User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Know the red flags for synaptic autoimmune psychosis
BARCELONA – Consider the possibility of an autoantibody-related etiology in all cases of first-onset psychosis, Josep Dalmau, MD, PhD, urged at the annual congress of the European College of Neuropsychopharmacology.
“There are patients in our clinics all of us – neurologists and psychiatrists – are missing. These patients are believed to have psychiatric presentations, but they do not. They are autoimmune,” said Dr. Dalmau, professor of neurology at the University of Barcelona.
Dr. Dalmau urged psychiatrists to become familiar with the red flags suggestive of synaptic autoimmunity as the underlying cause of first-episode, out-of-the-blue psychosis.
“If you have a patient with a classical presentation of schizophrenia or bipolar disorder, you probably won’t find antibodies,” according to the neurologist.
It’s important to have a high index of suspicion, because anti–NMDA receptor encephalitis is treatable with immunotherapy. And firm evidence shows that earlier recognition and treatment lead to improved outcomes. Also, the disorder is refractory to antipsychotics; indeed, 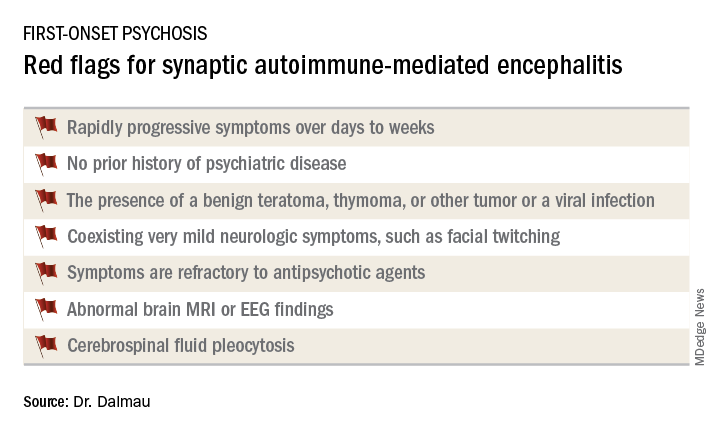
Manifestations of anti–NMDA receptor encephalitis follow a characteristic pattern, beginning with a prodromal flulike phase lasting several days to a week. This is followed by acute-onset bizarre behavioral changes, irritability, and psychosis with delusions and/or hallucinations, often progressing to catatonia. After 1-4 weeks of this, florid neurologic symptoms usually appear, including seizures, abnormal movements, autonomic dysregulation, and hypoventilation requiring prolonged ICU support for weeks to months. This is followed by a prolonged recovery phase lasting 5-24 months, and a period marked by deficits in executive function and working memory, impulsivity, and disinhibition. Impressively, the patient has no memory of the illness.
In one large series of patients with confirmed anti–NMDA receptor encephalitis reported by Dr. Dalmau and coinvestigators, psychiatric symptoms occurred in isolation without subsequent neurologic involvement in just 4% of cases (JAMA Neurol. 2013 Sep 1;70[9]:1133-9).
Dr. Dalmau was senior author of an international cohort study including 577 patients with anti-NMDA receptor encephalitis with serial follow-up for 24 months. The study provided an unprecedented picture of the epidemiology and clinical features of the disorder.
“It’s a disease predominantly of women and young people,” he observed.
Indeed, the median age of the study population was 21 years, and 37% of subjects were less than 18 years of age. Roughly 80% of patients were female and most of them had a benign ovarian teratoma, which played a key role in their neuropsychiatric disease (Lancet Neurol. 2013 Feb;12[2]:157-65). These benign tumors express the NMDA receptor in ectopic nerve tissue, triggering a systemic immune response.
One or more relapses – again treatable via immunotherapy – occurred in 12% of patients during 24 months of follow-up.
When a red flag suggestive of synaptic autoimmunity is present, it’s important to obtain a cerebrospinal fluid (CSF) sample for analysis, along with an EEG and/or brain MRI.
“I don’t know if you as psychiatrists are set up to do spinal taps in all persons with first presentation of psychosis, but this would be my suggestion. It’s extremely useful in this situation,” Dr. Dalmau said.
The vast majority of patients with anti–NMDA receptor encephalitis have CSF pleocytosis with a mild lymphocytic predominance. The MRI is abnormal in about 35% of cases. EEG abnormalities are common but nonspecific. The diagnosis is confirmed by identification of anti–NMDA receptor antibodies in the CSF.
First-line therapy is corticosteroids, intravenous immunoglobulin, and/or plasma exchange to remove the pathogenic antibodies, along with resection of the tumor if present. These treatments are effective in almost half of affected patients. When they’re not, the second-line options are rituximab (Rituxan) and cyclophosphamide, alone or combined.
Antibodies to the NMDA receptor are far and away the most common cause of synaptic autoimmunity-induced psychosis, but other targets of autoimmunity have been documented as well, including the alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor, contactin-associated protein-like 2 (CASPR2), and neurexin-3-alpha.
Dr. Dalmau and various collaborators continue to advance the understanding of this novel category of neuropsychiatric disease. They have developed a simple 5-point score, known as the NEOS score, that predicts 1-year functional status in patients with anti–NMDA receptor encephalitis (Neurology. 2018 Dec 21. doi: 10.1212/WNL.0000000000006783). He and his colleagues have also recently shown in a prospective study that herpes simplex encephalitis can result in an autoimmune encephalitis, with NMDA receptor antibodies present in most cases (Lancet Neurol. 2018 Sep;17[9]:760-72).
Dr. Dalmau’s research is supported by the U.S. National Institute of Neurological Disorders and Stroke, the Spanish Ministry of Health, and Spanish research foundations. He reported receiving royalties from the use of several neuronal antibody tests.
BARCELONA – Consider the possibility of an autoantibody-related etiology in all cases of first-onset psychosis, Josep Dalmau, MD, PhD, urged at the annual congress of the European College of Neuropsychopharmacology.
“There are patients in our clinics all of us – neurologists and psychiatrists – are missing. These patients are believed to have psychiatric presentations, but they do not. They are autoimmune,” said Dr. Dalmau, professor of neurology at the University of Barcelona.
Dr. Dalmau urged psychiatrists to become familiar with the red flags suggestive of synaptic autoimmunity as the underlying cause of first-episode, out-of-the-blue psychosis.
“If you have a patient with a classical presentation of schizophrenia or bipolar disorder, you probably won’t find antibodies,” according to the neurologist.
It’s important to have a high index of suspicion, because anti–NMDA receptor encephalitis is treatable with immunotherapy. And firm evidence shows that earlier recognition and treatment lead to improved outcomes. Also, the disorder is refractory to antipsychotics; indeed, 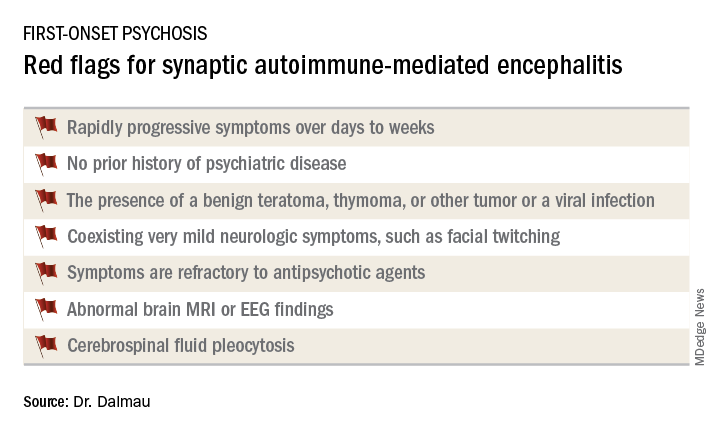
Manifestations of anti–NMDA receptor encephalitis follow a characteristic pattern, beginning with a prodromal flulike phase lasting several days to a week. This is followed by acute-onset bizarre behavioral changes, irritability, and psychosis with delusions and/or hallucinations, often progressing to catatonia. After 1-4 weeks of this, florid neurologic symptoms usually appear, including seizures, abnormal movements, autonomic dysregulation, and hypoventilation requiring prolonged ICU support for weeks to months. This is followed by a prolonged recovery phase lasting 5-24 months, and a period marked by deficits in executive function and working memory, impulsivity, and disinhibition. Impressively, the patient has no memory of the illness.
In one large series of patients with confirmed anti–NMDA receptor encephalitis reported by Dr. Dalmau and coinvestigators, psychiatric symptoms occurred in isolation without subsequent neurologic involvement in just 4% of cases (JAMA Neurol. 2013 Sep 1;70[9]:1133-9).
Dr. Dalmau was senior author of an international cohort study including 577 patients with anti-NMDA receptor encephalitis with serial follow-up for 24 months. The study provided an unprecedented picture of the epidemiology and clinical features of the disorder.
“It’s a disease predominantly of women and young people,” he observed.
Indeed, the median age of the study population was 21 years, and 37% of subjects were less than 18 years of age. Roughly 80% of patients were female and most of them had a benign ovarian teratoma, which played a key role in their neuropsychiatric disease (Lancet Neurol. 2013 Feb;12[2]:157-65). These benign tumors express the NMDA receptor in ectopic nerve tissue, triggering a systemic immune response.
One or more relapses – again treatable via immunotherapy – occurred in 12% of patients during 24 months of follow-up.
When a red flag suggestive of synaptic autoimmunity is present, it’s important to obtain a cerebrospinal fluid (CSF) sample for analysis, along with an EEG and/or brain MRI.
“I don’t know if you as psychiatrists are set up to do spinal taps in all persons with first presentation of psychosis, but this would be my suggestion. It’s extremely useful in this situation,” Dr. Dalmau said.
The vast majority of patients with anti–NMDA receptor encephalitis have CSF pleocytosis with a mild lymphocytic predominance. The MRI is abnormal in about 35% of cases. EEG abnormalities are common but nonspecific. The diagnosis is confirmed by identification of anti–NMDA receptor antibodies in the CSF.
First-line therapy is corticosteroids, intravenous immunoglobulin, and/or plasma exchange to remove the pathogenic antibodies, along with resection of the tumor if present. These treatments are effective in almost half of affected patients. When they’re not, the second-line options are rituximab (Rituxan) and cyclophosphamide, alone or combined.
Antibodies to the NMDA receptor are far and away the most common cause of synaptic autoimmunity-induced psychosis, but other targets of autoimmunity have been documented as well, including the alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor, contactin-associated protein-like 2 (CASPR2), and neurexin-3-alpha.
