User login
CHMP recommends rejection for betrixaban
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has issued a negative opinion recommending refusal of marketing authorization for the factor Xa inhibitor betrixaban (Dexxience).
Portola Pharmaceuticals, Inc. is seeking approval of betrixaban for the prevention of venous thromboembolism (VTE) in adults hospitalized for an acute medical illness with risk factors for VTE, including VTE-related death.
The marketing authorization application for betrixaban was supported by data from the phase 3 APEX study. In this study, researchers compared oral betrixaban to injectable enoxaparin for the prevention of VTE in patients with acute medical illnesses.
The CHMP said APEX did not satisfactorily show that betrixaban’s benefits outweigh its risk in this patient population. The study results were not considered reliable because some test results for VTEs were not available.
In addition, patients treated with betrixaban had more episodes of bleeding than those treated with enoxaparin. This was considered an important concern given that betrixaban was expected to be used in patients with serious underlying conditions.
For these reasons, the CHMP recommended that betrixaban be refused marketing authorization.
Portola Pharmaceuticals said it intends to appeal the CHMP’s opinion and ask the committee for a re-examination.
“We believe we have generated substantial evidence which demonstrates the clinically meaningful benefit of betrixaban in reducing VTE and VTE-related deaths in this vulnerable patient population, and we remain confident in its potential to have a major public health impact,” said Jack Lawrence, MD, chief medical officer of Portola Pharmaceuticals.
“The re-examination process allows us the opportunity to address the CHMP’s questions and provide further clarification as needed, with the goal of making betrixaban available to acute medically ill patients in Europe who are at risk for VTE.”
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has issued a negative opinion recommending refusal of marketing authorization for the factor Xa inhibitor betrixaban (Dexxience).
Portola Pharmaceuticals, Inc. is seeking approval of betrixaban for the prevention of venous thromboembolism (VTE) in adults hospitalized for an acute medical illness with risk factors for VTE, including VTE-related death.
The marketing authorization application for betrixaban was supported by data from the phase 3 APEX study. In this study, researchers compared oral betrixaban to injectable enoxaparin for the prevention of VTE in patients with acute medical illnesses.
The CHMP said APEX did not satisfactorily show that betrixaban’s benefits outweigh its risk in this patient population. The study results were not considered reliable because some test results for VTEs were not available.
In addition, patients treated with betrixaban had more episodes of bleeding than those treated with enoxaparin. This was considered an important concern given that betrixaban was expected to be used in patients with serious underlying conditions.
For these reasons, the CHMP recommended that betrixaban be refused marketing authorization.
Portola Pharmaceuticals said it intends to appeal the CHMP’s opinion and ask the committee for a re-examination.
“We believe we have generated substantial evidence which demonstrates the clinically meaningful benefit of betrixaban in reducing VTE and VTE-related deaths in this vulnerable patient population, and we remain confident in its potential to have a major public health impact,” said Jack Lawrence, MD, chief medical officer of Portola Pharmaceuticals.
“The re-examination process allows us the opportunity to address the CHMP’s questions and provide further clarification as needed, with the goal of making betrixaban available to acute medically ill patients in Europe who are at risk for VTE.”
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has issued a negative opinion recommending refusal of marketing authorization for the factor Xa inhibitor betrixaban (Dexxience).
Portola Pharmaceuticals, Inc. is seeking approval of betrixaban for the prevention of venous thromboembolism (VTE) in adults hospitalized for an acute medical illness with risk factors for VTE, including VTE-related death.
The marketing authorization application for betrixaban was supported by data from the phase 3 APEX study. In this study, researchers compared oral betrixaban to injectable enoxaparin for the prevention of VTE in patients with acute medical illnesses.
The CHMP said APEX did not satisfactorily show that betrixaban’s benefits outweigh its risk in this patient population. The study results were not considered reliable because some test results for VTEs were not available.
In addition, patients treated with betrixaban had more episodes of bleeding than those treated with enoxaparin. This was considered an important concern given that betrixaban was expected to be used in patients with serious underlying conditions.
For these reasons, the CHMP recommended that betrixaban be refused marketing authorization.
Portola Pharmaceuticals said it intends to appeal the CHMP’s opinion and ask the committee for a re-examination.
“We believe we have generated substantial evidence which demonstrates the clinically meaningful benefit of betrixaban in reducing VTE and VTE-related deaths in this vulnerable patient population, and we remain confident in its potential to have a major public health impact,” said Jack Lawrence, MD, chief medical officer of Portola Pharmaceuticals.
“The re-examination process allows us the opportunity to address the CHMP’s questions and provide further clarification as needed, with the goal of making betrixaban available to acute medically ill patients in Europe who are at risk for VTE.”
CBC data can predict immunotherapy responses in NSCLC
ORLANDO – Information readily available on complete blood count can help predict response to immunotherapy and outcomes in patients with advanced non–small cell lung cancer, according to findings from a review of 157 cases.
Specifically, absolute monocyte count of 0.63 or greater and absolute neutrophil count/absolute lymphocyte count of 5.9 or greater at baseline were significantly associated with poor progression-free survival (hazard ratios, 1.50 and 1.61, respectively) and overall survival (HRs, 1.71 and 1.87, respectively) in patients treated with anti–programmed death-1 (PD-1) antibodies, Aixa E. Soyano, MD, reported in a poster at the annual conference of the National Comprehensive Cancer Network.
Additionally, absolute neutrophil count of at least 7.5 and myeloid to lymphoid ratio of at least 11.3 at baseline were associated with poor overall survival (HRs, 1.86 and 2.31, respectively), according to Dr. Soyano of the Mayo Clinic, Jacksonville, Fla.
“The potential predictive value of these readily available biomarkers might help with risk stratification and treatment strategies,” she and her colleagues wrote.
Cases included in the review involved advanced non–small cell lung cancer (NSCLC) patients with a median age of 66 years who were treated with nivolumab or pembrolizumab at the Mayo Clinic from January 2010 to April 2017. Most (91%) were white, 4.5% were African American, 1.9% were Asian, 0.6% were native Hawaiian/Pacific Islander, and 1.9% were other ethnicities. Slightly more than half (53%) were men, and diagnoses included adenocarcinoma (69%), squamous disease (29%) and other (3%). Half had one prior line of chemotherapy, 22% had two prior lines, and 10% had three or more prior lines. The majority (72%) had Eastern Cooperative Oncology Group performance status of 1 or 2, and 34% had CNS disease.
Pembrolizumab was given intravenously at a dose of 2 mg/kg every 21 days (11 patients), and nivolumab was given intravenously at a dose of 3 mg/kg every 14 days (146 patients). Clinical response was assessed every 8-12 weeks by CT of the chest, abdomen and pelvis, and also – in some cases – by brain MRI.
The findings are notable because, although combination chemotherapy with a platinum-based doublet has, for the last decade, been the backbone of initial systemic therapy for patients whose tumor does not have driver mutations, monoclonal antibodies targeting PD-1 or its ligand PD-L1 have shown improvements in progression-free survival and overall survival in certain patients with metastatic or locally advanced lung cancer, the investigators explained.
Prior studies in melanoma patients treated with immunotherapy targeting the cytotoxic T-lymphocyte antigen 4 pathway and PD-1/PD-L1 pathways have identified predictive or prognostic hematological markers of outcomes. However, data with respect to hematologic markers in lung cancer are sparse, and given the high cost, significant immune-related side effects, and rapidly expanding number of indications for immunotherapy in NSCLC, there is a need for reliable biomarkers to help predict response and outcomes, they said.
In a separate presentation at the NCCN conference, John A. Thompson, MD, of the Fred Hutchinson Cancer Research Center, Seattle, noted that some progress has been made in the area of predicting response to immune checkpoint inhibitors in NSCLC patients. Namely, the value of tumor PD-L1 expression and tumor mutation burden for predicting outcomes was highlighted in a recent study by Rizvi et al., who concluded that “the incorporation of both TMB [tumor mutation burden] and PD-L1 expression into multivariable predictive models should result in greater predictive power.” .
“This is a first step in our evolution and our progress toward a better biomarker. I think when we add in other factors like gene expression, we may be able to develop an even more robust biomarker that will help us select appropriate patients for therapy,” he said.
Dr. Soyano and her colleagues noted, however, that these measures, as well as tumor infiltrating immune cells, which have also been shown to have predictive value, require special testing and/or processing.
Furthermore, the optimal cutoff with PD-L1 expression is debatable, they said.
CBC data is more readily available, and also appears to have predictive and prognostic value, they said, concluding that the findings warrant further investigation in a larger, prospective study.
The authors reported having no disclosures.
sworcester@frontlinemedcom.com
SOURCE: Soyano A et al. NCCN Poster 075.
ORLANDO – Information readily available on complete blood count can help predict response to immunotherapy and outcomes in patients with advanced non–small cell lung cancer, according to findings from a review of 157 cases.
Specifically, absolute monocyte count of 0.63 or greater and absolute neutrophil count/absolute lymphocyte count of 5.9 or greater at baseline were significantly associated with poor progression-free survival (hazard ratios, 1.50 and 1.61, respectively) and overall survival (HRs, 1.71 and 1.87, respectively) in patients treated with anti–programmed death-1 (PD-1) antibodies, Aixa E. Soyano, MD, reported in a poster at the annual conference of the National Comprehensive Cancer Network.
Additionally, absolute neutrophil count of at least 7.5 and myeloid to lymphoid ratio of at least 11.3 at baseline were associated with poor overall survival (HRs, 1.86 and 2.31, respectively), according to Dr. Soyano of the Mayo Clinic, Jacksonville, Fla.
“The potential predictive value of these readily available biomarkers might help with risk stratification and treatment strategies,” she and her colleagues wrote.
Cases included in the review involved advanced non–small cell lung cancer (NSCLC) patients with a median age of 66 years who were treated with nivolumab or pembrolizumab at the Mayo Clinic from January 2010 to April 2017. Most (91%) were white, 4.5% were African American, 1.9% were Asian, 0.6% were native Hawaiian/Pacific Islander, and 1.9% were other ethnicities. Slightly more than half (53%) were men, and diagnoses included adenocarcinoma (69%), squamous disease (29%) and other (3%). Half had one prior line of chemotherapy, 22% had two prior lines, and 10% had three or more prior lines. The majority (72%) had Eastern Cooperative Oncology Group performance status of 1 or 2, and 34% had CNS disease.
Pembrolizumab was given intravenously at a dose of 2 mg/kg every 21 days (11 patients), and nivolumab was given intravenously at a dose of 3 mg/kg every 14 days (146 patients). Clinical response was assessed every 8-12 weeks by CT of the chest, abdomen and pelvis, and also – in some cases – by brain MRI.
