User login
DACA lands before Supreme Court
Whether the Trump administration can rescind a safe-haven program for the children of first-generation immigrants will soon be decided by the U.S. Supreme Court.
Justices on Nov. 12, 2019, heard oral arguments in the case of Regents of the University of California v. Department of Homeland Security, which centers on the legality of the Deferred Action for Childhood Arrivals (DACA) policy.
The DACA case before the court, which consolidates three legal challenges, revolves around two primary legal arguments, said Austin, Tex., attorney Faye Kolly, who coauthored a brief in support of DACA. The plaintiffs argue that the decision to rescind the DACA program was arbitrary and capricious under the Administrative Procedure Act (APA) because there was no justification to end the policy. The DHS’s rescission memorandum did not acknowledge, nor weigh, the profound interests and devastating consequences that would be caused by the rescission to hundreds of thousands of DACA recipients and countless stakeholders who rely on the program, attorneys for the University of California wrote in its brief to the Supreme Court.
The DHS contends the DACA policy itself is unlawful because the Obama administration lacked the statutory authority to launch such a program. The government’s decision to revoke the program was based on the legal and practical implications of maintaining DACA in light of concerns about its legality and ongoing litigation challenging similar programs, attorneys for the DHS wrote in a brief to the Supreme Court.
With a conservative majority on the court, analysts say the Trump administration may have an upper hand in the case. However, Ms. Kolly noted that Chief Justice John G. Roberts Jr. is the wild card to watch.
Although Chief Justice Roberts tends to lean more conservatively, he recently sided with the court’s liberal justices last term in a case involving citizenship, said Ms. Kolly. In that case, Department of Commerce v. New York, Chief Justice Roberts voted to block the Department of Commerce from reinstating a citizenship question on the 2020 Census. In the majority ruling, Justice Roberts wrote that the department’s reasons for reinstating the citizenship question were “incongruent with what the record reveals about the agency’s priorities and decision making.”
Considering that the government’s rationale to end DACA is a key piece to the DACA dispute, it’s possible that Chief Justice Roberts could apply a similar line of reasoning to the case, Ms. Kolly said.
“I think the court will look very closely [at whether] the arbitrary and capricious standard has been violated by the government,” she said in an interview. “I do think they will split along [ideological] lines, but the surprise vote may be Roberts.”
A number of physician and health care organizations have weighed in on the DACA case, including the American Medical Association, the Association of American Medical Colleges, and the American College of Obstetricians and Gynecologists. In a joint brief to the Supreme Court, the organizations wrote that an estimated 27,000 health care workers and support staff depend on DACA for their authorization to work in the United States, including nearly 200 medical students, residents, and physicians. If these physicians and trainees retain their work eligibility, each will care for an average of 1,533-4,600 patients a year, according to the brief.
“Together, over the course of their careers, they will touch the lives of 1.7 [million] to 5.1 million U.S. patients,” the groups wrote. “If DACA is rescinded, however, almost none of these people will be able to serve the American public in their chosen fields. This action would therefore nullify the substantial and long-term investments that DACA recipients, educational institutions, and the public have made in educating and training those recipients to provide needed health care services to the nation.”
More than 25 other individuals and organizations have also submitted briefs – either in support or in opposition – regarding the case. In their brief, attorneys for the Immigration Law Reform Institute, wrote that the DACA policy is void because it was issued in violation of APA notice-and-comment requirements “by virtue of its creating rights and cabining discretion in a sufficiently binding manner to exceed its mere enforcement-discretion justification.”
“DACA also violates the [Immigration and Naturalization Act] on both substantive and procedural grounds, and either sort of violation renders DACA a nullity,” the brief states.
In a Nov. 12 tweet, President Trump indicated that, if the Supreme Court strikes down DACA, he will consider working with Democrats on a legislative remedy that would protect current DACA recipients from deportation.
“Many of the people in DACA, no longer very young, are far from ‘angels,’ ” President Trump tweeted. “Some are very tough, hardened criminals, President Obama said he had no legal right to sign order, but would anyway. If Supreme Court remedies with overturn, a deal will be made with Dems for them to stay!”
Whether the Trump administration can rescind a safe-haven program for the children of first-generation immigrants will soon be decided by the U.S. Supreme Court.
Justices on Nov. 12, 2019, heard oral arguments in the case of Regents of the University of California v. Department of Homeland Security, which centers on the legality of the Deferred Action for Childhood Arrivals (DACA) policy.
The DACA case before the court, which consolidates three legal challenges, revolves around two primary legal arguments, said Austin, Tex., attorney Faye Kolly, who coauthored a brief in support of DACA. The plaintiffs argue that the decision to rescind the DACA program was arbitrary and capricious under the Administrative Procedure Act (APA) because there was no justification to end the policy. The DHS’s rescission memorandum did not acknowledge, nor weigh, the profound interests and devastating consequences that would be caused by the rescission to hundreds of thousands of DACA recipients and countless stakeholders who rely on the program, attorneys for the University of California wrote in its brief to the Supreme Court.
The DHS contends the DACA policy itself is unlawful because the Obama administration lacked the statutory authority to launch such a program. The government’s decision to revoke the program was based on the legal and practical implications of maintaining DACA in light of concerns about its legality and ongoing litigation challenging similar programs, attorneys for the DHS wrote in a brief to the Supreme Court.
With a conservative majority on the court, analysts say the Trump administration may have an upper hand in the case. However, Ms. Kolly noted that Chief Justice John G. Roberts Jr. is the wild card to watch.
Although Chief Justice Roberts tends to lean more conservatively, he recently sided with the court’s liberal justices last term in a case involving citizenship, said Ms. Kolly. In that case, Department of Commerce v. New York, Chief Justice Roberts voted to block the Department of Commerce from reinstating a citizenship question on the 2020 Census. In the majority ruling, Justice Roberts wrote that the department’s reasons for reinstating the citizenship question were “incongruent with what the record reveals about the agency’s priorities and decision making.”
Considering that the government’s rationale to end DACA is a key piece to the DACA dispute, it’s possible that Chief Justice Roberts could apply a similar line of reasoning to the case, Ms. Kolly said.
“I think the court will look very closely [at whether] the arbitrary and capricious standard has been violated by the government,” she said in an interview. “I do think they will split along [ideological] lines, but the surprise vote may be Roberts.”
A number of physician and health care organizations have weighed in on the DACA case, including the American Medical Association, the Association of American Medical Colleges, and the American College of Obstetricians and Gynecologists. In a joint brief to the Supreme Court, the organizations wrote that an estimated 27,000 health care workers and support staff depend on DACA for their authorization to work in the United States, including nearly 200 medical students, residents, and physicians. If these physicians and trainees retain their work eligibility, each will care for an average of 1,533-4,600 patients a year, according to the brief.
“Together, over the course of their careers, they will touch the lives of 1.7 [million] to 5.1 million U.S. patients,” the groups wrote. “If DACA is rescinded, however, almost none of these people will be able to serve the American public in their chosen fields. This action would therefore nullify the substantial and long-term investments that DACA recipients, educational institutions, and the public have made in educating and training those recipients to provide needed health care services to the nation.”
More than 25 other individuals and organizations have also submitted briefs – either in support or in opposition – regarding the case. In their brief, attorneys for the Immigration Law Reform Institute, wrote that the DACA policy is void because it was issued in violation of APA notice-and-comment requirements “by virtue of its creating rights and cabining discretion in a sufficiently binding manner to exceed its mere enforcement-discretion justification.”
“DACA also violates the [Immigration and Naturalization Act] on both substantive and procedural grounds, and either sort of violation renders DACA a nullity,” the brief states.
In a Nov. 12 tweet, President Trump indicated that, if the Supreme Court strikes down DACA, he will consider working with Democrats on a legislative remedy that would protect current DACA recipients from deportation.
“Many of the people in DACA, no longer very young, are far from ‘angels,’ ” President Trump tweeted. “Some are very tough, hardened criminals, President Obama said he had no legal right to sign order, but would anyway. If Supreme Court remedies with overturn, a deal will be made with Dems for them to stay!”
Whether the Trump administration can rescind a safe-haven program for the children of first-generation immigrants will soon be decided by the U.S. Supreme Court.
Justices on Nov. 12, 2019, heard oral arguments in the case of Regents of the University of California v. Department of Homeland Security, which centers on the legality of the Deferred Action for Childhood Arrivals (DACA) policy.
The DACA case before the court, which consolidates three legal challenges, revolves around two primary legal arguments, said Austin, Tex., attorney Faye Kolly, who coauthored a brief in support of DACA. The plaintiffs argue that the decision to rescind the DACA program was arbitrary and capricious under the Administrative Procedure Act (APA) because there was no justification to end the policy. The DHS’s rescission memorandum did not acknowledge, nor weigh, the profound interests and devastating consequences that would be caused by the rescission to hundreds of thousands of DACA recipients and countless stakeholders who rely on the program, attorneys for the University of California wrote in its brief to the Supreme Court.
The DHS contends the DACA policy itself is unlawful because the Obama administration lacked the statutory authority to launch such a program. The government’s decision to revoke the program was based on the legal and practical implications of maintaining DACA in light of concerns about its legality and ongoing litigation challenging similar programs, attorneys for the DHS wrote in a brief to the Supreme Court.
With a conservative majority on the court, analysts say the Trump administration may have an upper hand in the case. However, Ms. Kolly noted that Chief Justice John G. Roberts Jr. is the wild card to watch.
Although Chief Justice Roberts tends to lean more conservatively, he recently sided with the court’s liberal justices last term in a case involving citizenship, said Ms. Kolly. In that case, Department of Commerce v. New York, Chief Justice Roberts voted to block the Department of Commerce from reinstating a citizenship question on the 2020 Census. In the majority ruling, Justice Roberts wrote that the department’s reasons for reinstating the citizenship question were “incongruent with what the record reveals about the agency’s priorities and decision making.”
Considering that the government’s rationale to end DACA is a key piece to the DACA dispute, it’s possible that Chief Justice Roberts could apply a similar line of reasoning to the case, Ms. Kolly said.
“I think the court will look very closely [at whether] the arbitrary and capricious standard has been violated by the government,” she said in an interview. “I do think they will split along [ideological] lines, but the surprise vote may be Roberts.”
A number of physician and health care organizations have weighed in on the DACA case, including the American Medical Association, the Association of American Medical Colleges, and the American College of Obstetricians and Gynecologists. In a joint brief to the Supreme Court, the organizations wrote that an estimated 27,000 health care workers and support staff depend on DACA for their authorization to work in the United States, including nearly 200 medical students, residents, and physicians. If these physicians and trainees retain their work eligibility, each will care for an average of 1,533-4,600 patients a year, according to the brief.
“Together, over the course of their careers, they will touch the lives of 1.7 [million] to 5.1 million U.S. patients,” the groups wrote. “If DACA is rescinded, however, almost none of these people will be able to serve the American public in their chosen fields. This action would therefore nullify the substantial and long-term investments that DACA recipients, educational institutions, and the public have made in educating and training those recipients to provide needed health care services to the nation.”
More than 25 other individuals and organizations have also submitted briefs – either in support or in opposition – regarding the case. In their brief, attorneys for the Immigration Law Reform Institute, wrote that the DACA policy is void because it was issued in violation of APA notice-and-comment requirements “by virtue of its creating rights and cabining discretion in a sufficiently binding manner to exceed its mere enforcement-discretion justification.”
“DACA also violates the [Immigration and Naturalization Act] on both substantive and procedural grounds, and either sort of violation renders DACA a nullity,” the brief states.
In a Nov. 12 tweet, President Trump indicated that, if the Supreme Court strikes down DACA, he will consider working with Democrats on a legislative remedy that would protect current DACA recipients from deportation.
“Many of the people in DACA, no longer very young, are far from ‘angels,’ ” President Trump tweeted. “Some are very tough, hardened criminals, President Obama said he had no legal right to sign order, but would anyway. If Supreme Court remedies with overturn, a deal will be made with Dems for them to stay!”
Long-term care insurance
A few years ago, my seemingly indestructible 94-year-old mother suffered a series of medical setbacks. As her health problems accumulated, so did the complexity and cost of her care, progressing from her home to an assisted-living facility to a nursing home. It was heartbreaking – and expensive. My wife likened it to “putting another kid through college” – an elite private college, at that.
Medicare, of course, did not cover any of this, except for physician visits and some of her medications. When it was finally over, my wife and I resolved that, should we face a similar situation in our final years, we could not put ourselves or our children through a similar financial ordeal.
, in-home services, and other end-of-life expenses. (Covered services vary by policy; and as always, I have no financial interest in any product or service mentioned here.)
According to the American Association for Long-Term Care Insurance (AALTCI), the average annual LTCI premium for a 60-year-old couple is $3,490. Not cheap; but there are ways to lower premiums without gutting your coverage.
The best way to keep costs down is to get in early. In general, the younger you are and the better health you are in, the lower your premiums will be. For example – again according to the AALTCI – that “average” annual premium of $3,490 for a hypothetical 60-year-old couple would increase 34%, to $4,675, if they waited until they were 65 to buy the policy. And if their health were to decline in the interim, they might not be able to obtain adequate coverage at all.
You can also lower premiums by decreasing daily benefits, or increasing the “elimination period” – the length of time after you become eligible for benefits that the policy starts paying them; 30-, 60-, and 90-day periods are common. As long as you have sufficient savings to realistically cover costs until the elimination period is over, choosing a longer one can reduce your costs significantly.