Dr. Dalmau and various collaborators continue to advance the understanding of this novel category of neuropsychiatric disease. They have developed a simple 5-point score, known as the NEOS score, that predicts 1-year functional status in patients with anti–NMDA receptor encephalitis (Neurology. 2018 Dec 21. doi: 10.1212/WNL.0000000000006783). He and his colleagues have also recently shown in a prospective study that herpes simplex encephalitis can result in an autoimmune encephalitis, with NMDA receptor antibodies present in most cases (Lancet Neurol. 2018 Sep;17[9]:760-72).
Dr. Dalmau’s research is supported by the U.S. National Institute of Neurological Disorders and Stroke, the Spanish Ministry of Health, and Spanish research foundations. He reported receiving royalties from the use of several neuronal antibody tests.
BARCELONA – Consider the possibility of an autoantibody-related etiology in all cases of first-onset psychosis, Josep Dalmau, MD, PhD, urged at the annual congress of the European College of Neuropsychopharmacology.
“There are patients in our clinics all of us – neurologists and psychiatrists – are missing. These patients are believed to have psychiatric presentations, but they do not. They are autoimmune,” said Dr. Dalmau, professor of neurology at the University of Barcelona.
Dr. Dalmau urged psychiatrists to become familiar with the red flags suggestive of synaptic autoimmunity as the underlying cause of first-episode, out-of-the-blue psychosis.
“If you have a patient with a classical presentation of schizophrenia or bipolar disorder, you probably won’t find antibodies,” according to the neurologist.
It’s important to have a high index of suspicion, because anti–NMDA receptor encephalitis is treatable with immunotherapy. And firm evidence shows that earlier recognition and treatment lead to improved outcomes. Also, the disorder is refractory to antipsychotics; indeed, 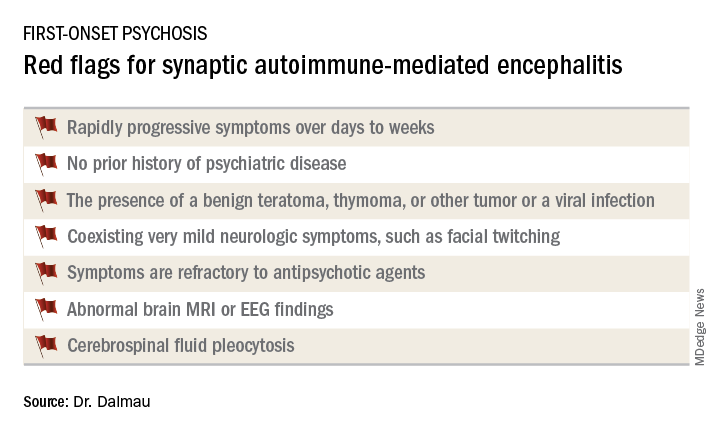
Manifestations of anti–NMDA receptor encephalitis follow a characteristic pattern, beginning with a prodromal flulike phase lasting several days to a week. This is followed by acute-onset bizarre behavioral changes, irritability, and psychosis with delusions and/or hallucinations, often progressing to catatonia. After 1-4 weeks of this, florid neurologic symptoms usually appear, including seizures, abnormal movements, autonomic dysregulation, and hypoventilation requiring prolonged ICU support for weeks to months. This is followed by a prolonged recovery phase lasting 5-24 months, and a period marked by deficits in executive function and working memory, impulsivity, and disinhibition. Impressively, the patient has no memory of the illness.
In one large series of patients with confirmed anti–NMDA receptor encephalitis reported by Dr. Dalmau and coinvestigators, psychiatric symptoms occurred in isolation without subsequent neurologic involvement in just 4% of cases (JAMA Neurol. 2013 Sep 1;70[9]:1133-9).
Dr. Dalmau was senior author of an international cohort study including 577 patients with anti-NMDA receptor encephalitis with serial follow-up for 24 months. The study provided an unprecedented picture of the epidemiology and clinical features of the disorder.
“It’s a disease predominantly of women and young people,” he observed.
Indeed, the median age of the study population was 21 years, and 37% of subjects were less than 18 years of age. Roughly 80% of patients were female and most of them had a benign ovarian teratoma, which played a key role in their neuropsychiatric disease (Lancet Neurol. 2013 Feb;12[2]:157-65). These benign tumors express the NMDA receptor in ectopic nerve tissue, triggering a systemic immune response.
One or more relapses – again treatable via immunotherapy – occurred in 12% of patients during 24 months of follow-up.
When a red flag suggestive of synaptic autoimmunity is present, it’s important to obtain a cerebrospinal fluid (CSF) sample for analysis, along with an EEG and/or brain MRI.
“I don’t know if you as psychiatrists are set up to do spinal taps in all persons with first presentation of psychosis, but this would be my suggestion. It’s extremely useful in this situation,” Dr. Dalmau said.
The vast majority of patients with anti–NMDA receptor encephalitis have CSF pleocytosis with a mild lymphocytic predominance. The MRI is abnormal in about 35% of cases. EEG abnormalities are common but nonspecific. The diagnosis is confirmed by identification of anti–NMDA receptor antibodies in the CSF.
First-line therapy is corticosteroids, intravenous immunoglobulin, and/or plasma exchange to remove the pathogenic antibodies, along with resection of the tumor if present. These treatments are effective in almost half of affected patients. When they’re not, the second-line options are rituximab (Rituxan) and cyclophosphamide, alone or combined.
Antibodies to the NMDA receptor are far and away the most common cause of synaptic autoimmunity-induced psychosis, but other targets of autoimmunity have been documented as well, including the alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor, contactin-associated protein-like 2 (CASPR2), and neurexin-3-alpha.
Dr. Dalmau and various collaborators continue to advance the understanding of this novel category of neuropsychiatric disease. They have developed a simple 5-point score, known as the NEOS score, that predicts 1-year functional status in patients with anti–NMDA receptor encephalitis (Neurology. 2018 Dec 21. doi: 10.1212/WNL.0000000000006783). He and his colleagues have also recently shown in a prospective study that herpes simplex encephalitis can result in an autoimmune encephalitis, with NMDA receptor antibodies present in most cases (Lancet Neurol. 2018 Sep;17[9]:760-72).
Dr. Dalmau’s research is supported by the U.S. National Institute of Neurological Disorders and Stroke, the Spanish Ministry of Health, and Spanish research foundations. He reported receiving royalties from the use of several neuronal antibody tests.
REPORTING FROM THE ECNP CONGRESS
Breast cancer study: No link between soy, all-cause mortality
Also today there is more benefit to chemoradiation earlier in small cell lung cancer, traditional jet nebulizers beat breath-enhanced nebulizers in pediatric asthma, and both new and existing drugs are fueling price inflation.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today there is more benefit to chemoradiation earlier in small cell lung cancer, traditional jet nebulizers beat breath-enhanced nebulizers in pediatric asthma, and both new and existing drugs are fueling price inflation.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today there is more benefit to chemoradiation earlier in small cell lung cancer, traditional jet nebulizers beat breath-enhanced nebulizers in pediatric asthma, and both new and existing drugs are fueling price inflation.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Phone etiquette, part 2
My recent column on proper telephone technique for front office employees triggered some interesting commentary. “What about the calls we take?” someone asked. “.”
How true! Haven’t we all answered a call from another physician, only to hear, “Please hold for Dr. ___________”?
Let’s begin with that, since it’s one of my major pet peeves: Long tradition, and common courtesy, dictate that the person initiating a call be on the line when the recipient picks up the receiver. So don’t ask an assistant to dial calls for you. Is it really that much bother to do it yourself? A peer should never answer and then be expected to wait while your employee tracks you down. It is impolite, and implies that you consider your time much more valuable than his or hers.
Speaking of common courtesy: Always give callers your undivided attention; they can tell if you are distracted. If it’s not a good time for you, say so honestly, at the outset. “Listen, I can give you a couple of minutes, but I’m right in the middle of office hours ...” That’s much more polite than abruptly cutting someone off, mid-conversation. If the caller needs more time, offer to call back.
By the same token, if you are the caller, be sure to ask, “Is this a good time for you?” Then, be aware of how long you keep the other person on the line. We all have a finite amount of time, and not everyone knows how to end a phone conversation gracefully. Respect others’ time and get to your point quickly.
When you reach an answering machine or voice mail, talk clearly and distinctly. Few things are more frustrating than a mumbled message that no one can decipher. I always repeat my name and phone number for clarity’s sake. And please don’t leave a callback number that no one answers, or that automatically rejects all unidentified callers.
Mobile phones have become so ubiquitous, it is hard to believe that they were relatively scarce only 15 years ago. A distinct set of faux pas has evolved around them; for example, few things are less professional than a loud, indiscreet, annoying, or profane ring tone. Your recorded voice mail message needs to sound professional too – especially if patients will be hearing it.
It should be obvious that cell phones be turned off in theaters and during meetings, but many still remain on. Vibrate mode doesn’t count; anyone close by will still hear it, and you’ll be tempted to answer it. If you get a call during a movie or show, or at a meeting, and you absolutely have to answer it, quietly excuse yourself, and don’t take the call until you are alone. If you miss the call, you can always call the person back.
Answering phone calls in a restaurant is my wife’s biggest pet peeve. She says it is rude and inappropriate, and she’s right – yet it is now, arguably, the most common etiquette mistake. Never take calls (or worse, answer texts or emails) while seated at the table – which leads to another issue: Don’t put your phone on the table! You can hear it just fine from your purse or pocket; and putting it on the table implies to your companions that you are looking for something – anything – more interesting than their company. If you must take a call or read a message, excuse yourself and go to a private area.
In fact, you shouldn’t answer any nonemergent calls or texts when you are with others; it makes your friends and colleagues feel unimportant and ignored. The people you are with should always take precedence over your phone, unless it is a medical emergency or otherwise extremely urgent. On those rare occasions when it is, be polite: “Do you mind if I take this call? It’s important.” Then, once again, excuse yourself to answer privately.
One final thought: Don’t walk around wearing one of those wireless Bluetooth earpieces on your ear, as if the Governor might call at any moment. Everyone around you has to guess whether you’re addressing them or some unseen caller; and frankly – with all respect – it looks ridiculous. And pretentious.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
My recent column on proper telephone technique for front office employees triggered some interesting commentary. “What about the calls we take?” someone asked. “.”
