User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
American Academy of Neurology cancels annual meeting amid COVID-19 pandemic
“Protecting the health, safety, and well-being of our members, attendees, and ultimately our neurology patients is paramount, and serves as the reason for our decision to cancel the AAN annual meeting for the first time in our 72-year history,” AAN President James Stevens, MD, said in a statement. “Put simply, canceling the AAN annual meeting is the right thing to do during this historic time.”
Dr. Stevens added that it is “important to keep our members in their communities – where you stand by to help patients during this time of uncertainty. We also have a professional responsibility to model social distancing and not contribute to the spread of the virus through a large public gathering.”
AAN said it is currently processing full registration fee refunds for those who had registered to attend. Information for exhibitors and sponsors will be forthcoming.
As for missed CME opportunities related to attending the annual meeting, AAN will provide different educational opportunities throughout the remainder of 2020.
Further questions should be directed via email to memberservices@aan.com. Additional information related to the cancellation will be posted to the AAN website and via social media.
“Protecting the health, safety, and well-being of our members, attendees, and ultimately our neurology patients is paramount, and serves as the reason for our decision to cancel the AAN annual meeting for the first time in our 72-year history,” AAN President James Stevens, MD, said in a statement. “Put simply, canceling the AAN annual meeting is the right thing to do during this historic time.”
Dr. Stevens added that it is “important to keep our members in their communities – where you stand by to help patients during this time of uncertainty. We also have a professional responsibility to model social distancing and not contribute to the spread of the virus through a large public gathering.”
AAN said it is currently processing full registration fee refunds for those who had registered to attend. Information for exhibitors and sponsors will be forthcoming.
As for missed CME opportunities related to attending the annual meeting, AAN will provide different educational opportunities throughout the remainder of 2020.
Further questions should be directed via email to memberservices@aan.com. Additional information related to the cancellation will be posted to the AAN website and via social media.
“Protecting the health, safety, and well-being of our members, attendees, and ultimately our neurology patients is paramount, and serves as the reason for our decision to cancel the AAN annual meeting for the first time in our 72-year history,” AAN President James Stevens, MD, said in a statement. “Put simply, canceling the AAN annual meeting is the right thing to do during this historic time.”
Dr. Stevens added that it is “important to keep our members in their communities – where you stand by to help patients during this time of uncertainty. We also have a professional responsibility to model social distancing and not contribute to the spread of the virus through a large public gathering.”
AAN said it is currently processing full registration fee refunds for those who had registered to attend. Information for exhibitors and sponsors will be forthcoming.
As for missed CME opportunities related to attending the annual meeting, AAN will provide different educational opportunities throughout the remainder of 2020.
Further questions should be directed via email to memberservices@aan.com. Additional information related to the cancellation will be posted to the AAN website and via social media.
Expert says progress in gut-brain research requires an open mind
A growing body of research links the gut with the brain and behavior, but compartmentalization within the medical community may be slowing investigation of the gut-brain axis, according to a leading expert.
Studies have shown that the microbiome may influence a diverse range of behavioral and neurological processes, from acute and chronic stress responses to development of Parkinson’s and Alzheimer’s disease, reported John F. Cryan, PhD, of University College Cork, Ireland.
Dr. Cryan began his presentation at the annual Gut Microbiota for Health World Summit by citing Hippocrates, who is thought to have stated that all diseases begin in the gut.
“That can be quite strange when I talk to my neurology or psychiatry colleagues,” Dr. Cryan said. “They sometimes look at me like I have two heads. Because in medicine we compartmentalize, and if you are studying neurology or psychiatry or [you are] in clinical practice, you are focusing on everything from the neck upwards.”
For more than a decade, Dr. Cryan and colleagues have been investigating the gut-brain axis, predominantly in mouse models, but also across animal species and in humans.
At the meeting, sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, Dr. Cryan reviewed a variety of representative studies.
For instance, in both mice and humans, research has shown that C-section, which is associated with poorer microbiome diversity than vaginal delivery, has also been linked with social deficits and elevated stress responses. And in the case of mice, coprophagia, in which cesarean-delivered mice eat the feces of vaginally born mice, has been shown to ameliorate these psychiatric effects.
Dr. Cryan likened this process to an “artificial fecal transplant.”
“You know, co-housing and eating each other’s poo is not the translational approach that we were advocating by any means,” Dr. Cryan said. “But at least it tells us – in a proof-of-concept way – that if we change the microbiome, then we can reverse what’s going on.”
While the mechanisms behind the gut-brain axis remain incompletely understood, Dr. Cryan noted that the vagus nerve, which travels from the gut to the brain, plays a central role, and that transecting this nerve in mice stops the microbiome from affecting the brain.
“What happens in vagus doesn’t just stay in vagus, but will actually affect our emotions in different ways,” Dr. Cryan said.
He emphasized that communication travels both ways along the gut-brain axis, and went on to describe how this phenomenon has been demonstrated across a wide array of animals.
“From insects all the way through to primates, if you start to interfere with social behavior, you change the microbiome,” Dr. Cryan said. “But the opposite is also true; if you start to change the microbiome you can start to have widespread effects on social behavior.”
In humans, manipulating the microbiome could open up new psychiatric frontiers, Dr. Cryan said.
“[In the past 30 years], there really have been no real advances in how we manage mental health,” he said. “That’s very sobering when we are having such a mental health problem across all ages right now. And so perhaps it’s time for what we’ve coined the ‘psychobiotic revolution’ – time for a new way of thinking about mental health.”
According to Dr. Cryan, psychobiotics are interventions that target the microbiome for mental health purposes, including fermented foods, probiotics, prebiotics, synbiotics, parabiotics, and postbiotics.
Among these, probiotics have been a focal point of interventional research. Although results have been mixed, Dr. Cryan suggested that negative probiotic studies are more likely due to bacterial strain than a failure of the concept as a whole.
“Most strains of bacteria will do absolutely nothing,” Dr. Cryan said. “Strain is really important.”
In demonstration of this concept, he recounted a 2017 study conducted at University College Cork in which 22 healthy volunteers were given Bifidobacterium longum 1714, and then subjected to a social stress test. The results, published in Translational Psychiatry, showed that the probiotic, compared with placebo, was associated with attenuated stress responses, reduced daily stress, and enhanced visuospatial memory.
In contrast, a similar study by Dr. Cryan and colleagues, which tested Lactobacillus rhamnosus (JB-1), fell short.
“You [could not have gotten] more negative data into one paper if you tried,” Dr. Cryan said, referring to the study. “It did absolutely nothing.”
To find out which psychobiotics may have an impact, and how, Dr. Cryan called for more research.
“It’s still early days,” he said. “We probably have more meta-analyses and systematic reviews of the field than we have primary research papers.
Dr. Cryan concluded his presentation on an optimistic note.
“Neurology is waking up ... to understand that the microbiome could be playing a key role in many, many other disorders. ... Overall, what we’re beginning to see is that our state of gut markedly affects our state of mind.”
Dr. Cryan disclosed relationships with Abbott Nutrition, Roche Pharma, Nutricia, and others.
A growing body of research links the gut with the brain and behavior, but compartmentalization within the medical community may be slowing investigation of the gut-brain axis, according to a leading expert.
Studies have shown that the microbiome may influence a diverse range of behavioral and neurological processes, from acute and chronic stress responses to development of Parkinson’s and Alzheimer’s disease, reported John F. Cryan, PhD, of University College Cork, Ireland.
Dr. Cryan began his presentation at the annual Gut Microbiota for Health World Summit by citing Hippocrates, who is thought to have stated that all diseases begin in the gut.
“That can be quite strange when I talk to my neurology or psychiatry colleagues,” Dr. Cryan said. “They sometimes look at me like I have two heads. Because in medicine we compartmentalize, and if you are studying neurology or psychiatry or [you are] in clinical practice, you are focusing on everything from the neck upwards.”
For more than a decade, Dr. Cryan and colleagues have been investigating the gut-brain axis, predominantly in mouse models, but also across animal species and in humans.
At the meeting, sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, Dr. Cryan reviewed a variety of representative studies.
For instance, in both mice and humans, research has shown that C-section, which is associated with poorer microbiome diversity than vaginal delivery, has also been linked with social deficits and elevated stress responses. And in the case of mice, coprophagia, in which cesarean-delivered mice eat the feces of vaginally born mice, has been shown to ameliorate these psychiatric effects.
Dr. Cryan likened this process to an “artificial fecal transplant.”
“You know, co-housing and eating each other’s poo is not the translational approach that we were advocating by any means,” Dr. Cryan said. “But at least it tells us – in a proof-of-concept way – that if we change the microbiome, then we can reverse what’s going on.”
While the mechanisms behind the gut-brain axis remain incompletely understood, Dr. Cryan noted that the vagus nerve, which travels from the gut to the brain, plays a central role, and that transecting this nerve in mice stops the microbiome from affecting the brain.
“What happens in vagus doesn’t just stay in vagus, but will actually affect our emotions in different ways,” Dr. Cryan said.
He emphasized that communication travels both ways along the gut-brain axis, and went on to describe how this phenomenon has been demonstrated across a wide array of animals.
“From insects all the way through to primates, if you start to interfere with social behavior, you change the microbiome,” Dr. Cryan said. “But the opposite is also true; if you start to change the microbiome you can start to have widespread effects on social behavior.”
In humans, manipulating the microbiome could open up new psychiatric frontiers, Dr. Cryan said.
“[In the past 30 years], there really have been no real advances in how we manage mental health,” he said. “That’s very sobering when we are having such a mental health problem across all ages right now. And so perhaps it’s time for what we’ve coined the ‘psychobiotic revolution’ – time for a new way of thinking about mental health.”
According to Dr. Cryan, psychobiotics are interventions that target the microbiome for mental health purposes, including fermented foods, probiotics, prebiotics, synbiotics, parabiotics, and postbiotics.
Among these, probiotics have been a focal point of interventional research. Although results have been mixed, Dr. Cryan suggested that negative probiotic studies are more likely due to bacterial strain than a failure of the concept as a whole.
“Most strains of bacteria will do absolutely nothing,” Dr. Cryan said. “Strain is really important.”
In demonstration of this concept, he recounted a 2017 study conducted at University College Cork in which 22 healthy volunteers were given Bifidobacterium longum 1714, and then subjected to a social stress test. The results, published in Translational Psychiatry, showed that the probiotic, compared with placebo, was associated with attenuated stress responses, reduced daily stress, and enhanced visuospatial memory.
In contrast, a similar study by Dr. Cryan and colleagues, which tested Lactobacillus rhamnosus (JB-1), fell short.
“You [could not have gotten] more negative data into one paper if you tried,” Dr. Cryan said, referring to the study. “It did absolutely nothing.”
To find out which psychobiotics may have an impact, and how, Dr. Cryan called for more research.
“It’s still early days,” he said. “We probably have more meta-analyses and systematic reviews of the field than we have primary research papers.
Dr. Cryan concluded his presentation on an optimistic note.
“Neurology is waking up ... to understand that the microbiome could be playing a key role in many, many other disorders. ... Overall, what we’re beginning to see is that our state of gut markedly affects our state of mind.”
Dr. Cryan disclosed relationships with Abbott Nutrition, Roche Pharma, Nutricia, and others.
A growing body of research links the gut with the brain and behavior, but compartmentalization within the medical community may be slowing investigation of the gut-brain axis, according to a leading expert.
Studies have shown that the microbiome may influence a diverse range of behavioral and neurological processes, from acute and chronic stress responses to development of Parkinson’s and Alzheimer’s disease, reported John F. Cryan, PhD, of University College Cork, Ireland.
Dr. Cryan began his presentation at the annual Gut Microbiota for Health World Summit by citing Hippocrates, who is thought to have stated that all diseases begin in the gut.
“That can be quite strange when I talk to my neurology or psychiatry colleagues,” Dr. Cryan said. “They sometimes look at me like I have two heads. Because in medicine we compartmentalize, and if you are studying neurology or psychiatry or [you are] in clinical practice, you are focusing on everything from the neck upwards.”
For more than a decade, Dr. Cryan and colleagues have been investigating the gut-brain axis, predominantly in mouse models, but also across animal species and in humans.
At the meeting, sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, Dr. Cryan reviewed a variety of representative studies.
For instance, in both mice and humans, research has shown that C-section, which is associated with poorer microbiome diversity than vaginal delivery, has also been linked with social deficits and elevated stress responses. And in the case of mice, coprophagia, in which cesarean-delivered mice eat the feces of vaginally born mice, has been shown to ameliorate these psychiatric effects.
Dr. Cryan likened this process to an “artificial fecal transplant.”
“You know, co-housing and eating each other’s poo is not the translational approach that we were advocating by any means,” Dr. Cryan said. “But at least it tells us – in a proof-of-concept way – that if we change the microbiome, then we can reverse what’s going on.”
While the mechanisms behind the gut-brain axis remain incompletely understood, Dr. Cryan noted that the vagus nerve, which travels from the gut to the brain, plays a central role, and that transecting this nerve in mice stops the microbiome from affecting the brain.
“What happens in vagus doesn’t just stay in vagus, but will actually affect our emotions in different ways,” Dr. Cryan said.
He emphasized that communication travels both ways along the gut-brain axis, and went on to describe how this phenomenon has been demonstrated across a wide array of animals.
“From insects all the way through to primates, if you start to interfere with social behavior, you change the microbiome,” Dr. Cryan said. “But the opposite is also true; if you start to change the microbiome you can start to have widespread effects on social behavior.”
In humans, manipulating the microbiome could open up new psychiatric frontiers, Dr. Cryan said.
“[In the past 30 years], there really have been no real advances in how we manage mental health,” he said. “That’s very sobering when we are having such a mental health problem across all ages right now. And so perhaps it’s time for what we’ve coined the ‘psychobiotic revolution’ – time for a new way of thinking about mental health.”
According to Dr. Cryan, psychobiotics are interventions that target the microbiome for mental health purposes, including fermented foods, probiotics, prebiotics, synbiotics, parabiotics, and postbiotics.
Among these, probiotics have been a focal point of interventional research. Although results have been mixed, Dr. Cryan suggested that negative probiotic studies are more likely due to bacterial strain than a failure of the concept as a whole.
“Most strains of bacteria will do absolutely nothing,” Dr. Cryan said. “Strain is really important.”
In demonstration of this concept, he recounted a 2017 study conducted at University College Cork in which 22 healthy volunteers were given Bifidobacterium longum 1714, and then subjected to a social stress test. The results, published in Translational Psychiatry, showed that the probiotic, compared with placebo, was associated with attenuated stress responses, reduced daily stress, and enhanced visuospatial memory.
In contrast, a similar study by Dr. Cryan and colleagues, which tested Lactobacillus rhamnosus (JB-1), fell short.
“You [could not have gotten] more negative data into one paper if you tried,” Dr. Cryan said, referring to the study. “It did absolutely nothing.”
To find out which psychobiotics may have an impact, and how, Dr. Cryan called for more research.
“It’s still early days,” he said. “We probably have more meta-analyses and systematic reviews of the field than we have primary research papers.
Dr. Cryan concluded his presentation on an optimistic note.
“Neurology is waking up ... to understand that the microbiome could be playing a key role in many, many other disorders. ... Overall, what we’re beginning to see is that our state of gut markedly affects our state of mind.”
Dr. Cryan disclosed relationships with Abbott Nutrition, Roche Pharma, Nutricia, and others.
FROM GMFH 2020
Lombardy ICU capacity stressed to breaking point by COVID-19 outbreak
The outbreak of COVID-19 in the Lombardy region of Italy has severely stressed the medical system and the current level of activity may not be sustainable for long, according to Maurizio Cecconi, MD, of the department of anesthesia and intensive care, Humanitas Research Hospital, Milan. Dr. Cecconi spoke via JAMA Live Stream interview with Howard Bauchner, MD, the Editor in Chief of JAMA.
A summary of comments by Dr. Cecconi and two colleagues was simultaneously published in JAMA (2020 Mar 13. doi: 10.1001/jama.2020.4031).
Dr. Cecconi discussed the progress and medical response to the swiftly expanding outbreak that began on Feb. 20. A man in his 30s was admitted to the Codogno Hospital, Lodi, Lombardy, Italy, in respiratory distress. He tested positive for a new coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19). In less than 24 hours, the hospital had 36 cases of COVID-19.