The findings are notable because, although combination chemotherapy with a platinum-based doublet has, for the last decade, been the backbone of initial systemic therapy for patients whose tumor does not have driver mutations, monoclonal antibodies targeting PD-1 or its ligand PD-L1 have shown improvements in progression-free survival and overall survival in certain patients with metastatic or locally advanced lung cancer, the investigators explained.
Prior studies in melanoma patients treated with immunotherapy targeting the cytotoxic T-lymphocyte antigen 4 pathway and PD-1/PD-L1 pathways have identified predictive or prognostic hematological markers of outcomes. However, data with respect to hematologic markers in lung cancer are sparse, and given the high cost, significant immune-related side effects, and rapidly expanding number of indications for immunotherapy in NSCLC, there is a need for reliable biomarkers to help predict response and outcomes, they said.
In a separate presentation at the NCCN conference, John A. Thompson, MD, of the Fred Hutchinson Cancer Research Center, Seattle, noted that some progress has been made in the area of predicting response to immune checkpoint inhibitors in NSCLC patients. Namely, the value of tumor PD-L1 expression and tumor mutation burden for predicting outcomes was highlighted in a recent study by Rizvi et al., who concluded that “the incorporation of both TMB [tumor mutation burden] and PD-L1 expression into multivariable predictive models should result in greater predictive power.” .
“This is a first step in our evolution and our progress toward a better biomarker. I think when we add in other factors like gene expression, we may be able to develop an even more robust biomarker that will help us select appropriate patients for therapy,” he said.
Dr. Soyano and her colleagues noted, however, that these measures, as well as tumor infiltrating immune cells, which have also been shown to have predictive value, require special testing and/or processing.
Furthermore, the optimal cutoff with PD-L1 expression is debatable, they said.
CBC data is more readily available, and also appears to have predictive and prognostic value, they said, concluding that the findings warrant further investigation in a larger, prospective study.
The authors reported having no disclosures.
sworcester@frontlinemedcom.com
SOURCE: Soyano A et al. NCCN Poster 075.
ORLANDO – Information readily available on complete blood count can help predict response to immunotherapy and outcomes in patients with advanced non–small cell lung cancer, according to findings from a review of 157 cases.
Specifically, absolute monocyte count of 0.63 or greater and absolute neutrophil count/absolute lymphocyte count of 5.9 or greater at baseline were significantly associated with poor progression-free survival (hazard ratios, 1.50 and 1.61, respectively) and overall survival (HRs, 1.71 and 1.87, respectively) in patients treated with anti–programmed death-1 (PD-1) antibodies, Aixa E. Soyano, MD, reported in a poster at the annual conference of the National Comprehensive Cancer Network.
Additionally, absolute neutrophil count of at least 7.5 and myeloid to lymphoid ratio of at least 11.3 at baseline were associated with poor overall survival (HRs, 1.86 and 2.31, respectively), according to Dr. Soyano of the Mayo Clinic, Jacksonville, Fla.
“The potential predictive value of these readily available biomarkers might help with risk stratification and treatment strategies,” she and her colleagues wrote.
Cases included in the review involved advanced non–small cell lung cancer (NSCLC) patients with a median age of 66 years who were treated with nivolumab or pembrolizumab at the Mayo Clinic from January 2010 to April 2017. Most (91%) were white, 4.5% were African American, 1.9% were Asian, 0.6% were native Hawaiian/Pacific Islander, and 1.9% were other ethnicities. Slightly more than half (53%) were men, and diagnoses included adenocarcinoma (69%), squamous disease (29%) and other (3%). Half had one prior line of chemotherapy, 22% had two prior lines, and 10% had three or more prior lines. The majority (72%) had Eastern Cooperative Oncology Group performance status of 1 or 2, and 34% had CNS disease.
Pembrolizumab was given intravenously at a dose of 2 mg/kg every 21 days (11 patients), and nivolumab was given intravenously at a dose of 3 mg/kg every 14 days (146 patients). Clinical response was assessed every 8-12 weeks by CT of the chest, abdomen and pelvis, and also – in some cases – by brain MRI.
The findings are notable because, although combination chemotherapy with a platinum-based doublet has, for the last decade, been the backbone of initial systemic therapy for patients whose tumor does not have driver mutations, monoclonal antibodies targeting PD-1 or its ligand PD-L1 have shown improvements in progression-free survival and overall survival in certain patients with metastatic or locally advanced lung cancer, the investigators explained.
Prior studies in melanoma patients treated with immunotherapy targeting the cytotoxic T-lymphocyte antigen 4 pathway and PD-1/PD-L1 pathways have identified predictive or prognostic hematological markers of outcomes. However, data with respect to hematologic markers in lung cancer are sparse, and given the high cost, significant immune-related side effects, and rapidly expanding number of indications for immunotherapy in NSCLC, there is a need for reliable biomarkers to help predict response and outcomes, they said.
In a separate presentation at the NCCN conference, John A. Thompson, MD, of the Fred Hutchinson Cancer Research Center, Seattle, noted that some progress has been made in the area of predicting response to immune checkpoint inhibitors in NSCLC patients. Namely, the value of tumor PD-L1 expression and tumor mutation burden for predicting outcomes was highlighted in a recent study by Rizvi et al., who concluded that “the incorporation of both TMB [tumor mutation burden] and PD-L1 expression into multivariable predictive models should result in greater predictive power.” .
“This is a first step in our evolution and our progress toward a better biomarker. I think when we add in other factors like gene expression, we may be able to develop an even more robust biomarker that will help us select appropriate patients for therapy,” he said.
Dr. Soyano and her colleagues noted, however, that these measures, as well as tumor infiltrating immune cells, which have also been shown to have predictive value, require special testing and/or processing.
Furthermore, the optimal cutoff with PD-L1 expression is debatable, they said.
CBC data is more readily available, and also appears to have predictive and prognostic value, they said, concluding that the findings warrant further investigation in a larger, prospective study.
The authors reported having no disclosures.
sworcester@frontlinemedcom.com
SOURCE: Soyano A et al. NCCN Poster 075.
REPORTING FROM THE NCCN ANNUAL CONFERENCE
Key clinical point:
Major finding: Hazard ratios for progression-free survival were 1.50 and 1.61 with absolute monocyte count of 0.63 or greater, absolute neutrophil count/absolute lymphocyte of 5.9 or greater at baseline.
Study details: A review of 157 NSCLC cases.
Disclosures: The authors reported having no disclosures.
Source: Soyano AE et al. NCCN poster 075.
VIDEO: Everolimus/letrozole promising for recurrent endometrial cancer
NEW ORLEANS – Combined treatment for 28 days with the mammalian target of rapamycin inhibitor everolimus plus the aromatase inhibitor letrozole in 37 women with recurrent endometrial cancer produced an overall objective response rate of 24% and an average progression-free survival rate of 6.3 months in a randomized phase 2 study with a total of 74 patients. The treatment was also relatively well tolerated, with more serious adverse vents of anemia and hyperglycemia.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
But the most attention-grabbing finding of this study was that, in the subset of 15 women who had received no prior chemotherapy, the objective response rate on this regimen was 53% and median progression-free survival was 21.6 months, Brian M. Slomovitz, MD, said at the annual meeting of the Society of Gynecologic Oncology.
This level of response in the chemotherapy-naive subgroup was “very high, and not what we expected,” Dr. Slomovitz, , professor of ob.gyn. and human genetics and director of gynecologic oncology at the University of Miami, said in a video interview. “This is something we need to further investigate to see if we can make this part of standard care.”
Although he conceded that the data from this study were too limited to warrant a regulatory indication, he suggested that it might be enough to gain the everolimus plus letrozole combination used in the study citation as a treatment option in clinical guidelines. The next step should be a phase 3 trial that compares the everolimus plus letrozole combination with the traditional chemotherapy regimen of carboplatin plus paclitaxel, Dr. Slomovitz added.
The Everolimus and Letrozole or Hormonal Therapy to Treat Endometrial Cancer phase 2 trial, initiated by the Gynecologic Oncology Group, ran at 26 U.S. centers, and randomized patients with stage III or IV recurrent, advanced, or persistent endometrial cancer who had either no or at most one prior course of chemotherapy. The study design also excluded patients who had previously been treated with an mammalian target of rapamycin inhibitor or hormonal therapy for their endometrial cancer. The control arm placed 37 patients on a standard hormonal therapy regimen of tamoxifen plus medroxyprogesterone, with 36 of patients in this subgroup evaluable.
The overall results in the two treatment arms were roughly similar, except for the striking benefit seen with everolimus(Afinitor) plus letrozole(Femara) in the chemotherapy-naive patents; 15 patients in each arm had not received any chemotherapy before entering the study. In this subgroup, among the patients who received conventional hormonal therapy, the objective response rate was 43% and progression-free survival was 6.6 months.
The two arms also differed by their pattern of grade 3 or 4 adverse events. Among the patients on everolimus plus letrozole, the most common were anemia (24%) and hyperglycemia (14%), both expected consequences of the regimen. The hormonal therapy arm led to an 8% incidence of thromboembolic events, which did not occur in the everolimus plus letrozole arm.
Another attraction of the everolimus and letrozole regimen is that it is oral and avoids the need for drug infusions, Dr. Slomovitz noted.
The investigator-initiated study received funding from Novartis, the company that markets everolimus and letrozole. Dr. Slomovitz has been an advisor to Advaxis, AstraZeneca, Clovis, Genmab, Jannsen, and Tesaro, and he has received research funding from Novartis.
SOURCE: Slomovitz BM et al. SGO 2018, abstract 1.
The results from this study are exciting, with fairly compelling response rates. The rate of progression-free survival with everolimus and letrozole treatment is very impressive, compared with traditional chemotherapy using carboplatin and paclitaxel. The median progression-free survival rate of 21.6 months seen among the chemotherapy naive patients who received everolimus and letrozole showed a 7-month edge over the 14-month median progression-free survival previously reported with chemotherapy. This difference is very provocative and could be practice changing, but it of course needs further evaluation.
Paola A. Gehrig, MD , is professor of ob.gyn. and director of gynecologic oncology at the University of North Carolina in Chapel Hill. She made these comments as designated discussant for the study. She had no disclosures.
The results from this study are exciting, with fairly compelling response rates. The rate of progression-free survival with everolimus and letrozole treatment is very impressive, compared with traditional chemotherapy using carboplatin and paclitaxel. The median progression-free survival rate of 21.6 months seen among the chemotherapy naive patients who received everolimus and letrozole showed a 7-month edge over the 14-month median progression-free survival previously reported with chemotherapy. This difference is very provocative and could be practice changing, but it of course needs further evaluation.
Paola A. Gehrig, MD , is professor of ob.gyn. and director of gynecologic oncology at the University of North Carolina in Chapel Hill. She made these comments as designated discussant for the study. She had no disclosures.
