User login
The Daycare Petri Dish
I can’t remember where I heard it. Maybe I made it up myself. But, one definition of a family is a group of folks with whom you share your genes and germs. In that same vein, one could define daycare as a group of germ-sharing children. Of course that’s news to almost no one. Parents who decide, or are forced, to send their children to daycare expect that those children will get more colds, “stomach flu,” and ear infections than the children who spend their days in isolation at home. Everyone from the pediatrician to the little old lady next door has warned parents of the inevitable reality of daycare. Of course there are upsides that parents can cling to, including increased socialization and the hope that getting sick young will build a more robust immunity in the long run.
However, there has been little research exploring the nuances of the germ sharing that we all know is happening in these and other social settings.
A team of evolutionary biologists at Harvard is working to better define the “social microbiome” and its “role in individuals’ susceptibility to, and resilience against, both communicable and noncommunicable diseases.” These researchers point out that while we harbor our own unique collection of microbes, we share those with the microbiomes of the people with whom we interact socially. They report that studies by other investigators have shown that residents of a household share a significant proportion of their gastrointestinal flora. There are other studies that have shown that villages can be identified by their own social biome. There are few social settings more intimately involved in microbe sharing than daycares. I have a friends who calls them “petri dishes.”
The biologists point out that antibiotic-resistant microbes can become part of an individual’s microbiome and can be shared with other individuals in their social group, who can then go on and share them in a different social environment. Imagine there is one popular physician in a community whose sense of antibiotic stewardship is, shall we say, somewhat lacking. By inappropriately prescribing antibiotics to a child or two in a daycare, he may be altering the social biome in that daycare, which could then jeopardize the health of all the children and eventually their own home-based social biomes, that may include an immune deficient individual.
The researchers also remind us that different cultures and countries may have different antibiotic usage patterns. Does this mean I am taking a risk by traveling in these “culture-dependent transmission landscapes”? Am I more likely to encounter an antibiotic-resistant microbe when I am visiting a country whose healthcare providers are less prudent prescribers?
However, as these evolutionary biologists point out, not all shared microbes are bad. There is some evidence in animals that individuals can share microbes that have been found to “increase resilience against colitis or improve their responsiveness to cancer therapy.” If a microbe can contribute to a disease that was once considered to be “noncommunicable,” we may need to redefine “communicable” in the light this more nuanced view of the social biome.
It became standard practice during the COVID pandemic to test dormitory and community sewage water to determine the level of infection. Can sewage water be used as a proxy for a social biome? If a parent is lucky enough to have a choice of daycares, would knowing each facility’s biome, as reflected in an analysis of its sewage effluent, help him or her decide? Should a daycare ask for a stool sample from each child before accepting him or her? Seems like this would raise some privacy issues, not to mention the logistical messiness of the process. As we learn more about social biomes, can we imagine a time when a daycare or country or region might proudly advertise itself as having the healthiest spectrum of microbes in its sewage system?
Communal living certainly has its benefits, not just for children but also adults as we realize how loneliness is eating its way into our society. However,
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
I can’t remember where I heard it. Maybe I made it up myself. But, one definition of a family is a group of folks with whom you share your genes and germs. In that same vein, one could define daycare as a group of germ-sharing children. Of course that’s news to almost no one. Parents who decide, or are forced, to send their children to daycare expect that those children will get more colds, “stomach flu,” and ear infections than the children who spend their days in isolation at home. Everyone from the pediatrician to the little old lady next door has warned parents of the inevitable reality of daycare. Of course there are upsides that parents can cling to, including increased socialization and the hope that getting sick young will build a more robust immunity in the long run.
However, there has been little research exploring the nuances of the germ sharing that we all know is happening in these and other social settings.
A team of evolutionary biologists at Harvard is working to better define the “social microbiome” and its “role in individuals’ susceptibility to, and resilience against, both communicable and noncommunicable diseases.” These researchers point out that while we harbor our own unique collection of microbes, we share those with the microbiomes of the people with whom we interact socially. They report that studies by other investigators have shown that residents of a household share a significant proportion of their gastrointestinal flora. There are other studies that have shown that villages can be identified by their own social biome. There are few social settings more intimately involved in microbe sharing than daycares. I have a friends who calls them “petri dishes.”
The biologists point out that antibiotic-resistant microbes can become part of an individual’s microbiome and can be shared with other individuals in their social group, who can then go on and share them in a different social environment. Imagine there is one popular physician in a community whose sense of antibiotic stewardship is, shall we say, somewhat lacking. By inappropriately prescribing antibiotics to a child or two in a daycare, he may be altering the social biome in that daycare, which could then jeopardize the health of all the children and eventually their own home-based social biomes, that may include an immune deficient individual.
The researchers also remind us that different cultures and countries may have different antibiotic usage patterns. Does this mean I am taking a risk by traveling in these “culture-dependent transmission landscapes”? Am I more likely to encounter an antibiotic-resistant microbe when I am visiting a country whose healthcare providers are less prudent prescribers?
However, as these evolutionary biologists point out, not all shared microbes are bad. There is some evidence in animals that individuals can share microbes that have been found to “increase resilience against colitis or improve their responsiveness to cancer therapy.” If a microbe can contribute to a disease that was once considered to be “noncommunicable,” we may need to redefine “communicable” in the light this more nuanced view of the social biome.
It became standard practice during the COVID pandemic to test dormitory and community sewage water to determine the level of infection. Can sewage water be used as a proxy for a social biome? If a parent is lucky enough to have a choice of daycares, would knowing each facility’s biome, as reflected in an analysis of its sewage effluent, help him or her decide? Should a daycare ask for a stool sample from each child before accepting him or her? Seems like this would raise some privacy issues, not to mention the logistical messiness of the process. As we learn more about social biomes, can we imagine a time when a daycare or country or region might proudly advertise itself as having the healthiest spectrum of microbes in its sewage system?
Communal living certainly has its benefits, not just for children but also adults as we realize how loneliness is eating its way into our society. However,
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
I can’t remember where I heard it. Maybe I made it up myself. But, one definition of a family is a group of folks with whom you share your genes and germs. In that same vein, one could define daycare as a group of germ-sharing children. Of course that’s news to almost no one. Parents who decide, or are forced, to send their children to daycare expect that those children will get more colds, “stomach flu,” and ear infections than the children who spend their days in isolation at home. Everyone from the pediatrician to the little old lady next door has warned parents of the inevitable reality of daycare. Of course there are upsides that parents can cling to, including increased socialization and the hope that getting sick young will build a more robust immunity in the long run.
However, there has been little research exploring the nuances of the germ sharing that we all know is happening in these and other social settings.
A team of evolutionary biologists at Harvard is working to better define the “social microbiome” and its “role in individuals’ susceptibility to, and resilience against, both communicable and noncommunicable diseases.” These researchers point out that while we harbor our own unique collection of microbes, we share those with the microbiomes of the people with whom we interact socially. They report that studies by other investigators have shown that residents of a household share a significant proportion of their gastrointestinal flora. There are other studies that have shown that villages can be identified by their own social biome. There are few social settings more intimately involved in microbe sharing than daycares. I have a friends who calls them “petri dishes.”
The biologists point out that antibiotic-resistant microbes can become part of an individual’s microbiome and can be shared with other individuals in their social group, who can then go on and share them in a different social environment. Imagine there is one popular physician in a community whose sense of antibiotic stewardship is, shall we say, somewhat lacking. By inappropriately prescribing antibiotics to a child or two in a daycare, he may be altering the social biome in that daycare, which could then jeopardize the health of all the children and eventually their own home-based social biomes, that may include an immune deficient individual.
The researchers also remind us that different cultures and countries may have different antibiotic usage patterns. Does this mean I am taking a risk by traveling in these “culture-dependent transmission landscapes”? Am I more likely to encounter an antibiotic-resistant microbe when I am visiting a country whose healthcare providers are less prudent prescribers?
However, as these evolutionary biologists point out, not all shared microbes are bad. There is some evidence in animals that individuals can share microbes that have been found to “increase resilience against colitis or improve their responsiveness to cancer therapy.” If a microbe can contribute to a disease that was once considered to be “noncommunicable,” we may need to redefine “communicable” in the light this more nuanced view of the social biome.
It became standard practice during the COVID pandemic to test dormitory and community sewage water to determine the level of infection. Can sewage water be used as a proxy for a social biome? If a parent is lucky enough to have a choice of daycares, would knowing each facility’s biome, as reflected in an analysis of its sewage effluent, help him or her decide? Should a daycare ask for a stool sample from each child before accepting him or her? Seems like this would raise some privacy issues, not to mention the logistical messiness of the process. As we learn more about social biomes, can we imagine a time when a daycare or country or region might proudly advertise itself as having the healthiest spectrum of microbes in its sewage system?
Communal living certainly has its benefits, not just for children but also adults as we realize how loneliness is eating its way into our society. However,
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Unleashing Our Immune Response to Quash Cancer
This article was originally published on February 10 in Eric Topol’s substack “Ground Truths.”
It’s astounding how devious cancer cells and tumor tissue can be. This week in Science we learned how certain lung cancer cells can function like “Catch Me If You Can” — changing their driver mutation and cell identity to escape targeted therapy. This histologic transformation, as seen in an experimental model, is just one of so many cancer tricks that we are learning about.
Recently, as shown by single-cell sequencing, cancer cells can steal the mitochondria from T cells, a double whammy that turbocharges cancer cells with the hijacked fuel supply and, at the same time, dismantles the immune response.
Last week, we saw how tumor cells can release a virus-like protein that unleashes a vicious autoimmune response.
And then there’s the finding that cancer cell spread predominantly is occurring while we sleep.
As I previously reviewed, the ability for cancer cells to hijack neurons and neural circuits is now well established, no less their ability to reprogram neurons to become adrenergic and stimulate tumor progression, and interfere with the immune response. Stay tuned on that for a new Ground Truths podcast with Prof Michelle Monje, a leader in cancer neuroscience, which will post soon.
Add advancing age’s immunosenescence as yet another challenge to the long and growing list of formidable ways that cancer cells, and the tumor microenvironment, evade our immune response.
An Ever-Expanding Armamentarium
Immune Checkpoint Inhibitors
The field of immunotherapies took off with the immune checkpoint inhibitors, first approved by the FDA in 2011, that take the brakes off of T cells, with the programmed death-1 (PD-1), PD-ligand1, and anti-CTLA-4 monoclonal antibodies.
But we’re clearly learning they are not enough to prevail over cancer with common recurrences, only short term success in most patients, with some notable exceptions. Adding other immune response strategies, such as a vaccine, or antibody-drug conjugates, or engineered T cells, are showing improved chances for success.
Therapeutic Cancer Vaccines
There are many therapeutic cancer vaccines in the works, as reviewed in depth here.
Here’s a list of ongoing clinical trials of cancer vaccines. You’ll note most of these are on top of a checkpoint inhibitor and use personalized neoantigens (cancer cell surface proteins) derived from sequencing (whole-exome or whole genome, RNA-sequencing and HLA-profiling) the patient’s tumor.
An example of positive findings is with the combination of an mRNA-nanoparticle vaccine with up to 34 personalized neoantigens and pembrolizumab (Keytruda) vs pembrolizumab alone in advanced melanoma after resection, with improved outcomes at 3-year follow-up, cutting death or relapse rate in half.
Antibody-Drug Conjugates (ADC)
There is considerable excitement about antibody-drug conjugates (ADC) whereby a linker is used to attach a chemotherapy agent to the checkpoint inhibitor antibody, specifically targeting the cancer cell and facilitating entry of the chemotherapy into the cell. Akin to these are bispecific antibodies (BiTEs, binding to a tumor antigen and T cell receptor simultaneously), both of these conjugates acting as “biologic” or “guided” missiles.
A very good example of the potency of an ADC was seen in a “HER2-low” breast cancer randomized trial. The absence or very low expression or amplification of the HER2 receptor is common in breast cancer and successful treatment has been elusive. A randomized trial of an ADC (trastuzumab deruxtecan) compared to physician’s choice therapy demonstrated a marked success for progression-free survival in HER2-low patients, which was characterized as “unheard-of success” by media coverage.
This strategy is being used to target some of the most difficult cancer driver mutations such as TP53 and KRAS.
Oncolytic Viruses
Modifying viruses to infect the tumor and make it more visible to the immune system, potentiating anti-tumor responses, known as oncolytic viruses, have been proposed as a way to rev up the immune response for a long time but without positive Phase 3 clinical trials.
After decades of failure, a recent trial in refractory bladder cancer showed marked success, along with others, summarized here, now providing very encouraging results. It looks like oncolytic viruses are on a comeback path.
Engineering T Cells (Chimeric Antigen Receptor [CAR-T])
As I recently reviewed, there are over 500 ongoing clinical trials to build on the success of the first CAR-T approval for leukemia 7 years ago. I won’t go through that all again here, but to reiterate most of the success to date has been in “liquid” blood (leukemia and lymphoma) cancer tumors. This week in Nature is the discovery of a T cell cancer mutation, a gene fusion CARD11-PIK3R3, from a T cell lymphoma that can potentially be used to augment CAR-T efficacy. It has pronounced and prolonged effects in the experimental model. Instead of 1 million cells needed for treatment, even 20,000 were enough to melt the tumor. This is a noteworthy discovery since CAR-T work to date has largely not exploited such naturally occurring mutations, while instead concentrating on those seen in the patient’s set of key tumor mutations.
As currently conceived, CAR-T, and what is being referred to more broadly as adoptive cell therapies, involves removing T cells from the patient’s body and engineering their activation, then reintroducing them back to the patient. This is laborious, technically difficult, and very expensive. Recently, the idea of achieving all of this via an injection of virus that specifically infects T cells and inserts the genes needed, was advanced by two biotech companies with preclinical results, one in non-human primates.
Gearing up to meet the challenge of solid tumor CAR-T intervention, there’s more work using CRISPR genome editing of T cell receptors. A.I. is increasingly being exploited to process the data from sequencing and identify optimal neoantigens.
Instead of just CAR-T, we’re seeing the emergence of CAR-macrophage and CAR-natural killer (NK) cells strategies, and rapidly expanding potential combinations of all the strategies I’ve mentioned. No less, there’s been maturation of on-off suicide switches programmed in, to limit cytokine release and promote safety of these interventions. Overall, major side effects of immunotherapies are not only cytokine release syndromes, but also include interstitial pneumonitis and neurotoxicity.
Summary
Given the multitude of ways cancer cells and tumor tissue can evade our immune response, durably successful treatment remains a daunting challenge. But the ingenuity of so many different approaches to unleash our immune response, and their combinations, provides considerable hope that we’ll increasingly meet the challenge in the years ahead. We have clearly learned that combining different immunotherapy strategies will be essential for many patients with the most resilient solid tumors.
Of concern, as noted by a recent editorial in The Lancet, entitled “Cancer Research Equity: Innovations For The Many, Not The Few,” is that these individualized, sophisticated strategies are not scalable; they will have limited reach and benefit. The movement towards “off the shelf” CAR-T and inexpensive, orally active checkpoint inhibitors may help mitigate this issue.
Notwithstanding this important concern, we’re seeing an array of diverse and potent immunotherapy strategies that are providing highly encouraging results, engendering more excitement than we’ve seen in this space for some time. These should propel substantial improvements in outcomes for patients in the years ahead. It can’t happen soon enough.
Thanks for reading this edition of Ground Truths. If you found it informative, please share it with your colleagues.
Dr. Topol has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for Dexcom; Illumina; Molecular Stethoscope; Quest Diagnostics; Blue Cross Blue Shield Association. Received research grant from National Institutes of Health.
A version of this article appeared on Medscape.com.
This article was originally published on February 10 in Eric Topol’s substack “Ground Truths.”
It’s astounding how devious cancer cells and tumor tissue can be. This week in Science we learned how certain lung cancer cells can function like “Catch Me If You Can” — changing their driver mutation and cell identity to escape targeted therapy. This histologic transformation, as seen in an experimental model, is just one of so many cancer tricks that we are learning about.
Recently, as shown by single-cell sequencing, cancer cells can steal the mitochondria from T cells, a double whammy that turbocharges cancer cells with the hijacked fuel supply and, at the same time, dismantles the immune response.
Last week, we saw how tumor cells can release a virus-like protein that unleashes a vicious autoimmune response.
And then there’s the finding that cancer cell spread predominantly is occurring while we sleep.
As I previously reviewed, the ability for cancer cells to hijack neurons and neural circuits is now well established, no less their ability to reprogram neurons to become adrenergic and stimulate tumor progression, and interfere with the immune response. Stay tuned on that for a new Ground Truths podcast with Prof Michelle Monje, a leader in cancer neuroscience, which will post soon.
Add advancing age’s immunosenescence as yet another challenge to the long and growing list of formidable ways that cancer cells, and the tumor microenvironment, evade our immune response.
An Ever-Expanding Armamentarium
Immune Checkpoint Inhibitors
The field of immunotherapies took off with the immune checkpoint inhibitors, first approved by the FDA in 2011, that take the brakes off of T cells, with the programmed death-1 (PD-1), PD-ligand1, and anti-CTLA-4 monoclonal antibodies.
But we’re clearly learning they are not enough to prevail over cancer with common recurrences, only short term success in most patients, with some notable exceptions. Adding other immune response strategies, such as a vaccine, or antibody-drug conjugates, or engineered T cells, are showing improved chances for success.
Therapeutic Cancer Vaccines
There are many therapeutic cancer vaccines in the works, as reviewed in depth here.
Here’s a list of ongoing clinical trials of cancer vaccines. You’ll note most of these are on top of a checkpoint inhibitor and use personalized neoantigens (cancer cell surface proteins) derived from sequencing (whole-exome or whole genome, RNA-sequencing and HLA-profiling) the patient’s tumor.
An example of positive findings is with the combination of an mRNA-nanoparticle vaccine with up to 34 personalized neoantigens and pembrolizumab (Keytruda) vs pembrolizumab alone in advanced melanoma after resection, with improved outcomes at 3-year follow-up, cutting death or relapse rate in half.
Antibody-Drug Conjugates (ADC)
There is considerable excitement about antibody-drug conjugates (ADC) whereby a linker is used to attach a chemotherapy agent to the checkpoint inhibitor antibody, specifically targeting the cancer cell and facilitating entry of the chemotherapy into the cell. Akin to these are bispecific antibodies (BiTEs, binding to a tumor antigen and T cell receptor simultaneously), both of these conjugates acting as “biologic” or “guided” missiles.
A very good example of the potency of an ADC was seen in a “HER2-low” breast cancer randomized trial. The absence or very low expression or amplification of the HER2 receptor is common in breast cancer and successful treatment has been elusive. A randomized trial of an ADC (trastuzumab deruxtecan) compared to physician’s choice therapy demonstrated a marked success for progression-free survival in HER2-low patients, which was characterized as “unheard-of success” by media coverage.
