User login
Learning about “No”
To say that the pandemic has dropped us into uncharted territory is an understatement of unmeasurable proportions. Every day we learn more about it, and every day that new information brings us new challenges. COVID-19 is playing by its own set of rules. To keep pace with it societies have been forced to adapt to them, and members of those societies have had to realize that these new rules must be obeyed or be prepared to suffer the consequences.
I’m not sure exactly when it happened but gradually over my 7 and a half decades on this planet it appears that following the rules and understanding the value of “No” have become concepts to be ignored and left to gather dust in the attics and basements of our society. The tug of war between well-considered rules and the often misinterpreted concept of freedom has been ebbing and flowing since Eve plucked a forbidden apple off that tree.
In some parts of the world, the twin skills of saying and responding to “No” have become lost arts. I think it is not by chance that, of the four books I have written for parents, the one titled “How to Say No to Your Toddler” has become the most widely distributed, having been translated into Italian, Polish, and Russian. It is only slightly comforting to learn that at least some parents understand that creating rules can be important, but realize they aren’t quite sure how go about it.
As it has become clear that social distancing and mask wearing are associated with curtailing the spread of COVID-19, state and local governments have had to bone up on their long-forgotten No-saying skills. This relearning process has been particularly painful for school administrators who may have been warned that “You’ll never be able to get first and second graders to wear masks” or that “College students just won’t obey the rules.”
Both of these cautions are based on observations by educators with years of experience and certainly have a ring of truth to them. But could it be that these pessimistic predictions reflect a society in which parents and educators have lost the talent for crafting sensible rules and linking them to enforceable and rational consequences?
As colleges throughout the country have reopened using a variety of learning and residential strategies, there have been numerous incidents that validate the gloomy predictions of student misbehavior. Smaller schools seem to be having less difficulty, which is not surprising given their relative ease in fostering a sense of community. Many schools have been forced to rollback their plans for in-person learning because students have failed to follow some very simple but unpopular rules.
In a swift and decisive response to student misbehavior, Northeastern University in Boston dismissed 11 first-year students and will not refund their tuition when officials discovered a prohibited social gathering in one of the resident facilities (“Northeastern Dismisses 11 Students for Gathering in Violation of COVID-19 Policies,” by Ian Thomsen, News at Northwestern). This response seemed to have come as a surprise to many students and parents around the country who have become accustomed a diet of warnings and minor sanctions.
Whether this action by Northeastern will trigger similar responses by other universities remains to be seen. But we can hope that it sets an example of how learning about “No” can be an important part of one’s education.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
To say that the pandemic has dropped us into uncharted territory is an understatement of unmeasurable proportions. Every day we learn more about it, and every day that new information brings us new challenges. COVID-19 is playing by its own set of rules. To keep pace with it societies have been forced to adapt to them, and members of those societies have had to realize that these new rules must be obeyed or be prepared to suffer the consequences.
I’m not sure exactly when it happened but gradually over my 7 and a half decades on this planet it appears that following the rules and understanding the value of “No” have become concepts to be ignored and left to gather dust in the attics and basements of our society. The tug of war between well-considered rules and the often misinterpreted concept of freedom has been ebbing and flowing since Eve plucked a forbidden apple off that tree.
In some parts of the world, the twin skills of saying and responding to “No” have become lost arts. I think it is not by chance that, of the four books I have written for parents, the one titled “How to Say No to Your Toddler” has become the most widely distributed, having been translated into Italian, Polish, and Russian. It is only slightly comforting to learn that at least some parents understand that creating rules can be important, but realize they aren’t quite sure how go about it.
As it has become clear that social distancing and mask wearing are associated with curtailing the spread of COVID-19, state and local governments have had to bone up on their long-forgotten No-saying skills. This relearning process has been particularly painful for school administrators who may have been warned that “You’ll never be able to get first and second graders to wear masks” or that “College students just won’t obey the rules.”
Both of these cautions are based on observations by educators with years of experience and certainly have a ring of truth to them. But could it be that these pessimistic predictions reflect a society in which parents and educators have lost the talent for crafting sensible rules and linking them to enforceable and rational consequences?
As colleges throughout the country have reopened using a variety of learning and residential strategies, there have been numerous incidents that validate the gloomy predictions of student misbehavior. Smaller schools seem to be having less difficulty, which is not surprising given their relative ease in fostering a sense of community. Many schools have been forced to rollback their plans for in-person learning because students have failed to follow some very simple but unpopular rules.
In a swift and decisive response to student misbehavior, Northeastern University in Boston dismissed 11 first-year students and will not refund their tuition when officials discovered a prohibited social gathering in one of the resident facilities (“Northeastern Dismisses 11 Students for Gathering in Violation of COVID-19 Policies,” by Ian Thomsen, News at Northwestern). This response seemed to have come as a surprise to many students and parents around the country who have become accustomed a diet of warnings and minor sanctions.
Whether this action by Northeastern will trigger similar responses by other universities remains to be seen. But we can hope that it sets an example of how learning about “No” can be an important part of one’s education.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
To say that the pandemic has dropped us into uncharted territory is an understatement of unmeasurable proportions. Every day we learn more about it, and every day that new information brings us new challenges. COVID-19 is playing by its own set of rules. To keep pace with it societies have been forced to adapt to them, and members of those societies have had to realize that these new rules must be obeyed or be prepared to suffer the consequences.
I’m not sure exactly when it happened but gradually over my 7 and a half decades on this planet it appears that following the rules and understanding the value of “No” have become concepts to be ignored and left to gather dust in the attics and basements of our society. The tug of war between well-considered rules and the often misinterpreted concept of freedom has been ebbing and flowing since Eve plucked a forbidden apple off that tree.
In some parts of the world, the twin skills of saying and responding to “No” have become lost arts. I think it is not by chance that, of the four books I have written for parents, the one titled “How to Say No to Your Toddler” has become the most widely distributed, having been translated into Italian, Polish, and Russian. It is only slightly comforting to learn that at least some parents understand that creating rules can be important, but realize they aren’t quite sure how go about it.
As it has become clear that social distancing and mask wearing are associated with curtailing the spread of COVID-19, state and local governments have had to bone up on their long-forgotten No-saying skills. This relearning process has been particularly painful for school administrators who may have been warned that “You’ll never be able to get first and second graders to wear masks” or that “College students just won’t obey the rules.”
Both of these cautions are based on observations by educators with years of experience and certainly have a ring of truth to them. But could it be that these pessimistic predictions reflect a society in which parents and educators have lost the talent for crafting sensible rules and linking them to enforceable and rational consequences?
As colleges throughout the country have reopened using a variety of learning and residential strategies, there have been numerous incidents that validate the gloomy predictions of student misbehavior. Smaller schools seem to be having less difficulty, which is not surprising given their relative ease in fostering a sense of community. Many schools have been forced to rollback their plans for in-person learning because students have failed to follow some very simple but unpopular rules.
In a swift and decisive response to student misbehavior, Northeastern University in Boston dismissed 11 first-year students and will not refund their tuition when officials discovered a prohibited social gathering in one of the resident facilities (“Northeastern Dismisses 11 Students for Gathering in Violation of COVID-19 Policies,” by Ian Thomsen, News at Northwestern). This response seemed to have come as a surprise to many students and parents around the country who have become accustomed a diet of warnings and minor sanctions.
Whether this action by Northeastern will trigger similar responses by other universities remains to be seen. But we can hope that it sets an example of how learning about “No” can be an important part of one’s education.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Returning to competition
As we continue to stumble around trying to find our way out of the COVID-19 pandemic, it has become clear that the journey has been a never-ending continuum of exercises in risk/benefit assessment. The population always has sorted itself into a bell-shaped curve from those who are risk averse to those who revel in risk taking. And, of course, with a paucity of facts on which we can base our assessment of risk, the discussion often shifts to our gut feelings about the benefits.
When faced with the question of when it is time for children to return to in-person schooling, there seems to be reasonably good agreement about the benefits of face-to-face learning. The level of risk is still to be determined.
When it comes to the issue of when to return to competitive school sports, the risks are equally indeterminate but there is less agreement on the benefits. This lack of uniformity reflects a long-standing dichotomy between those parents and students with a passion for competitive sports and those who see them as nonessential. This existential tug-of-war has gone on in almost every school system I am aware of when the school budget comes up for a vote.
The debate about a return to competitive sports on a collegiate and professional level unfortunately is colored by enormous revenues from media contracts, which means that high school and middle schools can’t look to what are essentially businesses for guidance. The delay created confusion, fluctuating angst and disappointment, but the end product made some sense. Volleyball (indoor) and football were indefinitely delayed. Heavy breathing between competitors separated by a couple of feet and protected only by a flimsy net or helmet cage seems like a risk not worth taking – at least until we have more information.
Other sports were allowed to start with restrictions based on existing social distancing mandates which include no locker rooms and no fans. Some rules such as no throw-ins for soccer didn’t make sense given what we are learning about the virus. But, for the most part, the compromises should result in a chance to reap the benefits of competition for the students whose families are willing to expose them to the yet to be fully determined risks.
There has been some grumbling from parents who see the no-fans mandate as a step too far. Until we know more about the risk of group gatherings outdoors, having no fans, including parents and grandparents, makes sense. In fact, to me it is a step long overdue and a rare sliver of silver lining to the pandemic. Competitive youth sports are for the kids. They are not meant to be entertainment events. Too often children are exposed to parental pressure (voiced and unvoiced) about their “performance” on the field. Neither my younger sister nor I can remember our parents going to any of my away football games in high school or any of my lacrosse games in college. I never felt the loss.
Will I miss watching my grandchildren compete? Of course I will miss it badly. However, giving kids some space to learn and enjoy the competition for itself in an atmosphere free of parental over-involvement will be a breath of fresh air. Something we need badly during this pandemic.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
As we continue to stumble around trying to find our way out of the COVID-19 pandemic, it has become clear that the journey has been a never-ending continuum of exercises in risk/benefit assessment. The population always has sorted itself into a bell-shaped curve from those who are risk averse to those who revel in risk taking. And, of course, with a paucity of facts on which we can base our assessment of risk, the discussion often shifts to our gut feelings about the benefits.
When faced with the question of when it is time for children to return to in-person schooling, there seems to be reasonably good agreement about the benefits of face-to-face learning. The level of risk is still to be determined.
When it comes to the issue of when to return to competitive school sports, the risks are equally indeterminate but there is less agreement on the benefits. This lack of uniformity reflects a long-standing dichotomy between those parents and students with a passion for competitive sports and those who see them as nonessential. This existential tug-of-war has gone on in almost every school system I am aware of when the school budget comes up for a vote.
The debate about a return to competitive sports on a collegiate and professional level unfortunately is colored by enormous revenues from media contracts, which means that high school and middle schools can’t look to what are essentially businesses for guidance. The delay created confusion, fluctuating angst and disappointment, but the end product made some sense. Volleyball (indoor) and football were indefinitely delayed. Heavy breathing between competitors separated by a couple of feet and protected only by a flimsy net or helmet cage seems like a risk not worth taking – at least until we have more information.
Other sports were allowed to start with restrictions based on existing social distancing mandates which include no locker rooms and no fans. Some rules such as no throw-ins for soccer didn’t make sense given what we are learning about the virus. But, for the most part, the compromises should result in a chance to reap the benefits of competition for the students whose families are willing to expose them to the yet to be fully determined risks.
There has been some grumbling from parents who see the no-fans mandate as a step too far. Until we know more about the risk of group gatherings outdoors, having no fans, including parents and grandparents, makes sense. In fact, to me it is a step long overdue and a rare sliver of silver lining to the pandemic. Competitive youth sports are for the kids. They are not meant to be entertainment events. Too often children are exposed to parental pressure (voiced and unvoiced) about their “performance” on the field. Neither my younger sister nor I can remember our parents going to any of my away football games in high school or any of my lacrosse games in college. I never felt the loss.
Will I miss watching my grandchildren compete? Of course I will miss it badly. However, giving kids some space to learn and enjoy the competition for itself in an atmosphere free of parental over-involvement will be a breath of fresh air. Something we need badly during this pandemic.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
As we continue to stumble around trying to find our way out of the COVID-19 pandemic, it has become clear that the journey has been a never-ending continuum of exercises in risk/benefit assessment. The population always has sorted itself into a bell-shaped curve from those who are risk averse to those who revel in risk taking. And, of course, with a paucity of facts on which we can base our assessment of risk, the discussion often shifts to our gut feelings about the benefits.
When faced with the question of when it is time for children to return to in-person schooling, there seems to be reasonably good agreement about the benefits of face-to-face learning. The level of risk is still to be determined.
When it comes to the issue of when to return to competitive school sports, the risks are equally indeterminate but there is less agreement on the benefits. This lack of uniformity reflects a long-standing dichotomy between those parents and students with a passion for competitive sports and those who see them as nonessential. This existential tug-of-war has gone on in almost every school system I am aware of when the school budget comes up for a vote.
The debate about a return to competitive sports on a collegiate and professional level unfortunately is colored by enormous revenues from media contracts, which means that high school and middle schools can’t look to what are essentially businesses for guidance. The delay created confusion, fluctuating angst and disappointment, but the end product made some sense. Volleyball (indoor) and football were indefinitely delayed. Heavy breathing between competitors separated by a couple of feet and protected only by a flimsy net or helmet cage seems like a risk not worth taking – at least until we have more information.
Other sports were allowed to start with restrictions based on existing social distancing mandates which include no locker rooms and no fans. Some rules such as no throw-ins for soccer didn’t make sense given what we are learning about the virus. But, for the most part, the compromises should result in a chance to reap the benefits of competition for the students whose families are willing to expose them to the yet to be fully determined risks.
There has been some grumbling from parents who see the no-fans mandate as a step too far. Until we know more about the risk of group gatherings outdoors, having no fans, including parents and grandparents, makes sense. In fact, to me it is a step long overdue and a rare sliver of silver lining to the pandemic. Competitive youth sports are for the kids. They are not meant to be entertainment events. Too often children are exposed to parental pressure (voiced and unvoiced) about their “performance” on the field. Neither my younger sister nor I can remember our parents going to any of my away football games in high school or any of my lacrosse games in college. I never felt the loss.
Will I miss watching my grandchildren compete? Of course I will miss it badly. However, giving kids some space to learn and enjoy the competition for itself in an atmosphere free of parental over-involvement will be a breath of fresh air. Something we need badly during this pandemic.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
Is depression contagious?
