User login
Axillary node dissection can be avoided with limited SLN involvement
SAN ANTONIO – Axillary dissection can be avoided in patients with early breast cancer and limited sentinel node involvement, investigators reported at the San Antonio Breast Cancer Symposium.
Both disease-free survival (DFS) and overall survival (OS) were similar in a population of patients with cT1-T2 N0M0 breast cancer and sentinel node micrometastases who underwent axillary dissection (AD), compared with those who did not. Complications associated with axillary surgery can be avoided in this population, without any adverse effect on survival.
“Our findings are fully consistent with those of the Z0011 trial, which after 10 years found no differences between the AD and no-AD groups for any endpoint in patients with moderate disease burden in the axilla undergoing conservative breast surgery,” said study author Viviana Galimberti, MD, of the European Institute of Oncology in Milan.
In the ACOSOG Z0011, trial, the use of sentinel node biopsy alone was not inferior to AD in patients with limited sentinel node metastasis treated with breast conservation and systemic therapy.
“We also suggest that non-AD is acceptable treatment in patients scheduled for mastectomy,” Dr. Galimberti said.
For patients with breast cancer and metastases in the sentinel nodes, AD has been the standard of care, but for those with limited sentinel node involvement, it was hypothesized that AD might not be necessary.
The phase 3 IBCSG 23-01 study was a multicenter, randomized, noninferiority trial that compared DFS in breast cancer patients with one or more micrometastases (greater than or equal to 2 mm) in the sentinel nodes who were randomized to either AD or no axillary dissection (no-AD). The 5-year results, which were published in 2013 in the Lancet Oncology (2013 Jun;14[7]:e251-2) showed no difference in DFS between the two groups.
At the meeting, Dr. Galimberti reported on outcomes after an extended median follow-up of 9.8 years. A cohort of 934 women (931 evaluable) were enrolled from 27 centers from 2001 to 2010 and randomized to either AD or no AD (467 in the no-AD group and 464 in the AD group).
The results were similar to those reported at 5 years. The 10-year DFS rates were similar for both cohorts; 77% for non-AD vs. 75% for AD (hazard ratio [no-AD vs. AD], 0.85; 95% confidence interval, 0.65-1.11; log-rank P = .23; noninferiority P = .002).
The rate of axillary failure in the no-AD group was low, Dr. Galimberti pointed out, at 1.7% and 0.8% among women who underwent breast-conserving surgery. There were nine ipsilateral axillary events in the no-AD group vs. three in the AD group, and 45 deaths in the no-AD group vs. 58 in the AD group. The 10-year OS was 91% (95% CI, 88%-94%) in the no-AD group and 88% (95% CI, 85%-92%) in the AD group (HR [no-AD vs. AD], 0.77; 95% CI, 0.56-1.07; log-rank P = .19).
There was no difference between groups for the main endpoint of DFS or the secondary endpoint of OS, said Dr. Galimberti.
In subgroup analyses, which included tumor size, estrogen-receptor status, progesterone-receptor status, tumor grade, and type of surgery, there were no subgroups identified that benefited from AD over no-AD.
“Our data fully support the change in clinical practice that started after the early published results,” Dr Galimberti concluded. “No AD is now standard treatment in early breast cancer when the sentinel node is only minimally involved.”
The study received no outside funding and the authors had no disclosures.
SOURCE: Galimberti et al. SABCS Abstract GS5-02
SAN ANTONIO – Axillary dissection can be avoided in patients with early breast cancer and limited sentinel node involvement, investigators reported at the San Antonio Breast Cancer Symposium.
Both disease-free survival (DFS) and overall survival (OS) were similar in a population of patients with cT1-T2 N0M0 breast cancer and sentinel node micrometastases who underwent axillary dissection (AD), compared with those who did not. Complications associated with axillary surgery can be avoided in this population, without any adverse effect on survival.
“Our findings are fully consistent with those of the Z0011 trial, which after 10 years found no differences between the AD and no-AD groups for any endpoint in patients with moderate disease burden in the axilla undergoing conservative breast surgery,” said study author Viviana Galimberti, MD, of the European Institute of Oncology in Milan.
In the ACOSOG Z0011, trial, the use of sentinel node biopsy alone was not inferior to AD in patients with limited sentinel node metastasis treated with breast conservation and systemic therapy.
“We also suggest that non-AD is acceptable treatment in patients scheduled for mastectomy,” Dr. Galimberti said.
For patients with breast cancer and metastases in the sentinel nodes, AD has been the standard of care, but for those with limited sentinel node involvement, it was hypothesized that AD might not be necessary.
The phase 3 IBCSG 23-01 study was a multicenter, randomized, noninferiority trial that compared DFS in breast cancer patients with one or more micrometastases (greater than or equal to 2 mm) in the sentinel nodes who were randomized to either AD or no axillary dissection (no-AD). The 5-year results, which were published in 2013 in the Lancet Oncology (2013 Jun;14[7]:e251-2) showed no difference in DFS between the two groups.
At the meeting, Dr. Galimberti reported on outcomes after an extended median follow-up of 9.8 years. A cohort of 934 women (931 evaluable) were enrolled from 27 centers from 2001 to 2010 and randomized to either AD or no AD (467 in the no-AD group and 464 in the AD group).
The results were similar to those reported at 5 years. The 10-year DFS rates were similar for both cohorts; 77% for non-AD vs. 75% for AD (hazard ratio [no-AD vs. AD], 0.85; 95% confidence interval, 0.65-1.11; log-rank P = .23; noninferiority P = .002).
The rate of axillary failure in the no-AD group was low, Dr. Galimberti pointed out, at 1.7% and 0.8% among women who underwent breast-conserving surgery. There were nine ipsilateral axillary events in the no-AD group vs. three in the AD group, and 45 deaths in the no-AD group vs. 58 in the AD group. The 10-year OS was 91% (95% CI, 88%-94%) in the no-AD group and 88% (95% CI, 85%-92%) in the AD group (HR [no-AD vs. AD], 0.77; 95% CI, 0.56-1.07; log-rank P = .19).
There was no difference between groups for the main endpoint of DFS or the secondary endpoint of OS, said Dr. Galimberti.
In subgroup analyses, which included tumor size, estrogen-receptor status, progesterone-receptor status, tumor grade, and type of surgery, there were no subgroups identified that benefited from AD over no-AD.
“Our data fully support the change in clinical practice that started after the early published results,” Dr Galimberti concluded. “No AD is now standard treatment in early breast cancer when the sentinel node is only minimally involved.”
The study received no outside funding and the authors had no disclosures.
SOURCE: Galimberti et al. SABCS Abstract GS5-02
SAN ANTONIO – Axillary dissection can be avoided in patients with early breast cancer and limited sentinel node involvement, investigators reported at the San Antonio Breast Cancer Symposium.
Both disease-free survival (DFS) and overall survival (OS) were similar in a population of patients with cT1-T2 N0M0 breast cancer and sentinel node micrometastases who underwent axillary dissection (AD), compared with those who did not. Complications associated with axillary surgery can be avoided in this population, without any adverse effect on survival.
“Our findings are fully consistent with those of the Z0011 trial, which after 10 years found no differences between the AD and no-AD groups for any endpoint in patients with moderate disease burden in the axilla undergoing conservative breast surgery,” said study author Viviana Galimberti, MD, of the European Institute of Oncology in Milan.
In the ACOSOG Z0011, trial, the use of sentinel node biopsy alone was not inferior to AD in patients with limited sentinel node metastasis treated with breast conservation and systemic therapy.
“We also suggest that non-AD is acceptable treatment in patients scheduled for mastectomy,” Dr. Galimberti said.
For patients with breast cancer and metastases in the sentinel nodes, AD has been the standard of care, but for those with limited sentinel node involvement, it was hypothesized that AD might not be necessary.
The phase 3 IBCSG 23-01 study was a multicenter, randomized, noninferiority trial that compared DFS in breast cancer patients with one or more micrometastases (greater than or equal to 2 mm) in the sentinel nodes who were randomized to either AD or no axillary dissection (no-AD). The 5-year results, which were published in 2013 in the Lancet Oncology (2013 Jun;14[7]:e251-2) showed no difference in DFS between the two groups.
At the meeting, Dr. Galimberti reported on outcomes after an extended median follow-up of 9.8 years. A cohort of 934 women (931 evaluable) were enrolled from 27 centers from 2001 to 2010 and randomized to either AD or no AD (467 in the no-AD group and 464 in the AD group).
The results were similar to those reported at 5 years. The 10-year DFS rates were similar for both cohorts; 77% for non-AD vs. 75% for AD (hazard ratio [no-AD vs. AD], 0.85; 95% confidence interval, 0.65-1.11; log-rank P = .23; noninferiority P = .002).
The rate of axillary failure in the no-AD group was low, Dr. Galimberti pointed out, at 1.7% and 0.8% among women who underwent breast-conserving surgery. There were nine ipsilateral axillary events in the no-AD group vs. three in the AD group, and 45 deaths in the no-AD group vs. 58 in the AD group. The 10-year OS was 91% (95% CI, 88%-94%) in the no-AD group and 88% (95% CI, 85%-92%) in the AD group (HR [no-AD vs. AD], 0.77; 95% CI, 0.56-1.07; log-rank P = .19).
There was no difference between groups for the main endpoint of DFS or the secondary endpoint of OS, said Dr. Galimberti.
In subgroup analyses, which included tumor size, estrogen-receptor status, progesterone-receptor status, tumor grade, and type of surgery, there were no subgroups identified that benefited from AD over no-AD.
“Our data fully support the change in clinical practice that started after the early published results,” Dr Galimberti concluded. “No AD is now standard treatment in early breast cancer when the sentinel node is only minimally involved.”
The study received no outside funding and the authors had no disclosures.
SOURCE: Galimberti et al. SABCS Abstract GS5-02
REPORTING FROM SABCS 2017
Key clinical point: Axillary dissection can be avoided in patients with early breast cancer and limited sentinel node involvement.
Major finding: At 10 years the disease-free rates were 77% for the no–axillary dissection group and 75% for the axillary dissection group (HR [no-AD vs. AD], 0.85; 95% CI, 0.65-1.11; log-rank P = .23; noninferiority P = .002).
Data source: Updated results of the phase 3 IBCSG 23-01 study, a multicenter, randomized, noninferiority trial that included 934 participants.
Disclosures: The study received no outside funding and the authors had no disclosures.
Source: Galimberti et al. SABCS Abstract GS5-02.
Single-agent daratumumab active in smoldering multiple myeloma
ATLANTA – Daratumumab monotherapy led to durable partial responses among intermediate to high-risk patients with smoldering multiple myeloma, according to results from the phase II CENTAURUS trial.
Although less than 5% of patients had complete responses, 27% had at least a very good partial response to long-term therapy (up to 20 treatment cycles lasting 8 weeks each), Craig C. Hofmeister, MD, of the Ohio State University Comprehensive Cancer Center, Columbus, said at the annual meeting of the American Society of Hematology. The coprimary endpoint, median progression-free survival, exceeded 24 months in all dose cohorts, and was the longest when patients were treated longest.
