User login
PTSD: Children, adolescents, and all of us may be at risk
Not everyone will suffer an episode of posttraumatic stress disorder, even though everyday American life is characterized by a lot of uncertainty these days, particularly considering the proliferation of gun violence.
Also, everyone who does experience a traumatic event will not suffer an episode of PTSD – just as not everyone develops a heart attack or cancer, nor will everyone get every illness.
The data suggest that of those exposed to trauma, up to 25% of people will develop PTSD, according to Massachusetts General/McLean Hospital, Belmont, psychiatrist Kerry J. Ressler, MD, PhD, chief of the division of depression and anxiety disorders.
As I wrote in December 2022, our “kids” are not all right and psychiatry can help. I would say that many adolescents, and adults as well, may not be all right as we are terrorized not only by mass school shootings, but shootings happening almost anywhere and everywhere in our country: in supermarkets, hospitals, and shopping malls, at graduation parties, and on the streets.
According to a report published in Clinical Psychiatry News, a poll conducted by the American Psychiatric Association showed that most American adults [70%] reported that they were anxious or extremely anxious about keeping themselves or their families safe. APA President Rebecca W. Brendel, MD, JD, pointed out that there is “a lot of worry out there about economic uncertainty, about violence and how we are going to come out of this time period.”
Meanwhile, PTSD is still defined in the DSM-5 as exposure to actual or threatened death, serious injury, or sexual violence experienced directly, witnessing the traumatic event as it occurs to others, learning that a traumatic event occurred to a close family member or friend, or experiencing of traumatic events plus extreme exposure to aversive details of the event.
Examples of traumatic events can be numerous. They include natural disasters, man-made disasters, various types of assaults, war trauma, and severe illness with ICU experiences. I would add encounters with racism and bigotry – including homophobia when one fears for their very life or physical injury. This list includes only a few triggers that may invoke this disorder.
Interestingly, the DSM-5 excludes aversive exposure through electronic media, television, movies, or pictures. Including these aspects of trauma exposure would indeed increase PTSD diagnoses, and I believe this type of exposure needs to be included, especially considering how different people process information. Some viewers of media remain “outside” the events depicted on television, movies, or electronic media while others fit directly “into” the film or TV show. Even, for example, a news program, as evidenced by those people suffering from PTSD after viewing the Sept. 11, 2001, disaster on TV.
I have interviewed numerous people who witnessed Sept. 11 tragedies on TV, some during and some after the event, and they genuinely had experienced key factors of PTSD, including nightmares and intrusive recollections of the event. It’s important to include the ways in which people process information and events in order to make a correct diagnosis, in that “one [diagnostic] size does not fit all.”
PTSD at school
In my December column, I noted the fear of death that my generation and beyond experienced with the endless threat of nuclear war, which by its very nature meant death, and if not, the saying went “the living would envy the dead” – that is, in post–nuclear war.
As I pointed out in the column, that war never came and hopefully never will, yet the intensity of those many decades of threatened terror with regular school exercises of “hide under the desk” and “don’t look at the flash” left some with intrusive fearful thoughts, nightmares, and even visualization of atomic destruction, as well as the many scenes of destruction portrayed in news casts and films of nuclear explosions.
Clearly, most U.S. school children who participate in school lockdown drills will not suffer from PTSD episodes, but some will. If that “some” approaches 20% or even 10% or less, that will amount to a lot of kids.
I decided to interview two of my grandchildren, each living in different communities and attending different school systems, but both experiencing “lockdown drills.”
Jack, who is 13 and going into eighth grade, was quite clear regarding the drills and reported that in his age group, both he and the kids in his class felt scared while in lockdown. He told me some kids looked nervous. He mentioned that they were taught in school that if the “real thing” happened, the message was “hide, run, and fight.” I was curious and asked why not run first. He was quick to answer and said if you run, you might run into danger, so it’s better to hide and wait for help to arrive. I said to myself, if not PTSD, then being scared or nervous may also lead to anxiety or even to an anxiety disorder.
Next, I interviewed almost 11-year-old Charley, who is going into sixth grade. She was very clear about not at all being fearful or nervous during these drills and was confident that her classmates felt the same way. Then she explained that the school did a great job with a security officer and had locked doors all around that only opened from the inside. She was proud of the school and not fearful or worried at all.
The diverse views of these two young people surprised me but confirm that PTSD is not at all a given based on what is occurring in society. However, it should always be considered by clinicians if a child or adolescent begins to show signs consistent with PTSD.
These two interviews were quite short, but after I finished talking with Charley, she reported spontaneously that while she and her classmates were neither worried nor scared, some of their teachers did look nervous and seemed scared.
I was quite impressed with her sharpness and nuanced observation, and as noted, adults as well may be adversely affected by the entire concept of school lockdowns, as the awareness of their purpose rests in the forefront of their minds.
The way forward
So how do we prepare kids and adolescents for potential emotional problems like PTSD arising from lockdowns, even though most children or adults will not suffer any of these PTSD issues?
First, I believe that Second, it is important that school children be aware that if they feel bad in any way emotionally, they should speak to their parents, guardians, teachers, or school nurses.
Clearly, communicating simple problems without embarrassment or shame can lead to solutions, often quickly. Larger, more complicated issues may need professional intervention. Equally important, many mental health interventions need not be long in duration but client-centered, focused, and short term.
But what needs to be emphasized is that speaking and addressing what’s going on, if your thoughts and emotions are troubling, are in themselves therapeutic. Talk therapy works – especially if you get a new perspective on the old set of problems.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Not everyone will suffer an episode of posttraumatic stress disorder, even though everyday American life is characterized by a lot of uncertainty these days, particularly considering the proliferation of gun violence.
Also, everyone who does experience a traumatic event will not suffer an episode of PTSD – just as not everyone develops a heart attack or cancer, nor will everyone get every illness.
The data suggest that of those exposed to trauma, up to 25% of people will develop PTSD, according to Massachusetts General/McLean Hospital, Belmont, psychiatrist Kerry J. Ressler, MD, PhD, chief of the division of depression and anxiety disorders.
As I wrote in December 2022, our “kids” are not all right and psychiatry can help. I would say that many adolescents, and adults as well, may not be all right as we are terrorized not only by mass school shootings, but shootings happening almost anywhere and everywhere in our country: in supermarkets, hospitals, and shopping malls, at graduation parties, and on the streets.
According to a report published in Clinical Psychiatry News, a poll conducted by the American Psychiatric Association showed that most American adults [70%] reported that they were anxious or extremely anxious about keeping themselves or their families safe. APA President Rebecca W. Brendel, MD, JD, pointed out that there is “a lot of worry out there about economic uncertainty, about violence and how we are going to come out of this time period.”
Meanwhile, PTSD is still defined in the DSM-5 as exposure to actual or threatened death, serious injury, or sexual violence experienced directly, witnessing the traumatic event as it occurs to others, learning that a traumatic event occurred to a close family member or friend, or experiencing of traumatic events plus extreme exposure to aversive details of the event.
Examples of traumatic events can be numerous. They include natural disasters, man-made disasters, various types of assaults, war trauma, and severe illness with ICU experiences. I would add encounters with racism and bigotry – including homophobia when one fears for their very life or physical injury. This list includes only a few triggers that may invoke this disorder.
Interestingly, the DSM-5 excludes aversive exposure through electronic media, television, movies, or pictures. Including these aspects of trauma exposure would indeed increase PTSD diagnoses, and I believe this type of exposure needs to be included, especially considering how different people process information. Some viewers of media remain “outside” the events depicted on television, movies, or electronic media while others fit directly “into” the film or TV show. Even, for example, a news program, as evidenced by those people suffering from PTSD after viewing the Sept. 11, 2001, disaster on TV.
I have interviewed numerous people who witnessed Sept. 11 tragedies on TV, some during and some after the event, and they genuinely had experienced key factors of PTSD, including nightmares and intrusive recollections of the event. It’s important to include the ways in which people process information and events in order to make a correct diagnosis, in that “one [diagnostic] size does not fit all.”
PTSD at school
In my December column, I noted the fear of death that my generation and beyond experienced with the endless threat of nuclear war, which by its very nature meant death, and if not, the saying went “the living would envy the dead” – that is, in post–nuclear war.
As I pointed out in the column, that war never came and hopefully never will, yet the intensity of those many decades of threatened terror with regular school exercises of “hide under the desk” and “don’t look at the flash” left some with intrusive fearful thoughts, nightmares, and even visualization of atomic destruction, as well as the many scenes of destruction portrayed in news casts and films of nuclear explosions.
Clearly, most U.S. school children who participate in school lockdown drills will not suffer from PTSD episodes, but some will. If that “some” approaches 20% or even 10% or less, that will amount to a lot of kids.
I decided to interview two of my grandchildren, each living in different communities and attending different school systems, but both experiencing “lockdown drills.”
Jack, who is 13 and going into eighth grade, was quite clear regarding the drills and reported that in his age group, both he and the kids in his class felt scared while in lockdown. He told me some kids looked nervous. He mentioned that they were taught in school that if the “real thing” happened, the message was “hide, run, and fight.” I was curious and asked why not run first. He was quick to answer and said if you run, you might run into danger, so it’s better to hide and wait for help to arrive. I said to myself, if not PTSD, then being scared or nervous may also lead to anxiety or even to an anxiety disorder.
Next, I interviewed almost 11-year-old Charley, who is going into sixth grade. She was very clear about not at all being fearful or nervous during these drills and was confident that her classmates felt the same way. Then she explained that the school did a great job with a security officer and had locked doors all around that only opened from the inside. She was proud of the school and not fearful or worried at all.
The diverse views of these two young people surprised me but confirm that PTSD is not at all a given based on what is occurring in society. However, it should always be considered by clinicians if a child or adolescent begins to show signs consistent with PTSD.
These two interviews were quite short, but after I finished talking with Charley, she reported spontaneously that while she and her classmates were neither worried nor scared, some of their teachers did look nervous and seemed scared.
I was quite impressed with her sharpness and nuanced observation, and as noted, adults as well may be adversely affected by the entire concept of school lockdowns, as the awareness of their purpose rests in the forefront of their minds.
The way forward
So how do we prepare kids and adolescents for potential emotional problems like PTSD arising from lockdowns, even though most children or adults will not suffer any of these PTSD issues?
First, I believe that Second, it is important that school children be aware that if they feel bad in any way emotionally, they should speak to their parents, guardians, teachers, or school nurses.
Clearly, communicating simple problems without embarrassment or shame can lead to solutions, often quickly. Larger, more complicated issues may need professional intervention. Equally important, many mental health interventions need not be long in duration but client-centered, focused, and short term.
But what needs to be emphasized is that speaking and addressing what’s going on, if your thoughts and emotions are troubling, are in themselves therapeutic. Talk therapy works – especially if you get a new perspective on the old set of problems.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Not everyone will suffer an episode of posttraumatic stress disorder, even though everyday American life is characterized by a lot of uncertainty these days, particularly considering the proliferation of gun violence.
Also, everyone who does experience a traumatic event will not suffer an episode of PTSD – just as not everyone develops a heart attack or cancer, nor will everyone get every illness.
The data suggest that of those exposed to trauma, up to 25% of people will develop PTSD, according to Massachusetts General/McLean Hospital, Belmont, psychiatrist Kerry J. Ressler, MD, PhD, chief of the division of depression and anxiety disorders.
As I wrote in December 2022, our “kids” are not all right and psychiatry can help. I would say that many adolescents, and adults as well, may not be all right as we are terrorized not only by mass school shootings, but shootings happening almost anywhere and everywhere in our country: in supermarkets, hospitals, and shopping malls, at graduation parties, and on the streets.
According to a report published in Clinical Psychiatry News, a poll conducted by the American Psychiatric Association showed that most American adults [70%] reported that they were anxious or extremely anxious about keeping themselves or their families safe. APA President Rebecca W. Brendel, MD, JD, pointed out that there is “a lot of worry out there about economic uncertainty, about violence and how we are going to come out of this time period.”
Meanwhile, PTSD is still defined in the DSM-5 as exposure to actual or threatened death, serious injury, or sexual violence experienced directly, witnessing the traumatic event as it occurs to others, learning that a traumatic event occurred to a close family member or friend, or experiencing of traumatic events plus extreme exposure to aversive details of the event.
Examples of traumatic events can be numerous. They include natural disasters, man-made disasters, various types of assaults, war trauma, and severe illness with ICU experiences. I would add encounters with racism and bigotry – including homophobia when one fears for their very life or physical injury. This list includes only a few triggers that may invoke this disorder.
Interestingly, the DSM-5 excludes aversive exposure through electronic media, television, movies, or pictures. Including these aspects of trauma exposure would indeed increase PTSD diagnoses, and I believe this type of exposure needs to be included, especially considering how different people process information. Some viewers of media remain “outside” the events depicted on television, movies, or electronic media while others fit directly “into” the film or TV show. Even, for example, a news program, as evidenced by those people suffering from PTSD after viewing the Sept. 11, 2001, disaster on TV.
I have interviewed numerous people who witnessed Sept. 11 tragedies on TV, some during and some after the event, and they genuinely had experienced key factors of PTSD, including nightmares and intrusive recollections of the event. It’s important to include the ways in which people process information and events in order to make a correct diagnosis, in that “one [diagnostic] size does not fit all.”
PTSD at school
In my December column, I noted the fear of death that my generation and beyond experienced with the endless threat of nuclear war, which by its very nature meant death, and if not, the saying went “the living would envy the dead” – that is, in post–nuclear war.
As I pointed out in the column, that war never came and hopefully never will, yet the intensity of those many decades of threatened terror with regular school exercises of “hide under the desk” and “don’t look at the flash” left some with intrusive fearful thoughts, nightmares, and even visualization of atomic destruction, as well as the many scenes of destruction portrayed in news casts and films of nuclear explosions.
Clearly, most U.S. school children who participate in school lockdown drills will not suffer from PTSD episodes, but some will. If that “some” approaches 20% or even 10% or less, that will amount to a lot of kids.
I decided to interview two of my grandchildren, each living in different communities and attending different school systems, but both experiencing “lockdown drills.”
Jack, who is 13 and going into eighth grade, was quite clear regarding the drills and reported that in his age group, both he and the kids in his class felt scared while in lockdown. He told me some kids looked nervous. He mentioned that they were taught in school that if the “real thing” happened, the message was “hide, run, and fight.” I was curious and asked why not run first. He was quick to answer and said if you run, you might run into danger, so it’s better to hide and wait for help to arrive. I said to myself, if not PTSD, then being scared or nervous may also lead to anxiety or even to an anxiety disorder.
Next, I interviewed almost 11-year-old Charley, who is going into sixth grade. She was very clear about not at all being fearful or nervous during these drills and was confident that her classmates felt the same way. Then she explained that the school did a great job with a security officer and had locked doors all around that only opened from the inside. She was proud of the school and not fearful or worried at all.
The diverse views of these two young people surprised me but confirm that PTSD is not at all a given based on what is occurring in society. However, it should always be considered by clinicians if a child or adolescent begins to show signs consistent with PTSD.
These two interviews were quite short, but after I finished talking with Charley, she reported spontaneously that while she and her classmates were neither worried nor scared, some of their teachers did look nervous and seemed scared.
I was quite impressed with her sharpness and nuanced observation, and as noted, adults as well may be adversely affected by the entire concept of school lockdowns, as the awareness of their purpose rests in the forefront of their minds.
The way forward
So how do we prepare kids and adolescents for potential emotional problems like PTSD arising from lockdowns, even though most children or adults will not suffer any of these PTSD issues?
First, I believe that Second, it is important that school children be aware that if they feel bad in any way emotionally, they should speak to their parents, guardians, teachers, or school nurses.
Clearly, communicating simple problems without embarrassment or shame can lead to solutions, often quickly. Larger, more complicated issues may need professional intervention. Equally important, many mental health interventions need not be long in duration but client-centered, focused, and short term.
But what needs to be emphasized is that speaking and addressing what’s going on, if your thoughts and emotions are troubling, are in themselves therapeutic. Talk therapy works – especially if you get a new perspective on the old set of problems.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Applications of ChatGPT and Large Language Models in Medicine and Health Care: Benefits and Pitfalls
The development of [artificial intelligence] is as fundamental as the creation of the microprocessor, the personal computer, the Internet, and the mobile phone. It will change the way people work, learn, travel, get health care, and communicate with each other.
Bill Gates 1
As the world emerges from the pandemic and the health care system faces new challenges, technology has become an increasingly important tool for health care professionals (HCPs). One such technology is the large language model (LLM), which has the potential to revolutionize the health care industry. ChatGPT, a popular LLM developed by OpenAI, has gained particular attention in the medical community for its ability to pass the United States Medical Licensing Exam.2 This article will explore the benefits and potential pitfalls of using LLMs like ChatGPT in medicine and health care.
Benefits
HCP burnout is a serious issue that can lead to lower productivity, increased medical errors, and decreased patient satisfaction.3 LLMs can alleviate some administrative burdens on HCPs, allowing them to focus on patient care. By assisting with billing, coding, insurance claims, and organizing schedules, LLMs like ChatGPT can free up time for HCPs to focus on what they do best: providing quality patient care.4 ChatGPT also can assist with diagnoses by providing accurate and reliable information based on a vast amount of clinical data. By learning the relationships between different medical conditions, symptoms, and treatment options, ChatGPT can provide an appropriate differential diagnosis (Figure 1).
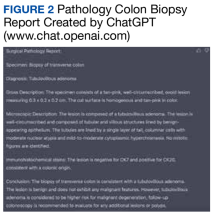
Imaging medical specialists like radiologists, pathologists, dermatologists, and others can benefit from combining computer vision diagnostics with ChatGPT report creation abilities to streamline the diagnostic workflow and improve diagnostic accuracy (Figure 2).
Although using ChatGPT and other LLMs in mental health care has potential benefits, it is essential to note that they are not a substitute for human interaction and personalized care. While ChatGPT can remember information from previous conversations, it cannot provide the same level of personalized, high-quality care that a professional therapist or HCP can. However, by augmenting the work of HCPs, ChatGPT and other LLMs have the potential to make mental health care more accessible and efficient. In addition to providing effective screening in underserved areas, ChatGPT technology may improve the competence of physician assistants and nurse practitioners in delivering mental health care. With the increased incidence of mental health problems in veterans, the pertinence of a ChatGPT-like feature will only increase with time.9
ChatGPT can also be integrated into health care organizations’ websites and mobile apps, providing patients instant access to medical information, self-care advice, symptom checkers, scheduling appointments, and arranging transportation. These features can reduce the burden on health care staff and help patients stay informed and motivated to take an active role in their health. Additionally, health care organizations can use ChatGPT to engage patients by providing reminders for medication renewals and assistance with self-care.4,6,10,11
The potential of artificial intelligence (AI) in the field of medical education and research is immense. According to a study by Gilson and colleagues, ChatGPT has shown promising results as a medical education tool.12 ChatGPT can simulate clinical scenarios, provide real-time feedback, and improve diagnostic skills. It also offers new interactive and personalized learning opportunities for medical students and HCPs.13 ChatGPT can help researchers by streamlining the process of data analysis. It can also administer surveys or questionnaires, facilitate data collection on preferences and experiences, and help in writing scientific publications.14 Nevertheless, to fully unlock the potential of these AI models, additional models that perform checks for factual accuracy, plagiarism, and copyright infringement must be developed.15,16
AI Bill of Rights
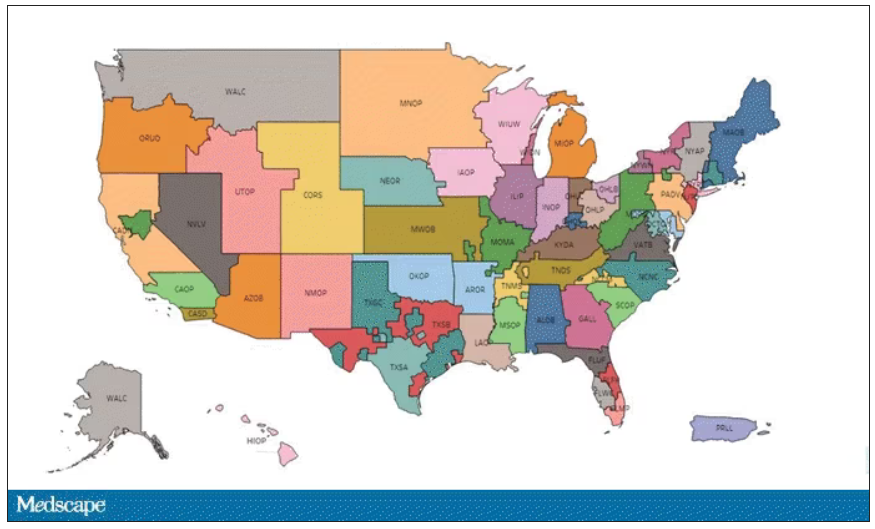
In order to protect the American public, the White House Office of Science and Technology Policy (OSTP) has released a blueprint for an AI Bill of Rights that emphasizes 5 principles to protect the public from the harmful effects of AI models, including safe and effective systems; algorithmic discrimination protection; data privacy; notice and explanation; and human alternatives, considerations, and fallback (Figure 3).17
One of the biggest challenges with LLMs like ChatGPT is the prevalence of inaccurate information or so-called hallucinations.16 These inaccuracies stem from the inability of LLMs to distinguish between real and fake information. To prevent hallucinations, researchers have proposed several methods, including training models on more diverse data, using adversarial training methods, and human-in-the-loop approaches.21 In addition, medicine-specific models like GatorTron, medPaLM, and Almanac were developed, increasing the accuracy of factual results.22-24 Unfortunately, only the GatorTron model is available to the public through the NVIDIA developers’ program.25
Despite these shortcomings, the future of LLMs in health care is promising. Although these models will not replace HCPs, they can help reduce the unnecessary burden on them, prevent burnout, and enable HCPs and patients spend more time together. Establishing an official hospital AI oversight governing body that would promote best practices could ensure the trustworthy implementation of these new technologies.26
Conclusions
The use of ChatGPT and other LLMs in health care has the potential to revolutionize the industry. By assisting HCPs with administrative tasks, improving the accuracy and reliability of diagnoses, and engaging patients, ChatGPT can help health care organizations provide better care to their patients. While LLMs are not a substitute for human interaction and personalized care, they can augment the work of HCPs, making health care more accessible and efficient. As the health care industry continues to evolve, it will be exciting to see how ChatGPT and other LLMs are used to improve patient outcomes and quality of care. In addition, AI technologies like ChatGPT offer enormous potential in medical education and research. To ensure that the benefits outweigh the risks, developing trustworthy AI health care products and establishing oversight governing bodies to ensure their implementation is essential. By doing so, we can help HCPs focus on what matters most, providing high-quality care to patients.
