User login
A 51-year-old woman presented for a routine full body skin exam after vacationing in Hawaii.
Primary adrenal insufficiency (Addison’s disease) results from a dysfunction of the adrenal glands, which may be secondary to autoimmune diseases, genetic conditions, infections, and vasculopathies,or may be drug-induced (e.g. checkpoint inhibitors), among others . In contrast, secondary adrenal insufficiency results from pituitary dysfunction of low adrenocorticotropic hormone (ACTH). The most common cause of primary adrenal insufficiency in developed countries is autoimmune adrenalitis, which accounts for upwards of 90% of cases. Typically, 21-hydroxylase autoantibodies are identified and account for destruction of the adrenal cortex through cell-mediated and humoral immune responses.
Palmar creases, subungual surfaces, sites of trauma, and joint spaces (including the knees, spine, elbows, and shoulders) are commonly affected. Hair depletes in the pubic area and axillary vaults. Nevi may also appear darker. In patients with autoimmune adrenalitis, vitiligo may be seen secondary to autoimmune destruction of melanocytes.
Diagnosis may be difficult in the early stages, but historical findings of fatigue and clinical findings of hyperpigmentation in classic areas may prompt appropriate lab screening workup. It is essential to determine whether adrenal insufficiency is primary or secondary. Evaluation of decreased cortisol production, determination of whether production is ACTH-dependent or -independent, and evaluation for the underlying causes of adrenal dysfunction are important. Lab screening includes morning serum cortisol, morning ACTH (cosyntropin) stimulation test, fasting CBC with differential, and CMP to evaluate for normocytic normochromic anemia, hyponatremia, hyperkalemia, hypoglycemia, plasma renin/aldosterone ratio, and 21-hydroxylase autoantibodies.
Management strategies of primary adrenal insufficiency require corticosteroid supplementation and multidisciplinary collaboration with endocrinology. If untreated, primary adrenal insufficiency can be fatal. Adrenal crisis is a critical condition following a precipitating event, such as GI infection, fever, acute stress, and/or untreated adrenal or pituitary disorders. Clinical findings include acute shock with hypotension, nausea, vomiting, abdominal pain, back or leg pain, and a change in mental status. In this scenario, increasing the dose of corticosteroid supplementation is essential for reducing mortality.
Upon examining this patient’s new skin findings of hyperpigmentation and discussing her fatigue, primary adrenal insufficiency was suspected. With further prompting, the patient reported an ICU hospitalization several months prior because of sepsis originating from a peritonsillar abscess. With these clinical and historical findings, preliminary workup was conducted by dermatology, which included morning cortisol level, ACTH, CBC with differential, CMP, plasma renin-aldosterone ratio, and 21-hydroxylase autoantibodies. Work up demonstrated a low morning cortisol level of 1.3 mcg/dL, an elevated ACTH of 2,739 pg/mL, and positive 21-hydroxylase autoantibodies. The patient was urgently referred to endocrinology and started on oral hydrocortisone. Her fatigue immediately improved, and at 1-year follow-up with dermatology, her mucocutaneous hyperpigmentation had subsided dramatically.
Dermatologists can play a major role in the early diagnosis of primary adrenal insufficiency, which is essential for reducing patient morbidity and mortality. Skin findings on full body skin exams can clue in dermatologists for ordering preliminary workup to expedite care for these patients.
The case and photos were submitted by Dr. Akhiyat, Scripps Clinic Medical Group, La Jolla, California. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
J Am Acad Dermatol. 2014 May;70(5):Supplement 1AB118. doi: 10.1016/j.jaad.2014.01.491.
Michels A, Michels N. Am Fam Physician. 2014 Apr 1;89(7):563-568.
Kauzman A et al. J Can Dent Assoc. 2004 Nov;70(10):682-683.
Primary adrenal insufficiency (Addison’s disease) results from a dysfunction of the adrenal glands, which may be secondary to autoimmune diseases, genetic conditions, infections, and vasculopathies,or may be drug-induced (e.g. checkpoint inhibitors), among others . In contrast, secondary adrenal insufficiency results from pituitary dysfunction of low adrenocorticotropic hormone (ACTH). The most common cause of primary adrenal insufficiency in developed countries is autoimmune adrenalitis, which accounts for upwards of 90% of cases. Typically, 21-hydroxylase autoantibodies are identified and account for destruction of the adrenal cortex through cell-mediated and humoral immune responses.
Palmar creases, subungual surfaces, sites of trauma, and joint spaces (including the knees, spine, elbows, and shoulders) are commonly affected. Hair depletes in the pubic area and axillary vaults. Nevi may also appear darker. In patients with autoimmune adrenalitis, vitiligo may be seen secondary to autoimmune destruction of melanocytes.
Diagnosis may be difficult in the early stages, but historical findings of fatigue and clinical findings of hyperpigmentation in classic areas may prompt appropriate lab screening workup. It is essential to determine whether adrenal insufficiency is primary or secondary. Evaluation of decreased cortisol production, determination of whether production is ACTH-dependent or -independent, and evaluation for the underlying causes of adrenal dysfunction are important. Lab screening includes morning serum cortisol, morning ACTH (cosyntropin) stimulation test, fasting CBC with differential, and CMP to evaluate for normocytic normochromic anemia, hyponatremia, hyperkalemia, hypoglycemia, plasma renin/aldosterone ratio, and 21-hydroxylase autoantibodies.
Management strategies of primary adrenal insufficiency require corticosteroid supplementation and multidisciplinary collaboration with endocrinology. If untreated, primary adrenal insufficiency can be fatal. Adrenal crisis is a critical condition following a precipitating event, such as GI infection, fever, acute stress, and/or untreated adrenal or pituitary disorders. Clinical findings include acute shock with hypotension, nausea, vomiting, abdominal pain, back or leg pain, and a change in mental status. In this scenario, increasing the dose of corticosteroid supplementation is essential for reducing mortality.
Upon examining this patient’s new skin findings of hyperpigmentation and discussing her fatigue, primary adrenal insufficiency was suspected. With further prompting, the patient reported an ICU hospitalization several months prior because of sepsis originating from a peritonsillar abscess. With these clinical and historical findings, preliminary workup was conducted by dermatology, which included morning cortisol level, ACTH, CBC with differential, CMP, plasma renin-aldosterone ratio, and 21-hydroxylase autoantibodies. Work up demonstrated a low morning cortisol level of 1.3 mcg/dL, an elevated ACTH of 2,739 pg/mL, and positive 21-hydroxylase autoantibodies. The patient was urgently referred to endocrinology and started on oral hydrocortisone. Her fatigue immediately improved, and at 1-year follow-up with dermatology, her mucocutaneous hyperpigmentation had subsided dramatically.
Dermatologists can play a major role in the early diagnosis of primary adrenal insufficiency, which is essential for reducing patient morbidity and mortality. Skin findings on full body skin exams can clue in dermatologists for ordering preliminary workup to expedite care for these patients.
The case and photos were submitted by Dr. Akhiyat, Scripps Clinic Medical Group, La Jolla, California. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
J Am Acad Dermatol. 2014 May;70(5):Supplement 1AB118. doi: 10.1016/j.jaad.2014.01.491.
Michels A, Michels N. Am Fam Physician. 2014 Apr 1;89(7):563-568.
Kauzman A et al. J Can Dent Assoc. 2004 Nov;70(10):682-683.
Primary adrenal insufficiency (Addison’s disease) results from a dysfunction of the adrenal glands, which may be secondary to autoimmune diseases, genetic conditions, infections, and vasculopathies,or may be drug-induced (e.g. checkpoint inhibitors), among others . In contrast, secondary adrenal insufficiency results from pituitary dysfunction of low adrenocorticotropic hormone (ACTH). The most common cause of primary adrenal insufficiency in developed countries is autoimmune adrenalitis, which accounts for upwards of 90% of cases. Typically, 21-hydroxylase autoantibodies are identified and account for destruction of the adrenal cortex through cell-mediated and humoral immune responses.
Palmar creases, subungual surfaces, sites of trauma, and joint spaces (including the knees, spine, elbows, and shoulders) are commonly affected. Hair depletes in the pubic area and axillary vaults. Nevi may also appear darker. In patients with autoimmune adrenalitis, vitiligo may be seen secondary to autoimmune destruction of melanocytes.
Diagnosis may be difficult in the early stages, but historical findings of fatigue and clinical findings of hyperpigmentation in classic areas may prompt appropriate lab screening workup. It is essential to determine whether adrenal insufficiency is primary or secondary. Evaluation of decreased cortisol production, determination of whether production is ACTH-dependent or -independent, and evaluation for the underlying causes of adrenal dysfunction are important. Lab screening includes morning serum cortisol, morning ACTH (cosyntropin) stimulation test, fasting CBC with differential, and CMP to evaluate for normocytic normochromic anemia, hyponatremia, hyperkalemia, hypoglycemia, plasma renin/aldosterone ratio, and 21-hydroxylase autoantibodies.
Management strategies of primary adrenal insufficiency require corticosteroid supplementation and multidisciplinary collaboration with endocrinology. If untreated, primary adrenal insufficiency can be fatal. Adrenal crisis is a critical condition following a precipitating event, such as GI infection, fever, acute stress, and/or untreated adrenal or pituitary disorders. Clinical findings include acute shock with hypotension, nausea, vomiting, abdominal pain, back or leg pain, and a change in mental status. In this scenario, increasing the dose of corticosteroid supplementation is essential for reducing mortality.
Upon examining this patient’s new skin findings of hyperpigmentation and discussing her fatigue, primary adrenal insufficiency was suspected. With further prompting, the patient reported an ICU hospitalization several months prior because of sepsis originating from a peritonsillar abscess. With these clinical and historical findings, preliminary workup was conducted by dermatology, which included morning cortisol level, ACTH, CBC with differential, CMP, plasma renin-aldosterone ratio, and 21-hydroxylase autoantibodies. Work up demonstrated a low morning cortisol level of 1.3 mcg/dL, an elevated ACTH of 2,739 pg/mL, and positive 21-hydroxylase autoantibodies. The patient was urgently referred to endocrinology and started on oral hydrocortisone. Her fatigue immediately improved, and at 1-year follow-up with dermatology, her mucocutaneous hyperpigmentation had subsided dramatically.
Dermatologists can play a major role in the early diagnosis of primary adrenal insufficiency, which is essential for reducing patient morbidity and mortality. Skin findings on full body skin exams can clue in dermatologists for ordering preliminary workup to expedite care for these patients.
The case and photos were submitted by Dr. Akhiyat, Scripps Clinic Medical Group, La Jolla, California. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
J Am Acad Dermatol. 2014 May;70(5):Supplement 1AB118. doi: 10.1016/j.jaad.2014.01.491.
Michels A, Michels N. Am Fam Physician. 2014 Apr 1;89(7):563-568.
Kauzman A et al. J Can Dent Assoc. 2004 Nov;70(10):682-683.
How Old Are You? Stand on One Leg and I’ll Tell You
This transcript has been edited for clarity.
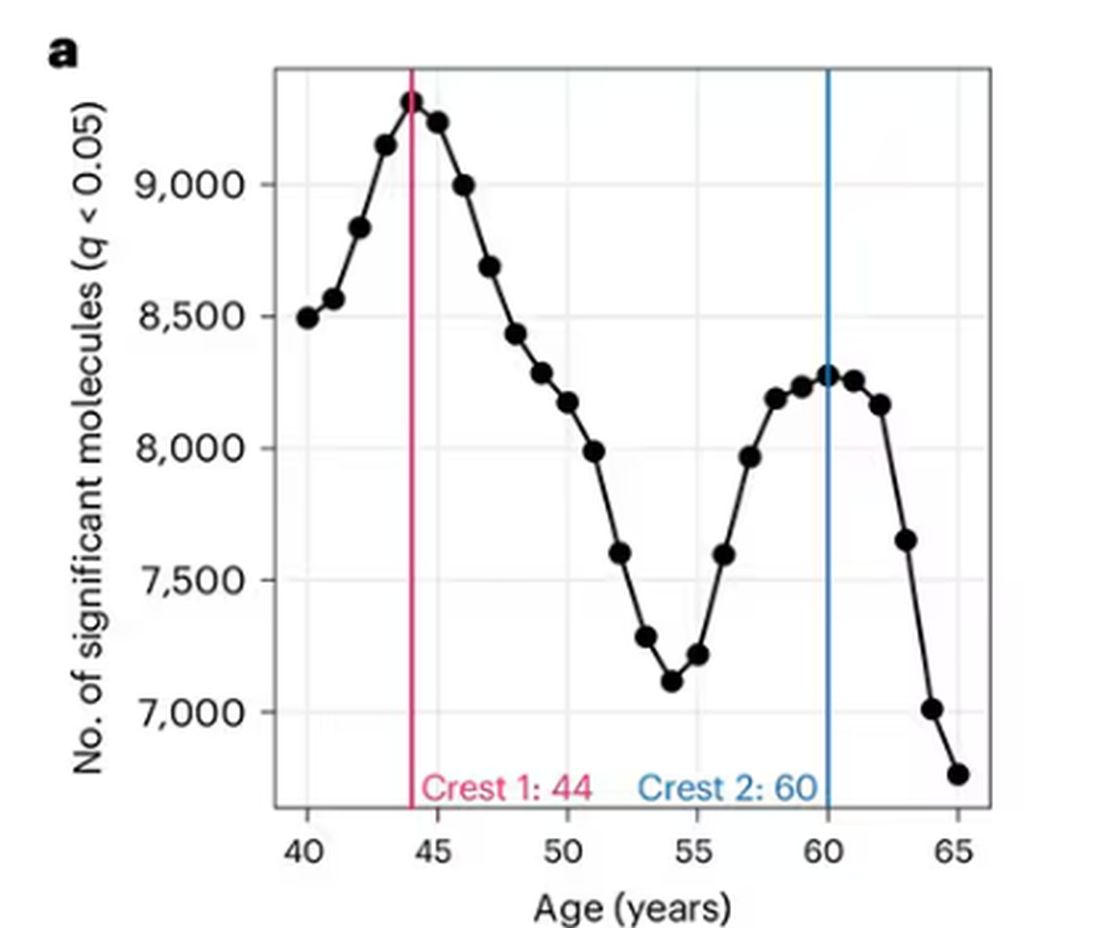
So I was lying in bed the other night, trying to read my phone, and started complaining to my wife about how my vision keeps getting worse, and then how stiff I feel when I wake up in the morning, and how a recent injury is taking too long to heal, and she said, “Well, yeah. You’re 44. That’s when things start to head downhill.”
And I was like, “Forty-four? That seems very specific. I thought 50 was what people complain about.” And she said, “No, it’s a thing — 44 years old and 60 years old. There’s a drop-off there.”
And you know what? She was right.
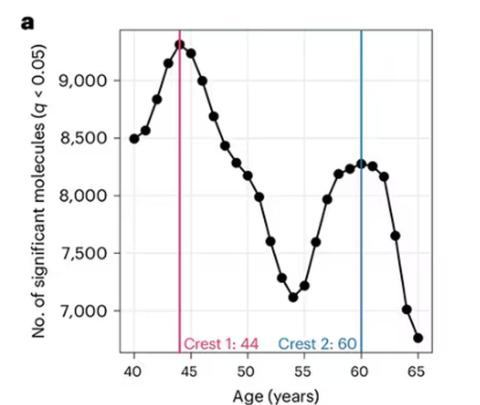
A study, “Nonlinear dynamics of multi-omics profiles during human aging,” published in Nature Aging in August 2024, analyzed a ton of proteins and metabolites in people of various ages and found, when you put it all together, that I should know better than to doubt my brilliant spouse.
But deep down, I believe the cliché that age is just a number. I don’t particularly care about being 44, or turning 50 or 60. I care about how my body and brain are aging. If I can be a happy, healthy, 80-year-old in full command of my faculties, I would consider that a major win no matter what the calendar says.
So I’m always interested in ways to quantify how my body is aging, independent of how many birthdays I have passed. And, according to a new study, there’s actually a really easy way to do this: Just stand on one leg.
The surprising results come from “Age-related changes in gait, balance, and strength parameters: A cross-sectional study,” appearing in PLOS One, which analyzed 40 individuals — half under age 65 and half over age 65 — across a variety of domains of strength, balance, and gait. The conceit of the study? We all know that things like strength and balance worsen over time, but what worsens fastest? What might be the best metric to tell us how our bodies are aging?
To that end, you have a variety of correlations between various metrics and calendar age.
