User login
For MD-IQ use only
A baby stops breathing at a grocery store – An ICU nurse steps in
My son needed a physical for his football team, and we couldn’t get an appointment. So, we went to the urgent care next to the H Mart in Cary, N.C. While I was waiting, I thought, let me go get a coffee or an iced tea at the H Mart. They have this French bakery in there.
I went in and ordered my drink, and I was waiting in line. I saw this woman pass me running with a baby. Another woman – I found out later it was her sister – was running after her, and she said: “Call 911!”
“I don’t have my phone,” I said. I left my phone with my son; he was using it.
I said: “Are you okay?” And she just handed me the baby. The baby was gray, and there was blood in her nose and mouth. The woman said: “She’s my baby. She’s 1 week old.”
I was trying to think very quickly. I didn’t see any bubbles in the blood around the baby’s nose or mouth to tell me if she was breathing. She was just limp. The mom was still screaming, but I couldn’t even hear her anymore. It was like I was having an out-of-body experience. All I could hear were my thoughts: “I need to put this baby down to start CPR. Someone was calling 911. I should go in the front of the store to save time, so EMS doesn’t have to look for me when they come.”
I started moving and trying to clean the blood from the baby’s face with her blanket. At the front of the store, I saw a display of rice bags. I put the baby on top of one of the bags. “Okay, where do I check for a pulse on a baby?” I took care of adults, never pediatric patients, never babies. She was so tiny. I put my hand on her chest and felt nothing. No heartbeat. She still wasn’t breathing.
People were around me, but I couldn’t see or hear anybody. All I was thinking was: “What can I do for this patient right now?” I started CPR with two fingers. Nothing was happening. It wasn’t that long, but it felt like forever for me. I couldn’t do mouth-to-mouth because there was so much blood on her face. I still don’t know what caused the bleeding.
It was COVID time, so I had my mask on. I was, like: “You know what? Screw this. She’s a 1-week-old baby. Her lungs are tiny. Maybe I don’t have to do mouth-to-mouth. I can just blow in her mouth.” I took off my mask and opened her mouth. I took a deep breath and blew a little bit of air in her mouth. I continued CPR for maybe 5 or 10 seconds.
And then she gasped! She opened her eyes, but they were rolled up. I was still doing CPR, and maybe 2 second after that, I could feel under my hand a very rapid heart rate. I took my hand away and lifted her up.
Just then the EMS got there. I gave them the baby and said: “I did CPR. I don’t know how long it lasted.” The EMS person looked at me, said: “Thank you for what you did. Now we need you to help us with mom.” I said, “okay.”
I turned around, and the mom was still screaming and crying. I asked one of the ladies that worked there, “Can you get me water?” She brought it, and I gave some to the mom, and she started talking to EMS.
People were asking me: “What happened? What happened?” It’s funny, I guess the nurse in me didn’t want to give out information. And I didn’t want to ask for information. I was thinking about privacy. I said, “I don’t know,” and walked away.
The mom’s sister came and hugged me and said thank you. I was still in this out-of-body zone, and I just wanted to get the hell out of there. So, I left. I went to my car and when I got in it, I started shaking and sweating and crying.
I had been so calm in the moment, not thinking about if the baby was going to survive or not. I didn’t know how long she was without oxygen, if she would have some anoxic brain injury or stroke. I’m a mom, too. I would have been just as terrified as that mom. I just hoped there was a chance that she could take her baby home.
I went back to the urgent care, and my son was, like, “are you okay?” I said: “You will not believe this. I just did CPR on a baby.” He said: “Oh. Okay.” I don’t think he even knew what that meant.
I’ve been an ICU nurse since 2008. I’ve been in very critical moments with patients, life or death situations. I help save people all the time at the hospital. Most of the time, you know what you’re getting. You can prepare. You have everything you need, and everyone knows what to do. You know what the worst will look like. You know the outcome.
But this was something else. You read about things like this. You hear about them. But you never think it’ll happen to you – until it happens.
I couldn’t stop thinking about the baby. So, 2 days later, I posted on Next Door to see if somebody would read it and say, “hey, the baby survived.” I was amazed at how many people responded, but no one knew the family.
The local news got hold of me and asked me to do a story. I told them, “the only way I can do a story is if the baby survived. I’m not going to do a story about a dead baby, and the mom has to live through it again.”
The reporter called me later on that day and said she had talked to the police. They said the family was visiting from out of state. The baby went to the hospital and was discharged home 2 days later. I said, “okay, then I can talk.”
When the news story came out, I started getting texts from people at work the same night. So many people were reaching out. Even people from out of state. But I never heard from the family. No one knew how to reach them.
Since I was very young, I wanted to work in a hospital, to help people. It really brings me joy, seeing somebody go home, knowing, yes, we did this. It’s a great feeling. I love this job. I wouldn’t trade it for anything.
I just wish I had asked the mom’s name. Because I always think about that baby. I always wonder, what did she become? I hope somebody reads this who might know that little girl. It would be so nice to meet her one day.
Ms. Diallo is an ICU nurse and now works as nurse care coordinator at the University of North Carolina’s Children’s Neurology Clinic in Chapel Hill.
A version of this article first appeared on Medscape.com.
My son needed a physical for his football team, and we couldn’t get an appointment. So, we went to the urgent care next to the H Mart in Cary, N.C. While I was waiting, I thought, let me go get a coffee or an iced tea at the H Mart. They have this French bakery in there.
I went in and ordered my drink, and I was waiting in line. I saw this woman pass me running with a baby. Another woman – I found out later it was her sister – was running after her, and she said: “Call 911!”
“I don’t have my phone,” I said. I left my phone with my son; he was using it.
I said: “Are you okay?” And she just handed me the baby. The baby was gray, and there was blood in her nose and mouth. The woman said: “She’s my baby. She’s 1 week old.”
I was trying to think very quickly. I didn’t see any bubbles in the blood around the baby’s nose or mouth to tell me if she was breathing. She was just limp. The mom was still screaming, but I couldn’t even hear her anymore. It was like I was having an out-of-body experience. All I could hear were my thoughts: “I need to put this baby down to start CPR. Someone was calling 911. I should go in the front of the store to save time, so EMS doesn’t have to look for me when they come.”
I started moving and trying to clean the blood from the baby’s face with her blanket. At the front of the store, I saw a display of rice bags. I put the baby on top of one of the bags. “Okay, where do I check for a pulse on a baby?” I took care of adults, never pediatric patients, never babies. She was so tiny. I put my hand on her chest and felt nothing. No heartbeat. She still wasn’t breathing.
People were around me, but I couldn’t see or hear anybody. All I was thinking was: “What can I do for this patient right now?” I started CPR with two fingers. Nothing was happening. It wasn’t that long, but it felt like forever for me. I couldn’t do mouth-to-mouth because there was so much blood on her face. I still don’t know what caused the bleeding.
It was COVID time, so I had my mask on. I was, like: “You know what? Screw this. She’s a 1-week-old baby. Her lungs are tiny. Maybe I don’t have to do mouth-to-mouth. I can just blow in her mouth.” I took off my mask and opened her mouth. I took a deep breath and blew a little bit of air in her mouth. I continued CPR for maybe 5 or 10 seconds.
And then she gasped! She opened her eyes, but they were rolled up. I was still doing CPR, and maybe 2 second after that, I could feel under my hand a very rapid heart rate. I took my hand away and lifted her up.
Just then the EMS got there. I gave them the baby and said: “I did CPR. I don’t know how long it lasted.” The EMS person looked at me, said: “Thank you for what you did. Now we need you to help us with mom.” I said, “okay.”
I turned around, and the mom was still screaming and crying. I asked one of the ladies that worked there, “Can you get me water?” She brought it, and I gave some to the mom, and she started talking to EMS.
People were asking me: “What happened? What happened?” It’s funny, I guess the nurse in me didn’t want to give out information. And I didn’t want to ask for information. I was thinking about privacy. I said, “I don’t know,” and walked away.
The mom’s sister came and hugged me and said thank you. I was still in this out-of-body zone, and I just wanted to get the hell out of there. So, I left. I went to my car and when I got in it, I started shaking and sweating and crying.
I had been so calm in the moment, not thinking about if the baby was going to survive or not. I didn’t know how long she was without oxygen, if she would have some anoxic brain injury or stroke. I’m a mom, too. I would have been just as terrified as that mom. I just hoped there was a chance that she could take her baby home.
I went back to the urgent care, and my son was, like, “are you okay?” I said: “You will not believe this. I just did CPR on a baby.” He said: “Oh. Okay.” I don’t think he even knew what that meant.
I’ve been an ICU nurse since 2008. I’ve been in very critical moments with patients, life or death situations. I help save people all the time at the hospital. Most of the time, you know what you’re getting. You can prepare. You have everything you need, and everyone knows what to do. You know what the worst will look like. You know the outcome.
But this was something else. You read about things like this. You hear about them. But you never think it’ll happen to you – until it happens.
I couldn’t stop thinking about the baby. So, 2 days later, I posted on Next Door to see if somebody would read it and say, “hey, the baby survived.” I was amazed at how many people responded, but no one knew the family.
The local news got hold of me and asked me to do a story. I told them, “the only way I can do a story is if the baby survived. I’m not going to do a story about a dead baby, and the mom has to live through it again.”
The reporter called me later on that day and said she had talked to the police. They said the family was visiting from out of state. The baby went to the hospital and was discharged home 2 days later. I said, “okay, then I can talk.”
When the news story came out, I started getting texts from people at work the same night. So many people were reaching out. Even people from out of state. But I never heard from the family. No one knew how to reach them.
Since I was very young, I wanted to work in a hospital, to help people. It really brings me joy, seeing somebody go home, knowing, yes, we did this. It’s a great feeling. I love this job. I wouldn’t trade it for anything.
I just wish I had asked the mom’s name. Because I always think about that baby. I always wonder, what did she become? I hope somebody reads this who might know that little girl. It would be so nice to meet her one day.
Ms. Diallo is an ICU nurse and now works as nurse care coordinator at the University of North Carolina’s Children’s Neurology Clinic in Chapel Hill.
A version of this article first appeared on Medscape.com.
My son needed a physical for his football team, and we couldn’t get an appointment. So, we went to the urgent care next to the H Mart in Cary, N.C. While I was waiting, I thought, let me go get a coffee or an iced tea at the H Mart. They have this French bakery in there.
I went in and ordered my drink, and I was waiting in line. I saw this woman pass me running with a baby. Another woman – I found out later it was her sister – was running after her, and she said: “Call 911!”
“I don’t have my phone,” I said. I left my phone with my son; he was using it.
I said: “Are you okay?” And she just handed me the baby. The baby was gray, and there was blood in her nose and mouth. The woman said: “She’s my baby. She’s 1 week old.”
I was trying to think very quickly. I didn’t see any bubbles in the blood around the baby’s nose or mouth to tell me if she was breathing. She was just limp. The mom was still screaming, but I couldn’t even hear her anymore. It was like I was having an out-of-body experience. All I could hear were my thoughts: “I need to put this baby down to start CPR. Someone was calling 911. I should go in the front of the store to save time, so EMS doesn’t have to look for me when they come.”
I started moving and trying to clean the blood from the baby’s face with her blanket. At the front of the store, I saw a display of rice bags. I put the baby on top of one of the bags. “Okay, where do I check for a pulse on a baby?” I took care of adults, never pediatric patients, never babies. She was so tiny. I put my hand on her chest and felt nothing. No heartbeat. She still wasn’t breathing.
People were around me, but I couldn’t see or hear anybody. All I was thinking was: “What can I do for this patient right now?” I started CPR with two fingers. Nothing was happening. It wasn’t that long, but it felt like forever for me. I couldn’t do mouth-to-mouth because there was so much blood on her face. I still don’t know what caused the bleeding.
It was COVID time, so I had my mask on. I was, like: “You know what? Screw this. She’s a 1-week-old baby. Her lungs are tiny. Maybe I don’t have to do mouth-to-mouth. I can just blow in her mouth.” I took off my mask and opened her mouth. I took a deep breath and blew a little bit of air in her mouth. I continued CPR for maybe 5 or 10 seconds.
And then she gasped! She opened her eyes, but they were rolled up. I was still doing CPR, and maybe 2 second after that, I could feel under my hand a very rapid heart rate. I took my hand away and lifted her up.
Just then the EMS got there. I gave them the baby and said: “I did CPR. I don’t know how long it lasted.” The EMS person looked at me, said: “Thank you for what you did. Now we need you to help us with mom.” I said, “okay.”
I turned around, and the mom was still screaming and crying. I asked one of the ladies that worked there, “Can you get me water?” She brought it, and I gave some to the mom, and she started talking to EMS.
People were asking me: “What happened? What happened?” It’s funny, I guess the nurse in me didn’t want to give out information. And I didn’t want to ask for information. I was thinking about privacy. I said, “I don’t know,” and walked away.
The mom’s sister came and hugged me and said thank you. I was still in this out-of-body zone, and I just wanted to get the hell out of there. So, I left. I went to my car and when I got in it, I started shaking and sweating and crying.
I had been so calm in the moment, not thinking about if the baby was going to survive or not. I didn’t know how long she was without oxygen, if she would have some anoxic brain injury or stroke. I’m a mom, too. I would have been just as terrified as that mom. I just hoped there was a chance that she could take her baby home.
I went back to the urgent care, and my son was, like, “are you okay?” I said: “You will not believe this. I just did CPR on a baby.” He said: “Oh. Okay.” I don’t think he even knew what that meant.
I’ve been an ICU nurse since 2008. I’ve been in very critical moments with patients, life or death situations. I help save people all the time at the hospital. Most of the time, you know what you’re getting. You can prepare. You have everything you need, and everyone knows what to do. You know what the worst will look like. You know the outcome.
But this was something else. You read about things like this. You hear about them. But you never think it’ll happen to you – until it happens.
I couldn’t stop thinking about the baby. So, 2 days later, I posted on Next Door to see if somebody would read it and say, “hey, the baby survived.” I was amazed at how many people responded, but no one knew the family.
The local news got hold of me and asked me to do a story. I told them, “the only way I can do a story is if the baby survived. I’m not going to do a story about a dead baby, and the mom has to live through it again.”
The reporter called me later on that day and said she had talked to the police. They said the family was visiting from out of state. The baby went to the hospital and was discharged home 2 days later. I said, “okay, then I can talk.”
When the news story came out, I started getting texts from people at work the same night. So many people were reaching out. Even people from out of state. But I never heard from the family. No one knew how to reach them.
Since I was very young, I wanted to work in a hospital, to help people. It really brings me joy, seeing somebody go home, knowing, yes, we did this. It’s a great feeling. I love this job. I wouldn’t trade it for anything.
I just wish I had asked the mom’s name. Because I always think about that baby. I always wonder, what did she become? I hope somebody reads this who might know that little girl. It would be so nice to meet her one day.
Ms. Diallo is an ICU nurse and now works as nurse care coordinator at the University of North Carolina’s Children’s Neurology Clinic in Chapel Hill.
A version of this article first appeared on Medscape.com.
Living the introvert’s dream: Alone for 500 days, but never lonely
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
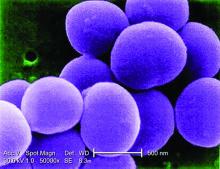
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Most adults, more than one in three children take dietary supplements: Report
The new figures continue a 15-year trend of small, steady increases in how many people in the United States use the products that can deliver essential nutrients, but their usage includes a risk of getting more nutrients than recommended. In 2007, 48% of adults took supplements, and that figure has reached nearly 59% in this latest count.
The new report looked at whether people took a multivitamin, as well as other more specific supplements. Among children and adolescents aged 19 and under, 23.5% took a multivitamin, while 31.5% of adults reported taking one. The most common specialized supplement that people took was vitamin D.
The report, released by the CDC’s National Center for Health Statistics, compiled survey data from 2017 through 2020 in which 15,548 people reported their household’s usage of dietary supplements. Dietary supplements include vitamins, minerals, herbs, or other botanicals that are taken by mouth in pill, capsule, tablet, or liquid form. The researchers said the vitamin and supplement market is large and growing, totaling $55.7 billion in sales in 2020.
More than one-third of adults (36%) reported taking more than one supplement, and one in four people aged 60 and older said they took four or more.
The data showed demographic trends in who uses dietary supplements. Women and girls were more likely to take supplements than men and boys, although there were similar usage levels for both genders among 1- to 2-year-olds. People with higher education or income levels were more likely to use supplements. Asian people and White people were more likely to take supplements, compared with Hispanic people and Black people.
The authors wrote that monitoring trends in supplement use is important because the products “contribute substantially to nutrient intake as well as increase the risk of excessive intake of certain micronutrients.”
A version of this article originally appeared on WebMD.com.
The new figures continue a 15-year trend of small, steady increases in how many people in the United States use the products that can deliver essential nutrients, but their usage includes a risk of getting more nutrients than recommended. In 2007, 48% of adults took supplements, and that figure has reached nearly 59% in this latest count.
The new report looked at whether people took a multivitamin, as well as other more specific supplements. Among children and adolescents aged 19 and under, 23.5% took a multivitamin, while 31.5% of adults reported taking one. The most common specialized supplement that people took was vitamin D.
The report, released by the CDC’s National Center for Health Statistics, compiled survey data from 2017 through 2020 in which 15,548 people reported their household’s usage of dietary supplements. Dietary supplements include vitamins, minerals, herbs, or other botanicals that are taken by mouth in pill, capsule, tablet, or liquid form. The researchers said the vitamin and supplement market is large and growing, totaling $55.7 billion in sales in 2020.
More than one-third of adults (36%) reported taking more than one supplement, and one in four people aged 60 and older said they took four or more.
The data showed demographic trends in who uses dietary supplements. Women and girls were more likely to take supplements than men and boys, although there were similar usage levels for both genders among 1- to 2-year-olds. People with higher education or income levels were more likely to use supplements. Asian people and White people were more likely to take supplements, compared with Hispanic people and Black people.
The authors wrote that monitoring trends in supplement use is important because the products “contribute substantially to nutrient intake as well as increase the risk of excessive intake of certain micronutrients.”
