User login
New evidence further supports starting CRC screening at age 45
SAN ANTONIO – The American Cancer Society’s 2018 qualified recommendation to lower the starting age for colorectal cancer screening from 50 to 45 years in average-risk individuals has picked up new support from a New Hampshire Colonoscopy Registry analysis.
Data from the population-based statewide colonoscopy registry demonstrated that the prevalence of both advanced adenomas and clinically significant serrated polyps was closely similar for average-risk New Hampshirites age 45-49 years and for those age 50-54, Lynn F. Butterly, MD, reported at the annual meeting of the American College of Gastroenterology.
“The clinical implication is that our data support the recommendation to begin average-risk colorectal cancer screening at age 45,” declared Dr. Butterly, a gastroenterologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
The American Cancer Society recommendation to lower the initial screening age was designed to address a disturbing national trend: the climbing incidence of colorectal cancer in young adults. Indeed, the incidence increased by 55% among 20- to 49-year-olds during 1995-2016, even while falling by 38% in individuals age 50 years and older. The 2018 recommendation was billed as “qualified” because it was based upon predictive modeling and National Cancer Institute Surveillance, Epidemiology, and End Results data which have been criticized as subject to potential bias. Several studies conducted in Korea and other Asian countries have reported a lower colorectal cancer risk in the younger adult population than in those age 50 or older, but questions have been raised about the applicability of such data to the U.S. population.
For Dr. Butterly and coinvestigators, the research imperative was clear: “We need to generate U.S. outcomes data for average-risk individuals age 45-49, versus those over age 50, for whom colorectal cancer screening is already strongly recommended.”
Toward that end, the investigators turned to the New Hampshire Colonoscopy Registry, which contains detailed data on 200,000 colonoscopies, with some 400 variables recorded per patient. To zero in on an average-risk population below age 50, they restricted the analysis to patients undergoing their first colonoscopy for evaluation of low-risk conditions including abdominal pain or constipation while excluding those with GI bleeding, iron-deficiency anemia, abnormal imaging, or a family history of colorectal cancer.
The final study population included 42,600 New Hampshire residents who underwent their first colonoscopy. The key outcomes were the prevalence of advanced adenomas, defined as adenomas more than 1 cm in size, or with high-grade dysplasia or villous elements, and the prevalence of clinically significant serrated polyps larger than 1 cm, or larger than 5 mm if proximally located, as well as traditional serrated adenomas and those with sessile features.
The prevalence of advanced adenomas in 1,870 average-risk patients aged 45-49 years was 3.7% and nearly identical at 3.6% in 22,160 individuals undergoing screening colonoscopy at age 50-54. The rate of clinically significant serrated polyps was 5.9% in the 45- to 49-year-olds, closely similar to the 6.1% rate in patients age 50-54.
Of note, the prevalence of advanced adenomas was just 1.1% in individuals younger than age 40 years, jumping to 3.0% among 40- to 44-year-olds, 5.1% in those age 55-59, and 6.9% at age 60 or more. Clinically significant serrated polyps followed a similar pattern, with rates of 3.0% before age 40, 5.1% in 40- to 44-year-olds, 6.6% in 55- to 59-year-olds, and 6.0% in those who were older.
In a multivariate logistic regression analysis adjusted for sex, body mass index, smoking, and other potential confounders, 45- to 49-year-olds were at a 243% increased risk of finding advanced adenomas on colonoscopy, compared with those less than 40 years old, while the 50- to 54-year-olds had a virtually identical 244% increased risk.
Dr. Butterly noted that there are now 15,000 cases of colorectal cancer occurring annually in individuals under age 50 in the United States, with 3,600 deaths.
“Prevention of colorectal cancer in young, productive individuals is an essential clinical imperative that must be addressed,” she concluded.
She reported having no financial conflicts regarding her study.
SAN ANTONIO – The American Cancer Society’s 2018 qualified recommendation to lower the starting age for colorectal cancer screening from 50 to 45 years in average-risk individuals has picked up new support from a New Hampshire Colonoscopy Registry analysis.
Data from the population-based statewide colonoscopy registry demonstrated that the prevalence of both advanced adenomas and clinically significant serrated polyps was closely similar for average-risk New Hampshirites age 45-49 years and for those age 50-54, Lynn F. Butterly, MD, reported at the annual meeting of the American College of Gastroenterology.
“The clinical implication is that our data support the recommendation to begin average-risk colorectal cancer screening at age 45,” declared Dr. Butterly, a gastroenterologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
The American Cancer Society recommendation to lower the initial screening age was designed to address a disturbing national trend: the climbing incidence of colorectal cancer in young adults. Indeed, the incidence increased by 55% among 20- to 49-year-olds during 1995-2016, even while falling by 38% in individuals age 50 years and older. The 2018 recommendation was billed as “qualified” because it was based upon predictive modeling and National Cancer Institute Surveillance, Epidemiology, and End Results data which have been criticized as subject to potential bias. Several studies conducted in Korea and other Asian countries have reported a lower colorectal cancer risk in the younger adult population than in those age 50 or older, but questions have been raised about the applicability of such data to the U.S. population.
For Dr. Butterly and coinvestigators, the research imperative was clear: “We need to generate U.S. outcomes data for average-risk individuals age 45-49, versus those over age 50, for whom colorectal cancer screening is already strongly recommended.”
Toward that end, the investigators turned to the New Hampshire Colonoscopy Registry, which contains detailed data on 200,000 colonoscopies, with some 400 variables recorded per patient. To zero in on an average-risk population below age 50, they restricted the analysis to patients undergoing their first colonoscopy for evaluation of low-risk conditions including abdominal pain or constipation while excluding those with GI bleeding, iron-deficiency anemia, abnormal imaging, or a family history of colorectal cancer.
The final study population included 42,600 New Hampshire residents who underwent their first colonoscopy. The key outcomes were the prevalence of advanced adenomas, defined as adenomas more than 1 cm in size, or with high-grade dysplasia or villous elements, and the prevalence of clinically significant serrated polyps larger than 1 cm, or larger than 5 mm if proximally located, as well as traditional serrated adenomas and those with sessile features.
The prevalence of advanced adenomas in 1,870 average-risk patients aged 45-49 years was 3.7% and nearly identical at 3.6% in 22,160 individuals undergoing screening colonoscopy at age 50-54. The rate of clinically significant serrated polyps was 5.9% in the 45- to 49-year-olds, closely similar to the 6.1% rate in patients age 50-54.
Of note, the prevalence of advanced adenomas was just 1.1% in individuals younger than age 40 years, jumping to 3.0% among 40- to 44-year-olds, 5.1% in those age 55-59, and 6.9% at age 60 or more. Clinically significant serrated polyps followed a similar pattern, with rates of 3.0% before age 40, 5.1% in 40- to 44-year-olds, 6.6% in 55- to 59-year-olds, and 6.0% in those who were older.
In a multivariate logistic regression analysis adjusted for sex, body mass index, smoking, and other potential confounders, 45- to 49-year-olds were at a 243% increased risk of finding advanced adenomas on colonoscopy, compared with those less than 40 years old, while the 50- to 54-year-olds had a virtually identical 244% increased risk.
Dr. Butterly noted that there are now 15,000 cases of colorectal cancer occurring annually in individuals under age 50 in the United States, with 3,600 deaths.
“Prevention of colorectal cancer in young, productive individuals is an essential clinical imperative that must be addressed,” she concluded.
She reported having no financial conflicts regarding her study.
SAN ANTONIO – The American Cancer Society’s 2018 qualified recommendation to lower the starting age for colorectal cancer screening from 50 to 45 years in average-risk individuals has picked up new support from a New Hampshire Colonoscopy Registry analysis.
Data from the population-based statewide colonoscopy registry demonstrated that the prevalence of both advanced adenomas and clinically significant serrated polyps was closely similar for average-risk New Hampshirites age 45-49 years and for those age 50-54, Lynn F. Butterly, MD, reported at the annual meeting of the American College of Gastroenterology.
“The clinical implication is that our data support the recommendation to begin average-risk colorectal cancer screening at age 45,” declared Dr. Butterly, a gastroenterologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
The American Cancer Society recommendation to lower the initial screening age was designed to address a disturbing national trend: the climbing incidence of colorectal cancer in young adults. Indeed, the incidence increased by 55% among 20- to 49-year-olds during 1995-2016, even while falling by 38% in individuals age 50 years and older. The 2018 recommendation was billed as “qualified” because it was based upon predictive modeling and National Cancer Institute Surveillance, Epidemiology, and End Results data which have been criticized as subject to potential bias. Several studies conducted in Korea and other Asian countries have reported a lower colorectal cancer risk in the younger adult population than in those age 50 or older, but questions have been raised about the applicability of such data to the U.S. population.
For Dr. Butterly and coinvestigators, the research imperative was clear: “We need to generate U.S. outcomes data for average-risk individuals age 45-49, versus those over age 50, for whom colorectal cancer screening is already strongly recommended.”
Toward that end, the investigators turned to the New Hampshire Colonoscopy Registry, which contains detailed data on 200,000 colonoscopies, with some 400 variables recorded per patient. To zero in on an average-risk population below age 50, they restricted the analysis to patients undergoing their first colonoscopy for evaluation of low-risk conditions including abdominal pain or constipation while excluding those with GI bleeding, iron-deficiency anemia, abnormal imaging, or a family history of colorectal cancer.
The final study population included 42,600 New Hampshire residents who underwent their first colonoscopy. The key outcomes were the prevalence of advanced adenomas, defined as adenomas more than 1 cm in size, or with high-grade dysplasia or villous elements, and the prevalence of clinically significant serrated polyps larger than 1 cm, or larger than 5 mm if proximally located, as well as traditional serrated adenomas and those with sessile features.
The prevalence of advanced adenomas in 1,870 average-risk patients aged 45-49 years was 3.7% and nearly identical at 3.6% in 22,160 individuals undergoing screening colonoscopy at age 50-54. The rate of clinically significant serrated polyps was 5.9% in the 45- to 49-year-olds, closely similar to the 6.1% rate in patients age 50-54.
Of note, the prevalence of advanced adenomas was just 1.1% in individuals younger than age 40 years, jumping to 3.0% among 40- to 44-year-olds, 5.1% in those age 55-59, and 6.9% at age 60 or more. Clinically significant serrated polyps followed a similar pattern, with rates of 3.0% before age 40, 5.1% in 40- to 44-year-olds, 6.6% in 55- to 59-year-olds, and 6.0% in those who were older.
In a multivariate logistic regression analysis adjusted for sex, body mass index, smoking, and other potential confounders, 45- to 49-year-olds were at a 243% increased risk of finding advanced adenomas on colonoscopy, compared with those less than 40 years old, while the 50- to 54-year-olds had a virtually identical 244% increased risk.
Dr. Butterly noted that there are now 15,000 cases of colorectal cancer occurring annually in individuals under age 50 in the United States, with 3,600 deaths.
“Prevention of colorectal cancer in young, productive individuals is an essential clinical imperative that must be addressed,” she concluded.
She reported having no financial conflicts regarding her study.
REPORTING FROM ACG 2019
Oral BTK inhibitor shows continued promise for pemphigus
MADRID – A novel Dedee F. Murrell, MD, said at the annual congress of the European Academy of Dermatology and Venereology.
“In pemphigus, we have a considerable unmet medical need. We could do with a treatment that has rapid onset, is steroid sparing or avoiding, safe for chronic administration, avoids chronic B cell depletion – which is an issue with rituxumab – is efficacious in both newly diagnosed as well as in our commonly relapsing patients, and is convenient to administer,” observed Dr. Murrell, professor of dermatology at the University of New South Wales in Sydney.
In the phase 2 BELIEVE trial, the BTK inhibitor known for now only as PRN1008 appeared to check all the boxes. However, definitive evidence of the drug’s efficacy and safety must await the results of the ongoing, double-bind, placebo-controlled, pivotal phase 3 PEGASUS trial, which is enrolling a planned 120 patients with pemphigus vulgaris or foliaceus in 19 countries.
Pemphigus is driven by autoantibodies against desmogleins 1 and 3. Even in contemporary practice, this blistering disease has roughly a 5% mortality rate. Current management of the disease with high-dose corticosteroids at 1 mg/kg per day or more with or without rituximab (Rituxan) is challenging because of the associated pronounced toxicities. And even when rituximab is utilized, patients need to be on high-dose steroids for at least 3-6 months before a rituximab response is achieved, Dr. Murrell said.
PRN1008 has three mechanisms of action targeting the drivers of pemphigus and other immune-mediated diseases, she explained. The drug blocks inflammatory B cells, neutrophils, and macrophages; eliminates downstream signalling by antidesmoglein autoantibodies; and prevents production of new autoantibodies. The drug has a double lock-and-key mechanism which makes it highly specific for its target, so treated patients are much less likely to experience bruising, diarrhea, and other off-target effects than is the case with other tyrosine kinase inhibitors.
“Also, PRN1008 is reversible. It comes off its target receptor after about 12 hours, at which point serum levels become low. So if any side effects do develop, the patient can recover quickly, unlike with rituximab, which involves ongoing inhibition of B cells for a long period of time,” the dermatologist noted.
BELIEVE was a phase 2 dose-ranging study of 27 patients with pemphigus treated open-label with PRN1008 for 12 weeks. The primary endpoint was control of disease activity, meaning no new lesions while established lesions showed some evidence of healing on no more than 0.5 mg/kg per day of prednisone. This outcome was achieved in 27% of participants at 2 weeks, 54% at 4 weeks, and 73% at 12 weeks. Autoantibody levels dropped by a mean of 65% at 12 weeks, with a median 70% reduction in Pemphigus Disease Activity Index scores while patients were on an average of just 12 mg of prednisone per day.
Phase 2b of BELIEVE included a separate group of 15 patients on PRN1008 for 24 weeks. Nine achieved a Pemphigus Disease Activity Index score of 0 or 1. Six patients had a complete response, meaning an absence of both new and established lesions while on no or a very low dose of prednisone. Another five patients were unable to achieve a complete response, and the jury was still out on another four still on treatment.
The side effect profile was benign in comparison with that of current standard therapies, she said. It consisted of a handful of cases of mild, transient nausea, headache, or upper abdominal pain and a few Grade 1 infections. There have been no severe treatment-related adverse events in BELIEVE participants.
Patients enrolled in the ongoing phase 3 PEGASUS trial start with a short course of high-dose corticosteroids, followed by double-blind randomization to PRN1008 at 400 mg twice a day or placebo, with a corticosteroid taper. The primary endpoint is durable complete remission at week 37, defined as no lesions being present for at least the previous 8 weeks while on no more than 5 mg/day of prednisone.
Secondary endpoints include cumulative corticosteroid dose through 36 weeks and patient-reported quality of life measures assessed out to 61 weeks. The trial is scheduled for completion in the spring of 2022.
Dr. Murrell reported serving as a consultant to the study sponsor, Principia Biopharma, as well as numerous other pharmaceutical companies.