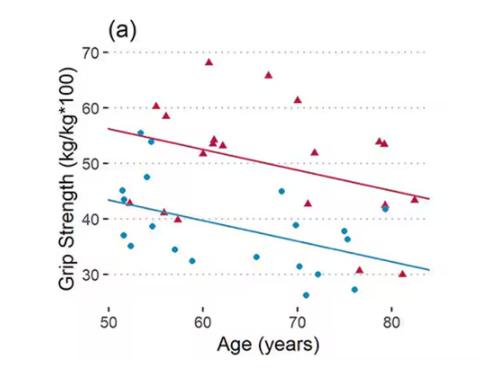
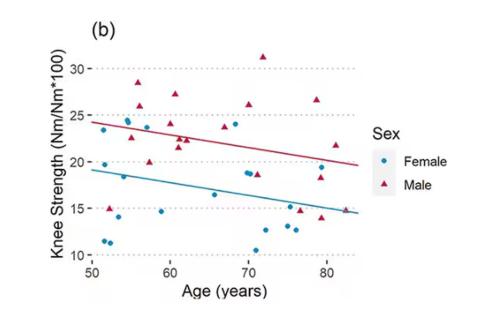
As age increases, grip strength goes down. Men (inexplicably in pink) have higher grip strength overall, and women (confusingly in blue) lower. Somewhat less strong correlations were seen for knee strength.
What about balance?
To assess this, the researchers had the participants stand on a pressure plate. In one scenario, they did this with eyes open, and the next with eyes closed. They then measured how much the pressure varied around the center of the individual on the plate — basically, how much the person swayed while they were standing there.
Sway increased as age increased. Sway increased a bit more with eyes closed than with eyes open.
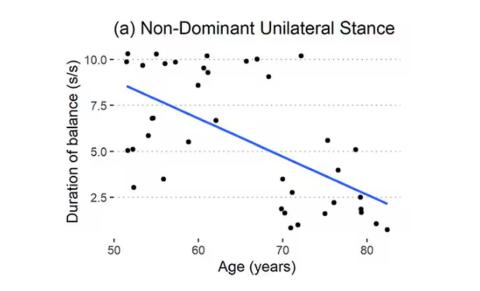
But the strongest correlation between any of these metrics and age was a simple one: How long can you stand on one leg?
Particularly for the nondominant leg, what you see here is a pretty dramatic drop-off in balance time around age 65, with younger people able to do 10 seconds with ease and some older people barely being able to make it to 2.
Of course, I had to try this for myself. And as I was standing around on one leg, it became clear to me exactly why this might be a good metric. It really integrates balance and strength in a way that the other tests don’t: balance, clearly, since you have to stay vertical over a relatively small base; but strength as well, because, well, one leg is holding up all the rest of you. You do feel it after a while.
So this metric passes the smell test to me, at least as a potential proxy for age-related physical decline.
But I should be careful to note that this was a cross-sectional study; the researchers looked at various people who were all different ages, not the same people over time to watch how these things change as they aged.
Also, the use of the correlation coefficient in graphs like this implies a certain linear relationship between age and standing-on-one-foot time. The raw data — the points on this graph — don’t appear that linear to me. As I mentioned above, it seems like there might be a bit of a sharp drop-off somewhere in the mid-60s. That means that we may not be able to use this as a sensitive test for aging that slowly changes as your body gets older. It might be that you’re able to essentially stand on one leg as long as you want until, one day, you can’t. That gives us less warning and less to act on.
And finally, we don’t know that changing this metric will change your health for the better. I’m sure a good physiatrist or physical therapist could design some exercises to increase any of our standing-on-one leg times. And no doubt, with practice, you could get your numbers way up. But that doesn’t necessarily mean you’re healthier. It’s like “teaching to the test”; you might score better on the standardized exam but you didn’t really learn the material.
So I am not adding one-leg standing to my daily exercise routine. But I won’t lie and tell you that, from time to time, and certainly on my 60th birthday, you may find me standing like a flamingo with a stopwatch in my hand.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
So I was lying in bed the other night, trying to read my phone, and started complaining to my wife about how my vision keeps getting worse, and then how stiff I feel when I wake up in the morning, and how a recent injury is taking too long to heal, and she said, “Well, yeah. You’re 44. That’s when things start to head downhill.”
And I was like, “Forty-four? That seems very specific. I thought 50 was what people complain about.” And she said, “No, it’s a thing — 44 years old and 60 years old. There’s a drop-off there.”
And you know what? She was right.
A study, “Nonlinear dynamics of multi-omics profiles during human aging,” published in Nature Aging in August 2024, analyzed a ton of proteins and metabolites in people of various ages and found, when you put it all together, that I should know better than to doubt my brilliant spouse.
But deep down, I believe the cliché that age is just a number. I don’t particularly care about being 44, or turning 50 or 60. I care about how my body and brain are aging. If I can be a happy, healthy, 80-year-old in full command of my faculties, I would consider that a major win no matter what the calendar says.
So I’m always interested in ways to quantify how my body is aging, independent of how many birthdays I have passed. And, according to a new study, there’s actually a really easy way to do this: Just stand on one leg.
The surprising results come from “Age-related changes in gait, balance, and strength parameters: A cross-sectional study,” appearing in PLOS One, which analyzed 40 individuals — half under age 65 and half over age 65 — across a variety of domains of strength, balance, and gait. The conceit of the study? We all know that things like strength and balance worsen over time, but what worsens fastest? What might be the best metric to tell us how our bodies are aging?
To that end, you have a variety of correlations between various metrics and calendar age.
As age increases, grip strength goes down. Men (inexplicably in pink) have higher grip strength overall, and women (confusingly in blue) lower. Somewhat less strong correlations were seen for knee strength.
What about balance?
To assess this, the researchers had the participants stand on a pressure plate. In one scenario, they did this with eyes open, and the next with eyes closed. They then measured how much the pressure varied around the center of the individual on the plate — basically, how much the person swayed while they were standing there.
Sway increased as age increased. Sway increased a bit more with eyes closed than with eyes open.
But the strongest correlation between any of these metrics and age was a simple one: How long can you stand on one leg?
Particularly for the nondominant leg, what you see here is a pretty dramatic drop-off in balance time around age 65, with younger people able to do 10 seconds with ease and some older people barely being able to make it to 2.
Of course, I had to try this for myself. And as I was standing around on one leg, it became clear to me exactly why this might be a good metric. It really integrates balance and strength in a way that the other tests don’t: balance, clearly, since you have to stay vertical over a relatively small base; but strength as well, because, well, one leg is holding up all the rest of you. You do feel it after a while.
So this metric passes the smell test to me, at least as a potential proxy for age-related physical decline.
But I should be careful to note that this was a cross-sectional study; the researchers looked at various people who were all different ages, not the same people over time to watch how these things change as they aged.
Also, the use of the correlation coefficient in graphs like this implies a certain linear relationship between age and standing-on-one-foot time. The raw data — the points on this graph — don’t appear that linear to me. As I mentioned above, it seems like there might be a bit of a sharp drop-off somewhere in the mid-60s. That means that we may not be able to use this as a sensitive test for aging that slowly changes as your body gets older. It might be that you’re able to essentially stand on one leg as long as you want until, one day, you can’t. That gives us less warning and less to act on.
And finally, we don’t know that changing this metric will change your health for the better. I’m sure a good physiatrist or physical therapist could design some exercises to increase any of our standing-on-one leg times. And no doubt, with practice, you could get your numbers way up. But that doesn’t necessarily mean you’re healthier. It’s like “teaching to the test”; you might score better on the standardized exam but you didn’t really learn the material.
So I am not adding one-leg standing to my daily exercise routine. But I won’t lie and tell you that, from time to time, and certainly on my 60th birthday, you may find me standing like a flamingo with a stopwatch in my hand.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
So I was lying in bed the other night, trying to read my phone, and started complaining to my wife about how my vision keeps getting worse, and then how stiff I feel when I wake up in the morning, and how a recent injury is taking too long to heal, and she said, “Well, yeah. You’re 44. That’s when things start to head downhill.”
And I was like, “Forty-four? That seems very specific. I thought 50 was what people complain about.” And she said, “No, it’s a thing — 44 years old and 60 years old. There’s a drop-off there.”
And you know what? She was right.
A study, “Nonlinear dynamics of multi-omics profiles during human aging,” published in Nature Aging in August 2024, analyzed a ton of proteins and metabolites in people of various ages and found, when you put it all together, that I should know better than to doubt my brilliant spouse.
But deep down, I believe the cliché that age is just a number. I don’t particularly care about being 44, or turning 50 or 60. I care about how my body and brain are aging. If I can be a happy, healthy, 80-year-old in full command of my faculties, I would consider that a major win no matter what the calendar says.
So I’m always interested in ways to quantify how my body is aging, independent of how many birthdays I have passed. And, according to a new study, there’s actually a really easy way to do this: Just stand on one leg.
The surprising results come from “Age-related changes in gait, balance, and strength parameters: A cross-sectional study,” appearing in PLOS One, which analyzed 40 individuals — half under age 65 and half over age 65 — across a variety of domains of strength, balance, and gait. The conceit of the study? We all know that things like strength and balance worsen over time, but what worsens fastest? What might be the best metric to tell us how our bodies are aging?
To that end, you have a variety of correlations between various metrics and calendar age.
As age increases, grip strength goes down. Men (inexplicably in pink) have higher grip strength overall, and women (confusingly in blue) lower. Somewhat less strong correlations were seen for knee strength.
What about balance?
To assess this, the researchers had the participants stand on a pressure plate. In one scenario, they did this with eyes open, and the next with eyes closed. They then measured how much the pressure varied around the center of the individual on the plate — basically, how much the person swayed while they were standing there.
Sway increased as age increased. Sway increased a bit more with eyes closed than with eyes open.
But the strongest correlation between any of these metrics and age was a simple one: How long can you stand on one leg?
Particularly for the nondominant leg, what you see here is a pretty dramatic drop-off in balance time around age 65, with younger people able to do 10 seconds with ease and some older people barely being able to make it to 2.
Of course, I had to try this for myself. And as I was standing around on one leg, it became clear to me exactly why this might be a good metric. It really integrates balance and strength in a way that the other tests don’t: balance, clearly, since you have to stay vertical over a relatively small base; but strength as well, because, well, one leg is holding up all the rest of you. You do feel it after a while.
So this metric passes the smell test to me, at least as a potential proxy for age-related physical decline.
But I should be careful to note that this was a cross-sectional study; the researchers looked at various people who were all different ages, not the same people over time to watch how these things change as they aged.
Also, the use of the correlation coefficient in graphs like this implies a certain linear relationship between age and standing-on-one-foot time. The raw data — the points on this graph — don’t appear that linear to me. As I mentioned above, it seems like there might be a bit of a sharp drop-off somewhere in the mid-60s. That means that we may not be able to use this as a sensitive test for aging that slowly changes as your body gets older. It might be that you’re able to essentially stand on one leg as long as you want until, one day, you can’t. That gives us less warning and less to act on.
And finally, we don’t know that changing this metric will change your health for the better. I’m sure a good physiatrist or physical therapist could design some exercises to increase any of our standing-on-one leg times. And no doubt, with practice, you could get your numbers way up. But that doesn’t necessarily mean you’re healthier. It’s like “teaching to the test”; you might score better on the standardized exam but you didn’t really learn the material.
So I am not adding one-leg standing to my daily exercise routine. But I won’t lie and tell you that, from time to time, and certainly on my 60th birthday, you may find me standing like a flamingo with a stopwatch in my hand.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
H pylori: ACG Guideline Advises New Approaches to Treatment
Helicobacter pylori is one of the most common human bacterial chronic infections globally. Its prevalence has actually decreased in North America in recent years, although its current range of approximately 30%-40% remains substantial given the potential clinical implications of infection.
Standards have changed considerably regarding the testing, treatment, and follow-up of H pylori. This is made clear by the just-published clinical practice guideline from the American College of Gastroenterology (ACG), which provides several new recommendations based on recent scientific evidence that should change your clinical approach to managing this common infection.
This discussion aims to synthesize and highlight key concepts from the ACG’s comprehensive publication.
Who Should Be Tested and Treated?
The cardinal diseases caused by H pylori have traditionally included peptic ulcer disease, marginal zone B-cell lymphoma, gastric adenocarcinoma, and dyspepsia.
Additional associations have been made with idiopathic thrombocytopenic purpura and otherwise unexplained iron deficiency.
New evidence suggests that patients taking long-term nonsteroidal anti-inflammatory drugs, including low-dose aspirin, are relatively more susceptible to infection.
The ACG’s guideline also recommends testing persons at an increased risk for gastric adenocarcinoma (eg, those with autoimmune gastritis, current or history of premalignant conditions, or first-degree relative with gastric cancer), as well as household members of patients with a positive nonserologic test for H pylori.
The authors note that those with an indication for testing should be offered treatment if determined to have an infection. These patients should also undergo a posttreatment test-of-cure, which should occur at least 4 weeks afterwards using a urea breath test, fecal antigen test, or gastric biopsy.
Caveats to Treatment
Patients with H pylori infections are advised to undergo treatment for a duration of 14 days. Some of the commercial prepackaged H pylori treatment options (eg, Pylera, which contains bismuth subcitrate/metronidazole/tetracycline) are dispensed in regimens lasting only 10 days and currently are viewed as inadequate.
In the United States, the patterns of antibiotic resistance for the previously used standard drugs in the treatment of H pylori have increased considerably. They range from 32% for clarithromycin, 38% for levofloxacin, and 42% for metronidazole, in contrast to 3% for amoxicillin, 1% for tetracycline, and 0% for rifabutin.
Clarithromycin- and levofloxacin-containing treatments should be avoided in treatment-naive patients unless specifically directed following the results of susceptibility tests with either a phenotypic method (culture-based) or a molecular method (polymerase chain reaction or next-generation sequencing). Notably, the mutations responsible for both clarithromycin and levofloxacin resistance may be detectable by stool-based testing.
Maintenance of intragastric acid suppression is key to H pylori eradication, as elevated intragastric pH promotes active replication of H pylori and makes it more susceptible to bactericidal antibiotics.
Therefore, the use of histamine-2 receptors is not recommended, as they are inadequate for achieving acid suppression. Instead, a dual-based therapy of either the potassium-competitive acid blocker (PCAB) vonoprazan (20 mg) or a high-dose proton pump inhibitor (PPI) and amoxicillin, administered twice daily, is effective, although this finding is based on limited evidence.
Treatment-Naive Patients
In treatment-naive patients without penicillin allergy and for whom antibiotic susceptibility testing has not been obtained, the guideline offers its strongest recommendation for bismuth quadruple therapy. This therapy typically consists of a PPI, bismuth subcitrate or subsalicylate, tetracycline, and metronidazole.
Among those with a penicillin allergy, bismuth quadruple therapy is also the primary treatment choice. The authors suggest that patients with a suspected allergy are referred to an allergist for possible penicillin desensitization, given that less than 1% of the population is thought to present with a “true” allergy.
The guideline also presented conditional recommendations, based on low- to moderate-quality evidence, for using a rifabutin-based triple regimen of omeprazole, amoxicillin, and rifabutin (Talicia); a PCAB-based dual regimen of vonoprazan and amoxicillin (Voquezna Dual Pak); and a PCAB-based triple regimen of vonoprazan, clarithromycin, and amoxicillin (Voquezna Triple Pak). In patients with unknown clarithromycin susceptibility, the PCAB-based triple therapy is preferred over PPI-clarithromycin triple therapy.
Although probiotics have been suggested to possibly lead to increased effectiveness or tolerability for H pylori eradication, this was based on studies with significant heterogeneity in their designs. At present, no high-quality data support probiotic therapy.
Clinicians may substitute doxycycline for tetracycline due to availability or cost, and also may prescribe metronidazole at a lower dose than recommended (1.5-2 g/d) to limit side effects. Both modifications have been associated with lower rates of H pylori eradication and are not recommended.
Treatment-Experienced Patients
Quadruple bismuth therapy is the optimal approach among treatment-experienced patients with persistent H pylori infection who have not previously received this therapy. However, this recommendation was rated as conditional, given that it was based on a low quality of evidence.
The guideline offered other recommendations for treatment-experienced patients with persistent infection who had received bismuth quadruple therapy — also conditionally based on a low quality of evidence.
In such patients, it is recommended to consider the use of a rifabutin-based triple therapy (ie, a PPI standard to double dose, amoxicillin, and rifabutin) and a levofloxacin-based triple therapy (ie, a PPI standard dose, levofloxacin, and amoxicillin or metronidazole).
Although significant evidence gaps prevented the authors from providing formal recommendations, they included a PCAB-based triple therapy of vonoprazan, clarithromycin, and amoxicillin (Voquezna Triple Pak) and a high-dose dual therapy of either vonoprazan (20 mg) or PPI (double dose) and amoxicillin among their suggested salvage regimens for these patients.
A New Standard
We must recognize, however, that there are still substantial evidence gaps, particularly around the use of a PCAB-based regimen and its relative advantages over a standard or high-dose PPI-based regimen. This may be of particular importance based on the variable prevalence of cytochrome P450 2C19 (CYP2C19) polymorphisms in the specific patient populations, as PCABs are not metabolized by CYP2C19.
