User login
Formerly Skin & Allergy News
ass lick
assault rifle
balls
ballsac
black jack
bleach
Boko Haram
bondage
causas
cheap
child abuse
cocaine
compulsive behaviors
cost of miracles
cunt
Daech
display network stats
drug paraphernalia
explosion
fart
fda and death
fda AND warn
fda AND warning
fda AND warns
feom
fuck
gambling
gfc
gun
human trafficking
humira AND expensive
illegal
ISIL
ISIS
Islamic caliphate
Islamic state
madvocate
masturbation
mixed martial arts
MMA
molestation
national rifle association
NRA
nsfw
nuccitelli
pedophile
pedophilia
poker
porn
porn
pornography
psychedelic drug
recreational drug
sex slave rings
shit
slot machine
snort
substance abuse
terrorism
terrorist
texarkana
Texas hold 'em
UFC
section[contains(@class, 'nav-hidden')]
section[contains(@class, 'nav-hidden active')]
The leading independent newspaper covering dermatology news and commentary.
Will monkeypox be the ‘syphilis of the 21st century’?
PARIS – France is boosting its vaccination campaign in response to the increase in cases of monkeypox. After a sluggish start, newly appointed French health minister François Braun has announced the release of 42,000 vaccine doses. At the same time, medical students will be able to lend a helping hand at vaccination sites. However, some experts have criticized the measures taken as being too lax to combat what the World Health Organization has designated a global health emergency.
For Benjamin Davido, MD, MSc, PhD, an infectious disease specialist at the Raymond-Poincaré Hospital (Paris Public Hospital Trust, AP-HP, Garches region), the risks of this disease have been minimized and the measures taken are not adequate, despite the ready availability of the tools needed to manage the epidemic. We must remain alert to the risks posed by this monkeypox epidemic, which seems different from the sporadic outbreaks that usually crop up in Central and West Africa, he said. Dr. Davido recently shared his opinions in an interview.
Question: What do you think about the monkeypox vaccination campaign currently underway in France?
Dr. Davido: It doesn’t go far enough, and I am surprised by the lack of a concrete and specific objective. It seems we have to wait until the fire is out of control before we can call the fire department. We should have been more reactive and taken a more drastic approach from the get-go. In France, as in other countries affected by this epidemic, we are still, unfortunately, in a phase of observation, reassuring ourselves that this will surely not become another pandemic, as that would be really bad luck.
Yet we find ourselves in an unprecedented situation: We have known about the disease in question for a long time, the target population has been identified, and we have a vaccine immediately available. So, we have all the tools and knowledge acquired from the COVID-19 pandemic at our disposal, yet we are choosing to wait and see. We have clearly underestimated the risks of failing after a stalled start to the vaccination campaign.
Question: What exactly are the risks, in your opinion? Should we already be worried about how the epidemic is progressing?
Dr. Davido: The situation is definitely worrying. I personally am convinced that this disease will be the syphilis of the 21st century. Although the risk is low, it is not beyond the bounds of possibility that this could be the start of a new pandemic. For the time being, its spread is limited to at-risk populations, mainly men who have sex with other men and who have multiple partners, which accounts for around 300,000 people in France. However, the risk for heterosexuals must not be minimized; we must not forget that this disease can also be transmitted through contact with an infected person and by respiratory droplets from people living in the same household. There have been recent cases of women and children infected with monkeypox. If monkeypox starts to spread in the community, rather than being a sexually transmitted infection, the epidemic could spread to the rest of the population. With the rise in cases, scientists are also concerned about transmission to animals. Monkeypox could become endemic like it is in Africa, where rodents are the main reservoir of the virus.
Question: What do we know about the dynamics of this epidemic? What can be done to effectively improve the situation?
Dr. Davido: Experience gained from African countries affected by monkeypox, as well as from the spate of cases that occurred in the United States in 2003, has shown us that the epidemic can be controlled once the cases have been contained. It is hoped that further waves of the epidemic can be avoided, providing the monkeypox vaccine achieves its objectives.
But we need to give ourselves the means to do so. The expansion of the vaccination program to the most at-risk populations in early July was the right decision. We have seen that ring vaccination targeting close-contact cases does not work with monkeypox. The current problem is that this vaccine is nearly exclusively restricted to hospital settings. We are making the same mistakes as [we did] at the start of the COVID-19 epidemic. We don’t have the right infrastructure in place for this vaccination program. We need to get doctors, paramedics, pharmacists, etc., involved. And cut back on the red tape. After embracing digital procedures during COVID-19, we find ourselves having to complete paper copies of documents for every single person attending a vaccination site. It just doesn’t make sense!
Question: You highlighted the lack of a clear objective with this vaccination campaign. What should we be aiming for?
Dr. Davido: During the COVID-19 vaccination campaign, there was a set number of people to be vaccinated within a given time frame. The approach demanded a fast pace and a desired outcome. Yes, it was an ambitious target from the get-go, but it was one that we stuck to. Currently, no figure, no target, has been set for the monkeypox vaccination program. Ideally, we would have completed the vaccination campaign before the start of the new school year to limit new infections.
As it stands now, only 10% of the target population has received the vaccine. There is talk of the summer period not being favorable. Yet I remember that last year, the COVID-19 vaccination program was strengthened in the middle of August. If the monkeypox vaccination campaign is not given a boost by the end of the summer, we run the risk of encouraging transmission of the virus between close contacts when different groups mix after being on holiday at the start of the new school year. I think that, first and foremost, we must make general practitioners aware of the disease and train them in how to diagnose it so that patients can be isolated and vaccinated as quickly as possible.
Question: There has also been talk of increasing the set 28-day period between the two doses, or even getting rid of it entirely. Would this perhaps lead to better vaccine uptake?
Dr. Davido: The United Kingdom has chosen to give a single dose and recommends a second dose after exposure. I am not sure that this is the best strategy. Although the efficacy data are still limited, the results are not as good after a single dose. According to initial data from the French National Agency for the Safety of Medicines and Health Products (the ANSM), the rate of seroconversion after one dose rises from 10% to 56% on D28 in healthy volunteers, but is between 77% and 89% 2 weeks after the second dose administered on D28.
So, the second dose is needed, especially as immunological memory seems to drop 2 years after the first injection. The U.S. Centers for Disease Control and Prevention proposes leaving 35 days between the two doses. I think this is a reasonable time frame. So, delaying the second dose makes administration of the first dose even easier because the second often fell in the middle of the holiday period and so we also save precious doses. If the time between doses is longer, we risk vaccinated individuals becoming lax and possibly being tempted to skip the “optional” booster or simply forgetting about it.
Question: Are people who have already had the smallpox vaccine better protected against monkeypox?
Dr. Davido: The efficacy of this vaccine against monkeypox is not perfect on a very long-term basis and, to be honest, we don’t really know the level of protection afforded by first-generation vaccines after 20 years. We must not forget that 20% of people infected with monkeypox were vaccinated against smallpox before mandatory vaccination for this disease was abolished [Editor’s note: The requirement of an initial dose of smallpox vaccine was lifted in 1979, once smallpox had been eradicated].
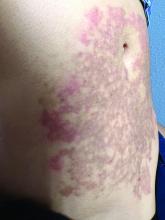
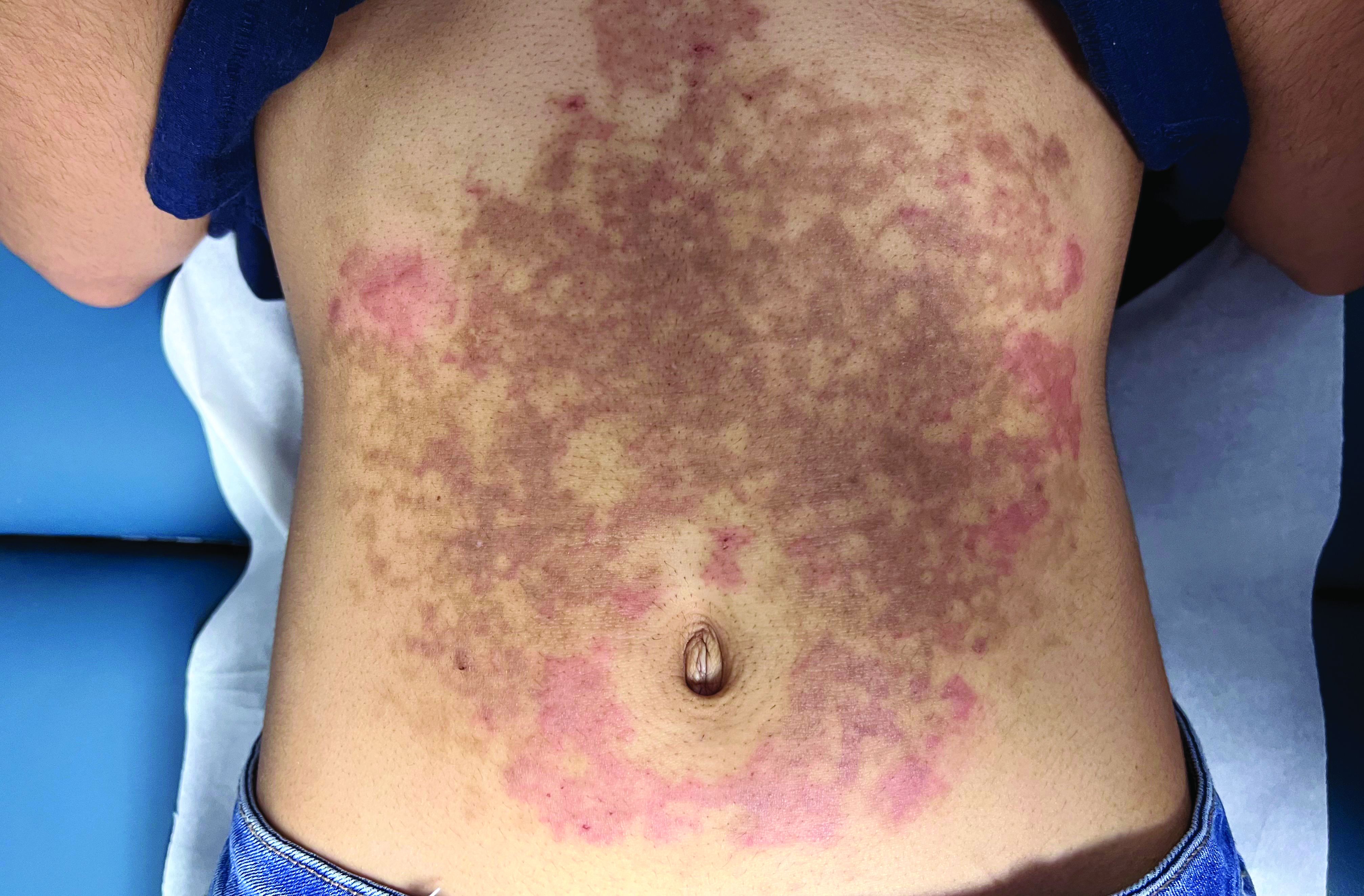
It is hoped that, as a minimum, this vaccine protects against serious illness. Yet in my department, we regularly see severe cases of monkeypox with widespread lesions in the over 45s, who are said to be vaccinated against smallpox.
Question: By comparison, is it likely that a third-generation vaccine would afford better protection against severe illness?
Dr. Davido: We still don’t have enough data or hindsight to assess the real-world impact of third-generation vaccines. This vaccine has a better tolerance profile than its predecessors, but we currently don’t know if it protects against severe forms of monkeypox. We also need to learn more about the disease causing the current epidemic, since it seems different from the sporadic outbreaks that usually crop up in Central and West Africa. The lesions seen are notably milder. The WHO has given this vaccine an efficacy level of 85% against infection by the monkeypox virus, but we must remain cautious: This figure is based on data from Africa. The epidemic in which we find ourselves is not the same. Overall, we must be wary of overly optimistic rhetoric around this new epidemic.
A version of this article appeared on Medscape.com. The article was translated from the Medscape French edition.
PARIS – France is boosting its vaccination campaign in response to the increase in cases of monkeypox. After a sluggish start, newly appointed French health minister François Braun has announced the release of 42,000 vaccine doses. At the same time, medical students will be able to lend a helping hand at vaccination sites. However, some experts have criticized the measures taken as being too lax to combat what the World Health Organization has designated a global health emergency.
For Benjamin Davido, MD, MSc, PhD, an infectious disease specialist at the Raymond-Poincaré Hospital (Paris Public Hospital Trust, AP-HP, Garches region), the risks of this disease have been minimized and the measures taken are not adequate, despite the ready availability of the tools needed to manage the epidemic. We must remain alert to the risks posed by this monkeypox epidemic, which seems different from the sporadic outbreaks that usually crop up in Central and West Africa, he said. Dr. Davido recently shared his opinions in an interview.
Question: What do you think about the monkeypox vaccination campaign currently underway in France?
Dr. Davido: It doesn’t go far enough, and I am surprised by the lack of a concrete and specific objective. It seems we have to wait until the fire is out of control before we can call the fire department. We should have been more reactive and taken a more drastic approach from the get-go. In France, as in other countries affected by this epidemic, we are still, unfortunately, in a phase of observation, reassuring ourselves that this will surely not become another pandemic, as that would be really bad luck.
Yet we find ourselves in an unprecedented situation: We have known about the disease in question for a long time, the target population has been identified, and we have a vaccine immediately available. So, we have all the tools and knowledge acquired from the COVID-19 pandemic at our disposal, yet we are choosing to wait and see. We have clearly underestimated the risks of failing after a stalled start to the vaccination campaign.
Question: What exactly are the risks, in your opinion? Should we already be worried about how the epidemic is progressing?
Dr. Davido: The situation is definitely worrying. I personally am convinced that this disease will be the syphilis of the 21st century. Although the risk is low, it is not beyond the bounds of possibility that this could be the start of a new pandemic. For the time being, its spread is limited to at-risk populations, mainly men who have sex with other men and who have multiple partners, which accounts for around 300,000 people in France. However, the risk for heterosexuals must not be minimized; we must not forget that this disease can also be transmitted through contact with an infected person and by respiratory droplets from people living in the same household. There have been recent cases of women and children infected with monkeypox. If monkeypox starts to spread in the community, rather than being a sexually transmitted infection, the epidemic could spread to the rest of the population. With the rise in cases, scientists are also concerned about transmission to animals. Monkeypox could become endemic like it is in Africa, where rodents are the main reservoir of the virus.
Question: What do we know about the dynamics of this epidemic? What can be done to effectively improve the situation?
Dr. Davido: Experience gained from African countries affected by monkeypox, as well as from the spate of cases that occurred in the United States in 2003, has shown us that the epidemic can be controlled once the cases have been contained. It is hoped that further waves of the epidemic can be avoided, providing the monkeypox vaccine achieves its objectives.
But we need to give ourselves the means to do so. The expansion of the vaccination program to the most at-risk populations in early July was the right decision. We have seen that ring vaccination targeting close-contact cases does not work with monkeypox. The current problem is that this vaccine is nearly exclusively restricted to hospital settings. We are making the same mistakes as [we did] at the start of the COVID-19 epidemic. We don’t have the right infrastructure in place for this vaccination program. We need to get doctors, paramedics, pharmacists, etc., involved. And cut back on the red tape. After embracing digital procedures during COVID-19, we find ourselves having to complete paper copies of documents for every single person attending a vaccination site. It just doesn’t make sense!
Question: You highlighted the lack of a clear objective with this vaccination campaign. What should we be aiming for?
Dr. Davido: During the COVID-19 vaccination campaign, there was a set number of people to be vaccinated within a given time frame. The approach demanded a fast pace and a desired outcome. Yes, it was an ambitious target from the get-go, but it was one that we stuck to. Currently, no figure, no target, has been set for the monkeypox vaccination program. Ideally, we would have completed the vaccination campaign before the start of the new school year to limit new infections.
As it stands now, only 10% of the target population has received the vaccine. There is talk of the summer period not being favorable. Yet I remember that last year, the COVID-19 vaccination program was strengthened in the middle of August. If the monkeypox vaccination campaign is not given a boost by the end of the summer, we run the risk of encouraging transmission of the virus between close contacts when different groups mix after being on holiday at the start of the new school year. I think that, first and foremost, we must make general practitioners aware of the disease and train them in how to diagnose it so that patients can be isolated and vaccinated as quickly as possible.
