User login
SHM expresses support for Fairness for High-Skilled Immigrants Act
Without immigrant hospitalists, health care accessibility would decrease tremendously.
The Society of Hospital Medicine recently expressed its support for the Fairness for High-Skilled Immigrants Act (H.R. 392). This legislation will ensure that highly-skilled medical professionals and their families will not be turned away from working in the United States based on per-country limitations.
What inspired the PPC – and more broadly, SHM – to express support for this bill?
SHM and the PPC have always taken pride in assuming a leadership role when it comes to policy issues affecting hospitalists and the patients they serve, ranging from observation status to addressing the opiate epidemic and now, immigration reform. We are one of the first medical societies to support this bill.
What inspired us to take action is that there are country-specific caps when applying for a green card for those immigrants currently in the United States on an H1B visa. In the current green card pool, no country can occupy more than 7% of applications. For more populated countries like India and China, two significant countries of origin for hospitalists practicing in the U.S., this creates a significant backlog. At the moment, the projected wait time for applicants from countries in this situation to receive their green cards could easily exceed 25 years.
What impact would this have on hospital medicine providers and patients?
The number of hospitalists trained in the U.S. who have come on visas from other countries is astounding. By virtue of what we do as hospital medicine providers, we are leaders in health care. We own major QI initiatives across the hospital and oversee health care outcomes that many other providers never become involved with. By stifling the ability of people to enter the country and stay here long-term, it would have a devastating impact on our communities. A large chunk of hospitalist staffing companies employ providers who are international medical graduates who completed their residencies in the U.S. Without them, health care accessibility would decrease tremendously – especially in rural areas like those in which I work.
This is more than just an issue of citizenship – these caps have a major impact on quality of life and morale for those affected by them. The high level of uncertainty surrounding the current process affects large-scale decision-making. For example, people who are waiting to be approved for their green cards often ask questions like, “Should I buy a house?” and “Can I visit my family abroad and still be able to get back into the U.S. without any unwarranted delays or hassles?” This demoralizes quality providers personally, and if they feel this way, I can’t see how it wouldn’t affect their performance professionally as hospital medicine providers.
How have the existing restrictions affected you?
I graduated from medical school in India and came to the U.S..initially as a student and eventually transitioned to an H1B visa. After waiting for many years and having participated in numerous QI initiatives, I was fortunate enough to have my green card petition approved under a higher application category termed “Aliens of Extraordinary Ability” with a lesser wait time. However, by nature of the work that they perform, most hospitalists usually are eligible to apply for their green cards under the “Exceptional Ability” or “Advanced Degree” category, the wait times of which are excruciatingly long, and that is what we at the PPC and at the SHM level are striving to address and correct.
If someone is reading and says, “I want to do more and help advocate,” what can they do?
You don’t have to be a member of the PPC to have an impact on policy. Every member of SHM can contact their local representatives and be informed using SHM’s Grassroots Network. I have even gone so far as to meet and talk with local representatives to help them understand how policy issues affect both me and my patients. It is imperative that we are on the right side of history for those affected by this bill, and all bills affecting our fellow providers in the future.
Without immigrant hospitalists, health care accessibility would decrease tremendously.
Without immigrant hospitalists, health care accessibility would decrease tremendously.
The Society of Hospital Medicine recently expressed its support for the Fairness for High-Skilled Immigrants Act (H.R. 392). This legislation will ensure that highly-skilled medical professionals and their families will not be turned away from working in the United States based on per-country limitations.
What inspired the PPC – and more broadly, SHM – to express support for this bill?
SHM and the PPC have always taken pride in assuming a leadership role when it comes to policy issues affecting hospitalists and the patients they serve, ranging from observation status to addressing the opiate epidemic and now, immigration reform. We are one of the first medical societies to support this bill.
What inspired us to take action is that there are country-specific caps when applying for a green card for those immigrants currently in the United States on an H1B visa. In the current green card pool, no country can occupy more than 7% of applications. For more populated countries like India and China, two significant countries of origin for hospitalists practicing in the U.S., this creates a significant backlog. At the moment, the projected wait time for applicants from countries in this situation to receive their green cards could easily exceed 25 years.
What impact would this have on hospital medicine providers and patients?
The number of hospitalists trained in the U.S. who have come on visas from other countries is astounding. By virtue of what we do as hospital medicine providers, we are leaders in health care. We own major QI initiatives across the hospital and oversee health care outcomes that many other providers never become involved with. By stifling the ability of people to enter the country and stay here long-term, it would have a devastating impact on our communities. A large chunk of hospitalist staffing companies employ providers who are international medical graduates who completed their residencies in the U.S. Without them, health care accessibility would decrease tremendously – especially in rural areas like those in which I work.
This is more than just an issue of citizenship – these caps have a major impact on quality of life and morale for those affected by them. The high level of uncertainty surrounding the current process affects large-scale decision-making. For example, people who are waiting to be approved for their green cards often ask questions like, “Should I buy a house?” and “Can I visit my family abroad and still be able to get back into the U.S. without any unwarranted delays or hassles?” This demoralizes quality providers personally, and if they feel this way, I can’t see how it wouldn’t affect their performance professionally as hospital medicine providers.
How have the existing restrictions affected you?
I graduated from medical school in India and came to the U.S..initially as a student and eventually transitioned to an H1B visa. After waiting for many years and having participated in numerous QI initiatives, I was fortunate enough to have my green card petition approved under a higher application category termed “Aliens of Extraordinary Ability” with a lesser wait time. However, by nature of the work that they perform, most hospitalists usually are eligible to apply for their green cards under the “Exceptional Ability” or “Advanced Degree” category, the wait times of which are excruciatingly long, and that is what we at the PPC and at the SHM level are striving to address and correct.
If someone is reading and says, “I want to do more and help advocate,” what can they do?
You don’t have to be a member of the PPC to have an impact on policy. Every member of SHM can contact their local representatives and be informed using SHM’s Grassroots Network. I have even gone so far as to meet and talk with local representatives to help them understand how policy issues affect both me and my patients. It is imperative that we are on the right side of history for those affected by this bill, and all bills affecting our fellow providers in the future.
The Society of Hospital Medicine recently expressed its support for the Fairness for High-Skilled Immigrants Act (H.R. 392). This legislation will ensure that highly-skilled medical professionals and their families will not be turned away from working in the United States based on per-country limitations.
What inspired the PPC – and more broadly, SHM – to express support for this bill?
SHM and the PPC have always taken pride in assuming a leadership role when it comes to policy issues affecting hospitalists and the patients they serve, ranging from observation status to addressing the opiate epidemic and now, immigration reform. We are one of the first medical societies to support this bill.
What inspired us to take action is that there are country-specific caps when applying for a green card for those immigrants currently in the United States on an H1B visa. In the current green card pool, no country can occupy more than 7% of applications. For more populated countries like India and China, two significant countries of origin for hospitalists practicing in the U.S., this creates a significant backlog. At the moment, the projected wait time for applicants from countries in this situation to receive their green cards could easily exceed 25 years.
What impact would this have on hospital medicine providers and patients?
The number of hospitalists trained in the U.S. who have come on visas from other countries is astounding. By virtue of what we do as hospital medicine providers, we are leaders in health care. We own major QI initiatives across the hospital and oversee health care outcomes that many other providers never become involved with. By stifling the ability of people to enter the country and stay here long-term, it would have a devastating impact on our communities. A large chunk of hospitalist staffing companies employ providers who are international medical graduates who completed their residencies in the U.S. Without them, health care accessibility would decrease tremendously – especially in rural areas like those in which I work.
This is more than just an issue of citizenship – these caps have a major impact on quality of life and morale for those affected by them. The high level of uncertainty surrounding the current process affects large-scale decision-making. For example, people who are waiting to be approved for their green cards often ask questions like, “Should I buy a house?” and “Can I visit my family abroad and still be able to get back into the U.S. without any unwarranted delays or hassles?” This demoralizes quality providers personally, and if they feel this way, I can’t see how it wouldn’t affect their performance professionally as hospital medicine providers.
How have the existing restrictions affected you?
I graduated from medical school in India and came to the U.S..initially as a student and eventually transitioned to an H1B visa. After waiting for many years and having participated in numerous QI initiatives, I was fortunate enough to have my green card petition approved under a higher application category termed “Aliens of Extraordinary Ability” with a lesser wait time. However, by nature of the work that they perform, most hospitalists usually are eligible to apply for their green cards under the “Exceptional Ability” or “Advanced Degree” category, the wait times of which are excruciatingly long, and that is what we at the PPC and at the SHM level are striving to address and correct.
If someone is reading and says, “I want to do more and help advocate,” what can they do?
You don’t have to be a member of the PPC to have an impact on policy. Every member of SHM can contact their local representatives and be informed using SHM’s Grassroots Network. I have even gone so far as to meet and talk with local representatives to help them understand how policy issues affect both me and my patients. It is imperative that we are on the right side of history for those affected by this bill, and all bills affecting our fellow providers in the future.
Medicare hospital deaths decline, hospice usage increases
Since 2000, Medicare beneficiaries have become less likely to die in hospitals, and more likely to die in their homes or in community health care facilities.
A review of Medicare records also determined that there was a decline in health care transitions in the final 3 days of life for these patients, Joan M. Teno, MD, and her colleagues wrote in JAMA.
It is not possible to identify a specific reason for the shift, wrote Dr. Teno, professor of medicine at the Oregon Health & Science University, Portland. Between the study years of 2000 and 2015, there were several large efforts to improve care at the end of life.
“Since 2009, programs ranging from ensuring informed patient decision making to enhanced care coordination have had the goal of improving care at the end of life. Specific interventions have included promoting conversations about the goals of care, continued growth of hospice services and palliative care, and the debate and passage of the Affordable Care Act … It is difficult to disentangle efforts such as public education, promotion of advance directives through the Patient Self- Determination Act, increased access to hospice and palliative care services, financial incentives of payment policies, and other secular changes.”
The study mined data from the Centers for Medicare & Medicaid Services, and examined end-of-life outcomes among two Medicare groups: Medicare fee-for-service recipients (1,361,870) during 2009-2015, and Medicare Advantage recipients (871,845), comparing 2011 and 2015. The mean age of both cohorts was 82 years.
Outcomes included site of death and “potentially burdensome transitions,” during the last days of life. These were defined as three or more hospitalizations in the previous 3 months, or two or more hospitalizations for pneumonia, urinary tract infection, dehydration, or sepsis during the last 120 days of life. Prolonged mechanical ventilation also was deemed potentially burdensome.
Among fee-for-service recipients, deaths in acute care hospitals declined from 32.6% to19.8%. Deaths in nursing homes remained steady, at 27.2% and 24.9%. Many of these deaths (42.9%) were preceded by a stay in an ICU. There was a transient increase in end-of-life ICU use, around 2009, but by 2015, the percentage was down to 29%, compared with 65.2% in 2000.
Transitions between a nursing home and hospital in the last 90 days of life were 0.49/person in 2000 and 0.33/person in 2015. Hospitalizations for infection or dehydration fell from 14.6% to12.2%. Hospitalization with prolonged ventilation fell from 3.1% to 2.5%.
Dying in hospice care increased from 21.6% to 50.4%, and people were taking advantage of hospice services longer: the proportion using short-term services (3 days or less) fell from 9.8% to 7.7%.
Among Medicare Advantage recipients, the numbers were somewhat different. More than 50% of recipients entered hospice care in both 2011 and 2015; in both years, 8% had services for more than 3 days. About 27% had ICU care in the last days of life, in both years. Compared to fee-for-service recipients, fewer Medicare Advantage patients were in nursing homes at the time of death, and that number declined from 2011 to 2015 (37.7% to 33.2%).
In each year, about 10% of these patients had a hospitalization for dehydration or infection, and 3% had a stay requiring prolonged mechanical ventilation in each year. The mean number of health care transitions remained steady, at 0.23 and 0.21 per person each year.
Dr. Teno had no financial disclosures.
SOURCE: Teno JM et al. JAMA. 2018 Jun 25. doi: 10.1001/jama.2018.8981.
Since 2000, Medicare beneficiaries have become less likely to die in hospitals, and more likely to die in their homes or in community health care facilities.
A review of Medicare records also determined that there was a decline in health care transitions in the final 3 days of life for these patients, Joan M. Teno, MD, and her colleagues wrote in JAMA.
It is not possible to identify a specific reason for the shift, wrote Dr. Teno, professor of medicine at the Oregon Health & Science University, Portland. Between the study years of 2000 and 2015, there were several large efforts to improve care at the end of life.
“Since 2009, programs ranging from ensuring informed patient decision making to enhanced care coordination have had the goal of improving care at the end of life. Specific interventions have included promoting conversations about the goals of care, continued growth of hospice services and palliative care, and the debate and passage of the Affordable Care Act … It is difficult to disentangle efforts such as public education, promotion of advance directives through the Patient Self- Determination Act, increased access to hospice and palliative care services, financial incentives of payment policies, and other secular changes.”
The study mined data from the Centers for Medicare & Medicaid Services, and examined end-of-life outcomes among two Medicare groups: Medicare fee-for-service recipients (1,361,870) during 2009-2015, and Medicare Advantage recipients (871,845), comparing 2011 and 2015. The mean age of both cohorts was 82 years.
Outcomes included site of death and “potentially burdensome transitions,” during the last days of life. These were defined as three or more hospitalizations in the previous 3 months, or two or more hospitalizations for pneumonia, urinary tract infection, dehydration, or sepsis during the last 120 days of life. Prolonged mechanical ventilation also was deemed potentially burdensome.
Among fee-for-service recipients, deaths in acute care hospitals declined from 32.6% to19.8%. Deaths in nursing homes remained steady, at 27.2% and 24.9%. Many of these deaths (42.9%) were preceded by a stay in an ICU. There was a transient increase in end-of-life ICU use, around 2009, but by 2015, the percentage was down to 29%, compared with 65.2% in 2000.
Transitions between a nursing home and hospital in the last 90 days of life were 0.49/person in 2000 and 0.33/person in 2015. Hospitalizations for infection or dehydration fell from 14.6% to12.2%. Hospitalization with prolonged ventilation fell from 3.1% to 2.5%.
Dying in hospice care increased from 21.6% to 50.4%, and people were taking advantage of hospice services longer: the proportion using short-term services (3 days or less) fell from 9.8% to 7.7%.
Among Medicare Advantage recipients, the numbers were somewhat different. More than 50% of recipients entered hospice care in both 2011 and 2015; in both years, 8% had services for more than 3 days. About 27% had ICU care in the last days of life, in both years. Compared to fee-for-service recipients, fewer Medicare Advantage patients were in nursing homes at the time of death, and that number declined from 2011 to 2015 (37.7% to 33.2%).
In each year, about 10% of these patients had a hospitalization for dehydration or infection, and 3% had a stay requiring prolonged mechanical ventilation in each year. The mean number of health care transitions remained steady, at 0.23 and 0.21 per person each year.
Dr. Teno had no financial disclosures.
SOURCE: Teno JM et al. JAMA. 2018 Jun 25. doi: 10.1001/jama.2018.8981.
Since 2000, Medicare beneficiaries have become less likely to die in hospitals, and more likely to die in their homes or in community health care facilities.
A review of Medicare records also determined that there was a decline in health care transitions in the final 3 days of life for these patients, Joan M. Teno, MD, and her colleagues wrote in JAMA.
It is not possible to identify a specific reason for the shift, wrote Dr. Teno, professor of medicine at the Oregon Health & Science University, Portland. Between the study years of 2000 and 2015, there were several large efforts to improve care at the end of life.
“Since 2009, programs ranging from ensuring informed patient decision making to enhanced care coordination have had the goal of improving care at the end of life. Specific interventions have included promoting conversations about the goals of care, continued growth of hospice services and palliative care, and the debate and passage of the Affordable Care Act … It is difficult to disentangle efforts such as public education, promotion of advance directives through the Patient Self- Determination Act, increased access to hospice and palliative care services, financial incentives of payment policies, and other secular changes.”
The study mined data from the Centers for Medicare & Medicaid Services, and examined end-of-life outcomes among two Medicare groups: Medicare fee-for-service recipients (1,361,870) during 2009-2015, and Medicare Advantage recipients (871,845), comparing 2011 and 2015. The mean age of both cohorts was 82 years.
Outcomes included site of death and “potentially burdensome transitions,” during the last days of life. These were defined as three or more hospitalizations in the previous 3 months, or two or more hospitalizations for pneumonia, urinary tract infection, dehydration, or sepsis during the last 120 days of life. Prolonged mechanical ventilation also was deemed potentially burdensome.
Among fee-for-service recipients, deaths in acute care hospitals declined from 32.6% to19.8%. Deaths in nursing homes remained steady, at 27.2% and 24.9%. Many of these deaths (42.9%) were preceded by a stay in an ICU. There was a transient increase in end-of-life ICU use, around 2009, but by 2015, the percentage was down to 29%, compared with 65.2% in 2000.
Transitions between a nursing home and hospital in the last 90 days of life were 0.49/person in 2000 and 0.33/person in 2015. Hospitalizations for infection or dehydration fell from 14.6% to12.2%. Hospitalization with prolonged ventilation fell from 3.1% to 2.5%.
Dying in hospice care increased from 21.6% to 50.4%, and people were taking advantage of hospice services longer: the proportion using short-term services (3 days or less) fell from 9.8% to 7.7%.
Among Medicare Advantage recipients, the numbers were somewhat different. More than 50% of recipients entered hospice care in both 2011 and 2015; in both years, 8% had services for more than 3 days. About 27% had ICU care in the last days of life, in both years. Compared to fee-for-service recipients, fewer Medicare Advantage patients were in nursing homes at the time of death, and that number declined from 2011 to 2015 (37.7% to 33.2%).
In each year, about 10% of these patients had a hospitalization for dehydration or infection, and 3% had a stay requiring prolonged mechanical ventilation in each year. The mean number of health care transitions remained steady, at 0.23 and 0.21 per person each year.
Dr. Teno had no financial disclosures.
SOURCE: Teno JM et al. JAMA. 2018 Jun 25. doi: 10.1001/jama.2018.8981.
FROM JAMA
Key clinical point: During 2000-2015, Medicare recipients became less likely to die in hospitals.
Major finding:
Study details: The retrospective study comprised more than 2.3 million Medicare recipients.
Disclosures: Dr. Teno had no financial disclosures.