This strategy is being used to target some of the most difficult cancer driver mutations such as TP53 and KRAS.
Oncolytic Viruses
Modifying viruses to infect the tumor and make it more visible to the immune system, potentiating anti-tumor responses, known as oncolytic viruses, have been proposed as a way to rev up the immune response for a long time but without positive Phase 3 clinical trials.
After decades of failure, a recent trial in refractory bladder cancer showed marked success, along with others, summarized here, now providing very encouraging results. It looks like oncolytic viruses are on a comeback path.
Engineering T Cells (Chimeric Antigen Receptor [CAR-T])
As I recently reviewed, there are over 500 ongoing clinical trials to build on the success of the first CAR-T approval for leukemia 7 years ago. I won’t go through that all again here, but to reiterate most of the success to date has been in “liquid” blood (leukemia and lymphoma) cancer tumors. This week in Nature is the discovery of a T cell cancer mutation, a gene fusion CARD11-PIK3R3, from a T cell lymphoma that can potentially be used to augment CAR-T efficacy. It has pronounced and prolonged effects in the experimental model. Instead of 1 million cells needed for treatment, even 20,000 were enough to melt the tumor. This is a noteworthy discovery since CAR-T work to date has largely not exploited such naturally occurring mutations, while instead concentrating on those seen in the patient’s set of key tumor mutations.
As currently conceived, CAR-T, and what is being referred to more broadly as adoptive cell therapies, involves removing T cells from the patient’s body and engineering their activation, then reintroducing them back to the patient. This is laborious, technically difficult, and very expensive. Recently, the idea of achieving all of this via an injection of virus that specifically infects T cells and inserts the genes needed, was advanced by two biotech companies with preclinical results, one in non-human primates.
Gearing up to meet the challenge of solid tumor CAR-T intervention, there’s more work using CRISPR genome editing of T cell receptors. A.I. is increasingly being exploited to process the data from sequencing and identify optimal neoantigens.
Instead of just CAR-T, we’re seeing the emergence of CAR-macrophage and CAR-natural killer (NK) cells strategies, and rapidly expanding potential combinations of all the strategies I’ve mentioned. No less, there’s been maturation of on-off suicide switches programmed in, to limit cytokine release and promote safety of these interventions. Overall, major side effects of immunotherapies are not only cytokine release syndromes, but also include interstitial pneumonitis and neurotoxicity.
Summary
Given the multitude of ways cancer cells and tumor tissue can evade our immune response, durably successful treatment remains a daunting challenge. But the ingenuity of so many different approaches to unleash our immune response, and their combinations, provides considerable hope that we’ll increasingly meet the challenge in the years ahead. We have clearly learned that combining different immunotherapy strategies will be essential for many patients with the most resilient solid tumors.
Of concern, as noted by a recent editorial in The Lancet, entitled “Cancer Research Equity: Innovations For The Many, Not The Few,” is that these individualized, sophisticated strategies are not scalable; they will have limited reach and benefit. The movement towards “off the shelf” CAR-T and inexpensive, orally active checkpoint inhibitors may help mitigate this issue.
Notwithstanding this important concern, we’re seeing an array of diverse and potent immunotherapy strategies that are providing highly encouraging results, engendering more excitement than we’ve seen in this space for some time. These should propel substantial improvements in outcomes for patients in the years ahead. It can’t happen soon enough.
Thanks for reading this edition of Ground Truths. If you found it informative, please share it with your colleagues.
Dr. Topol has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for Dexcom; Illumina; Molecular Stethoscope; Quest Diagnostics; Blue Cross Blue Shield Association. Received research grant from National Institutes of Health.
A version of this article appeared on Medscape.com.
This article was originally published on February 10 in Eric Topol’s substack “Ground Truths.”
It’s astounding how devious cancer cells and tumor tissue can be. This week in Science we learned how certain lung cancer cells can function like “Catch Me If You Can” — changing their driver mutation and cell identity to escape targeted therapy. This histologic transformation, as seen in an experimental model, is just one of so many cancer tricks that we are learning about.
Recently, as shown by single-cell sequencing, cancer cells can steal the mitochondria from T cells, a double whammy that turbocharges cancer cells with the hijacked fuel supply and, at the same time, dismantles the immune response.
Last week, we saw how tumor cells can release a virus-like protein that unleashes a vicious autoimmune response.
And then there’s the finding that cancer cell spread predominantly is occurring while we sleep.
As I previously reviewed, the ability for cancer cells to hijack neurons and neural circuits is now well established, no less their ability to reprogram neurons to become adrenergic and stimulate tumor progression, and interfere with the immune response. Stay tuned on that for a new Ground Truths podcast with Prof Michelle Monje, a leader in cancer neuroscience, which will post soon.
Add advancing age’s immunosenescence as yet another challenge to the long and growing list of formidable ways that cancer cells, and the tumor microenvironment, evade our immune response.
An Ever-Expanding Armamentarium
Immune Checkpoint Inhibitors
The field of immunotherapies took off with the immune checkpoint inhibitors, first approved by the FDA in 2011, that take the brakes off of T cells, with the programmed death-1 (PD-1), PD-ligand1, and anti-CTLA-4 monoclonal antibodies.
But we’re clearly learning they are not enough to prevail over cancer with common recurrences, only short term success in most patients, with some notable exceptions. Adding other immune response strategies, such as a vaccine, or antibody-drug conjugates, or engineered T cells, are showing improved chances for success.
Therapeutic Cancer Vaccines
There are many therapeutic cancer vaccines in the works, as reviewed in depth here.
Here’s a list of ongoing clinical trials of cancer vaccines. You’ll note most of these are on top of a checkpoint inhibitor and use personalized neoantigens (cancer cell surface proteins) derived from sequencing (whole-exome or whole genome, RNA-sequencing and HLA-profiling) the patient’s tumor.
An example of positive findings is with the combination of an mRNA-nanoparticle vaccine with up to 34 personalized neoantigens and pembrolizumab (Keytruda) vs pembrolizumab alone in advanced melanoma after resection, with improved outcomes at 3-year follow-up, cutting death or relapse rate in half.
Antibody-Drug Conjugates (ADC)
There is considerable excitement about antibody-drug conjugates (ADC) whereby a linker is used to attach a chemotherapy agent to the checkpoint inhibitor antibody, specifically targeting the cancer cell and facilitating entry of the chemotherapy into the cell. Akin to these are bispecific antibodies (BiTEs, binding to a tumor antigen and T cell receptor simultaneously), both of these conjugates acting as “biologic” or “guided” missiles.
A very good example of the potency of an ADC was seen in a “HER2-low” breast cancer randomized trial. The absence or very low expression or amplification of the HER2 receptor is common in breast cancer and successful treatment has been elusive. A randomized trial of an ADC (trastuzumab deruxtecan) compared to physician’s choice therapy demonstrated a marked success for progression-free survival in HER2-low patients, which was characterized as “unheard-of success” by media coverage.
This strategy is being used to target some of the most difficult cancer driver mutations such as TP53 and KRAS.
Oncolytic Viruses
Modifying viruses to infect the tumor and make it more visible to the immune system, potentiating anti-tumor responses, known as oncolytic viruses, have been proposed as a way to rev up the immune response for a long time but without positive Phase 3 clinical trials.
After decades of failure, a recent trial in refractory bladder cancer showed marked success, along with others, summarized here, now providing very encouraging results. It looks like oncolytic viruses are on a comeback path.
Engineering T Cells (Chimeric Antigen Receptor [CAR-T])
As I recently reviewed, there are over 500 ongoing clinical trials to build on the success of the first CAR-T approval for leukemia 7 years ago. I won’t go through that all again here, but to reiterate most of the success to date has been in “liquid” blood (leukemia and lymphoma) cancer tumors. This week in Nature is the discovery of a T cell cancer mutation, a gene fusion CARD11-PIK3R3, from a T cell lymphoma that can potentially be used to augment CAR-T efficacy. It has pronounced and prolonged effects in the experimental model. Instead of 1 million cells needed for treatment, even 20,000 were enough to melt the tumor. This is a noteworthy discovery since CAR-T work to date has largely not exploited such naturally occurring mutations, while instead concentrating on those seen in the patient’s set of key tumor mutations.
As currently conceived, CAR-T, and what is being referred to more broadly as adoptive cell therapies, involves removing T cells from the patient’s body and engineering their activation, then reintroducing them back to the patient. This is laborious, technically difficult, and very expensive. Recently, the idea of achieving all of this via an injection of virus that specifically infects T cells and inserts the genes needed, was advanced by two biotech companies with preclinical results, one in non-human primates.
Gearing up to meet the challenge of solid tumor CAR-T intervention, there’s more work using CRISPR genome editing of T cell receptors. A.I. is increasingly being exploited to process the data from sequencing and identify optimal neoantigens.
Instead of just CAR-T, we’re seeing the emergence of CAR-macrophage and CAR-natural killer (NK) cells strategies, and rapidly expanding potential combinations of all the strategies I’ve mentioned. No less, there’s been maturation of on-off suicide switches programmed in, to limit cytokine release and promote safety of these interventions. Overall, major side effects of immunotherapies are not only cytokine release syndromes, but also include interstitial pneumonitis and neurotoxicity.
Summary
Given the multitude of ways cancer cells and tumor tissue can evade our immune response, durably successful treatment remains a daunting challenge. But the ingenuity of so many different approaches to unleash our immune response, and their combinations, provides considerable hope that we’ll increasingly meet the challenge in the years ahead. We have clearly learned that combining different immunotherapy strategies will be essential for many patients with the most resilient solid tumors.
Of concern, as noted by a recent editorial in The Lancet, entitled “Cancer Research Equity: Innovations For The Many, Not The Few,” is that these individualized, sophisticated strategies are not scalable; they will have limited reach and benefit. The movement towards “off the shelf” CAR-T and inexpensive, orally active checkpoint inhibitors may help mitigate this issue.
Notwithstanding this important concern, we’re seeing an array of diverse and potent immunotherapy strategies that are providing highly encouraging results, engendering more excitement than we’ve seen in this space for some time. These should propel substantial improvements in outcomes for patients in the years ahead. It can’t happen soon enough.
Thanks for reading this edition of Ground Truths. If you found it informative, please share it with your colleagues.
Dr. Topol has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for Dexcom; Illumina; Molecular Stethoscope; Quest Diagnostics; Blue Cross Blue Shield Association. Received research grant from National Institutes of Health.
A version of this article appeared on Medscape.com.
Long-Term Follow-Up Emphasizes HPV Vaccination Importance
This transcript has been edited for clarity.
I want to briefly discuss a critically important topic that cannot be overly emphasized. It is the relevance, the importance, the benefits, and the outcome of HPV vaccination.
The paper I’m referring to was published in Pediatrics in October 2023. It’s titled, “Ten-Year Follow-up of 9-Valent Human Papillomavirus Vaccine: Immunogenicity, Effectiveness, and Safety.”
Let me emphasize that we’re talking about a 10-year follow-up. In this particular paper and analysis, 301 boys — I emphasize boys — were included and 971 girls at 40 different sites in 13 countries, who received the 9-valent vaccine, which includes HPV 16, 18, and seven other types.
Most importantly, there was not a single case. Not one. Let me repeat this: There was not a single case of high-grade intraepithelial neoplasia, or worse, or condyloma in either males or females. There was not a single case in over 1000 individuals with a follow-up of more than 10 years.
It is difficult to overstate the magnitude of the benefit associated with HPV vaccination for our children and young adults on their risk of developing highly relevant, life-changing, potentially deadly cancers.
For those of you who are interested in this topic — which should include almost all of you, if not all of you — I encourage you to read this very important follow-up paper, again, demonstrating the simple, overwhelming magnitude of the benefit of HPV vaccination. I thank you for your attention.
Dr. Markman is a professor in the department of medical oncology and therapeutics research, City of Hope, Duarte, California, and president of medicine and science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline; AstraZeneca.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I want to briefly discuss a critically important topic that cannot be overly emphasized. It is the relevance, the importance, the benefits, and the outcome of HPV vaccination.
The paper I’m referring to was published in Pediatrics in October 2023. It’s titled, “Ten-Year Follow-up of 9-Valent Human Papillomavirus Vaccine: Immunogenicity, Effectiveness, and Safety.”
Let me emphasize that we’re talking about a 10-year follow-up. In this particular paper and analysis, 301 boys — I emphasize boys — were included and 971 girls at 40 different sites in 13 countries, who received the 9-valent vaccine, which includes HPV 16, 18, and seven other types.
Most importantly, there was not a single case. Not one. Let me repeat this: There was not a single case of high-grade intraepithelial neoplasia, or worse, or condyloma in either males or females. There was not a single case in over 1000 individuals with a follow-up of more than 10 years.
It is difficult to overstate the magnitude of the benefit associated with HPV vaccination for our children and young adults on their risk of developing highly relevant, life-changing, potentially deadly cancers.
For those of you who are interested in this topic — which should include almost all of you, if not all of you — I encourage you to read this very important follow-up paper, again, demonstrating the simple, overwhelming magnitude of the benefit of HPV vaccination. I thank you for your attention.
Dr. Markman is a professor in the department of medical oncology and therapeutics research, City of Hope, Duarte, California, and president of medicine and science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline; AstraZeneca.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I want to briefly discuss a critically important topic that cannot be overly emphasized. It is the relevance, the importance, the benefits, and the outcome of HPV vaccination.
The paper I’m referring to was published in Pediatrics in October 2023. It’s titled, “Ten-Year Follow-up of 9-Valent Human Papillomavirus Vaccine: Immunogenicity, Effectiveness, and Safety.”
Let me emphasize that we’re talking about a 10-year follow-up. In this particular paper and analysis, 301 boys — I emphasize boys — were included and 971 girls at 40 different sites in 13 countries, who received the 9-valent vaccine, which includes HPV 16, 18, and seven other types.
Most importantly, there was not a single case. Not one. Let me repeat this: There was not a single case of high-grade intraepithelial neoplasia, or worse, or condyloma in either males or females. There was not a single case in over 1000 individuals with a follow-up of more than 10 years.
It is difficult to overstate the magnitude of the benefit associated with HPV vaccination for our children and young adults on their risk of developing highly relevant, life-changing, potentially deadly cancers.
For those of you who are interested in this topic — which should include almost all of you, if not all of you — I encourage you to read this very important follow-up paper, again, demonstrating the simple, overwhelming magnitude of the benefit of HPV vaccination. I thank you for your attention.
Dr. Markman is a professor in the department of medical oncology and therapeutics research, City of Hope, Duarte, California, and president of medicine and science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline; AstraZeneca.
A version of this article appeared on Medscape.com.
Physicians as First Responders II
I recently wrote about a fledgling program here in Maine in which some emergency room physicians were being outfitted with equipment and communications gear that would allow them to respond on the fly to emergencies in the field when they weren’t working in the hospital. I questioned the rationale of using in-house personnel, already in short supply, for the few situations in which trained EMT personnel would usually be called. At the same time, I promised to return to the broader subject of the role of physicians as first responders in a future letter. And, here it is.
Have you ever been on a plane or at a large public gathering and the public addressed system crackled, “Is there a doctor on board” or in the audience? Or have you been on the highway and come upon a fresh accident in which it appears that there may have been injuries? Or at a youth soccer game in which a player has been injured and is still on the ground?
How do you usually respond in situations like this? Do you immediately identify yourself as a physician? Or, do you routinely shy away from involvement? What thoughts run through your head?
Do you feel your training and experience with emergencies is so outdated that you doubt you could be of any assistance? Has your practice become so specialized that you aren’t comfortable with anything outside of your specialty? Maybe getting involved is likely to throw your already tight travel schedule into disarray? Or are you afraid that should something go wrong while you were helping out you could be sued?
Keeping in mind that I am a retired septuagenarian pediatrician more than a decade removed from active practice, I would describe my usual response to these situations as “attentive hovering.” I position myself to have a good view of the victim and watch to see if there are any other responders. Either because of their personality or their experience, often there is someone who steps forward to help. Trained EMTs seem to have no hesitancy going into action. If I sense things aren’t going well, or the victim is a child, I will identify myself as a retired pediatrician and offer my assistance. Even if the response given by others seems appropriate, I may still eventually identify myself, maybe to lend an air of legitimacy to the process.
What are the roots of my hesitancy? I have found that I generally have little to add when there is a trained first responder on hand. They have been-there-and-done-that far more recently than I have. They know how to stabilize potential or obvious fractures. They know how to position the victim for transport. Even when I am in an environment where my medical background is already known, I yield to the more recently experienced first responders.
I don’t particularly worry about being sued. Every state has Good Samaritan laws. Although the laws vary from state to state, here in Maine I feel comfortable with the good sense of my fellow citizens. I understand if you live or practice in a more litigious environment you may be more concerned. On an airplane there is the Aviation Medical Assistant Act, which became law in 1998, and provides us with some extra protection.
What if there is a situation in which even with my outdated skills I seem to be the only show in town? Fortunately, that situation hasn’t occurred for me in quite a few years, but the odds are that one might occur. In almost 1 out of 600 airline flights, there is an inflight emergency. I tend to hang out with other septuagenarians and octogenarians doing active things. And I frequent youth athletic events where there is unlikely to be a first responder assigned to the event.
Should I be doing more to update my skills? It’s been a while since I refreshed by CPR techniques. I can’t recall the last time I handled a defibrillator. Should I be learning more about exsanguination prevention techniques?
Every so often there are some rumblings to mandate that all physicians should be required to update these first responder skills to maintain their license or certification. That wouldn’t cover those of us who are retired or who no longer practice medicine. And, I’m not sure we need to add another layer to the system. I think there are enough of us out there who would like to add ourselves to the first responder population, maybe not as fully trained experts but as folks who would like to be more ready to help by updating old or seldom-used skills.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
I recently wrote about a fledgling program here in Maine in which some emergency room physicians were being outfitted with equipment and communications gear that would allow them to respond on the fly to emergencies in the field when they weren’t working in the hospital. I questioned the rationale of using in-house personnel, already in short supply, for the few situations in which trained EMT personnel would usually be called. At the same time, I promised to return to the broader subject of the role of physicians as first responders in a future letter. And, here it is.
Have you ever been on a plane or at a large public gathering and the public addressed system crackled, “Is there a doctor on board” or in the audience? Or have you been on the highway and come upon a fresh accident in which it appears that there may have been injuries? Or at a youth soccer game in which a player has been injured and is still on the ground?
How do you usually respond in situations like this? Do you immediately identify yourself as a physician? Or, do you routinely shy away from involvement? What thoughts run through your head?
Do you feel your training and experience with emergencies is so outdated that you doubt you could be of any assistance? Has your practice become so specialized that you aren’t comfortable with anything outside of your specialty? Maybe getting involved is likely to throw your already tight travel schedule into disarray? Or are you afraid that should something go wrong while you were helping out you could be sued?