MADRID – A novel Dedee F. Murrell, MD, said at the annual congress of the European Academy of Dermatology and Venereology.
“In pemphigus, we have a considerable unmet medical need. We could do with a treatment that has rapid onset, is steroid sparing or avoiding, safe for chronic administration, avoids chronic B cell depletion – which is an issue with rituxumab – is efficacious in both newly diagnosed as well as in our commonly relapsing patients, and is convenient to administer,” observed Dr. Murrell, professor of dermatology at the University of New South Wales in Sydney.
In the phase 2 BELIEVE trial, the BTK inhibitor known for now only as PRN1008 appeared to check all the boxes. However, definitive evidence of the drug’s efficacy and safety must await the results of the ongoing, double-bind, placebo-controlled, pivotal phase 3 PEGASUS trial, which is enrolling a planned 120 patients with pemphigus vulgaris or foliaceus in 19 countries.
Pemphigus is driven by autoantibodies against desmogleins 1 and 3. Even in contemporary practice, this blistering disease has roughly a 5% mortality rate. Current management of the disease with high-dose corticosteroids at 1 mg/kg per day or more with or without rituximab (Rituxan) is challenging because of the associated pronounced toxicities. And even when rituximab is utilized, patients need to be on high-dose steroids for at least 3-6 months before a rituximab response is achieved, Dr. Murrell said.
PRN1008 has three mechanisms of action targeting the drivers of pemphigus and other immune-mediated diseases, she explained. The drug blocks inflammatory B cells, neutrophils, and macrophages; eliminates downstream signalling by antidesmoglein autoantibodies; and prevents production of new autoantibodies. The drug has a double lock-and-key mechanism which makes it highly specific for its target, so treated patients are much less likely to experience bruising, diarrhea, and other off-target effects than is the case with other tyrosine kinase inhibitors.
“Also, PRN1008 is reversible. It comes off its target receptor after about 12 hours, at which point serum levels become low. So if any side effects do develop, the patient can recover quickly, unlike with rituximab, which involves ongoing inhibition of B cells for a long period of time,” the dermatologist noted.
BELIEVE was a phase 2 dose-ranging study of 27 patients with pemphigus treated open-label with PRN1008 for 12 weeks. The primary endpoint was control of disease activity, meaning no new lesions while established lesions showed some evidence of healing on no more than 0.5 mg/kg per day of prednisone. This outcome was achieved in 27% of participants at 2 weeks, 54% at 4 weeks, and 73% at 12 weeks. Autoantibody levels dropped by a mean of 65% at 12 weeks, with a median 70% reduction in Pemphigus Disease Activity Index scores while patients were on an average of just 12 mg of prednisone per day.
Phase 2b of BELIEVE included a separate group of 15 patients on PRN1008 for 24 weeks. Nine achieved a Pemphigus Disease Activity Index score of 0 or 1. Six patients had a complete response, meaning an absence of both new and established lesions while on no or a very low dose of prednisone. Another five patients were unable to achieve a complete response, and the jury was still out on another four still on treatment.
The side effect profile was benign in comparison with that of current standard therapies, she said. It consisted of a handful of cases of mild, transient nausea, headache, or upper abdominal pain and a few Grade 1 infections. There have been no severe treatment-related adverse events in BELIEVE participants.
Patients enrolled in the ongoing phase 3 PEGASUS trial start with a short course of high-dose corticosteroids, followed by double-blind randomization to PRN1008 at 400 mg twice a day or placebo, with a corticosteroid taper. The primary endpoint is durable complete remission at week 37, defined as no lesions being present for at least the previous 8 weeks while on no more than 5 mg/day of prednisone.
Secondary endpoints include cumulative corticosteroid dose through 36 weeks and patient-reported quality of life measures assessed out to 61 weeks. The trial is scheduled for completion in the spring of 2022.
Dr. Murrell reported serving as a consultant to the study sponsor, Principia Biopharma, as well as numerous other pharmaceutical companies.
MADRID – A novel Dedee F. Murrell, MD, said at the annual congress of the European Academy of Dermatology and Venereology.
“In pemphigus, we have a considerable unmet medical need. We could do with a treatment that has rapid onset, is steroid sparing or avoiding, safe for chronic administration, avoids chronic B cell depletion – which is an issue with rituxumab – is efficacious in both newly diagnosed as well as in our commonly relapsing patients, and is convenient to administer,” observed Dr. Murrell, professor of dermatology at the University of New South Wales in Sydney.
In the phase 2 BELIEVE trial, the BTK inhibitor known for now only as PRN1008 appeared to check all the boxes. However, definitive evidence of the drug’s efficacy and safety must await the results of the ongoing, double-bind, placebo-controlled, pivotal phase 3 PEGASUS trial, which is enrolling a planned 120 patients with pemphigus vulgaris or foliaceus in 19 countries.
Pemphigus is driven by autoantibodies against desmogleins 1 and 3. Even in contemporary practice, this blistering disease has roughly a 5% mortality rate. Current management of the disease with high-dose corticosteroids at 1 mg/kg per day or more with or without rituximab (Rituxan) is challenging because of the associated pronounced toxicities. And even when rituximab is utilized, patients need to be on high-dose steroids for at least 3-6 months before a rituximab response is achieved, Dr. Murrell said.
PRN1008 has three mechanisms of action targeting the drivers of pemphigus and other immune-mediated diseases, she explained. The drug blocks inflammatory B cells, neutrophils, and macrophages; eliminates downstream signalling by antidesmoglein autoantibodies; and prevents production of new autoantibodies. The drug has a double lock-and-key mechanism which makes it highly specific for its target, so treated patients are much less likely to experience bruising, diarrhea, and other off-target effects than is the case with other tyrosine kinase inhibitors.
“Also, PRN1008 is reversible. It comes off its target receptor after about 12 hours, at which point serum levels become low. So if any side effects do develop, the patient can recover quickly, unlike with rituximab, which involves ongoing inhibition of B cells for a long period of time,” the dermatologist noted.
BELIEVE was a phase 2 dose-ranging study of 27 patients with pemphigus treated open-label with PRN1008 for 12 weeks. The primary endpoint was control of disease activity, meaning no new lesions while established lesions showed some evidence of healing on no more than 0.5 mg/kg per day of prednisone. This outcome was achieved in 27% of participants at 2 weeks, 54% at 4 weeks, and 73% at 12 weeks. Autoantibody levels dropped by a mean of 65% at 12 weeks, with a median 70% reduction in Pemphigus Disease Activity Index scores while patients were on an average of just 12 mg of prednisone per day.
Phase 2b of BELIEVE included a separate group of 15 patients on PRN1008 for 24 weeks. Nine achieved a Pemphigus Disease Activity Index score of 0 or 1. Six patients had a complete response, meaning an absence of both new and established lesions while on no or a very low dose of prednisone. Another five patients were unable to achieve a complete response, and the jury was still out on another four still on treatment.
The side effect profile was benign in comparison with that of current standard therapies, she said. It consisted of a handful of cases of mild, transient nausea, headache, or upper abdominal pain and a few Grade 1 infections. There have been no severe treatment-related adverse events in BELIEVE participants.
Patients enrolled in the ongoing phase 3 PEGASUS trial start with a short course of high-dose corticosteroids, followed by double-blind randomization to PRN1008 at 400 mg twice a day or placebo, with a corticosteroid taper. The primary endpoint is durable complete remission at week 37, defined as no lesions being present for at least the previous 8 weeks while on no more than 5 mg/day of prednisone.
Secondary endpoints include cumulative corticosteroid dose through 36 weeks and patient-reported quality of life measures assessed out to 61 weeks. The trial is scheduled for completion in the spring of 2022.
Dr. Murrell reported serving as a consultant to the study sponsor, Principia Biopharma, as well as numerous other pharmaceutical companies.
REPORTING FROM THE EADV CONGRESS
A triple-antibiotic cure for Crohn’s disease?
SAN ANTONIO – A proprietary oral fixed-dose, triple-antibiotic combination pill offers a promising new approach to the treatment of Crohn’s disease, David Y. Graham, MD, declared at the annual meeting of the American College of Gastroenterology.
In the phase 3 MAP US trial, patients with Crohn’s disease who were randomized to the fixed-dose combination of 45 mg rifabutin, 95 mg clarithromycin, and 10 mg clofazimine, known for now as RHB-104, experienced significantly higher rates of clinical remission and improvement in inflammation as assessed endoscopically and via biomarkers, compared with placebo-treated controls, reported Dr. Graham, professor of medicine at Baylor College of Medicine, Houston.
RHB-104 is effective against Mycobacterium avium paratuberculosis (MAP) – and therein hangs a tale.
“MAP has been considered as a possible cause of Crohn’s disease since the disease was described by Crohn in 1932,” the gastroenterologist noted. “These randomized trial data provide further evidence suggesting an important role for MAP or similar microorganisms in the pathogenesis of Crohn’s disease.”
For Dr. Graham, this is a case of deja vu all over again. More than a quarter century ago he was lead author of a highly influential randomized, controlled trial which established that treatment with antibiotics directed against Helicobacter pylori cured peptic ulcer disease. As such, he became internationally recognized as a key figure in the resultant revolution in peptic ulcer treatment. He hears an echo of that earlier transformative change in the MAP US results.
“This is either an additional therapy or it’s the beginning of a paradigm shift. I mean, I see this as we’re standing at the same place now as we were standing with Helicobacter pylori 30 years ago, when the question was: Have we found something that we can eradicate and change the natural history of the disease and cure it? You can say this [MAP-directed therapy] is going in that direction, but it certainly hasn’t gotten to the point of proof yet. The results have to be reproduced,” he said.
The MAP US trial included 331 patients with moderate to severely active Crohn’s disease at 92 sites who had failed to achieve an adequate response with conventional therapies. Participants were randomized double blind to twice-daily RHB-104 or placebo for 52 weeks. Those not in remission at 26 weeks could opt for open-label RHB-104. Background concomitant treatment with corticosteroids, tumor necrosis factor inhibitors, and immunosuppressives was permitted.
The primary outcome was clinical remission as defined by a Crohn’s Disease Activity Index (CDAI) score below 150 at week 26. This was achieved in 36.7% of the active treatment group and 23% of controls, a highly significant difference. The clinical remission rates at week 16 were 42.2% and 29.1%, respectively. At week 26, 44% of RHB-104-treated patients had achieved at least a 100-point reduction in CDAI score, compared with baseline, as did 30.9% of controls. The key symptom score provided by the sum of the abdominal pain and bowel movement components of the CDAI was significantly lower in the RHB-104 group than in controls from week 16 on.
The remission rate at week 26 in the group on RHB-104 was similarly favorable regardless of whether or not they were on anti–tumor necrosis factor therapy.
“This suggests that RHB-104 can be used effectively and safely as an adjunct treatment to other medications to enhance the response to medical therapy,” according to Dr. Graham, who was principal investigator for MAP US.
The composite endpoint of clinical remission plus at least a 50% reduction from baseline in fecal calprotectin or C-reactive protein was achieved in 21.1% of the RHB-104 group and 9.1% of controls at week 26, and by 16.9% on RHB-104 and 7.9% on placebo at week 52.
In the 35 patients who underwent endoscopy at week 26, a 50% or greater reduction in the Simple Endoscopic Score in Crohn’s Disease was documented in 28.6% of patients on RHB-104 versus 4.8% of controls.
Durable remission, defined as a CDAI score below 150 at all study visits from week 16 to week 52, was achieved in 18.7% of the RHB-104 group, compared with 8.5% of controls.
The side effect profiles of RHB-104 and placebo were similar, with no serious adverse events recorded in the 52-week study. An increase in the QT interval on ECG was noted in the RHB-104 group from week 4 on, but it wasn’t associated with any clinical findings. Further study of this ECG finding is underway.
Several audience members rose to urge caution in interpreting the MAP US data.
“We must adhere to Koch’s postulates before we make conclusions about causative agents of an infectious disease, and I didn’t see those data here. So I look forward to a future presentation that shares that,” one gastroenterologist commented.
“I haven’t seen any data here that shows Mycobacterium was present in these patients,” noted another.
Dr. Graham replied that MAP US was a hypothesis-driven clinical trial: Crohn’s disease has much in common with an inflammatory bowel disease occurring in ruminant animals, where RHB-104 has shown treatment efficacy.
“This is a Mycobacterium avium organism, so it’s not something you’re going to cure in 2 weeks or 2 months. But the question is, do you have an effect on the disease, and the answer in MAP US was unquestionably yes. It’s very positive data to further pursue the hypothesis, but the study doesn’t provide a definitive answer,” he said.
Dr. Graham reported serving as a consultant to RedHill Biopharma, the study sponsor.
SAN ANTONIO – A proprietary oral fixed-dose, triple-antibiotic combination pill offers a promising new approach to the treatment of Crohn’s disease, David Y. Graham, MD, declared at the annual meeting of the American College of Gastroenterology.
In the phase 3 MAP US trial, patients with Crohn’s disease who were randomized to the fixed-dose combination of 45 mg rifabutin, 95 mg clarithromycin, and 10 mg clofazimine, known for now as RHB-104, experienced significantly higher rates of clinical remission and improvement in inflammation as assessed endoscopically and via biomarkers, compared with placebo-treated controls, reported Dr. Graham, professor of medicine at Baylor College of Medicine, Houston.
RHB-104 is effective against Mycobacterium avium paratuberculosis (MAP) – and therein hangs a tale.
“MAP has been considered as a possible cause of Crohn’s disease since the disease was described by Crohn in 1932,” the gastroenterologist noted. “These randomized trial data provide further evidence suggesting an important role for MAP or similar microorganisms in the pathogenesis of Crohn’s disease.”
For Dr. Graham, this is a case of deja vu all over again. More than a quarter century ago he was lead author of a highly influential randomized, controlled trial which established that treatment with antibiotics directed against Helicobacter pylori cured peptic ulcer disease. As such, he became internationally recognized as a key figure in the resultant revolution in peptic ulcer treatment. He hears an echo of that earlier transformative change in the MAP US results.
“This is either an additional therapy or it’s the beginning of a paradigm shift. I mean, I see this as we’re standing at the same place now as we were standing with Helicobacter pylori 30 years ago, when the question was: Have we found something that we can eradicate and change the natural history of the disease and cure it? You can say this [MAP-directed therapy] is going in that direction, but it certainly hasn’t gotten to the point of proof yet. The results have to be reproduced,” he said.
The MAP US trial included 331 patients with moderate to severely active Crohn’s disease at 92 sites who had failed to achieve an adequate response with conventional therapies. Participants were randomized double blind to twice-daily RHB-104 or placebo for 52 weeks. Those not in remission at 26 weeks could opt for open-label RHB-104. Background concomitant treatment with corticosteroids, tumor necrosis factor inhibitors, and immunosuppressives was permitted.