Source: Teno JM et al. JAMA. 2018 Jun 25. doi: 10.1001/jama.2018.8981.
Health care, technology, and the future
Major forces combining to reshape care delivery
What will be the role of humans in the future health system?
At first blush, this is a peculiar question. Health care is all about humans. How could one doubt their presence or role? It is working with and for people that attracted many to this profession.
On the cusp of a significant health system reformulation, it is the very question that hospitalists now must ponder. Just as ATMs replaced bank cashiers, online shopping replaced retail stores, and autonomous cars will soon replace drivers, the human landscape of health care is about to change. What pressures will force the changes?
On one hand, there is increasing demand. The Affordable Care Act opened the insurance door for people previously uncovered. Aging is delivering the baby boomer bubble into their sicker years. Hospitalists witness this phenomenon every day in the ballooning parade of patients they serve. At times, those pressures can overwhelm.
On the other hand, the political will to provide government subsidized health coverage is waning. Washington is tripping over itself to dismantle Obamacare with glancing concern for how it will inflate the ranks of the uninsured. Employers are eager to free themselves from the burden of providing increasingly expensive health coverage benefits. By removing the mandate to buy health care insurance, the current political health system architects are liberating the healthy paying population from their contributions to the overall insurance pool. Simply put, there is and will be less money and less of all that it buys.
Combine building demand with decreasing budget into a system that does not follow general market forces: You get that earthquake. A consumer can forgo that new phone in hard times but not that cardiac procedure. People will be caught in the fissures of the system. Waits, quality, burnout, morale problems, and financial losses will all trend in the wrong directions. The process will evolve in slow motion. Some might argue that we have already arrived.
Enter entrepreneurs, technologic advances, and a growing savvy and willingness to engage tech solutions to everyday problems. If Alexa can turn on your toaster, could it take your blood pressure? If a robot can vacuum your rug, could a different robot provide personal care services? And, if an algorithm can drive your car, could it similarly diagnose what ails you?
On Jan. 30, 2018, one of the greatest disrupters of all time, Amazon, announced that it is joining forces with Berkshire Hathaway and JPMorgan Chase to leap into health care. While they are initially experimenting with health care changes for their corporate employees, the ultimate marketwide goal is to apply technology to both reduce costs and improve patient care. Warren Buffet, Berkshire Hathaway’s founder, said in a statement, “The ballooning costs of health care act as a hungry tapeworm on the American economy.” (And yes, I imagine that many hospitalists would take umbrage with that characterization.) In addition to the Amazon alliance, CVS Health and Aetna also recently agreed to join forces.
The rising health care interest by Amazon begs the imagination. Technology already is far along in automating routine procedures, elevating patient safety protocols, and recalculating patient flows and information. This added corporate interest and investment will further expand new ideas and innovative technologies. And, for sure, it will challenge long held beliefs and practices that shape the health system we have today.
Hospitalist insight needed
What is the role of hospitalist leaders in this shifting equation? Hospitalists already can claim significant credit for introducing major changes in the landscape of hospital care in this country, with all the concomitant improvements in the efficiencies and quality of more integrated service delivery. Can you also guide the system in strategically selecting where and how technology can best be applied to automate and reconfigure service delivery?
The most important questions are: What is it that humans in health care uniquely do that cannot otherwise be accomplished? Are we able to hold onto the humane sides of health care, even as we seek to introduce cost-saving efficiencies?
Top of mind come the most personal sides of health service delivery: touch, empathy, understanding, and care itself. Next come human analysis, understanding, and translation. And beyond that, leadership, direction, and the vision to craft a health care system that meets our societal expectations – not just for the wealthy who cannot afford it – but for everyone.
It would be easy to dismiss this conversation. Society never decided whether those bank tellers, travel agents, or journalists were critical to our functioning. Along these same lines, you and your patients are more than mere algorithms.
As I often share in my leadership seminars, one key function of leaders is to identify and ask the right questions and to be at the decision-making table. What are those questions?
As a hospitalist leader, which part of your work and your activities could be eased by automation? Where might technology ease pressures and enhance your interactions with patients? How do we improve the efficiencies and effectiveness of health service delivery while we preserve the very human qualities that are fundamental to its values? No patient wants to speak to a physician who stares at a computer screen without eye contact, reassurance, or genuine interest. We can do better than that.
Business stakeholders in the system – and clearly, they are positioning and are powerful – will hold great sway on the contours of our future health care system. They could see humans – with all their costs, imperfections, and distractions – as replaceable.
Know that as you lead and pose your questions, there are people interested in listening. Certainly, the tech industry is looking for opportunities to generate broad market appeal. Similarly, health system decision makers looking to enhance how the system functions likewise seek guidance on what could – and could not – work. And who knows: Those decision makers could very well be you.
This is a conversation the country deserves. There is nothing more intimate, more personally important, and more professionally satisfying than the genuine person-to-person quality of what we do in health care. What we arrive at in the end should be achieved by intent, not by accident.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration,” 2nd ed. (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at ljmarcus@hsph.harvard.edu.
Major forces combining to reshape care delivery
Major forces combining to reshape care delivery
What will be the role of humans in the future health system?
At first blush, this is a peculiar question. Health care is all about humans. How could one doubt their presence or role? It is working with and for people that attracted many to this profession.
On the cusp of a significant health system reformulation, it is the very question that hospitalists now must ponder. Just as ATMs replaced bank cashiers, online shopping replaced retail stores, and autonomous cars will soon replace drivers, the human landscape of health care is about to change. What pressures will force the changes?
On one hand, there is increasing demand. The Affordable Care Act opened the insurance door for people previously uncovered. Aging is delivering the baby boomer bubble into their sicker years. Hospitalists witness this phenomenon every day in the ballooning parade of patients they serve. At times, those pressures can overwhelm.
On the other hand, the political will to provide government subsidized health coverage is waning. Washington is tripping over itself to dismantle Obamacare with glancing concern for how it will inflate the ranks of the uninsured. Employers are eager to free themselves from the burden of providing increasingly expensive health coverage benefits. By removing the mandate to buy health care insurance, the current political health system architects are liberating the healthy paying population from their contributions to the overall insurance pool. Simply put, there is and will be less money and less of all that it buys.
Combine building demand with decreasing budget into a system that does not follow general market forces: You get that earthquake. A consumer can forgo that new phone in hard times but not that cardiac procedure. People will be caught in the fissures of the system. Waits, quality, burnout, morale problems, and financial losses will all trend in the wrong directions. The process will evolve in slow motion. Some might argue that we have already arrived.
Enter entrepreneurs, technologic advances, and a growing savvy and willingness to engage tech solutions to everyday problems. If Alexa can turn on your toaster, could it take your blood pressure? If a robot can vacuum your rug, could a different robot provide personal care services? And, if an algorithm can drive your car, could it similarly diagnose what ails you?
On Jan. 30, 2018, one of the greatest disrupters of all time, Amazon, announced that it is joining forces with Berkshire Hathaway and JPMorgan Chase to leap into health care. While they are initially experimenting with health care changes for their corporate employees, the ultimate marketwide goal is to apply technology to both reduce costs and improve patient care. Warren Buffet, Berkshire Hathaway’s founder, said in a statement, “The ballooning costs of health care act as a hungry tapeworm on the American economy.” (And yes, I imagine that many hospitalists would take umbrage with that characterization.) In addition to the Amazon alliance, CVS Health and Aetna also recently agreed to join forces.
The rising health care interest by Amazon begs the imagination. Technology already is far along in automating routine procedures, elevating patient safety protocols, and recalculating patient flows and information. This added corporate interest and investment will further expand new ideas and innovative technologies. And, for sure, it will challenge long held beliefs and practices that shape the health system we have today.
Hospitalist insight needed
What is the role of hospitalist leaders in this shifting equation? Hospitalists already can claim significant credit for introducing major changes in the landscape of hospital care in this country, with all the concomitant improvements in the efficiencies and quality of more integrated service delivery. Can you also guide the system in strategically selecting where and how technology can best be applied to automate and reconfigure service delivery?
The most important questions are: What is it that humans in health care uniquely do that cannot otherwise be accomplished? Are we able to hold onto the humane sides of health care, even as we seek to introduce cost-saving efficiencies?
Top of mind come the most personal sides of health service delivery: touch, empathy, understanding, and care itself. Next come human analysis, understanding, and translation. And beyond that, leadership, direction, and the vision to craft a health care system that meets our societal expectations – not just for the wealthy who cannot afford it – but for everyone.
It would be easy to dismiss this conversation. Society never decided whether those bank tellers, travel agents, or journalists were critical to our functioning. Along these same lines, you and your patients are more than mere algorithms.
As I often share in my leadership seminars, one key function of leaders is to identify and ask the right questions and to be at the decision-making table. What are those questions?
As a hospitalist leader, which part of your work and your activities could be eased by automation? Where might technology ease pressures and enhance your interactions with patients? How do we improve the efficiencies and effectiveness of health service delivery while we preserve the very human qualities that are fundamental to its values? No patient wants to speak to a physician who stares at a computer screen without eye contact, reassurance, or genuine interest. We can do better than that.
Business stakeholders in the system – and clearly, they are positioning and are powerful – will hold great sway on the contours of our future health care system. They could see humans – with all their costs, imperfections, and distractions – as replaceable.
Know that as you lead and pose your questions, there are people interested in listening. Certainly, the tech industry is looking for opportunities to generate broad market appeal. Similarly, health system decision makers looking to enhance how the system functions likewise seek guidance on what could – and could not – work. And who knows: Those decision makers could very well be you.
This is a conversation the country deserves. There is nothing more intimate, more personally important, and more professionally satisfying than the genuine person-to-person quality of what we do in health care. What we arrive at in the end should be achieved by intent, not by accident.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration,” 2nd ed. (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at ljmarcus@hsph.harvard.edu.
What will be the role of humans in the future health system?
At first blush, this is a peculiar question. Health care is all about humans. How could one doubt their presence or role? It is working with and for people that attracted many to this profession.
On the cusp of a significant health system reformulation, it is the very question that hospitalists now must ponder. Just as ATMs replaced bank cashiers, online shopping replaced retail stores, and autonomous cars will soon replace drivers, the human landscape of health care is about to change. What pressures will force the changes?
On one hand, there is increasing demand. The Affordable Care Act opened the insurance door for people previously uncovered. Aging is delivering the baby boomer bubble into their sicker years. Hospitalists witness this phenomenon every day in the ballooning parade of patients they serve. At times, those pressures can overwhelm.
On the other hand, the political will to provide government subsidized health coverage is waning. Washington is tripping over itself to dismantle Obamacare with glancing concern for how it will inflate the ranks of the uninsured. Employers are eager to free themselves from the burden of providing increasingly expensive health coverage benefits. By removing the mandate to buy health care insurance, the current political health system architects are liberating the healthy paying population from their contributions to the overall insurance pool. Simply put, there is and will be less money and less of all that it buys.
Combine building demand with decreasing budget into a system that does not follow general market forces: You get that earthquake. A consumer can forgo that new phone in hard times but not that cardiac procedure. People will be caught in the fissures of the system. Waits, quality, burnout, morale problems, and financial losses will all trend in the wrong directions. The process will evolve in slow motion. Some might argue that we have already arrived.
Enter entrepreneurs, technologic advances, and a growing savvy and willingness to engage tech solutions to everyday problems. If Alexa can turn on your toaster, could it take your blood pressure? If a robot can vacuum your rug, could a different robot provide personal care services? And, if an algorithm can drive your car, could it similarly diagnose what ails you?
On Jan. 30, 2018, one of the greatest disrupters of all time, Amazon, announced that it is joining forces with Berkshire Hathaway and JPMorgan Chase to leap into health care. While they are initially experimenting with health care changes for their corporate employees, the ultimate marketwide goal is to apply technology to both reduce costs and improve patient care. Warren Buffet, Berkshire Hathaway’s founder, said in a statement, “The ballooning costs of health care act as a hungry tapeworm on the American economy.” (And yes, I imagine that many hospitalists would take umbrage with that characterization.) In addition to the Amazon alliance, CVS Health and Aetna also recently agreed to join forces.
The rising health care interest by Amazon begs the imagination. Technology already is far along in automating routine procedures, elevating patient safety protocols, and recalculating patient flows and information. This added corporate interest and investment will further expand new ideas and innovative technologies. And, for sure, it will challenge long held beliefs and practices that shape the health system we have today.
Hospitalist insight needed
What is the role of hospitalist leaders in this shifting equation? Hospitalists already can claim significant credit for introducing major changes in the landscape of hospital care in this country, with all the concomitant improvements in the efficiencies and quality of more integrated service delivery. Can you also guide the system in strategically selecting where and how technology can best be applied to automate and reconfigure service delivery?
The most important questions are: What is it that humans in health care uniquely do that cannot otherwise be accomplished? Are we able to hold onto the humane sides of health care, even as we seek to introduce cost-saving efficiencies?
Top of mind come the most personal sides of health service delivery: touch, empathy, understanding, and care itself. Next come human analysis, understanding, and translation. And beyond that, leadership, direction, and the vision to craft a health care system that meets our societal expectations – not just for the wealthy who cannot afford it – but for everyone.
It would be easy to dismiss this conversation. Society never decided whether those bank tellers, travel agents, or journalists were critical to our functioning. Along these same lines, you and your patients are more than mere algorithms.
As I often share in my leadership seminars, one key function of leaders is to identify and ask the right questions and to be at the decision-making table. What are those questions?
As a hospitalist leader, which part of your work and your activities could be eased by automation? Where might technology ease pressures and enhance your interactions with patients? How do we improve the efficiencies and effectiveness of health service delivery while we preserve the very human qualities that are fundamental to its values? No patient wants to speak to a physician who stares at a computer screen without eye contact, reassurance, or genuine interest. We can do better than that.
Business stakeholders in the system – and clearly, they are positioning and are powerful – will hold great sway on the contours of our future health care system. They could see humans – with all their costs, imperfections, and distractions – as replaceable.
Know that as you lead and pose your questions, there are people interested in listening. Certainly, the tech industry is looking for opportunities to generate broad market appeal. Similarly, health system decision makers looking to enhance how the system functions likewise seek guidance on what could – and could not – work. And who knows: Those decision makers could very well be you.
This is a conversation the country deserves. There is nothing more intimate, more personally important, and more professionally satisfying than the genuine person-to-person quality of what we do in health care. What we arrive at in the end should be achieved by intent, not by accident.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration,” 2nd ed. (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at ljmarcus@hsph.harvard.edu.
CMS sepsis measure a challenge to report
Hospitalists can champion sepsis-improvement efforts
In October 2015, the Centers for Medicare & Medicaid Services implemented its first meaningful policy to attempt for addressing sepsis.
The condition – one of the leading causes of mortality among hospitalized patients – afflicts more than a million people each year in the United States, and between 15% and 30% of them die. Sepsis is one of the leading drivers of hospital readmissions, sending more patients back to the hospital than heart failure, pneumonia, and chronic obstructive pulmonary disease.1
However, while providers seem to agree that time to address sepsis is past due, not everyone has embraced the Sepsis CMS Core Measure program, or SEP-1, as the means to best achieve it. This is, in part, because of discrepancies in how sepsis is defined, the burden of reporting, and what some consider to be arbitrary clinical requirements that may not correlate with better patient outcomes.
“Sepsis is indeed a critical public health problem, and it’s appropriate and valuable that Medicare and other policy makers are focusing on sepsis,” said Jeremy Kahn, MD, professor of critical care medicine and health policy and management at the University of Pittsburgh. “This was really the first approach at that … but at 85-pages long, it really is an enormous effort for hospitals to adhere to this measure.”
This is because of the tension between the “intense desire to improve sepsis outcomes” and the “incredible burden” of keeping up with the necessary documentation while also providing quality care, Dr. Kahn said.
In December 2017, Dr. Kahn helped lead a study published in the Journal of Hospital Medicine aimed at trying to understand hospital perceptions of SEP-1. Over the course of 29 interviews with randomly selected hospital quality leaders across the United States, including physicians and nurses, the results came as a surprise.2
“Generally, hospitals were very supportive of the concept, and there was no pushback on the idea that we should be measuring and reporting sepsis quality to CMS,” he said.
However, the research team found that respondents believed the program’s requirements with respect to treatment and documentation were complex and not always linked to patient-centered outcomes. Meeting the SEP-1 bundles consistently required hospitals to dedicate resources that not all may have, especially those in small, rural communities and those serving as urban safety nets.
Some, like emergency medicine physician Annahieta Kalantari, DO (who did not participate in the survey), feel that SEP-1 forces providers to practice “check-box” medicine and undermines successful efforts that don’t necessarily align with the CMS policy.
She arrived at her institution, Aria-Jefferson Health in Philadelphia, before CMS adopted SEP-1; at that time, she took note of the fact that the rate of sepsis mortalities in her hospital was, in her words, not great when compared with that at similar institutions. And then she helped do something about it.
“I thought, ‘We’re a Premier reporting hospital,’ so we did a gap analysis as to why and put together protocols for the hospital to follow with our sepsis patients, including a sepsis alert and a lot of education,” said Dr. Kalantari, associate program director for the emergency medicine residency program at Aria-Jefferson and a former chair of its sepsis management committee. “Before you knew it, mortalities were below benchmark.”
But once SEP-1 began, she said, the hospital was unable to check all of the boxes all of the time.
“We kept track, but we weren’t hitting all the bundles exactly within the periods of time recommended, but our mortalities were still amazing,” she said. “CMS basically picked definitions [for sepsis], and most of us don’t know what they’re basing them on because no one can agree on a definition anyway. Now they’re penalizing hospitals if they don’t hit the check marks in time, but we’d already demonstrated that our mortality and patient care was exceptional.”
She added: “I am extremely dissatisfied, as someone who provides frontline patient care, with how CMS is choosing to measure us.”
Dr. Kalantari wrote a piece in the Western Journal of Emergency Medicine in July 2017 in which she and coauthors outline the issues they take with SEP-1. They lay out the tension among the varied definitions of what sepsis is – and isn’t – and they also illuminate the apparent conflict between what CMS has officially defined and what evidence-based studies conducted since 2001 have suggested.3
In particular, CMS defines severe sepsis as an initial lactate above 2 mmol/L and septic shock as an initial lactate presentation of greater than 4 mmol/L. However, Dr. Kalantari and here coauthors argue in the paper that there is no standard definition of sepsis and that decades of attempts to achieve one have failed to reach consensus among providers. CMS, she said, fails to acknowledge this.
