User login
Eluxadoline effective for IBS in loperamide nonresponders
SAN ANTONIO – Darren M. Brenner, MD, reported at the annual meeting of the American College of Gastroenterology.
“From the totality of the clinical trials data we have now, we believe that eluxadoline can be effective both in patients who are naive to other treatments and in patients who have failed loperamide therapy,” concluded Dr. Brenner, a gastroenterologist at Northwestern University, Chicago.
Eluxadoline (Viberzi) is a novel mixed mu- and kappa-opioid receptor agonist and delta-opioid receptor antagonist approved by the Food and Drug Administration for treatment of irritable bowel syndrome with diarrhea (IBS-D) in adults. In contrast, loperamide, a mu-opioid receptor agonist, is not approved for that indication. Yet loperamide is widely prescribed for this purpose, despite the fact that both the Canadian Association of Gastroenterology and the ACG now recommend against this practice.
“There is a lack of conclusive evidence to support the use of loperamide for the relief of global IBS-D symptoms. It works on the stool symptoms – stool frequency and texture – but has never been shown to be beneficial for the abdominal pain symptoms or discomfort or bloating. That being said, as practitioners we continue to see loperamide used as a first-line agent,” Dr. Brenner noted.
RELIEF was a multicenter, prospective, double-blind study which randomized 346 patients with moderate to severe IBS-D to eluxadoline at 100 mg twice daily or placebo for 12 weeks. All participants were required to have an intact gallbladder as per the drug’s labeling guidance, and all had a self-reported recent inadequate response to loperamide.
The primary composite endpoint in the RELIEF trial was a 40% or greater improvement from baseline in the 11-point Daily Worst Abdominal Pain score plus a Bristol Stool Form score below 5 on the same day for at least 50% of study days. At baseline, participants had an average Worst Abdominal Pain score of 6.2 on the 0-10 scale and a Bristol score of 6.2. The primary endpoint was achieved at week 12 in 23% of the eluxadoline group, significantly better than the 10% rate in controls. The eluxadoline group also showed significantly greater improvement on the many secondary endpoints having to do with urgency-free days, stool consistency, bowel movement frequency, abdominal discomfort, bloating, and the experience of adequate relief of symptoms.
The safety profile of eluxadoline mirrored that of placebo, with no serious adverse events recorded in either study arm and a 2.9% study discontinuation rate because of treatment-emergent adverse events in the eluxadoline group. Asked why he thinks eluxadoline was effective in improving the full range of IBS-D symptoms when loperamide wasn’t, even though both drugs are mu-opioid receptor agonists, Dr. Brenner replied, “The problem is mu receptors line the entire GI tract, so you can actually push somebody from diarrhea to opioid-induced constipation – and that’s not the goal. What delta does is alleviate some of the adverse events by binding to the receptor, which results in increased transit time, reduced secretion, and increased absorption. Delta brings things back towards the center. We also believe antagonism of delta potentiates analgesic effects at the mu receptor, improves the pain component, gut symptoms, and stool symptoms.”
Dr. Brenner reported serving as a consultant to and member of a speaker’s bureau for Allergan, which markets eluxadoline and sponsored the RELIEF trial.
SAN ANTONIO – Darren M. Brenner, MD, reported at the annual meeting of the American College of Gastroenterology.
“From the totality of the clinical trials data we have now, we believe that eluxadoline can be effective both in patients who are naive to other treatments and in patients who have failed loperamide therapy,” concluded Dr. Brenner, a gastroenterologist at Northwestern University, Chicago.
Eluxadoline (Viberzi) is a novel mixed mu- and kappa-opioid receptor agonist and delta-opioid receptor antagonist approved by the Food and Drug Administration for treatment of irritable bowel syndrome with diarrhea (IBS-D) in adults. In contrast, loperamide, a mu-opioid receptor agonist, is not approved for that indication. Yet loperamide is widely prescribed for this purpose, despite the fact that both the Canadian Association of Gastroenterology and the ACG now recommend against this practice.
“There is a lack of conclusive evidence to support the use of loperamide for the relief of global IBS-D symptoms. It works on the stool symptoms – stool frequency and texture – but has never been shown to be beneficial for the abdominal pain symptoms or discomfort or bloating. That being said, as practitioners we continue to see loperamide used as a first-line agent,” Dr. Brenner noted.
RELIEF was a multicenter, prospective, double-blind study which randomized 346 patients with moderate to severe IBS-D to eluxadoline at 100 mg twice daily or placebo for 12 weeks. All participants were required to have an intact gallbladder as per the drug’s labeling guidance, and all had a self-reported recent inadequate response to loperamide.
The primary composite endpoint in the RELIEF trial was a 40% or greater improvement from baseline in the 11-point Daily Worst Abdominal Pain score plus a Bristol Stool Form score below 5 on the same day for at least 50% of study days. At baseline, participants had an average Worst Abdominal Pain score of 6.2 on the 0-10 scale and a Bristol score of 6.2. The primary endpoint was achieved at week 12 in 23% of the eluxadoline group, significantly better than the 10% rate in controls. The eluxadoline group also showed significantly greater improvement on the many secondary endpoints having to do with urgency-free days, stool consistency, bowel movement frequency, abdominal discomfort, bloating, and the experience of adequate relief of symptoms.
The safety profile of eluxadoline mirrored that of placebo, with no serious adverse events recorded in either study arm and a 2.9% study discontinuation rate because of treatment-emergent adverse events in the eluxadoline group. Asked why he thinks eluxadoline was effective in improving the full range of IBS-D symptoms when loperamide wasn’t, even though both drugs are mu-opioid receptor agonists, Dr. Brenner replied, “The problem is mu receptors line the entire GI tract, so you can actually push somebody from diarrhea to opioid-induced constipation – and that’s not the goal. What delta does is alleviate some of the adverse events by binding to the receptor, which results in increased transit time, reduced secretion, and increased absorption. Delta brings things back towards the center. We also believe antagonism of delta potentiates analgesic effects at the mu receptor, improves the pain component, gut symptoms, and stool symptoms.”
Dr. Brenner reported serving as a consultant to and member of a speaker’s bureau for Allergan, which markets eluxadoline and sponsored the RELIEF trial.
SAN ANTONIO – Darren M. Brenner, MD, reported at the annual meeting of the American College of Gastroenterology.
“From the totality of the clinical trials data we have now, we believe that eluxadoline can be effective both in patients who are naive to other treatments and in patients who have failed loperamide therapy,” concluded Dr. Brenner, a gastroenterologist at Northwestern University, Chicago.
Eluxadoline (Viberzi) is a novel mixed mu- and kappa-opioid receptor agonist and delta-opioid receptor antagonist approved by the Food and Drug Administration for treatment of irritable bowel syndrome with diarrhea (IBS-D) in adults. In contrast, loperamide, a mu-opioid receptor agonist, is not approved for that indication. Yet loperamide is widely prescribed for this purpose, despite the fact that both the Canadian Association of Gastroenterology and the ACG now recommend against this practice.
“There is a lack of conclusive evidence to support the use of loperamide for the relief of global IBS-D symptoms. It works on the stool symptoms – stool frequency and texture – but has never been shown to be beneficial for the abdominal pain symptoms or discomfort or bloating. That being said, as practitioners we continue to see loperamide used as a first-line agent,” Dr. Brenner noted.
RELIEF was a multicenter, prospective, double-blind study which randomized 346 patients with moderate to severe IBS-D to eluxadoline at 100 mg twice daily or placebo for 12 weeks. All participants were required to have an intact gallbladder as per the drug’s labeling guidance, and all had a self-reported recent inadequate response to loperamide.
The primary composite endpoint in the RELIEF trial was a 40% or greater improvement from baseline in the 11-point Daily Worst Abdominal Pain score plus a Bristol Stool Form score below 5 on the same day for at least 50% of study days. At baseline, participants had an average Worst Abdominal Pain score of 6.2 on the 0-10 scale and a Bristol score of 6.2. The primary endpoint was achieved at week 12 in 23% of the eluxadoline group, significantly better than the 10% rate in controls. The eluxadoline group also showed significantly greater improvement on the many secondary endpoints having to do with urgency-free days, stool consistency, bowel movement frequency, abdominal discomfort, bloating, and the experience of adequate relief of symptoms.
The safety profile of eluxadoline mirrored that of placebo, with no serious adverse events recorded in either study arm and a 2.9% study discontinuation rate because of treatment-emergent adverse events in the eluxadoline group. Asked why he thinks eluxadoline was effective in improving the full range of IBS-D symptoms when loperamide wasn’t, even though both drugs are mu-opioid receptor agonists, Dr. Brenner replied, “The problem is mu receptors line the entire GI tract, so you can actually push somebody from diarrhea to opioid-induced constipation – and that’s not the goal. What delta does is alleviate some of the adverse events by binding to the receptor, which results in increased transit time, reduced secretion, and increased absorption. Delta brings things back towards the center. We also believe antagonism of delta potentiates analgesic effects at the mu receptor, improves the pain component, gut symptoms, and stool symptoms.”
Dr. Brenner reported serving as a consultant to and member of a speaker’s bureau for Allergan, which markets eluxadoline and sponsored the RELIEF trial.
REPORTING FROM ACG 2019
Bariatric surgery candidates show high prevalence of thrombophilia
LAS VEGAS – More than half the patients seeking laparoscopic sleeve gastrectomy at a pair of large U.S. programs tested positive for thrombophilia, and for most of these patients, their thrombophilia stemmed from an abnormally elevated level of clotting factor VIII. This thrombophilia seemed to link with a small, but potentially meaningful, excess of portomesenteric venous thrombosis that could warrant treating patients with an anticoagulation regimen for an extended, 30-day period post surgery, Manish S. Parikh, MD, said at a meeting presented by The Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Although measurement of factor VIII excess can be done with a test that costs about $25, Dr. Parikh suggested that giving extended, 30-day anticoagulant prophylaxis to all patients undergoing laparoscopic sleeve gastrectomy (LSG) is a reasonable alternative to screening all patients first. “You could use our data to support 30-day prophylaxis for all LSG patients,” said Dr. Parikh, a metabolic and bariatric surgeon at NYU Langone Health in New York. He acknowledged that some logistic barriers can hamper the efficacy of extended prophylaxis.
The factor VIII elevations seen in many of these obese patients seeking metabolic surgery seems to be inherent and independent of their current weight. Although Dr. Parikh and his associates do not have long-term follow-up for all their LSG patients, “we’ve followed some patients, and their factor VIII is still elevated years later, after they’ve lost weight. We encourage lifelong anticoagulation [for these patients] because of their high risk for recurrent clot. This reflects their factor VIII and is independent of weight,” he said.
For their study, the researchers considered a factor VIII level above 150% of the normal level as abnormally elevated and prothrombotic.
The increased rate of portomesenteric venous thrombosis (PMVT) seen in the thrombophilic patients after LSG “is strongly related to the sleeve specifically,” added Dr. Parikh. He suggested that “something related to redirection of blood flow by taking the branches of the gastroepiploic arcade may lead to this.”
The interest of Dr. Parikh and his associates in thrombophilia and factor VIII excess began with a review they ran of more than 25,000 patients who underwent bariatric surgery at six U.S. centers during 2006-2016 that identified 40 patients who developed PMVT, all from the subgroup of nearly 10,000 patients who had LSG for their bariatric procedure. The prevalence of thrombophilia among those 40 patients with PMVT was 92%, with 76% having excess factor VIII (Surg Obes Relat Dis. 2017;13[11]:1835-9).
Based on those findings, the researchers began a practice of prospectively testing for thrombophilia in all patients who were assessed for LSG at two New York centers during August 2018–March 2019, a total of 1,075 patients, of whom 745 subsequently underwent the procedure. They tested the patients for factor VIII and four additional proteins in the clotting cascade that flag thrombophilia, a test panel that cost $103 per patient. That identified 563 surgery candidates (52%) with any thrombophilia, of whom 92% had excess factor VIII (48% of the total cohort of 1,075). Those patients received an extended, 30-day anticoagulant regimen.
To estimate the impact of this approach, the researchers compared the incidence of PMVT among the recent 745 patients who underwent LSG with a historic control group of 4,228 patients who underwent LSG at the two centers during the 4.5 years before routine thrombophilia screening. None of those 4,228 controls received extended anticoagulation.
During 30-day follow-up, 1 patient in the recent group of 745 patients (0.1%) developed PMVT, whereas 18 of the controls (0.4%) had PMVT. The incidence of bleeding was 0.6% in the recent patients and 0.4% in the controls. The researchers did not report a statistical analysis of these data, because the number of PMVT episodes was too small to allow reliable calculations, Dr. Parikh said. He also cautioned that the generalizability of the finding of thrombophilia prevalence is uncertain because the study population of 1,075 patients considering LSG was 84% Hispanic and 15% non-Hispanic African American.
Dr. Parikh had no disclosures.
SOURCE: Parikh MS et al. Obesity Week 2019, Abstract A109.
Vivek N. Prachand, MD , is professor of surgery and director of minimally invasive surgery at the University of Chicago. He had no disclosures. He made these comments as designated discussant for the report.
Vivek N. Prachand, MD , is professor of surgery and director of minimally invasive surgery at the University of Chicago. He had no disclosures. He made these comments as designated discussant for the report.
Vivek N. Prachand, MD , is professor of surgery and director of minimally invasive surgery at the University of Chicago. He had no disclosures. He made these comments as designated discussant for the report.
LAS VEGAS – More than half the patients seeking laparoscopic sleeve gastrectomy at a pair of large U.S. programs tested positive for thrombophilia, and for most of these patients, their thrombophilia stemmed from an abnormally elevated level of clotting factor VIII. This thrombophilia seemed to link with a small, but potentially meaningful, excess of portomesenteric venous thrombosis that could warrant treating patients with an anticoagulation regimen for an extended, 30-day period post surgery, Manish S. Parikh, MD, said at a meeting presented by The Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Although measurement of factor VIII excess can be done with a test that costs about $25, Dr. Parikh suggested that giving extended, 30-day anticoagulant prophylaxis to all patients undergoing laparoscopic sleeve gastrectomy (LSG) is a reasonable alternative to screening all patients first. “You could use our data to support 30-day prophylaxis for all LSG patients,” said Dr. Parikh, a metabolic and bariatric surgeon at NYU Langone Health in New York. He acknowledged that some logistic barriers can hamper the efficacy of extended prophylaxis.
The factor VIII elevations seen in many of these obese patients seeking metabolic surgery seems to be inherent and independent of their current weight. Although Dr. Parikh and his associates do not have long-term follow-up for all their LSG patients, “we’ve followed some patients, and their factor VIII is still elevated years later, after they’ve lost weight. We encourage lifelong anticoagulation [for these patients] because of their high risk for recurrent clot. This reflects their factor VIII and is independent of weight,” he said.
For their study, the researchers considered a factor VIII level above 150% of the normal level as abnormally elevated and prothrombotic.
The increased rate of portomesenteric venous thrombosis (PMVT) seen in the thrombophilic patients after LSG “is strongly related to the sleeve specifically,” added Dr. Parikh. He suggested that “something related to redirection of blood flow by taking the branches of the gastroepiploic arcade may lead to this.”
The interest of Dr. Parikh and his associates in thrombophilia and factor VIII excess began with a review they ran of more than 25,000 patients who underwent bariatric surgery at six U.S. centers during 2006-2016 that identified 40 patients who developed PMVT, all from the subgroup of nearly 10,000 patients who had LSG for their bariatric procedure. The prevalence of thrombophilia among those 40 patients with PMVT was 92%, with 76% having excess factor VIII (Surg Obes Relat Dis. 2017;13[11]:1835-9).
Based on those findings, the researchers began a practice of prospectively testing for thrombophilia in all patients who were assessed for LSG at two New York centers during August 2018–March 2019, a total of 1,075 patients, of whom 745 subsequently underwent the procedure. They tested the patients for factor VIII and four additional proteins in the clotting cascade that flag thrombophilia, a test panel that cost $103 per patient. That identified 563 surgery candidates (52%) with any thrombophilia, of whom 92% had excess factor VIII (48% of the total cohort of 1,075). Those patients received an extended, 30-day anticoagulant regimen.
To estimate the impact of this approach, the researchers compared the incidence of PMVT among the recent 745 patients who underwent LSG with a historic control group of 4,228 patients who underwent LSG at the two centers during the 4.5 years before routine thrombophilia screening. None of those 4,228 controls received extended anticoagulation.
During 30-day follow-up, 1 patient in the recent group of 745 patients (0.1%) developed PMVT, whereas 18 of the controls (0.4%) had PMVT. The incidence of bleeding was 0.6% in the recent patients and 0.4% in the controls. The researchers did not report a statistical analysis of these data, because the number of PMVT episodes was too small to allow reliable calculations, Dr. Parikh said. He also cautioned that the generalizability of the finding of thrombophilia prevalence is uncertain because the study population of 1,075 patients considering LSG was 84% Hispanic and 15% non-Hispanic African American.