Reviewing the entirety of the ACG’s clinical guideline is encouraged for additional details about the management of H pylori beyond what is highlighted herein.
Dr. Johnson, Professor of Medicine, Chief of Gastroenterology, Eastern Virginia Medical School, Norfolk, Virginia, disclosed ties with ISOTHRIVE and Johnson & Johnson.
A version of this article appeared on Medscape.com.
Helicobacter pylori is one of the most common human bacterial chronic infections globally. Its prevalence has actually decreased in North America in recent years, although its current range of approximately 30%-40% remains substantial given the potential clinical implications of infection.
Standards have changed considerably regarding the testing, treatment, and follow-up of H pylori. This is made clear by the just-published clinical practice guideline from the American College of Gastroenterology (ACG), which provides several new recommendations based on recent scientific evidence that should change your clinical approach to managing this common infection.
This discussion aims to synthesize and highlight key concepts from the ACG’s comprehensive publication.
Who Should Be Tested and Treated?
The cardinal diseases caused by H pylori have traditionally included peptic ulcer disease, marginal zone B-cell lymphoma, gastric adenocarcinoma, and dyspepsia.
Additional associations have been made with idiopathic thrombocytopenic purpura and otherwise unexplained iron deficiency.
New evidence suggests that patients taking long-term nonsteroidal anti-inflammatory drugs, including low-dose aspirin, are relatively more susceptible to infection.
The ACG’s guideline also recommends testing persons at an increased risk for gastric adenocarcinoma (eg, those with autoimmune gastritis, current or history of premalignant conditions, or first-degree relative with gastric cancer), as well as household members of patients with a positive nonserologic test for H pylori.
The authors note that those with an indication for testing should be offered treatment if determined to have an infection. These patients should also undergo a posttreatment test-of-cure, which should occur at least 4 weeks afterwards using a urea breath test, fecal antigen test, or gastric biopsy.
Caveats to Treatment
Patients with H pylori infections are advised to undergo treatment for a duration of 14 days. Some of the commercial prepackaged H pylori treatment options (eg, Pylera, which contains bismuth subcitrate/metronidazole/tetracycline) are dispensed in regimens lasting only 10 days and currently are viewed as inadequate.
In the United States, the patterns of antibiotic resistance for the previously used standard drugs in the treatment of H pylori have increased considerably. They range from 32% for clarithromycin, 38% for levofloxacin, and 42% for metronidazole, in contrast to 3% for amoxicillin, 1% for tetracycline, and 0% for rifabutin.
Clarithromycin- and levofloxacin-containing treatments should be avoided in treatment-naive patients unless specifically directed following the results of susceptibility tests with either a phenotypic method (culture-based) or a molecular method (polymerase chain reaction or next-generation sequencing). Notably, the mutations responsible for both clarithromycin and levofloxacin resistance may be detectable by stool-based testing.
Maintenance of intragastric acid suppression is key to H pylori eradication, as elevated intragastric pH promotes active replication of H pylori and makes it more susceptible to bactericidal antibiotics.
Therefore, the use of histamine-2 receptors is not recommended, as they are inadequate for achieving acid suppression. Instead, a dual-based therapy of either the potassium-competitive acid blocker (PCAB) vonoprazan (20 mg) or a high-dose proton pump inhibitor (PPI) and amoxicillin, administered twice daily, is effective, although this finding is based on limited evidence.
Treatment-Naive Patients
In treatment-naive patients without penicillin allergy and for whom antibiotic susceptibility testing has not been obtained, the guideline offers its strongest recommendation for bismuth quadruple therapy. This therapy typically consists of a PPI, bismuth subcitrate or subsalicylate, tetracycline, and metronidazole.
Among those with a penicillin allergy, bismuth quadruple therapy is also the primary treatment choice. The authors suggest that patients with a suspected allergy are referred to an allergist for possible penicillin desensitization, given that less than 1% of the population is thought to present with a “true” allergy.
The guideline also presented conditional recommendations, based on low- to moderate-quality evidence, for using a rifabutin-based triple regimen of omeprazole, amoxicillin, and rifabutin (Talicia); a PCAB-based dual regimen of vonoprazan and amoxicillin (Voquezna Dual Pak); and a PCAB-based triple regimen of vonoprazan, clarithromycin, and amoxicillin (Voquezna Triple Pak). In patients with unknown clarithromycin susceptibility, the PCAB-based triple therapy is preferred over PPI-clarithromycin triple therapy.
Although probiotics have been suggested to possibly lead to increased effectiveness or tolerability for H pylori eradication, this was based on studies with significant heterogeneity in their designs. At present, no high-quality data support probiotic therapy.
Clinicians may substitute doxycycline for tetracycline due to availability or cost, and also may prescribe metronidazole at a lower dose than recommended (1.5-2 g/d) to limit side effects. Both modifications have been associated with lower rates of H pylori eradication and are not recommended.
Treatment-Experienced Patients
Quadruple bismuth therapy is the optimal approach among treatment-experienced patients with persistent H pylori infection who have not previously received this therapy. However, this recommendation was rated as conditional, given that it was based on a low quality of evidence.
The guideline offered other recommendations for treatment-experienced patients with persistent infection who had received bismuth quadruple therapy — also conditionally based on a low quality of evidence.
In such patients, it is recommended to consider the use of a rifabutin-based triple therapy (ie, a PPI standard to double dose, amoxicillin, and rifabutin) and a levofloxacin-based triple therapy (ie, a PPI standard dose, levofloxacin, and amoxicillin or metronidazole).
Although significant evidence gaps prevented the authors from providing formal recommendations, they included a PCAB-based triple therapy of vonoprazan, clarithromycin, and amoxicillin (Voquezna Triple Pak) and a high-dose dual therapy of either vonoprazan (20 mg) or PPI (double dose) and amoxicillin among their suggested salvage regimens for these patients.
A New Standard
We must recognize, however, that there are still substantial evidence gaps, particularly around the use of a PCAB-based regimen and its relative advantages over a standard or high-dose PPI-based regimen. This may be of particular importance based on the variable prevalence of cytochrome P450 2C19 (CYP2C19) polymorphisms in the specific patient populations, as PCABs are not metabolized by CYP2C19.
Reviewing the entirety of the ACG’s clinical guideline is encouraged for additional details about the management of H pylori beyond what is highlighted herein.
Dr. Johnson, Professor of Medicine, Chief of Gastroenterology, Eastern Virginia Medical School, Norfolk, Virginia, disclosed ties with ISOTHRIVE and Johnson & Johnson.
A version of this article appeared on Medscape.com.
Helicobacter pylori is one of the most common human bacterial chronic infections globally. Its prevalence has actually decreased in North America in recent years, although its current range of approximately 30%-40% remains substantial given the potential clinical implications of infection.
Standards have changed considerably regarding the testing, treatment, and follow-up of H pylori. This is made clear by the just-published clinical practice guideline from the American College of Gastroenterology (ACG), which provides several new recommendations based on recent scientific evidence that should change your clinical approach to managing this common infection.
This discussion aims to synthesize and highlight key concepts from the ACG’s comprehensive publication.
Who Should Be Tested and Treated?
The cardinal diseases caused by H pylori have traditionally included peptic ulcer disease, marginal zone B-cell lymphoma, gastric adenocarcinoma, and dyspepsia.
Additional associations have been made with idiopathic thrombocytopenic purpura and otherwise unexplained iron deficiency.
New evidence suggests that patients taking long-term nonsteroidal anti-inflammatory drugs, including low-dose aspirin, are relatively more susceptible to infection.
The ACG’s guideline also recommends testing persons at an increased risk for gastric adenocarcinoma (eg, those with autoimmune gastritis, current or history of premalignant conditions, or first-degree relative with gastric cancer), as well as household members of patients with a positive nonserologic test for H pylori.
The authors note that those with an indication for testing should be offered treatment if determined to have an infection. These patients should also undergo a posttreatment test-of-cure, which should occur at least 4 weeks afterwards using a urea breath test, fecal antigen test, or gastric biopsy.
Caveats to Treatment
Patients with H pylori infections are advised to undergo treatment for a duration of 14 days. Some of the commercial prepackaged H pylori treatment options (eg, Pylera, which contains bismuth subcitrate/metronidazole/tetracycline) are dispensed in regimens lasting only 10 days and currently are viewed as inadequate.
In the United States, the patterns of antibiotic resistance for the previously used standard drugs in the treatment of H pylori have increased considerably. They range from 32% for clarithromycin, 38% for levofloxacin, and 42% for metronidazole, in contrast to 3% for amoxicillin, 1% for tetracycline, and 0% for rifabutin.
Clarithromycin- and levofloxacin-containing treatments should be avoided in treatment-naive patients unless specifically directed following the results of susceptibility tests with either a phenotypic method (culture-based) or a molecular method (polymerase chain reaction or next-generation sequencing). Notably, the mutations responsible for both clarithromycin and levofloxacin resistance may be detectable by stool-based testing.
Maintenance of intragastric acid suppression is key to H pylori eradication, as elevated intragastric pH promotes active replication of H pylori and makes it more susceptible to bactericidal antibiotics.
Therefore, the use of histamine-2 receptors is not recommended, as they are inadequate for achieving acid suppression. Instead, a dual-based therapy of either the potassium-competitive acid blocker (PCAB) vonoprazan (20 mg) or a high-dose proton pump inhibitor (PPI) and amoxicillin, administered twice daily, is effective, although this finding is based on limited evidence.
Treatment-Naive Patients
In treatment-naive patients without penicillin allergy and for whom antibiotic susceptibility testing has not been obtained, the guideline offers its strongest recommendation for bismuth quadruple therapy. This therapy typically consists of a PPI, bismuth subcitrate or subsalicylate, tetracycline, and metronidazole.
Among those with a penicillin allergy, bismuth quadruple therapy is also the primary treatment choice. The authors suggest that patients with a suspected allergy are referred to an allergist for possible penicillin desensitization, given that less than 1% of the population is thought to present with a “true” allergy.
The guideline also presented conditional recommendations, based on low- to moderate-quality evidence, for using a rifabutin-based triple regimen of omeprazole, amoxicillin, and rifabutin (Talicia); a PCAB-based dual regimen of vonoprazan and amoxicillin (Voquezna Dual Pak); and a PCAB-based triple regimen of vonoprazan, clarithromycin, and amoxicillin (Voquezna Triple Pak). In patients with unknown clarithromycin susceptibility, the PCAB-based triple therapy is preferred over PPI-clarithromycin triple therapy.
Although probiotics have been suggested to possibly lead to increased effectiveness or tolerability for H pylori eradication, this was based on studies with significant heterogeneity in their designs. At present, no high-quality data support probiotic therapy.
Clinicians may substitute doxycycline for tetracycline due to availability or cost, and also may prescribe metronidazole at a lower dose than recommended (1.5-2 g/d) to limit side effects. Both modifications have been associated with lower rates of H pylori eradication and are not recommended.
Treatment-Experienced Patients
Quadruple bismuth therapy is the optimal approach among treatment-experienced patients with persistent H pylori infection who have not previously received this therapy. However, this recommendation was rated as conditional, given that it was based on a low quality of evidence.
The guideline offered other recommendations for treatment-experienced patients with persistent infection who had received bismuth quadruple therapy — also conditionally based on a low quality of evidence.
In such patients, it is recommended to consider the use of a rifabutin-based triple therapy (ie, a PPI standard to double dose, amoxicillin, and rifabutin) and a levofloxacin-based triple therapy (ie, a PPI standard dose, levofloxacin, and amoxicillin or metronidazole).
Although significant evidence gaps prevented the authors from providing formal recommendations, they included a PCAB-based triple therapy of vonoprazan, clarithromycin, and amoxicillin (Voquezna Triple Pak) and a high-dose dual therapy of either vonoprazan (20 mg) or PPI (double dose) and amoxicillin among their suggested salvage regimens for these patients.
A New Standard
We must recognize, however, that there are still substantial evidence gaps, particularly around the use of a PCAB-based regimen and its relative advantages over a standard or high-dose PPI-based regimen. This may be of particular importance based on the variable prevalence of cytochrome P450 2C19 (CYP2C19) polymorphisms in the specific patient populations, as PCABs are not metabolized by CYP2C19.
Reviewing the entirety of the ACG’s clinical guideline is encouraged for additional details about the management of H pylori beyond what is highlighted herein.
Dr. Johnson, Professor of Medicine, Chief of Gastroenterology, Eastern Virginia Medical School, Norfolk, Virginia, disclosed ties with ISOTHRIVE and Johnson & Johnson.
A version of this article appeared on Medscape.com.
Help Your Patients Reap the Benefits of Plant-Based Diets
Research pooled from nearly 100 studies has indicated that people who adhere to a vegan diet (ie, completely devoid of animal products) or a vegetarian diet (ie, devoid of meat, but may include dairy and eggs) are able to ward off some chronic diseases, such as cardiovascular disease, optimize glycemic control, and decrease their risk for cancer compared with those who consume omnivorous diets.
Vegan and vegetarian diets, or flexitarian diets — which are less reliant on animal protein than the standard US diet but do not completely exclude meat, fish, eggs, or dairy — may promote homeostasis and decrease inflammation by providing more fiber, antioxidants, and unsaturated fatty acids than the typical Western diet.
Inflammation and Obesity
Adipose tissue is a major producer of pro-inflammatory cytokines like interleukin (IL)-6, whose presence then triggers a rush of acute-phase reactants such as C-reactive protein (CRP) by the liver. This process develops into chronic low-grade inflammation that can increase a person’s chances of developing diabetes, cardiovascular disease, kidney disease, metabolic syndrome, and related complications.
Adopting a plant-based diet can improve markers of chronic low-grade inflammation that can lead to chronic disease and worsen existent chronic disease. A meta-analysis of 29 studies encompassing nearly 2700 participants found that initiation of a plant-based diet showed significant improvement in CRP, IL-6, and soluble intercellular adhesion molecule 1.
If we want to prevent these inflammatory disease states and their complications, the obvious response is to counsel patients to avoid excessive weight gain or to lose weight if obesity is their baseline. This can be tough for some patients, but it is nonetheless an important step in chronic disease prevention and management.
Plant-Based Diet for Type 2 Diabetes
According to a review of nine studies of patients living with type 2 diabetes who adhered to a plant-based diet, all but one found that this approach led to significantly lower A1c values than those seen in control groups. Six of the included studies reported that participants were able to decrease or discontinue medications for the management of diabetes. Researchers across all included studies also noted a decrease in total cholesterol, low-density lipoprotein cholesterol, and triglycerides, as well as increased weight loss in participants in each intervention group.
Such improvements are probably the result of the increase in fiber intake that occurs with a plant-based diet. A high-fiber diet is known to promote improved glucose and lipid metabolism as well as weight loss.
It is also worth noting that participants in the intervention groups also experienced improvements in depression and less chronic pain than did those in the control groups.
Plant-Based Diet for Chronic Kidney Disease (CKD)
Although the use of a plant-based diet in the prevention of CKD is well documented, adopting such diets for the treatment of CKD may intimidate both patients and practitioners owing to the high potassium and phosphorus content of many fruits and vegetables.
However, research indicates that the bioavailability of both potassium and phosphorus is lower in plant-based, whole foods than in preservatives and the highly processed food items that incorporate them. This makes a plant-based diet more viable than previously thought.
Diets rich in vegetables, whole grains, nuts, and legumes have been shown to decrease dietary acid load, both preventing and treating metabolic acidosis. Such diets have also been shown to decrease blood pressure and the risk for a decline in estimated glomerular filtration rate. This type of diet would also prioritize the unsaturated fatty acids and fiber-rich proteins such as avocados, beans, and nuts shown to improve dyslipidemia, which may occur alongside CKD.
Realistic Options for Patients on Medical Diets
There is one question that I always seem to get from when recommending a plant-based diet: “These patients already have so many restrictions. Why would you add more?” And my answer is also always the same: I don’t.
I rarely, if ever, recommend completely cutting out any food item or food group. Instead, I ask the patient to increase their intake of plant-based foods and only limit highly processed foods and fatty meats. By shifting a patient’s focus to beans; nuts; and low-carbohydrate, high-fiber fruits and vegetables, I am often opening up a whole new world of possibilities.
Instead of a sandwich with low-sodium turkey and cheese on white bread with a side of unsalted pretzels, I recommend a caprese salad with blueberries and almonds or a Southwest salad with black beans, corn, and avocado. I don’t encourage my patients to skip the foods that they love, but instead to only think about all the delicious plant-based options that will provide them with more than just calories.
Meat, dairy, seafood, and eggs can certainly be a part of a healthy diet, but what if our chronically ill patients, especially those with diabetes, had more options than just grilled chicken and green beans for every meal? What if we focus on decreasing dietary restrictions, incorporating a variety of nourishing foods, and educating our patients, instead of on portion control and moderation?
