User login
Managing the COVID-19 isolation floor at UCSF Medical Center
Robert Wachter, MD, MHM, chair of the department of medicine at UCSF, interviewed Armond Esmaili, MD, a hospitalist and assistant professor of medicine at UCSF, who is the leader of the Respiratory Isolation Unit at UCSF Medical Center, where the institution's COVID-19 and rule-out COVID-19 patients are being cohorted.
Robert Wachter, MD, MHM, chair of the department of medicine at UCSF, interviewed Armond Esmaili, MD, a hospitalist and assistant professor of medicine at UCSF, who is the leader of the Respiratory Isolation Unit at UCSF Medical Center, where the institution's COVID-19 and rule-out COVID-19 patients are being cohorted.
Robert Wachter, MD, MHM, chair of the department of medicine at UCSF, interviewed Armond Esmaili, MD, a hospitalist and assistant professor of medicine at UCSF, who is the leader of the Respiratory Isolation Unit at UCSF Medical Center, where the institution's COVID-19 and rule-out COVID-19 patients are being cohorted.
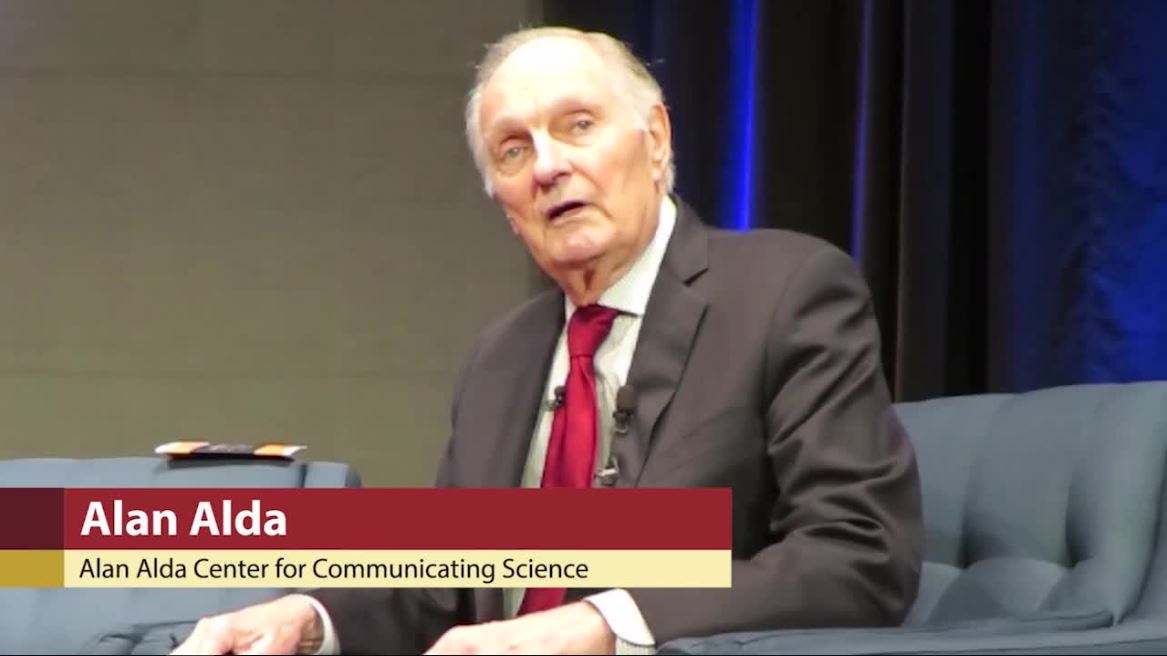
Actor Alan Alda discusses using empathy as an antidote to burnout
LA JOLLA, CALIF. – Physicians and other medical professionals who routinely foster empathic connections with patients may be helping themselves steer clear of burnout.
That’s what iconic actor Alan Alda suggested during a media briefing at Scripps Research on Jan. 16, 2020.
“There’s a tremendous pressure on doctors now to have shorter and shorter visits with their patients,” said the 83-year-old Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016 for his work as a champion of science. “A lot of that time is taken up with recording on a computer, which can only put pressure on the doctor.”
Practicing empathy, he continued, “kind of opens people up to one another, which inspirits them.”
Mr. Alda appeared on the research campus to announce that Scripps Research will serve as the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at Stony Brook (N.Y.) University, a nonprofit organization that Mr. Alda helped found in 2009.
“This will be a center where people can come to get training in effective communication,” Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards, told an audience of scientists and medical professionals prior to the media briefing.
“It’s an experiential kind of training,” he explained. “We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that, when you get a diagnosis, your life is over,” said Mr. Alda, who played army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H.”
“Under the burden of that belief, some people won’t tell their family or workplace colleagues,” he said. “There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – Physicians and other medical professionals who routinely foster empathic connections with patients may be helping themselves steer clear of burnout.
That’s what iconic actor Alan Alda suggested during a media briefing at Scripps Research on Jan. 16, 2020.
“There’s a tremendous pressure on doctors now to have shorter and shorter visits with their patients,” said the 83-year-old Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016 for his work as a champion of science. “A lot of that time is taken up with recording on a computer, which can only put pressure on the doctor.”
Practicing empathy, he continued, “kind of opens people up to one another, which inspirits them.”
Mr. Alda appeared on the research campus to announce that Scripps Research will serve as the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at Stony Brook (N.Y.) University, a nonprofit organization that Mr. Alda helped found in 2009.
“This will be a center where people can come to get training in effective communication,” Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards, told an audience of scientists and medical professionals prior to the media briefing.
“It’s an experiential kind of training,” he explained. “We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that, when you get a diagnosis, your life is over,” said Mr. Alda, who played army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H.”
“Under the burden of that belief, some people won’t tell their family or workplace colleagues,” he said. “There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – Physicians and other medical professionals who routinely foster empathic connections with patients may be helping themselves steer clear of burnout.
That’s what iconic actor Alan Alda suggested during a media briefing at Scripps Research on Jan. 16, 2020.
“There’s a tremendous pressure on doctors now to have shorter and shorter visits with their patients,” said the 83-year-old Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016 for his work as a champion of science. “A lot of that time is taken up with recording on a computer, which can only put pressure on the doctor.”
Practicing empathy, he continued, “kind of opens people up to one another, which inspirits them.”
Mr. Alda appeared on the research campus to announce that Scripps Research will serve as the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at Stony Brook (N.Y.) University, a nonprofit organization that Mr. Alda helped found in 2009.
“This will be a center where people can come to get training in effective communication,” Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards, told an audience of scientists and medical professionals prior to the media briefing.
“It’s an experiential kind of training,” he explained. “We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that, when you get a diagnosis, your life is over,” said Mr. Alda, who played army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H.”
“Under the burden of that belief, some people won’t tell their family or workplace colleagues,” he said. “There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
Experts break down latest CAR T-cell advances in lymphoma
ORLANDO – There’s now mature data surrounding the use of chimeric antigen receptor (CAR) T-cell therapy in lymphoma, and the annual meeting of the American Society of Hematology brought forth additional information from real-world studies, insights about what is driving relapse, and promising data on mantle cell lymphoma.

The roundtable participants included Brian Hill, MD, of the Cleveland Clinic Taussig Cancer Center; Frederick L. Locke, MD, of the Moffit Cancer Center in Tampa, Fla.; and Peter Riedell, MD, of the University of Chicago.
Among the studies highlighted by the panel was the Transcend NHL 001 study (Abstract 241), which looked at third-line use of lisocabtagene maraleucel (liso-cel) in patients with diffuse large B-cell lymphoma, transformed follicular lymphoma, and other indolent non-Hodgkin lymphoma subtypes. More than 300 patients were enrolled, and liso-cel met all primary and secondary efficacy endpoints, with an overall response rate of more than 70%. The notable take-home point from the study was the safety profile, Dr. Riedell noted. Liso-cel was associated with a lower rate of cytokine release syndrome and neurologic toxicity, compared with the currently approved products.
Since patients in the study had a lower incidence and later onset of cytokine release syndrome, liso-cel could be a candidate for outpatient administration, Dr. Locke said. However, doing that would require “significant infrastructure” in hospitals and clinics to properly support patients, especially given that the treatment-related mortality on the study was similar to approved CAR T-cell products at about 3%. “You have to be ready to admit the patient to the hospital very rapidly, and you have to have the providers and the nurses who are vigilant when the patient is not in the hospital,” he said.
Another notable study presented at ASH examined the characteristics and outcomes of patients receiving bridging therapy while awaiting treatment with axicabtagene ciloleucel (Abstract 245). This real-world study adds interesting information to the field because, in some of the studies that were pivotal to the approval of CAR T-cell therapy, bridging therapy was not allowed, Dr. Locke said.
In this analysis, researchers found that the overall survival was worse among patients who received bridging. This finding suggests that patients who received bridging therapy had a different biology or that the therapy itself may have had an effect on the host or tumor microenvironment that affected the efficacy of the CAR T-cell therapy, the researchers reported.
The panel also highlighted the Zuma-2 study, which looked at KTE-X19, an anti-CD19 CAR T-cell therapy, among more than 70 patients with relapsed/refractory mantle cell lymphoma who had failed treatment with a Bruton’s tyrosine kinase inhibitor (Abstract 754). “This was, I thought, kind of a sleeper study at ASH,” said Dr. Hill, who was one of the authors of the study.
The overall response rate was 93% with about two-thirds of patients achieving a complete response. Researchers found that the response was consistent across subgroups, including Ki-67 and patients with prior use of steroids or bridging therapy. Dr. Locke, who was also a study author, said the results are a “game changer.”
“I’m very excited about it,” Dr. Riedell said, noting that these are patients without a lot of treatment options.
The panel also discussed other studies from ASH, including an analysis of tumor tissue samples from patients in the ZUMA-1 trial who had responded and subsequently relapsed (Abstract 203); a multicenter prospective analysis of circulating tumor DNA in diffuse large B-cell lymphoma patients who had relapsed after treatment with axicabtagene ciloleucel (Abstract 884); and the early use of corticosteroids to prevent toxicities in patients in cohort 4 of the ZUMA-1 trial (Abstract 243).
Dr. Hill reported consulting with Juno/Celgene/BMS and Novartis and research and consulting for Kite/Gilead. Dr. Locke reported consulting for Cellular Biomedicine Group and being a scientific adviser to Kite/Gilead, Novartis, Celgene/BMS, GammaDelta Therapeutics, Calibr, and Allogene. Dr. Riedell reported consulting for Bayer and Verastem, consulting for and research funding from Novartis and BMS/Celgene, and consulting for, research funding from, and speaking for Kite.
ORLANDO – There’s now mature data surrounding the use of chimeric antigen receptor (CAR) T-cell therapy in lymphoma, and the annual meeting of the American Society of Hematology brought forth additional information from real-world studies, insights about what is driving relapse, and promising data on mantle cell lymphoma.

The roundtable participants included Brian Hill, MD, of the Cleveland Clinic Taussig Cancer Center; Frederick L. Locke, MD, of the Moffit Cancer Center in Tampa, Fla.; and Peter Riedell, MD, of the University of Chicago.
Among the studies highlighted by the panel was the Transcend NHL 001 study (Abstract 241), which looked at third-line use of lisocabtagene maraleucel (liso-cel) in patients with diffuse large B-cell lymphoma, transformed follicular lymphoma, and other indolent non-Hodgkin lymphoma subtypes. More than 300 patients were enrolled, and liso-cel met all primary and secondary efficacy endpoints, with an overall response rate of more than 70%. The notable take-home point from the study was the safety profile, Dr. Riedell noted. Liso-cel was associated with a lower rate of cytokine release syndrome and neurologic toxicity, compared with the currently approved products.
Since patients in the study had a lower incidence and later onset of cytokine release syndrome, liso-cel could be a candidate for outpatient administration, Dr. Locke said. However, doing that would require “significant infrastructure” in hospitals and clinics to properly support patients, especially given that the treatment-related mortality on the study was similar to approved CAR T-cell products at about 3%. “You have to be ready to admit the patient to the hospital very rapidly, and you have to have the providers and the nurses who are vigilant when the patient is not in the hospital,” he said.
Another notable study presented at ASH examined the characteristics and outcomes of patients receiving bridging therapy while awaiting treatment with axicabtagene ciloleucel (Abstract 245). This real-world study adds interesting information to the field because, in some of the studies that were pivotal to the approval of CAR T-cell therapy, bridging therapy was not allowed, Dr. Locke said.
In this analysis, researchers found that the overall survival was worse among patients who received bridging. This finding suggests that patients who received bridging therapy had a different biology or that the therapy itself may have had an effect on the host or tumor microenvironment that affected the efficacy of the CAR T-cell therapy, the researchers reported.
The panel also highlighted the Zuma-2 study, which looked at KTE-X19, an anti-CD19 CAR T-cell therapy, among more than 70 patients with relapsed/refractory mantle cell lymphoma who had failed treatment with a Bruton’s tyrosine kinase inhibitor (Abstract 754). “This was, I thought, kind of a sleeper study at ASH,” said Dr. Hill, who was one of the authors of the study.
The overall response rate was 93% with about two-thirds of patients achieving a complete response. Researchers found that the response was consistent across subgroups, including Ki-67 and patients with prior use of steroids or bridging therapy. Dr. Locke, who was also a study author, said the results are a “game changer.”
“I’m very excited about it,” Dr. Riedell said, noting that these are patients without a lot of treatment options.
The panel also discussed other studies from ASH, including an analysis of tumor tissue samples from patients in the ZUMA-1 trial who had responded and subsequently relapsed (Abstract 203); a multicenter prospective analysis of circulating tumor DNA in diffuse large B-cell lymphoma patients who had relapsed after treatment with axicabtagene ciloleucel (Abstract 884); and the early use of corticosteroids to prevent toxicities in patients in cohort 4 of the ZUMA-1 trial (Abstract 243).