Acknowledgments
This material is the result of work supported by resources and the use of facilities at the James A. Haley Veterans’ Hospital.
1. Bill Gates. The age of AI has begun. March 21, 2023. Accessed May 10, 2023. https://www.gatesnotes.com/the-age-of-ai-has-begun
2. Kung TH, Cheatham M, Medenilla A, et al. Performance of ChatGPT on USMLE: Potential for AI-assisted medical education using large language models. PLOS Digit Health. 2023;2(2):e0000198. Published 2023 Feb 9. doi:10.1371/journal.pdig.0000198
3. Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2020. Mayo Clin Proc. 2022;97(3):491-506. doi:10.1016/j.mayocp.2021.11.021
4. Goodman RS, Patrinely JR Jr, Osterman T, Wheless L, Johnson DB. On the cusp: considering the impact of artificial intelligence language models in healthcare. Med. 2023;4(3):139-140. doi:10.1016/j.medj.2023.02.008
5. Will ChatGPT transform healthcare? Nat Med. 2023;29(3):505-506. doi:10.1038/s41591-023-02289-5
6. Hopkins AM, Logan JM, Kichenadasse G, Sorich MJ. Artificial intelligence chatbots will revolutionize how cancer patients access information: ChatGPT represents a paradigm-shift. JNCI Cancer Spectr. 2023;7(2):pkad010. doi:10.1093/jncics/pkad010
7. Babar Z, van Laarhoven T, Zanzotto FM, Marchiori E. Evaluating diagnostic content of AI-generated radiology reports of chest X-rays. Artif Intell Med. 2021;116:102075. doi:10.1016/j.artmed.2021.102075
8. Lecler A, Duron L, Soyer P. Revolutionizing radiology with GPT-based models: current applications, future possibilities and limitations of ChatGPT. Diagn Interv Imaging. 2023;S2211-5684(23)00027-X. doi:10.1016/j.diii.2023.02.003
9. Germain JM. Is ChatGPT smart enough to practice mental health therapy? March 23, 2023. Accessed May 11, 2023. https://www.technewsworld.com/story/is-chatgpt-smart-enough-to-practice-mental-health-therapy-178064.html
10. Cascella M, Montomoli J, Bellini V, Bignami E. Evaluating the feasibility of ChatGPT in healthcare: an analysis of multiple clinical and research scenarios. J Med Syst. 2023;47(1):33. Published 2023 Mar 4. doi:10.1007/s10916-023-01925-4
11. Jungwirth D, Haluza D. Artificial intelligence and public health: an exploratory study. Int J Environ Res Public Health. 2023;20(5):4541. Published 2023 Mar 3. doi:10.3390/ijerph20054541
12. Gilson A, Safranek CW, Huang T, et al. How does ChatGPT perform on the United States Medical Licensing Examination? The implications of large language models for medical education and knowledge assessment. JMIR Med Educ. 2023;9:e45312. Published 2023 Feb 8. doi:10.2196/45312
13. Eysenbach G. The role of ChatGPT, generative language models, and artificial intelligence in medical education: a conversation with ChatGPT and a call for papers. JMIR Med Educ. 2023;9:e46885. Published 2023 Mar 6. doi:10.2196/46885
14. Macdonald C, Adeloye D, Sheikh A, Rudan I. Can ChatGPT draft a research article? An example of population-level vaccine effectiveness analysis. J Glob Health. 2023;13:01003. Published 2023 Feb 17. doi:10.7189/jogh.13.01003
15. Masters K. Ethical use of artificial intelligence in health professions education: AMEE Guide No.158. Med Teach. 2023;1-11. doi:10.1080/0142159X.2023.2186203
16. Smith CS. Hallucinations could blunt ChatGPT’s success. IEEE Spectrum. March 13, 2023. Accessed May 11, 2023. https://spectrum.ieee.org/ai-hallucination
17. Executive Office of the President, Office of Science and Technology Policy. Blueprint for an AI Bill of Rights. Accessed May 11, 2023. https://www.whitehouse.gov/ostp/ai-bill-of-rights
18. Executive office of the President. Executive Order 13960: promoting the use of trustworthy artificial intelligence in the federal government. Fed Regist. 2020;89(236):78939-78943.
19. US Department of Commerce, National institute of Standards and Technology. Artificial Intelligence Risk Management Framework (AI RMF 1.0). Published January 2023. doi:10.6028/NIST.AI.100-1
20. Microsoft. Azure Cognitive Search—Cloud Search Service. Accessed May 11, 2023. https://azure.microsoft.com/en-us/products/search
21. Aiyappa R, An J, Kwak H, Ahn YY. Can we trust the evaluation on ChatGPT? March 22, 2023. Accessed May 11, 2023. https://arxiv.org/abs/2303.12767v1
22. Yang X, Chen A, Pournejatian N, et al. GatorTron: a large clinical language model to unlock patient information from unstructured electronic health records. Updated December 16, 2022. Accessed May 11, 2023. https://arxiv.org/abs/2203.03540v3
23. Singhal K, Azizi S, Tu T, et al. Large language models encode clinical knowledge. December 26, 2022. Accessed May 11, 2023. https://arxiv.org/abs/2212.13138v1
24. Zakka C, Chaurasia A, Shad R, Hiesinger W. Almanac: knowledge-grounded language models for clinical medicine. March 1, 2023. Accessed May 11, 2023. https://arxiv.org/abs/2303.01229v1
25. NVIDIA. GatorTron-OG. Accessed May 11, 2023. https://catalog.ngc.nvidia.com/orgs/nvidia/teams/clara/models/gatortron_og
26. Borkowski AA, Jakey CE, Thomas LB, Viswanadhan N, Mastorides SM. Establishing a hospital artificial intelligence committee to improve patient care. Fed Pract. 2022;39(8):334-336. doi:10.12788/fp.0299
The development of [artificial intelligence] is as fundamental as the creation of the microprocessor, the personal computer, the Internet, and the mobile phone. It will change the way people work, learn, travel, get health care, and communicate with each other.
Bill Gates 1
As the world emerges from the pandemic and the health care system faces new challenges, technology has become an increasingly important tool for health care professionals (HCPs). One such technology is the large language model (LLM), which has the potential to revolutionize the health care industry. ChatGPT, a popular LLM developed by OpenAI, has gained particular attention in the medical community for its ability to pass the United States Medical Licensing Exam.2 This article will explore the benefits and potential pitfalls of using LLMs like ChatGPT in medicine and health care.
Benefits
HCP burnout is a serious issue that can lead to lower productivity, increased medical errors, and decreased patient satisfaction.3 LLMs can alleviate some administrative burdens on HCPs, allowing them to focus on patient care. By assisting with billing, coding, insurance claims, and organizing schedules, LLMs like ChatGPT can free up time for HCPs to focus on what they do best: providing quality patient care.4 ChatGPT also can assist with diagnoses by providing accurate and reliable information based on a vast amount of clinical data. By learning the relationships between different medical conditions, symptoms, and treatment options, ChatGPT can provide an appropriate differential diagnosis (Figure 1).
Imaging medical specialists like radiologists, pathologists, dermatologists, and others can benefit from combining computer vision diagnostics with ChatGPT report creation abilities to streamline the diagnostic workflow and improve diagnostic accuracy (Figure 2).
Although using ChatGPT and other LLMs in mental health care has potential benefits, it is essential to note that they are not a substitute for human interaction and personalized care. While ChatGPT can remember information from previous conversations, it cannot provide the same level of personalized, high-quality care that a professional therapist or HCP can. However, by augmenting the work of HCPs, ChatGPT and other LLMs have the potential to make mental health care more accessible and efficient. In addition to providing effective screening in underserved areas, ChatGPT technology may improve the competence of physician assistants and nurse practitioners in delivering mental health care. With the increased incidence of mental health problems in veterans, the pertinence of a ChatGPT-like feature will only increase with time.9
ChatGPT can also be integrated into health care organizations’ websites and mobile apps, providing patients instant access to medical information, self-care advice, symptom checkers, scheduling appointments, and arranging transportation. These features can reduce the burden on health care staff and help patients stay informed and motivated to take an active role in their health. Additionally, health care organizations can use ChatGPT to engage patients by providing reminders for medication renewals and assistance with self-care.4,6,10,11
The potential of artificial intelligence (AI) in the field of medical education and research is immense. According to a study by Gilson and colleagues, ChatGPT has shown promising results as a medical education tool.12 ChatGPT can simulate clinical scenarios, provide real-time feedback, and improve diagnostic skills. It also offers new interactive and personalized learning opportunities for medical students and HCPs.13 ChatGPT can help researchers by streamlining the process of data analysis. It can also administer surveys or questionnaires, facilitate data collection on preferences and experiences, and help in writing scientific publications.14 Nevertheless, to fully unlock the potential of these AI models, additional models that perform checks for factual accuracy, plagiarism, and copyright infringement must be developed.15,16
AI Bill of Rights
In order to protect the American public, the White House Office of Science and Technology Policy (OSTP) has released a blueprint for an AI Bill of Rights that emphasizes 5 principles to protect the public from the harmful effects of AI models, including safe and effective systems; algorithmic discrimination protection; data privacy; notice and explanation; and human alternatives, considerations, and fallback (Figure 3).17
One of the biggest challenges with LLMs like ChatGPT is the prevalence of inaccurate information or so-called hallucinations.16 These inaccuracies stem from the inability of LLMs to distinguish between real and fake information. To prevent hallucinations, researchers have proposed several methods, including training models on more diverse data, using adversarial training methods, and human-in-the-loop approaches.21 In addition, medicine-specific models like GatorTron, medPaLM, and Almanac were developed, increasing the accuracy of factual results.22-24 Unfortunately, only the GatorTron model is available to the public through the NVIDIA developers’ program.25
Despite these shortcomings, the future of LLMs in health care is promising. Although these models will not replace HCPs, they can help reduce the unnecessary burden on them, prevent burnout, and enable HCPs and patients spend more time together. Establishing an official hospital AI oversight governing body that would promote best practices could ensure the trustworthy implementation of these new technologies.26
Conclusions
The use of ChatGPT and other LLMs in health care has the potential to revolutionize the industry. By assisting HCPs with administrative tasks, improving the accuracy and reliability of diagnoses, and engaging patients, ChatGPT can help health care organizations provide better care to their patients. While LLMs are not a substitute for human interaction and personalized care, they can augment the work of HCPs, making health care more accessible and efficient. As the health care industry continues to evolve, it will be exciting to see how ChatGPT and other LLMs are used to improve patient outcomes and quality of care. In addition, AI technologies like ChatGPT offer enormous potential in medical education and research. To ensure that the benefits outweigh the risks, developing trustworthy AI health care products and establishing oversight governing bodies to ensure their implementation is essential. By doing so, we can help HCPs focus on what matters most, providing high-quality care to patients.
Acknowledgments
This material is the result of work supported by resources and the use of facilities at the James A. Haley Veterans’ Hospital.
The development of [artificial intelligence] is as fundamental as the creation of the microprocessor, the personal computer, the Internet, and the mobile phone. It will change the way people work, learn, travel, get health care, and communicate with each other.
Bill Gates 1
As the world emerges from the pandemic and the health care system faces new challenges, technology has become an increasingly important tool for health care professionals (HCPs). One such technology is the large language model (LLM), which has the potential to revolutionize the health care industry. ChatGPT, a popular LLM developed by OpenAI, has gained particular attention in the medical community for its ability to pass the United States Medical Licensing Exam.2 This article will explore the benefits and potential pitfalls of using LLMs like ChatGPT in medicine and health care.
Benefits
HCP burnout is a serious issue that can lead to lower productivity, increased medical errors, and decreased patient satisfaction.3 LLMs can alleviate some administrative burdens on HCPs, allowing them to focus on patient care. By assisting with billing, coding, insurance claims, and organizing schedules, LLMs like ChatGPT can free up time for HCPs to focus on what they do best: providing quality patient care.4 ChatGPT also can assist with diagnoses by providing accurate and reliable information based on a vast amount of clinical data. By learning the relationships between different medical conditions, symptoms, and treatment options, ChatGPT can provide an appropriate differential diagnosis (Figure 1).
Imaging medical specialists like radiologists, pathologists, dermatologists, and others can benefit from combining computer vision diagnostics with ChatGPT report creation abilities to streamline the diagnostic workflow and improve diagnostic accuracy (Figure 2).
Although using ChatGPT and other LLMs in mental health care has potential benefits, it is essential to note that they are not a substitute for human interaction and personalized care. While ChatGPT can remember information from previous conversations, it cannot provide the same level of personalized, high-quality care that a professional therapist or HCP can. However, by augmenting the work of HCPs, ChatGPT and other LLMs have the potential to make mental health care more accessible and efficient. In addition to providing effective screening in underserved areas, ChatGPT technology may improve the competence of physician assistants and nurse practitioners in delivering mental health care. With the increased incidence of mental health problems in veterans, the pertinence of a ChatGPT-like feature will only increase with time.9
ChatGPT can also be integrated into health care organizations’ websites and mobile apps, providing patients instant access to medical information, self-care advice, symptom checkers, scheduling appointments, and arranging transportation. These features can reduce the burden on health care staff and help patients stay informed and motivated to take an active role in their health. Additionally, health care organizations can use ChatGPT to engage patients by providing reminders for medication renewals and assistance with self-care.4,6,10,11
The potential of artificial intelligence (AI) in the field of medical education and research is immense. According to a study by Gilson and colleagues, ChatGPT has shown promising results as a medical education tool.12 ChatGPT can simulate clinical scenarios, provide real-time feedback, and improve diagnostic skills. It also offers new interactive and personalized learning opportunities for medical students and HCPs.13 ChatGPT can help researchers by streamlining the process of data analysis. It can also administer surveys or questionnaires, facilitate data collection on preferences and experiences, and help in writing scientific publications.14 Nevertheless, to fully unlock the potential of these AI models, additional models that perform checks for factual accuracy, plagiarism, and copyright infringement must be developed.15,16
AI Bill of Rights
In order to protect the American public, the White House Office of Science and Technology Policy (OSTP) has released a blueprint for an AI Bill of Rights that emphasizes 5 principles to protect the public from the harmful effects of AI models, including safe and effective systems; algorithmic discrimination protection; data privacy; notice and explanation; and human alternatives, considerations, and fallback (Figure 3).17
One of the biggest challenges with LLMs like ChatGPT is the prevalence of inaccurate information or so-called hallucinations.16 These inaccuracies stem from the inability of LLMs to distinguish between real and fake information. To prevent hallucinations, researchers have proposed several methods, including training models on more diverse data, using adversarial training methods, and human-in-the-loop approaches.21 In addition, medicine-specific models like GatorTron, medPaLM, and Almanac were developed, increasing the accuracy of factual results.22-24 Unfortunately, only the GatorTron model is available to the public through the NVIDIA developers’ program.25
Despite these shortcomings, the future of LLMs in health care is promising. Although these models will not replace HCPs, they can help reduce the unnecessary burden on them, prevent burnout, and enable HCPs and patients spend more time together. Establishing an official hospital AI oversight governing body that would promote best practices could ensure the trustworthy implementation of these new technologies.26
Conclusions
The use of ChatGPT and other LLMs in health care has the potential to revolutionize the industry. By assisting HCPs with administrative tasks, improving the accuracy and reliability of diagnoses, and engaging patients, ChatGPT can help health care organizations provide better care to their patients. While LLMs are not a substitute for human interaction and personalized care, they can augment the work of HCPs, making health care more accessible and efficient. As the health care industry continues to evolve, it will be exciting to see how ChatGPT and other LLMs are used to improve patient outcomes and quality of care. In addition, AI technologies like ChatGPT offer enormous potential in medical education and research. To ensure that the benefits outweigh the risks, developing trustworthy AI health care products and establishing oversight governing bodies to ensure their implementation is essential. By doing so, we can help HCPs focus on what matters most, providing high-quality care to patients.
Acknowledgments
This material is the result of work supported by resources and the use of facilities at the James A. Haley Veterans’ Hospital.
1. Bill Gates. The age of AI has begun. March 21, 2023. Accessed May 10, 2023. https://www.gatesnotes.com/the-age-of-ai-has-begun
2. Kung TH, Cheatham M, Medenilla A, et al. Performance of ChatGPT on USMLE: Potential for AI-assisted medical education using large language models. PLOS Digit Health. 2023;2(2):e0000198. Published 2023 Feb 9. doi:10.1371/journal.pdig.0000198
3. Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2020. Mayo Clin Proc. 2022;97(3):491-506. doi:10.1016/j.mayocp.2021.11.021
4. Goodman RS, Patrinely JR Jr, Osterman T, Wheless L, Johnson DB. On the cusp: considering the impact of artificial intelligence language models in healthcare. Med. 2023;4(3):139-140. doi:10.1016/j.medj.2023.02.008
5. Will ChatGPT transform healthcare? Nat Med. 2023;29(3):505-506. doi:10.1038/s41591-023-02289-5
6. Hopkins AM, Logan JM, Kichenadasse G, Sorich MJ. Artificial intelligence chatbots will revolutionize how cancer patients access information: ChatGPT represents a paradigm-shift. JNCI Cancer Spectr. 2023;7(2):pkad010. doi:10.1093/jncics/pkad010
7. Babar Z, van Laarhoven T, Zanzotto FM, Marchiori E. Evaluating diagnostic content of AI-generated radiology reports of chest X-rays. Artif Intell Med. 2021;116:102075. doi:10.1016/j.artmed.2021.102075
8. Lecler A, Duron L, Soyer P. Revolutionizing radiology with GPT-based models: current applications, future possibilities and limitations of ChatGPT. Diagn Interv Imaging. 2023;S2211-5684(23)00027-X. doi:10.1016/j.diii.2023.02.003
9. Germain JM. Is ChatGPT smart enough to practice mental health therapy? March 23, 2023. Accessed May 11, 2023. https://www.technewsworld.com/story/is-chatgpt-smart-enough-to-practice-mental-health-therapy-178064.html
10. Cascella M, Montomoli J, Bellini V, Bignami E. Evaluating the feasibility of ChatGPT in healthcare: an analysis of multiple clinical and research scenarios. J Med Syst. 2023;47(1):33. Published 2023 Mar 4. doi:10.1007/s10916-023-01925-4
11. Jungwirth D, Haluza D. Artificial intelligence and public health: an exploratory study. Int J Environ Res Public Health. 2023;20(5):4541. Published 2023 Mar 3. doi:10.3390/ijerph20054541
12. Gilson A, Safranek CW, Huang T, et al. How does ChatGPT perform on the United States Medical Licensing Examination? The implications of large language models for medical education and knowledge assessment. JMIR Med Educ. 2023;9:e45312. Published 2023 Feb 8. doi:10.2196/45312
13. Eysenbach G. The role of ChatGPT, generative language models, and artificial intelligence in medical education: a conversation with ChatGPT and a call for papers. JMIR Med Educ. 2023;9:e46885. Published 2023 Mar 6. doi:10.2196/46885
14. Macdonald C, Adeloye D, Sheikh A, Rudan I. Can ChatGPT draft a research article? An example of population-level vaccine effectiveness analysis. J Glob Health. 2023;13:01003. Published 2023 Feb 17. doi:10.7189/jogh.13.01003
15. Masters K. Ethical use of artificial intelligence in health professions education: AMEE Guide No.158. Med Teach. 2023;1-11. doi:10.1080/0142159X.2023.2186203
16. Smith CS. Hallucinations could blunt ChatGPT’s success. IEEE Spectrum. March 13, 2023. Accessed May 11, 2023. https://spectrum.ieee.org/ai-hallucination
17. Executive Office of the President, Office of Science and Technology Policy. Blueprint for an AI Bill of Rights. Accessed May 11, 2023. https://www.whitehouse.gov/ostp/ai-bill-of-rights
18. Executive office of the President. Executive Order 13960: promoting the use of trustworthy artificial intelligence in the federal government. Fed Regist. 2020;89(236):78939-78943.