The primary outcome was clinical remission as defined by a Crohn’s Disease Activity Index (CDAI) score below 150 at week 26. This was achieved in 36.7% of the active treatment group and 23% of controls, a highly significant difference. The clinical remission rates at week 16 were 42.2% and 29.1%, respectively. At week 26, 44% of RHB-104-treated patients had achieved at least a 100-point reduction in CDAI score, compared with baseline, as did 30.9% of controls. The key symptom score provided by the sum of the abdominal pain and bowel movement components of the CDAI was significantly lower in the RHB-104 group than in controls from week 16 on.
The remission rate at week 26 in the group on RHB-104 was similarly favorable regardless of whether or not they were on anti–tumor necrosis factor therapy.
“This suggests that RHB-104 can be used effectively and safely as an adjunct treatment to other medications to enhance the response to medical therapy,” according to Dr. Graham, who was principal investigator for MAP US.
The composite endpoint of clinical remission plus at least a 50% reduction from baseline in fecal calprotectin or C-reactive protein was achieved in 21.1% of the RHB-104 group and 9.1% of controls at week 26, and by 16.9% on RHB-104 and 7.9% on placebo at week 52.
In the 35 patients who underwent endoscopy at week 26, a 50% or greater reduction in the Simple Endoscopic Score in Crohn’s Disease was documented in 28.6% of patients on RHB-104 versus 4.8% of controls.
Durable remission, defined as a CDAI score below 150 at all study visits from week 16 to week 52, was achieved in 18.7% of the RHB-104 group, compared with 8.5% of controls.
The side effect profiles of RHB-104 and placebo were similar, with no serious adverse events recorded in the 52-week study. An increase in the QT interval on ECG was noted in the RHB-104 group from week 4 on, but it wasn’t associated with any clinical findings. Further study of this ECG finding is underway.
Several audience members rose to urge caution in interpreting the MAP US data.
“We must adhere to Koch’s postulates before we make conclusions about causative agents of an infectious disease, and I didn’t see those data here. So I look forward to a future presentation that shares that,” one gastroenterologist commented.
“I haven’t seen any data here that shows Mycobacterium was present in these patients,” noted another.
Dr. Graham replied that MAP US was a hypothesis-driven clinical trial: Crohn’s disease has much in common with an inflammatory bowel disease occurring in ruminant animals, where RHB-104 has shown treatment efficacy.
“This is a Mycobacterium avium organism, so it’s not something you’re going to cure in 2 weeks or 2 months. But the question is, do you have an effect on the disease, and the answer in MAP US was unquestionably yes. It’s very positive data to further pursue the hypothesis, but the study doesn’t provide a definitive answer,” he said.
Dr. Graham reported serving as a consultant to RedHill Biopharma, the study sponsor.
SAN ANTONIO – A proprietary oral fixed-dose, triple-antibiotic combination pill offers a promising new approach to the treatment of Crohn’s disease, David Y. Graham, MD, declared at the annual meeting of the American College of Gastroenterology.
In the phase 3 MAP US trial, patients with Crohn’s disease who were randomized to the fixed-dose combination of 45 mg rifabutin, 95 mg clarithromycin, and 10 mg clofazimine, known for now as RHB-104, experienced significantly higher rates of clinical remission and improvement in inflammation as assessed endoscopically and via biomarkers, compared with placebo-treated controls, reported Dr. Graham, professor of medicine at Baylor College of Medicine, Houston.
RHB-104 is effective against Mycobacterium avium paratuberculosis (MAP) – and therein hangs a tale.
“MAP has been considered as a possible cause of Crohn’s disease since the disease was described by Crohn in 1932,” the gastroenterologist noted. “These randomized trial data provide further evidence suggesting an important role for MAP or similar microorganisms in the pathogenesis of Crohn’s disease.”
For Dr. Graham, this is a case of deja vu all over again. More than a quarter century ago he was lead author of a highly influential randomized, controlled trial which established that treatment with antibiotics directed against Helicobacter pylori cured peptic ulcer disease. As such, he became internationally recognized as a key figure in the resultant revolution in peptic ulcer treatment. He hears an echo of that earlier transformative change in the MAP US results.
“This is either an additional therapy or it’s the beginning of a paradigm shift. I mean, I see this as we’re standing at the same place now as we were standing with Helicobacter pylori 30 years ago, when the question was: Have we found something that we can eradicate and change the natural history of the disease and cure it? You can say this [MAP-directed therapy] is going in that direction, but it certainly hasn’t gotten to the point of proof yet. The results have to be reproduced,” he said.
The MAP US trial included 331 patients with moderate to severely active Crohn’s disease at 92 sites who had failed to achieve an adequate response with conventional therapies. Participants were randomized double blind to twice-daily RHB-104 or placebo for 52 weeks. Those not in remission at 26 weeks could opt for open-label RHB-104. Background concomitant treatment with corticosteroids, tumor necrosis factor inhibitors, and immunosuppressives was permitted.
The primary outcome was clinical remission as defined by a Crohn’s Disease Activity Index (CDAI) score below 150 at week 26. This was achieved in 36.7% of the active treatment group and 23% of controls, a highly significant difference. The clinical remission rates at week 16 were 42.2% and 29.1%, respectively. At week 26, 44% of RHB-104-treated patients had achieved at least a 100-point reduction in CDAI score, compared with baseline, as did 30.9% of controls. The key symptom score provided by the sum of the abdominal pain and bowel movement components of the CDAI was significantly lower in the RHB-104 group than in controls from week 16 on.
The remission rate at week 26 in the group on RHB-104 was similarly favorable regardless of whether or not they were on anti–tumor necrosis factor therapy.
“This suggests that RHB-104 can be used effectively and safely as an adjunct treatment to other medications to enhance the response to medical therapy,” according to Dr. Graham, who was principal investigator for MAP US.
The composite endpoint of clinical remission plus at least a 50% reduction from baseline in fecal calprotectin or C-reactive protein was achieved in 21.1% of the RHB-104 group and 9.1% of controls at week 26, and by 16.9% on RHB-104 and 7.9% on placebo at week 52.
In the 35 patients who underwent endoscopy at week 26, a 50% or greater reduction in the Simple Endoscopic Score in Crohn’s Disease was documented in 28.6% of patients on RHB-104 versus 4.8% of controls.
Durable remission, defined as a CDAI score below 150 at all study visits from week 16 to week 52, was achieved in 18.7% of the RHB-104 group, compared with 8.5% of controls.
The side effect profiles of RHB-104 and placebo were similar, with no serious adverse events recorded in the 52-week study. An increase in the QT interval on ECG was noted in the RHB-104 group from week 4 on, but it wasn’t associated with any clinical findings. Further study of this ECG finding is underway.
Several audience members rose to urge caution in interpreting the MAP US data.
“We must adhere to Koch’s postulates before we make conclusions about causative agents of an infectious disease, and I didn’t see those data here. So I look forward to a future presentation that shares that,” one gastroenterologist commented.
“I haven’t seen any data here that shows Mycobacterium was present in these patients,” noted another.
Dr. Graham replied that MAP US was a hypothesis-driven clinical trial: Crohn’s disease has much in common with an inflammatory bowel disease occurring in ruminant animals, where RHB-104 has shown treatment efficacy.
“This is a Mycobacterium avium organism, so it’s not something you’re going to cure in 2 weeks or 2 months. But the question is, do you have an effect on the disease, and the answer in MAP US was unquestionably yes. It’s very positive data to further pursue the hypothesis, but the study doesn’t provide a definitive answer,” he said.
Dr. Graham reported serving as a consultant to RedHill Biopharma, the study sponsor.
REPORTING FROM ACG 2019
Effective NASH medications are coming ‘sooner than you think’
SAN ANTONIO – The therapeutic Dark Ages of nonalcoholic steatohepatitis (NASH) are finally drawing to a close.
“NASH-specific therapies are coming soon – sooner than you think,” Naim Alkhouri, MD, predicted at the annual meeting of the American College of Gastroenterology.
And that, he added, has important implications for clinical practice. Physicians are going to need to step up their game with regard to screening and staging patients with nonalcoholic fatty liver disease to identify the right candidates for the coming effective treatments.
The new treatment era in NASH could dawn as soon as the spring of 2020, by which time the Food and Drug Administration is expected to issue a decision on obeticholic acid, an oral FXR agonist for which the agency has granted breakthrough therapy status. Intercept Pharmaceuticals has filed for marketing approval of obeticholic acid for NASH on the strength of the positive 18-month histologic results of the pivotal phase 3 REGENERATE trial, the first-ever successful phase 3 study of a medication for NASH, noted Dr. Alkhouri, a gastroenterologist at the University of Texas, San Antonio, and director of the Metabolic Health Center at the Texas Liver Institute.
At present there are no FDA-approved pharmacotherapies for NASH. The unmet medical need is huge, since NASH is now recognized to be a full-blown, burgeoning epidemic. NASH will soon become the No. 1 indication for liver transplantation in the United States. A full-throttle race is on to find effective therapies targeting the various dimensions of NASH, with more than 70 drugs now in phase 2 studies. These drugs collectively address all four mechanisms of the disease’s development and progression: the metabolic targets, perturbations in the gut-liver axis, liver inflammation, and fibrosis.
Moreover, even as the FDA considers the application for approval of obeticholic acid in NASH, at least four other investigational drugs are in pivotal phase 3 clinical trials. These include elafibranor, aramchol, resmetirom, and cenicriviroc.
Cenicriviroc is a dual CCR 2/5 receptor antagonist that targets the hepatic inflammation and fibrosis dimensions of NASH. It is now being evaluated in the phase 3 AURORA trial on the strength of the earlier positive phase 2b Centaur study, in which patients randomized to cenicriviroc were twice as likely to experience significant improvement in fibrosis as were placebo-treated controls.
Elafibranor, aramchol, and resmetirom employ different mechanisms of action to address the metabolic derangements of NASH. What they share in common is their aim to reduce the influx of free fatty acids from adipose tissue to the liver, and/or to inhibit lipogenesis from carbohydrate building blocks. In so doing, these medications should result in reduced hepatocyte injury and liver inflammation.
Elafibranor is a peroxisome proliferator-activated receptor alpha/delta agonist that achieved significant biopsy-proven reversal of NASH in moderate- or severely affected patients in the phase 2 GOLDEN study. The phase 3 RESOLVE IT trial is underway.
Aramchol is a first-in-class synthetic fatty acid/bile acid conjugate that inhibits stearoyl-CoA desaturate activity. It’s designed to improve insulin resistance and curb accumulation of triglycerides in hepatocytes. In the 52-week, phase 2 ARREST trial, oral aramchol at 600 mg/day was 4.7-fold more likely than was placebo to achieve NASH resolution without worsening of fibrosis. The drug is now in phase 3 in the ARMOR study.
Resmetirom is a selective thyroid hormone receptor–beta agonist. Activation of the beta receptor lowers LDL cholesterol, triglycerides, and liver fat, whereas activation of the alpha receptor has the unwanted effects of promoting bone loss, thyrotoxicosis, and arrhythmias. In phase 2, 75% of patients on high-dose resmetirom achieved at least a 30% reduction in hepatic fat by MRI at week 12, compared with 18% of placebo-treated controls. And 39% of the high-dose resmetirom group showed histologic resolution of NASH on a week-36 liver biopsy, as did a mere 6% of controls. The phase 3 MAESTRO randomized trial is underway.
Obeticholic acid addresses the gut-liver axis abnormalities present in NASH, especially the exuberant bile acid circulation.
Clinical implications of the coming wave of medications
In Dr. Alkhouri’s view, .
“These are the patients with a high chance of progressing to cirrhosis and end-stage liver disease,” the gastroenterologist said.
Patients with earlier-stage nonalcoholic fatty liver disease are best managed via lifestyle changes, with particular emphasis upon 10% weight loss accompanied by exercise. And patients with more advanced disease – NASH with cirrhosis – appear thus far to be beyond the reach of the next-generation therapies.
None of the coming drugs is a cure-all. In the landmark phase 3 REGENERATE trial, for example, the rate of the primary outcome – fibrosis improvement of at least one stage plus no worsening of NASH at 18 months – was 23% in patients randomized to obeticholic acid at 25 mg/day, compared to 12% with placebo.
“These are not like hepatitis C medications, with 97% efficacy, so combination therapy targeting upstream and downstream for NASH is rational,” Dr. Alkhouri observed.
He reported serving on advisory boards for Allergan, Gilead, and Intercept, and receiving research grants from those companies as well as from Galmed, Genfit, and Madrigal.
*This story was updated on 12/5/2019.
SAN ANTONIO – The therapeutic Dark Ages of nonalcoholic steatohepatitis (NASH) are finally drawing to a close.
“NASH-specific therapies are coming soon – sooner than you think,” Naim Alkhouri, MD, predicted at the annual meeting of the American College of Gastroenterology.
And that, he added, has important implications for clinical practice. Physicians are going to need to step up their game with regard to screening and staging patients with nonalcoholic fatty liver disease to identify the right candidates for the coming effective treatments.
The new treatment era in NASH could dawn as soon as the spring of 2020, by which time the Food and Drug Administration is expected to issue a decision on obeticholic acid, an oral FXR agonist for which the agency has granted breakthrough therapy status. Intercept Pharmaceuticals has filed for marketing approval of obeticholic acid for NASH on the strength of the positive 18-month histologic results of the pivotal phase 3 REGENERATE trial, the first-ever successful phase 3 study of a medication for NASH, noted Dr. Alkhouri, a gastroenterologist at the University of Texas, San Antonio, and director of the Metabolic Health Center at the Texas Liver Institute.
At present there are no FDA-approved pharmacotherapies for NASH. The unmet medical need is huge, since NASH is now recognized to be a full-blown, burgeoning epidemic. NASH will soon become the No. 1 indication for liver transplantation in the United States. A full-throttle race is on to find effective therapies targeting the various dimensions of NASH, with more than 70 drugs now in phase 2 studies. These drugs collectively address all four mechanisms of the disease’s development and progression: the metabolic targets, perturbations in the gut-liver axis, liver inflammation, and fibrosis.
Moreover, even as the FDA considers the application for approval of obeticholic acid in NASH, at least four other investigational drugs are in pivotal phase 3 clinical trials. These include elafibranor, aramchol, resmetirom, and cenicriviroc.
Cenicriviroc is a dual CCR 2/5 receptor antagonist that targets the hepatic inflammation and fibrosis dimensions of NASH. It is now being evaluated in the phase 3 AURORA trial on the strength of the earlier positive phase 2b Centaur study, in which patients randomized to cenicriviroc were twice as likely to experience significant improvement in fibrosis as were placebo-treated controls.
Elafibranor, aramchol, and resmetirom employ different mechanisms of action to address the metabolic derangements of NASH. What they share in common is their aim to reduce the influx of free fatty acids from adipose tissue to the liver, and/or to inhibit lipogenesis from carbohydrate building blocks. In so doing, these medications should result in reduced hepatocyte injury and liver inflammation.