I previously wrote a column in which I discussed the possible relationship between television viewing and the risk of developing depression. In that column I mentioned that, while there is widespread suspicion that depression may have a genetic component, I was unaware of any strong evidence that this is the case. This week I encountered another study in the American Journal of Psychiatry that suggests that the environment in which a child is raised can play a significant role in whether he or she will develop depression.
All of the children in the study had been born to families in which at least one biological parent had been diagnosed with major depression. There were nearly 700 full sibships and 2,600 half sibships studied. The researchers found that children who had been adopted away and raised in families that had been selected for having high-quality childrearing standards were significantly less likely to develop depression (23% for full siblings, 19% for half siblings) than their siblings who had remained in the home of their biological parents. It is interesting that this protective effect of the adoptive home “disappeared when an adoptive parent or stepsibling had major depression or the adoptive home was disrupted by parental death or divorce.”
It is unlikely that this study ever will be replicated because of the unique manner in which these Swedish adoptions were managed and recorded. However, and probably even more of an influence than genetics.
Are you surprised by the results of this study? Or, like me, have you always suspected that a child growing up in a household with a depressed, missing, or divorced parent was at increased risk of becoming depressed, particularly they had a genetic vulnerability? How will you change your approach to families with a depressed parent or ones that are navigating through the stormy waters of even an amicable divorce? Will you be more diligent about screening children in these families for depression? Should the agencies that are responsible for managing adoption and foster home placement include this new information in their screening criteria?
It would be very interesting to see a similar study performed using families in which a biological parent had been diagnosed with anxiety or an attention-deficit disorder. Could it mean that we should be considering depression and these conditions as contagious disorders? The results from such studies might help provide clarity to why we are seeing more children with mental health complaints. They might explain why pediatricians are seeing an increasing frequency of mental health complaints in our offices. It may not be too far-fetched to use epidemiologic terms when we are talking about depression, anxiety, and ADHD. Should we be considering these conditions to be contagious under certain circumstances?
Since the human genome has been sequenced I sense that our attention has become overfocused on using what we are learning about our DNA to explain what makes us sick. It may be time to swing the pendulum back a few degrees and remind ourselves of the power of the family environment.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
I previously wrote a column in which I discussed the possible relationship between television viewing and the risk of developing depression. In that column I mentioned that, while there is widespread suspicion that depression may have a genetic component, I was unaware of any strong evidence that this is the case. This week I encountered another study in the American Journal of Psychiatry that suggests that the environment in which a child is raised can play a significant role in whether he or she will develop depression.
All of the children in the study had been born to families in which at least one biological parent had been diagnosed with major depression. There were nearly 700 full sibships and 2,600 half sibships studied. The researchers found that children who had been adopted away and raised in families that had been selected for having high-quality childrearing standards were significantly less likely to develop depression (23% for full siblings, 19% for half siblings) than their siblings who had remained in the home of their biological parents. It is interesting that this protective effect of the adoptive home “disappeared when an adoptive parent or stepsibling had major depression or the adoptive home was disrupted by parental death or divorce.”
It is unlikely that this study ever will be replicated because of the unique manner in which these Swedish adoptions were managed and recorded. However, and probably even more of an influence than genetics.
Are you surprised by the results of this study? Or, like me, have you always suspected that a child growing up in a household with a depressed, missing, or divorced parent was at increased risk of becoming depressed, particularly they had a genetic vulnerability? How will you change your approach to families with a depressed parent or ones that are navigating through the stormy waters of even an amicable divorce? Will you be more diligent about screening children in these families for depression? Should the agencies that are responsible for managing adoption and foster home placement include this new information in their screening criteria?
It would be very interesting to see a similar study performed using families in which a biological parent had been diagnosed with anxiety or an attention-deficit disorder. Could it mean that we should be considering depression and these conditions as contagious disorders? The results from such studies might help provide clarity to why we are seeing more children with mental health complaints. They might explain why pediatricians are seeing an increasing frequency of mental health complaints in our offices. It may not be too far-fetched to use epidemiologic terms when we are talking about depression, anxiety, and ADHD. Should we be considering these conditions to be contagious under certain circumstances?
Since the human genome has been sequenced I sense that our attention has become overfocused on using what we are learning about our DNA to explain what makes us sick. It may be time to swing the pendulum back a few degrees and remind ourselves of the power of the family environment.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
I previously wrote a column in which I discussed the possible relationship between television viewing and the risk of developing depression. In that column I mentioned that, while there is widespread suspicion that depression may have a genetic component, I was unaware of any strong evidence that this is the case. This week I encountered another study in the American Journal of Psychiatry that suggests that the environment in which a child is raised can play a significant role in whether he or she will develop depression.
All of the children in the study had been born to families in which at least one biological parent had been diagnosed with major depression. There were nearly 700 full sibships and 2,600 half sibships studied. The researchers found that children who had been adopted away and raised in families that had been selected for having high-quality childrearing standards were significantly less likely to develop depression (23% for full siblings, 19% for half siblings) than their siblings who had remained in the home of their biological parents. It is interesting that this protective effect of the adoptive home “disappeared when an adoptive parent or stepsibling had major depression or the adoptive home was disrupted by parental death or divorce.”
It is unlikely that this study ever will be replicated because of the unique manner in which these Swedish adoptions were managed and recorded. However, and probably even more of an influence than genetics.
Are you surprised by the results of this study? Or, like me, have you always suspected that a child growing up in a household with a depressed, missing, or divorced parent was at increased risk of becoming depressed, particularly they had a genetic vulnerability? How will you change your approach to families with a depressed parent or ones that are navigating through the stormy waters of even an amicable divorce? Will you be more diligent about screening children in these families for depression? Should the agencies that are responsible for managing adoption and foster home placement include this new information in their screening criteria?
It would be very interesting to see a similar study performed using families in which a biological parent had been diagnosed with anxiety or an attention-deficit disorder. Could it mean that we should be considering depression and these conditions as contagious disorders? The results from such studies might help provide clarity to why we are seeing more children with mental health complaints. They might explain why pediatricians are seeing an increasing frequency of mental health complaints in our offices. It may not be too far-fetched to use epidemiologic terms when we are talking about depression, anxiety, and ADHD. Should we be considering these conditions to be contagious under certain circumstances?
Since the human genome has been sequenced I sense that our attention has become overfocused on using what we are learning about our DNA to explain what makes us sick. It may be time to swing the pendulum back a few degrees and remind ourselves of the power of the family environment.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
Full-time, part-time, FTE: Know the differences
The wholesale to them. While rules vary from state to state, some generalizations can be made.
Even the definitions of full-time and part-time vary. For instance, under the Affordable Care Act (ACA), full time means working at least 30 hours per week. Under the Families First Coronavirus Response Act (FFCRA), it is 40 hours.
Full-time equivalent (FTE) is a concept designed to document a part-time workforce in terms of full-time employment, by taking the total hours worked by all part-time employees and dividing by the full-time schedule. Of course, the ACA and the Paycheck Protection Program (PPP) calculate that number differently: The ACA requires you to total all the hours worked by part-time employees per month, and divide by 120. For the PPP, you divide the total part-time hours per week by 40, and round to the nearest tenth. (You can also use a simplified method that assigns a 1.0 for employees who work 40 hours or more per week and 0.5 for those who work fewer; whichever method you choose, you must apply it consistently on all PPP forms.)
FTEs are important for the purposes of the ACA because employers with 50 or more full-timers plus FTEs must offer health coverage to their full-timers and dependents. But most private practitioners need an accurate FTE total to deal with the PPP: If staffing levels weren’t maintained after you received a PPP loan, your loan forgiveness amount may be reduced. Staffing levels are determined by comparing the average number of full-timers plus FTEs during the “covered period” to either the period from Feb. 15 through June 30, 2019, or Jan. 1 through Feb. 28, 2020.
The PPP aside, FTEs have created confusion over when an employee is entitled to overtime pay. Under federal law, overtime is due whenever an employee works more than 40 hours per week; up to 40 hours, the regular wage is paid. (There are exemptions, and a few states use a daily number.) For example, if a part-timer receiving $900 per week for a 30-hour workweek works more than 30 hours, the hours from 30 to 40 would be compensated at their normal wage of $30 per hour ($900 ÷ 30). If the employee worked more than 40 hours, you would pay overtime (in this case $45 per hour, $30 x 1.5) for the hours in excess of 40.
To address a few other employment questions that I am frequently asked:
Under the FFCRA, you must provide both full- and part-time employees with emergency paid sick leave (EPSL) if they’re unable to work from your office or their home because of illness attributable to COVID-19, quarantine, or caring for a sick family member or child whose school is closed. Full-time employees are entitled to up to 80 hours of EPSL, and part-timers an average of what they work every 2 weeks. Some states have their own laws independent from the FFCRA. Check your state or local laws.
- Some states require you to provide meal and rest breaks to both full- and part-time employees. In California, for example, employers must provide a 30-minute meal break after no more than 5 hours of work, unless the total workday is less than 6 hours and both employers and employees consent to waive breaks. California also requires rest breaks after every 4 hours worked. Check the laws in your state.
- You must include part-time employees in a 401(k) retirement plan if they work at least 1,000 hours in a year, which is about 20 hours per week. That rule is changing in 2021 to 500 hours for employees older than 21. There are state-run retirement programs in California, Connecticut, New Jersey, Washington, and Oregon, among other states. Check your state law for details.
- If you offer paid vacations to full-time employees, you do not have to do the same for part-timers. (In fact, there is no requirement in most states to offer vacation time at all.) My office does offer it to part-time employees on a pro rata basis, as do many others in my area. Again, check your state law.
As always, consult with your attorney if it’s not clear which rules apply in your specific situation.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. He has no relevant disclosures related to the topic of this column. Write to him at dermnews@mdedge.com.
The wholesale to them. While rules vary from state to state, some generalizations can be made.
Even the definitions of full-time and part-time vary. For instance, under the Affordable Care Act (ACA), full time means working at least 30 hours per week. Under the Families First Coronavirus Response Act (FFCRA), it is 40 hours.
Full-time equivalent (FTE) is a concept designed to document a part-time workforce in terms of full-time employment, by taking the total hours worked by all part-time employees and dividing by the full-time schedule. Of course, the ACA and the Paycheck Protection Program (PPP) calculate that number differently: The ACA requires you to total all the hours worked by part-time employees per month, and divide by 120. For the PPP, you divide the total part-time hours per week by 40, and round to the nearest tenth. (You can also use a simplified method that assigns a 1.0 for employees who work 40 hours or more per week and 0.5 for those who work fewer; whichever method you choose, you must apply it consistently on all PPP forms.)
FTEs are important for the purposes of the ACA because employers with 50 or more full-timers plus FTEs must offer health coverage to their full-timers and dependents. But most private practitioners need an accurate FTE total to deal with the PPP: If staffing levels weren’t maintained after you received a PPP loan, your loan forgiveness amount may be reduced. Staffing levels are determined by comparing the average number of full-timers plus FTEs during the “covered period” to either the period from Feb. 15 through June 30, 2019, or Jan. 1 through Feb. 28, 2020.
The PPP aside, FTEs have created confusion over when an employee is entitled to overtime pay. Under federal law, overtime is due whenever an employee works more than 40 hours per week; up to 40 hours, the regular wage is paid. (There are exemptions, and a few states use a daily number.) For example, if a part-timer receiving $900 per week for a 30-hour workweek works more than 30 hours, the hours from 30 to 40 would be compensated at their normal wage of $30 per hour ($900 ÷ 30). If the employee worked more than 40 hours, you would pay overtime (in this case $45 per hour, $30 x 1.5) for the hours in excess of 40.
To address a few other employment questions that I am frequently asked:
Under the FFCRA, you must provide both full- and part-time employees with emergency paid sick leave (EPSL) if they’re unable to work from your office or their home because of illness attributable to COVID-19, quarantine, or caring for a sick family member or child whose school is closed. Full-time employees are entitled to up to 80 hours of EPSL, and part-timers an average of what they work every 2 weeks. Some states have their own laws independent from the FFCRA. Check your state or local laws.
- Some states require you to provide meal and rest breaks to both full- and part-time employees. In California, for example, employers must provide a 30-minute meal break after no more than 5 hours of work, unless the total workday is less than 6 hours and both employers and employees consent to waive breaks. California also requires rest breaks after every 4 hours worked. Check the laws in your state.
- You must include part-time employees in a 401(k) retirement plan if they work at least 1,000 hours in a year, which is about 20 hours per week. That rule is changing in 2021 to 500 hours for employees older than 21. There are state-run retirement programs in California, Connecticut, New Jersey, Washington, and Oregon, among other states. Check your state law for details.
- If you offer paid vacations to full-time employees, you do not have to do the same for part-timers. (In fact, there is no requirement in most states to offer vacation time at all.) My office does offer it to part-time employees on a pro rata basis, as do many others in my area. Again, check your state law.
As always, consult with your attorney if it’s not clear which rules apply in your specific situation.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. He has no relevant disclosures related to the topic of this column. Write to him at dermnews@mdedge.com.
The wholesale to them. While rules vary from state to state, some generalizations can be made.
Even the definitions of full-time and part-time vary. For instance, under the Affordable Care Act (ACA), full time means working at least 30 hours per week. Under the Families First Coronavirus Response Act (FFCRA), it is 40 hours.
Full-time equivalent (FTE) is a concept designed to document a part-time workforce in terms of full-time employment, by taking the total hours worked by all part-time employees and dividing by the full-time schedule. Of course, the ACA and the Paycheck Protection Program (PPP) calculate that number differently: The ACA requires you to total all the hours worked by part-time employees per month, and divide by 120. For the PPP, you divide the total part-time hours per week by 40, and round to the nearest tenth. (You can also use a simplified method that assigns a 1.0 for employees who work 40 hours or more per week and 0.5 for those who work fewer; whichever method you choose, you must apply it consistently on all PPP forms.)
FTEs are important for the purposes of the ACA because employers with 50 or more full-timers plus FTEs must offer health coverage to their full-timers and dependents. But most private practitioners need an accurate FTE total to deal with the PPP: If staffing levels weren’t maintained after you received a PPP loan, your loan forgiveness amount may be reduced. Staffing levels are determined by comparing the average number of full-timers plus FTEs during the “covered period” to either the period from Feb. 15 through June 30, 2019, or Jan. 1 through Feb. 28, 2020.
