User login
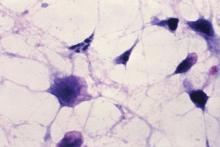
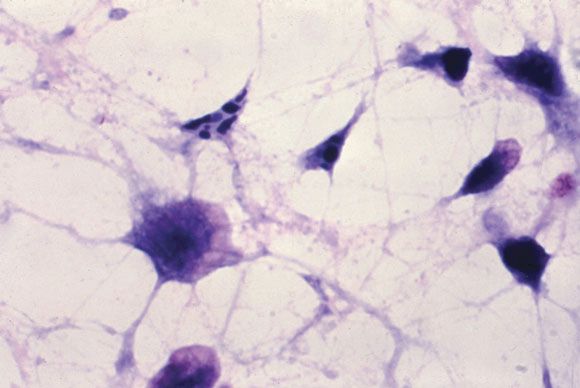
New C. difficile guidelines recommend fecal microbiota transplants
.
The updated Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children, published in the Feb. 15 edition of Clinical Infectious Diseases (doi: 10.1093/cid/cix1085), address changes in management and diagnosis of the infection, and include recommendations for pediatric infection. The guidelines from the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America were lasted published in 2010.
One of the strongest recommendations was on the use of FMTs to treat recurrent C. difficile infection after the failure of antibiotic therapy.
“Anecdotal treatment success rates of fecal microbiota transplantation for recurrent CDI [C. difficile infection] have been high regardless of route of instillation of feces, and have ranged between 77% and 94% with administration via the proximal small bowel; the highest success rates (80%-100%) have been associated with instillation of feces via the colon,” they wrote.
The guidelines also addressed what the authors described as the “evolving controversy” over the best methods for diagnosis, pointing out that there is little consensus about the best laboratory testing method.
“Given these various conundrums and the paucity of large prospective studies, the recommendations, while strong in some instances, are based upon a very low to low quality of evidence,” the authors said.
That aside, they advised that patients with unexplained and new-onset diarrhea (three or more unformed stools in 24 hours) were the preferred target population for testing for C. difficile infection. The most sensitive method of diagnosis in patients with clinical symptoms likely to be C. difficile infection was a nucleic acid amplification test, or a multistep algorithm, rather than a toxin test alone.
The guidelines committee also strongly advised against repeat testing within 7 days during the same episode of diarrhea, and against testing stool from asymptomatic patients, except for the purpose of epidemiologic study. They also noted there was insufficient evidence for the use of biologic markers such as fecal lactoferrin as an adjunct to testing.
The guidelines’ authors found there was not enough evidence to recommend discontinuing proton pump inhibitors to reduce the incidence of C. difficile infection, despite epidemiologic evidence of an association between proton pump inhibitor use and C. difficile infection. Similarly, there was a lack of evidence for the use of probiotics for primary prevention, but the authors noted that meta-analyses suggest probiotics may help prevent C. difficile infection in patients on antibiotics without a history of C. difficile infection.
With respect to antibiotic treatment, they recommended that patients diagnosed with C. difficile infection should first discontinue the inciting antibiotic treatment and then begin therapy with either vancomycin or fidaxomicin. For recurrent infection, they advised a tapered and pulsed regimen of oral vancomycin or a 10-day course of fidaxomicin. If patients had received metronidazole for the primary episode, they should be given a standard 10-day course of vancomycin for recurrent infection, the authors said.
In terms of diagnosis and management of pediatric C. difficile, the guidelines advised against routinely testing infants under 2 years of age with diarrhea, as the rate of C. difficile colonization even among asymptomatic infants can be higher than 40%. Even in children older than age 2, there was only a “weak” recommendation for C. difficile testing in patients with prolonged or worsening diarrhea and other risk factors such as inflammatory bowel disease or recent antibiotic exposure.
Children with a first episode or first recurrence of nonsevere C. difficile should be treated with either metronidazole or vancomycin, the authors wrote, but in the case of more severe illness or second recurrence, oral vancomycin was preferred over metronidazole.
The authors also suggested clinicians consider FMTs for children with recurrent infection that had failed to respond to antibiotics, but noted the quality of evidence for this was very low.
The guidelines were funded by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Six authors declared grants, consultancies, board positions, and other payments from the pharmaceutical industry outside the submitted work. One author also held patents relating to the treatment and prevention of C. difficile infection.
SOURCE: McDonald CL et al. Clin Infect Dis. 2018 Feb 15. doi: 10.1093/cid/cix1085.
.
The updated Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children, published in the Feb. 15 edition of Clinical Infectious Diseases (doi: 10.1093/cid/cix1085), address changes in management and diagnosis of the infection, and include recommendations for pediatric infection. The guidelines from the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America were lasted published in 2010.
One of the strongest recommendations was on the use of FMTs to treat recurrent C. difficile infection after the failure of antibiotic therapy.
“Anecdotal treatment success rates of fecal microbiota transplantation for recurrent CDI [C. difficile infection] have been high regardless of route of instillation of feces, and have ranged between 77% and 94% with administration via the proximal small bowel; the highest success rates (80%-100%) have been associated with instillation of feces via the colon,” they wrote.
The guidelines also addressed what the authors described as the “evolving controversy” over the best methods for diagnosis, pointing out that there is little consensus about the best laboratory testing method.
“Given these various conundrums and the paucity of large prospective studies, the recommendations, while strong in some instances, are based upon a very low to low quality of evidence,” the authors said.
That aside, they advised that patients with unexplained and new-onset diarrhea (three or more unformed stools in 24 hours) were the preferred target population for testing for C. difficile infection. The most sensitive method of diagnosis in patients with clinical symptoms likely to be C. difficile infection was a nucleic acid amplification test, or a multistep algorithm, rather than a toxin test alone.
The guidelines committee also strongly advised against repeat testing within 7 days during the same episode of diarrhea, and against testing stool from asymptomatic patients, except for the purpose of epidemiologic study. They also noted there was insufficient evidence for the use of biologic markers such as fecal lactoferrin as an adjunct to testing.
The guidelines’ authors found there was not enough evidence to recommend discontinuing proton pump inhibitors to reduce the incidence of C. difficile infection, despite epidemiologic evidence of an association between proton pump inhibitor use and C. difficile infection. Similarly, there was a lack of evidence for the use of probiotics for primary prevention, but the authors noted that meta-analyses suggest probiotics may help prevent C. difficile infection in patients on antibiotics without a history of C. difficile infection.
With respect to antibiotic treatment, they recommended that patients diagnosed with C. difficile infection should first discontinue the inciting antibiotic treatment and then begin therapy with either vancomycin or fidaxomicin. For recurrent infection, they advised a tapered and pulsed regimen of oral vancomycin or a 10-day course of fidaxomicin. If patients had received metronidazole for the primary episode, they should be given a standard 10-day course of vancomycin for recurrent infection, the authors said.
In terms of diagnosis and management of pediatric C. difficile, the guidelines advised against routinely testing infants under 2 years of age with diarrhea, as the rate of C. difficile colonization even among asymptomatic infants can be higher than 40%. Even in children older than age 2, there was only a “weak” recommendation for C. difficile testing in patients with prolonged or worsening diarrhea and other risk factors such as inflammatory bowel disease or recent antibiotic exposure.
Children with a first episode or first recurrence of nonsevere C. difficile should be treated with either metronidazole or vancomycin, the authors wrote, but in the case of more severe illness or second recurrence, oral vancomycin was preferred over metronidazole.
The authors also suggested clinicians consider FMTs for children with recurrent infection that had failed to respond to antibiotics, but noted the quality of evidence for this was very low.
The guidelines were funded by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Six authors declared grants, consultancies, board positions, and other payments from the pharmaceutical industry outside the submitted work. One author also held patents relating to the treatment and prevention of C. difficile infection.
SOURCE: McDonald CL et al. Clin Infect Dis. 2018 Feb 15. doi: 10.1093/cid/cix1085.
.
The updated Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children, published in the Feb. 15 edition of Clinical Infectious Diseases (doi: 10.1093/cid/cix1085), address changes in management and diagnosis of the infection, and include recommendations for pediatric infection. The guidelines from the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America were lasted published in 2010.
One of the strongest recommendations was on the use of FMTs to treat recurrent C. difficile infection after the failure of antibiotic therapy.
“Anecdotal treatment success rates of fecal microbiota transplantation for recurrent CDI [C. difficile infection] have been high regardless of route of instillation of feces, and have ranged between 77% and 94% with administration via the proximal small bowel; the highest success rates (80%-100%) have been associated with instillation of feces via the colon,” they wrote.
The guidelines also addressed what the authors described as the “evolving controversy” over the best methods for diagnosis, pointing out that there is little consensus about the best laboratory testing method.
“Given these various conundrums and the paucity of large prospective studies, the recommendations, while strong in some instances, are based upon a very low to low quality of evidence,” the authors said.
That aside, they advised that patients with unexplained and new-onset diarrhea (three or more unformed stools in 24 hours) were the preferred target population for testing for C. difficile infection. The most sensitive method of diagnosis in patients with clinical symptoms likely to be C. difficile infection was a nucleic acid amplification test, or a multistep algorithm, rather than a toxin test alone.
The guidelines committee also strongly advised against repeat testing within 7 days during the same episode of diarrhea, and against testing stool from asymptomatic patients, except for the purpose of epidemiologic study. They also noted there was insufficient evidence for the use of biologic markers such as fecal lactoferrin as an adjunct to testing.
The guidelines’ authors found there was not enough evidence to recommend discontinuing proton pump inhibitors to reduce the incidence of C. difficile infection, despite epidemiologic evidence of an association between proton pump inhibitor use and C. difficile infection. Similarly, there was a lack of evidence for the use of probiotics for primary prevention, but the authors noted that meta-analyses suggest probiotics may help prevent C. difficile infection in patients on antibiotics without a history of C. difficile infection.
With respect to antibiotic treatment, they recommended that patients diagnosed with C. difficile infection should first discontinue the inciting antibiotic treatment and then begin therapy with either vancomycin or fidaxomicin. For recurrent infection, they advised a tapered and pulsed regimen of oral vancomycin or a 10-day course of fidaxomicin. If patients had received metronidazole for the primary episode, they should be given a standard 10-day course of vancomycin for recurrent infection, the authors said.
In terms of diagnosis and management of pediatric C. difficile, the guidelines advised against routinely testing infants under 2 years of age with diarrhea, as the rate of C. difficile colonization even among asymptomatic infants can be higher than 40%. Even in children older than age 2, there was only a “weak” recommendation for C. difficile testing in patients with prolonged or worsening diarrhea and other risk factors such as inflammatory bowel disease or recent antibiotic exposure.
Children with a first episode or first recurrence of nonsevere C. difficile should be treated with either metronidazole or vancomycin, the authors wrote, but in the case of more severe illness or second recurrence, oral vancomycin was preferred over metronidazole.
The authors also suggested clinicians consider FMTs for children with recurrent infection that had failed to respond to antibiotics, but noted the quality of evidence for this was very low.
The guidelines were funded by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Six authors declared grants, consultancies, board positions, and other payments from the pharmaceutical industry outside the submitted work. One author also held patents relating to the treatment and prevention of C. difficile infection.