Another variable is the maximum length of time the policy will pay out benefits. Ideally, you would want a payout to continue for as long as necessary, but few if any companies are willing to write uncapped policies anymore. Two to five years of benefits is a common time frame. (The “average” premiums quoted above assume a benefit of $150 per day with a 3-year cap and a 90-day elimination period.)
As with any insurance, it is important not to overbuy LTCI. It isn’t necessary to obtain coverage that will pay for 100% of your long-term care costs – just the portion that your projected retirement income (Social Security, pensions, income from savings) may not be sufficient to cover. Buying only the amount of coverage you need will substantially reduce your premium costs over the life of the policy.
If you work for a hospital or a large group, it’s worth checking to see if your employer offers LTCI. Employer-sponsored plans are often offered at discounted group rates, and you can usually keep the policy even if you leave. If you’re a member of any social or religious groups, check their insurance plans as well.
To be sure, there is considerable debate about whether LTCI is worth the cost. Premiums for new policies are rising at a steep clip – 9% annually, according to the AALTCI – and insurers are allowed to raise premiums even after you buy the policy, so you’ll need to factor that possibility into your budget.
But forgoing coverage can be costly too: If you know you will have to cover your own long-term care costs, you won’t be able to spend that money on things you really care about – like your grandkids, or travel, or charitable work. You might even forgo necessary medical care for fear of running out of money.
Everyone must make their own decision. My wife and I decided that a few thousand dollars per year is a fair price to pay for the peace of mind of knowing we will be able to afford proper supportive care, without help from our children or anyone else, regardless of what happens in the years to come.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
A few years ago, my seemingly indestructible 94-year-old mother suffered a series of medical setbacks. As her health problems accumulated, so did the complexity and cost of her care, progressing from her home to an assisted-living facility to a nursing home. It was heartbreaking – and expensive. My wife likened it to “putting another kid through college” – an elite private college, at that.
Medicare, of course, did not cover any of this, except for physician visits and some of her medications. When it was finally over, my wife and I resolved that, should we face a similar situation in our final years, we could not put ourselves or our children through a similar financial ordeal.
, in-home services, and other end-of-life expenses. (Covered services vary by policy; and as always, I have no financial interest in any product or service mentioned here.)
According to the American Association for Long-Term Care Insurance (AALTCI), the average annual LTCI premium for a 60-year-old couple is $3,490. Not cheap; but there are ways to lower premiums without gutting your coverage.
The best way to keep costs down is to get in early. In general, the younger you are and the better health you are in, the lower your premiums will be. For example – again according to the AALTCI – that “average” annual premium of $3,490 for a hypothetical 60-year-old couple would increase 34%, to $4,675, if they waited until they were 65 to buy the policy. And if their health were to decline in the interim, they might not be able to obtain adequate coverage at all.
You can also lower premiums by decreasing daily benefits, or increasing the “elimination period” – the length of time after you become eligible for benefits that the policy starts paying them; 30-, 60-, and 90-day periods are common. As long as you have sufficient savings to realistically cover costs until the elimination period is over, choosing a longer one can reduce your costs significantly.
Another variable is the maximum length of time the policy will pay out benefits. Ideally, you would want a payout to continue for as long as necessary, but few if any companies are willing to write uncapped policies anymore. Two to five years of benefits is a common time frame. (The “average” premiums quoted above assume a benefit of $150 per day with a 3-year cap and a 90-day elimination period.)
As with any insurance, it is important not to overbuy LTCI. It isn’t necessary to obtain coverage that will pay for 100% of your long-term care costs – just the portion that your projected retirement income (Social Security, pensions, income from savings) may not be sufficient to cover. Buying only the amount of coverage you need will substantially reduce your premium costs over the life of the policy.
If you work for a hospital or a large group, it’s worth checking to see if your employer offers LTCI. Employer-sponsored plans are often offered at discounted group rates, and you can usually keep the policy even if you leave. If you’re a member of any social or religious groups, check their insurance plans as well.
To be sure, there is considerable debate about whether LTCI is worth the cost. Premiums for new policies are rising at a steep clip – 9% annually, according to the AALTCI – and insurers are allowed to raise premiums even after you buy the policy, so you’ll need to factor that possibility into your budget.
But forgoing coverage can be costly too: If you know you will have to cover your own long-term care costs, you won’t be able to spend that money on things you really care about – like your grandkids, or travel, or charitable work. You might even forgo necessary medical care for fear of running out of money.
Everyone must make their own decision. My wife and I decided that a few thousand dollars per year is a fair price to pay for the peace of mind of knowing we will be able to afford proper supportive care, without help from our children or anyone else, regardless of what happens in the years to come.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
A few years ago, my seemingly indestructible 94-year-old mother suffered a series of medical setbacks. As her health problems accumulated, so did the complexity and cost of her care, progressing from her home to an assisted-living facility to a nursing home. It was heartbreaking – and expensive. My wife likened it to “putting another kid through college” – an elite private college, at that.
Medicare, of course, did not cover any of this, except for physician visits and some of her medications. When it was finally over, my wife and I resolved that, should we face a similar situation in our final years, we could not put ourselves or our children through a similar financial ordeal.
, in-home services, and other end-of-life expenses. (Covered services vary by policy; and as always, I have no financial interest in any product or service mentioned here.)
According to the American Association for Long-Term Care Insurance (AALTCI), the average annual LTCI premium for a 60-year-old couple is $3,490. Not cheap; but there are ways to lower premiums without gutting your coverage.
The best way to keep costs down is to get in early. In general, the younger you are and the better health you are in, the lower your premiums will be. For example – again according to the AALTCI – that “average” annual premium of $3,490 for a hypothetical 60-year-old couple would increase 34%, to $4,675, if they waited until they were 65 to buy the policy. And if their health were to decline in the interim, they might not be able to obtain adequate coverage at all.
You can also lower premiums by decreasing daily benefits, or increasing the “elimination period” – the length of time after you become eligible for benefits that the policy starts paying them; 30-, 60-, and 90-day periods are common. As long as you have sufficient savings to realistically cover costs until the elimination period is over, choosing a longer one can reduce your costs significantly.
Another variable is the maximum length of time the policy will pay out benefits. Ideally, you would want a payout to continue for as long as necessary, but few if any companies are willing to write uncapped policies anymore. Two to five years of benefits is a common time frame. (The “average” premiums quoted above assume a benefit of $150 per day with a 3-year cap and a 90-day elimination period.)
As with any insurance, it is important not to overbuy LTCI. It isn’t necessary to obtain coverage that will pay for 100% of your long-term care costs – just the portion that your projected retirement income (Social Security, pensions, income from savings) may not be sufficient to cover. Buying only the amount of coverage you need will substantially reduce your premium costs over the life of the policy.
If you work for a hospital or a large group, it’s worth checking to see if your employer offers LTCI. Employer-sponsored plans are often offered at discounted group rates, and you can usually keep the policy even if you leave. If you’re a member of any social or religious groups, check their insurance plans as well.
To be sure, there is considerable debate about whether LTCI is worth the cost. Premiums for new policies are rising at a steep clip – 9% annually, according to the AALTCI – and insurers are allowed to raise premiums even after you buy the policy, so you’ll need to factor that possibility into your budget.
But forgoing coverage can be costly too: If you know you will have to cover your own long-term care costs, you won’t be able to spend that money on things you really care about – like your grandkids, or travel, or charitable work. You might even forgo necessary medical care for fear of running out of money.
Everyone must make their own decision. My wife and I decided that a few thousand dollars per year is a fair price to pay for the peace of mind of knowing we will be able to afford proper supportive care, without help from our children or anyone else, regardless of what happens in the years to come.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Product News November 2019
Aklief Cream Topical Retinoid Approved for Acne Vulgaris
Galderma Laboratories, LP, announces US Food and Drug Administration approval of Aklief (trifarotene) Cream 0.005% for the treatment of acne vulgaris in patients 9 years and older. Trifarotene is a retinoid that selectively targets retinoic acid receptor γ. Aklief Cream treats both facial and truncal acne. Aklief Cream is expected to be available in the United States in November 2019 in a 45-g pump. For more information, visit www.galderma.com.
Altreno Lotion Now Available in a 20-g Tube for Dermatologist Dispensing
Ortho Dermatologics launches a 20-g tube of Altreno (tretinoin) Lotion 0.05% for dermatologists to dispense in their offices. Offering the product in the physician’s office helps ensure that patients will be ready to begin their acne regimen, increasing patient compliance. Altreno Lotion is approved for the treatment of acne vulgaris in patients 9 years and older. It provides efficacy and tolerability in a once-daily dosing regimen. For more information, visit www.altrenohcp.com.
Amzeeq Topical Minocycline Approved for Acne
Foamix Pharmaceuticals Ltd receives US Food and Drug Administration approval of Amzeeq (minocycline) Foam 4% for the treatment of moderate to severe acne vulgaris in patients 9 years and older. Foamix’s proprietary Molecule Stabilizing Technology is used to effectively deliver minocycline—a broad-spectrum antibiotic—in a foam-based vehicle for once-daily application. Amzeeq is expected to be available for prescribing in January 2020. For more information, visit www.foamix.com.
FDA Clears Protego Antimicrobial Wound Dressing
Turn Therapeutics, Inc, receives US Food and Drug Administration clearance of Protego antimicrobial wound dressing for acute and chronic wound management. Protego wound dressings are single-use, sterile, antimicrobial gauze dressings impregnated with Hexagen, a proprietary petrolatum-based wound care emulsion. Protego offers patients the utility of traditional petrolatum-saturated gauze dressings with the added benefit of broad-spectrum antimicrobial protection against bacteria, fungi, and yeasts. For more information, visit www.turntherapeutics.com.
Skin Cancer Foundation Champions for Change Gala Raises More Than $700,000
The Skin Cancer Foundation held its 23rd annual Champions for Change Gala on October 17, 2019. The foundation’s signature fundraising event raised more than $700,000 to support educational campaigns, community programs, and research initiatives. More than 400 guests attended the event at The Plaza Hotel in New York, New York. The event was emceed by comedian Tom Kelly, and President Dr. Deborah S. Sarnoff reflected on the 40th birthday of the foundation, reinforcing the goal “to change behaviors and save lives.” For more information, visit www.
If you would like your product included in Product News, please email a press release to the Editorial Office at cutis@mdedge.com.
Aklief Cream Topical Retinoid Approved for Acne Vulgaris
Galderma Laboratories, LP, announces US Food and Drug Administration approval of Aklief (trifarotene) Cream 0.005% for the treatment of acne vulgaris in patients 9 years and older. Trifarotene is a retinoid that selectively targets retinoic acid receptor γ. Aklief Cream treats both facial and truncal acne. Aklief Cream is expected to be available in the United States in November 2019 in a 45-g pump. For more information, visit www.galderma.com.
Altreno Lotion Now Available in a 20-g Tube for Dermatologist Dispensing
Ortho Dermatologics launches a 20-g tube of Altreno (tretinoin) Lotion 0.05% for dermatologists to dispense in their offices. Offering the product in the physician’s office helps ensure that patients will be ready to begin their acne regimen, increasing patient compliance. Altreno Lotion is approved for the treatment of acne vulgaris in patients 9 years and older. It provides efficacy and tolerability in a once-daily dosing regimen. For more information, visit www.altrenohcp.com.
Amzeeq Topical Minocycline Approved for Acne
Foamix Pharmaceuticals Ltd receives US Food and Drug Administration approval of Amzeeq (minocycline) Foam 4% for the treatment of moderate to severe acne vulgaris in patients 9 years and older. Foamix’s proprietary Molecule Stabilizing Technology is used to effectively deliver minocycline—a broad-spectrum antibiotic—in a foam-based vehicle for once-daily application. Amzeeq is expected to be available for prescribing in January 2020. For more information, visit www.foamix.com.
FDA Clears Protego Antimicrobial Wound Dressing
Turn Therapeutics, Inc, receives US Food and Drug Administration clearance of Protego antimicrobial wound dressing for acute and chronic wound management. Protego wound dressings are single-use, sterile, antimicrobial gauze dressings impregnated with Hexagen, a proprietary petrolatum-based wound care emulsion. Protego offers patients the utility of traditional petrolatum-saturated gauze dressings with the added benefit of broad-spectrum antimicrobial protection against bacteria, fungi, and yeasts. For more information, visit www.turntherapeutics.com.
Skin Cancer Foundation Champions for Change Gala Raises More Than $700,000
The Skin Cancer Foundation held its 23rd annual Champions for Change Gala on October 17, 2019. The foundation’s signature fundraising event raised more than $700,000 to support educational campaigns, community programs, and research initiatives. More than 400 guests attended the event at The Plaza Hotel in New York, New York. The event was emceed by comedian Tom Kelly, and President Dr. Deborah S. Sarnoff reflected on the 40th birthday of the foundation, reinforcing the goal “to change behaviors and save lives.” For more information, visit www.
If you would like your product included in Product News, please email a press release to the Editorial Office at cutis@mdedge.com.
Aklief Cream Topical Retinoid Approved for Acne Vulgaris
Galderma Laboratories, LP, announces US Food and Drug Administration approval of Aklief (trifarotene) Cream 0.005% for the treatment of acne vulgaris in patients 9 years and older. Trifarotene is a retinoid that selectively targets retinoic acid receptor γ. Aklief Cream treats both facial and truncal acne. Aklief Cream is expected to be available in the United States in November 2019 in a 45-g pump. For more information, visit www.galderma.com.