A version of this article originally appeared on WebMD.com.
The new figures continue a 15-year trend of small, steady increases in how many people in the United States use the products that can deliver essential nutrients, but their usage includes a risk of getting more nutrients than recommended. In 2007, 48% of adults took supplements, and that figure has reached nearly 59% in this latest count.
The new report looked at whether people took a multivitamin, as well as other more specific supplements. Among children and adolescents aged 19 and under, 23.5% took a multivitamin, while 31.5% of adults reported taking one. The most common specialized supplement that people took was vitamin D.
The report, released by the CDC’s National Center for Health Statistics, compiled survey data from 2017 through 2020 in which 15,548 people reported their household’s usage of dietary supplements. Dietary supplements include vitamins, minerals, herbs, or other botanicals that are taken by mouth in pill, capsule, tablet, or liquid form. The researchers said the vitamin and supplement market is large and growing, totaling $55.7 billion in sales in 2020.
More than one-third of adults (36%) reported taking more than one supplement, and one in four people aged 60 and older said they took four or more.
The data showed demographic trends in who uses dietary supplements. Women and girls were more likely to take supplements than men and boys, although there were similar usage levels for both genders among 1- to 2-year-olds. People with higher education or income levels were more likely to use supplements. Asian people and White people were more likely to take supplements, compared with Hispanic people and Black people.
The authors wrote that monitoring trends in supplement use is important because the products “contribute substantially to nutrient intake as well as increase the risk of excessive intake of certain micronutrients.”
A version of this article originally appeared on WebMD.com.
Neuropsychiatric side effects of hormonal contraceptives: More common than you think!
Since its introduction in 1950, the combined oral contraceptive pill has been used by countless women as a method for birth control (Liao P. Can Fam Physician. 2012 Dec; 58[12]:e757-e760).
Hormonal contraception (HC) provides women with both contraceptive and noncontraceptive benefits, most notably a method for avoiding unintended pregnancy. In addition to being an effective method of contraception, oral contraceptive pills (OCPs) are well established for treating conditions such as hirsutism, pain symptoms associated with endometriosis and adenomyosis, and pelvic inflammatory disease, among others (Schindler A. Int J Endocrinol Metab. 2013 Winter;11[1]:41-7).
Combined hormonal contraceptives are also first-line treatment for women with menstrual disorders, and in women with polycystic ovary syndrome, can offer an effective long-term method to regulate their menstrual cycle, decrease androgens, clear up oily skin and acne, and reduce facial hair while also providing them with effective contraception (de Melo et al. Open Access J Contracept. 2017;8:13-23).
Associations between ‘the pill’ and mood effects remain controversial
More than 100 million women worldwide use hormonal contraceptives today, yet despite this, the data are mixed regarding the prevalence and extent of neuropsychiatric symptoms and mood changes associated with use of “the pill.” Some studies show combined oral contraceptives are associated with a decrease in general well-being, but had no effect on depression, in women compared with placebo (Zethraeus N et al. Fertil Steril. 2017 May;107[5]:1238-45).
However, a large Danish study published in JAMA Psychiatry of more than 1 million women found a significant association between use of hormonal contraception and antidepressant use or first diagnosis of depression, with adolescents having a higher rate of first depression diagnosis and antidepressant use compared with women 20–30 years old (Skovlund C et al. JAMA Psychiatry. 2016 Nov 1;73[11]:1154-62).
Studies have also shown long-term exposure to levonorgestrel is significantly associated with anxiety and sleep problems in women without a history of these issues (Slattery J et al. Drug Saf. 2018 Oct;41[10]:951-8). A recent small nationwide cohort study in France suggests this may also be true of levonorgestrel delivered by intrauterine devices (IUD) and the association may be dose-dependent (Roland N et al. JAMA. 2023;329[3]:257-9).
Of note, a study published in the American Journal of Psychiatry found a nearly twofold risk of suicide attempt and over threefold risk of suicide among women taking hormonal contraception compared with women who had never used hormonal contraceptives (Skovlund et al. Am J Psychiatry. 2017 Nov 17:appiajp201717060616).
Knowledge gaps make drawing conclusions difficult
The latest information on use of antidepressant and antianxiety medications in women of reproductive age (18-44 years) is sparse and, in some cases, outdated. According to data from the National Health and Nutrition Examination Survey, 18.6% of adult women 18 years or older reported using antidepressant medications within the last 30 days in 2017-2018, an increase from 13.8% in 2009-2010. Among women aged 15-44 year with private employer–sponsored insurance surveyed during 2008-2013, the results showed 15.4% of women filled a prescription for an antidepressant. We must look back further to find data on antianxiety medication use among women aged 18-44 years where use of antianxiety drugs (anxiolytics, sedatives, and hypnotics) was 4.3% between 2005 and 2008.
A lack of literature in this area is likely due to significant underreporting, and an inability to select patients who are sensitive to or at risk of developing neuropsychiatric symptoms resulting from hormonal contraception use because the true pathophysiology is unknown. Existing studies tend to use varying methods to assess mood changes, and do not usually specify hormonal contraceptive use type in their analyses (Schaffir J et al. Eur J Contracept Reprod Health Care. 2016 Oct;21[5]:347-55).
Studies of this nature also require large sample sizes, but the percentage of women who develop neuropsychiatric symptoms from hormonal contraceptive use has historically been relatively small. In the late 1990s, Rosenberg and colleagues found 46% of 1,657 women discontinued oral contraceptives due to side effects within 6 months of starting a new prescription; of these women, 5% reported mood changes as their reason for discontinuing oral contraceptives (Rosenberg M et al. Am J Obstet Gynecol. 1998 Sep;179[3 Pt 1]:577-82).
One might expect that, as lower dosage combined hormonal contraceptives were developed in the 1980s, that the rate of reporting psychological side effects would continue to decrease as well. Yet greater awareness of the potential for mood changes while on “the pill” as outlined by the lay press and social media may be leading to increased reporting of neuropsychiatric effects in women. In a recent cross-sectional survey of 188 women in New York, 43.6% said they experienced mood changes while on hormonal contraceptives, and 61.2% of women with histories of psychiatric illness reported mood changes they attributed to hormonal contraceptives (Martell S et al. Contracept Reprod Med. 2023;8:9).
Martell and colleagues found 48.3% of women cited side effects as a reason for discontinuing hormonal contraception, and 43 participants mentioned psychological side effects unprompted, including 2 patients with suicidal thoughts. The authors said this suggests “psychological side effects, at least in part, may have impacted” HC users’ decisions to switch from OCPs to an alternative method of contraception.
It is also not clear what risk factors exist for women who develop neuropsychiatric symptoms from hormonal contraceptive use. First, it is important to note that both progestin-only contraceptives and combined hormonal contraceptives are classified by the Centers for Disease Control and Prevention’s US Medical Eligibility Criteria for Contraceptive Use, 2016 as having no restrictions for use, including among patients with depression. While women in a smaller subgroup have significant neuropsychiatric symptoms related to their hormonal contraceptives, the underlying mechanism is unknown, and is thought to be largely related to the progestogen component of combined hormonal contraceptives or progestogen-only contraceptives (Mu E. Aust Prescr. 2022 Jun; 45[3]:75-9). We know that some women are hormone sensitive, while others are less so, and some not at all. Progestogens could affect mood as a direct action of the progestogen, because progestogens can be neurosteroids, or the progestogen effect could be mediated secondarily through a change in that woman’s own production of or bioavailability of androgens or naturally occurring estrogens (Giatti S. J Mol Endocrinol. 2016 Aug;57[2]:R109-26).
Here, we also find that currently available evidence limits our ability to draw firm conclusions. A study by Berry-Bibee and colleagues found a “low concern for clinically significant interactions” between hormonal contraception and psychotropic drugs, but was limited by quality/quantity of evidence (Berry-Bibee E et al. Contraception. 2016 Dec;94[6]:650-67). Interestingly, a study by Robinson and colleagues from the mid-2000s posited based on low evidence that “psychological response to the practice of contraception” was a potential explanation for the side effect profile of hormonal contraception (Robinson S et al. Med Hypotheses. 2004;63[2]:268-73).
Further, it may be that women with premenstrual dysphoric disorder (PMDD) might be selected for oral contraceptives, and they are predisposed to other neuropsychiatric problems. Estimates have placed the prevalence of comorbid psychiatric disorders such as anxiety, major depression, bipolar disorder, and posttraumatic stress disorder as high as 70% for women with PMDD (Sepede G et al. Neuropsychiatr Dis Treat. 2020;16:415-26). This phenomenon is not new, having been characterized in the lay literature nearly 20 years ago, by endocrinologist Geoffrey P. Redmond, MD (Redmond GP. The Hormonally Vulnerable Woman. New York: HarperCollins; 2005).
While the cause is not exactly idiosyncratic, They tend to have an entire spectrum of responses to the progestogens in combined or progestin-only contraceptives, ranging from just a flattened affect – which could easily be explained by their flattened level of endogenous hormones – to frank depression. Their frank depression, in turn, can be demonstrated to include suicidal ideation and actual suicide.
Compounding this issue is a woman’s perception of her sexuality. Some women with low sexual desire or sexual problems who are younger may have more distress about their problems compared with women of older reproductive age. While the reason for that is not clear, it may be that in the sexual arena, it is more important for some younger women to be a sexual person than in perimenopausal women, or that women who are younger are more likely to be partnered than women of older reproductive age. While the European Society of Sexual Medicine concluded in a 2019 position statement that there is inconclusive evidence whether hormonal contraception may be contributing to changes in sexual desire and sexual dysfunction, it appears that “a minority of women” experience “better or worse sexual functioning” from taking combined oral contraceptives (Both S et al. J Sex Med. 2019 Nov;16[11]:1681-95), suggesting that the majority of women report no significant changes.
Practitioners should discuss mood effects during consultation
An ob.gyn., primary care physicians, or others with prescriptive authority (i.e. nurse practitioners and physician assistants) in clinical practice may encounter a patient who seems to have mood side effects owing to progestogen-containing contraceptives that they prescribe. However, many ob.gyns. are likely unaware of the prevalence, or that some of those same patients can have such significant mood effects that they would become or are suicidal.
I believe questioning patients about mood effects during consultation and particularly during follow-up following the initiation of any hormonal contraceptive is worth a passing comment for every patient, which should include mood effects in broader discussion for anyone currently using an antidepressant, patients with a history of antidepressant use, and patients who have considered suicide. As we do with other drugs, these questions can be posed in the form of a questionnaire followed up by the practitioner in counseling.
Practitioners who encounter a patient with mood changes as a result of hormonal contraceptive use can consider changing to a nonhormonal method of birth control, or recommending the patient use a barrier method during sexual activity, as none of these options have neuropsychiatric side effects.
Ultimately, practitioners of all types need to engage in shared decision-making to identify the key benefits and risks of hormonal contraceptive use for each patient, which may involve trial and error to determine the ideal treatment. It is critical that practitioners of all types strike a balance between alleviating patient concerns about potential mood changes, monitoring patients with an appreciable risk of mood changes, and continuing patients on hormonal contraception for whom the benefits outweigh the risks.
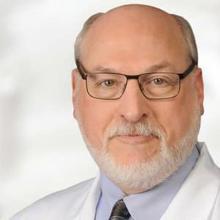
Dr. Simon is a clinical professor at George Washington University and the medical director and founder of IntimMedicine Specialists in Washington, which provides patient-focused care for women across the reproductive life cycle. He is a past president of the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Dr. Simon has been a consultant to, received grant and research support from, and served on the speakers bureau for various pharmaceutical companies that develop combination hormonal contraceptives. Email Dr. Simon at obnews@mdedge.com.
Since its introduction in 1950, the combined oral contraceptive pill has been used by countless women as a method for birth control (Liao P. Can Fam Physician. 2012 Dec; 58[12]:e757-e760).
Hormonal contraception (HC) provides women with both contraceptive and noncontraceptive benefits, most notably a method for avoiding unintended pregnancy. In addition to being an effective method of contraception, oral contraceptive pills (OCPs) are well established for treating conditions such as hirsutism, pain symptoms associated with endometriosis and adenomyosis, and pelvic inflammatory disease, among others (Schindler A. Int J Endocrinol Metab. 2013 Winter;11[1]:41-7).
Combined hormonal contraceptives are also first-line treatment for women with menstrual disorders, and in women with polycystic ovary syndrome, can offer an effective long-term method to regulate their menstrual cycle, decrease androgens, clear up oily skin and acne, and reduce facial hair while also providing them with effective contraception (de Melo et al. Open Access J Contracept. 2017;8:13-23).
Associations between ‘the pill’ and mood effects remain controversial
More than 100 million women worldwide use hormonal contraceptives today, yet despite this, the data are mixed regarding the prevalence and extent of neuropsychiatric symptoms and mood changes associated with use of “the pill.” Some studies show combined oral contraceptives are associated with a decrease in general well-being, but had no effect on depression, in women compared with placebo (Zethraeus N et al. Fertil Steril. 2017 May;107[5]:1238-45).
However, a large Danish study published in JAMA Psychiatry of more than 1 million women found a significant association between use of hormonal contraception and antidepressant use or first diagnosis of depression, with adolescents having a higher rate of first depression diagnosis and antidepressant use compared with women 20–30 years old (Skovlund C et al. JAMA Psychiatry. 2016 Nov 1;73[11]:1154-62).
Studies have also shown long-term exposure to levonorgestrel is significantly associated with anxiety and sleep problems in women without a history of these issues (Slattery J et al. Drug Saf. 2018 Oct;41[10]:951-8). A recent small nationwide cohort study in France suggests this may also be true of levonorgestrel delivered by intrauterine devices (IUD) and the association may be dose-dependent (Roland N et al. JAMA. 2023;329[3]:257-9).
Of note, a study published in the American Journal of Psychiatry found a nearly twofold risk of suicide attempt and over threefold risk of suicide among women taking hormonal contraception compared with women who had never used hormonal contraceptives (Skovlund et al. Am J Psychiatry. 2017 Nov 17:appiajp201717060616).
Knowledge gaps make drawing conclusions difficult
The latest information on use of antidepressant and antianxiety medications in women of reproductive age (18-44 years) is sparse and, in some cases, outdated. According to data from the National Health and Nutrition Examination Survey, 18.6% of adult women 18 years or older reported using antidepressant medications within the last 30 days in 2017-2018, an increase from 13.8% in 2009-2010. Among women aged 15-44 year with private employer–sponsored insurance surveyed during 2008-2013, the results showed 15.4% of women filled a prescription for an antidepressant. We must look back further to find data on antianxiety medication use among women aged 18-44 years where use of antianxiety drugs (anxiolytics, sedatives, and hypnotics) was 4.3% between 2005 and 2008.
A lack of literature in this area is likely due to significant underreporting, and an inability to select patients who are sensitive to or at risk of developing neuropsychiatric symptoms resulting from hormonal contraception use because the true pathophysiology is unknown. Existing studies tend to use varying methods to assess mood changes, and do not usually specify hormonal contraceptive use type in their analyses (Schaffir J et al. Eur J Contracept Reprod Health Care. 2016 Oct;21[5]:347-55).
Studies of this nature also require large sample sizes, but the percentage of women who develop neuropsychiatric symptoms from hormonal contraceptive use has historically been relatively small. In the late 1990s, Rosenberg and colleagues found 46% of 1,657 women discontinued oral contraceptives due to side effects within 6 months of starting a new prescription; of these women, 5% reported mood changes as their reason for discontinuing oral contraceptives (Rosenberg M et al. Am J Obstet Gynecol. 1998 Sep;179[3 Pt 1]:577-82).
One might expect that, as lower dosage combined hormonal contraceptives were developed in the 1980s, that the rate of reporting psychological side effects would continue to decrease as well. Yet greater awareness of the potential for mood changes while on “the pill” as outlined by the lay press and social media may be leading to increased reporting of neuropsychiatric effects in women. In a recent cross-sectional survey of 188 women in New York, 43.6% said they experienced mood changes while on hormonal contraceptives, and 61.2% of women with histories of psychiatric illness reported mood changes they attributed to hormonal contraceptives (Martell S et al. Contracept Reprod Med. 2023;8:9).
Martell and colleagues found 48.3% of women cited side effects as a reason for discontinuing hormonal contraception, and 43 participants mentioned psychological side effects unprompted, including 2 patients with suicidal thoughts. The authors said this suggests “psychological side effects, at least in part, may have impacted” HC users’ decisions to switch from OCPs to an alternative method of contraception.
It is also not clear what risk factors exist for women who develop neuropsychiatric symptoms from hormonal contraceptive use. First, it is important to note that both progestin-only contraceptives and combined hormonal contraceptives are classified by the Centers for Disease Control and Prevention’s US Medical Eligibility Criteria for Contraceptive Use, 2016 as having no restrictions for use, including among patients with depression. While women in a smaller subgroup have significant neuropsychiatric symptoms related to their hormonal contraceptives, the underlying mechanism is unknown, and is thought to be largely related to the progestogen component of combined hormonal contraceptives or progestogen-only contraceptives (Mu E. Aust Prescr. 2022 Jun; 45[3]:75-9). We know that some women are hormone sensitive, while others are less so, and some not at all. Progestogens could affect mood as a direct action of the progestogen, because progestogens can be neurosteroids, or the progestogen effect could be mediated secondarily through a change in that woman’s own production of or bioavailability of androgens or naturally occurring estrogens (Giatti S. J Mol Endocrinol. 2016 Aug;57[2]:R109-26).
Here, we also find that currently available evidence limits our ability to draw firm conclusions. A study by Berry-Bibee and colleagues found a “low concern for clinically significant interactions” between hormonal contraception and psychotropic drugs, but was limited by quality/quantity of evidence (Berry-Bibee E et al. Contraception. 2016 Dec;94[6]:650-67). Interestingly, a study by Robinson and colleagues from the mid-2000s posited based on low evidence that “psychological response to the practice of contraception” was a potential explanation for the side effect profile of hormonal contraception (Robinson S et al. Med Hypotheses. 2004;63[2]:268-73).