The PPP aside, FTEs have created confusion over when an employee is entitled to overtime pay. Under federal law, overtime is due whenever an employee works more than 40 hours per week; up to 40 hours, the regular wage is paid. (There are exemptions, and a few states use a daily number.) For example, if a part-timer receiving $900 per week for a 30-hour workweek works more than 30 hours, the hours from 30 to 40 would be compensated at their normal wage of $30 per hour ($900 ÷ 30). If the employee worked more than 40 hours, you would pay overtime (in this case $45 per hour, $30 x 1.5) for the hours in excess of 40.
To address a few other employment questions that I am frequently asked:
Under the FFCRA, you must provide both full- and part-time employees with emergency paid sick leave (EPSL) if they’re unable to work from your office or their home because of illness attributable to COVID-19, quarantine, or caring for a sick family member or child whose school is closed. Full-time employees are entitled to up to 80 hours of EPSL, and part-timers an average of what they work every 2 weeks. Some states have their own laws independent from the FFCRA. Check your state or local laws.
- Some states require you to provide meal and rest breaks to both full- and part-time employees. In California, for example, employers must provide a 30-minute meal break after no more than 5 hours of work, unless the total workday is less than 6 hours and both employers and employees consent to waive breaks. California also requires rest breaks after every 4 hours worked. Check the laws in your state.
- You must include part-time employees in a 401(k) retirement plan if they work at least 1,000 hours in a year, which is about 20 hours per week. That rule is changing in 2021 to 500 hours for employees older than 21. There are state-run retirement programs in California, Connecticut, New Jersey, Washington, and Oregon, among other states. Check your state law for details.
- If you offer paid vacations to full-time employees, you do not have to do the same for part-timers. (In fact, there is no requirement in most states to offer vacation time at all.) My office does offer it to part-time employees on a pro rata basis, as do many others in my area. Again, check your state law.
As always, consult with your attorney if it’s not clear which rules apply in your specific situation.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. He has no relevant disclosures related to the topic of this column. Write to him at dermnews@mdedge.com.
Hospital medicine, it’s time to vote
Whether physicians or advanced practice practitioners, we are the backbone of our nation’s network of acute care facilities, and on a daily basis, we see just about everything. We have valuable insight into how to improve our nation’s health care system, especially now, as our nation continues to battle COVID-19.
Our role, squarely on the front lines during this pandemic, has given us an important perspective that needs to be heard. We spend our days managing patients with complexity, coordinating with specialists and subspecialists, and advocating – at local, state, and national levels – so that our patients can more easily transition to their lives out of the hospital.
Our current polarized political climate makes it seem that individual voices will not make a difference. It is easy to feel frustrated and powerless. However, those in our specialty are actually in a perfect position to have an educated and influential say in how we move forward, not only about the immediate health crises, but also regarding future health care issues. That voice begins with voting.
Historically, physicians have had surprisingly low rates of voting. For example, a 2007 study found significantly lower rates of voting among physicians, compared with the general public.1 While physician voter turnout may have improved in the past decade, given the substantial changes in health care and the increasing amount of physician engagement in the public sphere, our participation should be greater still. Elected officials listen to, and follow up with, constituents who make their voices heard. Each of us can ensure that the health care policy priorities of our fast-growing specialty are addressed by mobilizing to the voting booth.
Candidates we elect shape our health care system for the future, directly impacting us and our patients. Cost, coverage, access to health care, the Centers for Medicare & Medicaid Services inpatient fee schedules, the ongoing pandemic response, surprise billing, use of telehealth, observation status, and the three-midnight rule are just a few of the issues most important to hospital medicine.
Therefore, we, the SHM Public Policy Committee, urge all of our colleagues, regardless of political sway, to make your voice heard this and every election henceforth. The first step is to register to vote, if you have not done so already.2 Next, exercise that privilege. Given the pandemic, this is not as simple a process as it has been in the past. Take the time to plan your approach to early voting, mail-in voting, or election day voting. Check your County Supervisor of Elections’ website for further information, including how to register, view candidate profiles, check your precinct, and request a mail-in ballot.
In addition to casting your vote, we encourage you to share your opinions and engage in dialogue about health care issues. Clinical fact can dispel rumor and misinformation, and daily experiences can personalize our patients’ health care stories and the impact laws and rules have on our ability to practice. We are part of a trusted profession and have a unique perspective; others need and want to hear it. They can only do that if we are part of the process. Arming yourself with information and voting are the first steps on the path of advocacy. Interpersonal advocacy can also be done on social media. For example, SHM has an active grassroots advocacy network on Twitter. Tag @SHMadvocacy in your tweets to share your thoughts with their network.
Finally, as advocates for our patients in health care, we can also help ensure their safety during this election, in particular regarding COVID-19. Some patients may not wish to engage us in politics, and we must respect their decision. Others may seek our counsel and we should provide it in an unbiased fashion. We can ask our patients if they have considered a safe voting plan, help patients review the alternatives to voting in person if desired, and inform those who wish to physically cast a vote on Election Day of how to mitigate the risk of in-person voting.
Every election is important and health care is front and center for a multitude of reasons. We who practice hospital medicine are integral to our communities and need to be more politically involved. This is our chance to share our voice through our vote, not just this year, but in future elections as well.
Ann Sheehy, MD, SFHM, is division chief of the Division of Hospital Medicine at the University of Wisconsin, Madison, and chair of the SHM Public Policy Committee. Other members of the SHM PPC include Marta Almli, MD; John Biebelhausen, MD; Robert Burke, MD, MS, FHM; George Cheely, MD; Hyung (Harry) Cho, MD, SFHM; Jennifer Cowart, MD, FHM; Suparna Dutta, MD, MS, MPH; Bradley Flansbaum, DO, MPH, MHM; Alain Folefack, MD; Rick Hilger MD SFHM; Melinda Johnson, MD; Sevan Karadolian, MD; Joshua D. Lenchus, DO, FACP, SFHM; Steve Phillipson, MD; Dahlia Rizk, DO; Kendall Rogers, MD, SFHM; Brett Stauffer, MD, MHS; Amit Vashist, MD, SFHM; Robert Zipper, MD, SFHM.
References
1. Grande D et al. Do doctors vote? J Gen Int Med. 2007 May;22(5):585-9.
2. How to register to vote, confirm or change your registration and get a voter registration card. https://www.usa.gov/voter-registration/.
Whether physicians or advanced practice practitioners, we are the backbone of our nation’s network of acute care facilities, and on a daily basis, we see just about everything. We have valuable insight into how to improve our nation’s health care system, especially now, as our nation continues to battle COVID-19.
Our role, squarely on the front lines during this pandemic, has given us an important perspective that needs to be heard. We spend our days managing patients with complexity, coordinating with specialists and subspecialists, and advocating – at local, state, and national levels – so that our patients can more easily transition to their lives out of the hospital.
Our current polarized political climate makes it seem that individual voices will not make a difference. It is easy to feel frustrated and powerless. However, those in our specialty are actually in a perfect position to have an educated and influential say in how we move forward, not only about the immediate health crises, but also regarding future health care issues. That voice begins with voting.
Historically, physicians have had surprisingly low rates of voting. For example, a 2007 study found significantly lower rates of voting among physicians, compared with the general public.1 While physician voter turnout may have improved in the past decade, given the substantial changes in health care and the increasing amount of physician engagement in the public sphere, our participation should be greater still. Elected officials listen to, and follow up with, constituents who make their voices heard. Each of us can ensure that the health care policy priorities of our fast-growing specialty are addressed by mobilizing to the voting booth.
Candidates we elect shape our health care system for the future, directly impacting us and our patients. Cost, coverage, access to health care, the Centers for Medicare & Medicaid Services inpatient fee schedules, the ongoing pandemic response, surprise billing, use of telehealth, observation status, and the three-midnight rule are just a few of the issues most important to hospital medicine.
Therefore, we, the SHM Public Policy Committee, urge all of our colleagues, regardless of political sway, to make your voice heard this and every election henceforth. The first step is to register to vote, if you have not done so already.2 Next, exercise that privilege. Given the pandemic, this is not as simple a process as it has been in the past. Take the time to plan your approach to early voting, mail-in voting, or election day voting. Check your County Supervisor of Elections’ website for further information, including how to register, view candidate profiles, check your precinct, and request a mail-in ballot.
In addition to casting your vote, we encourage you to share your opinions and engage in dialogue about health care issues. Clinical fact can dispel rumor and misinformation, and daily experiences can personalize our patients’ health care stories and the impact laws and rules have on our ability to practice. We are part of a trusted profession and have a unique perspective; others need and want to hear it. They can only do that if we are part of the process. Arming yourself with information and voting are the first steps on the path of advocacy. Interpersonal advocacy can also be done on social media. For example, SHM has an active grassroots advocacy network on Twitter. Tag @SHMadvocacy in your tweets to share your thoughts with their network.
Finally, as advocates for our patients in health care, we can also help ensure their safety during this election, in particular regarding COVID-19. Some patients may not wish to engage us in politics, and we must respect their decision. Others may seek our counsel and we should provide it in an unbiased fashion. We can ask our patients if they have considered a safe voting plan, help patients review the alternatives to voting in person if desired, and inform those who wish to physically cast a vote on Election Day of how to mitigate the risk of in-person voting.
Every election is important and health care is front and center for a multitude of reasons. We who practice hospital medicine are integral to our communities and need to be more politically involved. This is our chance to share our voice through our vote, not just this year, but in future elections as well.
Ann Sheehy, MD, SFHM, is division chief of the Division of Hospital Medicine at the University of Wisconsin, Madison, and chair of the SHM Public Policy Committee. Other members of the SHM PPC include Marta Almli, MD; John Biebelhausen, MD; Robert Burke, MD, MS, FHM; George Cheely, MD; Hyung (Harry) Cho, MD, SFHM; Jennifer Cowart, MD, FHM; Suparna Dutta, MD, MS, MPH; Bradley Flansbaum, DO, MPH, MHM; Alain Folefack, MD; Rick Hilger MD SFHM; Melinda Johnson, MD; Sevan Karadolian, MD; Joshua D. Lenchus, DO, FACP, SFHM; Steve Phillipson, MD; Dahlia Rizk, DO; Kendall Rogers, MD, SFHM; Brett Stauffer, MD, MHS; Amit Vashist, MD, SFHM; Robert Zipper, MD, SFHM.
References
1. Grande D et al. Do doctors vote? J Gen Int Med. 2007 May;22(5):585-9.
2. How to register to vote, confirm or change your registration and get a voter registration card. https://www.usa.gov/voter-registration/.
Whether physicians or advanced practice practitioners, we are the backbone of our nation’s network of acute care facilities, and on a daily basis, we see just about everything. We have valuable insight into how to improve our nation’s health care system, especially now, as our nation continues to battle COVID-19.
Our role, squarely on the front lines during this pandemic, has given us an important perspective that needs to be heard. We spend our days managing patients with complexity, coordinating with specialists and subspecialists, and advocating – at local, state, and national levels – so that our patients can more easily transition to their lives out of the hospital.
Our current polarized political climate makes it seem that individual voices will not make a difference. It is easy to feel frustrated and powerless. However, those in our specialty are actually in a perfect position to have an educated and influential say in how we move forward, not only about the immediate health crises, but also regarding future health care issues. That voice begins with voting.
Historically, physicians have had surprisingly low rates of voting. For example, a 2007 study found significantly lower rates of voting among physicians, compared with the general public.1 While physician voter turnout may have improved in the past decade, given the substantial changes in health care and the increasing amount of physician engagement in the public sphere, our participation should be greater still. Elected officials listen to, and follow up with, constituents who make their voices heard. Each of us can ensure that the health care policy priorities of our fast-growing specialty are addressed by mobilizing to the voting booth.
Candidates we elect shape our health care system for the future, directly impacting us and our patients. Cost, coverage, access to health care, the Centers for Medicare & Medicaid Services inpatient fee schedules, the ongoing pandemic response, surprise billing, use of telehealth, observation status, and the three-midnight rule are just a few of the issues most important to hospital medicine.
Therefore, we, the SHM Public Policy Committee, urge all of our colleagues, regardless of political sway, to make your voice heard this and every election henceforth. The first step is to register to vote, if you have not done so already.2 Next, exercise that privilege. Given the pandemic, this is not as simple a process as it has been in the past. Take the time to plan your approach to early voting, mail-in voting, or election day voting. Check your County Supervisor of Elections’ website for further information, including how to register, view candidate profiles, check your precinct, and request a mail-in ballot.
In addition to casting your vote, we encourage you to share your opinions and engage in dialogue about health care issues. Clinical fact can dispel rumor and misinformation, and daily experiences can personalize our patients’ health care stories and the impact laws and rules have on our ability to practice. We are part of a trusted profession and have a unique perspective; others need and want to hear it. They can only do that if we are part of the process. Arming yourself with information and voting are the first steps on the path of advocacy. Interpersonal advocacy can also be done on social media. For example, SHM has an active grassroots advocacy network on Twitter. Tag @SHMadvocacy in your tweets to share your thoughts with their network.
Finally, as advocates for our patients in health care, we can also help ensure their safety during this election, in particular regarding COVID-19. Some patients may not wish to engage us in politics, and we must respect their decision. Others may seek our counsel and we should provide it in an unbiased fashion. We can ask our patients if they have considered a safe voting plan, help patients review the alternatives to voting in person if desired, and inform those who wish to physically cast a vote on Election Day of how to mitigate the risk of in-person voting.
Every election is important and health care is front and center for a multitude of reasons. We who practice hospital medicine are integral to our communities and need to be more politically involved. This is our chance to share our voice through our vote, not just this year, but in future elections as well.
Ann Sheehy, MD, SFHM, is division chief of the Division of Hospital Medicine at the University of Wisconsin, Madison, and chair of the SHM Public Policy Committee. Other members of the SHM PPC include Marta Almli, MD; John Biebelhausen, MD; Robert Burke, MD, MS, FHM; George Cheely, MD; Hyung (Harry) Cho, MD, SFHM; Jennifer Cowart, MD, FHM; Suparna Dutta, MD, MS, MPH; Bradley Flansbaum, DO, MPH, MHM; Alain Folefack, MD; Rick Hilger MD SFHM; Melinda Johnson, MD; Sevan Karadolian, MD; Joshua D. Lenchus, DO, FACP, SFHM; Steve Phillipson, MD; Dahlia Rizk, DO; Kendall Rogers, MD, SFHM; Brett Stauffer, MD, MHS; Amit Vashist, MD, SFHM; Robert Zipper, MD, SFHM.
