User login
USPSTF statement on aspirin: poor messaging at best
: “The USPSTF concludes with moderate certainty that initiating aspirin use for the primary prevention of CVD events in adults age 60 years or older has no net benefit.” I take no issue with the data and appreciate the efforts of the researchers, but at a minimum the public statement is incomplete. At most, it’s dangerously poor messaging.
As physicians, we understand how best to apply this information, but most laypeople, some at significant cardiovascular risk, closed their medicine cabinets this morning and left their aspirin bottle unopened on the shelf. Some of these patients have never spent an hour in the hospital for cardiac-related issues, but they have mitigated their risk for myocardial infarction by purposely poisoning their platelets daily with 81 mg of aspirin. And they should continue to do so.
Don’t forget the calcium score
Take, for instance, my patient Jack, who is typical of many patients I’ve seen throughout the years. Jack is 68 years old and has never had a cardiac event or a gastrointestinal bleed. His daily routine includes a walk, a statin, and a baby aspirin because his CT coronary artery calcium (CAC) score was 10,000 at age 58.
He first visited me 10 years ago because his father died of a myocardial infarction in his late 50s. Jack’s left ventricular ejection fraction is normal and his stress ECG shows 1-mm ST-segment depression at 8 minutes on a Bruce protocol stress test, without angina. Because Jack is well-educated and keeps up with the latest cardiology recommendations, he is precisely the type of patient who may be harmed by this new USPSTF statement by stopping his aspirin.
In October 2020, an analysis from the DALLAS Heart Study showed that persons with a CAC score greater than 100 had a higher cumulative incidence of bleeding and of atherosclerotic cardiovascular disease (ASCVD) events compared with those with no coronary calcium. After adjustment for clinical risk factors, the association between CAC and bleeding was attenuated and no longer statistically significant, whereas the relationship between CAC and ASCVD remained.
I asked one of the investigators, Amit Khera, MD, MSc, from UT Southwestern Medical Center, about the latest recommendations. He emphasized that both the American College of Cardiology/American Heart Association prevention guidelines and the USPSTF statement say that aspirin could still be considered among patients who are at higher risk for cardiovascular events. The USPSTF delineated this as a 10-year ASCVD risk greater than 10%.
Dr. Khera, who was an author of the 2019 guidelines, explained that the guideline committee purposely did not make specific recommendations as to what demarcated higher risk because the data were not clear at that time. Since then, a couple of papers, including the Dallas Heart Study analysis published in JAMA Cardiology, showed that patients at low bleeding risk with a calcium score above 100 may get a net benefit from aspirin. “Thus, in my patients who have a high calcium score and low bleeding risk, I do discuss the option to start or continue aspirin,” he said.
One size does not fit all
I watched ABC World News Tonight on Tuesday, October 12, and was immediately troubled about the coverage of the USPSTF statement. With viewership for the “Big Three” networks in the millions, the message to discontinue aspirin may have unintended consequences for many at-risk patients. The blood-thinning effects of a single dose of aspirin last about 10 days; it will be interesting to see if the rates of myocardial infarction increase over time. This could have been avoided with a better-worded statement – I’m concerned that the lack of nuance could spell big trouble for some.
In JAMA Cardiology, Dr. Khera and colleagues wrote that, “Aspirin use is not a one-size-fits-all therapy.” All physicians likely agree with that opinion. The USPSTF statement should have included the point that if you have a high CT coronary artery calcium score and a low bleeding risk, aspirin still fits very well even if you haven’t experienced a cardiac event. At a minimum, the USPSTF statement should have included the suggestion for patients to consult their physician for advice before discontinuing aspirin therapy.
I hope patients like Jack get the right message.
Melissa Walton-Shirley, MD, is a native Kentuckian who retired from full-time invasive cardiology.
A version of this article first appeared on Medscape.com.
: “The USPSTF concludes with moderate certainty that initiating aspirin use for the primary prevention of CVD events in adults age 60 years or older has no net benefit.” I take no issue with the data and appreciate the efforts of the researchers, but at a minimum the public statement is incomplete. At most, it’s dangerously poor messaging.
As physicians, we understand how best to apply this information, but most laypeople, some at significant cardiovascular risk, closed their medicine cabinets this morning and left their aspirin bottle unopened on the shelf. Some of these patients have never spent an hour in the hospital for cardiac-related issues, but they have mitigated their risk for myocardial infarction by purposely poisoning their platelets daily with 81 mg of aspirin. And they should continue to do so.
Don’t forget the calcium score
Take, for instance, my patient Jack, who is typical of many patients I’ve seen throughout the years. Jack is 68 years old and has never had a cardiac event or a gastrointestinal bleed. His daily routine includes a walk, a statin, and a baby aspirin because his CT coronary artery calcium (CAC) score was 10,000 at age 58.
He first visited me 10 years ago because his father died of a myocardial infarction in his late 50s. Jack’s left ventricular ejection fraction is normal and his stress ECG shows 1-mm ST-segment depression at 8 minutes on a Bruce protocol stress test, without angina. Because Jack is well-educated and keeps up with the latest cardiology recommendations, he is precisely the type of patient who may be harmed by this new USPSTF statement by stopping his aspirin.
In October 2020, an analysis from the DALLAS Heart Study showed that persons with a CAC score greater than 100 had a higher cumulative incidence of bleeding and of atherosclerotic cardiovascular disease (ASCVD) events compared with those with no coronary calcium. After adjustment for clinical risk factors, the association between CAC and bleeding was attenuated and no longer statistically significant, whereas the relationship between CAC and ASCVD remained.
I asked one of the investigators, Amit Khera, MD, MSc, from UT Southwestern Medical Center, about the latest recommendations. He emphasized that both the American College of Cardiology/American Heart Association prevention guidelines and the USPSTF statement say that aspirin could still be considered among patients who are at higher risk for cardiovascular events. The USPSTF delineated this as a 10-year ASCVD risk greater than 10%.
Dr. Khera, who was an author of the 2019 guidelines, explained that the guideline committee purposely did not make specific recommendations as to what demarcated higher risk because the data were not clear at that time. Since then, a couple of papers, including the Dallas Heart Study analysis published in JAMA Cardiology, showed that patients at low bleeding risk with a calcium score above 100 may get a net benefit from aspirin. “Thus, in my patients who have a high calcium score and low bleeding risk, I do discuss the option to start or continue aspirin,” he said.
One size does not fit all
I watched ABC World News Tonight on Tuesday, October 12, and was immediately troubled about the coverage of the USPSTF statement. With viewership for the “Big Three” networks in the millions, the message to discontinue aspirin may have unintended consequences for many at-risk patients. The blood-thinning effects of a single dose of aspirin last about 10 days; it will be interesting to see if the rates of myocardial infarction increase over time. This could have been avoided with a better-worded statement – I’m concerned that the lack of nuance could spell big trouble for some.
In JAMA Cardiology, Dr. Khera and colleagues wrote that, “Aspirin use is not a one-size-fits-all therapy.” All physicians likely agree with that opinion. The USPSTF statement should have included the point that if you have a high CT coronary artery calcium score and a low bleeding risk, aspirin still fits very well even if you haven’t experienced a cardiac event. At a minimum, the USPSTF statement should have included the suggestion for patients to consult their physician for advice before discontinuing aspirin therapy.
I hope patients like Jack get the right message.
Melissa Walton-Shirley, MD, is a native Kentuckian who retired from full-time invasive cardiology.
A version of this article first appeared on Medscape.com.
: “The USPSTF concludes with moderate certainty that initiating aspirin use for the primary prevention of CVD events in adults age 60 years or older has no net benefit.” I take no issue with the data and appreciate the efforts of the researchers, but at a minimum the public statement is incomplete. At most, it’s dangerously poor messaging.
As physicians, we understand how best to apply this information, but most laypeople, some at significant cardiovascular risk, closed their medicine cabinets this morning and left their aspirin bottle unopened on the shelf. Some of these patients have never spent an hour in the hospital for cardiac-related issues, but they have mitigated their risk for myocardial infarction by purposely poisoning their platelets daily with 81 mg of aspirin. And they should continue to do so.
Don’t forget the calcium score
Take, for instance, my patient Jack, who is typical of many patients I’ve seen throughout the years. Jack is 68 years old and has never had a cardiac event or a gastrointestinal bleed. His daily routine includes a walk, a statin, and a baby aspirin because his CT coronary artery calcium (CAC) score was 10,000 at age 58.
He first visited me 10 years ago because his father died of a myocardial infarction in his late 50s. Jack’s left ventricular ejection fraction is normal and his stress ECG shows 1-mm ST-segment depression at 8 minutes on a Bruce protocol stress test, without angina. Because Jack is well-educated and keeps up with the latest cardiology recommendations, he is precisely the type of patient who may be harmed by this new USPSTF statement by stopping his aspirin.
In October 2020, an analysis from the DALLAS Heart Study showed that persons with a CAC score greater than 100 had a higher cumulative incidence of bleeding and of atherosclerotic cardiovascular disease (ASCVD) events compared with those with no coronary calcium. After adjustment for clinical risk factors, the association between CAC and bleeding was attenuated and no longer statistically significant, whereas the relationship between CAC and ASCVD remained.
I asked one of the investigators, Amit Khera, MD, MSc, from UT Southwestern Medical Center, about the latest recommendations. He emphasized that both the American College of Cardiology/American Heart Association prevention guidelines and the USPSTF statement say that aspirin could still be considered among patients who are at higher risk for cardiovascular events. The USPSTF delineated this as a 10-year ASCVD risk greater than 10%.
Dr. Khera, who was an author of the 2019 guidelines, explained that the guideline committee purposely did not make specific recommendations as to what demarcated higher risk because the data were not clear at that time. Since then, a couple of papers, including the Dallas Heart Study analysis published in JAMA Cardiology, showed that patients at low bleeding risk with a calcium score above 100 may get a net benefit from aspirin. “Thus, in my patients who have a high calcium score and low bleeding risk, I do discuss the option to start or continue aspirin,” he said.
One size does not fit all
I watched ABC World News Tonight on Tuesday, October 12, and was immediately troubled about the coverage of the USPSTF statement. With viewership for the “Big Three” networks in the millions, the message to discontinue aspirin may have unintended consequences for many at-risk patients. The blood-thinning effects of a single dose of aspirin last about 10 days; it will be interesting to see if the rates of myocardial infarction increase over time. This could have been avoided with a better-worded statement – I’m concerned that the lack of nuance could spell big trouble for some.
In JAMA Cardiology, Dr. Khera and colleagues wrote that, “Aspirin use is not a one-size-fits-all therapy.” All physicians likely agree with that opinion. The USPSTF statement should have included the point that if you have a high CT coronary artery calcium score and a low bleeding risk, aspirin still fits very well even if you haven’t experienced a cardiac event. At a minimum, the USPSTF statement should have included the suggestion for patients to consult their physician for advice before discontinuing aspirin therapy.
I hope patients like Jack get the right message.
Melissa Walton-Shirley, MD, is a native Kentuckian who retired from full-time invasive cardiology.
A version of this article first appeared on Medscape.com.
Guidelines for dementia and age-related cognitive changes
It is estimated that by the year 2060, 13.9 million Americans over the age of 65 will be diagnosed with dementia. Few good treatments are currently available.
Earlier this year, the American Psychological Association (APA) Task Force issued clinical guidelines “for the Evaluation of Dementia and Age-Related Cognitive Change.” While these 16 guidelines are aimed at psychologists, primary care doctors are often the first ones to evaluate a patient who may have dementia. As a family physician, I find having these guidelines especially helpful.
Neuropsychiatric testing and defining severity and type
This new guidance places emphasis on neuropsychiatric testing and defining the severity and type of dementia present.
Over the past 2 decades, diagnoses of mild neurocognitive disorders have increased, and this, in part, is due to diagnosing these problems earlier and with greater precision. It is also important to know that biomarkers are being increasingly researched, and it is imperative that we stay current with this research.
Cognitive decline may also occur with the coexistence of other mental health disorders, such as depression, so it is important that we screen for these as well. This is often difficult given the behavioral changes that can arise in dementia, but, as primary care doctors, we must differentiate these to treat our patients appropriately.
Informed consent
Informed consent can become an issue with patients with dementia. It must be assessed whether the patient has the capacity to make an informed decision and can competently communicate that decision.
The diagnosis of dementia alone does not preclude a patient from giving informed consent. A patient’s mental capacity must be determined, and if they are not capable of making an informed decision, the person legally responsible for giving informed consent on behalf of the patient must be identified.
Patients with dementia often have other medical comorbidities and take several medications. It is imperative to keep accurate medical records and medication lists. Sometimes, patients with dementia cannot provide this information. If that is the case, every attempt should be made to obtain records from every possible source.
Cultural competence
The guidelines also stress that there may be cultural differences when applying neuropsychiatric tests. It is our duty to maintain cultural competence and understand these differences. We all need to work to ensure we control our biases, and it is suggested that we review relevant evidence-based literature.
While ageism is common in our society, it shouldn’t be in our practices. For these reasons, outreach in at-risk populations is very important.
Pertinent data
The guidelines also suggest obtaining all possible information in our evaluation, especially when the patient is unable to give it to us.
Often, as primary care physicians, we refer these patients to other providers, and we should be providing all pertinent data to those we are referring these patients to. If all information is not available at the time of evaluation, follow-up visits should be scheduled.
If possible, family members should be present at the time of visit. They often provide valuable information regarding the extent and progression of the decline. Also, they know how the patient is functioning in the home setting and how much assistance they need with activities of daily living.
Caretaker support
Another important factor to consider is caretaker burnout. Caretakers are often under a lot of stress and have high rates of depression. It is important to provide them with education and support, as well as resources that may be available to them. For some, accepting the diagnosis that their loved one has dementia may be a struggle.
As doctors treating dementia patients, we need to know the resources that are available to assist dementia patients and their families. There are many local organizations that can help.
Also, research into dementia is ongoing and we need to stay current. The diagnosis of dementia should be made as early as possible using appropriate screening tools. The sooner the diagnosis is made, the quicker interventions can be started and the family members, as well as the patient, can come to accept the diagnosis.
As the population ages, we can expect the demands of dementia to rise as well. Primary care doctors are in a unique position to diagnose dementia once it starts to appear.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at fpnews@mdedge.com.
It is estimated that by the year 2060, 13.9 million Americans over the age of 65 will be diagnosed with dementia. Few good treatments are currently available.
Earlier this year, the American Psychological Association (APA) Task Force issued clinical guidelines “for the Evaluation of Dementia and Age-Related Cognitive Change.” While these 16 guidelines are aimed at psychologists, primary care doctors are often the first ones to evaluate a patient who may have dementia. As a family physician, I find having these guidelines especially helpful.
Neuropsychiatric testing and defining severity and type
This new guidance places emphasis on neuropsychiatric testing and defining the severity and type of dementia present.
Over the past 2 decades, diagnoses of mild neurocognitive disorders have increased, and this, in part, is due to diagnosing these problems earlier and with greater precision. It is also important to know that biomarkers are being increasingly researched, and it is imperative that we stay current with this research.
Cognitive decline may also occur with the coexistence of other mental health disorders, such as depression, so it is important that we screen for these as well. This is often difficult given the behavioral changes that can arise in dementia, but, as primary care doctors, we must differentiate these to treat our patients appropriately.
Informed consent
Informed consent can become an issue with patients with dementia. It must be assessed whether the patient has the capacity to make an informed decision and can competently communicate that decision.
The diagnosis of dementia alone does not preclude a patient from giving informed consent. A patient’s mental capacity must be determined, and if they are not capable of making an informed decision, the person legally responsible for giving informed consent on behalf of the patient must be identified.
Patients with dementia often have other medical comorbidities and take several medications. It is imperative to keep accurate medical records and medication lists. Sometimes, patients with dementia cannot provide this information. If that is the case, every attempt should be made to obtain records from every possible source.
Cultural competence
The guidelines also stress that there may be cultural differences when applying neuropsychiatric tests. It is our duty to maintain cultural competence and understand these differences. We all need to work to ensure we control our biases, and it is suggested that we review relevant evidence-based literature.
While ageism is common in our society, it shouldn’t be in our practices. For these reasons, outreach in at-risk populations is very important.
Pertinent data
The guidelines also suggest obtaining all possible information in our evaluation, especially when the patient is unable to give it to us.
Often, as primary care physicians, we refer these patients to other providers, and we should be providing all pertinent data to those we are referring these patients to. If all information is not available at the time of evaluation, follow-up visits should be scheduled.
If possible, family members should be present at the time of visit. They often provide valuable information regarding the extent and progression of the decline. Also, they know how the patient is functioning in the home setting and how much assistance they need with activities of daily living.
Caretaker support
Another important factor to consider is caretaker burnout. Caretakers are often under a lot of stress and have high rates of depression. It is important to provide them with education and support, as well as resources that may be available to them. For some, accepting the diagnosis that their loved one has dementia may be a struggle.
As doctors treating dementia patients, we need to know the resources that are available to assist dementia patients and their families. There are many local organizations that can help.
Also, research into dementia is ongoing and we need to stay current. The diagnosis of dementia should be made as early as possible using appropriate screening tools. The sooner the diagnosis is made, the quicker interventions can be started and the family members, as well as the patient, can come to accept the diagnosis.
As the population ages, we can expect the demands of dementia to rise as well. Primary care doctors are in a unique position to diagnose dementia once it starts to appear.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at fpnews@mdedge.com.
It is estimated that by the year 2060, 13.9 million Americans over the age of 65 will be diagnosed with dementia. Few good treatments are currently available.
Earlier this year, the American Psychological Association (APA) Task Force issued clinical guidelines “for the Evaluation of Dementia and Age-Related Cognitive Change.” While these 16 guidelines are aimed at psychologists, primary care doctors are often the first ones to evaluate a patient who may have dementia. As a family physician, I find having these guidelines especially helpful.
Neuropsychiatric testing and defining severity and type
This new guidance places emphasis on neuropsychiatric testing and defining the severity and type of dementia present.
Over the past 2 decades, diagnoses of mild neurocognitive disorders have increased, and this, in part, is due to diagnosing these problems earlier and with greater precision. It is also important to know that biomarkers are being increasingly researched, and it is imperative that we stay current with this research.
Cognitive decline may also occur with the coexistence of other mental health disorders, such as depression, so it is important that we screen for these as well. This is often difficult given the behavioral changes that can arise in dementia, but, as primary care doctors, we must differentiate these to treat our patients appropriately.
Informed consent
Informed consent can become an issue with patients with dementia. It must be assessed whether the patient has the capacity to make an informed decision and can competently communicate that decision.
The diagnosis of dementia alone does not preclude a patient from giving informed consent. A patient’s mental capacity must be determined, and if they are not capable of making an informed decision, the person legally responsible for giving informed consent on behalf of the patient must be identified.
Patients with dementia often have other medical comorbidities and take several medications. It is imperative to keep accurate medical records and medication lists. Sometimes, patients with dementia cannot provide this information. If that is the case, every attempt should be made to obtain records from every possible source.
Cultural competence
The guidelines also stress that there may be cultural differences when applying neuropsychiatric tests. It is our duty to maintain cultural competence and understand these differences. We all need to work to ensure we control our biases, and it is suggested that we review relevant evidence-based literature.
While ageism is common in our society, it shouldn’t be in our practices. For these reasons, outreach in at-risk populations is very important.
Pertinent data
The guidelines also suggest obtaining all possible information in our evaluation, especially when the patient is unable to give it to us.
Often, as primary care physicians, we refer these patients to other providers, and we should be providing all pertinent data to those we are referring these patients to. If all information is not available at the time of evaluation, follow-up visits should be scheduled.
If possible, family members should be present at the time of visit. They often provide valuable information regarding the extent and progression of the decline. Also, they know how the patient is functioning in the home setting and how much assistance they need with activities of daily living.
Caretaker support
Another important factor to consider is caretaker burnout. Caretakers are often under a lot of stress and have high rates of depression. It is important to provide them with education and support, as well as resources that may be available to them. For some, accepting the diagnosis that their loved one has dementia may be a struggle.
As doctors treating dementia patients, we need to know the resources that are available to assist dementia patients and their families. There are many local organizations that can help.
Also, research into dementia is ongoing and we need to stay current. The diagnosis of dementia should be made as early as possible using appropriate screening tools. The sooner the diagnosis is made, the quicker interventions can be started and the family members, as well as the patient, can come to accept the diagnosis.
As the population ages, we can expect the demands of dementia to rise as well. Primary care doctors are in a unique position to diagnose dementia once it starts to appear.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at fpnews@mdedge.com.
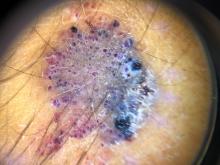
Teen boy’s knee lesion has changed
A biopsy of the lesion was performed which showed an increased number of eccrine glands and blood vessels within the dermis. Some areas showed an increase in adipocytes and smooth muscle bundles. The changes were consistent with eccrine angiomatous hamartoma (EAH).
The boy was referred to vascular laser therapy for treatment of the lesion.
