User login
Is ‘Med Ed’ changing for better or worse?
The next generation of physicians is learning much differently from how established doctors once did. Training has shifted from an acute focus on disease to a wider approach that considers patients within the larger context of their community and society. Although many, like myself, see this as progress, others have expressed doubts about this and many other changes.
Amid the madness that is the year 2020, I’m grateful to have a moment to reflect on this subject. Five years ago, in celebration of Medscape’s 20th anniversary, I spoke with various leaders in medical education to learn how med ed had evolved since they were in school. Since then, I’ve gone from student to faculty. This year, for Medscape’s 25th anniversary, I reached out to current medical trainees to reflect on how much things have changed in such a short time.
From adjustments forced on us by COVID-19 to trends that predated the pandemic – including an increased emphasis on social justice and a decreased emphasis on other material – becoming a doctor no longer looks like it did just a half-decade ago.
Social justice is now in the curricula
More than ever, medical training has shifted toward humanism, population health, and social justice. Students are now being shown not only how to treat the patient in front of them but how to “treat” the larger communities they serve. Research skills around social drivers of health, such as structural racism, are increasingly becoming status quo.
In reflecting on her current experience, Emily Kahoud, a third-year medical student at New Jersey Medical School, Newark, told me about a course she took that was devoted to health equity. She applauded how her professors have incorporated this education into their courses. “It’s so nice and refreshing to be in a community that appreciates that.”
I, too, have seen this change firsthand. In addition to caring for patients and teaching at the University of North Carolina at Chapel Hill, I work with a team that develops curricula around social justice. We strive to integrate this material into existing courses and rotations. I believe that this is not only the right thing to teach trainees in order to help their future patients, but that it also reduces harm that many students experience. The “hidden curriculum” of medical school has long marginalized anyone who isn’t White and/or male.
Children, women, and the elderly were often referred to as “special populations” during my training. Even now, content about social and structural drivers of health is still most often relegated to separate courses rather than integrated into existing material. I hope to help improve this at my institution and that others are doing the same elsewhere.
If the current students I spoke with are any indication, further integration will be a welcomed change. Travis Benson, a third-year medical student at Harvard Medical School, Boston, appreciates where medical training is headed. Specifically, he is interested in inequities in the care of transgender patients. He says he has loved what his school has done with education on issues not previously considered part of med ed. “In the first week of school, we go on tours and spend time in community health centers and learn about the ‘Family Van,’ a mobile health care clinic that offers free care. I even had an opportunity to have a longitudinal clinic experience at a jail.”
While some critics argue that this learning goes too far, others argue that it has not gone far enough fast enough. In general, I consider the progress made in this area since my time in med school to be a very good thing. Medical students are now being taught to think about the science of medicine in the context of the larger human condition.
More technology, less preclinical time and cost
Beyond evolution in curricular content, technical and logistical changes have dramatically reshaped med ed. Since I started my training in 2012, most medical schools now no longer formally require students to attend lectures. Instead, they make them available online for students to view on demand. This undoubtedly makes schedules more flexible, allows students to learn at their own pace, and helps accommodate students with different needs.
Another big change: Preclinical years may now be as short as 1.5 years or less. This is a big draw for some students. Most choose to go to medical school to take care of patients. Shortening the preclinical years means students have more time immersed in patient care and less time dealing with medical minutiae.
That also means that they can spend more time thinking about professional development. Ramie Fathy, a fourth-year student, told me, “I came to Penn [University of Pennsylvania in Philadelphia] because of the shortened preclinical curriculum. That allowed more time on the back end to explore different specialties.” Although some established doctors worry about what scientific details may be left out, providing more hands-on experience sure seems like a good thing to me. Learning from textbooks can only take you so far in this profession.
Another, and more expected, development is the use of ever-advancing technology. Some schools now offer 3D virtual modeling for the study of anatomy, as well as a myriad of electronic visual aids for subjects like pathology and microbiology. Adapting to technological changes can be challenging, however, especially because more nontraditional students are being admitted to medical school each year.
Kahoud is one such nontraditional – older – student. She had some concerns about reliance on newer resources going in. “It [medical school] has become increasingly dependent on technology, even before COVID,” she said. “When you are not well versed in these tools it can definitely be a struggle.”
Thanks to the pandemic, remote learning is now the name of the game for many. As a result, instructors have had to amend their teaching styles to suit distance education, various untested applications and programs have been integrated into the curriculum, and students and administrators alike have had to find alternative ways to build a sense of community.
Is this a glimpse at the future for med ed? And if so, what may be lost or gained from this transition? Tino Delamerced, a third-year student at the Brown University, Providence, R.I., shared a likely very widely held hope: “If the preclinical years can be totally remote permanently, then can tuition be cheaper?”
Med ed debt keeps growing and remains a huge deterrent for potential students, especially those who are the first in their family to pursue medicine, come from a disadvantaged background, or have other people for whom they are financially responsible. Is it possible that the restrictions of COVID-19 could finally lead to cost cutting?
A bigger solution – free medical school – predated the pandemic. Institutions such as New York University have completely eliminated tuition, whereas others such as the Icahn School of Medicine at Mount Sinai (my alma mater) have limited the amount of debt with which a student graduates. You can imagine my frustration that the debt limit policy was enacted after I graduated.
Still, as optimistic as some have been at this movement that developed in the past 5 years, many think this specific evolution is little more than a “pipe dream.”
Current students score big with USMLE change
Beyond med school cost, another universally despised part of medical training that has seen a dramatic change is the licensing examination. My dedicated study period for the United States Medical Licensing Examination (USMLE) Step 1 was my worst time of medical school. Well, it was second to holding a retractor in the operating room for hours at a time.
Like everyone, I suspected that Step 1 would not be an accurate indicator of my ability to actually care for patients. As a practicing physician, I can now tell you for sure that this is the case. How lucky for the next generation, then, that the test is going to a pass/fail grading system.
Step 1 has always been important, as residency programs rely on the score to weed out applicants. Even if that screening emphasis simply gets shifted to scores on other examinations, this change still feels like progress. As Fathy told me, “There will likely be more emphasis on USMLE Step 2. But I think, based on practice questions I’ve done, that is more relevant to clinical abilities.” From my new vantage point, I can confirm that.
Not everyone is excited, though. Delamerced told me that he fears that the pass/fail Step 1 score may disparately affect students outside of allopathic medical schools. He said that the new scoring system “does not allow students to distinguish themselves via a standardized test score. That may hurt IMGs or DO students.”
Even then, Delamerced conceded that the change has some clear benefits. “For med students’ mental health, it’s probably a good thing.” From a population-based perspective, a medical student’s mental health often declines throughout school. Standardized exams are not the only cause, but we all know that it is a big contributor. The Step 1 switch can only help with that.
Finish faster or learn more?
In addition to evolution in the content and methods used to teach and assess current med students, the duration of med ed has also changed. Today’s students can choose to complete medical school in less than 4 years.
At the school where I work, the Fully Integrated Readiness for Service Training (FIRST) program allows certain students to complete their education in just 3 years. This program is for students who already know early on that they want to pursue a specialty included on our curated list. The goal of the program is to ultimately train physicians in family medicine, psychiatry, pediatrics, or general surgery in order to provide crucial care to those who need it most in our state.
Other medical schools offer accelerated MD programs for students based on various admissions criteria and specialty interest. The benefit of these programs is that shortening training time cuts down on debt for students.
Accelerated MD programs also aim to quickly increase the number of practicing physicians. This is especially important for primary care, which expects to see a growing gap in the years to come. That aim has come under some criticism, as some believe that the 4-year program was the standard for a reason. But when I reflect on it, I often wonder whether my fourth year was really worth $60,000. I spent a lot of that year traveling for residency interviews and watching Netflix between clinic electives.
Instead of finishing medical school faster, some students now have an opportunity to integrate additional training and education. Benson told me that, at Harvard, many students take a year off to pursue other opportunities. He said, “About 40% of students end up taking a fifth year to do either a master’s degree, global health, or research.” Benson said the additional learning opportunities are broad. “Some classmates even go to other schools altogether to get additional education.” Widened areas of learning are likely to produce better doctors, in my opinion.
This chance to look back on medical education has shown me that the ways in which it has changed rapidly in just the past few years are largely positive. Although COVID-19 has been an unwanted bane, it has also forced schools to integrate new technology and has placed an even brighter spotlight on health inequities and other areas in which education further improved. I hope that, when I look back on med ed in another 5 years, it has grown even more flexible and nimble in meeting the ever-changing needs of students and patients alike.
Alexa Mieses Malchuk, MD, MPH, was born and raised in Queens, New York. Social justice is what drew her to family medicine. As an academic physician at the University of North Carolina, she practices inpatient and outpatient medicine and serves as a medical educator for students and residents.
This article first appeared on Medscape.com.
The next generation of physicians is learning much differently from how established doctors once did. Training has shifted from an acute focus on disease to a wider approach that considers patients within the larger context of their community and society. Although many, like myself, see this as progress, others have expressed doubts about this and many other changes.
Amid the madness that is the year 2020, I’m grateful to have a moment to reflect on this subject. Five years ago, in celebration of Medscape’s 20th anniversary, I spoke with various leaders in medical education to learn how med ed had evolved since they were in school. Since then, I’ve gone from student to faculty. This year, for Medscape’s 25th anniversary, I reached out to current medical trainees to reflect on how much things have changed in such a short time.
From adjustments forced on us by COVID-19 to trends that predated the pandemic – including an increased emphasis on social justice and a decreased emphasis on other material – becoming a doctor no longer looks like it did just a half-decade ago.
Social justice is now in the curricula
More than ever, medical training has shifted toward humanism, population health, and social justice. Students are now being shown not only how to treat the patient in front of them but how to “treat” the larger communities they serve. Research skills around social drivers of health, such as structural racism, are increasingly becoming status quo.
In reflecting on her current experience, Emily Kahoud, a third-year medical student at New Jersey Medical School, Newark, told me about a course she took that was devoted to health equity. She applauded how her professors have incorporated this education into their courses. “It’s so nice and refreshing to be in a community that appreciates that.”
I, too, have seen this change firsthand. In addition to caring for patients and teaching at the University of North Carolina at Chapel Hill, I work with a team that develops curricula around social justice. We strive to integrate this material into existing courses and rotations. I believe that this is not only the right thing to teach trainees in order to help their future patients, but that it also reduces harm that many students experience. The “hidden curriculum” of medical school has long marginalized anyone who isn’t White and/or male.
Children, women, and the elderly were often referred to as “special populations” during my training. Even now, content about social and structural drivers of health is still most often relegated to separate courses rather than integrated into existing material. I hope to help improve this at my institution and that others are doing the same elsewhere.
If the current students I spoke with are any indication, further integration will be a welcomed change. Travis Benson, a third-year medical student at Harvard Medical School, Boston, appreciates where medical training is headed. Specifically, he is interested in inequities in the care of transgender patients. He says he has loved what his school has done with education on issues not previously considered part of med ed. “In the first week of school, we go on tours and spend time in community health centers and learn about the ‘Family Van,’ a mobile health care clinic that offers free care. I even had an opportunity to have a longitudinal clinic experience at a jail.”
While some critics argue that this learning goes too far, others argue that it has not gone far enough fast enough. In general, I consider the progress made in this area since my time in med school to be a very good thing. Medical students are now being taught to think about the science of medicine in the context of the larger human condition.
More technology, less preclinical time and cost
Beyond evolution in curricular content, technical and logistical changes have dramatically reshaped med ed. Since I started my training in 2012, most medical schools now no longer formally require students to attend lectures. Instead, they make them available online for students to view on demand. This undoubtedly makes schedules more flexible, allows students to learn at their own pace, and helps accommodate students with different needs.
Another big change: Preclinical years may now be as short as 1.5 years or less. This is a big draw for some students. Most choose to go to medical school to take care of patients. Shortening the preclinical years means students have more time immersed in patient care and less time dealing with medical minutiae.
That also means that they can spend more time thinking about professional development. Ramie Fathy, a fourth-year student, told me, “I came to Penn [University of Pennsylvania in Philadelphia] because of the shortened preclinical curriculum. That allowed more time on the back end to explore different specialties.” Although some established doctors worry about what scientific details may be left out, providing more hands-on experience sure seems like a good thing to me. Learning from textbooks can only take you so far in this profession.
Another, and more expected, development is the use of ever-advancing technology. Some schools now offer 3D virtual modeling for the study of anatomy, as well as a myriad of electronic visual aids for subjects like pathology and microbiology. Adapting to technological changes can be challenging, however, especially because more nontraditional students are being admitted to medical school each year.
Kahoud is one such nontraditional – older – student. She had some concerns about reliance on newer resources going in. “It [medical school] has become increasingly dependent on technology, even before COVID,” she said. “When you are not well versed in these tools it can definitely be a struggle.”
Thanks to the pandemic, remote learning is now the name of the game for many. As a result, instructors have had to amend their teaching styles to suit distance education, various untested applications and programs have been integrated into the curriculum, and students and administrators alike have had to find alternative ways to build a sense of community.
Is this a glimpse at the future for med ed? And if so, what may be lost or gained from this transition? Tino Delamerced, a third-year student at the Brown University, Providence, R.I., shared a likely very widely held hope: “If the preclinical years can be totally remote permanently, then can tuition be cheaper?”
Med ed debt keeps growing and remains a huge deterrent for potential students, especially those who are the first in their family to pursue medicine, come from a disadvantaged background, or have other people for whom they are financially responsible. Is it possible that the restrictions of COVID-19 could finally lead to cost cutting?
A bigger solution – free medical school – predated the pandemic. Institutions such as New York University have completely eliminated tuition, whereas others such as the Icahn School of Medicine at Mount Sinai (my alma mater) have limited the amount of debt with which a student graduates. You can imagine my frustration that the debt limit policy was enacted after I graduated.
Still, as optimistic as some have been at this movement that developed in the past 5 years, many think this specific evolution is little more than a “pipe dream.”
Current students score big with USMLE change
Beyond med school cost, another universally despised part of medical training that has seen a dramatic change is the licensing examination. My dedicated study period for the United States Medical Licensing Examination (USMLE) Step 1 was my worst time of medical school. Well, it was second to holding a retractor in the operating room for hours at a time.
Like everyone, I suspected that Step 1 would not be an accurate indicator of my ability to actually care for patients. As a practicing physician, I can now tell you for sure that this is the case. How lucky for the next generation, then, that the test is going to a pass/fail grading system.
Step 1 has always been important, as residency programs rely on the score to weed out applicants. Even if that screening emphasis simply gets shifted to scores on other examinations, this change still feels like progress. As Fathy told me, “There will likely be more emphasis on USMLE Step 2. But I think, based on practice questions I’ve done, that is more relevant to clinical abilities.” From my new vantage point, I can confirm that.
Not everyone is excited, though. Delamerced told me that he fears that the pass/fail Step 1 score may disparately affect students outside of allopathic medical schools. He said that the new scoring system “does not allow students to distinguish themselves via a standardized test score. That may hurt IMGs or DO students.”
Even then, Delamerced conceded that the change has some clear benefits. “For med students’ mental health, it’s probably a good thing.” From a population-based perspective, a medical student’s mental health often declines throughout school. Standardized exams are not the only cause, but we all know that it is a big contributor. The Step 1 switch can only help with that.
Finish faster or learn more?
In addition to evolution in the content and methods used to teach and assess current med students, the duration of med ed has also changed. Today’s students can choose to complete medical school in less than 4 years.
At the school where I work, the Fully Integrated Readiness for Service Training (FIRST) program allows certain students to complete their education in just 3 years. This program is for students who already know early on that they want to pursue a specialty included on our curated list. The goal of the program is to ultimately train physicians in family medicine, psychiatry, pediatrics, or general surgery in order to provide crucial care to those who need it most in our state.
Other medical schools offer accelerated MD programs for students based on various admissions criteria and specialty interest. The benefit of these programs is that shortening training time cuts down on debt for students.
Accelerated MD programs also aim to quickly increase the number of practicing physicians. This is especially important for primary care, which expects to see a growing gap in the years to come. That aim has come under some criticism, as some believe that the 4-year program was the standard for a reason. But when I reflect on it, I often wonder whether my fourth year was really worth $60,000. I spent a lot of that year traveling for residency interviews and watching Netflix between clinic electives.
Instead of finishing medical school faster, some students now have an opportunity to integrate additional training and education. Benson told me that, at Harvard, many students take a year off to pursue other opportunities. He said, “About 40% of students end up taking a fifth year to do either a master’s degree, global health, or research.” Benson said the additional learning opportunities are broad. “Some classmates even go to other schools altogether to get additional education.” Widened areas of learning are likely to produce better doctors, in my opinion.
This chance to look back on medical education has shown me that the ways in which it has changed rapidly in just the past few years are largely positive. Although COVID-19 has been an unwanted bane, it has also forced schools to integrate new technology and has placed an even brighter spotlight on health inequities and other areas in which education further improved. I hope that, when I look back on med ed in another 5 years, it has grown even more flexible and nimble in meeting the ever-changing needs of students and patients alike.
Alexa Mieses Malchuk, MD, MPH, was born and raised in Queens, New York. Social justice is what drew her to family medicine. As an academic physician at the University of North Carolina, she practices inpatient and outpatient medicine and serves as a medical educator for students and residents.
This article first appeared on Medscape.com.
The next generation of physicians is learning much differently from how established doctors once did. Training has shifted from an acute focus on disease to a wider approach that considers patients within the larger context of their community and society. Although many, like myself, see this as progress, others have expressed doubts about this and many other changes.
Amid the madness that is the year 2020, I’m grateful to have a moment to reflect on this subject. Five years ago, in celebration of Medscape’s 20th anniversary, I spoke with various leaders in medical education to learn how med ed had evolved since they were in school. Since then, I’ve gone from student to faculty. This year, for Medscape’s 25th anniversary, I reached out to current medical trainees to reflect on how much things have changed in such a short time.
From adjustments forced on us by COVID-19 to trends that predated the pandemic – including an increased emphasis on social justice and a decreased emphasis on other material – becoming a doctor no longer looks like it did just a half-decade ago.
Social justice is now in the curricula
More than ever, medical training has shifted toward humanism, population health, and social justice. Students are now being shown not only how to treat the patient in front of them but how to “treat” the larger communities they serve. Research skills around social drivers of health, such as structural racism, are increasingly becoming status quo.
In reflecting on her current experience, Emily Kahoud, a third-year medical student at New Jersey Medical School, Newark, told me about a course she took that was devoted to health equity. She applauded how her professors have incorporated this education into their courses. “It’s so nice and refreshing to be in a community that appreciates that.”
I, too, have seen this change firsthand. In addition to caring for patients and teaching at the University of North Carolina at Chapel Hill, I work with a team that develops curricula around social justice. We strive to integrate this material into existing courses and rotations. I believe that this is not only the right thing to teach trainees in order to help their future patients, but that it also reduces harm that many students experience. The “hidden curriculum” of medical school has long marginalized anyone who isn’t White and/or male.
Children, women, and the elderly were often referred to as “special populations” during my training. Even now, content about social and structural drivers of health is still most often relegated to separate courses rather than integrated into existing material. I hope to help improve this at my institution and that others are doing the same elsewhere.
If the current students I spoke with are any indication, further integration will be a welcomed change. Travis Benson, a third-year medical student at Harvard Medical School, Boston, appreciates where medical training is headed. Specifically, he is interested in inequities in the care of transgender patients. He says he has loved what his school has done with education on issues not previously considered part of med ed. “In the first week of school, we go on tours and spend time in community health centers and learn about the ‘Family Van,’ a mobile health care clinic that offers free care. I even had an opportunity to have a longitudinal clinic experience at a jail.”
While some critics argue that this learning goes too far, others argue that it has not gone far enough fast enough. In general, I consider the progress made in this area since my time in med school to be a very good thing. Medical students are now being taught to think about the science of medicine in the context of the larger human condition.
More technology, less preclinical time and cost
Beyond evolution in curricular content, technical and logistical changes have dramatically reshaped med ed. Since I started my training in 2012, most medical schools now no longer formally require students to attend lectures. Instead, they make them available online for students to view on demand. This undoubtedly makes schedules more flexible, allows students to learn at their own pace, and helps accommodate students with different needs.
Another big change: Preclinical years may now be as short as 1.5 years or less. This is a big draw for some students. Most choose to go to medical school to take care of patients. Shortening the preclinical years means students have more time immersed in patient care and less time dealing with medical minutiae.
That also means that they can spend more time thinking about professional development. Ramie Fathy, a fourth-year student, told me, “I came to Penn [University of Pennsylvania in Philadelphia] because of the shortened preclinical curriculum. That allowed more time on the back end to explore different specialties.” Although some established doctors worry about what scientific details may be left out, providing more hands-on experience sure seems like a good thing to me. Learning from textbooks can only take you so far in this profession.
Another, and more expected, development is the use of ever-advancing technology. Some schools now offer 3D virtual modeling for the study of anatomy, as well as a myriad of electronic visual aids for subjects like pathology and microbiology. Adapting to technological changes can be challenging, however, especially because more nontraditional students are being admitted to medical school each year.
Kahoud is one such nontraditional – older – student. She had some concerns about reliance on newer resources going in. “It [medical school] has become increasingly dependent on technology, even before COVID,” she said. “When you are not well versed in these tools it can definitely be a struggle.”
Thanks to the pandemic, remote learning is now the name of the game for many. As a result, instructors have had to amend their teaching styles to suit distance education, various untested applications and programs have been integrated into the curriculum, and students and administrators alike have had to find alternative ways to build a sense of community.
Is this a glimpse at the future for med ed? And if so, what may be lost or gained from this transition? Tino Delamerced, a third-year student at the Brown University, Providence, R.I., shared a likely very widely held hope: “If the preclinical years can be totally remote permanently, then can tuition be cheaper?”
Med ed debt keeps growing and remains a huge deterrent for potential students, especially those who are the first in their family to pursue medicine, come from a disadvantaged background, or have other people for whom they are financially responsible. Is it possible that the restrictions of COVID-19 could finally lead to cost cutting?
A bigger solution – free medical school – predated the pandemic. Institutions such as New York University have completely eliminated tuition, whereas others such as the Icahn School of Medicine at Mount Sinai (my alma mater) have limited the amount of debt with which a student graduates. You can imagine my frustration that the debt limit policy was enacted after I graduated.
Still, as optimistic as some have been at this movement that developed in the past 5 years, many think this specific evolution is little more than a “pipe dream.”
Current students score big with USMLE change
Beyond med school cost, another universally despised part of medical training that has seen a dramatic change is the licensing examination. My dedicated study period for the United States Medical Licensing Examination (USMLE) Step 1 was my worst time of medical school. Well, it was second to holding a retractor in the operating room for hours at a time.
Like everyone, I suspected that Step 1 would not be an accurate indicator of my ability to actually care for patients. As a practicing physician, I can now tell you for sure that this is the case. How lucky for the next generation, then, that the test is going to a pass/fail grading system.
Step 1 has always been important, as residency programs rely on the score to weed out applicants. Even if that screening emphasis simply gets shifted to scores on other examinations, this change still feels like progress. As Fathy told me, “There will likely be more emphasis on USMLE Step 2. But I think, based on practice questions I’ve done, that is more relevant to clinical abilities.” From my new vantage point, I can confirm that.
Not everyone is excited, though. Delamerced told me that he fears that the pass/fail Step 1 score may disparately affect students outside of allopathic medical schools. He said that the new scoring system “does not allow students to distinguish themselves via a standardized test score. That may hurt IMGs or DO students.”
Even then, Delamerced conceded that the change has some clear benefits. “For med students’ mental health, it’s probably a good thing.” From a population-based perspective, a medical student’s mental health often declines throughout school. Standardized exams are not the only cause, but we all know that it is a big contributor. The Step 1 switch can only help with that.
Finish faster or learn more?
In addition to evolution in the content and methods used to teach and assess current med students, the duration of med ed has also changed. Today’s students can choose to complete medical school in less than 4 years.
At the school where I work, the Fully Integrated Readiness for Service Training (FIRST) program allows certain students to complete their education in just 3 years. This program is for students who already know early on that they want to pursue a specialty included on our curated list. The goal of the program is to ultimately train physicians in family medicine, psychiatry, pediatrics, or general surgery in order to provide crucial care to those who need it most in our state.
