User login
Vaccine delivery costs challenge physicians
, reported Mandy A. Allison, MD, of the University of Colorado at Denver, Aurora, and her associates.
Using the American Academy of Pediatrics’ recommended level of payment for first vaccine administration at that time – $25 – more than three-quarters of the practices surveyed said that all payer types paid less than the cost of vaccine administration, the researchers noted.
Those reporting that payment for vaccine administration was $11 or more was 74% for FFS, 74% for PPOs, 57% for MCOs/HMOs, 37% for CHIP, and 34% for Medicaid, the investigators reported.
In terms of how profit margins for vaccine delivery had changed in the last 3 years, an increase was reported by 25% of pediatric practices (Ped) and 15% of family physician practices (FP), no change was reported by 38% of Ped and 49% of FP, and a decrease by 37% of Ped and 36% of FP practices.
Of those practices that used strategies to reduce vaccine purchase cost or increase payment, 81% Ped and 36% FP used online purchasing discounts, 78% Ped and 49% FP used prompt pay discounts, 65% Ped and 49% FP used bulk order discounts, 69% Ped and 42% FP used group purchasing, and 69% Ped and 33% FP used promotional pricing.
Fewer than half of the practices said that they negotiated with private insurers regarding payment for vaccines (44% Ped, 33% FP) and administration fees (44% Ped, 35% FP).
When asked if they had stopped purchasing one or more pediatric vaccines for financial reasons, the answer was “yes” for 12% of Ped and 23% of FP, “no, but have seriously considered” for 24% of Ped and 26% of FP, and “no” for 64% of Ped and 51% of FP, reported Dr. Allison and her colleagues.
Read more in Academic Pediatrics (2017. doi: 10.1016/j.acap.2017.06.001).
, reported Mandy A. Allison, MD, of the University of Colorado at Denver, Aurora, and her associates.
Using the American Academy of Pediatrics’ recommended level of payment for first vaccine administration at that time – $25 – more than three-quarters of the practices surveyed said that all payer types paid less than the cost of vaccine administration, the researchers noted.
Those reporting that payment for vaccine administration was $11 or more was 74% for FFS, 74% for PPOs, 57% for MCOs/HMOs, 37% for CHIP, and 34% for Medicaid, the investigators reported.
In terms of how profit margins for vaccine delivery had changed in the last 3 years, an increase was reported by 25% of pediatric practices (Ped) and 15% of family physician practices (FP), no change was reported by 38% of Ped and 49% of FP, and a decrease by 37% of Ped and 36% of FP practices.
Of those practices that used strategies to reduce vaccine purchase cost or increase payment, 81% Ped and 36% FP used online purchasing discounts, 78% Ped and 49% FP used prompt pay discounts, 65% Ped and 49% FP used bulk order discounts, 69% Ped and 42% FP used group purchasing, and 69% Ped and 33% FP used promotional pricing.
Fewer than half of the practices said that they negotiated with private insurers regarding payment for vaccines (44% Ped, 33% FP) and administration fees (44% Ped, 35% FP).
When asked if they had stopped purchasing one or more pediatric vaccines for financial reasons, the answer was “yes” for 12% of Ped and 23% of FP, “no, but have seriously considered” for 24% of Ped and 26% of FP, and “no” for 64% of Ped and 51% of FP, reported Dr. Allison and her colleagues.
Read more in Academic Pediatrics (2017. doi: 10.1016/j.acap.2017.06.001).
, reported Mandy A. Allison, MD, of the University of Colorado at Denver, Aurora, and her associates.
Using the American Academy of Pediatrics’ recommended level of payment for first vaccine administration at that time – $25 – more than three-quarters of the practices surveyed said that all payer types paid less than the cost of vaccine administration, the researchers noted.
Those reporting that payment for vaccine administration was $11 or more was 74% for FFS, 74% for PPOs, 57% for MCOs/HMOs, 37% for CHIP, and 34% for Medicaid, the investigators reported.
In terms of how profit margins for vaccine delivery had changed in the last 3 years, an increase was reported by 25% of pediatric practices (Ped) and 15% of family physician practices (FP), no change was reported by 38% of Ped and 49% of FP, and a decrease by 37% of Ped and 36% of FP practices.
Of those practices that used strategies to reduce vaccine purchase cost or increase payment, 81% Ped and 36% FP used online purchasing discounts, 78% Ped and 49% FP used prompt pay discounts, 65% Ped and 49% FP used bulk order discounts, 69% Ped and 42% FP used group purchasing, and 69% Ped and 33% FP used promotional pricing.
Fewer than half of the practices said that they negotiated with private insurers regarding payment for vaccines (44% Ped, 33% FP) and administration fees (44% Ped, 35% FP).
When asked if they had stopped purchasing one or more pediatric vaccines for financial reasons, the answer was “yes” for 12% of Ped and 23% of FP, “no, but have seriously considered” for 24% of Ped and 26% of FP, and “no” for 64% of Ped and 51% of FP, reported Dr. Allison and her colleagues.
Read more in Academic Pediatrics (2017. doi: 10.1016/j.acap.2017.06.001).
FROM ACADEMIC PEDIATRICS
Painful Necrotic Ulcer on the Vulva
The Diagnosis: Mucormycosis
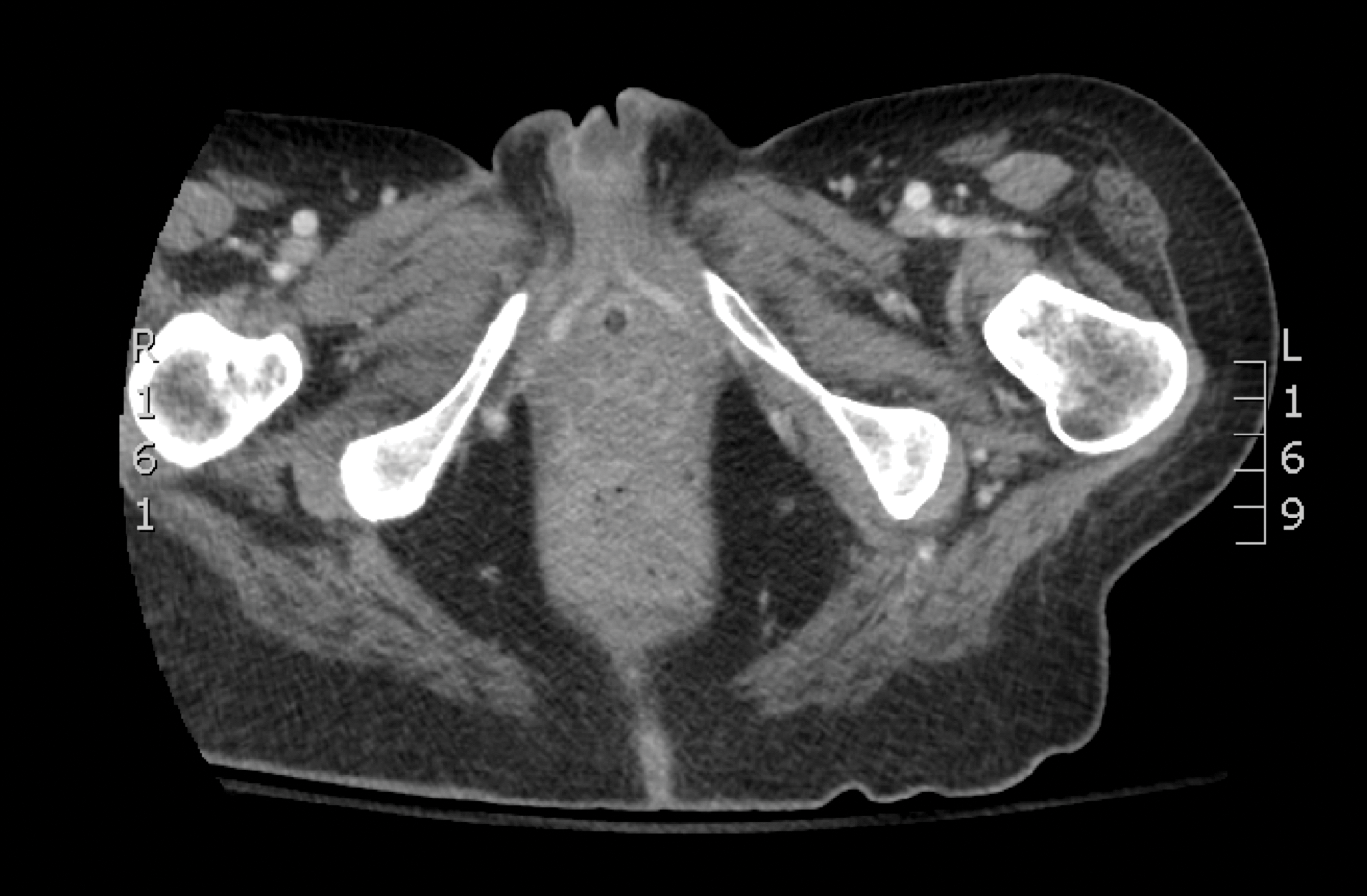
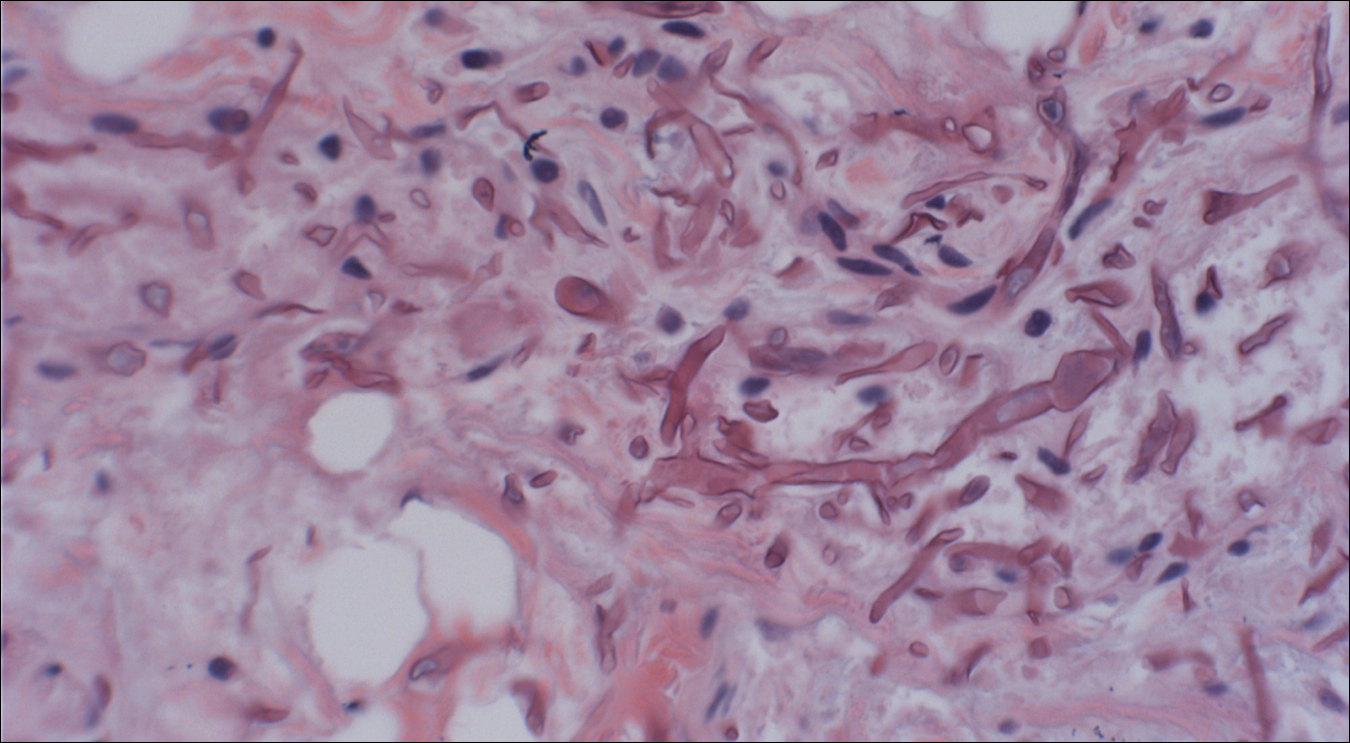
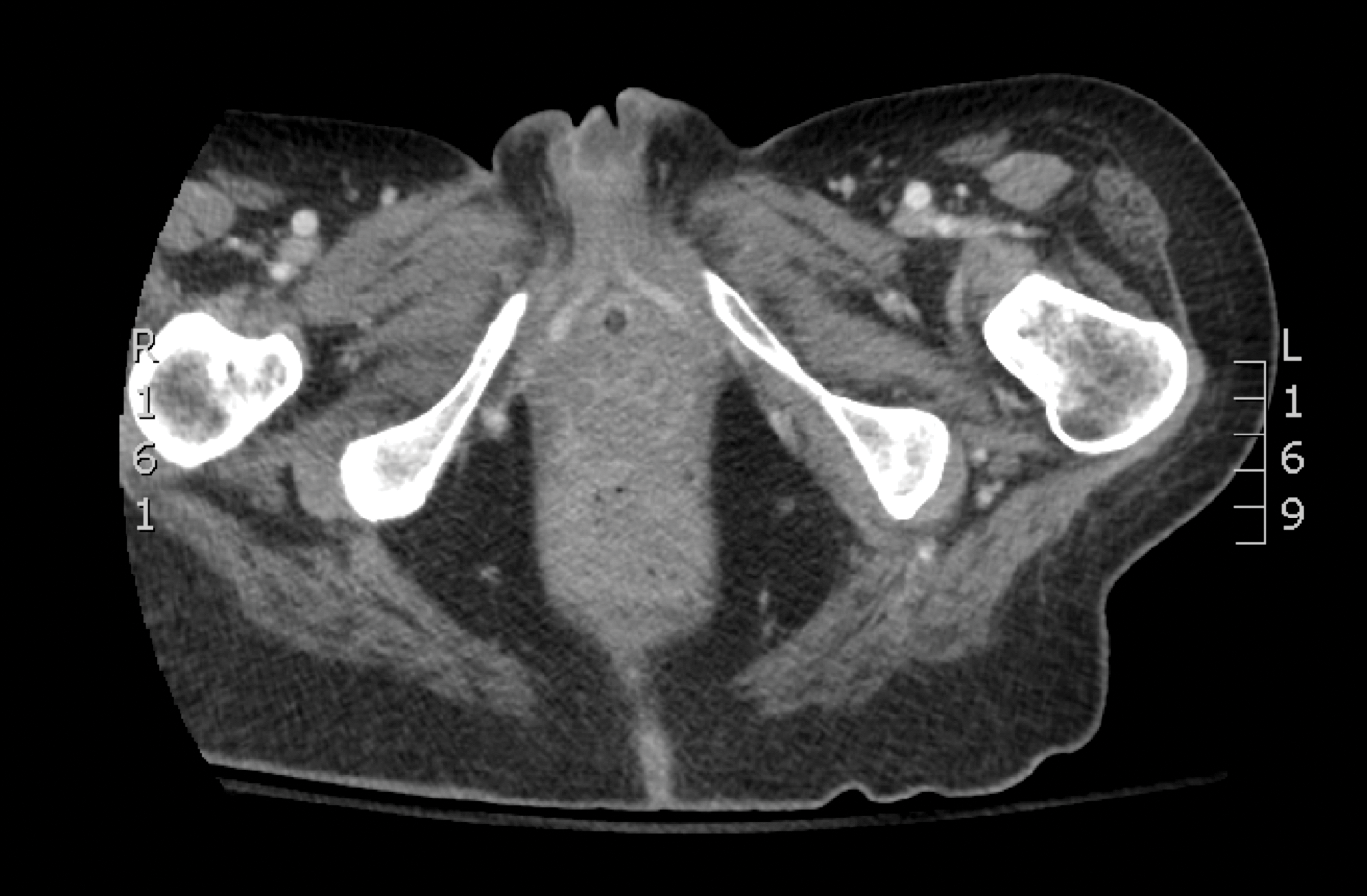
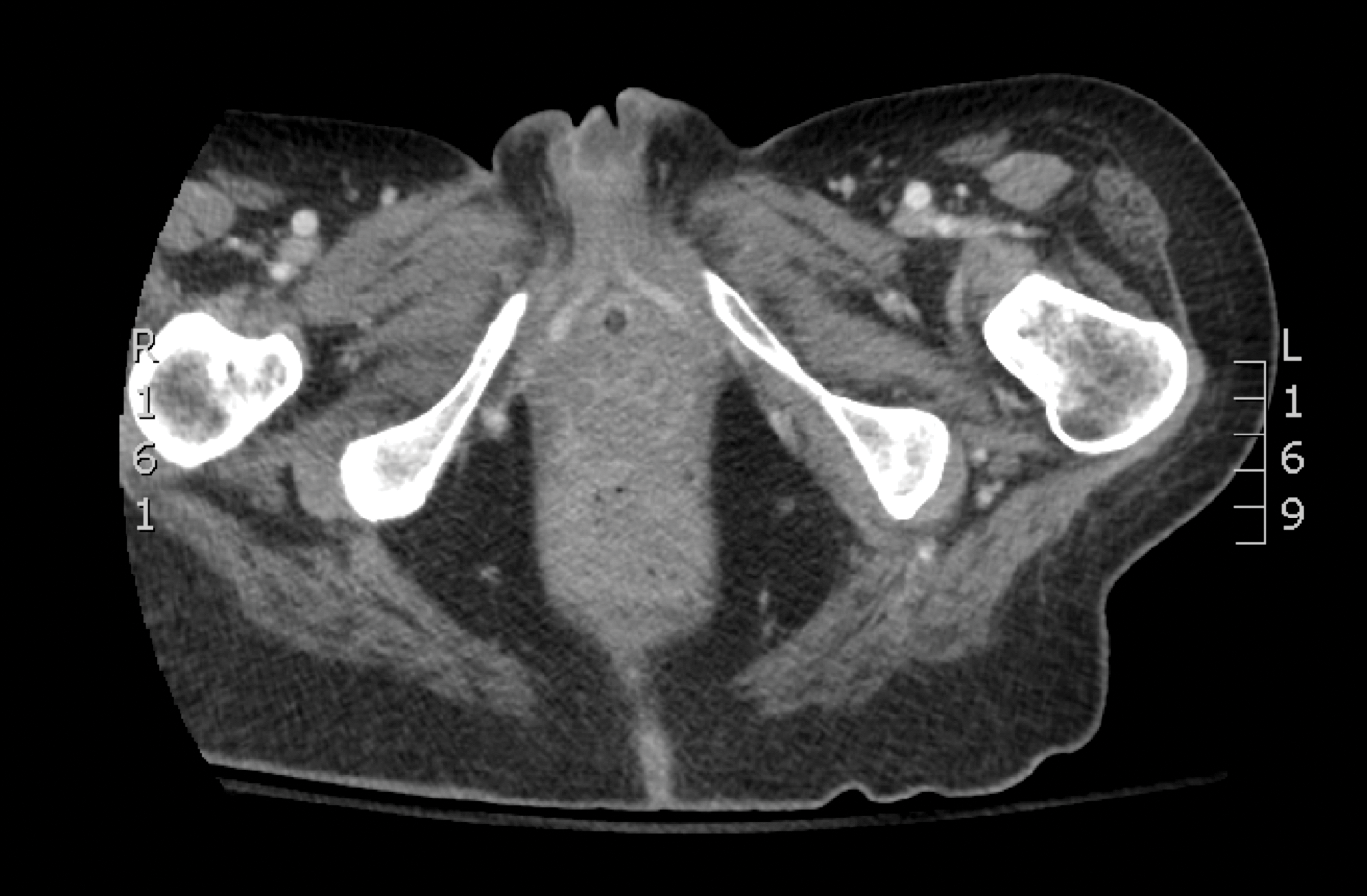
Skin biopsy and histology revealed broad, wide-angle, branched, nonseptate hyphae suggestive of mucormycosis infection (Figure 1). Computed tomography of the abdomen and pelvis revealed marked stranding in the vulvar region and urothelial thickening and enhancement suggestive of infection (Figure 2). Computed tomography of the chest demonstrated multiple irregular nodules in the bilateral upper lobes consistent with disseminated mucormycosis (Figure 3). The patient was started on intravenous amphotericin B and posaconazole. Surgery was not pursued given the poor prognosis of her refractory acute lymphoblastic leukemia, pancytopenia, and disseminated fungal infection. The patient was discharged home with hospice care.