Keeping in mind that I am a retired septuagenarian pediatrician more than a decade removed from active practice, I would describe my usual response to these situations as “attentive hovering.” I position myself to have a good view of the victim and watch to see if there are any other responders. Either because of their personality or their experience, often there is someone who steps forward to help. Trained EMTs seem to have no hesitancy going into action. If I sense things aren’t going well, or the victim is a child, I will identify myself as a retired pediatrician and offer my assistance. Even if the response given by others seems appropriate, I may still eventually identify myself, maybe to lend an air of legitimacy to the process.
What are the roots of my hesitancy? I have found that I generally have little to add when there is a trained first responder on hand. They have been-there-and-done-that far more recently than I have. They know how to stabilize potential or obvious fractures. They know how to position the victim for transport. Even when I am in an environment where my medical background is already known, I yield to the more recently experienced first responders.
I don’t particularly worry about being sued. Every state has Good Samaritan laws. Although the laws vary from state to state, here in Maine I feel comfortable with the good sense of my fellow citizens. I understand if you live or practice in a more litigious environment you may be more concerned. On an airplane there is the Aviation Medical Assistant Act, which became law in 1998, and provides us with some extra protection.
What if there is a situation in which even with my outdated skills I seem to be the only show in town? Fortunately, that situation hasn’t occurred for me in quite a few years, but the odds are that one might occur. In almost 1 out of 600 airline flights, there is an inflight emergency. I tend to hang out with other septuagenarians and octogenarians doing active things. And I frequent youth athletic events where there is unlikely to be a first responder assigned to the event.
Should I be doing more to update my skills? It’s been a while since I refreshed by CPR techniques. I can’t recall the last time I handled a defibrillator. Should I be learning more about exsanguination prevention techniques?
Every so often there are some rumblings to mandate that all physicians should be required to update these first responder skills to maintain their license or certification. That wouldn’t cover those of us who are retired or who no longer practice medicine. And, I’m not sure we need to add another layer to the system. I think there are enough of us out there who would like to add ourselves to the first responder population, maybe not as fully trained experts but as folks who would like to be more ready to help by updating old or seldom-used skills.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
I recently wrote about a fledgling program here in Maine in which some emergency room physicians were being outfitted with equipment and communications gear that would allow them to respond on the fly to emergencies in the field when they weren’t working in the hospital. I questioned the rationale of using in-house personnel, already in short supply, for the few situations in which trained EMT personnel would usually be called. At the same time, I promised to return to the broader subject of the role of physicians as first responders in a future letter. And, here it is.
Have you ever been on a plane or at a large public gathering and the public addressed system crackled, “Is there a doctor on board” or in the audience? Or have you been on the highway and come upon a fresh accident in which it appears that there may have been injuries? Or at a youth soccer game in which a player has been injured and is still on the ground?
How do you usually respond in situations like this? Do you immediately identify yourself as a physician? Or, do you routinely shy away from involvement? What thoughts run through your head?
Do you feel your training and experience with emergencies is so outdated that you doubt you could be of any assistance? Has your practice become so specialized that you aren’t comfortable with anything outside of your specialty? Maybe getting involved is likely to throw your already tight travel schedule into disarray? Or are you afraid that should something go wrong while you were helping out you could be sued?
Keeping in mind that I am a retired septuagenarian pediatrician more than a decade removed from active practice, I would describe my usual response to these situations as “attentive hovering.” I position myself to have a good view of the victim and watch to see if there are any other responders. Either because of their personality or their experience, often there is someone who steps forward to help. Trained EMTs seem to have no hesitancy going into action. If I sense things aren’t going well, or the victim is a child, I will identify myself as a retired pediatrician and offer my assistance. Even if the response given by others seems appropriate, I may still eventually identify myself, maybe to lend an air of legitimacy to the process.
What are the roots of my hesitancy? I have found that I generally have little to add when there is a trained first responder on hand. They have been-there-and-done-that far more recently than I have. They know how to stabilize potential or obvious fractures. They know how to position the victim for transport. Even when I am in an environment where my medical background is already known, I yield to the more recently experienced first responders.
I don’t particularly worry about being sued. Every state has Good Samaritan laws. Although the laws vary from state to state, here in Maine I feel comfortable with the good sense of my fellow citizens. I understand if you live or practice in a more litigious environment you may be more concerned. On an airplane there is the Aviation Medical Assistant Act, which became law in 1998, and provides us with some extra protection.
What if there is a situation in which even with my outdated skills I seem to be the only show in town? Fortunately, that situation hasn’t occurred for me in quite a few years, but the odds are that one might occur. In almost 1 out of 600 airline flights, there is an inflight emergency. I tend to hang out with other septuagenarians and octogenarians doing active things. And I frequent youth athletic events where there is unlikely to be a first responder assigned to the event.
Should I be doing more to update my skills? It’s been a while since I refreshed by CPR techniques. I can’t recall the last time I handled a defibrillator. Should I be learning more about exsanguination prevention techniques?
Every so often there are some rumblings to mandate that all physicians should be required to update these first responder skills to maintain their license or certification. That wouldn’t cover those of us who are retired or who no longer practice medicine. And, I’m not sure we need to add another layer to the system. I think there are enough of us out there who would like to add ourselves to the first responder population, maybe not as fully trained experts but as folks who would like to be more ready to help by updating old or seldom-used skills.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Bivalent Vaccines Protect Even Children Who’ve Had COVID
This transcript has been edited for clarity.
It was only 3 years ago when we called the pathogen we now refer to as the coronavirus “nCOV-19.” It was, in many ways, more descriptive than what we have today. The little “n” there stood for “novel” — and it was really that little “n” that caused us all the trouble.
You see, coronaviruses themselves were not really new to us. Understudied, perhaps, but with four strains running around the globe at any time giving rise to the common cold, these were viruses our bodies understood.
But Instead of acting like a cold, it acted like nothing we had seen before, at least in our lifetime. The story of the pandemic is very much a bildungsroman of our immune systems — a story of how our immunity grew up.
The difference between the start of 2020 and now, when infections with the coronavirus remain common but not as deadly, can be measured in terms of immune education. Some of our immune systems were educated by infection, some by vaccination, and many by both.
When the first vaccines emerged in December 2020, the opportunity to educate our immune systems was still huge. Though, at the time, an estimated 20 million had been infected in the US and 350,000 had died, there was a large population that remained immunologically naive. I was one of them.
If 2020 into early 2021 was the era of immune education, the postvaccine period was the era of the variant. From one COVID strain to two, to five, to innumerable, our immune memory — trained on a specific version of the virus or its spike protein — became imperfect again. Not naive; these variants were not “novel” in the way COVID-19 was novel, but they were different. And different enough to cause infection.
Following the playbook of another virus that loves to come dressed up in different outfits, the flu virus, we find ourselves in the booster era — a world where yearly doses of a vaccine, ideally matched to the variants circulating when the vaccine is given, are the recommendation if not the norm.
But questions remain about the vaccination program, particularly around who should get it. And two populations with big question marks over their heads are (1) people who have already been infected and (2) kids, because their risk for bad outcomes is so much lower.
This week, we finally have some evidence that can shed light on these questions. The study under the spotlight is this one, appearing in JAMA, which tries to analyze the ability of the bivalent vaccine — that’s the second one to come out, around September 2022 — to protect kids from COVID-19.
Now, right off the bat, this was not a randomized trial. The studies that established the viability of the mRNA vaccine platform were; they happened before the vaccine was authorized. But trials of the bivalent vaccine were mostly limited to proving immune response, not protection from disease.
Nevertheless, with some good observational methods and some statistics, we can try to tease out whether bivalent vaccines in kids worked.
The study combines three prospective cohort studies. The details are in the paper, but what you need to know is that the special sauce of these studies was that the kids were tested for COVID-19 on a weekly basis, whether they had symptoms or not. This is critical because asymptomatic infections can transmit COVID-19.
Let’s do the variables of interest. First and foremost, the bivalent vaccine. Some of these kids got the bivalent vaccine, some didn’t. Other key variables include prior vaccination with the monovalent vaccine. Some had been vaccinated with the monovalent vaccine before, some hadn’t. And, of course, prior infection. Some had been infected before (based on either nasal swabs or blood tests).
Let’s focus first on the primary exposure of interest: getting that bivalent vaccine. Again, this was not randomly assigned; kids who got the bivalent vaccine were different from those who did not. In general, they lived in smaller households, they were more likely to be White, less likely to have had a prior COVID infection, and quite a bit more likely to have at least one chronic condition.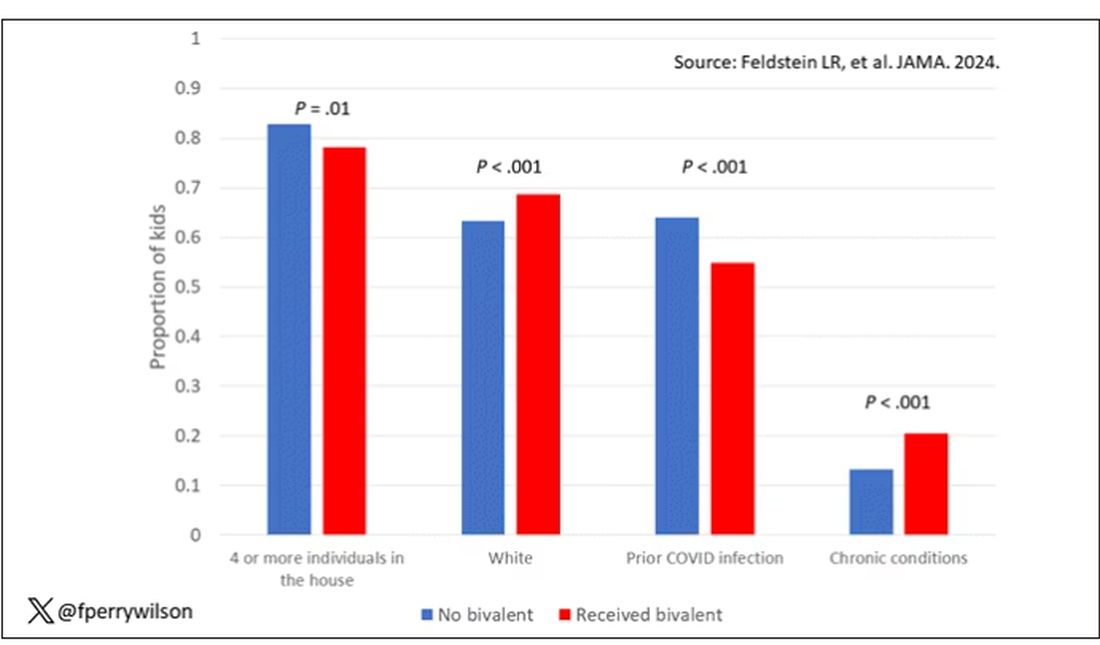
To me, this constellation of factors describes a slightly higher-risk group; it makes sense that they were more likely to get the second vaccine.
Given those factors, what were the rates of COVID infection? After nearly a year of follow-up, around 15% of the kids who hadn’t received the bivalent vaccine got infected compared with 5% of the vaccinated kids. Symptomatic infections represented roughly half of all infections in both groups.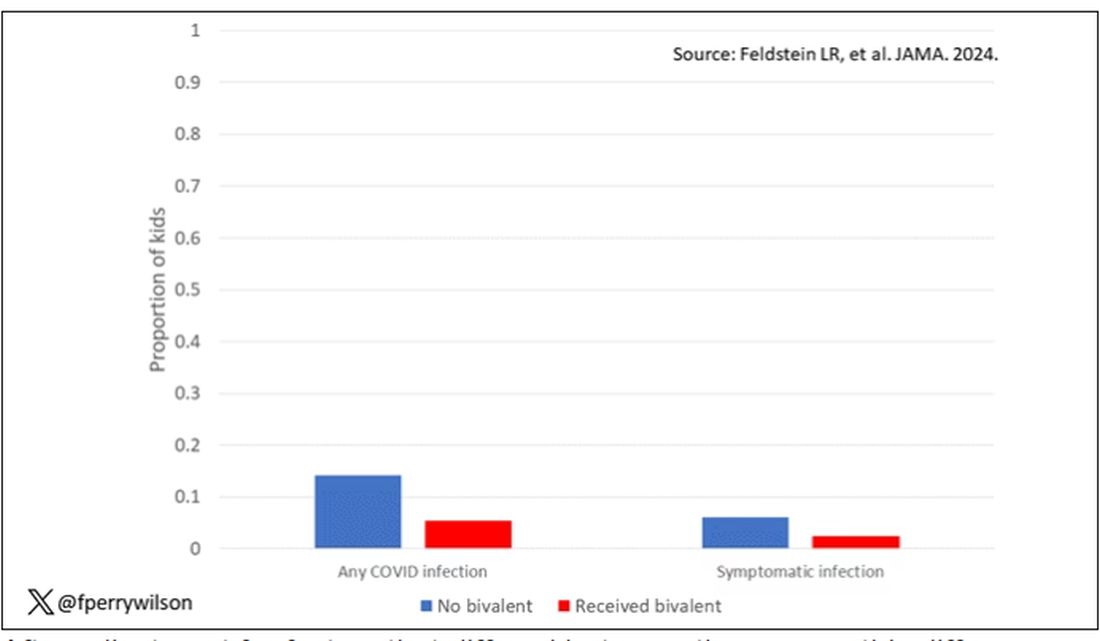
After adjustment for factors that differed between the groups, this difference translated into a vaccine efficacy of about 50% in this population. That’s our first data point. Yes, the bivalent vaccine worked. Not amazingly, of course. But it worked.
What about the kids who had had a prior COVID infection? Somewhat surprisingly, the vaccine was just as effective in this population, despite the fact that their immune systems already had some knowledge of COVID. Ten percent of unvaccinated kids got infected, even though they had been infected before. Just 2.5% of kids who received the bivalent vaccine got infected, suggesting some synergy between prior infection and vaccination.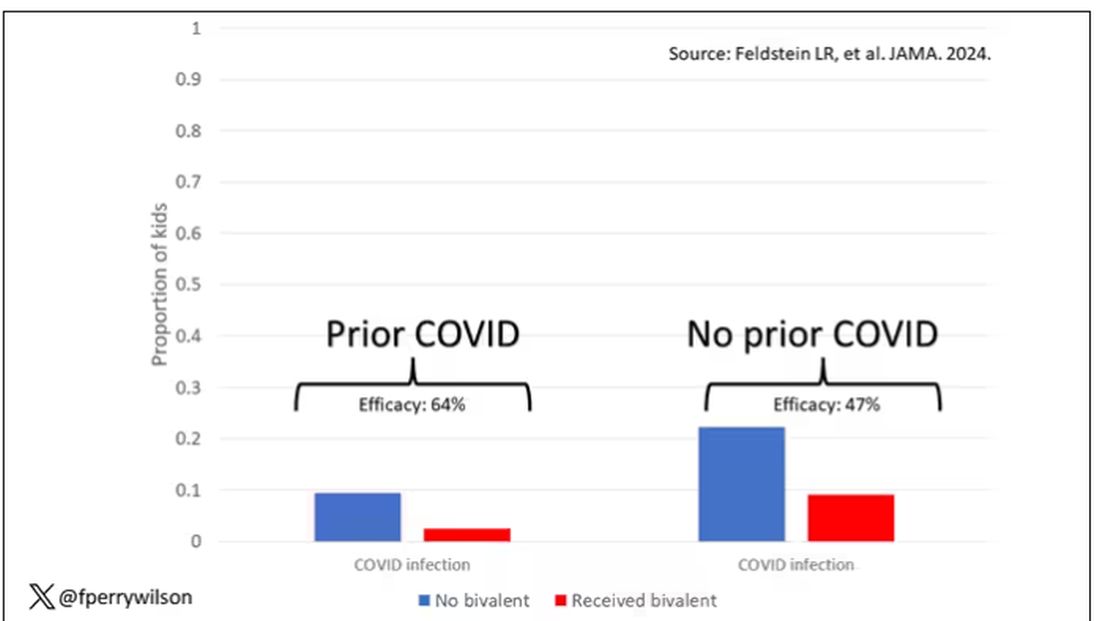
These data suggest that the bivalent vaccine did reduce the risk for COVID infection in kids. All good. But the piece still missing is how severe these infections were. It doesn’t appear that any of the 426 infections documented in this study resulted in hospitalization or death, fortunately. And no data are presented on the incidence of multisystem inflammatory syndrome of children, though given the rarity, I’d be surprised if any of these kids have this either.
So where are we? Well, it seems that the narrative out there that says “the vaccines don’t work” or “the vaccines don’t work if you’ve already been infected” is probably not true. They do work. This study and others in adults show that. If they work to reduce infections, as this study shows, they will also work to reduce deaths. It’s just that death is fortunately so rare in children that the number needed to vaccinate to prevent one death is very large. In that situation, the decision to vaccinate comes down to the risks associated with vaccination. So far, those risk seem very minimal.
Perhaps falling into a flu-like yearly vaccination schedule is not simply the result of old habits dying hard. Maybe it’s actually not a bad idea.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It was only 3 years ago when we called the pathogen we now refer to as the coronavirus “nCOV-19.” It was, in many ways, more descriptive than what we have today. The little “n” there stood for “novel” — and it was really that little “n” that caused us all the trouble.
You see, coronaviruses themselves were not really new to us. Understudied, perhaps, but with four strains running around the globe at any time giving rise to the common cold, these were viruses our bodies understood.
But Instead of acting like a cold, it acted like nothing we had seen before, at least in our lifetime. The story of the pandemic is very much a bildungsroman of our immune systems — a story of how our immunity grew up.
The difference between the start of 2020 and now, when infections with the coronavirus remain common but not as deadly, can be measured in terms of immune education. Some of our immune systems were educated by infection, some by vaccination, and many by both.
When the first vaccines emerged in December 2020, the opportunity to educate our immune systems was still huge. Though, at the time, an estimated 20 million had been infected in the US and 350,000 had died, there was a large population that remained immunologically naive. I was one of them.
If 2020 into early 2021 was the era of immune education, the postvaccine period was the era of the variant. From one COVID strain to two, to five, to innumerable, our immune memory — trained on a specific version of the virus or its spike protein — became imperfect again. Not naive; these variants were not “novel” in the way COVID-19 was novel, but they were different. And different enough to cause infection.
Following the playbook of another virus that loves to come dressed up in different outfits, the flu virus, we find ourselves in the booster era — a world where yearly doses of a vaccine, ideally matched to the variants circulating when the vaccine is given, are the recommendation if not the norm.
But questions remain about the vaccination program, particularly around who should get it. And two populations with big question marks over their heads are (1) people who have already been infected and (2) kids, because their risk for bad outcomes is so much lower.