Other medical schools offer accelerated MD programs for students based on various admissions criteria and specialty interest. The benefit of these programs is that shortening training time cuts down on debt for students.
Accelerated MD programs also aim to quickly increase the number of practicing physicians. This is especially important for primary care, which expects to see a growing gap in the years to come. That aim has come under some criticism, as some believe that the 4-year program was the standard for a reason. But when I reflect on it, I often wonder whether my fourth year was really worth $60,000. I spent a lot of that year traveling for residency interviews and watching Netflix between clinic electives.
Instead of finishing medical school faster, some students now have an opportunity to integrate additional training and education. Benson told me that, at Harvard, many students take a year off to pursue other opportunities. He said, “About 40% of students end up taking a fifth year to do either a master’s degree, global health, or research.” Benson said the additional learning opportunities are broad. “Some classmates even go to other schools altogether to get additional education.” Widened areas of learning are likely to produce better doctors, in my opinion.
This chance to look back on medical education has shown me that the ways in which it has changed rapidly in just the past few years are largely positive. Although COVID-19 has been an unwanted bane, it has also forced schools to integrate new technology and has placed an even brighter spotlight on health inequities and other areas in which education further improved. I hope that, when I look back on med ed in another 5 years, it has grown even more flexible and nimble in meeting the ever-changing needs of students and patients alike.
Alexa Mieses Malchuk, MD, MPH, was born and raised in Queens, New York. Social justice is what drew her to family medicine. As an academic physician at the University of North Carolina, she practices inpatient and outpatient medicine and serves as a medical educator for students and residents.
This article first appeared on Medscape.com.
Colorectal cancer screening guidelines: How to make best use of all of them
The recent death of “Black Panther” star Chadwick Boseman has resulted in colorectal cancer (CRC) screening guidelines receiving more attention. Mr. Boseman was diagnosed with Stage 3 CRC in 2016 and underwent treatment. He passed away 4 years later at the young age of 44.
Mr. Boseman’s death has highlighted two important concerns about current screening guidelines for CRC. These include racial disparities in patients with colon cancer and the fact that more younger patients are getting this disease.
There are at least three different sets of CRC screening recommendations from different trusted professional organizations that primary care physicians must decide how to follow. These organizations each published their guidelines indicating review of the best available evidence. On first glance there is discrepancy between these guidelines, but a closer look at them reveals they have a lot of similarities.
The U.S. Multi-Society Task Force of Colorectal Cancer (MSTF), which represents the American College of Gastroenterology, the American Gatroenterological Association, and the American Society for Gastrointestinal Endoscopy, is one of the organizations that offers guidelines. The MSTF recommends CRC screening for non-African American average risked persons at the age of 50 years (strong recommendation; moderate quality evidence). The first-tier options for this recommendation are to have a colonoscopy every 10 years or annual fecal immunochemial test. Additionally, the MSTF recommends beginning screening of African Americans at age 45 years (weak recommendation; very-low-quality evidence). This recommendation cites higher incidence rates, earlier mean age at onset, higher proportion of cancers before age 50 years and late-stage presentation. The MSTF indicates that the increased rate of CRC at an earlier age in African Americans is caused by a combination of biologic and societal factors, but do not point to what those are. This earlier screening is not backed by evidence that it in fact improves morbidity or mortality outcomes. The MSTF also address screening among high-risk individuals. Those with first degree relatives with CRC or advanced adenomas diagnosed before the age of 60 years should be screened beginning at age 40 years or 10 years younger than the age the relative was diagnosed, whichever comes first, according to the MSTF recommendations. These individuals should have a colonoscopy every 5 years, the MSTF says. Those with first degree relatives with CRC or advanced adenomas diagnosed at older than 60 years should have CRC beginning at 40 years, though with the same testing intervals as average-risk individuals.1
The American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP), however, endorse the guidelines set forth by the United States Preventive Services Task Force (USPSTF). These guidelines were published in 2016 in the JAMA and notably are currently under review. These guidelines recommend routine screening for those at average risk at the age of 50 years. In the publication of these guidelines, the increasing incidence of CRC in those under 50 was acknowledged. It is however stated that the modest benefit of earlier diagnosis made via screening is not better than the increased risk of increased lifetime colonoscopy.2
The publication specifically addresses the disparity among Black adults who have the highest incidence and mortality rates in comparison with other racial/ethnic groups. These guidelines specifically state that there are higher rates of colon cancer among black adults. They however clarify that they think it is because of decreased screening and treatment in this group. When compared with other groups and the screening and treatment is controlled for, there is no longer a difference. Lowering the age for starting screening, therefore, won’t help resolve the disparity because the higher cases in Black adults has resulted from not enough Black adults being screened at the recommended age of 50, according to the USPSTF recommendation statement. As such, rather than changing the age of screening for Black adults, this publication recommends efforts to ensure that screening, follow-up, and treatment are received.
The USPSTF specifically did not include adults with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC. They instead refer to other professional organizations for these recommendations.2
The American Cancer Society (ACS) also had a separate guideline published in CA: A Cancer Journal for Clinicians. It provides a qualified recommendation that CRC screening begin at age 45 years for those with average risk. The guideline also includes a strong recommendation for CRC screening beginning at age 50 years. The qualified recommendation for the younger age group is based on the incidence of colorectal cancer being similar between those aged 45-49 and those aged 50-54 years. The ACS also hypothesized that screening at an earlier age will decrease the disparity among population groups with a higher burden. Importantly, this updated guideline prioritized incidence reduction rather than mortality reduction. The ACS also stressed the need for a multipronged approach to mitigate barriers to CRC screening at the individual, provider, organizational, and policy levels. Similar to the USPSTF, the ACS did not address the screening of those with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC.3
In all of the publications discussing CRC screening guidelines, it is stressed that there is not sufficient uptake of any of these recommendations. Rather than conduct earlier screening, in my opinion, we should focus on programmatic ways to ensure that the existing screening recommendations are followed. This is a space in which we can help affect the disparity seen among population groups.
The most important screening test is the one that patients are willing to use. Primary care physicians can use any of these guidelines to have conversations with patients about risk and when to start screening. Although these guidelines may seem to be different from each other, each one includes strong recommendations with the same information.
Additional studies should be done to determine the benefits and harms of screening in patients with known risk factors such as obesity, cigarette smoking, diabetes, high consumption of alcohol, high consumption of red meat and processed food, inactivity, and low intake of dietary fiber, fruits, and vegetables. It is possible that the higher burden of disease among Black adults is related to societal factors leading to increased obesity and dietary habits that increase rates of CRC.
Primary care physicians would be better served by a tool that allows for risk stratification to help guide early screening for all patients. For certain patients, such a tool might result in them qualifying for screening that begins at a later age than the current guidelines recommend. Finally, primary care physicians must remember that these are just the guidelines for screening for CRC. They all specifically exclude patients experiencing any symptoms. As such, patients with unexplained bleeding, anemia, weight loss, and other symptoms should be evaluated fully, including being considered for colonoscopy to diagnose CRC. Primary care physicians should use these guidelines to screen their asymptomatic patients and should ensure that they provide evaluation of any of the symptoms of CRC.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is also program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on editorial advisory board of Family Practice News.
References
1. Rex DK et al. Gastrointest Endosc. 2017;86(1):18-33.
2. US Preventive Services Task Force. JAMA. 2016;315(23):2564-2575.
3. Wolf AMD et al. CA Cancer J Clin. 2018 Jul;68(4):250-281.
The recent death of “Black Panther” star Chadwick Boseman has resulted in colorectal cancer (CRC) screening guidelines receiving more attention. Mr. Boseman was diagnosed with Stage 3 CRC in 2016 and underwent treatment. He passed away 4 years later at the young age of 44.
Mr. Boseman’s death has highlighted two important concerns about current screening guidelines for CRC. These include racial disparities in patients with colon cancer and the fact that more younger patients are getting this disease.
There are at least three different sets of CRC screening recommendations from different trusted professional organizations that primary care physicians must decide how to follow. These organizations each published their guidelines indicating review of the best available evidence. On first glance there is discrepancy between these guidelines, but a closer look at them reveals they have a lot of similarities.
The U.S. Multi-Society Task Force of Colorectal Cancer (MSTF), which represents the American College of Gastroenterology, the American Gatroenterological Association, and the American Society for Gastrointestinal Endoscopy, is one of the organizations that offers guidelines. The MSTF recommends CRC screening for non-African American average risked persons at the age of 50 years (strong recommendation; moderate quality evidence). The first-tier options for this recommendation are to have a colonoscopy every 10 years or annual fecal immunochemial test. Additionally, the MSTF recommends beginning screening of African Americans at age 45 years (weak recommendation; very-low-quality evidence). This recommendation cites higher incidence rates, earlier mean age at onset, higher proportion of cancers before age 50 years and late-stage presentation. The MSTF indicates that the increased rate of CRC at an earlier age in African Americans is caused by a combination of biologic and societal factors, but do not point to what those are. This earlier screening is not backed by evidence that it in fact improves morbidity or mortality outcomes. The MSTF also address screening among high-risk individuals. Those with first degree relatives with CRC or advanced adenomas diagnosed before the age of 60 years should be screened beginning at age 40 years or 10 years younger than the age the relative was diagnosed, whichever comes first, according to the MSTF recommendations. These individuals should have a colonoscopy every 5 years, the MSTF says. Those with first degree relatives with CRC or advanced adenomas diagnosed at older than 60 years should have CRC beginning at 40 years, though with the same testing intervals as average-risk individuals.1
The American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP), however, endorse the guidelines set forth by the United States Preventive Services Task Force (USPSTF). These guidelines were published in 2016 in the JAMA and notably are currently under review. These guidelines recommend routine screening for those at average risk at the age of 50 years. In the publication of these guidelines, the increasing incidence of CRC in those under 50 was acknowledged. It is however stated that the modest benefit of earlier diagnosis made via screening is not better than the increased risk of increased lifetime colonoscopy.2
The publication specifically addresses the disparity among Black adults who have the highest incidence and mortality rates in comparison with other racial/ethnic groups. These guidelines specifically state that there are higher rates of colon cancer among black adults. They however clarify that they think it is because of decreased screening and treatment in this group. When compared with other groups and the screening and treatment is controlled for, there is no longer a difference. Lowering the age for starting screening, therefore, won’t help resolve the disparity because the higher cases in Black adults has resulted from not enough Black adults being screened at the recommended age of 50, according to the USPSTF recommendation statement. As such, rather than changing the age of screening for Black adults, this publication recommends efforts to ensure that screening, follow-up, and treatment are received.
The USPSTF specifically did not include adults with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC. They instead refer to other professional organizations for these recommendations.2
The American Cancer Society (ACS) also had a separate guideline published in CA: A Cancer Journal for Clinicians. It provides a qualified recommendation that CRC screening begin at age 45 years for those with average risk. The guideline also includes a strong recommendation for CRC screening beginning at age 50 years. The qualified recommendation for the younger age group is based on the incidence of colorectal cancer being similar between those aged 45-49 and those aged 50-54 years. The ACS also hypothesized that screening at an earlier age will decrease the disparity among population groups with a higher burden. Importantly, this updated guideline prioritized incidence reduction rather than mortality reduction. The ACS also stressed the need for a multipronged approach to mitigate barriers to CRC screening at the individual, provider, organizational, and policy levels. Similar to the USPSTF, the ACS did not address the screening of those with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC.3
In all of the publications discussing CRC screening guidelines, it is stressed that there is not sufficient uptake of any of these recommendations. Rather than conduct earlier screening, in my opinion, we should focus on programmatic ways to ensure that the existing screening recommendations are followed. This is a space in which we can help affect the disparity seen among population groups.
The most important screening test is the one that patients are willing to use. Primary care physicians can use any of these guidelines to have conversations with patients about risk and when to start screening. Although these guidelines may seem to be different from each other, each one includes strong recommendations with the same information.
Additional studies should be done to determine the benefits and harms of screening in patients with known risk factors such as obesity, cigarette smoking, diabetes, high consumption of alcohol, high consumption of red meat and processed food, inactivity, and low intake of dietary fiber, fruits, and vegetables. It is possible that the higher burden of disease among Black adults is related to societal factors leading to increased obesity and dietary habits that increase rates of CRC.
Primary care physicians would be better served by a tool that allows for risk stratification to help guide early screening for all patients. For certain patients, such a tool might result in them qualifying for screening that begins at a later age than the current guidelines recommend. Finally, primary care physicians must remember that these are just the guidelines for screening for CRC. They all specifically exclude patients experiencing any symptoms. As such, patients with unexplained bleeding, anemia, weight loss, and other symptoms should be evaluated fully, including being considered for colonoscopy to diagnose CRC. Primary care physicians should use these guidelines to screen their asymptomatic patients and should ensure that they provide evaluation of any of the symptoms of CRC.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is also program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on editorial advisory board of Family Practice News.
References
1. Rex DK et al. Gastrointest Endosc. 2017;86(1):18-33.
2. US Preventive Services Task Force. JAMA. 2016;315(23):2564-2575.
3. Wolf AMD et al. CA Cancer J Clin. 2018 Jul;68(4):250-281.
The recent death of “Black Panther” star Chadwick Boseman has resulted in colorectal cancer (CRC) screening guidelines receiving more attention. Mr. Boseman was diagnosed with Stage 3 CRC in 2016 and underwent treatment. He passed away 4 years later at the young age of 44.
Mr. Boseman’s death has highlighted two important concerns about current screening guidelines for CRC. These include racial disparities in patients with colon cancer and the fact that more younger patients are getting this disease.
There are at least three different sets of CRC screening recommendations from different trusted professional organizations that primary care physicians must decide how to follow. These organizations each published their guidelines indicating review of the best available evidence. On first glance there is discrepancy between these guidelines, but a closer look at them reveals they have a lot of similarities.
The U.S. Multi-Society Task Force of Colorectal Cancer (MSTF), which represents the American College of Gastroenterology, the American Gatroenterological Association, and the American Society for Gastrointestinal Endoscopy, is one of the organizations that offers guidelines. The MSTF recommends CRC screening for non-African American average risked persons at the age of 50 years (strong recommendation; moderate quality evidence). The first-tier options for this recommendation are to have a colonoscopy every 10 years or annual fecal immunochemial test. Additionally, the MSTF recommends beginning screening of African Americans at age 45 years (weak recommendation; very-low-quality evidence). This recommendation cites higher incidence rates, earlier mean age at onset, higher proportion of cancers before age 50 years and late-stage presentation. The MSTF indicates that the increased rate of CRC at an earlier age in African Americans is caused by a combination of biologic and societal factors, but do not point to what those are. This earlier screening is not backed by evidence that it in fact improves morbidity or mortality outcomes. The MSTF also address screening among high-risk individuals. Those with first degree relatives with CRC or advanced adenomas diagnosed before the age of 60 years should be screened beginning at age 40 years or 10 years younger than the age the relative was diagnosed, whichever comes first, according to the MSTF recommendations. These individuals should have a colonoscopy every 5 years, the MSTF says. Those with first degree relatives with CRC or advanced adenomas diagnosed at older than 60 years should have CRC beginning at 40 years, though with the same testing intervals as average-risk individuals.1
The American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP), however, endorse the guidelines set forth by the United States Preventive Services Task Force (USPSTF). These guidelines were published in 2016 in the JAMA and notably are currently under review. These guidelines recommend routine screening for those at average risk at the age of 50 years. In the publication of these guidelines, the increasing incidence of CRC in those under 50 was acknowledged. It is however stated that the modest benefit of earlier diagnosis made via screening is not better than the increased risk of increased lifetime colonoscopy.2
The publication specifically addresses the disparity among Black adults who have the highest incidence and mortality rates in comparison with other racial/ethnic groups. These guidelines specifically state that there are higher rates of colon cancer among black adults. They however clarify that they think it is because of decreased screening and treatment in this group. When compared with other groups and the screening and treatment is controlled for, there is no longer a difference. Lowering the age for starting screening, therefore, won’t help resolve the disparity because the higher cases in Black adults has resulted from not enough Black adults being screened at the recommended age of 50, according to the USPSTF recommendation statement. As such, rather than changing the age of screening for Black adults, this publication recommends efforts to ensure that screening, follow-up, and treatment are received.
The USPSTF specifically did not include adults with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC. They instead refer to other professional organizations for these recommendations.2
The American Cancer Society (ACS) also had a separate guideline published in CA: A Cancer Journal for Clinicians. It provides a qualified recommendation that CRC screening begin at age 45 years for those with average risk. The guideline also includes a strong recommendation for CRC screening beginning at age 50 years. The qualified recommendation for the younger age group is based on the incidence of colorectal cancer being similar between those aged 45-49 and those aged 50-54 years. The ACS also hypothesized that screening at an earlier age will decrease the disparity among population groups with a higher burden. Importantly, this updated guideline prioritized incidence reduction rather than mortality reduction. The ACS also stressed the need for a multipronged approach to mitigate barriers to CRC screening at the individual, provider, organizational, and policy levels. Similar to the USPSTF, the ACS did not address the screening of those with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC.3
In all of the publications discussing CRC screening guidelines, it is stressed that there is not sufficient uptake of any of these recommendations. Rather than conduct earlier screening, in my opinion, we should focus on programmatic ways to ensure that the existing screening recommendations are followed. This is a space in which we can help affect the disparity seen among population groups.
The most important screening test is the one that patients are willing to use. Primary care physicians can use any of these guidelines to have conversations with patients about risk and when to start screening. Although these guidelines may seem to be different from each other, each one includes strong recommendations with the same information.
Additional studies should be done to determine the benefits and harms of screening in patients with known risk factors such as obesity, cigarette smoking, diabetes, high consumption of alcohol, high consumption of red meat and processed food, inactivity, and low intake of dietary fiber, fruits, and vegetables. It is possible that the higher burden of disease among Black adults is related to societal factors leading to increased obesity and dietary habits that increase rates of CRC.
Primary care physicians would be better served by a tool that allows for risk stratification to help guide early screening for all patients. For certain patients, such a tool might result in them qualifying for screening that begins at a later age than the current guidelines recommend. Finally, primary care physicians must remember that these are just the guidelines for screening for CRC. They all specifically exclude patients experiencing any symptoms. As such, patients with unexplained bleeding, anemia, weight loss, and other symptoms should be evaluated fully, including being considered for colonoscopy to diagnose CRC. Primary care physicians should use these guidelines to screen their asymptomatic patients and should ensure that they provide evaluation of any of the symptoms of CRC.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is also program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on editorial advisory board of Family Practice News.
References
1. Rex DK et al. Gastrointest Endosc. 2017;86(1):18-33.
2. US Preventive Services Task Force. JAMA. 2016;315(23):2564-2575.
3. Wolf AMD et al. CA Cancer J Clin. 2018 Jul;68(4):250-281.
When the only clinical choices are ‘lose-lose’
Among the many tolls inflicted on health care workers by COVID-19 is one that is not as easily measured as rates of death or disease, but is no less tangible: moral injury. This is the term by which we describe the psychological, social, and spiritual impact of high-stakes situations that lead to the betrayal or transgression of our own deeply held moral beliefs and values.
The current pandemic has provided innumerable such situations that can increase the risk for moral injury, whether we deal directly with patients infected by the coronavirus or not. Telling family members they cannot visit critically ill loved ones. Delaying code activities, even momentarily, to get fully protected with personal protective equipment. Seeing patients who have delayed their necessary or preventive care. Using video rather than touch to reassure people.
Knowing that we are following guidelines from the Centers for Disease Control and Prevention does not stop our feelings of guilt. The longer this pandemic goes on, the more likely it is that these situations will begin to take a toll on us.
For most of us, being exposed to moral injuries is new; they have historically been most associated with severe traumatic wartime experiences. Soldiers, philosophers, and writers have described the ethical dilemmas inherent in war for as long as recorded history. But the use of this term is a more recent development, which the Moral Injury Project at Syracuse (N.Y.) University describes as probably originating in the Vietnam War–era writings of veteran and peace activist Camillo “Mac” Bica and psychiatrist Jonathan Shay. Examples of wartime events that have been thought to lead to moral injury include: causing the harm or death of civilians, knowingly but without alternatives, or accidentally; failing to provide medical aid to an injured civilian or service member; and following orders that were illegal, immoral, and/or against the rules of engagement or the Geneva Conventions.
However, the occurrence of moral injuries in modern health care is increasingly being reported, primarily as an adverse effect of health care inefficiencies that can contribute to burnout. COVID-19 has now provided an array of additional stressors that can cause moral injuries among health care workers. A recent guidance document on moral injury published by the American Psychiatric Association noted that, in the context of a public health disaster, such as COVID-19, it is sometimes necessary to transition from ordinary standards of care to those more appropriate in a crisis, as in wartime. This forces us all to confront challenging questions for which there may be no clear answers, and to make “lose-lose” choices in which no one involved – patients, family, or clinicians – ends up feeling satisfied or even comfortable.
Our lives have been altered significantly, and for many, completely turned upside down by enormous sacrifices and tragic losses. Globally, physicians account for over half of healthcare worker deaths. In the United States alone, over 900 health care workers have died of COVID-19.
Most of us have felt the symptoms of moral injury: frustration, anger, disgust, guilt. A recent report describes three levels of stressors in health care occurring during the pandemic, which are not dissimilar to those wartime events described previously.
- Severe moral stressors, such as the denial of treatment to a COVID-19 patient owing to lack of resources, the inability to provide optimal care to non–COVID-19 patients for many reasons, and concern about passing COVID to loved ones.
- Moderate moral stressors, such as preventing visitors, especially to dying patients, triaging patients for healthcare services with inadequate information, and trying to solve the tension between the need for self-preservation and the need to treat.
- Lower-level but common moral challenges, especially in the community – for example, seeing others not protecting the community by hoarding food, gathering for large parties, and not social distancing or wearing masks. Such stressors lead to frustration and contempt, especially from healthcare workers making personal sacrifices and who may be at risk for infection caused by these behaviors.
Every one of us is affected by these stressors. I certainly am.
What are the outcomes? We know that moral injuries are a risk factor for the development of mental health problems and burnout, and not surprisingly we are seeing that mental health problems, suicidality, and substance use disorders have increased markedly during COVID-19, as recently detailed by the CDC.
Common emotions that occur in response to moral injuries are: feelings of guilt, shame, anger, sadness, anxiety, and disgust; intrapersonal outcomes, including lowered self-esteem, high self-criticism, and beliefs about being bad, damaged, unworthy, failing, or weak; interpersonal outcomes, including loss of faith in people, avoidance of intimacy, and lack of trust in authority figures; and existential and spiritual outcomes, including loss of faith in previous religious beliefs and no longer believing in a just world.
Moral injuries tend to originate primarily from systems-based problems, as we have seen with the lack of concerted national approaches to the pandemic. On the positive side, solutions typically also involve systems-based changes, which in this case may mean changes in leadership styles nationally and locally, as well as changes in the culture of medicine and the way healthcare is practiced and managed in the modern era. We are starting to see some of those changes with the increased use of telemedicine and health technologies, as well as more of a focus on the well-being of health care workers, now deemed “essential.”
As individuals, we are not helpless. There are things we can do in our workplaces to create change. I suggest:
- Acknowledge that you, like me, are affected by these stressors. This is not a secret, and you should not be ashamed of your feelings.
- Talk with your colleagues, loved ones, and friends about how you and they are affected. You are not alone. Encourage others to share their thoughts, stories, and feelings.
- Put this topic on your meeting and departmental agendas and discuss these moral issues openly with your colleagues. Allow sufficient time to engage in open dialogue.
- Work out ways of assisting those who are in high-risk situations, especially for moderate to severe injuries. Be supportive toward those affected.
- Modify policies and change rosters and rotate staff between high- and low-stress roles. Protect and support at-risk colleagues.
- Think about difficult ethical decisions in advance so they can be made by groups, not individuals, and certainly not “on the fly.”
- Keep everyone in your workplace constantly informed, especially of impending staff or equipment shortages.
- Maintain your inherent self-care and resilience with rest, good nutrition, sleep, exercise, love, caring, socialization, and work-life balance.
- Be prepared to access the many professional support services available in our community if you are intensely distressed or if the above suggestions are not enough.
Remember, we are in this together and will find strength in each other. This too will pass.
This article first appeared on Medscape.com.