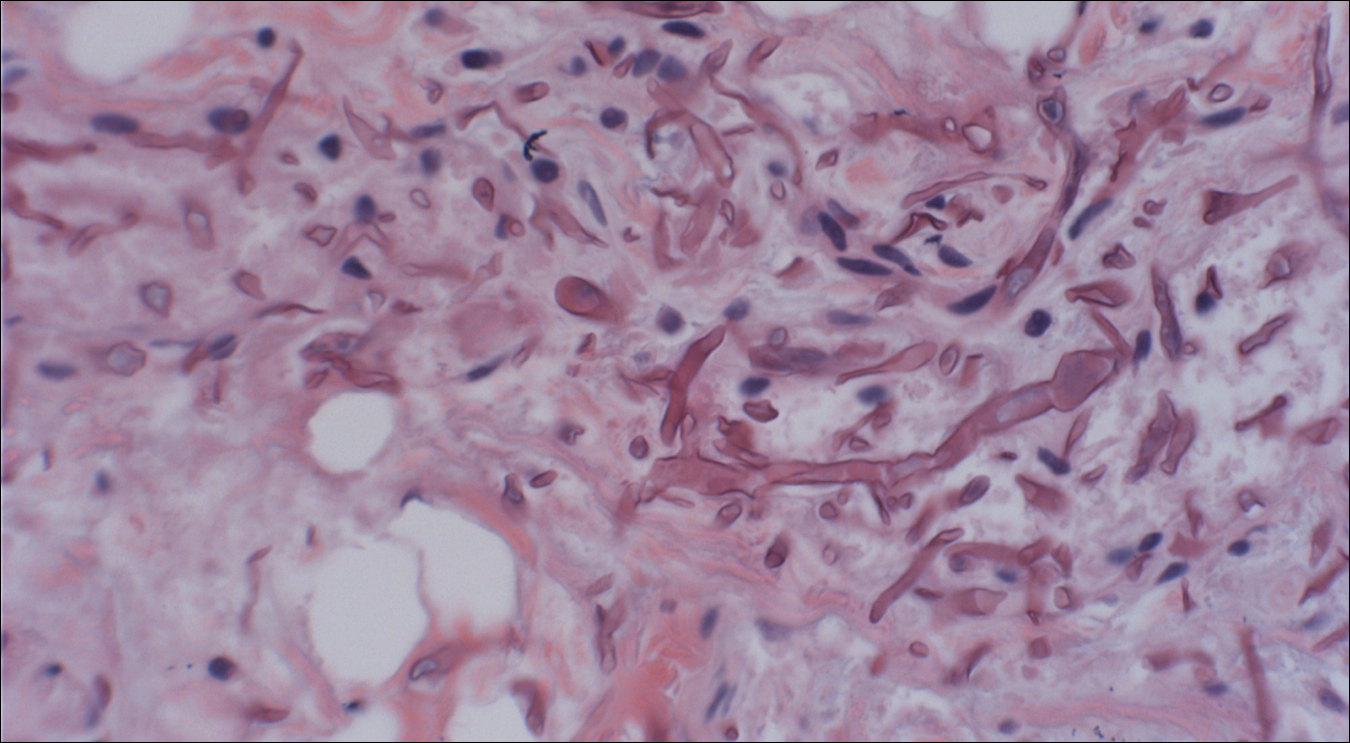

Mucormycosis is an infection caused by fungi that belong to the order Mucorales. The most common genera responsible for human disease are Rhizopus, Mucor, and Rhizomucor, which are organisms ubiquitous in nature and found in soil.1 Mucorales hyphae are widely branched and primarily nonseptate, which distinguishes them from hyphae of ascomycetous molds such as Aspergillus, which are narrowly branched and septate.
Mucormycosis primarily affects immunocompromised individuals. The overall incidence of mucormycosis is difficult to estimate, and the risk for infection varies based on the patient population. For example, the incidence of mucormycosis in hematologic malignancy ranges from 1% to 8% and from 0.4% to 16.0% in solid organ transplant recipients.2 One large series of 929 cases noted that the most common risk factors were associated with impaired immune function including diabetes mellitus and diabetic ketoacidosis (36% of cases), hematologic malignancy (17%), and solid organ (7%) or bone marrow transplantation (5%). Other risk factors include neutropenia, steroid therapy, and other immunocompromising conditions.3 Healthy individuals have a strong natural immunity to mucormycosis and rarely are affected by the disease.2
The host response to Mucorales is primarily driven by phagocyte-mediated killing via oxidative metabolites and cationic peptides called defensins.1 Thus, severely neutropenic patients are at high risk for developing mucormycosis.1 In contrast, it appears as though AIDS patients are not at increased risk for mucormycosis, supporting the theory that T lymphocytes are not involved in the host response.1 The conditions of diabetic ketoacidosis leave patients susceptible to mucormycosis for several reasons. First, hyperglycemia and low pH induce phagocyte dysfunction and thus inhibit the host response to Mucorales.4 Second, these organisms have an active ketone reductase system that may allow them to grow more readily in high glucose, acidic conditions.1 Third, diabetic ketoacidosis conditions increase serum free iron, and Mucorales utilizes host iron for cell growth and development.1 Individuals such as hemodialysis patients receiving the iron chelator deferoxamine also are at risk for mucormycosis, as Rhizopus can bind to this molecule and transport the bound iron intracellularly for growth utilization.1
Mucormycosis infection is characterized by infarction and rapid necrosis of host tissues resulting from vascular infiltration by fungal hyphae. The most common site of infection is rhino-orbital-cerebral (39%), followed by lungs (24%) and skin (19%).3 Dissemination occurs in 23% of cases.3 Inoculation most commonly occurs via inhalation of airborne fungal spores by an immunocompromised host with resultant fungal proliferation in the paranasal sinuses, bronchioles, or alveoli. Gastrointestinal tract infection is presumed to occur via ingestion of spores.5
Cutaneous infection, as in our patient, occurs via the inoculation of spores into the dermis through breaks in the skin such as from intravenous lines, urinary catheters, injection sites, surgical sites, and traumatic wounds. Cutaneous infections typically present as a single erythematous, painful, indurated papule that rapidly progresses to a necrotic ulcer with overlying black eschar. In some cases, the progression may be more indolent over the course of several weeks.2 There are few reported cases of primary vulvar mucormycosis, as in our patient.6,7 The previously reported cases involved severely immunocompromised patients who developed large necrotic lesions over the vulva that demonstrated widely branching, nonseptate hyphae on histologic examination. Each patient required extensive surgical debridement with systemic antifungal treatment.6,7
A timely diagnosis of mucormycosis often hinges on a high index of suspicion on behalf of the clinician. A fungal etiology always should be considered for an infection in an immunocompromised patient. Furthermore, nonresponse to antibiotic treatment should be an important diagnostic clue that the infection could be fungal in origin. The definitive diagnosis of mucormycosis is confirmed by tissue biopsy and the presence of broad, widely branching, nonseptate hyphae seen on histopathologic examination.
Treatment involves aggressive surgical debridement of all necrotic tissues and elimination of predisposing factors for infection such as hyperglycemia, metabolic acidosis, deferoxamine administration, and immunosuppressive medications. Early initiation of antifungal therapy with the lipid formulation of amphotericin B is recommended. Oral posaconazole or isavuconazole typically are used as step-down therapy after a favorable clinical response with initial amphotericin B treatment. Deferasirox, in contrast to deferoxamine, is an iron chelator that may reduce the pathogenicity of Mucorales and may help as an adjunctive therapy.8 In addition, hyperbaric oxygen therapy may have limited benefit in some cases.9 In spite of these treatments, the overall mortality of mucormycosis is 50% or higher and approaches nearly 100% in cases of disseminated disease, such as in our patient.1,3
- Ibrahim AS, Spellberg B, Walsh TJ, et al. Pathogenesis of mucormycosis. Clin Infect Dis. 2012;54(suppl 1):S16-S22.
- Petrikkos G, Skiada A, Lortholary O, et al. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 2012;54(suppl 1):S23-S34.
- Roden MM, Zaoutis TE, Buchanan WL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41:634-653.
- Chinn RY, Diamond RD. Generation of chemotactic factors by Rhizopus oryzae in the presence and absence of serum: relationship to hyphal damage mediated by human neutrophils and effects of hyperglycemia and ketoacidosis. Infect Immun. 1982;38:1123-1129.
- Cheng VC, Chan JF, Ngan AH, et al. Outbreak of intestinal infection due to Rhizopus microsporus [published online July 29, 2009]. J Clin Microbiol. 2009;47:2834-2843.
- Colon M, Romaguera J, Mendez K, et al. Mucormycosis of the vulva in an immunocompromised pediatric patient. Bol Asoc Med P R. 2013;105:65-67.
- Nomura J, Ruskin J, Sahebi F, et al. Mucormycosis of the vulva following bone marrow transplantation. Bone Marrow Transplant. 1997;19:859-860.
- Spellberg B, Andes D, Perez M, et al. Safety and outcomes of open-label deferasirox iron chelation therapy for mucormycosis. Antimicrob Agents Chemother. 2009;53:3122-3125.
- Ferguson BJ, Mitchell TG, Moon R, et al. Adjunctive hyperbaric oxygen for treatment of rhinocerebral mucormycosis. Rev Infect Dis. 1988;10:551-559.
The Diagnosis: Mucormycosis
Skin biopsy and histology revealed broad, wide-angle, branched, nonseptate hyphae suggestive of mucormycosis infection (Figure 1). Computed tomography of the abdomen and pelvis revealed marked stranding in the vulvar region and urothelial thickening and enhancement suggestive of infection (Figure 2). Computed tomography of the chest demonstrated multiple irregular nodules in the bilateral upper lobes consistent with disseminated mucormycosis (Figure 3). The patient was started on intravenous amphotericin B and posaconazole. Surgery was not pursued given the poor prognosis of her refractory acute lymphoblastic leukemia, pancytopenia, and disseminated fungal infection. The patient was discharged home with hospice care.

Mucormycosis is an infection caused by fungi that belong to the order Mucorales. The most common genera responsible for human disease are Rhizopus, Mucor, and Rhizomucor, which are organisms ubiquitous in nature and found in soil.1 Mucorales hyphae are widely branched and primarily nonseptate, which distinguishes them from hyphae of ascomycetous molds such as Aspergillus, which are narrowly branched and septate.
Mucormycosis primarily affects immunocompromised individuals. The overall incidence of mucormycosis is difficult to estimate, and the risk for infection varies based on the patient population. For example, the incidence of mucormycosis in hematologic malignancy ranges from 1% to 8% and from 0.4% to 16.0% in solid organ transplant recipients.2 One large series of 929 cases noted that the most common risk factors were associated with impaired immune function including diabetes mellitus and diabetic ketoacidosis (36% of cases), hematologic malignancy (17%), and solid organ (7%) or bone marrow transplantation (5%). Other risk factors include neutropenia, steroid therapy, and other immunocompromising conditions.3 Healthy individuals have a strong natural immunity to mucormycosis and rarely are affected by the disease.2
The host response to Mucorales is primarily driven by phagocyte-mediated killing via oxidative metabolites and cationic peptides called defensins.1 Thus, severely neutropenic patients are at high risk for developing mucormycosis.1 In contrast, it appears as though AIDS patients are not at increased risk for mucormycosis, supporting the theory that T lymphocytes are not involved in the host response.1 The conditions of diabetic ketoacidosis leave patients susceptible to mucormycosis for several reasons. First, hyperglycemia and low pH induce phagocyte dysfunction and thus inhibit the host response to Mucorales.4 Second, these organisms have an active ketone reductase system that may allow them to grow more readily in high glucose, acidic conditions.1 Third, diabetic ketoacidosis conditions increase serum free iron, and Mucorales utilizes host iron for cell growth and development.1 Individuals such as hemodialysis patients receiving the iron chelator deferoxamine also are at risk for mucormycosis, as Rhizopus can bind to this molecule and transport the bound iron intracellularly for growth utilization.1
Mucormycosis infection is characterized by infarction and rapid necrosis of host tissues resulting from vascular infiltration by fungal hyphae. The most common site of infection is rhino-orbital-cerebral (39%), followed by lungs (24%) and skin (19%).3 Dissemination occurs in 23% of cases.3 Inoculation most commonly occurs via inhalation of airborne fungal spores by an immunocompromised host with resultant fungal proliferation in the paranasal sinuses, bronchioles, or alveoli. Gastrointestinal tract infection is presumed to occur via ingestion of spores.5
Cutaneous infection, as in our patient, occurs via the inoculation of spores into the dermis through breaks in the skin such as from intravenous lines, urinary catheters, injection sites, surgical sites, and traumatic wounds. Cutaneous infections typically present as a single erythematous, painful, indurated papule that rapidly progresses to a necrotic ulcer with overlying black eschar. In some cases, the progression may be more indolent over the course of several weeks.2 There are few reported cases of primary vulvar mucormycosis, as in our patient.6,7 The previously reported cases involved severely immunocompromised patients who developed large necrotic lesions over the vulva that demonstrated widely branching, nonseptate hyphae on histologic examination. Each patient required extensive surgical debridement with systemic antifungal treatment.6,7
A timely diagnosis of mucormycosis often hinges on a high index of suspicion on behalf of the clinician. A fungal etiology always should be considered for an infection in an immunocompromised patient. Furthermore, nonresponse to antibiotic treatment should be an important diagnostic clue that the infection could be fungal in origin. The definitive diagnosis of mucormycosis is confirmed by tissue biopsy and the presence of broad, widely branching, nonseptate hyphae seen on histopathologic examination.
Treatment involves aggressive surgical debridement of all necrotic tissues and elimination of predisposing factors for infection such as hyperglycemia, metabolic acidosis, deferoxamine administration, and immunosuppressive medications. Early initiation of antifungal therapy with the lipid formulation of amphotericin B is recommended. Oral posaconazole or isavuconazole typically are used as step-down therapy after a favorable clinical response with initial amphotericin B treatment. Deferasirox, in contrast to deferoxamine, is an iron chelator that may reduce the pathogenicity of Mucorales and may help as an adjunctive therapy.8 In addition, hyperbaric oxygen therapy may have limited benefit in some cases.9 In spite of these treatments, the overall mortality of mucormycosis is 50% or higher and approaches nearly 100% in cases of disseminated disease, such as in our patient.1,3
The Diagnosis: Mucormycosis
Skin biopsy and histology revealed broad, wide-angle, branched, nonseptate hyphae suggestive of mucormycosis infection (Figure 1). Computed tomography of the abdomen and pelvis revealed marked stranding in the vulvar region and urothelial thickening and enhancement suggestive of infection (Figure 2). Computed tomography of the chest demonstrated multiple irregular nodules in the bilateral upper lobes consistent with disseminated mucormycosis (Figure 3). The patient was started on intravenous amphotericin B and posaconazole. Surgery was not pursued given the poor prognosis of her refractory acute lymphoblastic leukemia, pancytopenia, and disseminated fungal infection. The patient was discharged home with hospice care.
