User login
Hemophilia A drug heads toward approval in Europe
The European Medicines Agency’s Committee for Medicinal Products for Human Use recommended granting marketing authorization to the drug in January 2018, according to a statement. The recommendation will now be considered by the European Commission.
Emicizumab, which is marketed in the United States as Hemlibra, was approved by the Food and Drug Administration for adult and pediatric patients with hemophilia A with Factor VIII inhibitors in November. It is the first monoclonal antibody to be recommended for use in patients with hemophilia A with inhibitors, says the statement.
The European Medicines Agency’s Committee for Medicinal Products for Human Use recommended granting marketing authorization to the drug in January 2018, according to a statement. The recommendation will now be considered by the European Commission.
Emicizumab, which is marketed in the United States as Hemlibra, was approved by the Food and Drug Administration for adult and pediatric patients with hemophilia A with Factor VIII inhibitors in November. It is the first monoclonal antibody to be recommended for use in patients with hemophilia A with inhibitors, says the statement.
The European Medicines Agency’s Committee for Medicinal Products for Human Use recommended granting marketing authorization to the drug in January 2018, according to a statement. The recommendation will now be considered by the European Commission.
Emicizumab, which is marketed in the United States as Hemlibra, was approved by the Food and Drug Administration for adult and pediatric patients with hemophilia A with Factor VIII inhibitors in November. It is the first monoclonal antibody to be recommended for use in patients with hemophilia A with inhibitors, says the statement.
Obesity affects diagnosis of liver fibrosis with imaging techniques
, according to a study from the University of California, San Diego.
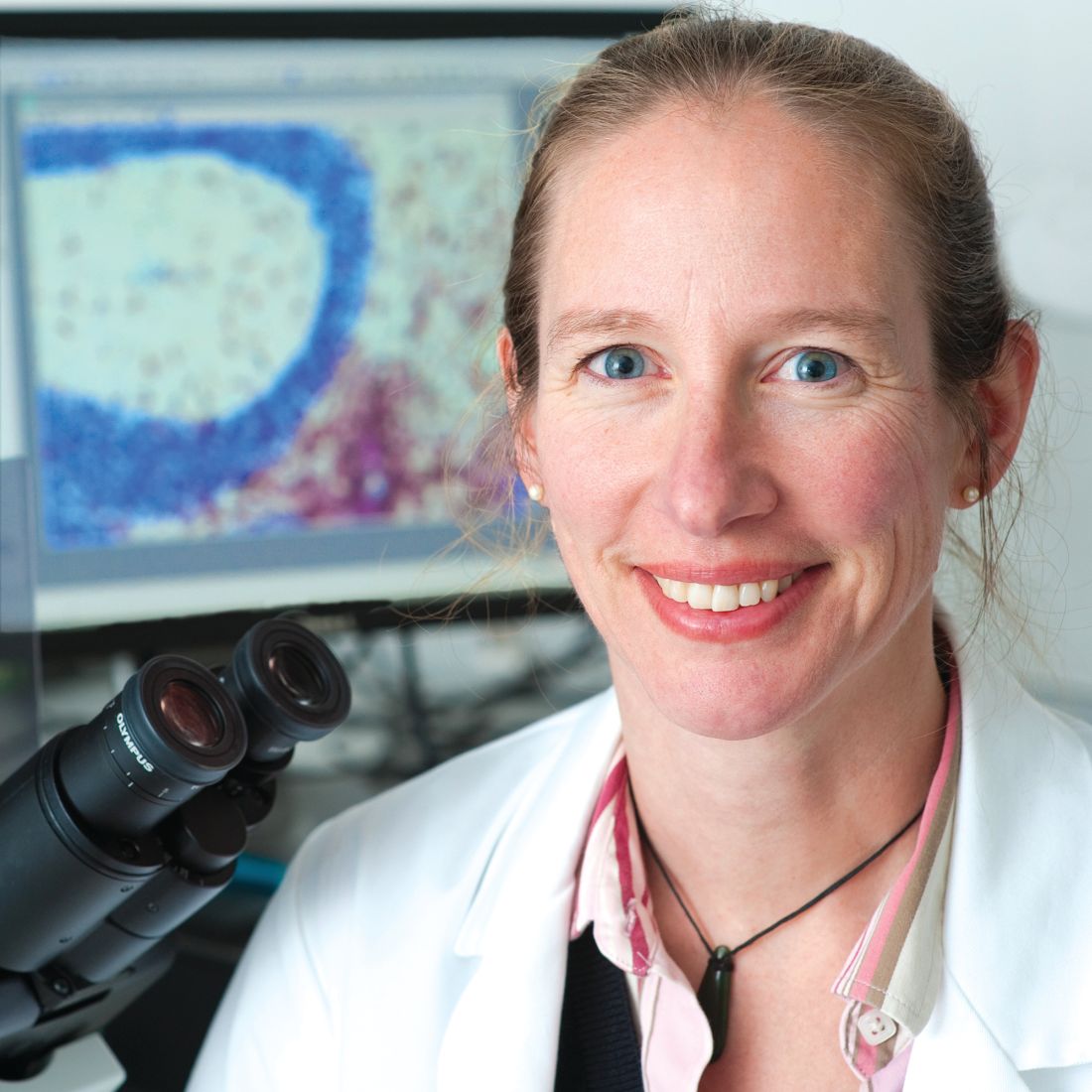
“This study demonstrates that BMI is a significant factor of discordancy between MRE and TE for the stage of significant fibrosis (2-4 vs. 0-1),” wrote Cyrielle Caussy, MD, and her colleagues (Clin Gastrolenterol Hepatol. 2018 Jan 15. doi: 10.1016/j.cgh.2017.10.037). “Furthermore, this study showed that the grade of obesity is also a significant predictor of discordancy between MRE and TE because the discordance rate between MRE and TE increases with the increase in BMI.”
Dr. Caussy of the University of California, San Diego, and her colleagues had noted that MRE and TE had discordant findings in obese patients. To ascertain under what conditions TE and MRE produce the same readings, Dr. Caussy and her associates conducted a cross-sectional study of two cohorts with nonalcoholic fatty liver disease (NAFLD) who underwent contemporaneous MRE, TE, and liver biopsy. TE utilized both M and XL probes during imaging. The training cohort involved 119 adult patients undergoing NAFLD testing from October 2011 through January 2017. The validation cohort, consisting of 75 adults with NAFLD undergoing liver imaging from March 2010 through May 2013, was formed to validate the findings of the training cohort.
The study revealed that BMI was a significant predictor of the difference between MRE and TE results and made it difficult to assess the stage of liver fibrosis (2-4 vs. 0-1). After adjustment for age and sex, BMI accounted for a 5-unit increase of 1.694 (95% confidence interval, 1.145-2.507; P = .008). This was not a static relationship, and as BMI increased, so did the discordance between MRE and TE (P = .0309). Interestingly, the discordance rate was significantly higher in participants with BMIs greater than 35 kg/m2, compared with participants with BMIs below 35 (63.0% vs. 38.0%; P = .022), the investigators reported. In severely obese adults with liver disease caused mainly by NAFLD, the accuracy of MRE was higher than TE for diagnosing significant fibrosis and advanced fibrosis.
While the study revealed valuable information, it had both strengths and limitations. A strength of the study was the use of two cohorts, specifically the validation cohort. The use of the liver biopsy as a reference, which is the standard for assessing fibrosis, was also a strength of the study. A limitation was that the study was conducted at specialized, tertiary care centers using advanced imaging techniques that may not be available at other clinics. Additionally, the cohorts included a small number of patients with advanced fibrosis.
“The integration of the BMI in the screening strategy for the noninvasive detection of liver fibrosis in NAFLD should be considered, and this parameter would help to determine when MRE is not needed in future guidelines” wrote Dr. Caussy and her associates. “Further cost-effectiveness studies are necessary to evaluate the clinical utility of MRE, TE, and/or liver biopsy to develop optimal screening strategies for diagnosing NAFLD-associated fibrosis.”
Jun Chen, MD, Meng Yin, MD, and Richard L. Ehman, MD, all have intellectual property rights and financial interests in elastography technology. Dr. Ehman also serves as an noncompensated CEO of Resoundant. Claude B. Sirlin, MD, has served as a consultant to Bayer and GE Healthcare. All other authors did not disclose any conflicts.
SOURCE: Caussy C et al. Clin Gastrolenterol Hepatol. 2018 Jan 15. doi: 10.1016/j.cgh.2017.10.037.
, according to a study from the University of California, San Diego.
“This study demonstrates that BMI is a significant factor of discordancy between MRE and TE for the stage of significant fibrosis (2-4 vs. 0-1),” wrote Cyrielle Caussy, MD, and her colleagues (Clin Gastrolenterol Hepatol. 2018 Jan 15. doi: 10.1016/j.cgh.2017.10.037). “Furthermore, this study showed that the grade of obesity is also a significant predictor of discordancy between MRE and TE because the discordance rate between MRE and TE increases with the increase in BMI.”
Dr. Caussy of the University of California, San Diego, and her colleagues had noted that MRE and TE had discordant findings in obese patients. To ascertain under what conditions TE and MRE produce the same readings, Dr. Caussy and her associates conducted a cross-sectional study of two cohorts with nonalcoholic fatty liver disease (NAFLD) who underwent contemporaneous MRE, TE, and liver biopsy. TE utilized both M and XL probes during imaging. The training cohort involved 119 adult patients undergoing NAFLD testing from October 2011 through January 2017. The validation cohort, consisting of 75 adults with NAFLD undergoing liver imaging from March 2010 through May 2013, was formed to validate the findings of the training cohort.
The study revealed that BMI was a significant predictor of the difference between MRE and TE results and made it difficult to assess the stage of liver fibrosis (2-4 vs. 0-1). After adjustment for age and sex, BMI accounted for a 5-unit increase of 1.694 (95% confidence interval, 1.145-2.507; P = .008). This was not a static relationship, and as BMI increased, so did the discordance between MRE and TE (P = .0309). Interestingly, the discordance rate was significantly higher in participants with BMIs greater than 35 kg/m2, compared with participants with BMIs below 35 (63.0% vs. 38.0%; P = .022), the investigators reported. In severely obese adults with liver disease caused mainly by NAFLD, the accuracy of MRE was higher than TE for diagnosing significant fibrosis and advanced fibrosis.
While the study revealed valuable information, it had both strengths and limitations. A strength of the study was the use of two cohorts, specifically the validation cohort. The use of the liver biopsy as a reference, which is the standard for assessing fibrosis, was also a strength of the study. A limitation was that the study was conducted at specialized, tertiary care centers using advanced imaging techniques that may not be available at other clinics. Additionally, the cohorts included a small number of patients with advanced fibrosis.
“The integration of the BMI in the screening strategy for the noninvasive detection of liver fibrosis in NAFLD should be considered, and this parameter would help to determine when MRE is not needed in future guidelines” wrote Dr. Caussy and her associates. “Further cost-effectiveness studies are necessary to evaluate the clinical utility of MRE, TE, and/or liver biopsy to develop optimal screening strategies for diagnosing NAFLD-associated fibrosis.”
Jun Chen, MD, Meng Yin, MD, and Richard L. Ehman, MD, all have intellectual property rights and financial interests in elastography technology. Dr. Ehman also serves as an noncompensated CEO of Resoundant. Claude B. Sirlin, MD, has served as a consultant to Bayer and GE Healthcare. All other authors did not disclose any conflicts.
SOURCE: Caussy C et al. Clin Gastrolenterol Hepatol. 2018 Jan 15. doi: 10.1016/j.cgh.2017.10.037.
, according to a study from the University of California, San Diego.
“This study demonstrates that BMI is a significant factor of discordancy between MRE and TE for the stage of significant fibrosis (2-4 vs. 0-1),” wrote Cyrielle Caussy, MD, and her colleagues (Clin Gastrolenterol Hepatol. 2018 Jan 15. doi: 10.1016/j.cgh.2017.10.037). “Furthermore, this study showed that the grade of obesity is also a significant predictor of discordancy between MRE and TE because the discordance rate between MRE and TE increases with the increase in BMI.”
Dr. Caussy of the University of California, San Diego, and her colleagues had noted that MRE and TE had discordant findings in obese patients. To ascertain under what conditions TE and MRE produce the same readings, Dr. Caussy and her associates conducted a cross-sectional study of two cohorts with nonalcoholic fatty liver disease (NAFLD) who underwent contemporaneous MRE, TE, and liver biopsy. TE utilized both M and XL probes during imaging. The training cohort involved 119 adult patients undergoing NAFLD testing from October 2011 through January 2017. The validation cohort, consisting of 75 adults with NAFLD undergoing liver imaging from March 2010 through May 2013, was formed to validate the findings of the training cohort.