How true! Haven’t we all answered a call from another physician, only to hear, “Please hold for Dr. ___________”?
Let’s begin with that, since it’s one of my major pet peeves: Long tradition, and common courtesy, dictate that the person initiating a call be on the line when the recipient picks up the receiver. So don’t ask an assistant to dial calls for you. Is it really that much bother to do it yourself? A peer should never answer and then be expected to wait while your employee tracks you down. It is impolite, and implies that you consider your time much more valuable than his or hers.
Speaking of common courtesy: Always give callers your undivided attention; they can tell if you are distracted. If it’s not a good time for you, say so honestly, at the outset. “Listen, I can give you a couple of minutes, but I’m right in the middle of office hours ...” That’s much more polite than abruptly cutting someone off, mid-conversation. If the caller needs more time, offer to call back.
By the same token, if you are the caller, be sure to ask, “Is this a good time for you?” Then, be aware of how long you keep the other person on the line. We all have a finite amount of time, and not everyone knows how to end a phone conversation gracefully. Respect others’ time and get to your point quickly.
When you reach an answering machine or voice mail, talk clearly and distinctly. Few things are more frustrating than a mumbled message that no one can decipher. I always repeat my name and phone number for clarity’s sake. And please don’t leave a callback number that no one answers, or that automatically rejects all unidentified callers.
Mobile phones have become so ubiquitous, it is hard to believe that they were relatively scarce only 15 years ago. A distinct set of faux pas has evolved around them; for example, few things are less professional than a loud, indiscreet, annoying, or profane ring tone. Your recorded voice mail message needs to sound professional too – especially if patients will be hearing it.
It should be obvious that cell phones be turned off in theaters and during meetings, but many still remain on. Vibrate mode doesn’t count; anyone close by will still hear it, and you’ll be tempted to answer it. If you get a call during a movie or show, or at a meeting, and you absolutely have to answer it, quietly excuse yourself, and don’t take the call until you are alone. If you miss the call, you can always call the person back.
Answering phone calls in a restaurant is my wife’s biggest pet peeve. She says it is rude and inappropriate, and she’s right – yet it is now, arguably, the most common etiquette mistake. Never take calls (or worse, answer texts or emails) while seated at the table – which leads to another issue: Don’t put your phone on the table! You can hear it just fine from your purse or pocket; and putting it on the table implies to your companions that you are looking for something – anything – more interesting than their company. If you must take a call or read a message, excuse yourself and go to a private area.
In fact, you shouldn’t answer any nonemergent calls or texts when you are with others; it makes your friends and colleagues feel unimportant and ignored. The people you are with should always take precedence over your phone, unless it is a medical emergency or otherwise extremely urgent. On those rare occasions when it is, be polite: “Do you mind if I take this call? It’s important.” Then, once again, excuse yourself to answer privately.
One final thought: Don’t walk around wearing one of those wireless Bluetooth earpieces on your ear, as if the Governor might call at any moment. Everyone around you has to guess whether you’re addressing them or some unseen caller; and frankly – with all respect – it looks ridiculous. And pretentious.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
My recent column on proper telephone technique for front office employees triggered some interesting commentary. “What about the calls we take?” someone asked. “.”
How true! Haven’t we all answered a call from another physician, only to hear, “Please hold for Dr. ___________”?
Let’s begin with that, since it’s one of my major pet peeves: Long tradition, and common courtesy, dictate that the person initiating a call be on the line when the recipient picks up the receiver. So don’t ask an assistant to dial calls for you. Is it really that much bother to do it yourself? A peer should never answer and then be expected to wait while your employee tracks you down. It is impolite, and implies that you consider your time much more valuable than his or hers.
Speaking of common courtesy: Always give callers your undivided attention; they can tell if you are distracted. If it’s not a good time for you, say so honestly, at the outset. “Listen, I can give you a couple of minutes, but I’m right in the middle of office hours ...” That’s much more polite than abruptly cutting someone off, mid-conversation. If the caller needs more time, offer to call back.
By the same token, if you are the caller, be sure to ask, “Is this a good time for you?” Then, be aware of how long you keep the other person on the line. We all have a finite amount of time, and not everyone knows how to end a phone conversation gracefully. Respect others’ time and get to your point quickly.
When you reach an answering machine or voice mail, talk clearly and distinctly. Few things are more frustrating than a mumbled message that no one can decipher. I always repeat my name and phone number for clarity’s sake. And please don’t leave a callback number that no one answers, or that automatically rejects all unidentified callers.
Mobile phones have become so ubiquitous, it is hard to believe that they were relatively scarce only 15 years ago. A distinct set of faux pas has evolved around them; for example, few things are less professional than a loud, indiscreet, annoying, or profane ring tone. Your recorded voice mail message needs to sound professional too – especially if patients will be hearing it.
It should be obvious that cell phones be turned off in theaters and during meetings, but many still remain on. Vibrate mode doesn’t count; anyone close by will still hear it, and you’ll be tempted to answer it. If you get a call during a movie or show, or at a meeting, and you absolutely have to answer it, quietly excuse yourself, and don’t take the call until you are alone. If you miss the call, you can always call the person back.
Answering phone calls in a restaurant is my wife’s biggest pet peeve. She says it is rude and inappropriate, and she’s right – yet it is now, arguably, the most common etiquette mistake. Never take calls (or worse, answer texts or emails) while seated at the table – which leads to another issue: Don’t put your phone on the table! You can hear it just fine from your purse or pocket; and putting it on the table implies to your companions that you are looking for something – anything – more interesting than their company. If you must take a call or read a message, excuse yourself and go to a private area.
In fact, you shouldn’t answer any nonemergent calls or texts when you are with others; it makes your friends and colleagues feel unimportant and ignored. The people you are with should always take precedence over your phone, unless it is a medical emergency or otherwise extremely urgent. On those rare occasions when it is, be polite: “Do you mind if I take this call? It’s important.” Then, once again, excuse yourself to answer privately.
One final thought: Don’t walk around wearing one of those wireless Bluetooth earpieces on your ear, as if the Governor might call at any moment. Everyone around you has to guess whether you’re addressing them or some unseen caller; and frankly – with all respect – it looks ridiculous. And pretentious.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Too much, too little sleep linked to atherosclerosis
in healthy middle-aged men and women in a Spanish investigation of bank employees.
“Overall, our findings support the potential role of healthy sleeping in protecting against atherosclerosis. Thus, recommending a good sleep hygiene” – 7-8 hours a night – “should be part of the lifestyle modifications provided in our daily clinical practice,” said investigators led by Fernando Domínguez, MD, PhD, of Centro Nacional de Investigaciones Cardiovasculares Carlos III (CNIC), Madrid. The report is in the Journal of the American College of Cardiology.
Studies have linked sleep problems to increased cardiovascular risk before, but the investigations tended to focus on patients with obstructive sleep apnea (OSA) and other problems, and often relied on patient self-report. The investors wanted to see if the relationship held in healthy adults, using an objective measure.
The participants – all with no known cardiovascular disease – wore Acti Trainers accelerometers (Actigraph, Pensacola, Fla.) around their waists for 7 days to record sleep duration and quality. Subjects also had their plaque burdens assessed by 3-dimensional vascular ultrasound (VUS) at their carotid and femoral arteries bilaterally. Cardiac CT was used to assess coronary artery calcification as a surrogate for coronary artery atherosclerosis.
The 3,974 participants had a mean age of 46 years, and a third were women; they had a low prevalence of both hypertension and diabetes. OSA patients were excluded from the study. Overall, 27% had very short sleep duration (VSSD), less than 6 hours a night; 38% had short sleep duration (SSD), 31% slept from 7 to 8 hours per night, and served as the reference group for healthy sleep habits; and 4% had long sleep duration (LSD), greater than 8 hours.
After adjustment for a wide range of cardiovascular risk factors, including body mass index, hypertension, and smoking, VSSD was independently associated with a higher atherosclerotic burden, compared to the reference group (odds ratio, 1.27; 95% confidence interval, 1.06-1.52; P = 0.008). Participants in the highest quintile of sleep fragmentation were more likely to have plaques at multiple sites (OR, 1.34; 95% CI, 1.09-1.64; P = 0.006). The Framingham risk score at both 10 and 30 years was significantly higher in participants with VSSD or SSD, and in the highest quintiles of sleep fragmentation.
LSD was also associated with a higher plaque burden, which reached statistical significance in women. “Too-long sleep duration may not be healthy either ... Recommendations should be restricted to 7 to 8 hours,” the investigators said.
Sleep duration and quality were not associated with inflammation markers or coronary artery calcification. The investigators noted that CT for coronary artery calcification might not be as sensitive as VUS for picking up subclinical atherosclerosis.
Short sleepers tended to have higher intakes of alcohol and caffeine than did those in the 7- to 8-hour group.
The work was funded by CNIC and Banco Santander, among others. Dr. Domínguez had no disclosures. Investigator Hector Bueno, MD, PhD, reported research funding and fees from a number of companies, including AstraZeneca and Novartis. The second author, Valentín Fuster, MD, PhD, is the editor of the Journal of the American College of Cardiology, which published the report.
SOURCE: Domínguez F et al. J Am Coll Cardiol 2019;73:134-44.
This study extends the published reports on sleep duration and vascular disease to an early middle-aged cohort by using an objective measure of sleep duration and sensitive measures of atherosclerosis in multiple vascular territories.
Ultimately, studies of sleep extension are needed to determine whether modification of sleep behaviors will improve vascular health outcomes. The potentially enormous impact of sleep deprivation and disruption on population health, reinforced by the present study, is ample justification for such trials, which are needed to place sleep with confidence alongside diet and exercise as a key pillar of a healthy lifestyle.
However, both hypertension and diabetes were more common in the group sleeping fewer than 6 hours per night, but neither blood pressure nor glucose metabolism was assessed with sufficiently comprehensive measures to explore these factors as potential effect mediators.
More importantly, the causes of short sleep duration and sleep fragmentation in this cohort are unknown. It is unclear to what extent short sleep duration in this cohort reflects voluntary behaviors that limit time available for sleep versus insomnia. Insomnia is itself associated with increased risk of vascular disease.