This is how I choose to incorporate plant-based diets into my practice to treat and prevent these chronic inflammatory conditions and promote sustainable, realistic change in my clients’ health.
Brandy Winfree Root, a renal dietitian in private practice in Mary Esther, Florida, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Research pooled from nearly 100 studies has indicated that people who adhere to a vegan diet (ie, completely devoid of animal products) or a vegetarian diet (ie, devoid of meat, but may include dairy and eggs) are able to ward off some chronic diseases, such as cardiovascular disease, optimize glycemic control, and decrease their risk for cancer compared with those who consume omnivorous diets.
Vegan and vegetarian diets, or flexitarian diets — which are less reliant on animal protein than the standard US diet but do not completely exclude meat, fish, eggs, or dairy — may promote homeostasis and decrease inflammation by providing more fiber, antioxidants, and unsaturated fatty acids than the typical Western diet.
Inflammation and Obesity
Adipose tissue is a major producer of pro-inflammatory cytokines like interleukin (IL)-6, whose presence then triggers a rush of acute-phase reactants such as C-reactive protein (CRP) by the liver. This process develops into chronic low-grade inflammation that can increase a person’s chances of developing diabetes, cardiovascular disease, kidney disease, metabolic syndrome, and related complications.
Adopting a plant-based diet can improve markers of chronic low-grade inflammation that can lead to chronic disease and worsen existent chronic disease. A meta-analysis of 29 studies encompassing nearly 2700 participants found that initiation of a plant-based diet showed significant improvement in CRP, IL-6, and soluble intercellular adhesion molecule 1.
If we want to prevent these inflammatory disease states and their complications, the obvious response is to counsel patients to avoid excessive weight gain or to lose weight if obesity is their baseline. This can be tough for some patients, but it is nonetheless an important step in chronic disease prevention and management.
Plant-Based Diet for Type 2 Diabetes
According to a review of nine studies of patients living with type 2 diabetes who adhered to a plant-based diet, all but one found that this approach led to significantly lower A1c values than those seen in control groups. Six of the included studies reported that participants were able to decrease or discontinue medications for the management of diabetes. Researchers across all included studies also noted a decrease in total cholesterol, low-density lipoprotein cholesterol, and triglycerides, as well as increased weight loss in participants in each intervention group.
Such improvements are probably the result of the increase in fiber intake that occurs with a plant-based diet. A high-fiber diet is known to promote improved glucose and lipid metabolism as well as weight loss.
It is also worth noting that participants in the intervention groups also experienced improvements in depression and less chronic pain than did those in the control groups.
Plant-Based Diet for Chronic Kidney Disease (CKD)
Although the use of a plant-based diet in the prevention of CKD is well documented, adopting such diets for the treatment of CKD may intimidate both patients and practitioners owing to the high potassium and phosphorus content of many fruits and vegetables.
However, research indicates that the bioavailability of both potassium and phosphorus is lower in plant-based, whole foods than in preservatives and the highly processed food items that incorporate them. This makes a plant-based diet more viable than previously thought.
Diets rich in vegetables, whole grains, nuts, and legumes have been shown to decrease dietary acid load, both preventing and treating metabolic acidosis. Such diets have also been shown to decrease blood pressure and the risk for a decline in estimated glomerular filtration rate. This type of diet would also prioritize the unsaturated fatty acids and fiber-rich proteins such as avocados, beans, and nuts shown to improve dyslipidemia, which may occur alongside CKD.
Realistic Options for Patients on Medical Diets
There is one question that I always seem to get from when recommending a plant-based diet: “These patients already have so many restrictions. Why would you add more?” And my answer is also always the same: I don’t.
I rarely, if ever, recommend completely cutting out any food item or food group. Instead, I ask the patient to increase their intake of plant-based foods and only limit highly processed foods and fatty meats. By shifting a patient’s focus to beans; nuts; and low-carbohydrate, high-fiber fruits and vegetables, I am often opening up a whole new world of possibilities.
Instead of a sandwich with low-sodium turkey and cheese on white bread with a side of unsalted pretzels, I recommend a caprese salad with blueberries and almonds or a Southwest salad with black beans, corn, and avocado. I don’t encourage my patients to skip the foods that they love, but instead to only think about all the delicious plant-based options that will provide them with more than just calories.
Meat, dairy, seafood, and eggs can certainly be a part of a healthy diet, but what if our chronically ill patients, especially those with diabetes, had more options than just grilled chicken and green beans for every meal? What if we focus on decreasing dietary restrictions, incorporating a variety of nourishing foods, and educating our patients, instead of on portion control and moderation?
This is how I choose to incorporate plant-based diets into my practice to treat and prevent these chronic inflammatory conditions and promote sustainable, realistic change in my clients’ health.
Brandy Winfree Root, a renal dietitian in private practice in Mary Esther, Florida, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Research pooled from nearly 100 studies has indicated that people who adhere to a vegan diet (ie, completely devoid of animal products) or a vegetarian diet (ie, devoid of meat, but may include dairy and eggs) are able to ward off some chronic diseases, such as cardiovascular disease, optimize glycemic control, and decrease their risk for cancer compared with those who consume omnivorous diets.
Vegan and vegetarian diets, or flexitarian diets — which are less reliant on animal protein than the standard US diet but do not completely exclude meat, fish, eggs, or dairy — may promote homeostasis and decrease inflammation by providing more fiber, antioxidants, and unsaturated fatty acids than the typical Western diet.
Inflammation and Obesity
Adipose tissue is a major producer of pro-inflammatory cytokines like interleukin (IL)-6, whose presence then triggers a rush of acute-phase reactants such as C-reactive protein (CRP) by the liver. This process develops into chronic low-grade inflammation that can increase a person’s chances of developing diabetes, cardiovascular disease, kidney disease, metabolic syndrome, and related complications.
Adopting a plant-based diet can improve markers of chronic low-grade inflammation that can lead to chronic disease and worsen existent chronic disease. A meta-analysis of 29 studies encompassing nearly 2700 participants found that initiation of a plant-based diet showed significant improvement in CRP, IL-6, and soluble intercellular adhesion molecule 1.
If we want to prevent these inflammatory disease states and their complications, the obvious response is to counsel patients to avoid excessive weight gain or to lose weight if obesity is their baseline. This can be tough for some patients, but it is nonetheless an important step in chronic disease prevention and management.
Plant-Based Diet for Type 2 Diabetes
According to a review of nine studies of patients living with type 2 diabetes who adhered to a plant-based diet, all but one found that this approach led to significantly lower A1c values than those seen in control groups. Six of the included studies reported that participants were able to decrease or discontinue medications for the management of diabetes. Researchers across all included studies also noted a decrease in total cholesterol, low-density lipoprotein cholesterol, and triglycerides, as well as increased weight loss in participants in each intervention group.
Such improvements are probably the result of the increase in fiber intake that occurs with a plant-based diet. A high-fiber diet is known to promote improved glucose and lipid metabolism as well as weight loss.
It is also worth noting that participants in the intervention groups also experienced improvements in depression and less chronic pain than did those in the control groups.
Plant-Based Diet for Chronic Kidney Disease (CKD)
Although the use of a plant-based diet in the prevention of CKD is well documented, adopting such diets for the treatment of CKD may intimidate both patients and practitioners owing to the high potassium and phosphorus content of many fruits and vegetables.
However, research indicates that the bioavailability of both potassium and phosphorus is lower in plant-based, whole foods than in preservatives and the highly processed food items that incorporate them. This makes a plant-based diet more viable than previously thought.
Diets rich in vegetables, whole grains, nuts, and legumes have been shown to decrease dietary acid load, both preventing and treating metabolic acidosis. Such diets have also been shown to decrease blood pressure and the risk for a decline in estimated glomerular filtration rate. This type of diet would also prioritize the unsaturated fatty acids and fiber-rich proteins such as avocados, beans, and nuts shown to improve dyslipidemia, which may occur alongside CKD.
Realistic Options for Patients on Medical Diets
There is one question that I always seem to get from when recommending a plant-based diet: “These patients already have so many restrictions. Why would you add more?” And my answer is also always the same: I don’t.
I rarely, if ever, recommend completely cutting out any food item or food group. Instead, I ask the patient to increase their intake of plant-based foods and only limit highly processed foods and fatty meats. By shifting a patient’s focus to beans; nuts; and low-carbohydrate, high-fiber fruits and vegetables, I am often opening up a whole new world of possibilities.
Instead of a sandwich with low-sodium turkey and cheese on white bread with a side of unsalted pretzels, I recommend a caprese salad with blueberries and almonds or a Southwest salad with black beans, corn, and avocado. I don’t encourage my patients to skip the foods that they love, but instead to only think about all the delicious plant-based options that will provide them with more than just calories.
Meat, dairy, seafood, and eggs can certainly be a part of a healthy diet, but what if our chronically ill patients, especially those with diabetes, had more options than just grilled chicken and green beans for every meal? What if we focus on decreasing dietary restrictions, incorporating a variety of nourishing foods, and educating our patients, instead of on portion control and moderation?
This is how I choose to incorporate plant-based diets into my practice to treat and prevent these chronic inflammatory conditions and promote sustainable, realistic change in my clients’ health.
Brandy Winfree Root, a renal dietitian in private practice in Mary Esther, Florida, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Is CGM the New CBT?
Lauren is a 45-year-old corporate lawyer who managed to excel in every aspect of her life, including parenting her three children while working full-time as a corporate lawyer. A math major at Harvard, she loves data.
Suffice it to say, given that I was treating her for a thyroid condition rather than diabetes, I was a little surprised when she requested I prescribe her a FreeStyle Libre (Abbott) monitor. She explained she was struggling to lose 10 pounds, and she thought continuous glucose monitoring (CGM) would help her determine which foods were impeding her weight loss journey.
While I didn’t see much downside to acquiescing, I felt she had probably been spending too much time on Reddit. What information could CGM give someone without diabetes that couldn’t be gleaned from a food label? Nevertheless, Lauren filled the prescription and began her foray into this relatively uncharted world. When she returned for a follow-up visit several months later, I was shocked to see that she had lost her intended weight. With my tail between my legs, I decided to review the theories and science behind the use of CGM in patients without insulin resistance.
Although it’s not rocket science, CGM can help patients through a “carrot and stick” approach to dieting. Lean proteins, nonstarchy vegetables, and monounsaturated fats such as nuts and avocado all support weight loss and tend to keep blood glucose levels stable. In contrast, foods known to cause weight gain (eg, sugary foods, refined starches, and processed foods) cause sugar spikes in real time. Similarly, large portion sizes are more likely to result in sugar spikes, and pairing proteins with carbohydrates minimizes blood glucose excursions.
Though all of this is basic common sense, . And because blood glucose is influenced by myriad factors including stress, genetics and metabolism, CGM can also potentially help create personal guidance for food choices.
In addition, CGM can reveal the effect of poor sleep and stress on blood glucose levels, thereby encouraging healthier lifestyle choices. The data collected also may provide information on how different modalities of physical activity affect blood glucose levels. A recent study compared the effect of high-intensity interval training (HIIT) and continuous moderate-intensity exercise on postmeal blood glucose in overweight individuals without diabetes. CGM revealed that HIIT is more advantageous for preventing postmeal spikes.
Although CGM appears to be a sophisticated form of cognitive-behavioral therapy, I do worry that the incessant stream of information can lead to worsening anxiety, obsessive compulsive behaviors, or restrictive eating tendencies. Still, thanks to Lauren, I now believe that real-time CGM may lead to behavior modification in food selection and physical activity.
Dr. Messer, Clinical Assistant Professor, Mount Sinai School of Medicine; Associate Professor, Hofstra School of Medicine, New York, NY, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Lauren is a 45-year-old corporate lawyer who managed to excel in every aspect of her life, including parenting her three children while working full-time as a corporate lawyer. A math major at Harvard, she loves data.
Suffice it to say, given that I was treating her for a thyroid condition rather than diabetes, I was a little surprised when she requested I prescribe her a FreeStyle Libre (Abbott) monitor. She explained she was struggling to lose 10 pounds, and she thought continuous glucose monitoring (CGM) would help her determine which foods were impeding her weight loss journey.
While I didn’t see much downside to acquiescing, I felt she had probably been spending too much time on Reddit. What information could CGM give someone without diabetes that couldn’t be gleaned from a food label? Nevertheless, Lauren filled the prescription and began her foray into this relatively uncharted world. When she returned for a follow-up visit several months later, I was shocked to see that she had lost her intended weight. With my tail between my legs, I decided to review the theories and science behind the use of CGM in patients without insulin resistance.
Although it’s not rocket science, CGM can help patients through a “carrot and stick” approach to dieting. Lean proteins, nonstarchy vegetables, and monounsaturated fats such as nuts and avocado all support weight loss and tend to keep blood glucose levels stable. In contrast, foods known to cause weight gain (eg, sugary foods, refined starches, and processed foods) cause sugar spikes in real time. Similarly, large portion sizes are more likely to result in sugar spikes, and pairing proteins with carbohydrates minimizes blood glucose excursions.
Though all of this is basic common sense, . And because blood glucose is influenced by myriad factors including stress, genetics and metabolism, CGM can also potentially help create personal guidance for food choices.
In addition, CGM can reveal the effect of poor sleep and stress on blood glucose levels, thereby encouraging healthier lifestyle choices. The data collected also may provide information on how different modalities of physical activity affect blood glucose levels. A recent study compared the effect of high-intensity interval training (HIIT) and continuous moderate-intensity exercise on postmeal blood glucose in overweight individuals without diabetes. CGM revealed that HIIT is more advantageous for preventing postmeal spikes.
Although CGM appears to be a sophisticated form of cognitive-behavioral therapy, I do worry that the incessant stream of information can lead to worsening anxiety, obsessive compulsive behaviors, or restrictive eating tendencies. Still, thanks to Lauren, I now believe that real-time CGM may lead to behavior modification in food selection and physical activity.
Dr. Messer, Clinical Assistant Professor, Mount Sinai School of Medicine; Associate Professor, Hofstra School of Medicine, New York, NY, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Lauren is a 45-year-old corporate lawyer who managed to excel in every aspect of her life, including parenting her three children while working full-time as a corporate lawyer. A math major at Harvard, she loves data.
Suffice it to say, given that I was treating her for a thyroid condition rather than diabetes, I was a little surprised when she requested I prescribe her a FreeStyle Libre (Abbott) monitor. She explained she was struggling to lose 10 pounds, and she thought continuous glucose monitoring (CGM) would help her determine which foods were impeding her weight loss journey.
While I didn’t see much downside to acquiescing, I felt she had probably been spending too much time on Reddit. What information could CGM give someone without diabetes that couldn’t be gleaned from a food label? Nevertheless, Lauren filled the prescription and began her foray into this relatively uncharted world. When she returned for a follow-up visit several months later, I was shocked to see that she had lost her intended weight. With my tail between my legs, I decided to review the theories and science behind the use of CGM in patients without insulin resistance.
Although it’s not rocket science, CGM can help patients through a “carrot and stick” approach to dieting. Lean proteins, nonstarchy vegetables, and monounsaturated fats such as nuts and avocado all support weight loss and tend to keep blood glucose levels stable. In contrast, foods known to cause weight gain (eg, sugary foods, refined starches, and processed foods) cause sugar spikes in real time. Similarly, large portion sizes are more likely to result in sugar spikes, and pairing proteins with carbohydrates minimizes blood glucose excursions.
Though all of this is basic common sense, . And because blood glucose is influenced by myriad factors including stress, genetics and metabolism, CGM can also potentially help create personal guidance for food choices.
In addition, CGM can reveal the effect of poor sleep and stress on blood glucose levels, thereby encouraging healthier lifestyle choices. The data collected also may provide information on how different modalities of physical activity affect blood glucose levels. A recent study compared the effect of high-intensity interval training (HIIT) and continuous moderate-intensity exercise on postmeal blood glucose in overweight individuals without diabetes. CGM revealed that HIIT is more advantageous for preventing postmeal spikes.
Although CGM appears to be a sophisticated form of cognitive-behavioral therapy, I do worry that the incessant stream of information can lead to worsening anxiety, obsessive compulsive behaviors, or restrictive eating tendencies. Still, thanks to Lauren, I now believe that real-time CGM may lead to behavior modification in food selection and physical activity.
Dr. Messer, Clinical Assistant Professor, Mount Sinai School of Medicine; Associate Professor, Hofstra School of Medicine, New York, NY, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Home HPV Testing: A New Frontier in Primary Care
Human papillomavirus (HPV) is one of the most common sexually transmitted infections and persistent infection with high-risk strains is the leading cause of cervical cancer. Fortunately, vaccines are available to prevent many HPV-related diseases, but they haven’t fully eliminated the risks. Cervical cancer screening remains essential for early detection and prevention.