Among the many tolls inflicted on health care workers by COVID-19 is one that is not as easily measured as rates of death or disease, but is no less tangible: moral injury. This is the term by which we describe the psychological, social, and spiritual impact of high-stakes situations that lead to the betrayal or transgression of our own deeply held moral beliefs and values.
The current pandemic has provided innumerable such situations that can increase the risk for moral injury, whether we deal directly with patients infected by the coronavirus or not. Telling family members they cannot visit critically ill loved ones. Delaying code activities, even momentarily, to get fully protected with personal protective equipment. Seeing patients who have delayed their necessary or preventive care. Using video rather than touch to reassure people.
Knowing that we are following guidelines from the Centers for Disease Control and Prevention does not stop our feelings of guilt. The longer this pandemic goes on, the more likely it is that these situations will begin to take a toll on us.
For most of us, being exposed to moral injuries is new; they have historically been most associated with severe traumatic wartime experiences. Soldiers, philosophers, and writers have described the ethical dilemmas inherent in war for as long as recorded history. But the use of this term is a more recent development, which the Moral Injury Project at Syracuse (N.Y.) University describes as probably originating in the Vietnam War–era writings of veteran and peace activist Camillo “Mac” Bica and psychiatrist Jonathan Shay. Examples of wartime events that have been thought to lead to moral injury include: causing the harm or death of civilians, knowingly but without alternatives, or accidentally; failing to provide medical aid to an injured civilian or service member; and following orders that were illegal, immoral, and/or against the rules of engagement or the Geneva Conventions.
However, the occurrence of moral injuries in modern health care is increasingly being reported, primarily as an adverse effect of health care inefficiencies that can contribute to burnout. COVID-19 has now provided an array of additional stressors that can cause moral injuries among health care workers. A recent guidance document on moral injury published by the American Psychiatric Association noted that, in the context of a public health disaster, such as COVID-19, it is sometimes necessary to transition from ordinary standards of care to those more appropriate in a crisis, as in wartime. This forces us all to confront challenging questions for which there may be no clear answers, and to make “lose-lose” choices in which no one involved – patients, family, or clinicians – ends up feeling satisfied or even comfortable.
Our lives have been altered significantly, and for many, completely turned upside down by enormous sacrifices and tragic losses. Globally, physicians account for over half of healthcare worker deaths. In the United States alone, over 900 health care workers have died of COVID-19.
Most of us have felt the symptoms of moral injury: frustration, anger, disgust, guilt. A recent report describes three levels of stressors in health care occurring during the pandemic, which are not dissimilar to those wartime events described previously.
- Severe moral stressors, such as the denial of treatment to a COVID-19 patient owing to lack of resources, the inability to provide optimal care to non–COVID-19 patients for many reasons, and concern about passing COVID to loved ones.
- Moderate moral stressors, such as preventing visitors, especially to dying patients, triaging patients for healthcare services with inadequate information, and trying to solve the tension between the need for self-preservation and the need to treat.
- Lower-level but common moral challenges, especially in the community – for example, seeing others not protecting the community by hoarding food, gathering for large parties, and not social distancing or wearing masks. Such stressors lead to frustration and contempt, especially from healthcare workers making personal sacrifices and who may be at risk for infection caused by these behaviors.
Every one of us is affected by these stressors. I certainly am.
What are the outcomes? We know that moral injuries are a risk factor for the development of mental health problems and burnout, and not surprisingly we are seeing that mental health problems, suicidality, and substance use disorders have increased markedly during COVID-19, as recently detailed by the CDC.
Common emotions that occur in response to moral injuries are: feelings of guilt, shame, anger, sadness, anxiety, and disgust; intrapersonal outcomes, including lowered self-esteem, high self-criticism, and beliefs about being bad, damaged, unworthy, failing, or weak; interpersonal outcomes, including loss of faith in people, avoidance of intimacy, and lack of trust in authority figures; and existential and spiritual outcomes, including loss of faith in previous religious beliefs and no longer believing in a just world.
Moral injuries tend to originate primarily from systems-based problems, as we have seen with the lack of concerted national approaches to the pandemic. On the positive side, solutions typically also involve systems-based changes, which in this case may mean changes in leadership styles nationally and locally, as well as changes in the culture of medicine and the way healthcare is practiced and managed in the modern era. We are starting to see some of those changes with the increased use of telemedicine and health technologies, as well as more of a focus on the well-being of health care workers, now deemed “essential.”
As individuals, we are not helpless. There are things we can do in our workplaces to create change. I suggest:
- Acknowledge that you, like me, are affected by these stressors. This is not a secret, and you should not be ashamed of your feelings.
- Talk with your colleagues, loved ones, and friends about how you and they are affected. You are not alone. Encourage others to share their thoughts, stories, and feelings.
- Put this topic on your meeting and departmental agendas and discuss these moral issues openly with your colleagues. Allow sufficient time to engage in open dialogue.
- Work out ways of assisting those who are in high-risk situations, especially for moderate to severe injuries. Be supportive toward those affected.
- Modify policies and change rosters and rotate staff between high- and low-stress roles. Protect and support at-risk colleagues.
- Think about difficult ethical decisions in advance so they can be made by groups, not individuals, and certainly not “on the fly.”
- Keep everyone in your workplace constantly informed, especially of impending staff or equipment shortages.
- Maintain your inherent self-care and resilience with rest, good nutrition, sleep, exercise, love, caring, socialization, and work-life balance.
- Be prepared to access the many professional support services available in our community if you are intensely distressed or if the above suggestions are not enough.
Remember, we are in this together and will find strength in each other. This too will pass.
This article first appeared on Medscape.com.
Among the many tolls inflicted on health care workers by COVID-19 is one that is not as easily measured as rates of death or disease, but is no less tangible: moral injury. This is the term by which we describe the psychological, social, and spiritual impact of high-stakes situations that lead to the betrayal or transgression of our own deeply held moral beliefs and values.
The current pandemic has provided innumerable such situations that can increase the risk for moral injury, whether we deal directly with patients infected by the coronavirus or not. Telling family members they cannot visit critically ill loved ones. Delaying code activities, even momentarily, to get fully protected with personal protective equipment. Seeing patients who have delayed their necessary or preventive care. Using video rather than touch to reassure people.
Knowing that we are following guidelines from the Centers for Disease Control and Prevention does not stop our feelings of guilt. The longer this pandemic goes on, the more likely it is that these situations will begin to take a toll on us.
For most of us, being exposed to moral injuries is new; they have historically been most associated with severe traumatic wartime experiences. Soldiers, philosophers, and writers have described the ethical dilemmas inherent in war for as long as recorded history. But the use of this term is a more recent development, which the Moral Injury Project at Syracuse (N.Y.) University describes as probably originating in the Vietnam War–era writings of veteran and peace activist Camillo “Mac” Bica and psychiatrist Jonathan Shay. Examples of wartime events that have been thought to lead to moral injury include: causing the harm or death of civilians, knowingly but without alternatives, or accidentally; failing to provide medical aid to an injured civilian or service member; and following orders that were illegal, immoral, and/or against the rules of engagement or the Geneva Conventions.
However, the occurrence of moral injuries in modern health care is increasingly being reported, primarily as an adverse effect of health care inefficiencies that can contribute to burnout. COVID-19 has now provided an array of additional stressors that can cause moral injuries among health care workers. A recent guidance document on moral injury published by the American Psychiatric Association noted that, in the context of a public health disaster, such as COVID-19, it is sometimes necessary to transition from ordinary standards of care to those more appropriate in a crisis, as in wartime. This forces us all to confront challenging questions for which there may be no clear answers, and to make “lose-lose” choices in which no one involved – patients, family, or clinicians – ends up feeling satisfied or even comfortable.
Our lives have been altered significantly, and for many, completely turned upside down by enormous sacrifices and tragic losses. Globally, physicians account for over half of healthcare worker deaths. In the United States alone, over 900 health care workers have died of COVID-19.
Most of us have felt the symptoms of moral injury: frustration, anger, disgust, guilt. A recent report describes three levels of stressors in health care occurring during the pandemic, which are not dissimilar to those wartime events described previously.
- Severe moral stressors, such as the denial of treatment to a COVID-19 patient owing to lack of resources, the inability to provide optimal care to non–COVID-19 patients for many reasons, and concern about passing COVID to loved ones.
- Moderate moral stressors, such as preventing visitors, especially to dying patients, triaging patients for healthcare services with inadequate information, and trying to solve the tension between the need for self-preservation and the need to treat.
- Lower-level but common moral challenges, especially in the community – for example, seeing others not protecting the community by hoarding food, gathering for large parties, and not social distancing or wearing masks. Such stressors lead to frustration and contempt, especially from healthcare workers making personal sacrifices and who may be at risk for infection caused by these behaviors.
Every one of us is affected by these stressors. I certainly am.
What are the outcomes? We know that moral injuries are a risk factor for the development of mental health problems and burnout, and not surprisingly we are seeing that mental health problems, suicidality, and substance use disorders have increased markedly during COVID-19, as recently detailed by the CDC.
Common emotions that occur in response to moral injuries are: feelings of guilt, shame, anger, sadness, anxiety, and disgust; intrapersonal outcomes, including lowered self-esteem, high self-criticism, and beliefs about being bad, damaged, unworthy, failing, or weak; interpersonal outcomes, including loss of faith in people, avoidance of intimacy, and lack of trust in authority figures; and existential and spiritual outcomes, including loss of faith in previous religious beliefs and no longer believing in a just world.
Moral injuries tend to originate primarily from systems-based problems, as we have seen with the lack of concerted national approaches to the pandemic. On the positive side, solutions typically also involve systems-based changes, which in this case may mean changes in leadership styles nationally and locally, as well as changes in the culture of medicine and the way healthcare is practiced and managed in the modern era. We are starting to see some of those changes with the increased use of telemedicine and health technologies, as well as more of a focus on the well-being of health care workers, now deemed “essential.”
As individuals, we are not helpless. There are things we can do in our workplaces to create change. I suggest:
- Acknowledge that you, like me, are affected by these stressors. This is not a secret, and you should not be ashamed of your feelings.
- Talk with your colleagues, loved ones, and friends about how you and they are affected. You are not alone. Encourage others to share their thoughts, stories, and feelings.
- Put this topic on your meeting and departmental agendas and discuss these moral issues openly with your colleagues. Allow sufficient time to engage in open dialogue.
- Work out ways of assisting those who are in high-risk situations, especially for moderate to severe injuries. Be supportive toward those affected.
- Modify policies and change rosters and rotate staff between high- and low-stress roles. Protect and support at-risk colleagues.
- Think about difficult ethical decisions in advance so they can be made by groups, not individuals, and certainly not “on the fly.”
- Keep everyone in your workplace constantly informed, especially of impending staff or equipment shortages.
- Maintain your inherent self-care and resilience with rest, good nutrition, sleep, exercise, love, caring, socialization, and work-life balance.
- Be prepared to access the many professional support services available in our community if you are intensely distressed or if the above suggestions are not enough.
Remember, we are in this together and will find strength in each other. This too will pass.
This article first appeared on Medscape.com.
Increasing racial diversity in hospital medicine’s leadership ranks
Have you ever done something where you’re not quite sure why you did it at the time, but later on you realize it was part of some larger cosmic purpose, and you go, “Ahhh, now I understand…that’s why!”? Call it a fortuitous coincidence. Or a subconscious act of anticipation. Maybe a little push from God.
Last summer, as SHM’s Practice Analysis Committee was planning the State of Hospital Medicine survey for 2020, we received a request from SHM’s Diversity, Equity & Inclusion (DEI) Special Interest Group (SIG) to include a series of questions related to hospitalist gender, race and ethnic distribution in the new survey. We’ve generally resisted doing things like this because the SoHM is designed to capture data at the group level, not the individual level – and honestly, it’s as much as a lot of groups can do to tell us reliably how many FTEs they have, much less provide details about individual providers. In addition, the survey is already really long, and we are always looking for ways to make it shorter and easier for participants while still collecting the information report users care most about.
But we wanted to take the asks from the DEI SIG seriously, and as we considered their request, we realized that though it wasn’t practical to collect this information for individual hospital medicine group (HMG) members, we could collect it for group leaders. Little did we know last summer that issues of gender and racial diversity and equity would be so front-and-center right now, as we prepare to release the 2020 SoHM Report in early September. Ahhh, now I understand…that’s why – with the prompting of the DEI SIG – we so fortuitously chose to include those questions this year!
Here’s a sneak preview of what we learned. Among SoHM respondents, 57.1% reported that the highest-ranking leader in their HMG is White, and 23.5% of highest-ranking leaders are Asian. Only 5.5% of HMG leaders were Black/African American. Ethnicity was a separate question, and only 2.2% of HMG leaders were reported as Hispanic/Latino.
I have been profoundly moved by the wretched deaths of George Floyd and other people of color at the hands of police in recent months, and by the subsequent protests and our growing national reckoning over issues of racial equity and justice. In my efforts to understand more about race in America, I have been challenged by my friend Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., and others to go beyond just learning about these issues. I want to use my voice to advocate for change, and my actions to participate in effecting change, within the context of my sphere of influence.
So, what does that have to do with the SoHM data on HMG leader demographics? Well, it’s clear that Black and brown people are woefully underrepresented in the ranks of hospital medicine leadership.
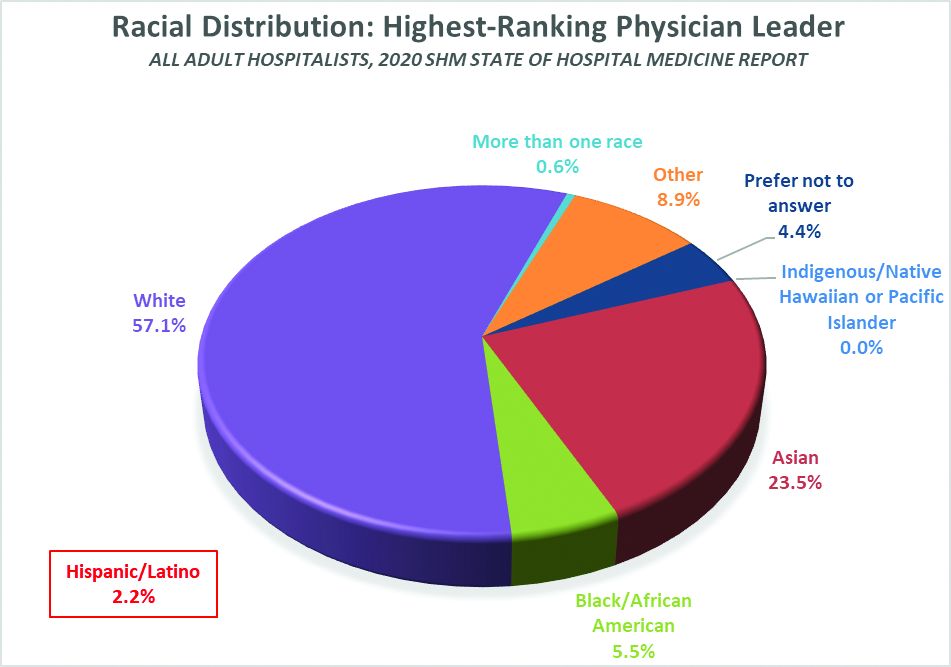
Unfortunately, we don’t have good information on racial diversity for hospitalists as a specialty, though I understand that SHM is working on plans to update membership profiles to begin collecting this information. In searching the Internet, I found a 2018 paper from the Journal of Health Care for the Poor and Underserved that studied racial and ethnic distribution of U.S. primary care physicians (doi: 10.1353/hpu.2018.0036). It reported that, in 2012, 7.8% of general internists were Black, along with 5.8% of family medicine/general practice physicians and 6.8% of pediatricians. A separate data set issued by the Association of American Medical Colleges reported that, in 2019, 6.4% of all actively practicing general internal medicine doctors were Black (5.5% of male IM physicians and 7.9% of female IM physicians). While this doesn’t mean hospitalists have the same racial and ethnic distribution, this is probably the best proxy we can come up with.
At first glance, having 5.5% of HMG leaders who are Black doesn’t seem terribly out of line with the reported range of 6.4 to 7.8% in the general population of internal medicine physicians (apologies to the family medicine and pediatric hospitalists reading this, but I’ll confine my discussion to internists for ease and brevity, since they represent the vast majority of the nation’s hospitalists). But do the math. It means Black hospitalists are likely underrepresented in HMG leadership ranks by something like 14% to 29% compared to their likely presence among hospitalists in general.
The real problem, of course, is that according the U.S. Census Bureau, 13.4% of the U.S. population is Black. So even if the racial distribution of HMG leaders catches up to the general hospitalist population, hospital medicine is still woefully underrepresenting the racial and ethnic distribution of our patient population.
The disconnect between the ethnic distribution of HMG leaders vs. hospitalists (based on general internal medicine distribution) is even more pronounced for Latinos. The JHCPU paper reported that, in 2012, 5.6% of general internists were Hispanic. The AAMC data set reported 5.8% of IM doctors were Hispanic/Latino. But only 2.2% of SoHM respondent HMGs reported a Hispanic/Latino leader, which means Latinos are underrepresented by somewhere around 61% or so relative to the likely hospitalist population, and by a whole lot more considering the fact that Latinos make up about 18.5% of the U.S. population.
I’m not saying that a White or Asian doctor can’t provide skilled, compassionate care to a Black or Latino patient, or vice-versa. It happens every day. I guess what I am saying is that we as a country and in the medical profession need to do a better job of creating pathways and promoting careers in medicine for people of color. A JAMA paper from 2019 reported that while the numbers and proportions of minority medical school matriculants has slowly been increasing from 2002 to 2017, the rate of increase was “slower than their age-matched counterparts in the U.S. population, resulting in increased underrepresentation” (doi:10.1001/jamanetworkopen.2019.10490). This means we’re falling behind, not catching up.
We need to make sure that people like Dr. Ryan Brown aren’t discouraged from pursuing medicine by teachers or school counselors because of their skin color or accent, or their gender or sexual orientation. And among those who become doctors, we need to promote hospital medicine as a desirable specialty for people of color and actively invite them in.
In my view, much of this starts with creating more and better paths to leadership within hospital medicine for people of color. Hospital medicine group leaders wield enormous – and increasing – influence, not only within their HMGs and within SHM, but within their institutions and health care systems. We need their voices and their influence to promote diversity within their groups, their institutions, within hospital medicine, and within medicine and the U.S. health care system more broadly.
The Society of Hospital Medicine is already taking steps to promote diversity, equity and inclusion. These include issuing a formal Diversity and Inclusion Statement, creating the DEI SIG, and the recent formation of a Board-designated DEI task force charged with making recommendations to promote DEI within SHM and in hospital medicine more broadly. But I want to challenge SHM to do more, particularly with regard to promoting diversity in leadership. Here are a few ideas to consider:
- Create and sponsor a mentoring program in which hospitalists volunteer to mentor minority junior high and high school students and help them prepare to pursue a career in medicine.
- Develop a formal, structured advocacy or collaboration effort with organizations like AAMC and the Accreditation Council for Graduate Medical Education designed to promote meaningful increases in the proportion of medical school students and residents who are people of color, and in the proportion who choose primary care – and ultimately, hospital medicine.
- Work hard to collect reliable racial, ethnic and gender information about SHM members and consider collaborating with MGMA to incorporate demographic questions into its survey tool for individual hospitalist compensation and productivity data. Challenge us on the Practice Analysis Committee who are responsible for the SoHM survey to continue surveying leadership demographics, and to consider how we can expand our collection of DEI information in 2022.
- Undertake a public relations campaign to highlight to health systems and other employers the under-representation of Black and Latino hospitalists in leadership positions, and to promote conscious efforts to increase those ranks.
- Create scholarships for hospitalists from underrepresented racial and ethnic groups to attend SHM-sponsored leadership development programs such as Leadership Academy, Academic Hospitalist Academy, and Quality and Safety Educators Academy, with the goal of increasing their ranks in positions of influence throughout healthcare. A scholarship program might even include raising funds to help minority hospitalists pursue Master’s-level programs such as an MBA, MHA, or MMM.
- Develop an educational track, mentoring program, or other support initiative for early-career hospitalist leaders and those interested in developing leadership skills, and ensure it gives specific attention to strategies for increasing the proportion of hospitalists of color in leadership positions.
- Review and revise existing SHM documents such as The Key Principles and Characteristics of an Effective Hospital Medicine Group, the Core Competencies in Hospital Medicine, and various white papers and position statements to ensure they address diversity, equity and inclusion – both with regard to the hospital medicine workforce and leadership, and with regard to patient care and eliminating health disparities.
I’m sure there are plenty of other similar actions we can take that I haven’t thought of. But we need to start the conversation about concrete steps our Society, and the medical specialty we represent, can take to foster real change. And then, we need to follow our words up with actions.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Have you ever done something where you’re not quite sure why you did it at the time, but later on you realize it was part of some larger cosmic purpose, and you go, “Ahhh, now I understand…that’s why!”? Call it a fortuitous coincidence. Or a subconscious act of anticipation. Maybe a little push from God.
Last summer, as SHM’s Practice Analysis Committee was planning the State of Hospital Medicine survey for 2020, we received a request from SHM’s Diversity, Equity & Inclusion (DEI) Special Interest Group (SIG) to include a series of questions related to hospitalist gender, race and ethnic distribution in the new survey. We’ve generally resisted doing things like this because the SoHM is designed to capture data at the group level, not the individual level – and honestly, it’s as much as a lot of groups can do to tell us reliably how many FTEs they have, much less provide details about individual providers. In addition, the survey is already really long, and we are always looking for ways to make it shorter and easier for participants while still collecting the information report users care most about.
But we wanted to take the asks from the DEI SIG seriously, and as we considered their request, we realized that though it wasn’t practical to collect this information for individual hospital medicine group (HMG) members, we could collect it for group leaders. Little did we know last summer that issues of gender and racial diversity and equity would be so front-and-center right now, as we prepare to release the 2020 SoHM Report in early September. Ahhh, now I understand…that’s why – with the prompting of the DEI SIG – we so fortuitously chose to include those questions this year!
Here’s a sneak preview of what we learned. Among SoHM respondents, 57.1% reported that the highest-ranking leader in their HMG is White, and 23.5% of highest-ranking leaders are Asian. Only 5.5% of HMG leaders were Black/African American. Ethnicity was a separate question, and only 2.2% of HMG leaders were reported as Hispanic/Latino.
I have been profoundly moved by the wretched deaths of George Floyd and other people of color at the hands of police in recent months, and by the subsequent protests and our growing national reckoning over issues of racial equity and justice. In my efforts to understand more about race in America, I have been challenged by my friend Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., and others to go beyond just learning about these issues. I want to use my voice to advocate for change, and my actions to participate in effecting change, within the context of my sphere of influence.
So, what does that have to do with the SoHM data on HMG leader demographics? Well, it’s clear that Black and brown people are woefully underrepresented in the ranks of hospital medicine leadership.
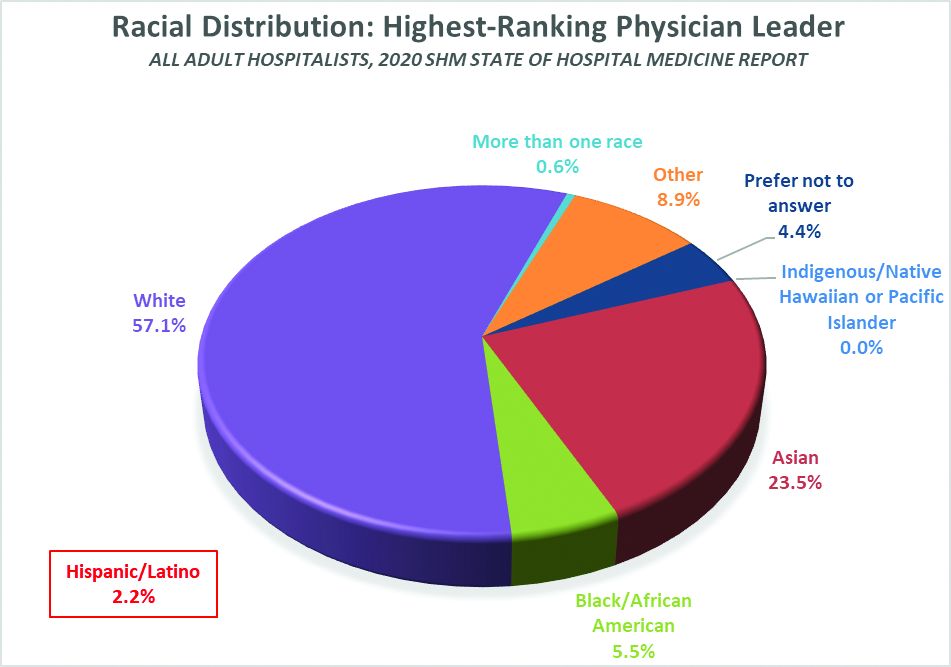
Unfortunately, we don’t have good information on racial diversity for hospitalists as a specialty, though I understand that SHM is working on plans to update membership profiles to begin collecting this information. In searching the Internet, I found a 2018 paper from the Journal of Health Care for the Poor and Underserved that studied racial and ethnic distribution of U.S. primary care physicians (doi: 10.1353/hpu.2018.0036). It reported that, in 2012, 7.8% of general internists were Black, along with 5.8% of family medicine/general practice physicians and 6.8% of pediatricians. A separate data set issued by the Association of American Medical Colleges reported that, in 2019, 6.4% of all actively practicing general internal medicine doctors were Black (5.5% of male IM physicians and 7.9% of female IM physicians). While this doesn’t mean hospitalists have the same racial and ethnic distribution, this is probably the best proxy we can come up with.