19. US Department of Commerce, National institute of Standards and Technology. Artificial Intelligence Risk Management Framework (AI RMF 1.0). Published January 2023. doi:10.6028/NIST.AI.100-1
20. Microsoft. Azure Cognitive Search—Cloud Search Service. Accessed May 11, 2023. https://azure.microsoft.com/en-us/products/search
21. Aiyappa R, An J, Kwak H, Ahn YY. Can we trust the evaluation on ChatGPT? March 22, 2023. Accessed May 11, 2023. https://arxiv.org/abs/2303.12767v1
22. Yang X, Chen A, Pournejatian N, et al. GatorTron: a large clinical language model to unlock patient information from unstructured electronic health records. Updated December 16, 2022. Accessed May 11, 2023. https://arxiv.org/abs/2203.03540v3
23. Singhal K, Azizi S, Tu T, et al. Large language models encode clinical knowledge. December 26, 2022. Accessed May 11, 2023. https://arxiv.org/abs/2212.13138v1
24. Zakka C, Chaurasia A, Shad R, Hiesinger W. Almanac: knowledge-grounded language models for clinical medicine. March 1, 2023. Accessed May 11, 2023. https://arxiv.org/abs/2303.01229v1
25. NVIDIA. GatorTron-OG. Accessed May 11, 2023. https://catalog.ngc.nvidia.com/orgs/nvidia/teams/clara/models/gatortron_og
26. Borkowski AA, Jakey CE, Thomas LB, Viswanadhan N, Mastorides SM. Establishing a hospital artificial intelligence committee to improve patient care. Fed Pract. 2022;39(8):334-336. doi:10.12788/fp.0299
1. Bill Gates. The age of AI has begun. March 21, 2023. Accessed May 10, 2023. https://www.gatesnotes.com/the-age-of-ai-has-begun
2. Kung TH, Cheatham M, Medenilla A, et al. Performance of ChatGPT on USMLE: Potential for AI-assisted medical education using large language models. PLOS Digit Health. 2023;2(2):e0000198. Published 2023 Feb 9. doi:10.1371/journal.pdig.0000198
3. Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2020. Mayo Clin Proc. 2022;97(3):491-506. doi:10.1016/j.mayocp.2021.11.021
4. Goodman RS, Patrinely JR Jr, Osterman T, Wheless L, Johnson DB. On the cusp: considering the impact of artificial intelligence language models in healthcare. Med. 2023;4(3):139-140. doi:10.1016/j.medj.2023.02.008
5. Will ChatGPT transform healthcare? Nat Med. 2023;29(3):505-506. doi:10.1038/s41591-023-02289-5
6. Hopkins AM, Logan JM, Kichenadasse G, Sorich MJ. Artificial intelligence chatbots will revolutionize how cancer patients access information: ChatGPT represents a paradigm-shift. JNCI Cancer Spectr. 2023;7(2):pkad010. doi:10.1093/jncics/pkad010
7. Babar Z, van Laarhoven T, Zanzotto FM, Marchiori E. Evaluating diagnostic content of AI-generated radiology reports of chest X-rays. Artif Intell Med. 2021;116:102075. doi:10.1016/j.artmed.2021.102075
8. Lecler A, Duron L, Soyer P. Revolutionizing radiology with GPT-based models: current applications, future possibilities and limitations of ChatGPT. Diagn Interv Imaging. 2023;S2211-5684(23)00027-X. doi:10.1016/j.diii.2023.02.003
9. Germain JM. Is ChatGPT smart enough to practice mental health therapy? March 23, 2023. Accessed May 11, 2023. https://www.technewsworld.com/story/is-chatgpt-smart-enough-to-practice-mental-health-therapy-178064.html
10. Cascella M, Montomoli J, Bellini V, Bignami E. Evaluating the feasibility of ChatGPT in healthcare: an analysis of multiple clinical and research scenarios. J Med Syst. 2023;47(1):33. Published 2023 Mar 4. doi:10.1007/s10916-023-01925-4
11. Jungwirth D, Haluza D. Artificial intelligence and public health: an exploratory study. Int J Environ Res Public Health. 2023;20(5):4541. Published 2023 Mar 3. doi:10.3390/ijerph20054541
12. Gilson A, Safranek CW, Huang T, et al. How does ChatGPT perform on the United States Medical Licensing Examination? The implications of large language models for medical education and knowledge assessment. JMIR Med Educ. 2023;9:e45312. Published 2023 Feb 8. doi:10.2196/45312
13. Eysenbach G. The role of ChatGPT, generative language models, and artificial intelligence in medical education: a conversation with ChatGPT and a call for papers. JMIR Med Educ. 2023;9:e46885. Published 2023 Mar 6. doi:10.2196/46885
14. Macdonald C, Adeloye D, Sheikh A, Rudan I. Can ChatGPT draft a research article? An example of population-level vaccine effectiveness analysis. J Glob Health. 2023;13:01003. Published 2023 Feb 17. doi:10.7189/jogh.13.01003
15. Masters K. Ethical use of artificial intelligence in health professions education: AMEE Guide No.158. Med Teach. 2023;1-11. doi:10.1080/0142159X.2023.2186203
16. Smith CS. Hallucinations could blunt ChatGPT’s success. IEEE Spectrum. March 13, 2023. Accessed May 11, 2023. https://spectrum.ieee.org/ai-hallucination
17. Executive Office of the President, Office of Science and Technology Policy. Blueprint for an AI Bill of Rights. Accessed May 11, 2023. https://www.whitehouse.gov/ostp/ai-bill-of-rights
18. Executive office of the President. Executive Order 13960: promoting the use of trustworthy artificial intelligence in the federal government. Fed Regist. 2020;89(236):78939-78943.
19. US Department of Commerce, National institute of Standards and Technology. Artificial Intelligence Risk Management Framework (AI RMF 1.0). Published January 2023. doi:10.6028/NIST.AI.100-1
20. Microsoft. Azure Cognitive Search—Cloud Search Service. Accessed May 11, 2023. https://azure.microsoft.com/en-us/products/search
21. Aiyappa R, An J, Kwak H, Ahn YY. Can we trust the evaluation on ChatGPT? March 22, 2023. Accessed May 11, 2023. https://arxiv.org/abs/2303.12767v1
22. Yang X, Chen A, Pournejatian N, et al. GatorTron: a large clinical language model to unlock patient information from unstructured electronic health records. Updated December 16, 2022. Accessed May 11, 2023. https://arxiv.org/abs/2203.03540v3
23. Singhal K, Azizi S, Tu T, et al. Large language models encode clinical knowledge. December 26, 2022. Accessed May 11, 2023. https://arxiv.org/abs/2212.13138v1
24. Zakka C, Chaurasia A, Shad R, Hiesinger W. Almanac: knowledge-grounded language models for clinical medicine. March 1, 2023. Accessed May 11, 2023. https://arxiv.org/abs/2303.01229v1
25. NVIDIA. GatorTron-OG. Accessed May 11, 2023. https://catalog.ngc.nvidia.com/orgs/nvidia/teams/clara/models/gatortron_og
26. Borkowski AA, Jakey CE, Thomas LB, Viswanadhan N, Mastorides SM. Establishing a hospital artificial intelligence committee to improve patient care. Fed Pract. 2022;39(8):334-336. doi:10.12788/fp.0299
WOW! You spend that much time on the EHR?
Unlike many of you, maybe even most of you, I can recall when my office records were handwritten, some would say scribbled, on pieces of paper. They were decipherable by a select few. Some veteran assistants never mastered the skill. Pages were sometimes lavishly illustrated with drawings of body parts, often because I couldn’t remember or spell the correct anatomic term. When I needed to send a referring letter to another provider I typed it myself because dictating never quite suited my personality.
When I joined a small primary care group, the computer-savvy lead physician and a programmer developed our own homegrown EHR. It relied on scanning documents, as so many of us still generated handwritten notes. Even the most vociferous Luddites among us loved the system from day 2.
However, for a variety of reasons, some defensible some just plain bad, our beloved system needed to be replaced after 7 years. We then invested in an off-the-shelf EHR system that promised more capabilities. We were told there would be a learning curve but the plateau would come quickly and we would enjoy our new electronic assistant.
You’ve lived the rest of the story. The learning curve was steep and long and the plateau was a time gobbler. I was probably the most efficient provider in the group, and after 6 months I was leaving the office an hour later than I had been and was seeing the same number of patients. Most of my coworkers were staying and/or working on the computer at home for an extra 2 hours. This change could be easily documented by speaking with our spouses and children. I understand from my colleagues who have stayed in the business that over the ensuing decade and a half since my first experience with the EHR, its insatiable appetite for a clinician’s time has not abated.
The authors of a recent article in Annals of Family Medicine offer up some advice on how this tragic situation might be brought under control. First, the investigators point out that the phenomenon of after-hours EHR work, sometimes referred to as WOW (work outside of work), has not gone unnoticed by health system administrators and vendors who develop and sell the EHRs. However, analyzing the voluminous data necessary is not any easy task and for the most part has resulted in metrics that cannot be easily applied over a variety of practice scenarios. Many health care organizations, even large ones, have simply given up and rely on the WOW data and recommendations provided by the vendors, obviously lending the situation a faint odor of conflict of interest.
The bottom line is that . It would seem to me just asking the spouses and significant others of the clinicians would be sufficient. But, authors of the paper have more specific recommendations. First, they suggest that time working on the computer outside of scheduled time with patients should be separated from any other calculation of EHR usage. They encourage vendors and time-management researchers to develop standardized and validated methods for measuring active EHR use. And, finally they recommend that all EHR work done outside of time scheduled with patients be attributed to WOW. They feel that clearly labeling it work outside of work offers health care organizations a better chance of developing policies that will address the scourge of burnout.
This, unfortunately, is another tragic example of how clinicians have lost control of our work environments. The fact that 20 years have passed and there is still no standardized method for determining how much time we spend on the computer is more evidence we need to raise our voices.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Unlike many of you, maybe even most of you, I can recall when my office records were handwritten, some would say scribbled, on pieces of paper. They were decipherable by a select few. Some veteran assistants never mastered the skill. Pages were sometimes lavishly illustrated with drawings of body parts, often because I couldn’t remember or spell the correct anatomic term. When I needed to send a referring letter to another provider I typed it myself because dictating never quite suited my personality.
When I joined a small primary care group, the computer-savvy lead physician and a programmer developed our own homegrown EHR. It relied on scanning documents, as so many of us still generated handwritten notes. Even the most vociferous Luddites among us loved the system from day 2.
However, for a variety of reasons, some defensible some just plain bad, our beloved system needed to be replaced after 7 years. We then invested in an off-the-shelf EHR system that promised more capabilities. We were told there would be a learning curve but the plateau would come quickly and we would enjoy our new electronic assistant.
You’ve lived the rest of the story. The learning curve was steep and long and the plateau was a time gobbler. I was probably the most efficient provider in the group, and after 6 months I was leaving the office an hour later than I had been and was seeing the same number of patients. Most of my coworkers were staying and/or working on the computer at home for an extra 2 hours. This change could be easily documented by speaking with our spouses and children. I understand from my colleagues who have stayed in the business that over the ensuing decade and a half since my first experience with the EHR, its insatiable appetite for a clinician’s time has not abated.
The authors of a recent article in Annals of Family Medicine offer up some advice on how this tragic situation might be brought under control. First, the investigators point out that the phenomenon of after-hours EHR work, sometimes referred to as WOW (work outside of work), has not gone unnoticed by health system administrators and vendors who develop and sell the EHRs. However, analyzing the voluminous data necessary is not any easy task and for the most part has resulted in metrics that cannot be easily applied over a variety of practice scenarios. Many health care organizations, even large ones, have simply given up and rely on the WOW data and recommendations provided by the vendors, obviously lending the situation a faint odor of conflict of interest.
The bottom line is that . It would seem to me just asking the spouses and significant others of the clinicians would be sufficient. But, authors of the paper have more specific recommendations. First, they suggest that time working on the computer outside of scheduled time with patients should be separated from any other calculation of EHR usage. They encourage vendors and time-management researchers to develop standardized and validated methods for measuring active EHR use. And, finally they recommend that all EHR work done outside of time scheduled with patients be attributed to WOW. They feel that clearly labeling it work outside of work offers health care organizations a better chance of developing policies that will address the scourge of burnout.
This, unfortunately, is another tragic example of how clinicians have lost control of our work environments. The fact that 20 years have passed and there is still no standardized method for determining how much time we spend on the computer is more evidence we need to raise our voices.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Unlike many of you, maybe even most of you, I can recall when my office records were handwritten, some would say scribbled, on pieces of paper. They were decipherable by a select few. Some veteran assistants never mastered the skill. Pages were sometimes lavishly illustrated with drawings of body parts, often because I couldn’t remember or spell the correct anatomic term. When I needed to send a referring letter to another provider I typed it myself because dictating never quite suited my personality.
When I joined a small primary care group, the computer-savvy lead physician and a programmer developed our own homegrown EHR. It relied on scanning documents, as so many of us still generated handwritten notes. Even the most vociferous Luddites among us loved the system from day 2.
However, for a variety of reasons, some defensible some just plain bad, our beloved system needed to be replaced after 7 years. We then invested in an off-the-shelf EHR system that promised more capabilities. We were told there would be a learning curve but the plateau would come quickly and we would enjoy our new electronic assistant.
You’ve lived the rest of the story. The learning curve was steep and long and the plateau was a time gobbler. I was probably the most efficient provider in the group, and after 6 months I was leaving the office an hour later than I had been and was seeing the same number of patients. Most of my coworkers were staying and/or working on the computer at home for an extra 2 hours. This change could be easily documented by speaking with our spouses and children. I understand from my colleagues who have stayed in the business that over the ensuing decade and a half since my first experience with the EHR, its insatiable appetite for a clinician’s time has not abated.
The authors of a recent article in Annals of Family Medicine offer up some advice on how this tragic situation might be brought under control. First, the investigators point out that the phenomenon of after-hours EHR work, sometimes referred to as WOW (work outside of work), has not gone unnoticed by health system administrators and vendors who develop and sell the EHRs. However, analyzing the voluminous data necessary is not any easy task and for the most part has resulted in metrics that cannot be easily applied over a variety of practice scenarios. Many health care organizations, even large ones, have simply given up and rely on the WOW data and recommendations provided by the vendors, obviously lending the situation a faint odor of conflict of interest.
The bottom line is that . It would seem to me just asking the spouses and significant others of the clinicians would be sufficient. But, authors of the paper have more specific recommendations. First, they suggest that time working on the computer outside of scheduled time with patients should be separated from any other calculation of EHR usage. They encourage vendors and time-management researchers to develop standardized and validated methods for measuring active EHR use. And, finally they recommend that all EHR work done outside of time scheduled with patients be attributed to WOW. They feel that clearly labeling it work outside of work offers health care organizations a better chance of developing policies that will address the scourge of burnout.
This, unfortunately, is another tragic example of how clinicians have lost control of our work environments. The fact that 20 years have passed and there is still no standardized method for determining how much time we spend on the computer is more evidence we need to raise our voices.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Daily multivitamins boost memory in older adults: A randomized trial
This transcript has been edited for clarity.
This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital. , known as COSMOS (Cocoa Supplement and Multivitamins Outcome Study). This is the second COSMOS trial to show a benefit of multivitamins on memory and cognition. This trial involved a collaboration between Brigham and Columbia University and was published in the American Journal of Clinical Nutrition. I’d like to acknowledge that I am a coauthor of this study, together with Dr. Howard Sesso, who co-leads the main COSMOS trial with me.
Preserving memory and cognitive function is of critical importance to older adults. Nutritional interventions play an important role because we know the brain requires several nutrients for optimal health, and deficiencies in one or more of these nutrients may accelerate cognitive decline. Some of the micronutrients that are known to be important for brain health include vitamin B12, thiamin, other B vitamins, lutein, magnesium, and zinc, among others.
The current trial included 3,500 participants aged 60 or older, looking at performance on a web-based memory test. The multivitamin group did significantly better than the placebo group on memory tests and word recall, a finding that was estimated as the equivalent of slowing age-related memory loss by about 3 years. The benefit was first seen at 1 year and was sustained across the 3 years of the trial.
Intriguingly, in both COSMOS and COSMOS-Web, and the earlier COSMOS-Mind study, which was done in collaboration with Wake Forest, the participants with a history of cardiovascular disease showed the greatest benefits from multivitamins, perhaps due to lower nutrient status. But the basis for this finding needs to be explored further.
A few important caveats need to be emphasized. First, multivitamins and other dietary supplements will never be a substitute for a healthy diet and healthy lifestyle and should not distract from those goals. But multivitamins may have a role as a complementary strategy. Another caveat is that the randomized trials tested recommended dietary allowances and not megadoses of these micronutrients. In fact, randomized trials of high doses of isolated micronutrients have not clearly shown cognitive benefits, and this suggests that more is not necessarily better and may be worse. High doses also may be associated with toxicity, or they may interfere with absorption or bioavailability of other nutrients.
In COSMOS, over the average 3.6 years of follow-up and in the earlier Physicians’ Health Study II, over 1 year of supplementation, multivitamins were found to be safe without any clear risks or safety concerns. A further caveat is that although Centrum Silver was tested in this trial, we would not expect that this is a brand-specific benefit, and other high-quality multivitamin brands would be expected to confer similar benefits. Of course, it’s important to check bottles for quality-control documentation such as the seals of the U.S. Pharmacopeia, National Science Foundation, ConsumerLab.com, and other auditors.
Overall, the finding that a daily multivitamin improved memory and slowed cognitive decline in two separate COSMOS randomized trials is exciting, suggesting that multivitamin supplementation holds promise as a safe, accessible, and affordable approach to protecting cognitive health in older adults. Further research will be needed to understand who is most likely to benefit and the biological mechanisms involved. Expert committees will have to look at the research and decide whether any changes in guidelines are indicated in the future.
Dr. Manson is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School and director of the Division of Preventive Medicine, Brigham and Women’s Hospital, both in Boston. She reported receiving funding/donations from Mars Symbioscience.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital. , known as COSMOS (Cocoa Supplement and Multivitamins Outcome Study). This is the second COSMOS trial to show a benefit of multivitamins on memory and cognition. This trial involved a collaboration between Brigham and Columbia University and was published in the American Journal of Clinical Nutrition. I’d like to acknowledge that I am a coauthor of this study, together with Dr. Howard Sesso, who co-leads the main COSMOS trial with me.
Preserving memory and cognitive function is of critical importance to older adults. Nutritional interventions play an important role because we know the brain requires several nutrients for optimal health, and deficiencies in one or more of these nutrients may accelerate cognitive decline. Some of the micronutrients that are known to be important for brain health include vitamin B12, thiamin, other B vitamins, lutein, magnesium, and zinc, among others.
The current trial included 3,500 participants aged 60 or older, looking at performance on a web-based memory test. The multivitamin group did significantly better than the placebo group on memory tests and word recall, a finding that was estimated as the equivalent of slowing age-related memory loss by about 3 years. The benefit was first seen at 1 year and was sustained across the 3 years of the trial.
Intriguingly, in both COSMOS and COSMOS-Web, and the earlier COSMOS-Mind study, which was done in collaboration with Wake Forest, the participants with a history of cardiovascular disease showed the greatest benefits from multivitamins, perhaps due to lower nutrient status. But the basis for this finding needs to be explored further.
A few important caveats need to be emphasized. First, multivitamins and other dietary supplements will never be a substitute for a healthy diet and healthy lifestyle and should not distract from those goals. But multivitamins may have a role as a complementary strategy. Another caveat is that the randomized trials tested recommended dietary allowances and not megadoses of these micronutrients. In fact, randomized trials of high doses of isolated micronutrients have not clearly shown cognitive benefits, and this suggests that more is not necessarily better and may be worse. High doses also may be associated with toxicity, or they may interfere with absorption or bioavailability of other nutrients.
In COSMOS, over the average 3.6 years of follow-up and in the earlier Physicians’ Health Study II, over 1 year of supplementation, multivitamins were found to be safe without any clear risks or safety concerns. A further caveat is that although Centrum Silver was tested in this trial, we would not expect that this is a brand-specific benefit, and other high-quality multivitamin brands would be expected to confer similar benefits. Of course, it’s important to check bottles for quality-control documentation such as the seals of the U.S. Pharmacopeia, National Science Foundation, ConsumerLab.com, and other auditors.
