User login
USPSTF recommends screening children, adolescents for obesity
Children and adolescents aged 6 years and older should be screened for obesity and referred to comprehensive, intensive behavioral interventions with at least 26 hours of intervention contact, according to a U.S. Preventive Services Task Force Recommendation Statement that was published online June 20 in JAMA.
This updated recommendation is largely consistent with the previous 2010 recommendation “but includes the word ‘adolescents’ to further clarify the population to which this recommendation applies,” according to a press release accompanying the Recommendation Statement and the Evidence Report on which it is based.
The behavioral interventions that proved most beneficial included at least 26 hours of contact over a period of 2-12 months. Those that included 52 or more hours of contact achieved even greater weight loss, as well as some improvements in cardiovascular and metabolic risk factors (JAMA. 2017 Jun 20. doi: 10.1001/jama.2017.6803).
In general, children and adolescents who received intensive behavioral intervention showed absolute reductions in BMI z scores of 0.20 and maintained their baseline weight within approximately 5 pounds, while control subjects showed small or no reductions in BMI z scores and typically gained a mean of 5-17 pounds.
The components of these comprehensive interventions varied, but the most successful ones included sessions involving both the child and the parent (separately, together, or both); offered both family and group sessions; provided education regarding healthy eating, exercising, and reading food labels; encouraged stimulus-control measures such as limiting access to unhealthy foods and limiting screen time (that is, physical inactivity); and included supervised physical activity. Additional beneficial components are assisting patients to identify and accomplish goals, self-monitor, and problem-solve, as well as teaching them coping skills and addressing their body image.
In contrast to behavioral interventions, pharmacotherapy was not endorsed by the USPSTF. The current evidence was deemed inadequate to determine whether the slight weight loss achieved with pharmacotherapy is clinically significant and whether it outweighs the harms of the medications.
The two agents currently used in this regard are metformin, which is not Food and Drug Administration–approved for this purpose, and orlistat, which is approved for patients aged 12 years and older. Orlistat in particular frequently causes adverse events including fatty or oily stools, abdominal pain or cramping, flatus with stool discharge, and fecal incontinence, Dr. Grossman and his associates said.
The USPSTF is an independent voluntary group supported by the U.S. Agency for Healthcare Research and Quality as mandated by Congress. The authors’ conflicts of interest are available at https://www.uspreventiveservicestaskforce.org/Page/Name/conflict-of-interest-disclosures.
Letter to the Editor
It is not surprising that there are so many overweight and obese children, despite the fact that in order to prevent bad feelings, children have to be much more overweight than adults to be classified as obese or overweight.
If one is waiting until age 6 years to screen for obesity, that horse will be long out of the barn. The problem begins when the rapid weight gain of infants does not slow down in the 2nd and 3rd years of life. This is also when bad food choices and eating habits often begin.
The other problem is that body mass index is a terrible tool and so is any indicator that tries to define obesity using only height and weight. None of these distinguish between the muscular child and the slender child with a large belly. Waist to height or body volume measurements are far better indicators.
Lastly, parents have come to see the mildly overweight child as the norm because so many children are. Until parents see pictures of children from a few decades ago and are educated as to what normal looks like, we will have great difficulty making a dent in this problem.
Richard H. Feuille Jr., MD
This USPSTF recommendation simply confirms what pediatric clinicians always do in the everyday care for children and adolescents: monitor growth, counsel on healthy lifestyles, and refer for specialized care when appropriate.
Intensive behavioral interventions are impractical for many families and frequently aren’t covered by insurance. At best, implementing this recommendation will have only a modest effect on obesity in the United States. At worst, it could divert attention and resources away from population-health approaches to prevention and toward weight management programs that are not well equipped to meet the demand and very often don’t exist within local communities.
Improving neighborhood walkability, increasing the availability of healthy foods, and providing safe physical spaces would be more effective at reducing childhood obesity, as would improving school nutrition and curtailing the marketing of sugar-sweetened drinks and other unhealthy foods to children.
Rachel L. J. Thornton, MD, PhD, Raquel G. Hernandez, MD, MPH; Tina L. Cheng, MD, MPH, are in the department of pediatrics at Johns Hopkins University, Baltimore. They reported having no relevant financial disclosures. They made these remarks in an editorial accompanying the USPSTF report (JAMA. 2017;317:2378-80).
This USPSTF recommendation simply confirms what pediatric clinicians always do in the everyday care for children and adolescents: monitor growth, counsel on healthy lifestyles, and refer for specialized care when appropriate.
Intensive behavioral interventions are impractical for many families and frequently aren’t covered by insurance. At best, implementing this recommendation will have only a modest effect on obesity in the United States. At worst, it could divert attention and resources away from population-health approaches to prevention and toward weight management programs that are not well equipped to meet the demand and very often don’t exist within local communities.
Improving neighborhood walkability, increasing the availability of healthy foods, and providing safe physical spaces would be more effective at reducing childhood obesity, as would improving school nutrition and curtailing the marketing of sugar-sweetened drinks and other unhealthy foods to children.
Rachel L. J. Thornton, MD, PhD, Raquel G. Hernandez, MD, MPH; Tina L. Cheng, MD, MPH, are in the department of pediatrics at Johns Hopkins University, Baltimore. They reported having no relevant financial disclosures. They made these remarks in an editorial accompanying the USPSTF report (JAMA. 2017;317:2378-80).
This USPSTF recommendation simply confirms what pediatric clinicians always do in the everyday care for children and adolescents: monitor growth, counsel on healthy lifestyles, and refer for specialized care when appropriate.
Intensive behavioral interventions are impractical for many families and frequently aren’t covered by insurance. At best, implementing this recommendation will have only a modest effect on obesity in the United States. At worst, it could divert attention and resources away from population-health approaches to prevention and toward weight management programs that are not well equipped to meet the demand and very often don’t exist within local communities.
Improving neighborhood walkability, increasing the availability of healthy foods, and providing safe physical spaces would be more effective at reducing childhood obesity, as would improving school nutrition and curtailing the marketing of sugar-sweetened drinks and other unhealthy foods to children.
Rachel L. J. Thornton, MD, PhD, Raquel G. Hernandez, MD, MPH; Tina L. Cheng, MD, MPH, are in the department of pediatrics at Johns Hopkins University, Baltimore. They reported having no relevant financial disclosures. They made these remarks in an editorial accompanying the USPSTF report (JAMA. 2017;317:2378-80).
Children and adolescents aged 6 years and older should be screened for obesity and referred to comprehensive, intensive behavioral interventions with at least 26 hours of intervention contact, according to a U.S. Preventive Services Task Force Recommendation Statement that was published online June 20 in JAMA.
This updated recommendation is largely consistent with the previous 2010 recommendation “but includes the word ‘adolescents’ to further clarify the population to which this recommendation applies,” according to a press release accompanying the Recommendation Statement and the Evidence Report on which it is based.
The behavioral interventions that proved most beneficial included at least 26 hours of contact over a period of 2-12 months. Those that included 52 or more hours of contact achieved even greater weight loss, as well as some improvements in cardiovascular and metabolic risk factors (JAMA. 2017 Jun 20. doi: 10.1001/jama.2017.6803).
In general, children and adolescents who received intensive behavioral intervention showed absolute reductions in BMI z scores of 0.20 and maintained their baseline weight within approximately 5 pounds, while control subjects showed small or no reductions in BMI z scores and typically gained a mean of 5-17 pounds.
The components of these comprehensive interventions varied, but the most successful ones included sessions involving both the child and the parent (separately, together, or both); offered both family and group sessions; provided education regarding healthy eating, exercising, and reading food labels; encouraged stimulus-control measures such as limiting access to unhealthy foods and limiting screen time (that is, physical inactivity); and included supervised physical activity. Additional beneficial components are assisting patients to identify and accomplish goals, self-monitor, and problem-solve, as well as teaching them coping skills and addressing their body image.
In contrast to behavioral interventions, pharmacotherapy was not endorsed by the USPSTF. The current evidence was deemed inadequate to determine whether the slight weight loss achieved with pharmacotherapy is clinically significant and whether it outweighs the harms of the medications.
The two agents currently used in this regard are metformin, which is not Food and Drug Administration–approved for this purpose, and orlistat, which is approved for patients aged 12 years and older. Orlistat in particular frequently causes adverse events including fatty or oily stools, abdominal pain or cramping, flatus with stool discharge, and fecal incontinence, Dr. Grossman and his associates said.
The USPSTF is an independent voluntary group supported by the U.S. Agency for Healthcare Research and Quality as mandated by Congress. The authors’ conflicts of interest are available at https://www.uspreventiveservicestaskforce.org/Page/Name/conflict-of-interest-disclosures.
Letter to the Editor
It is not surprising that there are so many overweight and obese children, despite the fact that in order to prevent bad feelings, children have to be much more overweight than adults to be classified as obese or overweight.
If one is waiting until age 6 years to screen for obesity, that horse will be long out of the barn. The problem begins when the rapid weight gain of infants does not slow down in the 2nd and 3rd years of life. This is also when bad food choices and eating habits often begin.
The other problem is that body mass index is a terrible tool and so is any indicator that tries to define obesity using only height and weight. None of these distinguish between the muscular child and the slender child with a large belly. Waist to height or body volume measurements are far better indicators.
Lastly, parents have come to see the mildly overweight child as the norm because so many children are. Until parents see pictures of children from a few decades ago and are educated as to what normal looks like, we will have great difficulty making a dent in this problem.
Richard H. Feuille Jr., MD
Children and adolescents aged 6 years and older should be screened for obesity and referred to comprehensive, intensive behavioral interventions with at least 26 hours of intervention contact, according to a U.S. Preventive Services Task Force Recommendation Statement that was published online June 20 in JAMA.
This updated recommendation is largely consistent with the previous 2010 recommendation “but includes the word ‘adolescents’ to further clarify the population to which this recommendation applies,” according to a press release accompanying the Recommendation Statement and the Evidence Report on which it is based.
The behavioral interventions that proved most beneficial included at least 26 hours of contact over a period of 2-12 months. Those that included 52 or more hours of contact achieved even greater weight loss, as well as some improvements in cardiovascular and metabolic risk factors (JAMA. 2017 Jun 20. doi: 10.1001/jama.2017.6803).
In general, children and adolescents who received intensive behavioral intervention showed absolute reductions in BMI z scores of 0.20 and maintained their baseline weight within approximately 5 pounds, while control subjects showed small or no reductions in BMI z scores and typically gained a mean of 5-17 pounds.
The components of these comprehensive interventions varied, but the most successful ones included sessions involving both the child and the parent (separately, together, or both); offered both family and group sessions; provided education regarding healthy eating, exercising, and reading food labels; encouraged stimulus-control measures such as limiting access to unhealthy foods and limiting screen time (that is, physical inactivity); and included supervised physical activity. Additional beneficial components are assisting patients to identify and accomplish goals, self-monitor, and problem-solve, as well as teaching them coping skills and addressing their body image.
In contrast to behavioral interventions, pharmacotherapy was not endorsed by the USPSTF. The current evidence was deemed inadequate to determine whether the slight weight loss achieved with pharmacotherapy is clinically significant and whether it outweighs the harms of the medications.
The two agents currently used in this regard are metformin, which is not Food and Drug Administration–approved for this purpose, and orlistat, which is approved for patients aged 12 years and older. Orlistat in particular frequently causes adverse events including fatty or oily stools, abdominal pain or cramping, flatus with stool discharge, and fecal incontinence, Dr. Grossman and his associates said.
The USPSTF is an independent voluntary group supported by the U.S. Agency for Healthcare Research and Quality as mandated by Congress. The authors’ conflicts of interest are available at https://www.uspreventiveservicestaskforce.org/Page/Name/conflict-of-interest-disclosures.
Letter to the Editor
It is not surprising that there are so many overweight and obese children, despite the fact that in order to prevent bad feelings, children have to be much more overweight than adults to be classified as obese or overweight.
If one is waiting until age 6 years to screen for obesity, that horse will be long out of the barn. The problem begins when the rapid weight gain of infants does not slow down in the 2nd and 3rd years of life. This is also when bad food choices and eating habits often begin.
The other problem is that body mass index is a terrible tool and so is any indicator that tries to define obesity using only height and weight. None of these distinguish between the muscular child and the slender child with a large belly. Waist to height or body volume measurements are far better indicators.
Lastly, parents have come to see the mildly overweight child as the norm because so many children are. Until parents see pictures of children from a few decades ago and are educated as to what normal looks like, we will have great difficulty making a dent in this problem.
Richard H. Feuille Jr., MD
FROM JAMA
Key clinical point: with at least 26 hours of contact.
Major finding: Children and adolescents who received intensive behavioral intervention showed absolute reductions in BMI z scores of 0.20 and maintained their baseline weight within approximately 5 pounds, while control subjects showed small or no reductions in BMI z scores and typically gained a mean of 5-17 pounds.
Data source: A review of the literature since the previous USPSTF recommendation statement in 2010, including 45 studies of lifestyle-based interventions involving 7,099 overweight and obese children.
Disclosures: The USPSTF is an independent voluntary group supported by the U.S. Agency for Healthcare Research and Quality as mandated by Congress. The authors’ conflicts of interest are available at www.uspreventiveservicestaskforce.org.
MMR vaccine cut hospitalizations for unrelated respiratory infections
, said Giuseppe La Torre of the Sapienza University of Rome and his associates.
The 2-year retrospective database study included 11,004 children, 21% of whom did not receive the MMR vaccine; 49% received one dose, and 30% received two doses. There were 12 hospitalizations for measles (9 in unvaccinated children, 3 in those who received one dose, and none in those who received two doses), 2 hospitalizations for mumps (1 among vaccinated and 1 among unvaccinated children), and no hospitalizations for rubella (P less than .001).
There were 414 hospitalizations for all infectious diseases, 11% in unvaccinated children, 1.5% in those who had received one dose of vaccine, and 1% in those who had received two doses (P less than .001). MMR vaccine also was highly protective against hospitalizations for all infectious diseases (HR, 0.29).
Of 809 hospitalizations for respiratory diseases, 18% involved children who had not been vaccinated, 4% involved children who had received one dose, and 5.5% involved children vaccinated with two doses (P less than .001). MMR likewise was highly protective against hospitalizations for respiratory diseases (HR, 0.18).
Read more in the journal Human Vaccines & Immunotherapeutics (2017 Jun 12. doi: 10.1080/21645515.2017.1330733).
, said Giuseppe La Torre of the Sapienza University of Rome and his associates.
The 2-year retrospective database study included 11,004 children, 21% of whom did not receive the MMR vaccine; 49% received one dose, and 30% received two doses. There were 12 hospitalizations for measles (9 in unvaccinated children, 3 in those who received one dose, and none in those who received two doses), 2 hospitalizations for mumps (1 among vaccinated and 1 among unvaccinated children), and no hospitalizations for rubella (P less than .001).