At first glance, having 5.5% of HMG leaders who are Black doesn’t seem terribly out of line with the reported range of 6.4 to 7.8% in the general population of internal medicine physicians (apologies to the family medicine and pediatric hospitalists reading this, but I’ll confine my discussion to internists for ease and brevity, since they represent the vast majority of the nation’s hospitalists). But do the math. It means Black hospitalists are likely underrepresented in HMG leadership ranks by something like 14% to 29% compared to their likely presence among hospitalists in general.
The real problem, of course, is that according the U.S. Census Bureau, 13.4% of the U.S. population is Black. So even if the racial distribution of HMG leaders catches up to the general hospitalist population, hospital medicine is still woefully underrepresenting the racial and ethnic distribution of our patient population.
The disconnect between the ethnic distribution of HMG leaders vs. hospitalists (based on general internal medicine distribution) is even more pronounced for Latinos. The JHCPU paper reported that, in 2012, 5.6% of general internists were Hispanic. The AAMC data set reported 5.8% of IM doctors were Hispanic/Latino. But only 2.2% of SoHM respondent HMGs reported a Hispanic/Latino leader, which means Latinos are underrepresented by somewhere around 61% or so relative to the likely hospitalist population, and by a whole lot more considering the fact that Latinos make up about 18.5% of the U.S. population.
I’m not saying that a White or Asian doctor can’t provide skilled, compassionate care to a Black or Latino patient, or vice-versa. It happens every day. I guess what I am saying is that we as a country and in the medical profession need to do a better job of creating pathways and promoting careers in medicine for people of color. A JAMA paper from 2019 reported that while the numbers and proportions of minority medical school matriculants has slowly been increasing from 2002 to 2017, the rate of increase was “slower than their age-matched counterparts in the U.S. population, resulting in increased underrepresentation” (doi:10.1001/jamanetworkopen.2019.10490). This means we’re falling behind, not catching up.
We need to make sure that people like Dr. Ryan Brown aren’t discouraged from pursuing medicine by teachers or school counselors because of their skin color or accent, or their gender or sexual orientation. And among those who become doctors, we need to promote hospital medicine as a desirable specialty for people of color and actively invite them in.
In my view, much of this starts with creating more and better paths to leadership within hospital medicine for people of color. Hospital medicine group leaders wield enormous – and increasing – influence, not only within their HMGs and within SHM, but within their institutions and health care systems. We need their voices and their influence to promote diversity within their groups, their institutions, within hospital medicine, and within medicine and the U.S. health care system more broadly.
The Society of Hospital Medicine is already taking steps to promote diversity, equity and inclusion. These include issuing a formal Diversity and Inclusion Statement, creating the DEI SIG, and the recent formation of a Board-designated DEI task force charged with making recommendations to promote DEI within SHM and in hospital medicine more broadly. But I want to challenge SHM to do more, particularly with regard to promoting diversity in leadership. Here are a few ideas to consider:
- Create and sponsor a mentoring program in which hospitalists volunteer to mentor minority junior high and high school students and help them prepare to pursue a career in medicine.
- Develop a formal, structured advocacy or collaboration effort with organizations like AAMC and the Accreditation Council for Graduate Medical Education designed to promote meaningful increases in the proportion of medical school students and residents who are people of color, and in the proportion who choose primary care – and ultimately, hospital medicine.
- Work hard to collect reliable racial, ethnic and gender information about SHM members and consider collaborating with MGMA to incorporate demographic questions into its survey tool for individual hospitalist compensation and productivity data. Challenge us on the Practice Analysis Committee who are responsible for the SoHM survey to continue surveying leadership demographics, and to consider how we can expand our collection of DEI information in 2022.
- Undertake a public relations campaign to highlight to health systems and other employers the under-representation of Black and Latino hospitalists in leadership positions, and to promote conscious efforts to increase those ranks.
- Create scholarships for hospitalists from underrepresented racial and ethnic groups to attend SHM-sponsored leadership development programs such as Leadership Academy, Academic Hospitalist Academy, and Quality and Safety Educators Academy, with the goal of increasing their ranks in positions of influence throughout healthcare. A scholarship program might even include raising funds to help minority hospitalists pursue Master’s-level programs such as an MBA, MHA, or MMM.
- Develop an educational track, mentoring program, or other support initiative for early-career hospitalist leaders and those interested in developing leadership skills, and ensure it gives specific attention to strategies for increasing the proportion of hospitalists of color in leadership positions.
- Review and revise existing SHM documents such as The Key Principles and Characteristics of an Effective Hospital Medicine Group, the Core Competencies in Hospital Medicine, and various white papers and position statements to ensure they address diversity, equity and inclusion – both with regard to the hospital medicine workforce and leadership, and with regard to patient care and eliminating health disparities.
I’m sure there are plenty of other similar actions we can take that I haven’t thought of. But we need to start the conversation about concrete steps our Society, and the medical specialty we represent, can take to foster real change. And then, we need to follow our words up with actions.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Have you ever done something where you’re not quite sure why you did it at the time, but later on you realize it was part of some larger cosmic purpose, and you go, “Ahhh, now I understand…that’s why!”? Call it a fortuitous coincidence. Or a subconscious act of anticipation. Maybe a little push from God.
Last summer, as SHM’s Practice Analysis Committee was planning the State of Hospital Medicine survey for 2020, we received a request from SHM’s Diversity, Equity & Inclusion (DEI) Special Interest Group (SIG) to include a series of questions related to hospitalist gender, race and ethnic distribution in the new survey. We’ve generally resisted doing things like this because the SoHM is designed to capture data at the group level, not the individual level – and honestly, it’s as much as a lot of groups can do to tell us reliably how many FTEs they have, much less provide details about individual providers. In addition, the survey is already really long, and we are always looking for ways to make it shorter and easier for participants while still collecting the information report users care most about.
But we wanted to take the asks from the DEI SIG seriously, and as we considered their request, we realized that though it wasn’t practical to collect this information for individual hospital medicine group (HMG) members, we could collect it for group leaders. Little did we know last summer that issues of gender and racial diversity and equity would be so front-and-center right now, as we prepare to release the 2020 SoHM Report in early September. Ahhh, now I understand…that’s why – with the prompting of the DEI SIG – we so fortuitously chose to include those questions this year!
Here’s a sneak preview of what we learned. Among SoHM respondents, 57.1% reported that the highest-ranking leader in their HMG is White, and 23.5% of highest-ranking leaders are Asian. Only 5.5% of HMG leaders were Black/African American. Ethnicity was a separate question, and only 2.2% of HMG leaders were reported as Hispanic/Latino.
I have been profoundly moved by the wretched deaths of George Floyd and other people of color at the hands of police in recent months, and by the subsequent protests and our growing national reckoning over issues of racial equity and justice. In my efforts to understand more about race in America, I have been challenged by my friend Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., and others to go beyond just learning about these issues. I want to use my voice to advocate for change, and my actions to participate in effecting change, within the context of my sphere of influence.
So, what does that have to do with the SoHM data on HMG leader demographics? Well, it’s clear that Black and brown people are woefully underrepresented in the ranks of hospital medicine leadership.
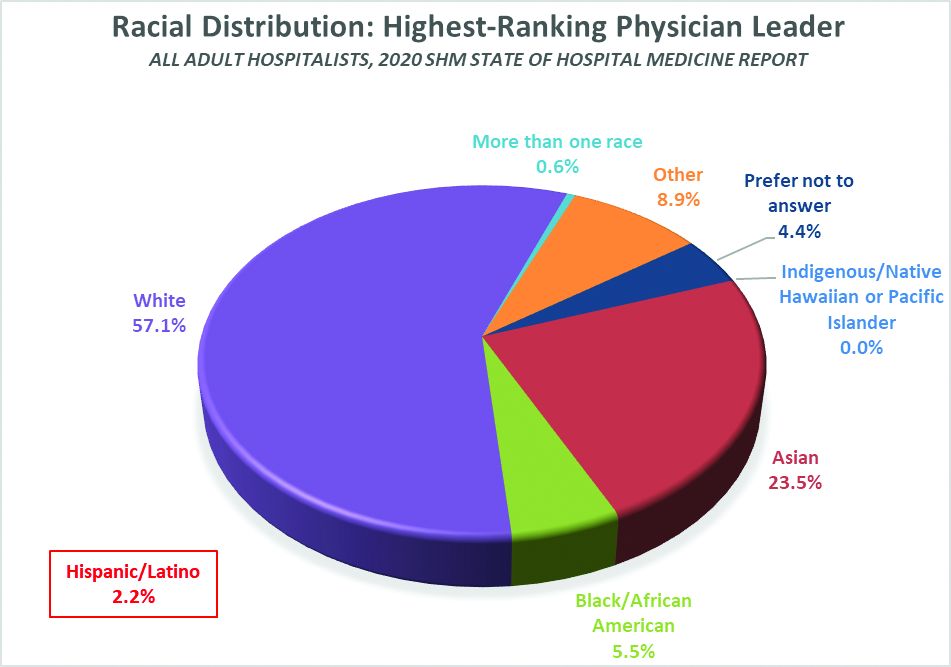
Unfortunately, we don’t have good information on racial diversity for hospitalists as a specialty, though I understand that SHM is working on plans to update membership profiles to begin collecting this information. In searching the Internet, I found a 2018 paper from the Journal of Health Care for the Poor and Underserved that studied racial and ethnic distribution of U.S. primary care physicians (doi: 10.1353/hpu.2018.0036). It reported that, in 2012, 7.8% of general internists were Black, along with 5.8% of family medicine/general practice physicians and 6.8% of pediatricians. A separate data set issued by the Association of American Medical Colleges reported that, in 2019, 6.4% of all actively practicing general internal medicine doctors were Black (5.5% of male IM physicians and 7.9% of female IM physicians). While this doesn’t mean hospitalists have the same racial and ethnic distribution, this is probably the best proxy we can come up with.
At first glance, having 5.5% of HMG leaders who are Black doesn’t seem terribly out of line with the reported range of 6.4 to 7.8% in the general population of internal medicine physicians (apologies to the family medicine and pediatric hospitalists reading this, but I’ll confine my discussion to internists for ease and brevity, since they represent the vast majority of the nation’s hospitalists). But do the math. It means Black hospitalists are likely underrepresented in HMG leadership ranks by something like 14% to 29% compared to their likely presence among hospitalists in general.
The real problem, of course, is that according the U.S. Census Bureau, 13.4% of the U.S. population is Black. So even if the racial distribution of HMG leaders catches up to the general hospitalist population, hospital medicine is still woefully underrepresenting the racial and ethnic distribution of our patient population.
The disconnect between the ethnic distribution of HMG leaders vs. hospitalists (based on general internal medicine distribution) is even more pronounced for Latinos. The JHCPU paper reported that, in 2012, 5.6% of general internists were Hispanic. The AAMC data set reported 5.8% of IM doctors were Hispanic/Latino. But only 2.2% of SoHM respondent HMGs reported a Hispanic/Latino leader, which means Latinos are underrepresented by somewhere around 61% or so relative to the likely hospitalist population, and by a whole lot more considering the fact that Latinos make up about 18.5% of the U.S. population.
I’m not saying that a White or Asian doctor can’t provide skilled, compassionate care to a Black or Latino patient, or vice-versa. It happens every day. I guess what I am saying is that we as a country and in the medical profession need to do a better job of creating pathways and promoting careers in medicine for people of color. A JAMA paper from 2019 reported that while the numbers and proportions of minority medical school matriculants has slowly been increasing from 2002 to 2017, the rate of increase was “slower than their age-matched counterparts in the U.S. population, resulting in increased underrepresentation” (doi:10.1001/jamanetworkopen.2019.10490). This means we’re falling behind, not catching up.
We need to make sure that people like Dr. Ryan Brown aren’t discouraged from pursuing medicine by teachers or school counselors because of their skin color or accent, or their gender or sexual orientation. And among those who become doctors, we need to promote hospital medicine as a desirable specialty for people of color and actively invite them in.
In my view, much of this starts with creating more and better paths to leadership within hospital medicine for people of color. Hospital medicine group leaders wield enormous – and increasing – influence, not only within their HMGs and within SHM, but within their institutions and health care systems. We need their voices and their influence to promote diversity within their groups, their institutions, within hospital medicine, and within medicine and the U.S. health care system more broadly.
The Society of Hospital Medicine is already taking steps to promote diversity, equity and inclusion. These include issuing a formal Diversity and Inclusion Statement, creating the DEI SIG, and the recent formation of a Board-designated DEI task force charged with making recommendations to promote DEI within SHM and in hospital medicine more broadly. But I want to challenge SHM to do more, particularly with regard to promoting diversity in leadership. Here are a few ideas to consider:
- Create and sponsor a mentoring program in which hospitalists volunteer to mentor minority junior high and high school students and help them prepare to pursue a career in medicine.
- Develop a formal, structured advocacy or collaboration effort with organizations like AAMC and the Accreditation Council for Graduate Medical Education designed to promote meaningful increases in the proportion of medical school students and residents who are people of color, and in the proportion who choose primary care – and ultimately, hospital medicine.
- Work hard to collect reliable racial, ethnic and gender information about SHM members and consider collaborating with MGMA to incorporate demographic questions into its survey tool for individual hospitalist compensation and productivity data. Challenge us on the Practice Analysis Committee who are responsible for the SoHM survey to continue surveying leadership demographics, and to consider how we can expand our collection of DEI information in 2022.
- Undertake a public relations campaign to highlight to health systems and other employers the under-representation of Black and Latino hospitalists in leadership positions, and to promote conscious efforts to increase those ranks.
- Create scholarships for hospitalists from underrepresented racial and ethnic groups to attend SHM-sponsored leadership development programs such as Leadership Academy, Academic Hospitalist Academy, and Quality and Safety Educators Academy, with the goal of increasing their ranks in positions of influence throughout healthcare. A scholarship program might even include raising funds to help minority hospitalists pursue Master’s-level programs such as an MBA, MHA, or MMM.
- Develop an educational track, mentoring program, or other support initiative for early-career hospitalist leaders and those interested in developing leadership skills, and ensure it gives specific attention to strategies for increasing the proportion of hospitalists of color in leadership positions.
- Review and revise existing SHM documents such as The Key Principles and Characteristics of an Effective Hospital Medicine Group, the Core Competencies in Hospital Medicine, and various white papers and position statements to ensure they address diversity, equity and inclusion – both with regard to the hospital medicine workforce and leadership, and with regard to patient care and eliminating health disparities.
I’m sure there are plenty of other similar actions we can take that I haven’t thought of. But we need to start the conversation about concrete steps our Society, and the medical specialty we represent, can take to foster real change. And then, we need to follow our words up with actions.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Efforts to close the ‘AYA gap’ in lymphoma
In the 1970s, cancer survival was poor for young children and older adults in the United States, as shown by data published in the Journal of the National Cancer Institute.
Great progress has been made since the 1970s, but improvements in outcome have been less impressive for cancer patients aged 15-39 years, as shown by research published in Cancer.
Patients aged 15-39 years have been designated by the National Institutes of Health (NIH) as “adolescents and young adults (AYAs),” and the lag in survival benefit has been termed “the AYA gap.”
The AYA gap persists in lymphoma patients, and an expert panel recently outlined differences between lymphoma in AYAs and lymphoma in other age groups.
The experts spoke at a special session of the AACR Virtual Meeting: Advances in Malignant Lymphoma moderated by Somali M. Smith, MD, of the University of Chicago.
Factors that contribute to the AYA gap
About 89,000 AYAs are diagnosed with cancer each year in the United States, according to data from the National Cancer Institute (NCI). Lymphomas and thyroid cancer are the most common cancers among younger AYAs, aged 15-24 years.
In a report commissioned by the NIH in 2006, many factors contributing to the AYA gap were identified. Chief among them were:
- Limitations in access to care.
- Delayed diagnosis.
- Inconsistency in treatment and follow-up.
- Long-term toxicity (fertility, second malignancies, and cardiovascular disease).
These factors compromise health-related survival, even when cancer-specific survival is improved.
Panelist Kara Kelly, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., noted that there are additional unique challenges for AYAs with cancer. These include:
- Pubertal changes.
- Developmental transition to independence.
- Societal impediments such as insurance coverage and disparities in access to specialized centers.
- Psychosocial factors such as health literacy and adherence to treatment and follow-up.
Focusing on lymphoma specifically, Dr. Kelly noted that lymphoma biology differs across the age spectrum and by race and ethnicity. Both tumor and host factors require further study, she said.
Clinical trial access for AYAs
Dr. Kelly emphasized that, unfortunately, clinical research participation is low among AYAs. A major impediment is that adult clinical trials historically required participants to be at least 18 years old.
In addition, there has not been a focused effort to educate AYAs about regulatory safeguards to ensure safety and the promise of enhanced benefit to them in NCI Cancer Trials Network (NCTN) trials. As a result, the refusal rate is high.
A multi-stakeholder workshop, convened in May 2016 by the American Society of Clinical Oncology and Friends of Cancer Research, outlined opportunities for expanding trial eligibility to include children younger than 18 years in first-in-human and other adult cancer clinical trials, enhancing their access to new agents, without compromising safety.
Recently, collaborative efforts between the adult and children’s NCTN research groups have included AYAs in studies addressing cancers that span the age spectrum, including lymphoma.
However, as Dr. Kelly noted, there are differences in AYA lymphoid malignancy types with a transition from more pediatric to more adult types.
Hodgkin lymphoma and primary mediastinal B-cell lymphoma
Panelist Lisa G. Roth, MD, of Weill Cornell Medicine, New York, reviewed the genomic landscape of Hodgkin lymphoma (HL) and primary mediastinal B-cell lymphoma (PMBCL).
Dr. Roth explained that both HL and PMBCL are derived from thymic B cells, predominantly affect the mediastinum, and are CD30-positive lymphomas. Both are characterized by upregulation of JAK/STAT and NF-kappaB as well as overexpression of PD-L1.
Dr. Roth noted that HL is challenging to sequence by standard methods because Reed Sternberg (HRS) cells represent less than 1% of the cellular infiltrate. Recurrently mutated genes in HL cluster by histologic subtype.
Whole-exome sequencing of HRS cells show loss of beta-2 microglobulin and MHC-1 expression, HLA-B, NF-kappaB signaling, and JAK-STAT signaling, according to data published in Blood Advances in 2019.
Dr. Roth’s lab performed immunohistochemistry on tissue microarrays in 145 cases of HL (unpublished data). Results showed that loss of beta-2 microglobulin is more common in younger HL patients. For other alterations, there were too few cases to know.
Dr. Roth’s lab is a member of a pediatric/AYA HL sequencing multi-institutional consortium that has been able to extract DNA and RNA from samples submitted for whole-exome sequencing. The consortium’s goal is to shed light on implications of other genomic alterations that may differ by age in HL patients.
Dr. Roth cited research showing that PMBCL shares molecular alterations similar to those of HL. Alterations in PMBCL suggest dysregulated cellular signaling and immune evasion mechanisms (e.g., deletions in MHC type 1 and 2, beta-2 microglobulin, JAK-STAT, and NF-kappaB mutations) that provide opportunities to study novel agents, according to data published in Blood in 2019.
By early 2021, the S1826 and ANHL1931 studies, which have no age restriction, will be available to AYA lymphoma patients with HL and PMBCL, respectively, Dr. Roth said.
Follicular lymphoma: Clinical features by age
Panelist Abner Louissaint Jr, MD, PhD, of Massachusetts General Hospital in Boston, discussed age-related differences in follicular lymphoma (FL).
He noted that FL typically presents at an advanced stage, with low- or high-grade histology. It is increasingly common in adults in their 50s and 60s, representing 20% of all lymphomas. FL is rare in children and AYAs.
Dr. Louissaint explained that the typical flow cytometric findings in FL are BCL2 translocations, occurring in up to 85%-90% of low-grade and 50% of high-grade cases. The t(14;18)(q32;q21) translocation juxtaposes BCL2 on 18q21 to regulatory sequences and enhances the expression of elements of the Ig heavy chain.
Malignant cells in FL patients express CD20, CD10, CD21, and BCL2 (in contrast to normal germinal centers) and overexpress BCL6 (in contrast to normal follicles), Dr. Louissaint noted. He said the Ki-67 proliferative index of the malignant cells is typically low.
Pediatric-type FL is rare, but case series show clinical, pathologic, and molecular features that are distinctive from adult FL, Dr. Louissaint explained.
He then discussed the features of pediatric-type FL in multiple domains. In the clinical domain, there is a male predilection, and stage tends to be low. There is frequent involvement of nodes of the head and neck region and rare involvement of internal lymph node chains.
Pathologically, the malignant cells appear high grade, with architectural effacement, expansile follicular pattern, large lymphocyte size, and an elevated proliferation index. In contrast to adult FL, malignant cells in pediatric-type FL lack aberrant BCL2 expression.
Most importantly, for pediatric-type FL, the prognosis is excellent with durable remissions after surgical excision, Dr. Louissaint said.
Follicular lymphoma: Molecular features by age
Because of the excellent prognosis in pediatric-type FL, it is important to assess whether young adults with FL have adult-type or pediatric-type lesions, Dr. Louissaint said.
He cited many studies showing differences in adult and pediatric-type FL. In adult FL, the mutational landscape is characterized by frequent chromatin-modifying mutations in genes such as CREBBP, KM22D, and EP300.
In contrast, in pediatric-type FL, there are frequent activating MAPK pathway mutations, including mutations in the negative regulatory domain of MAP2K1. These mutations are not seen in adult FL.
Dr. Louissaint noted that there may be mutations in epigenetic modifiers (CREBBP, TNFRSF14) in both adult and pediatric-type FL. However, CREBBP is very unusual in pediatric-type FL and common in adult FL. This suggests the alterations in pediatric-type FL do not simply represent an early stage of the same disease as adult FL.
Despite a high proliferating fraction and absence of BCL2/BCL6/IRF4 rearrangements in pediatric-type FL, the presence of these features was associated with dramatic difference in progression-free survival, according to research published in Blood in 2012.
A distinct entity
In 2016, the World Health Organization recognized pediatric-type FL as a distinct entity, with the following diagnostic criteria (published in Blood):
- At least partial effacement of nodal architecture, expansile follicles, intermediate-size blastoid cells, and no component of diffuse large B-cell lymphoma.
- Immunohistochemistry showing BCL6 positivity, BCL2 negativity or weak positivity, and a high proliferative fraction.
- Genomic studies showing no BCL2 amplification.
- Clinical features of nodal disease in the head and neck region, early clinical stage, age younger than 40 years, typically in a male with no internal nodes involved.
When FL occurs in AYAs, the diagnostic findings of pediatric-type FL suggest the patient will do well with conservative management (e.g., excision alone), Dr. Louissaint noted.
Two sizes do not fit all
The strategies that have improved cancer outcomes since the 1970s for children and older adults have been much less successful for AYAs with cancer.
As an oncologic community, we should not allow the AYA gap to persist. As always, the solutions are likely to involve focused clinical research, education, and communication. Effort will need to be targeted specifically to the AYA population.
