User login
Gender affirmation surgery has become more common
, and private insurers and Medicare and Medicaid are covering more of them, according to a review of the National Inpatient Sample from 2000 to 2014.
“As coverage for these procedures increases, likely so will demand for qualified surgeons to perform them,” said investigators led by Joseph Canner, MHS, of Johns Hopkins University, Baltimore (JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231).
The team sought to correct a glaring lack of demographic, hospital, and surgical data on transgender people, a problem due mainly to “the absence of routine, standardized collection and reporting of gender identity in health care settings,” the investigators said.
The Affordable Care Act banned gender identity discrimination, and state and federal governments – as well as private insurers – are expanding coverage of gender affirmation surgery and care. Given the trend, it’s essential that quality improvement agencies begin to “focus on adopting a new set of patient-centered measures to better monitor transgender care and identify opportunities for advancing transition-related services,” the researchers said.
The team identified 37,827 hospital encounters in the national database that had ICD-9 diagnosis codes of transsexualism or gender identity disorder that were listed in the National Inpatient Sample. The rate of those codes increased from 3.87/100,000 patients in 2000 to 14.22 /100,000 patients in 2014.
Mental health was the leading cause of hospitalization, accounting for 40.5% of admissions, a finding that “is consistent with the high prevalence of depression, anxiety, and suicidal ideation in this population,” the investigators said.
Patients were a median age of 38 years old; 57.1% identified as white; and 54.3% were categorized as male, 38.3% as female, and most of the rest as “inconsistent,” meaning their sex in the medical record did not match their procedures.
Almost 11% were hospitalized for gender affirmation surgery, including penile or vaginal construction. From 2000 to 2005, 72% of patients who underwent affirmation procedures had genital surgery; the number increased to 83.9% from 2006 to 2011. More than half of the patients weren’t covered by insurance, but the number covered by Medicare or Medicaid increased from 25 patients in 2012-2013 to 70 in 2014. Meanwhile, no one died in the hospital from gender reassignment surgery, and the median stay was 4 days.
“Our data suggest that genital surgery is the most common type of inpatient gender-affirming surgery; however, these data do not include gender-affirming surgical procedures performed in outpatient settings, which likely include most chest, breast, and facial surgery,” the investigators wrote.
Surgery patients in high-volume centers (performing more than 50 gender-affirming procedures per year) were mostly self-pay, while those admitted to low-volume centers were not. “It is possible that self-paying patients may be getting higher-quality care at high-volume centers, as has been observed in other types of surgery,” according to the investigators. There is a need for national clinical and patient-reported outcomes data to assess and improve the quality of gender-affirming surgery. Gender identity information should be a part of all electronic health records and reported back to national data repositories, they said.
The investigators are supported by the Patient-Centered Outcomes Research Institute, the Agency for Healthcare Research and Quality, and the National Institutes of Health, among others. They had no industry disclosures.
SOURCE: Canner JK et al. JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231.
The study is thought provoking and suggests many areas for future study.
Gender-affirming surgery is the final step in a spectrum of treatments for gender identity disorders or transsexualism, including psychological counseling, hormonal therapies, and pubertal hormone blockers. Referrals for these treatments are increasing, and likely the demand for surgical treatment will also continue to increase.
A comprehensive database or other prospective tool to assess the comparative efficacy of these treatments, create quality metrics, and address long-term health or psychiatric outcomes should be pursued.
Future research must address cost effectiveness and cost burdens, given increased public funding for gender affirmation surgeries. Most longitudinal studies of patients who have undergone gender affirmation procedures have found high satisfaction rates with low rates of regret (less than 5%). However, when regret occurs, it can be surgically challenging and costly to reverse these procedures.
Marie Crandall , MD, is a professor of surgery at the University of Florida, Jacksonville. She made her comments in an editorial and had no industry disclosures (JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6232).
The study is thought provoking and suggests many areas for future study.
Gender-affirming surgery is the final step in a spectrum of treatments for gender identity disorders or transsexualism, including psychological counseling, hormonal therapies, and pubertal hormone blockers. Referrals for these treatments are increasing, and likely the demand for surgical treatment will also continue to increase.
A comprehensive database or other prospective tool to assess the comparative efficacy of these treatments, create quality metrics, and address long-term health or psychiatric outcomes should be pursued.
Future research must address cost effectiveness and cost burdens, given increased public funding for gender affirmation surgeries. Most longitudinal studies of patients who have undergone gender affirmation procedures have found high satisfaction rates with low rates of regret (less than 5%). However, when regret occurs, it can be surgically challenging and costly to reverse these procedures.
Marie Crandall , MD, is a professor of surgery at the University of Florida, Jacksonville. She made her comments in an editorial and had no industry disclosures (JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6232).
The study is thought provoking and suggests many areas for future study.
Gender-affirming surgery is the final step in a spectrum of treatments for gender identity disorders or transsexualism, including psychological counseling, hormonal therapies, and pubertal hormone blockers. Referrals for these treatments are increasing, and likely the demand for surgical treatment will also continue to increase.
A comprehensive database or other prospective tool to assess the comparative efficacy of these treatments, create quality metrics, and address long-term health or psychiatric outcomes should be pursued.
Future research must address cost effectiveness and cost burdens, given increased public funding for gender affirmation surgeries. Most longitudinal studies of patients who have undergone gender affirmation procedures have found high satisfaction rates with low rates of regret (less than 5%). However, when regret occurs, it can be surgically challenging and costly to reverse these procedures.
Marie Crandall , MD, is a professor of surgery at the University of Florida, Jacksonville. She made her comments in an editorial and had no industry disclosures (JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6232).
, and private insurers and Medicare and Medicaid are covering more of them, according to a review of the National Inpatient Sample from 2000 to 2014.
“As coverage for these procedures increases, likely so will demand for qualified surgeons to perform them,” said investigators led by Joseph Canner, MHS, of Johns Hopkins University, Baltimore (JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231).
The team sought to correct a glaring lack of demographic, hospital, and surgical data on transgender people, a problem due mainly to “the absence of routine, standardized collection and reporting of gender identity in health care settings,” the investigators said.
The Affordable Care Act banned gender identity discrimination, and state and federal governments – as well as private insurers – are expanding coverage of gender affirmation surgery and care. Given the trend, it’s essential that quality improvement agencies begin to “focus on adopting a new set of patient-centered measures to better monitor transgender care and identify opportunities for advancing transition-related services,” the researchers said.
The team identified 37,827 hospital encounters in the national database that had ICD-9 diagnosis codes of transsexualism or gender identity disorder that were listed in the National Inpatient Sample. The rate of those codes increased from 3.87/100,000 patients in 2000 to 14.22 /100,000 patients in 2014.
Mental health was the leading cause of hospitalization, accounting for 40.5% of admissions, a finding that “is consistent with the high prevalence of depression, anxiety, and suicidal ideation in this population,” the investigators said.
Patients were a median age of 38 years old; 57.1% identified as white; and 54.3% were categorized as male, 38.3% as female, and most of the rest as “inconsistent,” meaning their sex in the medical record did not match their procedures.
Almost 11% were hospitalized for gender affirmation surgery, including penile or vaginal construction. From 2000 to 2005, 72% of patients who underwent affirmation procedures had genital surgery; the number increased to 83.9% from 2006 to 2011. More than half of the patients weren’t covered by insurance, but the number covered by Medicare or Medicaid increased from 25 patients in 2012-2013 to 70 in 2014. Meanwhile, no one died in the hospital from gender reassignment surgery, and the median stay was 4 days.
“Our data suggest that genital surgery is the most common type of inpatient gender-affirming surgery; however, these data do not include gender-affirming surgical procedures performed in outpatient settings, which likely include most chest, breast, and facial surgery,” the investigators wrote.
Surgery patients in high-volume centers (performing more than 50 gender-affirming procedures per year) were mostly self-pay, while those admitted to low-volume centers were not. “It is possible that self-paying patients may be getting higher-quality care at high-volume centers, as has been observed in other types of surgery,” according to the investigators. There is a need for national clinical and patient-reported outcomes data to assess and improve the quality of gender-affirming surgery. Gender identity information should be a part of all electronic health records and reported back to national data repositories, they said.
The investigators are supported by the Patient-Centered Outcomes Research Institute, the Agency for Healthcare Research and Quality, and the National Institutes of Health, among others. They had no industry disclosures.
SOURCE: Canner JK et al. JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231.
, and private insurers and Medicare and Medicaid are covering more of them, according to a review of the National Inpatient Sample from 2000 to 2014.
“As coverage for these procedures increases, likely so will demand for qualified surgeons to perform them,” said investigators led by Joseph Canner, MHS, of Johns Hopkins University, Baltimore (JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231).
The team sought to correct a glaring lack of demographic, hospital, and surgical data on transgender people, a problem due mainly to “the absence of routine, standardized collection and reporting of gender identity in health care settings,” the investigators said.
The Affordable Care Act banned gender identity discrimination, and state and federal governments – as well as private insurers – are expanding coverage of gender affirmation surgery and care. Given the trend, it’s essential that quality improvement agencies begin to “focus on adopting a new set of patient-centered measures to better monitor transgender care and identify opportunities for advancing transition-related services,” the researchers said.
The team identified 37,827 hospital encounters in the national database that had ICD-9 diagnosis codes of transsexualism or gender identity disorder that were listed in the National Inpatient Sample. The rate of those codes increased from 3.87/100,000 patients in 2000 to 14.22 /100,000 patients in 2014.
Mental health was the leading cause of hospitalization, accounting for 40.5% of admissions, a finding that “is consistent with the high prevalence of depression, anxiety, and suicidal ideation in this population,” the investigators said.
Patients were a median age of 38 years old; 57.1% identified as white; and 54.3% were categorized as male, 38.3% as female, and most of the rest as “inconsistent,” meaning their sex in the medical record did not match their procedures.
