust into an environment they had never before traversed.
These individuals are praised as “brave,” “dedicated,” “selfless.” A few even provided insight into their experiences through various publications highlighting their appreciation and gratitude toward such a treacherous, albeit, tremendous experience. Even though their words are an honest perspective of life through one of the worst health care crises in 100 years, in effect, they perpetuate the noble hero; the myth of the super doctor.
In a profession that has borne witness to multiple suicides over the past few months, why do we not encourage open dialogue of our victories as well as our defeats? Our wins as much as our losses? Why does an esteemed veteran physician feel guilt over declining to provide emergency services to patients whom they have long forgotten how to manage? What drives the guilt and the self-doubt? Are we ashamed of what others will think? Is it that the fear of not living up to our cherished medical oath outweighs our own boundaries and acknowledgment of our limitations?
A hero is an entity, a person encompassing a state of being, yet health care professionals are bestowed this title and this burden on a near-daily basis. We are perfectly imperfect. The more in tune we are to vulnerability, the more honest we can become with ourselves and one another.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
Let us begin with a thought exercise. Close your eyes and picture the word, “hero.” What comes to mind? A relative, a teacher, a fictional character wielding a hammer or flying gracefully through the air?
Several months ago, our country was introduced to a foe that brought us to our knees. Before that time, the idea of a hero had fluctuated with circumstance and had been guided by aging and maturity; however, since the moment COVID-19 struck, a new image has emerged. Not all heroes wear capes, but some wield stethoscopes.
Over these past months the phrase, “Health Care Heroes” has spread throughout our collective consciousness, highlighted everywhere from talk shows and news media to billboards and journals. Doctors, nurses, and other health care professionals are lauded for their strength, dedication, resilience, and compassion. Citizens line up to clap, honk horns, and shower praise in recognition of those who have risked their health, sacrificed their personal lives, and committed themselves to the greater good. Yet, what does it mean to be a hero, and what is the cost of hero worship?
The focus of medical training has gradually shifted to include the physical as well as mental well-being of future physicians, but the remnants of traditional doctrine linger. Hours of focused training through study and direct clinical interaction reinforce dedication to patient care. Rewards are given for time spent and compassion lent, and research is lauded, but family time is rarely applauded. We are encouraged to do our greatest, work our hardest, be the best, rise and defeat every test. Failure (or the perception thereof) is not an option.
According to Rikinkumar S. Patel, MD, MPH, and associates, physicians have nearly twice the burnout rate of other professionals (Behav Sci. [Basel]. 2018 Nov;8[11]:98). The dedication to our craft propels excellence as well as sacrifice. When COVID-19 entered our lives, many of my colleagues did not hesitate to heed to the call for action. They immersed themselves in the ICU, led triage units, and extended work hours in the service of the sick and dying. Several were years removed from emergency/intensive care, while others were allocated from their chosen residency programs and voluntarily thrust into an environment they had never before traversed.
These individuals are praised as “brave,” “dedicated,” “selfless.” A few even provided insight into their experiences through various publications highlighting their appreciation and gratitude toward such a treacherous, albeit, tremendous experience. Even though their words are an honest perspective of life through one of the worst health care crises in 100 years, in effect, they perpetuate the noble hero; the myth of the super doctor.
In a profession that has borne witness to multiple suicides over the past few months, why do we not encourage open dialogue of our victories as well as our defeats? Our wins as much as our losses? Why does an esteemed veteran physician feel guilt over declining to provide emergency services to patients whom they have long forgotten how to manage? What drives the guilt and the self-doubt? Are we ashamed of what others will think? Is it that the fear of not living up to our cherished medical oath outweighs our own boundaries and acknowledgment of our limitations?
A hero is an entity, a person encompassing a state of being, yet health care professionals are bestowed this title and this burden on a near-daily basis. We are perfectly imperfect. The more in tune we are to vulnerability, the more honest we can become with ourselves and one another.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
Fetal movement education: Time to change the status quo
Every antepartum record, whether it is on paper or EMR, has a space asking whether the patient feels fetal movement at the visit. Every provider inherently knows that fetal movement is important and worth asking about at each visit. Yet the education for patients about fetal movement and when to alert a provider to changes is not currently standardized in the United States. There is no practice bulletin or guideline from the American College of Obstetricians and Gynecologists and, therefore, there is a wide variation in clinical practice. An Australian study found that 97% of women were asked about fetal movement, but only 62% reported formal education regarding fetal movement. More concerning, only 40% were advised to call immediately if concerned about fetal movement change. A quarter were told to call only if baby moved fewer than 10 times in an hour.1
We have a standardized approach to most aspects of prenatal care. We know what to do if the patient has contractions, or protein in their urine, or an increased blood pressure. Our management and education regarding fetal movement must be standardized as well. In this article I will go through the incorrect education that often is given and the data that do not support this. We need a similar care plan or model for fetal movement education in the United States.
Myth one: Kick counts
When education is done, kick counts are far and away what providers and nurses advise in the clinic and hospital triage when women present with complaint of decreased fetal movement. The standard approach to this is advising the patient to perform a kick count several times per day to check in on the baby and call if less than 10 kicks per hour. This is not bad advice as it may help create awareness for the mom about what is “normal” for her baby and may help her to “check in” on the baby when she is occupied at work or with older children. However, advising that a kick count should be done to reassure a patient about a concerning change in fetal movement is not supported in the literature. A meta-analysis in the February 2020 issue of the Green Journal found that advised kick count monitoring did not significantly reduce stillbirth risk.2 Research shows that most moms will get 10 kicks normally within an hour, but there are no data showing what percentage of moms with perceived decreased fetal movement also will get a “passing” result despite their concern. For example, take a patient who normally feels 50 movements in an hour and is not reassured by 10 movements in an hour, but because she is told that 10 movements is okay, she tries not to worry about the concerning change. Many mothers in the stillbirth community report “passing kick counts” in the days leading up to the diagnosis. We need to move away from kick count education to a much simpler plan. We must tell patients if they are worried about a concerning change in fetal movement, they should call their provider.
Myth 2: Fetuses slow down at the end of pregnancy
There is a very common myth that fetuses slow down at the end of pregnancy, especially once labor has started. A study in the Journal of Physiology continuously monitored term fetuses when mom was both awake and asleep. The study also looked at the effect on fetal heart rate and fetal activity based on different maternal positions. The study found the fetuses spent around 90% of the day with active movements and with reactive nonstress tests (NSTs).3 A 2019 study looking at fetal movement at term and preterm in third-trimester patients illustrated that fetal movement does not decrease in frequency or strength at term. It found that only 6% of patients noted decreased strength and 14% decreased frequency of movements at term. Furthermore, 59% reported an increase in strength, and nearly 39% reported an increase in frequency of fetal movements at term.4 We must educate patients that a change in frequency or strength of movements is not normal or expected, and they must call if concerned about a change.
Myth 3: Try juice, ice water, or food before coming in for evaluation
A common set of advice when a patient calls with a complaint of decreased fetal movement is to suggest a meal or something sugary, although there is little or no evidence to support this. A randomized controlled trial found maternal perception of increased fetal movement was similar among the two groups. Giving something sugary at NST also was not shown in this study to improve reactivity.5 Another randomized, double placebo blind study was done to answer the question of whether glucose via IV helped improve fetal movements and decreased the need for admission for induction or further monitoring. In this study, no difference in outcome is found.6
When a patient calls with decreased fetal movement, advice should be to come and be evaluated, not recommendation of measures like ice water, orange juice, or sugary meal because it is not supported by the literature. This incorrect message also may further the false impression that a baby who is not moving is most likely sleeping or is simply in need of sugar, not that the baby may be at risk for impending stillbirth. The Perinatal Society of Australia and New Zealand and Royal College of Obstetricians and Gynecologists have fetal movement protocol that both discourage this advice and encourage immediate evaluation of patients with complaint of concerning fetal movement change.7,8
Myth 4: An increase in fetal movement is not of concern
I used to believe that increased fetal movement is never of concern. However, the STARS study illustrated that a concerning increase in fetal movement often is noted just before the diagnosis of stillbirth. A single episode of excessively vigorous activity which often is described as frantic or crazy is associated with an odds ratio for stillbirth of 4.3. In the study, 30% of cases reported this, compared with 7% of controls.9 In our practice, we manage mothers who call with this concern the same way as a decreased fetal movement complaint, and bring the mother in immediately for evaluation.
Myth 5: Patients all know that a concerning change in fetal movement is a risk factor for stillbirth
Decreased fetal movement has been associated with an increased OR for stillbirth of 4.51.10 However, patients often do not know of this association. A study in the United States of providers and stillbirth families showed fear of anxiety kept providers from talking about stillbirth and that it still happens. Because of this patients were completely surprised by the diagnosis.11 We tell patients that stillbirth still happens because research by Dr Suzanne Pullen found that 77% of families said they never worried their baby could die outside of the first trimester. Our patients have received this information without increased anxiety and are very appreciative and reassured about the education and protocol (based on the U.K. Saving Babies Lives Care Bundle Version 2) that we have implemented in our practice.
Fact: Fetal movement education guidelines exist and are easy to implement
The practice I am a partner at has been using a formalized method for educating patients about fetal movement over the past year. As mentioned earlier the U.K. and Australia have formal fetal movement education and management guidelines.7,8 Both protocols encourage formal education around 20-24 weeks and education for the patient to call immediately with concerns; the patient should be evaluated within 2 hours of the complaint. The formal education we provide is quite simple. The Star Legacy Foundation (United States) and Still Aware (Australia) have created a simple card to educate patients.
These patient-centric materials were devised from the results of the case/control cohort STARS study by Heazell et al. The STARS study demonstrated that patient report of reduced fetal movement in the 2 weeks prior to loss was associated with an OR of 12.9 for stillbirth, that decreased strength of fetal movement was associated with stillbirth OR of 2.83, and that decreased night time activity was strongly associated with impending stillbirth (74% of cases felt their fetuses died at night).12 This card also addresses sleep position data, supported by a 2018 meta-analysis in the journal Sleep Medicine. The study identified an OR for stillbirth of 2.45 for supine sleepers with LGA or average sized babies. Furthermore, if the baby was SGA and the mother slept supine, the OR for stillbirth increased to 15.66.13
Conclusions
When I think about the patients I have cared for who have presented with a stillborn baby, I think often that they usually presented for a complaint other than decreased fetal movement such as labor check or routine prenatal visit. When asked when they last felt fetal movement they will often say days before. This does not need to happen. Protocols in Norway for fetal movement education have shown that patients call sooner with decreased fetal movement when they have received a formal education.14
Not all stillbirth can be prevented but proper education about fetal movement and not perpetuating dangerous myths about fetal movement, may keep presentations like this from happening. I hope we may soon have a formal protocol for fetal movement education, but until then, I hope some will take these educational tips to heart.
Dr. Heather Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, NY. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures.
References
1. Aust N Z J Obstet Gynaecol. 2012 Oct;52(5):445-9.
2. Obstet Gynecol. 2020 Feb;135(2):453-62.
3. J Physiol. 2017 Feb 15;595(4):1213-21.
4. PLOS One. 2019 Jun 12. doi: 10.1371/journal.pone.0217583.
5. J Matern Fetal Neonatal Med. 2013 Jun;26(9):915-9.
6. J Perinatol. 2016 Aug;36(8):598-600.
7. Aust N Z J Obstet Gynaecol. 2018 Aug;58(4):463-8.
8. Reduced fetal movements: Green top #57, Royal College of Obstetricians and Gynaecologists.
9. BMC Pregnancy Childb. 2017. doi: 10.1186/s12884-017-1555-6.
10. BMJ Open. 2018. doi: 10.1136/bmjopen-2017-020031.
11. BMC Pregnancy Childb. 2012. doi: 10.1186/1471-2393-12-137.
12. BMC Pregnancy Childb. 2015. doi: 10.1186/s12884-015-0602-4.
13. EClinicalMedicine. 2019 Apr. doi: 10.1016/j.eclinm.2019.03.014.
14. BMC Pregnancy Childb. 2009. doi: 10.1186/1471-2393-9-32.
Every antepartum record, whether it is on paper or EMR, has a space asking whether the patient feels fetal movement at the visit. Every provider inherently knows that fetal movement is important and worth asking about at each visit. Yet the education for patients about fetal movement and when to alert a provider to changes is not currently standardized in the United States. There is no practice bulletin or guideline from the American College of Obstetricians and Gynecologists and, therefore, there is a wide variation in clinical practice. An Australian study found that 97% of women were asked about fetal movement, but only 62% reported formal education regarding fetal movement. More concerning, only 40% were advised to call immediately if concerned about fetal movement change. A quarter were told to call only if baby moved fewer than 10 times in an hour.1
We have a standardized approach to most aspects of prenatal care. We know what to do if the patient has contractions, or protein in their urine, or an increased blood pressure. Our management and education regarding fetal movement must be standardized as well. In this article I will go through the incorrect education that often is given and the data that do not support this. We need a similar care plan or model for fetal movement education in the United States.
Myth one: Kick counts
When education is done, kick counts are far and away what providers and nurses advise in the clinic and hospital triage when women present with complaint of decreased fetal movement. The standard approach to this is advising the patient to perform a kick count several times per day to check in on the baby and call if less than 10 kicks per hour. This is not bad advice as it may help create awareness for the mom about what is “normal” for her baby and may help her to “check in” on the baby when she is occupied at work or with older children. However, advising that a kick count should be done to reassure a patient about a concerning change in fetal movement is not supported in the literature. A meta-analysis in the February 2020 issue of the Green Journal found that advised kick count monitoring did not significantly reduce stillbirth risk.2 Research shows that most moms will get 10 kicks normally within an hour, but there are no data showing what percentage of moms with perceived decreased fetal movement also will get a “passing” result despite their concern. For example, take a patient who normally feels 50 movements in an hour and is not reassured by 10 movements in an hour, but because she is told that 10 movements is okay, she tries not to worry about the concerning change. Many mothers in the stillbirth community report “passing kick counts” in the days leading up to the diagnosis. We need to move away from kick count education to a much simpler plan. We must tell patients if they are worried about a concerning change in fetal movement, they should call their provider.
Myth 2: Fetuses slow down at the end of pregnancy
There is a very common myth that fetuses slow down at the end of pregnancy, especially once labor has started. A study in the Journal of Physiology continuously monitored term fetuses when mom was both awake and asleep. The study also looked at the effect on fetal heart rate and fetal activity based on different maternal positions. The study found the fetuses spent around 90% of the day with active movements and with reactive nonstress tests (NSTs).3 A 2019 study looking at fetal movement at term and preterm in third-trimester patients illustrated that fetal movement does not decrease in frequency or strength at term. It found that only 6% of patients noted decreased strength and 14% decreased frequency of movements at term. Furthermore, 59% reported an increase in strength, and nearly 39% reported an increase in frequency of fetal movements at term.4 We must educate patients that a change in frequency or strength of movements is not normal or expected, and they must call if concerned about a change.
Myth 3: Try juice, ice water, or food before coming in for evaluation
A common set of advice when a patient calls with a complaint of decreased fetal movement is to suggest a meal or something sugary, although there is little or no evidence to support this. A randomized controlled trial found maternal perception of increased fetal movement was similar among the two groups. Giving something sugary at NST also was not shown in this study to improve reactivity.5 Another randomized, double placebo blind study was done to answer the question of whether glucose via IV helped improve fetal movements and decreased the need for admission for induction or further monitoring. In this study, no difference in outcome is found.6
When a patient calls with decreased fetal movement, advice should be to come and be evaluated, not recommendation of measures like ice water, orange juice, or sugary meal because it is not supported by the literature. This incorrect message also may further the false impression that a baby who is not moving is most likely sleeping or is simply in need of sugar, not that the baby may be at risk for impending stillbirth. The Perinatal Society of Australia and New Zealand and Royal College of Obstetricians and Gynecologists have fetal movement protocol that both discourage this advice and encourage immediate evaluation of patients with complaint of concerning fetal movement change.7,8
Myth 4: An increase in fetal movement is not of concern
I used to believe that increased fetal movement is never of concern. However, the STARS study illustrated that a concerning increase in fetal movement often is noted just before the diagnosis of stillbirth. A single episode of excessively vigorous activity which often is described as frantic or crazy is associated with an odds ratio for stillbirth of 4.3. In the study, 30% of cases reported this, compared with 7% of controls.9 In our practice, we manage mothers who call with this concern the same way as a decreased fetal movement complaint, and bring the mother in immediately for evaluation.
Myth 5: Patients all know that a concerning change in fetal movement is a risk factor for stillbirth
Decreased fetal movement has been associated with an increased OR for stillbirth of 4.51.10 However, patients often do not know of this association. A study in the United States of providers and stillbirth families showed fear of anxiety kept providers from talking about stillbirth and that it still happens. Because of this patients were completely surprised by the diagnosis.11 We tell patients that stillbirth still happens because research by Dr Suzanne Pullen found that 77% of families said they never worried their baby could die outside of the first trimester. Our patients have received this information without increased anxiety and are very appreciative and reassured about the education and protocol (based on the U.K. Saving Babies Lives Care Bundle Version 2) that we have implemented in our practice.
Fact: Fetal movement education guidelines exist and are easy to implement
The practice I am a partner at has been using a formalized method for educating patients about fetal movement over the past year. As mentioned earlier the U.K. and Australia have formal fetal movement education and management guidelines.7,8 Both protocols encourage formal education around 20-24 weeks and education for the patient to call immediately with concerns; the patient should be evaluated within 2 hours of the complaint. The formal education we provide is quite simple. The Star Legacy Foundation (United States) and Still Aware (Australia) have created a simple card to educate patients.
These patient-centric materials were devised from the results of the case/control cohort STARS study by Heazell et al. The STARS study demonstrated that patient report of reduced fetal movement in the 2 weeks prior to loss was associated with an OR of 12.9 for stillbirth, that decreased strength of fetal movement was associated with stillbirth OR of 2.83, and that decreased night time activity was strongly associated with impending stillbirth (74% of cases felt their fetuses died at night).12 This card also addresses sleep position data, supported by a 2018 meta-analysis in the journal Sleep Medicine. The study identified an OR for stillbirth of 2.45 for supine sleepers with LGA or average sized babies. Furthermore, if the baby was SGA and the mother slept supine, the OR for stillbirth increased to 15.66.13
Conclusions
When I think about the patients I have cared for who have presented with a stillborn baby, I think often that they usually presented for a complaint other than decreased fetal movement such as labor check or routine prenatal visit. When asked when they last felt fetal movement they will often say days before. This does not need to happen. Protocols in Norway for fetal movement education have shown that patients call sooner with decreased fetal movement when they have received a formal education.14
Not all stillbirth can be prevented but proper education about fetal movement and not perpetuating dangerous myths about fetal movement, may keep presentations like this from happening. I hope we may soon have a formal protocol for fetal movement education, but until then, I hope some will take these educational tips to heart.
Dr. Heather Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, NY. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures.
References
1. Aust N Z J Obstet Gynaecol. 2012 Oct;52(5):445-9.
2. Obstet Gynecol. 2020 Feb;135(2):453-62.
3. J Physiol. 2017 Feb 15;595(4):1213-21.
4. PLOS One. 2019 Jun 12. doi: 10.1371/journal.pone.0217583.
5. J Matern Fetal Neonatal Med. 2013 Jun;26(9):915-9.
6. J Perinatol. 2016 Aug;36(8):598-600.
7. Aust N Z J Obstet Gynaecol. 2018 Aug;58(4):463-8.
8. Reduced fetal movements: Green top #57, Royal College of Obstetricians and Gynaecologists.
9. BMC Pregnancy Childb. 2017. doi: 10.1186/s12884-017-1555-6.
10. BMJ Open. 2018. doi: 10.1136/bmjopen-2017-020031.
11. BMC Pregnancy Childb. 2012. doi: 10.1186/1471-2393-12-137.
12. BMC Pregnancy Childb. 2015. doi: 10.1186/s12884-015-0602-4.
13. EClinicalMedicine. 2019 Apr. doi: 10.1016/j.eclinm.2019.03.014.
14. BMC Pregnancy Childb. 2009. doi: 10.1186/1471-2393-9-32.
Every antepartum record, whether it is on paper or EMR, has a space asking whether the patient feels fetal movement at the visit. Every provider inherently knows that fetal movement is important and worth asking about at each visit. Yet the education for patients about fetal movement and when to alert a provider to changes is not currently standardized in the United States. There is no practice bulletin or guideline from the American College of Obstetricians and Gynecologists and, therefore, there is a wide variation in clinical practice. An Australian study found that 97% of women were asked about fetal movement, but only 62% reported formal education regarding fetal movement. More concerning, only 40% were advised to call immediately if concerned about fetal movement change. A quarter were told to call only if baby moved fewer than 10 times in an hour.1
We have a standardized approach to most aspects of prenatal care. We know what to do if the patient has contractions, or protein in their urine, or an increased blood pressure. Our management and education regarding fetal movement must be standardized as well. In this article I will go through the incorrect education that often is given and the data that do not support this. We need a similar care plan or model for fetal movement education in the United States.
Myth one: Kick counts
When education is done, kick counts are far and away what providers and nurses advise in the clinic and hospital triage when women present with complaint of decreased fetal movement. The standard approach to this is advising the patient to perform a kick count several times per day to check in on the baby and call if less than 10 kicks per hour. This is not bad advice as it may help create awareness for the mom about what is “normal” for her baby and may help her to “check in” on the baby when she is occupied at work or with older children. However, advising that a kick count should be done to reassure a patient about a concerning change in fetal movement is not supported in the literature. A meta-analysis in the February 2020 issue of the Green Journal found that advised kick count monitoring did not significantly reduce stillbirth risk.2 Research shows that most moms will get 10 kicks normally within an hour, but there are no data showing what percentage of moms with perceived decreased fetal movement also will get a “passing” result despite their concern. For example, take a patient who normally feels 50 movements in an hour and is not reassured by 10 movements in an hour, but because she is told that 10 movements is okay, she tries not to worry about the concerning change. Many mothers in the stillbirth community report “passing kick counts” in the days leading up to the diagnosis. We need to move away from kick count education to a much simpler plan. We must tell patients if they are worried about a concerning change in fetal movement, they should call their provider.