There were 414 hospitalizations for all infectious diseases, 11% in unvaccinated children, 1.5% in those who had received one dose of vaccine, and 1% in those who had received two doses (P less than .001). MMR vaccine also was highly protective against hospitalizations for all infectious diseases (HR, 0.29).
Of 809 hospitalizations for respiratory diseases, 18% involved children who had not been vaccinated, 4% involved children who had received one dose, and 5.5% involved children vaccinated with two doses (P less than .001). MMR likewise was highly protective against hospitalizations for respiratory diseases (HR, 0.18).
Read more in the journal Human Vaccines & Immunotherapeutics (2017 Jun 12. doi: 10.1080/21645515.2017.1330733).
, said Giuseppe La Torre of the Sapienza University of Rome and his associates.
The 2-year retrospective database study included 11,004 children, 21% of whom did not receive the MMR vaccine; 49% received one dose, and 30% received two doses. There were 12 hospitalizations for measles (9 in unvaccinated children, 3 in those who received one dose, and none in those who received two doses), 2 hospitalizations for mumps (1 among vaccinated and 1 among unvaccinated children), and no hospitalizations for rubella (P less than .001).
There were 414 hospitalizations for all infectious diseases, 11% in unvaccinated children, 1.5% in those who had received one dose of vaccine, and 1% in those who had received two doses (P less than .001). MMR vaccine also was highly protective against hospitalizations for all infectious diseases (HR, 0.29).
Of 809 hospitalizations for respiratory diseases, 18% involved children who had not been vaccinated, 4% involved children who had received one dose, and 5.5% involved children vaccinated with two doses (P less than .001). MMR likewise was highly protective against hospitalizations for respiratory diseases (HR, 0.18).
Read more in the journal Human Vaccines & Immunotherapeutics (2017 Jun 12. doi: 10.1080/21645515.2017.1330733).
FROM HUMAN VACCINES & IMMUNOTHERAPEUTICS
Massive blood transfusions increase risk with CRS/HIPEC
Massive allogenic blood transfusion during cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (CRS/HIPEC) increased the risk of major complications and reduced overall survival in a review of 936 cases at St. George Hospital near Sydney, Australia.
CRS/HIPEC is a long, complex procedure for peritoneal carcinomatosis, pseudomyxoma peritonei, peritoneal mesothelioma, and other abdominal cancers. The abdomen is opened, the cancer is debulked as much as possible, and the cavity is filled with heated chemotherapy drugs. Because CRS/HIPEC often requires multivisceral resection and dissection in multiple abdominal regions, up to 77% of patients require intraoperative transfusions, and up to 37% require massive allogenic blood transfusions (MABT) with five or more units.
Blood transfusions are known to be associated with poorer cancer surgery outcomes, but their effect in CRS/HIPEC hasn’t been much studied, which is “surprising given the extent to which blood products are used in” the procedure, said investigators led by Akshat Saxena, MD, a surgeon at St. George Hospital (J Gastrointest Surg. 2017 May 30. doi: 10.1007/s11605-017-3444-8).
Based on their findings, the researchers concluded that “there is a real need to evaluate new strategies to reduce the rate of MABT during CRS/HIPEC.”
The procedures in the study were performed from 1996 to 2016. The in-hospital mortality rate was 0.3% in patients who did not have MABT but 4.4% among the 337 patients (36%) who did. Even after adjusting for confounders on multivariate analysis, including the fact that MABT patients had more extensive disease and longer surgeries, MABT significantly increased the risk of in-hospital mortality (relative risk, 7.72; P = .021). In patients requiring MABT had a 5-year survival of 5%. In patients not requiring MABT, 5-year survival was at 36%. The difference remained significant on multivariate analysis.
MABT patients also had twice the risk of life-threatening complications and complications requiring surgical, endoscopic, or radiological intervention (62% versus 30%; RR, 2.05; P less than .001). MABT patients were more likely to stay in the ICU for 4 or more days and in the hospital for 28 or more days.
Worse overall survival with MABT was driven at least in part by patients who had CRS/HIPEC for colorectal cancer peritoneal carcinomatosis and pseudomyxoma peritonei. MABT did not seem to contribute to lower survival in patients who had the procedure for appendiceal or ovarian cancer. “It seems that the impact of long-term immunomodulation induced by blood transfusion” – the suspected mechanism through which transfusions cause problems – “varies according to the disease subtype. This warrants further investigation,” the investigators said.
Several strategies have been tried to reduce the need for transfusions during CRS/HIPEC. The study team previously reported that preemptive clotting factor replacement helps. Others have had success with preemptive tranexamic acid and cryoprecipitate to address low serum fibrinogen levels during CRS/HIPEC. “Further evaluation of both these strategies is warranted,” the researchers said.
Funding source and disclosure information were not included in the study report.
Massive allogenic blood transfusion during cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (CRS/HIPEC) increased the risk of major complications and reduced overall survival in a review of 936 cases at St. George Hospital near Sydney, Australia.
CRS/HIPEC is a long, complex procedure for peritoneal carcinomatosis, pseudomyxoma peritonei, peritoneal mesothelioma, and other abdominal cancers. The abdomen is opened, the cancer is debulked as much as possible, and the cavity is filled with heated chemotherapy drugs. Because CRS/HIPEC often requires multivisceral resection and dissection in multiple abdominal regions, up to 77% of patients require intraoperative transfusions, and up to 37% require massive allogenic blood transfusions (MABT) with five or more units.
Blood transfusions are known to be associated with poorer cancer surgery outcomes, but their effect in CRS/HIPEC hasn’t been much studied, which is “surprising given the extent to which blood products are used in” the procedure, said investigators led by Akshat Saxena, MD, a surgeon at St. George Hospital (J Gastrointest Surg. 2017 May 30. doi: 10.1007/s11605-017-3444-8).
Based on their findings, the researchers concluded that “there is a real need to evaluate new strategies to reduce the rate of MABT during CRS/HIPEC.”
The procedures in the study were performed from 1996 to 2016. The in-hospital mortality rate was 0.3% in patients who did not have MABT but 4.4% among the 337 patients (36%) who did. Even after adjusting for confounders on multivariate analysis, including the fact that MABT patients had more extensive disease and longer surgeries, MABT significantly increased the risk of in-hospital mortality (relative risk, 7.72; P = .021). In patients requiring MABT had a 5-year survival of 5%. In patients not requiring MABT, 5-year survival was at 36%. The difference remained significant on multivariate analysis.
MABT patients also had twice the risk of life-threatening complications and complications requiring surgical, endoscopic, or radiological intervention (62% versus 30%; RR, 2.05; P less than .001). MABT patients were more likely to stay in the ICU for 4 or more days and in the hospital for 28 or more days.
Worse overall survival with MABT was driven at least in part by patients who had CRS/HIPEC for colorectal cancer peritoneal carcinomatosis and pseudomyxoma peritonei. MABT did not seem to contribute to lower survival in patients who had the procedure for appendiceal or ovarian cancer. “It seems that the impact of long-term immunomodulation induced by blood transfusion” – the suspected mechanism through which transfusions cause problems – “varies according to the disease subtype. This warrants further investigation,” the investigators said.
Several strategies have been tried to reduce the need for transfusions during CRS/HIPEC. The study team previously reported that preemptive clotting factor replacement helps. Others have had success with preemptive tranexamic acid and cryoprecipitate to address low serum fibrinogen levels during CRS/HIPEC. “Further evaluation of both these strategies is warranted,” the researchers said.
Funding source and disclosure information were not included in the study report.
Massive allogenic blood transfusion during cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (CRS/HIPEC) increased the risk of major complications and reduced overall survival in a review of 936 cases at St. George Hospital near Sydney, Australia.
CRS/HIPEC is a long, complex procedure for peritoneal carcinomatosis, pseudomyxoma peritonei, peritoneal mesothelioma, and other abdominal cancers. The abdomen is opened, the cancer is debulked as much as possible, and the cavity is filled with heated chemotherapy drugs. Because CRS/HIPEC often requires multivisceral resection and dissection in multiple abdominal regions, up to 77% of patients require intraoperative transfusions, and up to 37% require massive allogenic blood transfusions (MABT) with five or more units.
Blood transfusions are known to be associated with poorer cancer surgery outcomes, but their effect in CRS/HIPEC hasn’t been much studied, which is “surprising given the extent to which blood products are used in” the procedure, said investigators led by Akshat Saxena, MD, a surgeon at St. George Hospital (J Gastrointest Surg. 2017 May 30. doi: 10.1007/s11605-017-3444-8).
Based on their findings, the researchers concluded that “there is a real need to evaluate new strategies to reduce the rate of MABT during CRS/HIPEC.”
The procedures in the study were performed from 1996 to 2016. The in-hospital mortality rate was 0.3% in patients who did not have MABT but 4.4% among the 337 patients (36%) who did. Even after adjusting for confounders on multivariate analysis, including the fact that MABT patients had more extensive disease and longer surgeries, MABT significantly increased the risk of in-hospital mortality (relative risk, 7.72; P = .021). In patients requiring MABT had a 5-year survival of 5%. In patients not requiring MABT, 5-year survival was at 36%. The difference remained significant on multivariate analysis.
MABT patients also had twice the risk of life-threatening complications and complications requiring surgical, endoscopic, or radiological intervention (62% versus 30%; RR, 2.05; P less than .001). MABT patients were more likely to stay in the ICU for 4 or more days and in the hospital for 28 or more days.
Worse overall survival with MABT was driven at least in part by patients who had CRS/HIPEC for colorectal cancer peritoneal carcinomatosis and pseudomyxoma peritonei. MABT did not seem to contribute to lower survival in patients who had the procedure for appendiceal or ovarian cancer. “It seems that the impact of long-term immunomodulation induced by blood transfusion” – the suspected mechanism through which transfusions cause problems – “varies according to the disease subtype. This warrants further investigation,” the investigators said.
Several strategies have been tried to reduce the need for transfusions during CRS/HIPEC. The study team previously reported that preemptive clotting factor replacement helps. Others have had success with preemptive tranexamic acid and cryoprecipitate to address low serum fibrinogen levels during CRS/HIPEC. “Further evaluation of both these strategies is warranted,” the researchers said.
Funding source and disclosure information were not included in the study report.
FROM THE JOURNAL OF GASTROINTESTINAL SURGERY
Key clinical point:
Major finding: Even after adjusting for confounders, MABT significantly increased the risk of in-hospital mortality (RR, 7.72; P = .021).
Data source: A single institution review of 936 cases.
Disclosures: Funding source and disclosure information were not included in the study report.
Sneak Peek: Journal of Hospital Medicine – July 2017
BACKGROUND: Medicare patients account for approximately 50% of hospital days. Hospitalization in older adults often results in poor outcomes.
OBJECTIVE: To test the feasibility and impact of using Assessing Care of Vulnerable Elders (ACOVE) quality indicators (QIs) as a therapeutic intervention to improve care of hospitalized older adults.
SETTING: Large tertiary hospital in the greater New York Metropolitan area.
PATIENTS: Hospitalized patients, 75 and over, admitted to medical units.
INTERVENTION: A checklist, comprised of four ACOVE QIs, administered during daily interdisciplinary rounds: venous thrombosis prophylaxis (VTE) (QI 1), indwelling bladder catheters (QI 2), mobilization (QI 3), and delirium evaluation (QI 4).
MEASUREMENTS: Variables were extracted from electronic medical records with QI compliance as the primary outcome, and length of stay (LOS), discharge disposition, and readmissions as secondary outcomes. Generalized linear mixed models for binary clustered data were used to estimate compliance rates for each group (intervention group or control group) in the postintervention period, along with their corresponding 95% confidence intervals.
RESULTS: Of the 2,396 patients, 530 were on an intervention unit. In those patients not already compliant with VTE, the compliance rate was 57% in intervention vs. 39% in control (P less than .0056). For indwelling catheters, mobilization, and delirium evaluation, overall compliance was significantly higher in the intervention group 72.2% vs. 54.4% (P = .1061), 62.9% vs. 48.2% (P less than .0001), and 27.9% vs. 21.7% (P = .0027), respectively.
CONCLUSIONS: The study demonstrates the feasibility and effectiveness of integrating ACOVE QIs to improve the quality of care in hospitalized older adults.
Also in JHM
Use of simulation to assess incoming interns’ recognition of opportunities to choose wisely
AUTHORS: Kathleen M. Wiest, Jeanne M. Farnan, MD, MHPE, Ellen Byrne, Lukas Matern, Melissa Cappaert, MA, Kristen Hirsch, Vineet M. Arora, MD, MAPP
Clinician attitudes regarding ICD deactivation in DNR/DNI patients
AUTHORS: Andrew J. Bradley, MD, Adam D. Marks, MD, MPH
Using standardized patients to assess hospitalist communication skills
AUTHORS: Dennis T. Chang, MD, Micah Mann, MD, Terry Sommer, BFA, Robert Fallar, PhD, Alan Weinberg, MS, Erica Friedman, MD
Techniques and behaviors associated with exemplary inpatient general medicine teaching: An exploratory qualitative study
AUTHORS: Nathan Houchens, MD, Molly Harrod, PhD, Stephanie Moody, PhD, Karen E. Fowler, MPH, Sanjay Saint, MD, MPH
A simple algorithm for predicting bacteremia using food consumption and shaking chills: A prospective observational study
AUTHORS: Takayuki Komatsu, MD, PhD, Erika Takahashi, MD, Kentaro Mishima, MD, Takeo Toyoda, MD, Fumihiro Saitoh, MD, Akari Yasuda, RN, Joe Matsuoka, PhD, Manabu Sugita, MD, PhD, Joel Branch, MD, Makoto Aoki, MD, Lawrence M. Tierney Jr., MD, Kenji Inoue, MD, PhD
For more articles and subscription information, visit www.journalofhospitalmedicine.com.
BACKGROUND: Medicare patients account for approximately 50% of hospital days. Hospitalization in older adults often results in poor outcomes.
OBJECTIVE: To test the feasibility and impact of using Assessing Care of Vulnerable Elders (ACOVE) quality indicators (QIs) as a therapeutic intervention to improve care of hospitalized older adults.
SETTING: Large tertiary hospital in the greater New York Metropolitan area.
PATIENTS: Hospitalized patients, 75 and over, admitted to medical units.
INTERVENTION: A checklist, comprised of four ACOVE QIs, administered during daily interdisciplinary rounds: venous thrombosis prophylaxis (VTE) (QI 1), indwelling bladder catheters (QI 2), mobilization (QI 3), and delirium evaluation (QI 4).
MEASUREMENTS: Variables were extracted from electronic medical records with QI compliance as the primary outcome, and length of stay (LOS), discharge disposition, and readmissions as secondary outcomes. Generalized linear mixed models for binary clustered data were used to estimate compliance rates for each group (intervention group or control group) in the postintervention period, along with their corresponding 95% confidence intervals.