The study revealed that BMI was a significant predictor of the difference between MRE and TE results and made it difficult to assess the stage of liver fibrosis (2-4 vs. 0-1). After adjustment for age and sex, BMI accounted for a 5-unit increase of 1.694 (95% confidence interval, 1.145-2.507; P = .008). This was not a static relationship, and as BMI increased, so did the discordance between MRE and TE (P = .0309). Interestingly, the discordance rate was significantly higher in participants with BMIs greater than 35 kg/m2, compared with participants with BMIs below 35 (63.0% vs. 38.0%; P = .022), the investigators reported. In severely obese adults with liver disease caused mainly by NAFLD, the accuracy of MRE was higher than TE for diagnosing significant fibrosis and advanced fibrosis.
While the study revealed valuable information, it had both strengths and limitations. A strength of the study was the use of two cohorts, specifically the validation cohort. The use of the liver biopsy as a reference, which is the standard for assessing fibrosis, was also a strength of the study. A limitation was that the study was conducted at specialized, tertiary care centers using advanced imaging techniques that may not be available at other clinics. Additionally, the cohorts included a small number of patients with advanced fibrosis.
“The integration of the BMI in the screening strategy for the noninvasive detection of liver fibrosis in NAFLD should be considered, and this parameter would help to determine when MRE is not needed in future guidelines” wrote Dr. Caussy and her associates. “Further cost-effectiveness studies are necessary to evaluate the clinical utility of MRE, TE, and/or liver biopsy to develop optimal screening strategies for diagnosing NAFLD-associated fibrosis.”
Jun Chen, MD, Meng Yin, MD, and Richard L. Ehman, MD, all have intellectual property rights and financial interests in elastography technology. Dr. Ehman also serves as an noncompensated CEO of Resoundant. Claude B. Sirlin, MD, has served as a consultant to Bayer and GE Healthcare. All other authors did not disclose any conflicts.
SOURCE: Caussy C et al. Clin Gastrolenterol Hepatol. 2018 Jan 15. doi: 10.1016/j.cgh.2017.10.037.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Higher BMIs make it difficult to diagnose liver fibrosis with imaging techniques.
Major finding: The discordance rate between magnetic resonance elastography and transient elastrography was 43.7% in this study.
Study details: A cross-sectional study of two cohorts with nonalcoholic fatty liver disease patients who underwent contemporaneous MRE, TE, and liver biopsy; one with 119 adults, the other with 75.
Disclosures: Jun Chen, MD, Meng Yin, MD, and Richard L. Ehman, MD, all have intellectual property rights and financial interests in elastography technology. Dr. Ehman also serves as an noncompensated CEO of Resoundant. Claude B. Sirlin, MD, has served as a consultant to Bayer and GE Healthcare. All other authors did not disclose any conflicts.
Source: Caussy C et al. Clin Gastrolenterol Hepatol. 2018 Jan 15. doi: 10.1016/j.cgh.2017.10.037.
AAN Recommends Exercise for People With MCI
Neurologists should recommend twice-weekly exercise to patients diagnosed with mild cognitive impairment (MCI) as part of an overall approach to management, according to a practice guideline update from the American Academy of Neurology (AAN). The Level B recommendation is based on six-month studies that suggest that such exercise possibly improves cognition. The update was published online ahead of print December 27, 2017, in Neurology.
“Regular physical exercise has long been shown to have heart health benefits, and now we can say exercise also may help improve memory for people with MCI,” said Ronald Petersen, MD, PhD, Director of the Alzheimer’s Disease Research Center at the Mayo Clinic in Rochester, Minnesota, and lead author of the update. “What is good for your heart can be good for your brain.”
The update also states that clinicians may recommend cognitive training for people with MCI (Level C). The evidence, however, is insufficient “to support or refute the use of any individual cognitive intervention strategy,” according to the guideline. “When various cognitive interventions are considered as a group, for patients with MCI, cognitive interventions may improve select measures of cognitive function.”
Document Updates 2001 Practice Parameter
The current practice guideline update revises the AAN’s 2001 practice parameter that provided recommendations for the diagnosis and treatment of MCI. Dr. Petersen and colleagues based the update on a systematic review of articles about MCI prevalence, prognosis, and treatment. They classified evidence according to AAN criteria and based recommendations on modified Delphi consensus.
The authors found that the prevalence of MCI is 6.7% for people between ages 60 and 64, 8.4% for people between ages 65 and 69, 10.1% for people between ages 70 and 74, 14.8% for people between ages 75 and 79, and 25.2% for people between ages 80 and 84. Approximately 15% of people with MCI who are older than 65 develop dementia during two years of follow-up.
No Evidence for Pharmacologic Treatment
Evidence does not support a symptomatic cognitive benefit in MCI for any pharmacologic or dietary agents, according to the authors. The FDA has not approved any medication for treating MCI. If clinicians offer cholinesterase inhibitors to their patients with MCI, they must first discuss the fact that the treatment is off label and not backed by empirical evidence, according to the update. Gastrointestinal symptoms and cardiac concerns are common side effects of cholinesterase inhibitors.
Assessment for MCI is appropriate for patients who complain of impaired memory or cognition, as well as those who present for a Medicare Annual Wellness Visit, according to the update. Clinicians should evaluate patients with MCI for risk factors that are potentially modifiable. Patients with MCI also should undergo serial assessments over time so that clinicians can monitor them for changes in cognitive status.
—Erik Greb
Suggested Reading
Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA. 2014;312(23):2551-2561.
Petersen RC, Lopez O, Armstrong MJ, et al. Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2017 Dec 27 [Epub ahead of print].
Vega JN, Newhouse PA. Mild cognitive impairment: diagnosis, longitudinal course, and emerging treatments. Curr Psychiatry Rep. 2014;16(10):490.
Neurologists should recommend twice-weekly exercise to patients diagnosed with mild cognitive impairment (MCI) as part of an overall approach to management, according to a practice guideline update from the American Academy of Neurology (AAN). The Level B recommendation is based on six-month studies that suggest that such exercise possibly improves cognition. The update was published online ahead of print December 27, 2017, in Neurology.
“Regular physical exercise has long been shown to have heart health benefits, and now we can say exercise also may help improve memory for people with MCI,” said Ronald Petersen, MD, PhD, Director of the Alzheimer’s Disease Research Center at the Mayo Clinic in Rochester, Minnesota, and lead author of the update. “What is good for your heart can be good for your brain.”
The update also states that clinicians may recommend cognitive training for people with MCI (Level C). The evidence, however, is insufficient “to support or refute the use of any individual cognitive intervention strategy,” according to the guideline. “When various cognitive interventions are considered as a group, for patients with MCI, cognitive interventions may improve select measures of cognitive function.”
Document Updates 2001 Practice Parameter
The current practice guideline update revises the AAN’s 2001 practice parameter that provided recommendations for the diagnosis and treatment of MCI. Dr. Petersen and colleagues based the update on a systematic review of articles about MCI prevalence, prognosis, and treatment. They classified evidence according to AAN criteria and based recommendations on modified Delphi consensus.
The authors found that the prevalence of MCI is 6.7% for people between ages 60 and 64, 8.4% for people between ages 65 and 69, 10.1% for people between ages 70 and 74, 14.8% for people between ages 75 and 79, and 25.2% for people between ages 80 and 84. Approximately 15% of people with MCI who are older than 65 develop dementia during two years of follow-up.
No Evidence for Pharmacologic Treatment
Evidence does not support a symptomatic cognitive benefit in MCI for any pharmacologic or dietary agents, according to the authors. The FDA has not approved any medication for treating MCI. If clinicians offer cholinesterase inhibitors to their patients with MCI, they must first discuss the fact that the treatment is off label and not backed by empirical evidence, according to the update. Gastrointestinal symptoms and cardiac concerns are common side effects of cholinesterase inhibitors.
Assessment for MCI is appropriate for patients who complain of impaired memory or cognition, as well as those who present for a Medicare Annual Wellness Visit, according to the update. Clinicians should evaluate patients with MCI for risk factors that are potentially modifiable. Patients with MCI also should undergo serial assessments over time so that clinicians can monitor them for changes in cognitive status.
—Erik Greb
Suggested Reading
Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA. 2014;312(23):2551-2561.
Petersen RC, Lopez O, Armstrong MJ, et al. Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2017 Dec 27 [Epub ahead of print].
Vega JN, Newhouse PA. Mild cognitive impairment: diagnosis, longitudinal course, and emerging treatments. Curr Psychiatry Rep. 2014;16(10):490.
Neurologists should recommend twice-weekly exercise to patients diagnosed with mild cognitive impairment (MCI) as part of an overall approach to management, according to a practice guideline update from the American Academy of Neurology (AAN). The Level B recommendation is based on six-month studies that suggest that such exercise possibly improves cognition. The update was published online ahead of print December 27, 2017, in Neurology.
“Regular physical exercise has long been shown to have heart health benefits, and now we can say exercise also may help improve memory for people with MCI,” said Ronald Petersen, MD, PhD, Director of the Alzheimer’s Disease Research Center at the Mayo Clinic in Rochester, Minnesota, and lead author of the update. “What is good for your heart can be good for your brain.”
The update also states that clinicians may recommend cognitive training for people with MCI (Level C). The evidence, however, is insufficient “to support or refute the use of any individual cognitive intervention strategy,” according to the guideline. “When various cognitive interventions are considered as a group, for patients with MCI, cognitive interventions may improve select measures of cognitive function.”
Document Updates 2001 Practice Parameter
The current practice guideline update revises the AAN’s 2001 practice parameter that provided recommendations for the diagnosis and treatment of MCI. Dr. Petersen and colleagues based the update on a systematic review of articles about MCI prevalence, prognosis, and treatment. They classified evidence according to AAN criteria and based recommendations on modified Delphi consensus.
The authors found that the prevalence of MCI is 6.7% for people between ages 60 and 64, 8.4% for people between ages 65 and 69, 10.1% for people between ages 70 and 74, 14.8% for people between ages 75 and 79, and 25.2% for people between ages 80 and 84. Approximately 15% of people with MCI who are older than 65 develop dementia during two years of follow-up.
No Evidence for Pharmacologic Treatment
Evidence does not support a symptomatic cognitive benefit in MCI for any pharmacologic or dietary agents, according to the authors. The FDA has not approved any medication for treating MCI. If clinicians offer cholinesterase inhibitors to their patients with MCI, they must first discuss the fact that the treatment is off label and not backed by empirical evidence, according to the update. Gastrointestinal symptoms and cardiac concerns are common side effects of cholinesterase inhibitors.
Assessment for MCI is appropriate for patients who complain of impaired memory or cognition, as well as those who present for a Medicare Annual Wellness Visit, according to the update. Clinicians should evaluate patients with MCI for risk factors that are potentially modifiable. Patients with MCI also should undergo serial assessments over time so that clinicians can monitor them for changes in cognitive status.
—Erik Greb
Suggested Reading
Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA. 2014;312(23):2551-2561.
Petersen RC, Lopez O, Armstrong MJ, et al. Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2017 Dec 27 [Epub ahead of print].
Vega JN, Newhouse PA. Mild cognitive impairment: diagnosis, longitudinal course, and emerging treatments. Curr Psychiatry Rep. 2014;16(10):490.
The shrinking role of surgical aortic valve replacement
SNOWMASS, COLO. – Michael J. Mack, MD, predicted at the Annual Cardiovascular Conference at Snowmass.
That’s assuming, hypothetically, that two ongoing randomized trials – PARTNER 3 and EVOLUT R – comparing TAVR (transcatheter aortic valve replacement) and SAVR (surgical aortic valve replacement) in low-surgical-risk patients have positive results. If so, TAVR will be proven noninferior to SAVR, as has already been convincingly shown in randomized trials conducted in high- and intermediate-surgical-risk patients.
Several factors are working against universal adoption of TAVR. There are unresolved concerns about TAVR’s durability, its issues with valve thrombosis, and its greater need for new pacemaker implantation relative to SAVR. Those questions are among the issues being addressed in nearly two dozen ongoing or upcoming TAVR trials, said Dr. Mack, director of the cardiovascular service line at Baylor Scott & White Health System, Houston.
Here are the patients Dr. Mack predicts will likely stick with SAVR for the foreseeable future:
- Younger patients. Many younger, low-surgical-risk patients will be concerned about TAVR valves’ durability and the current higher pacemaker rate.
“We have some idea of what durability is in the surgical population. What we usually quote is 12-15 years. There has been no major signal of early valve deterioration in TAVR, but there aren’t yet a significant number of patients alive for more than 5 years. Be that as it may, no significant concerns yet, but the other shoe hasn’t dropped,” the cardiothoracic surgeon observed.
Both PARTNER 3 and the EVOLUT R low-risk trial will follow participants annually for 10 years, eventually providing a robust, combined 2,000-patient database to assess comparative device durability.