The results from this study are exciting, with fairly compelling response rates. The rate of progression-free survival with everolimus and letrozole treatment is very impressive, compared with traditional chemotherapy using carboplatin and paclitaxel. The median progression-free survival rate of 21.6 months seen among the chemotherapy naive patients who received everolimus and letrozole showed a 7-month edge over the 14-month median progression-free survival previously reported with chemotherapy. This difference is very provocative and could be practice changing, but it of course needs further evaluation.
Paola A. Gehrig, MD , is professor of ob.gyn. and director of gynecologic oncology at the University of North Carolina in Chapel Hill. She made these comments as designated discussant for the study. She had no disclosures.
NEW ORLEANS – Combined treatment for 28 days with the mammalian target of rapamycin inhibitor everolimus plus the aromatase inhibitor letrozole in 37 women with recurrent endometrial cancer produced an overall objective response rate of 24% and an average progression-free survival rate of 6.3 months in a randomized phase 2 study with a total of 74 patients. The treatment was also relatively well tolerated, with more serious adverse vents of anemia and hyperglycemia.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
But the most attention-grabbing finding of this study was that, in the subset of 15 women who had received no prior chemotherapy, the objective response rate on this regimen was 53% and median progression-free survival was 21.6 months, Brian M. Slomovitz, MD, said at the annual meeting of the Society of Gynecologic Oncology.
This level of response in the chemotherapy-naive subgroup was “very high, and not what we expected,” Dr. Slomovitz, , professor of ob.gyn. and human genetics and director of gynecologic oncology at the University of Miami, said in a video interview. “This is something we need to further investigate to see if we can make this part of standard care.”
Although he conceded that the data from this study were too limited to warrant a regulatory indication, he suggested that it might be enough to gain the everolimus plus letrozole combination used in the study citation as a treatment option in clinical guidelines. The next step should be a phase 3 trial that compares the everolimus plus letrozole combination with the traditional chemotherapy regimen of carboplatin plus paclitaxel, Dr. Slomovitz added.
The Everolimus and Letrozole or Hormonal Therapy to Treat Endometrial Cancer phase 2 trial, initiated by the Gynecologic Oncology Group, ran at 26 U.S. centers, and randomized patients with stage III or IV recurrent, advanced, or persistent endometrial cancer who had either no or at most one prior course of chemotherapy. The study design also excluded patients who had previously been treated with an mammalian target of rapamycin inhibitor or hormonal therapy for their endometrial cancer. The control arm placed 37 patients on a standard hormonal therapy regimen of tamoxifen plus medroxyprogesterone, with 36 of patients in this subgroup evaluable.
The overall results in the two treatment arms were roughly similar, except for the striking benefit seen with everolimus(Afinitor) plus letrozole(Femara) in the chemotherapy-naive patents; 15 patients in each arm had not received any chemotherapy before entering the study. In this subgroup, among the patients who received conventional hormonal therapy, the objective response rate was 43% and progression-free survival was 6.6 months.
The two arms also differed by their pattern of grade 3 or 4 adverse events. Among the patients on everolimus plus letrozole, the most common were anemia (24%) and hyperglycemia (14%), both expected consequences of the regimen. The hormonal therapy arm led to an 8% incidence of thromboembolic events, which did not occur in the everolimus plus letrozole arm.
Another attraction of the everolimus and letrozole regimen is that it is oral and avoids the need for drug infusions, Dr. Slomovitz noted.
The investigator-initiated study received funding from Novartis, the company that markets everolimus and letrozole. Dr. Slomovitz has been an advisor to Advaxis, AstraZeneca, Clovis, Genmab, Jannsen, and Tesaro, and he has received research funding from Novartis.
SOURCE: Slomovitz BM et al. SGO 2018, abstract 1.
NEW ORLEANS – Combined treatment for 28 days with the mammalian target of rapamycin inhibitor everolimus plus the aromatase inhibitor letrozole in 37 women with recurrent endometrial cancer produced an overall objective response rate of 24% and an average progression-free survival rate of 6.3 months in a randomized phase 2 study with a total of 74 patients. The treatment was also relatively well tolerated, with more serious adverse vents of anemia and hyperglycemia.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
But the most attention-grabbing finding of this study was that, in the subset of 15 women who had received no prior chemotherapy, the objective response rate on this regimen was 53% and median progression-free survival was 21.6 months, Brian M. Slomovitz, MD, said at the annual meeting of the Society of Gynecologic Oncology.
This level of response in the chemotherapy-naive subgroup was “very high, and not what we expected,” Dr. Slomovitz, , professor of ob.gyn. and human genetics and director of gynecologic oncology at the University of Miami, said in a video interview. “This is something we need to further investigate to see if we can make this part of standard care.”
Although he conceded that the data from this study were too limited to warrant a regulatory indication, he suggested that it might be enough to gain the everolimus plus letrozole combination used in the study citation as a treatment option in clinical guidelines. The next step should be a phase 3 trial that compares the everolimus plus letrozole combination with the traditional chemotherapy regimen of carboplatin plus paclitaxel, Dr. Slomovitz added.
The Everolimus and Letrozole or Hormonal Therapy to Treat Endometrial Cancer phase 2 trial, initiated by the Gynecologic Oncology Group, ran at 26 U.S. centers, and randomized patients with stage III or IV recurrent, advanced, or persistent endometrial cancer who had either no or at most one prior course of chemotherapy. The study design also excluded patients who had previously been treated with an mammalian target of rapamycin inhibitor or hormonal therapy for their endometrial cancer. The control arm placed 37 patients on a standard hormonal therapy regimen of tamoxifen plus medroxyprogesterone, with 36 of patients in this subgroup evaluable.
The overall results in the two treatment arms were roughly similar, except for the striking benefit seen with everolimus(Afinitor) plus letrozole(Femara) in the chemotherapy-naive patents; 15 patients in each arm had not received any chemotherapy before entering the study. In this subgroup, among the patients who received conventional hormonal therapy, the objective response rate was 43% and progression-free survival was 6.6 months.
The two arms also differed by their pattern of grade 3 or 4 adverse events. Among the patients on everolimus plus letrozole, the most common were anemia (24%) and hyperglycemia (14%), both expected consequences of the regimen. The hormonal therapy arm led to an 8% incidence of thromboembolic events, which did not occur in the everolimus plus letrozole arm.
Another attraction of the everolimus and letrozole regimen is that it is oral and avoids the need for drug infusions, Dr. Slomovitz noted.
The investigator-initiated study received funding from Novartis, the company that markets everolimus and letrozole. Dr. Slomovitz has been an advisor to Advaxis, AstraZeneca, Clovis, Genmab, Jannsen, and Tesaro, and he has received research funding from Novartis.
SOURCE: Slomovitz BM et al. SGO 2018, abstract 1.
REPORTING FROM SGO 2018
Key clinical point: Treatment of recurrent endometrial cancer with everolimus and letrozole shows promise.
Major finding: Among 15 chemotherapy-naive patients, objective responses occurred in 53% and median progression-free survival was 21.6 months.
Study details: A multicenter, phase 2 randomized study in 74 patients.
Disclosures: The investigator-initiated study received funding from Novartis, the company that markets everolimus(Afinitor) and letrozole(Femara). Dr. Slomovitz has been an advisor to Advaxis, AstraZeneca, Clovis, Genmab, Jannsen, and Tesaro, and he has received research funding from Novartis.
Source: Slomovitz BM et al. SGO 2018, abstract 1.
Drug coated balloons may match stents for small coronary lesions
WASHINGTON – For treating de novo coronary lesions in vessels smaller than 2.75 mm, drug coated balloon angioplasty is as safe and may be as effective as drug-eluting stents, according to a multicenter randomized trial presented as a late-breaker at CRT 2018 sponsored by the Cardiovascular Research Institute at Washington Hospital Center.
“The aim of PCI [percutaneous coronary intervention] without leaving any metal behind seems to be feasible and safe with drug coated balloons,” reported Victor A. Jimenez Diaz, MD, of the department of cardiology at University Hospital, Vigo, Spain.
In this study, 94 patients with de novo coronary lesions in small diameter vessels were randomized to treatment with a paclitaxel drug coated balloon (DCB) (IN.PACT Falcon, Medtronic) or a zotarolimus drug-eluting stent (DES) (Resolute Integrity, Medtronic). Lesions in vessels between 2.0 and 2.75 mm in diameter were eligible; 137 lesions were treated in a study with seven participating centers in Spain.
For entry, target lesions had to have a stenosis of at least 70% by visual estimation or at least 50% by quantitative coronary angiography. Lesion length was limited to less than 25 mm, and severely calcified lesions were excluded.
The primary endpoint was a composite major adverse coronary event (MACE) endpoint of cardiac death, myocardial infarction, or revascularization at 12 months of follow-up. Crossovers by discretion of the interventional team were permitted.
At 12 months, MACE had occurred in 4.4% of those in the DCB group and 11.1% of those in the DES group. All primary endpoint events in both groups involved revascularizations. The two events in the DCB group were clinically driven target vessel revascularizations. Only one of the five events in the DES group was a clinically driven target lesion revascularization; the remaining four were revascularizations performed for nontarget vessels.
Four patients (8%) in the DCB group crossed over, each because of a dissection and managed with a bare-metal stent. There were four other dissections in the DCB group; one type F dissection resulted in a bailout and three dissections were managed conservatively. There were no crossovers in the DES group, and of the two dissections in the group, both were managed with the originally assigned stenting strategy.
Calling DCB a safe strategy for small de novo coronary stenosis, Dr. Jimenez Diaz said, “The procedural success rates were comparable.” However, he acknowledged that because of low enrollment, the study was “underpowered for clinical events.” The original power calculation called for a study of 200 patients.
“We can say results are encouraging,” Dr. Jimenez Diaz said.
Several discussants at the late-breaker abstracts agreed that DCB is an intriguing option for a difficult problem. They also agreed that restoring blood flow without leaving a permanent device is an attractive concept. However, they emphasized that a larger study is needed to declare that DCB and DES are equivalent strategies in regard to risk of MACE.
While agreeing that more data powered for events are needed, Cindy Grines, MD, chief of cardiology, Hofstra University, Hempstead, N.Y., was among those who suggested that this approach might be “worth a try.” She indicated that this study, which involved interventionalists at multiple centers, does provide support for the safety of DCB.
SOURCE: Jimenez Diaz VA. CRT 2018.
WASHINGTON – For treating de novo coronary lesions in vessels smaller than 2.75 mm, drug coated balloon angioplasty is as safe and may be as effective as drug-eluting stents, according to a multicenter randomized trial presented as a late-breaker at CRT 2018 sponsored by the Cardiovascular Research Institute at Washington Hospital Center.
