User login
Obesity tied to worse brain health in children
CHICAGO – Higher weight and body mass index (BMI) in preadolescents are linked with poor brain health, new research suggests.
Poor brain health has been linked with obesity in adults, but little has been known about the link in children.
Lead author Simone Kaltenhauser, a postgraduate research fellow in radiology and biomedical imaging at the Yale School of Medicine, New Haven, Conn., presented her findings at the annual meeting of the Radiological Society of North America.
To represent the national sociodemographic makeup, the researchers used baseline information from the Adolescent Brain Cognitive Development (ABCD) study, which included 11,878 children aged 9 and 10 years from 21 centers across the United States.
This study included 5,169 children (51.9% girls). Children who had had traumatic brain injury, eating disorders, neurodevelopmental problems, and psychiatric diseases were excluded from the final analysis.
The researchers analyzed information from structural MRI and resting-state functional MRI, which allowed them to measure brain activity by detecting changes in blood flow.
“We analyzed the average fractional anisotropy (FA), mean (MD), axial (AD) and radial diffusivity (RD), and neurite density (ND) of 35 white matter (WM) tracts; cortical thickness and surface of 68 regions; and functional connectivity of 91 predefined network correlations,” the authors explained.
They adjusted for age, sex, race/ethnicity, handedness, and socioeconomic status. They used linear models to determine associations between weight and BMI z-scores and the imaging metrics.
Loss of white matter integrity
Among children with obesity, there was pervasive loss of white matter integrity and neurite density, cortical gray matter thinning, and decreased connectivity within and between networks that have been associated with impulse control and reward-based decision-making.
“These changes persisted in a similar pattern also 2 years later,” she said.
A member of the audience asked whether a reverse relationship might be at work – that poor brain health might drive obesity rather than the other way around.
Ms. Kaltenhauser agreed that other factors could be driving the link and acknowledged as a limitation that they did not have access to genetic information on the children.
Information on the effects of overweight and obesity is critical, especially in the United States, where an estimated 1 in 5 children are obese.
Ms. Kaltenhauser said she hopes her study raises awareness of potential brain health consequences as well as the physical consequences of childhood obesity.
Senior author Sam Payabvash, MD, a neuroradiologist and assistant professor of radiology and biomedical imaging at the Yale School of Medicine, said in a press release that the study may help explain the findings from previous studies that show an association between higher BMI in children and poor cognitive functioning and academic performance.
“The longitudinal ABCD study gives us the opportunity to observe any changes that occur in children with higher weight and BMI z-scores,” Dr. Payabvash said. “We’ll need to watch over the next 6-10 years.”
Avenues for future research
Amit B. Desai, MD, a neuroradiologist with Mayo Clinic in Jacksonville, Fla., who was not part of the study, said that while the research demonstrates an association between brain structure and BMI and obesity, “there may be other lurking variables.”
“What’s happening at an earlier stage in life could be causing both,” he said.
He noted that he would like to see future studies involving children at even earlier ages, along with investigations of the role of genetics or socioeconomic factors.
Including older children would be interesting as well, he said.
“Myelination doesn’t complete until you’re in your late teens or early 20s, so there are structural changes happening in the brain much later on into adolescence and early adulthood,” Dr. Desai said.
It would be premature, he said, to conclude from these findings that if children have obesity, there must be something wrong with their brain.
He would like to see whether there are changes in this link if a child is obese early on and later has normal weight or if a child has normal weight early and then becomes obese.
“It’s definitely an eye-opening study, but [it] needs additional work to expand upon it,” he said.
Ms. Kaltenhauser and Dr. Desai report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CHICAGO – Higher weight and body mass index (BMI) in preadolescents are linked with poor brain health, new research suggests.
Poor brain health has been linked with obesity in adults, but little has been known about the link in children.
Lead author Simone Kaltenhauser, a postgraduate research fellow in radiology and biomedical imaging at the Yale School of Medicine, New Haven, Conn., presented her findings at the annual meeting of the Radiological Society of North America.
To represent the national sociodemographic makeup, the researchers used baseline information from the Adolescent Brain Cognitive Development (ABCD) study, which included 11,878 children aged 9 and 10 years from 21 centers across the United States.
This study included 5,169 children (51.9% girls). Children who had had traumatic brain injury, eating disorders, neurodevelopmental problems, and psychiatric diseases were excluded from the final analysis.
The researchers analyzed information from structural MRI and resting-state functional MRI, which allowed them to measure brain activity by detecting changes in blood flow.
“We analyzed the average fractional anisotropy (FA), mean (MD), axial (AD) and radial diffusivity (RD), and neurite density (ND) of 35 white matter (WM) tracts; cortical thickness and surface of 68 regions; and functional connectivity of 91 predefined network correlations,” the authors explained.
They adjusted for age, sex, race/ethnicity, handedness, and socioeconomic status. They used linear models to determine associations between weight and BMI z-scores and the imaging metrics.
Loss of white matter integrity
Among children with obesity, there was pervasive loss of white matter integrity and neurite density, cortical gray matter thinning, and decreased connectivity within and between networks that have been associated with impulse control and reward-based decision-making.
“These changes persisted in a similar pattern also 2 years later,” she said.
A member of the audience asked whether a reverse relationship might be at work – that poor brain health might drive obesity rather than the other way around.
Ms. Kaltenhauser agreed that other factors could be driving the link and acknowledged as a limitation that they did not have access to genetic information on the children.
Information on the effects of overweight and obesity is critical, especially in the United States, where an estimated 1 in 5 children are obese.
Ms. Kaltenhauser said she hopes her study raises awareness of potential brain health consequences as well as the physical consequences of childhood obesity.
Senior author Sam Payabvash, MD, a neuroradiologist and assistant professor of radiology and biomedical imaging at the Yale School of Medicine, said in a press release that the study may help explain the findings from previous studies that show an association between higher BMI in children and poor cognitive functioning and academic performance.
“The longitudinal ABCD study gives us the opportunity to observe any changes that occur in children with higher weight and BMI z-scores,” Dr. Payabvash said. “We’ll need to watch over the next 6-10 years.”
Avenues for future research
Amit B. Desai, MD, a neuroradiologist with Mayo Clinic in Jacksonville, Fla., who was not part of the study, said that while the research demonstrates an association between brain structure and BMI and obesity, “there may be other lurking variables.”
“What’s happening at an earlier stage in life could be causing both,” he said.
He noted that he would like to see future studies involving children at even earlier ages, along with investigations of the role of genetics or socioeconomic factors.
Including older children would be interesting as well, he said.
“Myelination doesn’t complete until you’re in your late teens or early 20s, so there are structural changes happening in the brain much later on into adolescence and early adulthood,” Dr. Desai said.
It would be premature, he said, to conclude from these findings that if children have obesity, there must be something wrong with their brain.
He would like to see whether there are changes in this link if a child is obese early on and later has normal weight or if a child has normal weight early and then becomes obese.
“It’s definitely an eye-opening study, but [it] needs additional work to expand upon it,” he said.
Ms. Kaltenhauser and Dr. Desai report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CHICAGO – Higher weight and body mass index (BMI) in preadolescents are linked with poor brain health, new research suggests.
Poor brain health has been linked with obesity in adults, but little has been known about the link in children.
Lead author Simone Kaltenhauser, a postgraduate research fellow in radiology and biomedical imaging at the Yale School of Medicine, New Haven, Conn., presented her findings at the annual meeting of the Radiological Society of North America.
To represent the national sociodemographic makeup, the researchers used baseline information from the Adolescent Brain Cognitive Development (ABCD) study, which included 11,878 children aged 9 and 10 years from 21 centers across the United States.
This study included 5,169 children (51.9% girls). Children who had had traumatic brain injury, eating disorders, neurodevelopmental problems, and psychiatric diseases were excluded from the final analysis.
The researchers analyzed information from structural MRI and resting-state functional MRI, which allowed them to measure brain activity by detecting changes in blood flow.
“We analyzed the average fractional anisotropy (FA), mean (MD), axial (AD) and radial diffusivity (RD), and neurite density (ND) of 35 white matter (WM) tracts; cortical thickness and surface of 68 regions; and functional connectivity of 91 predefined network correlations,” the authors explained.
They adjusted for age, sex, race/ethnicity, handedness, and socioeconomic status. They used linear models to determine associations between weight and BMI z-scores and the imaging metrics.
Loss of white matter integrity
Among children with obesity, there was pervasive loss of white matter integrity and neurite density, cortical gray matter thinning, and decreased connectivity within and between networks that have been associated with impulse control and reward-based decision-making.
“These changes persisted in a similar pattern also 2 years later,” she said.
A member of the audience asked whether a reverse relationship might be at work – that poor brain health might drive obesity rather than the other way around.
Ms. Kaltenhauser agreed that other factors could be driving the link and acknowledged as a limitation that they did not have access to genetic information on the children.
Information on the effects of overweight and obesity is critical, especially in the United States, where an estimated 1 in 5 children are obese.
Ms. Kaltenhauser said she hopes her study raises awareness of potential brain health consequences as well as the physical consequences of childhood obesity.
Senior author Sam Payabvash, MD, a neuroradiologist and assistant professor of radiology and biomedical imaging at the Yale School of Medicine, said in a press release that the study may help explain the findings from previous studies that show an association between higher BMI in children and poor cognitive functioning and academic performance.
“The longitudinal ABCD study gives us the opportunity to observe any changes that occur in children with higher weight and BMI z-scores,” Dr. Payabvash said. “We’ll need to watch over the next 6-10 years.”
Avenues for future research
Amit B. Desai, MD, a neuroradiologist with Mayo Clinic in Jacksonville, Fla., who was not part of the study, said that while the research demonstrates an association between brain structure and BMI and obesity, “there may be other lurking variables.”
“What’s happening at an earlier stage in life could be causing both,” he said.
He noted that he would like to see future studies involving children at even earlier ages, along with investigations of the role of genetics or socioeconomic factors.
Including older children would be interesting as well, he said.
“Myelination doesn’t complete until you’re in your late teens or early 20s, so there are structural changes happening in the brain much later on into adolescence and early adulthood,” Dr. Desai said.
It would be premature, he said, to conclude from these findings that if children have obesity, there must be something wrong with their brain.
He would like to see whether there are changes in this link if a child is obese early on and later has normal weight or if a child has normal weight early and then becomes obese.
“It’s definitely an eye-opening study, but [it] needs additional work to expand upon it,” he said.
Ms. Kaltenhauser and Dr. Desai report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT RSNA 2022
Pregnancy not a barrier to interventional cardiology career
A new collaborative position paper on radiation exposure during pregnancy states that pregnant women can safely work in an ionizing radiation environment if exposure to the fetus does not exceed certain dose thresholds.
The position paper aims to “avoid discouraging” women from pursuing careers in interventional cardiology/electrophysiology (IC/EP) and to “dismantle” a barrier that says, “activity under x-rays, without any weighting, is incompatible with continuation of pregnancy,” lead author Stéphane Manzo-Silberman, MD, of AP-HP, Sorbonne Université, Paris, told this news organization.
“The main point of the statement is to show that it is possible and safe to maintain activity under radiation during pregnancy, [given] the data we have on the risk for the fetus at exposed doses, the regulations, and feedback from practice,” she said. “The data we currently have allowed us to be largely reassuring.”
The research showed that adverse effects on a fetus generally occur when radiation exposure is greater than 100 mGy. Most countries that permit pregnant women to work in IC/EP require that the cumulative dose during the pregnancy be less than 1 mSv. An exception is the United States, which permits a cumulative dose of less than 5 mSv.
The position paper, a collaboration among the European Association of Percutaneous Cardiovascular Interventions, the European Heart Rhythm Association, the European Association of Cardiovascular Imaging, the European Society of Cardiology Regulatory Affairs Committee, and Women as One, was published online in EuroIntervention.
The position paper covers regulations in various countries; fetal radiation doses that have been associated with ill effects, including abortion, malformations, and intelligence quotient reductions; the spontaneous probability of having a newborn with a congenital malformation or childhood cancer; and proposals to improve practice.
Highlights include the following:
- European, North American, Japanese, and Australian regulations permit pregnant women to work if closely monitored with an abdominal dosimeter; some countries, such as Austria, Hungary, Portugal, and Romania, do not allow women to work in IC/EP during pregnancy or breastfeeding.
- The maximum fetal dose exposure during pregnancy is 1 mSv in Europe, Australia, and Israel; 2 mSv in Japan; and 5 mSv in the United States.
- Doses associated with fetal harm are 100 times higher than those allowed during an interventional cardiologist’s entire pregnancy.
- There is a negligible risk increase in the spontaneous probability of a newborn having a congenital malformation or childhood cancer when the occupational exposure range of the mother respects a country’s limits.
- No studies have shown an increased risk of noncancerous adverse effects from prenatal radiation exposure less than 50 mSv.
To improve practice, the position paper suggests the following:
- Fluoroscopy operators must be guided by the “as low as reasonably achievable” principle: Obtaining optimal images must be balanced with procedure safety.
- Scatter radiation emitted from the patient is the main source of radiation exposure to the operator and personnel; reducing radiation to the patient will reduce exposure for staff.
- The three fundamentals of radiation safety for an operator are (1) time, (2) distance, and (3) shielding and dosimeter monitoring. Time refers to the amount of time the operator spends using the x-ray system; distance means maximizing distance from the x-ray source; and shielding includes personal, tableside, or external protection, with each form having a degree of lead equivalence defining its radiation protective effect.
- Changes in medical school curricula and creating a friendlier workplace environment for families and pregnant interventionists are among the strategies that will promote gender equity in the profession.
“Institutional radiation protection programs should be established to increase knowledge about radiation exposure and improve specific safety requirements for everyone. This would ensure safe exposure for all physicians, [including] during pregnancy,” Dr. Manzo-Silberman concluded.
Furthermore, she said, “As has already been demonstrated in the business world, improving representation and gender equity and diversity is key to improving results and efficiency. In the field of health, this translates into better care for our patients and better working conditions for health care professionals.”
No commercial funding was disclosed. Dr. Manzo-Silberman has received consulting fees from Bayer, Organon, and Exeltis; lecture fees from Bayer, BMS, Exeltis, and Organon; and has served on the adjudication board for a study for Biotronik.
A version of this article first appeared on Medscape.com.
A new collaborative position paper on radiation exposure during pregnancy states that pregnant women can safely work in an ionizing radiation environment if exposure to the fetus does not exceed certain dose thresholds.
The position paper aims to “avoid discouraging” women from pursuing careers in interventional cardiology/electrophysiology (IC/EP) and to “dismantle” a barrier that says, “activity under x-rays, without any weighting, is incompatible with continuation of pregnancy,” lead author Stéphane Manzo-Silberman, MD, of AP-HP, Sorbonne Université, Paris, told this news organization.
“The main point of the statement is to show that it is possible and safe to maintain activity under radiation during pregnancy, [given] the data we have on the risk for the fetus at exposed doses, the regulations, and feedback from practice,” she said. “The data we currently have allowed us to be largely reassuring.”
The research showed that adverse effects on a fetus generally occur when radiation exposure is greater than 100 mGy. Most countries that permit pregnant women to work in IC/EP require that the cumulative dose during the pregnancy be less than 1 mSv. An exception is the United States, which permits a cumulative dose of less than 5 mSv.
The position paper, a collaboration among the European Association of Percutaneous Cardiovascular Interventions, the European Heart Rhythm Association, the European Association of Cardiovascular Imaging, the European Society of Cardiology Regulatory Affairs Committee, and Women as One, was published online in EuroIntervention.
The position paper covers regulations in various countries; fetal radiation doses that have been associated with ill effects, including abortion, malformations, and intelligence quotient reductions; the spontaneous probability of having a newborn with a congenital malformation or childhood cancer; and proposals to improve practice.
Highlights include the following:
- European, North American, Japanese, and Australian regulations permit pregnant women to work if closely monitored with an abdominal dosimeter; some countries, such as Austria, Hungary, Portugal, and Romania, do not allow women to work in IC/EP during pregnancy or breastfeeding.
- The maximum fetal dose exposure during pregnancy is 1 mSv in Europe, Australia, and Israel; 2 mSv in Japan; and 5 mSv in the United States.
- Doses associated with fetal harm are 100 times higher than those allowed during an interventional cardiologist’s entire pregnancy.
- There is a negligible risk increase in the spontaneous probability of a newborn having a congenital malformation or childhood cancer when the occupational exposure range of the mother respects a country’s limits.
- No studies have shown an increased risk of noncancerous adverse effects from prenatal radiation exposure less than 50 mSv.
To improve practice, the position paper suggests the following:
- Fluoroscopy operators must be guided by the “as low as reasonably achievable” principle: Obtaining optimal images must be balanced with procedure safety.
- Scatter radiation emitted from the patient is the main source of radiation exposure to the operator and personnel; reducing radiation to the patient will reduce exposure for staff.
- The three fundamentals of radiation safety for an operator are (1) time, (2) distance, and (3) shielding and dosimeter monitoring. Time refers to the amount of time the operator spends using the x-ray system; distance means maximizing distance from the x-ray source; and shielding includes personal, tableside, or external protection, with each form having a degree of lead equivalence defining its radiation protective effect.
- Changes in medical school curricula and creating a friendlier workplace environment for families and pregnant interventionists are among the strategies that will promote gender equity in the profession.
“Institutional radiation protection programs should be established to increase knowledge about radiation exposure and improve specific safety requirements for everyone. This would ensure safe exposure for all physicians, [including] during pregnancy,” Dr. Manzo-Silberman concluded.
Furthermore, she said, “As has already been demonstrated in the business world, improving representation and gender equity and diversity is key to improving results and efficiency. In the field of health, this translates into better care for our patients and better working conditions for health care professionals.”
No commercial funding was disclosed. Dr. Manzo-Silberman has received consulting fees from Bayer, Organon, and Exeltis; lecture fees from Bayer, BMS, Exeltis, and Organon; and has served on the adjudication board for a study for Biotronik.
A version of this article first appeared on Medscape.com.
A new collaborative position paper on radiation exposure during pregnancy states that pregnant women can safely work in an ionizing radiation environment if exposure to the fetus does not exceed certain dose thresholds.
The position paper aims to “avoid discouraging” women from pursuing careers in interventional cardiology/electrophysiology (IC/EP) and to “dismantle” a barrier that says, “activity under x-rays, without any weighting, is incompatible with continuation of pregnancy,” lead author Stéphane Manzo-Silberman, MD, of AP-HP, Sorbonne Université, Paris, told this news organization.
“The main point of the statement is to show that it is possible and safe to maintain activity under radiation during pregnancy, [given] the data we have on the risk for the fetus at exposed doses, the regulations, and feedback from practice,” she said. “The data we currently have allowed us to be largely reassuring.”