Elafibranor is a peroxisome proliferator-activated receptor alpha/delta agonist that achieved significant biopsy-proven reversal of NASH in moderate- or severely affected patients in the phase 2 GOLDEN study. The phase 3 RESOLVE IT trial is underway.
Aramchol is a first-in-class synthetic fatty acid/bile acid conjugate that inhibits stearoyl-CoA desaturate activity. It’s designed to improve insulin resistance and curb accumulation of triglycerides in hepatocytes. In the 52-week, phase 2 ARREST trial, oral aramchol at 600 mg/day was 4.7-fold more likely than was placebo to achieve NASH resolution without worsening of fibrosis. The drug is now in phase 3 in the ARMOR study.
Resmetirom is a selective thyroid hormone receptor–beta agonist. Activation of the beta receptor lowers LDL cholesterol, triglycerides, and liver fat, whereas activation of the alpha receptor has the unwanted effects of promoting bone loss, thyrotoxicosis, and arrhythmias. In phase 2, 75% of patients on high-dose resmetirom achieved at least a 30% reduction in hepatic fat by MRI at week 12, compared with 18% of placebo-treated controls. And 39% of the high-dose resmetirom group showed histologic resolution of NASH on a week-36 liver biopsy, as did a mere 6% of controls. The phase 3 MAESTRO randomized trial is underway.
Obeticholic acid addresses the gut-liver axis abnormalities present in NASH, especially the exuberant bile acid circulation.
Clinical implications of the coming wave of medications
In Dr. Alkhouri’s view, .
“These are the patients with a high chance of progressing to cirrhosis and end-stage liver disease,” the gastroenterologist said.
Patients with earlier-stage nonalcoholic fatty liver disease are best managed via lifestyle changes, with particular emphasis upon 10% weight loss accompanied by exercise. And patients with more advanced disease – NASH with cirrhosis – appear thus far to be beyond the reach of the next-generation therapies.
None of the coming drugs is a cure-all. In the landmark phase 3 REGENERATE trial, for example, the rate of the primary outcome – fibrosis improvement of at least one stage plus no worsening of NASH at 18 months – was 23% in patients randomized to obeticholic acid at 25 mg/day, compared to 12% with placebo.
“These are not like hepatitis C medications, with 97% efficacy, so combination therapy targeting upstream and downstream for NASH is rational,” Dr. Alkhouri observed.
He reported serving on advisory boards for Allergan, Gilead, and Intercept, and receiving research grants from those companies as well as from Galmed, Genfit, and Madrigal.
*This story was updated on 12/5/2019.
SAN ANTONIO – The therapeutic Dark Ages of nonalcoholic steatohepatitis (NASH) are finally drawing to a close.
“NASH-specific therapies are coming soon – sooner than you think,” Naim Alkhouri, MD, predicted at the annual meeting of the American College of Gastroenterology.
And that, he added, has important implications for clinical practice. Physicians are going to need to step up their game with regard to screening and staging patients with nonalcoholic fatty liver disease to identify the right candidates for the coming effective treatments.
The new treatment era in NASH could dawn as soon as the spring of 2020, by which time the Food and Drug Administration is expected to issue a decision on obeticholic acid, an oral FXR agonist for which the agency has granted breakthrough therapy status. Intercept Pharmaceuticals has filed for marketing approval of obeticholic acid for NASH on the strength of the positive 18-month histologic results of the pivotal phase 3 REGENERATE trial, the first-ever successful phase 3 study of a medication for NASH, noted Dr. Alkhouri, a gastroenterologist at the University of Texas, San Antonio, and director of the Metabolic Health Center at the Texas Liver Institute.
At present there are no FDA-approved pharmacotherapies for NASH. The unmet medical need is huge, since NASH is now recognized to be a full-blown, burgeoning epidemic. NASH will soon become the No. 1 indication for liver transplantation in the United States. A full-throttle race is on to find effective therapies targeting the various dimensions of NASH, with more than 70 drugs now in phase 2 studies. These drugs collectively address all four mechanisms of the disease’s development and progression: the metabolic targets, perturbations in the gut-liver axis, liver inflammation, and fibrosis.
Moreover, even as the FDA considers the application for approval of obeticholic acid in NASH, at least four other investigational drugs are in pivotal phase 3 clinical trials. These include elafibranor, aramchol, resmetirom, and cenicriviroc.
Cenicriviroc is a dual CCR 2/5 receptor antagonist that targets the hepatic inflammation and fibrosis dimensions of NASH. It is now being evaluated in the phase 3 AURORA trial on the strength of the earlier positive phase 2b Centaur study, in which patients randomized to cenicriviroc were twice as likely to experience significant improvement in fibrosis as were placebo-treated controls.
Elafibranor, aramchol, and resmetirom employ different mechanisms of action to address the metabolic derangements of NASH. What they share in common is their aim to reduce the influx of free fatty acids from adipose tissue to the liver, and/or to inhibit lipogenesis from carbohydrate building blocks. In so doing, these medications should result in reduced hepatocyte injury and liver inflammation.
Elafibranor is a peroxisome proliferator-activated receptor alpha/delta agonist that achieved significant biopsy-proven reversal of NASH in moderate- or severely affected patients in the phase 2 GOLDEN study. The phase 3 RESOLVE IT trial is underway.
Aramchol is a first-in-class synthetic fatty acid/bile acid conjugate that inhibits stearoyl-CoA desaturate activity. It’s designed to improve insulin resistance and curb accumulation of triglycerides in hepatocytes. In the 52-week, phase 2 ARREST trial, oral aramchol at 600 mg/day was 4.7-fold more likely than was placebo to achieve NASH resolution without worsening of fibrosis. The drug is now in phase 3 in the ARMOR study.
Resmetirom is a selective thyroid hormone receptor–beta agonist. Activation of the beta receptor lowers LDL cholesterol, triglycerides, and liver fat, whereas activation of the alpha receptor has the unwanted effects of promoting bone loss, thyrotoxicosis, and arrhythmias. In phase 2, 75% of patients on high-dose resmetirom achieved at least a 30% reduction in hepatic fat by MRI at week 12, compared with 18% of placebo-treated controls. And 39% of the high-dose resmetirom group showed histologic resolution of NASH on a week-36 liver biopsy, as did a mere 6% of controls. The phase 3 MAESTRO randomized trial is underway.
Obeticholic acid addresses the gut-liver axis abnormalities present in NASH, especially the exuberant bile acid circulation.
Clinical implications of the coming wave of medications
In Dr. Alkhouri’s view, .
“These are the patients with a high chance of progressing to cirrhosis and end-stage liver disease,” the gastroenterologist said.
Patients with earlier-stage nonalcoholic fatty liver disease are best managed via lifestyle changes, with particular emphasis upon 10% weight loss accompanied by exercise. And patients with more advanced disease – NASH with cirrhosis – appear thus far to be beyond the reach of the next-generation therapies.
None of the coming drugs is a cure-all. In the landmark phase 3 REGENERATE trial, for example, the rate of the primary outcome – fibrosis improvement of at least one stage plus no worsening of NASH at 18 months – was 23% in patients randomized to obeticholic acid at 25 mg/day, compared to 12% with placebo.
“These are not like hepatitis C medications, with 97% efficacy, so combination therapy targeting upstream and downstream for NASH is rational,” Dr. Alkhouri observed.
He reported serving on advisory boards for Allergan, Gilead, and Intercept, and receiving research grants from those companies as well as from Galmed, Genfit, and Madrigal.
*This story was updated on 12/5/2019.
REPORTING FROM ACG 2019
Endoscopic radiofrequency ablation excels for pancreatic tumors
SAN ANTONIO – Endoscopic ultrasound-guided radiofrequency ablation is ready for a prime time proper definitive test in a randomized controlled trial for treatment of unresectable pancreatic tumors, Amaninder Dhaliwal, MD, declared at the annual meeting of the American College of Gastroenterology.
He backed this assertion by presenting his meta-analysis of 13 published studies of endoscopic ultrasound radiofrequency ablation (EUS-RFA) therapy applied to 127 patients with unresectable pancreatic tumors. Most of the studies were small, single center, and prospective, with a mean 5.2 months of follow-up. Fifty-three percent of the patients had locally advanced unresectable pancreatic ductal adenocarcinoma and 30% had pancreatic neuroendocrine tumors, with a smattering of rarer pancreatic tumors making up the balance. The median lesion size was 28.2 mm. The majority of target lesions were located on the pancreatic head.
EUS-RFA is a relatively new approach to the treatment of unresectable pancreatic tumors. It’s a minimally invasive treatment strategy guided by high-quality, real-time imaging. , according to Dr. Dhaliwal, a gastroenterology fellow at the University of Nebraska, Omaha.
The patients collectively underwent 156 EUS-RFA procedures, with a 98% technical success rate. The pooled clinical success rate was 84.5% as defined by reduction in lesion size, symptomatic improvement, and radiologic evidence of necrosis on imaging the day following the procedure.
”Symptoms improved as early as the next day, including hypoglycemia in patients with insulinomas,” he said.
The 7-day early adverse event rate was 13.4%, with mild to moderate abdominal pain accounting for nearly three-quarters of such events. Notably, no perforations or infections occurred. Late adverse events consisted of two cases of jaundice, two cases of mild pancreatitis, one duodenal stricture, and one cystic fluid pocket.
All of the studies utilized specialized 18- or 19-gauge needle electrodes. The mean energy delivered was 30 watts.
“I think [these] data give us some hope that we can go forward with multicenter trials in patients with unresectable pancreatic cancer and benign lesions. These patients are very sick and have limited options,” Dr. Dhaliwal observed.
He reported no financial conflicts regarding his study.
SOURCE: Dhaliwal A. ACG Abstract 30.
SAN ANTONIO – Endoscopic ultrasound-guided radiofrequency ablation is ready for a prime time proper definitive test in a randomized controlled trial for treatment of unresectable pancreatic tumors, Amaninder Dhaliwal, MD, declared at the annual meeting of the American College of Gastroenterology.
He backed this assertion by presenting his meta-analysis of 13 published studies of endoscopic ultrasound radiofrequency ablation (EUS-RFA) therapy applied to 127 patients with unresectable pancreatic tumors. Most of the studies were small, single center, and prospective, with a mean 5.2 months of follow-up. Fifty-three percent of the patients had locally advanced unresectable pancreatic ductal adenocarcinoma and 30% had pancreatic neuroendocrine tumors, with a smattering of rarer pancreatic tumors making up the balance. The median lesion size was 28.2 mm. The majority of target lesions were located on the pancreatic head.
EUS-RFA is a relatively new approach to the treatment of unresectable pancreatic tumors. It’s a minimally invasive treatment strategy guided by high-quality, real-time imaging. , according to Dr. Dhaliwal, a gastroenterology fellow at the University of Nebraska, Omaha.
The patients collectively underwent 156 EUS-RFA procedures, with a 98% technical success rate. The pooled clinical success rate was 84.5% as defined by reduction in lesion size, symptomatic improvement, and radiologic evidence of necrosis on imaging the day following the procedure.
”Symptoms improved as early as the next day, including hypoglycemia in patients with insulinomas,” he said.
The 7-day early adverse event rate was 13.4%, with mild to moderate abdominal pain accounting for nearly three-quarters of such events. Notably, no perforations or infections occurred. Late adverse events consisted of two cases of jaundice, two cases of mild pancreatitis, one duodenal stricture, and one cystic fluid pocket.
All of the studies utilized specialized 18- or 19-gauge needle electrodes. The mean energy delivered was 30 watts.
“I think [these] data give us some hope that we can go forward with multicenter trials in patients with unresectable pancreatic cancer and benign lesions. These patients are very sick and have limited options,” Dr. Dhaliwal observed.
He reported no financial conflicts regarding his study.
SOURCE: Dhaliwal A. ACG Abstract 30.
SAN ANTONIO – Endoscopic ultrasound-guided radiofrequency ablation is ready for a prime time proper definitive test in a randomized controlled trial for treatment of unresectable pancreatic tumors, Amaninder Dhaliwal, MD, declared at the annual meeting of the American College of Gastroenterology.
He backed this assertion by presenting his meta-analysis of 13 published studies of endoscopic ultrasound radiofrequency ablation (EUS-RFA) therapy applied to 127 patients with unresectable pancreatic tumors. Most of the studies were small, single center, and prospective, with a mean 5.2 months of follow-up. Fifty-three percent of the patients had locally advanced unresectable pancreatic ductal adenocarcinoma and 30% had pancreatic neuroendocrine tumors, with a smattering of rarer pancreatic tumors making up the balance. The median lesion size was 28.2 mm. The majority of target lesions were located on the pancreatic head.
EUS-RFA is a relatively new approach to the treatment of unresectable pancreatic tumors. It’s a minimally invasive treatment strategy guided by high-quality, real-time imaging. , according to Dr. Dhaliwal, a gastroenterology fellow at the University of Nebraska, Omaha.
The patients collectively underwent 156 EUS-RFA procedures, with a 98% technical success rate. The pooled clinical success rate was 84.5% as defined by reduction in lesion size, symptomatic improvement, and radiologic evidence of necrosis on imaging the day following the procedure.
”Symptoms improved as early as the next day, including hypoglycemia in patients with insulinomas,” he said.
The 7-day early adverse event rate was 13.4%, with mild to moderate abdominal pain accounting for nearly three-quarters of such events. Notably, no perforations or infections occurred. Late adverse events consisted of two cases of jaundice, two cases of mild pancreatitis, one duodenal stricture, and one cystic fluid pocket.
All of the studies utilized specialized 18- or 19-gauge needle electrodes. The mean energy delivered was 30 watts.
“I think [these] data give us some hope that we can go forward with multicenter trials in patients with unresectable pancreatic cancer and benign lesions. These patients are very sick and have limited options,” Dr. Dhaliwal observed.
He reported no financial conflicts regarding his study.
SOURCE: Dhaliwal A. ACG Abstract 30.
REPORTING FROM ACG 2019
Endoscopy-related occupational injuries run rampant in gastroenterology
SAN ANTONIO – Swati Pawa, MD, reported at the annual meeting of the American College of Gastroenterology.
Moreover, most respondents said they received zero training in ergonomic strategies for endoscopy-related injury (ERI) prevention during their fellowship training. And there’s been none since. Eighty-one percent of respondents indicated they would welcome such training, added Dr. Pawa, a gastroenterologist at Wake Forest University, Winston-Salem, N.C.
The survey results expose a glaring unmet need in clinical practice, she said: “There have been no published guidelines from any of the major professional GI societies to date addressing how to prevent endoscopy-related injuries.”
The 38-item survey was created by the ACG Women in GI Committee and sponsored by the ACG governing board.
Among the key findings was the identification of sex differences in the types of ERIs reported, which suggests different contributory mechanisms. For example, female gastroenterologists were more likely than were their male colleagues to have experienced ERIs involving the upper back, by a margin of 49% to 36%. Upper extremity pain was more common among the women, too, with 63% reporting hand or finger pain, compared with 53% of men. Twenty-four percent of women reported carpal tunnel syndrome and an equal percentage developed tendonitis, compared with 18% and 17% of men, respectively.