RESULTS: Of the 2,396 patients, 530 were on an intervention unit. In those patients not already compliant with VTE, the compliance rate was 57% in intervention vs. 39% in control (P less than .0056). For indwelling catheters, mobilization, and delirium evaluation, overall compliance was significantly higher in the intervention group 72.2% vs. 54.4% (P = .1061), 62.9% vs. 48.2% (P less than .0001), and 27.9% vs. 21.7% (P = .0027), respectively.
CONCLUSIONS: The study demonstrates the feasibility and effectiveness of integrating ACOVE QIs to improve the quality of care in hospitalized older adults.
Also in JHM
Use of simulation to assess incoming interns’ recognition of opportunities to choose wisely
AUTHORS: Kathleen M. Wiest, Jeanne M. Farnan, MD, MHPE, Ellen Byrne, Lukas Matern, Melissa Cappaert, MA, Kristen Hirsch, Vineet M. Arora, MD, MAPP
Clinician attitudes regarding ICD deactivation in DNR/DNI patients
AUTHORS: Andrew J. Bradley, MD, Adam D. Marks, MD, MPH
Using standardized patients to assess hospitalist communication skills
AUTHORS: Dennis T. Chang, MD, Micah Mann, MD, Terry Sommer, BFA, Robert Fallar, PhD, Alan Weinberg, MS, Erica Friedman, MD
Techniques and behaviors associated with exemplary inpatient general medicine teaching: An exploratory qualitative study
AUTHORS: Nathan Houchens, MD, Molly Harrod, PhD, Stephanie Moody, PhD, Karen E. Fowler, MPH, Sanjay Saint, MD, MPH
A simple algorithm for predicting bacteremia using food consumption and shaking chills: A prospective observational study
AUTHORS: Takayuki Komatsu, MD, PhD, Erika Takahashi, MD, Kentaro Mishima, MD, Takeo Toyoda, MD, Fumihiro Saitoh, MD, Akari Yasuda, RN, Joe Matsuoka, PhD, Manabu Sugita, MD, PhD, Joel Branch, MD, Makoto Aoki, MD, Lawrence M. Tierney Jr., MD, Kenji Inoue, MD, PhD
For more articles and subscription information, visit www.journalofhospitalmedicine.com.
BACKGROUND: Medicare patients account for approximately 50% of hospital days. Hospitalization in older adults often results in poor outcomes.
OBJECTIVE: To test the feasibility and impact of using Assessing Care of Vulnerable Elders (ACOVE) quality indicators (QIs) as a therapeutic intervention to improve care of hospitalized older adults.
SETTING: Large tertiary hospital in the greater New York Metropolitan area.
PATIENTS: Hospitalized patients, 75 and over, admitted to medical units.
INTERVENTION: A checklist, comprised of four ACOVE QIs, administered during daily interdisciplinary rounds: venous thrombosis prophylaxis (VTE) (QI 1), indwelling bladder catheters (QI 2), mobilization (QI 3), and delirium evaluation (QI 4).
MEASUREMENTS: Variables were extracted from electronic medical records with QI compliance as the primary outcome, and length of stay (LOS), discharge disposition, and readmissions as secondary outcomes. Generalized linear mixed models for binary clustered data were used to estimate compliance rates for each group (intervention group or control group) in the postintervention period, along with their corresponding 95% confidence intervals.
RESULTS: Of the 2,396 patients, 530 were on an intervention unit. In those patients not already compliant with VTE, the compliance rate was 57% in intervention vs. 39% in control (P less than .0056). For indwelling catheters, mobilization, and delirium evaluation, overall compliance was significantly higher in the intervention group 72.2% vs. 54.4% (P = .1061), 62.9% vs. 48.2% (P less than .0001), and 27.9% vs. 21.7% (P = .0027), respectively.
CONCLUSIONS: The study demonstrates the feasibility and effectiveness of integrating ACOVE QIs to improve the quality of care in hospitalized older adults.
Also in JHM
Use of simulation to assess incoming interns’ recognition of opportunities to choose wisely
AUTHORS: Kathleen M. Wiest, Jeanne M. Farnan, MD, MHPE, Ellen Byrne, Lukas Matern, Melissa Cappaert, MA, Kristen Hirsch, Vineet M. Arora, MD, MAPP
Clinician attitudes regarding ICD deactivation in DNR/DNI patients
AUTHORS: Andrew J. Bradley, MD, Adam D. Marks, MD, MPH
Using standardized patients to assess hospitalist communication skills
AUTHORS: Dennis T. Chang, MD, Micah Mann, MD, Terry Sommer, BFA, Robert Fallar, PhD, Alan Weinberg, MS, Erica Friedman, MD
Techniques and behaviors associated with exemplary inpatient general medicine teaching: An exploratory qualitative study
AUTHORS: Nathan Houchens, MD, Molly Harrod, PhD, Stephanie Moody, PhD, Karen E. Fowler, MPH, Sanjay Saint, MD, MPH
A simple algorithm for predicting bacteremia using food consumption and shaking chills: A prospective observational study
AUTHORS: Takayuki Komatsu, MD, PhD, Erika Takahashi, MD, Kentaro Mishima, MD, Takeo Toyoda, MD, Fumihiro Saitoh, MD, Akari Yasuda, RN, Joe Matsuoka, PhD, Manabu Sugita, MD, PhD, Joel Branch, MD, Makoto Aoki, MD, Lawrence M. Tierney Jr., MD, Kenji Inoue, MD, PhD
For more articles and subscription information, visit www.journalofhospitalmedicine.com.
Multimodality Approach to a Stener Lesion: Radiographic, Ultrasound, Magnetic Resonance Imaging, and Surgical Correlation
Take-Home Points
- Torn, displaced, and entrapped UCL is a Stener lesion.
- Hyperabduction injury with pain and joint laxity on examination.
- MRI and ultrasound are useful in evaluating UCL tears.
- Ultrasound offers dynamic evaluation.
- Must be treated appropriately to avoid pain, instability, and osteoarthritis.
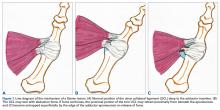
In the literature, hyperabduction injuries to the thumb metacarpophalangeal (MCP) joint have been referred to interchangeably as gamekeeper’s thumb and skier’s thumb. Historically, though, gamekeeper’s thumb was initially described in hunters with chronic injury to the ulnar collateral ligament (UCL),1 and skier’s thumb typically has been described as an acute hyperabduction injury of the UCL.2-5 The proximal portion of a torn UCL may retract with further abduction and displace dorsally, becoming entrapped by the adductor pollicis aponeurosis insertion, known as a Stener lesion.6
The first MCP joint is stabilized by static and dynamic structures that contribute in varying degrees in flexion and extension of the joint. The static stabilizers include the proper and accessory radial and UCLs, the palmar plate, and the dorsal capsule. The UCL originates at the dorsal ulnar aspect of the first metacarpal head at the metacarpal tubercle about 5 mm proximal to the articular surface. The UCL courses distally in the palmar direction to insert volar and proximal to the medial tubercle of the proximal phalanx about 3 mm distal to the articular surface.7 In flexion, the proper collateral ligament is taut and is the primary static stabilizer. In extension, the accessory collateral ligament, which inserts on the palmar plate, is taut and is the primary static stabilizer.8-11
The dynamic stabilizers include the extrinsic muscles (flexor pollicis longus, extensor pollicis longus and brevis) and the intrinsic muscles (abductor pollicis brevis, adductor pollicis, flexor pollicis brevis) inserting on the thumb at the distal phalanx and proximal phalanx and at the base of the first metacarpal.8-10
We report the case of an acute hyperabduction injury of the thumb MCP joint with radiographic, ultrasound, and magnetic resonance imaging (MRI) findings consistent with a Stener lesion and subsequently confirmed with intraoperative photographs. The patient provided written informed consent for print and electronic publication of this case report.
Clinical Findings
A 33-year-old healthy man had persistent left hand pain and grip weakness after performing a handstand. He presented to the orthopedic hand clinic 20 days after injury, having failed nonoperative management (use of nonsteroidal anti-inflammatory drugs and soft thumb spica splint). Physical examination revealed soft-tissue swelling and focal tenderness to palpation at the ulnar aspect of the thumb MCP joint. Despite bilateral first MCP joint laxity on varus and valgus stress without identification of a firm endpoint, pain was elicited only on valgus stress of the left first MCP joint. Given the laxity and the left thumb soft-tissue swelling with pain, plain radiographs, ultrasound, and MRI were used to evaluate for severity of presumed left thumb UCL injury.
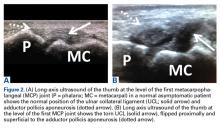
Imaging Findings
Plain radiographs showed normal bony anatomy without fracture, normal joint space, and mild soft-tissue swelling at the left thumb MCP level (Figures 3A, 3B).
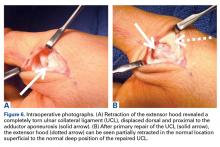
Surgical Findings
Given laxity with pain at the UCL on stress testing, MRI and ultrasound findings, and continued pain and instability of the thumb with pinching and grasping during activities of daily living, the patient and orthopedic hand surgeon proceeded with surgical intervention. Preoperative examination under anesthesia confirmed significant laxity on valgus stress without a palpable endpoint (Figures 5A, 5B).
Discussion
Hyperabduction injuries to the thumb may rupture the UCL of the MCP joint of the thumb or cause a bony avulsion of the base of the proximal phalanx. Injury to the UCL, most often at its distal portion,4,14,15 may result in a sprain or full-thickness tear of the ligament.
It is vital for the radiologist to identify a Stener lesion because a nondisplaced tear of the UCL is often treated nonsurgically, but UCL tears displaced more than 3 mm and Stener lesions usually must be operated on to avoid chronic instability, pain, and osteoarthritis.2-5,8,12-23 Sensitivity and specificity of MRI in evaluating UCL injuries are reported to be almost 100%, with resolution of 1 mm using current surface coils.23 There are various UCL injury patterns, including partial tears, displaced and nondisplaced complete tears, and even complex injuries, such as an incomplete tear with the torn portion retracted as a Stener lesion.22 MRI is needed to establish the extent of injury, as 90% of complete tears that are displaced at least 3 mm, and all tears with retraction proximal and superficial to the aponeurosis (true Stener lesions), failed immobilization and required surgical treatment.23Although they vary in the literature, mean sensitivity and specificity of ultrasound in detecting UCL tears in level I studies have been reported as 76% and 81%, respectively.24 When Melville and colleagues21 applied their ultrasound criteria—including absence of normal UCL fibers traversing the first MCP joint as well as heterogeneous masslike tissue at least partially proximal to the apex of the metacarpal lateral tubercle—they were able to distinguish displaced full-thickness tears from nondisplaced full-thickness tears with 100% accuracy. Hergan and colleagues25 found that the diagnostic accuracy of MRI was superior to that of ultrasound; while MRI accuracy was perfect, 12% of patients were incorrectly diagnosed with ultrasound, with false-positive or false-negative tendon-edge displacement. In our experience, ultrasound is uniquely useful in its ability to characterize the real-time dynamic interaction of the UCL with the adductor aponeurosis. It has been observed that passive flexion of the first interphalangeal joint moves the adductor aponeurosis in isolation, allowing differentiation from the subjacent UCL.21 Had a partial tear been in the differential diagnosis of our patient’s Stener lesion, such a maneuver under ultrasound visualization would have solved the dilemma. In addition, ultrasound allows for comparison with the contralateral ligament at the time of examination should a diagnostic dilemma arise.
As many have reported both bony avulsion of the base of the proximal phalanx and concomitant injury to the UCL, identification of a bony avulsion does not exclude a ligamentous injury and the possibility of a Stener lesion (Figure 7).16,19
Conclusion
A Stener lesion—retraction of a completely torn UCL becoming entrapped dorsally and proximally to the adductor insertion—can cause pain, instability, and ultimately osteoarthritis if not treated appropriately. The orthopedic surgeon should have a high index of suspicion for a Stener lesion in the appropriate clinical scenario and consider all imaging modalities for diagnosis. Likewise, it is of utmost importance for the radiologist to identify imaging findings of a Stener lesion, as physical examination alone may be limited in its ability to characterize injury severity. Both MRI and ultrasound are useful in evaluating UCL tears, and ultrasound provides the additional benefit of dynamic visualization and comparison with the contralateral side.
Am J Orthop. 2017;46(3):E195-E199. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Campbell CS. Gamekeeper’s thumb. J Bone Joint Surg Br. 1955;37(1):148-149.
2. Anderson D. Skier’s thumb. Aust Family Physician. 2010;39(8):575-577.
3. Heim D. The skier’s thumb. Acta Orthop Belg. 1999;65(4):440-446.
4. Lohman M, Vasenius J, Kivisaari A, Kivisaari L. MR imaging in chronic rupture of the ulnar collateral ligament of the thumb. Acta Radiol. 2001;42(1):10-14.
5. Kundu N, Asfaw S, Polster J, Lohman R. The Stener lesion. Eplasty. 2012;12:ic11.
6. Stener B. Displacement of the ruptured ulnar collateral ligament of the metacarpophalangeal joint of the thumb. J Bone Joint Surg Br. 1962;44:869-879.
7. Carlson MG, Warner KK, Meyers KN, Hearns KA, Kok PL. Anatomy of the thumb metacarpophalangeal ulnar and radial collateral ligaments. J Hand Surg Am. 2012;37(10):2021-2026.
8. Heyman P. Injuries to the ulnar collateral ligament of the thumb metacarpophalangeal joint. J Am Acad Orthop Surg. 1997;5(4):224-229.
9. Minami A, An KN, Cooney WP 3rd, Linscheid RL, Chao EY. Ligamentous structures of the metacarpophalangeal joint: a quantitative anatomic study. J Orthop Res. 1984;1(4):361-368.
10. Heyman P, Gelberman RH, Duncan K, Hipp JA. Injuries of the ulnar collateral ligament of the thumb metacarpophalangeal joint. Biomechanical and prospective clinical studies on the usefulness of valgus stress testing. Clin Orthop Relat Res. 1993;(292):165-171.
11. Patel S, Potty A, Taylor EJ, Sorene ED. Collateral ligament injuries of the metacarpophalangeal joint of the thumb: a treatment algorithm. Strategies Trauma Limb Reconstr. 2010;5(1):1-10.
12. O’Callaghan BI, Kohut G, Hoogewoud HM. Gamekeeper thumb: identification of the Stener lesion with US. Radiology. 1994;192(2):477-480.
13. Ebrahim FS, De Maeseneer M, Jager T, Marcelis S, Jamadar DA, Jacobson JA. US diagnosis of UCL tears of the thumb and Stener lesions: technique, pattern-based approach, and differential diagnosis. Radiographics. 2006;26(4):1007-1020.
14. Haramati N, Hiller N, Dowdle J, et al. MRI of the Stener lesion. Skeletal Radiol. 1995;24(7):515-518.
15. Shinohara T, Horii E, Majima M, et al. Sonographic diagnosis of acute injuries of the ulnar collateral ligament of the metacarpophalangeal joint of the thumb. J Clin Ultrasound. 2007;35(2):73-77.