References
1. Grande D et al. Do doctors vote? J Gen Int Med. 2007 May;22(5):585-9.
2. How to register to vote, confirm or change your registration and get a voter registration card. https://www.usa.gov/voter-registration/.
COVID-19 and the superspreaders: Teens
Although cases of COVID-19 in children is reported to be low, we are seeing a surge in Wisconsin with a 27.6% positivity rate reported on Sept. 27. Numerous other states across the country are reporting similar jumps of 10% or more.
According to the Wisconsin Department of Health Services as of Sept. 20, 2020, there were 10,644 cumulative cases in persons aged less than 18 years. This rise in cases is consistent with a return to school and sports. This cumulative case load amounts to 836.7/100, 000 cases. This population may not experience the level of illness seen in the older populations with hospitalization rates of only 3% under the age of 9 years and 13% of those age 10- 19-years, yet exposing older family and members of the community is driving the death rates. The combined influenza and COVID-19 season may greatly impact hospitalization rates of young and old. Additionally, we may see a surge in pediatric cancer rates and autoimmune diseases secondary to these trends.
I believe the overall number of adolescents with COVID-19 is underreported. Teens admit to a lack of understanding of symptoms. Many do not realize they have COVID-19 until someone points out the symptoms they describe such as a loss of taste or smell are COVID-19 symptoms. Others report they do not report symptoms to prevent quarantine. Additionally, others endorse ridicule from peers if they have tested positive and contract tracing identifies others potentially exposed and forced to sit out of sports because of quarantine. They have been bullied into amnesia when contract tracers call to prevent identifying others at school or in the community. All these behaviors proliferate the spread of disease within the community and will continue to drive both exposures and death rates.
Teens in high schools require increased education of the symptoms of COVID-19, promotion of the flu vaccine, and knowledge of the impact they can have on preventing the spread of viruses.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She is a member of the Pediatric News editorial advisory board. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
Reference
COVID-19: Wisconsin Cases, Wisconsin Department of Health Services. Accessed 2020 Sep 27.
Although cases of COVID-19 in children is reported to be low, we are seeing a surge in Wisconsin with a 27.6% positivity rate reported on Sept. 27. Numerous other states across the country are reporting similar jumps of 10% or more.
According to the Wisconsin Department of Health Services as of Sept. 20, 2020, there were 10,644 cumulative cases in persons aged less than 18 years. This rise in cases is consistent with a return to school and sports. This cumulative case load amounts to 836.7/100, 000 cases. This population may not experience the level of illness seen in the older populations with hospitalization rates of only 3% under the age of 9 years and 13% of those age 10- 19-years, yet exposing older family and members of the community is driving the death rates. The combined influenza and COVID-19 season may greatly impact hospitalization rates of young and old. Additionally, we may see a surge in pediatric cancer rates and autoimmune diseases secondary to these trends.
I believe the overall number of adolescents with COVID-19 is underreported. Teens admit to a lack of understanding of symptoms. Many do not realize they have COVID-19 until someone points out the symptoms they describe such as a loss of taste or smell are COVID-19 symptoms. Others report they do not report symptoms to prevent quarantine. Additionally, others endorse ridicule from peers if they have tested positive and contract tracing identifies others potentially exposed and forced to sit out of sports because of quarantine. They have been bullied into amnesia when contract tracers call to prevent identifying others at school or in the community. All these behaviors proliferate the spread of disease within the community and will continue to drive both exposures and death rates.
Teens in high schools require increased education of the symptoms of COVID-19, promotion of the flu vaccine, and knowledge of the impact they can have on preventing the spread of viruses.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She is a member of the Pediatric News editorial advisory board. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
Reference
COVID-19: Wisconsin Cases, Wisconsin Department of Health Services. Accessed 2020 Sep 27.
Although cases of COVID-19 in children is reported to be low, we are seeing a surge in Wisconsin with a 27.6% positivity rate reported on Sept. 27. Numerous other states across the country are reporting similar jumps of 10% or more.
According to the Wisconsin Department of Health Services as of Sept. 20, 2020, there were 10,644 cumulative cases in persons aged less than 18 years. This rise in cases is consistent with a return to school and sports. This cumulative case load amounts to 836.7/100, 000 cases. This population may not experience the level of illness seen in the older populations with hospitalization rates of only 3% under the age of 9 years and 13% of those age 10- 19-years, yet exposing older family and members of the community is driving the death rates. The combined influenza and COVID-19 season may greatly impact hospitalization rates of young and old. Additionally, we may see a surge in pediatric cancer rates and autoimmune diseases secondary to these trends.
I believe the overall number of adolescents with COVID-19 is underreported. Teens admit to a lack of understanding of symptoms. Many do not realize they have COVID-19 until someone points out the symptoms they describe such as a loss of taste or smell are COVID-19 symptoms. Others report they do not report symptoms to prevent quarantine. Additionally, others endorse ridicule from peers if they have tested positive and contract tracing identifies others potentially exposed and forced to sit out of sports because of quarantine. They have been bullied into amnesia when contract tracers call to prevent identifying others at school or in the community. All these behaviors proliferate the spread of disease within the community and will continue to drive both exposures and death rates.
Teens in high schools require increased education of the symptoms of COVID-19, promotion of the flu vaccine, and knowledge of the impact they can have on preventing the spread of viruses.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She is a member of the Pediatric News editorial advisory board. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
Reference
COVID-19: Wisconsin Cases, Wisconsin Department of Health Services. Accessed 2020 Sep 27.
2020 has been quite a year
I remember New Year’s Day 2020, full of hope and wonderment of what the year would bring. I was coming into the Society of Hospital Medicine as the incoming President, taking the 2020 reins in the organization’s 20th year. It would be a year of transitioning to a new CEO, reinvigorating our membership engagement efforts, and renewing a strategic plan for forward progress into the next decade. It would be a year chock full of travel, speaking engagements, and meetings with thousands of hospitalists around the globe.
What I didn’t know is that we would soon face the grim reality that the long-voiced concern of infectious disease experts and epidemiologists would come true. That our colleagues and friends and families would be infected, hospitalized, and die from this new disease, for which there were no good, effective treatments. That our ability to come together as a nation to implement basic infection control and epidemiologic practices would be fractured, uncoordinated, and ineffective. That within 6 months of the first case on U.S. soil, we would witness 5,270,000 people being infected from the disease, and 167,000 dying from it. And that the stunning toll of the disease would ripple into every nook and cranny of our society, from the economy to the fabric of our families and to the mental and physical health of all of our citizens.
However, what I couldn’t have known on this past New Year’s Day is how incredibly resilient and innovative our hospital medicine society and community would be to not only endure this new way of working and living, but also to find ways to improve upon how we care for all patients, despite COVID-19. What I couldn’t have known is how hospitalists would pivot to new arenas of care settings, including the EDs, ICUs, “COVID units,” and telehealth – flawlessly and seamlessly filling care gaps that would otherwise be catastrophically unfilled.
What I couldn’t have known is how we would be willing to come back into work, day after day, to care for our patients, despite the risks to ourselves and our families. What I couldn’t have known is how hospitalists would come together as a community to network and share knowledge in unprecedented ways, both humbly and proactively – knowing that we would not have all the answers but that we probably had better answers than most. What I couldn’t have known is that the SHM staff would pivot our entire SHM team away from previous “staple” offerings (e.g., live meetings) to virtual learning and network opportunities, which would be attended at rates higher than ever seen before, including live webinars, HMX exchanges, and e-learnings. What I couldn’t have known is that we would figure out, in a matter of weeks, what treatments were and were not effective for our patients and get those treatments to them despite the difficulties. And what I couldn’t have known is how much prouder I would be, more than ever before, to tell people: “I am a hospitalist.”
I took my son to the dentist recently, and when we were just about to leave, the dentist asked: “What do you do for a living?” and I stated: “I am a hospitalist.” He slowly breathed in and replied: “Oh … wow … you have really seen things …” Yes, we have.
So, is 2020 shaping up as expected? Absolutely not! But I am more inspired, humbled, and motivated than ever to proudly serve SHM with more energy and enthusiasm than I would have dreamed on New Year’s Day. And even if we can’t see each other in person (as we so naively planned), through virtual meetings (national, regional, and chapter), webinars, social media, and other listening modes, we will still be able to connect as a community and share ideas and issues as we muddle through the remainder of 2020 and beyond. We need each other more than ever before, and I am so proud to be a part of this SHM family.
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is president of SHM.
I remember New Year’s Day 2020, full of hope and wonderment of what the year would bring. I was coming into the Society of Hospital Medicine as the incoming President, taking the 2020 reins in the organization’s 20th year. It would be a year of transitioning to a new CEO, reinvigorating our membership engagement efforts, and renewing a strategic plan for forward progress into the next decade. It would be a year chock full of travel, speaking engagements, and meetings with thousands of hospitalists around the globe.
What I didn’t know is that we would soon face the grim reality that the long-voiced concern of infectious disease experts and epidemiologists would come true. That our colleagues and friends and families would be infected, hospitalized, and die from this new disease, for which there were no good, effective treatments. That our ability to come together as a nation to implement basic infection control and epidemiologic practices would be fractured, uncoordinated, and ineffective. That within 6 months of the first case on U.S. soil, we would witness 5,270,000 people being infected from the disease, and 167,000 dying from it. And that the stunning toll of the disease would ripple into every nook and cranny of our society, from the economy to the fabric of our families and to the mental and physical health of all of our citizens.
However, what I couldn’t have known on this past New Year’s Day is how incredibly resilient and innovative our hospital medicine society and community would be to not only endure this new way of working and living, but also to find ways to improve upon how we care for all patients, despite COVID-19. What I couldn’t have known is how hospitalists would pivot to new arenas of care settings, including the EDs, ICUs, “COVID units,” and telehealth – flawlessly and seamlessly filling care gaps that would otherwise be catastrophically unfilled.
What I couldn’t have known is how we would be willing to come back into work, day after day, to care for our patients, despite the risks to ourselves and our families. What I couldn’t have known is how hospitalists would come together as a community to network and share knowledge in unprecedented ways, both humbly and proactively – knowing that we would not have all the answers but that we probably had better answers than most. What I couldn’t have known is that the SHM staff would pivot our entire SHM team away from previous “staple” offerings (e.g., live meetings) to virtual learning and network opportunities, which would be attended at rates higher than ever seen before, including live webinars, HMX exchanges, and e-learnings. What I couldn’t have known is that we would figure out, in a matter of weeks, what treatments were and were not effective for our patients and get those treatments to them despite the difficulties. And what I couldn’t have known is how much prouder I would be, more than ever before, to tell people: “I am a hospitalist.”
I took my son to the dentist recently, and when we were just about to leave, the dentist asked: “What do you do for a living?” and I stated: “I am a hospitalist.” He slowly breathed in and replied: “Oh … wow … you have really seen things …” Yes, we have.
So, is 2020 shaping up as expected? Absolutely not! But I am more inspired, humbled, and motivated than ever to proudly serve SHM with more energy and enthusiasm than I would have dreamed on New Year’s Day. And even if we can’t see each other in person (as we so naively planned), through virtual meetings (national, regional, and chapter), webinars, social media, and other listening modes, we will still be able to connect as a community and share ideas and issues as we muddle through the remainder of 2020 and beyond. We need each other more than ever before, and I am so proud to be a part of this SHM family.
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is president of SHM.
I remember New Year’s Day 2020, full of hope and wonderment of what the year would bring. I was coming into the Society of Hospital Medicine as the incoming President, taking the 2020 reins in the organization’s 20th year. It would be a year of transitioning to a new CEO, reinvigorating our membership engagement efforts, and renewing a strategic plan for forward progress into the next decade. It would be a year chock full of travel, speaking engagements, and meetings with thousands of hospitalists around the globe.
What I didn’t know is that we would soon face the grim reality that the long-voiced concern of infectious disease experts and epidemiologists would come true. That our colleagues and friends and families would be infected, hospitalized, and die from this new disease, for which there were no good, effective treatments. That our ability to come together as a nation to implement basic infection control and epidemiologic practices would be fractured, uncoordinated, and ineffective. That within 6 months of the first case on U.S. soil, we would witness 5,270,000 people being infected from the disease, and 167,000 dying from it. And that the stunning toll of the disease would ripple into every nook and cranny of our society, from the economy to the fabric of our families and to the mental and physical health of all of our citizens.
However, what I couldn’t have known on this past New Year’s Day is how incredibly resilient and innovative our hospital medicine society and community would be to not only endure this new way of working and living, but also to find ways to improve upon how we care for all patients, despite COVID-19. What I couldn’t have known is how hospitalists would pivot to new arenas of care settings, including the EDs, ICUs, “COVID units,” and telehealth – flawlessly and seamlessly filling care gaps that would otherwise be catastrophically unfilled.
What I couldn’t have known is how we would be willing to come back into work, day after day, to care for our patients, despite the risks to ourselves and our families. What I couldn’t have known is how hospitalists would come together as a community to network and share knowledge in unprecedented ways, both humbly and proactively – knowing that we would not have all the answers but that we probably had better answers than most. What I couldn’t have known is that the SHM staff would pivot our entire SHM team away from previous “staple” offerings (e.g., live meetings) to virtual learning and network opportunities, which would be attended at rates higher than ever seen before, including live webinars, HMX exchanges, and e-learnings. What I couldn’t have known is that we would figure out, in a matter of weeks, what treatments were and were not effective for our patients and get those treatments to them despite the difficulties. And what I couldn’t have known is how much prouder I would be, more than ever before, to tell people: “I am a hospitalist.”
I took my son to the dentist recently, and when we were just about to leave, the dentist asked: “What do you do for a living?” and I stated: “I am a hospitalist.” He slowly breathed in and replied: “Oh … wow … you have really seen things …” Yes, we have.
So, is 2020 shaping up as expected? Absolutely not! But I am more inspired, humbled, and motivated than ever to proudly serve SHM with more energy and enthusiasm than I would have dreamed on New Year’s Day. And even if we can’t see each other in person (as we so naively planned), through virtual meetings (national, regional, and chapter), webinars, social media, and other listening modes, we will still be able to connect as a community and share ideas and issues as we muddle through the remainder of 2020 and beyond. We need each other more than ever before, and I am so proud to be a part of this SHM family.