Seventy-one percent of women attributed their ERI to torquing with their right hand, as did 63% of men. Women also more frequently cited having to deal with a nonadjustable bed or monitor as contributing to injury. In contrast, roughly twice as many men as women attributed their ERI to wearing a lead apron or use of the elevator on the duodenoscope.
Equally common causes of ERIs in men and women included standing in awkward positions while supporting an endoscope, standing for a long time, and adjusting tip angulation with the left hand.
Male and female gastroenterologists differed in their practice patterns. The men had been performing endoscopy for a mean of 23 years, compared with 13 years for the women. Fifty-six percent of the men were in private practice, compared with 35% of the women. In contrast, 43% of the women worked in academic settings versus 28% of the men. Thirty percent of the male gastroenterologists characterized themselves as interventional specialists, a rate more than twice that in women, who more commonly specialized in inflammatory bowel disease.
The survey was sent to nearly 16,000 ACG members. It generated a 14% response rate. Roughly two-thirds of responses were provided by male gastroenterologists.
Dr. Pawa and her coinvestigators are now drilling down through the survey data in an effort to identify an appropriate endoscopy workload limit that’s associated with reduced ERI risk.
One audience member commented, “The incidence of ERI in your survey is much higher than most of us would expect.” He speculated that response bias might be at work, with gastroenterologists who have personally experienced an ERI being perhaps more highly motivated to be among the 14% who completed the 38-question survey. Dr. Pawa replied that the survey figures are in line with other, smaller studies.
She reported having no financial conflicts regarding her study.
Visit https://www.ddwnews.org/
SAN ANTONIO – Swati Pawa, MD, reported at the annual meeting of the American College of Gastroenterology.
Moreover, most respondents said they received zero training in ergonomic strategies for endoscopy-related injury (ERI) prevention during their fellowship training. And there’s been none since. Eighty-one percent of respondents indicated they would welcome such training, added Dr. Pawa, a gastroenterologist at Wake Forest University, Winston-Salem, N.C.
The survey results expose a glaring unmet need in clinical practice, she said: “There have been no published guidelines from any of the major professional GI societies to date addressing how to prevent endoscopy-related injuries.”
The 38-item survey was created by the ACG Women in GI Committee and sponsored by the ACG governing board.
Among the key findings was the identification of sex differences in the types of ERIs reported, which suggests different contributory mechanisms. For example, female gastroenterologists were more likely than were their male colleagues to have experienced ERIs involving the upper back, by a margin of 49% to 36%. Upper extremity pain was more common among the women, too, with 63% reporting hand or finger pain, compared with 53% of men. Twenty-four percent of women reported carpal tunnel syndrome and an equal percentage developed tendonitis, compared with 18% and 17% of men, respectively.
Seventy-one percent of women attributed their ERI to torquing with their right hand, as did 63% of men. Women also more frequently cited having to deal with a nonadjustable bed or monitor as contributing to injury. In contrast, roughly twice as many men as women attributed their ERI to wearing a lead apron or use of the elevator on the duodenoscope.
Equally common causes of ERIs in men and women included standing in awkward positions while supporting an endoscope, standing for a long time, and adjusting tip angulation with the left hand.
Male and female gastroenterologists differed in their practice patterns. The men had been performing endoscopy for a mean of 23 years, compared with 13 years for the women. Fifty-six percent of the men were in private practice, compared with 35% of the women. In contrast, 43% of the women worked in academic settings versus 28% of the men. Thirty percent of the male gastroenterologists characterized themselves as interventional specialists, a rate more than twice that in women, who more commonly specialized in inflammatory bowel disease.
The survey was sent to nearly 16,000 ACG members. It generated a 14% response rate. Roughly two-thirds of responses were provided by male gastroenterologists.
Dr. Pawa and her coinvestigators are now drilling down through the survey data in an effort to identify an appropriate endoscopy workload limit that’s associated with reduced ERI risk.
One audience member commented, “The incidence of ERI in your survey is much higher than most of us would expect.” He speculated that response bias might be at work, with gastroenterologists who have personally experienced an ERI being perhaps more highly motivated to be among the 14% who completed the 38-question survey. Dr. Pawa replied that the survey figures are in line with other, smaller studies.
She reported having no financial conflicts regarding her study.
Visit https://www.ddwnews.org/
SAN ANTONIO – Swati Pawa, MD, reported at the annual meeting of the American College of Gastroenterology.
Moreover, most respondents said they received zero training in ergonomic strategies for endoscopy-related injury (ERI) prevention during their fellowship training. And there’s been none since. Eighty-one percent of respondents indicated they would welcome such training, added Dr. Pawa, a gastroenterologist at Wake Forest University, Winston-Salem, N.C.
The survey results expose a glaring unmet need in clinical practice, she said: “There have been no published guidelines from any of the major professional GI societies to date addressing how to prevent endoscopy-related injuries.”
The 38-item survey was created by the ACG Women in GI Committee and sponsored by the ACG governing board.
Among the key findings was the identification of sex differences in the types of ERIs reported, which suggests different contributory mechanisms. For example, female gastroenterologists were more likely than were their male colleagues to have experienced ERIs involving the upper back, by a margin of 49% to 36%. Upper extremity pain was more common among the women, too, with 63% reporting hand or finger pain, compared with 53% of men. Twenty-four percent of women reported carpal tunnel syndrome and an equal percentage developed tendonitis, compared with 18% and 17% of men, respectively.
Seventy-one percent of women attributed their ERI to torquing with their right hand, as did 63% of men. Women also more frequently cited having to deal with a nonadjustable bed or monitor as contributing to injury. In contrast, roughly twice as many men as women attributed their ERI to wearing a lead apron or use of the elevator on the duodenoscope.
Equally common causes of ERIs in men and women included standing in awkward positions while supporting an endoscope, standing for a long time, and adjusting tip angulation with the left hand.
Male and female gastroenterologists differed in their practice patterns. The men had been performing endoscopy for a mean of 23 years, compared with 13 years for the women. Fifty-six percent of the men were in private practice, compared with 35% of the women. In contrast, 43% of the women worked in academic settings versus 28% of the men. Thirty percent of the male gastroenterologists characterized themselves as interventional specialists, a rate more than twice that in women, who more commonly specialized in inflammatory bowel disease.
The survey was sent to nearly 16,000 ACG members. It generated a 14% response rate. Roughly two-thirds of responses were provided by male gastroenterologists.
Dr. Pawa and her coinvestigators are now drilling down through the survey data in an effort to identify an appropriate endoscopy workload limit that’s associated with reduced ERI risk.
One audience member commented, “The incidence of ERI in your survey is much higher than most of us would expect.” He speculated that response bias might be at work, with gastroenterologists who have personally experienced an ERI being perhaps more highly motivated to be among the 14% who completed the 38-question survey. Dr. Pawa replied that the survey figures are in line with other, smaller studies.
She reported having no financial conflicts regarding her study.
Visit https://www.ddwnews.org/
REPORTING FROM ACG 2019
Endoscopy-related occupational injuries run rampant in gastroenterology
SAN ANTONIO – Swati Pawa, MD, reported at the annual meeting of the American College of Gastroenterology.
Moreover, most respondents said they received zero training in ergonomic strategies for endoscopy-related injury (ERI) prevention during their fellowship training. And there’s been none since. Eighty-one percent of respondents indicated they would welcome such training, added Dr. Pawa, a gastroenterologist at Wake Forest University, Winston-Salem, N.C.
The survey results expose a glaring unmet need in clinical practice, she said: “There have been no published guidelines from any of the major professional GI societies to date addressing how to prevent endoscopy-related injuries.”
The 38-item survey was created by the ACG Women in GI Committee and sponsored by the ACG governing board.
Among the key findings was the identification of sex differences in the types of ERIs reported, which suggests different contributory mechanisms. For example, female gastroenterologists were more likely than were their male colleagues to have experienced ERIs involving the upper back, by a margin of 49% to 36%. Upper extremity pain was more common among the women, too, with 63% reporting hand or finger pain, compared with 53% of men. Twenty-four percent of women reported carpal tunnel syndrome and an equal percentage developed tendonitis, compared with 18% and 17% of men, respectively.
Seventy-one percent of women attributed their ERI to torquing with their right hand, as did 63% of men. Women also more frequently cited having to deal with a nonadjustable bed or monitor as contributing to injury. In contrast, roughly twice as many men as women attributed their ERI to wearing a lead apron or use of the elevator on the duodenoscope.
Equally common causes of ERIs in men and women included standing in awkward positions while supporting an endoscope, standing for a long time, and adjusting tip angulation with the left hand.
Male and female gastroenterologists differed in their practice patterns. The men had been performing endoscopy for a mean of 23 years, compared with 13 years for the women. Fifty-six percent of the men were in private practice, compared with 35% of the women. In contrast, 43% of the women worked in academic settings versus 28% of the men. Thirty percent of the male gastroenterologists characterized themselves as interventional specialists, a rate more than twice that in women, who more commonly specialized in inflammatory bowel disease.
The survey was sent to nearly 16,000 ACG members. It generated a 14% response rate. Roughly two-thirds of responses were provided by male gastroenterologists.
Dr. Pawa and her coinvestigators are now drilling down through the survey data in an effort to identify an appropriate endoscopy workload limit that’s associated with reduced ERI risk.
One audience member commented, “The incidence of ERI in your survey is much higher than most of us would expect.” He speculated that response bias might be at work, with gastroenterologists who have personally experienced an ERI being perhaps more highly motivated to be among the 14% who completed the 38-question survey. Dr. Pawa replied that the survey figures are in line with other, smaller studies.
She reported having no financial conflicts regarding her study.
SAN ANTONIO – Swati Pawa, MD, reported at the annual meeting of the American College of Gastroenterology.
Moreover, most respondents said they received zero training in ergonomic strategies for endoscopy-related injury (ERI) prevention during their fellowship training. And there’s been none since. Eighty-one percent of respondents indicated they would welcome such training, added Dr. Pawa, a gastroenterologist at Wake Forest University, Winston-Salem, N.C.
The survey results expose a glaring unmet need in clinical practice, she said: “There have been no published guidelines from any of the major professional GI societies to date addressing how to prevent endoscopy-related injuries.”
The 38-item survey was created by the ACG Women in GI Committee and sponsored by the ACG governing board.
Among the key findings was the identification of sex differences in the types of ERIs reported, which suggests different contributory mechanisms. For example, female gastroenterologists were more likely than were their male colleagues to have experienced ERIs involving the upper back, by a margin of 49% to 36%. Upper extremity pain was more common among the women, too, with 63% reporting hand or finger pain, compared with 53% of men. Twenty-four percent of women reported carpal tunnel syndrome and an equal percentage developed tendonitis, compared with 18% and 17% of men, respectively.
Seventy-one percent of women attributed their ERI to torquing with their right hand, as did 63% of men. Women also more frequently cited having to deal with a nonadjustable bed or monitor as contributing to injury. In contrast, roughly twice as many men as women attributed their ERI to wearing a lead apron or use of the elevator on the duodenoscope.
Equally common causes of ERIs in men and women included standing in awkward positions while supporting an endoscope, standing for a long time, and adjusting tip angulation with the left hand.
Male and female gastroenterologists differed in their practice patterns. The men had been performing endoscopy for a mean of 23 years, compared with 13 years for the women. Fifty-six percent of the men were in private practice, compared with 35% of the women. In contrast, 43% of the women worked in academic settings versus 28% of the men. Thirty percent of the male gastroenterologists characterized themselves as interventional specialists, a rate more than twice that in women, who more commonly specialized in inflammatory bowel disease.
The survey was sent to nearly 16,000 ACG members. It generated a 14% response rate. Roughly two-thirds of responses were provided by male gastroenterologists.
Dr. Pawa and her coinvestigators are now drilling down through the survey data in an effort to identify an appropriate endoscopy workload limit that’s associated with reduced ERI risk.
One audience member commented, “The incidence of ERI in your survey is much higher than most of us would expect.” He speculated that response bias might be at work, with gastroenterologists who have personally experienced an ERI being perhaps more highly motivated to be among the 14% who completed the 38-question survey. Dr. Pawa replied that the survey figures are in line with other, smaller studies.
She reported having no financial conflicts regarding her study.
SAN ANTONIO – Swati Pawa, MD, reported at the annual meeting of the American College of Gastroenterology.
Moreover, most respondents said they received zero training in ergonomic strategies for endoscopy-related injury (ERI) prevention during their fellowship training. And there’s been none since. Eighty-one percent of respondents indicated they would welcome such training, added Dr. Pawa, a gastroenterologist at Wake Forest University, Winston-Salem, N.C.
The survey results expose a glaring unmet need in clinical practice, she said: “There have been no published guidelines from any of the major professional GI societies to date addressing how to prevent endoscopy-related injuries.”
The 38-item survey was created by the ACG Women in GI Committee and sponsored by the ACG governing board.
Among the key findings was the identification of sex differences in the types of ERIs reported, which suggests different contributory mechanisms. For example, female gastroenterologists were more likely than were their male colleagues to have experienced ERIs involving the upper back, by a margin of 49% to 36%. Upper extremity pain was more common among the women, too, with 63% reporting hand or finger pain, compared with 53% of men. Twenty-four percent of women reported carpal tunnel syndrome and an equal percentage developed tendonitis, compared with 18% and 17% of men, respectively.
Seventy-one percent of women attributed their ERI to torquing with their right hand, as did 63% of men. Women also more frequently cited having to deal with a nonadjustable bed or monitor as contributing to injury. In contrast, roughly twice as many men as women attributed their ERI to wearing a lead apron or use of the elevator on the duodenoscope.
Equally common causes of ERIs in men and women included standing in awkward positions while supporting an endoscope, standing for a long time, and adjusting tip angulation with the left hand.
Male and female gastroenterologists differed in their practice patterns. The men had been performing endoscopy for a mean of 23 years, compared with 13 years for the women. Fifty-six percent of the men were in private practice, compared with 35% of the women. In contrast, 43% of the women worked in academic settings versus 28% of the men. Thirty percent of the male gastroenterologists characterized themselves as interventional specialists, a rate more than twice that in women, who more commonly specialized in inflammatory bowel disease.
The survey was sent to nearly 16,000 ACG members. It generated a 14% response rate. Roughly two-thirds of responses were provided by male gastroenterologists.
Dr. Pawa and her coinvestigators are now drilling down through the survey data in an effort to identify an appropriate endoscopy workload limit that’s associated with reduced ERI risk.
One audience member commented, “The incidence of ERI in your survey is much higher than most of us would expect.” He speculated that response bias might be at work, with gastroenterologists who have personally experienced an ERI being perhaps more highly motivated to be among the 14% who completed the 38-question survey. Dr. Pawa replied that the survey figures are in line with other, smaller studies.
She reported having no financial conflicts regarding her study.