SOURCE: McDonald CL et al. Clin Infect Dis. 2018 Feb 15. doi: 10.1093/cid/cix1085.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: Fecal microbiota transplants should be considered for use in patients with recurrent Clostridium difficile infection that has not responded to antibiotic therapy.
Major finding: One of the strongest recommendations in the new guidelines on C. difficile infection is to consider use of fecal microbiota transplants in patients with recurrent infection.
Data source: Clinical practice guidelines.
Disclosures: The guidelines were funded by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Six authors declared grants, consultancies, board positions, and other payments from the pharmaceutical industry outside the submitted work. One author also held patents relating to the treatment and prevention of C. difficile infection.
Source: McDonald CL et al. Clin Infect Dis. 2018 Feb 15. doi: 10.1093/cid/cix1085.
CPR decision support videos can serve as a supplement to CPR preference discussions for inpatients
Clinical question: Does the use of a CPR decision support video impact patients’ code status preferences?
Background: Discussions about cardiopulmonary resuscitation are an important aspect of inpatient care but may be difficult to complete for several reasons, including poor patient understanding of the CPR process and its expected outcomes. This study sought to evaluate the impact of a CPR decision support video on patient CPR preferences.
Setting: General medicine wards at the Minneapolis Veterans Affairs from Sept. 28, 2015, to Oct. 23, 2015.
Synopsis: One hundred and nineteen patients older than 65 were randomized to receive standard care plus viewing a CPR decision support video or standard care alone. The primary outcome was patient code status preference. Patients completed a survey assessing trust in their care team.
Among the patients who viewed the video, 37% chose full code, compared with 71% of patients in the usual care arm. Patients who viewed the video were more likely to choose DNR/DNI (56%, compared with 17% in the control group). There was no significant difference in patient trust of the care team.
Study conclusions are limited by a study population consisting predominantly of white males. Though the study was randomized, it was not blinded.
Bottom line: A CPR decision support video led to a decrease in full code preference and an increase in DNR/DNI preference among hospitalized patients.
Citation: Merino AM et al. A randomized controlled trial of a CPR decision support video for patients admitted to the general medicine service. J Hosp Med. 2017;12(9):700-4.
Dr. Rodriguez is a hospitalist and a clinical informatics fellow, Beth Israel Deaconess Medical Center, Boston.
Clinical question: Does the use of a CPR decision support video impact patients’ code status preferences?
Background: Discussions about cardiopulmonary resuscitation are an important aspect of inpatient care but may be difficult to complete for several reasons, including poor patient understanding of the CPR process and its expected outcomes. This study sought to evaluate the impact of a CPR decision support video on patient CPR preferences.
Setting: General medicine wards at the Minneapolis Veterans Affairs from Sept. 28, 2015, to Oct. 23, 2015.
Synopsis: One hundred and nineteen patients older than 65 were randomized to receive standard care plus viewing a CPR decision support video or standard care alone. The primary outcome was patient code status preference. Patients completed a survey assessing trust in their care team.
Among the patients who viewed the video, 37% chose full code, compared with 71% of patients in the usual care arm. Patients who viewed the video were more likely to choose DNR/DNI (56%, compared with 17% in the control group). There was no significant difference in patient trust of the care team.
Study conclusions are limited by a study population consisting predominantly of white males. Though the study was randomized, it was not blinded.
Bottom line: A CPR decision support video led to a decrease in full code preference and an increase in DNR/DNI preference among hospitalized patients.
Citation: Merino AM et al. A randomized controlled trial of a CPR decision support video for patients admitted to the general medicine service. J Hosp Med. 2017;12(9):700-4.
Dr. Rodriguez is a hospitalist and a clinical informatics fellow, Beth Israel Deaconess Medical Center, Boston.
Clinical question: Does the use of a CPR decision support video impact patients’ code status preferences?
Background: Discussions about cardiopulmonary resuscitation are an important aspect of inpatient care but may be difficult to complete for several reasons, including poor patient understanding of the CPR process and its expected outcomes. This study sought to evaluate the impact of a CPR decision support video on patient CPR preferences.
Setting: General medicine wards at the Minneapolis Veterans Affairs from Sept. 28, 2015, to Oct. 23, 2015.
Synopsis: One hundred and nineteen patients older than 65 were randomized to receive standard care plus viewing a CPR decision support video or standard care alone. The primary outcome was patient code status preference. Patients completed a survey assessing trust in their care team.
Among the patients who viewed the video, 37% chose full code, compared with 71% of patients in the usual care arm. Patients who viewed the video were more likely to choose DNR/DNI (56%, compared with 17% in the control group). There was no significant difference in patient trust of the care team.
Study conclusions are limited by a study population consisting predominantly of white males. Though the study was randomized, it was not blinded.
Bottom line: A CPR decision support video led to a decrease in full code preference and an increase in DNR/DNI preference among hospitalized patients.
Citation: Merino AM et al. A randomized controlled trial of a CPR decision support video for patients admitted to the general medicine service. J Hosp Med. 2017;12(9):700-4.
Dr. Rodriguez is a hospitalist and a clinical informatics fellow, Beth Israel Deaconess Medical Center, Boston.
Consent and DNR orders
Question: Paramedics brought an unconscious 70-year-old man to a Florida hospital emergency department. The patient had the words “Do Not Resuscitate” tattooed onto his chest. No one accompanied him, and he had no identifications on his person. His blood alcohol level was elevated, and a few hours after his arrival, he lapsed into severe metabolic acidosis and hypotensive shock. The treating team decided to enter a DNR order, and the patient died shortly thereafter without benefit of cardiopulmonary resuscitation.
Which of the following is best?
A. An ethics consult may suggest honoring the patient’s DNR wishes, as it is reasonable to infer that the tattoo expressed an authentic preference.
B. It has been said, but remains debatable, that tattoos might represent “permanent reminders of regretted decisions made while the person was intoxicated.”
C. An earlier case report in the literature cautioned that the tattooed expression of a DNR request did not reflect that particular patient’s current wishes.
D. If this patient’s Florida Department of Health out-of-hospital DNR order confirms his DNR preference, then it is appropriate to withhold resuscitation.
E. All are correct.
ANSWER: E. The above hypothetical situation is modified from a recent case report in the correspondence section of the New England Journal of Medicine.1 It can be read as offering a sharp and dramatic focus on the issue of consent surrounding decisions to withhold CPR.
In 1983, the President’s Commission for the Study of Ethical Problems in Medicine supported DNR protocols (“no code”) based on three value considerations: self-determination, well-being, and equity.2
The physician is obligated to discuss with the patient or surrogate the procedure, risks, and benefits of CPR so that an informed choice can be made. DNR means that, in the event of a cardiac or respiratory arrest, no CPR efforts would be undertaken. DNR orders are not exclusive to the in-hospital setting, as some states, for example, Florida and Texas, have also enacted statutes that allow such orders to be valid outside the hospital.
Critics lament that problems – many surrounding the consent issue – continue to plague DNR orders.3 Discussions are often vague, and they may not meet the threshold of informed consent requirements, because they frequently omit risks and complications. A resident, rather than the attending physician, typically performs this important task. This is compounded by ill-timed discussions and wrong assumptions about patients’ preferences, which may in fact be ignored.4
Physicians sometimes extrapolate DNR orders to limit other treatments. Or, they perform CPR in contraindicated situations such as terminal illnesses, where death is expected, which amounts to “a positive violation of an individual’s right to die with dignity.” In some situations, physicians are known to override a patient’s DNR request.
Take the operating-room conundrum. There, the immediate availability of drugs, heightened skills, and in-place procedures significantly improve survival following a cardiopulmonary arrest. Studies show a 50% survival rate, versus 8%-14% elsewhere in the hospital. A Swedish study showed that 65% of the patients who had a cardiac arrest perioperatively were successfully resuscitated. When anesthesia caused the arrest, for example, esophageal intubation, disconnection from mechanical ventilation, or prolonged exposure to high concentrations of anesthetics, the recovery rate jumped to 92%.
Terminally ill patients typically disavow CPR when choosing a palliative course of action. However, surgery can be a part of palliation. In 1991, approximately 15% of patients with DNR orders had a surgical procedure, with most interventions targeting comfort and/or nursing care. When a terminally ill patient with a DNR order undergoes surgery, how should physicians deal with the patient’s no-code status, especially if an iatrogenic cardiac arrest should occur?
Because overriding a patient’s DNR wish violates the right of self-determination, a reasonable rule is to require the surgeon and/or anesthesiologist to discuss preoperatively the increased risk of a cardiac arrest during surgery, as well as the markedly improved chance of a successful resuscitation. The patient will then decide whether to retain his/her original DNR intent, or to suspend its execution in the perioperative period.5
What about iatrogenesis?
In 1999, David Casarett, MD, and Lainie F. Ross, MD, PhD, assessed whether physicians were more likely to override a DNR order if a hypothetical cardiac arrest was caused iatrogenically.6 Their survey revealed that 69% of physicians were very likely to do so. The authors suggested three explanations: 1) concern for malpractice litigation, 2) feelings of guilt or responsibility, and 3) the belief that patients do not consider the possibility of an iatrogenic cardiac arrest when they consent to a DNR order. Physicians may also believe a “properly negotiated DNR order does not apply to all foreseeable circumstances.”
However, some ethicists believe that an iatrogenic mishap does not make it permissible to override a patient’s prior refusal of treatment, because errors should not alter ethical obligations to respect a patient’s wishes to forgo treatment, including CPR.
Can a DNR order exist if it is against a patient’s wishes?7 In Gilgunn v. Massachusetts General Hospital, a 71-year-old diabetic woman with heart disease, breast cancer, and a hip fracture suffered two grand mal seizures and lapsed into a coma.8 Her daughter was the surrogate decision maker, and she made it clear that her mother always said she wanted everything done. After several weeks, the physicians decided that further treatment would be futile.
The chair of the ethics committee felt that the daughter’s opinion was not relevant because CPR was not a genuine therapeutic option and would be “medically contraindicated, inhumane, and unethical.” Accordingly, the attending physician entered a DNR order despite strong protest from the daughter. The patient died shortly thereafter without receiving CPR, and the daughter filed a negligence lawsuit against the hospital.
Still, there are state and federal statutes touching on DNR orders that warrant careful attention. For example, New York Public Health Law Section 2962, paragraph 1, states: “Every person admitted to a hospital shall be presumed to consent to the administration of cardiopulmonary resuscitation in the event of cardiac or respiratory arrest, unless there is consent to the issuance of an order not to resuscitate ...” This raises the question as to whether it is ever legally permissible in New York to enter a unilateral DNR order against the wishes of the patient.
And the federal “anti-dumping” law governing emergency treatment, widely known as EMTALA (Emergency Medical Treatment and Labor Act), requires all emergency departments to provide treatment necessary to prevent the material deterioration of the individual’s condition. This would always include the use of CPR unless specifically rejected by the patient or surrogate, as the law does not contain a “standard of care” or “futility” exception.9
Dr. Tan is emeritus professor of medicine and a former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu.
