User login
Microbleeds, age contribute to ARIA risk with aducanumab
Though primary efficacy results have yet to be published,
Amyloid-related imaging abnormalities, or ARIA, have been seen linked to a variety of experimental amyloid-lowering treatments for Alzheimer’s disease. The abnormalities include brain bleeding (ARIA-H) and brain edema (ARIA-E), detected on magnetic resonance imaging.
Safety findings
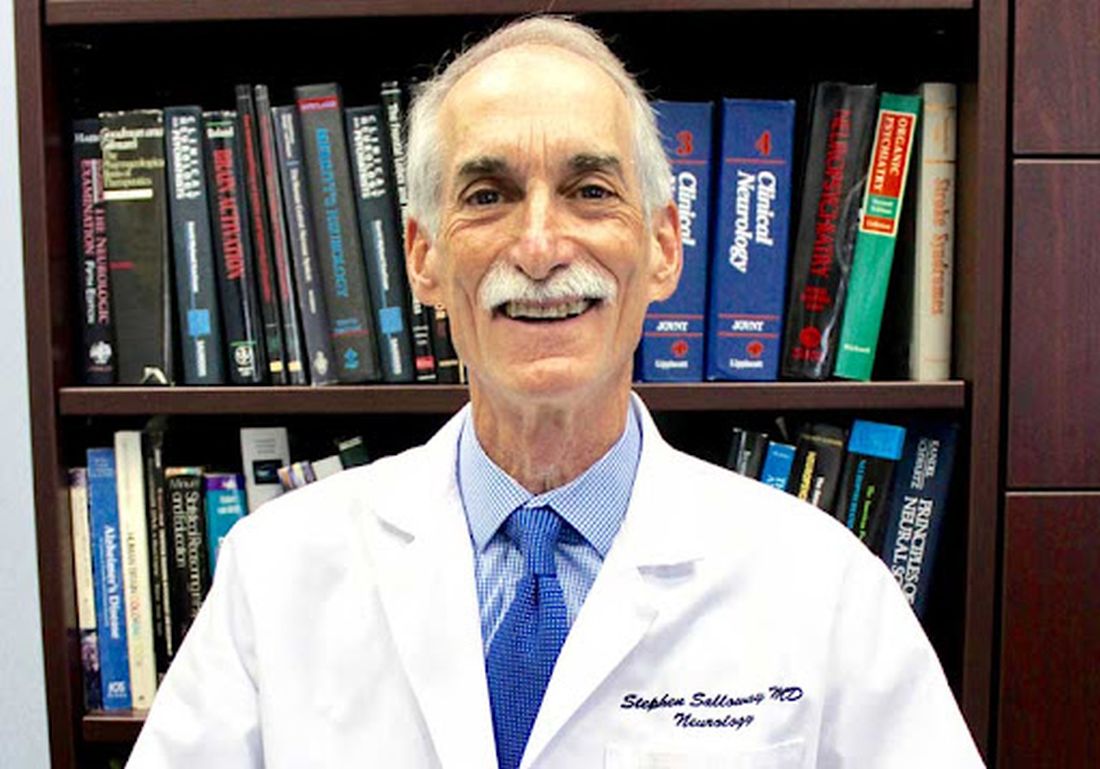
In a study published Nov. 22 in JAMA Neurology, Stephen Salloway, MD, director of neurology and the memory and aging program at Butler Hospital and the Martin M. Zucker Professor of Psychiatry and Human Behavior and Professor of Neurology at the Warren Alpert Medical School of Brown University in Providence, R.I., and his colleagues, reported that 41% of 1,029 patients in the high-dose (10 mg/kg) treatment groups of aducanumab (Aduhelm, Biogen) developed ARIA.
Thirty-five percent of the high-dose patients (n = 362) developed ARIA-E, and 94 had symptoms, with headache the most commonly reported, followed by confusion. ARIA-E occurred only sporadically in the placebo groups, while ARIA-H was more common. Microbleeds were seen in 19% of the high-dose patients compared with 6.6% in the placebo group, while superficial siderosis occurred in about 15%, versus 2.2% on placebo. Most of the ARIA-E events occurred during the first eight doses of the infusion treatment. People with one or more copies of the APOE4 genetic variant saw higher risk of ARIA-E associated with treatment compared with noncarriers (hazard ratio [HR] 2.5; 95% confidence interval [CI], 1.90-3.20). Evidence of brain micro-hemorrhages at baseline was associated with higher risk of ARIA-E (HR 1.7; 95% CI, 1.31-2.27) compared with patients without MRI evidence of brain bleeds in the year before treatment began.
Older age independently increased risk of ARIA-H, with a risk that was seen increasing 6% with each additional year of age.
The identically designed EMERGE and ENGAGE trials of aducanumab enrolled nearly 3,300 patients worldwide (mean age 70.4, 52% female). Participants were screened to include only those with amyloid-positive mild cognitive impairment (81% of the cohort) or mild Alzheimer’s dementia. Both trials were halted early after a futility analysis concluded that treatment was unlikely to result in benefit.
A post hoc analysis later determined that patients in one trial, EMERGE, showed slight clinical benefit on follow-up in the high-dose group only. The Food and Drug Administration approved the drug in July 2021 on the basis of that finding, overriding the consensus of its independent advisory committee, which was not persuaded. Since then the drug has become synonymous with controversy, not aided by its high list price of more than $50,000 per year, with many insurers and large health care systems refusing to deliver it. The recent reported death of a woman participating in an open-label extension trial of aducanumab, who was admitted to the hospital with brain swelling, has added to safety concerns.
Brain bleeds and age affect risk
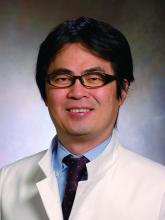
In an interview with MDedge Neurology, neurologist Madhav Thambisetty, MD, PhD, a senior investigator with the National Institute on Aging in Baltimore, and a member of the FDA advisory committee that recommended against approval for aducanumab, said that while physicians are aware that APOE4 carriers face higher risks of treatment-related complications, the new safety findings offer additional guidance on patient selection.
“The older you are the greater your risk of ARIA, and the more micro-hemorrhages you have at baseline the greater your risk. Those are important findings that were not previously well publicized before,” Dr. Thambisetty said.
In the EMERGE and ENGAGE trials, Dr. Thambisetty pointed out, patients with four or more micro-hemorrhages at baseline were excluded. The new findings reveal that even a small number of bleeds at baseline can contribute to ARIA risk.
“Patients in real-world clinical practice are going to be very different from the tightly controlled, well-screened participants who were enrolled in these trials. Microbleeds are very common in Alzheimer’s patients, occurring in 18-32%. Now that these findings are available, it’s important for a practicing physician to obtain a baseline MRI scan and really pay attention to microbleeds, because that will affect treatment decisions.”
Additional concerns
Dr. Thambisetty cautioned that the new results made no mention of another important safety outcome: loss of brain volume associated with treatment.
Changes in brain volume have been seen associated with other amyloid-lowering treatments, though the reasons for this are poorly understood. Participants in EMERGE and ENGAGE “received numerous MRI scans,” Dr. Thambisetty said. “This was one of the strengths of the trials. Thanks to an open-label extension we now have more than 2 years of MRI data from meticulously monitored patients, and there has been no mention of brain volume changes despite this being a prespecified outcome. This, for me, is one of the glaring omissions of this paper, and the fact that it’s not even mentioned is really worrisome.”
The sponsor of the aducanumab trials, Biogen, has yet to publish efficacy findings in a peer-reviewed journal, instead presenting them piecemeal at conferences.
“The current paper was a secondary analysis,” Dr. Thambisetty said. “The authors say the primary analysis will be published elsewhere. I think it’s important to reflect upon the fact that these clinical trials enrolled more than 3,000 participants at more than 300 trial centers in 20 countries. We now have an approved drug that’s commercially available. And yet we don’t have a single peer-reviewed publication discussing the efficacy data. None of this is in the interest of our patients, or in advancing the science.”
The EMERGE and ENGAGE trials were funded by Biogen. Eight of the current paper’s 14 authors are Biogen employees. Dr. Salloway, the lead author, disclosed financial support from Biogen and other manufacturers, as did two of his coauthors. Dr. Thambisetty disclosed no financial conflicts of interest.
Though primary efficacy results have yet to be published,
Amyloid-related imaging abnormalities, or ARIA, have been seen linked to a variety of experimental amyloid-lowering treatments for Alzheimer’s disease. The abnormalities include brain bleeding (ARIA-H) and brain edema (ARIA-E), detected on magnetic resonance imaging.
Safety findings
In a study published Nov. 22 in JAMA Neurology, Stephen Salloway, MD, director of neurology and the memory and aging program at Butler Hospital and the Martin M. Zucker Professor of Psychiatry and Human Behavior and Professor of Neurology at the Warren Alpert Medical School of Brown University in Providence, R.I., and his colleagues, reported that 41% of 1,029 patients in the high-dose (10 mg/kg) treatment groups of aducanumab (Aduhelm, Biogen) developed ARIA.
Thirty-five percent of the high-dose patients (n = 362) developed ARIA-E, and 94 had symptoms, with headache the most commonly reported, followed by confusion. ARIA-E occurred only sporadically in the placebo groups, while ARIA-H was more common. Microbleeds were seen in 19% of the high-dose patients compared with 6.6% in the placebo group, while superficial siderosis occurred in about 15%, versus 2.2% on placebo. Most of the ARIA-E events occurred during the first eight doses of the infusion treatment. People with one or more copies of the APOE4 genetic variant saw higher risk of ARIA-E associated with treatment compared with noncarriers (hazard ratio [HR] 2.5; 95% confidence interval [CI], 1.90-3.20). Evidence of brain micro-hemorrhages at baseline was associated with higher risk of ARIA-E (HR 1.7; 95% CI, 1.31-2.27) compared with patients without MRI evidence of brain bleeds in the year before treatment began.
Older age independently increased risk of ARIA-H, with a risk that was seen increasing 6% with each additional year of age.
The identically designed EMERGE and ENGAGE trials of aducanumab enrolled nearly 3,300 patients worldwide (mean age 70.4, 52% female). Participants were screened to include only those with amyloid-positive mild cognitive impairment (81% of the cohort) or mild Alzheimer’s dementia. Both trials were halted early after a futility analysis concluded that treatment was unlikely to result in benefit.
A post hoc analysis later determined that patients in one trial, EMERGE, showed slight clinical benefit on follow-up in the high-dose group only. The Food and Drug Administration approved the drug in July 2021 on the basis of that finding, overriding the consensus of its independent advisory committee, which was not persuaded. Since then the drug has become synonymous with controversy, not aided by its high list price of more than $50,000 per year, with many insurers and large health care systems refusing to deliver it. The recent reported death of a woman participating in an open-label extension trial of aducanumab, who was admitted to the hospital with brain swelling, has added to safety concerns.
Brain bleeds and age affect risk
In an interview with MDedge Neurology, neurologist Madhav Thambisetty, MD, PhD, a senior investigator with the National Institute on Aging in Baltimore, and a member of the FDA advisory committee that recommended against approval for aducanumab, said that while physicians are aware that APOE4 carriers face higher risks of treatment-related complications, the new safety findings offer additional guidance on patient selection.
“The older you are the greater your risk of ARIA, and the more micro-hemorrhages you have at baseline the greater your risk. Those are important findings that were not previously well publicized before,” Dr. Thambisetty said.
In the EMERGE and ENGAGE trials, Dr. Thambisetty pointed out, patients with four or more micro-hemorrhages at baseline were excluded. The new findings reveal that even a small number of bleeds at baseline can contribute to ARIA risk.
“Patients in real-world clinical practice are going to be very different from the tightly controlled, well-screened participants who were enrolled in these trials. Microbleeds are very common in Alzheimer’s patients, occurring in 18-32%. Now that these findings are available, it’s important for a practicing physician to obtain a baseline MRI scan and really pay attention to microbleeds, because that will affect treatment decisions.”
Additional concerns
Dr. Thambisetty cautioned that the new results made no mention of another important safety outcome: loss of brain volume associated with treatment.
Changes in brain volume have been seen associated with other amyloid-lowering treatments, though the reasons for this are poorly understood. Participants in EMERGE and ENGAGE “received numerous MRI scans,” Dr. Thambisetty said. “This was one of the strengths of the trials. Thanks to an open-label extension we now have more than 2 years of MRI data from meticulously monitored patients, and there has been no mention of brain volume changes despite this being a prespecified outcome. This, for me, is one of the glaring omissions of this paper, and the fact that it’s not even mentioned is really worrisome.”
The sponsor of the aducanumab trials, Biogen, has yet to publish efficacy findings in a peer-reviewed journal, instead presenting them piecemeal at conferences.
“The current paper was a secondary analysis,” Dr. Thambisetty said. “The authors say the primary analysis will be published elsewhere. I think it’s important to reflect upon the fact that these clinical trials enrolled more than 3,000 participants at more than 300 trial centers in 20 countries. We now have an approved drug that’s commercially available. And yet we don’t have a single peer-reviewed publication discussing the efficacy data. None of this is in the interest of our patients, or in advancing the science.”
The EMERGE and ENGAGE trials were funded by Biogen. Eight of the current paper’s 14 authors are Biogen employees. Dr. Salloway, the lead author, disclosed financial support from Biogen and other manufacturers, as did two of his coauthors. Dr. Thambisetty disclosed no financial conflicts of interest.