This week, we finally have some evidence that can shed light on these questions. The study under the spotlight is this one, appearing in JAMA, which tries to analyze the ability of the bivalent vaccine — that’s the second one to come out, around September 2022 — to protect kids from COVID-19.
Now, right off the bat, this was not a randomized trial. The studies that established the viability of the mRNA vaccine platform were; they happened before the vaccine was authorized. But trials of the bivalent vaccine were mostly limited to proving immune response, not protection from disease.
Nevertheless, with some good observational methods and some statistics, we can try to tease out whether bivalent vaccines in kids worked.
The study combines three prospective cohort studies. The details are in the paper, but what you need to know is that the special sauce of these studies was that the kids were tested for COVID-19 on a weekly basis, whether they had symptoms or not. This is critical because asymptomatic infections can transmit COVID-19.
Let’s do the variables of interest. First and foremost, the bivalent vaccine. Some of these kids got the bivalent vaccine, some didn’t. Other key variables include prior vaccination with the monovalent vaccine. Some had been vaccinated with the monovalent vaccine before, some hadn’t. And, of course, prior infection. Some had been infected before (based on either nasal swabs or blood tests).
Let’s focus first on the primary exposure of interest: getting that bivalent vaccine. Again, this was not randomly assigned; kids who got the bivalent vaccine were different from those who did not. In general, they lived in smaller households, they were more likely to be White, less likely to have had a prior COVID infection, and quite a bit more likely to have at least one chronic condition.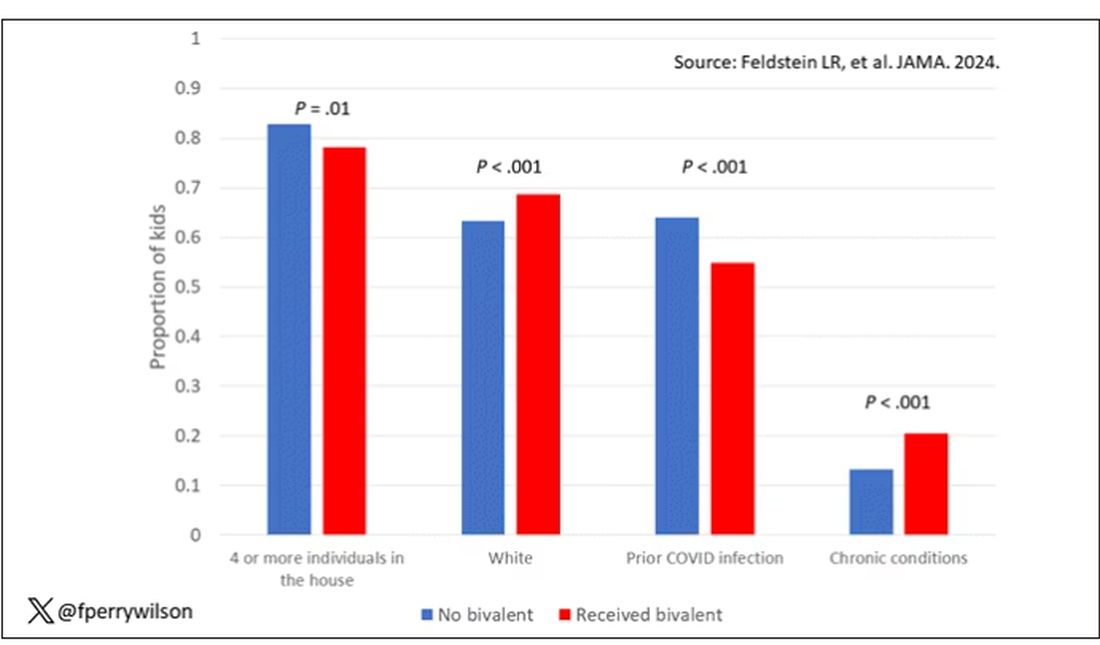
To me, this constellation of factors describes a slightly higher-risk group; it makes sense that they were more likely to get the second vaccine.
Given those factors, what were the rates of COVID infection? After nearly a year of follow-up, around 15% of the kids who hadn’t received the bivalent vaccine got infected compared with 5% of the vaccinated kids. Symptomatic infections represented roughly half of all infections in both groups.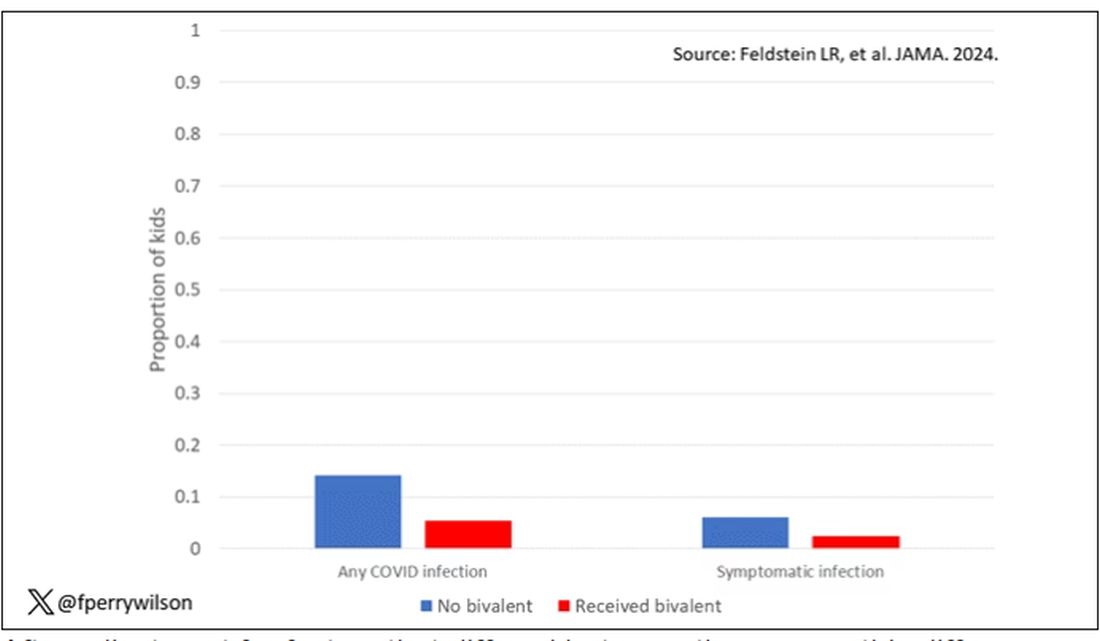
After adjustment for factors that differed between the groups, this difference translated into a vaccine efficacy of about 50% in this population. That’s our first data point. Yes, the bivalent vaccine worked. Not amazingly, of course. But it worked.
What about the kids who had had a prior COVID infection? Somewhat surprisingly, the vaccine was just as effective in this population, despite the fact that their immune systems already had some knowledge of COVID. Ten percent of unvaccinated kids got infected, even though they had been infected before. Just 2.5% of kids who received the bivalent vaccine got infected, suggesting some synergy between prior infection and vaccination.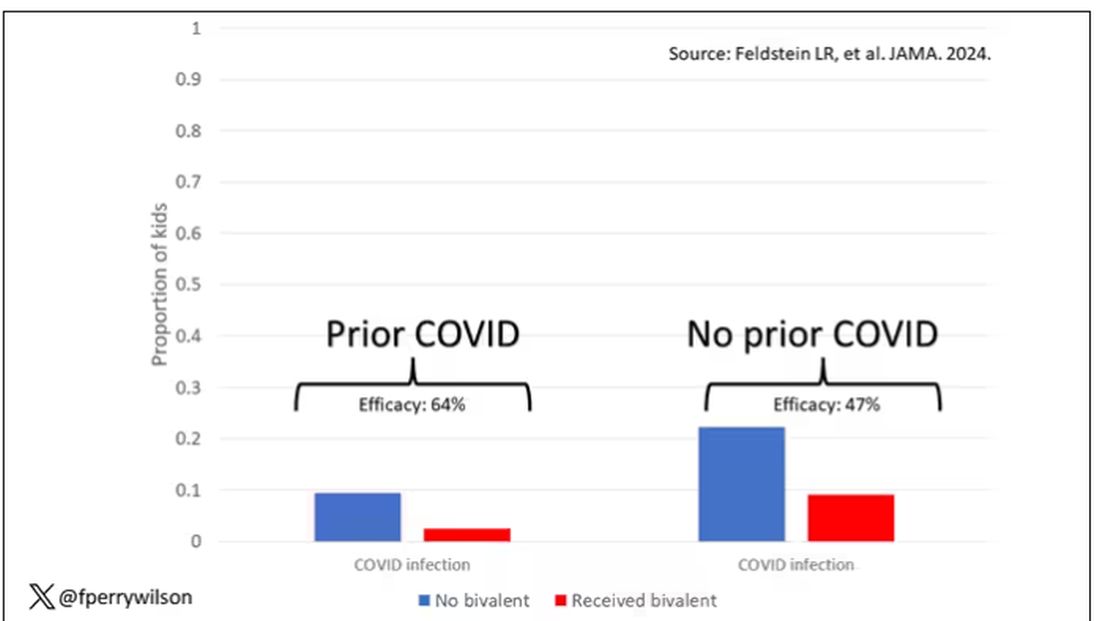
These data suggest that the bivalent vaccine did reduce the risk for COVID infection in kids. All good. But the piece still missing is how severe these infections were. It doesn’t appear that any of the 426 infections documented in this study resulted in hospitalization or death, fortunately. And no data are presented on the incidence of multisystem inflammatory syndrome of children, though given the rarity, I’d be surprised if any of these kids have this either.
So where are we? Well, it seems that the narrative out there that says “the vaccines don’t work” or “the vaccines don’t work if you’ve already been infected” is probably not true. They do work. This study and others in adults show that. If they work to reduce infections, as this study shows, they will also work to reduce deaths. It’s just that death is fortunately so rare in children that the number needed to vaccinate to prevent one death is very large. In that situation, the decision to vaccinate comes down to the risks associated with vaccination. So far, those risk seem very minimal.
Perhaps falling into a flu-like yearly vaccination schedule is not simply the result of old habits dying hard. Maybe it’s actually not a bad idea.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It was only 3 years ago when we called the pathogen we now refer to as the coronavirus “nCOV-19.” It was, in many ways, more descriptive than what we have today. The little “n” there stood for “novel” — and it was really that little “n” that caused us all the trouble.
You see, coronaviruses themselves were not really new to us. Understudied, perhaps, but with four strains running around the globe at any time giving rise to the common cold, these were viruses our bodies understood.
But Instead of acting like a cold, it acted like nothing we had seen before, at least in our lifetime. The story of the pandemic is very much a bildungsroman of our immune systems — a story of how our immunity grew up.
The difference between the start of 2020 and now, when infections with the coronavirus remain common but not as deadly, can be measured in terms of immune education. Some of our immune systems were educated by infection, some by vaccination, and many by both.
When the first vaccines emerged in December 2020, the opportunity to educate our immune systems was still huge. Though, at the time, an estimated 20 million had been infected in the US and 350,000 had died, there was a large population that remained immunologically naive. I was one of them.
If 2020 into early 2021 was the era of immune education, the postvaccine period was the era of the variant. From one COVID strain to two, to five, to innumerable, our immune memory — trained on a specific version of the virus or its spike protein — became imperfect again. Not naive; these variants were not “novel” in the way COVID-19 was novel, but they were different. And different enough to cause infection.
Following the playbook of another virus that loves to come dressed up in different outfits, the flu virus, we find ourselves in the booster era — a world where yearly doses of a vaccine, ideally matched to the variants circulating when the vaccine is given, are the recommendation if not the norm.
But questions remain about the vaccination program, particularly around who should get it. And two populations with big question marks over their heads are (1) people who have already been infected and (2) kids, because their risk for bad outcomes is so much lower.
This week, we finally have some evidence that can shed light on these questions. The study under the spotlight is this one, appearing in JAMA, which tries to analyze the ability of the bivalent vaccine — that’s the second one to come out, around September 2022 — to protect kids from COVID-19.
Now, right off the bat, this was not a randomized trial. The studies that established the viability of the mRNA vaccine platform were; they happened before the vaccine was authorized. But trials of the bivalent vaccine were mostly limited to proving immune response, not protection from disease.
Nevertheless, with some good observational methods and some statistics, we can try to tease out whether bivalent vaccines in kids worked.
The study combines three prospective cohort studies. The details are in the paper, but what you need to know is that the special sauce of these studies was that the kids were tested for COVID-19 on a weekly basis, whether they had symptoms or not. This is critical because asymptomatic infections can transmit COVID-19.
Let’s do the variables of interest. First and foremost, the bivalent vaccine. Some of these kids got the bivalent vaccine, some didn’t. Other key variables include prior vaccination with the monovalent vaccine. Some had been vaccinated with the monovalent vaccine before, some hadn’t. And, of course, prior infection. Some had been infected before (based on either nasal swabs or blood tests).
Let’s focus first on the primary exposure of interest: getting that bivalent vaccine. Again, this was not randomly assigned; kids who got the bivalent vaccine were different from those who did not. In general, they lived in smaller households, they were more likely to be White, less likely to have had a prior COVID infection, and quite a bit more likely to have at least one chronic condition.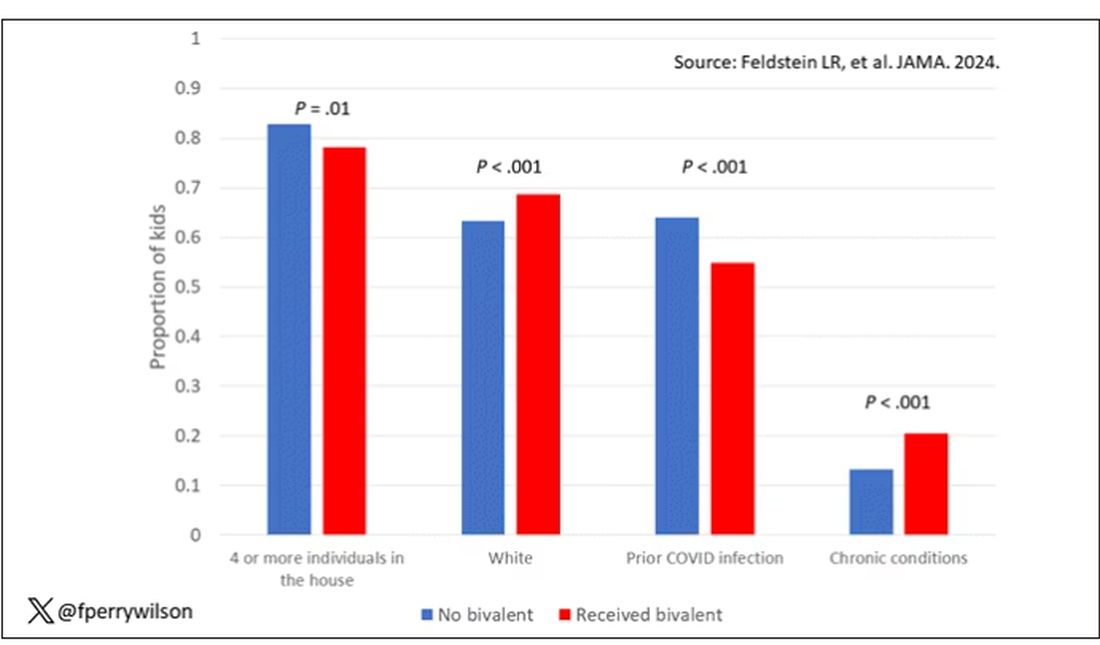
To me, this constellation of factors describes a slightly higher-risk group; it makes sense that they were more likely to get the second vaccine.
Given those factors, what were the rates of COVID infection? After nearly a year of follow-up, around 15% of the kids who hadn’t received the bivalent vaccine got infected compared with 5% of the vaccinated kids. Symptomatic infections represented roughly half of all infections in both groups.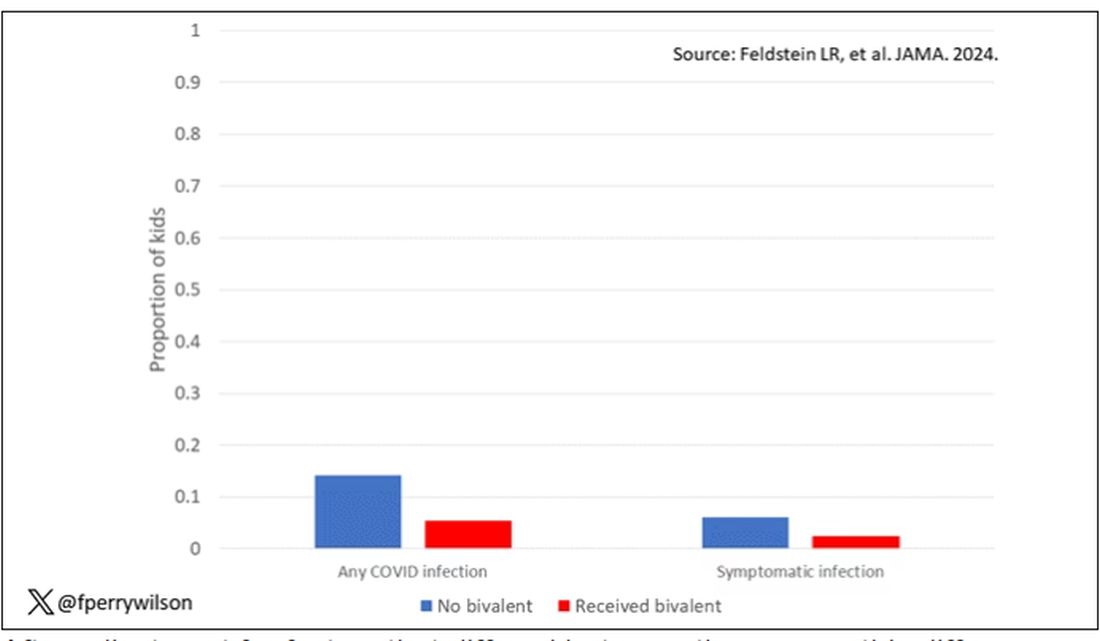
After adjustment for factors that differed between the groups, this difference translated into a vaccine efficacy of about 50% in this population. That’s our first data point. Yes, the bivalent vaccine worked. Not amazingly, of course. But it worked.