References
1. N Engl J Med. 2017 Nov 30;377(22):2192-3.
2. President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Deciding to Forego Life-Sustaining Treatment. Washington, DC: Government Printing Office, 1983.
3. J Gen Intern Med. 2011 Jul;26(7):791-7.
4. JAMA. 1995 Nov 22-29;274(20):1591-8.
5. Hawaii Med J. 2001 Mar;60(3):64-7.
6. N Engl J Med. 1997 Jun 26;336(26):1908-10.
7. Tan SY. Futility and DNR Orders. Internal Medicine News, March 21, 2014.
8. Gilgunn v. Mass. General Hosp. No. 92-4820 (Mass. Super Ct. Apr. 21, 1995).
9. In re Baby K, 16 F.3d 590 (4th Cir. 1994).
Question: Paramedics brought an unconscious 70-year-old man to a Florida hospital emergency department. The patient had the words “Do Not Resuscitate” tattooed onto his chest. No one accompanied him, and he had no identifications on his person. His blood alcohol level was elevated, and a few hours after his arrival, he lapsed into severe metabolic acidosis and hypotensive shock. The treating team decided to enter a DNR order, and the patient died shortly thereafter without benefit of cardiopulmonary resuscitation.
Which of the following is best?
A. An ethics consult may suggest honoring the patient’s DNR wishes, as it is reasonable to infer that the tattoo expressed an authentic preference.
B. It has been said, but remains debatable, that tattoos might represent “permanent reminders of regretted decisions made while the person was intoxicated.”
C. An earlier case report in the literature cautioned that the tattooed expression of a DNR request did not reflect that particular patient’s current wishes.
D. If this patient’s Florida Department of Health out-of-hospital DNR order confirms his DNR preference, then it is appropriate to withhold resuscitation.
E. All are correct.
ANSWER: E. The above hypothetical situation is modified from a recent case report in the correspondence section of the New England Journal of Medicine.1 It can be read as offering a sharp and dramatic focus on the issue of consent surrounding decisions to withhold CPR.
In 1983, the President’s Commission for the Study of Ethical Problems in Medicine supported DNR protocols (“no code”) based on three value considerations: self-determination, well-being, and equity.2
The physician is obligated to discuss with the patient or surrogate the procedure, risks, and benefits of CPR so that an informed choice can be made. DNR means that, in the event of a cardiac or respiratory arrest, no CPR efforts would be undertaken. DNR orders are not exclusive to the in-hospital setting, as some states, for example, Florida and Texas, have also enacted statutes that allow such orders to be valid outside the hospital.
Critics lament that problems – many surrounding the consent issue – continue to plague DNR orders.3 Discussions are often vague, and they may not meet the threshold of informed consent requirements, because they frequently omit risks and complications. A resident, rather than the attending physician, typically performs this important task. This is compounded by ill-timed discussions and wrong assumptions about patients’ preferences, which may in fact be ignored.4
Physicians sometimes extrapolate DNR orders to limit other treatments. Or, they perform CPR in contraindicated situations such as terminal illnesses, where death is expected, which amounts to “a positive violation of an individual’s right to die with dignity.” In some situations, physicians are known to override a patient’s DNR request.
Take the operating-room conundrum. There, the immediate availability of drugs, heightened skills, and in-place procedures significantly improve survival following a cardiopulmonary arrest. Studies show a 50% survival rate, versus 8%-14% elsewhere in the hospital. A Swedish study showed that 65% of the patients who had a cardiac arrest perioperatively were successfully resuscitated. When anesthesia caused the arrest, for example, esophageal intubation, disconnection from mechanical ventilation, or prolonged exposure to high concentrations of anesthetics, the recovery rate jumped to 92%.
Terminally ill patients typically disavow CPR when choosing a palliative course of action. However, surgery can be a part of palliation. In 1991, approximately 15% of patients with DNR orders had a surgical procedure, with most interventions targeting comfort and/or nursing care. When a terminally ill patient with a DNR order undergoes surgery, how should physicians deal with the patient’s no-code status, especially if an iatrogenic cardiac arrest should occur?
Because overriding a patient’s DNR wish violates the right of self-determination, a reasonable rule is to require the surgeon and/or anesthesiologist to discuss preoperatively the increased risk of a cardiac arrest during surgery, as well as the markedly improved chance of a successful resuscitation. The patient will then decide whether to retain his/her original DNR intent, or to suspend its execution in the perioperative period.5
What about iatrogenesis?
In 1999, David Casarett, MD, and Lainie F. Ross, MD, PhD, assessed whether physicians were more likely to override a DNR order if a hypothetical cardiac arrest was caused iatrogenically.6 Their survey revealed that 69% of physicians were very likely to do so. The authors suggested three explanations: 1) concern for malpractice litigation, 2) feelings of guilt or responsibility, and 3) the belief that patients do not consider the possibility of an iatrogenic cardiac arrest when they consent to a DNR order. Physicians may also believe a “properly negotiated DNR order does not apply to all foreseeable circumstances.”
However, some ethicists believe that an iatrogenic mishap does not make it permissible to override a patient’s prior refusal of treatment, because errors should not alter ethical obligations to respect a patient’s wishes to forgo treatment, including CPR.
Can a DNR order exist if it is against a patient’s wishes?7 In Gilgunn v. Massachusetts General Hospital, a 71-year-old diabetic woman with heart disease, breast cancer, and a hip fracture suffered two grand mal seizures and lapsed into a coma.8 Her daughter was the surrogate decision maker, and she made it clear that her mother always said she wanted everything done. After several weeks, the physicians decided that further treatment would be futile.
The chair of the ethics committee felt that the daughter’s opinion was not relevant because CPR was not a genuine therapeutic option and would be “medically contraindicated, inhumane, and unethical.” Accordingly, the attending physician entered a DNR order despite strong protest from the daughter. The patient died shortly thereafter without receiving CPR, and the daughter filed a negligence lawsuit against the hospital.
Still, there are state and federal statutes touching on DNR orders that warrant careful attention. For example, New York Public Health Law Section 2962, paragraph 1, states: “Every person admitted to a hospital shall be presumed to consent to the administration of cardiopulmonary resuscitation in the event of cardiac or respiratory arrest, unless there is consent to the issuance of an order not to resuscitate ...” This raises the question as to whether it is ever legally permissible in New York to enter a unilateral DNR order against the wishes of the patient.
And the federal “anti-dumping” law governing emergency treatment, widely known as EMTALA (Emergency Medical Treatment and Labor Act), requires all emergency departments to provide treatment necessary to prevent the material deterioration of the individual’s condition. This would always include the use of CPR unless specifically rejected by the patient or surrogate, as the law does not contain a “standard of care” or “futility” exception.9
Dr. Tan is emeritus professor of medicine and a former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu.
References
1. N Engl J Med. 2017 Nov 30;377(22):2192-3.
2. President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Deciding to Forego Life-Sustaining Treatment. Washington, DC: Government Printing Office, 1983.
3. J Gen Intern Med. 2011 Jul;26(7):791-7.
4. JAMA. 1995 Nov 22-29;274(20):1591-8.
5. Hawaii Med J. 2001 Mar;60(3):64-7.
6. N Engl J Med. 1997 Jun 26;336(26):1908-10.
7. Tan SY. Futility and DNR Orders. Internal Medicine News, March 21, 2014.
8. Gilgunn v. Mass. General Hosp. No. 92-4820 (Mass. Super Ct. Apr. 21, 1995).
9. In re Baby K, 16 F.3d 590 (4th Cir. 1994).
Question: Paramedics brought an unconscious 70-year-old man to a Florida hospital emergency department. The patient had the words “Do Not Resuscitate” tattooed onto his chest. No one accompanied him, and he had no identifications on his person. His blood alcohol level was elevated, and a few hours after his arrival, he lapsed into severe metabolic acidosis and hypotensive shock. The treating team decided to enter a DNR order, and the patient died shortly thereafter without benefit of cardiopulmonary resuscitation.
Which of the following is best?
A. An ethics consult may suggest honoring the patient’s DNR wishes, as it is reasonable to infer that the tattoo expressed an authentic preference.
B. It has been said, but remains debatable, that tattoos might represent “permanent reminders of regretted decisions made while the person was intoxicated.”
C. An earlier case report in the literature cautioned that the tattooed expression of a DNR request did not reflect that particular patient’s current wishes.
D. If this patient’s Florida Department of Health out-of-hospital DNR order confirms his DNR preference, then it is appropriate to withhold resuscitation.
E. All are correct.
ANSWER: E. The above hypothetical situation is modified from a recent case report in the correspondence section of the New England Journal of Medicine.1 It can be read as offering a sharp and dramatic focus on the issue of consent surrounding decisions to withhold CPR.
In 1983, the President’s Commission for the Study of Ethical Problems in Medicine supported DNR protocols (“no code”) based on three value considerations: self-determination, well-being, and equity.2
The physician is obligated to discuss with the patient or surrogate the procedure, risks, and benefits of CPR so that an informed choice can be made. DNR means that, in the event of a cardiac or respiratory arrest, no CPR efforts would be undertaken. DNR orders are not exclusive to the in-hospital setting, as some states, for example, Florida and Texas, have also enacted statutes that allow such orders to be valid outside the hospital.
Critics lament that problems – many surrounding the consent issue – continue to plague DNR orders.3 Discussions are often vague, and they may not meet the threshold of informed consent requirements, because they frequently omit risks and complications. A resident, rather than the attending physician, typically performs this important task. This is compounded by ill-timed discussions and wrong assumptions about patients’ preferences, which may in fact be ignored.4
Physicians sometimes extrapolate DNR orders to limit other treatments. Or, they perform CPR in contraindicated situations such as terminal illnesses, where death is expected, which amounts to “a positive violation of an individual’s right to die with dignity.” In some situations, physicians are known to override a patient’s DNR request.
Take the operating-room conundrum. There, the immediate availability of drugs, heightened skills, and in-place procedures significantly improve survival following a cardiopulmonary arrest. Studies show a 50% survival rate, versus 8%-14% elsewhere in the hospital. A Swedish study showed that 65% of the patients who had a cardiac arrest perioperatively were successfully resuscitated. When anesthesia caused the arrest, for example, esophageal intubation, disconnection from mechanical ventilation, or prolonged exposure to high concentrations of anesthetics, the recovery rate jumped to 92%.
Terminally ill patients typically disavow CPR when choosing a palliative course of action. However, surgery can be a part of palliation. In 1991, approximately 15% of patients with DNR orders had a surgical procedure, with most interventions targeting comfort and/or nursing care. When a terminally ill patient with a DNR order undergoes surgery, how should physicians deal with the patient’s no-code status, especially if an iatrogenic cardiac arrest should occur?
Because overriding a patient’s DNR wish violates the right of self-determination, a reasonable rule is to require the surgeon and/or anesthesiologist to discuss preoperatively the increased risk of a cardiac arrest during surgery, as well as the markedly improved chance of a successful resuscitation. The patient will then decide whether to retain his/her original DNR intent, or to suspend its execution in the perioperative period.5
What about iatrogenesis?
