User login
Malaria vaccine gets special delivery by tiny health personnel
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Recurrent drainage from an old gunshot wound

An x-ray revealed a metal density in the area of concern that was consistent with a bullet fragment or other metallic foreign body. Since there were no lucencies on x-ray or tracking from the area of concern to the metacarpal, the diagnosis was confirmed as an infected foreign body. The history was very concerning for osteomyelitis, given that the patient had sustained a GSW and had undergone surgical repair with hardware. (Shifting hardware can also lead to callus formation and skin breakdown.)
The patient was told that he’d retained a bullet fragment or foreign body that caused a chronic infection and the recurrent drainage. In addition, the hardware spanning the gap between the remnants of his proximal and distal metacarpal had broken as a result of fatigue. He was referred to a surgeon to remove the foreign body and treat the infection. The patient was advised that he might also need replacement hardware and a bone graft.
Images and text courtesy of Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker MD School of Medicine, Kalamazoo.

An x-ray revealed a metal density in the area of concern that was consistent with a bullet fragment or other metallic foreign body. Since there were no lucencies on x-ray or tracking from the area of concern to the metacarpal, the diagnosis was confirmed as an infected foreign body. The history was very concerning for osteomyelitis, given that the patient had sustained a GSW and had undergone surgical repair with hardware. (Shifting hardware can also lead to callus formation and skin breakdown.)
The patient was told that he’d retained a bullet fragment or foreign body that caused a chronic infection and the recurrent drainage. In addition, the hardware spanning the gap between the remnants of his proximal and distal metacarpal had broken as a result of fatigue. He was referred to a surgeon to remove the foreign body and treat the infection. The patient was advised that he might also need replacement hardware and a bone graft.
Images and text courtesy of Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker MD School of Medicine, Kalamazoo.

An x-ray revealed a metal density in the area of concern that was consistent with a bullet fragment or other metallic foreign body. Since there were no lucencies on x-ray or tracking from the area of concern to the metacarpal, the diagnosis was confirmed as an infected foreign body. The history was very concerning for osteomyelitis, given that the patient had sustained a GSW and had undergone surgical repair with hardware. (Shifting hardware can also lead to callus formation and skin breakdown.)
The patient was told that he’d retained a bullet fragment or foreign body that caused a chronic infection and the recurrent drainage. In addition, the hardware spanning the gap between the remnants of his proximal and distal metacarpal had broken as a result of fatigue. He was referred to a surgeon to remove the foreign body and treat the infection. The patient was advised that he might also need replacement hardware and a bone graft.
Images and text courtesy of Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker MD School of Medicine, Kalamazoo.
Children and COVID: Weekly cases dropped by 57% in September
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.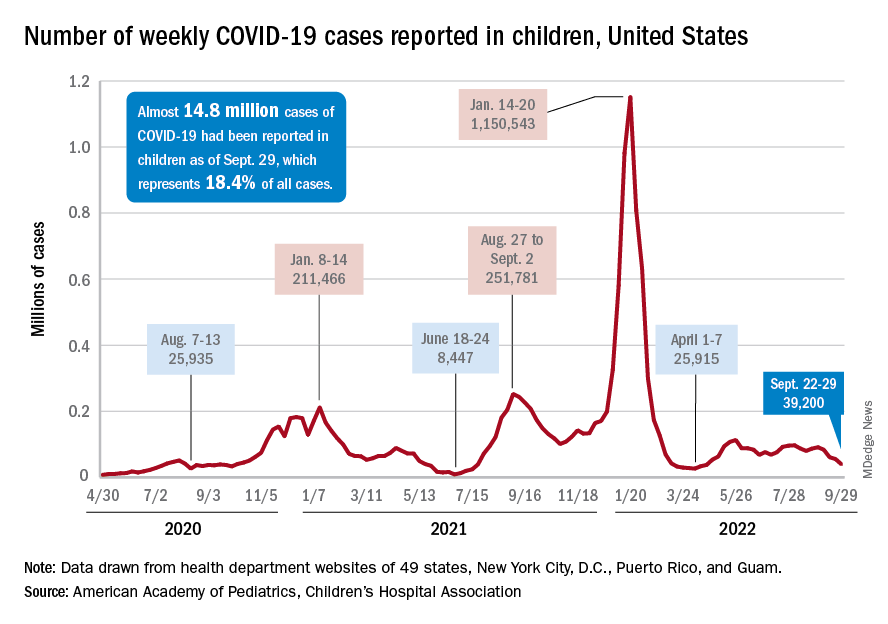
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.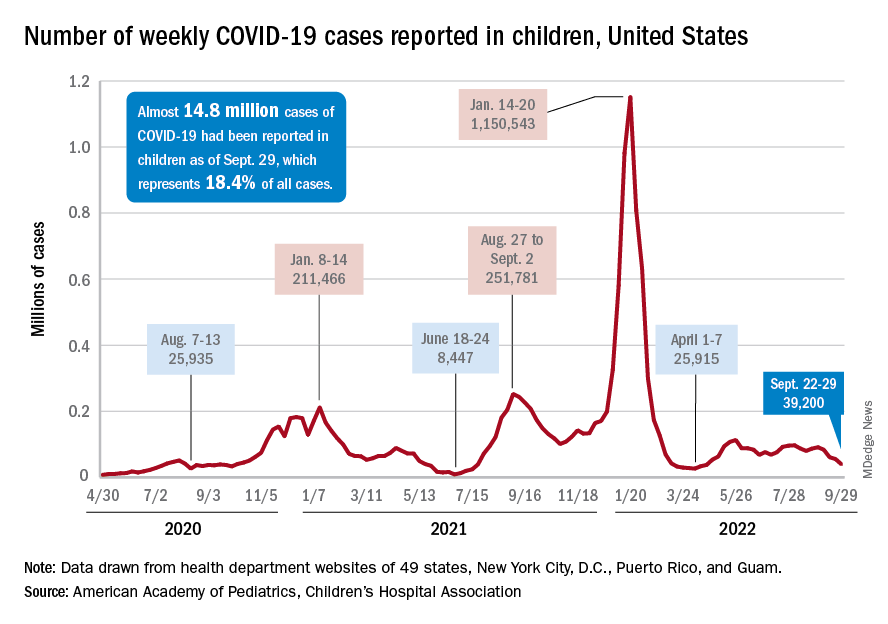
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.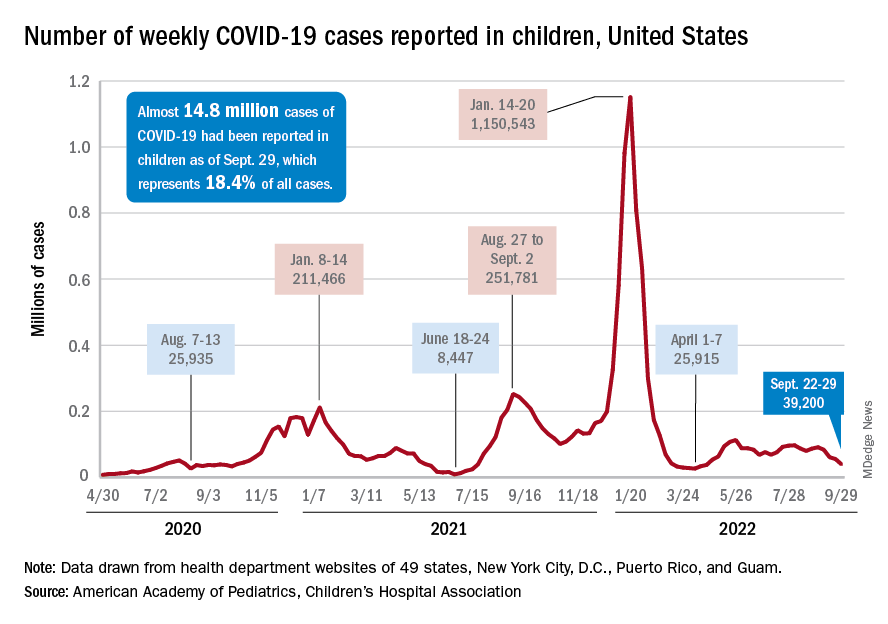
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
What is known about sexual dysfunction after breast cancer?
PARIS – What do doctors know about their patients’ sexual health? Not a lot. What about oncologists who treat women with breast cancer? Not much more.
To determine the extent of sexual dysfunction among women with breast cancer, Maria Alice Franzoi, MD, an oncologist at Gustave Roussy Hospital, Villejuif, France, analyzed data concerning sexuality from the CANTO cohort study. She showed that sexual dysfunction often predates the cancer diagnosis and doesn’t improve but rather worsens in the following 2 years. She presented her results at the annual meeting of the European Society for Medical Oncology.
Present at diagnosis
Dr. Franzoi, whose research projects have focused on patient monitoring post cancer, drew her conclusions from the data provided by CANTO, a longitudinal, prospective cohort study that monitors women being treated for localized breast cancer. Study participants answered the EORTC-QLQ-BR23 quality-of-life questionnaire at the time of diagnosis (T0), 1 year after diagnosis (T1), and 2 years after diagnosis (T2). Four factors were employed to better define women’s sex-related problems: poor body image, poor sexual functioning (activity and desire), lack of sexual pleasure, and a complete lack of sexual activity.
The analysis focused on the responses of 7,895 patients in the CANTO cohort study on sexual activity; 4,523 of those patients answered questions about sexual pleasure. Female respondents who reported engaging in no sexual activity did not have to answer the questions in this second section.
“Seventy-five percent of patients reported at least one of the four concerns during the study,” noted Dr. Franzoi during her presentation. This finding highlights the fact that “sexual problems are already present at the time of diagnosis in a considerable number of patients,” she said. More than a third of participants complained of at least one of the four items.
Developments after diagnosis
The proportion of women who reported no arousal or poor sexual function remained stable at around 30% over time, meaning that the sexual problems were reported in similar numbers at T0, T1, and T2. “However, after cancer, more patients are worried about a lack of sexual pleasure (38.7% at T1 and 38.1% at T2, vs. 29.1% at T0) or report having a negative body image (57.8% at T1 and 52.5% at T2, vs. 32.1% at T0),” said Dr. Franzoi.
She identified the following three variables as being associated with sexual dysfunction 2 years after diagnosis: the existence of this problem at the time of diagnosis, the use of adjuvant hormone therapy, and severe depression or a very high stress level after the first year of treatment.
Inadequate specific treatment
“Sexual dysfunction is a major unmet need with a significant impact on quality of life,” said Maryam Lustberg, MD, an oncologist at Yale School of Medicine, New Haven, Conn., who was invited to discuss the results at the conference.
Dr. Franzoi observed that most participants with sexual dysfunction that had continued 2 years after diagnosis had not been referred to a doctor for this problem. “In terms of sexual function, it’s better at T2 than at T1, but only 41% of these women have been seen by a gynecologist, and only 15% have received specific treatment,” she reported, emphasizing the need to assess and treat these issues “proactively” at the time of diagnosis and during and after treatment.
“Now we need to work out what the best treatment approach is,” commented Dr. Lustberg. She said that cancers other than breast and gynecologic cancers should also be taken into consideration. She cited the Sexual Health Assessment in Women With Lung Cancer study, which recently revealed that after being diagnosed with lung cancer, female patients experienced a drop in sexual desire (31% vs. 15% before diagnosis) and an increase in vaginal discomfort or dryness (43% vs. 13% before diagnosis). This study, presented in August to the 2022 International Association for the Study of Lung Cancer World Conference on Lung Cancer, also revealed that different parameters affect satisfaction in one’s sex life, including fatigue, sadness, relationship problems with a partner, and even breathing. Dr. Lustberg concluded from this study that a multidisciplinary approach is needed for cancer survivors.
Dr. Franzoi received research funding from Resilience Care. Dr. Lustberg has links with AstraZeneca, Pfizer, Novartis, Sanofi, and Lilly.
This article was translated from the Medscape French edition.
PARIS – What do doctors know about their patients’ sexual health? Not a lot. What about oncologists who treat women with breast cancer? Not much more.
To determine the extent of sexual dysfunction among women with breast cancer, Maria Alice Franzoi, MD, an oncologist at Gustave Roussy Hospital, Villejuif, France, analyzed data concerning sexuality from the CANTO cohort study. She showed that sexual dysfunction often predates the cancer diagnosis and doesn’t improve but rather worsens in the following 2 years. She presented her results at the annual meeting of the European Society for Medical Oncology.
Present at diagnosis
Dr. Franzoi, whose research projects have focused on patient monitoring post cancer, drew her conclusions from the data provided by CANTO, a longitudinal, prospective cohort study that monitors women being treated for localized breast cancer. Study participants answered the EORTC-QLQ-BR23 quality-of-life questionnaire at the time of diagnosis (T0), 1 year after diagnosis (T1), and 2 years after diagnosis (T2). Four factors were employed to better define women’s sex-related problems: poor body image, poor sexual functioning (activity and desire), lack of sexual pleasure, and a complete lack of sexual activity.
The analysis focused on the responses of 7,895 patients in the CANTO cohort study on sexual activity; 4,523 of those patients answered questions about sexual pleasure. Female respondents who reported engaging in no sexual activity did not have to answer the questions in this second section.
“Seventy-five percent of patients reported at least one of the four concerns during the study,” noted Dr. Franzoi during her presentation. This finding highlights the fact that “sexual problems are already present at the time of diagnosis in a considerable number of patients,” she said. More than a third of participants complained of at least one of the four items.
Developments after diagnosis
The proportion of women who reported no arousal or poor sexual function remained stable at around 30% over time, meaning that the sexual problems were reported in similar numbers at T0, T1, and T2. “However, after cancer, more patients are worried about a lack of sexual pleasure (38.7% at T1 and 38.1% at T2, vs. 29.1% at T0) or report having a negative body image (57.8% at T1 and 52.5% at T2, vs. 32.1% at T0),” said Dr. Franzoi.
She identified the following three variables as being associated with sexual dysfunction 2 years after diagnosis: the existence of this problem at the time of diagnosis, the use of adjuvant hormone therapy, and severe depression or a very high stress level after the first year of treatment.
Inadequate specific treatment
“Sexual dysfunction is a major unmet need with a significant impact on quality of life,” said Maryam Lustberg, MD, an oncologist at Yale School of Medicine, New Haven, Conn., who was invited to discuss the results at the conference.