Question: There has also been talk of increasing the set 28-day period between the two doses, or even getting rid of it entirely. Would this perhaps lead to better vaccine uptake?
Dr. Davido: The United Kingdom has chosen to give a single dose and recommends a second dose after exposure. I am not sure that this is the best strategy. Although the efficacy data are still limited, the results are not as good after a single dose. According to initial data from the French National Agency for the Safety of Medicines and Health Products (the ANSM), the rate of seroconversion after one dose rises from 10% to 56% on D28 in healthy volunteers, but is between 77% and 89% 2 weeks after the second dose administered on D28.
So, the second dose is needed, especially as immunological memory seems to drop 2 years after the first injection. The U.S. Centers for Disease Control and Prevention proposes leaving 35 days between the two doses. I think this is a reasonable time frame. So, delaying the second dose makes administration of the first dose even easier because the second often fell in the middle of the holiday period and so we also save precious doses. If the time between doses is longer, we risk vaccinated individuals becoming lax and possibly being tempted to skip the “optional” booster or simply forgetting about it.
Question: Are people who have already had the smallpox vaccine better protected against monkeypox?
Dr. Davido: The efficacy of this vaccine against monkeypox is not perfect on a very long-term basis and, to be honest, we don’t really know the level of protection afforded by first-generation vaccines after 20 years. We must not forget that 20% of people infected with monkeypox were vaccinated against smallpox before mandatory vaccination for this disease was abolished [Editor’s note: The requirement of an initial dose of smallpox vaccine was lifted in 1979, once smallpox had been eradicated].
It is hoped that, as a minimum, this vaccine protects against serious illness. Yet in my department, we regularly see severe cases of monkeypox with widespread lesions in the over 45s, who are said to be vaccinated against smallpox.
Question: By comparison, is it likely that a third-generation vaccine would afford better protection against severe illness?
Dr. Davido: We still don’t have enough data or hindsight to assess the real-world impact of third-generation vaccines. This vaccine has a better tolerance profile than its predecessors, but we currently don’t know if it protects against severe forms of monkeypox. We also need to learn more about the disease causing the current epidemic, since it seems different from the sporadic outbreaks that usually crop up in Central and West Africa. The lesions seen are notably milder. The WHO has given this vaccine an efficacy level of 85% against infection by the monkeypox virus, but we must remain cautious: This figure is based on data from Africa. The epidemic in which we find ourselves is not the same. Overall, we must be wary of overly optimistic rhetoric around this new epidemic.
A version of this article appeared on Medscape.com. The article was translated from the Medscape French edition.
PARIS – France is boosting its vaccination campaign in response to the increase in cases of monkeypox. After a sluggish start, newly appointed French health minister François Braun has announced the release of 42,000 vaccine doses. At the same time, medical students will be able to lend a helping hand at vaccination sites. However, some experts have criticized the measures taken as being too lax to combat what the World Health Organization has designated a global health emergency.
For Benjamin Davido, MD, MSc, PhD, an infectious disease specialist at the Raymond-Poincaré Hospital (Paris Public Hospital Trust, AP-HP, Garches region), the risks of this disease have been minimized and the measures taken are not adequate, despite the ready availability of the tools needed to manage the epidemic. We must remain alert to the risks posed by this monkeypox epidemic, which seems different from the sporadic outbreaks that usually crop up in Central and West Africa, he said. Dr. Davido recently shared his opinions in an interview.
Question: What do you think about the monkeypox vaccination campaign currently underway in France?
Dr. Davido: It doesn’t go far enough, and I am surprised by the lack of a concrete and specific objective. It seems we have to wait until the fire is out of control before we can call the fire department. We should have been more reactive and taken a more drastic approach from the get-go. In France, as in other countries affected by this epidemic, we are still, unfortunately, in a phase of observation, reassuring ourselves that this will surely not become another pandemic, as that would be really bad luck.
Yet we find ourselves in an unprecedented situation: We have known about the disease in question for a long time, the target population has been identified, and we have a vaccine immediately available. So, we have all the tools and knowledge acquired from the COVID-19 pandemic at our disposal, yet we are choosing to wait and see. We have clearly underestimated the risks of failing after a stalled start to the vaccination campaign.
Question: What exactly are the risks, in your opinion? Should we already be worried about how the epidemic is progressing?
Dr. Davido: The situation is definitely worrying. I personally am convinced that this disease will be the syphilis of the 21st century. Although the risk is low, it is not beyond the bounds of possibility that this could be the start of a new pandemic. For the time being, its spread is limited to at-risk populations, mainly men who have sex with other men and who have multiple partners, which accounts for around 300,000 people in France. However, the risk for heterosexuals must not be minimized; we must not forget that this disease can also be transmitted through contact with an infected person and by respiratory droplets from people living in the same household. There have been recent cases of women and children infected with monkeypox. If monkeypox starts to spread in the community, rather than being a sexually transmitted infection, the epidemic could spread to the rest of the population. With the rise in cases, scientists are also concerned about transmission to animals. Monkeypox could become endemic like it is in Africa, where rodents are the main reservoir of the virus.
Question: What do we know about the dynamics of this epidemic? What can be done to effectively improve the situation?
Dr. Davido: Experience gained from African countries affected by monkeypox, as well as from the spate of cases that occurred in the United States in 2003, has shown us that the epidemic can be controlled once the cases have been contained. It is hoped that further waves of the epidemic can be avoided, providing the monkeypox vaccine achieves its objectives.
But we need to give ourselves the means to do so. The expansion of the vaccination program to the most at-risk populations in early July was the right decision. We have seen that ring vaccination targeting close-contact cases does not work with monkeypox. The current problem is that this vaccine is nearly exclusively restricted to hospital settings. We are making the same mistakes as [we did] at the start of the COVID-19 epidemic. We don’t have the right infrastructure in place for this vaccination program. We need to get doctors, paramedics, pharmacists, etc., involved. And cut back on the red tape. After embracing digital procedures during COVID-19, we find ourselves having to complete paper copies of documents for every single person attending a vaccination site. It just doesn’t make sense!
Question: You highlighted the lack of a clear objective with this vaccination campaign. What should we be aiming for?
Dr. Davido: During the COVID-19 vaccination campaign, there was a set number of people to be vaccinated within a given time frame. The approach demanded a fast pace and a desired outcome. Yes, it was an ambitious target from the get-go, but it was one that we stuck to. Currently, no figure, no target, has been set for the monkeypox vaccination program. Ideally, we would have completed the vaccination campaign before the start of the new school year to limit new infections.
As it stands now, only 10% of the target population has received the vaccine. There is talk of the summer period not being favorable. Yet I remember that last year, the COVID-19 vaccination program was strengthened in the middle of August. If the monkeypox vaccination campaign is not given a boost by the end of the summer, we run the risk of encouraging transmission of the virus between close contacts when different groups mix after being on holiday at the start of the new school year. I think that, first and foremost, we must make general practitioners aware of the disease and train them in how to diagnose it so that patients can be isolated and vaccinated as quickly as possible.
Question: There has also been talk of increasing the set 28-day period between the two doses, or even getting rid of it entirely. Would this perhaps lead to better vaccine uptake?
Dr. Davido: The United Kingdom has chosen to give a single dose and recommends a second dose after exposure. I am not sure that this is the best strategy. Although the efficacy data are still limited, the results are not as good after a single dose. According to initial data from the French National Agency for the Safety of Medicines and Health Products (the ANSM), the rate of seroconversion after one dose rises from 10% to 56% on D28 in healthy volunteers, but is between 77% and 89% 2 weeks after the second dose administered on D28.
So, the second dose is needed, especially as immunological memory seems to drop 2 years after the first injection. The U.S. Centers for Disease Control and Prevention proposes leaving 35 days between the two doses. I think this is a reasonable time frame. So, delaying the second dose makes administration of the first dose even easier because the second often fell in the middle of the holiday period and so we also save precious doses. If the time between doses is longer, we risk vaccinated individuals becoming lax and possibly being tempted to skip the “optional” booster or simply forgetting about it.
Question: Are people who have already had the smallpox vaccine better protected against monkeypox?
Dr. Davido: The efficacy of this vaccine against monkeypox is not perfect on a very long-term basis and, to be honest, we don’t really know the level of protection afforded by first-generation vaccines after 20 years. We must not forget that 20% of people infected with monkeypox were vaccinated against smallpox before mandatory vaccination for this disease was abolished [Editor’s note: The requirement of an initial dose of smallpox vaccine was lifted in 1979, once smallpox had been eradicated].
It is hoped that, as a minimum, this vaccine protects against serious illness. Yet in my department, we regularly see severe cases of monkeypox with widespread lesions in the over 45s, who are said to be vaccinated against smallpox.
Question: By comparison, is it likely that a third-generation vaccine would afford better protection against severe illness?
Dr. Davido: We still don’t have enough data or hindsight to assess the real-world impact of third-generation vaccines. This vaccine has a better tolerance profile than its predecessors, but we currently don’t know if it protects against severe forms of monkeypox. We also need to learn more about the disease causing the current epidemic, since it seems different from the sporadic outbreaks that usually crop up in Central and West Africa. The lesions seen are notably milder. The WHO has given this vaccine an efficacy level of 85% against infection by the monkeypox virus, but we must remain cautious: This figure is based on data from Africa. The epidemic in which we find ourselves is not the same. Overall, we must be wary of overly optimistic rhetoric around this new epidemic.
A version of this article appeared on Medscape.com. The article was translated from the Medscape French edition.
Consider essential oil allergy in patient with dermatitis
PORTLAND, ORE. – When patients present to Brandon L. Adler, MD, with dermatitis on the eyelid, face, or neck, he routinely asks them if they apply essential oils on their skin, or if they have an essential oil diffuser or nebulizer in their home.
“The answer is frequently ‘yes,’ ” Dr. Adler, clinical assistant professor of dermatology at the University of Southern California, Los Angeles, said at the annual meeting of the Pacific Dermatologic Association. “Essential oils are widely used throughout the wellness industry. They are contained in personal care products, beauty products, natural cleaning products, and they’re being diffused by our patients into the air. More than 75 essential oils are reported to cause allergic contact dermatitis.”
“Linalool is most classically associated with lavender, while limonene is associated with citrus, but they’re found in many different plants,” said Dr. Adler, who directs USC’s contact dermatitis clinic. “On their own, linalool and limonene are not particularly allergenic; they’re not a big deal in the patch test clinic. The problem comes when we add air to the mix, because they oxidize to hydroperoxides of linalool and limonene. These are quite potent allergens.”
According to the most recent North American Contact Dermatitis Group data, 8.9% of patients undergoing patch testing tested positive to linalool hydroperoxides and 2.6% were positive to limonene hydroperoxides.
Dr. Adler discussed the case of a female massage therapist who presented with refractory hand dermatitis and was on methotrexate and dupilumab at the time of consultation but was still symptomatic. She patch-tested positive to limonene and linalool hydroperoxides as well as multiple essential oils that she had been using with her clients, ranging from sacred frankincense oil to basil oil, and she was advised to massage using only coconut or vegetable oils.
Essential oil allergy may also be related to cannabis allergy. According to Dr. Adler, allergic contact dermatitis to cannabis has been rarely reported, but in an analysis of 103 commercial topical cannabinoid preparations that he published with Vincent DeLeo, MD, also with USC, 84% contained a NACDG allergen, frequently essential oils.
More recently, Dr. Adler and colleagues reported the case of a 40-year-old woman who was referred for patch testing for nummular dermatitis that wasn’t responding to treatment. The patient was found to be using topical cannabis and also grew cannabis at home. “She asked to be patch-tested to her homegrown cannabis and had a strong positive patch test to the cannabis, linalool and limonene hydroperoxides, and other essential oils,” Dr. Adler recalled. “We sent her cannabis sample for analysis at a commercial lab and found that it contained limonene and other allergenic terpene chemicals.
“We’re just starting to unravel what this means in terms of our patients and how to manage them, but many are using topical cannabis and topical CBD. I suspect this is a lot less rare than we realize.”
Another recent case from Europe reported allergic contact dermatitis to Cannabis sativa (hemp) seed oil following topical application, with positive patch testing.
Dr. Adler disclosed that he has received research grants from the American Contact Dermatitis Society. He is also an investigator for AbbVie and a consultant for the Skin Research Institute.
PORTLAND, ORE. – When patients present to Brandon L. Adler, MD, with dermatitis on the eyelid, face, or neck, he routinely asks them if they apply essential oils on their skin, or if they have an essential oil diffuser or nebulizer in their home.
“The answer is frequently ‘yes,’ ” Dr. Adler, clinical assistant professor of dermatology at the University of Southern California, Los Angeles, said at the annual meeting of the Pacific Dermatologic Association. “Essential oils are widely used throughout the wellness industry. They are contained in personal care products, beauty products, natural cleaning products, and they’re being diffused by our patients into the air. More than 75 essential oils are reported to cause allergic contact dermatitis.”
“Linalool is most classically associated with lavender, while limonene is associated with citrus, but they’re found in many different plants,” said Dr. Adler, who directs USC’s contact dermatitis clinic. “On their own, linalool and limonene are not particularly allergenic; they’re not a big deal in the patch test clinic. The problem comes when we add air to the mix, because they oxidize to hydroperoxides of linalool and limonene. These are quite potent allergens.”
According to the most recent North American Contact Dermatitis Group data, 8.9% of patients undergoing patch testing tested positive to linalool hydroperoxides and 2.6% were positive to limonene hydroperoxides.
Dr. Adler discussed the case of a female massage therapist who presented with refractory hand dermatitis and was on methotrexate and dupilumab at the time of consultation but was still symptomatic. She patch-tested positive to limonene and linalool hydroperoxides as well as multiple essential oils that she had been using with her clients, ranging from sacred frankincense oil to basil oil, and she was advised to massage using only coconut or vegetable oils.
Essential oil allergy may also be related to cannabis allergy. According to Dr. Adler, allergic contact dermatitis to cannabis has been rarely reported, but in an analysis of 103 commercial topical cannabinoid preparations that he published with Vincent DeLeo, MD, also with USC, 84% contained a NACDG allergen, frequently essential oils.
More recently, Dr. Adler and colleagues reported the case of a 40-year-old woman who was referred for patch testing for nummular dermatitis that wasn’t responding to treatment. The patient was found to be using topical cannabis and also grew cannabis at home. “She asked to be patch-tested to her homegrown cannabis and had a strong positive patch test to the cannabis, linalool and limonene hydroperoxides, and other essential oils,” Dr. Adler recalled. “We sent her cannabis sample for analysis at a commercial lab and found that it contained limonene and other allergenic terpene chemicals.
“We’re just starting to unravel what this means in terms of our patients and how to manage them, but many are using topical cannabis and topical CBD. I suspect this is a lot less rare than we realize.”
Another recent case from Europe reported allergic contact dermatitis to Cannabis sativa (hemp) seed oil following topical application, with positive patch testing.
Dr. Adler disclosed that he has received research grants from the American Contact Dermatitis Society. He is also an investigator for AbbVie and a consultant for the Skin Research Institute.
PORTLAND, ORE. – When patients present to Brandon L. Adler, MD, with dermatitis on the eyelid, face, or neck, he routinely asks them if they apply essential oils on their skin, or if they have an essential oil diffuser or nebulizer in their home.
“The answer is frequently ‘yes,’ ” Dr. Adler, clinical assistant professor of dermatology at the University of Southern California, Los Angeles, said at the annual meeting of the Pacific Dermatologic Association. “Essential oils are widely used throughout the wellness industry. They are contained in personal care products, beauty products, natural cleaning products, and they’re being diffused by our patients into the air. More than 75 essential oils are reported to cause allergic contact dermatitis.”
“Linalool is most classically associated with lavender, while limonene is associated with citrus, but they’re found in many different plants,” said Dr. Adler, who directs USC’s contact dermatitis clinic. “On their own, linalool and limonene are not particularly allergenic; they’re not a big deal in the patch test clinic. The problem comes when we add air to the mix, because they oxidize to hydroperoxides of linalool and limonene. These are quite potent allergens.”
According to the most recent North American Contact Dermatitis Group data, 8.9% of patients undergoing patch testing tested positive to linalool hydroperoxides and 2.6% were positive to limonene hydroperoxides.