Almost 11% were hospitalized for gender affirmation surgery, including penile or vaginal construction. From 2000 to 2005, 72% of patients who underwent affirmation procedures had genital surgery; the number increased to 83.9% from 2006 to 2011. More than half of the patients weren’t covered by insurance, but the number covered by Medicare or Medicaid increased from 25 patients in 2012-2013 to 70 in 2014. Meanwhile, no one died in the hospital from gender reassignment surgery, and the median stay was 4 days.
“Our data suggest that genital surgery is the most common type of inpatient gender-affirming surgery; however, these data do not include gender-affirming surgical procedures performed in outpatient settings, which likely include most chest, breast, and facial surgery,” the investigators wrote.
Surgery patients in high-volume centers (performing more than 50 gender-affirming procedures per year) were mostly self-pay, while those admitted to low-volume centers were not. “It is possible that self-paying patients may be getting higher-quality care at high-volume centers, as has been observed in other types of surgery,” according to the investigators. There is a need for national clinical and patient-reported outcomes data to assess and improve the quality of gender-affirming surgery. Gender identity information should be a part of all electronic health records and reported back to national data repositories, they said.
The investigators are supported by the Patient-Centered Outcomes Research Institute, the Agency for Healthcare Research and Quality, and the National Institutes of Health, among others. They had no industry disclosures.
SOURCE: Canner JK et al. JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231.
FROM JAMA SURGERY
Key clinical point: With gender affirmation surgeries on the rise in the United States, it’s time for a more rigorous system to track outcomes.
Major finding: The rate of transsexual and gender identity disorder codes in the National Inpatient Sample increased from 3.87/100,000 patients in 2000 to 14.22/100,000 patients in 2014.
Study details: A review of 37,827 hospital encounters reported in the National Inpatient Sample.
Disclosures: The investigators are supported by the Patient-Centered Outcomes Research Institute, the Agency for Healthcare Research and Quality, and the National Institutes of Health, among others. They had no industry disclosures.
Source: Canner JK et al. JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231.
DDSEP® 8 Quick Quiz - March 2018 Question 1
Q1. Correct answer: C
Rationale
The initial management of dyspepsia depends on symptoms and presence of any “alarm features.” In patients without “alarm features” presenting with symptoms suggestive of hepatobiliary or pancreatic causes, the initial diagnostic tests should include liver/pancreatic blood tests and abdominal imaging. For other dyspeptic patients without alarm features, initial management would include H. pylori testing (breath, stool antigen, or antibody) and/or empiric antisecretory (PPI) therapy. However, for patients who present with “alarm features” such as dysphagia, anemia, GI bleeding, anorexia, significant weight loss, etc., an upper endoscopy should be performed to evaluate for the presence of any upper GI tract malignancy. In this patient, the presence of microcytic anemia is an alarm feature. Tricyclic antidepressants such as amitriptyline may be used as treatment for functional dyspepsia, after organic causes have been ruled out.
Reference
1. Talley N.J., Vakil N.B., Moayyedi P. American Gastroenterological Association technical review on the evaluation of dyspepsia. Gastroenterology 2005;129:1756-80.
Q1. Correct answer: C
Rationale
The initial management of dyspepsia depends on symptoms and presence of any “alarm features.” In patients without “alarm features” presenting with symptoms suggestive of hepatobiliary or pancreatic causes, the initial diagnostic tests should include liver/pancreatic blood tests and abdominal imaging. For other dyspeptic patients without alarm features, initial management would include H. pylori testing (breath, stool antigen, or antibody) and/or empiric antisecretory (PPI) therapy. However, for patients who present with “alarm features” such as dysphagia, anemia, GI bleeding, anorexia, significant weight loss, etc., an upper endoscopy should be performed to evaluate for the presence of any upper GI tract malignancy. In this patient, the presence of microcytic anemia is an alarm feature. Tricyclic antidepressants such as amitriptyline may be used as treatment for functional dyspepsia, after organic causes have been ruled out.
Reference
1. Talley N.J., Vakil N.B., Moayyedi P. American Gastroenterological Association technical review on the evaluation of dyspepsia. Gastroenterology 2005;129:1756-80.
Q1. Correct answer: C
Rationale
The initial management of dyspepsia depends on symptoms and presence of any “alarm features.” In patients without “alarm features” presenting with symptoms suggestive of hepatobiliary or pancreatic causes, the initial diagnostic tests should include liver/pancreatic blood tests and abdominal imaging. For other dyspeptic patients without alarm features, initial management would include H. pylori testing (breath, stool antigen, or antibody) and/or empiric antisecretory (PPI) therapy. However, for patients who present with “alarm features” such as dysphagia, anemia, GI bleeding, anorexia, significant weight loss, etc., an upper endoscopy should be performed to evaluate for the presence of any upper GI tract malignancy. In this patient, the presence of microcytic anemia is an alarm feature. Tricyclic antidepressants such as amitriptyline may be used as treatment for functional dyspepsia, after organic causes have been ruled out.
Reference
1. Talley N.J., Vakil N.B., Moayyedi P. American Gastroenterological Association technical review on the evaluation of dyspepsia. Gastroenterology 2005;129:1756-80.
A 37-year-old man with no significant past medical history presents with a dull, nonradiating epigastric pain for 3 months. The pain is not associated with eating or positional changes. He denies any heartburn, regurgitation, chest pain, nausea, vomiting, dysphagia, odynophagia, or weight loss. He currently does not take any medications or supplements. Social and family history are not significant. Physical examination reveals minimal tenderness to deep palpation in the epigastrum, but otherwise it is unremarkable. A complete blood count reveals a white blood cell count of 6, hemoglobin 10 g/dL, MCV 72 fL, and platelet count of 200 x 103/mcL. What is the most important next step of management?
Survey Highlights Challenges in Asian Americans With Stroke
LOS ANGELES—A large survey of Asian Americans suggests that the group experiences more severe ischemic strokes and is less likely to receive IV t-PA than white patients, according to research presented at the International Stroke Conference 2018. Investigators also found that stroke severity declined for whites between 2004 and 2016, but not for Asian Americans.
The research encompassed all self-identified Asian Americans in the Get With the Guidelines stroke database, which is a voluntary quality improvement program begun by the American Heart Association in 2003. The analysis included 64,337 Asian Americans and 1,707,962 white Americans at 2,171 hospitals nationwide that participated in the program from 2004 to 2016.
Largest Analysis of Asian Americans With Stroke
“There have been some limited studies, and studies in Asia, but this is the largest analysis of Asian-American stroke patients,” said Sarah Song, MD, Assistant Professor of Neurology at Rush University Medical Center in Chicago. “I think the most important finding is that they are not getting as much t-PA and [are] having more t-PA complications, such as bleeding more. I think it gives it an urgency that maybe was lacking, an urgency that we really need to address this issue by finding
One particular finding suggested a need for better education among Asian American communities. Asian Americans were less likely than whites to report a clinical history of having heightened levels of low-density lipoproteins (LDL). Asian Americans “did not know that they had high cholesterol, but they had a higher LDL [cholesterol level] than Caucasians on average,” said Dr. Song. The mean LDL cholesterol value was 101 mg/dL in Asian Americans, compared with 95 mg/dL in white patients, which was a statistically significant difference, said the researchers.
In addition, white patients had higher rates of atrial fibrillation (21.2% vs 16.0%), coronary artery disease (27.8% vs 17.5%), and stenosis (4.7% vs 2.0%), while Asian Americans were more likely to have diabetes (38.0% vs 29.2%). Severe strokes (defined as an NIH Stroke Scale score of 16 or greater) were more common among Asian Americans (odds ratio [OR], 1.35) than whites. After adjusting for stroke severity, the researchers found that Asian Americans were less likely to receive t-PA (OR, 0.90) and more likely to experience symptomatic intracerebral hemorrhage within 36 hours of receiving t-PA (OR, 1.23). “I think that may have something to do with the pathophysiology … that we do not quite understand yet, but we can see there is a problem,” Dr. Song said.
Although in-hospital mortality initially appeared to be higher among Asian Americans, this trend was reversed after researchers corrected the analysis for stroke severity, which suggested better outcome for Asian Americans (OR, 0.95). Some quality-of-care measures also favored Asian Americans, including receipt of stroke education (OR, 1.08), receipt of IV t-PA within 60 minutes of arrival (OR, 1.14), LDL cholesterol documentation (OR, 1.19), and receipt of intensive statin therapy (OR, 1.15). Asian Americans were less likely to receive a CT scan within 25 minutes of arrival, however (OR, 0.92).
Between 2004 and 2016, both groups benefited from similar improvements, but not in the same ways. In 2016, a stroke in a white patient was less likely to be severe than in 2004 (OR, 0.97), while there was no change in Asian Americans (OR, 1.00).
Study Limitations
One study limitation was that participation in the database was voluntary, which could lead to selection bias. Another limitation was that all Asian Americans were combined into one group. Stroke pathophysiology and outcomes may vary between Asian countries.
Still, the study suggests challenges that must be addressed. “I think it highlights the problem that Asian ischemic stroke patients do not do as well, they bleed more, and they receive less t-PA,” said Dr. Song.
—Jim Kling
LOS ANGELES—A large survey of Asian Americans suggests that the group experiences more severe ischemic strokes and is less likely to receive IV t-PA than white patients, according to research presented at the International Stroke Conference 2018. Investigators also found that stroke severity declined for whites between 2004 and 2016, but not for Asian Americans.
The research encompassed all self-identified Asian Americans in the Get With the Guidelines stroke database, which is a voluntary quality improvement program begun by the American Heart Association in 2003. The analysis included 64,337 Asian Americans and 1,707,962 white Americans at 2,171 hospitals nationwide that participated in the program from 2004 to 2016.