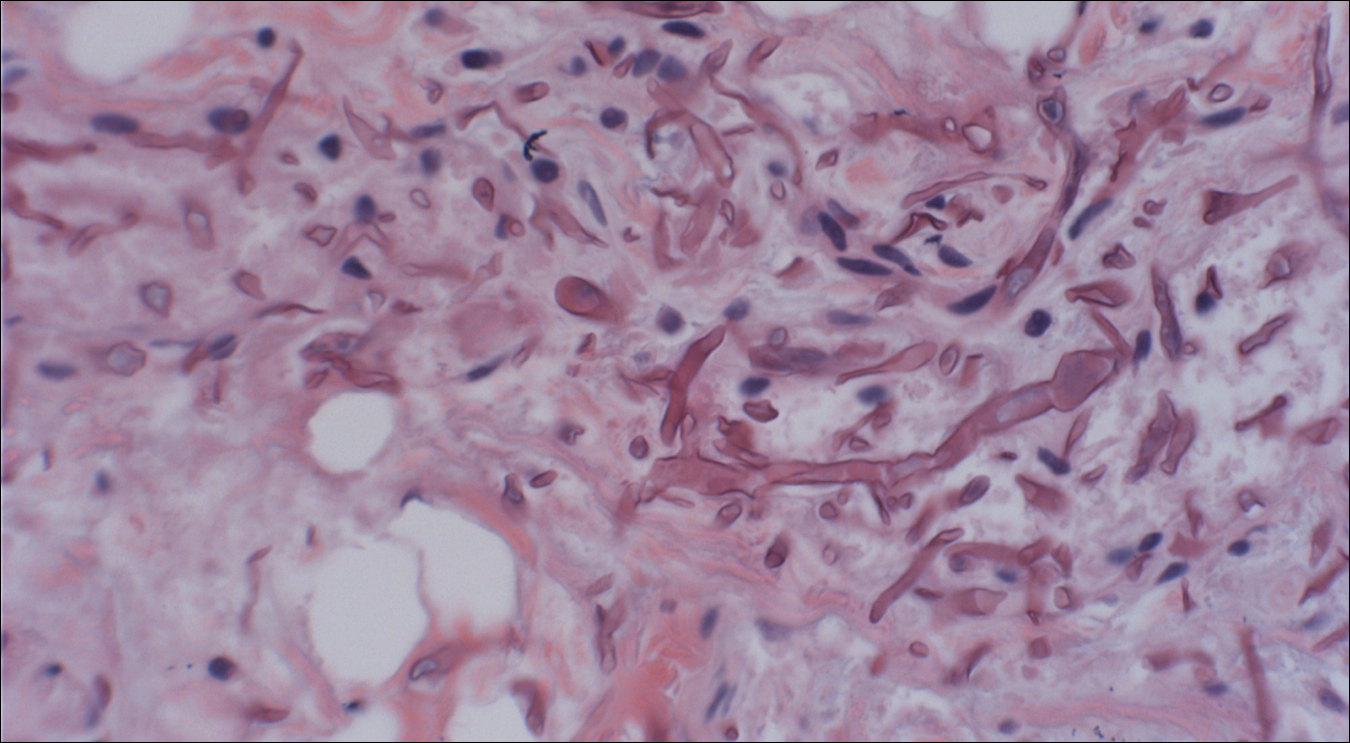

Mucormycosis is an infection caused by fungi that belong to the order Mucorales. The most common genera responsible for human disease are Rhizopus, Mucor, and Rhizomucor, which are organisms ubiquitous in nature and found in soil.1 Mucorales hyphae are widely branched and primarily nonseptate, which distinguishes them from hyphae of ascomycetous molds such as Aspergillus, which are narrowly branched and septate.
Mucormycosis primarily affects immunocompromised individuals. The overall incidence of mucormycosis is difficult to estimate, and the risk for infection varies based on the patient population. For example, the incidence of mucormycosis in hematologic malignancy ranges from 1% to 8% and from 0.4% to 16.0% in solid organ transplant recipients.2 One large series of 929 cases noted that the most common risk factors were associated with impaired immune function including diabetes mellitus and diabetic ketoacidosis (36% of cases), hematologic malignancy (17%), and solid organ (7%) or bone marrow transplantation (5%). Other risk factors include neutropenia, steroid therapy, and other immunocompromising conditions.3 Healthy individuals have a strong natural immunity to mucormycosis and rarely are affected by the disease.2
The host response to Mucorales is primarily driven by phagocyte-mediated killing via oxidative metabolites and cationic peptides called defensins.1 Thus, severely neutropenic patients are at high risk for developing mucormycosis.1 In contrast, it appears as though AIDS patients are not at increased risk for mucormycosis, supporting the theory that T lymphocytes are not involved in the host response.1 The conditions of diabetic ketoacidosis leave patients susceptible to mucormycosis for several reasons. First, hyperglycemia and low pH induce phagocyte dysfunction and thus inhibit the host response to Mucorales.4 Second, these organisms have an active ketone reductase system that may allow them to grow more readily in high glucose, acidic conditions.1 Third, diabetic ketoacidosis conditions increase serum free iron, and Mucorales utilizes host iron for cell growth and development.1 Individuals such as hemodialysis patients receiving the iron chelator deferoxamine also are at risk for mucormycosis, as Rhizopus can bind to this molecule and transport the bound iron intracellularly for growth utilization.1
Mucormycosis infection is characterized by infarction and rapid necrosis of host tissues resulting from vascular infiltration by fungal hyphae. The most common site of infection is rhino-orbital-cerebral (39%), followed by lungs (24%) and skin (19%).3 Dissemination occurs in 23% of cases.3 Inoculation most commonly occurs via inhalation of airborne fungal spores by an immunocompromised host with resultant fungal proliferation in the paranasal sinuses, bronchioles, or alveoli. Gastrointestinal tract infection is presumed to occur via ingestion of spores.5
Cutaneous infection, as in our patient, occurs via the inoculation of spores into the dermis through breaks in the skin such as from intravenous lines, urinary catheters, injection sites, surgical sites, and traumatic wounds. Cutaneous infections typically present as a single erythematous, painful, indurated papule that rapidly progresses to a necrotic ulcer with overlying black eschar. In some cases, the progression may be more indolent over the course of several weeks.2 There are few reported cases of primary vulvar mucormycosis, as in our patient.6,7 The previously reported cases involved severely immunocompromised patients who developed large necrotic lesions over the vulva that demonstrated widely branching, nonseptate hyphae on histologic examination. Each patient required extensive surgical debridement with systemic antifungal treatment.6,7
A timely diagnosis of mucormycosis often hinges on a high index of suspicion on behalf of the clinician. A fungal etiology always should be considered for an infection in an immunocompromised patient. Furthermore, nonresponse to antibiotic treatment should be an important diagnostic clue that the infection could be fungal in origin. The definitive diagnosis of mucormycosis is confirmed by tissue biopsy and the presence of broad, widely branching, nonseptate hyphae seen on histopathologic examination.
Treatment involves aggressive surgical debridement of all necrotic tissues and elimination of predisposing factors for infection such as hyperglycemia, metabolic acidosis, deferoxamine administration, and immunosuppressive medications. Early initiation of antifungal therapy with the lipid formulation of amphotericin B is recommended. Oral posaconazole or isavuconazole typically are used as step-down therapy after a favorable clinical response with initial amphotericin B treatment. Deferasirox, in contrast to deferoxamine, is an iron chelator that may reduce the pathogenicity of Mucorales and may help as an adjunctive therapy.8 In addition, hyperbaric oxygen therapy may have limited benefit in some cases.9 In spite of these treatments, the overall mortality of mucormycosis is 50% or higher and approaches nearly 100% in cases of disseminated disease, such as in our patient.1,3
- Ibrahim AS, Spellberg B, Walsh TJ, et al. Pathogenesis of mucormycosis. Clin Infect Dis. 2012;54(suppl 1):S16-S22.
- Petrikkos G, Skiada A, Lortholary O, et al. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 2012;54(suppl 1):S23-S34.
- Roden MM, Zaoutis TE, Buchanan WL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41:634-653.
- Chinn RY, Diamond RD. Generation of chemotactic factors by Rhizopus oryzae in the presence and absence of serum: relationship to hyphal damage mediated by human neutrophils and effects of hyperglycemia and ketoacidosis. Infect Immun. 1982;38:1123-1129.
- Cheng VC, Chan JF, Ngan AH, et al. Outbreak of intestinal infection due to Rhizopus microsporus [published online July 29, 2009]. J Clin Microbiol. 2009;47:2834-2843.
- Colon M, Romaguera J, Mendez K, et al. Mucormycosis of the vulva in an immunocompromised pediatric patient. Bol Asoc Med P R. 2013;105:65-67.
- Nomura J, Ruskin J, Sahebi F, et al. Mucormycosis of the vulva following bone marrow transplantation. Bone Marrow Transplant. 1997;19:859-860.
- Spellberg B, Andes D, Perez M, et al. Safety and outcomes of open-label deferasirox iron chelation therapy for mucormycosis. Antimicrob Agents Chemother. 2009;53:3122-3125.
- Ferguson BJ, Mitchell TG, Moon R, et al. Adjunctive hyperbaric oxygen for treatment of rhinocerebral mucormycosis. Rev Infect Dis. 1988;10:551-559.
- Ibrahim AS, Spellberg B, Walsh TJ, et al. Pathogenesis of mucormycosis. Clin Infect Dis. 2012;54(suppl 1):S16-S22.
- Petrikkos G, Skiada A, Lortholary O, et al. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 2012;54(suppl 1):S23-S34.
- Roden MM, Zaoutis TE, Buchanan WL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41:634-653.
- Chinn RY, Diamond RD. Generation of chemotactic factors by Rhizopus oryzae in the presence and absence of serum: relationship to hyphal damage mediated by human neutrophils and effects of hyperglycemia and ketoacidosis. Infect Immun. 1982;38:1123-1129.
- Cheng VC, Chan JF, Ngan AH, et al. Outbreak of intestinal infection due to Rhizopus microsporus [published online July 29, 2009]. J Clin Microbiol. 2009;47:2834-2843.
- Colon M, Romaguera J, Mendez K, et al. Mucormycosis of the vulva in an immunocompromised pediatric patient. Bol Asoc Med P R. 2013;105:65-67.
- Nomura J, Ruskin J, Sahebi F, et al. Mucormycosis of the vulva following bone marrow transplantation. Bone Marrow Transplant. 1997;19:859-860.
- Spellberg B, Andes D, Perez M, et al. Safety and outcomes of open-label deferasirox iron chelation therapy for mucormycosis. Antimicrob Agents Chemother. 2009;53:3122-3125.
- Ferguson BJ, Mitchell TG, Moon R, et al. Adjunctive hyperbaric oxygen for treatment of rhinocerebral mucormycosis. Rev Infect Dis. 1988;10:551-559.

A 48-year-old woman with relapsed T-cell acute lymphoblastic leukemia was admitted to the oncology service for salvage chemotherapy and allogeneic stem cell transplant. Her admission was complicated by extended-spectrum β-lactamase-producing Escherichia coli sepsis and persistent pancytopenia, which required transfer to the intensive care unit. After 2 weeks and while still in the intensive care unit, she developed a painful necrotic vulvar ulcer over the right labia and clitoris that progressed and formed an overlying black eschar.
Patients report issues with home O2
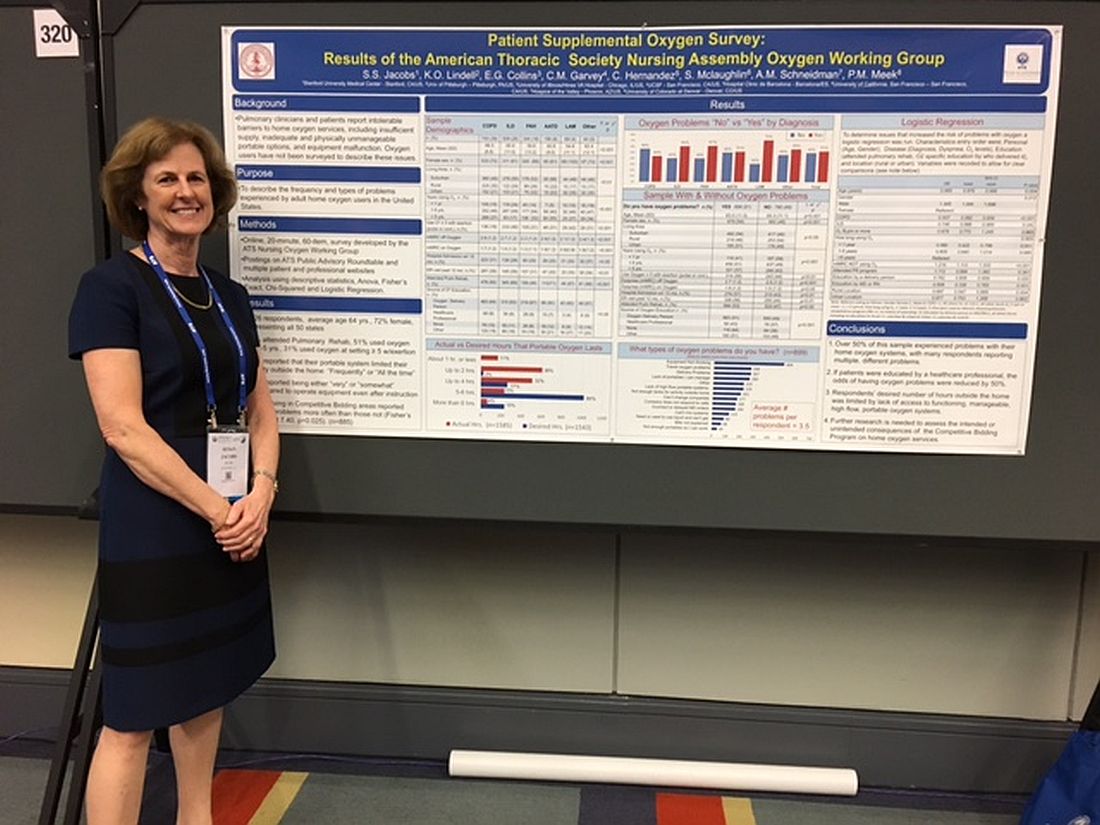
WASHINGTON – Patient education in the use of home oxygen halves the number of system use issues reported by patients, based on results of a survey of nearly 2,000 patients.
Pulmonary clinicians and patients report “intolerable barriers to home oxygen services,” lead researcher Susan S. Jacobs, RN, MS, said in a poster session at an international conference of the American Thoracic Society. These barriers include insufficient oxygen supply, inadequate and physically unmanageable portable options, and equipment malfunction.
“We’ve demonstrated that, if the patients are educated by a health care professional, the problems with oxygen go down, Ms. Jacobs, who is a nurse coordinator in the division of pulmonary and critical care medicine at Stanford (Calif.) University, said in an interview. “While physicians can provide oxygen for their patients, the patient oxygen education will most likely lie with the nurses and respiratory therapists.”
Of patients who responded to the survey question "Do you have oxygen problems?" 51% (899) said yes*. On average, these patients said they had experienced 3.5 types of problems with their systems.
Patients who were educated by a health care professional reported fewer problems and were more likely to report having no problems with their oxygen system. Of the patients who received oxygen therapy instruction from a health care professional, 76 (57%) did not report having any issues with their system. In contrast, of the patients who received no instruction, 116 (64%) said they had problems with their oxygen.
Most survey participants (1,113 patients) received oxygen therapy instruction from an oxygen delivery person instead of a health care professional. This group’s opinions about their oxygen systems were split, with 51% (563 patients) experiencing issues with their systems. The other 49% reported no problems.
Survey participants most frequently complained that their equipment was not working; 499 selected this response to the question, “What types of oxygen problems do you have?”
Many patients also reported being unable to spend as much time out of their homes as they wanted. This limitation resulted from their lack of access to functioning, manageable, high flow, portable oxygen systems, according to the researchers. Further, 43% of patients reported that their portable system limited their activity outside the home frequently or all of the time.
“Most of the reported problems were related to respondents not having portable systems that let them be out of their house for more than 2 to 4 hours or [to systems that] were too heavy for the patients to lift up and down their stairs and out of their cars, and they had problems operating them,” said Ms. Jacobs, who is a nurse coordinator in the division of pulmonary and critical care medicine at Stanford (Calif.) University.
The survey respondents also reported experiencing delivery problems, not being able to change the company providing them with oxygen, receiving incorrect or delayed orders from a physician, or being unable to get liquid oxygen. These responses were provided by 267, 177, 166, and 68 patients, respectively.
“There is a lot of confusion for the physicians as well as the nurses about what types of systems the patients can use [and] the pros and cons of each system. There’s lots of confusion and time spent about getting the initial orders right, getting them set up with a supplier, and ensuring the patient gets the equipment that was ordered. There is a lot of back and forth, which results in a delay to the patient, and the patients are upset because they are waiting for their oxygen supply,” she explained. “So, I think that physicians are very much wanting clarification to streamline the process and identify what patient systems are appropriate, which are high flow, [and] what their patients’ needs are to help physicians spend less time on this and help the patients get their oxygen set up in a timely manner.”
The study participants came from all 50 states and were 64 years of age on average and mostly women. A high percentage (39%) of the sample had chronic obstructive pulmonary disease, while 26% had interstitial lung diseases, 18% had pulmonary arterial hypertension, 8% had alpha-1 antitrypsin deficiency, and 4% had lymphangioleiomyomatosis.
Ms. Jacobs noted that she thought patients would benefit from greater physician knowledge of their prescribing options.
“A physician can dictate exactly what system they want. ... You can try to give [patients] a lighter system, a backpack, a smaller tank, more tanks per week, depending on their lifestyle and their needs. But physicians, a lot of times, like all of us and our patients, [are] not aware of all these choices,” she said, during the interview.
An online resource providing all of the pros and cons of the different types of portable oxygen systems that would be appropriate for physicians, nurses, and patients, as well as an examination of the quality standards of the oxygen suppliers, are needed, she noted
Ms. Jacobs reported no financial disclosures.
*This article was corrected June 16, 2017
WASHINGTON – Patient education in the use of home oxygen halves the number of system use issues reported by patients, based on results of a survey of nearly 2,000 patients.
Pulmonary clinicians and patients report “intolerable barriers to home oxygen services,” lead researcher Susan S. Jacobs, RN, MS, said in a poster session at an international conference of the American Thoracic Society. These barriers include insufficient oxygen supply, inadequate and physically unmanageable portable options, and equipment malfunction.