Dr. Franzoi observed that most participants with sexual dysfunction that had continued 2 years after diagnosis had not been referred to a doctor for this problem. “In terms of sexual function, it’s better at T2 than at T1, but only 41% of these women have been seen by a gynecologist, and only 15% have received specific treatment,” she reported, emphasizing the need to assess and treat these issues “proactively” at the time of diagnosis and during and after treatment.
“Now we need to work out what the best treatment approach is,” commented Dr. Lustberg. She said that cancers other than breast and gynecologic cancers should also be taken into consideration. She cited the Sexual Health Assessment in Women With Lung Cancer study, which recently revealed that after being diagnosed with lung cancer, female patients experienced a drop in sexual desire (31% vs. 15% before diagnosis) and an increase in vaginal discomfort or dryness (43% vs. 13% before diagnosis). This study, presented in August to the 2022 International Association for the Study of Lung Cancer World Conference on Lung Cancer, also revealed that different parameters affect satisfaction in one’s sex life, including fatigue, sadness, relationship problems with a partner, and even breathing. Dr. Lustberg concluded from this study that a multidisciplinary approach is needed for cancer survivors.
Dr. Franzoi received research funding from Resilience Care. Dr. Lustberg has links with AstraZeneca, Pfizer, Novartis, Sanofi, and Lilly.
This article was translated from the Medscape French edition.
PARIS – What do doctors know about their patients’ sexual health? Not a lot. What about oncologists who treat women with breast cancer? Not much more.
To determine the extent of sexual dysfunction among women with breast cancer, Maria Alice Franzoi, MD, an oncologist at Gustave Roussy Hospital, Villejuif, France, analyzed data concerning sexuality from the CANTO cohort study. She showed that sexual dysfunction often predates the cancer diagnosis and doesn’t improve but rather worsens in the following 2 years. She presented her results at the annual meeting of the European Society for Medical Oncology.
Present at diagnosis
Dr. Franzoi, whose research projects have focused on patient monitoring post cancer, drew her conclusions from the data provided by CANTO, a longitudinal, prospective cohort study that monitors women being treated for localized breast cancer. Study participants answered the EORTC-QLQ-BR23 quality-of-life questionnaire at the time of diagnosis (T0), 1 year after diagnosis (T1), and 2 years after diagnosis (T2). Four factors were employed to better define women’s sex-related problems: poor body image, poor sexual functioning (activity and desire), lack of sexual pleasure, and a complete lack of sexual activity.
The analysis focused on the responses of 7,895 patients in the CANTO cohort study on sexual activity; 4,523 of those patients answered questions about sexual pleasure. Female respondents who reported engaging in no sexual activity did not have to answer the questions in this second section.
“Seventy-five percent of patients reported at least one of the four concerns during the study,” noted Dr. Franzoi during her presentation. This finding highlights the fact that “sexual problems are already present at the time of diagnosis in a considerable number of patients,” she said. More than a third of participants complained of at least one of the four items.
Developments after diagnosis
The proportion of women who reported no arousal or poor sexual function remained stable at around 30% over time, meaning that the sexual problems were reported in similar numbers at T0, T1, and T2. “However, after cancer, more patients are worried about a lack of sexual pleasure (38.7% at T1 and 38.1% at T2, vs. 29.1% at T0) or report having a negative body image (57.8% at T1 and 52.5% at T2, vs. 32.1% at T0),” said Dr. Franzoi.
She identified the following three variables as being associated with sexual dysfunction 2 years after diagnosis: the existence of this problem at the time of diagnosis, the use of adjuvant hormone therapy, and severe depression or a very high stress level after the first year of treatment.
Inadequate specific treatment
“Sexual dysfunction is a major unmet need with a significant impact on quality of life,” said Maryam Lustberg, MD, an oncologist at Yale School of Medicine, New Haven, Conn., who was invited to discuss the results at the conference.
Dr. Franzoi observed that most participants with sexual dysfunction that had continued 2 years after diagnosis had not been referred to a doctor for this problem. “In terms of sexual function, it’s better at T2 than at T1, but only 41% of these women have been seen by a gynecologist, and only 15% have received specific treatment,” she reported, emphasizing the need to assess and treat these issues “proactively” at the time of diagnosis and during and after treatment.
“Now we need to work out what the best treatment approach is,” commented Dr. Lustberg. She said that cancers other than breast and gynecologic cancers should also be taken into consideration. She cited the Sexual Health Assessment in Women With Lung Cancer study, which recently revealed that after being diagnosed with lung cancer, female patients experienced a drop in sexual desire (31% vs. 15% before diagnosis) and an increase in vaginal discomfort or dryness (43% vs. 13% before diagnosis). This study, presented in August to the 2022 International Association for the Study of Lung Cancer World Conference on Lung Cancer, also revealed that different parameters affect satisfaction in one’s sex life, including fatigue, sadness, relationship problems with a partner, and even breathing. Dr. Lustberg concluded from this study that a multidisciplinary approach is needed for cancer survivors.
Dr. Franzoi received research funding from Resilience Care. Dr. Lustberg has links with AstraZeneca, Pfizer, Novartis, Sanofi, and Lilly.
This article was translated from the Medscape French edition.
AT ESMO CONGRESS 2022
2022 billing and coding updates
Telehealth and Teaching Physician Services and ICD-10 codes updates
In my previous article in June, 2022, we plowed through the billing and coding updates regarding critical care services, and, I hope that it helped our readers get more acquainted with the nuances of billing and coding in the ICU. In this piece, I would like to briefly elucidate three other areas of practice, which will be relevant to all physicians across various specialties.
Telehealth services
(PHE). Initially, the plan was to remove these from the list of covered services by the latter end of the COVID-19 PHE, which, created some uncertainty, or by December 31, 2021. Fortunately, CMS finalized that they will extend it through the end of the calendar year (CY) 2023. So, now all the telehealth services will remain on the CMS list until December 31, 2023. The general principle behind this ruling is to allow for more time for CMS and stakeholders to gather data and to submit support for requesting these services to be permanently added to the Medicare telehealth services list.
Not only has CMS extended the deadline for telehealth services but also they have gone far and beyond to extend some of the codes for cardiac and intensive cardiac rehabilitation until December 31, 2023, as well.
There has been a lot of debate regarding the geographic restrictions when it comes to telehealth visits for diagnosis, evaluation, or treatment of a mental health disorder. As per the latest Consolidated Appropriations Act of 2021 (Section 123), the home of the patient is a permissible site. But, the caveat is that there must be an in-person service with the practitioner/physician within 6 months prior to the initial telehealth visit. Additionally, there has to be a set frequency for subsequent in-person visits. And, usually the subsequent visits will need to be provided at least every 12 months. These requirements are not set in stone and can be changed on a case-by-case basis provided there is appropriate documentation in the chart.
Lastly, it is important to understand and use the appropriate telecommunication systems for the telehealth visits and the modifiers that are associated with them. By definition, it has to be audio and video equipment that allows two-way, real-time interactive communication between the patient and the provider when used for telehealth services for the diagnosis, evaluation, or treatment of mental health disorders. But, CMS is in the process of amending it to include audio-only communications technology. At this time, the use of audio-only interactive telecommunications system is limited to practitioners who have the capability to provide two-way audio/video communications but, where the patient is not capable, or does not consent to, the use of two-way audio/video technology. Modifier FQ should be attached to all the mental health services that were furnished using audio-only communications. And, mental health services can include services for treatment of substance use disorders (SUD). Please do not confuse modifier FQ with modifier 93 as FQ is only for behavioral health services. And, remember that the totality of the communication of information exchanged between the provider and the patient during the course of the synchronous telemedicine service (rendered via telephone or other real-time interactive audio only telecommunication system) must be of an amount and nature that is sufficient to meet the key components and/or requirements of the same service when rendered via a face-to-face interaction.
Teaching physician services
As a general rule, a teaching physician can bill for the resident services only if they are present for the critical (key) portion of the service. But, there is one exception called the “primary care exception” under which in certain teaching hospital primary care centers, the teaching physician can bill for certain services as furnished independently by the resident without the teaching physician being physically present, but with the teaching physician’s review.
The current model to bill for office/outpatient E/M visit level is either based on either total time spent (personally) or medical-decision-making (MDM). When time is used to select the visit level only the time spent by the teaching physician in qualifying activities can be included for the purposes of the visit level selection. And, this includes the time the teaching physician was present with the resident performing those qualifying activities. Also, under the primary care exception, time cannot be used to select the visit level. This is to guard against the possibility of inappropriate coding that reflects residents’ inefficiencies rather than a measure of the total medically necessary time required to furnish the E/M services.
ICD-10 updates
Usually, the ICD-10 codes are updated annually and take effect every October 1. Some of the most relevant updates are as follows:
1. U09.9 Post COVID-19 condition, unspecified: This should be used to document sequelae of COVID-19 or “long COVID” conditions, after the acute illness has resolved. But, remember to code the conditions related to COVID-19 first and do not use this code with an active or current COVID-19 infection.
2. U07.0 Vaping-related disorder: This should be used for all vaping-related illnesses. However, additional codes for other diagnoses such as acute respiratory failure, acute respiratory distress syndrome, or pneumonitis can also be used with this code. Other respiratory signs and symptoms such as cough and shortness of breath should not be coded separately.
3. Cough is one of the most common reasons for referral to a pulmonologist. The CDC has expanded these codes so please remember to code the most specific diagnosis as deemed appropriate.
R05.1 Acute cough
R05.2 Subacute cough
R05.3 Chronic cough
R05.4 Cough, syncope
R05.8 Other specified cough
R05.9 Cough, unspecified
We will be back with some more exciting and intriguing billing and coding updates in our next article and hope to see everyone at CHEST 2022 in Nashville., TN.
Telehealth and Teaching Physician Services and ICD-10 codes updates
Telehealth and Teaching Physician Services and ICD-10 codes updates
In my previous article in June, 2022, we plowed through the billing and coding updates regarding critical care services, and, I hope that it helped our readers get more acquainted with the nuances of billing and coding in the ICU. In this piece, I would like to briefly elucidate three other areas of practice, which will be relevant to all physicians across various specialties.
Telehealth services
(PHE). Initially, the plan was to remove these from the list of covered services by the latter end of the COVID-19 PHE, which, created some uncertainty, or by December 31, 2021. Fortunately, CMS finalized that they will extend it through the end of the calendar year (CY) 2023. So, now all the telehealth services will remain on the CMS list until December 31, 2023. The general principle behind this ruling is to allow for more time for CMS and stakeholders to gather data and to submit support for requesting these services to be permanently added to the Medicare telehealth services list.
Not only has CMS extended the deadline for telehealth services but also they have gone far and beyond to extend some of the codes for cardiac and intensive cardiac rehabilitation until December 31, 2023, as well.
There has been a lot of debate regarding the geographic restrictions when it comes to telehealth visits for diagnosis, evaluation, or treatment of a mental health disorder. As per the latest Consolidated Appropriations Act of 2021 (Section 123), the home of the patient is a permissible site. But, the caveat is that there must be an in-person service with the practitioner/physician within 6 months prior to the initial telehealth visit. Additionally, there has to be a set frequency for subsequent in-person visits. And, usually the subsequent visits will need to be provided at least every 12 months. These requirements are not set in stone and can be changed on a case-by-case basis provided there is appropriate documentation in the chart.
Lastly, it is important to understand and use the appropriate telecommunication systems for the telehealth visits and the modifiers that are associated with them. By definition, it has to be audio and video equipment that allows two-way, real-time interactive communication between the patient and the provider when used for telehealth services for the diagnosis, evaluation, or treatment of mental health disorders. But, CMS is in the process of amending it to include audio-only communications technology. At this time, the use of audio-only interactive telecommunications system is limited to practitioners who have the capability to provide two-way audio/video communications but, where the patient is not capable, or does not consent to, the use of two-way audio/video technology. Modifier FQ should be attached to all the mental health services that were furnished using audio-only communications. And, mental health services can include services for treatment of substance use disorders (SUD). Please do not confuse modifier FQ with modifier 93 as FQ is only for behavioral health services. And, remember that the totality of the communication of information exchanged between the provider and the patient during the course of the synchronous telemedicine service (rendered via telephone or other real-time interactive audio only telecommunication system) must be of an amount and nature that is sufficient to meet the key components and/or requirements of the same service when rendered via a face-to-face interaction.
Teaching physician services
As a general rule, a teaching physician can bill for the resident services only if they are present for the critical (key) portion of the service. But, there is one exception called the “primary care exception” under which in certain teaching hospital primary care centers, the teaching physician can bill for certain services as furnished independently by the resident without the teaching physician being physically present, but with the teaching physician’s review.
The current model to bill for office/outpatient E/M visit level is either based on either total time spent (personally) or medical-decision-making (MDM). When time is used to select the visit level only the time spent by the teaching physician in qualifying activities can be included for the purposes of the visit level selection. And, this includes the time the teaching physician was present with the resident performing those qualifying activities. Also, under the primary care exception, time cannot be used to select the visit level. This is to guard against the possibility of inappropriate coding that reflects residents’ inefficiencies rather than a measure of the total medically necessary time required to furnish the E/M services.
ICD-10 updates
Usually, the ICD-10 codes are updated annually and take effect every October 1. Some of the most relevant updates are as follows:
1. U09.9 Post COVID-19 condition, unspecified: This should be used to document sequelae of COVID-19 or “long COVID” conditions, after the acute illness has resolved. But, remember to code the conditions related to COVID-19 first and do not use this code with an active or current COVID-19 infection.
2. U07.0 Vaping-related disorder: This should be used for all vaping-related illnesses. However, additional codes for other diagnoses such as acute respiratory failure, acute respiratory distress syndrome, or pneumonitis can also be used with this code. Other respiratory signs and symptoms such as cough and shortness of breath should not be coded separately.
3. Cough is one of the most common reasons for referral to a pulmonologist. The CDC has expanded these codes so please remember to code the most specific diagnosis as deemed appropriate.
R05.1 Acute cough
R05.2 Subacute cough
R05.3 Chronic cough
R05.4 Cough, syncope
R05.8 Other specified cough
R05.9 Cough, unspecified
We will be back with some more exciting and intriguing billing and coding updates in our next article and hope to see everyone at CHEST 2022 in Nashville., TN.
