User login
Sealing the envelope
Mike died last week.
He was a long-retired doc, in his mid-90s. One of my favorite patients to just chat with about nothing in particular. I learned more from him about restoring old grandfather clocks than I ever dreamed I’d know.
After receiving the sad news, I sat down, as I often do, to write a letter to his family. After 23 years I have a pretty standard idea of what I want to say, but it still always takes some thought.
Sealing the envelopes on these letters always seems to be more than just paperwork. There’s a symbolism to it, that I’m closing out my relationship, sometimes of 10-20 years, with the person involved.
Some patients become friends after a time. It’s a matter of chemistry. I don’t socialize with them outside my office, but still enjoy seeing them and talking about nonmedical stuff in the space around clinical questions and answers. They’re the ones it’s hardest to say goodbye to.
I’ll miss my 2-3 visits a year with Mike. We swapped medical war stories, family anecdotes, and the occasional tip about clock restoration that I’ll probably never use (but who knows, he didn’t start until after he retired).
Closing the envelope comes with the realization that I won’t be seeing him again. I don’t go to patient funerals, as I believe those are for families and close friends, and so writing the letter is the closest I’ll get to saying goodbye.
Medicine, and how we practice, is focused on what we do for the patient – which is what it should be.
But lost in the shuffle sometimes is realizing what the patient does for us. That’s also important, but harder to quantify. And sometimes we don’t realize it until we seal the envelope.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mike died last week.
He was a long-retired doc, in his mid-90s. One of my favorite patients to just chat with about nothing in particular. I learned more from him about restoring old grandfather clocks than I ever dreamed I’d know.
After receiving the sad news, I sat down, as I often do, to write a letter to his family. After 23 years I have a pretty standard idea of what I want to say, but it still always takes some thought.
Sealing the envelopes on these letters always seems to be more than just paperwork. There’s a symbolism to it, that I’m closing out my relationship, sometimes of 10-20 years, with the person involved.
Some patients become friends after a time. It’s a matter of chemistry. I don’t socialize with them outside my office, but still enjoy seeing them and talking about nonmedical stuff in the space around clinical questions and answers. They’re the ones it’s hardest to say goodbye to.
I’ll miss my 2-3 visits a year with Mike. We swapped medical war stories, family anecdotes, and the occasional tip about clock restoration that I’ll probably never use (but who knows, he didn’t start until after he retired).
Closing the envelope comes with the realization that I won’t be seeing him again. I don’t go to patient funerals, as I believe those are for families and close friends, and so writing the letter is the closest I’ll get to saying goodbye.
Medicine, and how we practice, is focused on what we do for the patient – which is what it should be.
But lost in the shuffle sometimes is realizing what the patient does for us. That’s also important, but harder to quantify. And sometimes we don’t realize it until we seal the envelope.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mike died last week.
He was a long-retired doc, in his mid-90s. One of my favorite patients to just chat with about nothing in particular. I learned more from him about restoring old grandfather clocks than I ever dreamed I’d know.
After receiving the sad news, I sat down, as I often do, to write a letter to his family. After 23 years I have a pretty standard idea of what I want to say, but it still always takes some thought.
Sealing the envelopes on these letters always seems to be more than just paperwork. There’s a symbolism to it, that I’m closing out my relationship, sometimes of 10-20 years, with the person involved.
Some patients become friends after a time. It’s a matter of chemistry. I don’t socialize with them outside my office, but still enjoy seeing them and talking about nonmedical stuff in the space around clinical questions and answers. They’re the ones it’s hardest to say goodbye to.
I’ll miss my 2-3 visits a year with Mike. We swapped medical war stories, family anecdotes, and the occasional tip about clock restoration that I’ll probably never use (but who knows, he didn’t start until after he retired).
Closing the envelope comes with the realization that I won’t be seeing him again. I don’t go to patient funerals, as I believe those are for families and close friends, and so writing the letter is the closest I’ll get to saying goodbye.
Medicine, and how we practice, is focused on what we do for the patient – which is what it should be.
But lost in the shuffle sometimes is realizing what the patient does for us. That’s also important, but harder to quantify. And sometimes we don’t realize it until we seal the envelope.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In Zambia, PCR tracks pertussis
In the periurban slum of Lusaka, Zambia, asymptomatic pertussis infections were common among both mothers and infants, a surprising finding since asymptomatic infections are assumed to be rare in infants. The findings suggested that pertussis should be considered in cases of chronic cough, and that current standards of treating pertussis infections in low-resource settings may need to be reexamined.
The results come from testing of 1,320 infant-mother pairs who were first enrolled at a public health clinic, then followed over at least four visits. The researchers tracked pertussis infection using quantitative PCR (qPCR) on nasopharyngeal swabs. Over the course of the study, 8.9% tested positive, although only one infant developed clinical pertussis during the study.
The study was presented by Christian Gunning, a postdoctoral researcher at the University of Georgia, at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. The group also included researchers at Boston University and the University of Zambia, where PCR tests were conducted.
“That was amazing,” said session moderator Vana Spoulou, MD, PhD, professor of pediatric infectious diseases at National and Kapodistrian University of Athens, who is associated with Aghia Sofia Children’s Hospital of Athens. She noted that the study found that many physicians misdiagnosed coughs, believing them to be caused by another agent. “It was very interesting that there was so much pertussis spreading around in that community, and that nobody knew that it was around,” said Dr. Spoulou.
It’s important that physicians provide appropriate treatment, since ampicillin, which is typically prescribed for childhood upper respiratory illnesses, is believed to be ineffective against pertussis, while macrolides are effective and can prevent transmission.
Dr. Spoulou also noted that Zambia uses a whole cell vaccine, which is contraindicated in pregnant women because of potential side effects. “The good thing, despite that there was [a lot of] infection, there were no deaths, which means that maybe because the mother was infected, maybe some antibodies of the mother had passed to the child and could help the child to develop milder symptoms. So these are the pros and cons of natural infection,” said Dr. Spoulou.
The study took place in 2015, and participants were seen at the Chawama Public Health Clinic from about age 1 week to 4 months (with a target of seven clinic visits). Researchers recorded respiratory symptoms and antibiotics use at each visit, and collected a nasopharyngeal swab that was tested retrospectively using qPCR for Bordetella pertussis.
Real-time PCR analysis of the samples yields the CT value, which represents the number of amplification cycles that the PCR test must complete before Bordetella pertussis is detectable. The fewer the cycles (and the lower the CT value), the more infectious particles must have been present in the sample. For pertussis testing, a value below 35 is considered a clinically positive result. Tests that come back with higher CT values are increasingly likely to be false positives.
The researchers plotted a value called evidence for infection (EFI), which combined a range of CT values with the number of positive tests over the seven clinic visits to group patients into none, weak, or strong EFI. Among infants with no symptoms, 77% were in the no EFI category, 16% were in the weak category, and 7% were in the strong EFI group. Of infants with minimal respiratory symptoms, 18% were in the strong group, and 20% with moderate to severe symptoms were in the strong EFI group. Among mothers, 13% with no symptoms were in the strong group. 19% in the minimal symptom group were categorized as strong EFI, as were 11% in the moderate to severe symptom group.
The study used a full range of CT, not just positive test results (for pertussis, CT ≤ 35). Beyond contributing to composite measures such as EFI, CT values can serve as leading indicators of infectious disease outbreaks in a population, according to Dr. Gunning. That’s because weaker qPCR signals (CT > 35) can provide additional information within a large sample population. Higher CT values are successively more prone to false positives, but that’s less important for disease surveillance where sensitivity is of the highest importance. The false positive “noise” tends to cancel out over time. “It may be the case that you don’t make that call (correctly) 100% of the time for 100% of the people, but if you get it right in 80 out of 100 people, that’s sufficient to say we see this pathogen circulating in the population,” said Dr. Gunning.