Current guidelines recommend monitoring smoldering multiple myeloma every 3-6 months and treating only after patients progress. However, some experts pursue earlier treatment in the premalignant setting.
In CENTAURUS, 123 adults with smoldering multiple myeloma were randomly assigned to receive daratumumab (16 mg/kg IV) in 8-week cycles according to a long, intermediate, or short/intense schedule. The long schedule consisted of treatment weekly for cycle 1, every other week for cycles 2-3, monthly for cycles 4-7, and once every 8 weeks for up to 13 more cycles. The intermediate schedule consisted of treatment weekly in cycle 1 and every 8 weeks for up to 20 cycles. The short, intense schedule consisted of weekly treatment for 8 weeks (one cycle). Patients were followed for up to 4 years or until they progressed to multiple myeloma based on International Myeloma Working Group guidelines.
Over a median follow-up period of 15.8 months (range, 0 to 24 months), rates of complete response were 2% in the long treatment arm, 5% in the intermediate treatment arm, and 0% in the short treatment arm. Rates of at least very good partial response were 29%, 24%, and 15%, respectively. Overall response rates were 56%, 54%, and 38%, respectively. Median PFS was not reached in any arm, exceeding 24 months.
Treatment was generally well tolerated, said Dr. Hofmeister. The most common treatment-related adverse effects were fatigue, cough, upper respiratory tract infection, headache, and insomnia. Hypertension and hyperglycemia were the most common grade 3-4 treatment-emergent adverse events, affecting up to 5% of patients per arm. Fewer than 10% of patients in any arm developed treatment-emergent hematologic adverse events, and fewer than 5% developed grade 3-4 pneumonia or sepsis. There were three cases of a second primary malignancy, including one case of breast cancer and two cases of melanoma.
Rates of infusion-related reactions did not correlate with treatment duration. Grade 3-4 infusion-related reactions affected 0% to 3% of patients per arm. The sole death in this trial resulted from disease progression in a patient from the short treatment arm. “Taken together, efficacy and safety data support long dosing compared to intermediate and short dosing,” Dr. Hofmeister said.
The three arms were demographically similar. Patients tended to be white, in their late 50s to 60s, and to have ECOG scores of 0 with at least two risk factors for progression. About 70% had IgG disease and nearly half had less than 20% plasma cells in bone marrow.
Janssen, the maker of daratumumab, sponsored the trial. Dr. Hofmeister disclosed research funding from Janssen and research support, honoraria, and advisory relationships with Adaptive Biotechnologies, Thrasos, Celgene, Karyopharm, Takeda, and other pharmaceutical companies.
SOURCE: Hofmeister C et al, ASH 2017, Abstract 510.
ATLANTA – Daratumumab monotherapy led to durable partial responses among intermediate to high-risk patients with smoldering multiple myeloma, according to results from the phase II CENTAURUS trial.
Although less than 5% of patients had complete responses, 27% had at least a very good partial response to long-term therapy (up to 20 treatment cycles lasting 8 weeks each), Craig C. Hofmeister, MD, of the Ohio State University Comprehensive Cancer Center, Columbus, said at the annual meeting of the American Society of Hematology. The coprimary endpoint, median progression-free survival, exceeded 24 months in all dose cohorts, and was the longest when patients were treated longest.
Current guidelines recommend monitoring smoldering multiple myeloma every 3-6 months and treating only after patients progress. However, some experts pursue earlier treatment in the premalignant setting.
In CENTAURUS, 123 adults with smoldering multiple myeloma were randomly assigned to receive daratumumab (16 mg/kg IV) in 8-week cycles according to a long, intermediate, or short/intense schedule. The long schedule consisted of treatment weekly for cycle 1, every other week for cycles 2-3, monthly for cycles 4-7, and once every 8 weeks for up to 13 more cycles. The intermediate schedule consisted of treatment weekly in cycle 1 and every 8 weeks for up to 20 cycles. The short, intense schedule consisted of weekly treatment for 8 weeks (one cycle). Patients were followed for up to 4 years or until they progressed to multiple myeloma based on International Myeloma Working Group guidelines.
Over a median follow-up period of 15.8 months (range, 0 to 24 months), rates of complete response were 2% in the long treatment arm, 5% in the intermediate treatment arm, and 0% in the short treatment arm. Rates of at least very good partial response were 29%, 24%, and 15%, respectively. Overall response rates were 56%, 54%, and 38%, respectively. Median PFS was not reached in any arm, exceeding 24 months.
Treatment was generally well tolerated, said Dr. Hofmeister. The most common treatment-related adverse effects were fatigue, cough, upper respiratory tract infection, headache, and insomnia. Hypertension and hyperglycemia were the most common grade 3-4 treatment-emergent adverse events, affecting up to 5% of patients per arm. Fewer than 10% of patients in any arm developed treatment-emergent hematologic adverse events, and fewer than 5% developed grade 3-4 pneumonia or sepsis. There were three cases of a second primary malignancy, including one case of breast cancer and two cases of melanoma.
Rates of infusion-related reactions did not correlate with treatment duration. Grade 3-4 infusion-related reactions affected 0% to 3% of patients per arm. The sole death in this trial resulted from disease progression in a patient from the short treatment arm. “Taken together, efficacy and safety data support long dosing compared to intermediate and short dosing,” Dr. Hofmeister said.
The three arms were demographically similar. Patients tended to be white, in their late 50s to 60s, and to have ECOG scores of 0 with at least two risk factors for progression. About 70% had IgG disease and nearly half had less than 20% plasma cells in bone marrow.
Janssen, the maker of daratumumab, sponsored the trial. Dr. Hofmeister disclosed research funding from Janssen and research support, honoraria, and advisory relationships with Adaptive Biotechnologies, Thrasos, Celgene, Karyopharm, Takeda, and other pharmaceutical companies.
SOURCE: Hofmeister C et al, ASH 2017, Abstract 510.
ATLANTA – Daratumumab monotherapy led to durable partial responses among intermediate to high-risk patients with smoldering multiple myeloma, according to results from the phase II CENTAURUS trial.
Although less than 5% of patients had complete responses, 27% had at least a very good partial response to long-term therapy (up to 20 treatment cycles lasting 8 weeks each), Craig C. Hofmeister, MD, of the Ohio State University Comprehensive Cancer Center, Columbus, said at the annual meeting of the American Society of Hematology. The coprimary endpoint, median progression-free survival, exceeded 24 months in all dose cohorts, and was the longest when patients were treated longest.
Current guidelines recommend monitoring smoldering multiple myeloma every 3-6 months and treating only after patients progress. However, some experts pursue earlier treatment in the premalignant setting.
In CENTAURUS, 123 adults with smoldering multiple myeloma were randomly assigned to receive daratumumab (16 mg/kg IV) in 8-week cycles according to a long, intermediate, or short/intense schedule. The long schedule consisted of treatment weekly for cycle 1, every other week for cycles 2-3, monthly for cycles 4-7, and once every 8 weeks for up to 13 more cycles. The intermediate schedule consisted of treatment weekly in cycle 1 and every 8 weeks for up to 20 cycles. The short, intense schedule consisted of weekly treatment for 8 weeks (one cycle). Patients were followed for up to 4 years or until they progressed to multiple myeloma based on International Myeloma Working Group guidelines.
Over a median follow-up period of 15.8 months (range, 0 to 24 months), rates of complete response were 2% in the long treatment arm, 5% in the intermediate treatment arm, and 0% in the short treatment arm. Rates of at least very good partial response were 29%, 24%, and 15%, respectively. Overall response rates were 56%, 54%, and 38%, respectively. Median PFS was not reached in any arm, exceeding 24 months.
Treatment was generally well tolerated, said Dr. Hofmeister. The most common treatment-related adverse effects were fatigue, cough, upper respiratory tract infection, headache, and insomnia. Hypertension and hyperglycemia were the most common grade 3-4 treatment-emergent adverse events, affecting up to 5% of patients per arm. Fewer than 10% of patients in any arm developed treatment-emergent hematologic adverse events, and fewer than 5% developed grade 3-4 pneumonia or sepsis. There were three cases of a second primary malignancy, including one case of breast cancer and two cases of melanoma.
Rates of infusion-related reactions did not correlate with treatment duration. Grade 3-4 infusion-related reactions affected 0% to 3% of patients per arm. The sole death in this trial resulted from disease progression in a patient from the short treatment arm. “Taken together, efficacy and safety data support long dosing compared to intermediate and short dosing,” Dr. Hofmeister said.
The three arms were demographically similar. Patients tended to be white, in their late 50s to 60s, and to have ECOG scores of 0 with at least two risk factors for progression. About 70% had IgG disease and nearly half had less than 20% plasma cells in bone marrow.
Janssen, the maker of daratumumab, sponsored the trial. Dr. Hofmeister disclosed research funding from Janssen and research support, honoraria, and advisory relationships with Adaptive Biotechnologies, Thrasos, Celgene, Karyopharm, Takeda, and other pharmaceutical companies.
SOURCE: Hofmeister C et al, ASH 2017, Abstract 510.
REPORTING FROM ASH 2017
Key clinical point: Single-agent daratumumab therapy was active and its safety profile was acceptable in patients with smoldering multiple myeloma.
Major finding: Rates of at least very good partial response were 29%, 24%, and 15% among patients who received long, intermediate, and short/intense treatment schedules, respectively. Median progression-free survival exceeded 24 months in all three arms.
Data source: CENTAURUS, a phase II trial of 123 patients with smoldering multiple myeloma.
Disclosures: Janssen sponsored the trial. Dr. Hofmeister disclosed research funding from Janssen and research support, honoraria, and advisory relationships with Adaptive Biotechnologies, Thrasos, Celgene, Karyopharm, Takeda, and other pharmaceutical companies.
Source: Hofmeister C et al, ASH 2017, Abstract 510.
ERBB2 expression predicts pCR in HER2+ breast cancer
SAN ANTONIO – Among patients receiving trastuzumab plus lapatinib neoadjuvant therapy for HER2-positive early breast cancer, amplification of ERBB2 was predictive of a pathologic complete response (pCR), according to findings presented at the San Antonio Breast Cancer Symposium.
However, ERBB2 mRNA expression and PAM50-enriched HER2 better predicted pCR, said lead study author Cristos Sotiriou, MD, of the Breast Cancer Translational Research Laboratory at the Institut Jules Bordet in Belgium
High genomic instability was associated with a higher pCR rate in patients with estrogen receptor–positive tumors, but copy number alterations (CNAs) were not associated with event-free survival (EFS).
In the large phase 3 NeoALTTO trial, lapatinib combined with trastuzumab in the neoadjuvant setting nearly doubled the pCR rate as compared with either agent used alone. The 3-year EFS was also improved with dual HER2 blockage versus single HER2 therapy (84% for the combination, hazard ratio, 0.78; P = .33 vs. 78% for lapatinib alone and 76% for trastuzumab alone, HR, 1.06; P = .81 for both).
The researchers of this trial also found that pCR was a surrogate for long-term outcome.
“Expression of ERBB2, ESR1, and immune signatures were the main drivers of pCR,” said Dr. Sotiriou.