“The aim of PCI [percutaneous coronary intervention] without leaving any metal behind seems to be feasible and safe with drug coated balloons,” reported Victor A. Jimenez Diaz, MD, of the department of cardiology at University Hospital, Vigo, Spain.
In this study, 94 patients with de novo coronary lesions in small diameter vessels were randomized to treatment with a paclitaxel drug coated balloon (DCB) (IN.PACT Falcon, Medtronic) or a zotarolimus drug-eluting stent (DES) (Resolute Integrity, Medtronic). Lesions in vessels between 2.0 and 2.75 mm in diameter were eligible; 137 lesions were treated in a study with seven participating centers in Spain.
For entry, target lesions had to have a stenosis of at least 70% by visual estimation or at least 50% by quantitative coronary angiography. Lesion length was limited to less than 25 mm, and severely calcified lesions were excluded.
The primary endpoint was a composite major adverse coronary event (MACE) endpoint of cardiac death, myocardial infarction, or revascularization at 12 months of follow-up. Crossovers by discretion of the interventional team were permitted.
At 12 months, MACE had occurred in 4.4% of those in the DCB group and 11.1% of those in the DES group. All primary endpoint events in both groups involved revascularizations. The two events in the DCB group were clinically driven target vessel revascularizations. Only one of the five events in the DES group was a clinically driven target lesion revascularization; the remaining four were revascularizations performed for nontarget vessels.
Four patients (8%) in the DCB group crossed over, each because of a dissection and managed with a bare-metal stent. There were four other dissections in the DCB group; one type F dissection resulted in a bailout and three dissections were managed conservatively. There were no crossovers in the DES group, and of the two dissections in the group, both were managed with the originally assigned stenting strategy.
Calling DCB a safe strategy for small de novo coronary stenosis, Dr. Jimenez Diaz said, “The procedural success rates were comparable.” However, he acknowledged that because of low enrollment, the study was “underpowered for clinical events.” The original power calculation called for a study of 200 patients.
“We can say results are encouraging,” Dr. Jimenez Diaz said.
Several discussants at the late-breaker abstracts agreed that DCB is an intriguing option for a difficult problem. They also agreed that restoring blood flow without leaving a permanent device is an attractive concept. However, they emphasized that a larger study is needed to declare that DCB and DES are equivalent strategies in regard to risk of MACE.
While agreeing that more data powered for events are needed, Cindy Grines, MD, chief of cardiology, Hofstra University, Hempstead, N.Y., was among those who suggested that this approach might be “worth a try.” She indicated that this study, which involved interventionalists at multiple centers, does provide support for the safety of DCB.
SOURCE: Jimenez Diaz VA. CRT 2018.
WASHINGTON – For treating de novo coronary lesions in vessels smaller than 2.75 mm, drug coated balloon angioplasty is as safe and may be as effective as drug-eluting stents, according to a multicenter randomized trial presented as a late-breaker at CRT 2018 sponsored by the Cardiovascular Research Institute at Washington Hospital Center.
“The aim of PCI [percutaneous coronary intervention] without leaving any metal behind seems to be feasible and safe with drug coated balloons,” reported Victor A. Jimenez Diaz, MD, of the department of cardiology at University Hospital, Vigo, Spain.
In this study, 94 patients with de novo coronary lesions in small diameter vessels were randomized to treatment with a paclitaxel drug coated balloon (DCB) (IN.PACT Falcon, Medtronic) or a zotarolimus drug-eluting stent (DES) (Resolute Integrity, Medtronic). Lesions in vessels between 2.0 and 2.75 mm in diameter were eligible; 137 lesions were treated in a study with seven participating centers in Spain.
For entry, target lesions had to have a stenosis of at least 70% by visual estimation or at least 50% by quantitative coronary angiography. Lesion length was limited to less than 25 mm, and severely calcified lesions were excluded.
The primary endpoint was a composite major adverse coronary event (MACE) endpoint of cardiac death, myocardial infarction, or revascularization at 12 months of follow-up. Crossovers by discretion of the interventional team were permitted.
At 12 months, MACE had occurred in 4.4% of those in the DCB group and 11.1% of those in the DES group. All primary endpoint events in both groups involved revascularizations. The two events in the DCB group were clinically driven target vessel revascularizations. Only one of the five events in the DES group was a clinically driven target lesion revascularization; the remaining four were revascularizations performed for nontarget vessels.
Four patients (8%) in the DCB group crossed over, each because of a dissection and managed with a bare-metal stent. There were four other dissections in the DCB group; one type F dissection resulted in a bailout and three dissections were managed conservatively. There were no crossovers in the DES group, and of the two dissections in the group, both were managed with the originally assigned stenting strategy.
Calling DCB a safe strategy for small de novo coronary stenosis, Dr. Jimenez Diaz said, “The procedural success rates were comparable.” However, he acknowledged that because of low enrollment, the study was “underpowered for clinical events.” The original power calculation called for a study of 200 patients.
“We can say results are encouraging,” Dr. Jimenez Diaz said.
Several discussants at the late-breaker abstracts agreed that DCB is an intriguing option for a difficult problem. They also agreed that restoring blood flow without leaving a permanent device is an attractive concept. However, they emphasized that a larger study is needed to declare that DCB and DES are equivalent strategies in regard to risk of MACE.
While agreeing that more data powered for events are needed, Cindy Grines, MD, chief of cardiology, Hofstra University, Hempstead, N.Y., was among those who suggested that this approach might be “worth a try.” She indicated that this study, which involved interventionalists at multiple centers, does provide support for the safety of DCB.
SOURCE: Jimenez Diaz VA. CRT 2018.
REPORTING FROM CRT 2018
Key clinical point: Drug-coated balloon stents were as safe and effective as drug-eluting stents for treatment of small de novo coronary lesions in a randomized trial.
Major finding: (4.4% vs. 11%).
Study details: A multicenter randomized trial.
Disclosures: Dr. Jimenez Diaz reports no potential conflicts of interest.
Source: Jimenez Diaz VA. CRT 2018.
Debris left after TAVR varies by device
WASHINGTON – All transcatheter aortic valve replacement devices generate debris into the bloodstream, including debris larger than 1 mm, but the amount of the debris differs between devices, according to a study based on collections from a cerebral embolic protection system.
“The quantity of the debris measured by different methods and techniques revealed more debris in patients receiving the Evolut R or Lotus TAVR [transcatheter aortic valve replacement] devices than in patients receiving a Sapien 3 or Sapien XT prosthesis,” reported Tobias Schmidt, MD, a cardiologist at Asklepios Klinik St. Georg, Hamburg, Germany.
Of the 246 patients, 145 (59%) received a Sapien 3 device, 40 (16%) received an Evolut R, 36 (14%) received a Lotus, and 25 (10%) received a Sapien XT. Particle features based on histopathological and histomorphological analyses were compared. A multivariate analysis was conducted to test for interaction with the amount of debris according to patient demographics and procedural characteristics, which differed for the devices evaluated.
Debris was captured in essentially all patients (99%) and with every TAVR device. On automated histomorphometry, the Lotus device had significantly higher median particle counts relative to the Evolut R (P = .004), the Sapien S3 (P less than .001), and the Sapien XT (P = .02) devices. When stratified by particle size, the Evolut R generated significantly more particles greater than 500 mcm than either the Sapien S3 or the Sapien XT (both P less than .05).
For particle sizes greater than 1 mm, there were significantly higher counts for both the Lotus and Evolut R (both P less than .05) relative to the Sapien S3, but Dr. Schmidt emphasized all devices generated at least some debris this size and that particles greater than 1 mm were retrieved from 53% of all patients. Similarly, when median total particle area was calculated by histomorphometry, the Lotus (P = .0007) and Evolut R (P = .0009) devices were more likely to have particles greater than 1 mm than the Sapien devices, but again, debris with a large total particle area was retrieved from at least some patients in all device groups.
There were significant differences in patient demographics and procedural characteristics by device. For example, patients receiving an Evolut R were significantly more likely than those receiving the Lotus or Sapien S3 valves to have undergone dilation prior to TAVR. Patients receiving the Sapien XT were significantly older than patients receiving any of the other valve types.
In an effort to control for these differences, “multivariate analysis was performed to text for interaction with the amount of debris captured,” Dr. Schmidt explained. “This analysis showed that transcatheter valve type was the only significant predictor for the morphometric findings.”
In this study, most of the debris was found to come from the vascular bed, but foreign body debris and debris from myocardium was also identified. One hypothesis for the greater debris from the Lotus and Evolut R devices is that these are positionable, raising the possibility that manipulation of the devices was the source of the debris, according to Dr. Schmidt. However, this hypothesis needs verification.
One message from this study is that “capture of debris is universal across different transcatheter valve types,” Dr. Schmidt said, adding that this “supports the benefit of using a CPS device in all TAVR procedures.”
Several commentators, including Jeffrey Popma, MD, director of the Interventional Cardiology Clinical Service at Beth Israel Deaconess Hospital, Boston, observed that it would be inappropriate to conclude that the greater debris observed in this study would necessarily translate into a difference in risk of embolic events for the devices evaluated with or without a CPS device. He and others emphasized no relationship to clinical risk was demonstrated in this study.
Dr. Schmidt reports no potential conflicts of interest.
SOURCE: Schmidt T et al. CROI 2018.
WASHINGTON – All transcatheter aortic valve replacement devices generate debris into the bloodstream, including debris larger than 1 mm, but the amount of the debris differs between devices, according to a study based on collections from a cerebral embolic protection system.
“The quantity of the debris measured by different methods and techniques revealed more debris in patients receiving the Evolut R or Lotus TAVR [transcatheter aortic valve replacement] devices than in patients receiving a Sapien 3 or Sapien XT prosthesis,” reported Tobias Schmidt, MD, a cardiologist at Asklepios Klinik St. Georg, Hamburg, Germany.
Of the 246 patients, 145 (59%) received a Sapien 3 device, 40 (16%) received an Evolut R, 36 (14%) received a Lotus, and 25 (10%) received a Sapien XT. Particle features based on histopathological and histomorphological analyses were compared. A multivariate analysis was conducted to test for interaction with the amount of debris according to patient demographics and procedural characteristics, which differed for the devices evaluated.
Debris was captured in essentially all patients (99%) and with every TAVR device. On automated histomorphometry, the Lotus device had significantly higher median particle counts relative to the Evolut R (P = .004), the Sapien S3 (P less than .001), and the Sapien XT (P = .02) devices. When stratified by particle size, the Evolut R generated significantly more particles greater than 500 mcm than either the Sapien S3 or the Sapien XT (both P less than .05).