Though primary efficacy results have yet to be published,
Amyloid-related imaging abnormalities, or ARIA, have been seen linked to a variety of experimental amyloid-lowering treatments for Alzheimer’s disease. The abnormalities include brain bleeding (ARIA-H) and brain edema (ARIA-E), detected on magnetic resonance imaging.
Safety findings
In a study published Nov. 22 in JAMA Neurology, Stephen Salloway, MD, director of neurology and the memory and aging program at Butler Hospital and the Martin M. Zucker Professor of Psychiatry and Human Behavior and Professor of Neurology at the Warren Alpert Medical School of Brown University in Providence, R.I., and his colleagues, reported that 41% of 1,029 patients in the high-dose (10 mg/kg) treatment groups of aducanumab (Aduhelm, Biogen) developed ARIA.
Thirty-five percent of the high-dose patients (n = 362) developed ARIA-E, and 94 had symptoms, with headache the most commonly reported, followed by confusion. ARIA-E occurred only sporadically in the placebo groups, while ARIA-H was more common. Microbleeds were seen in 19% of the high-dose patients compared with 6.6% in the placebo group, while superficial siderosis occurred in about 15%, versus 2.2% on placebo. Most of the ARIA-E events occurred during the first eight doses of the infusion treatment. People with one or more copies of the APOE4 genetic variant saw higher risk of ARIA-E associated with treatment compared with noncarriers (hazard ratio [HR] 2.5; 95% confidence interval [CI], 1.90-3.20). Evidence of brain micro-hemorrhages at baseline was associated with higher risk of ARIA-E (HR 1.7; 95% CI, 1.31-2.27) compared with patients without MRI evidence of brain bleeds in the year before treatment began.
Older age independently increased risk of ARIA-H, with a risk that was seen increasing 6% with each additional year of age.
The identically designed EMERGE and ENGAGE trials of aducanumab enrolled nearly 3,300 patients worldwide (mean age 70.4, 52% female). Participants were screened to include only those with amyloid-positive mild cognitive impairment (81% of the cohort) or mild Alzheimer’s dementia. Both trials were halted early after a futility analysis concluded that treatment was unlikely to result in benefit.
A post hoc analysis later determined that patients in one trial, EMERGE, showed slight clinical benefit on follow-up in the high-dose group only. The Food and Drug Administration approved the drug in July 2021 on the basis of that finding, overriding the consensus of its independent advisory committee, which was not persuaded. Since then the drug has become synonymous with controversy, not aided by its high list price of more than $50,000 per year, with many insurers and large health care systems refusing to deliver it. The recent reported death of a woman participating in an open-label extension trial of aducanumab, who was admitted to the hospital with brain swelling, has added to safety concerns.
Brain bleeds and age affect risk
In an interview with MDedge Neurology, neurologist Madhav Thambisetty, MD, PhD, a senior investigator with the National Institute on Aging in Baltimore, and a member of the FDA advisory committee that recommended against approval for aducanumab, said that while physicians are aware that APOE4 carriers face higher risks of treatment-related complications, the new safety findings offer additional guidance on patient selection.
“The older you are the greater your risk of ARIA, and the more micro-hemorrhages you have at baseline the greater your risk. Those are important findings that were not previously well publicized before,” Dr. Thambisetty said.
In the EMERGE and ENGAGE trials, Dr. Thambisetty pointed out, patients with four or more micro-hemorrhages at baseline were excluded. The new findings reveal that even a small number of bleeds at baseline can contribute to ARIA risk.
“Patients in real-world clinical practice are going to be very different from the tightly controlled, well-screened participants who were enrolled in these trials. Microbleeds are very common in Alzheimer’s patients, occurring in 18-32%. Now that these findings are available, it’s important for a practicing physician to obtain a baseline MRI scan and really pay attention to microbleeds, because that will affect treatment decisions.”
Additional concerns
Dr. Thambisetty cautioned that the new results made no mention of another important safety outcome: loss of brain volume associated with treatment.
Changes in brain volume have been seen associated with other amyloid-lowering treatments, though the reasons for this are poorly understood. Participants in EMERGE and ENGAGE “received numerous MRI scans,” Dr. Thambisetty said. “This was one of the strengths of the trials. Thanks to an open-label extension we now have more than 2 years of MRI data from meticulously monitored patients, and there has been no mention of brain volume changes despite this being a prespecified outcome. This, for me, is one of the glaring omissions of this paper, and the fact that it’s not even mentioned is really worrisome.”
The sponsor of the aducanumab trials, Biogen, has yet to publish efficacy findings in a peer-reviewed journal, instead presenting them piecemeal at conferences.
“The current paper was a secondary analysis,” Dr. Thambisetty said. “The authors say the primary analysis will be published elsewhere. I think it’s important to reflect upon the fact that these clinical trials enrolled more than 3,000 participants at more than 300 trial centers in 20 countries. We now have an approved drug that’s commercially available. And yet we don’t have a single peer-reviewed publication discussing the efficacy data. None of this is in the interest of our patients, or in advancing the science.”
The EMERGE and ENGAGE trials were funded by Biogen. Eight of the current paper’s 14 authors are Biogen employees. Dr. Salloway, the lead author, disclosed financial support from Biogen and other manufacturers, as did two of his coauthors. Dr. Thambisetty disclosed no financial conflicts of interest.
FROM JAMA NEUROLOGY
Ulcerative colitis: Donor-derived strains predict response in FMT
The Odoribacter splanchnicus strain of human donor-derived bacteria correlated with clinical response to ulcerative colitis in study in which mouse models were colonized with patient-derived strains.
Although some recent trials have shown the effectiveness of fecal microbiota transplantation (FMT) for patients with ulcerative colitis (UC), the current process is limited by the used of crude donor fecal material, which increases the risk of infection and decreases potential effectiveness, Svetlana Lima, MD, of Weill Cornell Medicine, New York, and colleagues wrote.
“Rational selection and production of specific microbial strains or communities could improve efficacy, minimize the risk of adverse reactions as well as increase the acceptance of microbiome-based therapies,” the researchers wrote.
In a study published in Gastroenterology, the researchers used metagenomic analysis and IgA sequencing (for sorting and sequencing IgA-coated microbiota) to identify a core of transferable and IgA-coated microbiota. They conducted metagenomic sequencing on 60 stool samples, including 20 recipient-participants with active UC who were treated with FMT, and another 20 FMT recipients with data from 4 weeks after FMT from a previously reported trial.
The core transferable microbiota (CTM) included 22 species of bacteria at 4 weeks after FMT. To determine a relationship between CTM and clinical response to FMT, the researchers defined clinical response as a decrease in Mayo score of 3 or greater with a rectal bleeding score of 1 or less by 4 weeks after FMT; 35% of study participants met this endpoint.* A total of 20 species were unique to the responders. “Of the donor-derived genera, only the relative abundance of Odoribacter at [week 4] post FMT and its increase post FMT was found to significantly correlate with decrease in Mayo score,” the researchers noted.
The researchers then colonized germ-free or genetically engineered mice with patient-derived bacterial strains.
O. splanchnicus also increased induction of interleukin-10, and increased the production of short-chain fatty acids. Taken together, these factors allowed for O. splanchnicus to limit colitis in the mice.
The study findings represent the first strain-level analysis of FMT in UC participants, and define a transferable microbiota associated with clinical response that could serve as a prognostic biomarker, the researchers noted in their discussion section. Although analysis revealed 12 donor-derived bacterial species that predicted clinical response, further IgA analysis identified O. splanchnicus as “the only microbe within the responders core that correlates with clinical response and highlights the potential impact of this taxa seen in independent cohorts, as well as mouse models of colitis and colorectal cancer,” the researchers emphasized.
The study findings were limited by the small sample size and the lack of prospective data. However, “collectively, this work provides the first evidence of transferable, donor-derived strains that correlate with clinical response to FMT in UC and reveals O. splanchnicus as a key component, which mechanistically promotes protection through both cellular and metabolic function,” the researchers said. “These mechanistic features will help enable desperately needed strategies to enhance therapeutic efficacy of microbial therapy for UC.”
Study strains improve effectiveness
“There is an accumulating body of evidence that suggests that gut dysbiosis, or the imbalance between good and bad microbes, plays an important role in the pathogenesis and progression of ulcerative colitis,” Jeffrey Berinstein, MD, of the University of Michigan, Ann Arbor, said in an interview. “It is for this reason that therapeutic manipulation of gut microbiota with fecal microbiota transplant is being explored as a potential treatment option for UC. FMT has demonstrated promise for ulcerative colitis, however little is known about the specific microbiota strains contributing to this observed improvement. In this study, the authors aimed to better understand the mechanisms and the specific strains in FMT contributing to this observed improvement, which is an important step toward improving efficacy and minimizing the risk of adverse events related to FMT in the future.”
Dr. Berinstein was surprised that O. splanchnicus was the only microbe identified that correlated with clinical response. “Previous studies have suggested that microbial diversity is a key factor in successful response to FMT,” he noted. “FMT remains an important potential nonpharmacologic treatment strategy for ulcerative colitis, however more research is needed to understand the mechanism and to develop safer and more efficacious methods for delivering FMT.” Specifically, prospective studies are needed to explore the efficacy and safety of FMT enriched in strains of O. splanchnicus to confirm the current study findings.
The current study is important at this time because, although microbial transferability has emerged as a potential to treat IBD, “the mechanistic understanding of microbial transferability and engraftment has been lacking,” Atsushi Sakuraba, MD, PhD of the University of Chicago, said in an interview. “I was surprised that the effectiveness of FMT in UC could be narrowed down to O. splanchnicus.” The current take-home message for clinicians is that, although FMT currently uses crude donor fecal material, it may soon use more selected microbial strains. However, “whether transfer of O. splanchnicus alone or enriched fecal material provide improved efficacy and safety need to be analyzed,” he added.
The study was supported by Boehringer Ingelheim, the National Institutes of Health, the Kenneth Rainin Foundation, and the Charina Foundation. One coauthor disclosed grant support from Boehringer Ingelheim for this study, and several coauthors are employees of Boehringer Ingelheim. Neither Dr. Berinstein nor Dr. Sakuraba had no financial conflicts to disclose.
This article was updated Dec. 1, 2021.
*Correction, 4/11/22: An earlier version of this article misstated the definition of clinical response.
The Odoribacter splanchnicus strain of human donor-derived bacteria correlated with clinical response to ulcerative colitis in study in which mouse models were colonized with patient-derived strains.
Although some recent trials have shown the effectiveness of fecal microbiota transplantation (FMT) for patients with ulcerative colitis (UC), the current process is limited by the used of crude donor fecal material, which increases the risk of infection and decreases potential effectiveness, Svetlana Lima, MD, of Weill Cornell Medicine, New York, and colleagues wrote.
“Rational selection and production of specific microbial strains or communities could improve efficacy, minimize the risk of adverse reactions as well as increase the acceptance of microbiome-based therapies,” the researchers wrote.
In a study published in Gastroenterology, the researchers used metagenomic analysis and IgA sequencing (for sorting and sequencing IgA-coated microbiota) to identify a core of transferable and IgA-coated microbiota. They conducted metagenomic sequencing on 60 stool samples, including 20 recipient-participants with active UC who were treated with FMT, and another 20 FMT recipients with data from 4 weeks after FMT from a previously reported trial.
The core transferable microbiota (CTM) included 22 species of bacteria at 4 weeks after FMT. To determine a relationship between CTM and clinical response to FMT, the researchers defined clinical response as a decrease in Mayo score of 3 or greater with a rectal bleeding score of 1 or less by 4 weeks after FMT; 35% of study participants met this endpoint.* A total of 20 species were unique to the responders. “Of the donor-derived genera, only the relative abundance of Odoribacter at [week 4] post FMT and its increase post FMT was found to significantly correlate with decrease in Mayo score,” the researchers noted.
The researchers then colonized germ-free or genetically engineered mice with patient-derived bacterial strains.
O. splanchnicus also increased induction of interleukin-10, and increased the production of short-chain fatty acids. Taken together, these factors allowed for O. splanchnicus to limit colitis in the mice.
The study findings represent the first strain-level analysis of FMT in UC participants, and define a transferable microbiota associated with clinical response that could serve as a prognostic biomarker, the researchers noted in their discussion section. Although analysis revealed 12 donor-derived bacterial species that predicted clinical response, further IgA analysis identified O. splanchnicus as “the only microbe within the responders core that correlates with clinical response and highlights the potential impact of this taxa seen in independent cohorts, as well as mouse models of colitis and colorectal cancer,” the researchers emphasized.
The study findings were limited by the small sample size and the lack of prospective data. However, “collectively, this work provides the first evidence of transferable, donor-derived strains that correlate with clinical response to FMT in UC and reveals O. splanchnicus as a key component, which mechanistically promotes protection through both cellular and metabolic function,” the researchers said. “These mechanistic features will help enable desperately needed strategies to enhance therapeutic efficacy of microbial therapy for UC.”
Study strains improve effectiveness
“There is an accumulating body of evidence that suggests that gut dysbiosis, or the imbalance between good and bad microbes, plays an important role in the pathogenesis and progression of ulcerative colitis,” Jeffrey Berinstein, MD, of the University of Michigan, Ann Arbor, said in an interview. “It is for this reason that therapeutic manipulation of gut microbiota with fecal microbiota transplant is being explored as a potential treatment option for UC. FMT has demonstrated promise for ulcerative colitis, however little is known about the specific microbiota strains contributing to this observed improvement. In this study, the authors aimed to better understand the mechanisms and the specific strains in FMT contributing to this observed improvement, which is an important step toward improving efficacy and minimizing the risk of adverse events related to FMT in the future.”