Largest Analysis of Asian Americans With Stroke
“There have been some limited studies, and studies in Asia, but this is the largest analysis of Asian-American stroke patients,” said Sarah Song, MD, Assistant Professor of Neurology at Rush University Medical Center in Chicago. “I think the most important finding is that they are not getting as much t-PA and [are] having more t-PA complications, such as bleeding more. I think it gives it an urgency that maybe was lacking, an urgency that we really need to address this issue by finding
One particular finding suggested a need for better education among Asian American communities. Asian Americans were less likely than whites to report a clinical history of having heightened levels of low-density lipoproteins (LDL). Asian Americans “did not know that they had high cholesterol, but they had a higher LDL [cholesterol level] than Caucasians on average,” said Dr. Song. The mean LDL cholesterol value was 101 mg/dL in Asian Americans, compared with 95 mg/dL in white patients, which was a statistically significant difference, said the researchers.
In addition, white patients had higher rates of atrial fibrillation (21.2% vs 16.0%), coronary artery disease (27.8% vs 17.5%), and stenosis (4.7% vs 2.0%), while Asian Americans were more likely to have diabetes (38.0% vs 29.2%). Severe strokes (defined as an NIH Stroke Scale score of 16 or greater) were more common among Asian Americans (odds ratio [OR], 1.35) than whites. After adjusting for stroke severity, the researchers found that Asian Americans were less likely to receive t-PA (OR, 0.90) and more likely to experience symptomatic intracerebral hemorrhage within 36 hours of receiving t-PA (OR, 1.23). “I think that may have something to do with the pathophysiology … that we do not quite understand yet, but we can see there is a problem,” Dr. Song said.
Although in-hospital mortality initially appeared to be higher among Asian Americans, this trend was reversed after researchers corrected the analysis for stroke severity, which suggested better outcome for Asian Americans (OR, 0.95). Some quality-of-care measures also favored Asian Americans, including receipt of stroke education (OR, 1.08), receipt of IV t-PA within 60 minutes of arrival (OR, 1.14), LDL cholesterol documentation (OR, 1.19), and receipt of intensive statin therapy (OR, 1.15). Asian Americans were less likely to receive a CT scan within 25 minutes of arrival, however (OR, 0.92).
Between 2004 and 2016, both groups benefited from similar improvements, but not in the same ways. In 2016, a stroke in a white patient was less likely to be severe than in 2004 (OR, 0.97), while there was no change in Asian Americans (OR, 1.00).
Study Limitations
One study limitation was that participation in the database was voluntary, which could lead to selection bias. Another limitation was that all Asian Americans were combined into one group. Stroke pathophysiology and outcomes may vary between Asian countries.
Still, the study suggests challenges that must be addressed. “I think it highlights the problem that Asian ischemic stroke patients do not do as well, they bleed more, and they receive less t-PA,” said Dr. Song.
—Jim Kling
LOS ANGELES—A large survey of Asian Americans suggests that the group experiences more severe ischemic strokes and is less likely to receive IV t-PA than white patients, according to research presented at the International Stroke Conference 2018. Investigators also found that stroke severity declined for whites between 2004 and 2016, but not for Asian Americans.
The research encompassed all self-identified Asian Americans in the Get With the Guidelines stroke database, which is a voluntary quality improvement program begun by the American Heart Association in 2003. The analysis included 64,337 Asian Americans and 1,707,962 white Americans at 2,171 hospitals nationwide that participated in the program from 2004 to 2016.
Largest Analysis of Asian Americans With Stroke
“There have been some limited studies, and studies in Asia, but this is the largest analysis of Asian-American stroke patients,” said Sarah Song, MD, Assistant Professor of Neurology at Rush University Medical Center in Chicago. “I think the most important finding is that they are not getting as much t-PA and [are] having more t-PA complications, such as bleeding more. I think it gives it an urgency that maybe was lacking, an urgency that we really need to address this issue by finding
One particular finding suggested a need for better education among Asian American communities. Asian Americans were less likely than whites to report a clinical history of having heightened levels of low-density lipoproteins (LDL). Asian Americans “did not know that they had high cholesterol, but they had a higher LDL [cholesterol level] than Caucasians on average,” said Dr. Song. The mean LDL cholesterol value was 101 mg/dL in Asian Americans, compared with 95 mg/dL in white patients, which was a statistically significant difference, said the researchers.
In addition, white patients had higher rates of atrial fibrillation (21.2% vs 16.0%), coronary artery disease (27.8% vs 17.5%), and stenosis (4.7% vs 2.0%), while Asian Americans were more likely to have diabetes (38.0% vs 29.2%). Severe strokes (defined as an NIH Stroke Scale score of 16 or greater) were more common among Asian Americans (odds ratio [OR], 1.35) than whites. After adjusting for stroke severity, the researchers found that Asian Americans were less likely to receive t-PA (OR, 0.90) and more likely to experience symptomatic intracerebral hemorrhage within 36 hours of receiving t-PA (OR, 1.23). “I think that may have something to do with the pathophysiology … that we do not quite understand yet, but we can see there is a problem,” Dr. Song said.
Although in-hospital mortality initially appeared to be higher among Asian Americans, this trend was reversed after researchers corrected the analysis for stroke severity, which suggested better outcome for Asian Americans (OR, 0.95). Some quality-of-care measures also favored Asian Americans, including receipt of stroke education (OR, 1.08), receipt of IV t-PA within 60 minutes of arrival (OR, 1.14), LDL cholesterol documentation (OR, 1.19), and receipt of intensive statin therapy (OR, 1.15). Asian Americans were less likely to receive a CT scan within 25 minutes of arrival, however (OR, 0.92).
Between 2004 and 2016, both groups benefited from similar improvements, but not in the same ways. In 2016, a stroke in a white patient was less likely to be severe than in 2004 (OR, 0.97), while there was no change in Asian Americans (OR, 1.00).
Study Limitations
One study limitation was that participation in the database was voluntary, which could lead to selection bias. Another limitation was that all Asian Americans were combined into one group. Stroke pathophysiology and outcomes may vary between Asian countries.
Still, the study suggests challenges that must be addressed. “I think it highlights the problem that Asian ischemic stroke patients do not do as well, they bleed more, and they receive less t-PA,” said Dr. Song.
—Jim Kling
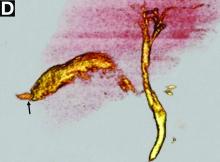
Clinical Challenges - March 2018 What's your diagnosis?
The diagnosis: Spontaneous gallbladder perforation
References
1. Ausania, F., Guzman Suarez, S., Alvarez Garcia, H. et al. Gallbladder perforation: morbidity, mortality and preoperative risk prediction. Surg Endosc. 2015;29:955-60.
2. Niemeier, O.W. Acute free perforation of the gall-bladder. Ann Surg. 1934;99:922-4.
3. Hyodo, T., Kumano, S., Kushihata, F. et al. CT and MR cholangiography: advantages and pitfalls in perioperative evaluation of biliary tree. Br J Radiol. 2012;85:887-96.
The diagnosis: Spontaneous gallbladder perforation
References
1. Ausania, F., Guzman Suarez, S., Alvarez Garcia, H. et al. Gallbladder perforation: morbidity, mortality and preoperative risk prediction. Surg Endosc. 2015;29:955-60.
2. Niemeier, O.W. Acute free perforation of the gall-bladder. Ann Surg. 1934;99:922-4.
3. Hyodo, T., Kumano, S., Kushihata, F. et al. CT and MR cholangiography: advantages and pitfalls in perioperative evaluation of biliary tree. Br J Radiol. 2012;85:887-96.
The diagnosis: Spontaneous gallbladder perforation
References
1. Ausania, F., Guzman Suarez, S., Alvarez Garcia, H. et al. Gallbladder perforation: morbidity, mortality and preoperative risk prediction. Surg Endosc. 2015;29:955-60.
2. Niemeier, O.W. Acute free perforation of the gall-bladder. Ann Surg. 1934;99:922-4.
3. Hyodo, T., Kumano, S., Kushihata, F. et al. CT and MR cholangiography: advantages and pitfalls in perioperative evaluation of biliary tree. Br J Radiol. 2012;85:887-96.
Published previously in Gastroenterology (2016;151[1]:40-2).
What is your diagnosis and treatment?
Can Online Patient Journals Improve MS Care?
SAN DIEGO—Continuous collection of patient-reported outcomes via a web-based platform may help neurologists identify patients with multiple sclerosis (MS) with active disease who would benefit from additional care coordination, according to a study described at the ACTRIMS 2018 Forum.
MS has a “variable and unpredictable disease course,” said Alexis Ahmad, Director of Clinical Trials for the Georgetown University Department of Neurology in Washington, DC, and colleagues. “Given the chronic and complex nature of MS, patients living with this disease require continuous and specialized care.”
The MS and Neuroimmunology Center at Georgetown University aims to become the first MS center recognized as a Patient-Centered Specialty Practice by the National Committee for Quality Assurance.
To assess whether a web-based platform to capture patient-reported outcomes can help MS practices meet Patient-Centered Specialty Practice standards and achieve MS care goals, the researchers analyzed patient responses in their center’s MS-Advance Study. The MS-Advance Study includes patients from the practice who use a web-based platform to relay patient-reported outcomes in between and at clinic visits.
Patients completed scales and questionnaires at baseline (eg, Modified Fatigue Impact Scale, Patient Health Questionnaire-9, Work Productivity and Activity Improvement Questionnaire, and Treatment Satisfaction Questionnaire for Medication) and journal entries about relapses, mood, energy, nutrition, sleep, and health service or resource utilization. The investigators analyzed responses from patients who completed at least one patient-reported outcome or journal entry between January and August 2017.
Five hundred twenty patients agreed to report outcomes using the online platform; 310 patients completed one or more patient-reported outcome or journal entry. In all, 259 patients reported daily MS sympto
“It is challenging for providers and clinicians to incorporate routine review of patient-reported outcomes into their clinic schedules,” the researchers noted. Strategies for reviewing patient-reported outcomes in clinic and eliciting more complete and timely patient reports are warranted, they said.