The 30-day rates of permanent pacemaker implantation in TAVR recipients without a preexisting pacemaker is in the 12%-16% range with the newer-generation Evolut R and Sapien 3 valves. The indication is often new-onset left bundle branch block or complete heart block.
“I don’t think the increased pacemaker incidence is a huge problem now, but with the younger population I think it’s going to be more of an issue,” according to Dr. Mack. “It’s one thing to need a pacemaker if you’re 80-85 years old, but it’s totally different in somebody who’s 55 or 65 that has 30-35 years to live. Pacemaker leads are not benign in that population.”
“On the other hand, there is a thought that younger patients have less intrinsic conduction system disease. It may be that they are less prone to needing a new pacemaker afterward,” he added.
TAVR valve leaflet thrombosis is a concern. While a change in transvalvular gradient on echocardiography provides a signal for this complication, the actual diagnosis of valve thrombosis requires four-dimensional CT. Much better data on the true incidence and clinical ramifications of valve thrombosis in both TAVR and SAVR are coming. For example, the PARTNER 3 and EVOLUT R LR trials will each include 400-patient substudies with four-dimensional CT aimed at answering questions about valve thrombosis. The GALILEO trial, involving 1,520 TAVR patients, is designed to determine whether low-dose rivaroxaban prevents valve thrombosis and periprocedural embolization. Results of this randomized trial are due in about a year. Similarly, the 1,509-patient randomized ATLANTIS trial is looking at the effects of apixaban versus warfarin versus dual or single antiplatelet therapy.
If long-term anticoagulation in TAVR patients is found to be beneficial, that may steer some patients toward SAVR, especially if they are physically active or at high bleeding risk.
- Aortic stenosis patients with a high Syntax score and multivessel coronary artery disease. This group is best served by concomitant SAVR and coronary artery bypass grafting surgery.
- Patients with low or intermediate surgical risk with multivalve disease. “We know that patients with moderate to severe mitral regurgitation and/or moderate to severe tricuspid regurgitation do not do well after TAVR,” the surgeon said.
- Rheumatic valve disease patients.
- Patients who present at a site that offers SAVR only. “There are about 1,150 cardiac surgery programs in the United States and about 560 TAVR programs. There is concern that patients who don’t come in to a center that offers TAVR will not be offered TAVR as an option. I think there’s probably some truth to that,” Dr. Mack said.
- Patients going to sites without a well-functioning collaborative heart team. “In institutions where surgeons and cardiologists don’t get along, turf is much more of an issue, and surgeons are going to hold on to those patients more closely,” he observed.
- Patient’s with certain preferences. “All other things being equal, the patient is always going to choose the less invasive option. However, we do see some patients – I think it’s about 1 out of 10 – who express a preference to stay with the tried and true surgery,” according to Dr. Mack.
He reported receiving research grants from Abbott Vascular, Edwards Lifesciences, and Medtronic.
SNOWMASS, COLO. – Michael J. Mack, MD, predicted at the Annual Cardiovascular Conference at Snowmass.
That’s assuming, hypothetically, that two ongoing randomized trials – PARTNER 3 and EVOLUT R – comparing TAVR (transcatheter aortic valve replacement) and SAVR (surgical aortic valve replacement) in low-surgical-risk patients have positive results. If so, TAVR will be proven noninferior to SAVR, as has already been convincingly shown in randomized trials conducted in high- and intermediate-surgical-risk patients.
Several factors are working against universal adoption of TAVR. There are unresolved concerns about TAVR’s durability, its issues with valve thrombosis, and its greater need for new pacemaker implantation relative to SAVR. Those questions are among the issues being addressed in nearly two dozen ongoing or upcoming TAVR trials, said Dr. Mack, director of the cardiovascular service line at Baylor Scott & White Health System, Houston.
Here are the patients Dr. Mack predicts will likely stick with SAVR for the foreseeable future:
- Younger patients. Many younger, low-surgical-risk patients will be concerned about TAVR valves’ durability and the current higher pacemaker rate.
“We have some idea of what durability is in the surgical population. What we usually quote is 12-15 years. There has been no major signal of early valve deterioration in TAVR, but there aren’t yet a significant number of patients alive for more than 5 years. Be that as it may, no significant concerns yet, but the other shoe hasn’t dropped,” the cardiothoracic surgeon observed.
Both PARTNER 3 and the EVOLUT R low-risk trial will follow participants annually for 10 years, eventually providing a robust, combined 2,000-patient database to assess comparative device durability.
The 30-day rates of permanent pacemaker implantation in TAVR recipients without a preexisting pacemaker is in the 12%-16% range with the newer-generation Evolut R and Sapien 3 valves. The indication is often new-onset left bundle branch block or complete heart block.
“I don’t think the increased pacemaker incidence is a huge problem now, but with the younger population I think it’s going to be more of an issue,” according to Dr. Mack. “It’s one thing to need a pacemaker if you’re 80-85 years old, but it’s totally different in somebody who’s 55 or 65 that has 30-35 years to live. Pacemaker leads are not benign in that population.”
“On the other hand, there is a thought that younger patients have less intrinsic conduction system disease. It may be that they are less prone to needing a new pacemaker afterward,” he added.
TAVR valve leaflet thrombosis is a concern. While a change in transvalvular gradient on echocardiography provides a signal for this complication, the actual diagnosis of valve thrombosis requires four-dimensional CT. Much better data on the true incidence and clinical ramifications of valve thrombosis in both TAVR and SAVR are coming. For example, the PARTNER 3 and EVOLUT R LR trials will each include 400-patient substudies with four-dimensional CT aimed at answering questions about valve thrombosis. The GALILEO trial, involving 1,520 TAVR patients, is designed to determine whether low-dose rivaroxaban prevents valve thrombosis and periprocedural embolization. Results of this randomized trial are due in about a year. Similarly, the 1,509-patient randomized ATLANTIS trial is looking at the effects of apixaban versus warfarin versus dual or single antiplatelet therapy.
If long-term anticoagulation in TAVR patients is found to be beneficial, that may steer some patients toward SAVR, especially if they are physically active or at high bleeding risk.
- Aortic stenosis patients with a high Syntax score and multivessel coronary artery disease. This group is best served by concomitant SAVR and coronary artery bypass grafting surgery.
- Patients with low or intermediate surgical risk with multivalve disease. “We know that patients with moderate to severe mitral regurgitation and/or moderate to severe tricuspid regurgitation do not do well after TAVR,” the surgeon said.
- Rheumatic valve disease patients.
- Patients who present at a site that offers SAVR only. “There are about 1,150 cardiac surgery programs in the United States and about 560 TAVR programs. There is concern that patients who don’t come in to a center that offers TAVR will not be offered TAVR as an option. I think there’s probably some truth to that,” Dr. Mack said.
- Patients going to sites without a well-functioning collaborative heart team. “In institutions where surgeons and cardiologists don’t get along, turf is much more of an issue, and surgeons are going to hold on to those patients more closely,” he observed.
- Patient’s with certain preferences. “All other things being equal, the patient is always going to choose the less invasive option. However, we do see some patients – I think it’s about 1 out of 10 – who express a preference to stay with the tried and true surgery,” according to Dr. Mack.
He reported receiving research grants from Abbott Vascular, Edwards Lifesciences, and Medtronic.
SNOWMASS, COLO. – Michael J. Mack, MD, predicted at the Annual Cardiovascular Conference at Snowmass.
That’s assuming, hypothetically, that two ongoing randomized trials – PARTNER 3 and EVOLUT R – comparing TAVR (transcatheter aortic valve replacement) and SAVR (surgical aortic valve replacement) in low-surgical-risk patients have positive results. If so, TAVR will be proven noninferior to SAVR, as has already been convincingly shown in randomized trials conducted in high- and intermediate-surgical-risk patients.
Several factors are working against universal adoption of TAVR. There are unresolved concerns about TAVR’s durability, its issues with valve thrombosis, and its greater need for new pacemaker implantation relative to SAVR. Those questions are among the issues being addressed in nearly two dozen ongoing or upcoming TAVR trials, said Dr. Mack, director of the cardiovascular service line at Baylor Scott & White Health System, Houston.
Here are the patients Dr. Mack predicts will likely stick with SAVR for the foreseeable future:
- Younger patients. Many younger, low-surgical-risk patients will be concerned about TAVR valves’ durability and the current higher pacemaker rate.
“We have some idea of what durability is in the surgical population. What we usually quote is 12-15 years. There has been no major signal of early valve deterioration in TAVR, but there aren’t yet a significant number of patients alive for more than 5 years. Be that as it may, no significant concerns yet, but the other shoe hasn’t dropped,” the cardiothoracic surgeon observed.
Both PARTNER 3 and the EVOLUT R low-risk trial will follow participants annually for 10 years, eventually providing a robust, combined 2,000-patient database to assess comparative device durability.
The 30-day rates of permanent pacemaker implantation in TAVR recipients without a preexisting pacemaker is in the 12%-16% range with the newer-generation Evolut R and Sapien 3 valves. The indication is often new-onset left bundle branch block or complete heart block.
“I don’t think the increased pacemaker incidence is a huge problem now, but with the younger population I think it’s going to be more of an issue,” according to Dr. Mack. “It’s one thing to need a pacemaker if you’re 80-85 years old, but it’s totally different in somebody who’s 55 or 65 that has 30-35 years to live. Pacemaker leads are not benign in that population.”
“On the other hand, there is a thought that younger patients have less intrinsic conduction system disease. It may be that they are less prone to needing a new pacemaker afterward,” he added.
TAVR valve leaflet thrombosis is a concern. While a change in transvalvular gradient on echocardiography provides a signal for this complication, the actual diagnosis of valve thrombosis requires four-dimensional CT. Much better data on the true incidence and clinical ramifications of valve thrombosis in both TAVR and SAVR are coming. For example, the PARTNER 3 and EVOLUT R LR trials will each include 400-patient substudies with four-dimensional CT aimed at answering questions about valve thrombosis. The GALILEO trial, involving 1,520 TAVR patients, is designed to determine whether low-dose rivaroxaban prevents valve thrombosis and periprocedural embolization. Results of this randomized trial are due in about a year. Similarly, the 1,509-patient randomized ATLANTIS trial is looking at the effects of apixaban versus warfarin versus dual or single antiplatelet therapy.
If long-term anticoagulation in TAVR patients is found to be beneficial, that may steer some patients toward SAVR, especially if they are physically active or at high bleeding risk.
- Aortic stenosis patients with a high Syntax score and multivessel coronary artery disease. This group is best served by concomitant SAVR and coronary artery bypass grafting surgery.
- Patients with low or intermediate surgical risk with multivalve disease. “We know that patients with moderate to severe mitral regurgitation and/or moderate to severe tricuspid regurgitation do not do well after TAVR,” the surgeon said.
- Rheumatic valve disease patients.
- Patients who present at a site that offers SAVR only. “There are about 1,150 cardiac surgery programs in the United States and about 560 TAVR programs. There is concern that patients who don’t come in to a center that offers TAVR will not be offered TAVR as an option. I think there’s probably some truth to that,” Dr. Mack said.
- Patients going to sites without a well-functioning collaborative heart team. “In institutions where surgeons and cardiologists don’t get along, turf is much more of an issue, and surgeons are going to hold on to those patients more closely,” he observed.
- Patient’s with certain preferences. “All other things being equal, the patient is always going to choose the less invasive option. However, we do see some patients – I think it’s about 1 out of 10 – who express a preference to stay with the tried and true surgery,” according to Dr. Mack.
He reported receiving research grants from Abbott Vascular, Edwards Lifesciences, and Medtronic.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Low Serum Caffeine Level Could Indicate Early Parkinson’s Disease
Low serum caffeine and caffeine metabolite levels after an overnight fast may be a sensitive way to detect Parkinson’s disease, according to the results of a case–control study published online ahead of print January 3 in Neurology.
In the study, levels of caffeine and its metabolites were lower in patients with Parkinson’s disease and motor dysfunction, compared with those without motor dysfunction. The investigators detected no differences in serum levels of caffeine metabolites between patients with mild Parkinson’s disease and those with severe Parkinson’s disease, said Motoki Fujimaki, MD, of Juntendo University School of Medicine in Tokyo, and colleagues.
A Single-Center Study
Previous research had shown that people drinking four or more cups of coffee per day had a greater than fivefold reduction in the risk of developing Parkinson’s disease. Mouse models of Parkinson’s disease showed that caffeine and two of its metabolites have a neuroprotective effect. Those results suggested that serum caffeine might be useful as a blood marker for Parkinson’s disease.
To test that idea, Dr. Fujimaki and associates recruited 31 healthy controls (18 women) and 108 patients with Parkinson’s disease but no dementia (50 women). The control group’s mean caffeine intake of 115.81 mg/day was similar to that of patients with Parkinson’s disease (107.50 mg/day).