The main goal of the current study was to investigate the relevance of CNAs for pCR and EFS in this population. A total of 455 patients were enrolled in the NeoALTTO study, and of this cohort, 270 had tumor content that was sufficient to assay for CNAs. Tumor-infiltrating lymphocytes and gene expression were also obtained and the genome instability index was calculated, and 184 samples were included in the final analysis.
Of the cancer genes, only ERBB2 was predictive of pCR.
A total of 159 recurrent CNA regions were identified. ERBB2 amplification was associated with high pCR (P = .0007), but less than ERBB2 expression, and it lost its significance after correcting for ERBB2 expression.
The genome instability index (GII) was defined as the “median absolute deviation of the normalized copy number” and independent of ERBB2 amplification, the pCR rate increased with the GII (P = .03.
Amplification of two regions on 6q23-24 was significantly associated with higher pCR (P = .00005 and P = .00087). One of the segments harbored 39 genes, some with an expression level that was also predictive of pCR. The 6q23-24 segment was associated with pCR in estrogen receptor–positive tumors only (interaction test P = .04).
After multiple testing correction, there were no amplified regions or genes found to be predictive of EFS.
“A novel amplified region on 6q23-24 was shown to be predictive of pCR, in particular for estrogen receptor–positive tumors,” said Dr. Sotiriou. “This may warrant further investigation.”
SOURCE: Sotiriou et al. SABCS Abstract GS1-04
SAN ANTONIO – Among patients receiving trastuzumab plus lapatinib neoadjuvant therapy for HER2-positive early breast cancer, amplification of ERBB2 was predictive of a pathologic complete response (pCR), according to findings presented at the San Antonio Breast Cancer Symposium.
However, ERBB2 mRNA expression and PAM50-enriched HER2 better predicted pCR, said lead study author Cristos Sotiriou, MD, of the Breast Cancer Translational Research Laboratory at the Institut Jules Bordet in Belgium
High genomic instability was associated with a higher pCR rate in patients with estrogen receptor–positive tumors, but copy number alterations (CNAs) were not associated with event-free survival (EFS).
In the large phase 3 NeoALTTO trial, lapatinib combined with trastuzumab in the neoadjuvant setting nearly doubled the pCR rate as compared with either agent used alone. The 3-year EFS was also improved with dual HER2 blockage versus single HER2 therapy (84% for the combination, hazard ratio, 0.78; P = .33 vs. 78% for lapatinib alone and 76% for trastuzumab alone, HR, 1.06; P = .81 for both).
The researchers of this trial also found that pCR was a surrogate for long-term outcome.
“Expression of ERBB2, ESR1, and immune signatures were the main drivers of pCR,” said Dr. Sotiriou.
The main goal of the current study was to investigate the relevance of CNAs for pCR and EFS in this population. A total of 455 patients were enrolled in the NeoALTTO study, and of this cohort, 270 had tumor content that was sufficient to assay for CNAs. Tumor-infiltrating lymphocytes and gene expression were also obtained and the genome instability index was calculated, and 184 samples were included in the final analysis.
Of the cancer genes, only ERBB2 was predictive of pCR.
A total of 159 recurrent CNA regions were identified. ERBB2 amplification was associated with high pCR (P = .0007), but less than ERBB2 expression, and it lost its significance after correcting for ERBB2 expression.
The genome instability index (GII) was defined as the “median absolute deviation of the normalized copy number” and independent of ERBB2 amplification, the pCR rate increased with the GII (P = .03.
Amplification of two regions on 6q23-24 was significantly associated with higher pCR (P = .00005 and P = .00087). One of the segments harbored 39 genes, some with an expression level that was also predictive of pCR. The 6q23-24 segment was associated with pCR in estrogen receptor–positive tumors only (interaction test P = .04).
After multiple testing correction, there were no amplified regions or genes found to be predictive of EFS.
“A novel amplified region on 6q23-24 was shown to be predictive of pCR, in particular for estrogen receptor–positive tumors,” said Dr. Sotiriou. “This may warrant further investigation.”
SOURCE: Sotiriou et al. SABCS Abstract GS1-04
SAN ANTONIO – Among patients receiving trastuzumab plus lapatinib neoadjuvant therapy for HER2-positive early breast cancer, amplification of ERBB2 was predictive of a pathologic complete response (pCR), according to findings presented at the San Antonio Breast Cancer Symposium.
However, ERBB2 mRNA expression and PAM50-enriched HER2 better predicted pCR, said lead study author Cristos Sotiriou, MD, of the Breast Cancer Translational Research Laboratory at the Institut Jules Bordet in Belgium
High genomic instability was associated with a higher pCR rate in patients with estrogen receptor–positive tumors, but copy number alterations (CNAs) were not associated with event-free survival (EFS).
In the large phase 3 NeoALTTO trial, lapatinib combined with trastuzumab in the neoadjuvant setting nearly doubled the pCR rate as compared with either agent used alone. The 3-year EFS was also improved with dual HER2 blockage versus single HER2 therapy (84% for the combination, hazard ratio, 0.78; P = .33 vs. 78% for lapatinib alone and 76% for trastuzumab alone, HR, 1.06; P = .81 for both).
The researchers of this trial also found that pCR was a surrogate for long-term outcome.
“Expression of ERBB2, ESR1, and immune signatures were the main drivers of pCR,” said Dr. Sotiriou.
The main goal of the current study was to investigate the relevance of CNAs for pCR and EFS in this population. A total of 455 patients were enrolled in the NeoALTTO study, and of this cohort, 270 had tumor content that was sufficient to assay for CNAs. Tumor-infiltrating lymphocytes and gene expression were also obtained and the genome instability index was calculated, and 184 samples were included in the final analysis.
Of the cancer genes, only ERBB2 was predictive of pCR.
A total of 159 recurrent CNA regions were identified. ERBB2 amplification was associated with high pCR (P = .0007), but less than ERBB2 expression, and it lost its significance after correcting for ERBB2 expression.
The genome instability index (GII) was defined as the “median absolute deviation of the normalized copy number” and independent of ERBB2 amplification, the pCR rate increased with the GII (P = .03.
Amplification of two regions on 6q23-24 was significantly associated with higher pCR (P = .00005 and P = .00087). One of the segments harbored 39 genes, some with an expression level that was also predictive of pCR. The 6q23-24 segment was associated with pCR in estrogen receptor–positive tumors only (interaction test P = .04).
After multiple testing correction, there were no amplified regions or genes found to be predictive of EFS.
“A novel amplified region on 6q23-24 was shown to be predictive of pCR, in particular for estrogen receptor–positive tumors,” said Dr. Sotiriou. “This may warrant further investigation.”
SOURCE: Sotiriou et al. SABCS Abstract GS1-04
REPORTING FROM SABCS 2017
Key clinical point: ERBB2 mRNA expression and PAM50-enriched HER2 better predicted pathologic complete response than did EEBB2 amplification.
Major finding: Of the cancer genes, only ERBB2 was predictive of pCR, and amplification of two regions on 6q23-24 was significantly associated with higher pCR (P = .00005 and P = .00087).
Data source: An analysis of the large phase 3 NeoALTTO trial, in which lapatinib was combined with trastuzumab in the neoadjuvant setting to investigate the relevance of copy number alterations on outcome.
Disclosures: The NeoALTTO trial was funded by GlaxoSmithKline. Dr. Sotiriou did not make any disclosures.
Source: Sotiriou et al. SABCS Abstract GS1-04
HealthCare.gov enrollment for 2018 nearly doubled in final week
A busy final week of open enrollment at HealthCare.gov almost doubled the total number of health insurance plans selected and nearly equaled the total for last year’s much longer period, according to data from the Centers for Medicare & Medicaid Services.
After the first 6 weeks of enrollment, the total number of plans selected for 2018 stood at 4.68 million. Just 1 week later, . That works out to 6.43 million plans selected by consumers who renewed their coverage on 1 of the 39 state exchanges that use the HealthCare.gov platform and 2.39 million plans selected by new consumers (those who did not have coverage in 2017), the CMS reported.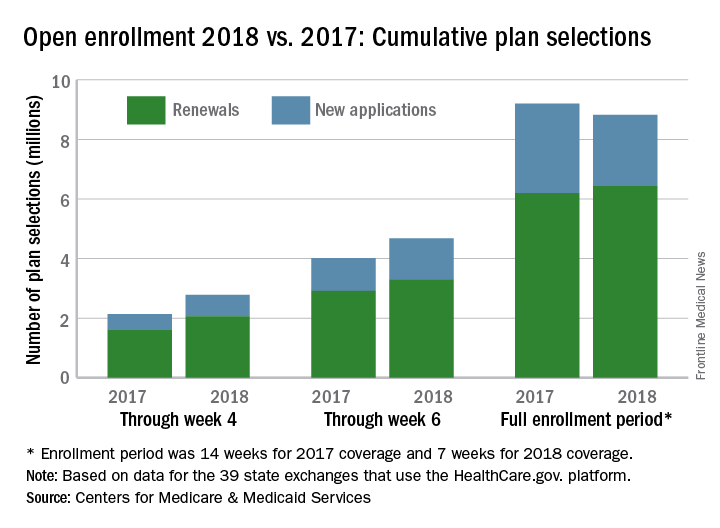
The CMS noted that the numbers for 2018 are estimates that represent plans selected and not the number of consumers who have paid premiums to effectuate their enrollment.
SOURCE: CMS.gov Fact Sheet
A busy final week of open enrollment at HealthCare.gov almost doubled the total number of health insurance plans selected and nearly equaled the total for last year’s much longer period, according to data from the Centers for Medicare & Medicaid Services.
After the first 6 weeks of enrollment, the total number of plans selected for 2018 stood at 4.68 million. Just 1 week later, . That works out to 6.43 million plans selected by consumers who renewed their coverage on 1 of the 39 state exchanges that use the HealthCare.gov platform and 2.39 million plans selected by new consumers (those who did not have coverage in 2017), the CMS reported.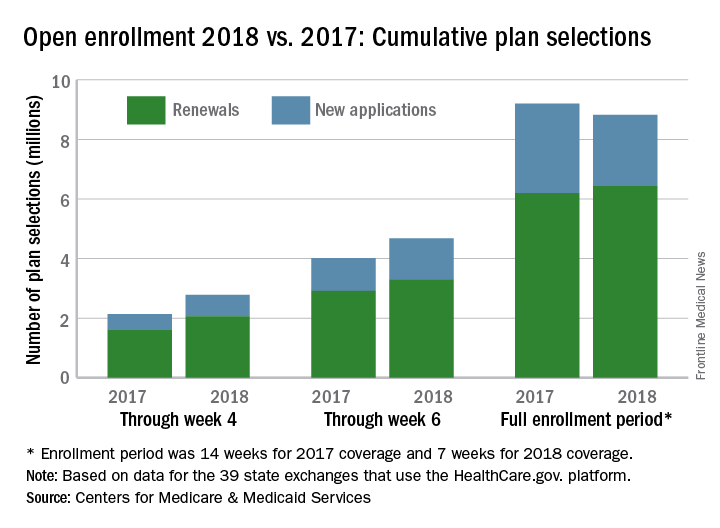
The CMS noted that the numbers for 2018 are estimates that represent plans selected and not the number of consumers who have paid premiums to effectuate their enrollment.