Since health-related mortality is high even when cancer-specific outcomes improve, adopting and maintaining a healthy lifestyle must be a key part of the discussion with these young patients.
The biologic differences associated with AYA lymphomas demand participation in clinical trials.
Oncologists should vigorously support removing impediments to the participation of AYAs in prospective clinical trials, stratified (but unrestricted) by age, with careful analysis of patient-reported outcomes, late adverse effects, and biospecimen collection.
As Dr. Kelly noted in the question-and-answer period, the Children’s Oncology Group has an existing biobank of paraffin-embedded tumor samples, DNA from lymphoma specimens, plasma, and sera with clinically annotated data that can be given to investigators upon request and justification.
Going beyond eligibility for clinical trials
Unfortunately, we will likely find that broadening eligibility criteria is the “low-hanging fruit.” There are protocol-, patient-, and physician-related obstacles, according to a review published in Cancer in 2019.
Patient-related obstacles include fear of toxicity, uncertainty about placebos, a steep learning curve for health literacy, insurance-related impediments, and other access-related issues.
Discussions will need to be tailored to the AYA population. Frank, early conversations about fertility, sexuality, financial hardship, career advancement, work-life balance, and cognitive risks may not only facilitate treatment planning but also encourage the trust that is essential for patients to enroll in trials.
The investment in time, multidisciplinary staff and physician involvement, and potential delays in treatment initiation may be painful and inconvenient, but the benefits for long-term health outcomes and personal-professional relationships will be gratifying beyond measure.
Dr. Smith disclosed relationships with Genentech/Roche, Celgene, TGTX, Karyopharm, Janssen, and Bantem. Dr. Roth disclosed relationships with Janssen, ADC Therapeutics, and Celgene. Dr. Kelly and Dr. Louissaint had no financial relationships to disclose.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
In the 1970s, cancer survival was poor for young children and older adults in the United States, as shown by data published in the Journal of the National Cancer Institute.
Great progress has been made since the 1970s, but improvements in outcome have been less impressive for cancer patients aged 15-39 years, as shown by research published in Cancer.
Patients aged 15-39 years have been designated by the National Institutes of Health (NIH) as “adolescents and young adults (AYAs),” and the lag in survival benefit has been termed “the AYA gap.”
The AYA gap persists in lymphoma patients, and an expert panel recently outlined differences between lymphoma in AYAs and lymphoma in other age groups.
The experts spoke at a special session of the AACR Virtual Meeting: Advances in Malignant Lymphoma moderated by Somali M. Smith, MD, of the University of Chicago.
Factors that contribute to the AYA gap
About 89,000 AYAs are diagnosed with cancer each year in the United States, according to data from the National Cancer Institute (NCI). Lymphomas and thyroid cancer are the most common cancers among younger AYAs, aged 15-24 years.
In a report commissioned by the NIH in 2006, many factors contributing to the AYA gap were identified. Chief among them were:
- Limitations in access to care.
- Delayed diagnosis.
- Inconsistency in treatment and follow-up.
- Long-term toxicity (fertility, second malignancies, and cardiovascular disease).
These factors compromise health-related survival, even when cancer-specific survival is improved.
Panelist Kara Kelly, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., noted that there are additional unique challenges for AYAs with cancer. These include:
- Pubertal changes.
- Developmental transition to independence.
- Societal impediments such as insurance coverage and disparities in access to specialized centers.
- Psychosocial factors such as health literacy and adherence to treatment and follow-up.
Focusing on lymphoma specifically, Dr. Kelly noted that lymphoma biology differs across the age spectrum and by race and ethnicity. Both tumor and host factors require further study, she said.
Clinical trial access for AYAs
Dr. Kelly emphasized that, unfortunately, clinical research participation is low among AYAs. A major impediment is that adult clinical trials historically required participants to be at least 18 years old.
In addition, there has not been a focused effort to educate AYAs about regulatory safeguards to ensure safety and the promise of enhanced benefit to them in NCI Cancer Trials Network (NCTN) trials. As a result, the refusal rate is high.
A multi-stakeholder workshop, convened in May 2016 by the American Society of Clinical Oncology and Friends of Cancer Research, outlined opportunities for expanding trial eligibility to include children younger than 18 years in first-in-human and other adult cancer clinical trials, enhancing their access to new agents, without compromising safety.
Recently, collaborative efforts between the adult and children’s NCTN research groups have included AYAs in studies addressing cancers that span the age spectrum, including lymphoma.
However, as Dr. Kelly noted, there are differences in AYA lymphoid malignancy types with a transition from more pediatric to more adult types.
Hodgkin lymphoma and primary mediastinal B-cell lymphoma
Panelist Lisa G. Roth, MD, of Weill Cornell Medicine, New York, reviewed the genomic landscape of Hodgkin lymphoma (HL) and primary mediastinal B-cell lymphoma (PMBCL).
Dr. Roth explained that both HL and PMBCL are derived from thymic B cells, predominantly affect the mediastinum, and are CD30-positive lymphomas. Both are characterized by upregulation of JAK/STAT and NF-kappaB as well as overexpression of PD-L1.
Dr. Roth noted that HL is challenging to sequence by standard methods because Reed Sternberg (HRS) cells represent less than 1% of the cellular infiltrate. Recurrently mutated genes in HL cluster by histologic subtype.
Whole-exome sequencing of HRS cells show loss of beta-2 microglobulin and MHC-1 expression, HLA-B, NF-kappaB signaling, and JAK-STAT signaling, according to data published in Blood Advances in 2019.
Dr. Roth’s lab performed immunohistochemistry on tissue microarrays in 145 cases of HL (unpublished data). Results showed that loss of beta-2 microglobulin is more common in younger HL patients. For other alterations, there were too few cases to know.
Dr. Roth’s lab is a member of a pediatric/AYA HL sequencing multi-institutional consortium that has been able to extract DNA and RNA from samples submitted for whole-exome sequencing. The consortium’s goal is to shed light on implications of other genomic alterations that may differ by age in HL patients.
Dr. Roth cited research showing that PMBCL shares molecular alterations similar to those of HL. Alterations in PMBCL suggest dysregulated cellular signaling and immune evasion mechanisms (e.g., deletions in MHC type 1 and 2, beta-2 microglobulin, JAK-STAT, and NF-kappaB mutations) that provide opportunities to study novel agents, according to data published in Blood in 2019.
By early 2021, the S1826 and ANHL1931 studies, which have no age restriction, will be available to AYA lymphoma patients with HL and PMBCL, respectively, Dr. Roth said.
Follicular lymphoma: Clinical features by age
Panelist Abner Louissaint Jr, MD, PhD, of Massachusetts General Hospital in Boston, discussed age-related differences in follicular lymphoma (FL).
He noted that FL typically presents at an advanced stage, with low- or high-grade histology. It is increasingly common in adults in their 50s and 60s, representing 20% of all lymphomas. FL is rare in children and AYAs.
Dr. Louissaint explained that the typical flow cytometric findings in FL are BCL2 translocations, occurring in up to 85%-90% of low-grade and 50% of high-grade cases. The t(14;18)(q32;q21) translocation juxtaposes BCL2 on 18q21 to regulatory sequences and enhances the expression of elements of the Ig heavy chain.
Malignant cells in FL patients express CD20, CD10, CD21, and BCL2 (in contrast to normal germinal centers) and overexpress BCL6 (in contrast to normal follicles), Dr. Louissaint noted. He said the Ki-67 proliferative index of the malignant cells is typically low.
Pediatric-type FL is rare, but case series show clinical, pathologic, and molecular features that are distinctive from adult FL, Dr. Louissaint explained.
He then discussed the features of pediatric-type FL in multiple domains. In the clinical domain, there is a male predilection, and stage tends to be low. There is frequent involvement of nodes of the head and neck region and rare involvement of internal lymph node chains.
Pathologically, the malignant cells appear high grade, with architectural effacement, expansile follicular pattern, large lymphocyte size, and an elevated proliferation index. In contrast to adult FL, malignant cells in pediatric-type FL lack aberrant BCL2 expression.
Most importantly, for pediatric-type FL, the prognosis is excellent with durable remissions after surgical excision, Dr. Louissaint said.
Follicular lymphoma: Molecular features by age
Because of the excellent prognosis in pediatric-type FL, it is important to assess whether young adults with FL have adult-type or pediatric-type lesions, Dr. Louissaint said.
He cited many studies showing differences in adult and pediatric-type FL. In adult FL, the mutational landscape is characterized by frequent chromatin-modifying mutations in genes such as CREBBP, KM22D, and EP300.
In contrast, in pediatric-type FL, there are frequent activating MAPK pathway mutations, including mutations in the negative regulatory domain of MAP2K1. These mutations are not seen in adult FL.
Dr. Louissaint noted that there may be mutations in epigenetic modifiers (CREBBP, TNFRSF14) in both adult and pediatric-type FL. However, CREBBP is very unusual in pediatric-type FL and common in adult FL. This suggests the alterations in pediatric-type FL do not simply represent an early stage of the same disease as adult FL.
Despite a high proliferating fraction and absence of BCL2/BCL6/IRF4 rearrangements in pediatric-type FL, the presence of these features was associated with dramatic difference in progression-free survival, according to research published in Blood in 2012.
A distinct entity
In 2016, the World Health Organization recognized pediatric-type FL as a distinct entity, with the following diagnostic criteria (published in Blood):
- At least partial effacement of nodal architecture, expansile follicles, intermediate-size blastoid cells, and no component of diffuse large B-cell lymphoma.
- Immunohistochemistry showing BCL6 positivity, BCL2 negativity or weak positivity, and a high proliferative fraction.
- Genomic studies showing no BCL2 amplification.
- Clinical features of nodal disease in the head and neck region, early clinical stage, age younger than 40 years, typically in a male with no internal nodes involved.
When FL occurs in AYAs, the diagnostic findings of pediatric-type FL suggest the patient will do well with conservative management (e.g., excision alone), Dr. Louissaint noted.
Two sizes do not fit all
The strategies that have improved cancer outcomes since the 1970s for children and older adults have been much less successful for AYAs with cancer.
As an oncologic community, we should not allow the AYA gap to persist. As always, the solutions are likely to involve focused clinical research, education, and communication. Effort will need to be targeted specifically to the AYA population.
Since health-related mortality is high even when cancer-specific outcomes improve, adopting and maintaining a healthy lifestyle must be a key part of the discussion with these young patients.
The biologic differences associated with AYA lymphomas demand participation in clinical trials.
Oncologists should vigorously support removing impediments to the participation of AYAs in prospective clinical trials, stratified (but unrestricted) by age, with careful analysis of patient-reported outcomes, late adverse effects, and biospecimen collection.
As Dr. Kelly noted in the question-and-answer period, the Children’s Oncology Group has an existing biobank of paraffin-embedded tumor samples, DNA from lymphoma specimens, plasma, and sera with clinically annotated data that can be given to investigators upon request and justification.
Going beyond eligibility for clinical trials
Unfortunately, we will likely find that broadening eligibility criteria is the “low-hanging fruit.” There are protocol-, patient-, and physician-related obstacles, according to a review published in Cancer in 2019.
Patient-related obstacles include fear of toxicity, uncertainty about placebos, a steep learning curve for health literacy, insurance-related impediments, and other access-related issues.
Discussions will need to be tailored to the AYA population. Frank, early conversations about fertility, sexuality, financial hardship, career advancement, work-life balance, and cognitive risks may not only facilitate treatment planning but also encourage the trust that is essential for patients to enroll in trials.
The investment in time, multidisciplinary staff and physician involvement, and potential delays in treatment initiation may be painful and inconvenient, but the benefits for long-term health outcomes and personal-professional relationships will be gratifying beyond measure.
Dr. Smith disclosed relationships with Genentech/Roche, Celgene, TGTX, Karyopharm, Janssen, and Bantem. Dr. Roth disclosed relationships with Janssen, ADC Therapeutics, and Celgene. Dr. Kelly and Dr. Louissaint had no financial relationships to disclose.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
In the 1970s, cancer survival was poor for young children and older adults in the United States, as shown by data published in the Journal of the National Cancer Institute.
Great progress has been made since the 1970s, but improvements in outcome have been less impressive for cancer patients aged 15-39 years, as shown by research published in Cancer.
Patients aged 15-39 years have been designated by the National Institutes of Health (NIH) as “adolescents and young adults (AYAs),” and the lag in survival benefit has been termed “the AYA gap.”
The AYA gap persists in lymphoma patients, and an expert panel recently outlined differences between lymphoma in AYAs and lymphoma in other age groups.
The experts spoke at a special session of the AACR Virtual Meeting: Advances in Malignant Lymphoma moderated by Somali M. Smith, MD, of the University of Chicago.
Factors that contribute to the AYA gap
About 89,000 AYAs are diagnosed with cancer each year in the United States, according to data from the National Cancer Institute (NCI). Lymphomas and thyroid cancer are the most common cancers among younger AYAs, aged 15-24 years.
In a report commissioned by the NIH in 2006, many factors contributing to the AYA gap were identified. Chief among them were:
- Limitations in access to care.
- Delayed diagnosis.
- Inconsistency in treatment and follow-up.
- Long-term toxicity (fertility, second malignancies, and cardiovascular disease).
These factors compromise health-related survival, even when cancer-specific survival is improved.
Panelist Kara Kelly, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., noted that there are additional unique challenges for AYAs with cancer. These include:
- Pubertal changes.
- Developmental transition to independence.
- Societal impediments such as insurance coverage and disparities in access to specialized centers.
- Psychosocial factors such as health literacy and adherence to treatment and follow-up.
Focusing on lymphoma specifically, Dr. Kelly noted that lymphoma biology differs across the age spectrum and by race and ethnicity. Both tumor and host factors require further study, she said.
Clinical trial access for AYAs
Dr. Kelly emphasized that, unfortunately, clinical research participation is low among AYAs. A major impediment is that adult clinical trials historically required participants to be at least 18 years old.
In addition, there has not been a focused effort to educate AYAs about regulatory safeguards to ensure safety and the promise of enhanced benefit to them in NCI Cancer Trials Network (NCTN) trials. As a result, the refusal rate is high.
A multi-stakeholder workshop, convened in May 2016 by the American Society of Clinical Oncology and Friends of Cancer Research, outlined opportunities for expanding trial eligibility to include children younger than 18 years in first-in-human and other adult cancer clinical trials, enhancing their access to new agents, without compromising safety.
Recently, collaborative efforts between the adult and children’s NCTN research groups have included AYAs in studies addressing cancers that span the age spectrum, including lymphoma.
However, as Dr. Kelly noted, there are differences in AYA lymphoid malignancy types with a transition from more pediatric to more adult types.
Hodgkin lymphoma and primary mediastinal B-cell lymphoma
Panelist Lisa G. Roth, MD, of Weill Cornell Medicine, New York, reviewed the genomic landscape of Hodgkin lymphoma (HL) and primary mediastinal B-cell lymphoma (PMBCL).
Dr. Roth explained that both HL and PMBCL are derived from thymic B cells, predominantly affect the mediastinum, and are CD30-positive lymphomas. Both are characterized by upregulation of JAK/STAT and NF-kappaB as well as overexpression of PD-L1.
Dr. Roth noted that HL is challenging to sequence by standard methods because Reed Sternberg (HRS) cells represent less than 1% of the cellular infiltrate. Recurrently mutated genes in HL cluster by histologic subtype.
Whole-exome sequencing of HRS cells show loss of beta-2 microglobulin and MHC-1 expression, HLA-B, NF-kappaB signaling, and JAK-STAT signaling, according to data published in Blood Advances in 2019.
Dr. Roth’s lab performed immunohistochemistry on tissue microarrays in 145 cases of HL (unpublished data). Results showed that loss of beta-2 microglobulin is more common in younger HL patients. For other alterations, there were too few cases to know.
Dr. Roth’s lab is a member of a pediatric/AYA HL sequencing multi-institutional consortium that has been able to extract DNA and RNA from samples submitted for whole-exome sequencing. The consortium’s goal is to shed light on implications of other genomic alterations that may differ by age in HL patients.
Dr. Roth cited research showing that PMBCL shares molecular alterations similar to those of HL. Alterations in PMBCL suggest dysregulated cellular signaling and immune evasion mechanisms (e.g., deletions in MHC type 1 and 2, beta-2 microglobulin, JAK-STAT, and NF-kappaB mutations) that provide opportunities to study novel agents, according to data published in Blood in 2019.
By early 2021, the S1826 and ANHL1931 studies, which have no age restriction, will be available to AYA lymphoma patients with HL and PMBCL, respectively, Dr. Roth said.
Follicular lymphoma: Clinical features by age
Panelist Abner Louissaint Jr, MD, PhD, of Massachusetts General Hospital in Boston, discussed age-related differences in follicular lymphoma (FL).
He noted that FL typically presents at an advanced stage, with low- or high-grade histology. It is increasingly common in adults in their 50s and 60s, representing 20% of all lymphomas. FL is rare in children and AYAs.
Dr. Louissaint explained that the typical flow cytometric findings in FL are BCL2 translocations, occurring in up to 85%-90% of low-grade and 50% of high-grade cases. The t(14;18)(q32;q21) translocation juxtaposes BCL2 on 18q21 to regulatory sequences and enhances the expression of elements of the Ig heavy chain.
Malignant cells in FL patients express CD20, CD10, CD21, and BCL2 (in contrast to normal germinal centers) and overexpress BCL6 (in contrast to normal follicles), Dr. Louissaint noted. He said the Ki-67 proliferative index of the malignant cells is typically low.
Pediatric-type FL is rare, but case series show clinical, pathologic, and molecular features that are distinctive from adult FL, Dr. Louissaint explained.
He then discussed the features of pediatric-type FL in multiple domains. In the clinical domain, there is a male predilection, and stage tends to be low. There is frequent involvement of nodes of the head and neck region and rare involvement of internal lymph node chains.
Pathologically, the malignant cells appear high grade, with architectural effacement, expansile follicular pattern, large lymphocyte size, and an elevated proliferation index. In contrast to adult FL, malignant cells in pediatric-type FL lack aberrant BCL2 expression.
Most importantly, for pediatric-type FL, the prognosis is excellent with durable remissions after surgical excision, Dr. Louissaint said.
Follicular lymphoma: Molecular features by age
Because of the excellent prognosis in pediatric-type FL, it is important to assess whether young adults with FL have adult-type or pediatric-type lesions, Dr. Louissaint said.
He cited many studies showing differences in adult and pediatric-type FL. In adult FL, the mutational landscape is characterized by frequent chromatin-modifying mutations in genes such as CREBBP, KM22D, and EP300.
In contrast, in pediatric-type FL, there are frequent activating MAPK pathway mutations, including mutations in the negative regulatory domain of MAP2K1. These mutations are not seen in adult FL.
Dr. Louissaint noted that there may be mutations in epigenetic modifiers (CREBBP, TNFRSF14) in both adult and pediatric-type FL. However, CREBBP is very unusual in pediatric-type FL and common in adult FL. This suggests the alterations in pediatric-type FL do not simply represent an early stage of the same disease as adult FL.
Despite a high proliferating fraction and absence of BCL2/BCL6/IRF4 rearrangements in pediatric-type FL, the presence of these features was associated with dramatic difference in progression-free survival, according to research published in Blood in 2012.
A distinct entity
In 2016, the World Health Organization recognized pediatric-type FL as a distinct entity, with the following diagnostic criteria (published in Blood):
- At least partial effacement of nodal architecture, expansile follicles, intermediate-size blastoid cells, and no component of diffuse large B-cell lymphoma.
- Immunohistochemistry showing BCL6 positivity, BCL2 negativity or weak positivity, and a high proliferative fraction.
- Genomic studies showing no BCL2 amplification.
- Clinical features of nodal disease in the head and neck region, early clinical stage, age younger than 40 years, typically in a male with no internal nodes involved.
When FL occurs in AYAs, the diagnostic findings of pediatric-type FL suggest the patient will do well with conservative management (e.g., excision alone), Dr. Louissaint noted.
Two sizes do not fit all
The strategies that have improved cancer outcomes since the 1970s for children and older adults have been much less successful for AYAs with cancer.
As an oncologic community, we should not allow the AYA gap to persist. As always, the solutions are likely to involve focused clinical research, education, and communication. Effort will need to be targeted specifically to the AYA population.
Since health-related mortality is high even when cancer-specific outcomes improve, adopting and maintaining a healthy lifestyle must be a key part of the discussion with these young patients.
The biologic differences associated with AYA lymphomas demand participation in clinical trials.
Oncologists should vigorously support removing impediments to the participation of AYAs in prospective clinical trials, stratified (but unrestricted) by age, with careful analysis of patient-reported outcomes, late adverse effects, and biospecimen collection.
As Dr. Kelly noted in the question-and-answer period, the Children’s Oncology Group has an existing biobank of paraffin-embedded tumor samples, DNA from lymphoma specimens, plasma, and sera with clinically annotated data that can be given to investigators upon request and justification.
Going beyond eligibility for clinical trials
Unfortunately, we will likely find that broadening eligibility criteria is the “low-hanging fruit.” There are protocol-, patient-, and physician-related obstacles, according to a review published in Cancer in 2019.
Patient-related obstacles include fear of toxicity, uncertainty about placebos, a steep learning curve for health literacy, insurance-related impediments, and other access-related issues.
Discussions will need to be tailored to the AYA population. Frank, early conversations about fertility, sexuality, financial hardship, career advancement, work-life balance, and cognitive risks may not only facilitate treatment planning but also encourage the trust that is essential for patients to enroll in trials.
The investment in time, multidisciplinary staff and physician involvement, and potential delays in treatment initiation may be painful and inconvenient, but the benefits for long-term health outcomes and personal-professional relationships will be gratifying beyond measure.
Dr. Smith disclosed relationships with Genentech/Roche, Celgene, TGTX, Karyopharm, Janssen, and Bantem. Dr. Roth disclosed relationships with Janssen, ADC Therapeutics, and Celgene. Dr. Kelly and Dr. Louissaint had no financial relationships to disclose.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
FROM AACR ADVANCES IN MALIGNANT LYMPHOMA 2020
New Americans: Considerations for culturally collaborative care
Adam is a 14-year-old who presents for “behavioral concerns” as recommended by his teacher. He is in the eighth grade and is struggling academically and socially. He has intermittent outbursts and poor engagement with other children, and often refuses to do schoolwork. He is seen in the outpatient primary care clinic, usually with his mother and two older siblings, one of whom typically translates for his Arabic-speaking mother. Adam is bilingual, although he prefers Arabic. It is difficult to understand the presenting concern as Adam states that he is doing well and is unsure why the teacher would have made such a report. Mother notes that she does not see these behaviors at home either.
What must we consider? Are there potential barriers, alternate ways to engage, and what role may culture have?
There are many things to consider in the above case, including language barriers, nuanced interactions, and cultural expectations and norms. To understand the scope, statistics reveal that the United States leads the world in its immigrant population with about 44.8 million foreign-born persons in 2018, which accounts for approximately 13.7% of the U.S. population.1 In 2019, 30,000 refugees were resettled in the United States.2 In 2017, immigrant children made up 27% (19.6 million) of U.S. children, of which second-generation children (born in the United States to immigrant parents) were the vast majority at 16.7 million.3 Given this information,
Culture is defined as a set of shared beliefs, norms, values, and behaviors exhibited by a group. Culture plays a role and impacts children in various ways throughout their development. Health care providers would benefit from aspiring to exude cultural humility – learning with and from patients and their families with openness, kindness, and a desire for collaboration. The provider also must consider a family’s history of migration as the response to migration may vary based on age, personal experiences, age at which migration occurred, language abilities, and amount of cultural engagement in the new country (i.e. acculturation).4,5
Cultural framework model
One example of a potential framework to use to engage within a cultural context includes the LEARN (Listen, Explain, Acknowledge, Recommend, Negotiate) model,6,7 which initially was developed to be used within a family medicine clinic. It includes the following:
Listen with sympathy and understanding to the patient’s perception of the problem. Try to understand their perspective of symptoms through considering their thoughts regarding etiology and treatment options.
Explain your perception of the problem. Have a dialogue about what you perceive is the likely cause based on a medical perspective.