“Use of an online platform provides an opportunity to learn about patients’ daily experiences. Understanding these experiences can inform care strategies to address total functionality and other clinical outcomes.”
—Jake Remaly
SAN DIEGO—Continuous collection of patient-reported outcomes via a web-based platform may help neurologists identify patients with multiple sclerosis (MS) with active disease who would benefit from additional care coordination, according to a study described at the ACTRIMS 2018 Forum.
MS has a “variable and unpredictable disease course,” said Alexis Ahmad, Director of Clinical Trials for the Georgetown University Department of Neurology in Washington, DC, and colleagues. “Given the chronic and complex nature of MS, patients living with this disease require continuous and specialized care.”
The MS and Neuroimmunology Center at Georgetown University aims to become the first MS center recognized as a Patient-Centered Specialty Practice by the National Committee for Quality Assurance.
To assess whether a web-based platform to capture patient-reported outcomes can help MS practices meet Patient-Centered Specialty Practice standards and achieve MS care goals, the researchers analyzed patient responses in their center’s MS-Advance Study. The MS-Advance Study includes patients from the practice who use a web-based platform to relay patient-reported outcomes in between and at clinic visits.
Patients completed scales and questionnaires at baseline (eg, Modified Fatigue Impact Scale, Patient Health Questionnaire-9, Work Productivity and Activity Improvement Questionnaire, and Treatment Satisfaction Questionnaire for Medication) and journal entries about relapses, mood, energy, nutrition, sleep, and health service or resource utilization. The investigators analyzed responses from patients who completed at least one patient-reported outcome or journal entry between January and August 2017.
Five hundred twenty patients agreed to report outcomes using the online platform; 310 patients completed one or more patient-reported outcome or journal entry. In all, 259 patients reported daily MS sympto
“It is challenging for providers and clinicians to incorporate routine review of patient-reported outcomes into their clinic schedules,” the researchers noted. Strategies for reviewing patient-reported outcomes in clinic and eliciting more complete and timely patient reports are warranted, they said.
“Use of an online platform provides an opportunity to learn about patients’ daily experiences. Understanding these experiences can inform care strategies to address total functionality and other clinical outcomes.”
—Jake Remaly
SAN DIEGO—Continuous collection of patient-reported outcomes via a web-based platform may help neurologists identify patients with multiple sclerosis (MS) with active disease who would benefit from additional care coordination, according to a study described at the ACTRIMS 2018 Forum.
MS has a “variable and unpredictable disease course,” said Alexis Ahmad, Director of Clinical Trials for the Georgetown University Department of Neurology in Washington, DC, and colleagues. “Given the chronic and complex nature of MS, patients living with this disease require continuous and specialized care.”
The MS and Neuroimmunology Center at Georgetown University aims to become the first MS center recognized as a Patient-Centered Specialty Practice by the National Committee for Quality Assurance.
To assess whether a web-based platform to capture patient-reported outcomes can help MS practices meet Patient-Centered Specialty Practice standards and achieve MS care goals, the researchers analyzed patient responses in their center’s MS-Advance Study. The MS-Advance Study includes patients from the practice who use a web-based platform to relay patient-reported outcomes in between and at clinic visits.
Patients completed scales and questionnaires at baseline (eg, Modified Fatigue Impact Scale, Patient Health Questionnaire-9, Work Productivity and Activity Improvement Questionnaire, and Treatment Satisfaction Questionnaire for Medication) and journal entries about relapses, mood, energy, nutrition, sleep, and health service or resource utilization. The investigators analyzed responses from patients who completed at least one patient-reported outcome or journal entry between January and August 2017.
Five hundred twenty patients agreed to report outcomes using the online platform; 310 patients completed one or more patient-reported outcome or journal entry. In all, 259 patients reported daily MS sympto
“It is challenging for providers and clinicians to incorporate routine review of patient-reported outcomes into their clinic schedules,” the researchers noted. Strategies for reviewing patient-reported outcomes in clinic and eliciting more complete and timely patient reports are warranted, they said.
“Use of an online platform provides an opportunity to learn about patients’ daily experiences. Understanding these experiences can inform care strategies to address total functionality and other clinical outcomes.”
—Jake Remaly
Tenecteplase May Be Superior to Alteplase Before Thrombectomy
LOS ANGELES—Tenecteplase may be superior to alteplase for thrombolysis in patients with acute ischemic stroke who are scheduled to undergo thrombectomy, according to research presented at the International Stroke Conference 2018.
Comparing Two Thrombolytic Agents
The results came from the Tenecteplase Versus Alteplase Before Endovascular Therapy for Ischemic Stroke (EXTEND-IA TNK) trial, a multicenter study of 202 patients in Australia and New Zealand. It was conducted from 2015 to 2017 at 18 hospitals. All enrolled patients received thrombolytic treatment within 4.5 hours of stroke onset and underwent endovascular thrombectomy within six hours of onset.
Investigators examined patients’ blood flow after they had received thrombolysis and undergone an initial angiogram, but before they underwent thrombectomy. The proportion of patients with robust blood flow, which was defined as a Thrombolysis in Cerebral Infarction (TICI) score of 2b or 3 or no retrievable thrombus, was 22% in the patients treated with
After the researchers adjusted the data, they found that tenecteplase was associated with 2.6 times greater odds of robust reperfusion, compared with alteplase. The result was statistically significant for the noninferiority and superiority of tenecteplase, said Bruce C. Campbell, MBBS, PhD, Professor of Neurology at the University of Melbourne and head of hyperacute stroke at Royal Melbourne Hospital.
These results, however, failed to show a significant between-group difference for improvement in NIH Stroke Scale score at three days after enrollment. This outcome occurred in 72% of the patients who received tenecteplase and 69% of patients who received alteplase. The 90-day modified Rankin Scale score was 0 to 2 or unchanged from baseline in 65% of the tenecteplase group and 52% of the alteplase group, a difference that did not reach statistical significance. All patients who enrolled were selected to undergo thrombectomy if their angiogram showed continued occlusion. Dr. Campbell did not report the number of patients who underwent this intervention, however.
The safety outcomes of death, symptomatic intracranial hemorrhage, and parenchymal hematoma occurred at statistically similar rates in both treatment arms.
Ongoing Research
Tenecteplase is a genetically modified tissue plasminogen activator with enhanced fibrin specificity that increases the drug’s half-life and allows for bolus administration, unlike alteplase, which needs continuous infusion. In the United States, the wholesale price per vial of tenecteplase is about $3,000 cheaper than that of alteplase, said Dr. Campbell.
Further data are needed before tenecteplase is ready for routine use, said Dr. Campbell. Two studies in progress are comparing tenecteplase with alteplase in patients with acute ischemic stroke who will not undergo endovascular thrombectomy. Dr. Campbell is leading a study that compares 0.25-mg/kg and 0.40-mg/kg doses of tenecteplase.
“I don’t think the data [that Dr. Campbell reported] are sufficient to say that tenecteplase is equivalent to alteplase. This [question] was studied in a select group of patients who had large-vessel occlusions and were transported to receive mechanical thrombectomy,” said William J. Powers, MD, Professor and Chair of Neurology at the University of North Carolina in Chapel Hill, who was not involved in the study. Most of the data on the efficacy of thrombolysis in patients with ischemic stroke have involved alteplase, he noted. Tenecteplase has FDA marketing approval only for treating patients with an acute myocardial infarction. Alteplase has FDA approval for treating acute ischemic stroke. Both drugs are marketed by Genentech.
Reports in recent years have suggested that treatment with tenecteplase appears to be at least as good as treatment with alteplase in patients with ischemic stroke. For example, a randomized trial that included 75 patients with ischemic stroke selected by imaging at three Australian centers found that treatment with tenecteplase produced a significant 24% improvement in the rate of arterial reperfusion and an average five-point improvement in NIH Stroke Scale score.
In addition, results from the NOR-TEST study showed that among 1,100 patients randomized at 13 Norwegian centers, the primary outcome of a 90-day modified Rankin Scale score of 0 to 1 was achieved by 64% of patients who received tenecteplase and 63% of patients who received alteplase.
In the EXTEND-IA TNK trial, tenecteplase appeared to act better than alteplase and had the extra advantage of being administered as a bolus injection, said Jeffrey L. Saver, MD, Professor of Neurology and Director of the Stroke Unit at the University of California, Los Angeles, in an interview at the meeting. “Alteplase is delivered as a drip, and it is often hard to get patients with an IV infusion out of the hospital quickly when you have to transport the patient. You need a nurse in the ambulance monitoring the drip. With tenecteplase, you administer the bolus and can then send the patient without an IV line, said Dr. Saver, who was not involved in the EXTEND-IA TNK study.
“Two other trials of tenecteplase, compared with alteplase, are now underway, so we will soon have a much larger evidence base for tenecteplase. This is the first large, multicenter, randomized trial to show an advantage for tenecteplase, but it failed to show a significant advantage for change in NIH Stroke Scale score. The results show a strong signal of benefit, but we need additional data from other trials.”
—Mitchel L. Zoler
Suggested Reading
Campbell BC, Mitchell PJ, Churilov L, et al. Tenecteplase versus alteplase before endovascular thrombectomy (EXTEND-IA TNK): A multicenter, randomized, controlled study. Int J Stroke. 2017 Sep 27 [Epub ahead of print].
Logallo N, Kvistad CE, Thomassen L. Therapeutic potential of tenecteplase in the management of acute ischemic stroke. CNS Drugs. 2015;29(10):811-818.
Logallo N, Novotny V, Assmus J, et al. Tenecteplase versus alteplase for management of acute ischaemic stroke (NOR-TEST): a phase 3, randomised, open-label, blinded endpoint trial. Lancet Neurol. 2017;16(10):781-788.