Serum caffeine levels measured after an overnight fast showed that a cutoff of 33.04 pmol/10 µL identified Parkinson’s disease with an area under the curve (AUC) of 0.78 (sensitivity, 76.9%; specificity, 74.2%). Inclusion of the primary caffeine metabolites theophylline, theobromine, and paraxanthine increased the AUC to 0.87. When the researchers included all 11 measurable metabolites, the AUC increased further to 0.98.
Genetic analyses revealed no significant differences in the frequencies of caffeine metabolism–associated genetic variants between patients and controls.
The study was limited by the fact that it was conducted at a single university hospital, and the patient population did not include many severe cases. The association should also be studied in other Parkinson’s disease patient populations, according to the authors.
Did Treatment Effects Influence the Findings?
A key question that the study raises is what caused the decrease in serum concentration found in patients with Parkinson’s disease, said David G. Munoz, MD, of the Department of Laboratory Medicine and Pathobiology at the University of Toronto, and Shinsuke Fujioka, MD, of the Department of Neurology at Fukuoka University in Japan, in an accompanying editorial. Almost all of the patients were receiving treatment, which could have affected serum levels, they added. The researchers looked for, but did not find, an association between serum caffeine metabolite levels and levodopa equivalent doses.
“The validity of the study depends on whether caffeine metabolism may be affected by treatment,” said Drs. Munoz and Fujioka. “To demonstrate the utility of caffeine metabolites unequivocally, a future study will have to reproduce these results in patients with untreated Parkinson’s disease or subjects at high risk of Parkinson’s disease, such as those with prodromal signs of Parkinson’s disease.”
—Jim Kling
Suggested Reading
Fujimaki M, Saiki S, Li Y, et al. Serum caffeine and metabolites are reliable biomarkers of early Parkinson disease. Neurology. 2018 Jan 3 [Epub ahead of print].
Munoz DG, Fujioka S. Caffeine and Parkinson disease: A possible diagnostic and pathogenic breakthrough. Neurology. 2018 Jan 3 [Epub ahead of print].
Low serum caffeine and caffeine metabolite levels after an overnight fast may be a sensitive way to detect Parkinson’s disease, according to the results of a case–control study published online ahead of print January 3 in Neurology.
In the study, levels of caffeine and its metabolites were lower in patients with Parkinson’s disease and motor dysfunction, compared with those without motor dysfunction. The investigators detected no differences in serum levels of caffeine metabolites between patients with mild Parkinson’s disease and those with severe Parkinson’s disease, said Motoki Fujimaki, MD, of Juntendo University School of Medicine in Tokyo, and colleagues.
A Single-Center Study
Previous research had shown that people drinking four or more cups of coffee per day had a greater than fivefold reduction in the risk of developing Parkinson’s disease. Mouse models of Parkinson’s disease showed that caffeine and two of its metabolites have a neuroprotective effect. Those results suggested that serum caffeine might be useful as a blood marker for Parkinson’s disease.
To test that idea, Dr. Fujimaki and associates recruited 31 healthy controls (18 women) and 108 patients with Parkinson’s disease but no dementia (50 women). The control group’s mean caffeine intake of 115.81 mg/day was similar to that of patients with Parkinson’s disease (107.50 mg/day).
Serum caffeine levels measured after an overnight fast showed that a cutoff of 33.04 pmol/10 µL identified Parkinson’s disease with an area under the curve (AUC) of 0.78 (sensitivity, 76.9%; specificity, 74.2%). Inclusion of the primary caffeine metabolites theophylline, theobromine, and paraxanthine increased the AUC to 0.87. When the researchers included all 11 measurable metabolites, the AUC increased further to 0.98.
Genetic analyses revealed no significant differences in the frequencies of caffeine metabolism–associated genetic variants between patients and controls.
The study was limited by the fact that it was conducted at a single university hospital, and the patient population did not include many severe cases. The association should also be studied in other Parkinson’s disease patient populations, according to the authors.
Did Treatment Effects Influence the Findings?
A key question that the study raises is what caused the decrease in serum concentration found in patients with Parkinson’s disease, said David G. Munoz, MD, of the Department of Laboratory Medicine and Pathobiology at the University of Toronto, and Shinsuke Fujioka, MD, of the Department of Neurology at Fukuoka University in Japan, in an accompanying editorial. Almost all of the patients were receiving treatment, which could have affected serum levels, they added. The researchers looked for, but did not find, an association between serum caffeine metabolite levels and levodopa equivalent doses.
“The validity of the study depends on whether caffeine metabolism may be affected by treatment,” said Drs. Munoz and Fujioka. “To demonstrate the utility of caffeine metabolites unequivocally, a future study will have to reproduce these results in patients with untreated Parkinson’s disease or subjects at high risk of Parkinson’s disease, such as those with prodromal signs of Parkinson’s disease.”
—Jim Kling
Suggested Reading
Fujimaki M, Saiki S, Li Y, et al. Serum caffeine and metabolites are reliable biomarkers of early Parkinson disease. Neurology. 2018 Jan 3 [Epub ahead of print].
Munoz DG, Fujioka S. Caffeine and Parkinson disease: A possible diagnostic and pathogenic breakthrough. Neurology. 2018 Jan 3 [Epub ahead of print].
Low serum caffeine and caffeine metabolite levels after an overnight fast may be a sensitive way to detect Parkinson’s disease, according to the results of a case–control study published online ahead of print January 3 in Neurology.
In the study, levels of caffeine and its metabolites were lower in patients with Parkinson’s disease and motor dysfunction, compared with those without motor dysfunction. The investigators detected no differences in serum levels of caffeine metabolites between patients with mild Parkinson’s disease and those with severe Parkinson’s disease, said Motoki Fujimaki, MD, of Juntendo University School of Medicine in Tokyo, and colleagues.
A Single-Center Study
Previous research had shown that people drinking four or more cups of coffee per day had a greater than fivefold reduction in the risk of developing Parkinson’s disease. Mouse models of Parkinson’s disease showed that caffeine and two of its metabolites have a neuroprotective effect. Those results suggested that serum caffeine might be useful as a blood marker for Parkinson’s disease.
To test that idea, Dr. Fujimaki and associates recruited 31 healthy controls (18 women) and 108 patients with Parkinson’s disease but no dementia (50 women). The control group’s mean caffeine intake of 115.81 mg/day was similar to that of patients with Parkinson’s disease (107.50 mg/day).
Serum caffeine levels measured after an overnight fast showed that a cutoff of 33.04 pmol/10 µL identified Parkinson’s disease with an area under the curve (AUC) of 0.78 (sensitivity, 76.9%; specificity, 74.2%). Inclusion of the primary caffeine metabolites theophylline, theobromine, and paraxanthine increased the AUC to 0.87. When the researchers included all 11 measurable metabolites, the AUC increased further to 0.98.
Genetic analyses revealed no significant differences in the frequencies of caffeine metabolism–associated genetic variants between patients and controls.
The study was limited by the fact that it was conducted at a single university hospital, and the patient population did not include many severe cases. The association should also be studied in other Parkinson’s disease patient populations, according to the authors.
Did Treatment Effects Influence the Findings?
A key question that the study raises is what caused the decrease in serum concentration found in patients with Parkinson’s disease, said David G. Munoz, MD, of the Department of Laboratory Medicine and Pathobiology at the University of Toronto, and Shinsuke Fujioka, MD, of the Department of Neurology at Fukuoka University in Japan, in an accompanying editorial. Almost all of the patients were receiving treatment, which could have affected serum levels, they added. The researchers looked for, but did not find, an association between serum caffeine metabolite levels and levodopa equivalent doses.
“The validity of the study depends on whether caffeine metabolism may be affected by treatment,” said Drs. Munoz and Fujioka. “To demonstrate the utility of caffeine metabolites unequivocally, a future study will have to reproduce these results in patients with untreated Parkinson’s disease or subjects at high risk of Parkinson’s disease, such as those with prodromal signs of Parkinson’s disease.”
—Jim Kling
Suggested Reading
Fujimaki M, Saiki S, Li Y, et al. Serum caffeine and metabolites are reliable biomarkers of early Parkinson disease. Neurology. 2018 Jan 3 [Epub ahead of print].
Munoz DG, Fujioka S. Caffeine and Parkinson disease: A possible diagnostic and pathogenic breakthrough. Neurology. 2018 Jan 3 [Epub ahead of print].
Embracing Life’s Simple 7 slashes PAD risk
ANAHEIM, CALIF. – Adherence to the American Heart Association’s widely publicized “Life’s Simple 7” program addressing key modifiable cardiovascular health factors substantially reduces the risk of developing peripheral arterial disease, Parveen Garg, MD, said at the American Heart Association scientific sessions.
This is new evidence-supported information. Until this new analysis from the landmark ARIC (Atherosclerosis Risk in Communities) study, the relationship between Life’s Simple 7 and peripheral arterial disease (PAD) hadn’t been studied. It’s a relationship worthy of examination, considering that more than 8 million Americans have PAD, and nearly 40% of them don’t have concomitant coronary or cerebrovascular disease, which raised the question of whether Life’s Simple 7 applied to PAD risk, noted Dr. Garg of the University of Southern California, Los Angeles.
ARIC is a National Heart, Lung, and Blood Institute–sponsored prospective study of nearly 16,000 black or white individuals who were middle-aged at enrollment and have been followed for more than 2 decades. Dr. Garg’s analysis focused on 12,865 participants who were free of CHD, heart failure, prior stroke, and PAD at baseline, and have been followed for a median of 24 years.
As background, the metrics for Life’s Simple 7 consist of total cholesterol, blood pressure, blood glucose, smoking status, body mass index, physical activity, and adherence to a healthy diet score. Each element can be scored 2 points for ideal, 1 for intermediate, and 0 for poor. The composite Life’s Simple 7 score is rated optimal at 10-14 points, average at 5-9, and inadequate at 0-4.
During follow-up, 3.4% of ARIC participants developed PAD sufficiently severe to involve hospitalization. The incidence rate was 5.2 cases per 1,000 person-years for the 1,008 subjects categorized as having an inadequate Life’s Simple 7 score, 1.1/1,000 person-years for the 8,395 people in the average category, and just 0.4 cases/1,000 person-years for the 3,462 individuals in the optimal Life’s Simple 7 group.
Compared with subjects in the inadequate category, those in the average group were 56% less likely to develop PAD. Those in the optimal Life’s Simple 7 category had an 86% reduction in risk.
For each of the seven components of Life’s Simple 7 a person scored ideally in, the risk of incident PAD was reduced by 28% in a multivariate analysis fully adjusted for demographics, alcohol consumption, aspirin use, study site, left ventricular hypertrophy, and other potential confounders.
The inverse relationship between Life’s Simple 7 score and PAD risk was stronger in women than men. However, the association didn’t differ by race.
Dr. Garg noted that his study undoubtedly underestimates the true incidence of PAD in the ARIC population, since a hospital diagnosis was required. Also, to date he and his coinvestigators have only analyzed the results in terms of baseline Life’s Simple 7 score. It would be useful to also document the impact of change in the score over time.
Session moderator David C. Goff Jr., MD, observed, “This is very consistent with evidence in CHD that people who are in ideal cardiovascular health status have about an 80%-90% lower risk of cardiovascular mortality and a 70%-80% reduction in risk of total mortality compared with people who are in poor cardiovascular health status.”
“This study really does provide additional evidence that if we could get more people into the ideal cardiovascular health range, we’d probably see less atherosclerotic cardiovascular disease in general,” added Dr. Goff, who is director of the division of cardiovascular sciences at the National Heart, Lung, and Blood Institute.
Dr. Garg reported having no financial conflicts of interest.
ANAHEIM, CALIF. – Adherence to the American Heart Association’s widely publicized “Life’s Simple 7” program addressing key modifiable cardiovascular health factors substantially reduces the risk of developing peripheral arterial disease, Parveen Garg, MD, said at the American Heart Association scientific sessions.
This is new evidence-supported information. Until this new analysis from the landmark ARIC (Atherosclerosis Risk in Communities) study, the relationship between Life’s Simple 7 and peripheral arterial disease (PAD) hadn’t been studied. It’s a relationship worthy of examination, considering that more than 8 million Americans have PAD, and nearly 40% of them don’t have concomitant coronary or cerebrovascular disease, which raised the question of whether Life’s Simple 7 applied to PAD risk, noted Dr. Garg of the University of Southern California, Los Angeles.
ARIC is a National Heart, Lung, and Blood Institute–sponsored prospective study of nearly 16,000 black or white individuals who were middle-aged at enrollment and have been followed for more than 2 decades. Dr. Garg’s analysis focused on 12,865 participants who were free of CHD, heart failure, prior stroke, and PAD at baseline, and have been followed for a median of 24 years.