What about the kids who had had a prior COVID infection? Somewhat surprisingly, the vaccine was just as effective in this population, despite the fact that their immune systems already had some knowledge of COVID. Ten percent of unvaccinated kids got infected, even though they had been infected before. Just 2.5% of kids who received the bivalent vaccine got infected, suggesting some synergy between prior infection and vaccination.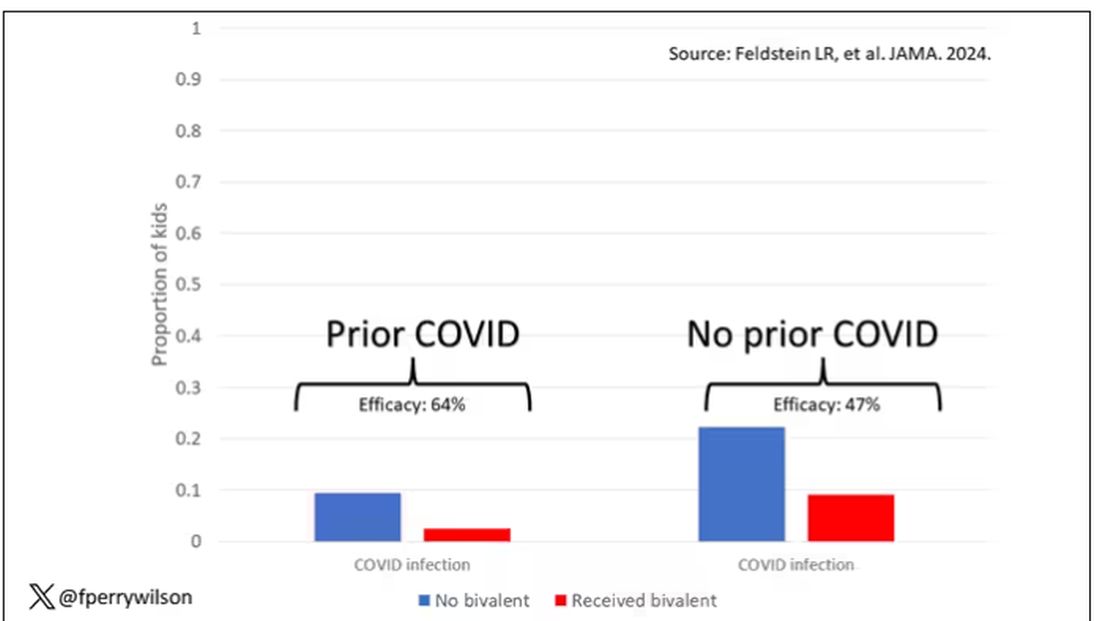
These data suggest that the bivalent vaccine did reduce the risk for COVID infection in kids. All good. But the piece still missing is how severe these infections were. It doesn’t appear that any of the 426 infections documented in this study resulted in hospitalization or death, fortunately. And no data are presented on the incidence of multisystem inflammatory syndrome of children, though given the rarity, I’d be surprised if any of these kids have this either.
So where are we? Well, it seems that the narrative out there that says “the vaccines don’t work” or “the vaccines don’t work if you’ve already been infected” is probably not true. They do work. This study and others in adults show that. If they work to reduce infections, as this study shows, they will also work to reduce deaths. It’s just that death is fortunately so rare in children that the number needed to vaccinate to prevent one death is very large. In that situation, the decision to vaccinate comes down to the risks associated with vaccination. So far, those risk seem very minimal.
Perhaps falling into a flu-like yearly vaccination schedule is not simply the result of old habits dying hard. Maybe it’s actually not a bad idea.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Weighing the Big Decisions
In my mind’s calendar, two dates stand out. Both far enough away that I don’t have to think about them too much right now, but near enough that they can’t be forgotten about, either.
On September 30, 2028, my office lease ends, and in 2029 my neurology board certification has to be renewed. I’ll be in my early 60s then and I’ve been a practicing neurologist for 30 years.
I have no idea what I’m going to do. Of course, a lot can happen between now and then, and a lot of variables come into the calculus of when to retire.
After all these years, I still enjoy my job. It gives me the purpose that I wanted so long ago when I applied to medical school. The late William Pancoe, associate dean when I was at Creighton, always told us to remember how we felt when we got that acceptance letter — we’d need it to keep us going through medical school.
And, even now, I still remember the call from my dad that it had arrived. What a moment that was. I have no regrets. I can’t imagine doing anything else.
But in 4 years how much longer will I want to practice? Hopefully I’ll be faced with that decision. Will I want to renew the lease for 2 years? 5 years? I like my little office. It’s far from gleaming, there’s no TV or Keurig in the lobby, the carpet, paint, and furnishings are still from the early 90s when the place was built. But it’s my home away from home. I spend anywhere from 40-60 hours/week there. It’s quiet and (at least for me) cozy. Would I want to give that up and move to a smaller, shared place, for the remainder of my career? Or just close down?
Likewise, will I want to renew my board certification? Granted, that isn’t necessary to practice, but it certainly looks better to have it. To do that I’ll have to fork over a decent chunk of change to take the test, more money for a review course, and spend some time studying. Strange to think that at 63 I might be back at my desk (same desk, by the way) studying for a test like I did in college and medical school. But, if I want to keep playing doctor, that’s what I’ll have to do.
Four years to think about this. The same amount of time I spent each in high school, medical school, and residency. For that matter, the same amount of time since we all went into quarantine.
Doesn’t seem that long, does it?
I guess I’ve got some thinking to do.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In my mind’s calendar, two dates stand out. Both far enough away that I don’t have to think about them too much right now, but near enough that they can’t be forgotten about, either.
On September 30, 2028, my office lease ends, and in 2029 my neurology board certification has to be renewed. I’ll be in my early 60s then and I’ve been a practicing neurologist for 30 years.
I have no idea what I’m going to do. Of course, a lot can happen between now and then, and a lot of variables come into the calculus of when to retire.
After all these years, I still enjoy my job. It gives me the purpose that I wanted so long ago when I applied to medical school. The late William Pancoe, associate dean when I was at Creighton, always told us to remember how we felt when we got that acceptance letter — we’d need it to keep us going through medical school.
And, even now, I still remember the call from my dad that it had arrived. What a moment that was. I have no regrets. I can’t imagine doing anything else.
But in 4 years how much longer will I want to practice? Hopefully I’ll be faced with that decision. Will I want to renew the lease for 2 years? 5 years? I like my little office. It’s far from gleaming, there’s no TV or Keurig in the lobby, the carpet, paint, and furnishings are still from the early 90s when the place was built. But it’s my home away from home. I spend anywhere from 40-60 hours/week there. It’s quiet and (at least for me) cozy. Would I want to give that up and move to a smaller, shared place, for the remainder of my career? Or just close down?
Likewise, will I want to renew my board certification? Granted, that isn’t necessary to practice, but it certainly looks better to have it. To do that I’ll have to fork over a decent chunk of change to take the test, more money for a review course, and spend some time studying. Strange to think that at 63 I might be back at my desk (same desk, by the way) studying for a test like I did in college and medical school. But, if I want to keep playing doctor, that’s what I’ll have to do.
Four years to think about this. The same amount of time I spent each in high school, medical school, and residency. For that matter, the same amount of time since we all went into quarantine.
Doesn’t seem that long, does it?
I guess I’ve got some thinking to do.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In my mind’s calendar, two dates stand out. Both far enough away that I don’t have to think about them too much right now, but near enough that they can’t be forgotten about, either.
On September 30, 2028, my office lease ends, and in 2029 my neurology board certification has to be renewed. I’ll be in my early 60s then and I’ve been a practicing neurologist for 30 years.
I have no idea what I’m going to do. Of course, a lot can happen between now and then, and a lot of variables come into the calculus of when to retire.
After all these years, I still enjoy my job. It gives me the purpose that I wanted so long ago when I applied to medical school. The late William Pancoe, associate dean when I was at Creighton, always told us to remember how we felt when we got that acceptance letter — we’d need it to keep us going through medical school.
And, even now, I still remember the call from my dad that it had arrived. What a moment that was. I have no regrets. I can’t imagine doing anything else.
But in 4 years how much longer will I want to practice? Hopefully I’ll be faced with that decision. Will I want to renew the lease for 2 years? 5 years? I like my little office. It’s far from gleaming, there’s no TV or Keurig in the lobby, the carpet, paint, and furnishings are still from the early 90s when the place was built. But it’s my home away from home. I spend anywhere from 40-60 hours/week there. It’s quiet and (at least for me) cozy. Would I want to give that up and move to a smaller, shared place, for the remainder of my career? Or just close down?
Likewise, will I want to renew my board certification? Granted, that isn’t necessary to practice, but it certainly looks better to have it. To do that I’ll have to fork over a decent chunk of change to take the test, more money for a review course, and spend some time studying. Strange to think that at 63 I might be back at my desk (same desk, by the way) studying for a test like I did in college and medical school. But, if I want to keep playing doctor, that’s what I’ll have to do.
Four years to think about this. The same amount of time I spent each in high school, medical school, and residency. For that matter, the same amount of time since we all went into quarantine.
Doesn’t seem that long, does it?
I guess I’ve got some thinking to do.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Long COVID: Another Great Pretender
Has COVID replaced syphilis as the great imitator? At the turn of the 20th century, Sir William Osler was quoted as saying, “He who knows syphilis knows medicine.”
If you have any doubts about the “imitator” analogy, simply use any broad search engine or AI portal and enter “what is the differential diagnosis of primary syphilis, or secondary syphilis, or tertiary syphilis?” A plethora of diseases across many body systems appears.
Another Great Pretender?
Did you or do you now have long COVID? How do you know? Do you even know what long COVID is? How would you diagnosis it?
When asked about long COVID, this is what large language model source bard.google.com had to say:
Long COVID, also known as post-COVID conditions or PASC, is a complex condition that can occur in people who have had COVID-19, even if their initial illness was mild or even asymptomatic. It’s characterized by a wide range of symptoms that can last for weeks, months, or even years after the initial infection.
Symptoms of long COVID can include: fatigue, shortness of breath, brain fog (trouble thinking or concentrating), loss of smell or taste, sleep problems, muscle pain, joint pain, headache, dizziness, depression or anxiety, heart palpitations, gastrointestinal problems.
Duh!!! It reads much like a continuation of the symptoms of acute COVID. Bard continued:
The exact cause of long COVID is still unknown, but there are several theories. One possibility is that the virus itself can damage organs and tissues, leading to ongoing symptoms. Another possibility is that the immune system’s response to the virus can continue to cause inflammation even after the virus is gone.
Human intelligence source Wikipedia says this:
Long COVID or long-haul COVID is a group of health problems persisting or developing after an initial COVID-19 infection. Symptoms can last weeks, months or years and are often debilitating. The World Health Organization defines long COVID as starting three months after infection, but other definitions put the start of long COVID at four weeks.
Highly varied, including post-exertional malaise (symptoms made worse with effort), fatigue, muscle pain, shortness of breath, chest pain, and cognitive dysfunction (brain fog).
Acute COVID to Long COVID
The World Health Organization estimates that 36 million people in the European region have developed long COVID in the first 3 years of the pandemic. That›s a lot.
We all know that the common signs and symptoms of acute COVID-19 include fever or chills, a dry cough and shortness of breath, feeling very tired, muscle or body aches, headache, loss of taste or smell, sore throat, congestion, runny nose, nausea, vomiting, and diarrhea. Except for the taste and smell findings, every one of these symptoms or signs could indicate a different virus infection or even some type of allergy. My point is the nonspecificity in this list.
Uncommon signs and symptoms of acute COVID include a flat skin rash covered with small bumps, discolored swollen areas on the fingers and toes (COVID toes), and hives. The skin of hands, wrists, or ankles also can be affected. Blisters, itchiness, rough skin, or pus can be seen.
Severe confusion (delirium) might be the main or only symptom of COVID-19 in older people. This COVID-19 symptom is linked with a high risk for poor outcomes, including death. Pink eye (conjunctivitis) can be a COVID-19 symptom. Other eye problems linked to COVID-19 are light sensitivity, sore eyes, and itchy eyes. Acute myocarditis, tinnitus, vertigo, and hearing loss have been reported. And 1-4 weeks after the onset of COVID-19 infection, a patient may experience de novo reactive synovitis and arthritis of any joints.
So, take your pick. Myriad symptoms, signs, diseases, diagnoses, and organ systems — still present, recurring, just appearing, apparently de novo, or after asymptomatic infection. We have so much still to learn.
What big-time symptoms, signs, and major diseases are not on any of these lists? Obviously, cancer, atherosclerotic cardiovascular diseases, obesity, bone diseases, and competitive infections. But be patient; the lingering effects of direct tissue invasion by the virus as well as a wide range of immunologic reactions may just be getting started. Mitochondrial damage, especially in muscles, is increasingly a pathophysiologic suspect.
Human diseases can be physical or mental; and in COVID, that twain not only meet but mix and mingle freely, and may even merge into psychosoma. Don’t ever forget that. Consider “fatigue.” Who among us, COVID or NOVID, does not experience that from time to time?
Or consider brain fog as a common reported symptom of COVID. What on earth is that actually? How can a person know they have brain fog, or whether they had it and are over it?
We need one or more lab or other diagnostic tests that can objectively confirm the diagnosis of long COVID.
Useful Progress?
A recent research paper in Science reported intriguing chemical findings that seemed to point a finger at some form of complement dysregulation as a potential disease marker for long COVID. Unfortunately, some critics have pointed out that this entire study may be invalid or irrelevant because the New York cohort was recruited in 2020, before vaccines were available. The Zurich cohort was recruited up until April 2021, so some may have been vaccinated.
Then this news organization came along in early January 2024 with an article about COVID causing not only more than a million American deaths but also more than 5000 deaths from long COVID. We physicians don’t really know what long COVID even is, but we have to sign death certificates blaming thousands of deaths on it anyway? And rolling back the clock to 2020: Are patients dying from COVID or with COVID, according to death certificates?Now, armed with the knowledge that “documented serious post–COVID-19 conditions include cardiovascular, pulmonary, neurological, renal, endocrine, hematological, and gastrointestinal complications, as well as death,” CDC has published clear and fairly concise instructions on how to address post-acute COVID sequelae on death certificates.
In late January, this news organization painted a hopeful picture by naming four phenotypes of long COVID, suggesting that such divisions might further our understanding, including prognosis, and even therapy for this condition. Among the clinical phenotypes of (1) chronic fatigue–like syndrome, headache, and memory loss; (2) respiratory syndrome (which includes cough and difficulty breathing); (3) chronic pain; and (4) neurosensorial syndrome (which causes an altered sense of taste and smell), overlap is clearly possible but isn›t addressed.
I see these recent developments as needed and useful progress, but we are still left with…not much. So, when you tell me that you do or do not have long COVID, I will say to you, “How do you know?”
I also say: She/he/they who know COVID know medicine.
A version of this article first appeared on Medscape.com.
Has COVID replaced syphilis as the great imitator? At the turn of the 20th century, Sir William Osler was quoted as saying, “He who knows syphilis knows medicine.”
If you have any doubts about the “imitator” analogy, simply use any broad search engine or AI portal and enter “what is the differential diagnosis of primary syphilis, or secondary syphilis, or tertiary syphilis?” A plethora of diseases across many body systems appears.
Another Great Pretender?
Did you or do you now have long COVID? How do you know? Do you even know what long COVID is? How would you diagnosis it?
When asked about long COVID, this is what large language model source bard.google.com had to say:
Long COVID, also known as post-COVID conditions or PASC, is a complex condition that can occur in people who have had COVID-19, even if their initial illness was mild or even asymptomatic. It’s characterized by a wide range of symptoms that can last for weeks, months, or even years after the initial infection.
Symptoms of long COVID can include: fatigue, shortness of breath, brain fog (trouble thinking or concentrating), loss of smell or taste, sleep problems, muscle pain, joint pain, headache, dizziness, depression or anxiety, heart palpitations, gastrointestinal problems.
Duh!!! It reads much like a continuation of the symptoms of acute COVID. Bard continued:
The exact cause of long COVID is still unknown, but there are several theories. One possibility is that the virus itself can damage organs and tissues, leading to ongoing symptoms. Another possibility is that the immune system’s response to the virus can continue to cause inflammation even after the virus is gone.
Human intelligence source Wikipedia says this:
Long COVID or long-haul COVID is a group of health problems persisting or developing after an initial COVID-19 infection. Symptoms can last weeks, months or years and are often debilitating. The World Health Organization defines long COVID as starting three months after infection, but other definitions put the start of long COVID at four weeks.
Highly varied, including post-exertional malaise (symptoms made worse with effort), fatigue, muscle pain, shortness of breath, chest pain, and cognitive dysfunction (brain fog).
Acute COVID to Long COVID
The World Health Organization estimates that 36 million people in the European region have developed long COVID in the first 3 years of the pandemic. That›s a lot.
We all know that the common signs and symptoms of acute COVID-19 include fever or chills, a dry cough and shortness of breath, feeling very tired, muscle or body aches, headache, loss of taste or smell, sore throat, congestion, runny nose, nausea, vomiting, and diarrhea. Except for the taste and smell findings, every one of these symptoms or signs could indicate a different virus infection or even some type of allergy. My point is the nonspecificity in this list.
Uncommon signs and symptoms of acute COVID include a flat skin rash covered with small bumps, discolored swollen areas on the fingers and toes (COVID toes), and hives. The skin of hands, wrists, or ankles also can be affected. Blisters, itchiness, rough skin, or pus can be seen.
Severe confusion (delirium) might be the main or only symptom of COVID-19 in older people. This COVID-19 symptom is linked with a high risk for poor outcomes, including death. Pink eye (conjunctivitis) can be a COVID-19 symptom. Other eye problems linked to COVID-19 are light sensitivity, sore eyes, and itchy eyes. Acute myocarditis, tinnitus, vertigo, and hearing loss have been reported. And 1-4 weeks after the onset of COVID-19 infection, a patient may experience de novo reactive synovitis and arthritis of any joints.
So, take your pick. Myriad symptoms, signs, diseases, diagnoses, and organ systems — still present, recurring, just appearing, apparently de novo, or after asymptomatic infection. We have so much still to learn.
What big-time symptoms, signs, and major diseases are not on any of these lists? Obviously, cancer, atherosclerotic cardiovascular diseases, obesity, bone diseases, and competitive infections. But be patient; the lingering effects of direct tissue invasion by the virus as well as a wide range of immunologic reactions may just be getting started. Mitochondrial damage, especially in muscles, is increasingly a pathophysiologic suspect.
Human diseases can be physical or mental; and in COVID, that twain not only meet but mix and mingle freely, and may even merge into psychosoma. Don’t ever forget that. Consider “fatigue.” Who among us, COVID or NOVID, does not experience that from time to time?
Or consider brain fog as a common reported symptom of COVID. What on earth is that actually? How can a person know they have brain fog, or whether they had it and are over it?
We need one or more lab or other diagnostic tests that can objectively confirm the diagnosis of long COVID.
Useful Progress?
A recent research paper in Science reported intriguing chemical findings that seemed to point a finger at some form of complement dysregulation as a potential disease marker for long COVID. Unfortunately, some critics have pointed out that this entire study may be invalid or irrelevant because the New York cohort was recruited in 2020, before vaccines were available. The Zurich cohort was recruited up until April 2021, so some may have been vaccinated.