Further, it may be that women with premenstrual dysphoric disorder (PMDD) might be selected for oral contraceptives, and they are predisposed to other neuropsychiatric problems. Estimates have placed the prevalence of comorbid psychiatric disorders such as anxiety, major depression, bipolar disorder, and posttraumatic stress disorder as high as 70% for women with PMDD (Sepede G et al. Neuropsychiatr Dis Treat. 2020;16:415-26). This phenomenon is not new, having been characterized in the lay literature nearly 20 years ago, by endocrinologist Geoffrey P. Redmond, MD (Redmond GP. The Hormonally Vulnerable Woman. New York: HarperCollins; 2005).
While the cause is not exactly idiosyncratic, They tend to have an entire spectrum of responses to the progestogens in combined or progestin-only contraceptives, ranging from just a flattened affect – which could easily be explained by their flattened level of endogenous hormones – to frank depression. Their frank depression, in turn, can be demonstrated to include suicidal ideation and actual suicide.
Compounding this issue is a woman’s perception of her sexuality. Some women with low sexual desire or sexual problems who are younger may have more distress about their problems compared with women of older reproductive age. While the reason for that is not clear, it may be that in the sexual arena, it is more important for some younger women to be a sexual person than in perimenopausal women, or that women who are younger are more likely to be partnered than women of older reproductive age. While the European Society of Sexual Medicine concluded in a 2019 position statement that there is inconclusive evidence whether hormonal contraception may be contributing to changes in sexual desire and sexual dysfunction, it appears that “a minority of women” experience “better or worse sexual functioning” from taking combined oral contraceptives (Both S et al. J Sex Med. 2019 Nov;16[11]:1681-95), suggesting that the majority of women report no significant changes.
Practitioners should discuss mood effects during consultation
An ob.gyn., primary care physicians, or others with prescriptive authority (i.e. nurse practitioners and physician assistants) in clinical practice may encounter a patient who seems to have mood side effects owing to progestogen-containing contraceptives that they prescribe. However, many ob.gyns. are likely unaware of the prevalence, or that some of those same patients can have such significant mood effects that they would become or are suicidal.
I believe questioning patients about mood effects during consultation and particularly during follow-up following the initiation of any hormonal contraceptive is worth a passing comment for every patient, which should include mood effects in broader discussion for anyone currently using an antidepressant, patients with a history of antidepressant use, and patients who have considered suicide. As we do with other drugs, these questions can be posed in the form of a questionnaire followed up by the practitioner in counseling.
Practitioners who encounter a patient with mood changes as a result of hormonal contraceptive use can consider changing to a nonhormonal method of birth control, or recommending the patient use a barrier method during sexual activity, as none of these options have neuropsychiatric side effects.
Ultimately, practitioners of all types need to engage in shared decision-making to identify the key benefits and risks of hormonal contraceptive use for each patient, which may involve trial and error to determine the ideal treatment. It is critical that practitioners of all types strike a balance between alleviating patient concerns about potential mood changes, monitoring patients with an appreciable risk of mood changes, and continuing patients on hormonal contraception for whom the benefits outweigh the risks.
Dr. Simon is a clinical professor at George Washington University and the medical director and founder of IntimMedicine Specialists in Washington, which provides patient-focused care for women across the reproductive life cycle. He is a past president of the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Dr. Simon has been a consultant to, received grant and research support from, and served on the speakers bureau for various pharmaceutical companies that develop combination hormonal contraceptives. Email Dr. Simon at obnews@mdedge.com.
Since its introduction in 1950, the combined oral contraceptive pill has been used by countless women as a method for birth control (Liao P. Can Fam Physician. 2012 Dec; 58[12]:e757-e760).
Hormonal contraception (HC) provides women with both contraceptive and noncontraceptive benefits, most notably a method for avoiding unintended pregnancy. In addition to being an effective method of contraception, oral contraceptive pills (OCPs) are well established for treating conditions such as hirsutism, pain symptoms associated with endometriosis and adenomyosis, and pelvic inflammatory disease, among others (Schindler A. Int J Endocrinol Metab. 2013 Winter;11[1]:41-7).
Combined hormonal contraceptives are also first-line treatment for women with menstrual disorders, and in women with polycystic ovary syndrome, can offer an effective long-term method to regulate their menstrual cycle, decrease androgens, clear up oily skin and acne, and reduce facial hair while also providing them with effective contraception (de Melo et al. Open Access J Contracept. 2017;8:13-23).
Associations between ‘the pill’ and mood effects remain controversial
More than 100 million women worldwide use hormonal contraceptives today, yet despite this, the data are mixed regarding the prevalence and extent of neuropsychiatric symptoms and mood changes associated with use of “the pill.” Some studies show combined oral contraceptives are associated with a decrease in general well-being, but had no effect on depression, in women compared with placebo (Zethraeus N et al. Fertil Steril. 2017 May;107[5]:1238-45).
However, a large Danish study published in JAMA Psychiatry of more than 1 million women found a significant association between use of hormonal contraception and antidepressant use or first diagnosis of depression, with adolescents having a higher rate of first depression diagnosis and antidepressant use compared with women 20–30 years old (Skovlund C et al. JAMA Psychiatry. 2016 Nov 1;73[11]:1154-62).
Studies have also shown long-term exposure to levonorgestrel is significantly associated with anxiety and sleep problems in women without a history of these issues (Slattery J et al. Drug Saf. 2018 Oct;41[10]:951-8). A recent small nationwide cohort study in France suggests this may also be true of levonorgestrel delivered by intrauterine devices (IUD) and the association may be dose-dependent (Roland N et al. JAMA. 2023;329[3]:257-9).
Of note, a study published in the American Journal of Psychiatry found a nearly twofold risk of suicide attempt and over threefold risk of suicide among women taking hormonal contraception compared with women who had never used hormonal contraceptives (Skovlund et al. Am J Psychiatry. 2017 Nov 17:appiajp201717060616).
Knowledge gaps make drawing conclusions difficult
The latest information on use of antidepressant and antianxiety medications in women of reproductive age (18-44 years) is sparse and, in some cases, outdated. According to data from the National Health and Nutrition Examination Survey, 18.6% of adult women 18 years or older reported using antidepressant medications within the last 30 days in 2017-2018, an increase from 13.8% in 2009-2010. Among women aged 15-44 year with private employer–sponsored insurance surveyed during 2008-2013, the results showed 15.4% of women filled a prescription for an antidepressant. We must look back further to find data on antianxiety medication use among women aged 18-44 years where use of antianxiety drugs (anxiolytics, sedatives, and hypnotics) was 4.3% between 2005 and 2008.
A lack of literature in this area is likely due to significant underreporting, and an inability to select patients who are sensitive to or at risk of developing neuropsychiatric symptoms resulting from hormonal contraception use because the true pathophysiology is unknown. Existing studies tend to use varying methods to assess mood changes, and do not usually specify hormonal contraceptive use type in their analyses (Schaffir J et al. Eur J Contracept Reprod Health Care. 2016 Oct;21[5]:347-55).
Studies of this nature also require large sample sizes, but the percentage of women who develop neuropsychiatric symptoms from hormonal contraceptive use has historically been relatively small. In the late 1990s, Rosenberg and colleagues found 46% of 1,657 women discontinued oral contraceptives due to side effects within 6 months of starting a new prescription; of these women, 5% reported mood changes as their reason for discontinuing oral contraceptives (Rosenberg M et al. Am J Obstet Gynecol. 1998 Sep;179[3 Pt 1]:577-82).
One might expect that, as lower dosage combined hormonal contraceptives were developed in the 1980s, that the rate of reporting psychological side effects would continue to decrease as well. Yet greater awareness of the potential for mood changes while on “the pill” as outlined by the lay press and social media may be leading to increased reporting of neuropsychiatric effects in women. In a recent cross-sectional survey of 188 women in New York, 43.6% said they experienced mood changes while on hormonal contraceptives, and 61.2% of women with histories of psychiatric illness reported mood changes they attributed to hormonal contraceptives (Martell S et al. Contracept Reprod Med. 2023;8:9).
Martell and colleagues found 48.3% of women cited side effects as a reason for discontinuing hormonal contraception, and 43 participants mentioned psychological side effects unprompted, including 2 patients with suicidal thoughts. The authors said this suggests “psychological side effects, at least in part, may have impacted” HC users’ decisions to switch from OCPs to an alternative method of contraception.
It is also not clear what risk factors exist for women who develop neuropsychiatric symptoms from hormonal contraceptive use. First, it is important to note that both progestin-only contraceptives and combined hormonal contraceptives are classified by the Centers for Disease Control and Prevention’s US Medical Eligibility Criteria for Contraceptive Use, 2016 as having no restrictions for use, including among patients with depression. While women in a smaller subgroup have significant neuropsychiatric symptoms related to their hormonal contraceptives, the underlying mechanism is unknown, and is thought to be largely related to the progestogen component of combined hormonal contraceptives or progestogen-only contraceptives (Mu E. Aust Prescr. 2022 Jun; 45[3]:75-9). We know that some women are hormone sensitive, while others are less so, and some not at all. Progestogens could affect mood as a direct action of the progestogen, because progestogens can be neurosteroids, or the progestogen effect could be mediated secondarily through a change in that woman’s own production of or bioavailability of androgens or naturally occurring estrogens (Giatti S. J Mol Endocrinol. 2016 Aug;57[2]:R109-26).
Here, we also find that currently available evidence limits our ability to draw firm conclusions. A study by Berry-Bibee and colleagues found a “low concern for clinically significant interactions” between hormonal contraception and psychotropic drugs, but was limited by quality/quantity of evidence (Berry-Bibee E et al. Contraception. 2016 Dec;94[6]:650-67). Interestingly, a study by Robinson and colleagues from the mid-2000s posited based on low evidence that “psychological response to the practice of contraception” was a potential explanation for the side effect profile of hormonal contraception (Robinson S et al. Med Hypotheses. 2004;63[2]:268-73).
Further, it may be that women with premenstrual dysphoric disorder (PMDD) might be selected for oral contraceptives, and they are predisposed to other neuropsychiatric problems. Estimates have placed the prevalence of comorbid psychiatric disorders such as anxiety, major depression, bipolar disorder, and posttraumatic stress disorder as high as 70% for women with PMDD (Sepede G et al. Neuropsychiatr Dis Treat. 2020;16:415-26). This phenomenon is not new, having been characterized in the lay literature nearly 20 years ago, by endocrinologist Geoffrey P. Redmond, MD (Redmond GP. The Hormonally Vulnerable Woman. New York: HarperCollins; 2005).
While the cause is not exactly idiosyncratic, They tend to have an entire spectrum of responses to the progestogens in combined or progestin-only contraceptives, ranging from just a flattened affect – which could easily be explained by their flattened level of endogenous hormones – to frank depression. Their frank depression, in turn, can be demonstrated to include suicidal ideation and actual suicide.
Compounding this issue is a woman’s perception of her sexuality. Some women with low sexual desire or sexual problems who are younger may have more distress about their problems compared with women of older reproductive age. While the reason for that is not clear, it may be that in the sexual arena, it is more important for some younger women to be a sexual person than in perimenopausal women, or that women who are younger are more likely to be partnered than women of older reproductive age. While the European Society of Sexual Medicine concluded in a 2019 position statement that there is inconclusive evidence whether hormonal contraception may be contributing to changes in sexual desire and sexual dysfunction, it appears that “a minority of women” experience “better or worse sexual functioning” from taking combined oral contraceptives (Both S et al. J Sex Med. 2019 Nov;16[11]:1681-95), suggesting that the majority of women report no significant changes.
Practitioners should discuss mood effects during consultation
An ob.gyn., primary care physicians, or others with prescriptive authority (i.e. nurse practitioners and physician assistants) in clinical practice may encounter a patient who seems to have mood side effects owing to progestogen-containing contraceptives that they prescribe. However, many ob.gyns. are likely unaware of the prevalence, or that some of those same patients can have such significant mood effects that they would become or are suicidal.
I believe questioning patients about mood effects during consultation and particularly during follow-up following the initiation of any hormonal contraceptive is worth a passing comment for every patient, which should include mood effects in broader discussion for anyone currently using an antidepressant, patients with a history of antidepressant use, and patients who have considered suicide. As we do with other drugs, these questions can be posed in the form of a questionnaire followed up by the practitioner in counseling.
Practitioners who encounter a patient with mood changes as a result of hormonal contraceptive use can consider changing to a nonhormonal method of birth control, or recommending the patient use a barrier method during sexual activity, as none of these options have neuropsychiatric side effects.
Ultimately, practitioners of all types need to engage in shared decision-making to identify the key benefits and risks of hormonal contraceptive use for each patient, which may involve trial and error to determine the ideal treatment. It is critical that practitioners of all types strike a balance between alleviating patient concerns about potential mood changes, monitoring patients with an appreciable risk of mood changes, and continuing patients on hormonal contraception for whom the benefits outweigh the risks.
Dr. Simon is a clinical professor at George Washington University and the medical director and founder of IntimMedicine Specialists in Washington, which provides patient-focused care for women across the reproductive life cycle. He is a past president of the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Dr. Simon has been a consultant to, received grant and research support from, and served on the speakers bureau for various pharmaceutical companies that develop combination hormonal contraceptives. Email Dr. Simon at obnews@mdedge.com.
Physical exercise tied to a reduction in suicide attempts
A meta-analysis of 17 randomized controlled trials (RCTs), which included more than 1,000 participants with mental or physical illnesses, showed there was a significant reduction in suicide attempts in participants randomly assigned to receive exercise interventions, compared with inactive controls. However, there were no differences between the exercise and the control groups in suicidal ideation or mortality.
On the other hand, there was also no significant difference in dropout rates between those randomly assigned to exercise versus inactive controls, suggesting that people with mental or physical impairments are able to adhere to exercise regimens.
“A common misconception is that patients, particularly those suffering from mental of physical illness, are not willing or motivated enough to participate in an exercise [regimen], and this has led to primary care providers underprescribing exercise to those with mental or physical illness,” lead author Nicholas Fabiano, MD, a resident in the department of psychiatry at the University of Ottawa, told this news organization.
As a result of the study findings, “we recommend that providers do not have apprehension about prescribing exercise to patients with physical or mental illness. Exercise may be an effective way to reduce suicidal behaviors” in these patients, he said.
The study was published online in the Journal of Affective Disorders.
Physical, mental health strongly linked
Existing literature has “demonstrated a protective effect of physical activity on suicidal ideation in the general population,” but to date there have been no systematic reviews or meta-analyses investigating its impact on suicide-related outcomes in patients with physical or mental illness, the authors write.
“Those with mental or physical illness are at increased risk of suicide, compared to the general population,” Dr. Fabiano commented.
“We often split up ‘mental health’ and ‘physical health’ in medicine; however, I believe that the two are more on a continuum and a holistic term, such as ‘health,’ should be used instead,” he added.
He noted that mental and physical health are “inexorably intertwined” and those with physical illness are more prone to developing mental illness, whereas those with mental illness are more likely to suffer from a variety of other medical conditions. “Therefore, when treating those with mental illness, it is also imperative that we bolster one’s physical health through easily accessible activities such as exercise,” he said.
The goal of the study was to determine whether individuals with “any mental, physical, clinical, or subclinical condition” might benefit from exercise, particularly in relation to suicide-related outcomes. They searched multiple databases from inception to June 2022 to identify RCTs investigating exercise and suicidal ideation in participants with physical or mental conditions.
Of 673 studies, 17 met the inclusion criteria (total of 1,021 participants). Participants’ mean age was 42.7 years, 82% were female, and 54% were randomly assigned to an exercise intervention.
Most studies (82%) focused on clinical versus subclinical outcomes. Depression was the most commonly included condition (59%). Aerobic exercise (53%) was the most common form of exercise used in the active study groups. This was followed by mind-body exercise and strength training (53%, 17.6%, and 17.6%, respectively). The mean follow-up time was 10 weeks.
Reduced impulsivity
The researchers found a difference in post-intervention suicidal ideation when they compared exercise participants to all control and inactive control participants (standardized mean difference, –1.09; 95% confidence interval, –3.08 to 0.90; P = .20, k = 5). However, the difference was not statistically significant.
Similarly, there was no significant difference (P = .60) in suicidal ideation incidence for subgroup analyses that stratified data among participants with depression, sickle cell disease, and suicidality.
All-cause discontinuation also did not significantly differ between participants who were randomly assigned to exercise interventions versus all controls or inactive controls (odds ratio, 0.85; 95% CI, 0.38-1.94; P = .86, k = 12 and OR, 0.81; 95% CI, 0.25-2.68; P = .70). All-cause discontinuation also did not differ between participants randomized to exercise versus active controls (OR, 0.94; 95% CI, 0.38-2.32; P = .79, k = 3).
Likewise, there were nonsignificant differences between participants who underwent aerobic exercise and strength training (P = .20).
However, there were some nonsignificant differences when comparing participants with depression and stress who received the exercise intervention versus controls (P = .46).
There was a significant reduction in suicide attempts in individuals who participated in exercise interventions versus inactive controls (OR, 0.23; 95% CI, 0.09-0.67; P = .04, k = 2). On the other hand, there was no significant difference in mortality (P = .70).
Most of the studies (82%) were “at high risk of bias,” the authors note. In addition, the analysis was limited because the included studies were “few, underpowered, and heterogeneous.”
Dr. Fabiano hypothesized that the lack of effect on suicidal ideation or mortality is “likely due to the limited sample size.” As additional RCTs are conducted, Dr. Fabiano expects to see decreases in both suicidal ideation and suicide attempts.
The findings may “be explained by the ideation-to-action framework, which suggests that the development of suicidal ideation and the progression to suicide attempts are distinct processes with different influential factors,” he said.
Increased levels of exercise have been “shown to reduce emotional impulsivity and, as it has been shown that most suicide attempts are characterized by impulsivity and low lethality, we hypothesize that regular exercise serves as a protective factor against suicide attempts,” he said.
Not useful?
Commenting on the study, Fabien Legrand, PhD, a lecturer in clinical psychology, University of Reims Champagne-Ardenne, Reims, France, said that the impact of physical activity is of “particular interest” to him because it is closely linked to his research activity, where he has “been exploring the antidepressant effects of exercise for more than 15 years.”