16. Giele H, Martin J. The two-level ulnar collateral ligament injury of the metacarpophalangeal joint of the thumb. J Hand Surg Br. 2003;28(1):92-93.
17. Kaplan SJ. The Stener lesion revisited: a case report. J Hand Surg Am. 1998;23(5):833-836.
18. Thirkannad S, Wolff TW. The “two fleck sign” for an occult Stener lesion. J Hand Surg Eur Vol. 2008;33(2):208-211.
19. Badawi RA, Hussain S, Compson JP. Two in one: a variant of the Stener lesion. Injury. 2002;33(4):379-380.
20. McKeon KE, Gelberman RH, Calfee RP. Ulnar collateral ligament injuries of the thumb: phalangeal translation during valgus stress in human cadavera. J Bone Joint Surg Am. 2013;95(10):881-887.
21. Melville D, Jacobson JA, Haase S, Brandon C, Brigido MK, Fessell D. Ultrasound of displaced ulnar collateral ligament tears of the thumb: the Stener lesion revisited. Skeletal Radiol. 2013;42(5):667-673.
22. Romano WM, Garvin G, Bhayana D, Chaudhary O. The spectrum of ulnar collateral ligament injuries as viewed on magnetic resonance imaging of the metacarpophalangeal joint of the thumb. Can Assoc Radiol J. 2003;54(4):243-248.
23. Milner CS, Manon-Matos Y, Thirkannad SM. Gamekeeper’s thumb—a treatment-oriented magnetic resonance imaging classification. J Hand Surg Am. 2015;40(1):90-95.
24. Papandrea RF, Fowler T. Injury at the thumb UCL: is there a Stener lesion? J Hand Surg Am. 2008;33(10):1882-1884.
25. Hergan K, Mittler C, Oser W. Ulnar collateral ligament: differentiation of displaced and nondisplaced tears with US and MR imaging. Radiology. 1995;194(1):65-71.
Take-Home Points
- Torn, displaced, and entrapped UCL is a Stener lesion.
- Hyperabduction injury with pain and joint laxity on examination.
- MRI and ultrasound are useful in evaluating UCL tears.
- Ultrasound offers dynamic evaluation.
- Must be treated appropriately to avoid pain, instability, and osteoarthritis.
In the literature, hyperabduction injuries to the thumb metacarpophalangeal (MCP) joint have been referred to interchangeably as gamekeeper’s thumb and skier’s thumb. Historically, though, gamekeeper’s thumb was initially described in hunters with chronic injury to the ulnar collateral ligament (UCL),1 and skier’s thumb typically has been described as an acute hyperabduction injury of the UCL.2-5 The proximal portion of a torn UCL may retract with further abduction and displace dorsally, becoming entrapped by the adductor pollicis aponeurosis insertion, known as a Stener lesion.6
The first MCP joint is stabilized by static and dynamic structures that contribute in varying degrees in flexion and extension of the joint. The static stabilizers include the proper and accessory radial and UCLs, the palmar plate, and the dorsal capsule. The UCL originates at the dorsal ulnar aspect of the first metacarpal head at the metacarpal tubercle about 5 mm proximal to the articular surface. The UCL courses distally in the palmar direction to insert volar and proximal to the medial tubercle of the proximal phalanx about 3 mm distal to the articular surface.7 In flexion, the proper collateral ligament is taut and is the primary static stabilizer. In extension, the accessory collateral ligament, which inserts on the palmar plate, is taut and is the primary static stabilizer.8-11
The dynamic stabilizers include the extrinsic muscles (flexor pollicis longus, extensor pollicis longus and brevis) and the intrinsic muscles (abductor pollicis brevis, adductor pollicis, flexor pollicis brevis) inserting on the thumb at the distal phalanx and proximal phalanx and at the base of the first metacarpal.8-10
We report the case of an acute hyperabduction injury of the thumb MCP joint with radiographic, ultrasound, and magnetic resonance imaging (MRI) findings consistent with a Stener lesion and subsequently confirmed with intraoperative photographs. The patient provided written informed consent for print and electronic publication of this case report.
Clinical Findings
A 33-year-old healthy man had persistent left hand pain and grip weakness after performing a handstand. He presented to the orthopedic hand clinic 20 days after injury, having failed nonoperative management (use of nonsteroidal anti-inflammatory drugs and soft thumb spica splint). Physical examination revealed soft-tissue swelling and focal tenderness to palpation at the ulnar aspect of the thumb MCP joint. Despite bilateral first MCP joint laxity on varus and valgus stress without identification of a firm endpoint, pain was elicited only on valgus stress of the left first MCP joint. Given the laxity and the left thumb soft-tissue swelling with pain, plain radiographs, ultrasound, and MRI were used to evaluate for severity of presumed left thumb UCL injury.
Imaging Findings
Plain radiographs showed normal bony anatomy without fracture, normal joint space, and mild soft-tissue swelling at the left thumb MCP level (Figures 3A, 3B).
Surgical Findings
Given laxity with pain at the UCL on stress testing, MRI and ultrasound findings, and continued pain and instability of the thumb with pinching and grasping during activities of daily living, the patient and orthopedic hand surgeon proceeded with surgical intervention. Preoperative examination under anesthesia confirmed significant laxity on valgus stress without a palpable endpoint (Figures 5A, 5B).
Discussion
Hyperabduction injuries to the thumb may rupture the UCL of the MCP joint of the thumb or cause a bony avulsion of the base of the proximal phalanx. Injury to the UCL, most often at its distal portion,4,14,15 may result in a sprain or full-thickness tear of the ligament.
It is vital for the radiologist to identify a Stener lesion because a nondisplaced tear of the UCL is often treated nonsurgically, but UCL tears displaced more than 3 mm and Stener lesions usually must be operated on to avoid chronic instability, pain, and osteoarthritis.2-5,8,12-23 Sensitivity and specificity of MRI in evaluating UCL injuries are reported to be almost 100%, with resolution of 1 mm using current surface coils.23 There are various UCL injury patterns, including partial tears, displaced and nondisplaced complete tears, and even complex injuries, such as an incomplete tear with the torn portion retracted as a Stener lesion.22 MRI is needed to establish the extent of injury, as 90% of complete tears that are displaced at least 3 mm, and all tears with retraction proximal and superficial to the aponeurosis (true Stener lesions), failed immobilization and required surgical treatment.23Although they vary in the literature, mean sensitivity and specificity of ultrasound in detecting UCL tears in level I studies have been reported as 76% and 81%, respectively.24 When Melville and colleagues21 applied their ultrasound criteria—including absence of normal UCL fibers traversing the first MCP joint as well as heterogeneous masslike tissue at least partially proximal to the apex of the metacarpal lateral tubercle—they were able to distinguish displaced full-thickness tears from nondisplaced full-thickness tears with 100% accuracy. Hergan and colleagues25 found that the diagnostic accuracy of MRI was superior to that of ultrasound; while MRI accuracy was perfect, 12% of patients were incorrectly diagnosed with ultrasound, with false-positive or false-negative tendon-edge displacement. In our experience, ultrasound is uniquely useful in its ability to characterize the real-time dynamic interaction of the UCL with the adductor aponeurosis. It has been observed that passive flexion of the first interphalangeal joint moves the adductor aponeurosis in isolation, allowing differentiation from the subjacent UCL.21 Had a partial tear been in the differential diagnosis of our patient’s Stener lesion, such a maneuver under ultrasound visualization would have solved the dilemma. In addition, ultrasound allows for comparison with the contralateral ligament at the time of examination should a diagnostic dilemma arise.
As many have reported both bony avulsion of the base of the proximal phalanx and concomitant injury to the UCL, identification of a bony avulsion does not exclude a ligamentous injury and the possibility of a Stener lesion (Figure 7).16,19
Conclusion
A Stener lesion—retraction of a completely torn UCL becoming entrapped dorsally and proximally to the adductor insertion—can cause pain, instability, and ultimately osteoarthritis if not treated appropriately. The orthopedic surgeon should have a high index of suspicion for a Stener lesion in the appropriate clinical scenario and consider all imaging modalities for diagnosis. Likewise, it is of utmost importance for the radiologist to identify imaging findings of a Stener lesion, as physical examination alone may be limited in its ability to characterize injury severity. Both MRI and ultrasound are useful in evaluating UCL tears, and ultrasound provides the additional benefit of dynamic visualization and comparison with the contralateral side.
Am J Orthop. 2017;46(3):E195-E199. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Take-Home Points
- Torn, displaced, and entrapped UCL is a Stener lesion.
- Hyperabduction injury with pain and joint laxity on examination.
- MRI and ultrasound are useful in evaluating UCL tears.
- Ultrasound offers dynamic evaluation.
- Must be treated appropriately to avoid pain, instability, and osteoarthritis.
In the literature, hyperabduction injuries to the thumb metacarpophalangeal (MCP) joint have been referred to interchangeably as gamekeeper’s thumb and skier’s thumb. Historically, though, gamekeeper’s thumb was initially described in hunters with chronic injury to the ulnar collateral ligament (UCL),1 and skier’s thumb typically has been described as an acute hyperabduction injury of the UCL.2-5 The proximal portion of a torn UCL may retract with further abduction and displace dorsally, becoming entrapped by the adductor pollicis aponeurosis insertion, known as a Stener lesion.6
The first MCP joint is stabilized by static and dynamic structures that contribute in varying degrees in flexion and extension of the joint. The static stabilizers include the proper and accessory radial and UCLs, the palmar plate, and the dorsal capsule. The UCL originates at the dorsal ulnar aspect of the first metacarpal head at the metacarpal tubercle about 5 mm proximal to the articular surface. The UCL courses distally in the palmar direction to insert volar and proximal to the medial tubercle of the proximal phalanx about 3 mm distal to the articular surface.7 In flexion, the proper collateral ligament is taut and is the primary static stabilizer. In extension, the accessory collateral ligament, which inserts on the palmar plate, is taut and is the primary static stabilizer.8-11
The dynamic stabilizers include the extrinsic muscles (flexor pollicis longus, extensor pollicis longus and brevis) and the intrinsic muscles (abductor pollicis brevis, adductor pollicis, flexor pollicis brevis) inserting on the thumb at the distal phalanx and proximal phalanx and at the base of the first metacarpal.8-10
We report the case of an acute hyperabduction injury of the thumb MCP joint with radiographic, ultrasound, and magnetic resonance imaging (MRI) findings consistent with a Stener lesion and subsequently confirmed with intraoperative photographs. The patient provided written informed consent for print and electronic publication of this case report.
Clinical Findings
A 33-year-old healthy man had persistent left hand pain and grip weakness after performing a handstand. He presented to the orthopedic hand clinic 20 days after injury, having failed nonoperative management (use of nonsteroidal anti-inflammatory drugs and soft thumb spica splint). Physical examination revealed soft-tissue swelling and focal tenderness to palpation at the ulnar aspect of the thumb MCP joint. Despite bilateral first MCP joint laxity on varus and valgus stress without identification of a firm endpoint, pain was elicited only on valgus stress of the left first MCP joint. Given the laxity and the left thumb soft-tissue swelling with pain, plain radiographs, ultrasound, and MRI were used to evaluate for severity of presumed left thumb UCL injury.
Imaging Findings
Plain radiographs showed normal bony anatomy without fracture, normal joint space, and mild soft-tissue swelling at the left thumb MCP level (Figures 3A, 3B).
Surgical Findings
Given laxity with pain at the UCL on stress testing, MRI and ultrasound findings, and continued pain and instability of the thumb with pinching and grasping during activities of daily living, the patient and orthopedic hand surgeon proceeded with surgical intervention. Preoperative examination under anesthesia confirmed significant laxity on valgus stress without a palpable endpoint (Figures 5A, 5B).
Discussion
Hyperabduction injuries to the thumb may rupture the UCL of the MCP joint of the thumb or cause a bony avulsion of the base of the proximal phalanx. Injury to the UCL, most often at its distal portion,4,14,15 may result in a sprain or full-thickness tear of the ligament.
It is vital for the radiologist to identify a Stener lesion because a nondisplaced tear of the UCL is often treated nonsurgically, but UCL tears displaced more than 3 mm and Stener lesions usually must be operated on to avoid chronic instability, pain, and osteoarthritis.2-5,8,12-23 Sensitivity and specificity of MRI in evaluating UCL injuries are reported to be almost 100%, with resolution of 1 mm using current surface coils.23 There are various UCL injury patterns, including partial tears, displaced and nondisplaced complete tears, and even complex injuries, such as an incomplete tear with the torn portion retracted as a Stener lesion.22 MRI is needed to establish the extent of injury, as 90% of complete tears that are displaced at least 3 mm, and all tears with retraction proximal and superficial to the aponeurosis (true Stener lesions), failed immobilization and required surgical treatment.23Although they vary in the literature, mean sensitivity and specificity of ultrasound in detecting UCL tears in level I studies have been reported as 76% and 81%, respectively.24 When Melville and colleagues21 applied their ultrasound criteria—including absence of normal UCL fibers traversing the first MCP joint as well as heterogeneous masslike tissue at least partially proximal to the apex of the metacarpal lateral tubercle—they were able to distinguish displaced full-thickness tears from nondisplaced full-thickness tears with 100% accuracy. Hergan and colleagues25 found that the diagnostic accuracy of MRI was superior to that of ultrasound; while MRI accuracy was perfect, 12% of patients were incorrectly diagnosed with ultrasound, with false-positive or false-negative tendon-edge displacement. In our experience, ultrasound is uniquely useful in its ability to characterize the real-time dynamic interaction of the UCL with the adductor aponeurosis. It has been observed that passive flexion of the first interphalangeal joint moves the adductor aponeurosis in isolation, allowing differentiation from the subjacent UCL.21 Had a partial tear been in the differential diagnosis of our patient’s Stener lesion, such a maneuver under ultrasound visualization would have solved the dilemma. In addition, ultrasound allows for comparison with the contralateral ligament at the time of examination should a diagnostic dilemma arise.
As many have reported both bony avulsion of the base of the proximal phalanx and concomitant injury to the UCL, identification of a bony avulsion does not exclude a ligamentous injury and the possibility of a Stener lesion (Figure 7).16,19
Conclusion
A Stener lesion—retraction of a completely torn UCL becoming entrapped dorsally and proximally to the adductor insertion—can cause pain, instability, and ultimately osteoarthritis if not treated appropriately. The orthopedic surgeon should have a high index of suspicion for a Stener lesion in the appropriate clinical scenario and consider all imaging modalities for diagnosis. Likewise, it is of utmost importance for the radiologist to identify imaging findings of a Stener lesion, as physical examination alone may be limited in its ability to characterize injury severity. Both MRI and ultrasound are useful in evaluating UCL tears, and ultrasound provides the additional benefit of dynamic visualization and comparison with the contralateral side.