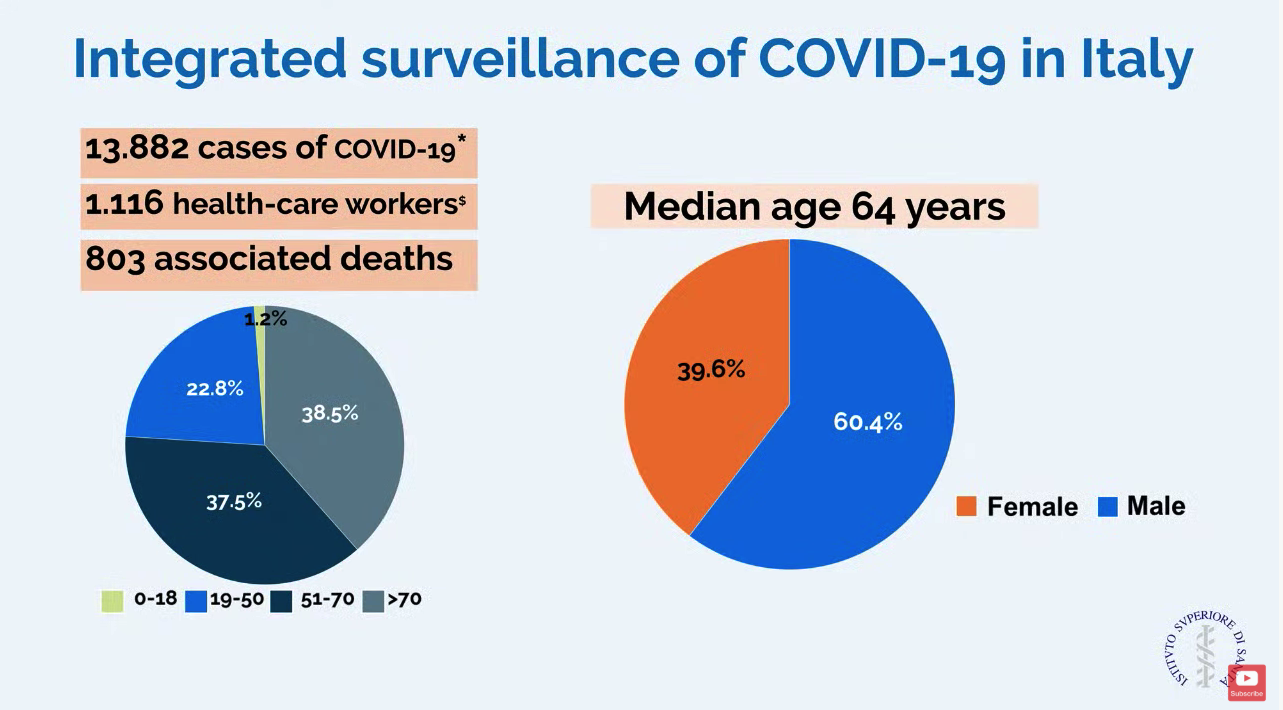
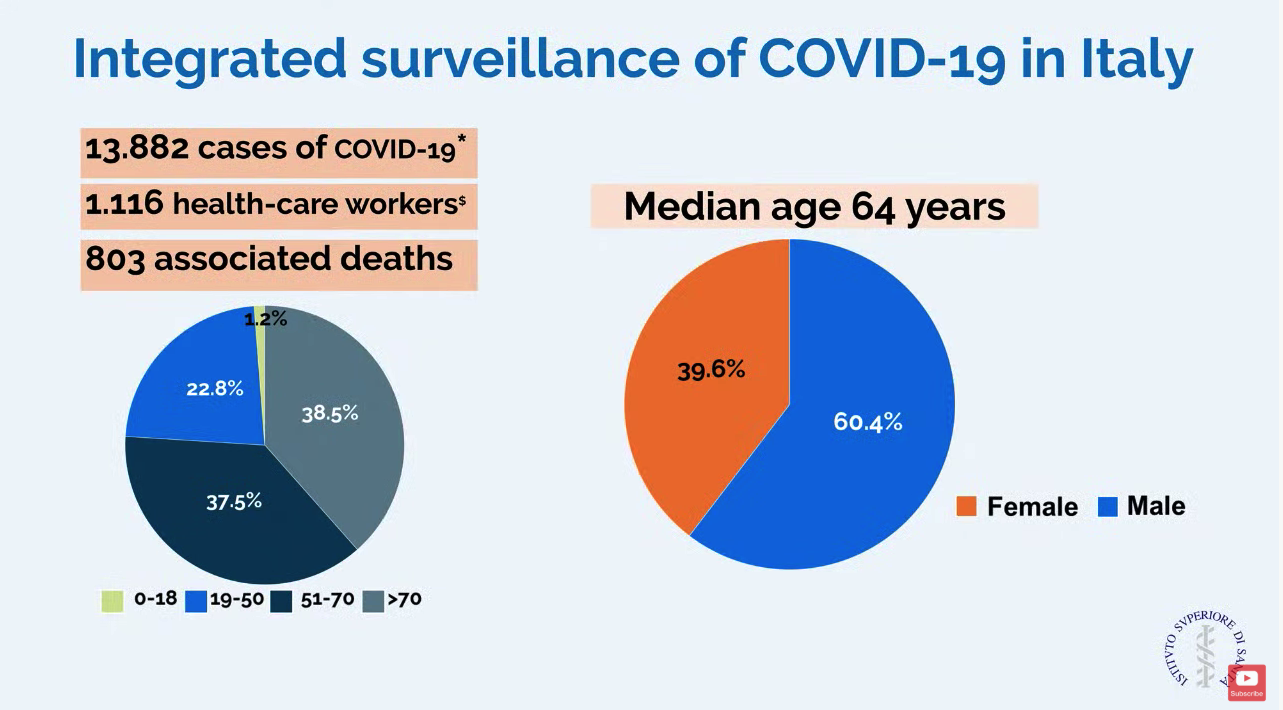
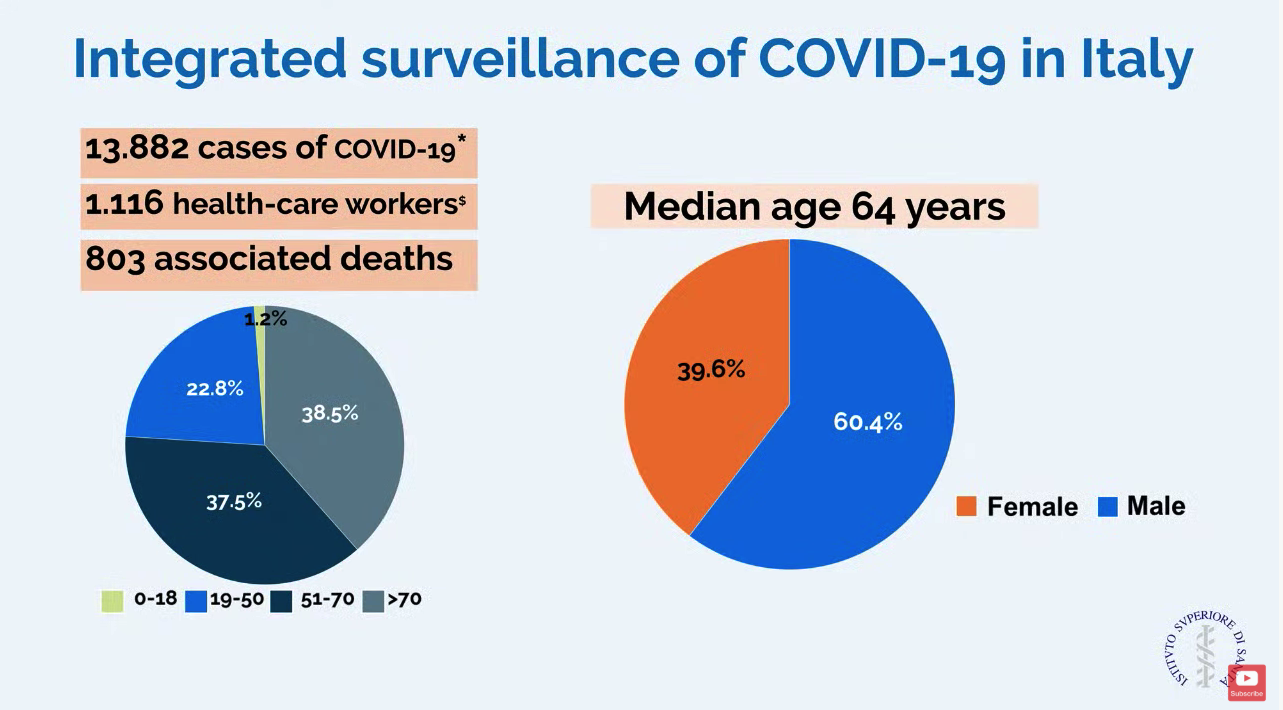
In a slide provided by the Italian National Health Service, the number of cases in Italy stands at 13,882 with 803 associated deaths.
ICU resources have been severely stressed. Before the outbreak, Lombardy had 720 ICU beds (about 5% of total beds). Within 48 hours of the first case, ICU cohorts were formed in 15 hub hospitals totaling 130 COVID-19 ICU beds. By March 7, the total number of dedicated cohorted COVID-19 ICU beds was 482.
“The proportion of ICU admissions represents 12% of the total positive cases, and 16% of all hospitalized patients,” compared with about 5% of ICU admissions reported from China. The difference may be attributable to different criteria for ICU admissions in Italy, compared with China, according to Dr. Cecconi and colleagues.
Dr. Cecconi mentioned that there were relatively few cases in children, and they had relatively mild disease. The death rate among patients remained under 1% up to age 59. For patients aged 60-69 years, the rate was 2.7%; for patients aged 70-79 years, the rate was 9.6%; for those aged 80-89, the rate was much higher at 16.6%.
Modeled forecasts of the potential number of cases in Lombardy are daunting. “The linear model forecasts that approximately 869 ICU admissions could occur by March 20, 2020, whereas the exponential model growth projects that approximately 14,542 ICU admissions could occur by then. Even though these projections are hypothetical and involve various assumptions, any substantial increase in the number of critically ill patients would rapidly exceed total ICU capacity, without even considering other critical admissions, such as for trauma, stroke, and other emergencies,” wrote Dr. Cecconi and his colleagues in JAMA. He said, “We could be on our knees very soon,” referring to the potential dramatic increase in cases.
Dr. Cecconi had some recommendations for other countries in which a major outbreak has not yet occurred. He recommended going beyond expanding ICU and isolation capacity and focus on training staff with simulation for treating these highly contagious patients. His medical center has worked hard to protect staff but 1,116 health care workers have tested positive for the virus. Conditions for staff are very difficult in full protective gear, and Dr. Cecconi commended the heroic work by these doctors and nurses.
In addition, Dr. Cecconi is focused on supportive care for patients and does not recommend using untried approaches on these patients that could cause harm. “Everyone wants to find a specific drug for these patients, but I say there is not particular drug at the moment.” He stressed that, despite the crisis, doctors should focus on evidence-based treatment and tried-and-true supportive care.
Disclosures by Dr. Cecconi are available on the JAMA website.
CORRECTION 3/13/2020 2.18 P.M. The death rate for patients aged 70-79 was corrected.
The outbreak of COVID-19 in the Lombardy region of Italy has severely stressed the medical system and the current level of activity may not be sustainable for long, according to Maurizio Cecconi, MD, of the department of anesthesia and intensive care, Humanitas Research Hospital, Milan. Dr. Cecconi spoke via JAMA Live Stream interview with Howard Bauchner, MD, the Editor in Chief of JAMA.
A summary of comments by Dr. Cecconi and two colleagues was simultaneously published in JAMA (2020 Mar 13. doi: 10.1001/jama.2020.4031).
Dr. Cecconi discussed the progress and medical response to the swiftly expanding outbreak that began on Feb. 20. A man in his 30s was admitted to the Codogno Hospital, Lodi, Lombardy, Italy, in respiratory distress. He tested positive for a new coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19). In less than 24 hours, the hospital had 36 cases of COVID-19.
In a slide provided by the Italian National Health Service, the number of cases in Italy stands at 13,882 with 803 associated deaths.
ICU resources have been severely stressed. Before the outbreak, Lombardy had 720 ICU beds (about 5% of total beds). Within 48 hours of the first case, ICU cohorts were formed in 15 hub hospitals totaling 130 COVID-19 ICU beds. By March 7, the total number of dedicated cohorted COVID-19 ICU beds was 482.
“The proportion of ICU admissions represents 12% of the total positive cases, and 16% of all hospitalized patients,” compared with about 5% of ICU admissions reported from China. The difference may be attributable to different criteria for ICU admissions in Italy, compared with China, according to Dr. Cecconi and colleagues.
Dr. Cecconi mentioned that there were relatively few cases in children, and they had relatively mild disease. The death rate among patients remained under 1% up to age 59. For patients aged 60-69 years, the rate was 2.7%; for patients aged 70-79 years, the rate was 9.6%; for those aged 80-89, the rate was much higher at 16.6%.
Modeled forecasts of the potential number of cases in Lombardy are daunting. “The linear model forecasts that approximately 869 ICU admissions could occur by March 20, 2020, whereas the exponential model growth projects that approximately 14,542 ICU admissions could occur by then. Even though these projections are hypothetical and involve various assumptions, any substantial increase in the number of critically ill patients would rapidly exceed total ICU capacity, without even considering other critical admissions, such as for trauma, stroke, and other emergencies,” wrote Dr. Cecconi and his colleagues in JAMA. He said, “We could be on our knees very soon,” referring to the potential dramatic increase in cases.
Dr. Cecconi had some recommendations for other countries in which a major outbreak has not yet occurred. He recommended going beyond expanding ICU and isolation capacity and focus on training staff with simulation for treating these highly contagious patients. His medical center has worked hard to protect staff but 1,116 health care workers have tested positive for the virus. Conditions for staff are very difficult in full protective gear, and Dr. Cecconi commended the heroic work by these doctors and nurses.
In addition, Dr. Cecconi is focused on supportive care for patients and does not recommend using untried approaches on these patients that could cause harm. “Everyone wants to find a specific drug for these patients, but I say there is not particular drug at the moment.” He stressed that, despite the crisis, doctors should focus on evidence-based treatment and tried-and-true supportive care.
Disclosures by Dr. Cecconi are available on the JAMA website.
CORRECTION 3/13/2020 2.18 P.M. The death rate for patients aged 70-79 was corrected.
The outbreak of COVID-19 in the Lombardy region of Italy has severely stressed the medical system and the current level of activity may not be sustainable for long, according to Maurizio Cecconi, MD, of the department of anesthesia and intensive care, Humanitas Research Hospital, Milan. Dr. Cecconi spoke via JAMA Live Stream interview with Howard Bauchner, MD, the Editor in Chief of JAMA.
A summary of comments by Dr. Cecconi and two colleagues was simultaneously published in JAMA (2020 Mar 13. doi: 10.1001/jama.2020.4031).
Dr. Cecconi discussed the progress and medical response to the swiftly expanding outbreak that began on Feb. 20. A man in his 30s was admitted to the Codogno Hospital, Lodi, Lombardy, Italy, in respiratory distress. He tested positive for a new coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19). In less than 24 hours, the hospital had 36 cases of COVID-19.
In a slide provided by the Italian National Health Service, the number of cases in Italy stands at 13,882 with 803 associated deaths.
ICU resources have been severely stressed. Before the outbreak, Lombardy had 720 ICU beds (about 5% of total beds). Within 48 hours of the first case, ICU cohorts were formed in 15 hub hospitals totaling 130 COVID-19 ICU beds. By March 7, the total number of dedicated cohorted COVID-19 ICU beds was 482.
“The proportion of ICU admissions represents 12% of the total positive cases, and 16% of all hospitalized patients,” compared with about 5% of ICU admissions reported from China. The difference may be attributable to different criteria for ICU admissions in Italy, compared with China, according to Dr. Cecconi and colleagues.
Dr. Cecconi mentioned that there were relatively few cases in children, and they had relatively mild disease. The death rate among patients remained under 1% up to age 59. For patients aged 60-69 years, the rate was 2.7%; for patients aged 70-79 years, the rate was 9.6%; for those aged 80-89, the rate was much higher at 16.6%.
Modeled forecasts of the potential number of cases in Lombardy are daunting. “The linear model forecasts that approximately 869 ICU admissions could occur by March 20, 2020, whereas the exponential model growth projects that approximately 14,542 ICU admissions could occur by then. Even though these projections are hypothetical and involve various assumptions, any substantial increase in the number of critically ill patients would rapidly exceed total ICU capacity, without even considering other critical admissions, such as for trauma, stroke, and other emergencies,” wrote Dr. Cecconi and his colleagues in JAMA. He said, “We could be on our knees very soon,” referring to the potential dramatic increase in cases.
Dr. Cecconi had some recommendations for other countries in which a major outbreak has not yet occurred. He recommended going beyond expanding ICU and isolation capacity and focus on training staff with simulation for treating these highly contagious patients. His medical center has worked hard to protect staff but 1,116 health care workers have tested positive for the virus. Conditions for staff are very difficult in full protective gear, and Dr. Cecconi commended the heroic work by these doctors and nurses.
In addition, Dr. Cecconi is focused on supportive care for patients and does not recommend using untried approaches on these patients that could cause harm. “Everyone wants to find a specific drug for these patients, but I say there is not particular drug at the moment.” He stressed that, despite the crisis, doctors should focus on evidence-based treatment and tried-and-true supportive care.
Disclosures by Dr. Cecconi are available on the JAMA website.
CORRECTION 3/13/2020 2.18 P.M. The death rate for patients aged 70-79 was corrected.
REPORTING FROM JAMA LIVE STREAM
Internist reports from COVID-19 front lines near Seattle
KENT, WASHINGTON – The first thing I learned in this outbreak is that my sense of alarm has been deadened by years of medical practice. As a primary care doctor working south of Seattle, in the University of Washington’s Kent neighborhood clinic, I have dealt with long hours, the sometimes-insurmountable problems of the patients I care for, and the constant, gnawing fear of missing something and doing harm. To get through my day, I’ve done my best to rationalize that fear, to explain it away.
I can’t explain how, when I heard the news of the coronavirus epidemic in China, I didn’t think it would affect me. I can’t explain how news of the first patient presenting to an urgent care north of Seattle didn’t cause me, or all health care providers, to think about how we would respond. I can’t explain why so many doctors were dismissive of the very real threat that was about to explode. I can’t explain why it took 6 weeks for the COVID-19 outbreak to seem real to me.
If you work in a doctor’s office, emergency department, hospital, or urgent care center and have not seen a coronavirus case yet, you may have time to think through what is likely to happen in your community. We did not activate a chain of command or decide how information was going to be communicated to the front line and back to leadership. Few of us ran worst-case scenarios.
By March 12, we had 376 confirmed cases, and likely more than a thousand are undetected. The moment of realization of the severity of the outbreak didn’t come to me until Saturday, Feb. 29. In the week prior, several patients had come into the clinic with symptoms and potential exposures, but not meeting the narrow Centers for Disease Control and Prevention testing criteria. They were all advised by the Washington Department of Health to go home. At the time, it seemed like decent advice. Frontline providers didn’t know that there had been two cases of community transmission weeks before, or that one was about to become the first death in Washington state. I still advised patients to quarantine themselves. In the absence of testing, we had to assume everyone was positive and should stay home until 72 hours after their symptoms resolved. Studying the state’s FMLA [Family and Medical Leave Act] intently, I wrote insistent letters to inflexible bosses, explaining that their employees needed to stay home.
I worked that Saturday. Half of my patients had coughs. Our team insisted that they wear masks. One woman refused, and I refused to see her until she did. In a customer service–oriented health care system, I had been schooled to accommodate almost any patient request. But I was not about to put my staff and other patients at risk. Reluctantly, she complied.
On my lunch break, my partner called me to tell me he was at the grocery store. “Why?” I asked, since we usually went together. It became clear he was worried about an outbreak. He had been following the news closely and tried to tell me how deadly this could get and how quickly the disease could spread. I brushed his fears aside, as more evidence of his sweet and overly cautious nature. “It’ll be fine,” I said with misplaced confidence.
Later that day, I heard about the first death and the outbreak at Life Care, a nursing home north of Seattle. I learned that firefighters who had responded to distress calls were under quarantine. I learned through an epidemiologist that there were likely hundreds of undetected cases throughout Washington.
On Monday, our clinic decided to convert all cases with symptoms into telemedicine visits. Luckily, we had been building the capacity to see and treat patients virtually for a while. We have ramped up quickly, but there have been bumps along the way. It’s difficult to convince those who are anxious about their symptoms to allow us to use telemedicine for everyone’s safety. It is unclear how much liability we are taking on as individual providers with this approach or who will speak up for us if something goes wrong.
Patients don’t seem to know where to get their information, and they have been turning to increasingly bizarre sources. For the poorest, who have had so much trouble accessing care, I cannot blame them for not knowing whom to trust. I post what I know on Twitter and Facebook, but I know I’m no match for cynical social media algorithms.