The research showed that adverse effects on a fetus generally occur when radiation exposure is greater than 100 mGy. Most countries that permit pregnant women to work in IC/EP require that the cumulative dose during the pregnancy be less than 1 mSv. An exception is the United States, which permits a cumulative dose of less than 5 mSv.
The position paper, a collaboration among the European Association of Percutaneous Cardiovascular Interventions, the European Heart Rhythm Association, the European Association of Cardiovascular Imaging, the European Society of Cardiology Regulatory Affairs Committee, and Women as One, was published online in EuroIntervention.
The position paper covers regulations in various countries; fetal radiation doses that have been associated with ill effects, including abortion, malformations, and intelligence quotient reductions; the spontaneous probability of having a newborn with a congenital malformation or childhood cancer; and proposals to improve practice.
Highlights include the following:
- European, North American, Japanese, and Australian regulations permit pregnant women to work if closely monitored with an abdominal dosimeter; some countries, such as Austria, Hungary, Portugal, and Romania, do not allow women to work in IC/EP during pregnancy or breastfeeding.
- The maximum fetal dose exposure during pregnancy is 1 mSv in Europe, Australia, and Israel; 2 mSv in Japan; and 5 mSv in the United States.
- Doses associated with fetal harm are 100 times higher than those allowed during an interventional cardiologist’s entire pregnancy.
- There is a negligible risk increase in the spontaneous probability of a newborn having a congenital malformation or childhood cancer when the occupational exposure range of the mother respects a country’s limits.
- No studies have shown an increased risk of noncancerous adverse effects from prenatal radiation exposure less than 50 mSv.
To improve practice, the position paper suggests the following:
- Fluoroscopy operators must be guided by the “as low as reasonably achievable” principle: Obtaining optimal images must be balanced with procedure safety.
- Scatter radiation emitted from the patient is the main source of radiation exposure to the operator and personnel; reducing radiation to the patient will reduce exposure for staff.
- The three fundamentals of radiation safety for an operator are (1) time, (2) distance, and (3) shielding and dosimeter monitoring. Time refers to the amount of time the operator spends using the x-ray system; distance means maximizing distance from the x-ray source; and shielding includes personal, tableside, or external protection, with each form having a degree of lead equivalence defining its radiation protective effect.
- Changes in medical school curricula and creating a friendlier workplace environment for families and pregnant interventionists are among the strategies that will promote gender equity in the profession.
“Institutional radiation protection programs should be established to increase knowledge about radiation exposure and improve specific safety requirements for everyone. This would ensure safe exposure for all physicians, [including] during pregnancy,” Dr. Manzo-Silberman concluded.
Furthermore, she said, “As has already been demonstrated in the business world, improving representation and gender equity and diversity is key to improving results and efficiency. In the field of health, this translates into better care for our patients and better working conditions for health care professionals.”
No commercial funding was disclosed. Dr. Manzo-Silberman has received consulting fees from Bayer, Organon, and Exeltis; lecture fees from Bayer, BMS, Exeltis, and Organon; and has served on the adjudication board for a study for Biotronik.
A version of this article first appeared on Medscape.com.
FROM EUROINTERVENTION
Lp(a) tied to more early CV events than familial hypercholesterolemia
Many more people are at risk for early cardiovascular events because of raised lipoprotein(a) levels than from having familial hypercholesterolemia (FH), a new study suggests.
The Danish study set out to try and establish a level of Lp(a) that would be associated with a cardiovascular risk similar to that seen with FH. As there are many different definitions of FH, results showed a large range of Lp(a) values that corresponded to risk levels of the different FH definitions.
However, if considering one of the broadest FH definitions (from MEDPED – Make Early Diagnoses, Prevent Early Deaths), which is the one most commonly used in the United States, results showed that the level of cardiovascular risk in patients with this definition of FH is similar to that associated with Lp(a) levels of around 70 mg/dL (0.7 g/L).
“While FH is fairly unusual, occurring in less than 1% of the population, levels of Lp(a) of 70 mg/dL or above are much more common, occurring in around 10% of the White population,” Børge Nordestgaard, MD, Copenhagen University Hospital, said in an interview. Around 20% of the Black population have such high levels, while levels in Hispanics are in between.
“Our results suggest that there will be many more individuals at risk of premature MI or cardiovascular death because of raised Lp(a) levels than because of FH,” added Dr. Nordestgaard, the senior author of the current study.
Dr. Nordestgaard explained that FH is well established to be a serious condition. “We consider FH to be the genetic disease that causes the most cases of early heart disease and early death worldwide.”
“But we know now that raised levels of Lp(a), which is also genetically determined, can also lead to an increased risk of cardiovascular events relatively early in life, and when you look into the numbers, it seems like high levels of Lp(a) could be more common than FH. We wanted to try and find the levels of Lp(a) that corresponded to similar cardiovascular risk as FH.”
The Danish study was published in the Journal of the American College of Cardiology.
The authors note that the 2019 joint European Society of Cardiology and European Atherosclerosis Society guidelines suggested that an Lp(a) level greater than 180 mg/dL (0.8 g/L) may confer a lifetime risk for heart disease equivalent to the risk associated with heterozygous FH, but they point out that this value was speculative and not based on a direct comparison of risk associated with the two conditions in the same population.
For their study, Dr. Nordestgaard and colleagues analyzed information from a large database of the Danish population, the Copenhagen General Population Study, including 69,644 individuals for whom data on FH and Lp(a) levels were available. As these conditions are genetically determined, and the study held records on individuals going back several decades, the researchers were able to analyze event rates over a median follow up time of 42 years. During this time, there were 4,166 cases of myocardial infarction and 11,464 cases of atherosclerotic cardiovascular disease (ASCVD).
Results showed that Lp(a) levels associated with MI risk equivalent to that of clinical FH ranged from 67 to 402 mg/dL depending on the definition used for FH. The Lp(a) level corresponding to the MI risk of genetically determined FH was 180 mg/dL.
In terms of risk of ASCVD events, the levels of Lp(a) corresponding to the risk associated with clinical FH ranged from 130 to 391 mg/dL, and the Lp(a) level corresponding to the ASCVD risk of genetically determined FH was 175 mg/dL.
“All these different definitions of FH may cause some confusion, but basically we are saying that if an individual is found to have an Lp(a) above 70 mg/dL, then they have a similar level of cardiovascular risk as that associated with the broadest definition of FH, and they should be taken as seriously as a patient diagnosed with FH,” Dr. Nordestgaard said.
He estimated that these individuals have approximately a doubling of cardiovascular risk, compared with the general population, and risk increases further with rising Lp(a) levels.
The researchers also found that if an individual has both FH and raised Lp(a) they are at very high risk, as these two conditions are independent of each other.
Although a specific treatment for lowering Lp(a) levels is not yet available, Dr. Nordestgaard stresses that it is still worth identifying individuals with raised Lp(a) as efforts can be made to address other cardiovascular risk factors.
“We know raised Lp(a) increases cardiovascular risk, but there are also many other factors that likewise increase this risk, and they are all additive. So, it is very important that individuals with raised Lp(a) levels address these other risk factors,” he said. “These include stopping smoking, being at healthy weight, exercising regularly, eating a heart-healthy diet, and aggressive treatment of raised LDL, hypertension, and diabetes. All these things will lower their overall risk of cardiovascular disease.”
And there is the promise of new drugs to lower Lp(a) on the horizon, with several such products now in clinical development.
Dr. Nordestgaard also points out that as Lp(a) is genetically determined, cascade screening of close relatives of the individual with raised Lp(a) should also take place to detect others who may be at risk.
Although a level of Lp(a) of around 70 mg/dL confers similar cardiovascular risk than some definitions of FH, Dr. Nordestgaard says lower levels than this should also be a signal for concern.
“We usually say Lp(a) levels of 50 mg/dL are when we need to start to take this seriously. And it’s estimated that about 20% of the White population will have levels of 50 mg/dL or over and even more in the Black population,” he added.
‘Screen for both conditions’
In an accompanying editorial, Pamela Morris, MD, Medical University of South Carolina, Charleston; Jagat Narula, MD, Icahn School of Medicine, New York; and Sotirios Tsimikas, MD, University of California, San Diego, say “the weight of evidence strongly supports that both genetic lipid disorders, elevated Lp(a) levels and FH, are causally associated with an increased risk of premature ASCVD and should be carefully considered in risk assessment and management for ASCVD risk reduction.”
Dr. Morris told this news organization that the current study found a very large range of Lp(a) levels that conferred a similar cardiovascular risk to FH, because of the many different definitions of FH in use.
“But this should not take away the importance of screening for raised Lp(a) levels,” she stressed.
“We know that increased Lp(a) levels signal a high risk of cardiovascular disease. A diagnosis of FH is also a high-risk condition,” she said. “Both are important, and we need to screen for both, but it is difficult to directly compare the two conditions because the different definitions of FH get in the way.”
Dr. Morris agrees with Dr. Nordestgaard that raised levels of Lp(a) may actually be more important for the population risk of cardiovascular disease than FH, as the prevalence of increased Lp(a) levels is higher.
“Because raised Lp(a) levels are more prevalent than confirmed FH, the risk to the population is greater,” she said.
Dr. Morris points out that cardiovascular risk starts to increase at Lp(a) levels of 30 mg/dL (75 nmol/L).
The editorialists recommend that “in addition to performing a lipid panel periodically according to evidence-based guidelines, measurement of Lp(a) levels should also be performed at least once in an individual’s lifetime for ASCVD risk assessment.”
They conclude that “it is vital to continue to raise awareness among clinicians and patients of these high-risk genetic lipid disorders. Our understanding of both disorders is rapidly expanding, and promising novel therapeutics may offer hope for prevention of cardiovascular disease in patients with elevated Lp(a) levels in the future.”
This work was supported by Copenhagen University Hospital – Herlev Gentofte, Denmark, and the Danish Beckett-Foundation. The Copenhagen General Population Study is supported by the Copenhagen County Foundation and Copenhagen University Hospital – Herlev Gentofte. Dr. Nordestgaard has been a consultant and a speaker for AstraZeneca, Sanofi, Regeneron, Akcea, Amgen, Kowa, Denka, Amarin, Novartis, Novo Nordisk, Silence Therapeutics, Abbott, and Esperion.
A version of this article first appeared on Medscape.com.
Many more people are at risk for early cardiovascular events because of raised lipoprotein(a) levels than from having familial hypercholesterolemia (FH), a new study suggests.
The Danish study set out to try and establish a level of Lp(a) that would be associated with a cardiovascular risk similar to that seen with FH. As there are many different definitions of FH, results showed a large range of Lp(a) values that corresponded to risk levels of the different FH definitions.
However, if considering one of the broadest FH definitions (from MEDPED – Make Early Diagnoses, Prevent Early Deaths), which is the one most commonly used in the United States, results showed that the level of cardiovascular risk in patients with this definition of FH is similar to that associated with Lp(a) levels of around 70 mg/dL (0.7 g/L).
“While FH is fairly unusual, occurring in less than 1% of the population, levels of Lp(a) of 70 mg/dL or above are much more common, occurring in around 10% of the White population,” Børge Nordestgaard, MD, Copenhagen University Hospital, said in an interview. Around 20% of the Black population have such high levels, while levels in Hispanics are in between.
“Our results suggest that there will be many more individuals at risk of premature MI or cardiovascular death because of raised Lp(a) levels than because of FH,” added Dr. Nordestgaard, the senior author of the current study.
Dr. Nordestgaard explained that FH is well established to be a serious condition. “We consider FH to be the genetic disease that causes the most cases of early heart disease and early death worldwide.”
“But we know now that raised levels of Lp(a), which is also genetically determined, can also lead to an increased risk of cardiovascular events relatively early in life, and when you look into the numbers, it seems like high levels of Lp(a) could be more common than FH. We wanted to try and find the levels of Lp(a) that corresponded to similar cardiovascular risk as FH.”
The Danish study was published in the Journal of the American College of Cardiology.
The authors note that the 2019 joint European Society of Cardiology and European Atherosclerosis Society guidelines suggested that an Lp(a) level greater than 180 mg/dL (0.8 g/L) may confer a lifetime risk for heart disease equivalent to the risk associated with heterozygous FH, but they point out that this value was speculative and not based on a direct comparison of risk associated with the two conditions in the same population.
For their study, Dr. Nordestgaard and colleagues analyzed information from a large database of the Danish population, the Copenhagen General Population Study, including 69,644 individuals for whom data on FH and Lp(a) levels were available. As these conditions are genetically determined, and the study held records on individuals going back several decades, the researchers were able to analyze event rates over a median follow up time of 42 years. During this time, there were 4,166 cases of myocardial infarction and 11,464 cases of atherosclerotic cardiovascular disease (ASCVD).
Results showed that Lp(a) levels associated with MI risk equivalent to that of clinical FH ranged from 67 to 402 mg/dL depending on the definition used for FH. The Lp(a) level corresponding to the MI risk of genetically determined FH was 180 mg/dL.
In terms of risk of ASCVD events, the levels of Lp(a) corresponding to the risk associated with clinical FH ranged from 130 to 391 mg/dL, and the Lp(a) level corresponding to the ASCVD risk of genetically determined FH was 175 mg/dL.
“All these different definitions of FH may cause some confusion, but basically we are saying that if an individual is found to have an Lp(a) above 70 mg/dL, then they have a similar level of cardiovascular risk as that associated with the broadest definition of FH, and they should be taken as seriously as a patient diagnosed with FH,” Dr. Nordestgaard said.
He estimated that these individuals have approximately a doubling of cardiovascular risk, compared with the general population, and risk increases further with rising Lp(a) levels.
The researchers also found that if an individual has both FH and raised Lp(a) they are at very high risk, as these two conditions are independent of each other.
Although a specific treatment for lowering Lp(a) levels is not yet available, Dr. Nordestgaard stresses that it is still worth identifying individuals with raised Lp(a) as efforts can be made to address other cardiovascular risk factors.
“We know raised Lp(a) increases cardiovascular risk, but there are also many other factors that likewise increase this risk, and they are all additive. So, it is very important that individuals with raised Lp(a) levels address these other risk factors,” he said. “These include stopping smoking, being at healthy weight, exercising regularly, eating a heart-healthy diet, and aggressive treatment of raised LDL, hypertension, and diabetes. All these things will lower their overall risk of cardiovascular disease.”
And there is the promise of new drugs to lower Lp(a) on the horizon, with several such products now in clinical development.
Dr. Nordestgaard also points out that as Lp(a) is genetically determined, cascade screening of close relatives of the individual with raised Lp(a) should also take place to detect others who may be at risk.
Although a level of Lp(a) of around 70 mg/dL confers similar cardiovascular risk than some definitions of FH, Dr. Nordestgaard says lower levels than this should also be a signal for concern.
“We usually say Lp(a) levels of 50 mg/dL are when we need to start to take this seriously. And it’s estimated that about 20% of the White population will have levels of 50 mg/dL or over and even more in the Black population,” he added.
‘Screen for both conditions’
In an accompanying editorial, Pamela Morris, MD, Medical University of South Carolina, Charleston; Jagat Narula, MD, Icahn School of Medicine, New York; and Sotirios Tsimikas, MD, University of California, San Diego, say “the weight of evidence strongly supports that both genetic lipid disorders, elevated Lp(a) levels and FH, are causally associated with an increased risk of premature ASCVD and should be carefully considered in risk assessment and management for ASCVD risk reduction.”
Dr. Morris told this news organization that the current study found a very large range of Lp(a) levels that conferred a similar cardiovascular risk to FH, because of the many different definitions of FH in use.
“But this should not take away the importance of screening for raised Lp(a) levels,” she stressed.
“We know that increased Lp(a) levels signal a high risk of cardiovascular disease. A diagnosis of FH is also a high-risk condition,” she said. “Both are important, and we need to screen for both, but it is difficult to directly compare the two conditions because the different definitions of FH get in the way.”
Dr. Morris agrees with Dr. Nordestgaard that raised levels of Lp(a) may actually be more important for the population risk of cardiovascular disease than FH, as the prevalence of increased Lp(a) levels is higher.
“Because raised Lp(a) levels are more prevalent than confirmed FH, the risk to the population is greater,” she said.
Dr. Morris points out that cardiovascular risk starts to increase at Lp(a) levels of 30 mg/dL (75 nmol/L).
The editorialists recommend that “in addition to performing a lipid panel periodically according to evidence-based guidelines, measurement of Lp(a) levels should also be performed at least once in an individual’s lifetime for ASCVD risk assessment.”
They conclude that “it is vital to continue to raise awareness among clinicians and patients of these high-risk genetic lipid disorders. Our understanding of both disorders is rapidly expanding, and promising novel therapeutics may offer hope for prevention of cardiovascular disease in patients with elevated Lp(a) levels in the future.”
This work was supported by Copenhagen University Hospital – Herlev Gentofte, Denmark, and the Danish Beckett-Foundation. The Copenhagen General Population Study is supported by the Copenhagen County Foundation and Copenhagen University Hospital – Herlev Gentofte. Dr. Nordestgaard has been a consultant and a speaker for AstraZeneca, Sanofi, Regeneron, Akcea, Amgen, Kowa, Denka, Amarin, Novartis, Novo Nordisk, Silence Therapeutics, Abbott, and Esperion.
A version of this article first appeared on Medscape.com.
Many more people are at risk for early cardiovascular events because of raised lipoprotein(a) levels than from having familial hypercholesterolemia (FH), a new study suggests.
The Danish study set out to try and establish a level of Lp(a) that would be associated with a cardiovascular risk similar to that seen with FH. As there are many different definitions of FH, results showed a large range of Lp(a) values that corresponded to risk levels of the different FH definitions.
However, if considering one of the broadest FH definitions (from MEDPED – Make Early Diagnoses, Prevent Early Deaths), which is the one most commonly used in the United States, results showed that the level of cardiovascular risk in patients with this definition of FH is similar to that associated with Lp(a) levels of around 70 mg/dL (0.7 g/L).
“While FH is fairly unusual, occurring in less than 1% of the population, levels of Lp(a) of 70 mg/dL or above are much more common, occurring in around 10% of the White population,” Børge Nordestgaard, MD, Copenhagen University Hospital, said in an interview. Around 20% of the Black population have such high levels, while levels in Hispanics are in between.
“Our results suggest that there will be many more individuals at risk of premature MI or cardiovascular death because of raised Lp(a) levels than because of FH,” added Dr. Nordestgaard, the senior author of the current study.
Dr. Nordestgaard explained that FH is well established to be a serious condition. “We consider FH to be the genetic disease that causes the most cases of early heart disease and early death worldwide.”