Then this news organization came along in early January 2024 with an article about COVID causing not only more than a million American deaths but also more than 5000 deaths from long COVID. We physicians don’t really know what long COVID even is, but we have to sign death certificates blaming thousands of deaths on it anyway? And rolling back the clock to 2020: Are patients dying from COVID or with COVID, according to death certificates?Now, armed with the knowledge that “documented serious post–COVID-19 conditions include cardiovascular, pulmonary, neurological, renal, endocrine, hematological, and gastrointestinal complications, as well as death,” CDC has published clear and fairly concise instructions on how to address post-acute COVID sequelae on death certificates.
In late January, this news organization painted a hopeful picture by naming four phenotypes of long COVID, suggesting that such divisions might further our understanding, including prognosis, and even therapy for this condition. Among the clinical phenotypes of (1) chronic fatigue–like syndrome, headache, and memory loss; (2) respiratory syndrome (which includes cough and difficulty breathing); (3) chronic pain; and (4) neurosensorial syndrome (which causes an altered sense of taste and smell), overlap is clearly possible but isn›t addressed.
I see these recent developments as needed and useful progress, but we are still left with…not much. So, when you tell me that you do or do not have long COVID, I will say to you, “How do you know?”
I also say: She/he/they who know COVID know medicine.
A version of this article first appeared on Medscape.com.
Has COVID replaced syphilis as the great imitator? At the turn of the 20th century, Sir William Osler was quoted as saying, “He who knows syphilis knows medicine.”
If you have any doubts about the “imitator” analogy, simply use any broad search engine or AI portal and enter “what is the differential diagnosis of primary syphilis, or secondary syphilis, or tertiary syphilis?” A plethora of diseases across many body systems appears.
Another Great Pretender?
Did you or do you now have long COVID? How do you know? Do you even know what long COVID is? How would you diagnosis it?
When asked about long COVID, this is what large language model source bard.google.com had to say:
Long COVID, also known as post-COVID conditions or PASC, is a complex condition that can occur in people who have had COVID-19, even if their initial illness was mild or even asymptomatic. It’s characterized by a wide range of symptoms that can last for weeks, months, or even years after the initial infection.
Symptoms of long COVID can include: fatigue, shortness of breath, brain fog (trouble thinking or concentrating), loss of smell or taste, sleep problems, muscle pain, joint pain, headache, dizziness, depression or anxiety, heart palpitations, gastrointestinal problems.
Duh!!! It reads much like a continuation of the symptoms of acute COVID. Bard continued:
The exact cause of long COVID is still unknown, but there are several theories. One possibility is that the virus itself can damage organs and tissues, leading to ongoing symptoms. Another possibility is that the immune system’s response to the virus can continue to cause inflammation even after the virus is gone.
Human intelligence source Wikipedia says this:
Long COVID or long-haul COVID is a group of health problems persisting or developing after an initial COVID-19 infection. Symptoms can last weeks, months or years and are often debilitating. The World Health Organization defines long COVID as starting three months after infection, but other definitions put the start of long COVID at four weeks.
Highly varied, including post-exertional malaise (symptoms made worse with effort), fatigue, muscle pain, shortness of breath, chest pain, and cognitive dysfunction (brain fog).
Acute COVID to Long COVID
The World Health Organization estimates that 36 million people in the European region have developed long COVID in the first 3 years of the pandemic. That›s a lot.
We all know that the common signs and symptoms of acute COVID-19 include fever or chills, a dry cough and shortness of breath, feeling very tired, muscle or body aches, headache, loss of taste or smell, sore throat, congestion, runny nose, nausea, vomiting, and diarrhea. Except for the taste and smell findings, every one of these symptoms or signs could indicate a different virus infection or even some type of allergy. My point is the nonspecificity in this list.
Uncommon signs and symptoms of acute COVID include a flat skin rash covered with small bumps, discolored swollen areas on the fingers and toes (COVID toes), and hives. The skin of hands, wrists, or ankles also can be affected. Blisters, itchiness, rough skin, or pus can be seen.
Severe confusion (delirium) might be the main or only symptom of COVID-19 in older people. This COVID-19 symptom is linked with a high risk for poor outcomes, including death. Pink eye (conjunctivitis) can be a COVID-19 symptom. Other eye problems linked to COVID-19 are light sensitivity, sore eyes, and itchy eyes. Acute myocarditis, tinnitus, vertigo, and hearing loss have been reported. And 1-4 weeks after the onset of COVID-19 infection, a patient may experience de novo reactive synovitis and arthritis of any joints.
So, take your pick. Myriad symptoms, signs, diseases, diagnoses, and organ systems — still present, recurring, just appearing, apparently de novo, or after asymptomatic infection. We have so much still to learn.
What big-time symptoms, signs, and major diseases are not on any of these lists? Obviously, cancer, atherosclerotic cardiovascular diseases, obesity, bone diseases, and competitive infections. But be patient; the lingering effects of direct tissue invasion by the virus as well as a wide range of immunologic reactions may just be getting started. Mitochondrial damage, especially in muscles, is increasingly a pathophysiologic suspect.
Human diseases can be physical or mental; and in COVID, that twain not only meet but mix and mingle freely, and may even merge into psychosoma. Don’t ever forget that. Consider “fatigue.” Who among us, COVID or NOVID, does not experience that from time to time?
Or consider brain fog as a common reported symptom of COVID. What on earth is that actually? How can a person know they have brain fog, or whether they had it and are over it?
We need one or more lab or other diagnostic tests that can objectively confirm the diagnosis of long COVID.
Useful Progress?
A recent research paper in Science reported intriguing chemical findings that seemed to point a finger at some form of complement dysregulation as a potential disease marker for long COVID. Unfortunately, some critics have pointed out that this entire study may be invalid or irrelevant because the New York cohort was recruited in 2020, before vaccines were available. The Zurich cohort was recruited up until April 2021, so some may have been vaccinated.
Then this news organization came along in early January 2024 with an article about COVID causing not only more than a million American deaths but also more than 5000 deaths from long COVID. We physicians don’t really know what long COVID even is, but we have to sign death certificates blaming thousands of deaths on it anyway? And rolling back the clock to 2020: Are patients dying from COVID or with COVID, according to death certificates?Now, armed with the knowledge that “documented serious post–COVID-19 conditions include cardiovascular, pulmonary, neurological, renal, endocrine, hematological, and gastrointestinal complications, as well as death,” CDC has published clear and fairly concise instructions on how to address post-acute COVID sequelae on death certificates.
In late January, this news organization painted a hopeful picture by naming four phenotypes of long COVID, suggesting that such divisions might further our understanding, including prognosis, and even therapy for this condition. Among the clinical phenotypes of (1) chronic fatigue–like syndrome, headache, and memory loss; (2) respiratory syndrome (which includes cough and difficulty breathing); (3) chronic pain; and (4) neurosensorial syndrome (which causes an altered sense of taste and smell), overlap is clearly possible but isn›t addressed.
I see these recent developments as needed and useful progress, but we are still left with…not much. So, when you tell me that you do or do not have long COVID, I will say to you, “How do you know?”
I also say: She/he/they who know COVID know medicine.
A version of this article first appeared on Medscape.com.
Freedom of Speech and Gender-Affirming Care
Blue Hill is a small idyllic town a little less than two and a half hours Down East the coast from where I am sitting here in Harpswell. Thanks to gentrification it tends to lean left politically, but like the rest of Maine most folks in the surrounding communities often don’t know or care much about their neighbor’s party affiliation. Its library, founded in 1796, is well funded and a source of civic pride.
One day a couple of years ago, the library director received a donated book from a patron. Although he personally didn’t agree with the book’s message, he felt it deserved a space in their collection dealing with the subject. What happened in the wake of this donation is an ugly tale. Some community members objected to the book and asked that it be removed from the shelves, or at least kept under the desk and loaned out only on request.
The objectors, many of whom knew the director, were confrontational. The collections committee unanimously supported his decision. Some committee members also received similar responses from community members. Remember, this is a small town.
A request for support sent to the American Library Association was basically ignored. Over the next 2 years things have quieted, but fractured friendships and relationships in this quiet coastal Maine town have not been repaired. However, as the librarian has observed, “intellectual freedom or the freedom of speech isn’t there just to protect the ideas that we like.”
While the title of the book may feel inflammatory to some, every publisher hopes to grab the market’s attention with a hot title. The cause of this sad situation in Blue Hill was not a white supremacist’s polemic offering specific ways to create genocide. This was a book suggesting that gender dysphoria presenting in adolescence may have multiple causes and raises concerns about the wisdom of the pace of some gender-affirming care.
Clearly the topic of gender dysphoria in adolescence has become a third rail that must be approached with caution or completely avoided. A recent opinion piece in the New York Times provides even more concerning examples of this peril. Again, the eye-catching title of the article — As Kids, They Thought They Were Trans. They No Longer Do — draws in the audience eager to read about some unfortunate individuals who have regretted their decision to transition and are now detransitioning.
If you are interested in hearing anecdotal evidence and opinions supporting the notion that there is such a thing as rapid-onset gender dysphoria, I suggest you read the entire piece. However, the article’s most troubling message for me comes when I read about the professionals who were former gender-related care providers who left the field because of “pushback, the accusations of being transphobic, from being pro-assessment and wanting a more thorough process.”
One therapist trained in gender-affirming care who began to have doubts about the model and spoke out in favor of a more measured approach was investigated by her licensing board after transgender advocates threatened to report her. Ultimately, her case was dismissed, but she continues to fear for her safety.
Gender-related healthcare is another sad example of how in this country it is the noise coming from the advocates on the extremes of the issue that is drowning out the “vast ideological middle” that is seeking civil and rational discussions.
In this situation there are those who want to make it illegal for the healthcare providers to help patients who might benefit from transitioning. On the other end of the spectrum are those advocates who are unwilling to acknowledge that there may be some adolescents with what has been called by some “rapid-onset gender dysphoria.”
The landscape on which this tragedy is being played out is changing so quickly that there will be no correct answers in the short term. There just isn’t enough data. However, there is enough anecdotal evidence from professionals who were and still are practicing gender-related care to raise a concern that something is happening in the adolescent population that suggests some individuals with gender dysphoria should be managed in a different way than the currently accepted gender-affirming model. The size of this subgroup is up for debate and we may never learn it because of reporting bias and privacy concerns.
The American Academy of Pediatrics has recently authorized a systematic review of gender-affirming care. I hope that, like the librarian in Blue Hill, it will have the courage to include all the evidence available even though, as we have seen here in Maine, some of it may spark a firestorm of vehement responses.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Blue Hill is a small idyllic town a little less than two and a half hours Down East the coast from where I am sitting here in Harpswell. Thanks to gentrification it tends to lean left politically, but like the rest of Maine most folks in the surrounding communities often don’t know or care much about their neighbor’s party affiliation. Its library, founded in 1796, is well funded and a source of civic pride.
One day a couple of years ago, the library director received a donated book from a patron. Although he personally didn’t agree with the book’s message, he felt it deserved a space in their collection dealing with the subject. What happened in the wake of this donation is an ugly tale. Some community members objected to the book and asked that it be removed from the shelves, or at least kept under the desk and loaned out only on request.
The objectors, many of whom knew the director, were confrontational. The collections committee unanimously supported his decision. Some committee members also received similar responses from community members. Remember, this is a small town.
A request for support sent to the American Library Association was basically ignored. Over the next 2 years things have quieted, but fractured friendships and relationships in this quiet coastal Maine town have not been repaired. However, as the librarian has observed, “intellectual freedom or the freedom of speech isn’t there just to protect the ideas that we like.”
While the title of the book may feel inflammatory to some, every publisher hopes to grab the market’s attention with a hot title. The cause of this sad situation in Blue Hill was not a white supremacist’s polemic offering specific ways to create genocide. This was a book suggesting that gender dysphoria presenting in adolescence may have multiple causes and raises concerns about the wisdom of the pace of some gender-affirming care.
Clearly the topic of gender dysphoria in adolescence has become a third rail that must be approached with caution or completely avoided. A recent opinion piece in the New York Times provides even more concerning examples of this peril. Again, the eye-catching title of the article — As Kids, They Thought They Were Trans. They No Longer Do — draws in the audience eager to read about some unfortunate individuals who have regretted their decision to transition and are now detransitioning.
If you are interested in hearing anecdotal evidence and opinions supporting the notion that there is such a thing as rapid-onset gender dysphoria, I suggest you read the entire piece. However, the article’s most troubling message for me comes when I read about the professionals who were former gender-related care providers who left the field because of “pushback, the accusations of being transphobic, from being pro-assessment and wanting a more thorough process.”
One therapist trained in gender-affirming care who began to have doubts about the model and spoke out in favor of a more measured approach was investigated by her licensing board after transgender advocates threatened to report her. Ultimately, her case was dismissed, but she continues to fear for her safety.
Gender-related healthcare is another sad example of how in this country it is the noise coming from the advocates on the extremes of the issue that is drowning out the “vast ideological middle” that is seeking civil and rational discussions.
In this situation there are those who want to make it illegal for the healthcare providers to help patients who might benefit from transitioning. On the other end of the spectrum are those advocates who are unwilling to acknowledge that there may be some adolescents with what has been called by some “rapid-onset gender dysphoria.”
The landscape on which this tragedy is being played out is changing so quickly that there will be no correct answers in the short term. There just isn’t enough data. However, there is enough anecdotal evidence from professionals who were and still are practicing gender-related care to raise a concern that something is happening in the adolescent population that suggests some individuals with gender dysphoria should be managed in a different way than the currently accepted gender-affirming model. The size of this subgroup is up for debate and we may never learn it because of reporting bias and privacy concerns.
The American Academy of Pediatrics has recently authorized a systematic review of gender-affirming care. I hope that, like the librarian in Blue Hill, it will have the courage to include all the evidence available even though, as we have seen here in Maine, some of it may spark a firestorm of vehement responses.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Blue Hill is a small idyllic town a little less than two and a half hours Down East the coast from where I am sitting here in Harpswell. Thanks to gentrification it tends to lean left politically, but like the rest of Maine most folks in the surrounding communities often don’t know or care much about their neighbor’s party affiliation. Its library, founded in 1796, is well funded and a source of civic pride.
One day a couple of years ago, the library director received a donated book from a patron. Although he personally didn’t agree with the book’s message, he felt it deserved a space in their collection dealing with the subject. What happened in the wake of this donation is an ugly tale. Some community members objected to the book and asked that it be removed from the shelves, or at least kept under the desk and loaned out only on request.
The objectors, many of whom knew the director, were confrontational. The collections committee unanimously supported his decision. Some committee members also received similar responses from community members. Remember, this is a small town.
A request for support sent to the American Library Association was basically ignored. Over the next 2 years things have quieted, but fractured friendships and relationships in this quiet coastal Maine town have not been repaired. However, as the librarian has observed, “intellectual freedom or the freedom of speech isn’t there just to protect the ideas that we like.”
While the title of the book may feel inflammatory to some, every publisher hopes to grab the market’s attention with a hot title. The cause of this sad situation in Blue Hill was not a white supremacist’s polemic offering specific ways to create genocide. This was a book suggesting that gender dysphoria presenting in adolescence may have multiple causes and raises concerns about the wisdom of the pace of some gender-affirming care.
Clearly the topic of gender dysphoria in adolescence has become a third rail that must be approached with caution or completely avoided. A recent opinion piece in the New York Times provides even more concerning examples of this peril. Again, the eye-catching title of the article — As Kids, They Thought They Were Trans. They No Longer Do — draws in the audience eager to read about some unfortunate individuals who have regretted their decision to transition and are now detransitioning.
If you are interested in hearing anecdotal evidence and opinions supporting the notion that there is such a thing as rapid-onset gender dysphoria, I suggest you read the entire piece. However, the article’s most troubling message for me comes when I read about the professionals who were former gender-related care providers who left the field because of “pushback, the accusations of being transphobic, from being pro-assessment and wanting a more thorough process.”
One therapist trained in gender-affirming care who began to have doubts about the model and spoke out in favor of a more measured approach was investigated by her licensing board after transgender advocates threatened to report her. Ultimately, her case was dismissed, but she continues to fear for her safety.
Gender-related healthcare is another sad example of how in this country it is the noise coming from the advocates on the extremes of the issue that is drowning out the “vast ideological middle” that is seeking civil and rational discussions.
In this situation there are those who want to make it illegal for the healthcare providers to help patients who might benefit from transitioning. On the other end of the spectrum are those advocates who are unwilling to acknowledge that there may be some adolescents with what has been called by some “rapid-onset gender dysphoria.”
The landscape on which this tragedy is being played out is changing so quickly that there will be no correct answers in the short term. There just isn’t enough data. However, there is enough anecdotal evidence from professionals who were and still are practicing gender-related care to raise a concern that something is happening in the adolescent population that suggests some individuals with gender dysphoria should be managed in a different way than the currently accepted gender-affirming model. The size of this subgroup is up for debate and we may never learn it because of reporting bias and privacy concerns.
The American Academy of Pediatrics has recently authorized a systematic review of gender-affirming care. I hope that, like the librarian in Blue Hill, it will have the courage to include all the evidence available even though, as we have seen here in Maine, some of it may spark a firestorm of vehement responses.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
How to Avoid the $400,000 Med School Debt Mistakes I Made
It’s not always great to be tops among your peers.
, according to Medscape Medical News’ 2023 Residents Salary and Debt Report.
I’m smack in that upper percentile. I amassed nearly a half million dollars in student debt and currently stand at roughly $400,000. Yay me.
As a naive twentysomething making a major life decision, I never thought my loans would amount to this inconceivable figure, the proverbial “mortgage without a roof” you hear student debt experts talk about.
This isn’t a story about how the student loan industry needs to be reformed or how education has become increasingly expensive or regrets about going to medical school.
It’s also not a story about how you should be handling basics like consolidating and refinancing and paying extra toward your principal.
It’s about my experience as a physician 13 years after signing that first promissory note. In short: I completely miscalculated the impact loans would have on my life.
I bought money to go to school. I can’t undo that. But over the past decade, I have learned a lot, particularly how those with their own mountain of debt — or who will inevitably wind up with one — can manage things better than I have.
Mistake #1: Loan Forgiveness Is More Complicated Than it Seems
My parents and I were aware of the Public Service Loan Forgiveness (PSLF) program which began in 2007 shortly before I started exploring medical school options. I wanted to help people, so working in the nonprofit sector sounded like a no-brainer. Making 120 payments while practicing at a qualifying institution didn’t sound hard.
Newsflash: Not all healthcare organizations are 501(c)3 programs that qualify as nonprofit for the PSLF program. You can’t just snap your fingers and land at one. I graduated from fellowship just as the COVID-19 pandemic began, which meant I was launching my medical career in the midst of hiring freezes and an overnight disappearance of job opportunities.