In my previous article in June, 2022, we plowed through the billing and coding updates regarding critical care services, and, I hope that it helped our readers get more acquainted with the nuances of billing and coding in the ICU. In this piece, I would like to briefly elucidate three other areas of practice, which will be relevant to all physicians across various specialties.
Telehealth services
(PHE). Initially, the plan was to remove these from the list of covered services by the latter end of the COVID-19 PHE, which, created some uncertainty, or by December 31, 2021. Fortunately, CMS finalized that they will extend it through the end of the calendar year (CY) 2023. So, now all the telehealth services will remain on the CMS list until December 31, 2023. The general principle behind this ruling is to allow for more time for CMS and stakeholders to gather data and to submit support for requesting these services to be permanently added to the Medicare telehealth services list.
Not only has CMS extended the deadline for telehealth services but also they have gone far and beyond to extend some of the codes for cardiac and intensive cardiac rehabilitation until December 31, 2023, as well.
There has been a lot of debate regarding the geographic restrictions when it comes to telehealth visits for diagnosis, evaluation, or treatment of a mental health disorder. As per the latest Consolidated Appropriations Act of 2021 (Section 123), the home of the patient is a permissible site. But, the caveat is that there must be an in-person service with the practitioner/physician within 6 months prior to the initial telehealth visit. Additionally, there has to be a set frequency for subsequent in-person visits. And, usually the subsequent visits will need to be provided at least every 12 months. These requirements are not set in stone and can be changed on a case-by-case basis provided there is appropriate documentation in the chart.
Lastly, it is important to understand and use the appropriate telecommunication systems for the telehealth visits and the modifiers that are associated with them. By definition, it has to be audio and video equipment that allows two-way, real-time interactive communication between the patient and the provider when used for telehealth services for the diagnosis, evaluation, or treatment of mental health disorders. But, CMS is in the process of amending it to include audio-only communications technology. At this time, the use of audio-only interactive telecommunications system is limited to practitioners who have the capability to provide two-way audio/video communications but, where the patient is not capable, or does not consent to, the use of two-way audio/video technology. Modifier FQ should be attached to all the mental health services that were furnished using audio-only communications. And, mental health services can include services for treatment of substance use disorders (SUD). Please do not confuse modifier FQ with modifier 93 as FQ is only for behavioral health services. And, remember that the totality of the communication of information exchanged between the provider and the patient during the course of the synchronous telemedicine service (rendered via telephone or other real-time interactive audio only telecommunication system) must be of an amount and nature that is sufficient to meet the key components and/or requirements of the same service when rendered via a face-to-face interaction.
Teaching physician services
As a general rule, a teaching physician can bill for the resident services only if they are present for the critical (key) portion of the service. But, there is one exception called the “primary care exception” under which in certain teaching hospital primary care centers, the teaching physician can bill for certain services as furnished independently by the resident without the teaching physician being physically present, but with the teaching physician’s review.
The current model to bill for office/outpatient E/M visit level is either based on either total time spent (personally) or medical-decision-making (MDM). When time is used to select the visit level only the time spent by the teaching physician in qualifying activities can be included for the purposes of the visit level selection. And, this includes the time the teaching physician was present with the resident performing those qualifying activities. Also, under the primary care exception, time cannot be used to select the visit level. This is to guard against the possibility of inappropriate coding that reflects residents’ inefficiencies rather than a measure of the total medically necessary time required to furnish the E/M services.
ICD-10 updates
Usually, the ICD-10 codes are updated annually and take effect every October 1. Some of the most relevant updates are as follows:
1. U09.9 Post COVID-19 condition, unspecified: This should be used to document sequelae of COVID-19 or “long COVID” conditions, after the acute illness has resolved. But, remember to code the conditions related to COVID-19 first and do not use this code with an active or current COVID-19 infection.
2. U07.0 Vaping-related disorder: This should be used for all vaping-related illnesses. However, additional codes for other diagnoses such as acute respiratory failure, acute respiratory distress syndrome, or pneumonitis can also be used with this code. Other respiratory signs and symptoms such as cough and shortness of breath should not be coded separately.
3. Cough is one of the most common reasons for referral to a pulmonologist. The CDC has expanded these codes so please remember to code the most specific diagnosis as deemed appropriate.
R05.1 Acute cough
R05.2 Subacute cough
R05.3 Chronic cough
R05.4 Cough, syncope
R05.8 Other specified cough
R05.9 Cough, unspecified
We will be back with some more exciting and intriguing billing and coding updates in our next article and hope to see everyone at CHEST 2022 in Nashville., TN.
Access unmatched asthma education from anywhere
CHEST is proud to announce the launch of the newest addition to our e-learning options: the CHEST Asthma Curriculum Pathway.
This unique offering combines a variety of bite-sized educational resources from among CHEST’s most popular and effective products, including case-based CHEST SEEK™ questions, podcasts and videos from asthma experts, the latest research from the journal CHEST®, and more.
The pathway comprises several different “paths,” or tracks, that enable clinicians to target their education based on their knowledge gaps and career level. Users can opt to follow the curriculum from start to finish to gain a comprehensive overview of asthma management. Or, they can select individual paths to focus their learning on topics including asthma pathophysiology, diagnosis and classification, exacerbations, phenotypes, and more.
According to early learners of the pathway: It helped a lot with the knowledge check-in.” Another commented: “It is very comprehensive on all aspects of asthma. I enjoyed the higher-level learning on the choice of biologics and asthma mimickers.” The education modalities were highlighted, as well, with this feedback: “I really enjoyed the variety of media (lectures, discussions, papers, games).”
Exploring the education
The Asthma Curriculum Pathway offers targeted education options to fit the career level and clinical interest of clinicians, ranging from trainees and early career physicians to experienced asthma specialists and advanced practice providers.
Paths include:
• Path 1: Pathophysiology
• Path 2: Diagnosis & Classification
• Path 3: Management
• Path 4: Mimickers
• Path 5: Comorbidities
• Path 6: Phenotypes
• Path 7: Exacerbations
• Path 8: Special Situations
Plus, each path offers claiming credit, including CME, for completion—all while driving clinicians to consistently advance best outcomes for their patients with asthma.
Visit (https://bit.ly/asthma-pathway) to access the best of CHEST’s asthma education with the new Asthma Curriculum Pathway, accessible via web or mobile device.
CHEST is proud to announce the launch of the newest addition to our e-learning options: the CHEST Asthma Curriculum Pathway.
This unique offering combines a variety of bite-sized educational resources from among CHEST’s most popular and effective products, including case-based CHEST SEEK™ questions, podcasts and videos from asthma experts, the latest research from the journal CHEST®, and more.
The pathway comprises several different “paths,” or tracks, that enable clinicians to target their education based on their knowledge gaps and career level. Users can opt to follow the curriculum from start to finish to gain a comprehensive overview of asthma management. Or, they can select individual paths to focus their learning on topics including asthma pathophysiology, diagnosis and classification, exacerbations, phenotypes, and more.
According to early learners of the pathway: It helped a lot with the knowledge check-in.” Another commented: “It is very comprehensive on all aspects of asthma. I enjoyed the higher-level learning on the choice of biologics and asthma mimickers.” The education modalities were highlighted, as well, with this feedback: “I really enjoyed the variety of media (lectures, discussions, papers, games).”
Exploring the education
The Asthma Curriculum Pathway offers targeted education options to fit the career level and clinical interest of clinicians, ranging from trainees and early career physicians to experienced asthma specialists and advanced practice providers.
Paths include:
• Path 1: Pathophysiology
• Path 2: Diagnosis & Classification
• Path 3: Management
• Path 4: Mimickers
• Path 5: Comorbidities
• Path 6: Phenotypes
• Path 7: Exacerbations
• Path 8: Special Situations
Plus, each path offers claiming credit, including CME, for completion—all while driving clinicians to consistently advance best outcomes for their patients with asthma.
Visit (https://bit.ly/asthma-pathway) to access the best of CHEST’s asthma education with the new Asthma Curriculum Pathway, accessible via web or mobile device.
CHEST is proud to announce the launch of the newest addition to our e-learning options: the CHEST Asthma Curriculum Pathway.
This unique offering combines a variety of bite-sized educational resources from among CHEST’s most popular and effective products, including case-based CHEST SEEK™ questions, podcasts and videos from asthma experts, the latest research from the journal CHEST®, and more.
The pathway comprises several different “paths,” or tracks, that enable clinicians to target their education based on their knowledge gaps and career level. Users can opt to follow the curriculum from start to finish to gain a comprehensive overview of asthma management. Or, they can select individual paths to focus their learning on topics including asthma pathophysiology, diagnosis and classification, exacerbations, phenotypes, and more.
According to early learners of the pathway: It helped a lot with the knowledge check-in.” Another commented: “It is very comprehensive on all aspects of asthma. I enjoyed the higher-level learning on the choice of biologics and asthma mimickers.” The education modalities were highlighted, as well, with this feedback: “I really enjoyed the variety of media (lectures, discussions, papers, games).”
Exploring the education
The Asthma Curriculum Pathway offers targeted education options to fit the career level and clinical interest of clinicians, ranging from trainees and early career physicians to experienced asthma specialists and advanced practice providers.
Paths include:
• Path 1: Pathophysiology
• Path 2: Diagnosis & Classification
• Path 3: Management
• Path 4: Mimickers
• Path 5: Comorbidities
• Path 6: Phenotypes
• Path 7: Exacerbations
• Path 8: Special Situations
Plus, each path offers claiming credit, including CME, for completion—all while driving clinicians to consistently advance best outcomes for their patients with asthma.
Visit (https://bit.ly/asthma-pathway) to access the best of CHEST’s asthma education with the new Asthma Curriculum Pathway, accessible via web or mobile device.
Advanced POCUS for us all?
Point-of-care ultrasound (POCUS) is a useful, practice-changing bedside tool that spans all medical and surgical specialties. While the definition of POCUS varies, most would agree it is an abbreviated exam that helps to answer a specific clinical question. With the expansion of POCUS training, the clinical questions being asked and answered have increased in scope and volume. The types of exams being utilized in “point of care ultrasound” have also increased and include transthoracic echocardiography; trans-esophageal echocardiography; and lung, gastric, abdominal, and ocular ultrasound. POCUS is used across multiple specialties, including critical care, anesthesiology, emergency medicine, and primary care.
Not only has POCUS become increasingly important clinically, but specialties now test these skills on their respective board examinations. Anesthesia is one of many such examples. The content outline for the American Board of Anesthesiology includes POCUS as a tested item on both the written and applied components of the exam. POCUS training must be directed toward both optimizing patient management and preparing learners for their board examination. A method for teaching this has yet to be defined (Naji A, et al. Cureus. 2021;13[5]:e15217).
One question – how should different specialties approach this educational challenge and should specialties train together? The answer is complicated. Many POCUS courses and certifications exist, and all vary in their content, didactics, and length. No true gold standard exists for POCUS certification for radiology or noncardiology providers. Additionally, there are no defined expectations or testing processes that certify a provider is “certified” to perform POCUS. While waiting for medical society guidelines to address these issues, many in graduate medical education (GME) are coming up with their own ways to incorporate POCUS into their respective training programs (Atkinson P, et al. CJEM. 2015 Mar;17[2]:161).
Who’s training whom?
Over the past decade, several expert committees, including those in critical care, have developed recommendations and consensus statements urging training facilities to independently create POCUS curriculums. The threshold for many programs to enter this realm of expertise is high and oftentimes unobtainable. We’ve seen emergency medicine and anesthesia raise the bar for ultrasound education in their residencies, but it’s unclear whether all fellowship-trained physicians can and should be tasked with obtaining official POCUS certification.
While specific specialties may require tailored certifications, there’s a considerable overlap in POCUS exam content across specialties. One approach to POCUS training could be developing and implementing a multidisciplinary curriculum. This would allow for pooling of resources (equipment, staff) and harnessing knowledge from providers familiar with different phases of patient care (ICU, perioperative, ED, outpatient clinics). By approaching POCUS from a multidisciplinary perspective, the quality of education may be enhanced (Mayo PH, et al. Intensive Care Med. 2014;40[5]:654). Is it then prudent for providers and trainees alike to share in didactics across all areas of the hospital and clinic? Would this close the knowledge gap between specialties who are facile with ultrasound and those not?
Determining the role of transesophageal echocardiography in a POCUS curriculum
This modality of imaging has been, until recently, reserved for cardiologists and anesthesiologists. More recently transesophageal echocardiography (TEE) has been utilized by emergency and critical care medicine physicians. TEE is part of recommended training for these specialties as a tool for diagnostic and rescue measures, including ventilator management, emergency procedures, and medication titration. Rescue TEE can also be utilized perioperatively where the transthoracic exam is limited by poor windows or the operative procedure precludes access to the chest. While transthoracic echocardiography (TTE) is often used in a point of care fashion, TEE is utilized less often. This may stem from the invasive nature of the procedure but likely also results from lack of equipment and training. Like POCUS overall, TEE POCUS will require incorporation into training programs to achieve widespread use and acceptance.
A deluge of research on TEE for the noncardiologist shows this modality is minimally invasive, safe, and effective. As it becomes more readily available and technology improves, there is no reason why an esophageal probe can’t be used in a patient with a secured airway (Wray TC, et al. J Intensive Care Med. 2021;36[1]:123).
Ultrasound for hemodynamic monitoring
There are many methods employed for hemodynamic monitoring in the ICU. Although echocardiographic and vascular parameters have been validated in the cardiac and perioperative fields, their application in the ICU setting for resuscitation and volume management remain somewhat controversial. The use of TEE and more advanced understanding of spectral doppler and pulmonary ultrasonography using TEE has revolutionized the way providers are managing critically ill patients. (Garcia YA, et al. Chest. 2017;152[4]:736).
In our opinion, physiology and imaging training for residents and fellows should be required for critical care medicine trainees. Delving into the nuances of frank-starling curves, stroke work, and diastolic function will enrich their understanding and highlight the applicability of ultrasonography. Furthermore, all clinicians caring for patients with critical illness should be privy to the nuances of physiologic derangement, and to that end, advanced echocardiographic principles and image acquisition. The heart-lung interactions are demonstrated in real time using POCUS and can clearly delineate treatment goals (Vieillard-Baron A, et al. Intensive Care Med. 2019;45[6]:770).