Dr. Berinstein was surprised that O. splanchnicus was the only microbe identified that correlated with clinical response. “Previous studies have suggested that microbial diversity is a key factor in successful response to FMT,” he noted. “FMT remains an important potential nonpharmacologic treatment strategy for ulcerative colitis, however more research is needed to understand the mechanism and to develop safer and more efficacious methods for delivering FMT.” Specifically, prospective studies are needed to explore the efficacy and safety of FMT enriched in strains of O. splanchnicus to confirm the current study findings.
The current study is important at this time because, although microbial transferability has emerged as a potential to treat IBD, “the mechanistic understanding of microbial transferability and engraftment has been lacking,” Atsushi Sakuraba, MD, PhD of the University of Chicago, said in an interview. “I was surprised that the effectiveness of FMT in UC could be narrowed down to O. splanchnicus.” The current take-home message for clinicians is that, although FMT currently uses crude donor fecal material, it may soon use more selected microbial strains. However, “whether transfer of O. splanchnicus alone or enriched fecal material provide improved efficacy and safety need to be analyzed,” he added.
The study was supported by Boehringer Ingelheim, the National Institutes of Health, the Kenneth Rainin Foundation, and the Charina Foundation. One coauthor disclosed grant support from Boehringer Ingelheim for this study, and several coauthors are employees of Boehringer Ingelheim. Neither Dr. Berinstein nor Dr. Sakuraba had no financial conflicts to disclose.
This article was updated Dec. 1, 2021.
*Correction, 4/11/22: An earlier version of this article misstated the definition of clinical response.
The Odoribacter splanchnicus strain of human donor-derived bacteria correlated with clinical response to ulcerative colitis in study in which mouse models were colonized with patient-derived strains.
Although some recent trials have shown the effectiveness of fecal microbiota transplantation (FMT) for patients with ulcerative colitis (UC), the current process is limited by the used of crude donor fecal material, which increases the risk of infection and decreases potential effectiveness, Svetlana Lima, MD, of Weill Cornell Medicine, New York, and colleagues wrote.
“Rational selection and production of specific microbial strains or communities could improve efficacy, minimize the risk of adverse reactions as well as increase the acceptance of microbiome-based therapies,” the researchers wrote.
In a study published in Gastroenterology, the researchers used metagenomic analysis and IgA sequencing (for sorting and sequencing IgA-coated microbiota) to identify a core of transferable and IgA-coated microbiota. They conducted metagenomic sequencing on 60 stool samples, including 20 recipient-participants with active UC who were treated with FMT, and another 20 FMT recipients with data from 4 weeks after FMT from a previously reported trial.
The core transferable microbiota (CTM) included 22 species of bacteria at 4 weeks after FMT. To determine a relationship between CTM and clinical response to FMT, the researchers defined clinical response as a decrease in Mayo score of 3 or greater with a rectal bleeding score of 1 or less by 4 weeks after FMT; 35% of study participants met this endpoint.* A total of 20 species were unique to the responders. “Of the donor-derived genera, only the relative abundance of Odoribacter at [week 4] post FMT and its increase post FMT was found to significantly correlate with decrease in Mayo score,” the researchers noted.
The researchers then colonized germ-free or genetically engineered mice with patient-derived bacterial strains.
O. splanchnicus also increased induction of interleukin-10, and increased the production of short-chain fatty acids. Taken together, these factors allowed for O. splanchnicus to limit colitis in the mice.
The study findings represent the first strain-level analysis of FMT in UC participants, and define a transferable microbiota associated with clinical response that could serve as a prognostic biomarker, the researchers noted in their discussion section. Although analysis revealed 12 donor-derived bacterial species that predicted clinical response, further IgA analysis identified O. splanchnicus as “the only microbe within the responders core that correlates with clinical response and highlights the potential impact of this taxa seen in independent cohorts, as well as mouse models of colitis and colorectal cancer,” the researchers emphasized.
The study findings were limited by the small sample size and the lack of prospective data. However, “collectively, this work provides the first evidence of transferable, donor-derived strains that correlate with clinical response to FMT in UC and reveals O. splanchnicus as a key component, which mechanistically promotes protection through both cellular and metabolic function,” the researchers said. “These mechanistic features will help enable desperately needed strategies to enhance therapeutic efficacy of microbial therapy for UC.”
Study strains improve effectiveness
“There is an accumulating body of evidence that suggests that gut dysbiosis, or the imbalance between good and bad microbes, plays an important role in the pathogenesis and progression of ulcerative colitis,” Jeffrey Berinstein, MD, of the University of Michigan, Ann Arbor, said in an interview. “It is for this reason that therapeutic manipulation of gut microbiota with fecal microbiota transplant is being explored as a potential treatment option for UC. FMT has demonstrated promise for ulcerative colitis, however little is known about the specific microbiota strains contributing to this observed improvement. In this study, the authors aimed to better understand the mechanisms and the specific strains in FMT contributing to this observed improvement, which is an important step toward improving efficacy and minimizing the risk of adverse events related to FMT in the future.”
Dr. Berinstein was surprised that O. splanchnicus was the only microbe identified that correlated with clinical response. “Previous studies have suggested that microbial diversity is a key factor in successful response to FMT,” he noted. “FMT remains an important potential nonpharmacologic treatment strategy for ulcerative colitis, however more research is needed to understand the mechanism and to develop safer and more efficacious methods for delivering FMT.” Specifically, prospective studies are needed to explore the efficacy and safety of FMT enriched in strains of O. splanchnicus to confirm the current study findings.
The current study is important at this time because, although microbial transferability has emerged as a potential to treat IBD, “the mechanistic understanding of microbial transferability and engraftment has been lacking,” Atsushi Sakuraba, MD, PhD of the University of Chicago, said in an interview. “I was surprised that the effectiveness of FMT in UC could be narrowed down to O. splanchnicus.” The current take-home message for clinicians is that, although FMT currently uses crude donor fecal material, it may soon use more selected microbial strains. However, “whether transfer of O. splanchnicus alone or enriched fecal material provide improved efficacy and safety need to be analyzed,” he added.
The study was supported by Boehringer Ingelheim, the National Institutes of Health, the Kenneth Rainin Foundation, and the Charina Foundation. One coauthor disclosed grant support from Boehringer Ingelheim for this study, and several coauthors are employees of Boehringer Ingelheim. Neither Dr. Berinstein nor Dr. Sakuraba had no financial conflicts to disclose.
This article was updated Dec. 1, 2021.
*Correction, 4/11/22: An earlier version of this article misstated the definition of clinical response.
FROM GASTROENTEROLOGY
We physicians must pull together as a knowledge community
The COVID-19 pandemic is a biosocial phenomenon. Patients and doctors alike find themselves assigned to groups designated as responsible and wise, or selfish and irrational, based strictly upon their personal assessments of medical risk. This trend in our culture is represented by threats of disciplinary action issued by medical regulators against physicians who are perceived to be undermining the public health message by spreading “misinformation.”
Our review of the literature reveals many references to “misinformation” but no definition narrow and precise enough to be interpreted consistently in a disciplinary environment. More pressing, this ambiguous word’s use is correlated with negative meaning and innuendo, often discrediting valuable information a priori without actual data points.
The most basic definition available is Merriam Webster’s: “incorrect or misleading information.” This definition includes no point of reference against which competing scientific claims can be measured.
Claudia E. Haupt, PhD, a political scientist and law professor, articulates a useful framework for understanding the relationship between medicine and state regulators. In the Yale Law Journal, Dr. Haupt wrote: “Knowledge communities have specialized expertise and are closest to those affected; they must have the freedom to work things out for themselves. The professions as knowledge communities have a fundamental interest in not having the state (or anyone else, for that matter) corrupt or distort what amounts to the state of the art in their respective fields.”
Injecting the artificial term “misinformation” into the science information ecosystem obfuscates and impedes the very ability of this vital knowledge community to perform its raison d’être. , rather than attending to healing or promoting progress.
Time has certainly shown us that science is anything but settled on all things COVID. If the scientific community accepts disrespect as the response of choice to difference of opinion and practice, we lose the trust in one another as colleagues; we need to keep scientific inquiry and exploration alive. Curiosity, equanimity, and tolerance are key components of the professional attitude as we deftly maneuver against the virus together.
In the face of deadly disease, it is especially imperative that intelligent, thoughtful, highly respected scientists, researchers, and physicians have room to safely share their knowledge and clinical experience. The Association of American Physicians and Surgeons has published a statement on scientific integrity that can be used as a measuring stick for claims about misinformation in medicine. We call on physicians to pull together as a knowledge community. Kindness and respect for patients starts with kindness and respect for one another as colleagues.
Dr. Kohanski is in private practice in Somerset, N.J., and is a diplomate of the American Board of Psychiatry & Neurology. She disclosed no relevant financial relationships. Dr. Emmons is part-time clinical associate professor in the department of psychiatry at the University of Vermont, Burlington, and is a past chair of the Ethics Committee for the Vermont District Branch of the American Psychiatric Association. He is in private practice in Moretown, Vt., and disclosed no relevant financial relationships.
The COVID-19 pandemic is a biosocial phenomenon. Patients and doctors alike find themselves assigned to groups designated as responsible and wise, or selfish and irrational, based strictly upon their personal assessments of medical risk. This trend in our culture is represented by threats of disciplinary action issued by medical regulators against physicians who are perceived to be undermining the public health message by spreading “misinformation.”
Our review of the literature reveals many references to “misinformation” but no definition narrow and precise enough to be interpreted consistently in a disciplinary environment. More pressing, this ambiguous word’s use is correlated with negative meaning and innuendo, often discrediting valuable information a priori without actual data points.
The most basic definition available is Merriam Webster’s: “incorrect or misleading information.” This definition includes no point of reference against which competing scientific claims can be measured.
Claudia E. Haupt, PhD, a political scientist and law professor, articulates a useful framework for understanding the relationship between medicine and state regulators. In the Yale Law Journal, Dr. Haupt wrote: “Knowledge communities have specialized expertise and are closest to those affected; they must have the freedom to work things out for themselves. The professions as knowledge communities have a fundamental interest in not having the state (or anyone else, for that matter) corrupt or distort what amounts to the state of the art in their respective fields.”
Injecting the artificial term “misinformation” into the science information ecosystem obfuscates and impedes the very ability of this vital knowledge community to perform its raison d’être. , rather than attending to healing or promoting progress.
Time has certainly shown us that science is anything but settled on all things COVID. If the scientific community accepts disrespect as the response of choice to difference of opinion and practice, we lose the trust in one another as colleagues; we need to keep scientific inquiry and exploration alive. Curiosity, equanimity, and tolerance are key components of the professional attitude as we deftly maneuver against the virus together.
In the face of deadly disease, it is especially imperative that intelligent, thoughtful, highly respected scientists, researchers, and physicians have room to safely share their knowledge and clinical experience. The Association of American Physicians and Surgeons has published a statement on scientific integrity that can be used as a measuring stick for claims about misinformation in medicine. We call on physicians to pull together as a knowledge community. Kindness and respect for patients starts with kindness and respect for one another as colleagues.
Dr. Kohanski is in private practice in Somerset, N.J., and is a diplomate of the American Board of Psychiatry & Neurology. She disclosed no relevant financial relationships. Dr. Emmons is part-time clinical associate professor in the department of psychiatry at the University of Vermont, Burlington, and is a past chair of the Ethics Committee for the Vermont District Branch of the American Psychiatric Association. He is in private practice in Moretown, Vt., and disclosed no relevant financial relationships.
The COVID-19 pandemic is a biosocial phenomenon. Patients and doctors alike find themselves assigned to groups designated as responsible and wise, or selfish and irrational, based strictly upon their personal assessments of medical risk. This trend in our culture is represented by threats of disciplinary action issued by medical regulators against physicians who are perceived to be undermining the public health message by spreading “misinformation.”
Our review of the literature reveals many references to “misinformation” but no definition narrow and precise enough to be interpreted consistently in a disciplinary environment. More pressing, this ambiguous word’s use is correlated with negative meaning and innuendo, often discrediting valuable information a priori without actual data points.
The most basic definition available is Merriam Webster’s: “incorrect or misleading information.” This definition includes no point of reference against which competing scientific claims can be measured.
Claudia E. Haupt, PhD, a political scientist and law professor, articulates a useful framework for understanding the relationship between medicine and state regulators. In the Yale Law Journal, Dr. Haupt wrote: “Knowledge communities have specialized expertise and are closest to those affected; they must have the freedom to work things out for themselves. The professions as knowledge communities have a fundamental interest in not having the state (or anyone else, for that matter) corrupt or distort what amounts to the state of the art in their respective fields.”
Injecting the artificial term “misinformation” into the science information ecosystem obfuscates and impedes the very ability of this vital knowledge community to perform its raison d’être. , rather than attending to healing or promoting progress.
Time has certainly shown us that science is anything but settled on all things COVID. If the scientific community accepts disrespect as the response of choice to difference of opinion and practice, we lose the trust in one another as colleagues; we need to keep scientific inquiry and exploration alive. Curiosity, equanimity, and tolerance are key components of the professional attitude as we deftly maneuver against the virus together.
In the face of deadly disease, it is especially imperative that intelligent, thoughtful, highly respected scientists, researchers, and physicians have room to safely share their knowledge and clinical experience. The Association of American Physicians and Surgeons has published a statement on scientific integrity that can be used as a measuring stick for claims about misinformation in medicine. We call on physicians to pull together as a knowledge community. Kindness and respect for patients starts with kindness and respect for one another as colleagues.