Testing was still not available at my clinic the first week of March, and it remains largely unavailable throughout much of the country. We have lost weeks of opportunity to contain this. Luckily, on March 4, the University of Washington was finally allowed to use their homegrown test and bypass the limited supply from the CDC. But our capacity at UW is still limited, and the test remained unavailable to the majority of those potentially showing symptoms until March 9.
I am used to being less worried than my patients. I am used to reassuring them. But over the first week of March, I had an eerie sense that my alarm far outstripped theirs. I got relatively few questions about coronavirus, even as the number of cases continued to rise. It wasn’t until the end of the week that I noticed a few were truly fearful. Patients started stealing the gloves and the hand sanitizer, and we had to zealously guard them. My hands are raw from washing.
Throughout this time, I have been grateful for a centralized drive with clear protocols. I am grateful for clear messages at the beginning and end of the day from our CEO. I hope that other clinics model this and have daily in-person meetings, because too much cannot be conveyed in an email when the situation changes hourly.
But our health system nationally was already stretched thin before, and providers have sacrificed a lot, especially in the most critical settings, to provide decent patient care. Now we are asked to risk our health and safety, and our family’s, and I worry about the erosion of trust and work conditions for those on the front lines. I also worry our patients won’t believe us when we have allowed the costs of care to continue to rise and ruin their lives. I worry about the millions of people without doctors to call because they have no insurance, and because so many primary care physicians have left unsustainable jobs.
I am grateful that few of my colleagues have been sick and that those that were called out. I am grateful for the new nurse practitioners in our clinic who took the lion’s share of possibly affected patients and triaged hundreds of phone calls, creating note and message templates that we all use. I am grateful that my clinic manager insisted on doing a drill with all the staff members.
I am grateful that we were reminded that we are a team and that if the call center and cleaning crews and front desk are excluded, then our protocols are useless. I am grateful that our registered nurses quickly shifted to triage. I am grateful that I have testing available.
This week, for the first time since I started working, multiple patients asked how I am doing and expressed their thanks. I am most grateful for them.
I can’t tell you what to do or what is going to happen, but I can tell you that you need to prepare now. You need to run drills and catch the holes in your plans before the pandemic reaches you. You need to be creative and honest about the flaws in your organization that this pandemic will inevitably expose. You need to meet with your team every day and remember that we are all going to be stretched even thinner than before.
Most of us will get through this, but many of us won’t. And for those who do, we need to be honest about our successes and failures. We need to build a system that can do better next time. Because this is not the last pandemic we will face.
Dr. Elisabeth Poorman is a general internist at a University of Washington neighborhood clinic in Kent. She completed her residency at Cambridge (Mass.) Health Alliance and specializes in addiction medicine. She also serves on the editorial advisory board of Internal Medicine News.
KENT, WASHINGTON – The first thing I learned in this outbreak is that my sense of alarm has been deadened by years of medical practice. As a primary care doctor working south of Seattle, in the University of Washington’s Kent neighborhood clinic, I have dealt with long hours, the sometimes-insurmountable problems of the patients I care for, and the constant, gnawing fear of missing something and doing harm. To get through my day, I’ve done my best to rationalize that fear, to explain it away.
I can’t explain how, when I heard the news of the coronavirus epidemic in China, I didn’t think it would affect me. I can’t explain how news of the first patient presenting to an urgent care north of Seattle didn’t cause me, or all health care providers, to think about how we would respond. I can’t explain why so many doctors were dismissive of the very real threat that was about to explode. I can’t explain why it took 6 weeks for the COVID-19 outbreak to seem real to me.
If you work in a doctor’s office, emergency department, hospital, or urgent care center and have not seen a coronavirus case yet, you may have time to think through what is likely to happen in your community. We did not activate a chain of command or decide how information was going to be communicated to the front line and back to leadership. Few of us ran worst-case scenarios.
By March 12, we had 376 confirmed cases, and likely more than a thousand are undetected. The moment of realization of the severity of the outbreak didn’t come to me until Saturday, Feb. 29. In the week prior, several patients had come into the clinic with symptoms and potential exposures, but not meeting the narrow Centers for Disease Control and Prevention testing criteria. They were all advised by the Washington Department of Health to go home. At the time, it seemed like decent advice. Frontline providers didn’t know that there had been two cases of community transmission weeks before, or that one was about to become the first death in Washington state. I still advised patients to quarantine themselves. In the absence of testing, we had to assume everyone was positive and should stay home until 72 hours after their symptoms resolved. Studying the state’s FMLA [Family and Medical Leave Act] intently, I wrote insistent letters to inflexible bosses, explaining that their employees needed to stay home.
I worked that Saturday. Half of my patients had coughs. Our team insisted that they wear masks. One woman refused, and I refused to see her until she did. In a customer service–oriented health care system, I had been schooled to accommodate almost any patient request. But I was not about to put my staff and other patients at risk. Reluctantly, she complied.
On my lunch break, my partner called me to tell me he was at the grocery store. “Why?” I asked, since we usually went together. It became clear he was worried about an outbreak. He had been following the news closely and tried to tell me how deadly this could get and how quickly the disease could spread. I brushed his fears aside, as more evidence of his sweet and overly cautious nature. “It’ll be fine,” I said with misplaced confidence.
Later that day, I heard about the first death and the outbreak at Life Care, a nursing home north of Seattle. I learned that firefighters who had responded to distress calls were under quarantine. I learned through an epidemiologist that there were likely hundreds of undetected cases throughout Washington.
On Monday, our clinic decided to convert all cases with symptoms into telemedicine visits. Luckily, we had been building the capacity to see and treat patients virtually for a while. We have ramped up quickly, but there have been bumps along the way. It’s difficult to convince those who are anxious about their symptoms to allow us to use telemedicine for everyone’s safety. It is unclear how much liability we are taking on as individual providers with this approach or who will speak up for us if something goes wrong.
Patients don’t seem to know where to get their information, and they have been turning to increasingly bizarre sources. For the poorest, who have had so much trouble accessing care, I cannot blame them for not knowing whom to trust. I post what I know on Twitter and Facebook, but I know I’m no match for cynical social media algorithms.
Testing was still not available at my clinic the first week of March, and it remains largely unavailable throughout much of the country. We have lost weeks of opportunity to contain this. Luckily, on March 4, the University of Washington was finally allowed to use their homegrown test and bypass the limited supply from the CDC. But our capacity at UW is still limited, and the test remained unavailable to the majority of those potentially showing symptoms until March 9.
I am used to being less worried than my patients. I am used to reassuring them. But over the first week of March, I had an eerie sense that my alarm far outstripped theirs. I got relatively few questions about coronavirus, even as the number of cases continued to rise. It wasn’t until the end of the week that I noticed a few were truly fearful. Patients started stealing the gloves and the hand sanitizer, and we had to zealously guard them. My hands are raw from washing.
Throughout this time, I have been grateful for a centralized drive with clear protocols. I am grateful for clear messages at the beginning and end of the day from our CEO. I hope that other clinics model this and have daily in-person meetings, because too much cannot be conveyed in an email when the situation changes hourly.
But our health system nationally was already stretched thin before, and providers have sacrificed a lot, especially in the most critical settings, to provide decent patient care. Now we are asked to risk our health and safety, and our family’s, and I worry about the erosion of trust and work conditions for those on the front lines. I also worry our patients won’t believe us when we have allowed the costs of care to continue to rise and ruin their lives. I worry about the millions of people without doctors to call because they have no insurance, and because so many primary care physicians have left unsustainable jobs.
I am grateful that few of my colleagues have been sick and that those that were called out. I am grateful for the new nurse practitioners in our clinic who took the lion’s share of possibly affected patients and triaged hundreds of phone calls, creating note and message templates that we all use. I am grateful that my clinic manager insisted on doing a drill with all the staff members.
I am grateful that we were reminded that we are a team and that if the call center and cleaning crews and front desk are excluded, then our protocols are useless. I am grateful that our registered nurses quickly shifted to triage. I am grateful that I have testing available.
This week, for the first time since I started working, multiple patients asked how I am doing and expressed their thanks. I am most grateful for them.
I can’t tell you what to do or what is going to happen, but I can tell you that you need to prepare now. You need to run drills and catch the holes in your plans before the pandemic reaches you. You need to be creative and honest about the flaws in your organization that this pandemic will inevitably expose. You need to meet with your team every day and remember that we are all going to be stretched even thinner than before.
Most of us will get through this, but many of us won’t. And for those who do, we need to be honest about our successes and failures. We need to build a system that can do better next time. Because this is not the last pandemic we will face.
Dr. Elisabeth Poorman is a general internist at a University of Washington neighborhood clinic in Kent. She completed her residency at Cambridge (Mass.) Health Alliance and specializes in addiction medicine. She also serves on the editorial advisory board of Internal Medicine News.
KENT, WASHINGTON – The first thing I learned in this outbreak is that my sense of alarm has been deadened by years of medical practice. As a primary care doctor working south of Seattle, in the University of Washington’s Kent neighborhood clinic, I have dealt with long hours, the sometimes-insurmountable problems of the patients I care for, and the constant, gnawing fear of missing something and doing harm. To get through my day, I’ve done my best to rationalize that fear, to explain it away.
I can’t explain how, when I heard the news of the coronavirus epidemic in China, I didn’t think it would affect me. I can’t explain how news of the first patient presenting to an urgent care north of Seattle didn’t cause me, or all health care providers, to think about how we would respond. I can’t explain why so many doctors were dismissive of the very real threat that was about to explode. I can’t explain why it took 6 weeks for the COVID-19 outbreak to seem real to me.
If you work in a doctor’s office, emergency department, hospital, or urgent care center and have not seen a coronavirus case yet, you may have time to think through what is likely to happen in your community. We did not activate a chain of command or decide how information was going to be communicated to the front line and back to leadership. Few of us ran worst-case scenarios.
By March 12, we had 376 confirmed cases, and likely more than a thousand are undetected. The moment of realization of the severity of the outbreak didn’t come to me until Saturday, Feb. 29. In the week prior, several patients had come into the clinic with symptoms and potential exposures, but not meeting the narrow Centers for Disease Control and Prevention testing criteria. They were all advised by the Washington Department of Health to go home. At the time, it seemed like decent advice. Frontline providers didn’t know that there had been two cases of community transmission weeks before, or that one was about to become the first death in Washington state. I still advised patients to quarantine themselves. In the absence of testing, we had to assume everyone was positive and should stay home until 72 hours after their symptoms resolved. Studying the state’s FMLA [Family and Medical Leave Act] intently, I wrote insistent letters to inflexible bosses, explaining that their employees needed to stay home.
I worked that Saturday. Half of my patients had coughs. Our team insisted that they wear masks. One woman refused, and I refused to see her until she did. In a customer service–oriented health care system, I had been schooled to accommodate almost any patient request. But I was not about to put my staff and other patients at risk. Reluctantly, she complied.
On my lunch break, my partner called me to tell me he was at the grocery store. “Why?” I asked, since we usually went together. It became clear he was worried about an outbreak. He had been following the news closely and tried to tell me how deadly this could get and how quickly the disease could spread. I brushed his fears aside, as more evidence of his sweet and overly cautious nature. “It’ll be fine,” I said with misplaced confidence.
Later that day, I heard about the first death and the outbreak at Life Care, a nursing home north of Seattle. I learned that firefighters who had responded to distress calls were under quarantine. I learned through an epidemiologist that there were likely hundreds of undetected cases throughout Washington.
On Monday, our clinic decided to convert all cases with symptoms into telemedicine visits. Luckily, we had been building the capacity to see and treat patients virtually for a while. We have ramped up quickly, but there have been bumps along the way. It’s difficult to convince those who are anxious about their symptoms to allow us to use telemedicine for everyone’s safety. It is unclear how much liability we are taking on as individual providers with this approach or who will speak up for us if something goes wrong.
Patients don’t seem to know where to get their information, and they have been turning to increasingly bizarre sources. For the poorest, who have had so much trouble accessing care, I cannot blame them for not knowing whom to trust. I post what I know on Twitter and Facebook, but I know I’m no match for cynical social media algorithms.
Testing was still not available at my clinic the first week of March, and it remains largely unavailable throughout much of the country. We have lost weeks of opportunity to contain this. Luckily, on March 4, the University of Washington was finally allowed to use their homegrown test and bypass the limited supply from the CDC. But our capacity at UW is still limited, and the test remained unavailable to the majority of those potentially showing symptoms until March 9.
I am used to being less worried than my patients. I am used to reassuring them. But over the first week of March, I had an eerie sense that my alarm far outstripped theirs. I got relatively few questions about coronavirus, even as the number of cases continued to rise. It wasn’t until the end of the week that I noticed a few were truly fearful. Patients started stealing the gloves and the hand sanitizer, and we had to zealously guard them. My hands are raw from washing.
Throughout this time, I have been grateful for a centralized drive with clear protocols. I am grateful for clear messages at the beginning and end of the day from our CEO. I hope that other clinics model this and have daily in-person meetings, because too much cannot be conveyed in an email when the situation changes hourly.
But our health system nationally was already stretched thin before, and providers have sacrificed a lot, especially in the most critical settings, to provide decent patient care. Now we are asked to risk our health and safety, and our family’s, and I worry about the erosion of trust and work conditions for those on the front lines. I also worry our patients won’t believe us when we have allowed the costs of care to continue to rise and ruin their lives. I worry about the millions of people without doctors to call because they have no insurance, and because so many primary care physicians have left unsustainable jobs.
I am grateful that few of my colleagues have been sick and that those that were called out. I am grateful for the new nurse practitioners in our clinic who took the lion’s share of possibly affected patients and triaged hundreds of phone calls, creating note and message templates that we all use. I am grateful that my clinic manager insisted on doing a drill with all the staff members.
I am grateful that we were reminded that we are a team and that if the call center and cleaning crews and front desk are excluded, then our protocols are useless. I am grateful that our registered nurses quickly shifted to triage. I am grateful that I have testing available.
This week, for the first time since I started working, multiple patients asked how I am doing and expressed their thanks. I am most grateful for them.
I can’t tell you what to do or what is going to happen, but I can tell you that you need to prepare now. You need to run drills and catch the holes in your plans before the pandemic reaches you. You need to be creative and honest about the flaws in your organization that this pandemic will inevitably expose. You need to meet with your team every day and remember that we are all going to be stretched even thinner than before.
Most of us will get through this, but many of us won’t. And for those who do, we need to be honest about our successes and failures. We need to build a system that can do better next time. Because this is not the last pandemic we will face.
Dr. Elisabeth Poorman is a general internist at a University of Washington neighborhood clinic in Kent. She completed her residency at Cambridge (Mass.) Health Alliance and specializes in addiction medicine. She also serves on the editorial advisory board of Internal Medicine News.
Your medical conference is canceled. Now what?
Khadija Hafidh, MD, was already booked on a 14-hour, direct flight from Dubai to Los Angeles, when the American College of Physicians (ACP) announced it was canceling its internal medicine meeting scheduled for April.
Canceling her hotel reservation was not a problem, and she was assured a refund for the conference fee, but her airline ticket was another matter, said Dr. Hafidh, an internist and diabetologist with the Dubai Health Authority.
“The airline I booked my ticket with is willing to waive the change fees, but will deduct a cancellation fee if I choose not to take the trip,” Dr. Hafidh said in an interview. “The cancellation fees is $300. A bit steep I must admit.”
Dr. Hafidh now faces a dilemma: Lose the $300 and cancel, or change her flight dates to June for the American Diabetes Association meeting in Chicago.
“But then again, we aren’t sure if that meeting will take place,” Dr. Hafidh said. “A few weeks ago I thought this whole thing was just a storm in a tea cup. However when it was declared a pandemic yesterday, it brought about another dimension.”
More than 25 medical meetings and conferences across the globe have been canceled or postponed because of COVID-19 concerns. The sudden cancellations have caused reservation woes and travel headaches for thousands of physicians who planned to attend the meetings. Some societies are considering the idea of virtual conferences, while other associations have scrapped their meetings until next year.
For physicians facing a canceled conference, the most likely question is, what now? Read on for tips and suggestions.
Reservation refunds vary
Refunds on airfare because of conference cancellations differ, depending on the airline and where you were traveling. Some airlines, such as United Airlines, have waived all change fees for tickets issued March 3, 2020, through March 31, 2020, and passengers can change their dates for up to 12 months after the ticket was issued.
Full refunds often depend on whether your ticket was nonrefundable when purchased. Many airlines, such as Delta, are providing full refunds if the airline canceled your flight. JetBlue is waiving all change and cancellation fees for customers scheduled to travel March 10, 2020, through April 30, 2020.
Las Vegas–based dermatologist H.L. Greenberg, MD, was satisfied with the credit he received from Southwest Airlines after the American Academy of Dermatology (AAD) canceled its Denver meeting. He and his staff were looking forward to the gathering, but he noted that the meeting would likely have been limited, even if it had take place as scheduled.
“I am disappointed that I won’t be able to meet with colleagues and industry to explore what the latest advances and interests are in dermatology,” he said. “Because many academic institutions were forbidding their faculty from traveling, the content of the meeting was going to be severely diminished. It’s just a rough time for everyone.”
Meanwhile, Asa Radix, MD, PhD, a New York–based internist, received a full refund for his Amtrak ticket to Boston when the Conference on Retroviruses and Opportunistic Infections (CROI) scheduled for early March was converted to a virtual meeting. Dr. Radix, senior director of research and education at the Callen-Lorde Community Health Center in New York, left another meeting in Brazil early to get to the Boston conference, he said.
“I was packed, but really that was a minor inconvenience,” he said in an interview. “I appreciate that they prioritized health concerns and changed to a virtual meeting. I received full refunds, no issues whatsoever. [It was] really great since I had no travel insurance.”
Check with your individual airline or train line for information about ticket refunds and credits. Many airlines are currently making special accommodations because of COVID-19. If your flight was covered by trip insurance, also called travel assistance, you are generally protected against unforeseen financial losses such as cancellations. The U.S. Department of Transportation provides this general online resource about airline refunds.
Hotel refunds probable
Most meeting organizations who have made the decision to cancel or postpone a conference also have canceled block hotel reservations reserved for the meeting. Medical associations are not directly refunding the hotel costs, but the majority of hotels are refunding reservations with no questions asked. Physicians interviewed for this story all reported no trouble getting refunds for their hotel reservations. However, attendees who did not book a hotel in official housing blocks should contact the hotel directly to cancel.
What about registration fees?
In response to COVID-19 cancellations, most conference leaders are refunding registration fees in full for both attendees and exhibitors. The refund may not be automatic, some associations such as ACP and the American College of Obstetricians and Gynecologists state it may take up to 45 days for the funds to be credited, depending on the payment used.