SOURCE: CMS.gov Fact Sheet
A busy final week of open enrollment at HealthCare.gov almost doubled the total number of health insurance plans selected and nearly equaled the total for last year’s much longer period, according to data from the Centers for Medicare & Medicaid Services.
After the first 6 weeks of enrollment, the total number of plans selected for 2018 stood at 4.68 million. Just 1 week later, . That works out to 6.43 million plans selected by consumers who renewed their coverage on 1 of the 39 state exchanges that use the HealthCare.gov platform and 2.39 million plans selected by new consumers (those who did not have coverage in 2017), the CMS reported.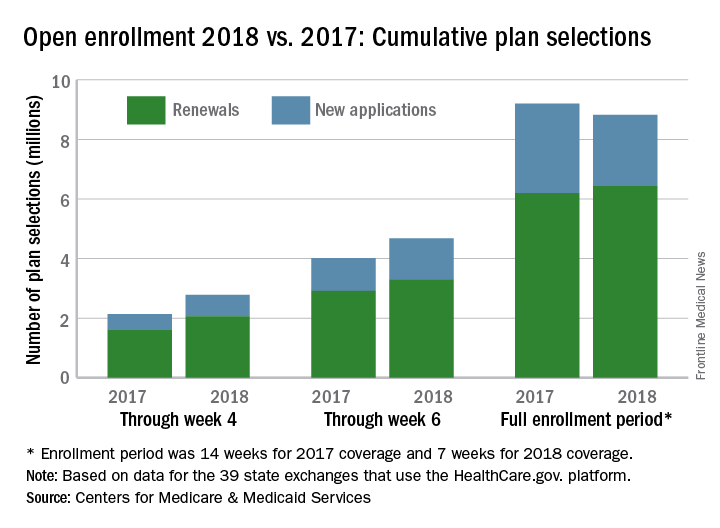
The CMS noted that the numbers for 2018 are estimates that represent plans selected and not the number of consumers who have paid premiums to effectuate their enrollment.
SOURCE: CMS.gov Fact Sheet
FDA approves hydroxyurea for pediatric patients with sickle cell anemia
to reduce the frequency of painful crises and the need for blood transfusions, the Food and Drug Administration announced on Dec. 21.
This is the first FDA approval of hydroxyurea for use in pediatric sickle cell patients. The recommended initial dose is 20 mg/kg once daily but can be changed based on blood count levels, the agency said in a press release.
The most common adverse reactions to hydroxyurea, infections and neutropenia, occurred in less than 10% of patients. Hydroxyurea causes severe myelosuppression and should not be administered to patients with depressed bone marrow function.
Hydroxyurea is manufactured as Siklos by Addmedica. More information concerning hydroxyurea indications, dosing, and precautions can be found here.
SOURCE: FDA press release.
to reduce the frequency of painful crises and the need for blood transfusions, the Food and Drug Administration announced on Dec. 21.
This is the first FDA approval of hydroxyurea for use in pediatric sickle cell patients. The recommended initial dose is 20 mg/kg once daily but can be changed based on blood count levels, the agency said in a press release.
The most common adverse reactions to hydroxyurea, infections and neutropenia, occurred in less than 10% of patients. Hydroxyurea causes severe myelosuppression and should not be administered to patients with depressed bone marrow function.
Hydroxyurea is manufactured as Siklos by Addmedica. More information concerning hydroxyurea indications, dosing, and precautions can be found here.
SOURCE: FDA press release.
to reduce the frequency of painful crises and the need for blood transfusions, the Food and Drug Administration announced on Dec. 21.
This is the first FDA approval of hydroxyurea for use in pediatric sickle cell patients. The recommended initial dose is 20 mg/kg once daily but can be changed based on blood count levels, the agency said in a press release.
The most common adverse reactions to hydroxyurea, infections and neutropenia, occurred in less than 10% of patients. Hydroxyurea causes severe myelosuppression and should not be administered to patients with depressed bone marrow function.
Hydroxyurea is manufactured as Siklos by Addmedica. More information concerning hydroxyurea indications, dosing, and precautions can be found here.
SOURCE: FDA press release.
Length of stay shorter with admission to family medicine, not hospitalist, service
MONTREAL – When a family medicine teaching service provided hospital care for local patients, length of stay was almost a third shorter than when care was provided by the hospitalist internal medicine service at a large tertiary care hospital.
What made the difference in length of stay? “,” said Gregory Garrison, MD, of the department of family medicine at the Mayo Clinic, Rochester, Minn. He noted that readmission rates weren’t higher for the patients cared for by the family medicine inpatient service.
The primary outcome measures were length of stay and readmission or death within 30 days of discharge, Dr. Garrison said at the annual meeting of the North American Primary Care Research Group.
A total of 3,125 admissions were seen for 2,138 unique patients. Most admissions (2,651; 84.8%) were for the family medicine service. Demographic characteristics and readmission rates were similar between admissions to the two services, but “hospitalist internal medicine patients were perhaps slightly sicker,” said Dr. Garrison. The mean Charlson comorbidity score was 4 for the family medicine admissions and 5.6 for the hospitalist internal medicine admissions (P less than .001). Also, the patients admitted to the hospitalist service were slightly more likely to have had a previous hospital admission within the prior 12 months.
Examining the unadjusted data, Dr. Garrison and his colleagues found that the family medicine patients had a shorter length of stay, with a mean 2.5 days and a median 1.8 days, compared with the mean 3.8 days and median 2.7 days spent in hospital for the hospitalist internal medicine patients.
The difference remained significant after multivariable analysis to control for several potentially confounding factors, including patient demographics, prior health care utilization, disposition, readmissions, and Charlson comorbidity score.
The adjusted figures showed that length of stay was 31.8% longer for admissions to the hospitalist internal medicine service than for the family medicine service.
In discussion, Dr. Garrison said that he and his colleagues believe that the physicians, social workers, and clinical assistants who make up the family medicine service really understand the “outpatient resources that can be marshaled to help local patients with the transition from hospital to home.”
In practical terms, this can mean that a social worker knows which skilled nursing facilities are likely to accept a Friday admission, or that a physician understands community resources that can help an elderly patient return to her home with a little extra support, he said.
Another practicality, is that “the lack of a census cap on the family medicine inpatient service may incentivize rapid turnover,” he added.
Dr. Garrison reported no outside sources of funding and no conflicts of interest.
SOURCE: Garrison G et al. NAPCRG 2017 Abstract AE32
MONTREAL – When a family medicine teaching service provided hospital care for local patients, length of stay was almost a third shorter than when care was provided by the hospitalist internal medicine service at a large tertiary care hospital.
What made the difference in length of stay? “,” said Gregory Garrison, MD, of the department of family medicine at the Mayo Clinic, Rochester, Minn. He noted that readmission rates weren’t higher for the patients cared for by the family medicine inpatient service.
The primary outcome measures were length of stay and readmission or death within 30 days of discharge, Dr. Garrison said at the annual meeting of the North American Primary Care Research Group.
A total of 3,125 admissions were seen for 2,138 unique patients. Most admissions (2,651; 84.8%) were for the family medicine service. Demographic characteristics and readmission rates were similar between admissions to the two services, but “hospitalist internal medicine patients were perhaps slightly sicker,” said Dr. Garrison. The mean Charlson comorbidity score was 4 for the family medicine admissions and 5.6 for the hospitalist internal medicine admissions (P less than .001). Also, the patients admitted to the hospitalist service were slightly more likely to have had a previous hospital admission within the prior 12 months.
Examining the unadjusted data, Dr. Garrison and his colleagues found that the family medicine patients had a shorter length of stay, with a mean 2.5 days and a median 1.8 days, compared with the mean 3.8 days and median 2.7 days spent in hospital for the hospitalist internal medicine patients.
The difference remained significant after multivariable analysis to control for several potentially confounding factors, including patient demographics, prior health care utilization, disposition, readmissions, and Charlson comorbidity score.
The adjusted figures showed that length of stay was 31.8% longer for admissions to the hospitalist internal medicine service than for the family medicine service.
In discussion, Dr. Garrison said that he and his colleagues believe that the physicians, social workers, and clinical assistants who make up the family medicine service really understand the “outpatient resources that can be marshaled to help local patients with the transition from hospital to home.”
In practical terms, this can mean that a social worker knows which skilled nursing facilities are likely to accept a Friday admission, or that a physician understands community resources that can help an elderly patient return to her home with a little extra support, he said.
Another practicality, is that “the lack of a census cap on the family medicine inpatient service may incentivize rapid turnover,” he added.
Dr. Garrison reported no outside sources of funding and no conflicts of interest.
SOURCE: Garrison G et al. NAPCRG 2017 Abstract AE32
MONTREAL – When a family medicine teaching service provided hospital care for local patients, length of stay was almost a third shorter than when care was provided by the hospitalist internal medicine service at a large tertiary care hospital.
What made the difference in length of stay? “,” said Gregory Garrison, MD, of the department of family medicine at the Mayo Clinic, Rochester, Minn. He noted that readmission rates weren’t higher for the patients cared for by the family medicine inpatient service.
The primary outcome measures were length of stay and readmission or death within 30 days of discharge, Dr. Garrison said at the annual meeting of the North American Primary Care Research Group.
A total of 3,125 admissions were seen for 2,138 unique patients. Most admissions (2,651; 84.8%) were for the family medicine service. Demographic characteristics and readmission rates were similar between admissions to the two services, but “hospitalist internal medicine patients were perhaps slightly sicker,” said Dr. Garrison. The mean Charlson comorbidity score was 4 for the family medicine admissions and 5.6 for the hospitalist internal medicine admissions (P less than .001). Also, the patients admitted to the hospitalist service were slightly more likely to have had a previous hospital admission within the prior 12 months.
Examining the unadjusted data, Dr. Garrison and his colleagues found that the family medicine patients had a shorter length of stay, with a mean 2.5 days and a median 1.8 days, compared with the mean 3.8 days and median 2.7 days spent in hospital for the hospitalist internal medicine patients.
The difference remained significant after multivariable analysis to control for several potentially confounding factors, including patient demographics, prior health care utilization, disposition, readmissions, and Charlson comorbidity score.
The adjusted figures showed that length of stay was 31.8% longer for admissions to the hospitalist internal medicine service than for the family medicine service.
In discussion, Dr. Garrison said that he and his colleagues believe that the physicians, social workers, and clinical assistants who make up the family medicine service really understand the “outpatient resources that can be marshaled to help local patients with the transition from hospital to home.”
In practical terms, this can mean that a social worker knows which skilled nursing facilities are likely to accept a Friday admission, or that a physician understands community resources that can help an elderly patient return to her home with a little extra support, he said.
Another practicality, is that “the lack of a census cap on the family medicine inpatient service may incentivize rapid turnover,” he added.
Dr. Garrison reported no outside sources of funding and no conflicts of interest.
SOURCE: Garrison G et al. NAPCRG 2017 Abstract AE32
REPORTING FROM NAPCRG 2017
Key clinical point: Patients’ length of stay was shorter when they were cared for by family medicine doctors and not hospitalists.