Myth 2: Fetuses slow down at the end of pregnancy
There is a very common myth that fetuses slow down at the end of pregnancy, especially once labor has started. A study in the Journal of Physiology continuously monitored term fetuses when mom was both awake and asleep. The study also looked at the effect on fetal heart rate and fetal activity based on different maternal positions. The study found the fetuses spent around 90% of the day with active movements and with reactive nonstress tests (NSTs).3 A 2019 study looking at fetal movement at term and preterm in third-trimester patients illustrated that fetal movement does not decrease in frequency or strength at term. It found that only 6% of patients noted decreased strength and 14% decreased frequency of movements at term. Furthermore, 59% reported an increase in strength, and nearly 39% reported an increase in frequency of fetal movements at term.4 We must educate patients that a change in frequency or strength of movements is not normal or expected, and they must call if concerned about a change.
Myth 3: Try juice, ice water, or food before coming in for evaluation
A common set of advice when a patient calls with a complaint of decreased fetal movement is to suggest a meal or something sugary, although there is little or no evidence to support this. A randomized controlled trial found maternal perception of increased fetal movement was similar among the two groups. Giving something sugary at NST also was not shown in this study to improve reactivity.5 Another randomized, double placebo blind study was done to answer the question of whether glucose via IV helped improve fetal movements and decreased the need for admission for induction or further monitoring. In this study, no difference in outcome is found.6
When a patient calls with decreased fetal movement, advice should be to come and be evaluated, not recommendation of measures like ice water, orange juice, or sugary meal because it is not supported by the literature. This incorrect message also may further the false impression that a baby who is not moving is most likely sleeping or is simply in need of sugar, not that the baby may be at risk for impending stillbirth. The Perinatal Society of Australia and New Zealand and Royal College of Obstetricians and Gynecologists have fetal movement protocol that both discourage this advice and encourage immediate evaluation of patients with complaint of concerning fetal movement change.7,8
Myth 4: An increase in fetal movement is not of concern
I used to believe that increased fetal movement is never of concern. However, the STARS study illustrated that a concerning increase in fetal movement often is noted just before the diagnosis of stillbirth. A single episode of excessively vigorous activity which often is described as frantic or crazy is associated with an odds ratio for stillbirth of 4.3. In the study, 30% of cases reported this, compared with 7% of controls.9 In our practice, we manage mothers who call with this concern the same way as a decreased fetal movement complaint, and bring the mother in immediately for evaluation.
Myth 5: Patients all know that a concerning change in fetal movement is a risk factor for stillbirth
Decreased fetal movement has been associated with an increased OR for stillbirth of 4.51.10 However, patients often do not know of this association. A study in the United States of providers and stillbirth families showed fear of anxiety kept providers from talking about stillbirth and that it still happens. Because of this patients were completely surprised by the diagnosis.11 We tell patients that stillbirth still happens because research by Dr Suzanne Pullen found that 77% of families said they never worried their baby could die outside of the first trimester. Our patients have received this information without increased anxiety and are very appreciative and reassured about the education and protocol (based on the U.K. Saving Babies Lives Care Bundle Version 2) that we have implemented in our practice.
Fact: Fetal movement education guidelines exist and are easy to implement
The practice I am a partner at has been using a formalized method for educating patients about fetal movement over the past year. As mentioned earlier the U.K. and Australia have formal fetal movement education and management guidelines.7,8 Both protocols encourage formal education around 20-24 weeks and education for the patient to call immediately with concerns; the patient should be evaluated within 2 hours of the complaint. The formal education we provide is quite simple. The Star Legacy Foundation (United States) and Still Aware (Australia) have created a simple card to educate patients.
These patient-centric materials were devised from the results of the case/control cohort STARS study by Heazell et al. The STARS study demonstrated that patient report of reduced fetal movement in the 2 weeks prior to loss was associated with an OR of 12.9 for stillbirth, that decreased strength of fetal movement was associated with stillbirth OR of 2.83, and that decreased night time activity was strongly associated with impending stillbirth (74% of cases felt their fetuses died at night).12 This card also addresses sleep position data, supported by a 2018 meta-analysis in the journal Sleep Medicine. The study identified an OR for stillbirth of 2.45 for supine sleepers with LGA or average sized babies. Furthermore, if the baby was SGA and the mother slept supine, the OR for stillbirth increased to 15.66.13
Conclusions
When I think about the patients I have cared for who have presented with a stillborn baby, I think often that they usually presented for a complaint other than decreased fetal movement such as labor check or routine prenatal visit. When asked when they last felt fetal movement they will often say days before. This does not need to happen. Protocols in Norway for fetal movement education have shown that patients call sooner with decreased fetal movement when they have received a formal education.14
Not all stillbirth can be prevented but proper education about fetal movement and not perpetuating dangerous myths about fetal movement, may keep presentations like this from happening. I hope we may soon have a formal protocol for fetal movement education, but until then, I hope some will take these educational tips to heart.
Dr. Heather Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, NY. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures.
References
1. Aust N Z J Obstet Gynaecol. 2012 Oct;52(5):445-9.
2. Obstet Gynecol. 2020 Feb;135(2):453-62.
3. J Physiol. 2017 Feb 15;595(4):1213-21.
4. PLOS One. 2019 Jun 12. doi: 10.1371/journal.pone.0217583.
5. J Matern Fetal Neonatal Med. 2013 Jun;26(9):915-9.
6. J Perinatol. 2016 Aug;36(8):598-600.
7. Aust N Z J Obstet Gynaecol. 2018 Aug;58(4):463-8.
8. Reduced fetal movements: Green top #57, Royal College of Obstetricians and Gynaecologists.
9. BMC Pregnancy Childb. 2017. doi: 10.1186/s12884-017-1555-6.
10. BMJ Open. 2018. doi: 10.1136/bmjopen-2017-020031.
11. BMC Pregnancy Childb. 2012. doi: 10.1186/1471-2393-12-137.
12. BMC Pregnancy Childb. 2015. doi: 10.1186/s12884-015-0602-4.
13. EClinicalMedicine. 2019 Apr. doi: 10.1016/j.eclinm.2019.03.014.
14. BMC Pregnancy Childb. 2009. doi: 10.1186/1471-2393-9-32.
How to truly connect with your patients
Introducing the ‘6H model’
I vividly remember the conversation that changed the way I practice medicine today.
During my medicine residency rounds, my attending at a Veterans Affairs hospital stated: “Remember Swati, there are three simple steps to gain your patients’ trust. The three questions they have are: No. 1, who are you? No. 2, are you any good? No. 3, do you really care about me?”
The first two questions are easier to address. The third question requires us bare our authentic human self often hiding behind our white coat and medical degree.
Who are you?
- Introduce yourself (everyone is wearing scrubs/white coats – state your full name and title)
- Describe your role in patient’s care plan
- Hand them your card (your name, photo, and a short description of the role of a hospitalist)
Are you any good?
- Briefly address your professional experience
- Explicitly state all the hard work you have done prior to entering the patient’s room (reviewing past medical records, hand off from ED provider or prior hospitalist)
- State your aim to collaborate with all people involved – their primary care provider, nurse, consultant
“Hello Mrs. Jones, my name is Dr. Swati Mehta. I will be your physician today. As a hospitalist, my role is to take care of your medical needs & worries. I will coordinate with your consultants, primary care physician, and other care teams to get you the answers you need. I have been working at XYZ Hospital for 6 years and have over 12 years of experience in medicine taking care of patients. I have reviewed your medical records, blood work, and x-rays before coming in. How are you feeling today? Do you mind if I ask you a few questions?”
Addressing the third question – Do you really care about me? – is the foundation of every human interaction. Answering this question involves addressing our patients’ many fears: Do you care about what I think is going on with my disease? Will you judge me by my socioeconomic status, gender, color of my skin, or addictions? Am I safe to open up and trust you? Are we equal partners in my health care journey? Do you really care?
A successful connection is achieved when we create a space of psychological safety and mutual respect. Once that happens, our patients open up to let us in their world and become more amenable to our opinion and recommendations. That is when true healing begins.
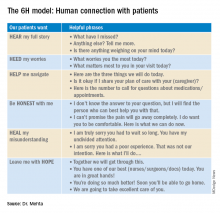
The “6H model” is an aide to form a strong human-centric connection.
The 6H model: Human connection with patients
Looking back at each patient interaction, good or bad, I have had in my almost 2 decades of practicing clinical medicine, the 6H model has brought me closer to my patients. We have formed a bond which has helped them navigate their arduous hospital journey, including medical and financial burdens, social and emotional needs. Utilizing this model, we were fortunate to receive the highest HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey scores for 3 consecutive years while I served as the medical director of a 40-provider hospitalist program in a busy 450-bed hospital in Oregon.
In 2020, we are in the process of embedding the 6H model in several hospitalist programs across California. We are optimistic this intuitive approach will strengthen patient-provider relationships and ultimately improve HCAHPS scores.
To form an authentic connection with our patients doesn’t necessary require a lot of our time. Hardwiring the 6H approach when addressing our patients’ three questions is the key. The answers can change slightly, but the core message remains the same.
While we might not have much influence on all the factors that make or break our patients’ experience, the patient encounter is where we can truly make a difference. Consider using this 6H model in your next clinical shift. Human connection in health care is the need of the hour. Let’s bring “care” back to health care.
Dr. Mehta is director of quality & performance and patient experience at Vituity in Emeryville, Calif., and vice chair of the SHM patient experience committee.
Introducing the ‘6H model’
Introducing the ‘6H model’
I vividly remember the conversation that changed the way I practice medicine today.
During my medicine residency rounds, my attending at a Veterans Affairs hospital stated: “Remember Swati, there are three simple steps to gain your patients’ trust. The three questions they have are: No. 1, who are you? No. 2, are you any good? No. 3, do you really care about me?”
The first two questions are easier to address. The third question requires us bare our authentic human self often hiding behind our white coat and medical degree.
Who are you?
- Introduce yourself (everyone is wearing scrubs/white coats – state your full name and title)
- Describe your role in patient’s care plan
- Hand them your card (your name, photo, and a short description of the role of a hospitalist)
Are you any good?
- Briefly address your professional experience
- Explicitly state all the hard work you have done prior to entering the patient’s room (reviewing past medical records, hand off from ED provider or prior hospitalist)
- State your aim to collaborate with all people involved – their primary care provider, nurse, consultant
“Hello Mrs. Jones, my name is Dr. Swati Mehta. I will be your physician today. As a hospitalist, my role is to take care of your medical needs & worries. I will coordinate with your consultants, primary care physician, and other care teams to get you the answers you need. I have been working at XYZ Hospital for 6 years and have over 12 years of experience in medicine taking care of patients. I have reviewed your medical records, blood work, and x-rays before coming in. How are you feeling today? Do you mind if I ask you a few questions?”
Addressing the third question – Do you really care about me? – is the foundation of every human interaction. Answering this question involves addressing our patients’ many fears: Do you care about what I think is going on with my disease? Will you judge me by my socioeconomic status, gender, color of my skin, or addictions? Am I safe to open up and trust you? Are we equal partners in my health care journey? Do you really care?
A successful connection is achieved when we create a space of psychological safety and mutual respect. Once that happens, our patients open up to let us in their world and become more amenable to our opinion and recommendations. That is when true healing begins.
The “6H model” is an aide to form a strong human-centric connection.
The 6H model: Human connection with patients
Looking back at each patient interaction, good or bad, I have had in my almost 2 decades of practicing clinical medicine, the 6H model has brought me closer to my patients. We have formed a bond which has helped them navigate their arduous hospital journey, including medical and financial burdens, social and emotional needs. Utilizing this model, we were fortunate to receive the highest HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey scores for 3 consecutive years while I served as the medical director of a 40-provider hospitalist program in a busy 450-bed hospital in Oregon.
In 2020, we are in the process of embedding the 6H model in several hospitalist programs across California. We are optimistic this intuitive approach will strengthen patient-provider relationships and ultimately improve HCAHPS scores.
To form an authentic connection with our patients doesn’t necessary require a lot of our time. Hardwiring the 6H approach when addressing our patients’ three questions is the key. The answers can change slightly, but the core message remains the same.
While we might not have much influence on all the factors that make or break our patients’ experience, the patient encounter is where we can truly make a difference. Consider using this 6H model in your next clinical shift. Human connection in health care is the need of the hour. Let’s bring “care” back to health care.
Dr. Mehta is director of quality & performance and patient experience at Vituity in Emeryville, Calif., and vice chair of the SHM patient experience committee.
I vividly remember the conversation that changed the way I practice medicine today.
During my medicine residency rounds, my attending at a Veterans Affairs hospital stated: “Remember Swati, there are three simple steps to gain your patients’ trust. The three questions they have are: No. 1, who are you? No. 2, are you any good? No. 3, do you really care about me?”
The first two questions are easier to address. The third question requires us bare our authentic human self often hiding behind our white coat and medical degree.
Who are you?
- Introduce yourself (everyone is wearing scrubs/white coats – state your full name and title)
- Describe your role in patient’s care plan
- Hand them your card (your name, photo, and a short description of the role of a hospitalist)
Are you any good?
- Briefly address your professional experience
- Explicitly state all the hard work you have done prior to entering the patient’s room (reviewing past medical records, hand off from ED provider or prior hospitalist)
- State your aim to collaborate with all people involved – their primary care provider, nurse, consultant
“Hello Mrs. Jones, my name is Dr. Swati Mehta. I will be your physician today. As a hospitalist, my role is to take care of your medical needs & worries. I will coordinate with your consultants, primary care physician, and other care teams to get you the answers you need. I have been working at XYZ Hospital for 6 years and have over 12 years of experience in medicine taking care of patients. I have reviewed your medical records, blood work, and x-rays before coming in. How are you feeling today? Do you mind if I ask you a few questions?”
Addressing the third question – Do you really care about me? – is the foundation of every human interaction. Answering this question involves addressing our patients’ many fears: Do you care about what I think is going on with my disease? Will you judge me by my socioeconomic status, gender, color of my skin, or addictions? Am I safe to open up and trust you? Are we equal partners in my health care journey? Do you really care?
A successful connection is achieved when we create a space of psychological safety and mutual respect. Once that happens, our patients open up to let us in their world and become more amenable to our opinion and recommendations. That is when true healing begins.
The “6H model” is an aide to form a strong human-centric connection.
The 6H model: Human connection with patients
Looking back at each patient interaction, good or bad, I have had in my almost 2 decades of practicing clinical medicine, the 6H model has brought me closer to my patients. We have formed a bond which has helped them navigate their arduous hospital journey, including medical and financial burdens, social and emotional needs. Utilizing this model, we were fortunate to receive the highest HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey scores for 3 consecutive years while I served as the medical director of a 40-provider hospitalist program in a busy 450-bed hospital in Oregon.
In 2020, we are in the process of embedding the 6H model in several hospitalist programs across California. We are optimistic this intuitive approach will strengthen patient-provider relationships and ultimately improve HCAHPS scores.
To form an authentic connection with our patients doesn’t necessary require a lot of our time. Hardwiring the 6H approach when addressing our patients’ three questions is the key. The answers can change slightly, but the core message remains the same.
While we might not have much influence on all the factors that make or break our patients’ experience, the patient encounter is where we can truly make a difference. Consider using this 6H model in your next clinical shift. Human connection in health care is the need of the hour. Let’s bring “care” back to health care.
Dr. Mehta is director of quality & performance and patient experience at Vituity in Emeryville, Calif., and vice chair of the SHM patient experience committee.
Deaths, despair tied to drug dependence are accelerating amid COVID-19
Patients with OUDs need assistance now more than ever.
The Centers for Disease Control and Prevention reported recently that opioid overdose deaths will increase to a new U.S. record, and more are expected as pandemic-related overdose deaths are yet to be counted.1
Specifically, according to the CDC, 70,980 people died from fatal overdoses in 2019,2 which is record high. Experts such as Bruce A. Goldberger, PhD, fear that the 2020 numbers could rise even higher, exacerbated by the coronavirus pandemic.
Deaths from drug overdoses remain higher than the peak yearly death totals ever recorded for car accidents, guns, or AIDS. Overdose deaths have accelerated further – pushing down overall life expectancy in the United States.3 Headlines purporting to identify good news in drug death figures don’t always get below top-level data. Deaths and despair tied to drug dependence are indeed accelerating. I am concerned about these alarmingly dangerous trends.
Synthetic opioids such as fentanyl accounted for about 3,000 deaths in 2013. By 2019, they accounted for more than 37,137.4 In addition, 16,539 deaths involved stimulants such as methamphetamine, and 16,196 deaths involved cocaine, the most recent CDC reporting shows. Opioids continue to play a role in U.S. “deaths of despair,” or rising fatalities from drugs, suicides, and alcohol among Americans without employment, hope of job opportunities, or college degrees.5 As the American Medical Association has warned,6 more people are dying from overdoses amid the COVID-19 pandemic. Clinicians need to be aware of trends so that we can help our patients navigate these challenges.
Fentanyl presents dangers
Experts had predicted that the pandemic, by limiting access to treatment, rescue, or overdose services, and increasing time at home and in the neighborhood, would result in more tragedy. In addition, the shift from prescription opioids to heroin and now to fentanyl has made deaths more common.
Fentanyls – synthetic opioids – are involved in more than half of overdose deaths, and in many of the cocaine and methamphetamine-related deaths, which also are on the rise. Fentanyl is about 100 times more potent than morphine and 50 times more potent than heroin. Breathing can stop after use of just 2 mg of fentanyl, which is about as much as trace amounts of table salt. Fentanyl has replaced heroin in many cities as the pandemic changed the relative ease of importing raw drugs such as heroin.
Another important trend is that fentanyl production and distribution throughout the United States have expanded. The ease of manufacture in unregulated sectors of the Chinese and Mexican economies is difficult for U.S. authorities to curb or eliminate. The Internet promotes novel strategies for synthesizing the substance, spreading its production across many labs; suppliers use the U.S. Postal Service for distribution, and e-commerce helps to get the drug from manufacturers to U.S. consumers for fentanyl transactions.
A recent RAND report observes that, for only $10 through the postal service, suppliers can ship a 1-kg parcel from China to the United States, and private shipments cost about $100.7 And with large volumes of legal trade between the two countries making rigorous scrutiny of products difficult, especially given the light weight of fentanyl, suppliers find it relatively easy to hide illicit substances in licit shipments. Opioid users have made the switch to fentanyl, and have seen fentanyl added to cocaine and methamphetamine they buy on the streets.
OUD and buprenorphine
Fentanyl is one part of the overdose crisis. Opioid use disorder (OUD) is the other. Both need to be addressed if we are to make any progress in this epidemic of death and dependency.
The OUD crisis continues amid the pandemic – and isn’t going away.8 Slips, relapses, and overdoses are all too common. Medication-assisted treatment (MAT) and OUD treatment programs are essential parts of our response to overdose initiatives. After naloxone rescue, the best anti-overdose response is to get the OUD patient into treatment with MATs. Patients with OUD have continuously high risks of overdose. The best outcomes appear to be related to treatment duration of greater than 2 years. But it is common to see patients with OUDs who have been in treatment multiple times, taking MATs, dropping out, overdosing, and dying. Some have been described as treatment resistant.9 It is clear that treatment can work, but also that even evidence-based treatments often fail.10
A recent study compared OUD patients who continued treatment for 6-9 months to those patients who had continued MAT treatment for 15-18 months. The longer the treatment, the fewer emergencies, prescriptions, or hospitalizations.11
But this study reminds us that all OUD patients, whether they are currently buprenorphine treated or not, experience overdoses and emergency department interventions. Short and longer treatment groups have a similar nonfatal overdose rate, about 6%, and went to the emergency department at a high rate, above 40%. Discontinuation of buprenorphine treatment is a major risk factor in opioid relapse, emergency department visits, and overdose. Cures are not common. Whether an OUD patient is being treated or has been treated in the past, carrying naloxone (brand name Narcan), makes sense and can save lives.
Methadone still considered most effective
Methadone is a synthetic opioid first studied as a treatment for OUD at Rockefeller University in New York City in the 1960s. Methadone may be the most effective treatment for OUD in promoting treatment retention for years, decreasing intravenous drug use, and decreasing deaths.12 It has been studied and safely used in treatment programs for decades. Methadone is typically administered in a clinic, daily, and with observation. In addition, methadone patients periodically take urine drug tests, which can distinguish methadone from substances of abuse. They also receive counseling. But methadone can be prescribed and administered only in methadone clinics in the United States. It is available for prescription in primary care clinics in Great Britain, Canada, and Australia.13 Numerous experts have suggested passing new legislation aimed at changing how methadone can be prescribed. Allowing primary care to administer methadone, just like buprenorphine, can improve access and benefit OUD patients.12
Availability of Narcan is critical
A comprehensive treatment model for OUDs includes prescribing naloxone, encouraging those patients with an OUD and their loved ones to have naloxone with them, and providing MATs and appropriate therapies, such as counseling.
As described by Allison L. Pitt and colleagues at Stanford (Calif.) University,14 the United States might be on track to have up to 500,000 deaths tied to opioid overdoses that might occur over the next 5 years. They modeled the effect on overdose of a long list of interventions, but only a few had an impact. At the top of the list was naloxone availability. We need to focus on saving lives by increasing naloxone availability, improving initiation, and expanding access to MAT, and increasing psychosocial treatment to improve outcomes, increase life-years and quality-adjusted life-years, and reduce opioid-related deaths. When Ms. Pitt and colleagues looked at what would make the most impact in reducing OUD deaths, it was naloxone. Pain patients on higher doses of opioids, nonprescription opioid users, OUD patients should be given naloxone prescriptions. While many can give a Heimlich to a choking person or CPR, few have naloxone to rescue a person who has overdosed on opioids. If an overdose is suspected, it should be administered by anyone who has it, as soon as possible. Then, the person who is intervening should call 911.