EAH is a rare benign vascular growth characterized by an increased number of mature eccrine glands and blood vessels in the dermis and subcutis. The lesions are mostly present on the extremities, but cases of diffuse congenital lesions and lesions on the face and trunk have also been described. The lesions can be seen at birth or during the first years of life in about half of the cases, and the others tend to occur later in puberty and rarely in adulthood.1
Clinically, EAH lesions present as red, yellow to brown papules and plaques. Different dermoscopic patterns have been described which include the popcorn pattern that presents as yellow, confluent nodules with popcornlike shapes over a background of erythema, and linear arborizing vessels. The spitzoid pattern are brown globules on a background of erythema and pseudoreticular pigmentation around the globules. The verrucous hemangiomalike pattern has a bluish-white hue, reddish-blue or bluish lacunae, as seen in our patient.2-4
Most of the lesions are asymptomatic, but in some patients, they can be associated with pain, hyperhidrosis, and sometimes bleeding. Hyperhidrosis has been reported early in the presentation or during puberty or pregnancy. Our patient had started on amphetamines when hyperhidrosis occurred. Hyperhidrosis is a knowns side effect of this type of medication and may have had a role in the increased sweating noted on the hamartoma.
EAH can clinically look like verrucous hemangiomas, angiokeratomas, and vascular malformations, and histopathology may be needed to differentiate between them. Eccrine nevi and EAH can be similar. Hyperhidrosis is an early and predominant component of eccrine nevi, compared with one-third of EAH.
The exact etiology of this lesion is not known. It is thought to be caused by an abnormal differentiation of the epithelium, adnexal structure, and the mesenchyme during organogenesis.3 No other associated conditions have been described with EAH.
EAH are benign lesions that rarely require treatment. If the lesions are symptomatic or because of cosmetic reasons, they can be removed surgically. There are some reports of successful treatment with pulse dual-wavelength sequential 595- and 1064-nm lasers.5 Botulinum toxin has also been used in cases of symptomatic hyperhidrosis.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. She has no conflicts. Email her at pdnews@mdedge.com.
References
1. Smith SD et al. Pediatr Dermatol. 2019 Nov;36(6):909-12.
2. Patterson AT et al. Am J Dermatopathol. 2016;38:413-7.
3. Garcıa-Garcıa SC et al. JAAD Case Rep. 2018;4(2):165-7.
4. Awatef Kelati et al. JAAD Case Rep. 2018;4(8)835-6.
5. Felgueiras J et al. Dermatol Surg. 2015 Mar;41(3):428-30.
A biopsy of the lesion was performed which showed an increased number of eccrine glands and blood vessels within the dermis. Some areas showed an increase in adipocytes and smooth muscle bundles. The changes were consistent with eccrine angiomatous hamartoma (EAH).
The boy was referred to vascular laser therapy for treatment of the lesion.
EAH is a rare benign vascular growth characterized by an increased number of mature eccrine glands and blood vessels in the dermis and subcutis. The lesions are mostly present on the extremities, but cases of diffuse congenital lesions and lesions on the face and trunk have also been described. The lesions can be seen at birth or during the first years of life in about half of the cases, and the others tend to occur later in puberty and rarely in adulthood.1
Clinically, EAH lesions present as red, yellow to brown papules and plaques. Different dermoscopic patterns have been described which include the popcorn pattern that presents as yellow, confluent nodules with popcornlike shapes over a background of erythema, and linear arborizing vessels. The spitzoid pattern are brown globules on a background of erythema and pseudoreticular pigmentation around the globules. The verrucous hemangiomalike pattern has a bluish-white hue, reddish-blue or bluish lacunae, as seen in our patient.2-4
Most of the lesions are asymptomatic, but in some patients, they can be associated with pain, hyperhidrosis, and sometimes bleeding. Hyperhidrosis has been reported early in the presentation or during puberty or pregnancy. Our patient had started on amphetamines when hyperhidrosis occurred. Hyperhidrosis is a knowns side effect of this type of medication and may have had a role in the increased sweating noted on the hamartoma.
EAH can clinically look like verrucous hemangiomas, angiokeratomas, and vascular malformations, and histopathology may be needed to differentiate between them. Eccrine nevi and EAH can be similar. Hyperhidrosis is an early and predominant component of eccrine nevi, compared with one-third of EAH.
The exact etiology of this lesion is not known. It is thought to be caused by an abnormal differentiation of the epithelium, adnexal structure, and the mesenchyme during organogenesis.3 No other associated conditions have been described with EAH.
EAH are benign lesions that rarely require treatment. If the lesions are symptomatic or because of cosmetic reasons, they can be removed surgically. There are some reports of successful treatment with pulse dual-wavelength sequential 595- and 1064-nm lasers.5 Botulinum toxin has also been used in cases of symptomatic hyperhidrosis.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. She has no conflicts. Email her at pdnews@mdedge.com.
References
1. Smith SD et al. Pediatr Dermatol. 2019 Nov;36(6):909-12.
2. Patterson AT et al. Am J Dermatopathol. 2016;38:413-7.
3. Garcıa-Garcıa SC et al. JAAD Case Rep. 2018;4(2):165-7.
4. Awatef Kelati et al. JAAD Case Rep. 2018;4(8)835-6.
5. Felgueiras J et al. Dermatol Surg. 2015 Mar;41(3):428-30.
A biopsy of the lesion was performed which showed an increased number of eccrine glands and blood vessels within the dermis. Some areas showed an increase in adipocytes and smooth muscle bundles. The changes were consistent with eccrine angiomatous hamartoma (EAH).
The boy was referred to vascular laser therapy for treatment of the lesion.
EAH is a rare benign vascular growth characterized by an increased number of mature eccrine glands and blood vessels in the dermis and subcutis. The lesions are mostly present on the extremities, but cases of diffuse congenital lesions and lesions on the face and trunk have also been described. The lesions can be seen at birth or during the first years of life in about half of the cases, and the others tend to occur later in puberty and rarely in adulthood.1
Clinically, EAH lesions present as red, yellow to brown papules and plaques. Different dermoscopic patterns have been described which include the popcorn pattern that presents as yellow, confluent nodules with popcornlike shapes over a background of erythema, and linear arborizing vessels. The spitzoid pattern are brown globules on a background of erythema and pseudoreticular pigmentation around the globules. The verrucous hemangiomalike pattern has a bluish-white hue, reddish-blue or bluish lacunae, as seen in our patient.2-4
Most of the lesions are asymptomatic, but in some patients, they can be associated with pain, hyperhidrosis, and sometimes bleeding. Hyperhidrosis has been reported early in the presentation or during puberty or pregnancy. Our patient had started on amphetamines when hyperhidrosis occurred. Hyperhidrosis is a knowns side effect of this type of medication and may have had a role in the increased sweating noted on the hamartoma.
EAH can clinically look like verrucous hemangiomas, angiokeratomas, and vascular malformations, and histopathology may be needed to differentiate between them. Eccrine nevi and EAH can be similar. Hyperhidrosis is an early and predominant component of eccrine nevi, compared with one-third of EAH.
The exact etiology of this lesion is not known. It is thought to be caused by an abnormal differentiation of the epithelium, adnexal structure, and the mesenchyme during organogenesis.3 No other associated conditions have been described with EAH.
EAH are benign lesions that rarely require treatment. If the lesions are symptomatic or because of cosmetic reasons, they can be removed surgically. There are some reports of successful treatment with pulse dual-wavelength sequential 595- and 1064-nm lasers.5 Botulinum toxin has also been used in cases of symptomatic hyperhidrosis.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. She has no conflicts. Email her at pdnews@mdedge.com.
References
1. Smith SD et al. Pediatr Dermatol. 2019 Nov;36(6):909-12.
2. Patterson AT et al. Am J Dermatopathol. 2016;38:413-7.
3. Garcıa-Garcıa SC et al. JAAD Case Rep. 2018;4(2):165-7.
4. Awatef Kelati et al. JAAD Case Rep. 2018;4(8)835-6.
5. Felgueiras J et al. Dermatol Surg. 2015 Mar;41(3):428-30.
A 14-year-old male was referred to our pediatric dermatology clinic for evaluation of a lesion on the left knee that appeared at 1 year of age. The lesion has been growing with him and was not symptomatic until 6 months prior to the consultation, when it started bleeding and feeling wet.
He has a history of attention-deficit/hyperactivity disorder managed with dextroamphetamine-amphetamine. The changes noted on the knee lesion seem to occur at the same time that his ADHD medication was started.
On physical exam he had a violaceous circular plaque on the left knee.
On dermoscopy the lesion showed multiple dilated red and violaceous lacunae and whitish blue hue.
Sleep apnea has many faces
Fortunately her problem stemmed from sleep apnea, and resolved with continuous positive airway pressure (CPAP) therapy.
Wallace and Bucks performed a meta analysis of 42 studies of memory in patients with sleep apnea and found sleep apnea patients were impaired when compared to healthy controls on verbal episodic memory (immediate recall, delayed recall, learning, and recognition) and visuospatial episodic memory (immediate and delayed recall).1 A meta-analysis by Olaithe and associates found an improvement in executive function in patients with sleep apnea who were treated with CPAP.2 I think this is worth considering especially in your patients who have subjective memory disturbances and do not appear to have a mild cognitive impairment or dementia.
About 15 years ago I saw a 74-year-old man for nocturia. He had seen two urologists and had a transurethral resection of the prostate (TURP) without any real change in his nocturia. I trialed him on all sorts of medications, and he seemed to improve temporarily a little on trazodone (went from seven episodes a night to four).
Eventually, after several years, I sent him for a sleep study. He had severe sleep apnea (Apnea Hypopnea Index, 65; O2 saturations as low as 60%). With treatment, his nocturia resolved. He went from seven episodes to two each night.
Zhou and colleagues performed a meta-analysis of 13 studies looking at the association of sleep apnea with nocturia.3 They found that men with sleep apnea have a high incidence of nocturia.
Miyazato and colleagues looked at the effect of CPAP treatment on nighttime urine production in patients with obstructive sleep apnea.4 In this small study of 40 patients, mean nighttime voiding episodes decreased from 2.1 to 1.2 (P < .01).
I have seen several patients with night sweats who ended up having sleep apnea. These patients have had a resolution of their night sweats with sleep apnea treatment.
Arnardottir and colleagues found that obstructive sleep apnea was associated with frequent nocturnal sweating.5 They found that 31% of men and 33% of women with OSA had nocturnal sweating, compared with about 10% of the general population.
When the OSA patients were treated with positive airway pressure, the prevalence of nocturnal sweating decreased to 11.5%, which is similar to general population numbers. Given how common both sleep apnea and night sweats are, this is an important consideration as you evaluate night sweats.
I have seen many patients who have had atrial fibrillation and sleep apnea. Shapira-Daniels and colleagues did a prospective study of 188 patients with atrial fibrillation without a history of sleep apnea who were referred for ablation.6 All patients had home sleep studies, and testing was consistent with sleep apnea in 82% of patients.
Kanagala and associates found that patients with untreated sleep apnea had a greater chance of recurrent atrial fibrillation after cardioversion.7 Recurrence of atrial fibrillation at 12 months was 82% in untreated OSA patients, higher than the 42% recurrence in the treated OSA group (P = .013) and the 53% recurrence in control patients.
I think sleep apnea evaluation should be strongly considered in patients with atrial fibrillation and should be done before referral for ablations.
Pearl: Consider sleep apnea as a possible cause of or contributing factor to the common primary care problems of cognitive concerns, nocturia, night sweats, and atrial fibrillation.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Wallace A and Bucks RS. Memory and obstructive sleep apnea: a meta-analysis. Sleep. 2013;36(2):203. Epub 2013 Feb 1.
2. Olaithe M and Bucks RS. Executive dysfunction in OSA before and after treatment: a meta-analysis. Sleep. 2013;36(9):1297. Epub 2013 Sep 1.
3. Zhou J et al. Association between obstructive sleep apnea syndrome and nocturia: a meta-analysis. Sleep Breath. 2020 Dec;24(4):1293-8.
4. Miyauchi Y et al. Effect of the continuous positive airway pressure on the nocturnal urine volume or night-time frequency in patients with obstructive sleep apnea syndrome. Urology 2015;85:333.
5. Arnardottir ES et al. Nocturnal sweating–a common symptom of obstructive sleep apnoea: the Icelandic sleep apnoea cohort. BMJ Open. 2013 May 14;3(5):e002795. BMJ Open 2013;3:e002795
6. Shapira-Daniels A et al. Prevalence of undiagnosed sleep apnea in patients with atrial fibrillation and its impact on therapy. JACC Clin Electrophysiol. 2020;6(12):1499. Epub 2020 Aug 12.
7. Kanagala R et al. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107(20):2589. Epub 2003 May 12.
Fortunately her problem stemmed from sleep apnea, and resolved with continuous positive airway pressure (CPAP) therapy.
Wallace and Bucks performed a meta analysis of 42 studies of memory in patients with sleep apnea and found sleep apnea patients were impaired when compared to healthy controls on verbal episodic memory (immediate recall, delayed recall, learning, and recognition) and visuospatial episodic memory (immediate and delayed recall).1 A meta-analysis by Olaithe and associates found an improvement in executive function in patients with sleep apnea who were treated with CPAP.2 I think this is worth considering especially in your patients who have subjective memory disturbances and do not appear to have a mild cognitive impairment or dementia.
About 15 years ago I saw a 74-year-old man for nocturia. He had seen two urologists and had a transurethral resection of the prostate (TURP) without any real change in his nocturia. I trialed him on all sorts of medications, and he seemed to improve temporarily a little on trazodone (went from seven episodes a night to four).
Eventually, after several years, I sent him for a sleep study. He had severe sleep apnea (Apnea Hypopnea Index, 65; O2 saturations as low as 60%). With treatment, his nocturia resolved. He went from seven episodes to two each night.
Zhou and colleagues performed a meta-analysis of 13 studies looking at the association of sleep apnea with nocturia.3 They found that men with sleep apnea have a high incidence of nocturia.
Miyazato and colleagues looked at the effect of CPAP treatment on nighttime urine production in patients with obstructive sleep apnea.4 In this small study of 40 patients, mean nighttime voiding episodes decreased from 2.1 to 1.2 (P < .01).
I have seen several patients with night sweats who ended up having sleep apnea. These patients have had a resolution of their night sweats with sleep apnea treatment.
Arnardottir and colleagues found that obstructive sleep apnea was associated with frequent nocturnal sweating.5 They found that 31% of men and 33% of women with OSA had nocturnal sweating, compared with about 10% of the general population.
When the OSA patients were treated with positive airway pressure, the prevalence of nocturnal sweating decreased to 11.5%, which is similar to general population numbers. Given how common both sleep apnea and night sweats are, this is an important consideration as you evaluate night sweats.
I have seen many patients who have had atrial fibrillation and sleep apnea. Shapira-Daniels and colleagues did a prospective study of 188 patients with atrial fibrillation without a history of sleep apnea who were referred for ablation.6 All patients had home sleep studies, and testing was consistent with sleep apnea in 82% of patients.
Kanagala and associates found that patients with untreated sleep apnea had a greater chance of recurrent atrial fibrillation after cardioversion.7 Recurrence of atrial fibrillation at 12 months was 82% in untreated OSA patients, higher than the 42% recurrence in the treated OSA group (P = .013) and the 53% recurrence in control patients.
I think sleep apnea evaluation should be strongly considered in patients with atrial fibrillation and should be done before referral for ablations.
Pearl: Consider sleep apnea as a possible cause of or contributing factor to the common primary care problems of cognitive concerns, nocturia, night sweats, and atrial fibrillation.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Wallace A and Bucks RS. Memory and obstructive sleep apnea: a meta-analysis. Sleep. 2013;36(2):203. Epub 2013 Feb 1.
2. Olaithe M and Bucks RS. Executive dysfunction in OSA before and after treatment: a meta-analysis. Sleep. 2013;36(9):1297. Epub 2013 Sep 1.
3. Zhou J et al. Association between obstructive sleep apnea syndrome and nocturia: a meta-analysis. Sleep Breath. 2020 Dec;24(4):1293-8.
4. Miyauchi Y et al. Effect of the continuous positive airway pressure on the nocturnal urine volume or night-time frequency in patients with obstructive sleep apnea syndrome. Urology 2015;85:333.
5. Arnardottir ES et al. Nocturnal sweating–a common symptom of obstructive sleep apnoea: the Icelandic sleep apnoea cohort. BMJ Open. 2013 May 14;3(5):e002795. BMJ Open 2013;3:e002795
6. Shapira-Daniels A et al. Prevalence of undiagnosed sleep apnea in patients with atrial fibrillation and its impact on therapy. JACC Clin Electrophysiol. 2020;6(12):1499. Epub 2020 Aug 12.
7. Kanagala R et al. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107(20):2589. Epub 2003 May 12.
Fortunately her problem stemmed from sleep apnea, and resolved with continuous positive airway pressure (CPAP) therapy.
Wallace and Bucks performed a meta analysis of 42 studies of memory in patients with sleep apnea and found sleep apnea patients were impaired when compared to healthy controls on verbal episodic memory (immediate recall, delayed recall, learning, and recognition) and visuospatial episodic memory (immediate and delayed recall).1 A meta-analysis by Olaithe and associates found an improvement in executive function in patients with sleep apnea who were treated with CPAP.2 I think this is worth considering especially in your patients who have subjective memory disturbances and do not appear to have a mild cognitive impairment or dementia.
About 15 years ago I saw a 74-year-old man for nocturia. He had seen two urologists and had a transurethral resection of the prostate (TURP) without any real change in his nocturia. I trialed him on all sorts of medications, and he seemed to improve temporarily a little on trazodone (went from seven episodes a night to four).
Eventually, after several years, I sent him for a sleep study. He had severe sleep apnea (Apnea Hypopnea Index, 65; O2 saturations as low as 60%). With treatment, his nocturia resolved. He went from seven episodes to two each night.
Zhou and colleagues performed a meta-analysis of 13 studies looking at the association of sleep apnea with nocturia.3 They found that men with sleep apnea have a high incidence of nocturia.
Miyazato and colleagues looked at the effect of CPAP treatment on nighttime urine production in patients with obstructive sleep apnea.4 In this small study of 40 patients, mean nighttime voiding episodes decreased from 2.1 to 1.2 (P < .01).
I have seen several patients with night sweats who ended up having sleep apnea. These patients have had a resolution of their night sweats with sleep apnea treatment.
Arnardottir and colleagues found that obstructive sleep apnea was associated with frequent nocturnal sweating.5 They found that 31% of men and 33% of women with OSA had nocturnal sweating, compared with about 10% of the general population.
When the OSA patients were treated with positive airway pressure, the prevalence of nocturnal sweating decreased to 11.5%, which is similar to general population numbers. Given how common both sleep apnea and night sweats are, this is an important consideration as you evaluate night sweats.
I have seen many patients who have had atrial fibrillation and sleep apnea. Shapira-Daniels and colleagues did a prospective study of 188 patients with atrial fibrillation without a history of sleep apnea who were referred for ablation.6 All patients had home sleep studies, and testing was consistent with sleep apnea in 82% of patients.
Kanagala and associates found that patients with untreated sleep apnea had a greater chance of recurrent atrial fibrillation after cardioversion.7 Recurrence of atrial fibrillation at 12 months was 82% in untreated OSA patients, higher than the 42% recurrence in the treated OSA group (P = .013) and the 53% recurrence in control patients.
I think sleep apnea evaluation should be strongly considered in patients with atrial fibrillation and should be done before referral for ablations.
Pearl: Consider sleep apnea as a possible cause of or contributing factor to the common primary care problems of cognitive concerns, nocturia, night sweats, and atrial fibrillation.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Wallace A and Bucks RS. Memory and obstructive sleep apnea: a meta-analysis. Sleep. 2013;36(2):203. Epub 2013 Feb 1.
2. Olaithe M and Bucks RS. Executive dysfunction in OSA before and after treatment: a meta-analysis. Sleep. 2013;36(9):1297. Epub 2013 Sep 1.
3. Zhou J et al. Association between obstructive sleep apnea syndrome and nocturia: a meta-analysis. Sleep Breath. 2020 Dec;24(4):1293-8.
4. Miyauchi Y et al. Effect of the continuous positive airway pressure on the nocturnal urine volume or night-time frequency in patients with obstructive sleep apnea syndrome. Urology 2015;85:333.
5. Arnardottir ES et al. Nocturnal sweating–a common symptom of obstructive sleep apnoea: the Icelandic sleep apnoea cohort. BMJ Open. 2013 May 14;3(5):e002795. BMJ Open 2013;3:e002795
6. Shapira-Daniels A et al. Prevalence of undiagnosed sleep apnea in patients with atrial fibrillation and its impact on therapy. JACC Clin Electrophysiol. 2020;6(12):1499. Epub 2020 Aug 12.
7. Kanagala R et al. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107(20):2589. Epub 2003 May 12.
Sorting out the meaning of misbehavior: The invisible culprit
You have probably heard that determining the A(ntecedent)s, B(ehavior)s, and C(onsequence)s of a behavior is basic to counseling about oppositionality or aggression. But sorting out the As is especially important to going beyond disciplining a misbehavior to building insight for both parents and children.