Documentation and billing
If clinicians are making medical decisions based off imaging gathered at the bedside and interpreted in real-time, documentation should reflect that. That documentation will invariably lead to billing and possibly audit or quality review by colleagues or other healthcare staff. Radiology and cardiology have perfected the billing process for image interpretation, but their form of documentation and interpretation may not easily be implemented in the perioperative or critical care settings. An abbreviated document with focused information should take the place of the formal study. With that, the credentialing and board certification process will allow providers to feel empowered to make clinical decisions based off these focused examinations.
Dr. Goertzen is Chief Fellow, Pulmonary/Critical Care; Dr. Knuf is Program Director, Department of Anesthesia; and Dr. Villalobos is Director of Medical ICU, Department of Internal Medicine, San Antonio Military Medical Center, San Antonio, Texas.
Point-of-care ultrasound (POCUS) is a useful, practice-changing bedside tool that spans all medical and surgical specialties. While the definition of POCUS varies, most would agree it is an abbreviated exam that helps to answer a specific clinical question. With the expansion of POCUS training, the clinical questions being asked and answered have increased in scope and volume. The types of exams being utilized in “point of care ultrasound” have also increased and include transthoracic echocardiography; trans-esophageal echocardiography; and lung, gastric, abdominal, and ocular ultrasound. POCUS is used across multiple specialties, including critical care, anesthesiology, emergency medicine, and primary care.
Not only has POCUS become increasingly important clinically, but specialties now test these skills on their respective board examinations. Anesthesia is one of many such examples. The content outline for the American Board of Anesthesiology includes POCUS as a tested item on both the written and applied components of the exam. POCUS training must be directed toward both optimizing patient management and preparing learners for their board examination. A method for teaching this has yet to be defined (Naji A, et al. Cureus. 2021;13[5]:e15217).
One question – how should different specialties approach this educational challenge and should specialties train together? The answer is complicated. Many POCUS courses and certifications exist, and all vary in their content, didactics, and length. No true gold standard exists for POCUS certification for radiology or noncardiology providers. Additionally, there are no defined expectations or testing processes that certify a provider is “certified” to perform POCUS. While waiting for medical society guidelines to address these issues, many in graduate medical education (GME) are coming up with their own ways to incorporate POCUS into their respective training programs (Atkinson P, et al. CJEM. 2015 Mar;17[2]:161).
Who’s training whom?
Over the past decade, several expert committees, including those in critical care, have developed recommendations and consensus statements urging training facilities to independently create POCUS curriculums. The threshold for many programs to enter this realm of expertise is high and oftentimes unobtainable. We’ve seen emergency medicine and anesthesia raise the bar for ultrasound education in their residencies, but it’s unclear whether all fellowship-trained physicians can and should be tasked with obtaining official POCUS certification.
While specific specialties may require tailored certifications, there’s a considerable overlap in POCUS exam content across specialties. One approach to POCUS training could be developing and implementing a multidisciplinary curriculum. This would allow for pooling of resources (equipment, staff) and harnessing knowledge from providers familiar with different phases of patient care (ICU, perioperative, ED, outpatient clinics). By approaching POCUS from a multidisciplinary perspective, the quality of education may be enhanced (Mayo PH, et al. Intensive Care Med. 2014;40[5]:654). Is it then prudent for providers and trainees alike to share in didactics across all areas of the hospital and clinic? Would this close the knowledge gap between specialties who are facile with ultrasound and those not?
Determining the role of transesophageal echocardiography in a POCUS curriculum
This modality of imaging has been, until recently, reserved for cardiologists and anesthesiologists. More recently transesophageal echocardiography (TEE) has been utilized by emergency and critical care medicine physicians. TEE is part of recommended training for these specialties as a tool for diagnostic and rescue measures, including ventilator management, emergency procedures, and medication titration. Rescue TEE can also be utilized perioperatively where the transthoracic exam is limited by poor windows or the operative procedure precludes access to the chest. While transthoracic echocardiography (TTE) is often used in a point of care fashion, TEE is utilized less often. This may stem from the invasive nature of the procedure but likely also results from lack of equipment and training. Like POCUS overall, TEE POCUS will require incorporation into training programs to achieve widespread use and acceptance.
A deluge of research on TEE for the noncardiologist shows this modality is minimally invasive, safe, and effective. As it becomes more readily available and technology improves, there is no reason why an esophageal probe can’t be used in a patient with a secured airway (Wray TC, et al. J Intensive Care Med. 2021;36[1]:123).
Ultrasound for hemodynamic monitoring
There are many methods employed for hemodynamic monitoring in the ICU. Although echocardiographic and vascular parameters have been validated in the cardiac and perioperative fields, their application in the ICU setting for resuscitation and volume management remain somewhat controversial. The use of TEE and more advanced understanding of spectral doppler and pulmonary ultrasonography using TEE has revolutionized the way providers are managing critically ill patients. (Garcia YA, et al. Chest. 2017;152[4]:736).
In our opinion, physiology and imaging training for residents and fellows should be required for critical care medicine trainees. Delving into the nuances of frank-starling curves, stroke work, and diastolic function will enrich their understanding and highlight the applicability of ultrasonography. Furthermore, all clinicians caring for patients with critical illness should be privy to the nuances of physiologic derangement, and to that end, advanced echocardiographic principles and image acquisition. The heart-lung interactions are demonstrated in real time using POCUS and can clearly delineate treatment goals (Vieillard-Baron A, et al. Intensive Care Med. 2019;45[6]:770).
Documentation and billing
If clinicians are making medical decisions based off imaging gathered at the bedside and interpreted in real-time, documentation should reflect that. That documentation will invariably lead to billing and possibly audit or quality review by colleagues or other healthcare staff. Radiology and cardiology have perfected the billing process for image interpretation, but their form of documentation and interpretation may not easily be implemented in the perioperative or critical care settings. An abbreviated document with focused information should take the place of the formal study. With that, the credentialing and board certification process will allow providers to feel empowered to make clinical decisions based off these focused examinations.
Dr. Goertzen is Chief Fellow, Pulmonary/Critical Care; Dr. Knuf is Program Director, Department of Anesthesia; and Dr. Villalobos is Director of Medical ICU, Department of Internal Medicine, San Antonio Military Medical Center, San Antonio, Texas.
Point-of-care ultrasound (POCUS) is a useful, practice-changing bedside tool that spans all medical and surgical specialties. While the definition of POCUS varies, most would agree it is an abbreviated exam that helps to answer a specific clinical question. With the expansion of POCUS training, the clinical questions being asked and answered have increased in scope and volume. The types of exams being utilized in “point of care ultrasound” have also increased and include transthoracic echocardiography; trans-esophageal echocardiography; and lung, gastric, abdominal, and ocular ultrasound. POCUS is used across multiple specialties, including critical care, anesthesiology, emergency medicine, and primary care.
Not only has POCUS become increasingly important clinically, but specialties now test these skills on their respective board examinations. Anesthesia is one of many such examples. The content outline for the American Board of Anesthesiology includes POCUS as a tested item on both the written and applied components of the exam. POCUS training must be directed toward both optimizing patient management and preparing learners for their board examination. A method for teaching this has yet to be defined (Naji A, et al. Cureus. 2021;13[5]:e15217).
One question – how should different specialties approach this educational challenge and should specialties train together? The answer is complicated. Many POCUS courses and certifications exist, and all vary in their content, didactics, and length. No true gold standard exists for POCUS certification for radiology or noncardiology providers. Additionally, there are no defined expectations or testing processes that certify a provider is “certified” to perform POCUS. While waiting for medical society guidelines to address these issues, many in graduate medical education (GME) are coming up with their own ways to incorporate POCUS into their respective training programs (Atkinson P, et al. CJEM. 2015 Mar;17[2]:161).
Who’s training whom?
Over the past decade, several expert committees, including those in critical care, have developed recommendations and consensus statements urging training facilities to independently create POCUS curriculums. The threshold for many programs to enter this realm of expertise is high and oftentimes unobtainable. We’ve seen emergency medicine and anesthesia raise the bar for ultrasound education in their residencies, but it’s unclear whether all fellowship-trained physicians can and should be tasked with obtaining official POCUS certification.
While specific specialties may require tailored certifications, there’s a considerable overlap in POCUS exam content across specialties. One approach to POCUS training could be developing and implementing a multidisciplinary curriculum. This would allow for pooling of resources (equipment, staff) and harnessing knowledge from providers familiar with different phases of patient care (ICU, perioperative, ED, outpatient clinics). By approaching POCUS from a multidisciplinary perspective, the quality of education may be enhanced (Mayo PH, et al. Intensive Care Med. 2014;40[5]:654). Is it then prudent for providers and trainees alike to share in didactics across all areas of the hospital and clinic? Would this close the knowledge gap between specialties who are facile with ultrasound and those not?
Determining the role of transesophageal echocardiography in a POCUS curriculum
This modality of imaging has been, until recently, reserved for cardiologists and anesthesiologists. More recently transesophageal echocardiography (TEE) has been utilized by emergency and critical care medicine physicians. TEE is part of recommended training for these specialties as a tool for diagnostic and rescue measures, including ventilator management, emergency procedures, and medication titration. Rescue TEE can also be utilized perioperatively where the transthoracic exam is limited by poor windows or the operative procedure precludes access to the chest. While transthoracic echocardiography (TTE) is often used in a point of care fashion, TEE is utilized less often. This may stem from the invasive nature of the procedure but likely also results from lack of equipment and training. Like POCUS overall, TEE POCUS will require incorporation into training programs to achieve widespread use and acceptance.
A deluge of research on TEE for the noncardiologist shows this modality is minimally invasive, safe, and effective. As it becomes more readily available and technology improves, there is no reason why an esophageal probe can’t be used in a patient with a secured airway (Wray TC, et al. J Intensive Care Med. 2021;36[1]:123).
Ultrasound for hemodynamic monitoring
There are many methods employed for hemodynamic monitoring in the ICU. Although echocardiographic and vascular parameters have been validated in the cardiac and perioperative fields, their application in the ICU setting for resuscitation and volume management remain somewhat controversial. The use of TEE and more advanced understanding of spectral doppler and pulmonary ultrasonography using TEE has revolutionized the way providers are managing critically ill patients. (Garcia YA, et al. Chest. 2017;152[4]:736).
In our opinion, physiology and imaging training for residents and fellows should be required for critical care medicine trainees. Delving into the nuances of frank-starling curves, stroke work, and diastolic function will enrich their understanding and highlight the applicability of ultrasonography. Furthermore, all clinicians caring for patients with critical illness should be privy to the nuances of physiologic derangement, and to that end, advanced echocardiographic principles and image acquisition. The heart-lung interactions are demonstrated in real time using POCUS and can clearly delineate treatment goals (Vieillard-Baron A, et al. Intensive Care Med. 2019;45[6]:770).
Documentation and billing
If clinicians are making medical decisions based off imaging gathered at the bedside and interpreted in real-time, documentation should reflect that. That documentation will invariably lead to billing and possibly audit or quality review by colleagues or other healthcare staff. Radiology and cardiology have perfected the billing process for image interpretation, but their form of documentation and interpretation may not easily be implemented in the perioperative or critical care settings. An abbreviated document with focused information should take the place of the formal study. With that, the credentialing and board certification process will allow providers to feel empowered to make clinical decisions based off these focused examinations.
Dr. Goertzen is Chief Fellow, Pulmonary/Critical Care; Dr. Knuf is Program Director, Department of Anesthesia; and Dr. Villalobos is Director of Medical ICU, Department of Internal Medicine, San Antonio Military Medical Center, San Antonio, Texas.
The possibilities are endless: A chat with the incoming CHEST Foundation President, Robert De Marco, MD, FCCP
As the presidency of the American College of Chest Physicians changes hands in January 2023, so will the role of President of the CHEST Foundation. To get to know the incoming President of the CHEST Foundation, we spoke with Robert (Bob) De Marco, MD, FCCP, about his philanthropy work and his goals for the philanthropic arm of CHEST.
Tell me about your history with philanthropy work.
My philanthropy work started long before the CHEST Foundation. While I’ve been a member of CHEST since my second year of fellowship, it wasn’t until much later that I became involved with the philanthropic side of the organization. Earlier in my career, I was involved more so with the American Cancer Society. I had gotten involved with them by chance – participating in an event of theirs – and was encouraged to get more involved by one of their board members. Being involved with them made a lot of sense seeing as a strong percentage of my patients at the time were being treated for lung cancer. My most notable accomplishments with the American Cancer Society were in serving as the Chairmen of my local Relay for Life program for 10 years, as a board member, and then as a president of my local chapter.
When did you get involved with the CHEST Foundation?
I had served in a handful of positions within CHEST, including Chair of the (since reinvented) Practice Management Committee, so I was deeply involved in the association, and I thought to myself, “I have experience in fundraising through my work with the American Cancer Society, why don’t I use it to help our association?” When I moved to Florida, I no longer had the local connection to the American Cancer Society, so it was an opportune time to transition over to the CHEST Foundation.
How has the Foundation changed in the time that you’ve been involved?
The Foundation has changed drastically since I first joined the Board of Trustees 9 years ago. When I first got involved, the primary goal of the Foundation was staying “out of the red.” At that time, we were an organization that gave away more than we made.
After years of building a corpus to fund our own projects, we’re in a really good place now with some phenomenal goals and some excellent initiatives to fundraise around, including a CHEST diversity initiative, First 5 Minutes™, and Bridging Specialties™: Timely Diagnosis for ILD Patients, which seeks to break down silos within medicine to improve patient care.
What will be a focus of your Foundation presidency?
You know, one thing I always appreciated about the American Cancer Society was that there were always notable accomplishments to point back to when supporting fundraising efforts. You could say, “Did you know that bone marrow transplantation was initially funded by the American Cancer Society?” and other examples that would truly inspire someone to want to get involved in supporting those efforts.
The CHEST Foundation may not have funded bone marrow transplantation, but in 25 years of awarding grants, there are equally good stories to share. The impact of the Foundation is tremendous, and we’ve only just begun to share examples of where grant recipients went with their research or community service projects.
A recent grant story that was shared with me was that of Panagis Galiatsatos, MD, MHS, who received a community service grant to start a program educating children in the Baltimore community about lung health. This program was so moving that it inspired one of the Baltimore teachers to pursue a career in medicine and that individual is now a practicing MD.