Acknowledge and discuss the differences and similarities. Engage in open conversation while being cognizant that there may be similarities and differences in the perception you may have versus your patient’s perception. Try to find areas that can be engaged in and an alliance built upon, as well as respectfully and humbly addressing any concerns about potentially harmful patient understandings.
Recommend treatment. Present a treatment recommendation that considers both yours and the patient’s perspectives.
Negotiate agreement. Discuss, collaborate, and finalize a treatment plan that considers a biopsychosocial and spiritual/religious model of care that is patient-centered and personalized such that the main goal is optimal health and wellness for the patient/family.
The following are tips to consider in the life-long process of becoming more culturally aware:
- Be willing to learn with your patients and be thoughtful about your own feelings/thoughts/behaviors that may be positively or negatively impacting those interactions.
- Be aware of your own identity and what that may contribute to the clinical space.
- Recognize that you are not meant to know everything, but being open to the journey and learning process will go a long way.
- Try to shift the focus from paternalistic medicine to collaborative and patient-centered approaches.
The case at hand
In returning to our case and applying the LEARN model and cultural humility, we may be able to uncover more of the story. Adam is seen at a subsequent appointment, and you determine it best to obtain an in-person interpreter for this appointment. As you listen to the story, you learn that his father was killed early in Adam’s life, his mother has suffered from depression, and they moved here 3 years ago from a refugee camp, where most of their family continues to reside. He notes that at times he feels that he is back in that space and that he also feels frustrated. He is accustomed to doing well academically, but English has been difficult to learn.
You explain your understanding and acknowledge concerns for his past experiences playing a role, the importance of having community supports, and that learning a new language is challenging. You recommend that the school offer culturally appropriate interventions, trauma-informed assessments, and English-language opportunities. Adam and his mother note willingness to engage in this plan but would like to speak to their local religious leader as well.
Collaborating in a manner similar to this will likely build a therapeutic alliance between the patient, their family, and caretakers, thus leading to improved outcomes.
For further reading, consider AACAP Finding Mental Healthcare for Children of Immigrants and the American Academy of Pediatrics Providing Culturally Effective Care Toolkit.
Dr. Abdul-Karim, a child and adolescent psychiatrist, is assistant professor of psychiatry at the University of Vermont, Burlington. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. “Key findings about U.S. immigrants.” Pew Research Center, Washington, D.C. (2020)
2. “Key facts about refugees to the U.S.” Pew Research Center, Washington, D.C. (2019)
3. “Immigrant Children.” Child Trends, Bethesda, MD (2018).
4. Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, 11th ed. (Philadelphia: Lippincott Williams & Wilkins, 2015, pp. 139-45).
5. Lewis’sChild and Adolescent Psychiatry: A Comprehensive Textbook, 5th ed. (Philadelphia: Lippincott Williams & Wilkins, 2017, pp. 111-22).
6. Berlin EA, Fowkes WA Jr.A teaching framework for cross-cultural health care. Application in family practice. West J Med 1983;139(6):934-8.
7. Paediatr Child Health. 2018 Feb;23(1):66-9.
Adam is a 14-year-old who presents for “behavioral concerns” as recommended by his teacher. He is in the eighth grade and is struggling academically and socially. He has intermittent outbursts and poor engagement with other children, and often refuses to do schoolwork. He is seen in the outpatient primary care clinic, usually with his mother and two older siblings, one of whom typically translates for his Arabic-speaking mother. Adam is bilingual, although he prefers Arabic. It is difficult to understand the presenting concern as Adam states that he is doing well and is unsure why the teacher would have made such a report. Mother notes that she does not see these behaviors at home either.
What must we consider? Are there potential barriers, alternate ways to engage, and what role may culture have?
There are many things to consider in the above case, including language barriers, nuanced interactions, and cultural expectations and norms. To understand the scope, statistics reveal that the United States leads the world in its immigrant population with about 44.8 million foreign-born persons in 2018, which accounts for approximately 13.7% of the U.S. population.1 In 2019, 30,000 refugees were resettled in the United States.2 In 2017, immigrant children made up 27% (19.6 million) of U.S. children, of which second-generation children (born in the United States to immigrant parents) were the vast majority at 16.7 million.3 Given this information,
Culture is defined as a set of shared beliefs, norms, values, and behaviors exhibited by a group. Culture plays a role and impacts children in various ways throughout their development. Health care providers would benefit from aspiring to exude cultural humility – learning with and from patients and their families with openness, kindness, and a desire for collaboration. The provider also must consider a family’s history of migration as the response to migration may vary based on age, personal experiences, age at which migration occurred, language abilities, and amount of cultural engagement in the new country (i.e. acculturation).4,5
Cultural framework model
One example of a potential framework to use to engage within a cultural context includes the LEARN (Listen, Explain, Acknowledge, Recommend, Negotiate) model,6,7 which initially was developed to be used within a family medicine clinic. It includes the following:
Listen with sympathy and understanding to the patient’s perception of the problem. Try to understand their perspective of symptoms through considering their thoughts regarding etiology and treatment options.
Explain your perception of the problem. Have a dialogue about what you perceive is the likely cause based on a medical perspective.
Acknowledge and discuss the differences and similarities. Engage in open conversation while being cognizant that there may be similarities and differences in the perception you may have versus your patient’s perception. Try to find areas that can be engaged in and an alliance built upon, as well as respectfully and humbly addressing any concerns about potentially harmful patient understandings.
Recommend treatment. Present a treatment recommendation that considers both yours and the patient’s perspectives.
Negotiate agreement. Discuss, collaborate, and finalize a treatment plan that considers a biopsychosocial and spiritual/religious model of care that is patient-centered and personalized such that the main goal is optimal health and wellness for the patient/family.
The following are tips to consider in the life-long process of becoming more culturally aware:
- Be willing to learn with your patients and be thoughtful about your own feelings/thoughts/behaviors that may be positively or negatively impacting those interactions.
- Be aware of your own identity and what that may contribute to the clinical space.
- Recognize that you are not meant to know everything, but being open to the journey and learning process will go a long way.
- Try to shift the focus from paternalistic medicine to collaborative and patient-centered approaches.
The case at hand
In returning to our case and applying the LEARN model and cultural humility, we may be able to uncover more of the story. Adam is seen at a subsequent appointment, and you determine it best to obtain an in-person interpreter for this appointment. As you listen to the story, you learn that his father was killed early in Adam’s life, his mother has suffered from depression, and they moved here 3 years ago from a refugee camp, where most of their family continues to reside. He notes that at times he feels that he is back in that space and that he also feels frustrated. He is accustomed to doing well academically, but English has been difficult to learn.
You explain your understanding and acknowledge concerns for his past experiences playing a role, the importance of having community supports, and that learning a new language is challenging. You recommend that the school offer culturally appropriate interventions, trauma-informed assessments, and English-language opportunities. Adam and his mother note willingness to engage in this plan but would like to speak to their local religious leader as well.
Collaborating in a manner similar to this will likely build a therapeutic alliance between the patient, their family, and caretakers, thus leading to improved outcomes.
For further reading, consider AACAP Finding Mental Healthcare for Children of Immigrants and the American Academy of Pediatrics Providing Culturally Effective Care Toolkit.
Dr. Abdul-Karim, a child and adolescent psychiatrist, is assistant professor of psychiatry at the University of Vermont, Burlington. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. “Key findings about U.S. immigrants.” Pew Research Center, Washington, D.C. (2020)
2. “Key facts about refugees to the U.S.” Pew Research Center, Washington, D.C. (2019)
3. “Immigrant Children.” Child Trends, Bethesda, MD (2018).
4. Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, 11th ed. (Philadelphia: Lippincott Williams & Wilkins, 2015, pp. 139-45).
5. Lewis’sChild and Adolescent Psychiatry: A Comprehensive Textbook, 5th ed. (Philadelphia: Lippincott Williams & Wilkins, 2017, pp. 111-22).
6. Berlin EA, Fowkes WA Jr.A teaching framework for cross-cultural health care. Application in family practice. West J Med 1983;139(6):934-8.
7. Paediatr Child Health. 2018 Feb;23(1):66-9.
Adam is a 14-year-old who presents for “behavioral concerns” as recommended by his teacher. He is in the eighth grade and is struggling academically and socially. He has intermittent outbursts and poor engagement with other children, and often refuses to do schoolwork. He is seen in the outpatient primary care clinic, usually with his mother and two older siblings, one of whom typically translates for his Arabic-speaking mother. Adam is bilingual, although he prefers Arabic. It is difficult to understand the presenting concern as Adam states that he is doing well and is unsure why the teacher would have made such a report. Mother notes that she does not see these behaviors at home either.
What must we consider? Are there potential barriers, alternate ways to engage, and what role may culture have?
There are many things to consider in the above case, including language barriers, nuanced interactions, and cultural expectations and norms. To understand the scope, statistics reveal that the United States leads the world in its immigrant population with about 44.8 million foreign-born persons in 2018, which accounts for approximately 13.7% of the U.S. population.1 In 2019, 30,000 refugees were resettled in the United States.2 In 2017, immigrant children made up 27% (19.6 million) of U.S. children, of which second-generation children (born in the United States to immigrant parents) were the vast majority at 16.7 million.3 Given this information,
Culture is defined as a set of shared beliefs, norms, values, and behaviors exhibited by a group. Culture plays a role and impacts children in various ways throughout their development. Health care providers would benefit from aspiring to exude cultural humility – learning with and from patients and their families with openness, kindness, and a desire for collaboration. The provider also must consider a family’s history of migration as the response to migration may vary based on age, personal experiences, age at which migration occurred, language abilities, and amount of cultural engagement in the new country (i.e. acculturation).4,5
Cultural framework model
One example of a potential framework to use to engage within a cultural context includes the LEARN (Listen, Explain, Acknowledge, Recommend, Negotiate) model,6,7 which initially was developed to be used within a family medicine clinic. It includes the following:
Listen with sympathy and understanding to the patient’s perception of the problem. Try to understand their perspective of symptoms through considering their thoughts regarding etiology and treatment options.
Explain your perception of the problem. Have a dialogue about what you perceive is the likely cause based on a medical perspective.
Acknowledge and discuss the differences and similarities. Engage in open conversation while being cognizant that there may be similarities and differences in the perception you may have versus your patient’s perception. Try to find areas that can be engaged in and an alliance built upon, as well as respectfully and humbly addressing any concerns about potentially harmful patient understandings.
Recommend treatment. Present a treatment recommendation that considers both yours and the patient’s perspectives.
Negotiate agreement. Discuss, collaborate, and finalize a treatment plan that considers a biopsychosocial and spiritual/religious model of care that is patient-centered and personalized such that the main goal is optimal health and wellness for the patient/family.
The following are tips to consider in the life-long process of becoming more culturally aware:
- Be willing to learn with your patients and be thoughtful about your own feelings/thoughts/behaviors that may be positively or negatively impacting those interactions.
- Be aware of your own identity and what that may contribute to the clinical space.
- Recognize that you are not meant to know everything, but being open to the journey and learning process will go a long way.
- Try to shift the focus from paternalistic medicine to collaborative and patient-centered approaches.
The case at hand
In returning to our case and applying the LEARN model and cultural humility, we may be able to uncover more of the story. Adam is seen at a subsequent appointment, and you determine it best to obtain an in-person interpreter for this appointment. As you listen to the story, you learn that his father was killed early in Adam’s life, his mother has suffered from depression, and they moved here 3 years ago from a refugee camp, where most of their family continues to reside. He notes that at times he feels that he is back in that space and that he also feels frustrated. He is accustomed to doing well academically, but English has been difficult to learn.
You explain your understanding and acknowledge concerns for his past experiences playing a role, the importance of having community supports, and that learning a new language is challenging. You recommend that the school offer culturally appropriate interventions, trauma-informed assessments, and English-language opportunities. Adam and his mother note willingness to engage in this plan but would like to speak to their local religious leader as well.
Collaborating in a manner similar to this will likely build a therapeutic alliance between the patient, their family, and caretakers, thus leading to improved outcomes.
For further reading, consider AACAP Finding Mental Healthcare for Children of Immigrants and the American Academy of Pediatrics Providing Culturally Effective Care Toolkit.
Dr. Abdul-Karim, a child and adolescent psychiatrist, is assistant professor of psychiatry at the University of Vermont, Burlington. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
References
1. “Key findings about U.S. immigrants.” Pew Research Center, Washington, D.C. (2020)
2. “Key facts about refugees to the U.S.” Pew Research Center, Washington, D.C. (2019)
3. “Immigrant Children.” Child Trends, Bethesda, MD (2018).
4. Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, 11th ed. (Philadelphia: Lippincott Williams & Wilkins, 2015, pp. 139-45).
5. Lewis’sChild and Adolescent Psychiatry: A Comprehensive Textbook, 5th ed. (Philadelphia: Lippincott Williams & Wilkins, 2017, pp. 111-22).
6. Berlin EA, Fowkes WA Jr.A teaching framework for cross-cultural health care. Application in family practice. West J Med 1983;139(6):934-8.
7. Paediatr Child Health. 2018 Feb;23(1):66-9.
The unsteady state
As the COVID-19 pandemic continues to chug along, some communities feel it slowing to a pace at which they might feel comfortable about a return to, if not quite “business as usual,” at least “business as sort of normal-ish.” They are ready to accept a level of disease that signals they have reached a steady state. However, in other communities, the virus has picked up speed and is threatening to overwhelm the medical infrastructure. If you are in one of those fortunate and skillfully managed states in which folks are beginning to talk seriously, but with little evidence, that it is time to return to normal, it is probably far too early.
Eons ago in pandemic terms, the World Health Organization in Thailand published a list of criteria to aid in determining when a community could consider lifting the limits that seemed to have been effective in halting transmission of the virus (“Transitioning to and maintaining a steady state of low-level or no transmission,” WHO, Thailand, 2020 Apr 18). While much more has been learned about the behavior of the virus since the spring of 2020, the criteria from the WHO in Thailand are worth considering.
Here is my summary of their criteria for returning to normalcy. First, virus transmission is controlled to the point that only sporadic cases and small clusters exist, and that all of these are traceable in origin. Second, health care and public health systems are in place with sufficient capacities to manage a shift from detection to treatment should the case load increase dramatically; this capacity should include detection, testing, isolation, and quarantine. Third, outbreaks in high-risk populations such as nursing homes have been minimized. Fourth, workplace prevention strategies are in place and have been demonstrated to be effective. Fifth, risk of imported cases is at manageable levels. Finally, communities are engaged.
It is hard to argue with the rationale behind each of these criteria. However, the United States is not Thailand, and just thinking about how this country would go about meeting those criteria provides a window into some of the reasons why we have done so poorly and will continue to be challenged in dealing with the pandemic.
First, notice that the criteria make no mention of a vaccine. One gets the sense that from the top down our country is banking too heavily on the effectiveness and widespread delivery of a vaccine. Even if and when a vaccine is developed and delivered, all of these criteria still must be met and kept in mind for a future pandemic.
Second, the criteria call for an effective health care system, but it is abundantly clear that the United States does not have a cohesive health care system and probably won’t for the foreseeable future. The best we can hope for is individual states cobbling together their own systems, which may in turn serve as examples for those states who haven’t had the foresight. We have had a public health system of sorts, but its credibility and effectiveness has been neutered to the point that again we must rely on each state’s ability to see through the haze and create it’s own systems for detection, testing, tracking, isolating, and quarantining – often with little help in materiel support from the federal government. The sliver of good news is that, after a bit of a stumbling start, detecting and limiting the importation of cases from abroad is being addressed.
We continue to hear and see evidence that there are segments of the population who are not engaged in the activities that we have learned are necessary to stabilize the pandemic. My sense is that those people represent a very small minority. But, it is probably large enough to make the route to a steady state on a national level long and painful. This unfortunately is to be expected in a country that was built on a framework of personal freedoms. The best you can hope for in achieving a steady state is to live in one of the states that seems to be achieving the fine balance between personal freedoms and the common good.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
As the COVID-19 pandemic continues to chug along, some communities feel it slowing to a pace at which they might feel comfortable about a return to, if not quite “business as usual,” at least “business as sort of normal-ish.” They are ready to accept a level of disease that signals they have reached a steady state. However, in other communities, the virus has picked up speed and is threatening to overwhelm the medical infrastructure. If you are in one of those fortunate and skillfully managed states in which folks are beginning to talk seriously, but with little evidence, that it is time to return to normal, it is probably far too early.
Eons ago in pandemic terms, the World Health Organization in Thailand published a list of criteria to aid in determining when a community could consider lifting the limits that seemed to have been effective in halting transmission of the virus (“Transitioning to and maintaining a steady state of low-level or no transmission,” WHO, Thailand, 2020 Apr 18). While much more has been learned about the behavior of the virus since the spring of 2020, the criteria from the WHO in Thailand are worth considering.
Here is my summary of their criteria for returning to normalcy. First, virus transmission is controlled to the point that only sporadic cases and small clusters exist, and that all of these are traceable in origin. Second, health care and public health systems are in place with sufficient capacities to manage a shift from detection to treatment should the case load increase dramatically; this capacity should include detection, testing, isolation, and quarantine. Third, outbreaks in high-risk populations such as nursing homes have been minimized. Fourth, workplace prevention strategies are in place and have been demonstrated to be effective. Fifth, risk of imported cases is at manageable levels. Finally, communities are engaged.
It is hard to argue with the rationale behind each of these criteria. However, the United States is not Thailand, and just thinking about how this country would go about meeting those criteria provides a window into some of the reasons why we have done so poorly and will continue to be challenged in dealing with the pandemic.
First, notice that the criteria make no mention of a vaccine. One gets the sense that from the top down our country is banking too heavily on the effectiveness and widespread delivery of a vaccine. Even if and when a vaccine is developed and delivered, all of these criteria still must be met and kept in mind for a future pandemic.
Second, the criteria call for an effective health care system, but it is abundantly clear that the United States does not have a cohesive health care system and probably won’t for the foreseeable future. The best we can hope for is individual states cobbling together their own systems, which may in turn serve as examples for those states who haven’t had the foresight. We have had a public health system of sorts, but its credibility and effectiveness has been neutered to the point that again we must rely on each state’s ability to see through the haze and create it’s own systems for detection, testing, tracking, isolating, and quarantining – often with little help in materiel support from the federal government. The sliver of good news is that, after a bit of a stumbling start, detecting and limiting the importation of cases from abroad is being addressed.
We continue to hear and see evidence that there are segments of the population who are not engaged in the activities that we have learned are necessary to stabilize the pandemic. My sense is that those people represent a very small minority. But, it is probably large enough to make the route to a steady state on a national level long and painful. This unfortunately is to be expected in a country that was built on a framework of personal freedoms. The best you can hope for in achieving a steady state is to live in one of the states that seems to be achieving the fine balance between personal freedoms and the common good.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
As the COVID-19 pandemic continues to chug along, some communities feel it slowing to a pace at which they might feel comfortable about a return to, if not quite “business as usual,” at least “business as sort of normal-ish.” They are ready to accept a level of disease that signals they have reached a steady state. However, in other communities, the virus has picked up speed and is threatening to overwhelm the medical infrastructure. If you are in one of those fortunate and skillfully managed states in which folks are beginning to talk seriously, but with little evidence, that it is time to return to normal, it is probably far too early.
Eons ago in pandemic terms, the World Health Organization in Thailand published a list of criteria to aid in determining when a community could consider lifting the limits that seemed to have been effective in halting transmission of the virus (“Transitioning to and maintaining a steady state of low-level or no transmission,” WHO, Thailand, 2020 Apr 18). While much more has been learned about the behavior of the virus since the spring of 2020, the criteria from the WHO in Thailand are worth considering.
Here is my summary of their criteria for returning to normalcy. First, virus transmission is controlled to the point that only sporadic cases and small clusters exist, and that all of these are traceable in origin. Second, health care and public health systems are in place with sufficient capacities to manage a shift from detection to treatment should the case load increase dramatically; this capacity should include detection, testing, isolation, and quarantine. Third, outbreaks in high-risk populations such as nursing homes have been minimized. Fourth, workplace prevention strategies are in place and have been demonstrated to be effective. Fifth, risk of imported cases is at manageable levels. Finally, communities are engaged.
It is hard to argue with the rationale behind each of these criteria. However, the United States is not Thailand, and just thinking about how this country would go about meeting those criteria provides a window into some of the reasons why we have done so poorly and will continue to be challenged in dealing with the pandemic.
First, notice that the criteria make no mention of a vaccine. One gets the sense that from the top down our country is banking too heavily on the effectiveness and widespread delivery of a vaccine. Even if and when a vaccine is developed and delivered, all of these criteria still must be met and kept in mind for a future pandemic.
Second, the criteria call for an effective health care system, but it is abundantly clear that the United States does not have a cohesive health care system and probably won’t for the foreseeable future. The best we can hope for is individual states cobbling together their own systems, which may in turn serve as examples for those states who haven’t had the foresight. We have had a public health system of sorts, but its credibility and effectiveness has been neutered to the point that again we must rely on each state’s ability to see through the haze and create it’s own systems for detection, testing, tracking, isolating, and quarantining – often with little help in materiel support from the federal government. The sliver of good news is that, after a bit of a stumbling start, detecting and limiting the importation of cases from abroad is being addressed.
We continue to hear and see evidence that there are segments of the population who are not engaged in the activities that we have learned are necessary to stabilize the pandemic. My sense is that those people represent a very small minority. But, it is probably large enough to make the route to a steady state on a national level long and painful. This unfortunately is to be expected in a country that was built on a framework of personal freedoms. The best you can hope for in achieving a steady state is to live in one of the states that seems to be achieving the fine balance between personal freedoms and the common good.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Manners matter
Have you been surprised and impressed by a child who says after a visit, “Thank you, Doctor [Howard]”? While it may seem antiquated to teach such manners to children these days, there are several important benefits to this education.
Manners serve important functions in benefiting a person’s group with cohesiveness and the individuals themselves with acceptance in the group. Use of manners instantly suggests a more trustworthy person.
There are three main categories of manners: hygiene, courtesy, and cultural norm manners.
Hygiene manners, from using the toilet to refraining from picking one’s nose, have obvious health benefits of not spreading disease. Hygiene manners take time to teach, but parents are motivated and helped by natural reactions of disgust that even infants recognize.
Courtesy manners, on the other hand, are habits of self-control and good-faith behaviors that signal that one is putting the interests of others ahead of one’s own for the moment. Taking another’s comfort into account, basic to kindness and respect, does not require agreeing with or submitting to the other. Courtesy manners require a developing self-awareness (I can choose to act this way) and awareness of social status (I am not more important than everyone else) that begins in toddlerhood. Modeling manners around the child is the most important way to teach courtesy. Parents usually start actively teaching the child to say “please” and “thank you,” and show pride in this apparent “demonstration of appreciation” even when it is simply reinforced behavior at first. The delight of grandparents reinforces both the parents and children, and reflects manners as building tribe cohesiveness.
Good manners become a habit
Manners such as warm greetings, a firm handshake (before COVID-19), and prompt thanks are most believable when occurring promptly when appropriate – when they come from habit. This immediate reaction, a result of so-called “fast thinking,” develops when behaviors learned from “slow thinking” are instilled early and often until they are automatic. The other benefit of this overlearning is that the behavior then looks unambivalent; a lag of too many milliseconds makes the recipient doubt genuineness.
Parents often ask us how to handle their child‘s rude or disrespectful behavior. Praise for manners is a simple start. Toddlers and preschoolers are taught manners best by adult modeling, but also by reinforcement and praise for the basics: to say “Hello,” ask “Please,” and say “Thank you,” “Excuse me,” “You’re welcome,” or “Would you help me, please?” The behaviors also include avoiding raising one’s voice, suppressing interrupting, and apologizing when appropriate. Even shy children can learn eye contact by making a game of figuring out the other’s eye color. Shaming, yelling, and punishing for poor manners usually backfires because it shows disrespect of the child who will likely give this back.
Older children can be taught to offer other people the opportunity to go through a door first, to be first to select a seat, speak first and without interruption, or order first. There are daily opportunities for these manners of showing respect. Opening doors for others, or standing when a guest enters the room are more formal but still appreciated. Parents who use and expect courtesy manners with everyone – irrespective of gender, race, ethnicity, or role as a server versus professional – show that they value others and build antiracism.