Dr. Adler discussed the case of a female massage therapist who presented with refractory hand dermatitis and was on methotrexate and dupilumab at the time of consultation but was still symptomatic. She patch-tested positive to limonene and linalool hydroperoxides as well as multiple essential oils that she had been using with her clients, ranging from sacred frankincense oil to basil oil, and she was advised to massage using only coconut or vegetable oils.
Essential oil allergy may also be related to cannabis allergy. According to Dr. Adler, allergic contact dermatitis to cannabis has been rarely reported, but in an analysis of 103 commercial topical cannabinoid preparations that he published with Vincent DeLeo, MD, also with USC, 84% contained a NACDG allergen, frequently essential oils.
More recently, Dr. Adler and colleagues reported the case of a 40-year-old woman who was referred for patch testing for nummular dermatitis that wasn’t responding to treatment. The patient was found to be using topical cannabis and also grew cannabis at home. “She asked to be patch-tested to her homegrown cannabis and had a strong positive patch test to the cannabis, linalool and limonene hydroperoxides, and other essential oils,” Dr. Adler recalled. “We sent her cannabis sample for analysis at a commercial lab and found that it contained limonene and other allergenic terpene chemicals.
“We’re just starting to unravel what this means in terms of our patients and how to manage them, but many are using topical cannabis and topical CBD. I suspect this is a lot less rare than we realize.”
Another recent case from Europe reported allergic contact dermatitis to Cannabis sativa (hemp) seed oil following topical application, with positive patch testing.
Dr. Adler disclosed that he has received research grants from the American Contact Dermatitis Society. He is also an investigator for AbbVie and a consultant for the Skin Research Institute.
AT PDA 2022
Why it’s important for dermatologists to learn about JAK inhibitors
PORTLAND, ORE. – according to Andrew Blauvelt, MD, MBA.
“In dermatology, you need to know about JAK inhibitors, and you need to know how to use them,” Dr. Blauvelt, president of Oregon Medical Research Center, Portland, said at the annual meeting of the Pacific Dermatologic Association. “Making the choice, ‘I’m not going to use those drugs because of safety concerns,’ may be okay in 2022, but we are going to be getting a lot more indications for these drugs. So instead of avoiding JAK inhibitors, I would say try to learn [about] them, understand them, and get your messaging out on safety.”
It’s difficult to imagine a clinician-researcher who has more experience with the use of biologics and JAK inhibitors in AD than Dr. Blauvelt, who has been the international investigator on several important trials of treatments that include dupilumab, tralokinumab, abrocitinib, and upadacitinib for AD such as CHRONOS, ECZTEND, JADE REGIMEN, and HEADS UP. At the meeting, he discussed his clinical approach to selecting systemic agents for AD and shared prescribing tips. He began by noting that the approval of dupilumab for moderate to severe AD in 2017 ushered in a new era of treating the disease systemically.
“When it was approved, experts went right to dupilumab if they could, and avoided the use of cyclosporine or methotrexate,” said Dr. Blauvelt, who is also an elected member of the American Society for Clinical Investigation and the International Eczema Council. “I still think that dupilumab is a great agent to start with. We’ve had a bit of difficulty improving upon it.”
Following dupilumab’s approval, three other systemic options became available for patients with moderate to severe AD: the human IgG4 monoclonal antibody tralokinumab that binds to interleukin-13, which is administered subcutaneously; and, more recently, the oral JAK inhibitors abrocitinib and upadacitinib, approved in January for moderate to severe AD.
“I’m a big fan of JAK inhibitors because I think they offer things that biologic and topical therapies can’t offer,” Dr. Blauvelt said. “Patients like the pills versus shots. They also like the speed; JAK inhibitors work faster than dupilumab and tralokinumab. So, if you have a patient with bad AD who wants to get better quickly, that would be a reason to choose a JAK inhibitor over a biologic if you can.”
When Dr. Blauvelt has asked AD clinical trial participants if they’d rather be treated with a biologic agent or with a JAK inhibitor, about half choose one over the other.
“Patients who shy away from the safety issues would choose the biologic trial while the ones who wanted the fast relief would choose the JAK trial,” he said. “But if you present both options and the patients prefer a pill, I think the JAK inhibitors do better with a rapid control of inflammation as well as pruritus – the latter within 2 days of taking the pills.”
When counseling patients initiating a JAK inhibitor, Dr. Blauvelt mentioned three advantages, compared with biologics: the pill formulation, the rapidity of response in pruritus control, and better efficacy. “The downside is the safety,” he said. “Safety is the elephant in the room for the JAK inhibitors.”
The risks listed in the boxed warning in the labeling for JAK inhibitors include: an increased risk of serious bacterial, fungal, and opportunistic infections such as TB; a higher rate of all-cause mortality, including cardiovascular death; a higher rate of MACE (major adverse cardiovascular events, defined as cardiovascular death, MI, and stroke); the potential for malignancy, including lymphoma; and the potential for thrombosis, including an increased incidence of pulmonary embolism (PE).
“Risk of thrombosis seems to be a class effect for all JAK inhibitors,” Dr. Blauvelt said. “As far as I know, it’s idiosyncratic. For nearly all the DVT [deep vein thrombosis] cases that have been reported, patients had baseline risk factors for DVT and PE, which are obesity, smoking, and use of oral contraceptives.”
Dr. Blauvelt pointed out that the boxed warning related to mortality, malignancies, and MACE stemmed from a long-term trial of the JAK inhibitor tofacitinib in RA patients. “Those patients had to be at least 50 years old, 75% of them were on concomitant methotrexate and/or prednisone, and they had to have at least one cardiac risk factor to get into the trial,” he said.
“I’m not saying those things can’t happen in dermatology patients, but if you look at the safety data of JAK inhibitors in the AD studies and in the alopecia areata studies, we are seeing a few cases of these things here and there, but not major signals,” he said. To date, “they look safer in dermatologic diseases compared to tofacitinib in RA data in older populations.”
He emphasized the importance of discussing each of the risks in the boxed warning with patients who are candidates for JAK inhibitor therapy.
Dr. Blauvelt likened the lab monitoring required for JAK inhibitors to that required for methotrexate. This means ordering at baseline, a CBC with differential, a chem-20, a lipid panel, and a QuantiFERON-TB Gold test. The JAK inhibitor labels do not include information on the frequency of monitoring, “but I have a distinct opinion on this because of my blood test monitoring experience in the trials for many years,” he said.
“I think it’s good to do follow-up testing at 1 month, then every 3 months in the first year. In my experience, the people who drop blood cell counts or increase their lipids tend to do it in the first year.”
After 1 year of treatment, he continued, follow-up testing once every 6 months is reasonable. “If CPK [creatine phosphokinase] goes up, I don’t worry about it; it’s not clinically relevant. There is no recommendation for CPK monitoring, so if you’re getting that on your chem-20, I’d say don’t worry about it.”
Dr. Blauvelt reported that he is an investigator and a scientific adviser for several pharmaceutical companies developing treatments for AD, including companies that are evaluating or marketing JAK inhibitors for AD, including AbbVie, Incyte, and Pfizer, as well as dupilumab’s joint developers Sanofi and Regeneron.
PORTLAND, ORE. – according to Andrew Blauvelt, MD, MBA.
“In dermatology, you need to know about JAK inhibitors, and you need to know how to use them,” Dr. Blauvelt, president of Oregon Medical Research Center, Portland, said at the annual meeting of the Pacific Dermatologic Association. “Making the choice, ‘I’m not going to use those drugs because of safety concerns,’ may be okay in 2022, but we are going to be getting a lot more indications for these drugs. So instead of avoiding JAK inhibitors, I would say try to learn [about] them, understand them, and get your messaging out on safety.”
It’s difficult to imagine a clinician-researcher who has more experience with the use of biologics and JAK inhibitors in AD than Dr. Blauvelt, who has been the international investigator on several important trials of treatments that include dupilumab, tralokinumab, abrocitinib, and upadacitinib for AD such as CHRONOS, ECZTEND, JADE REGIMEN, and HEADS UP. At the meeting, he discussed his clinical approach to selecting systemic agents for AD and shared prescribing tips. He began by noting that the approval of dupilumab for moderate to severe AD in 2017 ushered in a new era of treating the disease systemically.
“When it was approved, experts went right to dupilumab if they could, and avoided the use of cyclosporine or methotrexate,” said Dr. Blauvelt, who is also an elected member of the American Society for Clinical Investigation and the International Eczema Council. “I still think that dupilumab is a great agent to start with. We’ve had a bit of difficulty improving upon it.”
Following dupilumab’s approval, three other systemic options became available for patients with moderate to severe AD: the human IgG4 monoclonal antibody tralokinumab that binds to interleukin-13, which is administered subcutaneously; and, more recently, the oral JAK inhibitors abrocitinib and upadacitinib, approved in January for moderate to severe AD.
“I’m a big fan of JAK inhibitors because I think they offer things that biologic and topical therapies can’t offer,” Dr. Blauvelt said. “Patients like the pills versus shots. They also like the speed; JAK inhibitors work faster than dupilumab and tralokinumab. So, if you have a patient with bad AD who wants to get better quickly, that would be a reason to choose a JAK inhibitor over a biologic if you can.”
When Dr. Blauvelt has asked AD clinical trial participants if they’d rather be treated with a biologic agent or with a JAK inhibitor, about half choose one over the other.
“Patients who shy away from the safety issues would choose the biologic trial while the ones who wanted the fast relief would choose the JAK trial,” he said. “But if you present both options and the patients prefer a pill, I think the JAK inhibitors do better with a rapid control of inflammation as well as pruritus – the latter within 2 days of taking the pills.”
When counseling patients initiating a JAK inhibitor, Dr. Blauvelt mentioned three advantages, compared with biologics: the pill formulation, the rapidity of response in pruritus control, and better efficacy. “The downside is the safety,” he said. “Safety is the elephant in the room for the JAK inhibitors.”
The risks listed in the boxed warning in the labeling for JAK inhibitors include: an increased risk of serious bacterial, fungal, and opportunistic infections such as TB; a higher rate of all-cause mortality, including cardiovascular death; a higher rate of MACE (major adverse cardiovascular events, defined as cardiovascular death, MI, and stroke); the potential for malignancy, including lymphoma; and the potential for thrombosis, including an increased incidence of pulmonary embolism (PE).
“Risk of thrombosis seems to be a class effect for all JAK inhibitors,” Dr. Blauvelt said. “As far as I know, it’s idiosyncratic. For nearly all the DVT [deep vein thrombosis] cases that have been reported, patients had baseline risk factors for DVT and PE, which are obesity, smoking, and use of oral contraceptives.”
Dr. Blauvelt pointed out that the boxed warning related to mortality, malignancies, and MACE stemmed from a long-term trial of the JAK inhibitor tofacitinib in RA patients. “Those patients had to be at least 50 years old, 75% of them were on concomitant methotrexate and/or prednisone, and they had to have at least one cardiac risk factor to get into the trial,” he said.
“I’m not saying those things can’t happen in dermatology patients, but if you look at the safety data of JAK inhibitors in the AD studies and in the alopecia areata studies, we are seeing a few cases of these things here and there, but not major signals,” he said. To date, “they look safer in dermatologic diseases compared to tofacitinib in RA data in older populations.”
He emphasized the importance of discussing each of the risks in the boxed warning with patients who are candidates for JAK inhibitor therapy.
Dr. Blauvelt likened the lab monitoring required for JAK inhibitors to that required for methotrexate. This means ordering at baseline, a CBC with differential, a chem-20, a lipid panel, and a QuantiFERON-TB Gold test. The JAK inhibitor labels do not include information on the frequency of monitoring, “but I have a distinct opinion on this because of my blood test monitoring experience in the trials for many years,” he said.
“I think it’s good to do follow-up testing at 1 month, then every 3 months in the first year. In my experience, the people who drop blood cell counts or increase their lipids tend to do it in the first year.”
After 1 year of treatment, he continued, follow-up testing once every 6 months is reasonable. “If CPK [creatine phosphokinase] goes up, I don’t worry about it; it’s not clinically relevant. There is no recommendation for CPK monitoring, so if you’re getting that on your chem-20, I’d say don’t worry about it.”
Dr. Blauvelt reported that he is an investigator and a scientific adviser for several pharmaceutical companies developing treatments for AD, including companies that are evaluating or marketing JAK inhibitors for AD, including AbbVie, Incyte, and Pfizer, as well as dupilumab’s joint developers Sanofi and Regeneron.
PORTLAND, ORE. – according to Andrew Blauvelt, MD, MBA.
“In dermatology, you need to know about JAK inhibitors, and you need to know how to use them,” Dr. Blauvelt, president of Oregon Medical Research Center, Portland, said at the annual meeting of the Pacific Dermatologic Association. “Making the choice, ‘I’m not going to use those drugs because of safety concerns,’ may be okay in 2022, but we are going to be getting a lot more indications for these drugs. So instead of avoiding JAK inhibitors, I would say try to learn [about] them, understand them, and get your messaging out on safety.”
It’s difficult to imagine a clinician-researcher who has more experience with the use of biologics and JAK inhibitors in AD than Dr. Blauvelt, who has been the international investigator on several important trials of treatments that include dupilumab, tralokinumab, abrocitinib, and upadacitinib for AD such as CHRONOS, ECZTEND, JADE REGIMEN, and HEADS UP. At the meeting, he discussed his clinical approach to selecting systemic agents for AD and shared prescribing tips. He began by noting that the approval of dupilumab for moderate to severe AD in 2017 ushered in a new era of treating the disease systemically.
“When it was approved, experts went right to dupilumab if they could, and avoided the use of cyclosporine or methotrexate,” said Dr. Blauvelt, who is also an elected member of the American Society for Clinical Investigation and the International Eczema Council. “I still think that dupilumab is a great agent to start with. We’ve had a bit of difficulty improving upon it.”
Following dupilumab’s approval, three other systemic options became available for patients with moderate to severe AD: the human IgG4 monoclonal antibody tralokinumab that binds to interleukin-13, which is administered subcutaneously; and, more recently, the oral JAK inhibitors abrocitinib and upadacitinib, approved in January for moderate to severe AD.
“I’m a big fan of JAK inhibitors because I think they offer things that biologic and topical therapies can’t offer,” Dr. Blauvelt said. “Patients like the pills versus shots. They also like the speed; JAK inhibitors work faster than dupilumab and tralokinumab. So, if you have a patient with bad AD who wants to get better quickly, that would be a reason to choose a JAK inhibitor over a biologic if you can.”
When Dr. Blauvelt has asked AD clinical trial participants if they’d rather be treated with a biologic agent or with a JAK inhibitor, about half choose one over the other.
“Patients who shy away from the safety issues would choose the biologic trial while the ones who wanted the fast relief would choose the JAK trial,” he said. “But if you present both options and the patients prefer a pill, I think the JAK inhibitors do better with a rapid control of inflammation as well as pruritus – the latter within 2 days of taking the pills.”
When counseling patients initiating a JAK inhibitor, Dr. Blauvelt mentioned three advantages, compared with biologics: the pill formulation, the rapidity of response in pruritus control, and better efficacy. “The downside is the safety,” he said. “Safety is the elephant in the room for the JAK inhibitors.”
The risks listed in the boxed warning in the labeling for JAK inhibitors include: an increased risk of serious bacterial, fungal, and opportunistic infections such as TB; a higher rate of all-cause mortality, including cardiovascular death; a higher rate of MACE (major adverse cardiovascular events, defined as cardiovascular death, MI, and stroke); the potential for malignancy, including lymphoma; and the potential for thrombosis, including an increased incidence of pulmonary embolism (PE).
“Risk of thrombosis seems to be a class effect for all JAK inhibitors,” Dr. Blauvelt said. “As far as I know, it’s idiosyncratic. For nearly all the DVT [deep vein thrombosis] cases that have been reported, patients had baseline risk factors for DVT and PE, which are obesity, smoking, and use of oral contraceptives.”
Dr. Blauvelt pointed out that the boxed warning related to mortality, malignancies, and MACE stemmed from a long-term trial of the JAK inhibitor tofacitinib in RA patients. “Those patients had to be at least 50 years old, 75% of them were on concomitant methotrexate and/or prednisone, and they had to have at least one cardiac risk factor to get into the trial,” he said.
“I’m not saying those things can’t happen in dermatology patients, but if you look at the safety data of JAK inhibitors in the AD studies and in the alopecia areata studies, we are seeing a few cases of these things here and there, but not major signals,” he said. To date, “they look safer in dermatologic diseases compared to tofacitinib in RA data in older populations.”