This is just one example of the Foundation’s impact and it’s through these stories that we share the “why” behind every dollar that is raised, and my first goal is to tell these stories.
Another key focus of not only my presidency, but Dr. Ian Nathanson’s, as well, as we collaborated a lot on our roles, will be on member involvement and awareness. Even I wasn’t involved in the CHEST Foundation until years into my CHEST membership, so I understand that there are competing demands. But I also know that there is a lot to be gained from the work with the Foundation. I want the CHEST members to be excited about the Foundation and to want to support its efforts.
These two goals go hand in hand, and I look forward to sharing the Foundation’s impact with a new audience and reinvigorating the support of our existing donors.
Is there anything else you’d like to say to the reader?
We cannot accomplish anything without the support of our donors, and I want to sincerely thank everyone who has donated to the CHEST Foundation. I also encourage those who have never donated or have yet to donate this year to visit the Foundation’s website (foundation.chestnet.org) and explore some of the inspiring initiatives you can support to strengthen the impact of the CHEST Foundation because the possibilities are truly endless.
As the presidency of the American College of Chest Physicians changes hands in January 2023, so will the role of President of the CHEST Foundation. To get to know the incoming President of the CHEST Foundation, we spoke with Robert (Bob) De Marco, MD, FCCP, about his philanthropy work and his goals for the philanthropic arm of CHEST.
Tell me about your history with philanthropy work.
My philanthropy work started long before the CHEST Foundation. While I’ve been a member of CHEST since my second year of fellowship, it wasn’t until much later that I became involved with the philanthropic side of the organization. Earlier in my career, I was involved more so with the American Cancer Society. I had gotten involved with them by chance – participating in an event of theirs – and was encouraged to get more involved by one of their board members. Being involved with them made a lot of sense seeing as a strong percentage of my patients at the time were being treated for lung cancer. My most notable accomplishments with the American Cancer Society were in serving as the Chairmen of my local Relay for Life program for 10 years, as a board member, and then as a president of my local chapter.
When did you get involved with the CHEST Foundation?
I had served in a handful of positions within CHEST, including Chair of the (since reinvented) Practice Management Committee, so I was deeply involved in the association, and I thought to myself, “I have experience in fundraising through my work with the American Cancer Society, why don’t I use it to help our association?” When I moved to Florida, I no longer had the local connection to the American Cancer Society, so it was an opportune time to transition over to the CHEST Foundation.
How has the Foundation changed in the time that you’ve been involved?
The Foundation has changed drastically since I first joined the Board of Trustees 9 years ago. When I first got involved, the primary goal of the Foundation was staying “out of the red.” At that time, we were an organization that gave away more than we made.
After years of building a corpus to fund our own projects, we’re in a really good place now with some phenomenal goals and some excellent initiatives to fundraise around, including a CHEST diversity initiative, First 5 Minutes™, and Bridging Specialties™: Timely Diagnosis for ILD Patients, which seeks to break down silos within medicine to improve patient care.
What will be a focus of your Foundation presidency?
You know, one thing I always appreciated about the American Cancer Society was that there were always notable accomplishments to point back to when supporting fundraising efforts. You could say, “Did you know that bone marrow transplantation was initially funded by the American Cancer Society?” and other examples that would truly inspire someone to want to get involved in supporting those efforts.
The CHEST Foundation may not have funded bone marrow transplantation, but in 25 years of awarding grants, there are equally good stories to share. The impact of the Foundation is tremendous, and we’ve only just begun to share examples of where grant recipients went with their research or community service projects.
A recent grant story that was shared with me was that of Panagis Galiatsatos, MD, MHS, who received a community service grant to start a program educating children in the Baltimore community about lung health. This program was so moving that it inspired one of the Baltimore teachers to pursue a career in medicine and that individual is now a practicing MD.
This is just one example of the Foundation’s impact and it’s through these stories that we share the “why” behind every dollar that is raised, and my first goal is to tell these stories.
Another key focus of not only my presidency, but Dr. Ian Nathanson’s, as well, as we collaborated a lot on our roles, will be on member involvement and awareness. Even I wasn’t involved in the CHEST Foundation until years into my CHEST membership, so I understand that there are competing demands. But I also know that there is a lot to be gained from the work with the Foundation. I want the CHEST members to be excited about the Foundation and to want to support its efforts.
These two goals go hand in hand, and I look forward to sharing the Foundation’s impact with a new audience and reinvigorating the support of our existing donors.
Is there anything else you’d like to say to the reader?
We cannot accomplish anything without the support of our donors, and I want to sincerely thank everyone who has donated to the CHEST Foundation. I also encourage those who have never donated or have yet to donate this year to visit the Foundation’s website (foundation.chestnet.org) and explore some of the inspiring initiatives you can support to strengthen the impact of the CHEST Foundation because the possibilities are truly endless.
As the presidency of the American College of Chest Physicians changes hands in January 2023, so will the role of President of the CHEST Foundation. To get to know the incoming President of the CHEST Foundation, we spoke with Robert (Bob) De Marco, MD, FCCP, about his philanthropy work and his goals for the philanthropic arm of CHEST.
Tell me about your history with philanthropy work.
My philanthropy work started long before the CHEST Foundation. While I’ve been a member of CHEST since my second year of fellowship, it wasn’t until much later that I became involved with the philanthropic side of the organization. Earlier in my career, I was involved more so with the American Cancer Society. I had gotten involved with them by chance – participating in an event of theirs – and was encouraged to get more involved by one of their board members. Being involved with them made a lot of sense seeing as a strong percentage of my patients at the time were being treated for lung cancer. My most notable accomplishments with the American Cancer Society were in serving as the Chairmen of my local Relay for Life program for 10 years, as a board member, and then as a president of my local chapter.
When did you get involved with the CHEST Foundation?
I had served in a handful of positions within CHEST, including Chair of the (since reinvented) Practice Management Committee, so I was deeply involved in the association, and I thought to myself, “I have experience in fundraising through my work with the American Cancer Society, why don’t I use it to help our association?” When I moved to Florida, I no longer had the local connection to the American Cancer Society, so it was an opportune time to transition over to the CHEST Foundation.
How has the Foundation changed in the time that you’ve been involved?
The Foundation has changed drastically since I first joined the Board of Trustees 9 years ago. When I first got involved, the primary goal of the Foundation was staying “out of the red.” At that time, we were an organization that gave away more than we made.
After years of building a corpus to fund our own projects, we’re in a really good place now with some phenomenal goals and some excellent initiatives to fundraise around, including a CHEST diversity initiative, First 5 Minutes™, and Bridging Specialties™: Timely Diagnosis for ILD Patients, which seeks to break down silos within medicine to improve patient care.
What will be a focus of your Foundation presidency?
You know, one thing I always appreciated about the American Cancer Society was that there were always notable accomplishments to point back to when supporting fundraising efforts. You could say, “Did you know that bone marrow transplantation was initially funded by the American Cancer Society?” and other examples that would truly inspire someone to want to get involved in supporting those efforts.
The CHEST Foundation may not have funded bone marrow transplantation, but in 25 years of awarding grants, there are equally good stories to share. The impact of the Foundation is tremendous, and we’ve only just begun to share examples of where grant recipients went with their research or community service projects.
A recent grant story that was shared with me was that of Panagis Galiatsatos, MD, MHS, who received a community service grant to start a program educating children in the Baltimore community about lung health. This program was so moving that it inspired one of the Baltimore teachers to pursue a career in medicine and that individual is now a practicing MD.
This is just one example of the Foundation’s impact and it’s through these stories that we share the “why” behind every dollar that is raised, and my first goal is to tell these stories.
Another key focus of not only my presidency, but Dr. Ian Nathanson’s, as well, as we collaborated a lot on our roles, will be on member involvement and awareness. Even I wasn’t involved in the CHEST Foundation until years into my CHEST membership, so I understand that there are competing demands. But I also know that there is a lot to be gained from the work with the Foundation. I want the CHEST members to be excited about the Foundation and to want to support its efforts.
These two goals go hand in hand, and I look forward to sharing the Foundation’s impact with a new audience and reinvigorating the support of our existing donors.
Is there anything else you’d like to say to the reader?
We cannot accomplish anything without the support of our donors, and I want to sincerely thank everyone who has donated to the CHEST Foundation. I also encourage those who have never donated or have yet to donate this year to visit the Foundation’s website (foundation.chestnet.org) and explore some of the inspiring initiatives you can support to strengthen the impact of the CHEST Foundation because the possibilities are truly endless.
Reverse-Grip Technique of Scissors in Dermatologic Surgery: Tips to Improve Undermining Efficiency
Practice Gap
One of the most important elements of successful reconstruction is effective undermining prior to placement of buried sutures. The main benefit of an evenly undermined plane is that tension is reduced, thus permitting seamless tissue mobilization and wound edge approximation.1
However, achieving a consistent and appropriate plane can present challenges in certain blind spots within one’s field of work. A right hand–dominant surgeon might find it difficult to undermine tissue between the 3-o’clock and 6-o’clock positions (Figure 1) and often must resort to unnatural positioning to obtain adequate reach.

We propose a technique of reversing the grip on undermining scissors that improves efficiency without sacrificing technique.
Technique
The surgeon simply grasps the ring handles with the ring finger and thumb with the tip pointing to the wrist (Figure 2). Most of the control comes from rotating the wrist while spreading with the thumb (Figure 3).

The main advantage of the reverse-grip technique is that it prevents abduction of the arm at the shoulder joint, which reduces shoulder fatigue and keeps the elbow close to the trunk and away from the sterile surgical field. Achieving optimal ergonomics during surgery has been shown to reduce pain and likely prolong the surgeon’s career.2

A limitation of the reverse-grip technique is that direct visualization of the undermining plane is not achieved; however, direct visualization also is not obtained when undermining in the standard fashion unless the instruments are passed to the surgical assistant or the surgeon moves to the other side of the table.
Undermining can be performed safely without direct visualization as long as several rules are followed:
• The undermining plane is first established under direct visualization on the far side of the wound—at the 6-o’clock to 12-o’clock positions—and then followed to the area where direct visualization is not obtained.
• A blunt-tipped scissor is used to prevent penetrating trauma to neurovascular bundles. Blunt-tipped instruments allow more “feel” through tactile feedback to the surgeon and prevent accidental injury to these critical structures.
• A curved scissor is used with “tips up,” such that the surgeon does not unintentionally make the undermining plane deeper than anticipated.
Practice Implications
With practice, one can perform circumferential undermining independently with few alterations in stance and while maintaining a natural position throughout. Use of skin hooks to elevate the skin can further aid in visualizing the correct depth of undermining. If executed correctly, the reverse-grip technique can expand the surgeon’s work field, thus providing ease of dissection in difficult-to-reach areas.
- Chen DL, Carlson EO, Fathi R, et al. Undermining and hemostasis. Dermatol Surg. 2015;41(suppl 10):S201-S215. doi:10.1097/DSS.0000000000000489
- Chan J, Kim DJ, Kassira-Carley S, et al. Ergonomics in dermatologic surgery: lessons learned across related specialties and opportunities for improvement. Dermatol Surg. 2020;46:763-772. doi:10.1097/DSS.0000000000002295
Practice Gap
One of the most important elements of successful reconstruction is effective undermining prior to placement of buried sutures. The main benefit of an evenly undermined plane is that tension is reduced, thus permitting seamless tissue mobilization and wound edge approximation.1
However, achieving a consistent and appropriate plane can present challenges in certain blind spots within one’s field of work. A right hand–dominant surgeon might find it difficult to undermine tissue between the 3-o’clock and 6-o’clock positions (Figure 1) and often must resort to unnatural positioning to obtain adequate reach.

We propose a technique of reversing the grip on undermining scissors that improves efficiency without sacrificing technique.
Technique
The surgeon simply grasps the ring handles with the ring finger and thumb with the tip pointing to the wrist (Figure 2). Most of the control comes from rotating the wrist while spreading with the thumb (Figure 3).

The main advantage of the reverse-grip technique is that it prevents abduction of the arm at the shoulder joint, which reduces shoulder fatigue and keeps the elbow close to the trunk and away from the sterile surgical field. Achieving optimal ergonomics during surgery has been shown to reduce pain and likely prolong the surgeon’s career.2

A limitation of the reverse-grip technique is that direct visualization of the undermining plane is not achieved; however, direct visualization also is not obtained when undermining in the standard fashion unless the instruments are passed to the surgical assistant or the surgeon moves to the other side of the table.
Undermining can be performed safely without direct visualization as long as several rules are followed:
• The undermining plane is first established under direct visualization on the far side of the wound—at the 6-o’clock to 12-o’clock positions—and then followed to the area where direct visualization is not obtained.
• A blunt-tipped scissor is used to prevent penetrating trauma to neurovascular bundles. Blunt-tipped instruments allow more “feel” through tactile feedback to the surgeon and prevent accidental injury to these critical structures.
• A curved scissor is used with “tips up,” such that the surgeon does not unintentionally make the undermining plane deeper than anticipated.
Practice Implications
With practice, one can perform circumferential undermining independently with few alterations in stance and while maintaining a natural position throughout. Use of skin hooks to elevate the skin can further aid in visualizing the correct depth of undermining. If executed correctly, the reverse-grip technique can expand the surgeon’s work field, thus providing ease of dissection in difficult-to-reach areas.
Practice Gap
One of the most important elements of successful reconstruction is effective undermining prior to placement of buried sutures. The main benefit of an evenly undermined plane is that tension is reduced, thus permitting seamless tissue mobilization and wound edge approximation.1
However, achieving a consistent and appropriate plane can present challenges in certain blind spots within one’s field of work. A right hand–dominant surgeon might find it difficult to undermine tissue between the 3-o’clock and 6-o’clock positions (Figure 1) and often must resort to unnatural positioning to obtain adequate reach.

We propose a technique of reversing the grip on undermining scissors that improves efficiency without sacrificing technique.
Technique
The surgeon simply grasps the ring handles with the ring finger and thumb with the tip pointing to the wrist (Figure 2). Most of the control comes from rotating the wrist while spreading with the thumb (Figure 3).

The main advantage of the reverse-grip technique is that it prevents abduction of the arm at the shoulder joint, which reduces shoulder fatigue and keeps the elbow close to the trunk and away from the sterile surgical field. Achieving optimal ergonomics during surgery has been shown to reduce pain and likely prolong the surgeon’s career.2

A limitation of the reverse-grip technique is that direct visualization of the undermining plane is not achieved; however, direct visualization also is not obtained when undermining in the standard fashion unless the instruments are passed to the surgical assistant or the surgeon moves to the other side of the table.