Antecedents are of two types: triggers such as actions, words, or feelings that happen just before the behavior, and “setting events” that can occur intermittently hours or even days beforehand and lower the threshold for a trigger to cause a child to act out. Lack of sleep, hunger, or fatigue are common setting events that parents recognize and take into account as in “Oh, he missed his nap” to excuse a tantrum in younger children, but is less often considered or excused in older children in whom self-regulation is expected. Often, behavioral specialists in schools are asked to observe a child to identify the triggers and create a “functional behavioral assessment” based on what is observed.
While a functional behavioral assessment requires observations, invisible antecedents to consider include internal thoughts and feelings (meaning). A child feeling shame from a failed math test the day before may be on edge, then, when called on, may uncharacteristically talk back. The child may regard punishment for this “justified” response as unfair, accelerating anger. Feelings of shame or humiliation for failing one’s own standards (or perceived expectations of others the child cares about) are major setups for eliciting defiance.
Even more subtle are meanings the child creates for situations and people, whether real or imagined. A child’s behavior has meaning for the child and the family and can be initiated or maintained by that meaning. For example, a child may “live down” to what the family thinks of him/her; if you think I am bad, I will act badly.
Children may feel guilty about some real or imagined offense, such as divorce or death they think may be their fault, and act up with the family to elicit punishment as payment. When children feel conflicted in a relationship, such as a late adolescent feeling dependent on their mother when their age expectation is independence, they may act up expecting to be ejected from home when they are unable to gather the courage to voluntarily leave. This acting out may also occur with nonconflicted adults, who are actually safer targets. For example, school is often a safer place to express anger through aggression or bullying than home, the real source of the feelings, because family is the “lifeboat” of food and shelter they dare not upset.
Conflicted relationships may be present in blended families, especially if the ex speaks negatively about the other parent. The child of divorce, feeling himself composed of parts of each parent, has diminished self-esteem and anger on behalf of that side being put down. Marital conflict may set children up to feel they have to take sides to angrily defend the parent of like-gender by being oppositional to the other.
Just as we ponder whether the color blue looks the same to someone else, neurologically based differences in perception may make a child misinterpret or act inflexibly or explode in situations that seem normal to adults. While people joke about “being a little OCD,” for some children the distress caused by a change in routine, a messy room, a delayed bus, or loud music is enough to disrupt their functioning and coping enough to explode. Such hypersensitivity can be part of autism or obsessive compulsive disorder or a subthreshold variant. Children vary by age and individually in their ability to understand language, especially sarcastic humor, and often misinterpret it as insulting, threatening, or scary and act accordingly. While most common in children with autism, those with a language learning disability, intellectual disability, or who have English as a second language, or are anxious or vigilant may also take sarcasm the wrong way. Anxious children also may react aggressively from a “hostile bias attribution” of expecting the worst from others.
Another possible meaning of a behavior is that it is being used by the child to manage their feelings. I have found it useful to remind depressed children and parents that it “feels better to be mad than sad” as a reason for irritability. Anger can also push away a person whose otherwise sympathetic approach might release a collapse into tears the child can’t tolerate or would find embarrassing.
The meaning of a child’s misbehavior also resides in the minds of the adults. In addition to all the categories of meaning just described, a parent may be reminded by the child of someone else for whom the adult has strong or conflicted feelings (“projection”) such as a now-hated ex, a sibling of whom the adult is jealous, or a bully from childhood, thus eliciting a reaction falsely triggered by that connection rather than the actual child. Asking parents whom the child “takes after” may elicit such parental projections based on appearance, behavior, or temperament. Helping them pick a feature of the child to focus on to differentiate him/her can serve as an anchor to remind them to control these reactions. Other useful questions to detect meanings of behavior might include asking the child “What’s up with that?” or “What did that make you think/feel?” We can ask parents “How is that for you?” or “What do you think things will be like in 10 years?” to determine despair, mood disorders, or family discord contributing to maladaptive responses possibly maintaining unwanted behaviors.
Throughout life, putting feelings into words is the main way meanings that are contributing to misbehaviors or parenting dysfunction can be uncovered and shifted. For this, the child or adult must feel emotionally safe to talk with a person who conveys curiosity rather than judgment. Helping families explain that divorce is not the child’s fault; admit they also make mistakes; rebuild conflicted relationships through play or talking; identify hypersensitivities or triggers to avoid; and express confidence that the child is a good person, still young, and sure to do better over time, are all things we pediatricians can do to help sort out the meanings of behaviors.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
You have probably heard that determining the A(ntecedent)s, B(ehavior)s, and C(onsequence)s of a behavior is basic to counseling about oppositionality or aggression. But sorting out the As is especially important to going beyond disciplining a misbehavior to building insight for both parents and children.
Antecedents are of two types: triggers such as actions, words, or feelings that happen just before the behavior, and “setting events” that can occur intermittently hours or even days beforehand and lower the threshold for a trigger to cause a child to act out. Lack of sleep, hunger, or fatigue are common setting events that parents recognize and take into account as in “Oh, he missed his nap” to excuse a tantrum in younger children, but is less often considered or excused in older children in whom self-regulation is expected. Often, behavioral specialists in schools are asked to observe a child to identify the triggers and create a “functional behavioral assessment” based on what is observed.
While a functional behavioral assessment requires observations, invisible antecedents to consider include internal thoughts and feelings (meaning). A child feeling shame from a failed math test the day before may be on edge, then, when called on, may uncharacteristically talk back. The child may regard punishment for this “justified” response as unfair, accelerating anger. Feelings of shame or humiliation for failing one’s own standards (or perceived expectations of others the child cares about) are major setups for eliciting defiance.
Even more subtle are meanings the child creates for situations and people, whether real or imagined. A child’s behavior has meaning for the child and the family and can be initiated or maintained by that meaning. For example, a child may “live down” to what the family thinks of him/her; if you think I am bad, I will act badly.
Children may feel guilty about some real or imagined offense, such as divorce or death they think may be their fault, and act up with the family to elicit punishment as payment. When children feel conflicted in a relationship, such as a late adolescent feeling dependent on their mother when their age expectation is independence, they may act up expecting to be ejected from home when they are unable to gather the courage to voluntarily leave. This acting out may also occur with nonconflicted adults, who are actually safer targets. For example, school is often a safer place to express anger through aggression or bullying than home, the real source of the feelings, because family is the “lifeboat” of food and shelter they dare not upset.
Conflicted relationships may be present in blended families, especially if the ex speaks negatively about the other parent. The child of divorce, feeling himself composed of parts of each parent, has diminished self-esteem and anger on behalf of that side being put down. Marital conflict may set children up to feel they have to take sides to angrily defend the parent of like-gender by being oppositional to the other.
Just as we ponder whether the color blue looks the same to someone else, neurologically based differences in perception may make a child misinterpret or act inflexibly or explode in situations that seem normal to adults. While people joke about “being a little OCD,” for some children the distress caused by a change in routine, a messy room, a delayed bus, or loud music is enough to disrupt their functioning and coping enough to explode. Such hypersensitivity can be part of autism or obsessive compulsive disorder or a subthreshold variant. Children vary by age and individually in their ability to understand language, especially sarcastic humor, and often misinterpret it as insulting, threatening, or scary and act accordingly. While most common in children with autism, those with a language learning disability, intellectual disability, or who have English as a second language, or are anxious or vigilant may also take sarcasm the wrong way. Anxious children also may react aggressively from a “hostile bias attribution” of expecting the worst from others.
Another possible meaning of a behavior is that it is being used by the child to manage their feelings. I have found it useful to remind depressed children and parents that it “feels better to be mad than sad” as a reason for irritability. Anger can also push away a person whose otherwise sympathetic approach might release a collapse into tears the child can’t tolerate or would find embarrassing.
The meaning of a child’s misbehavior also resides in the minds of the adults. In addition to all the categories of meaning just described, a parent may be reminded by the child of someone else for whom the adult has strong or conflicted feelings (“projection”) such as a now-hated ex, a sibling of whom the adult is jealous, or a bully from childhood, thus eliciting a reaction falsely triggered by that connection rather than the actual child. Asking parents whom the child “takes after” may elicit such parental projections based on appearance, behavior, or temperament. Helping them pick a feature of the child to focus on to differentiate him/her can serve as an anchor to remind them to control these reactions. Other useful questions to detect meanings of behavior might include asking the child “What’s up with that?” or “What did that make you think/feel?” We can ask parents “How is that for you?” or “What do you think things will be like in 10 years?” to determine despair, mood disorders, or family discord contributing to maladaptive responses possibly maintaining unwanted behaviors.
Throughout life, putting feelings into words is the main way meanings that are contributing to misbehaviors or parenting dysfunction can be uncovered and shifted. For this, the child or adult must feel emotionally safe to talk with a person who conveys curiosity rather than judgment. Helping families explain that divorce is not the child’s fault; admit they also make mistakes; rebuild conflicted relationships through play or talking; identify hypersensitivities or triggers to avoid; and express confidence that the child is a good person, still young, and sure to do better over time, are all things we pediatricians can do to help sort out the meanings of behaviors.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
You have probably heard that determining the A(ntecedent)s, B(ehavior)s, and C(onsequence)s of a behavior is basic to counseling about oppositionality or aggression. But sorting out the As is especially important to going beyond disciplining a misbehavior to building insight for both parents and children.
Antecedents are of two types: triggers such as actions, words, or feelings that happen just before the behavior, and “setting events” that can occur intermittently hours or even days beforehand and lower the threshold for a trigger to cause a child to act out. Lack of sleep, hunger, or fatigue are common setting events that parents recognize and take into account as in “Oh, he missed his nap” to excuse a tantrum in younger children, but is less often considered or excused in older children in whom self-regulation is expected. Often, behavioral specialists in schools are asked to observe a child to identify the triggers and create a “functional behavioral assessment” based on what is observed.
While a functional behavioral assessment requires observations, invisible antecedents to consider include internal thoughts and feelings (meaning). A child feeling shame from a failed math test the day before may be on edge, then, when called on, may uncharacteristically talk back. The child may regard punishment for this “justified” response as unfair, accelerating anger. Feelings of shame or humiliation for failing one’s own standards (or perceived expectations of others the child cares about) are major setups for eliciting defiance.
Even more subtle are meanings the child creates for situations and people, whether real or imagined. A child’s behavior has meaning for the child and the family and can be initiated or maintained by that meaning. For example, a child may “live down” to what the family thinks of him/her; if you think I am bad, I will act badly.
Children may feel guilty about some real or imagined offense, such as divorce or death they think may be their fault, and act up with the family to elicit punishment as payment. When children feel conflicted in a relationship, such as a late adolescent feeling dependent on their mother when their age expectation is independence, they may act up expecting to be ejected from home when they are unable to gather the courage to voluntarily leave. This acting out may also occur with nonconflicted adults, who are actually safer targets. For example, school is often a safer place to express anger through aggression or bullying than home, the real source of the feelings, because family is the “lifeboat” of food and shelter they dare not upset.
Conflicted relationships may be present in blended families, especially if the ex speaks negatively about the other parent. The child of divorce, feeling himself composed of parts of each parent, has diminished self-esteem and anger on behalf of that side being put down. Marital conflict may set children up to feel they have to take sides to angrily defend the parent of like-gender by being oppositional to the other.
Just as we ponder whether the color blue looks the same to someone else, neurologically based differences in perception may make a child misinterpret or act inflexibly or explode in situations that seem normal to adults. While people joke about “being a little OCD,” for some children the distress caused by a change in routine, a messy room, a delayed bus, or loud music is enough to disrupt their functioning and coping enough to explode. Such hypersensitivity can be part of autism or obsessive compulsive disorder or a subthreshold variant. Children vary by age and individually in their ability to understand language, especially sarcastic humor, and often misinterpret it as insulting, threatening, or scary and act accordingly. While most common in children with autism, those with a language learning disability, intellectual disability, or who have English as a second language, or are anxious or vigilant may also take sarcasm the wrong way. Anxious children also may react aggressively from a “hostile bias attribution” of expecting the worst from others.
Another possible meaning of a behavior is that it is being used by the child to manage their feelings. I have found it useful to remind depressed children and parents that it “feels better to be mad than sad” as a reason for irritability. Anger can also push away a person whose otherwise sympathetic approach might release a collapse into tears the child can’t tolerate or would find embarrassing.
The meaning of a child’s misbehavior also resides in the minds of the adults. In addition to all the categories of meaning just described, a parent may be reminded by the child of someone else for whom the adult has strong or conflicted feelings (“projection”) such as a now-hated ex, a sibling of whom the adult is jealous, or a bully from childhood, thus eliciting a reaction falsely triggered by that connection rather than the actual child. Asking parents whom the child “takes after” may elicit such parental projections based on appearance, behavior, or temperament. Helping them pick a feature of the child to focus on to differentiate him/her can serve as an anchor to remind them to control these reactions. Other useful questions to detect meanings of behavior might include asking the child “What’s up with that?” or “What did that make you think/feel?” We can ask parents “How is that for you?” or “What do you think things will be like in 10 years?” to determine despair, mood disorders, or family discord contributing to maladaptive responses possibly maintaining unwanted behaviors.
Throughout life, putting feelings into words is the main way meanings that are contributing to misbehaviors or parenting dysfunction can be uncovered and shifted. For this, the child or adult must feel emotionally safe to talk with a person who conveys curiosity rather than judgment. Helping families explain that divorce is not the child’s fault; admit they also make mistakes; rebuild conflicted relationships through play or talking; identify hypersensitivities or triggers to avoid; and express confidence that the child is a good person, still young, and sure to do better over time, are all things we pediatricians can do to help sort out the meanings of behaviors.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
Call them by their names in your office
Given that approximately 9.5% of youth aged 13-17 in the United States identify as lesbian, gay, bisexual, transgender, or queer (LGBTQ),1 it is likely that a general pediatrician or pediatric subspecialist is going to encounter at least one LGBTQ patient during the course of the average workweek. By having an easy way to identify these patients and store this data in a user-friendly manner, you can ensure that your practice is LGBTQ friendly and an affirming environment for all sexual- and gender-minority youth.
One way to do this is to look over any paper or electronic forms your practice uses and make sure that they provide patients and families a range of options to identify themselves. For example, you could provide more options for gender, other than male or female, including a nonbinary or “other” (with a free text line) option. This allows your patients to give you an accurate description of what their affirmed gender is. Instead of having a space for mother’s name and father’s name, you could list these fields as “parent/guardian #1” and “parent/guardian #2.” These labels allow for more inclusivity and to reflect the diverse makeup of modern families. Providing a space for a patient to put the name and pronouns that they use allows your staff to make sure that you are calling a patient by the correct name and using the correct pronouns.
Within your EMR, there may be editable fields that allow for you or your staff to list the patient’s affirmed name and pronouns. Making this small change allows any staff member who accesses the chart to have that information displayed correctly for them and reduces the chances of staff misgendering or dead-naming a patient. Underscoring the importance of this, Sequeira et al. found that in a sample of youth from a gender clinic, only 9% of those adolescents reported that they were asked their name/pronouns outside of the gender clinic.2 If those fields are not there, you may check with your IT staff or your EMR vendor to see if these fields may be added in. However, staff needs to make sure that they check with the child/adolescent first to discern with whom the patient has discussed their gender identity. If you were to put a patient’s affirmed name into the chart and then call the patient by that name in front of the parent/guardian, the parent/guardian may look at you quizzically about why you are calling their child by that name. This could then cause an uncomfortable conversation in the exam room or result in harm to the patient after the visit.
It is not just good clinical practice to ensure that you use a patient’s affirmed name and pronouns. Russell et al. looked at the relationship between depressive symptoms and suicidal ideation and whether an adolescent’s name/pronouns were used in the context of their home, school, work, and/or friend group. They found that use of an adolescent’s affirmed name in at least one of these contexts was associated with a decrease in depressive symptoms and a 29% decrease in suicidal ideation.3 Therefore, the use of an adolescent’s affirmed name and pronouns in your office contributes to the overall mental well-being of your patients.
Fortunately, there are many guides to help you and your practice be successful at implementing some of these changes. The Gay, Lesbian, Bisexual and Transgender Health Access Project put together its “Community Standards of Practice for the Provision of Quality Health Care Services to Lesbian, Gay, Bisexual, and Transgender Clients” to aid practices in developing environments that are LGBTQ affirming. The National LGBTQIA+ Health Education Center, a part of the Fenway Institute, has a series of learning modules that you and your staff can view for interactive training and tips for best practices. These resources offer pediatricians and their practices free resources to improve their policies and procedures. By instituting these small changes, you can ensure that your practice continues to be an affirming environment for your LGBTQ children and adolescents.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Conran KJ. LGBT youth population in the United States, UCLA School of Law, Williams Institute, 2020 Sep.
2. Sequeira GM et al. Affirming transgender youths’ names and pronouns in the electronic medical record. JAMA Pediatr. 2020;174(5):501-3.
3. Russell ST et al. Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. J Adolesc Health. 2018;63(4):503-5.
Given that approximately 9.5% of youth aged 13-17 in the United States identify as lesbian, gay, bisexual, transgender, or queer (LGBTQ),1 it is likely that a general pediatrician or pediatric subspecialist is going to encounter at least one LGBTQ patient during the course of the average workweek. By having an easy way to identify these patients and store this data in a user-friendly manner, you can ensure that your practice is LGBTQ friendly and an affirming environment for all sexual- and gender-minority youth.
One way to do this is to look over any paper or electronic forms your practice uses and make sure that they provide patients and families a range of options to identify themselves. For example, you could provide more options for gender, other than male or female, including a nonbinary or “other” (with a free text line) option. This allows your patients to give you an accurate description of what their affirmed gender is. Instead of having a space for mother’s name and father’s name, you could list these fields as “parent/guardian #1” and “parent/guardian #2.” These labels allow for more inclusivity and to reflect the diverse makeup of modern families. Providing a space for a patient to put the name and pronouns that they use allows your staff to make sure that you are calling a patient by the correct name and using the correct pronouns.
Within your EMR, there may be editable fields that allow for you or your staff to list the patient’s affirmed name and pronouns. Making this small change allows any staff member who accesses the chart to have that information displayed correctly for them and reduces the chances of staff misgendering or dead-naming a patient. Underscoring the importance of this, Sequeira et al. found that in a sample of youth from a gender clinic, only 9% of those adolescents reported that they were asked their name/pronouns outside of the gender clinic.2 If those fields are not there, you may check with your IT staff or your EMR vendor to see if these fields may be added in. However, staff needs to make sure that they check with the child/adolescent first to discern with whom the patient has discussed their gender identity. If you were to put a patient’s affirmed name into the chart and then call the patient by that name in front of the parent/guardian, the parent/guardian may look at you quizzically about why you are calling their child by that name. This could then cause an uncomfortable conversation in the exam room or result in harm to the patient after the visit.
It is not just good clinical practice to ensure that you use a patient’s affirmed name and pronouns. Russell et al. looked at the relationship between depressive symptoms and suicidal ideation and whether an adolescent’s name/pronouns were used in the context of their home, school, work, and/or friend group. They found that use of an adolescent’s affirmed name in at least one of these contexts was associated with a decrease in depressive symptoms and a 29% decrease in suicidal ideation.3 Therefore, the use of an adolescent’s affirmed name and pronouns in your office contributes to the overall mental well-being of your patients.
Fortunately, there are many guides to help you and your practice be successful at implementing some of these changes. The Gay, Lesbian, Bisexual and Transgender Health Access Project put together its “Community Standards of Practice for the Provision of Quality Health Care Services to Lesbian, Gay, Bisexual, and Transgender Clients” to aid practices in developing environments that are LGBTQ affirming. The National LGBTQIA+ Health Education Center, a part of the Fenway Institute, has a series of learning modules that you and your staff can view for interactive training and tips for best practices. These resources offer pediatricians and their practices free resources to improve their policies and procedures. By instituting these small changes, you can ensure that your practice continues to be an affirming environment for your LGBTQ children and adolescents.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Conran KJ. LGBT youth population in the United States, UCLA School of Law, Williams Institute, 2020 Sep.
2. Sequeira GM et al. Affirming transgender youths’ names and pronouns in the electronic medical record. JAMA Pediatr. 2020;174(5):501-3.
3. Russell ST et al. Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. J Adolesc Health. 2018;63(4):503-5.
Given that approximately 9.5% of youth aged 13-17 in the United States identify as lesbian, gay, bisexual, transgender, or queer (LGBTQ),1 it is likely that a general pediatrician or pediatric subspecialist is going to encounter at least one LGBTQ patient during the course of the average workweek. By having an easy way to identify these patients and store this data in a user-friendly manner, you can ensure that your practice is LGBTQ friendly and an affirming environment for all sexual- and gender-minority youth.
One way to do this is to look over any paper or electronic forms your practice uses and make sure that they provide patients and families a range of options to identify themselves. For example, you could provide more options for gender, other than male or female, including a nonbinary or “other” (with a free text line) option. This allows your patients to give you an accurate description of what their affirmed gender is. Instead of having a space for mother’s name and father’s name, you could list these fields as “parent/guardian #1” and “parent/guardian #2.” These labels allow for more inclusivity and to reflect the diverse makeup of modern families. Providing a space for a patient to put the name and pronouns that they use allows your staff to make sure that you are calling a patient by the correct name and using the correct pronouns.