Deepak Bhatt , MD, professor of cardiovascular medicine, and Daniel Gottlieb , MD, an associate professor of medicine at Harvard Medical School, Boston, made these comments in an accompanying editorial ( J Am Coll Cardiol. 2019 Jan 14;73[2]:145-7 ). Dr. Gottlieb is also the director of the Boston Veterans Affairs Sleep Disorders Center. Dr. Bhatt reported research funding and income from a number of companies, including Abbott, Boehringer Ingelheim, and Medtronic.
This study extends the published reports on sleep duration and vascular disease to an early middle-aged cohort by using an objective measure of sleep duration and sensitive measures of atherosclerosis in multiple vascular territories.
Ultimately, studies of sleep extension are needed to determine whether modification of sleep behaviors will improve vascular health outcomes. The potentially enormous impact of sleep deprivation and disruption on population health, reinforced by the present study, is ample justification for such trials, which are needed to place sleep with confidence alongside diet and exercise as a key pillar of a healthy lifestyle.
However, both hypertension and diabetes were more common in the group sleeping fewer than 6 hours per night, but neither blood pressure nor glucose metabolism was assessed with sufficiently comprehensive measures to explore these factors as potential effect mediators.
More importantly, the causes of short sleep duration and sleep fragmentation in this cohort are unknown. It is unclear to what extent short sleep duration in this cohort reflects voluntary behaviors that limit time available for sleep versus insomnia. Insomnia is itself associated with increased risk of vascular disease.
Deepak Bhatt , MD, professor of cardiovascular medicine, and Daniel Gottlieb , MD, an associate professor of medicine at Harvard Medical School, Boston, made these comments in an accompanying editorial ( J Am Coll Cardiol. 2019 Jan 14;73[2]:145-7 ). Dr. Gottlieb is also the director of the Boston Veterans Affairs Sleep Disorders Center. Dr. Bhatt reported research funding and income from a number of companies, including Abbott, Boehringer Ingelheim, and Medtronic.
This study extends the published reports on sleep duration and vascular disease to an early middle-aged cohort by using an objective measure of sleep duration and sensitive measures of atherosclerosis in multiple vascular territories.
Ultimately, studies of sleep extension are needed to determine whether modification of sleep behaviors will improve vascular health outcomes. The potentially enormous impact of sleep deprivation and disruption on population health, reinforced by the present study, is ample justification for such trials, which are needed to place sleep with confidence alongside diet and exercise as a key pillar of a healthy lifestyle.
However, both hypertension and diabetes were more common in the group sleeping fewer than 6 hours per night, but neither blood pressure nor glucose metabolism was assessed with sufficiently comprehensive measures to explore these factors as potential effect mediators.
More importantly, the causes of short sleep duration and sleep fragmentation in this cohort are unknown. It is unclear to what extent short sleep duration in this cohort reflects voluntary behaviors that limit time available for sleep versus insomnia. Insomnia is itself associated with increased risk of vascular disease.
Deepak Bhatt , MD, professor of cardiovascular medicine, and Daniel Gottlieb , MD, an associate professor of medicine at Harvard Medical School, Boston, made these comments in an accompanying editorial ( J Am Coll Cardiol. 2019 Jan 14;73[2]:145-7 ). Dr. Gottlieb is also the director of the Boston Veterans Affairs Sleep Disorders Center. Dr. Bhatt reported research funding and income from a number of companies, including Abbott, Boehringer Ingelheim, and Medtronic.
in healthy middle-aged men and women in a Spanish investigation of bank employees.
“Overall, our findings support the potential role of healthy sleeping in protecting against atherosclerosis. Thus, recommending a good sleep hygiene” – 7-8 hours a night – “should be part of the lifestyle modifications provided in our daily clinical practice,” said investigators led by Fernando Domínguez, MD, PhD, of Centro Nacional de Investigaciones Cardiovasculares Carlos III (CNIC), Madrid. The report is in the Journal of the American College of Cardiology.
Studies have linked sleep problems to increased cardiovascular risk before, but the investigations tended to focus on patients with obstructive sleep apnea (OSA) and other problems, and often relied on patient self-report. The investors wanted to see if the relationship held in healthy adults, using an objective measure.
The participants – all with no known cardiovascular disease – wore Acti Trainers accelerometers (Actigraph, Pensacola, Fla.) around their waists for 7 days to record sleep duration and quality. Subjects also had their plaque burdens assessed by 3-dimensional vascular ultrasound (VUS) at their carotid and femoral arteries bilaterally. Cardiac CT was used to assess coronary artery calcification as a surrogate for coronary artery atherosclerosis.
The 3,974 participants had a mean age of 46 years, and a third were women; they had a low prevalence of both hypertension and diabetes. OSA patients were excluded from the study. Overall, 27% had very short sleep duration (VSSD), less than 6 hours a night; 38% had short sleep duration (SSD), 31% slept from 7 to 8 hours per night, and served as the reference group for healthy sleep habits; and 4% had long sleep duration (LSD), greater than 8 hours.
After adjustment for a wide range of cardiovascular risk factors, including body mass index, hypertension, and smoking, VSSD was independently associated with a higher atherosclerotic burden, compared to the reference group (odds ratio, 1.27; 95% confidence interval, 1.06-1.52; P = 0.008). Participants in the highest quintile of sleep fragmentation were more likely to have plaques at multiple sites (OR, 1.34; 95% CI, 1.09-1.64; P = 0.006). The Framingham risk score at both 10 and 30 years was significantly higher in participants with VSSD or SSD, and in the highest quintiles of sleep fragmentation.
LSD was also associated with a higher plaque burden, which reached statistical significance in women. “Too-long sleep duration may not be healthy either ... Recommendations should be restricted to 7 to 8 hours,” the investigators said.
Sleep duration and quality were not associated with inflammation markers or coronary artery calcification. The investigators noted that CT for coronary artery calcification might not be as sensitive as VUS for picking up subclinical atherosclerosis.
Short sleepers tended to have higher intakes of alcohol and caffeine than did those in the 7- to 8-hour group.
The work was funded by CNIC and Banco Santander, among others. Dr. Domínguez had no disclosures. Investigator Hector Bueno, MD, PhD, reported research funding and fees from a number of companies, including AstraZeneca and Novartis. The second author, Valentín Fuster, MD, PhD, is the editor of the Journal of the American College of Cardiology, which published the report.
SOURCE: Domínguez F et al. J Am Coll Cardiol 2019;73:134-44.
in healthy middle-aged men and women in a Spanish investigation of bank employees.
“Overall, our findings support the potential role of healthy sleeping in protecting against atherosclerosis. Thus, recommending a good sleep hygiene” – 7-8 hours a night – “should be part of the lifestyle modifications provided in our daily clinical practice,” said investigators led by Fernando Domínguez, MD, PhD, of Centro Nacional de Investigaciones Cardiovasculares Carlos III (CNIC), Madrid. The report is in the Journal of the American College of Cardiology.
Studies have linked sleep problems to increased cardiovascular risk before, but the investigations tended to focus on patients with obstructive sleep apnea (OSA) and other problems, and often relied on patient self-report. The investors wanted to see if the relationship held in healthy adults, using an objective measure.
The participants – all with no known cardiovascular disease – wore Acti Trainers accelerometers (Actigraph, Pensacola, Fla.) around their waists for 7 days to record sleep duration and quality. Subjects also had their plaque burdens assessed by 3-dimensional vascular ultrasound (VUS) at their carotid and femoral arteries bilaterally. Cardiac CT was used to assess coronary artery calcification as a surrogate for coronary artery atherosclerosis.
The 3,974 participants had a mean age of 46 years, and a third were women; they had a low prevalence of both hypertension and diabetes. OSA patients were excluded from the study. Overall, 27% had very short sleep duration (VSSD), less than 6 hours a night; 38% had short sleep duration (SSD), 31% slept from 7 to 8 hours per night, and served as the reference group for healthy sleep habits; and 4% had long sleep duration (LSD), greater than 8 hours.
After adjustment for a wide range of cardiovascular risk factors, including body mass index, hypertension, and smoking, VSSD was independently associated with a higher atherosclerotic burden, compared to the reference group (odds ratio, 1.27; 95% confidence interval, 1.06-1.52; P = 0.008). Participants in the highest quintile of sleep fragmentation were more likely to have plaques at multiple sites (OR, 1.34; 95% CI, 1.09-1.64; P = 0.006). The Framingham risk score at both 10 and 30 years was significantly higher in participants with VSSD or SSD, and in the highest quintiles of sleep fragmentation.
LSD was also associated with a higher plaque burden, which reached statistical significance in women. “Too-long sleep duration may not be healthy either ... Recommendations should be restricted to 7 to 8 hours,” the investigators said.
Sleep duration and quality were not associated with inflammation markers or coronary artery calcification. The investigators noted that CT for coronary artery calcification might not be as sensitive as VUS for picking up subclinical atherosclerosis.
Short sleepers tended to have higher intakes of alcohol and caffeine than did those in the 7- to 8-hour group.
The work was funded by CNIC and Banco Santander, among others. Dr. Domínguez had no disclosures. Investigator Hector Bueno, MD, PhD, reported research funding and fees from a number of companies, including AstraZeneca and Novartis. The second author, Valentín Fuster, MD, PhD, is the editor of the Journal of the American College of Cardiology, which published the report.
SOURCE: Domínguez F et al. J Am Coll Cardiol 2019;73:134-44.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: Even among healthy men and women, both too much and too little sleep are associated with atherosclerosis.
Major finding: Sleeping less than 6 hours a night was independently associated with a higher noncardiac atherosclerotic burden (OR ,1.27; 95% CI, 1.06-1.52; P = .008)
Study details: Spanish study of 3,974 bank employees.
Disclosures: The work was funded by CNIC and Banco Santander, among others. The study lead had no disclosures. Investigator Hector Bueno, MD, PhD, reported research funding and fees from a number of companies, including AstraZeneca and Novartis. The second author, Valentín Fuster, MD, PhD, is the editor of the Journal of the American College of Cardiology, which published the report.
Source: Domínguez F et al. J Am Coll Cardiol. 2019;73:134-44.
Back pain persists in one in five patients
according to data from a population-based study of more than 12,000 adults in Canada.
“Given that back pain [BP] is often recurrent, it is important to understand the course of back pain over time as this can provide additional insights on risk factors for nonfavorable outcomes,” wrote Mayilee Canizares, PhD, and her colleagues at the University Health Network’s Krembil Research Institute in Toronto.