In 1999, David Casarett, MD, and Lainie F. Ross, MD, PhD, assessed whether physicians were more likely to override a DNR order if a hypothetical cardiac arrest was caused iatrogenically.6 Their survey revealed that 69% of physicians were very likely to do so. The authors suggested three explanations: 1) concern for malpractice litigation, 2) feelings of guilt or responsibility, and 3) the belief that patients do not consider the possibility of an iatrogenic cardiac arrest when they consent to a DNR order. Physicians may also believe a “properly negotiated DNR order does not apply to all foreseeable circumstances.”
However, some ethicists believe that an iatrogenic mishap does not make it permissible to override a patient’s prior refusal of treatment, because errors should not alter ethical obligations to respect a patient’s wishes to forgo treatment, including CPR.
Can a DNR order exist if it is against a patient’s wishes?7 In Gilgunn v. Massachusetts General Hospital, a 71-year-old diabetic woman with heart disease, breast cancer, and a hip fracture suffered two grand mal seizures and lapsed into a coma.8 Her daughter was the surrogate decision maker, and she made it clear that her mother always said she wanted everything done. After several weeks, the physicians decided that further treatment would be futile.
The chair of the ethics committee felt that the daughter’s opinion was not relevant because CPR was not a genuine therapeutic option and would be “medically contraindicated, inhumane, and unethical.” Accordingly, the attending physician entered a DNR order despite strong protest from the daughter. The patient died shortly thereafter without receiving CPR, and the daughter filed a negligence lawsuit against the hospital.
Still, there are state and federal statutes touching on DNR orders that warrant careful attention. For example, New York Public Health Law Section 2962, paragraph 1, states: “Every person admitted to a hospital shall be presumed to consent to the administration of cardiopulmonary resuscitation in the event of cardiac or respiratory arrest, unless there is consent to the issuance of an order not to resuscitate ...” This raises the question as to whether it is ever legally permissible in New York to enter a unilateral DNR order against the wishes of the patient.
And the federal “anti-dumping” law governing emergency treatment, widely known as EMTALA (Emergency Medical Treatment and Labor Act), requires all emergency departments to provide treatment necessary to prevent the material deterioration of the individual’s condition. This would always include the use of CPR unless specifically rejected by the patient or surrogate, as the law does not contain a “standard of care” or “futility” exception.9
Dr. Tan is emeritus professor of medicine and a former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu.
References
1. N Engl J Med. 2017 Nov 30;377(22):2192-3.
2. President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Deciding to Forego Life-Sustaining Treatment. Washington, DC: Government Printing Office, 1983.
3. J Gen Intern Med. 2011 Jul;26(7):791-7.
4. JAMA. 1995 Nov 22-29;274(20):1591-8.
5. Hawaii Med J. 2001 Mar;60(3):64-7.
6. N Engl J Med. 1997 Jun 26;336(26):1908-10.
7. Tan SY. Futility and DNR Orders. Internal Medicine News, March 21, 2014.
8. Gilgunn v. Mass. General Hosp. No. 92-4820 (Mass. Super Ct. Apr. 21, 1995).
9. In re Baby K, 16 F.3d 590 (4th Cir. 1994).
Radiation exposure in MICU may exceed recommended limit
according to results of a recent observational study.
These “substantial” radiation doses in some patients suggest that efforts are warranted to “justify, restrict and optimize” the use of radiological resources when possible, said Sudhir Krishnan, MD, of the Cleveland Clinic, and his coauthors.
The retrospective, observational study included 4,155 adult admissions to a medical intensive care unit (MICU) at an academic medical center in 2013. Investigators calculated the cumulative effective dose (CED) of radiation based on reported ionizing radiological studies for each patient.
With a median length of stay of just 6.4 days, a total of 131 admissions (3%) accrued a CED of radiation of at least 50 millisieverts (mSv), the annual limit recommended by the National Commission on Radiation Protection, and 47 of those patients (1%) accrued a CED of radiation of at least 100 mSv, the 5-year cumulative exposure limit, the authors reported.
These findings suggest that “MICU patients could be subjected to radiation doses in a matter of days that are equivalent to or more than [the] CED observed in patients with chronic diseases and patients with trauma,” wrote Dr. Krishnan and his coauthors.
As hypothesized, patients with higher severity of illness scores (APACHE III scores) received a higher CED of radiation, according to the report. Using a multivariable linear regression model, investigators found that higher CED was predicted by higher APACHE III scores, sepsis, longer MICU stay, and gastrointestinal disorders and bleeding.
CT scans were the most common source of radiation exposure in patients who exceeded a 50 mSv of radiation, accounting for 49% of the total accrued dose, with interventional radiology accounting for 38%, authors reported.
Despite concerns about “the statistical risk of latent radiogenic cancer,” radiologic studies performed in the critically ill have the potential to reduce morbidity and mortality, the authors acknowledged in a discussion of the results.
“This understandably shifts the risk-benefit ratio towards radiation exposure,” the researchers wrote. “However, complacency in this regard cannot be entirely justified.”
Of the patients in the study who were exposed to a CED of at least 50 mSv, 81% survived the hospital admission and could be subjected to even more radiation as a part of ongoing medical care, they noted.
“Robust tools for monitoring CED prospectively per episode of clinical care, counseling patients exposed to high doses of radiation, and prospective studies exploring radiogenic risk associated with medical radiation are urgently required,” the authors said.
Dr. Krishnan and his coauthors reported no significant conflicts of interest.
SOURCE: Krishnan S et al. Chest. 2018 Feb 4. doi: 10.1016/j.chest.2018.01.019.
according to results of a recent observational study.
These “substantial” radiation doses in some patients suggest that efforts are warranted to “justify, restrict and optimize” the use of radiological resources when possible, said Sudhir Krishnan, MD, of the Cleveland Clinic, and his coauthors.
The retrospective, observational study included 4,155 adult admissions to a medical intensive care unit (MICU) at an academic medical center in 2013. Investigators calculated the cumulative effective dose (CED) of radiation based on reported ionizing radiological studies for each patient.
With a median length of stay of just 6.4 days, a total of 131 admissions (3%) accrued a CED of radiation of at least 50 millisieverts (mSv), the annual limit recommended by the National Commission on Radiation Protection, and 47 of those patients (1%) accrued a CED of radiation of at least 100 mSv, the 5-year cumulative exposure limit, the authors reported.
These findings suggest that “MICU patients could be subjected to radiation doses in a matter of days that are equivalent to or more than [the] CED observed in patients with chronic diseases and patients with trauma,” wrote Dr. Krishnan and his coauthors.
As hypothesized, patients with higher severity of illness scores (APACHE III scores) received a higher CED of radiation, according to the report. Using a multivariable linear regression model, investigators found that higher CED was predicted by higher APACHE III scores, sepsis, longer MICU stay, and gastrointestinal disorders and bleeding.
CT scans were the most common source of radiation exposure in patients who exceeded a 50 mSv of radiation, accounting for 49% of the total accrued dose, with interventional radiology accounting for 38%, authors reported.
Despite concerns about “the statistical risk of latent radiogenic cancer,” radiologic studies performed in the critically ill have the potential to reduce morbidity and mortality, the authors acknowledged in a discussion of the results.
“This understandably shifts the risk-benefit ratio towards radiation exposure,” the researchers wrote. “However, complacency in this regard cannot be entirely justified.”
Of the patients in the study who were exposed to a CED of at least 50 mSv, 81% survived the hospital admission and could be subjected to even more radiation as a part of ongoing medical care, they noted.
“Robust tools for monitoring CED prospectively per episode of clinical care, counseling patients exposed to high doses of radiation, and prospective studies exploring radiogenic risk associated with medical radiation are urgently required,” the authors said.
Dr. Krishnan and his coauthors reported no significant conflicts of interest.
SOURCE: Krishnan S et al. Chest. 2018 Feb 4. doi: 10.1016/j.chest.2018.01.019.
according to results of a recent observational study.
These “substantial” radiation doses in some patients suggest that efforts are warranted to “justify, restrict and optimize” the use of radiological resources when possible, said Sudhir Krishnan, MD, of the Cleveland Clinic, and his coauthors.
The retrospective, observational study included 4,155 adult admissions to a medical intensive care unit (MICU) at an academic medical center in 2013. Investigators calculated the cumulative effective dose (CED) of radiation based on reported ionizing radiological studies for each patient.
With a median length of stay of just 6.4 days, a total of 131 admissions (3%) accrued a CED of radiation of at least 50 millisieverts (mSv), the annual limit recommended by the National Commission on Radiation Protection, and 47 of those patients (1%) accrued a CED of radiation of at least 100 mSv, the 5-year cumulative exposure limit, the authors reported.
These findings suggest that “MICU patients could be subjected to radiation doses in a matter of days that are equivalent to or more than [the] CED observed in patients with chronic diseases and patients with trauma,” wrote Dr. Krishnan and his coauthors.
As hypothesized, patients with higher severity of illness scores (APACHE III scores) received a higher CED of radiation, according to the report. Using a multivariable linear regression model, investigators found that higher CED was predicted by higher APACHE III scores, sepsis, longer MICU stay, and gastrointestinal disorders and bleeding.
CT scans were the most common source of radiation exposure in patients who exceeded a 50 mSv of radiation, accounting for 49% of the total accrued dose, with interventional radiology accounting for 38%, authors reported.
Despite concerns about “the statistical risk of latent radiogenic cancer,” radiologic studies performed in the critically ill have the potential to reduce morbidity and mortality, the authors acknowledged in a discussion of the results.
“This understandably shifts the risk-benefit ratio towards radiation exposure,” the researchers wrote. “However, complacency in this regard cannot be entirely justified.”
Of the patients in the study who were exposed to a CED of at least 50 mSv, 81% survived the hospital admission and could be subjected to even more radiation as a part of ongoing medical care, they noted.
“Robust tools for monitoring CED prospectively per episode of clinical care, counseling patients exposed to high doses of radiation, and prospective studies exploring radiogenic risk associated with medical radiation are urgently required,” the authors said.
Dr. Krishnan and his coauthors reported no significant conflicts of interest.
SOURCE: Krishnan S et al. Chest. 2018 Feb 4. doi: 10.1016/j.chest.2018.01.019.
FROM CHEST
Key clinical point: Patients admitted to MICUs may be exposed to doses of radiation that are substantial and may exceed federal occupational health limits.
Major finding: In a short span of time (median 6.4 days length of stay), 3% of MICU patients received a cumulative dose of radiation that exceeded the U.S. recommended limit, and 1% accrued enough exposure to exceed the 5-year cumulative limit.
Data source: A retrospective, observational study including 4,155 adult admissions to the MICU at an academic medical center in 2013.
Disclosures: The study authors reported no significant conflicts of interest.
Source: Krishnan S et al. Chest. 2018 Feb 4. doi: 10.1016/j.chest.2018.01.019.
Evidence-based care processes decrease mortality in Staphylococcus aureus bacteremia
Clinical questions: What are the trends in patient outcome for Staphylococcus aureus bacteremia (SAB)? Does the use of evidence-based care processes decrease mortality in SAB?