“But we know now that raised levels of Lp(a), which is also genetically determined, can also lead to an increased risk of cardiovascular events relatively early in life, and when you look into the numbers, it seems like high levels of Lp(a) could be more common than FH. We wanted to try and find the levels of Lp(a) that corresponded to similar cardiovascular risk as FH.”
The Danish study was published in the Journal of the American College of Cardiology.
The authors note that the 2019 joint European Society of Cardiology and European Atherosclerosis Society guidelines suggested that an Lp(a) level greater than 180 mg/dL (0.8 g/L) may confer a lifetime risk for heart disease equivalent to the risk associated with heterozygous FH, but they point out that this value was speculative and not based on a direct comparison of risk associated with the two conditions in the same population.
For their study, Dr. Nordestgaard and colleagues analyzed information from a large database of the Danish population, the Copenhagen General Population Study, including 69,644 individuals for whom data on FH and Lp(a) levels were available. As these conditions are genetically determined, and the study held records on individuals going back several decades, the researchers were able to analyze event rates over a median follow up time of 42 years. During this time, there were 4,166 cases of myocardial infarction and 11,464 cases of atherosclerotic cardiovascular disease (ASCVD).
Results showed that Lp(a) levels associated with MI risk equivalent to that of clinical FH ranged from 67 to 402 mg/dL depending on the definition used for FH. The Lp(a) level corresponding to the MI risk of genetically determined FH was 180 mg/dL.
In terms of risk of ASCVD events, the levels of Lp(a) corresponding to the risk associated with clinical FH ranged from 130 to 391 mg/dL, and the Lp(a) level corresponding to the ASCVD risk of genetically determined FH was 175 mg/dL.
“All these different definitions of FH may cause some confusion, but basically we are saying that if an individual is found to have an Lp(a) above 70 mg/dL, then they have a similar level of cardiovascular risk as that associated with the broadest definition of FH, and they should be taken as seriously as a patient diagnosed with FH,” Dr. Nordestgaard said.
He estimated that these individuals have approximately a doubling of cardiovascular risk, compared with the general population, and risk increases further with rising Lp(a) levels.
The researchers also found that if an individual has both FH and raised Lp(a) they are at very high risk, as these two conditions are independent of each other.
Although a specific treatment for lowering Lp(a) levels is not yet available, Dr. Nordestgaard stresses that it is still worth identifying individuals with raised Lp(a) as efforts can be made to address other cardiovascular risk factors.
“We know raised Lp(a) increases cardiovascular risk, but there are also many other factors that likewise increase this risk, and they are all additive. So, it is very important that individuals with raised Lp(a) levels address these other risk factors,” he said. “These include stopping smoking, being at healthy weight, exercising regularly, eating a heart-healthy diet, and aggressive treatment of raised LDL, hypertension, and diabetes. All these things will lower their overall risk of cardiovascular disease.”
And there is the promise of new drugs to lower Lp(a) on the horizon, with several such products now in clinical development.
Dr. Nordestgaard also points out that as Lp(a) is genetically determined, cascade screening of close relatives of the individual with raised Lp(a) should also take place to detect others who may be at risk.
Although a level of Lp(a) of around 70 mg/dL confers similar cardiovascular risk than some definitions of FH, Dr. Nordestgaard says lower levels than this should also be a signal for concern.
“We usually say Lp(a) levels of 50 mg/dL are when we need to start to take this seriously. And it’s estimated that about 20% of the White population will have levels of 50 mg/dL or over and even more in the Black population,” he added.
‘Screen for both conditions’
In an accompanying editorial, Pamela Morris, MD, Medical University of South Carolina, Charleston; Jagat Narula, MD, Icahn School of Medicine, New York; and Sotirios Tsimikas, MD, University of California, San Diego, say “the weight of evidence strongly supports that both genetic lipid disorders, elevated Lp(a) levels and FH, are causally associated with an increased risk of premature ASCVD and should be carefully considered in risk assessment and management for ASCVD risk reduction.”
Dr. Morris told this news organization that the current study found a very large range of Lp(a) levels that conferred a similar cardiovascular risk to FH, because of the many different definitions of FH in use.
“But this should not take away the importance of screening for raised Lp(a) levels,” she stressed.
“We know that increased Lp(a) levels signal a high risk of cardiovascular disease. A diagnosis of FH is also a high-risk condition,” she said. “Both are important, and we need to screen for both, but it is difficult to directly compare the two conditions because the different definitions of FH get in the way.”
Dr. Morris agrees with Dr. Nordestgaard that raised levels of Lp(a) may actually be more important for the population risk of cardiovascular disease than FH, as the prevalence of increased Lp(a) levels is higher.
“Because raised Lp(a) levels are more prevalent than confirmed FH, the risk to the population is greater,” she said.
Dr. Morris points out that cardiovascular risk starts to increase at Lp(a) levels of 30 mg/dL (75 nmol/L).
The editorialists recommend that “in addition to performing a lipid panel periodically according to evidence-based guidelines, measurement of Lp(a) levels should also be performed at least once in an individual’s lifetime for ASCVD risk assessment.”
They conclude that “it is vital to continue to raise awareness among clinicians and patients of these high-risk genetic lipid disorders. Our understanding of both disorders is rapidly expanding, and promising novel therapeutics may offer hope for prevention of cardiovascular disease in patients with elevated Lp(a) levels in the future.”
This work was supported by Copenhagen University Hospital – Herlev Gentofte, Denmark, and the Danish Beckett-Foundation. The Copenhagen General Population Study is supported by the Copenhagen County Foundation and Copenhagen University Hospital – Herlev Gentofte. Dr. Nordestgaard has been a consultant and a speaker for AstraZeneca, Sanofi, Regeneron, Akcea, Amgen, Kowa, Denka, Amarin, Novartis, Novo Nordisk, Silence Therapeutics, Abbott, and Esperion.
A version of this article first appeared on Medscape.com.
The surprising failure of vitamin D in deficient kids
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
My basic gripe is that you’ve got all these observational studies linking lower levels of vitamin D to everything from dementia to falls to cancer to COVID infection, and then you do a big randomized trial of supplementation and don’t see an effect.
And the explanation is that vitamin D is not necessarily the thing causing these bad outcomes; it’s a bystander – a canary in the coal mine. Your vitamin D level is a marker of your lifestyle; it’s higher in people who eat healthier foods, who exercise, and who spend more time out in the sun.
And yet ... if you were to ask me whether supplementing vitamin D in children with vitamin D deficiency would help them grow better and be healthier, I probably would have been on board for the idea.
And, it looks like, I would have been wrong.
Yes, it’s another negative randomized trial of vitamin D supplementation to add to the seemingly ever-growing body of literature suggesting that your money is better spent on a day at the park rather than buying D3 from your local GNC.
We are talking about this study, appearing in JAMA Pediatrics.
Briefly, 8,851 children from around Ulaanbaatar, Mongolia, were randomized to receive 14,000 international units of vitamin D3 or placebo every week for 3 years.
Before we get into the results of the study, I need to point out that this part of Mongolia has a high rate of vitamin D deficiency. Beyond that, a prior observational study by these authors had shown that lower vitamin D levels were linked to the risk of acquiring latent tuberculosis infection in this area. Other studies have linked vitamin D deficiency with poorer growth metrics in children. Given the global scourge that is TB (around 2 million deaths a year) and childhood malnutrition (around 10% of children around the world), vitamin D supplementation is incredibly attractive as a public health intervention. It is relatively low on side effects and, importantly, it is cheap – and thus scalable.
Back to the study. These kids had pretty poor vitamin D levels at baseline; 95% of them were deficient, based on the accepted standard of levels less than 20 ng/mL. Over 30% were severely deficient, with levels less than 10 ng/mL.
The initial purpose of this study was to see if supplementation would prevent TB, but that analysis, which was published a few months ago, was negative. Vitamin D levels went up dramatically in the intervention group – they were taking their pills – but there was no difference in the rate of latent TB infection, active TB, other respiratory infections, or even serum interferon gamma levels.
Nothing.
But to be fair, the TB seroconversion rate was lower than expected, potentially leading to an underpowered study.
Which brings us to the just-published analysis which moves away from infectious disease to something where vitamin D should have some stronger footing: growth.
Would the kids who were randomized to vitamin D, those same kids who got their vitamin D levels into the normal range over 3 years of supplementation, grow more or grow better than the kids who didn’t?
And, unfortunately, the answer is still no.
At the end of follow-up, height z scores were not different between the groups. BMI z scores were not different between the groups. Pubertal development was not different between the groups. This was true not only overall, but across various subgroups, including analyses of those kids who had vitamin D levels less than 10 ng/mL to start with.
So, what’s going on? There are two very broad possibilities we can endorse. First, there’s the idea that vitamin D supplementation simply doesn’t do much for health. This is supported, now, by a long string of large clinical trials that show no effect across a variety of disease states and predisease states. In other words, the observational data linking low vitamin D to bad outcomes is correlation, not causation.
Or we can take the tack of some vitamin D apologists and decide that this trial just got it wrong. Perhaps the dose wasn’t given correctly, or 3 years isn’t long enough to see a real difference, or the growth metrics were wrong, or vitamin D needs to be given alongside something else to really work and so on. This is fine; no study is perfect and there is always something to criticize, believe me. But we need to be careful not to fall into the baby-and-bathwater fallacy. Just because we think a study could have done something better, or differently, doesn’t mean we can ignore all the results. And as each new randomized trial of vitamin D supplementation comes out, it’s getting harder and harder to believe that these trialists keep getting their methods wrong. Maybe they are just testing something that doesn’t work.
What to do? Well, it should be obvious. If low vitamin D levels are linked to TB rates and poor growth but supplementation doesn’t fix the problem, then we have to fix what is upstream of the problem. We need to boost vitamin D levels not through supplements, but through nutrition, exercise, activity, and getting outside. That’s a randomized trial you can sign me up for any day.
Dr. Wilson is associate professor, department of medicine, Yale University, New Haven, Conn. He reported no relevant conflicts of interest.
A version of this video transcript first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
My basic gripe is that you’ve got all these observational studies linking lower levels of vitamin D to everything from dementia to falls to cancer to COVID infection, and then you do a big randomized trial of supplementation and don’t see an effect.
And the explanation is that vitamin D is not necessarily the thing causing these bad outcomes; it’s a bystander – a canary in the coal mine. Your vitamin D level is a marker of your lifestyle; it’s higher in people who eat healthier foods, who exercise, and who spend more time out in the sun.
And yet ... if you were to ask me whether supplementing vitamin D in children with vitamin D deficiency would help them grow better and be healthier, I probably would have been on board for the idea.
And, it looks like, I would have been wrong.
Yes, it’s another negative randomized trial of vitamin D supplementation to add to the seemingly ever-growing body of literature suggesting that your money is better spent on a day at the park rather than buying D3 from your local GNC.
We are talking about this study, appearing in JAMA Pediatrics.
Briefly, 8,851 children from around Ulaanbaatar, Mongolia, were randomized to receive 14,000 international units of vitamin D3 or placebo every week for 3 years.
Before we get into the results of the study, I need to point out that this part of Mongolia has a high rate of vitamin D deficiency. Beyond that, a prior observational study by these authors had shown that lower vitamin D levels were linked to the risk of acquiring latent tuberculosis infection in this area. Other studies have linked vitamin D deficiency with poorer growth metrics in children. Given the global scourge that is TB (around 2 million deaths a year) and childhood malnutrition (around 10% of children around the world), vitamin D supplementation is incredibly attractive as a public health intervention. It is relatively low on side effects and, importantly, it is cheap – and thus scalable.
Back to the study. These kids had pretty poor vitamin D levels at baseline; 95% of them were deficient, based on the accepted standard of levels less than 20 ng/mL. Over 30% were severely deficient, with levels less than 10 ng/mL.
The initial purpose of this study was to see if supplementation would prevent TB, but that analysis, which was published a few months ago, was negative. Vitamin D levels went up dramatically in the intervention group – they were taking their pills – but there was no difference in the rate of latent TB infection, active TB, other respiratory infections, or even serum interferon gamma levels.
Nothing.
But to be fair, the TB seroconversion rate was lower than expected, potentially leading to an underpowered study.
Which brings us to the just-published analysis which moves away from infectious disease to something where vitamin D should have some stronger footing: growth.
Would the kids who were randomized to vitamin D, those same kids who got their vitamin D levels into the normal range over 3 years of supplementation, grow more or grow better than the kids who didn’t?
And, unfortunately, the answer is still no.
At the end of follow-up, height z scores were not different between the groups. BMI z scores were not different between the groups. Pubertal development was not different between the groups. This was true not only overall, but across various subgroups, including analyses of those kids who had vitamin D levels less than 10 ng/mL to start with.
So, what’s going on? There are two very broad possibilities we can endorse. First, there’s the idea that vitamin D supplementation simply doesn’t do much for health. This is supported, now, by a long string of large clinical trials that show no effect across a variety of disease states and predisease states. In other words, the observational data linking low vitamin D to bad outcomes is correlation, not causation.
Or we can take the tack of some vitamin D apologists and decide that this trial just got it wrong. Perhaps the dose wasn’t given correctly, or 3 years isn’t long enough to see a real difference, or the growth metrics were wrong, or vitamin D needs to be given alongside something else to really work and so on. This is fine; no study is perfect and there is always something to criticize, believe me. But we need to be careful not to fall into the baby-and-bathwater fallacy. Just because we think a study could have done something better, or differently, doesn’t mean we can ignore all the results. And as each new randomized trial of vitamin D supplementation comes out, it’s getting harder and harder to believe that these trialists keep getting their methods wrong. Maybe they are just testing something that doesn’t work.
What to do? Well, it should be obvious. If low vitamin D levels are linked to TB rates and poor growth but supplementation doesn’t fix the problem, then we have to fix what is upstream of the problem. We need to boost vitamin D levels not through supplements, but through nutrition, exercise, activity, and getting outside. That’s a randomized trial you can sign me up for any day.
Dr. Wilson is associate professor, department of medicine, Yale University, New Haven, Conn. He reported no relevant conflicts of interest.
A version of this video transcript first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
My basic gripe is that you’ve got all these observational studies linking lower levels of vitamin D to everything from dementia to falls to cancer to COVID infection, and then you do a big randomized trial of supplementation and don’t see an effect.
And the explanation is that vitamin D is not necessarily the thing causing these bad outcomes; it’s a bystander – a canary in the coal mine. Your vitamin D level is a marker of your lifestyle; it’s higher in people who eat healthier foods, who exercise, and who spend more time out in the sun.
And yet ... if you were to ask me whether supplementing vitamin D in children with vitamin D deficiency would help them grow better and be healthier, I probably would have been on board for the idea.
And, it looks like, I would have been wrong.
Yes, it’s another negative randomized trial of vitamin D supplementation to add to the seemingly ever-growing body of literature suggesting that your money is better spent on a day at the park rather than buying D3 from your local GNC.
We are talking about this study, appearing in JAMA Pediatrics.
Briefly, 8,851 children from around Ulaanbaatar, Mongolia, were randomized to receive 14,000 international units of vitamin D3 or placebo every week for 3 years.
Before we get into the results of the study, I need to point out that this part of Mongolia has a high rate of vitamin D deficiency. Beyond that, a prior observational study by these authors had shown that lower vitamin D levels were linked to the risk of acquiring latent tuberculosis infection in this area. Other studies have linked vitamin D deficiency with poorer growth metrics in children. Given the global scourge that is TB (around 2 million deaths a year) and childhood malnutrition (around 10% of children around the world), vitamin D supplementation is incredibly attractive as a public health intervention. It is relatively low on side effects and, importantly, it is cheap – and thus scalable.
Back to the study. These kids had pretty poor vitamin D levels at baseline; 95% of them were deficient, based on the accepted standard of levels less than 20 ng/mL. Over 30% were severely deficient, with levels less than 10 ng/mL.
The initial purpose of this study was to see if supplementation would prevent TB, but that analysis, which was published a few months ago, was negative. Vitamin D levels went up dramatically in the intervention group – they were taking their pills – but there was no difference in the rate of latent TB infection, active TB, other respiratory infections, or even serum interferon gamma levels.
Nothing.
But to be fair, the TB seroconversion rate was lower than expected, potentially leading to an underpowered study.
Which brings us to the just-published analysis which moves away from infectious disease to something where vitamin D should have some stronger footing: growth.
Would the kids who were randomized to vitamin D, those same kids who got their vitamin D levels into the normal range over 3 years of supplementation, grow more or grow better than the kids who didn’t?
And, unfortunately, the answer is still no.
At the end of follow-up, height z scores were not different between the groups. BMI z scores were not different between the groups. Pubertal development was not different between the groups. This was true not only overall, but across various subgroups, including analyses of those kids who had vitamin D levels less than 10 ng/mL to start with.
So, what’s going on? There are two very broad possibilities we can endorse. First, there’s the idea that vitamin D supplementation simply doesn’t do much for health. This is supported, now, by a long string of large clinical trials that show no effect across a variety of disease states and predisease states. In other words, the observational data linking low vitamin D to bad outcomes is correlation, not causation.
Or we can take the tack of some vitamin D apologists and decide that this trial just got it wrong. Perhaps the dose wasn’t given correctly, or 3 years isn’t long enough to see a real difference, or the growth metrics were wrong, or vitamin D needs to be given alongside something else to really work and so on. This is fine; no study is perfect and there is always something to criticize, believe me. But we need to be careful not to fall into the baby-and-bathwater fallacy. Just because we think a study could have done something better, or differently, doesn’t mean we can ignore all the results. And as each new randomized trial of vitamin D supplementation comes out, it’s getting harder and harder to believe that these trialists keep getting their methods wrong. Maybe they are just testing something that doesn’t work.
What to do? Well, it should be obvious. If low vitamin D levels are linked to TB rates and poor growth but supplementation doesn’t fix the problem, then we have to fix what is upstream of the problem. We need to boost vitamin D levels not through supplements, but through nutrition, exercise, activity, and getting outside. That’s a randomized trial you can sign me up for any day.
Dr. Wilson is associate professor, department of medicine, Yale University, New Haven, Conn. He reported no relevant conflicts of interest.
A version of this video transcript first appeared on Medscape.com.
‘Modest’ benefit for lecanemab in Alzheimer’s disease, but adverse events are common
SAN FRANCISCO –
In the CLARITY AD trial, adverse events (AEs) were common compared with placebo, including amyloid-related edema and effusions; and a recent news report linked a second death to the drug.
Moving forward, “longer trials are warranted to determine the efficacy and safety of lecanemab in early Alzheimer’s disease,” wrote Christopher H. van Dyck, MD, Yale University, New Haven, Conn., and colleagues.