Dr. Hill reported consulting with Juno/Celgene/BMS and Novartis and research and consulting for Kite/Gilead. Dr. Locke reported consulting for Cellular Biomedicine Group and being a scientific adviser to Kite/Gilead, Novartis, Celgene/BMS, GammaDelta Therapeutics, Calibr, and Allogene. Dr. Riedell reported consulting for Bayer and Verastem, consulting for and research funding from Novartis and BMS/Celgene, and consulting for, research funding from, and speaking for Kite.
ORLANDO – There’s now mature data surrounding the use of chimeric antigen receptor (CAR) T-cell therapy in lymphoma, and the annual meeting of the American Society of Hematology brought forth additional information from real-world studies, insights about what is driving relapse, and promising data on mantle cell lymphoma.

The roundtable participants included Brian Hill, MD, of the Cleveland Clinic Taussig Cancer Center; Frederick L. Locke, MD, of the Moffit Cancer Center in Tampa, Fla.; and Peter Riedell, MD, of the University of Chicago.
Among the studies highlighted by the panel was the Transcend NHL 001 study (Abstract 241), which looked at third-line use of lisocabtagene maraleucel (liso-cel) in patients with diffuse large B-cell lymphoma, transformed follicular lymphoma, and other indolent non-Hodgkin lymphoma subtypes. More than 300 patients were enrolled, and liso-cel met all primary and secondary efficacy endpoints, with an overall response rate of more than 70%. The notable take-home point from the study was the safety profile, Dr. Riedell noted. Liso-cel was associated with a lower rate of cytokine release syndrome and neurologic toxicity, compared with the currently approved products.
Since patients in the study had a lower incidence and later onset of cytokine release syndrome, liso-cel could be a candidate for outpatient administration, Dr. Locke said. However, doing that would require “significant infrastructure” in hospitals and clinics to properly support patients, especially given that the treatment-related mortality on the study was similar to approved CAR T-cell products at about 3%. “You have to be ready to admit the patient to the hospital very rapidly, and you have to have the providers and the nurses who are vigilant when the patient is not in the hospital,” he said.
Another notable study presented at ASH examined the characteristics and outcomes of patients receiving bridging therapy while awaiting treatment with axicabtagene ciloleucel (Abstract 245). This real-world study adds interesting information to the field because, in some of the studies that were pivotal to the approval of CAR T-cell therapy, bridging therapy was not allowed, Dr. Locke said.
In this analysis, researchers found that the overall survival was worse among patients who received bridging. This finding suggests that patients who received bridging therapy had a different biology or that the therapy itself may have had an effect on the host or tumor microenvironment that affected the efficacy of the CAR T-cell therapy, the researchers reported.
The panel also highlighted the Zuma-2 study, which looked at KTE-X19, an anti-CD19 CAR T-cell therapy, among more than 70 patients with relapsed/refractory mantle cell lymphoma who had failed treatment with a Bruton’s tyrosine kinase inhibitor (Abstract 754). “This was, I thought, kind of a sleeper study at ASH,” said Dr. Hill, who was one of the authors of the study.
The overall response rate was 93% with about two-thirds of patients achieving a complete response. Researchers found that the response was consistent across subgroups, including Ki-67 and patients with prior use of steroids or bridging therapy. Dr. Locke, who was also a study author, said the results are a “game changer.”
“I’m very excited about it,” Dr. Riedell said, noting that these are patients without a lot of treatment options.
The panel also discussed other studies from ASH, including an analysis of tumor tissue samples from patients in the ZUMA-1 trial who had responded and subsequently relapsed (Abstract 203); a multicenter prospective analysis of circulating tumor DNA in diffuse large B-cell lymphoma patients who had relapsed after treatment with axicabtagene ciloleucel (Abstract 884); and the early use of corticosteroids to prevent toxicities in patients in cohort 4 of the ZUMA-1 trial (Abstract 243).
Dr. Hill reported consulting with Juno/Celgene/BMS and Novartis and research and consulting for Kite/Gilead. Dr. Locke reported consulting for Cellular Biomedicine Group and being a scientific adviser to Kite/Gilead, Novartis, Celgene/BMS, GammaDelta Therapeutics, Calibr, and Allogene. Dr. Riedell reported consulting for Bayer and Verastem, consulting for and research funding from Novartis and BMS/Celgene, and consulting for, research funding from, and speaking for Kite.
EXPERT ANALYSIS FROM ASH 2019
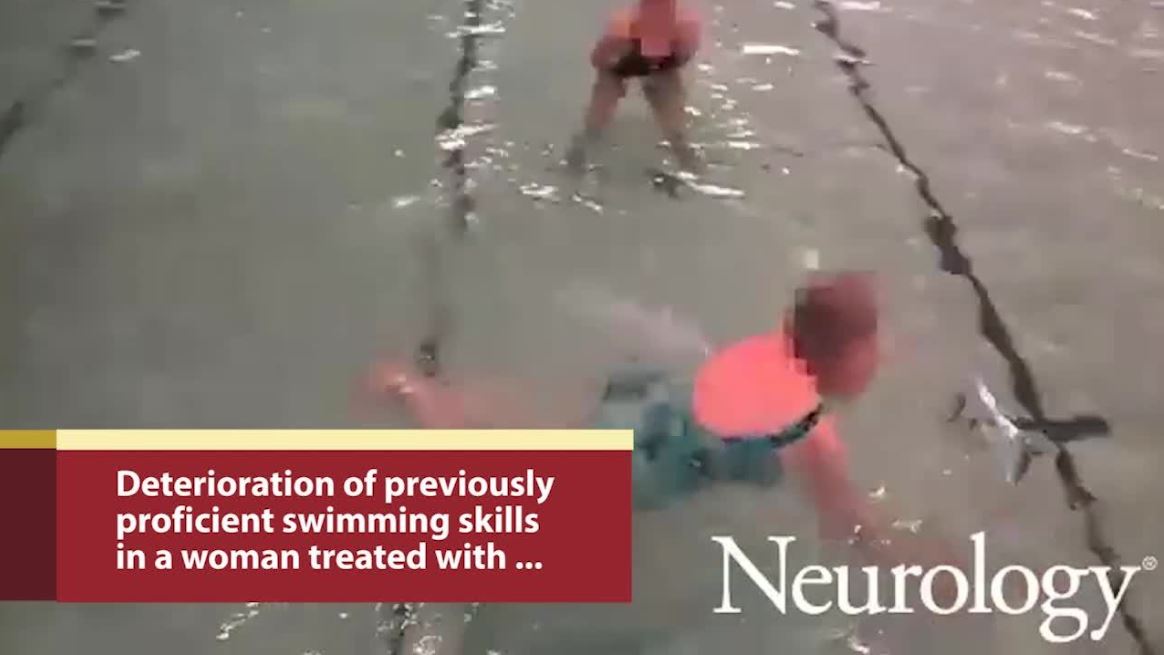
Parkinson’s patients can lose swimming ability after deep brain stimulation
Successful deep brain stimulation of the subthalamic nucleus may have unforeseen effects on the ability to swim in some patients with Parkinson’s disease, according to findings from a case series of nine patients published in Neurology.
All nine patients in the report were experienced swimmers, including two who competed in several competition-level races. They reported losing their ability to swim after successful deep brain stimulation of the subthalamic nucleus (STN-DBS) procedures. The Neurology paper focuses on three of the patients.
All of the patients achieved good to excellent motor control and cut their L-dopa dosage by impressive amounts. But they also lost the ability to coordinate limb movement when in the water, reported Daniel Waldvogel, MD, of the University of Zurich, and associates.
“All found their ability to swim came back immediately, with improved coordination of the limbs,” when stimulation was discontinued, the team noted. But soon after the stimulation ceased, their motor symptoms also rapidly returned, leading all to resume continuous stimulation.
One possible explanation is that STN-DBS does not strongly improve dopamine levels in the supplementary motor area, which controls independent limb movements.
It “may be that DBS affects the supplementary motor area (SMA) differently than levodopa. The SMA is a main output area of the basal ganglia, with connections to the primary motor cortex and the spinal cord,” wrote Dr. Waldvogel and associates. “Functionally, the SMA is thought to be crucial for facilitating independent movements of the limbs, which is a key requirement for swimming.”
Although the SMA also partly manages gait, walking was unaffected in all nine of the patients.
The authors described three patients in more detail:
- Case 1 was a 69-year-old man who was a proficient swimmer before DBS. His Unified Parkinson’s Disease Rating Scale (UPDRS) motor score on medication fell from 28 with dyskinesia before DBS to 17 after DBS, and his levodopa-equivalent dosage declined from 1,570 mg to 920 mg. The man almost drowned after he jumped into a lake and had to be rescued by another swimmer.
- Case 4 was a 59-year-old woman who was an accomplished and competitive swimmer and had been swimming up until the DBS procedure. After DBS, her UPDRS motor score on medication fell from 9 with dyskinesia to 6, and her levodopa-equivalent dosage dropped from 825 mg to 150 mg. She had good motor outcome after DBS but lost the ability to swim. “She regularly practiced swimming with her physiotherapist, but never came close to her previous level,” the authors said.
- Case 5 was a 61-year-old woman who was a competitive swimmer, including swimming across Lake Zurich, and held a lifesaving certification. Her UPDRS motor score on medication fell from 11 with dyskinesia to 9, and her levodopa-equivalent dosage decreased from 800 mg to 180 mg. After DBS, she could swim only a quarter of a kilometer and complained of “awkward posture” during her efforts.
The phenomenon has been reported just one other time by a group from the University of Western Australia. This reported patient was a 68-year-old man with a 5-year history of medication-refractory, tremor-predominant Parkinson’s. He received DBS of the posterior subthalamic area (PSA-DBS).
The patient was a dedicated lap swimmer at his local pool. When he returned to his hobby, “he quickly realized he could not propel himself adequately and that he required assistance to get to safety. In a supervised swimming situation, he was unable to float or perform freestyle, breaststroke, or back stroke. With the stimulator turned off for 30 minutes, he regained swimming ability and lost it when the stimulator was turned on.
The Australian team noted that three similar cases presented to them, but they did not discuss those cases in the paper.
Dr. Waldvogel and coauthors wrote that they might also have unreported cases in their cohort of patients with STN-DBS.
“Our cohort of patients with PD who underwent STN-DBS at the time of this retrospective study consisted of 217 patients, but we did not assess patients systematically for their swimming skills or loss thereof,” the authors said. “Until the mechanism of the reported deterioration of the ability to swim after STN-DBS is elucidated, it is crucial that we advise patients of the potential risk of drowning and the need for a carefully supervised assessment of their swimming skills before going into deep water.”
The report received no funding, and one author disclosed financial relationships with industry.
SOURCE: Waldvogel D et al Neurology. 2019 Nov 27. doi: 10.1212/WNL.0000000000008664.
Successful deep brain stimulation of the subthalamic nucleus may have unforeseen effects on the ability to swim in some patients with Parkinson’s disease, according to findings from a case series of nine patients published in Neurology.
All nine patients in the report were experienced swimmers, including two who competed in several competition-level races. They reported losing their ability to swim after successful deep brain stimulation of the subthalamic nucleus (STN-DBS) procedures. The Neurology paper focuses on three of the patients.
All of the patients achieved good to excellent motor control and cut their L-dopa dosage by impressive amounts. But they also lost the ability to coordinate limb movement when in the water, reported Daniel Waldvogel, MD, of the University of Zurich, and associates.
“All found their ability to swim came back immediately, with improved coordination of the limbs,” when stimulation was discontinued, the team noted. But soon after the stimulation ceased, their motor symptoms also rapidly returned, leading all to resume continuous stimulation.
One possible explanation is that STN-DBS does not strongly improve dopamine levels in the supplementary motor area, which controls independent limb movements.
It “may be that DBS affects the supplementary motor area (SMA) differently than levodopa. The SMA is a main output area of the basal ganglia, with connections to the primary motor cortex and the spinal cord,” wrote Dr. Waldvogel and associates. “Functionally, the SMA is thought to be crucial for facilitating independent movements of the limbs, which is a key requirement for swimming.”
Although the SMA also partly manages gait, walking was unaffected in all nine of the patients.
The authors described three patients in more detail:
- Case 1 was a 69-year-old man who was a proficient swimmer before DBS. His Unified Parkinson’s Disease Rating Scale (UPDRS) motor score on medication fell from 28 with dyskinesia before DBS to 17 after DBS, and his levodopa-equivalent dosage declined from 1,570 mg to 920 mg. The man almost drowned after he jumped into a lake and had to be rescued by another swimmer.
- Case 4 was a 59-year-old woman who was an accomplished and competitive swimmer and had been swimming up until the DBS procedure. After DBS, her UPDRS motor score on medication fell from 9 with dyskinesia to 6, and her levodopa-equivalent dosage dropped from 825 mg to 150 mg. She had good motor outcome after DBS but lost the ability to swim. “She regularly practiced swimming with her physiotherapist, but never came close to her previous level,” the authors said.
- Case 5 was a 61-year-old woman who was a competitive swimmer, including swimming across Lake Zurich, and held a lifesaving certification. Her UPDRS motor score on medication fell from 11 with dyskinesia to 9, and her levodopa-equivalent dosage decreased from 800 mg to 180 mg. After DBS, she could swim only a quarter of a kilometer and complained of “awkward posture” during her efforts.
The phenomenon has been reported just one other time by a group from the University of Western Australia. This reported patient was a 68-year-old man with a 5-year history of medication-refractory, tremor-predominant Parkinson’s. He received DBS of the posterior subthalamic area (PSA-DBS).