Major finding: After multivariable analysis, the adjusted length of stay was 31.8% longer for patients on the hospitalist service than on the family medicine inpatient service.
Study details: A retrospective review of records from 3,125 admissions of 2,138 patients.
Disclosures: Dr. Garrison reported no conflicts of interest and no outside sources of funding.
Source: Garrison G et al. NAPCRG 2017 Abstract AE32.
Study identifies predictors of acquired von Willebrand disease
ATLANTA – Waldenström macroglobulinemia can present as acquired von Willebrand disease (VWD), and when it does, the finding strongly correlates with high serum IgM levels and the presence of CXCR4 mutations, according to the results of a large, single-center retrospective study.
Further, successfully treating Waldenström macroglobulinemia often resolves acquired VWD, and the depth of treatment response predicts the degree of improvement, Jorge J. Castillo, MD, and his associates wrote in a poster presented at the annual meeting of the American Society of Hematology.
Acquired VWD is an uncommon, poorly understood presentation of Waldenström macroglobulinemia. Because affected patients require treatment, better characterizing this subgroup is important, the investigators noted.
At the Bing Center for Waldenström Macroglobulinemia at Dana-Farber Cancer Institute in Boston, the researchers retrospectively studied 320 individuals with newly diagnosed Waldenström macroglobulinemia and used logistic regression analysis to seek predictors of acquired VWD, which they evaluated by measuring levels of VW factor antigen, VW factor activity, and factor VIII. Levels under 30% were considered VWD and levels between 30% and 50% were considered low-level VWD.
In all, 49 individuals had acquired VWD while 271 patients did not. These two groups were similar in terms of age, sex, hemoglobin level, platelet count, and bone marrow involvement. However, 45% of patients with acquired VWD had serum IgM levels above 6,000 mg/dL versus 6% of patients without acquired VWD (P less than .001), and 47% of patients with acquired VWD had serum IgM levels between 3,000 and 5,999 versus 31% of patients without acquired VWD (P less than .001). Also, 77% of patients with acquired VWD tested positive for CXCR4 mutation versus 37% of patients without acquired VWD (P less than .001).
A significantly higher proportion of patients without acquired VWD had white blood cell concentrations above 6,000/mcL (29% vs. 50%; P = .006). This finding lost statistical significance in the logistic regression model, but all the other variables remained significantly associated. Serum IgM levels above 6,000 mg/dL conferred a 55-fold increase in the odds of having acquired VWD (95% confidence interval, 17-177; P less than .001), and serum IgM levels between 3,000 and 5,999 mg/dL led to an 11-fold increase in these odds (95% CI, 4-34). The presence of CXCR4 mutations was associated with a sixfold increased odds of acquired VWD (95% CI, 2-15). The P value for each of these three associations was at or below .001.
Therapy for Waldenström macroglobulinemia led to statistically significant increases in levels of factor VIII, VW factor antigen, and VW factor activity (P less than .001) and the median of each level improved by at least 35% after treatment. After treatment, 78% of patients with acquired VWD had levels of all three measures above 50% (versus 0% before treatment; P less than .001). Patients with acquired VWD with the best responses to treatment had about a 90% decrease in IgM levels, while those with a partial response had about a two-thirds decrease and patients with stable disease had about a 20% decrease. A linear regression model confirmed that depth of treatment response, based on change in IgM level, correlated with degree of improvement in VWD – that is, the extent of improvement in levels of VW factor antigen, VW factor activity, and factor VIII.
No external funding sources were reported. Dr. Castillo disclosed consulting ties and research funding from Pharmacyclics and Janssen, and research funding from Millenium and Abbvie.
SOURCE: Castillo J, et al. ASH 2017 Abstract 1088.
ATLANTA – Waldenström macroglobulinemia can present as acquired von Willebrand disease (VWD), and when it does, the finding strongly correlates with high serum IgM levels and the presence of CXCR4 mutations, according to the results of a large, single-center retrospective study.
Further, successfully treating Waldenström macroglobulinemia often resolves acquired VWD, and the depth of treatment response predicts the degree of improvement, Jorge J. Castillo, MD, and his associates wrote in a poster presented at the annual meeting of the American Society of Hematology.
Acquired VWD is an uncommon, poorly understood presentation of Waldenström macroglobulinemia. Because affected patients require treatment, better characterizing this subgroup is important, the investigators noted.
At the Bing Center for Waldenström Macroglobulinemia at Dana-Farber Cancer Institute in Boston, the researchers retrospectively studied 320 individuals with newly diagnosed Waldenström macroglobulinemia and used logistic regression analysis to seek predictors of acquired VWD, which they evaluated by measuring levels of VW factor antigen, VW factor activity, and factor VIII. Levels under 30% were considered VWD and levels between 30% and 50% were considered low-level VWD.
In all, 49 individuals had acquired VWD while 271 patients did not. These two groups were similar in terms of age, sex, hemoglobin level, platelet count, and bone marrow involvement. However, 45% of patients with acquired VWD had serum IgM levels above 6,000 mg/dL versus 6% of patients without acquired VWD (P less than .001), and 47% of patients with acquired VWD had serum IgM levels between 3,000 and 5,999 versus 31% of patients without acquired VWD (P less than .001). Also, 77% of patients with acquired VWD tested positive for CXCR4 mutation versus 37% of patients without acquired VWD (P less than .001).
A significantly higher proportion of patients without acquired VWD had white blood cell concentrations above 6,000/mcL (29% vs. 50%; P = .006). This finding lost statistical significance in the logistic regression model, but all the other variables remained significantly associated. Serum IgM levels above 6,000 mg/dL conferred a 55-fold increase in the odds of having acquired VWD (95% confidence interval, 17-177; P less than .001), and serum IgM levels between 3,000 and 5,999 mg/dL led to an 11-fold increase in these odds (95% CI, 4-34). The presence of CXCR4 mutations was associated with a sixfold increased odds of acquired VWD (95% CI, 2-15). The P value for each of these three associations was at or below .001.
Therapy for Waldenström macroglobulinemia led to statistically significant increases in levels of factor VIII, VW factor antigen, and VW factor activity (P less than .001) and the median of each level improved by at least 35% after treatment. After treatment, 78% of patients with acquired VWD had levels of all three measures above 50% (versus 0% before treatment; P less than .001). Patients with acquired VWD with the best responses to treatment had about a 90% decrease in IgM levels, while those with a partial response had about a two-thirds decrease and patients with stable disease had about a 20% decrease. A linear regression model confirmed that depth of treatment response, based on change in IgM level, correlated with degree of improvement in VWD – that is, the extent of improvement in levels of VW factor antigen, VW factor activity, and factor VIII.
No external funding sources were reported. Dr. Castillo disclosed consulting ties and research funding from Pharmacyclics and Janssen, and research funding from Millenium and Abbvie.
SOURCE: Castillo J, et al. ASH 2017 Abstract 1088.
ATLANTA – Waldenström macroglobulinemia can present as acquired von Willebrand disease (VWD), and when it does, the finding strongly correlates with high serum IgM levels and the presence of CXCR4 mutations, according to the results of a large, single-center retrospective study.
Further, successfully treating Waldenström macroglobulinemia often resolves acquired VWD, and the depth of treatment response predicts the degree of improvement, Jorge J. Castillo, MD, and his associates wrote in a poster presented at the annual meeting of the American Society of Hematology.
Acquired VWD is an uncommon, poorly understood presentation of Waldenström macroglobulinemia. Because affected patients require treatment, better characterizing this subgroup is important, the investigators noted.
At the Bing Center for Waldenström Macroglobulinemia at Dana-Farber Cancer Institute in Boston, the researchers retrospectively studied 320 individuals with newly diagnosed Waldenström macroglobulinemia and used logistic regression analysis to seek predictors of acquired VWD, which they evaluated by measuring levels of VW factor antigen, VW factor activity, and factor VIII. Levels under 30% were considered VWD and levels between 30% and 50% were considered low-level VWD.
In all, 49 individuals had acquired VWD while 271 patients did not. These two groups were similar in terms of age, sex, hemoglobin level, platelet count, and bone marrow involvement. However, 45% of patients with acquired VWD had serum IgM levels above 6,000 mg/dL versus 6% of patients without acquired VWD (P less than .001), and 47% of patients with acquired VWD had serum IgM levels between 3,000 and 5,999 versus 31% of patients without acquired VWD (P less than .001). Also, 77% of patients with acquired VWD tested positive for CXCR4 mutation versus 37% of patients without acquired VWD (P less than .001).
A significantly higher proportion of patients without acquired VWD had white blood cell concentrations above 6,000/mcL (29% vs. 50%; P = .006). This finding lost statistical significance in the logistic regression model, but all the other variables remained significantly associated. Serum IgM levels above 6,000 mg/dL conferred a 55-fold increase in the odds of having acquired VWD (95% confidence interval, 17-177; P less than .001), and serum IgM levels between 3,000 and 5,999 mg/dL led to an 11-fold increase in these odds (95% CI, 4-34). The presence of CXCR4 mutations was associated with a sixfold increased odds of acquired VWD (95% CI, 2-15). The P value for each of these three associations was at or below .001.
Therapy for Waldenström macroglobulinemia led to statistically significant increases in levels of factor VIII, VW factor antigen, and VW factor activity (P less than .001) and the median of each level improved by at least 35% after treatment. After treatment, 78% of patients with acquired VWD had levels of all three measures above 50% (versus 0% before treatment; P less than .001). Patients with acquired VWD with the best responses to treatment had about a 90% decrease in IgM levels, while those with a partial response had about a two-thirds decrease and patients with stable disease had about a 20% decrease. A linear regression model confirmed that depth of treatment response, based on change in IgM level, correlated with degree of improvement in VWD – that is, the extent of improvement in levels of VW factor antigen, VW factor activity, and factor VIII.
No external funding sources were reported. Dr. Castillo disclosed consulting ties and research funding from Pharmacyclics and Janssen, and research funding from Millenium and Abbvie.
SOURCE: Castillo J, et al. ASH 2017 Abstract 1088.
AT ASH 2017
Key clinical point: Successfully treating Waldenström macroglobulinemia often resolves acquired von Willebrand disease.
Major finding: Therapy for Waldenström macroglobulinemia led to statistically significant increases in levels of factor VIII, VW factor antigen, and VW factor activity (P less than .001) and the median of each level improved by at least 35% after treatment.
Data source: A single-center retrospective study of 320 patients with newly diagnosed Waldenström macroglobulinemia.
Disclosures: No external funding sources were reported. Dr. Castillo disclosed consultancy and research funding from Pharmacyclics and Janssen. He also disclosed research funding from Millenium and Abbvie.
Source: Castillo J, et al. ASH 2017 Abstract 1088.
Enhanced recovery protocols after colectomy safely cut LOS
, at 15 hospitals in a pilot study of the Enhanced Recovery in National Surgical Quality Improvement Program.
Guidance from experts, engaged multidisciplinary team leadership, continuous data collection and auditing, and collaboration across institutions were all key to success. “The pilot may serve to inform future implementation efforts across hospitals varied in size, location, and resource availability,” investigators led by Julia R. Berian, MD, a surgery resident at the University of Chicago, wrote in a study published online in JAMA Surgery.