The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Gunning and Dr. Spoulou have no relevant financial disclosures.
In the periurban slum of Lusaka, Zambia, asymptomatic pertussis infections were common among both mothers and infants, a surprising finding since asymptomatic infections are assumed to be rare in infants. The findings suggested that pertussis should be considered in cases of chronic cough, and that current standards of treating pertussis infections in low-resource settings may need to be reexamined.
The results come from testing of 1,320 infant-mother pairs who were first enrolled at a public health clinic, then followed over at least four visits. The researchers tracked pertussis infection using quantitative PCR (qPCR) on nasopharyngeal swabs. Over the course of the study, 8.9% tested positive, although only one infant developed clinical pertussis during the study.
The study was presented by Christian Gunning, a postdoctoral researcher at the University of Georgia, at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. The group also included researchers at Boston University and the University of Zambia, where PCR tests were conducted.
“That was amazing,” said session moderator Vana Spoulou, MD, PhD, professor of pediatric infectious diseases at National and Kapodistrian University of Athens, who is associated with Aghia Sofia Children’s Hospital of Athens. She noted that the study found that many physicians misdiagnosed coughs, believing them to be caused by another agent. “It was very interesting that there was so much pertussis spreading around in that community, and that nobody knew that it was around,” said Dr. Spoulou.
It’s important that physicians provide appropriate treatment, since ampicillin, which is typically prescribed for childhood upper respiratory illnesses, is believed to be ineffective against pertussis, while macrolides are effective and can prevent transmission.
Dr. Spoulou also noted that Zambia uses a whole cell vaccine, which is contraindicated in pregnant women because of potential side effects. “The good thing, despite that there was [a lot of] infection, there were no deaths, which means that maybe because the mother was infected, maybe some antibodies of the mother had passed to the child and could help the child to develop milder symptoms. So these are the pros and cons of natural infection,” said Dr. Spoulou.
The study took place in 2015, and participants were seen at the Chawama Public Health Clinic from about age 1 week to 4 months (with a target of seven clinic visits). Researchers recorded respiratory symptoms and antibiotics use at each visit, and collected a nasopharyngeal swab that was tested retrospectively using qPCR for Bordetella pertussis.
Real-time PCR analysis of the samples yields the CT value, which represents the number of amplification cycles that the PCR test must complete before Bordetella pertussis is detectable. The fewer the cycles (and the lower the CT value), the more infectious particles must have been present in the sample. For pertussis testing, a value below 35 is considered a clinically positive result. Tests that come back with higher CT values are increasingly likely to be false positives.
The researchers plotted a value called evidence for infection (EFI), which combined a range of CT values with the number of positive tests over the seven clinic visits to group patients into none, weak, or strong EFI. Among infants with no symptoms, 77% were in the no EFI category, 16% were in the weak category, and 7% were in the strong EFI group. Of infants with minimal respiratory symptoms, 18% were in the strong group, and 20% with moderate to severe symptoms were in the strong EFI group. Among mothers, 13% with no symptoms were in the strong group. 19% in the minimal symptom group were categorized as strong EFI, as were 11% in the moderate to severe symptom group.
The study used a full range of CT, not just positive test results (for pertussis, CT ≤ 35). Beyond contributing to composite measures such as EFI, CT values can serve as leading indicators of infectious disease outbreaks in a population, according to Dr. Gunning. That’s because weaker qPCR signals (CT > 35) can provide additional information within a large sample population. Higher CT values are successively more prone to false positives, but that’s less important for disease surveillance where sensitivity is of the highest importance. The false positive “noise” tends to cancel out over time. “It may be the case that you don’t make that call (correctly) 100% of the time for 100% of the people, but if you get it right in 80 out of 100 people, that’s sufficient to say we see this pathogen circulating in the population,” said Dr. Gunning.
The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Gunning and Dr. Spoulou have no relevant financial disclosures.
In the periurban slum of Lusaka, Zambia, asymptomatic pertussis infections were common among both mothers and infants, a surprising finding since asymptomatic infections are assumed to be rare in infants. The findings suggested that pertussis should be considered in cases of chronic cough, and that current standards of treating pertussis infections in low-resource settings may need to be reexamined.
The results come from testing of 1,320 infant-mother pairs who were first enrolled at a public health clinic, then followed over at least four visits. The researchers tracked pertussis infection using quantitative PCR (qPCR) on nasopharyngeal swabs. Over the course of the study, 8.9% tested positive, although only one infant developed clinical pertussis during the study.
The study was presented by Christian Gunning, a postdoctoral researcher at the University of Georgia, at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. The group also included researchers at Boston University and the University of Zambia, where PCR tests were conducted.
“That was amazing,” said session moderator Vana Spoulou, MD, PhD, professor of pediatric infectious diseases at National and Kapodistrian University of Athens, who is associated with Aghia Sofia Children’s Hospital of Athens. She noted that the study found that many physicians misdiagnosed coughs, believing them to be caused by another agent. “It was very interesting that there was so much pertussis spreading around in that community, and that nobody knew that it was around,” said Dr. Spoulou.
It’s important that physicians provide appropriate treatment, since ampicillin, which is typically prescribed for childhood upper respiratory illnesses, is believed to be ineffective against pertussis, while macrolides are effective and can prevent transmission.
Dr. Spoulou also noted that Zambia uses a whole cell vaccine, which is contraindicated in pregnant women because of potential side effects. “The good thing, despite that there was [a lot of] infection, there were no deaths, which means that maybe because the mother was infected, maybe some antibodies of the mother had passed to the child and could help the child to develop milder symptoms. So these are the pros and cons of natural infection,” said Dr. Spoulou.
The study took place in 2015, and participants were seen at the Chawama Public Health Clinic from about age 1 week to 4 months (with a target of seven clinic visits). Researchers recorded respiratory symptoms and antibiotics use at each visit, and collected a nasopharyngeal swab that was tested retrospectively using qPCR for Bordetella pertussis.
Real-time PCR analysis of the samples yields the CT value, which represents the number of amplification cycles that the PCR test must complete before Bordetella pertussis is detectable. The fewer the cycles (and the lower the CT value), the more infectious particles must have been present in the sample. For pertussis testing, a value below 35 is considered a clinically positive result. Tests that come back with higher CT values are increasingly likely to be false positives.
The researchers plotted a value called evidence for infection (EFI), which combined a range of CT values with the number of positive tests over the seven clinic visits to group patients into none, weak, or strong EFI. Among infants with no symptoms, 77% were in the no EFI category, 16% were in the weak category, and 7% were in the strong EFI group. Of infants with minimal respiratory symptoms, 18% were in the strong group, and 20% with moderate to severe symptoms were in the strong EFI group. Among mothers, 13% with no symptoms were in the strong group. 19% in the minimal symptom group were categorized as strong EFI, as were 11% in the moderate to severe symptom group.
The study used a full range of CT, not just positive test results (for pertussis, CT ≤ 35). Beyond contributing to composite measures such as EFI, CT values can serve as leading indicators of infectious disease outbreaks in a population, according to Dr. Gunning. That’s because weaker qPCR signals (CT > 35) can provide additional information within a large sample population. Higher CT values are successively more prone to false positives, but that’s less important for disease surveillance where sensitivity is of the highest importance. The false positive “noise” tends to cancel out over time. “It may be the case that you don’t make that call (correctly) 100% of the time for 100% of the people, but if you get it right in 80 out of 100 people, that’s sufficient to say we see this pathogen circulating in the population,” said Dr. Gunning.
The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Gunning and Dr. Spoulou have no relevant financial disclosures.