What we can do today
At this moment, clinicians can follow the Surgeon General’s advice,15 and prescribe naloxone.
We should give naloxone to OUD patients and their families, to pain patients at dosages of greater than or equal to 50 MME. Our top priorities should be patients with comorbid pain syndromes, those being treated with benzodiazepines and sleeping medications, and patients with alcohol use disorders. This is also an important intervention for those who binge drink, and have sleep apnea, and heart and respiratory diseases.
Naloxone is available without a prescription in at least 43 states. Naloxone is available in harm reduction programs and in hospitals, and is carried by emergency medical staff, law enforcement, and EMTs. It also is available on the streets, though it does not appear to have a dollar value like opioids or even buprenorphine. Also, the availability of naloxone in pharmacies has made it easier for family members and caregivers of pain patients or those with OUD to have it to administer in an emergency.
An excellent place for MDs to start is to do more to encourage all patients with OUD to carry naloxone, for their loved ones to carry naloxone, and for their homes to have naloxone nearby in the bedroom or bathroom. It is not logical to expect a person with an OUD to rescue themselves. Current and past OUD patients, as well as their loved ones, are at high risk – and should have naloxone nearby at all times.
Naloxone reverses an opioid overdose, but it should be thought about like cardioversion or CPR rather than a treatment for an underlying disease. Increasing access to buprenorphine, buprenorphine + naloxone, and naltrexone treatment for OUDs is an important organizing principle. Initiation of MAT treatment in the emergency setting or most anywhere and any place a patient with an OUD can begin treatment is necessary. Treatment with buprenorphine or methadone reduces opioid overdose and opioid-related acute care use.16
Reducing racial disparities in OUD treatment is necessary, because buprenorphine treatment is concentrated among White patients who either use private insurance or are self-pay.17 Reducing barriers to methadone program licenses, expanding sites for distribution,18 prescribing methadone in an office setting might help. Clinicians can do a better job of explaining the risks associated with opioid prescriptions, including diversion and overdose, and the benefits of OUD treatment. So, To reduce opioid overdoses, we must increase physician competencies in addiction medicine.
Dr. Gold is professor of psychiatry (adjunct) at Washington University, St. Louis. He is the 17th Distinguished Alumni Professor at the University of Florida, Gainesville. For more than 40 years, Dr. Gold has worked on developing models for understanding the effects of opioid, tobacco, cocaine, and other drugs, as well as food, on the brain and behavior. He disclosed financial ties with ADAPT Pharma and Magstim Ltd.
References
1. Kamp J. Overdose deaths rise, may reach record level, federal data show. Wall Street Journal. 2020 Jul 15.
2. 12 month–ending provisional number of drug overdose drugs. Centers for Disease Control and Prevention. 2020 Jul 5.
3. Katz J et al. In shadow of pandemic, U.S. drug overdose deaths resurge to record. New York Times. 2020 Jul 15.
4. Gold MS. The fentanyl crisis is only getting worse. Addiction Policy Forum. Updated 2020 Mar 12.
5. Gold MS. Mo Med. 2020-Mar-Apr;117(2):99-101.
6. Reports of increases in opioid-related overdoses and other concerns during the COVID-19 pandemic. American Medical Association. Issue brief. Updated 2020 Jul 20.
7. Pardo B et al. The future of fentanyl and other synthetic opioids. RAND report.
8. Gold MS. New challenges in the opioid epidemic. Addiction Policy Forum. 2020 Jun 4.
9. Patterson Silver Wolf DA and Gold MS. J Neurol Sci. 2020;411:116718.
10. Oesterle TS et al. Mayo Clin Proc. 2019;94(10):2072-86.
11. Connery HS and Weiss RD. Am J Psychiatry. 2020;177(2):104-6.
12. Kleber HD. JAMA. 2008;300(19):2303-5.
13. Samet JH et al. N Engl J Med. 2018;379(1):7-8.
14. Pitt AL et al. Am J Public Health. 2018;108(10):1394-1400.
15. U.S. Surgeon General’s Advisory on Naloxone and Opioid Overdose. hhs.gov.
16. Wakeman SE et al. JAMA Netw Open. 2020;3(2):e1920622.
17. Lagisetty PA et al. JAMA Psychiatry. 2019;76(9):979-81.
18. Kleinman RA. JAMA Psychiatry. 2020 Jul 15. doi: 10.1001/jamapsychiatry.2020.1624.
Patients with OUDs need assistance now more than ever.
Patients with OUDs need assistance now more than ever.
The Centers for Disease Control and Prevention reported recently that opioid overdose deaths will increase to a new U.S. record, and more are expected as pandemic-related overdose deaths are yet to be counted.1
Specifically, according to the CDC, 70,980 people died from fatal overdoses in 2019,2 which is record high. Experts such as Bruce A. Goldberger, PhD, fear that the 2020 numbers could rise even higher, exacerbated by the coronavirus pandemic.
Deaths from drug overdoses remain higher than the peak yearly death totals ever recorded for car accidents, guns, or AIDS. Overdose deaths have accelerated further – pushing down overall life expectancy in the United States.3 Headlines purporting to identify good news in drug death figures don’t always get below top-level data. Deaths and despair tied to drug dependence are indeed accelerating. I am concerned about these alarmingly dangerous trends.
Synthetic opioids such as fentanyl accounted for about 3,000 deaths in 2013. By 2019, they accounted for more than 37,137.4 In addition, 16,539 deaths involved stimulants such as methamphetamine, and 16,196 deaths involved cocaine, the most recent CDC reporting shows. Opioids continue to play a role in U.S. “deaths of despair,” or rising fatalities from drugs, suicides, and alcohol among Americans without employment, hope of job opportunities, or college degrees.5 As the American Medical Association has warned,6 more people are dying from overdoses amid the COVID-19 pandemic. Clinicians need to be aware of trends so that we can help our patients navigate these challenges.
Fentanyl presents dangers
Experts had predicted that the pandemic, by limiting access to treatment, rescue, or overdose services, and increasing time at home and in the neighborhood, would result in more tragedy. In addition, the shift from prescription opioids to heroin and now to fentanyl has made deaths more common.
Fentanyls – synthetic opioids – are involved in more than half of overdose deaths, and in many of the cocaine and methamphetamine-related deaths, which also are on the rise. Fentanyl is about 100 times more potent than morphine and 50 times more potent than heroin. Breathing can stop after use of just 2 mg of fentanyl, which is about as much as trace amounts of table salt. Fentanyl has replaced heroin in many cities as the pandemic changed the relative ease of importing raw drugs such as heroin.
Another important trend is that fentanyl production and distribution throughout the United States have expanded. The ease of manufacture in unregulated sectors of the Chinese and Mexican economies is difficult for U.S. authorities to curb or eliminate. The Internet promotes novel strategies for synthesizing the substance, spreading its production across many labs; suppliers use the U.S. Postal Service for distribution, and e-commerce helps to get the drug from manufacturers to U.S. consumers for fentanyl transactions.
A recent RAND report observes that, for only $10 through the postal service, suppliers can ship a 1-kg parcel from China to the United States, and private shipments cost about $100.7 And with large volumes of legal trade between the two countries making rigorous scrutiny of products difficult, especially given the light weight of fentanyl, suppliers find it relatively easy to hide illicit substances in licit shipments. Opioid users have made the switch to fentanyl, and have seen fentanyl added to cocaine and methamphetamine they buy on the streets.
OUD and buprenorphine
Fentanyl is one part of the overdose crisis. Opioid use disorder (OUD) is the other. Both need to be addressed if we are to make any progress in this epidemic of death and dependency.
The OUD crisis continues amid the pandemic – and isn’t going away.8 Slips, relapses, and overdoses are all too common. Medication-assisted treatment (MAT) and OUD treatment programs are essential parts of our response to overdose initiatives. After naloxone rescue, the best anti-overdose response is to get the OUD patient into treatment with MATs. Patients with OUD have continuously high risks of overdose. The best outcomes appear to be related to treatment duration of greater than 2 years. But it is common to see patients with OUDs who have been in treatment multiple times, taking MATs, dropping out, overdosing, and dying. Some have been described as treatment resistant.9 It is clear that treatment can work, but also that even evidence-based treatments often fail.10
A recent study compared OUD patients who continued treatment for 6-9 months to those patients who had continued MAT treatment for 15-18 months. The longer the treatment, the fewer emergencies, prescriptions, or hospitalizations.11
But this study reminds us that all OUD patients, whether they are currently buprenorphine treated or not, experience overdoses and emergency department interventions. Short and longer treatment groups have a similar nonfatal overdose rate, about 6%, and went to the emergency department at a high rate, above 40%. Discontinuation of buprenorphine treatment is a major risk factor in opioid relapse, emergency department visits, and overdose. Cures are not common. Whether an OUD patient is being treated or has been treated in the past, carrying naloxone (brand name Narcan), makes sense and can save lives.
Methadone still considered most effective
Methadone is a synthetic opioid first studied as a treatment for OUD at Rockefeller University in New York City in the 1960s. Methadone may be the most effective treatment for OUD in promoting treatment retention for years, decreasing intravenous drug use, and decreasing deaths.12 It has been studied and safely used in treatment programs for decades. Methadone is typically administered in a clinic, daily, and with observation. In addition, methadone patients periodically take urine drug tests, which can distinguish methadone from substances of abuse. They also receive counseling. But methadone can be prescribed and administered only in methadone clinics in the United States. It is available for prescription in primary care clinics in Great Britain, Canada, and Australia.13 Numerous experts have suggested passing new legislation aimed at changing how methadone can be prescribed. Allowing primary care to administer methadone, just like buprenorphine, can improve access and benefit OUD patients.12
Availability of Narcan is critical
A comprehensive treatment model for OUDs includes prescribing naloxone, encouraging those patients with an OUD and their loved ones to have naloxone with them, and providing MATs and appropriate therapies, such as counseling.
As described by Allison L. Pitt and colleagues at Stanford (Calif.) University,14 the United States might be on track to have up to 500,000 deaths tied to opioid overdoses that might occur over the next 5 years. They modeled the effect on overdose of a long list of interventions, but only a few had an impact. At the top of the list was naloxone availability. We need to focus on saving lives by increasing naloxone availability, improving initiation, and expanding access to MAT, and increasing psychosocial treatment to improve outcomes, increase life-years and quality-adjusted life-years, and reduce opioid-related deaths. When Ms. Pitt and colleagues looked at what would make the most impact in reducing OUD deaths, it was naloxone. Pain patients on higher doses of opioids, nonprescription opioid users, OUD patients should be given naloxone prescriptions. While many can give a Heimlich to a choking person or CPR, few have naloxone to rescue a person who has overdosed on opioids. If an overdose is suspected, it should be administered by anyone who has it, as soon as possible. Then, the person who is intervening should call 911.
What we can do today
At this moment, clinicians can follow the Surgeon General’s advice,15 and prescribe naloxone.
We should give naloxone to OUD patients and their families, to pain patients at dosages of greater than or equal to 50 MME. Our top priorities should be patients with comorbid pain syndromes, those being treated with benzodiazepines and sleeping medications, and patients with alcohol use disorders. This is also an important intervention for those who binge drink, and have sleep apnea, and heart and respiratory diseases.
Naloxone is available without a prescription in at least 43 states. Naloxone is available in harm reduction programs and in hospitals, and is carried by emergency medical staff, law enforcement, and EMTs. It also is available on the streets, though it does not appear to have a dollar value like opioids or even buprenorphine. Also, the availability of naloxone in pharmacies has made it easier for family members and caregivers of pain patients or those with OUD to have it to administer in an emergency.
An excellent place for MDs to start is to do more to encourage all patients with OUD to carry naloxone, for their loved ones to carry naloxone, and for their homes to have naloxone nearby in the bedroom or bathroom. It is not logical to expect a person with an OUD to rescue themselves. Current and past OUD patients, as well as their loved ones, are at high risk – and should have naloxone nearby at all times.
Naloxone reverses an opioid overdose, but it should be thought about like cardioversion or CPR rather than a treatment for an underlying disease. Increasing access to buprenorphine, buprenorphine + naloxone, and naltrexone treatment for OUDs is an important organizing principle. Initiation of MAT treatment in the emergency setting or most anywhere and any place a patient with an OUD can begin treatment is necessary. Treatment with buprenorphine or methadone reduces opioid overdose and opioid-related acute care use.16
Reducing racial disparities in OUD treatment is necessary, because buprenorphine treatment is concentrated among White patients who either use private insurance or are self-pay.17 Reducing barriers to methadone program licenses, expanding sites for distribution,18 prescribing methadone in an office setting might help. Clinicians can do a better job of explaining the risks associated with opioid prescriptions, including diversion and overdose, and the benefits of OUD treatment. So, To reduce opioid overdoses, we must increase physician competencies in addiction medicine.
Dr. Gold is professor of psychiatry (adjunct) at Washington University, St. Louis. He is the 17th Distinguished Alumni Professor at the University of Florida, Gainesville. For more than 40 years, Dr. Gold has worked on developing models for understanding the effects of opioid, tobacco, cocaine, and other drugs, as well as food, on the brain and behavior. He disclosed financial ties with ADAPT Pharma and Magstim Ltd.
References
1. Kamp J. Overdose deaths rise, may reach record level, federal data show. Wall Street Journal. 2020 Jul 15.
2. 12 month–ending provisional number of drug overdose drugs. Centers for Disease Control and Prevention. 2020 Jul 5.
3. Katz J et al. In shadow of pandemic, U.S. drug overdose deaths resurge to record. New York Times. 2020 Jul 15.
4. Gold MS. The fentanyl crisis is only getting worse. Addiction Policy Forum. Updated 2020 Mar 12.
5. Gold MS. Mo Med. 2020-Mar-Apr;117(2):99-101.
6. Reports of increases in opioid-related overdoses and other concerns during the COVID-19 pandemic. American Medical Association. Issue brief. Updated 2020 Jul 20.
7. Pardo B et al. The future of fentanyl and other synthetic opioids. RAND report.
8. Gold MS. New challenges in the opioid epidemic. Addiction Policy Forum. 2020 Jun 4.
9. Patterson Silver Wolf DA and Gold MS. J Neurol Sci. 2020;411:116718.
10. Oesterle TS et al. Mayo Clin Proc. 2019;94(10):2072-86.
11. Connery HS and Weiss RD. Am J Psychiatry. 2020;177(2):104-6.
12. Kleber HD. JAMA. 2008;300(19):2303-5.
13. Samet JH et al. N Engl J Med. 2018;379(1):7-8.
14. Pitt AL et al. Am J Public Health. 2018;108(10):1394-1400.
15. U.S. Surgeon General’s Advisory on Naloxone and Opioid Overdose. hhs.gov.
16. Wakeman SE et al. JAMA Netw Open. 2020;3(2):e1920622.
17. Lagisetty PA et al. JAMA Psychiatry. 2019;76(9):979-81.
18. Kleinman RA. JAMA Psychiatry. 2020 Jul 15. doi: 10.1001/jamapsychiatry.2020.1624.
The Centers for Disease Control and Prevention reported recently that opioid overdose deaths will increase to a new U.S. record, and more are expected as pandemic-related overdose deaths are yet to be counted.1
Specifically, according to the CDC, 70,980 people died from fatal overdoses in 2019,2 which is record high. Experts such as Bruce A. Goldberger, PhD, fear that the 2020 numbers could rise even higher, exacerbated by the coronavirus pandemic.
Deaths from drug overdoses remain higher than the peak yearly death totals ever recorded for car accidents, guns, or AIDS. Overdose deaths have accelerated further – pushing down overall life expectancy in the United States.3 Headlines purporting to identify good news in drug death figures don’t always get below top-level data. Deaths and despair tied to drug dependence are indeed accelerating. I am concerned about these alarmingly dangerous trends.
Synthetic opioids such as fentanyl accounted for about 3,000 deaths in 2013. By 2019, they accounted for more than 37,137.4 In addition, 16,539 deaths involved stimulants such as methamphetamine, and 16,196 deaths involved cocaine, the most recent CDC reporting shows. Opioids continue to play a role in U.S. “deaths of despair,” or rising fatalities from drugs, suicides, and alcohol among Americans without employment, hope of job opportunities, or college degrees.5 As the American Medical Association has warned,6 more people are dying from overdoses amid the COVID-19 pandemic. Clinicians need to be aware of trends so that we can help our patients navigate these challenges.
Fentanyl presents dangers
Experts had predicted that the pandemic, by limiting access to treatment, rescue, or overdose services, and increasing time at home and in the neighborhood, would result in more tragedy. In addition, the shift from prescription opioids to heroin and now to fentanyl has made deaths more common.
Fentanyls – synthetic opioids – are involved in more than half of overdose deaths, and in many of the cocaine and methamphetamine-related deaths, which also are on the rise. Fentanyl is about 100 times more potent than morphine and 50 times more potent than heroin. Breathing can stop after use of just 2 mg of fentanyl, which is about as much as trace amounts of table salt. Fentanyl has replaced heroin in many cities as the pandemic changed the relative ease of importing raw drugs such as heroin.
Another important trend is that fentanyl production and distribution throughout the United States have expanded. The ease of manufacture in unregulated sectors of the Chinese and Mexican economies is difficult for U.S. authorities to curb or eliminate. The Internet promotes novel strategies for synthesizing the substance, spreading its production across many labs; suppliers use the U.S. Postal Service for distribution, and e-commerce helps to get the drug from manufacturers to U.S. consumers for fentanyl transactions.
A recent RAND report observes that, for only $10 through the postal service, suppliers can ship a 1-kg parcel from China to the United States, and private shipments cost about $100.7 And with large volumes of legal trade between the two countries making rigorous scrutiny of products difficult, especially given the light weight of fentanyl, suppliers find it relatively easy to hide illicit substances in licit shipments. Opioid users have made the switch to fentanyl, and have seen fentanyl added to cocaine and methamphetamine they buy on the streets.
OUD and buprenorphine
Fentanyl is one part of the overdose crisis. Opioid use disorder (OUD) is the other. Both need to be addressed if we are to make any progress in this epidemic of death and dependency.
The OUD crisis continues amid the pandemic – and isn’t going away.8 Slips, relapses, and overdoses are all too common. Medication-assisted treatment (MAT) and OUD treatment programs are essential parts of our response to overdose initiatives. After naloxone rescue, the best anti-overdose response is to get the OUD patient into treatment with MATs. Patients with OUD have continuously high risks of overdose. The best outcomes appear to be related to treatment duration of greater than 2 years. But it is common to see patients with OUDs who have been in treatment multiple times, taking MATs, dropping out, overdosing, and dying. Some have been described as treatment resistant.9 It is clear that treatment can work, but also that even evidence-based treatments often fail.10
A recent study compared OUD patients who continued treatment for 6-9 months to those patients who had continued MAT treatment for 15-18 months. The longer the treatment, the fewer emergencies, prescriptions, or hospitalizations.11
But this study reminds us that all OUD patients, whether they are currently buprenorphine treated or not, experience overdoses and emergency department interventions. Short and longer treatment groups have a similar nonfatal overdose rate, about 6%, and went to the emergency department at a high rate, above 40%. Discontinuation of buprenorphine treatment is a major risk factor in opioid relapse, emergency department visits, and overdose. Cures are not common. Whether an OUD patient is being treated or has been treated in the past, carrying naloxone (brand name Narcan), makes sense and can save lives.
Methadone still considered most effective
Methadone is a synthetic opioid first studied as a treatment for OUD at Rockefeller University in New York City in the 1960s. Methadone may be the most effective treatment for OUD in promoting treatment retention for years, decreasing intravenous drug use, and decreasing deaths.12 It has been studied and safely used in treatment programs for decades. Methadone is typically administered in a clinic, daily, and with observation. In addition, methadone patients periodically take urine drug tests, which can distinguish methadone from substances of abuse. They also receive counseling. But methadone can be prescribed and administered only in methadone clinics in the United States. It is available for prescription in primary care clinics in Great Britain, Canada, and Australia.13 Numerous experts have suggested passing new legislation aimed at changing how methadone can be prescribed. Allowing primary care to administer methadone, just like buprenorphine, can improve access and benefit OUD patients.12
Availability of Narcan is critical
A comprehensive treatment model for OUDs includes prescribing naloxone, encouraging those patients with an OUD and their loved ones to have naloxone with them, and providing MATs and appropriate therapies, such as counseling.
As described by Allison L. Pitt and colleagues at Stanford (Calif.) University,14 the United States might be on track to have up to 500,000 deaths tied to opioid overdoses that might occur over the next 5 years. They modeled the effect on overdose of a long list of interventions, but only a few had an impact. At the top of the list was naloxone availability. We need to focus on saving lives by increasing naloxone availability, improving initiation, and expanding access to MAT, and increasing psychosocial treatment to improve outcomes, increase life-years and quality-adjusted life-years, and reduce opioid-related deaths. When Ms. Pitt and colleagues looked at what would make the most impact in reducing OUD deaths, it was naloxone. Pain patients on higher doses of opioids, nonprescription opioid users, OUD patients should be given naloxone prescriptions. While many can give a Heimlich to a choking person or CPR, few have naloxone to rescue a person who has overdosed on opioids. If an overdose is suspected, it should be administered by anyone who has it, as soon as possible. Then, the person who is intervening should call 911.
What we can do today
At this moment, clinicians can follow the Surgeon General’s advice,15 and prescribe naloxone.
We should give naloxone to OUD patients and their families, to pain patients at dosages of greater than or equal to 50 MME. Our top priorities should be patients with comorbid pain syndromes, those being treated with benzodiazepines and sleeping medications, and patients with alcohol use disorders. This is also an important intervention for those who binge drink, and have sleep apnea, and heart and respiratory diseases.