Am J Orthop. 2017;46(3):E195-E199. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Campbell CS. Gamekeeper’s thumb. J Bone Joint Surg Br. 1955;37(1):148-149.
2. Anderson D. Skier’s thumb. Aust Family Physician. 2010;39(8):575-577.
3. Heim D. The skier’s thumb. Acta Orthop Belg. 1999;65(4):440-446.
4. Lohman M, Vasenius J, Kivisaari A, Kivisaari L. MR imaging in chronic rupture of the ulnar collateral ligament of the thumb. Acta Radiol. 2001;42(1):10-14.
5. Kundu N, Asfaw S, Polster J, Lohman R. The Stener lesion. Eplasty. 2012;12:ic11.
6. Stener B. Displacement of the ruptured ulnar collateral ligament of the metacarpophalangeal joint of the thumb. J Bone Joint Surg Br. 1962;44:869-879.
7. Carlson MG, Warner KK, Meyers KN, Hearns KA, Kok PL. Anatomy of the thumb metacarpophalangeal ulnar and radial collateral ligaments. J Hand Surg Am. 2012;37(10):2021-2026.
8. Heyman P. Injuries to the ulnar collateral ligament of the thumb metacarpophalangeal joint. J Am Acad Orthop Surg. 1997;5(4):224-229.
9. Minami A, An KN, Cooney WP 3rd, Linscheid RL, Chao EY. Ligamentous structures of the metacarpophalangeal joint: a quantitative anatomic study. J Orthop Res. 1984;1(4):361-368.
10. Heyman P, Gelberman RH, Duncan K, Hipp JA. Injuries of the ulnar collateral ligament of the thumb metacarpophalangeal joint. Biomechanical and prospective clinical studies on the usefulness of valgus stress testing. Clin Orthop Relat Res. 1993;(292):165-171.
11. Patel S, Potty A, Taylor EJ, Sorene ED. Collateral ligament injuries of the metacarpophalangeal joint of the thumb: a treatment algorithm. Strategies Trauma Limb Reconstr. 2010;5(1):1-10.
12. O’Callaghan BI, Kohut G, Hoogewoud HM. Gamekeeper thumb: identification of the Stener lesion with US. Radiology. 1994;192(2):477-480.
13. Ebrahim FS, De Maeseneer M, Jager T, Marcelis S, Jamadar DA, Jacobson JA. US diagnosis of UCL tears of the thumb and Stener lesions: technique, pattern-based approach, and differential diagnosis. Radiographics. 2006;26(4):1007-1020.
14. Haramati N, Hiller N, Dowdle J, et al. MRI of the Stener lesion. Skeletal Radiol. 1995;24(7):515-518.
15. Shinohara T, Horii E, Majima M, et al. Sonographic diagnosis of acute injuries of the ulnar collateral ligament of the metacarpophalangeal joint of the thumb. J Clin Ultrasound. 2007;35(2):73-77.
16. Giele H, Martin J. The two-level ulnar collateral ligament injury of the metacarpophalangeal joint of the thumb. J Hand Surg Br. 2003;28(1):92-93.
17. Kaplan SJ. The Stener lesion revisited: a case report. J Hand Surg Am. 1998;23(5):833-836.
18. Thirkannad S, Wolff TW. The “two fleck sign” for an occult Stener lesion. J Hand Surg Eur Vol. 2008;33(2):208-211.
19. Badawi RA, Hussain S, Compson JP. Two in one: a variant of the Stener lesion. Injury. 2002;33(4):379-380.
20. McKeon KE, Gelberman RH, Calfee RP. Ulnar collateral ligament injuries of the thumb: phalangeal translation during valgus stress in human cadavera. J Bone Joint Surg Am. 2013;95(10):881-887.
21. Melville D, Jacobson JA, Haase S, Brandon C, Brigido MK, Fessell D. Ultrasound of displaced ulnar collateral ligament tears of the thumb: the Stener lesion revisited. Skeletal Radiol. 2013;42(5):667-673.
22. Romano WM, Garvin G, Bhayana D, Chaudhary O. The spectrum of ulnar collateral ligament injuries as viewed on magnetic resonance imaging of the metacarpophalangeal joint of the thumb. Can Assoc Radiol J. 2003;54(4):243-248.
23. Milner CS, Manon-Matos Y, Thirkannad SM. Gamekeeper’s thumb—a treatment-oriented magnetic resonance imaging classification. J Hand Surg Am. 2015;40(1):90-95.
24. Papandrea RF, Fowler T. Injury at the thumb UCL: is there a Stener lesion? J Hand Surg Am. 2008;33(10):1882-1884.
25. Hergan K, Mittler C, Oser W. Ulnar collateral ligament: differentiation of displaced and nondisplaced tears with US and MR imaging. Radiology. 1995;194(1):65-71.
1. Campbell CS. Gamekeeper’s thumb. J Bone Joint Surg Br. 1955;37(1):148-149.
2. Anderson D. Skier’s thumb. Aust Family Physician. 2010;39(8):575-577.
3. Heim D. The skier’s thumb. Acta Orthop Belg. 1999;65(4):440-446.
4. Lohman M, Vasenius J, Kivisaari A, Kivisaari L. MR imaging in chronic rupture of the ulnar collateral ligament of the thumb. Acta Radiol. 2001;42(1):10-14.
5. Kundu N, Asfaw S, Polster J, Lohman R. The Stener lesion. Eplasty. 2012;12:ic11.
6. Stener B. Displacement of the ruptured ulnar collateral ligament of the metacarpophalangeal joint of the thumb. J Bone Joint Surg Br. 1962;44:869-879.
7. Carlson MG, Warner KK, Meyers KN, Hearns KA, Kok PL. Anatomy of the thumb metacarpophalangeal ulnar and radial collateral ligaments. J Hand Surg Am. 2012;37(10):2021-2026.
8. Heyman P. Injuries to the ulnar collateral ligament of the thumb metacarpophalangeal joint. J Am Acad Orthop Surg. 1997;5(4):224-229.
9. Minami A, An KN, Cooney WP 3rd, Linscheid RL, Chao EY. Ligamentous structures of the metacarpophalangeal joint: a quantitative anatomic study. J Orthop Res. 1984;1(4):361-368.
10. Heyman P, Gelberman RH, Duncan K, Hipp JA. Injuries of the ulnar collateral ligament of the thumb metacarpophalangeal joint. Biomechanical and prospective clinical studies on the usefulness of valgus stress testing. Clin Orthop Relat Res. 1993;(292):165-171.
11. Patel S, Potty A, Taylor EJ, Sorene ED. Collateral ligament injuries of the metacarpophalangeal joint of the thumb: a treatment algorithm. Strategies Trauma Limb Reconstr. 2010;5(1):1-10.
12. O’Callaghan BI, Kohut G, Hoogewoud HM. Gamekeeper thumb: identification of the Stener lesion with US. Radiology. 1994;192(2):477-480.
13. Ebrahim FS, De Maeseneer M, Jager T, Marcelis S, Jamadar DA, Jacobson JA. US diagnosis of UCL tears of the thumb and Stener lesions: technique, pattern-based approach, and differential diagnosis. Radiographics. 2006;26(4):1007-1020.
14. Haramati N, Hiller N, Dowdle J, et al. MRI of the Stener lesion. Skeletal Radiol. 1995;24(7):515-518.
15. Shinohara T, Horii E, Majima M, et al. Sonographic diagnosis of acute injuries of the ulnar collateral ligament of the metacarpophalangeal joint of the thumb. J Clin Ultrasound. 2007;35(2):73-77.
16. Giele H, Martin J. The two-level ulnar collateral ligament injury of the metacarpophalangeal joint of the thumb. J Hand Surg Br. 2003;28(1):92-93.
17. Kaplan SJ. The Stener lesion revisited: a case report. J Hand Surg Am. 1998;23(5):833-836.
18. Thirkannad S, Wolff TW. The “two fleck sign” for an occult Stener lesion. J Hand Surg Eur Vol. 2008;33(2):208-211.
19. Badawi RA, Hussain S, Compson JP. Two in one: a variant of the Stener lesion. Injury. 2002;33(4):379-380.
20. McKeon KE, Gelberman RH, Calfee RP. Ulnar collateral ligament injuries of the thumb: phalangeal translation during valgus stress in human cadavera. J Bone Joint Surg Am. 2013;95(10):881-887.
21. Melville D, Jacobson JA, Haase S, Brandon C, Brigido MK, Fessell D. Ultrasound of displaced ulnar collateral ligament tears of the thumb: the Stener lesion revisited. Skeletal Radiol. 2013;42(5):667-673.
22. Romano WM, Garvin G, Bhayana D, Chaudhary O. The spectrum of ulnar collateral ligament injuries as viewed on magnetic resonance imaging of the metacarpophalangeal joint of the thumb. Can Assoc Radiol J. 2003;54(4):243-248.
23. Milner CS, Manon-Matos Y, Thirkannad SM. Gamekeeper’s thumb—a treatment-oriented magnetic resonance imaging classification. J Hand Surg Am. 2015;40(1):90-95.
24. Papandrea RF, Fowler T. Injury at the thumb UCL: is there a Stener lesion? J Hand Surg Am. 2008;33(10):1882-1884.
25. Hergan K, Mittler C, Oser W. Ulnar collateral ligament: differentiation of displaced and nondisplaced tears with US and MR imaging. Radiology. 1995;194(1):65-71.
Treating Traumatic Injuries and the Issues They Cause
In the Madigan Intrepid Spirit Transitions (MIST) program, holistic treatment for traumatic brain injuries (TBIs) includes traditional and nontraditional therapies as well as a little help from friends.
MIST is a 6-week intensive outpatient group for service members who have TBIs and other traumatic injuries, along with coexisting conditions, such as chronic pain or posttraumatic stress. Coexisting conditions can make cases more complex, said U.S. Army Colonel Beverly Scott, medical and program director of Madigan Army Medical Center’s Traumatic Brain Injury Program and Intrepid Spirit Program in an interview with Health.mil News. But she adds, “It’s never too late to help [patients] address a number of issues they may be having following a traumatic brain injury, dealing with pain, dealing with behavior health issues.”
Related: Let’s Dance: A Holistic Approach to Treating Veterans With Posttraumatic Stress Disorder
The MIST program serves only active-duty service members with referral from their primary care managers and other specialty services at Madigan or throughout the Regional Health Command-Pacific. Commanders must sign memoranda of understanding that patients will be off duty rosters for the duration of the program. “They’re making a commitment to help that service member get better,” Scott said.
The MIST program enrolls 8 to 12 service members at a time. The holistic focus allows patients to address chronic pain, insomnia, and cognitive issues through traditional means as well as less traditional means that include mindfulness training; art; such as creating symbolic masks; and yoga. The variety of approaches lets them “cherry pick the methods they believe will help them the most,” the Health.mil News article reports, or what one member called “customizing their own multitool.”
Participants are encouraged to continue individual care within the TBI/Intrepid Spirit program. The MIST program aims to introduce them to the resources they can use going forward. Giving them tools they can use after they complete the program is an acknowledgment that the recovery process is ongoing. “We recognize it is a transition,” Scott said.
Related: Ideas for Helping TBI Patients
The MIST program has graduated 2 groups. Scott says, “We’ve seen incredible success,” both in wellness and in other areas, such as improved interpersonal relationships. Some of the credit goes to the peer support that MIST promotes. The curriculum is evidence based, but Scott says some “significant success is clearly related to soldiers helping soldiers.”
In the Madigan Intrepid Spirit Transitions (MIST) program, holistic treatment for traumatic brain injuries (TBIs) includes traditional and nontraditional therapies as well as a little help from friends.
MIST is a 6-week intensive outpatient group for service members who have TBIs and other traumatic injuries, along with coexisting conditions, such as chronic pain or posttraumatic stress. Coexisting conditions can make cases more complex, said U.S. Army Colonel Beverly Scott, medical and program director of Madigan Army Medical Center’s Traumatic Brain Injury Program and Intrepid Spirit Program in an interview with Health.mil News. But she adds, “It’s never too late to help [patients] address a number of issues they may be having following a traumatic brain injury, dealing with pain, dealing with behavior health issues.”
Related: Let’s Dance: A Holistic Approach to Treating Veterans With Posttraumatic Stress Disorder
The MIST program serves only active-duty service members with referral from their primary care managers and other specialty services at Madigan or throughout the Regional Health Command-Pacific. Commanders must sign memoranda of understanding that patients will be off duty rosters for the duration of the program. “They’re making a commitment to help that service member get better,” Scott said.
The MIST program enrolls 8 to 12 service members at a time. The holistic focus allows patients to address chronic pain, insomnia, and cognitive issues through traditional means as well as less traditional means that include mindfulness training; art; such as creating symbolic masks; and yoga. The variety of approaches lets them “cherry pick the methods they believe will help them the most,” the Health.mil News article reports, or what one member called “customizing their own multitool.”
Participants are encouraged to continue individual care within the TBI/Intrepid Spirit program. The MIST program aims to introduce them to the resources they can use going forward. Giving them tools they can use after they complete the program is an acknowledgment that the recovery process is ongoing. “We recognize it is a transition,” Scott said.
Related: Ideas for Helping TBI Patients
The MIST program has graduated 2 groups. Scott says, “We’ve seen incredible success,” both in wellness and in other areas, such as improved interpersonal relationships. Some of the credit goes to the peer support that MIST promotes. The curriculum is evidence based, but Scott says some “significant success is clearly related to soldiers helping soldiers.”
In the Madigan Intrepid Spirit Transitions (MIST) program, holistic treatment for traumatic brain injuries (TBIs) includes traditional and nontraditional therapies as well as a little help from friends.
MIST is a 6-week intensive outpatient group for service members who have TBIs and other traumatic injuries, along with coexisting conditions, such as chronic pain or posttraumatic stress. Coexisting conditions can make cases more complex, said U.S. Army Colonel Beverly Scott, medical and program director of Madigan Army Medical Center’s Traumatic Brain Injury Program and Intrepid Spirit Program in an interview with Health.mil News. But she adds, “It’s never too late to help [patients] address a number of issues they may be having following a traumatic brain injury, dealing with pain, dealing with behavior health issues.”
Related: Let’s Dance: A Holistic Approach to Treating Veterans With Posttraumatic Stress Disorder
The MIST program serves only active-duty service members with referral from their primary care managers and other specialty services at Madigan or throughout the Regional Health Command-Pacific. Commanders must sign memoranda of understanding that patients will be off duty rosters for the duration of the program. “They’re making a commitment to help that service member get better,” Scott said.
The MIST program enrolls 8 to 12 service members at a time. The holistic focus allows patients to address chronic pain, insomnia, and cognitive issues through traditional means as well as less traditional means that include mindfulness training; art; such as creating symbolic masks; and yoga. The variety of approaches lets them “cherry pick the methods they believe will help them the most,” the Health.mil News article reports, or what one member called “customizing their own multitool.”