“We’ve demonstrated that, if the patients are educated by a health care professional, the problems with oxygen go down, Ms. Jacobs, who is a nurse coordinator in the division of pulmonary and critical care medicine at Stanford (Calif.) University, said in an interview. “While physicians can provide oxygen for their patients, the patient oxygen education will most likely lie with the nurses and respiratory therapists.”
Of patients who responded to the survey question "Do you have oxygen problems?" 51% (899) said yes*. On average, these patients said they had experienced 3.5 types of problems with their systems.
Patients who were educated by a health care professional reported fewer problems and were more likely to report having no problems with their oxygen system. Of the patients who received oxygen therapy instruction from a health care professional, 76 (57%) did not report having any issues with their system. In contrast, of the patients who received no instruction, 116 (64%) said they had problems with their oxygen.
Most survey participants (1,113 patients) received oxygen therapy instruction from an oxygen delivery person instead of a health care professional. This group’s opinions about their oxygen systems were split, with 51% (563 patients) experiencing issues with their systems. The other 49% reported no problems.
Survey participants most frequently complained that their equipment was not working; 499 selected this response to the question, “What types of oxygen problems do you have?”
Many patients also reported being unable to spend as much time out of their homes as they wanted. This limitation resulted from their lack of access to functioning, manageable, high flow, portable oxygen systems, according to the researchers. Further, 43% of patients reported that their portable system limited their activity outside the home frequently or all of the time.
“Most of the reported problems were related to respondents not having portable systems that let them be out of their house for more than 2 to 4 hours or [to systems that] were too heavy for the patients to lift up and down their stairs and out of their cars, and they had problems operating them,” said Ms. Jacobs, who is a nurse coordinator in the division of pulmonary and critical care medicine at Stanford (Calif.) University.
The survey respondents also reported experiencing delivery problems, not being able to change the company providing them with oxygen, receiving incorrect or delayed orders from a physician, or being unable to get liquid oxygen. These responses were provided by 267, 177, 166, and 68 patients, respectively.
“There is a lot of confusion for the physicians as well as the nurses about what types of systems the patients can use [and] the pros and cons of each system. There’s lots of confusion and time spent about getting the initial orders right, getting them set up with a supplier, and ensuring the patient gets the equipment that was ordered. There is a lot of back and forth, which results in a delay to the patient, and the patients are upset because they are waiting for their oxygen supply,” she explained. “So, I think that physicians are very much wanting clarification to streamline the process and identify what patient systems are appropriate, which are high flow, [and] what their patients’ needs are to help physicians spend less time on this and help the patients get their oxygen set up in a timely manner.”
The study participants came from all 50 states and were 64 years of age on average and mostly women. A high percentage (39%) of the sample had chronic obstructive pulmonary disease, while 26% had interstitial lung diseases, 18% had pulmonary arterial hypertension, 8% had alpha-1 antitrypsin deficiency, and 4% had lymphangioleiomyomatosis.
Ms. Jacobs noted that she thought patients would benefit from greater physician knowledge of their prescribing options.
“A physician can dictate exactly what system they want. ... You can try to give [patients] a lighter system, a backpack, a smaller tank, more tanks per week, depending on their lifestyle and their needs. But physicians, a lot of times, like all of us and our patients, [are] not aware of all these choices,” she said, during the interview.
An online resource providing all of the pros and cons of the different types of portable oxygen systems that would be appropriate for physicians, nurses, and patients, as well as an examination of the quality standards of the oxygen suppliers, are needed, she noted
Ms. Jacobs reported no financial disclosures.
*This article was corrected June 16, 2017
WASHINGTON – Patient education in the use of home oxygen halves the number of system use issues reported by patients, based on results of a survey of nearly 2,000 patients.
Pulmonary clinicians and patients report “intolerable barriers to home oxygen services,” lead researcher Susan S. Jacobs, RN, MS, said in a poster session at an international conference of the American Thoracic Society. These barriers include insufficient oxygen supply, inadequate and physically unmanageable portable options, and equipment malfunction.
“We’ve demonstrated that, if the patients are educated by a health care professional, the problems with oxygen go down, Ms. Jacobs, who is a nurse coordinator in the division of pulmonary and critical care medicine at Stanford (Calif.) University, said in an interview. “While physicians can provide oxygen for their patients, the patient oxygen education will most likely lie with the nurses and respiratory therapists.”
Of patients who responded to the survey question "Do you have oxygen problems?" 51% (899) said yes*. On average, these patients said they had experienced 3.5 types of problems with their systems.
Patients who were educated by a health care professional reported fewer problems and were more likely to report having no problems with their oxygen system. Of the patients who received oxygen therapy instruction from a health care professional, 76 (57%) did not report having any issues with their system. In contrast, of the patients who received no instruction, 116 (64%) said they had problems with their oxygen.
Most survey participants (1,113 patients) received oxygen therapy instruction from an oxygen delivery person instead of a health care professional. This group’s opinions about their oxygen systems were split, with 51% (563 patients) experiencing issues with their systems. The other 49% reported no problems.
Survey participants most frequently complained that their equipment was not working; 499 selected this response to the question, “What types of oxygen problems do you have?”
Many patients also reported being unable to spend as much time out of their homes as they wanted. This limitation resulted from their lack of access to functioning, manageable, high flow, portable oxygen systems, according to the researchers. Further, 43% of patients reported that their portable system limited their activity outside the home frequently or all of the time.
“Most of the reported problems were related to respondents not having portable systems that let them be out of their house for more than 2 to 4 hours or [to systems that] were too heavy for the patients to lift up and down their stairs and out of their cars, and they had problems operating them,” said Ms. Jacobs, who is a nurse coordinator in the division of pulmonary and critical care medicine at Stanford (Calif.) University.
The survey respondents also reported experiencing delivery problems, not being able to change the company providing them with oxygen, receiving incorrect or delayed orders from a physician, or being unable to get liquid oxygen. These responses were provided by 267, 177, 166, and 68 patients, respectively.
“There is a lot of confusion for the physicians as well as the nurses about what types of systems the patients can use [and] the pros and cons of each system. There’s lots of confusion and time spent about getting the initial orders right, getting them set up with a supplier, and ensuring the patient gets the equipment that was ordered. There is a lot of back and forth, which results in a delay to the patient, and the patients are upset because they are waiting for their oxygen supply,” she explained. “So, I think that physicians are very much wanting clarification to streamline the process and identify what patient systems are appropriate, which are high flow, [and] what their patients’ needs are to help physicians spend less time on this and help the patients get their oxygen set up in a timely manner.”
The study participants came from all 50 states and were 64 years of age on average and mostly women. A high percentage (39%) of the sample had chronic obstructive pulmonary disease, while 26% had interstitial lung diseases, 18% had pulmonary arterial hypertension, 8% had alpha-1 antitrypsin deficiency, and 4% had lymphangioleiomyomatosis.
Ms. Jacobs noted that she thought patients would benefit from greater physician knowledge of their prescribing options.
“A physician can dictate exactly what system they want. ... You can try to give [patients] a lighter system, a backpack, a smaller tank, more tanks per week, depending on their lifestyle and their needs. But physicians, a lot of times, like all of us and our patients, [are] not aware of all these choices,” she said, during the interview.
An online resource providing all of the pros and cons of the different types of portable oxygen systems that would be appropriate for physicians, nurses, and patients, as well as an examination of the quality standards of the oxygen suppliers, are needed, she noted
Ms. Jacobs reported no financial disclosures.
*This article was corrected June 16, 2017
AT ATS 2017
Key clinical point:
Major finding: Patients reported experiencing an average of 3.5 types of problems with their home oxygen systems.
Data source: An analysis of 1,926 home-oxygen users’ responses to an online, 60-question survey.
Disclosures: Ms. Jacobs reported no financial disclosures.
Pregnancy and MS: How do they affect each other?
NEW ORLEANS – Multiple sclerosis has little to no impact on the ability to conceive, on pregnancy, or on fetal status, according to Patricia K. Coyle, MD.
“That’s very reassuring,” Dr. Coyle said at the annual meeting of the Consortium of Multiple Sclerosis Centers. “We don’t see an increase in birth defects just because the mother has MS. There is no consistent increase in abortions, ectopic pregnancies, or assisted vaginal/cesarean deliveries.”
Dr. Coyle, director of the MS Comprehensive Care Center at Stony Brook (N.Y.) University Medical Center, said that the most dramatic changes for pregnant patients with MS occur in the final trimester and mainly involve rising levels of multiple hormones: estrogens, cortisol, progesterone, norepinephrine, and 1,25-dihydroxyvitamin D, which increase late in pregnancy, then rapidly drop off postpartum. This has led to the evaluation of sex hormone therapy for MS.
The impact of other pregnancy factors on MS disease activity remains unknown. One is microchimerism, a maternal-fetal exchange of cells and DNA. “These cells can last for a long time; you can find them in the blood, as well as in the [central nervous system],” Dr. Coyle said. “It’s been reported that fetal microchimerism may be increased in immune-mediated diseases like MS, but we really don’t have a lot of good data.”
Researchers also are studying the impact of changes in the gut microbiota that occur during pregnancy. “Could this be a potential target for MS therapy?” Dr. Coyle asked. “This is in its infancy.”
Counseling tips
She went on to share counseling tips for MS patients of childbearing age, including the fact that some studies report slightly smaller babies born to mothers with MS, while others have not found that association. “This is a question mark, but it doesn’t seem to be a major issue,” she said. One thing you can tell patients for certain is that MS is not inherited. “There are well over 230 genes linked to MS, so there’s a genetic enrichment that can make somebody vulnerable to MS, but there’s no gene that passes on MS,” Dr. Coyle said. “The risk is slightly higher for a first-degree relative, so when a parent has MS, the risk for the child is in the range of 2% to 2.5%, compared with the expected 0.13% in the general population. But there’s a slightly higher risk when you’re a sibling than when you’re a parent – 2.7% – which is speaking to environmental factors having an important impact on genes.”
Controversial data exist as to whether a maternal deficiency in vitamin D poses a risk of MS in the offspring. Dr. Coyle makes it a point to “normalize” vitamin D levels in pregnant MS patients, particularly in white patients. “You’d want to have them on prenatal vitamins and folic acid and tell them not to smoke, to limit their alcohol use, and advise them to have good sleep hygiene.”
Dr. Coyle, vice chair of clinical affairs at Stony Brook University Medical Center, said that up until the 1950s, physicians advised women with MS against having children. “They were told not to get pregnant or to have an abortion, because it was thought to make MS worse,” she said. “It turns out that was fiction. That was completely wrong. Pregnancy has no negative effect on long-term MS prognosis. It may have long-term benefits for relapsing MS, but there are not enough data to comment on its impact on progressive MS. Pregnancy makes it less likely that someone will develop a clinically isolated syndrome, but it may increase the radiologically isolated syndrome risk for clinical attack. That’s based on 7 pregnant patients out of a cohort of 60, so we need further data to explain that.”
Disease-modifying therapies
When it comes to washouts of disease-modifying therapies (DMTs), no one-size-fits-all approach exists. Interferon betas and glatiramer acetate have more than 1,000 pregnancy exposures that yield no evidence for teratogenicity or negative fetal impact. No washout is needed prior to pregnancy. “These agents can be used during pregnancy and breastfeeding,” she said.
The other DMTs paint a somewhat different picture. “There is insufficient pregnancy exposure to the three available oral DMTs to comment definitively on their safety, but there is no clear human teratogenicity to date,” Dr. Coyle said. The conventional washout for fingolimod is 8 weeks. In Dr. Coyle’s opinion, no washout is required with dimethyl fumarate. “The half-life is 40 minutes. There are no good signs of issues. For teriflunomide, it can hang around in individuals for 18-24 months. You should go through an accelerated elimination procedure with oral cholestyramine 8 mg three times a day for 11 days until blood level of the agent is less than 0.02 mcg/mL. Avoid all the orals with breastfeeding.”
Monoclonal antibodies – another form of DMTs – lack sufficient pregnancy exposures to merit comment on safety, but they should not be used during breastfeeding. Natalizumab is a humanized IgG4 antibody that crosses the placenta. “This has been used in several dozen pregnancies because the patients got so bad when they were taken off that it required reinstituting natalizumab even though they were pregnant,” Dr. Coyle said. “Human pregnancy exposures have been associated with transient hematologic issues in the newborn, including anemia, thrombocytopenia, and pancytopenia.” Data indicate that the rate of spontaneous abortion among pregnant women treated with natalizumab was 9%, the rate of major birth defects was 5.05%, and no malformation pattern was observed. The drug is detected in human breast milk and has a half-life of 11 days.
Alemtuzumab is a humanized IgG1 monoclonal antibody that crosses the placenta. The half-life elimination is about 14 days. In transgenic mice, giving alemtuzumab during organogenesis was found to be embryolethal. In human pregnancy, hypothyroidism is a concern. “The recommendation has been to wait 4 months after the last treatment before you try to become pregnant. Alemtuzumab is considered a two-cycle treatment. You don’t get the maximum benefit after the first cycle of 5 days. The complete treatment is the second cycle 3 days.”
Daclizumab, another humanized IgG1 monoclonal antibody, also crosses the placenta. Monkey exposure during gestation led to embryofetal death and decreased fetal growth, “but this was at greater than 30 times the human dose,” she said. “It was found to be excreted in monkey breast milk and the half-life is 21 days.” In humans, there have been 36 exposed women who had 38 pregnancies and 20 live births. The rate of spontaneous abortions/miscarriages was 11%, there were eight elective terminations, two ectopic pregnancies, and one congenital heart defect. “This is very limited data, but nothing that would raise the level of concern,” Dr. Coyle said.
Ocrelizumab, another humanized IgG1 monoclonal antibody, was approved by the Food and Drug Administration in March 2017. Prior studies of anti-CD20 antibodies in human pregnancy noted transient lymphocytopenia and peripheral B cell depletion in the newborns. In studies of pregnant monkeys that used 2 and 10 times human doses during organogenesis, it was associated with B cell depletion in spleen/lymph nodes, Dr. Coyle said. “During organogenesis and throughout the neonatal period, treatment could be associated with perinatal death, some associated with bacterial infection; glomerulonephropathy with inflammation; a decrease in circulating B cells, a decrease in testicular weight, and bone marrow lymphoid follicle formation.” Ocrelizumab is excreted in monkey breast milk and the prescription label suggests a 6-month delay in pregnancy. The drug’s half-life is 26 days.
Dr. Coyle reported that she has served as a consultant for Accordant, Acorda, Bayer, Biogen, Celgene, Genentech/Roche, Genzyme/Sanofi, Novartis, Serono, and Teva. She has also received research support from Actelion, Alkermes, Genentech/Roche, MedDay, the National Institute of Neurological Disorders and Stroke, and Novartis.
NEW ORLEANS – Multiple sclerosis has little to no impact on the ability to conceive, on pregnancy, or on fetal status, according to Patricia K. Coyle, MD.
“That’s very reassuring,” Dr. Coyle said at the annual meeting of the Consortium of Multiple Sclerosis Centers. “We don’t see an increase in birth defects just because the mother has MS. There is no consistent increase in abortions, ectopic pregnancies, or assisted vaginal/cesarean deliveries.”
Dr. Coyle, director of the MS Comprehensive Care Center at Stony Brook (N.Y.) University Medical Center, said that the most dramatic changes for pregnant patients with MS occur in the final trimester and mainly involve rising levels of multiple hormones: estrogens, cortisol, progesterone, norepinephrine, and 1,25-dihydroxyvitamin D, which increase late in pregnancy, then rapidly drop off postpartum. This has led to the evaluation of sex hormone therapy for MS.
The impact of other pregnancy factors on MS disease activity remains unknown. One is microchimerism, a maternal-fetal exchange of cells and DNA. “These cells can last for a long time; you can find them in the blood, as well as in the [central nervous system],” Dr. Coyle said. “It’s been reported that fetal microchimerism may be increased in immune-mediated diseases like MS, but we really don’t have a lot of good data.”
Researchers also are studying the impact of changes in the gut microbiota that occur during pregnancy. “Could this be a potential target for MS therapy?” Dr. Coyle asked. “This is in its infancy.”
Counseling tips
She went on to share counseling tips for MS patients of childbearing age, including the fact that some studies report slightly smaller babies born to mothers with MS, while others have not found that association. “This is a question mark, but it doesn’t seem to be a major issue,” she said. One thing you can tell patients for certain is that MS is not inherited. “There are well over 230 genes linked to MS, so there’s a genetic enrichment that can make somebody vulnerable to MS, but there’s no gene that passes on MS,” Dr. Coyle said. “The risk is slightly higher for a first-degree relative, so when a parent has MS, the risk for the child is in the range of 2% to 2.5%, compared with the expected 0.13% in the general population. But there’s a slightly higher risk when you’re a sibling than when you’re a parent – 2.7% – which is speaking to environmental factors having an important impact on genes.”
Controversial data exist as to whether a maternal deficiency in vitamin D poses a risk of MS in the offspring. Dr. Coyle makes it a point to “normalize” vitamin D levels in pregnant MS patients, particularly in white patients. “You’d want to have them on prenatal vitamins and folic acid and tell them not to smoke, to limit their alcohol use, and advise them to have good sleep hygiene.”
Dr. Coyle, vice chair of clinical affairs at Stony Brook University Medical Center, said that up until the 1950s, physicians advised women with MS against having children. “They were told not to get pregnant or to have an abortion, because it was thought to make MS worse,” she said. “It turns out that was fiction. That was completely wrong. Pregnancy has no negative effect on long-term MS prognosis. It may have long-term benefits for relapsing MS, but there are not enough data to comment on its impact on progressive MS. Pregnancy makes it less likely that someone will develop a clinically isolated syndrome, but it may increase the radiologically isolated syndrome risk for clinical attack. That’s based on 7 pregnant patients out of a cohort of 60, so we need further data to explain that.”
Disease-modifying therapies
When it comes to washouts of disease-modifying therapies (DMTs), no one-size-fits-all approach exists. Interferon betas and glatiramer acetate have more than 1,000 pregnancy exposures that yield no evidence for teratogenicity or negative fetal impact. No washout is needed prior to pregnancy. “These agents can be used during pregnancy and breastfeeding,” she said.