Dr. Kohanski is in private practice in Somerset, N.J., and is a diplomate of the American Board of Psychiatry & Neurology. She disclosed no relevant financial relationships. Dr. Emmons is part-time clinical associate professor in the department of psychiatry at the University of Vermont, Burlington, and is a past chair of the Ethics Committee for the Vermont District Branch of the American Psychiatric Association. He is in private practice in Moretown, Vt., and disclosed no relevant financial relationships.
NAFLD, ALD prevalent among teens, young adults
Two-fifths of adolescents and young adults in the United States may have nonalcoholic fatty liver disease (NAFLD), many with significant or advanced fibrosis, results of a nationwide surveillance study suggest.
In addition, among those who drink alcohol in excess, slightly more than half may have alcohol-associated fatty liver disease (ALD) that may lead to moderate to severe fibrosis in a substantial proportion, said Naim Alkhouri, MD, from Arizona Liver Health, Peoria, during a presentation of the findings at The Liver Meeting 2021: American Association for the Study of Liver Diseases (AASLD), held online.
“Efforts should focus on increasing awareness of the burden of ALD and NAFLD in this population and [mitigating] modifiable risk factors to prevent disease development and disease progression to potentially advanced fibrosis and cirrhosis,” he said.
Liver stiffness measured
Unlike previous studies that relied on liver enzyme levels or ultrasonography to estimate the prevalence of fatty liver disease among adolescents and young adults in the United States, Dr. Alkhouri and colleagues used valid liver ultrasonographic elastography (FibroScan) measurements, recorded during 2017-2018, from the National Health and Nutrition Examination Survey (NHANES) database.
The sample included participants aged 15 to 39 years. Those with viral hepatitis, alanine aminotransferase (ALT) levels greater than 500 U/L, or pregnancy were excluded.
The investigators divided the participants into those with excessive alcohol consumption, defined using the NHANES Alcohol Use Questionnaire as having more than two drinks per day for males or more than one drink per day for females, and those with no excessive alcohol consumption.
The authors used controlled attenuation parameters to identify participants with suspected ALD or NAFLD.
They then used liver stiffness measurement cutoffs of greater than or equal to 7.5 kPa to identify moderate fibrosis and greater than or equal to 9.5 kPa to identify severe fibrosis in those with evidence of ALD and cutoffs of greater than or equal to 6.1 kPa and greater than or equal to 7.1 kPa, respectively, in those with suspected NAFLD.
The cutoffs were chosen to maximize sensitivity, as determined from published literature, Dr. Alkhouri said.
Uncovering a high prevalence of ALD and NAFLD
The final sample comprised 1,319 participants, including 100 with excessive alcohol use and 1,219 without.
The heavy drinkers were significantly more likely to be older, male, White, current smokers, have lower platelet counts, higher aspartate aminotransferase (AST) and ALT levels, and higher mean corpuscular volumes.
Among the excessive drinkers, 52% had ALD. Of this group, 87.7% had either no or mild fibrosis, and 12.3% had moderate to severe fibrosis.
Among patients with excessive alcohol consumption, significant predictors of ALD included male sex, higher body mass index, ALT greater than the upper limit of normal, and higher A1c percentage.
Among those who were moderate drinkers or abstemious, 40% had NAFLD. Of this subgroup, 68.9% had no or mild fibrosis, and 31.1% had moderate to severe fibrosis.
Predictors of NAFLD in this group included older age, male sex, higher body mass index, and elevated ALT, AST, albumin, platelet counts, and A1c.
Is drinking underreported?
In a question-and-answer session following the presentation, co-moderator Miriam B. Vos, MD, a pediatric hepatologist at Children’s Healthcare of Atlanta, asked Dr. Alkhouri about his confidence in the accuracy of the measurements of alcohol consumption and whether there could be significant overlap between the ALD and NAFLD populations.
Dr. Alkhouri noted that he and his colleagues relied on items 121 and 130 of the NHANES Alcohol Use Questionnaire, which are self-reported by participants.
“Obviously, we’re not going to get honest answers all the time,” he said. “We’ve seen even in NASH [nonalcoholic steatohepatitis] clinical trials that when patients say they do not drink any alcohol, if you actually look for alcohol metabolites, up to 20% may have some evidence of alcohol consumption.
“I’m sure there’s a lot of overlap, but there’s no formal assessment,” he added.
Dr. Alkhouri noted that among the cohort with ALD, obesity and increased A1c were prevalent, “so it goes both ways. I think NAFLD can also contribute to progression of ALD, and that’s why we need to study another entity called ‘both alcoholic and nonalcoholic fatty liver disease.’”
Dr. Vos suggested that biomarkers may be useful for detecting alcohol use among patients with NAFLD and for further study of the progression of NAFLD to ALD.
No source of funding for the study has been disclosed. Dr. Alkhouri and Dr. Vos reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Two-fifths of adolescents and young adults in the United States may have nonalcoholic fatty liver disease (NAFLD), many with significant or advanced fibrosis, results of a nationwide surveillance study suggest.
In addition, among those who drink alcohol in excess, slightly more than half may have alcohol-associated fatty liver disease (ALD) that may lead to moderate to severe fibrosis in a substantial proportion, said Naim Alkhouri, MD, from Arizona Liver Health, Peoria, during a presentation of the findings at The Liver Meeting 2021: American Association for the Study of Liver Diseases (AASLD), held online.
“Efforts should focus on increasing awareness of the burden of ALD and NAFLD in this population and [mitigating] modifiable risk factors to prevent disease development and disease progression to potentially advanced fibrosis and cirrhosis,” he said.
Liver stiffness measured
Unlike previous studies that relied on liver enzyme levels or ultrasonography to estimate the prevalence of fatty liver disease among adolescents and young adults in the United States, Dr. Alkhouri and colleagues used valid liver ultrasonographic elastography (FibroScan) measurements, recorded during 2017-2018, from the National Health and Nutrition Examination Survey (NHANES) database.
The sample included participants aged 15 to 39 years. Those with viral hepatitis, alanine aminotransferase (ALT) levels greater than 500 U/L, or pregnancy were excluded.
The investigators divided the participants into those with excessive alcohol consumption, defined using the NHANES Alcohol Use Questionnaire as having more than two drinks per day for males or more than one drink per day for females, and those with no excessive alcohol consumption.
The authors used controlled attenuation parameters to identify participants with suspected ALD or NAFLD.
They then used liver stiffness measurement cutoffs of greater than or equal to 7.5 kPa to identify moderate fibrosis and greater than or equal to 9.5 kPa to identify severe fibrosis in those with evidence of ALD and cutoffs of greater than or equal to 6.1 kPa and greater than or equal to 7.1 kPa, respectively, in those with suspected NAFLD.
The cutoffs were chosen to maximize sensitivity, as determined from published literature, Dr. Alkhouri said.
Uncovering a high prevalence of ALD and NAFLD
The final sample comprised 1,319 participants, including 100 with excessive alcohol use and 1,219 without.
The heavy drinkers were significantly more likely to be older, male, White, current smokers, have lower platelet counts, higher aspartate aminotransferase (AST) and ALT levels, and higher mean corpuscular volumes.
Among the excessive drinkers, 52% had ALD. Of this group, 87.7% had either no or mild fibrosis, and 12.3% had moderate to severe fibrosis.
Among patients with excessive alcohol consumption, significant predictors of ALD included male sex, higher body mass index, ALT greater than the upper limit of normal, and higher A1c percentage.
Among those who were moderate drinkers or abstemious, 40% had NAFLD. Of this subgroup, 68.9% had no or mild fibrosis, and 31.1% had moderate to severe fibrosis.
Predictors of NAFLD in this group included older age, male sex, higher body mass index, and elevated ALT, AST, albumin, platelet counts, and A1c.
Is drinking underreported?
In a question-and-answer session following the presentation, co-moderator Miriam B. Vos, MD, a pediatric hepatologist at Children’s Healthcare of Atlanta, asked Dr. Alkhouri about his confidence in the accuracy of the measurements of alcohol consumption and whether there could be significant overlap between the ALD and NAFLD populations.
Dr. Alkhouri noted that he and his colleagues relied on items 121 and 130 of the NHANES Alcohol Use Questionnaire, which are self-reported by participants.
“Obviously, we’re not going to get honest answers all the time,” he said. “We’ve seen even in NASH [nonalcoholic steatohepatitis] clinical trials that when patients say they do not drink any alcohol, if you actually look for alcohol metabolites, up to 20% may have some evidence of alcohol consumption.
“I’m sure there’s a lot of overlap, but there’s no formal assessment,” he added.
Dr. Alkhouri noted that among the cohort with ALD, obesity and increased A1c were prevalent, “so it goes both ways. I think NAFLD can also contribute to progression of ALD, and that’s why we need to study another entity called ‘both alcoholic and nonalcoholic fatty liver disease.’”
Dr. Vos suggested that biomarkers may be useful for detecting alcohol use among patients with NAFLD and for further study of the progression of NAFLD to ALD.
No source of funding for the study has been disclosed. Dr. Alkhouri and Dr. Vos reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Two-fifths of adolescents and young adults in the United States may have nonalcoholic fatty liver disease (NAFLD), many with significant or advanced fibrosis, results of a nationwide surveillance study suggest.
In addition, among those who drink alcohol in excess, slightly more than half may have alcohol-associated fatty liver disease (ALD) that may lead to moderate to severe fibrosis in a substantial proportion, said Naim Alkhouri, MD, from Arizona Liver Health, Peoria, during a presentation of the findings at The Liver Meeting 2021: American Association for the Study of Liver Diseases (AASLD), held online.
“Efforts should focus on increasing awareness of the burden of ALD and NAFLD in this population and [mitigating] modifiable risk factors to prevent disease development and disease progression to potentially advanced fibrosis and cirrhosis,” he said.
Liver stiffness measured
Unlike previous studies that relied on liver enzyme levels or ultrasonography to estimate the prevalence of fatty liver disease among adolescents and young adults in the United States, Dr. Alkhouri and colleagues used valid liver ultrasonographic elastography (FibroScan) measurements, recorded during 2017-2018, from the National Health and Nutrition Examination Survey (NHANES) database.
The sample included participants aged 15 to 39 years. Those with viral hepatitis, alanine aminotransferase (ALT) levels greater than 500 U/L, or pregnancy were excluded.
The investigators divided the participants into those with excessive alcohol consumption, defined using the NHANES Alcohol Use Questionnaire as having more than two drinks per day for males or more than one drink per day for females, and those with no excessive alcohol consumption.
The authors used controlled attenuation parameters to identify participants with suspected ALD or NAFLD.
They then used liver stiffness measurement cutoffs of greater than or equal to 7.5 kPa to identify moderate fibrosis and greater than or equal to 9.5 kPa to identify severe fibrosis in those with evidence of ALD and cutoffs of greater than or equal to 6.1 kPa and greater than or equal to 7.1 kPa, respectively, in those with suspected NAFLD.
The cutoffs were chosen to maximize sensitivity, as determined from published literature, Dr. Alkhouri said.
Uncovering a high prevalence of ALD and NAFLD
The final sample comprised 1,319 participants, including 100 with excessive alcohol use and 1,219 without.
The heavy drinkers were significantly more likely to be older, male, White, current smokers, have lower platelet counts, higher aspartate aminotransferase (AST) and ALT levels, and higher mean corpuscular volumes.
Among the excessive drinkers, 52% had ALD. Of this group, 87.7% had either no or mild fibrosis, and 12.3% had moderate to severe fibrosis.
Among patients with excessive alcohol consumption, significant predictors of ALD included male sex, higher body mass index, ALT greater than the upper limit of normal, and higher A1c percentage.
Among those who were moderate drinkers or abstemious, 40% had NAFLD. Of this subgroup, 68.9% had no or mild fibrosis, and 31.1% had moderate to severe fibrosis.
Predictors of NAFLD in this group included older age, male sex, higher body mass index, and elevated ALT, AST, albumin, platelet counts, and A1c.
Is drinking underreported?
In a question-and-answer session following the presentation, co-moderator Miriam B. Vos, MD, a pediatric hepatologist at Children’s Healthcare of Atlanta, asked Dr. Alkhouri about his confidence in the accuracy of the measurements of alcohol consumption and whether there could be significant overlap between the ALD and NAFLD populations.
Dr. Alkhouri noted that he and his colleagues relied on items 121 and 130 of the NHANES Alcohol Use Questionnaire, which are self-reported by participants.
“Obviously, we’re not going to get honest answers all the time,” he said. “We’ve seen even in NASH [nonalcoholic steatohepatitis] clinical trials that when patients say they do not drink any alcohol, if you actually look for alcohol metabolites, up to 20% may have some evidence of alcohol consumption.
“I’m sure there’s a lot of overlap, but there’s no formal assessment,” he added.
Dr. Alkhouri noted that among the cohort with ALD, obesity and increased A1c were prevalent, “so it goes both ways. I think NAFLD can also contribute to progression of ALD, and that’s why we need to study another entity called ‘both alcoholic and nonalcoholic fatty liver disease.’”
Dr. Vos suggested that biomarkers may be useful for detecting alcohol use among patients with NAFLD and for further study of the progression of NAFLD to ALD.
No source of funding for the study has been disclosed. Dr. Alkhouri and Dr. Vos reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patient risk, not disease duration, key to timing biologics in IBD
The decision to initiate biologics early in the treatment of Crohn’s disease (CD) and ulcerative colitis (UC) should be based on complication risk, not on the assumption that earlier treatment produces better results, new research suggests.