I had to take a 2-year hiatus from the nonprofit sector and found a part-time position with a local private practice group. It still stings. Had I been working for a qualified employer, I could have benefited from the student loan payment pause and been closer to applying for loan forgiveness.
Avoid it: Be brutally honest with yourself about what kind of medicine you want to practice — especially within the opportunities you have on hand. Private practice is very different from working for the nonprofit sector. I didn›t know that. When weighing career choices, immediately ask, “How will this impact how I pay my loans?” You may not like the answer, but you›ll always know where you stand financially.
Mistake #2: I Forgot to Factor in Life Goals
To be fair, some things were out of my control: Not getting into a state school with cheaper tuition rates, graduating at the start of a once-in-a-lifetime global pandemic. I wasn’t prepared for a changing job landscape. But there were also “expected” life events like getting married, developing a geographical preference, and having a child. I didn’t consider those either.
How about the “expected” goal of buying a home? For years I didn’t feel financially comfortable enough to take on a mortgage. For so long, my attitude has been don’t take on any more debt. (A special shout-out to my 6.8% interest rate which has contributed over a third of my total loan amount.)
This even affected how my husband and I would talk about what a future home might look like. There’s always a giant unwelcome guest casting a shadow over my thoughts.
Avoid it: Don’t compartmentalize your personal and professional lives. Your student loans will hang over both, and you need to be honest with yourself about what “upward mobility” really means to you while in debt. There’s a reason people say “live like a resident” until your loans are paid off. My husband and I finally worked our numbers to where we bought our first home this past year — a moment years in the making. I still drive around in my beloved Honda CR-V like it’s a Mercedes G-Wagon.
Mistake #3: I Didn’t Ask Questions
I regret not talking to a practicing physician about their experience with student loans. I didn’t know any. There weren’t any physicians in my extended family or my community network. I was a first-generation Pakistani American kid trying to figure it out.
It’s difficult because even today, many physicians aren’t comfortable discussing their financial circumstances. The lack of financial transparency and even financial literacy is astounding among young medical professionals. We live in a medical culture where no one talks about the money. I was too diffident and nervous to even try.
Avoid it: Don’t be afraid to have uncomfortable conversations about money. Don’t allow yourself to make even one passive decision. It’s your life.
If you can’t find someone in medicine to talk to about their financial journey, there are plenty of credible resources. Medscape Medical News has a Physician Business Academy with hot topics like personal finance. The White Coat Investor is literally bookmarked on all my electronic devices. KevinMD.com has a ton of resources and articles answering common financial questions about retirement, savings, and house buying. And Travis Hornsby with www.studentloanplanner.com has wonderful advice on all kinds of different loans.
There are no stupid questions. Just ask. You might be surprised by what people are willing to share.
Mistake #4: Playing it Casual With My Lenders
If $400,000 in debt doesn’t sound bad enough, imagine lots more. It turns out my loan carrier had me at a much higher loan balance because they’d inadvertently duplicated one of my loans in the total. I didn’t know that until I transferred my loans to another handler and it came to light.
Imagine my relief at having a lower total. Imagine my anger at myself for not checking sooner.
Avoid it: Do a thorough self-audit on all your loans more than once a year. Pretend they’re a patient with odd symptoms you can’t pin down and you have the luxury of doing every diagnostic test available. It’s not fun studying your own debt, but it’s the only way to really know how much you have.
Mistake #5: Not Leaving Room to Change My Mind
I underestimated how I would evolve and how my goals would change after having the letters “MD” after my name. I never dreamed that a nonprofit salary might not be enough.
A lot of us assume that the bedside is where we will find professional satisfaction. But you might be surprised. In a climate where we’re constantly being pushed to do more in a broken healthcare system, a landscape where misinformation and technology are forcing medicine to change, there might be little joy in working clinically full time. Then what do you do?
Because I elected to go the PSLF route, I’m tied to this decision. And while it still makes the most economic sense for me personally, it now limits my professional exploration and freedom.
Avoid it: Consider how much time you really want to spend in clinical medicine. Be mindful that you have to work at least 0.8 full time equivalent to qualify for the PSLF program. It’s very hard to predict the future, let alone your future, but just know you›ll have moments where you ask, “Do I really want to stay on this career track?” Will you be able to pivot? Can you live with it if the answer is no?
Looking Ahead
Let me be clear about one thing. Despite all the negativity I feel toward my student loans — guilt about the burden I brought to my marriage and my adult life, disappointment about the cost of becoming a successful physician, and frustration that this has turned out to be the most influential factor shaping my professional and personal choices — the one thing I don’t feel is shame.
I worked hard to get to this point in my life. I am proud of being a physician.
My student loan burden will follow me to the grave. But progress is also possible. I have friends that have paid their loans down by hustling, working hard, and dropping every penny toward them.
I also have friends that have had their loans forgiven. There are options. Everyone’s experience looks a little different. But don’t be naive: Student loans will color every financial decision you make.
I’m finding solace now in recently moving and finding work at a nonprofit institution. I’m back at it; 77 payments made, and 43 to go.
Well, technically I’ve made 93 payments. I’m still waiting for my loan servicer to get around to updating my account.
You really have to stay on top of those folks.
A version of this article appeared on Medscape.com.
It’s not always great to be tops among your peers.
, according to Medscape Medical News’ 2023 Residents Salary and Debt Report.
I’m smack in that upper percentile. I amassed nearly a half million dollars in student debt and currently stand at roughly $400,000. Yay me.
As a naive twentysomething making a major life decision, I never thought my loans would amount to this inconceivable figure, the proverbial “mortgage without a roof” you hear student debt experts talk about.
This isn’t a story about how the student loan industry needs to be reformed or how education has become increasingly expensive or regrets about going to medical school.
It’s also not a story about how you should be handling basics like consolidating and refinancing and paying extra toward your principal.
It’s about my experience as a physician 13 years after signing that first promissory note. In short: I completely miscalculated the impact loans would have on my life.
I bought money to go to school. I can’t undo that. But over the past decade, I have learned a lot, particularly how those with their own mountain of debt — or who will inevitably wind up with one — can manage things better than I have.
Mistake #1: Loan Forgiveness Is More Complicated Than it Seems
My parents and I were aware of the Public Service Loan Forgiveness (PSLF) program which began in 2007 shortly before I started exploring medical school options. I wanted to help people, so working in the nonprofit sector sounded like a no-brainer. Making 120 payments while practicing at a qualifying institution didn’t sound hard.
Newsflash: Not all healthcare organizations are 501(c)3 programs that qualify as nonprofit for the PSLF program. You can’t just snap your fingers and land at one. I graduated from fellowship just as the COVID-19 pandemic began, which meant I was launching my medical career in the midst of hiring freezes and an overnight disappearance of job opportunities.
I had to take a 2-year hiatus from the nonprofit sector and found a part-time position with a local private practice group. It still stings. Had I been working for a qualified employer, I could have benefited from the student loan payment pause and been closer to applying for loan forgiveness.
Avoid it: Be brutally honest with yourself about what kind of medicine you want to practice — especially within the opportunities you have on hand. Private practice is very different from working for the nonprofit sector. I didn›t know that. When weighing career choices, immediately ask, “How will this impact how I pay my loans?” You may not like the answer, but you›ll always know where you stand financially.
Mistake #2: I Forgot to Factor in Life Goals
To be fair, some things were out of my control: Not getting into a state school with cheaper tuition rates, graduating at the start of a once-in-a-lifetime global pandemic. I wasn’t prepared for a changing job landscape. But there were also “expected” life events like getting married, developing a geographical preference, and having a child. I didn’t consider those either.
How about the “expected” goal of buying a home? For years I didn’t feel financially comfortable enough to take on a mortgage. For so long, my attitude has been don’t take on any more debt. (A special shout-out to my 6.8% interest rate which has contributed over a third of my total loan amount.)
This even affected how my husband and I would talk about what a future home might look like. There’s always a giant unwelcome guest casting a shadow over my thoughts.
Avoid it: Don’t compartmentalize your personal and professional lives. Your student loans will hang over both, and you need to be honest with yourself about what “upward mobility” really means to you while in debt. There’s a reason people say “live like a resident” until your loans are paid off. My husband and I finally worked our numbers to where we bought our first home this past year — a moment years in the making. I still drive around in my beloved Honda CR-V like it’s a Mercedes G-Wagon.
Mistake #3: I Didn’t Ask Questions
I regret not talking to a practicing physician about their experience with student loans. I didn’t know any. There weren’t any physicians in my extended family or my community network. I was a first-generation Pakistani American kid trying to figure it out.
It’s difficult because even today, many physicians aren’t comfortable discussing their financial circumstances. The lack of financial transparency and even financial literacy is astounding among young medical professionals. We live in a medical culture where no one talks about the money. I was too diffident and nervous to even try.
Avoid it: Don’t be afraid to have uncomfortable conversations about money. Don’t allow yourself to make even one passive decision. It’s your life.
If you can’t find someone in medicine to talk to about their financial journey, there are plenty of credible resources. Medscape Medical News has a Physician Business Academy with hot topics like personal finance. The White Coat Investor is literally bookmarked on all my electronic devices. KevinMD.com has a ton of resources and articles answering common financial questions about retirement, savings, and house buying. And Travis Hornsby with www.studentloanplanner.com has wonderful advice on all kinds of different loans.
There are no stupid questions. Just ask. You might be surprised by what people are willing to share.
Mistake #4: Playing it Casual With My Lenders
If $400,000 in debt doesn’t sound bad enough, imagine lots more. It turns out my loan carrier had me at a much higher loan balance because they’d inadvertently duplicated one of my loans in the total. I didn’t know that until I transferred my loans to another handler and it came to light.
Imagine my relief at having a lower total. Imagine my anger at myself for not checking sooner.
Avoid it: Do a thorough self-audit on all your loans more than once a year. Pretend they’re a patient with odd symptoms you can’t pin down and you have the luxury of doing every diagnostic test available. It’s not fun studying your own debt, but it’s the only way to really know how much you have.
Mistake #5: Not Leaving Room to Change My Mind
I underestimated how I would evolve and how my goals would change after having the letters “MD” after my name. I never dreamed that a nonprofit salary might not be enough.
A lot of us assume that the bedside is where we will find professional satisfaction. But you might be surprised. In a climate where we’re constantly being pushed to do more in a broken healthcare system, a landscape where misinformation and technology are forcing medicine to change, there might be little joy in working clinically full time. Then what do you do?
Because I elected to go the PSLF route, I’m tied to this decision. And while it still makes the most economic sense for me personally, it now limits my professional exploration and freedom.
Avoid it: Consider how much time you really want to spend in clinical medicine. Be mindful that you have to work at least 0.8 full time equivalent to qualify for the PSLF program. It’s very hard to predict the future, let alone your future, but just know you›ll have moments where you ask, “Do I really want to stay on this career track?” Will you be able to pivot? Can you live with it if the answer is no?
Looking Ahead
Let me be clear about one thing. Despite all the negativity I feel toward my student loans — guilt about the burden I brought to my marriage and my adult life, disappointment about the cost of becoming a successful physician, and frustration that this has turned out to be the most influential factor shaping my professional and personal choices — the one thing I don’t feel is shame.
I worked hard to get to this point in my life. I am proud of being a physician.
My student loan burden will follow me to the grave. But progress is also possible. I have friends that have paid their loans down by hustling, working hard, and dropping every penny toward them.
I also have friends that have had their loans forgiven. There are options. Everyone’s experience looks a little different. But don’t be naive: Student loans will color every financial decision you make.
I’m finding solace now in recently moving and finding work at a nonprofit institution. I’m back at it; 77 payments made, and 43 to go.
Well, technically I’ve made 93 payments. I’m still waiting for my loan servicer to get around to updating my account.
You really have to stay on top of those folks.
A version of this article appeared on Medscape.com.
It’s not always great to be tops among your peers.
, according to Medscape Medical News’ 2023 Residents Salary and Debt Report.
I’m smack in that upper percentile. I amassed nearly a half million dollars in student debt and currently stand at roughly $400,000. Yay me.
As a naive twentysomething making a major life decision, I never thought my loans would amount to this inconceivable figure, the proverbial “mortgage without a roof” you hear student debt experts talk about.
This isn’t a story about how the student loan industry needs to be reformed or how education has become increasingly expensive or regrets about going to medical school.
It’s also not a story about how you should be handling basics like consolidating and refinancing and paying extra toward your principal.
It’s about my experience as a physician 13 years after signing that first promissory note. In short: I completely miscalculated the impact loans would have on my life.
I bought money to go to school. I can’t undo that. But over the past decade, I have learned a lot, particularly how those with their own mountain of debt — or who will inevitably wind up with one — can manage things better than I have.
Mistake #1: Loan Forgiveness Is More Complicated Than it Seems
My parents and I were aware of the Public Service Loan Forgiveness (PSLF) program which began in 2007 shortly before I started exploring medical school options. I wanted to help people, so working in the nonprofit sector sounded like a no-brainer. Making 120 payments while practicing at a qualifying institution didn’t sound hard.
Newsflash: Not all healthcare organizations are 501(c)3 programs that qualify as nonprofit for the PSLF program. You can’t just snap your fingers and land at one. I graduated from fellowship just as the COVID-19 pandemic began, which meant I was launching my medical career in the midst of hiring freezes and an overnight disappearance of job opportunities.
I had to take a 2-year hiatus from the nonprofit sector and found a part-time position with a local private practice group. It still stings. Had I been working for a qualified employer, I could have benefited from the student loan payment pause and been closer to applying for loan forgiveness.
Avoid it: Be brutally honest with yourself about what kind of medicine you want to practice — especially within the opportunities you have on hand. Private practice is very different from working for the nonprofit sector. I didn›t know that. When weighing career choices, immediately ask, “How will this impact how I pay my loans?” You may not like the answer, but you›ll always know where you stand financially.
Mistake #2: I Forgot to Factor in Life Goals
To be fair, some things were out of my control: Not getting into a state school with cheaper tuition rates, graduating at the start of a once-in-a-lifetime global pandemic. I wasn’t prepared for a changing job landscape. But there were also “expected” life events like getting married, developing a geographical preference, and having a child. I didn’t consider those either.
How about the “expected” goal of buying a home? For years I didn’t feel financially comfortable enough to take on a mortgage. For so long, my attitude has been don’t take on any more debt. (A special shout-out to my 6.8% interest rate which has contributed over a third of my total loan amount.)
This even affected how my husband and I would talk about what a future home might look like. There’s always a giant unwelcome guest casting a shadow over my thoughts.
Avoid it: Don’t compartmentalize your personal and professional lives. Your student loans will hang over both, and you need to be honest with yourself about what “upward mobility” really means to you while in debt. There’s a reason people say “live like a resident” until your loans are paid off. My husband and I finally worked our numbers to where we bought our first home this past year — a moment years in the making. I still drive around in my beloved Honda CR-V like it’s a Mercedes G-Wagon.
Mistake #3: I Didn’t Ask Questions
I regret not talking to a practicing physician about their experience with student loans. I didn’t know any. There weren’t any physicians in my extended family or my community network. I was a first-generation Pakistani American kid trying to figure it out.
It’s difficult because even today, many physicians aren’t comfortable discussing their financial circumstances. The lack of financial transparency and even financial literacy is astounding among young medical professionals. We live in a medical culture where no one talks about the money. I was too diffident and nervous to even try.
Avoid it: Don’t be afraid to have uncomfortable conversations about money. Don’t allow yourself to make even one passive decision. It’s your life.
If you can’t find someone in medicine to talk to about their financial journey, there are plenty of credible resources. Medscape Medical News has a Physician Business Academy with hot topics like personal finance. The White Coat Investor is literally bookmarked on all my electronic devices. KevinMD.com has a ton of resources and articles answering common financial questions about retirement, savings, and house buying. And Travis Hornsby with www.studentloanplanner.com has wonderful advice on all kinds of different loans.
There are no stupid questions. Just ask. You might be surprised by what people are willing to share.
Mistake #4: Playing it Casual With My Lenders
If $400,000 in debt doesn’t sound bad enough, imagine lots more. It turns out my loan carrier had me at a much higher loan balance because they’d inadvertently duplicated one of my loans in the total. I didn’t know that until I transferred my loans to another handler and it came to light.
Imagine my relief at having a lower total. Imagine my anger at myself for not checking sooner.
Avoid it: Do a thorough self-audit on all your loans more than once a year. Pretend they’re a patient with odd symptoms you can’t pin down and you have the luxury of doing every diagnostic test available. It’s not fun studying your own debt, but it’s the only way to really know how much you have.
Mistake #5: Not Leaving Room to Change My Mind
I underestimated how I would evolve and how my goals would change after having the letters “MD” after my name. I never dreamed that a nonprofit salary might not be enough.
A lot of us assume that the bedside is where we will find professional satisfaction. But you might be surprised. In a climate where we’re constantly being pushed to do more in a broken healthcare system, a landscape where misinformation and technology are forcing medicine to change, there might be little joy in working clinically full time. Then what do you do?
Because I elected to go the PSLF route, I’m tied to this decision. And while it still makes the most economic sense for me personally, it now limits my professional exploration and freedom.
Avoid it: Consider how much time you really want to spend in clinical medicine. Be mindful that you have to work at least 0.8 full time equivalent to qualify for the PSLF program. It’s very hard to predict the future, let alone your future, but just know you›ll have moments where you ask, “Do I really want to stay on this career track?” Will you be able to pivot? Can you live with it if the answer is no?
Looking Ahead
Let me be clear about one thing. Despite all the negativity I feel toward my student loans — guilt about the burden I brought to my marriage and my adult life, disappointment about the cost of becoming a successful physician, and frustration that this has turned out to be the most influential factor shaping my professional and personal choices — the one thing I don’t feel is shame.
I worked hard to get to this point in my life. I am proud of being a physician.
My student loan burden will follow me to the grave. But progress is also possible. I have friends that have paid their loans down by hustling, working hard, and dropping every penny toward them.
I also have friends that have had their loans forgiven. There are options. Everyone’s experience looks a little different. But don’t be naive: Student loans will color every financial decision you make.
I’m finding solace now in recently moving and finding work at a nonprofit institution. I’m back at it; 77 payments made, and 43 to go.
Well, technically I’ve made 93 payments. I’m still waiting for my loan servicer to get around to updating my account.
You really have to stay on top of those folks.
A version of this article appeared on Medscape.com.
‘It’s Time’ to Empower Care for Patients With Obesity
A few weeks ago, I made a patient who lost 100 pounds following a sleeve gastrectomy 9 months prior feel bad because I told her she lost too much weight. As I spoke to her, I realized that she found it hard to make life changes and that the surgery was a huge aide in changing her life and her lifestyle. I ended up apologizing for initially saying she lost too much weight.
For the first time in her life, she was successful in losing weight and keeping it off. The surgery allowed her body to defend a lower body weight by altering the secretion of gut hormones that lead to satiety in the brain. It’s not her fault that her body responded so well!