Undermining can be performed safely without direct visualization as long as several rules are followed:
• The undermining plane is first established under direct visualization on the far side of the wound—at the 6-o’clock to 12-o’clock positions—and then followed to the area where direct visualization is not obtained.
• A blunt-tipped scissor is used to prevent penetrating trauma to neurovascular bundles. Blunt-tipped instruments allow more “feel” through tactile feedback to the surgeon and prevent accidental injury to these critical structures.
• A curved scissor is used with “tips up,” such that the surgeon does not unintentionally make the undermining plane deeper than anticipated.
Practice Implications
With practice, one can perform circumferential undermining independently with few alterations in stance and while maintaining a natural position throughout. Use of skin hooks to elevate the skin can further aid in visualizing the correct depth of undermining. If executed correctly, the reverse-grip technique can expand the surgeon’s work field, thus providing ease of dissection in difficult-to-reach areas.
- Chen DL, Carlson EO, Fathi R, et al. Undermining and hemostasis. Dermatol Surg. 2015;41(suppl 10):S201-S215. doi:10.1097/DSS.0000000000000489
- Chan J, Kim DJ, Kassira-Carley S, et al. Ergonomics in dermatologic surgery: lessons learned across related specialties and opportunities for improvement. Dermatol Surg. 2020;46:763-772. doi:10.1097/DSS.0000000000002295
- Chen DL, Carlson EO, Fathi R, et al. Undermining and hemostasis. Dermatol Surg. 2015;41(suppl 10):S201-S215. doi:10.1097/DSS.0000000000000489
- Chan J, Kim DJ, Kassira-Carley S, et al. Ergonomics in dermatologic surgery: lessons learned across related specialties and opportunities for improvement. Dermatol Surg. 2020;46:763-772. doi:10.1097/DSS.0000000000002295
Medicare Part D Prescription Claims for Brodalumab: Analysis of Annual Trends for 2017-2019
To the Editor:
Brodalumab, a monoclonal antibody targeting IL-17RA, was approved by the US Food and Drug Administration (FDA) in 2017 for the treatment of moderate to severe chronic plaque psoriasis. The drug is the only biologic agent available for the treatment of psoriasis for which a psoriasis area severity index score of 100 is a primary end point.1,2 Brodalumab is associated with an FDA boxed warning due to an increased risk for suicidal ideation and behavior (SIB), including completed suicides, during clinical trials.
We sought to characterize national utilization of this effective yet underutilized drug among Medicare beneficiaries by surveying the Medicare Part D Prescriber dataset.3 We tabulated brodalumab utilization statistics and characteristics of high-volume prescribers who had 11 or more annual claims for brodalumab.
Despite its associated boxed warning, the number of Medicare D claims for brodalumab increased by 1756 from 2017 to 2019, surpassing $7 million in costs by 2019. The number of beneficiaries also increased from 11 to 292—a 415.2% annual increase in beneficiaries for whom brodalumab was prescribed (Table 1).
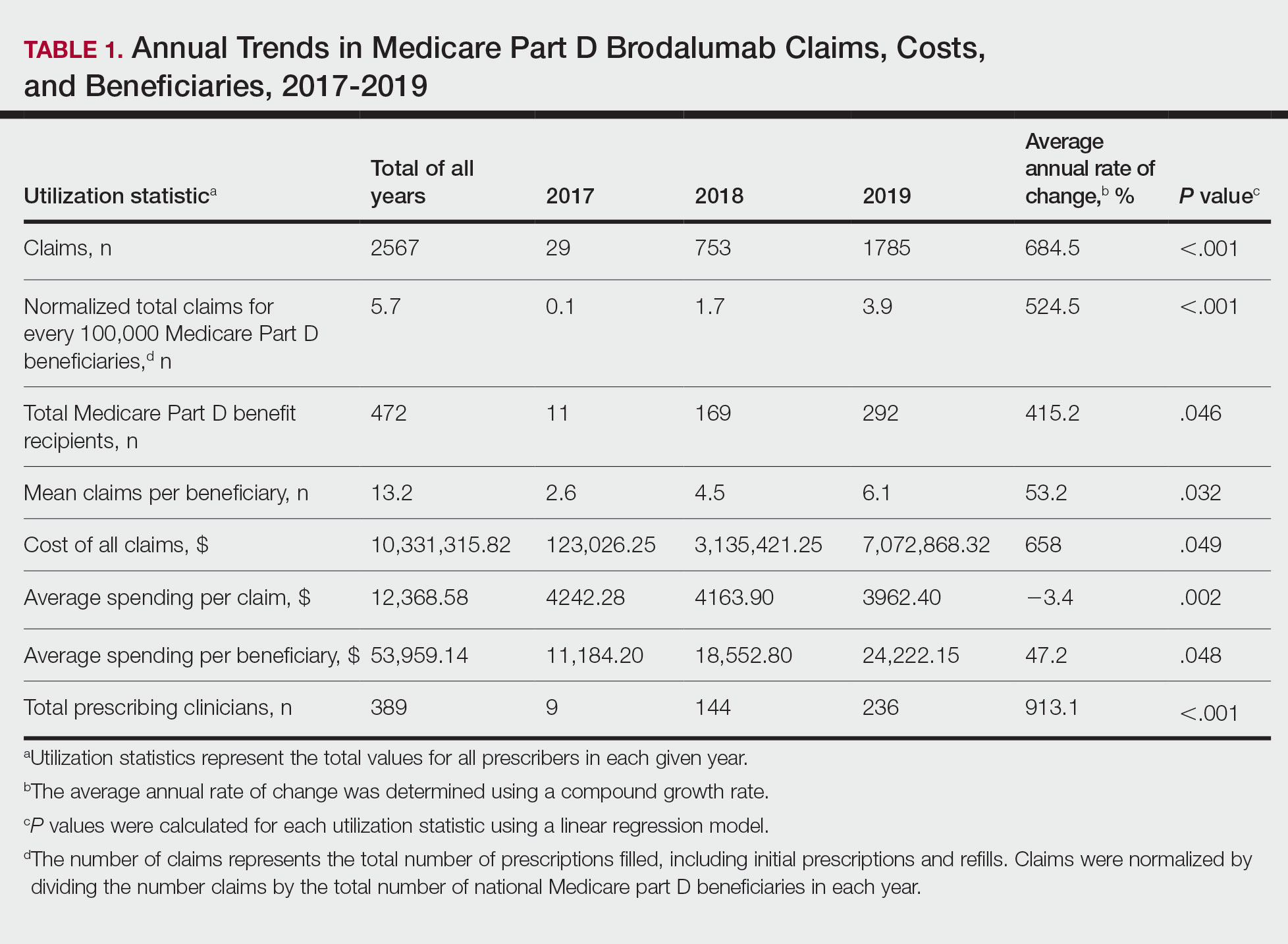
In addition, states in the West and South had the highest utilization rates of brodalumab in 2019. There also was an increasing trend toward high-volume prescribers of brodalumab, with private practice clinicians constituting the majority (Table 2).
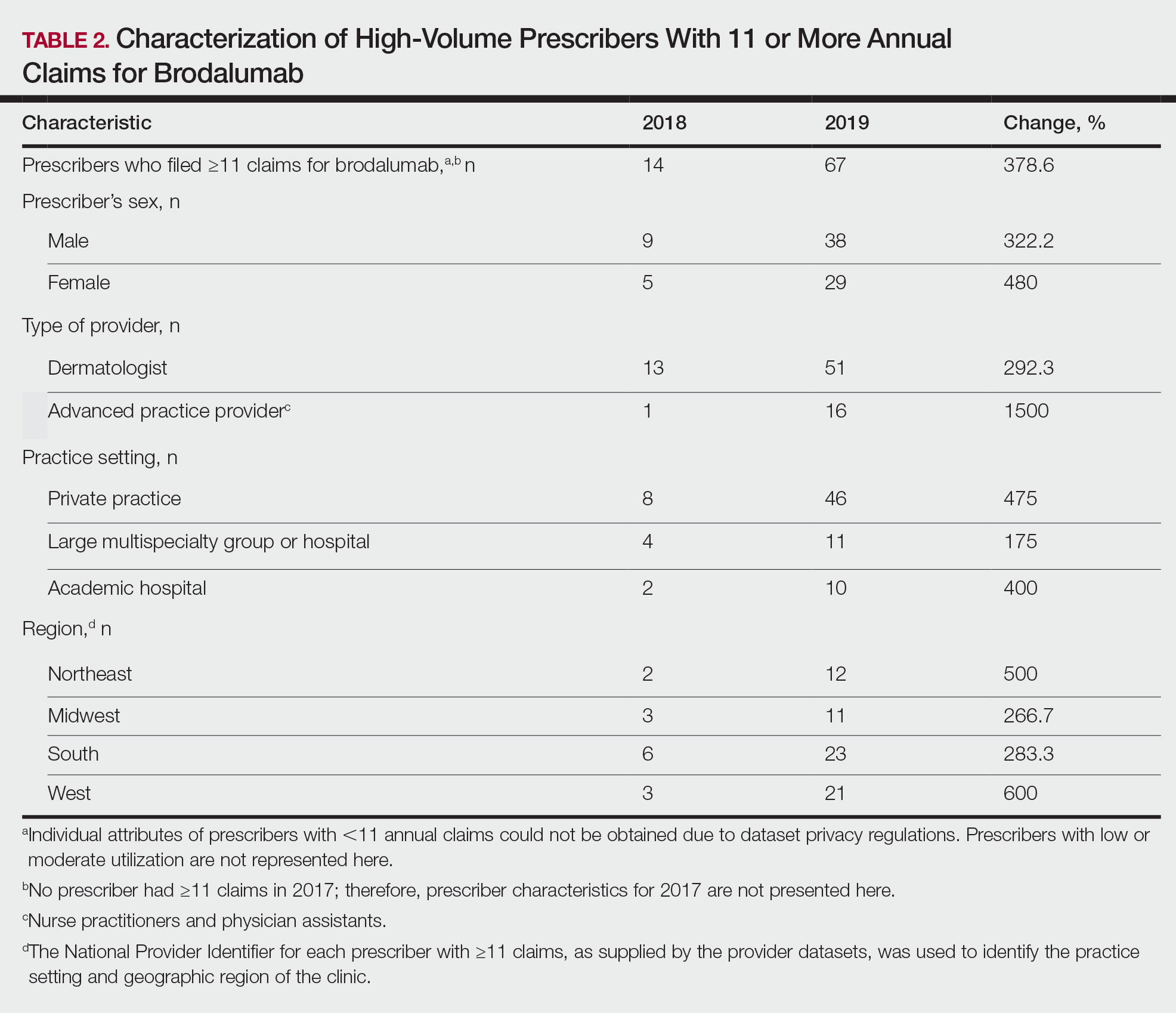
There was a substantial increase in advanced practice providers including nurse practitioners and physician assistants who were brodalumab prescribers. Although this trend might promote greater access to brodalumab, it is vital to ensure that advanced practice providers receive targeted training to properly understand the complexities of treatment with brodalumab.
Although the utilization of brodalumab has increased since 2017 (P<.001), it is still underutilized compared to the other IL-17 inhibitors secukinumab and ixekizumab. Secukinumab was FDA approved for the treatment of moderate to severe plaque psoriasis in 2015, followed by ixekizumab in 2016.4
According to the Medicare Part D database, both secukinumab and ixekizumab had a higher number of total claims and prescribers compared to brodalumab in the years of their debut.3 In 2015, there were 3593 claims for and 862 prescribers of secukinumab; in 2016, there were 1731 claims for and 681 prescribers of ixekizumab. In contrast, there were only 29 claims for and 11 prescribers of brodalumab in 2017, the year that the drug was approved by the FDA. During the same 3-year period, secukinumab and ixekizumab had a substantially greater number of claims—totals of 176,823 and 55,289, respectively—than brodalumab. The higher number of claims for secukinumab and ixekizumab compared to brodalumab may reflect clinicians’ increasing confidence in prescribing those drugs, given their long-term safety and efficacy. In addition, secukinumab and ixekizumab do not require completion of a Risk Evaluation and Mitigation Strategy (REMS) program, which makes them more readily prescribable.3
Overall, most experts agree that there is no increase in the risk for suicide associated with brodalumab compared to the general population. A 2-year pharmacovigilance report on brodalumab supports the safety of this drug.5 All participants who completed suicide during the clinical trials harbored an underlying psychiatric disorder or stressor(s).6
Although causation between brodalumab and SIB has not been demonstrated, it remains imperative that prescribers diligently assess patients’ risk of SIB and subsequently their access to appropriate psychiatric services as a precaution, if necessary. This is particularly important for private practice prescribers, who constitute the majority of Medicare D brodalumab claims, because they must ensure collaboration with a multidisciplinary team involving mental health providers. Lastly, considering that the highest number of brodalumab Medicare D claims were in western and southern states, it is critical to note that those 2 regions also harbor comparatively fewer mental health facilities that accept Medicare than other regions of the country.7 Prescribers in western and southern states must be mindful of mental health coverage limitations when treating psoriasis patients with brodalumab.
The increase in the number of claims, beneficiaries, and prescribers of brodalumab during its first 3 years of availability might be attributed to its efficacy and safety. On the other hand, the boxed warning and REMS associated with brodalumab might have led to underutilization of this drug compared to other IL-17 inhibitors.
Our analysis is limited by its representative restriction to Medicare patients. There also are limited data on brodalumab given its novelty. Individual attributes of prescribers with fewer than 11 annual claims for brodalumab could not be obtained because of dataset regulations; however, aggregated utilization statistics provide an indication of brodalumab prescribing patterns among all providers. Furthermore, during this analysis, data on the Medicare D database were limited to 2013 through 2020. Studies are needed to determine prescribing patterns of brodalumab since this study period.