Dr. Parikh had no disclosures.
SOURCE: Parikh MS et al. Obesity Week 2019, Abstract A109.
LAS VEGAS – More than half the patients seeking laparoscopic sleeve gastrectomy at a pair of large U.S. programs tested positive for thrombophilia, and for most of these patients, their thrombophilia stemmed from an abnormally elevated level of clotting factor VIII. This thrombophilia seemed to link with a small, but potentially meaningful, excess of portomesenteric venous thrombosis that could warrant treating patients with an anticoagulation regimen for an extended, 30-day period post surgery, Manish S. Parikh, MD, said at a meeting presented by The Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Although measurement of factor VIII excess can be done with a test that costs about $25, Dr. Parikh suggested that giving extended, 30-day anticoagulant prophylaxis to all patients undergoing laparoscopic sleeve gastrectomy (LSG) is a reasonable alternative to screening all patients first. “You could use our data to support 30-day prophylaxis for all LSG patients,” said Dr. Parikh, a metabolic and bariatric surgeon at NYU Langone Health in New York. He acknowledged that some logistic barriers can hamper the efficacy of extended prophylaxis.
The factor VIII elevations seen in many of these obese patients seeking metabolic surgery seems to be inherent and independent of their current weight. Although Dr. Parikh and his associates do not have long-term follow-up for all their LSG patients, “we’ve followed some patients, and their factor VIII is still elevated years later, after they’ve lost weight. We encourage lifelong anticoagulation [for these patients] because of their high risk for recurrent clot. This reflects their factor VIII and is independent of weight,” he said.
For their study, the researchers considered a factor VIII level above 150% of the normal level as abnormally elevated and prothrombotic.
The increased rate of portomesenteric venous thrombosis (PMVT) seen in the thrombophilic patients after LSG “is strongly related to the sleeve specifically,” added Dr. Parikh. He suggested that “something related to redirection of blood flow by taking the branches of the gastroepiploic arcade may lead to this.”
The interest of Dr. Parikh and his associates in thrombophilia and factor VIII excess began with a review they ran of more than 25,000 patients who underwent bariatric surgery at six U.S. centers during 2006-2016 that identified 40 patients who developed PMVT, all from the subgroup of nearly 10,000 patients who had LSG for their bariatric procedure. The prevalence of thrombophilia among those 40 patients with PMVT was 92%, with 76% having excess factor VIII (Surg Obes Relat Dis. 2017;13[11]:1835-9).
Based on those findings, the researchers began a practice of prospectively testing for thrombophilia in all patients who were assessed for LSG at two New York centers during August 2018–March 2019, a total of 1,075 patients, of whom 745 subsequently underwent the procedure. They tested the patients for factor VIII and four additional proteins in the clotting cascade that flag thrombophilia, a test panel that cost $103 per patient. That identified 563 surgery candidates (52%) with any thrombophilia, of whom 92% had excess factor VIII (48% of the total cohort of 1,075). Those patients received an extended, 30-day anticoagulant regimen.
To estimate the impact of this approach, the researchers compared the incidence of PMVT among the recent 745 patients who underwent LSG with a historic control group of 4,228 patients who underwent LSG at the two centers during the 4.5 years before routine thrombophilia screening. None of those 4,228 controls received extended anticoagulation.
During 30-day follow-up, 1 patient in the recent group of 745 patients (0.1%) developed PMVT, whereas 18 of the controls (0.4%) had PMVT. The incidence of bleeding was 0.6% in the recent patients and 0.4% in the controls. The researchers did not report a statistical analysis of these data, because the number of PMVT episodes was too small to allow reliable calculations, Dr. Parikh said. He also cautioned that the generalizability of the finding of thrombophilia prevalence is uncertain because the study population of 1,075 patients considering LSG was 84% Hispanic and 15% non-Hispanic African American.
Dr. Parikh had no disclosures.
SOURCE: Parikh MS et al. Obesity Week 2019, Abstract A109.
REPORTING FROM OBESITY WEEK 2019
Score predicts bariatric surgery’s benefits for obesity, type 2 diabetes
LAS VEGAS –
The Individualized Diabetes Complications risk score “can provide personalized, evidence-based risk information for patients with type 2 diabetes and obesity about their future cardiovascular disease outcomes and mortality with and without metabolic surgery,” Ali Aminian, MD, said at a meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Although the calculator needs validation in a prospective, randomized study to document its impact on practice, it is now available on two separate websites and as a downloadable app, said Dr. Aminian, a surgeon at the Cleveland Clinic.
The calculator inputs data for 26 distinct, “readily available” demographic and clinical entries, and based on that, estimates the patient’s 10-year risk for all-cause death, diabetic kidney disease, cerebrovascular disease, heart failure, and coronary artery disease if no surgery occurs or after some type of metabolic or bariatric surgery. The calculator does not currently have the ability to individualize predicted risks based on the specific type of metabolic surgery performed, but that is planned as a future refinement of the score.
“We validated the model in the nonsurgical patients, which showed it was very accurate. The next step is to run a randomized trial to see how useful the calculator is” for assisting in patients’ decision making, Dr. Aminian said.
The data for deriving the risk calculator, and for a preliminary validation of it, came from 13,722 patients with obesity (body mass index, 30 kg/m2 or greater) and type 2 diabetes, who were managed at the Cleveland Clinic during 1998-2017, drawn from more than 287,000 such patients in the clinic’s database. The study focused on 2,287 patients who underwent metabolic (bariatric) surgery and 11,435 patients from the same database who did not have surgery and matched by propensity scoring on a 5:1 basis with those who had surgery. The two cohorts this created matched well for age (about 54 years), sex (about two-thirds women), body mass index (about 44 kg/m2), and the prevalence of various comorbidities at baseline.
Dr. Aminian and associates then analyzed the incidence of all-cause mortality and various cardiovascular disease endpoints, as well as nephropathy during follow-up, through December 2018. Patients who had undergone metabolic surgery showed statistically significant reductions in the incidence of each of those events, compared with patients who did not have surgery (JAMA. 2019;322[13]:1271-82).
The investigators used these findings to create their model for calculating a patient’s risk score. For example, to calculate an estimate for the 10-year risk from all-cause mortality, the results showed that the most powerful risk factors were age; baseline body mass index, heart failure, and need for insulin; and smoking status. For the endpoint of nephropathy, the most important factors were estimated glomerular filtration rate at baseline and age. Identified risk factors could account for about 80% of the 10-year risk for all-cause death and for about 75% of the risk for developing nephropathy during 10 years, based on the area-under-the-curve values the model produced.
The risk score may help patients better understand the potential role that metabolic surgery can have in reducing their future event risk, thereby helping them better appreciate the benefit they stand to gain from undergoing surgery, Dr. Aminian said.
The calculator is available at a website maintained by the Cleveland Clinic, at a site of the American Society for Metabolic and Bariatric Surgery, and in app stores, he said.
The work was partially funded by Medtronic. Dr. Aminian has received grants from Medtronic.
SOURCE: Aminian A et al. Obesity Week 2019, Abstract A101.
LAS VEGAS –
The Individualized Diabetes Complications risk score “can provide personalized, evidence-based risk information for patients with type 2 diabetes and obesity about their future cardiovascular disease outcomes and mortality with and without metabolic surgery,” Ali Aminian, MD, said at a meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Although the calculator needs validation in a prospective, randomized study to document its impact on practice, it is now available on two separate websites and as a downloadable app, said Dr. Aminian, a surgeon at the Cleveland Clinic.
The calculator inputs data for 26 distinct, “readily available” demographic and clinical entries, and based on that, estimates the patient’s 10-year risk for all-cause death, diabetic kidney disease, cerebrovascular disease, heart failure, and coronary artery disease if no surgery occurs or after some type of metabolic or bariatric surgery. The calculator does not currently have the ability to individualize predicted risks based on the specific type of metabolic surgery performed, but that is planned as a future refinement of the score.
“We validated the model in the nonsurgical patients, which showed it was very accurate. The next step is to run a randomized trial to see how useful the calculator is” for assisting in patients’ decision making, Dr. Aminian said.
The data for deriving the risk calculator, and for a preliminary validation of it, came from 13,722 patients with obesity (body mass index, 30 kg/m2 or greater) and type 2 diabetes, who were managed at the Cleveland Clinic during 1998-2017, drawn from more than 287,000 such patients in the clinic’s database. The study focused on 2,287 patients who underwent metabolic (bariatric) surgery and 11,435 patients from the same database who did not have surgery and matched by propensity scoring on a 5:1 basis with those who had surgery. The two cohorts this created matched well for age (about 54 years), sex (about two-thirds women), body mass index (about 44 kg/m2), and the prevalence of various comorbidities at baseline.
Dr. Aminian and associates then analyzed the incidence of all-cause mortality and various cardiovascular disease endpoints, as well as nephropathy during follow-up, through December 2018. Patients who had undergone metabolic surgery showed statistically significant reductions in the incidence of each of those events, compared with patients who did not have surgery (JAMA. 2019;322[13]:1271-82).
The investigators used these findings to create their model for calculating a patient’s risk score. For example, to calculate an estimate for the 10-year risk from all-cause mortality, the results showed that the most powerful risk factors were age; baseline body mass index, heart failure, and need for insulin; and smoking status. For the endpoint of nephropathy, the most important factors were estimated glomerular filtration rate at baseline and age. Identified risk factors could account for about 80% of the 10-year risk for all-cause death and for about 75% of the risk for developing nephropathy during 10 years, based on the area-under-the-curve values the model produced.
The risk score may help patients better understand the potential role that metabolic surgery can have in reducing their future event risk, thereby helping them better appreciate the benefit they stand to gain from undergoing surgery, Dr. Aminian said.
The calculator is available at a website maintained by the Cleveland Clinic, at a site of the American Society for Metabolic and Bariatric Surgery, and in app stores, he said.
The work was partially funded by Medtronic. Dr. Aminian has received grants from Medtronic.
SOURCE: Aminian A et al. Obesity Week 2019, Abstract A101.
LAS VEGAS –
The Individualized Diabetes Complications risk score “can provide personalized, evidence-based risk information for patients with type 2 diabetes and obesity about their future cardiovascular disease outcomes and mortality with and without metabolic surgery,” Ali Aminian, MD, said at a meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Although the calculator needs validation in a prospective, randomized study to document its impact on practice, it is now available on two separate websites and as a downloadable app, said Dr. Aminian, a surgeon at the Cleveland Clinic.
The calculator inputs data for 26 distinct, “readily available” demographic and clinical entries, and based on that, estimates the patient’s 10-year risk for all-cause death, diabetic kidney disease, cerebrovascular disease, heart failure, and coronary artery disease if no surgery occurs or after some type of metabolic or bariatric surgery. The calculator does not currently have the ability to individualize predicted risks based on the specific type of metabolic surgery performed, but that is planned as a future refinement of the score.
“We validated the model in the nonsurgical patients, which showed it was very accurate. The next step is to run a randomized trial to see how useful the calculator is” for assisting in patients’ decision making, Dr. Aminian said.
The data for deriving the risk calculator, and for a preliminary validation of it, came from 13,722 patients with obesity (body mass index, 30 kg/m2 or greater) and type 2 diabetes, who were managed at the Cleveland Clinic during 1998-2017, drawn from more than 287,000 such patients in the clinic’s database. The study focused on 2,287 patients who underwent metabolic (bariatric) surgery and 11,435 patients from the same database who did not have surgery and matched by propensity scoring on a 5:1 basis with those who had surgery. The two cohorts this created matched well for age (about 54 years), sex (about two-thirds women), body mass index (about 44 kg/m2), and the prevalence of various comorbidities at baseline.
Dr. Aminian and associates then analyzed the incidence of all-cause mortality and various cardiovascular disease endpoints, as well as nephropathy during follow-up, through December 2018. Patients who had undergone metabolic surgery showed statistically significant reductions in the incidence of each of those events, compared with patients who did not have surgery (JAMA. 2019;322[13]:1271-82).
The investigators used these findings to create their model for calculating a patient’s risk score. For example, to calculate an estimate for the 10-year risk from all-cause mortality, the results showed that the most powerful risk factors were age; baseline body mass index, heart failure, and need for insulin; and smoking status. For the endpoint of nephropathy, the most important factors were estimated glomerular filtration rate at baseline and age. Identified risk factors could account for about 80% of the 10-year risk for all-cause death and for about 75% of the risk for developing nephropathy during 10 years, based on the area-under-the-curve values the model produced.
The risk score may help patients better understand the potential role that metabolic surgery can have in reducing their future event risk, thereby helping them better appreciate the benefit they stand to gain from undergoing surgery, Dr. Aminian said.
The calculator is available at a website maintained by the Cleveland Clinic, at a site of the American Society for Metabolic and Bariatric Surgery, and in app stores, he said.
The work was partially funded by Medtronic. Dr. Aminian has received grants from Medtronic.
SOURCE: Aminian A et al. Obesity Week 2019, Abstract A101.
REPORTING FROM OBESITY WEEK 2019
High response, survival rates with ponatinib/hCVAD in Ph-positive ALL
ORLANDO – For adults with newly diagnosed acute lymphoblastic leukemia positive for the Philadelphia chromosome (Ph+ALL), the combination of hyper-CVAD chemotherapy and ponatinib is associated with high complete molecular response and 5-year overall survival rates, investigators reported.
Long-term follow-up of 86 adults with Ph+ALL treated in the front line with chemotherapy plus ponatinib (Iclusig), a third-generation tyrosine kinase inhibitor (TKI), showed a complete remission (CR) rate of 100%, complete molecular remission (CMR) rate of 86%, and a 5-year overall survival (OS) rate of 74%, reported Nicholas J. Short, MD, from the University of Texas MD Anderson Cancer Center in Houston.
“Although we observed two treatment-related cardiovascular deaths with the original trial design, with almost 50 patients treated since instituting a risk-adapted dosing schedule with lower doses of ponatinib, no additional ponatinib-related deaths have been observed,” he said at the annual meeting of the American Society of Hematology.
The standard of care for adults with Ph+ALL is chemotherapy plus a TKI. With a first- or second-generation TKI plus chemotherapy, reported 5-year OS rates range from 35% to 50%.
“However, relapses are still common, and these are usually driven by the development of new resistance mutations in the ABL gene, particularly the T315I gatekeeper mutation which has been reported in up to 75% of patients at the time of relapse,” he said.
Ponatinib is a pan-BCR-ABL TKI with activity against ALL with T315I mutations, and the combination of this agent with hyper-CVAD chemotherapy (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) has been associated with higher response rates than those seen with earlier-generation TKIs, as well as higher levels of minimal residual disease (MRD) negativity, he noted.
Dr. Short and colleagues hypothesized that, compared with the standard of care, hyper-CVAD plus ponatinib would be associated with higher MRD levels, low relapse rates by suppression of T315I subclones, decreased reliance on stem cell transplantation in first remission, and improved long-term survival.
To test this, they treated 86 adults with newly diagnosed Ph+ALL, including those who had undergone one or two previous courses of chemotherapy with a TKI other than ponatinib. The patients had Eastern Cooperative Oncology Group performance status 0-2, adequate organ function, and no clinically significant cardiovascular disease.
The patients underwent eight cycles of hyper-CVAD alternating with high-dose methotrexate/cytarabine approximately every 21 days. The first 37 patients were treated with, ponatinib 45 mg daily for the first 14 days of cycle 1, then continuously for subsequent cycles. Patients with CD20 expression of 20% or greater also received rituximab during the first four cycles. CNS prophylaxis was also administered with 12 doses of intrathecal chemotherapy with alternating methotrexate and cytarabine.
Patients who had a CR received maintenance with ponatinib and vincristine/prednisone monthly for 2 years, followed by ponatinib indefinitely.
Out of concern for vascular toxicity with long-term use of high-dose ponatinib, including the two deaths mentioned before, the protocol was amended after the first 37 patients were treated. The amended protocol reduced ponatinib to 30 mg starting at cycle 2, with further reduction to 15 mg once a CMR (absence of BCR-ABL on polymerase chain reaction) was achieved.
At a median follow-up of 44 months, the event-free survival rates – the primary endpoint – were 71% at 3 years and 68% at 5 years. The 3-year OS rate was 78%, and the 5-year OS rate was 74%.
All patients had complete remission and complete cytogenetic remission as assessed by conventional karyotyping. Additionally, 73 of 85 evaluable patients (86%) achieved a CMR at some point during therapy.
“We had previously reported that achievement of a complete molecular response by 3 months is associated with superior outcomes. Approximately three quarters of patients achieved this milestone,” Dr. Short said.
Grade 3 or greater adverse events of particular concern included transaminase elevations in 29% of patients, elevated bilirubin and pancreatitis in 15% each, and hypertension in 14%.