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is president of SHM.
Breast cancer screening complexities
Breast cancer in women remains one of the most common types of cancer in the United States, affecting about one in eight women1 over the course of their lifetime. Despite its pervasiveness, the 5-year survival rate for women with breast cancer remains high, estimated at around 90%2 based on data from 2010-2016, in large part because of early detection and treatment through screening. However, many organizations disagree on when to start and how often to screen women at average risk.
Important to discussions about breast cancer screening is the trend that many women delay childbirth until their 30s and 40s. In 2018 the birth rate increased for women ages 35-44, and the mean age of first birth increased from the prior year across all racial and ethnic groups.3 Therefore, ob.gyns. may need to consider that their patients not only may have increased risk of developing breast cancer based on age alone – women aged 35-44 have four times greater risk of disease than women aged 20-342 – but that the pregnancy itself may further exacerbate risk in older women. A 2019 pooled analysis found that women who were older at first birth had a greater chance of developing breast cancer compared with women with no children.4
In addition, ob.gyns. should consider that their patients may have received a breast cancer diagnosis prior to initiation or completion of their family plans or that their patients are cancer survivors – in 2013-2017, breast cancer was the most common form of cancer in adolescents and young adults.5 Thus, practitioners should be prepared to discuss not only options for fertility preservation but the evidence regarding cancer recurrence after pregnancy.
We have invited Dr. Katherine Tkaczuk, professor of medicine at the University of Maryland School of Medicine* and director of the breast evaluation and treatment program at the Marlene and Stewart Greenebaum Comprehensive Cancer Center, to discuss the vital role of screening in the shared decision-making process of breast cancer prevention.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore,* as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at obnews@mdedge.com.
Correction, 1/8/21: *An earlier version of this article misstated the university affiliations for Dr. Tkaczuk and Dr. Reece.
References
1. U.S. Breast Cancer Statistics. breastcancer.org.
2. “Cancer Stat Facts: Female Breast Cancer,” Surveillance, Epidemiology, and End Results Program. National Cancer Institute.
3. Martin JA et al. “Births: Final Data for 2018.” National Vital Statistics Reports. 2019 Nov 27;68(13):1-46.
4. Nichols HB et al. Ann Intern Med. 2019 Jan;170(1):22-30.
5. “Cancer Stat Facts: Cancer Among Adolescents and Young Adults (AYAs) (Ages 15-39),” Surveillance, Epidemiology, and End Results Program. National Cancer Institute.
Breast cancer in women remains one of the most common types of cancer in the United States, affecting about one in eight women1 over the course of their lifetime. Despite its pervasiveness, the 5-year survival rate for women with breast cancer remains high, estimated at around 90%2 based on data from 2010-2016, in large part because of early detection and treatment through screening. However, many organizations disagree on when to start and how often to screen women at average risk.
Important to discussions about breast cancer screening is the trend that many women delay childbirth until their 30s and 40s. In 2018 the birth rate increased for women ages 35-44, and the mean age of first birth increased from the prior year across all racial and ethnic groups.3 Therefore, ob.gyns. may need to consider that their patients not only may have increased risk of developing breast cancer based on age alone – women aged 35-44 have four times greater risk of disease than women aged 20-342 – but that the pregnancy itself may further exacerbate risk in older women. A 2019 pooled analysis found that women who were older at first birth had a greater chance of developing breast cancer compared with women with no children.4
In addition, ob.gyns. should consider that their patients may have received a breast cancer diagnosis prior to initiation or completion of their family plans or that their patients are cancer survivors – in 2013-2017, breast cancer was the most common form of cancer in adolescents and young adults.5 Thus, practitioners should be prepared to discuss not only options for fertility preservation but the evidence regarding cancer recurrence after pregnancy.
We have invited Dr. Katherine Tkaczuk, professor of medicine at the University of Maryland School of Medicine* and director of the breast evaluation and treatment program at the Marlene and Stewart Greenebaum Comprehensive Cancer Center, to discuss the vital role of screening in the shared decision-making process of breast cancer prevention.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore,* as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at obnews@mdedge.com.
Correction, 1/8/21: *An earlier version of this article misstated the university affiliations for Dr. Tkaczuk and Dr. Reece.
References
1. U.S. Breast Cancer Statistics. breastcancer.org.
2. “Cancer Stat Facts: Female Breast Cancer,” Surveillance, Epidemiology, and End Results Program. National Cancer Institute.
3. Martin JA et al. “Births: Final Data for 2018.” National Vital Statistics Reports. 2019 Nov 27;68(13):1-46.
4. Nichols HB et al. Ann Intern Med. 2019 Jan;170(1):22-30.
5. “Cancer Stat Facts: Cancer Among Adolescents and Young Adults (AYAs) (Ages 15-39),” Surveillance, Epidemiology, and End Results Program. National Cancer Institute.
Breast cancer in women remains one of the most common types of cancer in the United States, affecting about one in eight women1 over the course of their lifetime. Despite its pervasiveness, the 5-year survival rate for women with breast cancer remains high, estimated at around 90%2 based on data from 2010-2016, in large part because of early detection and treatment through screening. However, many organizations disagree on when to start and how often to screen women at average risk.
Important to discussions about breast cancer screening is the trend that many women delay childbirth until their 30s and 40s. In 2018 the birth rate increased for women ages 35-44, and the mean age of first birth increased from the prior year across all racial and ethnic groups.3 Therefore, ob.gyns. may need to consider that their patients not only may have increased risk of developing breast cancer based on age alone – women aged 35-44 have four times greater risk of disease than women aged 20-342 – but that the pregnancy itself may further exacerbate risk in older women. A 2019 pooled analysis found that women who were older at first birth had a greater chance of developing breast cancer compared with women with no children.4
In addition, ob.gyns. should consider that their patients may have received a breast cancer diagnosis prior to initiation or completion of their family plans or that their patients are cancer survivors – in 2013-2017, breast cancer was the most common form of cancer in adolescents and young adults.5 Thus, practitioners should be prepared to discuss not only options for fertility preservation but the evidence regarding cancer recurrence after pregnancy.
We have invited Dr. Katherine Tkaczuk, professor of medicine at the University of Maryland School of Medicine* and director of the breast evaluation and treatment program at the Marlene and Stewart Greenebaum Comprehensive Cancer Center, to discuss the vital role of screening in the shared decision-making process of breast cancer prevention.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore,* as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at obnews@mdedge.com.
Correction, 1/8/21: *An earlier version of this article misstated the university affiliations for Dr. Tkaczuk and Dr. Reece.
References
1. U.S. Breast Cancer Statistics. breastcancer.org.
2. “Cancer Stat Facts: Female Breast Cancer,” Surveillance, Epidemiology, and End Results Program. National Cancer Institute.
3. Martin JA et al. “Births: Final Data for 2018.” National Vital Statistics Reports. 2019 Nov 27;68(13):1-46.
4. Nichols HB et al. Ann Intern Med. 2019 Jan;170(1):22-30.
5. “Cancer Stat Facts: Cancer Among Adolescents and Young Adults (AYAs) (Ages 15-39),” Surveillance, Epidemiology, and End Results Program. National Cancer Institute.
An oncologist’s view on screening mammography
Screening mammography has contributed to the lowering of mortality from breast cancer by facilitating earlier diagnosis and a lower stage at diagnosis. With more effective treatment options for women who are diagnosed with lower-stage breast cancer, the current 5-year survival rate has risen to 90% – significantly higher than the 5-year survival rate of 75% in 1975.1
Women who are at much higher risk for developing breast cancer – mainly because of family history, certain genetic mutations, or a history of radiation therapy to the chest – will benefit the most from earlier and more frequent screening mammography as well as enhanced screening with non-x-ray methods of breast imaging. It is important that ob.gyns. help to identify these women.
However, the majority of women who are screened with mammography are at “average risk,” with a lifetime risk for developing breast cancer of 12.9%, based on 2015-2017 data from the National Cancer Institute’s (NCI) Surveillance, Epidemiology, and End Results Program (SEER).1 The median age at diagnosis of breast cancer in the U.S. is 62 years,1 and advancing age is the most important risk factor for these women.
A 20% relative risk reduction in breast cancer mortality with screening mammography has been demonstrated both in systematic reviews of randomized and observational studies2 and in a meta-analysis of 11 randomized trials comparing screening and no screening.3 Even though the majority of randomized trials were done in the age of film mammography, experts believe that we still see at least a 20% reduction today.
Among average-risk women, those aged 50-74 with a life expectancy of at least 10 years will benefit the most from regular screening. According to the 2016 screening guideline of the United States Preventive Services Task Force (USPSTF), relative risk reductions in breast cancer mortality from mammography screening, by age group, are 0.88 (confidence interval, 0.73-1.003) for ages 39-49; 0.86 (CI, 0.68-0.97) for ages 50-59; 0.67 (CI, 0.55-0.91) for ages 60-69; and 0.80 (CI, 0.51 to 1.28) for ages 70-74.2
For women aged 40-49 years, most of the guidelines in the United States recommend individualized screening every 1 or 2 years – screening that is guided by shared decision-making that takes into account each woman’s values regarding relative harms and benefits. This is because their risk of developing breast cancer is relatively low while the risk of false-positive results can be higher.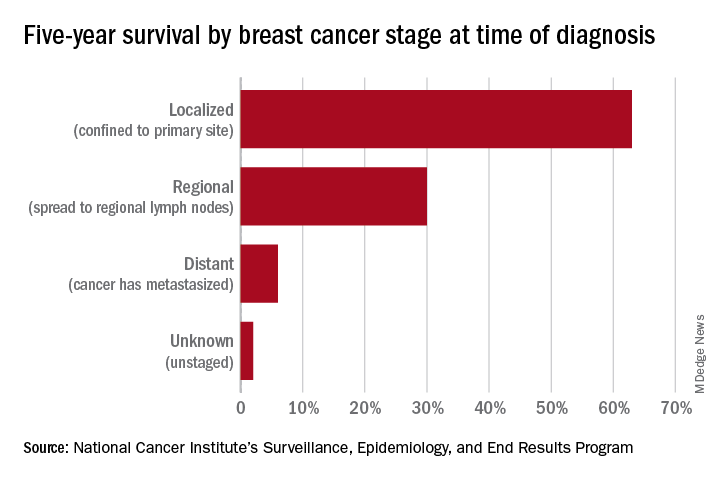
A few exceptions include guidelines by the National Comprehensive Cancer Network (NCCN) and the American College of Radiology, which recommend annual screening mammography starting at age 40 years for all average-risk women. In our program, we adhere to these latter recommendations and advise annual digital 3-D mammograms starting at age 40 and continuing until age 74, or longer if the woman is otherwise healthy with a life expectancy greater than 10 years.
Screening and overdiagnosis
Overdiagnosis – the diagnosis of cancers that may not actually cause mortality or may not even have become apparent without screening – is a concern for all women undergoing routine screening for breast cancer. There is significant uncertainty about its frequency, however.
Research cited by the USPSTF suggests that as many as one in five women diagnosed with breast cancer over approximately 10 years will be overdiagnosed. Other modeling studies have estimated one in eight overdiagnoses, for women aged 50-75 years specifically. By the more conservative estimate, according to the USPSTF, one breast cancer death will be prevented for every 2-3 cases of unnecessary treatment.2
Ductal carcinoma in situ is confined to the mammary ductal-lobular system and lacks the classic characteristics of cancer. Technically, it should not metastasize. But we do not know with certainty which cases of DCIS will or will not progress to invasive cancer. Therefore these women often are offered surgical approaches mirroring invasive cancer treatments (lumpectomy with radiation or even mastectomy in some cases), while for some, such treatments may be unnecessary.
Screening younger women (40-49)
Shared decision-making is always important for breast cancer screening, but in our program we routinely recommend annual screening in average-risk women starting at age 40 for several reasons. For one, younger women may present with more aggressive types of breast cancer such as triple-negative breast cancer. These are much less common than hormone-receptor positive breast cancers – they represent 15%-20% of all breast cancers – but they are faster growing and may develop in the interim if women are screened less often (at 2-year intervals).
In addition, finding an invasive breast cancer early is almost always beneficial. Earlier diagnosis (lower stage at diagnosis) is associated with increased breast cancer-specific and overall survival, as well as less-aggressive treatment approaches.
As a medical oncologist who treats women with breast cancer, I see these benefits firsthand. With earlier diagnosis, we are more likely to offer less aggressive surgical approaches such as partial mastectomy (lumpectomy) and sentinel lymph node biopsy as opposed to total mastectomy with axillary lymph node dissection, the latter of which is more likely to be associated with lymphedema and which can lead to postmastectomy chest wall pain syndromes.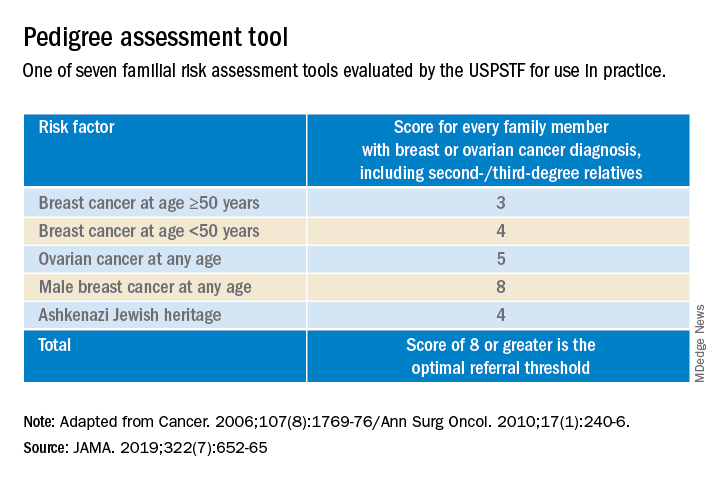
We also are able to use less aggressive radiation therapy approaches such as partial breast radiation, and less aggressive breast cancer–specific systemic treatments for women with a lower stage of breast cancer at diagnosis. In some cases, adjuvant or neoadjuvant chemotherapy may not be needed – and when it is necessary, shorter courses of chemotherapy or targeted chemotherapeutic regimens may be offered. This means lower systemic toxicities, both early and late, such as less cytopenias, risk of infections, mucositis, hair loss, cardiotoxicity, secondary malignancies/leukemia, and peripheral sensory neuropathy.