Results of a meta-analysis of randomized controlled trials show that “the proportional biologic/placebo treatment effect on remission and response to biologics was not influenced by disease duration in UC or CD patients,” the investigators note.
“Patients with Crohn’s disease treated with biologics early on show over 40% remission rate, compared [with] around 30% for those with disease of 20 years or more,” study investigator Shomron Ben-Horin, MD, Sheba Medical Center, Tel Aviv University, Israel, told this news organization.
The rates of remission with both biologics and placebo were higher for patients with short-duration CD compared with patients with disease of longer duration. However, for patients with UC, the remission rates with both biologics and placebo were similar regardless of disease duration.
“Our findings support the use of biologics in patients with Crohn’s disease early after diagnosis, if they are at high risk of disease progression and complications, but not just to achieve better efficacy,” Dr. Ben-Horin said.
The meta-analysis was published online in Gastroenterology.
Getting the timing right
Dr. Ben-Horin led the research with an international group of investigators who assessed individual data from 6,168 patients with CD and 3,227 patients with UC. The patients were participants in 25 placebo-controlled trials.
For patients with CD, the odds ratio of achieving remission with biologics in comparison with placebo was 1.47 (95% confidence interval, 1.01-2.15) for short-duration disease (≤18 months), which was not so different from the odds ratio for longer-duration disease (>18 months) (OR, 1.43; 95% CI, 1.19-1.72).
“These results remained similar when tested for other disease duration cutoffs or when accounting for individual patients’ characteristics, such as whether patients were previously exposed to biologics or not,” said Dr. Ben-Horin.
For patients with UC, the OR for remission with biologics in comparison with placebo was 1.82 (95% CI, 1.12-2.97) for those with short-duration disease and 2.21 (95% CI, 1.79-2.72) for those with long-duration disease.
What the optimal timing is for using biologics for patients with inflammatory bowel disease (IBD), which includes both CD and UC, and whether all patients with these conditions need them are very pertinent questions, said Dr. Ben-Horin.
About a decade ago, the treatment of IBD changed. At that time, patients were initially treated with immunomodulators or steroids; biologics were used only if those treatments failed. More recently, a top-down approach has been followed, in which biologics are brought in at the beginning of the treatment protocol, said Dr. Ben-Horin.
This top-down approach has been widely adopted to prevent complications, such as intestinal strictures, bowel obstruction, or fistulas, which can increase the odds that patients with CD will require surgery, he added.
Although treatment with biologics was more effective when initiated earlier than later, data to support this were limited, prompting the investigators to conduct the current review.
“A substantial fraction of patients with Crohn’s disease may be better off with biologics first if they are at a high risk of complications: for example, smokers, patients with extensive disease, or those with perianal fistula. But this may not be necessarily true for those with a low risk of complications,” said Dr. Ben-Horin.
For patients with UC, “the lack of better efficacy with biologics in short-duration disease forces us to rethink our protocols of an early start of biologics,” he added.
Possible reasons for the early response
The reasons for the higher response to both placebo and biologics for patients with early CD are unknown.
“It may be that there is plasticity in Crohn’s disease early in the course of disease, where the tissue is more amenable to return to normal whether the patient is on placebo or treatment,” said Dr. Ben-Horin.
He suspects that the more likely explanation is that the placebo response is higher in patients with CD of short duration.
“When we looked at levels of C-reactive protein, this was reduced by biologics at similar magnitude in early- and late-disease patients,” Dr. Ben-Horin said. He noted that more studies are needed to better understand disease dynamics with these conditions.
Commenting on the findings, Stephen B. Hanauer, MD, from Northwestern University Feinberg School of Medicine, Chicago, noted that they “absolutely support earlier intervention for moderate-severe Crohn’s disease from diagnosis, rather than waiting for transmural progression that will make disease more refractory to any mechanism of action.”
“Unfortunately, the average duration of disease in biologic trials is often close to 10 years, which implies a more refractory population,” Dr. Hanauer said.
“Furthermore, in the United States, clinicians and patients are hampered by inability to gain third-party authorization for biologics or advanced oral agents, such as JAK inhibitors or S1P modulators, until failure of so-called conventional agents despite labeling indication for moderate-severe disease,” he added.
Dr. Ben-Horin has received consultancy and/or advisory board fees from AbbVie, Novartis, Schering-Plough, Janssen, Celltrion, GSK, Pfizer, Galmed, and Takeda and research support from AbbVie, Janssen, Celltrion, Galmed, and Takeda. Dr. Hanauer is a consultant and speaker for AbbVie, Janssen, and Takeda.
A version of this article first appeared on Medscape.com.
The decision to initiate biologics early in the treatment of Crohn’s disease (CD) and ulcerative colitis (UC) should be based on complication risk, not on the assumption that earlier treatment produces better results, new research suggests.
Results of a meta-analysis of randomized controlled trials show that “the proportional biologic/placebo treatment effect on remission and response to biologics was not influenced by disease duration in UC or CD patients,” the investigators note.
“Patients with Crohn’s disease treated with biologics early on show over 40% remission rate, compared [with] around 30% for those with disease of 20 years or more,” study investigator Shomron Ben-Horin, MD, Sheba Medical Center, Tel Aviv University, Israel, told this news organization.
The rates of remission with both biologics and placebo were higher for patients with short-duration CD compared with patients with disease of longer duration. However, for patients with UC, the remission rates with both biologics and placebo were similar regardless of disease duration.
“Our findings support the use of biologics in patients with Crohn’s disease early after diagnosis, if they are at high risk of disease progression and complications, but not just to achieve better efficacy,” Dr. Ben-Horin said.
The meta-analysis was published online in Gastroenterology.
Getting the timing right
Dr. Ben-Horin led the research with an international group of investigators who assessed individual data from 6,168 patients with CD and 3,227 patients with UC. The patients were participants in 25 placebo-controlled trials.
For patients with CD, the odds ratio of achieving remission with biologics in comparison with placebo was 1.47 (95% confidence interval, 1.01-2.15) for short-duration disease (≤18 months), which was not so different from the odds ratio for longer-duration disease (>18 months) (OR, 1.43; 95% CI, 1.19-1.72).
“These results remained similar when tested for other disease duration cutoffs or when accounting for individual patients’ characteristics, such as whether patients were previously exposed to biologics or not,” said Dr. Ben-Horin.
For patients with UC, the OR for remission with biologics in comparison with placebo was 1.82 (95% CI, 1.12-2.97) for those with short-duration disease and 2.21 (95% CI, 1.79-2.72) for those with long-duration disease.
What the optimal timing is for using biologics for patients with inflammatory bowel disease (IBD), which includes both CD and UC, and whether all patients with these conditions need them are very pertinent questions, said Dr. Ben-Horin.
About a decade ago, the treatment of IBD changed. At that time, patients were initially treated with immunomodulators or steroids; biologics were used only if those treatments failed. More recently, a top-down approach has been followed, in which biologics are brought in at the beginning of the treatment protocol, said Dr. Ben-Horin.
This top-down approach has been widely adopted to prevent complications, such as intestinal strictures, bowel obstruction, or fistulas, which can increase the odds that patients with CD will require surgery, he added.
Although treatment with biologics was more effective when initiated earlier than later, data to support this were limited, prompting the investigators to conduct the current review.
“A substantial fraction of patients with Crohn’s disease may be better off with biologics first if they are at a high risk of complications: for example, smokers, patients with extensive disease, or those with perianal fistula. But this may not be necessarily true for those with a low risk of complications,” said Dr. Ben-Horin.
For patients with UC, “the lack of better efficacy with biologics in short-duration disease forces us to rethink our protocols of an early start of biologics,” he added.
Possible reasons for the early response
The reasons for the higher response to both placebo and biologics for patients with early CD are unknown.
“It may be that there is plasticity in Crohn’s disease early in the course of disease, where the tissue is more amenable to return to normal whether the patient is on placebo or treatment,” said Dr. Ben-Horin.
He suspects that the more likely explanation is that the placebo response is higher in patients with CD of short duration.
“When we looked at levels of C-reactive protein, this was reduced by biologics at similar magnitude in early- and late-disease patients,” Dr. Ben-Horin said. He noted that more studies are needed to better understand disease dynamics with these conditions.
Commenting on the findings, Stephen B. Hanauer, MD, from Northwestern University Feinberg School of Medicine, Chicago, noted that they “absolutely support earlier intervention for moderate-severe Crohn’s disease from diagnosis, rather than waiting for transmural progression that will make disease more refractory to any mechanism of action.”
“Unfortunately, the average duration of disease in biologic trials is often close to 10 years, which implies a more refractory population,” Dr. Hanauer said.
“Furthermore, in the United States, clinicians and patients are hampered by inability to gain third-party authorization for biologics or advanced oral agents, such as JAK inhibitors or S1P modulators, until failure of so-called conventional agents despite labeling indication for moderate-severe disease,” he added.
Dr. Ben-Horin has received consultancy and/or advisory board fees from AbbVie, Novartis, Schering-Plough, Janssen, Celltrion, GSK, Pfizer, Galmed, and Takeda and research support from AbbVie, Janssen, Celltrion, Galmed, and Takeda. Dr. Hanauer is a consultant and speaker for AbbVie, Janssen, and Takeda.
A version of this article first appeared on Medscape.com.
The decision to initiate biologics early in the treatment of Crohn’s disease (CD) and ulcerative colitis (UC) should be based on complication risk, not on the assumption that earlier treatment produces better results, new research suggests.
Results of a meta-analysis of randomized controlled trials show that “the proportional biologic/placebo treatment effect on remission and response to biologics was not influenced by disease duration in UC or CD patients,” the investigators note.
“Patients with Crohn’s disease treated with biologics early on show over 40% remission rate, compared [with] around 30% for those with disease of 20 years or more,” study investigator Shomron Ben-Horin, MD, Sheba Medical Center, Tel Aviv University, Israel, told this news organization.
The rates of remission with both biologics and placebo were higher for patients with short-duration CD compared with patients with disease of longer duration. However, for patients with UC, the remission rates with both biologics and placebo were similar regardless of disease duration.
“Our findings support the use of biologics in patients with Crohn’s disease early after diagnosis, if they are at high risk of disease progression and complications, but not just to achieve better efficacy,” Dr. Ben-Horin said.
The meta-analysis was published online in Gastroenterology.
Getting the timing right
Dr. Ben-Horin led the research with an international group of investigators who assessed individual data from 6,168 patients with CD and 3,227 patients with UC. The patients were participants in 25 placebo-controlled trials.
For patients with CD, the odds ratio of achieving remission with biologics in comparison with placebo was 1.47 (95% confidence interval, 1.01-2.15) for short-duration disease (≤18 months), which was not so different from the odds ratio for longer-duration disease (>18 months) (OR, 1.43; 95% CI, 1.19-1.72).
“These results remained similar when tested for other disease duration cutoffs or when accounting for individual patients’ characteristics, such as whether patients were previously exposed to biologics or not,” said Dr. Ben-Horin.
For patients with UC, the OR for remission with biologics in comparison with placebo was 1.82 (95% CI, 1.12-2.97) for those with short-duration disease and 2.21 (95% CI, 1.79-2.72) for those with long-duration disease.
What the optimal timing is for using biologics for patients with inflammatory bowel disease (IBD), which includes both CD and UC, and whether all patients with these conditions need them are very pertinent questions, said Dr. Ben-Horin.
About a decade ago, the treatment of IBD changed. At that time, patients were initially treated with immunomodulators or steroids; biologics were used only if those treatments failed. More recently, a top-down approach has been followed, in which biologics are brought in at the beginning of the treatment protocol, said Dr. Ben-Horin.
This top-down approach has been widely adopted to prevent complications, such as intestinal strictures, bowel obstruction, or fistulas, which can increase the odds that patients with CD will require surgery, he added.
Although treatment with biologics was more effective when initiated earlier than later, data to support this were limited, prompting the investigators to conduct the current review.
“A substantial fraction of patients with Crohn’s disease may be better off with biologics first if they are at a high risk of complications: for example, smokers, patients with extensive disease, or those with perianal fistula. But this may not be necessarily true for those with a low risk of complications,” said Dr. Ben-Horin.
For patients with UC, “the lack of better efficacy with biologics in short-duration disease forces us to rethink our protocols of an early start of biologics,” he added.
Possible reasons for the early response
The reasons for the higher response to both placebo and biologics for patients with early CD are unknown.
“It may be that there is plasticity in Crohn’s disease early in the course of disease, where the tissue is more amenable to return to normal whether the patient is on placebo or treatment,” said Dr. Ben-Horin.
He suspects that the more likely explanation is that the placebo response is higher in patients with CD of short duration.
“When we looked at levels of C-reactive protein, this was reduced by biologics at similar magnitude in early- and late-disease patients,” Dr. Ben-Horin said. He noted that more studies are needed to better understand disease dynamics with these conditions.
Commenting on the findings, Stephen B. Hanauer, MD, from Northwestern University Feinberg School of Medicine, Chicago, noted that they “absolutely support earlier intervention for moderate-severe Crohn’s disease from diagnosis, rather than waiting for transmural progression that will make disease more refractory to any mechanism of action.”
“Unfortunately, the average duration of disease in biologic trials is often close to 10 years, which implies a more refractory population,” Dr. Hanauer said.
“Furthermore, in the United States, clinicians and patients are hampered by inability to gain third-party authorization for biologics or advanced oral agents, such as JAK inhibitors or S1P modulators, until failure of so-called conventional agents despite labeling indication for moderate-severe disease,” he added.