The patient was a dedicated lap swimmer at his local pool. When he returned to his hobby, “he quickly realized he could not propel himself adequately and that he required assistance to get to safety. In a supervised swimming situation, he was unable to float or perform freestyle, breaststroke, or back stroke. With the stimulator turned off for 30 minutes, he regained swimming ability and lost it when the stimulator was turned on.
The Australian team noted that three similar cases presented to them, but they did not discuss those cases in the paper.
Dr. Waldvogel and coauthors wrote that they might also have unreported cases in their cohort of patients with STN-DBS.
“Our cohort of patients with PD who underwent STN-DBS at the time of this retrospective study consisted of 217 patients, but we did not assess patients systematically for their swimming skills or loss thereof,” the authors said. “Until the mechanism of the reported deterioration of the ability to swim after STN-DBS is elucidated, it is crucial that we advise patients of the potential risk of drowning and the need for a carefully supervised assessment of their swimming skills before going into deep water.”
The report received no funding, and one author disclosed financial relationships with industry.
SOURCE: Waldvogel D et al Neurology. 2019 Nov 27. doi: 10.1212/WNL.0000000000008664.
Successful deep brain stimulation of the subthalamic nucleus may have unforeseen effects on the ability to swim in some patients with Parkinson’s disease, according to findings from a case series of nine patients published in Neurology.
All nine patients in the report were experienced swimmers, including two who competed in several competition-level races. They reported losing their ability to swim after successful deep brain stimulation of the subthalamic nucleus (STN-DBS) procedures. The Neurology paper focuses on three of the patients.
All of the patients achieved good to excellent motor control and cut their L-dopa dosage by impressive amounts. But they also lost the ability to coordinate limb movement when in the water, reported Daniel Waldvogel, MD, of the University of Zurich, and associates.
“All found their ability to swim came back immediately, with improved coordination of the limbs,” when stimulation was discontinued, the team noted. But soon after the stimulation ceased, their motor symptoms also rapidly returned, leading all to resume continuous stimulation.
One possible explanation is that STN-DBS does not strongly improve dopamine levels in the supplementary motor area, which controls independent limb movements.
It “may be that DBS affects the supplementary motor area (SMA) differently than levodopa. The SMA is a main output area of the basal ganglia, with connections to the primary motor cortex and the spinal cord,” wrote Dr. Waldvogel and associates. “Functionally, the SMA is thought to be crucial for facilitating independent movements of the limbs, which is a key requirement for swimming.”
Although the SMA also partly manages gait, walking was unaffected in all nine of the patients.
The authors described three patients in more detail:
- Case 1 was a 69-year-old man who was a proficient swimmer before DBS. His Unified Parkinson’s Disease Rating Scale (UPDRS) motor score on medication fell from 28 with dyskinesia before DBS to 17 after DBS, and his levodopa-equivalent dosage declined from 1,570 mg to 920 mg. The man almost drowned after he jumped into a lake and had to be rescued by another swimmer.
- Case 4 was a 59-year-old woman who was an accomplished and competitive swimmer and had been swimming up until the DBS procedure. After DBS, her UPDRS motor score on medication fell from 9 with dyskinesia to 6, and her levodopa-equivalent dosage dropped from 825 mg to 150 mg. She had good motor outcome after DBS but lost the ability to swim. “She regularly practiced swimming with her physiotherapist, but never came close to her previous level,” the authors said.
- Case 5 was a 61-year-old woman who was a competitive swimmer, including swimming across Lake Zurich, and held a lifesaving certification. Her UPDRS motor score on medication fell from 11 with dyskinesia to 9, and her levodopa-equivalent dosage decreased from 800 mg to 180 mg. After DBS, she could swim only a quarter of a kilometer and complained of “awkward posture” during her efforts.
The phenomenon has been reported just one other time by a group from the University of Western Australia. This reported patient was a 68-year-old man with a 5-year history of medication-refractory, tremor-predominant Parkinson’s. He received DBS of the posterior subthalamic area (PSA-DBS).
The patient was a dedicated lap swimmer at his local pool. When he returned to his hobby, “he quickly realized he could not propel himself adequately and that he required assistance to get to safety. In a supervised swimming situation, he was unable to float or perform freestyle, breaststroke, or back stroke. With the stimulator turned off for 30 minutes, he regained swimming ability and lost it when the stimulator was turned on.
The Australian team noted that three similar cases presented to them, but they did not discuss those cases in the paper.
Dr. Waldvogel and coauthors wrote that they might also have unreported cases in their cohort of patients with STN-DBS.
“Our cohort of patients with PD who underwent STN-DBS at the time of this retrospective study consisted of 217 patients, but we did not assess patients systematically for their swimming skills or loss thereof,” the authors said. “Until the mechanism of the reported deterioration of the ability to swim after STN-DBS is elucidated, it is crucial that we advise patients of the potential risk of drowning and the need for a carefully supervised assessment of their swimming skills before going into deep water.”
The report received no funding, and one author disclosed financial relationships with industry.
SOURCE: Waldvogel D et al Neurology. 2019 Nov 27. doi: 10.1212/WNL.0000000000008664.
FROM NEUROLOGY
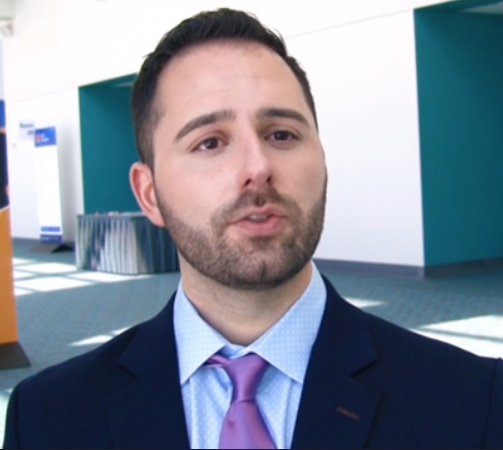
DAPA-HF: Dapagliflozin’s HFrEF efficacy confirmed in nondiabetics
PHILADELPHIA – The primary outcome results from the practice-changing DAPA-HF trial gave clinicians strong evidence that the diabetes drug dapagliflozin was equally effective at reducing cardiovascular death and acute exacerbations in patients with heart failure with reduced ejection fraction, whether or not they also had type 2 diabetes. More detailed findings from the 2,605 enrolled patients in DAPA-HF who lacked diabetes (55% of the total study population) have now sealed the deal.
“The relative and absolute reductions in cardiovascular death and hospitalizations or urgent visits for heart failure were substantial, clinically important, and consistent in patients with or without type 2 diabetes,” John McMurray, MD, declared at the American Heart Association scientific sessions as he summarized new trial results that confirmed the initial finding he reported previously.
While the initial report of the DAPA-HF (Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure) by the study’s lead investigator, Dr. McMurray, was limited to the finding that the relative risk reduction for the study’s primary endpoint was a highly statistically significant 25% in heart failure patients with diabetes and an equally strongly significant 27% relative cut among patients without diabetes (N Engl J Med. 2019 Sep 19;doi: 10.1056/NEJMoa1911303), the new data showed that same consistency across the range of outcomes studied in the trial as well as across the range of glycosylated hemoglobin levels that patients had at study entry.
In an analysis that divided the entire study population of 4,744 patients with heart failure with reduced ejection fraction (HFrEF) into tertiles based on their entry blood level of hemoglobin A1c, patients with a normal level at or below 5.6% had a 26% relative reduction in the study’s primary endpoint, essentially the same response as the 29% relative cut in adverse events in the tertile of patients with a glycosylated hemoglobin level of 5.7%-5.9% and the relative 28% relative reduction in events in patients diagnosed with type 2 diabetes and having a hemoglobin A1c of 6.0% or greater, reported Dr. McMurray, professor of cardiology at the University of Glasgow. The results also showed a very benign safety profile in the patients without diabetes, similar to patients with diabetes and to placebo, and with no episodes of major hypoglycemia or diabetic ketoacidosis.
“It’s quite impressive that the result was consistent regardless of the level of hemoglobin A1c,” commented Larry A. Allen, MD, professor of medicine at the University of Colorado in Aurora and designated discussant for the report. Even though the patients without diabetes constituted just over half of the full DAPA-HF enrollment, the comparison of the effect of dapagliflozin in patients with or without diabetes was prespecified in a trial that enrolled a relatively large number of patients into each of the two subgroups by diabetes status. “I think there a good chance dapagliflozin will get an indication” for treating HFrEF patients without diabetes, Dr. Allen suggested in a video interview.
If the DAPA-HF results persuade the U.S. Food and Drug Administration to grant a supplemental indication to dapagliflozin for use in cutting cardiovascular deaths and acute heart failure exacerbations in patients without diabetes, it would pave the way for health insurers to pay for the drug. Right now, even though Dr. Allen and other heart failure physicians have been impressed by the DAPA-HF findings and are eager to add the drug to the list of agents that HFrEF patients routinely receive, he’s been stymied so far by patients’ out-of pocket cost for using dapagliflozin off-label, roughly $500 a month.
“The DAPA-HF results suggest there is strong reason to consider dapagliflozin for patients without diabetes, and for payers to pay for it. I’m not prescribing dapagliflozin to HFrEF patients without diabetes right now; not because of the data, but because of noncoverage. Payers have not yet caught up with the data,” he said, and they likely will continue to not pay for the drug when used by patients without diabetes until a new labeled indication appears for those patients.
The immediate availability of dapagliflozin (Farxiga) and the two other approved members of the sodium-glucose co-transporter 2 inhibitor class of drugs, empagliflozin (Jardiance) and canagliflozin (Invokana), to treat patients with HFrEF, and the prospect of soon having dapagliflozin and possibly the other drugs in this class to treat patients with HFrEF but without diabetes also raises issues of drug sequencing in these patients and the overall number of drugs that HFrEF patients must now take to be on optimized medical therapy, Dr. Allen noted.
The already-existing lineup of medications for HFrEF patients includes starting on an ACE inhibitor or angiotensin receptor blocker and adding a beta-blocker, a mineralocorticoid receptor antagonist, then swapping out the initial renin-angiotensin system inhibitor for sacubitril/valsartan, and then, on top of all this, adding dapagliflozin or another drug in the same class. It raises questions of what is objectively the best way to introduce all these drugs into patients, and how to do it without subjecting patients to “financial toxicity,” Dr. Allen said during his discussion of the trial’s results.
DAPA-HF was sponsored by AstraZeneca, which markets dapagliflozin (Farxiga). The University of Glasgow received payment from AstraZeneca to compensate for the time Dr. McMurray spent running the study. Dr. Allen has been a consultant to ACI Clinical, Boston Scientific, and Janssen.
SOURCE: McMurray JJV. AHA 19, Late-Breaking Science 1.
A labeling change for dapagliflozin that says the drug is approved for use in patients with heart failure with reduced ejection fraction (HFrEF) and without diabetes is critical so that payers will get on board with this new and important treatment. The evidence for efficacy and safety in patients without diabetes was so strong in the DAPA-HF trial that I don’t think a second trial will be needed for the Food and Drug Administration to add this indication to dapagliflozin’s label.
For patients with type 2 diabetes as well as HFrEF, it’s already full steam ahead to use dapagliflozin or another drug from the class of sodium glucose co-transporter 2 (SGLT2) inhibitors, empagliflozin and canagliflozin. However, so far these drugs are not being widely prescribed by clinicians to patients with HFrEF but without diabetes. We need to build up the familiarity of clinicians with the SGLT2 inhibitor drugs so that primary care physicians will feel comfortable starting HFrEF patients on them. It’s relatively easy to start patients on the drugs in this class because of their good safety and no signal of problems when using them with other HFrEF medications.
The growing list of key drugs to use on patients with HFrEF means that we need to become smarter on how we start patients on these agents. Currently it’s done without evidence for which order of introduction works best. We also need to confirm that all five types of drugs that now appear indicated for HFrEF patients are all truly additive: an angiotensin receptor blocker coupled with the angiotensin receptor neprilysin inhibitor sacubitril, a beta-blocker, a mineralocorticoid receptor antagonist, and now an SGLT2 inhibitor. I propose that researchers run studies that systematically stop one of these drugs to see whether the overall benefit to HFrEF patients remains unchanged, thereby identifying an agent that could be dropped from what is a growing list of drug classes, with possibly more classes to follow depending on results from studies now underway.
Christopher M. O’Connor, MD, is a heart failure physician and president of the Inova Heart and Vascular Institute in Falls Church, Va. He has been a consultant to Arena, Bayer, Bristol-Meyers Squibb, Merck, and Windtree Therapeutics. He made these comments in an interview.
A labeling change for dapagliflozin that says the drug is approved for use in patients with heart failure with reduced ejection fraction (HFrEF) and without diabetes is critical so that payers will get on board with this new and important treatment. The evidence for efficacy and safety in patients without diabetes was so strong in the DAPA-HF trial that I don’t think a second trial will be needed for the Food and Drug Administration to add this indication to dapagliflozin’s label.
For patients with type 2 diabetes as well as HFrEF, it’s already full steam ahead to use dapagliflozin or another drug from the class of sodium glucose co-transporter 2 (SGLT2) inhibitors, empagliflozin and canagliflozin. However, so far these drugs are not being widely prescribed by clinicians to patients with HFrEF but without diabetes. We need to build up the familiarity of clinicians with the SGLT2 inhibitor drugs so that primary care physicians will feel comfortable starting HFrEF patients on them. It’s relatively easy to start patients on the drugs in this class because of their good safety and no signal of problems when using them with other HFrEF medications.
The growing list of key drugs to use on patients with HFrEF means that we need to become smarter on how we start patients on these agents. Currently it’s done without evidence for which order of introduction works best. We also need to confirm that all five types of drugs that now appear indicated for HFrEF patients are all truly additive: an angiotensin receptor blocker coupled with the angiotensin receptor neprilysin inhibitor sacubitril, a beta-blocker, a mineralocorticoid receptor antagonist, and now an SGLT2 inhibitor. I propose that researchers run studies that systematically stop one of these drugs to see whether the overall benefit to HFrEF patients remains unchanged, thereby identifying an agent that could be dropped from what is a growing list of drug classes, with possibly more classes to follow depending on results from studies now underway.