FROM ESPID 2021
Children aged 12-15 years continue to close COVID-19 vaccination gap
More children aged 12-15 years already have received at least one dose of a COVID-19 vaccine than have 16- and 17-year-olds, based on data from the Centers for Disease Control and Prevention.
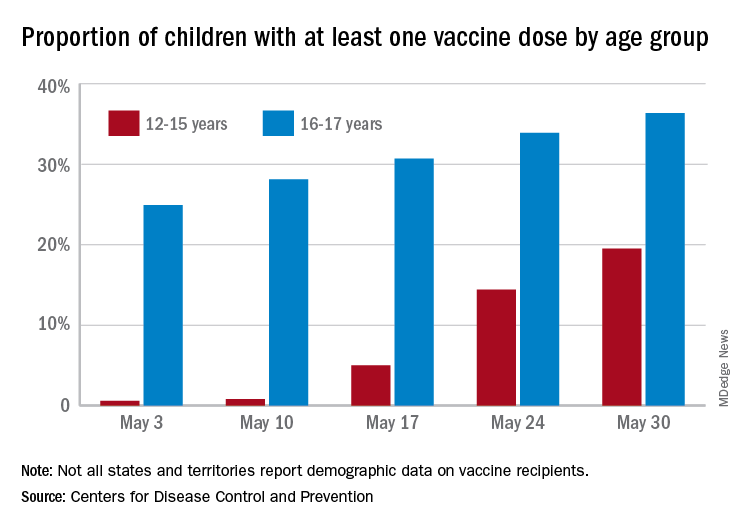
with those figures representing increases of 31.6% and 6.6% in the past week, respectively. Since the overall size of the 12-15 population is much larger, however, the proportion vaccinated is still smaller: 19.5% to 36.4%, according to the CDC’s COVID Data Tracker.
A look at full vaccination status shows that only 0.7% of those aged 12-15 years have received both doses of a two-dose vaccine or one dose of the single-shot variety, compared with 24% of those aged 16-17. For the country as a whole, 50.5% of all ages have received at least one dose and 40.7% are fully vaccinated, the CDC said.
Children aged 12-15 represent the largest share of the U.S. population (23.4%) initiating vaccination in the 14 days ending May 30, while children aged 16-17 made up just 4.5% of those getting their first dose. The younger group’s later entry into the vaccination pool shows up again when looking at completion rates, though, representing just 0.4% of all Americans who reached full vaccination during that same 14-day period, compared with 4.6% of the older children, the CDC data show.
Not all states are reporting data such as age for vaccine recipients, the CDC noted, and there are other variables that affect data collection. “Demographic data ... might differ by populations prioritized within each state or jurisdiction’s vaccination phase. Every geographic area has a different racial and ethnic composition, and not all are in the same vaccination phase,” the CDC said.
More children aged 12-15 years already have received at least one dose of a COVID-19 vaccine than have 16- and 17-year-olds, based on data from the Centers for Disease Control and Prevention.
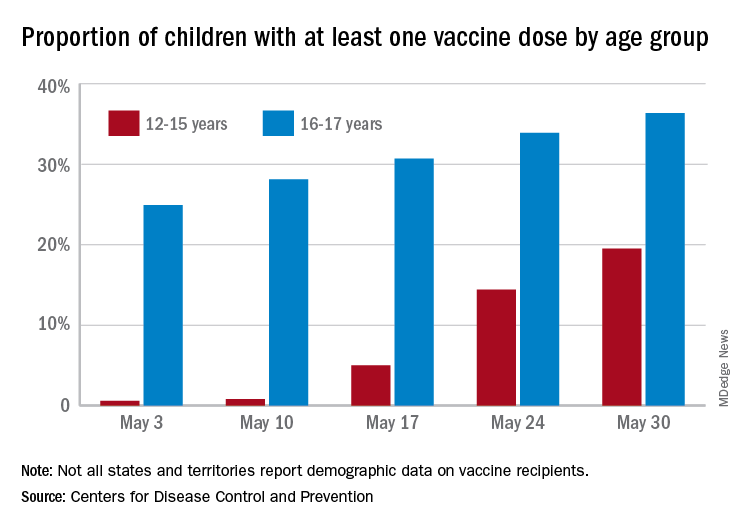
with those figures representing increases of 31.6% and 6.6% in the past week, respectively. Since the overall size of the 12-15 population is much larger, however, the proportion vaccinated is still smaller: 19.5% to 36.4%, according to the CDC’s COVID Data Tracker.
A look at full vaccination status shows that only 0.7% of those aged 12-15 years have received both doses of a two-dose vaccine or one dose of the single-shot variety, compared with 24% of those aged 16-17. For the country as a whole, 50.5% of all ages have received at least one dose and 40.7% are fully vaccinated, the CDC said.
Children aged 12-15 represent the largest share of the U.S. population (23.4%) initiating vaccination in the 14 days ending May 30, while children aged 16-17 made up just 4.5% of those getting their first dose. The younger group’s later entry into the vaccination pool shows up again when looking at completion rates, though, representing just 0.4% of all Americans who reached full vaccination during that same 14-day period, compared with 4.6% of the older children, the CDC data show.
Not all states are reporting data such as age for vaccine recipients, the CDC noted, and there are other variables that affect data collection. “Demographic data ... might differ by populations prioritized within each state or jurisdiction’s vaccination phase. Every geographic area has a different racial and ethnic composition, and not all are in the same vaccination phase,” the CDC said.
More children aged 12-15 years already have received at least one dose of a COVID-19 vaccine than have 16- and 17-year-olds, based on data from the Centers for Disease Control and Prevention.
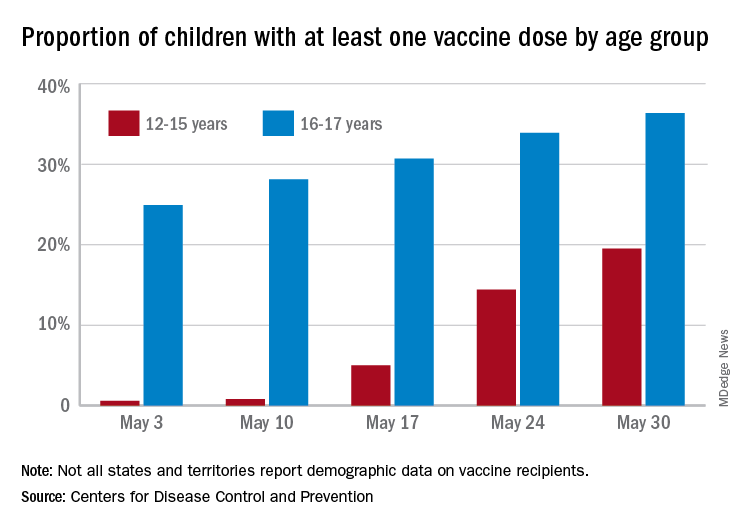
with those figures representing increases of 31.6% and 6.6% in the past week, respectively. Since the overall size of the 12-15 population is much larger, however, the proportion vaccinated is still smaller: 19.5% to 36.4%, according to the CDC’s COVID Data Tracker.
A look at full vaccination status shows that only 0.7% of those aged 12-15 years have received both doses of a two-dose vaccine or one dose of the single-shot variety, compared with 24% of those aged 16-17. For the country as a whole, 50.5% of all ages have received at least one dose and 40.7% are fully vaccinated, the CDC said.
Children aged 12-15 represent the largest share of the U.S. population (23.4%) initiating vaccination in the 14 days ending May 30, while children aged 16-17 made up just 4.5% of those getting their first dose. The younger group’s later entry into the vaccination pool shows up again when looking at completion rates, though, representing just 0.4% of all Americans who reached full vaccination during that same 14-day period, compared with 4.6% of the older children, the CDC data show.