Within your EMR, there may be editable fields that allow for you or your staff to list the patient’s affirmed name and pronouns. Making this small change allows any staff member who accesses the chart to have that information displayed correctly for them and reduces the chances of staff misgendering or dead-naming a patient. Underscoring the importance of this, Sequeira et al. found that in a sample of youth from a gender clinic, only 9% of those adolescents reported that they were asked their name/pronouns outside of the gender clinic.2 If those fields are not there, you may check with your IT staff or your EMR vendor to see if these fields may be added in. However, staff needs to make sure that they check with the child/adolescent first to discern with whom the patient has discussed their gender identity. If you were to put a patient’s affirmed name into the chart and then call the patient by that name in front of the parent/guardian, the parent/guardian may look at you quizzically about why you are calling their child by that name. This could then cause an uncomfortable conversation in the exam room or result in harm to the patient after the visit.
It is not just good clinical practice to ensure that you use a patient’s affirmed name and pronouns. Russell et al. looked at the relationship between depressive symptoms and suicidal ideation and whether an adolescent’s name/pronouns were used in the context of their home, school, work, and/or friend group. They found that use of an adolescent’s affirmed name in at least one of these contexts was associated with a decrease in depressive symptoms and a 29% decrease in suicidal ideation.3 Therefore, the use of an adolescent’s affirmed name and pronouns in your office contributes to the overall mental well-being of your patients.
Fortunately, there are many guides to help you and your practice be successful at implementing some of these changes. The Gay, Lesbian, Bisexual and Transgender Health Access Project put together its “Community Standards of Practice for the Provision of Quality Health Care Services to Lesbian, Gay, Bisexual, and Transgender Clients” to aid practices in developing environments that are LGBTQ affirming. The National LGBTQIA+ Health Education Center, a part of the Fenway Institute, has a series of learning modules that you and your staff can view for interactive training and tips for best practices. These resources offer pediatricians and their practices free resources to improve their policies and procedures. By instituting these small changes, you can ensure that your practice continues to be an affirming environment for your LGBTQ children and adolescents.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Conran KJ. LGBT youth population in the United States, UCLA School of Law, Williams Institute, 2020 Sep.
2. Sequeira GM et al. Affirming transgender youths’ names and pronouns in the electronic medical record. JAMA Pediatr. 2020;174(5):501-3.
3. Russell ST et al. Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. J Adolesc Health. 2018;63(4):503-5.
What’s behind the rise in youth anxiety and depression?
It’s well known that levels of anxiety and depression in youth are on the rise. While some of this increase may be because of other things, such as a lowering of the threshold for what counts as clinically relevant symptoms and decreased stigma when it comes to seeking out mental health services, there seems little debate that the number of children and adolescents who are actually struggling with their mental health is taking a sharp turn for the worse.
What is much less certain are the causes behind this surge. The answer to this important question will likely defy a clear answer from a definitive study. In its place then are a number of different theories that have been circulated and discussed. Each comes with some evidence to support the hypothesis, but none seems able to make a truly compelling argument as the single driving force behind this trend. This column briefly describes and examines some of the factors that may be contributing to the rise in anxiety and depression while providing some explanation for why each factor is unlikely to be the sole culprit.
Some of the biggest suggested causes for the rise in child and adolescent mental health problems include the following:
- COVID. Multiple studies have documented increases in mood and anxiety associated with the pandemic, which in turn, may be because of a number of factors such as social isolation, loss of family members, family financial stressors, and many other contributors.1 Yet, while it certainly makes sense that COVID is a powerful instigator of mood and anxiety problems, there is good evidence that the upward tic in emotional-behavioral problems began well before the COVID pandemic.2
- Smartphones. In 2017, psychologist Jean Twenge penned a provocative essay in the Atlantic with the title “Have Smartphones Destroyed a Generation?” and the basic answer was yes.3 The foundation for this conclusion was the tracking between the rise in mood and anxiety problems and the meteoric rise of smartphone use in youth. None of these associations, however, can be proven as casual, and more experimental data on the link between smartphone usage and mental health have been inconsistent.
- Bullying. The toxic effect of bullying and, in particular, online or “cyberbullying” has frequently been brought up as a potential cause. Yet while the negative effects of bullying have been well documented, there is evidence that overall bullying has actually decreased over recent years.4
These three factors have arguably been the most discussed, but a few others also probably deserve mention.
- Helicopter parenting. Critics of this common and increasingly popular approach to parenting are concerned that all the parental hovering and stepping in convey the message that the world is a very dangerous place while depriving children of opportunities to gain the exposure and competence they need to succeed. The critique is certainly logical and even has been supported in some studies but lacks the needed evidence for a more definitive conclusion.5
- Medications. Of course there will be stories blaming the mental health treatment itself, rather than the reasons people seek treatment, for this disturbing trend. And while it is always important to consider that medications can be part of the problem rather than the solution, the majority of evidence points overall to a lack of treatment rather than too much. A recent important study, for example, found that the peak of suicidal thoughts and behaviors occurred a month before medications were started, rather than after.6
- Cannabis. While there seems to be a lot of geographic variability with regard to whether or not the number of youth using cannabis is increasing or not, it’s clear that the product now being consumed is considerably stronger than what was used in decades past. This high-potency cannabis now being used has been shown to increase the risk for later mental health problems including psychosis and suicidal behavior.7 Unfortunately, these risks are not being heard as a powerful industry fights to increase their market share.
Putting all this together, it seems likely that a tidy and simple explanation for the alarming increase in youth mental health problems will be hard to pin down. It’s also worth pointing out that many of the above factors could work in a synergistic manner. For example, helicopter parenting may be keeping kids more confined to their rooms where they interact more and more on their phones and are exposed to higher amounts of online bullying, all of which has been magnified recently with the COVID pandemic. Obviously, understanding the causes behind this surge is much more than an academic exercise as the amount of stress and suffering rises and treatment resources get overwhelmed. In the meantime, addressing all of the above factors in both primary and specialty care is worthwhile in an effort to reverse this worrying and wide-ranging pattern.
Dr. Rettew is a child and adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Ore. He is the author of the 2021 book, “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
References
1. Hawes MT et al. Psychol Med. 2021;13:1-9.
2. Twenge JM et al. J Abnorm Psych. 2019;128(3):185-99.
3. Twenge JM. Have Smartphones Destroyed a Generation? The Atlantic. 2017:September.
4. Rettew DC. Bullying: An update. Child Psych Clin North Am. 2021; in press.
5. Van Der Bruggen CO et al. J Child Psychol Psychiatry. 2008;49(12):1257-69.
6. Lagerberg T et al. Selective serotonin reuptake inhibitors and suicidal behaviour: A population-based cohort study. Neuropsychopharmacology 2021 Sep 24.
7. Gobbi G et al. JAMA Psychiatry. 2019;76(4):426-34.
It’s well known that levels of anxiety and depression in youth are on the rise. While some of this increase may be because of other things, such as a lowering of the threshold for what counts as clinically relevant symptoms and decreased stigma when it comes to seeking out mental health services, there seems little debate that the number of children and adolescents who are actually struggling with their mental health is taking a sharp turn for the worse.
What is much less certain are the causes behind this surge. The answer to this important question will likely defy a clear answer from a definitive study. In its place then are a number of different theories that have been circulated and discussed. Each comes with some evidence to support the hypothesis, but none seems able to make a truly compelling argument as the single driving force behind this trend. This column briefly describes and examines some of the factors that may be contributing to the rise in anxiety and depression while providing some explanation for why each factor is unlikely to be the sole culprit.
Some of the biggest suggested causes for the rise in child and adolescent mental health problems include the following:
- COVID. Multiple studies have documented increases in mood and anxiety associated with the pandemic, which in turn, may be because of a number of factors such as social isolation, loss of family members, family financial stressors, and many other contributors.1 Yet, while it certainly makes sense that COVID is a powerful instigator of mood and anxiety problems, there is good evidence that the upward tic in emotional-behavioral problems began well before the COVID pandemic.2
- Smartphones. In 2017, psychologist Jean Twenge penned a provocative essay in the Atlantic with the title “Have Smartphones Destroyed a Generation?” and the basic answer was yes.3 The foundation for this conclusion was the tracking between the rise in mood and anxiety problems and the meteoric rise of smartphone use in youth. None of these associations, however, can be proven as casual, and more experimental data on the link between smartphone usage and mental health have been inconsistent.
- Bullying. The toxic effect of bullying and, in particular, online or “cyberbullying” has frequently been brought up as a potential cause. Yet while the negative effects of bullying have been well documented, there is evidence that overall bullying has actually decreased over recent years.4
These three factors have arguably been the most discussed, but a few others also probably deserve mention.
- Helicopter parenting. Critics of this common and increasingly popular approach to parenting are concerned that all the parental hovering and stepping in convey the message that the world is a very dangerous place while depriving children of opportunities to gain the exposure and competence they need to succeed. The critique is certainly logical and even has been supported in some studies but lacks the needed evidence for a more definitive conclusion.5
- Medications. Of course there will be stories blaming the mental health treatment itself, rather than the reasons people seek treatment, for this disturbing trend. And while it is always important to consider that medications can be part of the problem rather than the solution, the majority of evidence points overall to a lack of treatment rather than too much. A recent important study, for example, found that the peak of suicidal thoughts and behaviors occurred a month before medications were started, rather than after.6
- Cannabis. While there seems to be a lot of geographic variability with regard to whether or not the number of youth using cannabis is increasing or not, it’s clear that the product now being consumed is considerably stronger than what was used in decades past. This high-potency cannabis now being used has been shown to increase the risk for later mental health problems including psychosis and suicidal behavior.7 Unfortunately, these risks are not being heard as a powerful industry fights to increase their market share.
Putting all this together, it seems likely that a tidy and simple explanation for the alarming increase in youth mental health problems will be hard to pin down. It’s also worth pointing out that many of the above factors could work in a synergistic manner. For example, helicopter parenting may be keeping kids more confined to their rooms where they interact more and more on their phones and are exposed to higher amounts of online bullying, all of which has been magnified recently with the COVID pandemic. Obviously, understanding the causes behind this surge is much more than an academic exercise as the amount of stress and suffering rises and treatment resources get overwhelmed. In the meantime, addressing all of the above factors in both primary and specialty care is worthwhile in an effort to reverse this worrying and wide-ranging pattern.
Dr. Rettew is a child and adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Ore. He is the author of the 2021 book, “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
References
1. Hawes MT et al. Psychol Med. 2021;13:1-9.
2. Twenge JM et al. J Abnorm Psych. 2019;128(3):185-99.
3. Twenge JM. Have Smartphones Destroyed a Generation? The Atlantic. 2017:September.
4. Rettew DC. Bullying: An update. Child Psych Clin North Am. 2021; in press.
5. Van Der Bruggen CO et al. J Child Psychol Psychiatry. 2008;49(12):1257-69.
6. Lagerberg T et al. Selective serotonin reuptake inhibitors and suicidal behaviour: A population-based cohort study. Neuropsychopharmacology 2021 Sep 24.
7. Gobbi G et al. JAMA Psychiatry. 2019;76(4):426-34.
It’s well known that levels of anxiety and depression in youth are on the rise. While some of this increase may be because of other things, such as a lowering of the threshold for what counts as clinically relevant symptoms and decreased stigma when it comes to seeking out mental health services, there seems little debate that the number of children and adolescents who are actually struggling with their mental health is taking a sharp turn for the worse.
What is much less certain are the causes behind this surge. The answer to this important question will likely defy a clear answer from a definitive study. In its place then are a number of different theories that have been circulated and discussed. Each comes with some evidence to support the hypothesis, but none seems able to make a truly compelling argument as the single driving force behind this trend. This column briefly describes and examines some of the factors that may be contributing to the rise in anxiety and depression while providing some explanation for why each factor is unlikely to be the sole culprit.
Some of the biggest suggested causes for the rise in child and adolescent mental health problems include the following:
- COVID. Multiple studies have documented increases in mood and anxiety associated with the pandemic, which in turn, may be because of a number of factors such as social isolation, loss of family members, family financial stressors, and many other contributors.1 Yet, while it certainly makes sense that COVID is a powerful instigator of mood and anxiety problems, there is good evidence that the upward tic in emotional-behavioral problems began well before the COVID pandemic.2
- Smartphones. In 2017, psychologist Jean Twenge penned a provocative essay in the Atlantic with the title “Have Smartphones Destroyed a Generation?” and the basic answer was yes.3 The foundation for this conclusion was the tracking between the rise in mood and anxiety problems and the meteoric rise of smartphone use in youth. None of these associations, however, can be proven as casual, and more experimental data on the link between smartphone usage and mental health have been inconsistent.
- Bullying. The toxic effect of bullying and, in particular, online or “cyberbullying” has frequently been brought up as a potential cause. Yet while the negative effects of bullying have been well documented, there is evidence that overall bullying has actually decreased over recent years.4
These three factors have arguably been the most discussed, but a few others also probably deserve mention.
- Helicopter parenting. Critics of this common and increasingly popular approach to parenting are concerned that all the parental hovering and stepping in convey the message that the world is a very dangerous place while depriving children of opportunities to gain the exposure and competence they need to succeed. The critique is certainly logical and even has been supported in some studies but lacks the needed evidence for a more definitive conclusion.5
- Medications. Of course there will be stories blaming the mental health treatment itself, rather than the reasons people seek treatment, for this disturbing trend. And while it is always important to consider that medications can be part of the problem rather than the solution, the majority of evidence points overall to a lack of treatment rather than too much. A recent important study, for example, found that the peak of suicidal thoughts and behaviors occurred a month before medications were started, rather than after.6
- Cannabis. While there seems to be a lot of geographic variability with regard to whether or not the number of youth using cannabis is increasing or not, it’s clear that the product now being consumed is considerably stronger than what was used in decades past. This high-potency cannabis now being used has been shown to increase the risk for later mental health problems including psychosis and suicidal behavior.7 Unfortunately, these risks are not being heard as a powerful industry fights to increase their market share.
Putting all this together, it seems likely that a tidy and simple explanation for the alarming increase in youth mental health problems will be hard to pin down. It’s also worth pointing out that many of the above factors could work in a synergistic manner. For example, helicopter parenting may be keeping kids more confined to their rooms where they interact more and more on their phones and are exposed to higher amounts of online bullying, all of which has been magnified recently with the COVID pandemic. Obviously, understanding the causes behind this surge is much more than an academic exercise as the amount of stress and suffering rises and treatment resources get overwhelmed. In the meantime, addressing all of the above factors in both primary and specialty care is worthwhile in an effort to reverse this worrying and wide-ranging pattern.
Dr. Rettew is a child and adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Ore. He is the author of the 2021 book, “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
References
1. Hawes MT et al. Psychol Med. 2021;13:1-9.
2. Twenge JM et al. J Abnorm Psych. 2019;128(3):185-99.
3. Twenge JM. Have Smartphones Destroyed a Generation? The Atlantic. 2017:September.
4. Rettew DC. Bullying: An update. Child Psych Clin North Am. 2021; in press.
5. Van Der Bruggen CO et al. J Child Psychol Psychiatry. 2008;49(12):1257-69.
6. Lagerberg T et al. Selective serotonin reuptake inhibitors and suicidal behaviour: A population-based cohort study. Neuropsychopharmacology 2021 Sep 24.
7. Gobbi G et al. JAMA Psychiatry. 2019;76(4):426-34.
You’ve been uneasy about the mother’s boyfriend: This may be why
The first patient of the afternoon is a 4-month-old in for his health maintenance visit. You’ve known his 20-year-old mother since she was a toddler. This infant has a 2-year-old sister. Also in the exam room is a young man you don’t recognize whom the mother introduces as Jason, her new boyfriend. He never makes eye contact and despite your best efforts you can’t get him to engage.
At the child’s next visit you are relieved to see the 6-month-old is alive and well and learn that your former patient and her two children have moved back in with her parents and Jason is no longer in the picture.
You don’t have to have been doing pediatrics very long to have learned that a “family” that includes an infant and a young adult male who is probably not the father is an environment in which the infant’s health and well-being is at significant risk. It is a situation in which child abuse even to the point of infanticide should be waving a red flag in your face.
Infanticide occurs in many animal species including our own. As abhorrent we may find the act, it occurs often enough to be, if not normal, at least not unexpected in certain circumstances. Theories abound as to what advantage the act of infanticide might convey to the success of a species. However, little if anything is known about any possible mechanisms that would allow it to occur.
Recently, a professor of molecular and cellular biology at Harvard University discovered a specific set of neurons in the mouse brain that controls aggressive behavior toward infants (Biological triggers for infant abuse, by Juan Siliezar, The Harvard Gazette, Sept 27, 2021). This same set of neurons also appears to trigger avoidance and neglect behaviors as well.
Research in other animal species has found that these antiparental behaviors occur in both virgins and sexually mature males who are strangers to the group. Interestingly, the behaviors switch off once individuals have their own offspring or have had the opportunity to familiarize themselves with infants. Not surprisingly, other studies have found that in some species environmental stress such as food shortage or threats of predation have triggered females to attack or ignore their offspring.
I think it is safe to assume a similar collection of neurons controlling aggressive behavior also exists in humans. One can imagine some well-read defense attorney dredging up this study and claiming that because his client had not yet fathered a child of his own that it was his nervous system’s normal response that made him toss his girlfriend’s baby against the wall.
The lead author of the study intends to study this collection of neurons in more depth to discover more about the process. It is conceivable that with more information her initial findings may help in the development of treatment and specific prevention strategies. Until that happens, we must rely on our intuition and keep our antennae tuned and alert for high-risk scenarios like the one I described at the opening of this letter.
We are left with leaning heavily on our community social work networks to keep close tabs on these high-risk families, offering both financial and emotional support. Parenting classes may be helpful, but some of this research leads me to suspect that immersing these young parents-to-be in hands-on child care situations might provide the best protection we can offer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
The first patient of the afternoon is a 4-month-old in for his health maintenance visit. You’ve known his 20-year-old mother since she was a toddler. This infant has a 2-year-old sister. Also in the exam room is a young man you don’t recognize whom the mother introduces as Jason, her new boyfriend. He never makes eye contact and despite your best efforts you can’t get him to engage.
At the child’s next visit you are relieved to see the 6-month-old is alive and well and learn that your former patient and her two children have moved back in with her parents and Jason is no longer in the picture.
You don’t have to have been doing pediatrics very long to have learned that a “family” that includes an infant and a young adult male who is probably not the father is an environment in which the infant’s health and well-being is at significant risk. It is a situation in which child abuse even to the point of infanticide should be waving a red flag in your face.
Infanticide occurs in many animal species including our own. As abhorrent we may find the act, it occurs often enough to be, if not normal, at least not unexpected in certain circumstances. Theories abound as to what advantage the act of infanticide might convey to the success of a species. However, little if anything is known about any possible mechanisms that would allow it to occur.
Recently, a professor of molecular and cellular biology at Harvard University discovered a specific set of neurons in the mouse brain that controls aggressive behavior toward infants (Biological triggers for infant abuse, by Juan Siliezar, The Harvard Gazette, Sept 27, 2021). This same set of neurons also appears to trigger avoidance and neglect behaviors as well.
Research in other animal species has found that these antiparental behaviors occur in both virgins and sexually mature males who are strangers to the group. Interestingly, the behaviors switch off once individuals have their own offspring or have had the opportunity to familiarize themselves with infants. Not surprisingly, other studies have found that in some species environmental stress such as food shortage or threats of predation have triggered females to attack or ignore their offspring.
I think it is safe to assume a similar collection of neurons controlling aggressive behavior also exists in humans. One can imagine some well-read defense attorney dredging up this study and claiming that because his client had not yet fathered a child of his own that it was his nervous system’s normal response that made him toss his girlfriend’s baby against the wall.
The lead author of the study intends to study this collection of neurons in more depth to discover more about the process. It is conceivable that with more information her initial findings may help in the development of treatment and specific prevention strategies. Until that happens, we must rely on our intuition and keep our antennae tuned and alert for high-risk scenarios like the one I described at the opening of this letter.
We are left with leaning heavily on our community social work networks to keep close tabs on these high-risk families, offering both financial and emotional support. Parenting classes may be helpful, but some of this research leads me to suspect that immersing these young parents-to-be in hands-on child care situations might provide the best protection we can offer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
The first patient of the afternoon is a 4-month-old in for his health maintenance visit. You’ve known his 20-year-old mother since she was a toddler. This infant has a 2-year-old sister. Also in the exam room is a young man you don’t recognize whom the mother introduces as Jason, her new boyfriend. He never makes eye contact and despite your best efforts you can’t get him to engage.
At the child’s next visit you are relieved to see the 6-month-old is alive and well and learn that your former patient and her two children have moved back in with her parents and Jason is no longer in the picture.
You don’t have to have been doing pediatrics very long to have learned that a “family” that includes an infant and a young adult male who is probably not the father is an environment in which the infant’s health and well-being is at significant risk. It is a situation in which child abuse even to the point of infanticide should be waving a red flag in your face.