Background: SAB is associated with poor clinical outcomes. Prior research has demonstrated that several evidence-based interventions, namely appropriate antibiotics, echocardiography, and infectious disease consults, have been associated with improved outcomes. The use of these interventions in clinical practice and their large-scale impact on SAB mortality is not known.
Setting: Veterans Health Administration acute care hospitals in the continental United States from January 1, 2003, to Dec. 31, 2014.
Synopsis: This study used the Veterans Affairs Informatics and Computing Infrastructure to identify 36,868 patients across 124 acute care hospitals with a first episode of SAB. Use of evidence-based care processes (specifically appropriate antibiotic use, echocardiography, and infectious disease consults) and patient mortality were recorded.
All-cause 30-day mortality decreased 25.7% in 2003 to 16.5% in 2014. Concurrently, the rate of evidence-based care processes increased from 2003 to 2014. There was lower risk-adjusted mortality when patients received all three evidence-based care processes compared to those who received none, with an odds ratio of 0.33 (95% confidence interval, 0.30-0.37); 57.3% of the decrease in mortality was attributable to use of all three evidence-based care processes.
Given the observational nature of the study, unmeasured confounders were not considered. Generalizability of the study is limited since the patients were primarily men.
Bottom line: The use of evidence-based care processes (appropriate antibiotic use, echocardiography, and infectious disease consultation) was associated with decreased SAB mortality.
Citation: Goto M et al. Association of evidence-based care processes with mortality in Staphylococcus aureus bacteremia at Veterans Health Administration hospitals, 2003-2014. JAMA Intern Med. 2017;177(10):1489-97.
Dr. Rodriguez is a hospitalist and a clinical informatics fellow, Beth Israel Deaconess Medical Center, Boston.
Clinical questions: What are the trends in patient outcome for Staphylococcus aureus bacteremia (SAB)? Does the use of evidence-based care processes decrease mortality in SAB?
Background: SAB is associated with poor clinical outcomes. Prior research has demonstrated that several evidence-based interventions, namely appropriate antibiotics, echocardiography, and infectious disease consults, have been associated with improved outcomes. The use of these interventions in clinical practice and their large-scale impact on SAB mortality is not known.
Setting: Veterans Health Administration acute care hospitals in the continental United States from January 1, 2003, to Dec. 31, 2014.
Synopsis: This study used the Veterans Affairs Informatics and Computing Infrastructure to identify 36,868 patients across 124 acute care hospitals with a first episode of SAB. Use of evidence-based care processes (specifically appropriate antibiotic use, echocardiography, and infectious disease consults) and patient mortality were recorded.
All-cause 30-day mortality decreased 25.7% in 2003 to 16.5% in 2014. Concurrently, the rate of evidence-based care processes increased from 2003 to 2014. There was lower risk-adjusted mortality when patients received all three evidence-based care processes compared to those who received none, with an odds ratio of 0.33 (95% confidence interval, 0.30-0.37); 57.3% of the decrease in mortality was attributable to use of all three evidence-based care processes.
Given the observational nature of the study, unmeasured confounders were not considered. Generalizability of the study is limited since the patients were primarily men.
Bottom line: The use of evidence-based care processes (appropriate antibiotic use, echocardiography, and infectious disease consultation) was associated with decreased SAB mortality.
Citation: Goto M et al. Association of evidence-based care processes with mortality in Staphylococcus aureus bacteremia at Veterans Health Administration hospitals, 2003-2014. JAMA Intern Med. 2017;177(10):1489-97.
Dr. Rodriguez is a hospitalist and a clinical informatics fellow, Beth Israel Deaconess Medical Center, Boston.
Clinical questions: What are the trends in patient outcome for Staphylococcus aureus bacteremia (SAB)? Does the use of evidence-based care processes decrease mortality in SAB?
Background: SAB is associated with poor clinical outcomes. Prior research has demonstrated that several evidence-based interventions, namely appropriate antibiotics, echocardiography, and infectious disease consults, have been associated with improved outcomes. The use of these interventions in clinical practice and their large-scale impact on SAB mortality is not known.
Setting: Veterans Health Administration acute care hospitals in the continental United States from January 1, 2003, to Dec. 31, 2014.
Synopsis: This study used the Veterans Affairs Informatics and Computing Infrastructure to identify 36,868 patients across 124 acute care hospitals with a first episode of SAB. Use of evidence-based care processes (specifically appropriate antibiotic use, echocardiography, and infectious disease consults) and patient mortality were recorded.
All-cause 30-day mortality decreased 25.7% in 2003 to 16.5% in 2014. Concurrently, the rate of evidence-based care processes increased from 2003 to 2014. There was lower risk-adjusted mortality when patients received all three evidence-based care processes compared to those who received none, with an odds ratio of 0.33 (95% confidence interval, 0.30-0.37); 57.3% of the decrease in mortality was attributable to use of all three evidence-based care processes.
Given the observational nature of the study, unmeasured confounders were not considered. Generalizability of the study is limited since the patients were primarily men.
Bottom line: The use of evidence-based care processes (appropriate antibiotic use, echocardiography, and infectious disease consultation) was associated with decreased SAB mortality.
Citation: Goto M et al. Association of evidence-based care processes with mortality in Staphylococcus aureus bacteremia at Veterans Health Administration hospitals, 2003-2014. JAMA Intern Med. 2017;177(10):1489-97.
Dr. Rodriguez is a hospitalist and a clinical informatics fellow, Beth Israel Deaconess Medical Center, Boston.
Short Takes
Fluoroquinolone use tied to higher risk of aortic dissection and aneurysm
A meta-analysis of two observational studies found that current fluoroquinolone use was associated with modestly higher risk of aortic dissection (OR 2.79, 95% CI 2.31-3.37) and aortic aneurysm (OR 2.25, 95% CI 2.03-2.49).
Citation: Singh S, Nautiyal A. Aortic dissection and aortic aneurysms associated with fluoroquinolones: A systematic review and meta-analysis. Am J Med [online ahead of print, July 21, 2017].
Optimal lengths of postoperative opioid prescription range from 4 to 15 days
Citation: Scully RE, Schoenfeld AJ, Jiang W, et al. Defining optimal length of opioid pain medication prescription after common surgical procedures. JAMA Surg. Sept 2017.
Increased mortality in weekend and holiday hospital admissions
A meta-analysis of 97 studies showed a greater relative risk of mortality for patients admitted during the weekend or holidays compared to those admitted during the week. Subgroup analyses did not reveal significant effect modification by staffing level and other hospital factors. Further research to identify contributing factors and potential interventions is needed.
Citation: Pauls LA, Johnson-Paben R, McGready J, Murphy JD, Pronovost PJ, Wu CL. The weekend effect in hospitalized patients: a meta-analysis. J Hosp Med. 2017;12(9):760-6.
Kayexalate should not be taken at the same time as other medications
The Food and Drug Administration has released a drug safety communication on kayexalate (sodium polystyrene sulfonate). Given recent research showing that kayexalate may decrease the absorption and effectiveness of many oral medications, the FDA recommended that when prescribing kayexalate, it should be given at least 3 hours before or after administration of other oral medications. This time should be increased to 6 hours for those with conditions that result in delayed gastric emptying.
Citation: Food and Drug Administration. Kayexalate (sodium polystyrene sulfonate): Drug Safety Communication. 09/06/2017.
Most thrombophilia testing done in the hospital does not add value
A retrospective cohort study among emergency department and hospitalized patients at an academic medical center examined 163 patients and 1,451 thrombophilia tests; 63% of tests were of “minimal clinical utility.”
Citation: Cox N, Johnson SA, Vazquez S, et al. Patterns and appropriateness of thrombophilia testing in an academic medical center. J Hosp Med. 2017;12(9):705-709.
Fluoroquinolone use tied to higher risk of aortic dissection and aneurysm
A meta-analysis of two observational studies found that current fluoroquinolone use was associated with modestly higher risk of aortic dissection (OR 2.79, 95% CI 2.31-3.37) and aortic aneurysm (OR 2.25, 95% CI 2.03-2.49).
Citation: Singh S, Nautiyal A. Aortic dissection and aortic aneurysms associated with fluoroquinolones: A systematic review and meta-analysis. Am J Med [online ahead of print, July 21, 2017].
Optimal lengths of postoperative opioid prescription range from 4 to 15 days
Citation: Scully RE, Schoenfeld AJ, Jiang W, et al. Defining optimal length of opioid pain medication prescription after common surgical procedures. JAMA Surg. Sept 2017.
Increased mortality in weekend and holiday hospital admissions
A meta-analysis of 97 studies showed a greater relative risk of mortality for patients admitted during the weekend or holidays compared to those admitted during the week. Subgroup analyses did not reveal significant effect modification by staffing level and other hospital factors. Further research to identify contributing factors and potential interventions is needed.
Citation: Pauls LA, Johnson-Paben R, McGready J, Murphy JD, Pronovost PJ, Wu CL. The weekend effect in hospitalized patients: a meta-analysis. J Hosp Med. 2017;12(9):760-6.
Kayexalate should not be taken at the same time as other medications
The Food and Drug Administration has released a drug safety communication on kayexalate (sodium polystyrene sulfonate). Given recent research showing that kayexalate may decrease the absorption and effectiveness of many oral medications, the FDA recommended that when prescribing kayexalate, it should be given at least 3 hours before or after administration of other oral medications. This time should be increased to 6 hours for those with conditions that result in delayed gastric emptying.
Citation: Food and Drug Administration. Kayexalate (sodium polystyrene sulfonate): Drug Safety Communication. 09/06/2017.
Most thrombophilia testing done in the hospital does not add value
A retrospective cohort study among emergency department and hospitalized patients at an academic medical center examined 163 patients and 1,451 thrombophilia tests; 63% of tests were of “minimal clinical utility.”
Citation: Cox N, Johnson SA, Vazquez S, et al. Patterns and appropriateness of thrombophilia testing in an academic medical center. J Hosp Med. 2017;12(9):705-709.
Fluoroquinolone use tied to higher risk of aortic dissection and aneurysm
A meta-analysis of two observational studies found that current fluoroquinolone use was associated with modestly higher risk of aortic dissection (OR 2.79, 95% CI 2.31-3.37) and aortic aneurysm (OR 2.25, 95% CI 2.03-2.49).
Citation: Singh S, Nautiyal A. Aortic dissection and aortic aneurysms associated with fluoroquinolones: A systematic review and meta-analysis. Am J Med [online ahead of print, July 21, 2017].
Optimal lengths of postoperative opioid prescription range from 4 to 15 days
Citation: Scully RE, Schoenfeld AJ, Jiang W, et al. Defining optimal length of opioid pain medication prescription after common surgical procedures. JAMA Surg. Sept 2017.
Increased mortality in weekend and holiday hospital admissions
A meta-analysis of 97 studies showed a greater relative risk of mortality for patients admitted during the weekend or holidays compared to those admitted during the week. Subgroup analyses did not reveal significant effect modification by staffing level and other hospital factors. Further research to identify contributing factors and potential interventions is needed.
Citation: Pauls LA, Johnson-Paben R, McGready J, Murphy JD, Pronovost PJ, Wu CL. The weekend effect in hospitalized patients: a meta-analysis. J Hosp Med. 2017;12(9):760-6.