He emphasized the importance of discussing each of the risks in the boxed warning with patients who are candidates for JAK inhibitor therapy.
Dr. Blauvelt likened the lab monitoring required for JAK inhibitors to that required for methotrexate. This means ordering at baseline, a CBC with differential, a chem-20, a lipid panel, and a QuantiFERON-TB Gold test. The JAK inhibitor labels do not include information on the frequency of monitoring, “but I have a distinct opinion on this because of my blood test monitoring experience in the trials for many years,” he said.
“I think it’s good to do follow-up testing at 1 month, then every 3 months in the first year. In my experience, the people who drop blood cell counts or increase their lipids tend to do it in the first year.”
After 1 year of treatment, he continued, follow-up testing once every 6 months is reasonable. “If CPK [creatine phosphokinase] goes up, I don’t worry about it; it’s not clinically relevant. There is no recommendation for CPK monitoring, so if you’re getting that on your chem-20, I’d say don’t worry about it.”
Dr. Blauvelt reported that he is an investigator and a scientific adviser for several pharmaceutical companies developing treatments for AD, including companies that are evaluating or marketing JAK inhibitors for AD, including AbbVie, Incyte, and Pfizer, as well as dupilumab’s joint developers Sanofi and Regeneron.
AT PDA 2022
Is it COVID or long COVID? Your organs may know
There’s little doubt long COVID is real. The federal government recognizes long COVID as a condition and said in two reports issued in August that one in five adult COVID-19 survivors have a health condition related to their illness.
COVID-19 can damage multiple organs in the body. Sometimes this damage leads to long COVID; sometimes other reasons are at play. Doctors are beginning to sort it out.
“COVID itself can actually cause prolonged illness, and we don’t really call that long COVID,” said Nisha Viswanathan, MD, a doctor at UCLA Health in Los Angeles. But if symptoms extend beyond 12 weeks, that puts patients in the realm of long COVID.
Symptoms can range from mild to severe and can keep people from resuming their normal lives and jobs. Sometimes they last for months, according to the U.S. Department of Health & Human Services.
Multiorgan damage
Lung scarring and other lung problems are common after COVID, said Leora Horwitz, MD, an internal medicine specialist at New York University. Even after a mild case, people can have breathing issues for months, a team at Johns Hopkins Medicine, Baltimore, said in an online briefing. One study published in the journal Radiology found damage in people a full year after a COVID-19 diagnosis.
Some people have persistent heart, kidney, liver, and nervous system problems after COVID-19. A study published in 2020 in JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation. Nearly a third of people hospitalized for COVID-19 get kidney damage that can become chronic, and some end up needing dialysis or a transplant, said C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine.
This might be, in part, because SARS-CoV-2, the virus that causes COVID-19, directly infects the cells in many organs.
Nicole Bhave, MD, a cardiologist at University of Michigan Health, Ann Arbor is concerned that COVID-19 appears to increase the risk of heart problems in some people.
“Some of the uptick may just be recognition bias, in that people with symptoms are seeking care,” she said. “But there’s definitely a biological basis by which COVID could tip people over into a new diagnosis of heart failure.”
Inflammation
Inflammation is probably a key part of the long-term effects of COVID-19.
Some people have a serious immune reaction to COVID-19 called a cytokine storm, said Nitra Aggarwal Gilotra, MD, a cardiologist at Johns Hopkins Medicine. This release of inflammation-causing molecules called cytokines is meant to attack the invading virus. But it can be so severe that it wreaks havoc on healthy tissues and organs and causes lasting damage – if patients even survive it.
In some people, inflammation can affect the heart, causing myocarditis. Myocarditis symptoms include chest pain, breathlessness, and heart palpitations. Though rare, it can be serious and can raise the risk of other heart problems, including heart failure, down the line.
Long COVID may also trigger an autoimmune condition, said Eline Luning Prak, MD, PhD, a pathologist at the Hospital of the University of Pennsylvania, Philadelphia. Long COVID can share many hallmark symptoms with autoimmune diseases, including fatigue, widespread pain, memory problems, and mood disorders.
Blood clots
Studies have shown the overcharged inflammatory response to COVID-19 can cause blood clots. This sometimes overwhelming clotting was an early hallmark of COVID-19 infection, and when clots restrict blood flow in the brain, lungs, kidneys, or limbs, they can cause long-term damage. Some can be deadly. Researchers in Sweden found patients were at risk of deep vein thrombosis – a blood clot usually in the leg – up to 3 months after infection and at higher risk of a blood clot in the lung, called pulmonary embolism, for as long as 3 months.
Viral reservoirs
The virus itself may also linger in a patient’s body, causing continued symptoms and, potentially, new flare-ups. Zoe Swank, PhD, of Harvard Medical School, Boston, and colleagues reported in a preprint study that they found pieces of the SARS-CoV-2 virus in the blood of most patients with long COVID symptoms they tested – some as long as a year after infection. The study has not yet been peer reviewed.
Another team found evidence of the virus in stool up to 7 months later, which suggests the virus hides out in the gut. Other early studies have found bits of viral RNA in the appendix, breast tissue, heart, eyes, and brain.
Diabetes
Diabetes is a risk factor for getting severe COVID-19, and multiple studies have shown people can get diabetes both while battling infection and afterward. One study of veterans, published in The Lancet Diabetes and Endocrinology, found COVID-19 survivors were about 40% more likely to get diabetes over the next year.
There are a few ways this might happen. Insulin-producing cells in the pancreas have SARS-CoV-2 receptors – a type of molecular doorway the coronavirus can attach to. Damage to these cells could make the body less able to produce insulin, which in turn can lead to diabetes. The virus could also disrupt the balance in the body or cause inflammation that leads to insulin resistance, which can develop into diabetes, Ziad Al-Aly, MD, of the Veterans Affairs St. Louis Health Care System, and colleagues wrote.
Nervous system issues
People who get COVID-19 are also more vulnerable to postural orthostatic tachycardia syndrome (POTS). This affects what’s known as the autonomic nervous system, which regulates blood circulation, and includes those things that happen in your body without your having to think about them, like breathing, heartbeat, and digestion. POTS can cause common long COVID neurologic symptoms, including headaches, fatigue, brain fog, insomnia, and problems thinking and concentrating. “This was a known condition prior to COVID, but it was incredibly rare,” said Dr. Viswanathan. “After COVID, I’ve seen it with increasing frequency.”
Long-term outlook
Lasting issues after COVID-19 are much more likely after a moderate or severe infection. Still, plenty of people are battling them even after a mild illness. “As for why, that’s the billion-dollar question,” said Dr. Horwitz. “It’s well known that viral infections can cause long-term dysregulation. Why that is, we really just don’t know.”
Whether it’s virus hiding out in the body, long-term organ damage, or an autoimmune reaction likely differs from person to person. “I’m believing, increasingly, that it’s a combination of all of these, just based on how different patients are responding to different medications,” said Dr. Viswanathan. “One patient will respond to something beautifully, and another patient won’t at all.”
But it’s clear a significant number of people are facing long-term health struggles because of COVID-19, which has infected at least 580 million people globally and 92 million – likely many more – in the United States, according to Johns Hopkins University.
Even a small increased risk of conditions like heart disease or diabetes translates to a huge number of people, Dr. Horwitz said. “If even 1% of people getting COVID have long-term symptoms, that’s a major public health crisis, because that’s 1% of pretty much everybody in the country.”
A version of this article first appeared on WebMD.com.
There’s little doubt long COVID is real. The federal government recognizes long COVID as a condition and said in two reports issued in August that one in five adult COVID-19 survivors have a health condition related to their illness.
COVID-19 can damage multiple organs in the body. Sometimes this damage leads to long COVID; sometimes other reasons are at play. Doctors are beginning to sort it out.
“COVID itself can actually cause prolonged illness, and we don’t really call that long COVID,” said Nisha Viswanathan, MD, a doctor at UCLA Health in Los Angeles. But if symptoms extend beyond 12 weeks, that puts patients in the realm of long COVID.
Symptoms can range from mild to severe and can keep people from resuming their normal lives and jobs. Sometimes they last for months, according to the U.S. Department of Health & Human Services.
Multiorgan damage
Lung scarring and other lung problems are common after COVID, said Leora Horwitz, MD, an internal medicine specialist at New York University. Even after a mild case, people can have breathing issues for months, a team at Johns Hopkins Medicine, Baltimore, said in an online briefing. One study published in the journal Radiology found damage in people a full year after a COVID-19 diagnosis.
Some people have persistent heart, kidney, liver, and nervous system problems after COVID-19. A study published in 2020 in JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation. Nearly a third of people hospitalized for COVID-19 get kidney damage that can become chronic, and some end up needing dialysis or a transplant, said C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine.
This might be, in part, because SARS-CoV-2, the virus that causes COVID-19, directly infects the cells in many organs.
Nicole Bhave, MD, a cardiologist at University of Michigan Health, Ann Arbor is concerned that COVID-19 appears to increase the risk of heart problems in some people.
“Some of the uptick may just be recognition bias, in that people with symptoms are seeking care,” she said. “But there’s definitely a biological basis by which COVID could tip people over into a new diagnosis of heart failure.”
Inflammation
Inflammation is probably a key part of the long-term effects of COVID-19.
Some people have a serious immune reaction to COVID-19 called a cytokine storm, said Nitra Aggarwal Gilotra, MD, a cardiologist at Johns Hopkins Medicine. This release of inflammation-causing molecules called cytokines is meant to attack the invading virus. But it can be so severe that it wreaks havoc on healthy tissues and organs and causes lasting damage – if patients even survive it.
In some people, inflammation can affect the heart, causing myocarditis. Myocarditis symptoms include chest pain, breathlessness, and heart palpitations. Though rare, it can be serious and can raise the risk of other heart problems, including heart failure, down the line.
Long COVID may also trigger an autoimmune condition, said Eline Luning Prak, MD, PhD, a pathologist at the Hospital of the University of Pennsylvania, Philadelphia. Long COVID can share many hallmark symptoms with autoimmune diseases, including fatigue, widespread pain, memory problems, and mood disorders.
Blood clots
Studies have shown the overcharged inflammatory response to COVID-19 can cause blood clots. This sometimes overwhelming clotting was an early hallmark of COVID-19 infection, and when clots restrict blood flow in the brain, lungs, kidneys, or limbs, they can cause long-term damage. Some can be deadly. Researchers in Sweden found patients were at risk of deep vein thrombosis – a blood clot usually in the leg – up to 3 months after infection and at higher risk of a blood clot in the lung, called pulmonary embolism, for as long as 3 months.
Viral reservoirs
The virus itself may also linger in a patient’s body, causing continued symptoms and, potentially, new flare-ups. Zoe Swank, PhD, of Harvard Medical School, Boston, and colleagues reported in a preprint study that they found pieces of the SARS-CoV-2 virus in the blood of most patients with long COVID symptoms they tested – some as long as a year after infection. The study has not yet been peer reviewed.
Another team found evidence of the virus in stool up to 7 months later, which suggests the virus hides out in the gut. Other early studies have found bits of viral RNA in the appendix, breast tissue, heart, eyes, and brain.
Diabetes
Diabetes is a risk factor for getting severe COVID-19, and multiple studies have shown people can get diabetes both while battling infection and afterward. One study of veterans, published in The Lancet Diabetes and Endocrinology, found COVID-19 survivors were about 40% more likely to get diabetes over the next year.
There are a few ways this might happen. Insulin-producing cells in the pancreas have SARS-CoV-2 receptors – a type of molecular doorway the coronavirus can attach to. Damage to these cells could make the body less able to produce insulin, which in turn can lead to diabetes. The virus could also disrupt the balance in the body or cause inflammation that leads to insulin resistance, which can develop into diabetes, Ziad Al-Aly, MD, of the Veterans Affairs St. Louis Health Care System, and colleagues wrote.
Nervous system issues
People who get COVID-19 are also more vulnerable to postural orthostatic tachycardia syndrome (POTS). This affects what’s known as the autonomic nervous system, which regulates blood circulation, and includes those things that happen in your body without your having to think about them, like breathing, heartbeat, and digestion. POTS can cause common long COVID neurologic symptoms, including headaches, fatigue, brain fog, insomnia, and problems thinking and concentrating. “This was a known condition prior to COVID, but it was incredibly rare,” said Dr. Viswanathan. “After COVID, I’ve seen it with increasing frequency.”
Long-term outlook
Lasting issues after COVID-19 are much more likely after a moderate or severe infection. Still, plenty of people are battling them even after a mild illness. “As for why, that’s the billion-dollar question,” said Dr. Horwitz. “It’s well known that viral infections can cause long-term dysregulation. Why that is, we really just don’t know.”
Whether it’s virus hiding out in the body, long-term organ damage, or an autoimmune reaction likely differs from person to person. “I’m believing, increasingly, that it’s a combination of all of these, just based on how different patients are responding to different medications,” said Dr. Viswanathan. “One patient will respond to something beautifully, and another patient won’t at all.”
But it’s clear a significant number of people are facing long-term health struggles because of COVID-19, which has infected at least 580 million people globally and 92 million – likely many more – in the United States, according to Johns Hopkins University.
Even a small increased risk of conditions like heart disease or diabetes translates to a huge number of people, Dr. Horwitz said. “If even 1% of people getting COVID have long-term symptoms, that’s a major public health crisis, because that’s 1% of pretty much everybody in the country.”
A version of this article first appeared on WebMD.com.
There’s little doubt long COVID is real. The federal government recognizes long COVID as a condition and said in two reports issued in August that one in five adult COVID-19 survivors have a health condition related to their illness.
COVID-19 can damage multiple organs in the body. Sometimes this damage leads to long COVID; sometimes other reasons are at play. Doctors are beginning to sort it out.
“COVID itself can actually cause prolonged illness, and we don’t really call that long COVID,” said Nisha Viswanathan, MD, a doctor at UCLA Health in Los Angeles. But if symptoms extend beyond 12 weeks, that puts patients in the realm of long COVID.
Symptoms can range from mild to severe and can keep people from resuming their normal lives and jobs. Sometimes they last for months, according to the U.S. Department of Health & Human Services.
Multiorgan damage
Lung scarring and other lung problems are common after COVID, said Leora Horwitz, MD, an internal medicine specialist at New York University. Even after a mild case, people can have breathing issues for months, a team at Johns Hopkins Medicine, Baltimore, said in an online briefing. One study published in the journal Radiology found damage in people a full year after a COVID-19 diagnosis.
Some people have persistent heart, kidney, liver, and nervous system problems after COVID-19. A study published in 2020 in JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation. Nearly a third of people hospitalized for COVID-19 get kidney damage that can become chronic, and some end up needing dialysis or a transplant, said C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine.
This might be, in part, because SARS-CoV-2, the virus that causes COVID-19, directly infects the cells in many organs.
Nicole Bhave, MD, a cardiologist at University of Michigan Health, Ann Arbor is concerned that COVID-19 appears to increase the risk of heart problems in some people.
“Some of the uptick may just be recognition bias, in that people with symptoms are seeking care,” she said. “But there’s definitely a biological basis by which COVID could tip people over into a new diagnosis of heart failure.”
Inflammation
Inflammation is probably a key part of the long-term effects of COVID-19.
Some people have a serious immune reaction to COVID-19 called a cytokine storm, said Nitra Aggarwal Gilotra, MD, a cardiologist at Johns Hopkins Medicine. This release of inflammation-causing molecules called cytokines is meant to attack the invading virus. But it can be so severe that it wreaks havoc on healthy tissues and organs and causes lasting damage – if patients even survive it.
In some people, inflammation can affect the heart, causing myocarditis. Myocarditis symptoms include chest pain, breathlessness, and heart palpitations. Though rare, it can be serious and can raise the risk of other heart problems, including heart failure, down the line.
Long COVID may also trigger an autoimmune condition, said Eline Luning Prak, MD, PhD, a pathologist at the Hospital of the University of Pennsylvania, Philadelphia. Long COVID can share many hallmark symptoms with autoimmune diseases, including fatigue, widespread pain, memory problems, and mood disorders.