The US Preventive Services Task Force (USPSTF) currently recommends regular cervical cancer screenings for women aged 21-65. These screenings can include a Pap test every 3 years, a combination of HPV testing and Pap smear every 5 years, or high-risk HPV testing alone every 5 years, depending on age and individual risk factors.
Although these guidelines are currently under review, routine screenings have been instrumental in reducing cervical cancer rates. However, many patients still face barriers that prevent them from accessing these services. Common challenges include discomfort with pelvic exams, lack of time, and limited access to healthcare services. In recent years, advancements in home-based diagnostic testing have opened new avenues for preventative care.
Home HPV testing is one such advancement, offering an alternative to traditional in-office screening methods. While the US Food and Drug Administration (FDA) has not yet approved home HPV testing, self-collection in clinical settings is available and gaining traction. Primary care physicians can integrate this self-collection method into their practices, helping to close the screening gap, especially for underserved populations.
If approved, home HPV testing could be a game-changer for patients who have difficulty attending in-person visits. Geographical barriers, transportation issues, and personal discomfort with in-office exams can prevent patients from receiving the care they need. Home testing eliminates many of these hurdles, enabling patients to perform the test in the comfort of their own homes at a time that works for them. This flexibility is particularly beneficial for rural and underserved populations, where access to healthcare is limited.
Similarly, in-office self-collection offers a comfortable alternative for those who find traditional pelvic exams uncomfortable or distressing. Self-administered HPV tests allow patients to take control of their cervical cancer screening, fostering empowerment and personal responsibility for their health. By reducing the discomfort and inconvenience of traditional screening, self-collection can improve adherence to screening guidelines, leading to earlier detection and prevention of cervical cancer.
Primary care physicians may soon offer both in-office and at-home testing options, tailoring the approach to each patient’s unique needs. Virtual appointments provide an excellent opportunity to educate patients about the importance of cervical cancer screening and offer guidance on using home HPV testing kits. This personalized care ensures patients feel supported even without in-person visits. If home testing becomes FDA approved, patients could receive test kits by mail, perform the test, and send it back to the lab for analysis. For those with positive results, primary care physicians can ensure timely follow-up, including Pap smears or colposcopies, to further evaluate cervical health.
Although home HPV testing offers many benefits, there are valid concerns about accuracy and follow-up care. Studies show that self-collected samples for HPV testing are highly accurate, with sensitivity and specificity comparable with clinician-collected samples, echoing the success of self-swabbing for other sexually transmitted infections.
It is crucial, however, that patients receive clear instructions on proper sample collection to maintain this accuracy. Follow-up care is another essential aspect of the screening process. While many HPV infections resolve on their own, high-risk strains require closer monitoring to prevent progression to cervical cancer. Primary care physicians must establish clear protocols for notifying patients of their results and ensuring appropriate follow-up appointments.
Additionally, there may be concerns about the cost and insurance coverage of home HPV tests. However, home testing could prove more cost-effective than multiple in-office visits, especially when factoring in travel expenses and missed work. Physicians should work to make home testing accessible to all patients, including those in low-income and rural communities.
Should these options become more widely available, it will be important to communicate that this does not fully eliminate the need for pelvic exams. As primary care physicians, we will still need to advise patients that they should bring up concerns of vaginal bleeding, vaginal discharge, and other symptoms. Pelvic exams will still be necessary for diagnosis when symptoms are present. Home HPV tests also will not replace in-office clinician collected exams for those who do not feel comfortable with self-collection.
Home and in-office self-collection for HPV testing are promising tools for improving cervical cancer screening rates and patient satisfaction. By offering a convenient, private, and accessible option, primary care physicians can help more patients stay on track with their preventive care and reduce their risk of cervical cancer. As this technology continues to evolve, embracing both in-office and home HPV testing will be essential to ensuring all patients benefit from these innovations.
Dr. Wheat is Vice Chair of Diversity, Equity, and Inclusion, Department of Family and Community Medicine and Associate Professor, Family and Community Medicine Feinberg School of Medicine, Northwestern University, Chicago. She serves on the editorial advisory board of Family Practice News. You can contact her at fpnews@mdedge.com.
References
Daponte N et al. HPV-Based Self-Sampling in Cervical Cancer Screening: An Updated Review of the Current Evidence in the Literature. Cancers (Basel). 2023 Mar 8;15(6):1669.
Di Gennaro G et al. Does self-sampling for human papilloma virus testing have the potential to increase cervical cancer screening? An updated meta-analysis of observational studies and randomized clinical trials. Front Public Health. 2022 Dec 8;10:1003461.
US Preventive Services Task Force. Screening for Cervical Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(7):674-686.
Human papillomavirus (HPV) is one of the most common sexually transmitted infections and persistent infection with high-risk strains is the leading cause of cervical cancer. Fortunately, vaccines are available to prevent many HPV-related diseases, but they haven’t fully eliminated the risks. Cervical cancer screening remains essential for early detection and prevention.
The US Preventive Services Task Force (USPSTF) currently recommends regular cervical cancer screenings for women aged 21-65. These screenings can include a Pap test every 3 years, a combination of HPV testing and Pap smear every 5 years, or high-risk HPV testing alone every 5 years, depending on age and individual risk factors.
Although these guidelines are currently under review, routine screenings have been instrumental in reducing cervical cancer rates. However, many patients still face barriers that prevent them from accessing these services. Common challenges include discomfort with pelvic exams, lack of time, and limited access to healthcare services. In recent years, advancements in home-based diagnostic testing have opened new avenues for preventative care.
Home HPV testing is one such advancement, offering an alternative to traditional in-office screening methods. While the US Food and Drug Administration (FDA) has not yet approved home HPV testing, self-collection in clinical settings is available and gaining traction. Primary care physicians can integrate this self-collection method into their practices, helping to close the screening gap, especially for underserved populations.
If approved, home HPV testing could be a game-changer for patients who have difficulty attending in-person visits. Geographical barriers, transportation issues, and personal discomfort with in-office exams can prevent patients from receiving the care they need. Home testing eliminates many of these hurdles, enabling patients to perform the test in the comfort of their own homes at a time that works for them. This flexibility is particularly beneficial for rural and underserved populations, where access to healthcare is limited.
Similarly, in-office self-collection offers a comfortable alternative for those who find traditional pelvic exams uncomfortable or distressing. Self-administered HPV tests allow patients to take control of their cervical cancer screening, fostering empowerment and personal responsibility for their health. By reducing the discomfort and inconvenience of traditional screening, self-collection can improve adherence to screening guidelines, leading to earlier detection and prevention of cervical cancer.
Primary care physicians may soon offer both in-office and at-home testing options, tailoring the approach to each patient’s unique needs. Virtual appointments provide an excellent opportunity to educate patients about the importance of cervical cancer screening and offer guidance on using home HPV testing kits. This personalized care ensures patients feel supported even without in-person visits. If home testing becomes FDA approved, patients could receive test kits by mail, perform the test, and send it back to the lab for analysis. For those with positive results, primary care physicians can ensure timely follow-up, including Pap smears or colposcopies, to further evaluate cervical health.
Although home HPV testing offers many benefits, there are valid concerns about accuracy and follow-up care. Studies show that self-collected samples for HPV testing are highly accurate, with sensitivity and specificity comparable with clinician-collected samples, echoing the success of self-swabbing for other sexually transmitted infections.
It is crucial, however, that patients receive clear instructions on proper sample collection to maintain this accuracy. Follow-up care is another essential aspect of the screening process. While many HPV infections resolve on their own, high-risk strains require closer monitoring to prevent progression to cervical cancer. Primary care physicians must establish clear protocols for notifying patients of their results and ensuring appropriate follow-up appointments.
Additionally, there may be concerns about the cost and insurance coverage of home HPV tests. However, home testing could prove more cost-effective than multiple in-office visits, especially when factoring in travel expenses and missed work. Physicians should work to make home testing accessible to all patients, including those in low-income and rural communities.
Should these options become more widely available, it will be important to communicate that this does not fully eliminate the need for pelvic exams. As primary care physicians, we will still need to advise patients that they should bring up concerns of vaginal bleeding, vaginal discharge, and other symptoms. Pelvic exams will still be necessary for diagnosis when symptoms are present. Home HPV tests also will not replace in-office clinician collected exams for those who do not feel comfortable with self-collection.
Home and in-office self-collection for HPV testing are promising tools for improving cervical cancer screening rates and patient satisfaction. By offering a convenient, private, and accessible option, primary care physicians can help more patients stay on track with their preventive care and reduce their risk of cervical cancer. As this technology continues to evolve, embracing both in-office and home HPV testing will be essential to ensuring all patients benefit from these innovations.
Dr. Wheat is Vice Chair of Diversity, Equity, and Inclusion, Department of Family and Community Medicine and Associate Professor, Family and Community Medicine Feinberg School of Medicine, Northwestern University, Chicago. She serves on the editorial advisory board of Family Practice News. You can contact her at fpnews@mdedge.com.
References
Daponte N et al. HPV-Based Self-Sampling in Cervical Cancer Screening: An Updated Review of the Current Evidence in the Literature. Cancers (Basel). 2023 Mar 8;15(6):1669.
Di Gennaro G et al. Does self-sampling for human papilloma virus testing have the potential to increase cervical cancer screening? An updated meta-analysis of observational studies and randomized clinical trials. Front Public Health. 2022 Dec 8;10:1003461.
US Preventive Services Task Force. Screening for Cervical Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(7):674-686.
Human papillomavirus (HPV) is one of the most common sexually transmitted infections and persistent infection with high-risk strains is the leading cause of cervical cancer. Fortunately, vaccines are available to prevent many HPV-related diseases, but they haven’t fully eliminated the risks. Cervical cancer screening remains essential for early detection and prevention.
The US Preventive Services Task Force (USPSTF) currently recommends regular cervical cancer screenings for women aged 21-65. These screenings can include a Pap test every 3 years, a combination of HPV testing and Pap smear every 5 years, or high-risk HPV testing alone every 5 years, depending on age and individual risk factors.
Although these guidelines are currently under review, routine screenings have been instrumental in reducing cervical cancer rates. However, many patients still face barriers that prevent them from accessing these services. Common challenges include discomfort with pelvic exams, lack of time, and limited access to healthcare services. In recent years, advancements in home-based diagnostic testing have opened new avenues for preventative care.
Home HPV testing is one such advancement, offering an alternative to traditional in-office screening methods. While the US Food and Drug Administration (FDA) has not yet approved home HPV testing, self-collection in clinical settings is available and gaining traction. Primary care physicians can integrate this self-collection method into their practices, helping to close the screening gap, especially for underserved populations.
If approved, home HPV testing could be a game-changer for patients who have difficulty attending in-person visits. Geographical barriers, transportation issues, and personal discomfort with in-office exams can prevent patients from receiving the care they need. Home testing eliminates many of these hurdles, enabling patients to perform the test in the comfort of their own homes at a time that works for them. This flexibility is particularly beneficial for rural and underserved populations, where access to healthcare is limited.
Similarly, in-office self-collection offers a comfortable alternative for those who find traditional pelvic exams uncomfortable or distressing. Self-administered HPV tests allow patients to take control of their cervical cancer screening, fostering empowerment and personal responsibility for their health. By reducing the discomfort and inconvenience of traditional screening, self-collection can improve adherence to screening guidelines, leading to earlier detection and prevention of cervical cancer.
Primary care physicians may soon offer both in-office and at-home testing options, tailoring the approach to each patient’s unique needs. Virtual appointments provide an excellent opportunity to educate patients about the importance of cervical cancer screening and offer guidance on using home HPV testing kits. This personalized care ensures patients feel supported even without in-person visits. If home testing becomes FDA approved, patients could receive test kits by mail, perform the test, and send it back to the lab for analysis. For those with positive results, primary care physicians can ensure timely follow-up, including Pap smears or colposcopies, to further evaluate cervical health.
Although home HPV testing offers many benefits, there are valid concerns about accuracy and follow-up care. Studies show that self-collected samples for HPV testing are highly accurate, with sensitivity and specificity comparable with clinician-collected samples, echoing the success of self-swabbing for other sexually transmitted infections.
It is crucial, however, that patients receive clear instructions on proper sample collection to maintain this accuracy. Follow-up care is another essential aspect of the screening process. While many HPV infections resolve on their own, high-risk strains require closer monitoring to prevent progression to cervical cancer. Primary care physicians must establish clear protocols for notifying patients of their results and ensuring appropriate follow-up appointments.
Additionally, there may be concerns about the cost and insurance coverage of home HPV tests. However, home testing could prove more cost-effective than multiple in-office visits, especially when factoring in travel expenses and missed work. Physicians should work to make home testing accessible to all patients, including those in low-income and rural communities.
Should these options become more widely available, it will be important to communicate that this does not fully eliminate the need for pelvic exams. As primary care physicians, we will still need to advise patients that they should bring up concerns of vaginal bleeding, vaginal discharge, and other symptoms. Pelvic exams will still be necessary for diagnosis when symptoms are present. Home HPV tests also will not replace in-office clinician collected exams for those who do not feel comfortable with self-collection.
Home and in-office self-collection for HPV testing are promising tools for improving cervical cancer screening rates and patient satisfaction. By offering a convenient, private, and accessible option, primary care physicians can help more patients stay on track with their preventive care and reduce their risk of cervical cancer. As this technology continues to evolve, embracing both in-office and home HPV testing will be essential to ensuring all patients benefit from these innovations.
Dr. Wheat is Vice Chair of Diversity, Equity, and Inclusion, Department of Family and Community Medicine and Associate Professor, Family and Community Medicine Feinberg School of Medicine, Northwestern University, Chicago. She serves on the editorial advisory board of Family Practice News. You can contact her at fpnews@mdedge.com.
References
Daponte N et al. HPV-Based Self-Sampling in Cervical Cancer Screening: An Updated Review of the Current Evidence in the Literature. Cancers (Basel). 2023 Mar 8;15(6):1669.
Di Gennaro G et al. Does self-sampling for human papilloma virus testing have the potential to increase cervical cancer screening? An updated meta-analysis of observational studies and randomized clinical trials. Front Public Health. 2022 Dec 8;10:1003461.
US Preventive Services Task Force. Screening for Cervical Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(7):674-686.
How Are Doctors Using Tirzepatide vs Semaglutide? A Q&A
When prescribing glucagon-like peptide 1 (GLP-1) medications, many physicians prefer tirzepatide over the more well-known semaglutide due to its superior efficacy in weight loss and A1c reduction. Studies indicated that tirzepatide can lead to greater weight loss than semaglutide.
Factors like insurance coverage, drug availability, and side effects also influence physicians’ choices, with some patients benefiting from the broader dosing options that tirzepatide offers.
In this Q&A, Medscape Medical News explored how physicians can make the best decisions with their patients when choosing between GLP-1 medications tirzepatide and semaglutide for the treatment for type 2 diabetes and obesity.
We spoke to physicians who specialize in medical weight loss on things to consider when choosing between these two medications, such as patient profiles, drug access and availability, and financial considerations. We also discussed the side effect profiles of the medications based on current data in the literature.
Medscape Medical News: How are you deciding which of the two drugs to prescribe?
Caroline Messer, MD, endocrinologist at Lenox Hill Hospital, Northwell, New York City: To some degree, it’s based on insurance. But in general, I’m pushing most patients toward tirzepatide just because the data show that there’s more weight loss and more A1c reduction on tirzepatide. But the research shows that there are more side effects. But I think every practicing clinician who uses these medications knows that there are actually fewer side effects despite what the trial showed.
Sue Decotiis, MD, weight loss doctor, New York City: I think that many doctors that are prescribing these drugs are not really weight loss specialists. It’s just like one of many drugs that they prescribe. And semaglutide (Ozempic) is more well known. I think it’s because they don’t really know that it’s not as good as the other drugs. There are still massive shortages of these drugs. So that’s another reason why a doctor may choose one drug over another. Also, if a patient’s reliant on insurance to cover it, they may go with whatever the insurance company is willing to cover.
Kathleen Dungan, MD, professor of internal medicine, Division of Endocrinology, Diabetes and Metabolism, The Ohio State University Wexner Medical Center and College of Medicine: Some patients may have preferences with the delivery device. In the past year, in particular, availability of these drugs was limited and varied from time to time and geographically, and therefore, patients needed to substitute one drug for another in order to maintain treatment.
Maria Teresa Anton, MD, endocrinologist and educator, Pritikin Longevity Center, Miami: While I do not prescribe these medications, I do focus on integrating them into a comprehensive lifestyle program that empowers patients to make sustainable changes. By fostering an environment of education and support, we enhance their well-being and promote long-term health outcomes. In my practice, I’ve found that the most successful outcomes occur when these medications are combined with a comprehensive approach, including dietary changes, physical activity, and behavioral support.