A small pilot study conducted by Dr. Legrand and colleagues found rigorous physical activity to be helpful in reducing hopelessness in psychiatric patients, compared with controls. “This result is of particular relevance for suicidal patients, since it has long been documented that hopelessness is one of the main triggers of suicide ideation and suicide attempts,” he said.
Initially, Dr. Legrand “warmly welcomed” the current review and meta-analysis on the exercise and suicide. However, he felt that the paper fell short in accomplishing its intended goal. “After a thorough reading of the paper, I don’t think that the information provided can be used in any way,” he stated.
“The paper’s title – ‘Effects of Physical Exercise on Suicidal Ideation and Behavior’ – does not do justice to its content, since 9 of the included 17 RCTs did not measure changes in suicidal ideation and/or suicidal behavior following participation in an exercise program,” noted Dr. Legrand, who was not involved with authorship or the current analysis.
The study was funded by the University of Ottawa department of psychiatry. Dr. Fabiano declares no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. Legrand declares no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A meta-analysis of 17 randomized controlled trials (RCTs), which included more than 1,000 participants with mental or physical illnesses, showed there was a significant reduction in suicide attempts in participants randomly assigned to receive exercise interventions, compared with inactive controls. However, there were no differences between the exercise and the control groups in suicidal ideation or mortality.
On the other hand, there was also no significant difference in dropout rates between those randomly assigned to exercise versus inactive controls, suggesting that people with mental or physical impairments are able to adhere to exercise regimens.
“A common misconception is that patients, particularly those suffering from mental of physical illness, are not willing or motivated enough to participate in an exercise [regimen], and this has led to primary care providers underprescribing exercise to those with mental or physical illness,” lead author Nicholas Fabiano, MD, a resident in the department of psychiatry at the University of Ottawa, told this news organization.
As a result of the study findings, “we recommend that providers do not have apprehension about prescribing exercise to patients with physical or mental illness. Exercise may be an effective way to reduce suicidal behaviors” in these patients, he said.
The study was published online in the Journal of Affective Disorders.
Physical, mental health strongly linked
Existing literature has “demonstrated a protective effect of physical activity on suicidal ideation in the general population,” but to date there have been no systematic reviews or meta-analyses investigating its impact on suicide-related outcomes in patients with physical or mental illness, the authors write.
“Those with mental or physical illness are at increased risk of suicide, compared to the general population,” Dr. Fabiano commented.
“We often split up ‘mental health’ and ‘physical health’ in medicine; however, I believe that the two are more on a continuum and a holistic term, such as ‘health,’ should be used instead,” he added.
He noted that mental and physical health are “inexorably intertwined” and those with physical illness are more prone to developing mental illness, whereas those with mental illness are more likely to suffer from a variety of other medical conditions. “Therefore, when treating those with mental illness, it is also imperative that we bolster one’s physical health through easily accessible activities such as exercise,” he said.
The goal of the study was to determine whether individuals with “any mental, physical, clinical, or subclinical condition” might benefit from exercise, particularly in relation to suicide-related outcomes. They searched multiple databases from inception to June 2022 to identify RCTs investigating exercise and suicidal ideation in participants with physical or mental conditions.
Of 673 studies, 17 met the inclusion criteria (total of 1,021 participants). Participants’ mean age was 42.7 years, 82% were female, and 54% were randomly assigned to an exercise intervention.
Most studies (82%) focused on clinical versus subclinical outcomes. Depression was the most commonly included condition (59%). Aerobic exercise (53%) was the most common form of exercise used in the active study groups. This was followed by mind-body exercise and strength training (53%, 17.6%, and 17.6%, respectively). The mean follow-up time was 10 weeks.
Reduced impulsivity
The researchers found a difference in post-intervention suicidal ideation when they compared exercise participants to all control and inactive control participants (standardized mean difference, –1.09; 95% confidence interval, –3.08 to 0.90; P = .20, k = 5). However, the difference was not statistically significant.
Similarly, there was no significant difference (P = .60) in suicidal ideation incidence for subgroup analyses that stratified data among participants with depression, sickle cell disease, and suicidality.
All-cause discontinuation also did not significantly differ between participants who were randomly assigned to exercise interventions versus all controls or inactive controls (odds ratio, 0.85; 95% CI, 0.38-1.94; P = .86, k = 12 and OR, 0.81; 95% CI, 0.25-2.68; P = .70). All-cause discontinuation also did not differ between participants randomized to exercise versus active controls (OR, 0.94; 95% CI, 0.38-2.32; P = .79, k = 3).
Likewise, there were nonsignificant differences between participants who underwent aerobic exercise and strength training (P = .20).
However, there were some nonsignificant differences when comparing participants with depression and stress who received the exercise intervention versus controls (P = .46).
There was a significant reduction in suicide attempts in individuals who participated in exercise interventions versus inactive controls (OR, 0.23; 95% CI, 0.09-0.67; P = .04, k = 2). On the other hand, there was no significant difference in mortality (P = .70).
Most of the studies (82%) were “at high risk of bias,” the authors note. In addition, the analysis was limited because the included studies were “few, underpowered, and heterogeneous.”
Dr. Fabiano hypothesized that the lack of effect on suicidal ideation or mortality is “likely due to the limited sample size.” As additional RCTs are conducted, Dr. Fabiano expects to see decreases in both suicidal ideation and suicide attempts.
The findings may “be explained by the ideation-to-action framework, which suggests that the development of suicidal ideation and the progression to suicide attempts are distinct processes with different influential factors,” he said.
Increased levels of exercise have been “shown to reduce emotional impulsivity and, as it has been shown that most suicide attempts are characterized by impulsivity and low lethality, we hypothesize that regular exercise serves as a protective factor against suicide attempts,” he said.
Not useful?
Commenting on the study, Fabien Legrand, PhD, a lecturer in clinical psychology, University of Reims Champagne-Ardenne, Reims, France, said that the impact of physical activity is of “particular interest” to him because it is closely linked to his research activity, where he has “been exploring the antidepressant effects of exercise for more than 15 years.”
A small pilot study conducted by Dr. Legrand and colleagues found rigorous physical activity to be helpful in reducing hopelessness in psychiatric patients, compared with controls. “This result is of particular relevance for suicidal patients, since it has long been documented that hopelessness is one of the main triggers of suicide ideation and suicide attempts,” he said.
Initially, Dr. Legrand “warmly welcomed” the current review and meta-analysis on the exercise and suicide. However, he felt that the paper fell short in accomplishing its intended goal. “After a thorough reading of the paper, I don’t think that the information provided can be used in any way,” he stated.
“The paper’s title – ‘Effects of Physical Exercise on Suicidal Ideation and Behavior’ – does not do justice to its content, since 9 of the included 17 RCTs did not measure changes in suicidal ideation and/or suicidal behavior following participation in an exercise program,” noted Dr. Legrand, who was not involved with authorship or the current analysis.
The study was funded by the University of Ottawa department of psychiatry. Dr. Fabiano declares no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. Legrand declares no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A meta-analysis of 17 randomized controlled trials (RCTs), which included more than 1,000 participants with mental or physical illnesses, showed there was a significant reduction in suicide attempts in participants randomly assigned to receive exercise interventions, compared with inactive controls. However, there were no differences between the exercise and the control groups in suicidal ideation or mortality.
On the other hand, there was also no significant difference in dropout rates between those randomly assigned to exercise versus inactive controls, suggesting that people with mental or physical impairments are able to adhere to exercise regimens.
“A common misconception is that patients, particularly those suffering from mental of physical illness, are not willing or motivated enough to participate in an exercise [regimen], and this has led to primary care providers underprescribing exercise to those with mental or physical illness,” lead author Nicholas Fabiano, MD, a resident in the department of psychiatry at the University of Ottawa, told this news organization.
As a result of the study findings, “we recommend that providers do not have apprehension about prescribing exercise to patients with physical or mental illness. Exercise may be an effective way to reduce suicidal behaviors” in these patients, he said.
The study was published online in the Journal of Affective Disorders.
Physical, mental health strongly linked
Existing literature has “demonstrated a protective effect of physical activity on suicidal ideation in the general population,” but to date there have been no systematic reviews or meta-analyses investigating its impact on suicide-related outcomes in patients with physical or mental illness, the authors write.
“Those with mental or physical illness are at increased risk of suicide, compared to the general population,” Dr. Fabiano commented.
“We often split up ‘mental health’ and ‘physical health’ in medicine; however, I believe that the two are more on a continuum and a holistic term, such as ‘health,’ should be used instead,” he added.
He noted that mental and physical health are “inexorably intertwined” and those with physical illness are more prone to developing mental illness, whereas those with mental illness are more likely to suffer from a variety of other medical conditions. “Therefore, when treating those with mental illness, it is also imperative that we bolster one’s physical health through easily accessible activities such as exercise,” he said.
The goal of the study was to determine whether individuals with “any mental, physical, clinical, or subclinical condition” might benefit from exercise, particularly in relation to suicide-related outcomes. They searched multiple databases from inception to June 2022 to identify RCTs investigating exercise and suicidal ideation in participants with physical or mental conditions.
Of 673 studies, 17 met the inclusion criteria (total of 1,021 participants). Participants’ mean age was 42.7 years, 82% were female, and 54% were randomly assigned to an exercise intervention.
Most studies (82%) focused on clinical versus subclinical outcomes. Depression was the most commonly included condition (59%). Aerobic exercise (53%) was the most common form of exercise used in the active study groups. This was followed by mind-body exercise and strength training (53%, 17.6%, and 17.6%, respectively). The mean follow-up time was 10 weeks.
Reduced impulsivity
The researchers found a difference in post-intervention suicidal ideation when they compared exercise participants to all control and inactive control participants (standardized mean difference, –1.09; 95% confidence interval, –3.08 to 0.90; P = .20, k = 5). However, the difference was not statistically significant.
Similarly, there was no significant difference (P = .60) in suicidal ideation incidence for subgroup analyses that stratified data among participants with depression, sickle cell disease, and suicidality.
All-cause discontinuation also did not significantly differ between participants who were randomly assigned to exercise interventions versus all controls or inactive controls (odds ratio, 0.85; 95% CI, 0.38-1.94; P = .86, k = 12 and OR, 0.81; 95% CI, 0.25-2.68; P = .70). All-cause discontinuation also did not differ between participants randomized to exercise versus active controls (OR, 0.94; 95% CI, 0.38-2.32; P = .79, k = 3).
Likewise, there were nonsignificant differences between participants who underwent aerobic exercise and strength training (P = .20).
However, there were some nonsignificant differences when comparing participants with depression and stress who received the exercise intervention versus controls (P = .46).
There was a significant reduction in suicide attempts in individuals who participated in exercise interventions versus inactive controls (OR, 0.23; 95% CI, 0.09-0.67; P = .04, k = 2). On the other hand, there was no significant difference in mortality (P = .70).
Most of the studies (82%) were “at high risk of bias,” the authors note. In addition, the analysis was limited because the included studies were “few, underpowered, and heterogeneous.”
Dr. Fabiano hypothesized that the lack of effect on suicidal ideation or mortality is “likely due to the limited sample size.” As additional RCTs are conducted, Dr. Fabiano expects to see decreases in both suicidal ideation and suicide attempts.
The findings may “be explained by the ideation-to-action framework, which suggests that the development of suicidal ideation and the progression to suicide attempts are distinct processes with different influential factors,” he said.
Increased levels of exercise have been “shown to reduce emotional impulsivity and, as it has been shown that most suicide attempts are characterized by impulsivity and low lethality, we hypothesize that regular exercise serves as a protective factor against suicide attempts,” he said.
Not useful?
Commenting on the study, Fabien Legrand, PhD, a lecturer in clinical psychology, University of Reims Champagne-Ardenne, Reims, France, said that the impact of physical activity is of “particular interest” to him because it is closely linked to his research activity, where he has “been exploring the antidepressant effects of exercise for more than 15 years.”
A small pilot study conducted by Dr. Legrand and colleagues found rigorous physical activity to be helpful in reducing hopelessness in psychiatric patients, compared with controls. “This result is of particular relevance for suicidal patients, since it has long been documented that hopelessness is one of the main triggers of suicide ideation and suicide attempts,” he said.
Initially, Dr. Legrand “warmly welcomed” the current review and meta-analysis on the exercise and suicide. However, he felt that the paper fell short in accomplishing its intended goal. “After a thorough reading of the paper, I don’t think that the information provided can be used in any way,” he stated.
“The paper’s title – ‘Effects of Physical Exercise on Suicidal Ideation and Behavior’ – does not do justice to its content, since 9 of the included 17 RCTs did not measure changes in suicidal ideation and/or suicidal behavior following participation in an exercise program,” noted Dr. Legrand, who was not involved with authorship or the current analysis.
The study was funded by the University of Ottawa department of psychiatry. Dr. Fabiano declares no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. Legrand declares no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Weight loss linked to early death in older but healthy adults
suggesting the need for clinicians to be alert to such changes.
“Our study emphasizes the importance of weight loss even in relatively healthy individuals who are free from evident cardiovascular disease [CVD], dementia, physical disability, or life-limiting chronic illness,” first author Monira Hussain, MBBS, MPH, PhD, said in an interview.
“Clinicians should be aware that even minor weight loss of 5% or more in older adults without life-limiting illnesses can increase mortality risk,” Dr. Hussain said. “Regular monitoring of weight changes can help early identification of associated risks.”
The study was published online in JAMA Network Open.
The researchers noted that data on the significance of weight changes among older individuals who are otherwise relatively healthy and not diagnosed with life-limited diseases are limited, with the exception that “it is widely acknowledged that weight loss may precede a diagnosis of cancer.” But the association with the other types of non–cancer-related premature death is notable.
“In our study, weight loss also preceded an increased mortality from CVD and other causes, [such as] deaths from trauma, dementia, Parkinson disease, and other less common causes.”
Therefore, “a likely explanation for these findings is that weight loss can be an early prodromal indicator of the presence of various life-shortening diseases,” Dr. Hussain, of Monash University, Melbourne, and colleagues wrote.
In terms of why weight loss shows such a stronger link to mortality in older men, compared with women, Dr. Hussain speculated that this may be caused by “differences in body composition,” between the two sexes. “Men have a higher proportion of muscle and bone mass, and weight loss [in men] primarily involves loss of these tissues.”
10% weight loss quadrupled risk of premature death among men
To investigate this phenomenon, the researchers conducted a post hoc analysis of the Aspirin in Reducing Events in the Elderly (ASPREE) randomized trial, which included information on a variety of body size parameters, such as weight and waist circumference, measured annually, from a large population of healthy individuals with no evident CVD, dementia, physical disability, or life-limiting chronic illness.
The 16,523 participants included in the study had a mean age of 75 years and 55.6% were women. During a mean follow-up of 4.4 years, 1,256 deaths occurred in the cohort.
Looking at rates of all-cause mortality, stratified by gender, the results showed that among men who had a 5%-10% decrease in weight over the course of the study, the risk of all-cause mortality was 33% higher than that of men who had a stable weight (less than 5% change; hazard ratio, 1.33).
Among men who had a more than 10% decrease in weight, the mortality risk was as much as 289%, or nearly four times higher compared with those with a stable weight (HR, 3.89).
For women, the mortality risk was also increased, however, to a lesser degree. A 5%-10% loss of body weight was associated with a 26% increased mortality risk (HR, 1.26), and a loss of more than 10% was linked to a 114% increased risk of all-cause mortality (HR, 2.14).
In terms of cancer-specific deaths, the risk was significantly increased only among men who had a greater than 10% weight decrease (HR, 3.49), while the increased risk in women was observed with a 5%-10% decrease in weight (HR, 1.44) as well as a more than 10% decrease (HR, 2.78).
The risk of CVD-specific death was significantly increased with a more than 10% decrease in weight in both sexes, but the risk was again higher among men (HR, 3.14) than women (HR, 1.92), compared with stable weight groups.
And the noncancer, non–CVD-specific mortality risk was nearly five times higher among men who had a more than 10% decrease in weight versus stable weight (HR, 4.98); however, the association was not significant among women (HR, 1.49).
Looking at the effects of change in waist circumference, a decrease of more than 10% was associated with a higher risk in all-cause mortality that was again higher for men (HR, 2.14) versus women (HR, 1.34); however, no link with all-cause mortality was observed with a less than 10% decrease in either sex.
A greater than 10% decrease in waist circumference was also associated with higher risk of cancer death for men and women, and higher noncancer, non-CVD death among men, but not women, while there was no association between waist circumference and CVD mortality in men or women.
Association with mortality remained after adjustment for hospitalization
The results persisted after adjustment for age, frailty status, baseline body mass index, country of birth, smoking, hypertension, diabetes, and hospitalization in the previous 24 months.
The adjustment for recent hospitalization was especially important for ruling out weight loss that may have occurred because of hospitalization for acute conditions that could have contributed to mortality, the authors noted.
The authors reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
suggesting the need for clinicians to be alert to such changes.
“Our study emphasizes the importance of weight loss even in relatively healthy individuals who are free from evident cardiovascular disease [CVD], dementia, physical disability, or life-limiting chronic illness,” first author Monira Hussain, MBBS, MPH, PhD, said in an interview.
“Clinicians should be aware that even minor weight loss of 5% or more in older adults without life-limiting illnesses can increase mortality risk,” Dr. Hussain said. “Regular monitoring of weight changes can help early identification of associated risks.”
The study was published online in JAMA Network Open.
The researchers noted that data on the significance of weight changes among older individuals who are otherwise relatively healthy and not diagnosed with life-limited diseases are limited, with the exception that “it is widely acknowledged that weight loss may precede a diagnosis of cancer.” But the association with the other types of non–cancer-related premature death is notable.
“In our study, weight loss also preceded an increased mortality from CVD and other causes, [such as] deaths from trauma, dementia, Parkinson disease, and other less common causes.”
Therefore, “a likely explanation for these findings is that weight loss can be an early prodromal indicator of the presence of various life-shortening diseases,” Dr. Hussain, of Monash University, Melbourne, and colleagues wrote.