It is important to note that Black women in the United States have the highest death rate from breast cancer – 27.3 per 100,000 per year, versus 19.6 per 100,000 per year for White women1 – and that younger Black women appear to have a higher risk of developing triple-negative breast cancer, a more aggressive type of breast cancer. The higher breast cancer mortality in Black women is likely multifactorial and may be attributed partly to disparities in health care and partly to tumor biology. The case for annual screening in this population thus seems especially strong.
Screening modalities
Digital 3-D mammography, or digital breast tomosynthesis (DBT), is widely considered to be a more sensitive screening tool than conventional digital mammography alone. The NCCN recommends DBT for women with an average risk of developing breast cancer starting at age 40,4,5 and the USPSTF, while offering no recommendation on DBT as a primary screening method (“insufficient evidence”), says that DBT appears to increase cancer detection rates.2 So, I do routinely recommend it.
DBT may be especially beneficial for women with dense breast tissue (determined mammographically), who are most often premenopausal women – particularly non-Hispanic White women. Dense breast tissue itself can contribute to an increased risk of breast cancer – an approximately 20% higher relative risk in an average-risk woman with heterogeneously dense breast tissue, and an approximately 100% higher relative risk in a woman with extremely dense breasts6 – but unfortunately it affects the sensitivity and specificity of screening mammography.
I do not recommend routine supplemental screening with other methods (breast ultrasonography or MRI) for women at average risk of breast cancer who have dense breasts. MRI with gadolinium contrast is recommended as an adjunct to mammography for women who have a lifetime risk of developing breast cancer of more than 20%-25% (e.g., women with known BRCA1/2 mutations or radiation to breast tissue), and can be done annually at the same time as the screening mammogram is done. Some clinicians and patients prefer to alternate these two tests – one every 6 months.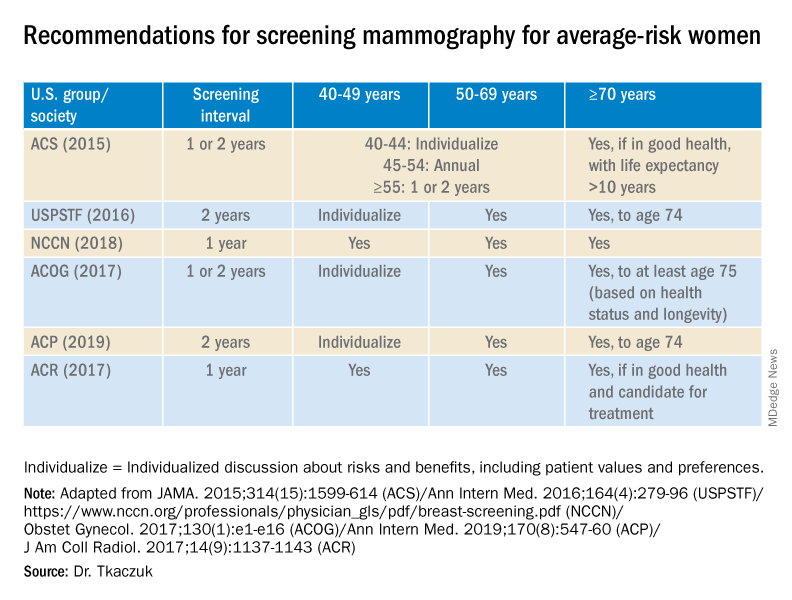
Screening breast MRI is more sensitive but less specific than mammography; combining the two screening modalities leads to overall increased sensitivity and specificity in high-risk populations.
Risk assessment
Identifying higher-risk women who need to be sent to a genetic counselor is critically important. The USPSTF recommends that women who have family members with breast, ovarian, tubal or peritoneal cancer, or who have an ancestry associated with BRCA1/2 gene mutations, be assessed with a brief familial risk assessment tool such as the Pedigree Assessment Tool. This and other validated tools have been evaluated by the USPSTF and can be used to guide referrals to genetic counseling for more definitive risk assessment.7
These tools are different from general breast cancer risk assessment models, such as the NCI’s Breast Cancer Risk Assessment Tool,8 which are designed to calculate the 5-year and lifetime risk of developing invasive breast cancer for an average-risk woman but not to identify BRCA-related cancer risk. (The NCI’s tool is based on the Gail model, which has been widely used over the years.)
The general risk assessment models use a women’s personal medical and reproductive history as well as the history of breast cancer among her first-degree relatives to estimate her risk.
Dr. Tkaczuk reported that she has no disclosures.
References
1. “Cancer Stat Facts: Female Breast Cancer.” Surveillance, Epidemiology, and End Results Program. National Cancer Institute.
2. Siu AL et al. Ann Intern Med. 2016 Feb 16. doi: 10.7326/M15-2886.
3. Independent UK Panel on Breast Cancer Screening. Lancet. 2012 Nov 17;380(9855):1778-86.
4. NCCN guidelines for Detection, Prevention, & Risk Reduction: Breast Cancer Screening and Diagnosis. National Comprehensive Cancer Network.
5. NCCN guidelines for Detection, Prevention, & Risk Reduction: Breast Cancer Risk Reduction. National Comprehensive Cancer Network.
6. Ziv E et al. Cancer Epidemiol Biomarkers Prev. 2004;13(12):2090-5.
7. USPSTF. JAMA. 2019;322(7):652-65.
8. The Breast Cancer Risk Assessment Tool. National Cancer Institute.
Screening mammography has contributed to the lowering of mortality from breast cancer by facilitating earlier diagnosis and a lower stage at diagnosis. With more effective treatment options for women who are diagnosed with lower-stage breast cancer, the current 5-year survival rate has risen to 90% – significantly higher than the 5-year survival rate of 75% in 1975.1
Women who are at much higher risk for developing breast cancer – mainly because of family history, certain genetic mutations, or a history of radiation therapy to the chest – will benefit the most from earlier and more frequent screening mammography as well as enhanced screening with non-x-ray methods of breast imaging. It is important that ob.gyns. help to identify these women.
However, the majority of women who are screened with mammography are at “average risk,” with a lifetime risk for developing breast cancer of 12.9%, based on 2015-2017 data from the National Cancer Institute’s (NCI) Surveillance, Epidemiology, and End Results Program (SEER).1 The median age at diagnosis of breast cancer in the U.S. is 62 years,1 and advancing age is the most important risk factor for these women.
A 20% relative risk reduction in breast cancer mortality with screening mammography has been demonstrated both in systematic reviews of randomized and observational studies2 and in a meta-analysis of 11 randomized trials comparing screening and no screening.3 Even though the majority of randomized trials were done in the age of film mammography, experts believe that we still see at least a 20% reduction today.
Among average-risk women, those aged 50-74 with a life expectancy of at least 10 years will benefit the most from regular screening. According to the 2016 screening guideline of the United States Preventive Services Task Force (USPSTF), relative risk reductions in breast cancer mortality from mammography screening, by age group, are 0.88 (confidence interval, 0.73-1.003) for ages 39-49; 0.86 (CI, 0.68-0.97) for ages 50-59; 0.67 (CI, 0.55-0.91) for ages 60-69; and 0.80 (CI, 0.51 to 1.28) for ages 70-74.2
For women aged 40-49 years, most of the guidelines in the United States recommend individualized screening every 1 or 2 years – screening that is guided by shared decision-making that takes into account each woman’s values regarding relative harms and benefits. This is because their risk of developing breast cancer is relatively low while the risk of false-positive results can be higher.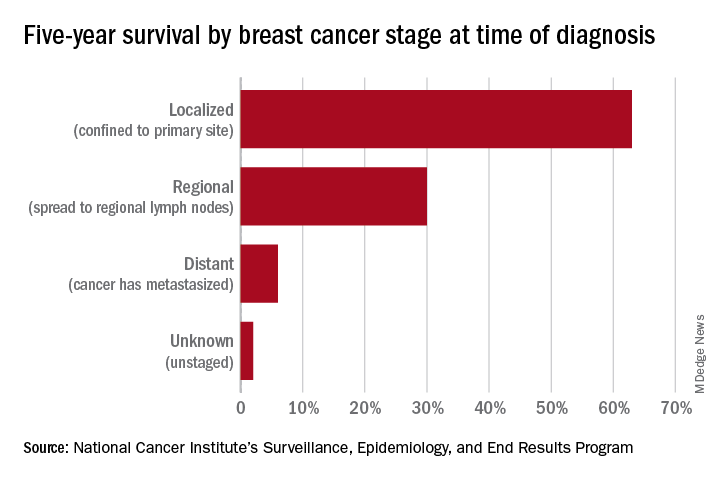
A few exceptions include guidelines by the National Comprehensive Cancer Network (NCCN) and the American College of Radiology, which recommend annual screening mammography starting at age 40 years for all average-risk women. In our program, we adhere to these latter recommendations and advise annual digital 3-D mammograms starting at age 40 and continuing until age 74, or longer if the woman is otherwise healthy with a life expectancy greater than 10 years.
Screening and overdiagnosis
Overdiagnosis – the diagnosis of cancers that may not actually cause mortality or may not even have become apparent without screening – is a concern for all women undergoing routine screening for breast cancer. There is significant uncertainty about its frequency, however.
Research cited by the USPSTF suggests that as many as one in five women diagnosed with breast cancer over approximately 10 years will be overdiagnosed. Other modeling studies have estimated one in eight overdiagnoses, for women aged 50-75 years specifically. By the more conservative estimate, according to the USPSTF, one breast cancer death will be prevented for every 2-3 cases of unnecessary treatment.2
Ductal carcinoma in situ is confined to the mammary ductal-lobular system and lacks the classic characteristics of cancer. Technically, it should not metastasize. But we do not know with certainty which cases of DCIS will or will not progress to invasive cancer. Therefore these women often are offered surgical approaches mirroring invasive cancer treatments (lumpectomy with radiation or even mastectomy in some cases), while for some, such treatments may be unnecessary.
Screening younger women (40-49)
Shared decision-making is always important for breast cancer screening, but in our program we routinely recommend annual screening in average-risk women starting at age 40 for several reasons. For one, younger women may present with more aggressive types of breast cancer such as triple-negative breast cancer. These are much less common than hormone-receptor positive breast cancers – they represent 15%-20% of all breast cancers – but they are faster growing and may develop in the interim if women are screened less often (at 2-year intervals).
In addition, finding an invasive breast cancer early is almost always beneficial. Earlier diagnosis (lower stage at diagnosis) is associated with increased breast cancer-specific and overall survival, as well as less-aggressive treatment approaches.
As a medical oncologist who treats women with breast cancer, I see these benefits firsthand. With earlier diagnosis, we are more likely to offer less aggressive surgical approaches such as partial mastectomy (lumpectomy) and sentinel lymph node biopsy as opposed to total mastectomy with axillary lymph node dissection, the latter of which is more likely to be associated with lymphedema and which can lead to postmastectomy chest wall pain syndromes.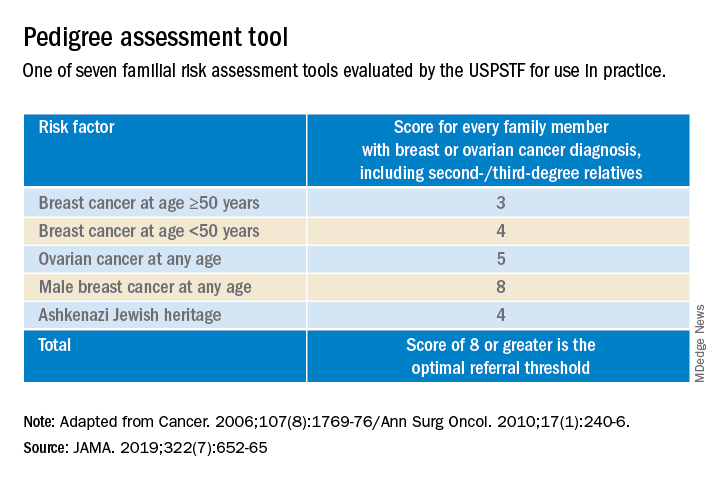
We also are able to use less aggressive radiation therapy approaches such as partial breast radiation, and less aggressive breast cancer–specific systemic treatments for women with a lower stage of breast cancer at diagnosis. In some cases, adjuvant or neoadjuvant chemotherapy may not be needed – and when it is necessary, shorter courses of chemotherapy or targeted chemotherapeutic regimens may be offered. This means lower systemic toxicities, both early and late, such as less cytopenias, risk of infections, mucositis, hair loss, cardiotoxicity, secondary malignancies/leukemia, and peripheral sensory neuropathy.
It is important to note that Black women in the United States have the highest death rate from breast cancer – 27.3 per 100,000 per year, versus 19.6 per 100,000 per year for White women1 – and that younger Black women appear to have a higher risk of developing triple-negative breast cancer, a more aggressive type of breast cancer. The higher breast cancer mortality in Black women is likely multifactorial and may be attributed partly to disparities in health care and partly to tumor biology. The case for annual screening in this population thus seems especially strong.
Screening modalities
Digital 3-D mammography, or digital breast tomosynthesis (DBT), is widely considered to be a more sensitive screening tool than conventional digital mammography alone. The NCCN recommends DBT for women with an average risk of developing breast cancer starting at age 40,4,5 and the USPSTF, while offering no recommendation on DBT as a primary screening method (“insufficient evidence”), says that DBT appears to increase cancer detection rates.2 So, I do routinely recommend it.
DBT may be especially beneficial for women with dense breast tissue (determined mammographically), who are most often premenopausal women – particularly non-Hispanic White women. Dense breast tissue itself can contribute to an increased risk of breast cancer – an approximately 20% higher relative risk in an average-risk woman with heterogeneously dense breast tissue, and an approximately 100% higher relative risk in a woman with extremely dense breasts6 – but unfortunately it affects the sensitivity and specificity of screening mammography.