Four patients had grade 3 or greater venous thromboembolic or arterial events, including the two previously noted deaths from myocardial infarction, both of which occurred prior to the protocol amendment.
At the most recent follow-up, 11 patients had experienced relapse (no CNS-only relapses), and of this group, 5 died and 6 were still alive. Nineteen patients underwent hematopoietic stem cell transplant, and of this group, 13 were still alive and 6 died.
Causes of death in the nine patients who died while in CR included the two myocardial infarction deaths on study, three deaths from sepsis during consolidation, one from lung cancer, one from a head injury after a fall, one from myocardial infarction in a 79-year-old patient 4 years after stopping ponatinib (off study), and one from preexisting congestive heart failure in a 74-year-old patient.
In all, 47 patients were either in ongoing therapy or observation at last follow-up, including three patients who were transitioned to MRD-directed therapy including blinatumomab (Blincyto).
“As a next step, we are now evaluating lower-intensity regimens with ponatinib and blinatumomab in both the frontline and relapsed/refractory settings, with the goals of decreased chemotherapy-related toxicity, increased MRD-negativity rates, further decreased reliance on transplant, and improved long-term outcomes,” Dr. Short said.
The study was sponsored by MD Anderson with support from the National Cancer Institute. Dr. Short reported consulting for AstraZenca, honoraria from Amgen, and consulting and receiving research funding from Takeda Oncology.
SOURCE: Short NJ et al. ASH 2019, Abstract 283.
ORLANDO – For adults with newly diagnosed acute lymphoblastic leukemia positive for the Philadelphia chromosome (Ph+ALL), the combination of hyper-CVAD chemotherapy and ponatinib is associated with high complete molecular response and 5-year overall survival rates, investigators reported.
Long-term follow-up of 86 adults with Ph+ALL treated in the front line with chemotherapy plus ponatinib (Iclusig), a third-generation tyrosine kinase inhibitor (TKI), showed a complete remission (CR) rate of 100%, complete molecular remission (CMR) rate of 86%, and a 5-year overall survival (OS) rate of 74%, reported Nicholas J. Short, MD, from the University of Texas MD Anderson Cancer Center in Houston.
“Although we observed two treatment-related cardiovascular deaths with the original trial design, with almost 50 patients treated since instituting a risk-adapted dosing schedule with lower doses of ponatinib, no additional ponatinib-related deaths have been observed,” he said at the annual meeting of the American Society of Hematology.
The standard of care for adults with Ph+ALL is chemotherapy plus a TKI. With a first- or second-generation TKI plus chemotherapy, reported 5-year OS rates range from 35% to 50%.
“However, relapses are still common, and these are usually driven by the development of new resistance mutations in the ABL gene, particularly the T315I gatekeeper mutation which has been reported in up to 75% of patients at the time of relapse,” he said.
Ponatinib is a pan-BCR-ABL TKI with activity against ALL with T315I mutations, and the combination of this agent with hyper-CVAD chemotherapy (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) has been associated with higher response rates than those seen with earlier-generation TKIs, as well as higher levels of minimal residual disease (MRD) negativity, he noted.
Dr. Short and colleagues hypothesized that, compared with the standard of care, hyper-CVAD plus ponatinib would be associated with higher MRD levels, low relapse rates by suppression of T315I subclones, decreased reliance on stem cell transplantation in first remission, and improved long-term survival.
To test this, they treated 86 adults with newly diagnosed Ph+ALL, including those who had undergone one or two previous courses of chemotherapy with a TKI other than ponatinib. The patients had Eastern Cooperative Oncology Group performance status 0-2, adequate organ function, and no clinically significant cardiovascular disease.
The patients underwent eight cycles of hyper-CVAD alternating with high-dose methotrexate/cytarabine approximately every 21 days. The first 37 patients were treated with, ponatinib 45 mg daily for the first 14 days of cycle 1, then continuously for subsequent cycles. Patients with CD20 expression of 20% or greater also received rituximab during the first four cycles. CNS prophylaxis was also administered with 12 doses of intrathecal chemotherapy with alternating methotrexate and cytarabine.
Patients who had a CR received maintenance with ponatinib and vincristine/prednisone monthly for 2 years, followed by ponatinib indefinitely.
Out of concern for vascular toxicity with long-term use of high-dose ponatinib, including the two deaths mentioned before, the protocol was amended after the first 37 patients were treated. The amended protocol reduced ponatinib to 30 mg starting at cycle 2, with further reduction to 15 mg once a CMR (absence of BCR-ABL on polymerase chain reaction) was achieved.
At a median follow-up of 44 months, the event-free survival rates – the primary endpoint – were 71% at 3 years and 68% at 5 years. The 3-year OS rate was 78%, and the 5-year OS rate was 74%.
All patients had complete remission and complete cytogenetic remission as assessed by conventional karyotyping. Additionally, 73 of 85 evaluable patients (86%) achieved a CMR at some point during therapy.
“We had previously reported that achievement of a complete molecular response by 3 months is associated with superior outcomes. Approximately three quarters of patients achieved this milestone,” Dr. Short said.
Grade 3 or greater adverse events of particular concern included transaminase elevations in 29% of patients, elevated bilirubin and pancreatitis in 15% each, and hypertension in 14%.
Four patients had grade 3 or greater venous thromboembolic or arterial events, including the two previously noted deaths from myocardial infarction, both of which occurred prior to the protocol amendment.
At the most recent follow-up, 11 patients had experienced relapse (no CNS-only relapses), and of this group, 5 died and 6 were still alive. Nineteen patients underwent hematopoietic stem cell transplant, and of this group, 13 were still alive and 6 died.
Causes of death in the nine patients who died while in CR included the two myocardial infarction deaths on study, three deaths from sepsis during consolidation, one from lung cancer, one from a head injury after a fall, one from myocardial infarction in a 79-year-old patient 4 years after stopping ponatinib (off study), and one from preexisting congestive heart failure in a 74-year-old patient.
In all, 47 patients were either in ongoing therapy or observation at last follow-up, including three patients who were transitioned to MRD-directed therapy including blinatumomab (Blincyto).
“As a next step, we are now evaluating lower-intensity regimens with ponatinib and blinatumomab in both the frontline and relapsed/refractory settings, with the goals of decreased chemotherapy-related toxicity, increased MRD-negativity rates, further decreased reliance on transplant, and improved long-term outcomes,” Dr. Short said.
The study was sponsored by MD Anderson with support from the National Cancer Institute. Dr. Short reported consulting for AstraZenca, honoraria from Amgen, and consulting and receiving research funding from Takeda Oncology.
SOURCE: Short NJ et al. ASH 2019, Abstract 283.
ORLANDO – For adults with newly diagnosed acute lymphoblastic leukemia positive for the Philadelphia chromosome (Ph+ALL), the combination of hyper-CVAD chemotherapy and ponatinib is associated with high complete molecular response and 5-year overall survival rates, investigators reported.
Long-term follow-up of 86 adults with Ph+ALL treated in the front line with chemotherapy plus ponatinib (Iclusig), a third-generation tyrosine kinase inhibitor (TKI), showed a complete remission (CR) rate of 100%, complete molecular remission (CMR) rate of 86%, and a 5-year overall survival (OS) rate of 74%, reported Nicholas J. Short, MD, from the University of Texas MD Anderson Cancer Center in Houston.
“Although we observed two treatment-related cardiovascular deaths with the original trial design, with almost 50 patients treated since instituting a risk-adapted dosing schedule with lower doses of ponatinib, no additional ponatinib-related deaths have been observed,” he said at the annual meeting of the American Society of Hematology.
The standard of care for adults with Ph+ALL is chemotherapy plus a TKI. With a first- or second-generation TKI plus chemotherapy, reported 5-year OS rates range from 35% to 50%.
“However, relapses are still common, and these are usually driven by the development of new resistance mutations in the ABL gene, particularly the T315I gatekeeper mutation which has been reported in up to 75% of patients at the time of relapse,” he said.
Ponatinib is a pan-BCR-ABL TKI with activity against ALL with T315I mutations, and the combination of this agent with hyper-CVAD chemotherapy (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) has been associated with higher response rates than those seen with earlier-generation TKIs, as well as higher levels of minimal residual disease (MRD) negativity, he noted.
Dr. Short and colleagues hypothesized that, compared with the standard of care, hyper-CVAD plus ponatinib would be associated with higher MRD levels, low relapse rates by suppression of T315I subclones, decreased reliance on stem cell transplantation in first remission, and improved long-term survival.
To test this, they treated 86 adults with newly diagnosed Ph+ALL, including those who had undergone one or two previous courses of chemotherapy with a TKI other than ponatinib. The patients had Eastern Cooperative Oncology Group performance status 0-2, adequate organ function, and no clinically significant cardiovascular disease.
The patients underwent eight cycles of hyper-CVAD alternating with high-dose methotrexate/cytarabine approximately every 21 days. The first 37 patients were treated with, ponatinib 45 mg daily for the first 14 days of cycle 1, then continuously for subsequent cycles. Patients with CD20 expression of 20% or greater also received rituximab during the first four cycles. CNS prophylaxis was also administered with 12 doses of intrathecal chemotherapy with alternating methotrexate and cytarabine.
Patients who had a CR received maintenance with ponatinib and vincristine/prednisone monthly for 2 years, followed by ponatinib indefinitely.
Out of concern for vascular toxicity with long-term use of high-dose ponatinib, including the two deaths mentioned before, the protocol was amended after the first 37 patients were treated. The amended protocol reduced ponatinib to 30 mg starting at cycle 2, with further reduction to 15 mg once a CMR (absence of BCR-ABL on polymerase chain reaction) was achieved.
At a median follow-up of 44 months, the event-free survival rates – the primary endpoint – were 71% at 3 years and 68% at 5 years. The 3-year OS rate was 78%, and the 5-year OS rate was 74%.
All patients had complete remission and complete cytogenetic remission as assessed by conventional karyotyping. Additionally, 73 of 85 evaluable patients (86%) achieved a CMR at some point during therapy.
“We had previously reported that achievement of a complete molecular response by 3 months is associated with superior outcomes. Approximately three quarters of patients achieved this milestone,” Dr. Short said.
Grade 3 or greater adverse events of particular concern included transaminase elevations in 29% of patients, elevated bilirubin and pancreatitis in 15% each, and hypertension in 14%.
Four patients had grade 3 or greater venous thromboembolic or arterial events, including the two previously noted deaths from myocardial infarction, both of which occurred prior to the protocol amendment.
At the most recent follow-up, 11 patients had experienced relapse (no CNS-only relapses), and of this group, 5 died and 6 were still alive. Nineteen patients underwent hematopoietic stem cell transplant, and of this group, 13 were still alive and 6 died.
Causes of death in the nine patients who died while in CR included the two myocardial infarction deaths on study, three deaths from sepsis during consolidation, one from lung cancer, one from a head injury after a fall, one from myocardial infarction in a 79-year-old patient 4 years after stopping ponatinib (off study), and one from preexisting congestive heart failure in a 74-year-old patient.
In all, 47 patients were either in ongoing therapy or observation at last follow-up, including three patients who were transitioned to MRD-directed therapy including blinatumomab (Blincyto).
“As a next step, we are now evaluating lower-intensity regimens with ponatinib and blinatumomab in both the frontline and relapsed/refractory settings, with the goals of decreased chemotherapy-related toxicity, increased MRD-negativity rates, further decreased reliance on transplant, and improved long-term outcomes,” Dr. Short said.
The study was sponsored by MD Anderson with support from the National Cancer Institute. Dr. Short reported consulting for AstraZenca, honoraria from Amgen, and consulting and receiving research funding from Takeda Oncology.
SOURCE: Short NJ et al. ASH 2019, Abstract 283.
REPORTING FROM ASH 2019
Is elagolix effective at reducing HMB for women with varying fibroid sizes and types?
Whether or not women experience symptoms from uterine fibroid(s) can be dependent on a fibroid’s size and location. Heavy menstrual bleeding (HMB) is the most common symptom resulting from fibroids, and it occurs in up to one-third of women with fibroids. For fibroids that are large (>10 cm), “bulk” symptoms may occur, including pelvic pressure, urinary urgency or frequency, incontinence, constipation, abdominal protrusion, etc.1
Elagolix, an oral gonadotropin-releasing hormone (GnRH) receptor antagonist, was US Food and Drug Administration–approved in 2018 to treat moderate to severe pain caused by endometriosis. 2 Elagolix is being evaluated in 2 phase 3 randomized, double-blind trials for the additional treatment of HMB associated with uterine fibroids. The results of these studies were presented at the 2019 AAGL meeting on November 12, in Vancouver, Canada.
Phase 3 study details
Premenopausal women aged 18 to 51 years were included in the Elaris UF-1 and UF-2 studies if they had HMB (defined using the alkaline hematin methodology as menstrual blood loss [MBL] >80 mL/cycle) and uterine fibroids as confirmed through ultrasound. Because elagolix suppresses estrogen and progesterone, treatment results in dose- and duration-dependent decreases in bone mineral density (BMD),2 and add-back therapy can lessen these adverse effects. Subsequently, participants were randomly assigned 1:1:2 to placebo, elagolix 300 mg twice daily, or elagolix 300 mg twice daily with add-back therapy (1 mg estradiol/0.5 mg norethidrone acetate [E2/NETA]) once daily. Uterine volume and size and location of uterine fibroid(s) were assessed by ultrasound. Subgroups were defined by baseline FIGO categories, grouped FIGO 0-3, FIGO 4, or FIGO 5-8.3
Over the 6-month studies, 72.2% (95% confidence interval [CI], 67.65–76.73) of the 395 women who received elagolix plus E2/NETA achieved < 80 mL MBL during the final month and ≥ 50% MBL reduction from baseline to the final month. When stratified by FIGO classification, the results were similar for all subgroups: FIGO 0-3, 77.7% (95% CI, 67.21–80.85). Similar results were seen in women with a primary fibroid volume of either greater or less than 36.2 cm3 (median).3
The most frequently reported adverse events among women taking elagolix plus E2/NETA were hot flushes, night sweats, nausea, and headache. Changes in BMD among these women were not significant compared with women taking placebo.3
The Elaris UF-1 and UF-2 studies are funded by AbbVie Inc.
- Al-Hendy A, Myers ER, Stewart E. Uterine fibroids: burden and unmet medical need. Semin Reprod Med. 2017;35:473-480.
- Orilissa [package insert]. North Chicago, IL: AbbVie; August 2019.
- Al-Hendy A, Simon J, Hurtado S, et al. Effect of fibroid location and size on efficacy in elagolix: results from phase 3 clinical trials. Paper presented at: 48th Annual Meeting of the AAGL; November 2019; Vancouver, Canada.
Whether or not women experience symptoms from uterine fibroid(s) can be dependent on a fibroid’s size and location. Heavy menstrual bleeding (HMB) is the most common symptom resulting from fibroids, and it occurs in up to one-third of women with fibroids. For fibroids that are large (>10 cm), “bulk” symptoms may occur, including pelvic pressure, urinary urgency or frequency, incontinence, constipation, abdominal protrusion, etc.1
Elagolix, an oral gonadotropin-releasing hormone (GnRH) receptor antagonist, was US Food and Drug Administration–approved in 2018 to treat moderate to severe pain caused by endometriosis. 2 Elagolix is being evaluated in 2 phase 3 randomized, double-blind trials for the additional treatment of HMB associated with uterine fibroids. The results of these studies were presented at the 2019 AAGL meeting on November 12, in Vancouver, Canada.
Phase 3 study details
Premenopausal women aged 18 to 51 years were included in the Elaris UF-1 and UF-2 studies if they had HMB (defined using the alkaline hematin methodology as menstrual blood loss [MBL] >80 mL/cycle) and uterine fibroids as confirmed through ultrasound. Because elagolix suppresses estrogen and progesterone, treatment results in dose- and duration-dependent decreases in bone mineral density (BMD),2 and add-back therapy can lessen these adverse effects. Subsequently, participants were randomly assigned 1:1:2 to placebo, elagolix 300 mg twice daily, or elagolix 300 mg twice daily with add-back therapy (1 mg estradiol/0.5 mg norethidrone acetate [E2/NETA]) once daily. Uterine volume and size and location of uterine fibroid(s) were assessed by ultrasound. Subgroups were defined by baseline FIGO categories, grouped FIGO 0-3, FIGO 4, or FIGO 5-8.3
Over the 6-month studies, 72.2% (95% confidence interval [CI], 67.65–76.73) of the 395 women who received elagolix plus E2/NETA achieved < 80 mL MBL during the final month and ≥ 50% MBL reduction from baseline to the final month. When stratified by FIGO classification, the results were similar for all subgroups: FIGO 0-3, 77.7% (95% CI, 67.21–80.85). Similar results were seen in women with a primary fibroid volume of either greater or less than 36.2 cm3 (median).3
The most frequently reported adverse events among women taking elagolix plus E2/NETA were hot flushes, night sweats, nausea, and headache. Changes in BMD among these women were not significant compared with women taking placebo.3
The Elaris UF-1 and UF-2 studies are funded by AbbVie Inc.