In terms of why weight loss shows such a stronger link to mortality in older men, compared with women, Dr. Hussain speculated that this may be caused by “differences in body composition,” between the two sexes. “Men have a higher proportion of muscle and bone mass, and weight loss [in men] primarily involves loss of these tissues.”
10% weight loss quadrupled risk of premature death among men
To investigate this phenomenon, the researchers conducted a post hoc analysis of the Aspirin in Reducing Events in the Elderly (ASPREE) randomized trial, which included information on a variety of body size parameters, such as weight and waist circumference, measured annually, from a large population of healthy individuals with no evident CVD, dementia, physical disability, or life-limiting chronic illness.
The 16,523 participants included in the study had a mean age of 75 years and 55.6% were women. During a mean follow-up of 4.4 years, 1,256 deaths occurred in the cohort.
Looking at rates of all-cause mortality, stratified by gender, the results showed that among men who had a 5%-10% decrease in weight over the course of the study, the risk of all-cause mortality was 33% higher than that of men who had a stable weight (less than 5% change; hazard ratio, 1.33).
Among men who had a more than 10% decrease in weight, the mortality risk was as much as 289%, or nearly four times higher compared with those with a stable weight (HR, 3.89).
For women, the mortality risk was also increased, however, to a lesser degree. A 5%-10% loss of body weight was associated with a 26% increased mortality risk (HR, 1.26), and a loss of more than 10% was linked to a 114% increased risk of all-cause mortality (HR, 2.14).
In terms of cancer-specific deaths, the risk was significantly increased only among men who had a greater than 10% weight decrease (HR, 3.49), while the increased risk in women was observed with a 5%-10% decrease in weight (HR, 1.44) as well as a more than 10% decrease (HR, 2.78).
The risk of CVD-specific death was significantly increased with a more than 10% decrease in weight in both sexes, but the risk was again higher among men (HR, 3.14) than women (HR, 1.92), compared with stable weight groups.
And the noncancer, non–CVD-specific mortality risk was nearly five times higher among men who had a more than 10% decrease in weight versus stable weight (HR, 4.98); however, the association was not significant among women (HR, 1.49).
Looking at the effects of change in waist circumference, a decrease of more than 10% was associated with a higher risk in all-cause mortality that was again higher for men (HR, 2.14) versus women (HR, 1.34); however, no link with all-cause mortality was observed with a less than 10% decrease in either sex.
A greater than 10% decrease in waist circumference was also associated with higher risk of cancer death for men and women, and higher noncancer, non-CVD death among men, but not women, while there was no association between waist circumference and CVD mortality in men or women.
Association with mortality remained after adjustment for hospitalization
The results persisted after adjustment for age, frailty status, baseline body mass index, country of birth, smoking, hypertension, diabetes, and hospitalization in the previous 24 months.
The adjustment for recent hospitalization was especially important for ruling out weight loss that may have occurred because of hospitalization for acute conditions that could have contributed to mortality, the authors noted.
The authors reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
suggesting the need for clinicians to be alert to such changes.
“Our study emphasizes the importance of weight loss even in relatively healthy individuals who are free from evident cardiovascular disease [CVD], dementia, physical disability, or life-limiting chronic illness,” first author Monira Hussain, MBBS, MPH, PhD, said in an interview.
“Clinicians should be aware that even minor weight loss of 5% or more in older adults without life-limiting illnesses can increase mortality risk,” Dr. Hussain said. “Regular monitoring of weight changes can help early identification of associated risks.”
The study was published online in JAMA Network Open.
The researchers noted that data on the significance of weight changes among older individuals who are otherwise relatively healthy and not diagnosed with life-limited diseases are limited, with the exception that “it is widely acknowledged that weight loss may precede a diagnosis of cancer.” But the association with the other types of non–cancer-related premature death is notable.
“In our study, weight loss also preceded an increased mortality from CVD and other causes, [such as] deaths from trauma, dementia, Parkinson disease, and other less common causes.”
Therefore, “a likely explanation for these findings is that weight loss can be an early prodromal indicator of the presence of various life-shortening diseases,” Dr. Hussain, of Monash University, Melbourne, and colleagues wrote.
In terms of why weight loss shows such a stronger link to mortality in older men, compared with women, Dr. Hussain speculated that this may be caused by “differences in body composition,” between the two sexes. “Men have a higher proportion of muscle and bone mass, and weight loss [in men] primarily involves loss of these tissues.”
10% weight loss quadrupled risk of premature death among men
To investigate this phenomenon, the researchers conducted a post hoc analysis of the Aspirin in Reducing Events in the Elderly (ASPREE) randomized trial, which included information on a variety of body size parameters, such as weight and waist circumference, measured annually, from a large population of healthy individuals with no evident CVD, dementia, physical disability, or life-limiting chronic illness.
The 16,523 participants included in the study had a mean age of 75 years and 55.6% were women. During a mean follow-up of 4.4 years, 1,256 deaths occurred in the cohort.
Looking at rates of all-cause mortality, stratified by gender, the results showed that among men who had a 5%-10% decrease in weight over the course of the study, the risk of all-cause mortality was 33% higher than that of men who had a stable weight (less than 5% change; hazard ratio, 1.33).
Among men who had a more than 10% decrease in weight, the mortality risk was as much as 289%, or nearly four times higher compared with those with a stable weight (HR, 3.89).
For women, the mortality risk was also increased, however, to a lesser degree. A 5%-10% loss of body weight was associated with a 26% increased mortality risk (HR, 1.26), and a loss of more than 10% was linked to a 114% increased risk of all-cause mortality (HR, 2.14).
In terms of cancer-specific deaths, the risk was significantly increased only among men who had a greater than 10% weight decrease (HR, 3.49), while the increased risk in women was observed with a 5%-10% decrease in weight (HR, 1.44) as well as a more than 10% decrease (HR, 2.78).
The risk of CVD-specific death was significantly increased with a more than 10% decrease in weight in both sexes, but the risk was again higher among men (HR, 3.14) than women (HR, 1.92), compared with stable weight groups.
And the noncancer, non–CVD-specific mortality risk was nearly five times higher among men who had a more than 10% decrease in weight versus stable weight (HR, 4.98); however, the association was not significant among women (HR, 1.49).
Looking at the effects of change in waist circumference, a decrease of more than 10% was associated with a higher risk in all-cause mortality that was again higher for men (HR, 2.14) versus women (HR, 1.34); however, no link with all-cause mortality was observed with a less than 10% decrease in either sex.
A greater than 10% decrease in waist circumference was also associated with higher risk of cancer death for men and women, and higher noncancer, non-CVD death among men, but not women, while there was no association between waist circumference and CVD mortality in men or women.
Association with mortality remained after adjustment for hospitalization
The results persisted after adjustment for age, frailty status, baseline body mass index, country of birth, smoking, hypertension, diabetes, and hospitalization in the previous 24 months.
The adjustment for recent hospitalization was especially important for ruling out weight loss that may have occurred because of hospitalization for acute conditions that could have contributed to mortality, the authors noted.
The authors reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN
More states nix nonconsensual pelvic exams by med students
Performing intimate exams under anesthesia (EUA) is a standard part of medical training. Yet,
“Whenever I talk about this at conferences around the country, people always come up to me and say it’s still happening at their institutions,” Lori Bruce, MA, MBE, HEC-C, associate director of the Interdisciplinary Center for Bioethics at Yale University, New Haven, Conn., told this news organization.
Most think this is a women’s issue, which occurs only in unconscious patients, she said. But Ms. Bruce found otherwise in a survey last year in which she polled the general public about their intimate exam experiences.
“Unconsented exams happen much more than we imagined, and they happen as often to men [having] prostate exams without consent as to women. Black [respondents] were nearly four times more likely to have reported receiving an unconsented intimate pelvic or prostate exam,” she said, based on her research. And Ms. Bruce believes it can happen across the economic spectrum.
Concern about unconsented EUAs arose in the early 2000s. In a study at that time, 75% of medical students reported that their patients had not given consent to be examined during surgical procedures. An ethics committee of the American College of Obstetricians and Gynecologists published guidelines for EUAs and states began passing legislation with patient protections and medical training consent policies.
California is believed to be the first to adopt legislation outlawing unconsented pelvic exams for training purposes in 2003, followed by Virginia in 2007, along with a handful of other states.
In 2019, on the heels of the #MeToo movement and renewed calls to end unconsented exams, more patients and providers began to speak publicly about their experiences with the practice. Some posted on social media using the #MeTooPelvic hashtag. In 2022, an award-winning documentary was also released about consent, “At Your Cervix.”More states subsequently passed legislation, and some medical schools strengthened their EUA consent policies.
Today, nearly half the states in the country have enacted laws against unconsented intimate EUAs, with some carrying misdemeanor charges for both the individual conducting the exam and the supervising physician. Other states leave open the option to fine the physician and revoke or suspend medical licenses.
Much of the new legislation requires explicit consent for intimate exams involving the pelvis, prostate, and rectum, with exceptions for emergency procedures and, in some cases, the collection of court-ordered forensic evidence. In addition, several states, including Colorado, Indiana, and Ohio, have pending or recently introduced bills. Last month, sister bills in Missouri passed the House and Senate, gaining more traction than previous legislative attempts. A similar bill was introduced in the Kansas House several times, including this year, and is expected to be on the agenda again in the next session.
Intimate exams on patients without consent are “unethical and unacceptable,” said Alison Whelan, MD, chief academic officer of the Association of American Medical Colleges. Although medical students learn sensitive procedures through simulation labs and gynecological teaching associates – individuals specifically trained to help students develop physical exam skills – EUAs require strict adherence to widely accepted guidelines.
“Learners in the clinical setting should only perform such examinations for teaching purposes when the exam is explicitly consented to, related to the planned procedure, performed by a student who is recognized by the patient as a part of their care team, and done under direct supervision by an educator,” Dr. Whelan said.
Medical students bear moral burden
Arthur Caplan, PhD, director of medical ethics at New York University, has called unconsented intimate exams a “cousin issue” to abusive predatory behavior.
If the public is outraged that physicians “have misused their authority with athletes, then we should be equally outraged if that authority, even for a higher purpose [like] teaching and training, is still misused in terms of getting permission and consent,” he said in a video discussing Connecticut’s legislation to strengthen intimate exam requirements, which went into effect Jan. 1.
Advocates of stricter EUA consent policies say the variability in consent practices destroys patient trust by ignoring the basic principles of respect and autonomy. Because patients are usually unaware a violation has occurred, reporting typically depends on medical students raising questions with educators and attendings, which they may hesitate to do for fear of repercussions.
Current practices, such as patients signing consent documents in the outpatient setting where students aren’t always privy to the discussion, contribute to the lack of transparency, Karampreet Kaur, MD, a 2nd-year ob.gyn. resident at the Hospital of the University of Pennsylvania, Philadelphia, said.
A 2019 survey of medical students by Elle magazine found that nearly half did not meet patients before conducting an intimate EUA. Of the 92% who performed a pelvic EUA, 61% reported doing so without obtaining explicit patient consent.
Dr. Kaur recently coauthored a survey of students from six medical schools and found that 84% completed at least one pelvic EUA during their ob.gyn. clerkships. About half of the students surveyed observed patients giving informed consent most or every time. Of those, 67% reported they never or rarely witnessed an explicit explanation that a medical student may perform a pelvic EUA.
This burden weighs on the consciences of medical students. Respondents reported that they wanted to honor patient autonomy but felt they lacked the authority to object to pelvic EUAs when consent was unclear, which led to significant emotional distress.
“It’s not that physicians don’t care,” Dr. Kaur said. “I think most want to make sure patients feel safe and fully informed of the care they are receiving.”
To consent or not
Incorporating a separate EUA consent form, typically signed during a preoperative visit but occasionally on the day of surgery, offers one potential solution as it ensures “clear and consistent language is used and forces documentation of this conversation,” said Dr. Kaur. At her current institution, providers and medical students must review charted EUA documentation, then that information is “made clear to attendings, fellows, residents, students, and even the OR staff,” she said.
In Dr. Kaur’s survey, 11% of respondents supported a separate consent. Another study of 3rd- and 4th-year medical students published last year found that 45% agreed with having a separate signature line on the surgical consent form.
Legislation introduced recently in Colorado states that medical students must meet the patient, and patients must receive a written or electronic document titled, in at least 18-point bolded font, “consent for examination of breasts, pelvic region, rectum, and/or prostate.” The form must also include the names of medical students performing or observing an intimate exam for educational purposes.
Elizabeth Newman, MPP, public policy director at the Colorado Coalition Against Sexual Assault and supporter of the state’s intimate exam bill, said the legislation will allow medical students to learn the intricacies of these sensitive body systems and provide better patient care, particularly following the rollback of Roe v. Wade.
“Abortion is available and accessible in Colorado, and we are surrounded by states where it’s not,” said Ms. Newman. “Medical students in states where it’s outright banned are coming to Colorado to learn how to provide abortion care in their residencies and fellowships, so we want to maintain that access and not take those learning opportunities away with this law.”
Opponents of a separate form say it complicates the consent process. Dr. Kaur said she originally thought it would involve a lot of extra work, but it only takes 3-5 minutes. Few patients decline the exam after the conversation, and students benefit from the clear guidelines and transparency, she said.
“I had hoped that the many medical association guidelines [supporting] explicit consent would have influenced hospital policy, but it did not have that effect,” said Ms. Bruce, adding that recent legislative efforts have largely been driven by concerned bioethicists, lawmakers, and some medical students and physicians. “It all circles back to the patient having the right to refuse; it’s their body.”
A version of this article first appeared on Medscape.com.
Performing intimate exams under anesthesia (EUA) is a standard part of medical training. Yet,
“Whenever I talk about this at conferences around the country, people always come up to me and say it’s still happening at their institutions,” Lori Bruce, MA, MBE, HEC-C, associate director of the Interdisciplinary Center for Bioethics at Yale University, New Haven, Conn., told this news organization.
Most think this is a women’s issue, which occurs only in unconscious patients, she said. But Ms. Bruce found otherwise in a survey last year in which she polled the general public about their intimate exam experiences.
“Unconsented exams happen much more than we imagined, and they happen as often to men [having] prostate exams without consent as to women. Black [respondents] were nearly four times more likely to have reported receiving an unconsented intimate pelvic or prostate exam,” she said, based on her research. And Ms. Bruce believes it can happen across the economic spectrum.
Concern about unconsented EUAs arose in the early 2000s. In a study at that time, 75% of medical students reported that their patients had not given consent to be examined during surgical procedures. An ethics committee of the American College of Obstetricians and Gynecologists published guidelines for EUAs and states began passing legislation with patient protections and medical training consent policies.
California is believed to be the first to adopt legislation outlawing unconsented pelvic exams for training purposes in 2003, followed by Virginia in 2007, along with a handful of other states.
In 2019, on the heels of the #MeToo movement and renewed calls to end unconsented exams, more patients and providers began to speak publicly about their experiences with the practice. Some posted on social media using the #MeTooPelvic hashtag. In 2022, an award-winning documentary was also released about consent, “At Your Cervix.”More states subsequently passed legislation, and some medical schools strengthened their EUA consent policies.
Today, nearly half the states in the country have enacted laws against unconsented intimate EUAs, with some carrying misdemeanor charges for both the individual conducting the exam and the supervising physician. Other states leave open the option to fine the physician and revoke or suspend medical licenses.
Much of the new legislation requires explicit consent for intimate exams involving the pelvis, prostate, and rectum, with exceptions for emergency procedures and, in some cases, the collection of court-ordered forensic evidence. In addition, several states, including Colorado, Indiana, and Ohio, have pending or recently introduced bills. Last month, sister bills in Missouri passed the House and Senate, gaining more traction than previous legislative attempts. A similar bill was introduced in the Kansas House several times, including this year, and is expected to be on the agenda again in the next session.
Intimate exams on patients without consent are “unethical and unacceptable,” said Alison Whelan, MD, chief academic officer of the Association of American Medical Colleges. Although medical students learn sensitive procedures through simulation labs and gynecological teaching associates – individuals specifically trained to help students develop physical exam skills – EUAs require strict adherence to widely accepted guidelines.
“Learners in the clinical setting should only perform such examinations for teaching purposes when the exam is explicitly consented to, related to the planned procedure, performed by a student who is recognized by the patient as a part of their care team, and done under direct supervision by an educator,” Dr. Whelan said.
Medical students bear moral burden
Arthur Caplan, PhD, director of medical ethics at New York University, has called unconsented intimate exams a “cousin issue” to abusive predatory behavior.
If the public is outraged that physicians “have misused their authority with athletes, then we should be equally outraged if that authority, even for a higher purpose [like] teaching and training, is still misused in terms of getting permission and consent,” he said in a video discussing Connecticut’s legislation to strengthen intimate exam requirements, which went into effect Jan. 1.
Advocates of stricter EUA consent policies say the variability in consent practices destroys patient trust by ignoring the basic principles of respect and autonomy. Because patients are usually unaware a violation has occurred, reporting typically depends on medical students raising questions with educators and attendings, which they may hesitate to do for fear of repercussions.
Current practices, such as patients signing consent documents in the outpatient setting where students aren’t always privy to the discussion, contribute to the lack of transparency, Karampreet Kaur, MD, a 2nd-year ob.gyn. resident at the Hospital of the University of Pennsylvania, Philadelphia, said.
A 2019 survey of medical students by Elle magazine found that nearly half did not meet patients before conducting an intimate EUA. Of the 92% who performed a pelvic EUA, 61% reported doing so without obtaining explicit patient consent.
Dr. Kaur recently coauthored a survey of students from six medical schools and found that 84% completed at least one pelvic EUA during their ob.gyn. clerkships. About half of the students surveyed observed patients giving informed consent most or every time. Of those, 67% reported they never or rarely witnessed an explicit explanation that a medical student may perform a pelvic EUA.
This burden weighs on the consciences of medical students. Respondents reported that they wanted to honor patient autonomy but felt they lacked the authority to object to pelvic EUAs when consent was unclear, which led to significant emotional distress.