Defining sepsis
In fact, in 2016, another new definition of sepsis emerged by way of a 19-member task-force of experts: The Third International Consensus Definitions for Sepsis and Septic Shock, also called Sepsis-3.4 In March 2017, the Surviving Sepsis Campaign adopted this definition, which defined sepsis as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.”5
“I think the definition has always been a challenging part of sepsis,” said Kencee Graves, MD, a hospitalist at the University of Utah, Salt Lake City. “The definitions came about for research purposes, so … they are not perfectly sensitive nor specific.”
However, Dr. Graves believes SEP-1 is a step in the right direction in that it brings awareness to sepsis and holds providers accountable. Several years ago, she and her colleague Devin Horton, MD, also a hospitalist at the University of Utah, embarked on a massive undertaking to address sepsis in their hospital. It was, at the time, lacking in “sepsis culture,” Dr. Horton said.
“One of the big things that motivated both of us was that we started doing chart review together and – it’s always easier with 20/20 hindsight – we were noticing that residents were missing the signs of sepsis,” Dr. Horton explained. “The clinical criteria would be there, but no one would say the word.” This is important, he said, because sepsis is time critical.
So the pair set out to create a cultural change by sharing data and collecting input from each service and unit, which relied heavily on nursing staff to perpetuate change. They created an early warning system in the medical record and worked with units to achieve flexibility in their criteria.
While the early warning system seemed helpful on the floor, SEP-1 adherence rates changed little in the emergency department. So Dr. Graves and Dr. Horton worked out an ED-specific process map that started at triage and was modeled after myocardial infarction STEMI protocols. From April through December 2016, the ED achieved between 29.5% adherence to the SEP-1 bundles, they said according to CMS abstractor data. After the change, between January and March 2017, the ED saw 52.2% adherence.
Dr. Kalantari would like to see CMS allow hospitals to evaluate and alter their processes more individually, with the required result being lower sepsis mortality. Hospitalists, said Dr. Kahn, are well poised to champion these sepsis improvement efforts.
“Hospitalists are uniquely positioned to lead in this area because they are a visible presence and a link between providers doing multidisciplinary acute care,” he said. “The other thing hospitalists can do is insist on rolling out approaches that are evidence based and not likely to cause harm by leading to over resuscitation, or ensuring patients are receiving central-line insertions only when needed.”
This is currently a moment for hospitals to innovate and provide meaningful feedback to CMS, which, he said, is listening.
“It’s a myth that CMS rolls out policy without listening to the clinical community, but what they want is constructive criticism, not just to hear ‘We’re not ready and we have to push this down the road,’ ” Dr. Kahn said. “The time is now in the era of accountability in health care.”
References
1. Sepsis. National Institute of General Medical Sciences. https://www.nigms.nih.gov/education/pages/factsheet_sepsis.aspx. Updated Sept 2017. Accessed Jan 4, 2018.
2. Barbash I et al. Hospital perceptions of Medicare’s sepsis quality reporting initiative. J Hosp Med. 2017;12;963-8.
3. Kalantari A et al. Sepsis Definitions: The search for gold and what CMS got wrong. West J Emerg Med. 2017 Aug;18(5):951-6.
4. Singer M et. al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016 Feb 23;315(8):801-10.
5. Rhodes A et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43:304.
Hospitalists can champion sepsis-improvement efforts
Hospitalists can champion sepsis-improvement efforts
In October 2015, the Centers for Medicare & Medicaid Services implemented its first meaningful policy to attempt for addressing sepsis.
The condition – one of the leading causes of mortality among hospitalized patients – afflicts more than a million people each year in the United States, and between 15% and 30% of them die. Sepsis is one of the leading drivers of hospital readmissions, sending more patients back to the hospital than heart failure, pneumonia, and chronic obstructive pulmonary disease.1
However, while providers seem to agree that time to address sepsis is past due, not everyone has embraced the Sepsis CMS Core Measure program, or SEP-1, as the means to best achieve it. This is, in part, because of discrepancies in how sepsis is defined, the burden of reporting, and what some consider to be arbitrary clinical requirements that may not correlate with better patient outcomes.
“Sepsis is indeed a critical public health problem, and it’s appropriate and valuable that Medicare and other policy makers are focusing on sepsis,” said Jeremy Kahn, MD, professor of critical care medicine and health policy and management at the University of Pittsburgh. “This was really the first approach at that … but at 85-pages long, it really is an enormous effort for hospitals to adhere to this measure.”
This is because of the tension between the “intense desire to improve sepsis outcomes” and the “incredible burden” of keeping up with the necessary documentation while also providing quality care, Dr. Kahn said.
In December 2017, Dr. Kahn helped lead a study published in the Journal of Hospital Medicine aimed at trying to understand hospital perceptions of SEP-1. Over the course of 29 interviews with randomly selected hospital quality leaders across the United States, including physicians and nurses, the results came as a surprise.2
“Generally, hospitals were very supportive of the concept, and there was no pushback on the idea that we should be measuring and reporting sepsis quality to CMS,” he said.
However, the research team found that respondents believed the program’s requirements with respect to treatment and documentation were complex and not always linked to patient-centered outcomes. Meeting the SEP-1 bundles consistently required hospitals to dedicate resources that not all may have, especially those in small, rural communities and those serving as urban safety nets.
Some, like emergency medicine physician Annahieta Kalantari, DO (who did not participate in the survey), feel that SEP-1 forces providers to practice “check-box” medicine and undermines successful efforts that don’t necessarily align with the CMS policy.
She arrived at her institution, Aria-Jefferson Health in Philadelphia, before CMS adopted SEP-1; at that time, she took note of the fact that the rate of sepsis mortalities in her hospital was, in her words, not great when compared with that at similar institutions. And then she helped do something about it.
“I thought, ‘We’re a Premier reporting hospital,’ so we did a gap analysis as to why and put together protocols for the hospital to follow with our sepsis patients, including a sepsis alert and a lot of education,” said Dr. Kalantari, associate program director for the emergency medicine residency program at Aria-Jefferson and a former chair of its sepsis management committee. “Before you knew it, mortalities were below benchmark.”
But once SEP-1 began, she said, the hospital was unable to check all of the boxes all of the time.
“We kept track, but we weren’t hitting all the bundles exactly within the periods of time recommended, but our mortalities were still amazing,” she said. “CMS basically picked definitions [for sepsis], and most of us don’t know what they’re basing them on because no one can agree on a definition anyway. Now they’re penalizing hospitals if they don’t hit the check marks in time, but we’d already demonstrated that our mortality and patient care was exceptional.”
She added: “I am extremely dissatisfied, as someone who provides frontline patient care, with how CMS is choosing to measure us.”
Dr. Kalantari wrote a piece in the Western Journal of Emergency Medicine in July 2017 in which she and coauthors outline the issues they take with SEP-1. They lay out the tension among the varied definitions of what sepsis is – and isn’t – and they also illuminate the apparent conflict between what CMS has officially defined and what evidence-based studies conducted since 2001 have suggested.3
In particular, CMS defines severe sepsis as an initial lactate above 2 mmol/L and septic shock as an initial lactate presentation of greater than 4 mmol/L. However, Dr. Kalantari and here coauthors argue in the paper that there is no standard definition of sepsis and that decades of attempts to achieve one have failed to reach consensus among providers. CMS, she said, fails to acknowledge this.
Defining sepsis
In fact, in 2016, another new definition of sepsis emerged by way of a 19-member task-force of experts: The Third International Consensus Definitions for Sepsis and Septic Shock, also called Sepsis-3.4 In March 2017, the Surviving Sepsis Campaign adopted this definition, which defined sepsis as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.”5
“I think the definition has always been a challenging part of sepsis,” said Kencee Graves, MD, a hospitalist at the University of Utah, Salt Lake City. “The definitions came about for research purposes, so … they are not perfectly sensitive nor specific.”
However, Dr. Graves believes SEP-1 is a step in the right direction in that it brings awareness to sepsis and holds providers accountable. Several years ago, she and her colleague Devin Horton, MD, also a hospitalist at the University of Utah, embarked on a massive undertaking to address sepsis in their hospital. It was, at the time, lacking in “sepsis culture,” Dr. Horton said.
“One of the big things that motivated both of us was that we started doing chart review together and – it’s always easier with 20/20 hindsight – we were noticing that residents were missing the signs of sepsis,” Dr. Horton explained. “The clinical criteria would be there, but no one would say the word.” This is important, he said, because sepsis is time critical.
So the pair set out to create a cultural change by sharing data and collecting input from each service and unit, which relied heavily on nursing staff to perpetuate change. They created an early warning system in the medical record and worked with units to achieve flexibility in their criteria.
While the early warning system seemed helpful on the floor, SEP-1 adherence rates changed little in the emergency department. So Dr. Graves and Dr. Horton worked out an ED-specific process map that started at triage and was modeled after myocardial infarction STEMI protocols. From April through December 2016, the ED achieved between 29.5% adherence to the SEP-1 bundles, they said according to CMS abstractor data. After the change, between January and March 2017, the ED saw 52.2% adherence.
Dr. Kalantari would like to see CMS allow hospitals to evaluate and alter their processes more individually, with the required result being lower sepsis mortality. Hospitalists, said Dr. Kahn, are well poised to champion these sepsis improvement efforts.
“Hospitalists are uniquely positioned to lead in this area because they are a visible presence and a link between providers doing multidisciplinary acute care,” he said. “The other thing hospitalists can do is insist on rolling out approaches that are evidence based and not likely to cause harm by leading to over resuscitation, or ensuring patients are receiving central-line insertions only when needed.”
This is currently a moment for hospitals to innovate and provide meaningful feedback to CMS, which, he said, is listening.
“It’s a myth that CMS rolls out policy without listening to the clinical community, but what they want is constructive criticism, not just to hear ‘We’re not ready and we have to push this down the road,’ ” Dr. Kahn said. “The time is now in the era of accountability in health care.”
References
1. Sepsis. National Institute of General Medical Sciences. https://www.nigms.nih.gov/education/pages/factsheet_sepsis.aspx. Updated Sept 2017. Accessed Jan 4, 2018.
2. Barbash I et al. Hospital perceptions of Medicare’s sepsis quality reporting initiative. J Hosp Med. 2017;12;963-8.
3. Kalantari A et al. Sepsis Definitions: The search for gold and what CMS got wrong. West J Emerg Med. 2017 Aug;18(5):951-6.
4. Singer M et. al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016 Feb 23;315(8):801-10.
5. Rhodes A et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43:304.
In October 2015, the Centers for Medicare & Medicaid Services implemented its first meaningful policy to attempt for addressing sepsis.
The condition – one of the leading causes of mortality among hospitalized patients – afflicts more than a million people each year in the United States, and between 15% and 30% of them die. Sepsis is one of the leading drivers of hospital readmissions, sending more patients back to the hospital than heart failure, pneumonia, and chronic obstructive pulmonary disease.1
However, while providers seem to agree that time to address sepsis is past due, not everyone has embraced the Sepsis CMS Core Measure program, or SEP-1, as the means to best achieve it. This is, in part, because of discrepancies in how sepsis is defined, the burden of reporting, and what some consider to be arbitrary clinical requirements that may not correlate with better patient outcomes.
“Sepsis is indeed a critical public health problem, and it’s appropriate and valuable that Medicare and other policy makers are focusing on sepsis,” said Jeremy Kahn, MD, professor of critical care medicine and health policy and management at the University of Pittsburgh. “This was really the first approach at that … but at 85-pages long, it really is an enormous effort for hospitals to adhere to this measure.”
This is because of the tension between the “intense desire to improve sepsis outcomes” and the “incredible burden” of keeping up with the necessary documentation while also providing quality care, Dr. Kahn said.
In December 2017, Dr. Kahn helped lead a study published in the Journal of Hospital Medicine aimed at trying to understand hospital perceptions of SEP-1. Over the course of 29 interviews with randomly selected hospital quality leaders across the United States, including physicians and nurses, the results came as a surprise.2
“Generally, hospitals were very supportive of the concept, and there was no pushback on the idea that we should be measuring and reporting sepsis quality to CMS,” he said.
However, the research team found that respondents believed the program’s requirements with respect to treatment and documentation were complex and not always linked to patient-centered outcomes. Meeting the SEP-1 bundles consistently required hospitals to dedicate resources that not all may have, especially those in small, rural communities and those serving as urban safety nets.
Some, like emergency medicine physician Annahieta Kalantari, DO (who did not participate in the survey), feel that SEP-1 forces providers to practice “check-box” medicine and undermines successful efforts that don’t necessarily align with the CMS policy.
She arrived at her institution, Aria-Jefferson Health in Philadelphia, before CMS adopted SEP-1; at that time, she took note of the fact that the rate of sepsis mortalities in her hospital was, in her words, not great when compared with that at similar institutions. And then she helped do something about it.
“I thought, ‘We’re a Premier reporting hospital,’ so we did a gap analysis as to why and put together protocols for the hospital to follow with our sepsis patients, including a sepsis alert and a lot of education,” said Dr. Kalantari, associate program director for the emergency medicine residency program at Aria-Jefferson and a former chair of its sepsis management committee. “Before you knew it, mortalities were below benchmark.”
But once SEP-1 began, she said, the hospital was unable to check all of the boxes all of the time.
“We kept track, but we weren’t hitting all the bundles exactly within the periods of time recommended, but our mortalities were still amazing,” she said. “CMS basically picked definitions [for sepsis], and most of us don’t know what they’re basing them on because no one can agree on a definition anyway. Now they’re penalizing hospitals if they don’t hit the check marks in time, but we’d already demonstrated that our mortality and patient care was exceptional.”
She added: “I am extremely dissatisfied, as someone who provides frontline patient care, with how CMS is choosing to measure us.”
Dr. Kalantari wrote a piece in the Western Journal of Emergency Medicine in July 2017 in which she and coauthors outline the issues they take with SEP-1. They lay out the tension among the varied definitions of what sepsis is – and isn’t – and they also illuminate the apparent conflict between what CMS has officially defined and what evidence-based studies conducted since 2001 have suggested.3
In particular, CMS defines severe sepsis as an initial lactate above 2 mmol/L and septic shock as an initial lactate presentation of greater than 4 mmol/L. However, Dr. Kalantari and here coauthors argue in the paper that there is no standard definition of sepsis and that decades of attempts to achieve one have failed to reach consensus among providers. CMS, she said, fails to acknowledge this.
Defining sepsis
In fact, in 2016, another new definition of sepsis emerged by way of a 19-member task-force of experts: The Third International Consensus Definitions for Sepsis and Septic Shock, also called Sepsis-3.4 In March 2017, the Surviving Sepsis Campaign adopted this definition, which defined sepsis as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.”5
“I think the definition has always been a challenging part of sepsis,” said Kencee Graves, MD, a hospitalist at the University of Utah, Salt Lake City. “The definitions came about for research purposes, so … they are not perfectly sensitive nor specific.”
However, Dr. Graves believes SEP-1 is a step in the right direction in that it brings awareness to sepsis and holds providers accountable. Several years ago, she and her colleague Devin Horton, MD, also a hospitalist at the University of Utah, embarked on a massive undertaking to address sepsis in their hospital. It was, at the time, lacking in “sepsis culture,” Dr. Horton said.
“One of the big things that motivated both of us was that we started doing chart review together and – it’s always easier with 20/20 hindsight – we were noticing that residents were missing the signs of sepsis,” Dr. Horton explained. “The clinical criteria would be there, but no one would say the word.” This is important, he said, because sepsis is time critical.
So the pair set out to create a cultural change by sharing data and collecting input from each service and unit, which relied heavily on nursing staff to perpetuate change. They created an early warning system in the medical record and worked with units to achieve flexibility in their criteria.
While the early warning system seemed helpful on the floor, SEP-1 adherence rates changed little in the emergency department. So Dr. Graves and Dr. Horton worked out an ED-specific process map that started at triage and was modeled after myocardial infarction STEMI protocols. From April through December 2016, the ED achieved between 29.5% adherence to the SEP-1 bundles, they said according to CMS abstractor data. After the change, between January and March 2017, the ED saw 52.2% adherence.
Dr. Kalantari would like to see CMS allow hospitals to evaluate and alter their processes more individually, with the required result being lower sepsis mortality. Hospitalists, said Dr. Kahn, are well poised to champion these sepsis improvement efforts.
“Hospitalists are uniquely positioned to lead in this area because they are a visible presence and a link between providers doing multidisciplinary acute care,” he said. “The other thing hospitalists can do is insist on rolling out approaches that are evidence based and not likely to cause harm by leading to over resuscitation, or ensuring patients are receiving central-line insertions only when needed.”
This is currently a moment for hospitals to innovate and provide meaningful feedback to CMS, which, he said, is listening.
“It’s a myth that CMS rolls out policy without listening to the clinical community, but what they want is constructive criticism, not just to hear ‘We’re not ready and we have to push this down the road,’ ” Dr. Kahn said. “The time is now in the era of accountability in health care.”
References
1. Sepsis. National Institute of General Medical Sciences. https://www.nigms.nih.gov/education/pages/factsheet_sepsis.aspx. Updated Sept 2017. Accessed Jan 4, 2018.
2. Barbash I et al. Hospital perceptions of Medicare’s sepsis quality reporting initiative. J Hosp Med. 2017;12;963-8.
3. Kalantari A et al. Sepsis Definitions: The search for gold and what CMS got wrong. West J Emerg Med. 2017 Aug;18(5):951-6.
4. Singer M et. al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016 Feb 23;315(8):801-10.
5. Rhodes A et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43:304.
CMS floats Medicare direct provider contracting
Under a direct provider contracting (DPC) arrangement, Medicare could pay physicians or physician groups a monthly fee to deliver a specific set of services to beneficiaries, who would gain greater access to the physicians. The physicians would be accountable for those Medicare patients’ costs and care quality.
CMS is looking at how to incorporate this concept into the Medicare ranks. On April 23, CMS issued a request for information (RFI) seeking input across a wide range of topics, including provider/state participation, beneficiary participation, payment, general model design, program integrity and beneficiary protection, and how such models would fit within the existing accountable care organization framework.
The RFI offered one possible vision on how a direct provider contracting model could work.