Infanticide occurs in many animal species including our own. As abhorrent we may find the act, it occurs often enough to be, if not normal, at least not unexpected in certain circumstances. Theories abound as to what advantage the act of infanticide might convey to the success of a species. However, little if anything is known about any possible mechanisms that would allow it to occur.
Recently, a professor of molecular and cellular biology at Harvard University discovered a specific set of neurons in the mouse brain that controls aggressive behavior toward infants (Biological triggers for infant abuse, by Juan Siliezar, The Harvard Gazette, Sept 27, 2021). This same set of neurons also appears to trigger avoidance and neglect behaviors as well.
Research in other animal species has found that these antiparental behaviors occur in both virgins and sexually mature males who are strangers to the group. Interestingly, the behaviors switch off once individuals have their own offspring or have had the opportunity to familiarize themselves with infants. Not surprisingly, other studies have found that in some species environmental stress such as food shortage or threats of predation have triggered females to attack or ignore their offspring.
I think it is safe to assume a similar collection of neurons controlling aggressive behavior also exists in humans. One can imagine some well-read defense attorney dredging up this study and claiming that because his client had not yet fathered a child of his own that it was his nervous system’s normal response that made him toss his girlfriend’s baby against the wall.
The lead author of the study intends to study this collection of neurons in more depth to discover more about the process. It is conceivable that with more information her initial findings may help in the development of treatment and specific prevention strategies. Until that happens, we must rely on our intuition and keep our antennae tuned and alert for high-risk scenarios like the one I described at the opening of this letter.
We are left with leaning heavily on our community social work networks to keep close tabs on these high-risk families, offering both financial and emotional support. Parenting classes may be helpful, but some of this research leads me to suspect that immersing these young parents-to-be in hands-on child care situations might provide the best protection we can offer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Effect of COVID-19 pandemic on respiratory infectious diseases in primary care practice
A secondary consequence of public health measures to prevent the spread of SARS-CoV-2 included a concurrent reduction in risk for children to acquire and spread other respiratory viral infectious diseases. In the Rochester, N.Y., area, we had an ongoing prospective study in primary care pediatric practices that afforded an opportunity to assess the effect of the pandemic control measures on all infectious disease illness visits in young children. Specifically, in children aged 6-36 months old, our study was in place when the pandemic began with a primary objective to evaluate the changing epidemiology of acute otitis media (AOM) and nasopharyngeal colonization by potential bacterial respiratory pathogens in community-based primary care pediatric practices. As the public health measures mandated by New York State Department of Health were implemented, we prospectively quantified their effect on physician-diagnosed infectious disease illness visits. The incidence of infectious disease visits by a cohort of young children during the COVID-19 pandemic period March 15, 2020, through Dec. 31, 2020, was compared with the same time frame in the preceding year, 2019.1
Recommendations of the New York State Department of Health for public health, changes in school and day care attendance, and clinical practice during the study time frame
On March 7, 2020, a state of emergency was declared in New York because of the COVID-19 pandemic. All schools were required to close. A mandated order for public use of masks in adults and children more than 2 years of age was enacted. In the Finger Lakes region of Upstate New York, where the two primary care pediatric practices reside, complete lockdown was partially lifted on May 15, 2020, and further lifted on June 26, 2020. Almost all regional school districts opened to at least hybrid learning models for all students starting Sept. 8, 2020. On March 6, 2020, video telehealth and telephone call visits were introduced as routine practice. Well-child visits were limited to those less than 2 years of age, then gradually expanded to all ages by late May 2020. During the “stay at home” phase of the New York State lockdown, day care services were considered an essential business. Day care child density was limited. All children less than 2 years old were required to wear a mask while in the facility. Upon arrival, children with any respiratory symptoms or fever were excluded. For the school year commencing September 2020, almost all regional school districts opened to virtual, hybrid, or in-person learning models. Exclusion occurred similar to that of the day care facilities.
Incidence of respiratory infectious disease illnesses
Clinical diagnoses and healthy visits of 144 children from March 15 to Dec. 31, 2020 (beginning of the pandemic) were compared to 215 children during the same months in 2019 (prepandemic). Pediatric SARS-CoV-2 positivity rates trended up alongside community spread. Pediatric practice positivity rates rose from 1.9% in October 2020 to 19% in December 2020.
The table shows the incidence of significantly different infectious disease illness visits in the two study cohorts.
During the pandemic, 258 infection visits occurred among 144 pandemic cohort children, compared with 687 visits among 215 prepandemic cohort children, a 1.8-fold decrease (P < .0001). The proportion of children with visits for AOM (3.7-fold; P < .0001), bronchiolitis (7.4-fold; P = .036), croup (27.5-fold; P < .0001), and viral upper respiratory infection (3.8-fold; P < .0001) decreased significantly. Fever without a source (1.4-fold decrease; P = .009) and skin/soft tissue infection (2.1-fold decrease; P = .042) represented a higher proportion of visits during the pandemic.
Prescription of antibiotics significantly decreased (P < .001) during the pandemic.
Change in care practices
In the prepandemic period, virtual visits, leading to a diagnosis and treatment and referring children to an urgent care or hospital emergency department during regular office hours were rare. During the pandemic, this changed. Significantly increased use of telemedicine visits (P < .0001) and significantly decreased office and urgent care visits (P < .0001) occurred during the pandemic. Telehealth visits peaked the week of April 12, 2020, at 45% of all pediatric visits. In-person illness visits gradually returned to year-to-year volumes in August-September 2020 with school opening. Early in the pandemic, both pediatric offices limited patient encounters to well-child visits in the first 2 years of life to not miss opportunities for childhood vaccinations. However, some parents were reluctant to bring their children to those visits. There was no significant change in frequency of healthy child visits during the pandemic.
To our knowledge, this was the first study from primary care pediatric practices in the United States to analyze the effect on infectious diseases during the first 9 months of the pandemic, including the 6-month time period after the reopening from the first 3 months of lockdown. One prior study from a primary care network in Massachusetts reported significant decreases in respiratory infectious diseases for children aged 0-17 years during the first months of the pandemic during lockdown.2 A study in Tennessee that included hospital emergency department, urgent care, primary care, and retail health clinics also reported respiratory infection diagnoses as well as antibiotic prescription were reduced in the early months of the pandemic.3
Our study shows an overall reduction in frequency of respiratory illness visits in children 6-36 months old during the first 9 months of the COVID-19 pandemic. We learned the value of using technology in the form of virtual visits to render care. Perhaps as the pandemic subsides, many of the hand-washing and sanitizing practices will remain in place and lead to less frequent illness in children in the future. However, there may be temporary negative consequences from the “immune debt” that has occurred from a prolonged time span when children were not becoming infected with respiratory pathogens.4 We will see what unfolds in the future.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. Dr. Schulz is pediatric medical director at Rochester (N.Y.) Regional Health. Dr. Pichichero and Dr. Schulz have no conflicts of interest to disclose. This study was funded in part by the Centers for Disease Control and Prevention.
References
1. Kaur R et al. Front Pediatr. 2021;(9)722483:1-8.
2. Hatoun J et al. Pediatrics. 2020;146(4):e2020006460.
3. Katz SE et al. J Pediatric Infect Dis Soc. 2021;10(1):62-4.
4. Cohen R et al. Infect. Dis Now. 2021; 51(5)418-23.
A secondary consequence of public health measures to prevent the spread of SARS-CoV-2 included a concurrent reduction in risk for children to acquire and spread other respiratory viral infectious diseases. In the Rochester, N.Y., area, we had an ongoing prospective study in primary care pediatric practices that afforded an opportunity to assess the effect of the pandemic control measures on all infectious disease illness visits in young children. Specifically, in children aged 6-36 months old, our study was in place when the pandemic began with a primary objective to evaluate the changing epidemiology of acute otitis media (AOM) and nasopharyngeal colonization by potential bacterial respiratory pathogens in community-based primary care pediatric practices. As the public health measures mandated by New York State Department of Health were implemented, we prospectively quantified their effect on physician-diagnosed infectious disease illness visits. The incidence of infectious disease visits by a cohort of young children during the COVID-19 pandemic period March 15, 2020, through Dec. 31, 2020, was compared with the same time frame in the preceding year, 2019.1
Recommendations of the New York State Department of Health for public health, changes in school and day care attendance, and clinical practice during the study time frame
On March 7, 2020, a state of emergency was declared in New York because of the COVID-19 pandemic. All schools were required to close. A mandated order for public use of masks in adults and children more than 2 years of age was enacted. In the Finger Lakes region of Upstate New York, where the two primary care pediatric practices reside, complete lockdown was partially lifted on May 15, 2020, and further lifted on June 26, 2020. Almost all regional school districts opened to at least hybrid learning models for all students starting Sept. 8, 2020. On March 6, 2020, video telehealth and telephone call visits were introduced as routine practice. Well-child visits were limited to those less than 2 years of age, then gradually expanded to all ages by late May 2020. During the “stay at home” phase of the New York State lockdown, day care services were considered an essential business. Day care child density was limited. All children less than 2 years old were required to wear a mask while in the facility. Upon arrival, children with any respiratory symptoms or fever were excluded. For the school year commencing September 2020, almost all regional school districts opened to virtual, hybrid, or in-person learning models. Exclusion occurred similar to that of the day care facilities.
Incidence of respiratory infectious disease illnesses
Clinical diagnoses and healthy visits of 144 children from March 15 to Dec. 31, 2020 (beginning of the pandemic) were compared to 215 children during the same months in 2019 (prepandemic). Pediatric SARS-CoV-2 positivity rates trended up alongside community spread. Pediatric practice positivity rates rose from 1.9% in October 2020 to 19% in December 2020.
The table shows the incidence of significantly different infectious disease illness visits in the two study cohorts.
During the pandemic, 258 infection visits occurred among 144 pandemic cohort children, compared with 687 visits among 215 prepandemic cohort children, a 1.8-fold decrease (P < .0001). The proportion of children with visits for AOM (3.7-fold; P < .0001), bronchiolitis (7.4-fold; P = .036), croup (27.5-fold; P < .0001), and viral upper respiratory infection (3.8-fold; P < .0001) decreased significantly. Fever without a source (1.4-fold decrease; P = .009) and skin/soft tissue infection (2.1-fold decrease; P = .042) represented a higher proportion of visits during the pandemic.
Prescription of antibiotics significantly decreased (P < .001) during the pandemic.
Change in care practices
In the prepandemic period, virtual visits, leading to a diagnosis and treatment and referring children to an urgent care or hospital emergency department during regular office hours were rare. During the pandemic, this changed. Significantly increased use of telemedicine visits (P < .0001) and significantly decreased office and urgent care visits (P < .0001) occurred during the pandemic. Telehealth visits peaked the week of April 12, 2020, at 45% of all pediatric visits. In-person illness visits gradually returned to year-to-year volumes in August-September 2020 with school opening. Early in the pandemic, both pediatric offices limited patient encounters to well-child visits in the first 2 years of life to not miss opportunities for childhood vaccinations. However, some parents were reluctant to bring their children to those visits. There was no significant change in frequency of healthy child visits during the pandemic.
To our knowledge, this was the first study from primary care pediatric practices in the United States to analyze the effect on infectious diseases during the first 9 months of the pandemic, including the 6-month time period after the reopening from the first 3 months of lockdown. One prior study from a primary care network in Massachusetts reported significant decreases in respiratory infectious diseases for children aged 0-17 years during the first months of the pandemic during lockdown.2 A study in Tennessee that included hospital emergency department, urgent care, primary care, and retail health clinics also reported respiratory infection diagnoses as well as antibiotic prescription were reduced in the early months of the pandemic.3
Our study shows an overall reduction in frequency of respiratory illness visits in children 6-36 months old during the first 9 months of the COVID-19 pandemic. We learned the value of using technology in the form of virtual visits to render care. Perhaps as the pandemic subsides, many of the hand-washing and sanitizing practices will remain in place and lead to less frequent illness in children in the future. However, there may be temporary negative consequences from the “immune debt” that has occurred from a prolonged time span when children were not becoming infected with respiratory pathogens.4 We will see what unfolds in the future.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. Dr. Schulz is pediatric medical director at Rochester (N.Y.) Regional Health. Dr. Pichichero and Dr. Schulz have no conflicts of interest to disclose. This study was funded in part by the Centers for Disease Control and Prevention.
References
1. Kaur R et al. Front Pediatr. 2021;(9)722483:1-8.
2. Hatoun J et al. Pediatrics. 2020;146(4):e2020006460.
3. Katz SE et al. J Pediatric Infect Dis Soc. 2021;10(1):62-4.
4. Cohen R et al. Infect. Dis Now. 2021; 51(5)418-23.
A secondary consequence of public health measures to prevent the spread of SARS-CoV-2 included a concurrent reduction in risk for children to acquire and spread other respiratory viral infectious diseases. In the Rochester, N.Y., area, we had an ongoing prospective study in primary care pediatric practices that afforded an opportunity to assess the effect of the pandemic control measures on all infectious disease illness visits in young children. Specifically, in children aged 6-36 months old, our study was in place when the pandemic began with a primary objective to evaluate the changing epidemiology of acute otitis media (AOM) and nasopharyngeal colonization by potential bacterial respiratory pathogens in community-based primary care pediatric practices. As the public health measures mandated by New York State Department of Health were implemented, we prospectively quantified their effect on physician-diagnosed infectious disease illness visits. The incidence of infectious disease visits by a cohort of young children during the COVID-19 pandemic period March 15, 2020, through Dec. 31, 2020, was compared with the same time frame in the preceding year, 2019.1
Recommendations of the New York State Department of Health for public health, changes in school and day care attendance, and clinical practice during the study time frame
On March 7, 2020, a state of emergency was declared in New York because of the COVID-19 pandemic. All schools were required to close. A mandated order for public use of masks in adults and children more than 2 years of age was enacted. In the Finger Lakes region of Upstate New York, where the two primary care pediatric practices reside, complete lockdown was partially lifted on May 15, 2020, and further lifted on June 26, 2020. Almost all regional school districts opened to at least hybrid learning models for all students starting Sept. 8, 2020. On March 6, 2020, video telehealth and telephone call visits were introduced as routine practice. Well-child visits were limited to those less than 2 years of age, then gradually expanded to all ages by late May 2020. During the “stay at home” phase of the New York State lockdown, day care services were considered an essential business. Day care child density was limited. All children less than 2 years old were required to wear a mask while in the facility. Upon arrival, children with any respiratory symptoms or fever were excluded. For the school year commencing September 2020, almost all regional school districts opened to virtual, hybrid, or in-person learning models. Exclusion occurred similar to that of the day care facilities.
Incidence of respiratory infectious disease illnesses
Clinical diagnoses and healthy visits of 144 children from March 15 to Dec. 31, 2020 (beginning of the pandemic) were compared to 215 children during the same months in 2019 (prepandemic). Pediatric SARS-CoV-2 positivity rates trended up alongside community spread. Pediatric practice positivity rates rose from 1.9% in October 2020 to 19% in December 2020.
The table shows the incidence of significantly different infectious disease illness visits in the two study cohorts.
During the pandemic, 258 infection visits occurred among 144 pandemic cohort children, compared with 687 visits among 215 prepandemic cohort children, a 1.8-fold decrease (P < .0001). The proportion of children with visits for AOM (3.7-fold; P < .0001), bronchiolitis (7.4-fold; P = .036), croup (27.5-fold; P < .0001), and viral upper respiratory infection (3.8-fold; P < .0001) decreased significantly. Fever without a source (1.4-fold decrease; P = .009) and skin/soft tissue infection (2.1-fold decrease; P = .042) represented a higher proportion of visits during the pandemic.
Prescription of antibiotics significantly decreased (P < .001) during the pandemic.
Change in care practices
In the prepandemic period, virtual visits, leading to a diagnosis and treatment and referring children to an urgent care or hospital emergency department during regular office hours were rare. During the pandemic, this changed. Significantly increased use of telemedicine visits (P < .0001) and significantly decreased office and urgent care visits (P < .0001) occurred during the pandemic. Telehealth visits peaked the week of April 12, 2020, at 45% of all pediatric visits. In-person illness visits gradually returned to year-to-year volumes in August-September 2020 with school opening. Early in the pandemic, both pediatric offices limited patient encounters to well-child visits in the first 2 years of life to not miss opportunities for childhood vaccinations. However, some parents were reluctant to bring their children to those visits. There was no significant change in frequency of healthy child visits during the pandemic.
To our knowledge, this was the first study from primary care pediatric practices in the United States to analyze the effect on infectious diseases during the first 9 months of the pandemic, including the 6-month time period after the reopening from the first 3 months of lockdown. One prior study from a primary care network in Massachusetts reported significant decreases in respiratory infectious diseases for children aged 0-17 years during the first months of the pandemic during lockdown.2 A study in Tennessee that included hospital emergency department, urgent care, primary care, and retail health clinics also reported respiratory infection diagnoses as well as antibiotic prescription were reduced in the early months of the pandemic.3
Our study shows an overall reduction in frequency of respiratory illness visits in children 6-36 months old during the first 9 months of the COVID-19 pandemic. We learned the value of using technology in the form of virtual visits to render care. Perhaps as the pandemic subsides, many of the hand-washing and sanitizing practices will remain in place and lead to less frequent illness in children in the future. However, there may be temporary negative consequences from the “immune debt” that has occurred from a prolonged time span when children were not becoming infected with respiratory pathogens.4 We will see what unfolds in the future.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. Dr. Schulz is pediatric medical director at Rochester (N.Y.) Regional Health. Dr. Pichichero and Dr. Schulz have no conflicts of interest to disclose. This study was funded in part by the Centers for Disease Control and Prevention.
References
1. Kaur R et al. Front Pediatr. 2021;(9)722483:1-8.
2. Hatoun J et al. Pediatrics. 2020;146(4):e2020006460.
3. Katz SE et al. J Pediatric Infect Dis Soc. 2021;10(1):62-4.
4. Cohen R et al. Infect. Dis Now. 2021; 51(5)418-23.
Operational Curriculum and Research Initiatives: Shaping the Future of Military Medicine
It is a time of significant change as the Military Health System (MHS) transitions to the purview of the Defense Health Agency (DHA). Additionally, the landscape of combat is ever changing, and military medicine needs to evolve to ensure that the lessons learned are utilized to optimize care of the war fighters. The purpose of this review is to evaluate the available literature on existing operational medicine curriculums and make recommendations to restructure current military medicine training to produce operationally prepared clinicians who are informed in operationally focused research principles.
Operational Medicine
Before diving into the importance of creating a curriculum and investing in training for scholarly activity proficiency, operational medicine needs to be defined. It can be defined as medical care provided in an austere environment with limited resources and possibly under hostile conditions. Another way to look at operational medicine is as the evaluation of normal human physiology and pathology under abnormal conditions. The mission set of each of the services is unique. The Marines and Army may operate forward past the wire vulnerable to the environment, gunfire, and improvised explosive devices, remote from fixed medical facilities. The Navy has divers exposed to the risks of decompression sickness. The Air Force has pilots exposed to altitude changes and strains of G-forces during flight. Locations vary from cold high-altitude mountainous regions to high-temperature desolate deserts. Many times, medical practitioners may be remotely stationed, far from specialty or immediate definitive care. Patient care may consist of low-acuity management of individual patients in sick call to mass casualty events where patient numbers and morbidity may outstrip available resources, making the difficult task of triage necessary.
Despite the challenges of being a uniformed physician, the benefits of being embedded is a better understanding of the roles and capability of the unit. Military physicians need to have the unique knowledge of the type of injuries sustained in that particular theater of war, such as differentiating between the trauma pattern and care required for blast injuries vs high-velocity missiles. There are also chemical, biologic, radiologic, and nuclear threats that military physicians need to recognize. Much of what disables a military fighting force is not a direct relationship to combat-related injuries; however, entire units have been taken down by infectious diarrhea or trench foot. There is also a need for familiarity of the infections and parasitology endemic to the particular theater with the aim of implementation of prevention whenever possible.
Military medicine does not fit in any box. Military physicians need to know the job requirements of various specialties, including elements of occupational medicine, such as aircrew piloting high-performance fighters or ground troops fully loaded with body armor and 80-lb backpacks. There are musculoskeletal injuries from the stressors of various military occupations. Working around weaponry and contact with hostile forces will create scenarios requiring emergent and critical care. In addition to physical injuries, there is the mental strain of combat with the risk of imminent personal injury, the guilt of survivorship, dealing with the scars and permanent physical damage of combat, and prolonged separation from family and other support systems.
The National Defense Authorization Act 2017 mandated the establishment of a standardized process to oversee all military graduate medical education (GME) programs with the goal of ensuring medical operational readiness.1 This is no small task with > 3000 residents in more than 70 specialties, comprising approximately 12% of US residents.1,2 Presently, 26 to 32% of the medical corps is enrolled in full-time training compared with 12% of the total force.2 With significant time and resources expended during this period, it is vital to maximize the potential of the training.