- Foulkes AC, Warren RB. Brodalumab in psoriasis: evidence to date and clinical potential. Drugs Context. 2019;8:212570. doi:10.7573/dic.212570
- Beck KM, Koo J. Brodalumab for the treatment of plaque psoriasis: up-to-date. Expert Opin Biol Ther. 2019;19:287-292. doi:10.1080/14712598.2019.1579794
- Centers for Medicare & Medicaid Services. Medicare Part D Prescribers. Updated July 27, 2022. Accessed September 23, 2022. https://data.cms.gov/provider-summary-by-type-of-service/medicare-part-d-prescribers/medicare-part-d-prescribers-by-provider
- Drugs. US Food and Drug Administration website. Accessed September 23, 2022. https://www.fda.gov/drugs
- Lebwohl M, Leonardi C, Wu JJ, et al. Two-year US pharmacovigilance report on brodalumab. Dermatol Ther (Heidelb). 2021;11:173-180. doi:10.1007/s13555-020-00472-x
- Lebwohl MG, Papp KA, Marangell LB, et al. Psychiatric adverse events during treatment with brodalumab: analysis of psoriasis clinical trials. J Am Acad Dermatol. 2018;78:81-89.e5. doi:10.1016/j.jaad.2017.08.024
- Substance Abuse and Mental Health Services Administration. National Mental Health Services Survey (N-MHSS): 2019, Data On Mental Health Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration; August 13, 2020. Accessed September 21, 2022. https://www.samhsa.gov/data/report/national-mental-health-services-survey-n-mhss-2019-data-mental-health-treatment-facilities
To the Editor:
Brodalumab, a monoclonal antibody targeting IL-17RA, was approved by the US Food and Drug Administration (FDA) in 2017 for the treatment of moderate to severe chronic plaque psoriasis. The drug is the only biologic agent available for the treatment of psoriasis for which a psoriasis area severity index score of 100 is a primary end point.1,2 Brodalumab is associated with an FDA boxed warning due to an increased risk for suicidal ideation and behavior (SIB), including completed suicides, during clinical trials.
We sought to characterize national utilization of this effective yet underutilized drug among Medicare beneficiaries by surveying the Medicare Part D Prescriber dataset.3 We tabulated brodalumab utilization statistics and characteristics of high-volume prescribers who had 11 or more annual claims for brodalumab.
Despite its associated boxed warning, the number of Medicare D claims for brodalumab increased by 1756 from 2017 to 2019, surpassing $7 million in costs by 2019. The number of beneficiaries also increased from 11 to 292—a 415.2% annual increase in beneficiaries for whom brodalumab was prescribed (Table 1).
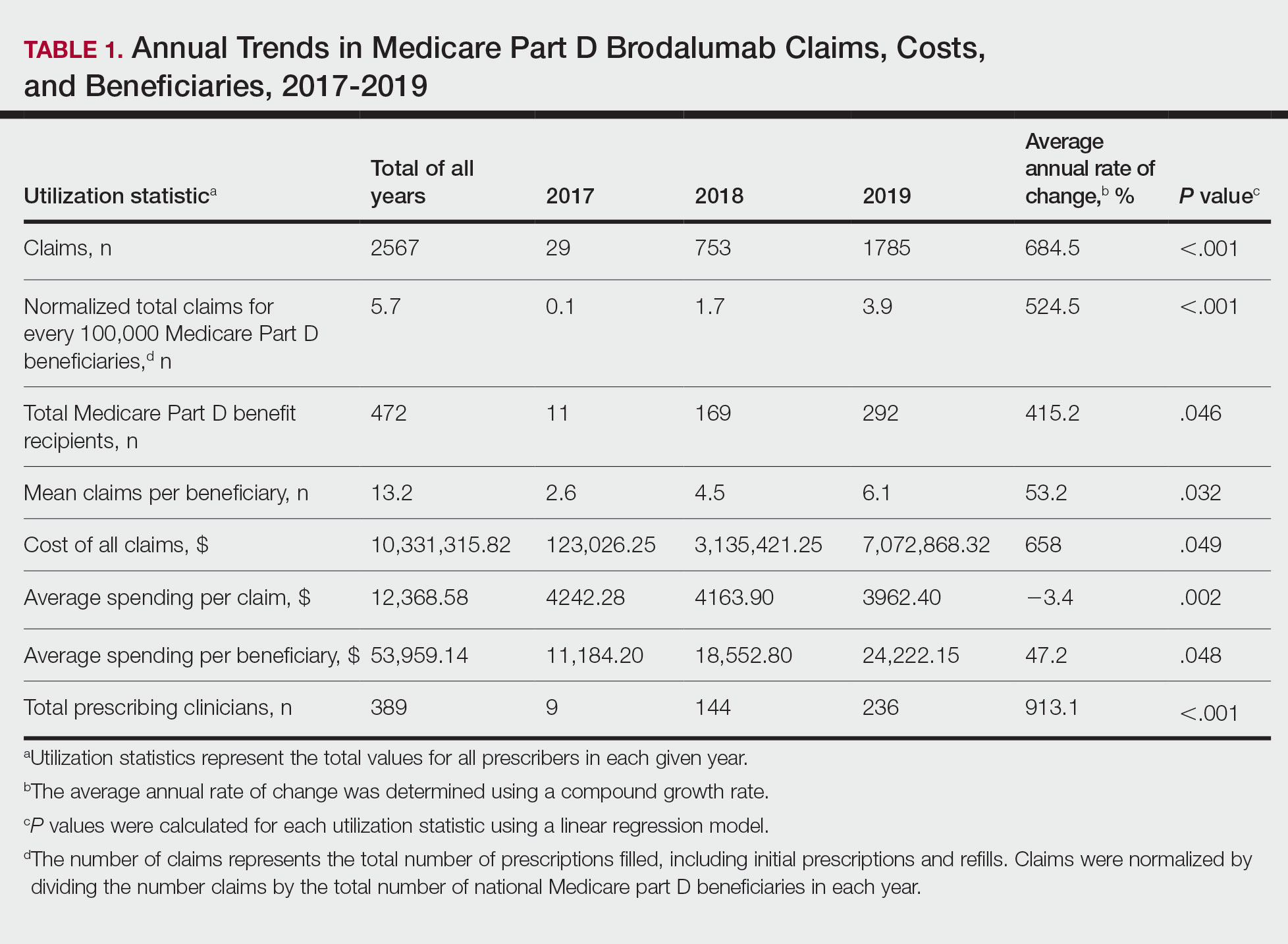
In addition, states in the West and South had the highest utilization rates of brodalumab in 2019. There also was an increasing trend toward high-volume prescribers of brodalumab, with private practice clinicians constituting the majority (Table 2).
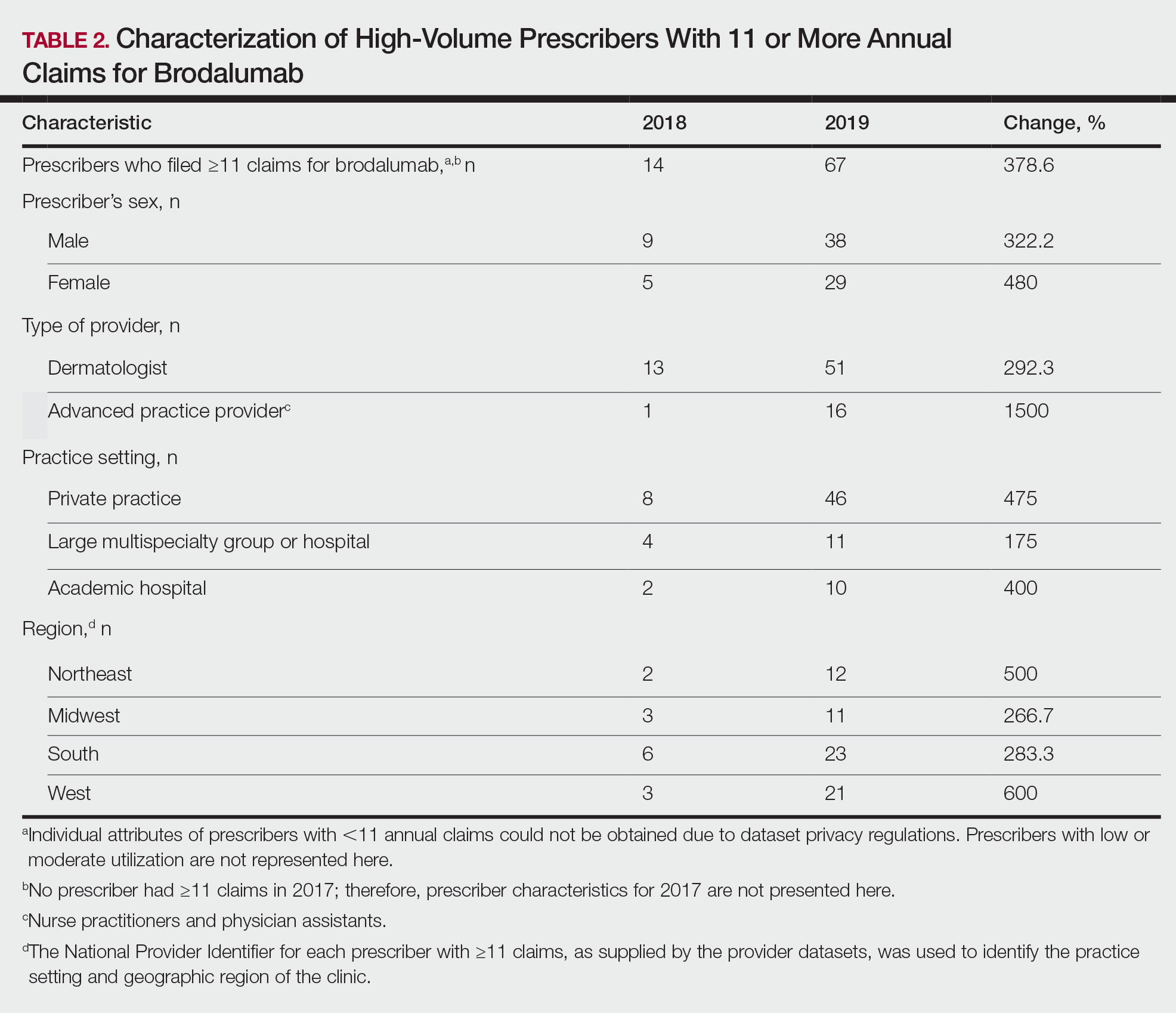
There was a substantial increase in advanced practice providers including nurse practitioners and physician assistants who were brodalumab prescribers. Although this trend might promote greater access to brodalumab, it is vital to ensure that advanced practice providers receive targeted training to properly understand the complexities of treatment with brodalumab.
Although the utilization of brodalumab has increased since 2017 (P<.001), it is still underutilized compared to the other IL-17 inhibitors secukinumab and ixekizumab. Secukinumab was FDA approved for the treatment of moderate to severe plaque psoriasis in 2015, followed by ixekizumab in 2016.4
According to the Medicare Part D database, both secukinumab and ixekizumab had a higher number of total claims and prescribers compared to brodalumab in the years of their debut.3 In 2015, there were 3593 claims for and 862 prescribers of secukinumab; in 2016, there were 1731 claims for and 681 prescribers of ixekizumab. In contrast, there were only 29 claims for and 11 prescribers of brodalumab in 2017, the year that the drug was approved by the FDA. During the same 3-year period, secukinumab and ixekizumab had a substantially greater number of claims—totals of 176,823 and 55,289, respectively—than brodalumab. The higher number of claims for secukinumab and ixekizumab compared to brodalumab may reflect clinicians’ increasing confidence in prescribing those drugs, given their long-term safety and efficacy. In addition, secukinumab and ixekizumab do not require completion of a Risk Evaluation and Mitigation Strategy (REMS) program, which makes them more readily prescribable.3
Overall, most experts agree that there is no increase in the risk for suicide associated with brodalumab compared to the general population. A 2-year pharmacovigilance report on brodalumab supports the safety of this drug.5 All participants who completed suicide during the clinical trials harbored an underlying psychiatric disorder or stressor(s).6
Although causation between brodalumab and SIB has not been demonstrated, it remains imperative that prescribers diligently assess patients’ risk of SIB and subsequently their access to appropriate psychiatric services as a precaution, if necessary. This is particularly important for private practice prescribers, who constitute the majority of Medicare D brodalumab claims, because they must ensure collaboration with a multidisciplinary team involving mental health providers. Lastly, considering that the highest number of brodalumab Medicare D claims were in western and southern states, it is critical to note that those 2 regions also harbor comparatively fewer mental health facilities that accept Medicare than other regions of the country.7 Prescribers in western and southern states must be mindful of mental health coverage limitations when treating psoriasis patients with brodalumab.
The increase in the number of claims, beneficiaries, and prescribers of brodalumab during its first 3 years of availability might be attributed to its efficacy and safety. On the other hand, the boxed warning and REMS associated with brodalumab might have led to underutilization of this drug compared to other IL-17 inhibitors.
Our analysis is limited by its representative restriction to Medicare patients. There also are limited data on brodalumab given its novelty. Individual attributes of prescribers with fewer than 11 annual claims for brodalumab could not be obtained because of dataset regulations; however, aggregated utilization statistics provide an indication of brodalumab prescribing patterns among all providers. Furthermore, during this analysis, data on the Medicare D database were limited to 2013 through 2020. Studies are needed to determine prescribing patterns of brodalumab since this study period.
To the Editor:
Brodalumab, a monoclonal antibody targeting IL-17RA, was approved by the US Food and Drug Administration (FDA) in 2017 for the treatment of moderate to severe chronic plaque psoriasis. The drug is the only biologic agent available for the treatment of psoriasis for which a psoriasis area severity index score of 100 is a primary end point.1,2 Brodalumab is associated with an FDA boxed warning due to an increased risk for suicidal ideation and behavior (SIB), including completed suicides, during clinical trials.
We sought to characterize national utilization of this effective yet underutilized drug among Medicare beneficiaries by surveying the Medicare Part D Prescriber dataset.3 We tabulated brodalumab utilization statistics and characteristics of high-volume prescribers who had 11 or more annual claims for brodalumab.
Despite its associated boxed warning, the number of Medicare D claims for brodalumab increased by 1756 from 2017 to 2019, surpassing $7 million in costs by 2019. The number of beneficiaries also increased from 11 to 292—a 415.2% annual increase in beneficiaries for whom brodalumab was prescribed (Table 1).