Medscape Medical News: How do you make the decision of tirzepatide vs semaglutide?
Messer: There’s no guideline per se. Sometimes when I don’t want a patient to lose too much weight, I might consider Ozempic or Wegovy if you know they only have 5 lb to lose. If diabetes, then I might go for the Ozempic instead, just because the weight loss is so drastic with tirzepatide with any kind of appetite.
Decotiis: If somebody has a lot of weight to lose and they’re highly insulin resistant, as most people are when they start these drugs, I really prefer tirzepatide ... because I think patients are going to lose more weight, they’re going to lose more fat. I also see that patients have less side effects because before tirzepatide came out, I was prescribing mostly semaglutide, and there were a lot of side effects. But semaglutide is fine. I mean, it’s a good drug. Maybe it’s better for people that don’t have as much weight to lose. So I don’t have to worry about them hitting that wall after a certain period of time. But it’s a good drug. I mean, I certainly still use it.
Medscape Medical News: What of the data and the literature on the differences in the outcomes and the side effect profile?
Messer: In terms of outcomes, the weight loss is almost double [with tirzepatide]. It depends what trial you’re looking at, but we tend to see like about 15% of your body weight you lose with the semaglutide and 25%-30% with the tirzepatide. The big difference, I suppose…is semaglutide now has a cardiovascular indication and the tirzepatide doesn’t, but I’m very confident that tirzepatide is going to get the same indication.
Decotiis: When that first Lilly study came out in June of 2022, it really blew everybody away. I mean, some patients lost up to 25% of their weight on tirzepatide, whereas on Ozempic, it was really like 15%. Now, in my practice, I really monitor everyone with a body composition scale. I’m not just looking at somebody’s weight or body mass index, I am looking at how much body fat they have, how much muscle mass they have, how much water they have, and how much bone they have.
The golden rule here is make sure the patient loses fat, and you want to make sure they’re not losing muscle or too much water. The patient really needs to be adequately hydrated. So what I’m saying is a lot of people who have lost weight have not reached the promised land because they haven’t lost enough body fat to get them into that healthy zone. But once they reduce the body fat to a certain percentage, let’s say for a woman about 20%, or a man in the low teens, they’re less likely to regain that weight because they haven’t really lost fat. And that’s how we gain health.
A version of this article first appeared on Medscape.com.
When prescribing glucagon-like peptide 1 (GLP-1) medications, many physicians prefer tirzepatide over the more well-known semaglutide due to its superior efficacy in weight loss and A1c reduction. Studies indicated that tirzepatide can lead to greater weight loss than semaglutide.
Factors like insurance coverage, drug availability, and side effects also influence physicians’ choices, with some patients benefiting from the broader dosing options that tirzepatide offers.
In this Q&A, Medscape Medical News explored how physicians can make the best decisions with their patients when choosing between GLP-1 medications tirzepatide and semaglutide for the treatment for type 2 diabetes and obesity.
We spoke to physicians who specialize in medical weight loss on things to consider when choosing between these two medications, such as patient profiles, drug access and availability, and financial considerations. We also discussed the side effect profiles of the medications based on current data in the literature.
Medscape Medical News: How are you deciding which of the two drugs to prescribe?
Caroline Messer, MD, endocrinologist at Lenox Hill Hospital, Northwell, New York City: To some degree, it’s based on insurance. But in general, I’m pushing most patients toward tirzepatide just because the data show that there’s more weight loss and more A1c reduction on tirzepatide. But the research shows that there are more side effects. But I think every practicing clinician who uses these medications knows that there are actually fewer side effects despite what the trial showed.
Sue Decotiis, MD, weight loss doctor, New York City: I think that many doctors that are prescribing these drugs are not really weight loss specialists. It’s just like one of many drugs that they prescribe. And semaglutide (Ozempic) is more well known. I think it’s because they don’t really know that it’s not as good as the other drugs. There are still massive shortages of these drugs. So that’s another reason why a doctor may choose one drug over another. Also, if a patient’s reliant on insurance to cover it, they may go with whatever the insurance company is willing to cover.
Kathleen Dungan, MD, professor of internal medicine, Division of Endocrinology, Diabetes and Metabolism, The Ohio State University Wexner Medical Center and College of Medicine: Some patients may have preferences with the delivery device. In the past year, in particular, availability of these drugs was limited and varied from time to time and geographically, and therefore, patients needed to substitute one drug for another in order to maintain treatment.
Maria Teresa Anton, MD, endocrinologist and educator, Pritikin Longevity Center, Miami: While I do not prescribe these medications, I do focus on integrating them into a comprehensive lifestyle program that empowers patients to make sustainable changes. By fostering an environment of education and support, we enhance their well-being and promote long-term health outcomes. In my practice, I’ve found that the most successful outcomes occur when these medications are combined with a comprehensive approach, including dietary changes, physical activity, and behavioral support.
Medscape Medical News: How do you make the decision of tirzepatide vs semaglutide?
Messer: There’s no guideline per se. Sometimes when I don’t want a patient to lose too much weight, I might consider Ozempic or Wegovy if you know they only have 5 lb to lose. If diabetes, then I might go for the Ozempic instead, just because the weight loss is so drastic with tirzepatide with any kind of appetite.
Decotiis: If somebody has a lot of weight to lose and they’re highly insulin resistant, as most people are when they start these drugs, I really prefer tirzepatide ... because I think patients are going to lose more weight, they’re going to lose more fat. I also see that patients have less side effects because before tirzepatide came out, I was prescribing mostly semaglutide, and there were a lot of side effects. But semaglutide is fine. I mean, it’s a good drug. Maybe it’s better for people that don’t have as much weight to lose. So I don’t have to worry about them hitting that wall after a certain period of time. But it’s a good drug. I mean, I certainly still use it.
Medscape Medical News: What of the data and the literature on the differences in the outcomes and the side effect profile?
Messer: In terms of outcomes, the weight loss is almost double [with tirzepatide]. It depends what trial you’re looking at, but we tend to see like about 15% of your body weight you lose with the semaglutide and 25%-30% with the tirzepatide. The big difference, I suppose…is semaglutide now has a cardiovascular indication and the tirzepatide doesn’t, but I’m very confident that tirzepatide is going to get the same indication.
Decotiis: When that first Lilly study came out in June of 2022, it really blew everybody away. I mean, some patients lost up to 25% of their weight on tirzepatide, whereas on Ozempic, it was really like 15%. Now, in my practice, I really monitor everyone with a body composition scale. I’m not just looking at somebody’s weight or body mass index, I am looking at how much body fat they have, how much muscle mass they have, how much water they have, and how much bone they have.
The golden rule here is make sure the patient loses fat, and you want to make sure they’re not losing muscle or too much water. The patient really needs to be adequately hydrated. So what I’m saying is a lot of people who have lost weight have not reached the promised land because they haven’t lost enough body fat to get them into that healthy zone. But once they reduce the body fat to a certain percentage, let’s say for a woman about 20%, or a man in the low teens, they’re less likely to regain that weight because they haven’t really lost fat. And that’s how we gain health.
A version of this article first appeared on Medscape.com.
When prescribing glucagon-like peptide 1 (GLP-1) medications, many physicians prefer tirzepatide over the more well-known semaglutide due to its superior efficacy in weight loss and A1c reduction. Studies indicated that tirzepatide can lead to greater weight loss than semaglutide.
Factors like insurance coverage, drug availability, and side effects also influence physicians’ choices, with some patients benefiting from the broader dosing options that tirzepatide offers.
In this Q&A, Medscape Medical News explored how physicians can make the best decisions with their patients when choosing between GLP-1 medications tirzepatide and semaglutide for the treatment for type 2 diabetes and obesity.
We spoke to physicians who specialize in medical weight loss on things to consider when choosing between these two medications, such as patient profiles, drug access and availability, and financial considerations. We also discussed the side effect profiles of the medications based on current data in the literature.
Medscape Medical News: How are you deciding which of the two drugs to prescribe?
Caroline Messer, MD, endocrinologist at Lenox Hill Hospital, Northwell, New York City: To some degree, it’s based on insurance. But in general, I’m pushing most patients toward tirzepatide just because the data show that there’s more weight loss and more A1c reduction on tirzepatide. But the research shows that there are more side effects. But I think every practicing clinician who uses these medications knows that there are actually fewer side effects despite what the trial showed.
Sue Decotiis, MD, weight loss doctor, New York City: I think that many doctors that are prescribing these drugs are not really weight loss specialists. It’s just like one of many drugs that they prescribe. And semaglutide (Ozempic) is more well known. I think it’s because they don’t really know that it’s not as good as the other drugs. There are still massive shortages of these drugs. So that’s another reason why a doctor may choose one drug over another. Also, if a patient’s reliant on insurance to cover it, they may go with whatever the insurance company is willing to cover.
Kathleen Dungan, MD, professor of internal medicine, Division of Endocrinology, Diabetes and Metabolism, The Ohio State University Wexner Medical Center and College of Medicine: Some patients may have preferences with the delivery device. In the past year, in particular, availability of these drugs was limited and varied from time to time and geographically, and therefore, patients needed to substitute one drug for another in order to maintain treatment.
Maria Teresa Anton, MD, endocrinologist and educator, Pritikin Longevity Center, Miami: While I do not prescribe these medications, I do focus on integrating them into a comprehensive lifestyle program that empowers patients to make sustainable changes. By fostering an environment of education and support, we enhance their well-being and promote long-term health outcomes. In my practice, I’ve found that the most successful outcomes occur when these medications are combined with a comprehensive approach, including dietary changes, physical activity, and behavioral support.
Medscape Medical News: How do you make the decision of tirzepatide vs semaglutide?
Messer: There’s no guideline per se. Sometimes when I don’t want a patient to lose too much weight, I might consider Ozempic or Wegovy if you know they only have 5 lb to lose. If diabetes, then I might go for the Ozempic instead, just because the weight loss is so drastic with tirzepatide with any kind of appetite.
Decotiis: If somebody has a lot of weight to lose and they’re highly insulin resistant, as most people are when they start these drugs, I really prefer tirzepatide ... because I think patients are going to lose more weight, they’re going to lose more fat. I also see that patients have less side effects because before tirzepatide came out, I was prescribing mostly semaglutide, and there were a lot of side effects. But semaglutide is fine. I mean, it’s a good drug. Maybe it’s better for people that don’t have as much weight to lose. So I don’t have to worry about them hitting that wall after a certain period of time. But it’s a good drug. I mean, I certainly still use it.
Medscape Medical News: What of the data and the literature on the differences in the outcomes and the side effect profile?
Messer: In terms of outcomes, the weight loss is almost double [with tirzepatide]. It depends what trial you’re looking at, but we tend to see like about 15% of your body weight you lose with the semaglutide and 25%-30% with the tirzepatide. The big difference, I suppose…is semaglutide now has a cardiovascular indication and the tirzepatide doesn’t, but I’m very confident that tirzepatide is going to get the same indication.
Decotiis: When that first Lilly study came out in June of 2022, it really blew everybody away. I mean, some patients lost up to 25% of their weight on tirzepatide, whereas on Ozempic, it was really like 15%. Now, in my practice, I really monitor everyone with a body composition scale. I’m not just looking at somebody’s weight or body mass index, I am looking at how much body fat they have, how much muscle mass they have, how much water they have, and how much bone they have.
The golden rule here is make sure the patient loses fat, and you want to make sure they’re not losing muscle or too much water. The patient really needs to be adequately hydrated. So what I’m saying is a lot of people who have lost weight have not reached the promised land because they haven’t lost enough body fat to get them into that healthy zone. But once they reduce the body fat to a certain percentage, let’s say for a woman about 20%, or a man in the low teens, they’re less likely to regain that weight because they haven’t really lost fat. And that’s how we gain health.
A version of this article first appeared on Medscape.com.
Sex After Pregnancy: Why It Matters and How to Start the Conversation
Sarah, a new mom who’s thrilled about her 3-month-old baby, is struggling with her sex life. Her once vibrant physical relationship with her partner has dwindled, and she’s dealing with painful intercourse and a notable drop in desire.
Pregnancy and childbirth are transformative experiences that affect every facet of a person’s life, including their sexual well-being. Despite this fact, clinicians frequently ignore sexual well-being, beyond contraception, in prenatal and postpartum care. In peripartum care, anticipatory guidance is recognized to be crucial to the well-being of new parents and their babies. Why should sexual well-being get the shaft?
Why Talk About Sex?
Sex is a fundamental aspect of many people’s lives and relationships and can significantly affect overall well-being. Despite cultural narratives that often exclude the sexual function and pleasure aspect of sexual health from peripartum discussions, many new parents face sexual challenges that can worsen their physical and emotional health.
While up to 88% of new parents report problems with sexual well-being, less than 30% report receiving anticipatory guidance about sexual function changes. One study found only 15% of postpartum women reported discussing sexual concerns with their medical providers. And, when new parents receive more information about sexual health, they tend to report improved sexual well-being. Clearly, a gap needs bridging.
Sexual health doesn’t just affect individual well-being; it intertwines with relationship satisfaction. Attending to satisfaction in one’s relationship may be an important component of child health as well.
Declines in the frequency of sexual engagement and desire are common after childbirth. Changes in arousal, orgasm, and sexual pleasure, often accompanied by pain, are also reported by many women. Some birthing parents report changes to the sensation of their genitals that are thought to be related to stretch of the pudendal nerve during parturition. Most experience resolution of these concerns within the first year after childbirth, although some women report persistent problems, including up to 33% with persistent sexual pain.
Many factors can contribute to postpartum sexual issues, including hormonal changes, body image concerns, and mental health conditions. Breastfeeding, for instance, can lead to vaginal dryness and reduced sexual arousal due to hormonal shifts. Body image issues and mood disorders like depression and anxiety can also adversely affect sexual function. Women with postpartum depression are more likely to experience sexual concerns, and the relationship between sexual difficulties and depression can be bidirectional.
Empowerment and Expectations
One commonly cited recommendation is to wait until 6 weeks postpartum before resuming penetrative intercourse after a normal vaginal delivery. However, this guideline lacks robust scientific backing. Many people might feel ready for sexual intercourse much sooner or, conversely, might not feel comfortable at the 6-week mark. As clinicians, we must empower our patients to trust their own bodies and make decisions based on their comfort and readiness.
The 6-week advice can sometimes unintentionally convey to women that they are not experts on their own bodies, or that any kind of sex is risky. Acknowledging the recovery timeline for every person is unique and various forms of sexual expression are safe can help foster a healthier approach to resuming sexual activities. In one study of postpartum sexual behavior, in the first 6 weeks after delivery, the most common kinds of sexual play included giving oral sex to a partner and solo sex. Between 80% and 90% have resumed vaginal-receiving sexual play (including intercourse) by 3 months.
While recognizing that changes to sexual experience occur, we need to reinforce that gradual recovery is expected. And if women express distress about a sexual change, or if those changes persist, primary care providers should be prepared to help them with their concerns.
Parents need to know experiencing pain is not something they should “just deal with” or ignore. Attempting to repeatedly endure sexual pain can cause new issues, such as high-tone dysfunction of the pelvic floor or an understandable decrease in willingness or receptiveness to sexual play of any kind. Encouraging open communication about these issues can help couples navigate these changes more smoothly.
Partners, especially new fathers, also experience sexual and emotional challenges. They can feel blindsided by the changes in their relationship and might struggle with feelings of jealousy or inadequacy. Understanding partners also face difficulties can help in providing a more comprehensive approach to sexual health care.
Starting the Conversation
So, how can we initiate these important conversations with new parents? Start by providing permission. As healthcare providers, we need to create an environment where discussing sexual health is normalized and welcomed. Simple, nonjudgmental statements can open the door to these discussions. For example, saying, “Many people notice changes in their sexual desire or pleasure after childbirth. Has anything like this happened to you or your partner?” can encourage patients to share their concerns.
Assessing the importance to patients of sexual problems can help direct the need for intervention. Follow up on these concerns and offer support, whether through counseling, pelvic floor physical therapy, or a referral to a sexual medicine specialist, a sex therapist, or other appropriate resource.
Let’s return to Sarah. In the ideal world, at 3 months postpartum she will already have had a handful of clinical conversations about her sexual well-being with her healthcare team — at prenatal visits, at well-baby visits, and at her postpartum checkups. Several of these conversations included her partner. They both understand the transition to parenthood could be rocky for their sex lives. They’ve set aside time to connect and stay physically close. She’s listened to her body and only engaged in sexual play for which she feels ready. Now, noting that some aspects of sexual play are persistently uncomfortable, she knows it’s time to follow up. Without shame or anxiety, she books an appointment with you, knowing that you understand how important this issue is for her, her partner, and her baby.
If you’re working with new parents, remember: Open dialogue about sexual health is not just beneficial — it’s essential. Let’s bridge the gap in care by embracing these conversations and offering the support new parents truly need.