Altreno Lotion Now Available in a 20-g Tube for Dermatologist Dispensing
Ortho Dermatologics launches a 20-g tube of Altreno (tretinoin) Lotion 0.05% for dermatologists to dispense in their offices. Offering the product in the physician’s office helps ensure that patients will be ready to begin their acne regimen, increasing patient compliance. Altreno Lotion is approved for the treatment of acne vulgaris in patients 9 years and older. It provides efficacy and tolerability in a once-daily dosing regimen. For more information, visit www.altrenohcp.com.
Amzeeq Topical Minocycline Approved for Acne
Foamix Pharmaceuticals Ltd receives US Food and Drug Administration approval of Amzeeq (minocycline) Foam 4% for the treatment of moderate to severe acne vulgaris in patients 9 years and older. Foamix’s proprietary Molecule Stabilizing Technology is used to effectively deliver minocycline—a broad-spectrum antibiotic—in a foam-based vehicle for once-daily application. Amzeeq is expected to be available for prescribing in January 2020. For more information, visit www.foamix.com.
FDA Clears Protego Antimicrobial Wound Dressing
Turn Therapeutics, Inc, receives US Food and Drug Administration clearance of Protego antimicrobial wound dressing for acute and chronic wound management. Protego wound dressings are single-use, sterile, antimicrobial gauze dressings impregnated with Hexagen, a proprietary petrolatum-based wound care emulsion. Protego offers patients the utility of traditional petrolatum-saturated gauze dressings with the added benefit of broad-spectrum antimicrobial protection against bacteria, fungi, and yeasts. For more information, visit www.turntherapeutics.com.
Skin Cancer Foundation Champions for Change Gala Raises More Than $700,000
The Skin Cancer Foundation held its 23rd annual Champions for Change Gala on October 17, 2019. The foundation’s signature fundraising event raised more than $700,000 to support educational campaigns, community programs, and research initiatives. More than 400 guests attended the event at The Plaza Hotel in New York, New York. The event was emceed by comedian Tom Kelly, and President Dr. Deborah S. Sarnoff reflected on the 40th birthday of the foundation, reinforcing the goal “to change behaviors and save lives.” For more information, visit www.
If you would like your product included in Product News, please email a press release to the Editorial Office at cutis@mdedge.com.
Orthopedic ambulatory surgery centers beat inpatient services on cost
NATIONAL HARBOR, MD. – Hospital outpatient departments (HOPDs) and (IPs) with similar levels of postoperative opioid use, according to a new study.
Fanta Waterman, PhD, director of medical and health sciences at Pacira Pharmaceuticals, and colleagues retrospectively published the results of their investigation in the Journal of Managed Care & Specialty Pharmacy supplement for the annual meeting of the Academy of Managed Care Pharmacy.
Investigators evaluated data from 126,172 commercially insured patients who underwent one of six orthopedic surgical procedures between April 2012 and December 2017. Using the Optum Research Database, they pooled data from patients who had received total knee arthroplasty (TKA), partial knee arthroplasty, total hip arthroplasty (THA), rotator cuff repair (RCR), total shoulder arthroplasty, and lumbar spine fusion.
More than half (51%) of the patients were male, and the patients averaged 58 years of age. Most patients who underwent any of the six surgical interventions had the procedures performed at IPs (68%), while 18% had their operations at HOPDs and 14% were perfomed at ASCs.
TKA, RCR, and THA were the most common procedures performed (32%, 27%, and 20%, respectively). While no fluctuation was observed in the total number of IP procedures performed during 2012-2017, researchers noted a marked increase in ASCs (58%) and HOPDs (15%).
At the 30-day mark, the total all-cause postsurgical costs associated with IPs ($44,566) were more than double that of HOPDs ($20,468) and ASCs ($19,110; P less than .001). Moreover, multivariate adjustment showed that postsurgical costs accrued 30 days after surgery for HOPDs and ASCs were 14% and 27% lower than IPs (P less than .001), respectively.
Additionally, each group exhibited similar evidence of opioid use in the 12-month period prior to undergoing surgery, ranging from 63% to 65%. Postsurgical opioid use among opioid-naive patients was the highest in the HOPD group at 96% prevalence, with IPs and ASCs trailing with 91% and 90% (P less than .001), respectively. However, the postsurgical prevalence of opioid use in patients who had used opioids before surgery was 95% for IPs and HOPDs and 82% for ASCs (P less than .001).
SOURCE: Waterman F et al. AMCP NEXUS 2019, Abstract U12.
NATIONAL HARBOR, MD. – Hospital outpatient departments (HOPDs) and (IPs) with similar levels of postoperative opioid use, according to a new study.
Fanta Waterman, PhD, director of medical and health sciences at Pacira Pharmaceuticals, and colleagues retrospectively published the results of their investigation in the Journal of Managed Care & Specialty Pharmacy supplement for the annual meeting of the Academy of Managed Care Pharmacy.
Investigators evaluated data from 126,172 commercially insured patients who underwent one of six orthopedic surgical procedures between April 2012 and December 2017. Using the Optum Research Database, they pooled data from patients who had received total knee arthroplasty (TKA), partial knee arthroplasty, total hip arthroplasty (THA), rotator cuff repair (RCR), total shoulder arthroplasty, and lumbar spine fusion.
More than half (51%) of the patients were male, and the patients averaged 58 years of age. Most patients who underwent any of the six surgical interventions had the procedures performed at IPs (68%), while 18% had their operations at HOPDs and 14% were perfomed at ASCs.
TKA, RCR, and THA were the most common procedures performed (32%, 27%, and 20%, respectively). While no fluctuation was observed in the total number of IP procedures performed during 2012-2017, researchers noted a marked increase in ASCs (58%) and HOPDs (15%).
At the 30-day mark, the total all-cause postsurgical costs associated with IPs ($44,566) were more than double that of HOPDs ($20,468) and ASCs ($19,110; P less than .001). Moreover, multivariate adjustment showed that postsurgical costs accrued 30 days after surgery for HOPDs and ASCs were 14% and 27% lower than IPs (P less than .001), respectively.
Additionally, each group exhibited similar evidence of opioid use in the 12-month period prior to undergoing surgery, ranging from 63% to 65%. Postsurgical opioid use among opioid-naive patients was the highest in the HOPD group at 96% prevalence, with IPs and ASCs trailing with 91% and 90% (P less than .001), respectively. However, the postsurgical prevalence of opioid use in patients who had used opioids before surgery was 95% for IPs and HOPDs and 82% for ASCs (P less than .001).
SOURCE: Waterman F et al. AMCP NEXUS 2019, Abstract U12.
NATIONAL HARBOR, MD. – Hospital outpatient departments (HOPDs) and (IPs) with similar levels of postoperative opioid use, according to a new study.
Fanta Waterman, PhD, director of medical and health sciences at Pacira Pharmaceuticals, and colleagues retrospectively published the results of their investigation in the Journal of Managed Care & Specialty Pharmacy supplement for the annual meeting of the Academy of Managed Care Pharmacy.
Investigators evaluated data from 126,172 commercially insured patients who underwent one of six orthopedic surgical procedures between April 2012 and December 2017. Using the Optum Research Database, they pooled data from patients who had received total knee arthroplasty (TKA), partial knee arthroplasty, total hip arthroplasty (THA), rotator cuff repair (RCR), total shoulder arthroplasty, and lumbar spine fusion.
More than half (51%) of the patients were male, and the patients averaged 58 years of age. Most patients who underwent any of the six surgical interventions had the procedures performed at IPs (68%), while 18% had their operations at HOPDs and 14% were perfomed at ASCs.
TKA, RCR, and THA were the most common procedures performed (32%, 27%, and 20%, respectively). While no fluctuation was observed in the total number of IP procedures performed during 2012-2017, researchers noted a marked increase in ASCs (58%) and HOPDs (15%).
At the 30-day mark, the total all-cause postsurgical costs associated with IPs ($44,566) were more than double that of HOPDs ($20,468) and ASCs ($19,110; P less than .001). Moreover, multivariate adjustment showed that postsurgical costs accrued 30 days after surgery for HOPDs and ASCs were 14% and 27% lower than IPs (P less than .001), respectively.
Additionally, each group exhibited similar evidence of opioid use in the 12-month period prior to undergoing surgery, ranging from 63% to 65%. Postsurgical opioid use among opioid-naive patients was the highest in the HOPD group at 96% prevalence, with IPs and ASCs trailing with 91% and 90% (P less than .001), respectively. However, the postsurgical prevalence of opioid use in patients who had used opioids before surgery was 95% for IPs and HOPDs and 82% for ASCs (P less than .001).
SOURCE: Waterman F et al. AMCP NEXUS 2019, Abstract U12.
REPORTING FROM AMCP NEXUS 2019
Adding mental health clinicians to your practice is full of benefits
NEW ORLEANS – The way Jay Rabinowitz, MD, MPH, sees it, providing mental and behavioral health care services in your primary care pediatrics practice is a win-win for patients, parents, and clinicians.
For one thing, children with mental and behavioral issues – especially depression and anxiety – make up a good chunk of any pediatrician’s workday. Dr. Rabinowitz, clinical professor of pediatrics at the University of Colorado, Aurora, said at the annual meeting of the American Academy of Pediatrics. “It is the most costly issue in children’s health care today.”
According to “Behavioral Health Integration in Pediatric Primary Care,” a report supported by the Milbank Memorial Fund, one in five children aged 9-17 years have a diagnosable psychiatric disorder, and up to 70% of children in the juvenile justice system have a mental health disorder. The report also found that the treatment of mental health disorders accounts for the most costly childhood medical expenditure, and that between 15% and 20% of children with psychiatric disorders receive specialty care; the rest see their primary care provider. A long-term cost analysis showed significant cost savings: $1 spent on collaborative care saves $6.50 on health care costs.
More recently, the Guidelines for Adolescent Depression in Primary Care (GLAD-PC) found that only 50% of adolescents with depression are diagnosed before reaching adulthood (Pediatrics. March 2018;141[3]:e20174081). As many as two out of three youth with depression are not identified by their pediatrician and do not receive any kind of care.
“Even when diagnosed, only half of these patients are treated appropriately,” said Dr. Rabinowitz, who also practices at Parker (Colo.) Pediatrics and Adolescents.
The guidelines also found that reliance on self-report depression checklists alone lead to substantial numbers of false-positive and false-negative cases. “Primary care providers will benefit from having access to ongoing consultation with mental health providers,” according to the guidelines.
“Integrative care was associated with significant decreases in depression scores, and improved response and remission rates at 12 months, compared with treatment as usual,” Dr. Rabinowitz said.
Providing mental health services in a primary care pediatrics setting also makes sense because there’s a shortage of psychiatrists and psychologists to see them, and it enables patients to get evaluated quicker. “It’s convenient, and it reduces stigma,” he added. “It’s a familiar setting, a familiar provider, and they’re more likely to initiate counseling. Nationwide, 50% of patients who are referred for mental health do not make their initial appointment. Think about that. If you had diabetics in your practice and only 50% would go to the endocrinologist, what would you think?”
How Dr. Rabinowitz and his partners got started
Dr. Rabinowitz and his colleagues created an integrated care model in 2008 by adding a psychologist to their practice, but before doing that, they asked parents of children with mental and behavioral health issues what type of insurance they had. Then they obtained a referral list from the family’s insurer and hoped for the best. “Sometimes I referred to someone I may not have heard of,” Dr. Rabinowitz said. “Usually I did not get follow-up reports, or even know for sure if the patient ever went.”
Today, Parker Pediatrics and Adolescents employs three doctoral-level psychologists: one full-time, one three-quarter time, and one half-time, as well as one master’s-level therapist who works half-time.
“On any given day, we have at least two counselors in our office,” said Lindsey Einhorn, PhD, a licensed clinical psychologist who joined the practice in 2011. She and her colleagues care for children and teens with ADHD, depression, anxiety, behavioral and adjustment disorders, drug counseling, behavioral addictions, social struggles such as bullying, obsessive compulsive disorder (OCD), loss, hair or eyelash pulling, mood dysregulation, and sibling conflict. They refer for educational testing, comprehensive psychological evaluations, difficult divorce cases, play therapy, complex cases requiring more than 20 sessions, and children of staff employed by the practice.
The practice features a separate waiting room for psychology patients and front office staff dedicated to managing their schedules. “For anyone who’s trying to make a psychology appointment but can’t be seen in an efficient manner or wants a different day or time, we keep an ongoing move-up list,” Dr. Einhorn said. “If a family calls to cancel an appointment, the front desk person who makes that cancellation will fill out a slip and give it to one of our psychology schedulers. That person will create a move-up list and start filling that appointment. If there’s a cancellation, it’s rare that it goes unfilled.”
Key forms for parents to complete include informed consent, a notice of privacy practices, a late cancel/no show policy, an initial intake agreement, and a summary of parent concerns.
Patient and clinician reaction
According to results from a recent survey of parents whose children were seen by a psychologist at Parker Pediatrics and Adolescents, 89% said it was important for their children to receive mental health services in the same location as their medical care, and 96% were satisfied with the services provided. In addition, 93% said that the experience benefited their child, 72% were satisfied with appointment times, and 55% expressed interest in virtual visits via telemedicine. Meanwhile, a survey of parents whose children have not been seen by a psychologist at the practice found that 65% knew a psychologist was on staff, and only 9% said that there were barriers to their child seeing a psychologist there.