REPORTING FROM ACG 2019
Certolizumab safety profile varies widely across indications
MADRID – , Andrew Blauvelt, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
He presented a comprehensive analysis of safety data from all 49 clinical trials of the tumor necrosis factor inhibitor for its approved indications. The data set included 11,317 patients who received certolizumab for a collective 21,695 person-years in 27 trials in rheumatoid arthritis patients, 5 in psoriasis, 15 for Crohn’s disease, and one trial each for axial spondyloarthritis and psoriatic arthritis.
“It’s not real-world data, but it is a large group of patients [studied] over many years,” noted Dr. Blauvelt, a dermatologist and president of the Oregon Medical Research Center, Portland.
As a renowned authority on psoriasis, he was part of a multidisciplinary expert panel commissioned by UCB to analyze serious adverse events in the complete clinical trials experience involving the company’s tumor necrosis factor inhibitor certolizumab (Cimzia). The panel included experts from rheumatology, gastroenterology, epidemiology, and other disciplines.
The key takeaway: “When you think about the serious side effects of the drug, you have to think about what the indication is, whether the patients are on systemic corticosteroids, and whether they’re heavy or not,” Dr. Blauvelt said.
Take, for example, the risk of serious infections requiring treatment with intravenous antibiotics. The incidence rates ranged from a low of 1.5 per 100 patient-years in psoriasis patients on certolizumab to a high of 5.97 in those with Crohn’s disease, with rates of 3.44 cases per 100 patient-years among rheumatoid arthritis patients and 1.64-1.67 in those with psoriatic arthritis and ankylosing spondylitis, respectively. Patients with Crohn’s disease were 2.22-fold more likely than were those with rheumatoid arthritis to experience a serious infection during their clinical trial experience on certolizumab. In contrast, psoriasis patients had a 52% relative risk reduction and those with psoriatic arthritis were 31% less likely to develop a serious infection compared with those with rheumatoid arthritis.
The explanation for these highly variable serious infection rates lies in part on the huge differences in the concurrent use of systemic corticosteroids with certolizumab across indications. A mere 3.3% of psoriasis patients were also on steroids, compared with 46.2% of rheumatoid arthritis patients, 50.8% of those with ankylosing spondylitis, and about 25% of the Crohn’s disease and psoriatic arthritis patients, he noted.
Advanced age was independently associated with increased risk of serious infections. Patients aged 65 or older were 1.68-fold more likely to experience this event than were those under age 45. And patients whose disease duration was 10 years or more at baseline had a 1.36-fold increased serious infection risk compared with those who had less than a 1-year-long disease history, independent of which disease they had.
The prevalence of baseline obesity varied by indication. The mean body mass index was 30.1 kg/m2 in the psoriasis patients, 29.8 kg/m2 in those with psoriatic arthritis, lowest at 24 kg/m2 in Crohn’s disease patients, and a bit over 27 kg/m2 in those with rheumatoid arthritis or ankylosing spondylitis.
Obesity alone was not an independent risk factor for serious infection in certolizumab-treated patients; however, the combination of a BMI of 30 kg/m2 or more plus systemic corticosteroid use was associated with a greater risk than with steroids alone.
Based upon a multivariate regression analysis adjusted for age, sex, indication, disease duration, use of methotrexate, and prior use of other TNF inhibitors, the investigators calculated that in patients with Crohn’s disease 16.6% of serious infections in patients on certolizumab were attributable to systemic corticosteroid use.
Risks of major adverse cardiovascular events and cancer on certolizumab
The risk of major adverse cardiovascular events (MACE) while on certolizumab ranged from a high of 0.62 MACE events per 100 patient-years in the rheumatoid arthritis population to a low of 0.1 per 100 patient-years in patients treated for Crohn’s disease or ankylosing spondylitis. Psoriasis and psoriatic arthritis patients had MACE rates of 0.27 and 0.54, respectively.
Obesity was independently associated with increased risk of an acute MI and other MACEs. So was advanced age. No surprises there. The investigators calculated that 16.7% of MACEs in patients on certolizumab were attributable to obesity and another 20.9% were attributable to use of systemic corticosteroids.
The incidence rate for all malignancies, including nonmelanoma skin cancer, ranged from a low of 0.46 cases per 100 patient-years in the psoriatic arthritis cohort on certolizumab to a high of 0.93 in those with rheumatoid arthritis, with rates of 0.68, 0.73, and 0.51 in patients with psoriasis, Crohn’s disease, and ankylosing spondylitis, respectively.
Neither systemic corticosteroids, obesity, disease duration, or prior exposure to a TNF inhibitor was linked to increased risk of cancer in patients on certolizumab. The standout risk factor was age: Patients who were 65 or older at baseline were 11.4-fold more likely to develop cancer during participation in their clinical trial than were those younger than 45. Those who were 45 to 65 years old were 4.3-fold more likely to be diagnosed with a malignancy than were those younger than age 45.
Of note, concomitant use of methotrexate was associated with a statistically significant 28% reduction in malignancy risk.
Dr. Blauvelt reported serving as a consultant to and receiving research funding from UCB, the study sponsor, as well as more than two dozen other pharmaceutical companies.
SOURCE: Blauvelt A. EADV Congress, Abstract FC04.06.
MADRID – , Andrew Blauvelt, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
He presented a comprehensive analysis of safety data from all 49 clinical trials of the tumor necrosis factor inhibitor for its approved indications. The data set included 11,317 patients who received certolizumab for a collective 21,695 person-years in 27 trials in rheumatoid arthritis patients, 5 in psoriasis, 15 for Crohn’s disease, and one trial each for axial spondyloarthritis and psoriatic arthritis.
“It’s not real-world data, but it is a large group of patients [studied] over many years,” noted Dr. Blauvelt, a dermatologist and president of the Oregon Medical Research Center, Portland.
As a renowned authority on psoriasis, he was part of a multidisciplinary expert panel commissioned by UCB to analyze serious adverse events in the complete clinical trials experience involving the company’s tumor necrosis factor inhibitor certolizumab (Cimzia). The panel included experts from rheumatology, gastroenterology, epidemiology, and other disciplines.
The key takeaway: “When you think about the serious side effects of the drug, you have to think about what the indication is, whether the patients are on systemic corticosteroids, and whether they’re heavy or not,” Dr. Blauvelt said.
Take, for example, the risk of serious infections requiring treatment with intravenous antibiotics. The incidence rates ranged from a low of 1.5 per 100 patient-years in psoriasis patients on certolizumab to a high of 5.97 in those with Crohn’s disease, with rates of 3.44 cases per 100 patient-years among rheumatoid arthritis patients and 1.64-1.67 in those with psoriatic arthritis and ankylosing spondylitis, respectively. Patients with Crohn’s disease were 2.22-fold more likely than were those with rheumatoid arthritis to experience a serious infection during their clinical trial experience on certolizumab. In contrast, psoriasis patients had a 52% relative risk reduction and those with psoriatic arthritis were 31% less likely to develop a serious infection compared with those with rheumatoid arthritis.
The explanation for these highly variable serious infection rates lies in part on the huge differences in the concurrent use of systemic corticosteroids with certolizumab across indications. A mere 3.3% of psoriasis patients were also on steroids, compared with 46.2% of rheumatoid arthritis patients, 50.8% of those with ankylosing spondylitis, and about 25% of the Crohn’s disease and psoriatic arthritis patients, he noted.
Advanced age was independently associated with increased risk of serious infections. Patients aged 65 or older were 1.68-fold more likely to experience this event than were those under age 45. And patients whose disease duration was 10 years or more at baseline had a 1.36-fold increased serious infection risk compared with those who had less than a 1-year-long disease history, independent of which disease they had.
The prevalence of baseline obesity varied by indication. The mean body mass index was 30.1 kg/m2 in the psoriasis patients, 29.8 kg/m2 in those with psoriatic arthritis, lowest at 24 kg/m2 in Crohn’s disease patients, and a bit over 27 kg/m2 in those with rheumatoid arthritis or ankylosing spondylitis.
Obesity alone was not an independent risk factor for serious infection in certolizumab-treated patients; however, the combination of a BMI of 30 kg/m2 or more plus systemic corticosteroid use was associated with a greater risk than with steroids alone.
Based upon a multivariate regression analysis adjusted for age, sex, indication, disease duration, use of methotrexate, and prior use of other TNF inhibitors, the investigators calculated that in patients with Crohn’s disease 16.6% of serious infections in patients on certolizumab were attributable to systemic corticosteroid use.
Risks of major adverse cardiovascular events and cancer on certolizumab
The risk of major adverse cardiovascular events (MACE) while on certolizumab ranged from a high of 0.62 MACE events per 100 patient-years in the rheumatoid arthritis population to a low of 0.1 per 100 patient-years in patients treated for Crohn’s disease or ankylosing spondylitis. Psoriasis and psoriatic arthritis patients had MACE rates of 0.27 and 0.54, respectively.
Obesity was independently associated with increased risk of an acute MI and other MACEs. So was advanced age. No surprises there. The investigators calculated that 16.7% of MACEs in patients on certolizumab were attributable to obesity and another 20.9% were attributable to use of systemic corticosteroids.
The incidence rate for all malignancies, including nonmelanoma skin cancer, ranged from a low of 0.46 cases per 100 patient-years in the psoriatic arthritis cohort on certolizumab to a high of 0.93 in those with rheumatoid arthritis, with rates of 0.68, 0.73, and 0.51 in patients with psoriasis, Crohn’s disease, and ankylosing spondylitis, respectively.
Neither systemic corticosteroids, obesity, disease duration, or prior exposure to a TNF inhibitor was linked to increased risk of cancer in patients on certolizumab. The standout risk factor was age: Patients who were 65 or older at baseline were 11.4-fold more likely to develop cancer during participation in their clinical trial than were those younger than 45. Those who were 45 to 65 years old were 4.3-fold more likely to be diagnosed with a malignancy than were those younger than age 45.
Of note, concomitant use of methotrexate was associated with a statistically significant 28% reduction in malignancy risk.
Dr. Blauvelt reported serving as a consultant to and receiving research funding from UCB, the study sponsor, as well as more than two dozen other pharmaceutical companies.
SOURCE: Blauvelt A. EADV Congress, Abstract FC04.06.
MADRID – , Andrew Blauvelt, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
He presented a comprehensive analysis of safety data from all 49 clinical trials of the tumor necrosis factor inhibitor for its approved indications. The data set included 11,317 patients who received certolizumab for a collective 21,695 person-years in 27 trials in rheumatoid arthritis patients, 5 in psoriasis, 15 for Crohn’s disease, and one trial each for axial spondyloarthritis and psoriatic arthritis.
“It’s not real-world data, but it is a large group of patients [studied] over many years,” noted Dr. Blauvelt, a dermatologist and president of the Oregon Medical Research Center, Portland.
As a renowned authority on psoriasis, he was part of a multidisciplinary expert panel commissioned by UCB to analyze serious adverse events in the complete clinical trials experience involving the company’s tumor necrosis factor inhibitor certolizumab (Cimzia). The panel included experts from rheumatology, gastroenterology, epidemiology, and other disciplines.
The key takeaway: “When you think about the serious side effects of the drug, you have to think about what the indication is, whether the patients are on systemic corticosteroids, and whether they’re heavy or not,” Dr. Blauvelt said.
Take, for example, the risk of serious infections requiring treatment with intravenous antibiotics. The incidence rates ranged from a low of 1.5 per 100 patient-years in psoriasis patients on certolizumab to a high of 5.97 in those with Crohn’s disease, with rates of 3.44 cases per 100 patient-years among rheumatoid arthritis patients and 1.64-1.67 in those with psoriatic arthritis and ankylosing spondylitis, respectively. Patients with Crohn’s disease were 2.22-fold more likely than were those with rheumatoid arthritis to experience a serious infection during their clinical trial experience on certolizumab. In contrast, psoriasis patients had a 52% relative risk reduction and those with psoriatic arthritis were 31% less likely to develop a serious infection compared with those with rheumatoid arthritis.
The explanation for these highly variable serious infection rates lies in part on the huge differences in the concurrent use of systemic corticosteroids with certolizumab across indications. A mere 3.3% of psoriasis patients were also on steroids, compared with 46.2% of rheumatoid arthritis patients, 50.8% of those with ankylosing spondylitis, and about 25% of the Crohn’s disease and psoriatic arthritis patients, he noted.
Advanced age was independently associated with increased risk of serious infections. Patients aged 65 or older were 1.68-fold more likely to experience this event than were those under age 45. And patients whose disease duration was 10 years or more at baseline had a 1.36-fold increased serious infection risk compared with those who had less than a 1-year-long disease history, independent of which disease they had.
The prevalence of baseline obesity varied by indication. The mean body mass index was 30.1 kg/m2 in the psoriasis patients, 29.8 kg/m2 in those with psoriatic arthritis, lowest at 24 kg/m2 in Crohn’s disease patients, and a bit over 27 kg/m2 in those with rheumatoid arthritis or ankylosing spondylitis.
Obesity alone was not an independent risk factor for serious infection in certolizumab-treated patients; however, the combination of a BMI of 30 kg/m2 or more plus systemic corticosteroid use was associated with a greater risk than with steroids alone.
Based upon a multivariate regression analysis adjusted for age, sex, indication, disease duration, use of methotrexate, and prior use of other TNF inhibitors, the investigators calculated that in patients with Crohn’s disease 16.6% of serious infections in patients on certolizumab were attributable to systemic corticosteroid use.
Risks of major adverse cardiovascular events and cancer on certolizumab
The risk of major adverse cardiovascular events (MACE) while on certolizumab ranged from a high of 0.62 MACE events per 100 patient-years in the rheumatoid arthritis population to a low of 0.1 per 100 patient-years in patients treated for Crohn’s disease or ankylosing spondylitis. Psoriasis and psoriatic arthritis patients had MACE rates of 0.27 and 0.54, respectively.
Obesity was independently associated with increased risk of an acute MI and other MACEs. So was advanced age. No surprises there. The investigators calculated that 16.7% of MACEs in patients on certolizumab were attributable to obesity and another 20.9% were attributable to use of systemic corticosteroids.
The incidence rate for all malignancies, including nonmelanoma skin cancer, ranged from a low of 0.46 cases per 100 patient-years in the psoriatic arthritis cohort on certolizumab to a high of 0.93 in those with rheumatoid arthritis, with rates of 0.68, 0.73, and 0.51 in patients with psoriasis, Crohn’s disease, and ankylosing spondylitis, respectively.
Neither systemic corticosteroids, obesity, disease duration, or prior exposure to a TNF inhibitor was linked to increased risk of cancer in patients on certolizumab. The standout risk factor was age: Patients who were 65 or older at baseline were 11.4-fold more likely to develop cancer during participation in their clinical trial than were those younger than 45. Those who were 45 to 65 years old were 4.3-fold more likely to be diagnosed with a malignancy than were those younger than age 45.
Of note, concomitant use of methotrexate was associated with a statistically significant 28% reduction in malignancy risk.