In a longitudinal study published in Arthritis Care & Research, the investigators followed 12,782 adults from 1994 to 2011. The study population was a representative sample of the Canadian population via the National Population Health Survey, which collected data every 2 years for a total of nine cycles of data. They included people aged 15 years or older in 1994-1995 who had at least three cycles of data from baseline onward.
Over the 16-year study period, 46% of the participants reported at least one episode of back pain. Of these, 18% were identified as persistent, 28% as developing, 21% as recovering, and 33% as occasional.
“A major finding from this study is the negative impact of persistent BP on a range of health-related outcomes, including health care use, after adjustments for sociodemographic, behavior-related factors, and comorbidities,” the researchers wrote.
They examined several sociodemographic variables, including age, gender, educational level, and household income, as well as behavior-related variables including physical activity, work activity, smoking status, and obesity. The average age of the participants at baseline was 39 years; 51% were female.
Individuals who reported any back pain were more likely than those with no back pain to be overweight or obese, to smoke, to engage in moderate to heavy physical activity each day, and to have chronic conditions, including arthritis, depression, high blood pressure, and migraine.
Overall, individuals with persistent or developing BP had more pain, disability, health care visits, and medication use, compared with those in the recovery and occasional BP groups. However, individuals in the recovery group showed increased use of opioids and antidepressants over time as well, suggesting a need for long-term monitoring of back pain patients.
The trend in general disability was greatest for individuals in the persistent group followed by the developing group, recovery group, and occasional BP group.
The study findings were limited by several factors, including the use of self-reports, potential selection bias, and the inability to differentiate the specific types of back pain, the researchers noted. However, the results support and extend data from previous studies and provide clinical implications for understanding back pain.
The researchers concluded that “the different trajectory patterns potentially represent subgroups in the population that may require different interventions. In light of the trend of marked worsening outcomes, particularly for the persistent and developing groups, studies are needed to determine the nature of these groups.”
The authors reported no relevant financial conflicts.
SOURCE: Canizares M et al. Arthritis Care Res. 2019 Jan 14. doi: 10.1002/acr.23811.
according to data from a population-based study of more than 12,000 adults in Canada.
“Given that back pain [BP] is often recurrent, it is important to understand the course of back pain over time as this can provide additional insights on risk factors for nonfavorable outcomes,” wrote Mayilee Canizares, PhD, and her colleagues at the University Health Network’s Krembil Research Institute in Toronto.
In a longitudinal study published in Arthritis Care & Research, the investigators followed 12,782 adults from 1994 to 2011. The study population was a representative sample of the Canadian population via the National Population Health Survey, which collected data every 2 years for a total of nine cycles of data. They included people aged 15 years or older in 1994-1995 who had at least three cycles of data from baseline onward.
Over the 16-year study period, 46% of the participants reported at least one episode of back pain. Of these, 18% were identified as persistent, 28% as developing, 21% as recovering, and 33% as occasional.
“A major finding from this study is the negative impact of persistent BP on a range of health-related outcomes, including health care use, after adjustments for sociodemographic, behavior-related factors, and comorbidities,” the researchers wrote.
They examined several sociodemographic variables, including age, gender, educational level, and household income, as well as behavior-related variables including physical activity, work activity, smoking status, and obesity. The average age of the participants at baseline was 39 years; 51% were female.
Individuals who reported any back pain were more likely than those with no back pain to be overweight or obese, to smoke, to engage in moderate to heavy physical activity each day, and to have chronic conditions, including arthritis, depression, high blood pressure, and migraine.
Overall, individuals with persistent or developing BP had more pain, disability, health care visits, and medication use, compared with those in the recovery and occasional BP groups. However, individuals in the recovery group showed increased use of opioids and antidepressants over time as well, suggesting a need for long-term monitoring of back pain patients.
The trend in general disability was greatest for individuals in the persistent group followed by the developing group, recovery group, and occasional BP group.
The study findings were limited by several factors, including the use of self-reports, potential selection bias, and the inability to differentiate the specific types of back pain, the researchers noted. However, the results support and extend data from previous studies and provide clinical implications for understanding back pain.
The researchers concluded that “the different trajectory patterns potentially represent subgroups in the population that may require different interventions. In light of the trend of marked worsening outcomes, particularly for the persistent and developing groups, studies are needed to determine the nature of these groups.”
The authors reported no relevant financial conflicts.
SOURCE: Canizares M et al. Arthritis Care Res. 2019 Jan 14. doi: 10.1002/acr.23811.
according to data from a population-based study of more than 12,000 adults in Canada.
“Given that back pain [BP] is often recurrent, it is important to understand the course of back pain over time as this can provide additional insights on risk factors for nonfavorable outcomes,” wrote Mayilee Canizares, PhD, and her colleagues at the University Health Network’s Krembil Research Institute in Toronto.
In a longitudinal study published in Arthritis Care & Research, the investigators followed 12,782 adults from 1994 to 2011. The study population was a representative sample of the Canadian population via the National Population Health Survey, which collected data every 2 years for a total of nine cycles of data. They included people aged 15 years or older in 1994-1995 who had at least three cycles of data from baseline onward.
Over the 16-year study period, 46% of the participants reported at least one episode of back pain. Of these, 18% were identified as persistent, 28% as developing, 21% as recovering, and 33% as occasional.
“A major finding from this study is the negative impact of persistent BP on a range of health-related outcomes, including health care use, after adjustments for sociodemographic, behavior-related factors, and comorbidities,” the researchers wrote.
They examined several sociodemographic variables, including age, gender, educational level, and household income, as well as behavior-related variables including physical activity, work activity, smoking status, and obesity. The average age of the participants at baseline was 39 years; 51% were female.
Individuals who reported any back pain were more likely than those with no back pain to be overweight or obese, to smoke, to engage in moderate to heavy physical activity each day, and to have chronic conditions, including arthritis, depression, high blood pressure, and migraine.
Overall, individuals with persistent or developing BP had more pain, disability, health care visits, and medication use, compared with those in the recovery and occasional BP groups. However, individuals in the recovery group showed increased use of opioids and antidepressants over time as well, suggesting a need for long-term monitoring of back pain patients.
The trend in general disability was greatest for individuals in the persistent group followed by the developing group, recovery group, and occasional BP group.
The study findings were limited by several factors, including the use of self-reports, potential selection bias, and the inability to differentiate the specific types of back pain, the researchers noted. However, the results support and extend data from previous studies and provide clinical implications for understanding back pain.
The researchers concluded that “the different trajectory patterns potentially represent subgroups in the population that may require different interventions. In light of the trend of marked worsening outcomes, particularly for the persistent and developing groups, studies are needed to determine the nature of these groups.”
The authors reported no relevant financial conflicts.
SOURCE: Canizares M et al. Arthritis Care Res. 2019 Jan 14. doi: 10.1002/acr.23811.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point: Back pain is a common health problem, and one in five Canadian adults reported persistent back pain.
Major finding: Approximately half (46%) of Canadian adults reported some type of back pain over a 16-year period.
Study details: The data come from a population-based study of 12,782 adults followed from 1994 to 2011.
Disclosures: The authors reported no relevant financial conflicts.
Source: Canizares M et al. Arthritis Care Res. 2019 Jan 14. doi: 10.1002/acr.23811.
Tic disorders are associated with obesity and diabetes
The movement disorders are associated with cardiometabolic problems “even after taking into account a number of covariates and shared familial confounders and excluding relevant psychiatric comorbidities,” the researchers wrote. “The results highlight the importance of carefully monitoring cardiometabolic health in patients with Tourette syndrome or chronic tic disorder across the lifespan, particularly in those with comorbid attention-deficit/hyperactivity disorder (ADHD).”
Gustaf Brander, a researcher in the department of clinical neuroscience at Karolinska Institutet in Stockholm, and his colleagues conducted a longitudinal population-based cohort study of individuals living in Sweden between Jan. 1, 1973, and Dec. 31, 2013. The researchers assessed outcomes for patients with previously validated diagnoses of Tourette syndrome or chronic tic disorder in the Swedish National Patient Register. Main outcomes included obesity, dyslipidemia, hypertension, T2DM, and cardiovascular diseases, including ischemic heart diseases, arrhythmia, cerebrovascular diseases, transient ischemic attack, and arteriosclerosis. In addition, the researchers identified families with full siblings discordant for Tourette syndrome or chronic tic disorder.
Of the more than 14 million individuals in the cohort, 7,804 (76.4% male; median age at first diagnosis, 13.3 years) had a diagnosis of Tourette syndrome or chronic tic disorder in specialist care. Furthermore, the cohort included 5,141 families with full siblings who were discordant for these disorders.
Individuals with Tourette syndrome or chronic tic disorder had a higher risk for any metabolic or cardiovascular disorder, compared with the general population (hazard ratio adjusted by sex and birth year [aHR], 1.99) and sibling controls (aHR, 1.37). Specifically, individuals with Tourette syndrome or chronic tic disorder had higher risks for obesity (aHR, 2.76), T2DM(aHR, 1.67), and circulatory system diseases (aHR, 1.76).
The increased risk of any cardiometabolic disorder was significantly greater for males than it was for females (aHRs, 2.13 vs. 1.79), as was the risk of obesity (aHRs, 3.24 vs. 1.97).
The increased risk for cardiometabolic disorders in this patient population was evident by age 8 years. Exclusion of those patients with comorbid ADHD reduced but did not eliminate the risk (aHR, 1.52). The exclusion of other comorbidities did not significantly affect the results. Among patients with Tourette syndrome or chronic tic disorder, those who had received antipsychotic treatment for more than 1 year were significantly less likely to have metabolic and cardiovascular disorders, compared with patients not taking antipsychotic medication. This association may be related to “greater medical vigilance” and “should not be taken as evidence that antipsychotics are free from cardiometabolic adverse effects,” the authors noted.
The study was supported by a research grant from Tourettes Action. In addition, authors reported support from the Swedish Research Council and a Karolinska Institutet PhD stipend. Two authors disclosed personal fees from publishers, and one author disclosed grants and other funding from Shire.
jremaly@mdedge.com
SOURCE: Brander G et al. JAMA Neurol. 2019 Jan 14. doi: 10.1001/jamaneurol.2018.4279.
The movement disorders are associated with cardiometabolic problems “even after taking into account a number of covariates and shared familial confounders and excluding relevant psychiatric comorbidities,” the researchers wrote. “The results highlight the importance of carefully monitoring cardiometabolic health in patients with Tourette syndrome or chronic tic disorder across the lifespan, particularly in those with comorbid attention-deficit/hyperactivity disorder (ADHD).”