The full trial findings were presented at the Clinical Trials on Alzheimer’s Disease (CTAD) conference, with simultaneous publication on Nov. 29 in the New England Journal of Medicine.
Complications in the field
The phase 3 trial of lecanemab has been closely watched in AD circles, especially considering positive early data released in September and reported by this news organization at that time.
The Food and Drug Administration is expected to make a decision about possible approval of the drug in January 2023. Only one other antiamyloid treatment, the highly controversial and expensive aducanumab (Aduhelm), is currently approved by the FDA.
For the new 18-month, randomized, double-blind CLARITY AD trial, researchers enrolled 1,795 patients aged 50-90 years (average age, 71 years) with early AD. All were randomly assigned to receive either a placebo (n = 898) or intravenous lecanemab, a humanized immunoglobulin G1 (IgG1) monoclonal antibody that selectively targets amyloid beta (A-beta) protofibrils, at 10 mg/kg of body weight every 2 weeks (n = 897).
The study ran from 2019 to 2021. The participants (52% women, 20% non-White) were recruited in North America, Europe, and Asia. Safety data included all participants, and the modified intention-to-treat group included 1,734 participants, with 859 receiving lecanemab and 875 receiving placebo.
The primary endpoint was the Clinical Dementia Rating–Sum of Boxes (CDR-SB). Scores from 0.5 to 6 are signs of early AD, according to the study. The mean baseline score for both groups was 3.2. The adjusted mean change at 18 months was 1.21 for lecanemab versus 1.66 for placebo (difference, –0.45; 95% confidence interval [CI], –0.67 to –0.23; P < .001).
As Dr. van Dyck noted in his presentation at the CTAD meting, this represents a 27% slowing of the decline in the lecanemab group.
The published findings do not speculate about how this difference would affect the day-to-day life of participants who took the drug, although it does refer to “modestly less decline” of cognition/function in the lecanemab group.
Other measurements that suggest cognitive improvements in the lecanemab group versus placebo include the Alzheimer’s Disease Assessment Scale–Cognitive Subscale score (mean difference, –1.44; 95% CI, –2.27 to –0.61), the Alzheimer’s Disease Composite Score (mean difference, –0.05; 95% CI, –.074 to –.027,), and the Alzheimer’s Disease Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment score (mean difference, 2.0; 95% CI, 1.2-2.8; all, P < .001).
Overall, Dr. van Dyck said, “Lecanemab met the primary and secondary endpoints versus placebo at 18 months, with highly significant differences starting at 6 months.”
In a substudy of 698 participants, results showed that amyloid burden fell at a higher rate in the lecanemab group than in the placebo group (difference, –59.1 centiloids; 95% CI, –62.6 to –55.6).
“Lecanemab has high selectivity for soluble aggregated species of A-beta as compared with monomeric amyloid, with moderate selectivity for fibrillar amyloid; this profile is considered to target the most toxic pathologic amyloid species,” the researchers wrote.
Concerning AE data
With respect to AEs, deaths occurred in both groups (0.7% in those who took lecanemab and 0.8% in those who took the placebo). The researchers did not attribute any deaths to the drug. However, according to a report in the journal Science published Nov. 27, a 65-year-old woman who was taking the drug as part of a clinical trial “recently died from a massive brain hemorrhage that some researchers link to the drug.”
The woman, the second person “whose death was linked to lecanemab,” died after suffering a stroke. Researchers summarized a case report as saying that the drug “contributed to her brain hemorrhage after biweekly infusions of lecanemab inflamed and weakened the blood vessels.”
Eisai, which sponsored the new trial, told Science that “all the available safety information indicates that lecanemab therapy is not associated with an increased risk of death overall or from any specific cause.”
In a CTAD presentation, study coauthor Marwan Sabbagh, MD, Barrow Neurological Institute, Phoenix, said two hemorrhage-related deaths occurred in an open-label extension. One was in the context of a tissue plasminogen activator treatment for a stroke, which fits with the description of the case in the Science report. “Causality with lecanemab is a little difficult ...,” he said. “Patients on anticoagulation might need further consideration.”
In the CLARITY AD Trial, serious AEs occurred in 14% of the lecanemab group, leading to discontinuation 6.9% of the time, and in 11.3% of the placebo group, leading to discontinuation 2.9% of the time, the investigators reported.
They added that, in the lecanemab group, the most common AEs, defined as affecting more than 10% of participants, were infusion-related reactions (26.4% vs. 7.4% for placebo); amyloid-related imaging abnormalities with cerebral microhemorrhages, cerebral macrohemorrhages, or superficial siderosis (17.3% vs. 9%, respectively); amyloid-related imaging abnormalities with edema or effusions (12.6% vs. 1.7%); headache (11.1% vs. 8.1%); and falls (10.4% vs. 9.6%).
In addition, macrohemorrhage was reported in 0.6% of the lecanemab group and 0.1% of the placebo group.
Cautious optimism
In separate interviews, two Alzheimer’s specialists who weren’t involved in the study praised the trial and described the findings as “exciting.” But they also highlighted its limitations.
Alvaro Pascual-Leone, MD, PhD, professor of neurology at Harvard Medical School and chief medical officer of Linus Health, said the study represents impressive progress after 60-plus trials examining anti-amyloid monoclonal antibodies. “This is the first trial that shows a clinical benefit that can be measured,” he said.
However, it’s unclear whether the changes “are really going to make a difference in people’s lives,” he said. The drug is likely to be expensive, owing to the large investment needed for research, he added, and patients will have to undergo costly testing, such as PET scans and spinal taps.
Still, “this could be a valuable adjunct to the armamentarium we have,” which includes interventions such as lifestyle changes, he said.
Howard Fillit, MD, cofounder and chief science officer at the Alzheimer’s Drug Discovery Foundation, noted that the trial reached its primary and secondary endpoints and that the drug had what he called a “modest” effect on cognition.
However, the drugmaker will need to explore the adverse effects, he said, especially among patients with atrial fibrillation who take anticoagulants. And, he said, medicine is still far from the ultimate goal – fully reversing cognitive decline.
Michael Weiner, MD, president of the CTAD22 Scientific Committee, noted in a press release that there is “growing evidence” that some antiamyloid therapies, “especially lecanemab and donanemab” have shown promising results.
“Unfortunately, these treatments are also associated with abnormal differences seen in imaging, including brain swelling and bleeding in the brain,” said Dr. Weiner, professor of radiology, medicine, and neurology at the University of California, San Francisco.
“There is considerable controversy concerning the significance and impact of these findings, including whether or not governments and medical insurance will provide financial coverage for such treatments,” he added.
Rave reviews from the Alzheimer’s Association
In a statement, the Alzheimer’s Association raved about lecanemab and declared that the FDA should approve lecanemab on an accelerated basis. The study “confirms this treatment can meaningfully change the course of the disease for people in the earliest stages of Alzheimer’s disease ...” the association said, adding that “it could mean many months more of recognizing their spouse, children and grandchildren.”
The association, which is a staunch supporter of aducanumab, called on the Centers for Medicare & Medicaid Services to cover the drug if the FDA approves it. The association’s statement did not address the drug’s potential high cost, the adverse effects, or the two reported deaths.
The trial was supported by Eisai (regulatory sponsor) with partial funding from Biogen. Dr. van Dyck reports having received research grants from Biogen, Eisai, Biohaven, Cerevel Therapeutics, Eli Lilly, Genentech, Janssen, Novartis, and UCB. He has been a consultant to Cerevel, Eisai, Ono Pharmaceutical, and Roche. Relevant financial relationships for the other investigators are fully listed in the original article.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO –
In the CLARITY AD trial, adverse events (AEs) were common compared with placebo, including amyloid-related edema and effusions; and a recent news report linked a second death to the drug.
Moving forward, “longer trials are warranted to determine the efficacy and safety of lecanemab in early Alzheimer’s disease,” wrote Christopher H. van Dyck, MD, Yale University, New Haven, Conn., and colleagues.
The full trial findings were presented at the Clinical Trials on Alzheimer’s Disease (CTAD) conference, with simultaneous publication on Nov. 29 in the New England Journal of Medicine.
Complications in the field
The phase 3 trial of lecanemab has been closely watched in AD circles, especially considering positive early data released in September and reported by this news organization at that time.
The Food and Drug Administration is expected to make a decision about possible approval of the drug in January 2023. Only one other antiamyloid treatment, the highly controversial and expensive aducanumab (Aduhelm), is currently approved by the FDA.
For the new 18-month, randomized, double-blind CLARITY AD trial, researchers enrolled 1,795 patients aged 50-90 years (average age, 71 years) with early AD. All were randomly assigned to receive either a placebo (n = 898) or intravenous lecanemab, a humanized immunoglobulin G1 (IgG1) monoclonal antibody that selectively targets amyloid beta (A-beta) protofibrils, at 10 mg/kg of body weight every 2 weeks (n = 897).
The study ran from 2019 to 2021. The participants (52% women, 20% non-White) were recruited in North America, Europe, and Asia. Safety data included all participants, and the modified intention-to-treat group included 1,734 participants, with 859 receiving lecanemab and 875 receiving placebo.
The primary endpoint was the Clinical Dementia Rating–Sum of Boxes (CDR-SB). Scores from 0.5 to 6 are signs of early AD, according to the study. The mean baseline score for both groups was 3.2. The adjusted mean change at 18 months was 1.21 for lecanemab versus 1.66 for placebo (difference, –0.45; 95% confidence interval [CI], –0.67 to –0.23; P < .001).
As Dr. van Dyck noted in his presentation at the CTAD meting, this represents a 27% slowing of the decline in the lecanemab group.
The published findings do not speculate about how this difference would affect the day-to-day life of participants who took the drug, although it does refer to “modestly less decline” of cognition/function in the lecanemab group.
Other measurements that suggest cognitive improvements in the lecanemab group versus placebo include the Alzheimer’s Disease Assessment Scale–Cognitive Subscale score (mean difference, –1.44; 95% CI, –2.27 to –0.61), the Alzheimer’s Disease Composite Score (mean difference, –0.05; 95% CI, –.074 to –.027,), and the Alzheimer’s Disease Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment score (mean difference, 2.0; 95% CI, 1.2-2.8; all, P < .001).
Overall, Dr. van Dyck said, “Lecanemab met the primary and secondary endpoints versus placebo at 18 months, with highly significant differences starting at 6 months.”
In a substudy of 698 participants, results showed that amyloid burden fell at a higher rate in the lecanemab group than in the placebo group (difference, –59.1 centiloids; 95% CI, –62.6 to –55.6).
“Lecanemab has high selectivity for soluble aggregated species of A-beta as compared with monomeric amyloid, with moderate selectivity for fibrillar amyloid; this profile is considered to target the most toxic pathologic amyloid species,” the researchers wrote.
Concerning AE data
With respect to AEs, deaths occurred in both groups (0.7% in those who took lecanemab and 0.8% in those who took the placebo). The researchers did not attribute any deaths to the drug. However, according to a report in the journal Science published Nov. 27, a 65-year-old woman who was taking the drug as part of a clinical trial “recently died from a massive brain hemorrhage that some researchers link to the drug.”
The woman, the second person “whose death was linked to lecanemab,” died after suffering a stroke. Researchers summarized a case report as saying that the drug “contributed to her brain hemorrhage after biweekly infusions of lecanemab inflamed and weakened the blood vessels.”
Eisai, which sponsored the new trial, told Science that “all the available safety information indicates that lecanemab therapy is not associated with an increased risk of death overall or from any specific cause.”
In a CTAD presentation, study coauthor Marwan Sabbagh, MD, Barrow Neurological Institute, Phoenix, said two hemorrhage-related deaths occurred in an open-label extension. One was in the context of a tissue plasminogen activator treatment for a stroke, which fits with the description of the case in the Science report. “Causality with lecanemab is a little difficult ...,” he said. “Patients on anticoagulation might need further consideration.”
In the CLARITY AD Trial, serious AEs occurred in 14% of the lecanemab group, leading to discontinuation 6.9% of the time, and in 11.3% of the placebo group, leading to discontinuation 2.9% of the time, the investigators reported.
They added that, in the lecanemab group, the most common AEs, defined as affecting more than 10% of participants, were infusion-related reactions (26.4% vs. 7.4% for placebo); amyloid-related imaging abnormalities with cerebral microhemorrhages, cerebral macrohemorrhages, or superficial siderosis (17.3% vs. 9%, respectively); amyloid-related imaging abnormalities with edema or effusions (12.6% vs. 1.7%); headache (11.1% vs. 8.1%); and falls (10.4% vs. 9.6%).
In addition, macrohemorrhage was reported in 0.6% of the lecanemab group and 0.1% of the placebo group.
Cautious optimism
In separate interviews, two Alzheimer’s specialists who weren’t involved in the study praised the trial and described the findings as “exciting.” But they also highlighted its limitations.
Alvaro Pascual-Leone, MD, PhD, professor of neurology at Harvard Medical School and chief medical officer of Linus Health, said the study represents impressive progress after 60-plus trials examining anti-amyloid monoclonal antibodies. “This is the first trial that shows a clinical benefit that can be measured,” he said.
However, it’s unclear whether the changes “are really going to make a difference in people’s lives,” he said. The drug is likely to be expensive, owing to the large investment needed for research, he added, and patients will have to undergo costly testing, such as PET scans and spinal taps.
Still, “this could be a valuable adjunct to the armamentarium we have,” which includes interventions such as lifestyle changes, he said.
Howard Fillit, MD, cofounder and chief science officer at the Alzheimer’s Drug Discovery Foundation, noted that the trial reached its primary and secondary endpoints and that the drug had what he called a “modest” effect on cognition.
However, the drugmaker will need to explore the adverse effects, he said, especially among patients with atrial fibrillation who take anticoagulants. And, he said, medicine is still far from the ultimate goal – fully reversing cognitive decline.
Michael Weiner, MD, president of the CTAD22 Scientific Committee, noted in a press release that there is “growing evidence” that some antiamyloid therapies, “especially lecanemab and donanemab” have shown promising results.
“Unfortunately, these treatments are also associated with abnormal differences seen in imaging, including brain swelling and bleeding in the brain,” said Dr. Weiner, professor of radiology, medicine, and neurology at the University of California, San Francisco.
“There is considerable controversy concerning the significance and impact of these findings, including whether or not governments and medical insurance will provide financial coverage for such treatments,” he added.
Rave reviews from the Alzheimer’s Association
In a statement, the Alzheimer’s Association raved about lecanemab and declared that the FDA should approve lecanemab on an accelerated basis. The study “confirms this treatment can meaningfully change the course of the disease for people in the earliest stages of Alzheimer’s disease ...” the association said, adding that “it could mean many months more of recognizing their spouse, children and grandchildren.”
The association, which is a staunch supporter of aducanumab, called on the Centers for Medicare & Medicaid Services to cover the drug if the FDA approves it. The association’s statement did not address the drug’s potential high cost, the adverse effects, or the two reported deaths.
The trial was supported by Eisai (regulatory sponsor) with partial funding from Biogen. Dr. van Dyck reports having received research grants from Biogen, Eisai, Biohaven, Cerevel Therapeutics, Eli Lilly, Genentech, Janssen, Novartis, and UCB. He has been a consultant to Cerevel, Eisai, Ono Pharmaceutical, and Roche. Relevant financial relationships for the other investigators are fully listed in the original article.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO –
In the CLARITY AD trial, adverse events (AEs) were common compared with placebo, including amyloid-related edema and effusions; and a recent news report linked a second death to the drug.
Moving forward, “longer trials are warranted to determine the efficacy and safety of lecanemab in early Alzheimer’s disease,” wrote Christopher H. van Dyck, MD, Yale University, New Haven, Conn., and colleagues.
The full trial findings were presented at the Clinical Trials on Alzheimer’s Disease (CTAD) conference, with simultaneous publication on Nov. 29 in the New England Journal of Medicine.
Complications in the field
The phase 3 trial of lecanemab has been closely watched in AD circles, especially considering positive early data released in September and reported by this news organization at that time.
The Food and Drug Administration is expected to make a decision about possible approval of the drug in January 2023. Only one other antiamyloid treatment, the highly controversial and expensive aducanumab (Aduhelm), is currently approved by the FDA.
For the new 18-month, randomized, double-blind CLARITY AD trial, researchers enrolled 1,795 patients aged 50-90 years (average age, 71 years) with early AD. All were randomly assigned to receive either a placebo (n = 898) or intravenous lecanemab, a humanized immunoglobulin G1 (IgG1) monoclonal antibody that selectively targets amyloid beta (A-beta) protofibrils, at 10 mg/kg of body weight every 2 weeks (n = 897).
The study ran from 2019 to 2021. The participants (52% women, 20% non-White) were recruited in North America, Europe, and Asia. Safety data included all participants, and the modified intention-to-treat group included 1,734 participants, with 859 receiving lecanemab and 875 receiving placebo.
The primary endpoint was the Clinical Dementia Rating–Sum of Boxes (CDR-SB). Scores from 0.5 to 6 are signs of early AD, according to the study. The mean baseline score for both groups was 3.2. The adjusted mean change at 18 months was 1.21 for lecanemab versus 1.66 for placebo (difference, –0.45; 95% confidence interval [CI], –0.67 to –0.23; P < .001).
As Dr. van Dyck noted in his presentation at the CTAD meting, this represents a 27% slowing of the decline in the lecanemab group.
The published findings do not speculate about how this difference would affect the day-to-day life of participants who took the drug, although it does refer to “modestly less decline” of cognition/function in the lecanemab group.
Other measurements that suggest cognitive improvements in the lecanemab group versus placebo include the Alzheimer’s Disease Assessment Scale–Cognitive Subscale score (mean difference, –1.44; 95% CI, –2.27 to –0.61), the Alzheimer’s Disease Composite Score (mean difference, –0.05; 95% CI, –.074 to –.027,), and the Alzheimer’s Disease Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment score (mean difference, 2.0; 95% CI, 1.2-2.8; all, P < .001).
Overall, Dr. van Dyck said, “Lecanemab met the primary and secondary endpoints versus placebo at 18 months, with highly significant differences starting at 6 months.”
In a substudy of 698 participants, results showed that amyloid burden fell at a higher rate in the lecanemab group than in the placebo group (difference, –59.1 centiloids; 95% CI, –62.6 to –55.6).
“Lecanemab has high selectivity for soluble aggregated species of A-beta as compared with monomeric amyloid, with moderate selectivity for fibrillar amyloid; this profile is considered to target the most toxic pathologic amyloid species,” the researchers wrote.
Concerning AE data
With respect to AEs, deaths occurred in both groups (0.7% in those who took lecanemab and 0.8% in those who took the placebo). The researchers did not attribute any deaths to the drug. However, according to a report in the journal Science published Nov. 27, a 65-year-old woman who was taking the drug as part of a clinical trial “recently died from a massive brain hemorrhage that some researchers link to the drug.”