Not all states are reporting data such as age for vaccine recipients, the CDC noted, and there are other variables that affect data collection. “Demographic data ... might differ by populations prioritized within each state or jurisdiction’s vaccination phase. Every geographic area has a different racial and ethnic composition, and not all are in the same vaccination phase,” the CDC said.
Clinical Edge Journal Scan Commentary: EPI June 2021
In the study, 60 patients were classified as having EPI based on the gold standard test of PABA excretion, then the FBHC of the two groups were compared. According to the study findings FBHC levels were higher in the EPI group 15.70 (1.4 to 77.0) ppm than in the non-PEI group 2.80 (0.7 to 28.2) ppm (P < 0.0001). The cutoff value for FBHC of 10.7 ppm (95% CI: 0.678–0.913; P < 0.001) showed a sensitivity of 73.3% and a specificity of 83.3% for PEI diagnosis. Interestingly, to prove biologic plausibility, the researchers also looked at microbiome analysis and found that there was a significant increase of relative abundance of phylum Firmicutes (P < 0.05) and the genus Clostridium (P < 0.05) in the EPI group. The researchers suggested that the flow of undigested food in EPI may select for Clorstridia species, which are the main hydrogen producing bacteria in the intestine.
In AZN Journal of Surgery, Chan-Min Choi, et al looked at management of palliative stage pancreatic ductal adenocarcinomas (PDAC) in 67 patients with locally advanced or metastatic pancreatic cancer at Western Health in Melbourne.2 Weight loss and steatorrhea were present in 83.6% and 13.4% of patients, respectively, and median body mass index decreased by 13.3% from pre-illness to cancer diagnosis. Yet, despite high rates of referral to dieticians (79.1%), only 24 patients were prescribed pancreatic enzyme replacement therapy. The researchers concluded that the "study shows a lack of clear guideline for diagnosis and management of EPI for palliative PDAC.”
Finally a study by Johnston et al. in Gastroenterology looked at predictors of exocrine pancreatic insufficiency in 68 patients who underwent pancreatectomy (distal, n=23; pancreaticoduodenectomy, n=45).3 EPI, requiring pancreatic enzyme replacement therapy, developed in 50% of patients at 1-year postpancreatectomy. The researchers looked at predictors of EPI including variables such as preoperative A1c, smoking status, neoadjuvant chemo and radio therapy, and age, among others. In the final multivariate analysis, the only factor associated with EPI development was postoperative remnant pancreas volume (odds ratio, 0.93; 95% CI, 0.88-0.98; P < 0.01). While these studies may not immediately change practice, they offer further steps in the direction towards better diagnostics and more appropriate management of EPI.
References
1. Uetsuki K, Kawashima H, Ohno E, et al. Measurement of fasting breath hydrogen concentration as a simple diagnostic method for pancreatic exocrine insufficiency. BMC Gastroenterol 2021;21(1):211.
2. Choi CC-M, Choi J, Houli N, et al. Evaluation of palliative treatments in unresectable pancreatic cancer. ANZ J Surg 2021;
3. Johnston ME, Wahab SA, Turner K, et al. 298 post-pancreatectomy volumetric analysis: a missing variable in the development of post-operative endocrine and exocrine dysfunction. Gastroenterology 2021;160(6):S-878.
In the study, 60 patients were classified as having EPI based on the gold standard test of PABA excretion, then the FBHC of the two groups were compared. According to the study findings FBHC levels were higher in the EPI group 15.70 (1.4 to 77.0) ppm than in the non-PEI group 2.80 (0.7 to 28.2) ppm (P < 0.0001). The cutoff value for FBHC of 10.7 ppm (95% CI: 0.678–0.913; P < 0.001) showed a sensitivity of 73.3% and a specificity of 83.3% for PEI diagnosis. Interestingly, to prove biologic plausibility, the researchers also looked at microbiome analysis and found that there was a significant increase of relative abundance of phylum Firmicutes (P < 0.05) and the genus Clostridium (P < 0.05) in the EPI group. The researchers suggested that the flow of undigested food in EPI may select for Clorstridia species, which are the main hydrogen producing bacteria in the intestine.
In AZN Journal of Surgery, Chan-Min Choi, et al looked at management of palliative stage pancreatic ductal adenocarcinomas (PDAC) in 67 patients with locally advanced or metastatic pancreatic cancer at Western Health in Melbourne.2 Weight loss and steatorrhea were present in 83.6% and 13.4% of patients, respectively, and median body mass index decreased by 13.3% from pre-illness to cancer diagnosis. Yet, despite high rates of referral to dieticians (79.1%), only 24 patients were prescribed pancreatic enzyme replacement therapy. The researchers concluded that the "study shows a lack of clear guideline for diagnosis and management of EPI for palliative PDAC.”
Finally a study by Johnston et al. in Gastroenterology looked at predictors of exocrine pancreatic insufficiency in 68 patients who underwent pancreatectomy (distal, n=23; pancreaticoduodenectomy, n=45).3 EPI, requiring pancreatic enzyme replacement therapy, developed in 50% of patients at 1-year postpancreatectomy. The researchers looked at predictors of EPI including variables such as preoperative A1c, smoking status, neoadjuvant chemo and radio therapy, and age, among others. In the final multivariate analysis, the only factor associated with EPI development was postoperative remnant pancreas volume (odds ratio, 0.93; 95% CI, 0.88-0.98; P < 0.01). While these studies may not immediately change practice, they offer further steps in the direction towards better diagnostics and more appropriate management of EPI.
References
1. Uetsuki K, Kawashima H, Ohno E, et al. Measurement of fasting breath hydrogen concentration as a simple diagnostic method for pancreatic exocrine insufficiency. BMC Gastroenterol 2021;21(1):211.
2. Choi CC-M, Choi J, Houli N, et al. Evaluation of palliative treatments in unresectable pancreatic cancer. ANZ J Surg 2021;
3. Johnston ME, Wahab SA, Turner K, et al. 298 post-pancreatectomy volumetric analysis: a missing variable in the development of post-operative endocrine and exocrine dysfunction. Gastroenterology 2021;160(6):S-878.
In the study, 60 patients were classified as having EPI based on the gold standard test of PABA excretion, then the FBHC of the two groups were compared. According to the study findings FBHC levels were higher in the EPI group 15.70 (1.4 to 77.0) ppm than in the non-PEI group 2.80 (0.7 to 28.2) ppm (P < 0.0001). The cutoff value for FBHC of 10.7 ppm (95% CI: 0.678–0.913; P < 0.001) showed a sensitivity of 73.3% and a specificity of 83.3% for PEI diagnosis. Interestingly, to prove biologic plausibility, the researchers also looked at microbiome analysis and found that there was a significant increase of relative abundance of phylum Firmicutes (P < 0.05) and the genus Clostridium (P < 0.05) in the EPI group. The researchers suggested that the flow of undigested food in EPI may select for Clorstridia species, which are the main hydrogen producing bacteria in the intestine.
In AZN Journal of Surgery, Chan-Min Choi, et al looked at management of palliative stage pancreatic ductal adenocarcinomas (PDAC) in 67 patients with locally advanced or metastatic pancreatic cancer at Western Health in Melbourne.2 Weight loss and steatorrhea were present in 83.6% and 13.4% of patients, respectively, and median body mass index decreased by 13.3% from pre-illness to cancer diagnosis. Yet, despite high rates of referral to dieticians (79.1%), only 24 patients were prescribed pancreatic enzyme replacement therapy. The researchers concluded that the "study shows a lack of clear guideline for diagnosis and management of EPI for palliative PDAC.”