As background, the metrics for Life’s Simple 7 consist of total cholesterol, blood pressure, blood glucose, smoking status, body mass index, physical activity, and adherence to a healthy diet score. Each element can be scored 2 points for ideal, 1 for intermediate, and 0 for poor. The composite Life’s Simple 7 score is rated optimal at 10-14 points, average at 5-9, and inadequate at 0-4.
During follow-up, 3.4% of ARIC participants developed PAD sufficiently severe to involve hospitalization. The incidence rate was 5.2 cases per 1,000 person-years for the 1,008 subjects categorized as having an inadequate Life’s Simple 7 score, 1.1/1,000 person-years for the 8,395 people in the average category, and just 0.4 cases/1,000 person-years for the 3,462 individuals in the optimal Life’s Simple 7 group.
Compared with subjects in the inadequate category, those in the average group were 56% less likely to develop PAD. Those in the optimal Life’s Simple 7 category had an 86% reduction in risk.
For each of the seven components of Life’s Simple 7 a person scored ideally in, the risk of incident PAD was reduced by 28% in a multivariate analysis fully adjusted for demographics, alcohol consumption, aspirin use, study site, left ventricular hypertrophy, and other potential confounders.
The inverse relationship between Life’s Simple 7 score and PAD risk was stronger in women than men. However, the association didn’t differ by race.
Dr. Garg noted that his study undoubtedly underestimates the true incidence of PAD in the ARIC population, since a hospital diagnosis was required. Also, to date he and his coinvestigators have only analyzed the results in terms of baseline Life’s Simple 7 score. It would be useful to also document the impact of change in the score over time.
Session moderator David C. Goff Jr., MD, observed, “This is very consistent with evidence in CHD that people who are in ideal cardiovascular health status have about an 80%-90% lower risk of cardiovascular mortality and a 70%-80% reduction in risk of total mortality compared with people who are in poor cardiovascular health status.”
“This study really does provide additional evidence that if we could get more people into the ideal cardiovascular health range, we’d probably see less atherosclerotic cardiovascular disease in general,” added Dr. Goff, who is director of the division of cardiovascular sciences at the National Heart, Lung, and Blood Institute.
Dr. Garg reported having no financial conflicts of interest.
ANAHEIM, CALIF. – Adherence to the American Heart Association’s widely publicized “Life’s Simple 7” program addressing key modifiable cardiovascular health factors substantially reduces the risk of developing peripheral arterial disease, Parveen Garg, MD, said at the American Heart Association scientific sessions.
This is new evidence-supported information. Until this new analysis from the landmark ARIC (Atherosclerosis Risk in Communities) study, the relationship between Life’s Simple 7 and peripheral arterial disease (PAD) hadn’t been studied. It’s a relationship worthy of examination, considering that more than 8 million Americans have PAD, and nearly 40% of them don’t have concomitant coronary or cerebrovascular disease, which raised the question of whether Life’s Simple 7 applied to PAD risk, noted Dr. Garg of the University of Southern California, Los Angeles.
ARIC is a National Heart, Lung, and Blood Institute–sponsored prospective study of nearly 16,000 black or white individuals who were middle-aged at enrollment and have been followed for more than 2 decades. Dr. Garg’s analysis focused on 12,865 participants who were free of CHD, heart failure, prior stroke, and PAD at baseline, and have been followed for a median of 24 years.
As background, the metrics for Life’s Simple 7 consist of total cholesterol, blood pressure, blood glucose, smoking status, body mass index, physical activity, and adherence to a healthy diet score. Each element can be scored 2 points for ideal, 1 for intermediate, and 0 for poor. The composite Life’s Simple 7 score is rated optimal at 10-14 points, average at 5-9, and inadequate at 0-4.
During follow-up, 3.4% of ARIC participants developed PAD sufficiently severe to involve hospitalization. The incidence rate was 5.2 cases per 1,000 person-years for the 1,008 subjects categorized as having an inadequate Life’s Simple 7 score, 1.1/1,000 person-years for the 8,395 people in the average category, and just 0.4 cases/1,000 person-years for the 3,462 individuals in the optimal Life’s Simple 7 group.
Compared with subjects in the inadequate category, those in the average group were 56% less likely to develop PAD. Those in the optimal Life’s Simple 7 category had an 86% reduction in risk.
For each of the seven components of Life’s Simple 7 a person scored ideally in, the risk of incident PAD was reduced by 28% in a multivariate analysis fully adjusted for demographics, alcohol consumption, aspirin use, study site, left ventricular hypertrophy, and other potential confounders.
The inverse relationship between Life’s Simple 7 score and PAD risk was stronger in women than men. However, the association didn’t differ by race.
Dr. Garg noted that his study undoubtedly underestimates the true incidence of PAD in the ARIC population, since a hospital diagnosis was required. Also, to date he and his coinvestigators have only analyzed the results in terms of baseline Life’s Simple 7 score. It would be useful to also document the impact of change in the score over time.
Session moderator David C. Goff Jr., MD, observed, “This is very consistent with evidence in CHD that people who are in ideal cardiovascular health status have about an 80%-90% lower risk of cardiovascular mortality and a 70%-80% reduction in risk of total mortality compared with people who are in poor cardiovascular health status.”
“This study really does provide additional evidence that if we could get more people into the ideal cardiovascular health range, we’d probably see less atherosclerotic cardiovascular disease in general,” added Dr. Goff, who is director of the division of cardiovascular sciences at the National Heart, Lung, and Blood Institute.
Dr. Garg reported having no financial conflicts of interest.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: The Life’s Simple 7 public health program points the way to reduced risk of PAD.
Major finding: Being in the top tertile of cardiovascular health by the American Heart Association’s Life’s Simple 7 metric is associated with an 86% lower risk of developing PAD than for those in poor cardiovascular health.
Study details: This biracial prospective observational study includes nearly 16,000 white and black Americans.
Disclosures: The ARIC study is funded by the NHLBI. The presenter reported having no financial conflicts.
Can Walking Protect Cognition in Amyloid-Positive Older Adults?
BOSTON—Walking appears to moderate cognitive decline in people with elevated levels of amyloid in the brain, according to a four-year observational study described at the Clinical Trials on Alzheimer’s Disease conference.
Among a group of cognitively normal older adults with beta-amyloid brain plaques, those who walked the most had significantly less decline in memory and thinking than those who walked little, said Dylan Kirn, MPH. Walking did not affect any biomarkers of Alzheimer’s disease, such as brain glucose utilization, amyloid accumulation, or hippocampal volume, but it was associated with significantly better cognitive scores on a composite measure of memory over time.
“We should be careful in interpreting these data, because this is an observational cohort, and we cannot make claims regarding causality or the mechanism by which physical activity may be influencing cognitive decline,” said Mr. Kirn, Clinical Research Project Manager at the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital in Boston. “But I find these results interesting and novel, and I think they support further investigation.”
The Harvard Aging Brain Study
The research is part of the ongoing Harvard Aging Brain Study, which is a longitudinal investigation of cognitively normal elderly individuals that seeks to identify the earliest changes in molecular, functional, and structural imaging markers that signal a transition from normal cognition to progressive cognitive decline and preclinical Alzheimer’s disease. The walking study included 255 subjects with a mean age of 73. Participants were highly educated, with a mean of 16 years’ schooling. About 24% of the population was amyloid-positive on PET imaging. All patients were cognitively normal, with a Clinical Dementia Rating scale score of 0. Activity was measured at baseline with a pedometer, which was worn for seven consecutive days; only people who walked at least 100 steps per day were included in the analysis.
In addition to amyloid PET imaging, subjects underwent an 18F-fluorodeoxyglucose (FDG) PET scan to assess brain glucose utilization, and MRI to measure hippocampal volume changes and white matter hyperintensities (WMHs). Changes in all of these biomarkers can herald the onset of Alzheimer’s disease.
The study’s primary outcome was the relationship between physical activity, as measured by number of walking steps per day, and changes on the Preclinical Alzheimer’s Cognitive Composite (PACC) test. This relatively new cognitive scale is gaining increasing use in clinical trials. The PACC is a composite of the Digit Symbol Substitution Test score from the Wechsler Adult Intelligence Scale–Revised, the Mini-Mental State Examination, the Total Recall score from the Free and Cued Selective Reminding Test, and the Delayed Recall score on the Logical Memory IIa subtest of the Wechsler Memory Scale. It correlates well with amyloid accumulation in the brain, said Mr. Kirn.
The cohort was followed for as long as six years (median follow-up, four years), and PACC scores were calculated annually. The investigators examined the relationship between walking at baseline and PACC decline during the study period in two multivariate models. One model controlled for age, sex, and years of education, and the second controlled for those variables plus cortical WMHs, bilateral hippocampal volume (HV), and FDG PET in brain regions typically affected by Alzheimer’s disease.
The investigators sorted physical activity into tertiles by the average number of steps per day over the seven-day measuring period. The middle tertile was the mean (ie, 5,616 steps/day), the top tertile was one standard deviation above the mean (ie, 8,482 steps/day), and the bottom tertile was one standard deviation below the mean (ie, 2,751 steps/day). Amyloid-positive patients were further categorized as having high or low brain amyloid load.
No Relationship Between Activity and Biomarkers
The researchers found no significant relationships between any of the biomarkers and any level of physical activity in either of the analyses, said Mr. Kirn. When looking at the time-linked changes in the PACC, however, they found significant differences. Subjects who walked at least the mean number of steps per day were much more likely to maintain a stable cognitive score, while those who walked the fewest steps declined by about a quarter of a point on the PACC. The difference in decline between the high-activity and low-activity subjects was statistically significant, even when the investigators controlled for amyloid burden and other Alzheimer’s disease biomarkers.
The level of physical activity at baseline was a particularly strong predictor of cognitive health among amyloid-positive subjects. Those in the high-activity group maintained a steady score on the PACC. Those in the mean activity group declined slightly, and those in the low activity group showed a sharp decline, losing almost a full point on the PACC by the end of follow-up.
In the amyloid-negative group, the researchers found no association between cognition and activity. PACC scores improved for all groups during the study period, which probably reflects a practice effect, said Mr. Kirn.
“We observed that physical activity was significantly predictive of cognitive decline in high-amyloid participants, but not in low-amyloid participants,” he said. “Individuals with high amyloid and low physical activity at baseline had the steepest decline in cognition over time. But in those with high amyloid and high physical activity at baseline, we did not see a tremendous amount of decline.”
The study suggests that pedometers may help stratify patients for clinical trials or assess cognitive risk in elderly subjects. “Most studies that have looked at physical activity and dementia use a self-reported activity level, so the results have been varied,” said Mr. Kirn. “These findings support consideration of objectively measured physical activity in clinical research, and perhaps in stratification for risk of cognitive decline.”
—Michele G. Sullivan
BOSTON—Walking appears to moderate cognitive decline in people with elevated levels of amyloid in the brain, according to a four-year observational study described at the Clinical Trials on Alzheimer’s Disease conference.
Among a group of cognitively normal older adults with beta-amyloid brain plaques, those who walked the most had significantly less decline in memory and thinking than those who walked little, said Dylan Kirn, MPH. Walking did not affect any biomarkers of Alzheimer’s disease, such as brain glucose utilization, amyloid accumulation, or hippocampal volume, but it was associated with significantly better cognitive scores on a composite measure of memory over time.
“We should be careful in interpreting these data, because this is an observational cohort, and we cannot make claims regarding causality or the mechanism by which physical activity may be influencing cognitive decline,” said Mr. Kirn, Clinical Research Project Manager at the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital in Boston. “But I find these results interesting and novel, and I think they support further investigation.”
The Harvard Aging Brain Study
The research is part of the ongoing Harvard Aging Brain Study, which is a longitudinal investigation of cognitively normal elderly individuals that seeks to identify the earliest changes in molecular, functional, and structural imaging markers that signal a transition from normal cognition to progressive cognitive decline and preclinical Alzheimer’s disease. The walking study included 255 subjects with a mean age of 73. Participants were highly educated, with a mean of 16 years’ schooling. About 24% of the population was amyloid-positive on PET imaging. All patients were cognitively normal, with a Clinical Dementia Rating scale score of 0. Activity was measured at baseline with a pedometer, which was worn for seven consecutive days; only people who walked at least 100 steps per day were included in the analysis.
In addition to amyloid PET imaging, subjects underwent an 18F-fluorodeoxyglucose (FDG) PET scan to assess brain glucose utilization, and MRI to measure hippocampal volume changes and white matter hyperintensities (WMHs). Changes in all of these biomarkers can herald the onset of Alzheimer’s disease.