Overall, the finding that a daily multivitamin improved memory and slowed cognitive decline in two separate COSMOS randomized trials is exciting, suggesting that multivitamin supplementation holds promise as a safe, accessible, and affordable approach to protecting cognitive health in older adults. Further research will be needed to understand who is most likely to benefit and the biological mechanisms involved. Expert committees will have to look at the research and decide whether any changes in guidelines are indicated in the future.
Dr. Manson is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School and director of the Division of Preventive Medicine, Brigham and Women’s Hospital, both in Boston. She reported receiving funding/donations from Mars Symbioscience.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital. , known as COSMOS (Cocoa Supplement and Multivitamins Outcome Study). This is the second COSMOS trial to show a benefit of multivitamins on memory and cognition. This trial involved a collaboration between Brigham and Columbia University and was published in the American Journal of Clinical Nutrition. I’d like to acknowledge that I am a coauthor of this study, together with Dr. Howard Sesso, who co-leads the main COSMOS trial with me.
Preserving memory and cognitive function is of critical importance to older adults. Nutritional interventions play an important role because we know the brain requires several nutrients for optimal health, and deficiencies in one or more of these nutrients may accelerate cognitive decline. Some of the micronutrients that are known to be important for brain health include vitamin B12, thiamin, other B vitamins, lutein, magnesium, and zinc, among others.
The current trial included 3,500 participants aged 60 or older, looking at performance on a web-based memory test. The multivitamin group did significantly better than the placebo group on memory tests and word recall, a finding that was estimated as the equivalent of slowing age-related memory loss by about 3 years. The benefit was first seen at 1 year and was sustained across the 3 years of the trial.
Intriguingly, in both COSMOS and COSMOS-Web, and the earlier COSMOS-Mind study, which was done in collaboration with Wake Forest, the participants with a history of cardiovascular disease showed the greatest benefits from multivitamins, perhaps due to lower nutrient status. But the basis for this finding needs to be explored further.
A few important caveats need to be emphasized. First, multivitamins and other dietary supplements will never be a substitute for a healthy diet and healthy lifestyle and should not distract from those goals. But multivitamins may have a role as a complementary strategy. Another caveat is that the randomized trials tested recommended dietary allowances and not megadoses of these micronutrients. In fact, randomized trials of high doses of isolated micronutrients have not clearly shown cognitive benefits, and this suggests that more is not necessarily better and may be worse. High doses also may be associated with toxicity, or they may interfere with absorption or bioavailability of other nutrients.
In COSMOS, over the average 3.6 years of follow-up and in the earlier Physicians’ Health Study II, over 1 year of supplementation, multivitamins were found to be safe without any clear risks or safety concerns. A further caveat is that although Centrum Silver was tested in this trial, we would not expect that this is a brand-specific benefit, and other high-quality multivitamin brands would be expected to confer similar benefits. Of course, it’s important to check bottles for quality-control documentation such as the seals of the U.S. Pharmacopeia, National Science Foundation, ConsumerLab.com, and other auditors.
Overall, the finding that a daily multivitamin improved memory and slowed cognitive decline in two separate COSMOS randomized trials is exciting, suggesting that multivitamin supplementation holds promise as a safe, accessible, and affordable approach to protecting cognitive health in older adults. Further research will be needed to understand who is most likely to benefit and the biological mechanisms involved. Expert committees will have to look at the research and decide whether any changes in guidelines are indicated in the future.
Dr. Manson is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School and director of the Division of Preventive Medicine, Brigham and Women’s Hospital, both in Boston. She reported receiving funding/donations from Mars Symbioscience.
A version of this article first appeared on Medscape.com.
Feeling disconnected? Focus on what you can do
This is the exciting time of year when we graduate new classes of medical students and residents. Med school graduation brings mixed emotions; the new doctors and I both know residency will bring growth and challenges. Residency graduation is a wistful passage as well. It is so rewarding to welcome the newly board-certified family physicians to family medicine, but we miss them even as we orient a new class.
Every year, a few months (or even a few years) after graduation, I hear from a former resident, sometimes several. They ask to talk and, although it can be hard for them to explain exactly the ennui and disillusionment they’re feeling, their concerns boil down to: Is this all there is?
They are not burnt out, exactly, but they were hoping for more from their careers in family medicine.1 They find their hopes and expectations are not fulfilled by seeing patients in the office 8 hours per day, 4.5 days per week. Even those who report rewarding relationships with patients express less overall enthusiasm for jobs they were excited to start just months or years earlier.
Some of the difficulties I hear the graduates report are expected growing pains. It is a transition to go from supervised practice with attending backup to a setting where you are on your own, typically with a 4-fold increase in volume compared with residency. But the monotony is real for family physicians in full-time outpatient practice.
Research suggests an expanded scope of practice—including hospital medicine, obstetrics, and procedures—is associated with physician well-being.2,3 A broad scope of practice can bring stress, but it also brings meaning, and that meaning is protective to our well-being. However, a robust scope of practice is not always supported by medical groups or hospital systems, who prefer a more compartmentalized, widgetized physician.4 It would be easier for their algorithms if family physicians picked a lane and stayed in it. Alas, the broader our scope of practice, the healthier our population, the more equitable our care,5,6 and the happier our physicians.
The disconnect and hopelessness experienced by family physicians is more concerning. Many of my graduates report feeling disconnected from their patients, because they begin to feel disillusioned by the demands and requests that practice and patients place on them. The paperwork, “permission slips,” and requests for tests and studies not only feel overwhelming and exhausting but also create distance between physicians and patients.7 We want to help our patients, so we do the forms and order the tests. As the quantity of forms, slips, and requests adds up, we begin to feel resentful at what the forms take away: time with our patients, perhaps, or time with our families. We get angry at the forms and the “asks,” and then begin to get angry at the patients simply for having needs. Administrative burden is a hassle, but it is also insidiously destructive.8
Family physicians confront hopelessness when, day after day, we diagnose problems that no physician is likely to fix in a single office visit: chronic stress, family dysfunction, violence, unemployment, poverty, racism, loneliness, and the hopelessness of the patients themselves. This is not to say that we ignore these concerns or their impact on health. It is because we see and feel them, and deeply understand their consequences for our patients, that we grow frustrated with the lack of solutions.9,10
Thankfully, we have strong teams working at the policy level to improve the primary care and public health infrastructure so that we can maintain some hope that it will be better in the future. Sometimes when I counsel a former resident, they decide to join those teams so that they can work on the solutions. Others decide to expand their scope of practice. Others seek out virtual scribes to streamline charting and regain time. Some build better boundaries with their EHR inboxes.
The key is figuring out what we can do and making peace with our limits. When disillusionment hits, what we can do includes seeking connection and social contact and remembering that we are not trapped in our situation, even if we are practicing in a less-than-functional health care system. There are many ways to “be” a family physician—if what you’re doing isn’t working for you, look for opportunities (big or small) that make it better. We can all reach out to coaches, therapists, colleagues, and friends for support to remain steadfast in our purpose as family physicians. This support and the power of change means that from residency to the latter parts of our careers, we will continue to bring the tremendous good of family medicine to the communities we serve.
1. Coutinho AJ, Cochrane A, Stelter K, et al. Comparison of intended scope of practice for family medicine residents with reported scope of practice among practicing family physicians. JAMA. 2015;314:2364-2372. doi: 10.1001/jama.2015.13734
2. Weidner AKH, Phillips RL, Fang B, et al. Burnout and scope of practice in new family physicians. Ann Fam Med. 2018;16:200-205. doi: 10.1370/afm.2221
3. Zomahoun HT, Samson I, Sawadogo J, et al. Effects of the scope of practice on family physicians: a systematic review. BMC Family Practice. 2021;22. doi: 10.1186/s12875-020-01328-1
4. Killeen D, Jetty A, Peterson LE, et al. The association of practice type and the scope of care of family physicians. J Am Board Fam Med. 2023;36:79-87. doi: 10.3122/jabfm.2022.220172R1
5. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457-502. doi: 10.1111/j.1468-0009.2005.00409.x
6. Ferrer RL. Pursuing equity: contact with primary care and specialist clinicians by demographics, insurance, and health status. Ann Fam Med. 2007;5:492-502. doi: 10.1370/afm.746
7. Rao SK, Kimball AB, Lehrhoff SR, et al. The impact of administrative burden on academic physicians: results of a hospital-wide physician survey. Acad Med. 2017;92:237-243. doi: 10.1097/ACM.0000000000001461
8. McMahon LF, Rize K, Irby-Johnson N, et al. Designed to fail? The future of primary care. J Gen Intern Med. 2021;36:515-517. doi: 10.1007/s11606-020-06077-6
9. Welles CC, Tong A, Brereton E, et al. Sources of clinician burnout in providing care for underserved patients in a safety-net healthcare system. J Gen Intern Med. 2023;38:1468-1475. doi: 10.1007/s11606-022-07896-5
10. Kung A, Cheung T, Knox M, et al. Capacity to address social needs affects primary care clinician burnout. Ann Fam Med. 2019;17:487-494. doi: 10.1370/afm.2470
This is the exciting time of year when we graduate new classes of medical students and residents. Med school graduation brings mixed emotions; the new doctors and I both know residency will bring growth and challenges. Residency graduation is a wistful passage as well. It is so rewarding to welcome the newly board-certified family physicians to family medicine, but we miss them even as we orient a new class.
Every year, a few months (or even a few years) after graduation, I hear from a former resident, sometimes several. They ask to talk and, although it can be hard for them to explain exactly the ennui and disillusionment they’re feeling, their concerns boil down to: Is this all there is?
They are not burnt out, exactly, but they were hoping for more from their careers in family medicine.1 They find their hopes and expectations are not fulfilled by seeing patients in the office 8 hours per day, 4.5 days per week. Even those who report rewarding relationships with patients express less overall enthusiasm for jobs they were excited to start just months or years earlier.
Some of the difficulties I hear the graduates report are expected growing pains. It is a transition to go from supervised practice with attending backup to a setting where you are on your own, typically with a 4-fold increase in volume compared with residency. But the monotony is real for family physicians in full-time outpatient practice.
Research suggests an expanded scope of practice—including hospital medicine, obstetrics, and procedures—is associated with physician well-being.2,3 A broad scope of practice can bring stress, but it also brings meaning, and that meaning is protective to our well-being. However, a robust scope of practice is not always supported by medical groups or hospital systems, who prefer a more compartmentalized, widgetized physician.4 It would be easier for their algorithms if family physicians picked a lane and stayed in it. Alas, the broader our scope of practice, the healthier our population, the more equitable our care,5,6 and the happier our physicians.
The disconnect and hopelessness experienced by family physicians is more concerning. Many of my graduates report feeling disconnected from their patients, because they begin to feel disillusioned by the demands and requests that practice and patients place on them. The paperwork, “permission slips,” and requests for tests and studies not only feel overwhelming and exhausting but also create distance between physicians and patients.7 We want to help our patients, so we do the forms and order the tests. As the quantity of forms, slips, and requests adds up, we begin to feel resentful at what the forms take away: time with our patients, perhaps, or time with our families. We get angry at the forms and the “asks,” and then begin to get angry at the patients simply for having needs. Administrative burden is a hassle, but it is also insidiously destructive.8
Family physicians confront hopelessness when, day after day, we diagnose problems that no physician is likely to fix in a single office visit: chronic stress, family dysfunction, violence, unemployment, poverty, racism, loneliness, and the hopelessness of the patients themselves. This is not to say that we ignore these concerns or their impact on health. It is because we see and feel them, and deeply understand their consequences for our patients, that we grow frustrated with the lack of solutions.9,10
Thankfully, we have strong teams working at the policy level to improve the primary care and public health infrastructure so that we can maintain some hope that it will be better in the future. Sometimes when I counsel a former resident, they decide to join those teams so that they can work on the solutions. Others decide to expand their scope of practice. Others seek out virtual scribes to streamline charting and regain time. Some build better boundaries with their EHR inboxes.
The key is figuring out what we can do and making peace with our limits. When disillusionment hits, what we can do includes seeking connection and social contact and remembering that we are not trapped in our situation, even if we are practicing in a less-than-functional health care system. There are many ways to “be” a family physician—if what you’re doing isn’t working for you, look for opportunities (big or small) that make it better. We can all reach out to coaches, therapists, colleagues, and friends for support to remain steadfast in our purpose as family physicians. This support and the power of change means that from residency to the latter parts of our careers, we will continue to bring the tremendous good of family medicine to the communities we serve.
This is the exciting time of year when we graduate new classes of medical students and residents. Med school graduation brings mixed emotions; the new doctors and I both know residency will bring growth and challenges. Residency graduation is a wistful passage as well. It is so rewarding to welcome the newly board-certified family physicians to family medicine, but we miss them even as we orient a new class.
Every year, a few months (or even a few years) after graduation, I hear from a former resident, sometimes several. They ask to talk and, although it can be hard for them to explain exactly the ennui and disillusionment they’re feeling, their concerns boil down to: Is this all there is?
They are not burnt out, exactly, but they were hoping for more from their careers in family medicine.1 They find their hopes and expectations are not fulfilled by seeing patients in the office 8 hours per day, 4.5 days per week. Even those who report rewarding relationships with patients express less overall enthusiasm for jobs they were excited to start just months or years earlier.
Some of the difficulties I hear the graduates report are expected growing pains. It is a transition to go from supervised practice with attending backup to a setting where you are on your own, typically with a 4-fold increase in volume compared with residency. But the monotony is real for family physicians in full-time outpatient practice.
Research suggests an expanded scope of practice—including hospital medicine, obstetrics, and procedures—is associated with physician well-being.2,3 A broad scope of practice can bring stress, but it also brings meaning, and that meaning is protective to our well-being. However, a robust scope of practice is not always supported by medical groups or hospital systems, who prefer a more compartmentalized, widgetized physician.4 It would be easier for their algorithms if family physicians picked a lane and stayed in it. Alas, the broader our scope of practice, the healthier our population, the more equitable our care,5,6 and the happier our physicians.
The disconnect and hopelessness experienced by family physicians is more concerning. Many of my graduates report feeling disconnected from their patients, because they begin to feel disillusioned by the demands and requests that practice and patients place on them. The paperwork, “permission slips,” and requests for tests and studies not only feel overwhelming and exhausting but also create distance between physicians and patients.7 We want to help our patients, so we do the forms and order the tests. As the quantity of forms, slips, and requests adds up, we begin to feel resentful at what the forms take away: time with our patients, perhaps, or time with our families. We get angry at the forms and the “asks,” and then begin to get angry at the patients simply for having needs. Administrative burden is a hassle, but it is also insidiously destructive.8
Family physicians confront hopelessness when, day after day, we diagnose problems that no physician is likely to fix in a single office visit: chronic stress, family dysfunction, violence, unemployment, poverty, racism, loneliness, and the hopelessness of the patients themselves. This is not to say that we ignore these concerns or their impact on health. It is because we see and feel them, and deeply understand their consequences for our patients, that we grow frustrated with the lack of solutions.9,10
Thankfully, we have strong teams working at the policy level to improve the primary care and public health infrastructure so that we can maintain some hope that it will be better in the future. Sometimes when I counsel a former resident, they decide to join those teams so that they can work on the solutions. Others decide to expand their scope of practice. Others seek out virtual scribes to streamline charting and regain time. Some build better boundaries with their EHR inboxes.
The key is figuring out what we can do and making peace with our limits. When disillusionment hits, what we can do includes seeking connection and social contact and remembering that we are not trapped in our situation, even if we are practicing in a less-than-functional health care system. There are many ways to “be” a family physician—if what you’re doing isn’t working for you, look for opportunities (big or small) that make it better. We can all reach out to coaches, therapists, colleagues, and friends for support to remain steadfast in our purpose as family physicians. This support and the power of change means that from residency to the latter parts of our careers, we will continue to bring the tremendous good of family medicine to the communities we serve.
1. Coutinho AJ, Cochrane A, Stelter K, et al. Comparison of intended scope of practice for family medicine residents with reported scope of practice among practicing family physicians. JAMA. 2015;314:2364-2372. doi: 10.1001/jama.2015.13734
2. Weidner AKH, Phillips RL, Fang B, et al. Burnout and scope of practice in new family physicians. Ann Fam Med. 2018;16:200-205. doi: 10.1370/afm.2221
3. Zomahoun HT, Samson I, Sawadogo J, et al. Effects of the scope of practice on family physicians: a systematic review. BMC Family Practice. 2021;22. doi: 10.1186/s12875-020-01328-1
4. Killeen D, Jetty A, Peterson LE, et al. The association of practice type and the scope of care of family physicians. J Am Board Fam Med. 2023;36:79-87. doi: 10.3122/jabfm.2022.220172R1
5. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457-502. doi: 10.1111/j.1468-0009.2005.00409.x
6. Ferrer RL. Pursuing equity: contact with primary care and specialist clinicians by demographics, insurance, and health status. Ann Fam Med. 2007;5:492-502. doi: 10.1370/afm.746
7. Rao SK, Kimball AB, Lehrhoff SR, et al. The impact of administrative burden on academic physicians: results of a hospital-wide physician survey. Acad Med. 2017;92:237-243. doi: 10.1097/ACM.0000000000001461
8. McMahon LF, Rize K, Irby-Johnson N, et al. Designed to fail? The future of primary care. J Gen Intern Med. 2021;36:515-517. doi: 10.1007/s11606-020-06077-6
9. Welles CC, Tong A, Brereton E, et al. Sources of clinician burnout in providing care for underserved patients in a safety-net healthcare system. J Gen Intern Med. 2023;38:1468-1475. doi: 10.1007/s11606-022-07896-5
10. Kung A, Cheung T, Knox M, et al. Capacity to address social needs affects primary care clinician burnout. Ann Fam Med. 2019;17:487-494. doi: 10.1370/afm.2470
1. Coutinho AJ, Cochrane A, Stelter K, et al. Comparison of intended scope of practice for family medicine residents with reported scope of practice among practicing family physicians. JAMA. 2015;314:2364-2372. doi: 10.1001/jama.2015.13734
2. Weidner AKH, Phillips RL, Fang B, et al. Burnout and scope of practice in new family physicians. Ann Fam Med. 2018;16:200-205. doi: 10.1370/afm.2221
3. Zomahoun HT, Samson I, Sawadogo J, et al. Effects of the scope of practice on family physicians: a systematic review. BMC Family Practice. 2021;22. doi: 10.1186/s12875-020-01328-1
4. Killeen D, Jetty A, Peterson LE, et al. The association of practice type and the scope of care of family physicians. J Am Board Fam Med. 2023;36:79-87. doi: 10.3122/jabfm.2022.220172R1
5. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457-502. doi: 10.1111/j.1468-0009.2005.00409.x
6. Ferrer RL. Pursuing equity: contact with primary care and specialist clinicians by demographics, insurance, and health status. Ann Fam Med. 2007;5:492-502. doi: 10.1370/afm.746
7. Rao SK, Kimball AB, Lehrhoff SR, et al. The impact of administrative burden on academic physicians: results of a hospital-wide physician survey. Acad Med. 2017;92:237-243. doi: 10.1097/ACM.0000000000001461
8. McMahon LF, Rize K, Irby-Johnson N, et al. Designed to fail? The future of primary care. J Gen Intern Med. 2021;36:515-517. doi: 10.1007/s11606-020-06077-6
9. Welles CC, Tong A, Brereton E, et al. Sources of clinician burnout in providing care for underserved patients in a safety-net healthcare system. J Gen Intern Med. 2023;38:1468-1475. doi: 10.1007/s11606-022-07896-5
10. Kung A, Cheung T, Knox M, et al. Capacity to address social needs affects primary care clinician burnout. Ann Fam Med. 2019;17:487-494. doi: 10.1370/afm.2470
Did an unfair system help ADAURA win on overall survival?
Barry Bonds and Roger Clemens are two world-class baseball players who played well enough to earn enduring respect and admiration. However, their reputations have been permanently tainted by their use of performance-enhancing drugs. Although they are both undeniably gifted, we’ll never know where their natural talent ended and their unfair advantage began.
The medical oncology version of this scenario played out in front of our eyes at the ASCO 2023 Plenary Session featuring the ADAURA trial. In this case, the unfair advantage was clear: Nearly two-thirds of patients in the control arm did not cross over to a standard-of-care treatment at relapse.
The ADAURA trial tested the value of the third-generation oral EGFR inhibitor osimertinib vs. placebo for up to 3 years in patients with a resected stage IB-IIIA non–small cell lung cancer (NSCLC) harboring an activating EGFR mutation. Initially presented in the ASCO 2020 Plenary Session, the preliminary analysis for ADAURA demonstrated a remarkably favorable improvement in disease-free survival (DFS) in the osimertinib arm, which led to its prompt Food and Drug Administration approval in this setting.