School age is a time to learn to wait before speaking to consider whether what they say could be experienced as hurtful to the other person. This requires taking someone else’s point of view, an ability that emerges around age 6 years and can be promoted when parents review with their child “How would you feel if it were you?” Role playing common scenarios of how to behave and speak when seeing a person who looks or acts different is also effective. Avoiding interrupting may be more difficult for very talkative or impulsive children, especially those with ADHD. Practicing waiting for permission to speak by being handed a “talking stick” at the dinner table can be good practice for everyone.
Manners are a group asset
Beyond personal benefits, manners are the basis of a civil society. Cultural norm manners are particular to groups, helping members feel affiliated, as well as identifying those with different manners as “other.”
Teens are particularly likely to use a different code of behavior to fit in with a subgroup. This may be acceptable if restricted to within their group (such as swear words) or within certain agreed-upon limits with family members. But teens need to understand the value of learning, practicing, and using manners for their own, as well as their group’s and nation’s, well-being.
As a developmental-behavioral pediatrician, I have cared for many children with intellectual disabilities and autism spectrum disorder (ASD). Deficits in social interaction skills are a basic criterion for the diagnosis of ASD. Overtraining is especially needed for children with ASD whose mirror movements, social attention, and imitation are weak. For children with these conditions, making manners a strong habit takes more effort but is even more vital than for neurotypical children. Temple Grandin, a famous adult with ASD, has described how her mother taught her manners as a survival skill. She reports incorporating manners very consciously and methodically because they did not come naturally. Children with even rote social skills are liked better by peers and teachers, their atypical behaviors is better tolerated, and they get more positive feedback that encourages integration inside and outside the classroom. Manners may make the difference between being allowed in or expelled from classrooms, libraries, clubs, teams, or religious institutions. When it is time to get a job, social skills are the key factor for employment for these individuals and a significant help for neurotypical individuals as well. Failure to signal socially appropriate behavior can make a person appear threatening and has had the rare but tragic result of rough or fatal handling by police.
Has the teaching of manners waned? Perhaps, because, for some families, the child is being socialized mostly by nonfamily caregivers who have low use of manners. Some parents have made teaching manners a low priority or even resisted using manners themselves as inauthentic. This may reflect prioritizing a “laid-back” lifestyle and speaking crudely as a sign of independence, perhaps in reaction to lack of autonomy at work. Mastering the careful interactions developed over time to avoid invoking an aggressive response depend on direct feedback from reactions of the recipient. With so much of our communication done electronically, asynchronously, even anonymously, the usual feedback has been reduced. Practicing curses, insults, and put-downs online easily extends to in-person interactions without the perpetrator even noticing and are generally reinforced and repeated without parental supervision. Disrespectful behavior from community leaders also reduces the threshold for society.
When people are ignorant of or choose not to use manners they may be perceived as “other” and hostile. This may lead to distrust, dislike, and lowered ability to find the common ground needed for making decisions that benefit the greater society. Oliver Wendell Holmes said “Under bad manners ... lies very commonly an overestimate of our special individuality, as distinguished from our generic humanity (“The Professor at the Breakfast Table,” 1858). Working for major goals that benefit all of humanity is essential to survival in our highly interconnected world. Considering all of humanity is a difficult concept for children, and even for many adults, but it starts with using civil behavior at home, in school, and in one’s community.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
Have you been surprised and impressed by a child who says after a visit, “Thank you, Doctor [Howard]”? While it may seem antiquated to teach such manners to children these days, there are several important benefits to this education.
Manners serve important functions in benefiting a person’s group with cohesiveness and the individuals themselves with acceptance in the group. Use of manners instantly suggests a more trustworthy person.
There are three main categories of manners: hygiene, courtesy, and cultural norm manners.
Hygiene manners, from using the toilet to refraining from picking one’s nose, have obvious health benefits of not spreading disease. Hygiene manners take time to teach, but parents are motivated and helped by natural reactions of disgust that even infants recognize.
Courtesy manners, on the other hand, are habits of self-control and good-faith behaviors that signal that one is putting the interests of others ahead of one’s own for the moment. Taking another’s comfort into account, basic to kindness and respect, does not require agreeing with or submitting to the other. Courtesy manners require a developing self-awareness (I can choose to act this way) and awareness of social status (I am not more important than everyone else) that begins in toddlerhood. Modeling manners around the child is the most important way to teach courtesy. Parents usually start actively teaching the child to say “please” and “thank you,” and show pride in this apparent “demonstration of appreciation” even when it is simply reinforced behavior at first. The delight of grandparents reinforces both the parents and children, and reflects manners as building tribe cohesiveness.
Good manners become a habit
Manners such as warm greetings, a firm handshake (before COVID-19), and prompt thanks are most believable when occurring promptly when appropriate – when they come from habit. This immediate reaction, a result of so-called “fast thinking,” develops when behaviors learned from “slow thinking” are instilled early and often until they are automatic. The other benefit of this overlearning is that the behavior then looks unambivalent; a lag of too many milliseconds makes the recipient doubt genuineness.
Parents often ask us how to handle their child‘s rude or disrespectful behavior. Praise for manners is a simple start. Toddlers and preschoolers are taught manners best by adult modeling, but also by reinforcement and praise for the basics: to say “Hello,” ask “Please,” and say “Thank you,” “Excuse me,” “You’re welcome,” or “Would you help me, please?” The behaviors also include avoiding raising one’s voice, suppressing interrupting, and apologizing when appropriate. Even shy children can learn eye contact by making a game of figuring out the other’s eye color. Shaming, yelling, and punishing for poor manners usually backfires because it shows disrespect of the child who will likely give this back.
Older children can be taught to offer other people the opportunity to go through a door first, to be first to select a seat, speak first and without interruption, or order first. There are daily opportunities for these manners of showing respect. Opening doors for others, or standing when a guest enters the room are more formal but still appreciated. Parents who use and expect courtesy manners with everyone – irrespective of gender, race, ethnicity, or role as a server versus professional – show that they value others and build antiracism.
School age is a time to learn to wait before speaking to consider whether what they say could be experienced as hurtful to the other person. This requires taking someone else’s point of view, an ability that emerges around age 6 years and can be promoted when parents review with their child “How would you feel if it were you?” Role playing common scenarios of how to behave and speak when seeing a person who looks or acts different is also effective. Avoiding interrupting may be more difficult for very talkative or impulsive children, especially those with ADHD. Practicing waiting for permission to speak by being handed a “talking stick” at the dinner table can be good practice for everyone.
Manners are a group asset
Beyond personal benefits, manners are the basis of a civil society. Cultural norm manners are particular to groups, helping members feel affiliated, as well as identifying those with different manners as “other.”
Teens are particularly likely to use a different code of behavior to fit in with a subgroup. This may be acceptable if restricted to within their group (such as swear words) or within certain agreed-upon limits with family members. But teens need to understand the value of learning, practicing, and using manners for their own, as well as their group’s and nation’s, well-being.
As a developmental-behavioral pediatrician, I have cared for many children with intellectual disabilities and autism spectrum disorder (ASD). Deficits in social interaction skills are a basic criterion for the diagnosis of ASD. Overtraining is especially needed for children with ASD whose mirror movements, social attention, and imitation are weak. For children with these conditions, making manners a strong habit takes more effort but is even more vital than for neurotypical children. Temple Grandin, a famous adult with ASD, has described how her mother taught her manners as a survival skill. She reports incorporating manners very consciously and methodically because they did not come naturally. Children with even rote social skills are liked better by peers and teachers, their atypical behaviors is better tolerated, and they get more positive feedback that encourages integration inside and outside the classroom. Manners may make the difference between being allowed in or expelled from classrooms, libraries, clubs, teams, or religious institutions. When it is time to get a job, social skills are the key factor for employment for these individuals and a significant help for neurotypical individuals as well. Failure to signal socially appropriate behavior can make a person appear threatening and has had the rare but tragic result of rough or fatal handling by police.
Has the teaching of manners waned? Perhaps, because, for some families, the child is being socialized mostly by nonfamily caregivers who have low use of manners. Some parents have made teaching manners a low priority or even resisted using manners themselves as inauthentic. This may reflect prioritizing a “laid-back” lifestyle and speaking crudely as a sign of independence, perhaps in reaction to lack of autonomy at work. Mastering the careful interactions developed over time to avoid invoking an aggressive response depend on direct feedback from reactions of the recipient. With so much of our communication done electronically, asynchronously, even anonymously, the usual feedback has been reduced. Practicing curses, insults, and put-downs online easily extends to in-person interactions without the perpetrator even noticing and are generally reinforced and repeated without parental supervision. Disrespectful behavior from community leaders also reduces the threshold for society.
When people are ignorant of or choose not to use manners they may be perceived as “other” and hostile. This may lead to distrust, dislike, and lowered ability to find the common ground needed for making decisions that benefit the greater society. Oliver Wendell Holmes said “Under bad manners ... lies very commonly an overestimate of our special individuality, as distinguished from our generic humanity (“The Professor at the Breakfast Table,” 1858). Working for major goals that benefit all of humanity is essential to survival in our highly interconnected world. Considering all of humanity is a difficult concept for children, and even for many adults, but it starts with using civil behavior at home, in school, and in one’s community.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
Have you been surprised and impressed by a child who says after a visit, “Thank you, Doctor [Howard]”? While it may seem antiquated to teach such manners to children these days, there are several important benefits to this education.
Manners serve important functions in benefiting a person’s group with cohesiveness and the individuals themselves with acceptance in the group. Use of manners instantly suggests a more trustworthy person.
There are three main categories of manners: hygiene, courtesy, and cultural norm manners.
Hygiene manners, from using the toilet to refraining from picking one’s nose, have obvious health benefits of not spreading disease. Hygiene manners take time to teach, but parents are motivated and helped by natural reactions of disgust that even infants recognize.
Courtesy manners, on the other hand, are habits of self-control and good-faith behaviors that signal that one is putting the interests of others ahead of one’s own for the moment. Taking another’s comfort into account, basic to kindness and respect, does not require agreeing with or submitting to the other. Courtesy manners require a developing self-awareness (I can choose to act this way) and awareness of social status (I am not more important than everyone else) that begins in toddlerhood. Modeling manners around the child is the most important way to teach courtesy. Parents usually start actively teaching the child to say “please” and “thank you,” and show pride in this apparent “demonstration of appreciation” even when it is simply reinforced behavior at first. The delight of grandparents reinforces both the parents and children, and reflects manners as building tribe cohesiveness.
Good manners become a habit
Manners such as warm greetings, a firm handshake (before COVID-19), and prompt thanks are most believable when occurring promptly when appropriate – when they come from habit. This immediate reaction, a result of so-called “fast thinking,” develops when behaviors learned from “slow thinking” are instilled early and often until they are automatic. The other benefit of this overlearning is that the behavior then looks unambivalent; a lag of too many milliseconds makes the recipient doubt genuineness.
Parents often ask us how to handle their child‘s rude or disrespectful behavior. Praise for manners is a simple start. Toddlers and preschoolers are taught manners best by adult modeling, but also by reinforcement and praise for the basics: to say “Hello,” ask “Please,” and say “Thank you,” “Excuse me,” “You’re welcome,” or “Would you help me, please?” The behaviors also include avoiding raising one’s voice, suppressing interrupting, and apologizing when appropriate. Even shy children can learn eye contact by making a game of figuring out the other’s eye color. Shaming, yelling, and punishing for poor manners usually backfires because it shows disrespect of the child who will likely give this back.
Older children can be taught to offer other people the opportunity to go through a door first, to be first to select a seat, speak first and without interruption, or order first. There are daily opportunities for these manners of showing respect. Opening doors for others, or standing when a guest enters the room are more formal but still appreciated. Parents who use and expect courtesy manners with everyone – irrespective of gender, race, ethnicity, or role as a server versus professional – show that they value others and build antiracism.
School age is a time to learn to wait before speaking to consider whether what they say could be experienced as hurtful to the other person. This requires taking someone else’s point of view, an ability that emerges around age 6 years and can be promoted when parents review with their child “How would you feel if it were you?” Role playing common scenarios of how to behave and speak when seeing a person who looks or acts different is also effective. Avoiding interrupting may be more difficult for very talkative or impulsive children, especially those with ADHD. Practicing waiting for permission to speak by being handed a “talking stick” at the dinner table can be good practice for everyone.
Manners are a group asset
Beyond personal benefits, manners are the basis of a civil society. Cultural norm manners are particular to groups, helping members feel affiliated, as well as identifying those with different manners as “other.”
Teens are particularly likely to use a different code of behavior to fit in with a subgroup. This may be acceptable if restricted to within their group (such as swear words) or within certain agreed-upon limits with family members. But teens need to understand the value of learning, practicing, and using manners for their own, as well as their group’s and nation’s, well-being.
As a developmental-behavioral pediatrician, I have cared for many children with intellectual disabilities and autism spectrum disorder (ASD). Deficits in social interaction skills are a basic criterion for the diagnosis of ASD. Overtraining is especially needed for children with ASD whose mirror movements, social attention, and imitation are weak. For children with these conditions, making manners a strong habit takes more effort but is even more vital than for neurotypical children. Temple Grandin, a famous adult with ASD, has described how her mother taught her manners as a survival skill. She reports incorporating manners very consciously and methodically because they did not come naturally. Children with even rote social skills are liked better by peers and teachers, their atypical behaviors is better tolerated, and they get more positive feedback that encourages integration inside and outside the classroom. Manners may make the difference between being allowed in or expelled from classrooms, libraries, clubs, teams, or religious institutions. When it is time to get a job, social skills are the key factor for employment for these individuals and a significant help for neurotypical individuals as well. Failure to signal socially appropriate behavior can make a person appear threatening and has had the rare but tragic result of rough or fatal handling by police.
Has the teaching of manners waned? Perhaps, because, for some families, the child is being socialized mostly by nonfamily caregivers who have low use of manners. Some parents have made teaching manners a low priority or even resisted using manners themselves as inauthentic. This may reflect prioritizing a “laid-back” lifestyle and speaking crudely as a sign of independence, perhaps in reaction to lack of autonomy at work. Mastering the careful interactions developed over time to avoid invoking an aggressive response depend on direct feedback from reactions of the recipient. With so much of our communication done electronically, asynchronously, even anonymously, the usual feedback has been reduced. Practicing curses, insults, and put-downs online easily extends to in-person interactions without the perpetrator even noticing and are generally reinforced and repeated without parental supervision. Disrespectful behavior from community leaders also reduces the threshold for society.
When people are ignorant of or choose not to use manners they may be perceived as “other” and hostile. This may lead to distrust, dislike, and lowered ability to find the common ground needed for making decisions that benefit the greater society. Oliver Wendell Holmes said “Under bad manners ... lies very commonly an overestimate of our special individuality, as distinguished from our generic humanity (“The Professor at the Breakfast Table,” 1858). Working for major goals that benefit all of humanity is essential to survival in our highly interconnected world. Considering all of humanity is a difficult concept for children, and even for many adults, but it starts with using civil behavior at home, in school, and in one’s community.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
Medicine and the meritocracy
Addressing systemic bias, gender inequity and discrimination
There are many challenges facing modern medicine today. Recent events have highlighted important issues affecting our society as a whole – systemic racism, sexism, and implicit bias. In medicine, we have seen a renewed focus on health equity, health disparities and the implicit systemic bias that affect those who work in the field. It is truly troubling that it has taken the continued loss of black lives to police brutality and a pandemic for this conversation to happen at every level in society.
Systemic bias is present throughout corporate America, and it is no different within the physician workforce. Overall, there has been gradual interest in promoting and teaching diversity. Institutions have been slowly creating policies and administrative positions focused on inclusion and diversity over the last decade. So has diversity training objectively increased representation and advancement of women and minority groups? Do traditionally marginalized groups have better access to health? And are women and people of color (POC) represented equally in leadership positions in medicine?
Clearly, the answers are not straightforward.
Diving into the data
A guilty pleasure of mine is to assess how diverse and inclusive an institution is by looking at the wall of pictures recognizing top leadership in hospitals. Despite women accounting for 47.9% of graduates from medical school in 2018-2019, I still see very few women or POC elevated to this level. Of the total women graduates, 22.6% were Asian, 8% were Black and 5.4% were Hispanic.
Being of Indian descent, I am a woman of color (albeit one who may not be as profoundly affected by racism in medicine as my less represented colleagues). It is especially rare for me to see someone I can identify with in the ranks of top leadership. I find encouragement in seeing any woman on any leadership board because to me, it means that there is hope. The literature seems to support this degree of disparity as well. For example, a recent analysis shows that presidential leadership in medical societies are predominantly held by men (82.6% male vs. 17.4% female). Other datasets demonstrate that only 15% of deans and interim deans are women and AAMC’s report shows that women account for only 18% of all department chairs.
Growing up, my parents fueled my interest to pursue medicine. They described it as a noble profession that rewarded true merit and dedication to the cause. However, those that have been traditionally elevated in medicine are men. If merit knows no gender, why does a gender gap exist? If merit is blind to race, why are minorities so poorly represented in the workforce (much less in leadership)? My view of the wall leaves me wondering about the role of both sexism and racism in medicine.
These visual representations of the medical culture reinforce the acceptable norms and values – white and masculine – in medicine. The feminist movement over the last several decades has increased awareness about the need for equality of the sexes. However, it was not until the concept of intersectionality was introduced by Black feminist Professor Kimberle Crenshaw, that feminism become a more inclusive term. Professor Crenshaw’s paper details how every individual has intersecting factors – race, gender, sexual identity, socioeconomic status – that create the sum of their experience be it privilege, oppression, or discrimination.
For example, a White woman has privileges that a woman of color does not. Among non-white women, race and sexual identity are confounding factors – a Black woman, a Black LGBTQ woman, and an Asian woman, for example, will not experience discrimination in the same way. The farther you deviate from the accepted norms and values, the harder it is for you to obtain support and achieve recognition.
Addressing the patriarchal structure and systemic bias in medicine
Why do patriarchal structures still exist in medicine? How do we resolve systemic bias? Addressing them in isolation – race or gender or sexual identity – is unlikely to create long-lasting change. For change to occur, organizations and individuals need to be intrinsically motivated. Creating awareness and challenging the status quo is the first step.
Over the last decade, implicit bias training and diversity training have become mandatory in various industries and states. Diversity training has grown to be a multi-billion-dollar industry that corporate America has embraced over the last several years. And yet, research shows that mandating such training may not be the most effective. To get results, organizations need to implement programs that “spark engagement, increase contact between different groups and draw on people’s desire to look good to others.”
Historically, the medical curriculum has not included a discourse on feminist theories and the advancement of women in medicine. Cultural competency training is typically offered on an annual basis once we are in the workforce, but in my experience, it focuses more on our interactions with patients and other health care colleagues, and less with regards to our physician peers and leadership. Is this enough to change deep rooted beliefs and traditions?
We can take our cue from non-medical organizations and consider changing this culture of no culture in medicine – introducing diversity task forces that hold departments accountable for recruiting and promoting women and minorities; employing diversity managers; voluntary training; cross-training to increase contact among different groups and mentoring programs that match senior leadership to women and POC. While some medical institutions have implemented some of these principles, changing century-old traditions will require embracing concepts of organizational change and every available effective tool.
Committing to change
Change is especially hard when the target outcome is not accurately quantifiable – even if you can measure attitudes, values, and beliefs, these are subject to reporting bias and tokenism. At the organizational level, change management involves employing a systematic approach to change organizational values, goals, policies, and processes.
Individual change, self-reflection, and personal growth are key components in changing culture. Reflexivity is being aware of your own values, norms, position, and power – an important concept to understand and apply in our everyday interactions. Believing that one’s class, gender, race and sexual orientation are irrelevant to their practice of medicine would not foster the change that we direly need in medicine. Rather, identifying how your own values and professional identity are shaped by your medical training, your organization and the broader cultural context are critically important to developing a greater empathic sense to motivate systemic change.
There has been valuable discussion on bottom-up changes to ensure women and POC have support, encouragement and a pathway to advance in an organization. Some of these include policy and process changes including providing flexible working conditions for women and sponsorship of women and minorities to help them navigate the barriers and microaggressions they encounter at work. While technical (policy) changes form the foundation for any organizational change, it is important to remember that the people side of change – the resistance that you encounter for any change effort in an organization – is equally important to address at the organizational level. A top-down approach is also vital to ensure that change is permanent in an organization and does not end when the individuals responsible for the change leave the organization.
Lewin’s three-stage change management model provides a framework for structural and organizational change in hospital systems. The three-stages of this model are: unfreezing, changing, and refreezing. Unfreezing is the process of determining what needs to change and obtaining leadership support. The actual change process involves getting people on board, empowering them to change and communicating with them frequently. Refreezing cements this change into the organization’s culture by providing support and training to sustain changes. Research has shown that Lewin’s change management model has applicability in the hospital setting.
Industry research in change management methodologies in the business sector has identified sponsorship by CEOs/senior management of an organization and having a structured implementation model for change management as two important factors for ensuring that change efforts are successful and sustainable.
This can be extrapolated to health care organizations – top leadership committed to changing the status quo should solidify organizational commitment by incorporating new attainable and measurable goals into their vision for the organization. Designing a phased implementation of change management methodologies should follow an open discussion to identify an organization’s weaknesses, strengths, capacity, and readiness for change. Lastly, helping busy professionals adapt to change requires innovative and continuous improvement strategies using formal, systematic tools for organization-wide strategic deployment.
Without a concrete commitment at the organizational level, programs such as diversity training may end up being band-aids on wounds that run deep.
I believe that the combination of both individual and organizational commitment to change systemic bias in medicine can be quite powerful. One without the other will fail to permanently change the system. The work to true equality – regardless of the intersecting factors of discrimination – starts with a commitment to change. We may all have different opportunities because of the inequality that is apparent in our systems today, but if we unite around the goal of a bias-free, merit-based equality, it gives us the strength we need to overcome challenges that we once thought insurmountable.
Each one of us is a leader in our own right. Speaking up for those with less power or opportunity than us and supporting talent and hard work solidifies medicine as a meritocracy. Even if the magnitude of change that we fight for may not be realized during our time in medical practice, our commitment to eradicate sexism, racism and discrimination will shape the future of medicine.
Just as our children are a legacy that we leave behind, our work in correcting bias in medicine will pave the path for a better future for the doctors of tomorrow. After all, when I think that my young daughter will be affected by what I do or do not do to address the discrimination, there is no better motivation for me to break down every barrier for her success.
Dr. Kanikkannan is a practicing hospitalist and assistant professor of medicine at Albany Medical College in Albany, NY. This article first appeared on The Hospital Leader, the official blog of SHM.
Addressing systemic bias, gender inequity and discrimination
Addressing systemic bias, gender inequity and discrimination
There are many challenges facing modern medicine today. Recent events have highlighted important issues affecting our society as a whole – systemic racism, sexism, and implicit bias. In medicine, we have seen a renewed focus on health equity, health disparities and the implicit systemic bias that affect those who work in the field. It is truly troubling that it has taken the continued loss of black lives to police brutality and a pandemic for this conversation to happen at every level in society.
Systemic bias is present throughout corporate America, and it is no different within the physician workforce. Overall, there has been gradual interest in promoting and teaching diversity. Institutions have been slowly creating policies and administrative positions focused on inclusion and diversity over the last decade. So has diversity training objectively increased representation and advancement of women and minority groups? Do traditionally marginalized groups have better access to health? And are women and people of color (POC) represented equally in leadership positions in medicine?
Clearly, the answers are not straightforward.
Diving into the data
A guilty pleasure of mine is to assess how diverse and inclusive an institution is by looking at the wall of pictures recognizing top leadership in hospitals. Despite women accounting for 47.9% of graduates from medical school in 2018-2019, I still see very few women or POC elevated to this level. Of the total women graduates, 22.6% were Asian, 8% were Black and 5.4% were Hispanic.
Being of Indian descent, I am a woman of color (albeit one who may not be as profoundly affected by racism in medicine as my less represented colleagues). It is especially rare for me to see someone I can identify with in the ranks of top leadership. I find encouragement in seeing any woman on any leadership board because to me, it means that there is hope. The literature seems to support this degree of disparity as well. For example, a recent analysis shows that presidential leadership in medical societies are predominantly held by men (82.6% male vs. 17.4% female). Other datasets demonstrate that only 15% of deans and interim deans are women and AAMC’s report shows that women account for only 18% of all department chairs.