The woman, the second person “whose death was linked to lecanemab,” died after suffering a stroke. Researchers summarized a case report as saying that the drug “contributed to her brain hemorrhage after biweekly infusions of lecanemab inflamed and weakened the blood vessels.”
Eisai, which sponsored the new trial, told Science that “all the available safety information indicates that lecanemab therapy is not associated with an increased risk of death overall or from any specific cause.”
In a CTAD presentation, study coauthor Marwan Sabbagh, MD, Barrow Neurological Institute, Phoenix, said two hemorrhage-related deaths occurred in an open-label extension. One was in the context of a tissue plasminogen activator treatment for a stroke, which fits with the description of the case in the Science report. “Causality with lecanemab is a little difficult ...,” he said. “Patients on anticoagulation might need further consideration.”
In the CLARITY AD Trial, serious AEs occurred in 14% of the lecanemab group, leading to discontinuation 6.9% of the time, and in 11.3% of the placebo group, leading to discontinuation 2.9% of the time, the investigators reported.
They added that, in the lecanemab group, the most common AEs, defined as affecting more than 10% of participants, were infusion-related reactions (26.4% vs. 7.4% for placebo); amyloid-related imaging abnormalities with cerebral microhemorrhages, cerebral macrohemorrhages, or superficial siderosis (17.3% vs. 9%, respectively); amyloid-related imaging abnormalities with edema or effusions (12.6% vs. 1.7%); headache (11.1% vs. 8.1%); and falls (10.4% vs. 9.6%).
In addition, macrohemorrhage was reported in 0.6% of the lecanemab group and 0.1% of the placebo group.
Cautious optimism
In separate interviews, two Alzheimer’s specialists who weren’t involved in the study praised the trial and described the findings as “exciting.” But they also highlighted its limitations.
Alvaro Pascual-Leone, MD, PhD, professor of neurology at Harvard Medical School and chief medical officer of Linus Health, said the study represents impressive progress after 60-plus trials examining anti-amyloid monoclonal antibodies. “This is the first trial that shows a clinical benefit that can be measured,” he said.
However, it’s unclear whether the changes “are really going to make a difference in people’s lives,” he said. The drug is likely to be expensive, owing to the large investment needed for research, he added, and patients will have to undergo costly testing, such as PET scans and spinal taps.
Still, “this could be a valuable adjunct to the armamentarium we have,” which includes interventions such as lifestyle changes, he said.
Howard Fillit, MD, cofounder and chief science officer at the Alzheimer’s Drug Discovery Foundation, noted that the trial reached its primary and secondary endpoints and that the drug had what he called a “modest” effect on cognition.
However, the drugmaker will need to explore the adverse effects, he said, especially among patients with atrial fibrillation who take anticoagulants. And, he said, medicine is still far from the ultimate goal – fully reversing cognitive decline.
Michael Weiner, MD, president of the CTAD22 Scientific Committee, noted in a press release that there is “growing evidence” that some antiamyloid therapies, “especially lecanemab and donanemab” have shown promising results.
“Unfortunately, these treatments are also associated with abnormal differences seen in imaging, including brain swelling and bleeding in the brain,” said Dr. Weiner, professor of radiology, medicine, and neurology at the University of California, San Francisco.
“There is considerable controversy concerning the significance and impact of these findings, including whether or not governments and medical insurance will provide financial coverage for such treatments,” he added.
Rave reviews from the Alzheimer’s Association
In a statement, the Alzheimer’s Association raved about lecanemab and declared that the FDA should approve lecanemab on an accelerated basis. The study “confirms this treatment can meaningfully change the course of the disease for people in the earliest stages of Alzheimer’s disease ...” the association said, adding that “it could mean many months more of recognizing their spouse, children and grandchildren.”
The association, which is a staunch supporter of aducanumab, called on the Centers for Medicare & Medicaid Services to cover the drug if the FDA approves it. The association’s statement did not address the drug’s potential high cost, the adverse effects, or the two reported deaths.
The trial was supported by Eisai (regulatory sponsor) with partial funding from Biogen. Dr. van Dyck reports having received research grants from Biogen, Eisai, Biohaven, Cerevel Therapeutics, Eli Lilly, Genentech, Janssen, Novartis, and UCB. He has been a consultant to Cerevel, Eisai, Ono Pharmaceutical, and Roche. Relevant financial relationships for the other investigators are fully listed in the original article.
A version of this article first appeared on Medscape.com.
AT CTAD 2022
New studies change beliefs about cardiovascular disease
This transcript has been edited for clarity.
I’m going to review a few of these.
The first is the TIME study. The TIME study looked at whether it matters if you give antihypertensive agents in the morning or the evening. This was a prospective, pragmatic, parallel-group study that was performed in the U.K. and published in The Lancet.
Their question was whether evening dosing of antihypertensives has benefit in cardiovascular outcomes in adults. They enrolled over 21,000 people with hypertension who were taking at least one antihypertensive medication. Patients were randomized to morning or evening dosing.
The primary outcome was death or hospitalization due to myocardial infarction or stroke. There was no difference. It doesn’t matter if you take your antihypertensive agent in the morning or the evening. I think this is important because, clinically, the simpler the regimen for the patient, the greater the adherence, leading to better outcomes.
I know I can safely ask a patient when they would rather take their medicine. For many people, that may be the morning because they’re brushing their teeth and they remember. If they want to take it in the evening, that’s fine, too. We’re no longer slave to telling a patient to take their antihypertensive medications in the evening.
At the meeting of the American Society of Nephrology, results from a study on the use of renin-angiotensin system (RAS) inhibitors in advanced CKD was presented, called the STOP ACEi trial. Again, another interesting trial asking a simple question. This was a randomized controlled trial (RCT) in patients who had an estimated glomerular filtration rate (eGFR) less than 30, and they were randomized to stop or continue therapy with their RAS inhibitors.
The primary outcome was the eGFR at 3 years. They enrolled 411 patients with a median baseline eGFR of 18. At 3 years, there was no difference in the eGFR between the groups. In the discontinuation group, the eGFR was 12.6 versus 13.3 in the continuation group. There were no differences in complications or anything else. Their conclusion was that among patients with advanced and progressive CKD, the discontinuation of a RAS inhibitor was not associated with a significant difference in the long-term rate of decrease in eGFR.
I think this is important because it changes our paradigm a bit. You can stop the RAS inhibitor; reduce the need for excessive medication in these patients; and, hopefully, focus on some newer medications that have been shown to prevent the decline in eGFR that are now available.
Next is from a letter published in JAMA, which asks the following question: Is diabetes itself an equivalent cardiovascular risk factor to those who have had a prior cardiovascular event?
We used to put having diabetes in that same high-risk category as people who’d already had a cardiovascular disease event. Well, have we made that any different? These authors are from Canada, and they did a retrospective population-based study looking at administrative health claims from Ontario, Canada, to assess the association of diabetes and prior cardiovascular disease with cardiovascular events from 1994 to 2014.
What I think is kind of cool, because I’m a diabetologist, is that over time the magnitude of the association between diabetes and cardiovascular event rates decreased. In somebody with diabetes, they don’t have the same high risk that a person who’s already had a cardiovascular event rate does. Diabetes is less of a risk factor for cardiovascular disease than having established cardiovascular disease, which means we’re treating diabetes better and reducing the risk for cardiovascular disease.
If you look at people with diabetes and a prior cardiovascular event, that’s still the very highest risk. The risk of people having another event who have established cardiovascular disease is pretty flat. Those people didn’t get better and the people with preexisting diabetes and cardiovascular events at baseline didn’t get much better, but those who had diabetes alone did improve in terms of looking at cardiovascular event rates.
I think this is good news because diabetes itself isn’t as high a cardiovascular risk factor as we once thought. It doesn’t mean that it isn’t a cardiovascular risk factor, but I think we’ve done better at mitigating the risk.
Finally, there is a relatively small study that was presented at the American Heart Association and published in the Journal of the American College of Cardiology, which asks whether supplements that are often used to lower LDL cholesterol are equivalent to a statin.
They compared six supplements with a placebo and with rosuvastatin, and looked to see what happened. This is not an outcome study, but a very short study, at 28 days, that used a placebo. They included 190 people with no history of cardiovascular disease but an increased 10-year risk for sclerotic cardiovascular disease.
The agents studied were rosuvastatin, placebo, fish oil, cinnamon, garlic, turmeric, plant sterols, and red yeast rice. Well, not surprisingly, rosuvastatin worked. It showed a 35% reduction in LDL cholesterol, and there was no significant impact on cholesterol levels with any of the other agents. The supplements yielded a similar response, as did the placebo. Side effects were similar, but they were most common with plant sterols and red yeast rice.
Clearly, a statin is better if you want to lower cholesterol levels. My approach, when patients want to take supplements, is to tell them what I know factually, which basically is that they don’t really cause much in the way of LDL cholesterol lowering. If I think the supplement isn’t going to hurt someone, I don’t tell them not to use it. I certainly tell them that they need to use agents that we know can actually reduce cardiovascular risk.
I think these studies really go through the gamut of asking questions. When can we stop an agent? What time of day do we need to give an agent? What, really, is the risk for type 2 diabetes with regard to cardiovascular events? What’s the value of supplements?
I think this is interesting, because I really encourage researchers to ask and answer these kinds of questions because it helps us clinically decide what’s best for treating our patients.
Thank you.
Dr. Peters is a professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She reported conflicts of interest with numerous pharmaceutical companies.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’m going to review a few of these.
The first is the TIME study. The TIME study looked at whether it matters if you give antihypertensive agents in the morning or the evening. This was a prospective, pragmatic, parallel-group study that was performed in the U.K. and published in The Lancet.
Their question was whether evening dosing of antihypertensives has benefit in cardiovascular outcomes in adults. They enrolled over 21,000 people with hypertension who were taking at least one antihypertensive medication. Patients were randomized to morning or evening dosing.
The primary outcome was death or hospitalization due to myocardial infarction or stroke. There was no difference. It doesn’t matter if you take your antihypertensive agent in the morning or the evening. I think this is important because, clinically, the simpler the regimen for the patient, the greater the adherence, leading to better outcomes.
I know I can safely ask a patient when they would rather take their medicine. For many people, that may be the morning because they’re brushing their teeth and they remember. If they want to take it in the evening, that’s fine, too. We’re no longer slave to telling a patient to take their antihypertensive medications in the evening.
At the meeting of the American Society of Nephrology, results from a study on the use of renin-angiotensin system (RAS) inhibitors in advanced CKD was presented, called the STOP ACEi trial. Again, another interesting trial asking a simple question. This was a randomized controlled trial (RCT) in patients who had an estimated glomerular filtration rate (eGFR) less than 30, and they were randomized to stop or continue therapy with their RAS inhibitors.
The primary outcome was the eGFR at 3 years. They enrolled 411 patients with a median baseline eGFR of 18. At 3 years, there was no difference in the eGFR between the groups. In the discontinuation group, the eGFR was 12.6 versus 13.3 in the continuation group. There were no differences in complications or anything else. Their conclusion was that among patients with advanced and progressive CKD, the discontinuation of a RAS inhibitor was not associated with a significant difference in the long-term rate of decrease in eGFR.
I think this is important because it changes our paradigm a bit. You can stop the RAS inhibitor; reduce the need for excessive medication in these patients; and, hopefully, focus on some newer medications that have been shown to prevent the decline in eGFR that are now available.
Next is from a letter published in JAMA, which asks the following question: Is diabetes itself an equivalent cardiovascular risk factor to those who have had a prior cardiovascular event?
We used to put having diabetes in that same high-risk category as people who’d already had a cardiovascular disease event. Well, have we made that any different? These authors are from Canada, and they did a retrospective population-based study looking at administrative health claims from Ontario, Canada, to assess the association of diabetes and prior cardiovascular disease with cardiovascular events from 1994 to 2014.
What I think is kind of cool, because I’m a diabetologist, is that over time the magnitude of the association between diabetes and cardiovascular event rates decreased. In somebody with diabetes, they don’t have the same high risk that a person who’s already had a cardiovascular event rate does. Diabetes is less of a risk factor for cardiovascular disease than having established cardiovascular disease, which means we’re treating diabetes better and reducing the risk for cardiovascular disease.
If you look at people with diabetes and a prior cardiovascular event, that’s still the very highest risk. The risk of people having another event who have established cardiovascular disease is pretty flat. Those people didn’t get better and the people with preexisting diabetes and cardiovascular events at baseline didn’t get much better, but those who had diabetes alone did improve in terms of looking at cardiovascular event rates.
I think this is good news because diabetes itself isn’t as high a cardiovascular risk factor as we once thought. It doesn’t mean that it isn’t a cardiovascular risk factor, but I think we’ve done better at mitigating the risk.
Finally, there is a relatively small study that was presented at the American Heart Association and published in the Journal of the American College of Cardiology, which asks whether supplements that are often used to lower LDL cholesterol are equivalent to a statin.
They compared six supplements with a placebo and with rosuvastatin, and looked to see what happened. This is not an outcome study, but a very short study, at 28 days, that used a placebo. They included 190 people with no history of cardiovascular disease but an increased 10-year risk for sclerotic cardiovascular disease.
The agents studied were rosuvastatin, placebo, fish oil, cinnamon, garlic, turmeric, plant sterols, and red yeast rice. Well, not surprisingly, rosuvastatin worked. It showed a 35% reduction in LDL cholesterol, and there was no significant impact on cholesterol levels with any of the other agents. The supplements yielded a similar response, as did the placebo. Side effects were similar, but they were most common with plant sterols and red yeast rice.
Clearly, a statin is better if you want to lower cholesterol levels. My approach, when patients want to take supplements, is to tell them what I know factually, which basically is that they don’t really cause much in the way of LDL cholesterol lowering. If I think the supplement isn’t going to hurt someone, I don’t tell them not to use it. I certainly tell them that they need to use agents that we know can actually reduce cardiovascular risk.
I think these studies really go through the gamut of asking questions. When can we stop an agent? What time of day do we need to give an agent? What, really, is the risk for type 2 diabetes with regard to cardiovascular events? What’s the value of supplements?
I think this is interesting, because I really encourage researchers to ask and answer these kinds of questions because it helps us clinically decide what’s best for treating our patients.
Thank you.
Dr. Peters is a professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She reported conflicts of interest with numerous pharmaceutical companies.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’m going to review a few of these.
The first is the TIME study. The TIME study looked at whether it matters if you give antihypertensive agents in the morning or the evening. This was a prospective, pragmatic, parallel-group study that was performed in the U.K. and published in The Lancet.
Their question was whether evening dosing of antihypertensives has benefit in cardiovascular outcomes in adults. They enrolled over 21,000 people with hypertension who were taking at least one antihypertensive medication. Patients were randomized to morning or evening dosing.
The primary outcome was death or hospitalization due to myocardial infarction or stroke. There was no difference. It doesn’t matter if you take your antihypertensive agent in the morning or the evening. I think this is important because, clinically, the simpler the regimen for the patient, the greater the adherence, leading to better outcomes.
I know I can safely ask a patient when they would rather take their medicine. For many people, that may be the morning because they’re brushing their teeth and they remember. If they want to take it in the evening, that’s fine, too. We’re no longer slave to telling a patient to take their antihypertensive medications in the evening.
At the meeting of the American Society of Nephrology, results from a study on the use of renin-angiotensin system (RAS) inhibitors in advanced CKD was presented, called the STOP ACEi trial. Again, another interesting trial asking a simple question. This was a randomized controlled trial (RCT) in patients who had an estimated glomerular filtration rate (eGFR) less than 30, and they were randomized to stop or continue therapy with their RAS inhibitors.
The primary outcome was the eGFR at 3 years. They enrolled 411 patients with a median baseline eGFR of 18. At 3 years, there was no difference in the eGFR between the groups. In the discontinuation group, the eGFR was 12.6 versus 13.3 in the continuation group. There were no differences in complications or anything else. Their conclusion was that among patients with advanced and progressive CKD, the discontinuation of a RAS inhibitor was not associated with a significant difference in the long-term rate of decrease in eGFR.
I think this is important because it changes our paradigm a bit. You can stop the RAS inhibitor; reduce the need for excessive medication in these patients; and, hopefully, focus on some newer medications that have been shown to prevent the decline in eGFR that are now available.
Next is from a letter published in JAMA, which asks the following question: Is diabetes itself an equivalent cardiovascular risk factor to those who have had a prior cardiovascular event?
We used to put having diabetes in that same high-risk category as people who’d already had a cardiovascular disease event. Well, have we made that any different? These authors are from Canada, and they did a retrospective population-based study looking at administrative health claims from Ontario, Canada, to assess the association of diabetes and prior cardiovascular disease with cardiovascular events from 1994 to 2014.
What I think is kind of cool, because I’m a diabetologist, is that over time the magnitude of the association between diabetes and cardiovascular event rates decreased. In somebody with diabetes, they don’t have the same high risk that a person who’s already had a cardiovascular event rate does. Diabetes is less of a risk factor for cardiovascular disease than having established cardiovascular disease, which means we’re treating diabetes better and reducing the risk for cardiovascular disease.
If you look at people with diabetes and a prior cardiovascular event, that’s still the very highest risk. The risk of people having another event who have established cardiovascular disease is pretty flat. Those people didn’t get better and the people with preexisting diabetes and cardiovascular events at baseline didn’t get much better, but those who had diabetes alone did improve in terms of looking at cardiovascular event rates.
I think this is good news because diabetes itself isn’t as high a cardiovascular risk factor as we once thought. It doesn’t mean that it isn’t a cardiovascular risk factor, but I think we’ve done better at mitigating the risk.
Finally, there is a relatively small study that was presented at the American Heart Association and published in the Journal of the American College of Cardiology, which asks whether supplements that are often used to lower LDL cholesterol are equivalent to a statin.
They compared six supplements with a placebo and with rosuvastatin, and looked to see what happened. This is not an outcome study, but a very short study, at 28 days, that used a placebo. They included 190 people with no history of cardiovascular disease but an increased 10-year risk for sclerotic cardiovascular disease.
The agents studied were rosuvastatin, placebo, fish oil, cinnamon, garlic, turmeric, plant sterols, and red yeast rice. Well, not surprisingly, rosuvastatin worked. It showed a 35% reduction in LDL cholesterol, and there was no significant impact on cholesterol levels with any of the other agents. The supplements yielded a similar response, as did the placebo. Side effects were similar, but they were most common with plant sterols and red yeast rice.