The other DMTs paint a somewhat different picture. “There is insufficient pregnancy exposure to the three available oral DMTs to comment definitively on their safety, but there is no clear human teratogenicity to date,” Dr. Coyle said. The conventional washout for fingolimod is 8 weeks. In Dr. Coyle’s opinion, no washout is required with dimethyl fumarate. “The half-life is 40 minutes. There are no good signs of issues. For teriflunomide, it can hang around in individuals for 18-24 months. You should go through an accelerated elimination procedure with oral cholestyramine 8 mg three times a day for 11 days until blood level of the agent is less than 0.02 mcg/mL. Avoid all the orals with breastfeeding.”
Monoclonal antibodies – another form of DMTs – lack sufficient pregnancy exposures to merit comment on safety, but they should not be used during breastfeeding. Natalizumab is a humanized IgG4 antibody that crosses the placenta. “This has been used in several dozen pregnancies because the patients got so bad when they were taken off that it required reinstituting natalizumab even though they were pregnant,” Dr. Coyle said. “Human pregnancy exposures have been associated with transient hematologic issues in the newborn, including anemia, thrombocytopenia, and pancytopenia.” Data indicate that the rate of spontaneous abortion among pregnant women treated with natalizumab was 9%, the rate of major birth defects was 5.05%, and no malformation pattern was observed. The drug is detected in human breast milk and has a half-life of 11 days.
Alemtuzumab is a humanized IgG1 monoclonal antibody that crosses the placenta. The half-life elimination is about 14 days. In transgenic mice, giving alemtuzumab during organogenesis was found to be embryolethal. In human pregnancy, hypothyroidism is a concern. “The recommendation has been to wait 4 months after the last treatment before you try to become pregnant. Alemtuzumab is considered a two-cycle treatment. You don’t get the maximum benefit after the first cycle of 5 days. The complete treatment is the second cycle 3 days.”
Daclizumab, another humanized IgG1 monoclonal antibody, also crosses the placenta. Monkey exposure during gestation led to embryofetal death and decreased fetal growth, “but this was at greater than 30 times the human dose,” she said. “It was found to be excreted in monkey breast milk and the half-life is 21 days.” In humans, there have been 36 exposed women who had 38 pregnancies and 20 live births. The rate of spontaneous abortions/miscarriages was 11%, there were eight elective terminations, two ectopic pregnancies, and one congenital heart defect. “This is very limited data, but nothing that would raise the level of concern,” Dr. Coyle said.
Ocrelizumab, another humanized IgG1 monoclonal antibody, was approved by the Food and Drug Administration in March 2017. Prior studies of anti-CD20 antibodies in human pregnancy noted transient lymphocytopenia and peripheral B cell depletion in the newborns. In studies of pregnant monkeys that used 2 and 10 times human doses during organogenesis, it was associated with B cell depletion in spleen/lymph nodes, Dr. Coyle said. “During organogenesis and throughout the neonatal period, treatment could be associated with perinatal death, some associated with bacterial infection; glomerulonephropathy with inflammation; a decrease in circulating B cells, a decrease in testicular weight, and bone marrow lymphoid follicle formation.” Ocrelizumab is excreted in monkey breast milk and the prescription label suggests a 6-month delay in pregnancy. The drug’s half-life is 26 days.
Dr. Coyle reported that she has served as a consultant for Accordant, Acorda, Bayer, Biogen, Celgene, Genentech/Roche, Genzyme/Sanofi, Novartis, Serono, and Teva. She has also received research support from Actelion, Alkermes, Genentech/Roche, MedDay, the National Institute of Neurological Disorders and Stroke, and Novartis.
NEW ORLEANS – Multiple sclerosis has little to no impact on the ability to conceive, on pregnancy, or on fetal status, according to Patricia K. Coyle, MD.
“That’s very reassuring,” Dr. Coyle said at the annual meeting of the Consortium of Multiple Sclerosis Centers. “We don’t see an increase in birth defects just because the mother has MS. There is no consistent increase in abortions, ectopic pregnancies, or assisted vaginal/cesarean deliveries.”
Dr. Coyle, director of the MS Comprehensive Care Center at Stony Brook (N.Y.) University Medical Center, said that the most dramatic changes for pregnant patients with MS occur in the final trimester and mainly involve rising levels of multiple hormones: estrogens, cortisol, progesterone, norepinephrine, and 1,25-dihydroxyvitamin D, which increase late in pregnancy, then rapidly drop off postpartum. This has led to the evaluation of sex hormone therapy for MS.
The impact of other pregnancy factors on MS disease activity remains unknown. One is microchimerism, a maternal-fetal exchange of cells and DNA. “These cells can last for a long time; you can find them in the blood, as well as in the [central nervous system],” Dr. Coyle said. “It’s been reported that fetal microchimerism may be increased in immune-mediated diseases like MS, but we really don’t have a lot of good data.”
Researchers also are studying the impact of changes in the gut microbiota that occur during pregnancy. “Could this be a potential target for MS therapy?” Dr. Coyle asked. “This is in its infancy.”
Counseling tips
She went on to share counseling tips for MS patients of childbearing age, including the fact that some studies report slightly smaller babies born to mothers with MS, while others have not found that association. “This is a question mark, but it doesn’t seem to be a major issue,” she said. One thing you can tell patients for certain is that MS is not inherited. “There are well over 230 genes linked to MS, so there’s a genetic enrichment that can make somebody vulnerable to MS, but there’s no gene that passes on MS,” Dr. Coyle said. “The risk is slightly higher for a first-degree relative, so when a parent has MS, the risk for the child is in the range of 2% to 2.5%, compared with the expected 0.13% in the general population. But there’s a slightly higher risk when you’re a sibling than when you’re a parent – 2.7% – which is speaking to environmental factors having an important impact on genes.”
Controversial data exist as to whether a maternal deficiency in vitamin D poses a risk of MS in the offspring. Dr. Coyle makes it a point to “normalize” vitamin D levels in pregnant MS patients, particularly in white patients. “You’d want to have them on prenatal vitamins and folic acid and tell them not to smoke, to limit their alcohol use, and advise them to have good sleep hygiene.”
Dr. Coyle, vice chair of clinical affairs at Stony Brook University Medical Center, said that up until the 1950s, physicians advised women with MS against having children. “They were told not to get pregnant or to have an abortion, because it was thought to make MS worse,” she said. “It turns out that was fiction. That was completely wrong. Pregnancy has no negative effect on long-term MS prognosis. It may have long-term benefits for relapsing MS, but there are not enough data to comment on its impact on progressive MS. Pregnancy makes it less likely that someone will develop a clinically isolated syndrome, but it may increase the radiologically isolated syndrome risk for clinical attack. That’s based on 7 pregnant patients out of a cohort of 60, so we need further data to explain that.”
Disease-modifying therapies
When it comes to washouts of disease-modifying therapies (DMTs), no one-size-fits-all approach exists. Interferon betas and glatiramer acetate have more than 1,000 pregnancy exposures that yield no evidence for teratogenicity or negative fetal impact. No washout is needed prior to pregnancy. “These agents can be used during pregnancy and breastfeeding,” she said.
The other DMTs paint a somewhat different picture. “There is insufficient pregnancy exposure to the three available oral DMTs to comment definitively on their safety, but there is no clear human teratogenicity to date,” Dr. Coyle said. The conventional washout for fingolimod is 8 weeks. In Dr. Coyle’s opinion, no washout is required with dimethyl fumarate. “The half-life is 40 minutes. There are no good signs of issues. For teriflunomide, it can hang around in individuals for 18-24 months. You should go through an accelerated elimination procedure with oral cholestyramine 8 mg three times a day for 11 days until blood level of the agent is less than 0.02 mcg/mL. Avoid all the orals with breastfeeding.”
Monoclonal antibodies – another form of DMTs – lack sufficient pregnancy exposures to merit comment on safety, but they should not be used during breastfeeding. Natalizumab is a humanized IgG4 antibody that crosses the placenta. “This has been used in several dozen pregnancies because the patients got so bad when they were taken off that it required reinstituting natalizumab even though they were pregnant,” Dr. Coyle said. “Human pregnancy exposures have been associated with transient hematologic issues in the newborn, including anemia, thrombocytopenia, and pancytopenia.” Data indicate that the rate of spontaneous abortion among pregnant women treated with natalizumab was 9%, the rate of major birth defects was 5.05%, and no malformation pattern was observed. The drug is detected in human breast milk and has a half-life of 11 days.
Alemtuzumab is a humanized IgG1 monoclonal antibody that crosses the placenta. The half-life elimination is about 14 days. In transgenic mice, giving alemtuzumab during organogenesis was found to be embryolethal. In human pregnancy, hypothyroidism is a concern. “The recommendation has been to wait 4 months after the last treatment before you try to become pregnant. Alemtuzumab is considered a two-cycle treatment. You don’t get the maximum benefit after the first cycle of 5 days. The complete treatment is the second cycle 3 days.”
Daclizumab, another humanized IgG1 monoclonal antibody, also crosses the placenta. Monkey exposure during gestation led to embryofetal death and decreased fetal growth, “but this was at greater than 30 times the human dose,” she said. “It was found to be excreted in monkey breast milk and the half-life is 21 days.” In humans, there have been 36 exposed women who had 38 pregnancies and 20 live births. The rate of spontaneous abortions/miscarriages was 11%, there were eight elective terminations, two ectopic pregnancies, and one congenital heart defect. “This is very limited data, but nothing that would raise the level of concern,” Dr. Coyle said.
Ocrelizumab, another humanized IgG1 monoclonal antibody, was approved by the Food and Drug Administration in March 2017. Prior studies of anti-CD20 antibodies in human pregnancy noted transient lymphocytopenia and peripheral B cell depletion in the newborns. In studies of pregnant monkeys that used 2 and 10 times human doses during organogenesis, it was associated with B cell depletion in spleen/lymph nodes, Dr. Coyle said. “During organogenesis and throughout the neonatal period, treatment could be associated with perinatal death, some associated with bacterial infection; glomerulonephropathy with inflammation; a decrease in circulating B cells, a decrease in testicular weight, and bone marrow lymphoid follicle formation.” Ocrelizumab is excreted in monkey breast milk and the prescription label suggests a 6-month delay in pregnancy. The drug’s half-life is 26 days.
Dr. Coyle reported that she has served as a consultant for Accordant, Acorda, Bayer, Biogen, Celgene, Genentech/Roche, Genzyme/Sanofi, Novartis, Serono, and Teva. She has also received research support from Actelion, Alkermes, Genentech/Roche, MedDay, the National Institute of Neurological Disorders and Stroke, and Novartis.
EXPERT ANALYSIS AT THE CMSC ANNUAL MEETING
Mindfulness May Alleviate Chronic Migraine Associated With Medication Overuse
Mindfulness training is as effective as prophylactic medications for treating chronic migraine associated with medication overuse (CM-MO), according to research published online ahead of print February 4 in the Journal of Headache and Pain.
“Our results further suggest that a mindfulness-based treatment may be comparable to standard pharmacologic prophylaxis with regard to relevant primary outcomes such as headache frequency reduction and reduction in the consumption of acute medications,” said Licia Grazzi, MD, a neurologist at Istituto Neurologico Carlo Besta in Milan.
Research has suggested that mindfulness may be beneficial for headache. Previous studies, however, have been limited by inadequate consideration of several significant end points in chronic headache, such as frequency of headache and consumption of medications for acute headache management, said the authors.
To address these limitations, Dr. Grazzi and colleagues conducted an exploratory clinical trial that compared conventional prophylactic pharmacologic treatment with a mindfulness-based treatment for patients diagnosed with CM-MO. Researchers hypothesized that the mindfulness-based approach would be as effective as conventional prophylactic treatment.
Eligible participants were between ages 18 and 65 and had been diagnosed with CM-MO according to the International Classification of Headache Disorders, third edition (beta version), and had presented for treatment at the Headache Center of the Istituto Neurologico Carlo Besta between February 2014 and June 2015. In addition, participants had a history of chronic migraine for at least 10 years that was associated with overuse of triptans and nonsteroidal anti-inflammatory drugs for a minimum of the past five years.
All patients completed a five-day medication withdrawal program and were encouraged to exercise at least 45 minutes twice a week, to stay properly hydrated, and to consume three meals every day.
Participants were separated into two groups. In one group, patients were treated with prophylactic medications. In the second group, patients participated in a mindfulness-based training that consisted of six weekly sessions of guided mindfulness. Patients were invited to practice mindfulness training for seven to 10 minutes per day. At each follow-up visit, the Headache Impact Test, the Migraine Disability Assessment, the State and Trait Anxiety Inventory, and the Beck Depression Inventory were administered. Patients also kept headache diaries.
A total of 44 patients participated in the study. The average age was 44.5, the average headache frequency per month was 20.5, and the average monthly medication intake was 18.4 pills. Overall, data indicated a similar improvement over time in the mindfulness group and pharmacologic prophylaxis group for headache frequency, use of medication, Migraine Disability Assessment, Headache Impact Test, and Beck Depression Inventory. No changes on State and Trait Anxiety Inventory were reported. Both groups had significant and equivalent proportions of participants who achieved at least 50% reduction of headaches, compared with baseline. The majority of patients in each group no longer satisfied criteria for chronic migraine.
“Our findings support the value of conducting further … well-controlled studies (incorporating random assignment, larger sample sizes, and checks on integrity of treatment),” said Dr. Grazzi. “[Such studies] are warranted to more fully explore the benefits, boundaries, and mechanisms of action for mindfulness in treating chronic migraine by itself and when it is complicated by medication overuse and medical or psychological comorbidities.”
—Erica Tricarico
Suggested Reading
Grazzi L, Sansone E, Raggi A, et al. Mindfulness and pharmacological prophylaxis after withdrawal from medication overuse in patients with chronic migraine: an effectiveness trial with a one-year follow-up. J Headache Pain. 2017;18(1):15.
Mindfulness training is as effective as prophylactic medications for treating chronic migraine associated with medication overuse (CM-MO), according to research published online ahead of print February 4 in the Journal of Headache and Pain.
“Our results further suggest that a mindfulness-based treatment may be comparable to standard pharmacologic prophylaxis with regard to relevant primary outcomes such as headache frequency reduction and reduction in the consumption of acute medications,” said Licia Grazzi, MD, a neurologist at Istituto Neurologico Carlo Besta in Milan.
Research has suggested that mindfulness may be beneficial for headache. Previous studies, however, have been limited by inadequate consideration of several significant end points in chronic headache, such as frequency of headache and consumption of medications for acute headache management, said the authors.
To address these limitations, Dr. Grazzi and colleagues conducted an exploratory clinical trial that compared conventional prophylactic pharmacologic treatment with a mindfulness-based treatment for patients diagnosed with CM-MO. Researchers hypothesized that the mindfulness-based approach would be as effective as conventional prophylactic treatment.
Eligible participants were between ages 18 and 65 and had been diagnosed with CM-MO according to the International Classification of Headache Disorders, third edition (beta version), and had presented for treatment at the Headache Center of the Istituto Neurologico Carlo Besta between February 2014 and June 2015. In addition, participants had a history of chronic migraine for at least 10 years that was associated with overuse of triptans and nonsteroidal anti-inflammatory drugs for a minimum of the past five years.
All patients completed a five-day medication withdrawal program and were encouraged to exercise at least 45 minutes twice a week, to stay properly hydrated, and to consume three meals every day.
Participants were separated into two groups. In one group, patients were treated with prophylactic medications. In the second group, patients participated in a mindfulness-based training that consisted of six weekly sessions of guided mindfulness. Patients were invited to practice mindfulness training for seven to 10 minutes per day. At each follow-up visit, the Headache Impact Test, the Migraine Disability Assessment, the State and Trait Anxiety Inventory, and the Beck Depression Inventory were administered. Patients also kept headache diaries.
A total of 44 patients participated in the study. The average age was 44.5, the average headache frequency per month was 20.5, and the average monthly medication intake was 18.4 pills. Overall, data indicated a similar improvement over time in the mindfulness group and pharmacologic prophylaxis group for headache frequency, use of medication, Migraine Disability Assessment, Headache Impact Test, and Beck Depression Inventory. No changes on State and Trait Anxiety Inventory were reported. Both groups had significant and equivalent proportions of participants who achieved at least 50% reduction of headaches, compared with baseline. The majority of patients in each group no longer satisfied criteria for chronic migraine.
“Our findings support the value of conducting further … well-controlled studies (incorporating random assignment, larger sample sizes, and checks on integrity of treatment),” said Dr. Grazzi. “[Such studies] are warranted to more fully explore the benefits, boundaries, and mechanisms of action for mindfulness in treating chronic migraine by itself and when it is complicated by medication overuse and medical or psychological comorbidities.”
—Erica Tricarico
Suggested Reading
Grazzi L, Sansone E, Raggi A, et al. Mindfulness and pharmacological prophylaxis after withdrawal from medication overuse in patients with chronic migraine: an effectiveness trial with a one-year follow-up. J Headache Pain. 2017;18(1):15.
Mindfulness training is as effective as prophylactic medications for treating chronic migraine associated with medication overuse (CM-MO), according to research published online ahead of print February 4 in the Journal of Headache and Pain.
“Our results further suggest that a mindfulness-based treatment may be comparable to standard pharmacologic prophylaxis with regard to relevant primary outcomes such as headache frequency reduction and reduction in the consumption of acute medications,” said Licia Grazzi, MD, a neurologist at Istituto Neurologico Carlo Besta in Milan.
Research has suggested that mindfulness may be beneficial for headache. Previous studies, however, have been limited by inadequate consideration of several significant end points in chronic headache, such as frequency of headache and consumption of medications for acute headache management, said the authors.
To address these limitations, Dr. Grazzi and colleagues conducted an exploratory clinical trial that compared conventional prophylactic pharmacologic treatment with a mindfulness-based treatment for patients diagnosed with CM-MO. Researchers hypothesized that the mindfulness-based approach would be as effective as conventional prophylactic treatment.