Parsons M, Spratt N, Bivard A, et al. A randomized trial of tenecteplase versus alteplase for acute ischemic stroke. N Eng J Med. 2012;366(12):1099-1107.
LOS ANGELES—Tenecteplase may be superior to alteplase for thrombolysis in patients with acute ischemic stroke who are scheduled to undergo thrombectomy, according to research presented at the International Stroke Conference 2018.
Comparing Two Thrombolytic Agents
The results came from the Tenecteplase Versus Alteplase Before Endovascular Therapy for Ischemic Stroke (EXTEND-IA TNK) trial, a multicenter study of 202 patients in Australia and New Zealand. It was conducted from 2015 to 2017 at 18 hospitals. All enrolled patients received thrombolytic treatment within 4.5 hours of stroke onset and underwent endovascular thrombectomy within six hours of onset.
Investigators examined patients’ blood flow after they had received thrombolysis and undergone an initial angiogram, but before they underwent thrombectomy. The proportion of patients with robust blood flow, which was defined as a Thrombolysis in Cerebral Infarction (TICI) score of 2b or 3 or no retrievable thrombus, was 22% in the patients treated with
After the researchers adjusted the data, they found that tenecteplase was associated with 2.6 times greater odds of robust reperfusion, compared with alteplase. The result was statistically significant for the noninferiority and superiority of tenecteplase, said Bruce C. Campbell, MBBS, PhD, Professor of Neurology at the University of Melbourne and head of hyperacute stroke at Royal Melbourne Hospital.
These results, however, failed to show a significant between-group difference for improvement in NIH Stroke Scale score at three days after enrollment. This outcome occurred in 72% of the patients who received tenecteplase and 69% of patients who received alteplase. The 90-day modified Rankin Scale score was 0 to 2 or unchanged from baseline in 65% of the tenecteplase group and 52% of the alteplase group, a difference that did not reach statistical significance. All patients who enrolled were selected to undergo thrombectomy if their angiogram showed continued occlusion. Dr. Campbell did not report the number of patients who underwent this intervention, however.
The safety outcomes of death, symptomatic intracranial hemorrhage, and parenchymal hematoma occurred at statistically similar rates in both treatment arms.
Ongoing Research
Tenecteplase is a genetically modified tissue plasminogen activator with enhanced fibrin specificity that increases the drug’s half-life and allows for bolus administration, unlike alteplase, which needs continuous infusion. In the United States, the wholesale price per vial of tenecteplase is about $3,000 cheaper than that of alteplase, said Dr. Campbell.
Further data are needed before tenecteplase is ready for routine use, said Dr. Campbell. Two studies in progress are comparing tenecteplase with alteplase in patients with acute ischemic stroke who will not undergo endovascular thrombectomy. Dr. Campbell is leading a study that compares 0.25-mg/kg and 0.40-mg/kg doses of tenecteplase.
“I don’t think the data [that Dr. Campbell reported] are sufficient to say that tenecteplase is equivalent to alteplase. This [question] was studied in a select group of patients who had large-vessel occlusions and were transported to receive mechanical thrombectomy,” said William J. Powers, MD, Professor and Chair of Neurology at the University of North Carolina in Chapel Hill, who was not involved in the study. Most of the data on the efficacy of thrombolysis in patients with ischemic stroke have involved alteplase, he noted. Tenecteplase has FDA marketing approval only for treating patients with an acute myocardial infarction. Alteplase has FDA approval for treating acute ischemic stroke. Both drugs are marketed by Genentech.
Reports in recent years have suggested that treatment with tenecteplase appears to be at least as good as treatment with alteplase in patients with ischemic stroke. For example, a randomized trial that included 75 patients with ischemic stroke selected by imaging at three Australian centers found that treatment with tenecteplase produced a significant 24% improvement in the rate of arterial reperfusion and an average five-point improvement in NIH Stroke Scale score.
In addition, results from the NOR-TEST study showed that among 1,100 patients randomized at 13 Norwegian centers, the primary outcome of a 90-day modified Rankin Scale score of 0 to 1 was achieved by 64% of patients who received tenecteplase and 63% of patients who received alteplase.
In the EXTEND-IA TNK trial, tenecteplase appeared to act better than alteplase and had the extra advantage of being administered as a bolus injection, said Jeffrey L. Saver, MD, Professor of Neurology and Director of the Stroke Unit at the University of California, Los Angeles, in an interview at the meeting. “Alteplase is delivered as a drip, and it is often hard to get patients with an IV infusion out of the hospital quickly when you have to transport the patient. You need a nurse in the ambulance monitoring the drip. With tenecteplase, you administer the bolus and can then send the patient without an IV line, said Dr. Saver, who was not involved in the EXTEND-IA TNK study.
“Two other trials of tenecteplase, compared with alteplase, are now underway, so we will soon have a much larger evidence base for tenecteplase. This is the first large, multicenter, randomized trial to show an advantage for tenecteplase, but it failed to show a significant advantage for change in NIH Stroke Scale score. The results show a strong signal of benefit, but we need additional data from other trials.”
—Mitchel L. Zoler
Suggested Reading
Campbell BC, Mitchell PJ, Churilov L, et al. Tenecteplase versus alteplase before endovascular thrombectomy (EXTEND-IA TNK): A multicenter, randomized, controlled study. Int J Stroke. 2017 Sep 27 [Epub ahead of print].
Logallo N, Kvistad CE, Thomassen L. Therapeutic potential of tenecteplase in the management of acute ischemic stroke. CNS Drugs. 2015;29(10):811-818.
Logallo N, Novotny V, Assmus J, et al. Tenecteplase versus alteplase for management of acute ischaemic stroke (NOR-TEST): a phase 3, randomised, open-label, blinded endpoint trial. Lancet Neurol. 2017;16(10):781-788.
Parsons M, Spratt N, Bivard A, et al. A randomized trial of tenecteplase versus alteplase for acute ischemic stroke. N Eng J Med. 2012;366(12):1099-1107.
LOS ANGELES—Tenecteplase may be superior to alteplase for thrombolysis in patients with acute ischemic stroke who are scheduled to undergo thrombectomy, according to research presented at the International Stroke Conference 2018.
Comparing Two Thrombolytic Agents
The results came from the Tenecteplase Versus Alteplase Before Endovascular Therapy for Ischemic Stroke (EXTEND-IA TNK) trial, a multicenter study of 202 patients in Australia and New Zealand. It was conducted from 2015 to 2017 at 18 hospitals. All enrolled patients received thrombolytic treatment within 4.5 hours of stroke onset and underwent endovascular thrombectomy within six hours of onset.
Investigators examined patients’ blood flow after they had received thrombolysis and undergone an initial angiogram, but before they underwent thrombectomy. The proportion of patients with robust blood flow, which was defined as a Thrombolysis in Cerebral Infarction (TICI) score of 2b or 3 or no retrievable thrombus, was 22% in the patients treated with
After the researchers adjusted the data, they found that tenecteplase was associated with 2.6 times greater odds of robust reperfusion, compared with alteplase. The result was statistically significant for the noninferiority and superiority of tenecteplase, said Bruce C. Campbell, MBBS, PhD, Professor of Neurology at the University of Melbourne and head of hyperacute stroke at Royal Melbourne Hospital.
These results, however, failed to show a significant between-group difference for improvement in NIH Stroke Scale score at three days after enrollment. This outcome occurred in 72% of the patients who received tenecteplase and 69% of patients who received alteplase. The 90-day modified Rankin Scale score was 0 to 2 or unchanged from baseline in 65% of the tenecteplase group and 52% of the alteplase group, a difference that did not reach statistical significance. All patients who enrolled were selected to undergo thrombectomy if their angiogram showed continued occlusion. Dr. Campbell did not report the number of patients who underwent this intervention, however.
The safety outcomes of death, symptomatic intracranial hemorrhage, and parenchymal hematoma occurred at statistically similar rates in both treatment arms.
Ongoing Research
Tenecteplase is a genetically modified tissue plasminogen activator with enhanced fibrin specificity that increases the drug’s half-life and allows for bolus administration, unlike alteplase, which needs continuous infusion. In the United States, the wholesale price per vial of tenecteplase is about $3,000 cheaper than that of alteplase, said Dr. Campbell.
Further data are needed before tenecteplase is ready for routine use, said Dr. Campbell. Two studies in progress are comparing tenecteplase with alteplase in patients with acute ischemic stroke who will not undergo endovascular thrombectomy. Dr. Campbell is leading a study that compares 0.25-mg/kg and 0.40-mg/kg doses of tenecteplase.
“I don’t think the data [that Dr. Campbell reported] are sufficient to say that tenecteplase is equivalent to alteplase. This [question] was studied in a select group of patients who had large-vessel occlusions and were transported to receive mechanical thrombectomy,” said William J. Powers, MD, Professor and Chair of Neurology at the University of North Carolina in Chapel Hill, who was not involved in the study. Most of the data on the efficacy of thrombolysis in patients with ischemic stroke have involved alteplase, he noted. Tenecteplase has FDA marketing approval only for treating patients with an acute myocardial infarction. Alteplase has FDA approval for treating acute ischemic stroke. Both drugs are marketed by Genentech.
Reports in recent years have suggested that treatment with tenecteplase appears to be at least as good as treatment with alteplase in patients with ischemic stroke. For example, a randomized trial that included 75 patients with ischemic stroke selected by imaging at three Australian centers found that treatment with tenecteplase produced a significant 24% improvement in the rate of arterial reperfusion and an average five-point improvement in NIH Stroke Scale score.
In addition, results from the NOR-TEST study showed that among 1,100 patients randomized at 13 Norwegian centers, the primary outcome of a 90-day modified Rankin Scale score of 0 to 1 was achieved by 64% of patients who received tenecteplase and 63% of patients who received alteplase.