At the time, I was among the more vocal critics of the fanfare around this trial. The DFS improvement was impressive but, in this context, represented a low threshold for FDA approval. We already knew that prior trials of other, less effective adjuvant EGFR inhibitors routinely improved DFS but ultimately failed to improve overall survival.
Although in some cases, a DFS benefit can be sufficient to warrant changing practice, I would argue that overall survival is the most critical endpoint in a curative setting by a wide margin. I would also argue that cost should be a consideration for a drug priced at $440,000 over 3 years in the United States. At the very least, we – patients, oncologists, payers – should want to clarify what we get for $440,000 per patient, especially if that money could be better spent on other things.
Of note, we need to know whether the same overall survival may be achieved in this setting by treating only patients whose disease relapses, avoiding both the cost and toxicity of continuous treatment.
The relevance of this question became even more acute when an updated version of the ADAURA trial showed that the DFS benefit from osimertinib began to erode immediately after patients completed active treatment. Although the DFS benefit remained excellent,
The overall survival data – the critical test in my mind – were presented at the ASCO Plenary Session. The results were highly positive, with a hazard ratio for overall survival of 0.49 and a similar benefit observed across all eligible disease stages.
As with the presentation of the DFS data in 2020, these results were accompanied by adulation during the session and fawning in the media. However, a subset of people in the audience, and on Twitter, voiced a major concern: In the control arm, only 38.5% of the patients whose disease had relapsed (79 of 205) ever received osimertinib.
Post-protocol treatment included reassurances that patients in the control arm were offered crossover to osimertinib, but this only occurred starting in April 2020 and only when the treating investigator requested it.
The fact that only a minority of patients in the control arm ever received osimertinib means that ADAURA is not a trial that tests adjuvant osimertinib to osimertinib at relapse, the prevailing standard of care in the United States and the preferred treatment in this setting, based on NCCN guidelines for patients with relapsed/metastatic EGFR mutation–positive NSCLC since the FDA approval in April 2018.
The change in standard of care in the United States and some other countries did not lead to an amendment in the trial, based on the argument that the trial was designed with DFS as the primary endpoint and that patients in the control arm are effectively off trial at relapse. That means patients would receive their country’s standard of care, which may be below, or different from, the standard in the United States or other parts of the world.
While defensible, others considered the low rate of osimertinib delivery in the control arm a serious flaw in the trial design and arguably an ethical problem.
Given this trial design, it’s important to question whether the trial magnified the difference in overall survival between the two arms compared with the standard of care in countries where adjuvant osimertinib will ultimately be marketed. Although I strongly suspect that the overall survival difference would have been significant without the disparity in access to osimertinib in the control arm, we will never know the magnitude of that difference.
With the current design, the trial demonstrates that osimertinib is associated with improved survival in 100% of patients with EGFR mutation–positive NSCLC who receive the agent vs. 38.5% of patients receiving it at some point after relapse.
At the end of the day, ADAURA followed conventional trial rules, which led to a windfall of accolades at the cost of suboptimal care for many of the patients randomly assigned to the control arm.
We need to decide as an oncology community whether we want to accept a system that confers rewards for stakeholders at the expense of patients enrolled in the trial.
We have developed a system that not only permits but depends on global trials enrolling many patients from countries with staging and off-protocol oncology care below standards of care in other parts of the world – effectively condoning and perpetuating disparities in optimal care globally. I am also saddened that some of the most respected leaders in our field have become upset when I question the ethics of accepting this system, one that I believe we have agency to change.
The question here is not whether osimertinib is a good drug; it is remarkably effective for patients with EGFR mutation–positive NSCLC. The question is how to design trials in a fair and balanced way that doesn’t compromise patient care or ethical standards.
If people think my assessment is too harsh, I openly welcome debate.
Bottom line: The ADAURA trial lays bare deeper problems with clinical trial design, and I would challenge readers to reflect on our clinical trial culture in oncology, which offers a system of rules that rewards denying the best identified care for patients on our clinical trials.
At the very least, should we celebrate these wins without fully acknowledging these problems?
Dr. West is clinical associate professor, department of medical oncology, City of Hope Comprehensive Cancer Care, Duarte, Calif. He reported conflicts of interest with Bristol-Myers Squibb, Boehringer Ingelheim, Spectrum, AstraZeneca, Celgene, Genentech/Roche, Pfizer, Merck, and Eli Lilly.
A version of this article first appeared on Medscape.com.
Barry Bonds and Roger Clemens are two world-class baseball players who played well enough to earn enduring respect and admiration. However, their reputations have been permanently tainted by their use of performance-enhancing drugs. Although they are both undeniably gifted, we’ll never know where their natural talent ended and their unfair advantage began.
The medical oncology version of this scenario played out in front of our eyes at the ASCO 2023 Plenary Session featuring the ADAURA trial. In this case, the unfair advantage was clear: Nearly two-thirds of patients in the control arm did not cross over to a standard-of-care treatment at relapse.
The ADAURA trial tested the value of the third-generation oral EGFR inhibitor osimertinib vs. placebo for up to 3 years in patients with a resected stage IB-IIIA non–small cell lung cancer (NSCLC) harboring an activating EGFR mutation. Initially presented in the ASCO 2020 Plenary Session, the preliminary analysis for ADAURA demonstrated a remarkably favorable improvement in disease-free survival (DFS) in the osimertinib arm, which led to its prompt Food and Drug Administration approval in this setting.
At the time, I was among the more vocal critics of the fanfare around this trial. The DFS improvement was impressive but, in this context, represented a low threshold for FDA approval. We already knew that prior trials of other, less effective adjuvant EGFR inhibitors routinely improved DFS but ultimately failed to improve overall survival.
Although in some cases, a DFS benefit can be sufficient to warrant changing practice, I would argue that overall survival is the most critical endpoint in a curative setting by a wide margin. I would also argue that cost should be a consideration for a drug priced at $440,000 over 3 years in the United States. At the very least, we – patients, oncologists, payers – should want to clarify what we get for $440,000 per patient, especially if that money could be better spent on other things.
Of note, we need to know whether the same overall survival may be achieved in this setting by treating only patients whose disease relapses, avoiding both the cost and toxicity of continuous treatment.
The relevance of this question became even more acute when an updated version of the ADAURA trial showed that the DFS benefit from osimertinib began to erode immediately after patients completed active treatment. Although the DFS benefit remained excellent,
The overall survival data – the critical test in my mind – were presented at the ASCO Plenary Session. The results were highly positive, with a hazard ratio for overall survival of 0.49 and a similar benefit observed across all eligible disease stages.
As with the presentation of the DFS data in 2020, these results were accompanied by adulation during the session and fawning in the media. However, a subset of people in the audience, and on Twitter, voiced a major concern: In the control arm, only 38.5% of the patients whose disease had relapsed (79 of 205) ever received osimertinib.
Post-protocol treatment included reassurances that patients in the control arm were offered crossover to osimertinib, but this only occurred starting in April 2020 and only when the treating investigator requested it.
The fact that only a minority of patients in the control arm ever received osimertinib means that ADAURA is not a trial that tests adjuvant osimertinib to osimertinib at relapse, the prevailing standard of care in the United States and the preferred treatment in this setting, based on NCCN guidelines for patients with relapsed/metastatic EGFR mutation–positive NSCLC since the FDA approval in April 2018.
The change in standard of care in the United States and some other countries did not lead to an amendment in the trial, based on the argument that the trial was designed with DFS as the primary endpoint and that patients in the control arm are effectively off trial at relapse. That means patients would receive their country’s standard of care, which may be below, or different from, the standard in the United States or other parts of the world.
While defensible, others considered the low rate of osimertinib delivery in the control arm a serious flaw in the trial design and arguably an ethical problem.
Given this trial design, it’s important to question whether the trial magnified the difference in overall survival between the two arms compared with the standard of care in countries where adjuvant osimertinib will ultimately be marketed. Although I strongly suspect that the overall survival difference would have been significant without the disparity in access to osimertinib in the control arm, we will never know the magnitude of that difference.
With the current design, the trial demonstrates that osimertinib is associated with improved survival in 100% of patients with EGFR mutation–positive NSCLC who receive the agent vs. 38.5% of patients receiving it at some point after relapse.
At the end of the day, ADAURA followed conventional trial rules, which led to a windfall of accolades at the cost of suboptimal care for many of the patients randomly assigned to the control arm.
We need to decide as an oncology community whether we want to accept a system that confers rewards for stakeholders at the expense of patients enrolled in the trial.
We have developed a system that not only permits but depends on global trials enrolling many patients from countries with staging and off-protocol oncology care below standards of care in other parts of the world – effectively condoning and perpetuating disparities in optimal care globally. I am also saddened that some of the most respected leaders in our field have become upset when I question the ethics of accepting this system, one that I believe we have agency to change.
The question here is not whether osimertinib is a good drug; it is remarkably effective for patients with EGFR mutation–positive NSCLC. The question is how to design trials in a fair and balanced way that doesn’t compromise patient care or ethical standards.
If people think my assessment is too harsh, I openly welcome debate.
Bottom line: The ADAURA trial lays bare deeper problems with clinical trial design, and I would challenge readers to reflect on our clinical trial culture in oncology, which offers a system of rules that rewards denying the best identified care for patients on our clinical trials.
At the very least, should we celebrate these wins without fully acknowledging these problems?
Dr. West is clinical associate professor, department of medical oncology, City of Hope Comprehensive Cancer Care, Duarte, Calif. He reported conflicts of interest with Bristol-Myers Squibb, Boehringer Ingelheim, Spectrum, AstraZeneca, Celgene, Genentech/Roche, Pfizer, Merck, and Eli Lilly.
A version of this article first appeared on Medscape.com.
Barry Bonds and Roger Clemens are two world-class baseball players who played well enough to earn enduring respect and admiration. However, their reputations have been permanently tainted by their use of performance-enhancing drugs. Although they are both undeniably gifted, we’ll never know where their natural talent ended and their unfair advantage began.
The medical oncology version of this scenario played out in front of our eyes at the ASCO 2023 Plenary Session featuring the ADAURA trial. In this case, the unfair advantage was clear: Nearly two-thirds of patients in the control arm did not cross over to a standard-of-care treatment at relapse.
The ADAURA trial tested the value of the third-generation oral EGFR inhibitor osimertinib vs. placebo for up to 3 years in patients with a resected stage IB-IIIA non–small cell lung cancer (NSCLC) harboring an activating EGFR mutation. Initially presented in the ASCO 2020 Plenary Session, the preliminary analysis for ADAURA demonstrated a remarkably favorable improvement in disease-free survival (DFS) in the osimertinib arm, which led to its prompt Food and Drug Administration approval in this setting.
At the time, I was among the more vocal critics of the fanfare around this trial. The DFS improvement was impressive but, in this context, represented a low threshold for FDA approval. We already knew that prior trials of other, less effective adjuvant EGFR inhibitors routinely improved DFS but ultimately failed to improve overall survival.
Although in some cases, a DFS benefit can be sufficient to warrant changing practice, I would argue that overall survival is the most critical endpoint in a curative setting by a wide margin. I would also argue that cost should be a consideration for a drug priced at $440,000 over 3 years in the United States. At the very least, we – patients, oncologists, payers – should want to clarify what we get for $440,000 per patient, especially if that money could be better spent on other things.
Of note, we need to know whether the same overall survival may be achieved in this setting by treating only patients whose disease relapses, avoiding both the cost and toxicity of continuous treatment.
The relevance of this question became even more acute when an updated version of the ADAURA trial showed that the DFS benefit from osimertinib began to erode immediately after patients completed active treatment. Although the DFS benefit remained excellent,
The overall survival data – the critical test in my mind – were presented at the ASCO Plenary Session. The results were highly positive, with a hazard ratio for overall survival of 0.49 and a similar benefit observed across all eligible disease stages.
As with the presentation of the DFS data in 2020, these results were accompanied by adulation during the session and fawning in the media. However, a subset of people in the audience, and on Twitter, voiced a major concern: In the control arm, only 38.5% of the patients whose disease had relapsed (79 of 205) ever received osimertinib.
Post-protocol treatment included reassurances that patients in the control arm were offered crossover to osimertinib, but this only occurred starting in April 2020 and only when the treating investigator requested it.
The fact that only a minority of patients in the control arm ever received osimertinib means that ADAURA is not a trial that tests adjuvant osimertinib to osimertinib at relapse, the prevailing standard of care in the United States and the preferred treatment in this setting, based on NCCN guidelines for patients with relapsed/metastatic EGFR mutation–positive NSCLC since the FDA approval in April 2018.
The change in standard of care in the United States and some other countries did not lead to an amendment in the trial, based on the argument that the trial was designed with DFS as the primary endpoint and that patients in the control arm are effectively off trial at relapse. That means patients would receive their country’s standard of care, which may be below, or different from, the standard in the United States or other parts of the world.
While defensible, others considered the low rate of osimertinib delivery in the control arm a serious flaw in the trial design and arguably an ethical problem.
Given this trial design, it’s important to question whether the trial magnified the difference in overall survival between the two arms compared with the standard of care in countries where adjuvant osimertinib will ultimately be marketed. Although I strongly suspect that the overall survival difference would have been significant without the disparity in access to osimertinib in the control arm, we will never know the magnitude of that difference.
With the current design, the trial demonstrates that osimertinib is associated with improved survival in 100% of patients with EGFR mutation–positive NSCLC who receive the agent vs. 38.5% of patients receiving it at some point after relapse.
At the end of the day, ADAURA followed conventional trial rules, which led to a windfall of accolades at the cost of suboptimal care for many of the patients randomly assigned to the control arm.
We need to decide as an oncology community whether we want to accept a system that confers rewards for stakeholders at the expense of patients enrolled in the trial.
We have developed a system that not only permits but depends on global trials enrolling many patients from countries with staging and off-protocol oncology care below standards of care in other parts of the world – effectively condoning and perpetuating disparities in optimal care globally. I am also saddened that some of the most respected leaders in our field have become upset when I question the ethics of accepting this system, one that I believe we have agency to change.
The question here is not whether osimertinib is a good drug; it is remarkably effective for patients with EGFR mutation–positive NSCLC. The question is how to design trials in a fair and balanced way that doesn’t compromise patient care or ethical standards.
If people think my assessment is too harsh, I openly welcome debate.
Bottom line: The ADAURA trial lays bare deeper problems with clinical trial design, and I would challenge readers to reflect on our clinical trial culture in oncology, which offers a system of rules that rewards denying the best identified care for patients on our clinical trials.
At the very least, should we celebrate these wins without fully acknowledging these problems?
Dr. West is clinical associate professor, department of medical oncology, City of Hope Comprehensive Cancer Care, Duarte, Calif. He reported conflicts of interest with Bristol-Myers Squibb, Boehringer Ingelheim, Spectrum, AstraZeneca, Celgene, Genentech/Roche, Pfizer, Merck, and Eli Lilly.
A version of this article first appeared on Medscape.com.
Antibiotics for acute exacerbation of COPD: It’s still controversial
In late 2021, the Rome Proposal for diagnosing acute exacerbations of chronic obstructive pulmonary disease (AECOPD) and grading their severity was published. The 2023 Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease (GOLD) Report has adopted the Rome Proposal criteria. Given that an endorsement by GOLD is tantamount to acceptance by clinicians, researchers, and policymakers alike, I guess we’re all using them now.
Anyone who’s ever cared for patients with COPD knows that treatment and reduction of exacerbations is how we improve outcomes. AECOPD are associated with considerable morbidity, greater health care utilization and costs, and a long-term decline in lung function. While we hope our pharmacotherapies improve symptoms, we know they reduce AECOPD. If our pharmacotherapies have any impact on mortality, it’s probably via AECOPD prevention.
Since antibiotic indications are tied to severity, using the Rome Proposal criteria may affect management in unpredictable ways. As such, it’s worth reviewing the data on antibiotics for AECOPD.
What do the data reveal?
To start, it’s important to note that GOLD doesn’t equate having an AECOPD with needing an antibiotic. I myself have conflated the diagnosis with the indication and thereby overprescribed. The bar for diagnosis is quite low. In previous GOLD summaries, any “change in respiratory symptoms” would warrant the AECOPD label. Although the Rome Proposal definition is more specific, it leaves room for liberal interpretation. It’s likely to have a greater effect on research than on clinical practice. My guess is that AECOPD prevalence doesn’t change.
The antibiotic hurdle is slightly higher than that for diagnosis but is equally open to interpretation. In part, that’s related to the inherent subjectivity of judging symptoms, sputum production, and changes in color, but it’s also because the data are so poor. The meta-analyses that have been used to establish the indications include fewer than 1000 patients spread across 10 to 11 trials. Thus, the individual trials are small, and the sample size remains nominal even after adding them together. The addition of antibiotics – and it doesn’t seem to matter which class, type, or duration – will decrease mortality and hospital length of stay. One study says these effects are limited to inpatients while the other does not. After reading GOLD 2013, GOLD 2023, and both the meta-analyses they used to support their recommendations, I’m still not sure who benefits. Do you have to be hospitalized? Is some sort of ventilatory support required? Does C-reactive protein help or not?
In accordance with the classic Anthonisen criteria, GOLD relies on sputum volume and color as evidence of a bacterial infection. Soon after GOLD 2023 was published, a meta-analysis found that sputum color isn’t particularly accurate for detecting bacterial infection. Because it doesn’t seem to matter which antibiotic class is used, I always thought we were using antibiotics for their magical, pleiotropic anti-inflammatory effects anyway. I didn’t think the presence of an actual bacterial infection was important. If I saw an infiltrate on chest x-ray, I’d change my diagnosis from AECOPD to community-acquired pneumonia (CAP) and switch to CAP coverage. I’ve been doing this so long that I swear it’s in a guideline somewhere, though admittedly I couldn’t find said guideline while reading for this piece.
Key takeaways
In summary, I believe that the guidance reflects the data, which is muddy. The Rome Proposal should be seen as just that – a framework for moving forward with AECOPD classification and antibiotic indications that will need to be refined over time as better data become available. In fact, they allow for a more objective, point-of-care assessment of severity that can be validated and tied to antibiotic benefits. The Rome criteria aren’t evidence-based; they’re a necessary first step toward creating the evidence.
In the meantime, if your AECOPD patients are hospitalized, they probably warrant an antibiotic. If they’re not, sputum changes may be a reasonable surrogate for a bacterial infection. Considerable uncertainty remains.
Aaron B. Holley, MD, is a professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He reported conflicts of interest with Metapharm, CHEST College, and WebMD.
A version of this article first appeared on Medscape.com.
In late 2021, the Rome Proposal for diagnosing acute exacerbations of chronic obstructive pulmonary disease (AECOPD) and grading their severity was published. The 2023 Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease (GOLD) Report has adopted the Rome Proposal criteria. Given that an endorsement by GOLD is tantamount to acceptance by clinicians, researchers, and policymakers alike, I guess we’re all using them now.
Anyone who’s ever cared for patients with COPD knows that treatment and reduction of exacerbations is how we improve outcomes. AECOPD are associated with considerable morbidity, greater health care utilization and costs, and a long-term decline in lung function. While we hope our pharmacotherapies improve symptoms, we know they reduce AECOPD. If our pharmacotherapies have any impact on mortality, it’s probably via AECOPD prevention.
Since antibiotic indications are tied to severity, using the Rome Proposal criteria may affect management in unpredictable ways. As such, it’s worth reviewing the data on antibiotics for AECOPD.
What do the data reveal?
To start, it’s important to note that GOLD doesn’t equate having an AECOPD with needing an antibiotic. I myself have conflated the diagnosis with the indication and thereby overprescribed. The bar for diagnosis is quite low. In previous GOLD summaries, any “change in respiratory symptoms” would warrant the AECOPD label. Although the Rome Proposal definition is more specific, it leaves room for liberal interpretation. It’s likely to have a greater effect on research than on clinical practice. My guess is that AECOPD prevalence doesn’t change.
The antibiotic hurdle is slightly higher than that for diagnosis but is equally open to interpretation. In part, that’s related to the inherent subjectivity of judging symptoms, sputum production, and changes in color, but it’s also because the data are so poor. The meta-analyses that have been used to establish the indications include fewer than 1000 patients spread across 10 to 11 trials. Thus, the individual trials are small, and the sample size remains nominal even after adding them together. The addition of antibiotics – and it doesn’t seem to matter which class, type, or duration – will decrease mortality and hospital length of stay. One study says these effects are limited to inpatients while the other does not. After reading GOLD 2013, GOLD 2023, and both the meta-analyses they used to support their recommendations, I’m still not sure who benefits. Do you have to be hospitalized? Is some sort of ventilatory support required? Does C-reactive protein help or not?
In accordance with the classic Anthonisen criteria, GOLD relies on sputum volume and color as evidence of a bacterial infection. Soon after GOLD 2023 was published, a meta-analysis found that sputum color isn’t particularly accurate for detecting bacterial infection. Because it doesn’t seem to matter which antibiotic class is used, I always thought we were using antibiotics for their magical, pleiotropic anti-inflammatory effects anyway. I didn’t think the presence of an actual bacterial infection was important. If I saw an infiltrate on chest x-ray, I’d change my diagnosis from AECOPD to community-acquired pneumonia (CAP) and switch to CAP coverage. I’ve been doing this so long that I swear it’s in a guideline somewhere, though admittedly I couldn’t find said guideline while reading for this piece.