Naloxone is available without a prescription in at least 43 states. Naloxone is available in harm reduction programs and in hospitals, and is carried by emergency medical staff, law enforcement, and EMTs. It also is available on the streets, though it does not appear to have a dollar value like opioids or even buprenorphine. Also, the availability of naloxone in pharmacies has made it easier for family members and caregivers of pain patients or those with OUD to have it to administer in an emergency.
An excellent place for MDs to start is to do more to encourage all patients with OUD to carry naloxone, for their loved ones to carry naloxone, and for their homes to have naloxone nearby in the bedroom or bathroom. It is not logical to expect a person with an OUD to rescue themselves. Current and past OUD patients, as well as their loved ones, are at high risk – and should have naloxone nearby at all times.
Naloxone reverses an opioid overdose, but it should be thought about like cardioversion or CPR rather than a treatment for an underlying disease. Increasing access to buprenorphine, buprenorphine + naloxone, and naltrexone treatment for OUDs is an important organizing principle. Initiation of MAT treatment in the emergency setting or most anywhere and any place a patient with an OUD can begin treatment is necessary. Treatment with buprenorphine or methadone reduces opioid overdose and opioid-related acute care use.16
Reducing racial disparities in OUD treatment is necessary, because buprenorphine treatment is concentrated among White patients who either use private insurance or are self-pay.17 Reducing barriers to methadone program licenses, expanding sites for distribution,18 prescribing methadone in an office setting might help. Clinicians can do a better job of explaining the risks associated with opioid prescriptions, including diversion and overdose, and the benefits of OUD treatment. So, To reduce opioid overdoses, we must increase physician competencies in addiction medicine.
Dr. Gold is professor of psychiatry (adjunct) at Washington University, St. Louis. He is the 17th Distinguished Alumni Professor at the University of Florida, Gainesville. For more than 40 years, Dr. Gold has worked on developing models for understanding the effects of opioid, tobacco, cocaine, and other drugs, as well as food, on the brain and behavior. He disclosed financial ties with ADAPT Pharma and Magstim Ltd.
References
1. Kamp J. Overdose deaths rise, may reach record level, federal data show. Wall Street Journal. 2020 Jul 15.
2. 12 month–ending provisional number of drug overdose drugs. Centers for Disease Control and Prevention. 2020 Jul 5.
3. Katz J et al. In shadow of pandemic, U.S. drug overdose deaths resurge to record. New York Times. 2020 Jul 15.
4. Gold MS. The fentanyl crisis is only getting worse. Addiction Policy Forum. Updated 2020 Mar 12.
5. Gold MS. Mo Med. 2020-Mar-Apr;117(2):99-101.
6. Reports of increases in opioid-related overdoses and other concerns during the COVID-19 pandemic. American Medical Association. Issue brief. Updated 2020 Jul 20.
7. Pardo B et al. The future of fentanyl and other synthetic opioids. RAND report.
8. Gold MS. New challenges in the opioid epidemic. Addiction Policy Forum. 2020 Jun 4.
9. Patterson Silver Wolf DA and Gold MS. J Neurol Sci. 2020;411:116718.
10. Oesterle TS et al. Mayo Clin Proc. 2019;94(10):2072-86.
11. Connery HS and Weiss RD. Am J Psychiatry. 2020;177(2):104-6.
12. Kleber HD. JAMA. 2008;300(19):2303-5.
13. Samet JH et al. N Engl J Med. 2018;379(1):7-8.
14. Pitt AL et al. Am J Public Health. 2018;108(10):1394-1400.
15. U.S. Surgeon General’s Advisory on Naloxone and Opioid Overdose. hhs.gov.
16. Wakeman SE et al. JAMA Netw Open. 2020;3(2):e1920622.
17. Lagisetty PA et al. JAMA Psychiatry. 2019;76(9):979-81.
18. Kleinman RA. JAMA Psychiatry. 2020 Jul 15. doi: 10.1001/jamapsychiatry.2020.1624.
Action and awareness are needed to increase immunization rates
August was National Immunization Awareness Month. ... just in time to address the precipitous drop in immunization delivered during the early months of the pandemic.
In May, the Centers for Disease Control and Prevention reported substantial reductions in vaccine doses ordered through the Vaccines for Children program after the declaration of national emergency because of COVID-19 on March 13. Approximately 2.5 million fewer doses of routine, noninfluenza vaccines were administered between Jan. 6 and April 2020, compared with a similar period last year (MMWR Morb Mortal Wkly Rep. 2020 May 15;69[19]:591-3). Declines in immunization rates were echoed by states and municipalities across the United States. Last month, the health system in which I work reported 40,000 children behind on at least one vaccine.
We all know that, when immunization rates drop, outbreaks of vaccine-preventable diseases follow. In order and that is going to take more than a single month.
Identify patients who’ve missed vaccinations
Simply being open and ready to vaccinate is not enough. The Centers for Disease Control and Prevention urges providers to identify patients who have missed vaccines, and call them to schedule in-person visits. Proactively let parents know about strategies implemented in your office to ensure a safe environment.
Pediatricians are accustomed to an influx of patients in the summer, as parents make sure their children have all of the vaccines required for school attendance. As noted in a Washington Post article from Aug. 4, 2020, schools have traditionally served as a backstop for immunization rates. But as many school districts opt to take education online this fall, the implications for vaccine requirements are unclear. District of Columbia public schools continue to require immunization for virtual school attendance, but it is not clear how easily this can be enforced. To read about how other school districts have chosen to address – or not address – immunization requirements for school, visit the the Immunization Action Coalition’s Repository of Resources for Maintaining Immunization during the COVID-19 Pandemic. The repository links to international, national, and state-level policies and guidance and advocacy materials, including talking points, webinars, press releases, media articles from around the United States and social media posts, as well as telehealth resources.
Get some inspiration to talk about vaccination
Need a little inspiration for talking to parents about vaccines? Check out the CDC’s #HowIRecommend video series. These are short videos, most under a minute in length, that explain the importance of vaccination, how to effectively address questions from parents about vaccine safety, and how clinicians routinely recommend same day vaccination to their patients. These videos are part of the CDC’s National Immunization Awareness Month (NIAM) toolkit for communication with health care professionals. A companion toolkit for communicating with parents and patients contains sample social media messages with graphics, along with educational resources to share with parents.
The “Comprehensive Vaccine Education Program – From Training to Practice,” a free online program offered by the Pediatric Infectious Diseases Society, takes a deeper dive into strategies to combat vaccine misinformation and address vaccine hesitancy. Available modules cover vaccine fundamentals, vaccine safety, clinical manifestations of vaccine-preventable diseases, and communication skills that lead to more effective conversations with patients and parents. The curriculum also includes the newest edition of The Vaccine Handbook app, a comprehensive source of practical information for vaccine providers.
Educate young children about vaccines
Don’t leave young children out of the conversation. Vax-Force is a children’s book that explores how vaccination works inside the human body. Dr. Vaxson the pediatrician explains how trusted doctors and scientists made Vicky the Vaccine. Her mission is to tell Willy the White Blood Cell and his Antibuddies how to find and fight bad-guy germs like measles, tetanus, and polio. The book was written by Kelsey Rowe, MD, while she was a medical student at Saint Louis University School of Medicine. Dr. Rowe, now a pediatric resident, notes, “In a world where anti-vaccination rhetoric threatens the health of our global community, this book’s mission is to teach children and adults alike that getting vaccinations is a safe, effective, and even exciting thing to do.” The book is available for purchase at https://www.vax-force.com/, and a small part of every sale is donated to Unicef USA.
Consider vaccination advocacy in your communities
Vaccinate Your Family, a national, nonprofit organization dedicated to protecting people of all ages from vaccine-preventable diseases, suggests that health care providers need to take an active role in raising immunization rates, not just in their own practices, but in their communities. One way to do this is to submit an opinion piece or letter to the editor to a local newspaper describing why it’s important for parents to make sure their child’s immunizations are current. Those who have never written an opinion-editorial should look at the guidance developed by Voices for Vaccines.
How are we doing?
Early data suggest a rebound in immunization rates in May and June, but that is unlikely to close the gap created by disruptions in health care delivery earlier in the year. Collectively, we need to set ambitious goals. Are we just trying to reach prepandemic immunization levels? In Kentucky, where I practice, only 71% of kids aged 19-45 months had received all doses of seven routinely recommended vaccines (≥4 DTaP doses, ≥3 polio doses, ≥1 MMR dose, Hib full series, ≥3 HepB doses, ≥1 varicella dose, and ≥4 PCV doses) based on 2017 National Immunization Survey data. The Healthy People 2020 target goal is 80%. Only 55% of Kentucky girls aged 13-17 years received at least one dose of HPV vaccine, and rates in boys were even lower. Flu vaccine coverage in children 6 months to 17 years also was 55%. The status quo sets the bar too low. To see how your state is doing, check out the interactive map developed by the American Academy of Pediatrics.
Are we attempting to avoid disaster or can we seize the opportunity to protect more children than ever from vaccine-preventable diseases? The latter would really be something to celebrate.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
August was National Immunization Awareness Month. ... just in time to address the precipitous drop in immunization delivered during the early months of the pandemic.
In May, the Centers for Disease Control and Prevention reported substantial reductions in vaccine doses ordered through the Vaccines for Children program after the declaration of national emergency because of COVID-19 on March 13. Approximately 2.5 million fewer doses of routine, noninfluenza vaccines were administered between Jan. 6 and April 2020, compared with a similar period last year (MMWR Morb Mortal Wkly Rep. 2020 May 15;69[19]:591-3). Declines in immunization rates were echoed by states and municipalities across the United States. Last month, the health system in which I work reported 40,000 children behind on at least one vaccine.
We all know that, when immunization rates drop, outbreaks of vaccine-preventable diseases follow. In order and that is going to take more than a single month.
Identify patients who’ve missed vaccinations
Simply being open and ready to vaccinate is not enough. The Centers for Disease Control and Prevention urges providers to identify patients who have missed vaccines, and call them to schedule in-person visits. Proactively let parents know about strategies implemented in your office to ensure a safe environment.
Pediatricians are accustomed to an influx of patients in the summer, as parents make sure their children have all of the vaccines required for school attendance. As noted in a Washington Post article from Aug. 4, 2020, schools have traditionally served as a backstop for immunization rates. But as many school districts opt to take education online this fall, the implications for vaccine requirements are unclear. District of Columbia public schools continue to require immunization for virtual school attendance, but it is not clear how easily this can be enforced. To read about how other school districts have chosen to address – or not address – immunization requirements for school, visit the the Immunization Action Coalition’s Repository of Resources for Maintaining Immunization during the COVID-19 Pandemic. The repository links to international, national, and state-level policies and guidance and advocacy materials, including talking points, webinars, press releases, media articles from around the United States and social media posts, as well as telehealth resources.
Get some inspiration to talk about vaccination
Need a little inspiration for talking to parents about vaccines? Check out the CDC’s #HowIRecommend video series. These are short videos, most under a minute in length, that explain the importance of vaccination, how to effectively address questions from parents about vaccine safety, and how clinicians routinely recommend same day vaccination to their patients. These videos are part of the CDC’s National Immunization Awareness Month (NIAM) toolkit for communication with health care professionals. A companion toolkit for communicating with parents and patients contains sample social media messages with graphics, along with educational resources to share with parents.
The “Comprehensive Vaccine Education Program – From Training to Practice,” a free online program offered by the Pediatric Infectious Diseases Society, takes a deeper dive into strategies to combat vaccine misinformation and address vaccine hesitancy. Available modules cover vaccine fundamentals, vaccine safety, clinical manifestations of vaccine-preventable diseases, and communication skills that lead to more effective conversations with patients and parents. The curriculum also includes the newest edition of The Vaccine Handbook app, a comprehensive source of practical information for vaccine providers.
Educate young children about vaccines
Don’t leave young children out of the conversation. Vax-Force is a children’s book that explores how vaccination works inside the human body. Dr. Vaxson the pediatrician explains how trusted doctors and scientists made Vicky the Vaccine. Her mission is to tell Willy the White Blood Cell and his Antibuddies how to find and fight bad-guy germs like measles, tetanus, and polio. The book was written by Kelsey Rowe, MD, while she was a medical student at Saint Louis University School of Medicine. Dr. Rowe, now a pediatric resident, notes, “In a world where anti-vaccination rhetoric threatens the health of our global community, this book’s mission is to teach children and adults alike that getting vaccinations is a safe, effective, and even exciting thing to do.” The book is available for purchase at https://www.vax-force.com/, and a small part of every sale is donated to Unicef USA.
Consider vaccination advocacy in your communities
Vaccinate Your Family, a national, nonprofit organization dedicated to protecting people of all ages from vaccine-preventable diseases, suggests that health care providers need to take an active role in raising immunization rates, not just in their own practices, but in their communities. One way to do this is to submit an opinion piece or letter to the editor to a local newspaper describing why it’s important for parents to make sure their child’s immunizations are current. Those who have never written an opinion-editorial should look at the guidance developed by Voices for Vaccines.
How are we doing?
Early data suggest a rebound in immunization rates in May and June, but that is unlikely to close the gap created by disruptions in health care delivery earlier in the year. Collectively, we need to set ambitious goals. Are we just trying to reach prepandemic immunization levels? In Kentucky, where I practice, only 71% of kids aged 19-45 months had received all doses of seven routinely recommended vaccines (≥4 DTaP doses, ≥3 polio doses, ≥1 MMR dose, Hib full series, ≥3 HepB doses, ≥1 varicella dose, and ≥4 PCV doses) based on 2017 National Immunization Survey data. The Healthy People 2020 target goal is 80%. Only 55% of Kentucky girls aged 13-17 years received at least one dose of HPV vaccine, and rates in boys were even lower. Flu vaccine coverage in children 6 months to 17 years also was 55%. The status quo sets the bar too low. To see how your state is doing, check out the interactive map developed by the American Academy of Pediatrics.
Are we attempting to avoid disaster or can we seize the opportunity to protect more children than ever from vaccine-preventable diseases? The latter would really be something to celebrate.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
August was National Immunization Awareness Month. ... just in time to address the precipitous drop in immunization delivered during the early months of the pandemic.
In May, the Centers for Disease Control and Prevention reported substantial reductions in vaccine doses ordered through the Vaccines for Children program after the declaration of national emergency because of COVID-19 on March 13. Approximately 2.5 million fewer doses of routine, noninfluenza vaccines were administered between Jan. 6 and April 2020, compared with a similar period last year (MMWR Morb Mortal Wkly Rep. 2020 May 15;69[19]:591-3). Declines in immunization rates were echoed by states and municipalities across the United States. Last month, the health system in which I work reported 40,000 children behind on at least one vaccine.
We all know that, when immunization rates drop, outbreaks of vaccine-preventable diseases follow. In order and that is going to take more than a single month.
Identify patients who’ve missed vaccinations
Simply being open and ready to vaccinate is not enough. The Centers for Disease Control and Prevention urges providers to identify patients who have missed vaccines, and call them to schedule in-person visits. Proactively let parents know about strategies implemented in your office to ensure a safe environment.
Pediatricians are accustomed to an influx of patients in the summer, as parents make sure their children have all of the vaccines required for school attendance. As noted in a Washington Post article from Aug. 4, 2020, schools have traditionally served as a backstop for immunization rates. But as many school districts opt to take education online this fall, the implications for vaccine requirements are unclear. District of Columbia public schools continue to require immunization for virtual school attendance, but it is not clear how easily this can be enforced. To read about how other school districts have chosen to address – or not address – immunization requirements for school, visit the the Immunization Action Coalition’s Repository of Resources for Maintaining Immunization during the COVID-19 Pandemic. The repository links to international, national, and state-level policies and guidance and advocacy materials, including talking points, webinars, press releases, media articles from around the United States and social media posts, as well as telehealth resources.
Get some inspiration to talk about vaccination
Need a little inspiration for talking to parents about vaccines? Check out the CDC’s #HowIRecommend video series. These are short videos, most under a minute in length, that explain the importance of vaccination, how to effectively address questions from parents about vaccine safety, and how clinicians routinely recommend same day vaccination to their patients. These videos are part of the CDC’s National Immunization Awareness Month (NIAM) toolkit for communication with health care professionals. A companion toolkit for communicating with parents and patients contains sample social media messages with graphics, along with educational resources to share with parents.
The “Comprehensive Vaccine Education Program – From Training to Practice,” a free online program offered by the Pediatric Infectious Diseases Society, takes a deeper dive into strategies to combat vaccine misinformation and address vaccine hesitancy. Available modules cover vaccine fundamentals, vaccine safety, clinical manifestations of vaccine-preventable diseases, and communication skills that lead to more effective conversations with patients and parents. The curriculum also includes the newest edition of The Vaccine Handbook app, a comprehensive source of practical information for vaccine providers.
Educate young children about vaccines
Don’t leave young children out of the conversation. Vax-Force is a children’s book that explores how vaccination works inside the human body. Dr. Vaxson the pediatrician explains how trusted doctors and scientists made Vicky the Vaccine. Her mission is to tell Willy the White Blood Cell and his Antibuddies how to find and fight bad-guy germs like measles, tetanus, and polio. The book was written by Kelsey Rowe, MD, while she was a medical student at Saint Louis University School of Medicine. Dr. Rowe, now a pediatric resident, notes, “In a world where anti-vaccination rhetoric threatens the health of our global community, this book’s mission is to teach children and adults alike that getting vaccinations is a safe, effective, and even exciting thing to do.” The book is available for purchase at https://www.vax-force.com/, and a small part of every sale is donated to Unicef USA.
Consider vaccination advocacy in your communities
Vaccinate Your Family, a national, nonprofit organization dedicated to protecting people of all ages from vaccine-preventable diseases, suggests that health care providers need to take an active role in raising immunization rates, not just in their own practices, but in their communities. One way to do this is to submit an opinion piece or letter to the editor to a local newspaper describing why it’s important for parents to make sure their child’s immunizations are current. Those who have never written an opinion-editorial should look at the guidance developed by Voices for Vaccines.
How are we doing?
Early data suggest a rebound in immunization rates in May and June, but that is unlikely to close the gap created by disruptions in health care delivery earlier in the year. Collectively, we need to set ambitious goals. Are we just trying to reach prepandemic immunization levels? In Kentucky, where I practice, only 71% of kids aged 19-45 months had received all doses of seven routinely recommended vaccines (≥4 DTaP doses, ≥3 polio doses, ≥1 MMR dose, Hib full series, ≥3 HepB doses, ≥1 varicella dose, and ≥4 PCV doses) based on 2017 National Immunization Survey data. The Healthy People 2020 target goal is 80%. Only 55% of Kentucky girls aged 13-17 years received at least one dose of HPV vaccine, and rates in boys were even lower. Flu vaccine coverage in children 6 months to 17 years also was 55%. The status quo sets the bar too low. To see how your state is doing, check out the interactive map developed by the American Academy of Pediatrics.
Are we attempting to avoid disaster or can we seize the opportunity to protect more children than ever from vaccine-preventable diseases? The latter would really be something to celebrate.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
Back to school: How pediatricians can help LGBTQ youth
September every year means one thing to students across the country: Summer break is over, and it is time to go back to school. For LGBTQ youth, this can be both a blessing and a curse. Schools can be a refuge from being stuck at home with unsupportive family, but it also can mean returning to hallways full of harassment from other students and/or staff. Groups such as a gender-sexuality alliance (GSA) or a chapter of the Gay, Lesbian, and Straight Education Network (GLSEN) can provide a safe space for these students at school. Pediatricians can play an important role in ensuring that their patients know about access to these resources.
Gender-sexuality alliances, or gay-straight alliances as they have been more commonly known, have been around since the late 1980s. The first one was founded at Concord Academy in Massachusetts in 1988 by a straight student who was upset at how her gay classmates were being treated. Today’s GSAs continue this mission to create a welcoming environment for students of all gender identities and sexual orientations to gather, increase awareness on their campus of LGBTQ issues, and make the school environment safer for all students. According to the GSA network, there are over 4,000 active GSAs today in the United States located in 40 states.1
GLSEN was founded in 1990 initially as a network of gay and lesbian educators who wanted to create safer spaces in schools for LGBTQ students. Over the last 30 years, GLSEN continues to support this mission but has expanded into research and advocacy as well. There are currently 43 chapters of GLSEN in 30 states.2 GLSEN sponsors a number of national events throughout the year to raise awareness of LGBTQ issues in schools, including No Name Calling Week and the Day of Silence. Many chapters provide mentoring to local GSAs and volunteering as a mentor can be a great way for pediatricians to become involved in their local schools.
You may be asking yourself, why are GSAs important? According to GLSEN’s 2017 National School Climate Survey, nearly 35% of LGBTQ students missed at least 1 day of school in the previous month because of feeling unsafe, and nearly 57% of students reported hearing homophobic remarks from teachers and staff at their school.3 Around 10% of LGBTQ students reported being physically assaulted based on their sexual orientation and/or gender identity. Those LGBTQ students who experienced discrimination based on their sexual orientation and/or gender identity were more likely to have lower grade point averages and were more likely to be disciplined than those students who had not experienced discrimination.3 The cumulative effect of these negative experiences at school lead a sizable portion of affected students to drop out of school and possibly not pursue postsecondary education. This then leads to decreased job opportunities or career advancement, which could then lead to unemployment or low-wage jobs. Creating safe spaces for education to take place can have a lasting effect on the lives of LGBTQ students.