Kayexalate should not be taken at the same time as other medications
The Food and Drug Administration has released a drug safety communication on kayexalate (sodium polystyrene sulfonate). Given recent research showing that kayexalate may decrease the absorption and effectiveness of many oral medications, the FDA recommended that when prescribing kayexalate, it should be given at least 3 hours before or after administration of other oral medications. This time should be increased to 6 hours for those with conditions that result in delayed gastric emptying.
Citation: Food and Drug Administration. Kayexalate (sodium polystyrene sulfonate): Drug Safety Communication. 09/06/2017.
Most thrombophilia testing done in the hospital does not add value
A retrospective cohort study among emergency department and hospitalized patients at an academic medical center examined 163 patients and 1,451 thrombophilia tests; 63% of tests were of “minimal clinical utility.”
Citation: Cox N, Johnson SA, Vazquez S, et al. Patterns and appropriateness of thrombophilia testing in an academic medical center. J Hosp Med. 2017;12(9):705-709.
Rivaroxaban versus warfarin in mild acute ischemic stroke secondary to atrial fibrillation
Clinical question: Is rivaroxaban as effective and safe as warfarin immediately following minor acute ischemic stroke from atrial fibrillation?
Background: There is uncertainty regarding the best approach to anticoagulation acutely after ischemic stroke secondary to atrial fibrillation. To reduce the risk of intracranial hemorrhage, many physicians start aspirin immediately and delay initiating warfarin until days to weeks later. With their more predictable and rapid anticoagulant effect with potentially lower risk of intracranial hemorrhage, direct oral anticoagulants such as rivaroxaban are an attractive possible alternative to warfarin in the acute setting.
Study design: Multicenter, randomized, open-label superiority trial with blinded outcome assessment.
Setting: Fourteen academic hospitals in South Korea.
Synopsis: One hundred eighty-three patients with mild acute (within 5 days) ischemic stroke secondary to nonvalvular atrial fibrillation were randomized to immediately initiate either rivaroxaban or warfarin. The primary outcome (composite of new ischemic lesion or new intracranial hemorrhage on MRI at 4 weeks) occurred at similar frequency between groups (49.5% versus 54.5%, P = .49). Rates of adverse events were comparable in each group. Median hospitalization length was shorter in those randomized to rivaroxaban (4.0 versus 6.0 days, P less than .001). Limitations include a radiographic primary outcome that captured many asymptomatic lesions, homogenous study population, and lack of a delayed anticoagulation group.
Bottom line: In patients with mild acute stroke from nonvalvular atrial fibrillation, rivaroxaban and warfarin demonstrated comparable efficacy and safety. More study is needed to determine the optimal anticoagulation strategy in acute stroke.
Citation: Hong K-S et al. Rivaroxaban vs. warfarin sodium in the ultra-early period after atrial fibrillation-related mild ischemic stroke: A randomized clinical trial. JAMA Neurol. 2017; 74(10):1206-15.
Dr. Kanjee is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
Clinical question: Is rivaroxaban as effective and safe as warfarin immediately following minor acute ischemic stroke from atrial fibrillation?
Background: There is uncertainty regarding the best approach to anticoagulation acutely after ischemic stroke secondary to atrial fibrillation. To reduce the risk of intracranial hemorrhage, many physicians start aspirin immediately and delay initiating warfarin until days to weeks later. With their more predictable and rapid anticoagulant effect with potentially lower risk of intracranial hemorrhage, direct oral anticoagulants such as rivaroxaban are an attractive possible alternative to warfarin in the acute setting.
Study design: Multicenter, randomized, open-label superiority trial with blinded outcome assessment.
Setting: Fourteen academic hospitals in South Korea.
Synopsis: One hundred eighty-three patients with mild acute (within 5 days) ischemic stroke secondary to nonvalvular atrial fibrillation were randomized to immediately initiate either rivaroxaban or warfarin. The primary outcome (composite of new ischemic lesion or new intracranial hemorrhage on MRI at 4 weeks) occurred at similar frequency between groups (49.5% versus 54.5%, P = .49). Rates of adverse events were comparable in each group. Median hospitalization length was shorter in those randomized to rivaroxaban (4.0 versus 6.0 days, P less than .001). Limitations include a radiographic primary outcome that captured many asymptomatic lesions, homogenous study population, and lack of a delayed anticoagulation group.
Bottom line: In patients with mild acute stroke from nonvalvular atrial fibrillation, rivaroxaban and warfarin demonstrated comparable efficacy and safety. More study is needed to determine the optimal anticoagulation strategy in acute stroke.
Citation: Hong K-S et al. Rivaroxaban vs. warfarin sodium in the ultra-early period after atrial fibrillation-related mild ischemic stroke: A randomized clinical trial. JAMA Neurol. 2017; 74(10):1206-15.
Dr. Kanjee is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
Clinical question: Is rivaroxaban as effective and safe as warfarin immediately following minor acute ischemic stroke from atrial fibrillation?
Background: There is uncertainty regarding the best approach to anticoagulation acutely after ischemic stroke secondary to atrial fibrillation. To reduce the risk of intracranial hemorrhage, many physicians start aspirin immediately and delay initiating warfarin until days to weeks later. With their more predictable and rapid anticoagulant effect with potentially lower risk of intracranial hemorrhage, direct oral anticoagulants such as rivaroxaban are an attractive possible alternative to warfarin in the acute setting.
Study design: Multicenter, randomized, open-label superiority trial with blinded outcome assessment.
Setting: Fourteen academic hospitals in South Korea.
Synopsis: One hundred eighty-three patients with mild acute (within 5 days) ischemic stroke secondary to nonvalvular atrial fibrillation were randomized to immediately initiate either rivaroxaban or warfarin. The primary outcome (composite of new ischemic lesion or new intracranial hemorrhage on MRI at 4 weeks) occurred at similar frequency between groups (49.5% versus 54.5%, P = .49). Rates of adverse events were comparable in each group. Median hospitalization length was shorter in those randomized to rivaroxaban (4.0 versus 6.0 days, P less than .001). Limitations include a radiographic primary outcome that captured many asymptomatic lesions, homogenous study population, and lack of a delayed anticoagulation group.
Bottom line: In patients with mild acute stroke from nonvalvular atrial fibrillation, rivaroxaban and warfarin demonstrated comparable efficacy and safety. More study is needed to determine the optimal anticoagulation strategy in acute stroke.
Citation: Hong K-S et al. Rivaroxaban vs. warfarin sodium in the ultra-early period after atrial fibrillation-related mild ischemic stroke: A randomized clinical trial. JAMA Neurol. 2017; 74(10):1206-15.
Dr. Kanjee is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
This is what a flu pandemic looks like
For the week ending Feb. 3, 2018, the proportion of outpatient visits for influenza-like illness (ILI) was 7.7%, which would appear to equal the mark of 7.7% set in October of 2009. The earlier 7.7%, however, is rounded down from 7.715%, while the current mark is rounded up from 7.653%, data from the CDC’s Fluview website show.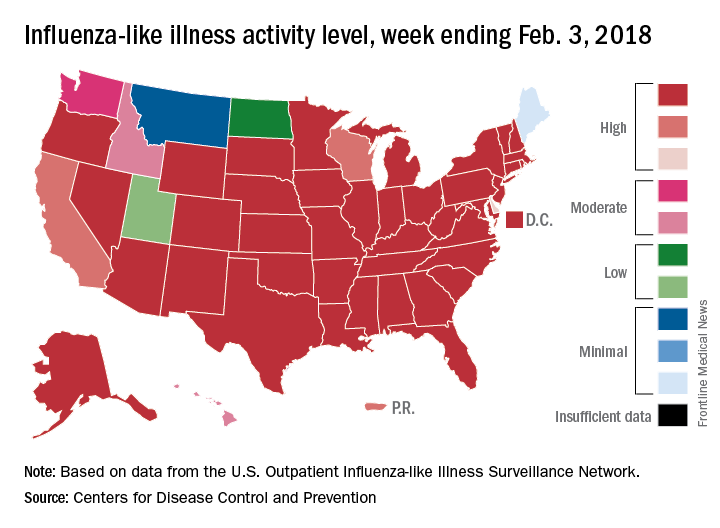
Deaths attributed to pneumonia and influenza were above the epidemic threshold set by the National Center for Health Statistics Mortality Surveillance system, acting CDC director Anne Schuchat, MD, said in a teleconference sponsored by the agency.
ILI activity was at level 10 on the CDC’s 1-10 scale in 41 states, compared with 34 the week before, and was categorized in the “high” range (levels 8-10) in another 3 states and Puerto Rico, according to data from the CDC’s Outpatient Influenza-like Illness Surveillance Network. In California, which was noted as a possible bright spot last week by Dr. Schuchat because activity there had been decreasing, the ILI level went back up to level 9 after being at 7 the week before.
Flu-related hospitalizations are continuing to rise at a record clip, with the cumulative rate for the week of Feb. 3 at 59.9 per 100,000 population, the CDC reported. A total of 1 in 10 hospital-based deaths last week were related to influenza. At this point in the 2014-2015 flu season – which has the highest number of hospitalizations at 710,000 – the hospitalization rate was only 50.9 per 100,000 population.
There were 10 pediatric deaths reported for the week ending Feb. 3, although 9 occurred in previous weeks. There have been 63 flu-related deaths among children so far during the 2017-2018 season.
Dr. Schuchat continued to recommend members of the public to get a flu shot and to stay home if they are feeling sick.
“What could be mild symptoms for you could be deadly for someone else,” Dr. Schuchat said, adding that antiviral medications remain important. “Physicians do not have to wait for confirmatory flu testing. They should begin treatment with antiviral drugs immediately in they suspect they have a severely ill or a high risk patient.”
“Flu vaccines often have lower effectiveness against H3N1 viruses. However, some protection is better than none. The vaccine’s effectiveness against other flu viruses, like B and H1N1, is better. Because of the ongoing intensity of the flu season and the increasing circulation of influenza B and h1n1, we do continue to recommend vaccination even this late in the season.”
Dr. Schuchat stressed the importance of the pneumococcal pneumonia vaccine. “Flu can make people more vulnerable to secondary infections like bacterial pneumonia. We recommend people aged 65 and over get a pneumococcal pneumonia vaccine,” she said.