“Under a primary care–focused DPC model, CMS could enter into arrangements with primary care practices under which CMS would pay these participating practices a fixed per beneficiary per month (PBPM) payment to cover the primary care services the practice would be expected to furnish under the model, which may include office visits, certain office-based procedures, and other non–visit-based services covered under the physician fee schedule, and flexibility in how otherwise billable services are delivered,” the RFI states.
Physicians could also earn performance bonuses, depending on how the DPC is structured, through “performance-based incentives for total cost of care and quality.”
CMS noted it also “could test ways to reduce administrative burden though innovative changes to claims submission processes for services included in the PBPM payment under these models.”
The direct provider contracting idea grew out of a previous RFI issued in 2017 by CMS’s Center for Medicare and Medicaid Innovation to collect ideas on new ways to deliver patient-centered care. The agency released the more than 1,000 comments received from that request on the same day it issued the RFI on direct provider contracting.
In those comments, a number of physician groups offered support for a direct-contracting approach.
For example, the American Academy of Family Physicians wrote that it “sees continued growth and interest in family physicians adopting this practice model in all settings types, including rural and underserved communities.” And the AAFP suggested that the innovation center should work with DPC organizations to learn more about them.
The American College of Physicians reiterated its previous position that it “supports physician and patient choice of practice and delivery models that are accessible, ethical, and viable and that strengthen the patient-physician relationship.” But the ACP raised a number of issues that could impede access to care or result in lower quality care.
The American Medical Association offered support for “testing of models in which physicians have the ability to deliver more or different services to patients who need them and to be paid more for doing so.”
The AMA suggested that some of the models to be tested include allowing patients to contract directly with physicians, with Medicare paying its fee schedule rates and patients paying the difference; allowing patients to receive their care from DPC practices and get reimbursed by Medicare; or allowing “physicians to define a team of providers who will provide all of the treatment needed for an acute condition or management of a chronic condition, and then allowing patients who select the team to receive all of the services related to their condition from the team in return for a single predefined cost-sharing amount.”
Comments on the RFI are due May 25.
Under a direct provider contracting (DPC) arrangement, Medicare could pay physicians or physician groups a monthly fee to deliver a specific set of services to beneficiaries, who would gain greater access to the physicians. The physicians would be accountable for those Medicare patients’ costs and care quality.
CMS is looking at how to incorporate this concept into the Medicare ranks. On April 23, CMS issued a request for information (RFI) seeking input across a wide range of topics, including provider/state participation, beneficiary participation, payment, general model design, program integrity and beneficiary protection, and how such models would fit within the existing accountable care organization framework.
The RFI offered one possible vision on how a direct provider contracting model could work.
“Under a primary care–focused DPC model, CMS could enter into arrangements with primary care practices under which CMS would pay these participating practices a fixed per beneficiary per month (PBPM) payment to cover the primary care services the practice would be expected to furnish under the model, which may include office visits, certain office-based procedures, and other non–visit-based services covered under the physician fee schedule, and flexibility in how otherwise billable services are delivered,” the RFI states.
Physicians could also earn performance bonuses, depending on how the DPC is structured, through “performance-based incentives for total cost of care and quality.”
CMS noted it also “could test ways to reduce administrative burden though innovative changes to claims submission processes for services included in the PBPM payment under these models.”
The direct provider contracting idea grew out of a previous RFI issued in 2017 by CMS’s Center for Medicare and Medicaid Innovation to collect ideas on new ways to deliver patient-centered care. The agency released the more than 1,000 comments received from that request on the same day it issued the RFI on direct provider contracting.
In those comments, a number of physician groups offered support for a direct-contracting approach.
For example, the American Academy of Family Physicians wrote that it “sees continued growth and interest in family physicians adopting this practice model in all settings types, including rural and underserved communities.” And the AAFP suggested that the innovation center should work with DPC organizations to learn more about them.
The American College of Physicians reiterated its previous position that it “supports physician and patient choice of practice and delivery models that are accessible, ethical, and viable and that strengthen the patient-physician relationship.” But the ACP raised a number of issues that could impede access to care or result in lower quality care.
The American Medical Association offered support for “testing of models in which physicians have the ability to deliver more or different services to patients who need them and to be paid more for doing so.”
The AMA suggested that some of the models to be tested include allowing patients to contract directly with physicians, with Medicare paying its fee schedule rates and patients paying the difference; allowing patients to receive their care from DPC practices and get reimbursed by Medicare; or allowing “physicians to define a team of providers who will provide all of the treatment needed for an acute condition or management of a chronic condition, and then allowing patients who select the team to receive all of the services related to their condition from the team in return for a single predefined cost-sharing amount.”
Comments on the RFI are due May 25.
Under a direct provider contracting (DPC) arrangement, Medicare could pay physicians or physician groups a monthly fee to deliver a specific set of services to beneficiaries, who would gain greater access to the physicians. The physicians would be accountable for those Medicare patients’ costs and care quality.
CMS is looking at how to incorporate this concept into the Medicare ranks. On April 23, CMS issued a request for information (RFI) seeking input across a wide range of topics, including provider/state participation, beneficiary participation, payment, general model design, program integrity and beneficiary protection, and how such models would fit within the existing accountable care organization framework.
The RFI offered one possible vision on how a direct provider contracting model could work.
“Under a primary care–focused DPC model, CMS could enter into arrangements with primary care practices under which CMS would pay these participating practices a fixed per beneficiary per month (PBPM) payment to cover the primary care services the practice would be expected to furnish under the model, which may include office visits, certain office-based procedures, and other non–visit-based services covered under the physician fee schedule, and flexibility in how otherwise billable services are delivered,” the RFI states.
Physicians could also earn performance bonuses, depending on how the DPC is structured, through “performance-based incentives for total cost of care and quality.”
CMS noted it also “could test ways to reduce administrative burden though innovative changes to claims submission processes for services included in the PBPM payment under these models.”
The direct provider contracting idea grew out of a previous RFI issued in 2017 by CMS’s Center for Medicare and Medicaid Innovation to collect ideas on new ways to deliver patient-centered care. The agency released the more than 1,000 comments received from that request on the same day it issued the RFI on direct provider contracting.
In those comments, a number of physician groups offered support for a direct-contracting approach.
For example, the American Academy of Family Physicians wrote that it “sees continued growth and interest in family physicians adopting this practice model in all settings types, including rural and underserved communities.” And the AAFP suggested that the innovation center should work with DPC organizations to learn more about them.
The American College of Physicians reiterated its previous position that it “supports physician and patient choice of practice and delivery models that are accessible, ethical, and viable and that strengthen the patient-physician relationship.” But the ACP raised a number of issues that could impede access to care or result in lower quality care.
The American Medical Association offered support for “testing of models in which physicians have the ability to deliver more or different services to patients who need them and to be paid more for doing so.”
The AMA suggested that some of the models to be tested include allowing patients to contract directly with physicians, with Medicare paying its fee schedule rates and patients paying the difference; allowing patients to receive their care from DPC practices and get reimbursed by Medicare; or allowing “physicians to define a team of providers who will provide all of the treatment needed for an acute condition or management of a chronic condition, and then allowing patients who select the team to receive all of the services related to their condition from the team in return for a single predefined cost-sharing amount.”
Comments on the RFI are due May 25.
MedPAC urges CMS to curb low-value care
according to a staff presentation at a meeting of the Medicare Payment Advisory Commission.
At the commission’s April meeting, MedPAC staff presented data from various literature searches, noting a “substantial use of low-value services in Medicare.” For example, they found that about 20% of Virginians, across all payers, received a low-value service in 2014, while 15% of Medicaid patients and 11% of commercially insured patients in Oregon received a low-value service in 2013.
“It is very hard to know at the beginning of coverage that something is going to be low value,” MedPAC commission member Kathy Buto, former vice president of global health policy at Johnson & Johnson, noted. “It may be covered for something narrow for which it is high value and then spreads. It’s important to have those kinds of tools once technologies and procedures are covered to be able to actually monitor what is going on and assess.”
But, she added, the Centers for Medicare & Medicaid Services needs to do more to routinely reexamine its coverage decisions.
Ms. Buto noted that noncoverage decisions are rarely issued and suggested that “there is an opportunity for us to take a look at whether we would advise CMS to take a look at using more of those tools more aggressively.”
Paul Ginsburg, PhD, commissioner and senior fellow in economic studies at the Brookings Institution, Washington, suggested that, for any new procedure or drug, initial coverage is always provisional for a certain length of time, which would force CMS to revisit coverage decisions.
“If there is no evidence, the coverage ends,” Dr Ginsburg said. “If there is positive evidence, the coverage proceeds.”
However, as commissioner Rita Redberg, MD, of the University of California, San Francisco, said of CMS, even with tools to cut coverage, its hands may be tied by outside forces. “CMS needs a lot more political cover.”
Dr. Redberg noted that there was extensive lobbying of local carriers, and within 6 months, despite the lack of evidence, everyone was covering cardiac CT.
“A few years later, CMS tried to walk back the coverage because it was just hemorrhaging money for cardiac CT, but there was no chance because it was a capital investment,” she added. “Even when there are restrictions on coverage, CMS doesn’t enforce them.”
Ms. Buto also raised the issue of how much influence CMS has over Medicare Part D prescription drug plan sponsors’ coverage decision policies, but suggested CMS could play a larger role in that.
Commissioner Amy Bricker, vice president of supply chain strategy at Express Scripts, St. Louis, suggested that, “We need to do more from a Part D perspective to allow plans to manage drug coverage more aggressively and in line with the commercial space. CMS has handcuffed them,” noting that FDA approval, regardless of value, generally means Medicare coverage.
Commissioner Jack Hoadley, PhD, of Georgetown University in Washington, cautioned that any discussion on these or possibly other tools needs to take into account the needs of those who will legitimately benefit from some of the low-value services so they do not inadvertently prevent access for those patients.
At press time, MedPAC had not scheduled a vote on specific recommendations to address low-value care.
according to a staff presentation at a meeting of the Medicare Payment Advisory Commission.
At the commission’s April meeting, MedPAC staff presented data from various literature searches, noting a “substantial use of low-value services in Medicare.” For example, they found that about 20% of Virginians, across all payers, received a low-value service in 2014, while 15% of Medicaid patients and 11% of commercially insured patients in Oregon received a low-value service in 2013.
“It is very hard to know at the beginning of coverage that something is going to be low value,” MedPAC commission member Kathy Buto, former vice president of global health policy at Johnson & Johnson, noted. “It may be covered for something narrow for which it is high value and then spreads. It’s important to have those kinds of tools once technologies and procedures are covered to be able to actually monitor what is going on and assess.”
But, she added, the Centers for Medicare & Medicaid Services needs to do more to routinely reexamine its coverage decisions.
Ms. Buto noted that noncoverage decisions are rarely issued and suggested that “there is an opportunity for us to take a look at whether we would advise CMS to take a look at using more of those tools more aggressively.”
Paul Ginsburg, PhD, commissioner and senior fellow in economic studies at the Brookings Institution, Washington, suggested that, for any new procedure or drug, initial coverage is always provisional for a certain length of time, which would force CMS to revisit coverage decisions.
“If there is no evidence, the coverage ends,” Dr Ginsburg said. “If there is positive evidence, the coverage proceeds.”
However, as commissioner Rita Redberg, MD, of the University of California, San Francisco, said of CMS, even with tools to cut coverage, its hands may be tied by outside forces. “CMS needs a lot more political cover.”
Dr. Redberg noted that there was extensive lobbying of local carriers, and within 6 months, despite the lack of evidence, everyone was covering cardiac CT.
“A few years later, CMS tried to walk back the coverage because it was just hemorrhaging money for cardiac CT, but there was no chance because it was a capital investment,” she added. “Even when there are restrictions on coverage, CMS doesn’t enforce them.”
Ms. Buto also raised the issue of how much influence CMS has over Medicare Part D prescription drug plan sponsors’ coverage decision policies, but suggested CMS could play a larger role in that.
Commissioner Amy Bricker, vice president of supply chain strategy at Express Scripts, St. Louis, suggested that, “We need to do more from a Part D perspective to allow plans to manage drug coverage more aggressively and in line with the commercial space. CMS has handcuffed them,” noting that FDA approval, regardless of value, generally means Medicare coverage.
Commissioner Jack Hoadley, PhD, of Georgetown University in Washington, cautioned that any discussion on these or possibly other tools needs to take into account the needs of those who will legitimately benefit from some of the low-value services so they do not inadvertently prevent access for those patients.
At press time, MedPAC had not scheduled a vote on specific recommendations to address low-value care.
according to a staff presentation at a meeting of the Medicare Payment Advisory Commission.
At the commission’s April meeting, MedPAC staff presented data from various literature searches, noting a “substantial use of low-value services in Medicare.” For example, they found that about 20% of Virginians, across all payers, received a low-value service in 2014, while 15% of Medicaid patients and 11% of commercially insured patients in Oregon received a low-value service in 2013.
“It is very hard to know at the beginning of coverage that something is going to be low value,” MedPAC commission member Kathy Buto, former vice president of global health policy at Johnson & Johnson, noted. “It may be covered for something narrow for which it is high value and then spreads. It’s important to have those kinds of tools once technologies and procedures are covered to be able to actually monitor what is going on and assess.”
But, she added, the Centers for Medicare & Medicaid Services needs to do more to routinely reexamine its coverage decisions.
Ms. Buto noted that noncoverage decisions are rarely issued and suggested that “there is an opportunity for us to take a look at whether we would advise CMS to take a look at using more of those tools more aggressively.”
Paul Ginsburg, PhD, commissioner and senior fellow in economic studies at the Brookings Institution, Washington, suggested that, for any new procedure or drug, initial coverage is always provisional for a certain length of time, which would force CMS to revisit coverage decisions.
“If there is no evidence, the coverage ends,” Dr Ginsburg said. “If there is positive evidence, the coverage proceeds.”
However, as commissioner Rita Redberg, MD, of the University of California, San Francisco, said of CMS, even with tools to cut coverage, its hands may be tied by outside forces. “CMS needs a lot more political cover.”
Dr. Redberg noted that there was extensive lobbying of local carriers, and within 6 months, despite the lack of evidence, everyone was covering cardiac CT.
“A few years later, CMS tried to walk back the coverage because it was just hemorrhaging money for cardiac CT, but there was no chance because it was a capital investment,” she added. “Even when there are restrictions on coverage, CMS doesn’t enforce them.”
Ms. Buto also raised the issue of how much influence CMS has over Medicare Part D prescription drug plan sponsors’ coverage decision policies, but suggested CMS could play a larger role in that.
Commissioner Amy Bricker, vice president of supply chain strategy at Express Scripts, St. Louis, suggested that, “We need to do more from a Part D perspective to allow plans to manage drug coverage more aggressively and in line with the commercial space. CMS has handcuffed them,” noting that FDA approval, regardless of value, generally means Medicare coverage.
Commissioner Jack Hoadley, PhD, of Georgetown University in Washington, cautioned that any discussion on these or possibly other tools needs to take into account the needs of those who will legitimately benefit from some of the low-value services so they do not inadvertently prevent access for those patients.
At press time, MedPAC had not scheduled a vote on specific recommendations to address low-value care.
REPORTING FROM MEDPAC
CMS finalizes measures to help combat opioid crisis
Federal agencies and leaders are taking a multipronged approach to the opioid crisis.
Efforts by the Centers for Medicare & Medicaid Services focus on changes to the Medicare Part D program and Medicare Advantage, via two policy changes issued April 2: The Part D/Medicare Advantage annual update and final calendar year 2019 guidance to insurers who provide coverage under those two programs.
The annual Part D/Medicare Advantage update implements provisions of the Comprehensive Addiction and Recovery Act of 2016 (S. 524), requiring “CMS to establish through regulation a framework that allows Part D sponsors to implement drug management programs,” according to a CMS fact sheet. “Under such programs, a sponsor can limit at-risk beneficiaries’ access to coverage for frequently abused drugs beginning with the 2019 plan year.” The update designates opioids and benzodiazepines as frequently abused drugs.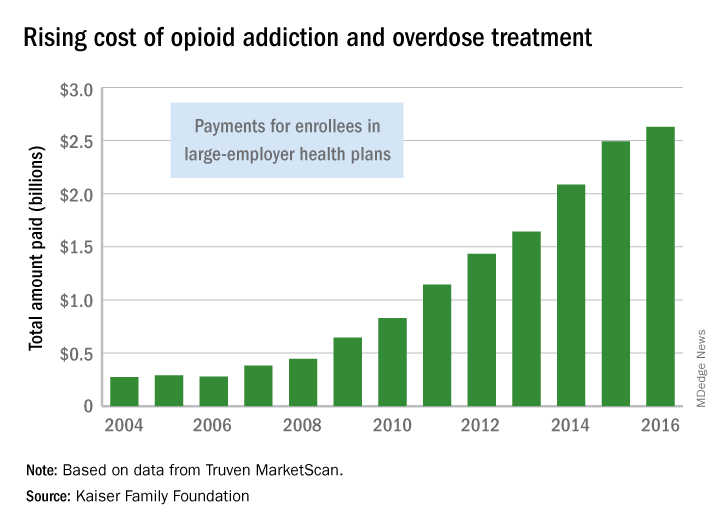
The agency is taking the further step of limiting special enrollment periods for dual eligibles – those beneficiaries eligible for both Medicare and Medicaid – if they are identified as at-risk or potentially at-risk for prescription drug abuse under the programs. Beneficiaries maintain the right to challenge the determination.
Patients who are being treated for cancer-related pain and those receiving hospice/palliative/end-of-life care are exempted from the drug management programs.
The policies also update opioid prescription limits. CMS is calling on “all Part D sponsors to implement a hard safety edit to limit initial opioid prescription fills for the treatment of acute pain to no more than a 7-day supply,” according to the fact sheet.
For chronic opioid users, CMS expects “all sponsors to implement an opioid care coordination edit at 90 morphine milligram equivalent (MME) per day. This formulary-level safety edit should trigger when a beneficiary’s cumulative MME per day across their opioid prescriptions reaches or exceeds 90 MME.”
There is flexibility: Pharmacists may contact prescribers and confirm that more pain medication is needed and then override the 90 MME/day threshold, if appropriate.
Finally, CMS expects “sponsors to implement additional soft safety edits to alert the pharmacist about duplicative opioid therapy and concurrent use of opioids and benzodiazepines,” according to the guidance.
The executive and legislative branches also are taking action.