If the conference you planned to attend was postponed, the registration fee may be assigned to the new meeting dates and the money may not be refunded. Registration fees for the Minimally Invasive Surgery Symposium, for example, delayed until an unconfirmed date, and for the European Association of Urology (EAU) meeting, postponed until July, will be automatically credited to the rescheduled meeting, according to the websites. If attendees cannot attend the rescheduled EAU meeting, the association will not provide a refund and the registration will not apply to the 2021 meeting, according to its website. However, the group is providing registrants with a free access code for the EAU20 Resource Centre, which contains websites of sessions and scientific content.
A number of physicians have expressed disappointment with the EAU’s postponement on social media. On Twitter, some doctors wrote that the rescheduled dates were bad timing, while others lamented the refund refusal.
The EAU said it regrets that some delegates will experience financial losses, but that the organization has already experienced a significant outlay that cannot be recovered including venue, logistics, travel, and accommodation costs.
"We are doing what we can to absorb costs, but we need to be realistic about what is affordable; should the organization have to refund all or even most registrations, it would significantly jeopardize the viability of the organization," the EAU said in a statement. "These are difficult times, not only for the EAU, but on a global scale. Where there are specific cases of hardship or very extenuating financial circumstances, we will be willing to review individual cases. So far, we believe that we have done what we can do to meet the conflicting demands presented by the postponement of the congress, but this is a situation which changes from day to day, and we need to continuously evaluate what might be the best course of action." *
Contact your medical association directly for details on postponements.
What if I’m a presenter?
In an attempt to save the hard work and time that planners and presenters have invested into now-canceled meetings, some conferences are moving to a digital format. The Conference on Retroviruses and Opportunistic Infections (CROI) was the first to convert its in-person conference to a virtual meeting, held from March 8 to 11, 2020. At-home attendees logged onto CROI’s digital platform to hear plenaries, oral abstracts, themed discussion sessions, and symposia.
Dr. Radix was one of many CROI speakers who changed his presentation on HIV prevalence among transgender men to a virtual format.
“We were provided with detailed instructions from CROI about how to do this,” said Dr. Radix, who tweeted about the experience. “For my presentation, I used the video option in PowerPoint; it seemed the most straightforward and didn’t require buying additional software. It was fairly easy to follow the instructions to create the video but it was disappointing to present to an empty room.”
Matthew Spinelli, MD, an HIV researcher with the University of California, San Francisco, who also presented virtually, said it was remarkable that CROI leaders were able to put together the virtual program in such a short time. He delivered his presentation on the accuracy of a real-time urine tenofovir test using PowerPoint and a podcast microphone.
“It seemed to work pretty well,” he said in an interview. “It’s not the same as being there in person, there’s a lot of networking and chance conversations that happen when you’re all in the same place, but it was the right decision to cancel. If I have to be at home or at work doing social distancing, this was the best possible way of doing it.”
Following in CROI’s footsteps, the National Kidney Foundation’s spring conference has moved to a live virtual conference. The 2020 Healthcare Information and Management Systems Society (HIMSS) global health conference also will move to a digital format. Other societies are considering similar virtual options. Check with your meeting website for more details on digital options and attendee access.
*The article was updated on 03/16/2020.
Khadija Hafidh, MD, was already booked on a 14-hour, direct flight from Dubai to Los Angeles, when the American College of Physicians (ACP) announced it was canceling its internal medicine meeting scheduled for April.
Canceling her hotel reservation was not a problem, and she was assured a refund for the conference fee, but her airline ticket was another matter, said Dr. Hafidh, an internist and diabetologist with the Dubai Health Authority.
“The airline I booked my ticket with is willing to waive the change fees, but will deduct a cancellation fee if I choose not to take the trip,” Dr. Hafidh said in an interview. “The cancellation fees is $300. A bit steep I must admit.”
Dr. Hafidh now faces a dilemma: Lose the $300 and cancel, or change her flight dates to June for the American Diabetes Association meeting in Chicago.
“But then again, we aren’t sure if that meeting will take place,” Dr. Hafidh said. “A few weeks ago I thought this whole thing was just a storm in a tea cup. However when it was declared a pandemic yesterday, it brought about another dimension.”
More than 25 medical meetings and conferences across the globe have been canceled or postponed because of COVID-19 concerns. The sudden cancellations have caused reservation woes and travel headaches for thousands of physicians who planned to attend the meetings. Some societies are considering the idea of virtual conferences, while other associations have scrapped their meetings until next year.
For physicians facing a canceled conference, the most likely question is, what now? Read on for tips and suggestions.
Reservation refunds vary
Refunds on airfare because of conference cancellations differ, depending on the airline and where you were traveling. Some airlines, such as United Airlines, have waived all change fees for tickets issued March 3, 2020, through March 31, 2020, and passengers can change their dates for up to 12 months after the ticket was issued.
Full refunds often depend on whether your ticket was nonrefundable when purchased. Many airlines, such as Delta, are providing full refunds if the airline canceled your flight. JetBlue is waiving all change and cancellation fees for customers scheduled to travel March 10, 2020, through April 30, 2020.
Las Vegas–based dermatologist H.L. Greenberg, MD, was satisfied with the credit he received from Southwest Airlines after the American Academy of Dermatology (AAD) canceled its Denver meeting. He and his staff were looking forward to the gathering, but he noted that the meeting would likely have been limited, even if it had take place as scheduled.
“I am disappointed that I won’t be able to meet with colleagues and industry to explore what the latest advances and interests are in dermatology,” he said. “Because many academic institutions were forbidding their faculty from traveling, the content of the meeting was going to be severely diminished. It’s just a rough time for everyone.”
Meanwhile, Asa Radix, MD, PhD, a New York–based internist, received a full refund for his Amtrak ticket to Boston when the Conference on Retroviruses and Opportunistic Infections (CROI) scheduled for early March was converted to a virtual meeting. Dr. Radix, senior director of research and education at the Callen-Lorde Community Health Center in New York, left another meeting in Brazil early to get to the Boston conference, he said.
“I was packed, but really that was a minor inconvenience,” he said in an interview. “I appreciate that they prioritized health concerns and changed to a virtual meeting. I received full refunds, no issues whatsoever. [It was] really great since I had no travel insurance.”
Check with your individual airline or train line for information about ticket refunds and credits. Many airlines are currently making special accommodations because of COVID-19. If your flight was covered by trip insurance, also called travel assistance, you are generally protected against unforeseen financial losses such as cancellations. The U.S. Department of Transportation provides this general online resource about airline refunds.
Hotel refunds probable
Most meeting organizations who have made the decision to cancel or postpone a conference also have canceled block hotel reservations reserved for the meeting. Medical associations are not directly refunding the hotel costs, but the majority of hotels are refunding reservations with no questions asked. Physicians interviewed for this story all reported no trouble getting refunds for their hotel reservations. However, attendees who did not book a hotel in official housing blocks should contact the hotel directly to cancel.
What about registration fees?
In response to COVID-19 cancellations, most conference leaders are refunding registration fees in full for both attendees and exhibitors. The refund may not be automatic, some associations such as ACP and the American College of Obstetricians and Gynecologists state it may take up to 45 days for the funds to be credited, depending on the payment used.
If the conference you planned to attend was postponed, the registration fee may be assigned to the new meeting dates and the money may not be refunded. Registration fees for the Minimally Invasive Surgery Symposium, for example, delayed until an unconfirmed date, and for the European Association of Urology (EAU) meeting, postponed until July, will be automatically credited to the rescheduled meeting, according to the websites. If attendees cannot attend the rescheduled EAU meeting, the association will not provide a refund and the registration will not apply to the 2021 meeting, according to its website. However, the group is providing registrants with a free access code for the EAU20 Resource Centre, which contains websites of sessions and scientific content.
A number of physicians have expressed disappointment with the EAU’s postponement on social media. On Twitter, some doctors wrote that the rescheduled dates were bad timing, while others lamented the refund refusal.
The EAU said it regrets that some delegates will experience financial losses, but that the organization has already experienced a significant outlay that cannot be recovered including venue, logistics, travel, and accommodation costs.
"We are doing what we can to absorb costs, but we need to be realistic about what is affordable; should the organization have to refund all or even most registrations, it would significantly jeopardize the viability of the organization," the EAU said in a statement. "These are difficult times, not only for the EAU, but on a global scale. Where there are specific cases of hardship or very extenuating financial circumstances, we will be willing to review individual cases. So far, we believe that we have done what we can do to meet the conflicting demands presented by the postponement of the congress, but this is a situation which changes from day to day, and we need to continuously evaluate what might be the best course of action." *
Contact your medical association directly for details on postponements.
What if I’m a presenter?
In an attempt to save the hard work and time that planners and presenters have invested into now-canceled meetings, some conferences are moving to a digital format. The Conference on Retroviruses and Opportunistic Infections (CROI) was the first to convert its in-person conference to a virtual meeting, held from March 8 to 11, 2020. At-home attendees logged onto CROI’s digital platform to hear plenaries, oral abstracts, themed discussion sessions, and symposia.
Dr. Radix was one of many CROI speakers who changed his presentation on HIV prevalence among transgender men to a virtual format.
“We were provided with detailed instructions from CROI about how to do this,” said Dr. Radix, who tweeted about the experience. “For my presentation, I used the video option in PowerPoint; it seemed the most straightforward and didn’t require buying additional software. It was fairly easy to follow the instructions to create the video but it was disappointing to present to an empty room.”
Matthew Spinelli, MD, an HIV researcher with the University of California, San Francisco, who also presented virtually, said it was remarkable that CROI leaders were able to put together the virtual program in such a short time. He delivered his presentation on the accuracy of a real-time urine tenofovir test using PowerPoint and a podcast microphone.
“It seemed to work pretty well,” he said in an interview. “It’s not the same as being there in person, there’s a lot of networking and chance conversations that happen when you’re all in the same place, but it was the right decision to cancel. If I have to be at home or at work doing social distancing, this was the best possible way of doing it.”
Following in CROI’s footsteps, the National Kidney Foundation’s spring conference has moved to a live virtual conference. The 2020 Healthcare Information and Management Systems Society (HIMSS) global health conference also will move to a digital format. Other societies are considering similar virtual options. Check with your meeting website for more details on digital options and attendee access.
*The article was updated on 03/16/2020.
Khadija Hafidh, MD, was already booked on a 14-hour, direct flight from Dubai to Los Angeles, when the American College of Physicians (ACP) announced it was canceling its internal medicine meeting scheduled for April.
Canceling her hotel reservation was not a problem, and she was assured a refund for the conference fee, but her airline ticket was another matter, said Dr. Hafidh, an internist and diabetologist with the Dubai Health Authority.
“The airline I booked my ticket with is willing to waive the change fees, but will deduct a cancellation fee if I choose not to take the trip,” Dr. Hafidh said in an interview. “The cancellation fees is $300. A bit steep I must admit.”
Dr. Hafidh now faces a dilemma: Lose the $300 and cancel, or change her flight dates to June for the American Diabetes Association meeting in Chicago.
“But then again, we aren’t sure if that meeting will take place,” Dr. Hafidh said. “A few weeks ago I thought this whole thing was just a storm in a tea cup. However when it was declared a pandemic yesterday, it brought about another dimension.”
More than 25 medical meetings and conferences across the globe have been canceled or postponed because of COVID-19 concerns. The sudden cancellations have caused reservation woes and travel headaches for thousands of physicians who planned to attend the meetings. Some societies are considering the idea of virtual conferences, while other associations have scrapped their meetings until next year.
For physicians facing a canceled conference, the most likely question is, what now? Read on for tips and suggestions.
Reservation refunds vary
Refunds on airfare because of conference cancellations differ, depending on the airline and where you were traveling. Some airlines, such as United Airlines, have waived all change fees for tickets issued March 3, 2020, through March 31, 2020, and passengers can change their dates for up to 12 months after the ticket was issued.
Full refunds often depend on whether your ticket was nonrefundable when purchased. Many airlines, such as Delta, are providing full refunds if the airline canceled your flight. JetBlue is waiving all change and cancellation fees for customers scheduled to travel March 10, 2020, through April 30, 2020.
Las Vegas–based dermatologist H.L. Greenberg, MD, was satisfied with the credit he received from Southwest Airlines after the American Academy of Dermatology (AAD) canceled its Denver meeting. He and his staff were looking forward to the gathering, but he noted that the meeting would likely have been limited, even if it had take place as scheduled.
“I am disappointed that I won’t be able to meet with colleagues and industry to explore what the latest advances and interests are in dermatology,” he said. “Because many academic institutions were forbidding their faculty from traveling, the content of the meeting was going to be severely diminished. It’s just a rough time for everyone.”
Meanwhile, Asa Radix, MD, PhD, a New York–based internist, received a full refund for his Amtrak ticket to Boston when the Conference on Retroviruses and Opportunistic Infections (CROI) scheduled for early March was converted to a virtual meeting. Dr. Radix, senior director of research and education at the Callen-Lorde Community Health Center in New York, left another meeting in Brazil early to get to the Boston conference, he said.
“I was packed, but really that was a minor inconvenience,” he said in an interview. “I appreciate that they prioritized health concerns and changed to a virtual meeting. I received full refunds, no issues whatsoever. [It was] really great since I had no travel insurance.”
Check with your individual airline or train line for information about ticket refunds and credits. Many airlines are currently making special accommodations because of COVID-19. If your flight was covered by trip insurance, also called travel assistance, you are generally protected against unforeseen financial losses such as cancellations. The U.S. Department of Transportation provides this general online resource about airline refunds.
Hotel refunds probable
Most meeting organizations who have made the decision to cancel or postpone a conference also have canceled block hotel reservations reserved for the meeting. Medical associations are not directly refunding the hotel costs, but the majority of hotels are refunding reservations with no questions asked. Physicians interviewed for this story all reported no trouble getting refunds for their hotel reservations. However, attendees who did not book a hotel in official housing blocks should contact the hotel directly to cancel.
What about registration fees?
In response to COVID-19 cancellations, most conference leaders are refunding registration fees in full for both attendees and exhibitors. The refund may not be automatic, some associations such as ACP and the American College of Obstetricians and Gynecologists state it may take up to 45 days for the funds to be credited, depending on the payment used.
If the conference you planned to attend was postponed, the registration fee may be assigned to the new meeting dates and the money may not be refunded. Registration fees for the Minimally Invasive Surgery Symposium, for example, delayed until an unconfirmed date, and for the European Association of Urology (EAU) meeting, postponed until July, will be automatically credited to the rescheduled meeting, according to the websites. If attendees cannot attend the rescheduled EAU meeting, the association will not provide a refund and the registration will not apply to the 2021 meeting, according to its website. However, the group is providing registrants with a free access code for the EAU20 Resource Centre, which contains websites of sessions and scientific content.
A number of physicians have expressed disappointment with the EAU’s postponement on social media. On Twitter, some doctors wrote that the rescheduled dates were bad timing, while others lamented the refund refusal.
The EAU said it regrets that some delegates will experience financial losses, but that the organization has already experienced a significant outlay that cannot be recovered including venue, logistics, travel, and accommodation costs.
"We are doing what we can to absorb costs, but we need to be realistic about what is affordable; should the organization have to refund all or even most registrations, it would significantly jeopardize the viability of the organization," the EAU said in a statement. "These are difficult times, not only for the EAU, but on a global scale. Where there are specific cases of hardship or very extenuating financial circumstances, we will be willing to review individual cases. So far, we believe that we have done what we can do to meet the conflicting demands presented by the postponement of the congress, but this is a situation which changes from day to day, and we need to continuously evaluate what might be the best course of action." *
Contact your medical association directly for details on postponements.
What if I’m a presenter?
In an attempt to save the hard work and time that planners and presenters have invested into now-canceled meetings, some conferences are moving to a digital format. The Conference on Retroviruses and Opportunistic Infections (CROI) was the first to convert its in-person conference to a virtual meeting, held from March 8 to 11, 2020. At-home attendees logged onto CROI’s digital platform to hear plenaries, oral abstracts, themed discussion sessions, and symposia.
Dr. Radix was one of many CROI speakers who changed his presentation on HIV prevalence among transgender men to a virtual format.
“We were provided with detailed instructions from CROI about how to do this,” said Dr. Radix, who tweeted about the experience. “For my presentation, I used the video option in PowerPoint; it seemed the most straightforward and didn’t require buying additional software. It was fairly easy to follow the instructions to create the video but it was disappointing to present to an empty room.”
Matthew Spinelli, MD, an HIV researcher with the University of California, San Francisco, who also presented virtually, said it was remarkable that CROI leaders were able to put together the virtual program in such a short time. He delivered his presentation on the accuracy of a real-time urine tenofovir test using PowerPoint and a podcast microphone.
“It seemed to work pretty well,” he said in an interview. “It’s not the same as being there in person, there’s a lot of networking and chance conversations that happen when you’re all in the same place, but it was the right decision to cancel. If I have to be at home or at work doing social distancing, this was the best possible way of doing it.”
Following in CROI’s footsteps, the National Kidney Foundation’s spring conference has moved to a live virtual conference. The 2020 Healthcare Information and Management Systems Society (HIMSS) global health conference also will move to a digital format. Other societies are considering similar virtual options. Check with your meeting website for more details on digital options and attendee access.
*The article was updated on 03/16/2020.
Wuhan case review: COVID-19 characteristics differ in children vs. adults
Pediatric cases of COVID-19 infection are typically mild, but underlying coinfection may be more common in children than in adults, according to an analysis of clinical, laboratory, and chest CT features of pediatric inpatients in Wuhan, China.

The findings point toward a need for early chest CT with corresponding pathogen detection in children with suspected COVID-19 infection, Wei Xia, MD, of Huazhong University of Science and Technology, Wuhan, China, and colleagues reported in Pediatric Pulmonology.
The most common symptoms in 20 pediatric patients hospitalized between Jan. 23 and Feb. 8, 2020, with COVID-19 infection confirmed by the pharyngeal swab COVID-19 nucleic acid test were fever and cough, which occurred in 60% and 65% of patients, respectively. Coinfection was detected in eight patients (40%), they noted.
Clinical manifestations were similar to those seen in adults, but overall symptoms were relatively mild and overall prognosis was good. Of particular note, 7 of the 20 (35%) patients had a previously diagnosed congenital or acquired diseases, suggesting that children with underlying conditions may be more susceptible, Dr. Xia and colleagues wrote.
Laboratory findings also were notable in that 80% of the children had procalcitonin (PCT) elevations not typically seen in adults with COVID-19. PCT is a marker for bacterial infection and “[this finding] may suggest that routine antibacterial treatment should be considered in pediatric patients,” the investigators wrote.
As for imaging results, chest CT findings in children were similar to those in adults.“The typical manifestations were unilateral or bilateral subpleural ground-glass opacities, and consolidations with surrounding halo signs,” Dr. Xia and associates wrote, adding that consolidations with surrounding halo sign accounted for about half the pediatric cases and should be considered as “typical signs in pediatric patients.”
Pediatric cases were “rather rare” in the early days of the COVID-19 outbreak in Wuhan, where the first cases of infection were reported.