The program suggested 13 measures aimed at improved pain control, reduced gut dysfunction, and early nutrition and physical activity. Recommendations included shorter fluid fasts and better preop patient counseling; discontinuation of IV fluids and mobilization of patients within 24 hours of surgery; and solid diets within 24-48 hours.
The measures weren’t mandatory; each hospital tailored its protocols, and timing of implementation was at their discretion.
The report didn’t name the 15 hospitals, but they varied by size and academic status. Hospitals were selected for the program because they were outliers on elective colectomy LOS. The study ran during 2013-2015.
There were 3,437 colectomies at the hospitals before implementation, and 1,538 after. Results were compared with those of 9,950 colectomies over the study period at hospitals not involved in the efforts. Emergency and septic cases were excluded.
ERPs decreased mean LOS by 1.7 days, from 6.9 to 5.2 days. After taking patient characteristics and other matters into account, the adjusted decrease was 1.1 days. LOS fell by 0.4 days in the control hospitals (P less than .001).
Serious morbidity or mortality in the ERP hospitals decreased from 485 cases (14.1%) before implementation to 162 (10.5%) afterward (P less than .001); there was no change in the control hospitals. After implementation, serious morbidity or mortality was significantly less likely in ERP hospitals (adjusted odds ratio, 0.76; 95% confidence interval, 0.60-0.96).
Meanwhile, there was no difference in readmission rates before and after implementation.
“The ERIN pilot study included hospitals of various sizes, indicating that both small and large hospitals can successfully decrease LOS with implementation of an ERP. ... Regardless of resource limitations, small hospitals may have the advantage of decreased bureaucracy and improved communication and collaboration across disciplines. ... We strongly believe that surgeon engagement and leadership in such initiatives are critical to sustained success,” the investigators wrote.
The ACS; Johns Hopkins’ Armstrong Institute for Patient Safety and Quality, Baltimore; and the Agency for Healthcare Research and Quality have recently launched the “Improving Surgical Care and Recovery” program to provide more than 750 hospitals with tools, experts, and other resources for implementing ERPs. “The program is one opportunity for hospitals seeking implementation guidance,” the investigators noted.
Dr. Berian reported receiving salary support from the John A. Hartford Foundation. Her coinvestigators reported receiving grant or salary support from the foundation and the Agency for Healthcare Research and Quality. One investigator reported relationships with a variety of drug and device companies.
SOURCE: Berian J et. al. JAMA Surg. 2017 Dec 20. doi: 10.1001/jamasurg.2017.4906
, at 15 hospitals in a pilot study of the Enhanced Recovery in National Surgical Quality Improvement Program.
Guidance from experts, engaged multidisciplinary team leadership, continuous data collection and auditing, and collaboration across institutions were all key to success. “The pilot may serve to inform future implementation efforts across hospitals varied in size, location, and resource availability,” investigators led by Julia R. Berian, MD, a surgery resident at the University of Chicago, wrote in a study published online in JAMA Surgery.
The program suggested 13 measures aimed at improved pain control, reduced gut dysfunction, and early nutrition and physical activity. Recommendations included shorter fluid fasts and better preop patient counseling; discontinuation of IV fluids and mobilization of patients within 24 hours of surgery; and solid diets within 24-48 hours.
The measures weren’t mandatory; each hospital tailored its protocols, and timing of implementation was at their discretion.
The report didn’t name the 15 hospitals, but they varied by size and academic status. Hospitals were selected for the program because they were outliers on elective colectomy LOS. The study ran during 2013-2015.
There were 3,437 colectomies at the hospitals before implementation, and 1,538 after. Results were compared with those of 9,950 colectomies over the study period at hospitals not involved in the efforts. Emergency and septic cases were excluded.
ERPs decreased mean LOS by 1.7 days, from 6.9 to 5.2 days. After taking patient characteristics and other matters into account, the adjusted decrease was 1.1 days. LOS fell by 0.4 days in the control hospitals (P less than .001).
Serious morbidity or mortality in the ERP hospitals decreased from 485 cases (14.1%) before implementation to 162 (10.5%) afterward (P less than .001); there was no change in the control hospitals. After implementation, serious morbidity or mortality was significantly less likely in ERP hospitals (adjusted odds ratio, 0.76; 95% confidence interval, 0.60-0.96).
Meanwhile, there was no difference in readmission rates before and after implementation.
“The ERIN pilot study included hospitals of various sizes, indicating that both small and large hospitals can successfully decrease LOS with implementation of an ERP. ... Regardless of resource limitations, small hospitals may have the advantage of decreased bureaucracy and improved communication and collaboration across disciplines. ... We strongly believe that surgeon engagement and leadership in such initiatives are critical to sustained success,” the investigators wrote.
The ACS; Johns Hopkins’ Armstrong Institute for Patient Safety and Quality, Baltimore; and the Agency for Healthcare Research and Quality have recently launched the “Improving Surgical Care and Recovery” program to provide more than 750 hospitals with tools, experts, and other resources for implementing ERPs. “The program is one opportunity for hospitals seeking implementation guidance,” the investigators noted.
Dr. Berian reported receiving salary support from the John A. Hartford Foundation. Her coinvestigators reported receiving grant or salary support from the foundation and the Agency for Healthcare Research and Quality. One investigator reported relationships with a variety of drug and device companies.
SOURCE: Berian J et. al. JAMA Surg. 2017 Dec 20. doi: 10.1001/jamasurg.2017.4906
, at 15 hospitals in a pilot study of the Enhanced Recovery in National Surgical Quality Improvement Program.
Guidance from experts, engaged multidisciplinary team leadership, continuous data collection and auditing, and collaboration across institutions were all key to success. “The pilot may serve to inform future implementation efforts across hospitals varied in size, location, and resource availability,” investigators led by Julia R. Berian, MD, a surgery resident at the University of Chicago, wrote in a study published online in JAMA Surgery.
The program suggested 13 measures aimed at improved pain control, reduced gut dysfunction, and early nutrition and physical activity. Recommendations included shorter fluid fasts and better preop patient counseling; discontinuation of IV fluids and mobilization of patients within 24 hours of surgery; and solid diets within 24-48 hours.
The measures weren’t mandatory; each hospital tailored its protocols, and timing of implementation was at their discretion.
The report didn’t name the 15 hospitals, but they varied by size and academic status. Hospitals were selected for the program because they were outliers on elective colectomy LOS. The study ran during 2013-2015.
There were 3,437 colectomies at the hospitals before implementation, and 1,538 after. Results were compared with those of 9,950 colectomies over the study period at hospitals not involved in the efforts. Emergency and septic cases were excluded.
ERPs decreased mean LOS by 1.7 days, from 6.9 to 5.2 days. After taking patient characteristics and other matters into account, the adjusted decrease was 1.1 days. LOS fell by 0.4 days in the control hospitals (P less than .001).
Serious morbidity or mortality in the ERP hospitals decreased from 485 cases (14.1%) before implementation to 162 (10.5%) afterward (P less than .001); there was no change in the control hospitals. After implementation, serious morbidity or mortality was significantly less likely in ERP hospitals (adjusted odds ratio, 0.76; 95% confidence interval, 0.60-0.96).
Meanwhile, there was no difference in readmission rates before and after implementation.
“The ERIN pilot study included hospitals of various sizes, indicating that both small and large hospitals can successfully decrease LOS with implementation of an ERP. ... Regardless of resource limitations, small hospitals may have the advantage of decreased bureaucracy and improved communication and collaboration across disciplines. ... We strongly believe that surgeon engagement and leadership in such initiatives are critical to sustained success,” the investigators wrote.
The ACS; Johns Hopkins’ Armstrong Institute for Patient Safety and Quality, Baltimore; and the Agency for Healthcare Research and Quality have recently launched the “Improving Surgical Care and Recovery” program to provide more than 750 hospitals with tools, experts, and other resources for implementing ERPs. “The program is one opportunity for hospitals seeking implementation guidance,” the investigators noted.
Dr. Berian reported receiving salary support from the John A. Hartford Foundation. Her coinvestigators reported receiving grant or salary support from the foundation and the Agency for Healthcare Research and Quality. One investigator reported relationships with a variety of drug and device companies.
SOURCE: Berian J et. al. JAMA Surg. 2017 Dec 20. doi: 10.1001/jamasurg.2017.4906
FROM JAMA SURGERY
Key clinical point: With the help of the Enhanced Recovery in National Surgical Quality Improvement Program, 15 hospitals enacted enhanced recovery protocols for elective colectomy that shortened length of stay and decreased complications, without increasing readmissions.
Major finding: After taking patient characteristics and other matters into account, the adjusted decrease in LOS was 1.1 days, versus 0.4 days in control hospitals (P less than .001).
Study details: The study compared 3,437 colectomies at 15 hospitals before ERP implementation to 1,538 after.
Disclosures: Dr. Berian reported receiving salary support from the John A. Hartford Foundation. Her coinvestigators reported receiving grant or salary support from the foundation and the Agency for Healthcare Research and Quality. One investigator reported relationships with a variety of drug and device companies.
Source: Berian J et. al. JAMA Surg. 2017 Dec 20. doi: 10.1001/jamasurg.2017.4906
Hospitalization risk twice as likely for veterans with mental illness
SAN DIEGO – compared with their peers who had no psychiatric or addiction diagnosis, according to results of a large VA database study.
“Our patients sit at the center of two public health crises,” David T. Moore, MD, PhD, said at the annual meeting and scientific symposium of the American Academy of Addiction Psychiatry. “One is the incredibly reduced life expectancy for adults with mental illnesses. There may be a 20-year reduced life expectancy. Their mortality rate for chronic medical conditions such as heart disease and COPD is increased by two- to fourfold, and is associated with greater hospitalization rates, longer lengths of stay, and increased readmission rates. The second part of this crisis is the incredible cost associated with medical hospitalizations. About 1 in every $20 in the entire U.S. economy goes toward inpatient medical hospitalization.”
The final analysis included 952,252 veterans with a mental illness and 1,064,140 without a psychiatric or addiction diagnosis. Dr. Moore reported that among veterans with mental illness, 100,191 (7.1%) were hospitalized on a medical unit at some point during the study period, compared with only 31,759 (2.9%) of veterans with no psychiatric or addiction diagnosis. The Charlson Comorbidity Index was significantly increased in veterans with mental health diagnoses, compared with those who did not have mental health diagnoses.
“There was more tobacco use; they were much more likely to receive an opioid prescription; [and] they used more outpatient medical services, whether it be primary care visits or specialty care visits,” Dr. Moore said of the hospitalized veterans. “They are sicker, but they also use more outpatient medical services, suggesting that they do not lack access to adequate outpatient medical care.”