Blood clots
Studies have shown the overcharged inflammatory response to COVID-19 can cause blood clots. This sometimes overwhelming clotting was an early hallmark of COVID-19 infection, and when clots restrict blood flow in the brain, lungs, kidneys, or limbs, they can cause long-term damage. Some can be deadly. Researchers in Sweden found patients were at risk of deep vein thrombosis – a blood clot usually in the leg – up to 3 months after infection and at higher risk of a blood clot in the lung, called pulmonary embolism, for as long as 3 months.
Viral reservoirs
The virus itself may also linger in a patient’s body, causing continued symptoms and, potentially, new flare-ups. Zoe Swank, PhD, of Harvard Medical School, Boston, and colleagues reported in a preprint study that they found pieces of the SARS-CoV-2 virus in the blood of most patients with long COVID symptoms they tested – some as long as a year after infection. The study has not yet been peer reviewed.
Another team found evidence of the virus in stool up to 7 months later, which suggests the virus hides out in the gut. Other early studies have found bits of viral RNA in the appendix, breast tissue, heart, eyes, and brain.
Diabetes
Diabetes is a risk factor for getting severe COVID-19, and multiple studies have shown people can get diabetes both while battling infection and afterward. One study of veterans, published in The Lancet Diabetes and Endocrinology, found COVID-19 survivors were about 40% more likely to get diabetes over the next year.
There are a few ways this might happen. Insulin-producing cells in the pancreas have SARS-CoV-2 receptors – a type of molecular doorway the coronavirus can attach to. Damage to these cells could make the body less able to produce insulin, which in turn can lead to diabetes. The virus could also disrupt the balance in the body or cause inflammation that leads to insulin resistance, which can develop into diabetes, Ziad Al-Aly, MD, of the Veterans Affairs St. Louis Health Care System, and colleagues wrote.
Nervous system issues
People who get COVID-19 are also more vulnerable to postural orthostatic tachycardia syndrome (POTS). This affects what’s known as the autonomic nervous system, which regulates blood circulation, and includes those things that happen in your body without your having to think about them, like breathing, heartbeat, and digestion. POTS can cause common long COVID neurologic symptoms, including headaches, fatigue, brain fog, insomnia, and problems thinking and concentrating. “This was a known condition prior to COVID, but it was incredibly rare,” said Dr. Viswanathan. “After COVID, I’ve seen it with increasing frequency.”
Long-term outlook
Lasting issues after COVID-19 are much more likely after a moderate or severe infection. Still, plenty of people are battling them even after a mild illness. “As for why, that’s the billion-dollar question,” said Dr. Horwitz. “It’s well known that viral infections can cause long-term dysregulation. Why that is, we really just don’t know.”
Whether it’s virus hiding out in the body, long-term organ damage, or an autoimmune reaction likely differs from person to person. “I’m believing, increasingly, that it’s a combination of all of these, just based on how different patients are responding to different medications,” said Dr. Viswanathan. “One patient will respond to something beautifully, and another patient won’t at all.”
But it’s clear a significant number of people are facing long-term health struggles because of COVID-19, which has infected at least 580 million people globally and 92 million – likely many more – in the United States, according to Johns Hopkins University.
Even a small increased risk of conditions like heart disease or diabetes translates to a huge number of people, Dr. Horwitz said. “If even 1% of people getting COVID have long-term symptoms, that’s a major public health crisis, because that’s 1% of pretty much everybody in the country.”
A version of this article first appeared on WebMD.com.
Most people with Omicron don’t know they’re infected
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
FROM JAMA NETWORK OPEN
Words, now actions: How medical associations try to fulfill pledges to combat racism in health care
– from health care outcomes, from the level and quality of patient treatment, from their own memberships. How have those pronouncements translated into programs that could have, or even have had, positive impacts?
For this article, this news organization asked several associations about tangible actions behind their vows to combat racism in health care. Meanwhile, a recent Medscape report focused on the degree to which physicians prioritize racial disparities as a leading social issue.
American Academy of Family Physicians
The American Academy of Family Physicians’ approach is to integrate diversity, equity, and inclusion (DEI) efforts into all existing and new projects rather than tackle racial disparities as a discrete problem.
“Our policies, our advocacy efforts, everything our commissions and staff do ... is through a lens of diversity, equity, and inclusiveness,” said AAFP Board Chair Ada D. Stewart, MD, FAAP.
That lens is ground by a DEI center the AAFP created in 2017. Run by AAFP staff, members, and chapters, the center focuses on five areas: policy, education and training, practice, diversifying the workplace, and strategic partnerships.
The center has established a special project called EveryONE to provide AAFP members with relevant research, policy templates, and other resources to address patient needs. One example is the Neighborhood Navigator, an online tool that shows food, housing, transportation, and other needs in a patient’s neighborhood.
Meanwhile, the DEI center has created training programs for AAFP members on topics like unconscious and implicit racial biases. And the AAFP has implemented several relevant governing policies regarding pushes to improve childbirth conditions and limit race-based treatment, among other areas.
In January, the AAFP established a new DEI commission for family medicine to set the academy’s agenda on racial issues moving forward. “We only had 10 physician positions available on the commission, and over 100 individuals applied, which gave us comfort that we were going in the right direction,” Dr. Stewart said.
Association of American Medical Colleges
The Association of American Medical Colleges, which represents nearly 600 U.S. and Canadian medical schools and teaching hospitals, has a “longstanding” focus on racial equity, said Philip Alberti, founder of the AAMC Center for Health Justice. However, in 2020 that focus became more detailed and layered.
Those layers include:
- Encouraging self-reflection by members on how personal racial biases and stereotypes can lead to systemic racism in health care.
- Working on the AAMC organizational structure. Priorities range from hiring a consultant to help guide antiracism efforts, to establishing a DEI council and advisors, to regularly seeking input from staff. In 2021, the AAMC launched a Center for Health Justice to work more closely with communities.
- Ramping up collaboration with national and local academic medicine organizations and partners. As one example, the AAMC and American Medical Association released a guide for physicians and health care professionals on language that could be interpreted as racist or disrespectful.
- Continuing to be outspoken about racial disparities in health care in society generally.
Meanwhile, the AAMC is supporting more specific, localized health equity efforts in cities such as Cincinnati and Boston.
Cincinnati Children’s Hospital research has found that children in poor neighborhoods are five times more likely to need hospital stays. AAMC members have helped identify “hot spots” for social needs among children and focused specifically on two neighborhoods in the city. The initiative has roped in partnerships with community and social service organizations as well as health care providers, and proponents say the number of child hospital stays in those neighborhoods has dropped by 20%.
Boston Medical Center researchers learned that Black and Latino patients experiencing problems with heart failure were less likely to be referred to a cardiologist. AAMC members assisted with a program to encourage physicians to make medically necessary referrals more often.
National Health Council
The National Health Council, an umbrella association of health organizations, similarly has made a “commitment, not just around policy work but anytime and anything the NHC is doing, to build around trying to identify and solve issues of health equity,” CEO Randall Rutta said.
The NHC has identified four strategic policy areas including race and in 2021 issued a statement signed by 45 other health care organizations vowing to take on systemic racism and advance equity, through public policy and law.
In relation to policy, Mr. Rutta said his organization is lobbying Congress and federal agencies to diversify clinical trials.
“We want to make sure that clinical trials are inclusive of people from different racial and ethnic groups, in order to understand how [they are] affected by a particular condition,” he said. “As you would imagine, some conditions hit certain groups harder than others for genetic or other reasons, or it may just be a reflection of other disparities that occur across health care.”
The organization has issued suggestions for policy change in the Food and Drug Administration’s clinical trial policy and separately targeted telemedicine policy to promote equity and greater patient access. For example, one initiative aims to ensure patients’ privacy and civil rights as telemedicine’s popularity grows after the COVID-19 pandemic. The NHC presented the initiative in a congressional briefing last year.
American Public Health Association
The American Public Health Association says it started focusing on racial disparities in health care in 2015, following a series of racially fueled violent acts. The APHA started with a four-part webinar series on racism in health (more than 10,000 live participants and 40,000 replays to date).
Shortly afterward, then-APHA President Camara Jones, MD, MPH, PhD, launched a national campaign encouraging APHA members, affiliates, and partners to name and address racism as a determinant of health.
More recently in 2021, the APHA adopted a “Truth, Racial Healing & Transformation” guiding framework and “Healing Through Policy” initiative that offer local leaders policy templates and best practices.
“We have identified a suite of policies that have actually been implemented successfully and are advancing racial equity,” said Regina Davis Moss, APHA’s associate executive director of health policy and practice. “You can’t advance health without having a policy that supports it.”
Montgomery County, Md., is one community that has used the framework (for racial equity training of county employees). Leaders in Evanston, Ill., also used it in crafting a resolution to end structural racism in the city.
A version of this article first appeared on Medscape.com.
– from health care outcomes, from the level and quality of patient treatment, from their own memberships. How have those pronouncements translated into programs that could have, or even have had, positive impacts?
For this article, this news organization asked several associations about tangible actions behind their vows to combat racism in health care. Meanwhile, a recent Medscape report focused on the degree to which physicians prioritize racial disparities as a leading social issue.
American Academy of Family Physicians
The American Academy of Family Physicians’ approach is to integrate diversity, equity, and inclusion (DEI) efforts into all existing and new projects rather than tackle racial disparities as a discrete problem.
“Our policies, our advocacy efforts, everything our commissions and staff do ... is through a lens of diversity, equity, and inclusiveness,” said AAFP Board Chair Ada D. Stewart, MD, FAAP.
That lens is ground by a DEI center the AAFP created in 2017. Run by AAFP staff, members, and chapters, the center focuses on five areas: policy, education and training, practice, diversifying the workplace, and strategic partnerships.
The center has established a special project called EveryONE to provide AAFP members with relevant research, policy templates, and other resources to address patient needs. One example is the Neighborhood Navigator, an online tool that shows food, housing, transportation, and other needs in a patient’s neighborhood.
Meanwhile, the DEI center has created training programs for AAFP members on topics like unconscious and implicit racial biases. And the AAFP has implemented several relevant governing policies regarding pushes to improve childbirth conditions and limit race-based treatment, among other areas.
In January, the AAFP established a new DEI commission for family medicine to set the academy’s agenda on racial issues moving forward. “We only had 10 physician positions available on the commission, and over 100 individuals applied, which gave us comfort that we were going in the right direction,” Dr. Stewart said.
Association of American Medical Colleges
The Association of American Medical Colleges, which represents nearly 600 U.S. and Canadian medical schools and teaching hospitals, has a “longstanding” focus on racial equity, said Philip Alberti, founder of the AAMC Center for Health Justice. However, in 2020 that focus became more detailed and layered.
Those layers include:
- Encouraging self-reflection by members on how personal racial biases and stereotypes can lead to systemic racism in health care.
- Working on the AAMC organizational structure. Priorities range from hiring a consultant to help guide antiracism efforts, to establishing a DEI council and advisors, to regularly seeking input from staff. In 2021, the AAMC launched a Center for Health Justice to work more closely with communities.
- Ramping up collaboration with national and local academic medicine organizations and partners. As one example, the AAMC and American Medical Association released a guide for physicians and health care professionals on language that could be interpreted as racist or disrespectful.
- Continuing to be outspoken about racial disparities in health care in society generally.
Meanwhile, the AAMC is supporting more specific, localized health equity efforts in cities such as Cincinnati and Boston.
Cincinnati Children’s Hospital research has found that children in poor neighborhoods are five times more likely to need hospital stays. AAMC members have helped identify “hot spots” for social needs among children and focused specifically on two neighborhoods in the city. The initiative has roped in partnerships with community and social service organizations as well as health care providers, and proponents say the number of child hospital stays in those neighborhoods has dropped by 20%.
Boston Medical Center researchers learned that Black and Latino patients experiencing problems with heart failure were less likely to be referred to a cardiologist. AAMC members assisted with a program to encourage physicians to make medically necessary referrals more often.
National Health Council
The National Health Council, an umbrella association of health organizations, similarly has made a “commitment, not just around policy work but anytime and anything the NHC is doing, to build around trying to identify and solve issues of health equity,” CEO Randall Rutta said.
The NHC has identified four strategic policy areas including race and in 2021 issued a statement signed by 45 other health care organizations vowing to take on systemic racism and advance equity, through public policy and law.
In relation to policy, Mr. Rutta said his organization is lobbying Congress and federal agencies to diversify clinical trials.
“We want to make sure that clinical trials are inclusive of people from different racial and ethnic groups, in order to understand how [they are] affected by a particular condition,” he said. “As you would imagine, some conditions hit certain groups harder than others for genetic or other reasons, or it may just be a reflection of other disparities that occur across health care.”
The organization has issued suggestions for policy change in the Food and Drug Administration’s clinical trial policy and separately targeted telemedicine policy to promote equity and greater patient access. For example, one initiative aims to ensure patients’ privacy and civil rights as telemedicine’s popularity grows after the COVID-19 pandemic. The NHC presented the initiative in a congressional briefing last year.
American Public Health Association
The American Public Health Association says it started focusing on racial disparities in health care in 2015, following a series of racially fueled violent acts. The APHA started with a four-part webinar series on racism in health (more than 10,000 live participants and 40,000 replays to date).
Shortly afterward, then-APHA President Camara Jones, MD, MPH, PhD, launched a national campaign encouraging APHA members, affiliates, and partners to name and address racism as a determinant of health.
More recently in 2021, the APHA adopted a “Truth, Racial Healing & Transformation” guiding framework and “Healing Through Policy” initiative that offer local leaders policy templates and best practices.
“We have identified a suite of policies that have actually been implemented successfully and are advancing racial equity,” said Regina Davis Moss, APHA’s associate executive director of health policy and practice. “You can’t advance health without having a policy that supports it.”
Montgomery County, Md., is one community that has used the framework (for racial equity training of county employees). Leaders in Evanston, Ill., also used it in crafting a resolution to end structural racism in the city.
A version of this article first appeared on Medscape.com.
– from health care outcomes, from the level and quality of patient treatment, from their own memberships. How have those pronouncements translated into programs that could have, or even have had, positive impacts?
For this article, this news organization asked several associations about tangible actions behind their vows to combat racism in health care. Meanwhile, a recent Medscape report focused on the degree to which physicians prioritize racial disparities as a leading social issue.
American Academy of Family Physicians
The American Academy of Family Physicians’ approach is to integrate diversity, equity, and inclusion (DEI) efforts into all existing and new projects rather than tackle racial disparities as a discrete problem.
“Our policies, our advocacy efforts, everything our commissions and staff do ... is through a lens of diversity, equity, and inclusiveness,” said AAFP Board Chair Ada D. Stewart, MD, FAAP.
That lens is ground by a DEI center the AAFP created in 2017. Run by AAFP staff, members, and chapters, the center focuses on five areas: policy, education and training, practice, diversifying the workplace, and strategic partnerships.
The center has established a special project called EveryONE to provide AAFP members with relevant research, policy templates, and other resources to address patient needs. One example is the Neighborhood Navigator, an online tool that shows food, housing, transportation, and other needs in a patient’s neighborhood.
Meanwhile, the DEI center has created training programs for AAFP members on topics like unconscious and implicit racial biases. And the AAFP has implemented several relevant governing policies regarding pushes to improve childbirth conditions and limit race-based treatment, among other areas.
In January, the AAFP established a new DEI commission for family medicine to set the academy’s agenda on racial issues moving forward. “We only had 10 physician positions available on the commission, and over 100 individuals applied, which gave us comfort that we were going in the right direction,” Dr. Stewart said.
Association of American Medical Colleges
The Association of American Medical Colleges, which represents nearly 600 U.S. and Canadian medical schools and teaching hospitals, has a “longstanding” focus on racial equity, said Philip Alberti, founder of the AAMC Center for Health Justice. However, in 2020 that focus became more detailed and layered.
Those layers include:
- Encouraging self-reflection by members on how personal racial biases and stereotypes can lead to systemic racism in health care.
- Working on the AAMC organizational structure. Priorities range from hiring a consultant to help guide antiracism efforts, to establishing a DEI council and advisors, to regularly seeking input from staff. In 2021, the AAMC launched a Center for Health Justice to work more closely with communities.
- Ramping up collaboration with national and local academic medicine organizations and partners. As one example, the AAMC and American Medical Association released a guide for physicians and health care professionals on language that could be interpreted as racist or disrespectful.
- Continuing to be outspoken about racial disparities in health care in society generally.
Meanwhile, the AAMC is supporting more specific, localized health equity efforts in cities such as Cincinnati and Boston.