Clinicians themselves benefit from having mental health specialists on site for referrals. “It enables you to be more efficient, and it saves time,” Dr. Rabinowitz said. “There’s knowledge and confidence gained, and it improves satisfaction because physicians don’t have to stay at the office later filling out referral forms. It meets the needs of your patients and their families, it attracts new patients, and you may be able to make some income on this.”
How to get started
Dr. Rabinowitz recommended that, once clinicians at a pediatric practice commit to expanding their services to include mental and behavioral health care, they should hold a corporate/partner meeting, assign responsibilities, and establish a timeline for implementation. “This is all very important,” he said. “Then you have to talk about what kind of arrangement you want to have. You could employ someone to join your practice, hire an independent contractor, establish a space share agreement, or have an out-of-office arrangement.”
For many years, clinicians at Parker Pediatrics and Adolescents had a psychologist perform ADHD evaluations on a consultative basis. “Then, as we saw a need for mental health services about a decade ago, we hired a part-time psychologist who did testing as well as counseling,” Dr. Rabinowitz said. “But that psychologist got very busy, so we hired a full-time psychologist. We continued to hire additional psychologists as need increased.”
Reimbursement issues
Numerous reimbursement barriers to providing mental health services in pediatric primary care exist, he noted, including a lack of payment if mental health codes are used, a lack of “incident to” payments in some areas of the country, existing reimbursement levels, and the fact that same-day billing of physical and mental health often is not allowed. “However, we have found that if we give flu shots during their mental health visit, [insurers] will cover the flu shot,” he said. “Reimbursement for screening is sometimes not covered very well.”
One reimbursement option is the fee-for-service/concierge model, “but that’s not an economic option for many,” he said. “You can’t see Medicaid patients in that model.” Joining a mental health networks is feasible, “but there is poor reimbursement,” he said. “It also creates another layer of administration.”
He recommends financial integration, “but you need to research your options because a lot of it is state dependent.” Other options include grants, insurance contracts, and seeking permission from Medicaid.
Mental health CPT codes that mental health clinicians at the practice commonly use include bill by time (CPT code 99214/15); psychotherapy session that lasts 16-37 minutes (CPT code 90832); psychotherapy session that lasts 38-52 minutes (CPT code 90834); and psychotherapy session that lasts more than 53 minutes (CPT code 90837). Clinicians also can bill by interactive complexity (CPT code 90785) and psychotherapy for crisis (CPT code 90839).
Dr. Rabinowitz and Dr. Einhorn reported having no financial disclosures.
NEW ORLEANS – The way Jay Rabinowitz, MD, MPH, sees it, providing mental and behavioral health care services in your primary care pediatrics practice is a win-win for patients, parents, and clinicians.
For one thing, children with mental and behavioral issues – especially depression and anxiety – make up a good chunk of any pediatrician’s workday. Dr. Rabinowitz, clinical professor of pediatrics at the University of Colorado, Aurora, said at the annual meeting of the American Academy of Pediatrics. “It is the most costly issue in children’s health care today.”
According to “Behavioral Health Integration in Pediatric Primary Care,” a report supported by the Milbank Memorial Fund, one in five children aged 9-17 years have a diagnosable psychiatric disorder, and up to 70% of children in the juvenile justice system have a mental health disorder. The report also found that the treatment of mental health disorders accounts for the most costly childhood medical expenditure, and that between 15% and 20% of children with psychiatric disorders receive specialty care; the rest see their primary care provider. A long-term cost analysis showed significant cost savings: $1 spent on collaborative care saves $6.50 on health care costs.
More recently, the Guidelines for Adolescent Depression in Primary Care (GLAD-PC) found that only 50% of adolescents with depression are diagnosed before reaching adulthood (Pediatrics. March 2018;141[3]:e20174081). As many as two out of three youth with depression are not identified by their pediatrician and do not receive any kind of care.
“Even when diagnosed, only half of these patients are treated appropriately,” said Dr. Rabinowitz, who also practices at Parker (Colo.) Pediatrics and Adolescents.
The guidelines also found that reliance on self-report depression checklists alone lead to substantial numbers of false-positive and false-negative cases. “Primary care providers will benefit from having access to ongoing consultation with mental health providers,” according to the guidelines.
“Integrative care was associated with significant decreases in depression scores, and improved response and remission rates at 12 months, compared with treatment as usual,” Dr. Rabinowitz said.
Providing mental health services in a primary care pediatrics setting also makes sense because there’s a shortage of psychiatrists and psychologists to see them, and it enables patients to get evaluated quicker. “It’s convenient, and it reduces stigma,” he added. “It’s a familiar setting, a familiar provider, and they’re more likely to initiate counseling. Nationwide, 50% of patients who are referred for mental health do not make their initial appointment. Think about that. If you had diabetics in your practice and only 50% would go to the endocrinologist, what would you think?”
How Dr. Rabinowitz and his partners got started
Dr. Rabinowitz and his colleagues created an integrated care model in 2008 by adding a psychologist to their practice, but before doing that, they asked parents of children with mental and behavioral health issues what type of insurance they had. Then they obtained a referral list from the family’s insurer and hoped for the best. “Sometimes I referred to someone I may not have heard of,” Dr. Rabinowitz said. “Usually I did not get follow-up reports, or even know for sure if the patient ever went.”
Today, Parker Pediatrics and Adolescents employs three doctoral-level psychologists: one full-time, one three-quarter time, and one half-time, as well as one master’s-level therapist who works half-time.
“On any given day, we have at least two counselors in our office,” said Lindsey Einhorn, PhD, a licensed clinical psychologist who joined the practice in 2011. She and her colleagues care for children and teens with ADHD, depression, anxiety, behavioral and adjustment disorders, drug counseling, behavioral addictions, social struggles such as bullying, obsessive compulsive disorder (OCD), loss, hair or eyelash pulling, mood dysregulation, and sibling conflict. They refer for educational testing, comprehensive psychological evaluations, difficult divorce cases, play therapy, complex cases requiring more than 20 sessions, and children of staff employed by the practice.
The practice features a separate waiting room for psychology patients and front office staff dedicated to managing their schedules. “For anyone who’s trying to make a psychology appointment but can’t be seen in an efficient manner or wants a different day or time, we keep an ongoing move-up list,” Dr. Einhorn said. “If a family calls to cancel an appointment, the front desk person who makes that cancellation will fill out a slip and give it to one of our psychology schedulers. That person will create a move-up list and start filling that appointment. If there’s a cancellation, it’s rare that it goes unfilled.”
Key forms for parents to complete include informed consent, a notice of privacy practices, a late cancel/no show policy, an initial intake agreement, and a summary of parent concerns.
Patient and clinician reaction
According to results from a recent survey of parents whose children were seen by a psychologist at Parker Pediatrics and Adolescents, 89% said it was important for their children to receive mental health services in the same location as their medical care, and 96% were satisfied with the services provided. In addition, 93% said that the experience benefited their child, 72% were satisfied with appointment times, and 55% expressed interest in virtual visits via telemedicine. Meanwhile, a survey of parents whose children have not been seen by a psychologist at the practice found that 65% knew a psychologist was on staff, and only 9% said that there were barriers to their child seeing a psychologist there.
Clinicians themselves benefit from having mental health specialists on site for referrals. “It enables you to be more efficient, and it saves time,” Dr. Rabinowitz said. “There’s knowledge and confidence gained, and it improves satisfaction because physicians don’t have to stay at the office later filling out referral forms. It meets the needs of your patients and their families, it attracts new patients, and you may be able to make some income on this.”
How to get started
Dr. Rabinowitz recommended that, once clinicians at a pediatric practice commit to expanding their services to include mental and behavioral health care, they should hold a corporate/partner meeting, assign responsibilities, and establish a timeline for implementation. “This is all very important,” he said. “Then you have to talk about what kind of arrangement you want to have. You could employ someone to join your practice, hire an independent contractor, establish a space share agreement, or have an out-of-office arrangement.”
For many years, clinicians at Parker Pediatrics and Adolescents had a psychologist perform ADHD evaluations on a consultative basis. “Then, as we saw a need for mental health services about a decade ago, we hired a part-time psychologist who did testing as well as counseling,” Dr. Rabinowitz said. “But that psychologist got very busy, so we hired a full-time psychologist. We continued to hire additional psychologists as need increased.”
Reimbursement issues
Numerous reimbursement barriers to providing mental health services in pediatric primary care exist, he noted, including a lack of payment if mental health codes are used, a lack of “incident to” payments in some areas of the country, existing reimbursement levels, and the fact that same-day billing of physical and mental health often is not allowed. “However, we have found that if we give flu shots during their mental health visit, [insurers] will cover the flu shot,” he said. “Reimbursement for screening is sometimes not covered very well.”
One reimbursement option is the fee-for-service/concierge model, “but that’s not an economic option for many,” he said. “You can’t see Medicaid patients in that model.” Joining a mental health networks is feasible, “but there is poor reimbursement,” he said. “It also creates another layer of administration.”
He recommends financial integration, “but you need to research your options because a lot of it is state dependent.” Other options include grants, insurance contracts, and seeking permission from Medicaid.
Mental health CPT codes that mental health clinicians at the practice commonly use include bill by time (CPT code 99214/15); psychotherapy session that lasts 16-37 minutes (CPT code 90832); psychotherapy session that lasts 38-52 minutes (CPT code 90834); and psychotherapy session that lasts more than 53 minutes (CPT code 90837). Clinicians also can bill by interactive complexity (CPT code 90785) and psychotherapy for crisis (CPT code 90839).
Dr. Rabinowitz and Dr. Einhorn reported having no financial disclosures.
NEW ORLEANS – The way Jay Rabinowitz, MD, MPH, sees it, providing mental and behavioral health care services in your primary care pediatrics practice is a win-win for patients, parents, and clinicians.
For one thing, children with mental and behavioral issues – especially depression and anxiety – make up a good chunk of any pediatrician’s workday. Dr. Rabinowitz, clinical professor of pediatrics at the University of Colorado, Aurora, said at the annual meeting of the American Academy of Pediatrics. “It is the most costly issue in children’s health care today.”
According to “Behavioral Health Integration in Pediatric Primary Care,” a report supported by the Milbank Memorial Fund, one in five children aged 9-17 years have a diagnosable psychiatric disorder, and up to 70% of children in the juvenile justice system have a mental health disorder. The report also found that the treatment of mental health disorders accounts for the most costly childhood medical expenditure, and that between 15% and 20% of children with psychiatric disorders receive specialty care; the rest see their primary care provider. A long-term cost analysis showed significant cost savings: $1 spent on collaborative care saves $6.50 on health care costs.
More recently, the Guidelines for Adolescent Depression in Primary Care (GLAD-PC) found that only 50% of adolescents with depression are diagnosed before reaching adulthood (Pediatrics. March 2018;141[3]:e20174081). As many as two out of three youth with depression are not identified by their pediatrician and do not receive any kind of care.
“Even when diagnosed, only half of these patients are treated appropriately,” said Dr. Rabinowitz, who also practices at Parker (Colo.) Pediatrics and Adolescents.
The guidelines also found that reliance on self-report depression checklists alone lead to substantial numbers of false-positive and false-negative cases. “Primary care providers will benefit from having access to ongoing consultation with mental health providers,” according to the guidelines.
“Integrative care was associated with significant decreases in depression scores, and improved response and remission rates at 12 months, compared with treatment as usual,” Dr. Rabinowitz said.
Providing mental health services in a primary care pediatrics setting also makes sense because there’s a shortage of psychiatrists and psychologists to see them, and it enables patients to get evaluated quicker. “It’s convenient, and it reduces stigma,” he added. “It’s a familiar setting, a familiar provider, and they’re more likely to initiate counseling. Nationwide, 50% of patients who are referred for mental health do not make their initial appointment. Think about that. If you had diabetics in your practice and only 50% would go to the endocrinologist, what would you think?”
How Dr. Rabinowitz and his partners got started
Dr. Rabinowitz and his colleagues created an integrated care model in 2008 by adding a psychologist to their practice, but before doing that, they asked parents of children with mental and behavioral health issues what type of insurance they had. Then they obtained a referral list from the family’s insurer and hoped for the best. “Sometimes I referred to someone I may not have heard of,” Dr. Rabinowitz said. “Usually I did not get follow-up reports, or even know for sure if the patient ever went.”
Today, Parker Pediatrics and Adolescents employs three doctoral-level psychologists: one full-time, one three-quarter time, and one half-time, as well as one master’s-level therapist who works half-time.
“On any given day, we have at least two counselors in our office,” said Lindsey Einhorn, PhD, a licensed clinical psychologist who joined the practice in 2011. She and her colleagues care for children and teens with ADHD, depression, anxiety, behavioral and adjustment disorders, drug counseling, behavioral addictions, social struggles such as bullying, obsessive compulsive disorder (OCD), loss, hair or eyelash pulling, mood dysregulation, and sibling conflict. They refer for educational testing, comprehensive psychological evaluations, difficult divorce cases, play therapy, complex cases requiring more than 20 sessions, and children of staff employed by the practice.
The practice features a separate waiting room for psychology patients and front office staff dedicated to managing their schedules. “For anyone who’s trying to make a psychology appointment but can’t be seen in an efficient manner or wants a different day or time, we keep an ongoing move-up list,” Dr. Einhorn said. “If a family calls to cancel an appointment, the front desk person who makes that cancellation will fill out a slip and give it to one of our psychology schedulers. That person will create a move-up list and start filling that appointment. If there’s a cancellation, it’s rare that it goes unfilled.”
Key forms for parents to complete include informed consent, a notice of privacy practices, a late cancel/no show policy, an initial intake agreement, and a summary of parent concerns.