The 53% of students who reported having a GSA at their school in the National School Climate survey were less likely to report hearing negative comments about LGBTQ students, were less likely to miss school, experienced lower levels of victimization, and reported higher levels of supportive teachers and staff. All of these factors taken together ensure that LGBTQ students are more likely to complete their high school education. Russell B. Toomey, PhD, and colleagues were able to show that LGBTQ students with a perceived effective GSA were two times more likely than those without an effective GSA to attain a college education.4 Research also has shown that the presence of a GSA can have a beneficial impact on reducing bullying in general for all students, whether they identify as LGBTQ or not.5
What active steps can a pediatrician take to support their LGBTQ students? First, If the families run into trouble from the school, have your social workers help them connect with legal resources, as many court cases have established precedent that public schools cannot have a blanket ban on GSAs solely because they focus on LGBTQ issues. Second, if your patient has a GSA at their school and seems to be struggling with his/her sexual orientation and/or gender identity, encourage that student to consider attending their GSA so that they are able to spend time with other students like themselves. Third, as many schools will be starting virtually this year, you can provide your LGBTQ patients with a list of local online groups that students can participate in virtually if their school’s GSA is not meeting (see my LGBTQ Youth Consult column entitled, “Resources for LGBTQ youth during challenging times” at mdedge.com/pediatrics for a few ideas).* Lastly, be an active advocate in your own local school district for the inclusion of comprehensive nondiscrimination policies and the presence of GSAs for students. These small steps can go a long way to helping your LGBTQ patients thrive and succeed in school.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas. Dr. Cooper has no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. gsanetwork.org/mission-vision-history/.
2. www.glsen.org/find_chapter?field_chapter_state_target_id=All.
3. live-glsen-website.pantheonsite.io/sites/default/files/2019-10/GLSEN-2017-National-School-Climate-Survey-NSCS-Full-Report.pdf.
4. Appl Dev Sci. 2011 Nov 7;15(4):175-85.
5.www.usnews.com/news/articles/2016-08-04/gay-straight-alliances-in-schools-pay-off-for-all-students-study-finds.
*This article was updated 8/17/2020.
September every year means one thing to students across the country: Summer break is over, and it is time to go back to school. For LGBTQ youth, this can be both a blessing and a curse. Schools can be a refuge from being stuck at home with unsupportive family, but it also can mean returning to hallways full of harassment from other students and/or staff. Groups such as a gender-sexuality alliance (GSA) or a chapter of the Gay, Lesbian, and Straight Education Network (GLSEN) can provide a safe space for these students at school. Pediatricians can play an important role in ensuring that their patients know about access to these resources.
Gender-sexuality alliances, or gay-straight alliances as they have been more commonly known, have been around since the late 1980s. The first one was founded at Concord Academy in Massachusetts in 1988 by a straight student who was upset at how her gay classmates were being treated. Today’s GSAs continue this mission to create a welcoming environment for students of all gender identities and sexual orientations to gather, increase awareness on their campus of LGBTQ issues, and make the school environment safer for all students. According to the GSA network, there are over 4,000 active GSAs today in the United States located in 40 states.1
GLSEN was founded in 1990 initially as a network of gay and lesbian educators who wanted to create safer spaces in schools for LGBTQ students. Over the last 30 years, GLSEN continues to support this mission but has expanded into research and advocacy as well. There are currently 43 chapters of GLSEN in 30 states.2 GLSEN sponsors a number of national events throughout the year to raise awareness of LGBTQ issues in schools, including No Name Calling Week and the Day of Silence. Many chapters provide mentoring to local GSAs and volunteering as a mentor can be a great way for pediatricians to become involved in their local schools.
You may be asking yourself, why are GSAs important? According to GLSEN’s 2017 National School Climate Survey, nearly 35% of LGBTQ students missed at least 1 day of school in the previous month because of feeling unsafe, and nearly 57% of students reported hearing homophobic remarks from teachers and staff at their school.3 Around 10% of LGBTQ students reported being physically assaulted based on their sexual orientation and/or gender identity. Those LGBTQ students who experienced discrimination based on their sexual orientation and/or gender identity were more likely to have lower grade point averages and were more likely to be disciplined than those students who had not experienced discrimination.3 The cumulative effect of these negative experiences at school lead a sizable portion of affected students to drop out of school and possibly not pursue postsecondary education. This then leads to decreased job opportunities or career advancement, which could then lead to unemployment or low-wage jobs. Creating safe spaces for education to take place can have a lasting effect on the lives of LGBTQ students.
The 53% of students who reported having a GSA at their school in the National School Climate survey were less likely to report hearing negative comments about LGBTQ students, were less likely to miss school, experienced lower levels of victimization, and reported higher levels of supportive teachers and staff. All of these factors taken together ensure that LGBTQ students are more likely to complete their high school education. Russell B. Toomey, PhD, and colleagues were able to show that LGBTQ students with a perceived effective GSA were two times more likely than those without an effective GSA to attain a college education.4 Research also has shown that the presence of a GSA can have a beneficial impact on reducing bullying in general for all students, whether they identify as LGBTQ or not.5
What active steps can a pediatrician take to support their LGBTQ students? First, If the families run into trouble from the school, have your social workers help them connect with legal resources, as many court cases have established precedent that public schools cannot have a blanket ban on GSAs solely because they focus on LGBTQ issues. Second, if your patient has a GSA at their school and seems to be struggling with his/her sexual orientation and/or gender identity, encourage that student to consider attending their GSA so that they are able to spend time with other students like themselves. Third, as many schools will be starting virtually this year, you can provide your LGBTQ patients with a list of local online groups that students can participate in virtually if their school’s GSA is not meeting (see my LGBTQ Youth Consult column entitled, “Resources for LGBTQ youth during challenging times” at mdedge.com/pediatrics for a few ideas).* Lastly, be an active advocate in your own local school district for the inclusion of comprehensive nondiscrimination policies and the presence of GSAs for students. These small steps can go a long way to helping your LGBTQ patients thrive and succeed in school.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas. Dr. Cooper has no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. gsanetwork.org/mission-vision-history/.
2. www.glsen.org/find_chapter?field_chapter_state_target_id=All.
3. live-glsen-website.pantheonsite.io/sites/default/files/2019-10/GLSEN-2017-National-School-Climate-Survey-NSCS-Full-Report.pdf.
4. Appl Dev Sci. 2011 Nov 7;15(4):175-85.
5.www.usnews.com/news/articles/2016-08-04/gay-straight-alliances-in-schools-pay-off-for-all-students-study-finds.
*This article was updated 8/17/2020.
September every year means one thing to students across the country: Summer break is over, and it is time to go back to school. For LGBTQ youth, this can be both a blessing and a curse. Schools can be a refuge from being stuck at home with unsupportive family, but it also can mean returning to hallways full of harassment from other students and/or staff. Groups such as a gender-sexuality alliance (GSA) or a chapter of the Gay, Lesbian, and Straight Education Network (GLSEN) can provide a safe space for these students at school. Pediatricians can play an important role in ensuring that their patients know about access to these resources.
Gender-sexuality alliances, or gay-straight alliances as they have been more commonly known, have been around since the late 1980s. The first one was founded at Concord Academy in Massachusetts in 1988 by a straight student who was upset at how her gay classmates were being treated. Today’s GSAs continue this mission to create a welcoming environment for students of all gender identities and sexual orientations to gather, increase awareness on their campus of LGBTQ issues, and make the school environment safer for all students. According to the GSA network, there are over 4,000 active GSAs today in the United States located in 40 states.1
GLSEN was founded in 1990 initially as a network of gay and lesbian educators who wanted to create safer spaces in schools for LGBTQ students. Over the last 30 years, GLSEN continues to support this mission but has expanded into research and advocacy as well. There are currently 43 chapters of GLSEN in 30 states.2 GLSEN sponsors a number of national events throughout the year to raise awareness of LGBTQ issues in schools, including No Name Calling Week and the Day of Silence. Many chapters provide mentoring to local GSAs and volunteering as a mentor can be a great way for pediatricians to become involved in their local schools.
You may be asking yourself, why are GSAs important? According to GLSEN’s 2017 National School Climate Survey, nearly 35% of LGBTQ students missed at least 1 day of school in the previous month because of feeling unsafe, and nearly 57% of students reported hearing homophobic remarks from teachers and staff at their school.3 Around 10% of LGBTQ students reported being physically assaulted based on their sexual orientation and/or gender identity. Those LGBTQ students who experienced discrimination based on their sexual orientation and/or gender identity were more likely to have lower grade point averages and were more likely to be disciplined than those students who had not experienced discrimination.3 The cumulative effect of these negative experiences at school lead a sizable portion of affected students to drop out of school and possibly not pursue postsecondary education. This then leads to decreased job opportunities or career advancement, which could then lead to unemployment or low-wage jobs. Creating safe spaces for education to take place can have a lasting effect on the lives of LGBTQ students.
The 53% of students who reported having a GSA at their school in the National School Climate survey were less likely to report hearing negative comments about LGBTQ students, were less likely to miss school, experienced lower levels of victimization, and reported higher levels of supportive teachers and staff. All of these factors taken together ensure that LGBTQ students are more likely to complete their high school education. Russell B. Toomey, PhD, and colleagues were able to show that LGBTQ students with a perceived effective GSA were two times more likely than those without an effective GSA to attain a college education.4 Research also has shown that the presence of a GSA can have a beneficial impact on reducing bullying in general for all students, whether they identify as LGBTQ or not.5
What active steps can a pediatrician take to support their LGBTQ students? First, If the families run into trouble from the school, have your social workers help them connect with legal resources, as many court cases have established precedent that public schools cannot have a blanket ban on GSAs solely because they focus on LGBTQ issues. Second, if your patient has a GSA at their school and seems to be struggling with his/her sexual orientation and/or gender identity, encourage that student to consider attending their GSA so that they are able to spend time with other students like themselves. Third, as many schools will be starting virtually this year, you can provide your LGBTQ patients with a list of local online groups that students can participate in virtually if their school’s GSA is not meeting (see my LGBTQ Youth Consult column entitled, “Resources for LGBTQ youth during challenging times” at mdedge.com/pediatrics for a few ideas).* Lastly, be an active advocate in your own local school district for the inclusion of comprehensive nondiscrimination policies and the presence of GSAs for students. These small steps can go a long way to helping your LGBTQ patients thrive and succeed in school.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas. Dr. Cooper has no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. gsanetwork.org/mission-vision-history/.
2. www.glsen.org/find_chapter?field_chapter_state_target_id=All.
3. live-glsen-website.pantheonsite.io/sites/default/files/2019-10/GLSEN-2017-National-School-Climate-Survey-NSCS-Full-Report.pdf.
4. Appl Dev Sci. 2011 Nov 7;15(4):175-85.
5.www.usnews.com/news/articles/2016-08-04/gay-straight-alliances-in-schools-pay-off-for-all-students-study-finds.
*This article was updated 8/17/2020.
Long-lasting COVID-19 symptoms: Patients want answers
Q&A with Dr. Sachin Gupta
For some patients, a bout of COVID-19 may not be over after hospital discharge, acute symptoms subside, or a couple of tests for SARS-CoV-2 come back negative. Those who have reached these milestones of conquering the disease may find that their recovery journey has only begun. Debilitating symptoms such as fatigue, headache, and dyspnea may linger for weeks or longer. Patients with persistent symptoms, often referred to as “long haulers” in reference to the duration of their recovery, are looking for answers about their condition and when their COVID-19 illness will finally resolve.
Long-haul patients organize
What started as an accumulation of anecdotal evidence in social media, blogs, and the mainstream press about slow recovery and long-lasting symptoms of COVID-19 is now the focus of clinical trials in the population of recovering patients. Projects such as the COVID Symptom Study, initiated by the Massachusetts General Hospital, Boston; the Harvard School of Public Health, Boston; King’s College London; and Stanford (Calif.) University, are collecting data on symptoms from millions of patients and will eventually contribute to a better understanding of prolonged recovery.
Patients looking for answers have created groups on social media such as Facebook to exchange information about their experiences (e.g., Survivor Corps, COVID-19 Support Group, COVID-19 Recovered Survivors). Recovering patients have created patient-led research organizations (Body Politic COVID-19 Support Group) to explore persistent symptoms and begin to create data for research.
Some data on lingering symptoms
A small study of 143 previously hospitalized, recovering patients in Italy found that 87.4% of the cohort had at least one persistent symptom 2 months or longer after initial onset and at more than a month after discharge. In this sample, only 5% had been intubated. (JAMA 2020 Jul 9. doi: 10.1001/jama.2020.12603).
One study found that even patients who have had relatively mild symptoms and were not hospitalized can have persistent symptoms. The Centers for Disease Control and Prevention conducted a survey of adults who tested positive for the positive reverse transcription–polymerase chain reaction test for SARS-CoV-2 and found that, among the 292 respondents, 35% were still feeling the impact of the disease 2-3 weeks after testing. Fatigue (71%), cough (61%), and headache (61%) were the most commonly reported symptoms. The survey found that delayed recovery was evident in nearly a quarter of 18- to 34-year-olds and in a third of 35- to 49-year-olds who were not sick enough to require hospitalization (MMWR. 2020 Jul 24. doi: 10.15585/mmwr.mm6930e1).
Sachin Gupta, MD, FCCP, ATSF, a pulmonologist and member of the CHEST Physician editorial advisory board, has treated patients with COVID-19 and shared some of his thoughts on the problem of prolonged symptoms of COVID-19.
Q: Should clinicians expect to see COVID-19 patients who have symptoms persisting weeks after they are diagnosed?
Dr. Gupta: I think clinicians, especially in primary care, are already seeing many patients with lingering symptoms, both respiratory and nonrespiratory related, and debility. A few patients here in the San Francisco Bay Area that I have spoken with 4-6 weeks out from their acute illness have complained of persisting, though improving, fatigue and cough. Early studies are confirming this as a topical issue. There may be other long-lasting sequelae of COVID-19 beyond the common mild lingering symptoms. It will also be important to consider (and get more data on) to what degree asymptomatic patients develop some degree of mild inflammatory and subsequent fibrotic changes in organs like the lungs and heart
Q: How does the recovery phase of COVID-19 compare with recovery from severe influenza or ARDS?
Dr. Gupta: Most prior influenza and acute respiratory distress syndrome (ARDS) studies have provided initial follow-up at 3 months and beyond, so technically speaking, it is a little difficult to compare the symptomatology patterns in the JAMA study of 2 months on follow-up. Nevertheless, the key takeaway is that, even though few patients in the study had ARDS requiring intubation (severe disease), many patients with milder disease had significant lingering symptoms (55% with three or more symptoms) at 2 months.
This fits logically with the premise, which we have some limited data on with ARDS (N Engl J Med. 2003;348:683-93. doi: 10.1056/NEJMoa022450) and severe influenza infection survivors (Nature Sci Rep. 2017;7:17275. doi: 10.1038/s41598-017-17497-6) that varying degrees of the inflammation cascade triggered by certain viruses can lead to changes in important patient-reported outcomes, and objective measures such as pulmonary function over the long term.
Q: What can you do for patients with lingering symptoms of COVID-19 or what can you tell them about their symptoms?
Dr. Gupta: For many patients, there is fear, given the novel nature of the virus/pandemic, that their symptoms may persist long term. Acknowledgment of their symptoms is validating and important for us to recognize as we learn more about the virus. As we are finding, many patients are going online to find answers, after sometimes feeling rushed or dismissed initially in the clinical setting.
In my experience, the bar is fairly high for most patients to reach out to their physicians with complaints of lingering symptoms after acute infection. For the ones who do reach out, they tend to have either a greater constellation of symptoms or higher severity of one or two key symptoms. After assessing and, when appropriate, ruling out secondary infections or newly developed conditions, I shift toward symptom management. I encourage such patients to build up slowly. I suggest they work first on their activities of daily living (bathing, grooming), then their instrumental activities of daily living (cooking, cleaning, checking the mail), and then to engage, based on their tolerance of symptoms, to light purposeful exercise. There are many online resources for at-home exercise activities that I recommend to patients who are more debilitated; some larger centers are beginning to offer some forms of telepulmonary rehab.
Based on what we know about other causes of viral pneumonitis and ARDS, I ask such symptomatic patients to expect a slow, gradual, and in most cases a complete recovery, and depending on the individual case, I recommend pulmonary function tests and imaging that may be helpful to track that progress.
I remind myself, and patients, that our understanding may change as we learn more over time. Checking in at set intervals, even if not in person but through a phone call, can go a long way in a setting where we do not have a specific therapy, other than gradual exercise training, to help these patients recover faster. Reassurance and encouragement are vital for patients who are struggling with the lingering burden of disease and who may find it difficult to return to work or function as usual at home. The final point is to be mindful of our patient’s mental health and, where our reassurance is not enough, to consider appropriate mental health referrals.
Q: Can you handle this kind of problem with telemedicine or which patients with lingering symptoms need to come into the office – or failing that, the ED?
Dr. Gupta: Telemedicine in the outpatient setting provides a helpful tool to assess and manage patients, in my experience, with limited and straightforward complaints. Its scope is limited diagnostically (assessing symptoms and signs) as is its reach (ability to connect with elderly, disabled, or patients without/limited telemedicine access). In many instances, telemedicine limits our ability to connect with patients emotionally and build trust. Many patients who have gone through the acute illness that we see in pulmonary clinic on follow-up are older in age, and for many, video visits are not a practical solution. Telemedicine visits can sometimes present challenges for me as well in terms of thoroughly conveying lifestyle and symptom management strategies. Health literacy is typically easier to gauge and address in person.
For patients with any degree of enduring dyspnea, more so in the acute phase, I recommend home pulse oximetry for monitoring their oxygen saturation if it is financially and technically feasible for them to obtain one. Sending a patient to the ED is an option of last resort, but one that is necessary in some cases. I expect patients with lingering symptoms to tell me that symptoms may be persisting, hopefully gradually improving, and not getting worse. If post–COVID-19 symptoms such as fever, dyspnea, fatigue, or lightheadedness are new or worsening, particularly rapidly, the safest and best option I advise patients is to go to the ED for further assessment and testing. Postviral bacterial pneumonia is something we should consider, and there is some potential for aspergillosis as well.
Q: Do you have any concerns about patients with asthma, chronic obstructive pulmonary disease, or other pulmonary issues having lingering symptoms that may mask exacerbations or may cause exacerbation of their disease?
Dr. Gupta: So far, patients with chronic lung conditions do not appear to have not been disproportionately affected by the pandemic in terms of absolute numbers or percentage wise compared to the general public. I think that sheltering in place has been readily followed by many of these patients, and in addition, I assume better adherence to their maintenance therapies has likely helped. The very few cases of patients with underlying chronic obstructive pulmonary disease and interstitial lung disease that I have seen have fared very poorly when they were diagnosed with COVID-19 in the hospital. There are emerging data about short-term outcomes from severe COVID-19 infection in patients with interstitial lung disease in Europe (medRxiv. 2020 Jul 17. doi: 10.1101/2020.07.15.20152967), and from physicians treating pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension (Ann Am Thorac Soc. 2020 Jul 29. doi: 10.1513/AnnalsATS.202005-521OC). But so far, little has been published on the outcomes of mild disease in these patients with chronic lung disease.
Q: It’s still early days to know the significance of lingering symptoms. But at what point do you begin to consider the possibility of some kind of relapse? And what is your next move if the symptoms get worse?
Dr. Gupta: COVID-19 recurrence, whether because of reinfection or relapse, is a potential concern but not one that is very commonly seen so far in my purview. Generally, symptoms of post–COVID-19 infection that are lingering trend toward getting better, even if slowly. If post–COVID-19 infection symptoms are progressing (particularly if rapidly), that would be a strong indication to evaluate that patient in the ED (less likely in clinic), reswab them for SARS-CoV-2, and obtain further testing such as blood work and imaging. A significant challenge from a research perspective will be determining if coinfection with another virus is playing a role as we move closer to the fall season.
Q&A with Dr. Sachin Gupta
Q&A with Dr. Sachin Gupta
For some patients, a bout of COVID-19 may not be over after hospital discharge, acute symptoms subside, or a couple of tests for SARS-CoV-2 come back negative. Those who have reached these milestones of conquering the disease may find that their recovery journey has only begun. Debilitating symptoms such as fatigue, headache, and dyspnea may linger for weeks or longer. Patients with persistent symptoms, often referred to as “long haulers” in reference to the duration of their recovery, are looking for answers about their condition and when their COVID-19 illness will finally resolve.
Long-haul patients organize
What started as an accumulation of anecdotal evidence in social media, blogs, and the mainstream press about slow recovery and long-lasting symptoms of COVID-19 is now the focus of clinical trials in the population of recovering patients. Projects such as the COVID Symptom Study, initiated by the Massachusetts General Hospital, Boston; the Harvard School of Public Health, Boston; King’s College London; and Stanford (Calif.) University, are collecting data on symptoms from millions of patients and will eventually contribute to a better understanding of prolonged recovery.
Patients looking for answers have created groups on social media such as Facebook to exchange information about their experiences (e.g., Survivor Corps, COVID-19 Support Group, COVID-19 Recovered Survivors). Recovering patients have created patient-led research organizations (Body Politic COVID-19 Support Group) to explore persistent symptoms and begin to create data for research.
Some data on lingering symptoms
A small study of 143 previously hospitalized, recovering patients in Italy found that 87.4% of the cohort had at least one persistent symptom 2 months or longer after initial onset and at more than a month after discharge. In this sample, only 5% had been intubated. (JAMA 2020 Jul 9. doi: 10.1001/jama.2020.12603).
One study found that even patients who have had relatively mild symptoms and were not hospitalized can have persistent symptoms. The Centers for Disease Control and Prevention conducted a survey of adults who tested positive for the positive reverse transcription–polymerase chain reaction test for SARS-CoV-2 and found that, among the 292 respondents, 35% were still feeling the impact of the disease 2-3 weeks after testing. Fatigue (71%), cough (61%), and headache (61%) were the most commonly reported symptoms. The survey found that delayed recovery was evident in nearly a quarter of 18- to 34-year-olds and in a third of 35- to 49-year-olds who were not sick enough to require hospitalization (MMWR. 2020 Jul 24. doi: 10.15585/mmwr.mm6930e1).
Sachin Gupta, MD, FCCP, ATSF, a pulmonologist and member of the CHEST Physician editorial advisory board, has treated patients with COVID-19 and shared some of his thoughts on the problem of prolonged symptoms of COVID-19.
Q: Should clinicians expect to see COVID-19 patients who have symptoms persisting weeks after they are diagnosed?