In the EXTEND-IA TNK trial, tenecteplase appeared to act better than alteplase and had the extra advantage of being administered as a bolus injection, said Jeffrey L. Saver, MD, Professor of Neurology and Director of the Stroke Unit at the University of California, Los Angeles, in an interview at the meeting. “Alteplase is delivered as a drip, and it is often hard to get patients with an IV infusion out of the hospital quickly when you have to transport the patient. You need a nurse in the ambulance monitoring the drip. With tenecteplase, you administer the bolus and can then send the patient without an IV line, said Dr. Saver, who was not involved in the EXTEND-IA TNK study.
“Two other trials of tenecteplase, compared with alteplase, are now underway, so we will soon have a much larger evidence base for tenecteplase. This is the first large, multicenter, randomized trial to show an advantage for tenecteplase, but it failed to show a significant advantage for change in NIH Stroke Scale score. The results show a strong signal of benefit, but we need additional data from other trials.”
—Mitchel L. Zoler
Suggested Reading
Campbell BC, Mitchell PJ, Churilov L, et al. Tenecteplase versus alteplase before endovascular thrombectomy (EXTEND-IA TNK): A multicenter, randomized, controlled study. Int J Stroke. 2017 Sep 27 [Epub ahead of print].
Logallo N, Kvistad CE, Thomassen L. Therapeutic potential of tenecteplase in the management of acute ischemic stroke. CNS Drugs. 2015;29(10):811-818.
Logallo N, Novotny V, Assmus J, et al. Tenecteplase versus alteplase for management of acute ischaemic stroke (NOR-TEST): a phase 3, randomised, open-label, blinded endpoint trial. Lancet Neurol. 2017;16(10):781-788.
Parsons M, Spratt N, Bivard A, et al. A randomized trial of tenecteplase versus alteplase for acute ischemic stroke. N Eng J Med. 2012;366(12):1099-1107.
Arm-placement indication for CGM approved by FDA
The Food and Drug Administration has approved a new indication for the Guardian Sensor 3 continuous glucose monitor (CGM), allowing patients to position it on their arms, according to an announcement by Medtronic, the sensor’s manufacturer.
Although previously only the abdomen had FDA approval as a CGM site, findings from at least one study have shown that most patients prefer to position their sensors elsewhere. This new indication gives these patients more flexibility in where they can place their CGMs. The site of CGM placement did not affect the failure rate or noncompliance.
The sensor works in tandem with an automated insulin delivery system known as the MiniMed 670G system, also manufactured by Medtronic. This system is approved for people with type 1 diabetes aged 14 years and older and adjusts basal insulin levels every 5 minutes – “based on real-time data delivered by the Guardian Sensor 3,” according to Medtronic.
Read more in Medtronic’s press release.
Correction, 3/21/18: A previous version of this article contained a photo of a device that was not the Guardian 3 Sensor.
The Food and Drug Administration has approved a new indication for the Guardian Sensor 3 continuous glucose monitor (CGM), allowing patients to position it on their arms, according to an announcement by Medtronic, the sensor’s manufacturer.
Although previously only the abdomen had FDA approval as a CGM site, findings from at least one study have shown that most patients prefer to position their sensors elsewhere. This new indication gives these patients more flexibility in where they can place their CGMs. The site of CGM placement did not affect the failure rate or noncompliance.
The sensor works in tandem with an automated insulin delivery system known as the MiniMed 670G system, also manufactured by Medtronic. This system is approved for people with type 1 diabetes aged 14 years and older and adjusts basal insulin levels every 5 minutes – “based on real-time data delivered by the Guardian Sensor 3,” according to Medtronic.
Read more in Medtronic’s press release.
Correction, 3/21/18: A previous version of this article contained a photo of a device that was not the Guardian 3 Sensor.
The Food and Drug Administration has approved a new indication for the Guardian Sensor 3 continuous glucose monitor (CGM), allowing patients to position it on their arms, according to an announcement by Medtronic, the sensor’s manufacturer.
Although previously only the abdomen had FDA approval as a CGM site, findings from at least one study have shown that most patients prefer to position their sensors elsewhere. This new indication gives these patients more flexibility in where they can place their CGMs. The site of CGM placement did not affect the failure rate or noncompliance.
The sensor works in tandem with an automated insulin delivery system known as the MiniMed 670G system, also manufactured by Medtronic. This system is approved for people with type 1 diabetes aged 14 years and older and adjusts basal insulin levels every 5 minutes – “based on real-time data delivered by the Guardian Sensor 3,” according to Medtronic.
Read more in Medtronic’s press release.
Correction, 3/21/18: A previous version of this article contained a photo of a device that was not the Guardian 3 Sensor.
Product Update: Vistara; Ultravision trocar; CompuFlo Epidural; and Philips ultrasound
PRENATAL SCREENING FOR SINGLE-GENE DISORDERS
Vistara®, a non-invasive prenatal test (NIPT) from Natera, Inc, screens for single-gene disorders after 9 weeks’ gestation. Complementing the Panorama® NIPT, Vistara tests for major anatomic abnormalities and chromosome imbalances that have a combined incidence rate of 1 in 600 (higher than Down syndrome). These mutations can cause severe conditions affecting skeletal, cardiac, and neurologic systems, such as Noonan syndrome, osteogenesis imperfecta, craniosynostosis syndromes, achondroplasia, and Rett syndrome. Standard NIPT commonly cannot detect these de novo (not inherited) mutations. Ultrasound exams may either completely miss the disorders or identify nonspecific findings later in pregnancy.
Natera says that Vistara has a combined analytical sensitivity of >99% and a combined analytical specificity of >99% in validation studies.
FOR MORE INFORMATION, VISIT: https://www.natera.com/vistara
ELECTROSTATIC SURGICAL SMOKE REMOVAL
The UltravisionTM Trocar device from Alesi Surgical Technologies uses a low-energy electrostatic charge to eliminate the surgical smoke generated by cutting instruments during laparoscopic surgery. Electrostatic precipitation accelerates the natural process of sedimentation; Ultravision creates negatively charged gas ions that draw water vapor and particulate matter away from the surgical site toward “positive” patient tissue.
Alesi says that bench studies comparing Ultravision with a vacuum-system when using monopolar, bipolar, and ultrasonic instruments show that its device is faster and more efficient than smoke evacuation. When switched on before cutting, Ultravision precipitates 99% of particles within 30 seconds. After 1 minute of continuous use, Ultravision precipitates 99.9% of particles, independent of particle size, from 7 nm to 10 µm. Smoke evacuation removes 30.2% of particles after 1 minute, according to Alesi.
FOR MORE INFORMATION, VISIT: http://www.alesi-surgical.com
PRESSURE-SENSING TECHNOLOGY FOR EPIDURALS
The CompuFlo®Epidural from Milestone Scientific uses pressure-sensing technology to identify the epidural space, and provides a computer-controlled drug delivery system.
Knowing the precise needle location during an epidural injection procedure provides a measure of safety not available to physicians who use conventional syringes. Milestone says that its CompuFlo Epidural allows anesthesiologists to use both hands to advance and direct the needle, and to confirm the epidural space with 99% accuracy on the first attempt.
CompuFlo Epidural differentiates tissue types for the medical professional via visual and audio feedback, leading to precise location guidance as the needle advances toward the intended area. It also allows for controlled needle exit pressure, precise flow rate and drug volumes, and patient treatment documentation.
FOR MORE INFORMATION, VISIT: https://www.milestonescientific.com/products/compuflo-epidural
OBGYN ULTRASOUND INNOVATIONS
Philips recently announced enhancements to its EPIQ 7 and 5 and Affiniti 70 ultrasound systems. According to Philips, the eL18-4 transducer provides high-detail resolution and image uniformity with penetration for enhanced diagnostic quality in 1st- and 2nd-trimester obstetric exams. aBiometry AssistAI, with anatomical intelligence of fetal anatomy, streamlines fetal measurement by preplacing measurement cursors on selected structures. The new TouchVue control-panel interface on TrueVue allows practitioners to interact with finger gestures and to direct 3D-volume rotation and internal light-source position. The 2D Tilt feature offered on the 3D9-v3 transducer provides lateral scanning of anatomic structures that are off-axis without having to manually angle the transducer.
These new features complement the existing suite of Philips ObGyn ultrasound visualization tools: TrueVue, GlassVue, aRevealAI, and MaxVue.
FOR MORE INFORMATION, VISIT: https://www.usa.philips.com/healthcare/resources/feature-detail/ultrasound-truevue-imaging
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
PRENATAL SCREENING FOR SINGLE-GENE DISORDERS
Vistara®, a non-invasive prenatal test (NIPT) from Natera, Inc, screens for single-gene disorders after 9 weeks’ gestation. Complementing the Panorama® NIPT, Vistara tests for major anatomic abnormalities and chromosome imbalances that have a combined incidence rate of 1 in 600 (higher than Down syndrome). These mutations can cause severe conditions affecting skeletal, cardiac, and neurologic systems, such as Noonan syndrome, osteogenesis imperfecta, craniosynostosis syndromes, achondroplasia, and Rett syndrome. Standard NIPT commonly cannot detect these de novo (not inherited) mutations. Ultrasound exams may either completely miss the disorders or identify nonspecific findings later in pregnancy.
Natera says that Vistara has a combined analytical sensitivity of >99% and a combined analytical specificity of >99% in validation studies.
FOR MORE INFORMATION, VISIT: https://www.natera.com/vistara
ELECTROSTATIC SURGICAL SMOKE REMOVAL
The UltravisionTM Trocar device from Alesi Surgical Technologies uses a low-energy electrostatic charge to eliminate the surgical smoke generated by cutting instruments during laparoscopic surgery. Electrostatic precipitation accelerates the natural process of sedimentation; Ultravision creates negatively charged gas ions that draw water vapor and particulate matter away from the surgical site toward “positive” patient tissue.