Christopher M. O’Connor, MD, is a heart failure physician and president of the Inova Heart and Vascular Institute in Falls Church, Va. He has been a consultant to Arena, Bayer, Bristol-Meyers Squibb, Merck, and Windtree Therapeutics. He made these comments in an interview.
A labeling change for dapagliflozin that says the drug is approved for use in patients with heart failure with reduced ejection fraction (HFrEF) and without diabetes is critical so that payers will get on board with this new and important treatment. The evidence for efficacy and safety in patients without diabetes was so strong in the DAPA-HF trial that I don’t think a second trial will be needed for the Food and Drug Administration to add this indication to dapagliflozin’s label.
For patients with type 2 diabetes as well as HFrEF, it’s already full steam ahead to use dapagliflozin or another drug from the class of sodium glucose co-transporter 2 (SGLT2) inhibitors, empagliflozin and canagliflozin. However, so far these drugs are not being widely prescribed by clinicians to patients with HFrEF but without diabetes. We need to build up the familiarity of clinicians with the SGLT2 inhibitor drugs so that primary care physicians will feel comfortable starting HFrEF patients on them. It’s relatively easy to start patients on the drugs in this class because of their good safety and no signal of problems when using them with other HFrEF medications.
The growing list of key drugs to use on patients with HFrEF means that we need to become smarter on how we start patients on these agents. Currently it’s done without evidence for which order of introduction works best. We also need to confirm that all five types of drugs that now appear indicated for HFrEF patients are all truly additive: an angiotensin receptor blocker coupled with the angiotensin receptor neprilysin inhibitor sacubitril, a beta-blocker, a mineralocorticoid receptor antagonist, and now an SGLT2 inhibitor. I propose that researchers run studies that systematically stop one of these drugs to see whether the overall benefit to HFrEF patients remains unchanged, thereby identifying an agent that could be dropped from what is a growing list of drug classes, with possibly more classes to follow depending on results from studies now underway.
Christopher M. O’Connor, MD, is a heart failure physician and president of the Inova Heart and Vascular Institute in Falls Church, Va. He has been a consultant to Arena, Bayer, Bristol-Meyers Squibb, Merck, and Windtree Therapeutics. He made these comments in an interview.
PHILADELPHIA – The primary outcome results from the practice-changing DAPA-HF trial gave clinicians strong evidence that the diabetes drug dapagliflozin was equally effective at reducing cardiovascular death and acute exacerbations in patients with heart failure with reduced ejection fraction, whether or not they also had type 2 diabetes. More detailed findings from the 2,605 enrolled patients in DAPA-HF who lacked diabetes (55% of the total study population) have now sealed the deal.
“The relative and absolute reductions in cardiovascular death and hospitalizations or urgent visits for heart failure were substantial, clinically important, and consistent in patients with or without type 2 diabetes,” John McMurray, MD, declared at the American Heart Association scientific sessions as he summarized new trial results that confirmed the initial finding he reported previously.
While the initial report of the DAPA-HF (Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure) by the study’s lead investigator, Dr. McMurray, was limited to the finding that the relative risk reduction for the study’s primary endpoint was a highly statistically significant 25% in heart failure patients with diabetes and an equally strongly significant 27% relative cut among patients without diabetes (N Engl J Med. 2019 Sep 19;doi: 10.1056/NEJMoa1911303), the new data showed that same consistency across the range of outcomes studied in the trial as well as across the range of glycosylated hemoglobin levels that patients had at study entry.
In an analysis that divided the entire study population of 4,744 patients with heart failure with reduced ejection fraction (HFrEF) into tertiles based on their entry blood level of hemoglobin A1c, patients with a normal level at or below 5.6% had a 26% relative reduction in the study’s primary endpoint, essentially the same response as the 29% relative cut in adverse events in the tertile of patients with a glycosylated hemoglobin level of 5.7%-5.9% and the relative 28% relative reduction in events in patients diagnosed with type 2 diabetes and having a hemoglobin A1c of 6.0% or greater, reported Dr. McMurray, professor of cardiology at the University of Glasgow. The results also showed a very benign safety profile in the patients without diabetes, similar to patients with diabetes and to placebo, and with no episodes of major hypoglycemia or diabetic ketoacidosis.
“It’s quite impressive that the result was consistent regardless of the level of hemoglobin A1c,” commented Larry A. Allen, MD, professor of medicine at the University of Colorado in Aurora and designated discussant for the report. Even though the patients without diabetes constituted just over half of the full DAPA-HF enrollment, the comparison of the effect of dapagliflozin in patients with or without diabetes was prespecified in a trial that enrolled a relatively large number of patients into each of the two subgroups by diabetes status. “I think there a good chance dapagliflozin will get an indication” for treating HFrEF patients without diabetes, Dr. Allen suggested in a video interview.
If the DAPA-HF results persuade the U.S. Food and Drug Administration to grant a supplemental indication to dapagliflozin for use in cutting cardiovascular deaths and acute heart failure exacerbations in patients without diabetes, it would pave the way for health insurers to pay for the drug. Right now, even though Dr. Allen and other heart failure physicians have been impressed by the DAPA-HF findings and are eager to add the drug to the list of agents that HFrEF patients routinely receive, he’s been stymied so far by patients’ out-of pocket cost for using dapagliflozin off-label, roughly $500 a month.
“The DAPA-HF results suggest there is strong reason to consider dapagliflozin for patients without diabetes, and for payers to pay for it. I’m not prescribing dapagliflozin to HFrEF patients without diabetes right now; not because of the data, but because of noncoverage. Payers have not yet caught up with the data,” he said, and they likely will continue to not pay for the drug when used by patients without diabetes until a new labeled indication appears for those patients.
The immediate availability of dapagliflozin (Farxiga) and the two other approved members of the sodium-glucose co-transporter 2 inhibitor class of drugs, empagliflozin (Jardiance) and canagliflozin (Invokana), to treat patients with HFrEF, and the prospect of soon having dapagliflozin and possibly the other drugs in this class to treat patients with HFrEF but without diabetes also raises issues of drug sequencing in these patients and the overall number of drugs that HFrEF patients must now take to be on optimized medical therapy, Dr. Allen noted.
The already-existing lineup of medications for HFrEF patients includes starting on an ACE inhibitor or angiotensin receptor blocker and adding a beta-blocker, a mineralocorticoid receptor antagonist, then swapping out the initial renin-angiotensin system inhibitor for sacubitril/valsartan, and then, on top of all this, adding dapagliflozin or another drug in the same class. It raises questions of what is objectively the best way to introduce all these drugs into patients, and how to do it without subjecting patients to “financial toxicity,” Dr. Allen said during his discussion of the trial’s results.
DAPA-HF was sponsored by AstraZeneca, which markets dapagliflozin (Farxiga). The University of Glasgow received payment from AstraZeneca to compensate for the time Dr. McMurray spent running the study. Dr. Allen has been a consultant to ACI Clinical, Boston Scientific, and Janssen.
SOURCE: McMurray JJV. AHA 19, Late-Breaking Science 1.
PHILADELPHIA – The primary outcome results from the practice-changing DAPA-HF trial gave clinicians strong evidence that the diabetes drug dapagliflozin was equally effective at reducing cardiovascular death and acute exacerbations in patients with heart failure with reduced ejection fraction, whether or not they also had type 2 diabetes. More detailed findings from the 2,605 enrolled patients in DAPA-HF who lacked diabetes (55% of the total study population) have now sealed the deal.
“The relative and absolute reductions in cardiovascular death and hospitalizations or urgent visits for heart failure were substantial, clinically important, and consistent in patients with or without type 2 diabetes,” John McMurray, MD, declared at the American Heart Association scientific sessions as he summarized new trial results that confirmed the initial finding he reported previously.
While the initial report of the DAPA-HF (Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure) by the study’s lead investigator, Dr. McMurray, was limited to the finding that the relative risk reduction for the study’s primary endpoint was a highly statistically significant 25% in heart failure patients with diabetes and an equally strongly significant 27% relative cut among patients without diabetes (N Engl J Med. 2019 Sep 19;doi: 10.1056/NEJMoa1911303), the new data showed that same consistency across the range of outcomes studied in the trial as well as across the range of glycosylated hemoglobin levels that patients had at study entry.
In an analysis that divided the entire study population of 4,744 patients with heart failure with reduced ejection fraction (HFrEF) into tertiles based on their entry blood level of hemoglobin A1c, patients with a normal level at or below 5.6% had a 26% relative reduction in the study’s primary endpoint, essentially the same response as the 29% relative cut in adverse events in the tertile of patients with a glycosylated hemoglobin level of 5.7%-5.9% and the relative 28% relative reduction in events in patients diagnosed with type 2 diabetes and having a hemoglobin A1c of 6.0% or greater, reported Dr. McMurray, professor of cardiology at the University of Glasgow. The results also showed a very benign safety profile in the patients without diabetes, similar to patients with diabetes and to placebo, and with no episodes of major hypoglycemia or diabetic ketoacidosis.
“It’s quite impressive that the result was consistent regardless of the level of hemoglobin A1c,” commented Larry A. Allen, MD, professor of medicine at the University of Colorado in Aurora and designated discussant for the report. Even though the patients without diabetes constituted just over half of the full DAPA-HF enrollment, the comparison of the effect of dapagliflozin in patients with or without diabetes was prespecified in a trial that enrolled a relatively large number of patients into each of the two subgroups by diabetes status. “I think there a good chance dapagliflozin will get an indication” for treating HFrEF patients without diabetes, Dr. Allen suggested in a video interview.
If the DAPA-HF results persuade the U.S. Food and Drug Administration to grant a supplemental indication to dapagliflozin for use in cutting cardiovascular deaths and acute heart failure exacerbations in patients without diabetes, it would pave the way for health insurers to pay for the drug. Right now, even though Dr. Allen and other heart failure physicians have been impressed by the DAPA-HF findings and are eager to add the drug to the list of agents that HFrEF patients routinely receive, he’s been stymied so far by patients’ out-of pocket cost for using dapagliflozin off-label, roughly $500 a month.
“The DAPA-HF results suggest there is strong reason to consider dapagliflozin for patients without diabetes, and for payers to pay for it. I’m not prescribing dapagliflozin to HFrEF patients without diabetes right now; not because of the data, but because of noncoverage. Payers have not yet caught up with the data,” he said, and they likely will continue to not pay for the drug when used by patients without diabetes until a new labeled indication appears for those patients.
The immediate availability of dapagliflozin (Farxiga) and the two other approved members of the sodium-glucose co-transporter 2 inhibitor class of drugs, empagliflozin (Jardiance) and canagliflozin (Invokana), to treat patients with HFrEF, and the prospect of soon having dapagliflozin and possibly the other drugs in this class to treat patients with HFrEF but without diabetes also raises issues of drug sequencing in these patients and the overall number of drugs that HFrEF patients must now take to be on optimized medical therapy, Dr. Allen noted.
The already-existing lineup of medications for HFrEF patients includes starting on an ACE inhibitor or angiotensin receptor blocker and adding a beta-blocker, a mineralocorticoid receptor antagonist, then swapping out the initial renin-angiotensin system inhibitor for sacubitril/valsartan, and then, on top of all this, adding dapagliflozin or another drug in the same class. It raises questions of what is objectively the best way to introduce all these drugs into patients, and how to do it without subjecting patients to “financial toxicity,” Dr. Allen said during his discussion of the trial’s results.
DAPA-HF was sponsored by AstraZeneca, which markets dapagliflozin (Farxiga). The University of Glasgow received payment from AstraZeneca to compensate for the time Dr. McMurray spent running the study. Dr. Allen has been a consultant to ACI Clinical, Boston Scientific, and Janssen.
SOURCE: McMurray JJV. AHA 19, Late-Breaking Science 1.
REPORTING FROM AHA 2019
Key clinical point: Dapaglifozin produced as much benefit in HFrEF patients without diabetes as it did in those with type 2 diabetes.
Major finding: The relative risk reduction with dapagliflozin was 26% in patients with a hemoglobin A1c of 5.6% or less.
Study details: DAPA-HF is a multicenter, randomized trial involving 4,744 patients with heart failure with reduced ejection fraction.
Disclosures: DAPA-HF was sponsored by AstraZeneca, which markets dapagliflozin (Farxiga). The University of Glasgow received payment from AstraZeneca to compensate for the time Dr. McMurray spent running the study. Dr. Allen has been a consultant to ACI Clinical, Boston Scientific, and Janssen.
Source: McMurray JJV et al. AHA 19, Late-Breaking Science 1.
Level of hepatitis B core–related antigen is risk factor for hepatocellular carcinoma
A high level of hepatitis B core–related antigen (HBcrAg) was a complementary risk factor for hepatocellular carcinoma, according to the results of a retrospective cohort study of more than 2,600 noncirrhotic adults with untreated hepatitis B virus (HBV) infection with a median of 16 years of follow-up.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
“Patients with an intermediate viral load and high levels of HBcrAg had a risk for hepatocellular carcinoma that did not differ significantly from that of patients with a high viral load. [An] HBcrAg of 10 KU/mL may serve as a novel biomarker for the management of patients with intermediate viral load in our clinical practice,” wrote Tai-Chung Tseng, MD, PhD, of National Taiwan University Hospital in Taipei and associates in Gastroenterology.
Deciding whether to start antiviral therapy is controversial for some patients with HBV infection. Typically, monitoring without treatment is recommended for patients who have both low hepatitis B surface antigen levels (less than 1,000 IU/mL) and low levels of HBV DNA (less than 2,000 IU/mL), and early antiviral therapy is recommended for patients who have high levels of HBV DNA (20,000 IU/mL or more). However, there is no clear evidence that early antiviral therapy benefits patients who have intermediate levels of HBV DNA (2,000-19,999 IU/mL) and are negative for hepatitis B e antigen. Biomarkers for risk-stratifying these patients also are lacking, the researchers noted.