For particle sizes greater than 1 mm, there were significantly higher counts for both the Lotus and Evolut R (both P less than .05) relative to the Sapien S3, but Dr. Schmidt emphasized all devices generated at least some debris this size and that particles greater than 1 mm were retrieved from 53% of all patients. Similarly, when median total particle area was calculated by histomorphometry, the Lotus (P = .0007) and Evolut R (P = .0009) devices were more likely to have particles greater than 1 mm than the Sapien devices, but again, debris with a large total particle area was retrieved from at least some patients in all device groups.
There were significant differences in patient demographics and procedural characteristics by device. For example, patients receiving an Evolut R were significantly more likely than those receiving the Lotus or Sapien S3 valves to have undergone dilation prior to TAVR. Patients receiving the Sapien XT were significantly older than patients receiving any of the other valve types.
In an effort to control for these differences, “multivariate analysis was performed to text for interaction with the amount of debris captured,” Dr. Schmidt explained. “This analysis showed that transcatheter valve type was the only significant predictor for the morphometric findings.”
In this study, most of the debris was found to come from the vascular bed, but foreign body debris and debris from myocardium was also identified. One hypothesis for the greater debris from the Lotus and Evolut R devices is that these are positionable, raising the possibility that manipulation of the devices was the source of the debris, according to Dr. Schmidt. However, this hypothesis needs verification.
One message from this study is that “capture of debris is universal across different transcatheter valve types,” Dr. Schmidt said, adding that this “supports the benefit of using a CPS device in all TAVR procedures.”
Several commentators, including Jeffrey Popma, MD, director of the Interventional Cardiology Clinical Service at Beth Israel Deaconess Hospital, Boston, observed that it would be inappropriate to conclude that the greater debris observed in this study would necessarily translate into a difference in risk of embolic events for the devices evaluated with or without a CPS device. He and others emphasized no relationship to clinical risk was demonstrated in this study.
Dr. Schmidt reports no potential conflicts of interest.
SOURCE: Schmidt T et al. CROI 2018.
WASHINGTON – All transcatheter aortic valve replacement devices generate debris into the bloodstream, including debris larger than 1 mm, but the amount of the debris differs between devices, according to a study based on collections from a cerebral embolic protection system.
“The quantity of the debris measured by different methods and techniques revealed more debris in patients receiving the Evolut R or Lotus TAVR [transcatheter aortic valve replacement] devices than in patients receiving a Sapien 3 or Sapien XT prosthesis,” reported Tobias Schmidt, MD, a cardiologist at Asklepios Klinik St. Georg, Hamburg, Germany.
Of the 246 patients, 145 (59%) received a Sapien 3 device, 40 (16%) received an Evolut R, 36 (14%) received a Lotus, and 25 (10%) received a Sapien XT. Particle features based on histopathological and histomorphological analyses were compared. A multivariate analysis was conducted to test for interaction with the amount of debris according to patient demographics and procedural characteristics, which differed for the devices evaluated.
Debris was captured in essentially all patients (99%) and with every TAVR device. On automated histomorphometry, the Lotus device had significantly higher median particle counts relative to the Evolut R (P = .004), the Sapien S3 (P less than .001), and the Sapien XT (P = .02) devices. When stratified by particle size, the Evolut R generated significantly more particles greater than 500 mcm than either the Sapien S3 or the Sapien XT (both P less than .05).
For particle sizes greater than 1 mm, there were significantly higher counts for both the Lotus and Evolut R (both P less than .05) relative to the Sapien S3, but Dr. Schmidt emphasized all devices generated at least some debris this size and that particles greater than 1 mm were retrieved from 53% of all patients. Similarly, when median total particle area was calculated by histomorphometry, the Lotus (P = .0007) and Evolut R (P = .0009) devices were more likely to have particles greater than 1 mm than the Sapien devices, but again, debris with a large total particle area was retrieved from at least some patients in all device groups.
There were significant differences in patient demographics and procedural characteristics by device. For example, patients receiving an Evolut R were significantly more likely than those receiving the Lotus or Sapien S3 valves to have undergone dilation prior to TAVR. Patients receiving the Sapien XT were significantly older than patients receiving any of the other valve types.
In an effort to control for these differences, “multivariate analysis was performed to text for interaction with the amount of debris captured,” Dr. Schmidt explained. “This analysis showed that transcatheter valve type was the only significant predictor for the morphometric findings.”
In this study, most of the debris was found to come from the vascular bed, but foreign body debris and debris from myocardium was also identified. One hypothesis for the greater debris from the Lotus and Evolut R devices is that these are positionable, raising the possibility that manipulation of the devices was the source of the debris, according to Dr. Schmidt. However, this hypothesis needs verification.
One message from this study is that “capture of debris is universal across different transcatheter valve types,” Dr. Schmidt said, adding that this “supports the benefit of using a CPS device in all TAVR procedures.”
Several commentators, including Jeffrey Popma, MD, director of the Interventional Cardiology Clinical Service at Beth Israel Deaconess Hospital, Boston, observed that it would be inappropriate to conclude that the greater debris observed in this study would necessarily translate into a difference in risk of embolic events for the devices evaluated with or without a CPS device. He and others emphasized no relationship to clinical risk was demonstrated in this study.
Dr. Schmidt reports no potential conflicts of interest.
SOURCE: Schmidt T et al. CROI 2018.
AT CRT 2018
Key clinical point: Based on a study with a cerebral embolic collection system, transcatheter aortic valve replacement devices generate unequal debris.
Major finding: .
Data source: Data analysis from two randomized trials.
Disclosures: Dr. Schmidt reports no potential conflicts of interest.
Source: Schmidt T et al. CROI 2018.
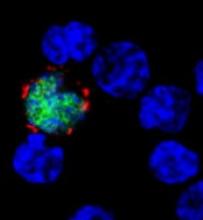
Mortality in patients with PTLD
LISBON—A review of recent studies has revealed a “significant burden” of mortality related to post-transplant lymphoproliferative disorder (PTLD), according to researchers.
Of the 120 PTLD patients studied, 64% died and 42.5% died with PTLD.
The median time from hematopoietic stem cell transplant (HSCT) to the development of PTLD was about 9 weeks in children and 11 weeks in adults.
The median time from PTLD diagnosis to death was about 6 weeks in adults and 8 weeks in children.
These findings were presented at 44th Annual Meeting of the EBMT (abstract A219).
The research was funded by Atara Biotherapeutics, Inc., which is developing tabelecleucel (formerly ATA129), a T-cell immunotherapy intended to treat patients with Epstein-Barr virus-associated PTLD who have failed treatment with rituximab.
The review included 9 articles, published in 2005 and later, detailing studies of patients who developed PTLD after HSCT.
There were 120 patients. They had a mean age of 28.97, 67% were male, and 79% had received rituximab.
The 31 pediatric patients had a mean age of 9.84, 81% were male, and 74% had received rituximab. The 89 adult patients had a mean age of 35.63, 62% were male, and 81% had received rituximab.
Among the 16 pediatric patients with available data, the median time from HSCT to PTLD diagnosis was 65 days, and the mean was 138 days.
For the 59 adults with available data, the median time from HSCT to PTLD was 76 days, and the mean was 132 days.
The all-cause mortality rate was 64% in the entire population (77/120), 71% in children (22/31), and 62% in adults (55/89).
Overall, 42.5% of patients (51/120) died with PTLD—35.5% of children (11/31) and 44.9% of adults (40/89).
Among the patients who died with PTLD, the median time from PTLD diagnosis to death was 55 days for children and 40 days for adults. The mean time from PTLD to death was 71 days and 51 days, respectively.
There were 110 patients with available overall survival data. The median survival time from PTLD diagnosis was 116 days in the entire cohort, 153 days in children, and 92 days in adults.
“Patients with PTLD following [HSCT] experience high mortality rates under the current standard of care due to aggressive disease that often rapidly progresses to death after diagnosis,” said Chris Haqq, MD, PhD, of Atara Biotherapeutics.
“Children and relatively young adults in their prime working years are disproportionately affected. Atara is dedicated to progressing tab‑cel™ development in the ongoing phase 3 clinical studies to potentially address the compelling medical need for patients with this life-threatening condition.”
LISBON—A review of recent studies has revealed a “significant burden” of mortality related to post-transplant lymphoproliferative disorder (PTLD), according to researchers.
Of the 120 PTLD patients studied, 64% died and 42.5% died with PTLD.
The median time from hematopoietic stem cell transplant (HSCT) to the development of PTLD was about 9 weeks in children and 11 weeks in adults.
The median time from PTLD diagnosis to death was about 6 weeks in adults and 8 weeks in children.
These findings were presented at 44th Annual Meeting of the EBMT (abstract A219).
The research was funded by Atara Biotherapeutics, Inc., which is developing tabelecleucel (formerly ATA129), a T-cell immunotherapy intended to treat patients with Epstein-Barr virus-associated PTLD who have failed treatment with rituximab.
The review included 9 articles, published in 2005 and later, detailing studies of patients who developed PTLD after HSCT.
There were 120 patients. They had a mean age of 28.97, 67% were male, and 79% had received rituximab.
The 31 pediatric patients had a mean age of 9.84, 81% were male, and 74% had received rituximab. The 89 adult patients had a mean age of 35.63, 62% were male, and 81% had received rituximab.
Among the 16 pediatric patients with available data, the median time from HSCT to PTLD diagnosis was 65 days, and the mean was 138 days.
For the 59 adults with available data, the median time from HSCT to PTLD was 76 days, and the mean was 132 days.
The all-cause mortality rate was 64% in the entire population (77/120), 71% in children (22/31), and 62% in adults (55/89).
Overall, 42.5% of patients (51/120) died with PTLD—35.5% of children (11/31) and 44.9% of adults (40/89).
Among the patients who died with PTLD, the median time from PTLD diagnosis to death was 55 days for children and 40 days for adults. The mean time from PTLD to death was 71 days and 51 days, respectively.
There were 110 patients with available overall survival data. The median survival time from PTLD diagnosis was 116 days in the entire cohort, 153 days in children, and 92 days in adults.
“Patients with PTLD following [HSCT] experience high mortality rates under the current standard of care due to aggressive disease that often rapidly progresses to death after diagnosis,” said Chris Haqq, MD, PhD, of Atara Biotherapeutics.
“Children and relatively young adults in their prime working years are disproportionately affected. Atara is dedicated to progressing tab‑cel™ development in the ongoing phase 3 clinical studies to potentially address the compelling medical need for patients with this life-threatening condition.”
LISBON—A review of recent studies has revealed a “significant burden” of mortality related to post-transplant lymphoproliferative disorder (PTLD), according to researchers.
Of the 120 PTLD patients studied, 64% died and 42.5% died with PTLD.
The median time from hematopoietic stem cell transplant (HSCT) to the development of PTLD was about 9 weeks in children and 11 weeks in adults.
The median time from PTLD diagnosis to death was about 6 weeks in adults and 8 weeks in children.