For the week ending Feb. 3, 2018, the proportion of outpatient visits for influenza-like illness (ILI) was 7.7%, which would appear to equal the mark of 7.7% set in October of 2009. The earlier 7.7%, however, is rounded down from 7.715%, while the current mark is rounded up from 7.653%, data from the CDC’s Fluview website show.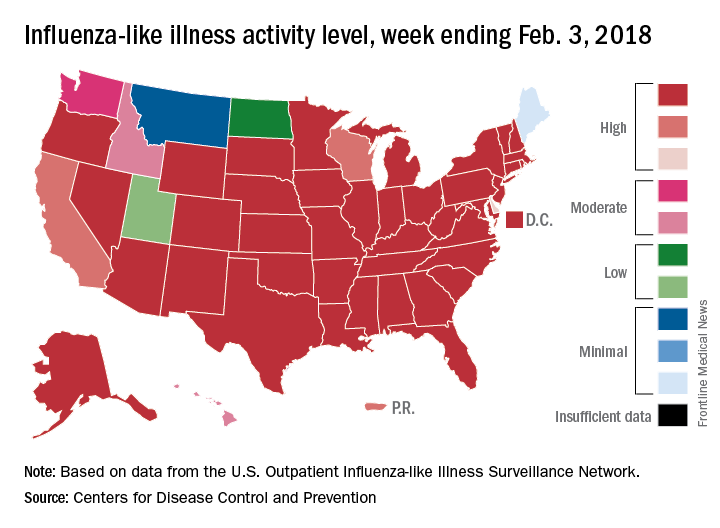
Deaths attributed to pneumonia and influenza were above the epidemic threshold set by the National Center for Health Statistics Mortality Surveillance system, acting CDC director Anne Schuchat, MD, said in a teleconference sponsored by the agency.
ILI activity was at level 10 on the CDC’s 1-10 scale in 41 states, compared with 34 the week before, and was categorized in the “high” range (levels 8-10) in another 3 states and Puerto Rico, according to data from the CDC’s Outpatient Influenza-like Illness Surveillance Network. In California, which was noted as a possible bright spot last week by Dr. Schuchat because activity there had been decreasing, the ILI level went back up to level 9 after being at 7 the week before.
Flu-related hospitalizations are continuing to rise at a record clip, with the cumulative rate for the week of Feb. 3 at 59.9 per 100,000 population, the CDC reported. A total of 1 in 10 hospital-based deaths last week were related to influenza. At this point in the 2014-2015 flu season – which has the highest number of hospitalizations at 710,000 – the hospitalization rate was only 50.9 per 100,000 population.
There were 10 pediatric deaths reported for the week ending Feb. 3, although 9 occurred in previous weeks. There have been 63 flu-related deaths among children so far during the 2017-2018 season.
Dr. Schuchat continued to recommend members of the public to get a flu shot and to stay home if they are feeling sick.
“What could be mild symptoms for you could be deadly for someone else,” Dr. Schuchat said, adding that antiviral medications remain important. “Physicians do not have to wait for confirmatory flu testing. They should begin treatment with antiviral drugs immediately in they suspect they have a severely ill or a high risk patient.”
“Flu vaccines often have lower effectiveness against H3N1 viruses. However, some protection is better than none. The vaccine’s effectiveness against other flu viruses, like B and H1N1, is better. Because of the ongoing intensity of the flu season and the increasing circulation of influenza B and h1n1, we do continue to recommend vaccination even this late in the season.”
Dr. Schuchat stressed the importance of the pneumococcal pneumonia vaccine. “Flu can make people more vulnerable to secondary infections like bacterial pneumonia. We recommend people aged 65 and over get a pneumococcal pneumonia vaccine,” she said.
For the week ending Feb. 3, 2018, the proportion of outpatient visits for influenza-like illness (ILI) was 7.7%, which would appear to equal the mark of 7.7% set in October of 2009. The earlier 7.7%, however, is rounded down from 7.715%, while the current mark is rounded up from 7.653%, data from the CDC’s Fluview website show.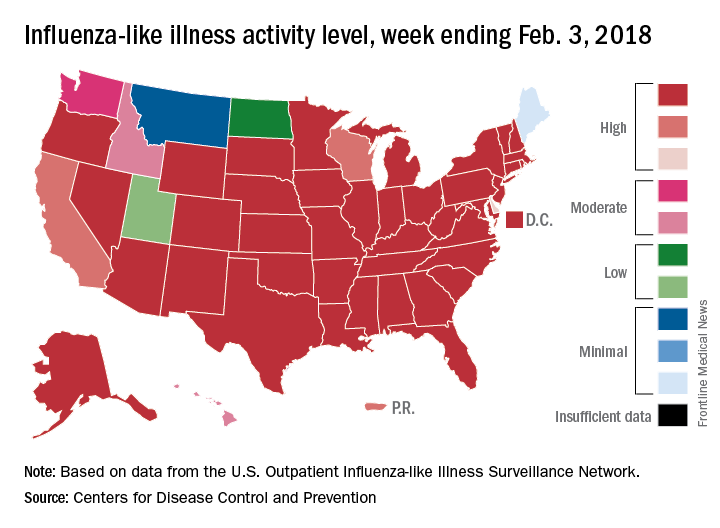
Deaths attributed to pneumonia and influenza were above the epidemic threshold set by the National Center for Health Statistics Mortality Surveillance system, acting CDC director Anne Schuchat, MD, said in a teleconference sponsored by the agency.
ILI activity was at level 10 on the CDC’s 1-10 scale in 41 states, compared with 34 the week before, and was categorized in the “high” range (levels 8-10) in another 3 states and Puerto Rico, according to data from the CDC’s Outpatient Influenza-like Illness Surveillance Network. In California, which was noted as a possible bright spot last week by Dr. Schuchat because activity there had been decreasing, the ILI level went back up to level 9 after being at 7 the week before.
Flu-related hospitalizations are continuing to rise at a record clip, with the cumulative rate for the week of Feb. 3 at 59.9 per 100,000 population, the CDC reported. A total of 1 in 10 hospital-based deaths last week were related to influenza. At this point in the 2014-2015 flu season – which has the highest number of hospitalizations at 710,000 – the hospitalization rate was only 50.9 per 100,000 population.
There were 10 pediatric deaths reported for the week ending Feb. 3, although 9 occurred in previous weeks. There have been 63 flu-related deaths among children so far during the 2017-2018 season.
Dr. Schuchat continued to recommend members of the public to get a flu shot and to stay home if they are feeling sick.
“What could be mild symptoms for you could be deadly for someone else,” Dr. Schuchat said, adding that antiviral medications remain important. “Physicians do not have to wait for confirmatory flu testing. They should begin treatment with antiviral drugs immediately in they suspect they have a severely ill or a high risk patient.”
“Flu vaccines often have lower effectiveness against H3N1 viruses. However, some protection is better than none. The vaccine’s effectiveness against other flu viruses, like B and H1N1, is better. Because of the ongoing intensity of the flu season and the increasing circulation of influenza B and h1n1, we do continue to recommend vaccination even this late in the season.”
Dr. Schuchat stressed the importance of the pneumococcal pneumonia vaccine. “Flu can make people more vulnerable to secondary infections like bacterial pneumonia. We recommend people aged 65 and over get a pneumococcal pneumonia vaccine,” she said.
FROM A CDC TELECONFERENCE
Hospitalist empathy associated with reduced patient anxiety
Clinical question: What effect does hospitalist empathy have on patient anxiety, ratings of physician communication, and duration of encounter?
Background: Physician empathy is associated with better patient-reported and medical outcomes in a number of settings. The effects of hospitalist empathy have been less well studied.
Study design: Observational study of audio recordings of hospitalist admission encounters.
Setting: General medical service at two urban hospitals within an academic medical center from August 2008 to March 2009.
Synopsis: Admission encounters (76 patients, 27 hospitalists) were recorded. Researchers detected negative emotional expressions from patients and characterized resultant physician replies as either empathic (“focuses toward further expression of emotion”), neutral (“focuses neither toward nor away from emotion”), or nonempathic (“focuses away from emotion”). Through use of regression models, response frequency was compared with change in pre/post-encounter patient anxiety, patient ratings of physician communication, and duration of encounter. Every additional empathic response was associated with a small decrease in anxiety, better ratings of physician communication, and no change in encounter duration. Nonempathic responses were associated with worse communication ratings. Limitations of the study include its observational nature, small sample size, exclusion of non–English-speaking patients, absence of data on nonverbal communication, and exclusively urban academic setting.
Bottom line: Empathic hospitalist responses during admission encounters are associated with reductions in patient anxiety and better ratings of physician communication without increases in encounter duration.
Citation: Weiss R et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12(10):805-10.
Dr. Kanjee is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
Clinical question: What effect does hospitalist empathy have on patient anxiety, ratings of physician communication, and duration of encounter?
Background: Physician empathy is associated with better patient-reported and medical outcomes in a number of settings. The effects of hospitalist empathy have been less well studied.
Study design: Observational study of audio recordings of hospitalist admission encounters.
Setting: General medical service at two urban hospitals within an academic medical center from August 2008 to March 2009.
Synopsis: Admission encounters (76 patients, 27 hospitalists) were recorded. Researchers detected negative emotional expressions from patients and characterized resultant physician replies as either empathic (“focuses toward further expression of emotion”), neutral (“focuses neither toward nor away from emotion”), or nonempathic (“focuses away from emotion”). Through use of regression models, response frequency was compared with change in pre/post-encounter patient anxiety, patient ratings of physician communication, and duration of encounter. Every additional empathic response was associated with a small decrease in anxiety, better ratings of physician communication, and no change in encounter duration. Nonempathic responses were associated with worse communication ratings. Limitations of the study include its observational nature, small sample size, exclusion of non–English-speaking patients, absence of data on nonverbal communication, and exclusively urban academic setting.
Bottom line: Empathic hospitalist responses during admission encounters are associated with reductions in patient anxiety and better ratings of physician communication without increases in encounter duration.
Citation: Weiss R et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12(10):805-10.
Dr. Kanjee is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
Clinical question: What effect does hospitalist empathy have on patient anxiety, ratings of physician communication, and duration of encounter?
Background: Physician empathy is associated with better patient-reported and medical outcomes in a number of settings. The effects of hospitalist empathy have been less well studied.
Study design: Observational study of audio recordings of hospitalist admission encounters.
Setting: General medical service at two urban hospitals within an academic medical center from August 2008 to March 2009.
Synopsis: Admission encounters (76 patients, 27 hospitalists) were recorded. Researchers detected negative emotional expressions from patients and characterized resultant physician replies as either empathic (“focuses toward further expression of emotion”), neutral (“focuses neither toward nor away from emotion”), or nonempathic (“focuses away from emotion”). Through use of regression models, response frequency was compared with change in pre/post-encounter patient anxiety, patient ratings of physician communication, and duration of encounter. Every additional empathic response was associated with a small decrease in anxiety, better ratings of physician communication, and no change in encounter duration. Nonempathic responses were associated with worse communication ratings. Limitations of the study include its observational nature, small sample size, exclusion of non–English-speaking patients, absence of data on nonverbal communication, and exclusively urban academic setting.
Bottom line: Empathic hospitalist responses during admission encounters are associated with reductions in patient anxiety and better ratings of physician communication without increases in encounter duration.
Citation: Weiss R et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12(10):805-10.
Dr. Kanjee is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
National Early Warning Score discriminates deterioration of inpatients with liver disease
, within 24 hours in hospitalized patients, according to a study published in the journal Clinical Gastroenterology and Hepatology.
Although existing predictive models estimate medium- and long-term prognosis in patients with liver disease, none are validated for short-term outcomes in inpatient settings. Despite the potential concern that patients with liver disease present with chronic physiological derangements affecting National Early Warning Score (NEWS) parameters, the score accurately discriminated patients at risk of death, admission to the ICU, or cardiac arrest within a 24-hour period for a range of liver-related diagnoses achieving an area under receiver operating characteristics (AUROC) curve of 0.894 (95% confidence intervals, 0.887-0.902), 0.857 (95% CI, 0.847-0.868), and 0.722 (95% CI, 0.685-0.759), respectively.