Therefore, they studied a cohort of 2,666 adults who had tested positive for hepatitis B surface antigen and were followed at National Taiwan University Hospital from 1985 through 2000. No patient had cirrhosis at baseline. In all, 209 patients developed hepatocellular carcinoma, yielding an incidence rate of 4.91 cases per 1,000 person-years.
Hepatitis B core–related antigen level remained an independent risk factor for hepatocellular carcinoma after accounting for age, sex, serum alanine aminotransferase (ALT) level, FIB-4 index, hepatitis B e antigen status, hepatitis B genotype (B, C, or undetermined), and HBV DNA level. Compared with patients whose HBcrAg level was less than 10 KU, a level of 10-99 KU/mL was associated with a nearly threefold increase in risk for hepatocellular carcinoma (HR, 2.93; 95% CI, 1.67-4.80), and this risk rose even further as HBcrAg levels increased.
In the subgroup of patients who tested negative for hepatitis B e antigen, had an intermediate HBV DNA load (2,000-19,999 IU/mL), and had a normal baseline ALT level (less than 40 U/L), a high HBcrAg level (10 KU/mL or more) was tied to a nearly fivefold greater risk for hepatocellular carcinoma (HR, 4.89; 95% CI, 2.18-10.93). This approximated the risk that is observed with high viral load (20,000 IU/mL), the researchers noted. In contrast, a low HBcrAg level was associated with a risk similar to that of minimal risk carriers (annual incidence rate, 0.10%; 95% CI, 0.04%-0.24%).
“To the best of our knowledge, this is the first study to report HBcrAg level as an independent viral biomarker to stratify hepatocellular risks in a large number of patients with intermediate viral load,” the researchers commented. Among the study limitations, 412 patients received antiviral therapy during follow-up. “This is a retrospective cohort study including Asian HBV patients with genotype B or C infection,” the investigators added. “It is unclear whether this finding could be extrapolated to populations with other HBV genotype infections. Nonetheless, we had a sound cohort, as several HBsAg-related clinical findings based on our cohort have already been validated by other prospective cohort studies, implying that our data were unlikely to be biased by the study design.”
Funders included National Taiwan University Hospital, the Ministry of Science and Technology, Executive Yuan in Taiwan, and National Health Research Institutes. The researchers reported having no conflicts of interest.
SOURCE: Tseng T-C et al. Gastroenterology. 2019 Aug 27. doi: 10.1053/j.gastro.2019.08.028.
A high level of hepatitis B core–related antigen (HBcrAg) was a complementary risk factor for hepatocellular carcinoma, according to the results of a retrospective cohort study of more than 2,600 noncirrhotic adults with untreated hepatitis B virus (HBV) infection with a median of 16 years of follow-up.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
“Patients with an intermediate viral load and high levels of HBcrAg had a risk for hepatocellular carcinoma that did not differ significantly from that of patients with a high viral load. [An] HBcrAg of 10 KU/mL may serve as a novel biomarker for the management of patients with intermediate viral load in our clinical practice,” wrote Tai-Chung Tseng, MD, PhD, of National Taiwan University Hospital in Taipei and associates in Gastroenterology.
Deciding whether to start antiviral therapy is controversial for some patients with HBV infection. Typically, monitoring without treatment is recommended for patients who have both low hepatitis B surface antigen levels (less than 1,000 IU/mL) and low levels of HBV DNA (less than 2,000 IU/mL), and early antiviral therapy is recommended for patients who have high levels of HBV DNA (20,000 IU/mL or more). However, there is no clear evidence that early antiviral therapy benefits patients who have intermediate levels of HBV DNA (2,000-19,999 IU/mL) and are negative for hepatitis B e antigen. Biomarkers for risk-stratifying these patients also are lacking, the researchers noted.
Therefore, they studied a cohort of 2,666 adults who had tested positive for hepatitis B surface antigen and were followed at National Taiwan University Hospital from 1985 through 2000. No patient had cirrhosis at baseline. In all, 209 patients developed hepatocellular carcinoma, yielding an incidence rate of 4.91 cases per 1,000 person-years.
Hepatitis B core–related antigen level remained an independent risk factor for hepatocellular carcinoma after accounting for age, sex, serum alanine aminotransferase (ALT) level, FIB-4 index, hepatitis B e antigen status, hepatitis B genotype (B, C, or undetermined), and HBV DNA level. Compared with patients whose HBcrAg level was less than 10 KU, a level of 10-99 KU/mL was associated with a nearly threefold increase in risk for hepatocellular carcinoma (HR, 2.93; 95% CI, 1.67-4.80), and this risk rose even further as HBcrAg levels increased.
In the subgroup of patients who tested negative for hepatitis B e antigen, had an intermediate HBV DNA load (2,000-19,999 IU/mL), and had a normal baseline ALT level (less than 40 U/L), a high HBcrAg level (10 KU/mL or more) was tied to a nearly fivefold greater risk for hepatocellular carcinoma (HR, 4.89; 95% CI, 2.18-10.93). This approximated the risk that is observed with high viral load (20,000 IU/mL), the researchers noted. In contrast, a low HBcrAg level was associated with a risk similar to that of minimal risk carriers (annual incidence rate, 0.10%; 95% CI, 0.04%-0.24%).
“To the best of our knowledge, this is the first study to report HBcrAg level as an independent viral biomarker to stratify hepatocellular risks in a large number of patients with intermediate viral load,” the researchers commented. Among the study limitations, 412 patients received antiviral therapy during follow-up. “This is a retrospective cohort study including Asian HBV patients with genotype B or C infection,” the investigators added. “It is unclear whether this finding could be extrapolated to populations with other HBV genotype infections. Nonetheless, we had a sound cohort, as several HBsAg-related clinical findings based on our cohort have already been validated by other prospective cohort studies, implying that our data were unlikely to be biased by the study design.”
Funders included National Taiwan University Hospital, the Ministry of Science and Technology, Executive Yuan in Taiwan, and National Health Research Institutes. The researchers reported having no conflicts of interest.
SOURCE: Tseng T-C et al. Gastroenterology. 2019 Aug 27. doi: 10.1053/j.gastro.2019.08.028.
A high level of hepatitis B core–related antigen (HBcrAg) was a complementary risk factor for hepatocellular carcinoma, according to the results of a retrospective cohort study of more than 2,600 noncirrhotic adults with untreated hepatitis B virus (HBV) infection with a median of 16 years of follow-up.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
“Patients with an intermediate viral load and high levels of HBcrAg had a risk for hepatocellular carcinoma that did not differ significantly from that of patients with a high viral load. [An] HBcrAg of 10 KU/mL may serve as a novel biomarker for the management of patients with intermediate viral load in our clinical practice,” wrote Tai-Chung Tseng, MD, PhD, of National Taiwan University Hospital in Taipei and associates in Gastroenterology.
Deciding whether to start antiviral therapy is controversial for some patients with HBV infection. Typically, monitoring without treatment is recommended for patients who have both low hepatitis B surface antigen levels (less than 1,000 IU/mL) and low levels of HBV DNA (less than 2,000 IU/mL), and early antiviral therapy is recommended for patients who have high levels of HBV DNA (20,000 IU/mL or more). However, there is no clear evidence that early antiviral therapy benefits patients who have intermediate levels of HBV DNA (2,000-19,999 IU/mL) and are negative for hepatitis B e antigen. Biomarkers for risk-stratifying these patients also are lacking, the researchers noted.
Therefore, they studied a cohort of 2,666 adults who had tested positive for hepatitis B surface antigen and were followed at National Taiwan University Hospital from 1985 through 2000. No patient had cirrhosis at baseline. In all, 209 patients developed hepatocellular carcinoma, yielding an incidence rate of 4.91 cases per 1,000 person-years.
Hepatitis B core–related antigen level remained an independent risk factor for hepatocellular carcinoma after accounting for age, sex, serum alanine aminotransferase (ALT) level, FIB-4 index, hepatitis B e antigen status, hepatitis B genotype (B, C, or undetermined), and HBV DNA level. Compared with patients whose HBcrAg level was less than 10 KU, a level of 10-99 KU/mL was associated with a nearly threefold increase in risk for hepatocellular carcinoma (HR, 2.93; 95% CI, 1.67-4.80), and this risk rose even further as HBcrAg levels increased.
In the subgroup of patients who tested negative for hepatitis B e antigen, had an intermediate HBV DNA load (2,000-19,999 IU/mL), and had a normal baseline ALT level (less than 40 U/L), a high HBcrAg level (10 KU/mL or more) was tied to a nearly fivefold greater risk for hepatocellular carcinoma (HR, 4.89; 95% CI, 2.18-10.93). This approximated the risk that is observed with high viral load (20,000 IU/mL), the researchers noted. In contrast, a low HBcrAg level was associated with a risk similar to that of minimal risk carriers (annual incidence rate, 0.10%; 95% CI, 0.04%-0.24%).
“To the best of our knowledge, this is the first study to report HBcrAg level as an independent viral biomarker to stratify hepatocellular risks in a large number of patients with intermediate viral load,” the researchers commented. Among the study limitations, 412 patients received antiviral therapy during follow-up. “This is a retrospective cohort study including Asian HBV patients with genotype B or C infection,” the investigators added. “It is unclear whether this finding could be extrapolated to populations with other HBV genotype infections. Nonetheless, we had a sound cohort, as several HBsAg-related clinical findings based on our cohort have already been validated by other prospective cohort studies, implying that our data were unlikely to be biased by the study design.”
Funders included National Taiwan University Hospital, the Ministry of Science and Technology, Executive Yuan in Taiwan, and National Health Research Institutes. The researchers reported having no conflicts of interest.
SOURCE: Tseng T-C et al. Gastroenterology. 2019 Aug 27. doi: 10.1053/j.gastro.2019.08.028.
FROM GASTROENTEROLOGY
Flu vaccine cuts infection severity in kids and adults
WASHINGTON –
During recent U.S. flu seasons, children and adults who contracted influenza despite vaccination had significantly fewer severe infections and infection complications, compared with unimmunized people, according to two separate reports from CDC researchers presented at an annual scientific meeting on infectious diseases.
One of the reports tracked the impact of flu vaccine in children using data that the CDC collected at seven medical centers that participated in the agency’s New Vaccine Surveillance Network, which provided information on children aged 6 months to 17 years who were hospitalized for an acute respiratory illness, including more than 1,700 children during the 2016-2017 flu season and more than 1,900 during the 2017-2018 season. Roughly 10% of these children tested positive for influenza, and the subsequent analysis focused on these cases and compared incidence rates among children who had been vaccinated during the index season and those who had remained unvaccinated.
Combined data from both seasons showed that vaccinated children were 50% less likely to have been hospitalized for an acute influenza infection, compared with unvaccinated kids, a pattern consistently seen both in children aged 6 months to 8 years and in those aged 9-17 years. The pattern of vaccine effectiveness also held regardless of which flu strain caused the infections, reported Angela P. Campbell, MD, a CDC medical officer.
“We saw a nice benefit from vaccination, both in previously healthy children and in those with an underlying medical condition,” a finding that adds to existing evidence of vaccine effectiveness, Dr. Campbell said in a video interview. The results confirmed that flu vaccination does not just prevent infections but also cuts the rate of more severe infections that lead to hospitalization, she explained.
Another CDC study looked at data collected by the agency’s Influenza Hospitalization Surveillance Network from adults at least 18 years old who were hospitalized for a laboratory-confirmed influenza infection during five flu seasons, 2013-2014 through 2017-18. The data, which came from more than 250 acute-care hospitals in 13 states, included more than 43,000 people hospitalized for an identified influenza strain and with a known vaccination history who were not institutionalized and had not received any antiviral treatment.
After propensity-weighted adjustment to create better parity between the vaccinated and unvaccinated patients, the results showed that people 18-64 years old with vaccination had statistically significant decreases in mortality of a relative 36%, need for mechanical ventilation of 34%, pneumonia of 20%, and need for ICU admission of a relative 19%, as well as an 18% drop in average ICU length of stay, Shikha Garg, MD, said at the meeting. The propensity-weighted analysis of data from people at least 65 years old showed statistically significant relative reductions linked with vaccination: 46% reduction in the need for mechanical ventilation, 28% reduction in ICU admissions, and 9% reduction in hospitalized length of stay.
Further analysis of these outcomes by the strains that caused these influenza infections showed that the statistically significant benefits from vaccination were seen only in patients infected with an H1N1 strain. Statistically significant effects on these severe outcomes were not apparent among people infected with the H3N2 or B strains, said Dr. Garg, a medical epidemiologist at the CDC.
“All adults should receive an annual flu vaccination as it can improve outcomes among those who develop influenza despite vaccination,” she concluded.
Results from a third CDC study reported at the meeting examined the importance of two vaccine doses (administered at least 4 weeks apart) given to children aged 6 months to 8 years for the first season they receive flu vaccination, which is the immunization approach for flu recommended by the CDC. The findings from a total of more than 7,500 children immunized during the 2014-2018 seasons showed a clear increment in vaccine protection among kids who received two doses during their first season vaccinated, especially in children who were 2 years old or younger. In that age group, administration of two doses produced vaccine effectiveness of 53% versus a 23% vaccine effectiveness after a single vaccine dose, reported Jessie Chung, a CDC epidemiologist.
WASHINGTON –
During recent U.S. flu seasons, children and adults who contracted influenza despite vaccination had significantly fewer severe infections and infection complications, compared with unimmunized people, according to two separate reports from CDC researchers presented at an annual scientific meeting on infectious diseases.