Gustaf Brander, a researcher in the department of clinical neuroscience at Karolinska Institutet in Stockholm, and his colleagues conducted a longitudinal population-based cohort study of individuals living in Sweden between Jan. 1, 1973, and Dec. 31, 2013. The researchers assessed outcomes for patients with previously validated diagnoses of Tourette syndrome or chronic tic disorder in the Swedish National Patient Register. Main outcomes included obesity, dyslipidemia, hypertension, T2DM, and cardiovascular diseases, including ischemic heart diseases, arrhythmia, cerebrovascular diseases, transient ischemic attack, and arteriosclerosis. In addition, the researchers identified families with full siblings discordant for Tourette syndrome or chronic tic disorder.
Of the more than 14 million individuals in the cohort, 7,804 (76.4% male; median age at first diagnosis, 13.3 years) had a diagnosis of Tourette syndrome or chronic tic disorder in specialist care. Furthermore, the cohort included 5,141 families with full siblings who were discordant for these disorders.
Individuals with Tourette syndrome or chronic tic disorder had a higher risk for any metabolic or cardiovascular disorder, compared with the general population (hazard ratio adjusted by sex and birth year [aHR], 1.99) and sibling controls (aHR, 1.37). Specifically, individuals with Tourette syndrome or chronic tic disorder had higher risks for obesity (aHR, 2.76), T2DM(aHR, 1.67), and circulatory system diseases (aHR, 1.76).
The increased risk of any cardiometabolic disorder was significantly greater for males than it was for females (aHRs, 2.13 vs. 1.79), as was the risk of obesity (aHRs, 3.24 vs. 1.97).
The increased risk for cardiometabolic disorders in this patient population was evident by age 8 years. Exclusion of those patients with comorbid ADHD reduced but did not eliminate the risk (aHR, 1.52). The exclusion of other comorbidities did not significantly affect the results. Among patients with Tourette syndrome or chronic tic disorder, those who had received antipsychotic treatment for more than 1 year were significantly less likely to have metabolic and cardiovascular disorders, compared with patients not taking antipsychotic medication. This association may be related to “greater medical vigilance” and “should not be taken as evidence that antipsychotics are free from cardiometabolic adverse effects,” the authors noted.
The study was supported by a research grant from Tourettes Action. In addition, authors reported support from the Swedish Research Council and a Karolinska Institutet PhD stipend. Two authors disclosed personal fees from publishers, and one author disclosed grants and other funding from Shire.
jremaly@mdedge.com
SOURCE: Brander G et al. JAMA Neurol. 2019 Jan 14. doi: 10.1001/jamaneurol.2018.4279.
The movement disorders are associated with cardiometabolic problems “even after taking into account a number of covariates and shared familial confounders and excluding relevant psychiatric comorbidities,” the researchers wrote. “The results highlight the importance of carefully monitoring cardiometabolic health in patients with Tourette syndrome or chronic tic disorder across the lifespan, particularly in those with comorbid attention-deficit/hyperactivity disorder (ADHD).”
Gustaf Brander, a researcher in the department of clinical neuroscience at Karolinska Institutet in Stockholm, and his colleagues conducted a longitudinal population-based cohort study of individuals living in Sweden between Jan. 1, 1973, and Dec. 31, 2013. The researchers assessed outcomes for patients with previously validated diagnoses of Tourette syndrome or chronic tic disorder in the Swedish National Patient Register. Main outcomes included obesity, dyslipidemia, hypertension, T2DM, and cardiovascular diseases, including ischemic heart diseases, arrhythmia, cerebrovascular diseases, transient ischemic attack, and arteriosclerosis. In addition, the researchers identified families with full siblings discordant for Tourette syndrome or chronic tic disorder.
Of the more than 14 million individuals in the cohort, 7,804 (76.4% male; median age at first diagnosis, 13.3 years) had a diagnosis of Tourette syndrome or chronic tic disorder in specialist care. Furthermore, the cohort included 5,141 families with full siblings who were discordant for these disorders.
Individuals with Tourette syndrome or chronic tic disorder had a higher risk for any metabolic or cardiovascular disorder, compared with the general population (hazard ratio adjusted by sex and birth year [aHR], 1.99) and sibling controls (aHR, 1.37). Specifically, individuals with Tourette syndrome or chronic tic disorder had higher risks for obesity (aHR, 2.76), T2DM(aHR, 1.67), and circulatory system diseases (aHR, 1.76).
The increased risk of any cardiometabolic disorder was significantly greater for males than it was for females (aHRs, 2.13 vs. 1.79), as was the risk of obesity (aHRs, 3.24 vs. 1.97).
The increased risk for cardiometabolic disorders in this patient population was evident by age 8 years. Exclusion of those patients with comorbid ADHD reduced but did not eliminate the risk (aHR, 1.52). The exclusion of other comorbidities did not significantly affect the results. Among patients with Tourette syndrome or chronic tic disorder, those who had received antipsychotic treatment for more than 1 year were significantly less likely to have metabolic and cardiovascular disorders, compared with patients not taking antipsychotic medication. This association may be related to “greater medical vigilance” and “should not be taken as evidence that antipsychotics are free from cardiometabolic adverse effects,” the authors noted.
The study was supported by a research grant from Tourettes Action. In addition, authors reported support from the Swedish Research Council and a Karolinska Institutet PhD stipend. Two authors disclosed personal fees from publishers, and one author disclosed grants and other funding from Shire.
jremaly@mdedge.com
SOURCE: Brander G et al. JAMA Neurol. 2019 Jan 14. doi: 10.1001/jamaneurol.2018.4279.
FROM JAMA NEUROLOGY
Key clinical point: Monitor cardiometabolic health in patients with Tourette syndrome or chronic tic disorder.
Major finding: Patients with Tourette syndrome or chronic tic disorder have a higher risk of metabolic or cardiovascular disorders, compared with the general population (adjusted hazard ratio, 1.99) and sibling controls (adjusted hazard ratio, 1.37).
Study details: A Swedish longitudinal, population-based cohort study of 7,804 individuals with Tourette syndrome or chronic tic disorder.
Disclosures: The study was supported by a research grant from Tourettes Action. Authors reported support from the Swedish Research Council and a Karolinska Institutet PhD stipend. Two authors disclosed personal fees from publishers, and one author disclosed grants and other funding from Shire.
Source: Brander G et al. JAMA Neurol. 2019 Jan 14. doi: 10.1001/jamaneurol.2018.4279.
Dermatologic comorbidities of atopic dermatitis
Also today, flu season is showing signs of slowing, BMI changes in adolescence is linked to cancer risk later in life, and does reduced degradation of insulin by the liver cause type 2 diabetes.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, flu season is showing signs of slowing, BMI changes in adolescence is linked to cancer risk later in life, and does reduced degradation of insulin by the liver cause type 2 diabetes.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, flu season is showing signs of slowing, BMI changes in adolescence is linked to cancer risk later in life, and does reduced degradation of insulin by the liver cause type 2 diabetes.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
New hypopnea criteria ID unique OSA patient subset
The latest recommended criteria for hypopnea define a distinct group of patients who report substantial daytime sleepiness but with no significant cardiovascular risk, investigators reported in a retrospective, cross-sectional analysis.
The number of obstructive sleep apnea (OSA) diagnoses increased by nearly 13% when using the 2012 American Academy of Sleep Medicine (AASM) criteria of ≥ 3% desaturation or arousal, instead of the 2007 criteria of ≥ 4% desaturation, according to investigators.
While cardiovascular disease risk did not appear to be elevated in those with an OSA diagnosis based on the newer, more inclusive criteria, reported lead author Christine H.J. Won, MD, of Yale University, New Haven, Conn., and her coinvestigators.
“Our findings suggest [that] a more inclusive hypopnea definition alters OSA severity categorization, identifies a new symptomatic group of patients with predominantly mild OSA without increased cardiovascular odds, and does not ameliorate the increased odds predicted by severe OSA for arrhythmias,” the investigators wrote in the Journal of Clinical Sleep Medicine.
The analysis by Dr. Won and her colleagues included 1,400 veterans who had polysomnography for suspected sleep-disordered breathing. Of those veterans, two-thirds (932; 66%) had an OSA diagnosis based on the ≥ 4% desaturation criteria.
With the newer criteria of ≥ 3% desaturation or arousal, another 175 OSA diagnoses were captured out of the remaining 468 previously negative studies, meaning that more than 37% of those patients would be recategorized as having OSA, Dr. Won and her coauthors said.
Compared with individuals with OSA classified by the older, more restrictive criteria, the 175 individuals in this “new OSA” group were younger and less likely to be obese, though they were still more likely to be obese, compared with individuals with no OSA diagnosis, according to the authors.
The new OSA group had more disrupted sleep architecture, significantly worse oxygen saturations, and more self-reported sleepiness on the Epworth Sleepiness Scale as compared with those with no OSA, they added.
Adding in the new OSA group redistributed disease severity, with a relative increase of 21.4% for mild and 21.3% for moderate OSA, but just 15.3% for severe OSA. “Most of the [new OSA] category consisted of mild sleep-disordered breathing,” said Dr. Won and her coauthors in the report.
While there was a statistically significant increase in odds ratio for arrhythmias using the older criteria, reclassifying OSA severity using the newer definition meant that mild and moderate disease lost predictive value. However, severe OSA by the new criteria remained a significant predictor of arrhythmias, the authors said.
Odds ratios for ischemic heart disease and heart failure were numerically higher in the new OSA group versus the no OSA group, though no statistically significant differences were found, according to investigators.
This is thought to be the first study to describe a unique group of patients who escape OSA diagnosis based on the ≥ 4% desaturation criteria but are captured ≥ 3% desaturation or arousal criteria, Dr. Won and her coauthors said.
Further studies would be helpful to evaluate other polysomnographic features in this group to see how they affect cardiovascular or other health risks, they added.
“It would also be important to assess whether treatment in any of these groups leads to improved cardiovascular health, or whether treatment of the [new OSA] group leads to improved daytime sleepiness or quality of life,” they said in the report.
The researchers reported no conflicts of interest related to their work, which was performed at the Veterans Affairs Healthcare System in West Haven, Conn.; Indianapolis; and Cleveland.
SOURCE: Won CHJ et al. J Clin Sleep Med. 2018 Dec 15;14[12]:1987-94.