“As a pediatric group is usually susceptible to upper respiratory tract infection, because of their developing immune system, the delayed presence of pediatric patients is confusing,” the investigators wrote, noting that a low detection rate of pharyngeal swab COVID-19 nucleic acid test, distinguishing the virus from other common respiratory tract infectious pathogens in pediatric patients, “is still a problem.”
To better characterize the clinical and imaging features in children versus adults with COVID-19, Dr. Xia and associates reviewed these 20 pediatric cases, including 13 boys and 7 girls with ages ranging from less than 1 month to 14 years, 7 months (median 2 years, 1.5 months). Thirteen had an identified close contact with a COVID-19–diagnosed family member, and all were treated in an isolation ward. A total of 18 children were cured and discharged after an average stay of 13 days, and 2 neonates remained under observation because of positive swab results with negative CT findings. The investigators speculated that the different findings in neonates were perhaps caused by the influence of delivery on sampling or the specific CT manifestations for neonates, adding that more samples are needed for further clarification.
Based on these findings, “the CT imaging of COVID-19 infection should be differentiated with other virus pneumonias such as influenza virus, parainfluenza virus, respiratory syncytial virus, and adenovirus,” they concluded. It also should “be differentiated from bacterial pneumonia, mycoplasma pneumonia, and chlamydia pneumonia ... the density of pneumonia lesions caused by the latter pathogens is relatively higher.”
However, Dr. Xia and colleagues noted that chest CT manifestations of pneumonia caused by different pathogens overlap, and COVID-19 pneumonia “can be superimposed with serious and complex imaging manifestations, so epidemiological and etiological examinations should be combined.”
The investigators concluded that COVID-19 virus pneumonia in children is generally mild, and that the characteristic changes of subpleural ground-glass opacities and consolidations with surrounding halo on chest CT provide an “effective means for follow-up and evaluating the changes of lung lesions.”
“In the case that the positive rate of COVID-19 nucleic acid test from pharyngeal swab samples is not high, the early detection of lesions by CT is conducive to reasonable management and early treatment for pediatric patients. However, the diagnosis of COVID-19 pneumonia by CT imaging alone is not sufficient enough, especially in the case of coinfection with other pathogens,” Dr. Xia and associates wrote. “Therefore, early chest CT screening and timely follow-up, combined with corresponding pathogen detection, is a feasible clinical protocol in children.”
An early study
In a separate retrospective analysis described in a letter to the editor of the New England Journal of Medicine, Weiyong Liu, PhD, of Tongji Hospital of Huazhong University of Science and Technology and colleagues found that the most frequently detected pathogens in 366 children under the age of 16 years hospitalized with respiratory infections in Wuhan during Jan. 7-15, 2020, were influenza A virus (6.3% of cases) and influenza B virus (5.5% of cases), whereas COVID-19 was detected in 1.6% of cases.
The median age of the COVID-19 patients in that series was 3 years (range 1-7 years), and in contrast to the findings of Xia et al., all previously had been “completely healthy.” Common characteristics were high fever and cough in all six patients, and vomiting in four patients. Five had pneumonia as assessed by X-ray, and CTs showed typical viral pneumonia patterns.
One patient was admitted to a pediatric ICU. All patients received antiviral agents, antibiotic agents, and supportive therapies; all recovered after a median hospital stay of 7.5 days (median range, 5-13 days).
In contrast with the findings of Xia et al., the findings of Liu et al. showed COVID-19 caused moderate to severe respiratory illness in children, and that infections in children were occurring early in the epidemic.
Some perspective
In an interview regarding the findings by Xia et al., Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University, and director of pediatric infectious diseases at Boston Medical Center, noted the absence of fever in 40% of cases.
“This is important, as the criteria for testing by public health departments has been high fever, cough, and shortness of breath,” he said. “The absence of fever is not inconsistent with COVID-19 disease.”
Another important point regarding the findings by Xia et al. is that the highest attack rates appear to be in children under 1 year of age, he said, further noting that the finding of concurrent influenza A, influenza B, or respiratory syncytial virus underscores that “concurrent infection can occur, and the presence of another virus in diagnostic tests does not mean that COVID-19 is not causal.”
As for whether the finding of elevated procalcitonin levels in 80% of cases reflects COVID-19 disease or coinfection with bacteria, the answer is unclear. But none of the children in the study were proven to have bacterial disease, he said, adding that “this marker will need to be interpreted with caution in the setting of COVID-19 disease.”
Dr. Xia and colleagues reported having no disclosures. Dr. Liu and associates also reported having no disclosures. The study by Liu et al. was supported by the Ministry of Science and Technology of China, the National Mega Project on Major Infectious Disease Prevention, and the National Key Research and Development Program of China.
SOURCES: Xia W et al. Ped Pulmonol. 2020 Mar 5. doi: 10.1002/ppul.24718; Liu W et al. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
Pediatric cases of COVID-19 infection are typically mild, but underlying coinfection may be more common in children than in adults, according to an analysis of clinical, laboratory, and chest CT features of pediatric inpatients in Wuhan, China.

The findings point toward a need for early chest CT with corresponding pathogen detection in children with suspected COVID-19 infection, Wei Xia, MD, of Huazhong University of Science and Technology, Wuhan, China, and colleagues reported in Pediatric Pulmonology.
The most common symptoms in 20 pediatric patients hospitalized between Jan. 23 and Feb. 8, 2020, with COVID-19 infection confirmed by the pharyngeal swab COVID-19 nucleic acid test were fever and cough, which occurred in 60% and 65% of patients, respectively. Coinfection was detected in eight patients (40%), they noted.
Clinical manifestations were similar to those seen in adults, but overall symptoms were relatively mild and overall prognosis was good. Of particular note, 7 of the 20 (35%) patients had a previously diagnosed congenital or acquired diseases, suggesting that children with underlying conditions may be more susceptible, Dr. Xia and colleagues wrote.
Laboratory findings also were notable in that 80% of the children had procalcitonin (PCT) elevations not typically seen in adults with COVID-19. PCT is a marker for bacterial infection and “[this finding] may suggest that routine antibacterial treatment should be considered in pediatric patients,” the investigators wrote.
As for imaging results, chest CT findings in children were similar to those in adults.“The typical manifestations were unilateral or bilateral subpleural ground-glass opacities, and consolidations with surrounding halo signs,” Dr. Xia and associates wrote, adding that consolidations with surrounding halo sign accounted for about half the pediatric cases and should be considered as “typical signs in pediatric patients.”
Pediatric cases were “rather rare” in the early days of the COVID-19 outbreak in Wuhan, where the first cases of infection were reported.
“As a pediatric group is usually susceptible to upper respiratory tract infection, because of their developing immune system, the delayed presence of pediatric patients is confusing,” the investigators wrote, noting that a low detection rate of pharyngeal swab COVID-19 nucleic acid test, distinguishing the virus from other common respiratory tract infectious pathogens in pediatric patients, “is still a problem.”
To better characterize the clinical and imaging features in children versus adults with COVID-19, Dr. Xia and associates reviewed these 20 pediatric cases, including 13 boys and 7 girls with ages ranging from less than 1 month to 14 years, 7 months (median 2 years, 1.5 months). Thirteen had an identified close contact with a COVID-19–diagnosed family member, and all were treated in an isolation ward. A total of 18 children were cured and discharged after an average stay of 13 days, and 2 neonates remained under observation because of positive swab results with negative CT findings. The investigators speculated that the different findings in neonates were perhaps caused by the influence of delivery on sampling or the specific CT manifestations for neonates, adding that more samples are needed for further clarification.
Based on these findings, “the CT imaging of COVID-19 infection should be differentiated with other virus pneumonias such as influenza virus, parainfluenza virus, respiratory syncytial virus, and adenovirus,” they concluded. It also should “be differentiated from bacterial pneumonia, mycoplasma pneumonia, and chlamydia pneumonia ... the density of pneumonia lesions caused by the latter pathogens is relatively higher.”
However, Dr. Xia and colleagues noted that chest CT manifestations of pneumonia caused by different pathogens overlap, and COVID-19 pneumonia “can be superimposed with serious and complex imaging manifestations, so epidemiological and etiological examinations should be combined.”
The investigators concluded that COVID-19 virus pneumonia in children is generally mild, and that the characteristic changes of subpleural ground-glass opacities and consolidations with surrounding halo on chest CT provide an “effective means for follow-up and evaluating the changes of lung lesions.”
“In the case that the positive rate of COVID-19 nucleic acid test from pharyngeal swab samples is not high, the early detection of lesions by CT is conducive to reasonable management and early treatment for pediatric patients. However, the diagnosis of COVID-19 pneumonia by CT imaging alone is not sufficient enough, especially in the case of coinfection with other pathogens,” Dr. Xia and associates wrote. “Therefore, early chest CT screening and timely follow-up, combined with corresponding pathogen detection, is a feasible clinical protocol in children.”
An early study
In a separate retrospective analysis described in a letter to the editor of the New England Journal of Medicine, Weiyong Liu, PhD, of Tongji Hospital of Huazhong University of Science and Technology and colleagues found that the most frequently detected pathogens in 366 children under the age of 16 years hospitalized with respiratory infections in Wuhan during Jan. 7-15, 2020, were influenza A virus (6.3% of cases) and influenza B virus (5.5% of cases), whereas COVID-19 was detected in 1.6% of cases.
The median age of the COVID-19 patients in that series was 3 years (range 1-7 years), and in contrast to the findings of Xia et al., all previously had been “completely healthy.” Common characteristics were high fever and cough in all six patients, and vomiting in four patients. Five had pneumonia as assessed by X-ray, and CTs showed typical viral pneumonia patterns.
One patient was admitted to a pediatric ICU. All patients received antiviral agents, antibiotic agents, and supportive therapies; all recovered after a median hospital stay of 7.5 days (median range, 5-13 days).
In contrast with the findings of Xia et al., the findings of Liu et al. showed COVID-19 caused moderate to severe respiratory illness in children, and that infections in children were occurring early in the epidemic.
Some perspective
In an interview regarding the findings by Xia et al., Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University, and director of pediatric infectious diseases at Boston Medical Center, noted the absence of fever in 40% of cases.
“This is important, as the criteria for testing by public health departments has been high fever, cough, and shortness of breath,” he said. “The absence of fever is not inconsistent with COVID-19 disease.”
Another important point regarding the findings by Xia et al. is that the highest attack rates appear to be in children under 1 year of age, he said, further noting that the finding of concurrent influenza A, influenza B, or respiratory syncytial virus underscores that “concurrent infection can occur, and the presence of another virus in diagnostic tests does not mean that COVID-19 is not causal.”
As for whether the finding of elevated procalcitonin levels in 80% of cases reflects COVID-19 disease or coinfection with bacteria, the answer is unclear. But none of the children in the study were proven to have bacterial disease, he said, adding that “this marker will need to be interpreted with caution in the setting of COVID-19 disease.”
Dr. Xia and colleagues reported having no disclosures. Dr. Liu and associates also reported having no disclosures. The study by Liu et al. was supported by the Ministry of Science and Technology of China, the National Mega Project on Major Infectious Disease Prevention, and the National Key Research and Development Program of China.
SOURCES: Xia W et al. Ped Pulmonol. 2020 Mar 5. doi: 10.1002/ppul.24718; Liu W et al. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
Pediatric cases of COVID-19 infection are typically mild, but underlying coinfection may be more common in children than in adults, according to an analysis of clinical, laboratory, and chest CT features of pediatric inpatients in Wuhan, China.

The findings point toward a need for early chest CT with corresponding pathogen detection in children with suspected COVID-19 infection, Wei Xia, MD, of Huazhong University of Science and Technology, Wuhan, China, and colleagues reported in Pediatric Pulmonology.
The most common symptoms in 20 pediatric patients hospitalized between Jan. 23 and Feb. 8, 2020, with COVID-19 infection confirmed by the pharyngeal swab COVID-19 nucleic acid test were fever and cough, which occurred in 60% and 65% of patients, respectively. Coinfection was detected in eight patients (40%), they noted.
Clinical manifestations were similar to those seen in adults, but overall symptoms were relatively mild and overall prognosis was good. Of particular note, 7 of the 20 (35%) patients had a previously diagnosed congenital or acquired diseases, suggesting that children with underlying conditions may be more susceptible, Dr. Xia and colleagues wrote.
Laboratory findings also were notable in that 80% of the children had procalcitonin (PCT) elevations not typically seen in adults with COVID-19. PCT is a marker for bacterial infection and “[this finding] may suggest that routine antibacterial treatment should be considered in pediatric patients,” the investigators wrote.
As for imaging results, chest CT findings in children were similar to those in adults.“The typical manifestations were unilateral or bilateral subpleural ground-glass opacities, and consolidations with surrounding halo signs,” Dr. Xia and associates wrote, adding that consolidations with surrounding halo sign accounted for about half the pediatric cases and should be considered as “typical signs in pediatric patients.”
Pediatric cases were “rather rare” in the early days of the COVID-19 outbreak in Wuhan, where the first cases of infection were reported.
“As a pediatric group is usually susceptible to upper respiratory tract infection, because of their developing immune system, the delayed presence of pediatric patients is confusing,” the investigators wrote, noting that a low detection rate of pharyngeal swab COVID-19 nucleic acid test, distinguishing the virus from other common respiratory tract infectious pathogens in pediatric patients, “is still a problem.”
To better characterize the clinical and imaging features in children versus adults with COVID-19, Dr. Xia and associates reviewed these 20 pediatric cases, including 13 boys and 7 girls with ages ranging from less than 1 month to 14 years, 7 months (median 2 years, 1.5 months). Thirteen had an identified close contact with a COVID-19–diagnosed family member, and all were treated in an isolation ward. A total of 18 children were cured and discharged after an average stay of 13 days, and 2 neonates remained under observation because of positive swab results with negative CT findings. The investigators speculated that the different findings in neonates were perhaps caused by the influence of delivery on sampling or the specific CT manifestations for neonates, adding that more samples are needed for further clarification.
Based on these findings, “the CT imaging of COVID-19 infection should be differentiated with other virus pneumonias such as influenza virus, parainfluenza virus, respiratory syncytial virus, and adenovirus,” they concluded. It also should “be differentiated from bacterial pneumonia, mycoplasma pneumonia, and chlamydia pneumonia ... the density of pneumonia lesions caused by the latter pathogens is relatively higher.”
However, Dr. Xia and colleagues noted that chest CT manifestations of pneumonia caused by different pathogens overlap, and COVID-19 pneumonia “can be superimposed with serious and complex imaging manifestations, so epidemiological and etiological examinations should be combined.”
The investigators concluded that COVID-19 virus pneumonia in children is generally mild, and that the characteristic changes of subpleural ground-glass opacities and consolidations with surrounding halo on chest CT provide an “effective means for follow-up and evaluating the changes of lung lesions.”
“In the case that the positive rate of COVID-19 nucleic acid test from pharyngeal swab samples is not high, the early detection of lesions by CT is conducive to reasonable management and early treatment for pediatric patients. However, the diagnosis of COVID-19 pneumonia by CT imaging alone is not sufficient enough, especially in the case of coinfection with other pathogens,” Dr. Xia and associates wrote. “Therefore, early chest CT screening and timely follow-up, combined with corresponding pathogen detection, is a feasible clinical protocol in children.”
An early study
In a separate retrospective analysis described in a letter to the editor of the New England Journal of Medicine, Weiyong Liu, PhD, of Tongji Hospital of Huazhong University of Science and Technology and colleagues found that the most frequently detected pathogens in 366 children under the age of 16 years hospitalized with respiratory infections in Wuhan during Jan. 7-15, 2020, were influenza A virus (6.3% of cases) and influenza B virus (5.5% of cases), whereas COVID-19 was detected in 1.6% of cases.
The median age of the COVID-19 patients in that series was 3 years (range 1-7 years), and in contrast to the findings of Xia et al., all previously had been “completely healthy.” Common characteristics were high fever and cough in all six patients, and vomiting in four patients. Five had pneumonia as assessed by X-ray, and CTs showed typical viral pneumonia patterns.
One patient was admitted to a pediatric ICU. All patients received antiviral agents, antibiotic agents, and supportive therapies; all recovered after a median hospital stay of 7.5 days (median range, 5-13 days).
In contrast with the findings of Xia et al., the findings of Liu et al. showed COVID-19 caused moderate to severe respiratory illness in children, and that infections in children were occurring early in the epidemic.
Some perspective
In an interview regarding the findings by Xia et al., Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University, and director of pediatric infectious diseases at Boston Medical Center, noted the absence of fever in 40% of cases.
“This is important, as the criteria for testing by public health departments has been high fever, cough, and shortness of breath,” he said. “The absence of fever is not inconsistent with COVID-19 disease.”
Another important point regarding the findings by Xia et al. is that the highest attack rates appear to be in children under 1 year of age, he said, further noting that the finding of concurrent influenza A, influenza B, or respiratory syncytial virus underscores that “concurrent infection can occur, and the presence of another virus in diagnostic tests does not mean that COVID-19 is not causal.”
As for whether the finding of elevated procalcitonin levels in 80% of cases reflects COVID-19 disease or coinfection with bacteria, the answer is unclear. But none of the children in the study were proven to have bacterial disease, he said, adding that “this marker will need to be interpreted with caution in the setting of COVID-19 disease.”
Dr. Xia and colleagues reported having no disclosures. Dr. Liu and associates also reported having no disclosures. The study by Liu et al. was supported by the Ministry of Science and Technology of China, the National Mega Project on Major Infectious Disease Prevention, and the National Key Research and Development Program of China.
SOURCES: Xia W et al. Ped Pulmonol. 2020 Mar 5. doi: 10.1002/ppul.24718; Liu W et al. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
FROM PEDIATRIC PULMONOLOGY
Teriflunomide increases the likelihood of achieving NEDA in relapsing-remitting MS
WEST PALM BEACH, FLA. – , according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. Teriflunomide reduces the risks of relapse, relapse resulting in hospital admission, and relapse resulting in prolonged hospitalization, compared with placebo.
Teriflunomide modulates the immune system and is an approved treatment for relapsing-remitting MS and clinically isolated syndrome. The phase 3 TEMSO study provided evidence that established the treatment’s safety and efficacy. In that study, significantly more patients who received a 14-mg dose of teriflunomide achieved NEDA, compared with patients who received placebo. Researchers generally weight all components of NEDA (i.e., confirmed disability worsening [CDW], relapse, and unique active MRI lesions) equally, but this approach could limit the interpretation of how each endpoint contributes to the effectiveness of a disease-modifying therapy.
A new analysis of TEMSO data
Keith R. Edwards, MD, director of the MS Center of Northeastern New York in Latham and colleagues conducted a win ratio matched-pairs analysis of TEMSO data to evaluate the efficacy of teriflunomide in enabling patients to achieve NEDA. In this analysis, the components of NEDA were assessed in order of priority, rather than as factors of equal weight.