Dr. Blauvelt reported serving as a consultant to and receiving research funding from UCB, the study sponsor, as well as more than two dozen other pharmaceutical companies.
SOURCE: Blauvelt A. EADV Congress, Abstract FC04.06.
REPORTING FROM THE EADV CONGRESS
Wide-area transepithelial sampling may be best method for detecting esophageal intestinal metaplasia
SAN ANTONIO – A wide-area transepithelial sampling (WATS) brush proved superior to standard forceps biopsies for detection of intestinal metaplasia (IM) in the esophagus and gastroesophageal junction in patients with no history of IM who had any visible columnar-lined esophagus on upper endoscopy in a large randomized trial.
“This suggests that WATS should in fact be the preferred method of sampling these patients,” Steven R. DeMeester, MD, commented in presenting the study results at the annual meeting of the American College of Gastroenterology.
With that specific exception, however, the two sampling methods proved similarly effective at detecting IM and dysplasia, suggesting either technology can otherwise reliably be used to detect these conditions, added Dr. DeMeester, a general and thoracic surgeon at the Oregon Clinic, Portland.
This is important new information for clinicians. A prior multicenter, randomized trial by other investigators demonstrated that adding WATS to biopsy sampling improved the detection rate of dysplasia and esophageal adenocarcinoma, compared with biopsies alone (Gastrointest Endosc. 2018 Feb;87[2]:348-55). However, this dual-sampling strategy is too time-consuming for routine use in a busy practice. Given the new evidence that the two sampling methods can reliably be used interchangeably except in patients with no history of IM who have endoscopically visible columnar-lined esophagus, WATS offers a clear advantage in that it’s much quicker, especially in patients with long-segment Barrett’s esophagus, the surgeon said.
Unlike brush cytology, which merely collects surface epithelial cells, the WATS brush collects sheets of esophageal mucosa, which then undergo computer-assisted three-dimensional analysis.
“When done appropriately, a wide area of the esophageal mucosa can be sampled with the WATS brush,” Dr. DeMeester explained.
He reported on 1,002 patients who presented at nine U.S. centers for upper endoscopy for Barrett’s esophagus surveillance or evaluation of foregut symptoms. They were randomized to WATS or forceps biopsies using the Seattle protocol. In the entire group, WATS and forceps biopsies were similarly effective, each finding IM – a potentially premalignant mucosal change – in about 21% of patients, and dysplasia or cancer in 0.8%. Among the 185 patients who underwent endoscopy for follow-up of Barrett’s esophagus or post ablation, the two sampling strategies also performed similarly, detecting IM in roughly 36% of the 151 patients with columnar-lined esophagus shorter than 3 cm and in 56% of those with columnar-lined esophagus of greater length.
However, in the 196 patients with no history of IM who had any length of visible columnar-lined esophagus on endoscopy, the frequency of IM detection was 32.7% with WATS, compared with 15.3% with biopsy.
Dr. DeMeester and coinvestigators were also eager to identify factors associated with detection of IM in the esophagus or gastroesophageal junction in patients undergoing elective endoscopy with no history of IM. They found that whites were at greater risk than blacks, by a margin of 10.1% (17.1% vs. 7%). Moreover, the 23% IM detection rate in patients aged over age 70 years was significantly higher than the 15.5% rate in those under age 70. And to their surprise, there was no significant difference between the IM detection rate in men and women.
Nearly 15% of study participants with no measurable columnar-lined esophagus turned out to have IM. And two patients with low-grade dysplasia and one with adenocarcinoma were found among the group with no history of IM and no visible columnar-lined esophagus on upper endoscopy.
“This demonstrates that the absence of a measurable columnar-lined esophagus does not exclude patients from the risk of having intestinal metaplasia, dysplasia, or cancer at the gastroesophageal junction. Therefore evaluation of the gastroesophageal junction by biopsy or WATS should be considered during upper endoscopy, particularly in patients at increased risk for having intestinal metaplasia,” he concluded.
Dr. DeMeester reported serving as a consultant to BARD and receiving research funding from and serving as a paid speaker for CDx Diagnostics, which funded the trial.
SAN ANTONIO – A wide-area transepithelial sampling (WATS) brush proved superior to standard forceps biopsies for detection of intestinal metaplasia (IM) in the esophagus and gastroesophageal junction in patients with no history of IM who had any visible columnar-lined esophagus on upper endoscopy in a large randomized trial.
“This suggests that WATS should in fact be the preferred method of sampling these patients,” Steven R. DeMeester, MD, commented in presenting the study results at the annual meeting of the American College of Gastroenterology.
With that specific exception, however, the two sampling methods proved similarly effective at detecting IM and dysplasia, suggesting either technology can otherwise reliably be used to detect these conditions, added Dr. DeMeester, a general and thoracic surgeon at the Oregon Clinic, Portland.
This is important new information for clinicians. A prior multicenter, randomized trial by other investigators demonstrated that adding WATS to biopsy sampling improved the detection rate of dysplasia and esophageal adenocarcinoma, compared with biopsies alone (Gastrointest Endosc. 2018 Feb;87[2]:348-55). However, this dual-sampling strategy is too time-consuming for routine use in a busy practice. Given the new evidence that the two sampling methods can reliably be used interchangeably except in patients with no history of IM who have endoscopically visible columnar-lined esophagus, WATS offers a clear advantage in that it’s much quicker, especially in patients with long-segment Barrett’s esophagus, the surgeon said.
Unlike brush cytology, which merely collects surface epithelial cells, the WATS brush collects sheets of esophageal mucosa, which then undergo computer-assisted three-dimensional analysis.
“When done appropriately, a wide area of the esophageal mucosa can be sampled with the WATS brush,” Dr. DeMeester explained.
He reported on 1,002 patients who presented at nine U.S. centers for upper endoscopy for Barrett’s esophagus surveillance or evaluation of foregut symptoms. They were randomized to WATS or forceps biopsies using the Seattle protocol. In the entire group, WATS and forceps biopsies were similarly effective, each finding IM – a potentially premalignant mucosal change – in about 21% of patients, and dysplasia or cancer in 0.8%. Among the 185 patients who underwent endoscopy for follow-up of Barrett’s esophagus or post ablation, the two sampling strategies also performed similarly, detecting IM in roughly 36% of the 151 patients with columnar-lined esophagus shorter than 3 cm and in 56% of those with columnar-lined esophagus of greater length.
However, in the 196 patients with no history of IM who had any length of visible columnar-lined esophagus on endoscopy, the frequency of IM detection was 32.7% with WATS, compared with 15.3% with biopsy.
Dr. DeMeester and coinvestigators were also eager to identify factors associated with detection of IM in the esophagus or gastroesophageal junction in patients undergoing elective endoscopy with no history of IM. They found that whites were at greater risk than blacks, by a margin of 10.1% (17.1% vs. 7%). Moreover, the 23% IM detection rate in patients aged over age 70 years was significantly higher than the 15.5% rate in those under age 70. And to their surprise, there was no significant difference between the IM detection rate in men and women.
Nearly 15% of study participants with no measurable columnar-lined esophagus turned out to have IM. And two patients with low-grade dysplasia and one with adenocarcinoma were found among the group with no history of IM and no visible columnar-lined esophagus on upper endoscopy.
“This demonstrates that the absence of a measurable columnar-lined esophagus does not exclude patients from the risk of having intestinal metaplasia, dysplasia, or cancer at the gastroesophageal junction. Therefore evaluation of the gastroesophageal junction by biopsy or WATS should be considered during upper endoscopy, particularly in patients at increased risk for having intestinal metaplasia,” he concluded.
Dr. DeMeester reported serving as a consultant to BARD and receiving research funding from and serving as a paid speaker for CDx Diagnostics, which funded the trial.
SAN ANTONIO – A wide-area transepithelial sampling (WATS) brush proved superior to standard forceps biopsies for detection of intestinal metaplasia (IM) in the esophagus and gastroesophageal junction in patients with no history of IM who had any visible columnar-lined esophagus on upper endoscopy in a large randomized trial.
“This suggests that WATS should in fact be the preferred method of sampling these patients,” Steven R. DeMeester, MD, commented in presenting the study results at the annual meeting of the American College of Gastroenterology.
With that specific exception, however, the two sampling methods proved similarly effective at detecting IM and dysplasia, suggesting either technology can otherwise reliably be used to detect these conditions, added Dr. DeMeester, a general and thoracic surgeon at the Oregon Clinic, Portland.
This is important new information for clinicians. A prior multicenter, randomized trial by other investigators demonstrated that adding WATS to biopsy sampling improved the detection rate of dysplasia and esophageal adenocarcinoma, compared with biopsies alone (Gastrointest Endosc. 2018 Feb;87[2]:348-55). However, this dual-sampling strategy is too time-consuming for routine use in a busy practice. Given the new evidence that the two sampling methods can reliably be used interchangeably except in patients with no history of IM who have endoscopically visible columnar-lined esophagus, WATS offers a clear advantage in that it’s much quicker, especially in patients with long-segment Barrett’s esophagus, the surgeon said.
Unlike brush cytology, which merely collects surface epithelial cells, the WATS brush collects sheets of esophageal mucosa, which then undergo computer-assisted three-dimensional analysis.
“When done appropriately, a wide area of the esophageal mucosa can be sampled with the WATS brush,” Dr. DeMeester explained.
He reported on 1,002 patients who presented at nine U.S. centers for upper endoscopy for Barrett’s esophagus surveillance or evaluation of foregut symptoms. They were randomized to WATS or forceps biopsies using the Seattle protocol. In the entire group, WATS and forceps biopsies were similarly effective, each finding IM – a potentially premalignant mucosal change – in about 21% of patients, and dysplasia or cancer in 0.8%. Among the 185 patients who underwent endoscopy for follow-up of Barrett’s esophagus or post ablation, the two sampling strategies also performed similarly, detecting IM in roughly 36% of the 151 patients with columnar-lined esophagus shorter than 3 cm and in 56% of those with columnar-lined esophagus of greater length.
However, in the 196 patients with no history of IM who had any length of visible columnar-lined esophagus on endoscopy, the frequency of IM detection was 32.7% with WATS, compared with 15.3% with biopsy.
Dr. DeMeester and coinvestigators were also eager to identify factors associated with detection of IM in the esophagus or gastroesophageal junction in patients undergoing elective endoscopy with no history of IM. They found that whites were at greater risk than blacks, by a margin of 10.1% (17.1% vs. 7%). Moreover, the 23% IM detection rate in patients aged over age 70 years was significantly higher than the 15.5% rate in those under age 70. And to their surprise, there was no significant difference between the IM detection rate in men and women.
Nearly 15% of study participants with no measurable columnar-lined esophagus turned out to have IM. And two patients with low-grade dysplasia and one with adenocarcinoma were found among the group with no history of IM and no visible columnar-lined esophagus on upper endoscopy.
“This demonstrates that the absence of a measurable columnar-lined esophagus does not exclude patients from the risk of having intestinal metaplasia, dysplasia, or cancer at the gastroesophageal junction. Therefore evaluation of the gastroesophageal junction by biopsy or WATS should be considered during upper endoscopy, particularly in patients at increased risk for having intestinal metaplasia,” he concluded.
Dr. DeMeester reported serving as a consultant to BARD and receiving research funding from and serving as a paid speaker for CDx Diagnostics, which funded the trial.
REPORTING FROM ACG 2019
Oral baricitinib performs well in phase 3 for atopic dermatitis
MADRID – Adding the oral Janus kinase (JAK) inhibitor baricitinib to standard atopic dermatitis therapy with low- and midpotency topical corticosteroids markedly improved disease severity and key patient-reported outcomes, compared with topical corticosteroids alone, in the phase 3, randomized, double-blind BREEZE-AD7 trial, Kristian Reich, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
in the phase 3 BREEZE-AD1 and -AD2 trials. But BREEZE-AD7 further advances the field because it’s the first phase 3 study testing the efficacy of a JAK inhibitor in combination with low- and midpotency topical steroids.
“I think this study is important because it looks into the situation that’s more like what happens in the real world, which is, as with dupilumab and other drugs, we use the systemic agent in combination with topical therapies and, in particular, with topical corticosteroids,” commented Dr. Reich, professor of dermatology at University Medical Center, Hamburg, and medical director at SCIderm, a scientific research company.
“This is what I think we can expect from existing and upcoming systemic therapies in atopic dermatitis: We will use them in combination with topical corticosteroids, and hopefully this will allow patients to dramatically reduce the concomitant use of topical corticosteroids, as shown here in BREEZE-AD7,” he added.
BREEZE-AD7 was a 16-week study that included 329 adults with moderate or severe atopic dermatitis who were randomized to low- and midpotency topical corticosteroids plus either baricitinib at 2 mg once daily, baricitinib at 4 mg once daily, or placebo. The group’s mean baseline Eczema Area and Severity Index (EASI) score was 29. Overall, 45% of participants had a baseline Investigator’s Global Assessment (IGA) of disease severity of 4 on a 0-4 scale.
The primary endpoint was achievement of an IGA of 0 or 1, meaning clear or almost clear, along with at least a 2-point IGA improvement from baseline at week 16. This was accomplished in 30.6% of those on 4 mg/day of baricitinib, 23.9% of patients in the 2-mg group, and 14.7% of controls.
The 4-mg dose of baricitinib was statistically superior to placebo; the 2-mg dose was not. However, Dr. Reich indicated he was untroubled by this because the primary endpoint was set at a high bar, and both doses of baricitinib proved to be significantly better than topical steroids plus placebo in terms of EASI 75 response rates, as well as reductions in itch, skin pain, and sleep problems, which aren’t captured in EASI scores (see graphic).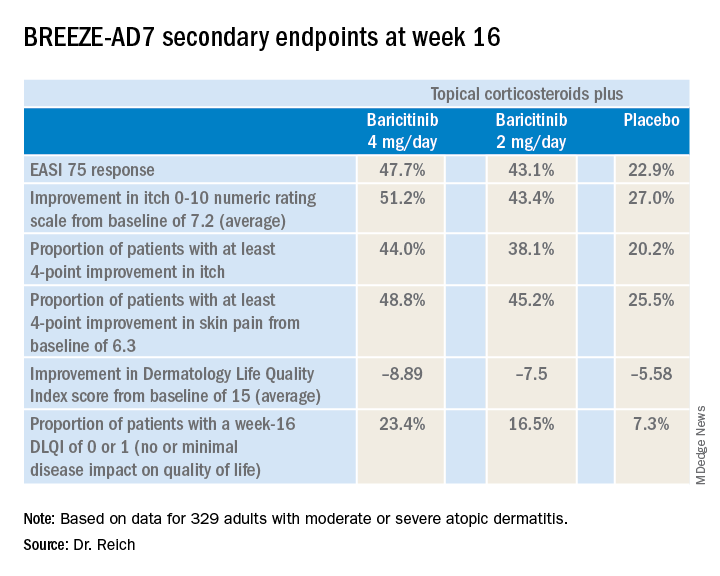
“One of my big learnings from this year’s EADV is that we have to rethink the dimensions of atopic dermatitis. I think we have underestimated the relevance of important symptoms such as itch, the impact atopic dermatitis has on pain, and the effect it has on sleeping problems,” the dermatologist said. “My feeling is that baricitinib is strongest in reducing itch, improving sleep, and reducing pain, but it also has good effects on the clinical signs of atopic dermatitis.”