Finally a study by Johnston et al. in Gastroenterology looked at predictors of exocrine pancreatic insufficiency in 68 patients who underwent pancreatectomy (distal, n=23; pancreaticoduodenectomy, n=45).3 EPI, requiring pancreatic enzyme replacement therapy, developed in 50% of patients at 1-year postpancreatectomy. The researchers looked at predictors of EPI including variables such as preoperative A1c, smoking status, neoadjuvant chemo and radio therapy, and age, among others. In the final multivariate analysis, the only factor associated with EPI development was postoperative remnant pancreas volume (odds ratio, 0.93; 95% CI, 0.88-0.98; P < 0.01). While these studies may not immediately change practice, they offer further steps in the direction towards better diagnostics and more appropriate management of EPI.
References
1. Uetsuki K, Kawashima H, Ohno E, et al. Measurement of fasting breath hydrogen concentration as a simple diagnostic method for pancreatic exocrine insufficiency. BMC Gastroenterol 2021;21(1):211.
2. Choi CC-M, Choi J, Houli N, et al. Evaluation of palliative treatments in unresectable pancreatic cancer. ANZ J Surg 2021;
3. Johnston ME, Wahab SA, Turner K, et al. 298 post-pancreatectomy volumetric analysis: a missing variable in the development of post-operative endocrine and exocrine dysfunction. Gastroenterology 2021;160(6):S-878.
Gastroenterologist follow-up improves EPI management in pancreatic disorders
Key clinical point: Patients with chronic pancreatitis, pancreatic cancer, and pancreatic resection, followed-up by a gastroenterologist had higher rates of screening for exocrine pancreatic insufficiency (EPI) and appropriate prescription of pancreatic enzyme replacement therapy (PERT).
Major finding: EPI screening by measurement of pancreatic elastase (odds ratio [OR], 5.94; P less than .001), PERT prescription (OR, 2.02; P less than .001), and prescription for a minimally effective dosage (OR, 1.5; P = .008) was higher in patients followed-up by gastroenterologist (n=470) vs. those who were not (n=994).
Study details: This retrospective study assessed 1,464 patients with either EPI, chronic pancreatitis, pancreatic cancer, or pancreatic resection at the University of Florida between February 2018 and February 2020.
Disclosures: No source of funding was identified.
Source: Ladna M et al. Gastroenterology. 2021 May 10. doi: 10.1016/S0016-5085(21)01015-5.
Key clinical point: Patients with chronic pancreatitis, pancreatic cancer, and pancreatic resection, followed-up by a gastroenterologist had higher rates of screening for exocrine pancreatic insufficiency (EPI) and appropriate prescription of pancreatic enzyme replacement therapy (PERT).
Major finding: EPI screening by measurement of pancreatic elastase (odds ratio [OR], 5.94; P less than .001), PERT prescription (OR, 2.02; P less than .001), and prescription for a minimally effective dosage (OR, 1.5; P = .008) was higher in patients followed-up by gastroenterologist (n=470) vs. those who were not (n=994).
Study details: This retrospective study assessed 1,464 patients with either EPI, chronic pancreatitis, pancreatic cancer, or pancreatic resection at the University of Florida between February 2018 and February 2020.
Disclosures: No source of funding was identified.
Source: Ladna M et al. Gastroenterology. 2021 May 10. doi: 10.1016/S0016-5085(21)01015-5.
Key clinical point: Patients with chronic pancreatitis, pancreatic cancer, and pancreatic resection, followed-up by a gastroenterologist had higher rates of screening for exocrine pancreatic insufficiency (EPI) and appropriate prescription of pancreatic enzyme replacement therapy (PERT).
Major finding: EPI screening by measurement of pancreatic elastase (odds ratio [OR], 5.94; P less than .001), PERT prescription (OR, 2.02; P less than .001), and prescription for a minimally effective dosage (OR, 1.5; P = .008) was higher in patients followed-up by gastroenterologist (n=470) vs. those who were not (n=994).
Study details: This retrospective study assessed 1,464 patients with either EPI, chronic pancreatitis, pancreatic cancer, or pancreatic resection at the University of Florida between February 2018 and February 2020.
Disclosures: No source of funding was identified.
Source: Ladna M et al. Gastroenterology. 2021 May 10. doi: 10.1016/S0016-5085(21)01015-5.
Postoperative pancreas remnant volume associated with EPI development after pancreatectomy
Key clinical point: Postoperative pancreas remnant volume was associated with the development of exocrine pancreatic insufficiency (EPI) after pancreatic resection.
Major finding: EPI, requiring pancreatic enzyme replacement therapy, developed in 50% of patients at 1-year postpancreatectomy. The incidence of EPI was higher in patients receiving Whipple vs. distal pancreatectomy (66% vs. 21%; P = .004). The only factor associated with EPI development was postoperative remnant pancreas volume (odds ratio, 0.93; 95% confidence interval, 0.88-0.98; P less than .01).
Study details: This study included 68 patients who underwent pancreatectomy (distal, n=23; pancreaticoduodenectomy, n=45) at a single institution between 2017 and 2018.
Disclosures: No source of funding was identified.
Source: Johnston ME et al. Gastroenterology. 2021 May 10. doi: 10.1016/S0016-5085(21)02827-4.
Key clinical point: Postoperative pancreas remnant volume was associated with the development of exocrine pancreatic insufficiency (EPI) after pancreatic resection.
Major finding: EPI, requiring pancreatic enzyme replacement therapy, developed in 50% of patients at 1-year postpancreatectomy. The incidence of EPI was higher in patients receiving Whipple vs. distal pancreatectomy (66% vs. 21%; P = .004). The only factor associated with EPI development was postoperative remnant pancreas volume (odds ratio, 0.93; 95% confidence interval, 0.88-0.98; P less than .01).
Study details: This study included 68 patients who underwent pancreatectomy (distal, n=23; pancreaticoduodenectomy, n=45) at a single institution between 2017 and 2018.
Disclosures: No source of funding was identified.
Source: Johnston ME et al. Gastroenterology. 2021 May 10. doi: 10.1016/S0016-5085(21)02827-4.
Key clinical point: Postoperative pancreas remnant volume was associated with the development of exocrine pancreatic insufficiency (EPI) after pancreatic resection.
Major finding: EPI, requiring pancreatic enzyme replacement therapy, developed in 50% of patients at 1-year postpancreatectomy. The incidence of EPI was higher in patients receiving Whipple vs. distal pancreatectomy (66% vs. 21%; P = .004). The only factor associated with EPI development was postoperative remnant pancreas volume (odds ratio, 0.93; 95% confidence interval, 0.88-0.98; P less than .01).
Study details: This study included 68 patients who underwent pancreatectomy (distal, n=23; pancreaticoduodenectomy, n=45) at a single institution between 2017 and 2018.
Disclosures: No source of funding was identified.
Source: Johnston ME et al. Gastroenterology. 2021 May 10. doi: 10.1016/S0016-5085(21)02827-4.
Semaglutide boosts weight loss following endoscopic gastroplasty
Combining minimally invasive endoscopic sleeve gastroplasty with a weekly injection of the glucagonlike peptide–1 agonist semaglutide (Ozempic, Novo Nordisk) leads to significantly greater weight loss than ESG alone in patients with diabetes and excess weight who are not candidates for bariatric surgery, new research shows.
During minimally invasive ESG, a flexible endoscope equipped with an endoscopic suturing device is inserted down the esophagus and into the stomach. The endoscopist then applies the sutures to the upper portion of the stomach, minimizing its size to restrict the amount of food a patient can ingest.
“Our stomachs can stretch back a bit, but we can use the suturing device again,” explained the lead investigator of the research Anna Carolina Hoff, MD, founder and clinical director of Angioskope Brazil in São José dos Campos.
“It’s important that patients with diabetes lose as much weight as possible because, if they lose about 10% of their total body weight, they have a great improvement in their glycemic levels, and some patients can even stop taking their [antidiabetic] medications,” Dr. Hoff said in an interview.