Clearly, a statin is better if you want to lower cholesterol levels. My approach, when patients want to take supplements, is to tell them what I know factually, which basically is that they don’t really cause much in the way of LDL cholesterol lowering. If I think the supplement isn’t going to hurt someone, I don’t tell them not to use it. I certainly tell them that they need to use agents that we know can actually reduce cardiovascular risk.
I think these studies really go through the gamut of asking questions. When can we stop an agent? What time of day do we need to give an agent? What, really, is the risk for type 2 diabetes with regard to cardiovascular events? What’s the value of supplements?
I think this is interesting, because I really encourage researchers to ask and answer these kinds of questions because it helps us clinically decide what’s best for treating our patients.
Thank you.
Dr. Peters is a professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She reported conflicts of interest with numerous pharmaceutical companies.
A version of this article first appeared on Medscape.com.
Buprenorphine linked with lower risk for neonatal harms than methadone
Using buprenorphine for opioid use disorder in pregnancy was linked with a lower risk of neonatal side effects than using methadone, but the risk of adverse maternal outcomes was similar between the two treatments, according to new research.
Elizabeth A. Suarez, PhD, MPH, with Brigham and Women’s Hospital in Boston, led the study published online in the New England Journal of Medicine.
Opioid use disorder in pregnant women has increased steadily in the United States since 2000, the authors write. As of 2017, about 8.2 per 1,000 deliveries were estimated to be affected by the disorder. The numbers were particularly high in people insured by Medicaid. In that group, an estimated 14.6 per 1,000 deliveries were affected.
Researchers studied pregnant women enrolled in public insurance programs in the United States from 2000 through 2018 in a dataset of 2,548,372 pregnancies that ended in live births. They analyzed outcomes in those who received buprenorphine as compared with those who received methadone.
They looked at different periods of exposure to the two medications: early pregnancy (through gestational week 19); late pregnancy (week 20 through the day before delivery); and the 30 days before delivery.
Highlighted differences in infants included:
- Neonatal abstinence syndrome in 52% of the infants who were exposed to buprenorphine in the 30 days before delivery as compared with 69.2% of those exposed to methadone (adjusted relative risk, 0.73).
- Preterm birth in 14.4% of infants exposed to buprenorphine in early pregnancy and in 24.9% of those exposed to methadone (ARR, 0.58).
- Small size for gestational age in 12.1% (buprenorphine) and 15.3% (methadone) (ARR, 0.72).
- Low birth weight in 8.3% (buprenorphine) and 14.9% (methadone) (ARR, 0.56).
- Delivery by cesarean section occurred in 33.6% of pregnant women exposed to buprenorphine in early pregnancy and 33.1% of those exposed to methadone (ARR, 1.02.).
Severe maternal complications developed in 3.3% of the women exposed to buprenorphine and 3.5% of those on methadone (ARR, 0.91.) Exposures in late pregnancy and early pregnancy yielded similar results, the authors say.
Michael Caucci, MD, of the department of psychiatry at Vanderbilt University Medical Center in Nashville, Tenn. who also runs the Women’s Mental Health Clinic at the university, said this paper supports preliminary findings from the Maternal Opioid Treatment: Human Experimental Research (MOTHER) study that suggested infants exposed to buprenorphine (compared with methadone) appeared to have lower rates of neonatal complications.
“It also supports buprenorphine as a relatively safe option for treatment of opioid use disorder during pregnancy,” said Dr. Caucci, who was not part of the study by Dr. Suarez and associates. “Reducing the fear of harming the fetus or neonate will help eliminate this barrier to perinatal substance use disorder treatment.”
But he cautions against concluding that, because buprenorphine has lower risks of fetal/neonatal complications, it is safer and therefore better than methadone in pregnancy.
“Some women do not tolerate buprenorphine and do much better on methadone, Dr. Caucci said. “Current recommendations are that both buprenorphine and methadone are relatively safe options for treatment of OUD [opioid use disorder] in pregnancy.”
Among the differences between the treatments is that while methadone is administered daily during in-person visits to federally regulated opioid treatment programs, buprenorphine can be prescribed by approved providers, which allows patients to administer buprenorphine themselves.
Dr. Caucci said he was intrigued by the finding that there was no difference in pregnancy, neonatal, and maternal outcomes depending on the time of exposure to the agents.
“I would have expected higher rates of neonatal abstinence syndrome (NAS) or poor fetal growth in those exposed later in pregnancy vs. those with early exposure,” he said.
The work was supported by the National Institute on Drug Abuse. Dr. Caucci reports no relevant financial relationships. The authors’ disclosures are available with the full text.
Using buprenorphine for opioid use disorder in pregnancy was linked with a lower risk of neonatal side effects than using methadone, but the risk of adverse maternal outcomes was similar between the two treatments, according to new research.
Elizabeth A. Suarez, PhD, MPH, with Brigham and Women’s Hospital in Boston, led the study published online in the New England Journal of Medicine.
Opioid use disorder in pregnant women has increased steadily in the United States since 2000, the authors write. As of 2017, about 8.2 per 1,000 deliveries were estimated to be affected by the disorder. The numbers were particularly high in people insured by Medicaid. In that group, an estimated 14.6 per 1,000 deliveries were affected.
Researchers studied pregnant women enrolled in public insurance programs in the United States from 2000 through 2018 in a dataset of 2,548,372 pregnancies that ended in live births. They analyzed outcomes in those who received buprenorphine as compared with those who received methadone.
They looked at different periods of exposure to the two medications: early pregnancy (through gestational week 19); late pregnancy (week 20 through the day before delivery); and the 30 days before delivery.
Highlighted differences in infants included:
- Neonatal abstinence syndrome in 52% of the infants who were exposed to buprenorphine in the 30 days before delivery as compared with 69.2% of those exposed to methadone (adjusted relative risk, 0.73).
- Preterm birth in 14.4% of infants exposed to buprenorphine in early pregnancy and in 24.9% of those exposed to methadone (ARR, 0.58).
- Small size for gestational age in 12.1% (buprenorphine) and 15.3% (methadone) (ARR, 0.72).
- Low birth weight in 8.3% (buprenorphine) and 14.9% (methadone) (ARR, 0.56).
- Delivery by cesarean section occurred in 33.6% of pregnant women exposed to buprenorphine in early pregnancy and 33.1% of those exposed to methadone (ARR, 1.02.).
Severe maternal complications developed in 3.3% of the women exposed to buprenorphine and 3.5% of those on methadone (ARR, 0.91.) Exposures in late pregnancy and early pregnancy yielded similar results, the authors say.
Michael Caucci, MD, of the department of psychiatry at Vanderbilt University Medical Center in Nashville, Tenn. who also runs the Women’s Mental Health Clinic at the university, said this paper supports preliminary findings from the Maternal Opioid Treatment: Human Experimental Research (MOTHER) study that suggested infants exposed to buprenorphine (compared with methadone) appeared to have lower rates of neonatal complications.
“It also supports buprenorphine as a relatively safe option for treatment of opioid use disorder during pregnancy,” said Dr. Caucci, who was not part of the study by Dr. Suarez and associates. “Reducing the fear of harming the fetus or neonate will help eliminate this barrier to perinatal substance use disorder treatment.”
But he cautions against concluding that, because buprenorphine has lower risks of fetal/neonatal complications, it is safer and therefore better than methadone in pregnancy.
“Some women do not tolerate buprenorphine and do much better on methadone, Dr. Caucci said. “Current recommendations are that both buprenorphine and methadone are relatively safe options for treatment of OUD [opioid use disorder] in pregnancy.”
Among the differences between the treatments is that while methadone is administered daily during in-person visits to federally regulated opioid treatment programs, buprenorphine can be prescribed by approved providers, which allows patients to administer buprenorphine themselves.
Dr. Caucci said he was intrigued by the finding that there was no difference in pregnancy, neonatal, and maternal outcomes depending on the time of exposure to the agents.
“I would have expected higher rates of neonatal abstinence syndrome (NAS) or poor fetal growth in those exposed later in pregnancy vs. those with early exposure,” he said.
The work was supported by the National Institute on Drug Abuse. Dr. Caucci reports no relevant financial relationships. The authors’ disclosures are available with the full text.
Using buprenorphine for opioid use disorder in pregnancy was linked with a lower risk of neonatal side effects than using methadone, but the risk of adverse maternal outcomes was similar between the two treatments, according to new research.
Elizabeth A. Suarez, PhD, MPH, with Brigham and Women’s Hospital in Boston, led the study published online in the New England Journal of Medicine.
Opioid use disorder in pregnant women has increased steadily in the United States since 2000, the authors write. As of 2017, about 8.2 per 1,000 deliveries were estimated to be affected by the disorder. The numbers were particularly high in people insured by Medicaid. In that group, an estimated 14.6 per 1,000 deliveries were affected.
Researchers studied pregnant women enrolled in public insurance programs in the United States from 2000 through 2018 in a dataset of 2,548,372 pregnancies that ended in live births. They analyzed outcomes in those who received buprenorphine as compared with those who received methadone.
They looked at different periods of exposure to the two medications: early pregnancy (through gestational week 19); late pregnancy (week 20 through the day before delivery); and the 30 days before delivery.
Highlighted differences in infants included:
- Neonatal abstinence syndrome in 52% of the infants who were exposed to buprenorphine in the 30 days before delivery as compared with 69.2% of those exposed to methadone (adjusted relative risk, 0.73).
- Preterm birth in 14.4% of infants exposed to buprenorphine in early pregnancy and in 24.9% of those exposed to methadone (ARR, 0.58).
- Small size for gestational age in 12.1% (buprenorphine) and 15.3% (methadone) (ARR, 0.72).
- Low birth weight in 8.3% (buprenorphine) and 14.9% (methadone) (ARR, 0.56).
- Delivery by cesarean section occurred in 33.6% of pregnant women exposed to buprenorphine in early pregnancy and 33.1% of those exposed to methadone (ARR, 1.02.).
Severe maternal complications developed in 3.3% of the women exposed to buprenorphine and 3.5% of those on methadone (ARR, 0.91.) Exposures in late pregnancy and early pregnancy yielded similar results, the authors say.
Michael Caucci, MD, of the department of psychiatry at Vanderbilt University Medical Center in Nashville, Tenn. who also runs the Women’s Mental Health Clinic at the university, said this paper supports preliminary findings from the Maternal Opioid Treatment: Human Experimental Research (MOTHER) study that suggested infants exposed to buprenorphine (compared with methadone) appeared to have lower rates of neonatal complications.
“It also supports buprenorphine as a relatively safe option for treatment of opioid use disorder during pregnancy,” said Dr. Caucci, who was not part of the study by Dr. Suarez and associates. “Reducing the fear of harming the fetus or neonate will help eliminate this barrier to perinatal substance use disorder treatment.”
But he cautions against concluding that, because buprenorphine has lower risks of fetal/neonatal complications, it is safer and therefore better than methadone in pregnancy.
“Some women do not tolerate buprenorphine and do much better on methadone, Dr. Caucci said. “Current recommendations are that both buprenorphine and methadone are relatively safe options for treatment of OUD [opioid use disorder] in pregnancy.”
Among the differences between the treatments is that while methadone is administered daily during in-person visits to federally regulated opioid treatment programs, buprenorphine can be prescribed by approved providers, which allows patients to administer buprenorphine themselves.
Dr. Caucci said he was intrigued by the finding that there was no difference in pregnancy, neonatal, and maternal outcomes depending on the time of exposure to the agents.
“I would have expected higher rates of neonatal abstinence syndrome (NAS) or poor fetal growth in those exposed later in pregnancy vs. those with early exposure,” he said.
The work was supported by the National Institute on Drug Abuse. Dr. Caucci reports no relevant financial relationships. The authors’ disclosures are available with the full text.
FROM NEW ENGLAND JOURNAL OF MEDICINE
U.S. flu activity already at mid-season levels
according to the Centers of Disease Control and Prevention.
Nationally, 6% of all outpatient visits were because of flu or flu-like illness for the week of Nov. 13-19, up from 5.8% the previous week, the CDC’s Influenza Division said in its weekly FluView report.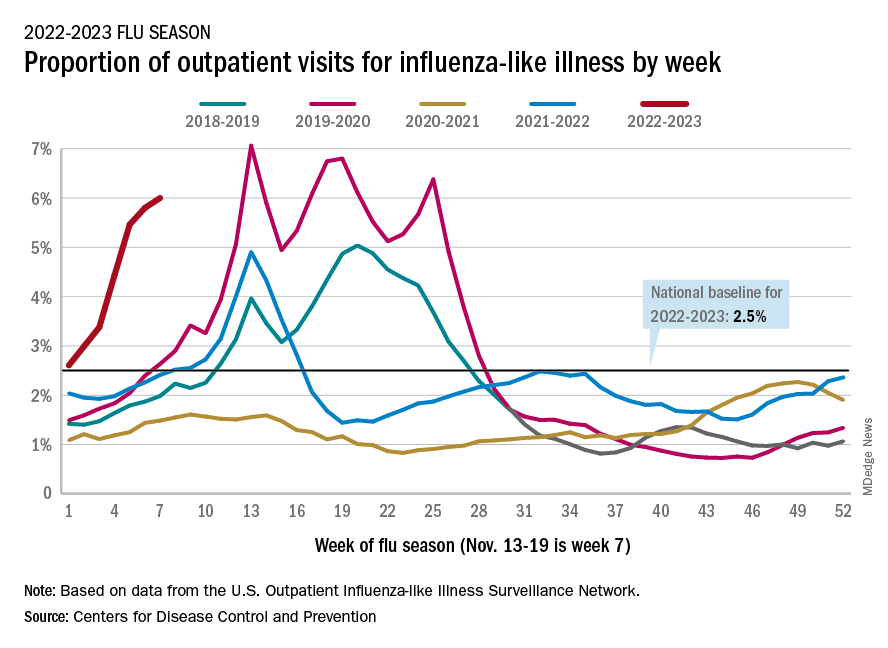
Those figures are the highest recorded in November since 2009, but the peak of the 2009-10 flu season occurred even earlier – the week of Oct. 18-24 – and the rate of flu-like illness had already dropped to just over 4.0% by Nov. 15-21 that year and continued to drop thereafter.
Although COVID-19 and respiratory syncytial virus (RSV) are included in the data from the CDC’s Outpatient Influenza-like Illness Surveillance Network, the agency did note that “seasonal influenza activity is elevated across the country” and estimated that “there have been at least 6.2 million illnesses, 53,000 hospitalizations, and 2,900 deaths from flu” during the 2022-23 season.
Total flu deaths include 11 reported in children as of Nov. 19, and children ages 0-4 had a higher proportion of visits for flu like-illness than other age groups.
The agency also said the cumulative hospitalization rate of 11.3 per 100,000 population “is higher than the rate observed in [the corresponding week of] every previous season since 2010-2011.” Adults 65 years and older have the highest cumulative rate, 25.9 per 100,000, for this year, compared with 20.7 for children 0-4; 11.1 for adults 50-64; 10.3 for children 5-17; and 5.6 for adults 18-49 years old, the CDC said.
A version of this article first appeared on WebMD.com.
according to the Centers of Disease Control and Prevention.
Nationally, 6% of all outpatient visits were because of flu or flu-like illness for the week of Nov. 13-19, up from 5.8% the previous week, the CDC’s Influenza Division said in its weekly FluView report.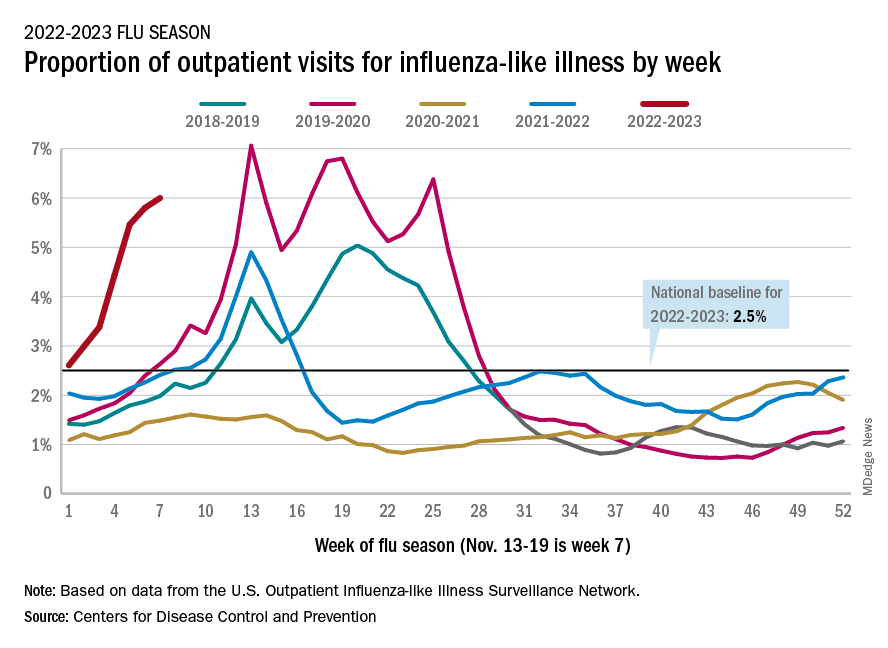
Those figures are the highest recorded in November since 2009, but the peak of the 2009-10 flu season occurred even earlier – the week of Oct. 18-24 – and the rate of flu-like illness had already dropped to just over 4.0% by Nov. 15-21 that year and continued to drop thereafter.
Although COVID-19 and respiratory syncytial virus (RSV) are included in the data from the CDC’s Outpatient Influenza-like Illness Surveillance Network, the agency did note that “seasonal influenza activity is elevated across the country” and estimated that “there have been at least 6.2 million illnesses, 53,000 hospitalizations, and 2,900 deaths from flu” during the 2022-23 season.
Total flu deaths include 11 reported in children as of Nov. 19, and children ages 0-4 had a higher proportion of visits for flu like-illness than other age groups.
The agency also said the cumulative hospitalization rate of 11.3 per 100,000 population “is higher than the rate observed in [the corresponding week of] every previous season since 2010-2011.” Adults 65 years and older have the highest cumulative rate, 25.9 per 100,000, for this year, compared with 20.7 for children 0-4; 11.1 for adults 50-64; 10.3 for children 5-17; and 5.6 for adults 18-49 years old, the CDC said.
A version of this article first appeared on WebMD.com.
according to the Centers of Disease Control and Prevention.