President Trump in March detailed initiatives to address the opioid crisis across three domains: reducing demand through education, awareness, and prevention of overprescribing; reducing illicit drug importation and distribution; and expanding opportunities for proven treatment options.
For prescribers, the president’s plan calls for a nationwide reduction in opioid prescriptions filled by one-third within 3 years. It also looks aims to ensure that 75% of opioid prescriptions paid for by the government are “issued using best practices within 3 years, and 95% within 5 years,” a White House fact sheet notes.
When it comes to federal health care providers, those standards are to be met by half within 2 years and all within 5.
The White House also is calling on states to transition to a nationally interoperable Prescription Drug Monitoring Program (PDMP) network.
The president’s plan also calls for ensuring first-responder access to naloxone, improving overdose tracking systems, and expanding access to medication-assisted treatment. It also aims to change the Medicaid law that prohibits reimbursement of residential treatment at certain facilities with more than 16 beds.
On the legislative side, the House Energy and Commerce Committee is in the process of hosting a series of hearings and is expected to introduce a comprehensive package of bills aimed at various aspects of the opioid crisis. Across the four hearings, more than 30 pieces of individual legislation have been examined.
In the Senate, the Health, Education, Labor and Pensions Committee on April 4 released a discussion draft of the Opioid Crisis Response Act of 2018 and has scheduled a hearing for April 11 to discuss it.
The bill would spur development of nonaddictive pain killers, clarify FDA authority on small-quantity blister packs for opioids, provide states with better PDMP support; increase access to mental health services in schools, and improve substance use disorder treatment in underserved areas.
Also on April 4, the National Institutes of Health launched the HEAL Initiative (Helping to End Addiction Long-Term) to increase research to help prevent addiction through advanced pain management, and improve treatments for opioid misuse disorder and addiction. NIH is nearly doubling funding into opioid misuse/addiction research from $600 million in fiscal 2016 to $1.1 billion in fiscal 2018.
Federal agencies and leaders are taking a multipronged approach to the opioid crisis.
Efforts by the Centers for Medicare & Medicaid Services focus on changes to the Medicare Part D program and Medicare Advantage, via two policy changes issued April 2: The Part D/Medicare Advantage annual update and final calendar year 2019 guidance to insurers who provide coverage under those two programs.
The annual Part D/Medicare Advantage update implements provisions of the Comprehensive Addiction and Recovery Act of 2016 (S. 524), requiring “CMS to establish through regulation a framework that allows Part D sponsors to implement drug management programs,” according to a CMS fact sheet. “Under such programs, a sponsor can limit at-risk beneficiaries’ access to coverage for frequently abused drugs beginning with the 2019 plan year.” The update designates opioids and benzodiazepines as frequently abused drugs.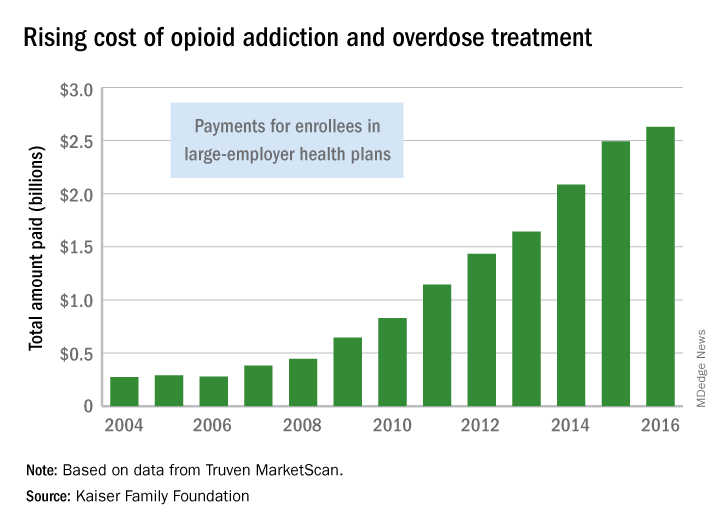
The agency is taking the further step of limiting special enrollment periods for dual eligibles – those beneficiaries eligible for both Medicare and Medicaid – if they are identified as at-risk or potentially at-risk for prescription drug abuse under the programs. Beneficiaries maintain the right to challenge the determination.
Patients who are being treated for cancer-related pain and those receiving hospice/palliative/end-of-life care are exempted from the drug management programs.
The policies also update opioid prescription limits. CMS is calling on “all Part D sponsors to implement a hard safety edit to limit initial opioid prescription fills for the treatment of acute pain to no more than a 7-day supply,” according to the fact sheet.
For chronic opioid users, CMS expects “all sponsors to implement an opioid care coordination edit at 90 morphine milligram equivalent (MME) per day. This formulary-level safety edit should trigger when a beneficiary’s cumulative MME per day across their opioid prescriptions reaches or exceeds 90 MME.”
There is flexibility: Pharmacists may contact prescribers and confirm that more pain medication is needed and then override the 90 MME/day threshold, if appropriate.
Finally, CMS expects “sponsors to implement additional soft safety edits to alert the pharmacist about duplicative opioid therapy and concurrent use of opioids and benzodiazepines,” according to the guidance.
The executive and legislative branches also are taking action.
President Trump in March detailed initiatives to address the opioid crisis across three domains: reducing demand through education, awareness, and prevention of overprescribing; reducing illicit drug importation and distribution; and expanding opportunities for proven treatment options.
For prescribers, the president’s plan calls for a nationwide reduction in opioid prescriptions filled by one-third within 3 years. It also looks aims to ensure that 75% of opioid prescriptions paid for by the government are “issued using best practices within 3 years, and 95% within 5 years,” a White House fact sheet notes.
When it comes to federal health care providers, those standards are to be met by half within 2 years and all within 5.
The White House also is calling on states to transition to a nationally interoperable Prescription Drug Monitoring Program (PDMP) network.
The president’s plan also calls for ensuring first-responder access to naloxone, improving overdose tracking systems, and expanding access to medication-assisted treatment. It also aims to change the Medicaid law that prohibits reimbursement of residential treatment at certain facilities with more than 16 beds.
On the legislative side, the House Energy and Commerce Committee is in the process of hosting a series of hearings and is expected to introduce a comprehensive package of bills aimed at various aspects of the opioid crisis. Across the four hearings, more than 30 pieces of individual legislation have been examined.
In the Senate, the Health, Education, Labor and Pensions Committee on April 4 released a discussion draft of the Opioid Crisis Response Act of 2018 and has scheduled a hearing for April 11 to discuss it.
The bill would spur development of nonaddictive pain killers, clarify FDA authority on small-quantity blister packs for opioids, provide states with better PDMP support; increase access to mental health services in schools, and improve substance use disorder treatment in underserved areas.
Also on April 4, the National Institutes of Health launched the HEAL Initiative (Helping to End Addiction Long-Term) to increase research to help prevent addiction through advanced pain management, and improve treatments for opioid misuse disorder and addiction. NIH is nearly doubling funding into opioid misuse/addiction research from $600 million in fiscal 2016 to $1.1 billion in fiscal 2018.
Federal agencies and leaders are taking a multipronged approach to the opioid crisis.
Efforts by the Centers for Medicare & Medicaid Services focus on changes to the Medicare Part D program and Medicare Advantage, via two policy changes issued April 2: The Part D/Medicare Advantage annual update and final calendar year 2019 guidance to insurers who provide coverage under those two programs.
The annual Part D/Medicare Advantage update implements provisions of the Comprehensive Addiction and Recovery Act of 2016 (S. 524), requiring “CMS to establish through regulation a framework that allows Part D sponsors to implement drug management programs,” according to a CMS fact sheet. “Under such programs, a sponsor can limit at-risk beneficiaries’ access to coverage for frequently abused drugs beginning with the 2019 plan year.” The update designates opioids and benzodiazepines as frequently abused drugs.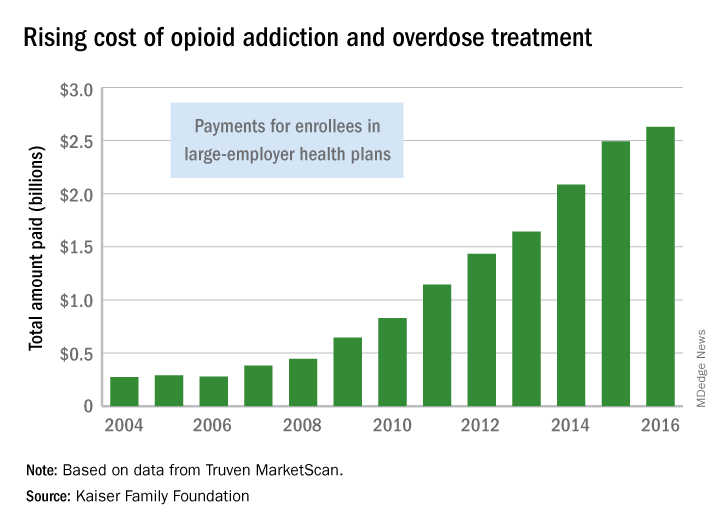
The agency is taking the further step of limiting special enrollment periods for dual eligibles – those beneficiaries eligible for both Medicare and Medicaid – if they are identified as at-risk or potentially at-risk for prescription drug abuse under the programs. Beneficiaries maintain the right to challenge the determination.
Patients who are being treated for cancer-related pain and those receiving hospice/palliative/end-of-life care are exempted from the drug management programs.
The policies also update opioid prescription limits. CMS is calling on “all Part D sponsors to implement a hard safety edit to limit initial opioid prescription fills for the treatment of acute pain to no more than a 7-day supply,” according to the fact sheet.
For chronic opioid users, CMS expects “all sponsors to implement an opioid care coordination edit at 90 morphine milligram equivalent (MME) per day. This formulary-level safety edit should trigger when a beneficiary’s cumulative MME per day across their opioid prescriptions reaches or exceeds 90 MME.”
There is flexibility: Pharmacists may contact prescribers and confirm that more pain medication is needed and then override the 90 MME/day threshold, if appropriate.
Finally, CMS expects “sponsors to implement additional soft safety edits to alert the pharmacist about duplicative opioid therapy and concurrent use of opioids and benzodiazepines,” according to the guidance.
The executive and legislative branches also are taking action.
President Trump in March detailed initiatives to address the opioid crisis across three domains: reducing demand through education, awareness, and prevention of overprescribing; reducing illicit drug importation and distribution; and expanding opportunities for proven treatment options.
For prescribers, the president’s plan calls for a nationwide reduction in opioid prescriptions filled by one-third within 3 years. It also looks aims to ensure that 75% of opioid prescriptions paid for by the government are “issued using best practices within 3 years, and 95% within 5 years,” a White House fact sheet notes.
When it comes to federal health care providers, those standards are to be met by half within 2 years and all within 5.
The White House also is calling on states to transition to a nationally interoperable Prescription Drug Monitoring Program (PDMP) network.
The president’s plan also calls for ensuring first-responder access to naloxone, improving overdose tracking systems, and expanding access to medication-assisted treatment. It also aims to change the Medicaid law that prohibits reimbursement of residential treatment at certain facilities with more than 16 beds.
On the legislative side, the House Energy and Commerce Committee is in the process of hosting a series of hearings and is expected to introduce a comprehensive package of bills aimed at various aspects of the opioid crisis. Across the four hearings, more than 30 pieces of individual legislation have been examined.
In the Senate, the Health, Education, Labor and Pensions Committee on April 4 released a discussion draft of the Opioid Crisis Response Act of 2018 and has scheduled a hearing for April 11 to discuss it.
The bill would spur development of nonaddictive pain killers, clarify FDA authority on small-quantity blister packs for opioids, provide states with better PDMP support; increase access to mental health services in schools, and improve substance use disorder treatment in underserved areas.
Also on April 4, the National Institutes of Health launched the HEAL Initiative (Helping to End Addiction Long-Term) to increase research to help prevent addiction through advanced pain management, and improve treatments for opioid misuse disorder and addiction. NIH is nearly doubling funding into opioid misuse/addiction research from $600 million in fiscal 2016 to $1.1 billion in fiscal 2018.
Understanding the new CMS bundle model
Hospitalists have been among the highest-volume participants in Medicare’s Bundled Payments for Care Improvement (BPCI) demonstration model, initiating over 200,000 episodes representing $4.7 billion in spending since the model began.1 On Jan. 9, the Centers for Medicare & Medicaid Services announced BPCI’s follow-on model, “BPCI Advanced.”2
BPCI launched in October 2013 and sunsets at the end of Q3 2018. BPCI Advanced starts immediately upon conclusion of BPCI (Q4 2018) and is slated to finish at year-end 2023.
CMS intends for the program to qualify as an Advanced Alternative Payment Model (APM). As BPCI Advanced focuses on episodes of care involving an inpatient stay (It also includes three outpatient episodes.) and the subsequent 90-day recovery period, it represents the first large-scale opportunity for hospitalists to meet criteria for Advanced APM participation. Qualifying for the Advanced APM track of the Quality Payment Program – which involves meeting patient volume or payment thresholds3 – comes with a 5% lump-sum bonus based on Medicare Part B fees and avoids exposure to penalties and reporting requirements of the Merit-based Incentive Payment System (MIPS).
Key program features
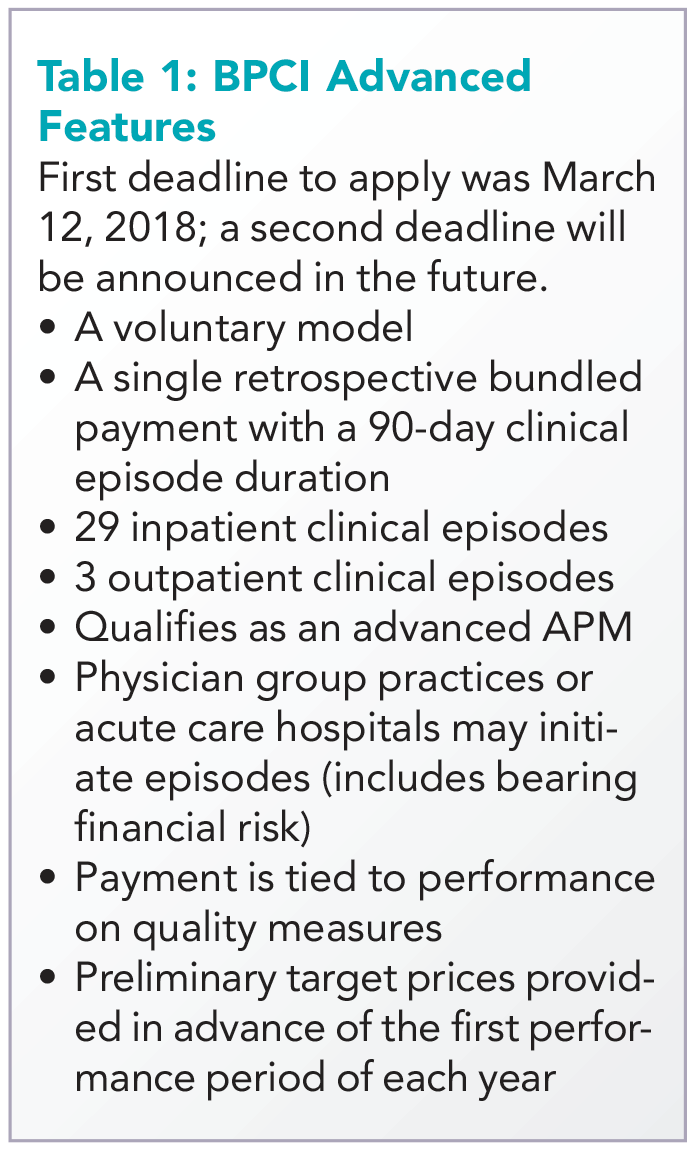
Acute care hospitals and physician groups may initiate episodes under BPCI Advanced, assuming financial risk under the model. Similar to its predecessor, BPCI Advanced assigns a target price based on past claims payments associated with the “episode initiator.”
During the performance period, if the initiator can beat the price in the aggregate for its bundles, it can keep the difference, and if it comes in over the price, it must pay the difference back to Medicare. Medicare discounts the target price by 3%, effectively paying itself that amount. After that, there is no sharing of savings with Medicare, as opposed to the permanent ACO programs, where there is sharing after the ACO meets the minimum savings rate.
The program allows physician groups and hospital initiators to go it alone or to work with a “convener,” which may share risk and reward with initiators, and may provide software, analytics, networks of high-performing providers like nursing facilities, and knowledge of specific care redesign approaches to enable program success. See Table 1 for a listing of other notable features of BPCI Advanced.
Quality measures
BPCI Advanced qualifies as an Advanced APM in part because payment is tied to performance on a set of quality measures (see Table 2). There are two measures applied to all episodes: all-cause hospital readmissions and advance care plan. These are notable because hospitalists may be especially focused on improvement activities in these areas.