Participants are encouraged to continue individual care within the TBI/Intrepid Spirit program. The MIST program aims to introduce them to the resources they can use going forward. Giving them tools they can use after they complete the program is an acknowledgment that the recovery process is ongoing. “We recognize it is a transition,” Scott said.
Related: Ideas for Helping TBI Patients
The MIST program has graduated 2 groups. Scott says, “We’ve seen incredible success,” both in wellness and in other areas, such as improved interpersonal relationships. Some of the credit goes to the peer support that MIST promotes. The curriculum is evidence based, but Scott says some “significant success is clearly related to soldiers helping soldiers.”
Patients With Cancer Have Higher Plasma Brain Natriuretic Peptide Levels
Natriuretic peptides have been shown to be valuable biomarkers for guiding diagnosis and treatment for cardiovascular disease. Recently, they also have been reported to inhibit progression of several cancers. The link is likely to be inflammation—which is usually a precursor to malignant changes, say researchers from Tokushima University and the National Cerebral and Cardiovascular Center Research Institute, both in Japan. To find out how reliable brain natriuretic peptide and C-reactive protein (CRP) levels might be in cancer, the researchers retrospectively studied 2,923 patients at their hospital who had had brain natriuretic peptide (BNP) measured to rule out heart disease.
Related: The Link Between Low-Density Lipoproteins and Chronic Lymphocytic Leukemia
Of 234 patients included in the final analysis, 80 were diagnosed with cancer. No patients with clinically evident heart failure and cardiac disease requiring medical treatment were included in the study. Both the plasma BNP and serum CRP levels were significantly higher in the patients with cancer (66.4 vs 44.0 pg/mL, and 0.99 vs 0.18 mg/dL, respectively). There were no significant differences in the echocardiographic parameters.
In 28 cured patients with solid cancers who underwent a radical surgery, the plasma BNP levels dropped significantly, from 70.7 to 45.0 pg/mL. However, the levels did not change after surgery in 7 relapsed or “insufficiently treated” patients with solid cancers. And although plasma BNP levels “tended to decrease” after chemotherapy in patients with hematologic cancers, in 13 patients plasma BNP levels did not change significantly.
Related: Novel Neuroendocrine Tumor in Multiple Endocrine Neoplasia Type 1
BNP levels were significantly higher in the patients with stage IV cancer, compared with those who had stages I, II, or III. This might be accompanied by systemic inflammation, the researchers say.
As far as the researchers know, no studies have shown that cancer cells generate BNP. Therefore, they think a higher plasma BNP level may reflect the elevated production from cardiomyocytes in association with inflammation in cancer patients.
Their findings suggest that it’s a good idea to consider the effect of cancer on the BNP levels when using BNP as an indicator of heart failure. Asymptomatic cancer patients with higher BNP levels should be diagnosed whether the elevated BNP is due to asymptomatic heart failure or cancer.
Source:
Bando S, Soeki T, Matsuura T, et al. PLoS One. 2017;12(6):e0178607
Natriuretic peptides have been shown to be valuable biomarkers for guiding diagnosis and treatment for cardiovascular disease. Recently, they also have been reported to inhibit progression of several cancers. The link is likely to be inflammation—which is usually a precursor to malignant changes, say researchers from Tokushima University and the National Cerebral and Cardiovascular Center Research Institute, both in Japan. To find out how reliable brain natriuretic peptide and C-reactive protein (CRP) levels might be in cancer, the researchers retrospectively studied 2,923 patients at their hospital who had had brain natriuretic peptide (BNP) measured to rule out heart disease.
Related: The Link Between Low-Density Lipoproteins and Chronic Lymphocytic Leukemia
Of 234 patients included in the final analysis, 80 were diagnosed with cancer. No patients with clinically evident heart failure and cardiac disease requiring medical treatment were included in the study. Both the plasma BNP and serum CRP levels were significantly higher in the patients with cancer (66.4 vs 44.0 pg/mL, and 0.99 vs 0.18 mg/dL, respectively). There were no significant differences in the echocardiographic parameters.
In 28 cured patients with solid cancers who underwent a radical surgery, the plasma BNP levels dropped significantly, from 70.7 to 45.0 pg/mL. However, the levels did not change after surgery in 7 relapsed or “insufficiently treated” patients with solid cancers. And although plasma BNP levels “tended to decrease” after chemotherapy in patients with hematologic cancers, in 13 patients plasma BNP levels did not change significantly.
Related: Novel Neuroendocrine Tumor in Multiple Endocrine Neoplasia Type 1
BNP levels were significantly higher in the patients with stage IV cancer, compared with those who had stages I, II, or III. This might be accompanied by systemic inflammation, the researchers say.
As far as the researchers know, no studies have shown that cancer cells generate BNP. Therefore, they think a higher plasma BNP level may reflect the elevated production from cardiomyocytes in association with inflammation in cancer patients.
Their findings suggest that it’s a good idea to consider the effect of cancer on the BNP levels when using BNP as an indicator of heart failure. Asymptomatic cancer patients with higher BNP levels should be diagnosed whether the elevated BNP is due to asymptomatic heart failure or cancer.
Source:
Bando S, Soeki T, Matsuura T, et al. PLoS One. 2017;12(6):e0178607
Natriuretic peptides have been shown to be valuable biomarkers for guiding diagnosis and treatment for cardiovascular disease. Recently, they also have been reported to inhibit progression of several cancers. The link is likely to be inflammation—which is usually a precursor to malignant changes, say researchers from Tokushima University and the National Cerebral and Cardiovascular Center Research Institute, both in Japan. To find out how reliable brain natriuretic peptide and C-reactive protein (CRP) levels might be in cancer, the researchers retrospectively studied 2,923 patients at their hospital who had had brain natriuretic peptide (BNP) measured to rule out heart disease.
Related: The Link Between Low-Density Lipoproteins and Chronic Lymphocytic Leukemia
Of 234 patients included in the final analysis, 80 were diagnosed with cancer. No patients with clinically evident heart failure and cardiac disease requiring medical treatment were included in the study. Both the plasma BNP and serum CRP levels were significantly higher in the patients with cancer (66.4 vs 44.0 pg/mL, and 0.99 vs 0.18 mg/dL, respectively). There were no significant differences in the echocardiographic parameters.
In 28 cured patients with solid cancers who underwent a radical surgery, the plasma BNP levels dropped significantly, from 70.7 to 45.0 pg/mL. However, the levels did not change after surgery in 7 relapsed or “insufficiently treated” patients with solid cancers. And although plasma BNP levels “tended to decrease” after chemotherapy in patients with hematologic cancers, in 13 patients plasma BNP levels did not change significantly.
Related: Novel Neuroendocrine Tumor in Multiple Endocrine Neoplasia Type 1
BNP levels were significantly higher in the patients with stage IV cancer, compared with those who had stages I, II, or III. This might be accompanied by systemic inflammation, the researchers say.
As far as the researchers know, no studies have shown that cancer cells generate BNP. Therefore, they think a higher plasma BNP level may reflect the elevated production from cardiomyocytes in association with inflammation in cancer patients.
Their findings suggest that it’s a good idea to consider the effect of cancer on the BNP levels when using BNP as an indicator of heart failure. Asymptomatic cancer patients with higher BNP levels should be diagnosed whether the elevated BNP is due to asymptomatic heart failure or cancer.
Source:
Bando S, Soeki T, Matsuura T, et al. PLoS One. 2017;12(6):e0178607
Company discontinues phase 3 trial of vadastuximab talirine in AML
Update as of June 21: The US Food and Drug Administration (FDA) has placed the Investigational New Drug (IND) application for vadastuximab talirine on hold. No clinical trial may resume under the IND until the FDA lifts the clinical hold.
On the advice of the Independent Data Monitoring Committee, Seattle Genetics is discontinuing the phase 3 CASCADE clinical trial of vadastuximab talirine as frontline treatment in older patients with acute myeloid leukemia (AML).
The company is also suspending patient enrollment and treatment in all its vadastuximab trials, including the ongoing phase 1/2 trial in frontline high-risk myelodysplastic syndromes (MDS).
In December last year, the US Food and Drug Administration (FDA) had placed the trials of vadastuximab on full and partial clinical holds due to the potential risk of hepatotoxicity.
The FDA lifted the hold in March of this year. However, concerns regarding a higher rate of deaths, including fatal infections but not liver toxicity, in the vadastuximab arm compared to control prompted the company to discontinue the phase 3 trial.
Vadastuximab talirene is an antibody-drug conjugate (ADC) targeted to CD33, which is expressed on most AML and MDS blasts. The ADC technology links anti-cancer compounds with targeting antibodies to precisely kill cancer cells and spare healthy ones.
Seattle Genetics’ ADC for Hodgkin lymphoma, brentuximab vedotin, was granted accelerated approval by the FDA in 2011.
The CASCADE trial was evaluating vadastuximab in combination with the hypomethylating agents (HMAs) azacytidine or decitabine compared to an HMA alone in older patients with newly diagnosed AML.
In addition to the MDS trial, the company is stopping enrollment onto the trial of vadastuximab in combination with 7+3 chemotherapy in newly diagnosed, younger AML patients and vadastuximab given prior to or after allogeneic hematopoietic stem cell transplant in AML patients.
Calling the decision “disappointing and unexpected,” Clay Siegall, PhD, president and CEO of Seattle Genetics, said, “Patient safety is our highest priority, and we will closely review the data and evaluate next steps.” ![]()
Update as of June 21: The US Food and Drug Administration (FDA) has placed the Investigational New Drug (IND) application for vadastuximab talirine on hold. No clinical trial may resume under the IND until the FDA lifts the clinical hold.
On the advice of the Independent Data Monitoring Committee, Seattle Genetics is discontinuing the phase 3 CASCADE clinical trial of vadastuximab talirine as frontline treatment in older patients with acute myeloid leukemia (AML).
The company is also suspending patient enrollment and treatment in all its vadastuximab trials, including the ongoing phase 1/2 trial in frontline high-risk myelodysplastic syndromes (MDS).
In December last year, the US Food and Drug Administration (FDA) had placed the trials of vadastuximab on full and partial clinical holds due to the potential risk of hepatotoxicity.
The FDA lifted the hold in March of this year. However, concerns regarding a higher rate of deaths, including fatal infections but not liver toxicity, in the vadastuximab arm compared to control prompted the company to discontinue the phase 3 trial.
Vadastuximab talirene is an antibody-drug conjugate (ADC) targeted to CD33, which is expressed on most AML and MDS blasts. The ADC technology links anti-cancer compounds with targeting antibodies to precisely kill cancer cells and spare healthy ones.
Seattle Genetics’ ADC for Hodgkin lymphoma, brentuximab vedotin, was granted accelerated approval by the FDA in 2011.
The CASCADE trial was evaluating vadastuximab in combination with the hypomethylating agents (HMAs) azacytidine or decitabine compared to an HMA alone in older patients with newly diagnosed AML.
In addition to the MDS trial, the company is stopping enrollment onto the trial of vadastuximab in combination with 7+3 chemotherapy in newly diagnosed, younger AML patients and vadastuximab given prior to or after allogeneic hematopoietic stem cell transplant in AML patients.
Calling the decision “disappointing and unexpected,” Clay Siegall, PhD, president and CEO of Seattle Genetics, said, “Patient safety is our highest priority, and we will closely review the data and evaluate next steps.” ![]()
Update as of June 21: The US Food and Drug Administration (FDA) has placed the Investigational New Drug (IND) application for vadastuximab talirine on hold. No clinical trial may resume under the IND until the FDA lifts the clinical hold.
On the advice of the Independent Data Monitoring Committee, Seattle Genetics is discontinuing the phase 3 CASCADE clinical trial of vadastuximab talirine as frontline treatment in older patients with acute myeloid leukemia (AML).
The company is also suspending patient enrollment and treatment in all its vadastuximab trials, including the ongoing phase 1/2 trial in frontline high-risk myelodysplastic syndromes (MDS).
In December last year, the US Food and Drug Administration (FDA) had placed the trials of vadastuximab on full and partial clinical holds due to the potential risk of hepatotoxicity.
The FDA lifted the hold in March of this year. However, concerns regarding a higher rate of deaths, including fatal infections but not liver toxicity, in the vadastuximab arm compared to control prompted the company to discontinue the phase 3 trial.
Vadastuximab talirene is an antibody-drug conjugate (ADC) targeted to CD33, which is expressed on most AML and MDS blasts. The ADC technology links anti-cancer compounds with targeting antibodies to precisely kill cancer cells and spare healthy ones.
Seattle Genetics’ ADC for Hodgkin lymphoma, brentuximab vedotin, was granted accelerated approval by the FDA in 2011.
The CASCADE trial was evaluating vadastuximab in combination with the hypomethylating agents (HMAs) azacytidine or decitabine compared to an HMA alone in older patients with newly diagnosed AML.
In addition to the MDS trial, the company is stopping enrollment onto the trial of vadastuximab in combination with 7+3 chemotherapy in newly diagnosed, younger AML patients and vadastuximab given prior to or after allogeneic hematopoietic stem cell transplant in AML patients.
Calling the decision “disappointing and unexpected,” Clay Siegall, PhD, president and CEO of Seattle Genetics, said, “Patient safety is our highest priority, and we will closely review the data and evaluate next steps.” ![]()
Biosimilar rituximab approved in Europe
The European Commission (EC) has approved the Sandoz biosimilar rituximab (Rixathon®) for use in the European Economic Area.
Rixathon is approved for all indications of the reference medicine, MabThera®, including follicular lymphoma, diffuse large B-cell lymphoma, chronic lymphocytic leukemia, and immunologic diseases such as rheumatoid arthritis, granulomatosis with polyangiitis, and microscopic polyangiitis.
This approval allows Rixathon to be marketed in the member states of the European Union and Iceland, Liechtenstein, and Norway, members of the European Free Trade Association.
The approval “represents a big win for patients in Europe with blood cancers or immunological diseases,” according to Carol Lynch, global head of Biopharmaceuticals at Sandoz.
“Rixathon will be one of the 5 major launches we plan in the next 4 years,” she said.
Earlier in the year, the European Medicines Agency’s Committee for Medicinal Products for Human Use had recommended marketing authorization for Rixathon.
The EC based its approval on a comprehensive development program generating analytical, preclinical, and clinical data. Clinical studies included ASSIST-RA and ASSIST-FL.
ASSIST-RA demonstrated that the biosimilar product has equivalent pharmacokinetic and pharmacodynamic profiles to the reference medicine, with no clinically meaningful differences in safety, tolerability, or immunogenicity in patients with rheumatoid arthritis.
ASSIST-FL was a phase 3 study confirming efficacy and safety. The study met its primary endpoint of equivalence in overall response rate between the biosimilar product and the reference medicine after 6 months.
ASSIST-FL also confirmed the comparable safety profiles of the 2 medicines.