Dr. Kranz, Clinical Assistant Professor of Obstetrics/Gynecology and Family Medicine, University of Rochester Medical Center, Rochester, New York, has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sarah, a new mom who’s thrilled about her 3-month-old baby, is struggling with her sex life. Her once vibrant physical relationship with her partner has dwindled, and she’s dealing with painful intercourse and a notable drop in desire.
Pregnancy and childbirth are transformative experiences that affect every facet of a person’s life, including their sexual well-being. Despite this fact, clinicians frequently ignore sexual well-being, beyond contraception, in prenatal and postpartum care. In peripartum care, anticipatory guidance is recognized to be crucial to the well-being of new parents and their babies. Why should sexual well-being get the shaft?
Why Talk About Sex?
Sex is a fundamental aspect of many people’s lives and relationships and can significantly affect overall well-being. Despite cultural narratives that often exclude the sexual function and pleasure aspect of sexual health from peripartum discussions, many new parents face sexual challenges that can worsen their physical and emotional health.
While up to 88% of new parents report problems with sexual well-being, less than 30% report receiving anticipatory guidance about sexual function changes. One study found only 15% of postpartum women reported discussing sexual concerns with their medical providers. And, when new parents receive more information about sexual health, they tend to report improved sexual well-being. Clearly, a gap needs bridging.
Sexual health doesn’t just affect individual well-being; it intertwines with relationship satisfaction. Attending to satisfaction in one’s relationship may be an important component of child health as well.
Declines in the frequency of sexual engagement and desire are common after childbirth. Changes in arousal, orgasm, and sexual pleasure, often accompanied by pain, are also reported by many women. Some birthing parents report changes to the sensation of their genitals that are thought to be related to stretch of the pudendal nerve during parturition. Most experience resolution of these concerns within the first year after childbirth, although some women report persistent problems, including up to 33% with persistent sexual pain.
Many factors can contribute to postpartum sexual issues, including hormonal changes, body image concerns, and mental health conditions. Breastfeeding, for instance, can lead to vaginal dryness and reduced sexual arousal due to hormonal shifts. Body image issues and mood disorders like depression and anxiety can also adversely affect sexual function. Women with postpartum depression are more likely to experience sexual concerns, and the relationship between sexual difficulties and depression can be bidirectional.
Empowerment and Expectations
One commonly cited recommendation is to wait until 6 weeks postpartum before resuming penetrative intercourse after a normal vaginal delivery. However, this guideline lacks robust scientific backing. Many people might feel ready for sexual intercourse much sooner or, conversely, might not feel comfortable at the 6-week mark. As clinicians, we must empower our patients to trust their own bodies and make decisions based on their comfort and readiness.
The 6-week advice can sometimes unintentionally convey to women that they are not experts on their own bodies, or that any kind of sex is risky. Acknowledging the recovery timeline for every person is unique and various forms of sexual expression are safe can help foster a healthier approach to resuming sexual activities. In one study of postpartum sexual behavior, in the first 6 weeks after delivery, the most common kinds of sexual play included giving oral sex to a partner and solo sex. Between 80% and 90% have resumed vaginal-receiving sexual play (including intercourse) by 3 months.
While recognizing that changes to sexual experience occur, we need to reinforce that gradual recovery is expected. And if women express distress about a sexual change, or if those changes persist, primary care providers should be prepared to help them with their concerns.
Parents need to know experiencing pain is not something they should “just deal with” or ignore. Attempting to repeatedly endure sexual pain can cause new issues, such as high-tone dysfunction of the pelvic floor or an understandable decrease in willingness or receptiveness to sexual play of any kind. Encouraging open communication about these issues can help couples navigate these changes more smoothly.
Partners, especially new fathers, also experience sexual and emotional challenges. They can feel blindsided by the changes in their relationship and might struggle with feelings of jealousy or inadequacy. Understanding partners also face difficulties can help in providing a more comprehensive approach to sexual health care.
Starting the Conversation
So, how can we initiate these important conversations with new parents? Start by providing permission. As healthcare providers, we need to create an environment where discussing sexual health is normalized and welcomed. Simple, nonjudgmental statements can open the door to these discussions. For example, saying, “Many people notice changes in their sexual desire or pleasure after childbirth. Has anything like this happened to you or your partner?” can encourage patients to share their concerns.
Assessing the importance to patients of sexual problems can help direct the need for intervention. Follow up on these concerns and offer support, whether through counseling, pelvic floor physical therapy, or a referral to a sexual medicine specialist, a sex therapist, or other appropriate resource.
Let’s return to Sarah. In the ideal world, at 3 months postpartum she will already have had a handful of clinical conversations about her sexual well-being with her healthcare team — at prenatal visits, at well-baby visits, and at her postpartum checkups. Several of these conversations included her partner. They both understand the transition to parenthood could be rocky for their sex lives. They’ve set aside time to connect and stay physically close. She’s listened to her body and only engaged in sexual play for which she feels ready. Now, noting that some aspects of sexual play are persistently uncomfortable, she knows it’s time to follow up. Without shame or anxiety, she books an appointment with you, knowing that you understand how important this issue is for her, her partner, and her baby.
If you’re working with new parents, remember: Open dialogue about sexual health is not just beneficial — it’s essential. Let’s bridge the gap in care by embracing these conversations and offering the support new parents truly need.
Dr. Kranz, Clinical Assistant Professor of Obstetrics/Gynecology and Family Medicine, University of Rochester Medical Center, Rochester, New York, has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sarah, a new mom who’s thrilled about her 3-month-old baby, is struggling with her sex life. Her once vibrant physical relationship with her partner has dwindled, and she’s dealing with painful intercourse and a notable drop in desire.
Pregnancy and childbirth are transformative experiences that affect every facet of a person’s life, including their sexual well-being. Despite this fact, clinicians frequently ignore sexual well-being, beyond contraception, in prenatal and postpartum care. In peripartum care, anticipatory guidance is recognized to be crucial to the well-being of new parents and their babies. Why should sexual well-being get the shaft?
Why Talk About Sex?
Sex is a fundamental aspect of many people’s lives and relationships and can significantly affect overall well-being. Despite cultural narratives that often exclude the sexual function and pleasure aspect of sexual health from peripartum discussions, many new parents face sexual challenges that can worsen their physical and emotional health.
While up to 88% of new parents report problems with sexual well-being, less than 30% report receiving anticipatory guidance about sexual function changes. One study found only 15% of postpartum women reported discussing sexual concerns with their medical providers. And, when new parents receive more information about sexual health, they tend to report improved sexual well-being. Clearly, a gap needs bridging.
Sexual health doesn’t just affect individual well-being; it intertwines with relationship satisfaction. Attending to satisfaction in one’s relationship may be an important component of child health as well.
Declines in the frequency of sexual engagement and desire are common after childbirth. Changes in arousal, orgasm, and sexual pleasure, often accompanied by pain, are also reported by many women. Some birthing parents report changes to the sensation of their genitals that are thought to be related to stretch of the pudendal nerve during parturition. Most experience resolution of these concerns within the first year after childbirth, although some women report persistent problems, including up to 33% with persistent sexual pain.
Many factors can contribute to postpartum sexual issues, including hormonal changes, body image concerns, and mental health conditions. Breastfeeding, for instance, can lead to vaginal dryness and reduced sexual arousal due to hormonal shifts. Body image issues and mood disorders like depression and anxiety can also adversely affect sexual function. Women with postpartum depression are more likely to experience sexual concerns, and the relationship between sexual difficulties and depression can be bidirectional.
Empowerment and Expectations
One commonly cited recommendation is to wait until 6 weeks postpartum before resuming penetrative intercourse after a normal vaginal delivery. However, this guideline lacks robust scientific backing. Many people might feel ready for sexual intercourse much sooner or, conversely, might not feel comfortable at the 6-week mark. As clinicians, we must empower our patients to trust their own bodies and make decisions based on their comfort and readiness.
The 6-week advice can sometimes unintentionally convey to women that they are not experts on their own bodies, or that any kind of sex is risky. Acknowledging the recovery timeline for every person is unique and various forms of sexual expression are safe can help foster a healthier approach to resuming sexual activities. In one study of postpartum sexual behavior, in the first 6 weeks after delivery, the most common kinds of sexual play included giving oral sex to a partner and solo sex. Between 80% and 90% have resumed vaginal-receiving sexual play (including intercourse) by 3 months.
While recognizing that changes to sexual experience occur, we need to reinforce that gradual recovery is expected. And if women express distress about a sexual change, or if those changes persist, primary care providers should be prepared to help them with their concerns.
Parents need to know experiencing pain is not something they should “just deal with” or ignore. Attempting to repeatedly endure sexual pain can cause new issues, such as high-tone dysfunction of the pelvic floor or an understandable decrease in willingness or receptiveness to sexual play of any kind. Encouraging open communication about these issues can help couples navigate these changes more smoothly.
Partners, especially new fathers, also experience sexual and emotional challenges. They can feel blindsided by the changes in their relationship and might struggle with feelings of jealousy or inadequacy. Understanding partners also face difficulties can help in providing a more comprehensive approach to sexual health care.
Starting the Conversation
So, how can we initiate these important conversations with new parents? Start by providing permission. As healthcare providers, we need to create an environment where discussing sexual health is normalized and welcomed. Simple, nonjudgmental statements can open the door to these discussions. For example, saying, “Many people notice changes in their sexual desire or pleasure after childbirth. Has anything like this happened to you or your partner?” can encourage patients to share their concerns.
Assessing the importance to patients of sexual problems can help direct the need for intervention. Follow up on these concerns and offer support, whether through counseling, pelvic floor physical therapy, or a referral to a sexual medicine specialist, a sex therapist, or other appropriate resource.
Let’s return to Sarah. In the ideal world, at 3 months postpartum she will already have had a handful of clinical conversations about her sexual well-being with her healthcare team — at prenatal visits, at well-baby visits, and at her postpartum checkups. Several of these conversations included her partner. They both understand the transition to parenthood could be rocky for their sex lives. They’ve set aside time to connect and stay physically close. She’s listened to her body and only engaged in sexual play for which she feels ready. Now, noting that some aspects of sexual play are persistently uncomfortable, she knows it’s time to follow up. Without shame or anxiety, she books an appointment with you, knowing that you understand how important this issue is for her, her partner, and her baby.
If you’re working with new parents, remember: Open dialogue about sexual health is not just beneficial — it’s essential. Let’s bridge the gap in care by embracing these conversations and offering the support new parents truly need.
Dr. Kranz, Clinical Assistant Professor of Obstetrics/Gynecology and Family Medicine, University of Rochester Medical Center, Rochester, New York, has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Genitals Are a Window Into Health: Sex as a Vital Sign
This transcript has been edited for clarity.
Rachel S. Rubin, MD: I’m Dr. Rachel Rubin, a urologist and sexual medicine specialist in the Washington, DC, area. And I am so thrilled because my co-fellow, the brilliant and famous Dr. Ashley Winter, a board-certified urologist and a certified menopause practitioner, who sees patients in our practice from Los Angeles, is joining us today to talk about sex as a vital sign.
Ashley Winter, MD: To have the best sexual function, you need many different systems to work. You need your hormones to be in the right place. You need your blood vessels to dilate when you want them to. You need your nerves to connect to your genitalia to make them responsive. The way people say, “The eyes are the window into the soul” — well, the genitals are the window into the cardiovascular system, the peripheral nervous system, and the hormonal system. It’s so dynamic. Patients can understand how this reflects their health. We just need healthcare providers to hammer home how those things connect.
Rubin: If you’re a primary care doctor seeing a patient and you want to educate them on diabetes or high blood pressure, how can you “ ‘sell it with ‘sex”? How can you use sex to educate them about these important medical conditions?
Winter: I hate using it as a fear tactic, but sometimes you have to. Time and again, I’ve seen men with severe profound erectile dysfunction at a young age, with chronically uncontrolled diabetes.
Diabetes can impair the peripheral nerves, resulting in peripheral neuropathy. The same way that it can affect the fingers and toes, diabetes can affect the penis, even before those other areas. Diabetes can also lead to other conditions such as low testosterone, which also affects the function of the penis.
I’m being brutally honest when I tell patients that diabetes control is critical to having a wonderful sexspan — the duration of your life where you’re able to be sexually active and have great sex and do it in the way that you want.
Chronic conditions such as high cholesterol or hypertension can affect your ability to become erect or aroused whether you have a penis or a vulva, and even your ability to have an orgasm.
Rubin: None of my doctors has ever asked me about these issues. But we have to bring them up with patients because they›re not going to bring them up to us. I always say in the review of systems, we shouldn›t just ask, “Do you have any sexual problems?” (which nobody ever does) and move past the question about men, women or both. We should be asking, “Do you have any issues with libido? Do you want to talk about it? Any issues with erection, arousal, orgasm, or sexual pain?”
When you can talk about those things, you can treat the patient from a whole physiologic perspective. For example, how does their sciatica affect their sexual pain? How does their antidepressant cause a delayed orgasm? How does their low testosterone level affect their energy level, their libido, and their desire?
We see so much shame and guilt in sexual health, to the extent that patients feel broken. We can help them understand the anatomy and physiology and explain that they aren’t broken. Instead, it’s “You need this medicine for your crippling anxiety, and that’s why your orgasm is delayed, and so can we augment it or add or subtract something to help you with it.”
Winter: In a primary care setting, where we are considering the patient›s overall health, we strive for medication compliance, but a huge part of medication noncompliance is sexual side effects, whether it›s antidepressants, beta-blockers, birth control, or this new world of GLP-1 agonists.
Rubin: I would add breast cancer treatments. Many patients go off their anastrozole or their tamoxifen because of the sexual side effects.
Winter: This is where we get to the crux of this discussion about sex being a vital sign — something you need to check routinely. We need to become comfortable with it, because then we are unlocking the ability to treat every patient like a whole person, give them better outcomes, improve their compliance, and have a really powerful tool for education.
Rubin: We have a growing toolbox for all genders when it comes to sexual health. We have FDA- approved medications for low libido in women. We use testosterone in men in an evidence-based way to safely improve libido. We use medications to help with the genitourinary syndrome of menopause. Orgasm is a challenging one, but we have devices that can help with those reflexes. And working with people who specialize in sexual pain can be extremely helpful for patients.
Dr. Winter, having practiced in different settings, what would you tell the primary care doctors who don’t want to talk about libido or who minimize sexual complaints because they don’t know how to navigate them?
Winter: I do not envy the challenge of being a primary care provider in the healthcare world we are living in. I think it is the hardest job. The ultimate takeaway is to just normalize the conversation and be able to validate what is happening. Have a few basic tools, and then have referrals. It›s not that you have to have all the time in the world or you have to treat every condition, but you have to start the conversation, be comfortable with it, and then get patients hooked up with the right resources.
Rubin: Every doctor of every kind can connect with patients and try to understand what they care about. What are their goals? What do they want for their families, for their relationships, for their quality of life? And how can we work collaboratively as a team to help them with those things?
Sex is a huge part of people’s lives. If we don’t ask about it; if we don’t look into it; and if we don’t admit that our physiology, our medications, and our surgeries can affect sexual health and functioning, how can we improve people’s lives? We can do so much as a team when we consider sex as a true vital sign.
Dr. Rubin, Assistant Clinical Professor, Department of Urology, Georgetown University, Washington, DC, has disclosed ties with Maternal Medical, Absorption Pharmaceuticals, GlaxoSmithKline, and Endo.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Rachel S. Rubin, MD: I’m Dr. Rachel Rubin, a urologist and sexual medicine specialist in the Washington, DC, area. And I am so thrilled because my co-fellow, the brilliant and famous Dr. Ashley Winter, a board-certified urologist and a certified menopause practitioner, who sees patients in our practice from Los Angeles, is joining us today to talk about sex as a vital sign.
Ashley Winter, MD: To have the best sexual function, you need many different systems to work. You need your hormones to be in the right place. You need your blood vessels to dilate when you want them to. You need your nerves to connect to your genitalia to make them responsive. The way people say, “The eyes are the window into the soul” — well, the genitals are the window into the cardiovascular system, the peripheral nervous system, and the hormonal system. It’s so dynamic. Patients can understand how this reflects their health. We just need healthcare providers to hammer home how those things connect.
Rubin: If you’re a primary care doctor seeing a patient and you want to educate them on diabetes or high blood pressure, how can you “ ‘sell it with ‘sex”? How can you use sex to educate them about these important medical conditions?
Winter: I hate using it as a fear tactic, but sometimes you have to. Time and again, I’ve seen men with severe profound erectile dysfunction at a young age, with chronically uncontrolled diabetes.
Diabetes can impair the peripheral nerves, resulting in peripheral neuropathy. The same way that it can affect the fingers and toes, diabetes can affect the penis, even before those other areas. Diabetes can also lead to other conditions such as low testosterone, which also affects the function of the penis.