I do not recommend routine supplemental screening with other methods (breast ultrasonography or MRI) for women at average risk of breast cancer who have dense breasts. MRI with gadolinium contrast is recommended as an adjunct to mammography for women who have a lifetime risk of developing breast cancer of more than 20%-25% (e.g., women with known BRCA1/2 mutations or radiation to breast tissue), and can be done annually at the same time as the screening mammogram is done. Some clinicians and patients prefer to alternate these two tests – one every 6 months.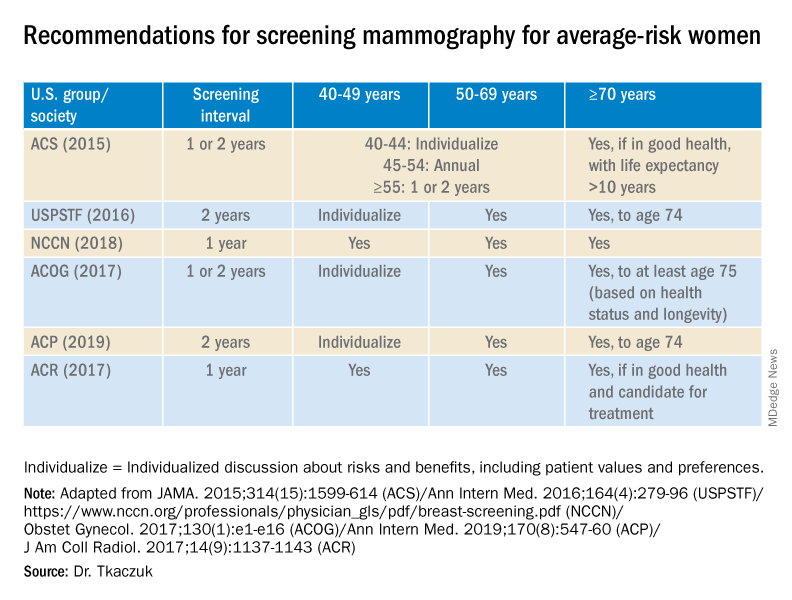
Screening breast MRI is more sensitive but less specific than mammography; combining the two screening modalities leads to overall increased sensitivity and specificity in high-risk populations.
Risk assessment
Identifying higher-risk women who need to be sent to a genetic counselor is critically important. The USPSTF recommends that women who have family members with breast, ovarian, tubal or peritoneal cancer, or who have an ancestry associated with BRCA1/2 gene mutations, be assessed with a brief familial risk assessment tool such as the Pedigree Assessment Tool. This and other validated tools have been evaluated by the USPSTF and can be used to guide referrals to genetic counseling for more definitive risk assessment.7
These tools are different from general breast cancer risk assessment models, such as the NCI’s Breast Cancer Risk Assessment Tool,8 which are designed to calculate the 5-year and lifetime risk of developing invasive breast cancer for an average-risk woman but not to identify BRCA-related cancer risk. (The NCI’s tool is based on the Gail model, which has been widely used over the years.)
The general risk assessment models use a women’s personal medical and reproductive history as well as the history of breast cancer among her first-degree relatives to estimate her risk.
Dr. Tkaczuk reported that she has no disclosures.
References
1. “Cancer Stat Facts: Female Breast Cancer.” Surveillance, Epidemiology, and End Results Program. National Cancer Institute.
2. Siu AL et al. Ann Intern Med. 2016 Feb 16. doi: 10.7326/M15-2886.
3. Independent UK Panel on Breast Cancer Screening. Lancet. 2012 Nov 17;380(9855):1778-86.
4. NCCN guidelines for Detection, Prevention, & Risk Reduction: Breast Cancer Screening and Diagnosis. National Comprehensive Cancer Network.
5. NCCN guidelines for Detection, Prevention, & Risk Reduction: Breast Cancer Risk Reduction. National Comprehensive Cancer Network.
6. Ziv E et al. Cancer Epidemiol Biomarkers Prev. 2004;13(12):2090-5.
7. USPSTF. JAMA. 2019;322(7):652-65.
8. The Breast Cancer Risk Assessment Tool. National Cancer Institute.
Screening mammography has contributed to the lowering of mortality from breast cancer by facilitating earlier diagnosis and a lower stage at diagnosis. With more effective treatment options for women who are diagnosed with lower-stage breast cancer, the current 5-year survival rate has risen to 90% – significantly higher than the 5-year survival rate of 75% in 1975.1
Women who are at much higher risk for developing breast cancer – mainly because of family history, certain genetic mutations, or a history of radiation therapy to the chest – will benefit the most from earlier and more frequent screening mammography as well as enhanced screening with non-x-ray methods of breast imaging. It is important that ob.gyns. help to identify these women.
However, the majority of women who are screened with mammography are at “average risk,” with a lifetime risk for developing breast cancer of 12.9%, based on 2015-2017 data from the National Cancer Institute’s (NCI) Surveillance, Epidemiology, and End Results Program (SEER).1 The median age at diagnosis of breast cancer in the U.S. is 62 years,1 and advancing age is the most important risk factor for these women.
A 20% relative risk reduction in breast cancer mortality with screening mammography has been demonstrated both in systematic reviews of randomized and observational studies2 and in a meta-analysis of 11 randomized trials comparing screening and no screening.3 Even though the majority of randomized trials were done in the age of film mammography, experts believe that we still see at least a 20% reduction today.
Among average-risk women, those aged 50-74 with a life expectancy of at least 10 years will benefit the most from regular screening. According to the 2016 screening guideline of the United States Preventive Services Task Force (USPSTF), relative risk reductions in breast cancer mortality from mammography screening, by age group, are 0.88 (confidence interval, 0.73-1.003) for ages 39-49; 0.86 (CI, 0.68-0.97) for ages 50-59; 0.67 (CI, 0.55-0.91) for ages 60-69; and 0.80 (CI, 0.51 to 1.28) for ages 70-74.2
For women aged 40-49 years, most of the guidelines in the United States recommend individualized screening every 1 or 2 years – screening that is guided by shared decision-making that takes into account each woman’s values regarding relative harms and benefits. This is because their risk of developing breast cancer is relatively low while the risk of false-positive results can be higher.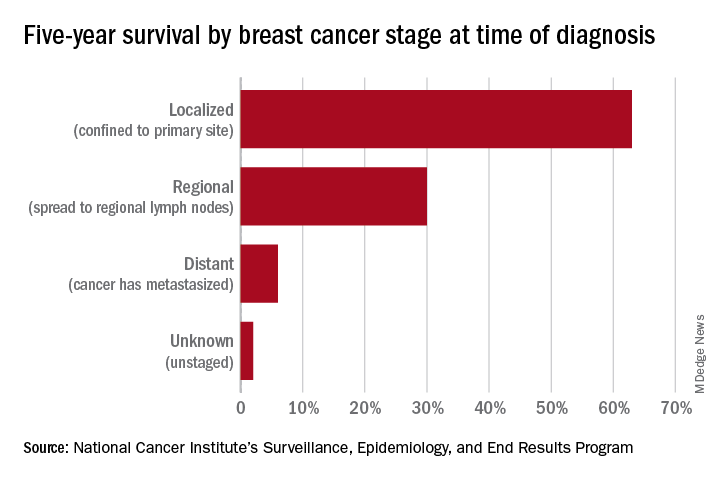
A few exceptions include guidelines by the National Comprehensive Cancer Network (NCCN) and the American College of Radiology, which recommend annual screening mammography starting at age 40 years for all average-risk women. In our program, we adhere to these latter recommendations and advise annual digital 3-D mammograms starting at age 40 and continuing until age 74, or longer if the woman is otherwise healthy with a life expectancy greater than 10 years.
Screening and overdiagnosis
Overdiagnosis – the diagnosis of cancers that may not actually cause mortality or may not even have become apparent without screening – is a concern for all women undergoing routine screening for breast cancer. There is significant uncertainty about its frequency, however.
Research cited by the USPSTF suggests that as many as one in five women diagnosed with breast cancer over approximately 10 years will be overdiagnosed. Other modeling studies have estimated one in eight overdiagnoses, for women aged 50-75 years specifically. By the more conservative estimate, according to the USPSTF, one breast cancer death will be prevented for every 2-3 cases of unnecessary treatment.2
Ductal carcinoma in situ is confined to the mammary ductal-lobular system and lacks the classic characteristics of cancer. Technically, it should not metastasize. But we do not know with certainty which cases of DCIS will or will not progress to invasive cancer. Therefore these women often are offered surgical approaches mirroring invasive cancer treatments (lumpectomy with radiation or even mastectomy in some cases), while for some, such treatments may be unnecessary.
Screening younger women (40-49)
Shared decision-making is always important for breast cancer screening, but in our program we routinely recommend annual screening in average-risk women starting at age 40 for several reasons. For one, younger women may present with more aggressive types of breast cancer such as triple-negative breast cancer. These are much less common than hormone-receptor positive breast cancers – they represent 15%-20% of all breast cancers – but they are faster growing and may develop in the interim if women are screened less often (at 2-year intervals).
In addition, finding an invasive breast cancer early is almost always beneficial. Earlier diagnosis (lower stage at diagnosis) is associated with increased breast cancer-specific and overall survival, as well as less-aggressive treatment approaches.
As a medical oncologist who treats women with breast cancer, I see these benefits firsthand. With earlier diagnosis, we are more likely to offer less aggressive surgical approaches such as partial mastectomy (lumpectomy) and sentinel lymph node biopsy as opposed to total mastectomy with axillary lymph node dissection, the latter of which is more likely to be associated with lymphedema and which can lead to postmastectomy chest wall pain syndromes.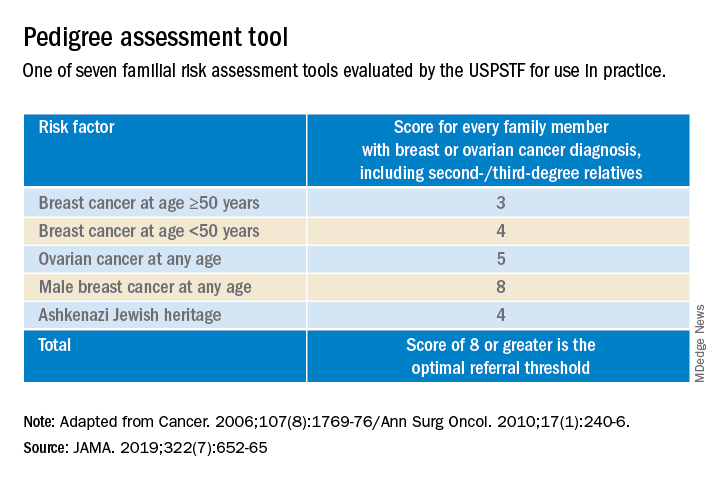
We also are able to use less aggressive radiation therapy approaches such as partial breast radiation, and less aggressive breast cancer–specific systemic treatments for women with a lower stage of breast cancer at diagnosis. In some cases, adjuvant or neoadjuvant chemotherapy may not be needed – and when it is necessary, shorter courses of chemotherapy or targeted chemotherapeutic regimens may be offered. This means lower systemic toxicities, both early and late, such as less cytopenias, risk of infections, mucositis, hair loss, cardiotoxicity, secondary malignancies/leukemia, and peripheral sensory neuropathy.
It is important to note that Black women in the United States have the highest death rate from breast cancer – 27.3 per 100,000 per year, versus 19.6 per 100,000 per year for White women1 – and that younger Black women appear to have a higher risk of developing triple-negative breast cancer, a more aggressive type of breast cancer. The higher breast cancer mortality in Black women is likely multifactorial and may be attributed partly to disparities in health care and partly to tumor biology. The case for annual screening in this population thus seems especially strong.
Screening modalities
Digital 3-D mammography, or digital breast tomosynthesis (DBT), is widely considered to be a more sensitive screening tool than conventional digital mammography alone. The NCCN recommends DBT for women with an average risk of developing breast cancer starting at age 40,4,5 and the USPSTF, while offering no recommendation on DBT as a primary screening method (“insufficient evidence”), says that DBT appears to increase cancer detection rates.2 So, I do routinely recommend it.
DBT may be especially beneficial for women with dense breast tissue (determined mammographically), who are most often premenopausal women – particularly non-Hispanic White women. Dense breast tissue itself can contribute to an increased risk of breast cancer – an approximately 20% higher relative risk in an average-risk woman with heterogeneously dense breast tissue, and an approximately 100% higher relative risk in a woman with extremely dense breasts6 – but unfortunately it affects the sensitivity and specificity of screening mammography.
I do not recommend routine supplemental screening with other methods (breast ultrasonography or MRI) for women at average risk of breast cancer who have dense breasts. MRI with gadolinium contrast is recommended as an adjunct to mammography for women who have a lifetime risk of developing breast cancer of more than 20%-25% (e.g., women with known BRCA1/2 mutations or radiation to breast tissue), and can be done annually at the same time as the screening mammogram is done. Some clinicians and patients prefer to alternate these two tests – one every 6 months.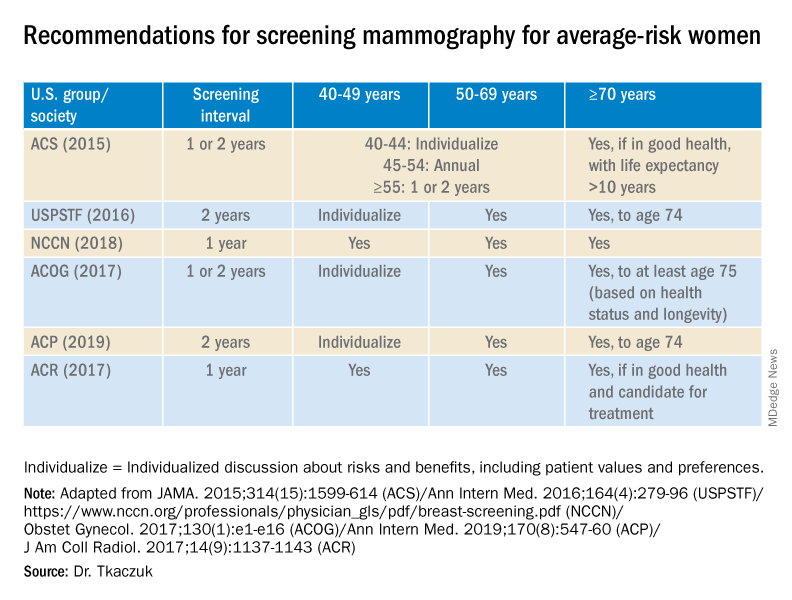
Screening breast MRI is more sensitive but less specific than mammography; combining the two screening modalities leads to overall increased sensitivity and specificity in high-risk populations.