Dr. Gupta: I think clinicians, especially in primary care, are already seeing many patients with lingering symptoms, both respiratory and nonrespiratory related, and debility. A few patients here in the San Francisco Bay Area that I have spoken with 4-6 weeks out from their acute illness have complained of persisting, though improving, fatigue and cough. Early studies are confirming this as a topical issue. There may be other long-lasting sequelae of COVID-19 beyond the common mild lingering symptoms. It will also be important to consider (and get more data on) to what degree asymptomatic patients develop some degree of mild inflammatory and subsequent fibrotic changes in organs like the lungs and heart
Q: How does the recovery phase of COVID-19 compare with recovery from severe influenza or ARDS?
Dr. Gupta: Most prior influenza and acute respiratory distress syndrome (ARDS) studies have provided initial follow-up at 3 months and beyond, so technically speaking, it is a little difficult to compare the symptomatology patterns in the JAMA study of 2 months on follow-up. Nevertheless, the key takeaway is that, even though few patients in the study had ARDS requiring intubation (severe disease), many patients with milder disease had significant lingering symptoms (55% with three or more symptoms) at 2 months.
This fits logically with the premise, which we have some limited data on with ARDS (N Engl J Med. 2003;348:683-93. doi: 10.1056/NEJMoa022450) and severe influenza infection survivors (Nature Sci Rep. 2017;7:17275. doi: 10.1038/s41598-017-17497-6) that varying degrees of the inflammation cascade triggered by certain viruses can lead to changes in important patient-reported outcomes, and objective measures such as pulmonary function over the long term.
Q: What can you do for patients with lingering symptoms of COVID-19 or what can you tell them about their symptoms?
Dr. Gupta: For many patients, there is fear, given the novel nature of the virus/pandemic, that their symptoms may persist long term. Acknowledgment of their symptoms is validating and important for us to recognize as we learn more about the virus. As we are finding, many patients are going online to find answers, after sometimes feeling rushed or dismissed initially in the clinical setting.
In my experience, the bar is fairly high for most patients to reach out to their physicians with complaints of lingering symptoms after acute infection. For the ones who do reach out, they tend to have either a greater constellation of symptoms or higher severity of one or two key symptoms. After assessing and, when appropriate, ruling out secondary infections or newly developed conditions, I shift toward symptom management. I encourage such patients to build up slowly. I suggest they work first on their activities of daily living (bathing, grooming), then their instrumental activities of daily living (cooking, cleaning, checking the mail), and then to engage, based on their tolerance of symptoms, to light purposeful exercise. There are many online resources for at-home exercise activities that I recommend to patients who are more debilitated; some larger centers are beginning to offer some forms of telepulmonary rehab.
Based on what we know about other causes of viral pneumonitis and ARDS, I ask such symptomatic patients to expect a slow, gradual, and in most cases a complete recovery, and depending on the individual case, I recommend pulmonary function tests and imaging that may be helpful to track that progress.
I remind myself, and patients, that our understanding may change as we learn more over time. Checking in at set intervals, even if not in person but through a phone call, can go a long way in a setting where we do not have a specific therapy, other than gradual exercise training, to help these patients recover faster. Reassurance and encouragement are vital for patients who are struggling with the lingering burden of disease and who may find it difficult to return to work or function as usual at home. The final point is to be mindful of our patient’s mental health and, where our reassurance is not enough, to consider appropriate mental health referrals.
Q: Can you handle this kind of problem with telemedicine or which patients with lingering symptoms need to come into the office – or failing that, the ED?
Dr. Gupta: Telemedicine in the outpatient setting provides a helpful tool to assess and manage patients, in my experience, with limited and straightforward complaints. Its scope is limited diagnostically (assessing symptoms and signs) as is its reach (ability to connect with elderly, disabled, or patients without/limited telemedicine access). In many instances, telemedicine limits our ability to connect with patients emotionally and build trust. Many patients who have gone through the acute illness that we see in pulmonary clinic on follow-up are older in age, and for many, video visits are not a practical solution. Telemedicine visits can sometimes present challenges for me as well in terms of thoroughly conveying lifestyle and symptom management strategies. Health literacy is typically easier to gauge and address in person.
For patients with any degree of enduring dyspnea, more so in the acute phase, I recommend home pulse oximetry for monitoring their oxygen saturation if it is financially and technically feasible for them to obtain one. Sending a patient to the ED is an option of last resort, but one that is necessary in some cases. I expect patients with lingering symptoms to tell me that symptoms may be persisting, hopefully gradually improving, and not getting worse. If post–COVID-19 symptoms such as fever, dyspnea, fatigue, or lightheadedness are new or worsening, particularly rapidly, the safest and best option I advise patients is to go to the ED for further assessment and testing. Postviral bacterial pneumonia is something we should consider, and there is some potential for aspergillosis as well.
Q: Do you have any concerns about patients with asthma, chronic obstructive pulmonary disease, or other pulmonary issues having lingering symptoms that may mask exacerbations or may cause exacerbation of their disease?
Dr. Gupta: So far, patients with chronic lung conditions do not appear to have not been disproportionately affected by the pandemic in terms of absolute numbers or percentage wise compared to the general public. I think that sheltering in place has been readily followed by many of these patients, and in addition, I assume better adherence to their maintenance therapies has likely helped. The very few cases of patients with underlying chronic obstructive pulmonary disease and interstitial lung disease that I have seen have fared very poorly when they were diagnosed with COVID-19 in the hospital. There are emerging data about short-term outcomes from severe COVID-19 infection in patients with interstitial lung disease in Europe (medRxiv. 2020 Jul 17. doi: 10.1101/2020.07.15.20152967), and from physicians treating pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension (Ann Am Thorac Soc. 2020 Jul 29. doi: 10.1513/AnnalsATS.202005-521OC). But so far, little has been published on the outcomes of mild disease in these patients with chronic lung disease.
Q: It’s still early days to know the significance of lingering symptoms. But at what point do you begin to consider the possibility of some kind of relapse? And what is your next move if the symptoms get worse?
Dr. Gupta: COVID-19 recurrence, whether because of reinfection or relapse, is a potential concern but not one that is very commonly seen so far in my purview. Generally, symptoms of post–COVID-19 infection that are lingering trend toward getting better, even if slowly. If post–COVID-19 infection symptoms are progressing (particularly if rapidly), that would be a strong indication to evaluate that patient in the ED (less likely in clinic), reswab them for SARS-CoV-2, and obtain further testing such as blood work and imaging. A significant challenge from a research perspective will be determining if coinfection with another virus is playing a role as we move closer to the fall season.
For some patients, a bout of COVID-19 may not be over after hospital discharge, acute symptoms subside, or a couple of tests for SARS-CoV-2 come back negative. Those who have reached these milestones of conquering the disease may find that their recovery journey has only begun. Debilitating symptoms such as fatigue, headache, and dyspnea may linger for weeks or longer. Patients with persistent symptoms, often referred to as “long haulers” in reference to the duration of their recovery, are looking for answers about their condition and when their COVID-19 illness will finally resolve.
Long-haul patients organize
What started as an accumulation of anecdotal evidence in social media, blogs, and the mainstream press about slow recovery and long-lasting symptoms of COVID-19 is now the focus of clinical trials in the population of recovering patients. Projects such as the COVID Symptom Study, initiated by the Massachusetts General Hospital, Boston; the Harvard School of Public Health, Boston; King’s College London; and Stanford (Calif.) University, are collecting data on symptoms from millions of patients and will eventually contribute to a better understanding of prolonged recovery.
Patients looking for answers have created groups on social media such as Facebook to exchange information about their experiences (e.g., Survivor Corps, COVID-19 Support Group, COVID-19 Recovered Survivors). Recovering patients have created patient-led research organizations (Body Politic COVID-19 Support Group) to explore persistent symptoms and begin to create data for research.
Some data on lingering symptoms
A small study of 143 previously hospitalized, recovering patients in Italy found that 87.4% of the cohort had at least one persistent symptom 2 months or longer after initial onset and at more than a month after discharge. In this sample, only 5% had been intubated. (JAMA 2020 Jul 9. doi: 10.1001/jama.2020.12603).
One study found that even patients who have had relatively mild symptoms and were not hospitalized can have persistent symptoms. The Centers for Disease Control and Prevention conducted a survey of adults who tested positive for the positive reverse transcription–polymerase chain reaction test for SARS-CoV-2 and found that, among the 292 respondents, 35% were still feeling the impact of the disease 2-3 weeks after testing. Fatigue (71%), cough (61%), and headache (61%) were the most commonly reported symptoms. The survey found that delayed recovery was evident in nearly a quarter of 18- to 34-year-olds and in a third of 35- to 49-year-olds who were not sick enough to require hospitalization (MMWR. 2020 Jul 24. doi: 10.15585/mmwr.mm6930e1).
Sachin Gupta, MD, FCCP, ATSF, a pulmonologist and member of the CHEST Physician editorial advisory board, has treated patients with COVID-19 and shared some of his thoughts on the problem of prolonged symptoms of COVID-19.
Q: Should clinicians expect to see COVID-19 patients who have symptoms persisting weeks after they are diagnosed?
Dr. Gupta: I think clinicians, especially in primary care, are already seeing many patients with lingering symptoms, both respiratory and nonrespiratory related, and debility. A few patients here in the San Francisco Bay Area that I have spoken with 4-6 weeks out from their acute illness have complained of persisting, though improving, fatigue and cough. Early studies are confirming this as a topical issue. There may be other long-lasting sequelae of COVID-19 beyond the common mild lingering symptoms. It will also be important to consider (and get more data on) to what degree asymptomatic patients develop some degree of mild inflammatory and subsequent fibrotic changes in organs like the lungs and heart
Q: How does the recovery phase of COVID-19 compare with recovery from severe influenza or ARDS?
Dr. Gupta: Most prior influenza and acute respiratory distress syndrome (ARDS) studies have provided initial follow-up at 3 months and beyond, so technically speaking, it is a little difficult to compare the symptomatology patterns in the JAMA study of 2 months on follow-up. Nevertheless, the key takeaway is that, even though few patients in the study had ARDS requiring intubation (severe disease), many patients with milder disease had significant lingering symptoms (55% with three or more symptoms) at 2 months.
This fits logically with the premise, which we have some limited data on with ARDS (N Engl J Med. 2003;348:683-93. doi: 10.1056/NEJMoa022450) and severe influenza infection survivors (Nature Sci Rep. 2017;7:17275. doi: 10.1038/s41598-017-17497-6) that varying degrees of the inflammation cascade triggered by certain viruses can lead to changes in important patient-reported outcomes, and objective measures such as pulmonary function over the long term.
Q: What can you do for patients with lingering symptoms of COVID-19 or what can you tell them about their symptoms?
Dr. Gupta: For many patients, there is fear, given the novel nature of the virus/pandemic, that their symptoms may persist long term. Acknowledgment of their symptoms is validating and important for us to recognize as we learn more about the virus. As we are finding, many patients are going online to find answers, after sometimes feeling rushed or dismissed initially in the clinical setting.
In my experience, the bar is fairly high for most patients to reach out to their physicians with complaints of lingering symptoms after acute infection. For the ones who do reach out, they tend to have either a greater constellation of symptoms or higher severity of one or two key symptoms. After assessing and, when appropriate, ruling out secondary infections or newly developed conditions, I shift toward symptom management. I encourage such patients to build up slowly. I suggest they work first on their activities of daily living (bathing, grooming), then their instrumental activities of daily living (cooking, cleaning, checking the mail), and then to engage, based on their tolerance of symptoms, to light purposeful exercise. There are many online resources for at-home exercise activities that I recommend to patients who are more debilitated; some larger centers are beginning to offer some forms of telepulmonary rehab.
Based on what we know about other causes of viral pneumonitis and ARDS, I ask such symptomatic patients to expect a slow, gradual, and in most cases a complete recovery, and depending on the individual case, I recommend pulmonary function tests and imaging that may be helpful to track that progress.
I remind myself, and patients, that our understanding may change as we learn more over time. Checking in at set intervals, even if not in person but through a phone call, can go a long way in a setting where we do not have a specific therapy, other than gradual exercise training, to help these patients recover faster. Reassurance and encouragement are vital for patients who are struggling with the lingering burden of disease and who may find it difficult to return to work or function as usual at home. The final point is to be mindful of our patient’s mental health and, where our reassurance is not enough, to consider appropriate mental health referrals.
Q: Can you handle this kind of problem with telemedicine or which patients with lingering symptoms need to come into the office – or failing that, the ED?
Dr. Gupta: Telemedicine in the outpatient setting provides a helpful tool to assess and manage patients, in my experience, with limited and straightforward complaints. Its scope is limited diagnostically (assessing symptoms and signs) as is its reach (ability to connect with elderly, disabled, or patients without/limited telemedicine access). In many instances, telemedicine limits our ability to connect with patients emotionally and build trust. Many patients who have gone through the acute illness that we see in pulmonary clinic on follow-up are older in age, and for many, video visits are not a practical solution. Telemedicine visits can sometimes present challenges for me as well in terms of thoroughly conveying lifestyle and symptom management strategies. Health literacy is typically easier to gauge and address in person.
For patients with any degree of enduring dyspnea, more so in the acute phase, I recommend home pulse oximetry for monitoring their oxygen saturation if it is financially and technically feasible for them to obtain one. Sending a patient to the ED is an option of last resort, but one that is necessary in some cases. I expect patients with lingering symptoms to tell me that symptoms may be persisting, hopefully gradually improving, and not getting worse. If post–COVID-19 symptoms such as fever, dyspnea, fatigue, or lightheadedness are new or worsening, particularly rapidly, the safest and best option I advise patients is to go to the ED for further assessment and testing. Postviral bacterial pneumonia is something we should consider, and there is some potential for aspergillosis as well.
Q: Do you have any concerns about patients with asthma, chronic obstructive pulmonary disease, or other pulmonary issues having lingering symptoms that may mask exacerbations or may cause exacerbation of their disease?
Dr. Gupta: So far, patients with chronic lung conditions do not appear to have not been disproportionately affected by the pandemic in terms of absolute numbers or percentage wise compared to the general public. I think that sheltering in place has been readily followed by many of these patients, and in addition, I assume better adherence to their maintenance therapies has likely helped. The very few cases of patients with underlying chronic obstructive pulmonary disease and interstitial lung disease that I have seen have fared very poorly when they were diagnosed with COVID-19 in the hospital. There are emerging data about short-term outcomes from severe COVID-19 infection in patients with interstitial lung disease in Europe (medRxiv. 2020 Jul 17. doi: 10.1101/2020.07.15.20152967), and from physicians treating pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension (Ann Am Thorac Soc. 2020 Jul 29. doi: 10.1513/AnnalsATS.202005-521OC). But so far, little has been published on the outcomes of mild disease in these patients with chronic lung disease.
Q: It’s still early days to know the significance of lingering symptoms. But at what point do you begin to consider the possibility of some kind of relapse? And what is your next move if the symptoms get worse?
Dr. Gupta: COVID-19 recurrence, whether because of reinfection or relapse, is a potential concern but not one that is very commonly seen so far in my purview. Generally, symptoms of post–COVID-19 infection that are lingering trend toward getting better, even if slowly. If post–COVID-19 infection symptoms are progressing (particularly if rapidly), that would be a strong indication to evaluate that patient in the ED (less likely in clinic), reswab them for SARS-CoV-2, and obtain further testing such as blood work and imaging. A significant challenge from a research perspective will be determining if coinfection with another virus is playing a role as we move closer to the fall season.
iResident: Virtual care on hospital medicine teaching services during a pandemic
At the start of each shift on his clinical service with rotating internal medicine residents, Benji Mathews, MD, SFHM, now adds a few components to his usual preparation. First, visiting the Minnesota Department of Health and various organizational websites to review the latest COVID-19 updates and guidelines. Next comes checking to see where he needs to pick up the surgical mask and eye protection that he will need to wear through the day. Last, he evaluates which of his patients are in telemedicine-equipped rooms; this last change has fast become a crucial part of working with his resident learners during a pandemic.
During the COVID-19 pandemic, residents and residency programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation (PUI). One increasingly available tool that can help protect trainees while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our internal medicine residents through the University of Minnesota Internal Medicine Residency program rotating at Regions Hospital in Saint Paul, Minn., we have used video visits to continue our mandate as both health care and education professionals.
Virtual care decision tree
Virtual care can mitigate exposure risk, minimize use of personal protective equipment (PPE), and improve communications with patients and their families. To guide our teaching teams on the optimal situations for telemedicine, we needed to select those patients who would be most appropriate for a virtual visit.
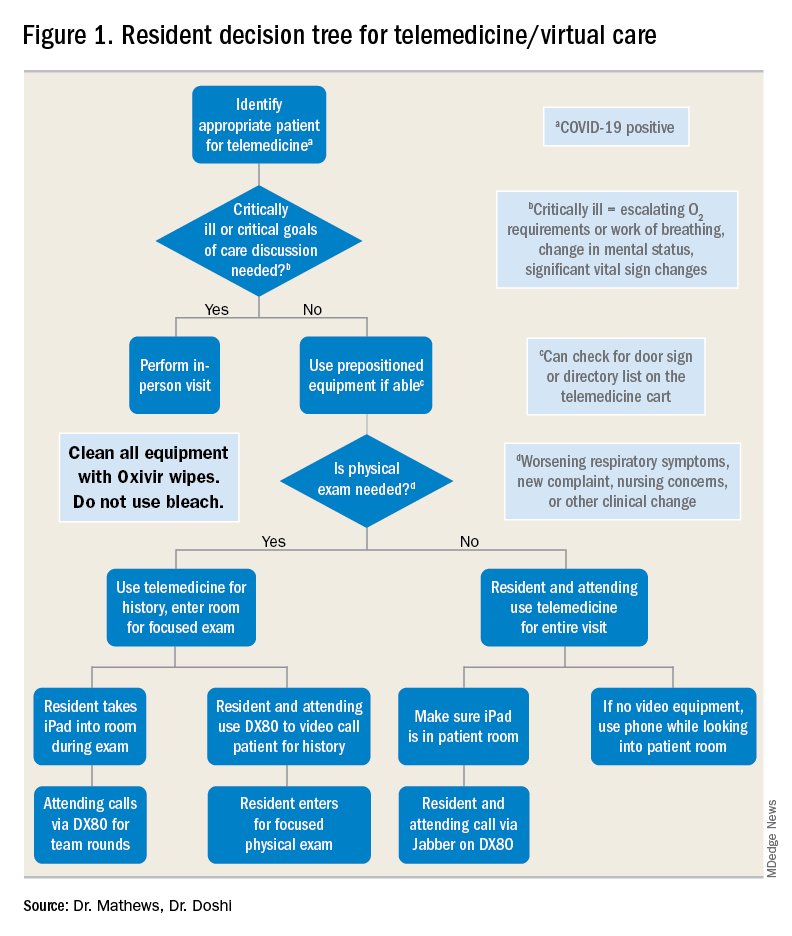
For example, patients with advanced dementia, or intubated in the intensive care unit, would have less utility from a real-time video encounter. Further, we implemented a simple decision tree (Figure 1). First, the team needs to decide whether the patient needs an immediate in-person assessment; for instance, for critically ill patients or those who need end-of-life care discussions, telemedicine would not be an appropriate modality. Next, the decision is made on whether a patient requires an in-person exam at that time. The idea of forgoing the in-person physical exam may run counterintuitive to the core training medical providers undergo, but in certain circumstances telemedicine can still provide the appropriate level of care a patient requires.
Virtual rounding with residents: Pros and cons
Through the course of this pandemic, there have many questions raised regarding how to handle inpatient teaching services: Should resident teams be assigned COVID-19 positives or PUIs? How do you optimize assessing and learning from patients’ conditions that require human touch? Should all members of the teaching team be donning PPE and entering the patient room?
Internal medicine residents in our hospital have been assigned COVID-19 positive and PUI patients. With proper PPE, and donning and doffing practices, residents may continue to learn from this important training opportunity while also optimizing care for patients supplemented by telemedicine. This pandemic has flattened the hierarchy; often residents are teaching their attendings much of the latest literature and best practices around COVID-19. Residents also benefit by joining the organization’s daily virtual interprofessional COVID-19 huddle where they partner with infectious disease, critical care, pharmacy, and other experts to collaborate in the care of these patients.
There have been counterarguments made for residents joining the front lines with COVID-19 patients. Some have conditions that limit them from seeing this subgroup of patients, such as their immune status or other issues. For these residents, we do not assign COVID-19–positive patients. However, they may continue to support in virtually updating COVID-19 patients and their families. A second argument has been the use of PPE. We have implemented telemedicine to limit the total number of exposures and have a protocol for the fewest number of providers possible to see any at-risk or confirmed COVID-19 patient. For example, a resident who sees a COVID-19 patient in person may also be simultaneously virtually supervised by the attending.
Webside manner
The physical exam is only one of several operational considerations when delivering virtual care, whether with a teaching or nonteaching service. One important aspect is the “webside manner” of the provider, the virtual analogue to bedside manner.
Inherent parts of in-person encounters, such as eye contact and allowing for patients to finish their sentences, have added nuances with virtual care. For instance, providers must adjust to looking into the web camera to make eye contact, even though the patient’s face may be on the screen below. Additionally, for patients who are hard of hearing or unfamiliar with video calling, providers must be cognizant of projecting well over an Internet connection and timing responses to avoid overlapping conversation.
Similarly, there are nuances to the virtual physical exam, some specific to care in the COVID-19 era. In our previous virtual care practice, a bedside facilitator assisted in using tools such a digital stethoscope. In contrast, our current practice aims to refine the observational skills of our learners in conjunction with chart review, vital signs, and actively incorporating the patient in the physical exam. This does not mean asking them to auscultate themselves, but is more toward allowing patients to participate in focused evaluations, such as assessing abdominal tenderness or working through range of motion. Remote guidance for virtual exams also extends itself to teaching teams; for example, in our practice, we have been able to conduct bedside ultrasound teaching with in-person team members and a virtual facilitator.
