User login
Vitamin D pearls
Case: A 56-year-old man with a history of type 2 diabetes, hypertension, hyperlipidemia, and obesity calls clinic to discuss concerns about COVID-19, stating: “I want to do everything I can to reduce my risk of infection.” In addition to physical distancing, mask wearing, hand hygiene, and control of chronic conditions, which of the following supplements would you recommend for this patient?
1. Coenzyme Q10 160 mg twice a day
2. Vitamin D 2,000 IU daily
3. Vitamin E 400 IU daily
4. Vitamin B12 1,000 mcg daily
Of these choices, vitamin D supplementation is likely the best option, based on the limited data that is available.
Risk factors for worse COVID-19 outcome, such as older age, obesity, and more pigmented skin are also risk factors for vitamin D deficiency. This makes the study of vitamin D and COVID-19 both challenging and relevant.
In a recent study of 7,807 people living in Israel, Merzon and colleagues found that low plasma vitamin D level was an independent risk factor for COVID-19 infection. Mean plasma vitamin D level was significantly lower among those who tested positive for COVID-19 (19.00 ng/mL) than negative (20.55 ng/ mL). After controlling for demographic variables and several medical conditions, the adjusted odds ratio of COVID-19 infection in those with lower vitamin D was 1.45 (95% confidence interval, 1.08-1.95; P < .001). However, the odds of hospitalization for COVID-19 was not significantly associated with vitamin D level.1
Prior studies have also looked at vitamin D and respiratory infection. Martineau and colleagues analyzed 25 randomized, controlled trials with a pooled number of 11,321 individuals, including healthy ones and those with comorbidities, and found that oral vitamin D supplementation in daily or weekly doses had a protective effect against acute respiratory infection (adjusted odds ratio, 0.88; 95% CI, 0.81-0.96; P < .001). Patients with vitamin D deficiency (less than 25 nmol/L) experienced the most protective benefit. Vitamin D did not influence respiratory infection outcome.2
These studies suggest an adequate vitamin D level may be protective against infection with COVID-19, but who will benefit from vitamin D supplementation, and in what dose? Per U.S. Preventive Services Task Force guidelines, there is insufficient evidence to recommend screening for vitamin D deficiency in asymptomatic adults. Regarding daily dietary intake, the Institute of Medicine recommends 600 IU for persons aged 1-70, and 800 IU for those aged over 70 years. Salmon (447 IU per 3 oz serving), tuna (154 IU), and fortified milk (116 IU) are among the most vitamin D–rich foods.3 The recommended upper level of intake is 4,000 IU/day.
Too much of a good thing?
Extra vitamin D is stored in adipose tissue. If it builds up over time, storage sites may be overwhelmed, causing a rise in serum D level. While one might expect a subsequent rise in calcium levels, studies have shown this happens inconsistently, and at very high vitamin D levels, over 120 ng/mL.4 Most people would have to take at least 50,000 IU daily for several months to see an effect. The main adverse outcome of vitamin D toxicity is kidney stones, mediated by increased calcium in the blood and urine.
Several animal models have demonstrated hypervitaminosis D–induced aortic and coronary artery calcification. Like with kidney stones, the mechanism appears to be through increased calcium and phosphate levels. Shroff and colleagues studied serum vitamin D levels and vascular disease in children with renal disease on dialysis and found a U-shaped distribution: Children with both low and high vitamin D levels had significantly increased carotid artery intima-media thickness and calcification.5 Given the specialized nature of this population, it’s unclear whether these results can be generalized to most people. More studies are warranted on this topic.
Other benefits
Vitamin D is perhaps most famous for helping to build strong bones. Avenell and colleagues performed a Cochrane meta-analysis of vitamin D supplementation in older adults and found that vitamin D alone did not significantly reduce the risk of hip or other new fracture. Vitamin D plus calcium supplementation did reduce the risk of hip fracture (nine trials, pooled number of individuals was 49,853; relative risk, 0.84; P = .01).6
A lesser-known benefit of vitamin D is muscle protection. A prospective study out of the Jewish Hospital of Cincinnati followed 146 adults who were intolerant to two or more statins because of muscle side effects and found to have a vitamin D level below 32 ng per mL. Subjects were given vitamin D replacement (50,000 units weekly) and followed for 2 years. On statin rechallenge, 88-95% tolerated a statin with vitamin D levels 53-55 ng/mL.7
Pearl
Vitamin D supplementation may protect against COVID-19 infection and has very low chance of harm at daily doses at or below 4,000 IU. Other benefits of taking vitamin D include bone protection and reduction in statin-induced myopathy. The main adverse effect is kidney stones.
Ms. Sharninghausen is a medical student at the University of Washington, Seattle. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Merzon E et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID‐19 infection: An Israeli population‐based study. FEBS J. 2020. doi: 10.1111/febs.15495.
2. Martineau AR et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583. doi:10.1136/bmj.i6583
3. “How to Get More Vitamin D From Your Food,” Cleveland Clinic. 2019 Oct 23. https://health.clevelandclinic.org/how-to-get-more-vitamin-d-from-your-food/.
4. Galior K et al. Development of vitamin d toxicity from overcorrection of vitamin D Deficiency: A review of case reports. Nutrients. 2018;10(8):953. doi: 10.3390/nu10080953
5. Shroff R et al. A bimodal association of vitamin D levels and vascular disease in children on dialysis. J Am Soc Nephrol. 2008;19(6):1239-46. doi: 10.1681/ASN.2007090993.
6. Avenell A et al. Vitamin D and vitamin D analogues for preventing fractures in post‐menopausal women and older men. Cochrane Database Syst Rev. 2014 Apr 14;2014(4):CD000227. doi: 10.1002/14651858.CD000227.pub4.
7. Khayznikov M et al. Statin intolerance because of myalgia, myositis, myopathy, or myonecrosis can in most cases be safely resolved by vitamin D supplementation. N Am J Med Sci. 2015;7(3):86-93. doi:10.4103/1947-2714.153919
Case: A 56-year-old man with a history of type 2 diabetes, hypertension, hyperlipidemia, and obesity calls clinic to discuss concerns about COVID-19, stating: “I want to do everything I can to reduce my risk of infection.” In addition to physical distancing, mask wearing, hand hygiene, and control of chronic conditions, which of the following supplements would you recommend for this patient?
1. Coenzyme Q10 160 mg twice a day
2. Vitamin D 2,000 IU daily
3. Vitamin E 400 IU daily
4. Vitamin B12 1,000 mcg daily
Of these choices, vitamin D supplementation is likely the best option, based on the limited data that is available.
Risk factors for worse COVID-19 outcome, such as older age, obesity, and more pigmented skin are also risk factors for vitamin D deficiency. This makes the study of vitamin D and COVID-19 both challenging and relevant.
In a recent study of 7,807 people living in Israel, Merzon and colleagues found that low plasma vitamin D level was an independent risk factor for COVID-19 infection. Mean plasma vitamin D level was significantly lower among those who tested positive for COVID-19 (19.00 ng/mL) than negative (20.55 ng/ mL). After controlling for demographic variables and several medical conditions, the adjusted odds ratio of COVID-19 infection in those with lower vitamin D was 1.45 (95% confidence interval, 1.08-1.95; P < .001). However, the odds of hospitalization for COVID-19 was not significantly associated with vitamin D level.1
Prior studies have also looked at vitamin D and respiratory infection. Martineau and colleagues analyzed 25 randomized, controlled trials with a pooled number of 11,321 individuals, including healthy ones and those with comorbidities, and found that oral vitamin D supplementation in daily or weekly doses had a protective effect against acute respiratory infection (adjusted odds ratio, 0.88; 95% CI, 0.81-0.96; P < .001). Patients with vitamin D deficiency (less than 25 nmol/L) experienced the most protective benefit. Vitamin D did not influence respiratory infection outcome.2
These studies suggest an adequate vitamin D level may be protective against infection with COVID-19, but who will benefit from vitamin D supplementation, and in what dose? Per U.S. Preventive Services Task Force guidelines, there is insufficient evidence to recommend screening for vitamin D deficiency in asymptomatic adults. Regarding daily dietary intake, the Institute of Medicine recommends 600 IU for persons aged 1-70, and 800 IU for those aged over 70 years. Salmon (447 IU per 3 oz serving), tuna (154 IU), and fortified milk (116 IU) are among the most vitamin D–rich foods.3 The recommended upper level of intake is 4,000 IU/day.
Too much of a good thing?
Extra vitamin D is stored in adipose tissue. If it builds up over time, storage sites may be overwhelmed, causing a rise in serum D level. While one might expect a subsequent rise in calcium levels, studies have shown this happens inconsistently, and at very high vitamin D levels, over 120 ng/mL.4 Most people would have to take at least 50,000 IU daily for several months to see an effect. The main adverse outcome of vitamin D toxicity is kidney stones, mediated by increased calcium in the blood and urine.
Several animal models have demonstrated hypervitaminosis D–induced aortic and coronary artery calcification. Like with kidney stones, the mechanism appears to be through increased calcium and phosphate levels. Shroff and colleagues studied serum vitamin D levels and vascular disease in children with renal disease on dialysis and found a U-shaped distribution: Children with both low and high vitamin D levels had significantly increased carotid artery intima-media thickness and calcification.5 Given the specialized nature of this population, it’s unclear whether these results can be generalized to most people. More studies are warranted on this topic.
Other benefits
Vitamin D is perhaps most famous for helping to build strong bones. Avenell and colleagues performed a Cochrane meta-analysis of vitamin D supplementation in older adults and found that vitamin D alone did not significantly reduce the risk of hip or other new fracture. Vitamin D plus calcium supplementation did reduce the risk of hip fracture (nine trials, pooled number of individuals was 49,853; relative risk, 0.84; P = .01).6
A lesser-known benefit of vitamin D is muscle protection. A prospective study out of the Jewish Hospital of Cincinnati followed 146 adults who were intolerant to two or more statins because of muscle side effects and found to have a vitamin D level below 32 ng per mL. Subjects were given vitamin D replacement (50,000 units weekly) and followed for 2 years. On statin rechallenge, 88-95% tolerated a statin with vitamin D levels 53-55 ng/mL.7
Pearl
Vitamin D supplementation may protect against COVID-19 infection and has very low chance of harm at daily doses at or below 4,000 IU. Other benefits of taking vitamin D include bone protection and reduction in statin-induced myopathy. The main adverse effect is kidney stones.
Ms. Sharninghausen is a medical student at the University of Washington, Seattle. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Merzon E et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID‐19 infection: An Israeli population‐based study. FEBS J. 2020. doi: 10.1111/febs.15495.
2. Martineau AR et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583. doi:10.1136/bmj.i6583
3. “How to Get More Vitamin D From Your Food,” Cleveland Clinic. 2019 Oct 23. https://health.clevelandclinic.org/how-to-get-more-vitamin-d-from-your-food/.
4. Galior K et al. Development of vitamin d toxicity from overcorrection of vitamin D Deficiency: A review of case reports. Nutrients. 2018;10(8):953. doi: 10.3390/nu10080953
5. Shroff R et al. A bimodal association of vitamin D levels and vascular disease in children on dialysis. J Am Soc Nephrol. 2008;19(6):1239-46. doi: 10.1681/ASN.2007090993.
6. Avenell A et al. Vitamin D and vitamin D analogues for preventing fractures in post‐menopausal women and older men. Cochrane Database Syst Rev. 2014 Apr 14;2014(4):CD000227. doi: 10.1002/14651858.CD000227.pub4.
7. Khayznikov M et al. Statin intolerance because of myalgia, myositis, myopathy, or myonecrosis can in most cases be safely resolved by vitamin D supplementation. N Am J Med Sci. 2015;7(3):86-93. doi:10.4103/1947-2714.153919
Case: A 56-year-old man with a history of type 2 diabetes, hypertension, hyperlipidemia, and obesity calls clinic to discuss concerns about COVID-19, stating: “I want to do everything I can to reduce my risk of infection.” In addition to physical distancing, mask wearing, hand hygiene, and control of chronic conditions, which of the following supplements would you recommend for this patient?
1. Coenzyme Q10 160 mg twice a day
2. Vitamin D 2,000 IU daily
3. Vitamin E 400 IU daily
4. Vitamin B12 1,000 mcg daily
Of these choices, vitamin D supplementation is likely the best option, based on the limited data that is available.
Risk factors for worse COVID-19 outcome, such as older age, obesity, and more pigmented skin are also risk factors for vitamin D deficiency. This makes the study of vitamin D and COVID-19 both challenging and relevant.
In a recent study of 7,807 people living in Israel, Merzon and colleagues found that low plasma vitamin D level was an independent risk factor for COVID-19 infection. Mean plasma vitamin D level was significantly lower among those who tested positive for COVID-19 (19.00 ng/mL) than negative (20.55 ng/ mL). After controlling for demographic variables and several medical conditions, the adjusted odds ratio of COVID-19 infection in those with lower vitamin D was 1.45 (95% confidence interval, 1.08-1.95; P < .001). However, the odds of hospitalization for COVID-19 was not significantly associated with vitamin D level.1
Prior studies have also looked at vitamin D and respiratory infection. Martineau and colleagues analyzed 25 randomized, controlled trials with a pooled number of 11,321 individuals, including healthy ones and those with comorbidities, and found that oral vitamin D supplementation in daily or weekly doses had a protective effect against acute respiratory infection (adjusted odds ratio, 0.88; 95% CI, 0.81-0.96; P < .001). Patients with vitamin D deficiency (less than 25 nmol/L) experienced the most protective benefit. Vitamin D did not influence respiratory infection outcome.2
These studies suggest an adequate vitamin D level may be protective against infection with COVID-19, but who will benefit from vitamin D supplementation, and in what dose? Per U.S. Preventive Services Task Force guidelines, there is insufficient evidence to recommend screening for vitamin D deficiency in asymptomatic adults. Regarding daily dietary intake, the Institute of Medicine recommends 600 IU for persons aged 1-70, and 800 IU for those aged over 70 years. Salmon (447 IU per 3 oz serving), tuna (154 IU), and fortified milk (116 IU) are among the most vitamin D–rich foods.3 The recommended upper level of intake is 4,000 IU/day.
Too much of a good thing?
Extra vitamin D is stored in adipose tissue. If it builds up over time, storage sites may be overwhelmed, causing a rise in serum D level. While one might expect a subsequent rise in calcium levels, studies have shown this happens inconsistently, and at very high vitamin D levels, over 120 ng/mL.4 Most people would have to take at least 50,000 IU daily for several months to see an effect. The main adverse outcome of vitamin D toxicity is kidney stones, mediated by increased calcium in the blood and urine.
Several animal models have demonstrated hypervitaminosis D–induced aortic and coronary artery calcification. Like with kidney stones, the mechanism appears to be through increased calcium and phosphate levels. Shroff and colleagues studied serum vitamin D levels and vascular disease in children with renal disease on dialysis and found a U-shaped distribution: Children with both low and high vitamin D levels had significantly increased carotid artery intima-media thickness and calcification.5 Given the specialized nature of this population, it’s unclear whether these results can be generalized to most people. More studies are warranted on this topic.
Other benefits
Vitamin D is perhaps most famous for helping to build strong bones. Avenell and colleagues performed a Cochrane meta-analysis of vitamin D supplementation in older adults and found that vitamin D alone did not significantly reduce the risk of hip or other new fracture. Vitamin D plus calcium supplementation did reduce the risk of hip fracture (nine trials, pooled number of individuals was 49,853; relative risk, 0.84; P = .01).6
A lesser-known benefit of vitamin D is muscle protection. A prospective study out of the Jewish Hospital of Cincinnati followed 146 adults who were intolerant to two or more statins because of muscle side effects and found to have a vitamin D level below 32 ng per mL. Subjects were given vitamin D replacement (50,000 units weekly) and followed for 2 years. On statin rechallenge, 88-95% tolerated a statin with vitamin D levels 53-55 ng/mL.7
Pearl
Vitamin D supplementation may protect against COVID-19 infection and has very low chance of harm at daily doses at or below 4,000 IU. Other benefits of taking vitamin D include bone protection and reduction in statin-induced myopathy. The main adverse effect is kidney stones.
Ms. Sharninghausen is a medical student at the University of Washington, Seattle. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Merzon E et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID‐19 infection: An Israeli population‐based study. FEBS J. 2020. doi: 10.1111/febs.15495.
2. Martineau AR et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583. doi:10.1136/bmj.i6583
3. “How to Get More Vitamin D From Your Food,” Cleveland Clinic. 2019 Oct 23. https://health.clevelandclinic.org/how-to-get-more-vitamin-d-from-your-food/.
4. Galior K et al. Development of vitamin d toxicity from overcorrection of vitamin D Deficiency: A review of case reports. Nutrients. 2018;10(8):953. doi: 10.3390/nu10080953
5. Shroff R et al. A bimodal association of vitamin D levels and vascular disease in children on dialysis. J Am Soc Nephrol. 2008;19(6):1239-46. doi: 10.1681/ASN.2007090993.
6. Avenell A et al. Vitamin D and vitamin D analogues for preventing fractures in post‐menopausal women and older men. Cochrane Database Syst Rev. 2014 Apr 14;2014(4):CD000227. doi: 10.1002/14651858.CD000227.pub4.
7. Khayznikov M et al. Statin intolerance because of myalgia, myositis, myopathy, or myonecrosis can in most cases be safely resolved by vitamin D supplementation. N Am J Med Sci. 2015;7(3):86-93. doi:10.4103/1947-2714.153919
Heart failure: Practice-changing developments for hospitalists
A recently validated, easy-to-use calculator of predicted 7-day mortality risk in patients presenting with acute decompensated heart failure is well worth incorporating into hospitalist clinical practice, Dustin T. Smith, MD, said at HM20 Virtual, hosted by the Society of Hospital Medicine.
In addition to the EHMRG, other highlights of his wide-ranging update on recent practice-changing developments in heart failure directly relevant to hospitalists included the introduction of a simple, evidence-based tool for differentiating heart failure with preserved ejection fraction from other potential causes of unexplained dyspnea on exertion in euvolemic patients, and a study debunking what has been called the potassium repletion reflex in patients with acute heart failure undergoing diuresis.
The ACUTE study
Heart failure is an area of special interest for Dr. Smith. He has been surprised to find that virtually no hospitalists, emergency medicine physicians, or cardiologists he has spoken with have heard of the EHMRG or its validation in the ACUTE (Acute Congestive Heart Failure Urgent Care Evaluation) study. Yet this is a very handy tool for hospitalists, he observed.
The EHMRG algorithm utilizes nine variables for which data is readily available for every patient who arrives at the emergency department with acute heart failure. The variables are age, arrival by ambulance, heart rate, systolic blood pressure, potassium level, oxygen saturation, troponin, serum creatine, and presence or absence of active cancer. The information is entered into a cell phone app, which spits out the patient’s estimated 7-day mortality risk. The algorithm divides patients into one of five risk groups ranging from very low to very high. With the addition of data input as to the presence or absence of ST-segment depression on the 12-lead ECG, the weighted algorithm will simultaneously generate an estimated 30-day mortality risk.
ACUTE was a prospective, observational, real-world validation study of EHMRG involving 1,983 patients seeking emergency department care for acute heart failure at nine Canadian hospitals. The actual 7-day mortality rate was 0% in the very-low-risk group, 0% in the low-risk group, 0.6% with an intermediate-risk EHMRG, 1.9% with high risk, and 3.9% in the very-high-risk group. The corresponding 30-day mortality rates were 0%, 1.9%, 3.9%, 5.9%, and 14.3%.
The University of Toronto investigators also asked participating physicians for their clinical estimates of 7-day mortality risk while blinded to the EHMRG predictions. The algorithm proved more accurate than physician predictions across the board. Indeed, physicians consistently overestimated the mortality risk for all categories except the very-high-risk one, where they underestimated the true risk (Circulation. 2019 Feb 26;139[9]:1146-56).
Given that heart failure remains year after year at the top of the list of most frequent causes for hospital admission, and that there is compelling evidence that many low-risk patients get hospitalized while potentially unsafe early discharges also occur, the EHMRG score fills an important unmet need.
“I think this can help inform us as to who with acute heart failure potentially needs to come into the hospital and who doesn’t,” Dr. Smith said. “I think the sweet spot here is that if you’re in the low- or very-low-risk category, your 7-day mortality is less than 1%; in fact, in this study it’s zero. But once you get to category 3 – the intermediate category – you’re talking about a 7-day mortality of 1%-2%, which I think is high enough to warrant hospital admission for treatment and to watch them, not just send them home.”
The H2FPEF score
Diagnosis of heart failure with preserved ejection fraction (HFpEF) is a challenge in euvolemic patients with clear lungs and dyspnea on exertion. Investigators at the Mayo Clinic have developed and subsequently validated a weighted score known as the H2FPEF score that’s of great assistance in this task. The score is based upon a set of six simple variables universally available in patients undergoing diagnostic workup for the numerous potential causes for dyspnea on exertion. Together these six variables comprise the acronym H2FPEF:
- Heavy: One point for a BMI greater than 30 kg/m2.
- Hypertension: One point for being on two or more antihypertensive drugs.
- Atrial fibrillation: Three points for paroxysmal or persistent AF.
- Pulmonary hypertension: One point for having a Doppler echocardiographic estimated pulmonary artery systolic pressure greater than 35 mm Hg.
- Elder: One point for age greater than 60 years.
- Filling pressure: One point for a Doppler echocardiographic E/e’ ratio above 9.
The total score can range from 0 to 9. (Circulation. 2018 Aug 28;138[9]:861-70).
Each 1-point increase in the score essentially doubled a patient’s risk of having HFpEF as opposed to pulmonary embolism or some other cause for the dyspnea.
“I really like this H2FPEF score. The score works very, very well. Once you get to a score of 6 or above, the probability of HFpEF is more than 90%, which is pretty powerful. I think this is worthwhile,” Dr. Smith said.
In their derivation and validation cohorts, the Mayo Clinic investigators used as their gold standard for diagnosis of HFpEF invasive hemodynamic exercise testing with a pulmonary artery catheter in place to measure pressures. A score that enables hospitalists to lessen the need for that kind of costly invasive testing is most welcome.
“Here’s how I’d use this score: With an H2FPEF score of 0-1, HFpEF is unlikely. With an intermediate score of 2-5, additional testing is warranted. If the score is high, 6-9, I think HFpEF is likely,” the hospitalist said.
Dr. Smith isn’t the only big fan of the H2FPEF score. In an editorial accompanying publication of the score’s validation study, Walter J. Paulus, MD, PhD, hailed the H2FPEF score as “a unique tour de force” which constitutes a major advance beyond the confusing diagnostic recommendations for HFpEF issued by the European Society of Cardiology and the American Society of Echocardiography, which he said have been “met by skepticism qualifying them as overcomplicated and even triggered disbelief in the existence of HFpEF.”
Particularly interesting were the variables rejected for inclusion in the H2FPEF score because they failed to achieve statistical significance as predictors, even though they’re often considered important in defining HFpEF, he noted. These included left atrial volume index, sex, and levels of circulating N-terminal probrain natriuretic peptide, wrote Dr. Paulus, professor of cardiac pathophysiology at VU University, Amsterdam.
Debunking the potassium repletion reflex
Longstanding conventional wisdom holds that patients hospitalized for heart failure need to maintain a serum potassium above 4.0 mEq/L.
“I’m sure you’ve all written orders to keep the potassium greater than 4.0 mEq/L and the magnesium above 2mEq/L about a million times, like I have,” Dr. Smith said.
But it turns out this traditional practice, which involves a huge cost in terms of time, money, and health care resources, is supported by weak evidence – and an important recent study has now debunked what the investigators termed the potassium “repletion reflex.”
The investigators at the University of Massachusetts identified 4,995 patients admitted with exacerbation of acute heart failure and a normal admission serum potassium level of 3.5-5.0 mEq/L. More than 70% received potassium repletion at least once within a 72-hour observation window, during which 2,080 patients maintained a low-normal serum potassium below 4.0 mEq/L, 2,326 had a mid-normal level of 4.0-4.5 mEq/L, and 589 had a high-normal level of more than 4.5 mEq/L but not more than 5.0 mEq/L.
The study had three endpoints: in-hospital mortality, transfer to the intensive care unit, and hospital length of stay. After statistical adjustment for comorbidities, demographics, and severity at admission, there was no difference between the low- and mid-normal serum potassium groups in any of the three endpoints. In contrast, the high-normal potassium group had a significantly longer length of stay, by a median of 0.6 extra days. The high-normal group also had a 78% increased likelihood of ICU transfer and a 51% increased risk of in-hospital mortality, although neither of these differences reached statistical significance (J Hosp Med. 2019 Dec 1;14[12]:729-36).
“A potassium greater than 4.5 mEq/L may be associated with increased risk of worse outcomes,” Dr. Smith observed. “I think the sweet spot may be 3.5-4.5 mEq/L based on this study.”
He reported having no financial conflicts regarding his presentation.
A recently validated, easy-to-use calculator of predicted 7-day mortality risk in patients presenting with acute decompensated heart failure is well worth incorporating into hospitalist clinical practice, Dustin T. Smith, MD, said at HM20 Virtual, hosted by the Society of Hospital Medicine.
In addition to the EHMRG, other highlights of his wide-ranging update on recent practice-changing developments in heart failure directly relevant to hospitalists included the introduction of a simple, evidence-based tool for differentiating heart failure with preserved ejection fraction from other potential causes of unexplained dyspnea on exertion in euvolemic patients, and a study debunking what has been called the potassium repletion reflex in patients with acute heart failure undergoing diuresis.
The ACUTE study
Heart failure is an area of special interest for Dr. Smith. He has been surprised to find that virtually no hospitalists, emergency medicine physicians, or cardiologists he has spoken with have heard of the EHMRG or its validation in the ACUTE (Acute Congestive Heart Failure Urgent Care Evaluation) study. Yet this is a very handy tool for hospitalists, he observed.
The EHMRG algorithm utilizes nine variables for which data is readily available for every patient who arrives at the emergency department with acute heart failure. The variables are age, arrival by ambulance, heart rate, systolic blood pressure, potassium level, oxygen saturation, troponin, serum creatine, and presence or absence of active cancer. The information is entered into a cell phone app, which spits out the patient’s estimated 7-day mortality risk. The algorithm divides patients into one of five risk groups ranging from very low to very high. With the addition of data input as to the presence or absence of ST-segment depression on the 12-lead ECG, the weighted algorithm will simultaneously generate an estimated 30-day mortality risk.
ACUTE was a prospective, observational, real-world validation study of EHMRG involving 1,983 patients seeking emergency department care for acute heart failure at nine Canadian hospitals. The actual 7-day mortality rate was 0% in the very-low-risk group, 0% in the low-risk group, 0.6% with an intermediate-risk EHMRG, 1.9% with high risk, and 3.9% in the very-high-risk group. The corresponding 30-day mortality rates were 0%, 1.9%, 3.9%, 5.9%, and 14.3%.
The University of Toronto investigators also asked participating physicians for their clinical estimates of 7-day mortality risk while blinded to the EHMRG predictions. The algorithm proved more accurate than physician predictions across the board. Indeed, physicians consistently overestimated the mortality risk for all categories except the very-high-risk one, where they underestimated the true risk (Circulation. 2019 Feb 26;139[9]:1146-56).
Given that heart failure remains year after year at the top of the list of most frequent causes for hospital admission, and that there is compelling evidence that many low-risk patients get hospitalized while potentially unsafe early discharges also occur, the EHMRG score fills an important unmet need.
“I think this can help inform us as to who with acute heart failure potentially needs to come into the hospital and who doesn’t,” Dr. Smith said. “I think the sweet spot here is that if you’re in the low- or very-low-risk category, your 7-day mortality is less than 1%; in fact, in this study it’s zero. But once you get to category 3 – the intermediate category – you’re talking about a 7-day mortality of 1%-2%, which I think is high enough to warrant hospital admission for treatment and to watch them, not just send them home.”
The H2FPEF score
Diagnosis of heart failure with preserved ejection fraction (HFpEF) is a challenge in euvolemic patients with clear lungs and dyspnea on exertion. Investigators at the Mayo Clinic have developed and subsequently validated a weighted score known as the H2FPEF score that’s of great assistance in this task. The score is based upon a set of six simple variables universally available in patients undergoing diagnostic workup for the numerous potential causes for dyspnea on exertion. Together these six variables comprise the acronym H2FPEF:
- Heavy: One point for a BMI greater than 30 kg/m2.
- Hypertension: One point for being on two or more antihypertensive drugs.
- Atrial fibrillation: Three points for paroxysmal or persistent AF.
- Pulmonary hypertension: One point for having a Doppler echocardiographic estimated pulmonary artery systolic pressure greater than 35 mm Hg.
- Elder: One point for age greater than 60 years.
- Filling pressure: One point for a Doppler echocardiographic E/e’ ratio above 9.
The total score can range from 0 to 9. (Circulation. 2018 Aug 28;138[9]:861-70).
Each 1-point increase in the score essentially doubled a patient’s risk of having HFpEF as opposed to pulmonary embolism or some other cause for the dyspnea.
“I really like this H2FPEF score. The score works very, very well. Once you get to a score of 6 or above, the probability of HFpEF is more than 90%, which is pretty powerful. I think this is worthwhile,” Dr. Smith said.
In their derivation and validation cohorts, the Mayo Clinic investigators used as their gold standard for diagnosis of HFpEF invasive hemodynamic exercise testing with a pulmonary artery catheter in place to measure pressures. A score that enables hospitalists to lessen the need for that kind of costly invasive testing is most welcome.
“Here’s how I’d use this score: With an H2FPEF score of 0-1, HFpEF is unlikely. With an intermediate score of 2-5, additional testing is warranted. If the score is high, 6-9, I think HFpEF is likely,” the hospitalist said.
Dr. Smith isn’t the only big fan of the H2FPEF score. In an editorial accompanying publication of the score’s validation study, Walter J. Paulus, MD, PhD, hailed the H2FPEF score as “a unique tour de force” which constitutes a major advance beyond the confusing diagnostic recommendations for HFpEF issued by the European Society of Cardiology and the American Society of Echocardiography, which he said have been “met by skepticism qualifying them as overcomplicated and even triggered disbelief in the existence of HFpEF.”
Particularly interesting were the variables rejected for inclusion in the H2FPEF score because they failed to achieve statistical significance as predictors, even though they’re often considered important in defining HFpEF, he noted. These included left atrial volume index, sex, and levels of circulating N-terminal probrain natriuretic peptide, wrote Dr. Paulus, professor of cardiac pathophysiology at VU University, Amsterdam.
Debunking the potassium repletion reflex
Longstanding conventional wisdom holds that patients hospitalized for heart failure need to maintain a serum potassium above 4.0 mEq/L.
“I’m sure you’ve all written orders to keep the potassium greater than 4.0 mEq/L and the magnesium above 2mEq/L about a million times, like I have,” Dr. Smith said.
But it turns out this traditional practice, which involves a huge cost in terms of time, money, and health care resources, is supported by weak evidence – and an important recent study has now debunked what the investigators termed the potassium “repletion reflex.”
The investigators at the University of Massachusetts identified 4,995 patients admitted with exacerbation of acute heart failure and a normal admission serum potassium level of 3.5-5.0 mEq/L. More than 70% received potassium repletion at least once within a 72-hour observation window, during which 2,080 patients maintained a low-normal serum potassium below 4.0 mEq/L, 2,326 had a mid-normal level of 4.0-4.5 mEq/L, and 589 had a high-normal level of more than 4.5 mEq/L but not more than 5.0 mEq/L.
The study had three endpoints: in-hospital mortality, transfer to the intensive care unit, and hospital length of stay. After statistical adjustment for comorbidities, demographics, and severity at admission, there was no difference between the low- and mid-normal serum potassium groups in any of the three endpoints. In contrast, the high-normal potassium group had a significantly longer length of stay, by a median of 0.6 extra days. The high-normal group also had a 78% increased likelihood of ICU transfer and a 51% increased risk of in-hospital mortality, although neither of these differences reached statistical significance (J Hosp Med. 2019 Dec 1;14[12]:729-36).
“A potassium greater than 4.5 mEq/L may be associated with increased risk of worse outcomes,” Dr. Smith observed. “I think the sweet spot may be 3.5-4.5 mEq/L based on this study.”
He reported having no financial conflicts regarding his presentation.
A recently validated, easy-to-use calculator of predicted 7-day mortality risk in patients presenting with acute decompensated heart failure is well worth incorporating into hospitalist clinical practice, Dustin T. Smith, MD, said at HM20 Virtual, hosted by the Society of Hospital Medicine.
In addition to the EHMRG, other highlights of his wide-ranging update on recent practice-changing developments in heart failure directly relevant to hospitalists included the introduction of a simple, evidence-based tool for differentiating heart failure with preserved ejection fraction from other potential causes of unexplained dyspnea on exertion in euvolemic patients, and a study debunking what has been called the potassium repletion reflex in patients with acute heart failure undergoing diuresis.
The ACUTE study
Heart failure is an area of special interest for Dr. Smith. He has been surprised to find that virtually no hospitalists, emergency medicine physicians, or cardiologists he has spoken with have heard of the EHMRG or its validation in the ACUTE (Acute Congestive Heart Failure Urgent Care Evaluation) study. Yet this is a very handy tool for hospitalists, he observed.
The EHMRG algorithm utilizes nine variables for which data is readily available for every patient who arrives at the emergency department with acute heart failure. The variables are age, arrival by ambulance, heart rate, systolic blood pressure, potassium level, oxygen saturation, troponin, serum creatine, and presence or absence of active cancer. The information is entered into a cell phone app, which spits out the patient’s estimated 7-day mortality risk. The algorithm divides patients into one of five risk groups ranging from very low to very high. With the addition of data input as to the presence or absence of ST-segment depression on the 12-lead ECG, the weighted algorithm will simultaneously generate an estimated 30-day mortality risk.
ACUTE was a prospective, observational, real-world validation study of EHMRG involving 1,983 patients seeking emergency department care for acute heart failure at nine Canadian hospitals. The actual 7-day mortality rate was 0% in the very-low-risk group, 0% in the low-risk group, 0.6% with an intermediate-risk EHMRG, 1.9% with high risk, and 3.9% in the very-high-risk group. The corresponding 30-day mortality rates were 0%, 1.9%, 3.9%, 5.9%, and 14.3%.
The University of Toronto investigators also asked participating physicians for their clinical estimates of 7-day mortality risk while blinded to the EHMRG predictions. The algorithm proved more accurate than physician predictions across the board. Indeed, physicians consistently overestimated the mortality risk for all categories except the very-high-risk one, where they underestimated the true risk (Circulation. 2019 Feb 26;139[9]:1146-56).
Given that heart failure remains year after year at the top of the list of most frequent causes for hospital admission, and that there is compelling evidence that many low-risk patients get hospitalized while potentially unsafe early discharges also occur, the EHMRG score fills an important unmet need.
“I think this can help inform us as to who with acute heart failure potentially needs to come into the hospital and who doesn’t,” Dr. Smith said. “I think the sweet spot here is that if you’re in the low- or very-low-risk category, your 7-day mortality is less than 1%; in fact, in this study it’s zero. But once you get to category 3 – the intermediate category – you’re talking about a 7-day mortality of 1%-2%, which I think is high enough to warrant hospital admission for treatment and to watch them, not just send them home.”
The H2FPEF score
Diagnosis of heart failure with preserved ejection fraction (HFpEF) is a challenge in euvolemic patients with clear lungs and dyspnea on exertion. Investigators at the Mayo Clinic have developed and subsequently validated a weighted score known as the H2FPEF score that’s of great assistance in this task. The score is based upon a set of six simple variables universally available in patients undergoing diagnostic workup for the numerous potential causes for dyspnea on exertion. Together these six variables comprise the acronym H2FPEF:
- Heavy: One point for a BMI greater than 30 kg/m2.
- Hypertension: One point for being on two or more antihypertensive drugs.
- Atrial fibrillation: Three points for paroxysmal or persistent AF.
- Pulmonary hypertension: One point for having a Doppler echocardiographic estimated pulmonary artery systolic pressure greater than 35 mm Hg.
- Elder: One point for age greater than 60 years.
- Filling pressure: One point for a Doppler echocardiographic E/e’ ratio above 9.
The total score can range from 0 to 9. (Circulation. 2018 Aug 28;138[9]:861-70).
Each 1-point increase in the score essentially doubled a patient’s risk of having HFpEF as opposed to pulmonary embolism or some other cause for the dyspnea.
“I really like this H2FPEF score. The score works very, very well. Once you get to a score of 6 or above, the probability of HFpEF is more than 90%, which is pretty powerful. I think this is worthwhile,” Dr. Smith said.
In their derivation and validation cohorts, the Mayo Clinic investigators used as their gold standard for diagnosis of HFpEF invasive hemodynamic exercise testing with a pulmonary artery catheter in place to measure pressures. A score that enables hospitalists to lessen the need for that kind of costly invasive testing is most welcome.
“Here’s how I’d use this score: With an H2FPEF score of 0-1, HFpEF is unlikely. With an intermediate score of 2-5, additional testing is warranted. If the score is high, 6-9, I think HFpEF is likely,” the hospitalist said.
Dr. Smith isn’t the only big fan of the H2FPEF score. In an editorial accompanying publication of the score’s validation study, Walter J. Paulus, MD, PhD, hailed the H2FPEF score as “a unique tour de force” which constitutes a major advance beyond the confusing diagnostic recommendations for HFpEF issued by the European Society of Cardiology and the American Society of Echocardiography, which he said have been “met by skepticism qualifying them as overcomplicated and even triggered disbelief in the existence of HFpEF.”
Particularly interesting were the variables rejected for inclusion in the H2FPEF score because they failed to achieve statistical significance as predictors, even though they’re often considered important in defining HFpEF, he noted. These included left atrial volume index, sex, and levels of circulating N-terminal probrain natriuretic peptide, wrote Dr. Paulus, professor of cardiac pathophysiology at VU University, Amsterdam.
Debunking the potassium repletion reflex
Longstanding conventional wisdom holds that patients hospitalized for heart failure need to maintain a serum potassium above 4.0 mEq/L.
“I’m sure you’ve all written orders to keep the potassium greater than 4.0 mEq/L and the magnesium above 2mEq/L about a million times, like I have,” Dr. Smith said.
But it turns out this traditional practice, which involves a huge cost in terms of time, money, and health care resources, is supported by weak evidence – and an important recent study has now debunked what the investigators termed the potassium “repletion reflex.”
The investigators at the University of Massachusetts identified 4,995 patients admitted with exacerbation of acute heart failure and a normal admission serum potassium level of 3.5-5.0 mEq/L. More than 70% received potassium repletion at least once within a 72-hour observation window, during which 2,080 patients maintained a low-normal serum potassium below 4.0 mEq/L, 2,326 had a mid-normal level of 4.0-4.5 mEq/L, and 589 had a high-normal level of more than 4.5 mEq/L but not more than 5.0 mEq/L.
The study had three endpoints: in-hospital mortality, transfer to the intensive care unit, and hospital length of stay. After statistical adjustment for comorbidities, demographics, and severity at admission, there was no difference between the low- and mid-normal serum potassium groups in any of the three endpoints. In contrast, the high-normal potassium group had a significantly longer length of stay, by a median of 0.6 extra days. The high-normal group also had a 78% increased likelihood of ICU transfer and a 51% increased risk of in-hospital mortality, although neither of these differences reached statistical significance (J Hosp Med. 2019 Dec 1;14[12]:729-36).
“A potassium greater than 4.5 mEq/L may be associated with increased risk of worse outcomes,” Dr. Smith observed. “I think the sweet spot may be 3.5-4.5 mEq/L based on this study.”
He reported having no financial conflicts regarding his presentation.
FROM HM20 VIRTUAL
Nine antihypertensive drugs associated with reduced risk of depression
The risk of depression is elevated in patients with cardiovascular diseases, but several specific antihypertensive therapies are associated with a reduced risk, and none appear to increase the risk, according to a population-based study that evaluated 10 years of data in nearly 4 million subjects.
“As the first study on individual antihypertensives and risk of depression, we found a decreased risk of depression with nine drugs,” reported a collaborative group of investigators from multiple institutions in Denmark where the study was undertaken.
In a study period spanning from 2005 to 2015, risk of a diagnosis of depression was evaluated in patients taking any of 41 antihypertensive therapies in four major categories. These were identified as angiotensin agents (ACE inhibitors or angiotensin II receptor blockers), calcium antagonists, beta-blockers, and diuretics.
Within these groups, agents associated with a reduced risk of depression were: two angiotensin agents, enalapril and ramipril; three calcium antagonists, amlodipine, verapamil, and verapamil combinations; and four beta-blockers, propranolol, atenolol, bisoprolol, and carvedilol. The remaining drugs in these classes and diuretics were not associated with a reduced risk of depression. However, no antihypertensive agent was linked to an increased risk of depression.
All people living in Denmark are assigned a unique personal identification number that permits health information to be tracked across multiple registers. In this study, information was linked for several registries, including the Danish Medical Register on Vital Statistics, the Medicinal Product Statistics, and the Danish Psychiatric Central Register.
Data from a total of 3.75 million patients exposed to antihypertensive therapy during the study period were evaluated. Roughly 1 million of them were exposed to angiotensin drugs and slightly more than a million were exposed to diuretics. For calcium antagonists or beta-blockers, the numbers were approximately 835,000 and 775,000, respectively.
After adjustment for such factors as concomitant somatic diagnoses, sex, age, and employment status, the hazard ratios for depression among drugs associated with protection identified a risk reduction of 10%-25% in most cases when those who had been given 6-10 prescriptions or more than 10 prescriptions were compared with those who received 2 or fewer.
At the level of 10 or more prescriptions, for example, the risk reductions were 17% for ramipril (HR, 0.83; 95% CI, 0.78-0.89), 8% for enalapril (HR, 0.92; 95% CI, 0.88-0.96), 18% for amlodipine (HR, 0.82; 95% CI, 0.79-0.86), 15% for verapamil (HR, 0.85; 95% CI, 0.79-0.83), 28% for propranolol (HR, 0.72; 95% CI, 0.67-0.77), 20% for atenolol (HR, 0.80; 95% CI, 0.74-0.86), 25% for bisoprolol (HR, 0.75; 95% CI, 0.67-0.84), and 16% for carvedilol (HR, 0.84; 95% CI, 0.75-0.95).
For verapamil combinations, the risk reduction was 67% (HR, 0.33; 95% CI, 0.17-0.63), but the investigators cautioned that only 130 individuals were exposed to verapamil combinations, limiting the reliability of this analysis.
Interpreting the findings
A study hypothesis, the observed protective effect against depression, was expected for angiotensin drugs and calcium-channel blockers, but not for beta-blockers, according to the investigators.
“The renin-angiotensin systems is one of the pathways known to modulate inflammation in the central nervous system and seems involved in the regulation of the stress response. Angiotensin agents may also exert anti-inflammatory effects,” the investigators explained. “Dysregulation of intracellular calcium is evident in depression, including receptor-regulated calcium signaling.”
In contrast, beta-blockers have been associated with increased risk of depression in some but not all studies, according to the investigators. They maintained that some clinicians avoid these agents in patients with a history of mood disorders.
In attempting to account for the variability within drug classes regarding protection and lack of protection against depression, the investigators speculated that differences in pharmacologic properties, such as relative lipophilicity or anti-inflammatory effect, might be important.
Despite the large amount of data, William B. White, MD, professor emeritus at the Calhoun Cardiology Center, University of Connecticut, Farmington, is not convinced.
“In observational studies, even those with very large samples sizes, bias and confounding are hard to extricate with controls and propensity-score matching,” Dr. White said. From his perspective, the protective effects of some but not all drugs within a class “give one the impression that the findings are likely random.”
A member of the editorial board of the journal in which this study appeared, Dr. White said he was not involved in the review of the manuscript. Ultimately, he believed that the results are difficult to interpret.
“For example, there is no plausible rationale for why 2 of the 16 ACE inhibitors or angiotensin II receptor blockers or 4 of the 15 beta-blockers or 3 of the 10 calcium-channel blockers would reduce depression while the others in the class would have no effect,” he said.
Despite the investigators’ conclusion that these data should drive drug choice for patients at risk of depression, “I would say the results of this analysis would not lead me to alter clinical practice,” Dr. White added.
According to the principal investigator of the study, Lars Vedel Kessing, MD, DSc, professor of psychiatry at the University of Copenhagen, many variables affect choice of antihypertensive drug. However, the depression risk is elevated in patients with cardiovascular or cerebrovascular disease and hypertension.
When risk of a mood disorder is a concern, use of one of the nine drugs associated with protection from depression should be considered, “especially in patients at increased risk of developing depression, including patients with prior depression or anxiety and patients with a family history of depression,” he and his coinvestigators concluded.
However, Dr. Kessing said in an interview that the data do not help with individual treatment choices. “We do not compare different antihypertensives against each other due to the risk of confounding by indications, so, no, it is not reasonable to consider relative risk among specific agents.”
The authors reported no potential conflicts of interest involving this topic.
SOURCE: Kessing LV et al. Hypertension. 2020 Aug 24. doi: 10.1161/HYPERTENSIONAHA.120.15605.
The risk of depression is elevated in patients with cardiovascular diseases, but several specific antihypertensive therapies are associated with a reduced risk, and none appear to increase the risk, according to a population-based study that evaluated 10 years of data in nearly 4 million subjects.
“As the first study on individual antihypertensives and risk of depression, we found a decreased risk of depression with nine drugs,” reported a collaborative group of investigators from multiple institutions in Denmark where the study was undertaken.
In a study period spanning from 2005 to 2015, risk of a diagnosis of depression was evaluated in patients taking any of 41 antihypertensive therapies in four major categories. These were identified as angiotensin agents (ACE inhibitors or angiotensin II receptor blockers), calcium antagonists, beta-blockers, and diuretics.
Within these groups, agents associated with a reduced risk of depression were: two angiotensin agents, enalapril and ramipril; three calcium antagonists, amlodipine, verapamil, and verapamil combinations; and four beta-blockers, propranolol, atenolol, bisoprolol, and carvedilol. The remaining drugs in these classes and diuretics were not associated with a reduced risk of depression. However, no antihypertensive agent was linked to an increased risk of depression.
All people living in Denmark are assigned a unique personal identification number that permits health information to be tracked across multiple registers. In this study, information was linked for several registries, including the Danish Medical Register on Vital Statistics, the Medicinal Product Statistics, and the Danish Psychiatric Central Register.
Data from a total of 3.75 million patients exposed to antihypertensive therapy during the study period were evaluated. Roughly 1 million of them were exposed to angiotensin drugs and slightly more than a million were exposed to diuretics. For calcium antagonists or beta-blockers, the numbers were approximately 835,000 and 775,000, respectively.
After adjustment for such factors as concomitant somatic diagnoses, sex, age, and employment status, the hazard ratios for depression among drugs associated with protection identified a risk reduction of 10%-25% in most cases when those who had been given 6-10 prescriptions or more than 10 prescriptions were compared with those who received 2 or fewer.
At the level of 10 or more prescriptions, for example, the risk reductions were 17% for ramipril (HR, 0.83; 95% CI, 0.78-0.89), 8% for enalapril (HR, 0.92; 95% CI, 0.88-0.96), 18% for amlodipine (HR, 0.82; 95% CI, 0.79-0.86), 15% for verapamil (HR, 0.85; 95% CI, 0.79-0.83), 28% for propranolol (HR, 0.72; 95% CI, 0.67-0.77), 20% for atenolol (HR, 0.80; 95% CI, 0.74-0.86), 25% for bisoprolol (HR, 0.75; 95% CI, 0.67-0.84), and 16% for carvedilol (HR, 0.84; 95% CI, 0.75-0.95).
For verapamil combinations, the risk reduction was 67% (HR, 0.33; 95% CI, 0.17-0.63), but the investigators cautioned that only 130 individuals were exposed to verapamil combinations, limiting the reliability of this analysis.
Interpreting the findings
A study hypothesis, the observed protective effect against depression, was expected for angiotensin drugs and calcium-channel blockers, but not for beta-blockers, according to the investigators.
“The renin-angiotensin systems is one of the pathways known to modulate inflammation in the central nervous system and seems involved in the regulation of the stress response. Angiotensin agents may also exert anti-inflammatory effects,” the investigators explained. “Dysregulation of intracellular calcium is evident in depression, including receptor-regulated calcium signaling.”
In contrast, beta-blockers have been associated with increased risk of depression in some but not all studies, according to the investigators. They maintained that some clinicians avoid these agents in patients with a history of mood disorders.
In attempting to account for the variability within drug classes regarding protection and lack of protection against depression, the investigators speculated that differences in pharmacologic properties, such as relative lipophilicity or anti-inflammatory effect, might be important.
Despite the large amount of data, William B. White, MD, professor emeritus at the Calhoun Cardiology Center, University of Connecticut, Farmington, is not convinced.
“In observational studies, even those with very large samples sizes, bias and confounding are hard to extricate with controls and propensity-score matching,” Dr. White said. From his perspective, the protective effects of some but not all drugs within a class “give one the impression that the findings are likely random.”
A member of the editorial board of the journal in which this study appeared, Dr. White said he was not involved in the review of the manuscript. Ultimately, he believed that the results are difficult to interpret.
“For example, there is no plausible rationale for why 2 of the 16 ACE inhibitors or angiotensin II receptor blockers or 4 of the 15 beta-blockers or 3 of the 10 calcium-channel blockers would reduce depression while the others in the class would have no effect,” he said.
Despite the investigators’ conclusion that these data should drive drug choice for patients at risk of depression, “I would say the results of this analysis would not lead me to alter clinical practice,” Dr. White added.
According to the principal investigator of the study, Lars Vedel Kessing, MD, DSc, professor of psychiatry at the University of Copenhagen, many variables affect choice of antihypertensive drug. However, the depression risk is elevated in patients with cardiovascular or cerebrovascular disease and hypertension.
When risk of a mood disorder is a concern, use of one of the nine drugs associated with protection from depression should be considered, “especially in patients at increased risk of developing depression, including patients with prior depression or anxiety and patients with a family history of depression,” he and his coinvestigators concluded.
However, Dr. Kessing said in an interview that the data do not help with individual treatment choices. “We do not compare different antihypertensives against each other due to the risk of confounding by indications, so, no, it is not reasonable to consider relative risk among specific agents.”
The authors reported no potential conflicts of interest involving this topic.
SOURCE: Kessing LV et al. Hypertension. 2020 Aug 24. doi: 10.1161/HYPERTENSIONAHA.120.15605.
The risk of depression is elevated in patients with cardiovascular diseases, but several specific antihypertensive therapies are associated with a reduced risk, and none appear to increase the risk, according to a population-based study that evaluated 10 years of data in nearly 4 million subjects.
“As the first study on individual antihypertensives and risk of depression, we found a decreased risk of depression with nine drugs,” reported a collaborative group of investigators from multiple institutions in Denmark where the study was undertaken.
In a study period spanning from 2005 to 2015, risk of a diagnosis of depression was evaluated in patients taking any of 41 antihypertensive therapies in four major categories. These were identified as angiotensin agents (ACE inhibitors or angiotensin II receptor blockers), calcium antagonists, beta-blockers, and diuretics.
Within these groups, agents associated with a reduced risk of depression were: two angiotensin agents, enalapril and ramipril; three calcium antagonists, amlodipine, verapamil, and verapamil combinations; and four beta-blockers, propranolol, atenolol, bisoprolol, and carvedilol. The remaining drugs in these classes and diuretics were not associated with a reduced risk of depression. However, no antihypertensive agent was linked to an increased risk of depression.
All people living in Denmark are assigned a unique personal identification number that permits health information to be tracked across multiple registers. In this study, information was linked for several registries, including the Danish Medical Register on Vital Statistics, the Medicinal Product Statistics, and the Danish Psychiatric Central Register.
Data from a total of 3.75 million patients exposed to antihypertensive therapy during the study period were evaluated. Roughly 1 million of them were exposed to angiotensin drugs and slightly more than a million were exposed to diuretics. For calcium antagonists or beta-blockers, the numbers were approximately 835,000 and 775,000, respectively.
After adjustment for such factors as concomitant somatic diagnoses, sex, age, and employment status, the hazard ratios for depression among drugs associated with protection identified a risk reduction of 10%-25% in most cases when those who had been given 6-10 prescriptions or more than 10 prescriptions were compared with those who received 2 or fewer.
At the level of 10 or more prescriptions, for example, the risk reductions were 17% for ramipril (HR, 0.83; 95% CI, 0.78-0.89), 8% for enalapril (HR, 0.92; 95% CI, 0.88-0.96), 18% for amlodipine (HR, 0.82; 95% CI, 0.79-0.86), 15% for verapamil (HR, 0.85; 95% CI, 0.79-0.83), 28% for propranolol (HR, 0.72; 95% CI, 0.67-0.77), 20% for atenolol (HR, 0.80; 95% CI, 0.74-0.86), 25% for bisoprolol (HR, 0.75; 95% CI, 0.67-0.84), and 16% for carvedilol (HR, 0.84; 95% CI, 0.75-0.95).
For verapamil combinations, the risk reduction was 67% (HR, 0.33; 95% CI, 0.17-0.63), but the investigators cautioned that only 130 individuals were exposed to verapamil combinations, limiting the reliability of this analysis.
Interpreting the findings
A study hypothesis, the observed protective effect against depression, was expected for angiotensin drugs and calcium-channel blockers, but not for beta-blockers, according to the investigators.
“The renin-angiotensin systems is one of the pathways known to modulate inflammation in the central nervous system and seems involved in the regulation of the stress response. Angiotensin agents may also exert anti-inflammatory effects,” the investigators explained. “Dysregulation of intracellular calcium is evident in depression, including receptor-regulated calcium signaling.”
In contrast, beta-blockers have been associated with increased risk of depression in some but not all studies, according to the investigators. They maintained that some clinicians avoid these agents in patients with a history of mood disorders.
In attempting to account for the variability within drug classes regarding protection and lack of protection against depression, the investigators speculated that differences in pharmacologic properties, such as relative lipophilicity or anti-inflammatory effect, might be important.
Despite the large amount of data, William B. White, MD, professor emeritus at the Calhoun Cardiology Center, University of Connecticut, Farmington, is not convinced.
“In observational studies, even those with very large samples sizes, bias and confounding are hard to extricate with controls and propensity-score matching,” Dr. White said. From his perspective, the protective effects of some but not all drugs within a class “give one the impression that the findings are likely random.”
A member of the editorial board of the journal in which this study appeared, Dr. White said he was not involved in the review of the manuscript. Ultimately, he believed that the results are difficult to interpret.
“For example, there is no plausible rationale for why 2 of the 16 ACE inhibitors or angiotensin II receptor blockers or 4 of the 15 beta-blockers or 3 of the 10 calcium-channel blockers would reduce depression while the others in the class would have no effect,” he said.
Despite the investigators’ conclusion that these data should drive drug choice for patients at risk of depression, “I would say the results of this analysis would not lead me to alter clinical practice,” Dr. White added.
According to the principal investigator of the study, Lars Vedel Kessing, MD, DSc, professor of psychiatry at the University of Copenhagen, many variables affect choice of antihypertensive drug. However, the depression risk is elevated in patients with cardiovascular or cerebrovascular disease and hypertension.
When risk of a mood disorder is a concern, use of one of the nine drugs associated with protection from depression should be considered, “especially in patients at increased risk of developing depression, including patients with prior depression or anxiety and patients with a family history of depression,” he and his coinvestigators concluded.
However, Dr. Kessing said in an interview that the data do not help with individual treatment choices. “We do not compare different antihypertensives against each other due to the risk of confounding by indications, so, no, it is not reasonable to consider relative risk among specific agents.”
The authors reported no potential conflicts of interest involving this topic.
SOURCE: Kessing LV et al. Hypertension. 2020 Aug 24. doi: 10.1161/HYPERTENSIONAHA.120.15605.
FROM HYPERTENSION
FDA pulls amputation boxed warning off canagliflozin label
The Food and Drug Administration has removed the boxed warning about the risk of leg and foot amputations for canagliflozin (Invokana, Invokamet, Janssen), a sodium-glucose cotransporter-2 (SGLT2) inhibitor for the treatment of type 2 diabetes, the agency announced Aug. 26.
As previously reported by Medscape Medical News, the FDA added the boxed warning to the canagliflozin label in May 2017, after an approximately doubled risk for lower-extremity amputations with the drug compared with placebo was seen during two trials.
The FDA said the decision to remove the boxed warning was made following a review of new data from three clinical trials, which demonstrated additional heart- and kidney-related benefits and led to additional approved uses for canagliflozin.
In 2018, canagliflozin was approved to reduce the risk of major adverse cardiovascular events in adults with type 2 diabetes who have established cardiovascular disease.
In 2019, canagliflozin was approved to reduce the risk of end-stage kidney disease, worsening of kidney function, cardiovascular death, and heart failure hospitalization, in adults with type 2 diabetes and diabetic kidney disease.
“Collectively, these newly identified effects of canagliflozin on heart and kidney disease show significantly enhanced benefit of this medicine,” the FDA said.
The safety information from these trials, the FDA said, suggests that the risk of amputation, “while still increased with canagliflozin, is lower than previously described, particularly when appropriately monitored.”
The agency added: “Based upon these considerations, FDA concluded that the boxed warning should be removed.”
The FDA announcement said clinicians and patients should continue to be aware of the importance of preventive foot care and to monitor for new pain, tenderness, sores, ulcers, and infections in the legs and feet. Risk factors that may predispose patients to amputation should be considered when choosing antidiabetic medicines.
Health care professionals are encouraged to report adverse reactions with canagliflozin to the FDA’s MedWatch program.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has removed the boxed warning about the risk of leg and foot amputations for canagliflozin (Invokana, Invokamet, Janssen), a sodium-glucose cotransporter-2 (SGLT2) inhibitor for the treatment of type 2 diabetes, the agency announced Aug. 26.
As previously reported by Medscape Medical News, the FDA added the boxed warning to the canagliflozin label in May 2017, after an approximately doubled risk for lower-extremity amputations with the drug compared with placebo was seen during two trials.
The FDA said the decision to remove the boxed warning was made following a review of new data from three clinical trials, which demonstrated additional heart- and kidney-related benefits and led to additional approved uses for canagliflozin.
In 2018, canagliflozin was approved to reduce the risk of major adverse cardiovascular events in adults with type 2 diabetes who have established cardiovascular disease.
In 2019, canagliflozin was approved to reduce the risk of end-stage kidney disease, worsening of kidney function, cardiovascular death, and heart failure hospitalization, in adults with type 2 diabetes and diabetic kidney disease.
“Collectively, these newly identified effects of canagliflozin on heart and kidney disease show significantly enhanced benefit of this medicine,” the FDA said.
The safety information from these trials, the FDA said, suggests that the risk of amputation, “while still increased with canagliflozin, is lower than previously described, particularly when appropriately monitored.”
The agency added: “Based upon these considerations, FDA concluded that the boxed warning should be removed.”
The FDA announcement said clinicians and patients should continue to be aware of the importance of preventive foot care and to monitor for new pain, tenderness, sores, ulcers, and infections in the legs and feet. Risk factors that may predispose patients to amputation should be considered when choosing antidiabetic medicines.
Health care professionals are encouraged to report adverse reactions with canagliflozin to the FDA’s MedWatch program.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has removed the boxed warning about the risk of leg and foot amputations for canagliflozin (Invokana, Invokamet, Janssen), a sodium-glucose cotransporter-2 (SGLT2) inhibitor for the treatment of type 2 diabetes, the agency announced Aug. 26.
As previously reported by Medscape Medical News, the FDA added the boxed warning to the canagliflozin label in May 2017, after an approximately doubled risk for lower-extremity amputations with the drug compared with placebo was seen during two trials.
The FDA said the decision to remove the boxed warning was made following a review of new data from three clinical trials, which demonstrated additional heart- and kidney-related benefits and led to additional approved uses for canagliflozin.
In 2018, canagliflozin was approved to reduce the risk of major adverse cardiovascular events in adults with type 2 diabetes who have established cardiovascular disease.
In 2019, canagliflozin was approved to reduce the risk of end-stage kidney disease, worsening of kidney function, cardiovascular death, and heart failure hospitalization, in adults with type 2 diabetes and diabetic kidney disease.
“Collectively, these newly identified effects of canagliflozin on heart and kidney disease show significantly enhanced benefit of this medicine,” the FDA said.
The safety information from these trials, the FDA said, suggests that the risk of amputation, “while still increased with canagliflozin, is lower than previously described, particularly when appropriately monitored.”
The agency added: “Based upon these considerations, FDA concluded that the boxed warning should be removed.”
The FDA announcement said clinicians and patients should continue to be aware of the importance of preventive foot care and to monitor for new pain, tenderness, sores, ulcers, and infections in the legs and feet. Risk factors that may predispose patients to amputation should be considered when choosing antidiabetic medicines.
Health care professionals are encouraged to report adverse reactions with canagliflozin to the FDA’s MedWatch program.
A version of this article originally appeared on Medscape.com.
ESC 2020 looks to make its mark in ‘new era’ of virtual meetings
The coronavirus may have quashed plans to socialize and stroll the canals of Amsterdam while at this year’s European Society of Cardiology (ESC) Congress, but organizers are promising a historic digital experience that will “once again, be a celebration of discovery and ground-breaking science.”
“My message — if I have to choose only one thing why ESC 2020 will be a historic event — is that the physician working at the Cleveland Clinic, who was planning to attend this year in Amsterdam, as well as the colleague in a bush hospital in Uganda, who would have never have dreamed to be part of the ESC Congress, both will have for the first time the same access at the same time to knowledge shared at the worldwide leading cardiovascular meeting,” Marco Roffi, MD, co-chair of the scientific program, told theheart.org | Medscape Cardiology.
Taking a page from the American College of Cardiology, which set the virtual bar early in the pandemic with its highly interactive ACC 2020, ESC is taking some 80 Hot Line, clinical practice guidelines, and special sessions live with question-and-answer interactions and panel discussions.
The latest COVID-19 research and four new guideline documents — including recommendations on atrial fibrillation (AF), non-ST-segment elevation acute coronary syndromes, sports cardiology and exercise in patients with cardiovascular disease, and adult congenital heart disease — will be featured at the ESC Congress 2020, scheduled for August 29 to September 1.
Presentations will be shorter and sessions more focused, but more than 500 scientific and educational sessions will be streamed in addition to more than 4000 abstracts available live or on demand as full presentations or e-posters, said Roffi, University Hospital of Geneva, Switzerland.
To pull off the virtual event, a digital studio in Amsterdam will host hundreds of key opinion leaders, and ESC employed more than 1000 satellite studios around the world to gather contributions from scientists and experts with the help of 70 behind-the-scenes experts.
Nevertheless, a “strategic decision” was made to provide free access to the event and its content for 30 days — a strategy that has attracted some 58,000 registrants thus far, up from a record 32,000 attendees at last year’s congress in Paris, Roffi said.
“Obviously, the income will not be the same as a physical congress, but we felt there was too much at stake to make a compromise,” he said. “We believe we are the leaders in cardiovascular meetings in the physical ones and we want to keep this position even in the new era. And we believe this is the beginning of a new era in whatever form will be.”
Hot Line Sessions 1-3, Saturday (14:00 CEST)
The Hot Line sessions will feature 13 clinical trials and kick off with EMPEROR-Reduced, which compared the sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (Jardiance, Boehringer Ingelheim/Eli Lilly) added to standard care in patients with heart failure with reduced ejection fraction (HFrEF), with and without diabetes.
Eli Lilly and Boehringer Ingelheim already announced the trial met its composite primary endpoint of reducing cardiovascular (CV) death or HF hospitalization risk but the details will be important given the SGLT2 inhibitors› rapid shift beyond diabetes to HF and chronic kidney disease (CKD).
Results presented at ESC 2019 from the landmark DAPA-HF trial led to the recent new indication for dapagliflozin (Farxiga, AstraZeneca) for HFrEF in the absence of diabetes. New data will be released in a Sunday Hot Line session looking at the SGLT2 inhibitor among diabetic and nondiabetic CKD patients in DAPA-CKD, which was halted early because of overwhelming efficacy.
As the indication evolved, the SGLT2 inhibitors became truly cardiovascular disease drugs, Roffi said, “so all the cardiologists will have to become familiar with these agents.”
Hot Line 2 will look at the oral cardiac myosin inhibitor mavacamten as an alternative to surgery or percutaneous interventions to treat obstructive hypertrophic cardiomyopathy (HCM). The first-in-class investigational agent is thought to reduce the hypercontractility characteristic of HCM by inhibiting excessive actin-myosin cross-bridges, and it showed promise in the recent phase 2 dose-finding MAVERICK HCM trial.
Investigators are expected to flesh out details from the 251-patient phase 3 EXPLORER-HCM trial, which reported functional and symptomatic gains with once-daily dosing in top-line results released by developer MyoKardia.
“This is really a revolutionary way to treat — hopefully successfully — this very complex disease,” Roffi said.
Rounding out the day is the EAST-AFNET 4 trial, which has been almost 10 years in the making and examined whether early rhythm control with antiarrhythmic drugs and catheter ablation can prevent adverse outcomes in patients with AF compared with usual care alone based on the ESC 2010 AF treatment guidelines.
Hot Line Sessions 4-6, Sunday (14:00 CEST)
Hot Line 4 features the ATPCI study examining the addition of the oral antianginal agent trimetazidine to standard of care in 6007 patients with angina after recent successful percutaneous coronary intervention.
Next up is POPULAR-TAVI looking at aspirin with or without clopidogrel in patients undergoing transcatheter aortic valve implantation (TAVI).
“This is a dilemma that we have every day in the cath lab when we perform a TAVI because we have in front of us patients who, by definition, are at high bleeding risk, are old, and have comorbidities such as renal insufficiencies,” Roffi said. “I like this very much because it’s a very practical study. Whatever the response will be of this study, it will impact clinical practice.”
Hot Line 6 is devoted to the PARALLAX trial comparing sacubitril/valsartan (Entresto, Novartis) with individualized medical therapy in 2569 heart failure with preserved ejection fraction (HFpEF) patients. The primary outcomes are 12-week change in N-terminal pro-brain natriuretic peptide and 24-week change in 6-minute walk distance.
Hot Line Sessions 7-9, Monday (14:00 CEST)
The next day starts with the timely topic of inflammation with the LoDoCo2 trial, in which 5522 patients with stable coronary artery disease were randomized to low-dose colchicine 0.5 mg daily or placebo on top of optimal medical therapy. The primary composite endpoint is CV death, myocardial infarction (MI), ischemic stroke, and ischemia-driven revascularization.
Additional colchicine data also will be presented in a late-breaking science session on Saturday that includes the Australian COPS trial in acute coronary syndromes and new analyses from COLCOT, which demonstrated a 23% reduction in the risk of first ischemic CV events following an MI but no mortality benefit. The low-cost anti-inflammatory drug is also being tested in the mammoth 6000-patient phase 3 Colchicine Coronavirus SARS-CoV-2 (COLCORONA) trial, expected to be completed by the end of September.
Hot Line 8 switches gears with the open-label randomized HOME-PE trial comparing outpatient management of pulmonary embolism (PE) in 1975 select patients based on either the simplified Pulmonary Embolism Severity Index (PESI) score, featured in the most recent ESC acute PE guidelines, or the HESTIA criteria, developed in the HESTIA study. The event-driven primary end point is the composite of recurrent venous thromboembolism, major bleeding, and all-cause death at 30 days.
Last up on Monday is a new analysis on the effects of lowering blood pressure for prevention of CV events across various BP levels from the BPLTTC, which is the largest resource of patient-level randomized clinical trial data, at more than 350,000 patients.
Tuesday Hot Line Sessions 10-12 (14:00 CEST)
The final day of the Congress ends with bang, with the randomized BRACE-CORONA trial examining the effect of continuing or suspending angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) in 700 patients with SARS-CoV-2 infection.
Although several cardiovascular societies including ESC recommend continuation of renin-angiotensin-aldosterone system (RAAS) antagonists in COVID-19 patients, randomized data are lacking and patients have been rattled by early observations suggesting that ACE2 upregulation from RAAS antagonists could increase the risk of developing severe COVID-19.
“BRACE-CORONA will answer the question that everybody’s been asking, whether or not you should continue ARBs and ACE inhibitors in COVID-19 patients. This is a randomized trial and we are all very excited about it,” Roffi said.
COVID-19 will also be discussed in a late-breaking science session on Sunday and in three industry Q&A sessions scattered over the 4 days.
Rounding out the last Hot Line session is IMPACT-AFib, a claims database analysis of early vs delayed educational interventions to improve oral anticoagulation use in a whopping 80,000 patients with AF, and REALITY, a much-needed cost-effectiveness analysis of liberal vs restrictive transfusion strategies in 630 patients with acute MI and anemia.
This article first appeared on Medscape.com.
The coronavirus may have quashed plans to socialize and stroll the canals of Amsterdam while at this year’s European Society of Cardiology (ESC) Congress, but organizers are promising a historic digital experience that will “once again, be a celebration of discovery and ground-breaking science.”
“My message — if I have to choose only one thing why ESC 2020 will be a historic event — is that the physician working at the Cleveland Clinic, who was planning to attend this year in Amsterdam, as well as the colleague in a bush hospital in Uganda, who would have never have dreamed to be part of the ESC Congress, both will have for the first time the same access at the same time to knowledge shared at the worldwide leading cardiovascular meeting,” Marco Roffi, MD, co-chair of the scientific program, told theheart.org | Medscape Cardiology.
Taking a page from the American College of Cardiology, which set the virtual bar early in the pandemic with its highly interactive ACC 2020, ESC is taking some 80 Hot Line, clinical practice guidelines, and special sessions live with question-and-answer interactions and panel discussions.
The latest COVID-19 research and four new guideline documents — including recommendations on atrial fibrillation (AF), non-ST-segment elevation acute coronary syndromes, sports cardiology and exercise in patients with cardiovascular disease, and adult congenital heart disease — will be featured at the ESC Congress 2020, scheduled for August 29 to September 1.
Presentations will be shorter and sessions more focused, but more than 500 scientific and educational sessions will be streamed in addition to more than 4000 abstracts available live or on demand as full presentations or e-posters, said Roffi, University Hospital of Geneva, Switzerland.
To pull off the virtual event, a digital studio in Amsterdam will host hundreds of key opinion leaders, and ESC employed more than 1000 satellite studios around the world to gather contributions from scientists and experts with the help of 70 behind-the-scenes experts.
Nevertheless, a “strategic decision” was made to provide free access to the event and its content for 30 days — a strategy that has attracted some 58,000 registrants thus far, up from a record 32,000 attendees at last year’s congress in Paris, Roffi said.
“Obviously, the income will not be the same as a physical congress, but we felt there was too much at stake to make a compromise,” he said. “We believe we are the leaders in cardiovascular meetings in the physical ones and we want to keep this position even in the new era. And we believe this is the beginning of a new era in whatever form will be.”
Hot Line Sessions 1-3, Saturday (14:00 CEST)
The Hot Line sessions will feature 13 clinical trials and kick off with EMPEROR-Reduced, which compared the sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (Jardiance, Boehringer Ingelheim/Eli Lilly) added to standard care in patients with heart failure with reduced ejection fraction (HFrEF), with and without diabetes.
Eli Lilly and Boehringer Ingelheim already announced the trial met its composite primary endpoint of reducing cardiovascular (CV) death or HF hospitalization risk but the details will be important given the SGLT2 inhibitors› rapid shift beyond diabetes to HF and chronic kidney disease (CKD).
Results presented at ESC 2019 from the landmark DAPA-HF trial led to the recent new indication for dapagliflozin (Farxiga, AstraZeneca) for HFrEF in the absence of diabetes. New data will be released in a Sunday Hot Line session looking at the SGLT2 inhibitor among diabetic and nondiabetic CKD patients in DAPA-CKD, which was halted early because of overwhelming efficacy.
As the indication evolved, the SGLT2 inhibitors became truly cardiovascular disease drugs, Roffi said, “so all the cardiologists will have to become familiar with these agents.”
Hot Line 2 will look at the oral cardiac myosin inhibitor mavacamten as an alternative to surgery or percutaneous interventions to treat obstructive hypertrophic cardiomyopathy (HCM). The first-in-class investigational agent is thought to reduce the hypercontractility characteristic of HCM by inhibiting excessive actin-myosin cross-bridges, and it showed promise in the recent phase 2 dose-finding MAVERICK HCM trial.
Investigators are expected to flesh out details from the 251-patient phase 3 EXPLORER-HCM trial, which reported functional and symptomatic gains with once-daily dosing in top-line results released by developer MyoKardia.
“This is really a revolutionary way to treat — hopefully successfully — this very complex disease,” Roffi said.
Rounding out the day is the EAST-AFNET 4 trial, which has been almost 10 years in the making and examined whether early rhythm control with antiarrhythmic drugs and catheter ablation can prevent adverse outcomes in patients with AF compared with usual care alone based on the ESC 2010 AF treatment guidelines.
Hot Line Sessions 4-6, Sunday (14:00 CEST)
Hot Line 4 features the ATPCI study examining the addition of the oral antianginal agent trimetazidine to standard of care in 6007 patients with angina after recent successful percutaneous coronary intervention.
Next up is POPULAR-TAVI looking at aspirin with or without clopidogrel in patients undergoing transcatheter aortic valve implantation (TAVI).
“This is a dilemma that we have every day in the cath lab when we perform a TAVI because we have in front of us patients who, by definition, are at high bleeding risk, are old, and have comorbidities such as renal insufficiencies,” Roffi said. “I like this very much because it’s a very practical study. Whatever the response will be of this study, it will impact clinical practice.”
Hot Line 6 is devoted to the PARALLAX trial comparing sacubitril/valsartan (Entresto, Novartis) with individualized medical therapy in 2569 heart failure with preserved ejection fraction (HFpEF) patients. The primary outcomes are 12-week change in N-terminal pro-brain natriuretic peptide and 24-week change in 6-minute walk distance.
Hot Line Sessions 7-9, Monday (14:00 CEST)
The next day starts with the timely topic of inflammation with the LoDoCo2 trial, in which 5522 patients with stable coronary artery disease were randomized to low-dose colchicine 0.5 mg daily or placebo on top of optimal medical therapy. The primary composite endpoint is CV death, myocardial infarction (MI), ischemic stroke, and ischemia-driven revascularization.
Additional colchicine data also will be presented in a late-breaking science session on Saturday that includes the Australian COPS trial in acute coronary syndromes and new analyses from COLCOT, which demonstrated a 23% reduction in the risk of first ischemic CV events following an MI but no mortality benefit. The low-cost anti-inflammatory drug is also being tested in the mammoth 6000-patient phase 3 Colchicine Coronavirus SARS-CoV-2 (COLCORONA) trial, expected to be completed by the end of September.
Hot Line 8 switches gears with the open-label randomized HOME-PE trial comparing outpatient management of pulmonary embolism (PE) in 1975 select patients based on either the simplified Pulmonary Embolism Severity Index (PESI) score, featured in the most recent ESC acute PE guidelines, or the HESTIA criteria, developed in the HESTIA study. The event-driven primary end point is the composite of recurrent venous thromboembolism, major bleeding, and all-cause death at 30 days.
Last up on Monday is a new analysis on the effects of lowering blood pressure for prevention of CV events across various BP levels from the BPLTTC, which is the largest resource of patient-level randomized clinical trial data, at more than 350,000 patients.
Tuesday Hot Line Sessions 10-12 (14:00 CEST)
The final day of the Congress ends with bang, with the randomized BRACE-CORONA trial examining the effect of continuing or suspending angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) in 700 patients with SARS-CoV-2 infection.
Although several cardiovascular societies including ESC recommend continuation of renin-angiotensin-aldosterone system (RAAS) antagonists in COVID-19 patients, randomized data are lacking and patients have been rattled by early observations suggesting that ACE2 upregulation from RAAS antagonists could increase the risk of developing severe COVID-19.
“BRACE-CORONA will answer the question that everybody’s been asking, whether or not you should continue ARBs and ACE inhibitors in COVID-19 patients. This is a randomized trial and we are all very excited about it,” Roffi said.
COVID-19 will also be discussed in a late-breaking science session on Sunday and in three industry Q&A sessions scattered over the 4 days.
Rounding out the last Hot Line session is IMPACT-AFib, a claims database analysis of early vs delayed educational interventions to improve oral anticoagulation use in a whopping 80,000 patients with AF, and REALITY, a much-needed cost-effectiveness analysis of liberal vs restrictive transfusion strategies in 630 patients with acute MI and anemia.
This article first appeared on Medscape.com.
The coronavirus may have quashed plans to socialize and stroll the canals of Amsterdam while at this year’s European Society of Cardiology (ESC) Congress, but organizers are promising a historic digital experience that will “once again, be a celebration of discovery and ground-breaking science.”
“My message — if I have to choose only one thing why ESC 2020 will be a historic event — is that the physician working at the Cleveland Clinic, who was planning to attend this year in Amsterdam, as well as the colleague in a bush hospital in Uganda, who would have never have dreamed to be part of the ESC Congress, both will have for the first time the same access at the same time to knowledge shared at the worldwide leading cardiovascular meeting,” Marco Roffi, MD, co-chair of the scientific program, told theheart.org | Medscape Cardiology.
Taking a page from the American College of Cardiology, which set the virtual bar early in the pandemic with its highly interactive ACC 2020, ESC is taking some 80 Hot Line, clinical practice guidelines, and special sessions live with question-and-answer interactions and panel discussions.
The latest COVID-19 research and four new guideline documents — including recommendations on atrial fibrillation (AF), non-ST-segment elevation acute coronary syndromes, sports cardiology and exercise in patients with cardiovascular disease, and adult congenital heart disease — will be featured at the ESC Congress 2020, scheduled for August 29 to September 1.
Presentations will be shorter and sessions more focused, but more than 500 scientific and educational sessions will be streamed in addition to more than 4000 abstracts available live or on demand as full presentations or e-posters, said Roffi, University Hospital of Geneva, Switzerland.
To pull off the virtual event, a digital studio in Amsterdam will host hundreds of key opinion leaders, and ESC employed more than 1000 satellite studios around the world to gather contributions from scientists and experts with the help of 70 behind-the-scenes experts.
Nevertheless, a “strategic decision” was made to provide free access to the event and its content for 30 days — a strategy that has attracted some 58,000 registrants thus far, up from a record 32,000 attendees at last year’s congress in Paris, Roffi said.
“Obviously, the income will not be the same as a physical congress, but we felt there was too much at stake to make a compromise,” he said. “We believe we are the leaders in cardiovascular meetings in the physical ones and we want to keep this position even in the new era. And we believe this is the beginning of a new era in whatever form will be.”
Hot Line Sessions 1-3, Saturday (14:00 CEST)
The Hot Line sessions will feature 13 clinical trials and kick off with EMPEROR-Reduced, which compared the sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (Jardiance, Boehringer Ingelheim/Eli Lilly) added to standard care in patients with heart failure with reduced ejection fraction (HFrEF), with and without diabetes.
Eli Lilly and Boehringer Ingelheim already announced the trial met its composite primary endpoint of reducing cardiovascular (CV) death or HF hospitalization risk but the details will be important given the SGLT2 inhibitors› rapid shift beyond diabetes to HF and chronic kidney disease (CKD).
Results presented at ESC 2019 from the landmark DAPA-HF trial led to the recent new indication for dapagliflozin (Farxiga, AstraZeneca) for HFrEF in the absence of diabetes. New data will be released in a Sunday Hot Line session looking at the SGLT2 inhibitor among diabetic and nondiabetic CKD patients in DAPA-CKD, which was halted early because of overwhelming efficacy.
As the indication evolved, the SGLT2 inhibitors became truly cardiovascular disease drugs, Roffi said, “so all the cardiologists will have to become familiar with these agents.”
Hot Line 2 will look at the oral cardiac myosin inhibitor mavacamten as an alternative to surgery or percutaneous interventions to treat obstructive hypertrophic cardiomyopathy (HCM). The first-in-class investigational agent is thought to reduce the hypercontractility characteristic of HCM by inhibiting excessive actin-myosin cross-bridges, and it showed promise in the recent phase 2 dose-finding MAVERICK HCM trial.
Investigators are expected to flesh out details from the 251-patient phase 3 EXPLORER-HCM trial, which reported functional and symptomatic gains with once-daily dosing in top-line results released by developer MyoKardia.
“This is really a revolutionary way to treat — hopefully successfully — this very complex disease,” Roffi said.
Rounding out the day is the EAST-AFNET 4 trial, which has been almost 10 years in the making and examined whether early rhythm control with antiarrhythmic drugs and catheter ablation can prevent adverse outcomes in patients with AF compared with usual care alone based on the ESC 2010 AF treatment guidelines.
Hot Line Sessions 4-6, Sunday (14:00 CEST)
Hot Line 4 features the ATPCI study examining the addition of the oral antianginal agent trimetazidine to standard of care in 6007 patients with angina after recent successful percutaneous coronary intervention.
Next up is POPULAR-TAVI looking at aspirin with or without clopidogrel in patients undergoing transcatheter aortic valve implantation (TAVI).
“This is a dilemma that we have every day in the cath lab when we perform a TAVI because we have in front of us patients who, by definition, are at high bleeding risk, are old, and have comorbidities such as renal insufficiencies,” Roffi said. “I like this very much because it’s a very practical study. Whatever the response will be of this study, it will impact clinical practice.”
Hot Line 6 is devoted to the PARALLAX trial comparing sacubitril/valsartan (Entresto, Novartis) with individualized medical therapy in 2569 heart failure with preserved ejection fraction (HFpEF) patients. The primary outcomes are 12-week change in N-terminal pro-brain natriuretic peptide and 24-week change in 6-minute walk distance.
Hot Line Sessions 7-9, Monday (14:00 CEST)
The next day starts with the timely topic of inflammation with the LoDoCo2 trial, in which 5522 patients with stable coronary artery disease were randomized to low-dose colchicine 0.5 mg daily or placebo on top of optimal medical therapy. The primary composite endpoint is CV death, myocardial infarction (MI), ischemic stroke, and ischemia-driven revascularization.
Additional colchicine data also will be presented in a late-breaking science session on Saturday that includes the Australian COPS trial in acute coronary syndromes and new analyses from COLCOT, which demonstrated a 23% reduction in the risk of first ischemic CV events following an MI but no mortality benefit. The low-cost anti-inflammatory drug is also being tested in the mammoth 6000-patient phase 3 Colchicine Coronavirus SARS-CoV-2 (COLCORONA) trial, expected to be completed by the end of September.
Hot Line 8 switches gears with the open-label randomized HOME-PE trial comparing outpatient management of pulmonary embolism (PE) in 1975 select patients based on either the simplified Pulmonary Embolism Severity Index (PESI) score, featured in the most recent ESC acute PE guidelines, or the HESTIA criteria, developed in the HESTIA study. The event-driven primary end point is the composite of recurrent venous thromboembolism, major bleeding, and all-cause death at 30 days.
Last up on Monday is a new analysis on the effects of lowering blood pressure for prevention of CV events across various BP levels from the BPLTTC, which is the largest resource of patient-level randomized clinical trial data, at more than 350,000 patients.
Tuesday Hot Line Sessions 10-12 (14:00 CEST)
The final day of the Congress ends with bang, with the randomized BRACE-CORONA trial examining the effect of continuing or suspending angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) in 700 patients with SARS-CoV-2 infection.
Although several cardiovascular societies including ESC recommend continuation of renin-angiotensin-aldosterone system (RAAS) antagonists in COVID-19 patients, randomized data are lacking and patients have been rattled by early observations suggesting that ACE2 upregulation from RAAS antagonists could increase the risk of developing severe COVID-19.
“BRACE-CORONA will answer the question that everybody’s been asking, whether or not you should continue ARBs and ACE inhibitors in COVID-19 patients. This is a randomized trial and we are all very excited about it,” Roffi said.
COVID-19 will also be discussed in a late-breaking science session on Sunday and in three industry Q&A sessions scattered over the 4 days.
Rounding out the last Hot Line session is IMPACT-AFib, a claims database analysis of early vs delayed educational interventions to improve oral anticoagulation use in a whopping 80,000 patients with AF, and REALITY, a much-needed cost-effectiveness analysis of liberal vs restrictive transfusion strategies in 630 patients with acute MI and anemia.
This article first appeared on Medscape.com.
First evidence of SARS-CoV-2 in heart cells
SARS-CoV-2 has been found in cardiac tissue of a child from Brazil with multisystem inflammatory syndrome (MIS-C) related to COVID-19 who presented with myocarditis and died of heart failure.
It’s believed to be the first evidence of direct infection of heart muscle cells by the virus; viral particles were identified in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells, and inflammatory cells.
The case was described in a report published online August 20 in The Lancet Child & Adolescent Health.
“The presence of the virus in various cell types of cardiac tissue, as evidenced by electron microscopy, shows that myocarditis in this case is likely a direct inflammatory response to the virus infection in the heart,” first author Marisa Dolhnikoff, MD, department of pathology, University of São Paulo, said in an interview.
There have been previous reports in adults with COVID-19 of both SARS-CoV-2 RNA by reverse transcription–polymerase chain reaction (RT-PCR) and viral particles by electron microscopy in cardiac tissue from endomyocardial specimens, the researchers noted. One of these reports, published in April by Tavazzi and colleagues, “detected viral particles in cardiac macrophages in an adult patient with acute cardiac injury associated with COVID-19; no viral particles were seen in cardiomyocytes or endothelial cells.
“Our case report is the first to our knowledge to document the presence of viral particles in the cardiac tissue of a child affected by MIS-C,” they added. “Moreover, viral particles were identified in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells, and inflammatory cells.”
‘Concerning’ case report
“This is a concerning report as it shows for the first time that the virus can actually invade the heart muscle cells themselves,” C. Michael Gibson, MD, CEO of the Baim Institute for Clinical Research in Boston, said in an interview.
“Previous reports of COVID-19 and the heart found that the virus was in the area outside the heart muscle cells. We do not know yet the relative contribution of the inflammatory cells invading the heart, the release of blood-borne inflammatory mediators, and the virus inside the heart muscle cells themselves to heart damage,” Dr. Gibson said.
The patient was a previously healthy 11-year-old girl of African descent with MIS-C related to COVID-19. She developed cardiac failure and died after 1 day in the hospital, despite aggressive treatment.
SARS-CoV-2 RNA was detected on a postmortem nasopharyngeal swab and in cardiac and pulmonary tissues by RT-PCR.
Postmortem ultrasound examination of the heart showed a “hyperechogenic and diffusely thickened endocardium (mean thickness, 10 mm), a thickened myocardium (18 mm thick in the left ventricle), and a small pericardial effusion,” Dr. Dolhnikoff and colleagues reported.
Histopathologic exam revealed myocarditis, pericarditis, and endocarditis characterized by infiltration of inflammatory cells. Inflammation was mainly interstitial and perivascular, associated with foci of cardiomyocyte necrosis and was mainly composed of CD68+ macrophages, a few CD45+ lymphocytes, and a few neutrophils and eosinophils.
Electron microscopy of cardiac tissue revealed spherical viral particles in shape and size consistent with the Coronaviridae family in the extracellular compartment and within cardiomyocytes, capillary endothelial cells, endocardium endothelial cells, macrophages, neutrophils, and fibroblasts.
Microthrombi in the pulmonary arterioles and renal glomerular capillaries were also seen at autopsy. SARS-CoV-2–associated pneumonia was mild.
Lymphoid depletion and signs of hemophagocytosis were observed in the spleen and lymph nodes. Acute tubular necrosis in the kidneys and hepatic centrilobular necrosis, secondary to shock, were also seen. Brain tissue showed microglial reactivity.
“Fortunately, MIS-C is a rare event and, although it can be severe and life threatening, most children recover,” Dr. Dolhnikoff commented.
“This case report comes at a time when the scientific community around the world calls attention to MIS-C and the need for it to be quickly recognized and treated by the pediatric community. Evidence of a direct relation between the virus and myocarditis confirms that MIS-C is one of the possible forms of presentation of COVID-19 and that the heart may be the target organ. It also alerts clinicians to possible cardiac sequelae in these children,” she added.
Experts weigh in
Scott Aydin, MD, medical director of pediatric cardiac intensive care, Mount Sinai Kravis Children’s Hospital in New York City, said that this case report is “unfortunately not all that surprising.
“Since the initial presentations of MIS-C several months ago, we have suspected mechanisms of direct and indirect injury to the myocardium. This important work is just the next step in further understanding the mechanisms of how COVID-19 creates havoc in the human body and the choices of possible therapies we have to treat children with COVID-19 and MIS-C,” said Dr. Aydin, who was not involved with the case report.
Anish Koka, MD, a cardiologist in private practice in Philadelphia, noted that, in these cases, endomyocardial biopsy is “rarely done because it is fairly invasive, but even when it has been done, the pathologic findings are of widespread inflammation rather than virus-induced cell necrosis.”
“While reports like this are sure to spawn viral tweets, it’s vital to understand that it’s not unusual to find widespread organ dissemination of virus in very sick patients. This does not mean that the virus is causing dysfunction of the organ it happens to be found in,” Dr. Koka said in an interview.
He noted that, in the case of the young girl who died, it took high PCR-cycle threshold values to isolate virus from the lung and heart samples.
“This means there was a low viral load in both organs, supporting the theory of SARS-CoV-2 as a potential trigger of a widespread inflammatory response that results in organ damage, rather than the virus itself infecting and destroying organs,” said Dr. Koka, who was also not associated with the case report.
This research had no specific funding. The authors declared no competing interests. Dr. Aydin disclosed no relevant financial relationships. Dr. Koka disclosed financial relationships with Boehringer Ingelheim and Jardiance.
This article first appeared on Medscape.com.
SARS-CoV-2 has been found in cardiac tissue of a child from Brazil with multisystem inflammatory syndrome (MIS-C) related to COVID-19 who presented with myocarditis and died of heart failure.
It’s believed to be the first evidence of direct infection of heart muscle cells by the virus; viral particles were identified in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells, and inflammatory cells.
The case was described in a report published online August 20 in The Lancet Child & Adolescent Health.
“The presence of the virus in various cell types of cardiac tissue, as evidenced by electron microscopy, shows that myocarditis in this case is likely a direct inflammatory response to the virus infection in the heart,” first author Marisa Dolhnikoff, MD, department of pathology, University of São Paulo, said in an interview.
There have been previous reports in adults with COVID-19 of both SARS-CoV-2 RNA by reverse transcription–polymerase chain reaction (RT-PCR) and viral particles by electron microscopy in cardiac tissue from endomyocardial specimens, the researchers noted. One of these reports, published in April by Tavazzi and colleagues, “detected viral particles in cardiac macrophages in an adult patient with acute cardiac injury associated with COVID-19; no viral particles were seen in cardiomyocytes or endothelial cells.
“Our case report is the first to our knowledge to document the presence of viral particles in the cardiac tissue of a child affected by MIS-C,” they added. “Moreover, viral particles were identified in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells, and inflammatory cells.”
‘Concerning’ case report
“This is a concerning report as it shows for the first time that the virus can actually invade the heart muscle cells themselves,” C. Michael Gibson, MD, CEO of the Baim Institute for Clinical Research in Boston, said in an interview.
“Previous reports of COVID-19 and the heart found that the virus was in the area outside the heart muscle cells. We do not know yet the relative contribution of the inflammatory cells invading the heart, the release of blood-borne inflammatory mediators, and the virus inside the heart muscle cells themselves to heart damage,” Dr. Gibson said.
The patient was a previously healthy 11-year-old girl of African descent with MIS-C related to COVID-19. She developed cardiac failure and died after 1 day in the hospital, despite aggressive treatment.
SARS-CoV-2 RNA was detected on a postmortem nasopharyngeal swab and in cardiac and pulmonary tissues by RT-PCR.
Postmortem ultrasound examination of the heart showed a “hyperechogenic and diffusely thickened endocardium (mean thickness, 10 mm), a thickened myocardium (18 mm thick in the left ventricle), and a small pericardial effusion,” Dr. Dolhnikoff and colleagues reported.
Histopathologic exam revealed myocarditis, pericarditis, and endocarditis characterized by infiltration of inflammatory cells. Inflammation was mainly interstitial and perivascular, associated with foci of cardiomyocyte necrosis and was mainly composed of CD68+ macrophages, a few CD45+ lymphocytes, and a few neutrophils and eosinophils.
Electron microscopy of cardiac tissue revealed spherical viral particles in shape and size consistent with the Coronaviridae family in the extracellular compartment and within cardiomyocytes, capillary endothelial cells, endocardium endothelial cells, macrophages, neutrophils, and fibroblasts.
Microthrombi in the pulmonary arterioles and renal glomerular capillaries were also seen at autopsy. SARS-CoV-2–associated pneumonia was mild.
Lymphoid depletion and signs of hemophagocytosis were observed in the spleen and lymph nodes. Acute tubular necrosis in the kidneys and hepatic centrilobular necrosis, secondary to shock, were also seen. Brain tissue showed microglial reactivity.
“Fortunately, MIS-C is a rare event and, although it can be severe and life threatening, most children recover,” Dr. Dolhnikoff commented.
“This case report comes at a time when the scientific community around the world calls attention to MIS-C and the need for it to be quickly recognized and treated by the pediatric community. Evidence of a direct relation between the virus and myocarditis confirms that MIS-C is one of the possible forms of presentation of COVID-19 and that the heart may be the target organ. It also alerts clinicians to possible cardiac sequelae in these children,” she added.
Experts weigh in
Scott Aydin, MD, medical director of pediatric cardiac intensive care, Mount Sinai Kravis Children’s Hospital in New York City, said that this case report is “unfortunately not all that surprising.
“Since the initial presentations of MIS-C several months ago, we have suspected mechanisms of direct and indirect injury to the myocardium. This important work is just the next step in further understanding the mechanisms of how COVID-19 creates havoc in the human body and the choices of possible therapies we have to treat children with COVID-19 and MIS-C,” said Dr. Aydin, who was not involved with the case report.
Anish Koka, MD, a cardiologist in private practice in Philadelphia, noted that, in these cases, endomyocardial biopsy is “rarely done because it is fairly invasive, but even when it has been done, the pathologic findings are of widespread inflammation rather than virus-induced cell necrosis.”
“While reports like this are sure to spawn viral tweets, it’s vital to understand that it’s not unusual to find widespread organ dissemination of virus in very sick patients. This does not mean that the virus is causing dysfunction of the organ it happens to be found in,” Dr. Koka said in an interview.
He noted that, in the case of the young girl who died, it took high PCR-cycle threshold values to isolate virus from the lung and heart samples.
“This means there was a low viral load in both organs, supporting the theory of SARS-CoV-2 as a potential trigger of a widespread inflammatory response that results in organ damage, rather than the virus itself infecting and destroying organs,” said Dr. Koka, who was also not associated with the case report.
This research had no specific funding. The authors declared no competing interests. Dr. Aydin disclosed no relevant financial relationships. Dr. Koka disclosed financial relationships with Boehringer Ingelheim and Jardiance.
This article first appeared on Medscape.com.
SARS-CoV-2 has been found in cardiac tissue of a child from Brazil with multisystem inflammatory syndrome (MIS-C) related to COVID-19 who presented with myocarditis and died of heart failure.
It’s believed to be the first evidence of direct infection of heart muscle cells by the virus; viral particles were identified in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells, and inflammatory cells.
The case was described in a report published online August 20 in The Lancet Child & Adolescent Health.
“The presence of the virus in various cell types of cardiac tissue, as evidenced by electron microscopy, shows that myocarditis in this case is likely a direct inflammatory response to the virus infection in the heart,” first author Marisa Dolhnikoff, MD, department of pathology, University of São Paulo, said in an interview.
There have been previous reports in adults with COVID-19 of both SARS-CoV-2 RNA by reverse transcription–polymerase chain reaction (RT-PCR) and viral particles by electron microscopy in cardiac tissue from endomyocardial specimens, the researchers noted. One of these reports, published in April by Tavazzi and colleagues, “detected viral particles in cardiac macrophages in an adult patient with acute cardiac injury associated with COVID-19; no viral particles were seen in cardiomyocytes or endothelial cells.
“Our case report is the first to our knowledge to document the presence of viral particles in the cardiac tissue of a child affected by MIS-C,” they added. “Moreover, viral particles were identified in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells, and inflammatory cells.”
‘Concerning’ case report
“This is a concerning report as it shows for the first time that the virus can actually invade the heart muscle cells themselves,” C. Michael Gibson, MD, CEO of the Baim Institute for Clinical Research in Boston, said in an interview.
“Previous reports of COVID-19 and the heart found that the virus was in the area outside the heart muscle cells. We do not know yet the relative contribution of the inflammatory cells invading the heart, the release of blood-borne inflammatory mediators, and the virus inside the heart muscle cells themselves to heart damage,” Dr. Gibson said.
The patient was a previously healthy 11-year-old girl of African descent with MIS-C related to COVID-19. She developed cardiac failure and died after 1 day in the hospital, despite aggressive treatment.
SARS-CoV-2 RNA was detected on a postmortem nasopharyngeal swab and in cardiac and pulmonary tissues by RT-PCR.
Postmortem ultrasound examination of the heart showed a “hyperechogenic and diffusely thickened endocardium (mean thickness, 10 mm), a thickened myocardium (18 mm thick in the left ventricle), and a small pericardial effusion,” Dr. Dolhnikoff and colleagues reported.
Histopathologic exam revealed myocarditis, pericarditis, and endocarditis characterized by infiltration of inflammatory cells. Inflammation was mainly interstitial and perivascular, associated with foci of cardiomyocyte necrosis and was mainly composed of CD68+ macrophages, a few CD45+ lymphocytes, and a few neutrophils and eosinophils.
Electron microscopy of cardiac tissue revealed spherical viral particles in shape and size consistent with the Coronaviridae family in the extracellular compartment and within cardiomyocytes, capillary endothelial cells, endocardium endothelial cells, macrophages, neutrophils, and fibroblasts.
Microthrombi in the pulmonary arterioles and renal glomerular capillaries were also seen at autopsy. SARS-CoV-2–associated pneumonia was mild.
Lymphoid depletion and signs of hemophagocytosis were observed in the spleen and lymph nodes. Acute tubular necrosis in the kidneys and hepatic centrilobular necrosis, secondary to shock, were also seen. Brain tissue showed microglial reactivity.
“Fortunately, MIS-C is a rare event and, although it can be severe and life threatening, most children recover,” Dr. Dolhnikoff commented.
“This case report comes at a time when the scientific community around the world calls attention to MIS-C and the need for it to be quickly recognized and treated by the pediatric community. Evidence of a direct relation between the virus and myocarditis confirms that MIS-C is one of the possible forms of presentation of COVID-19 and that the heart may be the target organ. It also alerts clinicians to possible cardiac sequelae in these children,” she added.
Experts weigh in
Scott Aydin, MD, medical director of pediatric cardiac intensive care, Mount Sinai Kravis Children’s Hospital in New York City, said that this case report is “unfortunately not all that surprising.
“Since the initial presentations of MIS-C several months ago, we have suspected mechanisms of direct and indirect injury to the myocardium. This important work is just the next step in further understanding the mechanisms of how COVID-19 creates havoc in the human body and the choices of possible therapies we have to treat children with COVID-19 and MIS-C,” said Dr. Aydin, who was not involved with the case report.
Anish Koka, MD, a cardiologist in private practice in Philadelphia, noted that, in these cases, endomyocardial biopsy is “rarely done because it is fairly invasive, but even when it has been done, the pathologic findings are of widespread inflammation rather than virus-induced cell necrosis.”
“While reports like this are sure to spawn viral tweets, it’s vital to understand that it’s not unusual to find widespread organ dissemination of virus in very sick patients. This does not mean that the virus is causing dysfunction of the organ it happens to be found in,” Dr. Koka said in an interview.
He noted that, in the case of the young girl who died, it took high PCR-cycle threshold values to isolate virus from the lung and heart samples.
“This means there was a low viral load in both organs, supporting the theory of SARS-CoV-2 as a potential trigger of a widespread inflammatory response that results in organ damage, rather than the virus itself infecting and destroying organs,” said Dr. Koka, who was also not associated with the case report.
This research had no specific funding. The authors declared no competing interests. Dr. Aydin disclosed no relevant financial relationships. Dr. Koka disclosed financial relationships with Boehringer Ingelheim and Jardiance.
This article first appeared on Medscape.com.
SYNTAXES: Female benefit with CABG vanishes by 10 years
The beneficial effect on all-cause mortality of coronary artery bypass grafting surgery observed at 4 and 5 years in women with complex coronary disease seen in the SYNTAX trial is gone at 10 years.
If anything, the results suggest a mortality benefit for coronary artery bypass grafting (CABG) over percutaneous coronary intervention (PCI) mainly for men (adjusted hazard ratio, 0.76; 95% confidence interval, 0.56-1.02) and not for women (adjusted HR, 0.90; 95% CI, 0.54-1.51) in the SYNTAX Extended Survival (SYNTAXES) study.
The sex-treatment interaction for all-cause mortality was significant at 5 years (P = .025) but not at 10 years (P = .952).
“I’m becoming very humble with trials because I’m not expecting the convergence of the curve. I was expecting like a surge, a further divergence,” senior author Patrick Serruys, MD, PhD, National University of Ireland, Galway, said in an interview. “You could say, at the end of the day, everybody dies. And that’s the life expectancy factor.”
Although female patients had slightly lower anatomic SYNTAX scores at randomization (27.0 vs. 29.2), they were on average 4 years older than men (mean age, 68 years) and had higher prevalence rates of diabetes, hypertension, and chronic kidney disease, he noted. “The other explanation is that we know that the bypass graft, the saphenous bypass graft, became vulnerable around 7 years; that’s probably the half-life.”
Overall, mortality in both men and women tended to be lower after CABG than after PCI, although the differences were not statistically significant, the authors reported August 17 in the Journal of the American College of Cardiology.
The 1,800-patient SYNTAX trial showed no difference in all-cause mortality at 5 years between CABG and PCI, although CABG was associated with fewer major adverse cardiac and cerebrovascular events (MACCE) and more favorable results among those with complex, three-vessel disease.
The findings were confirmed in 10-year follow-up reported last year from SYNTAXES, which analyzed only all-cause mortality.
Female sex, however, was an independent predictor of mortality with PCI at 4-years follow-up (HR, 2.87) in SYNTAX and led to sex being incorporated into the SYNTAX II score to help guide revascularization decisions. Notably, this interaction for all-cause mortality has not been seen in other studies.
Treatment effect by sex
In the new prespecified subgroup analysis, women had a higher crude rate of all-cause mortality at 10 years than men (32.8% vs. 24.7%; log-rank P = .002). This held true whether women were in the PCI group (33.0% vs. 27.0%; log-rank P = .053) or the CABG group (32.5% vs. 22.5%; log-rank P = .017).
In women, the mortality rate was significantly higher with PCI than with CABG at 5 years, but was no longer different at 10 years (33.0% vs. 32.5%; log-rank P = .601). This was largely caused by an uptick in deaths between 5 and 10 years in those treated with CABG, compared with PCI.
In men, the mortality rate was similar between PCI and CABG at 5 years, but tended to be higher with PCI at 10 years (27.0% vs. 22.5%; log-rank P = .082).
Asked about the possible late benefit for CABG in men, Dr. Serruys replied: “Of course, everyone had made a hypothesis – ‘let’s look at the use of internal mammary arteries in these patients, etc.’ – but I must be honest, we don’t have an explanation so far.”
Roxana Mehran, MD, Mount Sinai School of Medicine, New York City, said with just 402 women and using a no-longer-available, first-generation (Taxus) stent, the findings are, unfortunately, not informative.
“For me, it would be important for these investigators to share their data for women so we can do a patient-based analysis to better figure out the differential between first-generation stents and how well we’re doing,” Dr. Mehran said.
“What’s really important is to have a study where you actually collect female-specific risk factors that are never, ever looked at, [such as] age at menopause or having had pregnancy-related complications, that predispose these women to more of an atherosclerotic risk. And, even so, to better understand their anatomy and what suits them better,” she said. “I just don’t think we know enough or have put enough effort into understanding the biology that is sex specific and different for men and women.”
Revising SYNTAX II score
Given the lack of a sex-treatment interaction in the analysis, Dr. Serruys and colleagues suggest that the SYNTAX II score “should be reevaluated for the prediction of all-cause mortality at 10 years.”
Lending further support to this is the fact that SYNTAX II score was similar between women who died at 5-10 years and those who died in the first 5 years after CABG (31.8 vs. 31.6).
“The authors rightfully ask whether the SYNTAX II score should be revised to remove female sex, and given the current study result this appears warranted,” Arnold H. Seto, MD, MPA, Long Beach (Calif.) Veterans Administration Hospital, said in a related editorial.
He pointed out that women in SYNTAXES treated with CABG tended to have a survival time 0.51 years longer than women treated with PCI (P = .07). Nonetheless, the lack of confirmation for a sex-specific treatment interaction in any other study – EXCEL, FREEDOM, BEST, PRECOMBAT, BARI, or MASS – strongly suggests that the interaction seen in SYNTAX is likely a “type 1 error.”
Rather than focusing on early mortality, which may represent relatively rare events that are susceptible to chance, Dr. Seto suggested “other endpoints such years of life saved, quality adjusted life-years, and MACE may better capture the benefits of different revascularization decisions, even if they have a higher risk for bias.”
A new risk model, SYNTAX score 2020, has been developed and will be published imminently, Dr. Serruys said in an interview.
The SYNTAX Extended Survival study was supported by the German Foundation of Heart Research. The SYNTAX trial, during 0- to 5-years of follow-up, was funded by Boston Scientific. Both sponsors had no role in study design or data collection, analyses, and interpretation, nor were they involved in the decision to publish the final manuscript. Dr. Serruys has received personal fees from Biosensors, Micel Technologies, Sinomedical Sciences Technology, Philips/Volcano, Xeltis, and HeartFlow, outside the submitted work. Dr. Seto reported research grants from Philips and Acist, and honoraria from Terumo, Getinge, Boston Scientific, General Electric, and Janssen.
A version of this article originally appeared on Medscape.com.
The beneficial effect on all-cause mortality of coronary artery bypass grafting surgery observed at 4 and 5 years in women with complex coronary disease seen in the SYNTAX trial is gone at 10 years.
If anything, the results suggest a mortality benefit for coronary artery bypass grafting (CABG) over percutaneous coronary intervention (PCI) mainly for men (adjusted hazard ratio, 0.76; 95% confidence interval, 0.56-1.02) and not for women (adjusted HR, 0.90; 95% CI, 0.54-1.51) in the SYNTAX Extended Survival (SYNTAXES) study.
The sex-treatment interaction for all-cause mortality was significant at 5 years (P = .025) but not at 10 years (P = .952).
“I’m becoming very humble with trials because I’m not expecting the convergence of the curve. I was expecting like a surge, a further divergence,” senior author Patrick Serruys, MD, PhD, National University of Ireland, Galway, said in an interview. “You could say, at the end of the day, everybody dies. And that’s the life expectancy factor.”
Although female patients had slightly lower anatomic SYNTAX scores at randomization (27.0 vs. 29.2), they were on average 4 years older than men (mean age, 68 years) and had higher prevalence rates of diabetes, hypertension, and chronic kidney disease, he noted. “The other explanation is that we know that the bypass graft, the saphenous bypass graft, became vulnerable around 7 years; that’s probably the half-life.”
Overall, mortality in both men and women tended to be lower after CABG than after PCI, although the differences were not statistically significant, the authors reported August 17 in the Journal of the American College of Cardiology.
The 1,800-patient SYNTAX trial showed no difference in all-cause mortality at 5 years between CABG and PCI, although CABG was associated with fewer major adverse cardiac and cerebrovascular events (MACCE) and more favorable results among those with complex, three-vessel disease.
The findings were confirmed in 10-year follow-up reported last year from SYNTAXES, which analyzed only all-cause mortality.
Female sex, however, was an independent predictor of mortality with PCI at 4-years follow-up (HR, 2.87) in SYNTAX and led to sex being incorporated into the SYNTAX II score to help guide revascularization decisions. Notably, this interaction for all-cause mortality has not been seen in other studies.
Treatment effect by sex
In the new prespecified subgroup analysis, women had a higher crude rate of all-cause mortality at 10 years than men (32.8% vs. 24.7%; log-rank P = .002). This held true whether women were in the PCI group (33.0% vs. 27.0%; log-rank P = .053) or the CABG group (32.5% vs. 22.5%; log-rank P = .017).
In women, the mortality rate was significantly higher with PCI than with CABG at 5 years, but was no longer different at 10 years (33.0% vs. 32.5%; log-rank P = .601). This was largely caused by an uptick in deaths between 5 and 10 years in those treated with CABG, compared with PCI.
In men, the mortality rate was similar between PCI and CABG at 5 years, but tended to be higher with PCI at 10 years (27.0% vs. 22.5%; log-rank P = .082).
Asked about the possible late benefit for CABG in men, Dr. Serruys replied: “Of course, everyone had made a hypothesis – ‘let’s look at the use of internal mammary arteries in these patients, etc.’ – but I must be honest, we don’t have an explanation so far.”
Roxana Mehran, MD, Mount Sinai School of Medicine, New York City, said with just 402 women and using a no-longer-available, first-generation (Taxus) stent, the findings are, unfortunately, not informative.
“For me, it would be important for these investigators to share their data for women so we can do a patient-based analysis to better figure out the differential between first-generation stents and how well we’re doing,” Dr. Mehran said.
“What’s really important is to have a study where you actually collect female-specific risk factors that are never, ever looked at, [such as] age at menopause or having had pregnancy-related complications, that predispose these women to more of an atherosclerotic risk. And, even so, to better understand their anatomy and what suits them better,” she said. “I just don’t think we know enough or have put enough effort into understanding the biology that is sex specific and different for men and women.”
Revising SYNTAX II score
Given the lack of a sex-treatment interaction in the analysis, Dr. Serruys and colleagues suggest that the SYNTAX II score “should be reevaluated for the prediction of all-cause mortality at 10 years.”
Lending further support to this is the fact that SYNTAX II score was similar between women who died at 5-10 years and those who died in the first 5 years after CABG (31.8 vs. 31.6).
“The authors rightfully ask whether the SYNTAX II score should be revised to remove female sex, and given the current study result this appears warranted,” Arnold H. Seto, MD, MPA, Long Beach (Calif.) Veterans Administration Hospital, said in a related editorial.
He pointed out that women in SYNTAXES treated with CABG tended to have a survival time 0.51 years longer than women treated with PCI (P = .07). Nonetheless, the lack of confirmation for a sex-specific treatment interaction in any other study – EXCEL, FREEDOM, BEST, PRECOMBAT, BARI, or MASS – strongly suggests that the interaction seen in SYNTAX is likely a “type 1 error.”
Rather than focusing on early mortality, which may represent relatively rare events that are susceptible to chance, Dr. Seto suggested “other endpoints such years of life saved, quality adjusted life-years, and MACE may better capture the benefits of different revascularization decisions, even if they have a higher risk for bias.”
A new risk model, SYNTAX score 2020, has been developed and will be published imminently, Dr. Serruys said in an interview.
The SYNTAX Extended Survival study was supported by the German Foundation of Heart Research. The SYNTAX trial, during 0- to 5-years of follow-up, was funded by Boston Scientific. Both sponsors had no role in study design or data collection, analyses, and interpretation, nor were they involved in the decision to publish the final manuscript. Dr. Serruys has received personal fees from Biosensors, Micel Technologies, Sinomedical Sciences Technology, Philips/Volcano, Xeltis, and HeartFlow, outside the submitted work. Dr. Seto reported research grants from Philips and Acist, and honoraria from Terumo, Getinge, Boston Scientific, General Electric, and Janssen.
A version of this article originally appeared on Medscape.com.
The beneficial effect on all-cause mortality of coronary artery bypass grafting surgery observed at 4 and 5 years in women with complex coronary disease seen in the SYNTAX trial is gone at 10 years.
If anything, the results suggest a mortality benefit for coronary artery bypass grafting (CABG) over percutaneous coronary intervention (PCI) mainly for men (adjusted hazard ratio, 0.76; 95% confidence interval, 0.56-1.02) and not for women (adjusted HR, 0.90; 95% CI, 0.54-1.51) in the SYNTAX Extended Survival (SYNTAXES) study.
The sex-treatment interaction for all-cause mortality was significant at 5 years (P = .025) but not at 10 years (P = .952).
“I’m becoming very humble with trials because I’m not expecting the convergence of the curve. I was expecting like a surge, a further divergence,” senior author Patrick Serruys, MD, PhD, National University of Ireland, Galway, said in an interview. “You could say, at the end of the day, everybody dies. And that’s the life expectancy factor.”
Although female patients had slightly lower anatomic SYNTAX scores at randomization (27.0 vs. 29.2), they were on average 4 years older than men (mean age, 68 years) and had higher prevalence rates of diabetes, hypertension, and chronic kidney disease, he noted. “The other explanation is that we know that the bypass graft, the saphenous bypass graft, became vulnerable around 7 years; that’s probably the half-life.”
Overall, mortality in both men and women tended to be lower after CABG than after PCI, although the differences were not statistically significant, the authors reported August 17 in the Journal of the American College of Cardiology.
The 1,800-patient SYNTAX trial showed no difference in all-cause mortality at 5 years between CABG and PCI, although CABG was associated with fewer major adverse cardiac and cerebrovascular events (MACCE) and more favorable results among those with complex, three-vessel disease.
The findings were confirmed in 10-year follow-up reported last year from SYNTAXES, which analyzed only all-cause mortality.
Female sex, however, was an independent predictor of mortality with PCI at 4-years follow-up (HR, 2.87) in SYNTAX and led to sex being incorporated into the SYNTAX II score to help guide revascularization decisions. Notably, this interaction for all-cause mortality has not been seen in other studies.
Treatment effect by sex
In the new prespecified subgroup analysis, women had a higher crude rate of all-cause mortality at 10 years than men (32.8% vs. 24.7%; log-rank P = .002). This held true whether women were in the PCI group (33.0% vs. 27.0%; log-rank P = .053) or the CABG group (32.5% vs. 22.5%; log-rank P = .017).
In women, the mortality rate was significantly higher with PCI than with CABG at 5 years, but was no longer different at 10 years (33.0% vs. 32.5%; log-rank P = .601). This was largely caused by an uptick in deaths between 5 and 10 years in those treated with CABG, compared with PCI.
In men, the mortality rate was similar between PCI and CABG at 5 years, but tended to be higher with PCI at 10 years (27.0% vs. 22.5%; log-rank P = .082).
Asked about the possible late benefit for CABG in men, Dr. Serruys replied: “Of course, everyone had made a hypothesis – ‘let’s look at the use of internal mammary arteries in these patients, etc.’ – but I must be honest, we don’t have an explanation so far.”
Roxana Mehran, MD, Mount Sinai School of Medicine, New York City, said with just 402 women and using a no-longer-available, first-generation (Taxus) stent, the findings are, unfortunately, not informative.
“For me, it would be important for these investigators to share their data for women so we can do a patient-based analysis to better figure out the differential between first-generation stents and how well we’re doing,” Dr. Mehran said.
“What’s really important is to have a study where you actually collect female-specific risk factors that are never, ever looked at, [such as] age at menopause or having had pregnancy-related complications, that predispose these women to more of an atherosclerotic risk. And, even so, to better understand their anatomy and what suits them better,” she said. “I just don’t think we know enough or have put enough effort into understanding the biology that is sex specific and different for men and women.”
Revising SYNTAX II score
Given the lack of a sex-treatment interaction in the analysis, Dr. Serruys and colleagues suggest that the SYNTAX II score “should be reevaluated for the prediction of all-cause mortality at 10 years.”
Lending further support to this is the fact that SYNTAX II score was similar between women who died at 5-10 years and those who died in the first 5 years after CABG (31.8 vs. 31.6).
“The authors rightfully ask whether the SYNTAX II score should be revised to remove female sex, and given the current study result this appears warranted,” Arnold H. Seto, MD, MPA, Long Beach (Calif.) Veterans Administration Hospital, said in a related editorial.
He pointed out that women in SYNTAXES treated with CABG tended to have a survival time 0.51 years longer than women treated with PCI (P = .07). Nonetheless, the lack of confirmation for a sex-specific treatment interaction in any other study – EXCEL, FREEDOM, BEST, PRECOMBAT, BARI, or MASS – strongly suggests that the interaction seen in SYNTAX is likely a “type 1 error.”
Rather than focusing on early mortality, which may represent relatively rare events that are susceptible to chance, Dr. Seto suggested “other endpoints such years of life saved, quality adjusted life-years, and MACE may better capture the benefits of different revascularization decisions, even if they have a higher risk for bias.”
A new risk model, SYNTAX score 2020, has been developed and will be published imminently, Dr. Serruys said in an interview.
The SYNTAX Extended Survival study was supported by the German Foundation of Heart Research. The SYNTAX trial, during 0- to 5-years of follow-up, was funded by Boston Scientific. Both sponsors had no role in study design or data collection, analyses, and interpretation, nor were they involved in the decision to publish the final manuscript. Dr. Serruys has received personal fees from Biosensors, Micel Technologies, Sinomedical Sciences Technology, Philips/Volcano, Xeltis, and HeartFlow, outside the submitted work. Dr. Seto reported research grants from Philips and Acist, and honoraria from Terumo, Getinge, Boston Scientific, General Electric, and Janssen.
A version of this article originally appeared on Medscape.com.
FDA updates hydrochlorothiazide label to include nonmelanoma skin cancer risk
and undergo regular skin cancer screening, according to updates to the medication’s label.
The skin cancer risk is small, however, and patients should continue taking HCTZ, a commonly used diuretic and antihypertensive drug, unless their doctor says otherwise, according to a U.S. Food and Drug Administration announcement about the labeling changes, which the agency approved on Aug. 20.
HCTZ, first approved in 1959, is associated with photosensitivity. Researchers identified a relationship between HCTZ and nonmelanoma skin cancer in postmarketing studies. Investigators have described dose-response patterns for basal cell carcinoma and squamous cell carcinoma (SCC).
An FDA analysis found that the risk mostly was increased for SCC. The drug was associated with approximately one additional case of SCC per 16,000 patients per year. For white patients who received a cumulative dose of 50,000 mg or more, the risk was greater. In this patient population, HCTZ was associated with about one additional case of SCC per 6,700 patients per year, according to the label.
Reliably estimating the frequency of nonmelanoma skin cancer and establishing a causal relationship to drug exposure is not possible with the available postmarketing data, the label notes
“Treatment for nonmelanoma skin cancer is typically local and successful, with very low rates of death,” the FDA said. “Meanwhile, the risks of uncontrolled blood pressure can be severe and include life-threatening heart attacks or stroke. Given this information, patients should continue to use HCTZ and take protective skin care measures to reduce their risk of nonmelanoma skin cancer, unless directed otherwise from their health care provider.”
Patients can reduce sun exposure by using broad-spectrum sunscreens with a sun protection factor value of at least 15, limiting time in the sun, and wearing protective clothing, the agency advised.
and undergo regular skin cancer screening, according to updates to the medication’s label.
The skin cancer risk is small, however, and patients should continue taking HCTZ, a commonly used diuretic and antihypertensive drug, unless their doctor says otherwise, according to a U.S. Food and Drug Administration announcement about the labeling changes, which the agency approved on Aug. 20.
HCTZ, first approved in 1959, is associated with photosensitivity. Researchers identified a relationship between HCTZ and nonmelanoma skin cancer in postmarketing studies. Investigators have described dose-response patterns for basal cell carcinoma and squamous cell carcinoma (SCC).
An FDA analysis found that the risk mostly was increased for SCC. The drug was associated with approximately one additional case of SCC per 16,000 patients per year. For white patients who received a cumulative dose of 50,000 mg or more, the risk was greater. In this patient population, HCTZ was associated with about one additional case of SCC per 6,700 patients per year, according to the label.
Reliably estimating the frequency of nonmelanoma skin cancer and establishing a causal relationship to drug exposure is not possible with the available postmarketing data, the label notes
“Treatment for nonmelanoma skin cancer is typically local and successful, with very low rates of death,” the FDA said. “Meanwhile, the risks of uncontrolled blood pressure can be severe and include life-threatening heart attacks or stroke. Given this information, patients should continue to use HCTZ and take protective skin care measures to reduce their risk of nonmelanoma skin cancer, unless directed otherwise from their health care provider.”
Patients can reduce sun exposure by using broad-spectrum sunscreens with a sun protection factor value of at least 15, limiting time in the sun, and wearing protective clothing, the agency advised.
and undergo regular skin cancer screening, according to updates to the medication’s label.
The skin cancer risk is small, however, and patients should continue taking HCTZ, a commonly used diuretic and antihypertensive drug, unless their doctor says otherwise, according to a U.S. Food and Drug Administration announcement about the labeling changes, which the agency approved on Aug. 20.
HCTZ, first approved in 1959, is associated with photosensitivity. Researchers identified a relationship between HCTZ and nonmelanoma skin cancer in postmarketing studies. Investigators have described dose-response patterns for basal cell carcinoma and squamous cell carcinoma (SCC).
An FDA analysis found that the risk mostly was increased for SCC. The drug was associated with approximately one additional case of SCC per 16,000 patients per year. For white patients who received a cumulative dose of 50,000 mg or more, the risk was greater. In this patient population, HCTZ was associated with about one additional case of SCC per 6,700 patients per year, according to the label.
Reliably estimating the frequency of nonmelanoma skin cancer and establishing a causal relationship to drug exposure is not possible with the available postmarketing data, the label notes
“Treatment for nonmelanoma skin cancer is typically local and successful, with very low rates of death,” the FDA said. “Meanwhile, the risks of uncontrolled blood pressure can be severe and include life-threatening heart attacks or stroke. Given this information, patients should continue to use HCTZ and take protective skin care measures to reduce their risk of nonmelanoma skin cancer, unless directed otherwise from their health care provider.”
Patients can reduce sun exposure by using broad-spectrum sunscreens with a sun protection factor value of at least 15, limiting time in the sun, and wearing protective clothing, the agency advised.
HM20 Virtual product theaters: Aug. 25-27
Aug. 25, 2020. 12:00 p.m. – 1:00 p.m. ET
Medical Product Theater: Worsening Symptoms and Hospitalization for Heart Failure: Increased Risk of Poor Outcomes and Opportunities to Enhance Care
Objectives
- Discuss hospitalization as a pivotal point in the clinical trajectory of heart failure.
- Highlight strategies for improvement and optimization of the treatment plan for patients with heart failure.
- Provide practical guidance for identifying predictors of worsening heart failure and educating on the importance of patients’ self-management.
Speaker
William T. Abraham, MD, FACP, FACC, FAHA, FESC, FRCPE
Professor of Medicine, Physiology, and Cell Biology
College of Medicine Distinguished Professor
Division of Cardiovascular Medicine
The Ohio State University,
Columbus, Ohio
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 26, 2020. 12:00 p.m. – 1:00 p.m. ET
Commercial Product Theater: A First Choice Treatment for the Inpatient Management of Stabilized Systolic HF Patients: An Evidence-Based Approach
Description
Patients hospitalized due to heart failure with reduced ejection fraction (HFrEF) are at considerable risk of readmission and mortality. This program will review the benefits and risks of starting therapy in the hospital to help prevent rehospitalization and reduce patient mortality.
Speaker
Hameed Ali, DO, SFHM
Clinical Assistant Professor of Medicine
Baylor Scott and White Health
Dallas, Texas
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 27, 2020. 12:00 p.m. – 1:00 p.m. ET
Commercial Product Theater: Selecting A First-Choice Therapy for Systolic HF: Meeting the Burden of Proof
Description
What is the burden of proof that needs to be met before a therapy can be selected for the treatment of systolic heart failure? Hear from Dr. Javed Butler, chairman of the Department of Medicine at the University of Mississippi Medical Center, to learn more about selecting a first-choice therapy for your patients with systolic heart failure.
In this program, Dr. Butler will discuss how aligning your therapy selection to pathophysiologic pathways for HFrEF, it is possible to reduce mortality and morbidity while providing a proven safety and tolerability profile.
Regardless of your patients’ previous heart failure treatment history, following this program, you can feel confident selecting your first-choice therapy for your patients with HFrEF.
Speaker
Javed Butler, MD, MPH, MBA
Chairman, Department of Medicine
University of Mississippi Medical Center,
Jackson, Mississippi
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 25, 2020. 12:00 p.m. – 1:00 p.m. ET
Medical Product Theater: Worsening Symptoms and Hospitalization for Heart Failure: Increased Risk of Poor Outcomes and Opportunities to Enhance Care
Objectives
- Discuss hospitalization as a pivotal point in the clinical trajectory of heart failure.
- Highlight strategies for improvement and optimization of the treatment plan for patients with heart failure.
- Provide practical guidance for identifying predictors of worsening heart failure and educating on the importance of patients’ self-management.
Speaker
William T. Abraham, MD, FACP, FACC, FAHA, FESC, FRCPE
Professor of Medicine, Physiology, and Cell Biology
College of Medicine Distinguished Professor
Division of Cardiovascular Medicine
The Ohio State University,
Columbus, Ohio
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 26, 2020. 12:00 p.m. – 1:00 p.m. ET
Commercial Product Theater: A First Choice Treatment for the Inpatient Management of Stabilized Systolic HF Patients: An Evidence-Based Approach
Description
Patients hospitalized due to heart failure with reduced ejection fraction (HFrEF) are at considerable risk of readmission and mortality. This program will review the benefits and risks of starting therapy in the hospital to help prevent rehospitalization and reduce patient mortality.
Speaker
Hameed Ali, DO, SFHM
Clinical Assistant Professor of Medicine
Baylor Scott and White Health
Dallas, Texas
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 27, 2020. 12:00 p.m. – 1:00 p.m. ET
Commercial Product Theater: Selecting A First-Choice Therapy for Systolic HF: Meeting the Burden of Proof
Description
What is the burden of proof that needs to be met before a therapy can be selected for the treatment of systolic heart failure? Hear from Dr. Javed Butler, chairman of the Department of Medicine at the University of Mississippi Medical Center, to learn more about selecting a first-choice therapy for your patients with systolic heart failure.
In this program, Dr. Butler will discuss how aligning your therapy selection to pathophysiologic pathways for HFrEF, it is possible to reduce mortality and morbidity while providing a proven safety and tolerability profile.
Regardless of your patients’ previous heart failure treatment history, following this program, you can feel confident selecting your first-choice therapy for your patients with HFrEF.
Speaker
Javed Butler, MD, MPH, MBA
Chairman, Department of Medicine
University of Mississippi Medical Center,
Jackson, Mississippi
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 25, 2020. 12:00 p.m. – 1:00 p.m. ET
Medical Product Theater: Worsening Symptoms and Hospitalization for Heart Failure: Increased Risk of Poor Outcomes and Opportunities to Enhance Care
Objectives
- Discuss hospitalization as a pivotal point in the clinical trajectory of heart failure.
- Highlight strategies for improvement and optimization of the treatment plan for patients with heart failure.
- Provide practical guidance for identifying predictors of worsening heart failure and educating on the importance of patients’ self-management.
Speaker
William T. Abraham, MD, FACP, FACC, FAHA, FESC, FRCPE
Professor of Medicine, Physiology, and Cell Biology
College of Medicine Distinguished Professor
Division of Cardiovascular Medicine
The Ohio State University,
Columbus, Ohio
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 26, 2020. 12:00 p.m. – 1:00 p.m. ET
Commercial Product Theater: A First Choice Treatment for the Inpatient Management of Stabilized Systolic HF Patients: An Evidence-Based Approach
Description
Patients hospitalized due to heart failure with reduced ejection fraction (HFrEF) are at considerable risk of readmission and mortality. This program will review the benefits and risks of starting therapy in the hospital to help prevent rehospitalization and reduce patient mortality.
Speaker
Hameed Ali, DO, SFHM
Clinical Assistant Professor of Medicine
Baylor Scott and White Health
Dallas, Texas
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 27, 2020. 12:00 p.m. – 1:00 p.m. ET
Commercial Product Theater: Selecting A First-Choice Therapy for Systolic HF: Meeting the Burden of Proof
Description
What is the burden of proof that needs to be met before a therapy can be selected for the treatment of systolic heart failure? Hear from Dr. Javed Butler, chairman of the Department of Medicine at the University of Mississippi Medical Center, to learn more about selecting a first-choice therapy for your patients with systolic heart failure.
In this program, Dr. Butler will discuss how aligning your therapy selection to pathophysiologic pathways for HFrEF, it is possible to reduce mortality and morbidity while providing a proven safety and tolerability profile.
Regardless of your patients’ previous heart failure treatment history, following this program, you can feel confident selecting your first-choice therapy for your patients with HFrEF.
Speaker
Javed Butler, MD, MPH, MBA
Chairman, Department of Medicine
University of Mississippi Medical Center,
Jackson, Mississippi
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Humira topped drug-revenue list for 2019
Humira outsold all other drugs in 2019 in terms of revenue as cytokine inhibitor medications earned their way to three of the first four spots on the pharmaceutical best-seller list, according to a new analysis from the IQVIA Institute for Human Data Science.
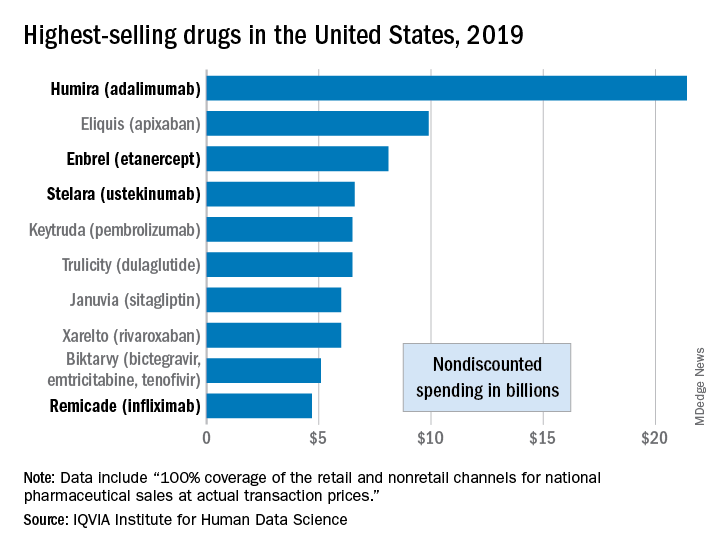
Sales of Humira (adalimumab) amounted to $21.4 billion before discounting, Murray Aitken, the institute’s executive director, and associates wrote in their analysis. That’s more than double the total of the anticoagulant Eliquis (apixaban), which brought in $9.9 billion in its last year before generic forms became available.
The next two spots were filled by the tumor necrosis factor inhibitor Enbrel (etanercept) with $8.1 billion in sales and the interleukin 12/23 inhibitor Stelara (ustekinumab) with sales totaling $6.6 billion, followed by the chemotherapy drug Keytruda (pembrolizumab) close behind after racking up $6.5 billion in sales, the researchers reported.
Total nondiscounted spending on all drugs in the U.S. market came to $511 billion in 2019, an increase of 5.7% over the $484 billion spent in 2018, based on data from the July 2020 IQVIA National Sales Perspectives.
These figures are “not adjusted for estimates of off-invoice discounts and rebates,” the authors noted, but they include “prescription and insulin products sold into chain and independent pharmacies, food store pharmacies, mail service pharmacies, long-term care facilities, hospitals, clinics, and other institutional settings.”
Those “discounts and rebates” do exist, however, and they can add up. Drug sales for 2019, “after deducting negotiated rebates, discounts, and other forms of price concessions, such as patient coupons or vouchers that offset out-of-pocket costs,” were $235 billion less than overall nondiscounted spending, the report noted.
Now that we’ve shown you the money, let’s take a quick look at volume. The leading drugs by number of dispensed prescriptions in 2019 were, not surprisingly, quite different. First, with 118 million prescriptions, was atorvastatin, followed by levothyroxine (113 million), lisinopril (96), amlodipine (89), and metoprolol (85), Mr. Aitken and associates reported.
Altogether, over 4.2 billion prescriptions were dispensed last year, with a couple of caveats: 90-day and 30-day fills were both counted as one prescription, and OTC drugs were not included, they pointed out.
Humira outsold all other drugs in 2019 in terms of revenue as cytokine inhibitor medications earned their way to three of the first four spots on the pharmaceutical best-seller list, according to a new analysis from the IQVIA Institute for Human Data Science.
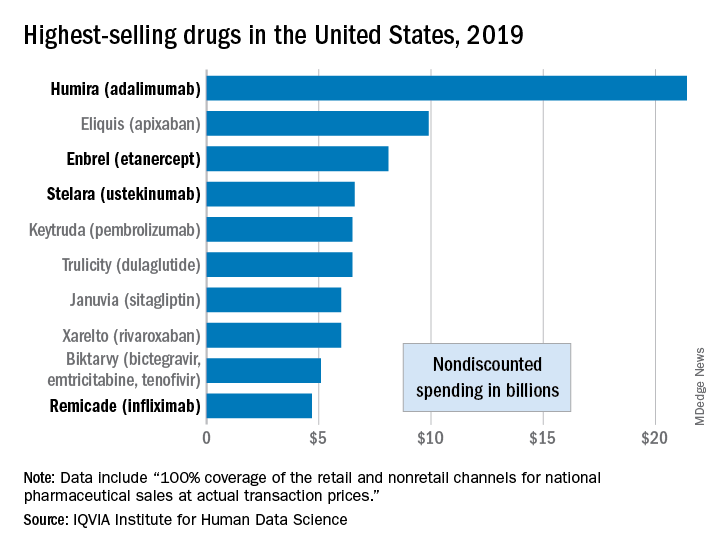
Sales of Humira (adalimumab) amounted to $21.4 billion before discounting, Murray Aitken, the institute’s executive director, and associates wrote in their analysis. That’s more than double the total of the anticoagulant Eliquis (apixaban), which brought in $9.9 billion in its last year before generic forms became available.
The next two spots were filled by the tumor necrosis factor inhibitor Enbrel (etanercept) with $8.1 billion in sales and the interleukin 12/23 inhibitor Stelara (ustekinumab) with sales totaling $6.6 billion, followed by the chemotherapy drug Keytruda (pembrolizumab) close behind after racking up $6.5 billion in sales, the researchers reported.
Total nondiscounted spending on all drugs in the U.S. market came to $511 billion in 2019, an increase of 5.7% over the $484 billion spent in 2018, based on data from the July 2020 IQVIA National Sales Perspectives.
These figures are “not adjusted for estimates of off-invoice discounts and rebates,” the authors noted, but they include “prescription and insulin products sold into chain and independent pharmacies, food store pharmacies, mail service pharmacies, long-term care facilities, hospitals, clinics, and other institutional settings.”
Those “discounts and rebates” do exist, however, and they can add up. Drug sales for 2019, “after deducting negotiated rebates, discounts, and other forms of price concessions, such as patient coupons or vouchers that offset out-of-pocket costs,” were $235 billion less than overall nondiscounted spending, the report noted.
Now that we’ve shown you the money, let’s take a quick look at volume. The leading drugs by number of dispensed prescriptions in 2019 were, not surprisingly, quite different. First, with 118 million prescriptions, was atorvastatin, followed by levothyroxine (113 million), lisinopril (96), amlodipine (89), and metoprolol (85), Mr. Aitken and associates reported.
Altogether, over 4.2 billion prescriptions were dispensed last year, with a couple of caveats: 90-day and 30-day fills were both counted as one prescription, and OTC drugs were not included, they pointed out.
Humira outsold all other drugs in 2019 in terms of revenue as cytokine inhibitor medications earned their way to three of the first four spots on the pharmaceutical best-seller list, according to a new analysis from the IQVIA Institute for Human Data Science.
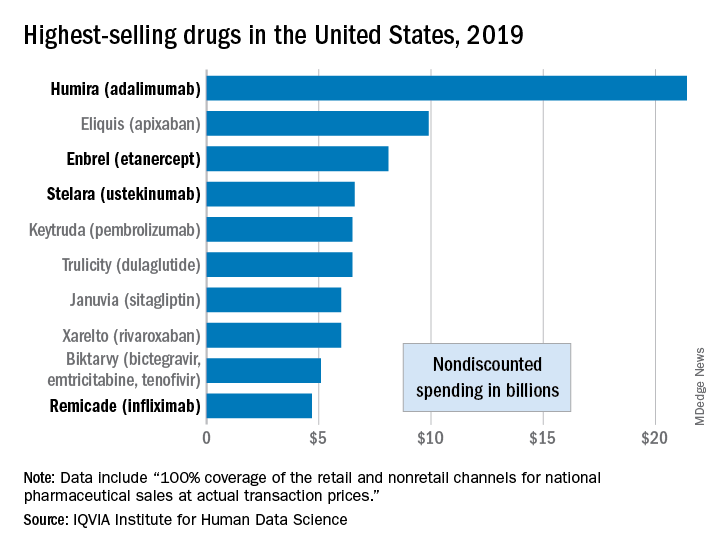
Sales of Humira (adalimumab) amounted to $21.4 billion before discounting, Murray Aitken, the institute’s executive director, and associates wrote in their analysis. That’s more than double the total of the anticoagulant Eliquis (apixaban), which brought in $9.9 billion in its last year before generic forms became available.
The next two spots were filled by the tumor necrosis factor inhibitor Enbrel (etanercept) with $8.1 billion in sales and the interleukin 12/23 inhibitor Stelara (ustekinumab) with sales totaling $6.6 billion, followed by the chemotherapy drug Keytruda (pembrolizumab) close behind after racking up $6.5 billion in sales, the researchers reported.
Total nondiscounted spending on all drugs in the U.S. market came to $511 billion in 2019, an increase of 5.7% over the $484 billion spent in 2018, based on data from the July 2020 IQVIA National Sales Perspectives.
These figures are “not adjusted for estimates of off-invoice discounts and rebates,” the authors noted, but they include “prescription and insulin products sold into chain and independent pharmacies, food store pharmacies, mail service pharmacies, long-term care facilities, hospitals, clinics, and other institutional settings.”
Those “discounts and rebates” do exist, however, and they can add up. Drug sales for 2019, “after deducting negotiated rebates, discounts, and other forms of price concessions, such as patient coupons or vouchers that offset out-of-pocket costs,” were $235 billion less than overall nondiscounted spending, the report noted.
Now that we’ve shown you the money, let’s take a quick look at volume. The leading drugs by number of dispensed prescriptions in 2019 were, not surprisingly, quite different. First, with 118 million prescriptions, was atorvastatin, followed by levothyroxine (113 million), lisinopril (96), amlodipine (89), and metoprolol (85), Mr. Aitken and associates reported.
Altogether, over 4.2 billion prescriptions were dispensed last year, with a couple of caveats: 90-day and 30-day fills were both counted as one prescription, and OTC drugs were not included, they pointed out.