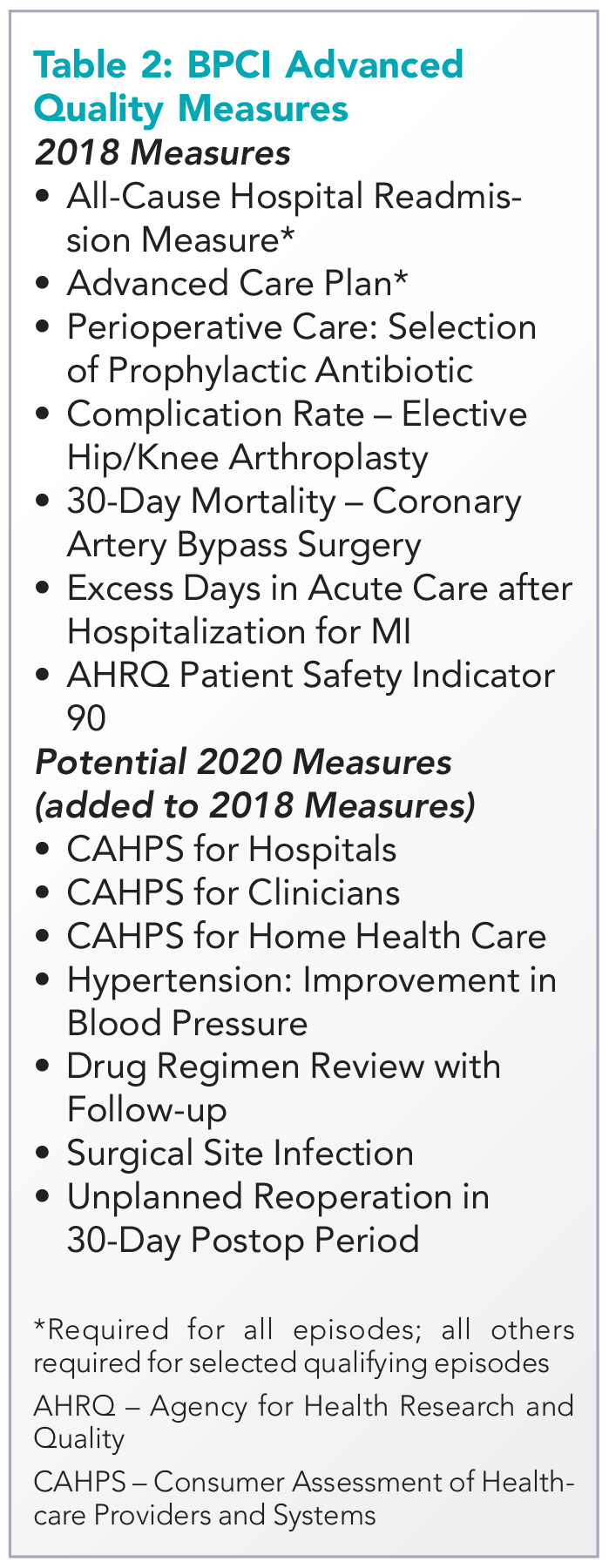
While the advance care plan measure refers to a process reflected by record documentation and is therefore directly under the control of hospitalists, readmissions – and most of the other measures – require a team approach. Because the outcome measures are risk adjusted, accurate and complete clinical documentation is crucial, as it drives how risk is adjusted. Of note, all the 2018 measures, collected directly through claims, will place no additional administrative burden for collection on providers.
Two ways for hospitalists to participate
Hospitalist groups – whether independent or employed – may be episode initiators in BPCI Advanced. In this case, any episodes in which the group participates that carry the name of a member of the hospitalist group in the “Attending Provider” field on the hospital bill claim form to Medicare (and the associated carrier claim) are attributed to that member’s physician group.
For example, if the group has chosen heart failure as an episode in which to participate at the program’s outset, a hospitalization is assigned the heart failure DRG (diagnosis-related group) and a group member is the Attending Provider on the claim form (and submits a claim for the physician services), then the episode is attributed to that group. This means that the group is responsible for payments represented by Medicare Part A and Part B claims (with a few exclusions like trauma and cancer) against the target price for the initial hospitalization and subsequent 90-day period. In practice, hospitalists are rewarded for actions aimed at optimizing location after discharge,4 avoiding readmissions, choosing efficient nursing facilities, and helping patients to maximize functional status.
The other way hospitalists may participate is through an agreement to share in savings with a hospital or physician group episode initiator. This requires hospitalist individuals or groups to enter into a contract with the initiator that meets certain program requirements – for example, report quality measures, engage in care redesign, use certified EHR technology (hospital-based clinicians automatically fulfill this criterion).
If there is broad participation, BPCI Advanced could represent a key milestone for hospitalists, as they seek to be recognized for the value they confer to the system as a whole instead of simply their professional billings. While there are legitimate concerns about the effect MIPS may have on health care value and the complexity of participation in APMs, barring a repeal of the law that created them, hospitalists now have the chance to extend their influence within and outside the hospital’s four walls and be more fairly rewarded for it.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of the Society of Hospital Medicine. Contact him at wfwhit@comcast.net. Disclosure: The author’s employer, Remedy Partners, is an Awardee Convener for the BPCI initiative and intends to apply as a Convener in BPCI Advanced.
References
1. Based on BPCI awardee convener Remedy Partners claims analysis.
2. https://innovation.cms.gov/initiatives/bpci-advanced.
3. https://qpp.cms.gov/apms/overview.
4. Whitcomb W. Choosing location after discharge wisely. The-hospitalist.org. 2018 Jan 3. Digital edition. Accessed Jan 13, 2018.
Hospitalists have been among the highest-volume participants in Medicare’s Bundled Payments for Care Improvement (BPCI) demonstration model, initiating over 200,000 episodes representing $4.7 billion in spending since the model began.1 On Jan. 9, the Centers for Medicare & Medicaid Services announced BPCI’s follow-on model, “BPCI Advanced.”2
BPCI launched in October 2013 and sunsets at the end of Q3 2018. BPCI Advanced starts immediately upon conclusion of BPCI (Q4 2018) and is slated to finish at year-end 2023.
CMS intends for the program to qualify as an Advanced Alternative Payment Model (APM). As BPCI Advanced focuses on episodes of care involving an inpatient stay (It also includes three outpatient episodes.) and the subsequent 90-day recovery period, it represents the first large-scale opportunity for hospitalists to meet criteria for Advanced APM participation. Qualifying for the Advanced APM track of the Quality Payment Program – which involves meeting patient volume or payment thresholds3 – comes with a 5% lump-sum bonus based on Medicare Part B fees and avoids exposure to penalties and reporting requirements of the Merit-based Incentive Payment System (MIPS).
Key program features
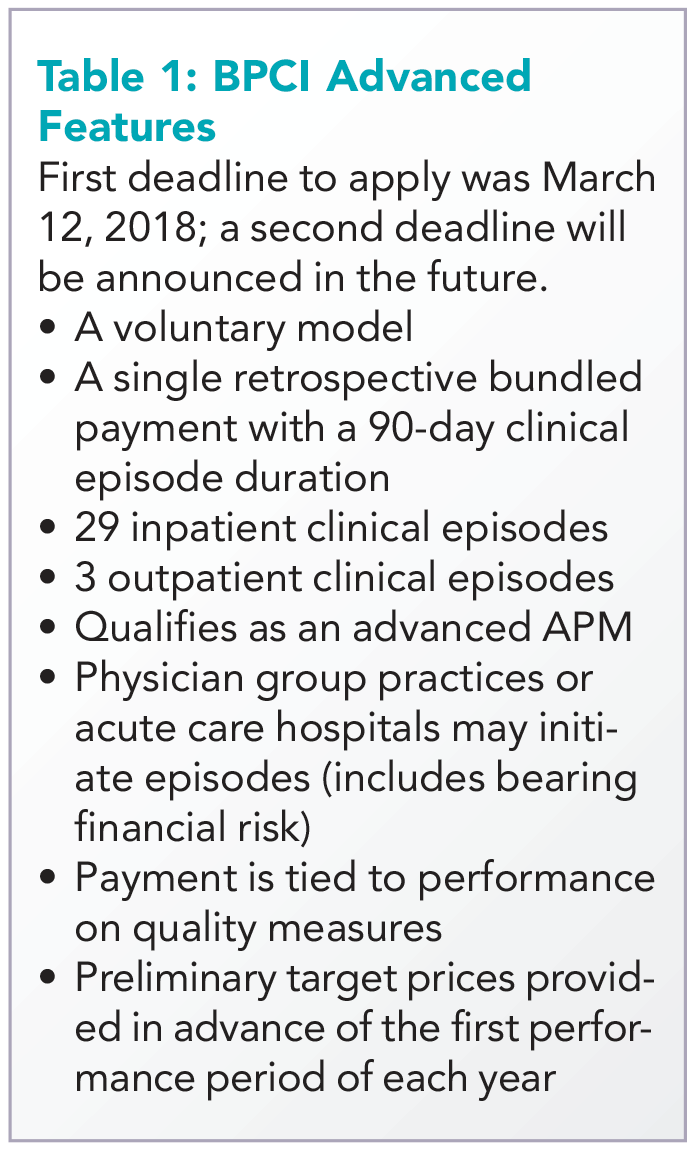
Acute care hospitals and physician groups may initiate episodes under BPCI Advanced, assuming financial risk under the model. Similar to its predecessor, BPCI Advanced assigns a target price based on past claims payments associated with the “episode initiator.”
During the performance period, if the initiator can beat the price in the aggregate for its bundles, it can keep the difference, and if it comes in over the price, it must pay the difference back to Medicare. Medicare discounts the target price by 3%, effectively paying itself that amount. After that, there is no sharing of savings with Medicare, as opposed to the permanent ACO programs, where there is sharing after the ACO meets the minimum savings rate.
The program allows physician groups and hospital initiators to go it alone or to work with a “convener,” which may share risk and reward with initiators, and may provide software, analytics, networks of high-performing providers like nursing facilities, and knowledge of specific care redesign approaches to enable program success. See Table 1 for a listing of other notable features of BPCI Advanced.
Quality measures
BPCI Advanced qualifies as an Advanced APM in part because payment is tied to performance on a set of quality measures (see Table 2). There are two measures applied to all episodes: all-cause hospital readmissions and advance care plan. These are notable because hospitalists may be especially focused on improvement activities in these areas.
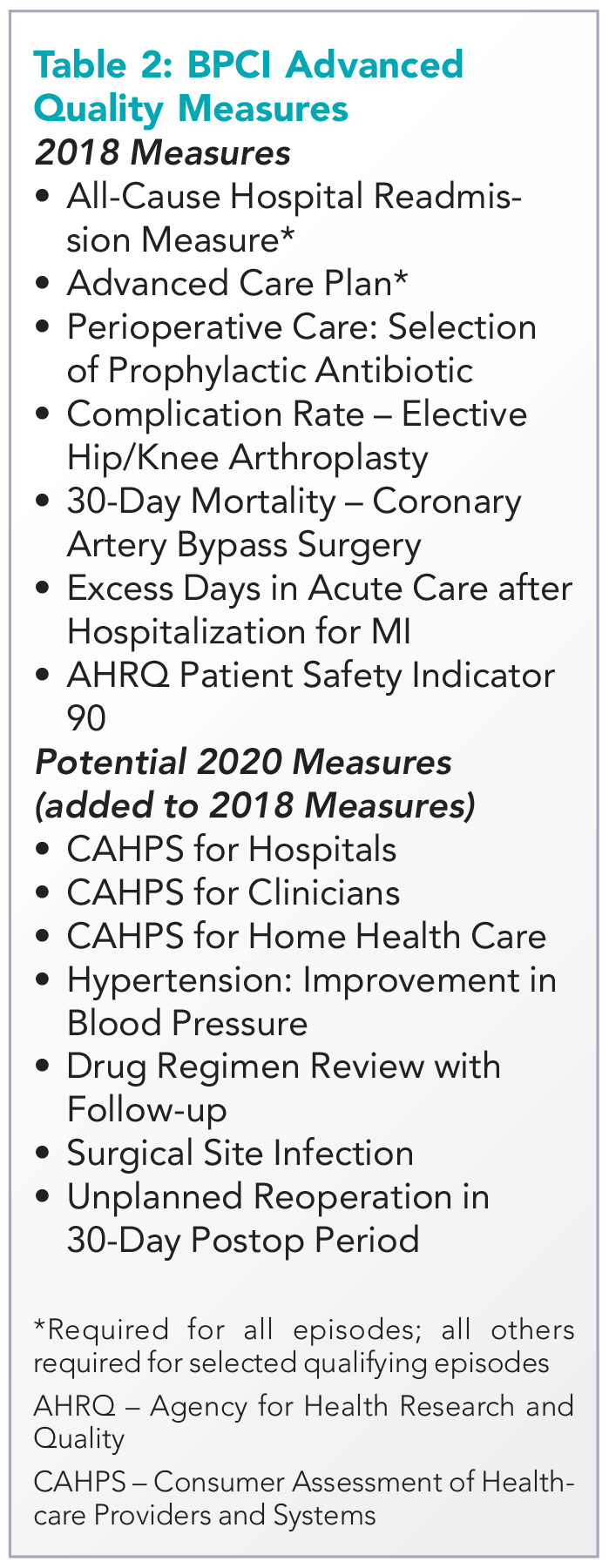
While the advance care plan measure refers to a process reflected by record documentation and is therefore directly under the control of hospitalists, readmissions – and most of the other measures – require a team approach. Because the outcome measures are risk adjusted, accurate and complete clinical documentation is crucial, as it drives how risk is adjusted. Of note, all the 2018 measures, collected directly through claims, will place no additional administrative burden for collection on providers.
Two ways for hospitalists to participate
Hospitalist groups – whether independent or employed – may be episode initiators in BPCI Advanced. In this case, any episodes in which the group participates that carry the name of a member of the hospitalist group in the “Attending Provider” field on the hospital bill claim form to Medicare (and the associated carrier claim) are attributed to that member’s physician group.
For example, if the group has chosen heart failure as an episode in which to participate at the program’s outset, a hospitalization is assigned the heart failure DRG (diagnosis-related group) and a group member is the Attending Provider on the claim form (and submits a claim for the physician services), then the episode is attributed to that group. This means that the group is responsible for payments represented by Medicare Part A and Part B claims (with a few exclusions like trauma and cancer) against the target price for the initial hospitalization and subsequent 90-day period. In practice, hospitalists are rewarded for actions aimed at optimizing location after discharge,4 avoiding readmissions, choosing efficient nursing facilities, and helping patients to maximize functional status.
The other way hospitalists may participate is through an agreement to share in savings with a hospital or physician group episode initiator. This requires hospitalist individuals or groups to enter into a contract with the initiator that meets certain program requirements – for example, report quality measures, engage in care redesign, use certified EHR technology (hospital-based clinicians automatically fulfill this criterion).
If there is broad participation, BPCI Advanced could represent a key milestone for hospitalists, as they seek to be recognized for the value they confer to the system as a whole instead of simply their professional billings. While there are legitimate concerns about the effect MIPS may have on health care value and the complexity of participation in APMs, barring a repeal of the law that created them, hospitalists now have the chance to extend their influence within and outside the hospital’s four walls and be more fairly rewarded for it.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of the Society of Hospital Medicine. Contact him at wfwhit@comcast.net. Disclosure: The author’s employer, Remedy Partners, is an Awardee Convener for the BPCI initiative and intends to apply as a Convener in BPCI Advanced.
References
1. Based on BPCI awardee convener Remedy Partners claims analysis.
2. https://innovation.cms.gov/initiatives/bpci-advanced.
3. https://qpp.cms.gov/apms/overview.
4. Whitcomb W. Choosing location after discharge wisely. The-hospitalist.org. 2018 Jan 3. Digital edition. Accessed Jan 13, 2018.
Hospitalists have been among the highest-volume participants in Medicare’s Bundled Payments for Care Improvement (BPCI) demonstration model, initiating over 200,000 episodes representing $4.7 billion in spending since the model began.1 On Jan. 9, the Centers for Medicare & Medicaid Services announced BPCI’s follow-on model, “BPCI Advanced.”2
BPCI launched in October 2013 and sunsets at the end of Q3 2018. BPCI Advanced starts immediately upon conclusion of BPCI (Q4 2018) and is slated to finish at year-end 2023.
CMS intends for the program to qualify as an Advanced Alternative Payment Model (APM). As BPCI Advanced focuses on episodes of care involving an inpatient stay (It also includes three outpatient episodes.) and the subsequent 90-day recovery period, it represents the first large-scale opportunity for hospitalists to meet criteria for Advanced APM participation. Qualifying for the Advanced APM track of the Quality Payment Program – which involves meeting patient volume or payment thresholds3 – comes with a 5% lump-sum bonus based on Medicare Part B fees and avoids exposure to penalties and reporting requirements of the Merit-based Incentive Payment System (MIPS).
Key program features
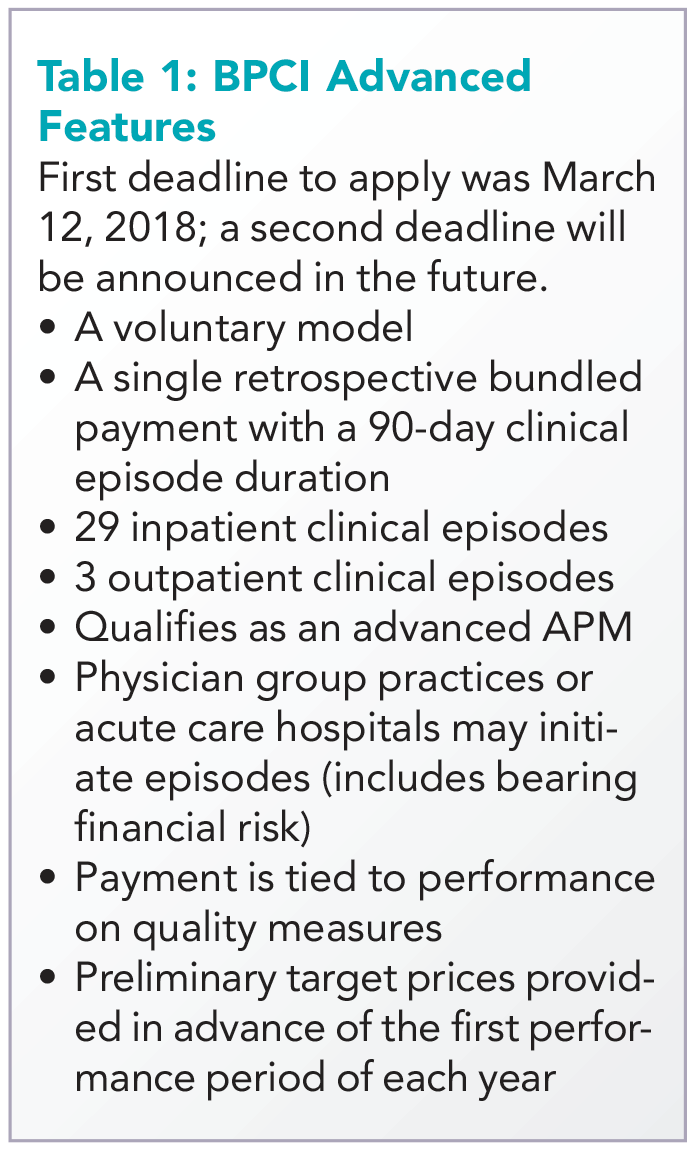
Acute care hospitals and physician groups may initiate episodes under BPCI Advanced, assuming financial risk under the model. Similar to its predecessor, BPCI Advanced assigns a target price based on past claims payments associated with the “episode initiator.”
During the performance period, if the initiator can beat the price in the aggregate for its bundles, it can keep the difference, and if it comes in over the price, it must pay the difference back to Medicare. Medicare discounts the target price by 3%, effectively paying itself that amount. After that, there is no sharing of savings with Medicare, as opposed to the permanent ACO programs, where there is sharing after the ACO meets the minimum savings rate.