Maskless connections: ‘Face-to-face’ visits with patients
As many hospitalists have witnessed, COVID-19 is so isolating for patients and their families. Patients have limited visitors, and their care team members are aiming to minimize exposures. Those who are entering the rooms wear masks and face shields that limit connecting with patients in a truly “face-to-face” manner. Telemedicine provides a face-to-face encounter that arguably improves upon portions of the traditional in-person encounter during this pandemic, with providers wearing PPE. For medical learners, gaining the interpersonal skills essential for health care professionals has been skewed with pandemic-related limitations; telemedicine can provide a tool to adapt to this unique era and augment this important educational piece.
Limitations, equity, and technological considerations
Realistically, the virtual exam during COVID-19 does have its limitations. An important part of virtual care and teaching services is instilling the appropriate times for use of telemedicine. If a patient has a clinical change (such as increase in FiO2 requirements) or other clinical need, there should be no hesitation for learners to conduct in-person assessments with appropriate PPE.
Nonexam indications are just as important – for example, if a patient requires extensive goals of care counseling, we recommend this not be done virtually. Other indications may vary between organizations; in our practice, we suggest at least one in-person assessment on the initial and discharge hospital days. Regardless of the specific indications, a successful virtual inpatient teaching service must be predicated on outlining the appropriate uses of telemedicine.
In the United States, there are already health care disparities for people of color and non–English speakers. If there is not a careful consideration for these marginalized groups, their health disparities could be further exacerbated – not just around COVID-19, but also for other inpatient conditions where telemedicine is being used. Groups whose equity must be thoughtfully managed include those who do not speak English and those who do not have access to smartphones or the Internet. Our HealthPartners organization has implemented the integration of interpreters for virtual three-way connections with patients and their clinicians to help mitigate this for non–English speakers. Additionally, utilizing easy-to-use tablets and telemedicine-capable carts has helped patients overcome technology barriers.
Last, the members of the teaching team must know the essential technical aspects of the technology they are using. Robust information technology (IT) support is also needed, but no matter how simple the equipment may be, staff and trainees must know how to both operate it and handle basic troubleshooting (such as audio or video disconnections). This also dovetails with the important element of on-boarding other members of the care team. In our practice, nursing staff, chaplains, interpreters, and dietitians also use virtual care as part of their workflow. However, even if it is used only by the teaching team, orienting other care team members will limit technical problems such as equipment being turned off or moved out of position.
Prior to the COVID-19 pandemic, telemedicine adoption was limited because of lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. The COVID-19 pandemic has resulted in a remarkable increase in the provision of telemedicine services in the inpatient hospital medicine services. Importantly, it is, and should be, a developing part of the education and training for health care learners. This pandemic has underscored the need for providing telemedicine services that will likely long outlast this crisis, and to support our health care learners in being effective “iResidents” on our care teams.
Takeaways
- The future of graduate medical education involves virtual care.
The COVID-19 pandemic response has demonstrated that virtual care plays an instrumental part in patient care, and its effects will not dissipate when the pandemic is done. The curriculum for health care trainees should incorporate telemedicine competencies so that they may more effectively leverage this technology for improving care delivery.
- Selection of telemedicine patients must be stratified.
In order to obtain the highest utility for medical learners on telemedicine, there needs to be a clear decision process for which patients can be seen virtually. This involves both clinical criteria, such as avoiding virtual care for end-of-life discussions, and patient criteria, such as those who are hard of hearing.
- Virtual communication requires new communication skills.
Seeing patients via telemedicine mandates a different skill set than in-person communication. Learners must improve their “webside manner” in order to build the patient-provider relationship. Instilling these tools can pay dividends in settings where telemedicine has high yield, such as maskless communication during a pandemic.
- Health disparities could be further exacerbated by telemedicine and should not be overlooked.
Equity in access to health care applies to telemedicine as it does to many other elements. There are multiple groups that can suffer from disparities, such as patients who need interpreters, or those who have lower technological literacy and access to digital devices. Creating awareness of these pitfalls in virtual care can help medical learners recognize and support in creative solutions for these factors.
Dr. Mathews is chief, hospital medicine, at Regions Hospital, HealthPartners, St. Paul, Minn. Dr. Doshi is telemedicine director, hospital medicine, HealthPartners.
At the start of each shift on his clinical service with rotating internal medicine residents, Benji Mathews, MD, SFHM, now adds a few components to his usual preparation. First, visiting the Minnesota Department of Health and various organizational websites to review the latest COVID-19 updates and guidelines. Next comes checking to see where he needs to pick up the surgical mask and eye protection that he will need to wear through the day. Last, he evaluates which of his patients are in telemedicine-equipped rooms; this last change has fast become a crucial part of working with his resident learners during a pandemic.
During the COVID-19 pandemic, residents and residency programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation (PUI). One increasingly available tool that can help protect trainees while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our internal medicine residents through the University of Minnesota Internal Medicine Residency program rotating at Regions Hospital in Saint Paul, Minn., we have used video visits to continue our mandate as both health care and education professionals.
Virtual care decision tree
Virtual care can mitigate exposure risk, minimize use of personal protective equipment (PPE), and improve communications with patients and their families. To guide our teaching teams on the optimal situations for telemedicine, we needed to select those patients who would be most appropriate for a virtual visit.
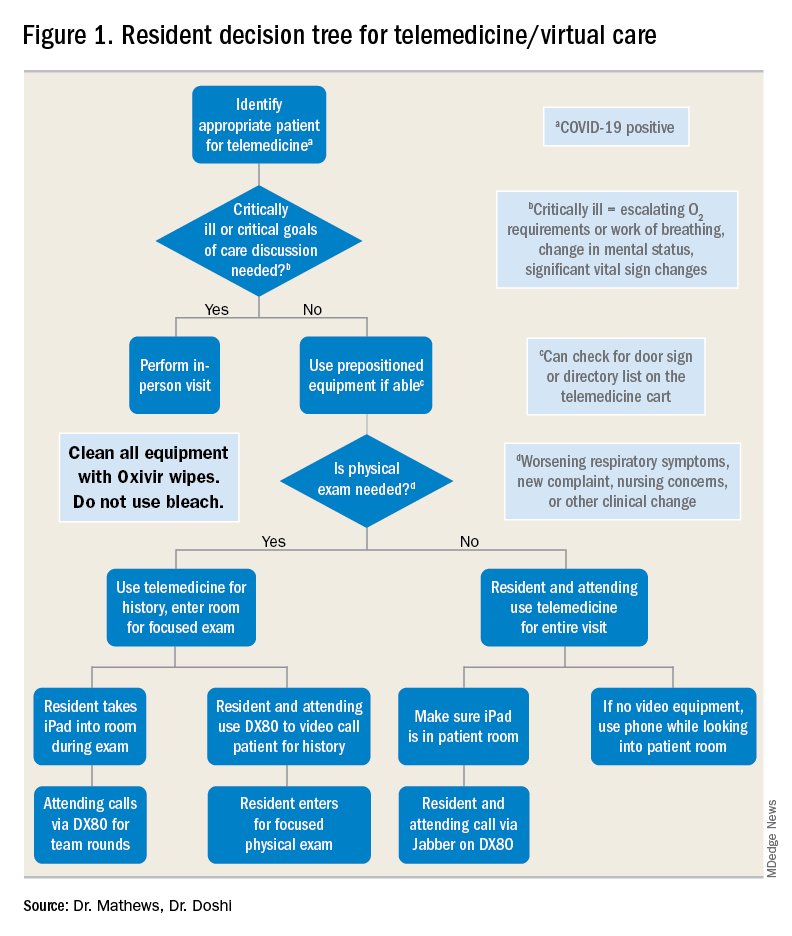
For example, patients with advanced dementia, or intubated in the intensive care unit, would have less utility from a real-time video encounter. Further, we implemented a simple decision tree (Figure 1). First, the team needs to decide whether the patient needs an immediate in-person assessment; for instance, for critically ill patients or those who need end-of-life care discussions, telemedicine would not be an appropriate modality. Next, the decision is made on whether a patient requires an in-person exam at that time. The idea of forgoing the in-person physical exam may run counterintuitive to the core training medical providers undergo, but in certain circumstances telemedicine can still provide the appropriate level of care a patient requires.
Virtual rounding with residents: Pros and cons
Through the course of this pandemic, there have many questions raised regarding how to handle inpatient teaching services: Should resident teams be assigned COVID-19 positives or PUIs? How do you optimize assessing and learning from patients’ conditions that require human touch? Should all members of the teaching team be donning PPE and entering the patient room?
Internal medicine residents in our hospital have been assigned COVID-19 positive and PUI patients. With proper PPE, and donning and doffing practices, residents may continue to learn from this important training opportunity while also optimizing care for patients supplemented by telemedicine. This pandemic has flattened the hierarchy; often residents are teaching their attendings much of the latest literature and best practices around COVID-19. Residents also benefit by joining the organization’s daily virtual interprofessional COVID-19 huddle where they partner with infectious disease, critical care, pharmacy, and other experts to collaborate in the care of these patients.
There have been counterarguments made for residents joining the front lines with COVID-19 patients. Some have conditions that limit them from seeing this subgroup of patients, such as their immune status or other issues. For these residents, we do not assign COVID-19–positive patients. However, they may continue to support in virtually updating COVID-19 patients and their families. A second argument has been the use of PPE. We have implemented telemedicine to limit the total number of exposures and have a protocol for the fewest number of providers possible to see any at-risk or confirmed COVID-19 patient. For example, a resident who sees a COVID-19 patient in person may also be simultaneously virtually supervised by the attending.
Webside manner
The physical exam is only one of several operational considerations when delivering virtual care, whether with a teaching or nonteaching service. One important aspect is the “webside manner” of the provider, the virtual analogue to bedside manner.
Inherent parts of in-person encounters, such as eye contact and allowing for patients to finish their sentences, have added nuances with virtual care. For instance, providers must adjust to looking into the web camera to make eye contact, even though the patient’s face may be on the screen below. Additionally, for patients who are hard of hearing or unfamiliar with video calling, providers must be cognizant of projecting well over an Internet connection and timing responses to avoid overlapping conversation.
Similarly, there are nuances to the virtual physical exam, some specific to care in the COVID-19 era. In our previous virtual care practice, a bedside facilitator assisted in using tools such a digital stethoscope. In contrast, our current practice aims to refine the observational skills of our learners in conjunction with chart review, vital signs, and actively incorporating the patient in the physical exam. This does not mean asking them to auscultate themselves, but is more toward allowing patients to participate in focused evaluations, such as assessing abdominal tenderness or working through range of motion. Remote guidance for virtual exams also extends itself to teaching teams; for example, in our practice, we have been able to conduct bedside ultrasound teaching with in-person team members and a virtual facilitator.
Maskless connections: ‘Face-to-face’ visits with patients
As many hospitalists have witnessed, COVID-19 is so isolating for patients and their families. Patients have limited visitors, and their care team members are aiming to minimize exposures. Those who are entering the rooms wear masks and face shields that limit connecting with patients in a truly “face-to-face” manner. Telemedicine provides a face-to-face encounter that arguably improves upon portions of the traditional in-person encounter during this pandemic, with providers wearing PPE. For medical learners, gaining the interpersonal skills essential for health care professionals has been skewed with pandemic-related limitations; telemedicine can provide a tool to adapt to this unique era and augment this important educational piece.
Limitations, equity, and technological considerations
Realistically, the virtual exam during COVID-19 does have its limitations. An important part of virtual care and teaching services is instilling the appropriate times for use of telemedicine. If a patient has a clinical change (such as increase in FiO2 requirements) or other clinical need, there should be no hesitation for learners to conduct in-person assessments with appropriate PPE.
Nonexam indications are just as important – for example, if a patient requires extensive goals of care counseling, we recommend this not be done virtually. Other indications may vary between organizations; in our practice, we suggest at least one in-person assessment on the initial and discharge hospital days. Regardless of the specific indications, a successful virtual inpatient teaching service must be predicated on outlining the appropriate uses of telemedicine.
In the United States, there are already health care disparities for people of color and non–English speakers. If there is not a careful consideration for these marginalized groups, their health disparities could be further exacerbated – not just around COVID-19, but also for other inpatient conditions where telemedicine is being used. Groups whose equity must be thoughtfully managed include those who do not speak English and those who do not have access to smartphones or the Internet. Our HealthPartners organization has implemented the integration of interpreters for virtual three-way connections with patients and their clinicians to help mitigate this for non–English speakers. Additionally, utilizing easy-to-use tablets and telemedicine-capable carts has helped patients overcome technology barriers.
Last, the members of the teaching team must know the essential technical aspects of the technology they are using. Robust information technology (IT) support is also needed, but no matter how simple the equipment may be, staff and trainees must know how to both operate it and handle basic troubleshooting (such as audio or video disconnections). This also dovetails with the important element of on-boarding other members of the care team. In our practice, nursing staff, chaplains, interpreters, and dietitians also use virtual care as part of their workflow. However, even if it is used only by the teaching team, orienting other care team members will limit technical problems such as equipment being turned off or moved out of position.
Prior to the COVID-19 pandemic, telemedicine adoption was limited because of lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. The COVID-19 pandemic has resulted in a remarkable increase in the provision of telemedicine services in the inpatient hospital medicine services. Importantly, it is, and should be, a developing part of the education and training for health care learners. This pandemic has underscored the need for providing telemedicine services that will likely long outlast this crisis, and to support our health care learners in being effective “iResidents” on our care teams.
Takeaways
- The future of graduate medical education involves virtual care.
The COVID-19 pandemic response has demonstrated that virtual care plays an instrumental part in patient care, and its effects will not dissipate when the pandemic is done. The curriculum for health care trainees should incorporate telemedicine competencies so that they may more effectively leverage this technology for improving care delivery.
- Selection of telemedicine patients must be stratified.
In order to obtain the highest utility for medical learners on telemedicine, there needs to be a clear decision process for which patients can be seen virtually. This involves both clinical criteria, such as avoiding virtual care for end-of-life discussions, and patient criteria, such as those who are hard of hearing.
- Virtual communication requires new communication skills.
Seeing patients via telemedicine mandates a different skill set than in-person communication. Learners must improve their “webside manner” in order to build the patient-provider relationship. Instilling these tools can pay dividends in settings where telemedicine has high yield, such as maskless communication during a pandemic.
- Health disparities could be further exacerbated by telemedicine and should not be overlooked.
Equity in access to health care applies to telemedicine as it does to many other elements. There are multiple groups that can suffer from disparities, such as patients who need interpreters, or those who have lower technological literacy and access to digital devices. Creating awareness of these pitfalls in virtual care can help medical learners recognize and support in creative solutions for these factors.
Dr. Mathews is chief, hospital medicine, at Regions Hospital, HealthPartners, St. Paul, Minn. Dr. Doshi is telemedicine director, hospital medicine, HealthPartners.
At the start of each shift on his clinical service with rotating internal medicine residents, Benji Mathews, MD, SFHM, now adds a few components to his usual preparation. First, visiting the Minnesota Department of Health and various organizational websites to review the latest COVID-19 updates and guidelines. Next comes checking to see where he needs to pick up the surgical mask and eye protection that he will need to wear through the day. Last, he evaluates which of his patients are in telemedicine-equipped rooms; this last change has fast become a crucial part of working with his resident learners during a pandemic.
During the COVID-19 pandemic, residents and residency programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation (PUI). One increasingly available tool that can help protect trainees while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our internal medicine residents through the University of Minnesota Internal Medicine Residency program rotating at Regions Hospital in Saint Paul, Minn., we have used video visits to continue our mandate as both health care and education professionals.
Virtual care decision tree
Virtual care can mitigate exposure risk, minimize use of personal protective equipment (PPE), and improve communications with patients and their families. To guide our teaching teams on the optimal situations for telemedicine, we needed to select those patients who would be most appropriate for a virtual visit.
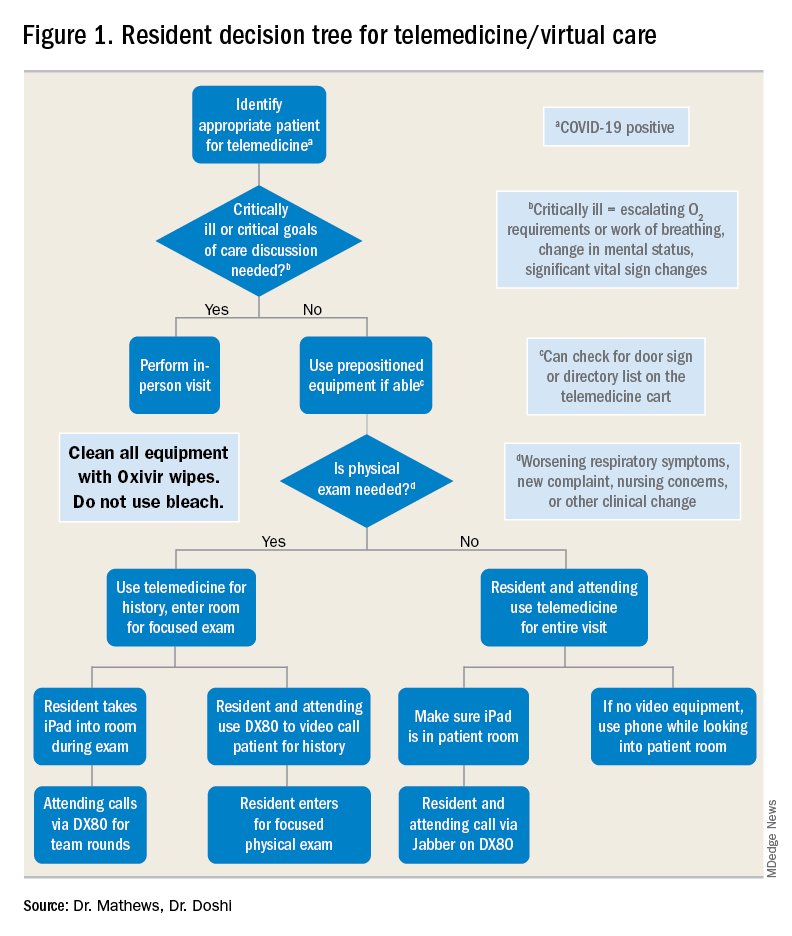
For example, patients with advanced dementia, or intubated in the intensive care unit, would have less utility from a real-time video encounter. Further, we implemented a simple decision tree (Figure 1). First, the team needs to decide whether the patient needs an immediate in-person assessment; for instance, for critically ill patients or those who need end-of-life care discussions, telemedicine would not be an appropriate modality. Next, the decision is made on whether a patient requires an in-person exam at that time. The idea of forgoing the in-person physical exam may run counterintuitive to the core training medical providers undergo, but in certain circumstances telemedicine can still provide the appropriate level of care a patient requires.
Virtual rounding with residents: Pros and cons
Through the course of this pandemic, there have many questions raised regarding how to handle inpatient teaching services: Should resident teams be assigned COVID-19 positives or PUIs? How do you optimize assessing and learning from patients’ conditions that require human touch? Should all members of the teaching team be donning PPE and entering the patient room?
Internal medicine residents in our hospital have been assigned COVID-19 positive and PUI patients. With proper PPE, and donning and doffing practices, residents may continue to learn from this important training opportunity while also optimizing care for patients supplemented by telemedicine. This pandemic has flattened the hierarchy; often residents are teaching their attendings much of the latest literature and best practices around COVID-19. Residents also benefit by joining the organization’s daily virtual interprofessional COVID-19 huddle where they partner with infectious disease, critical care, pharmacy, and other experts to collaborate in the care of these patients.
There have been counterarguments made for residents joining the front lines with COVID-19 patients. Some have conditions that limit them from seeing this subgroup of patients, such as their immune status or other issues. For these residents, we do not assign COVID-19–positive patients. However, they may continue to support in virtually updating COVID-19 patients and their families. A second argument has been the use of PPE. We have implemented telemedicine to limit the total number of exposures and have a protocol for the fewest number of providers possible to see any at-risk or confirmed COVID-19 patient. For example, a resident who sees a COVID-19 patient in person may also be simultaneously virtually supervised by the attending.
Webside manner
The physical exam is only one of several operational considerations when delivering virtual care, whether with a teaching or nonteaching service. One important aspect is the “webside manner” of the provider, the virtual analogue to bedside manner.
Inherent parts of in-person encounters, such as eye contact and allowing for patients to finish their sentences, have added nuances with virtual care. For instance, providers must adjust to looking into the web camera to make eye contact, even though the patient’s face may be on the screen below. Additionally, for patients who are hard of hearing or unfamiliar with video calling, providers must be cognizant of projecting well over an Internet connection and timing responses to avoid overlapping conversation.
Similarly, there are nuances to the virtual physical exam, some specific to care in the COVID-19 era. In our previous virtual care practice, a bedside facilitator assisted in using tools such a digital stethoscope. In contrast, our current practice aims to refine the observational skills of our learners in conjunction with chart review, vital signs, and actively incorporating the patient in the physical exam. This does not mean asking them to auscultate themselves, but is more toward allowing patients to participate in focused evaluations, such as assessing abdominal tenderness or working through range of motion. Remote guidance for virtual exams also extends itself to teaching teams; for example, in our practice, we have been able to conduct bedside ultrasound teaching with in-person team members and a virtual facilitator.
Maskless connections: ‘Face-to-face’ visits with patients
As many hospitalists have witnessed, COVID-19 is so isolating for patients and their families. Patients have limited visitors, and their care team members are aiming to minimize exposures. Those who are entering the rooms wear masks and face shields that limit connecting with patients in a truly “face-to-face” manner. Telemedicine provides a face-to-face encounter that arguably improves upon portions of the traditional in-person encounter during this pandemic, with providers wearing PPE. For medical learners, gaining the interpersonal skills essential for health care professionals has been skewed with pandemic-related limitations; telemedicine can provide a tool to adapt to this unique era and augment this important educational piece.