“It’s not that physicians don’t care,” Dr. Kaur said. “I think most want to make sure patients feel safe and fully informed of the care they are receiving.”
To consent or not
Incorporating a separate EUA consent form, typically signed during a preoperative visit but occasionally on the day of surgery, offers one potential solution as it ensures “clear and consistent language is used and forces documentation of this conversation,” said Dr. Kaur. At her current institution, providers and medical students must review charted EUA documentation, then that information is “made clear to attendings, fellows, residents, students, and even the OR staff,” she said.
In Dr. Kaur’s survey, 11% of respondents supported a separate consent. Another study of 3rd- and 4th-year medical students published last year found that 45% agreed with having a separate signature line on the surgical consent form.
Legislation introduced recently in Colorado states that medical students must meet the patient, and patients must receive a written or electronic document titled, in at least 18-point bolded font, “consent for examination of breasts, pelvic region, rectum, and/or prostate.” The form must also include the names of medical students performing or observing an intimate exam for educational purposes.
Elizabeth Newman, MPP, public policy director at the Colorado Coalition Against Sexual Assault and supporter of the state’s intimate exam bill, said the legislation will allow medical students to learn the intricacies of these sensitive body systems and provide better patient care, particularly following the rollback of Roe v. Wade.
“Abortion is available and accessible in Colorado, and we are surrounded by states where it’s not,” said Ms. Newman. “Medical students in states where it’s outright banned are coming to Colorado to learn how to provide abortion care in their residencies and fellowships, so we want to maintain that access and not take those learning opportunities away with this law.”
Opponents of a separate form say it complicates the consent process. Dr. Kaur said she originally thought it would involve a lot of extra work, but it only takes 3-5 minutes. Few patients decline the exam after the conversation, and students benefit from the clear guidelines and transparency, she said.
“I had hoped that the many medical association guidelines [supporting] explicit consent would have influenced hospital policy, but it did not have that effect,” said Ms. Bruce, adding that recent legislative efforts have largely been driven by concerned bioethicists, lawmakers, and some medical students and physicians. “It all circles back to the patient having the right to refuse; it’s their body.”
A version of this article first appeared on Medscape.com.
Performing intimate exams under anesthesia (EUA) is a standard part of medical training. Yet,
“Whenever I talk about this at conferences around the country, people always come up to me and say it’s still happening at their institutions,” Lori Bruce, MA, MBE, HEC-C, associate director of the Interdisciplinary Center for Bioethics at Yale University, New Haven, Conn., told this news organization.
Most think this is a women’s issue, which occurs only in unconscious patients, she said. But Ms. Bruce found otherwise in a survey last year in which she polled the general public about their intimate exam experiences.
“Unconsented exams happen much more than we imagined, and they happen as often to men [having] prostate exams without consent as to women. Black [respondents] were nearly four times more likely to have reported receiving an unconsented intimate pelvic or prostate exam,” she said, based on her research. And Ms. Bruce believes it can happen across the economic spectrum.
Concern about unconsented EUAs arose in the early 2000s. In a study at that time, 75% of medical students reported that their patients had not given consent to be examined during surgical procedures. An ethics committee of the American College of Obstetricians and Gynecologists published guidelines for EUAs and states began passing legislation with patient protections and medical training consent policies.
California is believed to be the first to adopt legislation outlawing unconsented pelvic exams for training purposes in 2003, followed by Virginia in 2007, along with a handful of other states.
In 2019, on the heels of the #MeToo movement and renewed calls to end unconsented exams, more patients and providers began to speak publicly about their experiences with the practice. Some posted on social media using the #MeTooPelvic hashtag. In 2022, an award-winning documentary was also released about consent, “At Your Cervix.”More states subsequently passed legislation, and some medical schools strengthened their EUA consent policies.
Today, nearly half the states in the country have enacted laws against unconsented intimate EUAs, with some carrying misdemeanor charges for both the individual conducting the exam and the supervising physician. Other states leave open the option to fine the physician and revoke or suspend medical licenses.
Much of the new legislation requires explicit consent for intimate exams involving the pelvis, prostate, and rectum, with exceptions for emergency procedures and, in some cases, the collection of court-ordered forensic evidence. In addition, several states, including Colorado, Indiana, and Ohio, have pending or recently introduced bills. Last month, sister bills in Missouri passed the House and Senate, gaining more traction than previous legislative attempts. A similar bill was introduced in the Kansas House several times, including this year, and is expected to be on the agenda again in the next session.
Intimate exams on patients without consent are “unethical and unacceptable,” said Alison Whelan, MD, chief academic officer of the Association of American Medical Colleges. Although medical students learn sensitive procedures through simulation labs and gynecological teaching associates – individuals specifically trained to help students develop physical exam skills – EUAs require strict adherence to widely accepted guidelines.
“Learners in the clinical setting should only perform such examinations for teaching purposes when the exam is explicitly consented to, related to the planned procedure, performed by a student who is recognized by the patient as a part of their care team, and done under direct supervision by an educator,” Dr. Whelan said.
Medical students bear moral burden
Arthur Caplan, PhD, director of medical ethics at New York University, has called unconsented intimate exams a “cousin issue” to abusive predatory behavior.
If the public is outraged that physicians “have misused their authority with athletes, then we should be equally outraged if that authority, even for a higher purpose [like] teaching and training, is still misused in terms of getting permission and consent,” he said in a video discussing Connecticut’s legislation to strengthen intimate exam requirements, which went into effect Jan. 1.
Advocates of stricter EUA consent policies say the variability in consent practices destroys patient trust by ignoring the basic principles of respect and autonomy. Because patients are usually unaware a violation has occurred, reporting typically depends on medical students raising questions with educators and attendings, which they may hesitate to do for fear of repercussions.
Current practices, such as patients signing consent documents in the outpatient setting where students aren’t always privy to the discussion, contribute to the lack of transparency, Karampreet Kaur, MD, a 2nd-year ob.gyn. resident at the Hospital of the University of Pennsylvania, Philadelphia, said.
A 2019 survey of medical students by Elle magazine found that nearly half did not meet patients before conducting an intimate EUA. Of the 92% who performed a pelvic EUA, 61% reported doing so without obtaining explicit patient consent.
Dr. Kaur recently coauthored a survey of students from six medical schools and found that 84% completed at least one pelvic EUA during their ob.gyn. clerkships. About half of the students surveyed observed patients giving informed consent most or every time. Of those, 67% reported they never or rarely witnessed an explicit explanation that a medical student may perform a pelvic EUA.
This burden weighs on the consciences of medical students. Respondents reported that they wanted to honor patient autonomy but felt they lacked the authority to object to pelvic EUAs when consent was unclear, which led to significant emotional distress.
“It’s not that physicians don’t care,” Dr. Kaur said. “I think most want to make sure patients feel safe and fully informed of the care they are receiving.”
To consent or not
Incorporating a separate EUA consent form, typically signed during a preoperative visit but occasionally on the day of surgery, offers one potential solution as it ensures “clear and consistent language is used and forces documentation of this conversation,” said Dr. Kaur. At her current institution, providers and medical students must review charted EUA documentation, then that information is “made clear to attendings, fellows, residents, students, and even the OR staff,” she said.
In Dr. Kaur’s survey, 11% of respondents supported a separate consent. Another study of 3rd- and 4th-year medical students published last year found that 45% agreed with having a separate signature line on the surgical consent form.
Legislation introduced recently in Colorado states that medical students must meet the patient, and patients must receive a written or electronic document titled, in at least 18-point bolded font, “consent for examination of breasts, pelvic region, rectum, and/or prostate.” The form must also include the names of medical students performing or observing an intimate exam for educational purposes.
Elizabeth Newman, MPP, public policy director at the Colorado Coalition Against Sexual Assault and supporter of the state’s intimate exam bill, said the legislation will allow medical students to learn the intricacies of these sensitive body systems and provide better patient care, particularly following the rollback of Roe v. Wade.
“Abortion is available and accessible in Colorado, and we are surrounded by states where it’s not,” said Ms. Newman. “Medical students in states where it’s outright banned are coming to Colorado to learn how to provide abortion care in their residencies and fellowships, so we want to maintain that access and not take those learning opportunities away with this law.”
Opponents of a separate form say it complicates the consent process. Dr. Kaur said she originally thought it would involve a lot of extra work, but it only takes 3-5 minutes. Few patients decline the exam after the conversation, and students benefit from the clear guidelines and transparency, she said.
“I had hoped that the many medical association guidelines [supporting] explicit consent would have influenced hospital policy, but it did not have that effect,” said Ms. Bruce, adding that recent legislative efforts have largely been driven by concerned bioethicists, lawmakers, and some medical students and physicians. “It all circles back to the patient having the right to refuse; it’s their body.”
A version of this article first appeared on Medscape.com.
Sentinel events in hospitals continue to rise, driven by increase in falls
Reporting sentinel events to The Joint Commission began in 1996 as a way to help health care organizations improve safety. The annual review is based on an aggregate database of reports analyzed each year, according to the review authors.
The Joint Commission defines a sentinel event as a patient safety event (not primarily related to the natural course of the patient’s illness or underlying condition) that reaches a patient and results in death, permanent harm (regardless of severity), or severe harm (regardless of duration).
Some of the specific events deemed sentinel include patient suicide while under care in a health care setting, unanticipated death of a full-term infant, homicide of any patient or staff member while on site at a health care organization, any intrapartum maternal death, severe maternal morbidity, sexual abuse or assault of any patient undergoing care in the health care setting, sexual abuse or assault of any staff member providing care, and physical assault of any patient or staff member in the health care setting.
Additional events considered sentinel are related to treatments and procedures. These include surgery in the wrong site; wrong patient or wrong procedure for a given patient; administration of blood or blood products incompatible with the patient that results in death, permanent harm, or severe harm; severe neonatal hyperbilirubinemia; and patient falls.
A total of 1,441 sentinel events were reported in 2022. Patient falls accounted for the majority (42%) of these events, continuing a trend in increasing rates of patient falls from previous years. Falls considered sentinel events were those resulting in any fracture, surgery, casting or traction, consultation or comfort care for neurologic or internal injury, the need for blood products, or death or permanent harm as a result of injuries sustained in the fall. The leading sentinel event types after falls included delay in treatment, unintended retention of a foreign object, and wrong surgery (6% for each). Other sentinel event types in the top 10 accounted for 5% or less of reports: suicide (5%), assault/rape/sexual assault/homicide (4%), fire/burns (3%), perinatal events (2%), self-harm (2%), and medication management (2%).
Overall, 20% of the 2022 events resulted in patient death, 6% in permanent harm or loss of function, 44% in severe temporary harm, and 13% in a need for additional care or an extended hospital stay.
The most common events that led to patient death were suicide (24%), treatment delays (21%), and patient falls (11%). Patient falls also accounted for nearly two-thirds of the events resulting in severe temporary harm (62%).
Most of the events (88%) occurred in hospital settings; of these, the most common were falls (45%), followed by the retention of foreign objects and incorrect surgeries (7% and 6%, respectively). Overall, 90% of sentinel events were reported by the health care organizations; the remaining 10% were reported by patients, families, or employees (current or former).
“Failures in communication, teamwork, and consistently following policies were leading causes for reported sentinel events,” the authors wrote. However, reporting sentinel events is voluntary; therefore “no conclusions should be drawn about the actual relative frequency of events or trends in events over time,” they noted.
Increased reporting may not reflect increased occurrence
“It is important to clarify that The Joint Commission saw an increase in reporting of sentinel events; whether this is indicative of an actual increase in occurrence of sentinel events across the country or not is difficult to say, as the reporting is voluntary,” said Haytham Kaafarani, MD, MPH, chief patient safety officer and medical director for The Joint Commission, in an interview.
“However, this is the highest number reported to The Joint Commission since the inception of the sentinel event policy: there were 547 health care organizations that reported sentinel events in 2022, compared to 500 in 2021 and 423 in 2020,” Dr. Kaafarani said. “Having said that, based on published literature, the COVID-19 pandemic stressed our health care systems in many ways including but not limited to staff shortage in times of increased needs, worsening of mental health conditions, and delay in presentation of non–COVID-related medical conditions during the pandemic,” he noted.
Dr. Kaafarani said that The Joint Commission was not surprised by the type of sentinel events reported, which has remained consistent with previous years.
However, The Joint Commission was surprised by the significant increase in the number of reported events, he said. “Since reporting is voluntarily, we welcome the increase in reporting of sentinel events, as it helps The Joint Commission better understand the patient safety landscape across the country, and better helps health care organizations during their difficult times.”
Based on the latest information, “The Joint Commission encourages health care organizations to create research that is focused on preventing patient falls in hospitals,” said Dr. Kaafarani. “With staff shortages reported within many health care organizations, it is now more essential than ever to establish systematic interventions to prevent patient falls and resultant harm.”
The review authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Reporting sentinel events to The Joint Commission began in 1996 as a way to help health care organizations improve safety. The annual review is based on an aggregate database of reports analyzed each year, according to the review authors.
The Joint Commission defines a sentinel event as a patient safety event (not primarily related to the natural course of the patient’s illness or underlying condition) that reaches a patient and results in death, permanent harm (regardless of severity), or severe harm (regardless of duration).
Some of the specific events deemed sentinel include patient suicide while under care in a health care setting, unanticipated death of a full-term infant, homicide of any patient or staff member while on site at a health care organization, any intrapartum maternal death, severe maternal morbidity, sexual abuse or assault of any patient undergoing care in the health care setting, sexual abuse or assault of any staff member providing care, and physical assault of any patient or staff member in the health care setting.
Additional events considered sentinel are related to treatments and procedures. These include surgery in the wrong site; wrong patient or wrong procedure for a given patient; administration of blood or blood products incompatible with the patient that results in death, permanent harm, or severe harm; severe neonatal hyperbilirubinemia; and patient falls.
A total of 1,441 sentinel events were reported in 2022. Patient falls accounted for the majority (42%) of these events, continuing a trend in increasing rates of patient falls from previous years. Falls considered sentinel events were those resulting in any fracture, surgery, casting or traction, consultation or comfort care for neurologic or internal injury, the need for blood products, or death or permanent harm as a result of injuries sustained in the fall. The leading sentinel event types after falls included delay in treatment, unintended retention of a foreign object, and wrong surgery (6% for each). Other sentinel event types in the top 10 accounted for 5% or less of reports: suicide (5%), assault/rape/sexual assault/homicide (4%), fire/burns (3%), perinatal events (2%), self-harm (2%), and medication management (2%).
Overall, 20% of the 2022 events resulted in patient death, 6% in permanent harm or loss of function, 44% in severe temporary harm, and 13% in a need for additional care or an extended hospital stay.
The most common events that led to patient death were suicide (24%), treatment delays (21%), and patient falls (11%). Patient falls also accounted for nearly two-thirds of the events resulting in severe temporary harm (62%).
Most of the events (88%) occurred in hospital settings; of these, the most common were falls (45%), followed by the retention of foreign objects and incorrect surgeries (7% and 6%, respectively). Overall, 90% of sentinel events were reported by the health care organizations; the remaining 10% were reported by patients, families, or employees (current or former).
“Failures in communication, teamwork, and consistently following policies were leading causes for reported sentinel events,” the authors wrote. However, reporting sentinel events is voluntary; therefore “no conclusions should be drawn about the actual relative frequency of events or trends in events over time,” they noted.
Increased reporting may not reflect increased occurrence
“It is important to clarify that The Joint Commission saw an increase in reporting of sentinel events; whether this is indicative of an actual increase in occurrence of sentinel events across the country or not is difficult to say, as the reporting is voluntary,” said Haytham Kaafarani, MD, MPH, chief patient safety officer and medical director for The Joint Commission, in an interview.
“However, this is the highest number reported to The Joint Commission since the inception of the sentinel event policy: there were 547 health care organizations that reported sentinel events in 2022, compared to 500 in 2021 and 423 in 2020,” Dr. Kaafarani said. “Having said that, based on published literature, the COVID-19 pandemic stressed our health care systems in many ways including but not limited to staff shortage in times of increased needs, worsening of mental health conditions, and delay in presentation of non–COVID-related medical conditions during the pandemic,” he noted.
Dr. Kaafarani said that The Joint Commission was not surprised by the type of sentinel events reported, which has remained consistent with previous years.
However, The Joint Commission was surprised by the significant increase in the number of reported events, he said. “Since reporting is voluntarily, we welcome the increase in reporting of sentinel events, as it helps The Joint Commission better understand the patient safety landscape across the country, and better helps health care organizations during their difficult times.”
Based on the latest information, “The Joint Commission encourages health care organizations to create research that is focused on preventing patient falls in hospitals,” said Dr. Kaafarani. “With staff shortages reported within many health care organizations, it is now more essential than ever to establish systematic interventions to prevent patient falls and resultant harm.”
The review authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Reporting sentinel events to The Joint Commission began in 1996 as a way to help health care organizations improve safety. The annual review is based on an aggregate database of reports analyzed each year, according to the review authors.
The Joint Commission defines a sentinel event as a patient safety event (not primarily related to the natural course of the patient’s illness or underlying condition) that reaches a patient and results in death, permanent harm (regardless of severity), or severe harm (regardless of duration).
Some of the specific events deemed sentinel include patient suicide while under care in a health care setting, unanticipated death of a full-term infant, homicide of any patient or staff member while on site at a health care organization, any intrapartum maternal death, severe maternal morbidity, sexual abuse or assault of any patient undergoing care in the health care setting, sexual abuse or assault of any staff member providing care, and physical assault of any patient or staff member in the health care setting.
Additional events considered sentinel are related to treatments and procedures. These include surgery in the wrong site; wrong patient or wrong procedure for a given patient; administration of blood or blood products incompatible with the patient that results in death, permanent harm, or severe harm; severe neonatal hyperbilirubinemia; and patient falls.