The baricitinib-treated patients’ rapidity of improvement in the various endpoints was particularly impressive. Both doses of the JAK 1/2 inhibitor showed significant separation from the control group in the first week, and the majority of improvement occurred by week 4.
A key finding was that patients on baricitinib at 2 mg/day and 4 mg/day used a mean total of 162 g and 137 g of midpotency topical steroids, respectively, during the 16 weeks, compared with 225 g in the control group. The higher-dose baricitinib group was topical corticosteroid-free on 33% of study days, compared with 25% of days for the baricitinib 2 mg patients and 17% of days for controls.
In terms of safety, there was a case of pulmonary embolism in the higher-dose baricitinib group and an opportunistic toxoplasmosis eye infection in the control population. The frequency of oral herpes and herpes simplex virus infections was 2.8% in controls, 4.6% in the baricitinib 2-mg group, and 6.3% in the 4-mg group. There was also a signal of a dose-dependent increased risk of new-onset acne, with rates of 0.9% in controls and patients on baricitinib 2 mg, climbing to 3.6% with baricitinib 4 mg.
“In phase 2 results with upadacitinib [another oral JAK inhibitor], we saw that more than 10% of patients in the highest-dose group developed what was classified as acne. I cannot explain this, but it’s something we will monitor in the future,” Dr. Reich promised.
A fuller picture of baricitinib’s safety profile in the setting of atopic dermatitis clearly requires larger and longer-term studies, he added.
Baricitinib at the 2 mg daily dose is already marketed as Olumiant for the treatment of rheumatoid arthritis, with labeling that includes a boxed warning about serious infections, malignancy, and thrombosis. The Food and Drug Administration did not approve the 4-mg dose after determining that its higher safety hazard outweighed the efficacy advantage over the lower dose.
The BREEZE-AD7 study was sponsored by Eli Lilly. Dr. Reich reported serving as an adviser to, paid speaker for, and recipient of research grants from that pharmaceutical company and more than two dozen others.
MADRID – Adding the oral Janus kinase (JAK) inhibitor baricitinib to standard atopic dermatitis therapy with low- and midpotency topical corticosteroids markedly improved disease severity and key patient-reported outcomes, compared with topical corticosteroids alone, in the phase 3, randomized, double-blind BREEZE-AD7 trial, Kristian Reich, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
in the phase 3 BREEZE-AD1 and -AD2 trials. But BREEZE-AD7 further advances the field because it’s the first phase 3 study testing the efficacy of a JAK inhibitor in combination with low- and midpotency topical steroids.
“I think this study is important because it looks into the situation that’s more like what happens in the real world, which is, as with dupilumab and other drugs, we use the systemic agent in combination with topical therapies and, in particular, with topical corticosteroids,” commented Dr. Reich, professor of dermatology at University Medical Center, Hamburg, and medical director at SCIderm, a scientific research company.
“This is what I think we can expect from existing and upcoming systemic therapies in atopic dermatitis: We will use them in combination with topical corticosteroids, and hopefully this will allow patients to dramatically reduce the concomitant use of topical corticosteroids, as shown here in BREEZE-AD7,” he added.
BREEZE-AD7 was a 16-week study that included 329 adults with moderate or severe atopic dermatitis who were randomized to low- and midpotency topical corticosteroids plus either baricitinib at 2 mg once daily, baricitinib at 4 mg once daily, or placebo. The group’s mean baseline Eczema Area and Severity Index (EASI) score was 29. Overall, 45% of participants had a baseline Investigator’s Global Assessment (IGA) of disease severity of 4 on a 0-4 scale.
The primary endpoint was achievement of an IGA of 0 or 1, meaning clear or almost clear, along with at least a 2-point IGA improvement from baseline at week 16. This was accomplished in 30.6% of those on 4 mg/day of baricitinib, 23.9% of patients in the 2-mg group, and 14.7% of controls.
The 4-mg dose of baricitinib was statistically superior to placebo; the 2-mg dose was not. However, Dr. Reich indicated he was untroubled by this because the primary endpoint was set at a high bar, and both doses of baricitinib proved to be significantly better than topical steroids plus placebo in terms of EASI 75 response rates, as well as reductions in itch, skin pain, and sleep problems, which aren’t captured in EASI scores (see graphic).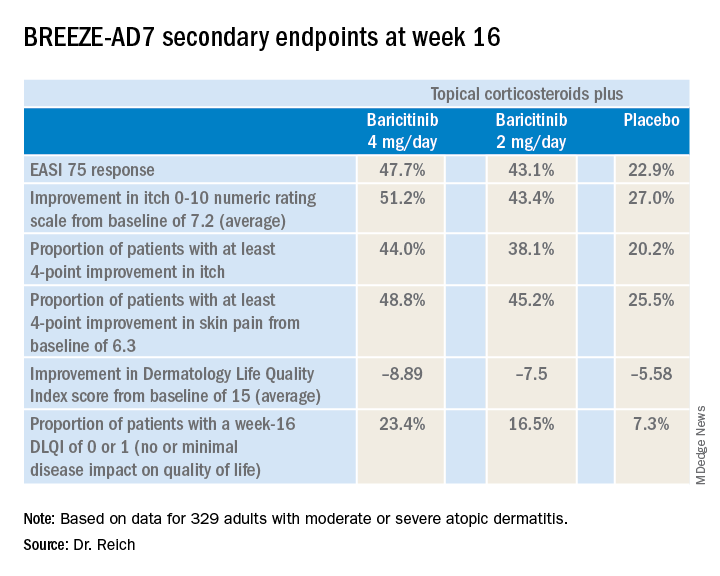
“One of my big learnings from this year’s EADV is that we have to rethink the dimensions of atopic dermatitis. I think we have underestimated the relevance of important symptoms such as itch, the impact atopic dermatitis has on pain, and the effect it has on sleeping problems,” the dermatologist said. “My feeling is that baricitinib is strongest in reducing itch, improving sleep, and reducing pain, but it also has good effects on the clinical signs of atopic dermatitis.”
The baricitinib-treated patients’ rapidity of improvement in the various endpoints was particularly impressive. Both doses of the JAK 1/2 inhibitor showed significant separation from the control group in the first week, and the majority of improvement occurred by week 4.
A key finding was that patients on baricitinib at 2 mg/day and 4 mg/day used a mean total of 162 g and 137 g of midpotency topical steroids, respectively, during the 16 weeks, compared with 225 g in the control group. The higher-dose baricitinib group was topical corticosteroid-free on 33% of study days, compared with 25% of days for the baricitinib 2 mg patients and 17% of days for controls.
In terms of safety, there was a case of pulmonary embolism in the higher-dose baricitinib group and an opportunistic toxoplasmosis eye infection in the control population. The frequency of oral herpes and herpes simplex virus infections was 2.8% in controls, 4.6% in the baricitinib 2-mg group, and 6.3% in the 4-mg group. There was also a signal of a dose-dependent increased risk of new-onset acne, with rates of 0.9% in controls and patients on baricitinib 2 mg, climbing to 3.6% with baricitinib 4 mg.
“In phase 2 results with upadacitinib [another oral JAK inhibitor], we saw that more than 10% of patients in the highest-dose group developed what was classified as acne. I cannot explain this, but it’s something we will monitor in the future,” Dr. Reich promised.
A fuller picture of baricitinib’s safety profile in the setting of atopic dermatitis clearly requires larger and longer-term studies, he added.
Baricitinib at the 2 mg daily dose is already marketed as Olumiant for the treatment of rheumatoid arthritis, with labeling that includes a boxed warning about serious infections, malignancy, and thrombosis. The Food and Drug Administration did not approve the 4-mg dose after determining that its higher safety hazard outweighed the efficacy advantage over the lower dose.
The BREEZE-AD7 study was sponsored by Eli Lilly. Dr. Reich reported serving as an adviser to, paid speaker for, and recipient of research grants from that pharmaceutical company and more than two dozen others.
MADRID – Adding the oral Janus kinase (JAK) inhibitor baricitinib to standard atopic dermatitis therapy with low- and midpotency topical corticosteroids markedly improved disease severity and key patient-reported outcomes, compared with topical corticosteroids alone, in the phase 3, randomized, double-blind BREEZE-AD7 trial, Kristian Reich, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
in the phase 3 BREEZE-AD1 and -AD2 trials. But BREEZE-AD7 further advances the field because it’s the first phase 3 study testing the efficacy of a JAK inhibitor in combination with low- and midpotency topical steroids.
“I think this study is important because it looks into the situation that’s more like what happens in the real world, which is, as with dupilumab and other drugs, we use the systemic agent in combination with topical therapies and, in particular, with topical corticosteroids,” commented Dr. Reich, professor of dermatology at University Medical Center, Hamburg, and medical director at SCIderm, a scientific research company.
“This is what I think we can expect from existing and upcoming systemic therapies in atopic dermatitis: We will use them in combination with topical corticosteroids, and hopefully this will allow patients to dramatically reduce the concomitant use of topical corticosteroids, as shown here in BREEZE-AD7,” he added.
BREEZE-AD7 was a 16-week study that included 329 adults with moderate or severe atopic dermatitis who were randomized to low- and midpotency topical corticosteroids plus either baricitinib at 2 mg once daily, baricitinib at 4 mg once daily, or placebo. The group’s mean baseline Eczema Area and Severity Index (EASI) score was 29. Overall, 45% of participants had a baseline Investigator’s Global Assessment (IGA) of disease severity of 4 on a 0-4 scale.
The primary endpoint was achievement of an IGA of 0 or 1, meaning clear or almost clear, along with at least a 2-point IGA improvement from baseline at week 16. This was accomplished in 30.6% of those on 4 mg/day of baricitinib, 23.9% of patients in the 2-mg group, and 14.7% of controls.
The 4-mg dose of baricitinib was statistically superior to placebo; the 2-mg dose was not. However, Dr. Reich indicated he was untroubled by this because the primary endpoint was set at a high bar, and both doses of baricitinib proved to be significantly better than topical steroids plus placebo in terms of EASI 75 response rates, as well as reductions in itch, skin pain, and sleep problems, which aren’t captured in EASI scores (see graphic).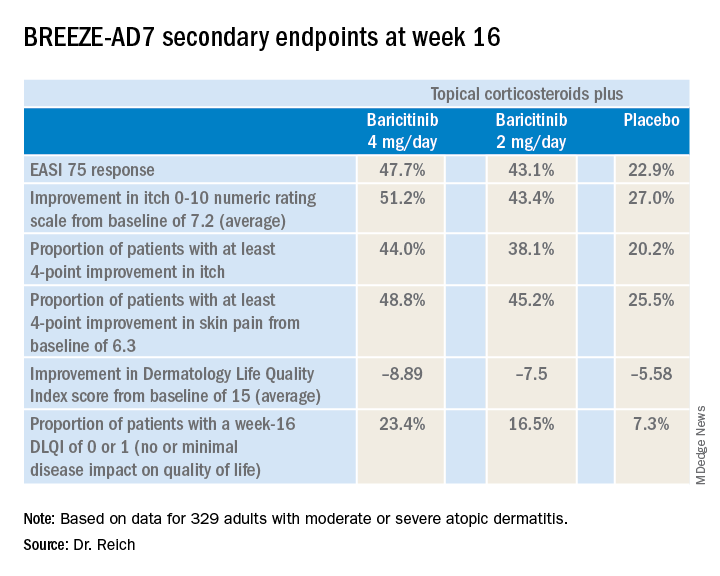
“One of my big learnings from this year’s EADV is that we have to rethink the dimensions of atopic dermatitis. I think we have underestimated the relevance of important symptoms such as itch, the impact atopic dermatitis has on pain, and the effect it has on sleeping problems,” the dermatologist said. “My feeling is that baricitinib is strongest in reducing itch, improving sleep, and reducing pain, but it also has good effects on the clinical signs of atopic dermatitis.”
The baricitinib-treated patients’ rapidity of improvement in the various endpoints was particularly impressive. Both doses of the JAK 1/2 inhibitor showed significant separation from the control group in the first week, and the majority of improvement occurred by week 4.
A key finding was that patients on baricitinib at 2 mg/day and 4 mg/day used a mean total of 162 g and 137 g of midpotency topical steroids, respectively, during the 16 weeks, compared with 225 g in the control group. The higher-dose baricitinib group was topical corticosteroid-free on 33% of study days, compared with 25% of days for the baricitinib 2 mg patients and 17% of days for controls.
In terms of safety, there was a case of pulmonary embolism in the higher-dose baricitinib group and an opportunistic toxoplasmosis eye infection in the control population. The frequency of oral herpes and herpes simplex virus infections was 2.8% in controls, 4.6% in the baricitinib 2-mg group, and 6.3% in the 4-mg group. There was also a signal of a dose-dependent increased risk of new-onset acne, with rates of 0.9% in controls and patients on baricitinib 2 mg, climbing to 3.6% with baricitinib 4 mg.
“In phase 2 results with upadacitinib [another oral JAK inhibitor], we saw that more than 10% of patients in the highest-dose group developed what was classified as acne. I cannot explain this, but it’s something we will monitor in the future,” Dr. Reich promised.
A fuller picture of baricitinib’s safety profile in the setting of atopic dermatitis clearly requires larger and longer-term studies, he added.
Baricitinib at the 2 mg daily dose is already marketed as Olumiant for the treatment of rheumatoid arthritis, with labeling that includes a boxed warning about serious infections, malignancy, and thrombosis. The Food and Drug Administration did not approve the 4-mg dose after determining that its higher safety hazard outweighed the efficacy advantage over the lower dose.
The BREEZE-AD7 study was sponsored by Eli Lilly. Dr. Reich reported serving as an adviser to, paid speaker for, and recipient of research grants from that pharmaceutical company and more than two dozen others.
REPORTING FROM EADV CONGRESS
Key clinical point: The Janus kinase 1/2 inhibitor baricitinib shows promise as a novel oral treatment for moderate or severe atopic dermatitis.
Major finding: Among atopic dermatitis patients on concomitant topical corticosteroids, a 75% improvement on Eczema Area and Severity Index at 16 weeks was achieved in 48% of those on baricitinib at 4 mg/day, 43% with baricitinib at 2 mg/day, and 23% on placebo.
Study details: BREEZE-AD7 was a phase 3, multicenter, 16-week, double-blind, three-arm study including 329 adults with moderate or severe atopic dermatitis.
Disclosures: The BREEZE-AD7 study was sponsored by Eli Lilly. The presenter reported serving as an adviser to, paid speaker for, and/or recipient of research grants from that pharmaceutical company and more than two dozen others.
Source: Reich K. EADV Congress, late breaker.