“And we found that by adding the GLP-1 agonist [semaglutide], we could increase weight loss from, on average, about 16%-18% of total body weight with ESG alone to up to 27%, so it’s a great metabolic combination,” she noted.
Dr. Hoff presented the findings at the annual Digestive Disease Week® (DDW).
Asked to comment, Scott Kahan, MD, MPH, director, National Center for Weight and Wellness, George Washington University, Washington, cautioned that it’s still early days for minimally invasive ESG.
“It is reasonable to assume that the long-term outcomes [with ESG] won’t be as good or durable over time as with bariatric surgery, but ... we will have to see.”
However, “we know that, typically, combinations of therapeutic options work better than a one-off option, so I think the real benefit of this study – outside the specific procedure and this specific medication – is that it is a very valuable proof-of-principle study showing that combinations do work better,” Dr. Kahan said in an interview.
Minimally invasive endoscopic sleeve gastroplasty
ESG is a surrogate for laparoscopic sleeve gastrectomy that can offer the benefits of such a procedure to those who don’t qualify for, or don’t wish to pursue, bariatric surgery. It can be performed at an earlier stage of disease, in those with a body mass index of 30 mg/kg2, whereas generally people are not offered bariatric procedures unless they have a BMI of at least 35 with comorbidities or a BMI of at least 40 if they do not have comorbidities.
Subcutaneous semaglutide is already approved for the treatment of type 2 diabetes in adults at doses of up to 1 mg/week; higher doses are needed for weight loss. Novo Nordisk has been investigating higher doses for weight loss in the STEP trial program, which is now complete, and the company has submitted the data to the Food and Drug Administration and European Medicines Agency for an additional indication of adults with obesity (BMI ≥30) or who are overweight (BMI ≥27) and who have at least one weight-related comorbidity, as an adjunct to a reduced-calorie diet and increased physical activity, with a decision expected soon.
Novo Nordisk has also developed an oral form of semaglutide, which has been approved as a once-daily agent for type 2 diabetes (Rybelsus) in doses of 7 mg and 14 mg to improve glycemic control along with diet and exercise. It is the first GLP-1 agonist available in tablet form.
Patients lost fat mass as well as excess weight
The Brazilian study involved 58 patients with obesity or overweight who also had diabetes and were undergoing minimally invasive ESG; they were further randomized to receive semaglutide or placebo.
The GLP-1 agonist (or sham placebo) was initiated 1 month after participants had undergone the procedure and patients were monitored each month for weight loss and type of fat loss achieved with the combination versus ESG alone. The initial dose of semaglutide used was 0.25 mg subcutaneous a week but could be titrated up to a maximum dose of 1.5 mg.
At the end of 11 months of active treatment versus placebo (12 months after ESG), patients who received additional semaglutide lost 86.3% of their excess body weight – the amount of weight patients needed to lose to reach normal BMI – compared with only 60.4% for ESG controls.
Specifically, the mean percentage total body weight loss at the end of 12 months was 25.2% for those in the combination group, compared with 18.6% for those treated with ESG alone (P < .001).
More importantly, patients in the combination group lost 12.6% of their body fat mass, compared with 9% for ESG controls, while mean A1c levels fell more in those treated with additional semaglutide compared with controls (P = .0394).
Indeed, five patients in the combination group reverted to a nondiabetic state and were able to discontinue antidiabetic medications altogether, Dr. Hoff noted.
“Our main goal is not just to lose weight but to lose body mass fat, which is very different from just losing weight,” she explained.
If patients lose weight but still maintain a high percentage of body fat mass, they have what she refers to as “sarcopenic obesity” because in this state patients have lost a lot of muscle mass but still have high levels of metabolically active visceral fat. Among many other inflammatory complexes, metabolically active visceral fat contains a large number of inflammasomes, and it is the latter that have been associated with obesity-related cancers.
“Obesity is a progressive disease, so what we are trying to do here is buy time for patients so they do not progress to [bariatric] surgery, and this approach gives patients a chance to act earlier before obesity takes over and more metabolic consequences occur,” Dr. Hoff emphasized.
So, when combined with semaglutide, “we now have a minimally invasive procedure that can be just as successful [as surgery] and which can be made available to even more people looking to lose a significant amount of weight,” she concluded.
Dr. Hoff and Dr. Kahan have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Combining minimally invasive endoscopic sleeve gastroplasty with a weekly injection of the glucagonlike peptide–1 agonist semaglutide (Ozempic, Novo Nordisk) leads to significantly greater weight loss than ESG alone in patients with diabetes and excess weight who are not candidates for bariatric surgery, new research shows.
During minimally invasive ESG, a flexible endoscope equipped with an endoscopic suturing device is inserted down the esophagus and into the stomach. The endoscopist then applies the sutures to the upper portion of the stomach, minimizing its size to restrict the amount of food a patient can ingest.
“Our stomachs can stretch back a bit, but we can use the suturing device again,” explained the lead investigator of the research Anna Carolina Hoff, MD, founder and clinical director of Angioskope Brazil in São José dos Campos.
“It’s important that patients with diabetes lose as much weight as possible because, if they lose about 10% of their total body weight, they have a great improvement in their glycemic levels, and some patients can even stop taking their [antidiabetic] medications,” Dr. Hoff said in an interview.
“And we found that by adding the GLP-1 agonist [semaglutide], we could increase weight loss from, on average, about 16%-18% of total body weight with ESG alone to up to 27%, so it’s a great metabolic combination,” she noted.
Dr. Hoff presented the findings at the annual Digestive Disease Week® (DDW).
Asked to comment, Scott Kahan, MD, MPH, director, National Center for Weight and Wellness, George Washington University, Washington, cautioned that it’s still early days for minimally invasive ESG.
“It is reasonable to assume that the long-term outcomes [with ESG] won’t be as good or durable over time as with bariatric surgery, but ... we will have to see.”
However, “we know that, typically, combinations of therapeutic options work better than a one-off option, so I think the real benefit of this study – outside the specific procedure and this specific medication – is that it is a very valuable proof-of-principle study showing that combinations do work better,” Dr. Kahan said in an interview.
Minimally invasive endoscopic sleeve gastroplasty
ESG is a surrogate for laparoscopic sleeve gastrectomy that can offer the benefits of such a procedure to those who don’t qualify for, or don’t wish to pursue, bariatric surgery. It can be performed at an earlier stage of disease, in those with a body mass index of 30 mg/kg2, whereas generally people are not offered bariatric procedures unless they have a BMI of at least 35 with comorbidities or a BMI of at least 40 if they do not have comorbidities.
Subcutaneous semaglutide is already approved for the treatment of type 2 diabetes in adults at doses of up to 1 mg/week; higher doses are needed for weight loss. Novo Nordisk has been investigating higher doses for weight loss in the STEP trial program, which is now complete, and the company has submitted the data to the Food and Drug Administration and European Medicines Agency for an additional indication of adults with obesity (BMI ≥30) or who are overweight (BMI ≥27) and who have at least one weight-related comorbidity, as an adjunct to a reduced-calorie diet and increased physical activity, with a decision expected soon.
Novo Nordisk has also developed an oral form of semaglutide, which has been approved as a once-daily agent for type 2 diabetes (Rybelsus) in doses of 7 mg and 14 mg to improve glycemic control along with diet and exercise. It is the first GLP-1 agonist available in tablet form.
Patients lost fat mass as well as excess weight
The Brazilian study involved 58 patients with obesity or overweight who also had diabetes and were undergoing minimally invasive ESG; they were further randomized to receive semaglutide or placebo.