I asked her to be on my next orientation virtual meeting with prospective weight management patients to urge those with a body mass index (BMI) > 40 to consider bariatric surgery as the most effective durable and safe treatment for their degree of obesity.
Metabolic bariatric surgery, primarily sleeve gastrectomy and Roux-en-Y gastric bypass , alters the gut hormone milieu such that the body defends a lower mass of adipose tissue and a lower weight. We have learned what it takes to alter body weight defense to a healthy lower weight by studying why metabolic bariatric surgery works so well. It turns out that there are several hormones secreted by the gut that allow the brain to register fullness.
One of these gut hormones, glucagon-like peptide (GLP)-1, has been researched as an analog to help reduce body weight by 16% and has also been shown to reduce cardiovascular risk in the SELECT trial, as published in The New England Journal of Medicine (NEJM).
It’s the first weight loss medication to be shown in a cardiovascular outcomes trial to be superior to placebo in reduction of major cardiovascular events, including cardiovascular deaths, nonfatal myocardial infarction, and nonfatal stroke. The results presented at the 2023 American Heart Association meetings in Philadelphia ended in wholehearted applause by a “standing only” audience even before the presentation’s conclusion.
As we pave the way for nutrient-stimulated hormone (NuSH) therapies to be prescribed to all Americans with a BMI > 30 to improve health, we need to remember what these medications actually do. We used to think that metabolic bariatric surgery worked by restricting the stomach contents and malabsorbing nutrients. We now know that the surgeries work by altering NuSH secretion, allowing for less secretion of the hunger hormone ghrelin and more secretion of GLP-1, glucose-dependent insulinotropic polypeptide (GIP), peptide YY (PYY), cholecystokinin (CCK), oxyntomodulin (OXM), and other satiety hormones with less food ingestion.
They have pleiotropic effects on many organ systems in the body, including the brain, heart, adipose tissue, and liver. They decrease inflammation and also increase satiety and delay gastric emptying. None of these effects automatically produce weight loss, but they certainly aid in the adoption of a healthier body weight and better health. The weight loss occurs because these medications steer the body toward behavioral changes that promote weight loss.
As we delve into the SELECT trial results, a 20% reduction in major cardiovascular events was accompanied by an average weight loss of 9.6%, without a behavioral component added to either the placebo or intervention arms, as is usual in antiobesity agent trials.
Does this mean that primary care providers (PCPs) don’t have to educate patients on behavior change, diet, and exercise therapy? Well, if we consider obesity a disease as we do type 2 diabetes and dyslipidemia or hypertension, then no — PCPs don’t have to, just like they don’t in treating these other diseases.
However, we should rethink this practice. The recently published SURMOUNT-3 trial looked at another NuSH, tirzepatide, with intensive behavioral therapy; it resulted in a 26.6% weight loss, which is comparable to results with bariatric surgery. The SURMOUNT-1 trial of tirzepatide with nonintensive behavioral therapy resulted in a 20.9% weight loss, which is still substantial, but SURMOUNT-3 showed how much more is achievable with robust behavior-change therapy.
In other words, it’s time that PCPs provide education on behavior change to maximize the power of the medications prescribed in practice for the most common diseases suffered in the United States: obesity, type 2 diabetes, cardiovascular disease, and hypertension. These are all chronic, relapsing diseases. Medication alone will improve numbers (weight, blood glucose, A1c, and blood pressure), but a relapsing disease continues relentlessly as patients age to overcome the medications prescribed.
Today I made another patient feel bad because she lost over 100 pounds on semaglutide (Wegovy) 2.4 mg over 1 year, reducing her BMI from 57 to 36. She wanted to keep losing, so I recommended sleeve gastrectomy to lose more weight. I told her she could always restart the Wegovy after the procedure if needed.
We really don’t have an answer to this issue of NuSH therapy not getting to goal and bariatric surgery following medication therapy. The reality is that bariatric surgery should be considered a safe, effective treatment for extreme obesity somewhere along the trajectory of treatments starting with behavior (diet, exercise) and medications. It is still considered a last resort, and for some, just too aggressive.
We have learned much about the incretin hormones and what they can accomplish for obesity from studying bariatric — now called metabolic — surgery. Surgery should be seen as we see stent placement for angina, only more effective for longevity. The COURAGE trial, published in 2007 in NEJM, showed that when compared with medication treatment alone for angina, stent placement plus medications resulted in no difference in mortality after a 7-year follow-up period. Compare this to bariatric surgery, which in many retrospective analyses shows a 20% reduction in cardiovascular mortality after 20-year follow-up (Swedish Obesity Study). In the United States, there are 2 million stent procedures performed per year vs 250,000 bariatric surgical procedures. There are millions of Americans with a BMI > 40 and, yes, millions of Americans with angina. I think I make my point that we need to do more bariatric surgeries to effectively treat extreme obesity.
The solution to this negligent medical practice in obesity treatment is to empower PCPs to treat obesity (at least uncomplicated obesity) and refer to obesity medicine practices for complicated obesity with multiple complications, such as type 2 diabetes and cardiovascular disease, and to refer to obesity medicine practices with a surgical component for BMIs > 40 or > 35 with type 2 diabetes, sleep apnea, and/or cardiovascular disease or other serious conditions.
How do we empower PCPs? Insurance coverage of NuSH therapies due to life-saving properties — as evidenced by the SELECT trial — without prior authorizations; and education on how and why metabolic surgery works, as well as education on behavioral approaches, such as healthy diet and exercise, as a core therapy for all BMI categories.
It’s time.
Caroline Apovian, MD, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, adviser, consultant, or trustee for Altimmune; Cowen and Company; Currax Pharmaceuticals; EPG Communication Holdings; Gelesis, Srl; L-Nutra; and NeuroBo Pharmaceuticals. Received research grant from: National Institutes of Health; Patient-Centered Outcomes Research Institute; and GI Dynamics. Received income in an amount equal to or greater than $250 from: Altimmune; Cowen and Company; NeuroBo Pharmaceuticals; and Novo Nordisk.
A version of this article appeared on Medscape.com.
A few weeks ago, I made a patient who lost 100 pounds following a sleeve gastrectomy 9 months prior feel bad because I told her she lost too much weight. As I spoke to her, I realized that she found it hard to make life changes and that the surgery was a huge aide in changing her life and her lifestyle. I ended up apologizing for initially saying she lost too much weight.
For the first time in her life, she was successful in losing weight and keeping it off. The surgery allowed her body to defend a lower body weight by altering the secretion of gut hormones that lead to satiety in the brain. It’s not her fault that her body responded so well!
I asked her to be on my next orientation virtual meeting with prospective weight management patients to urge those with a body mass index (BMI) > 40 to consider bariatric surgery as the most effective durable and safe treatment for their degree of obesity.
Metabolic bariatric surgery, primarily sleeve gastrectomy and Roux-en-Y gastric bypass , alters the gut hormone milieu such that the body defends a lower mass of adipose tissue and a lower weight. We have learned what it takes to alter body weight defense to a healthy lower weight by studying why metabolic bariatric surgery works so well. It turns out that there are several hormones secreted by the gut that allow the brain to register fullness.
One of these gut hormones, glucagon-like peptide (GLP)-1, has been researched as an analog to help reduce body weight by 16% and has also been shown to reduce cardiovascular risk in the SELECT trial, as published in The New England Journal of Medicine (NEJM).
It’s the first weight loss medication to be shown in a cardiovascular outcomes trial to be superior to placebo in reduction of major cardiovascular events, including cardiovascular deaths, nonfatal myocardial infarction, and nonfatal stroke. The results presented at the 2023 American Heart Association meetings in Philadelphia ended in wholehearted applause by a “standing only” audience even before the presentation’s conclusion.
As we pave the way for nutrient-stimulated hormone (NuSH) therapies to be prescribed to all Americans with a BMI > 30 to improve health, we need to remember what these medications actually do. We used to think that metabolic bariatric surgery worked by restricting the stomach contents and malabsorbing nutrients. We now know that the surgeries work by altering NuSH secretion, allowing for less secretion of the hunger hormone ghrelin and more secretion of GLP-1, glucose-dependent insulinotropic polypeptide (GIP), peptide YY (PYY), cholecystokinin (CCK), oxyntomodulin (OXM), and other satiety hormones with less food ingestion.
They have pleiotropic effects on many organ systems in the body, including the brain, heart, adipose tissue, and liver. They decrease inflammation and also increase satiety and delay gastric emptying. None of these effects automatically produce weight loss, but they certainly aid in the adoption of a healthier body weight and better health. The weight loss occurs because these medications steer the body toward behavioral changes that promote weight loss.
As we delve into the SELECT trial results, a 20% reduction in major cardiovascular events was accompanied by an average weight loss of 9.6%, without a behavioral component added to either the placebo or intervention arms, as is usual in antiobesity agent trials.
Does this mean that primary care providers (PCPs) don’t have to educate patients on behavior change, diet, and exercise therapy? Well, if we consider obesity a disease as we do type 2 diabetes and dyslipidemia or hypertension, then no — PCPs don’t have to, just like they don’t in treating these other diseases.
However, we should rethink this practice. The recently published SURMOUNT-3 trial looked at another NuSH, tirzepatide, with intensive behavioral therapy; it resulted in a 26.6% weight loss, which is comparable to results with bariatric surgery. The SURMOUNT-1 trial of tirzepatide with nonintensive behavioral therapy resulted in a 20.9% weight loss, which is still substantial, but SURMOUNT-3 showed how much more is achievable with robust behavior-change therapy.
In other words, it’s time that PCPs provide education on behavior change to maximize the power of the medications prescribed in practice for the most common diseases suffered in the United States: obesity, type 2 diabetes, cardiovascular disease, and hypertension. These are all chronic, relapsing diseases. Medication alone will improve numbers (weight, blood glucose, A1c, and blood pressure), but a relapsing disease continues relentlessly as patients age to overcome the medications prescribed.
Today I made another patient feel bad because she lost over 100 pounds on semaglutide (Wegovy) 2.4 mg over 1 year, reducing her BMI from 57 to 36. She wanted to keep losing, so I recommended sleeve gastrectomy to lose more weight. I told her she could always restart the Wegovy after the procedure if needed.
We really don’t have an answer to this issue of NuSH therapy not getting to goal and bariatric surgery following medication therapy. The reality is that bariatric surgery should be considered a safe, effective treatment for extreme obesity somewhere along the trajectory of treatments starting with behavior (diet, exercise) and medications. It is still considered a last resort, and for some, just too aggressive.
We have learned much about the incretin hormones and what they can accomplish for obesity from studying bariatric — now called metabolic — surgery. Surgery should be seen as we see stent placement for angina, only more effective for longevity. The COURAGE trial, published in 2007 in NEJM, showed that when compared with medication treatment alone for angina, stent placement plus medications resulted in no difference in mortality after a 7-year follow-up period. Compare this to bariatric surgery, which in many retrospective analyses shows a 20% reduction in cardiovascular mortality after 20-year follow-up (Swedish Obesity Study). In the United States, there are 2 million stent procedures performed per year vs 250,000 bariatric surgical procedures. There are millions of Americans with a BMI > 40 and, yes, millions of Americans with angina. I think I make my point that we need to do more bariatric surgeries to effectively treat extreme obesity.
The solution to this negligent medical practice in obesity treatment is to empower PCPs to treat obesity (at least uncomplicated obesity) and refer to obesity medicine practices for complicated obesity with multiple complications, such as type 2 diabetes and cardiovascular disease, and to refer to obesity medicine practices with a surgical component for BMIs > 40 or > 35 with type 2 diabetes, sleep apnea, and/or cardiovascular disease or other serious conditions.
How do we empower PCPs? Insurance coverage of NuSH therapies due to life-saving properties — as evidenced by the SELECT trial — without prior authorizations; and education on how and why metabolic surgery works, as well as education on behavioral approaches, such as healthy diet and exercise, as a core therapy for all BMI categories.
It’s time.
Caroline Apovian, MD, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, adviser, consultant, or trustee for Altimmune; Cowen and Company; Currax Pharmaceuticals; EPG Communication Holdings; Gelesis, Srl; L-Nutra; and NeuroBo Pharmaceuticals. Received research grant from: National Institutes of Health; Patient-Centered Outcomes Research Institute; and GI Dynamics. Received income in an amount equal to or greater than $250 from: Altimmune; Cowen and Company; NeuroBo Pharmaceuticals; and Novo Nordisk.
A version of this article appeared on Medscape.com.
A few weeks ago, I made a patient who lost 100 pounds following a sleeve gastrectomy 9 months prior feel bad because I told her she lost too much weight. As I spoke to her, I realized that she found it hard to make life changes and that the surgery was a huge aide in changing her life and her lifestyle. I ended up apologizing for initially saying she lost too much weight.
For the first time in her life, she was successful in losing weight and keeping it off. The surgery allowed her body to defend a lower body weight by altering the secretion of gut hormones that lead to satiety in the brain. It’s not her fault that her body responded so well!
I asked her to be on my next orientation virtual meeting with prospective weight management patients to urge those with a body mass index (BMI) > 40 to consider bariatric surgery as the most effective durable and safe treatment for their degree of obesity.
Metabolic bariatric surgery, primarily sleeve gastrectomy and Roux-en-Y gastric bypass , alters the gut hormone milieu such that the body defends a lower mass of adipose tissue and a lower weight. We have learned what it takes to alter body weight defense to a healthy lower weight by studying why metabolic bariatric surgery works so well. It turns out that there are several hormones secreted by the gut that allow the brain to register fullness.
One of these gut hormones, glucagon-like peptide (GLP)-1, has been researched as an analog to help reduce body weight by 16% and has also been shown to reduce cardiovascular risk in the SELECT trial, as published in The New England Journal of Medicine (NEJM).
It’s the first weight loss medication to be shown in a cardiovascular outcomes trial to be superior to placebo in reduction of major cardiovascular events, including cardiovascular deaths, nonfatal myocardial infarction, and nonfatal stroke. The results presented at the 2023 American Heart Association meetings in Philadelphia ended in wholehearted applause by a “standing only” audience even before the presentation’s conclusion.
As we pave the way for nutrient-stimulated hormone (NuSH) therapies to be prescribed to all Americans with a BMI > 30 to improve health, we need to remember what these medications actually do. We used to think that metabolic bariatric surgery worked by restricting the stomach contents and malabsorbing nutrients. We now know that the surgeries work by altering NuSH secretion, allowing for less secretion of the hunger hormone ghrelin and more secretion of GLP-1, glucose-dependent insulinotropic polypeptide (GIP), peptide YY (PYY), cholecystokinin (CCK), oxyntomodulin (OXM), and other satiety hormones with less food ingestion.
They have pleiotropic effects on many organ systems in the body, including the brain, heart, adipose tissue, and liver. They decrease inflammation and also increase satiety and delay gastric emptying. None of these effects automatically produce weight loss, but they certainly aid in the adoption of a healthier body weight and better health. The weight loss occurs because these medications steer the body toward behavioral changes that promote weight loss.
As we delve into the SELECT trial results, a 20% reduction in major cardiovascular events was accompanied by an average weight loss of 9.6%, without a behavioral component added to either the placebo or intervention arms, as is usual in antiobesity agent trials.
Does this mean that primary care providers (PCPs) don’t have to educate patients on behavior change, diet, and exercise therapy? Well, if we consider obesity a disease as we do type 2 diabetes and dyslipidemia or hypertension, then no — PCPs don’t have to, just like they don’t in treating these other diseases.
However, we should rethink this practice. The recently published SURMOUNT-3 trial looked at another NuSH, tirzepatide, with intensive behavioral therapy; it resulted in a 26.6% weight loss, which is comparable to results with bariatric surgery. The SURMOUNT-1 trial of tirzepatide with nonintensive behavioral therapy resulted in a 20.9% weight loss, which is still substantial, but SURMOUNT-3 showed how much more is achievable with robust behavior-change therapy.
In other words, it’s time that PCPs provide education on behavior change to maximize the power of the medications prescribed in practice for the most common diseases suffered in the United States: obesity, type 2 diabetes, cardiovascular disease, and hypertension. These are all chronic, relapsing diseases. Medication alone will improve numbers (weight, blood glucose, A1c, and blood pressure), but a relapsing disease continues relentlessly as patients age to overcome the medications prescribed.
Today I made another patient feel bad because she lost over 100 pounds on semaglutide (Wegovy) 2.4 mg over 1 year, reducing her BMI from 57 to 36. She wanted to keep losing, so I recommended sleeve gastrectomy to lose more weight. I told her she could always restart the Wegovy after the procedure if needed.
We really don’t have an answer to this issue of NuSH therapy not getting to goal and bariatric surgery following medication therapy. The reality is that bariatric surgery should be considered a safe, effective treatment for extreme obesity somewhere along the trajectory of treatments starting with behavior (diet, exercise) and medications. It is still considered a last resort, and for some, just too aggressive.
We have learned much about the incretin hormones and what they can accomplish for obesity from studying bariatric — now called metabolic — surgery. Surgery should be seen as we see stent placement for angina, only more effective for longevity. The COURAGE trial, published in 2007 in NEJM, showed that when compared with medication treatment alone for angina, stent placement plus medications resulted in no difference in mortality after a 7-year follow-up period. Compare this to bariatric surgery, which in many retrospective analyses shows a 20% reduction in cardiovascular mortality after 20-year follow-up (Swedish Obesity Study). In the United States, there are 2 million stent procedures performed per year vs 250,000 bariatric surgical procedures. There are millions of Americans with a BMI > 40 and, yes, millions of Americans with angina. I think I make my point that we need to do more bariatric surgeries to effectively treat extreme obesity.
The solution to this negligent medical practice in obesity treatment is to empower PCPs to treat obesity (at least uncomplicated obesity) and refer to obesity medicine practices for complicated obesity with multiple complications, such as type 2 diabetes and cardiovascular disease, and to refer to obesity medicine practices with a surgical component for BMIs > 40 or > 35 with type 2 diabetes, sleep apnea, and/or cardiovascular disease or other serious conditions.
How do we empower PCPs? Insurance coverage of NuSH therapies due to life-saving properties — as evidenced by the SELECT trial — without prior authorizations; and education on how and why metabolic surgery works, as well as education on behavioral approaches, such as healthy diet and exercise, as a core therapy for all BMI categories.
It’s time.
Caroline Apovian, MD, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, adviser, consultant, or trustee for Altimmune; Cowen and Company; Currax Pharmaceuticals; EPG Communication Holdings; Gelesis, Srl; L-Nutra; and NeuroBo Pharmaceuticals. Received research grant from: National Institutes of Health; Patient-Centered Outcomes Research Institute; and GI Dynamics. Received income in an amount equal to or greater than $250 from: Altimmune; Cowen and Company; NeuroBo Pharmaceuticals; and Novo Nordisk.
A version of this article appeared on Medscape.com.