Cincinnati Children’s Hospital research has found that children in poor neighborhoods are five times more likely to need hospital stays. AAMC members have helped identify “hot spots” for social needs among children and focused specifically on two neighborhoods in the city. The initiative has roped in partnerships with community and social service organizations as well as health care providers, and proponents say the number of child hospital stays in those neighborhoods has dropped by 20%.
Boston Medical Center researchers learned that Black and Latino patients experiencing problems with heart failure were less likely to be referred to a cardiologist. AAMC members assisted with a program to encourage physicians to make medically necessary referrals more often.
National Health Council
The National Health Council, an umbrella association of health organizations, similarly has made a “commitment, not just around policy work but anytime and anything the NHC is doing, to build around trying to identify and solve issues of health equity,” CEO Randall Rutta said.
The NHC has identified four strategic policy areas including race and in 2021 issued a statement signed by 45 other health care organizations vowing to take on systemic racism and advance equity, through public policy and law.
In relation to policy, Mr. Rutta said his organization is lobbying Congress and federal agencies to diversify clinical trials.
“We want to make sure that clinical trials are inclusive of people from different racial and ethnic groups, in order to understand how [they are] affected by a particular condition,” he said. “As you would imagine, some conditions hit certain groups harder than others for genetic or other reasons, or it may just be a reflection of other disparities that occur across health care.”
The organization has issued suggestions for policy change in the Food and Drug Administration’s clinical trial policy and separately targeted telemedicine policy to promote equity and greater patient access. For example, one initiative aims to ensure patients’ privacy and civil rights as telemedicine’s popularity grows after the COVID-19 pandemic. The NHC presented the initiative in a congressional briefing last year.
American Public Health Association
The American Public Health Association says it started focusing on racial disparities in health care in 2015, following a series of racially fueled violent acts. The APHA started with a four-part webinar series on racism in health (more than 10,000 live participants and 40,000 replays to date).
Shortly afterward, then-APHA President Camara Jones, MD, MPH, PhD, launched a national campaign encouraging APHA members, affiliates, and partners to name and address racism as a determinant of health.
More recently in 2021, the APHA adopted a “Truth, Racial Healing & Transformation” guiding framework and “Healing Through Policy” initiative that offer local leaders policy templates and best practices.
“We have identified a suite of policies that have actually been implemented successfully and are advancing racial equity,” said Regina Davis Moss, APHA’s associate executive director of health policy and practice. “You can’t advance health without having a policy that supports it.”
Montgomery County, Md., is one community that has used the framework (for racial equity training of county employees). Leaders in Evanston, Ill., also used it in crafting a resolution to end structural racism in the city.
A version of this article first appeared on Medscape.com.
Physicians’ bad behavior seen at work, online by colleagues: Survey
“The days of surgeons throwing retractors across the OR and screaming at nurses and medical students are hopefully gone now,” said Barron Lerner, MD, PhD, professor of medicine at New York University Langone Health and author of “The Good Doctor: A Father, a Son, and the Evolution of Medical Ethics” (Boston: Beacon Press, 2014). “We’re not going to tolerate that as an institution.”
But, Dr. Lerner said, bad behavior still happens. And according to a recent Medscape survey, it seems to be on the rise.
For the 2022 Physicians Behaving Badly Report, more than 1,500 physicians shared how often they see fellow doctors misbehaving in person or on social media, and shared some of the worse behavior they’ve seen.
Though misconduct is still relatively uncommon among doctors, and most physicians say they’re proud of the high standards and attitudes of their colleagues, respondents to the survey did say that they’re seeing more frequent incidents of other doctors acting disrespectfully toward patients and coworkers, taking too casual an approach to patient privacy, and even acting angrily or aggressively at work. While the uptick is not substantial, it’s nonetheless worrying.
“I have increased concern for my colleagues,” said Drew Ramsey, MD, an assistant clinical professor of psychiatry at Columbia University, New York. “People forget that COVID has made the physician workplace incredibly stressful. Physicians are struggling with their mental health.”
Bullying and harassment top bad behavior
When it comes to what kind of bad behavior was reported, bullying or harassing clinicians and staff was the runaway winner, with 86% of respondents saying they’d seen this type of behavior at work at some time. Making fun of or disparaging patients behind their backs was a close second, at 82%.
Dr. Ramsey thinks that these figures may reflect a deeper understanding of and sensitivity to harassment and bullying. “Five years ago, we weren’t talking about microaggression,” he said. This heightened awareness might explain the fact that doctors reported witnessing physicians mistreating other medical personnel and/or bullying or harassing patients somewhat more often than in 2021’s report.
Docs were caught using racist language by 55% of respondents, and 44% reported seeing colleagues becoming physically aggressive with patients, clinicians, or staff. Other disturbing behaviors respondents witnessed included bullying or harassing patients (45%), inebriation at work (43%), lying about credentials (34%), trying to date a patient (30%), and committing a crime, such as embezzling or stealing (27%).
Women were seen misbehaving about one-third as often as their male counterparts. This could be because women are more likely to seek help, rather than the bottle, when the stress piles up. “Some misbehavior stems from alcohol abuse, and a higher percentage of men have an alcoholism problem,” Dr. Ramsey pointed out. “Also, male physicians have historically been reluctant to seek mental health assistance.”
Speaking up
Doctors are behaving badly slightly more often, and their colleagues are slightly more willing to speak up about that behavior. In 2021, 35% of physicians said they did nothing upon witnessing inappropriate behavior. In 2022’s survey, that number fell to 29%.
Respondents largely agreed (49%) that doctors should be verbally warned when they’ve behaved badly at work, yet only 39% reported speaking to a colleague who acted inappropriately, and only 27% reported the bad behavior to an authority.
Dr. Lerner pointed out that it is very difficult for doctors to speak up, even though they know they should. There are several reasons for their reticence.
“For one thing, we all have bad days, and the reporting physician may worry that he or she could do something similar in the future,” he said. “Also, there is the liability question. A doctor might think: ‘What if I’m wrong? What if I think someone has a drinking problem and they don’t, or I can’t prove it?’ If you’re the doctor who reported the misbehavior, you’re potentially opening a can of worms. So there’s all sorts of reasons people convince themselves they don’t have to report it.” But, he added, “if you see it and don’t report it, you’re in the wrong.”
Off the job
Work isn’t the only place where doctors observe their colleagues misbehaving. About 66% of respondents had seen disparaging behavior, and 42% had heard racist language, away from the hospital or clinic, according to the survey.
Bullying and harassment weren’t limited to work, either, with 45% reporting seeing a colleague engage in this behavior off campus, and 52% reporting witnessing a colleague inebriated in public. That’s actually down from 2021 when 58% of respondents said they witnessed inebriated doctors in public.
The public sphere has broadened in recent years to include social media, and there, too, doctors sometimes behave badly. However, 47% of doctors surveyed said they saw more inappropriate behavior in person than on social media.
When doctors do act out online, they make the same mistakes other professionals make. One respondent reported seeing a fellow physician “copying and posting an interoffice memo from work and badmouthing the company and the person who wrote the memo.” Another said: “Someone got fired and stalked the supervisor and posted aggressive things.”
Not all social media transgressions were work related. One respondent reported that “a physician posted pictures of herself at a bar with multiple ER staff members, without masks during COVID restriction,” and another reported a colleague posting “unbelievable, antiscientific information expressed as valid, factual material.”
Though posting nonfactual, unscientific, and potentially unsafe information is clearly an ethics violation, Dr. Lerner said, the boundaries around posting personal peccadillos are less clear. This is a part of “digital professionalism,” he explained, adding that there is a broad range of opinions on this. “I think it’s important to discuss these things. Interestingly, while the rules for behavior at the hospital have become more strict, the culture has become less strict.”
As one respondent put it: “What exactly is bad behavior? If you’re saying physicians should be allowed to sexually assault people and use drugs, then no. Can they wear a tiny bathing suit on vacation and drink cocktails with friends? Yeah.”
A version of this article first appeared on Medscape.com.
“The days of surgeons throwing retractors across the OR and screaming at nurses and medical students are hopefully gone now,” said Barron Lerner, MD, PhD, professor of medicine at New York University Langone Health and author of “The Good Doctor: A Father, a Son, and the Evolution of Medical Ethics” (Boston: Beacon Press, 2014). “We’re not going to tolerate that as an institution.”
But, Dr. Lerner said, bad behavior still happens. And according to a recent Medscape survey, it seems to be on the rise.
For the 2022 Physicians Behaving Badly Report, more than 1,500 physicians shared how often they see fellow doctors misbehaving in person or on social media, and shared some of the worse behavior they’ve seen.
Though misconduct is still relatively uncommon among doctors, and most physicians say they’re proud of the high standards and attitudes of their colleagues, respondents to the survey did say that they’re seeing more frequent incidents of other doctors acting disrespectfully toward patients and coworkers, taking too casual an approach to patient privacy, and even acting angrily or aggressively at work. While the uptick is not substantial, it’s nonetheless worrying.
“I have increased concern for my colleagues,” said Drew Ramsey, MD, an assistant clinical professor of psychiatry at Columbia University, New York. “People forget that COVID has made the physician workplace incredibly stressful. Physicians are struggling with their mental health.”
Bullying and harassment top bad behavior
When it comes to what kind of bad behavior was reported, bullying or harassing clinicians and staff was the runaway winner, with 86% of respondents saying they’d seen this type of behavior at work at some time. Making fun of or disparaging patients behind their backs was a close second, at 82%.
Dr. Ramsey thinks that these figures may reflect a deeper understanding of and sensitivity to harassment and bullying. “Five years ago, we weren’t talking about microaggression,” he said. This heightened awareness might explain the fact that doctors reported witnessing physicians mistreating other medical personnel and/or bullying or harassing patients somewhat more often than in 2021’s report.
Docs were caught using racist language by 55% of respondents, and 44% reported seeing colleagues becoming physically aggressive with patients, clinicians, or staff. Other disturbing behaviors respondents witnessed included bullying or harassing patients (45%), inebriation at work (43%), lying about credentials (34%), trying to date a patient (30%), and committing a crime, such as embezzling or stealing (27%).
Women were seen misbehaving about one-third as often as their male counterparts. This could be because women are more likely to seek help, rather than the bottle, when the stress piles up. “Some misbehavior stems from alcohol abuse, and a higher percentage of men have an alcoholism problem,” Dr. Ramsey pointed out. “Also, male physicians have historically been reluctant to seek mental health assistance.”
Speaking up
Doctors are behaving badly slightly more often, and their colleagues are slightly more willing to speak up about that behavior. In 2021, 35% of physicians said they did nothing upon witnessing inappropriate behavior. In 2022’s survey, that number fell to 29%.
Respondents largely agreed (49%) that doctors should be verbally warned when they’ve behaved badly at work, yet only 39% reported speaking to a colleague who acted inappropriately, and only 27% reported the bad behavior to an authority.
Dr. Lerner pointed out that it is very difficult for doctors to speak up, even though they know they should. There are several reasons for their reticence.
“For one thing, we all have bad days, and the reporting physician may worry that he or she could do something similar in the future,” he said. “Also, there is the liability question. A doctor might think: ‘What if I’m wrong? What if I think someone has a drinking problem and they don’t, or I can’t prove it?’ If you’re the doctor who reported the misbehavior, you’re potentially opening a can of worms. So there’s all sorts of reasons people convince themselves they don’t have to report it.” But, he added, “if you see it and don’t report it, you’re in the wrong.”
Off the job
Work isn’t the only place where doctors observe their colleagues misbehaving. About 66% of respondents had seen disparaging behavior, and 42% had heard racist language, away from the hospital or clinic, according to the survey.
Bullying and harassment weren’t limited to work, either, with 45% reporting seeing a colleague engage in this behavior off campus, and 52% reporting witnessing a colleague inebriated in public. That’s actually down from 2021 when 58% of respondents said they witnessed inebriated doctors in public.
The public sphere has broadened in recent years to include social media, and there, too, doctors sometimes behave badly. However, 47% of doctors surveyed said they saw more inappropriate behavior in person than on social media.
When doctors do act out online, they make the same mistakes other professionals make. One respondent reported seeing a fellow physician “copying and posting an interoffice memo from work and badmouthing the company and the person who wrote the memo.” Another said: “Someone got fired and stalked the supervisor and posted aggressive things.”
Not all social media transgressions were work related. One respondent reported that “a physician posted pictures of herself at a bar with multiple ER staff members, without masks during COVID restriction,” and another reported a colleague posting “unbelievable, antiscientific information expressed as valid, factual material.”
Though posting nonfactual, unscientific, and potentially unsafe information is clearly an ethics violation, Dr. Lerner said, the boundaries around posting personal peccadillos are less clear. This is a part of “digital professionalism,” he explained, adding that there is a broad range of opinions on this. “I think it’s important to discuss these things. Interestingly, while the rules for behavior at the hospital have become more strict, the culture has become less strict.”
As one respondent put it: “What exactly is bad behavior? If you’re saying physicians should be allowed to sexually assault people and use drugs, then no. Can they wear a tiny bathing suit on vacation and drink cocktails with friends? Yeah.”
A version of this article first appeared on Medscape.com.
“The days of surgeons throwing retractors across the OR and screaming at nurses and medical students are hopefully gone now,” said Barron Lerner, MD, PhD, professor of medicine at New York University Langone Health and author of “The Good Doctor: A Father, a Son, and the Evolution of Medical Ethics” (Boston: Beacon Press, 2014). “We’re not going to tolerate that as an institution.”
But, Dr. Lerner said, bad behavior still happens. And according to a recent Medscape survey, it seems to be on the rise.
For the 2022 Physicians Behaving Badly Report, more than 1,500 physicians shared how often they see fellow doctors misbehaving in person or on social media, and shared some of the worse behavior they’ve seen.
Though misconduct is still relatively uncommon among doctors, and most physicians say they’re proud of the high standards and attitudes of their colleagues, respondents to the survey did say that they’re seeing more frequent incidents of other doctors acting disrespectfully toward patients and coworkers, taking too casual an approach to patient privacy, and even acting angrily or aggressively at work. While the uptick is not substantial, it’s nonetheless worrying.
“I have increased concern for my colleagues,” said Drew Ramsey, MD, an assistant clinical professor of psychiatry at Columbia University, New York. “People forget that COVID has made the physician workplace incredibly stressful. Physicians are struggling with their mental health.”
Bullying and harassment top bad behavior
When it comes to what kind of bad behavior was reported, bullying or harassing clinicians and staff was the runaway winner, with 86% of respondents saying they’d seen this type of behavior at work at some time. Making fun of or disparaging patients behind their backs was a close second, at 82%.
Dr. Ramsey thinks that these figures may reflect a deeper understanding of and sensitivity to harassment and bullying. “Five years ago, we weren’t talking about microaggression,” he said. This heightened awareness might explain the fact that doctors reported witnessing physicians mistreating other medical personnel and/or bullying or harassing patients somewhat more often than in 2021’s report.
Docs were caught using racist language by 55% of respondents, and 44% reported seeing colleagues becoming physically aggressive with patients, clinicians, or staff. Other disturbing behaviors respondents witnessed included bullying or harassing patients (45%), inebriation at work (43%), lying about credentials (34%), trying to date a patient (30%), and committing a crime, such as embezzling or stealing (27%).
Women were seen misbehaving about one-third as often as their male counterparts. This could be because women are more likely to seek help, rather than the bottle, when the stress piles up. “Some misbehavior stems from alcohol abuse, and a higher percentage of men have an alcoholism problem,” Dr. Ramsey pointed out. “Also, male physicians have historically been reluctant to seek mental health assistance.”
Speaking up
Doctors are behaving badly slightly more often, and their colleagues are slightly more willing to speak up about that behavior. In 2021, 35% of physicians said they did nothing upon witnessing inappropriate behavior. In 2022’s survey, that number fell to 29%.
Respondents largely agreed (49%) that doctors should be verbally warned when they’ve behaved badly at work, yet only 39% reported speaking to a colleague who acted inappropriately, and only 27% reported the bad behavior to an authority.
Dr. Lerner pointed out that it is very difficult for doctors to speak up, even though they know they should. There are several reasons for their reticence.