Key takeaways
In summary, I believe that the guidance reflects the data, which is muddy. The Rome Proposal should be seen as just that – a framework for moving forward with AECOPD classification and antibiotic indications that will need to be refined over time as better data become available. In fact, they allow for a more objective, point-of-care assessment of severity that can be validated and tied to antibiotic benefits. The Rome criteria aren’t evidence-based; they’re a necessary first step toward creating the evidence.
In the meantime, if your AECOPD patients are hospitalized, they probably warrant an antibiotic. If they’re not, sputum changes may be a reasonable surrogate for a bacterial infection. Considerable uncertainty remains.
Aaron B. Holley, MD, is a professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He reported conflicts of interest with Metapharm, CHEST College, and WebMD.
A version of this article first appeared on Medscape.com.
In late 2021, the Rome Proposal for diagnosing acute exacerbations of chronic obstructive pulmonary disease (AECOPD) and grading their severity was published. The 2023 Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease (GOLD) Report has adopted the Rome Proposal criteria. Given that an endorsement by GOLD is tantamount to acceptance by clinicians, researchers, and policymakers alike, I guess we’re all using them now.
Anyone who’s ever cared for patients with COPD knows that treatment and reduction of exacerbations is how we improve outcomes. AECOPD are associated with considerable morbidity, greater health care utilization and costs, and a long-term decline in lung function. While we hope our pharmacotherapies improve symptoms, we know they reduce AECOPD. If our pharmacotherapies have any impact on mortality, it’s probably via AECOPD prevention.
Since antibiotic indications are tied to severity, using the Rome Proposal criteria may affect management in unpredictable ways. As such, it’s worth reviewing the data on antibiotics for AECOPD.
What do the data reveal?
To start, it’s important to note that GOLD doesn’t equate having an AECOPD with needing an antibiotic. I myself have conflated the diagnosis with the indication and thereby overprescribed. The bar for diagnosis is quite low. In previous GOLD summaries, any “change in respiratory symptoms” would warrant the AECOPD label. Although the Rome Proposal definition is more specific, it leaves room for liberal interpretation. It’s likely to have a greater effect on research than on clinical practice. My guess is that AECOPD prevalence doesn’t change.
The antibiotic hurdle is slightly higher than that for diagnosis but is equally open to interpretation. In part, that’s related to the inherent subjectivity of judging symptoms, sputum production, and changes in color, but it’s also because the data are so poor. The meta-analyses that have been used to establish the indications include fewer than 1000 patients spread across 10 to 11 trials. Thus, the individual trials are small, and the sample size remains nominal even after adding them together. The addition of antibiotics – and it doesn’t seem to matter which class, type, or duration – will decrease mortality and hospital length of stay. One study says these effects are limited to inpatients while the other does not. After reading GOLD 2013, GOLD 2023, and both the meta-analyses they used to support their recommendations, I’m still not sure who benefits. Do you have to be hospitalized? Is some sort of ventilatory support required? Does C-reactive protein help or not?
In accordance with the classic Anthonisen criteria, GOLD relies on sputum volume and color as evidence of a bacterial infection. Soon after GOLD 2023 was published, a meta-analysis found that sputum color isn’t particularly accurate for detecting bacterial infection. Because it doesn’t seem to matter which antibiotic class is used, I always thought we were using antibiotics for their magical, pleiotropic anti-inflammatory effects anyway. I didn’t think the presence of an actual bacterial infection was important. If I saw an infiltrate on chest x-ray, I’d change my diagnosis from AECOPD to community-acquired pneumonia (CAP) and switch to CAP coverage. I’ve been doing this so long that I swear it’s in a guideline somewhere, though admittedly I couldn’t find said guideline while reading for this piece.
Key takeaways
In summary, I believe that the guidance reflects the data, which is muddy. The Rome Proposal should be seen as just that – a framework for moving forward with AECOPD classification and antibiotic indications that will need to be refined over time as better data become available. In fact, they allow for a more objective, point-of-care assessment of severity that can be validated and tied to antibiotic benefits. The Rome criteria aren’t evidence-based; they’re a necessary first step toward creating the evidence.
In the meantime, if your AECOPD patients are hospitalized, they probably warrant an antibiotic. If they’re not, sputum changes may be a reasonable surrogate for a bacterial infection. Considerable uncertainty remains.
Aaron B. Holley, MD, is a professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He reported conflicts of interest with Metapharm, CHEST College, and WebMD.
A version of this article first appeared on Medscape.com.
Transplant centers often skip the top spot on the kidney waitlist
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
The idea of rationing medical care is anathema to most doctors. Sure, we acknowledge that the realities of health care costs and insurance companies might limit our options, but there is always a sense that when something is truly, truly needed, we can get it done.
Except in one very particular situation, a situation where rationing of care is the norm. That situation? Organ transplantation.
There is no way around this: More patients need organ transplants than there are organs available to transplant. It is cold, hard arithmetic. No amount of negotiating with an insurance company or engaging in prior authorization can change that.
As a kidney doctor, this issue is close to my heart. There are around 100,000 people on the kidney transplant waiting list in the U.S., with 3,000 new patients being added per month. There are only 25,000 kidney transplants per year. And each year, around 5,000 people die while waiting for a transplant.
A world of scarcity, like the world of kidney transplant, is ripe for bias at best and abuse at worst. It is in part for that reason that the Kidney Allocation System exists. It answers the cold, hard arithmetic of transplant scarcity with the cold, hard arithmetic of a computer algorithm, ranking individuals on the waitlist on a variety of factors to ensure that those who will benefit most from a transplant get it first.
This area is a bit complex but I’ll try to break it down into what you need to know. There are 56 organ procurement organizations (OPOs) in the United States. These are nonprofits with the responsibility to recover organs from deceased donors in their area.
Each of those OPOs maintains a ranked list of those waiting for a kidney transplant. Depending on the OPO, the list may range from a couple hundred people to a couple thousand, but one thing is the same, no matter what: If you are at the top of the list, you should be the next to get a transplant.
Most OPOs have multiple transplant centers in them, and each center is going to prioritize its own patients. If a Yale patient is No. 1 on the list and a kidney offer comes in, it would be a good idea for us to accept, because if we reject the offer, the organ may go to a competing center whose patients is ranked No. 2.
But 11 OPOs around the country are served by only one center. This gives that center huge flexibility to determine who gets what kidney, because if they refuse an offer for whoever is at the top of their list, they can still give the kidney to the second person on their list, or third, or 30th, theoretically.
But in practice, does this phenomenon, known colloquially as “list diving,” actually happen? This manuscript from Sumit Mohan and colleagues suggests that it does, and at rates that are, frankly, eye-popping.
The Columbia team used data from the Scientific Registry of Transplant Recipients to conduct the analysis. The database tracks all aspects of the transplant process, from listing to ranking to, eventually, the transplant itself. With that data, they could determine how often, across these 11 OPOs, the No. 1 person on the list did not get the available kidney.
The answer? Out of 4,668 transplants conducted from 2015 to 2019, the transplant centers skipped their highest-ranked person 3,169 times – 68% of the time.
This graph shows the distribution of where on the list these kidneys went. You can see some centers diving down 100 or 200 places.
Transplant centers have lists of different lengths, so this graph shows you how far down on the percentage scale the centers dived. You can see centers skipping right to the bottom of their list in some cases.
Now, I should make it clear that transplant centers do have legitimate discretion here. Transplant centers may pass up a less-than-perfect kidney for their No. 1 spot, knowing that that individual will get more offers soon, in favor of someone further down the list who will not see an offer for a while. It’s gaming the system a bit, but not, you know, for evil. And the data support this. Top-ranked people who got skipped had received a lower-quality kidney offer than those who did not get skipped. But I will also note that those who were skipped were less likely to be White, less likely to be Hispanic, and more likely to be male. That should raise your eyebrows.
Interestingly, this practice may not be limited to those cases where the OPO has only one transplant center. Conducting the same analysis across all 231 kidney transplant centers in the U.S., the authors found that the top candidate was skipped 76% of the time.
So, what’s going on here? I’m sure that some of this list-skipping is for legitimate medical reasons. And it should be pointed out that recipients have a right to refuse an offer as well – and might be more picky if they know they are at the top of the list. But patient preference was listed as the reason for list diving in only about 14% of cases. The vast majority (65%) of reasons given were based on donor quality. The problem is that donor quality can be quite subjective. And remember, these organs were transplanted eventually so they couldn’t have been that bad.
Putting the data together, though, I can’t shake the sense that centers are using the list more for guidance than as a real mechanism to ensure an equitable allocation system. With all the flexibility that centers have to bypass individuals on the list, the list loses its meaning and its power.
I spoke to one transplant nephrologist who suggested that these data should prompt an investigation by the United Network for Organ Sharing, the body that governs all these OPOs. That may be a necessary step.
I hope there comes a day when this issue is moot, when growing kidneys in the lab – or regenerating one’s own kidneys – is a possibility. But that day is not yet here and we must deal with the scarcity we have. In this world, we need the list to prevent abuse. But the list only works if the list is followed.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He reported having no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
The idea of rationing medical care is anathema to most doctors. Sure, we acknowledge that the realities of health care costs and insurance companies might limit our options, but there is always a sense that when something is truly, truly needed, we can get it done.
Except in one very particular situation, a situation where rationing of care is the norm. That situation? Organ transplantation.
There is no way around this: More patients need organ transplants than there are organs available to transplant. It is cold, hard arithmetic. No amount of negotiating with an insurance company or engaging in prior authorization can change that.
As a kidney doctor, this issue is close to my heart. There are around 100,000 people on the kidney transplant waiting list in the U.S., with 3,000 new patients being added per month. There are only 25,000 kidney transplants per year. And each year, around 5,000 people die while waiting for a transplant.
A world of scarcity, like the world of kidney transplant, is ripe for bias at best and abuse at worst. It is in part for that reason that the Kidney Allocation System exists. It answers the cold, hard arithmetic of transplant scarcity with the cold, hard arithmetic of a computer algorithm, ranking individuals on the waitlist on a variety of factors to ensure that those who will benefit most from a transplant get it first.
This area is a bit complex but I’ll try to break it down into what you need to know. There are 56 organ procurement organizations (OPOs) in the United States. These are nonprofits with the responsibility to recover organs from deceased donors in their area.
Each of those OPOs maintains a ranked list of those waiting for a kidney transplant. Depending on the OPO, the list may range from a couple hundred people to a couple thousand, but one thing is the same, no matter what: If you are at the top of the list, you should be the next to get a transplant.
Most OPOs have multiple transplant centers in them, and each center is going to prioritize its own patients. If a Yale patient is No. 1 on the list and a kidney offer comes in, it would be a good idea for us to accept, because if we reject the offer, the organ may go to a competing center whose patients is ranked No. 2.
But 11 OPOs around the country are served by only one center. This gives that center huge flexibility to determine who gets what kidney, because if they refuse an offer for whoever is at the top of their list, they can still give the kidney to the second person on their list, or third, or 30th, theoretically.
But in practice, does this phenomenon, known colloquially as “list diving,” actually happen? This manuscript from Sumit Mohan and colleagues suggests that it does, and at rates that are, frankly, eye-popping.
The Columbia team used data from the Scientific Registry of Transplant Recipients to conduct the analysis. The database tracks all aspects of the transplant process, from listing to ranking to, eventually, the transplant itself. With that data, they could determine how often, across these 11 OPOs, the No. 1 person on the list did not get the available kidney.
The answer? Out of 4,668 transplants conducted from 2015 to 2019, the transplant centers skipped their highest-ranked person 3,169 times – 68% of the time.
This graph shows the distribution of where on the list these kidneys went. You can see some centers diving down 100 or 200 places.
Transplant centers have lists of different lengths, so this graph shows you how far down on the percentage scale the centers dived. You can see centers skipping right to the bottom of their list in some cases.
Now, I should make it clear that transplant centers do have legitimate discretion here. Transplant centers may pass up a less-than-perfect kidney for their No. 1 spot, knowing that that individual will get more offers soon, in favor of someone further down the list who will not see an offer for a while. It’s gaming the system a bit, but not, you know, for evil. And the data support this. Top-ranked people who got skipped had received a lower-quality kidney offer than those who did not get skipped. But I will also note that those who were skipped were less likely to be White, less likely to be Hispanic, and more likely to be male. That should raise your eyebrows.
Interestingly, this practice may not be limited to those cases where the OPO has only one transplant center. Conducting the same analysis across all 231 kidney transplant centers in the U.S., the authors found that the top candidate was skipped 76% of the time.
So, what’s going on here? I’m sure that some of this list-skipping is for legitimate medical reasons. And it should be pointed out that recipients have a right to refuse an offer as well – and might be more picky if they know they are at the top of the list. But patient preference was listed as the reason for list diving in only about 14% of cases. The vast majority (65%) of reasons given were based on donor quality. The problem is that donor quality can be quite subjective. And remember, these organs were transplanted eventually so they couldn’t have been that bad.
Putting the data together, though, I can’t shake the sense that centers are using the list more for guidance than as a real mechanism to ensure an equitable allocation system. With all the flexibility that centers have to bypass individuals on the list, the list loses its meaning and its power.
I spoke to one transplant nephrologist who suggested that these data should prompt an investigation by the United Network for Organ Sharing, the body that governs all these OPOs. That may be a necessary step.
I hope there comes a day when this issue is moot, when growing kidneys in the lab – or regenerating one’s own kidneys – is a possibility. But that day is not yet here and we must deal with the scarcity we have. In this world, we need the list to prevent abuse. But the list only works if the list is followed.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He reported having no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
The idea of rationing medical care is anathema to most doctors. Sure, we acknowledge that the realities of health care costs and insurance companies might limit our options, but there is always a sense that when something is truly, truly needed, we can get it done.
Except in one very particular situation, a situation where rationing of care is the norm. That situation? Organ transplantation.
There is no way around this: More patients need organ transplants than there are organs available to transplant. It is cold, hard arithmetic. No amount of negotiating with an insurance company or engaging in prior authorization can change that.
As a kidney doctor, this issue is close to my heart. There are around 100,000 people on the kidney transplant waiting list in the U.S., with 3,000 new patients being added per month. There are only 25,000 kidney transplants per year. And each year, around 5,000 people die while waiting for a transplant.
A world of scarcity, like the world of kidney transplant, is ripe for bias at best and abuse at worst. It is in part for that reason that the Kidney Allocation System exists. It answers the cold, hard arithmetic of transplant scarcity with the cold, hard arithmetic of a computer algorithm, ranking individuals on the waitlist on a variety of factors to ensure that those who will benefit most from a transplant get it first.
This area is a bit complex but I’ll try to break it down into what you need to know. There are 56 organ procurement organizations (OPOs) in the United States. These are nonprofits with the responsibility to recover organs from deceased donors in their area.
Each of those OPOs maintains a ranked list of those waiting for a kidney transplant. Depending on the OPO, the list may range from a couple hundred people to a couple thousand, but one thing is the same, no matter what: If you are at the top of the list, you should be the next to get a transplant.
Most OPOs have multiple transplant centers in them, and each center is going to prioritize its own patients. If a Yale patient is No. 1 on the list and a kidney offer comes in, it would be a good idea for us to accept, because if we reject the offer, the organ may go to a competing center whose patients is ranked No. 2.
But 11 OPOs around the country are served by only one center. This gives that center huge flexibility to determine who gets what kidney, because if they refuse an offer for whoever is at the top of their list, they can still give the kidney to the second person on their list, or third, or 30th, theoretically.
But in practice, does this phenomenon, known colloquially as “list diving,” actually happen? This manuscript from Sumit Mohan and colleagues suggests that it does, and at rates that are, frankly, eye-popping.
The Columbia team used data from the Scientific Registry of Transplant Recipients to conduct the analysis. The database tracks all aspects of the transplant process, from listing to ranking to, eventually, the transplant itself. With that data, they could determine how often, across these 11 OPOs, the No. 1 person on the list did not get the available kidney.
The answer? Out of 4,668 transplants conducted from 2015 to 2019, the transplant centers skipped their highest-ranked person 3,169 times – 68% of the time.
This graph shows the distribution of where on the list these kidneys went. You can see some centers diving down 100 or 200 places.
Transplant centers have lists of different lengths, so this graph shows you how far down on the percentage scale the centers dived. You can see centers skipping right to the bottom of their list in some cases.
Now, I should make it clear that transplant centers do have legitimate discretion here. Transplant centers may pass up a less-than-perfect kidney for their No. 1 spot, knowing that that individual will get more offers soon, in favor of someone further down the list who will not see an offer for a while. It’s gaming the system a bit, but not, you know, for evil. And the data support this. Top-ranked people who got skipped had received a lower-quality kidney offer than those who did not get skipped. But I will also note that those who were skipped were less likely to be White, less likely to be Hispanic, and more likely to be male. That should raise your eyebrows.
Interestingly, this practice may not be limited to those cases where the OPO has only one transplant center. Conducting the same analysis across all 231 kidney transplant centers in the U.S., the authors found that the top candidate was skipped 76% of the time.
So, what’s going on here? I’m sure that some of this list-skipping is for legitimate medical reasons. And it should be pointed out that recipients have a right to refuse an offer as well – and might be more picky if they know they are at the top of the list. But patient preference was listed as the reason for list diving in only about 14% of cases. The vast majority (65%) of reasons given were based on donor quality. The problem is that donor quality can be quite subjective. And remember, these organs were transplanted eventually so they couldn’t have been that bad.
Putting the data together, though, I can’t shake the sense that centers are using the list more for guidance than as a real mechanism to ensure an equitable allocation system. With all the flexibility that centers have to bypass individuals on the list, the list loses its meaning and its power.
I spoke to one transplant nephrologist who suggested that these data should prompt an investigation by the United Network for Organ Sharing, the body that governs all these OPOs. That may be a necessary step.
I hope there comes a day when this issue is moot, when growing kidneys in the lab – or regenerating one’s own kidneys – is a possibility. But that day is not yet here and we must deal with the scarcity we have. In this world, we need the list to prevent abuse. But the list only works if the list is followed.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He reported having no conflicts of interest.
A version of this article first appeared on Medscape.com.
How can we make medical training less ‘toxic’?
This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining me to discuss ways to address and reform the toxic culture associated with medical training is Dr. Amy Faith Ho, senior vice president of clinical informatics and analytics at Integrative Emergency Services in Dallas. Also joining us is Dr. Júlia Loyola Ferreira, a pediatric surgeon originally from Brazil, now practicing at Montreal Children’s and focused on advocacy for gender equity and patient-centered care.
Welcome to both of you. Thanks so much for joining me.
Amy Faith Ho, MD, MPH: Thanks so much for having us, Rob.
Dr. Glatter: Amy, I noticed a tweet recently where you talked about how your career choice was affected by the toxic environment in medical school, affecting your choice of residency. Can you elaborate on that?
Dr. Ho: In this instance, what we’re talking about is gender, but it can be directed toward any number of other groups as well.
What you’re alluding to is a tweet by Stanford Surgery Group showing the next residency class, and what was really stunning about this residency class was that it was almost all females. And this was something that took off on social media.
When I saw this, I was really brought back to one of my personal experiences that I chose to share, which was basically that, as a medical student, I really wanted to be a surgeon. I’m an emergency medicine doctor now, so you know that didn’t happen.
The story that I was sharing was that when I was a third-year medical student rotating on surgery, we had a male attending who was very well known at that school at the time who basically would take the female medical students, and instead of clinic, he would round us up. He would have us sit around him in the workplace room while everyone else was seeing patients, and he would have you look at news clippings of himself. He would tell you stories about himself, like he was holding court for the ladies.
It was this very weird culture where my takeaway as a med student was like, “Wow, this is kind of abusive patriarchy that is supported,” because everyone knew about it and was complicit. Even though I really liked surgery, this was just one instance and one example of where you see this culture that really resonates into the rest of life that I didn’t really want to be a part of.
I went into emergency medicine and loved it. It’s also highly procedural, and I was very happy with where I was. What was really interesting about this tweet to me, though, is that it really took off and garnered hundreds of thousands of views on a very niche topic, because what was most revealing is that everyone has a story like this.
It is not just surgery. It is definitely not just one specialty and it is not just one school. It is an endemic problem in medicine. Not only does it change the lives of young women, but it also says so much about the complicity and the culture that we have in medicine that many people were upset about just the same way I was.
Medical training experience in other countries vs. the United States
Dr. Glatter: Júlia, I want to hear about your experience in medical school, surgery, and then fellowship training and up to the present, if possible.
Júlia Loyola Ferreira, MD: In Brazil, as in many countries now, women have made up the majority of the medical students since 2010. It’s a more female-friendly environment when you’re going through medical school, and I was lucky enough to do rotations in areas of surgery where people were friendly to women.