Sandoz is a division of the Swiss pharmaceutical company Novartis. MabThera is a registered trademark of F. Hoffmann-La-Roche AG.
Another Sandoz biosimilar rituximab has been approved in the EU as Riximyo® under a duplicate marketing authorization. ![]()
The European Commission (EC) has approved the Sandoz biosimilar rituximab (Rixathon®) for use in the European Economic Area.
Rixathon is approved for all indications of the reference medicine, MabThera®, including follicular lymphoma, diffuse large B-cell lymphoma, chronic lymphocytic leukemia, and immunologic diseases such as rheumatoid arthritis, granulomatosis with polyangiitis, and microscopic polyangiitis.
This approval allows Rixathon to be marketed in the member states of the European Union and Iceland, Liechtenstein, and Norway, members of the European Free Trade Association.
The approval “represents a big win for patients in Europe with blood cancers or immunological diseases,” according to Carol Lynch, global head of Biopharmaceuticals at Sandoz.
“Rixathon will be one of the 5 major launches we plan in the next 4 years,” she said.
Earlier in the year, the European Medicines Agency’s Committee for Medicinal Products for Human Use had recommended marketing authorization for Rixathon.
The EC based its approval on a comprehensive development program generating analytical, preclinical, and clinical data. Clinical studies included ASSIST-RA and ASSIST-FL.
ASSIST-RA demonstrated that the biosimilar product has equivalent pharmacokinetic and pharmacodynamic profiles to the reference medicine, with no clinically meaningful differences in safety, tolerability, or immunogenicity in patients with rheumatoid arthritis.
ASSIST-FL was a phase 3 study confirming efficacy and safety. The study met its primary endpoint of equivalence in overall response rate between the biosimilar product and the reference medicine after 6 months.
ASSIST-FL also confirmed the comparable safety profiles of the 2 medicines.
Sandoz is a division of the Swiss pharmaceutical company Novartis. MabThera is a registered trademark of F. Hoffmann-La-Roche AG.
Another Sandoz biosimilar rituximab has been approved in the EU as Riximyo® under a duplicate marketing authorization. ![]()
The European Commission (EC) has approved the Sandoz biosimilar rituximab (Rixathon®) for use in the European Economic Area.
Rixathon is approved for all indications of the reference medicine, MabThera®, including follicular lymphoma, diffuse large B-cell lymphoma, chronic lymphocytic leukemia, and immunologic diseases such as rheumatoid arthritis, granulomatosis with polyangiitis, and microscopic polyangiitis.
This approval allows Rixathon to be marketed in the member states of the European Union and Iceland, Liechtenstein, and Norway, members of the European Free Trade Association.
The approval “represents a big win for patients in Europe with blood cancers or immunological diseases,” according to Carol Lynch, global head of Biopharmaceuticals at Sandoz.
“Rixathon will be one of the 5 major launches we plan in the next 4 years,” she said.
Earlier in the year, the European Medicines Agency’s Committee for Medicinal Products for Human Use had recommended marketing authorization for Rixathon.
The EC based its approval on a comprehensive development program generating analytical, preclinical, and clinical data. Clinical studies included ASSIST-RA and ASSIST-FL.
ASSIST-RA demonstrated that the biosimilar product has equivalent pharmacokinetic and pharmacodynamic profiles to the reference medicine, with no clinically meaningful differences in safety, tolerability, or immunogenicity in patients with rheumatoid arthritis.
ASSIST-FL was a phase 3 study confirming efficacy and safety. The study met its primary endpoint of equivalence in overall response rate between the biosimilar product and the reference medicine after 6 months.
ASSIST-FL also confirmed the comparable safety profiles of the 2 medicines.
Sandoz is a division of the Swiss pharmaceutical company Novartis. MabThera is a registered trademark of F. Hoffmann-La-Roche AG.
Another Sandoz biosimilar rituximab has been approved in the EU as Riximyo® under a duplicate marketing authorization. ![]()
Rest dyspnea dims as acute heart failure treatment target
PARIS – During the most recent pharmaceutical generation, drug development for heart failure largely focused on acute heart failure, and specifically on patients with rest dyspnea as the primary manifestation of their acute heart failure decompensation events.
That has now changed, agreed heart failure experts as they debated the upshot of sobering results from two neutral trials that failed to show a midterm mortality benefit in patients hospitalized for acute heart failure who underwent aggressive management of their congestion using 2 days of intravenous treatment with either of two potent vasodilating drugs. Results first reported in November 2016 failed to show a survival benefit from ularitide in the 2,100-patient TRUE-AHF (Efficacy and Safety of Ularitide for the Treatment of Acute Decompensated Heart Failure) trial (N Engl J Med. 2017 May 18;376[20]:1956-64). And results reported at a meeting of the Heart Failure Association of the ESC failed to show a survival benefit from serelaxin in more than 6,500 acute heart failure patients in the RELAX-AHF-2 (Efficacy, Safety and Tolerability of Serelaxin When Added to Standard Therapy in AHF) trial.
The failure of a 2-day infusion of serelaxin to produce a significant reduction in cardiovascular death in RELAX-AHF-2 was especially surprising because the predecessor trial, RELAX-AHF, which randomized only 1,160 patients and used a surrogate endpoint of dyspnea improvement, had shown significant benefit that hinted more clinically meaningful benefits might also result from serelaxin treatment (Lancet. 2013 Jan 5;381[9860]:29-39). The disappointing serelaxin and ularitide results also culminate a series of studies using several different agents or procedures to treat acute decompensated heart failure patients that all failed to produce a reduction in deaths.
“This is a sea change; make no mistake. We will need a more targeted, selective approach. It was always a daunting proposition to believe that short-term infusion could have an effect 6 months later. We were misled by the analogy [of acute heart failure] to acute coronary syndrome,” said Dr. Ruschitzka, professor of medicine at the University of Zürich.
The right time to intervene
Meeting attendees offered several hypotheses to explain why the acute ularitide and serelaxin trials both failed to show a mortality benefit, with timing of treatment the most common denominator.
Acute heart failure “is an event, not a disease,” declared Milton Packer, MD, lead investigator of TRUE-AHF, during a session devoted to vasodilator treatment of acute heart failure. Acute heart failure decompensations “are fluctuations in a chronic disease. It doesn’t matter what you do during the episode – it matters what you do between acute episodes. We focus all our attention on which vasodilator and which dose of Lasix [furosemide], but we send patients home on inadequate chronic therapy. It doesn’t matter what you do to the dyspnea, the shortness of breath will get better. Do we need a new drug that makes dyspnea go away an hour sooner and doesn’t cost a fortune? What really matters is what patients do between acute episodes and how to prevent them, ” said Dr. Packer, distinguished scholar in cardiovascular science at Baylor University Medical Center in Dallas.
Dr. Packer strongly urged clinicians to put heart failure patients on the full regimen of guideline-directed drugs and at full dosages, a step he thinks would go a long way toward preventing a majority of decompensation episodes. “Chronic heart failure treatment has improved dramatically, but implementation is abysmal,” he said.
Of course, at this phase of their disease heart failure patients are usually at home, which more or less demands that the treatments they take are oral or at least delivered by subcutaneous injection.
“We’ve had a mismatch of candidate drugs, which have mostly been IV infusions, with a clinical setting where an IV infusion is challenging to use.”
“We are killing good drugs by the way we’re testing them,” commented Javed Butler, MD, who bemoaned the ignominious outcome of serelaxin treatment in RELAX-AHF-2. “The available data show it makes no sense to treat for just 2 days. We should take true worsening heart failure patients, those who are truly failing standard treatment, and look at new chronic oral therapies to try on them.” Oral drugs similar to serelaxin and ularitide could be used chronically, suggested Dr. Butler, professor of medicine and chief of cardiology at Stony Brook (N.Y.) School of Medicine.
Wrong patients with the wrong presentation
Perhaps just as big a flaw of the acute heart failure trials has been their target patient population, patients with rest dyspnea at the time of admission. “Why do we think that dyspnea is a clinically relevant symptom for acute heart failure?” Dr. Packer asked.
Dr. Cleland and his associates analyzed data on 116,752 hospitalizations for acute heart failure in England and Wales during April 2007–March 2013, a database that included more than 90% of hospitals for these regions. “We found that a large proportion of admitted patients did not have breathlessness at rest as their primary reason for seeking hospitalization. For about half the patients, moderate or severe peripheral edema was the main problem,” he reported. Roughly a third of patients had rest dyspnea as their main symptom.
An unadjusted analysis also showed a stronger link between peripheral edema and the rate of mortality during a median follow-up of about a year following hospitalization, compared with rest dyspnea. Compared with the lowest-risk subgroup, the patients with severe peripheral edema (18% of the population) had more than twice the mortality. In contrast, the patients with the most severe rest dyspnea and no evidence at all of peripheral edema, just 6% of the population, had a 50% higher mortality rate than the lowest-risk patients.
”It’s peripheral edema rather than breathlessness that is the important determinant of length of stay and prognosis. The disastrous neutral trials for acute heart failure have all targeted the breathless subset of patients. Maybe a reason for the failures has been that they’ve been treating a problem that does not exist. The trials have looked at the wrong patients,” Dr. Cleland said.
‘We’ve told the wrong story to industry” about the importance of rest dyspnea to acute heart failure patients. “When we say acute heart failure, we mean an ambulance and oxygen and the emergency department and rapid IV treatment. That’s breathlessness. Patients with peripheral edema usually get driven in and walk from the car to a wheelchair and they wait 4 hours to be seen. I think that, following the TRUE-AHF and RELAX-AHF-2 results, we’ll see a radical change.”
But just because the focus should be on peripheral edema rather than dyspnea, that doesn’t mean better drugs aren’t needed, Dr. Cleland added.
“We need better treatments to deal with congestion. Once a patient is congested, we are not very good at getting rid of it. We depend on diuretics, which we don’t use properly. Ultimately I’d like to see agents as adjuncts to diuretics, to produce better kidney function.” But treatments for breathlessness are decent as they now exist: furosemide plus oxygen. When a simple, cheap drug works 80% of the time, it is really hard to improve on that.” The real unmet needs for treating acute decompensated heart failure are patients with rest dyspnea who don’t respond to conventional treatment, and especially patients with gross peripheral edema plus low blood pressure and renal dysfunction for whom no good treatments have been developed, Dr. Cleland said.
Another flaw in the patient selection criteria for the acute heart failure studies has been the focus on patients with elevated blood pressures, the logical target for vasodilator drugs that lower blood pressure, noted Dr. Felker. “But these are the patients at lowest risk. We’ve had a mismatch between the patients with the biggest need and the patients we actually study, which relates to the types of drugs we’ve developed.”
Acute heart failure remains a target
Despite all the talk of refocusing attention on chronic heart failure and peripheral edema, at least one expert remained steadfast in talking up the importance of new acute interventions.
Part of the problem in believing that existing treatments can adequately manage heart failure and prevent acute decompensations is that about 75% of acute heart failure episodes either occur as the first presentation of heart failure, or occur in patients with heart failure with preserved ejection fraction (HFpEF), a type of heart failure that, until recently, had no chronic drug regimens with widely acknowledged efficacy for HFpEF. (The 2017 U.S. heart failure management guidelines update listed aldosterone receptor antagonists as a class IIb recommendation for treating HFpEF, the first time guidelines have sanctioned a drug class for treating HFpEF [Circulation. 2017 Apr 28. doi: 10.1161/CIR.0000000000000509].)
“For patients with heart failure with reduced ejection fraction, you can give optimal treatments and [decompensations] are prevented,” noted Dr. Mebazaa, a professor of anesthesiology and resuscitation at Lariboisière Hospital in Paris. “But for the huge number of HFpEF patients we have nothing. Acute heart failure will remain prevalent, and we still don’t have the right drugs to use on these patients.”
The TRUE-AHF trial was sponsored by Cardiorentis. RELAX-AHF-2 was sponsored by Novartis. Dr. Ruschitzka has been a speaker on behalf of Novartis, and has been a speaker for or consultant to several companies and was a coinvestigator for TRUE-AHF and received fees from Cardiorentis for his participation. Dr. Packer is a consultant to and stockholder in Cardiorentis and has been a consultant to several other companies. Dr. Felker has been a consultant to Novartis and several other companies and was a coinvestigator on RELAX-AHF-2. Dr. Butler has been a consultant to several companies. Dr. Cleland has received research support from Novartis, and he has been a consultant to and received research support from several other companies. Dr. Mebazaa has received honoraria from Novartis and Cardiorentis as well as from several other companies and was a coinvestigator on TRUE-AHF.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
PARIS – During the most recent pharmaceutical generation, drug development for heart failure largely focused on acute heart failure, and specifically on patients with rest dyspnea as the primary manifestation of their acute heart failure decompensation events.
That has now changed, agreed heart failure experts as they debated the upshot of sobering results from two neutral trials that failed to show a midterm mortality benefit in patients hospitalized for acute heart failure who underwent aggressive management of their congestion using 2 days of intravenous treatment with either of two potent vasodilating drugs. Results first reported in November 2016 failed to show a survival benefit from ularitide in the 2,100-patient TRUE-AHF (Efficacy and Safety of Ularitide for the Treatment of Acute Decompensated Heart Failure) trial (N Engl J Med. 2017 May 18;376[20]:1956-64). And results reported at a meeting of the Heart Failure Association of the ESC failed to show a survival benefit from serelaxin in more than 6,500 acute heart failure patients in the RELAX-AHF-2 (Efficacy, Safety and Tolerability of Serelaxin When Added to Standard Therapy in AHF) trial.
The failure of a 2-day infusion of serelaxin to produce a significant reduction in cardiovascular death in RELAX-AHF-2 was especially surprising because the predecessor trial, RELAX-AHF, which randomized only 1,160 patients and used a surrogate endpoint of dyspnea improvement, had shown significant benefit that hinted more clinically meaningful benefits might also result from serelaxin treatment (Lancet. 2013 Jan 5;381[9860]:29-39). The disappointing serelaxin and ularitide results also culminate a series of studies using several different agents or procedures to treat acute decompensated heart failure patients that all failed to produce a reduction in deaths.
“This is a sea change; make no mistake. We will need a more targeted, selective approach. It was always a daunting proposition to believe that short-term infusion could have an effect 6 months later. We were misled by the analogy [of acute heart failure] to acute coronary syndrome,” said Dr. Ruschitzka, professor of medicine at the University of Zürich.
The right time to intervene
Meeting attendees offered several hypotheses to explain why the acute ularitide and serelaxin trials both failed to show a mortality benefit, with timing of treatment the most common denominator.
Acute heart failure “is an event, not a disease,” declared Milton Packer, MD, lead investigator of TRUE-AHF, during a session devoted to vasodilator treatment of acute heart failure. Acute heart failure decompensations “are fluctuations in a chronic disease. It doesn’t matter what you do during the episode – it matters what you do between acute episodes. We focus all our attention on which vasodilator and which dose of Lasix [furosemide], but we send patients home on inadequate chronic therapy. It doesn’t matter what you do to the dyspnea, the shortness of breath will get better. Do we need a new drug that makes dyspnea go away an hour sooner and doesn’t cost a fortune? What really matters is what patients do between acute episodes and how to prevent them, ” said Dr. Packer, distinguished scholar in cardiovascular science at Baylor University Medical Center in Dallas.
