User login
VIDEO: Revised guidelines raise lung cancer screening age ceiling
TORONTO – A proposed change to CHEST’s lung cancer screening guideline calls for raising the upper age for screening recent cigarette smokers to 77 years of age from 74 years of age.
This proposal is part of draft guideline that was unveiled during the CHEST annual meeting but is still subject to tweaking by peer review until formal release in early 2018. The draft also offers expanded guidance on how to implement screening, containing three times as many recommendations as the current lung cancer screening guidelines (Chest. 2013 May; 143[5 Suppl]:e78S-e92S).
“We want screening to expand in a safe and effective way,” said Peter J. Mazzone, MD, chair of the expert panel that is preparing the revision for CHEST and a pulmonologist at the Cleveland Clinic. “We are less restrictive with these guidelines” than in the 2013 version.
Dr. Mazzone cited two major changes that will produce modest broadening of the criteria that determine which patients can appropriately get screening. The clearest change was the age range, which expanded from 55-74 years of age set in 2013 to reflect the age criterion for enrollment in the National Lung Screening Trial (New Engl J Med. 2011 Aug 4; 365[5]:395-409). Dr. Mazzone explained, though it remains short of the 80-year old ceiling recommended by the U.S. Preventive Services Task Force.
The second, subtler change eased back on the outright ban that the 2013 guidelines placed on screening anyone who falls outside the target age range and smoking history (at least 30 pack years and either being a current smoker or having recently quit within the past 15 years) and who is without severe comorbidities.
The guidelines from 2013 said that screening people who fell outside these limits “should not be performed.” In contrast, the new draft guideline simply said that people who fall outside of the age and smoking-history criteria but who are still considered high risk for lung cancer based on a risk-prediction calculator should not “routinely” undergo screening. Additionally, exceptions could be made for certain patients whose high risk appears to warrant screening, Dr. Mazzone and others from the expert panel noted.
The revision specified that a high-risk person outside of the core criteria might still be a reasonable candidate for screening if this person tallies at least a 1.51% risk of developing lung cancer during the next 6 years according to the PLCOM2012 risk calculator (New Engl J Med. 2013 Feb 21; 368[8]:728-36).
“Some of the evidence allowed us to be a little more flexible,” though not to the point of “opening screening widely” to people who fall outside the core target population; rather, clinicians get to have a little more discretion, said Dr. Mazzone, who directs the Cleveland Clinic’s Lung Cancer Program. “We hope this will lead to more patients being screened in a high quality way,” he said in an interview. The panel strove to “look beyond the National Lung Screening Trial and find other groups of patients who could benefit” from screening. “We say that other high-risk people should not, on the whole, be screened” but that clinicians could consider individuals as appropriate for screening on a case-by-case basis.
The revision “fills in the outline” for screening that was established in the 2013 guidelines, said Gerard A. Silvestri, MD, a member of the revision panel, in a video interview. The updated guideline better detailed who benefits the most from screening and who benefits less, as well as the potential complications screening may cause, said Dr. Silvestri, a professor of medicine and lung cancer pulmonologist at the Medical University of South Carolina in Charleston.
“The sweet spot for screening is patients with a medium lung cancer risk without many comorbidities. We are trying to come up with individualized risk profiling,” explained Dr. Silvestri during the CHEST session. He noted that, in the screening program he runs in Charleston, every person who contacts the program and is interested in screening undergoes risk profiling. Are there people with a risk profile that justifies screening but fall outside the proposed criteria? “Absolutely,” Dr. Silvestri said.
People considering screening also need to recognize its potential harms, noted Renda Soylemez Wiener, MD, another member of the expert panel who spoke at the meeting. She cited five potential harms: death or complications from a biopsy of a screen-detected nodule, surgery for a screen-detected lesion that turns out to be benign, the psychosocial impact of finding a lung nodule, over diagnosis, and the cumulative radiation exposure from serial low-dose chest CT scans. “All of these dangers are real and may be magnified or mitigated as low-dose CT screening is implemented in real world practice,” said Dr. Wiener, a pulmonologist at Boston University.
In addition to four evidence-based recommendations that help define who is and isn’t an appropriate screening candidate, the revised guideline also included 11 mostly consensus-based “suggestions” about how screening programs should ideally operate. These covered issues such as identifying symptomatic patients who require diagnosis rather than screening, having strategies to encourage compliance with annual screening, including smoking cessation treatments in screening programs, and having strategies that minimize overtreatment of potentially indolent cancers.
The goal of these suggestions is to help in the design of high-quality screening programs, said Dr. Mazzone. “It’s not just who you screen but also how you screen.”
On Twitter @mitchelzoler
M. Patricia Rivera, MD, FCCP, comments: The revised ACCP screening guidelines recommend expanding the screening age from 55-74 years (age criterion used in the National Lung Screening Trial) to 55-77 years. While this may be interpreted as raising the screening age ceiling, the new recommendation is in line with the age range approved by Medicare. We should also keep in mind that after modeling studies to predict the benefits and harms of screening programs using different screening intervals, age ranges, and smoking histories (duration and time since quitting), the USPSTF concluded in their final recommendation that screening adults aged 55-80 years with same smoking history and time since quitting used in the National Lung Screening Trial (NLST) had a reasonable balance of benefits and harms. Implementing lung cancer screening has been challenging, and studies have reported many patient-, provider-, and system-based barriers including conflicting upper age range recommendations.
While age and smoking history are important in identifying individuals at risk for lung cancer, development of lung cancer is likely multifactorial and several other risk factors need to be considered. The ACCP's revised guidelines provide flexibility when evaluating patients who do not meet the age and smoking history criteria for screening but who have a high risk for developing lung cancer based on risk prediction models. Following publication of the NLST results, secondary analysis of the data using a risk prediction model that takes into account additional risk factors for the development of lung cancer (race, COPD, and family history of lung cancer, among others) suggests risk prediction modeling may be helpful at identifying the individuals who are at highest risk for developing lung cancer. As pointed out by Dr. Mazzone and Dr. Silvestri, the ACCP lung cancer screening guidelines promote the expansion of lung cancer screening in a safe and effective way and encourage individualized risk profiling to aid in the selection of all individuals who will benefit from lung cancer screening.
M. Patricia Rivera, MD, FCCP, comments: The revised ACCP screening guidelines recommend expanding the screening age from 55-74 years (age criterion used in the National Lung Screening Trial) to 55-77 years. While this may be interpreted as raising the screening age ceiling, the new recommendation is in line with the age range approved by Medicare. We should also keep in mind that after modeling studies to predict the benefits and harms of screening programs using different screening intervals, age ranges, and smoking histories (duration and time since quitting), the USPSTF concluded in their final recommendation that screening adults aged 55-80 years with same smoking history and time since quitting used in the National Lung Screening Trial (NLST) had a reasonable balance of benefits and harms. Implementing lung cancer screening has been challenging, and studies have reported many patient-, provider-, and system-based barriers including conflicting upper age range recommendations.
While age and smoking history are important in identifying individuals at risk for lung cancer, development of lung cancer is likely multifactorial and several other risk factors need to be considered. The ACCP's revised guidelines provide flexibility when evaluating patients who do not meet the age and smoking history criteria for screening but who have a high risk for developing lung cancer based on risk prediction models. Following publication of the NLST results, secondary analysis of the data using a risk prediction model that takes into account additional risk factors for the development of lung cancer (race, COPD, and family history of lung cancer, among others) suggests risk prediction modeling may be helpful at identifying the individuals who are at highest risk for developing lung cancer. As pointed out by Dr. Mazzone and Dr. Silvestri, the ACCP lung cancer screening guidelines promote the expansion of lung cancer screening in a safe and effective way and encourage individualized risk profiling to aid in the selection of all individuals who will benefit from lung cancer screening.
M. Patricia Rivera, MD, FCCP, comments: The revised ACCP screening guidelines recommend expanding the screening age from 55-74 years (age criterion used in the National Lung Screening Trial) to 55-77 years. While this may be interpreted as raising the screening age ceiling, the new recommendation is in line with the age range approved by Medicare. We should also keep in mind that after modeling studies to predict the benefits and harms of screening programs using different screening intervals, age ranges, and smoking histories (duration and time since quitting), the USPSTF concluded in their final recommendation that screening adults aged 55-80 years with same smoking history and time since quitting used in the National Lung Screening Trial (NLST) had a reasonable balance of benefits and harms. Implementing lung cancer screening has been challenging, and studies have reported many patient-, provider-, and system-based barriers including conflicting upper age range recommendations.
While age and smoking history are important in identifying individuals at risk for lung cancer, development of lung cancer is likely multifactorial and several other risk factors need to be considered. The ACCP's revised guidelines provide flexibility when evaluating patients who do not meet the age and smoking history criteria for screening but who have a high risk for developing lung cancer based on risk prediction models. Following publication of the NLST results, secondary analysis of the data using a risk prediction model that takes into account additional risk factors for the development of lung cancer (race, COPD, and family history of lung cancer, among others) suggests risk prediction modeling may be helpful at identifying the individuals who are at highest risk for developing lung cancer. As pointed out by Dr. Mazzone and Dr. Silvestri, the ACCP lung cancer screening guidelines promote the expansion of lung cancer screening in a safe and effective way and encourage individualized risk profiling to aid in the selection of all individuals who will benefit from lung cancer screening.
TORONTO – A proposed change to CHEST’s lung cancer screening guideline calls for raising the upper age for screening recent cigarette smokers to 77 years of age from 74 years of age.
This proposal is part of draft guideline that was unveiled during the CHEST annual meeting but is still subject to tweaking by peer review until formal release in early 2018. The draft also offers expanded guidance on how to implement screening, containing three times as many recommendations as the current lung cancer screening guidelines (Chest. 2013 May; 143[5 Suppl]:e78S-e92S).
“We want screening to expand in a safe and effective way,” said Peter J. Mazzone, MD, chair of the expert panel that is preparing the revision for CHEST and a pulmonologist at the Cleveland Clinic. “We are less restrictive with these guidelines” than in the 2013 version.
Dr. Mazzone cited two major changes that will produce modest broadening of the criteria that determine which patients can appropriately get screening. The clearest change was the age range, which expanded from 55-74 years of age set in 2013 to reflect the age criterion for enrollment in the National Lung Screening Trial (New Engl J Med. 2011 Aug 4; 365[5]:395-409). Dr. Mazzone explained, though it remains short of the 80-year old ceiling recommended by the U.S. Preventive Services Task Force.
The second, subtler change eased back on the outright ban that the 2013 guidelines placed on screening anyone who falls outside the target age range and smoking history (at least 30 pack years and either being a current smoker or having recently quit within the past 15 years) and who is without severe comorbidities.