The program allows physician groups and hospital initiators to go it alone or to work with a “convener,” which may share risk and reward with initiators, and may provide software, analytics, networks of high-performing providers like nursing facilities, and knowledge of specific care redesign approaches to enable program success. See Table 1 for a listing of other notable features of BPCI Advanced.
Quality measures
BPCI Advanced qualifies as an Advanced APM in part because payment is tied to performance on a set of quality measures (see Table 2). There are two measures applied to all episodes: all-cause hospital readmissions and advance care plan. These are notable because hospitalists may be especially focused on improvement activities in these areas.
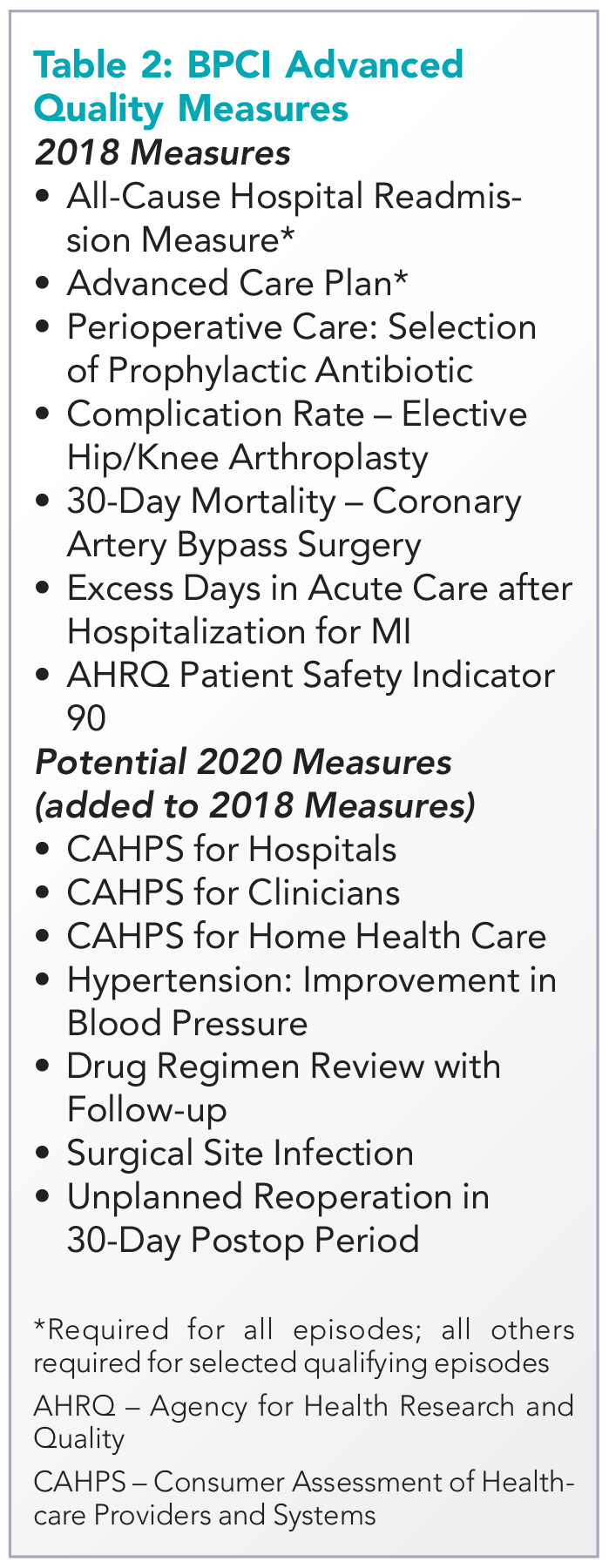
While the advance care plan measure refers to a process reflected by record documentation and is therefore directly under the control of hospitalists, readmissions – and most of the other measures – require a team approach. Because the outcome measures are risk adjusted, accurate and complete clinical documentation is crucial, as it drives how risk is adjusted. Of note, all the 2018 measures, collected directly through claims, will place no additional administrative burden for collection on providers.
Two ways for hospitalists to participate
Hospitalist groups – whether independent or employed – may be episode initiators in BPCI Advanced. In this case, any episodes in which the group participates that carry the name of a member of the hospitalist group in the “Attending Provider” field on the hospital bill claim form to Medicare (and the associated carrier claim) are attributed to that member’s physician group.
For example, if the group has chosen heart failure as an episode in which to participate at the program’s outset, a hospitalization is assigned the heart failure DRG (diagnosis-related group) and a group member is the Attending Provider on the claim form (and submits a claim for the physician services), then the episode is attributed to that group. This means that the group is responsible for payments represented by Medicare Part A and Part B claims (with a few exclusions like trauma and cancer) against the target price for the initial hospitalization and subsequent 90-day period. In practice, hospitalists are rewarded for actions aimed at optimizing location after discharge,4 avoiding readmissions, choosing efficient nursing facilities, and helping patients to maximize functional status.
The other way hospitalists may participate is through an agreement to share in savings with a hospital or physician group episode initiator. This requires hospitalist individuals or groups to enter into a contract with the initiator that meets certain program requirements – for example, report quality measures, engage in care redesign, use certified EHR technology (hospital-based clinicians automatically fulfill this criterion).
If there is broad participation, BPCI Advanced could represent a key milestone for hospitalists, as they seek to be recognized for the value they confer to the system as a whole instead of simply their professional billings. While there are legitimate concerns about the effect MIPS may have on health care value and the complexity of participation in APMs, barring a repeal of the law that created them, hospitalists now have the chance to extend their influence within and outside the hospital’s four walls and be more fairly rewarded for it.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of the Society of Hospital Medicine. Contact him at wfwhit@comcast.net. Disclosure: The author’s employer, Remedy Partners, is an Awardee Convener for the BPCI initiative and intends to apply as a Convener in BPCI Advanced.
References
1. Based on BPCI awardee convener Remedy Partners claims analysis.
2. https://innovation.cms.gov/initiatives/bpci-advanced.
3. https://qpp.cms.gov/apms/overview.
4. Whitcomb W. Choosing location after discharge wisely. The-hospitalist.org. 2018 Jan 3. Digital edition. Accessed Jan 13, 2018.
A public health approach to gun violence
In 2014, 33,594 people were killed by firearms in the United States. More than 21,000 of these deaths were suicides. The rest were primarily homicides and accidental shootings. Meanwhile, firearm deaths represented nearly 17% of injury deaths that year.1,2
In a 2015 Perspective published in the New England Journal of Medicine, author Chana Sacks, MD, pointed out that 20 children and adolescents are sent to the hospital daily for firearm injuries and 2,000 people each year suffer gunshot-related spinal cord injuries and “become lifelong patients.”3
At the same time, Federal Bureau of Investigation data show that the number of active shooter situations rose between 2000 and 2013, with an average of 6.4 incidents a year for the first 7 years of the study, conducted in 2013, and an average of 16.4 in the last 7 years of the study. More than 1,000 people were wounded or killed across 160 active shooter incidents, defined as an individual or individuals actively engaged in killing or trying to kill people in a populous area.4
“Gun violence is undeniably a public health issue,” said Dr. Sacks, a hospitalist at Massachusetts General Hospital and instructor at Harvard Medical School, both in Boston, and a vocal proponent of addressing firearms in the public health sphere. Her cousin’s 7-year-old son, Daniel Barden, was fatally shot at Sandy Hook Elementary School in Newtown, Conn., in December 2012.
Yet, the notion of firearm injuries and deaths as a public health issue is, in America, an issue of contention. How can hospitalists and other health care providers avoid wading into the political thicket while also looking out for their patients?
For one, it’s not the only controversial issue with which providers are confronted, Dr. Sacks and others say. From taking sexual histories, counseling patients about abortion and adoption, and discussing end-of-life issues, clinicians may routinely face uncomfortable interactions in the name of patient care.
“It’s not a question about their right to a weapon; it’s about how individuals can stay as safe as possible and keep their families as safe as possible,” said Dr. Sacks, who also wrote in a January 2017 opinion for the American Medical Association that: “Counseling about gun safety is not political – no more so than a physician counseling a patient about cutting down on sugary beverages is an act of declaring support for New York City’s attempted ban on large-sized sodas.”5
This idea is echoed by David Hemenway, PhD, director of the Harvard Injury Control Research Center, Boston. “You can talk about wearing your seat belt without advocating for mandatory seat belt laws,” he said.
Yet in a 2014 survey of internist members of the American College of Physicians, only 66% of respondents said they believed physicians have the right to counsel patients on gun violence prevention and 58% said they never ask patients about guns in their home. That same survey showed the public is also split: While two-thirds of respondents said it was at least sometimes appropriate for providers to ask about firearms during a visit, one-third believed it was never appropriate.6
In fact, Barbara Meyer, MD, MPH, a family physician in Seattle, said she once had a patient walk out of the office when he encountered a question about firearms on the intake forms for the health system at which she was employed at the time. Today, at NeighborCare Health, the presence of firearms in the home is a question in the well-child electronic health record.
The Harvard Injury Control Research Center runs a campaign called Means Matter, designed to address suicide by firearm, the most common method of suicide in America. The campaign – backed by decades of some of the best research available – reports that people die of suicide by gun more than all other methods combined, that suicide attempts using a firearm are almost always fatal, and that firearms used by youths who commit suicide almost always belong to a parent.
“Suicide is often an impulsive act,” said Dr. Sacks, which means preventing access to firearms for patients at risk can be a matter of life and death. “There is potential for intervention there … what can be more clearly medical than suicide prevention?”
For her, that means eliminating the partisan component and equipping providers with the best evidence-based research available and with best practices. Reliable studies show that having guns at home increases the danger to families, said Dr. Hemenway, and places with fewer guns and stronger gun laws are correlated with fewer gun fatalities.7,8
“In accordance with guidelines and the best evidence out there, we should be screening patients who might be at risk for gun violence,” he said. “In some cases, interventions can be as simple and straightforward as informing patients where to get gun locks and talking to them about how to store firearms safely.”
At Massachusetts General Hospital, Dr. Sacks helped found the Gun Violence Prevention Coalition, an interdisciplinary group of physicians, nurses, physical therapists, and others committed to raising awareness and preparing providers to address gun violence. She believes strongly that physicians can act locally to help address the issue.
In Seattle, Dr. Meyer has been involved with a local group called Washington Ceasefire, prompted both by her experience as a resident in Detroit – where she was routinely exposed to the traumas of gun violence – as well as a shooting that occurred outside her daughter’s high school in Seattle years ago. The group has recently begun advocating for smart guns, which are designed to be fired only by an authorized user.
Indeed, Dr. Hemenway said research by his group suggests 300,000-500,000 guns are stolen every year, though he points out that we know almost nothing about “who, what, when, why, and where.” That’s largely because of an effective ban on gun violence research, enacted by Congress in the 1990s.9
“It’s not like there’s no evidence, but compared to the size of the problem, you want good evidence,” Dr. Hemenway said. “America has lots of guns. How can we learn to live with them?”
Gun violence affects not just those shot and killed by firearms, but also those affected by the trauma it can leave in its wake. Dr. Sacks recounts a recent visit to Massachusetts General by survivors of the Pulse Nightclub shooting in Orlando, Fla., which took place on June 12, 2016.
“It was a moving, intense event where we all sat around and talked about this issue,” Dr. Sacks said. “The number of people dying is horrific enough, but it’s not just that. Here were a number of young people who survived and yet whose lives will never be the same. We are undercounting the number of people affected by gun violence.”
Studies also estimate the cost of medical care related to gun violence to be roughly $620 million per year, averaging between $9,000 and $18,000 per patient in 2014.10
Despite some arguments to the contrary, addressing gun violence as a public health issue is not a distraction from other important public health issues such as opioid abuse. “It is entirely a false choice that we must only take on one issue or another,” Dr. Sacks said.
Nor should efforts to address gun violence focus only on individuals, said Dr. Hemenway, who told the Harvard T.H. Chan School of Public Health in October 2017 that: “A lesson from public health is that it is usually more effective to change the environment than to try to change people. The U.S. should use the same harm reduction approach to gun violence that it uses to treat other public health threats, like automobile crashes or air pollution, employing a wide variety of methods to reduce the problem.”
The issue must be reframed, said Dr. Sacks. This remains one of her biggest goals. “If we can find a way to act and intervene and lower [the] number [of people affected by gun violence], what could be more fundamentally in line with what we try to do every day as physicians?” she asked. “How can we reduce morbidity and mortality? That’s an answerable question and we can make sure we have pathways and approaches we can put in place to understand this. This is a solvable problem.”
1. Centers for Disease Control and Prevention, National Center for Health Statistics. FastStats. Injuries. https://www.cdc.gov/nchs/fastats/injury.htm. Accessed Nov 20, 2017.
2. Centers for Disease Control and Prevention, National Center for Health Statistics. FastStats. Suicide. https://www.cdc.gov/nchs/fastats/suicide.htm. Accessed Nov 20, 2017.
3. Sacks CA. In memory of Daniel – Reviving research to prevent gun violence. N Engl J Med. 2015; 372:800-801. doi: 10.1056/NEJMp1415128.
4. U.S. Department of Justice, Federal Bureau of Investigation. A study of active shooter incidents in the United States between 2000 and 2013. Published Sept 16, 2013. Accessed Nov 20, 2017.
5. Sacks CA. The role of physicians in preventing firearm suicides. JAMA Int Med. doi: 10.001/jamainternmed.2016.6715. Published Nov 14, 2016. Accessed Nov 20, 2017.
6. Butkus R, Weissman A. Internists’ attitudes toward prevention of firearm injury. Ann Intern Med. 2014;160(12):821-827. doi: 10.7326/M13-1960.
7. Fleegler EW, Lee LK, Monuteaux MC, et al. Firearm Legislation and Firearm-Related Fatalities in the United States. JAMA Intern Med. 2013; 173(9):732-740. doi: 10.1001/jamaimternmed.2013.1286.
8. American Academy of Pediatricians. Addressing gun violence. The federal level. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Pages/Gun-Violence-Matrix--Intentional-(Federal).aspx. Accessed Nov 20, 2017.
9. Rubin R. Tale of 2 agencies: CDC avoids gun violence research bit NIH funds it. JAMA. 2016;315(16):1689-1692. doi:10.1001/jama.2016.1707.
10. Howell E and Gangopadhyaya A. State variation in the hospital costs of gun violence, 2010 and 2014. The Urban Institute, Health Policy Center.
In 2014, 33,594 people were killed by firearms in the United States. More than 21,000 of these deaths were suicides. The rest were primarily homicides and accidental shootings. Meanwhile, firearm deaths represented nearly 17% of injury deaths that year.1,2
In a 2015 Perspective published in the New England Journal of Medicine, author Chana Sacks, MD, pointed out that 20 children and adolescents are sent to the hospital daily for firearm injuries and 2,000 people each year suffer gunshot-related spinal cord injuries and “become lifelong patients.”3
At the same time, Federal Bureau of Investigation data show that the number of active shooter situations rose between 2000 and 2013, with an average of 6.4 incidents a year for the first 7 years of the study, conducted in 2013, and an average of 16.4 in the last 7 years of the study. More than 1,000 people were wounded or killed across 160 active shooter incidents, defined as an individual or individuals actively engaged in killing or trying to kill people in a populous area.4
“Gun violence is undeniably a public health issue,” said Dr. Sacks, a hospitalist at Massachusetts General Hospital and instructor at Harvard Medical School, both in Boston, and a vocal proponent of addressing firearms in the public health sphere. Her cousin’s 7-year-old son, Daniel Barden, was fatally shot at Sandy Hook Elementary School in Newtown, Conn., in December 2012.
Yet, the notion of firearm injuries and deaths as a public health issue is, in America, an issue of contention. How can hospitalists and other health care providers avoid wading into the political thicket while also looking out for their patients?
For one, it’s not the only controversial issue with which providers are confronted, Dr. Sacks and others say. From taking sexual histories, counseling patients about abortion and adoption, and discussing end-of-life issues, clinicians may routinely face uncomfortable interactions in the name of patient care.
“It’s not a question about their right to a weapon; it’s about how individuals can stay as safe as possible and keep their families as safe as possible,” said Dr. Sacks, who also wrote in a January 2017 opinion for the American Medical Association that: “Counseling about gun safety is not political – no more so than a physician counseling a patient about cutting down on sugary beverages is an act of declaring support for New York City’s attempted ban on large-sized sodas.”5
This idea is echoed by David Hemenway, PhD, director of the Harvard Injury Control Research Center, Boston. “You can talk about wearing your seat belt without advocating for mandatory seat belt laws,” he said.
Yet in a 2014 survey of internist members of the American College of Physicians, only 66% of respondents said they believed physicians have the right to counsel patients on gun violence prevention and 58% said they never ask patients about guns in their home. That same survey showed the public is also split: While two-thirds of respondents said it was at least sometimes appropriate for providers to ask about firearms during a visit, one-third believed it was never appropriate.6
In fact, Barbara Meyer, MD, MPH, a family physician in Seattle, said she once had a patient walk out of the office when he encountered a question about firearms on the intake forms for the health system at which she was employed at the time. Today, at NeighborCare Health, the presence of firearms in the home is a question in the well-child electronic health record.
The Harvard Injury Control Research Center runs a campaign called Means Matter, designed to address suicide by firearm, the most common method of suicide in America. The campaign – backed by decades of some of the best research available – reports that people die of suicide by gun more than all other methods combined, that suicide attempts using a firearm are almost always fatal, and that firearms used by youths who commit suicide almost always belong to a parent.
“Suicide is often an impulsive act,” said Dr. Sacks, which means preventing access to firearms for patients at risk can be a matter of life and death. “There is potential for intervention there … what can be more clearly medical than suicide prevention?”
For her, that means eliminating the partisan component and equipping providers with the best evidence-based research available and with best practices. Reliable studies show that having guns at home increases the danger to families, said Dr. Hemenway, and places with fewer guns and stronger gun laws are correlated with fewer gun fatalities.7,8
“In accordance with guidelines and the best evidence out there, we should be screening patients who might be at risk for gun violence,” he said. “In some cases, interventions can be as simple and straightforward as informing patients where to get gun locks and talking to them about how to store firearms safely.”