Patient and clinician reaction
According to results from a recent survey of parents whose children were seen by a psychologist at Parker Pediatrics and Adolescents, 89% said it was important for their children to receive mental health services in the same location as their medical care, and 96% were satisfied with the services provided. In addition, 93% said that the experience benefited their child, 72% were satisfied with appointment times, and 55% expressed interest in virtual visits via telemedicine. Meanwhile, a survey of parents whose children have not been seen by a psychologist at the practice found that 65% knew a psychologist was on staff, and only 9% said that there were barriers to their child seeing a psychologist there.
Clinicians themselves benefit from having mental health specialists on site for referrals. “It enables you to be more efficient, and it saves time,” Dr. Rabinowitz said. “There’s knowledge and confidence gained, and it improves satisfaction because physicians don’t have to stay at the office later filling out referral forms. It meets the needs of your patients and their families, it attracts new patients, and you may be able to make some income on this.”
How to get started
Dr. Rabinowitz recommended that, once clinicians at a pediatric practice commit to expanding their services to include mental and behavioral health care, they should hold a corporate/partner meeting, assign responsibilities, and establish a timeline for implementation. “This is all very important,” he said. “Then you have to talk about what kind of arrangement you want to have. You could employ someone to join your practice, hire an independent contractor, establish a space share agreement, or have an out-of-office arrangement.”
For many years, clinicians at Parker Pediatrics and Adolescents had a psychologist perform ADHD evaluations on a consultative basis. “Then, as we saw a need for mental health services about a decade ago, we hired a part-time psychologist who did testing as well as counseling,” Dr. Rabinowitz said. “But that psychologist got very busy, so we hired a full-time psychologist. We continued to hire additional psychologists as need increased.”
Reimbursement issues
Numerous reimbursement barriers to providing mental health services in pediatric primary care exist, he noted, including a lack of payment if mental health codes are used, a lack of “incident to” payments in some areas of the country, existing reimbursement levels, and the fact that same-day billing of physical and mental health often is not allowed. “However, we have found that if we give flu shots during their mental health visit, [insurers] will cover the flu shot,” he said. “Reimbursement for screening is sometimes not covered very well.”
One reimbursement option is the fee-for-service/concierge model, “but that’s not an economic option for many,” he said. “You can’t see Medicaid patients in that model.” Joining a mental health networks is feasible, “but there is poor reimbursement,” he said. “It also creates another layer of administration.”
He recommends financial integration, “but you need to research your options because a lot of it is state dependent.” Other options include grants, insurance contracts, and seeking permission from Medicaid.
Mental health CPT codes that mental health clinicians at the practice commonly use include bill by time (CPT code 99214/15); psychotherapy session that lasts 16-37 minutes (CPT code 90832); psychotherapy session that lasts 38-52 minutes (CPT code 90834); and psychotherapy session that lasts more than 53 minutes (CPT code 90837). Clinicians also can bill by interactive complexity (CPT code 90785) and psychotherapy for crisis (CPT code 90839).
Dr. Rabinowitz and Dr. Einhorn reported having no financial disclosures.
EXPERT ANALYSIS FROM AAP 2019
Medicare beneficiaries pay most for Alzheimer’s
according to the Kaiser Family Foundation.
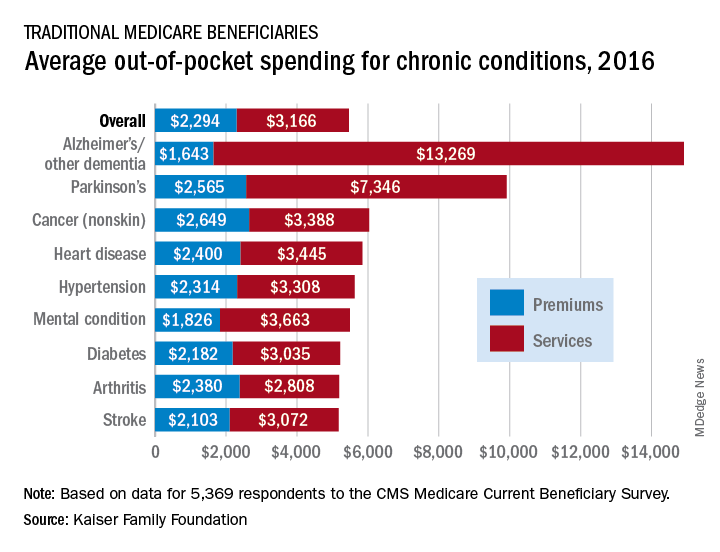
Out-of-pocket spending for Alzheimer’s disease or other dementia was higher than any other chronic condition, averaging $14,913 in 2016 (the latest year for which data are available), compared with $5,460 for all beneficiaries in traditional Medicare, Kaiser investigators said in a recent report based on data for 5,369 respondents to the Medicare Current Beneficiary Survey.
Those totals were divided between services – including long-term care facilities, medical providers and supplies, and prescription drugs – and premiums for Medicare and other types of supplemental insurance. The premium associated with Alzheimer’s, $1,643, was the lowest of any major chronic condition, but the average cost for services, $13,269, was almost twice as high as the next most expensive condition, Parkinson’s disease, and more than four times higher than the overall Medicare average, Juliette Cubanski, PhD, and associates said.
Out-of-pocket costs are higher for patients with Alzheimer’s and Parkinson’s because “these beneficiaries are more likely to reside in a long-term care facility than those with other conditions,” they said. In 2016, out-of-pocket spending on long-term care facility services averaged over $27,000 for Medicare beneficiaries with Alzheimer’s and other dementia and over $28,000 for those with Parkinson’s disease. For all traditional Medicare beneficiaries, average out-of-pocket spending on such services was $1,014.
“The fact that traditional Medicare does not have an annual out-of-pocket limit and does not cover certain services that older adults are more likely to need may undermine the financial security that Medicare provides, especially for people with significant needs and limited incomes. Addressing these gaps would help to alleviate the financial burden of health care for people with Medicare, although doing so would also increase federal spending and taxes,” Dr. Cubanski and associates wrote.
according to the Kaiser Family Foundation.
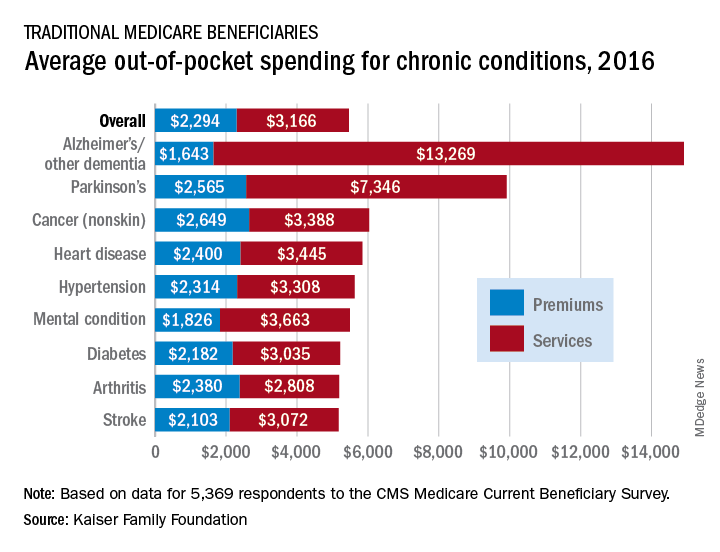
Out-of-pocket spending for Alzheimer’s disease or other dementia was higher than any other chronic condition, averaging $14,913 in 2016 (the latest year for which data are available), compared with $5,460 for all beneficiaries in traditional Medicare, Kaiser investigators said in a recent report based on data for 5,369 respondents to the Medicare Current Beneficiary Survey.
Those totals were divided between services – including long-term care facilities, medical providers and supplies, and prescription drugs – and premiums for Medicare and other types of supplemental insurance. The premium associated with Alzheimer’s, $1,643, was the lowest of any major chronic condition, but the average cost for services, $13,269, was almost twice as high as the next most expensive condition, Parkinson’s disease, and more than four times higher than the overall Medicare average, Juliette Cubanski, PhD, and associates said.
Out-of-pocket costs are higher for patients with Alzheimer’s and Parkinson’s because “these beneficiaries are more likely to reside in a long-term care facility than those with other conditions,” they said. In 2016, out-of-pocket spending on long-term care facility services averaged over $27,000 for Medicare beneficiaries with Alzheimer’s and other dementia and over $28,000 for those with Parkinson’s disease. For all traditional Medicare beneficiaries, average out-of-pocket spending on such services was $1,014.
“The fact that traditional Medicare does not have an annual out-of-pocket limit and does not cover certain services that older adults are more likely to need may undermine the financial security that Medicare provides, especially for people with significant needs and limited incomes. Addressing these gaps would help to alleviate the financial burden of health care for people with Medicare, although doing so would also increase federal spending and taxes,” Dr. Cubanski and associates wrote.
according to the Kaiser Family Foundation.
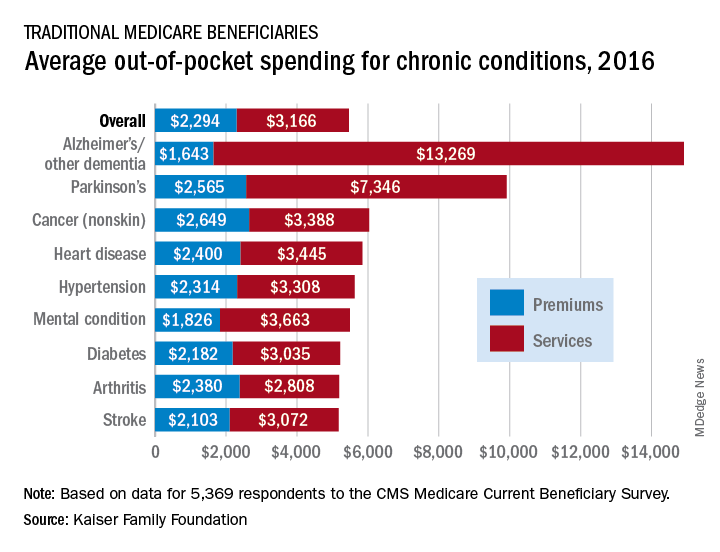
Out-of-pocket spending for Alzheimer’s disease or other dementia was higher than any other chronic condition, averaging $14,913 in 2016 (the latest year for which data are available), compared with $5,460 for all beneficiaries in traditional Medicare, Kaiser investigators said in a recent report based on data for 5,369 respondents to the Medicare Current Beneficiary Survey.
Those totals were divided between services – including long-term care facilities, medical providers and supplies, and prescription drugs – and premiums for Medicare and other types of supplemental insurance. The premium associated with Alzheimer’s, $1,643, was the lowest of any major chronic condition, but the average cost for services, $13,269, was almost twice as high as the next most expensive condition, Parkinson’s disease, and more than four times higher than the overall Medicare average, Juliette Cubanski, PhD, and associates said.
Out-of-pocket costs are higher for patients with Alzheimer’s and Parkinson’s because “these beneficiaries are more likely to reside in a long-term care facility than those with other conditions,” they said. In 2016, out-of-pocket spending on long-term care facility services averaged over $27,000 for Medicare beneficiaries with Alzheimer’s and other dementia and over $28,000 for those with Parkinson’s disease. For all traditional Medicare beneficiaries, average out-of-pocket spending on such services was $1,014.
“The fact that traditional Medicare does not have an annual out-of-pocket limit and does not cover certain services that older adults are more likely to need may undermine the financial security that Medicare provides, especially for people with significant needs and limited incomes. Addressing these gaps would help to alleviate the financial burden of health care for people with Medicare, although doing so would also increase federal spending and taxes,” Dr. Cubanski and associates wrote.
Study: Pediatricians support alternative MOC assessment
two recent surveys show.
Lead author Laurel K. Leslie, MD, of Tufts University, Boston, and colleagues analyzed the perceptions of 4,238 pediatricians who participated in a pilot MOC program in 2017 and completed a fourth-quarter survey, a voluntary end-of-year survey, or both surveys. The new MOC option was developed by the American Board of Pediatrics between 2015 and 2016 as an alternative to the current proctored, closed-book general pediatrics (GP) MOC examination. The Maintenance of Certification Assessment for Pediatrics (MOCA-Peds) includes timed, multiple-choice questions delivered quarterly through a Web-based interface, provides resources to help answer questions, and yields immediate feedback, rationale, and references pertaining to answers.
Of the pediatricians surveyed, 93% considered the MOCA-Peds to be a feasible and acceptable alternative to the traditional MOC GP examination, and 89% of pediatricians indicated they would chose the MOCA-Peds model over the proctored examination, according to the study, published in Pediatrics. Of doctors who completed the quarter 4 survey, 88% agreed or strongly agreed that assessment questions aligned with the stated learning objectives, 82% agreed the questions assessed clinical judgment, 82% agreed the questions were relevant to the practice of GP, and 59% agreed the questions were relevant to their specific practice setting, according to the study. For most pediatricians surveyed, the time to answer questions was sufficient (78%).
Regarding potential anxiety associated with MOC, 89% of doctors surveyed agreed that they felt less anxiety participating in the MOCA-Peds compared with the proctored examination, and that any anxiety they felt about the MOCA-Peds lessened during the pilot as their comfort with the assessment grew (81%). When asked whether they would partake in MOCA-Peds in the future, 97% of general pediatricians and 95% of subspecialists planned to participate in MOCA-Peds to maintain their GP certification; 95% of subspecialists said they would participate in MOCA-Peds to maintain their subspecialty certification.
In a second analysis of the same study population led by Adam L. Turner, MPH, of the American Board of Pediatrics, participants were asked whether the MOCA-Peds led to any practice or knowledge changes. Nearly all (98%) respondents reported they had “learned, refreshed, or enhanced their medical knowledge” because of the assessment and 62% of pediatricians reported a practice change associated with pilot participation, according to the study, published in Pediatrics. Of those who made a practice change, 70% were general pediatricians and 41% were subspecialists.
Of the 1,727 pediatricians who positively indicated a practice change, 84% reported details about the specific change made. The most common content domains associated with a practice change included ear, nose, and throat; preventive and well-child care; and mental and behavioral health.
Within the content domains, the three most frequently cited instances in which knowledge or a practice change took place included planning the management of a child with otitis media, managing a child with an acute asthma exacerbation, and planning the management of a child with influenza. Of 400 additional responses related to practice changes beyond answers associated with a specific content domain, the three most common subthemes were using evidence-based medicine, expanding review of materials or resource use, and improving differential diagnosis. Pediatricians reported that participation in MOCA-Peds exposed them to new material and encouraged them to review guidelines or standard care protocols and their application. Respondents also reported increased review of materials or resources in practice, updating the types of resources used, and/or an increased effort to stay more updated.
Dr. Turner and associates concluded that the results “support the notion that assessment and learning can be integrated into a single platform and need not be considered mutually exclusive activities, in turn adding value for practicing physicians.”
The studies were funded by the American Board of Pediatrics Foundation. Dr. Leslie, Dr. Linda Althouse, Mr. Andrew Bradford, and Mr. Adam L. Turner are employees of The American Board of Pediatrics. Dr. Victoria Dounoucos, Dr. Murrey G. Olmsted, and Ms. Amanda C. Smith are employees of RTI International, an international nonprofit research firm with whom the board contracted to conduct this evaluation.
SOURCE: Leslie LK et al. Pediatrics. Nov. 2019 Nov. doi: 10.1542/peds.2019-2303; Turner AL et al. Pediatrics. 2019 Nov. doi: 10.1542/peds.2019-2305.
two recent surveys show.
Lead author Laurel K. Leslie, MD, of Tufts University, Boston, and colleagues analyzed the perceptions of 4,238 pediatricians who participated in a pilot MOC program in 2017 and completed a fourth-quarter survey, a voluntary end-of-year survey, or both surveys. The new MOC option was developed by the American Board of Pediatrics between 2015 and 2016 as an alternative to the current proctored, closed-book general pediatrics (GP) MOC examination. The Maintenance of Certification Assessment for Pediatrics (MOCA-Peds) includes timed, multiple-choice questions delivered quarterly through a Web-based interface, provides resources to help answer questions, and yields immediate feedback, rationale, and references pertaining to answers.
Of the pediatricians surveyed, 93% considered the MOCA-Peds to be a feasible and acceptable alternative to the traditional MOC GP examination, and 89% of pediatricians indicated they would chose the MOCA-Peds model over the proctored examination, according to the study, published in Pediatrics. Of doctors who completed the quarter 4 survey, 88% agreed or strongly agreed that assessment questions aligned with the stated learning objectives, 82% agreed the questions assessed clinical judgment, 82% agreed the questions were relevant to the practice of GP, and 59% agreed the questions were relevant to their specific practice setting, according to the study. For most pediatricians surveyed, the time to answer questions was sufficient (78%).
Regarding potential anxiety associated with MOC, 89% of doctors surveyed agreed that they felt less anxiety participating in the MOCA-Peds compared with the proctored examination, and that any anxiety they felt about the MOCA-Peds lessened during the pilot as their comfort with the assessment grew (81%). When asked whether they would partake in MOCA-Peds in the future, 97% of general pediatricians and 95% of subspecialists planned to participate in MOCA-Peds to maintain their GP certification; 95% of subspecialists said they would participate in MOCA-Peds to maintain their subspecialty certification.
In a second analysis of the same study population led by Adam L. Turner, MPH, of the American Board of Pediatrics, participants were asked whether the MOCA-Peds led to any practice or knowledge changes. Nearly all (98%) respondents reported they had “learned, refreshed, or enhanced their medical knowledge” because of the assessment and 62% of pediatricians reported a practice change associated with pilot participation, according to the study, published in Pediatrics. Of those who made a practice change, 70% were general pediatricians and 41% were subspecialists.
Of the 1,727 pediatricians who positively indicated a practice change, 84% reported details about the specific change made. The most common content domains associated with a practice change included ear, nose, and throat; preventive and well-child care; and mental and behavioral health.
Within the content domains, the three most frequently cited instances in which knowledge or a practice change took place included planning the management of a child with otitis media, managing a child with an acute asthma exacerbation, and planning the management of a child with influenza. Of 400 additional responses related to practice changes beyond answers associated with a specific content domain, the three most common subthemes were using evidence-based medicine, expanding review of materials or resource use, and improving differential diagnosis. Pediatricians reported that participation in MOCA-Peds exposed them to new material and encouraged them to review guidelines or standard care protocols and their application. Respondents also reported increased review of materials or resources in practice, updating the types of resources used, and/or an increased effort to stay more updated.
Dr. Turner and associates concluded that the results “support the notion that assessment and learning can be integrated into a single platform and need not be considered mutually exclusive activities, in turn adding value for practicing physicians.”
The studies were funded by the American Board of Pediatrics Foundation. Dr. Leslie, Dr. Linda Althouse, Mr. Andrew Bradford, and Mr. Adam L. Turner are employees of The American Board of Pediatrics. Dr. Victoria Dounoucos, Dr. Murrey G. Olmsted, and Ms. Amanda C. Smith are employees of RTI International, an international nonprofit research firm with whom the board contracted to conduct this evaluation.
SOURCE: Leslie LK et al. Pediatrics. Nov. 2019 Nov. doi: 10.1542/peds.2019-2303; Turner AL et al. Pediatrics. 2019 Nov. doi: 10.1542/peds.2019-2305.
two recent surveys show.
Lead author Laurel K. Leslie, MD, of Tufts University, Boston, and colleagues analyzed the perceptions of 4,238 pediatricians who participated in a pilot MOC program in 2017 and completed a fourth-quarter survey, a voluntary end-of-year survey, or both surveys. The new MOC option was developed by the American Board of Pediatrics between 2015 and 2016 as an alternative to the current proctored, closed-book general pediatrics (GP) MOC examination. The Maintenance of Certification Assessment for Pediatrics (MOCA-Peds) includes timed, multiple-choice questions delivered quarterly through a Web-based interface, provides resources to help answer questions, and yields immediate feedback, rationale, and references pertaining to answers.
Of the pediatricians surveyed, 93% considered the MOCA-Peds to be a feasible and acceptable alternative to the traditional MOC GP examination, and 89% of pediatricians indicated they would chose the MOCA-Peds model over the proctored examination, according to the study, published in Pediatrics. Of doctors who completed the quarter 4 survey, 88% agreed or strongly agreed that assessment questions aligned with the stated learning objectives, 82% agreed the questions assessed clinical judgment, 82% agreed the questions were relevant to the practice of GP, and 59% agreed the questions were relevant to their specific practice setting, according to the study. For most pediatricians surveyed, the time to answer questions was sufficient (78%).
Regarding potential anxiety associated with MOC, 89% of doctors surveyed agreed that they felt less anxiety participating in the MOCA-Peds compared with the proctored examination, and that any anxiety they felt about the MOCA-Peds lessened during the pilot as their comfort with the assessment grew (81%). When asked whether they would partake in MOCA-Peds in the future, 97% of general pediatricians and 95% of subspecialists planned to participate in MOCA-Peds to maintain their GP certification; 95% of subspecialists said they would participate in MOCA-Peds to maintain their subspecialty certification.
In a second analysis of the same study population led by Adam L. Turner, MPH, of the American Board of Pediatrics, participants were asked whether the MOCA-Peds led to any practice or knowledge changes. Nearly all (98%) respondents reported they had “learned, refreshed, or enhanced their medical knowledge” because of the assessment and 62% of pediatricians reported a practice change associated with pilot participation, according to the study, published in Pediatrics. Of those who made a practice change, 70% were general pediatricians and 41% were subspecialists.
Of the 1,727 pediatricians who positively indicated a practice change, 84% reported details about the specific change made. The most common content domains associated with a practice change included ear, nose, and throat; preventive and well-child care; and mental and behavioral health.
Within the content domains, the three most frequently cited instances in which knowledge or a practice change took place included planning the management of a child with otitis media, managing a child with an acute asthma exacerbation, and planning the management of a child with influenza. Of 400 additional responses related to practice changes beyond answers associated with a specific content domain, the three most common subthemes were using evidence-based medicine, expanding review of materials or resource use, and improving differential diagnosis. Pediatricians reported that participation in MOCA-Peds exposed them to new material and encouraged them to review guidelines or standard care protocols and their application. Respondents also reported increased review of materials or resources in practice, updating the types of resources used, and/or an increased effort to stay more updated.
Dr. Turner and associates concluded that the results “support the notion that assessment and learning can be integrated into a single platform and need not be considered mutually exclusive activities, in turn adding value for practicing physicians.”
The studies were funded by the American Board of Pediatrics Foundation. Dr. Leslie, Dr. Linda Althouse, Mr. Andrew Bradford, and Mr. Adam L. Turner are employees of The American Board of Pediatrics. Dr. Victoria Dounoucos, Dr. Murrey G. Olmsted, and Ms. Amanda C. Smith are employees of RTI International, an international nonprofit research firm with whom the board contracted to conduct this evaluation.
SOURCE: Leslie LK et al. Pediatrics. Nov. 2019 Nov. doi: 10.1542/peds.2019-2303; Turner AL et al. Pediatrics. 2019 Nov. doi: 10.1542/peds.2019-2305.
Court strikes down Trump’s conscience rule
A federal court has struck down a Trump administration rule that would have allowed clinicians to refuse to provide medical care to patients for religious or moral reasons.
In a Nov. 6 decision, the U.S. District Court for the Southern District of New York vacated President Trump’s rule in its entirety, concluding that the rule had no justification and that its provisions were arbitrary and capricious. In his 147-page opinion, District Judge Paul Engelmayer wrote that the U.S. Department of Health & Human Services did not have the authority to enact such an expansive rule and that the measure conflicts with the Administrative Procedure Act, Title VII of the Civil Rights Act, and the Emergency Medical Treatment & Labor Act, among other laws.
“Had the court found only narrow parts of the rule infirm, a remedy tailoring the vacatur to only the problematic provision might well have been viable,” Judge Engelmayer wrote. “The [Administrative Procedure Act] violations that the court has found, however, are numerous, fundamental, and far reaching ... In these circumstances, a decision to leave standing isolated shards of the rule that have not been found specifically infirm would ignore the big picture: that the rulemaking exercise here was sufficiently shot through with glaring legal defects as to not justify a search for survivors [and] leaving stray nonsubstantive provisions intact would not serve a useful purpose.”
At press time, the Trump administration had not indicated whether they plan to file an appeal.
Clare Coleman, president & CEO for the National Family Planning & Reproductive Health Association, a plaintiff in the case, said the organization was heartened by the ruling and that the judge’s decision protects health care for millions of Americans.
“The court safeguarded the public’s health by striking down the Trump administration’s health care refusal rule,” Ms. Coleman said in a statement. “This unlawful rule is an outright attack on the health and wellness of millions of people across the country, and the court heard clear and compelling arguments about the harm communities face when our health care system is distorted to the point in which a patient’s health care needs are not paramount.”
The conscience rule, finalized in May 2019 by HHS, would have allowed clinicians to refuse care to patients if they deemed that care was in conflict with their religious or moral beliefs. The provisions principally – although not exclusively – addressed objections to abortion, sterilization, and assisted suicide, as well as counseling and referrals associated with these services.
According to HHS, the final rule fulfills President Trump’s promise to promote and protect rights of conscience and religious liberty. “This rule ensures that health care entities and professionals won’t be bullied out of the health care field because they decline to participate in actions that violate their conscience, including the taking of human life,” Roger Severino, director of the Office for Civil Rights, said in a statement. “Protecting conscience and religious freedom not only fosters greater diversity in health care, it’s the law.”
The judge’s order invalidating the rule consolidated three legal challenges against HHS over the rule. Plaintiffs included more than 15 states, Planned Parenthood Federation of America, and the National Family Planning & Reproductive Health Association, among others. The plaintiffs argued that the rule, scheduled to take effect on Nov. 22, would have threatened the ability of clinicians to provide essential, potentially life-saving medical care and would have exacerbated health disparities.
Stephanie Taub, senior counsel at the First Liberty Institute, an organization that represents religious freedom cases, said the court’s decision leaves health care professionals across America vulnerable to being forced “to perform, facilitate, or refer for procedures that violate their conscience.”
“The Trump administration’s HHS protections would ensure that health care professionals are free to work consistent with their religious beliefs while providing the best care to their patients,” Ms. Taub said in a statement.
The court’s decision comes less than a week after another district judge temporarily blocked an order by President Trump that would make having health insurance, or the ability to pay for medical care, a requirement for immigrants seeking U.S. visas. In that case, the judge said there are serious questions about whether President Trump’s immigration rule was arbitrary and capricious and, therefore, a violation of the Administrative Procedure Act. The order is on hold while the case continues through the courts.
A federal court has struck down a Trump administration rule that would have allowed clinicians to refuse to provide medical care to patients for religious or moral reasons.
In a Nov. 6 decision, the U.S. District Court for the Southern District of New York vacated President Trump’s rule in its entirety, concluding that the rule had no justification and that its provisions were arbitrary and capricious. In his 147-page opinion, District Judge Paul Engelmayer wrote that the U.S. Department of Health & Human Services did not have the authority to enact such an expansive rule and that the measure conflicts with the Administrative Procedure Act, Title VII of the Civil Rights Act, and the Emergency Medical Treatment & Labor Act, among other laws.
“Had the court found only narrow parts of the rule infirm, a remedy tailoring the vacatur to only the problematic provision might well have been viable,” Judge Engelmayer wrote. “The [Administrative Procedure Act] violations that the court has found, however, are numerous, fundamental, and far reaching ... In these circumstances, a decision to leave standing isolated shards of the rule that have not been found specifically infirm would ignore the big picture: that the rulemaking exercise here was sufficiently shot through with glaring legal defects as to not justify a search for survivors [and] leaving stray nonsubstantive provisions intact would not serve a useful purpose.”
At press time, the Trump administration had not indicated whether they plan to file an appeal.
Clare Coleman, president & CEO for the National Family Planning & Reproductive Health Association, a plaintiff in the case, said the organization was heartened by the ruling and that the judge’s decision protects health care for millions of Americans.
“The court safeguarded the public’s health by striking down the Trump administration’s health care refusal rule,” Ms. Coleman said in a statement. “This unlawful rule is an outright attack on the health and wellness of millions of people across the country, and the court heard clear and compelling arguments about the harm communities face when our health care system is distorted to the point in which a patient’s health care needs are not paramount.”
The conscience rule, finalized in May 2019 by HHS, would have allowed clinicians to refuse care to patients if they deemed that care was in conflict with their religious or moral beliefs. The provisions principally – although not exclusively – addressed objections to abortion, sterilization, and assisted suicide, as well as counseling and referrals associated with these services.
According to HHS, the final rule fulfills President Trump’s promise to promote and protect rights of conscience and religious liberty. “This rule ensures that health care entities and professionals won’t be bullied out of the health care field because they decline to participate in actions that violate their conscience, including the taking of human life,” Roger Severino, director of the Office for Civil Rights, said in a statement. “Protecting conscience and religious freedom not only fosters greater diversity in health care, it’s the law.”
The judge’s order invalidating the rule consolidated three legal challenges against HHS over the rule. Plaintiffs included more than 15 states, Planned Parenthood Federation of America, and the National Family Planning & Reproductive Health Association, among others. The plaintiffs argued that the rule, scheduled to take effect on Nov. 22, would have threatened the ability of clinicians to provide essential, potentially life-saving medical care and would have exacerbated health disparities.
Stephanie Taub, senior counsel at the First Liberty Institute, an organization that represents religious freedom cases, said the court’s decision leaves health care professionals across America vulnerable to being forced “to perform, facilitate, or refer for procedures that violate their conscience.”
“The Trump administration’s HHS protections would ensure that health care professionals are free to work consistent with their religious beliefs while providing the best care to their patients,” Ms. Taub said in a statement.
The court’s decision comes less than a week after another district judge temporarily blocked an order by President Trump that would make having health insurance, or the ability to pay for medical care, a requirement for immigrants seeking U.S. visas. In that case, the judge said there are serious questions about whether President Trump’s immigration rule was arbitrary and capricious and, therefore, a violation of the Administrative Procedure Act. The order is on hold while the case continues through the courts.
A federal court has struck down a Trump administration rule that would have allowed clinicians to refuse to provide medical care to patients for religious or moral reasons.
In a Nov. 6 decision, the U.S. District Court for the Southern District of New York vacated President Trump’s rule in its entirety, concluding that the rule had no justification and that its provisions were arbitrary and capricious. In his 147-page opinion, District Judge Paul Engelmayer wrote that the U.S. Department of Health & Human Services did not have the authority to enact such an expansive rule and that the measure conflicts with the Administrative Procedure Act, Title VII of the Civil Rights Act, and the Emergency Medical Treatment & Labor Act, among other laws.
“Had the court found only narrow parts of the rule infirm, a remedy tailoring the vacatur to only the problematic provision might well have been viable,” Judge Engelmayer wrote. “The [Administrative Procedure Act] violations that the court has found, however, are numerous, fundamental, and far reaching ... In these circumstances, a decision to leave standing isolated shards of the rule that have not been found specifically infirm would ignore the big picture: that the rulemaking exercise here was sufficiently shot through with glaring legal defects as to not justify a search for survivors [and] leaving stray nonsubstantive provisions intact would not serve a useful purpose.”
At press time, the Trump administration had not indicated whether they plan to file an appeal.
Clare Coleman, president & CEO for the National Family Planning & Reproductive Health Association, a plaintiff in the case, said the organization was heartened by the ruling and that the judge’s decision protects health care for millions of Americans.
“The court safeguarded the public’s health by striking down the Trump administration’s health care refusal rule,” Ms. Coleman said in a statement. “This unlawful rule is an outright attack on the health and wellness of millions of people across the country, and the court heard clear and compelling arguments about the harm communities face when our health care system is distorted to the point in which a patient’s health care needs are not paramount.”
The conscience rule, finalized in May 2019 by HHS, would have allowed clinicians to refuse care to patients if they deemed that care was in conflict with their religious or moral beliefs. The provisions principally – although not exclusively – addressed objections to abortion, sterilization, and assisted suicide, as well as counseling and referrals associated with these services.
According to HHS, the final rule fulfills President Trump’s promise to promote and protect rights of conscience and religious liberty. “This rule ensures that health care entities and professionals won’t be bullied out of the health care field because they decline to participate in actions that violate their conscience, including the taking of human life,” Roger Severino, director of the Office for Civil Rights, said in a statement. “Protecting conscience and religious freedom not only fosters greater diversity in health care, it’s the law.”
The judge’s order invalidating the rule consolidated three legal challenges against HHS over the rule. Plaintiffs included more than 15 states, Planned Parenthood Federation of America, and the National Family Planning & Reproductive Health Association, among others. The plaintiffs argued that the rule, scheduled to take effect on Nov. 22, would have threatened the ability of clinicians to provide essential, potentially life-saving medical care and would have exacerbated health disparities.
Stephanie Taub, senior counsel at the First Liberty Institute, an organization that represents religious freedom cases, said the court’s decision leaves health care professionals across America vulnerable to being forced “to perform, facilitate, or refer for procedures that violate their conscience.”
“The Trump administration’s HHS protections would ensure that health care professionals are free to work consistent with their religious beliefs while providing the best care to their patients,” Ms. Taub said in a statement.
The court’s decision comes less than a week after another district judge temporarily blocked an order by President Trump that would make having health insurance, or the ability to pay for medical care, a requirement for immigrants seeking U.S. visas. In that case, the judge said there are serious questions about whether President Trump’s immigration rule was arbitrary and capricious and, therefore, a violation of the Administrative Procedure Act. The order is on hold while the case continues through the courts.
The fundamental things apply
Dear Colleagues,
or questions about cosmetic procedures or skin care advice.
Needle nippers were around, but no elaborate, molded-plastic contraptions like the sharps containers now in wide use. You sent pathology specimens in plastic cylinders by U.S. mail; then you called the lab 2 weeks later to ask, “Where’s the report on Jane Smith, with the rule out melanoma,” and the lab said, “Jane who?”
Of course, some things about practice have not changed. Patients with atopic dermatitis still ask why eczema comes back and why we can’t give them something to make it go away once and for all. Some referring physicians still treat scaly rashes with ketoconazole cream (and when that fails, oral fluconazole, which doesn’t work either).
Of course the biggest change between then and now, coincident with the rise of computers and technology, is the advent and ubiquity of that great swindle foisted upon the profession and the public – electronic health records – with their unfulfilled promises of cost-savings and efficiency and unconceded consequences: turning healers into harried data-entry drudges too busy clicking mice to make eye contact with humans. Yes, the Emperor has clothes. The Emperor is wearing Depends.
I wrote my first column for this periodical 22 years ago; this will be my last. My wonderful editor, Elizabeth Mechcatie, has agreed to take under advisement a proposal that I go on sending occasional dispatches under the heading “Pruritus Emeritus.” My family used to refer to those in the anomalous state of being emeritus – it means, roughly, “Forgotten, but not gone” – by rhyming emeritus with sinusitis.
There is no way to remember 40 years of patients. Many came just once, others several times. Some moved away, some passed away, changed primary doctors, changed insurances. Some grew too old to visit, sent regretful notes apologizing for finding the drive too long, the parking too hard. Some returned after an absence of a decade or 3, having forgotten that they had once come for the same problem, or come at all.
But there have been other patients who formed a real bond, whose names and faces still come readily to mind, who visited over long periods, sent their spouses, family members, even children and grandchildren. The stories of their lives became part of mine, and sometimes mine part of theirs.
Though hardly an old-movie buff, I know the famous scene in Casablanca in which a radiant Ingrid Bergman (that skin!) asks Dooley Wilson – the piano player, Sam – to play the song Humphrey Bogart does not want to hear:
“You must remember this
A kiss is just a kiss
A sigh is just a sigh
The fundamental things apply
As time goes by.”
Over the last 40 years there have been substantial advances in the way we treat patients, though perhaps not enough to justify the endless noisy hype about imminent breakthroughs and looming disruptions, therapies, and apps that are sure to change practice and civilization as we know them. Altogether too much noise, at least for my taste. But not inside the examining room.
Outside the room rages the din of demographic updates, of online checks of insurance eligibility, referral status, prior authorizations, the blare of marketing and promotion, the cacophony of metrics and algorithms.
Inside the room, however, quiet reigns. A patient presents with a symptom or a sign, or the fear of a symptom or anxiety over the meaning of a sign, filtered through a jumble of ideas – misremembered, half understood, at times mutually contradictory – that amplify fears common to anyone who visits a practitioner, however minor the presenting complaint: pain, debility, decline, isolation, solitude, death.
And the practitioner attends, considers, contextualizes, counsels, consoles, and conveys a response to the patient’s questions, whether in so many words or by body language or tone of voice, offers answers not just to what the patient has asked but the ones the patient meant to ask but did not know how.
“Yes, sir, death waits for all of us in the end, but for you, perhaps, not today.”
“Yes, madam, illness can be a frightening affair, but your case is not as bad as you think it is and won’t move as fast as you imagine. And as to your being limited and alone – well, not yet. There are those you can rely on, people with a bit of knowledge and a little experience, who are committed to doing what can be done to bend the arc of illness in your favor.”
That fundamental role will, it seems to me, always apply as long people practice medicine.
With all good wishes for personal happiness and professional success,
Alan Rockoff
Dear Colleagues,
or questions about cosmetic procedures or skin care advice.
Needle nippers were around, but no elaborate, molded-plastic contraptions like the sharps containers now in wide use. You sent pathology specimens in plastic cylinders by U.S. mail; then you called the lab 2 weeks later to ask, “Where’s the report on Jane Smith, with the rule out melanoma,” and the lab said, “Jane who?”
Of course, some things about practice have not changed. Patients with atopic dermatitis still ask why eczema comes back and why we can’t give them something to make it go away once and for all. Some referring physicians still treat scaly rashes with ketoconazole cream (and when that fails, oral fluconazole, which doesn’t work either).
Of course the biggest change between then and now, coincident with the rise of computers and technology, is the advent and ubiquity of that great swindle foisted upon the profession and the public – electronic health records – with their unfulfilled promises of cost-savings and efficiency and unconceded consequences: turning healers into harried data-entry drudges too busy clicking mice to make eye contact with humans. Yes, the Emperor has clothes. The Emperor is wearing Depends.
I wrote my first column for this periodical 22 years ago; this will be my last. My wonderful editor, Elizabeth Mechcatie, has agreed to take under advisement a proposal that I go on sending occasional dispatches under the heading “Pruritus Emeritus.” My family used to refer to those in the anomalous state of being emeritus – it means, roughly, “Forgotten, but not gone” – by rhyming emeritus with sinusitis.
There is no way to remember 40 years of patients. Many came just once, others several times. Some moved away, some passed away, changed primary doctors, changed insurances. Some grew too old to visit, sent regretful notes apologizing for finding the drive too long, the parking too hard. Some returned after an absence of a decade or 3, having forgotten that they had once come for the same problem, or come at all.
But there have been other patients who formed a real bond, whose names and faces still come readily to mind, who visited over long periods, sent their spouses, family members, even children and grandchildren. The stories of their lives became part of mine, and sometimes mine part of theirs.
Though hardly an old-movie buff, I know the famous scene in Casablanca in which a radiant Ingrid Bergman (that skin!) asks Dooley Wilson – the piano player, Sam – to play the song Humphrey Bogart does not want to hear:
“You must remember this
A kiss is just a kiss
A sigh is just a sigh
The fundamental things apply
As time goes by.”
Over the last 40 years there have been substantial advances in the way we treat patients, though perhaps not enough to justify the endless noisy hype about imminent breakthroughs and looming disruptions, therapies, and apps that are sure to change practice and civilization as we know them. Altogether too much noise, at least for my taste. But not inside the examining room.
Outside the room rages the din of demographic updates, of online checks of insurance eligibility, referral status, prior authorizations, the blare of marketing and promotion, the cacophony of metrics and algorithms.