The study’s primary outcome was the relationship between physical activity, as measured by number of walking steps per day, and changes on the Preclinical Alzheimer’s Cognitive Composite (PACC) test. This relatively new cognitive scale is gaining increasing use in clinical trials. The PACC is a composite of the Digit Symbol Substitution Test score from the Wechsler Adult Intelligence Scale–Revised, the Mini-Mental State Examination, the Total Recall score from the Free and Cued Selective Reminding Test, and the Delayed Recall score on the Logical Memory IIa subtest of the Wechsler Memory Scale. It correlates well with amyloid accumulation in the brain, said Mr. Kirn.
The cohort was followed for as long as six years (median follow-up, four years), and PACC scores were calculated annually. The investigators examined the relationship between walking at baseline and PACC decline during the study period in two multivariate models. One model controlled for age, sex, and years of education, and the second controlled for those variables plus cortical WMHs, bilateral hippocampal volume (HV), and FDG PET in brain regions typically affected by Alzheimer’s disease.
The investigators sorted physical activity into tertiles by the average number of steps per day over the seven-day measuring period. The middle tertile was the mean (ie, 5,616 steps/day), the top tertile was one standard deviation above the mean (ie, 8,482 steps/day), and the bottom tertile was one standard deviation below the mean (ie, 2,751 steps/day). Amyloid-positive patients were further categorized as having high or low brain amyloid load.
No Relationship Between Activity and Biomarkers
The researchers found no significant relationships between any of the biomarkers and any level of physical activity in either of the analyses, said Mr. Kirn. When looking at the time-linked changes in the PACC, however, they found significant differences. Subjects who walked at least the mean number of steps per day were much more likely to maintain a stable cognitive score, while those who walked the fewest steps declined by about a quarter of a point on the PACC. The difference in decline between the high-activity and low-activity subjects was statistically significant, even when the investigators controlled for amyloid burden and other Alzheimer’s disease biomarkers.
The level of physical activity at baseline was a particularly strong predictor of cognitive health among amyloid-positive subjects. Those in the high-activity group maintained a steady score on the PACC. Those in the mean activity group declined slightly, and those in the low activity group showed a sharp decline, losing almost a full point on the PACC by the end of follow-up.
In the amyloid-negative group, the researchers found no association between cognition and activity. PACC scores improved for all groups during the study period, which probably reflects a practice effect, said Mr. Kirn.
“We observed that physical activity was significantly predictive of cognitive decline in high-amyloid participants, but not in low-amyloid participants,” he said. “Individuals with high amyloid and low physical activity at baseline had the steepest decline in cognition over time. But in those with high amyloid and high physical activity at baseline, we did not see a tremendous amount of decline.”
The study suggests that pedometers may help stratify patients for clinical trials or assess cognitive risk in elderly subjects. “Most studies that have looked at physical activity and dementia use a self-reported activity level, so the results have been varied,” said Mr. Kirn. “These findings support consideration of objectively measured physical activity in clinical research, and perhaps in stratification for risk of cognitive decline.”
—Michele G. Sullivan
BOSTON—Walking appears to moderate cognitive decline in people with elevated levels of amyloid in the brain, according to a four-year observational study described at the Clinical Trials on Alzheimer’s Disease conference.
Among a group of cognitively normal older adults with beta-amyloid brain plaques, those who walked the most had significantly less decline in memory and thinking than those who walked little, said Dylan Kirn, MPH. Walking did not affect any biomarkers of Alzheimer’s disease, such as brain glucose utilization, amyloid accumulation, or hippocampal volume, but it was associated with significantly better cognitive scores on a composite measure of memory over time.
“We should be careful in interpreting these data, because this is an observational cohort, and we cannot make claims regarding causality or the mechanism by which physical activity may be influencing cognitive decline,” said Mr. Kirn, Clinical Research Project Manager at the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital in Boston. “But I find these results interesting and novel, and I think they support further investigation.”
The Harvard Aging Brain Study
The research is part of the ongoing Harvard Aging Brain Study, which is a longitudinal investigation of cognitively normal elderly individuals that seeks to identify the earliest changes in molecular, functional, and structural imaging markers that signal a transition from normal cognition to progressive cognitive decline and preclinical Alzheimer’s disease. The walking study included 255 subjects with a mean age of 73. Participants were highly educated, with a mean of 16 years’ schooling. About 24% of the population was amyloid-positive on PET imaging. All patients were cognitively normal, with a Clinical Dementia Rating scale score of 0. Activity was measured at baseline with a pedometer, which was worn for seven consecutive days; only people who walked at least 100 steps per day were included in the analysis.
In addition to amyloid PET imaging, subjects underwent an 18F-fluorodeoxyglucose (FDG) PET scan to assess brain glucose utilization, and MRI to measure hippocampal volume changes and white matter hyperintensities (WMHs). Changes in all of these biomarkers can herald the onset of Alzheimer’s disease.
The study’s primary outcome was the relationship between physical activity, as measured by number of walking steps per day, and changes on the Preclinical Alzheimer’s Cognitive Composite (PACC) test. This relatively new cognitive scale is gaining increasing use in clinical trials. The PACC is a composite of the Digit Symbol Substitution Test score from the Wechsler Adult Intelligence Scale–Revised, the Mini-Mental State Examination, the Total Recall score from the Free and Cued Selective Reminding Test, and the Delayed Recall score on the Logical Memory IIa subtest of the Wechsler Memory Scale. It correlates well with amyloid accumulation in the brain, said Mr. Kirn.
The cohort was followed for as long as six years (median follow-up, four years), and PACC scores were calculated annually. The investigators examined the relationship between walking at baseline and PACC decline during the study period in two multivariate models. One model controlled for age, sex, and years of education, and the second controlled for those variables plus cortical WMHs, bilateral hippocampal volume (HV), and FDG PET in brain regions typically affected by Alzheimer’s disease.
The investigators sorted physical activity into tertiles by the average number of steps per day over the seven-day measuring period. The middle tertile was the mean (ie, 5,616 steps/day), the top tertile was one standard deviation above the mean (ie, 8,482 steps/day), and the bottom tertile was one standard deviation below the mean (ie, 2,751 steps/day). Amyloid-positive patients were further categorized as having high or low brain amyloid load.
No Relationship Between Activity and Biomarkers
The researchers found no significant relationships between any of the biomarkers and any level of physical activity in either of the analyses, said Mr. Kirn. When looking at the time-linked changes in the PACC, however, they found significant differences. Subjects who walked at least the mean number of steps per day were much more likely to maintain a stable cognitive score, while those who walked the fewest steps declined by about a quarter of a point on the PACC. The difference in decline between the high-activity and low-activity subjects was statistically significant, even when the investigators controlled for amyloid burden and other Alzheimer’s disease biomarkers.
The level of physical activity at baseline was a particularly strong predictor of cognitive health among amyloid-positive subjects. Those in the high-activity group maintained a steady score on the PACC. Those in the mean activity group declined slightly, and those in the low activity group showed a sharp decline, losing almost a full point on the PACC by the end of follow-up.
In the amyloid-negative group, the researchers found no association between cognition and activity. PACC scores improved for all groups during the study period, which probably reflects a practice effect, said Mr. Kirn.
“We observed that physical activity was significantly predictive of cognitive decline in high-amyloid participants, but not in low-amyloid participants,” he said. “Individuals with high amyloid and low physical activity at baseline had the steepest decline in cognition over time. But in those with high amyloid and high physical activity at baseline, we did not see a tremendous amount of decline.”
The study suggests that pedometers may help stratify patients for clinical trials or assess cognitive risk in elderly subjects. “Most studies that have looked at physical activity and dementia use a self-reported activity level, so the results have been varied,” said Mr. Kirn. “These findings support consideration of objectively measured physical activity in clinical research, and perhaps in stratification for risk of cognitive decline.”
—Michele G. Sullivan
Psychiatric issues common among hepatitis C inpatients
Adult inpatients with hepatitis C are much more likely to have mental health comorbidities, compared with those who do not have hepatitis C, according to the Agency for Healthcare Research and Quality.
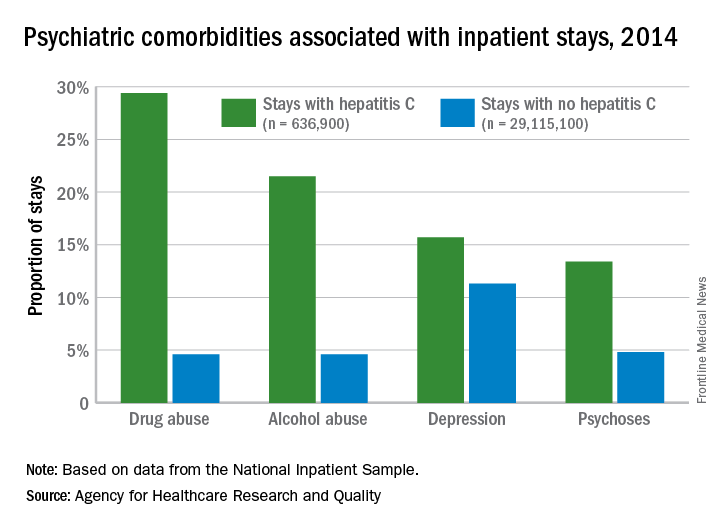
All four comorbidities skewed younger, and the oldest patients (73 years and older) with hepatitis C presented with each condition at about the same rate as the non–hepatitis C population. The proportions of hepatitis C–related inpatient stays with alcohol abuse by age, for example, were 20.5% for 18-51 years, 23.3% for those aged 52-72, and 5.8% for the 73-and-older group, according to data from the National Inpatient Sample, which includes more than 95% of all discharges from community (short-term, nonfederal, nonrehabilitation) hospitals in the United States.
Adult inpatients with hepatitis C are much more likely to have mental health comorbidities, compared with those who do not have hepatitis C, according to the Agency for Healthcare Research and Quality.
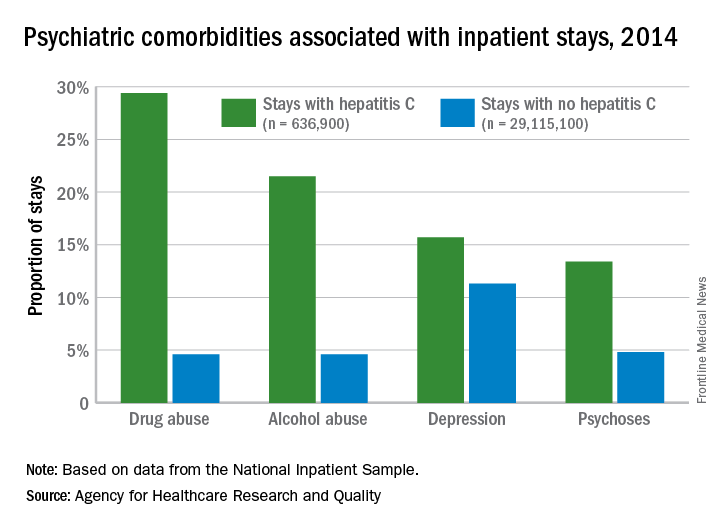
All four comorbidities skewed younger, and the oldest patients (73 years and older) with hepatitis C presented with each condition at about the same rate as the non–hepatitis C population. The proportions of hepatitis C–related inpatient stays with alcohol abuse by age, for example, were 20.5% for 18-51 years, 23.3% for those aged 52-72, and 5.8% for the 73-and-older group, according to data from the National Inpatient Sample, which includes more than 95% of all discharges from community (short-term, nonfederal, nonrehabilitation) hospitals in the United States.
Adult inpatients with hepatitis C are much more likely to have mental health comorbidities, compared with those who do not have hepatitis C, according to the Agency for Healthcare Research and Quality.
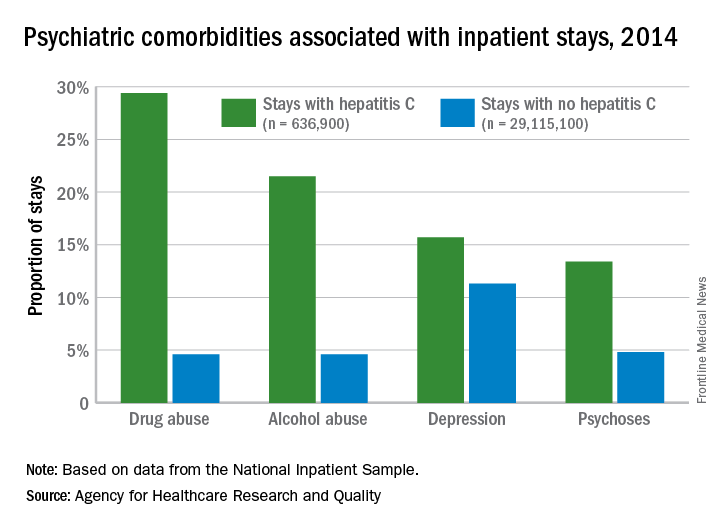
All four comorbidities skewed younger, and the oldest patients (73 years and older) with hepatitis C presented with each condition at about the same rate as the non–hepatitis C population. The proportions of hepatitis C–related inpatient stays with alcohol abuse by age, for example, were 20.5% for 18-51 years, 23.3% for those aged 52-72, and 5.8% for the 73-and-older group, according to data from the National Inpatient Sample, which includes more than 95% of all discharges from community (short-term, nonfederal, nonrehabilitation) hospitals in the United States.