Alesi says that bench studies comparing Ultravision with a vacuum-system when using monopolar, bipolar, and ultrasonic instruments show that its device is faster and more efficient than smoke evacuation. When switched on before cutting, Ultravision precipitates 99% of particles within 30 seconds. After 1 minute of continuous use, Ultravision precipitates 99.9% of particles, independent of particle size, from 7 nm to 10 µm. Smoke evacuation removes 30.2% of particles after 1 minute, according to Alesi.
FOR MORE INFORMATION, VISIT: http://www.alesi-surgical.com
PRESSURE-SENSING TECHNOLOGY FOR EPIDURALS
The CompuFlo®Epidural from Milestone Scientific uses pressure-sensing technology to identify the epidural space, and provides a computer-controlled drug delivery system.
Knowing the precise needle location during an epidural injection procedure provides a measure of safety not available to physicians who use conventional syringes. Milestone says that its CompuFlo Epidural allows anesthesiologists to use both hands to advance and direct the needle, and to confirm the epidural space with 99% accuracy on the first attempt.
CompuFlo Epidural differentiates tissue types for the medical professional via visual and audio feedback, leading to precise location guidance as the needle advances toward the intended area. It also allows for controlled needle exit pressure, precise flow rate and drug volumes, and patient treatment documentation.
FOR MORE INFORMATION, VISIT: https://www.milestonescientific.com/products/compuflo-epidural
OBGYN ULTRASOUND INNOVATIONS
Philips recently announced enhancements to its EPIQ 7 and 5 and Affiniti 70 ultrasound systems. According to Philips, the eL18-4 transducer provides high-detail resolution and image uniformity with penetration for enhanced diagnostic quality in 1st- and 2nd-trimester obstetric exams. aBiometry AssistAI, with anatomical intelligence of fetal anatomy, streamlines fetal measurement by preplacing measurement cursors on selected structures. The new TouchVue control-panel interface on TrueVue allows practitioners to interact with finger gestures and to direct 3D-volume rotation and internal light-source position. The 2D Tilt feature offered on the 3D9-v3 transducer provides lateral scanning of anatomic structures that are off-axis without having to manually angle the transducer.
These new features complement the existing suite of Philips ObGyn ultrasound visualization tools: TrueVue, GlassVue, aRevealAI, and MaxVue.
FOR MORE INFORMATION, VISIT: https://www.usa.philips.com/healthcare/resources/feature-detail/ultrasound-truevue-imaging
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
PRENATAL SCREENING FOR SINGLE-GENE DISORDERS
Vistara®, a non-invasive prenatal test (NIPT) from Natera, Inc, screens for single-gene disorders after 9 weeks’ gestation. Complementing the Panorama® NIPT, Vistara tests for major anatomic abnormalities and chromosome imbalances that have a combined incidence rate of 1 in 600 (higher than Down syndrome). These mutations can cause severe conditions affecting skeletal, cardiac, and neurologic systems, such as Noonan syndrome, osteogenesis imperfecta, craniosynostosis syndromes, achondroplasia, and Rett syndrome. Standard NIPT commonly cannot detect these de novo (not inherited) mutations. Ultrasound exams may either completely miss the disorders or identify nonspecific findings later in pregnancy.
Natera says that Vistara has a combined analytical sensitivity of >99% and a combined analytical specificity of >99% in validation studies.
FOR MORE INFORMATION, VISIT: https://www.natera.com/vistara
ELECTROSTATIC SURGICAL SMOKE REMOVAL
The UltravisionTM Trocar device from Alesi Surgical Technologies uses a low-energy electrostatic charge to eliminate the surgical smoke generated by cutting instruments during laparoscopic surgery. Electrostatic precipitation accelerates the natural process of sedimentation; Ultravision creates negatively charged gas ions that draw water vapor and particulate matter away from the surgical site toward “positive” patient tissue.
Alesi says that bench studies comparing Ultravision with a vacuum-system when using monopolar, bipolar, and ultrasonic instruments show that its device is faster and more efficient than smoke evacuation. When switched on before cutting, Ultravision precipitates 99% of particles within 30 seconds. After 1 minute of continuous use, Ultravision precipitates 99.9% of particles, independent of particle size, from 7 nm to 10 µm. Smoke evacuation removes 30.2% of particles after 1 minute, according to Alesi.
FOR MORE INFORMATION, VISIT: http://www.alesi-surgical.com
PRESSURE-SENSING TECHNOLOGY FOR EPIDURALS
The CompuFlo®Epidural from Milestone Scientific uses pressure-sensing technology to identify the epidural space, and provides a computer-controlled drug delivery system.
Knowing the precise needle location during an epidural injection procedure provides a measure of safety not available to physicians who use conventional syringes. Milestone says that its CompuFlo Epidural allows anesthesiologists to use both hands to advance and direct the needle, and to confirm the epidural space with 99% accuracy on the first attempt.
CompuFlo Epidural differentiates tissue types for the medical professional via visual and audio feedback, leading to precise location guidance as the needle advances toward the intended area. It also allows for controlled needle exit pressure, precise flow rate and drug volumes, and patient treatment documentation.
FOR MORE INFORMATION, VISIT: https://www.milestonescientific.com/products/compuflo-epidural
OBGYN ULTRASOUND INNOVATIONS
Philips recently announced enhancements to its EPIQ 7 and 5 and Affiniti 70 ultrasound systems. According to Philips, the eL18-4 transducer provides high-detail resolution and image uniformity with penetration for enhanced diagnostic quality in 1st- and 2nd-trimester obstetric exams. aBiometry AssistAI, with anatomical intelligence of fetal anatomy, streamlines fetal measurement by preplacing measurement cursors on selected structures. The new TouchVue control-panel interface on TrueVue allows practitioners to interact with finger gestures and to direct 3D-volume rotation and internal light-source position. The 2D Tilt feature offered on the 3D9-v3 transducer provides lateral scanning of anatomic structures that are off-axis without having to manually angle the transducer.
These new features complement the existing suite of Philips ObGyn ultrasound visualization tools: TrueVue, GlassVue, aRevealAI, and MaxVue.
FOR MORE INFORMATION, VISIT: https://www.usa.philips.com/healthcare/resources/feature-detail/ultrasound-truevue-imaging
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
VIDEO: Cannabinoids in dermatology
SAN DIEGO – To date, most of the research on cannabinoids has been outside of dermatology, but these agents may eventually play an important role in the treatment of dermatologic diseases, according to Adam Friedman, MD, director of translational research, department of dermatology, at George Washington University, Washington.
for diseases like dermatomyositis, scleroderma, and lupus, Dr. Friedman said in a video interview at the annual meeting of the American Academy of Dermatology.
In this area, most progress has been made with a synthetic cannabinoid, ajulemic acid (also known as anabasum), which is designed to go after CB2 cannabinoid receptors, which have the anti-inflammatory effects, and not the CB1 receptors, which have the psychoactive effects, he explained. Results of phase 2 studies of ajulemic acid in dermatomyositis and systemic sclerosis have been “very promising,” he noted.
In collaboration with Albert Einstein College of Medicine, New York, he and his associates have studied the topical application of an endocannabinoid, anandamide (AEA), in nanoparticles in an animal model of cutaneous lupus. “We found that we can actually reverse the very classic, almost chronic cutaneous-like symptoms that we see in these animals if they go untreated,” he said.
In the interview, Dr. Friedman, who spoke about the potential of cannabinoids for the treatment of inflammatory and neoplastic diseases of the skin at the meeting, said that it is actually surprising that most research with cannabinoids to date has been outside of dermatology, “because our skin is chock full of cannabinoids; chock full of expression of cannabinoid receptors.”
Dr. Friedman disclosed that he has invented the nanotechnology licensed to Zylo Therapeutics. He is a member of the Dermatology News advisory board.
SAN DIEGO – To date, most of the research on cannabinoids has been outside of dermatology, but these agents may eventually play an important role in the treatment of dermatologic diseases, according to Adam Friedman, MD, director of translational research, department of dermatology, at George Washington University, Washington.
for diseases like dermatomyositis, scleroderma, and lupus, Dr. Friedman said in a video interview at the annual meeting of the American Academy of Dermatology.
In this area, most progress has been made with a synthetic cannabinoid, ajulemic acid (also known as anabasum), which is designed to go after CB2 cannabinoid receptors, which have the anti-inflammatory effects, and not the CB1 receptors, which have the psychoactive effects, he explained. Results of phase 2 studies of ajulemic acid in dermatomyositis and systemic sclerosis have been “very promising,” he noted.
In collaboration with Albert Einstein College of Medicine, New York, he and his associates have studied the topical application of an endocannabinoid, anandamide (AEA), in nanoparticles in an animal model of cutaneous lupus. “We found that we can actually reverse the very classic, almost chronic cutaneous-like symptoms that we see in these animals if they go untreated,” he said.
In the interview, Dr. Friedman, who spoke about the potential of cannabinoids for the treatment of inflammatory and neoplastic diseases of the skin at the meeting, said that it is actually surprising that most research with cannabinoids to date has been outside of dermatology, “because our skin is chock full of cannabinoids; chock full of expression of cannabinoid receptors.”
Dr. Friedman disclosed that he has invented the nanotechnology licensed to Zylo Therapeutics. He is a member of the Dermatology News advisory board.
SAN DIEGO – To date, most of the research on cannabinoids has been outside of dermatology, but these agents may eventually play an important role in the treatment of dermatologic diseases, according to Adam Friedman, MD, director of translational research, department of dermatology, at George Washington University, Washington.
for diseases like dermatomyositis, scleroderma, and lupus, Dr. Friedman said in a video interview at the annual meeting of the American Academy of Dermatology.
In this area, most progress has been made with a synthetic cannabinoid, ajulemic acid (also known as anabasum), which is designed to go after CB2 cannabinoid receptors, which have the anti-inflammatory effects, and not the CB1 receptors, which have the psychoactive effects, he explained. Results of phase 2 studies of ajulemic acid in dermatomyositis and systemic sclerosis have been “very promising,” he noted.