I’m being brutally honest when I tell patients that diabetes control is critical to having a wonderful sexspan — the duration of your life where you’re able to be sexually active and have great sex and do it in the way that you want.
Chronic conditions such as high cholesterol or hypertension can affect your ability to become erect or aroused whether you have a penis or a vulva, and even your ability to have an orgasm.
Rubin: None of my doctors has ever asked me about these issues. But we have to bring them up with patients because they›re not going to bring them up to us. I always say in the review of systems, we shouldn›t just ask, “Do you have any sexual problems?” (which nobody ever does) and move past the question about men, women or both. We should be asking, “Do you have any issues with libido? Do you want to talk about it? Any issues with erection, arousal, orgasm, or sexual pain?”
When you can talk about those things, you can treat the patient from a whole physiologic perspective. For example, how does their sciatica affect their sexual pain? How does their antidepressant cause a delayed orgasm? How does their low testosterone level affect their energy level, their libido, and their desire?
We see so much shame and guilt in sexual health, to the extent that patients feel broken. We can help them understand the anatomy and physiology and explain that they aren’t broken. Instead, it’s “You need this medicine for your crippling anxiety, and that’s why your orgasm is delayed, and so can we augment it or add or subtract something to help you with it.”
Winter: In a primary care setting, where we are considering the patient›s overall health, we strive for medication compliance, but a huge part of medication noncompliance is sexual side effects, whether it›s antidepressants, beta-blockers, birth control, or this new world of GLP-1 agonists.
Rubin: I would add breast cancer treatments. Many patients go off their anastrozole or their tamoxifen because of the sexual side effects.
Winter: This is where we get to the crux of this discussion about sex being a vital sign — something you need to check routinely. We need to become comfortable with it, because then we are unlocking the ability to treat every patient like a whole person, give them better outcomes, improve their compliance, and have a really powerful tool for education.
Rubin: We have a growing toolbox for all genders when it comes to sexual health. We have FDA- approved medications for low libido in women. We use testosterone in men in an evidence-based way to safely improve libido. We use medications to help with the genitourinary syndrome of menopause. Orgasm is a challenging one, but we have devices that can help with those reflexes. And working with people who specialize in sexual pain can be extremely helpful for patients.
Dr. Winter, having practiced in different settings, what would you tell the primary care doctors who don’t want to talk about libido or who minimize sexual complaints because they don’t know how to navigate them?
Winter: I do not envy the challenge of being a primary care provider in the healthcare world we are living in. I think it is the hardest job. The ultimate takeaway is to just normalize the conversation and be able to validate what is happening. Have a few basic tools, and then have referrals. It›s not that you have to have all the time in the world or you have to treat every condition, but you have to start the conversation, be comfortable with it, and then get patients hooked up with the right resources.
Rubin: Every doctor of every kind can connect with patients and try to understand what they care about. What are their goals? What do they want for their families, for their relationships, for their quality of life? And how can we work collaboratively as a team to help them with those things?
Sex is a huge part of people’s lives. If we don’t ask about it; if we don’t look into it; and if we don’t admit that our physiology, our medications, and our surgeries can affect sexual health and functioning, how can we improve people’s lives? We can do so much as a team when we consider sex as a true vital sign.
Dr. Rubin, Assistant Clinical Professor, Department of Urology, Georgetown University, Washington, DC, has disclosed ties with Maternal Medical, Absorption Pharmaceuticals, GlaxoSmithKline, and Endo.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Rachel S. Rubin, MD: I’m Dr. Rachel Rubin, a urologist and sexual medicine specialist in the Washington, DC, area. And I am so thrilled because my co-fellow, the brilliant and famous Dr. Ashley Winter, a board-certified urologist and a certified menopause practitioner, who sees patients in our practice from Los Angeles, is joining us today to talk about sex as a vital sign.
Ashley Winter, MD: To have the best sexual function, you need many different systems to work. You need your hormones to be in the right place. You need your blood vessels to dilate when you want them to. You need your nerves to connect to your genitalia to make them responsive. The way people say, “The eyes are the window into the soul” — well, the genitals are the window into the cardiovascular system, the peripheral nervous system, and the hormonal system. It’s so dynamic. Patients can understand how this reflects their health. We just need healthcare providers to hammer home how those things connect.
Rubin: If you’re a primary care doctor seeing a patient and you want to educate them on diabetes or high blood pressure, how can you “ ‘sell it with ‘sex”? How can you use sex to educate them about these important medical conditions?
Winter: I hate using it as a fear tactic, but sometimes you have to. Time and again, I’ve seen men with severe profound erectile dysfunction at a young age, with chronically uncontrolled diabetes.
Diabetes can impair the peripheral nerves, resulting in peripheral neuropathy. The same way that it can affect the fingers and toes, diabetes can affect the penis, even before those other areas. Diabetes can also lead to other conditions such as low testosterone, which also affects the function of the penis.
I’m being brutally honest when I tell patients that diabetes control is critical to having a wonderful sexspan — the duration of your life where you’re able to be sexually active and have great sex and do it in the way that you want.
Chronic conditions such as high cholesterol or hypertension can affect your ability to become erect or aroused whether you have a penis or a vulva, and even your ability to have an orgasm.
Rubin: None of my doctors has ever asked me about these issues. But we have to bring them up with patients because they›re not going to bring them up to us. I always say in the review of systems, we shouldn›t just ask, “Do you have any sexual problems?” (which nobody ever does) and move past the question about men, women or both. We should be asking, “Do you have any issues with libido? Do you want to talk about it? Any issues with erection, arousal, orgasm, or sexual pain?”
When you can talk about those things, you can treat the patient from a whole physiologic perspective. For example, how does their sciatica affect their sexual pain? How does their antidepressant cause a delayed orgasm? How does their low testosterone level affect their energy level, their libido, and their desire?
We see so much shame and guilt in sexual health, to the extent that patients feel broken. We can help them understand the anatomy and physiology and explain that they aren’t broken. Instead, it’s “You need this medicine for your crippling anxiety, and that’s why your orgasm is delayed, and so can we augment it or add or subtract something to help you with it.”
Winter: In a primary care setting, where we are considering the patient›s overall health, we strive for medication compliance, but a huge part of medication noncompliance is sexual side effects, whether it›s antidepressants, beta-blockers, birth control, or this new world of GLP-1 agonists.
Rubin: I would add breast cancer treatments. Many patients go off their anastrozole or their tamoxifen because of the sexual side effects.
Winter: This is where we get to the crux of this discussion about sex being a vital sign — something you need to check routinely. We need to become comfortable with it, because then we are unlocking the ability to treat every patient like a whole person, give them better outcomes, improve their compliance, and have a really powerful tool for education.
Rubin: We have a growing toolbox for all genders when it comes to sexual health. We have FDA- approved medications for low libido in women. We use testosterone in men in an evidence-based way to safely improve libido. We use medications to help with the genitourinary syndrome of menopause. Orgasm is a challenging one, but we have devices that can help with those reflexes. And working with people who specialize in sexual pain can be extremely helpful for patients.
Dr. Winter, having practiced in different settings, what would you tell the primary care doctors who don’t want to talk about libido or who minimize sexual complaints because they don’t know how to navigate them?
Winter: I do not envy the challenge of being a primary care provider in the healthcare world we are living in. I think it is the hardest job. The ultimate takeaway is to just normalize the conversation and be able to validate what is happening. Have a few basic tools, and then have referrals. It›s not that you have to have all the time in the world or you have to treat every condition, but you have to start the conversation, be comfortable with it, and then get patients hooked up with the right resources.
Rubin: Every doctor of every kind can connect with patients and try to understand what they care about. What are their goals? What do they want for their families, for their relationships, for their quality of life? And how can we work collaboratively as a team to help them with those things?
Sex is a huge part of people’s lives. If we don’t ask about it; if we don’t look into it; and if we don’t admit that our physiology, our medications, and our surgeries can affect sexual health and functioning, how can we improve people’s lives? We can do so much as a team when we consider sex as a true vital sign.
Dr. Rubin, Assistant Clinical Professor, Department of Urology, Georgetown University, Washington, DC, has disclosed ties with Maternal Medical, Absorption Pharmaceuticals, GlaxoSmithKline, and Endo.
A version of this article first appeared on Medscape.com.
A Brief Glimpse Into 80,000 Years of Human History
Like millions of other modern humans, my daughter and I stood in the backyard recently and watched comet C/2023 A3 (Tsuchinshan–ATLAS) with binoculars. It took a few minutes to locate, but once you see it is unmistakable.
It’s got a long (at least in human terms) orbit, roughly 80,000 years. So what was going on here, on our pale blue dot, the last time it graced our skies?
Well, here in Phoenix, the people were ... not here. Nor were they in Arizona, or North America, or pretty much the entire Western Hemisphere.
In fact, Homo sapiens were confined to Africa. The hardier Neanderthals had successfully moved into Eurasia, but our lineage was just starting to migrate there. There’s some evidence that we numbered maybe 10,000-15,000 at that point. Far more people saw the comet that night in the United States than our entire population count last time it swung by.
But we were moving up in the world. Our ancestors at the time had developed the first forms of jewelry, using seashells. There’s evidence that we’d learned to trade with other, distant, communities. We were using spears to put dinner on the table with less risk to ourselves than clubs posed.
And, in what’s now Kenya, in the same time frame, a pair of grieving parents carefully buried their 3-year-old child, wrapped in a covering and gently placed on a pillow.
Sadly, this isn’t a scene we’re unfamiliar with. Possibly the most famous painting of a physician is “The Doctor” (1891) by Luke Fildes, showing a physician trying to treat a seriously ill child while the parents look on helplessly.

What did the Kenyan child die from? We’ll probably never know. Did they try to treat it? Most likely.
Humans, by nature, form societies. The size varies, but everyone has a role. There was probably some ancestor of Fildes’ doctor in the group who tried to help. Perhaps with prayers in an unknown tongue, or a preparation of certain leaves, or placing the child near a fire. When whatever they tried failed, the same person likely consoled the parents. Maybe they were involved in the burial, too.
The child would be found in 2017, giving us the first clear evidence of a ritual human burial in Africa. Just like today, we let go of our lost ones with ceremony. Perhaps the parents noticed the comet and thought it was their child’s spirit departing.
Now the comet is back. The planet hasn’t changed dramatically in 80,000 years (which isn’t much in geological time), but we have.
Would today’s doctors have been able to save the child? No idea, though we probably have a better chance than our professional ancestor did.
But our job hasn’t changed. Like us, the ancient practitioner probably tried to figure out why the child was sick and what could be done about it. When it was over they, and others, grieved with the parents.
The comet will be back in 80,000 years. On our scale, that’s a long time. The entire recorded history of our species is only 5,000 to 8,000 years. We’ve come a long way, but where we’re going in 80,000 years is anyone’s guess.
Will doctors in the year 82024 even know what we do now to care for people? Will they still be practicing on the third rock from the sun, or spread out across the galaxy? Will there even be doctors? (Probably, in one form or another.)
But We do our best to care, heal, and hope now, as we did then, and as our descendants will.
And, like my daughter and I did, no matter where we are, we will still look up at the sky with wonder.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
Like millions of other modern humans, my daughter and I stood in the backyard recently and watched comet C/2023 A3 (Tsuchinshan–ATLAS) with binoculars. It took a few minutes to locate, but once you see it is unmistakable.
It’s got a long (at least in human terms) orbit, roughly 80,000 years. So what was going on here, on our pale blue dot, the last time it graced our skies?
Well, here in Phoenix, the people were ... not here. Nor were they in Arizona, or North America, or pretty much the entire Western Hemisphere.
In fact, Homo sapiens were confined to Africa. The hardier Neanderthals had successfully moved into Eurasia, but our lineage was just starting to migrate there. There’s some evidence that we numbered maybe 10,000-15,000 at that point. Far more people saw the comet that night in the United States than our entire population count last time it swung by.
But we were moving up in the world. Our ancestors at the time had developed the first forms of jewelry, using seashells. There’s evidence that we’d learned to trade with other, distant, communities. We were using spears to put dinner on the table with less risk to ourselves than clubs posed.
And, in what’s now Kenya, in the same time frame, a pair of grieving parents carefully buried their 3-year-old child, wrapped in a covering and gently placed on a pillow.
Sadly, this isn’t a scene we’re unfamiliar with. Possibly the most famous painting of a physician is “The Doctor” (1891) by Luke Fildes, showing a physician trying to treat a seriously ill child while the parents look on helplessly.

What did the Kenyan child die from? We’ll probably never know. Did they try to treat it? Most likely.
Humans, by nature, form societies. The size varies, but everyone has a role. There was probably some ancestor of Fildes’ doctor in the group who tried to help. Perhaps with prayers in an unknown tongue, or a preparation of certain leaves, or placing the child near a fire. When whatever they tried failed, the same person likely consoled the parents. Maybe they were involved in the burial, too.
The child would be found in 2017, giving us the first clear evidence of a ritual human burial in Africa. Just like today, we let go of our lost ones with ceremony. Perhaps the parents noticed the comet and thought it was their child’s spirit departing.
Now the comet is back. The planet hasn’t changed dramatically in 80,000 years (which isn’t much in geological time), but we have.
Would today’s doctors have been able to save the child? No idea, though we probably have a better chance than our professional ancestor did.
But our job hasn’t changed. Like us, the ancient practitioner probably tried to figure out why the child was sick and what could be done about it. When it was over they, and others, grieved with the parents.
The comet will be back in 80,000 years. On our scale, that’s a long time. The entire recorded history of our species is only 5,000 to 8,000 years. We’ve come a long way, but where we’re going in 80,000 years is anyone’s guess.
Will doctors in the year 82024 even know what we do now to care for people? Will they still be practicing on the third rock from the sun, or spread out across the galaxy? Will there even be doctors? (Probably, in one form or another.)
But We do our best to care, heal, and hope now, as we did then, and as our descendants will.
And, like my daughter and I did, no matter where we are, we will still look up at the sky with wonder.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
Like millions of other modern humans, my daughter and I stood in the backyard recently and watched comet C/2023 A3 (Tsuchinshan–ATLAS) with binoculars. It took a few minutes to locate, but once you see it is unmistakable.
It’s got a long (at least in human terms) orbit, roughly 80,000 years. So what was going on here, on our pale blue dot, the last time it graced our skies?
Well, here in Phoenix, the people were ... not here. Nor were they in Arizona, or North America, or pretty much the entire Western Hemisphere.
In fact, Homo sapiens were confined to Africa. The hardier Neanderthals had successfully moved into Eurasia, but our lineage was just starting to migrate there. There’s some evidence that we numbered maybe 10,000-15,000 at that point. Far more people saw the comet that night in the United States than our entire population count last time it swung by.
But we were moving up in the world. Our ancestors at the time had developed the first forms of jewelry, using seashells. There’s evidence that we’d learned to trade with other, distant, communities. We were using spears to put dinner on the table with less risk to ourselves than clubs posed.
And, in what’s now Kenya, in the same time frame, a pair of grieving parents carefully buried their 3-year-old child, wrapped in a covering and gently placed on a pillow.
Sadly, this isn’t a scene we’re unfamiliar with. Possibly the most famous painting of a physician is “The Doctor” (1891) by Luke Fildes, showing a physician trying to treat a seriously ill child while the parents look on helplessly.

What did the Kenyan child die from? We’ll probably never know. Did they try to treat it? Most likely.
Humans, by nature, form societies. The size varies, but everyone has a role. There was probably some ancestor of Fildes’ doctor in the group who tried to help. Perhaps with prayers in an unknown tongue, or a preparation of certain leaves, or placing the child near a fire. When whatever they tried failed, the same person likely consoled the parents. Maybe they were involved in the burial, too.
The child would be found in 2017, giving us the first clear evidence of a ritual human burial in Africa. Just like today, we let go of our lost ones with ceremony. Perhaps the parents noticed the comet and thought it was their child’s spirit departing.
Now the comet is back. The planet hasn’t changed dramatically in 80,000 years (which isn’t much in geological time), but we have.
Would today’s doctors have been able to save the child? No idea, though we probably have a better chance than our professional ancestor did.
But our job hasn’t changed. Like us, the ancient practitioner probably tried to figure out why the child was sick and what could be done about it. When it was over they, and others, grieved with the parents.
The comet will be back in 80,000 years. On our scale, that’s a long time. The entire recorded history of our species is only 5,000 to 8,000 years. We’ve come a long way, but where we’re going in 80,000 years is anyone’s guess.
Will doctors in the year 82024 even know what we do now to care for people? Will they still be practicing on the third rock from the sun, or spread out across the galaxy? Will there even be doctors? (Probably, in one form or another.)
But We do our best to care, heal, and hope now, as we did then, and as our descendants will.
And, like my daughter and I did, no matter where we are, we will still look up at the sky with wonder.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.