One of the reports tracked the impact of flu vaccine in children using data that the CDC collected at seven medical centers that participated in the agency’s New Vaccine Surveillance Network, which provided information on children aged 6 months to 17 years who were hospitalized for an acute respiratory illness, including more than 1,700 children during the 2016-2017 flu season and more than 1,900 during the 2017-2018 season. Roughly 10% of these children tested positive for influenza, and the subsequent analysis focused on these cases and compared incidence rates among children who had been vaccinated during the index season and those who had remained unvaccinated.
Combined data from both seasons showed that vaccinated children were 50% less likely to have been hospitalized for an acute influenza infection, compared with unvaccinated kids, a pattern consistently seen both in children aged 6 months to 8 years and in those aged 9-17 years. The pattern of vaccine effectiveness also held regardless of which flu strain caused the infections, reported Angela P. Campbell, MD, a CDC medical officer.
“We saw a nice benefit from vaccination, both in previously healthy children and in those with an underlying medical condition,” a finding that adds to existing evidence of vaccine effectiveness, Dr. Campbell said in a video interview. The results confirmed that flu vaccination does not just prevent infections but also cuts the rate of more severe infections that lead to hospitalization, she explained.
Another CDC study looked at data collected by the agency’s Influenza Hospitalization Surveillance Network from adults at least 18 years old who were hospitalized for a laboratory-confirmed influenza infection during five flu seasons, 2013-2014 through 2017-18. The data, which came from more than 250 acute-care hospitals in 13 states, included more than 43,000 people hospitalized for an identified influenza strain and with a known vaccination history who were not institutionalized and had not received any antiviral treatment.
After propensity-weighted adjustment to create better parity between the vaccinated and unvaccinated patients, the results showed that people 18-64 years old with vaccination had statistically significant decreases in mortality of a relative 36%, need for mechanical ventilation of 34%, pneumonia of 20%, and need for ICU admission of a relative 19%, as well as an 18% drop in average ICU length of stay, Shikha Garg, MD, said at the meeting. The propensity-weighted analysis of data from people at least 65 years old showed statistically significant relative reductions linked with vaccination: 46% reduction in the need for mechanical ventilation, 28% reduction in ICU admissions, and 9% reduction in hospitalized length of stay.
Further analysis of these outcomes by the strains that caused these influenza infections showed that the statistically significant benefits from vaccination were seen only in patients infected with an H1N1 strain. Statistically significant effects on these severe outcomes were not apparent among people infected with the H3N2 or B strains, said Dr. Garg, a medical epidemiologist at the CDC.
“All adults should receive an annual flu vaccination as it can improve outcomes among those who develop influenza despite vaccination,” she concluded.
Results from a third CDC study reported at the meeting examined the importance of two vaccine doses (administered at least 4 weeks apart) given to children aged 6 months to 8 years for the first season they receive flu vaccination, which is the immunization approach for flu recommended by the CDC. The findings from a total of more than 7,500 children immunized during the 2014-2018 seasons showed a clear increment in vaccine protection among kids who received two doses during their first season vaccinated, especially in children who were 2 years old or younger. In that age group, administration of two doses produced vaccine effectiveness of 53% versus a 23% vaccine effectiveness after a single vaccine dose, reported Jessie Chung, a CDC epidemiologist.
WASHINGTON –
During recent U.S. flu seasons, children and adults who contracted influenza despite vaccination had significantly fewer severe infections and infection complications, compared with unimmunized people, according to two separate reports from CDC researchers presented at an annual scientific meeting on infectious diseases.
One of the reports tracked the impact of flu vaccine in children using data that the CDC collected at seven medical centers that participated in the agency’s New Vaccine Surveillance Network, which provided information on children aged 6 months to 17 years who were hospitalized for an acute respiratory illness, including more than 1,700 children during the 2016-2017 flu season and more than 1,900 during the 2017-2018 season. Roughly 10% of these children tested positive for influenza, and the subsequent analysis focused on these cases and compared incidence rates among children who had been vaccinated during the index season and those who had remained unvaccinated.
Combined data from both seasons showed that vaccinated children were 50% less likely to have been hospitalized for an acute influenza infection, compared with unvaccinated kids, a pattern consistently seen both in children aged 6 months to 8 years and in those aged 9-17 years. The pattern of vaccine effectiveness also held regardless of which flu strain caused the infections, reported Angela P. Campbell, MD, a CDC medical officer.
“We saw a nice benefit from vaccination, both in previously healthy children and in those with an underlying medical condition,” a finding that adds to existing evidence of vaccine effectiveness, Dr. Campbell said in a video interview. The results confirmed that flu vaccination does not just prevent infections but also cuts the rate of more severe infections that lead to hospitalization, she explained.
Another CDC study looked at data collected by the agency’s Influenza Hospitalization Surveillance Network from adults at least 18 years old who were hospitalized for a laboratory-confirmed influenza infection during five flu seasons, 2013-2014 through 2017-18. The data, which came from more than 250 acute-care hospitals in 13 states, included more than 43,000 people hospitalized for an identified influenza strain and with a known vaccination history who were not institutionalized and had not received any antiviral treatment.
After propensity-weighted adjustment to create better parity between the vaccinated and unvaccinated patients, the results showed that people 18-64 years old with vaccination had statistically significant decreases in mortality of a relative 36%, need for mechanical ventilation of 34%, pneumonia of 20%, and need for ICU admission of a relative 19%, as well as an 18% drop in average ICU length of stay, Shikha Garg, MD, said at the meeting. The propensity-weighted analysis of data from people at least 65 years old showed statistically significant relative reductions linked with vaccination: 46% reduction in the need for mechanical ventilation, 28% reduction in ICU admissions, and 9% reduction in hospitalized length of stay.
Further analysis of these outcomes by the strains that caused these influenza infections showed that the statistically significant benefits from vaccination were seen only in patients infected with an H1N1 strain. Statistically significant effects on these severe outcomes were not apparent among people infected with the H3N2 or B strains, said Dr. Garg, a medical epidemiologist at the CDC.
“All adults should receive an annual flu vaccination as it can improve outcomes among those who develop influenza despite vaccination,” she concluded.
Results from a third CDC study reported at the meeting examined the importance of two vaccine doses (administered at least 4 weeks apart) given to children aged 6 months to 8 years for the first season they receive flu vaccination, which is the immunization approach for flu recommended by the CDC. The findings from a total of more than 7,500 children immunized during the 2014-2018 seasons showed a clear increment in vaccine protection among kids who received two doses during their first season vaccinated, especially in children who were 2 years old or younger. In that age group, administration of two doses produced vaccine effectiveness of 53% versus a 23% vaccine effectiveness after a single vaccine dose, reported Jessie Chung, a CDC epidemiologist.
REPORTING FROM ID WEEK 2019
Cancer overtakes CVD as cause of death in high-income countries
PARIS – Though cardiovascular disease still accounts for 40% of deaths around the world, , according to new data from a global prospective study.
“Cancer deaths are becoming more frequent not because the rates of death from cancer are going up, but because we have decreased the deaths from cardiovascular disease,” said the study’s senior author, Salim Yusuf, MD, at the annual congress of the European Society of Cardiology.
A striking pattern emerged when cause of death was stratified by country income level, said fellow investigator Darryl P. Leong, MBBS, in presenting data regarding shifting global mortality patterns. Fully 55% of deaths in high-income nations were caused by cancer, compared with 30% in middle-income countries and 15% in low-income countries. In high-income countries, by contrast, cardiovascular disease (CVD) was the cause of death 23% of the time, while that figure was 42% and 43% for middle- and low-income countries, respectively.
Looking at the data slightly differently, the ratio of cardiovascular deaths to cancer deaths for high-income countries is 0.4; for middle-income countries, the ratio is 1.3, and “One is threefold more likely to die from cardiovascular disease as from cancer” in low-income countries, said Dr. Leong. Although the United States is not included in the PURE study, “recent data shows that some states in the U.S. also have higher cancer mortality than cardiovascular disease. This is a success story,” said Dr. Yusuf, since the shift is largely attributable to decreased mortality from CVD.
Dr. Leong and Dr. Yusuf each presented results from the PURE (Prospective Urban Rural Epidemiology) study, which has enrolled a total of 202,000 individuals from 27 countries on every inhabited continent but Australia. Follow-up data are available for 167,000 individuals in 21 countries. Canada, Russia, China, India, Brazil, and Chile are among the most populous national that are included. Their findings were published simultaneously in the Lancet with the congress presentations (2019 Sep 3; doi: 10.1016/S0140-6736(19)32008-2 and doi: 10.1016/S0140-6736(19)32007-0).
The INTERHEART risk score, an integrated cardiovascular risk score that uses non-laboratory values such as age, smoking status, family history, and comorbidities, was calculated for all participants. “We observed that the highest predicted cardiovascular risk is in high-income countries, and the lowest, in low-income countries,” said Dr. Leong, a cardiologist at McMaster University and the Population Health Research Institute, both in Hamilton, Ont.
Over the study period, 11,307 deaths occurred. Over 9,000 incident cardiovascular events were observed, as were over 5,000 new cancers.
“We have some interesting observations from these data,” said Dr. Leong. “Firstly, there is a gradient in the cardiovascular disease rates, moving from lowest in high-income countries – despite the fact that their INTERHEART risk score was highest – through to highest incident cardiovascular disease in low-income countries, despite their INTERHEART risk score being lowest.” This difference, said Dr. Leong, was driven by higher myocardial infarction rates in low-income countries and higher stroke rates in middle-income countries, when compared to high-income countries.
Once a participant was subject to one of the incident diseases, though, the patterns shifted. For CVD, cancer, chronic obstructive pulmonary disease, pneumonia, and injury, the likelihood of death within 1 year was highest in low-income countries – markedly higher, in the case of CVD. For all conditions, the one-year case-fatality rate after the occurrence of an incident disease was lowest in high-income countries.
“So we are seeing a new transition,” said Dr. Yusuf, the executive director of the Population Health Research Institute and Distinguished University Professor of Medicine, McMaster University, both in Hamilton, Ont. “The old transition was infectious diseases giving way to noncommunicable diseases. Now we are seeing a transition within noncommunicable diseases: In rich countries, cardiovascular disease is going down, perhaps due to better prevention, but I think even more importantly, due to better treatments.
“I want to hasten to add that the difference in risk between high-, middle-, and low-income countries in cardiovascular disease is not due to risk factors,” he went on. “Risk factors, if anything, are lower in the poor countries, compared to the higher-income countries.”
The shift away from cardiovascular disease mortality toward cancer mortality is also occurring in some countries that are in the upper tier of middle-income nations, including Chile, Argentina, Turkey, and Poland, said Dr. Yusuf, who presented data regarding the relative contributions of risk factors to cardiovascular disease and mortality.
Risk factors for cardiovascular disease in the PURE study were expressed by a measure called the population attributable fraction (PAF) that captures both the hazard ratio for a particular risk factor and the prevalence of the risk factor, explained Dr. Yusuf. “Hypertension, by far, was the biggest risk factor of cardiovascular disease globally,” he added, noting that the PAF for hypertension was over 20%. Hypertension far outstripped the next most significant risk factor, high non-HDL cholesterol, which had a PAF of less than 10%.
“This was a big surprise to us: Household pollution was a big factor,” said Dr. Yusuf, who later added that particulate matter from cooking, particularly with solid fuels such as wood or charcoal, was likely the source of much household air pollution, “a big problem in middle- and low-income countries.”
Tobacco usage is decreasing, as is its contribution to cardiovascular deaths, but other commonly cited culprits for cardiovascular disease were not significant contributors to cardiovascular disease in the PURE population.
“Abdominal obesity, and not BMI” contributes to cardiovascular risk. “BMI is not a good indicator of risk,” said Dr. Yusuf in a video interview. These results were presented separately at the congress.
“Grip strength is important; in fact, it is more important than low physical activity. People have focused on physical activity – how much you do. But strength seems to be more important…We haven’t focused on the importance of strength in the past.”
“Salt doesn’t figure in at all; salt has been exaggerated as a risk factor,” said Dr. Yusuf. “Diet needs to be rethought,” and conventional thinking challenged, he added, noting that consumption of full-fat dairy, nuts, and a moderate amount of meat all were protective among the PURE cohort.
Looking next at factors contributing to mortality in the global PURE population, low educational level had the highest attributable fraction of mortality of any single risk factor, at about 12%. “This has been ignored,” said Dr. Yusuf. “In most epidemiological studies, it’s been used as a covariate, or a stratifier,” rather than addressing low education itself as a risk factor, he said.
Tobacco use, low grip strength, and poor diet all had attributable fractions of just over 10%, said Dr. Yusuf, again noting that it wasn’t fat or meat consumption that made for the riskiest diet.
Overall, metabolic risk factors accounted for the largest fraction of risk of cardiovascular disease in the PURE population, with behavioral risk factors such as alcohol and tobacco use coming next. This held true across all income categories. However, in higher income nations where environmental factors and household air pollution are lower contributors to cardiovascular disease, metabolic and behavioral risk factors contributed more to cardiovascular disease risk.
Global differences in cardiovascular disease rates, stressed Dr. Yusuf, are not primarily attributable to metabolic risk factors. “The [World Health Organization] has focused on risk factors and has not focused on improved health care. Health care matters, and it matters in a big way.”
Adults aged 35-70 were recruited from 4 high-, 12 middle- and 5 low-income countries for PURE, and followed for a median 9.5 years. Cardiovascular disease and other health events salient to the study were documented both through direct contact and administrative record review, said Dr. Leong, and data about cardiovascular events and vital status were known for well over 90% of study participants.
Slightly less than half of participants were male, and over 108,000 participants were from middle income countries.