The guidelines from 2013 said that screening people who fell outside these limits “should not be performed.” In contrast, the new draft guideline simply said that people who fall outside of the age and smoking-history criteria but who are still considered high risk for lung cancer based on a risk-prediction calculator should not “routinely” undergo screening. Additionally, exceptions could be made for certain patients whose high risk appears to warrant screening, Dr. Mazzone and others from the expert panel noted.
The revision specified that a high-risk person outside of the core criteria might still be a reasonable candidate for screening if this person tallies at least a 1.51% risk of developing lung cancer during the next 6 years according to the PLCOM2012 risk calculator (New Engl J Med. 2013 Feb 21; 368[8]:728-36).
“Some of the evidence allowed us to be a little more flexible,” though not to the point of “opening screening widely” to people who fall outside the core target population; rather, clinicians get to have a little more discretion, said Dr. Mazzone, who directs the Cleveland Clinic’s Lung Cancer Program. “We hope this will lead to more patients being screened in a high quality way,” he said in an interview. The panel strove to “look beyond the National Lung Screening Trial and find other groups of patients who could benefit” from screening. “We say that other high-risk people should not, on the whole, be screened” but that clinicians could consider individuals as appropriate for screening on a case-by-case basis.
The revision “fills in the outline” for screening that was established in the 2013 guidelines, said Gerard A. Silvestri, MD, a member of the revision panel, in a video interview. The updated guideline better detailed who benefits the most from screening and who benefits less, as well as the potential complications screening may cause, said Dr. Silvestri, a professor of medicine and lung cancer pulmonologist at the Medical University of South Carolina in Charleston.
“The sweet spot for screening is patients with a medium lung cancer risk without many comorbidities. We are trying to come up with individualized risk profiling,” explained Dr. Silvestri during the CHEST session. He noted that, in the screening program he runs in Charleston, every person who contacts the program and is interested in screening undergoes risk profiling. Are there people with a risk profile that justifies screening but fall outside the proposed criteria? “Absolutely,” Dr. Silvestri said.
People considering screening also need to recognize its potential harms, noted Renda Soylemez Wiener, MD, another member of the expert panel who spoke at the meeting. She cited five potential harms: death or complications from a biopsy of a screen-detected nodule, surgery for a screen-detected lesion that turns out to be benign, the psychosocial impact of finding a lung nodule, over diagnosis, and the cumulative radiation exposure from serial low-dose chest CT scans. “All of these dangers are real and may be magnified or mitigated as low-dose CT screening is implemented in real world practice,” said Dr. Wiener, a pulmonologist at Boston University.
In addition to four evidence-based recommendations that help define who is and isn’t an appropriate screening candidate, the revised guideline also included 11 mostly consensus-based “suggestions” about how screening programs should ideally operate. These covered issues such as identifying symptomatic patients who require diagnosis rather than screening, having strategies to encourage compliance with annual screening, including smoking cessation treatments in screening programs, and having strategies that minimize overtreatment of potentially indolent cancers.
The goal of these suggestions is to help in the design of high-quality screening programs, said Dr. Mazzone. “It’s not just who you screen but also how you screen.”
On Twitter @mitchelzoler
TORONTO – A proposed change to CHEST’s lung cancer screening guideline calls for raising the upper age for screening recent cigarette smokers to 77 years of age from 74 years of age.
This proposal is part of draft guideline that was unveiled during the CHEST annual meeting but is still subject to tweaking by peer review until formal release in early 2018. The draft also offers expanded guidance on how to implement screening, containing three times as many recommendations as the current lung cancer screening guidelines (Chest. 2013 May; 143[5 Suppl]:e78S-e92S).
“We want screening to expand in a safe and effective way,” said Peter J. Mazzone, MD, chair of the expert panel that is preparing the revision for CHEST and a pulmonologist at the Cleveland Clinic. “We are less restrictive with these guidelines” than in the 2013 version.
Dr. Mazzone cited two major changes that will produce modest broadening of the criteria that determine which patients can appropriately get screening. The clearest change was the age range, which expanded from 55-74 years of age set in 2013 to reflect the age criterion for enrollment in the National Lung Screening Trial (New Engl J Med. 2011 Aug 4; 365[5]:395-409). Dr. Mazzone explained, though it remains short of the 80-year old ceiling recommended by the U.S. Preventive Services Task Force.
The second, subtler change eased back on the outright ban that the 2013 guidelines placed on screening anyone who falls outside the target age range and smoking history (at least 30 pack years and either being a current smoker or having recently quit within the past 15 years) and who is without severe comorbidities.
The guidelines from 2013 said that screening people who fell outside these limits “should not be performed.” In contrast, the new draft guideline simply said that people who fall outside of the age and smoking-history criteria but who are still considered high risk for lung cancer based on a risk-prediction calculator should not “routinely” undergo screening. Additionally, exceptions could be made for certain patients whose high risk appears to warrant screening, Dr. Mazzone and others from the expert panel noted.
The revision specified that a high-risk person outside of the core criteria might still be a reasonable candidate for screening if this person tallies at least a 1.51% risk of developing lung cancer during the next 6 years according to the PLCOM2012 risk calculator (New Engl J Med. 2013 Feb 21; 368[8]:728-36).
“Some of the evidence allowed us to be a little more flexible,” though not to the point of “opening screening widely” to people who fall outside the core target population; rather, clinicians get to have a little more discretion, said Dr. Mazzone, who directs the Cleveland Clinic’s Lung Cancer Program. “We hope this will lead to more patients being screened in a high quality way,” he said in an interview. The panel strove to “look beyond the National Lung Screening Trial and find other groups of patients who could benefit” from screening. “We say that other high-risk people should not, on the whole, be screened” but that clinicians could consider individuals as appropriate for screening on a case-by-case basis.
The revision “fills in the outline” for screening that was established in the 2013 guidelines, said Gerard A. Silvestri, MD, a member of the revision panel, in a video interview. The updated guideline better detailed who benefits the most from screening and who benefits less, as well as the potential complications screening may cause, said Dr. Silvestri, a professor of medicine and lung cancer pulmonologist at the Medical University of South Carolina in Charleston.
“The sweet spot for screening is patients with a medium lung cancer risk without many comorbidities. We are trying to come up with individualized risk profiling,” explained Dr. Silvestri during the CHEST session. He noted that, in the screening program he runs in Charleston, every person who contacts the program and is interested in screening undergoes risk profiling. Are there people with a risk profile that justifies screening but fall outside the proposed criteria? “Absolutely,” Dr. Silvestri said.
People considering screening also need to recognize its potential harms, noted Renda Soylemez Wiener, MD, another member of the expert panel who spoke at the meeting. She cited five potential harms: death or complications from a biopsy of a screen-detected nodule, surgery for a screen-detected lesion that turns out to be benign, the psychosocial impact of finding a lung nodule, over diagnosis, and the cumulative radiation exposure from serial low-dose chest CT scans. “All of these dangers are real and may be magnified or mitigated as low-dose CT screening is implemented in real world practice,” said Dr. Wiener, a pulmonologist at Boston University.
In addition to four evidence-based recommendations that help define who is and isn’t an appropriate screening candidate, the revised guideline also included 11 mostly consensus-based “suggestions” about how screening programs should ideally operate. These covered issues such as identifying symptomatic patients who require diagnosis rather than screening, having strategies to encourage compliance with annual screening, including smoking cessation treatments in screening programs, and having strategies that minimize overtreatment of potentially indolent cancers.
The goal of these suggestions is to help in the design of high-quality screening programs, said Dr. Mazzone. “It’s not just who you screen but also how you screen.”
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM CHEST 2017
Neoantigen profiling predicts response to immunotherapy
In antitumor immunity and immunotherapy, quality and fitness count.
Specifically, the quality and fitness of neoantigens – tumor-specific mutated peptides on the surface of cancer cells – can influence a patient’s response to immune checkpoint inhibitors, and mathematical models of neoantigen fitness can serve as biomarkers for response to immunotherapy, according to investigators of two separate but related studies published in Nature.
In one study, Marta Łuksza, PhD, from the Simons Center for Systems Biology at the Institute for Advanced Study in Princeton, N.J., and colleagues propose a neoantigen fitness model that can predict tumor response to checkpoint blockade immunotherapy.
Importantly, low-fitness neoantigens identified by our method may be leveraged for developing novel immunotherapies,” they wrote (Nature. 2017 Nov 8. doi: 10.1038/nature24473).
In a related study, Vinod P. Balachandran, MD, from the David M. Rubinstein Center for Pancreatic Cancer Research at Memorial Sloan Kettering Cancer Center in New York and colleagues, including Dr. Łuksza and others, looked at T-cell antigens in long-term survivors of pancreatic cancer and identified specific neoantigens as T-cell targets.
“More broadly, we identify neoantigen quality as a biomarker for immunogenic tumors that may guide the application of immunotherapies,” Dr. Balachandran and colleagues wrote (Nature. 2017 Nov 8. doi: 10.1038/nature24462).
Proof of concept
The studies provide a proof of concept that mathematical modeling of tumor evolution and the interactions of tumors with the immune system may soon provide clinicians with valuable and actionable information about responses to immunotherapy, Benjamin Greenbaum, PhD, senior author on the study by Łuksza et al., and a coauthor on the pancreatic cancer study said in an interview.
“We’re trying to come up with measures that take into account what we think the underlying processes are and what lies behind therapy response, and that should lead to better predictive models associated with response in the future,” said Dr. Greenbaum, of the Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai Medical Center, New York.
One of the key findings of the studies is that neoantigen quality – the ability of neoantigens to spark T-cell recognition – seems to be as or more important than neoantigen quantity for influencing immune responses during tumor evolution.
“The general logic behind the idea that mutational burden can be a good predictor of response is that the more mutations you have, the more likely that you have a neoantigen, a peptide generated by a tumor mutation, that elicits productive T-cell recognition. We tried to model that process that might lead to productive T-cell recognition, to assign a kind of number to every neoantigen to provide some estimate of how likely it was to undergo a productive process,” Dr. Greenbaum explained.
Melanoma and lung cancer survivors
In the study by Łuksza et al., the investigators created a mathematical fitness model that can predict how tumors respond to immunotherapy based on how neoantigens interact with the immune system and applied the model to data on three previously reported patient cohorts, including two groups of patients with malignant melanoma treated with a cytotoxic T-lymphocyte associated protein 4 (CTLA4) immune checkpoint such as ipilimumab (Yervoy), and one group of patients with non–small cell lung cancer treated with a programmed death-1 (PD-1) inhibitor (for example, nivolumab [Opdivo]).
They found that their proposed model is more accurate than genomic biomarkers for predicting how a specific tumor may respond to immunotherapy.
“Importantly, low-fitness neoantigens identified by our method may be leveraged for developing novel immunotherapies. By using an immune fitness model to study immunotherapy, we reveal broad similarities between the evolution of tumors and rapidly evolving pathogens,” they wrote.