I lived in this tiny bubble that also gave me the privilege of not facing some things that I can imagine that people in Brazil in different areas and smaller towns face. In Brazil, people try to not talk about this gender agenda. This is something that’s being talked about outside Brazil. But in Brazil, we are years back. People are not really engaging on this conversation. I thought it was going to be hard for me as a woman, because Brazil has around 20% female surgeons.
I knew it was going to be challenging, but I had no idea how bad it was. When I started and things started happening, the list was big. I have an example of everything that is written about – microaggression, implicit bias, discrimination, harassment.
Every time I would try to speak about it and talk to someone, I would be strongly gaslighted. It was the whole training, the whole 5 years. People would say, “Oh, I don’t think it was like that. I think you were overreacting.” People would come with all these different answers for what I was experiencing, and that was frustrating. That was even harder because I had to cope with everything that was happening and I had no one to turn to. I had no mentors.
When I looked up to women who were in surgery, they would be tougher on us young surgeons than the men and they would tell us that we should not complain because in their time it was even harder. Now, it’s getting better and we are supposed to accept whatever comes.
That was at least a little bit of what I experienced in my training. It was only after I finished and started to do research about it that I really encountered a field of people who would echo what I was trying to say to many people in different hospitals that I attended to.
That was the key for me to get out of that situation of being gaslighted and of not being able to really talk about it. Suddenly, I started to publish things about Brazil that nobody was even writing or studying. That gave me a large amount of responsibility, but also motivation to keep going and to see the change.
Valuing women in medicine
Dr. Glatter: This is a very important point that you’re raising about the environment of women being hard on other women. We know that men can be very difficult on and also judgmental toward their trainees.
Amy, how would you respond to that? Was your experience similar in emergency medicine training?
Dr. Ho: I actually don’t feel like it was. I think what Júlia is alluding to is this “mean girls” idea, of “I went through it and thus you have to go through it.” I think you do see this in many specialties. One of the classic ones we hear about, and I don’t want to speak to it too much because it’s not my specialty, is ob.gyn., where it is a very female-dominant surgery group. There’s almost a hazing level that you hear about in some of the more malignant workplaces.
I think that you speak to two really important things. Number one is the numbers game. As you were saying, Brazil actually has many women. That’s awesome. That’s actually different from the United States, especially for the historic, existing workplace and less so for the medical students and for residents. I think step one is having minorities like women just present and there.
Step two is actually including and valuing them. While I think it’s really easy to move away from the women discussion, because there are women when you look around in medicine, it doesn’t mean that women are actually being heard, that they’re actually being accepted, or that their viewpoints are being listened to. A big part of it is normalizing not only seeing women in medicine but also normalizing the narrative of women in medicine.
It’s not just about motherhood; it’s about things like normalizing talking about advancement, academic promotions, pay, culture, being called things like “too reactive,” “anxious,” or “too assertive.” These are all classic things that we hear about when we talk about women.
That’s why we’re looking to not only conversations like this, but also structured ways for women to discuss being women in medicine. There are many women in medicine groups in emergency medicine, including: Females Working in Emergency Medicine (FemInEM); the American College of Emergency Physicians (ACEP) and Society for Academic Emergency Medicine (SAEM) women’s groups, which are American Association of Women Emergency Physicians (AAWEP) and Academy for Women in Academic Emergency Medicine (AWAEM), respectively; and the American Medical Women’s Association (AMWA), which is the American Medical Association’s offshoot.
All of these groups are geared toward normalizing women in medicine, normalizing the narrative of women in medicine, and then working on mentoring and educating so that we can advance our initiatives.
Gender balance is not gender equity
Dr. Glatter: Amy, you bring up a very critical point that mentoring is sort of the antidote to gender-based discrimination. Júlia had written a paper back in November of 2022 that was published in the Journal of Surgical Research talking exactly about this and how important it is to develop mentoring. Part of her research showed that about 20% of medical students who took the survey, about 1,000 people, had mentors, which was very disturbing.
Dr. Loyola Ferreira: Mentorship is one of the ways of changing the reality about gender-based discrimination. Amy’s comment was very strong and we need to really keep saying it, which is that gender balance is not gender equity.
The idea of having more women is not the same as women being recognized as equals, as able as men, and as valued as men. To change this very long culture of male domination, we need support, and this support comes from mentorship.
Although I didn’t have one, I feel that since I started being a mentor for some students, it changed not only them but myself. It gave me strength to keep going, studying, publishing, and going further with this discussion. I feel like the relationship was as good for them as it is for me. That’s how things change.
Diversity, equity, and inclusion training
Dr. Glatter: We’re talking about the reality of gender equity in terms of the ability to have equal respect, recognition, opportunities, and access. That’s really an important point to realize, and for our audience, to understand that gender equity is not gender balance.
Amy, I want to talk about medical school curriculums. Are there advances that you’re aware of being made at certain schools, programs, even in residencies, to enforce these things and make it a priority?
Dr. Ho: We’re really lucky that, as a culture in the United States, medical training is certainly very geared toward diversity. Some of that is certainly unofficial. Some of that just means when they’re looking at a medical school class or looking at rank lists for residency, that they’re cognizant of the different backgrounds that people have. That’s still a step. That is a step, that we’re at least acknowledging it.
There are multiple medical schools and residencies that have more formal unconscious-bias training or diversity, equity, and inclusion (DEI) training, both of which are excellent not only for us in the workplace but also for our patients. Almost all of us will see patients of highly diverse backgrounds. I think the biggest push is looking toward the criteria that we use for selecting trainees and students into our programs. Historically, it’s been MCAT, GPA, and so on.
We’ve really started to ask the question of, are these sorts of “objective criteria” actually biased in institutional ways? They talk about this all the time where GPAs will bias against students from underrepresented minorities (URM). I think all medical students and residencies have really acknowledged that. Although there are still test cutoffs, we are putting an inquisitive eye to what those mean, why they exist, and what are the other things that we should consider. This is all very heartening from what I’m seeing in medical training.
Dr. Glatter: There’s no formal rating system for DEI curriculums right now, like ranking of this school, or this program has more advanced recognition in terms of DEI?
Dr. Ho: No, but on the flip side, the U.S. News & World Report was classically one of the major rankings for medical schools. What we saw fairly recently was that very high-tier schools like Harvard and University of Chicago pulled out of that ranking because that ranking did not acknowledge the value of diversity. That was an incredible stance for medical schools to take, to say, “Hey, you are not evaluating an important criterion of ours.”
Dr. Glatter: That’s a great point. Júlia, where are we now in Brazil in terms of awareness of DEI and curriculum in schools and training programs?
Dr. Loyola Ferreira: Our reality is not as good as in the U.S., unfortunately. I don’t see much discussion on residency programs or medical schools at the moment. I see many students bringing it out and trying to make their schools engage in that discussion. This is something that is coming from the bottom up and not from the top down. I think it can lead to change as well. It is a step and it’s a beginning. Institutions should take the responsibility of doing this from the beginning. This is something where Brazil is still years behind you guys.
Dr. Glatter: It’s unfortunate, but certainly it’s important to hear that. What about in Canada and certainly your institution, McGill, where you just completed a master’s degree?
Dr. Loyola Ferreira: Canada is very much like the U.S. This is something that is really happening and it’s happening fast. I see, at least at McGill, a large amount of DEI inclusion and everything on this discussion. They have institutional courses for us to do as students, and we are all obliged to do many courses, which I think is really educating, especially for people with different cultures and backgrounds.
Dr. Glatter: Amy, where do you think we are in emergency medicine to look at the other side of it? Comparing surgery with emergency medicine, do you think we’re well advanced in terms of DEI, inclusion criteria, respect, and dignity, or are we really far off?
Dr. Ho: I may be biased, but I think emergency medicine is one of the best in terms of this, and I think there are a couple of reasons for it. One is that we are an inherently team-based organization. The attending, the residents, and the students all work in line with one another. There’s less of a hierarchy.
The same is true for our nurses, pharmacists, techs, and EMS. We all work together as a team. Because of that fairly flat structure, it’s really easy for us to value one another as individuals with our diverse backgrounds. In a way, that’s harder for specialties that are more hierarchical, and I think surgery is certainly one of the most hierarchical.
The second reason why emergency medicine is fairly well off in this is that we’re, by nature, a safety-net specialty. We see patients of all-comers, all walks, all backgrounds. I think we both recognize the value of physician-patient concordance. When we share characteristics with our patients, we recognize that value immediately at the bedside.
It exposes us to so much diversity. I see a refugee one day and the next patient is someone who is incarcerated. The next patient after that is an important businessman in society. That diversity and whiplash in the type of patients that we see back-to-back helps us see the playing field in a really flat, diverse way. Because of that, I think our culture is much better, as is our understanding of the value and importance of diversity not only for our programs, but also for our patients.
Do female doctors have better patient outcomes?
Dr. Glatter: Specialties working together in the emergency department is so important. Building that team and that togetherness is so critical. Júlia, would you agree?
Dr. Loyola Ferreira: Definitely. Something Amy said that is beautiful is that you recognize yourself in these patients. In surgery, we are taught to try to be away from the patients and not to put ourselves in the same position. We are taught to be less engaging, and this is not good. The good thing is when we really have patient-centered care, when we listen to them, and when we are involved with them.
I saw a publication showing that female and male surgeons treating similar patients had the same surgical outcomes. Women are as good as men technically to do surgery and have the same surgical outcomes. However, there is research showing that surgical teams with greater representation of women have improved surgical outcomes because of patient-centered care and the way women conduct bedside attention to patients. And they have better patient experience measures afterward. That is not only from the women who are treating the patients, but the whole environment. Women end up bringing men [into the conversation] and this better improves patient-centered care, and that makes the whole team a better team attending patients. Definitely, we are in the moment of patient experience and satisfaction, and increasing women is a way of achieving better patient satisfaction and experience.
Dr. Ho: There’s much to be said about having female clinicians available for patients. It doesn’t have to be just for female patients, although again, concordance between physicians and patients is certainly beneficial. Besides outcomes benefit, there’s even just a communication benefit. The way that women and men communicate is inherently different. The way women and men experience certain things is also inherently different.
A classic example of this is women who are experiencing a heart attack may not actually have chest pain but present with nausea. As a female who’s sensitive to this, when I see a woman throwing up, I am very attuned to something actually being wrong, knowing that they may not present with classic pain for a syndrome, but actually may be presenting with nausea instead. It doesn’t have to be a woman who takes that knowledge and turns it into something at the bedside. It certainly doesn’t have to, but it is just a natural, easy thing to step into as a female.
While I’m really careful to not step into this “women are better than men” or “men are better than women” argument, there’s something to be said about how the availability of female clinicians for all patients, not just female patients, can have benefit. Again, it’s shown in studies with cardiovascular outcomes and cardiologists, it’s certainly shown in ob.gyn., particularly for underrepresented minorities as well for maternal outcomes of Black mothers. It’s certainly shown again in patient satisfaction, which is concordance.
There is a profound level of research already on this that goes beyond just the idea of stacking the bench and putting more women in there. That’s not the value. We’re not just here to check off the box. We’re here to actually lend some value to our patients and, again, to one another as well.
Dr. Glatter: Absolutely. These are excellent points. The point you make about patient presentation is so vital. The fact that women have nausea sometimes in ACS presentations, the research never was really attentive to this. It was biased. The symptoms that women may have that are not “typical” for ACS weren’t included in patient presentations. Educating everyone about, overall, the types of presentations that we can recognize is vital and important.
Dr. Ho: Yes. It’s worth saying that, when you look at how medicine and research developed, classically, who were the research participants? They were often White men. They were college students who, historically, because women were not allowed to go to college, were men.
I say that not to fault the institution, because that was the culture of our history, but to just say it is okay to question things. It is okay to realize that someone’s presenting outside of the box and that maybe we actually need to reframe what even created the walls of the box in the first place.
Dr. Glatter: Thank you again for joining us. I truly appreciate your insight and expertise.
Dr. Glatter is assistant professor of emergency medicine, department of emergency medicine, Hofstra/Northwell, New York. Dr. Ho is senior vice president of clinical informatics & analytics, department of emergency medicine, Integrative Emergency Services, Dallas. Dr. Loyola Ferreira is a master of science candidate, department of experimental surgery, McGill University, Montreal. They reported that they had no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining me to discuss ways to address and reform the toxic culture associated with medical training is Dr. Amy Faith Ho, senior vice president of clinical informatics and analytics at Integrative Emergency Services in Dallas. Also joining us is Dr. Júlia Loyola Ferreira, a pediatric surgeon originally from Brazil, now practicing at Montreal Children’s and focused on advocacy for gender equity and patient-centered care.
Welcome to both of you. Thanks so much for joining me.
Amy Faith Ho, MD, MPH: Thanks so much for having us, Rob.
Dr. Glatter: Amy, I noticed a tweet recently where you talked about how your career choice was affected by the toxic environment in medical school, affecting your choice of residency. Can you elaborate on that?
Dr. Ho: In this instance, what we’re talking about is gender, but it can be directed toward any number of other groups as well.
What you’re alluding to is a tweet by Stanford Surgery Group showing the next residency class, and what was really stunning about this residency class was that it was almost all females. And this was something that took off on social media.
When I saw this, I was really brought back to one of my personal experiences that I chose to share, which was basically that, as a medical student, I really wanted to be a surgeon. I’m an emergency medicine doctor now, so you know that didn’t happen.
The story that I was sharing was that when I was a third-year medical student rotating on surgery, we had a male attending who was very well known at that school at the time who basically would take the female medical students, and instead of clinic, he would round us up. He would have us sit around him in the workplace room while everyone else was seeing patients, and he would have you look at news clippings of himself. He would tell you stories about himself, like he was holding court for the ladies.
It was this very weird culture where my takeaway as a med student was like, “Wow, this is kind of abusive patriarchy that is supported,” because everyone knew about it and was complicit. Even though I really liked surgery, this was just one instance and one example of where you see this culture that really resonates into the rest of life that I didn’t really want to be a part of.
I went into emergency medicine and loved it. It’s also highly procedural, and I was very happy with where I was. What was really interesting about this tweet to me, though, is that it really took off and garnered hundreds of thousands of views on a very niche topic, because what was most revealing is that everyone has a story like this.
It is not just surgery. It is definitely not just one specialty and it is not just one school. It is an endemic problem in medicine. Not only does it change the lives of young women, but it also says so much about the complicity and the culture that we have in medicine that many people were upset about just the same way I was.
Medical training experience in other countries vs. the United States
Dr. Glatter: Júlia, I want to hear about your experience in medical school, surgery, and then fellowship training and up to the present, if possible.
Júlia Loyola Ferreira, MD: In Brazil, as in many countries now, women have made up the majority of the medical students since 2010. It’s a more female-friendly environment when you’re going through medical school, and I was lucky enough to do rotations in areas of surgery where people were friendly to women.
I lived in this tiny bubble that also gave me the privilege of not facing some things that I can imagine that people in Brazil in different areas and smaller towns face. In Brazil, people try to not talk about this gender agenda. This is something that’s being talked about outside Brazil. But in Brazil, we are years back. People are not really engaging on this conversation. I thought it was going to be hard for me as a woman, because Brazil has around 20% female surgeons.
I knew it was going to be challenging, but I had no idea how bad it was. When I started and things started happening, the list was big. I have an example of everything that is written about – microaggression, implicit bias, discrimination, harassment.
Every time I would try to speak about it and talk to someone, I would be strongly gaslighted. It was the whole training, the whole 5 years. People would say, “Oh, I don’t think it was like that. I think you were overreacting.” People would come with all these different answers for what I was experiencing, and that was frustrating. That was even harder because I had to cope with everything that was happening and I had no one to turn to. I had no mentors.
When I looked up to women who were in surgery, they would be tougher on us young surgeons than the men and they would tell us that we should not complain because in their time it was even harder. Now, it’s getting better and we are supposed to accept whatever comes.
That was at least a little bit of what I experienced in my training. It was only after I finished and started to do research about it that I really encountered a field of people who would echo what I was trying to say to many people in different hospitals that I attended to.
That was the key for me to get out of that situation of being gaslighted and of not being able to really talk about it. Suddenly, I started to publish things about Brazil that nobody was even writing or studying. That gave me a large amount of responsibility, but also motivation to keep going and to see the change.
Valuing women in medicine
Dr. Glatter: This is a very important point that you’re raising about the environment of women being hard on other women. We know that men can be very difficult on and also judgmental toward their trainees.
Amy, how would you respond to that? Was your experience similar in emergency medicine training?
Dr. Ho: I actually don’t feel like it was. I think what Júlia is alluding to is this “mean girls” idea, of “I went through it and thus you have to go through it.” I think you do see this in many specialties. One of the classic ones we hear about, and I don’t want to speak to it too much because it’s not my specialty, is ob.gyn., where it is a very female-dominant surgery group. There’s almost a hazing level that you hear about in some of the more malignant workplaces.
I think that you speak to two really important things. Number one is the numbers game. As you were saying, Brazil actually has many women. That’s awesome. That’s actually different from the United States, especially for the historic, existing workplace and less so for the medical students and for residents. I think step one is having minorities like women just present and there.
Step two is actually including and valuing them. While I think it’s really easy to move away from the women discussion, because there are women when you look around in medicine, it doesn’t mean that women are actually being heard, that they’re actually being accepted, or that their viewpoints are being listened to. A big part of it is normalizing not only seeing women in medicine but also normalizing the narrative of women in medicine.
It’s not just about motherhood; it’s about things like normalizing talking about advancement, academic promotions, pay, culture, being called things like “too reactive,” “anxious,” or “too assertive.” These are all classic things that we hear about when we talk about women.
That’s why we’re looking to not only conversations like this, but also structured ways for women to discuss being women in medicine. There are many women in medicine groups in emergency medicine, including: Females Working in Emergency Medicine (FemInEM); the American College of Emergency Physicians (ACEP) and Society for Academic Emergency Medicine (SAEM) women’s groups, which are American Association of Women Emergency Physicians (AAWEP) and Academy for Women in Academic Emergency Medicine (AWAEM), respectively; and the American Medical Women’s Association (AMWA), which is the American Medical Association’s offshoot.
All of these groups are geared toward normalizing women in medicine, normalizing the narrative of women in medicine, and then working on mentoring and educating so that we can advance our initiatives.
Gender balance is not gender equity
Dr. Glatter: Amy, you bring up a very critical point that mentoring is sort of the antidote to gender-based discrimination. Júlia had written a paper back in November of 2022 that was published in the Journal of Surgical Research talking exactly about this and how important it is to develop mentoring. Part of her research showed that about 20% of medical students who took the survey, about 1,000 people, had mentors, which was very disturbing.
Dr. Loyola Ferreira: Mentorship is one of the ways of changing the reality about gender-based discrimination. Amy’s comment was very strong and we need to really keep saying it, which is that gender balance is not gender equity.
The idea of having more women is not the same as women being recognized as equals, as able as men, and as valued as men. To change this very long culture of male domination, we need support, and this support comes from mentorship.
Although I didn’t have one, I feel that since I started being a mentor for some students, it changed not only them but myself. It gave me strength to keep going, studying, publishing, and going further with this discussion. I feel like the relationship was as good for them as it is for me. That’s how things change.
Diversity, equity, and inclusion training
Dr. Glatter: We’re talking about the reality of gender equity in terms of the ability to have equal respect, recognition, opportunities, and access. That’s really an important point to realize, and for our audience, to understand that gender equity is not gender balance.
Amy, I want to talk about medical school curriculums. Are there advances that you’re aware of being made at certain schools, programs, even in residencies, to enforce these things and make it a priority?
Dr. Ho: We’re really lucky that, as a culture in the United States, medical training is certainly very geared toward diversity. Some of that is certainly unofficial. Some of that just means when they’re looking at a medical school class or looking at rank lists for residency, that they’re cognizant of the different backgrounds that people have. That’s still a step. That is a step, that we’re at least acknowledging it.
There are multiple medical schools and residencies that have more formal unconscious-bias training or diversity, equity, and inclusion (DEI) training, both of which are excellent not only for us in the workplace but also for our patients. Almost all of us will see patients of highly diverse backgrounds. I think the biggest push is looking toward the criteria that we use for selecting trainees and students into our programs. Historically, it’s been MCAT, GPA, and so on.
We’ve really started to ask the question of, are these sorts of “objective criteria” actually biased in institutional ways? They talk about this all the time where GPAs will bias against students from underrepresented minorities (URM). I think all medical students and residencies have really acknowledged that. Although there are still test cutoffs, we are putting an inquisitive eye to what those mean, why they exist, and what are the other things that we should consider. This is all very heartening from what I’m seeing in medical training.
Dr. Glatter: There’s no formal rating system for DEI curriculums right now, like ranking of this school, or this program has more advanced recognition in terms of DEI?