Eligible participants were between ages 18 and 65 and had been diagnosed with CM-MO according to the International Classification of Headache Disorders, third edition (beta version), and had presented for treatment at the Headache Center of the Istituto Neurologico Carlo Besta between February 2014 and June 2015. In addition, participants had a history of chronic migraine for at least 10 years that was associated with overuse of triptans and nonsteroidal anti-inflammatory drugs for a minimum of the past five years.
All patients completed a five-day medication withdrawal program and were encouraged to exercise at least 45 minutes twice a week, to stay properly hydrated, and to consume three meals every day.
Participants were separated into two groups. In one group, patients were treated with prophylactic medications. In the second group, patients participated in a mindfulness-based training that consisted of six weekly sessions of guided mindfulness. Patients were invited to practice mindfulness training for seven to 10 minutes per day. At each follow-up visit, the Headache Impact Test, the Migraine Disability Assessment, the State and Trait Anxiety Inventory, and the Beck Depression Inventory were administered. Patients also kept headache diaries.
A total of 44 patients participated in the study. The average age was 44.5, the average headache frequency per month was 20.5, and the average monthly medication intake was 18.4 pills. Overall, data indicated a similar improvement over time in the mindfulness group and pharmacologic prophylaxis group for headache frequency, use of medication, Migraine Disability Assessment, Headache Impact Test, and Beck Depression Inventory. No changes on State and Trait Anxiety Inventory were reported. Both groups had significant and equivalent proportions of participants who achieved at least 50% reduction of headaches, compared with baseline. The majority of patients in each group no longer satisfied criteria for chronic migraine.
“Our findings support the value of conducting further … well-controlled studies (incorporating random assignment, larger sample sizes, and checks on integrity of treatment),” said Dr. Grazzi. “[Such studies] are warranted to more fully explore the benefits, boundaries, and mechanisms of action for mindfulness in treating chronic migraine by itself and when it is complicated by medication overuse and medical or psychological comorbidities.”
—Erica Tricarico
Suggested Reading
Grazzi L, Sansone E, Raggi A, et al. Mindfulness and pharmacological prophylaxis after withdrawal from medication overuse in patients with chronic migraine: an effectiveness trial with a one-year follow-up. J Headache Pain. 2017;18(1):15.
ABIM finds 69% concordance between MOC questions and common practice
, according to new research conducted and funded by the board.
“In this study comparing the percentages of 186 categories of medical conditions seen by general internists in office visits and hospital stays with the percentages of 3,461 questions on IM-MOC examinations from 2010 to 2013, 69% of examination questions were concordant with conditions seen,” Bradley Gray, PhD, ABIM senior health services researcher, Philadelphia, and his colleagues said in a report published in JAMA (2017 Jun 13;317[22]:2317-24).
Questions’ discordance with conditions seen specifically in the office outpatient setting and in the hospital was greater. Comparing questions and office-based practice, 58% of questions (2,010) involving 145 conditions were categorized as concordant. Comparing questions and hospital stays only, 42% of questions (1,456) involving 122 conditions were categorized as concordant.
The study did not evaluate the importance of the conditions that were found in questions that were in discordance with what physicians see in practice.
“Most of the discordant conditions where the frequency of questions on the exam was greater than the frequency of conditions seen were conditions that may have been uncommon but were rated as extremely important to patient care by internists responding to a survey involving review of exam blueprints,” Marianne Green, MD, study coauthor and ABIM board member, said in a statement. “An example of this is diagnosis of vasculitis, a rare but painful condition that can slow vital blood supply to tissues and organs. Based on physicians’ input, these conditions continue to be included on the exam.”
Conversely, there are questions that appear infrequently despite the fact that they cover conditions commonly seen in practice.
“For example, the question percentage for hypertension was judged to be concordant because it was similar to hospital stay percentage (1.91% vs. 1.84%), even though the question percentage was much lower than office visit percentage for this condition (1.91% vs. 13.87%),” the authors stated in the report.
ABIM researchers added that certain common conditions do not require more questions “because care guidelines are widely disseminated and more questions in these areas may be repetitive in terms of content and, therefore, do not contribute significantly to the assessment of a physician’s clinical judgment, especially when limited testing time is available.”
The overall percentage was a reasonable range, Andrea Paul, MD, chief medical officer of BoardVitals, a New York-based company that helps doctors prepare for MOC exams, said in an interview.
“Aiming for somewhere between 65% and 75% on commonly experienced patient conditions is reasonable,” Dr. Paul said. “The reason for that is that those common things that physicians see regularly in practice are just that – they are regularly practiced. So, they don’t necessarily need as much review and testing on topics that they are maintaining their own knowledge of on a daily basis.”
It is important for maintenance of certification exams to cover the rarer conditions, compared with what doctors see regularly, she added.
“I think the exams are aiming to cover those in greater detail because, if a rare condition were to walk into someone’s practice, there would be a great lapse in reviewing those obscure or rare conditions, and it might lead to a delay in diagnosing it or a delay in treating one of those conditions,” Dr. Paul said. “While people find it a nuisance to review something they don’t see regularly, that’s the reason that it’s important.”
The study’s findings have helped inform the review of the MOC testing blueprint that began in 2015, the ABIM noted, so the results may not match the current rate of concordance between questions asked and conditions that physicians are seeing. The report’s authors added that not enough new exams have been administered and not enough information on office visits has been made available to determine the latest concordance rates.
Dr. Paul suggested that, even in internal medicine, it might be better to offer examinations that are more specialized.
“Of people taking that exam, a great proportion of them don’t practice in general outpatient internal medicine,” she said. “They are either specialized in oncology or nephrology, or they practice in academia or are researchers. So, although you would think that everyone would have what they define as a general internal medicine practice, a great proportion doesn’t practice general internal medicine, especially outpatient internal medicine.
“The way to get that [concordance] number up would be to create different maintenance of certification exams based on people’s practice type,” Dr. Paul added. “To have an exam that tests what that person’s specific area is ... That would be a way that I could see to improve it.”
All of the researchers are either employed by or affiliated with ABIM. No additional conflicts of interest were disclosed.
In recent years, ABIM examinations have placed greater emphasis on evidence-based medicine. Yet, the ABIM has been too slow to develop rigorous evidence to support the validity of its recertification examination. There will never be a perfect examination, nor will there be a perfect way to assess physician knowledge, understanding, decision making, and clinical skills.
However, the study by Gray et al. represents an important effort to provide evidence on the validity of the recertification examination and its relevance to practicing internists.
The ABIM must strive for continuous improvement and is most relevant and useful when it asks for help and listens to its members, a process that it has been involved with for the past several years. Open, ongoing evaluation of the recertification examination will be essential, along with frank and productive discussion about how to ensure the continuous improvement, excellence, and relevance of the recertification process.
Adam B. Schwartz, MD, of New York University and J. Sanford Schwartz, MD, of the University of Pennsylvania, Philadelphia, made these comments in an editorial (JAMA. 2017 Jun 13;317[22]:2288-9).
In recent years, ABIM examinations have placed greater emphasis on evidence-based medicine. Yet, the ABIM has been too slow to develop rigorous evidence to support the validity of its recertification examination. There will never be a perfect examination, nor will there be a perfect way to assess physician knowledge, understanding, decision making, and clinical skills.
However, the study by Gray et al. represents an important effort to provide evidence on the validity of the recertification examination and its relevance to practicing internists.
The ABIM must strive for continuous improvement and is most relevant and useful when it asks for help and listens to its members, a process that it has been involved with for the past several years. Open, ongoing evaluation of the recertification examination will be essential, along with frank and productive discussion about how to ensure the continuous improvement, excellence, and relevance of the recertification process.
Adam B. Schwartz, MD, of New York University and J. Sanford Schwartz, MD, of the University of Pennsylvania, Philadelphia, made these comments in an editorial (JAMA. 2017 Jun 13;317[22]:2288-9).
In recent years, ABIM examinations have placed greater emphasis on evidence-based medicine. Yet, the ABIM has been too slow to develop rigorous evidence to support the validity of its recertification examination. There will never be a perfect examination, nor will there be a perfect way to assess physician knowledge, understanding, decision making, and clinical skills.
However, the study by Gray et al. represents an important effort to provide evidence on the validity of the recertification examination and its relevance to practicing internists.
The ABIM must strive for continuous improvement and is most relevant and useful when it asks for help and listens to its members, a process that it has been involved with for the past several years. Open, ongoing evaluation of the recertification examination will be essential, along with frank and productive discussion about how to ensure the continuous improvement, excellence, and relevance of the recertification process.
Adam B. Schwartz, MD, of New York University and J. Sanford Schwartz, MD, of the University of Pennsylvania, Philadelphia, made these comments in an editorial (JAMA. 2017 Jun 13;317[22]:2288-9).
, according to new research conducted and funded by the board.
“In this study comparing the percentages of 186 categories of medical conditions seen by general internists in office visits and hospital stays with the percentages of 3,461 questions on IM-MOC examinations from 2010 to 2013, 69% of examination questions were concordant with conditions seen,” Bradley Gray, PhD, ABIM senior health services researcher, Philadelphia, and his colleagues said in a report published in JAMA (2017 Jun 13;317[22]:2317-24).
Questions’ discordance with conditions seen specifically in the office outpatient setting and in the hospital was greater. Comparing questions and office-based practice, 58% of questions (2,010) involving 145 conditions were categorized as concordant. Comparing questions and hospital stays only, 42% of questions (1,456) involving 122 conditions were categorized as concordant.
The study did not evaluate the importance of the conditions that were found in questions that were in discordance with what physicians see in practice.
“Most of the discordant conditions where the frequency of questions on the exam was greater than the frequency of conditions seen were conditions that may have been uncommon but were rated as extremely important to patient care by internists responding to a survey involving review of exam blueprints,” Marianne Green, MD, study coauthor and ABIM board member, said in a statement. “An example of this is diagnosis of vasculitis, a rare but painful condition that can slow vital blood supply to tissues and organs. Based on physicians’ input, these conditions continue to be included on the exam.”
Conversely, there are questions that appear infrequently despite the fact that they cover conditions commonly seen in practice.
“For example, the question percentage for hypertension was judged to be concordant because it was similar to hospital stay percentage (1.91% vs. 1.84%), even though the question percentage was much lower than office visit percentage for this condition (1.91% vs. 13.87%),” the authors stated in the report.
ABIM researchers added that certain common conditions do not require more questions “because care guidelines are widely disseminated and more questions in these areas may be repetitive in terms of content and, therefore, do not contribute significantly to the assessment of a physician’s clinical judgment, especially when limited testing time is available.”
The overall percentage was a reasonable range, Andrea Paul, MD, chief medical officer of BoardVitals, a New York-based company that helps doctors prepare for MOC exams, said in an interview.
“Aiming for somewhere between 65% and 75% on commonly experienced patient conditions is reasonable,” Dr. Paul said. “The reason for that is that those common things that physicians see regularly in practice are just that – they are regularly practiced. So, they don’t necessarily need as much review and testing on topics that they are maintaining their own knowledge of on a daily basis.”
It is important for maintenance of certification exams to cover the rarer conditions, compared with what doctors see regularly, she added.
“I think the exams are aiming to cover those in greater detail because, if a rare condition were to walk into someone’s practice, there would be a great lapse in reviewing those obscure or rare conditions, and it might lead to a delay in diagnosing it or a delay in treating one of those conditions,” Dr. Paul said. “While people find it a nuisance to review something they don’t see regularly, that’s the reason that it’s important.”
The study’s findings have helped inform the review of the MOC testing blueprint that began in 2015, the ABIM noted, so the results may not match the current rate of concordance between questions asked and conditions that physicians are seeing. The report’s authors added that not enough new exams have been administered and not enough information on office visits has been made available to determine the latest concordance rates.
Dr. Paul suggested that, even in internal medicine, it might be better to offer examinations that are more specialized.
“Of people taking that exam, a great proportion of them don’t practice in general outpatient internal medicine,” she said. “They are either specialized in oncology or nephrology, or they practice in academia or are researchers. So, although you would think that everyone would have what they define as a general internal medicine practice, a great proportion doesn’t practice general internal medicine, especially outpatient internal medicine.
“The way to get that [concordance] number up would be to create different maintenance of certification exams based on people’s practice type,” Dr. Paul added. “To have an exam that tests what that person’s specific area is ... That would be a way that I could see to improve it.”
All of the researchers are either employed by or affiliated with ABIM. No additional conflicts of interest were disclosed.
, according to new research conducted and funded by the board.
“In this study comparing the percentages of 186 categories of medical conditions seen by general internists in office visits and hospital stays with the percentages of 3,461 questions on IM-MOC examinations from 2010 to 2013, 69% of examination questions were concordant with conditions seen,” Bradley Gray, PhD, ABIM senior health services researcher, Philadelphia, and his colleagues said in a report published in JAMA (2017 Jun 13;317[22]:2317-24).
Questions’ discordance with conditions seen specifically in the office outpatient setting and in the hospital was greater. Comparing questions and office-based practice, 58% of questions (2,010) involving 145 conditions were categorized as concordant. Comparing questions and hospital stays only, 42% of questions (1,456) involving 122 conditions were categorized as concordant.
The study did not evaluate the importance of the conditions that were found in questions that were in discordance with what physicians see in practice.
“Most of the discordant conditions where the frequency of questions on the exam was greater than the frequency of conditions seen were conditions that may have been uncommon but were rated as extremely important to patient care by internists responding to a survey involving review of exam blueprints,” Marianne Green, MD, study coauthor and ABIM board member, said in a statement. “An example of this is diagnosis of vasculitis, a rare but painful condition that can slow vital blood supply to tissues and organs. Based on physicians’ input, these conditions continue to be included on the exam.”
Conversely, there are questions that appear infrequently despite the fact that they cover conditions commonly seen in practice.
“For example, the question percentage for hypertension was judged to be concordant because it was similar to hospital stay percentage (1.91% vs. 1.84%), even though the question percentage was much lower than office visit percentage for this condition (1.91% vs. 13.87%),” the authors stated in the report.
ABIM researchers added that certain common conditions do not require more questions “because care guidelines are widely disseminated and more questions in these areas may be repetitive in terms of content and, therefore, do not contribute significantly to the assessment of a physician’s clinical judgment, especially when limited testing time is available.”
The overall percentage was a reasonable range, Andrea Paul, MD, chief medical officer of BoardVitals, a New York-based company that helps doctors prepare for MOC exams, said in an interview.
“Aiming for somewhere between 65% and 75% on commonly experienced patient conditions is reasonable,” Dr. Paul said. “The reason for that is that those common things that physicians see regularly in practice are just that – they are regularly practiced. So, they don’t necessarily need as much review and testing on topics that they are maintaining their own knowledge of on a daily basis.”
It is important for maintenance of certification exams to cover the rarer conditions, compared with what doctors see regularly, she added.
“I think the exams are aiming to cover those in greater detail because, if a rare condition were to walk into someone’s practice, there would be a great lapse in reviewing those obscure or rare conditions, and it might lead to a delay in diagnosing it or a delay in treating one of those conditions,” Dr. Paul said. “While people find it a nuisance to review something they don’t see regularly, that’s the reason that it’s important.”
The study’s findings have helped inform the review of the MOC testing blueprint that began in 2015, the ABIM noted, so the results may not match the current rate of concordance between questions asked and conditions that physicians are seeing. The report’s authors added that not enough new exams have been administered and not enough information on office visits has been made available to determine the latest concordance rates.
Dr. Paul suggested that, even in internal medicine, it might be better to offer examinations that are more specialized.
“Of people taking that exam, a great proportion of them don’t practice in general outpatient internal medicine,” she said. “They are either specialized in oncology or nephrology, or they practice in academia or are researchers. So, although you would think that everyone would have what they define as a general internal medicine practice, a great proportion doesn’t practice general internal medicine, especially outpatient internal medicine.
“The way to get that [concordance] number up would be to create different maintenance of certification exams based on people’s practice type,” Dr. Paul added. “To have an exam that tests what that person’s specific area is ... That would be a way that I could see to improve it.”
All of the researchers are either employed by or affiliated with ABIM. No additional conflicts of interest were disclosed.
FROM JAMA
EHR Report: Don’t let the electronic health record do the driving
The secret to the care of the patient ... is in caring for the patient.
-Francis W. Peabody, MD1
Last month I received a call from a man who was upset about the way he was treated in our office. He had presented with depression and felt insulted by one of our resident physicians in the way he had interacted with him during his visit. I offered to see him the next day.
When I walked into the exam room, I noticed that his eyes were bloodshot and he was fidgeting in his chair. He explained that it was difficult for him to address this issue, but he had been taken aback at his previous visit to our office when the doctor who saw him, after introducing himself, proceeded to sit down, open his computer, and start typing. The patient went on to describe that the physician – while staring at his computer screen – first acknowledged that he was being seen for depression and then immediately asked him if he had any plans to commit suicide. He did not have any suicidal plans, but he felt strongly that being asked about suicide as the first question in the doctor’s interview missed the point of his visit. He was having trouble concentrating, he felt down, and he was having difficulty sleeping at night, all contributing to trouble both at work and in his personal life. Suicide was not a concern of his. He shook his head. He said he understood that we, as doctors, had to put information into the computer, but he also felt that the doctor’s main goal during that visit appeared to be to get through the forms on the computer rather than taking care of him. He admonished that physicians also need to remember that there is a patient in the room and that we should pay attention to the patient first. The computer should be second. I couldn’t have said it better myself. I told him that I would look into what happened, and then we continued with his visit.
You can already see where this discussion is going. The odd thing about the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medicare’s quality payment program, is that, unless we are careful, the result of the program may be the opposite of what it’s intended to accomplish. By leading to an over-focus on documentation of the quality of care, we are at risk of diminishing the quality of care itself. In essence, many of the requirements appear to simply be more advanced versions of the meaningful (meaningless?) use provisions with which we have previously grappled. It is clear that we should assess the quality of care that is given and that physician payment should be influenced by that care. It is also clear that the only reasonable way to measure the care provided is by collecting data from the EHR. The problem is that the sophistication of the EHR has not caught up to the sophistication of our goals.