Pancreatic cancer survivors
Fewer than 7% of patients diagnosed with pancreatic ductal adenocarcinoma (PDAC) survive more than 5 years, despite the best surgical and medical therapy. But a few lucky patients are long-term survivors, and Dr. Balachandran and associates sought to examine what aspects of T-cell immunity contributed to their longevity.
Rather than relying on genomic analysis of tumor samples, however, they used a combination of genetic, immunohistochemical, and transcriptional immunoprofiling, as well as computational biophysics and function to identify T-cell antigens in the long-term survivors.
When they compared surgically resected patients matched by tumor stage, they found that tumors from those with a median overall survival (OS) of 6 years had a 3-fold greater density of CD8-positive T cells and a 12-fold greater density of cytolytic CD8-positive cells, as well as more mature dendritic cells, regulatory T cells, and macrophages, but decreased numbers of CD4-positive T cells, compared with patients with a more typical course of survival (median OS, 0.8 years). There were no differences between long- and short-term survivors in either B cells or major histocompatibility complex (MHC) class I–positive cells.
They then performed whole-exome sequencing on tumor samples to determine the frequency of neoantigens and found a median of 38 predicted neoantigens per tumor.
“Notably, patients with both the highest predicted neoantigen number and either the greatest CD3+, CD8+, or polyclonal T-cell repertoire, but neither alone, exhibited the longest survival,” they wrote.
When they looked for qualities of neoantigens responsible for promoting T-cell activation in the long-term survivors, they found that the tumors from the survivors, compared with others, were enriched in neoantigen qualities that could be described by a mathematical fitness model.
“Our results provide insight into the heterogeneous immunobiology of PDAC, a presumed poorly immunogenic and checkpoint blockade–refractory tumor, demonstrating that neoantigens may be T-cell targets in [long-term survivors]”, they wrote.
The investigators propose that immunity to neoantigens that are generated during the outgrowth of a primary tumor could at least partially explain the lower incidence of relapse and prolonged survival of a small minority of patients with pancreatic cancer.
“Our findings support the development of strategies to harness neoantigen-specific immunity to treat checkpoint blockade–refractory cancers, and the identification of immunogenic hot spots for directed neoantigen targeting,” they concluded.
The studies were supported by grants from Stand Up to Cancer, American Cancer Society, National Science Foundation, Lustgarten Foundation, Janssen Research & Development, the STARR Cancer Consortium, the Pershing Square Sohn Cancer Research Alliance, the National Institutes of Health, the V Foundation, Swim Across America, Ludwig Institute for Cancer Research, the Parker Institute for Cancer Immunotherapy, a National Cancer Institute Career Development Award, and a Memorial Sloan Kettering Cancer Center core grant. Dr. Łuksza and Dr. Greenbaum disclosed consulting for Merck. Dr. Balachandran disclosed research funding from Bristol-Myers Squibb.
In antitumor immunity and immunotherapy, quality and fitness count.
Specifically, the quality and fitness of neoantigens – tumor-specific mutated peptides on the surface of cancer cells – can influence a patient’s response to immune checkpoint inhibitors, and mathematical models of neoantigen fitness can serve as biomarkers for response to immunotherapy, according to investigators of two separate but related studies published in Nature.
In one study, Marta Łuksza, PhD, from the Simons Center for Systems Biology at the Institute for Advanced Study in Princeton, N.J., and colleagues propose a neoantigen fitness model that can predict tumor response to checkpoint blockade immunotherapy.
Importantly, low-fitness neoantigens identified by our method may be leveraged for developing novel immunotherapies,” they wrote (Nature. 2017 Nov 8. doi: 10.1038/nature24473).
In a related study, Vinod P. Balachandran, MD, from the David M. Rubinstein Center for Pancreatic Cancer Research at Memorial Sloan Kettering Cancer Center in New York and colleagues, including Dr. Łuksza and others, looked at T-cell antigens in long-term survivors of pancreatic cancer and identified specific neoantigens as T-cell targets.
“More broadly, we identify neoantigen quality as a biomarker for immunogenic tumors that may guide the application of immunotherapies,” Dr. Balachandran and colleagues wrote (Nature. 2017 Nov 8. doi: 10.1038/nature24462).
Proof of concept
The studies provide a proof of concept that mathematical modeling of tumor evolution and the interactions of tumors with the immune system may soon provide clinicians with valuable and actionable information about responses to immunotherapy, Benjamin Greenbaum, PhD, senior author on the study by Łuksza et al., and a coauthor on the pancreatic cancer study said in an interview.
“We’re trying to come up with measures that take into account what we think the underlying processes are and what lies behind therapy response, and that should lead to better predictive models associated with response in the future,” said Dr. Greenbaum, of the Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai Medical Center, New York.
One of the key findings of the studies is that neoantigen quality – the ability of neoantigens to spark T-cell recognition – seems to be as or more important than neoantigen quantity for influencing immune responses during tumor evolution.
“The general logic behind the idea that mutational burden can be a good predictor of response is that the more mutations you have, the more likely that you have a neoantigen, a peptide generated by a tumor mutation, that elicits productive T-cell recognition. We tried to model that process that might lead to productive T-cell recognition, to assign a kind of number to every neoantigen to provide some estimate of how likely it was to undergo a productive process,” Dr. Greenbaum explained.
Melanoma and lung cancer survivors
In the study by Łuksza et al., the investigators created a mathematical fitness model that can predict how tumors respond to immunotherapy based on how neoantigens interact with the immune system and applied the model to data on three previously reported patient cohorts, including two groups of patients with malignant melanoma treated with a cytotoxic T-lymphocyte associated protein 4 (CTLA4) immune checkpoint such as ipilimumab (Yervoy), and one group of patients with non–small cell lung cancer treated with a programmed death-1 (PD-1) inhibitor (for example, nivolumab [Opdivo]).
They found that their proposed model is more accurate than genomic biomarkers for predicting how a specific tumor may respond to immunotherapy.
“Importantly, low-fitness neoantigens identified by our method may be leveraged for developing novel immunotherapies. By using an immune fitness model to study immunotherapy, we reveal broad similarities between the evolution of tumors and rapidly evolving pathogens,” they wrote.
Pancreatic cancer survivors
Fewer than 7% of patients diagnosed with pancreatic ductal adenocarcinoma (PDAC) survive more than 5 years, despite the best surgical and medical therapy. But a few lucky patients are long-term survivors, and Dr. Balachandran and associates sought to examine what aspects of T-cell immunity contributed to their longevity.
Rather than relying on genomic analysis of tumor samples, however, they used a combination of genetic, immunohistochemical, and transcriptional immunoprofiling, as well as computational biophysics and function to identify T-cell antigens in the long-term survivors.
When they compared surgically resected patients matched by tumor stage, they found that tumors from those with a median overall survival (OS) of 6 years had a 3-fold greater density of CD8-positive T cells and a 12-fold greater density of cytolytic CD8-positive cells, as well as more mature dendritic cells, regulatory T cells, and macrophages, but decreased numbers of CD4-positive T cells, compared with patients with a more typical course of survival (median OS, 0.8 years). There were no differences between long- and short-term survivors in either B cells or major histocompatibility complex (MHC) class I–positive cells.
They then performed whole-exome sequencing on tumor samples to determine the frequency of neoantigens and found a median of 38 predicted neoantigens per tumor.
“Notably, patients with both the highest predicted neoantigen number and either the greatest CD3+, CD8+, or polyclonal T-cell repertoire, but neither alone, exhibited the longest survival,” they wrote.
When they looked for qualities of neoantigens responsible for promoting T-cell activation in the long-term survivors, they found that the tumors from the survivors, compared with others, were enriched in neoantigen qualities that could be described by a mathematical fitness model.
“Our results provide insight into the heterogeneous immunobiology of PDAC, a presumed poorly immunogenic and checkpoint blockade–refractory tumor, demonstrating that neoantigens may be T-cell targets in [long-term survivors]”, they wrote.
The investigators propose that immunity to neoantigens that are generated during the outgrowth of a primary tumor could at least partially explain the lower incidence of relapse and prolonged survival of a small minority of patients with pancreatic cancer.
“Our findings support the development of strategies to harness neoantigen-specific immunity to treat checkpoint blockade–refractory cancers, and the identification of immunogenic hot spots for directed neoantigen targeting,” they concluded.
The studies were supported by grants from Stand Up to Cancer, American Cancer Society, National Science Foundation, Lustgarten Foundation, Janssen Research & Development, the STARR Cancer Consortium, the Pershing Square Sohn Cancer Research Alliance, the National Institutes of Health, the V Foundation, Swim Across America, Ludwig Institute for Cancer Research, the Parker Institute for Cancer Immunotherapy, a National Cancer Institute Career Development Award, and a Memorial Sloan Kettering Cancer Center core grant. Dr. Łuksza and Dr. Greenbaum disclosed consulting for Merck. Dr. Balachandran disclosed research funding from Bristol-Myers Squibb.
In antitumor immunity and immunotherapy, quality and fitness count.
Specifically, the quality and fitness of neoantigens – tumor-specific mutated peptides on the surface of cancer cells – can influence a patient’s response to immune checkpoint inhibitors, and mathematical models of neoantigen fitness can serve as biomarkers for response to immunotherapy, according to investigators of two separate but related studies published in Nature.
In one study, Marta Łuksza, PhD, from the Simons Center for Systems Biology at the Institute for Advanced Study in Princeton, N.J., and colleagues propose a neoantigen fitness model that can predict tumor response to checkpoint blockade immunotherapy.
Importantly, low-fitness neoantigens identified by our method may be leveraged for developing novel immunotherapies,” they wrote (Nature. 2017 Nov 8. doi: 10.1038/nature24473).
In a related study, Vinod P. Balachandran, MD, from the David M. Rubinstein Center for Pancreatic Cancer Research at Memorial Sloan Kettering Cancer Center in New York and colleagues, including Dr. Łuksza and others, looked at T-cell antigens in long-term survivors of pancreatic cancer and identified specific neoantigens as T-cell targets.
“More broadly, we identify neoantigen quality as a biomarker for immunogenic tumors that may guide the application of immunotherapies,” Dr. Balachandran and colleagues wrote (Nature. 2017 Nov 8. doi: 10.1038/nature24462).
Proof of concept
The studies provide a proof of concept that mathematical modeling of tumor evolution and the interactions of tumors with the immune system may soon provide clinicians with valuable and actionable information about responses to immunotherapy, Benjamin Greenbaum, PhD, senior author on the study by Łuksza et al., and a coauthor on the pancreatic cancer study said in an interview.
“We’re trying to come up with measures that take into account what we think the underlying processes are and what lies behind therapy response, and that should lead to better predictive models associated with response in the future,” said Dr. Greenbaum, of the Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai Medical Center, New York.
One of the key findings of the studies is that neoantigen quality – the ability of neoantigens to spark T-cell recognition – seems to be as or more important than neoantigen quantity for influencing immune responses during tumor evolution.