Whether or not women experience symptoms from uterine fibroid(s) can be dependent on a fibroid’s size and location. Heavy menstrual bleeding (HMB) is the most common symptom resulting from fibroids, and it occurs in up to one-third of women with fibroids. For fibroids that are large (>10 cm), “bulk” symptoms may occur, including pelvic pressure, urinary urgency or frequency, incontinence, constipation, abdominal protrusion, etc.1
Elagolix, an oral gonadotropin-releasing hormone (GnRH) receptor antagonist, was US Food and Drug Administration–approved in 2018 to treat moderate to severe pain caused by endometriosis. 2 Elagolix is being evaluated in 2 phase 3 randomized, double-blind trials for the additional treatment of HMB associated with uterine fibroids. The results of these studies were presented at the 2019 AAGL meeting on November 12, in Vancouver, Canada.
Phase 3 study details
Premenopausal women aged 18 to 51 years were included in the Elaris UF-1 and UF-2 studies if they had HMB (defined using the alkaline hematin methodology as menstrual blood loss [MBL] >80 mL/cycle) and uterine fibroids as confirmed through ultrasound. Because elagolix suppresses estrogen and progesterone, treatment results in dose- and duration-dependent decreases in bone mineral density (BMD),2 and add-back therapy can lessen these adverse effects. Subsequently, participants were randomly assigned 1:1:2 to placebo, elagolix 300 mg twice daily, or elagolix 300 mg twice daily with add-back therapy (1 mg estradiol/0.5 mg norethidrone acetate [E2/NETA]) once daily. Uterine volume and size and location of uterine fibroid(s) were assessed by ultrasound. Subgroups were defined by baseline FIGO categories, grouped FIGO 0-3, FIGO 4, or FIGO 5-8.3
Over the 6-month studies, 72.2% (95% confidence interval [CI], 67.65–76.73) of the 395 women who received elagolix plus E2/NETA achieved < 80 mL MBL during the final month and ≥ 50% MBL reduction from baseline to the final month. When stratified by FIGO classification, the results were similar for all subgroups: FIGO 0-3, 77.7% (95% CI, 67.21–80.85). Similar results were seen in women with a primary fibroid volume of either greater or less than 36.2 cm3 (median).3
The most frequently reported adverse events among women taking elagolix plus E2/NETA were hot flushes, night sweats, nausea, and headache. Changes in BMD among these women were not significant compared with women taking placebo.3
The Elaris UF-1 and UF-2 studies are funded by AbbVie Inc.
- Al-Hendy A, Myers ER, Stewart E. Uterine fibroids: burden and unmet medical need. Semin Reprod Med. 2017;35:473-480.
- Orilissa [package insert]. North Chicago, IL: AbbVie; August 2019.
- Al-Hendy A, Simon J, Hurtado S, et al. Effect of fibroid location and size on efficacy in elagolix: results from phase 3 clinical trials. Paper presented at: 48th Annual Meeting of the AAGL; November 2019; Vancouver, Canada.
- Al-Hendy A, Myers ER, Stewart E. Uterine fibroids: burden and unmet medical need. Semin Reprod Med. 2017;35:473-480.
- Orilissa [package insert]. North Chicago, IL: AbbVie; August 2019.
- Al-Hendy A, Simon J, Hurtado S, et al. Effect of fibroid location and size on efficacy in elagolix: results from phase 3 clinical trials. Paper presented at: 48th Annual Meeting of the AAGL; November 2019; Vancouver, Canada.
Ideal management of RA in pregnancy improves outcomes
Women whose rheumatoid arthritis is carefully managed before and during pregnancy have a significantly lower risk of adverse pregnancy outcomes, including miscarriage or perinatal death, new research suggests.
A study published in Arthritis Care & Research presents the outcomes of a retrospective, observational study examining health care data from 443 first pregnancies in women with RA and 6,097 women without the disease.
First author Alessandra Bortoluzzi, MD, PhD, from the Rheumatology Unit at the University of Ferrara (Italy) and coauthors looked at seven diagnostic, therapeutic, and follow-up health care quality indicators during the prepregnancy and perinatal period. They included having at least one blood test in the 18 months before conception and during pregnancy, preconception musculoskeletal imaging, no exposure or wash-out from teratogenic drugs, and no exposure to biologic drugs between conception and delivery or end of pregnancy.
An ideal clinical pathway included at least one element from each of the diagnostic, therapeutic, and prenatal follow-up quality indicators.
Overall, women with RA had a significantly higher rate of thyroid diseases, adverse pregnancy outcomes, and miscarriage or perinatal death when compared with controls. However, those who followed the ideal clinical pathway for management of their disease during pregnancy had a 40% lower odds of adverse pregnancy outcomes (odds ratio, 0.60; 95% confidence interval, 0.39-0.94) and a 60% lower odds of miscarriage or perinatal death (OR, 0.40; 95% CI, 0.24-0.69) in comparison with women with RA who were not managed to the same standard. The researchers adjusted both comparisons for age, Charlson comorbidity index, and thyroid diseases.
Women with RA who met diagnostic, therapeutic, and prenatal follow-up quality indicators showed no significant differences from the general population in terms of the risk of adverse pregnancy outcomes, miscarriage, or perinatal death after adjusting for hypertension in addition to the same variables as before.
When researchers looked at some of the individual health care quality indicators, they found that testing for antiphospholipid (aPL) antibodies within 18 months of conception or pregnancy was associated with a 44% lower rate of adverse pregnancy outcomes. Similarly, antinuclear antibody or anti–extractable nuclear antigen antibody testing was associated with 36% lower odds of adverse pregnancy outcomes.
Dr. Bortoluzzi and her coauthors wrote that their findings pointed to the value of testing for aPL antibodies in women with RA who wish to get pregnant.
“In fact, despite the absence of formal recommendation or validated health care quality indicators focused on stratification of preconceptional obstetric risk in patients with RA, we started from the basic and universally accepted assumption that aPL antibodies are pathogenic autoantibodies and therefore recognized risk factors for adverse pregnancy outcome,” they wrote.
Women with RA who had either no exposure to methotrexate or leflunomide or who had a washout period from 6 months prior to conception had 72% lower odds of adverse pregnancy outcomes.
The authors also looked at the effects of drugs such as aspirin, glucocorticoids, and low-molecular-weight heparin that are used during pregnancy. They found that the relative risk of adverse pregnancy outcomes was 40% higher in women with RA who were taking glucocorticoids, compared with those with the disease but not taking that type of medication. However, low-molecular-weight heparin use was associated with an 80% lower relative risk of miscarriage or perinatal death in comparison with those not taking it. Researchers saw no significant effects of aspirin or conventional synthetic disease-modifying antirheumatic drugs on either adverse pregnancy outcomes or the risk of miscarriage or perinatal death.
“This reinforces the importance of adjustment of therapy for RA before conception and throughout pregnancy, because medication use could affect pregnancy course not only influencing maternal disease activity but also the gestational outcome,” the authors wrote. “Although this is a study conducted on administrative data, we can hypothesize that exposure to therapy represents a marker of high RA disease activity and severity. In our setting, it is possible that, the more active the disease, the greater the probability of being included in the ideal clinical pathway, but in any case, this resulted in a lower odds ratio of adverse pregnancy outcome and miscarriage/perinatal death.”
The study was supported by the Italian Society for Rheumatology. No conflicts of interest were declared.
SOURCE: Bortoluzzi A et al. Arthritis Care Res. 2020 Jan 8. doi: 10.1002/ACR.24116.
Women whose rheumatoid arthritis is carefully managed before and during pregnancy have a significantly lower risk of adverse pregnancy outcomes, including miscarriage or perinatal death, new research suggests.
A study published in Arthritis Care & Research presents the outcomes of a retrospective, observational study examining health care data from 443 first pregnancies in women with RA and 6,097 women without the disease.
First author Alessandra Bortoluzzi, MD, PhD, from the Rheumatology Unit at the University of Ferrara (Italy) and coauthors looked at seven diagnostic, therapeutic, and follow-up health care quality indicators during the prepregnancy and perinatal period. They included having at least one blood test in the 18 months before conception and during pregnancy, preconception musculoskeletal imaging, no exposure or wash-out from teratogenic drugs, and no exposure to biologic drugs between conception and delivery or end of pregnancy.
An ideal clinical pathway included at least one element from each of the diagnostic, therapeutic, and prenatal follow-up quality indicators.
Overall, women with RA had a significantly higher rate of thyroid diseases, adverse pregnancy outcomes, and miscarriage or perinatal death when compared with controls. However, those who followed the ideal clinical pathway for management of their disease during pregnancy had a 40% lower odds of adverse pregnancy outcomes (odds ratio, 0.60; 95% confidence interval, 0.39-0.94) and a 60% lower odds of miscarriage or perinatal death (OR, 0.40; 95% CI, 0.24-0.69) in comparison with women with RA who were not managed to the same standard. The researchers adjusted both comparisons for age, Charlson comorbidity index, and thyroid diseases.
Women with RA who met diagnostic, therapeutic, and prenatal follow-up quality indicators showed no significant differences from the general population in terms of the risk of adverse pregnancy outcomes, miscarriage, or perinatal death after adjusting for hypertension in addition to the same variables as before.
When researchers looked at some of the individual health care quality indicators, they found that testing for antiphospholipid (aPL) antibodies within 18 months of conception or pregnancy was associated with a 44% lower rate of adverse pregnancy outcomes. Similarly, antinuclear antibody or anti–extractable nuclear antigen antibody testing was associated with 36% lower odds of adverse pregnancy outcomes.
Dr. Bortoluzzi and her coauthors wrote that their findings pointed to the value of testing for aPL antibodies in women with RA who wish to get pregnant.
“In fact, despite the absence of formal recommendation or validated health care quality indicators focused on stratification of preconceptional obstetric risk in patients with RA, we started from the basic and universally accepted assumption that aPL antibodies are pathogenic autoantibodies and therefore recognized risk factors for adverse pregnancy outcome,” they wrote.
Women with RA who had either no exposure to methotrexate or leflunomide or who had a washout period from 6 months prior to conception had 72% lower odds of adverse pregnancy outcomes.
The authors also looked at the effects of drugs such as aspirin, glucocorticoids, and low-molecular-weight heparin that are used during pregnancy. They found that the relative risk of adverse pregnancy outcomes was 40% higher in women with RA who were taking glucocorticoids, compared with those with the disease but not taking that type of medication. However, low-molecular-weight heparin use was associated with an 80% lower relative risk of miscarriage or perinatal death in comparison with those not taking it. Researchers saw no significant effects of aspirin or conventional synthetic disease-modifying antirheumatic drugs on either adverse pregnancy outcomes or the risk of miscarriage or perinatal death.
“This reinforces the importance of adjustment of therapy for RA before conception and throughout pregnancy, because medication use could affect pregnancy course not only influencing maternal disease activity but also the gestational outcome,” the authors wrote. “Although this is a study conducted on administrative data, we can hypothesize that exposure to therapy represents a marker of high RA disease activity and severity. In our setting, it is possible that, the more active the disease, the greater the probability of being included in the ideal clinical pathway, but in any case, this resulted in a lower odds ratio of adverse pregnancy outcome and miscarriage/perinatal death.”
The study was supported by the Italian Society for Rheumatology. No conflicts of interest were declared.
SOURCE: Bortoluzzi A et al. Arthritis Care Res. 2020 Jan 8. doi: 10.1002/ACR.24116.
Women whose rheumatoid arthritis is carefully managed before and during pregnancy have a significantly lower risk of adverse pregnancy outcomes, including miscarriage or perinatal death, new research suggests.
A study published in Arthritis Care & Research presents the outcomes of a retrospective, observational study examining health care data from 443 first pregnancies in women with RA and 6,097 women without the disease.
First author Alessandra Bortoluzzi, MD, PhD, from the Rheumatology Unit at the University of Ferrara (Italy) and coauthors looked at seven diagnostic, therapeutic, and follow-up health care quality indicators during the prepregnancy and perinatal period. They included having at least one blood test in the 18 months before conception and during pregnancy, preconception musculoskeletal imaging, no exposure or wash-out from teratogenic drugs, and no exposure to biologic drugs between conception and delivery or end of pregnancy.
An ideal clinical pathway included at least one element from each of the diagnostic, therapeutic, and prenatal follow-up quality indicators.
Overall, women with RA had a significantly higher rate of thyroid diseases, adverse pregnancy outcomes, and miscarriage or perinatal death when compared with controls. However, those who followed the ideal clinical pathway for management of their disease during pregnancy had a 40% lower odds of adverse pregnancy outcomes (odds ratio, 0.60; 95% confidence interval, 0.39-0.94) and a 60% lower odds of miscarriage or perinatal death (OR, 0.40; 95% CI, 0.24-0.69) in comparison with women with RA who were not managed to the same standard. The researchers adjusted both comparisons for age, Charlson comorbidity index, and thyroid diseases.
Women with RA who met diagnostic, therapeutic, and prenatal follow-up quality indicators showed no significant differences from the general population in terms of the risk of adverse pregnancy outcomes, miscarriage, or perinatal death after adjusting for hypertension in addition to the same variables as before.
When researchers looked at some of the individual health care quality indicators, they found that testing for antiphospholipid (aPL) antibodies within 18 months of conception or pregnancy was associated with a 44% lower rate of adverse pregnancy outcomes. Similarly, antinuclear antibody or anti–extractable nuclear antigen antibody testing was associated with 36% lower odds of adverse pregnancy outcomes.
Dr. Bortoluzzi and her coauthors wrote that their findings pointed to the value of testing for aPL antibodies in women with RA who wish to get pregnant.
“In fact, despite the absence of formal recommendation or validated health care quality indicators focused on stratification of preconceptional obstetric risk in patients with RA, we started from the basic and universally accepted assumption that aPL antibodies are pathogenic autoantibodies and therefore recognized risk factors for adverse pregnancy outcome,” they wrote.
Women with RA who had either no exposure to methotrexate or leflunomide or who had a washout period from 6 months prior to conception had 72% lower odds of adverse pregnancy outcomes.
The authors also looked at the effects of drugs such as aspirin, glucocorticoids, and low-molecular-weight heparin that are used during pregnancy. They found that the relative risk of adverse pregnancy outcomes was 40% higher in women with RA who were taking glucocorticoids, compared with those with the disease but not taking that type of medication. However, low-molecular-weight heparin use was associated with an 80% lower relative risk of miscarriage or perinatal death in comparison with those not taking it. Researchers saw no significant effects of aspirin or conventional synthetic disease-modifying antirheumatic drugs on either adverse pregnancy outcomes or the risk of miscarriage or perinatal death.
“This reinforces the importance of adjustment of therapy for RA before conception and throughout pregnancy, because medication use could affect pregnancy course not only influencing maternal disease activity but also the gestational outcome,” the authors wrote. “Although this is a study conducted on administrative data, we can hypothesize that exposure to therapy represents a marker of high RA disease activity and severity. In our setting, it is possible that, the more active the disease, the greater the probability of being included in the ideal clinical pathway, but in any case, this resulted in a lower odds ratio of adverse pregnancy outcome and miscarriage/perinatal death.”
The study was supported by the Italian Society for Rheumatology. No conflicts of interest were declared.
SOURCE: Bortoluzzi A et al. Arthritis Care Res. 2020 Jan 8. doi: 10.1002/ACR.24116.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point: Well-managed rheumatoid arthritis during preconception and pregnancy is associated with improved pregnancy outcomes.
Major finding: Women who adhered to an ideal clinical pathway for their RA had significantly lower risk of adverse pregnancy outcomes and miscarriage and/or perinatal death.
Study details: Retrospective, observational study of 443 first pregnancies in women with RA and 6,097 women without.
Disclosures: The study was supported by the Italian Society for Rheumatology. No conflicts of interest were declared.
Source: Bortoluzzi A et al. Arthritis Care Res. 2020 Jan 8. doi: 10.1002/ACR.24116.
Barrett’s esophagus risk factors vary by patient sex
In males but not females, hyperinsulinemia, insulin resistance, and metabolic syndrome are independently associated with a higher risk of Barrett’s esophagus (BE), based on a recent case-control study.
These findings offer some insight into why men have higher rates of BE and esophageal adenocarcinoma than do women, reported lead author Bradley J. Kendall, MBBS, PhD, of the University of Queensland in Brisbane, Australia, and colleagues.
“Esophageal adenocarcinoma (EA) and its precursor lesion, Barrett’s esophagus (BE), are more common in males than females,” the investigators wrote in the Journal of Clinical Gastroenterology. “In contrast, gastroesophageal reflux (GER), the major risk factor for BE and EA occurs at similar frequencies in both sexes. In addition, 10% to 20% of BE and EA cases report no history of GER symptoms. This suggests that non-GER factors are important in the development of BE and EA.”