Our challenge as physicians who care for patients therefore occurs at an individual level for each of us. How do we provide the necessary documentation scattered throughout our digital charts to satisfy reporting requirements, yet still meet the very real needs of patients to have their voices heard and their emotions acknowledged? The Physician Charter by the American Board of Internal Medicine discusses “the primacy of patient welfare” as a core tenant of medical practice. It goes on to state that “administrative exigencies must not compromise this principle.”2 Given competing demands, how do we continue to accomplish these goals which are often in conflict with one another?
We cannot provide an answer to this question because unfortunately – or perhaps fortunately – the answer does not come in the form of a clear algorithm of behaviors or a form that we can click on. However that does not mean that it cannot be done. Simply being mindful of how important personal interaction is to our patients will help us stay focused on patient needs. In fact, one of the most exciting aspects of our digital age (and our use of EHRs) is that the need to actually connect with people is more important than ever, and prioritizing this stands to reward those individuals who continue to pay attention to patients. In a future column, we will discuss suggestions and strategies for integrating the EHR into truly patient-centered care. In the early 1920s, Dr. Francis W. Peabody said, “The treatment of a disease may be entirely impersonal: the care of the patient must be completely personal.”1 Medical competency is essential and documentation is required, but neither alone is sufficient for the care of patients.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
References
1. Peabody FW. The care of the patient. JAMA. 1927;88:877-82.
2. The Physician Charter. American Board of Internal Medicine Foundation at http://abimfoundation.org/what-we-do/physician-charter.
The secret to the care of the patient ... is in caring for the patient.
-Francis W. Peabody, MD1
Last month I received a call from a man who was upset about the way he was treated in our office. He had presented with depression and felt insulted by one of our resident physicians in the way he had interacted with him during his visit. I offered to see him the next day.
When I walked into the exam room, I noticed that his eyes were bloodshot and he was fidgeting in his chair. He explained that it was difficult for him to address this issue, but he had been taken aback at his previous visit to our office when the doctor who saw him, after introducing himself, proceeded to sit down, open his computer, and start typing. The patient went on to describe that the physician – while staring at his computer screen – first acknowledged that he was being seen for depression and then immediately asked him if he had any plans to commit suicide. He did not have any suicidal plans, but he felt strongly that being asked about suicide as the first question in the doctor’s interview missed the point of his visit. He was having trouble concentrating, he felt down, and he was having difficulty sleeping at night, all contributing to trouble both at work and in his personal life. Suicide was not a concern of his. He shook his head. He said he understood that we, as doctors, had to put information into the computer, but he also felt that the doctor’s main goal during that visit appeared to be to get through the forms on the computer rather than taking care of him. He admonished that physicians also need to remember that there is a patient in the room and that we should pay attention to the patient first. The computer should be second. I couldn’t have said it better myself. I told him that I would look into what happened, and then we continued with his visit.
You can already see where this discussion is going. The odd thing about the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medicare’s quality payment program, is that, unless we are careful, the result of the program may be the opposite of what it’s intended to accomplish. By leading to an over-focus on documentation of the quality of care, we are at risk of diminishing the quality of care itself. In essence, many of the requirements appear to simply be more advanced versions of the meaningful (meaningless?) use provisions with which we have previously grappled. It is clear that we should assess the quality of care that is given and that physician payment should be influenced by that care. It is also clear that the only reasonable way to measure the care provided is by collecting data from the EHR. The problem is that the sophistication of the EHR has not caught up to the sophistication of our goals.
Our challenge as physicians who care for patients therefore occurs at an individual level for each of us. How do we provide the necessary documentation scattered throughout our digital charts to satisfy reporting requirements, yet still meet the very real needs of patients to have their voices heard and their emotions acknowledged? The Physician Charter by the American Board of Internal Medicine discusses “the primacy of patient welfare” as a core tenant of medical practice. It goes on to state that “administrative exigencies must not compromise this principle.”2 Given competing demands, how do we continue to accomplish these goals which are often in conflict with one another?
We cannot provide an answer to this question because unfortunately – or perhaps fortunately – the answer does not come in the form of a clear algorithm of behaviors or a form that we can click on. However that does not mean that it cannot be done. Simply being mindful of how important personal interaction is to our patients will help us stay focused on patient needs. In fact, one of the most exciting aspects of our digital age (and our use of EHRs) is that the need to actually connect with people is more important than ever, and prioritizing this stands to reward those individuals who continue to pay attention to patients. In a future column, we will discuss suggestions and strategies for integrating the EHR into truly patient-centered care. In the early 1920s, Dr. Francis W. Peabody said, “The treatment of a disease may be entirely impersonal: the care of the patient must be completely personal.”1 Medical competency is essential and documentation is required, but neither alone is sufficient for the care of patients.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
References
1. Peabody FW. The care of the patient. JAMA. 1927;88:877-82.
2. The Physician Charter. American Board of Internal Medicine Foundation at http://abimfoundation.org/what-we-do/physician-charter.
The secret to the care of the patient ... is in caring for the patient.
-Francis W. Peabody, MD1
Last month I received a call from a man who was upset about the way he was treated in our office. He had presented with depression and felt insulted by one of our resident physicians in the way he had interacted with him during his visit. I offered to see him the next day.
When I walked into the exam room, I noticed that his eyes were bloodshot and he was fidgeting in his chair. He explained that it was difficult for him to address this issue, but he had been taken aback at his previous visit to our office when the doctor who saw him, after introducing himself, proceeded to sit down, open his computer, and start typing. The patient went on to describe that the physician – while staring at his computer screen – first acknowledged that he was being seen for depression and then immediately asked him if he had any plans to commit suicide. He did not have any suicidal plans, but he felt strongly that being asked about suicide as the first question in the doctor’s interview missed the point of his visit. He was having trouble concentrating, he felt down, and he was having difficulty sleeping at night, all contributing to trouble both at work and in his personal life. Suicide was not a concern of his. He shook his head. He said he understood that we, as doctors, had to put information into the computer, but he also felt that the doctor’s main goal during that visit appeared to be to get through the forms on the computer rather than taking care of him. He admonished that physicians also need to remember that there is a patient in the room and that we should pay attention to the patient first. The computer should be second. I couldn’t have said it better myself. I told him that I would look into what happened, and then we continued with his visit.
You can already see where this discussion is going. The odd thing about the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medicare’s quality payment program, is that, unless we are careful, the result of the program may be the opposite of what it’s intended to accomplish. By leading to an over-focus on documentation of the quality of care, we are at risk of diminishing the quality of care itself. In essence, many of the requirements appear to simply be more advanced versions of the meaningful (meaningless?) use provisions with which we have previously grappled. It is clear that we should assess the quality of care that is given and that physician payment should be influenced by that care. It is also clear that the only reasonable way to measure the care provided is by collecting data from the EHR. The problem is that the sophistication of the EHR has not caught up to the sophistication of our goals.
Our challenge as physicians who care for patients therefore occurs at an individual level for each of us. How do we provide the necessary documentation scattered throughout our digital charts to satisfy reporting requirements, yet still meet the very real needs of patients to have their voices heard and their emotions acknowledged? The Physician Charter by the American Board of Internal Medicine discusses “the primacy of patient welfare” as a core tenant of medical practice. It goes on to state that “administrative exigencies must not compromise this principle.”2 Given competing demands, how do we continue to accomplish these goals which are often in conflict with one another?
We cannot provide an answer to this question because unfortunately – or perhaps fortunately – the answer does not come in the form of a clear algorithm of behaviors or a form that we can click on. However that does not mean that it cannot be done. Simply being mindful of how important personal interaction is to our patients will help us stay focused on patient needs. In fact, one of the most exciting aspects of our digital age (and our use of EHRs) is that the need to actually connect with people is more important than ever, and prioritizing this stands to reward those individuals who continue to pay attention to patients. In a future column, we will discuss suggestions and strategies for integrating the EHR into truly patient-centered care. In the early 1920s, Dr. Francis W. Peabody said, “The treatment of a disease may be entirely impersonal: the care of the patient must be completely personal.”1 Medical competency is essential and documentation is required, but neither alone is sufficient for the care of patients.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
References
1. Peabody FW. The care of the patient. JAMA. 1927;88:877-82.
2. The Physician Charter. American Board of Internal Medicine Foundation at http://abimfoundation.org/what-we-do/physician-charter.
VIDEO: Social networking offers coping help for endometriosis patients
VANCOUVER – Nearly half of the discussion topics on the social networking site www.myendometriosisteam.com are about pain, but other uncontrolled symptoms are popular topics, including fatigue and depression.
The online social support network includes 30,000 women with endometriosis and offers them a chance to connect with other women with the condition, find a provider, and research treatments. Elise-Marie Menke, director of alliance management at MyHealthTeams, which runs the site, presented data at the World Congress on Endometriosis. Among the findings she presented was how symptoms mapped to a woman’s cycle.
In a video interview, Ms. Menke described how this type of patient-generated data can play a role in the management of disease and serve to highlight unmet needs to physicians.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VANCOUVER – Nearly half of the discussion topics on the social networking site www.myendometriosisteam.com are about pain, but other uncontrolled symptoms are popular topics, including fatigue and depression.
The online social support network includes 30,000 women with endometriosis and offers them a chance to connect with other women with the condition, find a provider, and research treatments. Elise-Marie Menke, director of alliance management at MyHealthTeams, which runs the site, presented data at the World Congress on Endometriosis. Among the findings she presented was how symptoms mapped to a woman’s cycle.
In a video interview, Ms. Menke described how this type of patient-generated data can play a role in the management of disease and serve to highlight unmet needs to physicians.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VANCOUVER – Nearly half of the discussion topics on the social networking site www.myendometriosisteam.com are about pain, but other uncontrolled symptoms are popular topics, including fatigue and depression.
The online social support network includes 30,000 women with endometriosis and offers them a chance to connect with other women with the condition, find a provider, and research treatments. Elise-Marie Menke, director of alliance management at MyHealthTeams, which runs the site, presented data at the World Congress on Endometriosis. Among the findings she presented was how symptoms mapped to a woman’s cycle.
In a video interview, Ms. Menke described how this type of patient-generated data can play a role in the management of disease and serve to highlight unmet needs to physicians.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT WCE 2017
PORTEC-3: Possible benefit with combined CT/RT in high-risk endometrial cancer
CHICAGO – Adjuvant chemotherapy given during and after pelvic radiotherapy in women with high-risk endometrial cancer provided no significant 5-year failure-free or overall survival benefit, compared with pelvic radiotherapy alone, in the randomized PORTEC-3 intergroup trial. It did, however, show a trend toward improved 5-year failure-free survival (FFS).
Further, study participants with stage III endometrial cancer experienced a statistically significant 11% improvement in FFS – defined as relapse or endometrial cancer-related death – at 5 years, Stephanie M. de Boer, MD, reported at the annual meeting of the American Society of Clinical Oncology.
The 5-year FFS rate in 330 women who received both chemotherapy and radiotherapy was 76%, vs. 69% in 330 women who received only radiotherapy (hazard ratio, 0.77). The respective 5-year overall survival rates were 82%, vs. 77% (HR, 0.79), said Dr. de Boer of Leiden University Medical Center, the Netherlands.
The differences did not reach statistical significance, but there was a “trend for better failure-free survival” beginning after 1 year and “a small suggestion for an overall survival benefit” after 3 years in patients treated with chemotherapy and radiotherapy, she said.
Among the 45% of study participants with stage III endometrial cancer, 5-year FFS and overall survival were significantly lower than in those with stage I-II disease (64% vs. 79% and 74% vs. 83%, respectively), but those with stage III disease experienced the greatest benefit with adjuvant chemotherapy.
“Five-year failure-free survival was 69% for those [with stage III disease] treated with radiotherapy and chemotherapy, vs. 58% for those treated with radiotherapy alone,” she said, noting that the hazard ratio was 0.66.
Five-year overall survival in the stage III patients was 79%, vs. 70% (HR, 0.69). Only the difference in FFS reached statistical significance, Dr. de Boer noted.
Study subjects were women with either Federation Internationale de Gynecologie et d’Obstetrique stage I grade 3 endometrial cancer with deep myometrial invasion and/or lymphovascular space invasion or with stage II or III disease or with serous/clear cell histology. They had a mean age of 62 years, good performance status, and no residual macroscopic tumor after surgery. They were randomly assigned to receive two cycles of cisplatin at 50 mg/m2 in week 1 and 4 of radiotherapy (48.6 Gy in 1.8 Gy fractions), followed by four cycles of carboplatin AUC5 and paclitaxel at 175 mg/m2 in 3-week intervals, or to receive radiotherapy alone.
Median follow-up was 60.2 months.
“The rationale of the PORTEC-3 trial was that 15% of endometrial cancer patients have high-risk disease features, and these patients are at increased risk of distant metastases and endometrial cancer–related death,” Dr. de Boer said.
Several trials have looked at intensified treatment in these patients and include some that have compared chemotherapy and radiation and that found no difference in progression-free survival or overall survival. A Radiation Therapy Oncology Group (RTOG) phase II trial of concurrent chemotherapy and radiotherapy, however, showed promising results and a feasible toxicity profile, she said.
A phase III Nordic Society of Gynecologic Oncology (SGO)/European Organization for Research and Treatment of Cancer (EORTC) trial suggested that sequential chemotherapy and radiotherapy was associated with improved progression-free survival.
“But, various chemotherapy schedules and sequences have been used in these trials, and no extensive quality of life analysis was done,” she noted.
In PORTEC-3, radiotherapy and two cycles of concurrent cisplatin followed by four cycles of carboplatin and paclitaxel showed some promise, and quality of life analyses showed no difference between groups at 1 and 2 years after randomization.
In fact, although the adverse events findings as reported in 2016 in Lancet Oncology showed that, during therapy and for the first 6 months after therapy, “significantly more and more severe toxicity” occurred in the chemotherapy and radiotherapy group, vs. the radiotherapy group alone, this effect was transient and not associated with long-term effects on quality of life.
“There was significant recovery without significant differences at 1 and 2 years after randomization,” Dr. de Boer said, adding that the toxicity translated to worse physical functioning and quality of life during and for 6 months after therapy but that no differences in quality of life, and only small differences in physical functioning, were seen at 1 and 2 years.
The residual effect on physical functioning may have been related to the tingling and numbness, which was the most important long-term side effect reported in the trial, she said, noting that 25% of patients in the chemotherapy and radiotherapy group reported tingling and numbness at 2 years, compared with 6% in the radiotherapy group.
Based on these findings, combined chemotherapy and radiotherapy cannot be recommended as standard for patients with stage I and II high-risk endometrial cancer, she said.
However, based on the 11% FFS benefit for stage III patients, “the combined chemotherapy and radiotherapy schedule is recommended to maximize failure-free survival,” she concluded, noting that interpretation of overall survival results may need longer follow-up.
Ritu Salani, MD, who was invited to discuss Dr. de Boer’s abstract, said the PORTEC-3 findings raise a number of questions for studies going forward, such as the role of therapy sequence.
“Radiation has always preceded chemotherapy, and I wonder if distant recurrences could actually be impacted if we do chemotherapy first, whether it’s a complete course or in a sandwich-approach style. I think these are questions that we need to continue to address,” said Dr. Salani of Ohio State University, Columbus.
Other questions posed by Dr. Salani focused on whether high risk early stage and advanced disease should be studied separately, whether maintenance therapy should be evaluated in this population, whether there was under-staging in PORTEC-3 as 42% of patients did not undergo lymphadenectomy, whether there is a role for sentinel node assessment, and whether residual disease status should be a surgical metric and if chemotherapy should be reserved for those with residual disease.
“I think we continue to have many treatment options, and I think our tumor board debates will continue. And I think PORTEC-3 will add to this discussion. But, at this point I think we’re left to individualize treatment and to continue to provide the best outcome for our patients while minimizing toxicity,” she concluded.
Dr. de Boer reported having no disclosures. Dr. Salani has received honoraria from Clovis Oncology and Lynparza and has served as a consultant or advisor for Genentech/Roche.
CHICAGO – Adjuvant chemotherapy given during and after pelvic radiotherapy in women with high-risk endometrial cancer provided no significant 5-year failure-free or overall survival benefit, compared with pelvic radiotherapy alone, in the randomized PORTEC-3 intergroup trial. It did, however, show a trend toward improved 5-year failure-free survival (FFS).
Further, study participants with stage III endometrial cancer experienced a statistically significant 11% improvement in FFS – defined as relapse or endometrial cancer-related death – at 5 years, Stephanie M. de Boer, MD, reported at the annual meeting of the American Society of Clinical Oncology.
The 5-year FFS rate in 330 women who received both chemotherapy and radiotherapy was 76%, vs. 69% in 330 women who received only radiotherapy (hazard ratio, 0.77). The respective 5-year overall survival rates were 82%, vs. 77% (HR, 0.79), said Dr. de Boer of Leiden University Medical Center, the Netherlands.
The differences did not reach statistical significance, but there was a “trend for better failure-free survival” beginning after 1 year and “a small suggestion for an overall survival benefit” after 3 years in patients treated with chemotherapy and radiotherapy, she said.
Among the 45% of study participants with stage III endometrial cancer, 5-year FFS and overall survival were significantly lower than in those with stage I-II disease (64% vs. 79% and 74% vs. 83%, respectively), but those with stage III disease experienced the greatest benefit with adjuvant chemotherapy.
“Five-year failure-free survival was 69% for those [with stage III disease] treated with radiotherapy and chemotherapy, vs. 58% for those treated with radiotherapy alone,” she said, noting that the hazard ratio was 0.66.
Five-year overall survival in the stage III patients was 79%, vs. 70% (HR, 0.69). Only the difference in FFS reached statistical significance, Dr. de Boer noted.
Study subjects were women with either Federation Internationale de Gynecologie et d’Obstetrique stage I grade 3 endometrial cancer with deep myometrial invasion and/or lymphovascular space invasion or with stage II or III disease or with serous/clear cell histology. They had a mean age of 62 years, good performance status, and no residual macroscopic tumor after surgery. They were randomly assigned to receive two cycles of cisplatin at 50 mg/m2 in week 1 and 4 of radiotherapy (48.6 Gy in 1.8 Gy fractions), followed by four cycles of carboplatin AUC5 and paclitaxel at 175 mg/m2 in 3-week intervals, or to receive radiotherapy alone.