Dr. Ho: No, but on the flip side, the U.S. News & World Report was classically one of the major rankings for medical schools. What we saw fairly recently was that very high-tier schools like Harvard and University of Chicago pulled out of that ranking because that ranking did not acknowledge the value of diversity. That was an incredible stance for medical schools to take, to say, “Hey, you are not evaluating an important criterion of ours.”
Dr. Glatter: That’s a great point. Júlia, where are we now in Brazil in terms of awareness of DEI and curriculum in schools and training programs?
Dr. Loyola Ferreira: Our reality is not as good as in the U.S., unfortunately. I don’t see much discussion on residency programs or medical schools at the moment. I see many students bringing it out and trying to make their schools engage in that discussion. This is something that is coming from the bottom up and not from the top down. I think it can lead to change as well. It is a step and it’s a beginning. Institutions should take the responsibility of doing this from the beginning. This is something where Brazil is still years behind you guys.
Dr. Glatter: It’s unfortunate, but certainly it’s important to hear that. What about in Canada and certainly your institution, McGill, where you just completed a master’s degree?
Dr. Loyola Ferreira: Canada is very much like the U.S. This is something that is really happening and it’s happening fast. I see, at least at McGill, a large amount of DEI inclusion and everything on this discussion. They have institutional courses for us to do as students, and we are all obliged to do many courses, which I think is really educating, especially for people with different cultures and backgrounds.
Dr. Glatter: Amy, where do you think we are in emergency medicine to look at the other side of it? Comparing surgery with emergency medicine, do you think we’re well advanced in terms of DEI, inclusion criteria, respect, and dignity, or are we really far off?
Dr. Ho: I may be biased, but I think emergency medicine is one of the best in terms of this, and I think there are a couple of reasons for it. One is that we are an inherently team-based organization. The attending, the residents, and the students all work in line with one another. There’s less of a hierarchy.
The same is true for our nurses, pharmacists, techs, and EMS. We all work together as a team. Because of that fairly flat structure, it’s really easy for us to value one another as individuals with our diverse backgrounds. In a way, that’s harder for specialties that are more hierarchical, and I think surgery is certainly one of the most hierarchical.
The second reason why emergency medicine is fairly well off in this is that we’re, by nature, a safety-net specialty. We see patients of all-comers, all walks, all backgrounds. I think we both recognize the value of physician-patient concordance. When we share characteristics with our patients, we recognize that value immediately at the bedside.
It exposes us to so much diversity. I see a refugee one day and the next patient is someone who is incarcerated. The next patient after that is an important businessman in society. That diversity and whiplash in the type of patients that we see back-to-back helps us see the playing field in a really flat, diverse way. Because of that, I think our culture is much better, as is our understanding of the value and importance of diversity not only for our programs, but also for our patients.
Do female doctors have better patient outcomes?
Dr. Glatter: Specialties working together in the emergency department is so important. Building that team and that togetherness is so critical. Júlia, would you agree?
Dr. Loyola Ferreira: Definitely. Something Amy said that is beautiful is that you recognize yourself in these patients. In surgery, we are taught to try to be away from the patients and not to put ourselves in the same position. We are taught to be less engaging, and this is not good. The good thing is when we really have patient-centered care, when we listen to them, and when we are involved with them.
I saw a publication showing that female and male surgeons treating similar patients had the same surgical outcomes. Women are as good as men technically to do surgery and have the same surgical outcomes. However, there is research showing that surgical teams with greater representation of women have improved surgical outcomes because of patient-centered care and the way women conduct bedside attention to patients. And they have better patient experience measures afterward. That is not only from the women who are treating the patients, but the whole environment. Women end up bringing men [into the conversation] and this better improves patient-centered care, and that makes the whole team a better team attending patients. Definitely, we are in the moment of patient experience and satisfaction, and increasing women is a way of achieving better patient satisfaction and experience.
Dr. Ho: There’s much to be said about having female clinicians available for patients. It doesn’t have to be just for female patients, although again, concordance between physicians and patients is certainly beneficial. Besides outcomes benefit, there’s even just a communication benefit. The way that women and men communicate is inherently different. The way women and men experience certain things is also inherently different.
A classic example of this is women who are experiencing a heart attack may not actually have chest pain but present with nausea. As a female who’s sensitive to this, when I see a woman throwing up, I am very attuned to something actually being wrong, knowing that they may not present with classic pain for a syndrome, but actually may be presenting with nausea instead. It doesn’t have to be a woman who takes that knowledge and turns it into something at the bedside. It certainly doesn’t have to, but it is just a natural, easy thing to step into as a female.
While I’m really careful to not step into this “women are better than men” or “men are better than women” argument, there’s something to be said about how the availability of female clinicians for all patients, not just female patients, can have benefit. Again, it’s shown in studies with cardiovascular outcomes and cardiologists, it’s certainly shown in ob.gyn., particularly for underrepresented minorities as well for maternal outcomes of Black mothers. It’s certainly shown again in patient satisfaction, which is concordance.
There is a profound level of research already on this that goes beyond just the idea of stacking the bench and putting more women in there. That’s not the value. We’re not just here to check off the box. We’re here to actually lend some value to our patients and, again, to one another as well.
Dr. Glatter: Absolutely. These are excellent points. The point you make about patient presentation is so vital. The fact that women have nausea sometimes in ACS presentations, the research never was really attentive to this. It was biased. The symptoms that women may have that are not “typical” for ACS weren’t included in patient presentations. Educating everyone about, overall, the types of presentations that we can recognize is vital and important.
Dr. Ho: Yes. It’s worth saying that, when you look at how medicine and research developed, classically, who were the research participants? They were often White men. They were college students who, historically, because women were not allowed to go to college, were men.
I say that not to fault the institution, because that was the culture of our history, but to just say it is okay to question things. It is okay to realize that someone’s presenting outside of the box and that maybe we actually need to reframe what even created the walls of the box in the first place.
Dr. Glatter: Thank you again for joining us. I truly appreciate your insight and expertise.
Dr. Glatter is assistant professor of emergency medicine, department of emergency medicine, Hofstra/Northwell, New York. Dr. Ho is senior vice president of clinical informatics & analytics, department of emergency medicine, Integrative Emergency Services, Dallas. Dr. Loyola Ferreira is a master of science candidate, department of experimental surgery, McGill University, Montreal. They reported that they had no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining me to discuss ways to address and reform the toxic culture associated with medical training is Dr. Amy Faith Ho, senior vice president of clinical informatics and analytics at Integrative Emergency Services in Dallas. Also joining us is Dr. Júlia Loyola Ferreira, a pediatric surgeon originally from Brazil, now practicing at Montreal Children’s and focused on advocacy for gender equity and patient-centered care.
Welcome to both of you. Thanks so much for joining me.
Amy Faith Ho, MD, MPH: Thanks so much for having us, Rob.
Dr. Glatter: Amy, I noticed a tweet recently where you talked about how your career choice was affected by the toxic environment in medical school, affecting your choice of residency. Can you elaborate on that?
Dr. Ho: In this instance, what we’re talking about is gender, but it can be directed toward any number of other groups as well.
What you’re alluding to is a tweet by Stanford Surgery Group showing the next residency class, and what was really stunning about this residency class was that it was almost all females. And this was something that took off on social media.
When I saw this, I was really brought back to one of my personal experiences that I chose to share, which was basically that, as a medical student, I really wanted to be a surgeon. I’m an emergency medicine doctor now, so you know that didn’t happen.
The story that I was sharing was that when I was a third-year medical student rotating on surgery, we had a male attending who was very well known at that school at the time who basically would take the female medical students, and instead of clinic, he would round us up. He would have us sit around him in the workplace room while everyone else was seeing patients, and he would have you look at news clippings of himself. He would tell you stories about himself, like he was holding court for the ladies.
It was this very weird culture where my takeaway as a med student was like, “Wow, this is kind of abusive patriarchy that is supported,” because everyone knew about it and was complicit. Even though I really liked surgery, this was just one instance and one example of where you see this culture that really resonates into the rest of life that I didn’t really want to be a part of.
I went into emergency medicine and loved it. It’s also highly procedural, and I was very happy with where I was. What was really interesting about this tweet to me, though, is that it really took off and garnered hundreds of thousands of views on a very niche topic, because what was most revealing is that everyone has a story like this.
It is not just surgery. It is definitely not just one specialty and it is not just one school. It is an endemic problem in medicine. Not only does it change the lives of young women, but it also says so much about the complicity and the culture that we have in medicine that many people were upset about just the same way I was.
Medical training experience in other countries vs. the United States
Dr. Glatter: Júlia, I want to hear about your experience in medical school, surgery, and then fellowship training and up to the present, if possible.
Júlia Loyola Ferreira, MD: In Brazil, as in many countries now, women have made up the majority of the medical students since 2010. It’s a more female-friendly environment when you’re going through medical school, and I was lucky enough to do rotations in areas of surgery where people were friendly to women.
I lived in this tiny bubble that also gave me the privilege of not facing some things that I can imagine that people in Brazil in different areas and smaller towns face. In Brazil, people try to not talk about this gender agenda. This is something that’s being talked about outside Brazil. But in Brazil, we are years back. People are not really engaging on this conversation. I thought it was going to be hard for me as a woman, because Brazil has around 20% female surgeons.
I knew it was going to be challenging, but I had no idea how bad it was. When I started and things started happening, the list was big. I have an example of everything that is written about – microaggression, implicit bias, discrimination, harassment.
Every time I would try to speak about it and talk to someone, I would be strongly gaslighted. It was the whole training, the whole 5 years. People would say, “Oh, I don’t think it was like that. I think you were overreacting.” People would come with all these different answers for what I was experiencing, and that was frustrating. That was even harder because I had to cope with everything that was happening and I had no one to turn to. I had no mentors.
When I looked up to women who were in surgery, they would be tougher on us young surgeons than the men and they would tell us that we should not complain because in their time it was even harder. Now, it’s getting better and we are supposed to accept whatever comes.
That was at least a little bit of what I experienced in my training. It was only after I finished and started to do research about it that I really encountered a field of people who would echo what I was trying to say to many people in different hospitals that I attended to.
That was the key for me to get out of that situation of being gaslighted and of not being able to really talk about it. Suddenly, I started to publish things about Brazil that nobody was even writing or studying. That gave me a large amount of responsibility, but also motivation to keep going and to see the change.
Valuing women in medicine
Dr. Glatter: This is a very important point that you’re raising about the environment of women being hard on other women. We know that men can be very difficult on and also judgmental toward their trainees.
Amy, how would you respond to that? Was your experience similar in emergency medicine training?
Dr. Ho: I actually don’t feel like it was. I think what Júlia is alluding to is this “mean girls” idea, of “I went through it and thus you have to go through it.” I think you do see this in many specialties. One of the classic ones we hear about, and I don’t want to speak to it too much because it’s not my specialty, is ob.gyn., where it is a very female-dominant surgery group. There’s almost a hazing level that you hear about in some of the more malignant workplaces.
I think that you speak to two really important things. Number one is the numbers game. As you were saying, Brazil actually has many women. That’s awesome. That’s actually different from the United States, especially for the historic, existing workplace and less so for the medical students and for residents. I think step one is having minorities like women just present and there.
Step two is actually including and valuing them. While I think it’s really easy to move away from the women discussion, because there are women when you look around in medicine, it doesn’t mean that women are actually being heard, that they’re actually being accepted, or that their viewpoints are being listened to. A big part of it is normalizing not only seeing women in medicine but also normalizing the narrative of women in medicine.
It’s not just about motherhood; it’s about things like normalizing talking about advancement, academic promotions, pay, culture, being called things like “too reactive,” “anxious,” or “too assertive.” These are all classic things that we hear about when we talk about women.
That’s why we’re looking to not only conversations like this, but also structured ways for women to discuss being women in medicine. There are many women in medicine groups in emergency medicine, including: Females Working in Emergency Medicine (FemInEM); the American College of Emergency Physicians (ACEP) and Society for Academic Emergency Medicine (SAEM) women’s groups, which are American Association of Women Emergency Physicians (AAWEP) and Academy for Women in Academic Emergency Medicine (AWAEM), respectively; and the American Medical Women’s Association (AMWA), which is the American Medical Association’s offshoot.
All of these groups are geared toward normalizing women in medicine, normalizing the narrative of women in medicine, and then working on mentoring and educating so that we can advance our initiatives.
Gender balance is not gender equity
Dr. Glatter: Amy, you bring up a very critical point that mentoring is sort of the antidote to gender-based discrimination. Júlia had written a paper back in November of 2022 that was published in the Journal of Surgical Research talking exactly about this and how important it is to develop mentoring. Part of her research showed that about 20% of medical students who took the survey, about 1,000 people, had mentors, which was very disturbing.
Dr. Loyola Ferreira: Mentorship is one of the ways of changing the reality about gender-based discrimination. Amy’s comment was very strong and we need to really keep saying it, which is that gender balance is not gender equity.
The idea of having more women is not the same as women being recognized as equals, as able as men, and as valued as men. To change this very long culture of male domination, we need support, and this support comes from mentorship.
Although I didn’t have one, I feel that since I started being a mentor for some students, it changed not only them but myself. It gave me strength to keep going, studying, publishing, and going further with this discussion. I feel like the relationship was as good for them as it is for me. That’s how things change.
Diversity, equity, and inclusion training
Dr. Glatter: We’re talking about the reality of gender equity in terms of the ability to have equal respect, recognition, opportunities, and access. That’s really an important point to realize, and for our audience, to understand that gender equity is not gender balance.
Amy, I want to talk about medical school curriculums. Are there advances that you’re aware of being made at certain schools, programs, even in residencies, to enforce these things and make it a priority?
Dr. Ho: We’re really lucky that, as a culture in the United States, medical training is certainly very geared toward diversity. Some of that is certainly unofficial. Some of that just means when they’re looking at a medical school class or looking at rank lists for residency, that they’re cognizant of the different backgrounds that people have. That’s still a step. That is a step, that we’re at least acknowledging it.
There are multiple medical schools and residencies that have more formal unconscious-bias training or diversity, equity, and inclusion (DEI) training, both of which are excellent not only for us in the workplace but also for our patients. Almost all of us will see patients of highly diverse backgrounds. I think the biggest push is looking toward the criteria that we use for selecting trainees and students into our programs. Historically, it’s been MCAT, GPA, and so on.
We’ve really started to ask the question of, are these sorts of “objective criteria” actually biased in institutional ways? They talk about this all the time where GPAs will bias against students from underrepresented minorities (URM). I think all medical students and residencies have really acknowledged that. Although there are still test cutoffs, we are putting an inquisitive eye to what those mean, why they exist, and what are the other things that we should consider. This is all very heartening from what I’m seeing in medical training.
Dr. Glatter: There’s no formal rating system for DEI curriculums right now, like ranking of this school, or this program has more advanced recognition in terms of DEI?
Dr. Ho: No, but on the flip side, the U.S. News & World Report was classically one of the major rankings for medical schools. What we saw fairly recently was that very high-tier schools like Harvard and University of Chicago pulled out of that ranking because that ranking did not acknowledge the value of diversity. That was an incredible stance for medical schools to take, to say, “Hey, you are not evaluating an important criterion of ours.”
Dr. Glatter: That’s a great point. Júlia, where are we now in Brazil in terms of awareness of DEI and curriculum in schools and training programs?
Dr. Loyola Ferreira: Our reality is not as good as in the U.S., unfortunately. I don’t see much discussion on residency programs or medical schools at the moment. I see many students bringing it out and trying to make their schools engage in that discussion. This is something that is coming from the bottom up and not from the top down. I think it can lead to change as well. It is a step and it’s a beginning. Institutions should take the responsibility of doing this from the beginning. This is something where Brazil is still years behind you guys.
Dr. Glatter: It’s unfortunate, but certainly it’s important to hear that. What about in Canada and certainly your institution, McGill, where you just completed a master’s degree?
Dr. Loyola Ferreira: Canada is very much like the U.S. This is something that is really happening and it’s happening fast. I see, at least at McGill, a large amount of DEI inclusion and everything on this discussion. They have institutional courses for us to do as students, and we are all obliged to do many courses, which I think is really educating, especially for people with different cultures and backgrounds.
Dr. Glatter: Amy, where do you think we are in emergency medicine to look at the other side of it? Comparing surgery with emergency medicine, do you think we’re well advanced in terms of DEI, inclusion criteria, respect, and dignity, or are we really far off?
Dr. Ho: I may be biased, but I think emergency medicine is one of the best in terms of this, and I think there are a couple of reasons for it. One is that we are an inherently team-based organization. The attending, the residents, and the students all work in line with one another. There’s less of a hierarchy.
The same is true for our nurses, pharmacists, techs, and EMS. We all work together as a team. Because of that fairly flat structure, it’s really easy for us to value one another as individuals with our diverse backgrounds. In a way, that’s harder for specialties that are more hierarchical, and I think surgery is certainly one of the most hierarchical.
The second reason why emergency medicine is fairly well off in this is that we’re, by nature, a safety-net specialty. We see patients of all-comers, all walks, all backgrounds. I think we both recognize the value of physician-patient concordance. When we share characteristics with our patients, we recognize that value immediately at the bedside.
It exposes us to so much diversity. I see a refugee one day and the next patient is someone who is incarcerated. The next patient after that is an important businessman in society. That diversity and whiplash in the type of patients that we see back-to-back helps us see the playing field in a really flat, diverse way. Because of that, I think our culture is much better, as is our understanding of the value and importance of diversity not only for our programs, but also for our patients.
Do female doctors have better patient outcomes?
Dr. Glatter: Specialties working together in the emergency department is so important. Building that team and that togetherness is so critical. Júlia, would you agree?
Dr. Loyola Ferreira: Definitely. Something Amy said that is beautiful is that you recognize yourself in these patients. In surgery, we are taught to try to be away from the patients and not to put ourselves in the same position. We are taught to be less engaging, and this is not good. The good thing is when we really have patient-centered care, when we listen to them, and when we are involved with them.
I saw a publication showing that female and male surgeons treating similar patients had the same surgical outcomes. Women are as good as men technically to do surgery and have the same surgical outcomes. However, there is research showing that surgical teams with greater representation of women have improved surgical outcomes because of patient-centered care and the way women conduct bedside attention to patients. And they have better patient experience measures afterward. That is not only from the women who are treating the patients, but the whole environment. Women end up bringing men [into the conversation] and this better improves patient-centered care, and that makes the whole team a better team attending patients. Definitely, we are in the moment of patient experience and satisfaction, and increasing women is a way of achieving better patient satisfaction and experience.
Dr. Ho: There’s much to be said about having female clinicians available for patients. It doesn’t have to be just for female patients, although again, concordance between physicians and patients is certainly beneficial. Besides outcomes benefit, there’s even just a communication benefit. The way that women and men communicate is inherently different. The way women and men experience certain things is also inherently different.
A classic example of this is women who are experiencing a heart attack may not actually have chest pain but present with nausea. As a female who’s sensitive to this, when I see a woman throwing up, I am very attuned to something actually being wrong, knowing that they may not present with classic pain for a syndrome, but actually may be presenting with nausea instead. It doesn’t have to be a woman who takes that knowledge and turns it into something at the bedside. It certainly doesn’t have to, but it is just a natural, easy thing to step into as a female.
While I’m really careful to not step into this “women are better than men” or “men are better than women” argument, there’s something to be said about how the availability of female clinicians for all patients, not just female patients, can have benefit. Again, it’s shown in studies with cardiovascular outcomes and cardiologists, it’s certainly shown in ob.gyn., particularly for underrepresented minorities as well for maternal outcomes of Black mothers. It’s certainly shown again in patient satisfaction, which is concordance.
There is a profound level of research already on this that goes beyond just the idea of stacking the bench and putting more women in there. That’s not the value. We’re not just here to check off the box. We’re here to actually lend some value to our patients and, again, to one another as well.
Dr. Glatter: Absolutely. These are excellent points. The point you make about patient presentation is so vital. The fact that women have nausea sometimes in ACS presentations, the research never was really attentive to this. It was biased. The symptoms that women may have that are not “typical” for ACS weren’t included in patient presentations. Educating everyone about, overall, the types of presentations that we can recognize is vital and important.
Dr. Ho: Yes. It’s worth saying that, when you look at how medicine and research developed, classically, who were the research participants? They were often White men. They were college students who, historically, because women were not allowed to go to college, were men.
I say that not to fault the institution, because that was the culture of our history, but to just say it is okay to question things. It is okay to realize that someone’s presenting outside of the box and that maybe we actually need to reframe what even created the walls of the box in the first place.
Dr. Glatter: Thank you again for joining us. I truly appreciate your insight and expertise.
Dr. Glatter is assistant professor of emergency medicine, department of emergency medicine, Hofstra/Northwell, New York. Dr. Ho is senior vice president of clinical informatics & analytics, department of emergency medicine, Integrative Emergency Services, Dallas. Dr. Loyola Ferreira is a master of science candidate, department of experimental surgery, McGill University, Montreal. They reported that they had no conflicts of interest.
A version of this article first appeared on Medscape.com.