To examine risk factors more closely, the investigators enrolled 227 patients with BE and 241 age- and sex-matched controls. Data were drawn from self-reported questionnaires, interviews, blood pressure readings, and anthropometric measurements, the latter of which included weight, height, and waist circumference. These patient characteristics were supplemented with fasted blood assays. The investigators looked for associations between BE and insulin level, Homeostatic Model Assessment of Insulin Resistance, metabolic syndrome, type 2 diabetes mellitus, insulin-like growth factors, and interleukin-6 (IL-6).
Across the entire population, independent associations were detected between BE and hyperinsulinemia (highest vs. lowest tertile; odds ratio, 1.9; P = .003), insulin resistance (OR, 1.9; P = .006) and metabolic syndrome (OR, 1.8; P = .004). For those with metabolic syndrome, risk of BE increased by 20% for each additional syndrome criterion (P = .02).
When stratifying by sex, however, all of the above risk factors remained statistically significant in men, but not in women. For male patients, compared with the population as a whole, risks were relatively higher for all three factors: hyperinsulinemia (OR, 2.1; P = .007), insulin resistance (OR, 2.1; P = .01), and metabolic syndrome (OR, 2.3; P = .001). Similarly, for men with metabolic syndrome, each additional syndrome criterion increased risk of BE by 40% (P = .005).
Regardless of sex stratification, the other evaluated characteristics (type 2 diabetes mellitus, insulin-like growth factors, and IL-6) were not associated with BE risk.
The investigators offered some possible mechanistic explanations for their findings.
“Hyperinsulinemia ... can result in increased insulin signaling, increased cellular proliferation, reduced apoptosis, oncogenic pathway activation, and enhanced cellular invasion,” they wrote. “In addition, abdominal obesity, which is the driver of these disorders of insulin homeostasis, also alters adipocytokine profiles and induces a chronic systemic inflammatory state. The inflammatory state can result in oncoprotein activation, angiogenesis, cellular proliferation, apoptosis, and metastasis.”
Concerning the difference between sexes, the investigators pointed to patterns of abdominal obesity. “[A]bdominal obesity and the associated metabolic sequelae are more common in males than females,” they wrote. “These observations give rise to the notion that the metabolic syndrome potentiates the inflammatory effects of the gastric refluxate in the distal esophagus and this may play a role in the male predominance of BE and EA.”
While these findings offer insight into the underlying processes that precipitate BE, the investigators suggested that more research is needed.
“The interactions of obesity hormones, GER, and the cells of the esophageal mucosa warrant further investigation,” they concluded.
The study was funded by the Queensland Cancer Fund, Queensland Government Smart State Fund, and the Princess Alexandra Hospital Research Foundation, and others. The investigators reported no disclosures.
SOURCE: Kendall BJ et al. J Clin Gastroenterol. 2019 Dec 24. doi: 10.1097/MCG.0000000000001307.
In males but not females, hyperinsulinemia, insulin resistance, and metabolic syndrome are independently associated with a higher risk of Barrett’s esophagus (BE), based on a recent case-control study.
These findings offer some insight into why men have higher rates of BE and esophageal adenocarcinoma than do women, reported lead author Bradley J. Kendall, MBBS, PhD, of the University of Queensland in Brisbane, Australia, and colleagues.
“Esophageal adenocarcinoma (EA) and its precursor lesion, Barrett’s esophagus (BE), are more common in males than females,” the investigators wrote in the Journal of Clinical Gastroenterology. “In contrast, gastroesophageal reflux (GER), the major risk factor for BE and EA occurs at similar frequencies in both sexes. In addition, 10% to 20% of BE and EA cases report no history of GER symptoms. This suggests that non-GER factors are important in the development of BE and EA.”
To examine risk factors more closely, the investigators enrolled 227 patients with BE and 241 age- and sex-matched controls. Data were drawn from self-reported questionnaires, interviews, blood pressure readings, and anthropometric measurements, the latter of which included weight, height, and waist circumference. These patient characteristics were supplemented with fasted blood assays. The investigators looked for associations between BE and insulin level, Homeostatic Model Assessment of Insulin Resistance, metabolic syndrome, type 2 diabetes mellitus, insulin-like growth factors, and interleukin-6 (IL-6).
Across the entire population, independent associations were detected between BE and hyperinsulinemia (highest vs. lowest tertile; odds ratio, 1.9; P = .003), insulin resistance (OR, 1.9; P = .006) and metabolic syndrome (OR, 1.8; P = .004). For those with metabolic syndrome, risk of BE increased by 20% for each additional syndrome criterion (P = .02).
When stratifying by sex, however, all of the above risk factors remained statistically significant in men, but not in women. For male patients, compared with the population as a whole, risks were relatively higher for all three factors: hyperinsulinemia (OR, 2.1; P = .007), insulin resistance (OR, 2.1; P = .01), and metabolic syndrome (OR, 2.3; P = .001). Similarly, for men with metabolic syndrome, each additional syndrome criterion increased risk of BE by 40% (P = .005).
Regardless of sex stratification, the other evaluated characteristics (type 2 diabetes mellitus, insulin-like growth factors, and IL-6) were not associated with BE risk.
The investigators offered some possible mechanistic explanations for their findings.
“Hyperinsulinemia ... can result in increased insulin signaling, increased cellular proliferation, reduced apoptosis, oncogenic pathway activation, and enhanced cellular invasion,” they wrote. “In addition, abdominal obesity, which is the driver of these disorders of insulin homeostasis, also alters adipocytokine profiles and induces a chronic systemic inflammatory state. The inflammatory state can result in oncoprotein activation, angiogenesis, cellular proliferation, apoptosis, and metastasis.”
Concerning the difference between sexes, the investigators pointed to patterns of abdominal obesity. “[A]bdominal obesity and the associated metabolic sequelae are more common in males than females,” they wrote. “These observations give rise to the notion that the metabolic syndrome potentiates the inflammatory effects of the gastric refluxate in the distal esophagus and this may play a role in the male predominance of BE and EA.”
While these findings offer insight into the underlying processes that precipitate BE, the investigators suggested that more research is needed.
“The interactions of obesity hormones, GER, and the cells of the esophageal mucosa warrant further investigation,” they concluded.
The study was funded by the Queensland Cancer Fund, Queensland Government Smart State Fund, and the Princess Alexandra Hospital Research Foundation, and others. The investigators reported no disclosures.
SOURCE: Kendall BJ et al. J Clin Gastroenterol. 2019 Dec 24. doi: 10.1097/MCG.0000000000001307.
In males but not females, hyperinsulinemia, insulin resistance, and metabolic syndrome are independently associated with a higher risk of Barrett’s esophagus (BE), based on a recent case-control study.
These findings offer some insight into why men have higher rates of BE and esophageal adenocarcinoma than do women, reported lead author Bradley J. Kendall, MBBS, PhD, of the University of Queensland in Brisbane, Australia, and colleagues.
“Esophageal adenocarcinoma (EA) and its precursor lesion, Barrett’s esophagus (BE), are more common in males than females,” the investigators wrote in the Journal of Clinical Gastroenterology. “In contrast, gastroesophageal reflux (GER), the major risk factor for BE and EA occurs at similar frequencies in both sexes. In addition, 10% to 20% of BE and EA cases report no history of GER symptoms. This suggests that non-GER factors are important in the development of BE and EA.”
To examine risk factors more closely, the investigators enrolled 227 patients with BE and 241 age- and sex-matched controls. Data were drawn from self-reported questionnaires, interviews, blood pressure readings, and anthropometric measurements, the latter of which included weight, height, and waist circumference. These patient characteristics were supplemented with fasted blood assays. The investigators looked for associations between BE and insulin level, Homeostatic Model Assessment of Insulin Resistance, metabolic syndrome, type 2 diabetes mellitus, insulin-like growth factors, and interleukin-6 (IL-6).
Across the entire population, independent associations were detected between BE and hyperinsulinemia (highest vs. lowest tertile; odds ratio, 1.9; P = .003), insulin resistance (OR, 1.9; P = .006) and metabolic syndrome (OR, 1.8; P = .004). For those with metabolic syndrome, risk of BE increased by 20% for each additional syndrome criterion (P = .02).
When stratifying by sex, however, all of the above risk factors remained statistically significant in men, but not in women. For male patients, compared with the population as a whole, risks were relatively higher for all three factors: hyperinsulinemia (OR, 2.1; P = .007), insulin resistance (OR, 2.1; P = .01), and metabolic syndrome (OR, 2.3; P = .001). Similarly, for men with metabolic syndrome, each additional syndrome criterion increased risk of BE by 40% (P = .005).
Regardless of sex stratification, the other evaluated characteristics (type 2 diabetes mellitus, insulin-like growth factors, and IL-6) were not associated with BE risk.
The investigators offered some possible mechanistic explanations for their findings.
“Hyperinsulinemia ... can result in increased insulin signaling, increased cellular proliferation, reduced apoptosis, oncogenic pathway activation, and enhanced cellular invasion,” they wrote. “In addition, abdominal obesity, which is the driver of these disorders of insulin homeostasis, also alters adipocytokine profiles and induces a chronic systemic inflammatory state. The inflammatory state can result in oncoprotein activation, angiogenesis, cellular proliferation, apoptosis, and metastasis.”
Concerning the difference between sexes, the investigators pointed to patterns of abdominal obesity. “[A]bdominal obesity and the associated metabolic sequelae are more common in males than females,” they wrote. “These observations give rise to the notion that the metabolic syndrome potentiates the inflammatory effects of the gastric refluxate in the distal esophagus and this may play a role in the male predominance of BE and EA.”
While these findings offer insight into the underlying processes that precipitate BE, the investigators suggested that more research is needed.
“The interactions of obesity hormones, GER, and the cells of the esophageal mucosa warrant further investigation,” they concluded.
The study was funded by the Queensland Cancer Fund, Queensland Government Smart State Fund, and the Princess Alexandra Hospital Research Foundation, and others. The investigators reported no disclosures.
SOURCE: Kendall BJ et al. J Clin Gastroenterol. 2019 Dec 24. doi: 10.1097/MCG.0000000000001307.
FROM JOURNAL OF CLINICAL GASTROENTEROLOGY
Reducing Surgical Patients’ Postoperative Exposure to Opioid Analgesics
Click here to access the transcript.
Panelists include:
MODERATOR
Chad Brummett, MD
Associate Professor, Anesthesiology,
Director, Anesthesia Clinical Research,
Director, Division of Pain Research,
Michigan Medicine Back & Pain Center
Ann Arbor, MI
PARTICIPANTS
Andrew C. Eppstein, MD
Assistant Professor of Clinical Surgery,
Indiana University School of Medicine
Chief of General Surgery,
Richard L. Roudebush VA Medical Center
Indianapolis, IN
Nicholas Giori MD, PhD
Professor of Orthopedic Surgery,
Stanford University
Chief of Orthopedic Surgery,
VA Palo Alto Health Care System
Palo Alto, CA
Georgine Lamvu, MD, MHP
Professor in Obstetrics and Gynecology,
University of Central Florida College of Medicine
Division of Surgery, Gynecology Section
Orlando VA Medical Center
Orlando, FL
Bryan Sakamoto, MD, PhD
Staff Physician,
Richard L. Roudebush VA Medical Center
Assistant Professor of Clinical Anesthesia
Indiana University School of Medicine
Indianapolis, IN
Jack D. Wright, PharmD
Chief of Pharmacy,
Beckley VA Medical Center
Beckley, WV
Click here to access the transcript.
Panelists include:
MODERATOR
Chad Brummett, MD
Associate Professor, Anesthesiology,
Director, Anesthesia Clinical Research,
Director, Division of Pain Research,
Michigan Medicine Back & Pain Center
Ann Arbor, MI
PARTICIPANTS
Andrew C. Eppstein, MD
Assistant Professor of Clinical Surgery,
Indiana University School of Medicine
Chief of General Surgery,
Richard L. Roudebush VA Medical Center
Indianapolis, IN
Nicholas Giori MD, PhD
Professor of Orthopedic Surgery,
Stanford University
Chief of Orthopedic Surgery,
VA Palo Alto Health Care System
Palo Alto, CA
Georgine Lamvu, MD, MHP
Professor in Obstetrics and Gynecology,
University of Central Florida College of Medicine
Division of Surgery, Gynecology Section
Orlando VA Medical Center
Orlando, FL
Bryan Sakamoto, MD, PhD
Staff Physician,
Richard L. Roudebush VA Medical Center
Assistant Professor of Clinical Anesthesia
Indiana University School of Medicine
Indianapolis, IN
Jack D. Wright, PharmD
Chief of Pharmacy,
Beckley VA Medical Center
Beckley, WV
Click here to access the transcript.
Panelists include:
MODERATOR
Chad Brummett, MD
Associate Professor, Anesthesiology,
Director, Anesthesia Clinical Research,
Director, Division of Pain Research,
Michigan Medicine Back & Pain Center
Ann Arbor, MI
PARTICIPANTS
Andrew C. Eppstein, MD
Assistant Professor of Clinical Surgery,
Indiana University School of Medicine
Chief of General Surgery,
Richard L. Roudebush VA Medical Center
Indianapolis, IN
Nicholas Giori MD, PhD
Professor of Orthopedic Surgery,
Stanford University
Chief of Orthopedic Surgery,
VA Palo Alto Health Care System
Palo Alto, CA
Georgine Lamvu, MD, MHP
Professor in Obstetrics and Gynecology,
University of Central Florida College of Medicine
Division of Surgery, Gynecology Section
Orlando VA Medical Center
Orlando, FL
Bryan Sakamoto, MD, PhD
Staff Physician,
Richard L. Roudebush VA Medical Center
Assistant Professor of Clinical Anesthesia
Indiana University School of Medicine
Indianapolis, IN
Jack D. Wright, PharmD
Chief of Pharmacy,
Beckley VA Medical Center
Beckley, WV
We can achieve opioid-free analgesia after childbirth: Stop prescribing opioids after vaginal delivery and reduce their use after cesarean
CASE New mother receives unneeded opioids after CD
A house officer wrote orders for a healthy patient who had just had an uncomplicated cesarean delivery (CD). The hospital’s tradition dictates orders for oxycodone plus acetaminophen tablets in addition to ibuprofen for all new mothers. At the time of the patient’s discharge, the same house officer prescribed 30 tablets of oxycodone plus acetaminophen “just in case,” although the patient had required only a few tablets while in the hospital on postoperative day 2 and none on the day of discharge.
Stuck in the habit
Prescribing postpartum opioids in the United States is almost habitual. Both optimizing patient satisfaction and minimizing patient phone calls may be driving this well-established pattern. Interestingly, a survey study of obstetric providers in 14 countries found that clinicians in 13 countries prescribe opioids “almost never” after vaginal delivery.1 The United States was the 1 outlier, with providers reporting prescribing opioids “on a regular basis” after vaginal birth. Similarly, providers in 10 countries reported prescribing opioids “almost never” after CD, while those in the United States reported prescribing opioids “almost always” in this context.
Moreover, mounting data suggest that many patients do not require the quantity of opioids prescribed and that our overprescribing may be causing more harm than good.
The problem of overprescribing opioids after childbirth
Opioid analgesia has long been the mainstay of treatment for postpartum pain, which when poorly controlled is associated with the development of postpartum depression and chronic pain.2 However, common adverse effects of opioids, including nausea, drowsiness, and dizziness, similarly can interfere with self-care and infant care. Of additional concern, a 2016 claims data study found that 1 of 300 opioid-naïve women who were prescribed opioids at discharge after CD used these medications persistently in the first year postpartum.3
Many women do not use the opioids that are prescribed to them at discharge, thus making tablets available for potential diversion into the community—a commonly recognized source of opioid misuse and abuse.4,5 In a 2018 Committee Opinion on postpartum pain management, the American College of Obstetricians and Gynecologists (ACOG) stated that “a stepwise, multimodal approach emphasizing nonopioid analgesia as first-line therapy is safe and effective for vaginal deliveries and cesarean deliveries.”6 The Committee Opinion also asserted that “opioid medication is an adjunct for patients with uncontrolled pain despite adequate first-line therapy.”6
Despite efforts by the Centers for Disease Control and Prevention (CDC) and ACOG to improve opioid prescribing patterns after childbirth, the vast majority of women receive opioids in the hospital and at discharge not only after CD, but after vaginal delivery as well.4,7 Why has tradition prevailed over data, and why have we not changed?
Continue to: Common misconceptions about reducing opioid use...
Common misconceptions about reducing opioid use
Two misconceptions persist regarding reducing opioid prescriptions for postpartum pain.