Nationally, 6% of all outpatient visits were because of flu or flu-like illness for the week of Nov. 13-19, up from 5.8% the previous week, the CDC’s Influenza Division said in its weekly FluView report.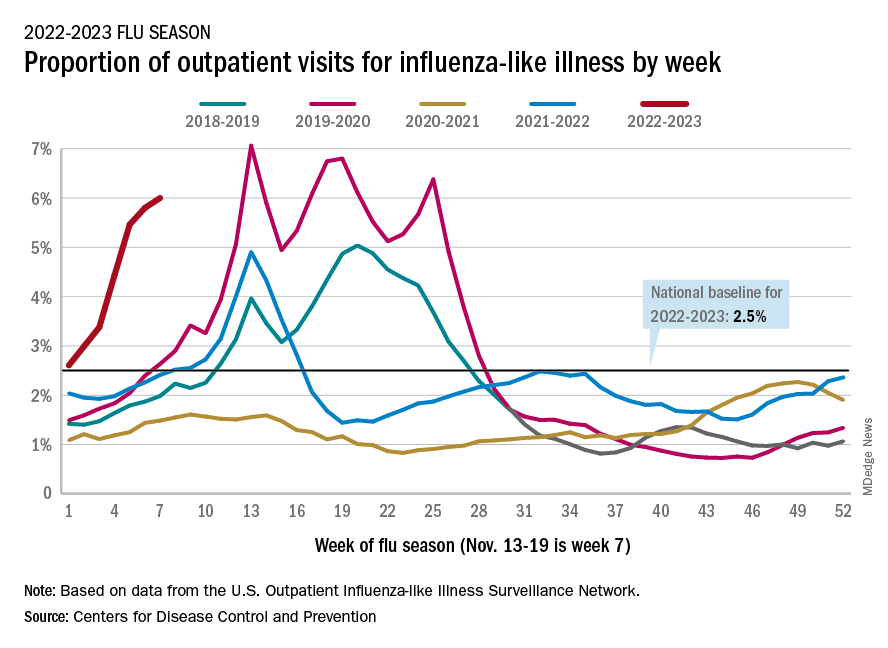
Those figures are the highest recorded in November since 2009, but the peak of the 2009-10 flu season occurred even earlier – the week of Oct. 18-24 – and the rate of flu-like illness had already dropped to just over 4.0% by Nov. 15-21 that year and continued to drop thereafter.
Although COVID-19 and respiratory syncytial virus (RSV) are included in the data from the CDC’s Outpatient Influenza-like Illness Surveillance Network, the agency did note that “seasonal influenza activity is elevated across the country” and estimated that “there have been at least 6.2 million illnesses, 53,000 hospitalizations, and 2,900 deaths from flu” during the 2022-23 season.
Total flu deaths include 11 reported in children as of Nov. 19, and children ages 0-4 had a higher proportion of visits for flu like-illness than other age groups.
The agency also said the cumulative hospitalization rate of 11.3 per 100,000 population “is higher than the rate observed in [the corresponding week of] every previous season since 2010-2011.” Adults 65 years and older have the highest cumulative rate, 25.9 per 100,000, for this year, compared with 20.7 for children 0-4; 11.1 for adults 50-64; 10.3 for children 5-17; and 5.6 for adults 18-49 years old, the CDC said.
A version of this article first appeared on WebMD.com.
Yellow Nodule on the Scalp
The Diagnosis: Solitary Sclerotic Fibroma
Based on the clinical and histologic findings, the patient was diagnosed with solitary sclerotic fibroma (SF). Sclerotic fibroma is a rare benign tumor that first was described in 1972 by Weary et al1 in the oral mucosa of a patient with Cowden syndrome, a genodermatosis associated with multiple benign and malignant tumors. Rapini and Golitz2 reported solitary SF in 11 otherwise-healthy individuals with no signs of multiple hamartoma syndrome. Solitary SF is a sporadic benign condition, whereas multiple lesions are suggestive of Cowden syndrome. Solitary SF most commonly appears as an asymptomatic white-yellow papule or nodule on the head or neck, though larger tumors have been reported on the trunk and extremities.3 Histologic features of solitary SF include a well-circumscribed dermal nodule composed of eosinophilic dense collagen bundles arranged in a plywoodlike pattern (Figure). Immunohistochemistry is positive for CD34 and vimentin but negative for S-100, epithelial membrane antigen, and neuron-specific enolase.4
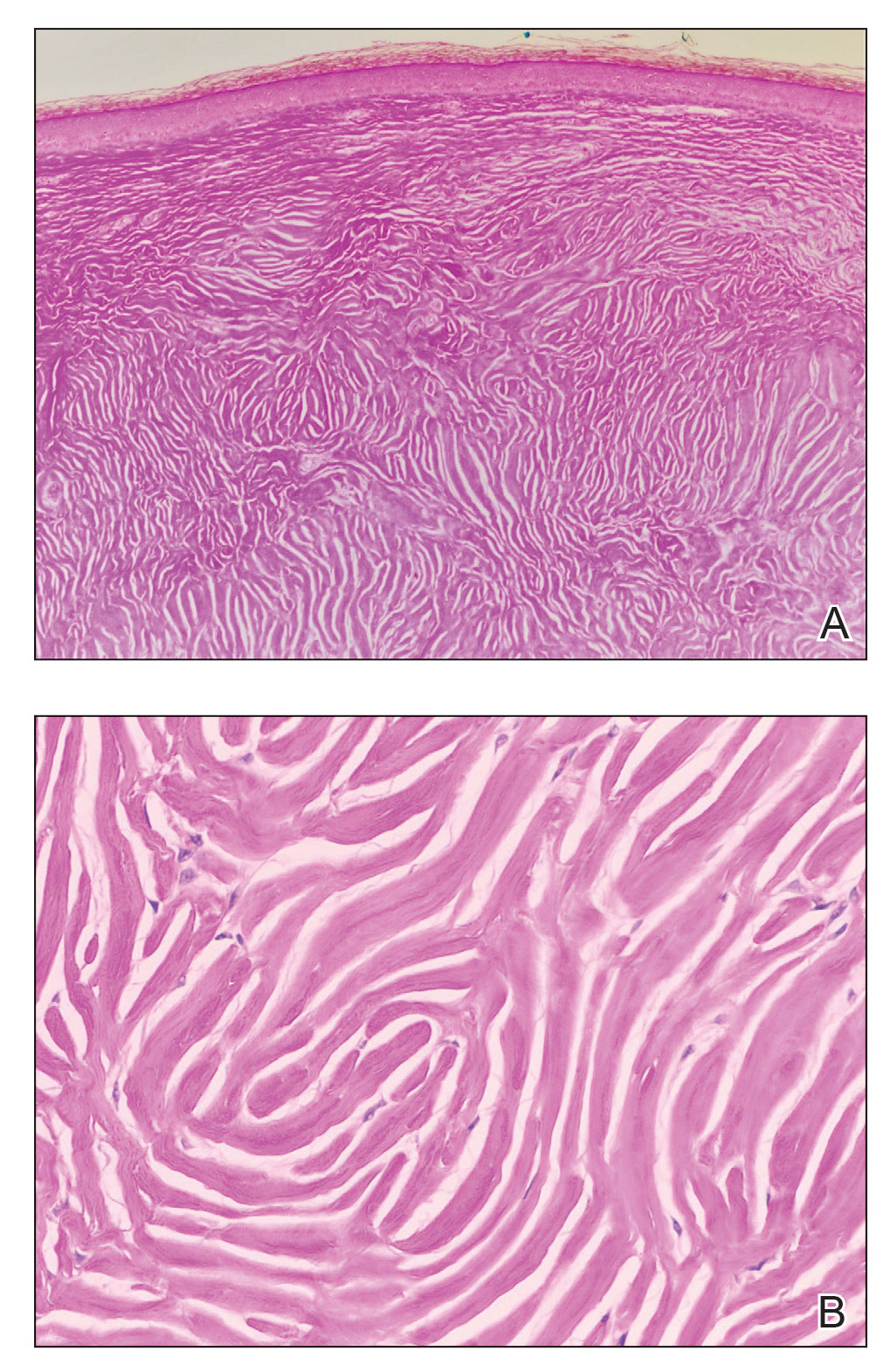
The differential diagnosis of solitary SF of the head and neck includes sebaceous adenoma, pilar cyst, nodular basal cell carcinoma, and giant molluscum contagiosum. Sebaceous adenomas usually are solitary yellow nodules less than 1 cm in diameter and located on the head and neck. They are the most common sebaceous neoplasm associated with Muir-Torre syndrome, an autosomal-dominant disorder characterized by sebaceous adenoma or carcinoma and colorectal cancer. Histopathology demonstrates well-circumscribed, round aggregations of mature lipid-filled sebocytes with a rim of basaloid germinative cells at the periphery. Pilar cysts typically are flesh-colored subcutaneous nodules on the scalp that are freely mobile over underlying tissue. Histopathology shows stratified squamous epithelium lining and trichilemmal keratinization. Nodular basal cell carcinoma has a pearly translucent appearance and arborizing telangiectases. Histopathology demonstrates nests of basaloid cells with palisading of the cells at the periphery. Giant solitary molluscum contagiosum is a dome-shaped, flesh-colored nodule with central umbilication. Histopathology reveals hyperplastic squamous epithelium with characteristic eosinophilic inclusion bodies above the basal layer.
Solitary SF can be difficult to diagnose based solely on the clinical presentation; thus biopsy with histologic evaluation is recommended. If SF is confirmed, the clinician should inquire about a family history of Cowden syndrome and then perform a total-body skin examination to check for multiple SF and other clinical hamartomas of Cowden syndrome such as trichilemmomas, acral keratosis, and oral papillomas.
- Weary PE, Gorlin RJ, Gentry Jr WC, et al. Multiple hamartoma syndrome (Cowden’s disease). Arch Dermatol. 1972;106:682-690.
- Rapini RP, Golitz LE. Sclerotic fibromas of the skin. J Am Acad Dermatol. 1989;20(2 pt 1):266-271.
- Tosa M, Ansai S, Kuwahara H, et al. Two cases of sclerotic fibroma of the skin that mimicked keloids clinically. J Nippon Med Sch. 2018;85:283-286.
- High WA, Stewart D, Essary LR, et al. Sclerotic fibroma-like changes in various neoplastic and inflammatory skin lesions: is sclerotic fibroma a distinct entity? J Cutan Pathol. 2004;31:373-378.
The Diagnosis: Solitary Sclerotic Fibroma
Based on the clinical and histologic findings, the patient was diagnosed with solitary sclerotic fibroma (SF). Sclerotic fibroma is a rare benign tumor that first was described in 1972 by Weary et al1 in the oral mucosa of a patient with Cowden syndrome, a genodermatosis associated with multiple benign and malignant tumors. Rapini and Golitz2 reported solitary SF in 11 otherwise-healthy individuals with no signs of multiple hamartoma syndrome. Solitary SF is a sporadic benign condition, whereas multiple lesions are suggestive of Cowden syndrome. Solitary SF most commonly appears as an asymptomatic white-yellow papule or nodule on the head or neck, though larger tumors have been reported on the trunk and extremities.3 Histologic features of solitary SF include a well-circumscribed dermal nodule composed of eosinophilic dense collagen bundles arranged in a plywoodlike pattern (Figure). Immunohistochemistry is positive for CD34 and vimentin but negative for S-100, epithelial membrane antigen, and neuron-specific enolase.4
The differential diagnosis of solitary SF of the head and neck includes sebaceous adenoma, pilar cyst, nodular basal cell carcinoma, and giant molluscum contagiosum. Sebaceous adenomas usually are solitary yellow nodules less than 1 cm in diameter and located on the head and neck. They are the most common sebaceous neoplasm associated with Muir-Torre syndrome, an autosomal-dominant disorder characterized by sebaceous adenoma or carcinoma and colorectal cancer. Histopathology demonstrates well-circumscribed, round aggregations of mature lipid-filled sebocytes with a rim of basaloid germinative cells at the periphery. Pilar cysts typically are flesh-colored subcutaneous nodules on the scalp that are freely mobile over underlying tissue. Histopathology shows stratified squamous epithelium lining and trichilemmal keratinization. Nodular basal cell carcinoma has a pearly translucent appearance and arborizing telangiectases. Histopathology demonstrates nests of basaloid cells with palisading of the cells at the periphery. Giant solitary molluscum contagiosum is a dome-shaped, flesh-colored nodule with central umbilication. Histopathology reveals hyperplastic squamous epithelium with characteristic eosinophilic inclusion bodies above the basal layer.
Solitary SF can be difficult to diagnose based solely on the clinical presentation; thus biopsy with histologic evaluation is recommended. If SF is confirmed, the clinician should inquire about a family history of Cowden syndrome and then perform a total-body skin examination to check for multiple SF and other clinical hamartomas of Cowden syndrome such as trichilemmomas, acral keratosis, and oral papillomas.
The Diagnosis: Solitary Sclerotic Fibroma
Based on the clinical and histologic findings, the patient was diagnosed with solitary sclerotic fibroma (SF). Sclerotic fibroma is a rare benign tumor that first was described in 1972 by Weary et al1 in the oral mucosa of a patient with Cowden syndrome, a genodermatosis associated with multiple benign and malignant tumors. Rapini and Golitz2 reported solitary SF in 11 otherwise-healthy individuals with no signs of multiple hamartoma syndrome. Solitary SF is a sporadic benign condition, whereas multiple lesions are suggestive of Cowden syndrome. Solitary SF most commonly appears as an asymptomatic white-yellow papule or nodule on the head or neck, though larger tumors have been reported on the trunk and extremities.3 Histologic features of solitary SF include a well-circumscribed dermal nodule composed of eosinophilic dense collagen bundles arranged in a plywoodlike pattern (Figure). Immunohistochemistry is positive for CD34 and vimentin but negative for S-100, epithelial membrane antigen, and neuron-specific enolase.4
The differential diagnosis of solitary SF of the head and neck includes sebaceous adenoma, pilar cyst, nodular basal cell carcinoma, and giant molluscum contagiosum. Sebaceous adenomas usually are solitary yellow nodules less than 1 cm in diameter and located on the head and neck. They are the most common sebaceous neoplasm associated with Muir-Torre syndrome, an autosomal-dominant disorder characterized by sebaceous adenoma or carcinoma and colorectal cancer. Histopathology demonstrates well-circumscribed, round aggregations of mature lipid-filled sebocytes with a rim of basaloid germinative cells at the periphery. Pilar cysts typically are flesh-colored subcutaneous nodules on the scalp that are freely mobile over underlying tissue. Histopathology shows stratified squamous epithelium lining and trichilemmal keratinization. Nodular basal cell carcinoma has a pearly translucent appearance and arborizing telangiectases. Histopathology demonstrates nests of basaloid cells with palisading of the cells at the periphery. Giant solitary molluscum contagiosum is a dome-shaped, flesh-colored nodule with central umbilication. Histopathology reveals hyperplastic squamous epithelium with characteristic eosinophilic inclusion bodies above the basal layer.
Solitary SF can be difficult to diagnose based solely on the clinical presentation; thus biopsy with histologic evaluation is recommended. If SF is confirmed, the clinician should inquire about a family history of Cowden syndrome and then perform a total-body skin examination to check for multiple SF and other clinical hamartomas of Cowden syndrome such as trichilemmomas, acral keratosis, and oral papillomas.
- Weary PE, Gorlin RJ, Gentry Jr WC, et al. Multiple hamartoma syndrome (Cowden’s disease). Arch Dermatol. 1972;106:682-690.
- Rapini RP, Golitz LE. Sclerotic fibromas of the skin. J Am Acad Dermatol. 1989;20(2 pt 1):266-271.
- Tosa M, Ansai S, Kuwahara H, et al. Two cases of sclerotic fibroma of the skin that mimicked keloids clinically. J Nippon Med Sch. 2018;85:283-286.
- High WA, Stewart D, Essary LR, et al. Sclerotic fibroma-like changes in various neoplastic and inflammatory skin lesions: is sclerotic fibroma a distinct entity? J Cutan Pathol. 2004;31:373-378.
- Weary PE, Gorlin RJ, Gentry Jr WC, et al. Multiple hamartoma syndrome (Cowden’s disease). Arch Dermatol. 1972;106:682-690.
- Rapini RP, Golitz LE. Sclerotic fibromas of the skin. J Am Acad Dermatol. 1989;20(2 pt 1):266-271.
- Tosa M, Ansai S, Kuwahara H, et al. Two cases of sclerotic fibroma of the skin that mimicked keloids clinically. J Nippon Med Sch. 2018;85:283-286.
- High WA, Stewart D, Essary LR, et al. Sclerotic fibroma-like changes in various neoplastic and inflammatory skin lesions: is sclerotic fibroma a distinct entity? J Cutan Pathol. 2004;31:373-378.
A 45-year-old woman was referred to dermatology by a primary care physician for evaluation of a raised skin lesion on the scalp. She was otherwise healthy. The lesion had been present for many years but recently grew in size. The patient reported that the lesion was subject to recurrent physical trauma and she wanted it removed. Physical examination revealed a 6×6-mm, domeshaped, yellow nodule on the left inferior parietal scalp. There were no similar lesions located elsewhere on the body. A shave removal was performed and sent for histopathologic evaluation.

DEI advances in dermatology unremarkable to date, studies find
suggest.
To evaluate diversity and career goals of graduating allopathic medical students pursuing careers in dermatology, corresponding author Matthew Mansh, MD, of the department of dermatology at the University of Minnesota, Minneapolis, and colleagues drew from the 2016-2019 Association of American Medical Colleges Graduation Questionnaire for their study. The main outcome measures were the proportion of female students, students from racial and ethnic groups underrepresented in medicine (URM), and sexual minority (SM) students pursuing dermatology versus those pursuing other specialties, as well as the proportions and multivariable adjusted odds of intended career goals between students pursuing dermatology and those pursuing other specialties, and by sex, race, and ethnicity, and sexual orientation among students pursuing dermatology.
Of the 58,077 graduating students, 49% were women, 15% were URM, and 6% were SM. The researchers found that women pursuing dermatology were significantly less likely than women pursuing other specialties to identify as URM (11.6% vs. 17.2%; P < .001) or SM (1.9% vs. 5.7%; P < .001).
In multivariable-adjusted analyses of all students, those pursuing dermatology compared with other specialties had decreased odds of intending to care for underserved populations (18.3% vs. 34%; adjusted odd ratio, 0.40; P < .001), practice in underserved areas (12.7% vs. 25.9%; aOR, 0.40; P < .001), and practice public health (17% vs. 30.2%; aOR, 0.44; P < .001). The odds for pursuing research in their careers was greater among those pursuing dermatology (64.7% vs. 51.7%; aOR, 1.76; P < .001).
“Addressing health inequities and improving care for underserved patients is the responsibility of all dermatologists, and efforts are needed to increase diversity and interest in careers focused on underserved care among trainees in the dermatology workforce pipeline,” the authors concluded. They acknowledged certain limitations of the analysis, including lack of data delineating sex, sex assigned at birth, and gender identity, and lack of intersectional analyses between multiple minority identities and multiple career goals. “Importantly, diversity factors and their relationship to underserved care is likely multidimensional, and many students pursuing dermatology identified with multiple minority identities, highlighting the need for future studies focused on intersectionality,” they wrote.