Next, the researchers performed a subset analysis of all veterans with any mental health diagnosis. Compared with those who were not hospitalized during the study period, those hospitalized were older (a mean age of 52 vs. 45 years, respectively), more likely to be homeless (21% vs. 12%; relative risk, 1.8), and receive a VA pension, which is correlated with poor functioning and disability (7.1% vs. 2.9%; RR, 2.4). The only psychiatric disorder correlated with correlated with medical hospitalization was personality disorder (6.3% vs. 3.7%; RR, 1.7). The researchers also observed that a higher proportion of hospitalized patients had an alcohol use disorder (34% vs. 23%; RR, 1.7) and drug use (31% vs. 17%; RR, 1.8). “The use of benzodiazepines had the greatest relative risk for medical hospitalizations,” Dr. Moore said.
In unadjusted analyses, veterans with the following diagnoses were at increased risk for hospitalization: drug use disorder (odds ratio, 4.58), alcohol use disorder (OR, 3.84), bipolar disorder (OR, 3.29), major depressive disorder (OR, 3.04), schizophrenia (OR, 2.98), and posttraumatic stress disorder (OR, 1.91).
After adjusting for other health factors in multiple regression, alcohol use disorder was the only psychiatric or addiction disorder strongly associated with medical hospitalizations (OR, 1.95). After accounting for sociodemographic characteristics, medical comorbidities, use of outpatient medical services, and alcohol use, the OR for medical hospitalizations among veterans with mental illness decreased from 2.52 to 1.24.
“It looks like a lot of the folks with drug use disorders who are being hospitalized may also have co-occurring alcohol use disorders,” Dr. Moore said. “That may partly account for their hospitalization risk.”
He concluded that the study’s overall findings “leave us with a lot of questions about what to do. The majority of patients who are hospitalized have a mental illness. Is this a setting where we should be engaging them and trying to connect them with outpatient services?”
Dr. Moore reported having no financial disclosures.
SOURCE: Moore et al. AAAP 2017. Paper session A1.
SAN DIEGO – compared with their peers who had no psychiatric or addiction diagnosis, according to results of a large VA database study.
“Our patients sit at the center of two public health crises,” David T. Moore, MD, PhD, said at the annual meeting and scientific symposium of the American Academy of Addiction Psychiatry. “One is the incredibly reduced life expectancy for adults with mental illnesses. There may be a 20-year reduced life expectancy. Their mortality rate for chronic medical conditions such as heart disease and COPD is increased by two- to fourfold, and is associated with greater hospitalization rates, longer lengths of stay, and increased readmission rates. The second part of this crisis is the incredible cost associated with medical hospitalizations. About 1 in every $20 in the entire U.S. economy goes toward inpatient medical hospitalization.”
The final analysis included 952,252 veterans with a mental illness and 1,064,140 without a psychiatric or addiction diagnosis. Dr. Moore reported that among veterans with mental illness, 100,191 (7.1%) were hospitalized on a medical unit at some point during the study period, compared with only 31,759 (2.9%) of veterans with no psychiatric or addiction diagnosis. The Charlson Comorbidity Index was significantly increased in veterans with mental health diagnoses, compared with those who did not have mental health diagnoses.
“There was more tobacco use; they were much more likely to receive an opioid prescription; [and] they used more outpatient medical services, whether it be primary care visits or specialty care visits,” Dr. Moore said of the hospitalized veterans. “They are sicker, but they also use more outpatient medical services, suggesting that they do not lack access to adequate outpatient medical care.”
Next, the researchers performed a subset analysis of all veterans with any mental health diagnosis. Compared with those who were not hospitalized during the study period, those hospitalized were older (a mean age of 52 vs. 45 years, respectively), more likely to be homeless (21% vs. 12%; relative risk, 1.8), and receive a VA pension, which is correlated with poor functioning and disability (7.1% vs. 2.9%; RR, 2.4). The only psychiatric disorder correlated with correlated with medical hospitalization was personality disorder (6.3% vs. 3.7%; RR, 1.7). The researchers also observed that a higher proportion of hospitalized patients had an alcohol use disorder (34% vs. 23%; RR, 1.7) and drug use (31% vs. 17%; RR, 1.8). “The use of benzodiazepines had the greatest relative risk for medical hospitalizations,” Dr. Moore said.
In unadjusted analyses, veterans with the following diagnoses were at increased risk for hospitalization: drug use disorder (odds ratio, 4.58), alcohol use disorder (OR, 3.84), bipolar disorder (OR, 3.29), major depressive disorder (OR, 3.04), schizophrenia (OR, 2.98), and posttraumatic stress disorder (OR, 1.91).
After adjusting for other health factors in multiple regression, alcohol use disorder was the only psychiatric or addiction disorder strongly associated with medical hospitalizations (OR, 1.95). After accounting for sociodemographic characteristics, medical comorbidities, use of outpatient medical services, and alcohol use, the OR for medical hospitalizations among veterans with mental illness decreased from 2.52 to 1.24.
“It looks like a lot of the folks with drug use disorders who are being hospitalized may also have co-occurring alcohol use disorders,” Dr. Moore said. “That may partly account for their hospitalization risk.”
He concluded that the study’s overall findings “leave us with a lot of questions about what to do. The majority of patients who are hospitalized have a mental illness. Is this a setting where we should be engaging them and trying to connect them with outpatient services?”
Dr. Moore reported having no financial disclosures.
SOURCE: Moore et al. AAAP 2017. Paper session A1.
SAN DIEGO – compared with their peers who had no psychiatric or addiction diagnosis, according to results of a large VA database study.
“Our patients sit at the center of two public health crises,” David T. Moore, MD, PhD, said at the annual meeting and scientific symposium of the American Academy of Addiction Psychiatry. “One is the incredibly reduced life expectancy for adults with mental illnesses. There may be a 20-year reduced life expectancy. Their mortality rate for chronic medical conditions such as heart disease and COPD is increased by two- to fourfold, and is associated with greater hospitalization rates, longer lengths of stay, and increased readmission rates. The second part of this crisis is the incredible cost associated with medical hospitalizations. About 1 in every $20 in the entire U.S. economy goes toward inpatient medical hospitalization.”
The final analysis included 952,252 veterans with a mental illness and 1,064,140 without a psychiatric or addiction diagnosis. Dr. Moore reported that among veterans with mental illness, 100,191 (7.1%) were hospitalized on a medical unit at some point during the study period, compared with only 31,759 (2.9%) of veterans with no psychiatric or addiction diagnosis. The Charlson Comorbidity Index was significantly increased in veterans with mental health diagnoses, compared with those who did not have mental health diagnoses.
“There was more tobacco use; they were much more likely to receive an opioid prescription; [and] they used more outpatient medical services, whether it be primary care visits or specialty care visits,” Dr. Moore said of the hospitalized veterans. “They are sicker, but they also use more outpatient medical services, suggesting that they do not lack access to adequate outpatient medical care.”
Next, the researchers performed a subset analysis of all veterans with any mental health diagnosis. Compared with those who were not hospitalized during the study period, those hospitalized were older (a mean age of 52 vs. 45 years, respectively), more likely to be homeless (21% vs. 12%; relative risk, 1.8), and receive a VA pension, which is correlated with poor functioning and disability (7.1% vs. 2.9%; RR, 2.4). The only psychiatric disorder correlated with correlated with medical hospitalization was personality disorder (6.3% vs. 3.7%; RR, 1.7). The researchers also observed that a higher proportion of hospitalized patients had an alcohol use disorder (34% vs. 23%; RR, 1.7) and drug use (31% vs. 17%; RR, 1.8). “The use of benzodiazepines had the greatest relative risk for medical hospitalizations,” Dr. Moore said.
In unadjusted analyses, veterans with the following diagnoses were at increased risk for hospitalization: drug use disorder (odds ratio, 4.58), alcohol use disorder (OR, 3.84), bipolar disorder (OR, 3.29), major depressive disorder (OR, 3.04), schizophrenia (OR, 2.98), and posttraumatic stress disorder (OR, 1.91).
After adjusting for other health factors in multiple regression, alcohol use disorder was the only psychiatric or addiction disorder strongly associated with medical hospitalizations (OR, 1.95). After accounting for sociodemographic characteristics, medical comorbidities, use of outpatient medical services, and alcohol use, the OR for medical hospitalizations among veterans with mental illness decreased from 2.52 to 1.24.
“It looks like a lot of the folks with drug use disorders who are being hospitalized may also have co-occurring alcohol use disorders,” Dr. Moore said. “That may partly account for their hospitalization risk.”
He concluded that the study’s overall findings “leave us with a lot of questions about what to do. The majority of patients who are hospitalized have a mental illness. Is this a setting where we should be engaging them and trying to connect them with outpatient services?”
Dr. Moore reported having no financial disclosures.
SOURCE: Moore et al. AAAP 2017. Paper session A1.
REPORTING FROM AAAP
Key clinical point: In order to improve the health of veterans with mental illness, more efforts are needed to target alcohol use.
Major finding: Among veterans with mental illnesses, 7.1% were hospitalized, compared with 2.9% of their peers with no psychiatric or addiction diagnosis.
Study details: A database analysis of 952,252 veterans with a mental illness and 1,064,140 without a psychiatric or addiction diagnosis.
Disclosures: Dr. Moore reported having no financial disclosures.
Source: Moore et al. AAAP 2017. Paper session A1.
Palliative care underutilized in dementia patients with acute abdomen
Despite high rates of in-hospital mortality and nonroutine discharge, palliative care is underutilized in patients with dementia and acute abdominal emergency, according to findings published in Surgery.
“Currently little is known about palliative care utilization among patients with dementia in possible need of surgical intervention. This raises the question of whether the acute surgical emergency represents an appropriate episode during which to introduce palliative care for patients with dementia,” wrote Ana Berlin, MD, FACS, of the department of surgery at New Jersey Medical School, Newark, N.J., and her coauthors (Surgery. 2017 Dec 4. doi: 10.1016/j.surg.2017.09.048).
Of 15,209 patients aged 50 years and older with dementia and acute abdomen, 7.5% received palliative care. Patients discharged nonroutinely and patients treated operatively were less likely to receive palliative care, the researchers reported.
Dr. Berlin and her colleagues used the National Inpatient Sample database to identify patients with dementia and acute abdomen who were admitted nonelectively between 2009 and 2013. They used ICD-9 primary and secondary codes to limit surgical diagnoses to gastrointestinal obstruction, ischemia, and perforation.
Overall, 50.9% of patients were admitted for gastrointestinal obstruction, 39.8% for perforation, 5.1% for bowel ischemia, and 4.3% for mixed pathology; 17.8% of patients were managed operatively.
Patients with intestinal ischemia had the highest rate of both operation and mortality, at 22.8% and 27.6%, respectively. These patients also had the lowest rate of routine discharge, at 15.9%, the authors said. In comparison, patients with obstruction had surgical intervention and in-hospital mortality rates of 17% and 10.1%, respectively, and a routine discharge rate of 20.9%. Patients with perforation had an operation rate of 13.8%, in-hospital mortality rate of 6.8%, and routine discharge rate of 26.9%.
The palliative care utilization rate overall was 7.5%. Patients with mixed pathology who did not have surgery were most likely to receive palliative care, at 21.1%, noted Dr. Berlin and her coauthors.
Patients who died postoperatively were less likely than were those who died without surgical intervention to have received palliative care (20.9% vs. 31.4%; odds ratio = 0.63, 95% confidence interval, 0.46-0.86; P = .0039), and those who were discharged nonroutinely after an operation were less likely than were patients who were discharged nonroutinely without an operation to receive palliative care (3.7% vs. 7.0%; OR = 0.44, 95% CI, 0.34-0.57; P less than .0001).