Dr. Ben-Horin has received consultancy and/or advisory board fees from AbbVie, Novartis, Schering-Plough, Janssen, Celltrion, GSK, Pfizer, Galmed, and Takeda and research support from AbbVie, Janssen, Celltrion, Galmed, and Takeda. Dr. Hanauer is a consultant and speaker for AbbVie, Janssen, and Takeda.
A version of this article first appeared on Medscape.com.
Change in testing protocol for cirrhosis
Patients with cirrhosis, or permanent liver damage, are at higher risk for coagulation disorders, which impact your body’s ability to control blood clotting. This puts cirrhosis patients at increased risk of morbidity and mortality when undergoing diagnostic or therapeutic invasive procedures. AGA has released new clinical guidelines to change how you identify and treat coagulation disorders in patients with cirrhosis. These guidelines, which were developed after a detailed review of available literature, are published in Gastroenterology, AGA’s official journal.
Key guideline recommendations:
- Extensive preprocedural testing, including measurements of prothrombin time/international normalized ratio or platelet count, should not routinely be performed in patients with stable cirrhosis undergoing common GI procedures.
- Blood products, including fresh frozen plasma or platelet transfusion, should not routinely be used for bleeding prophylaxis in patients with stable cirrhosis undergoing common GI procedures.
- Standard pharmacologic venous thromboembolism prophylaxis should be given to hospitalized patients with cirrhosis like other medical patients.
- Anticoagulation should be used to treat acute or subacute nontumoral portal vein thrombosis in patients with cirrhosis to improve patient outcomes.
Learn more in the AGA GI Patient Center. Read the AGA Clinical Practice Guidelines on the Management of Coagulation Disorders in Patients with Cirrhosis to review the complete recommendations.
Patients with cirrhosis, or permanent liver damage, are at higher risk for coagulation disorders, which impact your body’s ability to control blood clotting. This puts cirrhosis patients at increased risk of morbidity and mortality when undergoing diagnostic or therapeutic invasive procedures. AGA has released new clinical guidelines to change how you identify and treat coagulation disorders in patients with cirrhosis. These guidelines, which were developed after a detailed review of available literature, are published in Gastroenterology, AGA’s official journal.
Key guideline recommendations:
- Extensive preprocedural testing, including measurements of prothrombin time/international normalized ratio or platelet count, should not routinely be performed in patients with stable cirrhosis undergoing common GI procedures.
- Blood products, including fresh frozen plasma or platelet transfusion, should not routinely be used for bleeding prophylaxis in patients with stable cirrhosis undergoing common GI procedures.
- Standard pharmacologic venous thromboembolism prophylaxis should be given to hospitalized patients with cirrhosis like other medical patients.
- Anticoagulation should be used to treat acute or subacute nontumoral portal vein thrombosis in patients with cirrhosis to improve patient outcomes.
Learn more in the AGA GI Patient Center. Read the AGA Clinical Practice Guidelines on the Management of Coagulation Disorders in Patients with Cirrhosis to review the complete recommendations.
Patients with cirrhosis, or permanent liver damage, are at higher risk for coagulation disorders, which impact your body’s ability to control blood clotting. This puts cirrhosis patients at increased risk of morbidity and mortality when undergoing diagnostic or therapeutic invasive procedures. AGA has released new clinical guidelines to change how you identify and treat coagulation disorders in patients with cirrhosis. These guidelines, which were developed after a detailed review of available literature, are published in Gastroenterology, AGA’s official journal.
Key guideline recommendations:
- Extensive preprocedural testing, including measurements of prothrombin time/international normalized ratio or platelet count, should not routinely be performed in patients with stable cirrhosis undergoing common GI procedures.
- Blood products, including fresh frozen plasma or platelet transfusion, should not routinely be used for bleeding prophylaxis in patients with stable cirrhosis undergoing common GI procedures.
- Standard pharmacologic venous thromboembolism prophylaxis should be given to hospitalized patients with cirrhosis like other medical patients.
- Anticoagulation should be used to treat acute or subacute nontumoral portal vein thrombosis in patients with cirrhosis to improve patient outcomes.
Learn more in the AGA GI Patient Center. Read the AGA Clinical Practice Guidelines on the Management of Coagulation Disorders in Patients with Cirrhosis to review the complete recommendations.
Be cautious with HBV drug withdrawal
More than half of chronic hepatitis B e antigen–negative patients who withdraw from nucleoside or nucleotide analogue therapy experienced relapse within 4 years, according to a new study that looked at patients from 11 centers in Europe, North America, and Asia.
“We wanted to see if the patients stabilize after that year. Are they just having relapses within the first year, and then they’re inactive carriers? Especially patients who don’t achieve [hepatitis B surface antigen; HBsAg] loss. Is that mildly active disease? Would they have been better off being retreated, or are they better off [staying off] therapy? It is important to look at what happens among these patients who stop and if there is a way to tell which way they’re going to go,” said Grishma Hirode, who is a PhD candidate at the University of Toronto. Ms. Hirode presented the multinational study at the annual meeting of the American Association for the Study of Liver Diseases.
The study provided a clear picture: “They do not stabilize after 1 year. They have relapses, and these relapses aren’t mild fluctuations,” said Ms. Hirode. Another study, which was presented during the same session and investigated a national cohort in Taiwan, also found a high rate of flareups and retreatment out to 4 years.
The RETRACT-B study presented by Ms. Hirode collected data on 945 patients from 11 centers in North America, Europe, and Asia. Overall, 66% had at least one relapse within 1 year of drug withdrawal. At 2 years, 40% had a sustained remission without HBsAg loss, as had 20% at 4 years; 44% had sustained remission or HBsAg loss at 2 years, as did 30% at 4 years.
Subgroup analyses found differences between some populations: 48% of Whites and 28% of Asians had sustained remission or HBsAg loss, and 30% of Whites and 20% of Asians had sustained remission without HBsAg loss. Patients who were HBsAg positive at start of therapy were more likely to have a sustained remission or HBsAg loss (36% vs. 28%; P < .05) and to have a sustained remission without HBsAg loss (31% vs. 19%; P < .05). HBsAg levels below 100 IU/mL at cessation was also associated with a greater chance of sustained remission or HBsAg loss (58% vs. 24%; P < .05) and sustained remission without HBsAg loss (24% vs. 20%; P < .05). Not having a relapse within the first year after cessation was also associated with greater chance of sustained remission or HBsAg loss (50% versus 19%; P < .05) and sustained remission without HBsAg loss (37% vs. 13%; P < .05).
The Taiwan cohort study examined the repercussions of a government policy that limited reimbursement of nucleotide/nucleoside analogues to a fixed duration of time. Among 10,192 eligible patients, researchers at I-SHOU University found a 6.58% 4-year cumulative incidence of severe flare-ups after discontinuation (95% confidence interval, 5.91%-7.30%), defined as serum ALT levels higher than five times the upper limit of normal plus serum bilirubin levels above 2 mg/dL.
The overall incidence of flare-ups was 30.66% over 4 years (95% CI, 29.37%-31.96%). Higher risk of flareup was associated with older age (hazard ratio for each 10 years, 1.19; P<.0001), male sex (HR, 1.76; P < .0001), a diagnosis of cirrhosis (HR, 1.84; P < .0001), and a history of hepatic decompensation (HR, 1.45; P = .044).
The 4-year incidence of retreatment was 48.74% (95% CI, 46.55-50.90%)
The mortality rate was 0.63% at 4 years after a flareup (95% CI, 0.44-0.87%), and the combined rate of mortality or liver transplant was 0.79% (95% CI, 0.58-1.05%). Risk factors for higher mortality included older age (per 10 years; HR, 1.70; P < .0001), a diagnosis of cirrhosis (HR, 6.12; P < .0001), and hypertension (HR, 2.29; P = .029).
Selecting patients safely?
The results of both studies suggest that withdrawal from medication should be done cautiously, and patients monitored for relapse and retreatment, according to Anna Lok, MD, who was asked for comment. Dr. Lok is a professor of internal medicine, director of clinical hematology, and assistant dean for clinical research at the University of Michigan, Ann Arbor.
Between the two studies, “the message is that this approach can benefit some patients, but if the goal of treatment withdrawal is to increase the rate of hepatitis B surface antigen loss, only a small percentage of patients would benefit. Contrary to studies in Europe, the rates of HBsAg loss in studies with predominantly Asian patients are much lower,” said Dr. Lok.
The new studies provide guidance as for which patients might safely stop treatment; specifically, she suggested, young White patients who have a low HBsAg level when treatment is stopped. “But you probably shouldn’t be trying it in older Asian patients who still have high HBsAg titer, because the chance of them relapsing is very high and the chance of benefit is very low,” she said.
“One has to be very careful in selecting which patients you’re going to try this on. And if you do want to try, you’ve got to make sure that you monitor patients very carefully so treatment can be promptly resumed if necessary because some of the patients can have a severe flare and they can even develop liver failure, and this should never be tried in patients with cirrhosis” said Dr. Lok.
Ms. Hirode and Dr. Lok have no relevant financial disclosures.
More than half of chronic hepatitis B e antigen–negative patients who withdraw from nucleoside or nucleotide analogue therapy experienced relapse within 4 years, according to a new study that looked at patients from 11 centers in Europe, North America, and Asia.
“We wanted to see if the patients stabilize after that year. Are they just having relapses within the first year, and then they’re inactive carriers? Especially patients who don’t achieve [hepatitis B surface antigen; HBsAg] loss. Is that mildly active disease? Would they have been better off being retreated, or are they better off [staying off] therapy? It is important to look at what happens among these patients who stop and if there is a way to tell which way they’re going to go,” said Grishma Hirode, who is a PhD candidate at the University of Toronto. Ms. Hirode presented the multinational study at the annual meeting of the American Association for the Study of Liver Diseases.
The study provided a clear picture: “They do not stabilize after 1 year. They have relapses, and these relapses aren’t mild fluctuations,” said Ms. Hirode. Another study, which was presented during the same session and investigated a national cohort in Taiwan, also found a high rate of flareups and retreatment out to 4 years.
The RETRACT-B study presented by Ms. Hirode collected data on 945 patients from 11 centers in North America, Europe, and Asia. Overall, 66% had at least one relapse within 1 year of drug withdrawal. At 2 years, 40% had a sustained remission without HBsAg loss, as had 20% at 4 years; 44% had sustained remission or HBsAg loss at 2 years, as did 30% at 4 years.
Subgroup analyses found differences between some populations: 48% of Whites and 28% of Asians had sustained remission or HBsAg loss, and 30% of Whites and 20% of Asians had sustained remission without HBsAg loss. Patients who were HBsAg positive at start of therapy were more likely to have a sustained remission or HBsAg loss (36% vs. 28%; P < .05) and to have a sustained remission without HBsAg loss (31% vs. 19%; P < .05). HBsAg levels below 100 IU/mL at cessation was also associated with a greater chance of sustained remission or HBsAg loss (58% vs. 24%; P < .05) and sustained remission without HBsAg loss (24% vs. 20%; P < .05). Not having a relapse within the first year after cessation was also associated with greater chance of sustained remission or HBsAg loss (50% versus 19%; P < .05) and sustained remission without HBsAg loss (37% vs. 13%; P < .05).
The Taiwan cohort study examined the repercussions of a government policy that limited reimbursement of nucleotide/nucleoside analogues to a fixed duration of time. Among 10,192 eligible patients, researchers at I-SHOU University found a 6.58% 4-year cumulative incidence of severe flare-ups after discontinuation (95% confidence interval, 5.91%-7.30%), defined as serum ALT levels higher than five times the upper limit of normal plus serum bilirubin levels above 2 mg/dL.
The overall incidence of flare-ups was 30.66% over 4 years (95% CI, 29.37%-31.96%). Higher risk of flareup was associated with older age (hazard ratio for each 10 years, 1.19; P<.0001), male sex (HR, 1.76; P < .0001), a diagnosis of cirrhosis (HR, 1.84; P < .0001), and a history of hepatic decompensation (HR, 1.45; P = .044).
The 4-year incidence of retreatment was 48.74% (95% CI, 46.55-50.90%)
The mortality rate was 0.63% at 4 years after a flareup (95% CI, 0.44-0.87%), and the combined rate of mortality or liver transplant was 0.79% (95% CI, 0.58-1.05%). Risk factors for higher mortality included older age (per 10 years; HR, 1.70; P < .0001), a diagnosis of cirrhosis (HR, 6.12; P < .0001), and hypertension (HR, 2.29; P = .029).
Selecting patients safely?
The results of both studies suggest that withdrawal from medication should be done cautiously, and patients monitored for relapse and retreatment, according to Anna Lok, MD, who was asked for comment. Dr. Lok is a professor of internal medicine, director of clinical hematology, and assistant dean for clinical research at the University of Michigan, Ann Arbor.
Between the two studies, “the message is that this approach can benefit some patients, but if the goal of treatment withdrawal is to increase the rate of hepatitis B surface antigen loss, only a small percentage of patients would benefit. Contrary to studies in Europe, the rates of HBsAg loss in studies with predominantly Asian patients are much lower,” said Dr. Lok.
The new studies provide guidance as for which patients might safely stop treatment; specifically, she suggested, young White patients who have a low HBsAg level when treatment is stopped. “But you probably shouldn’t be trying it in older Asian patients who still have high HBsAg titer, because the chance of them relapsing is very high and the chance of benefit is very low,” she said.