Limitations, equity, and technological considerations
Realistically, the virtual exam during COVID-19 does have its limitations. An important part of virtual care and teaching services is instilling the appropriate times for use of telemedicine. If a patient has a clinical change (such as increase in FiO2 requirements) or other clinical need, there should be no hesitation for learners to conduct in-person assessments with appropriate PPE.
Nonexam indications are just as important – for example, if a patient requires extensive goals of care counseling, we recommend this not be done virtually. Other indications may vary between organizations; in our practice, we suggest at least one in-person assessment on the initial and discharge hospital days. Regardless of the specific indications, a successful virtual inpatient teaching service must be predicated on outlining the appropriate uses of telemedicine.
In the United States, there are already health care disparities for people of color and non–English speakers. If there is not a careful consideration for these marginalized groups, their health disparities could be further exacerbated – not just around COVID-19, but also for other inpatient conditions where telemedicine is being used. Groups whose equity must be thoughtfully managed include those who do not speak English and those who do not have access to smartphones or the Internet. Our HealthPartners organization has implemented the integration of interpreters for virtual three-way connections with patients and their clinicians to help mitigate this for non–English speakers. Additionally, utilizing easy-to-use tablets and telemedicine-capable carts has helped patients overcome technology barriers.
Last, the members of the teaching team must know the essential technical aspects of the technology they are using. Robust information technology (IT) support is also needed, but no matter how simple the equipment may be, staff and trainees must know how to both operate it and handle basic troubleshooting (such as audio or video disconnections). This also dovetails with the important element of on-boarding other members of the care team. In our practice, nursing staff, chaplains, interpreters, and dietitians also use virtual care as part of their workflow. However, even if it is used only by the teaching team, orienting other care team members will limit technical problems such as equipment being turned off or moved out of position.
Prior to the COVID-19 pandemic, telemedicine adoption was limited because of lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. The COVID-19 pandemic has resulted in a remarkable increase in the provision of telemedicine services in the inpatient hospital medicine services. Importantly, it is, and should be, a developing part of the education and training for health care learners. This pandemic has underscored the need for providing telemedicine services that will likely long outlast this crisis, and to support our health care learners in being effective “iResidents” on our care teams.
Takeaways
- The future of graduate medical education involves virtual care.
The COVID-19 pandemic response has demonstrated that virtual care plays an instrumental part in patient care, and its effects will not dissipate when the pandemic is done. The curriculum for health care trainees should incorporate telemedicine competencies so that they may more effectively leverage this technology for improving care delivery.
- Selection of telemedicine patients must be stratified.
In order to obtain the highest utility for medical learners on telemedicine, there needs to be a clear decision process for which patients can be seen virtually. This involves both clinical criteria, such as avoiding virtual care for end-of-life discussions, and patient criteria, such as those who are hard of hearing.
- Virtual communication requires new communication skills.
Seeing patients via telemedicine mandates a different skill set than in-person communication. Learners must improve their “webside manner” in order to build the patient-provider relationship. Instilling these tools can pay dividends in settings where telemedicine has high yield, such as maskless communication during a pandemic.
- Health disparities could be further exacerbated by telemedicine and should not be overlooked.
Equity in access to health care applies to telemedicine as it does to many other elements. There are multiple groups that can suffer from disparities, such as patients who need interpreters, or those who have lower technological literacy and access to digital devices. Creating awareness of these pitfalls in virtual care can help medical learners recognize and support in creative solutions for these factors.
Dr. Mathews is chief, hospital medicine, at Regions Hospital, HealthPartners, St. Paul, Minn. Dr. Doshi is telemedicine director, hospital medicine, HealthPartners.
Taming a terrible illness
Darth Vader is, to me, one of the most intimidating villains in movie history. I was 11 when Star Wars came out. I even cleaned my room so my mother would take me to see it.
When Darth Vader first walked on screen, it was striking. A tall, imposing figure in black, with harsh mechanical respirations. There was no question of who the bad guy was. As the movie progressed his darkness became more frightening until, in the first lightsaber battle any of us had seen, he cut down the benevolent Obi-Wan Kenobi.
Last year my family went to Disneyland. While browsing the park’s stores we saw numerous Darth Vader items ... with him now available as a teddy bear, and on T-shirts riding carousels and the Dumbo ride.
From terrifying villain to cutesy toy in 43 years.* Quite the fall from glory.
Diseases are often (and hopefully) like that. Syphilis, once the most common, feared, and incurable neurologic disease is now, for most, just a nuisance. The butt of jokes and sexual innuendos, rendered harmless by Alexander Fleming’s discoveries.
Bit by bit we see other diseases tamed. Multiple sclerosis, though still serious, becomes better controlled every year as new agents come out. The cure for Parkinson’s disease remains elusive, but agents to control the symptoms and improve quality of life are available. Even HIV, the most feared disease of the 80s and 90s, has been beaten back from a terrible death sentence to one where patients lead normal lives with antiviral therapy.
Today we face a new enemy, the COVID-19 pandemic. So far we have no definite treatments, nor shortage of ideas. Many companies are racing to develop a vaccine, and will likely, at some point, find one, but what and when are still in the future. too.
Alzheimer’s disease, for all practical purposes, remains untreatable and rightfully feared. Perhaps the only ones more terrifying are those we’ve reduced to just three letters: ALS (amyotrophic lateral sclerosis) and GBM (glioblastoma multiforme). Both have terrible courses and, in spite of years of research, nothing even close to an effective treatment.
I hope that changes, and soon, for all those affected by these (and many other) terrible disorders.
Like the Darth Vader teddy bear, I’ll be happy to see them become shells of their former selves, with the dread they bring now reduced to the lesser trepidation seen when facing a serious, but treatable, illness.
*Correction, 8/11/20: An earlier version of this column misstated the number of years since Star Wars debuted.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Darth Vader is, to me, one of the most intimidating villains in movie history. I was 11 when Star Wars came out. I even cleaned my room so my mother would take me to see it.
When Darth Vader first walked on screen, it was striking. A tall, imposing figure in black, with harsh mechanical respirations. There was no question of who the bad guy was. As the movie progressed his darkness became more frightening until, in the first lightsaber battle any of us had seen, he cut down the benevolent Obi-Wan Kenobi.
Last year my family went to Disneyland. While browsing the park’s stores we saw numerous Darth Vader items ... with him now available as a teddy bear, and on T-shirts riding carousels and the Dumbo ride.
From terrifying villain to cutesy toy in 43 years.* Quite the fall from glory.
Diseases are often (and hopefully) like that. Syphilis, once the most common, feared, and incurable neurologic disease is now, for most, just a nuisance. The butt of jokes and sexual innuendos, rendered harmless by Alexander Fleming’s discoveries.
Bit by bit we see other diseases tamed. Multiple sclerosis, though still serious, becomes better controlled every year as new agents come out. The cure for Parkinson’s disease remains elusive, but agents to control the symptoms and improve quality of life are available. Even HIV, the most feared disease of the 80s and 90s, has been beaten back from a terrible death sentence to one where patients lead normal lives with antiviral therapy.
Today we face a new enemy, the COVID-19 pandemic. So far we have no definite treatments, nor shortage of ideas. Many companies are racing to develop a vaccine, and will likely, at some point, find one, but what and when are still in the future. too.
Alzheimer’s disease, for all practical purposes, remains untreatable and rightfully feared. Perhaps the only ones more terrifying are those we’ve reduced to just three letters: ALS (amyotrophic lateral sclerosis) and GBM (glioblastoma multiforme). Both have terrible courses and, in spite of years of research, nothing even close to an effective treatment.
I hope that changes, and soon, for all those affected by these (and many other) terrible disorders.
Like the Darth Vader teddy bear, I’ll be happy to see them become shells of their former selves, with the dread they bring now reduced to the lesser trepidation seen when facing a serious, but treatable, illness.
*Correction, 8/11/20: An earlier version of this column misstated the number of years since Star Wars debuted.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Darth Vader is, to me, one of the most intimidating villains in movie history. I was 11 when Star Wars came out. I even cleaned my room so my mother would take me to see it.
When Darth Vader first walked on screen, it was striking. A tall, imposing figure in black, with harsh mechanical respirations. There was no question of who the bad guy was. As the movie progressed his darkness became more frightening until, in the first lightsaber battle any of us had seen, he cut down the benevolent Obi-Wan Kenobi.
Last year my family went to Disneyland. While browsing the park’s stores we saw numerous Darth Vader items ... with him now available as a teddy bear, and on T-shirts riding carousels and the Dumbo ride.
From terrifying villain to cutesy toy in 43 years.* Quite the fall from glory.
Diseases are often (and hopefully) like that. Syphilis, once the most common, feared, and incurable neurologic disease is now, for most, just a nuisance. The butt of jokes and sexual innuendos, rendered harmless by Alexander Fleming’s discoveries.
Bit by bit we see other diseases tamed. Multiple sclerosis, though still serious, becomes better controlled every year as new agents come out. The cure for Parkinson’s disease remains elusive, but agents to control the symptoms and improve quality of life are available. Even HIV, the most feared disease of the 80s and 90s, has been beaten back from a terrible death sentence to one where patients lead normal lives with antiviral therapy.
Today we face a new enemy, the COVID-19 pandemic. So far we have no definite treatments, nor shortage of ideas. Many companies are racing to develop a vaccine, and will likely, at some point, find one, but what and when are still in the future. too.
Alzheimer’s disease, for all practical purposes, remains untreatable and rightfully feared. Perhaps the only ones more terrifying are those we’ve reduced to just three letters: ALS (amyotrophic lateral sclerosis) and GBM (glioblastoma multiforme). Both have terrible courses and, in spite of years of research, nothing even close to an effective treatment.
I hope that changes, and soon, for all those affected by these (and many other) terrible disorders.
Like the Darth Vader teddy bear, I’ll be happy to see them become shells of their former selves, with the dread they bring now reduced to the lesser trepidation seen when facing a serious, but treatable, illness.
*Correction, 8/11/20: An earlier version of this column misstated the number of years since Star Wars debuted.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Coming soon: The 2020 SoHM Report!
On behalf of SHM’s Practice Analysis Committee, I am excited to announce the scheduled September 2020 release of the 2020 State of Hospital Medicine Report (SoHM)!
For reasons all too familiar, this year’s SoHM survey process was unlike any in SHM’s history. We were still collecting survey responses from a few stragglers in early March when the entire world shut down almost overnight to flatten the curve of a deadly pandemic. Hospital medicine group (HMG) leaders were suddenly either up to their eyeballs trying to figure out how to safely care for huge influxes of COVID-19 patients that overwhelmed established systems of care or were trying to figure out how to staff in a low-volume environment with few COVID patients, a relative trickle of ED admissions, and virtually no surgical care. And everywhere, hospitals and their HMGs were quickly stressed in ways that would have been unimaginable just a couple of months earlier – financially, operationally, epidemiologically, and culturally.
SHM offices closed, with all staff working from home. And the talented people who would normally have been working diligently on the survey data were suddenly redirected to focus on COVID-related issues, including tracking government announcements that were changing daily and providing needed resources to SHM members. By the time they could raise their heads and begin thinking about survey data, we were months behind schedule.
I need to give a huge shout-out to our survey manager extraordinaire Josh Lapps, SHM’s Director of Policy and Practice Management, and his survey support team including Luke Heisinger and Kim Schonberger. Once they were able to turn their focus back to the SoHM, they worked like demons to catch up. And in addition to the work of preparing the SoHM for publication, they helped issue and analyze a follow-up survey to investigate how HMGs adjusted their staffing and operations in response to COVID! As I write this, we appear to be back on schedule for a September SoHM release date, with the COVID supplemental survey report to follow soon after. Thanks also to PAC committee members who, despite their own stresses, rose to the challenge of participating in calls and planning the supplemental survey.
Despite the pandemic, HMGs found survey participation valuable. When all was said and done, we had a respectable number of respondent groups: 502 this year vs. 569 in 2018. Although the number of respondent groups is down, the average group size has increased, so that an all-time high of 10,122 employed/contracted full-time equivalent (FTE) hospitalists (plus 484 locum tenens FTEs) are represented in the data set. The respondents continue to be very diverse, representing all practice models and every state – and even a couple of other countries. One notable change is a significant increase in pediatric HM group participation, thanks to a recruitment charge led by PAC member Sandra Gage, associate division chief of hospital medicine at Phoenix Children’s Hospital, and supported by the inclusion of several new pediatric HM-specific questions to better capture unique attributes of these hospital medicine practices.
We had more multisite respondents than ever, and the multisite respondents overwhelmingly used the new “retake” feature in the online version of the survey. I’m happy to report that we received consistent positive feedback about our new electronic survey platform, and thanks to its capabilities data analysis has been significantly automated, enhancing both efficiency and data reliability.
The survey content is more wide ranging than ever. In addition to the usual topics such as scope of services, staffing and scheduling, compensation models, evaluation and management code distribution, and HM group finances, the 2020 report will include the afore-referenced information about HM groups serving children, expanded information on nurse practitioner (NPs)/physician assistant (PA) roles, and data on diversity in HM physician leadership. The follow-up COVID survey will be published separately as a supplement, available only to purchasers of the SoHM report.
Multiple options for SoHM report purchase. All survey participants will receive access to the online version of the survey. Others may purchase the hard copy report, online access, or both. The report has a colorful, easy-to-read layout, and many of the tables have been streamlined to make them easier to read. I encourage you to sign up to preorder your copy of the SoHM Report today at www.hospitalmedicine.org/sohm; you’ll almost certainly discover a treasure trove of worthwhile information.
Use the report to assess how your practice compares to other practices, but always keep in mind that surveys don’t tell you what should be; they only tell you what currently is the case – or at least, what was during the survey period. New best practices not yet reflected in survey data are emerging all the time, and that is probably more true today in the new world affected by this pandemic than ever before. And while the ways others do things won’t always be right for your group’s unique situation and needs, it always helps to know how you compare with others. Whether you are partners or employees, you and your colleagues “own” the success of your hospital medicine practice and, armed with the best available data, are the best judges of what is right for you.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
On behalf of SHM’s Practice Analysis Committee, I am excited to announce the scheduled September 2020 release of the 2020 State of Hospital Medicine Report (SoHM)!
For reasons all too familiar, this year’s SoHM survey process was unlike any in SHM’s history. We were still collecting survey responses from a few stragglers in early March when the entire world shut down almost overnight to flatten the curve of a deadly pandemic. Hospital medicine group (HMG) leaders were suddenly either up to their eyeballs trying to figure out how to safely care for huge influxes of COVID-19 patients that overwhelmed established systems of care or were trying to figure out how to staff in a low-volume environment with few COVID patients, a relative trickle of ED admissions, and virtually no surgical care. And everywhere, hospitals and their HMGs were quickly stressed in ways that would have been unimaginable just a couple of months earlier – financially, operationally, epidemiologically, and culturally.
SHM offices closed, with all staff working from home. And the talented people who would normally have been working diligently on the survey data were suddenly redirected to focus on COVID-related issues, including tracking government announcements that were changing daily and providing needed resources to SHM members. By the time they could raise their heads and begin thinking about survey data, we were months behind schedule.
I need to give a huge shout-out to our survey manager extraordinaire Josh Lapps, SHM’s Director of Policy and Practice Management, and his survey support team including Luke Heisinger and Kim Schonberger. Once they were able to turn their focus back to the SoHM, they worked like demons to catch up. And in addition to the work of preparing the SoHM for publication, they helped issue and analyze a follow-up survey to investigate how HMGs adjusted their staffing and operations in response to COVID! As I write this, we appear to be back on schedule for a September SoHM release date, with the COVID supplemental survey report to follow soon after. Thanks also to PAC committee members who, despite their own stresses, rose to the challenge of participating in calls and planning the supplemental survey.
Despite the pandemic, HMGs found survey participation valuable. When all was said and done, we had a respectable number of respondent groups: 502 this year vs. 569 in 2018. Although the number of respondent groups is down, the average group size has increased, so that an all-time high of 10,122 employed/contracted full-time equivalent (FTE) hospitalists (plus 484 locum tenens FTEs) are represented in the data set. The respondents continue to be very diverse, representing all practice models and every state – and even a couple of other countries. One notable change is a significant increase in pediatric HM group participation, thanks to a recruitment charge led by PAC member Sandra Gage, associate division chief of hospital medicine at Phoenix Children’s Hospital, and supported by the inclusion of several new pediatric HM-specific questions to better capture unique attributes of these hospital medicine practices.
We had more multisite respondents than ever, and the multisite respondents overwhelmingly used the new “retake” feature in the online version of the survey. I’m happy to report that we received consistent positive feedback about our new electronic survey platform, and thanks to its capabilities data analysis has been significantly automated, enhancing both efficiency and data reliability.
The survey content is more wide ranging than ever. In addition to the usual topics such as scope of services, staffing and scheduling, compensation models, evaluation and management code distribution, and HM group finances, the 2020 report will include the afore-referenced information about HM groups serving children, expanded information on nurse practitioner (NPs)/physician assistant (PA) roles, and data on diversity in HM physician leadership. The follow-up COVID survey will be published separately as a supplement, available only to purchasers of the SoHM report.
Multiple options for SoHM report purchase. All survey participants will receive access to the online version of the survey. Others may purchase the hard copy report, online access, or both. The report has a colorful, easy-to-read layout, and many of the tables have been streamlined to make them easier to read. I encourage you to sign up to preorder your copy of the SoHM Report today at www.hospitalmedicine.org/sohm; you’ll almost certainly discover a treasure trove of worthwhile information.
Use the report to assess how your practice compares to other practices, but always keep in mind that surveys don’t tell you what should be; they only tell you what currently is the case – or at least, what was during the survey period. New best practices not yet reflected in survey data are emerging all the time, and that is probably more true today in the new world affected by this pandemic than ever before. And while the ways others do things won’t always be right for your group’s unique situation and needs, it always helps to know how you compare with others. Whether you are partners or employees, you and your colleagues “own” the success of your hospital medicine practice and, armed with the best available data, are the best judges of what is right for you.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
On behalf of SHM’s Practice Analysis Committee, I am excited to announce the scheduled September 2020 release of the 2020 State of Hospital Medicine Report (SoHM)!
For reasons all too familiar, this year’s SoHM survey process was unlike any in SHM’s history. We were still collecting survey responses from a few stragglers in early March when the entire world shut down almost overnight to flatten the curve of a deadly pandemic. Hospital medicine group (HMG) leaders were suddenly either up to their eyeballs trying to figure out how to safely care for huge influxes of COVID-19 patients that overwhelmed established systems of care or were trying to figure out how to staff in a low-volume environment with few COVID patients, a relative trickle of ED admissions, and virtually no surgical care. And everywhere, hospitals and their HMGs were quickly stressed in ways that would have been unimaginable just a couple of months earlier – financially, operationally, epidemiologically, and culturally.
SHM offices closed, with all staff working from home. And the talented people who would normally have been working diligently on the survey data were suddenly redirected to focus on COVID-related issues, including tracking government announcements that were changing daily and providing needed resources to SHM members. By the time they could raise their heads and begin thinking about survey data, we were months behind schedule.
I need to give a huge shout-out to our survey manager extraordinaire Josh Lapps, SHM’s Director of Policy and Practice Management, and his survey support team including Luke Heisinger and Kim Schonberger. Once they were able to turn their focus back to the SoHM, they worked like demons to catch up. And in addition to the work of preparing the SoHM for publication, they helped issue and analyze a follow-up survey to investigate how HMGs adjusted their staffing and operations in response to COVID! As I write this, we appear to be back on schedule for a September SoHM release date, with the COVID supplemental survey report to follow soon after. Thanks also to PAC committee members who, despite their own stresses, rose to the challenge of participating in calls and planning the supplemental survey.
Despite the pandemic, HMGs found survey participation valuable. When all was said and done, we had a respectable number of respondent groups: 502 this year vs. 569 in 2018. Although the number of respondent groups is down, the average group size has increased, so that an all-time high of 10,122 employed/contracted full-time equivalent (FTE) hospitalists (plus 484 locum tenens FTEs) are represented in the data set. The respondents continue to be very diverse, representing all practice models and every state – and even a couple of other countries. One notable change is a significant increase in pediatric HM group participation, thanks to a recruitment charge led by PAC member Sandra Gage, associate division chief of hospital medicine at Phoenix Children’s Hospital, and supported by the inclusion of several new pediatric HM-specific questions to better capture unique attributes of these hospital medicine practices.
We had more multisite respondents than ever, and the multisite respondents overwhelmingly used the new “retake” feature in the online version of the survey. I’m happy to report that we received consistent positive feedback about our new electronic survey platform, and thanks to its capabilities data analysis has been significantly automated, enhancing both efficiency and data reliability.
The survey content is more wide ranging than ever. In addition to the usual topics such as scope of services, staffing and scheduling, compensation models, evaluation and management code distribution, and HM group finances, the 2020 report will include the afore-referenced information about HM groups serving children, expanded information on nurse practitioner (NPs)/physician assistant (PA) roles, and data on diversity in HM physician leadership. The follow-up COVID survey will be published separately as a supplement, available only to purchasers of the SoHM report.
Multiple options for SoHM report purchase. All survey participants will receive access to the online version of the survey. Others may purchase the hard copy report, online access, or both. The report has a colorful, easy-to-read layout, and many of the tables have been streamlined to make them easier to read. I encourage you to sign up to preorder your copy of the SoHM Report today at www.hospitalmedicine.org/sohm; you’ll almost certainly discover a treasure trove of worthwhile information.
Use the report to assess how your practice compares to other practices, but always keep in mind that surveys don’t tell you what should be; they only tell you what currently is the case – or at least, what was during the survey period. New best practices not yet reflected in survey data are emerging all the time, and that is probably more true today in the new world affected by this pandemic than ever before. And while the ways others do things won’t always be right for your group’s unique situation and needs, it always helps to know how you compare with others. Whether you are partners or employees, you and your colleagues “own” the success of your hospital medicine practice and, armed with the best available data, are the best judges of what is right for you.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.