NEWS was launched in 2012 to reduce variations among existing early warning scores by the Royal College of Physicians for use in all adults except pregnant women. Theresa J. Hydes MD, PhD, and her colleagues at the department of gastroenterology & hepatology, Portsmouth (England) Hospitals NHS Trust, sought to validate NEWS in 35,585 unselected medical patients.
The NEWS allocates weighted points, based on derangement of vital signs from defined normal ranges including pulse, respiratory rate, systolic blood pressure, an alert-verbal-painful-unresponsive scale, temperature, peripheral oxygen saturations, and use of supplemental oxygen. The summation of allocated points to directs changes in the level of care, for example, more frequent monitoring, involving senior staff, or calling a rapid response team.
The study was performed in a large, acute care hospital in southern England and analyzed a database of electronically captured vital signs recorded in real time from completed consecutive admissions of patients aged 16 years or older, during 2010-2014. International Classification of Diseases-10 codes were used to categorize patients for any finished consultant episode. The categories included patients with primary diagnosis of liver disease, those with nonprimary liver diagnosis (comorbidity), and patients not allocated any liver disease codes (controls). The NEWS performance was examined according to whether liver disease was acute or chronic, alcohol induced, or associated with portal hypertension, with four clinical subgroups: acute alcohol-induced liver injury, other acute injury, chronic liver disease without cirrhosis, or cirrhosis. The final dataset comprised 722 patients (1,112 episodes) with a primary liver diagnosis, and 2,339 patients (3,658 episodes) with a nonprimary liver diagnosis.
The primary study endpoint was any of the following events occurring within 24 hours of an observation set: in-hospital mortality, unanticipated ICU admission, or cardiac arrest. “The NEWS identified patients with primary, nonprimary, and no diagnoses of liver disease with AUROC values of 0.873 (95% CI, 0.860-0.886), 0.898 (95% CI, 0.891-0.905), and 0.879 (95% CI, 0.877-0.881), respectively. High AUROC values also were obtained for all clinical subgroups; the NEWS identified patients with alcohol-related liver disease with an AUROC value of 0.927 (95% CI, 0.912-0.941). The NEWS identified patients with liver diseases with higher AUROC values than [did] other early warning scoring systems,” according to Dr. Hydes and her colleagues.
“Because of its widespread use, the NEWS serves a ready-made, easy-to-use option for identifying patients with liver disease who require early assessment and intervention, without the need to modify parameters, weightings or escalation criteria,” wrote the authors.
The study was supported by VitalPAC, a collaborative development of the Learning Clinic and Portsmouth Hospitals NHS Trust. Dr. Schmidt, Dr. Aspinall, and Dr. Meredith are employed by PHT. Dr. Hydes had no conflicts of interest.
SOURCE: Hydes TJ et al. Clin Gastroenterol Hepatol. 2017 Dec 22. doi: 10.1016/j.cgh.2017.12.035.
, within 24 hours in hospitalized patients, according to a study published in the journal Clinical Gastroenterology and Hepatology.
Although existing predictive models estimate medium- and long-term prognosis in patients with liver disease, none are validated for short-term outcomes in inpatient settings. Despite the potential concern that patients with liver disease present with chronic physiological derangements affecting National Early Warning Score (NEWS) parameters, the score accurately discriminated patients at risk of death, admission to the ICU, or cardiac arrest within a 24-hour period for a range of liver-related diagnoses achieving an area under receiver operating characteristics (AUROC) curve of 0.894 (95% confidence intervals, 0.887-0.902), 0.857 (95% CI, 0.847-0.868), and 0.722 (95% CI, 0.685-0.759), respectively.
NEWS was launched in 2012 to reduce variations among existing early warning scores by the Royal College of Physicians for use in all adults except pregnant women. Theresa J. Hydes MD, PhD, and her colleagues at the department of gastroenterology & hepatology, Portsmouth (England) Hospitals NHS Trust, sought to validate NEWS in 35,585 unselected medical patients.
The NEWS allocates weighted points, based on derangement of vital signs from defined normal ranges including pulse, respiratory rate, systolic blood pressure, an alert-verbal-painful-unresponsive scale, temperature, peripheral oxygen saturations, and use of supplemental oxygen. The summation of allocated points to directs changes in the level of care, for example, more frequent monitoring, involving senior staff, or calling a rapid response team.
The study was performed in a large, acute care hospital in southern England and analyzed a database of electronically captured vital signs recorded in real time from completed consecutive admissions of patients aged 16 years or older, during 2010-2014. International Classification of Diseases-10 codes were used to categorize patients for any finished consultant episode. The categories included patients with primary diagnosis of liver disease, those with nonprimary liver diagnosis (comorbidity), and patients not allocated any liver disease codes (controls). The NEWS performance was examined according to whether liver disease was acute or chronic, alcohol induced, or associated with portal hypertension, with four clinical subgroups: acute alcohol-induced liver injury, other acute injury, chronic liver disease without cirrhosis, or cirrhosis. The final dataset comprised 722 patients (1,112 episodes) with a primary liver diagnosis, and 2,339 patients (3,658 episodes) with a nonprimary liver diagnosis.
The primary study endpoint was any of the following events occurring within 24 hours of an observation set: in-hospital mortality, unanticipated ICU admission, or cardiac arrest. “The NEWS identified patients with primary, nonprimary, and no diagnoses of liver disease with AUROC values of 0.873 (95% CI, 0.860-0.886), 0.898 (95% CI, 0.891-0.905), and 0.879 (95% CI, 0.877-0.881), respectively. High AUROC values also were obtained for all clinical subgroups; the NEWS identified patients with alcohol-related liver disease with an AUROC value of 0.927 (95% CI, 0.912-0.941). The NEWS identified patients with liver diseases with higher AUROC values than [did] other early warning scoring systems,” according to Dr. Hydes and her colleagues.
“Because of its widespread use, the NEWS serves a ready-made, easy-to-use option for identifying patients with liver disease who require early assessment and intervention, without the need to modify parameters, weightings or escalation criteria,” wrote the authors.
The study was supported by VitalPAC, a collaborative development of the Learning Clinic and Portsmouth Hospitals NHS Trust. Dr. Schmidt, Dr. Aspinall, and Dr. Meredith are employed by PHT. Dr. Hydes had no conflicts of interest.
SOURCE: Hydes TJ et al. Clin Gastroenterol Hepatol. 2017 Dec 22. doi: 10.1016/j.cgh.2017.12.035.
, within 24 hours in hospitalized patients, according to a study published in the journal Clinical Gastroenterology and Hepatology.
Although existing predictive models estimate medium- and long-term prognosis in patients with liver disease, none are validated for short-term outcomes in inpatient settings. Despite the potential concern that patients with liver disease present with chronic physiological derangements affecting National Early Warning Score (NEWS) parameters, the score accurately discriminated patients at risk of death, admission to the ICU, or cardiac arrest within a 24-hour period for a range of liver-related diagnoses achieving an area under receiver operating characteristics (AUROC) curve of 0.894 (95% confidence intervals, 0.887-0.902), 0.857 (95% CI, 0.847-0.868), and 0.722 (95% CI, 0.685-0.759), respectively.
NEWS was launched in 2012 to reduce variations among existing early warning scores by the Royal College of Physicians for use in all adults except pregnant women. Theresa J. Hydes MD, PhD, and her colleagues at the department of gastroenterology & hepatology, Portsmouth (England) Hospitals NHS Trust, sought to validate NEWS in 35,585 unselected medical patients.
The NEWS allocates weighted points, based on derangement of vital signs from defined normal ranges including pulse, respiratory rate, systolic blood pressure, an alert-verbal-painful-unresponsive scale, temperature, peripheral oxygen saturations, and use of supplemental oxygen. The summation of allocated points to directs changes in the level of care, for example, more frequent monitoring, involving senior staff, or calling a rapid response team.
The study was performed in a large, acute care hospital in southern England and analyzed a database of electronically captured vital signs recorded in real time from completed consecutive admissions of patients aged 16 years or older, during 2010-2014. International Classification of Diseases-10 codes were used to categorize patients for any finished consultant episode. The categories included patients with primary diagnosis of liver disease, those with nonprimary liver diagnosis (comorbidity), and patients not allocated any liver disease codes (controls). The NEWS performance was examined according to whether liver disease was acute or chronic, alcohol induced, or associated with portal hypertension, with four clinical subgroups: acute alcohol-induced liver injury, other acute injury, chronic liver disease without cirrhosis, or cirrhosis. The final dataset comprised 722 patients (1,112 episodes) with a primary liver diagnosis, and 2,339 patients (3,658 episodes) with a nonprimary liver diagnosis.
The primary study endpoint was any of the following events occurring within 24 hours of an observation set: in-hospital mortality, unanticipated ICU admission, or cardiac arrest. “The NEWS identified patients with primary, nonprimary, and no diagnoses of liver disease with AUROC values of 0.873 (95% CI, 0.860-0.886), 0.898 (95% CI, 0.891-0.905), and 0.879 (95% CI, 0.877-0.881), respectively. High AUROC values also were obtained for all clinical subgroups; the NEWS identified patients with alcohol-related liver disease with an AUROC value of 0.927 (95% CI, 0.912-0.941). The NEWS identified patients with liver diseases with higher AUROC values than [did] other early warning scoring systems,” according to Dr. Hydes and her colleagues.
“Because of its widespread use, the NEWS serves a ready-made, easy-to-use option for identifying patients with liver disease who require early assessment and intervention, without the need to modify parameters, weightings or escalation criteria,” wrote the authors.
The study was supported by VitalPAC, a collaborative development of the Learning Clinic and Portsmouth Hospitals NHS Trust. Dr. Schmidt, Dr. Aspinall, and Dr. Meredith are employed by PHT. Dr. Hydes had no conflicts of interest.
SOURCE: Hydes TJ et al. Clin Gastroenterol Hepatol. 2017 Dec 22. doi: 10.1016/j.cgh.2017.12.035.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: The performance of the National Early Warning Score, used to identify deteriorating adult hospital inpatients with acute and chronic liver diseases within 24 hours of admission, was assessed.
Major finding: NEWS accurately discriminates risk of death, ICU admission, or cardiac arrest within 24 hours in patients with liver-related diagnoses.
Study details: A database of electronically captured vital signs recorded in real-time from completed consecutive admissions (episodes) of patients aged at least 16 years between Jan. 1, 2010, and Oct. 31, 2014. Nurses recorded data at the bedside using electronic devices running VitalPAC software.
Disclosures: The study was supported by VitalPAC, a collaborative development of the Learning Clinic and Portsmouth Hospitals NHS Trust (PHT). Dr. Schmidt, Dr. Aspinall, and Dr. Meredith are employed by PHT. Dr. Hydes had no conflicts of interest.
Source: Hydes TJ et al. Clin Gastroenterol Hepatol. 2017 Dec 22. doi: 10.1016/j.cgh.2017.12.035