Misconception #1: Patients will be in pain
Randomized controlled trials that compared nonopioid with opioid regimens in the emergency room setting and opioid use after outpatient general surgery procedures have demonstrated that pain control for patients receiving opioids was equivalent to that for patients with pain managed with nonopioid regimens.8-10 In the obstetric setting, a survey study of 720 women who underwent CD found that higher quantities of opioid tablets prescribed at discharge were not associated with improved pain, higher satisfaction, or lower refill rates at 2 weeks postpartum.4 However, greater quantities of opioids prescribed at the time of discharge were associated with greater opioid consumption.
Recently, several quality improvement studies implemented various interventions and successfully decreased postpartum opioid consumption without compromising pain management. One quality improvement project eliminated the routine use of opioids after CD and decreased the proportion of patients using any opioids in the hospital from 68% to 45%, with no changes in pain scores.11 A similar study implemented an enhanced recovery after surgery (ERAS) program for women after CD; mean in-patient opioid use decreased from 10.7 to 5.4 average daily morphine equivalents, with improvement in the proportion of time that patients reported their pain as acceptable.12
Misconception #2: Clinicians will be overwhelmed with pages and phone calls
Providers commonly fear that decreasing opioid use will lead to an increased volume of pages and phone calls from patients requesting additional medication. However, data suggest otherwise. For example, a quality improvement study that eliminated the routine use of opioids after CD tracked the number of phone calls that were received requesting rescue opioid prescriptions after discharge.11 Although the percentage of women discharged with opioids decreased from 90.6% to 40.3%, the requests for rescue opioid prescriptions did not change. Of 191 women, 4 requested a rescue prescription prior to the intervention compared with no women after the intervention. At the same time, according to unpublished data (Dr. Holland), satisfaction among nurses, house staff, and faculty did not change.
Similarly, a quality improvement project that implemented shared decision-making to inform the quantity of opioids prescribed at discharge demonstrated that the number of tablets prescribed decreased from 33.2 to 26.5, and there was no change in the rate of patients requesting opioid refills.13
Success stories: Strategies for reducing opioid use after childbirth
While overall rates of opioid prescribing after vaginal delivery and CD remain high throughout the United States, various institutions have developed successful and reproducible strategies to reduce opioid use after childbirth both in the hospital and at discharge. We highlight 3 strategies below.
Strategy 1: ERAS initiatives
An integrated health care system in northern California studied the effects of an ERAS protocol for CD across 15 medical centers.12 The intervention centered on 4 pillars: multimodal pain management, early mobility, optimal nutrition, and patient engagement through education. Specifically, multimodal pain management consisted of the following:
- intrathecal opioids during CD
- scheduled intravenous acetaminophen for 24 hours followed by oral acetaminophen every 6 hours
- nonsteroidal anti-inflammatory drugs (NSAIDs) every 6 hours
- oral oxycodone for breakthrough pain
- decoupling of opioid medication from nonopioids in the post-CD order set
- decoupling of opioid and nonopioid medications in the discharge order set along with a reduction from 30 to 20 tablets as the default discharge quantity.
Continue to: Among 4,689 and 4,624 patients who underwent CD...
Among 4,689 and 4,624 patients who underwent CD before and after the intervention, the daily morphine milligram equivalents (MME) consumed in the hospital decreased from 10.7 to 5.4. The percentage of women who required no opioids while in the hospital increased from 8.3% to 21.4% after ERAS implementation, while the percentage of time that patients reported acceptable pain scores increased from 82.1% to 86.4%. The average number of opioid tablets prescribed at discharge also decreased, from 37 to 26 MME.12 (The TABLE shows oxycodone doses converted to MMEs.)
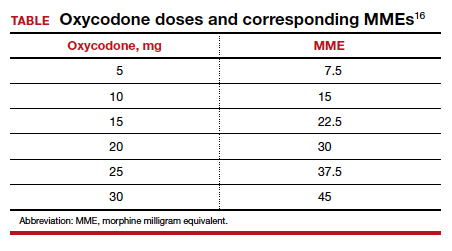
A similar initiative at a network of 5 hospitals in Texas showed that implementation of a “multimodal pain power plan” (which incorporated postpartum activity goals with standardized order sets) decreased opioid use after both vaginal delivery and CD.14
Strategy 2: Order set change to eliminate routine use of opioids
A tertiary care center in Boston, Massachusetts, implemented a quality improvement project aimed at eliminating the routine use of opioid medication after CD through an order set change.11 The intervention consisted of the following:
- intrathecal morphine
- multimodal postoperative pain management including scheduled oral acetaminophen for 72 hours followed by as-needed oral acetaminophen, scheduled NSAIDs for 72 hours followed by as-needed NSAIDs
- no postoperative order for opioids unless the patient had a contraindication to acetaminophen or NSAIDs, had a history of opioid dependence, or underwent complex surgery
- counseling patients that opioids were available for breakthrough pain if needed. In this case, nursing staff would page the responding clinician, who would order oxycodone 5 mg every 6 hours for 6 doses.
- specific criteria for discharge quantities of opioids: if the patient required no opioids in the hospital, she received no opioids at discharge; if the patient required opioids in the hospital but none at the time of discharge, she received no more than 10 tablets of oxycodone 5 mg; if the patient required opioids at the time of discharge, she received a maximum of 20 tablets of oxycodone 5 mg.
Among 191 and 181 women undergoing CD before and after the intervention, the percentage of patients who received any opioids in the hospital decreased from 68.1% to 45.3%.11 Similarly, the percentage of patients receiving a discharge prescription for opioids decreased from 90.6% to 40.3%, while patient pain scores and satisfaction with pain control remained unchanged.
Strategy 3: Shared decision-making tool
Another tertiary care center in Boston evaluated the effects of a shared decision-making tool on opioid discharge prescribing after CD.15 The intervention consisted of a 10-minute clinician-facilitated session incorporating:
- education around anticipated patterns of postoperative pain
- expected outpatient opioid use after CD
- risks and benefits of opioids and nonopioids
- education around opioid disposal and access to refills.
Among the 50 women enrolled in the study, the number of oxycodone 5-mg tablets prescribed at discharge decreased from the institutional standard of 40 to 20. Ninety percent of women reported being satisfied or very satisfied with their pain control, while only 4 of 50 women required an opioid refill. A follow-up quality improvement project, which implemented the shared decision-making model along with a standardized multimodal pain management protocol, demonstrated a similar decrease in the quantity of opioids prescribed at discharge.13
Continue to: Change is here to stay: A new culture of postpartum analgesia...
Change is here to stay: A new culture of postpartum analgesia
The CDC continues to champion responsible opioid prescribing, while ACOG advocates for a reassessment of the way that opioids are utilized postpartum. The majority of women in the United States, however, continue to receive opioids after both vaginal delivery and CD. Consciously or not, we clinicians may be contributing to an outdated tradition that is potentially harmful both to patients and society. Reproducible strategies exist to reduce opioid use without compromising pain control or overwhelming clinicians with phone calls. It is time to embrace the change.
- Wong CA, Girard T. Undertreated or overtreated? Opioids for postdelivery analgesia. Br J Anaesth. 2018;121:339-342.
- Eisenach JC, Pan PH, Smiley R, et al. Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain. 2008;140:87-94.
- Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naïve women. Am J Obstet Gynecol. 2016;215:353.e1- 353.e18.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130:29-35.
- Osmundson SS, Schornack LA, Grasch JL, et al. Postdischarge opioid use after cesarean delivery. Obstet Gynecol. 2017;130:36-41.
- American College of Obstetricians and Gynecologists. ACOG committee opinion no. 742: postpartum pain management. Obstet Gynecol. 2018;132:e35-e43.
- Mills JR, Huizinga MM, Robinson SB, et al. Draft opioid prescribing guidelines for uncomplicated normal spontaneous vaginal birth. Obstet Gynecol. 2019;133:81-90.
- Chang AK, Bijur PE, Esses D, et al. Effect of a single dose of oral opioid and nonopioid analgesics on acute extremity pain in the emergency department: a randomized clinical trial. JAMA. 2017;318:1661-1667.
- Mitchell A, van Zanten SV, Inglis K, et al. A randomized controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine after outpatient general surgery. J Am Coll Surg. 2008;206:472-479.
- Mitchell A, McCrea P, Inglis K, et al. A randomized, controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine (Tylenol 3) after outpatient breast surgery. Ann Surg Oncol. 2012;19:3792-3800.
- Holland E, Bateman BT, Cole N, et al. Evaluation of a quality improvement intervention that eliminated routine use of opioids after cesarean delivery. Obstet Gynecol. 2019;133:91-97.
- Hedderson M, Lee D, Hunt E, et al. Enhanced recovery after surgery to change process measures and reduce opioid use after cesarean delivery: a quality improvement initiative. Obstet Gynecol. 2019;134:511-519.
- Prabhu M, Dubois H, James K, et al. Implementation of a quality improvement initiative to decrease opioid prescribing after cesarean delivery. Obstet Gynecol. 2018;132:631-636.
- Rogers RG, Nix M, Chipman Z, et al. Decreasing opioid use postpartum: a quality improvement initiative. Obstet Gynecol. 2019;134:932-940.
- Prabhu M, McQuaid-Hanson E, Hopp S, et al. A shared decision-making intervention to guide opioid prescribing after cesarean delivery. Obstet Gynecol. 2017;130:42-46.
- Centers for Disease Control and Prevention. Calculating total daily dose of opioids for safer dosage. www.cdc.gov/ drugoverdose/pdf/calculating_total_daily_dose-a.pdf. Accessed December 31, 2019.
CASE New mother receives unneeded opioids after CD
A house officer wrote orders for a healthy patient who had just had an uncomplicated cesarean delivery (CD). The hospital’s tradition dictates orders for oxycodone plus acetaminophen tablets in addition to ibuprofen for all new mothers. At the time of the patient’s discharge, the same house officer prescribed 30 tablets of oxycodone plus acetaminophen “just in case,” although the patient had required only a few tablets while in the hospital on postoperative day 2 and none on the day of discharge.
Stuck in the habit
Prescribing postpartum opioids in the United States is almost habitual. Both optimizing patient satisfaction and minimizing patient phone calls may be driving this well-established pattern. Interestingly, a survey study of obstetric providers in 14 countries found that clinicians in 13 countries prescribe opioids “almost never” after vaginal delivery.1 The United States was the 1 outlier, with providers reporting prescribing opioids “on a regular basis” after vaginal birth. Similarly, providers in 10 countries reported prescribing opioids “almost never” after CD, while those in the United States reported prescribing opioids “almost always” in this context.
Moreover, mounting data suggest that many patients do not require the quantity of opioids prescribed and that our overprescribing may be causing more harm than good.
The problem of overprescribing opioids after childbirth
Opioid analgesia has long been the mainstay of treatment for postpartum pain, which when poorly controlled is associated with the development of postpartum depression and chronic pain.2 However, common adverse effects of opioids, including nausea, drowsiness, and dizziness, similarly can interfere with self-care and infant care. Of additional concern, a 2016 claims data study found that 1 of 300 opioid-naïve women who were prescribed opioids at discharge after CD used these medications persistently in the first year postpartum.3
Many women do not use the opioids that are prescribed to them at discharge, thus making tablets available for potential diversion into the community—a commonly recognized source of opioid misuse and abuse.4,5 In a 2018 Committee Opinion on postpartum pain management, the American College of Obstetricians and Gynecologists (ACOG) stated that “a stepwise, multimodal approach emphasizing nonopioid analgesia as first-line therapy is safe and effective for vaginal deliveries and cesarean deliveries.”6 The Committee Opinion also asserted that “opioid medication is an adjunct for patients with uncontrolled pain despite adequate first-line therapy.”6
Despite efforts by the Centers for Disease Control and Prevention (CDC) and ACOG to improve opioid prescribing patterns after childbirth, the vast majority of women receive opioids in the hospital and at discharge not only after CD, but after vaginal delivery as well.4,7 Why has tradition prevailed over data, and why have we not changed?
Continue to: Common misconceptions about reducing opioid use...
Common misconceptions about reducing opioid use
Two misconceptions persist regarding reducing opioid prescriptions for postpartum pain.
Misconception #1: Patients will be in pain
Randomized controlled trials that compared nonopioid with opioid regimens in the emergency room setting and opioid use after outpatient general surgery procedures have demonstrated that pain control for patients receiving opioids was equivalent to that for patients with pain managed with nonopioid regimens.8-10 In the obstetric setting, a survey study of 720 women who underwent CD found that higher quantities of opioid tablets prescribed at discharge were not associated with improved pain, higher satisfaction, or lower refill rates at 2 weeks postpartum.4 However, greater quantities of opioids prescribed at the time of discharge were associated with greater opioid consumption.
Recently, several quality improvement studies implemented various interventions and successfully decreased postpartum opioid consumption without compromising pain management. One quality improvement project eliminated the routine use of opioids after CD and decreased the proportion of patients using any opioids in the hospital from 68% to 45%, with no changes in pain scores.11 A similar study implemented an enhanced recovery after surgery (ERAS) program for women after CD; mean in-patient opioid use decreased from 10.7 to 5.4 average daily morphine equivalents, with improvement in the proportion of time that patients reported their pain as acceptable.12
Misconception #2: Clinicians will be overwhelmed with pages and phone calls
Providers commonly fear that decreasing opioid use will lead to an increased volume of pages and phone calls from patients requesting additional medication. However, data suggest otherwise. For example, a quality improvement study that eliminated the routine use of opioids after CD tracked the number of phone calls that were received requesting rescue opioid prescriptions after discharge.11 Although the percentage of women discharged with opioids decreased from 90.6% to 40.3%, the requests for rescue opioid prescriptions did not change. Of 191 women, 4 requested a rescue prescription prior to the intervention compared with no women after the intervention. At the same time, according to unpublished data (Dr. Holland), satisfaction among nurses, house staff, and faculty did not change.
Similarly, a quality improvement project that implemented shared decision-making to inform the quantity of opioids prescribed at discharge demonstrated that the number of tablets prescribed decreased from 33.2 to 26.5, and there was no change in the rate of patients requesting opioid refills.13
Success stories: Strategies for reducing opioid use after childbirth
While overall rates of opioid prescribing after vaginal delivery and CD remain high throughout the United States, various institutions have developed successful and reproducible strategies to reduce opioid use after childbirth both in the hospital and at discharge. We highlight 3 strategies below.
Strategy 1: ERAS initiatives
An integrated health care system in northern California studied the effects of an ERAS protocol for CD across 15 medical centers.12 The intervention centered on 4 pillars: multimodal pain management, early mobility, optimal nutrition, and patient engagement through education. Specifically, multimodal pain management consisted of the following:
- intrathecal opioids during CD
- scheduled intravenous acetaminophen for 24 hours followed by oral acetaminophen every 6 hours
- nonsteroidal anti-inflammatory drugs (NSAIDs) every 6 hours
- oral oxycodone for breakthrough pain
- decoupling of opioid medication from nonopioids in the post-CD order set
- decoupling of opioid and nonopioid medications in the discharge order set along with a reduction from 30 to 20 tablets as the default discharge quantity.
Continue to: Among 4,689 and 4,624 patients who underwent CD...
Among 4,689 and 4,624 patients who underwent CD before and after the intervention, the daily morphine milligram equivalents (MME) consumed in the hospital decreased from 10.7 to 5.4. The percentage of women who required no opioids while in the hospital increased from 8.3% to 21.4% after ERAS implementation, while the percentage of time that patients reported acceptable pain scores increased from 82.1% to 86.4%. The average number of opioid tablets prescribed at discharge also decreased, from 37 to 26 MME.12 (The TABLE shows oxycodone doses converted to MMEs.)
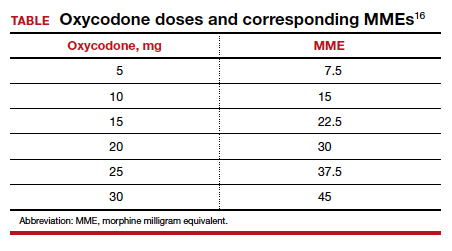
A similar initiative at a network of 5 hospitals in Texas showed that implementation of a “multimodal pain power plan” (which incorporated postpartum activity goals with standardized order sets) decreased opioid use after both vaginal delivery and CD.14
Strategy 2: Order set change to eliminate routine use of opioids
A tertiary care center in Boston, Massachusetts, implemented a quality improvement project aimed at eliminating the routine use of opioid medication after CD through an order set change.11 The intervention consisted of the following:
- intrathecal morphine
- multimodal postoperative pain management including scheduled oral acetaminophen for 72 hours followed by as-needed oral acetaminophen, scheduled NSAIDs for 72 hours followed by as-needed NSAIDs
- no postoperative order for opioids unless the patient had a contraindication to acetaminophen or NSAIDs, had a history of opioid dependence, or underwent complex surgery
- counseling patients that opioids were available for breakthrough pain if needed. In this case, nursing staff would page the responding clinician, who would order oxycodone 5 mg every 6 hours for 6 doses.