“For one thing, we all have bad days, and the reporting physician may worry that he or she could do something similar in the future,” he said. “Also, there is the liability question. A doctor might think: ‘What if I’m wrong? What if I think someone has a drinking problem and they don’t, or I can’t prove it?’ If you’re the doctor who reported the misbehavior, you’re potentially opening a can of worms. So there’s all sorts of reasons people convince themselves they don’t have to report it.” But, he added, “if you see it and don’t report it, you’re in the wrong.”
Off the job
Work isn’t the only place where doctors observe their colleagues misbehaving. About 66% of respondents had seen disparaging behavior, and 42% had heard racist language, away from the hospital or clinic, according to the survey.
Bullying and harassment weren’t limited to work, either, with 45% reporting seeing a colleague engage in this behavior off campus, and 52% reporting witnessing a colleague inebriated in public. That’s actually down from 2021 when 58% of respondents said they witnessed inebriated doctors in public.
The public sphere has broadened in recent years to include social media, and there, too, doctors sometimes behave badly. However, 47% of doctors surveyed said they saw more inappropriate behavior in person than on social media.
When doctors do act out online, they make the same mistakes other professionals make. One respondent reported seeing a fellow physician “copying and posting an interoffice memo from work and badmouthing the company and the person who wrote the memo.” Another said: “Someone got fired and stalked the supervisor and posted aggressive things.”
Not all social media transgressions were work related. One respondent reported that “a physician posted pictures of herself at a bar with multiple ER staff members, without masks during COVID restriction,” and another reported a colleague posting “unbelievable, antiscientific information expressed as valid, factual material.”
Though posting nonfactual, unscientific, and potentially unsafe information is clearly an ethics violation, Dr. Lerner said, the boundaries around posting personal peccadillos are less clear. This is a part of “digital professionalism,” he explained, adding that there is a broad range of opinions on this. “I think it’s important to discuss these things. Interestingly, while the rules for behavior at the hospital have become more strict, the culture has become less strict.”
As one respondent put it: “What exactly is bad behavior? If you’re saying physicians should be allowed to sexually assault people and use drugs, then no. Can they wear a tiny bathing suit on vacation and drink cocktails with friends? Yeah.”
A version of this article first appeared on Medscape.com.
A White female presented with pruritic, reticulated, erythematous plaques on the abdomen
It is characterized by pruritic, erythematous papules, papulovesicles, and vesicles that appear in a reticular pattern, most commonly on the trunk. The lesions are typically followed by postinflammatory hyperpigmentation (PIH).
Although PP has been described in people of all races, ages, and sexes, it is predominantly observed in Japan, often in female young adults. Triggers may include a ketogenic diet, diabetes mellitus, and pregnancy. Friction and contact allergic reactions to chrome or nickel have been proposed as exogenous trigger factors. Individual cases of Sjögren’s syndrome, Helicobacter pylori infections, and adult Still syndrome have also been associated with recurrent eruptions.
The diagnosis of PP is made both clinically and by biopsy. The histological features vary according to the stage of the disease. In early-stage disease, superficial and perivascular infiltration of neutrophils are prominent. Later stages are characterized by spongiosis and necrotic keratinocytes.
The first-line therapy for prurigo pigmentosa is oral minocycline. However, for some patients, doxycycline, macrolide antibiotics, or dapsone may be indicated. Adding carbohydrates to a keto diet may be helpful. In this patient, a punch biopsy was performed, which revealed an interface dermatitis with eosinophils and neutrophils, consistent with prurigo pigmentosa. The cause of her PP remains idiopathic. She was treated with 100 mg doxycycline twice a day, which resulted in a resolution of active lesions. The patient did have postinflammatory hyperpigmentation.
This case and photo were submitted by Brooke Resh Sateesh, MD, of San Diego Family Dermatology, San Diego, California, and Mina Zulal, University Medical Center Hamburg-Eppendorf (UKE), Hamburg, Germany. Dr. Bilu Martin edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Beutler et al. Am J Clin Dermatol. 2015 Dec;16(6):533-43.
2. Kim et al. J Dermatol. 2012 Nov;39(11):891-7.
3. Mufti et al. JAAD Int. 2021 Apr 10;3:79-87.
It is characterized by pruritic, erythematous papules, papulovesicles, and vesicles that appear in a reticular pattern, most commonly on the trunk. The lesions are typically followed by postinflammatory hyperpigmentation (PIH).
Although PP has been described in people of all races, ages, and sexes, it is predominantly observed in Japan, often in female young adults. Triggers may include a ketogenic diet, diabetes mellitus, and pregnancy. Friction and contact allergic reactions to chrome or nickel have been proposed as exogenous trigger factors. Individual cases of Sjögren’s syndrome, Helicobacter pylori infections, and adult Still syndrome have also been associated with recurrent eruptions.
The diagnosis of PP is made both clinically and by biopsy. The histological features vary according to the stage of the disease. In early-stage disease, superficial and perivascular infiltration of neutrophils are prominent. Later stages are characterized by spongiosis and necrotic keratinocytes.
The first-line therapy for prurigo pigmentosa is oral minocycline. However, for some patients, doxycycline, macrolide antibiotics, or dapsone may be indicated. Adding carbohydrates to a keto diet may be helpful. In this patient, a punch biopsy was performed, which revealed an interface dermatitis with eosinophils and neutrophils, consistent with prurigo pigmentosa. The cause of her PP remains idiopathic. She was treated with 100 mg doxycycline twice a day, which resulted in a resolution of active lesions. The patient did have postinflammatory hyperpigmentation.
This case and photo were submitted by Brooke Resh Sateesh, MD, of San Diego Family Dermatology, San Diego, California, and Mina Zulal, University Medical Center Hamburg-Eppendorf (UKE), Hamburg, Germany. Dr. Bilu Martin edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Beutler et al. Am J Clin Dermatol. 2015 Dec;16(6):533-43.
2. Kim et al. J Dermatol. 2012 Nov;39(11):891-7.
3. Mufti et al. JAAD Int. 2021 Apr 10;3:79-87.
It is characterized by pruritic, erythematous papules, papulovesicles, and vesicles that appear in a reticular pattern, most commonly on the trunk. The lesions are typically followed by postinflammatory hyperpigmentation (PIH).
Although PP has been described in people of all races, ages, and sexes, it is predominantly observed in Japan, often in female young adults. Triggers may include a ketogenic diet, diabetes mellitus, and pregnancy. Friction and contact allergic reactions to chrome or nickel have been proposed as exogenous trigger factors. Individual cases of Sjögren’s syndrome, Helicobacter pylori infections, and adult Still syndrome have also been associated with recurrent eruptions.
The diagnosis of PP is made both clinically and by biopsy. The histological features vary according to the stage of the disease. In early-stage disease, superficial and perivascular infiltration of neutrophils are prominent. Later stages are characterized by spongiosis and necrotic keratinocytes.
The first-line therapy for prurigo pigmentosa is oral minocycline. However, for some patients, doxycycline, macrolide antibiotics, or dapsone may be indicated. Adding carbohydrates to a keto diet may be helpful. In this patient, a punch biopsy was performed, which revealed an interface dermatitis with eosinophils and neutrophils, consistent with prurigo pigmentosa. The cause of her PP remains idiopathic. She was treated with 100 mg doxycycline twice a day, which resulted in a resolution of active lesions. The patient did have postinflammatory hyperpigmentation.
This case and photo were submitted by Brooke Resh Sateesh, MD, of San Diego Family Dermatology, San Diego, California, and Mina Zulal, University Medical Center Hamburg-Eppendorf (UKE), Hamburg, Germany. Dr. Bilu Martin edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Beutler et al. Am J Clin Dermatol. 2015 Dec;16(6):533-43.
2. Kim et al. J Dermatol. 2012 Nov;39(11):891-7.
3. Mufti et al. JAAD Int. 2021 Apr 10;3:79-87.
Primary care now offering physicians the 26.7-hour day
Taking ‘not enough hours in the day’ to new heights
It’s no secret that there’s a big doctor shortage in the United States. Going through medical school is long, expensive, and stressful, and it’s not like those long, stressful hours stop once you finally do get that degree. There is, however, an excellent reason to take that dive into doctorhood: You’ll gain mastery over time itself.
A study from the University of Chicago, Johns Hopkins University, and Imperial College London has revealed the truth. By using data pulled from the National Health and Nutrition Examination Survey, the researchers found that primary care physicians who see an average number of patients and follow all the current national guidelines for preventive care, chronic disease care, and acute care – plus administrative tasks – must work 26.7 hours a day. That works out to 14.1 hours of preventive care, 7.2 hours of chronic disease care, 2.2 hours of acute care, and 3.2 hours of documentation and inbox management.
Astute readers may note that this is a bit more than the traditional 8-hour workday. It is, in fact, more hours than there actually are in a day. As it turns out, Doctor Strange is more of a documentary than …
Hang on, we’re receiving word that doctors are not in fact wizards who can bend time and space to their will, nor are they sitting on a stash of Time-Turners they saved from the Ministry of Magic before Voldemort destroyed them all. They are, according to the study, overworked and overburdened with too many things and too little time. This is why outcomes haven’t improved despite technological advances and why burnout is so common. We’d be burned out too, having to work temporally impossible hours.
The study authors suggested a team-based approach to medicine that would spread the workload out to nurses, physician assistants, dietitians, etc., estimating that about two-thirds of what a primary care physician does can be handled by someone else. A team-based approach would reduce the physician’s required hours down to 9.3 hours a day, which is at least physically possible. It’s either that or we make the day longer, which sounds like the plot of an episode of Futurama. Swap overwork for global warming and a longer day for a longer year and it is actually the plot of an episode of Futurama.
After a hard day of thinking, brains need their rest
Do you ever feel like you have no more capacity to think or make any more decisions after a long day at work? Do you need a few extra cups of coffee to even make it through the day, even though you’re mostly just sitting around talking and typing? Have we got the research for you: Mental exhaustion is an actual thing. Imagine that double whammy of having a job that’s physically and mentally demanding.
A recent study in Current Biology explained why we feel so exhausted after doing something mentally demanding for several hours. Over that time, glutamate builds up in synapses of the prefrontal cortex, which affects our decision making and leads to cognitive lethargy. Your brain eventually becomes more interested in tasks that are less mentally fatiguing, and that’s probably why you’re reading this LOTME right now instead of getting back to work.
“Our findings show that cognitive work results in a true functional alteration – accumulation of noxious substances – so fatigue would indeed be a signal that makes us stop working but for a different purpose: to preserve the integrity of brain functioning,” senior author Mathias Pessiglione of Pitié-Salpêtrière University, Paris, said in a written statement.
The group of researchers conducted studies by using magnetic resonance spectroscopy to look at two groups of people over the course of a workday: One group had mentally tasking jobs and one didn’t. Those who had to think harder for their jobs had more signs of fatigue, such as reduced pupil dilation and glutamate in synapses of the prefrontal cortex. They also looked for more rewards that required less thinking.
For those whose mentally exhausting jobs probably won’t get better or change, the researchers suggest getting as much rest as possible. Those who don’t have that option will have to continue drinking those 7 cups of coffee a day. ... and reading LOTME.
Hmm, might be a new tagline for us in there somewhere. LOTME: Tired brains love us? When you’re too tired to think, think of LOTME? You can’t spell mental exhaustion without L-O-T-M-E?
Testosterone shows its warm and fuzzy side
Stereotypically, men are loud, knuckle-dragging Neanderthals. The hair coming out of our faces is kind of a dead giveaway, right? We grunt, we scratch, we start wars, we watch sports on TV. But why? It’s the testosterone. Everyone knows that. Testosterone makes men aggressive … or does it?
Since this sort of research generally isn’t done with actual men, investigators at Emory University used Mongolian gerbils. The advantage being that males exhibit cuddling behavior after females become pregnant and they don’t watch a lot of sports on TV. They introduced a male and female gerbil, who then formed a pair bond and the female became pregnant. When the male started displaying cuddling behaviors, the researchers injected him with testosterone, expecting to see his antisocial side.
“Instead, we were surprised that a male gerbil became even more cuddly and prosocial with his partner. He became like ‘super partner,’ ” lead author Aubrey Kelly, PhD, said in a written statement from the university.
For the next experiment, the female was removed and another male was introduced to a male who had already received a testosterone injection. That male was surprisingly unaggressive toward the intruder, at least initially. Then he received a second injection of testosterone. “It was like they suddenly woke up and realized they weren’t supposed to be friendly in that context,” Dr. Kelly said.
The testosterone seemed to influence the activity of oxytocin, the so-called “love hormone,” the investigators suggested. “It’s surprising because normally we think of testosterone as increasing sexual behaviors and aggression. But we’ve shown that it can have more nuanced effects, depending on the social context.”
The researchers were not as surprised when their use of the phrase “super partner” led to a bidding war between DC and Marvel. Then came the contact from the Department of Defense, wondering about weaponized testosterone: Would it be possible for some sort of bomb to turn Vlad “the Impaler” Putin into Vlad “the Cuddler” Putin?
Are instruments spreading the sounds of COVID?
COVID restrictions are practically a thing of the past now. With more people laxed on being in close proximity to each other and the CDC not even recommending social distancing anymore, live concerts and events are back in full swing. But with new variants on the rise and people being a little more cautious, should we be worried about musical instruments spreading COVID?
Yes and no.
A study published in Physics of Fluids looked at wind instruments specifically and how much aerosol is produced and dispersed when playing them. For the study, the investigators measured fog particles with a laser and aerosol concentration with a particle counter to see how fast these particles decay in the air from the distance of the instrument.
Musicians in an orchestra typically would sit close together to produce the best sound, but with COVID that became an issue, senior author Paulo Arratia of the University of Pennsylvania, Philadelphia, noted in a separate written statement. By looking at the distance traveled by the particles coming from a single instrument and how quickly they decayed, they could determine if sitting in close proximity is an actual threat.
Well, the threat was no greater than talking to someone face to face. Particle exit speeds were lower than for a cough or a sneeze, and the maximum decay length was 2 meters from the instrument’s opening.
But that’s just one instrument: What kind of impact does a whole orchestra have on a space? The researchers are looking into that too, but for now they suggest that musicians continue to stay 6 feet away from each other.
So, yeah, there is a threat, but it’s probably safer for you to see that orchestra than have someone sneeze on you.
Music to our ears.
Taking ‘not enough hours in the day’ to new heights
It’s no secret that there’s a big doctor shortage in the United States. Going through medical school is long, expensive, and stressful, and it’s not like those long, stressful hours stop once you finally do get that degree. There is, however, an excellent reason to take that dive into doctorhood: You’ll gain mastery over time itself.
A study from the University of Chicago, Johns Hopkins University, and Imperial College London has revealed the truth. By using data pulled from the National Health and Nutrition Examination Survey, the researchers found that primary care physicians who see an average number of patients and follow all the current national guidelines for preventive care, chronic disease care, and acute care – plus administrative tasks – must work 26.7 hours a day. That works out to 14.1 hours of preventive care, 7.2 hours of chronic disease care, 2.2 hours of acute care, and 3.2 hours of documentation and inbox management.
Astute readers may note that this is a bit more than the traditional 8-hour workday. It is, in fact, more hours than there actually are in a day. As it turns out, Doctor Strange is more of a documentary than …
Hang on, we’re receiving word that doctors are not in fact wizards who can bend time and space to their will, nor are they sitting on a stash of Time-Turners they saved from the Ministry of Magic before Voldemort destroyed them all. They are, according to the study, overworked and overburdened with too many things and too little time. This is why outcomes haven’t improved despite technological advances and why burnout is so common. We’d be burned out too, having to work temporally impossible hours.
The study authors suggested a team-based approach to medicine that would spread the workload out to nurses, physician assistants, dietitians, etc., estimating that about two-thirds of what a primary care physician does can be handled by someone else. A team-based approach would reduce the physician’s required hours down to 9.3 hours a day, which is at least physically possible. It’s either that or we make the day longer, which sounds like the plot of an episode of Futurama. Swap overwork for global warming and a longer day for a longer year and it is actually the plot of an episode of Futurama.
After a hard day of thinking, brains need their rest
Do you ever feel like you have no more capacity to think or make any more decisions after a long day at work? Do you need a few extra cups of coffee to even make it through the day, even though you’re mostly just sitting around talking and typing? Have we got the research for you: Mental exhaustion is an actual thing. Imagine that double whammy of having a job that’s physically and mentally demanding.