The GLP-1 agonist (or sham placebo) was initiated 1 month after participants had undergone the procedure and patients were monitored each month for weight loss and type of fat loss achieved with the combination versus ESG alone. The initial dose of semaglutide used was 0.25 mg subcutaneous a week but could be titrated up to a maximum dose of 1.5 mg.
At the end of 11 months of active treatment versus placebo (12 months after ESG), patients who received additional semaglutide lost 86.3% of their excess body weight – the amount of weight patients needed to lose to reach normal BMI – compared with only 60.4% for ESG controls.
Specifically, the mean percentage total body weight loss at the end of 12 months was 25.2% for those in the combination group, compared with 18.6% for those treated with ESG alone (P < .001).
More importantly, patients in the combination group lost 12.6% of their body fat mass, compared with 9% for ESG controls, while mean A1c levels fell more in those treated with additional semaglutide compared with controls (P = .0394).
Indeed, five patients in the combination group reverted to a nondiabetic state and were able to discontinue antidiabetic medications altogether, Dr. Hoff noted.
“Our main goal is not just to lose weight but to lose body mass fat, which is very different from just losing weight,” she explained.
If patients lose weight but still maintain a high percentage of body fat mass, they have what she refers to as “sarcopenic obesity” because in this state patients have lost a lot of muscle mass but still have high levels of metabolically active visceral fat. Among many other inflammatory complexes, metabolically active visceral fat contains a large number of inflammasomes, and it is the latter that have been associated with obesity-related cancers.
“Obesity is a progressive disease, so what we are trying to do here is buy time for patients so they do not progress to [bariatric] surgery, and this approach gives patients a chance to act earlier before obesity takes over and more metabolic consequences occur,” Dr. Hoff emphasized.
So, when combined with semaglutide, “we now have a minimally invasive procedure that can be just as successful [as surgery] and which can be made available to even more people looking to lose a significant amount of weight,” she concluded.
Dr. Hoff and Dr. Kahan have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Combining minimally invasive endoscopic sleeve gastroplasty with a weekly injection of the glucagonlike peptide–1 agonist semaglutide (Ozempic, Novo Nordisk) leads to significantly greater weight loss than ESG alone in patients with diabetes and excess weight who are not candidates for bariatric surgery, new research shows.
During minimally invasive ESG, a flexible endoscope equipped with an endoscopic suturing device is inserted down the esophagus and into the stomach. The endoscopist then applies the sutures to the upper portion of the stomach, minimizing its size to restrict the amount of food a patient can ingest.
“Our stomachs can stretch back a bit, but we can use the suturing device again,” explained the lead investigator of the research Anna Carolina Hoff, MD, founder and clinical director of Angioskope Brazil in São José dos Campos.
“It’s important that patients with diabetes lose as much weight as possible because, if they lose about 10% of their total body weight, they have a great improvement in their glycemic levels, and some patients can even stop taking their [antidiabetic] medications,” Dr. Hoff said in an interview.
“And we found that by adding the GLP-1 agonist [semaglutide], we could increase weight loss from, on average, about 16%-18% of total body weight with ESG alone to up to 27%, so it’s a great metabolic combination,” she noted.
Dr. Hoff presented the findings at the annual Digestive Disease Week® (DDW).
Asked to comment, Scott Kahan, MD, MPH, director, National Center for Weight and Wellness, George Washington University, Washington, cautioned that it’s still early days for minimally invasive ESG.
“It is reasonable to assume that the long-term outcomes [with ESG] won’t be as good or durable over time as with bariatric surgery, but ... we will have to see.”
However, “we know that, typically, combinations of therapeutic options work better than a one-off option, so I think the real benefit of this study – outside the specific procedure and this specific medication – is that it is a very valuable proof-of-principle study showing that combinations do work better,” Dr. Kahan said in an interview.
Minimally invasive endoscopic sleeve gastroplasty
ESG is a surrogate for laparoscopic sleeve gastrectomy that can offer the benefits of such a procedure to those who don’t qualify for, or don’t wish to pursue, bariatric surgery. It can be performed at an earlier stage of disease, in those with a body mass index of 30 mg/kg2, whereas generally people are not offered bariatric procedures unless they have a BMI of at least 35 with comorbidities or a BMI of at least 40 if they do not have comorbidities.
Subcutaneous semaglutide is already approved for the treatment of type 2 diabetes in adults at doses of up to 1 mg/week; higher doses are needed for weight loss. Novo Nordisk has been investigating higher doses for weight loss in the STEP trial program, which is now complete, and the company has submitted the data to the Food and Drug Administration and European Medicines Agency for an additional indication of adults with obesity (BMI ≥30) or who are overweight (BMI ≥27) and who have at least one weight-related comorbidity, as an adjunct to a reduced-calorie diet and increased physical activity, with a decision expected soon.
Novo Nordisk has also developed an oral form of semaglutide, which has been approved as a once-daily agent for type 2 diabetes (Rybelsus) in doses of 7 mg and 14 mg to improve glycemic control along with diet and exercise. It is the first GLP-1 agonist available in tablet form.
Patients lost fat mass as well as excess weight
The Brazilian study involved 58 patients with obesity or overweight who also had diabetes and were undergoing minimally invasive ESG; they were further randomized to receive semaglutide or placebo.
The GLP-1 agonist (or sham placebo) was initiated 1 month after participants had undergone the procedure and patients were monitored each month for weight loss and type of fat loss achieved with the combination versus ESG alone. The initial dose of semaglutide used was 0.25 mg subcutaneous a week but could be titrated up to a maximum dose of 1.5 mg.
At the end of 11 months of active treatment versus placebo (12 months after ESG), patients who received additional semaglutide lost 86.3% of their excess body weight – the amount of weight patients needed to lose to reach normal BMI – compared with only 60.4% for ESG controls.
Specifically, the mean percentage total body weight loss at the end of 12 months was 25.2% for those in the combination group, compared with 18.6% for those treated with ESG alone (P < .001).
More importantly, patients in the combination group lost 12.6% of their body fat mass, compared with 9% for ESG controls, while mean A1c levels fell more in those treated with additional semaglutide compared with controls (P = .0394).
Indeed, five patients in the combination group reverted to a nondiabetic state and were able to discontinue antidiabetic medications altogether, Dr. Hoff noted.
“Our main goal is not just to lose weight but to lose body mass fat, which is very different from just losing weight,” she explained.
If patients lose weight but still maintain a high percentage of body fat mass, they have what she refers to as “sarcopenic obesity” because in this state patients have lost a lot of muscle mass but still have high levels of metabolically active visceral fat. Among many other inflammatory complexes, metabolically active visceral fat contains a large number of inflammasomes, and it is the latter that have been associated with obesity-related cancers.
“Obesity is a progressive disease, so what we are trying to do here is buy time for patients so they do not progress to [bariatric] surgery, and this approach gives patients a chance to act earlier before obesity takes over and more metabolic consequences occur,” Dr. Hoff emphasized.
So, when combined with semaglutide, “we now have a minimally invasive procedure that can be just as successful [as surgery] and which can be made available to even more people looking to lose a significant amount of weight,” she concluded.
Dr. Hoff and Dr. Kahan have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term EPI management after pancreatic surgery needs specialist guidance
Key clinical point: Considerable proportion of patients suffer from exocrine pancreatic insufficiency (EPI)-associated complaints which persisted for 3 years or even more after pancreatoduodenectomy or left pancreatectomy, even in patients receiving pancreatic enzyme replacement therapy (PERT).
Major finding: EPI, indicated by PERT usage, was reported in 41% of patients, of which only 48% reported complete relief, whereas 35% reported decrease in EPI-related complaints. Patients with vs. without PERT had higher complaints of fatty stools (50% vs. 26%; P = .003) and unintentional weight loss (11% vs. 2%; P = .019).