In TEMSO, patients with relapsing-remitting MS received placebo or 14 mg of teriflunomide for 108 weeks. Dr. Edwards and colleagues matched active and control patients according to baseline characteristics. They compared the occurrence of disease activity events between the members of each pair. If a patient receiving teriflunomide had an event later than a control did, or did not have the event at all, teriflunomide was considered to “win.” If neither patient in a pair had a given event, the researchers omitted the pair from their analysis. Dr. Edwards and colleagues counted wins and summarized them as ratios. They conducted a second win ratio analysis of all relapses and relapses resulting in deaths, life-threatening events, prolonged hospitalizations, and hospital admissions.
NEDA components were ranked and assessed in the following order of decreasing priority: CDW, relapse, unique active MRI lesions. In a sensitivity analysis, the investigators ranked and assessed these components in the reverse order.
Sensitivity analysis supported primary analysis
Dr. Edwards and colleagues included 363 participants who received placebo and 358 who received teriflunomide in their analysis. Baseline characteristics did not differ significantly between the two groups. The population’s mean age was approximately 38 years, and about 73% of participants were female. The population’s mean baseline Expanded Disability Status Scale score was 2.7. Overall, about 72% of participants completed the study.
The researchers created 321 risk-matched pairs of participants. The win ratio analysis indicated that patients who received teriflunomide were significantly more likely to achieve NEDA, compared with controls (win ratio, 1.33). When the investigators analyzed the data by prioritizing the NEDA components in the reverse order, they found similar results (win ratio, 1.41).
When Dr. Edwards and colleagues analyzed relapse severity, they found that no relapses resulting in death or life-threatening events occurred in the active or control groups. Compared with placebo, teriflunomide significantly reduced the risk of relapse, relapses resulting in hospital admissions, and relapses resulting in prolonged hospitalizations (win ratio, 1.37).
The TEMSO study was funded by Sanofi. Dr. Edwards received grant or research support from Biogen, Genentech, Genzyme, and Novartis. Several authors received funding from Sanofi.
SOURCE: Edwards KR et al. ACTRIMS 2020, Abstract P036.
WEST PALM BEACH, FLA. – , according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. Teriflunomide reduces the risks of relapse, relapse resulting in hospital admission, and relapse resulting in prolonged hospitalization, compared with placebo.
Teriflunomide modulates the immune system and is an approved treatment for relapsing-remitting MS and clinically isolated syndrome. The phase 3 TEMSO study provided evidence that established the treatment’s safety and efficacy. In that study, significantly more patients who received a 14-mg dose of teriflunomide achieved NEDA, compared with patients who received placebo. Researchers generally weight all components of NEDA (i.e., confirmed disability worsening [CDW], relapse, and unique active MRI lesions) equally, but this approach could limit the interpretation of how each endpoint contributes to the effectiveness of a disease-modifying therapy.
A new analysis of TEMSO data
Keith R. Edwards, MD, director of the MS Center of Northeastern New York in Latham and colleagues conducted a win ratio matched-pairs analysis of TEMSO data to evaluate the efficacy of teriflunomide in enabling patients to achieve NEDA. In this analysis, the components of NEDA were assessed in order of priority, rather than as factors of equal weight.
In TEMSO, patients with relapsing-remitting MS received placebo or 14 mg of teriflunomide for 108 weeks. Dr. Edwards and colleagues matched active and control patients according to baseline characteristics. They compared the occurrence of disease activity events between the members of each pair. If a patient receiving teriflunomide had an event later than a control did, or did not have the event at all, teriflunomide was considered to “win.” If neither patient in a pair had a given event, the researchers omitted the pair from their analysis. Dr. Edwards and colleagues counted wins and summarized them as ratios. They conducted a second win ratio analysis of all relapses and relapses resulting in deaths, life-threatening events, prolonged hospitalizations, and hospital admissions.
NEDA components were ranked and assessed in the following order of decreasing priority: CDW, relapse, unique active MRI lesions. In a sensitivity analysis, the investigators ranked and assessed these components in the reverse order.
Sensitivity analysis supported primary analysis
Dr. Edwards and colleagues included 363 participants who received placebo and 358 who received teriflunomide in their analysis. Baseline characteristics did not differ significantly between the two groups. The population’s mean age was approximately 38 years, and about 73% of participants were female. The population’s mean baseline Expanded Disability Status Scale score was 2.7. Overall, about 72% of participants completed the study.
The researchers created 321 risk-matched pairs of participants. The win ratio analysis indicated that patients who received teriflunomide were significantly more likely to achieve NEDA, compared with controls (win ratio, 1.33). When the investigators analyzed the data by prioritizing the NEDA components in the reverse order, they found similar results (win ratio, 1.41).
When Dr. Edwards and colleagues analyzed relapse severity, they found that no relapses resulting in death or life-threatening events occurred in the active or control groups. Compared with placebo, teriflunomide significantly reduced the risk of relapse, relapses resulting in hospital admissions, and relapses resulting in prolonged hospitalizations (win ratio, 1.37).
The TEMSO study was funded by Sanofi. Dr. Edwards received grant or research support from Biogen, Genentech, Genzyme, and Novartis. Several authors received funding from Sanofi.
SOURCE: Edwards KR et al. ACTRIMS 2020, Abstract P036.
WEST PALM BEACH, FLA. – , according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. Teriflunomide reduces the risks of relapse, relapse resulting in hospital admission, and relapse resulting in prolonged hospitalization, compared with placebo.
Teriflunomide modulates the immune system and is an approved treatment for relapsing-remitting MS and clinically isolated syndrome. The phase 3 TEMSO study provided evidence that established the treatment’s safety and efficacy. In that study, significantly more patients who received a 14-mg dose of teriflunomide achieved NEDA, compared with patients who received placebo. Researchers generally weight all components of NEDA (i.e., confirmed disability worsening [CDW], relapse, and unique active MRI lesions) equally, but this approach could limit the interpretation of how each endpoint contributes to the effectiveness of a disease-modifying therapy.
A new analysis of TEMSO data
Keith R. Edwards, MD, director of the MS Center of Northeastern New York in Latham and colleagues conducted a win ratio matched-pairs analysis of TEMSO data to evaluate the efficacy of teriflunomide in enabling patients to achieve NEDA. In this analysis, the components of NEDA were assessed in order of priority, rather than as factors of equal weight.
In TEMSO, patients with relapsing-remitting MS received placebo or 14 mg of teriflunomide for 108 weeks. Dr. Edwards and colleagues matched active and control patients according to baseline characteristics. They compared the occurrence of disease activity events between the members of each pair. If a patient receiving teriflunomide had an event later than a control did, or did not have the event at all, teriflunomide was considered to “win.” If neither patient in a pair had a given event, the researchers omitted the pair from their analysis. Dr. Edwards and colleagues counted wins and summarized them as ratios. They conducted a second win ratio analysis of all relapses and relapses resulting in deaths, life-threatening events, prolonged hospitalizations, and hospital admissions.
NEDA components were ranked and assessed in the following order of decreasing priority: CDW, relapse, unique active MRI lesions. In a sensitivity analysis, the investigators ranked and assessed these components in the reverse order.
Sensitivity analysis supported primary analysis
Dr. Edwards and colleagues included 363 participants who received placebo and 358 who received teriflunomide in their analysis. Baseline characteristics did not differ significantly between the two groups. The population’s mean age was approximately 38 years, and about 73% of participants were female. The population’s mean baseline Expanded Disability Status Scale score was 2.7. Overall, about 72% of participants completed the study.
The researchers created 321 risk-matched pairs of participants. The win ratio analysis indicated that patients who received teriflunomide were significantly more likely to achieve NEDA, compared with controls (win ratio, 1.33). When the investigators analyzed the data by prioritizing the NEDA components in the reverse order, they found similar results (win ratio, 1.41).
When Dr. Edwards and colleagues analyzed relapse severity, they found that no relapses resulting in death or life-threatening events occurred in the active or control groups. Compared with placebo, teriflunomide significantly reduced the risk of relapse, relapses resulting in hospital admissions, and relapses resulting in prolonged hospitalizations (win ratio, 1.37).
The TEMSO study was funded by Sanofi. Dr. Edwards received grant or research support from Biogen, Genentech, Genzyme, and Novartis. Several authors received funding from Sanofi.
SOURCE: Edwards KR et al. ACTRIMS 2020, Abstract P036.
REPORTING FROM ACTRIMS Forum 2020
COVID-19: Older patients with cancer especially vulnerable
For oncologists and other clinicians caring for patients with cancer, the COVID-19 pandemic represents a dynamic clinical challenge that is changing daily and that can feel overwhelming at times, say experts.
“Oncology clinicians are well versed in caring for immunosuppressed patients with cancer, of all ages,” Merry-Jennifer Markham, MD, interim chief of the Division of Hematology and Oncology at the University of Florida Health, Gainesville, told Medscape Medical News.
However, she emphasized that, during this COVID-19 outbreak, “we must be especially diligent about screening for symptoms and exposure, and we must recognize that our older patients with cancer may be especially vulnerable.”
Patients with cancer who are in active treatment are immunosuppressed and are more susceptible to infection and to complications from infection, Markham pointed out. “While we don’t yet have much data on how COVID-19 impacts patients with cancer, I have to suspect that patients undergoing active cancer treatment may be especially vulnerable to the more severe illness associated with COVID-19,” she said.
Indeed, a recent report from China that was published in the Lancet Oncology supports this. The authors suggest that patients with cancer are at higher risk for COVID-19 and have a worse prognosis if they become infected than do those without cancer.
Commonsense rules
Commonsense rules apply for all patients with cancer, regardless of age, said Markham. Measures include thorough handwashing, staying home when sick, and avoiding sick contacts.
Markham, who acts as an expert spokesperson for the American Society of Clinical Oncology, provides information on what patients with cancer need to know about COVID-19 at Cancer.net, the society’s website for patients with cancer.
“Unfortunately, this outbreak of COVID-19 is happening rapidly and in real time,” Markham noted. “The entire medical community is learning as we go, rather than having the luxury of years of evidence-based literature to guide us.”
Another expert agrees. “Unfortunately, there are not a lot of data on how COVID-19 affects cancer patients,” Cardinale Smith, MD, PhD, director of Quality for Cancer Services in the Mount Sinai Health System, New York City, said in an interview.
“We need to minimize the risk for patients and minimize our own exposure by treating this situation like we would a really bad flu season,” Smith told Medscape Medical News. “Some patients have had a bad outcome, but the vast majority do not. The best we can do is stay calm and focused.”
At Mount Sinai, for patients with cancer, routine, nonurgent appointments are being rescheduled for May, Smith said. Those in active treatment are screened by telephone 24 to 48 hours before arrival, after which they undergo a full risk assessment in an isolation room. Those with a respiratory infection are given a mask.
“Patients are very anxious and worried about COVID-19,” said Smith, who has young children and an elderly parent at home. “We don’t have all the answers, and this can heighten anxiety.”
To help allay fears, social workers are asking patients with cancer who express anxiety to discuss their concerns and provide information. A one-page handout on both flu and COVID-10 is available in the waiting room.
The Web portal MyChart gives patients access to updated information on COVID-19 precautions and provides links to the hospital website and to the US Centers for Disease Control and Prevention. Patients who are not feeling well can speak to someone or get answers if they have additional questions.
When counseling patients, Smith advises them to use “an abundance of caution” and to be creative in efforts to minimize risk. “My suggestion is to use FaceTime and Skype to connect and communicate with your community,” she said.
Some churches are conducting services via teleconferencing to minimize risk, and seniors’ centers that offer yoga and other classes are also beginning to provide services virtually, she pointed out.
Data from China
A report published February 14 in the Lancet Oncology appears to be the first analysis in the literature to focus on COVID-19 in patients with cancer.
“Patients with cancer are more susceptible to infection than individuals without cancer because of their systemic immunosuppressive state caused by the malignancy and anticancer treatments, such as chemotherapy or surgery,” write the authors, led by Wenhua Liang, MD, of Guangzhou Medical University. However, in correspondence published in the Lancet Oncology, other experts in China question some of Liang’s and colleagues’ findings.
The report by Liang and colleagues concerns a prospective cohort of 1590 patients with COVID-19.
There were 2007 laboratory-confirmed cases of COVID-19 among patients admitted to 575 hospitals throughout China as of January 31. Of those cases, 417 were excluded from the analysis because of insufficient information regarding disease history.
The team reports that of 18 patients with cancer and COVID-19, 39% were at significantly higher risk for “severe events.” By comparison, of 1572 patients with COVID-19 who did not have cancer, 8% were at significantly higher risk (P = .0003). These events included rapid clinical deterioration that required admission to intensive care; invasive ventilation; or death.
Patients with cancer experienced a much more rapid deterioration in clinical status than did those without cancer. The median time to severe events was 13 days, vs 43 days (hazard ratio [HR] adjusted for age, 3.56; P < .0001).
The analysis also shows that patients who underwent chemotherapy or surgery in the past month had a 75% risk of experiencing clinically severe events, compared with a 43% risk for those who had not received recent treatment.
After adjusting for other risk factors, including age and smoking history, older age was the only risk factor for severe events (odds ratio [OR], 1.43; 95% confidence interval [CI], 0.97 – 2.12; P = .072), the study authors say.
Patients with lung cancer did not have a higher probability of severe events compared with patients with other cancer types (20% vs 62%, respectively; P = .294).
Liang and colleagues conclude that these findings provide “a timely reminder to physicians that more intensive attention should be paid to patients with cancer, in case of rapid deterioration.”
The team also proposes three strategies for managing patients with cancer who are at risk for COVID-19 or any other severe infectious disease. They recommend that intentional postponement of adjuvant chemotherapy or elective surgery be considered for patients with stable cancer who live in areas where disease is endemic. Stronger “personal protection provisions” could also be made for patients with cancer or for cancer survivors. Lastly, for patients with cancer who have COVID-19, especially those who are older or who have comorbidities, more intensive surveillance or treatment should be considered.
However, in comments in the Lancet Oncology, other authors in China say these findings should be interpreted with caution.
One group suggests that the increased susceptibility to COVID-19 in patients with cancer could be the result of higher rates of smoking compared with patients who did not have cancer. “Overall, current evidence remains insufficient to explain a conclusive association between cancer and COVID-19,” say Huahao Shen, PhD, of Zhejiang University School of Medicine, Hangzhou, Zhejiang, and colleagues.
Another group suggests that the significantly higher median age of patients with cancer compared with noncancer patients (63 years vs 49 years) may have contributed to poor prognosis.
These authors, led by Li Zhang, MD, PhD, and Hanping Wang, MD, of Peking Union Medical College and the Chinese Academy of Medical Sciences, Beijing, emphasize that patients with cancer need online medical counseling and that critical cases need to be identified and treated.
“In endemic areas outside Wuhan, decisions on whether or not to postpone cancer treatment need to made on a patient-by-patient basis and according to the risk to the patient and the prevailing situation because delays could lead to tumor progression and ultimately poorer outcomes,” they write.
The study was funded by the China National Science Foundation and the Key Project of Guangzhou Scientific Research Project. Liang and coauthors, Shen and coauthors, Zhang, Wang, and Smith have disclosed no relevant financial relationships. Markham has relationships with Aduro Biotech, Lilly, Tesaro, Novartis, and VBL Therapeutics.
This article first appeared on Medscape.com.
For oncologists and other clinicians caring for patients with cancer, the COVID-19 pandemic represents a dynamic clinical challenge that is changing daily and that can feel overwhelming at times, say experts.
“Oncology clinicians are well versed in caring for immunosuppressed patients with cancer, of all ages,” Merry-Jennifer Markham, MD, interim chief of the Division of Hematology and Oncology at the University of Florida Health, Gainesville, told Medscape Medical News.
However, she emphasized that, during this COVID-19 outbreak, “we must be especially diligent about screening for symptoms and exposure, and we must recognize that our older patients with cancer may be especially vulnerable.”
Patients with cancer who are in active treatment are immunosuppressed and are more susceptible to infection and to complications from infection, Markham pointed out. “While we don’t yet have much data on how COVID-19 impacts patients with cancer, I have to suspect that patients undergoing active cancer treatment may be especially vulnerable to the more severe illness associated with COVID-19,” she said.
Indeed, a recent report from China that was published in the Lancet Oncology supports this. The authors suggest that patients with cancer are at higher risk for COVID-19 and have a worse prognosis if they become infected than do those without cancer.
Commonsense rules
Commonsense rules apply for all patients with cancer, regardless of age, said Markham. Measures include thorough handwashing, staying home when sick, and avoiding sick contacts.
Markham, who acts as an expert spokesperson for the American Society of Clinical Oncology, provides information on what patients with cancer need to know about COVID-19 at Cancer.net, the society’s website for patients with cancer.
“Unfortunately, this outbreak of COVID-19 is happening rapidly and in real time,” Markham noted. “The entire medical community is learning as we go, rather than having the luxury of years of evidence-based literature to guide us.”
Another expert agrees. “Unfortunately, there are not a lot of data on how COVID-19 affects cancer patients,” Cardinale Smith, MD, PhD, director of Quality for Cancer Services in the Mount Sinai Health System, New York City, said in an interview.
“We need to minimize the risk for patients and minimize our own exposure by treating this situation like we would a really bad flu season,” Smith told Medscape Medical News. “Some patients have had a bad outcome, but the vast majority do not. The best we can do is stay calm and focused.”
At Mount Sinai, for patients with cancer, routine, nonurgent appointments are being rescheduled for May, Smith said. Those in active treatment are screened by telephone 24 to 48 hours before arrival, after which they undergo a full risk assessment in an isolation room. Those with a respiratory infection are given a mask.
“Patients are very anxious and worried about COVID-19,” said Smith, who has young children and an elderly parent at home. “We don’t have all the answers, and this can heighten anxiety.”
To help allay fears, social workers are asking patients with cancer who express anxiety to discuss their concerns and provide information. A one-page handout on both flu and COVID-10 is available in the waiting room.
The Web portal MyChart gives patients access to updated information on COVID-19 precautions and provides links to the hospital website and to the US Centers for Disease Control and Prevention. Patients who are not feeling well can speak to someone or get answers if they have additional questions.
When counseling patients, Smith advises them to use “an abundance of caution” and to be creative in efforts to minimize risk. “My suggestion is to use FaceTime and Skype to connect and communicate with your community,” she said.
Some churches are conducting services via teleconferencing to minimize risk, and seniors’ centers that offer yoga and other classes are also beginning to provide services virtually, she pointed out.
Data from China
A report published February 14 in the Lancet Oncology appears to be the first analysis in the literature to focus on COVID-19 in patients with cancer.