Growing up, my parents fueled my interest to pursue medicine. They described it as a noble profession that rewarded true merit and dedication to the cause. However, those that have been traditionally elevated in medicine are men. If merit knows no gender, why does a gender gap exist? If merit is blind to race, why are minorities so poorly represented in the workforce (much less in leadership)? My view of the wall leaves me wondering about the role of both sexism and racism in medicine.
These visual representations of the medical culture reinforce the acceptable norms and values – white and masculine – in medicine. The feminist movement over the last several decades has increased awareness about the need for equality of the sexes. However, it was not until the concept of intersectionality was introduced by Black feminist Professor Kimberle Crenshaw, that feminism become a more inclusive term. Professor Crenshaw’s paper details how every individual has intersecting factors – race, gender, sexual identity, socioeconomic status – that create the sum of their experience be it privilege, oppression, or discrimination.
For example, a White woman has privileges that a woman of color does not. Among non-white women, race and sexual identity are confounding factors – a Black woman, a Black LGBTQ woman, and an Asian woman, for example, will not experience discrimination in the same way. The farther you deviate from the accepted norms and values, the harder it is for you to obtain support and achieve recognition.
Addressing the patriarchal structure and systemic bias in medicine
Why do patriarchal structures still exist in medicine? How do we resolve systemic bias? Addressing them in isolation – race or gender or sexual identity – is unlikely to create long-lasting change. For change to occur, organizations and individuals need to be intrinsically motivated. Creating awareness and challenging the status quo is the first step.
Over the last decade, implicit bias training and diversity training have become mandatory in various industries and states. Diversity training has grown to be a multi-billion-dollar industry that corporate America has embraced over the last several years. And yet, research shows that mandating such training may not be the most effective. To get results, organizations need to implement programs that “spark engagement, increase contact between different groups and draw on people’s desire to look good to others.”
Historically, the medical curriculum has not included a discourse on feminist theories and the advancement of women in medicine. Cultural competency training is typically offered on an annual basis once we are in the workforce, but in my experience, it focuses more on our interactions with patients and other health care colleagues, and less with regards to our physician peers and leadership. Is this enough to change deep rooted beliefs and traditions?
We can take our cue from non-medical organizations and consider changing this culture of no culture in medicine – introducing diversity task forces that hold departments accountable for recruiting and promoting women and minorities; employing diversity managers; voluntary training; cross-training to increase contact among different groups and mentoring programs that match senior leadership to women and POC. While some medical institutions have implemented some of these principles, changing century-old traditions will require embracing concepts of organizational change and every available effective tool.
Committing to change
Change is especially hard when the target outcome is not accurately quantifiable – even if you can measure attitudes, values, and beliefs, these are subject to reporting bias and tokenism. At the organizational level, change management involves employing a systematic approach to change organizational values, goals, policies, and processes.
Individual change, self-reflection, and personal growth are key components in changing culture. Reflexivity is being aware of your own values, norms, position, and power – an important concept to understand and apply in our everyday interactions. Believing that one’s class, gender, race and sexual orientation are irrelevant to their practice of medicine would not foster the change that we direly need in medicine. Rather, identifying how your own values and professional identity are shaped by your medical training, your organization and the broader cultural context are critically important to developing a greater empathic sense to motivate systemic change.
There has been valuable discussion on bottom-up changes to ensure women and POC have support, encouragement and a pathway to advance in an organization. Some of these include policy and process changes including providing flexible working conditions for women and sponsorship of women and minorities to help them navigate the barriers and microaggressions they encounter at work. While technical (policy) changes form the foundation for any organizational change, it is important to remember that the people side of change – the resistance that you encounter for any change effort in an organization – is equally important to address at the organizational level. A top-down approach is also vital to ensure that change is permanent in an organization and does not end when the individuals responsible for the change leave the organization.
Lewin’s three-stage change management model provides a framework for structural and organizational change in hospital systems. The three-stages of this model are: unfreezing, changing, and refreezing. Unfreezing is the process of determining what needs to change and obtaining leadership support. The actual change process involves getting people on board, empowering them to change and communicating with them frequently. Refreezing cements this change into the organization’s culture by providing support and training to sustain changes. Research has shown that Lewin’s change management model has applicability in the hospital setting.
Industry research in change management methodologies in the business sector has identified sponsorship by CEOs/senior management of an organization and having a structured implementation model for change management as two important factors for ensuring that change efforts are successful and sustainable.
This can be extrapolated to health care organizations – top leadership committed to changing the status quo should solidify organizational commitment by incorporating new attainable and measurable goals into their vision for the organization. Designing a phased implementation of change management methodologies should follow an open discussion to identify an organization’s weaknesses, strengths, capacity, and readiness for change. Lastly, helping busy professionals adapt to change requires innovative and continuous improvement strategies using formal, systematic tools for organization-wide strategic deployment.
Without a concrete commitment at the organizational level, programs such as diversity training may end up being band-aids on wounds that run deep.
I believe that the combination of both individual and organizational commitment to change systemic bias in medicine can be quite powerful. One without the other will fail to permanently change the system. The work to true equality – regardless of the intersecting factors of discrimination – starts with a commitment to change. We may all have different opportunities because of the inequality that is apparent in our systems today, but if we unite around the goal of a bias-free, merit-based equality, it gives us the strength we need to overcome challenges that we once thought insurmountable.
Each one of us is a leader in our own right. Speaking up for those with less power or opportunity than us and supporting talent and hard work solidifies medicine as a meritocracy. Even if the magnitude of change that we fight for may not be realized during our time in medical practice, our commitment to eradicate sexism, racism and discrimination will shape the future of medicine.
Just as our children are a legacy that we leave behind, our work in correcting bias in medicine will pave the path for a better future for the doctors of tomorrow. After all, when I think that my young daughter will be affected by what I do or do not do to address the discrimination, there is no better motivation for me to break down every barrier for her success.
Dr. Kanikkannan is a practicing hospitalist and assistant professor of medicine at Albany Medical College in Albany, NY. This article first appeared on The Hospital Leader, the official blog of SHM.
There are many challenges facing modern medicine today. Recent events have highlighted important issues affecting our society as a whole – systemic racism, sexism, and implicit bias. In medicine, we have seen a renewed focus on health equity, health disparities and the implicit systemic bias that affect those who work in the field. It is truly troubling that it has taken the continued loss of black lives to police brutality and a pandemic for this conversation to happen at every level in society.
Systemic bias is present throughout corporate America, and it is no different within the physician workforce. Overall, there has been gradual interest in promoting and teaching diversity. Institutions have been slowly creating policies and administrative positions focused on inclusion and diversity over the last decade. So has diversity training objectively increased representation and advancement of women and minority groups? Do traditionally marginalized groups have better access to health? And are women and people of color (POC) represented equally in leadership positions in medicine?
Clearly, the answers are not straightforward.
Diving into the data
A guilty pleasure of mine is to assess how diverse and inclusive an institution is by looking at the wall of pictures recognizing top leadership in hospitals. Despite women accounting for 47.9% of graduates from medical school in 2018-2019, I still see very few women or POC elevated to this level. Of the total women graduates, 22.6% were Asian, 8% were Black and 5.4% were Hispanic.
Being of Indian descent, I am a woman of color (albeit one who may not be as profoundly affected by racism in medicine as my less represented colleagues). It is especially rare for me to see someone I can identify with in the ranks of top leadership. I find encouragement in seeing any woman on any leadership board because to me, it means that there is hope. The literature seems to support this degree of disparity as well. For example, a recent analysis shows that presidential leadership in medical societies are predominantly held by men (82.6% male vs. 17.4% female). Other datasets demonstrate that only 15% of deans and interim deans are women and AAMC’s report shows that women account for only 18% of all department chairs.
Growing up, my parents fueled my interest to pursue medicine. They described it as a noble profession that rewarded true merit and dedication to the cause. However, those that have been traditionally elevated in medicine are men. If merit knows no gender, why does a gender gap exist? If merit is blind to race, why are minorities so poorly represented in the workforce (much less in leadership)? My view of the wall leaves me wondering about the role of both sexism and racism in medicine.
These visual representations of the medical culture reinforce the acceptable norms and values – white and masculine – in medicine. The feminist movement over the last several decades has increased awareness about the need for equality of the sexes. However, it was not until the concept of intersectionality was introduced by Black feminist Professor Kimberle Crenshaw, that feminism become a more inclusive term. Professor Crenshaw’s paper details how every individual has intersecting factors – race, gender, sexual identity, socioeconomic status – that create the sum of their experience be it privilege, oppression, or discrimination.
For example, a White woman has privileges that a woman of color does not. Among non-white women, race and sexual identity are confounding factors – a Black woman, a Black LGBTQ woman, and an Asian woman, for example, will not experience discrimination in the same way. The farther you deviate from the accepted norms and values, the harder it is for you to obtain support and achieve recognition.
Addressing the patriarchal structure and systemic bias in medicine
Why do patriarchal structures still exist in medicine? How do we resolve systemic bias? Addressing them in isolation – race or gender or sexual identity – is unlikely to create long-lasting change. For change to occur, organizations and individuals need to be intrinsically motivated. Creating awareness and challenging the status quo is the first step.
Over the last decade, implicit bias training and diversity training have become mandatory in various industries and states. Diversity training has grown to be a multi-billion-dollar industry that corporate America has embraced over the last several years. And yet, research shows that mandating such training may not be the most effective. To get results, organizations need to implement programs that “spark engagement, increase contact between different groups and draw on people’s desire to look good to others.”
Historically, the medical curriculum has not included a discourse on feminist theories and the advancement of women in medicine. Cultural competency training is typically offered on an annual basis once we are in the workforce, but in my experience, it focuses more on our interactions with patients and other health care colleagues, and less with regards to our physician peers and leadership. Is this enough to change deep rooted beliefs and traditions?
We can take our cue from non-medical organizations and consider changing this culture of no culture in medicine – introducing diversity task forces that hold departments accountable for recruiting and promoting women and minorities; employing diversity managers; voluntary training; cross-training to increase contact among different groups and mentoring programs that match senior leadership to women and POC. While some medical institutions have implemented some of these principles, changing century-old traditions will require embracing concepts of organizational change and every available effective tool.
Committing to change
Change is especially hard when the target outcome is not accurately quantifiable – even if you can measure attitudes, values, and beliefs, these are subject to reporting bias and tokenism. At the organizational level, change management involves employing a systematic approach to change organizational values, goals, policies, and processes.
Individual change, self-reflection, and personal growth are key components in changing culture. Reflexivity is being aware of your own values, norms, position, and power – an important concept to understand and apply in our everyday interactions. Believing that one’s class, gender, race and sexual orientation are irrelevant to their practice of medicine would not foster the change that we direly need in medicine. Rather, identifying how your own values and professional identity are shaped by your medical training, your organization and the broader cultural context are critically important to developing a greater empathic sense to motivate systemic change.
There has been valuable discussion on bottom-up changes to ensure women and POC have support, encouragement and a pathway to advance in an organization. Some of these include policy and process changes including providing flexible working conditions for women and sponsorship of women and minorities to help them navigate the barriers and microaggressions they encounter at work. While technical (policy) changes form the foundation for any organizational change, it is important to remember that the people side of change – the resistance that you encounter for any change effort in an organization – is equally important to address at the organizational level. A top-down approach is also vital to ensure that change is permanent in an organization and does not end when the individuals responsible for the change leave the organization.
Lewin’s three-stage change management model provides a framework for structural and organizational change in hospital systems. The three-stages of this model are: unfreezing, changing, and refreezing. Unfreezing is the process of determining what needs to change and obtaining leadership support. The actual change process involves getting people on board, empowering them to change and communicating with them frequently. Refreezing cements this change into the organization’s culture by providing support and training to sustain changes. Research has shown that Lewin’s change management model has applicability in the hospital setting.
Industry research in change management methodologies in the business sector has identified sponsorship by CEOs/senior management of an organization and having a structured implementation model for change management as two important factors for ensuring that change efforts are successful and sustainable.
This can be extrapolated to health care organizations – top leadership committed to changing the status quo should solidify organizational commitment by incorporating new attainable and measurable goals into their vision for the organization. Designing a phased implementation of change management methodologies should follow an open discussion to identify an organization’s weaknesses, strengths, capacity, and readiness for change. Lastly, helping busy professionals adapt to change requires innovative and continuous improvement strategies using formal, systematic tools for organization-wide strategic deployment.
Without a concrete commitment at the organizational level, programs such as diversity training may end up being band-aids on wounds that run deep.
I believe that the combination of both individual and organizational commitment to change systemic bias in medicine can be quite powerful. One without the other will fail to permanently change the system. The work to true equality – regardless of the intersecting factors of discrimination – starts with a commitment to change. We may all have different opportunities because of the inequality that is apparent in our systems today, but if we unite around the goal of a bias-free, merit-based equality, it gives us the strength we need to overcome challenges that we once thought insurmountable.
Each one of us is a leader in our own right. Speaking up for those with less power or opportunity than us and supporting talent and hard work solidifies medicine as a meritocracy. Even if the magnitude of change that we fight for may not be realized during our time in medical practice, our commitment to eradicate sexism, racism and discrimination will shape the future of medicine.
Just as our children are a legacy that we leave behind, our work in correcting bias in medicine will pave the path for a better future for the doctors of tomorrow. After all, when I think that my young daughter will be affected by what I do or do not do to address the discrimination, there is no better motivation for me to break down every barrier for her success.
Dr. Kanikkannan is a practicing hospitalist and assistant professor of medicine at Albany Medical College in Albany, NY. This article first appeared on The Hospital Leader, the official blog of SHM.
Access to care: A nurse practitioner’s plea
Having been a reader of Pediatric News for years, I want to bring to light access-to-care issues involving COVID-19 medical facility restrictions for pediatric patients and their parents.
On March 27, 2020, I received a phone call from the Department of Human Services pleading with me to take a medically fragile child who was entering the foster care system that day. He had very specific needs, and they had no one available who could medically meet those needs. The week prior was my kids’ scheduled spring break; the week I got the call was the week that I was voluntarily furloughed from my job as a pediatric nurse practitioner so that I could stay home with my kids as their school would not be reopening for the year, and someone had to be with them. I was already home with my 3-year-old and 6-year-old, so why not add another?
Leo (name changed for privacy) came to me with a multitude of diagnoses, to say the least. Not only did he require physical, speech, and occupational therapy twice weekly, but he often had appointments with 10 different specialists at the local children’s hospital. The first few weeks he was in my care, we had almost daily visits to either therapists or specialists. Keeping up with these types of appointments in a normal world is difficult ... I was getting the crash course on how to navigate all of it in the COVID-19 world.
So now, I am the primary caregiver during the day for my two children and our medically fragile foster child who has multiple medical appointments a week. Our local children’s hospital allowed only the caregiver to accompany him to his visits. In theory this sounds great, right? Fewer people in a facility equals less exposure, less risk, and fewer COVID-19 infections.
But what about the negative consequences of these hospital policies? I have two other children I was caring for. I couldn’t take them to their grandparents’ house because people over age 65 years are at risk of having COVID-19 complications. I had been furloughed, so our income was half what it typically was. Regardless,
Now imagine if I were a single mom who had three kids and a lesser paying job. Schools are closed and she’s forced to work from home and homeschool her children. Or worse, she’s been laid off and living on unemployment. Do you think she is going to have the time or finances available to hire a babysitter so that she can take her medically fragile child in for his cardiology follow-up? Because not only does she have to pay the copays and whatever insurance doesn’t cover, but now she has to fork over $50 for child care. If you don’t know the answer already, it’s no, she does not have the time or the finances. So her child misses a cardiology appointment, which means that his meds weren’t increased according to his growth, which means his pulmonary hypertension is not controlled, which worsens his heart failure ... you get my drift.
Fast forward to Sept. 22, 2020. I had a cardiology appointment at our local heart hospital for myself. It’s 2020, people, I’ve been having some palpitations that I needed checked out and was going in to have a heart monitor patch placed. I had my 4-year-old son with me because he is on a hybrid schedule where we homeschool 2 days a week. We entered the building wearing masks, and I was immediately stopped by security and informed that, according to the COVID-19 policy for their hospital, children under 16 are not allowed to enter the building. After some discussion, I was ultimately refused care because my son was with me that day. Refused care because I had a masked 4-year-old with a normal temperature at my side.
These policies are not working. We are in health care. It should not matter what pandemic is on the table, we should not be refusing patients access to care based on who is by their side that day. We knew the risks when we entered our profession, and we know the proper measures to protect ourselves. Our patients also know the risks and can protect themselves accordingly.
So this is my plea to all medical facilities out there: Stop. Stop telling people their loved ones can’t accompany them to appointments. Stop telling caregivers to wait in their cars while their elderly, demented mothers have their annual physicals. Stop telling moms they need to leave their other children at home. This is now a huge access-to-care issue nationwide and it needs to stop. Excess deaths in our nation are soaring, and it’s not just because people don’t want to seek medical attention; it’s because medical facilities are making it almost impossible to seek help for many. People are dying, and it’s not only from COVID-19. This is on us as health care providers, and we need to step up to the plate and do what is right.
Ms. Baxendale is a nurse practitioner in Mustang, Okla. Email her at pdnews@mdedge.com.
Having been a reader of Pediatric News for years, I want to bring to light access-to-care issues involving COVID-19 medical facility restrictions for pediatric patients and their parents.
On March 27, 2020, I received a phone call from the Department of Human Services pleading with me to take a medically fragile child who was entering the foster care system that day. He had very specific needs, and they had no one available who could medically meet those needs. The week prior was my kids’ scheduled spring break; the week I got the call was the week that I was voluntarily furloughed from my job as a pediatric nurse practitioner so that I could stay home with my kids as their school would not be reopening for the year, and someone had to be with them. I was already home with my 3-year-old and 6-year-old, so why not add another?
Leo (name changed for privacy) came to me with a multitude of diagnoses, to say the least. Not only did he require physical, speech, and occupational therapy twice weekly, but he often had appointments with 10 different specialists at the local children’s hospital. The first few weeks he was in my care, we had almost daily visits to either therapists or specialists. Keeping up with these types of appointments in a normal world is difficult ... I was getting the crash course on how to navigate all of it in the COVID-19 world.
So now, I am the primary caregiver during the day for my two children and our medically fragile foster child who has multiple medical appointments a week. Our local children’s hospital allowed only the caregiver to accompany him to his visits. In theory this sounds great, right? Fewer people in a facility equals less exposure, less risk, and fewer COVID-19 infections.
But what about the negative consequences of these hospital policies? I have two other children I was caring for. I couldn’t take them to their grandparents’ house because people over age 65 years are at risk of having COVID-19 complications. I had been furloughed, so our income was half what it typically was. Regardless,
Now imagine if I were a single mom who had three kids and a lesser paying job. Schools are closed and she’s forced to work from home and homeschool her children. Or worse, she’s been laid off and living on unemployment. Do you think she is going to have the time or finances available to hire a babysitter so that she can take her medically fragile child in for his cardiology follow-up? Because not only does she have to pay the copays and whatever insurance doesn’t cover, but now she has to fork over $50 for child care. If you don’t know the answer already, it’s no, she does not have the time or the finances. So her child misses a cardiology appointment, which means that his meds weren’t increased according to his growth, which means his pulmonary hypertension is not controlled, which worsens his heart failure ... you get my drift.
Fast forward to Sept. 22, 2020. I had a cardiology appointment at our local heart hospital for myself. It’s 2020, people, I’ve been having some palpitations that I needed checked out and was going in to have a heart monitor patch placed. I had my 4-year-old son with me because he is on a hybrid schedule where we homeschool 2 days a week. We entered the building wearing masks, and I was immediately stopped by security and informed that, according to the COVID-19 policy for their hospital, children under 16 are not allowed to enter the building. After some discussion, I was ultimately refused care because my son was with me that day. Refused care because I had a masked 4-year-old with a normal temperature at my side.
These policies are not working. We are in health care. It should not matter what pandemic is on the table, we should not be refusing patients access to care based on who is by their side that day. We knew the risks when we entered our profession, and we know the proper measures to protect ourselves. Our patients also know the risks and can protect themselves accordingly.
So this is my plea to all medical facilities out there: Stop. Stop telling people their loved ones can’t accompany them to appointments. Stop telling caregivers to wait in their cars while their elderly, demented mothers have their annual physicals. Stop telling moms they need to leave their other children at home. This is now a huge access-to-care issue nationwide and it needs to stop. Excess deaths in our nation are soaring, and it’s not just because people don’t want to seek medical attention; it’s because medical facilities are making it almost impossible to seek help for many. People are dying, and it’s not only from COVID-19. This is on us as health care providers, and we need to step up to the plate and do what is right.
Ms. Baxendale is a nurse practitioner in Mustang, Okla. Email her at pdnews@mdedge.com.
Having been a reader of Pediatric News for years, I want to bring to light access-to-care issues involving COVID-19 medical facility restrictions for pediatric patients and their parents.
On March 27, 2020, I received a phone call from the Department of Human Services pleading with me to take a medically fragile child who was entering the foster care system that day. He had very specific needs, and they had no one available who could medically meet those needs. The week prior was my kids’ scheduled spring break; the week I got the call was the week that I was voluntarily furloughed from my job as a pediatric nurse practitioner so that I could stay home with my kids as their school would not be reopening for the year, and someone had to be with them. I was already home with my 3-year-old and 6-year-old, so why not add another?
Leo (name changed for privacy) came to me with a multitude of diagnoses, to say the least. Not only did he require physical, speech, and occupational therapy twice weekly, but he often had appointments with 10 different specialists at the local children’s hospital. The first few weeks he was in my care, we had almost daily visits to either therapists or specialists. Keeping up with these types of appointments in a normal world is difficult ... I was getting the crash course on how to navigate all of it in the COVID-19 world.
So now, I am the primary caregiver during the day for my two children and our medically fragile foster child who has multiple medical appointments a week. Our local children’s hospital allowed only the caregiver to accompany him to his visits. In theory this sounds great, right? Fewer people in a facility equals less exposure, less risk, and fewer COVID-19 infections.
But what about the negative consequences of these hospital policies? I have two other children I was caring for. I couldn’t take them to their grandparents’ house because people over age 65 years are at risk of having COVID-19 complications. I had been furloughed, so our income was half what it typically was. Regardless,
Now imagine if I were a single mom who had three kids and a lesser paying job. Schools are closed and she’s forced to work from home and homeschool her children. Or worse, she’s been laid off and living on unemployment. Do you think she is going to have the time or finances available to hire a babysitter so that she can take her medically fragile child in for his cardiology follow-up? Because not only does she have to pay the copays and whatever insurance doesn’t cover, but now she has to fork over $50 for child care. If you don’t know the answer already, it’s no, she does not have the time or the finances. So her child misses a cardiology appointment, which means that his meds weren’t increased according to his growth, which means his pulmonary hypertension is not controlled, which worsens his heart failure ... you get my drift.
Fast forward to Sept. 22, 2020. I had a cardiology appointment at our local heart hospital for myself. It’s 2020, people, I’ve been having some palpitations that I needed checked out and was going in to have a heart monitor patch placed. I had my 4-year-old son with me because he is on a hybrid schedule where we homeschool 2 days a week. We entered the building wearing masks, and I was immediately stopped by security and informed that, according to the COVID-19 policy for their hospital, children under 16 are not allowed to enter the building. After some discussion, I was ultimately refused care because my son was with me that day. Refused care because I had a masked 4-year-old with a normal temperature at my side.
These policies are not working. We are in health care. It should not matter what pandemic is on the table, we should not be refusing patients access to care based on who is by their side that day. We knew the risks when we entered our profession, and we know the proper measures to protect ourselves. Our patients also know the risks and can protect themselves accordingly.
So this is my plea to all medical facilities out there: Stop. Stop telling people their loved ones can’t accompany them to appointments. Stop telling caregivers to wait in their cars while their elderly, demented mothers have their annual physicals. Stop telling moms they need to leave their other children at home. This is now a huge access-to-care issue nationwide and it needs to stop. Excess deaths in our nation are soaring, and it’s not just because people don’t want to seek medical attention; it’s because medical facilities are making it almost impossible to seek help for many. People are dying, and it’s not only from COVID-19. This is on us as health care providers, and we need to step up to the plate and do what is right.
Ms. Baxendale is a nurse practitioner in Mustang, Okla. Email her at pdnews@mdedge.com.