The PURE study was supported by the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Ontaario Ministry of Health and Long-Term Care, Astra Zeneca, Boehringer Ingelheim, Sanofi-Aentis, Servier Laboratories, and Glaxo Smith Kline. The study also received additional support in individual participating countries. Dr. Yusuf and Dr. Leon reported that they had no relevant conflicts of interest.
koakes@mdedge.com
PARIS – Though cardiovascular disease still accounts for 40% of deaths around the world, , according to new data from a global prospective study.
“Cancer deaths are becoming more frequent not because the rates of death from cancer are going up, but because we have decreased the deaths from cardiovascular disease,” said the study’s senior author, Salim Yusuf, MD, at the annual congress of the European Society of Cardiology.
A striking pattern emerged when cause of death was stratified by country income level, said fellow investigator Darryl P. Leong, MBBS, in presenting data regarding shifting global mortality patterns. Fully 55% of deaths in high-income nations were caused by cancer, compared with 30% in middle-income countries and 15% in low-income countries. In high-income countries, by contrast, cardiovascular disease (CVD) was the cause of death 23% of the time, while that figure was 42% and 43% for middle- and low-income countries, respectively.
Looking at the data slightly differently, the ratio of cardiovascular deaths to cancer deaths for high-income countries is 0.4; for middle-income countries, the ratio is 1.3, and “One is threefold more likely to die from cardiovascular disease as from cancer” in low-income countries, said Dr. Leong. Although the United States is not included in the PURE study, “recent data shows that some states in the U.S. also have higher cancer mortality than cardiovascular disease. This is a success story,” said Dr. Yusuf, since the shift is largely attributable to decreased mortality from CVD.
Dr. Leong and Dr. Yusuf each presented results from the PURE (Prospective Urban Rural Epidemiology) study, which has enrolled a total of 202,000 individuals from 27 countries on every inhabited continent but Australia. Follow-up data are available for 167,000 individuals in 21 countries. Canada, Russia, China, India, Brazil, and Chile are among the most populous national that are included. Their findings were published simultaneously in the Lancet with the congress presentations (2019 Sep 3; doi: 10.1016/S0140-6736(19)32008-2 and doi: 10.1016/S0140-6736(19)32007-0).
The INTERHEART risk score, an integrated cardiovascular risk score that uses non-laboratory values such as age, smoking status, family history, and comorbidities, was calculated for all participants. “We observed that the highest predicted cardiovascular risk is in high-income countries, and the lowest, in low-income countries,” said Dr. Leong, a cardiologist at McMaster University and the Population Health Research Institute, both in Hamilton, Ont.
Over the study period, 11,307 deaths occurred. Over 9,000 incident cardiovascular events were observed, as were over 5,000 new cancers.
“We have some interesting observations from these data,” said Dr. Leong. “Firstly, there is a gradient in the cardiovascular disease rates, moving from lowest in high-income countries – despite the fact that their INTERHEART risk score was highest – through to highest incident cardiovascular disease in low-income countries, despite their INTERHEART risk score being lowest.” This difference, said Dr. Leong, was driven by higher myocardial infarction rates in low-income countries and higher stroke rates in middle-income countries, when compared to high-income countries.
Once a participant was subject to one of the incident diseases, though, the patterns shifted. For CVD, cancer, chronic obstructive pulmonary disease, pneumonia, and injury, the likelihood of death within 1 year was highest in low-income countries – markedly higher, in the case of CVD. For all conditions, the one-year case-fatality rate after the occurrence of an incident disease was lowest in high-income countries.
“So we are seeing a new transition,” said Dr. Yusuf, the executive director of the Population Health Research Institute and Distinguished University Professor of Medicine, McMaster University, both in Hamilton, Ont. “The old transition was infectious diseases giving way to noncommunicable diseases. Now we are seeing a transition within noncommunicable diseases: In rich countries, cardiovascular disease is going down, perhaps due to better prevention, but I think even more importantly, due to better treatments.
“I want to hasten to add that the difference in risk between high-, middle-, and low-income countries in cardiovascular disease is not due to risk factors,” he went on. “Risk factors, if anything, are lower in the poor countries, compared to the higher-income countries.”
The shift away from cardiovascular disease mortality toward cancer mortality is also occurring in some countries that are in the upper tier of middle-income nations, including Chile, Argentina, Turkey, and Poland, said Dr. Yusuf, who presented data regarding the relative contributions of risk factors to cardiovascular disease and mortality.
Risk factors for cardiovascular disease in the PURE study were expressed by a measure called the population attributable fraction (PAF) that captures both the hazard ratio for a particular risk factor and the prevalence of the risk factor, explained Dr. Yusuf. “Hypertension, by far, was the biggest risk factor of cardiovascular disease globally,” he added, noting that the PAF for hypertension was over 20%. Hypertension far outstripped the next most significant risk factor, high non-HDL cholesterol, which had a PAF of less than 10%.
“This was a big surprise to us: Household pollution was a big factor,” said Dr. Yusuf, who later added that particulate matter from cooking, particularly with solid fuels such as wood or charcoal, was likely the source of much household air pollution, “a big problem in middle- and low-income countries.”
Tobacco usage is decreasing, as is its contribution to cardiovascular deaths, but other commonly cited culprits for cardiovascular disease were not significant contributors to cardiovascular disease in the PURE population.
“Abdominal obesity, and not BMI” contributes to cardiovascular risk. “BMI is not a good indicator of risk,” said Dr. Yusuf in a video interview. These results were presented separately at the congress.
“Grip strength is important; in fact, it is more important than low physical activity. People have focused on physical activity – how much you do. But strength seems to be more important…We haven’t focused on the importance of strength in the past.”
“Salt doesn’t figure in at all; salt has been exaggerated as a risk factor,” said Dr. Yusuf. “Diet needs to be rethought,” and conventional thinking challenged, he added, noting that consumption of full-fat dairy, nuts, and a moderate amount of meat all were protective among the PURE cohort.
Looking next at factors contributing to mortality in the global PURE population, low educational level had the highest attributable fraction of mortality of any single risk factor, at about 12%. “This has been ignored,” said Dr. Yusuf. “In most epidemiological studies, it’s been used as a covariate, or a stratifier,” rather than addressing low education itself as a risk factor, he said.
Tobacco use, low grip strength, and poor diet all had attributable fractions of just over 10%, said Dr. Yusuf, again noting that it wasn’t fat or meat consumption that made for the riskiest diet.
Overall, metabolic risk factors accounted for the largest fraction of risk of cardiovascular disease in the PURE population, with behavioral risk factors such as alcohol and tobacco use coming next. This held true across all income categories. However, in higher income nations where environmental factors and household air pollution are lower contributors to cardiovascular disease, metabolic and behavioral risk factors contributed more to cardiovascular disease risk.
Global differences in cardiovascular disease rates, stressed Dr. Yusuf, are not primarily attributable to metabolic risk factors. “The [World Health Organization] has focused on risk factors and has not focused on improved health care. Health care matters, and it matters in a big way.”
Adults aged 35-70 were recruited from 4 high-, 12 middle- and 5 low-income countries for PURE, and followed for a median 9.5 years. Cardiovascular disease and other health events salient to the study were documented both through direct contact and administrative record review, said Dr. Leong, and data about cardiovascular events and vital status were known for well over 90% of study participants.
Slightly less than half of participants were male, and over 108,000 participants were from middle income countries.
The PURE study was supported by the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Ontaario Ministry of Health and Long-Term Care, Astra Zeneca, Boehringer Ingelheim, Sanofi-Aentis, Servier Laboratories, and Glaxo Smith Kline. The study also received additional support in individual participating countries. Dr. Yusuf and Dr. Leon reported that they had no relevant conflicts of interest.
koakes@mdedge.com
PARIS – Though cardiovascular disease still accounts for 40% of deaths around the world, , according to new data from a global prospective study.
“Cancer deaths are becoming more frequent not because the rates of death from cancer are going up, but because we have decreased the deaths from cardiovascular disease,” said the study’s senior author, Salim Yusuf, MD, at the annual congress of the European Society of Cardiology.
A striking pattern emerged when cause of death was stratified by country income level, said fellow investigator Darryl P. Leong, MBBS, in presenting data regarding shifting global mortality patterns. Fully 55% of deaths in high-income nations were caused by cancer, compared with 30% in middle-income countries and 15% in low-income countries. In high-income countries, by contrast, cardiovascular disease (CVD) was the cause of death 23% of the time, while that figure was 42% and 43% for middle- and low-income countries, respectively.
Looking at the data slightly differently, the ratio of cardiovascular deaths to cancer deaths for high-income countries is 0.4; for middle-income countries, the ratio is 1.3, and “One is threefold more likely to die from cardiovascular disease as from cancer” in low-income countries, said Dr. Leong. Although the United States is not included in the PURE study, “recent data shows that some states in the U.S. also have higher cancer mortality than cardiovascular disease. This is a success story,” said Dr. Yusuf, since the shift is largely attributable to decreased mortality from CVD.
Dr. Leong and Dr. Yusuf each presented results from the PURE (Prospective Urban Rural Epidemiology) study, which has enrolled a total of 202,000 individuals from 27 countries on every inhabited continent but Australia. Follow-up data are available for 167,000 individuals in 21 countries. Canada, Russia, China, India, Brazil, and Chile are among the most populous national that are included. Their findings were published simultaneously in the Lancet with the congress presentations (2019 Sep 3; doi: 10.1016/S0140-6736(19)32008-2 and doi: 10.1016/S0140-6736(19)32007-0).
The INTERHEART risk score, an integrated cardiovascular risk score that uses non-laboratory values such as age, smoking status, family history, and comorbidities, was calculated for all participants. “We observed that the highest predicted cardiovascular risk is in high-income countries, and the lowest, in low-income countries,” said Dr. Leong, a cardiologist at McMaster University and the Population Health Research Institute, both in Hamilton, Ont.
Over the study period, 11,307 deaths occurred. Over 9,000 incident cardiovascular events were observed, as were over 5,000 new cancers.
“We have some interesting observations from these data,” said Dr. Leong. “Firstly, there is a gradient in the cardiovascular disease rates, moving from lowest in high-income countries – despite the fact that their INTERHEART risk score was highest – through to highest incident cardiovascular disease in low-income countries, despite their INTERHEART risk score being lowest.” This difference, said Dr. Leong, was driven by higher myocardial infarction rates in low-income countries and higher stroke rates in middle-income countries, when compared to high-income countries.
Once a participant was subject to one of the incident diseases, though, the patterns shifted. For CVD, cancer, chronic obstructive pulmonary disease, pneumonia, and injury, the likelihood of death within 1 year was highest in low-income countries – markedly higher, in the case of CVD. For all conditions, the one-year case-fatality rate after the occurrence of an incident disease was lowest in high-income countries.
“So we are seeing a new transition,” said Dr. Yusuf, the executive director of the Population Health Research Institute and Distinguished University Professor of Medicine, McMaster University, both in Hamilton, Ont. “The old transition was infectious diseases giving way to noncommunicable diseases. Now we are seeing a transition within noncommunicable diseases: In rich countries, cardiovascular disease is going down, perhaps due to better prevention, but I think even more importantly, due to better treatments.
“I want to hasten to add that the difference in risk between high-, middle-, and low-income countries in cardiovascular disease is not due to risk factors,” he went on. “Risk factors, if anything, are lower in the poor countries, compared to the higher-income countries.”
The shift away from cardiovascular disease mortality toward cancer mortality is also occurring in some countries that are in the upper tier of middle-income nations, including Chile, Argentina, Turkey, and Poland, said Dr. Yusuf, who presented data regarding the relative contributions of risk factors to cardiovascular disease and mortality.
Risk factors for cardiovascular disease in the PURE study were expressed by a measure called the population attributable fraction (PAF) that captures both the hazard ratio for a particular risk factor and the prevalence of the risk factor, explained Dr. Yusuf. “Hypertension, by far, was the biggest risk factor of cardiovascular disease globally,” he added, noting that the PAF for hypertension was over 20%. Hypertension far outstripped the next most significant risk factor, high non-HDL cholesterol, which had a PAF of less than 10%.
“This was a big surprise to us: Household pollution was a big factor,” said Dr. Yusuf, who later added that particulate matter from cooking, particularly with solid fuels such as wood or charcoal, was likely the source of much household air pollution, “a big problem in middle- and low-income countries.”
Tobacco usage is decreasing, as is its contribution to cardiovascular deaths, but other commonly cited culprits for cardiovascular disease were not significant contributors to cardiovascular disease in the PURE population.
“Abdominal obesity, and not BMI” contributes to cardiovascular risk. “BMI is not a good indicator of risk,” said Dr. Yusuf in a video interview. These results were presented separately at the congress.
“Grip strength is important; in fact, it is more important than low physical activity. People have focused on physical activity – how much you do. But strength seems to be more important…We haven’t focused on the importance of strength in the past.”
“Salt doesn’t figure in at all; salt has been exaggerated as a risk factor,” said Dr. Yusuf. “Diet needs to be rethought,” and conventional thinking challenged, he added, noting that consumption of full-fat dairy, nuts, and a moderate amount of meat all were protective among the PURE cohort.
Looking next at factors contributing to mortality in the global PURE population, low educational level had the highest attributable fraction of mortality of any single risk factor, at about 12%. “This has been ignored,” said Dr. Yusuf. “In most epidemiological studies, it’s been used as a covariate, or a stratifier,” rather than addressing low education itself as a risk factor, he said.
Tobacco use, low grip strength, and poor diet all had attributable fractions of just over 10%, said Dr. Yusuf, again noting that it wasn’t fat or meat consumption that made for the riskiest diet.
Overall, metabolic risk factors accounted for the largest fraction of risk of cardiovascular disease in the PURE population, with behavioral risk factors such as alcohol and tobacco use coming next. This held true across all income categories. However, in higher income nations where environmental factors and household air pollution are lower contributors to cardiovascular disease, metabolic and behavioral risk factors contributed more to cardiovascular disease risk.