Literature Review
A literature review was performed, evaluating historical precedence of specialized military medical training and research as well as current operational curriculums. Literature search was conducted in the PubMed and Uniformed Services University (USU) Learning Resource databases using the terms “operational medicine curriculum,” “military medicine curriculum,” “operational medicine training,” “military medicine training,” “operational medicine research,” and “military medicine research,” and included all articles from 1997 to 2020. Inclusion criteria included studies that detailed military medicine training programs and/or outcomes. The source types used in this research project included peer-reviewed journal publications—both review articles and original research—from medical and military journals. The citations of these articles were also reviewed for additional usable publications. Secondary sources included official reports and studies by the RAND Corporation, the US Government Accountability Office, and the Institute for Defense Analysis (IDA). Due to lack of literature on the topic, other sources such as talking papers, letters, and formal presentations from subject matter experts were included to showcase the current state and gaps on this topic. Key findings from peer-reviewed publications are presented in Table 1.
Overall, the literature review showed that longitudinal deliberately mapped out curriculums can be well integrated into the existing medical curriculum.3 The military medicine course topics include environmental medicine, applied field medicine, combat casualty care, medical support planning, mass casualty incident preparation, and military-focused problem solving, decision making, and leadership.4
One 1997 study looked at the degree of implementation of military unique curriculum in 18 family medicine residencies. Only 30% of residents stated that their program had a specific operational medicine curriculum.5 Salerno and colleagues surveyed current residents and recently graduated internal medicine physicians at 14 facilities in the Army, Air Force, and Navy to determine confidence level with military medicine. More than half did not feel ready to practice deployment medicine; just 19% felt comfortable treating nuclear, biologic, and chemical warfare injuries; and 32% felt unfamiliar with the command and administrative duties. A subgroup analysis showed that USU graduates felt more prepared in these areas compared with civilian program graduates.6 Additional studies showed perceived smoother transition in the first active-duty tour after participation in an operational curriculum.7
Didactics can provide a foundation. However, just as the practice of medicine is learned in the clinic, the art of military medicine is learned in the field. Hands-on training in one study was accomplished through the Combat Casualty Care Course (C4), the USU Bushmaster exercise, and a field training exercise. The field exercise included components of mission planning, medical threat assessments, triage of a mass casualty situation, management of disease and nonbattle injuries, combat stress casualties, resource management, and patient evacuation.8
Another publication described a similar longitudinal curriculum with C4 after the first year of training and the Medical Management of Chemical and Biological Casualty Course during the second year. The operational curriculum 3-day capstone occurred at the end of medical training utilizing mannequins to realistically simulate combat casualty care, including emergency airways, chest tube, and tourniquets.9 Due to the current deployment tempo, just in time refresher courses like this could be valuable preparation.
While most of the operational curriculums evaluated assessed efficiency over a short time interval, one study looked at 1189 graduates from the military medical school from the past 20 years. Preparedness was perceived to be high for military-unique practice and leadership.10 The operational curriculum at USU had been purposefully structured to provide continuity. Didactics and casework were reinforced with hands-on training whether through realistic simulator training or field exercises. The authors note a weakness of many operational curriculums is inconsistency and fragmented training without deliberate longitudinal planning.
One of the more recent military GME curriculums include the creation of the operational medicine residency in 2013, which created a standardized longitudinal operational curriculum integrated along with the existing family medicine, emergency medicine, or internal medicine curriculum to create mission-ready military physicians upon graduation. Scheduled rotations include global medicine, aeromedical evacuation, occupational medicine, and tropical medicine. Completing military officer professional development and an operationally relevant research project is an expectation (Table 2).11
In addition to in-program training, other options include operational rotations offsite and military courses conducted outside the GME program.12 Some of these courses may include just-in-time training such as expeditionary medical support system training prior to scheduled deployments. Examples of experiential training are listed in Table 3.
Critical Analysis
Current gaps were identified in the military medicine training pipeline’s operational medicine curriculum and research programs. The analysis looked at specific components that make the operational medicine curriculum and research unique as well as current readiness goals, to determine how to best align both to meet the mission requirements. Some factors considered included efficiency, cost, program portability, duplication minimization, retention, and sustainability.
Efficiency
A well-created curriculum that meets objectives will require more than an assigned rotation and a few lectures. The most successful ones in the literature review were the ones that were deliberately planned and longitudinal, such as the ones at USU that combined a mixture of classroom and field exercises over the course of 4 years.4,8 In that way, the curriculum may not be considered time efficient, but if integrated well into the already existing medical training, the production of military physicians who are mission ready upon graduation—ready to serve as military medical leaders and deploy—will be invaluable.
Cost Comparison
Due to the associated overhead of running a training platform and the additional hours of operational training, military GME is more expensive initially compared with civilian outsourcing. In USU, for example, there is an additional 700 hours of operational curriculum alone. This cost difference more than doubles the cost of a USU education vs a Health Professional Scholarship Program (HPSP) scholarship at a civilian medical school. However, a causal analysis performed by the IDA to determine value basis noted that USU graduates deploy almost 3 times as much and serve 6 years longer on active duty.3
After graduating medical school through either accession source, physicians complete specialization training in a GME program. The IDA study noted an average $12,000 increased cost of military GME compared with civilian programs. The analysis included resident compensation and overhead costs of running the program as well as the net cost, which also accounted for resident productivity and workload by training in a military facility.3 Calculations due to mandated budget cuts estimated cost savings of closing the military medical school at < $100 million while significantly impacting the military physician pipeline and operational research output.3
Duplication of Effort
There are already established training programs such as Tactical Combat Casualty Care (TCCC) that could be incorporated into the curriculum to avoid expending additional resources to recreate the wheel. USU has a validated operational training curriculum and may be able to make opportunities available for outside trainees to participate in some of its military-unique training and leadership exercises. Other ways to decrease duplication of effort and improve cost efficiency include focusing on the creation of an academic health system (AHS) and consolidating similar programs to conserve resources. Increasing existing military program sizes will not only ensure the continuation of the military medicine pipeline, but will spread overhead costs over a larger cohort, decrease costs of civilian outsourcing, and ensure the less tangible benefits of military cultural exposure early in trainees’ careers. For example, increasing the class size of USU by 30 students actually reduces the cost per student to $239,000 per year from $253,000, while decreasing the need for HPSP accessions training in civilian programs, making the endeavor overall cost neutral.3
Program Portability
The operational medicine residency has proved that an operational curriculum can be remotely managed and reproduced at a variety of residency specialties.12 Remote education could be developed and distributed throughout the MHS, such as the proposed USU course Military Medicine and Leadership course.3 Centralized training programs like Global Medicine and C-STARS could be scheduled TDYs during the medical training calendar.
Retention
The military medical school, USU, is the largest military medicine accession source. An IDA report notes that retention of USU graduates is 15.2 years compared with 9.2 years served by civilian trainees. Due to the longevity in service, USU graduates also make up more than 25% of military medical leadership.4 The long-term outcome study that looked at the past 40 years of USU graduates observed that over 70% of graduates served until retirement eligibility and are overrepresented in special operations units.3,13 While some of this longevity may be attributed to the longer USU service contracts, military GME graduates were still noted to be 4 times more likely to commit to a multiyear service contract.14 A RAND study on the retention of military physicians in the Army, Air Force, and Navy noted that overall retention increased throughout all the services for physicians who went through the military GME pipeline.15 Conversely, civilian GME training was associated with a 45% chance in leaving active duty.16
It is theorized that early military acculturation during training increases the likelihood of instilling a sense of mission. Being involved in military GME on the teaching side also showed increased retention rates for 63% of survey respondents.17 Reduced burnout and increased work satisfaction for those involved in military GME was noted on another faculty satisfaction survey.17
Sustainability
Programs like USU, which have been around for decades, and the newer operational residency program evolving since 2013 have shown sustainability.4,11 Dissemination of proven curriculums as well as centralization of already validated training programs can help standardize operational medical training throughout the MHS. In order to flourish at individual programs, the faculty need to be well versed in a train the trainer model and have institutional support. The ability to engage with the line at individual locations may be a factor as well.18 In regard to research, once residents are taught the principles of scholarly activity, they will have the tools to continue operational medicine research advancements and mentoring students.
Discussion
The 2020 NDAA recommends the establishment of an AHS.3 This step will create a culture of military medical readiness from the top down as congressional mandates push reorganization of the MHS, including military GME programs. An overall restructuring of military medicine will require prioritization of resources toward operational requirements vs the historic significant division of attention to beneficiary care that has caused a lack of unity of effort and additional strain on an already heavily tasked medical force. The changes in military GME are just one aspect of that. It is vital to look at the restructuring with a comprehension of the unique challenges of combat health rather than only from an in-garrison, hospital-based aspect.19 Benefits of having a military medicine AHS include opportunities to share resources and successful business models as well as foster interdisciplinary teamwork and partnerships with civilian health care facilities and research institutions as a force multiplier.19
There has been recent discussion about budget cuts, including shutting down USU and military GME and transitioning all training to civilian programs to be cost-effective.4 If this were to happen, it would be a step backward from the goal of operational readiness. Maintaining US Department of Defense (DoD) control of the military medicine pipeline has innumerable benefits, including built-in mentorship from operationally-seasoned faculty, military leadership development, proficiency in MHS systems, open communication between GME programs and DoD, and curriculum control to ensure focus on readiness.20 Military GME programs are also a significant production source of military-related scholarly activity. Over fiscal year 2017/2018, 63% of the publications out of the San Antonio Uniformed Services Health Education Consortium—the largest Air Force GME platform and second largest multiservice GME platform—involved military relevant medical topics.17 Much of the volume of operational research as well as the relevant skills learned and future innovations secondary to conducting this research would be lost if military GME did not exist.17,21
Practically speaking, military GME provides the majority of the military medicine accessions. For example, a presentation by the Air Force Chief of Physician Education noted that the total military GME pipeline included 2875 students, but direct physician access averaged only 20 physicians a year.22 Even if the decision was made to defer to civilian education, capacity does not exist in civilian GME programs. This is worsened by the increased competitiveness of the GME match with the proliferation of medical schools without concurrent increase in residency spots. The 2018 National Resident Matching Program noted that there were more than 37,103 US and foreign applicants for only 33,000 residency positions, leaving many US applicants unmatched.17 It is doubtful that the civilian GME programs would be able to absorb the influx of military residents, affecting both the military and civilian medicine pipelines. As a secondary effect, the military treatment centers that house the military GME programs would have to close, with surrounding civilian medical facilities also likely unable to absorb the sudden influx of patients and residents losing the intangible benefits of caring for a military population.15 This was even recognized by the civilian president of the Accreditation Council for Graduate Medical Education:
Military physicians must be trained in the systems of care that are operative in military medicine, which is significantly unlike civilian medicine in many ways. It is often practiced in circumstances that are not seen in civilian medicine, within care structures that are not encountered in American medical practice… Military medicine has advanced research into the care of individuals suffering traumatic injury, critical care, rehabilitation medicine, prosthetics, psychiatric care of those traumatized, and closed head injury, to name a just a few. The sacrifices of our active military demand these advances, and the American Public benefit from these advances.21
Where deficiencies exist in military GME, it is possible to use the growing military-civilian training institution partnerships. Two prime examples are the just-in-time deployment training done with civilian trauma facilities by the Air Force Center for the Sustainment of Trauma Readiness Skills and the Air Force Special Operations Surgical Team-Special Operations Critical Care Evacuation Team being embedded in civilian facilities to maintain trauma, surgical, and emergency care skills. While military physicians can maintain competencies, at the same time, the civilian sector can benefit from the lessons learned in the military in regard to mass casualty and disaster responses. Fostering military and civilian training agreements can also enhance research opportunities.1
Just as the realities of operational medicine frequently require the military physician to think outside the box, the most successful methods of instruction of military medicine tend to be nontraditional. Classroom education should be involved beyond lectures and can include other methods, such as case-based, role-playing, small group discussion, and computer-based teaching. Maintaining flexibility in live vs distance learning as well as synchronous vs asynchronous learning can expand the capacity of available instructors and standardize material over several sites.23 Asking learners to consider operational concerns, such as whether certain medical conditions would be compatible with military duty in addition to the routine investigation is an easy way to incorporate military training in preexisting medical training.12 The advancement of technology has made simulation one of the best ways to engage in hands-on learning, whether through computer simulations, animal models, standardized or moulaged patients, or mannequins that can realistically mimic medical or trauma-related conditions.24 Many times, simulation can be combined with exercises in the field to create a realistic operational environment.23
There are 3 pillars of an operational curriculum that should be integrated into the existing residency curriculum—operational medicine, leadership, and research principles (Appendix).
Conclusions
Judging by the continuing operational tempo and evolution of warfare, maintaining enhanced military medical readiness will remain a priority. Operational medicine is a unique field that requires specialized preparation. Studies have shown that longitudinal deliberately mapped out curriculums are able to be integrated well into the existing medical curriculum. The recommendation moving forward is increasing the access of existing operational training structures that have well established programs and modeling individual GME program curriculums after those that have shown proven success with a focus on the 3 pillars of operational training, leadership, and research.
Acknowledgments
Previously submitted in April 2020 in expanded form as part of graduation requirements for the Masters of Military Arts and Science degree program at Air University, Maxwell Air Force Base in Alabama.
1. US Government Accountability Office. Defense Health Care: DoD’s proposed plan for oversight of graduate medical education program. Published March 2019. Accessed September 24, 2021. https://www.gao.gov/assets/700/698075.pdf
2. De Lorenzo RA. Accreditation status of U.S. military graduate medical education programs. Mil Med. 2008;173(7):635-640. doi:10.7205/milmed.173.7.635
3. John SK, Bishop JM, Hidreth LA, et al; Institute for Defense Analysis. Analysis of DoD accession alternatives for military physicians: readiness value and cost. Published October 2019. Accessed September 24, 2021. https://www.ida.org/-/media/feature/publications/a/an/analysis-of-dod-accession-alternatives-for-military-physicians-readiness-value-and-cost/p-10815.ashx.
4. O’Connor FG, Grunberg N, Kellermann AL, Schoomaker E. Leadership education and development at the Uniformed Services University. Mil Med. 2015;180(suppl 4):147-152. doi:10.7205/MILMED-D-14-00563
5. Suls H, Karnei K, Gardner JW, Fogarty JP, Llewellyn CH. The extent of military medicine topics taught in military family practice residency programs: Part II, a survey of residency graduates from 1987-1990. Mil Med. 1997;162(6):428-434. doi:10.1093/milmed/162.6.428
6. Salerno S, Cash B, Cranston M, Schoomaker E. Perceptions of current and recent military internal medicine residents on operational medicine, managed care, graduate medical education, and continued military service. Mil Med. 1998;163(6):392-397. doi:10.1093/milmed/163.6.392
7. Roop SA, Murray CK, Pugh AM, Phillips YY, Bolan CD. Operational medicine experience integrated into a military internal medicine residency curriculum. Mil Med. 2001;166(1):34-39. doi:10.1093/milmed/166.1.34
8. Perkins JG, Roy MJ, Bolan CD, Phillips YY. Operational experiences during medical residency: perspectives from the Walter Reed Army Medical Center Department of Medicine. Mil Med. 2001;166(12):1038-1045. doi:10.1093/milmed/166.12.1038
9. Murray CK, Reynolds JC, Boyer DA, et al. Development of a deployment course for graduating military internal medicine residents. Mil Med. 2006;171(10):933-936. doi:10.7205/milmed.171.10.933. doi:10.7205/milmed.171.10.933
10. Picho K, Gilliland WR, Artino AR Jr, et al. Assessing curriculum effectiveness: a survey of Uniformed Services University medical school graduates. Mil Med. 2015;180(suppl 4):113-128. doi:10.7205/MILMED-D-14-00570
11. Jacobson MD: Operational Aerospace medicine collaborative programs: past, present, and future. US Air Force School of Aerospace Medicine Presentation. November 1, 2018.
12. Roy MJ, Brietzke S, Hemmer P, Pangaro L, Goldstein R. Teaching military medicine: enhancing military relevance within the fabric of current medical training. Mil Med. 2002;167(4):277-280. doi:10.1093/miled.milmed.167.4.277
13. Durning SJ, Dong T, LaRochelle JL, et al. The long-term career outcome study: lessons learned and implications for educational practice. Mil Med. 2015;180(suppl 4):164-170. doi:10.7205/MILMED-D-14-00574
14. Keating EG, Brauner MK, Galway LA, Mele JD, Burks JJ, Saloner B. The Air Force Medical Corps’ status and how its physicians respond to multiyear special pay. Mil Med. 2009;174(11):1155-1162. doi:10.7205/milmed-d-01-4309
15. Mundell BF. Retention of military physicians: the differential effects of practice opportunities across the three services. RAND Corporation; 2010:74-77. Accessed September 24, 2021. https://www.rand.org/pubs/rgs_dissertations/RGSD275.html
16. Nagy CJ. The importance of a military-unique curriculum in active duty graduate medical education. Mil Med. 2012;177(3):243-244. doi:10.7205/milmed-d-11-00280
17. True M: The value of military graduate medical education. SAUSHEC interim dean talking paper. November 2, 2018.
18. Hatzfeld JJ, Khalili RA, Hendrickson TL, Reilly PA. Publishing military medical research: appreciating the process. Mil Med. 2016;181(suppl 5):5-6. doi:10.7205/MILMED-D-15-00517
19. Sauer SW, Robinson JB, Smith MP, et al. Lessons learned: saving lives on the battlefield. J Spec Oper Med. 2016;15(2). 25-41.
20. Tankersley MS: Air Force Physician Education Branch response to GME questions. Talking Paper. Feb 23, 2015.
21. Nasca TJ. [Letter] Published October 26, 2019. Accessed September 24, 2021. https://www.moaa.org/uploadedfiles/nasca-to-kellerman-a--cordts-p-2019-10-26.pdf
22. Forgione MA: USAF-SAM GME Brief. Air Force Personnel Center. October 2018.
23. Turner M, Wilson C, Gausman K, Roy MJ. Optimal methods of learning for military medical education. Mil Med. 2003;168(suppl 9):46-50. doi:10.1093/milmed/168.suppl_1.46
24. Goolsby C, Deering S. Hybrid simulation during military medical student field training--a novel curriculum. Mil Med. 2013;178(7):742-745. doi:10.7205/MILMED-D-12-00541
25. Hartzell JD, Yu CE, Cohee BM, Nelson MR, Wilson RL. Moving beyond accidental leadership: a graduate medical education leadership curriculum needs assessment. Mil Med. 2017;182(7):e1815-e1822. doi:10.7205/MILMED-D-16-00365
26. Barry ES, Dong T, Durning SJ, Schreiber-Gregory D, Torre D, Grunberg NE. Medical Student Leader Performance in an Applied Medical Field Practicum. Mil Med. 2019;184(11-12):653-660. doi:10.1093/milmed/usz121
27. Air Force Medical Corps Development Team: Medical corps integrated OPS career path. MC Pyramids 2019 Presentation. January 18, 2019. https://kx.health.mil [Nonpublic source, not verified]
28. Polski MM: Back to basics—research design for the operational level of war. Naval War College Rev. 2019;72(3):1-23. https://digital-commons.usnwc.edu/nwc-review/vol72/iss3/6.
It is a time of significant change as the Military Health System (MHS) transitions to the purview of the Defense Health Agency (DHA). Additionally, the landscape of combat is ever changing, and military medicine needs to evolve to ensure that the lessons learned are utilized to optimize care of the war fighters. The purpose of this review is to evaluate the available literature on existing operational medicine curriculums and make recommendations to restructure current military medicine training to produce operationally prepared clinicians who are informed in operationally focused research principles.
Operational Medicine
Before diving into the importance of creating a curriculum and investing in training for scholarly activity proficiency, operational medicine needs to be defined. It can be defined as medical care provided in an austere environment with limited resources and possibly under hostile conditions. Another way to look at operational medicine is as the evaluation of normal human physiology and pathology under abnormal conditions. The mission set of each of the services is unique. The Marines and Army may operate forward past the wire vulnerable to the environment, gunfire, and improvised explosive devices, remote from fixed medical facilities. The Navy has divers exposed to the risks of decompression sickness. The Air Force has pilots exposed to altitude changes and strains of G-forces during flight. Locations vary from cold high-altitude mountainous regions to high-temperature desolate deserts. Many times, medical practitioners may be remotely stationed, far from specialty or immediate definitive care. Patient care may consist of low-acuity management of individual patients in sick call to mass casualty events where patient numbers and morbidity may outstrip available resources, making the difficult task of triage necessary.
Despite the challenges of being a uniformed physician, the benefits of being embedded is a better understanding of the roles and capability of the unit. Military physicians need to have the unique knowledge of the type of injuries sustained in that particular theater of war, such as differentiating between the trauma pattern and care required for blast injuries vs high-velocity missiles. There are also chemical, biologic, radiologic, and nuclear threats that military physicians need to recognize. Much of what disables a military fighting force is not a direct relationship to combat-related injuries; however, entire units have been taken down by infectious diarrhea or trench foot. There is also a need for familiarity of the infections and parasitology endemic to the particular theater with the aim of implementation of prevention whenever possible.