Study details: This study included 153 patients who underwent pancreatoduodenectomy or left pancreatectomy for premalignant or benign diseases between 2006 and 2016.
Disclosures: This study was supported by the Dutch Cancer Society. The lead author reported research funding from Mylan and Allergan.
Source: Latenstein AEJ et al. HPB. 2021 Apr 27. doi: 10.1016/j.hpb.2021.04.012.
Key clinical point: Considerable proportion of patients suffer from exocrine pancreatic insufficiency (EPI)-associated complaints which persisted for 3 years or even more after pancreatoduodenectomy or left pancreatectomy, even in patients receiving pancreatic enzyme replacement therapy (PERT).
Major finding: EPI, indicated by PERT usage, was reported in 41% of patients, of which only 48% reported complete relief, whereas 35% reported decrease in EPI-related complaints. Patients with vs. without PERT had higher complaints of fatty stools (50% vs. 26%; P = .003) and unintentional weight loss (11% vs. 2%; P = .019).
Study details: This study included 153 patients who underwent pancreatoduodenectomy or left pancreatectomy for premalignant or benign diseases between 2006 and 2016.
Disclosures: This study was supported by the Dutch Cancer Society. The lead author reported research funding from Mylan and Allergan.
Source: Latenstein AEJ et al. HPB. 2021 Apr 27. doi: 10.1016/j.hpb.2021.04.012.
Key clinical point: Considerable proportion of patients suffer from exocrine pancreatic insufficiency (EPI)-associated complaints which persisted for 3 years or even more after pancreatoduodenectomy or left pancreatectomy, even in patients receiving pancreatic enzyme replacement therapy (PERT).
Major finding: EPI, indicated by PERT usage, was reported in 41% of patients, of which only 48% reported complete relief, whereas 35% reported decrease in EPI-related complaints. Patients with vs. without PERT had higher complaints of fatty stools (50% vs. 26%; P = .003) and unintentional weight loss (11% vs. 2%; P = .019).
Study details: This study included 153 patients who underwent pancreatoduodenectomy or left pancreatectomy for premalignant or benign diseases between 2006 and 2016.
Disclosures: This study was supported by the Dutch Cancer Society. The lead author reported research funding from Mylan and Allergan.
Source: Latenstein AEJ et al. HPB. 2021 Apr 27. doi: 10.1016/j.hpb.2021.04.012.
High incidence of EPI but not diabetes in childhood-onset hereditary pancreatitis
Key clinical point: Over half of the patients with childhood-onset hereditary pancreatitis developed exocrine pancreatic insufficiency (EPI). EPI development preceded loss of endocrine function in this rare patient population.
Major finding: Overall, EPI developed in 7 patients at an average age of 12.5±8.4 years, with fecal pancreatic elastase less than 100 mg/g in all patients at disease onset. No evidence of pancreoprive diabetes mellitus (type IIIc) was reported in any patient.
Study details: This retrospective study evaluated 11 patients with childhood-onset (mean age at onset, 7.5±4.2 years) hereditary pancreatitis.
Disclosures: No funding source was identified. The authors declared no conflicts of interest.
Source: Prommer R et al. Wien Klin Wochenschr. 2021 Apr 28. doi: 10.1007/s00508-021-01869-0.
Key clinical point: Over half of the patients with childhood-onset hereditary pancreatitis developed exocrine pancreatic insufficiency (EPI). EPI development preceded loss of endocrine function in this rare patient population.
Major finding: Overall, EPI developed in 7 patients at an average age of 12.5±8.4 years, with fecal pancreatic elastase less than 100 mg/g in all patients at disease onset. No evidence of pancreoprive diabetes mellitus (type IIIc) was reported in any patient.
Study details: This retrospective study evaluated 11 patients with childhood-onset (mean age at onset, 7.5±4.2 years) hereditary pancreatitis.
Disclosures: No funding source was identified. The authors declared no conflicts of interest.
Source: Prommer R et al. Wien Klin Wochenschr. 2021 Apr 28. doi: 10.1007/s00508-021-01869-0.
Key clinical point: Over half of the patients with childhood-onset hereditary pancreatitis developed exocrine pancreatic insufficiency (EPI). EPI development preceded loss of endocrine function in this rare patient population.
Major finding: Overall, EPI developed in 7 patients at an average age of 12.5±8.4 years, with fecal pancreatic elastase less than 100 mg/g in all patients at disease onset. No evidence of pancreoprive diabetes mellitus (type IIIc) was reported in any patient.
Study details: This retrospective study evaluated 11 patients with childhood-onset (mean age at onset, 7.5±4.2 years) hereditary pancreatitis.
Disclosures: No funding source was identified. The authors declared no conflicts of interest.
Source: Prommer R et al. Wien Klin Wochenschr. 2021 Apr 28. doi: 10.1007/s00508-021-01869-0.
EPI management needs attention in palliative care of pancreatic ductal adenocarcinomas
Key clinical point: Although locally advanced pancreatic cancer (LAPC) or metastatic pancreatic cancer (MPC) is associated with reduced exocrine function, there is a lack of clear guidelines for the diagnosis and management of exocrine pancreatic insufficiency (EPI) for palliative pancreatic ductal adenocarcinomas.
Major finding: Weight loss and steatorrhea were present in 83.6% and 13.4% of patients, respectively. Median body mass index decreased by 13.3% from preillness state to cancer diagnosis. Despite high rates of referral to dieticians (79.1%), only 24 patients were prescribed pancreatic enzyme replacement therapy. Pancrelipase dose varied from 10,000 to 50,000 units with each meal.
Study details: This retrospective study assessed palliative management in 67 patients with LAPC or MPC.
Disclosures: No specific funding source was identified. The authors declared no conflicts of interest.
Source: Choi CCM et al. ANZ J Surg. 2021 Apr 18. doi: 10.1111/ans.16669.
Key clinical point: Although locally advanced pancreatic cancer (LAPC) or metastatic pancreatic cancer (MPC) is associated with reduced exocrine function, there is a lack of clear guidelines for the diagnosis and management of exocrine pancreatic insufficiency (EPI) for palliative pancreatic ductal adenocarcinomas.
Major finding: Weight loss and steatorrhea were present in 83.6% and 13.4% of patients, respectively. Median body mass index decreased by 13.3% from preillness state to cancer diagnosis. Despite high rates of referral to dieticians (79.1%), only 24 patients were prescribed pancreatic enzyme replacement therapy. Pancrelipase dose varied from 10,000 to 50,000 units with each meal.
Study details: This retrospective study assessed palliative management in 67 patients with LAPC or MPC.
Disclosures: No specific funding source was identified. The authors declared no conflicts of interest.
Source: Choi CCM et al. ANZ J Surg. 2021 Apr 18. doi: 10.1111/ans.16669.
Key clinical point: Although locally advanced pancreatic cancer (LAPC) or metastatic pancreatic cancer (MPC) is associated with reduced exocrine function, there is a lack of clear guidelines for the diagnosis and management of exocrine pancreatic insufficiency (EPI) for palliative pancreatic ductal adenocarcinomas.
Major finding: Weight loss and steatorrhea were present in 83.6% and 13.4% of patients, respectively. Median body mass index decreased by 13.3% from preillness state to cancer diagnosis. Despite high rates of referral to dieticians (79.1%), only 24 patients were prescribed pancreatic enzyme replacement therapy. Pancrelipase dose varied from 10,000 to 50,000 units with each meal.
Study details: This retrospective study assessed palliative management in 67 patients with LAPC or MPC.
Disclosures: No specific funding source was identified. The authors declared no conflicts of interest.
Source: Choi CCM et al. ANZ J Surg. 2021 Apr 18. doi: 10.1111/ans.16669.