“One has to be very careful in selecting which patients you’re going to try this on. And if you do want to try, you’ve got to make sure that you monitor patients very carefully so treatment can be promptly resumed if necessary because some of the patients can have a severe flare and they can even develop liver failure, and this should never be tried in patients with cirrhosis” said Dr. Lok.
Ms. Hirode and Dr. Lok have no relevant financial disclosures.
More than half of chronic hepatitis B e antigen–negative patients who withdraw from nucleoside or nucleotide analogue therapy experienced relapse within 4 years, according to a new study that looked at patients from 11 centers in Europe, North America, and Asia.
“We wanted to see if the patients stabilize after that year. Are they just having relapses within the first year, and then they’re inactive carriers? Especially patients who don’t achieve [hepatitis B surface antigen; HBsAg] loss. Is that mildly active disease? Would they have been better off being retreated, or are they better off [staying off] therapy? It is important to look at what happens among these patients who stop and if there is a way to tell which way they’re going to go,” said Grishma Hirode, who is a PhD candidate at the University of Toronto. Ms. Hirode presented the multinational study at the annual meeting of the American Association for the Study of Liver Diseases.
The study provided a clear picture: “They do not stabilize after 1 year. They have relapses, and these relapses aren’t mild fluctuations,” said Ms. Hirode. Another study, which was presented during the same session and investigated a national cohort in Taiwan, also found a high rate of flareups and retreatment out to 4 years.
The RETRACT-B study presented by Ms. Hirode collected data on 945 patients from 11 centers in North America, Europe, and Asia. Overall, 66% had at least one relapse within 1 year of drug withdrawal. At 2 years, 40% had a sustained remission without HBsAg loss, as had 20% at 4 years; 44% had sustained remission or HBsAg loss at 2 years, as did 30% at 4 years.
Subgroup analyses found differences between some populations: 48% of Whites and 28% of Asians had sustained remission or HBsAg loss, and 30% of Whites and 20% of Asians had sustained remission without HBsAg loss. Patients who were HBsAg positive at start of therapy were more likely to have a sustained remission or HBsAg loss (36% vs. 28%; P < .05) and to have a sustained remission without HBsAg loss (31% vs. 19%; P < .05). HBsAg levels below 100 IU/mL at cessation was also associated with a greater chance of sustained remission or HBsAg loss (58% vs. 24%; P < .05) and sustained remission without HBsAg loss (24% vs. 20%; P < .05). Not having a relapse within the first year after cessation was also associated with greater chance of sustained remission or HBsAg loss (50% versus 19%; P < .05) and sustained remission without HBsAg loss (37% vs. 13%; P < .05).
The Taiwan cohort study examined the repercussions of a government policy that limited reimbursement of nucleotide/nucleoside analogues to a fixed duration of time. Among 10,192 eligible patients, researchers at I-SHOU University found a 6.58% 4-year cumulative incidence of severe flare-ups after discontinuation (95% confidence interval, 5.91%-7.30%), defined as serum ALT levels higher than five times the upper limit of normal plus serum bilirubin levels above 2 mg/dL.
The overall incidence of flare-ups was 30.66% over 4 years (95% CI, 29.37%-31.96%). Higher risk of flareup was associated with older age (hazard ratio for each 10 years, 1.19; P<.0001), male sex (HR, 1.76; P < .0001), a diagnosis of cirrhosis (HR, 1.84; P < .0001), and a history of hepatic decompensation (HR, 1.45; P = .044).
The 4-year incidence of retreatment was 48.74% (95% CI, 46.55-50.90%)
The mortality rate was 0.63% at 4 years after a flareup (95% CI, 0.44-0.87%), and the combined rate of mortality or liver transplant was 0.79% (95% CI, 0.58-1.05%). Risk factors for higher mortality included older age (per 10 years; HR, 1.70; P < .0001), a diagnosis of cirrhosis (HR, 6.12; P < .0001), and hypertension (HR, 2.29; P = .029).
Selecting patients safely?
The results of both studies suggest that withdrawal from medication should be done cautiously, and patients monitored for relapse and retreatment, according to Anna Lok, MD, who was asked for comment. Dr. Lok is a professor of internal medicine, director of clinical hematology, and assistant dean for clinical research at the University of Michigan, Ann Arbor.
Between the two studies, “the message is that this approach can benefit some patients, but if the goal of treatment withdrawal is to increase the rate of hepatitis B surface antigen loss, only a small percentage of patients would benefit. Contrary to studies in Europe, the rates of HBsAg loss in studies with predominantly Asian patients are much lower,” said Dr. Lok.
The new studies provide guidance as for which patients might safely stop treatment; specifically, she suggested, young White patients who have a low HBsAg level when treatment is stopped. “But you probably shouldn’t be trying it in older Asian patients who still have high HBsAg titer, because the chance of them relapsing is very high and the chance of benefit is very low,” she said.
“One has to be very careful in selecting which patients you’re going to try this on. And if you do want to try, you’ve got to make sure that you monitor patients very carefully so treatment can be promptly resumed if necessary because some of the patients can have a severe flare and they can even develop liver failure, and this should never be tried in patients with cirrhosis” said Dr. Lok.
Ms. Hirode and Dr. Lok have no relevant financial disclosures.
FROM THE LIVER MEETING
Virtual center boosts liver transplant listings in rural area
A “virtual” liver transplant center servicing Vermont and New Hampshire has improved access to liver transplant listing among patients in rural areas of the region, according to a new analysis.
The virtual center was established in 2016 at Dartmouth Hitchcock Medical Center, and it allows patients to receive pre–liver transplant evaluations, testing, and care and posttransplant follow-up there rather than at the liver transplant center that conducts the surgery. The center includes two hepatologists, two associate care providers, and a nurse liver transplant coordinator at DHMC, and led to increased transplant listing in the vicinity, according to Margaret Liu, MD, who presented the study at the virtual annual meeting of the American Association for the Study of Liver Diseases.
“The initiation of this Virtual Liver Transplant Center has been able to provide patients with the ability to get a full liver transplant workup and evaluation at a center near their home rather than the often time-consuming and costly process of potentially multiple trips to a liver transplant center up to 250 miles away for a full transplant evaluation,” said Dr. Liu in an interview. Dr. Liu is an internal medicine resident at Dartmouth Hitchcock Medical Center.
“Our results did show that the initiation of a virtual liver transplant center correlated with an increased and sustained liver transplant listing rate within 60 miles of Dartmouth over that particular study period. Conversely there was no significant change in the listing rate of New Hampshire zip codes that were within 60 miles of the nearest transplant center during the same study period,” said Dr. Liu.
The center receives referrals of patients who are potential candidates for liver transplant listing from practices throughout New Hampshire and Vermont, or from their own center. Their specialists conduct full testing, including a full liver transplant workup that includes evaluation of the patient’s general health and social factors, prior to sending the patient to the actual liver transplant center for their evaluation and transplant surgery. “We essentially do all of the pre–liver transplant workup, a formal liver transplant evaluation, and then the whole packet gets sent to an actual liver transplant center to expedite the process of getting listed for liver transplant. We’re able to streamline the process, so they get everything done here at a hospital near their home. If that requires multiple trips, it’s a lot more doable for the patients,” said Dr. Liu.
The researchers defined urban areas as having more than 50,000 people per square mile and within 30 miles of the nearest hospital, and rural as fewer than 10,000 and more than 60 miles from the nearest hospital. They used the Scientific Registry of Transplant Recipients to determine the number of liver transplant listings per zip code.
Between 2015 and 2019, the frequency of liver transplant listings per 10,000 people remained nearly unchanged in the metropolitan area of southern New Hampshire, ranging from around 0.36 to 0.75. In the rural area within 60 miles of DHMC, the frequency increased from about 0.7 per 10,000 in 2015 to about 1.4 in 2016 and 0.9 in 2017. There was an increase to nearly 3 in 10,000 in 2018, and the frequency was just over 2 in 2019.
The model has the potential to be used in other areas, according to Dr. Liu. “This could potentially be implemented in other rural areas that do not have a transplant center or don’t have a formal liver transplant evaluation process,” said Dr. Liu.
While other centers may have taken on some aspects of liver transplant evaluation and posttransplant care, the Virtual Liver Transplant Center is unique in that a great deal of effort has gone into covering all of a patient’s needs for the liver transplant evaluation. “It’s really the formalization that, from what I have researched, has not been done before,” said Dr. Liu.
The model addresses transplant-listing disparity, as well as improves patient quality of life through reduction in travel, according to Mayur Brahmania, MD, of Western University, London, Ont., who moderated the session. “They’ve proven that they can get more of their patients listed over the study period, which I think is amazing. The next step, I think, would be about whether getting them onto the transplant list actually made a difference in terms of outcome – looking at their wait list mortality, looking at how many of these patients actually got a liver transplantation. That’s the ultimate outcome,” said Dr. Brahmania.
He also noted the challenge of setting up a virtual center. “You have to have allied health staff – addiction counselors, physical therapists, dietitians, social workers. You need to have the appropriate ancillary services like cardiac testing, pulmonary function testing. It’s quite an endeavor, and if the program isn’t too enthusiastic or doesn’t have a local champion, it’s really hard to get something like this started off. So kudos to them for taking on this challenge and getting this up and running over the last 5 years,” said Dr. Brahmania.
Dr. Liu and Dr. Brahmania have no relevant financial disclosures.
A “virtual” liver transplant center servicing Vermont and New Hampshire has improved access to liver transplant listing among patients in rural areas of the region, according to a new analysis.
The virtual center was established in 2016 at Dartmouth Hitchcock Medical Center, and it allows patients to receive pre–liver transplant evaluations, testing, and care and posttransplant follow-up there rather than at the liver transplant center that conducts the surgery. The center includes two hepatologists, two associate care providers, and a nurse liver transplant coordinator at DHMC, and led to increased transplant listing in the vicinity, according to Margaret Liu, MD, who presented the study at the virtual annual meeting of the American Association for the Study of Liver Diseases.
“The initiation of this Virtual Liver Transplant Center has been able to provide patients with the ability to get a full liver transplant workup and evaluation at a center near their home rather than the often time-consuming and costly process of potentially multiple trips to a liver transplant center up to 250 miles away for a full transplant evaluation,” said Dr. Liu in an interview. Dr. Liu is an internal medicine resident at Dartmouth Hitchcock Medical Center.
“Our results did show that the initiation of a virtual liver transplant center correlated with an increased and sustained liver transplant listing rate within 60 miles of Dartmouth over that particular study period. Conversely there was no significant change in the listing rate of New Hampshire zip codes that were within 60 miles of the nearest transplant center during the same study period,” said Dr. Liu.
The center receives referrals of patients who are potential candidates for liver transplant listing from practices throughout New Hampshire and Vermont, or from their own center. Their specialists conduct full testing, including a full liver transplant workup that includes evaluation of the patient’s general health and social factors, prior to sending the patient to the actual liver transplant center for their evaluation and transplant surgery. “We essentially do all of the pre–liver transplant workup, a formal liver transplant evaluation, and then the whole packet gets sent to an actual liver transplant center to expedite the process of getting listed for liver transplant. We’re able to streamline the process, so they get everything done here at a hospital near their home. If that requires multiple trips, it’s a lot more doable for the patients,” said Dr. Liu.
The researchers defined urban areas as having more than 50,000 people per square mile and within 30 miles of the nearest hospital, and rural as fewer than 10,000 and more than 60 miles from the nearest hospital. They used the Scientific Registry of Transplant Recipients to determine the number of liver transplant listings per zip code.
Between 2015 and 2019, the frequency of liver transplant listings per 10,000 people remained nearly unchanged in the metropolitan area of southern New Hampshire, ranging from around 0.36 to 0.75. In the rural area within 60 miles of DHMC, the frequency increased from about 0.7 per 10,000 in 2015 to about 1.4 in 2016 and 0.9 in 2017. There was an increase to nearly 3 in 10,000 in 2018, and the frequency was just over 2 in 2019.
The model has the potential to be used in other areas, according to Dr. Liu. “This could potentially be implemented in other rural areas that do not have a transplant center or don’t have a formal liver transplant evaluation process,” said Dr. Liu.
While other centers may have taken on some aspects of liver transplant evaluation and posttransplant care, the Virtual Liver Transplant Center is unique in that a great deal of effort has gone into covering all of a patient’s needs for the liver transplant evaluation. “It’s really the formalization that, from what I have researched, has not been done before,” said Dr. Liu.
The model addresses transplant-listing disparity, as well as improves patient quality of life through reduction in travel, according to Mayur Brahmania, MD, of Western University, London, Ont., who moderated the session. “They’ve proven that they can get more of their patients listed over the study period, which I think is amazing. The next step, I think, would be about whether getting them onto the transplant list actually made a difference in terms of outcome – looking at their wait list mortality, looking at how many of these patients actually got a liver transplantation. That’s the ultimate outcome,” said Dr. Brahmania.
He also noted the challenge of setting up a virtual center. “You have to have allied health staff – addiction counselors, physical therapists, dietitians, social workers. You need to have the appropriate ancillary services like cardiac testing, pulmonary function testing. It’s quite an endeavor, and if the program isn’t too enthusiastic or doesn’t have a local champion, it’s really hard to get something like this started off. So kudos to them for taking on this challenge and getting this up and running over the last 5 years,” said Dr. Brahmania.
Dr. Liu and Dr. Brahmania have no relevant financial disclosures.
A “virtual” liver transplant center servicing Vermont and New Hampshire has improved access to liver transplant listing among patients in rural areas of the region, according to a new analysis.