Dr. Packer strongly urged clinicians to put heart failure patients on the full regimen of guideline-directed drugs and at full dosages, a step he thinks would go a long way toward preventing a majority of decompensation episodes. “Chronic heart failure treatment has improved dramatically, but implementation is abysmal,” he said.
Of course, at this phase of their disease heart failure patients are usually at home, which more or less demands that the treatments they take are oral or at least delivered by subcutaneous injection.
“We’ve had a mismatch of candidate drugs, which have mostly been IV infusions, with a clinical setting where an IV infusion is challenging to use.”
“We are killing good drugs by the way we’re testing them,” commented Javed Butler, MD, who bemoaned the ignominious outcome of serelaxin treatment in RELAX-AHF-2. “The available data show it makes no sense to treat for just 2 days. We should take true worsening heart failure patients, those who are truly failing standard treatment, and look at new chronic oral therapies to try on them.” Oral drugs similar to serelaxin and ularitide could be used chronically, suggested Dr. Butler, professor of medicine and chief of cardiology at Stony Brook (N.Y.) School of Medicine.
Wrong patients with the wrong presentation
Perhaps just as big a flaw of the acute heart failure trials has been their target patient population, patients with rest dyspnea at the time of admission. “Why do we think that dyspnea is a clinically relevant symptom for acute heart failure?” Dr. Packer asked.
Dr. Cleland and his associates analyzed data on 116,752 hospitalizations for acute heart failure in England and Wales during April 2007–March 2013, a database that included more than 90% of hospitals for these regions. “We found that a large proportion of admitted patients did not have breathlessness at rest as their primary reason for seeking hospitalization. For about half the patients, moderate or severe peripheral edema was the main problem,” he reported. Roughly a third of patients had rest dyspnea as their main symptom.
An unadjusted analysis also showed a stronger link between peripheral edema and the rate of mortality during a median follow-up of about a year following hospitalization, compared with rest dyspnea. Compared with the lowest-risk subgroup, the patients with severe peripheral edema (18% of the population) had more than twice the mortality. In contrast, the patients with the most severe rest dyspnea and no evidence at all of peripheral edema, just 6% of the population, had a 50% higher mortality rate than the lowest-risk patients.
”It’s peripheral edema rather than breathlessness that is the important determinant of length of stay and prognosis. The disastrous neutral trials for acute heart failure have all targeted the breathless subset of patients. Maybe a reason for the failures has been that they’ve been treating a problem that does not exist. The trials have looked at the wrong patients,” Dr. Cleland said.
‘We’ve told the wrong story to industry” about the importance of rest dyspnea to acute heart failure patients. “When we say acute heart failure, we mean an ambulance and oxygen and the emergency department and rapid IV treatment. That’s breathlessness. Patients with peripheral edema usually get driven in and walk from the car to a wheelchair and they wait 4 hours to be seen. I think that, following the TRUE-AHF and RELAX-AHF-2 results, we’ll see a radical change.”
But just because the focus should be on peripheral edema rather than dyspnea, that doesn’t mean better drugs aren’t needed, Dr. Cleland added.
“We need better treatments to deal with congestion. Once a patient is congested, we are not very good at getting rid of it. We depend on diuretics, which we don’t use properly. Ultimately I’d like to see agents as adjuncts to diuretics, to produce better kidney function.” But treatments for breathlessness are decent as they now exist: furosemide plus oxygen. When a simple, cheap drug works 80% of the time, it is really hard to improve on that.” The real unmet needs for treating acute decompensated heart failure are patients with rest dyspnea who don’t respond to conventional treatment, and especially patients with gross peripheral edema plus low blood pressure and renal dysfunction for whom no good treatments have been developed, Dr. Cleland said.
Another flaw in the patient selection criteria for the acute heart failure studies has been the focus on patients with elevated blood pressures, the logical target for vasodilator drugs that lower blood pressure, noted Dr. Felker. “But these are the patients at lowest risk. We’ve had a mismatch between the patients with the biggest need and the patients we actually study, which relates to the types of drugs we’ve developed.”
Acute heart failure remains a target
Despite all the talk of refocusing attention on chronic heart failure and peripheral edema, at least one expert remained steadfast in talking up the importance of new acute interventions.
Part of the problem in believing that existing treatments can adequately manage heart failure and prevent acute decompensations is that about 75% of acute heart failure episodes either occur as the first presentation of heart failure, or occur in patients with heart failure with preserved ejection fraction (HFpEF), a type of heart failure that, until recently, had no chronic drug regimens with widely acknowledged efficacy for HFpEF. (The 2017 U.S. heart failure management guidelines update listed aldosterone receptor antagonists as a class IIb recommendation for treating HFpEF, the first time guidelines have sanctioned a drug class for treating HFpEF [Circulation. 2017 Apr 28. doi: 10.1161/CIR.0000000000000509].)
“For patients with heart failure with reduced ejection fraction, you can give optimal treatments and [decompensations] are prevented,” noted Dr. Mebazaa, a professor of anesthesiology and resuscitation at Lariboisière Hospital in Paris. “But for the huge number of HFpEF patients we have nothing. Acute heart failure will remain prevalent, and we still don’t have the right drugs to use on these patients.”
The TRUE-AHF trial was sponsored by Cardiorentis. RELAX-AHF-2 was sponsored by Novartis. Dr. Ruschitzka has been a speaker on behalf of Novartis, and has been a speaker for or consultant to several companies and was a coinvestigator for TRUE-AHF and received fees from Cardiorentis for his participation. Dr. Packer is a consultant to and stockholder in Cardiorentis and has been a consultant to several other companies. Dr. Felker has been a consultant to Novartis and several other companies and was a coinvestigator on RELAX-AHF-2. Dr. Butler has been a consultant to several companies. Dr. Cleland has received research support from Novartis, and he has been a consultant to and received research support from several other companies. Dr. Mebazaa has received honoraria from Novartis and Cardiorentis as well as from several other companies and was a coinvestigator on TRUE-AHF.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
PARIS – During the most recent pharmaceutical generation, drug development for heart failure largely focused on acute heart failure, and specifically on patients with rest dyspnea as the primary manifestation of their acute heart failure decompensation events.
That has now changed, agreed heart failure experts as they debated the upshot of sobering results from two neutral trials that failed to show a midterm mortality benefit in patients hospitalized for acute heart failure who underwent aggressive management of their congestion using 2 days of intravenous treatment with either of two potent vasodilating drugs. Results first reported in November 2016 failed to show a survival benefit from ularitide in the 2,100-patient TRUE-AHF (Efficacy and Safety of Ularitide for the Treatment of Acute Decompensated Heart Failure) trial (N Engl J Med. 2017 May 18;376[20]:1956-64). And results reported at a meeting of the Heart Failure Association of the ESC failed to show a survival benefit from serelaxin in more than 6,500 acute heart failure patients in the RELAX-AHF-2 (Efficacy, Safety and Tolerability of Serelaxin When Added to Standard Therapy in AHF) trial.
The failure of a 2-day infusion of serelaxin to produce a significant reduction in cardiovascular death in RELAX-AHF-2 was especially surprising because the predecessor trial, RELAX-AHF, which randomized only 1,160 patients and used a surrogate endpoint of dyspnea improvement, had shown significant benefit that hinted more clinically meaningful benefits might also result from serelaxin treatment (Lancet. 2013 Jan 5;381[9860]:29-39). The disappointing serelaxin and ularitide results also culminate a series of studies using several different agents or procedures to treat acute decompensated heart failure patients that all failed to produce a reduction in deaths.
“This is a sea change; make no mistake. We will need a more targeted, selective approach. It was always a daunting proposition to believe that short-term infusion could have an effect 6 months later. We were misled by the analogy [of acute heart failure] to acute coronary syndrome,” said Dr. Ruschitzka, professor of medicine at the University of Zürich.
The right time to intervene
Meeting attendees offered several hypotheses to explain why the acute ularitide and serelaxin trials both failed to show a mortality benefit, with timing of treatment the most common denominator.
Acute heart failure “is an event, not a disease,” declared Milton Packer, MD, lead investigator of TRUE-AHF, during a session devoted to vasodilator treatment of acute heart failure. Acute heart failure decompensations “are fluctuations in a chronic disease. It doesn’t matter what you do during the episode – it matters what you do between acute episodes. We focus all our attention on which vasodilator and which dose of Lasix [furosemide], but we send patients home on inadequate chronic therapy. It doesn’t matter what you do to the dyspnea, the shortness of breath will get better. Do we need a new drug that makes dyspnea go away an hour sooner and doesn’t cost a fortune? What really matters is what patients do between acute episodes and how to prevent them, ” said Dr. Packer, distinguished scholar in cardiovascular science at Baylor University Medical Center in Dallas.
Dr. Packer strongly urged clinicians to put heart failure patients on the full regimen of guideline-directed drugs and at full dosages, a step he thinks would go a long way toward preventing a majority of decompensation episodes. “Chronic heart failure treatment has improved dramatically, but implementation is abysmal,” he said.
Of course, at this phase of their disease heart failure patients are usually at home, which more or less demands that the treatments they take are oral or at least delivered by subcutaneous injection.
“We’ve had a mismatch of candidate drugs, which have mostly been IV infusions, with a clinical setting where an IV infusion is challenging to use.”
“We are killing good drugs by the way we’re testing them,” commented Javed Butler, MD, who bemoaned the ignominious outcome of serelaxin treatment in RELAX-AHF-2. “The available data show it makes no sense to treat for just 2 days. We should take true worsening heart failure patients, those who are truly failing standard treatment, and look at new chronic oral therapies to try on them.” Oral drugs similar to serelaxin and ularitide could be used chronically, suggested Dr. Butler, professor of medicine and chief of cardiology at Stony Brook (N.Y.) School of Medicine.
Wrong patients with the wrong presentation
Perhaps just as big a flaw of the acute heart failure trials has been their target patient population, patients with rest dyspnea at the time of admission. “Why do we think that dyspnea is a clinically relevant symptom for acute heart failure?” Dr. Packer asked.
Dr. Cleland and his associates analyzed data on 116,752 hospitalizations for acute heart failure in England and Wales during April 2007–March 2013, a database that included more than 90% of hospitals for these regions. “We found that a large proportion of admitted patients did not have breathlessness at rest as their primary reason for seeking hospitalization. For about half the patients, moderate or severe peripheral edema was the main problem,” he reported. Roughly a third of patients had rest dyspnea as their main symptom.
An unadjusted analysis also showed a stronger link between peripheral edema and the rate of mortality during a median follow-up of about a year following hospitalization, compared with rest dyspnea. Compared with the lowest-risk subgroup, the patients with severe peripheral edema (18% of the population) had more than twice the mortality. In contrast, the patients with the most severe rest dyspnea and no evidence at all of peripheral edema, just 6% of the population, had a 50% higher mortality rate than the lowest-risk patients.
”It’s peripheral edema rather than breathlessness that is the important determinant of length of stay and prognosis. The disastrous neutral trials for acute heart failure have all targeted the breathless subset of patients. Maybe a reason for the failures has been that they’ve been treating a problem that does not exist. The trials have looked at the wrong patients,” Dr. Cleland said.
‘We’ve told the wrong story to industry” about the importance of rest dyspnea to acute heart failure patients. “When we say acute heart failure, we mean an ambulance and oxygen and the emergency department and rapid IV treatment. That’s breathlessness. Patients with peripheral edema usually get driven in and walk from the car to a wheelchair and they wait 4 hours to be seen. I think that, following the TRUE-AHF and RELAX-AHF-2 results, we’ll see a radical change.”
But just because the focus should be on peripheral edema rather than dyspnea, that doesn’t mean better drugs aren’t needed, Dr. Cleland added.
“We need better treatments to deal with congestion. Once a patient is congested, we are not very good at getting rid of it. We depend on diuretics, which we don’t use properly. Ultimately I’d like to see agents as adjuncts to diuretics, to produce better kidney function.” But treatments for breathlessness are decent as they now exist: furosemide plus oxygen. When a simple, cheap drug works 80% of the time, it is really hard to improve on that.” The real unmet needs for treating acute decompensated heart failure are patients with rest dyspnea who don’t respond to conventional treatment, and especially patients with gross peripheral edema plus low blood pressure and renal dysfunction for whom no good treatments have been developed, Dr. Cleland said.
Another flaw in the patient selection criteria for the acute heart failure studies has been the focus on patients with elevated blood pressures, the logical target for vasodilator drugs that lower blood pressure, noted Dr. Felker. “But these are the patients at lowest risk. We’ve had a mismatch between the patients with the biggest need and the patients we actually study, which relates to the types of drugs we’ve developed.”
Acute heart failure remains a target
Despite all the talk of refocusing attention on chronic heart failure and peripheral edema, at least one expert remained steadfast in talking up the importance of new acute interventions.
Part of the problem in believing that existing treatments can adequately manage heart failure and prevent acute decompensations is that about 75% of acute heart failure episodes either occur as the first presentation of heart failure, or occur in patients with heart failure with preserved ejection fraction (HFpEF), a type of heart failure that, until recently, had no chronic drug regimens with widely acknowledged efficacy for HFpEF. (The 2017 U.S. heart failure management guidelines update listed aldosterone receptor antagonists as a class IIb recommendation for treating HFpEF, the first time guidelines have sanctioned a drug class for treating HFpEF [Circulation. 2017 Apr 28. doi: 10.1161/CIR.0000000000000509].)
“For patients with heart failure with reduced ejection fraction, you can give optimal treatments and [decompensations] are prevented,” noted Dr. Mebazaa, a professor of anesthesiology and resuscitation at Lariboisière Hospital in Paris. “But for the huge number of HFpEF patients we have nothing. Acute heart failure will remain prevalent, and we still don’t have the right drugs to use on these patients.”
The TRUE-AHF trial was sponsored by Cardiorentis. RELAX-AHF-2 was sponsored by Novartis. Dr. Ruschitzka has been a speaker on behalf of Novartis, and has been a speaker for or consultant to several companies and was a coinvestigator for TRUE-AHF and received fees from Cardiorentis for his participation. Dr. Packer is a consultant to and stockholder in Cardiorentis and has been a consultant to several other companies. Dr. Felker has been a consultant to Novartis and several other companies and was a coinvestigator on RELAX-AHF-2. Dr. Butler has been a consultant to several companies. Dr. Cleland has received research support from Novartis, and he has been a consultant to and received research support from several other companies. Dr. Mebazaa has received honoraria from Novartis and Cardiorentis as well as from several other companies and was a coinvestigator on TRUE-AHF.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM HEART FAILURE 2017