ROBOT trial compares surgical approaches to esophagectomy
SAN FRANCISCO – Patients undergoing had less morbidity and pain and similarly good oncologic outcomes, when the surgery was performed by robot-assisted laparoscopy instead of by the open technique, a phase 3 clinical trial has found.
Investigators of the ROBOT (Robot-assisted Thoracolaparoscopic Esophagectomy vs. Open Transthoracic Esophagectomy) trial, led by Pieter C. van der Sluis, MD, a surgeon at the University Medical Center Utrecht, the Netherlands, randomized 112 patients with resectable esophageal cancer to open transthoracic esophagectomy – considered to be the gold standard – or robot-assisted minimally invasive thoracolaparoscopic esophagectomy.
“Robot-assisted minimally invasive thoracolaparoscopic esophagectomy versus open transthoracic esophagectomy improves postoperative outcome. There were no differences in oncologic outcomes, and our oncologic outcomes were in concordance with the highest standards nowadays,” Dr. van der Sluis summarized. “This trial provides evidence for the minimally invasive approach over the open approach, and especially the robot-assisted minimally invasive esophagectomy.”
The investigators will report a full cost comparison separately. “We see that costs are lower, though not significantly lower, with the robot,” he said, giving a preview. “We are going to show that the real costs of the operation are in the complications. When you have complications that involve the ICU and reoperations, some patients are in the hospital for months after the surgery. So by investing a little extra money in the surgical procedure, you might actually get it back by reducing the complications.”
When asked by an attendee why the trial did not compare robotic esophagectomy with thoracoscopic esophagectomy, Dr. van der Sluis noted that such comparison is complicated by many factors; for example, the challenge of finding surgeons skilled in both techniques, and the likelihood of small differences in outcomes, potentially requiring enrollment of thousands of patients to have adequate study power. “We concluded that such a trial might not be feasible,” he said.
Parsing the findings
“The complication rates [in this trial] are very high in the robotic and open groups, much higher than reported in some well-controlled prospective and retrospective studies,” commented session attendee Kenneth Meredith, MD, FACS, professor at Florida State University, Sarasota, and director of gastrointestinal oncology, Sarasota Memorial Institute for Cancer Care.
He wondered how extensive the investigators’ experience with robotics was and how many cases they had done on their learning curve. Data from his group suggest that surgeons must perform 29 cases of robotic esophagectomy before the complication rate drops (Dis Esophagus. 2017;30:1-7).
“That’s more then half of the patients in the robotic arm of their study,” he noted in an interview. “I find this needs to be explained. If the authors are past their learning curve, why were the complication rates so high?” Additionally, the 80% rate in the open group “is among the highest I’ve seen in many years.”
The lack of significant differences in complete resection rate and in lymph node harvest was also surprising, as he and other robotics users have found that this technique can improve these outcomes, Dr. Meredith added. This could likewise be a learning curve phenomenon.
Although ROBOT’s comparison of robotic with open esophagectomy is relevant, “it would have been more relevant to compare robotic to minimally invasive esophagectomy [MIE],” he maintained, as MIE has been shown to improve outcomes relative to open surgery (Lancet. 2012;379:1887-92).
“There are many high-volume centers in MIE but not necessarily robotics. The two are often mutually exclusive, and a multicenter trial in which each center performs high volumes of their respective technique, rather then mandating each center perform an operation they may not be facile in,” would be practical, Dr. Meredith concluded.
Study details
“The main objective in our trial was to reduce surgical trauma and reduce the percentage of complications,” Dr. van der Sluis told attendees of the symposium, sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Results showed that compared with peers in the open surgery group, patients in the robotic-assisted surgery group specifically had a lower rate of pulmonary complications (32% vs. 58%, P = .005), largely due to a reduction in rate of pneumonia (28% vs. 55%, P = .005), and a lower rate of cardiac complications (22% vs. 47%, P = .006), almost entirely due to a reduction in rate of atrial fibrillation (22% vs. 46%, P = .01).
There was a trend toward fewer wound infections with robotics (4% vs. 14%, P = .09), with a large difference in thoracic wound infections (0% vs. 9%, P = .06).
The two groups were statistically indistinguishable on rates of anastomotic leakage (24% and 20%) and recurrent laryngeal nerve injury (9% and 11%). The fairly high rate of anastomotic leakage was likely due to the center’s use of cervical anastomosis at the time of the trial, according to Dr. van der Sluis; they have since started using thoracic anastomosis, and will report results with that technique soon.
There was also no significant difference between groups in the rate of in-hospital mortality (4% with robotic surgery and 2% with open surgery), median hospital length of stay (14 and 16 days), and ICU length of stay (1 day in each group).
Patients in the robotics group more commonly had functional recovery within 2 weeks (70% vs. 51%, P = .04). And on the Quality of Life Questionnaire Core 30, they had better scores for health-related quality of life at discharge (57.9 vs 44.6, P = .02) and at 6 weeks (68.7 vs. 57.6, P = .03), and for physical functioning at discharge (54.5 vs. 41.0, P = .03) and 6 weeks (69.3 vs. 58.6, P = .049).
The two groups were similar on rates of R0 resection (93% and 96%) and median number of lymph nodes retrieved (27 and 25), reported Dr. van der Sluis. Pain during the first 14 days after surgery was lower for the robotics group (P = .003).
With a median follow-up of 40 months, the robotics and open groups did not differ significantly on disease-free survival (median, 26 and 28 months) and overall survival (not reached in either group).
Dr. van der Sluis disclosed no relevant conflicts of interest.
SOURCE: van der Sluis PC et al. 2018 GI Cancer Symposium, Abstract 156148
SAN FRANCISCO – Patients undergoing had less morbidity and pain and similarly good oncologic outcomes, when the surgery was performed by robot-assisted laparoscopy instead of by the open technique, a phase 3 clinical trial has found.
Investigators of the ROBOT (Robot-assisted Thoracolaparoscopic Esophagectomy vs. Open Transthoracic Esophagectomy) trial, led by Pieter C. van der Sluis, MD, a surgeon at the University Medical Center Utrecht, the Netherlands, randomized 112 patients with resectable esophageal cancer to open transthoracic esophagectomy – considered to be the gold standard – or robot-assisted minimally invasive thoracolaparoscopic esophagectomy.
“Robot-assisted minimally invasive thoracolaparoscopic esophagectomy versus open transthoracic esophagectomy improves postoperative outcome. There were no differences in oncologic outcomes, and our oncologic outcomes were in concordance with the highest standards nowadays,” Dr. van der Sluis summarized. “This trial provides evidence for the minimally invasive approach over the open approach, and especially the robot-assisted minimally invasive esophagectomy.”
The investigators will report a full cost comparison separately. “We see that costs are lower, though not significantly lower, with the robot,” he said, giving a preview. “We are going to show that the real costs of the operation are in the complications. When you have complications that involve the ICU and reoperations, some patients are in the hospital for months after the surgery. So by investing a little extra money in the surgical procedure, you might actually get it back by reducing the complications.”
When asked by an attendee why the trial did not compare robotic esophagectomy with thoracoscopic esophagectomy, Dr. van der Sluis noted that such comparison is complicated by many factors; for example, the challenge of finding surgeons skilled in both techniques, and the likelihood of small differences in outcomes, potentially requiring enrollment of thousands of patients to have adequate study power. “We concluded that such a trial might not be feasible,” he said.
Parsing the findings
“The complication rates [in this trial] are very high in the robotic and open groups, much higher than reported in some well-controlled prospective and retrospective studies,” commented session attendee Kenneth Meredith, MD, FACS, professor at Florida State University, Sarasota, and director of gastrointestinal oncology, Sarasota Memorial Institute for Cancer Care.
He wondered how extensive the investigators’ experience with robotics was and how many cases they had done on their learning curve. Data from his group suggest that surgeons must perform 29 cases of robotic esophagectomy before the complication rate drops (Dis Esophagus. 2017;30:1-7).
“That’s more then half of the patients in the robotic arm of their study,” he noted in an interview. “I find this needs to be explained. If the authors are past their learning curve, why were the complication rates so high?” Additionally, the 80% rate in the open group “is among the highest I’ve seen in many years.”
The lack of significant differences in complete resection rate and in lymph node harvest was also surprising, as he and other robotics users have found that this technique can improve these outcomes, Dr. Meredith added. This could likewise be a learning curve phenomenon.
Although ROBOT’s comparison of robotic with open esophagectomy is relevant, “it would have been more relevant to compare robotic to minimally invasive esophagectomy [MIE],” he maintained, as MIE has been shown to improve outcomes relative to open surgery (Lancet. 2012;379:1887-92).
“There are many high-volume centers in MIE but not necessarily robotics. The two are often mutually exclusive, and a multicenter trial in which each center performs high volumes of their respective technique, rather then mandating each center perform an operation they may not be facile in,” would be practical, Dr. Meredith concluded.
Study details
“The main objective in our trial was to reduce surgical trauma and reduce the percentage of complications,” Dr. van der Sluis told attendees of the symposium, sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Results showed that compared with peers in the open surgery group, patients in the robotic-assisted surgery group specifically had a lower rate of pulmonary complications (32% vs. 58%, P = .005), largely due to a reduction in rate of pneumonia (28% vs. 55%, P = .005), and a lower rate of cardiac complications (22% vs. 47%, P = .006), almost entirely due to a reduction in rate of atrial fibrillation (22% vs. 46%, P = .01).
There was a trend toward fewer wound infections with robotics (4% vs. 14%, P = .09), with a large difference in thoracic wound infections (0% vs. 9%, P = .06).
The two groups were statistically indistinguishable on rates of anastomotic leakage (24% and 20%) and recurrent laryngeal nerve injury (9% and 11%). The fairly high rate of anastomotic leakage was likely due to the center’s use of cervical anastomosis at the time of the trial, according to Dr. van der Sluis; they have since started using thoracic anastomosis, and will report results with that technique soon.
There was also no significant difference between groups in the rate of in-hospital mortality (4% with robotic surgery and 2% with open surgery), median hospital length of stay (14 and 16 days), and ICU length of stay (1 day in each group).
Patients in the robotics group more commonly had functional recovery within 2 weeks (70% vs. 51%, P = .04). And on the Quality of Life Questionnaire Core 30, they had better scores for health-related quality of life at discharge (57.9 vs 44.6, P = .02) and at 6 weeks (68.7 vs. 57.6, P = .03), and for physical functioning at discharge (54.5 vs. 41.0, P = .03) and 6 weeks (69.3 vs. 58.6, P = .049).
The two groups were similar on rates of R0 resection (93% and 96%) and median number of lymph nodes retrieved (27 and 25), reported Dr. van der Sluis. Pain during the first 14 days after surgery was lower for the robotics group (P = .003).
With a median follow-up of 40 months, the robotics and open groups did not differ significantly on disease-free survival (median, 26 and 28 months) and overall survival (not reached in either group).
Dr. van der Sluis disclosed no relevant conflicts of interest.
SOURCE: van der Sluis PC et al. 2018 GI Cancer Symposium, Abstract 156148
SAN FRANCISCO – Patients undergoing had less morbidity and pain and similarly good oncologic outcomes, when the surgery was performed by robot-assisted laparoscopy instead of by the open technique, a phase 3 clinical trial has found.
Investigators of the ROBOT (Robot-assisted Thoracolaparoscopic Esophagectomy vs. Open Transthoracic Esophagectomy) trial, led by Pieter C. van der Sluis, MD, a surgeon at the University Medical Center Utrecht, the Netherlands, randomized 112 patients with resectable esophageal cancer to open transthoracic esophagectomy – considered to be the gold standard – or robot-assisted minimally invasive thoracolaparoscopic esophagectomy.
“Robot-assisted minimally invasive thoracolaparoscopic esophagectomy versus open transthoracic esophagectomy improves postoperative outcome. There were no differences in oncologic outcomes, and our oncologic outcomes were in concordance with the highest standards nowadays,” Dr. van der Sluis summarized. “This trial provides evidence for the minimally invasive approach over the open approach, and especially the robot-assisted minimally invasive esophagectomy.”
The investigators will report a full cost comparison separately. “We see that costs are lower, though not significantly lower, with the robot,” he said, giving a preview. “We are going to show that the real costs of the operation are in the complications. When you have complications that involve the ICU and reoperations, some patients are in the hospital for months after the surgery. So by investing a little extra money in the surgical procedure, you might actually get it back by reducing the complications.”