“The general logic behind the idea that mutational burden can be a good predictor of response is that the more mutations you have, the more likely that you have a neoantigen, a peptide generated by a tumor mutation, that elicits productive T-cell recognition. We tried to model that process that might lead to productive T-cell recognition, to assign a kind of number to every neoantigen to provide some estimate of how likely it was to undergo a productive process,” Dr. Greenbaum explained.
Melanoma and lung cancer survivors
In the study by Łuksza et al., the investigators created a mathematical fitness model that can predict how tumors respond to immunotherapy based on how neoantigens interact with the immune system and applied the model to data on three previously reported patient cohorts, including two groups of patients with malignant melanoma treated with a cytotoxic T-lymphocyte associated protein 4 (CTLA4) immune checkpoint such as ipilimumab (Yervoy), and one group of patients with non–small cell lung cancer treated with a programmed death-1 (PD-1) inhibitor (for example, nivolumab [Opdivo]).
They found that their proposed model is more accurate than genomic biomarkers for predicting how a specific tumor may respond to immunotherapy.
“Importantly, low-fitness neoantigens identified by our method may be leveraged for developing novel immunotherapies. By using an immune fitness model to study immunotherapy, we reveal broad similarities between the evolution of tumors and rapidly evolving pathogens,” they wrote.
Pancreatic cancer survivors
Fewer than 7% of patients diagnosed with pancreatic ductal adenocarcinoma (PDAC) survive more than 5 years, despite the best surgical and medical therapy. But a few lucky patients are long-term survivors, and Dr. Balachandran and associates sought to examine what aspects of T-cell immunity contributed to their longevity.
Rather than relying on genomic analysis of tumor samples, however, they used a combination of genetic, immunohistochemical, and transcriptional immunoprofiling, as well as computational biophysics and function to identify T-cell antigens in the long-term survivors.
When they compared surgically resected patients matched by tumor stage, they found that tumors from those with a median overall survival (OS) of 6 years had a 3-fold greater density of CD8-positive T cells and a 12-fold greater density of cytolytic CD8-positive cells, as well as more mature dendritic cells, regulatory T cells, and macrophages, but decreased numbers of CD4-positive T cells, compared with patients with a more typical course of survival (median OS, 0.8 years). There were no differences between long- and short-term survivors in either B cells or major histocompatibility complex (MHC) class I–positive cells.
They then performed whole-exome sequencing on tumor samples to determine the frequency of neoantigens and found a median of 38 predicted neoantigens per tumor.
“Notably, patients with both the highest predicted neoantigen number and either the greatest CD3+, CD8+, or polyclonal T-cell repertoire, but neither alone, exhibited the longest survival,” they wrote.
When they looked for qualities of neoantigens responsible for promoting T-cell activation in the long-term survivors, they found that the tumors from the survivors, compared with others, were enriched in neoantigen qualities that could be described by a mathematical fitness model.
“Our results provide insight into the heterogeneous immunobiology of PDAC, a presumed poorly immunogenic and checkpoint blockade–refractory tumor, demonstrating that neoantigens may be T-cell targets in [long-term survivors]”, they wrote.
The investigators propose that immunity to neoantigens that are generated during the outgrowth of a primary tumor could at least partially explain the lower incidence of relapse and prolonged survival of a small minority of patients with pancreatic cancer.
“Our findings support the development of strategies to harness neoantigen-specific immunity to treat checkpoint blockade–refractory cancers, and the identification of immunogenic hot spots for directed neoantigen targeting,” they concluded.
The studies were supported by grants from Stand Up to Cancer, American Cancer Society, National Science Foundation, Lustgarten Foundation, Janssen Research & Development, the STARR Cancer Consortium, the Pershing Square Sohn Cancer Research Alliance, the National Institutes of Health, the V Foundation, Swim Across America, Ludwig Institute for Cancer Research, the Parker Institute for Cancer Immunotherapy, a National Cancer Institute Career Development Award, and a Memorial Sloan Kettering Cancer Center core grant. Dr. Łuksza and Dr. Greenbaum disclosed consulting for Merck. Dr. Balachandran disclosed research funding from Bristol-Myers Squibb.
FROM NATURE
Key clinical point: Proof-of-concept studies show that mathematical modeling of neoantigens can be used to predict tumor responses to immune checkpoint inhibitors.
Major finding: Neoantigen quality may be a better biomarker for guiding immunotherapy than tumor genomic profiling.
Data source: Basic science reports focusing on neoantigens and their potential influence on tumor interactions with the immune system.
Disclosures: The studies were supported by grants from Stand Up to Cancer, American Cancer Society, National Science Foundation, Lustgarten Foundation, Janssen Research & Development, the STARR Cancer Consortium, the Pershing Square Sohn Cancer Research Alliance, the National Institutes of Health, the V Foundation, Swim Across America, Ludwig Institute for Cancer Research, the Parker Institute for Cancer Immunotherapy, a National Cancer Institute Career Development Award, and a Memorial Sloan Kettering Cancer Center core grant. Dr. Łuksza and Dr. Greenbaum disclosed consulting for Merck. Dr. Balachandran disclosed research funding from Bristol-Myers Squibb.
FDA approves alectinib as frontline therapy for ALK-positive metastatic NSCLC
The Food and Drug Administration has approved frontline alectinib for the treatment of anaplastic lymphoma kinase (ALK)–positive metastatic non–small cell lung cancer (NSCLC) that has been detected by an FDA-approved test.
The drug previously received accelerated approval for treatment of patients with ALK-positive metastatic NSCLC whose disease progressed while receiving crizotinib or who were intolerant of that treatment.
There was also a lower incidence of progression to the central nervous system as first site of disease progression with alectinib: Incidence of progression to the CNS was 12% for patients receiving alectinib and 45% for patients receiving crizotinib.
The most common adverse events in patients receiving alectinib were fatigue, constipation, edema, myalgia, and anemia. Serious adverse events occurred in 28% of patients. Adverse events resulting in discontinuation occurred in 11% of patients.
“All patients in the trial were required to have evidence of ALK-rearrangement identified by the VENTANA ALK (D5F3) CDx Assay performed through central laboratory testing,” the FDA said in a press statement.
The recommended dose is 600 mg orally taken twice daily with food.
The Food and Drug Administration has approved frontline alectinib for the treatment of anaplastic lymphoma kinase (ALK)–positive metastatic non–small cell lung cancer (NSCLC) that has been detected by an FDA-approved test.
The drug previously received accelerated approval for treatment of patients with ALK-positive metastatic NSCLC whose disease progressed while receiving crizotinib or who were intolerant of that treatment.
There was also a lower incidence of progression to the central nervous system as first site of disease progression with alectinib: Incidence of progression to the CNS was 12% for patients receiving alectinib and 45% for patients receiving crizotinib.
The most common adverse events in patients receiving alectinib were fatigue, constipation, edema, myalgia, and anemia. Serious adverse events occurred in 28% of patients. Adverse events resulting in discontinuation occurred in 11% of patients.
“All patients in the trial were required to have evidence of ALK-rearrangement identified by the VENTANA ALK (D5F3) CDx Assay performed through central laboratory testing,” the FDA said in a press statement.
The recommended dose is 600 mg orally taken twice daily with food.
The Food and Drug Administration has approved frontline alectinib for the treatment of anaplastic lymphoma kinase (ALK)–positive metastatic non–small cell lung cancer (NSCLC) that has been detected by an FDA-approved test.
The drug previously received accelerated approval for treatment of patients with ALK-positive metastatic NSCLC whose disease progressed while receiving crizotinib or who were intolerant of that treatment.
There was also a lower incidence of progression to the central nervous system as first site of disease progression with alectinib: Incidence of progression to the CNS was 12% for patients receiving alectinib and 45% for patients receiving crizotinib.
The most common adverse events in patients receiving alectinib were fatigue, constipation, edema, myalgia, and anemia. Serious adverse events occurred in 28% of patients. Adverse events resulting in discontinuation occurred in 11% of patients.
“All patients in the trial were required to have evidence of ALK-rearrangement identified by the VENTANA ALK (D5F3) CDx Assay performed through central laboratory testing,” the FDA said in a press statement.
The recommended dose is 600 mg orally taken twice daily with food.
VIDEO: Rapid influenza test obviates empiric antivirals
TORONTO – A test that only requires a maximum 2-hour wait for results was highly accurate at detecting influenza and respiratory syncytial virus infection in lung transplant patients, according to research presented at the CHEST annual meeting on Oct. 30.
This rapid and highly accurate test for detecting three common respiratory viruses has dramatically cut the need for empiric treatments and the risk for causing nosocomial infections in lung transplant patients who develop severe upper respiratory infections, Macé M. Schuurmans, MD, noted during the presentation.
This study involved 100 consecutive lung transplant patients who presented at Zurich University Hospital with signs of severe upper respiratory infection. The researchers ran the rapid and standard diagnostic tests for each patient and found that, relative to the standard test, the rapid test had positive and negative predictive values of 95%.
The number of empiric treatments with oseltamivir (Tamiflu) and ribavirin to treat a suspected influenza or respiratory syncytial virus infection (RSV) has “strongly diminished” by about two-thirds, noted Dr. Schuurmans, who is a pulmonologist at the hospital.
Until the rapid test became available, Dr. Shuurmans and his associates used a standard polymerase chain reaction test that takes 36-48 hours to yield a result. Using this test made treating patients empirically with oseltamivir and oral antibiotics for a couple of days a necessity, he said in a video interview. The older test also required isolating patients to avoid the potential spread of influenza or RSV in the hospital.
The rapid test, which became available for U.S. use in early 2017, covers influenza A and B and RSV in a single test with a single mouth-swab specimen.
“We now routinely use the rapid test and don’t prescribe empiric antivirals or antibiotics as often,” Dr. Schuurmans said. “There is much less drug cost and fewer potential adverse effects from empiric treatment.” Specimens still also undergo conventional testing, however, because that can identify eight additional viruses that the rapid test doesn’t cover.
Dr. Schuurmans acknowledged that further study needs to assess the cost-benefit of the rapid test to confirm that its added expense is offset by reduced expenses for empiric treatment and hospital isolation.
He had no disclosures. The study received no commercial support.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
TORONTO – A test that only requires a maximum 2-hour wait for results was highly accurate at detecting influenza and respiratory syncytial virus infection in lung transplant patients, according to research presented at the CHEST annual meeting on Oct. 30.
This rapid and highly accurate test for detecting three common respiratory viruses has dramatically cut the need for empiric treatments and the risk for causing nosocomial infections in lung transplant patients who develop severe upper respiratory infections, Macé M. Schuurmans, MD, noted during the presentation.
This study involved 100 consecutive lung transplant patients who presented at Zurich University Hospital with signs of severe upper respiratory infection. The researchers ran the rapid and standard diagnostic tests for each patient and found that, relative to the standard test, the rapid test had positive and negative predictive values of 95%.