The virtual center was established in 2016 at Dartmouth Hitchcock Medical Center, and it allows patients to receive pre–liver transplant evaluations, testing, and care and posttransplant follow-up there rather than at the liver transplant center that conducts the surgery. The center includes two hepatologists, two associate care providers, and a nurse liver transplant coordinator at DHMC, and led to increased transplant listing in the vicinity, according to Margaret Liu, MD, who presented the study at the virtual annual meeting of the American Association for the Study of Liver Diseases.
“The initiation of this Virtual Liver Transplant Center has been able to provide patients with the ability to get a full liver transplant workup and evaluation at a center near their home rather than the often time-consuming and costly process of potentially multiple trips to a liver transplant center up to 250 miles away for a full transplant evaluation,” said Dr. Liu in an interview. Dr. Liu is an internal medicine resident at Dartmouth Hitchcock Medical Center.
“Our results did show that the initiation of a virtual liver transplant center correlated with an increased and sustained liver transplant listing rate within 60 miles of Dartmouth over that particular study period. Conversely there was no significant change in the listing rate of New Hampshire zip codes that were within 60 miles of the nearest transplant center during the same study period,” said Dr. Liu.
The center receives referrals of patients who are potential candidates for liver transplant listing from practices throughout New Hampshire and Vermont, or from their own center. Their specialists conduct full testing, including a full liver transplant workup that includes evaluation of the patient’s general health and social factors, prior to sending the patient to the actual liver transplant center for their evaluation and transplant surgery. “We essentially do all of the pre–liver transplant workup, a formal liver transplant evaluation, and then the whole packet gets sent to an actual liver transplant center to expedite the process of getting listed for liver transplant. We’re able to streamline the process, so they get everything done here at a hospital near their home. If that requires multiple trips, it’s a lot more doable for the patients,” said Dr. Liu.
The researchers defined urban areas as having more than 50,000 people per square mile and within 30 miles of the nearest hospital, and rural as fewer than 10,000 and more than 60 miles from the nearest hospital. They used the Scientific Registry of Transplant Recipients to determine the number of liver transplant listings per zip code.
Between 2015 and 2019, the frequency of liver transplant listings per 10,000 people remained nearly unchanged in the metropolitan area of southern New Hampshire, ranging from around 0.36 to 0.75. In the rural area within 60 miles of DHMC, the frequency increased from about 0.7 per 10,000 in 2015 to about 1.4 in 2016 and 0.9 in 2017. There was an increase to nearly 3 in 10,000 in 2018, and the frequency was just over 2 in 2019.
The model has the potential to be used in other areas, according to Dr. Liu. “This could potentially be implemented in other rural areas that do not have a transplant center or don’t have a formal liver transplant evaluation process,” said Dr. Liu.
While other centers may have taken on some aspects of liver transplant evaluation and posttransplant care, the Virtual Liver Transplant Center is unique in that a great deal of effort has gone into covering all of a patient’s needs for the liver transplant evaluation. “It’s really the formalization that, from what I have researched, has not been done before,” said Dr. Liu.
The model addresses transplant-listing disparity, as well as improves patient quality of life through reduction in travel, according to Mayur Brahmania, MD, of Western University, London, Ont., who moderated the session. “They’ve proven that they can get more of their patients listed over the study period, which I think is amazing. The next step, I think, would be about whether getting them onto the transplant list actually made a difference in terms of outcome – looking at their wait list mortality, looking at how many of these patients actually got a liver transplantation. That’s the ultimate outcome,” said Dr. Brahmania.
He also noted the challenge of setting up a virtual center. “You have to have allied health staff – addiction counselors, physical therapists, dietitians, social workers. You need to have the appropriate ancillary services like cardiac testing, pulmonary function testing. It’s quite an endeavor, and if the program isn’t too enthusiastic or doesn’t have a local champion, it’s really hard to get something like this started off. So kudos to them for taking on this challenge and getting this up and running over the last 5 years,” said Dr. Brahmania.
Dr. Liu and Dr. Brahmania have no relevant financial disclosures.
FROM THE LIVER MEETING
Merck’s COVID-19 pill may be less effective than first hoped
According to an analysis by scientists at the Food and Drug Administration, the experimental pill cut the risk of hospitalization or death from COVID-19 by about 30%, compared to a placebo, and the pill showed no benefit for people with antibodies against COVID-19 from prior infection.
The updated analysis showed 48 hospitalizations or deaths among study participants who were randomly assigned to take the antiviral drug, compared to 68 among those who took a placebo.
Those results come from the full set of 1,433 patients who were randomized in the clinical trial, which just became available last week.
Initial results from the first 775 patients enrolled in the clinical trial, which were issued in a company news release in October, had said the drug cut the risk of hospitalization or death for patients at high risk of severe disease by about 50%.
Merck has been producing millions of doses of molnupiravir, which is the first antiviral pill to treat COVID-19 infections. The United Kingdom’s drug regulator authorized use of the medication in early November. The company said it expected to distribute the medication globally by the end of 2021.
In October, two Indian drug companies halted late-stage clinical trials of a generic version of molnupiravir after the studies failed to find any benefit to patients with moderate COVID-19. Trials in patients with milder symptoms are still ongoing.
On Nov. 27, the New England Journal of Medicine postponed its planned early release of the molnupiravir study results, citing “new information.”
The medication is designed to be given as four pills taken every 12 hours for 5 days. It’s most effective when taken within the first few days of new symptoms, something that requires convenient and affordable testing.
The new results seem to put molnupiravir far below the effectiveness of existing treatments.
The infused monoclonal antibody cocktail REGEN-COV, which the FDA has already authorized for emergency use, is about 85% effective at preventing hospitalization or death in patients who are at risk for severe COVID-19 outcomes, and it appears to be just as effective in people who already have antibodies against COVID-19, which is why it is being given to both vaccinated and unvaccinated patients, the FDA said.
In early November, Pfizer said its experimental antiviral pill Paxlovid cut the risk of hospitalization or death by 89%.
In briefing documents posted ahead of an advisory committee meeting Nov. 30, the FDA highlights other potential safety issues with the Merck drug, which works by causing the virus to make mistakes as it copies itself, eventually causing the virus to mutate itself to death.
The agency has asked the advisory committee to weigh in on the right patient population for the drug: Should pregnant women get it? Could the drug harm a developing fetus?
Should vaccinated people with breakthrough infections get it? Would it work for them? People with reduced immune function are more likely to get a breakthrough infection. They’re also more likely to shed virus for a longer period of time, making them perfect incubators for variants. What could happen if we give this type of patient a drug that increases mutations?
And what about mutations caused by the medication? Could they increase the potential for more variants? The agency concluded the risk of this happening was low.
In animal studies, the drug impacted bone formation. For this reason, the agency has agreed with the drug company that molnupiravir should not be given to anyone under the age of 18.
Aside from these concerns, the FDA says there were no major safety issues among people who took part in the clinical trial, though they acknowledge that number is small.
A version of this article first appeared on WebMD.com.
According to an analysis by scientists at the Food and Drug Administration, the experimental pill cut the risk of hospitalization or death from COVID-19 by about 30%, compared to a placebo, and the pill showed no benefit for people with antibodies against COVID-19 from prior infection.
The updated analysis showed 48 hospitalizations or deaths among study participants who were randomly assigned to take the antiviral drug, compared to 68 among those who took a placebo.
Those results come from the full set of 1,433 patients who were randomized in the clinical trial, which just became available last week.
Initial results from the first 775 patients enrolled in the clinical trial, which were issued in a company news release in October, had said the drug cut the risk of hospitalization or death for patients at high risk of severe disease by about 50%.
Merck has been producing millions of doses of molnupiravir, which is the first antiviral pill to treat COVID-19 infections. The United Kingdom’s drug regulator authorized use of the medication in early November. The company said it expected to distribute the medication globally by the end of 2021.
In October, two Indian drug companies halted late-stage clinical trials of a generic version of molnupiravir after the studies failed to find any benefit to patients with moderate COVID-19. Trials in patients with milder symptoms are still ongoing.
On Nov. 27, the New England Journal of Medicine postponed its planned early release of the molnupiravir study results, citing “new information.”
The medication is designed to be given as four pills taken every 12 hours for 5 days. It’s most effective when taken within the first few days of new symptoms, something that requires convenient and affordable testing.
The new results seem to put molnupiravir far below the effectiveness of existing treatments.
The infused monoclonal antibody cocktail REGEN-COV, which the FDA has already authorized for emergency use, is about 85% effective at preventing hospitalization or death in patients who are at risk for severe COVID-19 outcomes, and it appears to be just as effective in people who already have antibodies against COVID-19, which is why it is being given to both vaccinated and unvaccinated patients, the FDA said.
In early November, Pfizer said its experimental antiviral pill Paxlovid cut the risk of hospitalization or death by 89%.
In briefing documents posted ahead of an advisory committee meeting Nov. 30, the FDA highlights other potential safety issues with the Merck drug, which works by causing the virus to make mistakes as it copies itself, eventually causing the virus to mutate itself to death.
The agency has asked the advisory committee to weigh in on the right patient population for the drug: Should pregnant women get it? Could the drug harm a developing fetus?
Should vaccinated people with breakthrough infections get it? Would it work for them? People with reduced immune function are more likely to get a breakthrough infection. They’re also more likely to shed virus for a longer period of time, making them perfect incubators for variants. What could happen if we give this type of patient a drug that increases mutations?
And what about mutations caused by the medication? Could they increase the potential for more variants? The agency concluded the risk of this happening was low.
In animal studies, the drug impacted bone formation. For this reason, the agency has agreed with the drug company that molnupiravir should not be given to anyone under the age of 18.
Aside from these concerns, the FDA says there were no major safety issues among people who took part in the clinical trial, though they acknowledge that number is small.
A version of this article first appeared on WebMD.com.
According to an analysis by scientists at the Food and Drug Administration, the experimental pill cut the risk of hospitalization or death from COVID-19 by about 30%, compared to a placebo, and the pill showed no benefit for people with antibodies against COVID-19 from prior infection.
The updated analysis showed 48 hospitalizations or deaths among study participants who were randomly assigned to take the antiviral drug, compared to 68 among those who took a placebo.
Those results come from the full set of 1,433 patients who were randomized in the clinical trial, which just became available last week.
Initial results from the first 775 patients enrolled in the clinical trial, which were issued in a company news release in October, had said the drug cut the risk of hospitalization or death for patients at high risk of severe disease by about 50%.
Merck has been producing millions of doses of molnupiravir, which is the first antiviral pill to treat COVID-19 infections. The United Kingdom’s drug regulator authorized use of the medication in early November. The company said it expected to distribute the medication globally by the end of 2021.
In October, two Indian drug companies halted late-stage clinical trials of a generic version of molnupiravir after the studies failed to find any benefit to patients with moderate COVID-19. Trials in patients with milder symptoms are still ongoing.
On Nov. 27, the New England Journal of Medicine postponed its planned early release of the molnupiravir study results, citing “new information.”
The medication is designed to be given as four pills taken every 12 hours for 5 days. It’s most effective when taken within the first few days of new symptoms, something that requires convenient and affordable testing.
The new results seem to put molnupiravir far below the effectiveness of existing treatments.
The infused monoclonal antibody cocktail REGEN-COV, which the FDA has already authorized for emergency use, is about 85% effective at preventing hospitalization or death in patients who are at risk for severe COVID-19 outcomes, and it appears to be just as effective in people who already have antibodies against COVID-19, which is why it is being given to both vaccinated and unvaccinated patients, the FDA said.
In early November, Pfizer said its experimental antiviral pill Paxlovid cut the risk of hospitalization or death by 89%.
In briefing documents posted ahead of an advisory committee meeting Nov. 30, the FDA highlights other potential safety issues with the Merck drug, which works by causing the virus to make mistakes as it copies itself, eventually causing the virus to mutate itself to death.
The agency has asked the advisory committee to weigh in on the right patient population for the drug: Should pregnant women get it? Could the drug harm a developing fetus?
Should vaccinated people with breakthrough infections get it? Would it work for them? People with reduced immune function are more likely to get a breakthrough infection. They’re also more likely to shed virus for a longer period of time, making them perfect incubators for variants. What could happen if we give this type of patient a drug that increases mutations?
And what about mutations caused by the medication? Could they increase the potential for more variants? The agency concluded the risk of this happening was low.
In animal studies, the drug impacted bone formation. For this reason, the agency has agreed with the drug company that molnupiravir should not be given to anyone under the age of 18.
Aside from these concerns, the FDA says there were no major safety issues among people who took part in the clinical trial, though they acknowledge that number is small.
A version of this article first appeared on WebMD.com.
Best of MS
Good data is lacking on best first-line MS drug strategies
Personalized medicine is just about the biggest buzzword in health. But neurologist Ellen M. Mowry, MD, of Johns Hopkins University, Baltimore, steers patients with multiple sclerosis (MS) away from the concept when she first starts talking to them about initial therapy options and possible ways to forestall disability down the line.
Good data is lacking on best first-line MS drug strategies
Personalized medicine is just about the biggest buzzword in health. But neurologist Ellen M. Mowry, MD, of Johns Hopkins University, Baltimore, steers patients with multiple sclerosis (MS) away from the concept when she first starts talking to them about initial therapy options and possible ways to forestall disability down the line.
Good data is lacking on best first-line MS drug strategies
Personalized medicine is just about the biggest buzzword in health. But neurologist Ellen M. Mowry, MD, of Johns Hopkins University, Baltimore, steers patients with multiple sclerosis (MS) away from the concept when she first starts talking to them about initial therapy options and possible ways to forestall disability down the line.