These findings were presented at 44th Annual Meeting of the EBMT (abstract A219).
The research was funded by Atara Biotherapeutics, Inc., which is developing tabelecleucel (formerly ATA129), a T-cell immunotherapy intended to treat patients with Epstein-Barr virus-associated PTLD who have failed treatment with rituximab.
The review included 9 articles, published in 2005 and later, detailing studies of patients who developed PTLD after HSCT.
There were 120 patients. They had a mean age of 28.97, 67% were male, and 79% had received rituximab.
The 31 pediatric patients had a mean age of 9.84, 81% were male, and 74% had received rituximab. The 89 adult patients had a mean age of 35.63, 62% were male, and 81% had received rituximab.
Among the 16 pediatric patients with available data, the median time from HSCT to PTLD diagnosis was 65 days, and the mean was 138 days.
For the 59 adults with available data, the median time from HSCT to PTLD was 76 days, and the mean was 132 days.
The all-cause mortality rate was 64% in the entire population (77/120), 71% in children (22/31), and 62% in adults (55/89).
Overall, 42.5% of patients (51/120) died with PTLD—35.5% of children (11/31) and 44.9% of adults (40/89).
Among the patients who died with PTLD, the median time from PTLD diagnosis to death was 55 days for children and 40 days for adults. The mean time from PTLD to death was 71 days and 51 days, respectively.
There were 110 patients with available overall survival data. The median survival time from PTLD diagnosis was 116 days in the entire cohort, 153 days in children, and 92 days in adults.
“Patients with PTLD following [HSCT] experience high mortality rates under the current standard of care due to aggressive disease that often rapidly progresses to death after diagnosis,” said Chris Haqq, MD, PhD, of Atara Biotherapeutics.
“Children and relatively young adults in their prime working years are disproportionately affected. Atara is dedicated to progressing tab‑cel™ development in the ongoing phase 3 clinical studies to potentially address the compelling medical need for patients with this life-threatening condition.”
Top hospital heart failure performance translates to longer survival
ORLANDO – Hospitals in the first quartile of short-term performance in treating heart failure patients had higher long-term survival rates for those patients, based on data from 317 hospitals that participated in a voluntary quality improvement program.
The burden of heart failure remains substantial in the United States, and health policies are increasingly focused on improving care for heart failure patients, said Ambarish Pandey, MD, of the University of Texas, Dallas, in a presentation at the annual meeting of the American College of Cardiology.
The researchers assessed hospital performance based on 30-day risk-standardized mortality rates (RSMR) in hospitals participating in the Get With the Guidelines–Heart Failure (GWTG-HF) registry, using a hierarchical, logistic regression model to calculate hospital-specific 30-day RSMRs.
Get With the Guidelines is a voluntary, observational quality improvement program that has been linked with CMS to capture long-term follow-up data, Dr. Pandey explained.
The study included 106,304 heart failure patients older than 65 years at 317 GWTG hospitals across the United States during 2005-2013. The hospitals were divided into performance quartiles based on 30-day RSMR. The 30-day RSMRs were 8.6%, 9.4%, 9.9%, and 10.7% in the first, second, third, and fourth quartiles, respectively.
There was a strong association between the top-performing hospitals and long-term survival rates for the patients that persisted beyond 30 days, said Dr. Pandey. The mortality rates after 5 years were 75.6%, 76.2%, 76.9%, and 79.6%, in the first, second, third, and fourth quartiles, respectively.
The hospitals in the first quartile were more likely than those in the fourth quartile to have primary percutaneous coronary intervention capabilities (80% vs. 73%), in-house cardiac surgery (66% vs. 57%), and a heart transplant center (13% vs. 2%).
In addition, the hospitals in the highest quartile had higher rates of adherence than those in the lowest quartile to guideline-directed heart failure therapies, including evidence-based beta-blocker use, ACE inhibitor and angiotensin receptor blocker use, postdischarge heart failure follow-up, implantable cardioverter defibrillator placement prior to discharge, and cardiac resynchronization therapy prior to discharge.The study was limited by a possible lack of generalizability to hospitals not participating in the GWTG program, Dr. Pandey said. In addition, “we cannot establish causation between hospital performance based on 30-day RSMR and long-term survival.”
However, the long-term survival advantage for heart failure patients treated at hospitals with the highest measures of short-term performance suggests that the 30-day RSMR could be used as an incentive for quality care and the improvement of long-term outcomes, he said.
Dr. Pandey had no financial conflicts to disclose. The Get With the Guidelines–Heart Failure program is supported by the American Heart Association, and has been previously funded by Medtronic, GlaxoSmithKline, Ortho-McNeil, and the AHA Pharmaceutical Roundtable. The findings were published simultaneously in JAMA Cardiology (2018 Mar 12. doi:10.1001/jamacardio.2018.0579).
SOURCE: Pandy A. ACC 2018.
ORLANDO – Hospitals in the first quartile of short-term performance in treating heart failure patients had higher long-term survival rates for those patients, based on data from 317 hospitals that participated in a voluntary quality improvement program.
The burden of heart failure remains substantial in the United States, and health policies are increasingly focused on improving care for heart failure patients, said Ambarish Pandey, MD, of the University of Texas, Dallas, in a presentation at the annual meeting of the American College of Cardiology.
The researchers assessed hospital performance based on 30-day risk-standardized mortality rates (RSMR) in hospitals participating in the Get With the Guidelines–Heart Failure (GWTG-HF) registry, using a hierarchical, logistic regression model to calculate hospital-specific 30-day RSMRs.
Get With the Guidelines is a voluntary, observational quality improvement program that has been linked with CMS to capture long-term follow-up data, Dr. Pandey explained.
The study included 106,304 heart failure patients older than 65 years at 317 GWTG hospitals across the United States during 2005-2013. The hospitals were divided into performance quartiles based on 30-day RSMR. The 30-day RSMRs were 8.6%, 9.4%, 9.9%, and 10.7% in the first, second, third, and fourth quartiles, respectively.
There was a strong association between the top-performing hospitals and long-term survival rates for the patients that persisted beyond 30 days, said Dr. Pandey. The mortality rates after 5 years were 75.6%, 76.2%, 76.9%, and 79.6%, in the first, second, third, and fourth quartiles, respectively.
The hospitals in the first quartile were more likely than those in the fourth quartile to have primary percutaneous coronary intervention capabilities (80% vs. 73%), in-house cardiac surgery (66% vs. 57%), and a heart transplant center (13% vs. 2%).
In addition, the hospitals in the highest quartile had higher rates of adherence than those in the lowest quartile to guideline-directed heart failure therapies, including evidence-based beta-blocker use, ACE inhibitor and angiotensin receptor blocker use, postdischarge heart failure follow-up, implantable cardioverter defibrillator placement prior to discharge, and cardiac resynchronization therapy prior to discharge.The study was limited by a possible lack of generalizability to hospitals not participating in the GWTG program, Dr. Pandey said. In addition, “we cannot establish causation between hospital performance based on 30-day RSMR and long-term survival.”
However, the long-term survival advantage for heart failure patients treated at hospitals with the highest measures of short-term performance suggests that the 30-day RSMR could be used as an incentive for quality care and the improvement of long-term outcomes, he said.
Dr. Pandey had no financial conflicts to disclose. The Get With the Guidelines–Heart Failure program is supported by the American Heart Association, and has been previously funded by Medtronic, GlaxoSmithKline, Ortho-McNeil, and the AHA Pharmaceutical Roundtable. The findings were published simultaneously in JAMA Cardiology (2018 Mar 12. doi:10.1001/jamacardio.2018.0579).
SOURCE: Pandy A. ACC 2018.
ORLANDO – Hospitals in the first quartile of short-term performance in treating heart failure patients had higher long-term survival rates for those patients, based on data from 317 hospitals that participated in a voluntary quality improvement program.
The burden of heart failure remains substantial in the United States, and health policies are increasingly focused on improving care for heart failure patients, said Ambarish Pandey, MD, of the University of Texas, Dallas, in a presentation at the annual meeting of the American College of Cardiology.
The researchers assessed hospital performance based on 30-day risk-standardized mortality rates (RSMR) in hospitals participating in the Get With the Guidelines–Heart Failure (GWTG-HF) registry, using a hierarchical, logistic regression model to calculate hospital-specific 30-day RSMRs.
Get With the Guidelines is a voluntary, observational quality improvement program that has been linked with CMS to capture long-term follow-up data, Dr. Pandey explained.
The study included 106,304 heart failure patients older than 65 years at 317 GWTG hospitals across the United States during 2005-2013. The hospitals were divided into performance quartiles based on 30-day RSMR. The 30-day RSMRs were 8.6%, 9.4%, 9.9%, and 10.7% in the first, second, third, and fourth quartiles, respectively.
There was a strong association between the top-performing hospitals and long-term survival rates for the patients that persisted beyond 30 days, said Dr. Pandey. The mortality rates after 5 years were 75.6%, 76.2%, 76.9%, and 79.6%, in the first, second, third, and fourth quartiles, respectively.
The hospitals in the first quartile were more likely than those in the fourth quartile to have primary percutaneous coronary intervention capabilities (80% vs. 73%), in-house cardiac surgery (66% vs. 57%), and a heart transplant center (13% vs. 2%).
In addition, the hospitals in the highest quartile had higher rates of adherence than those in the lowest quartile to guideline-directed heart failure therapies, including evidence-based beta-blocker use, ACE inhibitor and angiotensin receptor blocker use, postdischarge heart failure follow-up, implantable cardioverter defibrillator placement prior to discharge, and cardiac resynchronization therapy prior to discharge.The study was limited by a possible lack of generalizability to hospitals not participating in the GWTG program, Dr. Pandey said. In addition, “we cannot establish causation between hospital performance based on 30-day RSMR and long-term survival.”
However, the long-term survival advantage for heart failure patients treated at hospitals with the highest measures of short-term performance suggests that the 30-day RSMR could be used as an incentive for quality care and the improvement of long-term outcomes, he said.
Dr. Pandey had no financial conflicts to disclose. The Get With the Guidelines–Heart Failure program is supported by the American Heart Association, and has been previously funded by Medtronic, GlaxoSmithKline, Ortho-McNeil, and the AHA Pharmaceutical Roundtable. The findings were published simultaneously in JAMA Cardiology (2018 Mar 12. doi:10.1001/jamacardio.2018.0579).
SOURCE: Pandy A. ACC 2018.
REPORTING FROM ACC 2018
Key clinical point:
Major finding: Hospitals in the lowest quartile had a 22% higher 5-year mortality rate for heart failure patients compared with the highest quartile hospitals.
Study details: The data come from 106,304 heart failure patients admitted to 317 hospitals participating in a voluntary quality improvement program.