The number of empiric treatments with oseltamivir (Tamiflu) and ribavirin to treat a suspected influenza or respiratory syncytial virus infection (RSV) has “strongly diminished” by about two-thirds, noted Dr. Schuurmans, who is a pulmonologist at the hospital.
Until the rapid test became available, Dr. Shuurmans and his associates used a standard polymerase chain reaction test that takes 36-48 hours to yield a result. Using this test made treating patients empirically with oseltamivir and oral antibiotics for a couple of days a necessity, he said in a video interview. The older test also required isolating patients to avoid the potential spread of influenza or RSV in the hospital.
The rapid test, which became available for U.S. use in early 2017, covers influenza A and B and RSV in a single test with a single mouth-swab specimen.
“We now routinely use the rapid test and don’t prescribe empiric antivirals or antibiotics as often,” Dr. Schuurmans said. “There is much less drug cost and fewer potential adverse effects from empiric treatment.” Specimens still also undergo conventional testing, however, because that can identify eight additional viruses that the rapid test doesn’t cover.
Dr. Schuurmans acknowledged that further study needs to assess the cost-benefit of the rapid test to confirm that its added expense is offset by reduced expenses for empiric treatment and hospital isolation.
He had no disclosures. The study received no commercial support.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
TORONTO – A test that only requires a maximum 2-hour wait for results was highly accurate at detecting influenza and respiratory syncytial virus infection in lung transplant patients, according to research presented at the CHEST annual meeting on Oct. 30.
This rapid and highly accurate test for detecting three common respiratory viruses has dramatically cut the need for empiric treatments and the risk for causing nosocomial infections in lung transplant patients who develop severe upper respiratory infections, Macé M. Schuurmans, MD, noted during the presentation.
This study involved 100 consecutive lung transplant patients who presented at Zurich University Hospital with signs of severe upper respiratory infection. The researchers ran the rapid and standard diagnostic tests for each patient and found that, relative to the standard test, the rapid test had positive and negative predictive values of 95%.
The number of empiric treatments with oseltamivir (Tamiflu) and ribavirin to treat a suspected influenza or respiratory syncytial virus infection (RSV) has “strongly diminished” by about two-thirds, noted Dr. Schuurmans, who is a pulmonologist at the hospital.
Until the rapid test became available, Dr. Shuurmans and his associates used a standard polymerase chain reaction test that takes 36-48 hours to yield a result. Using this test made treating patients empirically with oseltamivir and oral antibiotics for a couple of days a necessity, he said in a video interview. The older test also required isolating patients to avoid the potential spread of influenza or RSV in the hospital.
The rapid test, which became available for U.S. use in early 2017, covers influenza A and B and RSV in a single test with a single mouth-swab specimen.
“We now routinely use the rapid test and don’t prescribe empiric antivirals or antibiotics as often,” Dr. Schuurmans said. “There is much less drug cost and fewer potential adverse effects from empiric treatment.” Specimens still also undergo conventional testing, however, because that can identify eight additional viruses that the rapid test doesn’t cover.
Dr. Schuurmans acknowledged that further study needs to assess the cost-benefit of the rapid test to confirm that its added expense is offset by reduced expenses for empiric treatment and hospital isolation.
He had no disclosures. The study received no commercial support.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT CHEST 2017
Key clinical point:
Major finding: The rapid test had positive and negative predictive values of 95%.
Data source: A single-center observational study of 100 consecutive lung transplant recipients who presented with severe, acute respiratory infection.
Disclosures: Dr. Schuurmans had no disclosures. The study received no commercial support.
CHEST Physician’s planned coverage of CHEST 2017
CHEST Physician is providing on-site coverage of the CHEST annual meeting in Toronto from Oct. 29 through Nov. 1.
We are planning to share findings from the latest research on treating COPD, sleep apnea, pulmonary hypertension, severe asthma, and other diseases that are part of pulmonary, critical care, and sleep medicine. Any improved methods for managing an ICU and updated recommendations on screening for lung cancer will also be on our radar.
The meeting’s agenda includes presentations of hundreds of study abstracts, and we thought you would be interested in hearing which ones grabbed the attention of some of CHEST Physician’s editorial advisory board members.
Board member Susan L. Millard, MD, FCCP, suggested attendees check out presentations of the following two studies:
- Impact of Race on Quality of Life of Families of Children with Asthma when Asthma Guidelines are Followed: Long-Term Follow-Up
- Results Of A Phase 3, Multicenter, Randomized, Placebo-controlled Trial of Remimazolam: A New Ultra Short Acting Benzodiazepine for Bronchoscopy
The first study is part of a session entitled Pediatrics, scheduled to run from 3:15 to 4:15 p.m. on Sunday, Oct. 29, in Convention Center - 606. Shahid Sheikh, MD, of Nationwide Children’s Hospital in New Albany, Ohio, is scheduled to present the abstract at 4:00 p.m.
Dr. Millard, who is Therapeutic Development Network director for the Pediatric CF Care Center and director of research for pediatric pulmonary and sleep medicine at the Helen DeVos Children’s Hospital in Grand Rapids, Mich., noted that she is interested in Dr. Sheikh’s research, “because cultural diversity is such a hot topic in general.”
Her other recommendation is part of the Late Breaking Abstracts 2 session, scheduled to occur on Wednesday, Nov. 1, from 2:45 to 4:15 p.m. in Convention Center - 603. CHEST President, Gerard A. Silvestri, MD, MS, FCCP, will present the abstract at 4:00 p.m.
Dr. Millard said she is interested in this study, because new drug options are so helpful for the frequently performed bronchoscopy.
Two sleep medicine experts on CHEST Physician’s editorial advisory board also selected a few presentations they expect to be newsworthy.
David Schulman, MD, MPH, FCCP, and professor of medicine at Emory University School of Medicine in Atlanta suggested CHEST Physician cover the following studies:
- Results of a Randomized, Placebo-Controlled, Double-Blind, 12-Week, Multicenter Study of JZP-110 for the Treatment Of Excessive Sleepiness in Patients with OSA, scheduled to be presented on Sunday, Oct. 29, at 1:30 p.m. in Convention Center - 601A. Dr. Kingman Strohl, MD, FCCP, of University Hospitals Case Medical Center-Sleep Center in Shaker Heights, Ohio, will present this research during a session entitled, Obstructive Sleep Apnea: Insights & Management, running from 1:30 to 3:00 p.m.
- History of Sleep Apnea and Cardiovascular Disease may Portend Improved Mortality in Patients With Acute Ischemic Stroke, scheduled to be presented on Tuesday, Oct. 31, at 11:15 a.m., in Convention Center - 601A. Nura Festic will present this research during the session, “Sleep, Heart, Brain and More,” running from 11:00 a.m. to 12:15 p.m.
- Ischemic Preconditioning in OSA Patients Manifested after Surviving a Cardiac Arrest? John Moss, MD, of Jacksonville, Fla., will present this study on Tuesday, Oct. 31, at 11:30 a.m., in Convention Center - 601A as part of the session “Sleep, Heart, Brain and More.”
Krishna M. Sundar, MD, FCCP, also recommended that CHEST Physician cover “A Prospective Cohort Study of Endothelial Function and its Relationship to Aspirin Responsiveness in OSA Patients.” Lirim Krveshi is scheduled to present this study on Sunday, Oct. 29, at 1:45 p.m. in Convention Center - 601A. This presentation is part of the Obstructive Sleep Apnea: Insights & Management session.
Dr. Sundar is an associate clinical professor of pulmonary, critical care and sleep medicine and medical director of the Sleep-Wake Center at the University of Utah, Salt Lake City.
To view the full agenda of the CHEST annual meeting, visit: chestmeeting.chestnet.org.
Look for CHEST Physician’s coverage of CHEST 2017 on our conference coverage page.
CHEST Physician is providing on-site coverage of the CHEST annual meeting in Toronto from Oct. 29 through Nov. 1.
We are planning to share findings from the latest research on treating COPD, sleep apnea, pulmonary hypertension, severe asthma, and other diseases that are part of pulmonary, critical care, and sleep medicine. Any improved methods for managing an ICU and updated recommendations on screening for lung cancer will also be on our radar.
The meeting’s agenda includes presentations of hundreds of study abstracts, and we thought you would be interested in hearing which ones grabbed the attention of some of CHEST Physician’s editorial advisory board members.
Board member Susan L. Millard, MD, FCCP, suggested attendees check out presentations of the following two studies:
- Impact of Race on Quality of Life of Families of Children with Asthma when Asthma Guidelines are Followed: Long-Term Follow-Up
- Results Of A Phase 3, Multicenter, Randomized, Placebo-controlled Trial of Remimazolam: A New Ultra Short Acting Benzodiazepine for Bronchoscopy
The first study is part of a session entitled Pediatrics, scheduled to run from 3:15 to 4:15 p.m. on Sunday, Oct. 29, in Convention Center - 606. Shahid Sheikh, MD, of Nationwide Children’s Hospital in New Albany, Ohio, is scheduled to present the abstract at 4:00 p.m.
Dr. Millard, who is Therapeutic Development Network director for the Pediatric CF Care Center and director of research for pediatric pulmonary and sleep medicine at the Helen DeVos Children’s Hospital in Grand Rapids, Mich., noted that she is interested in Dr. Sheikh’s research, “because cultural diversity is such a hot topic in general.”
Her other recommendation is part of the Late Breaking Abstracts 2 session, scheduled to occur on Wednesday, Nov. 1, from 2:45 to 4:15 p.m. in Convention Center - 603. CHEST President, Gerard A. Silvestri, MD, MS, FCCP, will present the abstract at 4:00 p.m.
Dr. Millard said she is interested in this study, because new drug options are so helpful for the frequently performed bronchoscopy.
Two sleep medicine experts on CHEST Physician’s editorial advisory board also selected a few presentations they expect to be newsworthy.
David Schulman, MD, MPH, FCCP, and professor of medicine at Emory University School of Medicine in Atlanta suggested CHEST Physician cover the following studies:
- Results of a Randomized, Placebo-Controlled, Double-Blind, 12-Week, Multicenter Study of JZP-110 for the Treatment Of Excessive Sleepiness in Patients with OSA, scheduled to be presented on Sunday, Oct. 29, at 1:30 p.m. in Convention Center - 601A. Dr. Kingman Strohl, MD, FCCP, of University Hospitals Case Medical Center-Sleep Center in Shaker Heights, Ohio, will present this research during a session entitled, Obstructive Sleep Apnea: Insights & Management, running from 1:30 to 3:00 p.m.
- History of Sleep Apnea and Cardiovascular Disease may Portend Improved Mortality in Patients With Acute Ischemic Stroke, scheduled to be presented on Tuesday, Oct. 31, at 11:15 a.m., in Convention Center - 601A. Nura Festic will present this research during the session, “Sleep, Heart, Brain and More,” running from 11:00 a.m. to 12:15 p.m.
- Ischemic Preconditioning in OSA Patients Manifested after Surviving a Cardiac Arrest? John Moss, MD, of Jacksonville, Fla., will present this study on Tuesday, Oct. 31, at 11:30 a.m., in Convention Center - 601A as part of the session “Sleep, Heart, Brain and More.”
Krishna M. Sundar, MD, FCCP, also recommended that CHEST Physician cover “A Prospective Cohort Study of Endothelial Function and its Relationship to Aspirin Responsiveness in OSA Patients.” Lirim Krveshi is scheduled to present this study on Sunday, Oct. 29, at 1:45 p.m. in Convention Center - 601A. This presentation is part of the Obstructive Sleep Apnea: Insights & Management session.
Dr. Sundar is an associate clinical professor of pulmonary, critical care and sleep medicine and medical director of the Sleep-Wake Center at the University of Utah, Salt Lake City.
To view the full agenda of the CHEST annual meeting, visit: chestmeeting.chestnet.org.
Look for CHEST Physician’s coverage of CHEST 2017 on our conference coverage page.
CHEST Physician is providing on-site coverage of the CHEST annual meeting in Toronto from Oct. 29 through Nov. 1.
We are planning to share findings from the latest research on treating COPD, sleep apnea, pulmonary hypertension, severe asthma, and other diseases that are part of pulmonary, critical care, and sleep medicine. Any improved methods for managing an ICU and updated recommendations on screening for lung cancer will also be on our radar.
The meeting’s agenda includes presentations of hundreds of study abstracts, and we thought you would be interested in hearing which ones grabbed the attention of some of CHEST Physician’s editorial advisory board members.
Board member Susan L. Millard, MD, FCCP, suggested attendees check out presentations of the following two studies:
- Impact of Race on Quality of Life of Families of Children with Asthma when Asthma Guidelines are Followed: Long-Term Follow-Up
- Results Of A Phase 3, Multicenter, Randomized, Placebo-controlled Trial of Remimazolam: A New Ultra Short Acting Benzodiazepine for Bronchoscopy
The first study is part of a session entitled Pediatrics, scheduled to run from 3:15 to 4:15 p.m. on Sunday, Oct. 29, in Convention Center - 606. Shahid Sheikh, MD, of Nationwide Children’s Hospital in New Albany, Ohio, is scheduled to present the abstract at 4:00 p.m.
Dr. Millard, who is Therapeutic Development Network director for the Pediatric CF Care Center and director of research for pediatric pulmonary and sleep medicine at the Helen DeVos Children’s Hospital in Grand Rapids, Mich., noted that she is interested in Dr. Sheikh’s research, “because cultural diversity is such a hot topic in general.”
Her other recommendation is part of the Late Breaking Abstracts 2 session, scheduled to occur on Wednesday, Nov. 1, from 2:45 to 4:15 p.m. in Convention Center - 603. CHEST President, Gerard A. Silvestri, MD, MS, FCCP, will present the abstract at 4:00 p.m.
Dr. Millard said she is interested in this study, because new drug options are so helpful for the frequently performed bronchoscopy.
Two sleep medicine experts on CHEST Physician’s editorial advisory board also selected a few presentations they expect to be newsworthy.
David Schulman, MD, MPH, FCCP, and professor of medicine at Emory University School of Medicine in Atlanta suggested CHEST Physician cover the following studies:
- Results of a Randomized, Placebo-Controlled, Double-Blind, 12-Week, Multicenter Study of JZP-110 for the Treatment Of Excessive Sleepiness in Patients with OSA, scheduled to be presented on Sunday, Oct. 29, at 1:30 p.m. in Convention Center - 601A. Dr. Kingman Strohl, MD, FCCP, of University Hospitals Case Medical Center-Sleep Center in Shaker Heights, Ohio, will present this research during a session entitled, Obstructive Sleep Apnea: Insights & Management, running from 1:30 to 3:00 p.m.
- History of Sleep Apnea and Cardiovascular Disease may Portend Improved Mortality in Patients With Acute Ischemic Stroke, scheduled to be presented on Tuesday, Oct. 31, at 11:15 a.m., in Convention Center - 601A. Nura Festic will present this research during the session, “Sleep, Heart, Brain and More,” running from 11:00 a.m. to 12:15 p.m.
- Ischemic Preconditioning in OSA Patients Manifested after Surviving a Cardiac Arrest? John Moss, MD, of Jacksonville, Fla., will present this study on Tuesday, Oct. 31, at 11:30 a.m., in Convention Center - 601A as part of the session “Sleep, Heart, Brain and More.”
Krishna M. Sundar, MD, FCCP, also recommended that CHEST Physician cover “A Prospective Cohort Study of Endothelial Function and its Relationship to Aspirin Responsiveness in OSA Patients.” Lirim Krveshi is scheduled to present this study on Sunday, Oct. 29, at 1:45 p.m. in Convention Center - 601A. This presentation is part of the Obstructive Sleep Apnea: Insights & Management session.
Dr. Sundar is an associate clinical professor of pulmonary, critical care and sleep medicine and medical director of the Sleep-Wake Center at the University of Utah, Salt Lake City.
To view the full agenda of the CHEST annual meeting, visit: chestmeeting.chestnet.org.
Look for CHEST Physician’s coverage of CHEST 2017 on our conference coverage page.
FROM CHEST 2017
Yoga benefits lung cancer patients and caregivers alike
Yoga provides physical and mental benefits for both lung cancer patients and their caregivers, according to results of a randomized study presented at the Palliative and Supportive Care in Oncology Symposium.
“Overall, we are encouraged by the findings,” said lead study author, Kathrin Milbury, PhD, of University of Texas MD Anderson Cancer Center, Houston.
This study provides preliminary evidence that a yoga program can provide a “buffer” and improve physical function for patients, as well as self-reported improved quality of life for both patients and their caregivers, she added.
All patients in the study had non–small cell lung cancer and were undergoing thoracic radiation therapy, which can cause respiratory toxicities that negatively affect quality of life and physical activity, according to Dr. Milbury and her coinvestigators.
A total of 32 patient-caregiver dyads were randomized to participate in 15 yoga sessions or to be in a “wait-list” control group, and 26 dyads completed all assessments.
Patients who practiced yoga had significantly better scores on a 6-minute walking test (478 vs. 402 for wait-list enrollees; P less than .05), plus better stamina and mental health. Caregivers had improved fatigue and better stamina at work.
Almost all patients (96%) rated the program as “very useful,” investigators reported at the symposium, which was cosponsored by AAHPM, ASCO, ASTRO, and MASCC.
This study provides additional evidence that yoga and other nonpharmacologic supportive therapies “can be integrated into not only the care of cancer patients, but also the family caregivers who support them,” according to Andrew S. Epstein, MD, of Memorial Sloan Kettering Cancer Center, New York.
Next, the researchers plan to conduct a larger, randomized, controlled trial with a more stringent comparison group, according to Dr. Milbury.
Yoga provides physical and mental benefits for both lung cancer patients and their caregivers, according to results of a randomized study presented at the Palliative and Supportive Care in Oncology Symposium.
“Overall, we are encouraged by the findings,” said lead study author, Kathrin Milbury, PhD, of University of Texas MD Anderson Cancer Center, Houston.
This study provides preliminary evidence that a yoga program can provide a “buffer” and improve physical function for patients, as well as self-reported improved quality of life for both patients and their caregivers, she added.
All patients in the study had non–small cell lung cancer and were undergoing thoracic radiation therapy, which can cause respiratory toxicities that negatively affect quality of life and physical activity, according to Dr. Milbury and her coinvestigators.
A total of 32 patient-caregiver dyads were randomized to participate in 15 yoga sessions or to be in a “wait-list” control group, and 26 dyads completed all assessments.
Patients who practiced yoga had significantly better scores on a 6-minute walking test (478 vs. 402 for wait-list enrollees; P less than .05), plus better stamina and mental health. Caregivers had improved fatigue and better stamina at work.
Almost all patients (96%) rated the program as “very useful,” investigators reported at the symposium, which was cosponsored by AAHPM, ASCO, ASTRO, and MASCC.
This study provides additional evidence that yoga and other nonpharmacologic supportive therapies “can be integrated into not only the care of cancer patients, but also the family caregivers who support them,” according to Andrew S. Epstein, MD, of Memorial Sloan Kettering Cancer Center, New York.
Next, the researchers plan to conduct a larger, randomized, controlled trial with a more stringent comparison group, according to Dr. Milbury.
Yoga provides physical and mental benefits for both lung cancer patients and their caregivers, according to results of a randomized study presented at the Palliative and Supportive Care in Oncology Symposium.
“Overall, we are encouraged by the findings,” said lead study author, Kathrin Milbury, PhD, of University of Texas MD Anderson Cancer Center, Houston.
This study provides preliminary evidence that a yoga program can provide a “buffer” and improve physical function for patients, as well as self-reported improved quality of life for both patients and their caregivers, she added.
All patients in the study had non–small cell lung cancer and were undergoing thoracic radiation therapy, which can cause respiratory toxicities that negatively affect quality of life and physical activity, according to Dr. Milbury and her coinvestigators.
A total of 32 patient-caregiver dyads were randomized to participate in 15 yoga sessions or to be in a “wait-list” control group, and 26 dyads completed all assessments.
Patients who practiced yoga had significantly better scores on a 6-minute walking test (478 vs. 402 for wait-list enrollees; P less than .05), plus better stamina and mental health. Caregivers had improved fatigue and better stamina at work.
Almost all patients (96%) rated the program as “very useful,” investigators reported at the symposium, which was cosponsored by AAHPM, ASCO, ASTRO, and MASCC.
This study provides additional evidence that yoga and other nonpharmacologic supportive therapies “can be integrated into not only the care of cancer patients, but also the family caregivers who support them,” according to Andrew S. Epstein, MD, of Memorial Sloan Kettering Cancer Center, New York.
Next, the researchers plan to conduct a larger, randomized, controlled trial with a more stringent comparison group, according to Dr. Milbury.
FROM PALLONC 2017
Key clinical point: Yoga provides both physical and mental benefits for lung cancer patients undergoing radiotherapy and their caregivers.
Major finding: Patients who practiced yoga had significantly better scores on a 6-minute walking test (478 vs. 402 for wait-list enrollees; P less than .05), plus better stamina and mental health. Caregivers had improved fatigue and better stamina at work.
Data source: Randomized study including 47 patient-caregiver dyads, of which 32 consented and 26 completed all assessments.
Disclosures: Funding for this study came from the National Institutes of Health. Lead author Kathrin Milbury, PhD, reported no potential conflicts of interest.
Robotic-assisted pulmonary lobectomy effective for large tumors
Robotic-assisted pulmonary lobectomy is a safe and effective way to remove large tumors in patients with non–small cell lung cancer (NSCLC), according to the abstract of a study scheduled to be presented at the CHEST annual meeting.
The study covers a retrospective analysis of 345 NSCLC patients with tumors who underwent robotic-assisted pulmonary lobectomy performed by one surgeon from September 2010 through August 2016. The participants were grouped into the following three cohorts: patients with tumors less than 5 cm in diameter, patients with tumors from 5 to 7 cm, and patients with tumors larger than 7 cm. The researchers excluded patients with pulmonary metastases or benign lesions from the study.
Patients with smaller tumors were more likely to have simple lobectomy or lobectomy plus wedge, while patients with larger tumors were more likely to require lobectomy with chest wall resection. Increased tumor size was also associated with increased intraoperative estimated blood loss, skin-to-skin operative time, hospital length of stay, and overall conversion to open lobectomy.
There was no association found between tumor size and increased overall intraoperative or postoperative complications, or in-hospital mortality.
Nirav Patel, MD, FCCP, of the Tampa Bay Sleep Center is scheduled to present his abstract on Sunday Oct. 29th, between 2:15 and 2:30 p.m. in Convention Center – 606. Dr. Patel’s research is part of the Cardiothoracic Surgery session, running from 1:30 p.m. to 3:00 p.m. at the CHEST annual meeting.
Robotic-assisted pulmonary lobectomy is a safe and effective way to remove large tumors in patients with non–small cell lung cancer (NSCLC), according to the abstract of a study scheduled to be presented at the CHEST annual meeting.
The study covers a retrospective analysis of 345 NSCLC patients with tumors who underwent robotic-assisted pulmonary lobectomy performed by one surgeon from September 2010 through August 2016. The participants were grouped into the following three cohorts: patients with tumors less than 5 cm in diameter, patients with tumors from 5 to 7 cm, and patients with tumors larger than 7 cm. The researchers excluded patients with pulmonary metastases or benign lesions from the study.
Patients with smaller tumors were more likely to have simple lobectomy or lobectomy plus wedge, while patients with larger tumors were more likely to require lobectomy with chest wall resection. Increased tumor size was also associated with increased intraoperative estimated blood loss, skin-to-skin operative time, hospital length of stay, and overall conversion to open lobectomy.
There was no association found between tumor size and increased overall intraoperative or postoperative complications, or in-hospital mortality.
Nirav Patel, MD, FCCP, of the Tampa Bay Sleep Center is scheduled to present his abstract on Sunday Oct. 29th, between 2:15 and 2:30 p.m. in Convention Center – 606. Dr. Patel’s research is part of the Cardiothoracic Surgery session, running from 1:30 p.m. to 3:00 p.m. at the CHEST annual meeting.
Robotic-assisted pulmonary lobectomy is a safe and effective way to remove large tumors in patients with non–small cell lung cancer (NSCLC), according to the abstract of a study scheduled to be presented at the CHEST annual meeting.
The study covers a retrospective analysis of 345 NSCLC patients with tumors who underwent robotic-assisted pulmonary lobectomy performed by one surgeon from September 2010 through August 2016. The participants were grouped into the following three cohorts: patients with tumors less than 5 cm in diameter, patients with tumors from 5 to 7 cm, and patients with tumors larger than 7 cm. The researchers excluded patients with pulmonary metastases or benign lesions from the study.
Patients with smaller tumors were more likely to have simple lobectomy or lobectomy plus wedge, while patients with larger tumors were more likely to require lobectomy with chest wall resection. Increased tumor size was also associated with increased intraoperative estimated blood loss, skin-to-skin operative time, hospital length of stay, and overall conversion to open lobectomy.
There was no association found between tumor size and increased overall intraoperative or postoperative complications, or in-hospital mortality.
Nirav Patel, MD, FCCP, of the Tampa Bay Sleep Center is scheduled to present his abstract on Sunday Oct. 29th, between 2:15 and 2:30 p.m. in Convention Center – 606. Dr. Patel’s research is part of the Cardiothoracic Surgery session, running from 1:30 p.m. to 3:00 p.m. at the CHEST annual meeting.
FROM CHEST 2017
VA Partnership Expands Access to Lung Screening Programs
Lung cancer has an 80% cure rate when caught early, and screening programs are key to providing this chance. The VA and the Bristol-Myers Squibb Foundation have established the VA-Partnership to increase Access to Lung Screening (VA-PALS) Implementation Network.
The initiative builds upon experience gained from other screening programs, the VA says, including those of the VA’s Office of Rural Health, which is supporting the project’s goal to reach veterans living in rural areas. It also adds to a portfolio of other major VA lung cancer initiatives, including the VALOR Trial (Veterans Affairs Lung Cancer Or Stereotactic Radiotherapy) and the APOLLO Network (Applied Proteogenomics OrganizationaL Learning and Outcomes).
“Research shows that with comprehensive lung screening programs, early identification of lung cancer leads to more effective treatments and, ultimately, saves lives,” said John Damonti, president of Bristol-Myers Squibb Foundation, the project’s sponsor.
The project will launch with lung-screening services at the Phoenix VA Health Care System in Arizona by December 2017, and then extend these services to 9 additional VA medical facilities starting in 2018.
Lung cancer has an 80% cure rate when caught early, and screening programs are key to providing this chance. The VA and the Bristol-Myers Squibb Foundation have established the VA-Partnership to increase Access to Lung Screening (VA-PALS) Implementation Network.
The initiative builds upon experience gained from other screening programs, the VA says, including those of the VA’s Office of Rural Health, which is supporting the project’s goal to reach veterans living in rural areas. It also adds to a portfolio of other major VA lung cancer initiatives, including the VALOR Trial (Veterans Affairs Lung Cancer Or Stereotactic Radiotherapy) and the APOLLO Network (Applied Proteogenomics OrganizationaL Learning and Outcomes).
“Research shows that with comprehensive lung screening programs, early identification of lung cancer leads to more effective treatments and, ultimately, saves lives,” said John Damonti, president of Bristol-Myers Squibb Foundation, the project’s sponsor.
The project will launch with lung-screening services at the Phoenix VA Health Care System in Arizona by December 2017, and then extend these services to 9 additional VA medical facilities starting in 2018.
Lung cancer has an 80% cure rate when caught early, and screening programs are key to providing this chance. The VA and the Bristol-Myers Squibb Foundation have established the VA-Partnership to increase Access to Lung Screening (VA-PALS) Implementation Network.
The initiative builds upon experience gained from other screening programs, the VA says, including those of the VA’s Office of Rural Health, which is supporting the project’s goal to reach veterans living in rural areas. It also adds to a portfolio of other major VA lung cancer initiatives, including the VALOR Trial (Veterans Affairs Lung Cancer Or Stereotactic Radiotherapy) and the APOLLO Network (Applied Proteogenomics OrganizationaL Learning and Outcomes).
“Research shows that with comprehensive lung screening programs, early identification of lung cancer leads to more effective treatments and, ultimately, saves lives,” said John Damonti, president of Bristol-Myers Squibb Foundation, the project’s sponsor.
The project will launch with lung-screening services at the Phoenix VA Health Care System in Arizona by December 2017, and then extend these services to 9 additional VA medical facilities starting in 2018.
Dabrafenib/trametinib bests docetaxel for advanced NSCLC in indirect comparison
CHICAGO – Compared with docetaxel in matched external controls, combination therapy with dabrafenib and trametinib was associated with significantly prolonged progression-free and overall survival in previously treated patients with metastatic non–small cell lung cancer in a phase 2 trial.
Median progression-free survival (PFS) was 9.7 months in 57 patients in an open-label, multicenter phase 2 trial that investigated dabrafenib/trametinib treatment for metastatic BRAF V600E–mutated NSCLC, compared with 4.2 months in 290 patients treated with docetaxel in the randomized phase 3 CheckMate057 trial, which compared nivolumab and docetaxel in similar patients (hazard ratio, 0.32). Overall survival in the groups was 19.2 vs. 9.3 months, respectively (HR, 0.41), Junlong Li, MD, of Analysis Group, Boston, reported at the Chicago Multidisciplinary Symposium in Thoracic Oncology.
Patients treated with the combination of dabrafenib and trametinib also had a significantly higher overall response rate (61% vs. 12%) and disease control rate (77% vs. 55%), Dr. Li said.
Patient-level data for the combination therapy patients and summary data for the docetaxel-treated patients were used for the current analysis. Patients and controls were matched based on age, sex, race, smoking history, performance score, tumor histology, prior regimens, prior radiotherapy, and prior maintenance therapy. The two trials used for the analysis (NCT01336634 and CheckMate 057) were comparable in design and inclusion/exclusion criteria, and both used RECIST v1.1 to evaluate response to therapy.
“In the absence of head-to-head trials ... this study contributes some comparative efficacy evidence in this area,” Dr. Li concluded.
Invited discussant, Thomas Eldridge Stinchcombe, MD, of Duke University, Durham, N.C., said that the findings are unsurprising but important in that they are confirmatory.
Dr. Li is a consultant for Novartis, which sponsored the analysis.
CHICAGO – Compared with docetaxel in matched external controls, combination therapy with dabrafenib and trametinib was associated with significantly prolonged progression-free and overall survival in previously treated patients with metastatic non–small cell lung cancer in a phase 2 trial.
Median progression-free survival (PFS) was 9.7 months in 57 patients in an open-label, multicenter phase 2 trial that investigated dabrafenib/trametinib treatment for metastatic BRAF V600E–mutated NSCLC, compared with 4.2 months in 290 patients treated with docetaxel in the randomized phase 3 CheckMate057 trial, which compared nivolumab and docetaxel in similar patients (hazard ratio, 0.32). Overall survival in the groups was 19.2 vs. 9.3 months, respectively (HR, 0.41), Junlong Li, MD, of Analysis Group, Boston, reported at the Chicago Multidisciplinary Symposium in Thoracic Oncology.
Patients treated with the combination of dabrafenib and trametinib also had a significantly higher overall response rate (61% vs. 12%) and disease control rate (77% vs. 55%), Dr. Li said.
Patient-level data for the combination therapy patients and summary data for the docetaxel-treated patients were used for the current analysis. Patients and controls were matched based on age, sex, race, smoking history, performance score, tumor histology, prior regimens, prior radiotherapy, and prior maintenance therapy. The two trials used for the analysis (NCT01336634 and CheckMate 057) were comparable in design and inclusion/exclusion criteria, and both used RECIST v1.1 to evaluate response to therapy.
“In the absence of head-to-head trials ... this study contributes some comparative efficacy evidence in this area,” Dr. Li concluded.
Invited discussant, Thomas Eldridge Stinchcombe, MD, of Duke University, Durham, N.C., said that the findings are unsurprising but important in that they are confirmatory.
Dr. Li is a consultant for Novartis, which sponsored the analysis.