When asked by an attendee why the trial did not compare robotic esophagectomy with thoracoscopic esophagectomy, Dr. van der Sluis noted that such comparison is complicated by many factors; for example, the challenge of finding surgeons skilled in both techniques, and the likelihood of small differences in outcomes, potentially requiring enrollment of thousands of patients to have adequate study power. “We concluded that such a trial might not be feasible,” he said.
Parsing the findings
“The complication rates [in this trial] are very high in the robotic and open groups, much higher than reported in some well-controlled prospective and retrospective studies,” commented session attendee Kenneth Meredith, MD, FACS, professor at Florida State University, Sarasota, and director of gastrointestinal oncology, Sarasota Memorial Institute for Cancer Care.
He wondered how extensive the investigators’ experience with robotics was and how many cases they had done on their learning curve. Data from his group suggest that surgeons must perform 29 cases of robotic esophagectomy before the complication rate drops (Dis Esophagus. 2017;30:1-7).
“That’s more then half of the patients in the robotic arm of their study,” he noted in an interview. “I find this needs to be explained. If the authors are past their learning curve, why were the complication rates so high?” Additionally, the 80% rate in the open group “is among the highest I’ve seen in many years.”
The lack of significant differences in complete resection rate and in lymph node harvest was also surprising, as he and other robotics users have found that this technique can improve these outcomes, Dr. Meredith added. This could likewise be a learning curve phenomenon.
Although ROBOT’s comparison of robotic with open esophagectomy is relevant, “it would have been more relevant to compare robotic to minimally invasive esophagectomy [MIE],” he maintained, as MIE has been shown to improve outcomes relative to open surgery (Lancet. 2012;379:1887-92).
“There are many high-volume centers in MIE but not necessarily robotics. The two are often mutually exclusive, and a multicenter trial in which each center performs high volumes of their respective technique, rather then mandating each center perform an operation they may not be facile in,” would be practical, Dr. Meredith concluded.
Study details
“The main objective in our trial was to reduce surgical trauma and reduce the percentage of complications,” Dr. van der Sluis told attendees of the symposium, sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Results showed that compared with peers in the open surgery group, patients in the robotic-assisted surgery group specifically had a lower rate of pulmonary complications (32% vs. 58%, P = .005), largely due to a reduction in rate of pneumonia (28% vs. 55%, P = .005), and a lower rate of cardiac complications (22% vs. 47%, P = .006), almost entirely due to a reduction in rate of atrial fibrillation (22% vs. 46%, P = .01).
There was a trend toward fewer wound infections with robotics (4% vs. 14%, P = .09), with a large difference in thoracic wound infections (0% vs. 9%, P = .06).
The two groups were statistically indistinguishable on rates of anastomotic leakage (24% and 20%) and recurrent laryngeal nerve injury (9% and 11%). The fairly high rate of anastomotic leakage was likely due to the center’s use of cervical anastomosis at the time of the trial, according to Dr. van der Sluis; they have since started using thoracic anastomosis, and will report results with that technique soon.
There was also no significant difference between groups in the rate of in-hospital mortality (4% with robotic surgery and 2% with open surgery), median hospital length of stay (14 and 16 days), and ICU length of stay (1 day in each group).
Patients in the robotics group more commonly had functional recovery within 2 weeks (70% vs. 51%, P = .04). And on the Quality of Life Questionnaire Core 30, they had better scores for health-related quality of life at discharge (57.9 vs 44.6, P = .02) and at 6 weeks (68.7 vs. 57.6, P = .03), and for physical functioning at discharge (54.5 vs. 41.0, P = .03) and 6 weeks (69.3 vs. 58.6, P = .049).
The two groups were similar on rates of R0 resection (93% and 96%) and median number of lymph nodes retrieved (27 and 25), reported Dr. van der Sluis. Pain during the first 14 days after surgery was lower for the robotics group (P = .003).
With a median follow-up of 40 months, the robotics and open groups did not differ significantly on disease-free survival (median, 26 and 28 months) and overall survival (not reached in either group).
Dr. van der Sluis disclosed no relevant conflicts of interest.
SOURCE: van der Sluis PC et al. 2018 GI Cancer Symposium, Abstract 156148
REPORTING FROM THE 2018 GI CANCERS SYMPOSIUM
Key clinical point: Patients with esophageal cancer undergoing esophagectomy are less likely to experience complications when the surgery is performed robotically.
Major finding: Compared with open transthoracic esophagectomy, robot-assisted minimally invasive thoracolaparoscopic esophagectomy had a lower rate of MCDC grade 2 or higher surgery-related postoperative complications (59% vs. 80%).
Data source: A single-center phase 3 randomized controlled trial among 112 patients with resectable esophageal cancer.
Disclosures: Dr. van der Sluis disclosed no relevant conflicts of interest.
Source: van der Sluis PC et al. 2018 GI Cancer Symposium, Abstract 156148
Trial of clozapine, risperidone halted in MS
SAN DIEGO – New Zealand researchers halted a small trial that was testing the use of the antipsychotics clozapine and risperidone to treat progressive multiple sclerosis because significant side effects caused participants to withdraw.
The adverse events appeared even though the doses were much smaller than those routinely given to patients with psychiatric illnesses. “The neurologists realized it was in the participants’ best interest to stop,” said study lead author Anne Camille La Flamme, PhD, of Victoria University of Wellington (New Zealand). “Adverse events included dizziness, muscle weakness, and falls.”
The researchers launched the study – a blinded, randomized, placebo-controlled trial – to learn whether the two antipsychotic drugs, also known by the brand names Clozaril and Risperdal, have potential as treatments for progressive multiple sclerosis.
Previous in-vitro research had linked the drugs to anti-inflammatory effects in the central nervous system, Dr. La Flamme said, and researchers believed that the progressive form of MS might be especially vulnerable to their effects because of high immune system involvement.
The researchers planned to randomly assign three groups of 12 patients per arm to placebo, clozapine, and risperidone.
For clozapine, “the doses were very low, much lower than you’d expect for psychiatric use,” Dr. La Flamme said. A typical dose for psychiatric disorders is about 350 mg/day, she said, and the trial aimed to use 100-150 mg/day with an eye toward preventing dose-dependent side effects.
As for risperidone, a typical dose is about 4 mg/day, and the trial began at 2 mg/day and would increase to 3.5 mg/day, she said.
Three subjects in the clozapine group had to withdraw within 2 weeks when their doses had only reached an average of 35 mg/day. Two of three in the risperidone group withdrew within 4 months.
In light of the adverse effects, “it was deemed not wise to continue,” Dr. La Flamme said.
The placebo group, meanwhile, completed the trial at 178 days and had adverse effects that were more indicative of MS, she said.
What happened? One possibility is that disability from MS made the adverse events more evident, Dr. La Flamme said. Another possible explanation is that the underlying MS physiology changed the targets of the medications, she said.
“We have no conclusive evidence that would suggest one over the other,” she said. “But a lot of the evidence supports the idea that it’s a change in the physiology, that something about those pathways has been altered.”
It’s clear, she said, that the doses of the drugs in the trial were not appropriate. However, a big question remains: “We do not know whether these medicines are effective at reducing neuroinflammation.”
It’s possible, she said, that a “whisper of a dose” could still be effective. “It may get back to how these agents metabolize and become an active form.”
The study was funded by New Zealand’s Ministry of Business, Innovation and Employment. Dr. La Flamme disclosed that the study team has a patent for repurposing of clozapine and risperidone to treat MS.
SOURCE: La Flamme A et al. ACTRIMS Forum 2018, abstract P031.
SAN DIEGO – New Zealand researchers halted a small trial that was testing the use of the antipsychotics clozapine and risperidone to treat progressive multiple sclerosis because significant side effects caused participants to withdraw.
The adverse events appeared even though the doses were much smaller than those routinely given to patients with psychiatric illnesses. “The neurologists realized it was in the participants’ best interest to stop,” said study lead author Anne Camille La Flamme, PhD, of Victoria University of Wellington (New Zealand). “Adverse events included dizziness, muscle weakness, and falls.”
The researchers launched the study – a blinded, randomized, placebo-controlled trial – to learn whether the two antipsychotic drugs, also known by the brand names Clozaril and Risperdal, have potential as treatments for progressive multiple sclerosis.
Previous in-vitro research had linked the drugs to anti-inflammatory effects in the central nervous system, Dr. La Flamme said, and researchers believed that the progressive form of MS might be especially vulnerable to their effects because of high immune system involvement.
The researchers planned to randomly assign three groups of 12 patients per arm to placebo, clozapine, and risperidone.
For clozapine, “the doses were very low, much lower than you’d expect for psychiatric use,” Dr. La Flamme said. A typical dose for psychiatric disorders is about 350 mg/day, she said, and the trial aimed to use 100-150 mg/day with an eye toward preventing dose-dependent side effects.
As for risperidone, a typical dose is about 4 mg/day, and the trial began at 2 mg/day and would increase to 3.5 mg/day, she said.
Three subjects in the clozapine group had to withdraw within 2 weeks when their doses had only reached an average of 35 mg/day. Two of three in the risperidone group withdrew within 4 months.
In light of the adverse effects, “it was deemed not wise to continue,” Dr. La Flamme said.
The placebo group, meanwhile, completed the trial at 178 days and had adverse effects that were more indicative of MS, she said.
What happened? One possibility is that disability from MS made the adverse events more evident, Dr. La Flamme said. Another possible explanation is that the underlying MS physiology changed the targets of the medications, she said.
“We have no conclusive evidence that would suggest one over the other,” she said. “But a lot of the evidence supports the idea that it’s a change in the physiology, that something about those pathways has been altered.”
It’s clear, she said, that the doses of the drugs in the trial were not appropriate. However, a big question remains: “We do not know whether these medicines are effective at reducing neuroinflammation.”
It’s possible, she said, that a “whisper of a dose” could still be effective. “It may get back to how these agents metabolize and become an active form.”
The study was funded by New Zealand’s Ministry of Business, Innovation and Employment. Dr. La Flamme disclosed that the study team has a patent for repurposing of clozapine and risperidone to treat MS.
SOURCE: La Flamme A et al. ACTRIMS Forum 2018, abstract P031.
SAN DIEGO – New Zealand researchers halted a small trial that was testing the use of the antipsychotics clozapine and risperidone to treat progressive multiple sclerosis because significant side effects caused participants to withdraw.
The adverse events appeared even though the doses were much smaller than those routinely given to patients with psychiatric illnesses. “The neurologists realized it was in the participants’ best interest to stop,” said study lead author Anne Camille La Flamme, PhD, of Victoria University of Wellington (New Zealand). “Adverse events included dizziness, muscle weakness, and falls.”
The researchers launched the study – a blinded, randomized, placebo-controlled trial – to learn whether the two antipsychotic drugs, also known by the brand names Clozaril and Risperdal, have potential as treatments for progressive multiple sclerosis.
Previous in-vitro research had linked the drugs to anti-inflammatory effects in the central nervous system, Dr. La Flamme said, and researchers believed that the progressive form of MS might be especially vulnerable to their effects because of high immune system involvement.
The researchers planned to randomly assign three groups of 12 patients per arm to placebo, clozapine, and risperidone.
For clozapine, “the doses were very low, much lower than you’d expect for psychiatric use,” Dr. La Flamme said. A typical dose for psychiatric disorders is about 350 mg/day, she said, and the trial aimed to use 100-150 mg/day with an eye toward preventing dose-dependent side effects.
As for risperidone, a typical dose is about 4 mg/day, and the trial began at 2 mg/day and would increase to 3.5 mg/day, she said.
Three subjects in the clozapine group had to withdraw within 2 weeks when their doses had only reached an average of 35 mg/day. Two of three in the risperidone group withdrew within 4 months.
In light of the adverse effects, “it was deemed not wise to continue,” Dr. La Flamme said.
The placebo group, meanwhile, completed the trial at 178 days and had adverse effects that were more indicative of MS, she said.
What happened? One possibility is that disability from MS made the adverse events more evident, Dr. La Flamme said. Another possible explanation is that the underlying MS physiology changed the targets of the medications, she said.
“We have no conclusive evidence that would suggest one over the other,” she said. “But a lot of the evidence supports the idea that it’s a change in the physiology, that something about those pathways has been altered.”
It’s clear, she said, that the doses of the drugs in the trial were not appropriate. However, a big question remains: “We do not know whether these medicines are effective at reducing neuroinflammation.”
It’s possible, she said, that a “whisper of a dose” could still be effective. “It may get back to how these agents metabolize and become an active form.”
The study was funded by New Zealand’s Ministry of Business, Innovation and Employment. Dr. La Flamme disclosed that the study team has a patent for repurposing of clozapine and risperidone to treat MS.
SOURCE: La Flamme A et al. ACTRIMS Forum 2018, abstract P031.
REPORTING FROM ACTRIMS Forum 2018