Risk assessment
Identifying higher-risk women who need to be sent to a genetic counselor is critically important. The USPSTF recommends that women who have family members with breast, ovarian, tubal or peritoneal cancer, or who have an ancestry associated with BRCA1/2 gene mutations, be assessed with a brief familial risk assessment tool such as the Pedigree Assessment Tool. This and other validated tools have been evaluated by the USPSTF and can be used to guide referrals to genetic counseling for more definitive risk assessment.7
These tools are different from general breast cancer risk assessment models, such as the NCI’s Breast Cancer Risk Assessment Tool,8 which are designed to calculate the 5-year and lifetime risk of developing invasive breast cancer for an average-risk woman but not to identify BRCA-related cancer risk. (The NCI’s tool is based on the Gail model, which has been widely used over the years.)
The general risk assessment models use a women’s personal medical and reproductive history as well as the history of breast cancer among her first-degree relatives to estimate her risk.
Dr. Tkaczuk reported that she has no disclosures.
References
1. “Cancer Stat Facts: Female Breast Cancer.” Surveillance, Epidemiology, and End Results Program. National Cancer Institute.
2. Siu AL et al. Ann Intern Med. 2016 Feb 16. doi: 10.7326/M15-2886.
3. Independent UK Panel on Breast Cancer Screening. Lancet. 2012 Nov 17;380(9855):1778-86.
4. NCCN guidelines for Detection, Prevention, & Risk Reduction: Breast Cancer Screening and Diagnosis. National Comprehensive Cancer Network.
5. NCCN guidelines for Detection, Prevention, & Risk Reduction: Breast Cancer Risk Reduction. National Comprehensive Cancer Network.
6. Ziv E et al. Cancer Epidemiol Biomarkers Prev. 2004;13(12):2090-5.
7. USPSTF. JAMA. 2019;322(7):652-65.
8. The Breast Cancer Risk Assessment Tool. National Cancer Institute.
Geriatric patients: My three rules for them
I have been in practice for 31 years, so many of my patients are now in their 80s and 90s. Practices age with us, and I have been seeing many of these patients for 25-30 years.
Absolutely, positively make sure you move!
Our older patients often have many reasons not to move, including pain from arthritis, deconditioning, muscle weakness, fatigue, and depression. “Keeping moving” is probably the most important thing a patient can do for their health.
Holme and Anderssen studied a large cohort of men for cardiovascular risk in 1972 and again in 2000. The surviving men were followed over an additional 12 years.1 They found that 30 minutes of physical activity 6 days a week was associated with a 40% reduction in mortality. Sedentary men had a reduced life expectancy of about 5 years, compared with men who were moderately to vigorously physically active.
Stewart etal. studied the benefit of physical activity in people with stable coronary disease.2 They concluded that, in patients with stable coronary heart disease, more physical activity was associated with lower mortality, and the largest benefit occurred in the sedentary patient groups and the highest cardiac risk groups.
Saint-Maurice et al. studied the effects of total daily step count and step intensity on mortality risk.3 They found that the risk of all-cause mortality decreases as the total number of daily steps increases, but that the speed of those steps did not make a difference. This is very encouraging data for our elderly patients. Moving is the secret, even if it may not be moving at a fast pace!
Never, ever get on a ladder!
This one should be part of every geriatric’s assessment and every Medicare wellness exam. I first experienced the horror of what can happen when elderly people climb when a 96-year-old healthy patient of mine fell off his roof and died. I never thought to tell him climbing on the roof was an awful idea.
Akland et al. looked at the epidemiology and outcomes of ladder-related falls that required ICU admission.4 Hospital mortality was 26%, and almost all of the mortalities occurred in older males in domestic falls, who died as a result of traumatic brain injury. Fewer than half of the survivors were living independently 1 year after the fall.
Valmuur et al. studied ladder related falls in Australia.5 They found that rates of ladder related falls requiring hospitalization rose from about 20/100,000 for men ages 15-29 years to 78/100,000 for men aged over 60 years. Of those who died from fall-related injury, 82% were over the age of 60, with more than 70% dying from head injuries.
Schaffarczyk et al. looked at the impact of nonoccupational falls from ladders in men aged over 50 years.6 The mean age of the patients in the study was 64 years (range, 50-85), with 27% suffering severe trauma. There was a striking impact on long-term function occurring in over half the study patients. The authors did interviews with patients in follow-up long after the falls and found that most never thought of themselves at risk for a fall, and after the experience of a bad fall, would never consider going on a ladder again. I think it is important for health care professionals to discuss the dangers of ladder use with our older patients, pointing out the higher risk of falling and the potential for the fall to be a life-changing or life-ending event.
Let them eat!
Many patients have a reduced appetite as they age. We work hard with our patients to choose a healthy diet throughout their lives, to help ward off obesity, treat hypertension, prevent or control diabetes, or provide heart health. Many patients just stop being interested in food, reduce intake, and may lose weight and muscle mass. When my patients pass the age of 85, I change my focus to encouraging them to eat for calories, socialization, and joy. I think the marginal benefits of more restrictive diets are small, compared with the benefits of helping your patients enjoy eating again. I ask patients what their very favorite foods are and encourage them to have them.
Pearl
Keep your patients eating and moving, except not onto a ladder!
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Holme I, Anderssen SA. Increases in physical activity is as important as smoking cessation for reduction in total mortality in elderly men: 12 years of follow-up of the Oslo II study. Br J Sports Med. 2015; 49:743-8.
2. Stewart RAH et al. Physical activity and mortality in patients with stable coronary heart disease. J Am Coll Cardiol. 2017 Oct 3;70(14):1689-1700..
3. Saint-Maurice PF et al. Association of daily step count and step intensity with mortality among U.S. adults. JAMA 2020;323:1151-60.
4. Ackland HM et al. Danger at every rung: Epidemiology and outcomes of ICU-admitted ladder-related trauma. Injury. 2016;47:1109-117.
5. Vallmuur K et al. Falls from ladders in Australia: comparing occupational and nonoccupational injuries across age groups. Aust N Z J Public Health. 2016 Dec;40(6):559-63.
6. Schaffarczyk K et al. Nonoccupational falls from ladders in men 50 years and over: Contributing factors and impact. Injury. 2020 Aug;51(8):1798-1804.
I have been in practice for 31 years, so many of my patients are now in their 80s and 90s. Practices age with us, and I have been seeing many of these patients for 25-30 years.
Absolutely, positively make sure you move!
Our older patients often have many reasons not to move, including pain from arthritis, deconditioning, muscle weakness, fatigue, and depression. “Keeping moving” is probably the most important thing a patient can do for their health.
Holme and Anderssen studied a large cohort of men for cardiovascular risk in 1972 and again in 2000. The surviving men were followed over an additional 12 years.1 They found that 30 minutes of physical activity 6 days a week was associated with a 40% reduction in mortality. Sedentary men had a reduced life expectancy of about 5 years, compared with men who were moderately to vigorously physically active.
Stewart etal. studied the benefit of physical activity in people with stable coronary disease.2 They concluded that, in patients with stable coronary heart disease, more physical activity was associated with lower mortality, and the largest benefit occurred in the sedentary patient groups and the highest cardiac risk groups.
Saint-Maurice et al. studied the effects of total daily step count and step intensity on mortality risk.3 They found that the risk of all-cause mortality decreases as the total number of daily steps increases, but that the speed of those steps did not make a difference. This is very encouraging data for our elderly patients. Moving is the secret, even if it may not be moving at a fast pace!
Never, ever get on a ladder!
This one should be part of every geriatric’s assessment and every Medicare wellness exam. I first experienced the horror of what can happen when elderly people climb when a 96-year-old healthy patient of mine fell off his roof and died. I never thought to tell him climbing on the roof was an awful idea.
Akland et al. looked at the epidemiology and outcomes of ladder-related falls that required ICU admission.4 Hospital mortality was 26%, and almost all of the mortalities occurred in older males in domestic falls, who died as a result of traumatic brain injury. Fewer than half of the survivors were living independently 1 year after the fall.
Valmuur et al. studied ladder related falls in Australia.5 They found that rates of ladder related falls requiring hospitalization rose from about 20/100,000 for men ages 15-29 years to 78/100,000 for men aged over 60 years. Of those who died from fall-related injury, 82% were over the age of 60, with more than 70% dying from head injuries.
Schaffarczyk et al. looked at the impact of nonoccupational falls from ladders in men aged over 50 years.6 The mean age of the patients in the study was 64 years (range, 50-85), with 27% suffering severe trauma. There was a striking impact on long-term function occurring in over half the study patients. The authors did interviews with patients in follow-up long after the falls and found that most never thought of themselves at risk for a fall, and after the experience of a bad fall, would never consider going on a ladder again. I think it is important for health care professionals to discuss the dangers of ladder use with our older patients, pointing out the higher risk of falling and the potential for the fall to be a life-changing or life-ending event.
Let them eat!
Many patients have a reduced appetite as they age. We work hard with our patients to choose a healthy diet throughout their lives, to help ward off obesity, treat hypertension, prevent or control diabetes, or provide heart health. Many patients just stop being interested in food, reduce intake, and may lose weight and muscle mass. When my patients pass the age of 85, I change my focus to encouraging them to eat for calories, socialization, and joy. I think the marginal benefits of more restrictive diets are small, compared with the benefits of helping your patients enjoy eating again. I ask patients what their very favorite foods are and encourage them to have them.
Pearl
Keep your patients eating and moving, except not onto a ladder!
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Holme I, Anderssen SA. Increases in physical activity is as important as smoking cessation for reduction in total mortality in elderly men: 12 years of follow-up of the Oslo II study. Br J Sports Med. 2015; 49:743-8.
2. Stewart RAH et al. Physical activity and mortality in patients with stable coronary heart disease. J Am Coll Cardiol. 2017 Oct 3;70(14):1689-1700..
3. Saint-Maurice PF et al. Association of daily step count and step intensity with mortality among U.S. adults. JAMA 2020;323:1151-60.
4. Ackland HM et al. Danger at every rung: Epidemiology and outcomes of ICU-admitted ladder-related trauma. Injury. 2016;47:1109-117.
5. Vallmuur K et al. Falls from ladders in Australia: comparing occupational and nonoccupational injuries across age groups. Aust N Z J Public Health. 2016 Dec;40(6):559-63.
6. Schaffarczyk K et al. Nonoccupational falls from ladders in men 50 years and over: Contributing factors and impact. Injury. 2020 Aug;51(8):1798-1804.
I have been in practice for 31 years, so many of my patients are now in their 80s and 90s. Practices age with us, and I have been seeing many of these patients for 25-30 years.
Absolutely, positively make sure you move!
Our older patients often have many reasons not to move, including pain from arthritis, deconditioning, muscle weakness, fatigue, and depression. “Keeping moving” is probably the most important thing a patient can do for their health.
Holme and Anderssen studied a large cohort of men for cardiovascular risk in 1972 and again in 2000. The surviving men were followed over an additional 12 years.1 They found that 30 minutes of physical activity 6 days a week was associated with a 40% reduction in mortality. Sedentary men had a reduced life expectancy of about 5 years, compared with men who were moderately to vigorously physically active.
Stewart etal. studied the benefit of physical activity in people with stable coronary disease.2 They concluded that, in patients with stable coronary heart disease, more physical activity was associated with lower mortality, and the largest benefit occurred in the sedentary patient groups and the highest cardiac risk groups.
Saint-Maurice et al. studied the effects of total daily step count and step intensity on mortality risk.3 They found that the risk of all-cause mortality decreases as the total number of daily steps increases, but that the speed of those steps did not make a difference. This is very encouraging data for our elderly patients. Moving is the secret, even if it may not be moving at a fast pace!
Never, ever get on a ladder!
This one should be part of every geriatric’s assessment and every Medicare wellness exam. I first experienced the horror of what can happen when elderly people climb when a 96-year-old healthy patient of mine fell off his roof and died. I never thought to tell him climbing on the roof was an awful idea.
Akland et al. looked at the epidemiology and outcomes of ladder-related falls that required ICU admission.4 Hospital mortality was 26%, and almost all of the mortalities occurred in older males in domestic falls, who died as a result of traumatic brain injury. Fewer than half of the survivors were living independently 1 year after the fall.
Valmuur et al. studied ladder related falls in Australia.5 They found that rates of ladder related falls requiring hospitalization rose from about 20/100,000 for men ages 15-29 years to 78/100,000 for men aged over 60 years. Of those who died from fall-related injury, 82% were over the age of 60, with more than 70% dying from head injuries.
Schaffarczyk et al. looked at the impact of nonoccupational falls from ladders in men aged over 50 years.6 The mean age of the patients in the study was 64 years (range, 50-85), with 27% suffering severe trauma. There was a striking impact on long-term function occurring in over half the study patients. The authors did interviews with patients in follow-up long after the falls and found that most never thought of themselves at risk for a fall, and after the experience of a bad fall, would never consider going on a ladder again. I think it is important for health care professionals to discuss the dangers of ladder use with our older patients, pointing out the higher risk of falling and the potential for the fall to be a life-changing or life-ending event.
Let them eat!
Many patients have a reduced appetite as they age. We work hard with our patients to choose a healthy diet throughout their lives, to help ward off obesity, treat hypertension, prevent or control diabetes, or provide heart health. Many patients just stop being interested in food, reduce intake, and may lose weight and muscle mass. When my patients pass the age of 85, I change my focus to encouraging them to eat for calories, socialization, and joy. I think the marginal benefits of more restrictive diets are small, compared with the benefits of helping your patients enjoy eating again. I ask patients what their very favorite foods are and encourage them to have them.
Pearl
Keep your patients eating and moving, except not onto a ladder!
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Holme I, Anderssen SA. Increases in physical activity is as important as smoking cessation for reduction in total mortality in elderly men: 12 years of follow-up of the Oslo II study. Br J Sports Med. 2015; 49:743-8.
2. Stewart RAH et al. Physical activity and mortality in patients with stable coronary heart disease. J Am Coll Cardiol. 2017 Oct 3;70(14):1689-1700..
3. Saint-Maurice PF et al. Association of daily step count and step intensity with mortality among U.S. adults. JAMA 2020;323:1151-60.
4. Ackland HM et al. Danger at every rung: Epidemiology and outcomes of ICU-admitted ladder-related trauma. Injury. 2016;47:1109-117.
5. Vallmuur K et al. Falls from ladders in Australia: comparing occupational and nonoccupational injuries across age groups. Aust N Z J Public Health. 2016 Dec;40(6):559-63.
6. Schaffarczyk K et al. Nonoccupational falls from ladders in men 50 years and over: Contributing factors and impact. Injury. 2020 Aug;51(8):1798-1804.




