At Massachusetts General Hospital, Dr. Sacks helped found the Gun Violence Prevention Coalition, an interdisciplinary group of physicians, nurses, physical therapists, and others committed to raising awareness and preparing providers to address gun violence. She believes strongly that physicians can act locally to help address the issue.
In Seattle, Dr. Meyer has been involved with a local group called Washington Ceasefire, prompted both by her experience as a resident in Detroit – where she was routinely exposed to the traumas of gun violence – as well as a shooting that occurred outside her daughter’s high school in Seattle years ago. The group has recently begun advocating for smart guns, which are designed to be fired only by an authorized user.
Indeed, Dr. Hemenway said research by his group suggests 300,000-500,000 guns are stolen every year, though he points out that we know almost nothing about “who, what, when, why, and where.” That’s largely because of an effective ban on gun violence research, enacted by Congress in the 1990s.9
“It’s not like there’s no evidence, but compared to the size of the problem, you want good evidence,” Dr. Hemenway said. “America has lots of guns. How can we learn to live with them?”
Gun violence affects not just those shot and killed by firearms, but also those affected by the trauma it can leave in its wake. Dr. Sacks recounts a recent visit to Massachusetts General by survivors of the Pulse Nightclub shooting in Orlando, Fla., which took place on June 12, 2016.
“It was a moving, intense event where we all sat around and talked about this issue,” Dr. Sacks said. “The number of people dying is horrific enough, but it’s not just that. Here were a number of young people who survived and yet whose lives will never be the same. We are undercounting the number of people affected by gun violence.”
Studies also estimate the cost of medical care related to gun violence to be roughly $620 million per year, averaging between $9,000 and $18,000 per patient in 2014.10
Despite some arguments to the contrary, addressing gun violence as a public health issue is not a distraction from other important public health issues such as opioid abuse. “It is entirely a false choice that we must only take on one issue or another,” Dr. Sacks said.
Nor should efforts to address gun violence focus only on individuals, said Dr. Hemenway, who told the Harvard T.H. Chan School of Public Health in October 2017 that: “A lesson from public health is that it is usually more effective to change the environment than to try to change people. The U.S. should use the same harm reduction approach to gun violence that it uses to treat other public health threats, like automobile crashes or air pollution, employing a wide variety of methods to reduce the problem.”
The issue must be reframed, said Dr. Sacks. This remains one of her biggest goals. “If we can find a way to act and intervene and lower [the] number [of people affected by gun violence], what could be more fundamentally in line with what we try to do every day as physicians?” she asked. “How can we reduce morbidity and mortality? That’s an answerable question and we can make sure we have pathways and approaches we can put in place to understand this. This is a solvable problem.”
In 2014, 33,594 people were killed by firearms in the United States. More than 21,000 of these deaths were suicides. The rest were primarily homicides and accidental shootings. Meanwhile, firearm deaths represented nearly 17% of injury deaths that year.1,2
In a 2015 Perspective published in the New England Journal of Medicine, author Chana Sacks, MD, pointed out that 20 children and adolescents are sent to the hospital daily for firearm injuries and 2,000 people each year suffer gunshot-related spinal cord injuries and “become lifelong patients.”3
At the same time, Federal Bureau of Investigation data show that the number of active shooter situations rose between 2000 and 2013, with an average of 6.4 incidents a year for the first 7 years of the study, conducted in 2013, and an average of 16.4 in the last 7 years of the study. More than 1,000 people were wounded or killed across 160 active shooter incidents, defined as an individual or individuals actively engaged in killing or trying to kill people in a populous area.4
“Gun violence is undeniably a public health issue,” said Dr. Sacks, a hospitalist at Massachusetts General Hospital and instructor at Harvard Medical School, both in Boston, and a vocal proponent of addressing firearms in the public health sphere. Her cousin’s 7-year-old son, Daniel Barden, was fatally shot at Sandy Hook Elementary School in Newtown, Conn., in December 2012.
Yet, the notion of firearm injuries and deaths as a public health issue is, in America, an issue of contention. How can hospitalists and other health care providers avoid wading into the political thicket while also looking out for their patients?
For one, it’s not the only controversial issue with which providers are confronted, Dr. Sacks and others say. From taking sexual histories, counseling patients about abortion and adoption, and discussing end-of-life issues, clinicians may routinely face uncomfortable interactions in the name of patient care.
“It’s not a question about their right to a weapon; it’s about how individuals can stay as safe as possible and keep their families as safe as possible,” said Dr. Sacks, who also wrote in a January 2017 opinion for the American Medical Association that: “Counseling about gun safety is not political – no more so than a physician counseling a patient about cutting down on sugary beverages is an act of declaring support for New York City’s attempted ban on large-sized sodas.”5
This idea is echoed by David Hemenway, PhD, director of the Harvard Injury Control Research Center, Boston. “You can talk about wearing your seat belt without advocating for mandatory seat belt laws,” he said.
Yet in a 2014 survey of internist members of the American College of Physicians, only 66% of respondents said they believed physicians have the right to counsel patients on gun violence prevention and 58% said they never ask patients about guns in their home. That same survey showed the public is also split: While two-thirds of respondents said it was at least sometimes appropriate for providers to ask about firearms during a visit, one-third believed it was never appropriate.6
In fact, Barbara Meyer, MD, MPH, a family physician in Seattle, said she once had a patient walk out of the office when he encountered a question about firearms on the intake forms for the health system at which she was employed at the time. Today, at NeighborCare Health, the presence of firearms in the home is a question in the well-child electronic health record.
The Harvard Injury Control Research Center runs a campaign called Means Matter, designed to address suicide by firearm, the most common method of suicide in America. The campaign – backed by decades of some of the best research available – reports that people die of suicide by gun more than all other methods combined, that suicide attempts using a firearm are almost always fatal, and that firearms used by youths who commit suicide almost always belong to a parent.
“Suicide is often an impulsive act,” said Dr. Sacks, which means preventing access to firearms for patients at risk can be a matter of life and death. “There is potential for intervention there … what can be more clearly medical than suicide prevention?”
For her, that means eliminating the partisan component and equipping providers with the best evidence-based research available and with best practices. Reliable studies show that having guns at home increases the danger to families, said Dr. Hemenway, and places with fewer guns and stronger gun laws are correlated with fewer gun fatalities.7,8
“In accordance with guidelines and the best evidence out there, we should be screening patients who might be at risk for gun violence,” he said. “In some cases, interventions can be as simple and straightforward as informing patients where to get gun locks and talking to them about how to store firearms safely.”
At Massachusetts General Hospital, Dr. Sacks helped found the Gun Violence Prevention Coalition, an interdisciplinary group of physicians, nurses, physical therapists, and others committed to raising awareness and preparing providers to address gun violence. She believes strongly that physicians can act locally to help address the issue.
In Seattle, Dr. Meyer has been involved with a local group called Washington Ceasefire, prompted both by her experience as a resident in Detroit – where she was routinely exposed to the traumas of gun violence – as well as a shooting that occurred outside her daughter’s high school in Seattle years ago. The group has recently begun advocating for smart guns, which are designed to be fired only by an authorized user.
Indeed, Dr. Hemenway said research by his group suggests 300,000-500,000 guns are stolen every year, though he points out that we know almost nothing about “who, what, when, why, and where.” That’s largely because of an effective ban on gun violence research, enacted by Congress in the 1990s.9
“It’s not like there’s no evidence, but compared to the size of the problem, you want good evidence,” Dr. Hemenway said. “America has lots of guns. How can we learn to live with them?”
Gun violence affects not just those shot and killed by firearms, but also those affected by the trauma it can leave in its wake. Dr. Sacks recounts a recent visit to Massachusetts General by survivors of the Pulse Nightclub shooting in Orlando, Fla., which took place on June 12, 2016.
“It was a moving, intense event where we all sat around and talked about this issue,” Dr. Sacks said. “The number of people dying is horrific enough, but it’s not just that. Here were a number of young people who survived and yet whose lives will never be the same. We are undercounting the number of people affected by gun violence.”
Studies also estimate the cost of medical care related to gun violence to be roughly $620 million per year, averaging between $9,000 and $18,000 per patient in 2014.10
Despite some arguments to the contrary, addressing gun violence as a public health issue is not a distraction from other important public health issues such as opioid abuse. “It is entirely a false choice that we must only take on one issue or another,” Dr. Sacks said.
Nor should efforts to address gun violence focus only on individuals, said Dr. Hemenway, who told the Harvard T.H. Chan School of Public Health in October 2017 that: “A lesson from public health is that it is usually more effective to change the environment than to try to change people. The U.S. should use the same harm reduction approach to gun violence that it uses to treat other public health threats, like automobile crashes or air pollution, employing a wide variety of methods to reduce the problem.”
The issue must be reframed, said Dr. Sacks. This remains one of her biggest goals. “If we can find a way to act and intervene and lower [the] number [of people affected by gun violence], what could be more fundamentally in line with what we try to do every day as physicians?” she asked. “How can we reduce morbidity and mortality? That’s an answerable question and we can make sure we have pathways and approaches we can put in place to understand this. This is a solvable problem.”
1. Centers for Disease Control and Prevention, National Center for Health Statistics. FastStats. Injuries. https://www.cdc.gov/nchs/fastats/injury.htm. Accessed Nov 20, 2017.
2. Centers for Disease Control and Prevention, National Center for Health Statistics. FastStats. Suicide. https://www.cdc.gov/nchs/fastats/suicide.htm. Accessed Nov 20, 2017.
3. Sacks CA. In memory of Daniel – Reviving research to prevent gun violence. N Engl J Med. 2015; 372:800-801. doi: 10.1056/NEJMp1415128.
4. U.S. Department of Justice, Federal Bureau of Investigation. A study of active shooter incidents in the United States between 2000 and 2013. Published Sept 16, 2013. Accessed Nov 20, 2017.
5. Sacks CA. The role of physicians in preventing firearm suicides. JAMA Int Med. doi: 10.001/jamainternmed.2016.6715. Published Nov 14, 2016. Accessed Nov 20, 2017.
6. Butkus R, Weissman A. Internists’ attitudes toward prevention of firearm injury. Ann Intern Med. 2014;160(12):821-827. doi: 10.7326/M13-1960.
7. Fleegler EW, Lee LK, Monuteaux MC, et al. Firearm Legislation and Firearm-Related Fatalities in the United States. JAMA Intern Med. 2013; 173(9):732-740. doi: 10.1001/jamaimternmed.2013.1286.
8. American Academy of Pediatricians. Addressing gun violence. The federal level. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Pages/Gun-Violence-Matrix--Intentional-(Federal).aspx. Accessed Nov 20, 2017.
9. Rubin R. Tale of 2 agencies: CDC avoids gun violence research bit NIH funds it. JAMA. 2016;315(16):1689-1692. doi:10.1001/jama.2016.1707.
10. Howell E and Gangopadhyaya A. State variation in the hospital costs of gun violence, 2010 and 2014. The Urban Institute, Health Policy Center.
1. Centers for Disease Control and Prevention, National Center for Health Statistics. FastStats. Injuries. https://www.cdc.gov/nchs/fastats/injury.htm. Accessed Nov 20, 2017.
2. Centers for Disease Control and Prevention, National Center for Health Statistics. FastStats. Suicide. https://www.cdc.gov/nchs/fastats/suicide.htm. Accessed Nov 20, 2017.
3. Sacks CA. In memory of Daniel – Reviving research to prevent gun violence. N Engl J Med. 2015; 372:800-801. doi: 10.1056/NEJMp1415128.
4. U.S. Department of Justice, Federal Bureau of Investigation. A study of active shooter incidents in the United States between 2000 and 2013. Published Sept 16, 2013. Accessed Nov 20, 2017.
5. Sacks CA. The role of physicians in preventing firearm suicides. JAMA Int Med. doi: 10.001/jamainternmed.2016.6715. Published Nov 14, 2016. Accessed Nov 20, 2017.
6. Butkus R, Weissman A. Internists’ attitudes toward prevention of firearm injury. Ann Intern Med. 2014;160(12):821-827. doi: 10.7326/M13-1960.
7. Fleegler EW, Lee LK, Monuteaux MC, et al. Firearm Legislation and Firearm-Related Fatalities in the United States. JAMA Intern Med. 2013; 173(9):732-740. doi: 10.1001/jamaimternmed.2013.1286.
8. American Academy of Pediatricians. Addressing gun violence. The federal level. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Pages/Gun-Violence-Matrix--Intentional-(Federal).aspx. Accessed Nov 20, 2017.
9. Rubin R. Tale of 2 agencies: CDC avoids gun violence research bit NIH funds it. JAMA. 2016;315(16):1689-1692. doi:10.1001/jama.2016.1707.
10. Howell E and Gangopadhyaya A. State variation in the hospital costs of gun violence, 2010 and 2014. The Urban Institute, Health Policy Center.
Synthetic opioids drive increase in overdose deaths
Opioid-related drug overdose deaths jumped 28% from 2015 to 2016, with the largest increase coming from synthetic opioids, such as illicitly manufactured fentanyl, according to the Centers for Disease Control and Prevention.
The age-adjusted death rate for opioid overdoses increased from 10.4 per 100,000 population in 2015 to 13.3 per 100,000 in 2016, and the 42,249 opioid deaths in 2016 represented more than 66% of all overdose deaths that year, Puja Seth, PhD, and her associates at the CDC reported in the Morbidity and Mortality Weekly Report.
Illegally manufactured fentanyl “is now being mixed into counterfeit opioid and benzodiazepine pills, heroin, and cocaine, likely contributing to increases in overdose death rates involving other substances,” they wrote. To illustrate that point, they reported that cocaine overdose deaths increased 52.4% from 2.1 per 100,000 in 2015 to 3.2 in 2016. The death rate for the other drug category covered in the report – psychostimulants with abuse potential – climbed from 1.8 per 100,000 in 2015 to 2.4 in 2016, for an increase of 33.3%, Dr. Seth and her associates noted.
Data presented from 31 states and the District of Columbia show that
CDC Principal Deputy Director Anne Schuchat, MD, said in a written statement.
Death rates from overdoses involving synthetic opioids increased in 21 states, with 10 states doubling their rates from 2015 to 2016, and 14 states had significant increases in death rates involving heroin. In D.C., for example, the death rate increased 392% (3.9 per 100,000 to 19.2) from synthetic opioid overdoses and 75% (9.9 per 100,000 to 17.3) for deaths related to heroin, the report showed.
“Effective, synchronized programs to prevent drug overdoses will require coordination of law enforcement, first responders, mental health/substance-abuse providers, public health agencies, and community partners,” Dr. Seth and her associates said.
SOURCE: Seth P et al. MMWR. 2018 Mar 30;67(12):349-58.
Opioid-related drug overdose deaths jumped 28% from 2015 to 2016, with the largest increase coming from synthetic opioids, such as illicitly manufactured fentanyl, according to the Centers for Disease Control and Prevention.
The age-adjusted death rate for opioid overdoses increased from 10.4 per 100,000 population in 2015 to 13.3 per 100,000 in 2016, and the 42,249 opioid deaths in 2016 represented more than 66% of all overdose deaths that year, Puja Seth, PhD, and her associates at the CDC reported in the Morbidity and Mortality Weekly Report.
Illegally manufactured fentanyl “is now being mixed into counterfeit opioid and benzodiazepine pills, heroin, and cocaine, likely contributing to increases in overdose death rates involving other substances,” they wrote. To illustrate that point, they reported that cocaine overdose deaths increased 52.4% from 2.1 per 100,000 in 2015 to 3.2 in 2016. The death rate for the other drug category covered in the report – psychostimulants with abuse potential – climbed from 1.8 per 100,000 in 2015 to 2.4 in 2016, for an increase of 33.3%, Dr. Seth and her associates noted.
Data presented from 31 states and the District of Columbia show that
CDC Principal Deputy Director Anne Schuchat, MD, said in a written statement.
Death rates from overdoses involving synthetic opioids increased in 21 states, with 10 states doubling their rates from 2015 to 2016, and 14 states had significant increases in death rates involving heroin. In D.C., for example, the death rate increased 392% (3.9 per 100,000 to 19.2) from synthetic opioid overdoses and 75% (9.9 per 100,000 to 17.3) for deaths related to heroin, the report showed.
“Effective, synchronized programs to prevent drug overdoses will require coordination of law enforcement, first responders, mental health/substance-abuse providers, public health agencies, and community partners,” Dr. Seth and her associates said.
SOURCE: Seth P et al. MMWR. 2018 Mar 30;67(12):349-58.
Opioid-related drug overdose deaths jumped 28% from 2015 to 2016, with the largest increase coming from synthetic opioids, such as illicitly manufactured fentanyl, according to the Centers for Disease Control and Prevention.
The age-adjusted death rate for opioid overdoses increased from 10.4 per 100,000 population in 2015 to 13.3 per 100,000 in 2016, and the 42,249 opioid deaths in 2016 represented more than 66% of all overdose deaths that year, Puja Seth, PhD, and her associates at the CDC reported in the Morbidity and Mortality Weekly Report.
Illegally manufactured fentanyl “is now being mixed into counterfeit opioid and benzodiazepine pills, heroin, and cocaine, likely contributing to increases in overdose death rates involving other substances,” they wrote. To illustrate that point, they reported that cocaine overdose deaths increased 52.4% from 2.1 per 100,000 in 2015 to 3.2 in 2016. The death rate for the other drug category covered in the report – psychostimulants with abuse potential – climbed from 1.8 per 100,000 in 2015 to 2.4 in 2016, for an increase of 33.3%, Dr. Seth and her associates noted.
Data presented from 31 states and the District of Columbia show that
CDC Principal Deputy Director Anne Schuchat, MD, said in a written statement.
Death rates from overdoses involving synthetic opioids increased in 21 states, with 10 states doubling their rates from 2015 to 2016, and 14 states had significant increases in death rates involving heroin. In D.C., for example, the death rate increased 392% (3.9 per 100,000 to 19.2) from synthetic opioid overdoses and 75% (9.9 per 100,000 to 17.3) for deaths related to heroin, the report showed.
“Effective, synchronized programs to prevent drug overdoses will require coordination of law enforcement, first responders, mental health/substance-abuse providers, public health agencies, and community partners,” Dr. Seth and her associates said.
SOURCE: Seth P et al. MMWR. 2018 Mar 30;67(12):349-58.
FROM MMWR