- specific criteria for discharge quantities of opioids: if the patient required no opioids in the hospital, she received no opioids at discharge; if the patient required opioids in the hospital but none at the time of discharge, she received no more than 10 tablets of oxycodone 5 mg; if the patient required opioids at the time of discharge, she received a maximum of 20 tablets of oxycodone 5 mg.
Among 191 and 181 women undergoing CD before and after the intervention, the percentage of patients who received any opioids in the hospital decreased from 68.1% to 45.3%.11 Similarly, the percentage of patients receiving a discharge prescription for opioids decreased from 90.6% to 40.3%, while patient pain scores and satisfaction with pain control remained unchanged.
Strategy 3: Shared decision-making tool
Another tertiary care center in Boston evaluated the effects of a shared decision-making tool on opioid discharge prescribing after CD.15 The intervention consisted of a 10-minute clinician-facilitated session incorporating:
- education around anticipated patterns of postoperative pain
- expected outpatient opioid use after CD
- risks and benefits of opioids and nonopioids
- education around opioid disposal and access to refills.
Among the 50 women enrolled in the study, the number of oxycodone 5-mg tablets prescribed at discharge decreased from the institutional standard of 40 to 20. Ninety percent of women reported being satisfied or very satisfied with their pain control, while only 4 of 50 women required an opioid refill. A follow-up quality improvement project, which implemented the shared decision-making model along with a standardized multimodal pain management protocol, demonstrated a similar decrease in the quantity of opioids prescribed at discharge.13
Continue to: Change is here to stay: A new culture of postpartum analgesia...
Change is here to stay: A new culture of postpartum analgesia
The CDC continues to champion responsible opioid prescribing, while ACOG advocates for a reassessment of the way that opioids are utilized postpartum. The majority of women in the United States, however, continue to receive opioids after both vaginal delivery and CD. Consciously or not, we clinicians may be contributing to an outdated tradition that is potentially harmful both to patients and society. Reproducible strategies exist to reduce opioid use without compromising pain control or overwhelming clinicians with phone calls. It is time to embrace the change.
CASE New mother receives unneeded opioids after CD
A house officer wrote orders for a healthy patient who had just had an uncomplicated cesarean delivery (CD). The hospital’s tradition dictates orders for oxycodone plus acetaminophen tablets in addition to ibuprofen for all new mothers. At the time of the patient’s discharge, the same house officer prescribed 30 tablets of oxycodone plus acetaminophen “just in case,” although the patient had required only a few tablets while in the hospital on postoperative day 2 and none on the day of discharge.
Stuck in the habit
Prescribing postpartum opioids in the United States is almost habitual. Both optimizing patient satisfaction and minimizing patient phone calls may be driving this well-established pattern. Interestingly, a survey study of obstetric providers in 14 countries found that clinicians in 13 countries prescribe opioids “almost never” after vaginal delivery.1 The United States was the 1 outlier, with providers reporting prescribing opioids “on a regular basis” after vaginal birth. Similarly, providers in 10 countries reported prescribing opioids “almost never” after CD, while those in the United States reported prescribing opioids “almost always” in this context.
Moreover, mounting data suggest that many patients do not require the quantity of opioids prescribed and that our overprescribing may be causing more harm than good.
The problem of overprescribing opioids after childbirth
Opioid analgesia has long been the mainstay of treatment for postpartum pain, which when poorly controlled is associated with the development of postpartum depression and chronic pain.2 However, common adverse effects of opioids, including nausea, drowsiness, and dizziness, similarly can interfere with self-care and infant care. Of additional concern, a 2016 claims data study found that 1 of 300 opioid-naïve women who were prescribed opioids at discharge after CD used these medications persistently in the first year postpartum.3
Many women do not use the opioids that are prescribed to them at discharge, thus making tablets available for potential diversion into the community—a commonly recognized source of opioid misuse and abuse.4,5 In a 2018 Committee Opinion on postpartum pain management, the American College of Obstetricians and Gynecologists (ACOG) stated that “a stepwise, multimodal approach emphasizing nonopioid analgesia as first-line therapy is safe and effective for vaginal deliveries and cesarean deliveries.”6 The Committee Opinion also asserted that “opioid medication is an adjunct for patients with uncontrolled pain despite adequate first-line therapy.”6
Despite efforts by the Centers for Disease Control and Prevention (CDC) and ACOG to improve opioid prescribing patterns after childbirth, the vast majority of women receive opioids in the hospital and at discharge not only after CD, but after vaginal delivery as well.4,7 Why has tradition prevailed over data, and why have we not changed?
Continue to: Common misconceptions about reducing opioid use...
Common misconceptions about reducing opioid use
Two misconceptions persist regarding reducing opioid prescriptions for postpartum pain.
Misconception #1: Patients will be in pain
Randomized controlled trials that compared nonopioid with opioid regimens in the emergency room setting and opioid use after outpatient general surgery procedures have demonstrated that pain control for patients receiving opioids was equivalent to that for patients with pain managed with nonopioid regimens.8-10 In the obstetric setting, a survey study of 720 women who underwent CD found that higher quantities of opioid tablets prescribed at discharge were not associated with improved pain, higher satisfaction, or lower refill rates at 2 weeks postpartum.4 However, greater quantities of opioids prescribed at the time of discharge were associated with greater opioid consumption.
Recently, several quality improvement studies implemented various interventions and successfully decreased postpartum opioid consumption without compromising pain management. One quality improvement project eliminated the routine use of opioids after CD and decreased the proportion of patients using any opioids in the hospital from 68% to 45%, with no changes in pain scores.11 A similar study implemented an enhanced recovery after surgery (ERAS) program for women after CD; mean in-patient opioid use decreased from 10.7 to 5.4 average daily morphine equivalents, with improvement in the proportion of time that patients reported their pain as acceptable.12
Misconception #2: Clinicians will be overwhelmed with pages and phone calls
Providers commonly fear that decreasing opioid use will lead to an increased volume of pages and phone calls from patients requesting additional medication. However, data suggest otherwise. For example, a quality improvement study that eliminated the routine use of opioids after CD tracked the number of phone calls that were received requesting rescue opioid prescriptions after discharge.11 Although the percentage of women discharged with opioids decreased from 90.6% to 40.3%, the requests for rescue opioid prescriptions did not change. Of 191 women, 4 requested a rescue prescription prior to the intervention compared with no women after the intervention. At the same time, according to unpublished data (Dr. Holland), satisfaction among nurses, house staff, and faculty did not change.
Similarly, a quality improvement project that implemented shared decision-making to inform the quantity of opioids prescribed at discharge demonstrated that the number of tablets prescribed decreased from 33.2 to 26.5, and there was no change in the rate of patients requesting opioid refills.13
Success stories: Strategies for reducing opioid use after childbirth
While overall rates of opioid prescribing after vaginal delivery and CD remain high throughout the United States, various institutions have developed successful and reproducible strategies to reduce opioid use after childbirth both in the hospital and at discharge. We highlight 3 strategies below.
Strategy 1: ERAS initiatives
An integrated health care system in northern California studied the effects of an ERAS protocol for CD across 15 medical centers.12 The intervention centered on 4 pillars: multimodal pain management, early mobility, optimal nutrition, and patient engagement through education. Specifically, multimodal pain management consisted of the following:
- intrathecal opioids during CD
- scheduled intravenous acetaminophen for 24 hours followed by oral acetaminophen every 6 hours
- nonsteroidal anti-inflammatory drugs (NSAIDs) every 6 hours
- oral oxycodone for breakthrough pain
- decoupling of opioid medication from nonopioids in the post-CD order set
- decoupling of opioid and nonopioid medications in the discharge order set along with a reduction from 30 to 20 tablets as the default discharge quantity.
Continue to: Among 4,689 and 4,624 patients who underwent CD...
Among 4,689 and 4,624 patients who underwent CD before and after the intervention, the daily morphine milligram equivalents (MME) consumed in the hospital decreased from 10.7 to 5.4. The percentage of women who required no opioids while in the hospital increased from 8.3% to 21.4% after ERAS implementation, while the percentage of time that patients reported acceptable pain scores increased from 82.1% to 86.4%. The average number of opioid tablets prescribed at discharge also decreased, from 37 to 26 MME.12 (The TABLE shows oxycodone doses converted to MMEs.)
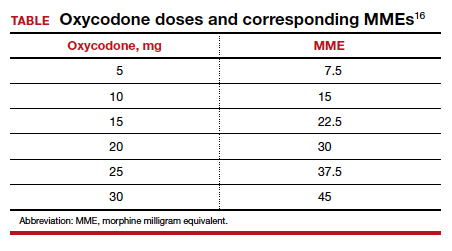
A similar initiative at a network of 5 hospitals in Texas showed that implementation of a “multimodal pain power plan” (which incorporated postpartum activity goals with standardized order sets) decreased opioid use after both vaginal delivery and CD.14
Strategy 2: Order set change to eliminate routine use of opioids
A tertiary care center in Boston, Massachusetts, implemented a quality improvement project aimed at eliminating the routine use of opioid medication after CD through an order set change.11 The intervention consisted of the following:
- intrathecal morphine
- multimodal postoperative pain management including scheduled oral acetaminophen for 72 hours followed by as-needed oral acetaminophen, scheduled NSAIDs for 72 hours followed by as-needed NSAIDs
- no postoperative order for opioids unless the patient had a contraindication to acetaminophen or NSAIDs, had a history of opioid dependence, or underwent complex surgery
- counseling patients that opioids were available for breakthrough pain if needed. In this case, nursing staff would page the responding clinician, who would order oxycodone 5 mg every 6 hours for 6 doses.
- specific criteria for discharge quantities of opioids: if the patient required no opioids in the hospital, she received no opioids at discharge; if the patient required opioids in the hospital but none at the time of discharge, she received no more than 10 tablets of oxycodone 5 mg; if the patient required opioids at the time of discharge, she received a maximum of 20 tablets of oxycodone 5 mg.
Among 191 and 181 women undergoing CD before and after the intervention, the percentage of patients who received any opioids in the hospital decreased from 68.1% to 45.3%.11 Similarly, the percentage of patients receiving a discharge prescription for opioids decreased from 90.6% to 40.3%, while patient pain scores and satisfaction with pain control remained unchanged.
Strategy 3: Shared decision-making tool
Another tertiary care center in Boston evaluated the effects of a shared decision-making tool on opioid discharge prescribing after CD.15 The intervention consisted of a 10-minute clinician-facilitated session incorporating:
- education around anticipated patterns of postoperative pain
- expected outpatient opioid use after CD
- risks and benefits of opioids and nonopioids
- education around opioid disposal and access to refills.
Among the 50 women enrolled in the study, the number of oxycodone 5-mg tablets prescribed at discharge decreased from the institutional standard of 40 to 20. Ninety percent of women reported being satisfied or very satisfied with their pain control, while only 4 of 50 women required an opioid refill. A follow-up quality improvement project, which implemented the shared decision-making model along with a standardized multimodal pain management protocol, demonstrated a similar decrease in the quantity of opioids prescribed at discharge.13
Continue to: Change is here to stay: A new culture of postpartum analgesia...
Change is here to stay: A new culture of postpartum analgesia
The CDC continues to champion responsible opioid prescribing, while ACOG advocates for a reassessment of the way that opioids are utilized postpartum. The majority of women in the United States, however, continue to receive opioids after both vaginal delivery and CD. Consciously or not, we clinicians may be contributing to an outdated tradition that is potentially harmful both to patients and society. Reproducible strategies exist to reduce opioid use without compromising pain control or overwhelming clinicians with phone calls. It is time to embrace the change.
- Wong CA, Girard T. Undertreated or overtreated? Opioids for postdelivery analgesia. Br J Anaesth. 2018;121:339-342.
- Eisenach JC, Pan PH, Smiley R, et al. Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain. 2008;140:87-94.
- Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naïve women. Am J Obstet Gynecol. 2016;215:353.e1- 353.e18.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130:29-35.
- Osmundson SS, Schornack LA, Grasch JL, et al. Postdischarge opioid use after cesarean delivery. Obstet Gynecol. 2017;130:36-41.
- American College of Obstetricians and Gynecologists. ACOG committee opinion no. 742: postpartum pain management. Obstet Gynecol. 2018;132:e35-e43.
- Mills JR, Huizinga MM, Robinson SB, et al. Draft opioid prescribing guidelines for uncomplicated normal spontaneous vaginal birth. Obstet Gynecol. 2019;133:81-90.
- Chang AK, Bijur PE, Esses D, et al. Effect of a single dose of oral opioid and nonopioid analgesics on acute extremity pain in the emergency department: a randomized clinical trial. JAMA. 2017;318:1661-1667.
- Mitchell A, van Zanten SV, Inglis K, et al. A randomized controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine after outpatient general surgery. J Am Coll Surg. 2008;206:472-479.
- Mitchell A, McCrea P, Inglis K, et al. A randomized, controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine (Tylenol 3) after outpatient breast surgery. Ann Surg Oncol. 2012;19:3792-3800.
- Holland E, Bateman BT, Cole N, et al. Evaluation of a quality improvement intervention that eliminated routine use of opioids after cesarean delivery. Obstet Gynecol. 2019;133:91-97.
- Hedderson M, Lee D, Hunt E, et al. Enhanced recovery after surgery to change process measures and reduce opioid use after cesarean delivery: a quality improvement initiative. Obstet Gynecol. 2019;134:511-519.
- Prabhu M, Dubois H, James K, et al. Implementation of a quality improvement initiative to decrease opioid prescribing after cesarean delivery. Obstet Gynecol. 2018;132:631-636.
- Rogers RG, Nix M, Chipman Z, et al. Decreasing opioid use postpartum: a quality improvement initiative. Obstet Gynecol. 2019;134:932-940.
- Prabhu M, McQuaid-Hanson E, Hopp S, et al. A shared decision-making intervention to guide opioid prescribing after cesarean delivery. Obstet Gynecol. 2017;130:42-46.
- Centers for Disease Control and Prevention. Calculating total daily dose of opioids for safer dosage. www.cdc.gov/ drugoverdose/pdf/calculating_total_daily_dose-a.pdf. Accessed December 31, 2019.
- Wong CA, Girard T. Undertreated or overtreated? Opioids for postdelivery analgesia. Br J Anaesth. 2018;121:339-342.
- Eisenach JC, Pan PH, Smiley R, et al. Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain. 2008;140:87-94.
- Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naïve women. Am J Obstet Gynecol. 2016;215:353.e1- 353.e18.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130:29-35.
- Osmundson SS, Schornack LA, Grasch JL, et al. Postdischarge opioid use after cesarean delivery. Obstet Gynecol. 2017;130:36-41.
- American College of Obstetricians and Gynecologists. ACOG committee opinion no. 742: postpartum pain management. Obstet Gynecol. 2018;132:e35-e43.
- Mills JR, Huizinga MM, Robinson SB, et al. Draft opioid prescribing guidelines for uncomplicated normal spontaneous vaginal birth. Obstet Gynecol. 2019;133:81-90.
- Chang AK, Bijur PE, Esses D, et al. Effect of a single dose of oral opioid and nonopioid analgesics on acute extremity pain in the emergency department: a randomized clinical trial. JAMA. 2017;318:1661-1667.
- Mitchell A, van Zanten SV, Inglis K, et al. A randomized controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine after outpatient general surgery. J Am Coll Surg. 2008;206:472-479.
- Mitchell A, McCrea P, Inglis K, et al. A randomized, controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine (Tylenol 3) after outpatient breast surgery. Ann Surg Oncol. 2012;19:3792-3800.
- Holland E, Bateman BT, Cole N, et al. Evaluation of a quality improvement intervention that eliminated routine use of opioids after cesarean delivery. Obstet Gynecol. 2019;133:91-97.
- Hedderson M, Lee D, Hunt E, et al. Enhanced recovery after surgery to change process measures and reduce opioid use after cesarean delivery: a quality improvement initiative. Obstet Gynecol. 2019;134:511-519.
- Prabhu M, Dubois H, James K, et al. Implementation of a quality improvement initiative to decrease opioid prescribing after cesarean delivery. Obstet Gynecol. 2018;132:631-636.
- Rogers RG, Nix M, Chipman Z, et al. Decreasing opioid use postpartum: a quality improvement initiative. Obstet Gynecol. 2019;134:932-940.
- Prabhu M, McQuaid-Hanson E, Hopp S, et al. A shared decision-making intervention to guide opioid prescribing after cesarean delivery. Obstet Gynecol. 2017;130:42-46.
- Centers for Disease Control and Prevention. Calculating total daily dose of opioids for safer dosage. www.cdc.gov/ drugoverdose/pdf/calculating_total_daily_dose-a.pdf. Accessed December 31, 2019.
CAR T cells produce complete responses in T-cell malignancies
ORLANDO – Anti-CD5 chimeric antigen receptor (CAR) T cells can produce complete responses (CRs) in patients with relapsed or refractory T-cell malignancies, according to findings from a phase 1 trial.