Lastly, patients who received palliative care had shorter median hospital stays than did those who did not receive palliative care (5 days vs. 6 days; P less than .0001). These patients also had lower median hospital charges ($29,500 vs. $31,600; P = .0403).
The results identify two subsets of patients with unmet palliative care needs: patients requiring operative intervention, and patients with a diagnosis of intestinal ischemia, the authors said. In addition, the findings suggest that “surgeons should consider initiating palliative care … early in the hospital course for patients with dementia presenting with acute surgical abdomen,” they wrote.
“Both hip fracture and intensive care unit admission in patients with dementia have been described as appropriate triggers for palliative care assessment. ... Acute abdominal emergency [may also represent] an appropriate episode during which to introduce palliative care for patients with dementia,” they concluded.
The study was funded by the Rutgers New Jersey Medical School department of surgery and the New Jersey Medical School Hispanic Center of Excellence, Health Resources, and Services Administration. No other disclosures were reported.
SOURCE: Surgery. 2017 Dec 4. doi: 10.1016/j.surg.2017.09.048.
Few surgeons would argue that a patient with dementia and an acute abdomen would be less appropriate for a palliative care consultation than demented patients with a hip fracture or ICU admission who have been shown to benefit from triggered palliative care consults. However, the dynamic interaction between patient, family, and surgeon, described by Thomas Miner as the “palliative triangle,” will likely prevent universal acceptance of triggered consults (Ann Surg Oncol. 2002;9[7]:696-709). Despite the current trend of increasingly algorithmic care, there is still a need for surgeon autonomy for treatment decisions even when the recommended triggered intervention is highly appropriate. A mentor of mine put it, “I never do things routinely, but there are some things I do all the time.” As the benefits of palliative care become more evident, the referrals for palliative care for this latest indication will become “some things I do all the time” just as pharmacokinetics referrals have become for antibiotics, anticoagulation, and total parenteral nutrition.
Few surgeons would argue that a patient with dementia and an acute abdomen would be less appropriate for a palliative care consultation than demented patients with a hip fracture or ICU admission who have been shown to benefit from triggered palliative care consults. However, the dynamic interaction between patient, family, and surgeon, described by Thomas Miner as the “palliative triangle,” will likely prevent universal acceptance of triggered consults (Ann Surg Oncol. 2002;9[7]:696-709). Despite the current trend of increasingly algorithmic care, there is still a need for surgeon autonomy for treatment decisions even when the recommended triggered intervention is highly appropriate. A mentor of mine put it, “I never do things routinely, but there are some things I do all the time.” As the benefits of palliative care become more evident, the referrals for palliative care for this latest indication will become “some things I do all the time” just as pharmacokinetics referrals have become for antibiotics, anticoagulation, and total parenteral nutrition.
Few surgeons would argue that a patient with dementia and an acute abdomen would be less appropriate for a palliative care consultation than demented patients with a hip fracture or ICU admission who have been shown to benefit from triggered palliative care consults. However, the dynamic interaction between patient, family, and surgeon, described by Thomas Miner as the “palliative triangle,” will likely prevent universal acceptance of triggered consults (Ann Surg Oncol. 2002;9[7]:696-709). Despite the current trend of increasingly algorithmic care, there is still a need for surgeon autonomy for treatment decisions even when the recommended triggered intervention is highly appropriate. A mentor of mine put it, “I never do things routinely, but there are some things I do all the time.” As the benefits of palliative care become more evident, the referrals for palliative care for this latest indication will become “some things I do all the time” just as pharmacokinetics referrals have become for antibiotics, anticoagulation, and total parenteral nutrition.
Despite high rates of in-hospital mortality and nonroutine discharge, palliative care is underutilized in patients with dementia and acute abdominal emergency, according to findings published in Surgery.
“Currently little is known about palliative care utilization among patients with dementia in possible need of surgical intervention. This raises the question of whether the acute surgical emergency represents an appropriate episode during which to introduce palliative care for patients with dementia,” wrote Ana Berlin, MD, FACS, of the department of surgery at New Jersey Medical School, Newark, N.J., and her coauthors (Surgery. 2017 Dec 4. doi: 10.1016/j.surg.2017.09.048).
Of 15,209 patients aged 50 years and older with dementia and acute abdomen, 7.5% received palliative care. Patients discharged nonroutinely and patients treated operatively were less likely to receive palliative care, the researchers reported.
Dr. Berlin and her colleagues used the National Inpatient Sample database to identify patients with dementia and acute abdomen who were admitted nonelectively between 2009 and 2013. They used ICD-9 primary and secondary codes to limit surgical diagnoses to gastrointestinal obstruction, ischemia, and perforation.
Overall, 50.9% of patients were admitted for gastrointestinal obstruction, 39.8% for perforation, 5.1% for bowel ischemia, and 4.3% for mixed pathology; 17.8% of patients were managed operatively.
Patients with intestinal ischemia had the highest rate of both operation and mortality, at 22.8% and 27.6%, respectively. These patients also had the lowest rate of routine discharge, at 15.9%, the authors said. In comparison, patients with obstruction had surgical intervention and in-hospital mortality rates of 17% and 10.1%, respectively, and a routine discharge rate of 20.9%. Patients with perforation had an operation rate of 13.8%, in-hospital mortality rate of 6.8%, and routine discharge rate of 26.9%.
The palliative care utilization rate overall was 7.5%. Patients with mixed pathology who did not have surgery were most likely to receive palliative care, at 21.1%, noted Dr. Berlin and her coauthors.
Patients who died postoperatively were less likely than were those who died without surgical intervention to have received palliative care (20.9% vs. 31.4%; odds ratio = 0.63, 95% confidence interval, 0.46-0.86; P = .0039), and those who were discharged nonroutinely after an operation were less likely than were patients who were discharged nonroutinely without an operation to receive palliative care (3.7% vs. 7.0%; OR = 0.44, 95% CI, 0.34-0.57; P less than .0001).
Lastly, patients who received palliative care had shorter median hospital stays than did those who did not receive palliative care (5 days vs. 6 days; P less than .0001). These patients also had lower median hospital charges ($29,500 vs. $31,600; P = .0403).
The results identify two subsets of patients with unmet palliative care needs: patients requiring operative intervention, and patients with a diagnosis of intestinal ischemia, the authors said. In addition, the findings suggest that “surgeons should consider initiating palliative care … early in the hospital course for patients with dementia presenting with acute surgical abdomen,” they wrote.
“Both hip fracture and intensive care unit admission in patients with dementia have been described as appropriate triggers for palliative care assessment. ... Acute abdominal emergency [may also represent] an appropriate episode during which to introduce palliative care for patients with dementia,” they concluded.
The study was funded by the Rutgers New Jersey Medical School department of surgery and the New Jersey Medical School Hispanic Center of Excellence, Health Resources, and Services Administration. No other disclosures were reported.
SOURCE: Surgery. 2017 Dec 4. doi: 10.1016/j.surg.2017.09.048.
Despite high rates of in-hospital mortality and nonroutine discharge, palliative care is underutilized in patients with dementia and acute abdominal emergency, according to findings published in Surgery.
“Currently little is known about palliative care utilization among patients with dementia in possible need of surgical intervention. This raises the question of whether the acute surgical emergency represents an appropriate episode during which to introduce palliative care for patients with dementia,” wrote Ana Berlin, MD, FACS, of the department of surgery at New Jersey Medical School, Newark, N.J., and her coauthors (Surgery. 2017 Dec 4. doi: 10.1016/j.surg.2017.09.048).
Of 15,209 patients aged 50 years and older with dementia and acute abdomen, 7.5% received palliative care. Patients discharged nonroutinely and patients treated operatively were less likely to receive palliative care, the researchers reported.
Dr. Berlin and her colleagues used the National Inpatient Sample database to identify patients with dementia and acute abdomen who were admitted nonelectively between 2009 and 2013. They used ICD-9 primary and secondary codes to limit surgical diagnoses to gastrointestinal obstruction, ischemia, and perforation.
Overall, 50.9% of patients were admitted for gastrointestinal obstruction, 39.8% for perforation, 5.1% for bowel ischemia, and 4.3% for mixed pathology; 17.8% of patients were managed operatively.
Patients with intestinal ischemia had the highest rate of both operation and mortality, at 22.8% and 27.6%, respectively. These patients also had the lowest rate of routine discharge, at 15.9%, the authors said. In comparison, patients with obstruction had surgical intervention and in-hospital mortality rates of 17% and 10.1%, respectively, and a routine discharge rate of 20.9%. Patients with perforation had an operation rate of 13.8%, in-hospital mortality rate of 6.8%, and routine discharge rate of 26.9%.
The palliative care utilization rate overall was 7.5%. Patients with mixed pathology who did not have surgery were most likely to receive palliative care, at 21.1%, noted Dr. Berlin and her coauthors.
Patients who died postoperatively were less likely than were those who died without surgical intervention to have received palliative care (20.9% vs. 31.4%; odds ratio = 0.63, 95% confidence interval, 0.46-0.86; P = .0039), and those who were discharged nonroutinely after an operation were less likely than were patients who were discharged nonroutinely without an operation to receive palliative care (3.7% vs. 7.0%; OR = 0.44, 95% CI, 0.34-0.57; P less than .0001).
Lastly, patients who received palliative care had shorter median hospital stays than did those who did not receive palliative care (5 days vs. 6 days; P less than .0001). These patients also had lower median hospital charges ($29,500 vs. $31,600; P = .0403).
The results identify two subsets of patients with unmet palliative care needs: patients requiring operative intervention, and patients with a diagnosis of intestinal ischemia, the authors said. In addition, the findings suggest that “surgeons should consider initiating palliative care … early in the hospital course for patients with dementia presenting with acute surgical abdomen,” they wrote.
“Both hip fracture and intensive care unit admission in patients with dementia have been described as appropriate triggers for palliative care assessment. ... Acute abdominal emergency [may also represent] an appropriate episode during which to introduce palliative care for patients with dementia,” they concluded.
The study was funded by the Rutgers New Jersey Medical School department of surgery and the New Jersey Medical School Hispanic Center of Excellence, Health Resources, and Services Administration. No other disclosures were reported.
SOURCE: Surgery. 2017 Dec 4. doi: 10.1016/j.surg.2017.09.048.
FROM SURGERY
Key clinical point: Despite high mortality and frequent nonroutine discharges, palliative care is underutilized in dementia patients with acute abdominal emergency.
Major finding: Among dementia patients with acute abdominal emergency, 7.5% received palliative care.
Data source: A retrospective analysis of 15,209 patients aged 50 years and older from the National Inpatient Sample, for the period of 2009-2013.
Disclosures: The study was funded by the Rutgers New Jersey Medical School Department of Surgery and the New Jersey Medical School Hispanic Center of Excellence, Health Resources, and Services Administration.
SOURCE: Surgery. 2017 Dec 4. doi: http://dx.doi.org/10.1016/j.surg.2017.09.048.