Disclosures: Dr. Pandey had no financial conflicts to disclose. The Get With the Guidelines–Heart Failure program is supported by the American Heart Association, and has been previously funded by Medtronic, GlaxoSmithKline, Ortho-McNeil, and the AHA Pharmaceutical Roundtable.
Source: Pandey A. ACC 2018.
Clinical pattern may help distinguish pediatric NMN from subungal melanoma
When longitudinal melanonychia appears as a sharply demarcated pigment band of even width against normal nail in a child, Hutchinson’s sign with longitudinal brushy pigmentation may be a useful clinical pattern suggesting a diagnosis of nail matrix nevus rather than subungual melanoma, said Jae Ho Lee, MD, of Sungkyunkwan University, Seoul, South Korea, and associates.
with 14 children having melanonychia greater than 20% the width of the nail, compared with 2 adults. Total melanonychia occurred just twice, in two children. A total of 12 children had nail dystrophy, while none of the adults did; nail dystrophy was more frequent in wider lesions.
Hutchinson’s sign was seen in seven pediatric patients, but no adult patients. In most cases, Hutchinson’s sign had hyponychial pigmentation, and on dermoscopy showed a pigment pattern presenting longitudinally and resembling a brush mark (longitudinal brushy pigmentation or LBP). LBP of nail matrix nevi is different from the Hutchinson’s sign that occurs in subungual melanoma (SUM), where it is typically a “haphazard pigmentation pattern involving periungual skin.
“We propose that Hutchinson’s sign occurs more commonly in pediatric NMN than in adult NMN, and that the presence of the LBP pattern can help distinguish pediatric NMN from SUM,” the investigators said.
Histologically, the biopsies of the NMN in this study showed some important differences from known SUM histology. All the study biopsies “showed a melanocytic proliferation exhibiting a predominantly nested growth pattern, with the nests mostly located at the dermoepithelial junction and with retraction artifact surrounding the nests. There were variable nuclear hyperchromatism, nuclear sizes, and cytologic atypia within the NMN biopsy specimens,” the researchers said. “In contrast, the histology of SUM demonstrates a predominance of atypical single melanocytes over nests, retraction artifacts around individual melanocytes, and uniform atypia of melanocytes throughout the biopsy specimen.”
SOURCE: Lee JH et al. J Am Acad Dermatol. 2018 Mar;78(3):479-89.
When longitudinal melanonychia appears as a sharply demarcated pigment band of even width against normal nail in a child, Hutchinson’s sign with longitudinal brushy pigmentation may be a useful clinical pattern suggesting a diagnosis of nail matrix nevus rather than subungual melanoma, said Jae Ho Lee, MD, of Sungkyunkwan University, Seoul, South Korea, and associates.
with 14 children having melanonychia greater than 20% the width of the nail, compared with 2 adults. Total melanonychia occurred just twice, in two children. A total of 12 children had nail dystrophy, while none of the adults did; nail dystrophy was more frequent in wider lesions.
Hutchinson’s sign was seen in seven pediatric patients, but no adult patients. In most cases, Hutchinson’s sign had hyponychial pigmentation, and on dermoscopy showed a pigment pattern presenting longitudinally and resembling a brush mark (longitudinal brushy pigmentation or LBP). LBP of nail matrix nevi is different from the Hutchinson’s sign that occurs in subungual melanoma (SUM), where it is typically a “haphazard pigmentation pattern involving periungual skin.
“We propose that Hutchinson’s sign occurs more commonly in pediatric NMN than in adult NMN, and that the presence of the LBP pattern can help distinguish pediatric NMN from SUM,” the investigators said.
Histologically, the biopsies of the NMN in this study showed some important differences from known SUM histology. All the study biopsies “showed a melanocytic proliferation exhibiting a predominantly nested growth pattern, with the nests mostly located at the dermoepithelial junction and with retraction artifact surrounding the nests. There were variable nuclear hyperchromatism, nuclear sizes, and cytologic atypia within the NMN biopsy specimens,” the researchers said. “In contrast, the histology of SUM demonstrates a predominance of atypical single melanocytes over nests, retraction artifacts around individual melanocytes, and uniform atypia of melanocytes throughout the biopsy specimen.”
SOURCE: Lee JH et al. J Am Acad Dermatol. 2018 Mar;78(3):479-89.
When longitudinal melanonychia appears as a sharply demarcated pigment band of even width against normal nail in a child, Hutchinson’s sign with longitudinal brushy pigmentation may be a useful clinical pattern suggesting a diagnosis of nail matrix nevus rather than subungual melanoma, said Jae Ho Lee, MD, of Sungkyunkwan University, Seoul, South Korea, and associates.
with 14 children having melanonychia greater than 20% the width of the nail, compared with 2 adults. Total melanonychia occurred just twice, in two children. A total of 12 children had nail dystrophy, while none of the adults did; nail dystrophy was more frequent in wider lesions.
Hutchinson’s sign was seen in seven pediatric patients, but no adult patients. In most cases, Hutchinson’s sign had hyponychial pigmentation, and on dermoscopy showed a pigment pattern presenting longitudinally and resembling a brush mark (longitudinal brushy pigmentation or LBP). LBP of nail matrix nevi is different from the Hutchinson’s sign that occurs in subungual melanoma (SUM), where it is typically a “haphazard pigmentation pattern involving periungual skin.
“We propose that Hutchinson’s sign occurs more commonly in pediatric NMN than in adult NMN, and that the presence of the LBP pattern can help distinguish pediatric NMN from SUM,” the investigators said.
Histologically, the biopsies of the NMN in this study showed some important differences from known SUM histology. All the study biopsies “showed a melanocytic proliferation exhibiting a predominantly nested growth pattern, with the nests mostly located at the dermoepithelial junction and with retraction artifact surrounding the nests. There were variable nuclear hyperchromatism, nuclear sizes, and cytologic atypia within the NMN biopsy specimens,” the researchers said. “In contrast, the histology of SUM demonstrates a predominance of atypical single melanocytes over nests, retraction artifacts around individual melanocytes, and uniform atypia of melanocytes throughout the biopsy specimen.”
SOURCE: Lee JH et al. J Am Acad Dermatol. 2018 Mar;78(3):479-89.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Psoriasis patients often have history of childhood trauma
reported Maria Luigia Crosta, of Catholic University of the Sacred Heart, Rome, and her associates.
Other studies have shown that among dermatologic disorders, psoriasis has the highest link to psychiatric illness such as mood, anxiety, and personality disorders, and that patients with psoriasis have an increased risk of suicidal ideation, the investigators said.
“Improving resilience with a multidisciplinary approach and an early psychological intervention could facilitate the management of psoriasis, by promoting the establishment of a stronger therapeutic alliance and a better acceptance of disease. Programs for psoriasis patients should focus on self-motivation and strengthening of self-efficacy,” Dr. Crosta and her associates concluded.
SOURCE: Crosta ML et al. J Psychosom Res. 2018;106:25-8.
reported Maria Luigia Crosta, of Catholic University of the Sacred Heart, Rome, and her associates.
Other studies have shown that among dermatologic disorders, psoriasis has the highest link to psychiatric illness such as mood, anxiety, and personality disorders, and that patients with psoriasis have an increased risk of suicidal ideation, the investigators said.
“Improving resilience with a multidisciplinary approach and an early psychological intervention could facilitate the management of psoriasis, by promoting the establishment of a stronger therapeutic alliance and a better acceptance of disease. Programs for psoriasis patients should focus on self-motivation and strengthening of self-efficacy,” Dr. Crosta and her associates concluded.
SOURCE: Crosta ML et al. J Psychosom Res. 2018;106:25-8.
reported Maria Luigia Crosta, of Catholic University of the Sacred Heart, Rome, and her associates.
Other studies have shown that among dermatologic disorders, psoriasis has the highest link to psychiatric illness such as mood, anxiety, and personality disorders, and that patients with psoriasis have an increased risk of suicidal ideation, the investigators said.
“Improving resilience with a multidisciplinary approach and an early psychological intervention could facilitate the management of psoriasis, by promoting the establishment of a stronger therapeutic alliance and a better acceptance of disease. Programs for psoriasis patients should focus on self-motivation and strengthening of self-efficacy,” Dr. Crosta and her associates concluded.
SOURCE: Crosta ML et al. J Psychosom Res. 2018;106:25-8.
FROM THE JOURNAL OF PSYCHOSOMATIC RESEARCH
Efavirenz-based ART may hamper vaginal ring contraception
BOSTON – Efavirenz-based antiretroviral therapy may significantly impair the effectiveness of vaginal ring contraceptives, investigators reported.
Over a 21-day period, levels of estrogen among women who used a vaginal ring (NuvaRing) while on efavirenz-based antiretroviral therapy (ART) were up to 79% lower, and levels of progestin were up to 57% lower, than in women with HIV infection who used the vaginal ring before starting ART, reported Kimberly K. Scarsi, PharmD, of the University of Nebraska, Omaha.
In contrast, women on an atazanavir-based ART regimen had lower estrogen levels than untreated controls who used a vaginal ring, but higher levels of progestin – the primary antiovulatory component of the ring – suggesting that it would retain contraceptive effectiveness, she said at the annual Conference on Retroviruses and Opportunistic Infections.
“In a broader context, these data can be applied to other drugs that behave similarly. So for example, erythromycins are also known to interfere with hormones in this way, as well as some anticonvulsant agents that may also impair the effectiveness of vaginal ring contraceptives,” she said at a brief, following her presentation of the data in an oral abstract session.
She noted that the findings have important implications for developers of vaginal rings designed to prevent HIV transmission as well as provide hormone-based contraception.
Dr. Scarsi and colleagues conducted a phase 2, international, nonrandomized, parallel pharmacokinetic study comparing levels of estrogen in the form of ethinyl estradiol (EE) and progestin in the form of etonogestrel among women with HIV infection who had not yet begun ART, as well as women on efavirenz- or atazanavir-based regimens.
Participants 16 years and older from centers in Africa, Asia, and North and South America were enrolled. The patients had to be willing to use a second, nonhormonal form of effective contraceptive, and if they were not on ART had to have CD4 cell counts of 350 cells/m3 or higher at screening. Participants on ART had to be on stable therapy for at least 30 days, and have HIV-1 RNA of 400 copies/mL or less.
A total of 25 control subjects, 25 women on efavirenz, and 24 on atazanavir were available for the primary pharmacokinetic analysis.
Over 21 days, EE levels among the efavirenz groups were 53%-57% lower than those of controls. Levels among the atazanavir groups were 29%-59% lower.
On days 7, 14, and 21, the EE geometric means ratios in efavirenz-treated patients versus controls were 0.47, 0.45, and 0.43, respectively (P less than .05 for each comparison).
In the atazanavir group, the EE geometric mean ratios versus controls at the same time points were 0.68 (P nonsignificant), 0.71 (P less than .05), and 0.65 (P less than .05).