Global differences in cardiovascular disease rates, stressed Dr. Yusuf, are not primarily attributable to metabolic risk factors. “The [World Health Organization] has focused on risk factors and has not focused on improved health care. Health care matters, and it matters in a big way.”
Adults aged 35-70 were recruited from 4 high-, 12 middle- and 5 low-income countries for PURE, and followed for a median 9.5 years. Cardiovascular disease and other health events salient to the study were documented both through direct contact and administrative record review, said Dr. Leong, and data about cardiovascular events and vital status were known for well over 90% of study participants.
Slightly less than half of participants were male, and over 108,000 participants were from middle income countries.
The PURE study was supported by the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Ontaario Ministry of Health and Long-Term Care, Astra Zeneca, Boehringer Ingelheim, Sanofi-Aentis, Servier Laboratories, and Glaxo Smith Kline. The study also received additional support in individual participating countries. Dr. Yusuf and Dr. Leon reported that they had no relevant conflicts of interest.
koakes@mdedge.com
REPORTING FROM ESC CONGRESS 2019
New borderline personality disorder intervention less intensive, works for most
SAN DIEGO – A relatively new treatment approach called good psychiatric management (GPM) is available for patients with borderline personality disorder.
It’s a solid option for “environments where people may not have many resources and might not be able to deliver treatments that are more resource intensive, like dialectical behavioral therapy,” the standard intervention, said James Jenkins, MD, a psychiatrist affiliated with Massachusetts General Hospital, Boston, in a video interview at the annual Psych Congress.
“GPM is a treatment, not a psychotherapy, that’s maybe a little bit more easily adaptable to a variety of different contexts and situations,” he said.
It’s an atheoretical, pragmatic approach that focuses on helping people establish a life outside of therapy. Clinicians actively engage with patients, encouraging them to start working and building successful relationships with other people. The model emphasizes the value of educating people about the condition and giving them hope. Typically, patients participate in GPM once each week (Curr Opin Psychol. 2018 Jun;21:127-31).
For most people, it works just as well as dialectical behavioral therapy, and when it doesn’t, patients can transition to that or another more intensive approach. Training is less intensive and sometimes free. GPM is offered at McLean Hospital in Boston, where the intervention originated. McLean also is Dr. Jenkins’s former institution.
Dr. Jenkins reported that he had no disclosures.
SAN DIEGO – A relatively new treatment approach called good psychiatric management (GPM) is available for patients with borderline personality disorder.
It’s a solid option for “environments where people may not have many resources and might not be able to deliver treatments that are more resource intensive, like dialectical behavioral therapy,” the standard intervention, said James Jenkins, MD, a psychiatrist affiliated with Massachusetts General Hospital, Boston, in a video interview at the annual Psych Congress.
“GPM is a treatment, not a psychotherapy, that’s maybe a little bit more easily adaptable to a variety of different contexts and situations,” he said.
It’s an atheoretical, pragmatic approach that focuses on helping people establish a life outside of therapy. Clinicians actively engage with patients, encouraging them to start working and building successful relationships with other people. The model emphasizes the value of educating people about the condition and giving them hope. Typically, patients participate in GPM once each week (Curr Opin Psychol. 2018 Jun;21:127-31).
For most people, it works just as well as dialectical behavioral therapy, and when it doesn’t, patients can transition to that or another more intensive approach. Training is less intensive and sometimes free. GPM is offered at McLean Hospital in Boston, where the intervention originated. McLean also is Dr. Jenkins’s former institution.
Dr. Jenkins reported that he had no disclosures.
SAN DIEGO – A relatively new treatment approach called good psychiatric management (GPM) is available for patients with borderline personality disorder.
It’s a solid option for “environments where people may not have many resources and might not be able to deliver treatments that are more resource intensive, like dialectical behavioral therapy,” the standard intervention, said James Jenkins, MD, a psychiatrist affiliated with Massachusetts General Hospital, Boston, in a video interview at the annual Psych Congress.
“GPM is a treatment, not a psychotherapy, that’s maybe a little bit more easily adaptable to a variety of different contexts and situations,” he said.
It’s an atheoretical, pragmatic approach that focuses on helping people establish a life outside of therapy. Clinicians actively engage with patients, encouraging them to start working and building successful relationships with other people. The model emphasizes the value of educating people about the condition and giving them hope. Typically, patients participate in GPM once each week (Curr Opin Psychol. 2018 Jun;21:127-31).
For most people, it works just as well as dialectical behavioral therapy, and when it doesn’t, patients can transition to that or another more intensive approach. Training is less intensive and sometimes free. GPM is offered at McLean Hospital in Boston, where the intervention originated. McLean also is Dr. Jenkins’s former institution.
Dr. Jenkins reported that he had no disclosures.
REPORTING FROM PSYCH CONGRESS 2019
Oral beta-lactams provide noninferior postdischarge pyelonephritis treatment
WASHINGTON – Patients hospitalized for pyelonephritis and discharged after receiving intravenous antibiotic treatment who then received step-down treatment with an oral beta-lactam had 30-day outcomes that were noninferior to patients who received an oral fluoroquinolone or trimethoprim-sulfamethoxazole as their discharge regimen, in a retrospective study of 211 patients managed at either of two U.S. hospitals.
This was the largest comparison reported on oral beta-lactam drugs for postdischarge treatment of pyelonephritis relative to the standard oral agents, fluoroquinolones and trimethoprim-sulfamethoxazole (Bactrim), Athena Hobbs, PharmD, said at an annual scientific meeting on infectious diseases. The superiority of an oral fluoroquinolone or trimethoprim-sulfamethoxazole and inferiority of oral beta-lactam drugs were cited in 2010 guidelines for managing pyelonephritis from the Infectious Diseases Society of America (Clin Infect Dis. 2011 March 1;52 [5]: e103-20).
Although limited as a nonrandomized, retrospective comparison, the finding of at least similar efficacy by beta-lactam agents “opens new treatment options” that avoid issues with drug resistance and adverse effects from treatment with fluoroquinolones or trimethoprim-sulfamethoxazole, Dr. Hobbs said in a video interview. Beta-lactams have already been embraced for this indication by some hospitalists, demonstrated by their use of beta-lactam antibiotics for 122 (58%) of the 211 patients included in the study. Among the 89 patients discharged on a non–beta-lactam, 69 (78%) had fluoroquinolone treatment and the remaining 20 patients went home taking trimethoprim-sulfamethoxazole. The new finding “confirms that we are not doing harm to patients,” with this existing practice of mostly prescribing an oral beta-lactam drug, noted Dr. Hobbs, an infectious diseases pharmacy specialist at Baptist Memorial Hospital in Memphis.
The study included patients aged 18-89 years hospitalized during 2014-2017 for a primary diagnosis of pyelonephritis at Baptist or at a second Hospital in Austin, Tex. The study excluded patients in intensive care, with a urologic abnormality, pregnant women, and patients treated with an intravenous antibiotic other than a beta-lactam for more than 24 hours. The most commonly used intravenous drugs were cefazolin and ceftriaxone. The enrolled patients averaged just over 40 years old, and more than 90% were women.
The study’s primary outcome was the 30-day rate of either hospital readmission or an ED visit for pyelonephritis or a urinary tract infection. This occurred in 4.9% of the patients discharged on an oral course of a beta-lactam drug, and in 5.6% of those discharged on either a fluoroquinolone or trimethoprim-sulfamethoxazole, a difference that was not statistically significant and that met the prespecified criteria for noninferiority, Dr. Hobbs reported. The most commonly prescribed oral beta-lactam was cefuroxime in about half the patients, followed by cephalexin or cefadroxil in about a quarter of patients, and amoxicillin with clavulanate in 19%. The two arms of the study also showed no significant difference in infection recurrences during 90-day follow-up.
The study received no commercial funding. Dr. Hobbs had no relevant disclosures.
WASHINGTON – Patients hospitalized for pyelonephritis and discharged after receiving intravenous antibiotic treatment who then received step-down treatment with an oral beta-lactam had 30-day outcomes that were noninferior to patients who received an oral fluoroquinolone or trimethoprim-sulfamethoxazole as their discharge regimen, in a retrospective study of 211 patients managed at either of two U.S. hospitals.
This was the largest comparison reported on oral beta-lactam drugs for postdischarge treatment of pyelonephritis relative to the standard oral agents, fluoroquinolones and trimethoprim-sulfamethoxazole (Bactrim), Athena Hobbs, PharmD, said at an annual scientific meeting on infectious diseases. The superiority of an oral fluoroquinolone or trimethoprim-sulfamethoxazole and inferiority of oral beta-lactam drugs were cited in 2010 guidelines for managing pyelonephritis from the Infectious Diseases Society of America (Clin Infect Dis. 2011 March 1;52 [5]: e103-20).
Although limited as a nonrandomized, retrospective comparison, the finding of at least similar efficacy by beta-lactam agents “opens new treatment options” that avoid issues with drug resistance and adverse effects from treatment with fluoroquinolones or trimethoprim-sulfamethoxazole, Dr. Hobbs said in a video interview. Beta-lactams have already been embraced for this indication by some hospitalists, demonstrated by their use of beta-lactam antibiotics for 122 (58%) of the 211 patients included in the study. Among the 89 patients discharged on a non–beta-lactam, 69 (78%) had fluoroquinolone treatment and the remaining 20 patients went home taking trimethoprim-sulfamethoxazole. The new finding “confirms that we are not doing harm to patients,” with this existing practice of mostly prescribing an oral beta-lactam drug, noted Dr. Hobbs, an infectious diseases pharmacy specialist at Baptist Memorial Hospital in Memphis.
The study included patients aged 18-89 years hospitalized during 2014-2017 for a primary diagnosis of pyelonephritis at Baptist or at a second Hospital in Austin, Tex. The study excluded patients in intensive care, with a urologic abnormality, pregnant women, and patients treated with an intravenous antibiotic other than a beta-lactam for more than 24 hours. The most commonly used intravenous drugs were cefazolin and ceftriaxone. The enrolled patients averaged just over 40 years old, and more than 90% were women.
The study’s primary outcome was the 30-day rate of either hospital readmission or an ED visit for pyelonephritis or a urinary tract infection. This occurred in 4.9% of the patients discharged on an oral course of a beta-lactam drug, and in 5.6% of those discharged on either a fluoroquinolone or trimethoprim-sulfamethoxazole, a difference that was not statistically significant and that met the prespecified criteria for noninferiority, Dr. Hobbs reported. The most commonly prescribed oral beta-lactam was cefuroxime in about half the patients, followed by cephalexin or cefadroxil in about a quarter of patients, and amoxicillin with clavulanate in 19%. The two arms of the study also showed no significant difference in infection recurrences during 90-day follow-up.
The study received no commercial funding. Dr. Hobbs had no relevant disclosures.
WASHINGTON – Patients hospitalized for pyelonephritis and discharged after receiving intravenous antibiotic treatment who then received step-down treatment with an oral beta-lactam had 30-day outcomes that were noninferior to patients who received an oral fluoroquinolone or trimethoprim-sulfamethoxazole as their discharge regimen, in a retrospective study of 211 patients managed at either of two U.S. hospitals.
This was the largest comparison reported on oral beta-lactam drugs for postdischarge treatment of pyelonephritis relative to the standard oral agents, fluoroquinolones and trimethoprim-sulfamethoxazole (Bactrim), Athena Hobbs, PharmD, said at an annual scientific meeting on infectious diseases. The superiority of an oral fluoroquinolone or trimethoprim-sulfamethoxazole and inferiority of oral beta-lactam drugs were cited in 2010 guidelines for managing pyelonephritis from the Infectious Diseases Society of America (Clin Infect Dis. 2011 March 1;52 [5]: e103-20).
Although limited as a nonrandomized, retrospective comparison, the finding of at least similar efficacy by beta-lactam agents “opens new treatment options” that avoid issues with drug resistance and adverse effects from treatment with fluoroquinolones or trimethoprim-sulfamethoxazole, Dr. Hobbs said in a video interview. Beta-lactams have already been embraced for this indication by some hospitalists, demonstrated by their use of beta-lactam antibiotics for 122 (58%) of the 211 patients included in the study. Among the 89 patients discharged on a non–beta-lactam, 69 (78%) had fluoroquinolone treatment and the remaining 20 patients went home taking trimethoprim-sulfamethoxazole. The new finding “confirms that we are not doing harm to patients,” with this existing practice of mostly prescribing an oral beta-lactam drug, noted Dr. Hobbs, an infectious diseases pharmacy specialist at Baptist Memorial Hospital in Memphis.
The study included patients aged 18-89 years hospitalized during 2014-2017 for a primary diagnosis of pyelonephritis at Baptist or at a second Hospital in Austin, Tex. The study excluded patients in intensive care, with a urologic abnormality, pregnant women, and patients treated with an intravenous antibiotic other than a beta-lactam for more than 24 hours. The most commonly used intravenous drugs were cefazolin and ceftriaxone. The enrolled patients averaged just over 40 years old, and more than 90% were women.
The study’s primary outcome was the 30-day rate of either hospital readmission or an ED visit for pyelonephritis or a urinary tract infection. This occurred in 4.9% of the patients discharged on an oral course of a beta-lactam drug, and in 5.6% of those discharged on either a fluoroquinolone or trimethoprim-sulfamethoxazole, a difference that was not statistically significant and that met the prespecified criteria for noninferiority, Dr. Hobbs reported. The most commonly prescribed oral beta-lactam was cefuroxime in about half the patients, followed by cephalexin or cefadroxil in about a quarter of patients, and amoxicillin with clavulanate in 19%. The two arms of the study also showed no significant difference in infection recurrences during 90-day follow-up.
The study received no commercial funding. Dr. Hobbs had no relevant disclosures.
REPORTING FROM IDWEEK 2019