Military medicine does not fit in any box. Military physicians need to know the job requirements of various specialties, including elements of occupational medicine, such as aircrew piloting high-performance fighters or ground troops fully loaded with body armor and 80-lb backpacks. There are musculoskeletal injuries from the stressors of various military occupations. Working around weaponry and contact with hostile forces will create scenarios requiring emergent and critical care. In addition to physical injuries, there is the mental strain of combat with the risk of imminent personal injury, the guilt of survivorship, dealing with the scars and permanent physical damage of combat, and prolonged separation from family and other support systems.
The National Defense Authorization Act 2017 mandated the establishment of a standardized process to oversee all military graduate medical education (GME) programs with the goal of ensuring medical operational readiness.1 This is no small task with > 3000 residents in more than 70 specialties, comprising approximately 12% of US residents.1,2 Presently, 26 to 32% of the medical corps is enrolled in full-time training compared with 12% of the total force.2 With significant time and resources expended during this period, it is vital to maximize the potential of the training.
Literature Review
A literature review was performed, evaluating historical precedence of specialized military medical training and research as well as current operational curriculums. Literature search was conducted in the PubMed and Uniformed Services University (USU) Learning Resource databases using the terms “operational medicine curriculum,” “military medicine curriculum,” “operational medicine training,” “military medicine training,” “operational medicine research,” and “military medicine research,” and included all articles from 1997 to 2020. Inclusion criteria included studies that detailed military medicine training programs and/or outcomes. The source types used in this research project included peer-reviewed journal publications—both review articles and original research—from medical and military journals. The citations of these articles were also reviewed for additional usable publications. Secondary sources included official reports and studies by the RAND Corporation, the US Government Accountability Office, and the Institute for Defense Analysis (IDA). Due to lack of literature on the topic, other sources such as talking papers, letters, and formal presentations from subject matter experts were included to showcase the current state and gaps on this topic. Key findings from peer-reviewed publications are presented in Table 1.
Overall, the literature review showed that longitudinal deliberately mapped out curriculums can be well integrated into the existing medical curriculum.3 The military medicine course topics include environmental medicine, applied field medicine, combat casualty care, medical support planning, mass casualty incident preparation, and military-focused problem solving, decision making, and leadership.4
One 1997 study looked at the degree of implementation of military unique curriculum in 18 family medicine residencies. Only 30% of residents stated that their program had a specific operational medicine curriculum.5 Salerno and colleagues surveyed current residents and recently graduated internal medicine physicians at 14 facilities in the Army, Air Force, and Navy to determine confidence level with military medicine. More than half did not feel ready to practice deployment medicine; just 19% felt comfortable treating nuclear, biologic, and chemical warfare injuries; and 32% felt unfamiliar with the command and administrative duties. A subgroup analysis showed that USU graduates felt more prepared in these areas compared with civilian program graduates.6 Additional studies showed perceived smoother transition in the first active-duty tour after participation in an operational curriculum.7
Didactics can provide a foundation. However, just as the practice of medicine is learned in the clinic, the art of military medicine is learned in the field. Hands-on training in one study was accomplished through the Combat Casualty Care Course (C4), the USU Bushmaster exercise, and a field training exercise. The field exercise included components of mission planning, medical threat assessments, triage of a mass casualty situation, management of disease and nonbattle injuries, combat stress casualties, resource management, and patient evacuation.8
Another publication described a similar longitudinal curriculum with C4 after the first year of training and the Medical Management of Chemical and Biological Casualty Course during the second year. The operational curriculum 3-day capstone occurred at the end of medical training utilizing mannequins to realistically simulate combat casualty care, including emergency airways, chest tube, and tourniquets.9 Due to the current deployment tempo, just in time refresher courses like this could be valuable preparation.
While most of the operational curriculums evaluated assessed efficiency over a short time interval, one study looked at 1189 graduates from the military medical school from the past 20 years. Preparedness was perceived to be high for military-unique practice and leadership.10 The operational curriculum at USU had been purposefully structured to provide continuity. Didactics and casework were reinforced with hands-on training whether through realistic simulator training or field exercises. The authors note a weakness of many operational curriculums is inconsistency and fragmented training without deliberate longitudinal planning.
One of the more recent military GME curriculums include the creation of the operational medicine residency in 2013, which created a standardized longitudinal operational curriculum integrated along with the existing family medicine, emergency medicine, or internal medicine curriculum to create mission-ready military physicians upon graduation. Scheduled rotations include global medicine, aeromedical evacuation, occupational medicine, and tropical medicine. Completing military officer professional development and an operationally relevant research project is an expectation (Table 2).11
In addition to in-program training, other options include operational rotations offsite and military courses conducted outside the GME program.12 Some of these courses may include just-in-time training such as expeditionary medical support system training prior to scheduled deployments. Examples of experiential training are listed in Table 3.
Critical Analysis
Current gaps were identified in the military medicine training pipeline’s operational medicine curriculum and research programs. The analysis looked at specific components that make the operational medicine curriculum and research unique as well as current readiness goals, to determine how to best align both to meet the mission requirements. Some factors considered included efficiency, cost, program portability, duplication minimization, retention, and sustainability.
Efficiency
A well-created curriculum that meets objectives will require more than an assigned rotation and a few lectures. The most successful ones in the literature review were the ones that were deliberately planned and longitudinal, such as the ones at USU that combined a mixture of classroom and field exercises over the course of 4 years.4,8 In that way, the curriculum may not be considered time efficient, but if integrated well into the already existing medical training, the production of military physicians who are mission ready upon graduation—ready to serve as military medical leaders and deploy—will be invaluable.
Cost Comparison
Due to the associated overhead of running a training platform and the additional hours of operational training, military GME is more expensive initially compared with civilian outsourcing. In USU, for example, there is an additional 700 hours of operational curriculum alone. This cost difference more than doubles the cost of a USU education vs a Health Professional Scholarship Program (HPSP) scholarship at a civilian medical school. However, a causal analysis performed by the IDA to determine value basis noted that USU graduates deploy almost 3 times as much and serve 6 years longer on active duty.3
After graduating medical school through either accession source, physicians complete specialization training in a GME program. The IDA study noted an average $12,000 increased cost of military GME compared with civilian programs. The analysis included resident compensation and overhead costs of running the program as well as the net cost, which also accounted for resident productivity and workload by training in a military facility.3 Calculations due to mandated budget cuts estimated cost savings of closing the military medical school at < $100 million while significantly impacting the military physician pipeline and operational research output.3
Duplication of Effort
There are already established training programs such as Tactical Combat Casualty Care (TCCC) that could be incorporated into the curriculum to avoid expending additional resources to recreate the wheel. USU has a validated operational training curriculum and may be able to make opportunities available for outside trainees to participate in some of its military-unique training and leadership exercises. Other ways to decrease duplication of effort and improve cost efficiency include focusing on the creation of an academic health system (AHS) and consolidating similar programs to conserve resources. Increasing existing military program sizes will not only ensure the continuation of the military medicine pipeline, but will spread overhead costs over a larger cohort, decrease costs of civilian outsourcing, and ensure the less tangible benefits of military cultural exposure early in trainees’ careers. For example, increasing the class size of USU by 30 students actually reduces the cost per student to $239,000 per year from $253,000, while decreasing the need for HPSP accessions training in civilian programs, making the endeavor overall cost neutral.3
Program Portability
The operational medicine residency has proved that an operational curriculum can be remotely managed and reproduced at a variety of residency specialties.12 Remote education could be developed and distributed throughout the MHS, such as the proposed USU course Military Medicine and Leadership course.3 Centralized training programs like Global Medicine and C-STARS could be scheduled TDYs during the medical training calendar.
Retention
The military medical school, USU, is the largest military medicine accession source. An IDA report notes that retention of USU graduates is 15.2 years compared with 9.2 years served by civilian trainees. Due to the longevity in service, USU graduates also make up more than 25% of military medical leadership.4 The long-term outcome study that looked at the past 40 years of USU graduates observed that over 70% of graduates served until retirement eligibility and are overrepresented in special operations units.3,13 While some of this longevity may be attributed to the longer USU service contracts, military GME graduates were still noted to be 4 times more likely to commit to a multiyear service contract.14 A RAND study on the retention of military physicians in the Army, Air Force, and Navy noted that overall retention increased throughout all the services for physicians who went through the military GME pipeline.15 Conversely, civilian GME training was associated with a 45% chance in leaving active duty.16
It is theorized that early military acculturation during training increases the likelihood of instilling a sense of mission. Being involved in military GME on the teaching side also showed increased retention rates for 63% of survey respondents.17 Reduced burnout and increased work satisfaction for those involved in military GME was noted on another faculty satisfaction survey.17
Sustainability
Programs like USU, which have been around for decades, and the newer operational residency program evolving since 2013 have shown sustainability.4,11 Dissemination of proven curriculums as well as centralization of already validated training programs can help standardize operational medical training throughout the MHS. In order to flourish at individual programs, the faculty need to be well versed in a train the trainer model and have institutional support. The ability to engage with the line at individual locations may be a factor as well.18 In regard to research, once residents are taught the principles of scholarly activity, they will have the tools to continue operational medicine research advancements and mentoring students.
Discussion
The 2020 NDAA recommends the establishment of an AHS.3 This step will create a culture of military medical readiness from the top down as congressional mandates push reorganization of the MHS, including military GME programs. An overall restructuring of military medicine will require prioritization of resources toward operational requirements vs the historic significant division of attention to beneficiary care that has caused a lack of unity of effort and additional strain on an already heavily tasked medical force. The changes in military GME are just one aspect of that. It is vital to look at the restructuring with a comprehension of the unique challenges of combat health rather than only from an in-garrison, hospital-based aspect.19 Benefits of having a military medicine AHS include opportunities to share resources and successful business models as well as foster interdisciplinary teamwork and partnerships with civilian health care facilities and research institutions as a force multiplier.19
There has been recent discussion about budget cuts, including shutting down USU and military GME and transitioning all training to civilian programs to be cost-effective.4 If this were to happen, it would be a step backward from the goal of operational readiness. Maintaining US Department of Defense (DoD) control of the military medicine pipeline has innumerable benefits, including built-in mentorship from operationally-seasoned faculty, military leadership development, proficiency in MHS systems, open communication between GME programs and DoD, and curriculum control to ensure focus on readiness.20 Military GME programs are also a significant production source of military-related scholarly activity. Over fiscal year 2017/2018, 63% of the publications out of the San Antonio Uniformed Services Health Education Consortium—the largest Air Force GME platform and second largest multiservice GME platform—involved military relevant medical topics.17 Much of the volume of operational research as well as the relevant skills learned and future innovations secondary to conducting this research would be lost if military GME did not exist.17,21
Practically speaking, military GME provides the majority of the military medicine accessions. For example, a presentation by the Air Force Chief of Physician Education noted that the total military GME pipeline included 2875 students, but direct physician access averaged only 20 physicians a year.22 Even if the decision was made to defer to civilian education, capacity does not exist in civilian GME programs. This is worsened by the increased competitiveness of the GME match with the proliferation of medical schools without concurrent increase in residency spots. The 2018 National Resident Matching Program noted that there were more than 37,103 US and foreign applicants for only 33,000 residency positions, leaving many US applicants unmatched.17 It is doubtful that the civilian GME programs would be able to absorb the influx of military residents, affecting both the military and civilian medicine pipelines. As a secondary effect, the military treatment centers that house the military GME programs would have to close, with surrounding civilian medical facilities also likely unable to absorb the sudden influx of patients and residents losing the intangible benefits of caring for a military population.15 This was even recognized by the civilian president of the Accreditation Council for Graduate Medical Education:
Military physicians must be trained in the systems of care that are operative in military medicine, which is significantly unlike civilian medicine in many ways. It is often practiced in circumstances that are not seen in civilian medicine, within care structures that are not encountered in American medical practice… Military medicine has advanced research into the care of individuals suffering traumatic injury, critical care, rehabilitation medicine, prosthetics, psychiatric care of those traumatized, and closed head injury, to name a just a few. The sacrifices of our active military demand these advances, and the American Public benefit from these advances.21
Where deficiencies exist in military GME, it is possible to use the growing military-civilian training institution partnerships. Two prime examples are the just-in-time deployment training done with civilian trauma facilities by the Air Force Center for the Sustainment of Trauma Readiness Skills and the Air Force Special Operations Surgical Team-Special Operations Critical Care Evacuation Team being embedded in civilian facilities to maintain trauma, surgical, and emergency care skills. While military physicians can maintain competencies, at the same time, the civilian sector can benefit from the lessons learned in the military in regard to mass casualty and disaster responses. Fostering military and civilian training agreements can also enhance research opportunities.1
Just as the realities of operational medicine frequently require the military physician to think outside the box, the most successful methods of instruction of military medicine tend to be nontraditional. Classroom education should be involved beyond lectures and can include other methods, such as case-based, role-playing, small group discussion, and computer-based teaching. Maintaining flexibility in live vs distance learning as well as synchronous vs asynchronous learning can expand the capacity of available instructors and standardize material over several sites.23 Asking learners to consider operational concerns, such as whether certain medical conditions would be compatible with military duty in addition to the routine investigation is an easy way to incorporate military training in preexisting medical training.12 The advancement of technology has made simulation one of the best ways to engage in hands-on learning, whether through computer simulations, animal models, standardized or moulaged patients, or mannequins that can realistically mimic medical or trauma-related conditions.24 Many times, simulation can be combined with exercises in the field to create a realistic operational environment.23
There are 3 pillars of an operational curriculum that should be integrated into the existing residency curriculum—operational medicine, leadership, and research principles (Appendix).
Conclusions
Judging by the continuing operational tempo and evolution of warfare, maintaining enhanced military medical readiness will remain a priority. Operational medicine is a unique field that requires specialized preparation. Studies have shown that longitudinal deliberately mapped out curriculums are able to be integrated well into the existing medical curriculum. The recommendation moving forward is increasing the access of existing operational training structures that have well established programs and modeling individual GME program curriculums after those that have shown proven success with a focus on the 3 pillars of operational training, leadership, and research.
Acknowledgments
Previously submitted in April 2020 in expanded form as part of graduation requirements for the Masters of Military Arts and Science degree program at Air University, Maxwell Air Force Base in Alabama.
It is a time of significant change as the Military Health System (MHS) transitions to the purview of the Defense Health Agency (DHA). Additionally, the landscape of combat is ever changing, and military medicine needs to evolve to ensure that the lessons learned are utilized to optimize care of the war fighters. The purpose of this review is to evaluate the available literature on existing operational medicine curriculums and make recommendations to restructure current military medicine training to produce operationally prepared clinicians who are informed in operationally focused research principles.
Operational Medicine
Before diving into the importance of creating a curriculum and investing in training for scholarly activity proficiency, operational medicine needs to be defined. It can be defined as medical care provided in an austere environment with limited resources and possibly under hostile conditions. Another way to look at operational medicine is as the evaluation of normal human physiology and pathology under abnormal conditions. The mission set of each of the services is unique. The Marines and Army may operate forward past the wire vulnerable to the environment, gunfire, and improvised explosive devices, remote from fixed medical facilities. The Navy has divers exposed to the risks of decompression sickness. The Air Force has pilots exposed to altitude changes and strains of G-forces during flight. Locations vary from cold high-altitude mountainous regions to high-temperature desolate deserts. Many times, medical practitioners may be remotely stationed, far from specialty or immediate definitive care. Patient care may consist of low-acuity management of individual patients in sick call to mass casualty events where patient numbers and morbidity may outstrip available resources, making the difficult task of triage necessary.
Despite the challenges of being a uniformed physician, the benefits of being embedded is a better understanding of the roles and capability of the unit. Military physicians need to have the unique knowledge of the type of injuries sustained in that particular theater of war, such as differentiating between the trauma pattern and care required for blast injuries vs high-velocity missiles. There are also chemical, biologic, radiologic, and nuclear threats that military physicians need to recognize. Much of what disables a military fighting force is not a direct relationship to combat-related injuries; however, entire units have been taken down by infectious diarrhea or trench foot. There is also a need for familiarity of the infections and parasitology endemic to the particular theater with the aim of implementation of prevention whenever possible.
Military medicine does not fit in any box. Military physicians need to know the job requirements of various specialties, including elements of occupational medicine, such as aircrew piloting high-performance fighters or ground troops fully loaded with body armor and 80-lb backpacks. There are musculoskeletal injuries from the stressors of various military occupations. Working around weaponry and contact with hostile forces will create scenarios requiring emergent and critical care. In addition to physical injuries, there is the mental strain of combat with the risk of imminent personal injury, the guilt of survivorship, dealing with the scars and permanent physical damage of combat, and prolonged separation from family and other support systems.
The National Defense Authorization Act 2017 mandated the establishment of a standardized process to oversee all military graduate medical education (GME) programs with the goal of ensuring medical operational readiness.1 This is no small task with > 3000 residents in more than 70 specialties, comprising approximately 12% of US residents.1,2 Presently, 26 to 32% of the medical corps is enrolled in full-time training compared with 12% of the total force.2 With significant time and resources expended during this period, it is vital to maximize the potential of the training.
Literature Review
A literature review was performed, evaluating historical precedence of specialized military medical training and research as well as current operational curriculums. Literature search was conducted in the PubMed and Uniformed Services University (USU) Learning Resource databases using the terms “operational medicine curriculum,” “military medicine curriculum,” “operational medicine training,” “military medicine training,” “operational medicine research,” and “military medicine research,” and included all articles from 1997 to 2020. Inclusion criteria included studies that detailed military medicine training programs and/or outcomes. The source types used in this research project included peer-reviewed journal publications—both review articles and original research—from medical and military journals. The citations of these articles were also reviewed for additional usable publications. Secondary sources included official reports and studies by the RAND Corporation, the US Government Accountability Office, and the Institute for Defense Analysis (IDA). Due to lack of literature on the topic, other sources such as talking papers, letters, and formal presentations from subject matter experts were included to showcase the current state and gaps on this topic. Key findings from peer-reviewed publications are presented in Table 1.
Overall, the literature review showed that longitudinal deliberately mapped out curriculums can be well integrated into the existing medical curriculum.3 The military medicine course topics include environmental medicine, applied field medicine, combat casualty care, medical support planning, mass casualty incident preparation, and military-focused problem solving, decision making, and leadership.4
One 1997 study looked at the degree of implementation of military unique curriculum in 18 family medicine residencies. Only 30% of residents stated that their program had a specific operational medicine curriculum.5 Salerno and colleagues surveyed current residents and recently graduated internal medicine physicians at 14 facilities in the Army, Air Force, and Navy to determine confidence level with military medicine. More than half did not feel ready to practice deployment medicine; just 19% felt comfortable treating nuclear, biologic, and chemical warfare injuries; and 32% felt unfamiliar with the command and administrative duties. A subgroup analysis showed that USU graduates felt more prepared in these areas compared with civilian program graduates.6 Additional studies showed perceived smoother transition in the first active-duty tour after participation in an operational curriculum.7
Didactics can provide a foundation. However, just as the practice of medicine is learned in the clinic, the art of military medicine is learned in the field. Hands-on training in one study was accomplished through the Combat Casualty Care Course (C4), the USU Bushmaster exercise, and a field training exercise. The field exercise included components of mission planning, medical threat assessments, triage of a mass casualty situation, management of disease and nonbattle injuries, combat stress casualties, resource management, and patient evacuation.8
Another publication described a similar longitudinal curriculum with C4 after the first year of training and the Medical Management of Chemical and Biological Casualty Course during the second year. The operational curriculum 3-day capstone occurred at the end of medical training utilizing mannequins to realistically simulate combat casualty care, including emergency airways, chest tube, and tourniquets.9 Due to the current deployment tempo, just in time refresher courses like this could be valuable preparation.
While most of the operational curriculums evaluated assessed efficiency over a short time interval, one study looked at 1189 graduates from the military medical school from the past 20 years. Preparedness was perceived to be high for military-unique practice and leadership.10 The operational curriculum at USU had been purposefully structured to provide continuity. Didactics and casework were reinforced with hands-on training whether through realistic simulator training or field exercises. The authors note a weakness of many operational curriculums is inconsistency and fragmented training without deliberate longitudinal planning.
One of the more recent military GME curriculums include the creation of the operational medicine residency in 2013, which created a standardized longitudinal operational curriculum integrated along with the existing family medicine, emergency medicine, or internal medicine curriculum to create mission-ready military physicians upon graduation. Scheduled rotations include global medicine, aeromedical evacuation, occupational medicine, and tropical medicine. Completing military officer professional development and an operationally relevant research project is an expectation (Table 2).11
In addition to in-program training, other options include operational rotations offsite and military courses conducted outside the GME program.12 Some of these courses may include just-in-time training such as expeditionary medical support system training prior to scheduled deployments. Examples of experiential training are listed in Table 3.
Critical Analysis
Current gaps were identified in the military medicine training pipeline’s operational medicine curriculum and research programs. The analysis looked at specific components that make the operational medicine curriculum and research unique as well as current readiness goals, to determine how to best align both to meet the mission requirements. Some factors considered included efficiency, cost, program portability, duplication minimization, retention, and sustainability.