A total of 1,441 sentinel events were reported in 2022. Patient falls accounted for the majority (42%) of these events, continuing a trend in increasing rates of patient falls from previous years. Falls considered sentinel events were those resulting in any fracture, surgery, casting or traction, consultation or comfort care for neurologic or internal injury, the need for blood products, or death or permanent harm as a result of injuries sustained in the fall. The leading sentinel event types after falls included delay in treatment, unintended retention of a foreign object, and wrong surgery (6% for each). Other sentinel event types in the top 10 accounted for 5% or less of reports: suicide (5%), assault/rape/sexual assault/homicide (4%), fire/burns (3%), perinatal events (2%), self-harm (2%), and medication management (2%).
Overall, 20% of the 2022 events resulted in patient death, 6% in permanent harm or loss of function, 44% in severe temporary harm, and 13% in a need for additional care or an extended hospital stay.
The most common events that led to patient death were suicide (24%), treatment delays (21%), and patient falls (11%). Patient falls also accounted for nearly two-thirds of the events resulting in severe temporary harm (62%).
Most of the events (88%) occurred in hospital settings; of these, the most common were falls (45%), followed by the retention of foreign objects and incorrect surgeries (7% and 6%, respectively). Overall, 90% of sentinel events were reported by the health care organizations; the remaining 10% were reported by patients, families, or employees (current or former).
“Failures in communication, teamwork, and consistently following policies were leading causes for reported sentinel events,” the authors wrote. However, reporting sentinel events is voluntary; therefore “no conclusions should be drawn about the actual relative frequency of events or trends in events over time,” they noted.
Increased reporting may not reflect increased occurrence
“It is important to clarify that The Joint Commission saw an increase in reporting of sentinel events; whether this is indicative of an actual increase in occurrence of sentinel events across the country or not is difficult to say, as the reporting is voluntary,” said Haytham Kaafarani, MD, MPH, chief patient safety officer and medical director for The Joint Commission, in an interview.
“However, this is the highest number reported to The Joint Commission since the inception of the sentinel event policy: there were 547 health care organizations that reported sentinel events in 2022, compared to 500 in 2021 and 423 in 2020,” Dr. Kaafarani said. “Having said that, based on published literature, the COVID-19 pandemic stressed our health care systems in many ways including but not limited to staff shortage in times of increased needs, worsening of mental health conditions, and delay in presentation of non–COVID-related medical conditions during the pandemic,” he noted.
Dr. Kaafarani said that The Joint Commission was not surprised by the type of sentinel events reported, which has remained consistent with previous years.
However, The Joint Commission was surprised by the significant increase in the number of reported events, he said. “Since reporting is voluntarily, we welcome the increase in reporting of sentinel events, as it helps The Joint Commission better understand the patient safety landscape across the country, and better helps health care organizations during their difficult times.”
Based on the latest information, “The Joint Commission encourages health care organizations to create research that is focused on preventing patient falls in hospitals,” said Dr. Kaafarani. “With staff shortages reported within many health care organizations, it is now more essential than ever to establish systematic interventions to prevent patient falls and resultant harm.”
The review authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Should you recommend e-cigs to help patients quit smoking?
In 2014, after smoking cigarettes for 40 years, Kati Markowitz decided to switch to vaping. She had heard the newer electronic cigarettes might be less harmful. And, at the time, she said, she wasn’t aware of other options to try to quit smoking.
For 7 years, she vaped every day.
Then Ms. Markowitz received news she’d hoped never to hear: She had lung cancer. A nodule detected in a CT scan had grown. She was scheduled for treatment – the removal of an entire lobe from her right lung. But first, she said, her surgeon told her she had to quit vaping, which reduces the risk for post-operative complications and enables a healthy recovery.
Ms. Markowitz had thought switching to vaping would be less harmful than smoking cigarettes. Now, she no longer believes that’s true.
“Did I fool myself by hoping to get lucky and not have any bad repercussions? Yes, I did,” Ms. Markowitz said, adding that she wonders if vaping contributed to her lung cancer or if she’ll experience other negative health effects in the future.
Researchers are divided on if e-cigarettes are as effective in smoking cessation as other nicotine replacement therapies like gums and lozenges. They also say more research is needed on the long-term health impacts of vaping to ultimately determine if vapes are a safe replacement for cigarettes.
“There is scientific research to support vaping as a cessation tool, but we wouldn’t use it as a first line of defense because we still need longitudinal studies to understand the long-term risk of e-cigarettes,” said Monica Hanna, MPH, assistant director of the Nicotine and Tobacco Recovery Program at RWJBarnabas Health’s Institute for Prevention and Recovery, Eatontown, N.J. “We also need research to understand exactly how we could use e-cigarettes as a cessation device.”
Vaping to quit
The first prototypes of e-cigarettes were developed in the 1930s, although what are now known as vapes weren’t sold by manufacturers until the 2000s in the United States, following an invention by a former health official in China. The vape was touted by both researchers and manufacturers over the years of development as a way to quit smoking cigarettes.
The Consumer Advocates for Smoke-free Alternatives Association, a nonprofit group that supports vaping and accepts donations from the e-cigarette industry, has compiled more than 13,000 testimonials from people who say vaping helped them give up smoking.
Studies show mixed results that using vapes can help traditional smokers quit.
A November 2022 Cochrane review showed a “high certainty of evidence that people are more likely to stop smoking traditional cigarettes for at least 6 months using e-cigarettes, or ‘vapes,’ than using nicotine replacement therapies, such as patches and gums.” The meta-analysis examined 78 studies with more than 22,000 participants. And a 2019 study with 886 participants, published in the New England Journal Medicine, found smokers who tried vaping to quit were twice as likely after a year to have stopped smoking cigarettes than those who used nicotine replacement therapy.
“In terms of the global research, it’s pretty clear that vaping can help smokers quit,” said Peter Shields, MD, a professor in the department of internal medicine at The Ohio State University College of Medicine, Columbus, who specializes in the treatment of lung cancer.
But a 2013 study published in the Lancet, and another from the Lancet in 2019, found only a modest improvement in cessation outcomes when participants used e-cigarettes paired with patches, compared with patches alone.
“For a disruptive technology that was supposed to end combustible tobacco use, there seems very little large-scale disruption,” said Thomas Eissenberg, PhD, co-director of Virginia Commonwealth University’s Center for the Study of Tobacco Products, Richmond.
Michael Joseph Blaha, MD, MPH, director of clinical research at the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease, Baltimore, pointed to research that shows a portion of people who start vaping to quit smoking end up using both products – or become so-called “dual” users.
“I do think there is fairly high-quality evidence that vaping can lead to more cessation, but at the tradeoff of more long-term dual users and more overall nicotine addiction,” Dr. Blaha said. “Vaping remains a third-line clinical tool after nicotine replacement therapy and FDA-approved cessation medications.”
The U.S. Food and Drug Administration has not approved any e-cigarette or vaping device for smoking cessation, like it has for patches and gums, which means manufacturers cannot market their products as helping tobacco smokers quit.
“ Ms. Hanna, from RWJBarnabas Health’s Institute for Prevention and Recovery, said.
Reducing harm and improving health?
Vapes have also been touted as a boon to individual and public health since cigarette smoking is the leading cause of preventable disease and disability in the United States, responsible for more than 480,000 deaths per year in the U.S., according to the U.S. Centers for Disease Control and Prevention.
Quitting smoking lowers the risk of developing various cancers, heart disease, stroke, and other serious diseases. The aim of nicotine replacement therapy is to help smokers quit by gradually providing the body with smaller doses of nicotine over time, without exposing the body to toxic chemicals found in cigarettes.
“No one should say that e-cigarettes are safe, but compared to cigarettes, the data is consistent: They are not as harmful, and when a smoker switches, it’s better for them,” Dr. Shields said. “Like with other nicotine replacement therapies, if there is a risk that someone stops vaping and returns to smoking, I would rather have them as long-term vapers since it is generally considered to be less harmful than combustible tobacco.”
The FDA has allowed a handful of companies to market their electronic nicotine delivery systems as safer than traditional cigarettes by gaining approval through the Premarket Tobacco Product Applications process. In 2021, the agency announced its first PMTA authorization of an electronic cigarette to R.J. Reynolds for three of its tobacco-flavored vaping products. Regulators approved more products from three additional companies in 2022.
But the FDA has also denied others, including two products in 2023 from R.J. Reynolds, stating that, “the applications lacked sufficient evidence to demonstrate that permitting the marketing of the products would be appropriate for the protection of the public health.”
Questions remain among some researchers on the effects of vaping if used long term. Data on the health effects of vapes are just beginning to emerge and are mainly from studies of animals or cells. Measuring health effects among vape users will entail decades more of study, since Americans only gained access to the products in the 2000s.
Dr. Eissenberg said vaping likely does not cause the same diseases as cigarette smoking, but that does not mean they are not harmful. Ingredients found in e-cigarettes, such as heated propylene glycol, vegetable glycerin, and flavors, have only been used as food ingredients. The potential diseases caused by vapes are still unknown, because inhaling these heated ingredients is new. He also said he had “no issue” with an adult smoker vaping to help them quit smoking – as long they do so for a short period.
“I am very concerned that long-term use in adults could lead to considerable disease and death,” Dr. Eissenberg said. “Simply put, the human lung evolved for one purpose: gas exchange of oxygen in, carbon dioxide out. Anything else that enters the lung is a challenge to the organ.”
But Kenneth Warner, PhD, dean emeritus at the University of Michigan School of Public Health, Ann Arbor, said breaking the addiction to traditional cigarettes could reduce high rates of lung cancer in lower income communities where rates of smoking are comparatively high.
About three times as many Americans smoked (12.6%) than vaped (4.7%) in 2021, but those who live in households with lower incomes are more likely to smoke. According to the CDC, use of tobacco is higher among adults who were uninsured (27.3%) or who had Medicaid coverage (28.6%) than among those with private insurance (16.4%). People with annual family incomes of less than $12,500 also are more likely to be diagnosed with lung cancer than those with family incomes of $50,000 or more. Public health researchers have attributed those disparities in part to higher rates of smoking in lower-income households.
Dr. Warner said many lower-income and other Americans may never quit smoking cigarettes because they believe making the switch to e-cigarettes will not benefit their health. A 2022 study, published in the American Journal of Preventive Medicine, found that the percent of Americans who thought vaping was more harmful than smoking quadrupled between 2018 and 2020, from 6.8% to 28.3%. A third of respondents thought vaping was as harmful as smoking.
“We’ve convinced a large percentage of the American public that vaping is as harmful as smoking when it could be helping people quit smoking,” Dr. Warner said. “People are dying right now.”
Ms. Markowitz did quit smoking by taking up vaping. But now she questions if her lung cancer prognosis would have been delayed, or even avoided, if she’d tried a traditional method like a lozenge or gum instead. She vaped once an hour for most of her 7 years of using the devices.
“For people who are trying to stop smoking, I would recommend something like the patch instead,” Ms. Markowitz said.
The Consumer Advocates for Smoke-free Alternatives receives funding from the vaping industry. Dr. Blaha, Dr. Eissenberg, Ms. Hanna, Dr. Shields, and Dr. Warner reported no funding from the tobacco or e-cigarette industry. Dr. Blaha and Dr. Warner receive tobacco-related research funding from the FDA. Dr. Warner is a member of the FDA’s Tobacco Products Scientific Advisory Committee.
A version of this article first appeared on Medscape.com.
In 2014, after smoking cigarettes for 40 years, Kati Markowitz decided to switch to vaping. She had heard the newer electronic cigarettes might be less harmful. And, at the time, she said, she wasn’t aware of other options to try to quit smoking.
For 7 years, she vaped every day.
Then Ms. Markowitz received news she’d hoped never to hear: She had lung cancer. A nodule detected in a CT scan had grown. She was scheduled for treatment – the removal of an entire lobe from her right lung. But first, she said, her surgeon told her she had to quit vaping, which reduces the risk for post-operative complications and enables a healthy recovery.
Ms. Markowitz had thought switching to vaping would be less harmful than smoking cigarettes. Now, she no longer believes that’s true.
“Did I fool myself by hoping to get lucky and not have any bad repercussions? Yes, I did,” Ms. Markowitz said, adding that she wonders if vaping contributed to her lung cancer or if she’ll experience other negative health effects in the future.
Researchers are divided on if e-cigarettes are as effective in smoking cessation as other nicotine replacement therapies like gums and lozenges. They also say more research is needed on the long-term health impacts of vaping to ultimately determine if vapes are a safe replacement for cigarettes.
“There is scientific research to support vaping as a cessation tool, but we wouldn’t use it as a first line of defense because we still need longitudinal studies to understand the long-term risk of e-cigarettes,” said Monica Hanna, MPH, assistant director of the Nicotine and Tobacco Recovery Program at RWJBarnabas Health’s Institute for Prevention and Recovery, Eatontown, N.J. “We also need research to understand exactly how we could use e-cigarettes as a cessation device.”
Vaping to quit
The first prototypes of e-cigarettes were developed in the 1930s, although what are now known as vapes weren’t sold by manufacturers until the 2000s in the United States, following an invention by a former health official in China. The vape was touted by both researchers and manufacturers over the years of development as a way to quit smoking cigarettes.
The Consumer Advocates for Smoke-free Alternatives Association, a nonprofit group that supports vaping and accepts donations from the e-cigarette industry, has compiled more than 13,000 testimonials from people who say vaping helped them give up smoking.
Studies show mixed results that using vapes can help traditional smokers quit.
A November 2022 Cochrane review showed a “high certainty of evidence that people are more likely to stop smoking traditional cigarettes for at least 6 months using e-cigarettes, or ‘vapes,’ than using nicotine replacement therapies, such as patches and gums.” The meta-analysis examined 78 studies with more than 22,000 participants. And a 2019 study with 886 participants, published in the New England Journal Medicine, found smokers who tried vaping to quit were twice as likely after a year to have stopped smoking cigarettes than those who used nicotine replacement therapy.
“In terms of the global research, it’s pretty clear that vaping can help smokers quit,” said Peter Shields, MD, a professor in the department of internal medicine at The Ohio State University College of Medicine, Columbus, who specializes in the treatment of lung cancer.
But a 2013 study published in the Lancet, and another from the Lancet in 2019, found only a modest improvement in cessation outcomes when participants used e-cigarettes paired with patches, compared with patches alone.
“For a disruptive technology that was supposed to end combustible tobacco use, there seems very little large-scale disruption,” said Thomas Eissenberg, PhD, co-director of Virginia Commonwealth University’s Center for the Study of Tobacco Products, Richmond.
Michael Joseph Blaha, MD, MPH, director of clinical research at the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease, Baltimore, pointed to research that shows a portion of people who start vaping to quit smoking end up using both products – or become so-called “dual” users.
“I do think there is fairly high-quality evidence that vaping can lead to more cessation, but at the tradeoff of more long-term dual users and more overall nicotine addiction,” Dr. Blaha said. “Vaping remains a third-line clinical tool after nicotine replacement therapy and FDA-approved cessation medications.”
The U.S. Food and Drug Administration has not approved any e-cigarette or vaping device for smoking cessation, like it has for patches and gums, which means manufacturers cannot market their products as helping tobacco smokers quit.
“ Ms. Hanna, from RWJBarnabas Health’s Institute for Prevention and Recovery, said.
Reducing harm and improving health?
Vapes have also been touted as a boon to individual and public health since cigarette smoking is the leading cause of preventable disease and disability in the United States, responsible for more than 480,000 deaths per year in the U.S., according to the U.S. Centers for Disease Control and Prevention.
Quitting smoking lowers the risk of developing various cancers, heart disease, stroke, and other serious diseases. The aim of nicotine replacement therapy is to help smokers quit by gradually providing the body with smaller doses of nicotine over time, without exposing the body to toxic chemicals found in cigarettes.
“No one should say that e-cigarettes are safe, but compared to cigarettes, the data is consistent: They are not as harmful, and when a smoker switches, it’s better for them,” Dr. Shields said. “Like with other nicotine replacement therapies, if there is a risk that someone stops vaping and returns to smoking, I would rather have them as long-term vapers since it is generally considered to be less harmful than combustible tobacco.”
The FDA has allowed a handful of companies to market their electronic nicotine delivery systems as safer than traditional cigarettes by gaining approval through the Premarket Tobacco Product Applications process. In 2021, the agency announced its first PMTA authorization of an electronic cigarette to R.J. Reynolds for three of its tobacco-flavored vaping products. Regulators approved more products from three additional companies in 2022.
But the FDA has also denied others, including two products in 2023 from R.J. Reynolds, stating that, “the applications lacked sufficient evidence to demonstrate that permitting the marketing of the products would be appropriate for the protection of the public health.”
Questions remain among some researchers on the effects of vaping if used long term. Data on the health effects of vapes are just beginning to emerge and are mainly from studies of animals or cells. Measuring health effects among vape users will entail decades more of study, since Americans only gained access to the products in the 2000s.
Dr. Eissenberg said vaping likely does not cause the same diseases as cigarette smoking, but that does not mean they are not harmful. Ingredients found in e-cigarettes, such as heated propylene glycol, vegetable glycerin, and flavors, have only been used as food ingredients. The potential diseases caused by vapes are still unknown, because inhaling these heated ingredients is new. He also said he had “no issue” with an adult smoker vaping to help them quit smoking – as long they do so for a short period.
“I am very concerned that long-term use in adults could lead to considerable disease and death,” Dr. Eissenberg said. “Simply put, the human lung evolved for one purpose: gas exchange of oxygen in, carbon dioxide out. Anything else that enters the lung is a challenge to the organ.”
But Kenneth Warner, PhD, dean emeritus at the University of Michigan School of Public Health, Ann Arbor, said breaking the addiction to traditional cigarettes could reduce high rates of lung cancer in lower income communities where rates of smoking are comparatively high.
About three times as many Americans smoked (12.6%) than vaped (4.7%) in 2021, but those who live in households with lower incomes are more likely to smoke. According to the CDC, use of tobacco is higher among adults who were uninsured (27.3%) or who had Medicaid coverage (28.6%) than among those with private insurance (16.4%). People with annual family incomes of less than $12,500 also are more likely to be diagnosed with lung cancer than those with family incomes of $50,000 or more. Public health researchers have attributed those disparities in part to higher rates of smoking in lower-income households.