“Patients with cancer are more susceptible to infection than individuals without cancer because of their systemic immunosuppressive state caused by the malignancy and anticancer treatments, such as chemotherapy or surgery,” write the authors, led by Wenhua Liang, MD, of Guangzhou Medical University. However, in correspondence published in the Lancet Oncology, other experts in China question some of Liang’s and colleagues’ findings.
The report by Liang and colleagues concerns a prospective cohort of 1590 patients with COVID-19.
There were 2007 laboratory-confirmed cases of COVID-19 among patients admitted to 575 hospitals throughout China as of January 31. Of those cases, 417 were excluded from the analysis because of insufficient information regarding disease history.
The team reports that of 18 patients with cancer and COVID-19, 39% were at significantly higher risk for “severe events.” By comparison, of 1572 patients with COVID-19 who did not have cancer, 8% were at significantly higher risk (P = .0003). These events included rapid clinical deterioration that required admission to intensive care; invasive ventilation; or death.
Patients with cancer experienced a much more rapid deterioration in clinical status than did those without cancer. The median time to severe events was 13 days, vs 43 days (hazard ratio [HR] adjusted for age, 3.56; P < .0001).
The analysis also shows that patients who underwent chemotherapy or surgery in the past month had a 75% risk of experiencing clinically severe events, compared with a 43% risk for those who had not received recent treatment.
After adjusting for other risk factors, including age and smoking history, older age was the only risk factor for severe events (odds ratio [OR], 1.43; 95% confidence interval [CI], 0.97 – 2.12; P = .072), the study authors say.
Patients with lung cancer did not have a higher probability of severe events compared with patients with other cancer types (20% vs 62%, respectively; P = .294).
Liang and colleagues conclude that these findings provide “a timely reminder to physicians that more intensive attention should be paid to patients with cancer, in case of rapid deterioration.”
The team also proposes three strategies for managing patients with cancer who are at risk for COVID-19 or any other severe infectious disease. They recommend that intentional postponement of adjuvant chemotherapy or elective surgery be considered for patients with stable cancer who live in areas where disease is endemic. Stronger “personal protection provisions” could also be made for patients with cancer or for cancer survivors. Lastly, for patients with cancer who have COVID-19, especially those who are older or who have comorbidities, more intensive surveillance or treatment should be considered.
However, in comments in the Lancet Oncology, other authors in China say these findings should be interpreted with caution.
One group suggests that the increased susceptibility to COVID-19 in patients with cancer could be the result of higher rates of smoking compared with patients who did not have cancer. “Overall, current evidence remains insufficient to explain a conclusive association between cancer and COVID-19,” say Huahao Shen, PhD, of Zhejiang University School of Medicine, Hangzhou, Zhejiang, and colleagues.
Another group suggests that the significantly higher median age of patients with cancer compared with noncancer patients (63 years vs 49 years) may have contributed to poor prognosis.
These authors, led by Li Zhang, MD, PhD, and Hanping Wang, MD, of Peking Union Medical College and the Chinese Academy of Medical Sciences, Beijing, emphasize that patients with cancer need online medical counseling and that critical cases need to be identified and treated.
“In endemic areas outside Wuhan, decisions on whether or not to postpone cancer treatment need to made on a patient-by-patient basis and according to the risk to the patient and the prevailing situation because delays could lead to tumor progression and ultimately poorer outcomes,” they write.
The study was funded by the China National Science Foundation and the Key Project of Guangzhou Scientific Research Project. Liang and coauthors, Shen and coauthors, Zhang, Wang, and Smith have disclosed no relevant financial relationships. Markham has relationships with Aduro Biotech, Lilly, Tesaro, Novartis, and VBL Therapeutics.
This article first appeared on Medscape.com.
For oncologists and other clinicians caring for patients with cancer, the COVID-19 pandemic represents a dynamic clinical challenge that is changing daily and that can feel overwhelming at times, say experts.
“Oncology clinicians are well versed in caring for immunosuppressed patients with cancer, of all ages,” Merry-Jennifer Markham, MD, interim chief of the Division of Hematology and Oncology at the University of Florida Health, Gainesville, told Medscape Medical News.
However, she emphasized that, during this COVID-19 outbreak, “we must be especially diligent about screening for symptoms and exposure, and we must recognize that our older patients with cancer may be especially vulnerable.”
Patients with cancer who are in active treatment are immunosuppressed and are more susceptible to infection and to complications from infection, Markham pointed out. “While we don’t yet have much data on how COVID-19 impacts patients with cancer, I have to suspect that patients undergoing active cancer treatment may be especially vulnerable to the more severe illness associated with COVID-19,” she said.
Indeed, a recent report from China that was published in the Lancet Oncology supports this. The authors suggest that patients with cancer are at higher risk for COVID-19 and have a worse prognosis if they become infected than do those without cancer.
Commonsense rules
Commonsense rules apply for all patients with cancer, regardless of age, said Markham. Measures include thorough handwashing, staying home when sick, and avoiding sick contacts.
Markham, who acts as an expert spokesperson for the American Society of Clinical Oncology, provides information on what patients with cancer need to know about COVID-19 at Cancer.net, the society’s website for patients with cancer.
“Unfortunately, this outbreak of COVID-19 is happening rapidly and in real time,” Markham noted. “The entire medical community is learning as we go, rather than having the luxury of years of evidence-based literature to guide us.”
Another expert agrees. “Unfortunately, there are not a lot of data on how COVID-19 affects cancer patients,” Cardinale Smith, MD, PhD, director of Quality for Cancer Services in the Mount Sinai Health System, New York City, said in an interview.
“We need to minimize the risk for patients and minimize our own exposure by treating this situation like we would a really bad flu season,” Smith told Medscape Medical News. “Some patients have had a bad outcome, but the vast majority do not. The best we can do is stay calm and focused.”
At Mount Sinai, for patients with cancer, routine, nonurgent appointments are being rescheduled for May, Smith said. Those in active treatment are screened by telephone 24 to 48 hours before arrival, after which they undergo a full risk assessment in an isolation room. Those with a respiratory infection are given a mask.
“Patients are very anxious and worried about COVID-19,” said Smith, who has young children and an elderly parent at home. “We don’t have all the answers, and this can heighten anxiety.”
To help allay fears, social workers are asking patients with cancer who express anxiety to discuss their concerns and provide information. A one-page handout on both flu and COVID-10 is available in the waiting room.
The Web portal MyChart gives patients access to updated information on COVID-19 precautions and provides links to the hospital website and to the US Centers for Disease Control and Prevention. Patients who are not feeling well can speak to someone or get answers if they have additional questions.
When counseling patients, Smith advises them to use “an abundance of caution” and to be creative in efforts to minimize risk. “My suggestion is to use FaceTime and Skype to connect and communicate with your community,” she said.
Some churches are conducting services via teleconferencing to minimize risk, and seniors’ centers that offer yoga and other classes are also beginning to provide services virtually, she pointed out.
Data from China
A report published February 14 in the Lancet Oncology appears to be the first analysis in the literature to focus on COVID-19 in patients with cancer.
“Patients with cancer are more susceptible to infection than individuals without cancer because of their systemic immunosuppressive state caused by the malignancy and anticancer treatments, such as chemotherapy or surgery,” write the authors, led by Wenhua Liang, MD, of Guangzhou Medical University. However, in correspondence published in the Lancet Oncology, other experts in China question some of Liang’s and colleagues’ findings.
The report by Liang and colleagues concerns a prospective cohort of 1590 patients with COVID-19.
There were 2007 laboratory-confirmed cases of COVID-19 among patients admitted to 575 hospitals throughout China as of January 31. Of those cases, 417 were excluded from the analysis because of insufficient information regarding disease history.
The team reports that of 18 patients with cancer and COVID-19, 39% were at significantly higher risk for “severe events.” By comparison, of 1572 patients with COVID-19 who did not have cancer, 8% were at significantly higher risk (P = .0003). These events included rapid clinical deterioration that required admission to intensive care; invasive ventilation; or death.
Patients with cancer experienced a much more rapid deterioration in clinical status than did those without cancer. The median time to severe events was 13 days, vs 43 days (hazard ratio [HR] adjusted for age, 3.56; P < .0001).
The analysis also shows that patients who underwent chemotherapy or surgery in the past month had a 75% risk of experiencing clinically severe events, compared with a 43% risk for those who had not received recent treatment.
After adjusting for other risk factors, including age and smoking history, older age was the only risk factor for severe events (odds ratio [OR], 1.43; 95% confidence interval [CI], 0.97 – 2.12; P = .072), the study authors say.
Patients with lung cancer did not have a higher probability of severe events compared with patients with other cancer types (20% vs 62%, respectively; P = .294).
Liang and colleagues conclude that these findings provide “a timely reminder to physicians that more intensive attention should be paid to patients with cancer, in case of rapid deterioration.”
The team also proposes three strategies for managing patients with cancer who are at risk for COVID-19 or any other severe infectious disease. They recommend that intentional postponement of adjuvant chemotherapy or elective surgery be considered for patients with stable cancer who live in areas where disease is endemic. Stronger “personal protection provisions” could also be made for patients with cancer or for cancer survivors. Lastly, for patients with cancer who have COVID-19, especially those who are older or who have comorbidities, more intensive surveillance or treatment should be considered.
However, in comments in the Lancet Oncology, other authors in China say these findings should be interpreted with caution.
One group suggests that the increased susceptibility to COVID-19 in patients with cancer could be the result of higher rates of smoking compared with patients who did not have cancer. “Overall, current evidence remains insufficient to explain a conclusive association between cancer and COVID-19,” say Huahao Shen, PhD, of Zhejiang University School of Medicine, Hangzhou, Zhejiang, and colleagues.
Another group suggests that the significantly higher median age of patients with cancer compared with noncancer patients (63 years vs 49 years) may have contributed to poor prognosis.
These authors, led by Li Zhang, MD, PhD, and Hanping Wang, MD, of Peking Union Medical College and the Chinese Academy of Medical Sciences, Beijing, emphasize that patients with cancer need online medical counseling and that critical cases need to be identified and treated.
“In endemic areas outside Wuhan, decisions on whether or not to postpone cancer treatment need to made on a patient-by-patient basis and according to the risk to the patient and the prevailing situation because delays could lead to tumor progression and ultimately poorer outcomes,” they write.
The study was funded by the China National Science Foundation and the Key Project of Guangzhou Scientific Research Project. Liang and coauthors, Shen and coauthors, Zhang, Wang, and Smith have disclosed no relevant financial relationships. Markham has relationships with Aduro Biotech, Lilly, Tesaro, Novartis, and VBL Therapeutics.
This article first appeared on Medscape.com.
Medical identity theft
In his book, “Scam Me If You Can,” fraud expert Frank Abagnale relates the case of a 5-year-old boy whose pediatrician’s computer was hacked, compromising his name, birth date, Social Security number, insurance information, and medical records. The result was a bureaucratic nightmare that may well continue for the rest of that unfortunate young patient’s life. One can only speculate on the difficulties he might have as adult in obtaining a line of credit, or in proving his medical identity to physicians and hospitals.
– your Social Security number, bank account numbers, etc. – sells for about $25 on the black market; add health insurance and medical records, and the price can jump to $1,000 or more. That’s because there is a far greater potential yield from medical identity theft – and once your personal information and medical records are breached, they are in the Cloud for the rest of your life, available to anyone who wants to buy them. Older patients are particularly vulnerable: Medicare billing scams cost taxpayers more than $60 billion a year.
If your office’s computer system does not have effective fraud protection, you could be held liable for any fraud committed with information stolen from it – and if the information is resold years later and reused to commit more fraud, you’ll be liable for that, too. That’s why I strongly recommend that you invest in high-quality security technology and software, so that in the event of a breach, the security company will at least share in the fault and the liability. (As always, I have no financial interest in any product or industry mentioned in this column.)
Even with adequate protection, breaches can still occur, so all medical offices should have a breach response plan in place, covering how to halt security breaches, and how to handle any lost or stolen data. Your computer and security vendors can help with formulating such a plan. Patients affected by a breach need to be contacted as well, so they may put a freeze on accounts or send out fraud alerts.
Patients also need to be aware of the risks. If your EHR includes an online portal to communicate protected information to patients, it may be secure on your end, but patients are unlikely to have similar protection on their home computers. If you offer online patient portal services, you should make your patients aware of measures they can take to protect their data once it arrives on their computers or phones.
Patients should also be warned of the risks that come with sharing medical information with others. If they are asked to reveal medical data via phone or email, they need to ask who is requesting it, and why. Any unsolicited calls inquiring about their medical information, from someone who can’t or won’t confirm their identity, should be considered extremely suspicious.
We tell our patients to protect their insurance numbers as carefully as they guard their Social Security number and other valuable data, and to shred any medical paperwork they no longer need, including labels on prescription bottles. And if they see something on an Explanation of Benefits that doesn’t look right, they should question it immediately. We encourage them to take advantage of the free services at MyMedicare.gov, including Medicare Summary Notices provided every 3 months (if any services or medical supplies are received during that period), to make sure they’re being billed only for services they have received.
Your staff should be made aware of the potential for “friendly fraud,” which is defined as theft of identity and medical information by patients’ friends or family members. (According to some studies, as much as 50% of all medical identity theft may be committed this way.) Staffers should never divulge insurance numbers, diagnoses, lab reports, or any other privileged information to family or friends, whether by phone, fax, mail, or in person, without written permission from the patient. And when callers claiming to be patients request information about themselves, your employees should be alert for “red flags.” For example, legitimate patients won’t stumble over simple questions (such as “What is your birth date?”) or request test results or diagnoses that they should already know about.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
In his book, “Scam Me If You Can,” fraud expert Frank Abagnale relates the case of a 5-year-old boy whose pediatrician’s computer was hacked, compromising his name, birth date, Social Security number, insurance information, and medical records. The result was a bureaucratic nightmare that may well continue for the rest of that unfortunate young patient’s life. One can only speculate on the difficulties he might have as adult in obtaining a line of credit, or in proving his medical identity to physicians and hospitals.
– your Social Security number, bank account numbers, etc. – sells for about $25 on the black market; add health insurance and medical records, and the price can jump to $1,000 or more. That’s because there is a far greater potential yield from medical identity theft – and once your personal information and medical records are breached, they are in the Cloud for the rest of your life, available to anyone who wants to buy them. Older patients are particularly vulnerable: Medicare billing scams cost taxpayers more than $60 billion a year.
If your office’s computer system does not have effective fraud protection, you could be held liable for any fraud committed with information stolen from it – and if the information is resold years later and reused to commit more fraud, you’ll be liable for that, too. That’s why I strongly recommend that you invest in high-quality security technology and software, so that in the event of a breach, the security company will at least share in the fault and the liability. (As always, I have no financial interest in any product or industry mentioned in this column.)
Even with adequate protection, breaches can still occur, so all medical offices should have a breach response plan in place, covering how to halt security breaches, and how to handle any lost or stolen data. Your computer and security vendors can help with formulating such a plan. Patients affected by a breach need to be contacted as well, so they may put a freeze on accounts or send out fraud alerts.
Patients also need to be aware of the risks. If your EHR includes an online portal to communicate protected information to patients, it may be secure on your end, but patients are unlikely to have similar protection on their home computers. If you offer online patient portal services, you should make your patients aware of measures they can take to protect their data once it arrives on their computers or phones.
Patients should also be warned of the risks that come with sharing medical information with others. If they are asked to reveal medical data via phone or email, they need to ask who is requesting it, and why. Any unsolicited calls inquiring about their medical information, from someone who can’t or won’t confirm their identity, should be considered extremely suspicious.
We tell our patients to protect their insurance numbers as carefully as they guard their Social Security number and other valuable data, and to shred any medical paperwork they no longer need, including labels on prescription bottles. And if they see something on an Explanation of Benefits that doesn’t look right, they should question it immediately. We encourage them to take advantage of the free services at MyMedicare.gov, including Medicare Summary Notices provided every 3 months (if any services or medical supplies are received during that period), to make sure they’re being billed only for services they have received.
Your staff should be made aware of the potential for “friendly fraud,” which is defined as theft of identity and medical information by patients’ friends or family members. (According to some studies, as much as 50% of all medical identity theft may be committed this way.) Staffers should never divulge insurance numbers, diagnoses, lab reports, or any other privileged information to family or friends, whether by phone, fax, mail, or in person, without written permission from the patient. And when callers claiming to be patients request information about themselves, your employees should be alert for “red flags.” For example, legitimate patients won’t stumble over simple questions (such as “What is your birth date?”) or request test results or diagnoses that they should already know about.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
In his book, “Scam Me If You Can,” fraud expert Frank Abagnale relates the case of a 5-year-old boy whose pediatrician’s computer was hacked, compromising his name, birth date, Social Security number, insurance information, and medical records. The result was a bureaucratic nightmare that may well continue for the rest of that unfortunate young patient’s life. One can only speculate on the difficulties he might have as adult in obtaining a line of credit, or in proving his medical identity to physicians and hospitals.
– your Social Security number, bank account numbers, etc. – sells for about $25 on the black market; add health insurance and medical records, and the price can jump to $1,000 or more. That’s because there is a far greater potential yield from medical identity theft – and once your personal information and medical records are breached, they are in the Cloud for the rest of your life, available to anyone who wants to buy them. Older patients are particularly vulnerable: Medicare billing scams cost taxpayers more than $60 billion a year.
If your office’s computer system does not have effective fraud protection, you could be held liable for any fraud committed with information stolen from it – and if the information is resold years later and reused to commit more fraud, you’ll be liable for that, too. That’s why I strongly recommend that you invest in high-quality security technology and software, so that in the event of a breach, the security company will at least share in the fault and the liability. (As always, I have no financial interest in any product or industry mentioned in this column.)
Even with adequate protection, breaches can still occur, so all medical offices should have a breach response plan in place, covering how to halt security breaches, and how to handle any lost or stolen data. Your computer and security vendors can help with formulating such a plan. Patients affected by a breach need to be contacted as well, so they may put a freeze on accounts or send out fraud alerts.
Patients also need to be aware of the risks. If your EHR includes an online portal to communicate protected information to patients, it may be secure on your end, but patients are unlikely to have similar protection on their home computers. If you offer online patient portal services, you should make your patients aware of measures they can take to protect their data once it arrives on their computers or phones.
Patients should also be warned of the risks that come with sharing medical information with others. If they are asked to reveal medical data via phone or email, they need to ask who is requesting it, and why. Any unsolicited calls inquiring about their medical information, from someone who can’t or won’t confirm their identity, should be considered extremely suspicious.
We tell our patients to protect their insurance numbers as carefully as they guard their Social Security number and other valuable data, and to shred any medical paperwork they no longer need, including labels on prescription bottles. And if they see something on an Explanation of Benefits that doesn’t look right, they should question it immediately. We encourage them to take advantage of the free services at MyMedicare.gov, including Medicare Summary Notices provided every 3 months (if any services or medical supplies are received during that period), to make sure they’re being billed only for services they have received.