The study by Won and colleagues provides a “useful perspective” on how hypopnea is defined by including outcome data based on the two different scoring criteria, according to Kenneth R. Casey, MD, MPH, and Rachna Tiwari, MBBS.
Results of the study suggest a rationale for using both the 2007 American Academy of Sleep Medicine hypopnea criteria based on ≥ 4% desaturation, and the updated 2012 AASM criteria based on ≥ 3% desaturation or arousal in the evaluation of polysomnography results, Dr. Casey and Dr. Tiwari said in a commentary accompanying the study.
“This perspective may ultimately be the solution to the confusion caused by competing functional definitions of hypopnea,” they said in the commentary published in the Journal of Clinical Sleep Medicine.
The 2007 recommended criteria of ≥ 4% desaturation seemed reasonable based on available evidence at the time, but was not rigorously based by today’s standards, the authors said.
At that time, they also proposed the new alternative criteria based on ≥ 3% desaturation or an arousal, which in 2012 became elevated to a recommended rule. However, the previous recommended rule was kept to accommodate patients who required Centers for Medicare & Medicaid Services reimbursement, according to Dr. Casey and Dr. Tiwari.
Subsequent studies demonstrated “significant differences” in apnea-hypopnea index results, depending on which scoring criteria were used, they added.
“This confusing, vacillating definition has created a rather bizarre, and perhaps unsettling, situation wherein the severity of the diagnosis of sleep-disordered breathing, and perhaps its presence or absence, is determined by the patient’s insurance coverage,” they said in the commentary.
Dr. Casey and Dr. Tiwari are with the University of Wisconsin and William S. Middleton Memorial Veterans Hospital, both in Madison. They reported no conflicts of interest related to their editorial, which appears in the Journal of Clinical Sleep Medicine.
The study by Won and colleagues provides a “useful perspective” on how hypopnea is defined by including outcome data based on the two different scoring criteria, according to Kenneth R. Casey, MD, MPH, and Rachna Tiwari, MBBS.
Results of the study suggest a rationale for using both the 2007 American Academy of Sleep Medicine hypopnea criteria based on ≥ 4% desaturation, and the updated 2012 AASM criteria based on ≥ 3% desaturation or arousal in the evaluation of polysomnography results, Dr. Casey and Dr. Tiwari said in a commentary accompanying the study.
“This perspective may ultimately be the solution to the confusion caused by competing functional definitions of hypopnea,” they said in the commentary published in the Journal of Clinical Sleep Medicine.
The 2007 recommended criteria of ≥ 4% desaturation seemed reasonable based on available evidence at the time, but was not rigorously based by today’s standards, the authors said.
At that time, they also proposed the new alternative criteria based on ≥ 3% desaturation or an arousal, which in 2012 became elevated to a recommended rule. However, the previous recommended rule was kept to accommodate patients who required Centers for Medicare & Medicaid Services reimbursement, according to Dr. Casey and Dr. Tiwari.
Subsequent studies demonstrated “significant differences” in apnea-hypopnea index results, depending on which scoring criteria were used, they added.
“This confusing, vacillating definition has created a rather bizarre, and perhaps unsettling, situation wherein the severity of the diagnosis of sleep-disordered breathing, and perhaps its presence or absence, is determined by the patient’s insurance coverage,” they said in the commentary.
Dr. Casey and Dr. Tiwari are with the University of Wisconsin and William S. Middleton Memorial Veterans Hospital, both in Madison. They reported no conflicts of interest related to their editorial, which appears in the Journal of Clinical Sleep Medicine.
The study by Won and colleagues provides a “useful perspective” on how hypopnea is defined by including outcome data based on the two different scoring criteria, according to Kenneth R. Casey, MD, MPH, and Rachna Tiwari, MBBS.
Results of the study suggest a rationale for using both the 2007 American Academy of Sleep Medicine hypopnea criteria based on ≥ 4% desaturation, and the updated 2012 AASM criteria based on ≥ 3% desaturation or arousal in the evaluation of polysomnography results, Dr. Casey and Dr. Tiwari said in a commentary accompanying the study.
“This perspective may ultimately be the solution to the confusion caused by competing functional definitions of hypopnea,” they said in the commentary published in the Journal of Clinical Sleep Medicine.
The 2007 recommended criteria of ≥ 4% desaturation seemed reasonable based on available evidence at the time, but was not rigorously based by today’s standards, the authors said.
At that time, they also proposed the new alternative criteria based on ≥ 3% desaturation or an arousal, which in 2012 became elevated to a recommended rule. However, the previous recommended rule was kept to accommodate patients who required Centers for Medicare & Medicaid Services reimbursement, according to Dr. Casey and Dr. Tiwari.
Subsequent studies demonstrated “significant differences” in apnea-hypopnea index results, depending on which scoring criteria were used, they added.
“This confusing, vacillating definition has created a rather bizarre, and perhaps unsettling, situation wherein the severity of the diagnosis of sleep-disordered breathing, and perhaps its presence or absence, is determined by the patient’s insurance coverage,” they said in the commentary.
Dr. Casey and Dr. Tiwari are with the University of Wisconsin and William S. Middleton Memorial Veterans Hospital, both in Madison. They reported no conflicts of interest related to their editorial, which appears in the Journal of Clinical Sleep Medicine.
The latest recommended criteria for hypopnea define a distinct group of patients who report substantial daytime sleepiness but with no significant cardiovascular risk, investigators reported in a retrospective, cross-sectional analysis.
The number of obstructive sleep apnea (OSA) diagnoses increased by nearly 13% when using the 2012 American Academy of Sleep Medicine (AASM) criteria of ≥ 3% desaturation or arousal, instead of the 2007 criteria of ≥ 4% desaturation, according to investigators.
While cardiovascular disease risk did not appear to be elevated in those with an OSA diagnosis based on the newer, more inclusive criteria, reported lead author Christine H.J. Won, MD, of Yale University, New Haven, Conn., and her coinvestigators.
“Our findings suggest [that] a more inclusive hypopnea definition alters OSA severity categorization, identifies a new symptomatic group of patients with predominantly mild OSA without increased cardiovascular odds, and does not ameliorate the increased odds predicted by severe OSA for arrhythmias,” the investigators wrote in the Journal of Clinical Sleep Medicine.
The analysis by Dr. Won and her colleagues included 1,400 veterans who had polysomnography for suspected sleep-disordered breathing. Of those veterans, two-thirds (932; 66%) had an OSA diagnosis based on the ≥ 4% desaturation criteria.
With the newer criteria of ≥ 3% desaturation or arousal, another 175 OSA diagnoses were captured out of the remaining 468 previously negative studies, meaning that more than 37% of those patients would be recategorized as having OSA, Dr. Won and her coauthors said.
Compared with individuals with OSA classified by the older, more restrictive criteria, the 175 individuals in this “new OSA” group were younger and less likely to be obese, though they were still more likely to be obese, compared with individuals with no OSA diagnosis, according to the authors.
The new OSA group had more disrupted sleep architecture, significantly worse oxygen saturations, and more self-reported sleepiness on the Epworth Sleepiness Scale as compared with those with no OSA, they added.
Adding in the new OSA group redistributed disease severity, with a relative increase of 21.4% for mild and 21.3% for moderate OSA, but just 15.3% for severe OSA. “Most of the [new OSA] category consisted of mild sleep-disordered breathing,” said Dr. Won and her coauthors in the report.
While there was a statistically significant increase in odds ratio for arrhythmias using the older criteria, reclassifying OSA severity using the newer definition meant that mild and moderate disease lost predictive value. However, severe OSA by the new criteria remained a significant predictor of arrhythmias, the authors said.
Odds ratios for ischemic heart disease and heart failure were numerically higher in the new OSA group versus the no OSA group, though no statistically significant differences were found, according to investigators.
This is thought to be the first study to describe a unique group of patients who escape OSA diagnosis based on the ≥ 4% desaturation criteria but are captured ≥ 3% desaturation or arousal criteria, Dr. Won and her coauthors said.
Further studies would be helpful to evaluate other polysomnographic features in this group to see how they affect cardiovascular or other health risks, they added.
“It would also be important to assess whether treatment in any of these groups leads to improved cardiovascular health, or whether treatment of the [new OSA] group leads to improved daytime sleepiness or quality of life,” they said in the report.
The researchers reported no conflicts of interest related to their work, which was performed at the Veterans Affairs Healthcare System in West Haven, Conn.; Indianapolis; and Cleveland.
SOURCE: Won CHJ et al. J Clin Sleep Med. 2018 Dec 15;14[12]:1987-94.
The latest recommended criteria for hypopnea define a distinct group of patients who report substantial daytime sleepiness but with no significant cardiovascular risk, investigators reported in a retrospective, cross-sectional analysis.
The number of obstructive sleep apnea (OSA) diagnoses increased by nearly 13% when using the 2012 American Academy of Sleep Medicine (AASM) criteria of ≥ 3% desaturation or arousal, instead of the 2007 criteria of ≥ 4% desaturation, according to investigators.
While cardiovascular disease risk did not appear to be elevated in those with an OSA diagnosis based on the newer, more inclusive criteria, reported lead author Christine H.J. Won, MD, of Yale University, New Haven, Conn., and her coinvestigators.
“Our findings suggest [that] a more inclusive hypopnea definition alters OSA severity categorization, identifies a new symptomatic group of patients with predominantly mild OSA without increased cardiovascular odds, and does not ameliorate the increased odds predicted by severe OSA for arrhythmias,” the investigators wrote in the Journal of Clinical Sleep Medicine.
The analysis by Dr. Won and her colleagues included 1,400 veterans who had polysomnography for suspected sleep-disordered breathing. Of those veterans, two-thirds (932; 66%) had an OSA diagnosis based on the ≥ 4% desaturation criteria.
With the newer criteria of ≥ 3% desaturation or arousal, another 175 OSA diagnoses were captured out of the remaining 468 previously negative studies, meaning that more than 37% of those patients would be recategorized as having OSA, Dr. Won and her coauthors said.
Compared with individuals with OSA classified by the older, more restrictive criteria, the 175 individuals in this “new OSA” group were younger and less likely to be obese, though they were still more likely to be obese, compared with individuals with no OSA diagnosis, according to the authors.
The new OSA group had more disrupted sleep architecture, significantly worse oxygen saturations, and more self-reported sleepiness on the Epworth Sleepiness Scale as compared with those with no OSA, they added.