Three of 11 patients achieved a CR after CAR T-cell therapy, and one patient achieved a mixed response that deepened to a CR after transplant. Three responders, all of whom had T-cell lymphoma, were still alive and in CR at last follow-up.
There were no cases of severe cytokine release syndrome (CRS) or severe neurotoxicity, no serious infectious complications, and no nonhematologic grade 4 adverse events in this trial.
LaQuisa C. Hill, MD, of Baylor College of Medicine, Houston, presented these results at the annual meeting of the American Society of Hematology.
“While CD19 CAR T cells have revolutionized the treatment of relapsed/refractory B-cell malignancies, development of CAR T-cell platforms targeting T-cell-driven malignancies have been hindered by three main factors: CAR T-cell fratricide due to shared expression of target antigens leading to impaired expansion, ablation of normal T cells continuing to cause profound immunodeficiency, and the potential of transduced tumor cells providing a means of tumor escape,” Dr. Hill said.
Researchers have theorized that anti-CD5 CAR T cells can overcome these obstacles. In preclinical studies, anti-CD5 CAR T cells eliminated malignant blasts in vitro and in vivo and resulted in “limited and transient” fratricide (Blood. 2015 Aug 20;126[8]:983-92).
With this in mind, Dr. Hill and her colleagues tested CD5.28z CAR T cells in a phase 1 trial (NCT03081910). Eleven patients have been treated thus far – five with T-cell acute lymphoblastic leukemia (T-ALL), three with peripheral T-cell lymphoma (PTCL), two with angioimmunoblastic T-cell lymphoma (AITL), and one with Sézary syndrome.
The patients’ median age at baseline was 62 years (range, 21-71 years), and 63% were men. They had received a median of 5 prior therapies (range, 3-18). Two patients had relapsed after allogeneic hematopoietic stem cell transplant (HSCT), three had relapsed after autologous HSCT, and five were primary refractory.
Patients underwent lymphodepletion with fludarabine and cyclophosphamide, then received CAR T cells at doses of 1 x 107 or 5 x 107.
Response
Three lymphoma patients – two with AITL and one with PTCL – were still alive and in CR at last follow-up. The PTCL patient achieved a CR after CAR T-cell therapy and declined a subsequent HSCT. The patient has not received additional therapy and has retained the CR for 7 months.
One AITL patient achieved a CR and declined transplant as well. He relapsed after 7 months but received subsequent therapy and achieved another CR. The other AITL patient had a mixed response to CAR T-cell therapy but proceeded to allogeneic HSCT and achieved a CR that has lasted 9 months.
The remaining three lymphoma patients – two with PTCL and one with Sézary syndrome – progressed and died.
One T-ALL patient achieved a CR lasting 6 weeks, but the patient died while undergoing transplant workup. Two T-ALL patients did not respond to treatment and died. The remaining two patients progressed, and one of them died. The other patient who progressed is still alive and in CR after receiving subsequent therapy.
Factors associated with response
Dr. Hill said a shortened manufacturing process may be associated with enhanced response, as all responders received CAR T cells produced via a shorter manufacturing process. The shortened process involves freezing cells on day 4-5 post transduction, as opposed to day 7.
“While the numbers are too small to make any definitive conclusions, this seems to correlate with less terminal differentiation, which might improve potency,” Dr. Hill said. “However, additional analyses are ongoing.”
Dr. Hill also pointed out that CAR T-cell expansion was observed in all patients, with higher peak levels observed at the higher dose. In addition, CAR T-cell persistence was durable at both dose levels.
“We have been able to detect the CAR transgene at all follow-up time points, out to 9 months for some patients,” Dr. Hill said. “While limited persistence may play a role in nonresponders, it does not appear to be the only factor.”
Safety
“Surprisingly, no selective ablation of normal T cells has been observed,” Dr. Hill said. “As CAR T cells dwindled [after infusion], we were able to see recovery of normal T cells, all of which expressed normal levels of CD5. This was observed in all patients on study, except for one patient who had prolonged pancytopenia.”
Cytopenias were the most common grade 3/4 adverse events, including neutropenia (n = 8), anemia (n = 7), and thrombocytopenia (n = 5). Other grade 3/4 events included elevated aspartate aminotransferase (n = 2), hypoalbuminemia (n = 1), hyponatremia (n = 1), hypophosphatemia (n = 1), and elevated alanine aminotransferase (n = 1). There were no grade 5 adverse events.
Two patients developed grade 1 CRS, and two had grade 2 CRS. Both patients with grade 2 CRS were treated with tocilizumab, and their symptoms resolved.
One patient developed grade 2 immune effector cell-associated neurotoxicity syndrome, but this resolved with supportive care.
One patient had a central line–associated bloodstream infection (coagulase-negative staphylococci), and one had cytomegalovirus and BK virus reactivation. There were no fungal infections.
“We have demonstrated that CD5 CAR T cells can be manufactured from heavily pretreated patients with T-cell malignancies, and therapy is well tolerated,” Dr. Hill said. “We have seen strong and promising activity in T-cell lymphoma, which we hope to be able to translate to T-ALL as well.”
Dr. Hill said she and her colleagues hope to improve upon these results with a higher dose level of CD5 CAR T cells (1 x 108), which the team plans to start testing soon. The researchers may also investigate other target antigens, such as CD7, as well as the use of donor-derived CAR T cells for patients who have relapsed after allogeneic HSCT.
Dr. Hill said she has no relevant disclosures. Baylor College of Medicine is sponsoring this trial.
SOURCE: Hill L et al. ASH 2019. Abstract 199.
ORLANDO – Anti-CD5 chimeric antigen receptor (CAR) T cells can produce complete responses (CRs) in patients with relapsed or refractory T-cell malignancies, according to findings from a phase 1 trial.
Three of 11 patients achieved a CR after CAR T-cell therapy, and one patient achieved a mixed response that deepened to a CR after transplant. Three responders, all of whom had T-cell lymphoma, were still alive and in CR at last follow-up.
There were no cases of severe cytokine release syndrome (CRS) or severe neurotoxicity, no serious infectious complications, and no nonhematologic grade 4 adverse events in this trial.
LaQuisa C. Hill, MD, of Baylor College of Medicine, Houston, presented these results at the annual meeting of the American Society of Hematology.
“While CD19 CAR T cells have revolutionized the treatment of relapsed/refractory B-cell malignancies, development of CAR T-cell platforms targeting T-cell-driven malignancies have been hindered by three main factors: CAR T-cell fratricide due to shared expression of target antigens leading to impaired expansion, ablation of normal T cells continuing to cause profound immunodeficiency, and the potential of transduced tumor cells providing a means of tumor escape,” Dr. Hill said.
Researchers have theorized that anti-CD5 CAR T cells can overcome these obstacles. In preclinical studies, anti-CD5 CAR T cells eliminated malignant blasts in vitro and in vivo and resulted in “limited and transient” fratricide (Blood. 2015 Aug 20;126[8]:983-92).
With this in mind, Dr. Hill and her colleagues tested CD5.28z CAR T cells in a phase 1 trial (NCT03081910). Eleven patients have been treated thus far – five with T-cell acute lymphoblastic leukemia (T-ALL), three with peripheral T-cell lymphoma (PTCL), two with angioimmunoblastic T-cell lymphoma (AITL), and one with Sézary syndrome.
The patients’ median age at baseline was 62 years (range, 21-71 years), and 63% were men. They had received a median of 5 prior therapies (range, 3-18). Two patients had relapsed after allogeneic hematopoietic stem cell transplant (HSCT), three had relapsed after autologous HSCT, and five were primary refractory.
Patients underwent lymphodepletion with fludarabine and cyclophosphamide, then received CAR T cells at doses of 1 x 107 or 5 x 107.
Response
Three lymphoma patients – two with AITL and one with PTCL – were still alive and in CR at last follow-up. The PTCL patient achieved a CR after CAR T-cell therapy and declined a subsequent HSCT. The patient has not received additional therapy and has retained the CR for 7 months.
One AITL patient achieved a CR and declined transplant as well. He relapsed after 7 months but received subsequent therapy and achieved another CR. The other AITL patient had a mixed response to CAR T-cell therapy but proceeded to allogeneic HSCT and achieved a CR that has lasted 9 months.
The remaining three lymphoma patients – two with PTCL and one with Sézary syndrome – progressed and died.
One T-ALL patient achieved a CR lasting 6 weeks, but the patient died while undergoing transplant workup. Two T-ALL patients did not respond to treatment and died. The remaining two patients progressed, and one of them died. The other patient who progressed is still alive and in CR after receiving subsequent therapy.
Factors associated with response
Dr. Hill said a shortened manufacturing process may be associated with enhanced response, as all responders received CAR T cells produced via a shorter manufacturing process. The shortened process involves freezing cells on day 4-5 post transduction, as opposed to day 7.
“While the numbers are too small to make any definitive conclusions, this seems to correlate with less terminal differentiation, which might improve potency,” Dr. Hill said. “However, additional analyses are ongoing.”
Dr. Hill also pointed out that CAR T-cell expansion was observed in all patients, with higher peak levels observed at the higher dose. In addition, CAR T-cell persistence was durable at both dose levels.
“We have been able to detect the CAR transgene at all follow-up time points, out to 9 months for some patients,” Dr. Hill said. “While limited persistence may play a role in nonresponders, it does not appear to be the only factor.”
Safety
“Surprisingly, no selective ablation of normal T cells has been observed,” Dr. Hill said. “As CAR T cells dwindled [after infusion], we were able to see recovery of normal T cells, all of which expressed normal levels of CD5. This was observed in all patients on study, except for one patient who had prolonged pancytopenia.”
Cytopenias were the most common grade 3/4 adverse events, including neutropenia (n = 8), anemia (n = 7), and thrombocytopenia (n = 5). Other grade 3/4 events included elevated aspartate aminotransferase (n = 2), hypoalbuminemia (n = 1), hyponatremia (n = 1), hypophosphatemia (n = 1), and elevated alanine aminotransferase (n = 1). There were no grade 5 adverse events.
Two patients developed grade 1 CRS, and two had grade 2 CRS. Both patients with grade 2 CRS were treated with tocilizumab, and their symptoms resolved.
One patient developed grade 2 immune effector cell-associated neurotoxicity syndrome, but this resolved with supportive care.
One patient had a central line–associated bloodstream infection (coagulase-negative staphylococci), and one had cytomegalovirus and BK virus reactivation. There were no fungal infections.
“We have demonstrated that CD5 CAR T cells can be manufactured from heavily pretreated patients with T-cell malignancies, and therapy is well tolerated,” Dr. Hill said. “We have seen strong and promising activity in T-cell lymphoma, which we hope to be able to translate to T-ALL as well.”
Dr. Hill said she and her colleagues hope to improve upon these results with a higher dose level of CD5 CAR T cells (1 x 108), which the team plans to start testing soon. The researchers may also investigate other target antigens, such as CD7, as well as the use of donor-derived CAR T cells for patients who have relapsed after allogeneic HSCT.
Dr. Hill said she has no relevant disclosures. Baylor College of Medicine is sponsoring this trial.
SOURCE: Hill L et al. ASH 2019. Abstract 199.
ORLANDO – Anti-CD5 chimeric antigen receptor (CAR) T cells can produce complete responses (CRs) in patients with relapsed or refractory T-cell malignancies, according to findings from a phase 1 trial.
Three of 11 patients achieved a CR after CAR T-cell therapy, and one patient achieved a mixed response that deepened to a CR after transplant. Three responders, all of whom had T-cell lymphoma, were still alive and in CR at last follow-up.
There were no cases of severe cytokine release syndrome (CRS) or severe neurotoxicity, no serious infectious complications, and no nonhematologic grade 4 adverse events in this trial.
LaQuisa C. Hill, MD, of Baylor College of Medicine, Houston, presented these results at the annual meeting of the American Society of Hematology.
“While CD19 CAR T cells have revolutionized the treatment of relapsed/refractory B-cell malignancies, development of CAR T-cell platforms targeting T-cell-driven malignancies have been hindered by three main factors: CAR T-cell fratricide due to shared expression of target antigens leading to impaired expansion, ablation of normal T cells continuing to cause profound immunodeficiency, and the potential of transduced tumor cells providing a means of tumor escape,” Dr. Hill said.
Researchers have theorized that anti-CD5 CAR T cells can overcome these obstacles. In preclinical studies, anti-CD5 CAR T cells eliminated malignant blasts in vitro and in vivo and resulted in “limited and transient” fratricide (Blood. 2015 Aug 20;126[8]:983-92).
With this in mind, Dr. Hill and her colleagues tested CD5.28z CAR T cells in a phase 1 trial (NCT03081910). Eleven patients have been treated thus far – five with T-cell acute lymphoblastic leukemia (T-ALL), three with peripheral T-cell lymphoma (PTCL), two with angioimmunoblastic T-cell lymphoma (AITL), and one with Sézary syndrome.
The patients’ median age at baseline was 62 years (range, 21-71 years), and 63% were men. They had received a median of 5 prior therapies (range, 3-18). Two patients had relapsed after allogeneic hematopoietic stem cell transplant (HSCT), three had relapsed after autologous HSCT, and five were primary refractory.
Patients underwent lymphodepletion with fludarabine and cyclophosphamide, then received CAR T cells at doses of 1 x 107 or 5 x 107.
Response
Three lymphoma patients – two with AITL and one with PTCL – were still alive and in CR at last follow-up. The PTCL patient achieved a CR after CAR T-cell therapy and declined a subsequent HSCT. The patient has not received additional therapy and has retained the CR for 7 months.
One AITL patient achieved a CR and declined transplant as well. He relapsed after 7 months but received subsequent therapy and achieved another CR. The other AITL patient had a mixed response to CAR T-cell therapy but proceeded to allogeneic HSCT and achieved a CR that has lasted 9 months.
The remaining three lymphoma patients – two with PTCL and one with Sézary syndrome – progressed and died.
One T-ALL patient achieved a CR lasting 6 weeks, but the patient died while undergoing transplant workup. Two T-ALL patients did not respond to treatment and died. The remaining two patients progressed, and one of them died. The other patient who progressed is still alive and in CR after receiving subsequent therapy.
Factors associated with response
Dr. Hill said a shortened manufacturing process may be associated with enhanced response, as all responders received CAR T cells produced via a shorter manufacturing process. The shortened process involves freezing cells on day 4-5 post transduction, as opposed to day 7.
“While the numbers are too small to make any definitive conclusions, this seems to correlate with less terminal differentiation, which might improve potency,” Dr. Hill said. “However, additional analyses are ongoing.”
Dr. Hill also pointed out that CAR T-cell expansion was observed in all patients, with higher peak levels observed at the higher dose. In addition, CAR T-cell persistence was durable at both dose levels.
“We have been able to detect the CAR transgene at all follow-up time points, out to 9 months for some patients,” Dr. Hill said. “While limited persistence may play a role in nonresponders, it does not appear to be the only factor.”
Safety
“Surprisingly, no selective ablation of normal T cells has been observed,” Dr. Hill said. “As CAR T cells dwindled [after infusion], we were able to see recovery of normal T cells, all of which expressed normal levels of CD5. This was observed in all patients on study, except for one patient who had prolonged pancytopenia.”
Cytopenias were the most common grade 3/4 adverse events, including neutropenia (n = 8), anemia (n = 7), and thrombocytopenia (n = 5). Other grade 3/4 events included elevated aspartate aminotransferase (n = 2), hypoalbuminemia (n = 1), hyponatremia (n = 1), hypophosphatemia (n = 1), and elevated alanine aminotransferase (n = 1). There were no grade 5 adverse events.
Two patients developed grade 1 CRS, and two had grade 2 CRS. Both patients with grade 2 CRS were treated with tocilizumab, and their symptoms resolved.
One patient developed grade 2 immune effector cell-associated neurotoxicity syndrome, but this resolved with supportive care.
One patient had a central line–associated bloodstream infection (coagulase-negative staphylococci), and one had cytomegalovirus and BK virus reactivation. There were no fungal infections.
“We have demonstrated that CD5 CAR T cells can be manufactured from heavily pretreated patients with T-cell malignancies, and therapy is well tolerated,” Dr. Hill said. “We have seen strong and promising activity in T-cell lymphoma, which we hope to be able to translate to T-ALL as well.”
Dr. Hill said she and her colleagues hope to improve upon these results with a higher dose level of CD5 CAR T cells (1 x 108), which the team plans to start testing soon. The researchers may also investigate other target antigens, such as CD7, as well as the use of donor-derived CAR T cells for patients who have relapsed after allogeneic HSCT.
Dr. Hill said she has no relevant disclosures. Baylor College of Medicine is sponsoring this trial.
SOURCE: Hill L et al. ASH 2019. Abstract 199.
REPORTING FROM ASH 2019













