User login
APA, others lobby to make COVID-19 telehealth waivers permanent
The American Psychiatric Association (APA) is calling on Congress to permanently lift restrictions that have allowed unfettered delivery of telehealth services during the COVID-19 pandemic, which experts say has been a boon to patients and physicians alike.
“We ask Congress to extend the telehealth waiver authority under COVID-19 beyond the emergency and to study its impact while doing so,” said APA President Jeffrey Geller, MD, in a May 27 video briefing with congressional staff and reporters.
The APA is also seeking to make permanent certain waivers granted by the Centers for Medicare & Medicaid Services on April 30, including elimination of geographic restrictions on behavioral health and allowing patients be seen at home, said Dr. Geller.
The APA also is asking for the elimination of the rule that requires clinicians to have an initial face-to-face meeting with patients before they can prescribe controlled substances, Dr. Geller said. The Drug Enforcement Administration waived that requirement, known as the Ryan Haight Act, on March 17 for the duration of the national emergency.
Telemedicine has supporters on both sides of the aisle in Congress, including Rep. Paul Tonko (D-N.Y.) who said at the APA briefing he would fight to make the waivers permanent.
“The expanded use of telehealth has enormous potential during normal times as well, especially in behavioral health,” said Mr. Tonko. “I am pushing fiercely for these current flexibilities to be extended for a reasonable time after the public health emergency so that we can have time to evaluate which should be made permanent,” he said.
Dr. Geller, other clinicians, and advocates in the briefing praised CMS for facilitating telepsychiatry for Medicare. That follows in the footsteps of most private insurers, who have also relaxed requirements into the summer, according to the Medical Group Management Association.
Game changer
The Medicare waivers “have dramatically changed the entire scene for someone like myself as a clinician to allow me to see my patients in a much easier way,” said Peter Yellowlees, MBBS, MD, chief wellness officer, University of California Davis Health. Within 2 weeks in March, the health system converted almost all of its regular outpatient visits to telemedicine, he said.
Dr. Yellowlees added government still needs to address, what he called, outdated HIPAA regulations that ban certain technologies.
“It makes no sense that I can talk to someone on an iPhone, but the moment I talk to them on FaceTime, it’s illegal,” said Dr. Yellowlees, a former president of the American Telemedicine Association.
Dr. Geller said that “psychiatric care provided by telehealth is as effective as in-person psychiatric services,” adding that “some patients prefer telepsychiatry because of its convenience and as a means of reducing stigma associated with seeking help for mental health.”
Shabana Khan, MD, a child psychiatrist and director of telepsychiatry at New York University Langone Health, said audio and video conferencing are helping address a shortage and maldistribution of child and adolescent psychiatrists.
Americans’ mental health is suffering during the pandemic. The U.S. Census Bureau recently released data showing that half of those surveyed reported depressed mood and that one-third are reporting anxiety, depression, or both, as reported by the Washington Post.
“At this very time that anxiety, depression, substance use, and other mental health problems are rising, our nation’s already strained mental health system is really being pushed to the brink,” said Jodi Kwarciany, manager for mental health policy for the National Alliance on Mental Illness, during the briefing.
Telemedicine can help “by connecting people to providers at the time and the place and using the technology that works best for them,” she said, adding that NAMI would press policymakers to address barriers to access.
The clinicians on the briefing said they’ve observed that some patients are more comfortable with video or audio interactions than with in-person visits.
Increased access to care
Telepsychiatry seems to be convincing some to reconsider therapy, since they can do it at home, said Dr. Yellowlees. he said.
For instance, he said, he has been able to consult by phone and video with several patients who receive care through the Indian Health Service who had not be able to get into the physical clinic.
Dr. Yellowlees said video sessions also may encourage patients to be more, not less, talkative. “Video is actually counterintuitively a very intimate experience,” he said, in part because of the perceived distance and people’s tendency to be less inhibited on technology platforms.“It’s less embarrassing,” he said. “If you’ve got really dramatic, difficult, traumatic things to talk about, it’s slightly easier to talk to someone who’s slightly further apart from you on video,” said Dr. Yellowlees.
“Individuals who have a significant amount of anxiety may actually feel more comfortable with the distance that this technology affords,” agreed Dr. Khan. She said telemedicine had made sessions more comfortable for some of her patients with autism spectrum disorder.
Dr. Geller said audio and video have been important to his practice during the pandemic. One of his patients never leaves the house and does not use computers. “He spends his time sequestered at home listening to records on his record player,” said Dr. Geller. But he’s been amenable to phone sessions. “What I’ve found with him, and I’ve found with several other patients, is that they actually talk more easily when they’re not face to face,” he said.
Far fewer no-shows
Another plus for his New England–based practice during the last few months: patients have not been anxious about missing sessions because of the weather. The clinicians all noted that telepsychiatry seemed to reduce missed visits.
Dr. Yellowlees said that no-show rates had decreased by half at UC Davis. “That means no significant loss of income,” during the pandemic, he said.
“The no-show rate is incredibly low, particularly because when you call the patients and they don’t remember they had an appointment, you have the appointment anyway, most of the time,” said Dr. Geller.
For Dr. Khan, being able to conduct audio and video sessions during the pandemic has meant keeping up continuity of care.
As a result of the pandemic, many college students in New York City had to go home – often to another state. The waivers granted by New York’s Medicaid program and other insurers have allowed Dr. Khan to continue care for these patients.
The NYU clinic also operates day programs in rural areas 5 hours from the city. Dr. Khan recently evaluated a 12-year-old girl with significant anxiety and low mood, both of which had worsened.
“She would not have been able to access care otherwise,” said Dr. Khan. And for rural patients who do not have access to broadband or smartphones, audio visits “have been immensely helpful,” she said.
Dr. Khan, Dr. Geller, and Dr. Yellowlees have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The American Psychiatric Association (APA) is calling on Congress to permanently lift restrictions that have allowed unfettered delivery of telehealth services during the COVID-19 pandemic, which experts say has been a boon to patients and physicians alike.
“We ask Congress to extend the telehealth waiver authority under COVID-19 beyond the emergency and to study its impact while doing so,” said APA President Jeffrey Geller, MD, in a May 27 video briefing with congressional staff and reporters.
The APA is also seeking to make permanent certain waivers granted by the Centers for Medicare & Medicaid Services on April 30, including elimination of geographic restrictions on behavioral health and allowing patients be seen at home, said Dr. Geller.
The APA also is asking for the elimination of the rule that requires clinicians to have an initial face-to-face meeting with patients before they can prescribe controlled substances, Dr. Geller said. The Drug Enforcement Administration waived that requirement, known as the Ryan Haight Act, on March 17 for the duration of the national emergency.
Telemedicine has supporters on both sides of the aisle in Congress, including Rep. Paul Tonko (D-N.Y.) who said at the APA briefing he would fight to make the waivers permanent.
“The expanded use of telehealth has enormous potential during normal times as well, especially in behavioral health,” said Mr. Tonko. “I am pushing fiercely for these current flexibilities to be extended for a reasonable time after the public health emergency so that we can have time to evaluate which should be made permanent,” he said.
Dr. Geller, other clinicians, and advocates in the briefing praised CMS for facilitating telepsychiatry for Medicare. That follows in the footsteps of most private insurers, who have also relaxed requirements into the summer, according to the Medical Group Management Association.
Game changer
The Medicare waivers “have dramatically changed the entire scene for someone like myself as a clinician to allow me to see my patients in a much easier way,” said Peter Yellowlees, MBBS, MD, chief wellness officer, University of California Davis Health. Within 2 weeks in March, the health system converted almost all of its regular outpatient visits to telemedicine, he said.
Dr. Yellowlees added government still needs to address, what he called, outdated HIPAA regulations that ban certain technologies.
“It makes no sense that I can talk to someone on an iPhone, but the moment I talk to them on FaceTime, it’s illegal,” said Dr. Yellowlees, a former president of the American Telemedicine Association.
Dr. Geller said that “psychiatric care provided by telehealth is as effective as in-person psychiatric services,” adding that “some patients prefer telepsychiatry because of its convenience and as a means of reducing stigma associated with seeking help for mental health.”
Shabana Khan, MD, a child psychiatrist and director of telepsychiatry at New York University Langone Health, said audio and video conferencing are helping address a shortage and maldistribution of child and adolescent psychiatrists.
Americans’ mental health is suffering during the pandemic. The U.S. Census Bureau recently released data showing that half of those surveyed reported depressed mood and that one-third are reporting anxiety, depression, or both, as reported by the Washington Post.
“At this very time that anxiety, depression, substance use, and other mental health problems are rising, our nation’s already strained mental health system is really being pushed to the brink,” said Jodi Kwarciany, manager for mental health policy for the National Alliance on Mental Illness, during the briefing.
Telemedicine can help “by connecting people to providers at the time and the place and using the technology that works best for them,” she said, adding that NAMI would press policymakers to address barriers to access.
The clinicians on the briefing said they’ve observed that some patients are more comfortable with video or audio interactions than with in-person visits.
Increased access to care
Telepsychiatry seems to be convincing some to reconsider therapy, since they can do it at home, said Dr. Yellowlees. he said.
For instance, he said, he has been able to consult by phone and video with several patients who receive care through the Indian Health Service who had not be able to get into the physical clinic.
Dr. Yellowlees said video sessions also may encourage patients to be more, not less, talkative. “Video is actually counterintuitively a very intimate experience,” he said, in part because of the perceived distance and people’s tendency to be less inhibited on technology platforms.“It’s less embarrassing,” he said. “If you’ve got really dramatic, difficult, traumatic things to talk about, it’s slightly easier to talk to someone who’s slightly further apart from you on video,” said Dr. Yellowlees.
“Individuals who have a significant amount of anxiety may actually feel more comfortable with the distance that this technology affords,” agreed Dr. Khan. She said telemedicine had made sessions more comfortable for some of her patients with autism spectrum disorder.
Dr. Geller said audio and video have been important to his practice during the pandemic. One of his patients never leaves the house and does not use computers. “He spends his time sequestered at home listening to records on his record player,” said Dr. Geller. But he’s been amenable to phone sessions. “What I’ve found with him, and I’ve found with several other patients, is that they actually talk more easily when they’re not face to face,” he said.
Far fewer no-shows
Another plus for his New England–based practice during the last few months: patients have not been anxious about missing sessions because of the weather. The clinicians all noted that telepsychiatry seemed to reduce missed visits.
Dr. Yellowlees said that no-show rates had decreased by half at UC Davis. “That means no significant loss of income,” during the pandemic, he said.
“The no-show rate is incredibly low, particularly because when you call the patients and they don’t remember they had an appointment, you have the appointment anyway, most of the time,” said Dr. Geller.
For Dr. Khan, being able to conduct audio and video sessions during the pandemic has meant keeping up continuity of care.
As a result of the pandemic, many college students in New York City had to go home – often to another state. The waivers granted by New York’s Medicaid program and other insurers have allowed Dr. Khan to continue care for these patients.
The NYU clinic also operates day programs in rural areas 5 hours from the city. Dr. Khan recently evaluated a 12-year-old girl with significant anxiety and low mood, both of which had worsened.
“She would not have been able to access care otherwise,” said Dr. Khan. And for rural patients who do not have access to broadband or smartphones, audio visits “have been immensely helpful,” she said.
Dr. Khan, Dr. Geller, and Dr. Yellowlees have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The American Psychiatric Association (APA) is calling on Congress to permanently lift restrictions that have allowed unfettered delivery of telehealth services during the COVID-19 pandemic, which experts say has been a boon to patients and physicians alike.
“We ask Congress to extend the telehealth waiver authority under COVID-19 beyond the emergency and to study its impact while doing so,” said APA President Jeffrey Geller, MD, in a May 27 video briefing with congressional staff and reporters.
The APA is also seeking to make permanent certain waivers granted by the Centers for Medicare & Medicaid Services on April 30, including elimination of geographic restrictions on behavioral health and allowing patients be seen at home, said Dr. Geller.
The APA also is asking for the elimination of the rule that requires clinicians to have an initial face-to-face meeting with patients before they can prescribe controlled substances, Dr. Geller said. The Drug Enforcement Administration waived that requirement, known as the Ryan Haight Act, on March 17 for the duration of the national emergency.
Telemedicine has supporters on both sides of the aisle in Congress, including Rep. Paul Tonko (D-N.Y.) who said at the APA briefing he would fight to make the waivers permanent.
“The expanded use of telehealth has enormous potential during normal times as well, especially in behavioral health,” said Mr. Tonko. “I am pushing fiercely for these current flexibilities to be extended for a reasonable time after the public health emergency so that we can have time to evaluate which should be made permanent,” he said.
Dr. Geller, other clinicians, and advocates in the briefing praised CMS for facilitating telepsychiatry for Medicare. That follows in the footsteps of most private insurers, who have also relaxed requirements into the summer, according to the Medical Group Management Association.
Game changer
The Medicare waivers “have dramatically changed the entire scene for someone like myself as a clinician to allow me to see my patients in a much easier way,” said Peter Yellowlees, MBBS, MD, chief wellness officer, University of California Davis Health. Within 2 weeks in March, the health system converted almost all of its regular outpatient visits to telemedicine, he said.
Dr. Yellowlees added government still needs to address, what he called, outdated HIPAA regulations that ban certain technologies.
“It makes no sense that I can talk to someone on an iPhone, but the moment I talk to them on FaceTime, it’s illegal,” said Dr. Yellowlees, a former president of the American Telemedicine Association.
Dr. Geller said that “psychiatric care provided by telehealth is as effective as in-person psychiatric services,” adding that “some patients prefer telepsychiatry because of its convenience and as a means of reducing stigma associated with seeking help for mental health.”
Shabana Khan, MD, a child psychiatrist and director of telepsychiatry at New York University Langone Health, said audio and video conferencing are helping address a shortage and maldistribution of child and adolescent psychiatrists.
Americans’ mental health is suffering during the pandemic. The U.S. Census Bureau recently released data showing that half of those surveyed reported depressed mood and that one-third are reporting anxiety, depression, or both, as reported by the Washington Post.
“At this very time that anxiety, depression, substance use, and other mental health problems are rising, our nation’s already strained mental health system is really being pushed to the brink,” said Jodi Kwarciany, manager for mental health policy for the National Alliance on Mental Illness, during the briefing.
Telemedicine can help “by connecting people to providers at the time and the place and using the technology that works best for them,” she said, adding that NAMI would press policymakers to address barriers to access.
The clinicians on the briefing said they’ve observed that some patients are more comfortable with video or audio interactions than with in-person visits.
Increased access to care
Telepsychiatry seems to be convincing some to reconsider therapy, since they can do it at home, said Dr. Yellowlees. he said.
For instance, he said, he has been able to consult by phone and video with several patients who receive care through the Indian Health Service who had not be able to get into the physical clinic.
Dr. Yellowlees said video sessions also may encourage patients to be more, not less, talkative. “Video is actually counterintuitively a very intimate experience,” he said, in part because of the perceived distance and people’s tendency to be less inhibited on technology platforms.“It’s less embarrassing,” he said. “If you’ve got really dramatic, difficult, traumatic things to talk about, it’s slightly easier to talk to someone who’s slightly further apart from you on video,” said Dr. Yellowlees.
“Individuals who have a significant amount of anxiety may actually feel more comfortable with the distance that this technology affords,” agreed Dr. Khan. She said telemedicine had made sessions more comfortable for some of her patients with autism spectrum disorder.
Dr. Geller said audio and video have been important to his practice during the pandemic. One of his patients never leaves the house and does not use computers. “He spends his time sequestered at home listening to records on his record player,” said Dr. Geller. But he’s been amenable to phone sessions. “What I’ve found with him, and I’ve found with several other patients, is that they actually talk more easily when they’re not face to face,” he said.
Far fewer no-shows
Another plus for his New England–based practice during the last few months: patients have not been anxious about missing sessions because of the weather. The clinicians all noted that telepsychiatry seemed to reduce missed visits.
Dr. Yellowlees said that no-show rates had decreased by half at UC Davis. “That means no significant loss of income,” during the pandemic, he said.
“The no-show rate is incredibly low, particularly because when you call the patients and they don’t remember they had an appointment, you have the appointment anyway, most of the time,” said Dr. Geller.
For Dr. Khan, being able to conduct audio and video sessions during the pandemic has meant keeping up continuity of care.
As a result of the pandemic, many college students in New York City had to go home – often to another state. The waivers granted by New York’s Medicaid program and other insurers have allowed Dr. Khan to continue care for these patients.
The NYU clinic also operates day programs in rural areas 5 hours from the city. Dr. Khan recently evaluated a 12-year-old girl with significant anxiety and low mood, both of which had worsened.
“She would not have been able to access care otherwise,” said Dr. Khan. And for rural patients who do not have access to broadband or smartphones, audio visits “have been immensely helpful,” she said.
Dr. Khan, Dr. Geller, and Dr. Yellowlees have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
‘Loss-frame’ approach makes psoriasis patients more agreeable to treatment
, held virtually.
“We typically explain to patients the benefits of treatment,” Ari A. Kassardjian, BS, of the University of Southern California, Los Angeles, said in his presentation. “However, explaining to them the harmful effects on their skin and joint diseases, such as exacerbation of psoriasis and/or psoriatic arthritis, could offer some patients a new perspective that may influence their treatment preferences; and ultimately, better communication may lead to better medication adherence in patients.”
In the study he presented, explaining to patients possible outcomes without treatment was more effective in getting them to agree to treatment than was messaging that focused on the positive effects of a therapy (reducing disease severity and pain, and improved health).
He noted that the impact of framing choices in terms of gain or loss on decision-making has been measured in other areas of medicine, including in patients with multiple sclerosis where medication adherence is an issue (J Health Commun. 2017 Jun;22[6]:523-31). “Gain-framed” messages focus on the benefits of taking a medication, while “loss-framed” messages highlight the potential consequences of not agreeing or adhering to treatment.
In the study, Mr. Kassardjian and coinvestigators evaluated 90 patients with psoriasis who were randomized to receive a gain-framed or loss-framed message about a hypothetical new biologic injectable medication for psoriasis and psoriatic arthritis (PsA). More than half were male (64.4%), white (53.3%), and non-Hispanic or Latino (55.6%); and about one-fourth of the participants (27.8%) also had psoriatic arthritis (PsA).
The gain-framed message emphasized “the chance to reduce psoriasis severity, reduce joint pain, and improve how you feel overall,” while the loss-framed message described the downsides of not taking medication – missing out “on the chance to improve your skin, your joints, and your overall health,” with the possibility that psoriasis may get worse, “with worsening pain in your joints from psoriatic arthritis,” and feeling “worse overall.” Both messages included the side effects of the theoretical injectable, a small risk of injection-site pain and skin infections. After receiving the message, participants ranked their likelihood of taking the medication on an 11-point Likert scale, with a score of 0 indicating that they would “definitely” not use the medication and a score of 10 indicating that they would “definitely” use the medication.
Scores among those who received the loss-framed message were a mean of 8.84, compared with 7.11 among patients who received the gain-framed message (between-group difference; 1.73; P less than .0001). When comparing patients with and without PsA, the between-group difference was 1.90 for patients with PsA (P less than .0001) and 1.08 for patients who did not have PsA (P = .002). Comparing the responses of those with PsA and those without PsA, the between-group difference was 1.08 (P = .03). While PsA and non-PsA patients favored the loss-framed messages, “regardless of the framing type, PsA patients always responded with a greater preference for the therapy,” Mr. Kassardjian said.
Gender also had an effect on responsiveness to gain-framed or loss-framed messaging. Both men and women ranked the loss-framed messaging as making them more likely to use the medication, but the between-group difference for women (2.00; P = .008) was higher than in men (1.49; P = .003). However, the total men compared with total women between-group differences were not significant.
“In clinical practice, physicians regularly weigh the benefits and risks of treatment. In order to communicate this information to patients, it is important to understand how framing these benefits and risks impacts patient preferences for therapy,” Mr. Kassardjian said. “While most available biologics are effective and have tolerable safety profiles, many psoriasis patients may be hesitant to initiate these therapies. Thus, it is important to convey the benefits and risks of these systemic agents in ways that resonate with patients.”
Mr. Kassardjian reports receiving the Dean’s Research Scholarship at the University of Southern California, funded by the Wright Foundation at the time of the study. Senior author April Armstrong, MD, disclosed serving as an investigator and/or consultant for AbbVie, BMS, Dermavant, Dermira, Eli Lilly, Janssen, Leo Pharma, Kyowa Hakko Kirin, Modernizing Medicine, Novartis, Ortho Dermatologics, Regeneron, Sanofi, Sun Pharma, and UCB.
SOURCE: Kassardjian A. SID 2020, Abstract 489.
, held virtually.
“We typically explain to patients the benefits of treatment,” Ari A. Kassardjian, BS, of the University of Southern California, Los Angeles, said in his presentation. “However, explaining to them the harmful effects on their skin and joint diseases, such as exacerbation of psoriasis and/or psoriatic arthritis, could offer some patients a new perspective that may influence their treatment preferences; and ultimately, better communication may lead to better medication adherence in patients.”
In the study he presented, explaining to patients possible outcomes without treatment was more effective in getting them to agree to treatment than was messaging that focused on the positive effects of a therapy (reducing disease severity and pain, and improved health).
He noted that the impact of framing choices in terms of gain or loss on decision-making has been measured in other areas of medicine, including in patients with multiple sclerosis where medication adherence is an issue (J Health Commun. 2017 Jun;22[6]:523-31). “Gain-framed” messages focus on the benefits of taking a medication, while “loss-framed” messages highlight the potential consequences of not agreeing or adhering to treatment.
In the study, Mr. Kassardjian and coinvestigators evaluated 90 patients with psoriasis who were randomized to receive a gain-framed or loss-framed message about a hypothetical new biologic injectable medication for psoriasis and psoriatic arthritis (PsA). More than half were male (64.4%), white (53.3%), and non-Hispanic or Latino (55.6%); and about one-fourth of the participants (27.8%) also had psoriatic arthritis (PsA).
The gain-framed message emphasized “the chance to reduce psoriasis severity, reduce joint pain, and improve how you feel overall,” while the loss-framed message described the downsides of not taking medication – missing out “on the chance to improve your skin, your joints, and your overall health,” with the possibility that psoriasis may get worse, “with worsening pain in your joints from psoriatic arthritis,” and feeling “worse overall.” Both messages included the side effects of the theoretical injectable, a small risk of injection-site pain and skin infections. After receiving the message, participants ranked their likelihood of taking the medication on an 11-point Likert scale, with a score of 0 indicating that they would “definitely” not use the medication and a score of 10 indicating that they would “definitely” use the medication.
Scores among those who received the loss-framed message were a mean of 8.84, compared with 7.11 among patients who received the gain-framed message (between-group difference; 1.73; P less than .0001). When comparing patients with and without PsA, the between-group difference was 1.90 for patients with PsA (P less than .0001) and 1.08 for patients who did not have PsA (P = .002). Comparing the responses of those with PsA and those without PsA, the between-group difference was 1.08 (P = .03). While PsA and non-PsA patients favored the loss-framed messages, “regardless of the framing type, PsA patients always responded with a greater preference for the therapy,” Mr. Kassardjian said.
Gender also had an effect on responsiveness to gain-framed or loss-framed messaging. Both men and women ranked the loss-framed messaging as making them more likely to use the medication, but the between-group difference for women (2.00; P = .008) was higher than in men (1.49; P = .003). However, the total men compared with total women between-group differences were not significant.
“In clinical practice, physicians regularly weigh the benefits and risks of treatment. In order to communicate this information to patients, it is important to understand how framing these benefits and risks impacts patient preferences for therapy,” Mr. Kassardjian said. “While most available biologics are effective and have tolerable safety profiles, many psoriasis patients may be hesitant to initiate these therapies. Thus, it is important to convey the benefits and risks of these systemic agents in ways that resonate with patients.”
Mr. Kassardjian reports receiving the Dean’s Research Scholarship at the University of Southern California, funded by the Wright Foundation at the time of the study. Senior author April Armstrong, MD, disclosed serving as an investigator and/or consultant for AbbVie, BMS, Dermavant, Dermira, Eli Lilly, Janssen, Leo Pharma, Kyowa Hakko Kirin, Modernizing Medicine, Novartis, Ortho Dermatologics, Regeneron, Sanofi, Sun Pharma, and UCB.
SOURCE: Kassardjian A. SID 2020, Abstract 489.
, held virtually.
“We typically explain to patients the benefits of treatment,” Ari A. Kassardjian, BS, of the University of Southern California, Los Angeles, said in his presentation. “However, explaining to them the harmful effects on their skin and joint diseases, such as exacerbation of psoriasis and/or psoriatic arthritis, could offer some patients a new perspective that may influence their treatment preferences; and ultimately, better communication may lead to better medication adherence in patients.”
In the study he presented, explaining to patients possible outcomes without treatment was more effective in getting them to agree to treatment than was messaging that focused on the positive effects of a therapy (reducing disease severity and pain, and improved health).
He noted that the impact of framing choices in terms of gain or loss on decision-making has been measured in other areas of medicine, including in patients with multiple sclerosis where medication adherence is an issue (J Health Commun. 2017 Jun;22[6]:523-31). “Gain-framed” messages focus on the benefits of taking a medication, while “loss-framed” messages highlight the potential consequences of not agreeing or adhering to treatment.
In the study, Mr. Kassardjian and coinvestigators evaluated 90 patients with psoriasis who were randomized to receive a gain-framed or loss-framed message about a hypothetical new biologic injectable medication for psoriasis and psoriatic arthritis (PsA). More than half were male (64.4%), white (53.3%), and non-Hispanic or Latino (55.6%); and about one-fourth of the participants (27.8%) also had psoriatic arthritis (PsA).
The gain-framed message emphasized “the chance to reduce psoriasis severity, reduce joint pain, and improve how you feel overall,” while the loss-framed message described the downsides of not taking medication – missing out “on the chance to improve your skin, your joints, and your overall health,” with the possibility that psoriasis may get worse, “with worsening pain in your joints from psoriatic arthritis,” and feeling “worse overall.” Both messages included the side effects of the theoretical injectable, a small risk of injection-site pain and skin infections. After receiving the message, participants ranked their likelihood of taking the medication on an 11-point Likert scale, with a score of 0 indicating that they would “definitely” not use the medication and a score of 10 indicating that they would “definitely” use the medication.
Scores among those who received the loss-framed message were a mean of 8.84, compared with 7.11 among patients who received the gain-framed message (between-group difference; 1.73; P less than .0001). When comparing patients with and without PsA, the between-group difference was 1.90 for patients with PsA (P less than .0001) and 1.08 for patients who did not have PsA (P = .002). Comparing the responses of those with PsA and those without PsA, the between-group difference was 1.08 (P = .03). While PsA and non-PsA patients favored the loss-framed messages, “regardless of the framing type, PsA patients always responded with a greater preference for the therapy,” Mr. Kassardjian said.
Gender also had an effect on responsiveness to gain-framed or loss-framed messaging. Both men and women ranked the loss-framed messaging as making them more likely to use the medication, but the between-group difference for women (2.00; P = .008) was higher than in men (1.49; P = .003). However, the total men compared with total women between-group differences were not significant.
“In clinical practice, physicians regularly weigh the benefits and risks of treatment. In order to communicate this information to patients, it is important to understand how framing these benefits and risks impacts patient preferences for therapy,” Mr. Kassardjian said. “While most available biologics are effective and have tolerable safety profiles, many psoriasis patients may be hesitant to initiate these therapies. Thus, it is important to convey the benefits and risks of these systemic agents in ways that resonate with patients.”
Mr. Kassardjian reports receiving the Dean’s Research Scholarship at the University of Southern California, funded by the Wright Foundation at the time of the study. Senior author April Armstrong, MD, disclosed serving as an investigator and/or consultant for AbbVie, BMS, Dermavant, Dermira, Eli Lilly, Janssen, Leo Pharma, Kyowa Hakko Kirin, Modernizing Medicine, Novartis, Ortho Dermatologics, Regeneron, Sanofi, Sun Pharma, and UCB.
SOURCE: Kassardjian A. SID 2020, Abstract 489.
FROM SID 2020
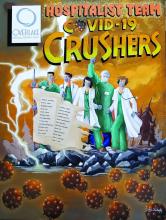
COVID-19 crushers: An appreciation of hospitalists
The hospitalist team at Overlake Medical Center and Clinics in Bellevue, Wash., has been a major partner of our Clinical Documentation Integrity Department in achieving its goal of accurately capturing the quality care patients receive on their records.
For many years, we have been witnesses of our hospitalists’ hard work, and the unique challenges of this pandemic further showed their tenacity and resilience. I thought that the best way to tell this story is through the poster accompanying this article.
To the viewer, this demonstrates the fierce battle raging between our hospitalists and the invisible foe, COVID-19. To my hospitalist colleagues, this is a constant reminder, albeit visually, that you are appreciated, admired and valued – not only by the CDI Department but by the whole organization as well.
Beyond my local colleagues, I would like to also thank the hospitalists working around the globe for their dedication and resolve in fighting this pandemic.
Mr. Valentin is a nurse and Certified Clinical Documentation Integrity Specialist at Overlake Medical Center and Clinics, Bellevue, Wash. His clinical specialties within nursing practice are in the OR, acute inpatient psychiatry, and the AIDS Unit.
The hospitalist team at Overlake Medical Center and Clinics in Bellevue, Wash., has been a major partner of our Clinical Documentation Integrity Department in achieving its goal of accurately capturing the quality care patients receive on their records.
For many years, we have been witnesses of our hospitalists’ hard work, and the unique challenges of this pandemic further showed their tenacity and resilience. I thought that the best way to tell this story is through the poster accompanying this article.
To the viewer, this demonstrates the fierce battle raging between our hospitalists and the invisible foe, COVID-19. To my hospitalist colleagues, this is a constant reminder, albeit visually, that you are appreciated, admired and valued – not only by the CDI Department but by the whole organization as well.
Beyond my local colleagues, I would like to also thank the hospitalists working around the globe for their dedication and resolve in fighting this pandemic.
Mr. Valentin is a nurse and Certified Clinical Documentation Integrity Specialist at Overlake Medical Center and Clinics, Bellevue, Wash. His clinical specialties within nursing practice are in the OR, acute inpatient psychiatry, and the AIDS Unit.
The hospitalist team at Overlake Medical Center and Clinics in Bellevue, Wash., has been a major partner of our Clinical Documentation Integrity Department in achieving its goal of accurately capturing the quality care patients receive on their records.
For many years, we have been witnesses of our hospitalists’ hard work, and the unique challenges of this pandemic further showed their tenacity and resilience. I thought that the best way to tell this story is through the poster accompanying this article.
To the viewer, this demonstrates the fierce battle raging between our hospitalists and the invisible foe, COVID-19. To my hospitalist colleagues, this is a constant reminder, albeit visually, that you are appreciated, admired and valued – not only by the CDI Department but by the whole organization as well.
Beyond my local colleagues, I would like to also thank the hospitalists working around the globe for their dedication and resolve in fighting this pandemic.
Mr. Valentin is a nurse and Certified Clinical Documentation Integrity Specialist at Overlake Medical Center and Clinics, Bellevue, Wash. His clinical specialties within nursing practice are in the OR, acute inpatient psychiatry, and the AIDS Unit.
COVID-19 may increase risk of preterm birth and cesarean delivery
Among 57 hospitalized patients with SARS-CoV-2 infection who underwent vaginal or cesarean delivery, 7 had spontaneous preterm or respiratory-indicated preterm delivery, a rate of 12%, according to a study published in Obstetrics & Gynecology. For comparison, 7% of patients had preterm delivery in 2019, researchers reported “We also noted a high cesarean delivery rate in the study population (39% vs. 27% in the same area in 2019), mainly as a result of maternal respiratory-indicated urgent delivery,” wrote Valeria M. Savasi, MD, PhD, of the University of Milan and Luigi Sacco Hospital, also in Milan, and colleagues.
Data do not indicate that pregnant women are more susceptible to severe COVID-19 infection, nor have studies suggested an increased risk of miscarriage, congenital anomalies, or early pregnancy loss in pregnant patients with COVID-19, the authors wrote. Studies have described an increased risk of preterm birth, however.
To study clinical features of maternal SARS-CoV-2 infection and potential factors associated with severe disease and iatrogenic delivery, Dr. Savasi and colleagues conducted a prospective study of 77 women with laboratory-confirmed SARS-CoV-2 infection who were admitted during pregnancy or the immediate postpartum period in 12 maternity hospitals in northern Italy between Feb. 23 and March 28, 2020.
The investigators classified patients as having severe disease if they underwent urgent delivery based on maternal respiratory function or if they were admitted to an ICU or subintensive care department. In all, 14 patients (18%) were classified as having severe disease.
“Three patients were intubated after emergency cesarean delivery performed for maternal deterioration, and one patient underwent extracorporeal membrane oxygenation,” Dr. Savasi and colleagues reported. The results are consistent with epidemiologic data in the nonpregnant population with COVID-19 disease.
Of 11 patients with severe disease who underwent urgent delivery for respiratory compromise, 6 had significant postpartum improvement in clinical conditions. No maternal deaths occurred.
“Increased BMI [body mass index] was a significant risk factor for severe disease,” Dr. Savasi and colleagues wrote. “Fever and dyspnea on admission were symptoms significantly associated with subsequent severe maternal respiratory deterioration.”
Most patients (65%) were admitted during the third trimester, and 20 patients were still pregnant at discharge.
“Nine newborns were admitted to the neonatal intensive care unit,” the authors wrote. “Interestingly, besides prematurity, fetal oxygenation and well-being at delivery were not apparently affected by the maternal acute conditions.” Three newborns with vaginal delivery and one with cesarean delivery tested positive for SARS-CoV-2. The newborns may have been infected after delivery, Dr. Savasi and colleagues added. For all newborns, rooming-in and breastfeeding were performed, and none developed respiratory symptoms.
Criteria for hospital admission and therapeutic protocols may have varied between hospitals, the authors noted. In addition, the study included 12 patients who were asymptomatic and admitted for obstetric indications. These patients were tested for SARS-CoV-2 because of contact with an infected individual. Most patients were symptomatic, however, which explains the high rate of maternal severe outcomes. Hospitals have since adopted a universal SARS-CoV-2 screening policy for hospitalized pregnant patients.
Kristina Adams Waldorf, MD, professor of obstetrics and gynecology at the University of Washington, Seattle, commented in an interview that Savasi et al. describe one of the larger COVID-19 in pregnancy cohorts to date with rates of severe disease and delivery for respiratory compromise, which is remarkably similar to Washington state (severe disease, 18% vs. nearly 15%; delivery for respiratory compromise, 16% vs. 20%). As in Washington state, Italian women with a higher prepregnancy BMI were overrepresented in the severe disease group.
“Data are beginning to emerge that identify women who were overweight or obese prior to pregnancy as a high risk group for developing severe COVID-19. These data are similar to known associations between obesity and critical illness in pregnancy during the 2009 ‘swine flu’ (influenza A virus, H1N1) pandemic,” she said.
“This study and others indicate that the late second and third trimesters may be a time when women are more likely to be symptomatic from COVID-19. It remains unclear if women in the first trimester are protected from severe COVID-19 outcomes or have outcomes similar to nonpregnant women,” concluded Dr. Waldorf.
One study author disclosed receiving funds from Lo Li Pharma and Zambongroup. The other authors did not report any potential conflicts of interest. Dr. Waldorf said she had no relevant financial disclosures.
SOURCE: Savasi VM et al. Obstet Gynecol. 2020 May 19. doi: 10.1097/AOG.0000000000003979.
Among 57 hospitalized patients with SARS-CoV-2 infection who underwent vaginal or cesarean delivery, 7 had spontaneous preterm or respiratory-indicated preterm delivery, a rate of 12%, according to a study published in Obstetrics & Gynecology. For comparison, 7% of patients had preterm delivery in 2019, researchers reported “We also noted a high cesarean delivery rate in the study population (39% vs. 27% in the same area in 2019), mainly as a result of maternal respiratory-indicated urgent delivery,” wrote Valeria M. Savasi, MD, PhD, of the University of Milan and Luigi Sacco Hospital, also in Milan, and colleagues.
Data do not indicate that pregnant women are more susceptible to severe COVID-19 infection, nor have studies suggested an increased risk of miscarriage, congenital anomalies, or early pregnancy loss in pregnant patients with COVID-19, the authors wrote. Studies have described an increased risk of preterm birth, however.
To study clinical features of maternal SARS-CoV-2 infection and potential factors associated with severe disease and iatrogenic delivery, Dr. Savasi and colleagues conducted a prospective study of 77 women with laboratory-confirmed SARS-CoV-2 infection who were admitted during pregnancy or the immediate postpartum period in 12 maternity hospitals in northern Italy between Feb. 23 and March 28, 2020.
The investigators classified patients as having severe disease if they underwent urgent delivery based on maternal respiratory function or if they were admitted to an ICU or subintensive care department. In all, 14 patients (18%) were classified as having severe disease.
“Three patients were intubated after emergency cesarean delivery performed for maternal deterioration, and one patient underwent extracorporeal membrane oxygenation,” Dr. Savasi and colleagues reported. The results are consistent with epidemiologic data in the nonpregnant population with COVID-19 disease.
Of 11 patients with severe disease who underwent urgent delivery for respiratory compromise, 6 had significant postpartum improvement in clinical conditions. No maternal deaths occurred.
“Increased BMI [body mass index] was a significant risk factor for severe disease,” Dr. Savasi and colleagues wrote. “Fever and dyspnea on admission were symptoms significantly associated with subsequent severe maternal respiratory deterioration.”
Most patients (65%) were admitted during the third trimester, and 20 patients were still pregnant at discharge.
“Nine newborns were admitted to the neonatal intensive care unit,” the authors wrote. “Interestingly, besides prematurity, fetal oxygenation and well-being at delivery were not apparently affected by the maternal acute conditions.” Three newborns with vaginal delivery and one with cesarean delivery tested positive for SARS-CoV-2. The newborns may have been infected after delivery, Dr. Savasi and colleagues added. For all newborns, rooming-in and breastfeeding were performed, and none developed respiratory symptoms.
Criteria for hospital admission and therapeutic protocols may have varied between hospitals, the authors noted. In addition, the study included 12 patients who were asymptomatic and admitted for obstetric indications. These patients were tested for SARS-CoV-2 because of contact with an infected individual. Most patients were symptomatic, however, which explains the high rate of maternal severe outcomes. Hospitals have since adopted a universal SARS-CoV-2 screening policy for hospitalized pregnant patients.
Kristina Adams Waldorf, MD, professor of obstetrics and gynecology at the University of Washington, Seattle, commented in an interview that Savasi et al. describe one of the larger COVID-19 in pregnancy cohorts to date with rates of severe disease and delivery for respiratory compromise, which is remarkably similar to Washington state (severe disease, 18% vs. nearly 15%; delivery for respiratory compromise, 16% vs. 20%). As in Washington state, Italian women with a higher prepregnancy BMI were overrepresented in the severe disease group.
“Data are beginning to emerge that identify women who were overweight or obese prior to pregnancy as a high risk group for developing severe COVID-19. These data are similar to known associations between obesity and critical illness in pregnancy during the 2009 ‘swine flu’ (influenza A virus, H1N1) pandemic,” she said.
“This study and others indicate that the late second and third trimesters may be a time when women are more likely to be symptomatic from COVID-19. It remains unclear if women in the first trimester are protected from severe COVID-19 outcomes or have outcomes similar to nonpregnant women,” concluded Dr. Waldorf.
One study author disclosed receiving funds from Lo Li Pharma and Zambongroup. The other authors did not report any potential conflicts of interest. Dr. Waldorf said she had no relevant financial disclosures.
SOURCE: Savasi VM et al. Obstet Gynecol. 2020 May 19. doi: 10.1097/AOG.0000000000003979.
Among 57 hospitalized patients with SARS-CoV-2 infection who underwent vaginal or cesarean delivery, 7 had spontaneous preterm or respiratory-indicated preterm delivery, a rate of 12%, according to a study published in Obstetrics & Gynecology. For comparison, 7% of patients had preterm delivery in 2019, researchers reported “We also noted a high cesarean delivery rate in the study population (39% vs. 27% in the same area in 2019), mainly as a result of maternal respiratory-indicated urgent delivery,” wrote Valeria M. Savasi, MD, PhD, of the University of Milan and Luigi Sacco Hospital, also in Milan, and colleagues.
Data do not indicate that pregnant women are more susceptible to severe COVID-19 infection, nor have studies suggested an increased risk of miscarriage, congenital anomalies, or early pregnancy loss in pregnant patients with COVID-19, the authors wrote. Studies have described an increased risk of preterm birth, however.
To study clinical features of maternal SARS-CoV-2 infection and potential factors associated with severe disease and iatrogenic delivery, Dr. Savasi and colleagues conducted a prospective study of 77 women with laboratory-confirmed SARS-CoV-2 infection who were admitted during pregnancy or the immediate postpartum period in 12 maternity hospitals in northern Italy between Feb. 23 and March 28, 2020.
The investigators classified patients as having severe disease if they underwent urgent delivery based on maternal respiratory function or if they were admitted to an ICU or subintensive care department. In all, 14 patients (18%) were classified as having severe disease.
“Three patients were intubated after emergency cesarean delivery performed for maternal deterioration, and one patient underwent extracorporeal membrane oxygenation,” Dr. Savasi and colleagues reported. The results are consistent with epidemiologic data in the nonpregnant population with COVID-19 disease.
Of 11 patients with severe disease who underwent urgent delivery for respiratory compromise, 6 had significant postpartum improvement in clinical conditions. No maternal deaths occurred.
“Increased BMI [body mass index] was a significant risk factor for severe disease,” Dr. Savasi and colleagues wrote. “Fever and dyspnea on admission were symptoms significantly associated with subsequent severe maternal respiratory deterioration.”
Most patients (65%) were admitted during the third trimester, and 20 patients were still pregnant at discharge.
“Nine newborns were admitted to the neonatal intensive care unit,” the authors wrote. “Interestingly, besides prematurity, fetal oxygenation and well-being at delivery were not apparently affected by the maternal acute conditions.” Three newborns with vaginal delivery and one with cesarean delivery tested positive for SARS-CoV-2. The newborns may have been infected after delivery, Dr. Savasi and colleagues added. For all newborns, rooming-in and breastfeeding were performed, and none developed respiratory symptoms.
Criteria for hospital admission and therapeutic protocols may have varied between hospitals, the authors noted. In addition, the study included 12 patients who were asymptomatic and admitted for obstetric indications. These patients were tested for SARS-CoV-2 because of contact with an infected individual. Most patients were symptomatic, however, which explains the high rate of maternal severe outcomes. Hospitals have since adopted a universal SARS-CoV-2 screening policy for hospitalized pregnant patients.
Kristina Adams Waldorf, MD, professor of obstetrics and gynecology at the University of Washington, Seattle, commented in an interview that Savasi et al. describe one of the larger COVID-19 in pregnancy cohorts to date with rates of severe disease and delivery for respiratory compromise, which is remarkably similar to Washington state (severe disease, 18% vs. nearly 15%; delivery for respiratory compromise, 16% vs. 20%). As in Washington state, Italian women with a higher prepregnancy BMI were overrepresented in the severe disease group.
“Data are beginning to emerge that identify women who were overweight or obese prior to pregnancy as a high risk group for developing severe COVID-19. These data are similar to known associations between obesity and critical illness in pregnancy during the 2009 ‘swine flu’ (influenza A virus, H1N1) pandemic,” she said.
“This study and others indicate that the late second and third trimesters may be a time when women are more likely to be symptomatic from COVID-19. It remains unclear if women in the first trimester are protected from severe COVID-19 outcomes or have outcomes similar to nonpregnant women,” concluded Dr. Waldorf.
One study author disclosed receiving funds from Lo Li Pharma and Zambongroup. The other authors did not report any potential conflicts of interest. Dr. Waldorf said she had no relevant financial disclosures.
SOURCE: Savasi VM et al. Obstet Gynecol. 2020 May 19. doi: 10.1097/AOG.0000000000003979.
FROM OBSTETRICS & GYNECOLOGY
Testing the limits of medical technology
On March 9 my team was given a directive by the chief medical officer of our health system. It seemed like an impossible task, involving the mobilization of people, processes, and technology at a scale and speed we had never before achieved. It turned out getting this done was impossible. In spite of our best efforts, we failed to meet the deadline – it actually took us 3 days. Still, by March 12, we had opened the doors on the first community testing site in our area and gained the attention of local and national news outlets for our accomplishment.
Now more than 2 months later, I’m quite proud of what our team was able to achieve for the health system, but I’m still quite frustrated at the state of COVID-19 testing nationwide – there’s simply not enough available, and there is tremendous variability in the reliability of the tests. In this column, we’d like to highlight some of the challenges we’ve faced and reflect on how the shortcomings of modern technology have once again proven that medicine is both a science and an art.
Our dangerous lack of preparation
Prior to the coronavirus pandemic, I had never considered surgical masks, face shields, and nasal swabs to be critical components of medical technology. My opinion quickly changed after opening our drive-through COVID-19 site. I now have a much greater appreciation for the importance of personal protective equipment and basic testing supplies.
I was shocked by how difficult obtaining it has been during the past few months. It seems that no one anticipated the possibility of a pandemic on this grand a scale, so stockpiles of equipment were depleted quickly and couldn’t be replenished. Also, most manufacturing occurs outside the United States, which creates additional barriers to controlling the supply chain. One need not look far to find stories of widespread price-gouging, black market racketeering, and even hijackings that have stood in the way of accessing the necessary supplies. Sadly, the lack of equipment is far from the only challenge we’ve faced. In some cases, it has been a mistrust of results that has prevented widespread testing and mitigation.
The risks of flying blind
When President Trump touted the introduction of a rapid COVID-19 test at the end of March, many people were excited. Promising positive results in as few as 5 minutes, the assay was granted an Emergency Use Authorization (EUA) by the Food and Drug Administration in order to expedite its availability in the market. According to the FDA’s website, an EUA allows “unapproved medical products or unapproved uses of approved medical products to be used in an emergency to diagnose, treat, or prevent serious or life-threatening diseases or conditions.” This rapid (though untested) approval was all that many health care providers needed to hear – immediately hospitals and physicians scrambled to get their hands on the testing devices. Unfortunately, on May 14th, the FDA issued a press release that raised concerns about that same test because it seemed to be reporting a high number of false-negative results. Just as quickly as the devices had been adopted, health care providers began backing away from them in favor of other assays, and a serious truth about COVID-19 testing was revealed: In many ways, we’re flying blind.
Laboratory manufacturers have been working overtime to create assays for SARS-CoV-2 (the coronavirus that causes COVID-19) and have used different technologies for detection. The most commonly used are polymerase chain reaction (PCR) tests. In these assays, viral RNA is converted to DNA by reverse transcriptase, then amplified through the addition of primers that enable detection. PCR technology has been available for years and is a reliable method for identifying DNA and RNA, but the required heating and cooling process takes time and results can take several hours to return. To address this and expedite testing, other methods of detection have been tried, such as the loop-mediated isothermal amplification (LAMP) technique employed by the rapid assay mentioned above. Regardless of methodology, all laboratory tests have one thing in common: None of them is perfect.
Every assay has a different level of reliability. When screening for a disease such as COVID-19, we are particularly interested in a test’s sensitivity (that is, it’s ability to detect disease); we’d love such a screening test to be 100% sensitive and thereby not miss a single case. In truth, no test’s sensitivity is 100%, and in this particular case even the best assays only score around 98%. This means that out of every 100 patients with COVID-19 who are evaluated, two might test negative for the virus. In a pandemic this can have dire consequences, so health care providers – unable to fully trust their instruments – must employ clinical acumen and years of experience to navigate these cloudy skies. We are hopeful that additional tools will complement our current methods, but with new assays also come new questions.
Is anyone safe?
We receive regular questions from physicians about the value of antibody testing, but it’s not yet clear how best to respond. While the assays seem to be reliable, the utility of the results are still ill defined. Antibodies to SARS-CoV-2 (both IgG and IgM) appear to peak about 2-3 weeks after symptom onset, but we don’t yet know if the presence of those antibodies confers long-term immunity. Therefore, patients should not use the information to change their masking or social-distancing practices, nor should they presume that they are safe from becoming reinfected with COVID-19. While new research looks promising, there are still too many unknowns to be able to confidently reassure providers or patients of the true value of antibody testing. This underscores our final point: Medicine remains an art.
As we are regularly reminded, we’ll never fully anticipate the challenges or barriers to success, and technology will never replace the value of clinical judgment and human experience. While the situation is unsettling in many ways, we are reassured and encouraged by the role we still get to play in keeping our patients healthy in this health care crisis, and we’ll continue to do so through whatever the future holds.
Dr. Notte is a family physician and chief medical officer of Abington Lansdale (Pa.) Hospital - Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
On March 9 my team was given a directive by the chief medical officer of our health system. It seemed like an impossible task, involving the mobilization of people, processes, and technology at a scale and speed we had never before achieved. It turned out getting this done was impossible. In spite of our best efforts, we failed to meet the deadline – it actually took us 3 days. Still, by March 12, we had opened the doors on the first community testing site in our area and gained the attention of local and national news outlets for our accomplishment.
Now more than 2 months later, I’m quite proud of what our team was able to achieve for the health system, but I’m still quite frustrated at the state of COVID-19 testing nationwide – there’s simply not enough available, and there is tremendous variability in the reliability of the tests. In this column, we’d like to highlight some of the challenges we’ve faced and reflect on how the shortcomings of modern technology have once again proven that medicine is both a science and an art.
Our dangerous lack of preparation
Prior to the coronavirus pandemic, I had never considered surgical masks, face shields, and nasal swabs to be critical components of medical technology. My opinion quickly changed after opening our drive-through COVID-19 site. I now have a much greater appreciation for the importance of personal protective equipment and basic testing supplies.
I was shocked by how difficult obtaining it has been during the past few months. It seems that no one anticipated the possibility of a pandemic on this grand a scale, so stockpiles of equipment were depleted quickly and couldn’t be replenished. Also, most manufacturing occurs outside the United States, which creates additional barriers to controlling the supply chain. One need not look far to find stories of widespread price-gouging, black market racketeering, and even hijackings that have stood in the way of accessing the necessary supplies. Sadly, the lack of equipment is far from the only challenge we’ve faced. In some cases, it has been a mistrust of results that has prevented widespread testing and mitigation.
The risks of flying blind
When President Trump touted the introduction of a rapid COVID-19 test at the end of March, many people were excited. Promising positive results in as few as 5 minutes, the assay was granted an Emergency Use Authorization (EUA) by the Food and Drug Administration in order to expedite its availability in the market. According to the FDA’s website, an EUA allows “unapproved medical products or unapproved uses of approved medical products to be used in an emergency to diagnose, treat, or prevent serious or life-threatening diseases or conditions.” This rapid (though untested) approval was all that many health care providers needed to hear – immediately hospitals and physicians scrambled to get their hands on the testing devices. Unfortunately, on May 14th, the FDA issued a press release that raised concerns about that same test because it seemed to be reporting a high number of false-negative results. Just as quickly as the devices had been adopted, health care providers began backing away from them in favor of other assays, and a serious truth about COVID-19 testing was revealed: In many ways, we’re flying blind.
Laboratory manufacturers have been working overtime to create assays for SARS-CoV-2 (the coronavirus that causes COVID-19) and have used different technologies for detection. The most commonly used are polymerase chain reaction (PCR) tests. In these assays, viral RNA is converted to DNA by reverse transcriptase, then amplified through the addition of primers that enable detection. PCR technology has been available for years and is a reliable method for identifying DNA and RNA, but the required heating and cooling process takes time and results can take several hours to return. To address this and expedite testing, other methods of detection have been tried, such as the loop-mediated isothermal amplification (LAMP) technique employed by the rapid assay mentioned above. Regardless of methodology, all laboratory tests have one thing in common: None of them is perfect.
Every assay has a different level of reliability. When screening for a disease such as COVID-19, we are particularly interested in a test’s sensitivity (that is, it’s ability to detect disease); we’d love such a screening test to be 100% sensitive and thereby not miss a single case. In truth, no test’s sensitivity is 100%, and in this particular case even the best assays only score around 98%. This means that out of every 100 patients with COVID-19 who are evaluated, two might test negative for the virus. In a pandemic this can have dire consequences, so health care providers – unable to fully trust their instruments – must employ clinical acumen and years of experience to navigate these cloudy skies. We are hopeful that additional tools will complement our current methods, but with new assays also come new questions.
Is anyone safe?
We receive regular questions from physicians about the value of antibody testing, but it’s not yet clear how best to respond. While the assays seem to be reliable, the utility of the results are still ill defined. Antibodies to SARS-CoV-2 (both IgG and IgM) appear to peak about 2-3 weeks after symptom onset, but we don’t yet know if the presence of those antibodies confers long-term immunity. Therefore, patients should not use the information to change their masking or social-distancing practices, nor should they presume that they are safe from becoming reinfected with COVID-19. While new research looks promising, there are still too many unknowns to be able to confidently reassure providers or patients of the true value of antibody testing. This underscores our final point: Medicine remains an art.
As we are regularly reminded, we’ll never fully anticipate the challenges or barriers to success, and technology will never replace the value of clinical judgment and human experience. While the situation is unsettling in many ways, we are reassured and encouraged by the role we still get to play in keeping our patients healthy in this health care crisis, and we’ll continue to do so through whatever the future holds.
Dr. Notte is a family physician and chief medical officer of Abington Lansdale (Pa.) Hospital - Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
On March 9 my team was given a directive by the chief medical officer of our health system. It seemed like an impossible task, involving the mobilization of people, processes, and technology at a scale and speed we had never before achieved. It turned out getting this done was impossible. In spite of our best efforts, we failed to meet the deadline – it actually took us 3 days. Still, by March 12, we had opened the doors on the first community testing site in our area and gained the attention of local and national news outlets for our accomplishment.
Now more than 2 months later, I’m quite proud of what our team was able to achieve for the health system, but I’m still quite frustrated at the state of COVID-19 testing nationwide – there’s simply not enough available, and there is tremendous variability in the reliability of the tests. In this column, we’d like to highlight some of the challenges we’ve faced and reflect on how the shortcomings of modern technology have once again proven that medicine is both a science and an art.
Our dangerous lack of preparation
Prior to the coronavirus pandemic, I had never considered surgical masks, face shields, and nasal swabs to be critical components of medical technology. My opinion quickly changed after opening our drive-through COVID-19 site. I now have a much greater appreciation for the importance of personal protective equipment and basic testing supplies.
I was shocked by how difficult obtaining it has been during the past few months. It seems that no one anticipated the possibility of a pandemic on this grand a scale, so stockpiles of equipment were depleted quickly and couldn’t be replenished. Also, most manufacturing occurs outside the United States, which creates additional barriers to controlling the supply chain. One need not look far to find stories of widespread price-gouging, black market racketeering, and even hijackings that have stood in the way of accessing the necessary supplies. Sadly, the lack of equipment is far from the only challenge we’ve faced. In some cases, it has been a mistrust of results that has prevented widespread testing and mitigation.
The risks of flying blind
When President Trump touted the introduction of a rapid COVID-19 test at the end of March, many people were excited. Promising positive results in as few as 5 minutes, the assay was granted an Emergency Use Authorization (EUA) by the Food and Drug Administration in order to expedite its availability in the market. According to the FDA’s website, an EUA allows “unapproved medical products or unapproved uses of approved medical products to be used in an emergency to diagnose, treat, or prevent serious or life-threatening diseases or conditions.” This rapid (though untested) approval was all that many health care providers needed to hear – immediately hospitals and physicians scrambled to get their hands on the testing devices. Unfortunately, on May 14th, the FDA issued a press release that raised concerns about that same test because it seemed to be reporting a high number of false-negative results. Just as quickly as the devices had been adopted, health care providers began backing away from them in favor of other assays, and a serious truth about COVID-19 testing was revealed: In many ways, we’re flying blind.
Laboratory manufacturers have been working overtime to create assays for SARS-CoV-2 (the coronavirus that causes COVID-19) and have used different technologies for detection. The most commonly used are polymerase chain reaction (PCR) tests. In these assays, viral RNA is converted to DNA by reverse transcriptase, then amplified through the addition of primers that enable detection. PCR technology has been available for years and is a reliable method for identifying DNA and RNA, but the required heating and cooling process takes time and results can take several hours to return. To address this and expedite testing, other methods of detection have been tried, such as the loop-mediated isothermal amplification (LAMP) technique employed by the rapid assay mentioned above. Regardless of methodology, all laboratory tests have one thing in common: None of them is perfect.
Every assay has a different level of reliability. When screening for a disease such as COVID-19, we are particularly interested in a test’s sensitivity (that is, it’s ability to detect disease); we’d love such a screening test to be 100% sensitive and thereby not miss a single case. In truth, no test’s sensitivity is 100%, and in this particular case even the best assays only score around 98%. This means that out of every 100 patients with COVID-19 who are evaluated, two might test negative for the virus. In a pandemic this can have dire consequences, so health care providers – unable to fully trust their instruments – must employ clinical acumen and years of experience to navigate these cloudy skies. We are hopeful that additional tools will complement our current methods, but with new assays also come new questions.
Is anyone safe?
We receive regular questions from physicians about the value of antibody testing, but it’s not yet clear how best to respond. While the assays seem to be reliable, the utility of the results are still ill defined. Antibodies to SARS-CoV-2 (both IgG and IgM) appear to peak about 2-3 weeks after symptom onset, but we don’t yet know if the presence of those antibodies confers long-term immunity. Therefore, patients should not use the information to change their masking or social-distancing practices, nor should they presume that they are safe from becoming reinfected with COVID-19. While new research looks promising, there are still too many unknowns to be able to confidently reassure providers or patients of the true value of antibody testing. This underscores our final point: Medicine remains an art.
As we are regularly reminded, we’ll never fully anticipate the challenges or barriers to success, and technology will never replace the value of clinical judgment and human experience. While the situation is unsettling in many ways, we are reassured and encouraged by the role we still get to play in keeping our patients healthy in this health care crisis, and we’ll continue to do so through whatever the future holds.
Dr. Notte is a family physician and chief medical officer of Abington Lansdale (Pa.) Hospital - Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
Scientific doubt tempers COVID-19 vaccine optimism
US government and industry projections that a COVID-19 vaccine will be ready by this fall or even January would take compressing what usually takes at least a decade into months, with little room for error or safety surprises.
“If all the cards fall into the right place and all the stars are aligned, you definitely could get a vaccine by December or January,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said last week.
But Fauci said a more realistic timeline is still 12 to 18 months, and experts interviewed by Medscape Medical News agree. They say that although recent developments are encouraging, history and scientific reason say the day when a COVID-19 vaccine is widely available will not come this year and may not come by the end of 2021.
The encouraging signals come primarily from two recent announcements: the $1.2 billion United States backing last week of one vaccine platform and the announcement on May 18 that the first human trials of another have produced some positive phase 1 results.
Recent developments
On May 21, the US Department of Health and Human Services (HHS) under “Operation Warp Speed” announced that the US will give AstraZeneca $1.2 billion “to make available at least 300 million doses of a coronavirus vaccine called AZD1222, with the first doses delivered as early as October 2020.”
On May 18, the Massachusetts-based biotechnology company Moderna announced that phase 1 clinical results showed that its vaccine candidate, which uses a new messenger RNA (mRNA) technology, appeared safe. Eight participants in the human trials were able to produce neutralizing antibodies that researchers believe are important in developing protection from the virus.
Moderna Chief Medical Officer Tal Zaks, MD, PhD told CNN that if the vaccine candidate does well in phase 2, “it could be ready by January 2021.”
The two candidates are among 10 in clinical trials for the SARS-CoV-2 virus, according to the World Health Organization (WHO). The AstraZeneca/ AZD1222 candidate (also called ChAdOx1 nCoV-19, in collaboration with the University of Oxford) has entered phase 2/3.
Moderna’s candidate and another being developed in Beijing, China, are in phase 2, WHO reports. As of yesterday, 115 other candidates are in preclinical evaluation.
Maria Elena Bottazzi, PhD, associate dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, Texas, told Medscape Medical News it’s important to realize that, in the case of the $1.2 billion US investment, “what they’re talking about is manufacturing.”
The idea, she said, is to pay AstraZeneca up front so that manufacturing can start before it is known whether the vaccine candidate is safe or effective, the reverse of how the clinical trial process usually works.
That way, if the candidate is deemed safe and effective, time is not lost by then deciding how to make it and distribute it.
By the end of this year, she said, “Maybe we will have many vaccines made and stored in a refrigerator somewhere. But between now and December, there’s absolutely no way you can show efficacy of the vaccine at the same time you confirm that it’s safe.”
“Take these things with a grain of salt”
Animal testing for the AstraZeneca candidate, made in partnership with the University of Oxford in the United Kingdom, has yielded lackluster results, according to results on the preprint server BioRxiv, which have not been peer-reviewed.
“The results were not bad, but they were not gangbusters,” Bottazzi said. The results show the vaccine offered only partial protection.
“Partial protection is better than no protection,” she noted. “You have to take these things with a grain of salt. We don’t know what’s going to happen in humans.”
As for the Moderna candidate, Bottazzi said, “the good news is they found an appropriate safety profile. But from an eight-person group to make the extrapolation that they have efficacy — it’s unrealistic.”
Nicole Lurie, MD, MSPH, is senior adviser to the CEO for the Coalition for Epidemic Preparedness Innovation (CEPI), a nongovernmental organization funded by the Wellcome Trust, the Bill and Melinda Gates Foundation, the European Commission, and eight countries (Australia, Belgium, Canada, Ethiopia, Germany, Japan, Norway, and the United Kingdom) charged with supporting development of vaccines for pathogens on WHO’s priority list.
She and her colleagues write in a paper published online in the New England Journal of Medicine on March 30 that “it typically takes multiple candidates and many years to produce a licensed vaccine.”
The fastest time for developing a vaccine to date is 4 years, for the mumps vaccine, licensed in 1967.
As to whether she would expect a rollout of any vaccine by the end of the year, Lurie told Medscape Medical News, “If everything goes according to plan in every way, shape or form, well then maybe you can get there. But I wouldn’t hold my breath.”
Lurie and her colleagues write that “it’s far from certain that these new platforms will be scalable or that existing capacity can provide sufficient quantities of vaccine fast enough.”
On a call with reporters today, leaders of some of the words largest pharmaceutical companies said that one of the key bottlenecks is the sheer number of vials needed in order to distribute billions of doses of a successful vaccine.
Pfizer CEO Albert Bourla, DVM, PhD, said, “Typically we are producing vaccines in single-dose vials. We are exploring with governments right now if it would be more convenient if there were 5-dose vials or 10-dose vials. I think we can resolve a significant part of the bottleneck.”
Despite the challenges, experts interviewed for this article agree that it will be possible to make a vaccine for COVID-19. They don’t expect attempts to meet the same complications that HIV researchers have seen over decades as the virus continues to confound with mutations.
Fred Ledley, MD, director of the Center for Integration of Science and Industry at Bentley University in Waltham, Massachusetts, told Medscape Medical News, “There doesn’t appear to be anything terribly diabolical about this virus. The mutation rate doesn’t appear to be anything like HIV. It appears to have some big, ugly proteins on the surface, which is good for vaccines — proteins with a lot of physical features look distinguishable from healthy cells. Signs all point to that it should be possible to make a vaccine.”
History raises safety concerns
However, Ledley said, “The idea of doing it in 6 months is largely unrealistic.”
He says 18 months is more realistic, primarily because of the sheer number of people that would have to be enrolled in a phase 3 study to truly test whether the endpoints are being met.
Vaccines are given to healthy volunteers. If safety signals arise, they may not be apparent until massive numbers of people are tested in phase 3.
“You’re never going to see the rates cut to 0%, but to see the difference between 10 people getting sick and seven people getting sick, takes very, very large numbers,” Ledley said. “There’s no way that can be done in 6 months. You’re talking about tens of thousands of people enrolled.”
He notes at this point it’s unclear what the endpoints will be and what the safety thresholds will be after consideration of risks and benefit.
Another big question for Ledley: “We don’t know what type of immunity we need to protect us against the virus. Do you just need the antibodies in your blood or do you need cells that are primed to attack the virus? Is it more of a chemical clearance or do the cells need to physically go in and digest the virus?”
History also points to the need for rigorous safety precautions that scientists fear could be compromised as trial phases overlap and processes are run in parallel instead of one step at a time.
An early batch of the Salk vaccine for polio in 1955, for example, turned out to be contaminated and caused paralysis in some children and 10 deaths, he points out.
CEPI’s Lurie adds that early candidates for another coronavirus, severe acute respiratory syndrome (SARS), “caused a reaction in the lungs that was very dangerous” before development was halted.
She also pointed to previous findings that a vaccine for dengue fever could worsen the disease in some people through a phenomenon called antibody-dependent enhancement.
Lurie and colleagues write in their paper that “it’s critical that vaccines also be developed using the tried-and-true methods, even if they may take longer to enter clinical trials or to result in large numbers of doses.”
Live attenuated vaccine
Raul Andino, PhD, a virologist at the University of California San Francisco, is among the scientists working with a tried-and-true method — a live attenuated vaccine — and he told Medscape Medical News he’s predicting it will take 2 years to develop.
He said it is cheaper to produce because scientists just have to learn how to grow the virus. Because the technology is already proven, a live attenuated vaccine could be rapidly produced on a worldwide scale.
The hope is also that a live attenuated vaccine would be given once in a lifetime and therefore be more affordable, especially in poorer countries.
“While a Moderna vaccine might be good for Europe and the United States,” he said, “It’s not going to be good for Africa, India, Brazil.”
Andino said, “I would bet money” that the front-runner vaccines so far will not be one-time vaccines.
He points out that most of the vaccine candidates are trying to protect people from disease. While there’s nothing wrong with that, he said, “In my opinion that is the lower-hanging fruit.”
“In my mind we need something that interrupts the chain of transmission and induces protection,” Andino said, important for developing herd immunity.
The reason this type of approach takes longer is because you are introducing a weakened form of the virus to the body and you have to make sure it doesn’t cause disease, not just in a small test population, but in populations who may be more susceptible to the disease, Andino said.
A call for unified strategies
Universities, countries, international consortiums, and public-private partnerships are all racing to find several safe and effective vaccines as no one entity will likely be able to provide the global solution.
Some of the efforts involve overlap of entities but with different focuses.
Along with “Operation Warp Speed” and CEPI, other collaborations include Gavi the Vaccine Alliance, whose core partners include WHO, UNICEF, the World Bank, and the Gates Foundation; and “Accelerating Therapeutic Interventions and Vaccines (ACTIV) partnership,” led by the National Institutes of Health.
Industry partners in ACTIV (18 biopharmaceutical companies), according to a May 18 article published online in the Journal of the American Medical Association, have said they will contribute their respective clinical trial capacities, regardless of which agent is studied.
Some, however, have called for more streamlining of efforts.
“Ideally we’d be working together,” Lurie told Medscape Medical News.
“I’m hopeful we will find ways to collaborate scientifically,” she said. “The US government’s responsibility is to make doses for the US. CEPI’s responsibility is to make doses for the world. A big focus of CEPI is to make sure we have manufacturing capacity outside of the US so those doses can be available to the world and they don’t get seized by wealthy countries.”
Bottazzi, Ledley, Lurie, and Andino report no relevant financial relationships.
This article first appeared on Medscape.com.
US government and industry projections that a COVID-19 vaccine will be ready by this fall or even January would take compressing what usually takes at least a decade into months, with little room for error or safety surprises.
“If all the cards fall into the right place and all the stars are aligned, you definitely could get a vaccine by December or January,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said last week.
But Fauci said a more realistic timeline is still 12 to 18 months, and experts interviewed by Medscape Medical News agree. They say that although recent developments are encouraging, history and scientific reason say the day when a COVID-19 vaccine is widely available will not come this year and may not come by the end of 2021.
The encouraging signals come primarily from two recent announcements: the $1.2 billion United States backing last week of one vaccine platform and the announcement on May 18 that the first human trials of another have produced some positive phase 1 results.
Recent developments
On May 21, the US Department of Health and Human Services (HHS) under “Operation Warp Speed” announced that the US will give AstraZeneca $1.2 billion “to make available at least 300 million doses of a coronavirus vaccine called AZD1222, with the first doses delivered as early as October 2020.”
On May 18, the Massachusetts-based biotechnology company Moderna announced that phase 1 clinical results showed that its vaccine candidate, which uses a new messenger RNA (mRNA) technology, appeared safe. Eight participants in the human trials were able to produce neutralizing antibodies that researchers believe are important in developing protection from the virus.
Moderna Chief Medical Officer Tal Zaks, MD, PhD told CNN that if the vaccine candidate does well in phase 2, “it could be ready by January 2021.”
The two candidates are among 10 in clinical trials for the SARS-CoV-2 virus, according to the World Health Organization (WHO). The AstraZeneca/ AZD1222 candidate (also called ChAdOx1 nCoV-19, in collaboration with the University of Oxford) has entered phase 2/3.
Moderna’s candidate and another being developed in Beijing, China, are in phase 2, WHO reports. As of yesterday, 115 other candidates are in preclinical evaluation.
Maria Elena Bottazzi, PhD, associate dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, Texas, told Medscape Medical News it’s important to realize that, in the case of the $1.2 billion US investment, “what they’re talking about is manufacturing.”
The idea, she said, is to pay AstraZeneca up front so that manufacturing can start before it is known whether the vaccine candidate is safe or effective, the reverse of how the clinical trial process usually works.
That way, if the candidate is deemed safe and effective, time is not lost by then deciding how to make it and distribute it.
By the end of this year, she said, “Maybe we will have many vaccines made and stored in a refrigerator somewhere. But between now and December, there’s absolutely no way you can show efficacy of the vaccine at the same time you confirm that it’s safe.”
“Take these things with a grain of salt”
Animal testing for the AstraZeneca candidate, made in partnership with the University of Oxford in the United Kingdom, has yielded lackluster results, according to results on the preprint server BioRxiv, which have not been peer-reviewed.
“The results were not bad, but they were not gangbusters,” Bottazzi said. The results show the vaccine offered only partial protection.
“Partial protection is better than no protection,” she noted. “You have to take these things with a grain of salt. We don’t know what’s going to happen in humans.”
As for the Moderna candidate, Bottazzi said, “the good news is they found an appropriate safety profile. But from an eight-person group to make the extrapolation that they have efficacy — it’s unrealistic.”
Nicole Lurie, MD, MSPH, is senior adviser to the CEO for the Coalition for Epidemic Preparedness Innovation (CEPI), a nongovernmental organization funded by the Wellcome Trust, the Bill and Melinda Gates Foundation, the European Commission, and eight countries (Australia, Belgium, Canada, Ethiopia, Germany, Japan, Norway, and the United Kingdom) charged with supporting development of vaccines for pathogens on WHO’s priority list.
She and her colleagues write in a paper published online in the New England Journal of Medicine on March 30 that “it typically takes multiple candidates and many years to produce a licensed vaccine.”
The fastest time for developing a vaccine to date is 4 years, for the mumps vaccine, licensed in 1967.
As to whether she would expect a rollout of any vaccine by the end of the year, Lurie told Medscape Medical News, “If everything goes according to plan in every way, shape or form, well then maybe you can get there. But I wouldn’t hold my breath.”
Lurie and her colleagues write that “it’s far from certain that these new platforms will be scalable or that existing capacity can provide sufficient quantities of vaccine fast enough.”
On a call with reporters today, leaders of some of the words largest pharmaceutical companies said that one of the key bottlenecks is the sheer number of vials needed in order to distribute billions of doses of a successful vaccine.
Pfizer CEO Albert Bourla, DVM, PhD, said, “Typically we are producing vaccines in single-dose vials. We are exploring with governments right now if it would be more convenient if there were 5-dose vials or 10-dose vials. I think we can resolve a significant part of the bottleneck.”
Despite the challenges, experts interviewed for this article agree that it will be possible to make a vaccine for COVID-19. They don’t expect attempts to meet the same complications that HIV researchers have seen over decades as the virus continues to confound with mutations.
Fred Ledley, MD, director of the Center for Integration of Science and Industry at Bentley University in Waltham, Massachusetts, told Medscape Medical News, “There doesn’t appear to be anything terribly diabolical about this virus. The mutation rate doesn’t appear to be anything like HIV. It appears to have some big, ugly proteins on the surface, which is good for vaccines — proteins with a lot of physical features look distinguishable from healthy cells. Signs all point to that it should be possible to make a vaccine.”
History raises safety concerns
However, Ledley said, “The idea of doing it in 6 months is largely unrealistic.”
He says 18 months is more realistic, primarily because of the sheer number of people that would have to be enrolled in a phase 3 study to truly test whether the endpoints are being met.
Vaccines are given to healthy volunteers. If safety signals arise, they may not be apparent until massive numbers of people are tested in phase 3.
“You’re never going to see the rates cut to 0%, but to see the difference between 10 people getting sick and seven people getting sick, takes very, very large numbers,” Ledley said. “There’s no way that can be done in 6 months. You’re talking about tens of thousands of people enrolled.”
He notes at this point it’s unclear what the endpoints will be and what the safety thresholds will be after consideration of risks and benefit.
Another big question for Ledley: “We don’t know what type of immunity we need to protect us against the virus. Do you just need the antibodies in your blood or do you need cells that are primed to attack the virus? Is it more of a chemical clearance or do the cells need to physically go in and digest the virus?”
History also points to the need for rigorous safety precautions that scientists fear could be compromised as trial phases overlap and processes are run in parallel instead of one step at a time.
An early batch of the Salk vaccine for polio in 1955, for example, turned out to be contaminated and caused paralysis in some children and 10 deaths, he points out.
CEPI’s Lurie adds that early candidates for another coronavirus, severe acute respiratory syndrome (SARS), “caused a reaction in the lungs that was very dangerous” before development was halted.
She also pointed to previous findings that a vaccine for dengue fever could worsen the disease in some people through a phenomenon called antibody-dependent enhancement.
Lurie and colleagues write in their paper that “it’s critical that vaccines also be developed using the tried-and-true methods, even if they may take longer to enter clinical trials or to result in large numbers of doses.”
Live attenuated vaccine
Raul Andino, PhD, a virologist at the University of California San Francisco, is among the scientists working with a tried-and-true method — a live attenuated vaccine — and he told Medscape Medical News he’s predicting it will take 2 years to develop.
He said it is cheaper to produce because scientists just have to learn how to grow the virus. Because the technology is already proven, a live attenuated vaccine could be rapidly produced on a worldwide scale.
The hope is also that a live attenuated vaccine would be given once in a lifetime and therefore be more affordable, especially in poorer countries.
“While a Moderna vaccine might be good for Europe and the United States,” he said, “It’s not going to be good for Africa, India, Brazil.”
Andino said, “I would bet money” that the front-runner vaccines so far will not be one-time vaccines.
He points out that most of the vaccine candidates are trying to protect people from disease. While there’s nothing wrong with that, he said, “In my opinion that is the lower-hanging fruit.”
“In my mind we need something that interrupts the chain of transmission and induces protection,” Andino said, important for developing herd immunity.
The reason this type of approach takes longer is because you are introducing a weakened form of the virus to the body and you have to make sure it doesn’t cause disease, not just in a small test population, but in populations who may be more susceptible to the disease, Andino said.
A call for unified strategies
Universities, countries, international consortiums, and public-private partnerships are all racing to find several safe and effective vaccines as no one entity will likely be able to provide the global solution.
Some of the efforts involve overlap of entities but with different focuses.
Along with “Operation Warp Speed” and CEPI, other collaborations include Gavi the Vaccine Alliance, whose core partners include WHO, UNICEF, the World Bank, and the Gates Foundation; and “Accelerating Therapeutic Interventions and Vaccines (ACTIV) partnership,” led by the National Institutes of Health.
Industry partners in ACTIV (18 biopharmaceutical companies), according to a May 18 article published online in the Journal of the American Medical Association, have said they will contribute their respective clinical trial capacities, regardless of which agent is studied.
Some, however, have called for more streamlining of efforts.
“Ideally we’d be working together,” Lurie told Medscape Medical News.
“I’m hopeful we will find ways to collaborate scientifically,” she said. “The US government’s responsibility is to make doses for the US. CEPI’s responsibility is to make doses for the world. A big focus of CEPI is to make sure we have manufacturing capacity outside of the US so those doses can be available to the world and they don’t get seized by wealthy countries.”
Bottazzi, Ledley, Lurie, and Andino report no relevant financial relationships.
This article first appeared on Medscape.com.
US government and industry projections that a COVID-19 vaccine will be ready by this fall or even January would take compressing what usually takes at least a decade into months, with little room for error or safety surprises.
“If all the cards fall into the right place and all the stars are aligned, you definitely could get a vaccine by December or January,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said last week.
But Fauci said a more realistic timeline is still 12 to 18 months, and experts interviewed by Medscape Medical News agree. They say that although recent developments are encouraging, history and scientific reason say the day when a COVID-19 vaccine is widely available will not come this year and may not come by the end of 2021.
The encouraging signals come primarily from two recent announcements: the $1.2 billion United States backing last week of one vaccine platform and the announcement on May 18 that the first human trials of another have produced some positive phase 1 results.
Recent developments
On May 21, the US Department of Health and Human Services (HHS) under “Operation Warp Speed” announced that the US will give AstraZeneca $1.2 billion “to make available at least 300 million doses of a coronavirus vaccine called AZD1222, with the first doses delivered as early as October 2020.”
On May 18, the Massachusetts-based biotechnology company Moderna announced that phase 1 clinical results showed that its vaccine candidate, which uses a new messenger RNA (mRNA) technology, appeared safe. Eight participants in the human trials were able to produce neutralizing antibodies that researchers believe are important in developing protection from the virus.
Moderna Chief Medical Officer Tal Zaks, MD, PhD told CNN that if the vaccine candidate does well in phase 2, “it could be ready by January 2021.”
The two candidates are among 10 in clinical trials for the SARS-CoV-2 virus, according to the World Health Organization (WHO). The AstraZeneca/ AZD1222 candidate (also called ChAdOx1 nCoV-19, in collaboration with the University of Oxford) has entered phase 2/3.
Moderna’s candidate and another being developed in Beijing, China, are in phase 2, WHO reports. As of yesterday, 115 other candidates are in preclinical evaluation.
Maria Elena Bottazzi, PhD, associate dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, Texas, told Medscape Medical News it’s important to realize that, in the case of the $1.2 billion US investment, “what they’re talking about is manufacturing.”
The idea, she said, is to pay AstraZeneca up front so that manufacturing can start before it is known whether the vaccine candidate is safe or effective, the reverse of how the clinical trial process usually works.
That way, if the candidate is deemed safe and effective, time is not lost by then deciding how to make it and distribute it.
By the end of this year, she said, “Maybe we will have many vaccines made and stored in a refrigerator somewhere. But between now and December, there’s absolutely no way you can show efficacy of the vaccine at the same time you confirm that it’s safe.”
“Take these things with a grain of salt”
Animal testing for the AstraZeneca candidate, made in partnership with the University of Oxford in the United Kingdom, has yielded lackluster results, according to results on the preprint server BioRxiv, which have not been peer-reviewed.
“The results were not bad, but they were not gangbusters,” Bottazzi said. The results show the vaccine offered only partial protection.
“Partial protection is better than no protection,” she noted. “You have to take these things with a grain of salt. We don’t know what’s going to happen in humans.”
As for the Moderna candidate, Bottazzi said, “the good news is they found an appropriate safety profile. But from an eight-person group to make the extrapolation that they have efficacy — it’s unrealistic.”
Nicole Lurie, MD, MSPH, is senior adviser to the CEO for the Coalition for Epidemic Preparedness Innovation (CEPI), a nongovernmental organization funded by the Wellcome Trust, the Bill and Melinda Gates Foundation, the European Commission, and eight countries (Australia, Belgium, Canada, Ethiopia, Germany, Japan, Norway, and the United Kingdom) charged with supporting development of vaccines for pathogens on WHO’s priority list.
She and her colleagues write in a paper published online in the New England Journal of Medicine on March 30 that “it typically takes multiple candidates and many years to produce a licensed vaccine.”
The fastest time for developing a vaccine to date is 4 years, for the mumps vaccine, licensed in 1967.
As to whether she would expect a rollout of any vaccine by the end of the year, Lurie told Medscape Medical News, “If everything goes according to plan in every way, shape or form, well then maybe you can get there. But I wouldn’t hold my breath.”
Lurie and her colleagues write that “it’s far from certain that these new platforms will be scalable or that existing capacity can provide sufficient quantities of vaccine fast enough.”
On a call with reporters today, leaders of some of the words largest pharmaceutical companies said that one of the key bottlenecks is the sheer number of vials needed in order to distribute billions of doses of a successful vaccine.
Pfizer CEO Albert Bourla, DVM, PhD, said, “Typically we are producing vaccines in single-dose vials. We are exploring with governments right now if it would be more convenient if there were 5-dose vials or 10-dose vials. I think we can resolve a significant part of the bottleneck.”
Despite the challenges, experts interviewed for this article agree that it will be possible to make a vaccine for COVID-19. They don’t expect attempts to meet the same complications that HIV researchers have seen over decades as the virus continues to confound with mutations.
Fred Ledley, MD, director of the Center for Integration of Science and Industry at Bentley University in Waltham, Massachusetts, told Medscape Medical News, “There doesn’t appear to be anything terribly diabolical about this virus. The mutation rate doesn’t appear to be anything like HIV. It appears to have some big, ugly proteins on the surface, which is good for vaccines — proteins with a lot of physical features look distinguishable from healthy cells. Signs all point to that it should be possible to make a vaccine.”
History raises safety concerns
However, Ledley said, “The idea of doing it in 6 months is largely unrealistic.”
He says 18 months is more realistic, primarily because of the sheer number of people that would have to be enrolled in a phase 3 study to truly test whether the endpoints are being met.
Vaccines are given to healthy volunteers. If safety signals arise, they may not be apparent until massive numbers of people are tested in phase 3.
“You’re never going to see the rates cut to 0%, but to see the difference between 10 people getting sick and seven people getting sick, takes very, very large numbers,” Ledley said. “There’s no way that can be done in 6 months. You’re talking about tens of thousands of people enrolled.”
He notes at this point it’s unclear what the endpoints will be and what the safety thresholds will be after consideration of risks and benefit.
Another big question for Ledley: “We don’t know what type of immunity we need to protect us against the virus. Do you just need the antibodies in your blood or do you need cells that are primed to attack the virus? Is it more of a chemical clearance or do the cells need to physically go in and digest the virus?”
History also points to the need for rigorous safety precautions that scientists fear could be compromised as trial phases overlap and processes are run in parallel instead of one step at a time.
An early batch of the Salk vaccine for polio in 1955, for example, turned out to be contaminated and caused paralysis in some children and 10 deaths, he points out.
CEPI’s Lurie adds that early candidates for another coronavirus, severe acute respiratory syndrome (SARS), “caused a reaction in the lungs that was very dangerous” before development was halted.
She also pointed to previous findings that a vaccine for dengue fever could worsen the disease in some people through a phenomenon called antibody-dependent enhancement.
Lurie and colleagues write in their paper that “it’s critical that vaccines also be developed using the tried-and-true methods, even if they may take longer to enter clinical trials or to result in large numbers of doses.”
Live attenuated vaccine
Raul Andino, PhD, a virologist at the University of California San Francisco, is among the scientists working with a tried-and-true method — a live attenuated vaccine — and he told Medscape Medical News he’s predicting it will take 2 years to develop.
He said it is cheaper to produce because scientists just have to learn how to grow the virus. Because the technology is already proven, a live attenuated vaccine could be rapidly produced on a worldwide scale.
The hope is also that a live attenuated vaccine would be given once in a lifetime and therefore be more affordable, especially in poorer countries.
“While a Moderna vaccine might be good for Europe and the United States,” he said, “It’s not going to be good for Africa, India, Brazil.”
Andino said, “I would bet money” that the front-runner vaccines so far will not be one-time vaccines.
He points out that most of the vaccine candidates are trying to protect people from disease. While there’s nothing wrong with that, he said, “In my opinion that is the lower-hanging fruit.”
“In my mind we need something that interrupts the chain of transmission and induces protection,” Andino said, important for developing herd immunity.
The reason this type of approach takes longer is because you are introducing a weakened form of the virus to the body and you have to make sure it doesn’t cause disease, not just in a small test population, but in populations who may be more susceptible to the disease, Andino said.
A call for unified strategies
Universities, countries, international consortiums, and public-private partnerships are all racing to find several safe and effective vaccines as no one entity will likely be able to provide the global solution.
Some of the efforts involve overlap of entities but with different focuses.
Along with “Operation Warp Speed” and CEPI, other collaborations include Gavi the Vaccine Alliance, whose core partners include WHO, UNICEF, the World Bank, and the Gates Foundation; and “Accelerating Therapeutic Interventions and Vaccines (ACTIV) partnership,” led by the National Institutes of Health.
Industry partners in ACTIV (18 biopharmaceutical companies), according to a May 18 article published online in the Journal of the American Medical Association, have said they will contribute their respective clinical trial capacities, regardless of which agent is studied.
Some, however, have called for more streamlining of efforts.
“Ideally we’d be working together,” Lurie told Medscape Medical News.
“I’m hopeful we will find ways to collaborate scientifically,” she said. “The US government’s responsibility is to make doses for the US. CEPI’s responsibility is to make doses for the world. A big focus of CEPI is to make sure we have manufacturing capacity outside of the US so those doses can be available to the world and they don’t get seized by wealthy countries.”
Bottazzi, Ledley, Lurie, and Andino report no relevant financial relationships.
This article first appeared on Medscape.com.
Clinicians still unaware of need for genetic testing in NSCLC
Moreover, the majority of these clinicians believe that fewer than 50% of patients in their country undergo molecular testing, the same survey showed.
The survey was conducted by the International Association for the Study of Lung Cancer (IASLC); 2537 questionnaires from 102 countries were returned and analyzed.
It was published online May 20 in the Journal of Thoracic Oncology.
The results are concerning because “the risk of death for patients with NSCLC is substantially reduced when a gene alteration is identified and the available targeted therapy is administered,” the authors emphasize.
“Specific protocols to initiate reflex testing for guideline-recommended molecular markers would help providers consider molecular testing earlier and optimize tissue,” they suggest.
Surprised that clinicians were unaware of guidelines
“I was not surprised that we found suboptimal testing rates based on other research that has demonstrated the need to improve the quality of lung cancer in some areas,” corresponding author Matthew Smeltzer, PhD, University of Memphis, Tennessee, told Medscape Medical News in an email.
“However, I was surprised that so many respondents were unaware of guidelines,” he said.
The College of American Pathologists, IASLC, and Association for Molecular Pathology established evidence-based standards for the selection of NSCLC patients for molecular testing in 2013, and these guidelines were subsequently endorsed by the American Society of Clinical Oncology.
“We suspect that the level of access a provider has to targeted therapies does affect molecular testing rates,” Smeltzer acknowledged.
Molecular testing survey
“The survey included a seven-question introduction for all respondents and then divided respondents into one of three tracks,” the authors explain.
These tracks included respondents who requested tests and who treated patients (medical oncologists), those who analyzed and interpreted assays (pathologists), and those who acquired tissue samples (surgeons, pulmonologists, radiologists).
Countries were also grouped into five geographic regions — Asia, Europe, Latin America, United States, and Canada — and the rest of the world (ROW).
“Overall, respondents reported that molecular testing rates were lower than we would like but they were not satisfied with the current state of testing, and they reported higher testing rates in their own clinics,” Smeltzer noted.
However, when tests were ordered, “we found 99% of respondents in the requesting/treating track ordered tests for EGFR, 95% for ALK, 79% for ROS1, and < 50% ordered other tests,” the authors observe.
Indeed, EGFR, ALK, and ROS1 were the top three tests ordered across all regions, though less frequently so in the ROW, they add.
More than half of requesting/treating track respondents also order multiplex assays, although Latin America and the ROW did this less frequently than other regions.
Over 90% of respondents who perform or interpret assays indicated that they perform EGFR testing, while 83% of the same group do ALK testing; 69% tested for KRAS; 68% for BRAF, 64% for ROS1, and 56% for HER2. Fewer than half of them performed other tests.
Survey results also showed that EGFR, ALK, and KRAS are the top three tests performed across all regions, with no regional differences.
“Respondents also reported on the acquisition and testing of liquid biopsies,” survey authors point out.
Here, 87% of requesting/treating track respondents indicated that they “sometimes” request molecular testing on liquid biopsies, but the proportions of those who sometimes use liquid biopsy varied by region and were lowest in Latin America and the ROW.
A lower proportion of those who perform and interpret assays, at 69%, also offer tests on liquid biopsies, but this percentage, too, varied significantly by region, being the least frequently done in the United States and Canada, as well as in the ROW.
All the above tests are for genetic mutations or alterations that guide clinicians on use of targeted therapy directed at particular mutations, for example, drugs like erlotinib for EGFR and crizotinib for ALK.
However, immunotherapy with checkpoint inhibitors has also made a big impact on the treatment of NSCLC, and the use of these agents is sometimes guided by testing for programmed cell-death ligand (PD-L1).
PD-L1 is not a molecular marker per se, the authors note.
Nevertheless, “we found that 84% of respondents in the requesting/treating track ordered PD-L1 and 68% of respondents who perform or interpret assays report PD-L1 is offered in their own lab,” the authors observe.
Smeltzer commented that both approaches — targeted therapies and immunotherapy — have made inroads into the treatment of NSCLC, in some cases replacing chemotherapy.
He emphasized that “it is important to know if a specific oncogene driver is present before initiating immunotherapy treatment,” and noted that when tissue is sent out for both types of testing, the results for PD-L1 are usually available before the results for the full molecular testing panel are back.
Barriers to testing
“The most frequent barrier to molecular testing in every region was cost,” the survey authors note.
Insufficient amount of tumor cells was the main reason for molecular testing failures along with inadequate tissue quality.
The majority of respondents who order tests and treat patients were sure that the laboratories they use perform appropriate validation of molecular tests, while almost all of those who perform or interpret assays said they perform validation tests in their labs.
Only 30% of respondents who request tests and treat patients have access to molecular testing labs within their own institutions; the remaining respondents have to outsource testing completely or partially.
Most respondents who test and treat patients also have multidisciplinary tumor boards to discuss patients with NSCLC, but almost one quarter of the same group indicated their board met less than once a month.
“Turnaround time is a barrier to molecular testing across the world,” the authors continue, with 29% of those who request tests and treat patients reporting that it typically takes 10 days or more to receive molecular testing results.
Interestingly, the highest percentage of respondents who reported this long turnaround time were in North America.
Perhaps encouragingly, 41% of respondents who perform or interpret assays indicated they were dissatisfied with the condition of molecular testing in their country, although in this regard, the United States and Canada had the lowest rates of dissatisfaction.
In fact, 39% of those who request tests and treat patients ranked the conditions of molecular testing in their country as “average or below,” while 42% of respondents in the tissue acquisition track ranked the conditions of molecular testing as average or below, the worst rankings coming from Latin America and the ROW.
Low quality of tissue samples was another reason respondents expressed dissatisfaction with the current state of molecular testing in their country.
Smeltzer is a research consultant for the Association of Community Cancer Centers.
This article first appeared on Medscape.com.
Moreover, the majority of these clinicians believe that fewer than 50% of patients in their country undergo molecular testing, the same survey showed.
The survey was conducted by the International Association for the Study of Lung Cancer (IASLC); 2537 questionnaires from 102 countries were returned and analyzed.
It was published online May 20 in the Journal of Thoracic Oncology.
The results are concerning because “the risk of death for patients with NSCLC is substantially reduced when a gene alteration is identified and the available targeted therapy is administered,” the authors emphasize.
“Specific protocols to initiate reflex testing for guideline-recommended molecular markers would help providers consider molecular testing earlier and optimize tissue,” they suggest.
Surprised that clinicians were unaware of guidelines
“I was not surprised that we found suboptimal testing rates based on other research that has demonstrated the need to improve the quality of lung cancer in some areas,” corresponding author Matthew Smeltzer, PhD, University of Memphis, Tennessee, told Medscape Medical News in an email.
“However, I was surprised that so many respondents were unaware of guidelines,” he said.
The College of American Pathologists, IASLC, and Association for Molecular Pathology established evidence-based standards for the selection of NSCLC patients for molecular testing in 2013, and these guidelines were subsequently endorsed by the American Society of Clinical Oncology.
“We suspect that the level of access a provider has to targeted therapies does affect molecular testing rates,” Smeltzer acknowledged.
Molecular testing survey
“The survey included a seven-question introduction for all respondents and then divided respondents into one of three tracks,” the authors explain.
These tracks included respondents who requested tests and who treated patients (medical oncologists), those who analyzed and interpreted assays (pathologists), and those who acquired tissue samples (surgeons, pulmonologists, radiologists).
Countries were also grouped into five geographic regions — Asia, Europe, Latin America, United States, and Canada — and the rest of the world (ROW).
“Overall, respondents reported that molecular testing rates were lower than we would like but they were not satisfied with the current state of testing, and they reported higher testing rates in their own clinics,” Smeltzer noted.
However, when tests were ordered, “we found 99% of respondents in the requesting/treating track ordered tests for EGFR, 95% for ALK, 79% for ROS1, and < 50% ordered other tests,” the authors observe.
Indeed, EGFR, ALK, and ROS1 were the top three tests ordered across all regions, though less frequently so in the ROW, they add.
More than half of requesting/treating track respondents also order multiplex assays, although Latin America and the ROW did this less frequently than other regions.
Over 90% of respondents who perform or interpret assays indicated that they perform EGFR testing, while 83% of the same group do ALK testing; 69% tested for KRAS; 68% for BRAF, 64% for ROS1, and 56% for HER2. Fewer than half of them performed other tests.
Survey results also showed that EGFR, ALK, and KRAS are the top three tests performed across all regions, with no regional differences.
“Respondents also reported on the acquisition and testing of liquid biopsies,” survey authors point out.
Here, 87% of requesting/treating track respondents indicated that they “sometimes” request molecular testing on liquid biopsies, but the proportions of those who sometimes use liquid biopsy varied by region and were lowest in Latin America and the ROW.
A lower proportion of those who perform and interpret assays, at 69%, also offer tests on liquid biopsies, but this percentage, too, varied significantly by region, being the least frequently done in the United States and Canada, as well as in the ROW.
All the above tests are for genetic mutations or alterations that guide clinicians on use of targeted therapy directed at particular mutations, for example, drugs like erlotinib for EGFR and crizotinib for ALK.
However, immunotherapy with checkpoint inhibitors has also made a big impact on the treatment of NSCLC, and the use of these agents is sometimes guided by testing for programmed cell-death ligand (PD-L1).
PD-L1 is not a molecular marker per se, the authors note.
Nevertheless, “we found that 84% of respondents in the requesting/treating track ordered PD-L1 and 68% of respondents who perform or interpret assays report PD-L1 is offered in their own lab,” the authors observe.
Smeltzer commented that both approaches — targeted therapies and immunotherapy — have made inroads into the treatment of NSCLC, in some cases replacing chemotherapy.
He emphasized that “it is important to know if a specific oncogene driver is present before initiating immunotherapy treatment,” and noted that when tissue is sent out for both types of testing, the results for PD-L1 are usually available before the results for the full molecular testing panel are back.
Barriers to testing
“The most frequent barrier to molecular testing in every region was cost,” the survey authors note.
Insufficient amount of tumor cells was the main reason for molecular testing failures along with inadequate tissue quality.
The majority of respondents who order tests and treat patients were sure that the laboratories they use perform appropriate validation of molecular tests, while almost all of those who perform or interpret assays said they perform validation tests in their labs.
Only 30% of respondents who request tests and treat patients have access to molecular testing labs within their own institutions; the remaining respondents have to outsource testing completely or partially.
Most respondents who test and treat patients also have multidisciplinary tumor boards to discuss patients with NSCLC, but almost one quarter of the same group indicated their board met less than once a month.
“Turnaround time is a barrier to molecular testing across the world,” the authors continue, with 29% of those who request tests and treat patients reporting that it typically takes 10 days or more to receive molecular testing results.
Interestingly, the highest percentage of respondents who reported this long turnaround time were in North America.
Perhaps encouragingly, 41% of respondents who perform or interpret assays indicated they were dissatisfied with the condition of molecular testing in their country, although in this regard, the United States and Canada had the lowest rates of dissatisfaction.
In fact, 39% of those who request tests and treat patients ranked the conditions of molecular testing in their country as “average or below,” while 42% of respondents in the tissue acquisition track ranked the conditions of molecular testing as average or below, the worst rankings coming from Latin America and the ROW.
Low quality of tissue samples was another reason respondents expressed dissatisfaction with the current state of molecular testing in their country.
Smeltzer is a research consultant for the Association of Community Cancer Centers.
This article first appeared on Medscape.com.
Moreover, the majority of these clinicians believe that fewer than 50% of patients in their country undergo molecular testing, the same survey showed.
The survey was conducted by the International Association for the Study of Lung Cancer (IASLC); 2537 questionnaires from 102 countries were returned and analyzed.
It was published online May 20 in the Journal of Thoracic Oncology.
The results are concerning because “the risk of death for patients with NSCLC is substantially reduced when a gene alteration is identified and the available targeted therapy is administered,” the authors emphasize.
“Specific protocols to initiate reflex testing for guideline-recommended molecular markers would help providers consider molecular testing earlier and optimize tissue,” they suggest.
Surprised that clinicians were unaware of guidelines
“I was not surprised that we found suboptimal testing rates based on other research that has demonstrated the need to improve the quality of lung cancer in some areas,” corresponding author Matthew Smeltzer, PhD, University of Memphis, Tennessee, told Medscape Medical News in an email.
“However, I was surprised that so many respondents were unaware of guidelines,” he said.
The College of American Pathologists, IASLC, and Association for Molecular Pathology established evidence-based standards for the selection of NSCLC patients for molecular testing in 2013, and these guidelines were subsequently endorsed by the American Society of Clinical Oncology.
“We suspect that the level of access a provider has to targeted therapies does affect molecular testing rates,” Smeltzer acknowledged.
Molecular testing survey
“The survey included a seven-question introduction for all respondents and then divided respondents into one of three tracks,” the authors explain.
These tracks included respondents who requested tests and who treated patients (medical oncologists), those who analyzed and interpreted assays (pathologists), and those who acquired tissue samples (surgeons, pulmonologists, radiologists).
Countries were also grouped into five geographic regions — Asia, Europe, Latin America, United States, and Canada — and the rest of the world (ROW).
“Overall, respondents reported that molecular testing rates were lower than we would like but they were not satisfied with the current state of testing, and they reported higher testing rates in their own clinics,” Smeltzer noted.
However, when tests were ordered, “we found 99% of respondents in the requesting/treating track ordered tests for EGFR, 95% for ALK, 79% for ROS1, and < 50% ordered other tests,” the authors observe.
Indeed, EGFR, ALK, and ROS1 were the top three tests ordered across all regions, though less frequently so in the ROW, they add.
More than half of requesting/treating track respondents also order multiplex assays, although Latin America and the ROW did this less frequently than other regions.
Over 90% of respondents who perform or interpret assays indicated that they perform EGFR testing, while 83% of the same group do ALK testing; 69% tested for KRAS; 68% for BRAF, 64% for ROS1, and 56% for HER2. Fewer than half of them performed other tests.
Survey results also showed that EGFR, ALK, and KRAS are the top three tests performed across all regions, with no regional differences.
“Respondents also reported on the acquisition and testing of liquid biopsies,” survey authors point out.
Here, 87% of requesting/treating track respondents indicated that they “sometimes” request molecular testing on liquid biopsies, but the proportions of those who sometimes use liquid biopsy varied by region and were lowest in Latin America and the ROW.
A lower proportion of those who perform and interpret assays, at 69%, also offer tests on liquid biopsies, but this percentage, too, varied significantly by region, being the least frequently done in the United States and Canada, as well as in the ROW.
All the above tests are for genetic mutations or alterations that guide clinicians on use of targeted therapy directed at particular mutations, for example, drugs like erlotinib for EGFR and crizotinib for ALK.
However, immunotherapy with checkpoint inhibitors has also made a big impact on the treatment of NSCLC, and the use of these agents is sometimes guided by testing for programmed cell-death ligand (PD-L1).
PD-L1 is not a molecular marker per se, the authors note.
Nevertheless, “we found that 84% of respondents in the requesting/treating track ordered PD-L1 and 68% of respondents who perform or interpret assays report PD-L1 is offered in their own lab,” the authors observe.
Smeltzer commented that both approaches — targeted therapies and immunotherapy — have made inroads into the treatment of NSCLC, in some cases replacing chemotherapy.
He emphasized that “it is important to know if a specific oncogene driver is present before initiating immunotherapy treatment,” and noted that when tissue is sent out for both types of testing, the results for PD-L1 are usually available before the results for the full molecular testing panel are back.
Barriers to testing
“The most frequent barrier to molecular testing in every region was cost,” the survey authors note.
Insufficient amount of tumor cells was the main reason for molecular testing failures along with inadequate tissue quality.
The majority of respondents who order tests and treat patients were sure that the laboratories they use perform appropriate validation of molecular tests, while almost all of those who perform or interpret assays said they perform validation tests in their labs.
Only 30% of respondents who request tests and treat patients have access to molecular testing labs within their own institutions; the remaining respondents have to outsource testing completely or partially.
Most respondents who test and treat patients also have multidisciplinary tumor boards to discuss patients with NSCLC, but almost one quarter of the same group indicated their board met less than once a month.
“Turnaround time is a barrier to molecular testing across the world,” the authors continue, with 29% of those who request tests and treat patients reporting that it typically takes 10 days or more to receive molecular testing results.
Interestingly, the highest percentage of respondents who reported this long turnaround time were in North America.
Perhaps encouragingly, 41% of respondents who perform or interpret assays indicated they were dissatisfied with the condition of molecular testing in their country, although in this regard, the United States and Canada had the lowest rates of dissatisfaction.
In fact, 39% of those who request tests and treat patients ranked the conditions of molecular testing in their country as “average or below,” while 42% of respondents in the tissue acquisition track ranked the conditions of molecular testing as average or below, the worst rankings coming from Latin America and the ROW.
Low quality of tissue samples was another reason respondents expressed dissatisfaction with the current state of molecular testing in their country.
Smeltzer is a research consultant for the Association of Community Cancer Centers.
This article first appeared on Medscape.com.
Nilotinib is safe in moderate and advanced Parkinson’s disease
according to investigators. Nevertheless, other drugs that – like nilotinib – inhibit tyrosine kinase (c-Abl) may have a neuroprotective effect, they added. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Research using preclinical models of Parkinson’s disease has indicated that nilotinib offers neuroprotection. Tanya Simuni, MD, the Arthur C. Nielsen Jr., Research Professor of Parkinson’s Disease and Movement Disorders at Northwestern University in Chicago, and colleagues conducted a prospective study to evaluate the safety and tolerability of oral nilotinib in patients with moderate or advanced Parkinson’s disease. The investigators also sought to examine nilotinib’s symptomatic effect, as measured by the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III. In addition, Dr. Simuni and colleagues analyzed the drug’s effect on progression of disability, as measured by various other Parkinson’s disease scales. The study’s exploratory outcomes included cognitive function, quality of life, pharmacokinetic profile, and a battery of serum and spinal fluid biomarkers.
The researchers conducted their randomized, double-blind, placebo-controlled, parallel-group study at 25 sites in the United States. They randomized 76 patients with Parkinson’s disease in approximately equal groups to a daily dose of placebo, 150 mg of nilotinib, or 300 mg of nilotinib. Safety visits occurred monthly. Patient assessments occurred at 3 months and at 6 months, which was the end of the treatment period. Patients presented off study medication at 1 month and 2 months after the end of the treatment period.
Treatment did not change dopamine levels
Baseline demographics and disease characteristics were balanced between groups. Mean age was about 66 years in the placebo group, 61 years in the 150-mg group, and 67 years in the 300-mg group. The proportion of male participants was 64% in the placebo group, 60% in the 150-mg group, and 81% in the 300-mg group. Disease duration was 9 years in the placebo group, approximately 9 years in the 150-mg group, and approximately 12 years in the 300-mg group. Mean MDS-UPDRS total on score was 46 in the placebo group, 47 in the 150-mg group, and 52 in the 300-mg group.
Tolerability was 84% in the placebo group, 76% in the in the 150-mg group, and 77% in the 300-mg group. The sole treatment-related serious adverse event, arrhythmia, occurred in one patient in the 300-mg group. The rate of any adverse event was 88% in the placebo group, 92% in the 150-mg group, and 88% in the 300-mg group. The rate of any serious adverse event was 8% in the placebo group and 4% in each nilotinib group.
From baseline to 1 month, MDS-UPDRS part III on scores decreased by 0.49 points in the placebo group, increased by 2.08 in the 150-mg group, and increased by 4.67 in the 300-mg group. Differences in other secondary measures (e.g., change in MDS-UPDRS part III on scores from baseline to 6 months and change in MDS-UPDRS part III off score from baseline to 6 months) were not statistically significant.
At 3 months, CSF levels of nilotinib were well below the threshold for c-Abl inhibition (approximately 11 ng/mL). The arithmetic mean levels were 0.91 ng/mL in the 150-mg group and 1.69 ng/mL in the 300-mg group. Nilotinib also failed to alter CSF levels of dopamine or its metabolites at 3 months. Dr. Simuni and colleagues did not see significant differences between treatment groups in the exploratory outcomes of cognitive function and quality of life.
“Nilotinib is not an optimal molecule to assess the therapeutic potential of c-Abl inhibition for Parkinson’s disease,” the investigators concluded.
Nilotinib may be an inappropriate candidate
The data “suggest that the hypothesis wasn’t tested, since the CSF and serum concentration of the drug were insufficient for enzyme inhibition,” said Peter LeWitt, MD, Sastry Foundation Endowed Chair in Neurology and professor of neurology at Wayne State University, Detroit. “A higher dose or a more CNS-penetrant drug would be needed for adequate testing of the hypothesis that c-Abl inhibition could provide disease modification.”
Nilotinib might not be an appropriate drug for this investigation, he continued. “There may be better choices among c-Abl inhibitors for penetration into the CNS, such as dasatinib, or for increased potency of effect, such as imatinib.”
Sun Pharma Advanced Research Company is conducting a clinical trial of KO706, another c-Abl inhibitor, added Dr. LeWitt, who is a researcher in that trial and an editorial adviser to Neurology Reviews. “The studies published recently in JAMA Neurology by Pagan et al. claiming target engagement with nilotinib in Parkinson’s disease patients need to be contrasted with the results of the current investigation. Disease modification with c-Abl inhibition continues to be a promising therapeutic avenue, but both positive and negative study results need careful reassessment and validation.”
The Michael J. Fox Foundation, the Cure Parkinson’s Trust, and Van Andel Research Institute funded the study. Novartis provided the study drug and placebo. The investigators reported no conflicts of interest.
SOURCE: Simuni T et al. AAN 2020. Abstract 43617.
according to investigators. Nevertheless, other drugs that – like nilotinib – inhibit tyrosine kinase (c-Abl) may have a neuroprotective effect, they added. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Research using preclinical models of Parkinson’s disease has indicated that nilotinib offers neuroprotection. Tanya Simuni, MD, the Arthur C. Nielsen Jr., Research Professor of Parkinson’s Disease and Movement Disorders at Northwestern University in Chicago, and colleagues conducted a prospective study to evaluate the safety and tolerability of oral nilotinib in patients with moderate or advanced Parkinson’s disease. The investigators also sought to examine nilotinib’s symptomatic effect, as measured by the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III. In addition, Dr. Simuni and colleagues analyzed the drug’s effect on progression of disability, as measured by various other Parkinson’s disease scales. The study’s exploratory outcomes included cognitive function, quality of life, pharmacokinetic profile, and a battery of serum and spinal fluid biomarkers.
The researchers conducted their randomized, double-blind, placebo-controlled, parallel-group study at 25 sites in the United States. They randomized 76 patients with Parkinson’s disease in approximately equal groups to a daily dose of placebo, 150 mg of nilotinib, or 300 mg of nilotinib. Safety visits occurred monthly. Patient assessments occurred at 3 months and at 6 months, which was the end of the treatment period. Patients presented off study medication at 1 month and 2 months after the end of the treatment period.
Treatment did not change dopamine levels
Baseline demographics and disease characteristics were balanced between groups. Mean age was about 66 years in the placebo group, 61 years in the 150-mg group, and 67 years in the 300-mg group. The proportion of male participants was 64% in the placebo group, 60% in the 150-mg group, and 81% in the 300-mg group. Disease duration was 9 years in the placebo group, approximately 9 years in the 150-mg group, and approximately 12 years in the 300-mg group. Mean MDS-UPDRS total on score was 46 in the placebo group, 47 in the 150-mg group, and 52 in the 300-mg group.
Tolerability was 84% in the placebo group, 76% in the in the 150-mg group, and 77% in the 300-mg group. The sole treatment-related serious adverse event, arrhythmia, occurred in one patient in the 300-mg group. The rate of any adverse event was 88% in the placebo group, 92% in the 150-mg group, and 88% in the 300-mg group. The rate of any serious adverse event was 8% in the placebo group and 4% in each nilotinib group.
From baseline to 1 month, MDS-UPDRS part III on scores decreased by 0.49 points in the placebo group, increased by 2.08 in the 150-mg group, and increased by 4.67 in the 300-mg group. Differences in other secondary measures (e.g., change in MDS-UPDRS part III on scores from baseline to 6 months and change in MDS-UPDRS part III off score from baseline to 6 months) were not statistically significant.
At 3 months, CSF levels of nilotinib were well below the threshold for c-Abl inhibition (approximately 11 ng/mL). The arithmetic mean levels were 0.91 ng/mL in the 150-mg group and 1.69 ng/mL in the 300-mg group. Nilotinib also failed to alter CSF levels of dopamine or its metabolites at 3 months. Dr. Simuni and colleagues did not see significant differences between treatment groups in the exploratory outcomes of cognitive function and quality of life.
“Nilotinib is not an optimal molecule to assess the therapeutic potential of c-Abl inhibition for Parkinson’s disease,” the investigators concluded.
Nilotinib may be an inappropriate candidate
The data “suggest that the hypothesis wasn’t tested, since the CSF and serum concentration of the drug were insufficient for enzyme inhibition,” said Peter LeWitt, MD, Sastry Foundation Endowed Chair in Neurology and professor of neurology at Wayne State University, Detroit. “A higher dose or a more CNS-penetrant drug would be needed for adequate testing of the hypothesis that c-Abl inhibition could provide disease modification.”
Nilotinib might not be an appropriate drug for this investigation, he continued. “There may be better choices among c-Abl inhibitors for penetration into the CNS, such as dasatinib, or for increased potency of effect, such as imatinib.”
Sun Pharma Advanced Research Company is conducting a clinical trial of KO706, another c-Abl inhibitor, added Dr. LeWitt, who is a researcher in that trial and an editorial adviser to Neurology Reviews. “The studies published recently in JAMA Neurology by Pagan et al. claiming target engagement with nilotinib in Parkinson’s disease patients need to be contrasted with the results of the current investigation. Disease modification with c-Abl inhibition continues to be a promising therapeutic avenue, but both positive and negative study results need careful reassessment and validation.”
The Michael J. Fox Foundation, the Cure Parkinson’s Trust, and Van Andel Research Institute funded the study. Novartis provided the study drug and placebo. The investigators reported no conflicts of interest.
SOURCE: Simuni T et al. AAN 2020. Abstract 43617.
according to investigators. Nevertheless, other drugs that – like nilotinib – inhibit tyrosine kinase (c-Abl) may have a neuroprotective effect, they added. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Research using preclinical models of Parkinson’s disease has indicated that nilotinib offers neuroprotection. Tanya Simuni, MD, the Arthur C. Nielsen Jr., Research Professor of Parkinson’s Disease and Movement Disorders at Northwestern University in Chicago, and colleagues conducted a prospective study to evaluate the safety and tolerability of oral nilotinib in patients with moderate or advanced Parkinson’s disease. The investigators also sought to examine nilotinib’s symptomatic effect, as measured by the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III. In addition, Dr. Simuni and colleagues analyzed the drug’s effect on progression of disability, as measured by various other Parkinson’s disease scales. The study’s exploratory outcomes included cognitive function, quality of life, pharmacokinetic profile, and a battery of serum and spinal fluid biomarkers.
The researchers conducted their randomized, double-blind, placebo-controlled, parallel-group study at 25 sites in the United States. They randomized 76 patients with Parkinson’s disease in approximately equal groups to a daily dose of placebo, 150 mg of nilotinib, or 300 mg of nilotinib. Safety visits occurred monthly. Patient assessments occurred at 3 months and at 6 months, which was the end of the treatment period. Patients presented off study medication at 1 month and 2 months after the end of the treatment period.
Treatment did not change dopamine levels
Baseline demographics and disease characteristics were balanced between groups. Mean age was about 66 years in the placebo group, 61 years in the 150-mg group, and 67 years in the 300-mg group. The proportion of male participants was 64% in the placebo group, 60% in the 150-mg group, and 81% in the 300-mg group. Disease duration was 9 years in the placebo group, approximately 9 years in the 150-mg group, and approximately 12 years in the 300-mg group. Mean MDS-UPDRS total on score was 46 in the placebo group, 47 in the 150-mg group, and 52 in the 300-mg group.
Tolerability was 84% in the placebo group, 76% in the in the 150-mg group, and 77% in the 300-mg group. The sole treatment-related serious adverse event, arrhythmia, occurred in one patient in the 300-mg group. The rate of any adverse event was 88% in the placebo group, 92% in the 150-mg group, and 88% in the 300-mg group. The rate of any serious adverse event was 8% in the placebo group and 4% in each nilotinib group.
From baseline to 1 month, MDS-UPDRS part III on scores decreased by 0.49 points in the placebo group, increased by 2.08 in the 150-mg group, and increased by 4.67 in the 300-mg group. Differences in other secondary measures (e.g., change in MDS-UPDRS part III on scores from baseline to 6 months and change in MDS-UPDRS part III off score from baseline to 6 months) were not statistically significant.
At 3 months, CSF levels of nilotinib were well below the threshold for c-Abl inhibition (approximately 11 ng/mL). The arithmetic mean levels were 0.91 ng/mL in the 150-mg group and 1.69 ng/mL in the 300-mg group. Nilotinib also failed to alter CSF levels of dopamine or its metabolites at 3 months. Dr. Simuni and colleagues did not see significant differences between treatment groups in the exploratory outcomes of cognitive function and quality of life.
“Nilotinib is not an optimal molecule to assess the therapeutic potential of c-Abl inhibition for Parkinson’s disease,” the investigators concluded.
Nilotinib may be an inappropriate candidate
The data “suggest that the hypothesis wasn’t tested, since the CSF and serum concentration of the drug were insufficient for enzyme inhibition,” said Peter LeWitt, MD, Sastry Foundation Endowed Chair in Neurology and professor of neurology at Wayne State University, Detroit. “A higher dose or a more CNS-penetrant drug would be needed for adequate testing of the hypothesis that c-Abl inhibition could provide disease modification.”
Nilotinib might not be an appropriate drug for this investigation, he continued. “There may be better choices among c-Abl inhibitors for penetration into the CNS, such as dasatinib, or for increased potency of effect, such as imatinib.”
Sun Pharma Advanced Research Company is conducting a clinical trial of KO706, another c-Abl inhibitor, added Dr. LeWitt, who is a researcher in that trial and an editorial adviser to Neurology Reviews. “The studies published recently in JAMA Neurology by Pagan et al. claiming target engagement with nilotinib in Parkinson’s disease patients need to be contrasted with the results of the current investigation. Disease modification with c-Abl inhibition continues to be a promising therapeutic avenue, but both positive and negative study results need careful reassessment and validation.”
The Michael J. Fox Foundation, the Cure Parkinson’s Trust, and Van Andel Research Institute funded the study. Novartis provided the study drug and placebo. The investigators reported no conflicts of interest.
SOURCE: Simuni T et al. AAN 2020. Abstract 43617.
FROM AAN 2020
Early or delayed cardioversion in recent-onset atrial fibrillation
Background: Often atrial fibrillation terminates spontaneously and occasionally recurs; therefore, the advantage of immediate electric or pharmacologic cardioversion over watchful waiting and subsequent delayed cardioversion is not clear.
Study design: Multicenter, randomized, open-label, noninferiority trial.
Setting: 15 hospitals in the Netherlands (3 academic, 8 nonacademic teaching, and 4 nonteaching).
Synopsis: Randomizing 437 patients with early-onset (less than 36 hours) symptomatic AFib presenting to 15 hospitals, the authors showed that, at 4 weeks’ follow-up, a similar number of patients remained in sinus rhythm whether they were assigned to an immediate cardioversion strategy or to a delayed one where rate control was attempted first and cardioversion was done if patients remained in fibrillation after 48 hours. Specifically the presence of sinus rhythm occurred in 94% in the early cardioversion group and in 91% of the delayed one (95% confidence interval, –8.2 to 2.2; P = .005 for noninferiority). Both groups received anticoagulation per current standards.
This was a noninferiority, open-label study that was not powered enough to study harm between the two strategies. It showed a 30% incidence of recurrence of AFib regardless of study assignment. Hospitalists should not feel pressured to initiate early cardioversion for new-onset AFib. Rate control, anticoagulation (if applicable), prompt follow-up, and early discharge (even from the ED) seem to be a safe and practical approach.
Bottom line: In patients presenting with symptomatic recent-onset AFib, delayed cardioversion in a wait-and-see approach was noninferior to early cardioversion in achieving sinus rhythm at 4 weeks’ follow-up.
Citation: Pluymaekers NA et al. Early or delayed cardioversion in recent-onset atrial fibrillation. N Engl J Med.
Dr. Abdo is a hospitalist at Duke University Health System.
Background: Often atrial fibrillation terminates spontaneously and occasionally recurs; therefore, the advantage of immediate electric or pharmacologic cardioversion over watchful waiting and subsequent delayed cardioversion is not clear.
Study design: Multicenter, randomized, open-label, noninferiority trial.
Setting: 15 hospitals in the Netherlands (3 academic, 8 nonacademic teaching, and 4 nonteaching).
Synopsis: Randomizing 437 patients with early-onset (less than 36 hours) symptomatic AFib presenting to 15 hospitals, the authors showed that, at 4 weeks’ follow-up, a similar number of patients remained in sinus rhythm whether they were assigned to an immediate cardioversion strategy or to a delayed one where rate control was attempted first and cardioversion was done if patients remained in fibrillation after 48 hours. Specifically the presence of sinus rhythm occurred in 94% in the early cardioversion group and in 91% of the delayed one (95% confidence interval, –8.2 to 2.2; P = .005 for noninferiority). Both groups received anticoagulation per current standards.
This was a noninferiority, open-label study that was not powered enough to study harm between the two strategies. It showed a 30% incidence of recurrence of AFib regardless of study assignment. Hospitalists should not feel pressured to initiate early cardioversion for new-onset AFib. Rate control, anticoagulation (if applicable), prompt follow-up, and early discharge (even from the ED) seem to be a safe and practical approach.
Bottom line: In patients presenting with symptomatic recent-onset AFib, delayed cardioversion in a wait-and-see approach was noninferior to early cardioversion in achieving sinus rhythm at 4 weeks’ follow-up.
Citation: Pluymaekers NA et al. Early or delayed cardioversion in recent-onset atrial fibrillation. N Engl J Med.
Dr. Abdo is a hospitalist at Duke University Health System.
Background: Often atrial fibrillation terminates spontaneously and occasionally recurs; therefore, the advantage of immediate electric or pharmacologic cardioversion over watchful waiting and subsequent delayed cardioversion is not clear.
Study design: Multicenter, randomized, open-label, noninferiority trial.
Setting: 15 hospitals in the Netherlands (3 academic, 8 nonacademic teaching, and 4 nonteaching).
Synopsis: Randomizing 437 patients with early-onset (less than 36 hours) symptomatic AFib presenting to 15 hospitals, the authors showed that, at 4 weeks’ follow-up, a similar number of patients remained in sinus rhythm whether they were assigned to an immediate cardioversion strategy or to a delayed one where rate control was attempted first and cardioversion was done if patients remained in fibrillation after 48 hours. Specifically the presence of sinus rhythm occurred in 94% in the early cardioversion group and in 91% of the delayed one (95% confidence interval, –8.2 to 2.2; P = .005 for noninferiority). Both groups received anticoagulation per current standards.
This was a noninferiority, open-label study that was not powered enough to study harm between the two strategies. It showed a 30% incidence of recurrence of AFib regardless of study assignment. Hospitalists should not feel pressured to initiate early cardioversion for new-onset AFib. Rate control, anticoagulation (if applicable), prompt follow-up, and early discharge (even from the ED) seem to be a safe and practical approach.
Bottom line: In patients presenting with symptomatic recent-onset AFib, delayed cardioversion in a wait-and-see approach was noninferior to early cardioversion in achieving sinus rhythm at 4 weeks’ follow-up.
Citation: Pluymaekers NA et al. Early or delayed cardioversion in recent-onset atrial fibrillation. N Engl J Med.
Dr. Abdo is a hospitalist at Duke University Health System.
Improving care for women who have experienced stillbirth
Think of the current standard of care and do the opposite
One of hardest parts of being an obstetrician is taking care of patients who experience a stillbirth. I am very comfortable with the care of a grieving patient and I always have been, although I am not sure why. I have a model of care that I have evolved in my 16 years since medical school graduation. This model is not based on formal instruction because I received none, but on my natural instincts of what a grieving mom and her family need to hear and receive in the worst moments of their lives. All obstetrics providers grieve the loss of the baby, but often not with the patient but on our own. We may do this because we want to respect the patient’s privacy or because we are not sure of the words to say. I hope I can provide some guidance for those who struggle with what to do.
I delivered my first stillborn baby as a third-year medical student. My mentor, a chief resident, saw something in me and encouraged me to care for this mother. She had twins and one baby was still living, but the prognosis was poor since this was the surviving twin from a monochorionic diamniotic pregnancy. On the day of the mom’s induction, I just pulled up a chair and talked with her. We talked about her life, the loss of the first baby several weeks before, and her hope that her surviving son would be okay. She felt so bonded to me that she refused to push until I was there. Her delivery is still firm in my mind. I still remember 17 years later the room she delivered in.
My first loss (stillbirth) as a resident was my intern year – a beautiful baby named Jude, who was stillborn at 39 weeks. After delivering Jude, I asked the family about the funeral arrangements. Three days later, I attended his funeral. I looked all around for the mother’s attending doctors but none of them were there. I remember thinking then that it was a given that they would be there, but now I know that it is rare. I also learned a lot about the grief a stillborn baby brings while listening to Jude’s father’s eulogy. He talked about how Jude would never bake cookies with Aunt Jane, ride the slide with cousin Chris, or put on a yellow backpack and ride the bus on the first day of school. Because of this eulogy, I understood this unique kind of grief that these losses bring early in my training.
I delivered many losses in my residency. The attendings left soon after the birth and I stayed behind with the family. I sat and counseled the families, and I helped them make memories. I realized that to care for these patients, I would need to trust my instincts because there was no formal and little informal training on how to care for families who lost their babies.
Once I completed residency, I was really able to do my “thing.” At loss deliveries, I was able to model for residents my method of care. I showed them that families want and need attention, support, and guidance. I modeled for them how to deliver and greet the baby. That it is not necessary to leave the room right after the birth, and it is okay to grieve and help families meet their babies. I modeled commenting on the baby’s features, on who they looked like. I showed how laughing about how the baby has grandma’s nose is okay. I showed them that it is okay to ask to hold and get a picture taken with the baby. I showed them that these are the only moments these families will get with their babies, and it is our job to help them do this. The family will have many moments alone in the days and weeks to come. They need our support and guidance. It is a part of being an ob.gyn. to care for families after stillbirths, and we do not want our patients to feel abandoned during this time by those they entrust to care for them.
I also was able to create a model for aftercare. I call my families often after they go home. Sometimes I catch them in the anger stage of the grief process and I let them vent. I work through this with them, and I answer their hardest and sometimes accusatory questions regarding care leading up to the diagnosis. I am not saying this is easy for me or for them. I think fear of these tough conversations is a barrier to giving the emotional support that these families need. I work through this with them in an honest and open manner. I also call to check on the patients as much as possible, especially on anniversaries. I am not saying that all providers must follow this model. This is my passion and is natural for me, but data clearly show that the standard of emotional care we provide is not what patients need at this time. Thankfully, there is an amazing resource of grief counselors, social workers, online resources, and support groups for these families to help them get through the tragedy. These resources, however, are not the provider who spent this precious time with them and their beloved baby, and our emotional support is invaluable.