Adding in the new OSA group redistributed disease severity, with a relative increase of 21.4% for mild and 21.3% for moderate OSA, but just 15.3% for severe OSA. “Most of the [new OSA] category consisted of mild sleep-disordered breathing,” said Dr. Won and her coauthors in the report.
While there was a statistically significant increase in odds ratio for arrhythmias using the older criteria, reclassifying OSA severity using the newer definition meant that mild and moderate disease lost predictive value. However, severe OSA by the new criteria remained a significant predictor of arrhythmias, the authors said.
Odds ratios for ischemic heart disease and heart failure were numerically higher in the new OSA group versus the no OSA group, though no statistically significant differences were found, according to investigators.
This is thought to be the first study to describe a unique group of patients who escape OSA diagnosis based on the ≥ 4% desaturation criteria but are captured ≥ 3% desaturation or arousal criteria, Dr. Won and her coauthors said.
Further studies would be helpful to evaluate other polysomnographic features in this group to see how they affect cardiovascular or other health risks, they added.
“It would also be important to assess whether treatment in any of these groups leads to improved cardiovascular health, or whether treatment of the [new OSA] group leads to improved daytime sleepiness or quality of life,” they said in the report.
The researchers reported no conflicts of interest related to their work, which was performed at the Veterans Affairs Healthcare System in West Haven, Conn.; Indianapolis; and Cleveland.
SOURCE: Won CHJ et al. J Clin Sleep Med. 2018 Dec 15;14[12]:1987-94.
FROM THE CLINICAL JOURNAL OF SLEEP MEDICINE
Key clinical point: The latest AASM criteria for hypopnea identify a subset of obstructive sleep apnea patients with substantial daytime sleepiness but no apparent significant increase in cardiovascular risk.
Major finding: The number of obstructive sleep apnea (OSA) diagnoses increased by nearly 13% when using the 2012 AASM criteria of ≥ 3% desaturation or an arousal, instead of the 2007 criteria of ≥ 4% desaturation.
Study details: Retrospective, cross-sectional, observational study that includes 1,400 veterans evaluated for suspected sleep-disordered breathing.
Disclosures: Authors reported no conflicts of interest.
Source: Won CHJ et al. J Clin Sleep Med. 2018 Dec 15;14(12):1987-94.
New or existing drugs? Both fuel price inflation
Inflation in existing drugs’ prices and the debut of new drugs are both contributing to the overall rising costs of pharmaceuticals.
.
For oral and injectable specialty drugs, costs increased 20.6% and 12.5%, respectively, with 71.1% and 52.4% attributable to new drugs. Costs of oral and injectable generic drugs grew by 4.4% and 7.3%, also driven by entrants into the market.
Researchers looked at monthly wholesale acquisition costs of 24,877 National Drug Codes for oral drugs and 3,049 injectable drugs from 2005 to 2016. They compared them with pharmacy claims from the UPMC Health Plan, which offers insurance products to more than 3.2 million members across the spectrum of private and public arenas.
“Our analyses yielded three main findings,” explained Inmaculada Hernandez, PharmD, PhD, University of Pittsburgh, and her colleagues in a report published in the January 2019 issue of Health Affairs.
“First, costs increased considerably faster than inflation across all drug classes, and increases were highest for oral specialty drugs and lowest for oral generics,” Dr. Hernandez and her colleagues wrote.
“Second, rising costs of brand-name drugs were driven by inflation in the prices of widely used existing drugs,” they added. A combination of new products and price inflation in existing drugs drove the rising costs of specialty drugs, with new drugs accounting for a larger share of the price increases.
Third, “existing generics tended to decrease the average cost of generic drugs,” Dr. Hernandez noted. However, new generic products cost more than those already on the market, which fueled the annual increases in average costs.
The authors noted that their estimates demonstrate the role of inflation on pharmaceutical cost increases and support policy efforts to control that inflation.
“In the current value-based landscape, increasing drug costs attributable to new products can sometimes be justified on the basis of improved outcomes,” Dr. Hernandez and colleagues stated. “However, rising costs due to inflation do not reflect improved value for patients.”
The researchers noted that the data are limited by the lack of rebate information, which is generally proprietary. Thus, “the contribution of existing drugs may have been lower than we estimated,” they noted. In addition, “because the magnitude of rebates has increased in the past decade, our findings likely overestimated cost increases for brand-name drugs.” The researchers also didn’t examine the effect of drugs transitioning from brand to generic offerings.
The authors provided no disclosures.
gtwachtman@mdedge.com
SOURCE: Hernandez I et al. Health Aff (Millwood). 2019 Jan 2019. doi: 10.1377/hlthaff.2018.05147.
Inflation in existing drugs’ prices and the debut of new drugs are both contributing to the overall rising costs of pharmaceuticals.
.
For oral and injectable specialty drugs, costs increased 20.6% and 12.5%, respectively, with 71.1% and 52.4% attributable to new drugs. Costs of oral and injectable generic drugs grew by 4.4% and 7.3%, also driven by entrants into the market.
Researchers looked at monthly wholesale acquisition costs of 24,877 National Drug Codes for oral drugs and 3,049 injectable drugs from 2005 to 2016. They compared them with pharmacy claims from the UPMC Health Plan, which offers insurance products to more than 3.2 million members across the spectrum of private and public arenas.
“Our analyses yielded three main findings,” explained Inmaculada Hernandez, PharmD, PhD, University of Pittsburgh, and her colleagues in a report published in the January 2019 issue of Health Affairs.
“First, costs increased considerably faster than inflation across all drug classes, and increases were highest for oral specialty drugs and lowest for oral generics,” Dr. Hernandez and her colleagues wrote.
“Second, rising costs of brand-name drugs were driven by inflation in the prices of widely used existing drugs,” they added. A combination of new products and price inflation in existing drugs drove the rising costs of specialty drugs, with new drugs accounting for a larger share of the price increases.
Third, “existing generics tended to decrease the average cost of generic drugs,” Dr. Hernandez noted. However, new generic products cost more than those already on the market, which fueled the annual increases in average costs.
The authors noted that their estimates demonstrate the role of inflation on pharmaceutical cost increases and support policy efforts to control that inflation.
“In the current value-based landscape, increasing drug costs attributable to new products can sometimes be justified on the basis of improved outcomes,” Dr. Hernandez and colleagues stated. “However, rising costs due to inflation do not reflect improved value for patients.”
The researchers noted that the data are limited by the lack of rebate information, which is generally proprietary. Thus, “the contribution of existing drugs may have been lower than we estimated,” they noted. In addition, “because the magnitude of rebates has increased in the past decade, our findings likely overestimated cost increases for brand-name drugs.” The researchers also didn’t examine the effect of drugs transitioning from brand to generic offerings.
The authors provided no disclosures.
gtwachtman@mdedge.com
SOURCE: Hernandez I et al. Health Aff (Millwood). 2019 Jan 2019. doi: 10.1377/hlthaff.2018.05147.
Inflation in existing drugs’ prices and the debut of new drugs are both contributing to the overall rising costs of pharmaceuticals.
.
For oral and injectable specialty drugs, costs increased 20.6% and 12.5%, respectively, with 71.1% and 52.4% attributable to new drugs. Costs of oral and injectable generic drugs grew by 4.4% and 7.3%, also driven by entrants into the market.
Researchers looked at monthly wholesale acquisition costs of 24,877 National Drug Codes for oral drugs and 3,049 injectable drugs from 2005 to 2016. They compared them with pharmacy claims from the UPMC Health Plan, which offers insurance products to more than 3.2 million members across the spectrum of private and public arenas.
“Our analyses yielded three main findings,” explained Inmaculada Hernandez, PharmD, PhD, University of Pittsburgh, and her colleagues in a report published in the January 2019 issue of Health Affairs.
“First, costs increased considerably faster than inflation across all drug classes, and increases were highest for oral specialty drugs and lowest for oral generics,” Dr. Hernandez and her colleagues wrote.
“Second, rising costs of brand-name drugs were driven by inflation in the prices of widely used existing drugs,” they added. A combination of new products and price inflation in existing drugs drove the rising costs of specialty drugs, with new drugs accounting for a larger share of the price increases.
Third, “existing generics tended to decrease the average cost of generic drugs,” Dr. Hernandez noted. However, new generic products cost more than those already on the market, which fueled the annual increases in average costs.
The authors noted that their estimates demonstrate the role of inflation on pharmaceutical cost increases and support policy efforts to control that inflation.
“In the current value-based landscape, increasing drug costs attributable to new products can sometimes be justified on the basis of improved outcomes,” Dr. Hernandez and colleagues stated. “However, rising costs due to inflation do not reflect improved value for patients.”
The researchers noted that the data are limited by the lack of rebate information, which is generally proprietary. Thus, “the contribution of existing drugs may have been lower than we estimated,” they noted. In addition, “because the magnitude of rebates has increased in the past decade, our findings likely overestimated cost increases for brand-name drugs.” The researchers also didn’t examine the effect of drugs transitioning from brand to generic offerings.
The authors provided no disclosures.
gtwachtman@mdedge.com
SOURCE: Hernandez I et al. Health Aff (Millwood). 2019 Jan 2019. doi: 10.1377/hlthaff.2018.05147.
FROM HEALTH AFFAIRS
Key clinical point: Price inflation in existing drugs and new product introductions are driving increases in pharmaceutical costs.
Major finding: 71% of oral specialty drug price increases during 2005-2019 are attributable to new products.
Study details: Researchers analyzed the wholesale acquisition prices of 24,877 oral drugs and 3,049 injectable drugs and compared them with pharmacy claims across all public and private insurance products offered by the UPMC Health Plan.
Disclosures: The authors provided no disclosures.
Source: Hernandez I et al. Health Aff (Millwood). 2019 Jan. doi: 10.1377/hlthaff.2018.05147.
Daily News Special: SABCS
Stories include: uUing low-dose tamoxifen, the latest findings from the KATHERINE trial, results of a meta-analysis of neoadjuvant chemotherapy, and capecitabine in early stage triple negative breast cancer.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Stories include: uUing low-dose tamoxifen, the latest findings from the KATHERINE trial, results of a meta-analysis of neoadjuvant chemotherapy, and capecitabine in early stage triple negative breast cancer.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Stories include: uUing low-dose tamoxifen, the latest findings from the KATHERINE trial, results of a meta-analysis of neoadjuvant chemotherapy, and capecitabine in early stage triple negative breast cancer.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify