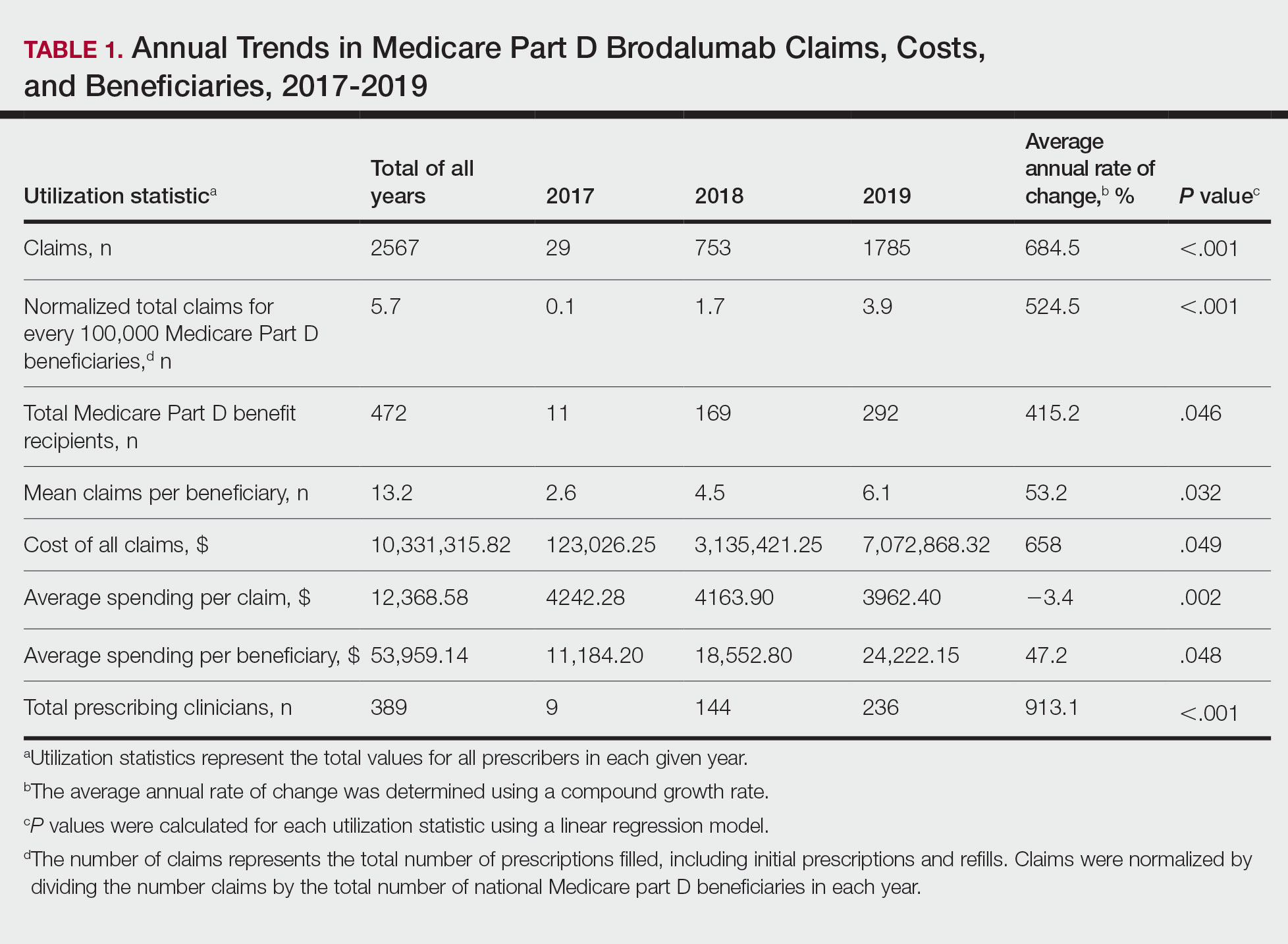
In addition, states in the West and South had the highest utilization rates of brodalumab in 2019. There also was an increasing trend toward high-volume prescribers of brodalumab, with private practice clinicians constituting the majority (Table 2).
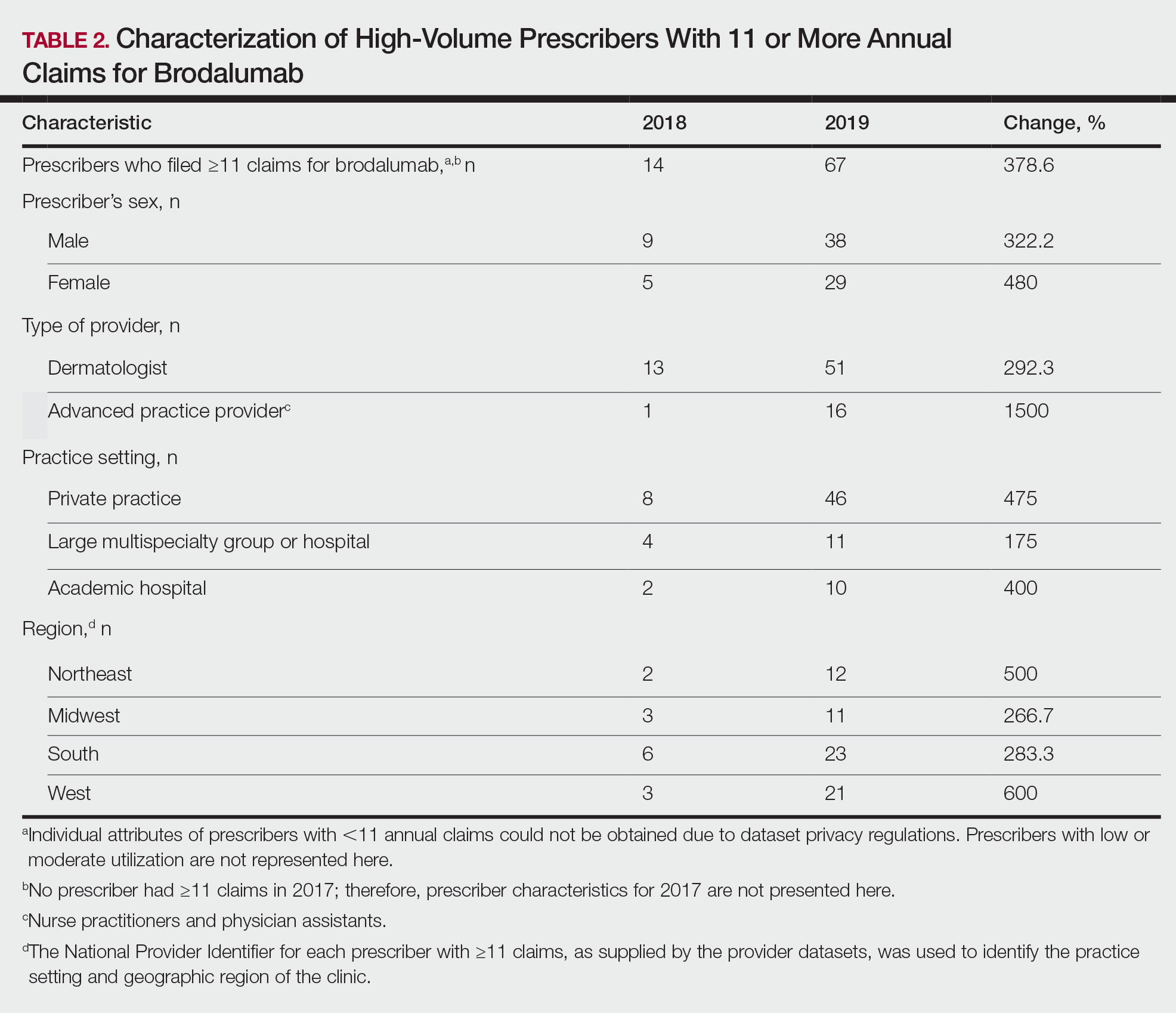
There was a substantial increase in advanced practice providers including nurse practitioners and physician assistants who were brodalumab prescribers. Although this trend might promote greater access to brodalumab, it is vital to ensure that advanced practice providers receive targeted training to properly understand the complexities of treatment with brodalumab.
Although the utilization of brodalumab has increased since 2017 (P<.001), it is still underutilized compared to the other IL-17 inhibitors secukinumab and ixekizumab. Secukinumab was FDA approved for the treatment of moderate to severe plaque psoriasis in 2015, followed by ixekizumab in 2016.4
According to the Medicare Part D database, both secukinumab and ixekizumab had a higher number of total claims and prescribers compared to brodalumab in the years of their debut.3 In 2015, there were 3593 claims for and 862 prescribers of secukinumab; in 2016, there were 1731 claims for and 681 prescribers of ixekizumab. In contrast, there were only 29 claims for and 11 prescribers of brodalumab in 2017, the year that the drug was approved by the FDA. During the same 3-year period, secukinumab and ixekizumab had a substantially greater number of claims—totals of 176,823 and 55,289, respectively—than brodalumab. The higher number of claims for secukinumab and ixekizumab compared to brodalumab may reflect clinicians’ increasing confidence in prescribing those drugs, given their long-term safety and efficacy. In addition, secukinumab and ixekizumab do not require completion of a Risk Evaluation and Mitigation Strategy (REMS) program, which makes them more readily prescribable.3
Overall, most experts agree that there is no increase in the risk for suicide associated with brodalumab compared to the general population. A 2-year pharmacovigilance report on brodalumab supports the safety of this drug.5 All participants who completed suicide during the clinical trials harbored an underlying psychiatric disorder or stressor(s).6
Although causation between brodalumab and SIB has not been demonstrated, it remains imperative that prescribers diligently assess patients’ risk of SIB and subsequently their access to appropriate psychiatric services as a precaution, if necessary. This is particularly important for private practice prescribers, who constitute the majority of Medicare D brodalumab claims, because they must ensure collaboration with a multidisciplinary team involving mental health providers. Lastly, considering that the highest number of brodalumab Medicare D claims were in western and southern states, it is critical to note that those 2 regions also harbor comparatively fewer mental health facilities that accept Medicare than other regions of the country.7 Prescribers in western and southern states must be mindful of mental health coverage limitations when treating psoriasis patients with brodalumab.
The increase in the number of claims, beneficiaries, and prescribers of brodalumab during its first 3 years of availability might be attributed to its efficacy and safety. On the other hand, the boxed warning and REMS associated with brodalumab might have led to underutilization of this drug compared to other IL-17 inhibitors.
Our analysis is limited by its representative restriction to Medicare patients. There also are limited data on brodalumab given its novelty. Individual attributes of prescribers with fewer than 11 annual claims for brodalumab could not be obtained because of dataset regulations; however, aggregated utilization statistics provide an indication of brodalumab prescribing patterns among all providers. Furthermore, during this analysis, data on the Medicare D database were limited to 2013 through 2020. Studies are needed to determine prescribing patterns of brodalumab since this study period.
- Foulkes AC, Warren RB. Brodalumab in psoriasis: evidence to date and clinical potential. Drugs Context. 2019;8:212570. doi:10.7573/dic.212570
- Beck KM, Koo J. Brodalumab for the treatment of plaque psoriasis: up-to-date. Expert Opin Biol Ther. 2019;19:287-292. doi:10.1080/14712598.2019.1579794
- Centers for Medicare & Medicaid Services. Medicare Part D Prescribers. Updated July 27, 2022. Accessed September 23, 2022. https://data.cms.gov/provider-summary-by-type-of-service/medicare-part-d-prescribers/medicare-part-d-prescribers-by-provider
- Drugs. US Food and Drug Administration website. Accessed September 23, 2022. https://www.fda.gov/drugs
- Lebwohl M, Leonardi C, Wu JJ, et al. Two-year US pharmacovigilance report on brodalumab. Dermatol Ther (Heidelb). 2021;11:173-180. doi:10.1007/s13555-020-00472-x
- Lebwohl MG, Papp KA, Marangell LB, et al. Psychiatric adverse events during treatment with brodalumab: analysis of psoriasis clinical trials. J Am Acad Dermatol. 2018;78:81-89.e5. doi:10.1016/j.jaad.2017.08.024
- Substance Abuse and Mental Health Services Administration. National Mental Health Services Survey (N-MHSS): 2019, Data On Mental Health Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration; August 13, 2020. Accessed September 21, 2022. https://www.samhsa.gov/data/report/national-mental-health-services-survey-n-mhss-2019-data-mental-health-treatment-facilities
- Foulkes AC, Warren RB. Brodalumab in psoriasis: evidence to date and clinical potential. Drugs Context. 2019;8:212570. doi:10.7573/dic.212570
- Beck KM, Koo J. Brodalumab for the treatment of plaque psoriasis: up-to-date. Expert Opin Biol Ther. 2019;19:287-292. doi:10.1080/14712598.2019.1579794
- Centers for Medicare & Medicaid Services. Medicare Part D Prescribers. Updated July 27, 2022. Accessed September 23, 2022. https://data.cms.gov/provider-summary-by-type-of-service/medicare-part-d-prescribers/medicare-part-d-prescribers-by-provider
- Drugs. US Food and Drug Administration website. Accessed September 23, 2022. https://www.fda.gov/drugs
- Lebwohl M, Leonardi C, Wu JJ, et al. Two-year US pharmacovigilance report on brodalumab. Dermatol Ther (Heidelb). 2021;11:173-180. doi:10.1007/s13555-020-00472-x
- Lebwohl MG, Papp KA, Marangell LB, et al. Psychiatric adverse events during treatment with brodalumab: analysis of psoriasis clinical trials. J Am Acad Dermatol. 2018;78:81-89.e5. doi:10.1016/j.jaad.2017.08.024
- Substance Abuse and Mental Health Services Administration. National Mental Health Services Survey (N-MHSS): 2019, Data On Mental Health Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration; August 13, 2020. Accessed September 21, 2022. https://www.samhsa.gov/data/report/national-mental-health-services-survey-n-mhss-2019-data-mental-health-treatment-facilities
Practice Points
- Brodalumab is associated with a boxed warning due to increased suicidal ideation and behavior (SIB), including completed suicides, during clinical trials.
- Brodalumab is underutilized compared to the other US Food and Drug Administration–approved IL-17 inhibitors used to treat psoriasis.
- Most experts agree that there is no increased risk for suicide associated with brodalumab. However, it remains imperative that prescribers assess patients’ risk of SIB and subsequently their access to appropriate psychiatric services prior to initiating and during treatment with brodalumab.