This past year has been very eventful for me. One of my patients delivered a new baby, after a prior loss, and asked if we could teach together. I had mentioned that everything I do with stillbirths is not based on my residency education, but on my experience and instinctual feeling of what families need. She knew from friends in bereavement circles that they felt that their care was different. We started teaching last summer and have done 10 training sessions to date; hopefully we will continue to teach new groups of nurses, residents, medical students, doulas, and physician assistant students each year.
This year also was eventful because I discovered the Star Legacy Foundation, a national not-for-profit organization with the goal of spreading awareness, education, and prevention regarding stillbirth. I attended their 2019 Summit in Minnesota. I thought I would meet many more doctors and midwives like myself, and I would learn even more about care for bereaved patients. However, that summer I learned preventing stillbirth may be possible from the then chief medical officer of Scotland, Catherine Calderwood, MB ChB. She talked about the preventive protocol she had created that had reduced the stillbirth rate by 23%. Because I was one of only five ob.gyn. nonspeaker attendees in a room of 400, I realized I had a real opportunity to try to bring some model for prevention to the United States. I brought the U.K. protocol to my practice and we have been doing it now for 9 months. (See “Decreased fetal movement: Time to educate patients and ourselves” at mdedge.com/pediatrics.)
I have had a year to think about why the U.S. stillbirth rate is higher than that of many high-income nations and why we have the lowest annual rate of reduction in the 2016 Lancet series among high resource nations.1 I think it is due to lack of education and training for providers in stillbirth prevention and care, which has led to further marginalization and stigmatization of bereaved moms. This has pushed them further into the shadows and makes it taboo to share their stories. It is providers being fearful to even mention to patients that stillbirth still happens. It is the lack of any protocol on how to educate patients and providers about fetal movement, and what to do if pregnant women complain about a decrease or change in fetal movement. I think a lot of this stems from an innate discomfort that obstetric providers have in the care of these patients. That if women felt cared for and empowered to tell their stories, there would be more efforts at stillbirth education and prevention.
I often think of an experience that the founder of Star Legacy, Lindsey Wimmer, experienced when she lost her son, Garrett, 16 years ago. She told a story in the documentary, “Don’t talk about the baby.” She tells that on the first night of the induction, the nurse came in and told her that the attending wanted to turn off the oxytocin so “she could get her rest.” I heard this and immediately knew the attending’s true reason for turning off the oxytocin. Lindsey then said she knew it was because the attending did not want to wake up to deliver a dead baby. I wrote Lindsey that day and told her I completely agreed and apologized on behalf of my profession for that care. She wrote me back that she had waited 16 years to have a provider validate her feelings about this. I told her I think her doctor was fearful and uncomfortable with this birth and was avoiding it, but I believe with better education and training this can change. I want to deliver babies like Garrett during my shift, because it is giving this vital care that reminds me why I became a doctor in the first place.
I know there are many providers out there who follow a similar model, but I want more providers to do so, and so does the bereavement community. In one study of 20 parents, all but 2 were frustrated about how the ob.gyn. and staff handled their deliveries.2 I truly believe that every person who delivers babies does it because they love it. Part of doing this job we love is realizing there will be times of great sadness. I also believe if this model of care is attempted by wary providers, they will quickly realize that this is what patients and their families need. With this care, stillbirth may become less of a taboo subject, and our stillbirth rate may fall.
Dr. Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, N.Y. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures. Email her a obnews@mdedge.com.
References
1. “Stillbirths 2016: ending preventable stillbirths.” Series from The Lancet journals. Published: Jan. 20, 2016.
2. BMC Pregnancy Childbirth. 2012 Nov 27. doi: 10.1186/1471-2393-12-137.
Think of the current standard of care and do the opposite
Think of the current standard of care and do the opposite
One of hardest parts of being an obstetrician is taking care of patients who experience a stillbirth. I am very comfortable with the care of a grieving patient and I always have been, although I am not sure why. I have a model of care that I have evolved in my 16 years since medical school graduation. This model is not based on formal instruction because I received none, but on my natural instincts of what a grieving mom and her family need to hear and receive in the worst moments of their lives. All obstetrics providers grieve the loss of the baby, but often not with the patient but on our own. We may do this because we want to respect the patient’s privacy or because we are not sure of the words to say. I hope I can provide some guidance for those who struggle with what to do.
I delivered my first stillborn baby as a third-year medical student. My mentor, a chief resident, saw something in me and encouraged me to care for this mother. She had twins and one baby was still living, but the prognosis was poor since this was the surviving twin from a monochorionic diamniotic pregnancy. On the day of the mom’s induction, I just pulled up a chair and talked with her. We talked about her life, the loss of the first baby several weeks before, and her hope that her surviving son would be okay. She felt so bonded to me that she refused to push until I was there. Her delivery is still firm in my mind. I still remember 17 years later the room she delivered in.
My first loss (stillbirth) as a resident was my intern year – a beautiful baby named Jude, who was stillborn at 39 weeks. After delivering Jude, I asked the family about the funeral arrangements. Three days later, I attended his funeral. I looked all around for the mother’s attending doctors but none of them were there. I remember thinking then that it was a given that they would be there, but now I know that it is rare. I also learned a lot about the grief a stillborn baby brings while listening to Jude’s father’s eulogy. He talked about how Jude would never bake cookies with Aunt Jane, ride the slide with cousin Chris, or put on a yellow backpack and ride the bus on the first day of school. Because of this eulogy, I understood this unique kind of grief that these losses bring early in my training.
I delivered many losses in my residency. The attendings left soon after the birth and I stayed behind with the family. I sat and counseled the families, and I helped them make memories. I realized that to care for these patients, I would need to trust my instincts because there was no formal and little informal training on how to care for families who lost their babies.
Once I completed residency, I was really able to do my “thing.” At loss deliveries, I was able to model for residents my method of care. I showed them that families want and need attention, support, and guidance. I modeled for them how to deliver and greet the baby. That it is not necessary to leave the room right after the birth, and it is okay to grieve and help families meet their babies. I modeled commenting on the baby’s features, on who they looked like. I showed how laughing about how the baby has grandma’s nose is okay. I showed them that it is okay to ask to hold and get a picture taken with the baby. I showed them that these are the only moments these families will get with their babies, and it is our job to help them do this. The family will have many moments alone in the days and weeks to come. They need our support and guidance. It is a part of being an ob.gyn. to care for families after stillbirths, and we do not want our patients to feel abandoned during this time by those they entrust to care for them.
I also was able to create a model for aftercare. I call my families often after they go home. Sometimes I catch them in the anger stage of the grief process and I let them vent. I work through this with them, and I answer their hardest and sometimes accusatory questions regarding care leading up to the diagnosis. I am not saying this is easy for me or for them. I think fear of these tough conversations is a barrier to giving the emotional support that these families need. I work through this with them in an honest and open manner. I also call to check on the patients as much as possible, especially on anniversaries. I am not saying that all providers must follow this model. This is my passion and is natural for me, but data clearly show that the standard of emotional care we provide is not what patients need at this time. Thankfully, there is an amazing resource of grief counselors, social workers, online resources, and support groups for these families to help them get through the tragedy. These resources, however, are not the provider who spent this precious time with them and their beloved baby, and our emotional support is invaluable.
This past year has been very eventful for me. One of my patients delivered a new baby, after a prior loss, and asked if we could teach together. I had mentioned that everything I do with stillbirths is not based on my residency education, but on my experience and instinctual feeling of what families need. She knew from friends in bereavement circles that they felt that their care was different. We started teaching last summer and have done 10 training sessions to date; hopefully we will continue to teach new groups of nurses, residents, medical students, doulas, and physician assistant students each year.
This year also was eventful because I discovered the Star Legacy Foundation, a national not-for-profit organization with the goal of spreading awareness, education, and prevention regarding stillbirth. I attended their 2019 Summit in Minnesota. I thought I would meet many more doctors and midwives like myself, and I would learn even more about care for bereaved patients. However, that summer I learned preventing stillbirth may be possible from the then chief medical officer of Scotland, Catherine Calderwood, MB ChB. She talked about the preventive protocol she had created that had reduced the stillbirth rate by 23%. Because I was one of only five ob.gyn. nonspeaker attendees in a room of 400, I realized I had a real opportunity to try to bring some model for prevention to the United States. I brought the U.K. protocol to my practice and we have been doing it now for 9 months. (See “Decreased fetal movement: Time to educate patients and ourselves” at mdedge.com/pediatrics.)
I have had a year to think about why the U.S. stillbirth rate is higher than that of many high-income nations and why we have the lowest annual rate of reduction in the 2016 Lancet series among high resource nations.1 I think it is due to lack of education and training for providers in stillbirth prevention and care, which has led to further marginalization and stigmatization of bereaved moms. This has pushed them further into the shadows and makes it taboo to share their stories. It is providers being fearful to even mention to patients that stillbirth still happens. It is the lack of any protocol on how to educate patients and providers about fetal movement, and what to do if pregnant women complain about a decrease or change in fetal movement. I think a lot of this stems from an innate discomfort that obstetric providers have in the care of these patients. That if women felt cared for and empowered to tell their stories, there would be more efforts at stillbirth education and prevention.
I often think of an experience that the founder of Star Legacy, Lindsey Wimmer, experienced when she lost her son, Garrett, 16 years ago. She told a story in the documentary, “Don’t talk about the baby.” She tells that on the first night of the induction, the nurse came in and told her that the attending wanted to turn off the oxytocin so “she could get her rest.” I heard this and immediately knew the attending’s true reason for turning off the oxytocin. Lindsey then said she knew it was because the attending did not want to wake up to deliver a dead baby. I wrote Lindsey that day and told her I completely agreed and apologized on behalf of my profession for that care. She wrote me back that she had waited 16 years to have a provider validate her feelings about this. I told her I think her doctor was fearful and uncomfortable with this birth and was avoiding it, but I believe with better education and training this can change. I want to deliver babies like Garrett during my shift, because it is giving this vital care that reminds me why I became a doctor in the first place.
I know there are many providers out there who follow a similar model, but I want more providers to do so, and so does the bereavement community. In one study of 20 parents, all but 2 were frustrated about how the ob.gyn. and staff handled their deliveries.2 I truly believe that every person who delivers babies does it because they love it. Part of doing this job we love is realizing there will be times of great sadness. I also believe if this model of care is attempted by wary providers, they will quickly realize that this is what patients and their families need. With this care, stillbirth may become less of a taboo subject, and our stillbirth rate may fall.
Dr. Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, N.Y. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures. Email her a obnews@mdedge.com.
References
1. “Stillbirths 2016: ending preventable stillbirths.” Series from The Lancet journals. Published: Jan. 20, 2016.
2. BMC Pregnancy Childbirth. 2012 Nov 27. doi: 10.1186/1471-2393-12-137.
One of hardest parts of being an obstetrician is taking care of patients who experience a stillbirth. I am very comfortable with the care of a grieving patient and I always have been, although I am not sure why. I have a model of care that I have evolved in my 16 years since medical school graduation. This model is not based on formal instruction because I received none, but on my natural instincts of what a grieving mom and her family need to hear and receive in the worst moments of their lives. All obstetrics providers grieve the loss of the baby, but often not with the patient but on our own. We may do this because we want to respect the patient’s privacy or because we are not sure of the words to say. I hope I can provide some guidance for those who struggle with what to do.
I delivered my first stillborn baby as a third-year medical student. My mentor, a chief resident, saw something in me and encouraged me to care for this mother. She had twins and one baby was still living, but the prognosis was poor since this was the surviving twin from a monochorionic diamniotic pregnancy. On the day of the mom’s induction, I just pulled up a chair and talked with her. We talked about her life, the loss of the first baby several weeks before, and her hope that her surviving son would be okay. She felt so bonded to me that she refused to push until I was there. Her delivery is still firm in my mind. I still remember 17 years later the room she delivered in.
My first loss (stillbirth) as a resident was my intern year – a beautiful baby named Jude, who was stillborn at 39 weeks. After delivering Jude, I asked the family about the funeral arrangements. Three days later, I attended his funeral. I looked all around for the mother’s attending doctors but none of them were there. I remember thinking then that it was a given that they would be there, but now I know that it is rare. I also learned a lot about the grief a stillborn baby brings while listening to Jude’s father’s eulogy. He talked about how Jude would never bake cookies with Aunt Jane, ride the slide with cousin Chris, or put on a yellow backpack and ride the bus on the first day of school. Because of this eulogy, I understood this unique kind of grief that these losses bring early in my training.
I delivered many losses in my residency. The attendings left soon after the birth and I stayed behind with the family. I sat and counseled the families, and I helped them make memories. I realized that to care for these patients, I would need to trust my instincts because there was no formal and little informal training on how to care for families who lost their babies.
Once I completed residency, I was really able to do my “thing.” At loss deliveries, I was able to model for residents my method of care. I showed them that families want and need attention, support, and guidance. I modeled for them how to deliver and greet the baby. That it is not necessary to leave the room right after the birth, and it is okay to grieve and help families meet their babies. I modeled commenting on the baby’s features, on who they looked like. I showed how laughing about how the baby has grandma’s nose is okay. I showed them that it is okay to ask to hold and get a picture taken with the baby. I showed them that these are the only moments these families will get with their babies, and it is our job to help them do this. The family will have many moments alone in the days and weeks to come. They need our support and guidance. It is a part of being an ob.gyn. to care for families after stillbirths, and we do not want our patients to feel abandoned during this time by those they entrust to care for them.
I also was able to create a model for aftercare. I call my families often after they go home. Sometimes I catch them in the anger stage of the grief process and I let them vent. I work through this with them, and I answer their hardest and sometimes accusatory questions regarding care leading up to the diagnosis. I am not saying this is easy for me or for them. I think fear of these tough conversations is a barrier to giving the emotional support that these families need. I work through this with them in an honest and open manner. I also call to check on the patients as much as possible, especially on anniversaries. I am not saying that all providers must follow this model. This is my passion and is natural for me, but data clearly show that the standard of emotional care we provide is not what patients need at this time. Thankfully, there is an amazing resource of grief counselors, social workers, online resources, and support groups for these families to help them get through the tragedy. These resources, however, are not the provider who spent this precious time with them and their beloved baby, and our emotional support is invaluable.
This past year has been very eventful for me. One of my patients delivered a new baby, after a prior loss, and asked if we could teach together. I had mentioned that everything I do with stillbirths is not based on my residency education, but on my experience and instinctual feeling of what families need. She knew from friends in bereavement circles that they felt that their care was different. We started teaching last summer and have done 10 training sessions to date; hopefully we will continue to teach new groups of nurses, residents, medical students, doulas, and physician assistant students each year.
This year also was eventful because I discovered the Star Legacy Foundation, a national not-for-profit organization with the goal of spreading awareness, education, and prevention regarding stillbirth. I attended their 2019 Summit in Minnesota. I thought I would meet many more doctors and midwives like myself, and I would learn even more about care for bereaved patients. However, that summer I learned preventing stillbirth may be possible from the then chief medical officer of Scotland, Catherine Calderwood, MB ChB. She talked about the preventive protocol she had created that had reduced the stillbirth rate by 23%. Because I was one of only five ob.gyn. nonspeaker attendees in a room of 400, I realized I had a real opportunity to try to bring some model for prevention to the United States. I brought the U.K. protocol to my practice and we have been doing it now for 9 months. (See “Decreased fetal movement: Time to educate patients and ourselves” at mdedge.com/pediatrics.)
I have had a year to think about why the U.S. stillbirth rate is higher than that of many high-income nations and why we have the lowest annual rate of reduction in the 2016 Lancet series among high resource nations.1 I think it is due to lack of education and training for providers in stillbirth prevention and care, which has led to further marginalization and stigmatization of bereaved moms. This has pushed them further into the shadows and makes it taboo to share their stories. It is providers being fearful to even mention to patients that stillbirth still happens. It is the lack of any protocol on how to educate patients and providers about fetal movement, and what to do if pregnant women complain about a decrease or change in fetal movement. I think a lot of this stems from an innate discomfort that obstetric providers have in the care of these patients. That if women felt cared for and empowered to tell their stories, there would be more efforts at stillbirth education and prevention.
I often think of an experience that the founder of Star Legacy, Lindsey Wimmer, experienced when she lost her son, Garrett, 16 years ago. She told a story in the documentary, “Don’t talk about the baby.” She tells that on the first night of the induction, the nurse came in and told her that the attending wanted to turn off the oxytocin so “she could get her rest.” I heard this and immediately knew the attending’s true reason for turning off the oxytocin. Lindsey then said she knew it was because the attending did not want to wake up to deliver a dead baby. I wrote Lindsey that day and told her I completely agreed and apologized on behalf of my profession for that care. She wrote me back that she had waited 16 years to have a provider validate her feelings about this. I told her I think her doctor was fearful and uncomfortable with this birth and was avoiding it, but I believe with better education and training this can change. I want to deliver babies like Garrett during my shift, because it is giving this vital care that reminds me why I became a doctor in the first place.
I know there are many providers out there who follow a similar model, but I want more providers to do so, and so does the bereavement community. In one study of 20 parents, all but 2 were frustrated about how the ob.gyn. and staff handled their deliveries.2 I truly believe that every person who delivers babies does it because they love it. Part of doing this job we love is realizing there will be times of great sadness. I also believe if this model of care is attempted by wary providers, they will quickly realize that this is what patients and their families need. With this care, stillbirth may become less of a taboo subject, and our stillbirth rate may fall.
Dr. Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, N.Y. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures. Email her a obnews@mdedge.com.
References
1. “Stillbirths 2016: ending preventable stillbirths.” Series from The Lancet journals. Published: Jan. 20, 2016.
2. BMC Pregnancy Childbirth. 2012 Nov 27. doi: 10.1186/1471-2393-12-137.