For those in the efavirenz group, etonogestrel levels over 21 days were 76%-79% lower than in controls. In contrast, levels in the atazanavir group were 71%-79% higher than in controls.
The geometric mean ratios for the efavirenz group at 7, 14, and 21 days versus controls were 0.21, 0.22, and 0.24 (P less than .05 for all comparisons). In the atazanavir group, the respective geometric mean ratios were 1.71, 1.79, and 1.74 (P less than .05 for all comparisons).
Safety and tolerability of the ring, a secondary endpoint, was similar among the groups, with slightly more than one-fourth of participants in each arm having a mild adverse event, most commonly associated with abnormal vaginal discharge or menstrual irregularities such as spotting.
The investigators also looked at endogenous progesterone levels as a surrogate for ovulation. Although the ring’s package insert recommends to start using it within the first 5 days after the start of menses, the median enrollment time was 9 days after menses in all groups. Nonetheless, all participants in the control and atazanavir groups had undetectable progesterone values (less than 5 ng/mL) by day 14.
In contrast, among women in the efavirenz group, all women had undetectable progesterone values only at day 21.
The findings suggest that, when considering contraception and ART in HIV-infected women, developers of intravaginally administered drugs should consider systemic drug-drug interactions, because hormones released from a vaginal ring are extensively absorbed and act systemically. It is also important to consider local drug-drug interactions with the microbiome, because although it is known that dapivirine released from a vaginal ring can concentrate in the vaginal tract, possible interactions with the local microbiome, local drug transporters, and local drug-metabolizing enzymes are not known, Dr. Scarsi cautioned.
The study was supported by the National Institutes of Health. Merck provided the vaginal ring used in the study. Dr. Scarsi reported having no conflicts of interest to disclose.
SOURCE: Scarsi KK et al. CROI 2018, Abstract 141.
BOSTON – Efavirenz-based antiretroviral therapy may significantly impair the effectiveness of vaginal ring contraceptives, investigators reported.
Over a 21-day period, levels of estrogen among women who used a vaginal ring (NuvaRing) while on efavirenz-based antiretroviral therapy (ART) were up to 79% lower, and levels of progestin were up to 57% lower, than in women with HIV infection who used the vaginal ring before starting ART, reported Kimberly K. Scarsi, PharmD, of the University of Nebraska, Omaha.
In contrast, women on an atazanavir-based ART regimen had lower estrogen levels than untreated controls who used a vaginal ring, but higher levels of progestin – the primary antiovulatory component of the ring – suggesting that it would retain contraceptive effectiveness, she said at the annual Conference on Retroviruses and Opportunistic Infections.
“In a broader context, these data can be applied to other drugs that behave similarly. So for example, erythromycins are also known to interfere with hormones in this way, as well as some anticonvulsant agents that may also impair the effectiveness of vaginal ring contraceptives,” she said at a brief, following her presentation of the data in an oral abstract session.
She noted that the findings have important implications for developers of vaginal rings designed to prevent HIV transmission as well as provide hormone-based contraception.
Dr. Scarsi and colleagues conducted a phase 2, international, nonrandomized, parallel pharmacokinetic study comparing levels of estrogen in the form of ethinyl estradiol (EE) and progestin in the form of etonogestrel among women with HIV infection who had not yet begun ART, as well as women on efavirenz- or atazanavir-based regimens.
Participants 16 years and older from centers in Africa, Asia, and North and South America were enrolled. The patients had to be willing to use a second, nonhormonal form of effective contraceptive, and if they were not on ART had to have CD4 cell counts of 350 cells/m3 or higher at screening. Participants on ART had to be on stable therapy for at least 30 days, and have HIV-1 RNA of 400 copies/mL or less.
A total of 25 control subjects, 25 women on efavirenz, and 24 on atazanavir were available for the primary pharmacokinetic analysis.
Over 21 days, EE levels among the efavirenz groups were 53%-57% lower than those of controls. Levels among the atazanavir groups were 29%-59% lower.
On days 7, 14, and 21, the EE geometric means ratios in efavirenz-treated patients versus controls were 0.47, 0.45, and 0.43, respectively (P less than .05 for each comparison).
In the atazanavir group, the EE geometric mean ratios versus controls at the same time points were 0.68 (P nonsignificant), 0.71 (P less than .05), and 0.65 (P less than .05).
For those in the efavirenz group, etonogestrel levels over 21 days were 76%-79% lower than in controls. In contrast, levels in the atazanavir group were 71%-79% higher than in controls.
The geometric mean ratios for the efavirenz group at 7, 14, and 21 days versus controls were 0.21, 0.22, and 0.24 (P less than .05 for all comparisons). In the atazanavir group, the respective geometric mean ratios were 1.71, 1.79, and 1.74 (P less than .05 for all comparisons).
Safety and tolerability of the ring, a secondary endpoint, was similar among the groups, with slightly more than one-fourth of participants in each arm having a mild adverse event, most commonly associated with abnormal vaginal discharge or menstrual irregularities such as spotting.
The investigators also looked at endogenous progesterone levels as a surrogate for ovulation. Although the ring’s package insert recommends to start using it within the first 5 days after the start of menses, the median enrollment time was 9 days after menses in all groups. Nonetheless, all participants in the control and atazanavir groups had undetectable progesterone values (less than 5 ng/mL) by day 14.
In contrast, among women in the efavirenz group, all women had undetectable progesterone values only at day 21.
The findings suggest that, when considering contraception and ART in HIV-infected women, developers of intravaginally administered drugs should consider systemic drug-drug interactions, because hormones released from a vaginal ring are extensively absorbed and act systemically. It is also important to consider local drug-drug interactions with the microbiome, because although it is known that dapivirine released from a vaginal ring can concentrate in the vaginal tract, possible interactions with the local microbiome, local drug transporters, and local drug-metabolizing enzymes are not known, Dr. Scarsi cautioned.
The study was supported by the National Institutes of Health. Merck provided the vaginal ring used in the study. Dr. Scarsi reported having no conflicts of interest to disclose.
SOURCE: Scarsi KK et al. CROI 2018, Abstract 141.
BOSTON – Efavirenz-based antiretroviral therapy may significantly impair the effectiveness of vaginal ring contraceptives, investigators reported.
Over a 21-day period, levels of estrogen among women who used a vaginal ring (NuvaRing) while on efavirenz-based antiretroviral therapy (ART) were up to 79% lower, and levels of progestin were up to 57% lower, than in women with HIV infection who used the vaginal ring before starting ART, reported Kimberly K. Scarsi, PharmD, of the University of Nebraska, Omaha.
In contrast, women on an atazanavir-based ART regimen had lower estrogen levels than untreated controls who used a vaginal ring, but higher levels of progestin – the primary antiovulatory component of the ring – suggesting that it would retain contraceptive effectiveness, she said at the annual Conference on Retroviruses and Opportunistic Infections.
“In a broader context, these data can be applied to other drugs that behave similarly. So for example, erythromycins are also known to interfere with hormones in this way, as well as some anticonvulsant agents that may also impair the effectiveness of vaginal ring contraceptives,” she said at a brief, following her presentation of the data in an oral abstract session.
She noted that the findings have important implications for developers of vaginal rings designed to prevent HIV transmission as well as provide hormone-based contraception.
Dr. Scarsi and colleagues conducted a phase 2, international, nonrandomized, parallel pharmacokinetic study comparing levels of estrogen in the form of ethinyl estradiol (EE) and progestin in the form of etonogestrel among women with HIV infection who had not yet begun ART, as well as women on efavirenz- or atazanavir-based regimens.
Participants 16 years and older from centers in Africa, Asia, and North and South America were enrolled. The patients had to be willing to use a second, nonhormonal form of effective contraceptive, and if they were not on ART had to have CD4 cell counts of 350 cells/m3 or higher at screening. Participants on ART had to be on stable therapy for at least 30 days, and have HIV-1 RNA of 400 copies/mL or less.
A total of 25 control subjects, 25 women on efavirenz, and 24 on atazanavir were available for the primary pharmacokinetic analysis.
Over 21 days, EE levels among the efavirenz groups were 53%-57% lower than those of controls. Levels among the atazanavir groups were 29%-59% lower.
On days 7, 14, and 21, the EE geometric means ratios in efavirenz-treated patients versus controls were 0.47, 0.45, and 0.43, respectively (P less than .05 for each comparison).
In the atazanavir group, the EE geometric mean ratios versus controls at the same time points were 0.68 (P nonsignificant), 0.71 (P less than .05), and 0.65 (P less than .05).
For those in the efavirenz group, etonogestrel levels over 21 days were 76%-79% lower than in controls. In contrast, levels in the atazanavir group were 71%-79% higher than in controls.
The geometric mean ratios for the efavirenz group at 7, 14, and 21 days versus controls were 0.21, 0.22, and 0.24 (P less than .05 for all comparisons). In the atazanavir group, the respective geometric mean ratios were 1.71, 1.79, and 1.74 (P less than .05 for all comparisons).
Safety and tolerability of the ring, a secondary endpoint, was similar among the groups, with slightly more than one-fourth of participants in each arm having a mild adverse event, most commonly associated with abnormal vaginal discharge or menstrual irregularities such as spotting.
The investigators also looked at endogenous progesterone levels as a surrogate for ovulation. Although the ring’s package insert recommends to start using it within the first 5 days after the start of menses, the median enrollment time was 9 days after menses in all groups. Nonetheless, all participants in the control and atazanavir groups had undetectable progesterone values (less than 5 ng/mL) by day 14.
In contrast, among women in the efavirenz group, all women had undetectable progesterone values only at day 21.
The findings suggest that, when considering contraception and ART in HIV-infected women, developers of intravaginally administered drugs should consider systemic drug-drug interactions, because hormones released from a vaginal ring are extensively absorbed and act systemically. It is also important to consider local drug-drug interactions with the microbiome, because although it is known that dapivirine released from a vaginal ring can concentrate in the vaginal tract, possible interactions with the local microbiome, local drug transporters, and local drug-metabolizing enzymes are not known, Dr. Scarsi cautioned.
The study was supported by the National Institutes of Health. Merck provided the vaginal ring used in the study. Dr. Scarsi reported having no conflicts of interest to disclose.
SOURCE: Scarsi KK et al. CROI 2018, Abstract 141.
REPORTING FROM CROI 2018
Key clinical point:
Major finding: Estrogen exposure in women on efavirenz was 53%-57% lower than among controls.
Study details: A pharmacokinetic study in 74 HIV-infected women.
Disclosures: The study was supported by the National Institutes of Health. Merck provided the vaginal ring used in the study. Dr. Scarsi reported having no conflicts of interest to disclose.
Source: Scarsi KK et al. CROI 2018, Abstract 141.