CHICAGO – Compared with docetaxel in matched external controls, combination therapy with dabrafenib and trametinib was associated with significantly prolonged progression-free and overall survival in previously treated patients with metastatic non–small cell lung cancer in a phase 2 trial.
Median progression-free survival (PFS) was 9.7 months in 57 patients in an open-label, multicenter phase 2 trial that investigated dabrafenib/trametinib treatment for metastatic BRAF V600E–mutated NSCLC, compared with 4.2 months in 290 patients treated with docetaxel in the randomized phase 3 CheckMate057 trial, which compared nivolumab and docetaxel in similar patients (hazard ratio, 0.32). Overall survival in the groups was 19.2 vs. 9.3 months, respectively (HR, 0.41), Junlong Li, MD, of Analysis Group, Boston, reported at the Chicago Multidisciplinary Symposium in Thoracic Oncology.
Patients treated with the combination of dabrafenib and trametinib also had a significantly higher overall response rate (61% vs. 12%) and disease control rate (77% vs. 55%), Dr. Li said.
Patient-level data for the combination therapy patients and summary data for the docetaxel-treated patients were used for the current analysis. Patients and controls were matched based on age, sex, race, smoking history, performance score, tumor histology, prior regimens, prior radiotherapy, and prior maintenance therapy. The two trials used for the analysis (NCT01336634 and CheckMate 057) were comparable in design and inclusion/exclusion criteria, and both used RECIST v1.1 to evaluate response to therapy.
“In the absence of head-to-head trials ... this study contributes some comparative efficacy evidence in this area,” Dr. Li concluded.
Invited discussant, Thomas Eldridge Stinchcombe, MD, of Duke University, Durham, N.C., said that the findings are unsurprising but important in that they are confirmatory.
Dr. Li is a consultant for Novartis, which sponsored the analysis.
AT A SYMPOSIUM IN THORACIC ONCOLOGY
Key clinical point:
Major finding: Median PFS with dabrafenib and trametinib vs. docetaxel: 9.7 vs. 4.2 months (HR, 0.32); overall survival: 19.2 vs. 9.3 months (HR, 0.41).
Data source: An adjusted indirect comparison of data from 347 patients from two separate studies.
Disclosures: Dr. Li is a consultant for Novartis, which sponsored the analysis.
Lifesaving future seen for electronic cigarettes
A switch from cigarettes to e-cigarettes has the potential to prevent almost 90,000 premature deaths in the United States in the year 2026, according to a study examining e-cigarette substitution scenarios.
The investigators’ “optimistic scenario” – in which new smokers use e-cigarettes instead of cigarettes, smoking prevalence falls to 5% over a 10-year period, and e-cigarettes have a 5% excess risk over regular cigarettes – projects 380,832 premature deaths from smoking in the year 2026. Under a “status quo scenario,” which projected current cigarette initiation and cessation rates and did not include e-cigarettes or other tobacco products, there would be 470,743 deaths, reported David T. Levy, PhD, and his associates (Tob Control. 2017 Oct 2. doi: 10.1136/tobaccocontrol-2017-053759).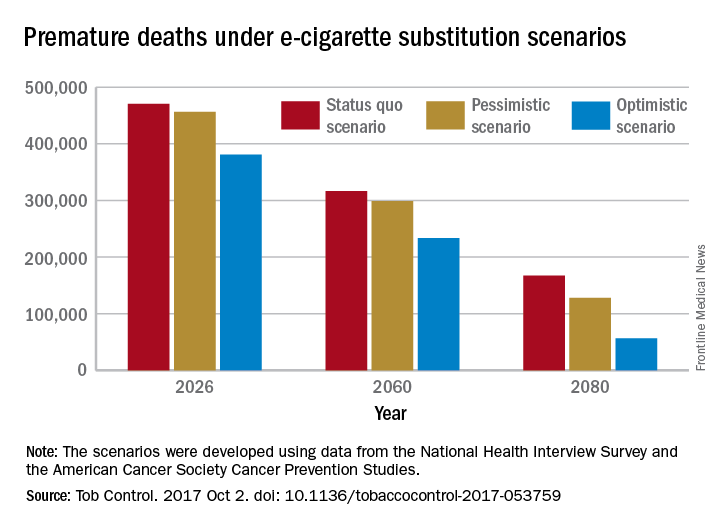
Further projections suggest that the optimistic scenario could result in almost 6.6 million fewer premature deaths and 86.7 million years of life gained by the year 2100, compared with the status quo scenario, while the pessimistic scenario would prevent 1.6 million deaths and add an extra 20.8 million years of life, they noted.
Since “a strategy of replacing cigarette by e-cigarette use can yield substantial gains, even with conservative assumptions about related risks … an endgame scenario for cigarettes might well be within reach, if new technologies for delivering nicotine with substantially less harm, but sufficient satisfaction, are harnessed with sufficient passion and political will to aggressively phase out tobacco cigarettes,” Dr. Levy and his associates wrote.
The study was funded by grants from the National Institute on Drug Abuse and the National Cancer Institute. One investigator received a research grant from Pfizer and served as an advisory board member to Johnson & Johnson, which manufactures smoking cessation medications. No other conflicts of interest were declared.
A switch from cigarettes to e-cigarettes has the potential to prevent almost 90,000 premature deaths in the United States in the year 2026, according to a study examining e-cigarette substitution scenarios.
The investigators’ “optimistic scenario” – in which new smokers use e-cigarettes instead of cigarettes, smoking prevalence falls to 5% over a 10-year period, and e-cigarettes have a 5% excess risk over regular cigarettes – projects 380,832 premature deaths from smoking in the year 2026. Under a “status quo scenario,” which projected current cigarette initiation and cessation rates and did not include e-cigarettes or other tobacco products, there would be 470,743 deaths, reported David T. Levy, PhD, and his associates (Tob Control. 2017 Oct 2. doi: 10.1136/tobaccocontrol-2017-053759).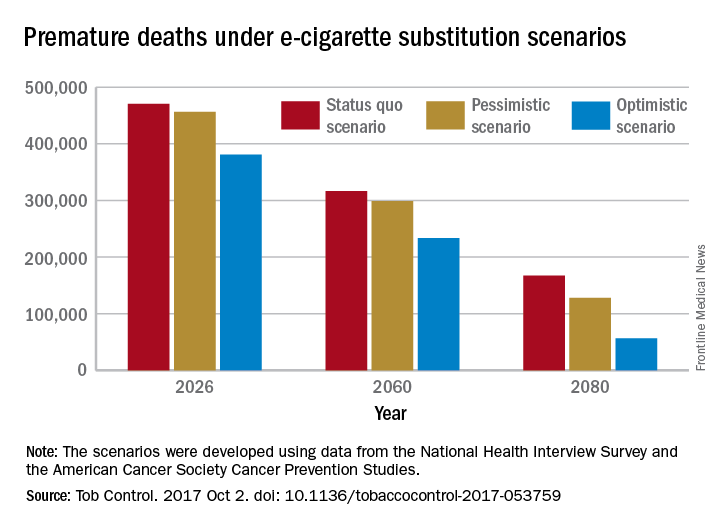
Further projections suggest that the optimistic scenario could result in almost 6.6 million fewer premature deaths and 86.7 million years of life gained by the year 2100, compared with the status quo scenario, while the pessimistic scenario would prevent 1.6 million deaths and add an extra 20.8 million years of life, they noted.
Since “a strategy of replacing cigarette by e-cigarette use can yield substantial gains, even with conservative assumptions about related risks … an endgame scenario for cigarettes might well be within reach, if new technologies for delivering nicotine with substantially less harm, but sufficient satisfaction, are harnessed with sufficient passion and political will to aggressively phase out tobacco cigarettes,” Dr. Levy and his associates wrote.
The study was funded by grants from the National Institute on Drug Abuse and the National Cancer Institute. One investigator received a research grant from Pfizer and served as an advisory board member to Johnson & Johnson, which manufactures smoking cessation medications. No other conflicts of interest were declared.
A switch from cigarettes to e-cigarettes has the potential to prevent almost 90,000 premature deaths in the United States in the year 2026, according to a study examining e-cigarette substitution scenarios.
The investigators’ “optimistic scenario” – in which new smokers use e-cigarettes instead of cigarettes, smoking prevalence falls to 5% over a 10-year period, and e-cigarettes have a 5% excess risk over regular cigarettes – projects 380,832 premature deaths from smoking in the year 2026. Under a “status quo scenario,” which projected current cigarette initiation and cessation rates and did not include e-cigarettes or other tobacco products, there would be 470,743 deaths, reported David T. Levy, PhD, and his associates (Tob Control. 2017 Oct 2. doi: 10.1136/tobaccocontrol-2017-053759).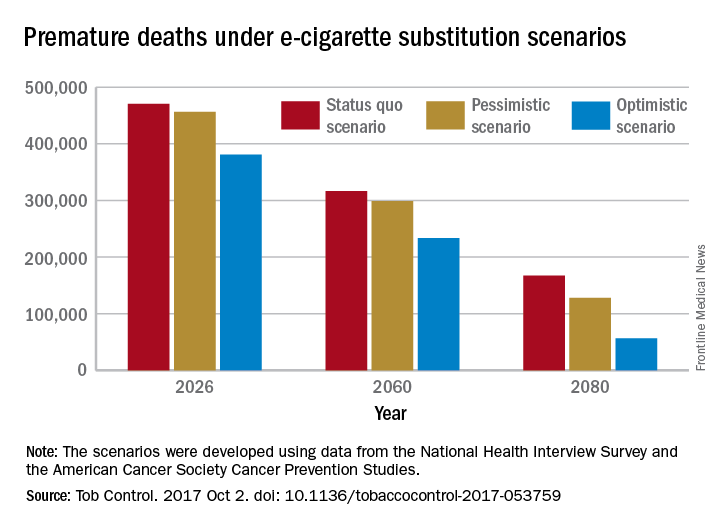
Further projections suggest that the optimistic scenario could result in almost 6.6 million fewer premature deaths and 86.7 million years of life gained by the year 2100, compared with the status quo scenario, while the pessimistic scenario would prevent 1.6 million deaths and add an extra 20.8 million years of life, they noted.
Since “a strategy of replacing cigarette by e-cigarette use can yield substantial gains, even with conservative assumptions about related risks … an endgame scenario for cigarettes might well be within reach, if new technologies for delivering nicotine with substantially less harm, but sufficient satisfaction, are harnessed with sufficient passion and political will to aggressively phase out tobacco cigarettes,” Dr. Levy and his associates wrote.
The study was funded by grants from the National Institute on Drug Abuse and the National Cancer Institute. One investigator received a research grant from Pfizer and served as an advisory board member to Johnson & Johnson, which manufactures smoking cessation medications. No other conflicts of interest were declared.
FROM TOBACCO CONTROL