A recent study in Current Biology explained why we feel so exhausted after doing something mentally demanding for several hours. Over that time, glutamate builds up in synapses of the prefrontal cortex, which affects our decision making and leads to cognitive lethargy. Your brain eventually becomes more interested in tasks that are less mentally fatiguing, and that’s probably why you’re reading this LOTME right now instead of getting back to work.
“Our findings show that cognitive work results in a true functional alteration – accumulation of noxious substances – so fatigue would indeed be a signal that makes us stop working but for a different purpose: to preserve the integrity of brain functioning,” senior author Mathias Pessiglione of Pitié-Salpêtrière University, Paris, said in a written statement.
The group of researchers conducted studies by using magnetic resonance spectroscopy to look at two groups of people over the course of a workday: One group had mentally tasking jobs and one didn’t. Those who had to think harder for their jobs had more signs of fatigue, such as reduced pupil dilation and glutamate in synapses of the prefrontal cortex. They also looked for more rewards that required less thinking.
For those whose mentally exhausting jobs probably won’t get better or change, the researchers suggest getting as much rest as possible. Those who don’t have that option will have to continue drinking those 7 cups of coffee a day. ... and reading LOTME.
Hmm, might be a new tagline for us in there somewhere. LOTME: Tired brains love us? When you’re too tired to think, think of LOTME? You can’t spell mental exhaustion without L-O-T-M-E?
Testosterone shows its warm and fuzzy side
Stereotypically, men are loud, knuckle-dragging Neanderthals. The hair coming out of our faces is kind of a dead giveaway, right? We grunt, we scratch, we start wars, we watch sports on TV. But why? It’s the testosterone. Everyone knows that. Testosterone makes men aggressive … or does it?
Since this sort of research generally isn’t done with actual men, investigators at Emory University used Mongolian gerbils. The advantage being that males exhibit cuddling behavior after females become pregnant and they don’t watch a lot of sports on TV. They introduced a male and female gerbil, who then formed a pair bond and the female became pregnant. When the male started displaying cuddling behaviors, the researchers injected him with testosterone, expecting to see his antisocial side.
“Instead, we were surprised that a male gerbil became even more cuddly and prosocial with his partner. He became like ‘super partner,’ ” lead author Aubrey Kelly, PhD, said in a written statement from the university.
For the next experiment, the female was removed and another male was introduced to a male who had already received a testosterone injection. That male was surprisingly unaggressive toward the intruder, at least initially. Then he received a second injection of testosterone. “It was like they suddenly woke up and realized they weren’t supposed to be friendly in that context,” Dr. Kelly said.
The testosterone seemed to influence the activity of oxytocin, the so-called “love hormone,” the investigators suggested. “It’s surprising because normally we think of testosterone as increasing sexual behaviors and aggression. But we’ve shown that it can have more nuanced effects, depending on the social context.”
The researchers were not as surprised when their use of the phrase “super partner” led to a bidding war between DC and Marvel. Then came the contact from the Department of Defense, wondering about weaponized testosterone: Would it be possible for some sort of bomb to turn Vlad “the Impaler” Putin into Vlad “the Cuddler” Putin?
Are instruments spreading the sounds of COVID?
COVID restrictions are practically a thing of the past now. With more people laxed on being in close proximity to each other and the CDC not even recommending social distancing anymore, live concerts and events are back in full swing. But with new variants on the rise and people being a little more cautious, should we be worried about musical instruments spreading COVID?
Yes and no.
A study published in Physics of Fluids looked at wind instruments specifically and how much aerosol is produced and dispersed when playing them. For the study, the investigators measured fog particles with a laser and aerosol concentration with a particle counter to see how fast these particles decay in the air from the distance of the instrument.
Musicians in an orchestra typically would sit close together to produce the best sound, but with COVID that became an issue, senior author Paulo Arratia of the University of Pennsylvania, Philadelphia, noted in a separate written statement. By looking at the distance traveled by the particles coming from a single instrument and how quickly they decayed, they could determine if sitting in close proximity is an actual threat.
Well, the threat was no greater than talking to someone face to face. Particle exit speeds were lower than for a cough or a sneeze, and the maximum decay length was 2 meters from the instrument’s opening.
But that’s just one instrument: What kind of impact does a whole orchestra have on a space? The researchers are looking into that too, but for now they suggest that musicians continue to stay 6 feet away from each other.
So, yeah, there is a threat, but it’s probably safer for you to see that orchestra than have someone sneeze on you.
Music to our ears.
Taking ‘not enough hours in the day’ to new heights
It’s no secret that there’s a big doctor shortage in the United States. Going through medical school is long, expensive, and stressful, and it’s not like those long, stressful hours stop once you finally do get that degree. There is, however, an excellent reason to take that dive into doctorhood: You’ll gain mastery over time itself.
A study from the University of Chicago, Johns Hopkins University, and Imperial College London has revealed the truth. By using data pulled from the National Health and Nutrition Examination Survey, the researchers found that primary care physicians who see an average number of patients and follow all the current national guidelines for preventive care, chronic disease care, and acute care – plus administrative tasks – must work 26.7 hours a day. That works out to 14.1 hours of preventive care, 7.2 hours of chronic disease care, 2.2 hours of acute care, and 3.2 hours of documentation and inbox management.
Astute readers may note that this is a bit more than the traditional 8-hour workday. It is, in fact, more hours than there actually are in a day. As it turns out, Doctor Strange is more of a documentary than …
Hang on, we’re receiving word that doctors are not in fact wizards who can bend time and space to their will, nor are they sitting on a stash of Time-Turners they saved from the Ministry of Magic before Voldemort destroyed them all. They are, according to the study, overworked and overburdened with too many things and too little time. This is why outcomes haven’t improved despite technological advances and why burnout is so common. We’d be burned out too, having to work temporally impossible hours.
The study authors suggested a team-based approach to medicine that would spread the workload out to nurses, physician assistants, dietitians, etc., estimating that about two-thirds of what a primary care physician does can be handled by someone else. A team-based approach would reduce the physician’s required hours down to 9.3 hours a day, which is at least physically possible. It’s either that or we make the day longer, which sounds like the plot of an episode of Futurama. Swap overwork for global warming and a longer day for a longer year and it is actually the plot of an episode of Futurama.
After a hard day of thinking, brains need their rest
Do you ever feel like you have no more capacity to think or make any more decisions after a long day at work? Do you need a few extra cups of coffee to even make it through the day, even though you’re mostly just sitting around talking and typing? Have we got the research for you: Mental exhaustion is an actual thing. Imagine that double whammy of having a job that’s physically and mentally demanding.
A recent study in Current Biology explained why we feel so exhausted after doing something mentally demanding for several hours. Over that time, glutamate builds up in synapses of the prefrontal cortex, which affects our decision making and leads to cognitive lethargy. Your brain eventually becomes more interested in tasks that are less mentally fatiguing, and that’s probably why you’re reading this LOTME right now instead of getting back to work.
“Our findings show that cognitive work results in a true functional alteration – accumulation of noxious substances – so fatigue would indeed be a signal that makes us stop working but for a different purpose: to preserve the integrity of brain functioning,” senior author Mathias Pessiglione of Pitié-Salpêtrière University, Paris, said in a written statement.
The group of researchers conducted studies by using magnetic resonance spectroscopy to look at two groups of people over the course of a workday: One group had mentally tasking jobs and one didn’t. Those who had to think harder for their jobs had more signs of fatigue, such as reduced pupil dilation and glutamate in synapses of the prefrontal cortex. They also looked for more rewards that required less thinking.
For those whose mentally exhausting jobs probably won’t get better or change, the researchers suggest getting as much rest as possible. Those who don’t have that option will have to continue drinking those 7 cups of coffee a day. ... and reading LOTME.
Hmm, might be a new tagline for us in there somewhere. LOTME: Tired brains love us? When you’re too tired to think, think of LOTME? You can’t spell mental exhaustion without L-O-T-M-E?
Testosterone shows its warm and fuzzy side
Stereotypically, men are loud, knuckle-dragging Neanderthals. The hair coming out of our faces is kind of a dead giveaway, right? We grunt, we scratch, we start wars, we watch sports on TV. But why? It’s the testosterone. Everyone knows that. Testosterone makes men aggressive … or does it?
Since this sort of research generally isn’t done with actual men, investigators at Emory University used Mongolian gerbils. The advantage being that males exhibit cuddling behavior after females become pregnant and they don’t watch a lot of sports on TV. They introduced a male and female gerbil, who then formed a pair bond and the female became pregnant. When the male started displaying cuddling behaviors, the researchers injected him with testosterone, expecting to see his antisocial side.
“Instead, we were surprised that a male gerbil became even more cuddly and prosocial with his partner. He became like ‘super partner,’ ” lead author Aubrey Kelly, PhD, said in a written statement from the university.
For the next experiment, the female was removed and another male was introduced to a male who had already received a testosterone injection. That male was surprisingly unaggressive toward the intruder, at least initially. Then he received a second injection of testosterone. “It was like they suddenly woke up and realized they weren’t supposed to be friendly in that context,” Dr. Kelly said.
The testosterone seemed to influence the activity of oxytocin, the so-called “love hormone,” the investigators suggested. “It’s surprising because normally we think of testosterone as increasing sexual behaviors and aggression. But we’ve shown that it can have more nuanced effects, depending on the social context.”
The researchers were not as surprised when their use of the phrase “super partner” led to a bidding war between DC and Marvel. Then came the contact from the Department of Defense, wondering about weaponized testosterone: Would it be possible for some sort of bomb to turn Vlad “the Impaler” Putin into Vlad “the Cuddler” Putin?
Are instruments spreading the sounds of COVID?
COVID restrictions are practically a thing of the past now. With more people laxed on being in close proximity to each other and the CDC not even recommending social distancing anymore, live concerts and events are back in full swing. But with new variants on the rise and people being a little more cautious, should we be worried about musical instruments spreading COVID?
Yes and no.
A study published in Physics of Fluids looked at wind instruments specifically and how much aerosol is produced and dispersed when playing them. For the study, the investigators measured fog particles with a laser and aerosol concentration with a particle counter to see how fast these particles decay in the air from the distance of the instrument.
Musicians in an orchestra typically would sit close together to produce the best sound, but with COVID that became an issue, senior author Paulo Arratia of the University of Pennsylvania, Philadelphia, noted in a separate written statement. By looking at the distance traveled by the particles coming from a single instrument and how quickly they decayed, they could determine if sitting in close proximity is an actual threat.
Well, the threat was no greater than talking to someone face to face. Particle exit speeds were lower than for a cough or a sneeze, and the maximum decay length was 2 meters from the instrument’s opening.
But that’s just one instrument: What kind of impact does a whole orchestra have on a space? The researchers are looking into that too, but for now they suggest that musicians continue to stay 6 feet away from each other.
So, yeah, there is a threat, but it’s probably safer for you to see that orchestra than have someone sneeze on you.
Music to our ears.
FDA approves adalimumab-bwwd biosimilar (Hadlima) in high-concentration form
The U.S. Food and Drug Administration today approved a citrate-free, high-concentration formulation of adalimumab-bwwd (Hadlima), the manufacturer, Samsung Bioepis, and its commercialization partner Organon said in an announcement.
Hadlima is a biosimilar of the tumor necrosis factor inhibitor reference product adalimumab (Humira).
Hadlima was first approved in July 2019 in a citrated, 50-mg/mL formulation. The new citrate-free, 100-mg/mL version will be available in prefilled syringe and autoinjector options.
The 100-mg/mL formulation is indicated for the same seven conditions as its 50-mg/mL counterpart: rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, plaque psoriasis, psoriatic arthritis, ankylosing spondylitis, adult and pediatric Crohn’s disease, and ulcerative colitis.
The approval was based on clinical data from a randomized, single-blind, two-arm, parallel group, single-dose study that compared the pharmacokinetics, safety, tolerability, and immunogenicity of the 100-mg/mL and 50-mg/mL formulations of Hadlima in healthy volunteers.
Both low- and high-concentration formulations of Humira are currently marketed in the United States. Organon said that it expects to market Hadlima in the United States on or after July 1, 2023, in accordance with a licensing agreement with AbbVie.
The prescribing information for Hadlima includes specific warnings and areas of concern. The drug should not be administered to individuals who are known to be hypersensitive to adalimumab. The drug may lower the ability of the immune system to fight infections and may increase risk of infections, including serious infections leading to hospitalization or death, such as tuberculosis, bacterial sepsis, invasive fungal infections (such as histoplasmosis), and infections attributable to other opportunistic pathogens.
A test for latent TB infection should be given before administration, and treatment of TB should begin before administration of Hadlima.
Patients taking Hadlima should not take a live vaccine.
The most common adverse effects (incidence > 10%) include infections (for example, upper respiratory infections, sinusitis), injection site reactions, headache, and rash.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration today approved a citrate-free, high-concentration formulation of adalimumab-bwwd (Hadlima), the manufacturer, Samsung Bioepis, and its commercialization partner Organon said in an announcement.
Hadlima is a biosimilar of the tumor necrosis factor inhibitor reference product adalimumab (Humira).
Hadlima was first approved in July 2019 in a citrated, 50-mg/mL formulation. The new citrate-free, 100-mg/mL version will be available in prefilled syringe and autoinjector options.
The 100-mg/mL formulation is indicated for the same seven conditions as its 50-mg/mL counterpart: rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, plaque psoriasis, psoriatic arthritis, ankylosing spondylitis, adult and pediatric Crohn’s disease, and ulcerative colitis.
The approval was based on clinical data from a randomized, single-blind, two-arm, parallel group, single-dose study that compared the pharmacokinetics, safety, tolerability, and immunogenicity of the 100-mg/mL and 50-mg/mL formulations of Hadlima in healthy volunteers.
Both low- and high-concentration formulations of Humira are currently marketed in the United States. Organon said that it expects to market Hadlima in the United States on or after July 1, 2023, in accordance with a licensing agreement with AbbVie.
The prescribing information for Hadlima includes specific warnings and areas of concern. The drug should not be administered to individuals who are known to be hypersensitive to adalimumab. The drug may lower the ability of the immune system to fight infections and may increase risk of infections, including serious infections leading to hospitalization or death, such as tuberculosis, bacterial sepsis, invasive fungal infections (such as histoplasmosis), and infections attributable to other opportunistic pathogens.
A test for latent TB infection should be given before administration, and treatment of TB should begin before administration of Hadlima.
Patients taking Hadlima should not take a live vaccine.
The most common adverse effects (incidence > 10%) include infections (for example, upper respiratory infections, sinusitis), injection site reactions, headache, and rash.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration today approved a citrate-free, high-concentration formulation of adalimumab-bwwd (Hadlima), the manufacturer, Samsung Bioepis, and its commercialization partner Organon said in an announcement.
Hadlima is a biosimilar of the tumor necrosis factor inhibitor reference product adalimumab (Humira).
Hadlima was first approved in July 2019 in a citrated, 50-mg/mL formulation. The new citrate-free, 100-mg/mL version will be available in prefilled syringe and autoinjector options.
The 100-mg/mL formulation is indicated for the same seven conditions as its 50-mg/mL counterpart: rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, plaque psoriasis, psoriatic arthritis, ankylosing spondylitis, adult and pediatric Crohn’s disease, and ulcerative colitis.
The approval was based on clinical data from a randomized, single-blind, two-arm, parallel group, single-dose study that compared the pharmacokinetics, safety, tolerability, and immunogenicity of the 100-mg/mL and 50-mg/mL formulations of Hadlima in healthy volunteers.
Both low- and high-concentration formulations of Humira are currently marketed in the United States. Organon said that it expects to market Hadlima in the United States on or after July 1, 2023, in accordance with a licensing agreement with AbbVie.
The prescribing information for Hadlima includes specific warnings and areas of concern. The drug should not be administered to individuals who are known to be hypersensitive to adalimumab. The drug may lower the ability of the immune system to fight infections and may increase risk of infections, including serious infections leading to hospitalization or death, such as tuberculosis, bacterial sepsis, invasive fungal infections (such as histoplasmosis), and infections attributable to other opportunistic pathogens.
A test for latent TB infection should be given before administration, and treatment of TB should begin before administration of Hadlima.
Patients taking Hadlima should not take a live vaccine.
The most common adverse effects (incidence > 10%) include infections (for example, upper respiratory infections, sinusitis), injection site reactions, headache, and rash.
A version of this article first appeared on Medscape.com.