Inside the room, however, quiet reigns. A patient presents with a symptom or a sign, or the fear of a symptom or anxiety over the meaning of a sign, filtered through a jumble of ideas – misremembered, half understood, at times mutually contradictory – that amplify fears common to anyone who visits a practitioner, however minor the presenting complaint: pain, debility, decline, isolation, solitude, death.
And the practitioner attends, considers, contextualizes, counsels, consoles, and conveys a response to the patient’s questions, whether in so many words or by body language or tone of voice, offers answers not just to what the patient has asked but the ones the patient meant to ask but did not know how.
“Yes, sir, death waits for all of us in the end, but for you, perhaps, not today.”
“Yes, madam, illness can be a frightening affair, but your case is not as bad as you think it is and won’t move as fast as you imagine. And as to your being limited and alone – well, not yet. There are those you can rely on, people with a bit of knowledge and a little experience, who are committed to doing what can be done to bend the arc of illness in your favor.”
That fundamental role will, it seems to me, always apply as long people practice medicine.
With all good wishes for personal happiness and professional success,
Alan Rockoff
Dear Colleagues,
or questions about cosmetic procedures or skin care advice.
Needle nippers were around, but no elaborate, molded-plastic contraptions like the sharps containers now in wide use. You sent pathology specimens in plastic cylinders by U.S. mail; then you called the lab 2 weeks later to ask, “Where’s the report on Jane Smith, with the rule out melanoma,” and the lab said, “Jane who?”
Of course, some things about practice have not changed. Patients with atopic dermatitis still ask why eczema comes back and why we can’t give them something to make it go away once and for all. Some referring physicians still treat scaly rashes with ketoconazole cream (and when that fails, oral fluconazole, which doesn’t work either).
Of course the biggest change between then and now, coincident with the rise of computers and technology, is the advent and ubiquity of that great swindle foisted upon the profession and the public – electronic health records – with their unfulfilled promises of cost-savings and efficiency and unconceded consequences: turning healers into harried data-entry drudges too busy clicking mice to make eye contact with humans. Yes, the Emperor has clothes. The Emperor is wearing Depends.
I wrote my first column for this periodical 22 years ago; this will be my last. My wonderful editor, Elizabeth Mechcatie, has agreed to take under advisement a proposal that I go on sending occasional dispatches under the heading “Pruritus Emeritus.” My family used to refer to those in the anomalous state of being emeritus – it means, roughly, “Forgotten, but not gone” – by rhyming emeritus with sinusitis.
There is no way to remember 40 years of patients. Many came just once, others several times. Some moved away, some passed away, changed primary doctors, changed insurances. Some grew too old to visit, sent regretful notes apologizing for finding the drive too long, the parking too hard. Some returned after an absence of a decade or 3, having forgotten that they had once come for the same problem, or come at all.
But there have been other patients who formed a real bond, whose names and faces still come readily to mind, who visited over long periods, sent their spouses, family members, even children and grandchildren. The stories of their lives became part of mine, and sometimes mine part of theirs.
Though hardly an old-movie buff, I know the famous scene in Casablanca in which a radiant Ingrid Bergman (that skin!) asks Dooley Wilson – the piano player, Sam – to play the song Humphrey Bogart does not want to hear:
“You must remember this
A kiss is just a kiss
A sigh is just a sigh
The fundamental things apply
As time goes by.”
Over the last 40 years there have been substantial advances in the way we treat patients, though perhaps not enough to justify the endless noisy hype about imminent breakthroughs and looming disruptions, therapies, and apps that are sure to change practice and civilization as we know them. Altogether too much noise, at least for my taste. But not inside the examining room.
Outside the room rages the din of demographic updates, of online checks of insurance eligibility, referral status, prior authorizations, the blare of marketing and promotion, the cacophony of metrics and algorithms.
Inside the room, however, quiet reigns. A patient presents with a symptom or a sign, or the fear of a symptom or anxiety over the meaning of a sign, filtered through a jumble of ideas – misremembered, half understood, at times mutually contradictory – that amplify fears common to anyone who visits a practitioner, however minor the presenting complaint: pain, debility, decline, isolation, solitude, death.
And the practitioner attends, considers, contextualizes, counsels, consoles, and conveys a response to the patient’s questions, whether in so many words or by body language or tone of voice, offers answers not just to what the patient has asked but the ones the patient meant to ask but did not know how.
“Yes, sir, death waits for all of us in the end, but for you, perhaps, not today.”
“Yes, madam, illness can be a frightening affair, but your case is not as bad as you think it is and won’t move as fast as you imagine. And as to your being limited and alone – well, not yet. There are those you can rely on, people with a bit of knowledge and a little experience, who are committed to doing what can be done to bend the arc of illness in your favor.”
That fundamental role will, it seems to me, always apply as long people practice medicine.
With all good wishes for personal happiness and professional success,
Alan Rockoff
Strategy critical to surviving drug shortages
NATIONAL HARBOR, MD. –
“Statistically speaking, there is no proof that patients are worse off from drug shortages,” Matt Grissinger, RPh, director of error-reporting programs at the Institute for Safe Medication Practices, told the audience at the annual conference of the Academy of Managed Care Pharmacy. The data and anecdotes he presented suggest the contrary.
As Mr. Grissinger pointed out, drug shortages can create a sequela of events that stress health care workers seeking to find the next-best available and most appropriate therapy for their patients. In the process, numerous medication-related errors can occur, resulting in patient harm, including adverse drug events and even death.
One potential problems is erroneous or inappropriate drug substitution stemming from mis- or uncalculated doses because of factors such as incorrect labeling and lack of knowledge regarding acceptable therapeutic interchanges. Other potential errors include non–therapeutically equivalent drug substitutions, resulting in supraoptimal therapy or overdoses, and unfamiliarity with drug labeling from outsourced facilities.
As a result, patients may experience worse outcomes as a consequence of the drug shortage: Worsening of the disease, disease prolongation, side effects stemming from alternative drug selections, untreated pain, psychological effects, severe electrolyte imbalances, severe acid/base imbalances, and death.
While a paper trail can help piece together clues regarding how a medication error occurred, documentation or lack thereof can also introduce errors when drug shortages occur.
Any changes to a drug order or prescription that deviate from the prescriber’s original request require prescriber approval but can still create opportunities for error. While documenting these changes and updating labeling is essential, appropriate documentation does not always occur and raises the question of who is responsible for making such changes.
Drug shortages also challenge a clinician’s professional judgment. Mr. Grissinger cited an example in which a nurse used half of a 0.5-mg single-use vial of promethazine for a patient requiring a 0.25 mg dose. The nurse wrote on the label that the remainder should be saved. While the vial was manufactured for one-time use, whether to discard the unused contents in a situation of drug shortages required the nurse to make a judgment call. In this case, the nurse chose to save the balance of the drug – a choice Mr. Grissinger stated he might have made had he been in a similar situation.
Additionally, drug shortages can create a climate in which more ethical questions arise – especially with regard to disease states such as cancer.
“If you only have 10 vials of vincristine, who gets it?” Mr. Grissinger asked the audience.
To help answer these difficult life-or-death questions, hospital settings need to engage the ethics committees and social workers.
While education plays a vital role in bringing attention to and addressing errors stemming from drug shortages, Mr. Grissinger cautioned the audience not to rely on education as the solution.
“Education is a poor strategy for addressing drug shortages,” he said. While education can draw awareness to drug shortages and subsequent medication-related errors, Mr. Grissinger recommends that organizations implement strategies to help ameliorate the havoc created by drug shortages.
Drug shortage assessment checklists can help organizations evaluate the impact of shortages by verifying inventory, and proactively searching for alternatives. From there, they can enact strategies such as assigning priority to patients who have the greatest need, altering packaging and concentrations, and finding suitable therapeutic substitutions.
NATIONAL HARBOR, MD. –
“Statistically speaking, there is no proof that patients are worse off from drug shortages,” Matt Grissinger, RPh, director of error-reporting programs at the Institute for Safe Medication Practices, told the audience at the annual conference of the Academy of Managed Care Pharmacy. The data and anecdotes he presented suggest the contrary.
As Mr. Grissinger pointed out, drug shortages can create a sequela of events that stress health care workers seeking to find the next-best available and most appropriate therapy for their patients. In the process, numerous medication-related errors can occur, resulting in patient harm, including adverse drug events and even death.
One potential problems is erroneous or inappropriate drug substitution stemming from mis- or uncalculated doses because of factors such as incorrect labeling and lack of knowledge regarding acceptable therapeutic interchanges. Other potential errors include non–therapeutically equivalent drug substitutions, resulting in supraoptimal therapy or overdoses, and unfamiliarity with drug labeling from outsourced facilities.
As a result, patients may experience worse outcomes as a consequence of the drug shortage: Worsening of the disease, disease prolongation, side effects stemming from alternative drug selections, untreated pain, psychological effects, severe electrolyte imbalances, severe acid/base imbalances, and death.
While a paper trail can help piece together clues regarding how a medication error occurred, documentation or lack thereof can also introduce errors when drug shortages occur.
Any changes to a drug order or prescription that deviate from the prescriber’s original request require prescriber approval but can still create opportunities for error. While documenting these changes and updating labeling is essential, appropriate documentation does not always occur and raises the question of who is responsible for making such changes.
Drug shortages also challenge a clinician’s professional judgment. Mr. Grissinger cited an example in which a nurse used half of a 0.5-mg single-use vial of promethazine for a patient requiring a 0.25 mg dose. The nurse wrote on the label that the remainder should be saved. While the vial was manufactured for one-time use, whether to discard the unused contents in a situation of drug shortages required the nurse to make a judgment call. In this case, the nurse chose to save the balance of the drug – a choice Mr. Grissinger stated he might have made had he been in a similar situation.
Additionally, drug shortages can create a climate in which more ethical questions arise – especially with regard to disease states such as cancer.
“If you only have 10 vials of vincristine, who gets it?” Mr. Grissinger asked the audience.
To help answer these difficult life-or-death questions, hospital settings need to engage the ethics committees and social workers.
While education plays a vital role in bringing attention to and addressing errors stemming from drug shortages, Mr. Grissinger cautioned the audience not to rely on education as the solution.
“Education is a poor strategy for addressing drug shortages,” he said. While education can draw awareness to drug shortages and subsequent medication-related errors, Mr. Grissinger recommends that organizations implement strategies to help ameliorate the havoc created by drug shortages.
Drug shortage assessment checklists can help organizations evaluate the impact of shortages by verifying inventory, and proactively searching for alternatives. From there, they can enact strategies such as assigning priority to patients who have the greatest need, altering packaging and concentrations, and finding suitable therapeutic substitutions.
NATIONAL HARBOR, MD. –
“Statistically speaking, there is no proof that patients are worse off from drug shortages,” Matt Grissinger, RPh, director of error-reporting programs at the Institute for Safe Medication Practices, told the audience at the annual conference of the Academy of Managed Care Pharmacy. The data and anecdotes he presented suggest the contrary.
As Mr. Grissinger pointed out, drug shortages can create a sequela of events that stress health care workers seeking to find the next-best available and most appropriate therapy for their patients. In the process, numerous medication-related errors can occur, resulting in patient harm, including adverse drug events and even death.
One potential problems is erroneous or inappropriate drug substitution stemming from mis- or uncalculated doses because of factors such as incorrect labeling and lack of knowledge regarding acceptable therapeutic interchanges. Other potential errors include non–therapeutically equivalent drug substitutions, resulting in supraoptimal therapy or overdoses, and unfamiliarity with drug labeling from outsourced facilities.
As a result, patients may experience worse outcomes as a consequence of the drug shortage: Worsening of the disease, disease prolongation, side effects stemming from alternative drug selections, untreated pain, psychological effects, severe electrolyte imbalances, severe acid/base imbalances, and death.
While a paper trail can help piece together clues regarding how a medication error occurred, documentation or lack thereof can also introduce errors when drug shortages occur.
Any changes to a drug order or prescription that deviate from the prescriber’s original request require prescriber approval but can still create opportunities for error. While documenting these changes and updating labeling is essential, appropriate documentation does not always occur and raises the question of who is responsible for making such changes.
Drug shortages also challenge a clinician’s professional judgment. Mr. Grissinger cited an example in which a nurse used half of a 0.5-mg single-use vial of promethazine for a patient requiring a 0.25 mg dose. The nurse wrote on the label that the remainder should be saved. While the vial was manufactured for one-time use, whether to discard the unused contents in a situation of drug shortages required the nurse to make a judgment call. In this case, the nurse chose to save the balance of the drug – a choice Mr. Grissinger stated he might have made had he been in a similar situation.
Additionally, drug shortages can create a climate in which more ethical questions arise – especially with regard to disease states such as cancer.
“If you only have 10 vials of vincristine, who gets it?” Mr. Grissinger asked the audience.
To help answer these difficult life-or-death questions, hospital settings need to engage the ethics committees and social workers.
While education plays a vital role in bringing attention to and addressing errors stemming from drug shortages, Mr. Grissinger cautioned the audience not to rely on education as the solution.
“Education is a poor strategy for addressing drug shortages,” he said. While education can draw awareness to drug shortages and subsequent medication-related errors, Mr. Grissinger recommends that organizations implement strategies to help ameliorate the havoc created by drug shortages.
Drug shortage assessment checklists can help organizations evaluate the impact of shortages by verifying inventory, and proactively searching for alternatives. From there, they can enact strategies such as assigning priority to patients who have the greatest need, altering packaging and concentrations, and finding suitable therapeutic substitutions.
REPORTING FROM AMCP NEXUS 2019