Efficiency
A well-created curriculum that meets objectives will require more than an assigned rotation and a few lectures. The most successful ones in the literature review were the ones that were deliberately planned and longitudinal, such as the ones at USU that combined a mixture of classroom and field exercises over the course of 4 years.4,8 In that way, the curriculum may not be considered time efficient, but if integrated well into the already existing medical training, the production of military physicians who are mission ready upon graduation—ready to serve as military medical leaders and deploy—will be invaluable.
Cost Comparison
Due to the associated overhead of running a training platform and the additional hours of operational training, military GME is more expensive initially compared with civilian outsourcing. In USU, for example, there is an additional 700 hours of operational curriculum alone. This cost difference more than doubles the cost of a USU education vs a Health Professional Scholarship Program (HPSP) scholarship at a civilian medical school. However, a causal analysis performed by the IDA to determine value basis noted that USU graduates deploy almost 3 times as much and serve 6 years longer on active duty.3
After graduating medical school through either accession source, physicians complete specialization training in a GME program. The IDA study noted an average $12,000 increased cost of military GME compared with civilian programs. The analysis included resident compensation and overhead costs of running the program as well as the net cost, which also accounted for resident productivity and workload by training in a military facility.3 Calculations due to mandated budget cuts estimated cost savings of closing the military medical school at < $100 million while significantly impacting the military physician pipeline and operational research output.3
Duplication of Effort
There are already established training programs such as Tactical Combat Casualty Care (TCCC) that could be incorporated into the curriculum to avoid expending additional resources to recreate the wheel. USU has a validated operational training curriculum and may be able to make opportunities available for outside trainees to participate in some of its military-unique training and leadership exercises. Other ways to decrease duplication of effort and improve cost efficiency include focusing on the creation of an academic health system (AHS) and consolidating similar programs to conserve resources. Increasing existing military program sizes will not only ensure the continuation of the military medicine pipeline, but will spread overhead costs over a larger cohort, decrease costs of civilian outsourcing, and ensure the less tangible benefits of military cultural exposure early in trainees’ careers. For example, increasing the class size of USU by 30 students actually reduces the cost per student to $239,000 per year from $253,000, while decreasing the need for HPSP accessions training in civilian programs, making the endeavor overall cost neutral.3
Program Portability
The operational medicine residency has proved that an operational curriculum can be remotely managed and reproduced at a variety of residency specialties.12 Remote education could be developed and distributed throughout the MHS, such as the proposed USU course Military Medicine and Leadership course.3 Centralized training programs like Global Medicine and C-STARS could be scheduled TDYs during the medical training calendar.
Retention
The military medical school, USU, is the largest military medicine accession source. An IDA report notes that retention of USU graduates is 15.2 years compared with 9.2 years served by civilian trainees. Due to the longevity in service, USU graduates also make up more than 25% of military medical leadership.4 The long-term outcome study that looked at the past 40 years of USU graduates observed that over 70% of graduates served until retirement eligibility and are overrepresented in special operations units.3,13 While some of this longevity may be attributed to the longer USU service contracts, military GME graduates were still noted to be 4 times more likely to commit to a multiyear service contract.14 A RAND study on the retention of military physicians in the Army, Air Force, and Navy noted that overall retention increased throughout all the services for physicians who went through the military GME pipeline.15 Conversely, civilian GME training was associated with a 45% chance in leaving active duty.16
It is theorized that early military acculturation during training increases the likelihood of instilling a sense of mission. Being involved in military GME on the teaching side also showed increased retention rates for 63% of survey respondents.17 Reduced burnout and increased work satisfaction for those involved in military GME was noted on another faculty satisfaction survey.17
Sustainability
Programs like USU, which have been around for decades, and the newer operational residency program evolving since 2013 have shown sustainability.4,11 Dissemination of proven curriculums as well as centralization of already validated training programs can help standardize operational medical training throughout the MHS. In order to flourish at individual programs, the faculty need to be well versed in a train the trainer model and have institutional support. The ability to engage with the line at individual locations may be a factor as well.18 In regard to research, once residents are taught the principles of scholarly activity, they will have the tools to continue operational medicine research advancements and mentoring students.
Discussion
The 2020 NDAA recommends the establishment of an AHS.3 This step will create a culture of military medical readiness from the top down as congressional mandates push reorganization of the MHS, including military GME programs. An overall restructuring of military medicine will require prioritization of resources toward operational requirements vs the historic significant division of attention to beneficiary care that has caused a lack of unity of effort and additional strain on an already heavily tasked medical force. The changes in military GME are just one aspect of that. It is vital to look at the restructuring with a comprehension of the unique challenges of combat health rather than only from an in-garrison, hospital-based aspect.19 Benefits of having a military medicine AHS include opportunities to share resources and successful business models as well as foster interdisciplinary teamwork and partnerships with civilian health care facilities and research institutions as a force multiplier.19
There has been recent discussion about budget cuts, including shutting down USU and military GME and transitioning all training to civilian programs to be cost-effective.4 If this were to happen, it would be a step backward from the goal of operational readiness. Maintaining US Department of Defense (DoD) control of the military medicine pipeline has innumerable benefits, including built-in mentorship from operationally-seasoned faculty, military leadership development, proficiency in MHS systems, open communication between GME programs and DoD, and curriculum control to ensure focus on readiness.20 Military GME programs are also a significant production source of military-related scholarly activity. Over fiscal year 2017/2018, 63% of the publications out of the San Antonio Uniformed Services Health Education Consortium—the largest Air Force GME platform and second largest multiservice GME platform—involved military relevant medical topics.17 Much of the volume of operational research as well as the relevant skills learned and future innovations secondary to conducting this research would be lost if military GME did not exist.17,21
Practically speaking, military GME provides the majority of the military medicine accessions. For example, a presentation by the Air Force Chief of Physician Education noted that the total military GME pipeline included 2875 students, but direct physician access averaged only 20 physicians a year.22 Even if the decision was made to defer to civilian education, capacity does not exist in civilian GME programs. This is worsened by the increased competitiveness of the GME match with the proliferation of medical schools without concurrent increase in residency spots. The 2018 National Resident Matching Program noted that there were more than 37,103 US and foreign applicants for only 33,000 residency positions, leaving many US applicants unmatched.17 It is doubtful that the civilian GME programs would be able to absorb the influx of military residents, affecting both the military and civilian medicine pipelines. As a secondary effect, the military treatment centers that house the military GME programs would have to close, with surrounding civilian medical facilities also likely unable to absorb the sudden influx of patients and residents losing the intangible benefits of caring for a military population.15 This was even recognized by the civilian president of the Accreditation Council for Graduate Medical Education:
Military physicians must be trained in the systems of care that are operative in military medicine, which is significantly unlike civilian medicine in many ways. It is often practiced in circumstances that are not seen in civilian medicine, within care structures that are not encountered in American medical practice… Military medicine has advanced research into the care of individuals suffering traumatic injury, critical care, rehabilitation medicine, prosthetics, psychiatric care of those traumatized, and closed head injury, to name a just a few. The sacrifices of our active military demand these advances, and the American Public benefit from these advances.21
Where deficiencies exist in military GME, it is possible to use the growing military-civilian training institution partnerships. Two prime examples are the just-in-time deployment training done with civilian trauma facilities by the Air Force Center for the Sustainment of Trauma Readiness Skills and the Air Force Special Operations Surgical Team-Special Operations Critical Care Evacuation Team being embedded in civilian facilities to maintain trauma, surgical, and emergency care skills. While military physicians can maintain competencies, at the same time, the civilian sector can benefit from the lessons learned in the military in regard to mass casualty and disaster responses. Fostering military and civilian training agreements can also enhance research opportunities.1
Just as the realities of operational medicine frequently require the military physician to think outside the box, the most successful methods of instruction of military medicine tend to be nontraditional. Classroom education should be involved beyond lectures and can include other methods, such as case-based, role-playing, small group discussion, and computer-based teaching. Maintaining flexibility in live vs distance learning as well as synchronous vs asynchronous learning can expand the capacity of available instructors and standardize material over several sites.23 Asking learners to consider operational concerns, such as whether certain medical conditions would be compatible with military duty in addition to the routine investigation is an easy way to incorporate military training in preexisting medical training.12 The advancement of technology has made simulation one of the best ways to engage in hands-on learning, whether through computer simulations, animal models, standardized or moulaged patients, or mannequins that can realistically mimic medical or trauma-related conditions.24 Many times, simulation can be combined with exercises in the field to create a realistic operational environment.23
There are 3 pillars of an operational curriculum that should be integrated into the existing residency curriculum—operational medicine, leadership, and research principles (Appendix).
Conclusions
Judging by the continuing operational tempo and evolution of warfare, maintaining enhanced military medical readiness will remain a priority. Operational medicine is a unique field that requires specialized preparation. Studies have shown that longitudinal deliberately mapped out curriculums are able to be integrated well into the existing medical curriculum. The recommendation moving forward is increasing the access of existing operational training structures that have well established programs and modeling individual GME program curriculums after those that have shown proven success with a focus on the 3 pillars of operational training, leadership, and research.
Acknowledgments
Previously submitted in April 2020 in expanded form as part of graduation requirements for the Masters of Military Arts and Science degree program at Air University, Maxwell Air Force Base in Alabama.
1. US Government Accountability Office. Defense Health Care: DoD’s proposed plan for oversight of graduate medical education program. Published March 2019. Accessed September 24, 2021. https://www.gao.gov/assets/700/698075.pdf
2. De Lorenzo RA. Accreditation status of U.S. military graduate medical education programs. Mil Med. 2008;173(7):635-640. doi:10.7205/milmed.173.7.635
3. John SK, Bishop JM, Hidreth LA, et al; Institute for Defense Analysis. Analysis of DoD accession alternatives for military physicians: readiness value and cost. Published October 2019. Accessed September 24, 2021. https://www.ida.org/-/media/feature/publications/a/an/analysis-of-dod-accession-alternatives-for-military-physicians-readiness-value-and-cost/p-10815.ashx.
4. O’Connor FG, Grunberg N, Kellermann AL, Schoomaker E. Leadership education and development at the Uniformed Services University. Mil Med. 2015;180(suppl 4):147-152. doi:10.7205/MILMED-D-14-00563
5. Suls H, Karnei K, Gardner JW, Fogarty JP, Llewellyn CH. The extent of military medicine topics taught in military family practice residency programs: Part II, a survey of residency graduates from 1987-1990. Mil Med. 1997;162(6):428-434. doi:10.1093/milmed/162.6.428
6. Salerno S, Cash B, Cranston M, Schoomaker E. Perceptions of current and recent military internal medicine residents on operational medicine, managed care, graduate medical education, and continued military service. Mil Med. 1998;163(6):392-397. doi:10.1093/milmed/163.6.392
7. Roop SA, Murray CK, Pugh AM, Phillips YY, Bolan CD. Operational medicine experience integrated into a military internal medicine residency curriculum. Mil Med. 2001;166(1):34-39. doi:10.1093/milmed/166.1.34
8. Perkins JG, Roy MJ, Bolan CD, Phillips YY. Operational experiences during medical residency: perspectives from the Walter Reed Army Medical Center Department of Medicine. Mil Med. 2001;166(12):1038-1045. doi:10.1093/milmed/166.12.1038
9. Murray CK, Reynolds JC, Boyer DA, et al. Development of a deployment course for graduating military internal medicine residents. Mil Med. 2006;171(10):933-936. doi:10.7205/milmed.171.10.933. doi:10.7205/milmed.171.10.933
10. Picho K, Gilliland WR, Artino AR Jr, et al. Assessing curriculum effectiveness: a survey of Uniformed Services University medical school graduates. Mil Med. 2015;180(suppl 4):113-128. doi:10.7205/MILMED-D-14-00570
11. Jacobson MD: Operational Aerospace medicine collaborative programs: past, present, and future. US Air Force School of Aerospace Medicine Presentation. November 1, 2018.
12. Roy MJ, Brietzke S, Hemmer P, Pangaro L, Goldstein R. Teaching military medicine: enhancing military relevance within the fabric of current medical training. Mil Med. 2002;167(4):277-280. doi:10.1093/miled.milmed.167.4.277
13. Durning SJ, Dong T, LaRochelle JL, et al. The long-term career outcome study: lessons learned and implications for educational practice. Mil Med. 2015;180(suppl 4):164-170. doi:10.7205/MILMED-D-14-00574
14. Keating EG, Brauner MK, Galway LA, Mele JD, Burks JJ, Saloner B. The Air Force Medical Corps’ status and how its physicians respond to multiyear special pay. Mil Med. 2009;174(11):1155-1162. doi:10.7205/milmed-d-01-4309
15. Mundell BF. Retention of military physicians: the differential effects of practice opportunities across the three services. RAND Corporation; 2010:74-77. Accessed September 24, 2021. https://www.rand.org/pubs/rgs_dissertations/RGSD275.html
16. Nagy CJ. The importance of a military-unique curriculum in active duty graduate medical education. Mil Med. 2012;177(3):243-244. doi:10.7205/milmed-d-11-00280
17. True M: The value of military graduate medical education. SAUSHEC interim dean talking paper. November 2, 2018.
18. Hatzfeld JJ, Khalili RA, Hendrickson TL, Reilly PA. Publishing military medical research: appreciating the process. Mil Med. 2016;181(suppl 5):5-6. doi:10.7205/MILMED-D-15-00517
19. Sauer SW, Robinson JB, Smith MP, et al. Lessons learned: saving lives on the battlefield. J Spec Oper Med. 2016;15(2). 25-41.
20. Tankersley MS: Air Force Physician Education Branch response to GME questions. Talking Paper. Feb 23, 2015.
21. Nasca TJ. [Letter] Published October 26, 2019. Accessed September 24, 2021. https://www.moaa.org/uploadedfiles/nasca-to-kellerman-a--cordts-p-2019-10-26.pdf
22. Forgione MA: USAF-SAM GME Brief. Air Force Personnel Center. October 2018.
23. Turner M, Wilson C, Gausman K, Roy MJ. Optimal methods of learning for military medical education. Mil Med. 2003;168(suppl 9):46-50. doi:10.1093/milmed/168.suppl_1.46
24. Goolsby C, Deering S. Hybrid simulation during military medical student field training--a novel curriculum. Mil Med. 2013;178(7):742-745. doi:10.7205/MILMED-D-12-00541
25. Hartzell JD, Yu CE, Cohee BM, Nelson MR, Wilson RL. Moving beyond accidental leadership: a graduate medical education leadership curriculum needs assessment. Mil Med. 2017;182(7):e1815-e1822. doi:10.7205/MILMED-D-16-00365
26. Barry ES, Dong T, Durning SJ, Schreiber-Gregory D, Torre D, Grunberg NE. Medical Student Leader Performance in an Applied Medical Field Practicum. Mil Med. 2019;184(11-12):653-660. doi:10.1093/milmed/usz121
27. Air Force Medical Corps Development Team: Medical corps integrated OPS career path. MC Pyramids 2019 Presentation. January 18, 2019. https://kx.health.mil [Nonpublic source, not verified]
28. Polski MM: Back to basics—research design for the operational level of war. Naval War College Rev. 2019;72(3):1-23. https://digital-commons.usnwc.edu/nwc-review/vol72/iss3/6.
1. US Government Accountability Office. Defense Health Care: DoD’s proposed plan for oversight of graduate medical education program. Published March 2019. Accessed September 24, 2021. https://www.gao.gov/assets/700/698075.pdf
2. De Lorenzo RA. Accreditation status of U.S. military graduate medical education programs. Mil Med. 2008;173(7):635-640. doi:10.7205/milmed.173.7.635
3. John SK, Bishop JM, Hidreth LA, et al; Institute for Defense Analysis. Analysis of DoD accession alternatives for military physicians: readiness value and cost. Published October 2019. Accessed September 24, 2021. https://www.ida.org/-/media/feature/publications/a/an/analysis-of-dod-accession-alternatives-for-military-physicians-readiness-value-and-cost/p-10815.ashx.
4. O’Connor FG, Grunberg N, Kellermann AL, Schoomaker E. Leadership education and development at the Uniformed Services University. Mil Med. 2015;180(suppl 4):147-152. doi:10.7205/MILMED-D-14-00563
5. Suls H, Karnei K, Gardner JW, Fogarty JP, Llewellyn CH. The extent of military medicine topics taught in military family practice residency programs: Part II, a survey of residency graduates from 1987-1990. Mil Med. 1997;162(6):428-434. doi:10.1093/milmed/162.6.428
6. Salerno S, Cash B, Cranston M, Schoomaker E. Perceptions of current and recent military internal medicine residents on operational medicine, managed care, graduate medical education, and continued military service. Mil Med. 1998;163(6):392-397. doi:10.1093/milmed/163.6.392
7. Roop SA, Murray CK, Pugh AM, Phillips YY, Bolan CD. Operational medicine experience integrated into a military internal medicine residency curriculum. Mil Med. 2001;166(1):34-39. doi:10.1093/milmed/166.1.34
8. Perkins JG, Roy MJ, Bolan CD, Phillips YY. Operational experiences during medical residency: perspectives from the Walter Reed Army Medical Center Department of Medicine. Mil Med. 2001;166(12):1038-1045. doi:10.1093/milmed/166.12.1038
9. Murray CK, Reynolds JC, Boyer DA, et al. Development of a deployment course for graduating military internal medicine residents. Mil Med. 2006;171(10):933-936. doi:10.7205/milmed.171.10.933. doi:10.7205/milmed.171.10.933
10. Picho K, Gilliland WR, Artino AR Jr, et al. Assessing curriculum effectiveness: a survey of Uniformed Services University medical school graduates. Mil Med. 2015;180(suppl 4):113-128. doi:10.7205/MILMED-D-14-00570
11. Jacobson MD: Operational Aerospace medicine collaborative programs: past, present, and future. US Air Force School of Aerospace Medicine Presentation. November 1, 2018.
12. Roy MJ, Brietzke S, Hemmer P, Pangaro L, Goldstein R. Teaching military medicine: enhancing military relevance within the fabric of current medical training. Mil Med. 2002;167(4):277-280. doi:10.1093/miled.milmed.167.4.277
13. Durning SJ, Dong T, LaRochelle JL, et al. The long-term career outcome study: lessons learned and implications for educational practice. Mil Med. 2015;180(suppl 4):164-170. doi:10.7205/MILMED-D-14-00574
14. Keating EG, Brauner MK, Galway LA, Mele JD, Burks JJ, Saloner B. The Air Force Medical Corps’ status and how its physicians respond to multiyear special pay. Mil Med. 2009;174(11):1155-1162. doi:10.7205/milmed-d-01-4309
15. Mundell BF. Retention of military physicians: the differential effects of practice opportunities across the three services. RAND Corporation; 2010:74-77. Accessed September 24, 2021. https://www.rand.org/pubs/rgs_dissertations/RGSD275.html
16. Nagy CJ. The importance of a military-unique curriculum in active duty graduate medical education. Mil Med. 2012;177(3):243-244. doi:10.7205/milmed-d-11-00280
17. True M: The value of military graduate medical education. SAUSHEC interim dean talking paper. November 2, 2018.
18. Hatzfeld JJ, Khalili RA, Hendrickson TL, Reilly PA. Publishing military medical research: appreciating the process. Mil Med. 2016;181(suppl 5):5-6. doi:10.7205/MILMED-D-15-00517
19. Sauer SW, Robinson JB, Smith MP, et al. Lessons learned: saving lives on the battlefield. J Spec Oper Med. 2016;15(2). 25-41.
20. Tankersley MS: Air Force Physician Education Branch response to GME questions. Talking Paper. Feb 23, 2015.
21. Nasca TJ. [Letter] Published October 26, 2019. Accessed September 24, 2021. https://www.moaa.org/uploadedfiles/nasca-to-kellerman-a--cordts-p-2019-10-26.pdf
22. Forgione MA: USAF-SAM GME Brief. Air Force Personnel Center. October 2018.
23. Turner M, Wilson C, Gausman K, Roy MJ. Optimal methods of learning for military medical education. Mil Med. 2003;168(suppl 9):46-50. doi:10.1093/milmed/168.suppl_1.46
24. Goolsby C, Deering S. Hybrid simulation during military medical student field training--a novel curriculum. Mil Med. 2013;178(7):742-745. doi:10.7205/MILMED-D-12-00541
25. Hartzell JD, Yu CE, Cohee BM, Nelson MR, Wilson RL. Moving beyond accidental leadership: a graduate medical education leadership curriculum needs assessment. Mil Med. 2017;182(7):e1815-e1822. doi:10.7205/MILMED-D-16-00365
26. Barry ES, Dong T, Durning SJ, Schreiber-Gregory D, Torre D, Grunberg NE. Medical Student Leader Performance in an Applied Medical Field Practicum. Mil Med. 2019;184(11-12):653-660. doi:10.1093/milmed/usz121
27. Air Force Medical Corps Development Team: Medical corps integrated OPS career path. MC Pyramids 2019 Presentation. January 18, 2019. https://kx.health.mil [Nonpublic source, not verified]
28. Polski MM: Back to basics—research design for the operational level of war. Naval War College Rev. 2019;72(3):1-23. https://digital-commons.usnwc.edu/nwc-review/vol72/iss3/6.