In collaboration with Albert Einstein College of Medicine, New York, he and his associates have studied the topical application of an endocannabinoid, anandamide (AEA), in nanoparticles in an animal model of cutaneous lupus. “We found that we can actually reverse the very classic, almost chronic cutaneous-like symptoms that we see in these animals if they go untreated,” he said.
In the interview, Dr. Friedman, who spoke about the potential of cannabinoids for the treatment of inflammatory and neoplastic diseases of the skin at the meeting, said that it is actually surprising that most research with cannabinoids to date has been outside of dermatology, “because our skin is chock full of cannabinoids; chock full of expression of cannabinoid receptors.”
Dr. Friedman disclosed that he has invented the nanotechnology licensed to Zylo Therapeutics. He is a member of the Dermatology News advisory board.
REPORTING FROM AAD 18
Health Care Use May Elucidate MS Prodrome
SAN DIEGO—In the five years before multiple sclerosis (MS) symptom onset, patients are more likely to see a physician or be admitted to the hospital for problems related to the nervous system, sensory organs, musculoskeletal system, and genitourinary system, compared with controls, according to research presented at the ACTRIMS 2018 Forum.
In addition, patients with MS are more likely to see psychiatrists and urologists and to fill prescriptions related to the musculoskeletal system or the genitourinary system in the five years before MS onset.
“It is possible to measure and phenotype the MS prodrome five years before the clinical recognition of MS,” said Elaine Kingwell, PhD, a research associate in the Division of Neurology at the University of British Columbia in Vancouver, and colleagues. “Our findings inform the etiologically relevant time window and suggest that an earlier recognition and diagnosis of MS is feasible.”
A prior study by the researchers had identified increased health care use before a first demyelinating event among patients
Phenotypic Characteristics
To investigate the phenotypic characteristics of the MS prodrome, Dr. Kingwell and colleagues examined the medical diagnoses and therapeutic drug classes related to inpatient and outpatient health care encounters five years before the clinical recognition of MS. The researchers performed a population-based matched cohort study using linked health administrative and clinical data in four Canadian provinces between 1989 and 2014.
The investigators compared the reasons for physician and hospital encounters, using ICD-10 chapters or physician specialty, and prescriptions filled, using Anatomical Therapeutic Chemical System, level 1 drug classes. The researchers matched people with MS with as many as five people without any demyelinating disease by sex, year of birth, and postal code.
The study included two cohorts of people with MS. One cohort encompassed patients with a first demyelinating disease–related claim (ie, the administrative cohort), and the other cohort comprised patients with a neurologist-confirmed diagnosis of MS (ie, the clinical cohort). The researchers compared inpatient and outpatient encounters between cases and controls in the five years before the cases’ first demyelinating claim or clinically reported symptom onset.
Fewer Pregnancy-Related Encounters
The administrative cohort included 13,951 cases and 66,940 controls (about 73% women; average age, 43). The clinical cohort included 3,202 cases and 16,006 controls (about 74% women; average age, 36.5). Compared with controls, in the five years before the first demyelinating claim or symptom onset, cases had more physician and hospital encounters for the nervous system (rate ratio [RR] = 1.70–4.75), sensory organs (RR = 1.40–2.28), musculoskeletal system (RR = 1.19–1.70), and genitourinary system (RR = 1.17–1.59). Cases also had more encounters with psychiatrists (RR = 1.48–1.66) and urologists (RR = 1.49–1.80), and a higher proportion of filled prescriptions for hormonal preparations and for drugs related to the musculoskeletal or genitourinary systems (1.1–1.5 times higher). In contrast, cases had fewer pregnancy-related encounters, compared with controls (RR = 0.78–0.88).
“Research into factors that might cause or prevent MS should take the MS prodrome into account,” the researchers said.
—Jake Remaly
Suggested Reading
Wijnands JMA, Kingwell E, Zhu F, et al. Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study. Lancet Neurol. 2017;16(6):445-451.
SAN DIEGO—In the five years before multiple sclerosis (MS) symptom onset, patients are more likely to see a physician or be admitted to the hospital for problems related to the nervous system, sensory organs, musculoskeletal system, and genitourinary system, compared with controls, according to research presented at the ACTRIMS 2018 Forum.
In addition, patients with MS are more likely to see psychiatrists and urologists and to fill prescriptions related to the musculoskeletal system or the genitourinary system in the five years before MS onset.
“It is possible to measure and phenotype the MS prodrome five years before the clinical recognition of MS,” said Elaine Kingwell, PhD, a research associate in the Division of Neurology at the University of British Columbia in Vancouver, and colleagues. “Our findings inform the etiologically relevant time window and suggest that an earlier recognition and diagnosis of MS is feasible.”
A prior study by the researchers had identified increased health care use before a first demyelinating event among patients
Phenotypic Characteristics
To investigate the phenotypic characteristics of the MS prodrome, Dr. Kingwell and colleagues examined the medical diagnoses and therapeutic drug classes related to inpatient and outpatient health care encounters five years before the clinical recognition of MS. The researchers performed a population-based matched cohort study using linked health administrative and clinical data in four Canadian provinces between 1989 and 2014.
The investigators compared the reasons for physician and hospital encounters, using ICD-10 chapters or physician specialty, and prescriptions filled, using Anatomical Therapeutic Chemical System, level 1 drug classes. The researchers matched people with MS with as many as five people without any demyelinating disease by sex, year of birth, and postal code.
The study included two cohorts of people with MS. One cohort encompassed patients with a first demyelinating disease–related claim (ie, the administrative cohort), and the other cohort comprised patients with a neurologist-confirmed diagnosis of MS (ie, the clinical cohort). The researchers compared inpatient and outpatient encounters between cases and controls in the five years before the cases’ first demyelinating claim or clinically reported symptom onset.
Fewer Pregnancy-Related Encounters
The administrative cohort included 13,951 cases and 66,940 controls (about 73% women; average age, 43). The clinical cohort included 3,202 cases and 16,006 controls (about 74% women; average age, 36.5). Compared with controls, in the five years before the first demyelinating claim or symptom onset, cases had more physician and hospital encounters for the nervous system (rate ratio [RR] = 1.70–4.75), sensory organs (RR = 1.40–2.28), musculoskeletal system (RR = 1.19–1.70), and genitourinary system (RR = 1.17–1.59). Cases also had more encounters with psychiatrists (RR = 1.48–1.66) and urologists (RR = 1.49–1.80), and a higher proportion of filled prescriptions for hormonal preparations and for drugs related to the musculoskeletal or genitourinary systems (1.1–1.5 times higher). In contrast, cases had fewer pregnancy-related encounters, compared with controls (RR = 0.78–0.88).
“Research into factors that might cause or prevent MS should take the MS prodrome into account,” the researchers said.
—Jake Remaly
Suggested Reading
Wijnands JMA, Kingwell E, Zhu F, et al. Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study. Lancet Neurol. 2017;16(6):445-451.
SAN DIEGO—In the five years before multiple sclerosis (MS) symptom onset, patients are more likely to see a physician or be admitted to the hospital for problems related to the nervous system, sensory organs, musculoskeletal system, and genitourinary system, compared with controls, according to research presented at the ACTRIMS 2018 Forum.
In addition, patients with MS are more likely to see psychiatrists and urologists and to fill prescriptions related to the musculoskeletal system or the genitourinary system in the five years before MS onset.
“It is possible to measure and phenotype the MS prodrome five years before the clinical recognition of MS,” said Elaine Kingwell, PhD, a research associate in the Division of Neurology at the University of British Columbia in Vancouver, and colleagues. “Our findings inform the etiologically relevant time window and suggest that an earlier recognition and diagnosis of MS is feasible.”
A prior study by the researchers had identified increased health care use before a first demyelinating event among patients
Phenotypic Characteristics
To investigate the phenotypic characteristics of the MS prodrome, Dr. Kingwell and colleagues examined the medical diagnoses and therapeutic drug classes related to inpatient and outpatient health care encounters five years before the clinical recognition of MS. The researchers performed a population-based matched cohort study using linked health administrative and clinical data in four Canadian provinces between 1989 and 2014.
The investigators compared the reasons for physician and hospital encounters, using ICD-10 chapters or physician specialty, and prescriptions filled, using Anatomical Therapeutic Chemical System, level 1 drug classes. The researchers matched people with MS with as many as five people without any demyelinating disease by sex, year of birth, and postal code.
The study included two cohorts of people with MS. One cohort encompassed patients with a first demyelinating disease–related claim (ie, the administrative cohort), and the other cohort comprised patients with a neurologist-confirmed diagnosis of MS (ie, the clinical cohort). The researchers compared inpatient and outpatient encounters between cases and controls in the five years before the cases’ first demyelinating claim or clinically reported symptom onset.
Fewer Pregnancy-Related Encounters
The administrative cohort included 13,951 cases and 66,940 controls (about 73% women; average age, 43). The clinical cohort included 3,202 cases and 16,006 controls (about 74% women; average age, 36.5). Compared with controls, in the five years before the first demyelinating claim or symptom onset, cases had more physician and hospital encounters for the nervous system (rate ratio [RR] = 1.70–4.75), sensory organs (RR = 1.40–2.28), musculoskeletal system (RR = 1.19–1.70), and genitourinary system (RR = 1.17–1.59). Cases also had more encounters with psychiatrists (RR = 1.48–1.66) and urologists (RR = 1.49–1.80), and a higher proportion of filled prescriptions for hormonal preparations and for drugs related to the musculoskeletal or genitourinary systems (1.1–1.5 times higher). In contrast, cases had fewer pregnancy-related encounters, compared with controls (RR = 0.78–0.88).
“Research into factors that might cause or prevent MS should take the MS prodrome into account,” the researchers said.
—Jake Remaly
Suggested Reading
Wijnands JMA, Kingwell E, Zhu F, et al. Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study. Lancet Neurol. 2017;16(6):445-451.