Median follow-up was 60.2 months.
“The rationale of the PORTEC-3 trial was that 15% of endometrial cancer patients have high-risk disease features, and these patients are at increased risk of distant metastases and endometrial cancer–related death,” Dr. de Boer said.
Several trials have looked at intensified treatment in these patients and include some that have compared chemotherapy and radiation and that found no difference in progression-free survival or overall survival. A Radiation Therapy Oncology Group (RTOG) phase II trial of concurrent chemotherapy and radiotherapy, however, showed promising results and a feasible toxicity profile, she said.
A phase III Nordic Society of Gynecologic Oncology (SGO)/European Organization for Research and Treatment of Cancer (EORTC) trial suggested that sequential chemotherapy and radiotherapy was associated with improved progression-free survival.
“But, various chemotherapy schedules and sequences have been used in these trials, and no extensive quality of life analysis was done,” she noted.
In PORTEC-3, radiotherapy and two cycles of concurrent cisplatin followed by four cycles of carboplatin and paclitaxel showed some promise, and quality of life analyses showed no difference between groups at 1 and 2 years after randomization.
In fact, although the adverse events findings as reported in 2016 in Lancet Oncology showed that, during therapy and for the first 6 months after therapy, “significantly more and more severe toxicity” occurred in the chemotherapy and radiotherapy group, vs. the radiotherapy group alone, this effect was transient and not associated with long-term effects on quality of life.
“There was significant recovery without significant differences at 1 and 2 years after randomization,” Dr. de Boer said, adding that the toxicity translated to worse physical functioning and quality of life during and for 6 months after therapy but that no differences in quality of life, and only small differences in physical functioning, were seen at 1 and 2 years.
The residual effect on physical functioning may have been related to the tingling and numbness, which was the most important long-term side effect reported in the trial, she said, noting that 25% of patients in the chemotherapy and radiotherapy group reported tingling and numbness at 2 years, compared with 6% in the radiotherapy group.
Based on these findings, combined chemotherapy and radiotherapy cannot be recommended as standard for patients with stage I and II high-risk endometrial cancer, she said.
However, based on the 11% FFS benefit for stage III patients, “the combined chemotherapy and radiotherapy schedule is recommended to maximize failure-free survival,” she concluded, noting that interpretation of overall survival results may need longer follow-up.
Ritu Salani, MD, who was invited to discuss Dr. de Boer’s abstract, said the PORTEC-3 findings raise a number of questions for studies going forward, such as the role of therapy sequence.
“Radiation has always preceded chemotherapy, and I wonder if distant recurrences could actually be impacted if we do chemotherapy first, whether it’s a complete course or in a sandwich-approach style. I think these are questions that we need to continue to address,” said Dr. Salani of Ohio State University, Columbus.
Other questions posed by Dr. Salani focused on whether high risk early stage and advanced disease should be studied separately, whether maintenance therapy should be evaluated in this population, whether there was under-staging in PORTEC-3 as 42% of patients did not undergo lymphadenectomy, whether there is a role for sentinel node assessment, and whether residual disease status should be a surgical metric and if chemotherapy should be reserved for those with residual disease.
“I think we continue to have many treatment options, and I think our tumor board debates will continue. And I think PORTEC-3 will add to this discussion. But, at this point I think we’re left to individualize treatment and to continue to provide the best outcome for our patients while minimizing toxicity,” she concluded.
Dr. de Boer reported having no disclosures. Dr. Salani has received honoraria from Clovis Oncology and Lynparza and has served as a consultant or advisor for Genentech/Roche.
CHICAGO – Adjuvant chemotherapy given during and after pelvic radiotherapy in women with high-risk endometrial cancer provided no significant 5-year failure-free or overall survival benefit, compared with pelvic radiotherapy alone, in the randomized PORTEC-3 intergroup trial. It did, however, show a trend toward improved 5-year failure-free survival (FFS).
Further, study participants with stage III endometrial cancer experienced a statistically significant 11% improvement in FFS – defined as relapse or endometrial cancer-related death – at 5 years, Stephanie M. de Boer, MD, reported at the annual meeting of the American Society of Clinical Oncology.
The 5-year FFS rate in 330 women who received both chemotherapy and radiotherapy was 76%, vs. 69% in 330 women who received only radiotherapy (hazard ratio, 0.77). The respective 5-year overall survival rates were 82%, vs. 77% (HR, 0.79), said Dr. de Boer of Leiden University Medical Center, the Netherlands.
The differences did not reach statistical significance, but there was a “trend for better failure-free survival” beginning after 1 year and “a small suggestion for an overall survival benefit” after 3 years in patients treated with chemotherapy and radiotherapy, she said.
Among the 45% of study participants with stage III endometrial cancer, 5-year FFS and overall survival were significantly lower than in those with stage I-II disease (64% vs. 79% and 74% vs. 83%, respectively), but those with stage III disease experienced the greatest benefit with adjuvant chemotherapy.
“Five-year failure-free survival was 69% for those [with stage III disease] treated with radiotherapy and chemotherapy, vs. 58% for those treated with radiotherapy alone,” she said, noting that the hazard ratio was 0.66.
Five-year overall survival in the stage III patients was 79%, vs. 70% (HR, 0.69). Only the difference in FFS reached statistical significance, Dr. de Boer noted.
Study subjects were women with either Federation Internationale de Gynecologie et d’Obstetrique stage I grade 3 endometrial cancer with deep myometrial invasion and/or lymphovascular space invasion or with stage II or III disease or with serous/clear cell histology. They had a mean age of 62 years, good performance status, and no residual macroscopic tumor after surgery. They were randomly assigned to receive two cycles of cisplatin at 50 mg/m2 in week 1 and 4 of radiotherapy (48.6 Gy in 1.8 Gy fractions), followed by four cycles of carboplatin AUC5 and paclitaxel at 175 mg/m2 in 3-week intervals, or to receive radiotherapy alone.
Median follow-up was 60.2 months.
“The rationale of the PORTEC-3 trial was that 15% of endometrial cancer patients have high-risk disease features, and these patients are at increased risk of distant metastases and endometrial cancer–related death,” Dr. de Boer said.
Several trials have looked at intensified treatment in these patients and include some that have compared chemotherapy and radiation and that found no difference in progression-free survival or overall survival. A Radiation Therapy Oncology Group (RTOG) phase II trial of concurrent chemotherapy and radiotherapy, however, showed promising results and a feasible toxicity profile, she said.
A phase III Nordic Society of Gynecologic Oncology (SGO)/European Organization for Research and Treatment of Cancer (EORTC) trial suggested that sequential chemotherapy and radiotherapy was associated with improved progression-free survival.
“But, various chemotherapy schedules and sequences have been used in these trials, and no extensive quality of life analysis was done,” she noted.
In PORTEC-3, radiotherapy and two cycles of concurrent cisplatin followed by four cycles of carboplatin and paclitaxel showed some promise, and quality of life analyses showed no difference between groups at 1 and 2 years after randomization.
In fact, although the adverse events findings as reported in 2016 in Lancet Oncology showed that, during therapy and for the first 6 months after therapy, “significantly more and more severe toxicity” occurred in the chemotherapy and radiotherapy group, vs. the radiotherapy group alone, this effect was transient and not associated with long-term effects on quality of life.
“There was significant recovery without significant differences at 1 and 2 years after randomization,” Dr. de Boer said, adding that the toxicity translated to worse physical functioning and quality of life during and for 6 months after therapy but that no differences in quality of life, and only small differences in physical functioning, were seen at 1 and 2 years.
The residual effect on physical functioning may have been related to the tingling and numbness, which was the most important long-term side effect reported in the trial, she said, noting that 25% of patients in the chemotherapy and radiotherapy group reported tingling and numbness at 2 years, compared with 6% in the radiotherapy group.
Based on these findings, combined chemotherapy and radiotherapy cannot be recommended as standard for patients with stage I and II high-risk endometrial cancer, she said.
However, based on the 11% FFS benefit for stage III patients, “the combined chemotherapy and radiotherapy schedule is recommended to maximize failure-free survival,” she concluded, noting that interpretation of overall survival results may need longer follow-up.
Ritu Salani, MD, who was invited to discuss Dr. de Boer’s abstract, said the PORTEC-3 findings raise a number of questions for studies going forward, such as the role of therapy sequence.
“Radiation has always preceded chemotherapy, and I wonder if distant recurrences could actually be impacted if we do chemotherapy first, whether it’s a complete course or in a sandwich-approach style. I think these are questions that we need to continue to address,” said Dr. Salani of Ohio State University, Columbus.
Other questions posed by Dr. Salani focused on whether high risk early stage and advanced disease should be studied separately, whether maintenance therapy should be evaluated in this population, whether there was under-staging in PORTEC-3 as 42% of patients did not undergo lymphadenectomy, whether there is a role for sentinel node assessment, and whether residual disease status should be a surgical metric and if chemotherapy should be reserved for those with residual disease.
“I think we continue to have many treatment options, and I think our tumor board debates will continue. And I think PORTEC-3 will add to this discussion. But, at this point I think we’re left to individualize treatment and to continue to provide the best outcome for our patients while minimizing toxicity,” she concluded.
Dr. de Boer reported having no disclosures. Dr. Salani has received honoraria from Clovis Oncology and Lynparza and has served as a consultant or advisor for Genentech/Roche.
AT ASCO 2017
Key clinical point:
Major finding: The 5-year FFS rate in 330 women who received both chemotherapy and radiotherapy was 76%, vs. 69% in 330 women who received only radiotherapy (HR, 0.77).
Data source: The randomized PORTEC-3 trial of 660 patients.
Disclosures: Dr. de Boer reported having no disclosures. Dr. Salani has received honoraria from Clovis Oncology and Lynparza and has served as a consultant or advisor for Genentech/Roche.
Hiring the right employees
Many of the personnel questions I receive concern the dreaded “marginal employee” – a person who has never done anything truly heinous to merit firing but also hasn’t done anything special to merit continued employment. I always advise getting rid of such people and then changing the hiring criteria that all too often result in poor hires.
Most bad hires come about because employers do not have a clear vision of the kind of employee they want. Many office manuals do not contain detailed job descriptions. If you don’t know exactly what you are looking for, your entire selection process will be inadequate from initial screening of applicants through assessments of their skills and personalities. Many physicians compound the problem with poor interview techniques and inadequate checking of references.
Once you have a clear job description in mind (and in print), take all the time you need to find the best possible match for it. This is not a place to cut corners. Screen your candidates carefully, and avoid lowering your expectations. This is the point at which it might be tempting to settle for a marginal candidate just to get the process over with.
It is also sometimes tempting to hire the candidate that you have the “best feeling” about, even though he or she is a poor match for the job, and then try to mold the job to that person. Every doctor knows that hunches are no substitute for hard data.
Be alert for red flags in resumes: significant time gaps between jobs, positions at companies that are no longer in business or are otherwise impossible to verify, job titles that don’t make sense given the applicant’s qualifications.
Background checks are a dicey subject, but publicly available information can be found, cheap or free, on multiple web sites created for that purpose. Be sure to tell applicants that you will be verifying facts in their resumes. It’s usually wise to get their written consent to do so.
Many employers skip the essential step of calling references, and many applicants know that. Some old bosses will be reluctant to tell you anything substantive, so I always ask, “Would you hire this person again?” You can interpret a lot from the answer – or lack of one.
Interviews often get short shrift as well. Many doctors tend to do all the talking. As I’ve observed numerous times, listening is not our strong suit, as a general rule. The purpose of an interview is to allow you to size up the prospective employee, not to deliver a lecture on the sterling attributes of your office. Important interview topics include educational background, skills, experience, and unrelated job history.
By law, you cannot ask an applicant’s age, date of birth, gender, creed, color, religion, or national origin. Other forbidden subjects include disabilities, marital status, military record, number of children (or who cares for them), addiction history, citizenship, criminal record, psychiatric history, absenteeism, or workman’s compensation.
However, there are acceptable alternatives to some of those questions. You can ask if applicants have ever gone by another name (for your background check), for example. You can ask if they are legally authorized to work in this country and whether they will be physically able to perform the duties specified in the job description. While past addictions are off limits, you do have a right to know about current addictions to illegal substances.
Once you have hired people whose skills and personalities best fit your needs, train them well. Then, give them the opportunity to succeed. “The best executive,” wrote Theodore Roosevelt, “is one who has sense enough to pick good people to do what he [or she] wants done and self-restraint enough to keep from meddling with them while they do it.” ”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@frontlinemedcom.com.
Many of the personnel questions I receive concern the dreaded “marginal employee” – a person who has never done anything truly heinous to merit firing but also hasn’t done anything special to merit continued employment. I always advise getting rid of such people and then changing the hiring criteria that all too often result in poor hires.
Most bad hires come about because employers do not have a clear vision of the kind of employee they want. Many office manuals do not contain detailed job descriptions. If you don’t know exactly what you are looking for, your entire selection process will be inadequate from initial screening of applicants through assessments of their skills and personalities. Many physicians compound the problem with poor interview techniques and inadequate checking of references.
Once you have a clear job description in mind (and in print), take all the time you need to find the best possible match for it. This is not a place to cut corners. Screen your candidates carefully, and avoid lowering your expectations. This is the point at which it might be tempting to settle for a marginal candidate just to get the process over with.
It is also sometimes tempting to hire the candidate that you have the “best feeling” about, even though he or she is a poor match for the job, and then try to mold the job to that person. Every doctor knows that hunches are no substitute for hard data.
Be alert for red flags in resumes: significant time gaps between jobs, positions at companies that are no longer in business or are otherwise impossible to verify, job titles that don’t make sense given the applicant’s qualifications.
Background checks are a dicey subject, but publicly available information can be found, cheap or free, on multiple web sites created for that purpose. Be sure to tell applicants that you will be verifying facts in their resumes. It’s usually wise to get their written consent to do so.
Many employers skip the essential step of calling references, and many applicants know that. Some old bosses will be reluctant to tell you anything substantive, so I always ask, “Would you hire this person again?” You can interpret a lot from the answer – or lack of one.
Interviews often get short shrift as well. Many doctors tend to do all the talking. As I’ve observed numerous times, listening is not our strong suit, as a general rule. The purpose of an interview is to allow you to size up the prospective employee, not to deliver a lecture on the sterling attributes of your office. Important interview topics include educational background, skills, experience, and unrelated job history.
By law, you cannot ask an applicant’s age, date of birth, gender, creed, color, religion, or national origin. Other forbidden subjects include disabilities, marital status, military record, number of children (or who cares for them), addiction history, citizenship, criminal record, psychiatric history, absenteeism, or workman’s compensation.
However, there are acceptable alternatives to some of those questions. You can ask if applicants have ever gone by another name (for your background check), for example. You can ask if they are legally authorized to work in this country and whether they will be physically able to perform the duties specified in the job description. While past addictions are off limits, you do have a right to know about current addictions to illegal substances.
Once you have hired people whose skills and personalities best fit your needs, train them well. Then, give them the opportunity to succeed. “The best executive,” wrote Theodore Roosevelt, “is one who has sense enough to pick good people to do what he [or she] wants done and self-restraint enough to keep from meddling with them while they do it.” ”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@frontlinemedcom.com.
Many of the personnel questions I receive concern the dreaded “marginal employee” – a person who has never done anything truly heinous to merit firing but also hasn’t done anything special to merit continued employment. I always advise getting rid of such people and then changing the hiring criteria that all too often result in poor hires.
Most bad hires come about because employers do not have a clear vision of the kind of employee they want. Many office manuals do not contain detailed job descriptions. If you don’t know exactly what you are looking for, your entire selection process will be inadequate from initial screening of applicants through assessments of their skills and personalities. Many physicians compound the problem with poor interview techniques and inadequate checking of references.
Once you have a clear job description in mind (and in print), take all the time you need to find the best possible match for it. This is not a place to cut corners. Screen your candidates carefully, and avoid lowering your expectations. This is the point at which it might be tempting to settle for a marginal candidate just to get the process over with.
It is also sometimes tempting to hire the candidate that you have the “best feeling” about, even though he or she is a poor match for the job, and then try to mold the job to that person. Every doctor knows that hunches are no substitute for hard data.
Be alert for red flags in resumes: significant time gaps between jobs, positions at companies that are no longer in business or are otherwise impossible to verify, job titles that don’t make sense given the applicant’s qualifications.
Background checks are a dicey subject, but publicly available information can be found, cheap or free, on multiple web sites created for that purpose. Be sure to tell applicants that you will be verifying facts in their resumes. It’s usually wise to get their written consent to do so.
Many employers skip the essential step of calling references, and many applicants know that. Some old bosses will be reluctant to tell you anything substantive, so I always ask, “Would you hire this person again?” You can interpret a lot from the answer – or lack of one.
Interviews often get short shrift as well. Many doctors tend to do all the talking. As I’ve observed numerous times, listening is not our strong suit, as a general rule. The purpose of an interview is to allow you to size up the prospective employee, not to deliver a lecture on the sterling attributes of your office. Important interview topics include educational background, skills, experience, and unrelated job history.
By law, you cannot ask an applicant’s age, date of birth, gender, creed, color, religion, or national origin. Other forbidden subjects include disabilities, marital status, military record, number of children (or who cares for them), addiction history, citizenship, criminal record, psychiatric history, absenteeism, or workman’s compensation.
However, there are acceptable alternatives to some of those questions. You can ask if applicants have ever gone by another name (for your background check), for example. You can ask if they are legally authorized to work in this country and whether they will be physically able to perform the duties specified in the job description. While past addictions are off limits, you do have a right to know about current addictions to illegal substances.
Once you have hired people whose skills and personalities best fit your needs, train them well. Then, give them the opportunity to succeed. “The best executive,” wrote Theodore Roosevelt, “is one who has sense enough to pick good people to do what he [or she] wants done and self-restraint enough to keep from meddling with them while they do it.” ”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@frontlinemedcom.com.