Trends over 15 years
In a separate study, Jazzmin C. Williams, a medical student at the University of California, San Francisco, and coauthors drew from an Association of American Medical Colleges report of trainees’ and applicants’ self-reported race and ethnicity by specialty from 2005 to 2020 to evaluate diversity trends over the 15-year period. They found that Black and Latinx trainees were underrepresented in all specialties, but even more so in dermatology (mean annual rate ratios of 0.32 and 0.14, respectively), compared with those in primary care (mean annual RRs of 0.54 and 0.23) and those in specialty care (mean annual RRs of 0.39 and 0.18).
In other findings, the annual representation of Black trainees remained unchanged in dermatology between 2005 and 2020, but down-trended for primary (P < .001) and specialty care (P = .001). At the same time, representation of Latinx trainees remained unchanged in dermatology and specialty care but increased in primary care (P < .001). Finally, Black and Latinx race and ethnicity comprised a lower mean proportion of matriculating dermatology trainees (postgraduate year-2s) compared with annual dermatology applicants (4.01% vs. 5.97%, respectively, and 2.06% vs. 6.37% among Latinx; P < .001 for all associations).
“Much of these disparities can be attributed to the leaky pipeline – the disproportionate, stepwise reduction in racial and ethnic minority representation along the path to medicine,” the authors wrote. “This leaky pipeline is the direct result of structural racism, which includes, but is not limited to, historical and contemporary economic disinvestment from majority-minority schools, kindergarten through grade 12.” They concluded by stating that “dermatologists must intervene throughout the educational pipeline, including residency selection and mentorship, to effectively increase diversity.”
Solutions to address diversity
In an editorial accompanying the two studies published in the same issue of JAMA Dermatology, Ellen N. Pritchett, MD, MPH, of the department of dermatology at Howard University, Washington, and Andrew J. Park, MD, MBA, and Rebecca Vasquez, MD, of the department of dermatology at the University of Texas Southwestern Medical Center, Dallas, offered several solutions to address diversity in the dermatology work force. They include:
Go beyond individual bias in recruitment. “A residency selection framework that meaningfully incorporates diversity, equity, and inclusion (DEI) will require more than strategies that address individual bias,” they wrote. “Departmental recruitment committees must become familiar with systems that serve to perpetuate individual bias, like institutional racism or practices that disproportionately favor non-URM versus URM individuals.”
Challenge the myth of meritocracy. “The inaccurate notion of meritocracy – that success purely derives from individual effort has become the foundation of residency selection,” the authors wrote. “Unfortunately, this view ignores the inequitably distributed sociostructural resources that limit the rewards of individual effort.”
Avoid tokenism in retention strategies. Tokenism, which they defined as “a symbolic addition of members from a marginalized group to give the impression of social inclusiveness and diversity without meaningful incorporation of DEI in the policies, processes, and culture,” can lead to depression, burnout, and attrition, they wrote. They advise leaders of dermatology departments to “review their residency selection framework to ensure that it allows for meaningful representation, inclusion, and equity among trainees and faculty to better support URM individuals at all levels.”
Omar N. Qutub, MD, a Portland, Ore.–based dermatologist who was asked to comment on the studies, characterized the findings by Dr. Mansh and colleagues as sobering. “It appears that there is work to do as far as improving diversity in the dermatology workforce that will likely benefit greatly from an honest and steadfast approach to equitable application standards as well as mentorship during all stages of the application process,” such as medical school and residency, said Dr. Qutub, who is the director of equity, diversity, and inclusion of the ODAC Dermatology, Aesthetic & Surgical Conference. “With a focused attempt, we are likely to matriculate more racial minorities into our residency programs, maximizing patient outcomes.”
As for the study by Ms. Williams and colleagues, he told this news organization that efforts toward recruiting URM students as well as sexual minority students “is likely to not only improve health inequities in underserved areas, but will also enrich the specialty as a whole, allowing for better understanding of our diverse patient population and [for us to] to deliver quality care more readily for people and in areas where the focus has often been limited.”
In an interview, Chesahna Kindred, MD, a Columbia, Md.–based dermatologist and immediate past chair of the National Medical Association dermatology section, pointed out that the number of Black physicians in the United States has increased by only 4% in the last 120 years. The study by Dr. Mansh and colleagues, she commented, “underscores what I’ve recognized in the last couple of years: Where are the Black male dermatologists? NMA Derm started recruiting this demographic aggressively about a year ago and started the Black Men in Derm events. Black male members of NMA Derm travel to the Student National Medical Association and NMA conference and hold a panel to expose Black male students into dermatology. This article provides the numbers needed to measure how successful this and other programs are to closing the equity gap.”
Ms. Williams reported having no financial disclosures. Dr. Mansh reported receiving grants from National Institute of Environmental Health Sciences outside the submitted work. Dr. Pritchett and colleagues reported having no relevant financial disclosures, as did Dr. Qutub and Dr. Kindred.
suggest.
To evaluate diversity and career goals of graduating allopathic medical students pursuing careers in dermatology, corresponding author Matthew Mansh, MD, of the department of dermatology at the University of Minnesota, Minneapolis, and colleagues drew from the 2016-2019 Association of American Medical Colleges Graduation Questionnaire for their study. The main outcome measures were the proportion of female students, students from racial and ethnic groups underrepresented in medicine (URM), and sexual minority (SM) students pursuing dermatology versus those pursuing other specialties, as well as the proportions and multivariable adjusted odds of intended career goals between students pursuing dermatology and those pursuing other specialties, and by sex, race, and ethnicity, and sexual orientation among students pursuing dermatology.
Of the 58,077 graduating students, 49% were women, 15% were URM, and 6% were SM. The researchers found that women pursuing dermatology were significantly less likely than women pursuing other specialties to identify as URM (11.6% vs. 17.2%; P < .001) or SM (1.9% vs. 5.7%; P < .001).
In multivariable-adjusted analyses of all students, those pursuing dermatology compared with other specialties had decreased odds of intending to care for underserved populations (18.3% vs. 34%; adjusted odd ratio, 0.40; P < .001), practice in underserved areas (12.7% vs. 25.9%; aOR, 0.40; P < .001), and practice public health (17% vs. 30.2%; aOR, 0.44; P < .001). The odds for pursuing research in their careers was greater among those pursuing dermatology (64.7% vs. 51.7%; aOR, 1.76; P < .001).
“Addressing health inequities and improving care for underserved patients is the responsibility of all dermatologists, and efforts are needed to increase diversity and interest in careers focused on underserved care among trainees in the dermatology workforce pipeline,” the authors concluded. They acknowledged certain limitations of the analysis, including lack of data delineating sex, sex assigned at birth, and gender identity, and lack of intersectional analyses between multiple minority identities and multiple career goals. “Importantly, diversity factors and their relationship to underserved care is likely multidimensional, and many students pursuing dermatology identified with multiple minority identities, highlighting the need for future studies focused on intersectionality,” they wrote.
Trends over 15 years
In a separate study, Jazzmin C. Williams, a medical student at the University of California, San Francisco, and coauthors drew from an Association of American Medical Colleges report of trainees’ and applicants’ self-reported race and ethnicity by specialty from 2005 to 2020 to evaluate diversity trends over the 15-year period. They found that Black and Latinx trainees were underrepresented in all specialties, but even more so in dermatology (mean annual rate ratios of 0.32 and 0.14, respectively), compared with those in primary care (mean annual RRs of 0.54 and 0.23) and those in specialty care (mean annual RRs of 0.39 and 0.18).
In other findings, the annual representation of Black trainees remained unchanged in dermatology between 2005 and 2020, but down-trended for primary (P < .001) and specialty care (P = .001). At the same time, representation of Latinx trainees remained unchanged in dermatology and specialty care but increased in primary care (P < .001). Finally, Black and Latinx race and ethnicity comprised a lower mean proportion of matriculating dermatology trainees (postgraduate year-2s) compared with annual dermatology applicants (4.01% vs. 5.97%, respectively, and 2.06% vs. 6.37% among Latinx; P < .001 for all associations).
“Much of these disparities can be attributed to the leaky pipeline – the disproportionate, stepwise reduction in racial and ethnic minority representation along the path to medicine,” the authors wrote. “This leaky pipeline is the direct result of structural racism, which includes, but is not limited to, historical and contemporary economic disinvestment from majority-minority schools, kindergarten through grade 12.” They concluded by stating that “dermatologists must intervene throughout the educational pipeline, including residency selection and mentorship, to effectively increase diversity.”
Solutions to address diversity
In an editorial accompanying the two studies published in the same issue of JAMA Dermatology, Ellen N. Pritchett, MD, MPH, of the department of dermatology at Howard University, Washington, and Andrew J. Park, MD, MBA, and Rebecca Vasquez, MD, of the department of dermatology at the University of Texas Southwestern Medical Center, Dallas, offered several solutions to address diversity in the dermatology work force. They include:
Go beyond individual bias in recruitment. “A residency selection framework that meaningfully incorporates diversity, equity, and inclusion (DEI) will require more than strategies that address individual bias,” they wrote. “Departmental recruitment committees must become familiar with systems that serve to perpetuate individual bias, like institutional racism or practices that disproportionately favor non-URM versus URM individuals.”
Challenge the myth of meritocracy. “The inaccurate notion of meritocracy – that success purely derives from individual effort has become the foundation of residency selection,” the authors wrote. “Unfortunately, this view ignores the inequitably distributed sociostructural resources that limit the rewards of individual effort.”
Avoid tokenism in retention strategies. Tokenism, which they defined as “a symbolic addition of members from a marginalized group to give the impression of social inclusiveness and diversity without meaningful incorporation of DEI in the policies, processes, and culture,” can lead to depression, burnout, and attrition, they wrote. They advise leaders of dermatology departments to “review their residency selection framework to ensure that it allows for meaningful representation, inclusion, and equity among trainees and faculty to better support URM individuals at all levels.”
Omar N. Qutub, MD, a Portland, Ore.–based dermatologist who was asked to comment on the studies, characterized the findings by Dr. Mansh and colleagues as sobering. “It appears that there is work to do as far as improving diversity in the dermatology workforce that will likely benefit greatly from an honest and steadfast approach to equitable application standards as well as mentorship during all stages of the application process,” such as medical school and residency, said Dr. Qutub, who is the director of equity, diversity, and inclusion of the ODAC Dermatology, Aesthetic & Surgical Conference. “With a focused attempt, we are likely to matriculate more racial minorities into our residency programs, maximizing patient outcomes.”
As for the study by Ms. Williams and colleagues, he told this news organization that efforts toward recruiting URM students as well as sexual minority students “is likely to not only improve health inequities in underserved areas, but will also enrich the specialty as a whole, allowing for better understanding of our diverse patient population and [for us to] to deliver quality care more readily for people and in areas where the focus has often been limited.”
In an interview, Chesahna Kindred, MD, a Columbia, Md.–based dermatologist and immediate past chair of the National Medical Association dermatology section, pointed out that the number of Black physicians in the United States has increased by only 4% in the last 120 years. The study by Dr. Mansh and colleagues, she commented, “underscores what I’ve recognized in the last couple of years: Where are the Black male dermatologists? NMA Derm started recruiting this demographic aggressively about a year ago and started the Black Men in Derm events. Black male members of NMA Derm travel to the Student National Medical Association and NMA conference and hold a panel to expose Black male students into dermatology. This article provides the numbers needed to measure how successful this and other programs are to closing the equity gap.”
Ms. Williams reported having no financial disclosures. Dr. Mansh reported receiving grants from National Institute of Environmental Health Sciences outside the submitted work. Dr. Pritchett and colleagues reported having no relevant financial disclosures, as did Dr. Qutub and Dr. Kindred.
suggest.
To evaluate diversity and career goals of graduating allopathic medical students pursuing careers in dermatology, corresponding author Matthew Mansh, MD, of the department of dermatology at the University of Minnesota, Minneapolis, and colleagues drew from the 2016-2019 Association of American Medical Colleges Graduation Questionnaire for their study. The main outcome measures were the proportion of female students, students from racial and ethnic groups underrepresented in medicine (URM), and sexual minority (SM) students pursuing dermatology versus those pursuing other specialties, as well as the proportions and multivariable adjusted odds of intended career goals between students pursuing dermatology and those pursuing other specialties, and by sex, race, and ethnicity, and sexual orientation among students pursuing dermatology.
Of the 58,077 graduating students, 49% were women, 15% were URM, and 6% were SM. The researchers found that women pursuing dermatology were significantly less likely than women pursuing other specialties to identify as URM (11.6% vs. 17.2%; P < .001) or SM (1.9% vs. 5.7%; P < .001).
In multivariable-adjusted analyses of all students, those pursuing dermatology compared with other specialties had decreased odds of intending to care for underserved populations (18.3% vs. 34%; adjusted odd ratio, 0.40; P < .001), practice in underserved areas (12.7% vs. 25.9%; aOR, 0.40; P < .001), and practice public health (17% vs. 30.2%; aOR, 0.44; P < .001). The odds for pursuing research in their careers was greater among those pursuing dermatology (64.7% vs. 51.7%; aOR, 1.76; P < .001).
“Addressing health inequities and improving care for underserved patients is the responsibility of all dermatologists, and efforts are needed to increase diversity and interest in careers focused on underserved care among trainees in the dermatology workforce pipeline,” the authors concluded. They acknowledged certain limitations of the analysis, including lack of data delineating sex, sex assigned at birth, and gender identity, and lack of intersectional analyses between multiple minority identities and multiple career goals. “Importantly, diversity factors and their relationship to underserved care is likely multidimensional, and many students pursuing dermatology identified with multiple minority identities, highlighting the need for future studies focused on intersectionality,” they wrote.
Trends over 15 years
In a separate study, Jazzmin C. Williams, a medical student at the University of California, San Francisco, and coauthors drew from an Association of American Medical Colleges report of trainees’ and applicants’ self-reported race and ethnicity by specialty from 2005 to 2020 to evaluate diversity trends over the 15-year period. They found that Black and Latinx trainees were underrepresented in all specialties, but even more so in dermatology (mean annual rate ratios of 0.32 and 0.14, respectively), compared with those in primary care (mean annual RRs of 0.54 and 0.23) and those in specialty care (mean annual RRs of 0.39 and 0.18).
In other findings, the annual representation of Black trainees remained unchanged in dermatology between 2005 and 2020, but down-trended for primary (P < .001) and specialty care (P = .001). At the same time, representation of Latinx trainees remained unchanged in dermatology and specialty care but increased in primary care (P < .001). Finally, Black and Latinx race and ethnicity comprised a lower mean proportion of matriculating dermatology trainees (postgraduate year-2s) compared with annual dermatology applicants (4.01% vs. 5.97%, respectively, and 2.06% vs. 6.37% among Latinx; P < .001 for all associations).
“Much of these disparities can be attributed to the leaky pipeline – the disproportionate, stepwise reduction in racial and ethnic minority representation along the path to medicine,” the authors wrote. “This leaky pipeline is the direct result of structural racism, which includes, but is not limited to, historical and contemporary economic disinvestment from majority-minority schools, kindergarten through grade 12.” They concluded by stating that “dermatologists must intervene throughout the educational pipeline, including residency selection and mentorship, to effectively increase diversity.”
Solutions to address diversity
In an editorial accompanying the two studies published in the same issue of JAMA Dermatology, Ellen N. Pritchett, MD, MPH, of the department of dermatology at Howard University, Washington, and Andrew J. Park, MD, MBA, and Rebecca Vasquez, MD, of the department of dermatology at the University of Texas Southwestern Medical Center, Dallas, offered several solutions to address diversity in the dermatology work force. They include:
Go beyond individual bias in recruitment. “A residency selection framework that meaningfully incorporates diversity, equity, and inclusion (DEI) will require more than strategies that address individual bias,” they wrote. “Departmental recruitment committees must become familiar with systems that serve to perpetuate individual bias, like institutional racism or practices that disproportionately favor non-URM versus URM individuals.”
Challenge the myth of meritocracy. “The inaccurate notion of meritocracy – that success purely derives from individual effort has become the foundation of residency selection,” the authors wrote. “Unfortunately, this view ignores the inequitably distributed sociostructural resources that limit the rewards of individual effort.”
Avoid tokenism in retention strategies. Tokenism, which they defined as “a symbolic addition of members from a marginalized group to give the impression of social inclusiveness and diversity without meaningful incorporation of DEI in the policies, processes, and culture,” can lead to depression, burnout, and attrition, they wrote. They advise leaders of dermatology departments to “review their residency selection framework to ensure that it allows for meaningful representation, inclusion, and equity among trainees and faculty to better support URM individuals at all levels.”
Omar N. Qutub, MD, a Portland, Ore.–based dermatologist who was asked to comment on the studies, characterized the findings by Dr. Mansh and colleagues as sobering. “It appears that there is work to do as far as improving diversity in the dermatology workforce that will likely benefit greatly from an honest and steadfast approach to equitable application standards as well as mentorship during all stages of the application process,” such as medical school and residency, said Dr. Qutub, who is the director of equity, diversity, and inclusion of the ODAC Dermatology, Aesthetic & Surgical Conference. “With a focused attempt, we are likely to matriculate more racial minorities into our residency programs, maximizing patient outcomes.”
As for the study by Ms. Williams and colleagues, he told this news organization that efforts toward recruiting URM students as well as sexual minority students “is likely to not only improve health inequities in underserved areas, but will also enrich the specialty as a whole, allowing for better understanding of our diverse patient population and [for us to] to deliver quality care more readily for people and in areas where the focus has often been limited.”
In an interview, Chesahna Kindred, MD, a Columbia, Md.–based dermatologist and immediate past chair of the National Medical Association dermatology section, pointed out that the number of Black physicians in the United States has increased by only 4% in the last 120 years. The study by Dr. Mansh and colleagues, she commented, “underscores what I’ve recognized in the last couple of years: Where are the Black male dermatologists? NMA Derm started recruiting this demographic aggressively about a year ago and started the Black Men in Derm events. Black male members of NMA Derm travel to the Student National Medical Association and NMA conference and hold a panel to expose Black male students into dermatology. This article provides the numbers needed to measure how successful this and other programs are to closing the equity gap.”
Ms. Williams reported having no financial disclosures. Dr. Mansh reported receiving grants from National Institute of Environmental Health Sciences outside the submitted work. Dr. Pritchett and colleagues reported having no relevant financial disclosures, as did Dr. Qutub and Dr. Kindred.
FROM JAMA DERMATOLOGY