Your staff should be made aware of the potential for “friendly fraud,” which is defined as theft of identity and medical information by patients’ friends or family members. (According to some studies, as much as 50% of all medical identity theft may be committed this way.) Staffers should never divulge insurance numbers, diagnoses, lab reports, or any other privileged information to family or friends, whether by phone, fax, mail, or in person, without written permission from the patient. And when callers claiming to be patients request information about themselves, your employees should be alert for “red flags.” For example, legitimate patients won’t stumble over simple questions (such as “What is your birth date?”) or request test results or diagnoses that they should already know about.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Scientific community ‘shocked’ by loss of MIND diet pioneer
Martha Clare Morris, ScD, a pioneer in research linking nutrition to brain health and a creator of the breakthrough MIND diet, has died of cancer at the age of 64.
Morris was a professor in the Department of Internal Medicine, assistant provost of community research, and director of the Rush Institute for Healthy Aging at Rush University, in Chicago, Illinois. She was also a director of the internal medicine department’s Section of Community Epidemiology.
Long-time friend and colleague Julie A. Schneider, MD, the Deborah R. and Edgar D. Jannotta Presidential Professor of Pathology and Neurological Sciences, Rush University Medical Center, described Morris as creative, passionate, and adventurous.
Her death was “a shock” to the scientific community, Schneider told Medscape Medical News.
“It’s a tragic loss in so many ways,” said Schneider, who is also associate director of the Rush Alzheimer’s Disease Center. She was a very well-respected nutritional epidemiologist and was passionate about her work; she had just so much unwavering commitment to it.
Diet, said Schneider, is “notoriously a hard thing to study” because “it’s so intertwined with lifestyle” and other factors that create “barriers” to conducting such research.
But Morris had a unique and creative talent for filtering out what might be the individual contribution of a particular modifiable risk factor, said Heather Snyder, PhD, vice president of medical and scientific relations, Alzheimer’s Association, who also knew Morris both personally and professionally.
“Humble” trailblazer
Morris’s pioneering research examined the connection between nutrition and the prevention of cognitive decline. Taking results from this research, she developed the MIND diet – a hybrid of the Mediterranean diet and the Dietary Approaches to Stop Hypertension – along with colleagues at both Rush and Harvard Universities.
The MIND diet – an acronym for Mediterranean-DASH Intervention for Neurodegenerative Delay – emphasizes brain-healthy foods, including leafy green vegetables, nuts, berries, chicken, fish, whole grains, beans, olive oil, and moderate amounts of red wine. The diet limits consumption of red meat, butter, margarine, and processed foods.
In 2015, Morris published her initial findings on the MIND diet in Alzheimer’s and Dementia. Reported by Medscape Medical News at that time, the study showed that the diet protected cardiovascular health and slowed cognitive decline in older individuals.
The excitement around the findings inspired Morris to write “Diet for the Mind,” which was published in 2017. The book summarizes the benefits of the MIND diet and includes brain-healthy recipes created by her daughter Laura, who is a chef. Despite many accolades, Morris was “humble” about this project, said Schneider.
“This was not about publicity and trying to get a book out; she wanted to see if this diet really was going to change people’s lives. She wanted to bring it into the community,” she said.
Proud legacy
Since 2017, Morris had led a large clinical trial of the effectiveness of the MIND diet in preventing cognitive decline. The first study of its kind, the trial received a $14.5 million grant from the National Institutes of Health (NIH). Results of this study are expected in 2021.
The MIND diet was ranked among the top 10 diets for five consecutive years in US News and World Report.
Morris’s nutrition-related research went beyond diets and examined the impact of individual nutrients. One of her studies, published in 2018 and reported by Medscape Medical News, suggested that the presence of folate, phylloquinone, and lutein – nutrients found in relatively large amounts in green leafy vegetables – may account for why consuming a daily serving of these vegetables slows cognitive decline.
One of the most recent studies from Morris’ group, published in January 2020 and reported by Medscape Medical News at that time, provided the first evidence that dietary flavonols, which are found in many fruits and vegetables, are associated with a significantly reduced risk for dementia.
What Morris did so well was to “look at the big picture” and “think about commonalities that cross nutritional components” of diets such as MIND, DASH, the Mediterranean diet, and the Nordic diet, which is similar to the Mediterranean diet but highlights local foods such as fish from Nordic regions, Snyder told Medscape Medical News.
Morris was instrumental in getting the Alzheimer’s Association’s US POINTER (US Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk) study off the ground. The 2-year clinical trial is testing whether combining a healthy diet with exercise, cognitive and social stimulation, and the management of cardiovascular conditions protects cognitive function in older adults who are at increased risk for cognitive decline.
This study will be part of her legacy, said Snyder.
“She will be remembered for her perseverance to get us to a place where we can be looking at nutrition as a modifiable risk factor and now testing it in trials that she helped to set up,” she said.
Even before her involvement with US POINTER, Morris had long been an active volunteer for the Alzheimer’s Association, said Snyder.
“She contributed significant time and expertise as we looked at the state of the evidence around nutrition and other lifestyle and behavioral interventions.”
We’ll ‘always have Paris’
While Morris was “truly passionate” about diet and health “both professionally and personally,” she also had a fun side, said Schneider. She remembers she and Morris had a chance meeting in Paris, where they spent an entire day going to museums and restaurants and just talking about life and their travels. To the end, they joked they would “always have Paris,” said Schneider.
She was also a loyal friend. Morris threw a baby shower when Schneider was pregnant, organizing every detail, despite her extremely busy schedule.
Family was another of Morris’s passions. Snyder recalls Morris’s face lighting up when she talked about her children and grandchildren. She also remembers her friend’s zest for life. “She had an energy that was contagious.”
Morris also loved the outdoors and was a keen adventurer. She once trained for weeks before a long bike trip with her daughter and would take a helicopter to access remote backcountry on hiking excursions.
“She wanted to try everything,” said Schneider.
An author or contributor to more than 80 articles in peer-reviewed journals, Morris also served two terms (from 2011 to 2013) as chair of the NIH’s Neurological, Aging and Musculoskeletal Epidemiology Study Section.
She left behind multiple grants for various studies. One unique study, said Schneider, investigated the relationship between iron and other metals in the brain and the neuropathology of Alzheimer disease.
“She was really in the prime of her career,” noted Schneider. “She had so much left to give and to offer, so this is tremendously sad.”
According to news reports, Morris (nee Chinn) grew up in Homewood, Illinois, and earned bachelor’s and master’s degrees in sociology from the University of Iowa in Iowa City, where she met her husband, James Morris. The two married in 1978 and had three children.
Morris completed a doctorate in epidemiology at the Harvard School of Public Health. James died in 2012, also from cancer. Morris passed away peacefully at her home on February 15.
Martha Clare Morris, ScD, a pioneer in research linking nutrition to brain health and a creator of the breakthrough MIND diet, has died of cancer at the age of 64.
Morris was a professor in the Department of Internal Medicine, assistant provost of community research, and director of the Rush Institute for Healthy Aging at Rush University, in Chicago, Illinois. She was also a director of the internal medicine department’s Section of Community Epidemiology.
Long-time friend and colleague Julie A. Schneider, MD, the Deborah R. and Edgar D. Jannotta Presidential Professor of Pathology and Neurological Sciences, Rush University Medical Center, described Morris as creative, passionate, and adventurous.
Her death was “a shock” to the scientific community, Schneider told Medscape Medical News.
“It’s a tragic loss in so many ways,” said Schneider, who is also associate director of the Rush Alzheimer’s Disease Center. She was a very well-respected nutritional epidemiologist and was passionate about her work; she had just so much unwavering commitment to it.
Diet, said Schneider, is “notoriously a hard thing to study” because “it’s so intertwined with lifestyle” and other factors that create “barriers” to conducting such research.
But Morris had a unique and creative talent for filtering out what might be the individual contribution of a particular modifiable risk factor, said Heather Snyder, PhD, vice president of medical and scientific relations, Alzheimer’s Association, who also knew Morris both personally and professionally.
“Humble” trailblazer
Morris’s pioneering research examined the connection between nutrition and the prevention of cognitive decline. Taking results from this research, she developed the MIND diet – a hybrid of the Mediterranean diet and the Dietary Approaches to Stop Hypertension – along with colleagues at both Rush and Harvard Universities.
The MIND diet – an acronym for Mediterranean-DASH Intervention for Neurodegenerative Delay – emphasizes brain-healthy foods, including leafy green vegetables, nuts, berries, chicken, fish, whole grains, beans, olive oil, and moderate amounts of red wine. The diet limits consumption of red meat, butter, margarine, and processed foods.
In 2015, Morris published her initial findings on the MIND diet in Alzheimer’s and Dementia. Reported by Medscape Medical News at that time, the study showed that the diet protected cardiovascular health and slowed cognitive decline in older individuals.
The excitement around the findings inspired Morris to write “Diet for the Mind,” which was published in 2017. The book summarizes the benefits of the MIND diet and includes brain-healthy recipes created by her daughter Laura, who is a chef. Despite many accolades, Morris was “humble” about this project, said Schneider.
“This was not about publicity and trying to get a book out; she wanted to see if this diet really was going to change people’s lives. She wanted to bring it into the community,” she said.
Proud legacy
Since 2017, Morris had led a large clinical trial of the effectiveness of the MIND diet in preventing cognitive decline. The first study of its kind, the trial received a $14.5 million grant from the National Institutes of Health (NIH). Results of this study are expected in 2021.
The MIND diet was ranked among the top 10 diets for five consecutive years in US News and World Report.
Morris’s nutrition-related research went beyond diets and examined the impact of individual nutrients. One of her studies, published in 2018 and reported by Medscape Medical News, suggested that the presence of folate, phylloquinone, and lutein – nutrients found in relatively large amounts in green leafy vegetables – may account for why consuming a daily serving of these vegetables slows cognitive decline.
One of the most recent studies from Morris’ group, published in January 2020 and reported by Medscape Medical News at that time, provided the first evidence that dietary flavonols, which are found in many fruits and vegetables, are associated with a significantly reduced risk for dementia.
What Morris did so well was to “look at the big picture” and “think about commonalities that cross nutritional components” of diets such as MIND, DASH, the Mediterranean diet, and the Nordic diet, which is similar to the Mediterranean diet but highlights local foods such as fish from Nordic regions, Snyder told Medscape Medical News.
Morris was instrumental in getting the Alzheimer’s Association’s US POINTER (US Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk) study off the ground. The 2-year clinical trial is testing whether combining a healthy diet with exercise, cognitive and social stimulation, and the management of cardiovascular conditions protects cognitive function in older adults who are at increased risk for cognitive decline.
This study will be part of her legacy, said Snyder.
“She will be remembered for her perseverance to get us to a place where we can be looking at nutrition as a modifiable risk factor and now testing it in trials that she helped to set up,” she said.
Even before her involvement with US POINTER, Morris had long been an active volunteer for the Alzheimer’s Association, said Snyder.
“She contributed significant time and expertise as we looked at the state of the evidence around nutrition and other lifestyle and behavioral interventions.”
We’ll ‘always have Paris’
While Morris was “truly passionate” about diet and health “both professionally and personally,” she also had a fun side, said Schneider. She remembers she and Morris had a chance meeting in Paris, where they spent an entire day going to museums and restaurants and just talking about life and their travels. To the end, they joked they would “always have Paris,” said Schneider.
She was also a loyal friend. Morris threw a baby shower when Schneider was pregnant, organizing every detail, despite her extremely busy schedule.
Family was another of Morris’s passions. Snyder recalls Morris’s face lighting up when she talked about her children and grandchildren. She also remembers her friend’s zest for life. “She had an energy that was contagious.”
Morris also loved the outdoors and was a keen adventurer. She once trained for weeks before a long bike trip with her daughter and would take a helicopter to access remote backcountry on hiking excursions.
“She wanted to try everything,” said Schneider.
An author or contributor to more than 80 articles in peer-reviewed journals, Morris also served two terms (from 2011 to 2013) as chair of the NIH’s Neurological, Aging and Musculoskeletal Epidemiology Study Section.
She left behind multiple grants for various studies. One unique study, said Schneider, investigated the relationship between iron and other metals in the brain and the neuropathology of Alzheimer disease.
“She was really in the prime of her career,” noted Schneider. “She had so much left to give and to offer, so this is tremendously sad.”
According to news reports, Morris (nee Chinn) grew up in Homewood, Illinois, and earned bachelor’s and master’s degrees in sociology from the University of Iowa in Iowa City, where she met her husband, James Morris. The two married in 1978 and had three children.
Morris completed a doctorate in epidemiology at the Harvard School of Public Health. James died in 2012, also from cancer. Morris passed away peacefully at her home on February 15.
Martha Clare Morris, ScD, a pioneer in research linking nutrition to brain health and a creator of the breakthrough MIND diet, has died of cancer at the age of 64.
Morris was a professor in the Department of Internal Medicine, assistant provost of community research, and director of the Rush Institute for Healthy Aging at Rush University, in Chicago, Illinois. She was also a director of the internal medicine department’s Section of Community Epidemiology.
Long-time friend and colleague Julie A. Schneider, MD, the Deborah R. and Edgar D. Jannotta Presidential Professor of Pathology and Neurological Sciences, Rush University Medical Center, described Morris as creative, passionate, and adventurous.
Her death was “a shock” to the scientific community, Schneider told Medscape Medical News.
“It’s a tragic loss in so many ways,” said Schneider, who is also associate director of the Rush Alzheimer’s Disease Center. She was a very well-respected nutritional epidemiologist and was passionate about her work; she had just so much unwavering commitment to it.
Diet, said Schneider, is “notoriously a hard thing to study” because “it’s so intertwined with lifestyle” and other factors that create “barriers” to conducting such research.
But Morris had a unique and creative talent for filtering out what might be the individual contribution of a particular modifiable risk factor, said Heather Snyder, PhD, vice president of medical and scientific relations, Alzheimer’s Association, who also knew Morris both personally and professionally.
“Humble” trailblazer
Morris’s pioneering research examined the connection between nutrition and the prevention of cognitive decline. Taking results from this research, she developed the MIND diet – a hybrid of the Mediterranean diet and the Dietary Approaches to Stop Hypertension – along with colleagues at both Rush and Harvard Universities.
The MIND diet – an acronym for Mediterranean-DASH Intervention for Neurodegenerative Delay – emphasizes brain-healthy foods, including leafy green vegetables, nuts, berries, chicken, fish, whole grains, beans, olive oil, and moderate amounts of red wine. The diet limits consumption of red meat, butter, margarine, and processed foods.
In 2015, Morris published her initial findings on the MIND diet in Alzheimer’s and Dementia. Reported by Medscape Medical News at that time, the study showed that the diet protected cardiovascular health and slowed cognitive decline in older individuals.
The excitement around the findings inspired Morris to write “Diet for the Mind,” which was published in 2017. The book summarizes the benefits of the MIND diet and includes brain-healthy recipes created by her daughter Laura, who is a chef. Despite many accolades, Morris was “humble” about this project, said Schneider.
“This was not about publicity and trying to get a book out; she wanted to see if this diet really was going to change people’s lives. She wanted to bring it into the community,” she said.
Proud legacy
Since 2017, Morris had led a large clinical trial of the effectiveness of the MIND diet in preventing cognitive decline. The first study of its kind, the trial received a $14.5 million grant from the National Institutes of Health (NIH). Results of this study are expected in 2021.
The MIND diet was ranked among the top 10 diets for five consecutive years in US News and World Report.
Morris’s nutrition-related research went beyond diets and examined the impact of individual nutrients. One of her studies, published in 2018 and reported by Medscape Medical News, suggested that the presence of folate, phylloquinone, and lutein – nutrients found in relatively large amounts in green leafy vegetables – may account for why consuming a daily serving of these vegetables slows cognitive decline.
One of the most recent studies from Morris’ group, published in January 2020 and reported by Medscape Medical News at that time, provided the first evidence that dietary flavonols, which are found in many fruits and vegetables, are associated with a significantly reduced risk for dementia.
What Morris did so well was to “look at the big picture” and “think about commonalities that cross nutritional components” of diets such as MIND, DASH, the Mediterranean diet, and the Nordic diet, which is similar to the Mediterranean diet but highlights local foods such as fish from Nordic regions, Snyder told Medscape Medical News.
Morris was instrumental in getting the Alzheimer’s Association’s US POINTER (US Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk) study off the ground. The 2-year clinical trial is testing whether combining a healthy diet with exercise, cognitive and social stimulation, and the management of cardiovascular conditions protects cognitive function in older adults who are at increased risk for cognitive decline.
This study will be part of her legacy, said Snyder.
“She will be remembered for her perseverance to get us to a place where we can be looking at nutrition as a modifiable risk factor and now testing it in trials that she helped to set up,” she said.
Even before her involvement with US POINTER, Morris had long been an active volunteer for the Alzheimer’s Association, said Snyder.
“She contributed significant time and expertise as we looked at the state of the evidence around nutrition and other lifestyle and behavioral interventions.”
We’ll ‘always have Paris’
While Morris was “truly passionate” about diet and health “both professionally and personally,” she also had a fun side, said Schneider. She remembers she and Morris had a chance meeting in Paris, where they spent an entire day going to museums and restaurants and just talking about life and their travels. To the end, they joked they would “always have Paris,” said Schneider.
She was also a loyal friend. Morris threw a baby shower when Schneider was pregnant, organizing every detail, despite her extremely busy schedule.
Family was another of Morris’s passions. Snyder recalls Morris’s face lighting up when she talked about her children and grandchildren. She also remembers her friend’s zest for life. “She had an energy that was contagious.”
Morris also loved the outdoors and was a keen adventurer. She once trained for weeks before a long bike trip with her daughter and would take a helicopter to access remote backcountry on hiking excursions.
“She wanted to try everything,” said Schneider.
An author or contributor to more than 80 articles in peer-reviewed journals, Morris also served two terms (from 2011 to 2013) as chair of the NIH’s Neurological, Aging and Musculoskeletal Epidemiology Study Section.
She left behind multiple grants for various studies. One unique study, said Schneider, investigated the relationship between iron and other metals in the brain and the neuropathology of Alzheimer disease.
“She was really in the prime of her career,” noted Schneider. “She had so much left to give and to offer, so this is tremendously sad.”
According to news reports, Morris (nee Chinn) grew up in Homewood, Illinois, and earned bachelor’s and master’s degrees in sociology from the University of Iowa in Iowa City, where she met her husband, James Morris. The two married in 1978 and had three children.
Morris completed a doctorate in epidemiology at the Harvard School of Public Health. James died in 2012, also from cancer. Morris passed away peacefully at her home on February 15.