Dr. Warner said many lower-income and other Americans may never quit smoking cigarettes because they believe making the switch to e-cigarettes will not benefit their health. A 2022 study, published in the American Journal of Preventive Medicine, found that the percent of Americans who thought vaping was more harmful than smoking quadrupled between 2018 and 2020, from 6.8% to 28.3%. A third of respondents thought vaping was as harmful as smoking.
“We’ve convinced a large percentage of the American public that vaping is as harmful as smoking when it could be helping people quit smoking,” Dr. Warner said. “People are dying right now.”
Ms. Markowitz did quit smoking by taking up vaping. But now she questions if her lung cancer prognosis would have been delayed, or even avoided, if she’d tried a traditional method like a lozenge or gum instead. She vaped once an hour for most of her 7 years of using the devices.
“For people who are trying to stop smoking, I would recommend something like the patch instead,” Ms. Markowitz said.
The Consumer Advocates for Smoke-free Alternatives receives funding from the vaping industry. Dr. Blaha, Dr. Eissenberg, Ms. Hanna, Dr. Shields, and Dr. Warner reported no funding from the tobacco or e-cigarette industry. Dr. Blaha and Dr. Warner receive tobacco-related research funding from the FDA. Dr. Warner is a member of the FDA’s Tobacco Products Scientific Advisory Committee.
A version of this article first appeared on Medscape.com.
In 2014, after smoking cigarettes for 40 years, Kati Markowitz decided to switch to vaping. She had heard the newer electronic cigarettes might be less harmful. And, at the time, she said, she wasn’t aware of other options to try to quit smoking.
For 7 years, she vaped every day.
Then Ms. Markowitz received news she’d hoped never to hear: She had lung cancer. A nodule detected in a CT scan had grown. She was scheduled for treatment – the removal of an entire lobe from her right lung. But first, she said, her surgeon told her she had to quit vaping, which reduces the risk for post-operative complications and enables a healthy recovery.
Ms. Markowitz had thought switching to vaping would be less harmful than smoking cigarettes. Now, she no longer believes that’s true.
“Did I fool myself by hoping to get lucky and not have any bad repercussions? Yes, I did,” Ms. Markowitz said, adding that she wonders if vaping contributed to her lung cancer or if she’ll experience other negative health effects in the future.
Researchers are divided on if e-cigarettes are as effective in smoking cessation as other nicotine replacement therapies like gums and lozenges. They also say more research is needed on the long-term health impacts of vaping to ultimately determine if vapes are a safe replacement for cigarettes.
“There is scientific research to support vaping as a cessation tool, but we wouldn’t use it as a first line of defense because we still need longitudinal studies to understand the long-term risk of e-cigarettes,” said Monica Hanna, MPH, assistant director of the Nicotine and Tobacco Recovery Program at RWJBarnabas Health’s Institute for Prevention and Recovery, Eatontown, N.J. “We also need research to understand exactly how we could use e-cigarettes as a cessation device.”
Vaping to quit
The first prototypes of e-cigarettes were developed in the 1930s, although what are now known as vapes weren’t sold by manufacturers until the 2000s in the United States, following an invention by a former health official in China. The vape was touted by both researchers and manufacturers over the years of development as a way to quit smoking cigarettes.
The Consumer Advocates for Smoke-free Alternatives Association, a nonprofit group that supports vaping and accepts donations from the e-cigarette industry, has compiled more than 13,000 testimonials from people who say vaping helped them give up smoking.
Studies show mixed results that using vapes can help traditional smokers quit.
A November 2022 Cochrane review showed a “high certainty of evidence that people are more likely to stop smoking traditional cigarettes for at least 6 months using e-cigarettes, or ‘vapes,’ than using nicotine replacement therapies, such as patches and gums.” The meta-analysis examined 78 studies with more than 22,000 participants. And a 2019 study with 886 participants, published in the New England Journal Medicine, found smokers who tried vaping to quit were twice as likely after a year to have stopped smoking cigarettes than those who used nicotine replacement therapy.
“In terms of the global research, it’s pretty clear that vaping can help smokers quit,” said Peter Shields, MD, a professor in the department of internal medicine at The Ohio State University College of Medicine, Columbus, who specializes in the treatment of lung cancer.
But a 2013 study published in the Lancet, and another from the Lancet in 2019, found only a modest improvement in cessation outcomes when participants used e-cigarettes paired with patches, compared with patches alone.
“For a disruptive technology that was supposed to end combustible tobacco use, there seems very little large-scale disruption,” said Thomas Eissenberg, PhD, co-director of Virginia Commonwealth University’s Center for the Study of Tobacco Products, Richmond.
Michael Joseph Blaha, MD, MPH, director of clinical research at the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease, Baltimore, pointed to research that shows a portion of people who start vaping to quit smoking end up using both products – or become so-called “dual” users.
“I do think there is fairly high-quality evidence that vaping can lead to more cessation, but at the tradeoff of more long-term dual users and more overall nicotine addiction,” Dr. Blaha said. “Vaping remains a third-line clinical tool after nicotine replacement therapy and FDA-approved cessation medications.”
The U.S. Food and Drug Administration has not approved any e-cigarette or vaping device for smoking cessation, like it has for patches and gums, which means manufacturers cannot market their products as helping tobacco smokers quit.
“ Ms. Hanna, from RWJBarnabas Health’s Institute for Prevention and Recovery, said.
Reducing harm and improving health?
Vapes have also been touted as a boon to individual and public health since cigarette smoking is the leading cause of preventable disease and disability in the United States, responsible for more than 480,000 deaths per year in the U.S., according to the U.S. Centers for Disease Control and Prevention.
Quitting smoking lowers the risk of developing various cancers, heart disease, stroke, and other serious diseases. The aim of nicotine replacement therapy is to help smokers quit by gradually providing the body with smaller doses of nicotine over time, without exposing the body to toxic chemicals found in cigarettes.
“No one should say that e-cigarettes are safe, but compared to cigarettes, the data is consistent: They are not as harmful, and when a smoker switches, it’s better for them,” Dr. Shields said. “Like with other nicotine replacement therapies, if there is a risk that someone stops vaping and returns to smoking, I would rather have them as long-term vapers since it is generally considered to be less harmful than combustible tobacco.”
The FDA has allowed a handful of companies to market their electronic nicotine delivery systems as safer than traditional cigarettes by gaining approval through the Premarket Tobacco Product Applications process. In 2021, the agency announced its first PMTA authorization of an electronic cigarette to R.J. Reynolds for three of its tobacco-flavored vaping products. Regulators approved more products from three additional companies in 2022.
But the FDA has also denied others, including two products in 2023 from R.J. Reynolds, stating that, “the applications lacked sufficient evidence to demonstrate that permitting the marketing of the products would be appropriate for the protection of the public health.”
Questions remain among some researchers on the effects of vaping if used long term. Data on the health effects of vapes are just beginning to emerge and are mainly from studies of animals or cells. Measuring health effects among vape users will entail decades more of study, since Americans only gained access to the products in the 2000s.
Dr. Eissenberg said vaping likely does not cause the same diseases as cigarette smoking, but that does not mean they are not harmful. Ingredients found in e-cigarettes, such as heated propylene glycol, vegetable glycerin, and flavors, have only been used as food ingredients. The potential diseases caused by vapes are still unknown, because inhaling these heated ingredients is new. He also said he had “no issue” with an adult smoker vaping to help them quit smoking – as long they do so for a short period.
“I am very concerned that long-term use in adults could lead to considerable disease and death,” Dr. Eissenberg said. “Simply put, the human lung evolved for one purpose: gas exchange of oxygen in, carbon dioxide out. Anything else that enters the lung is a challenge to the organ.”
But Kenneth Warner, PhD, dean emeritus at the University of Michigan School of Public Health, Ann Arbor, said breaking the addiction to traditional cigarettes could reduce high rates of lung cancer in lower income communities where rates of smoking are comparatively high.
About three times as many Americans smoked (12.6%) than vaped (4.7%) in 2021, but those who live in households with lower incomes are more likely to smoke. According to the CDC, use of tobacco is higher among adults who were uninsured (27.3%) or who had Medicaid coverage (28.6%) than among those with private insurance (16.4%). People with annual family incomes of less than $12,500 also are more likely to be diagnosed with lung cancer than those with family incomes of $50,000 or more. Public health researchers have attributed those disparities in part to higher rates of smoking in lower-income households.
Dr. Warner said many lower-income and other Americans may never quit smoking cigarettes because they believe making the switch to e-cigarettes will not benefit their health. A 2022 study, published in the American Journal of Preventive Medicine, found that the percent of Americans who thought vaping was more harmful than smoking quadrupled between 2018 and 2020, from 6.8% to 28.3%. A third of respondents thought vaping was as harmful as smoking.
“We’ve convinced a large percentage of the American public that vaping is as harmful as smoking when it could be helping people quit smoking,” Dr. Warner said. “People are dying right now.”
Ms. Markowitz did quit smoking by taking up vaping. But now she questions if her lung cancer prognosis would have been delayed, or even avoided, if she’d tried a traditional method like a lozenge or gum instead. She vaped once an hour for most of her 7 years of using the devices.
“For people who are trying to stop smoking, I would recommend something like the patch instead,” Ms. Markowitz said.
The Consumer Advocates for Smoke-free Alternatives receives funding from the vaping industry. Dr. Blaha, Dr. Eissenberg, Ms. Hanna, Dr. Shields, and Dr. Warner reported no funding from the tobacco or e-cigarette industry. Dr. Blaha and Dr. Warner receive tobacco-related research funding from the FDA. Dr. Warner is a member of the FDA’s Tobacco Products Scientific Advisory Committee.
A version of this article first appeared on Medscape.com.
Previously unknown viral families hide in the darnedest places
You and me and baby makes 10,003
If you were a virus hunter, looking for your next big virus discovery, where would you go? The wholesale seafood market in Wuhan? A gathering of unmasked anti-vaxxers in the heartland of America? The frozen snot fields of northwest Siberia?
How about babies? Well, it’s too late now, because that’s what Dennis Sandris Nielsen, PhD, of the University of Copenhagen, and his associates did, and they hit the mother lode. Actually, it was more like the infant load, if we’re being honest here.
“We found an exceptional number of unknown viruses in the faeces of these babies,” Dr. Nielsen said in a written statement from the university. (The study was published in Nature Microbiology, so we get the English spelling of feces.)
The investigators mapped the gut “viromes” of 647 healthy Danish 1-year-old children over the course of 5 years and found 10,000 species of viruses distributed across 248 different viral families, of which only 16 were already known. Incredible stuff, but then things took a turn for the cute. “The researchers named the remaining 232 unknown viral families after the children whose diapers made the study possible. As a result, new viral families include names like Sylvesterviridae, Rigmorviridae and Tristanviridae,” the university said.
About 90% of the viruses found in the feces are bacterial viruses, aka bacteriophages, which have bacteria as their hosts and don’t attack the children’s cells, so they don’t cause disease. The other 10%, however, are eukaryotic: They use human cells as hosts, so they can be either friend or foe. “It is thought-provoking that all children run around with 10-20 of these virus types that infect human cells. So, there is a constant viral infection taking place, which apparently doesn’t make them sick,” Dr. Nielsen said.
Doesn’t make them sick? Riiiight. The thought that this gives rise to now? People love babies. Everyone wants to pick up the baby. Now we know why. Because the viruses want us to! Well, those cute little faces aren’t fooling us anymore. No more babies for us. Everyone should stay away from babies and their evil little eukaryotic viruses. STOP THE BABIES!
[Editor’s note: After a short timeout, we explained to the staff that the human species actually needs babies for its survival. They calmed down, picked up their crayons, and quietly went back to work.]
Fooled them. Stop the babies!
At least someone out there appreciates hospital food
Life in Alaska is not for the meek. It’s dark half the year. Summer is 3 weeks in July. And somehow, there’s a moose in line ahead of you at the doctor’s office. To make matters worse, it’s arguing about insurance. “What do you mean, you’ve heard the Moo Cross Moo Shield joke before?”
One might expect that Providence Alaska Health Park, located near downtown Anchorage, the largest city in Alaska by a massive margin, might be safe from ungulate invasion. Nope. In recent days, a young moose has taken to hanging around Providence campus, and it just could not find anything to eat. Remember, it may be early April, but this is Alaska. It’s still winter there. The ground’s still covered in snow.
Eventually, the gears in our young moose friend’s mind turned and it settled on a course of action: “Hey, those are some nice-looking plants behind that door over there. …” And that’s how Providence Alaska Health ended up with a moose munching on decorative potted plants in the hospital lobby.
Funnily enough, the moose didn’t even make a big scene. It just walked through the automatic doors and started chowing down. Security only found out because a tenant called them. Naturally though, once security made the announcement that a massive wild animal had been spotted in the building, the lobby was evacuated. … What do you mean, half the hospital came around to see it? Apparently, even though Alaskans have to fight moose herds on their daily commute, a lot of people wanted to see our moose friend do its thing.
“That’s crazy,” a woman in scrubs said in a video as she snapped a photo with her phone.
“This is the best. Like, what’s the code for this?” asked another bystander.
Despite security’s best efforts to shoo the moose out with barricades and offers of tasty branches, our furry friend left of its own volition, presumably irritated that his breakfast had become a spectator sport. But it didn’t go far. It hung around the front drive for a while, then went around the back of the building for a nap. What has four hooves and still doesn’t give a crap? Bob Moose-o! How you doing?
That click sounded stressed
How can people tell that you’re stressed? Maybe you get irritable and a little snappy. Some people have an inability to concentrate or focus. Eating that muffin when you weren’t really hungry could be a sign you’re not relaxed.
Did you know that your computer can be an indicator of your stress levels?
We tend to be working when we’re using computers, right? That can be a stressor in itself. Well, some researchers at ETH Zürich decided to have a look at the situation. Surprisingly, at least to us, one in three Swiss employees experience workplace stress, which makes us wonder what the percentage is in this country.
The Swiss researchers developed a model that tells how stressed someone is just by the way they use their computer mouse or type. The results of their study showed that those who were stressed clicked and tapped differently than participants who were more relaxed.
Stressed people click “more often and less precisely and cover longer distances on the screen,” while the relaxed take “shorter, more direct routes to reach their destination and take more time doing so,” study author Mara Nägelin explained in a written statement from ETH (Eidgenössische Technische Hochschule, or Swiss Federal Institute of Technology) Zürich.
Ever find when you’re frustrated and in a rush you end up making more mistakes? Same deal. Coauthor Jasmine Kerr noted that “increased levels of stress negatively impact our brain’s ability to process information.” Which totally is going to affect how we move.
Hopefully, these results can give insight to companies on how stressed their employees are and the effect it has on their work performance, eventually leading to, guess what, more research on how to alleviate workplace stress in general, which can benefit us all.
So if you find yourself in the office working on your computer like it’s a game of Perfection and time is running out, take a beat. Maybe try a stress-relieving breathing technique. Nonstressed people, according to the study, take fewer and longer pauses on their computers. Perfection on the job may mean relaxing first.
You and me and baby makes 10,003
If you were a virus hunter, looking for your next big virus discovery, where would you go? The wholesale seafood market in Wuhan? A gathering of unmasked anti-vaxxers in the heartland of America? The frozen snot fields of northwest Siberia?
How about babies? Well, it’s too late now, because that’s what Dennis Sandris Nielsen, PhD, of the University of Copenhagen, and his associates did, and they hit the mother lode. Actually, it was more like the infant load, if we’re being honest here.
“We found an exceptional number of unknown viruses in the faeces of these babies,” Dr. Nielsen said in a written statement from the university. (The study was published in Nature Microbiology, so we get the English spelling of feces.)
The investigators mapped the gut “viromes” of 647 healthy Danish 1-year-old children over the course of 5 years and found 10,000 species of viruses distributed across 248 different viral families, of which only 16 were already known. Incredible stuff, but then things took a turn for the cute. “The researchers named the remaining 232 unknown viral families after the children whose diapers made the study possible. As a result, new viral families include names like Sylvesterviridae, Rigmorviridae and Tristanviridae,” the university said.
About 90% of the viruses found in the feces are bacterial viruses, aka bacteriophages, which have bacteria as their hosts and don’t attack the children’s cells, so they don’t cause disease. The other 10%, however, are eukaryotic: They use human cells as hosts, so they can be either friend or foe. “It is thought-provoking that all children run around with 10-20 of these virus types that infect human cells. So, there is a constant viral infection taking place, which apparently doesn’t make them sick,” Dr. Nielsen said.
Doesn’t make them sick? Riiiight. The thought that this gives rise to now? People love babies. Everyone wants to pick up the baby. Now we know why. Because the viruses want us to! Well, those cute little faces aren’t fooling us anymore. No more babies for us. Everyone should stay away from babies and their evil little eukaryotic viruses. STOP THE BABIES!
[Editor’s note: After a short timeout, we explained to the staff that the human species actually needs babies for its survival. They calmed down, picked up their crayons, and quietly went back to work.]
Fooled them. Stop the babies!
At least someone out there appreciates hospital food
Life in Alaska is not for the meek. It’s dark half the year. Summer is 3 weeks in July. And somehow, there’s a moose in line ahead of you at the doctor’s office. To make matters worse, it’s arguing about insurance. “What do you mean, you’ve heard the Moo Cross Moo Shield joke before?”
One might expect that Providence Alaska Health Park, located near downtown Anchorage, the largest city in Alaska by a massive margin, might be safe from ungulate invasion. Nope. In recent days, a young moose has taken to hanging around Providence campus, and it just could not find anything to eat. Remember, it may be early April, but this is Alaska. It’s still winter there. The ground’s still covered in snow.
Eventually, the gears in our young moose friend’s mind turned and it settled on a course of action: “Hey, those are some nice-looking plants behind that door over there. …” And that’s how Providence Alaska Health ended up with a moose munching on decorative potted plants in the hospital lobby.
Funnily enough, the moose didn’t even make a big scene. It just walked through the automatic doors and started chowing down. Security only found out because a tenant called them. Naturally though, once security made the announcement that a massive wild animal had been spotted in the building, the lobby was evacuated. … What do you mean, half the hospital came around to see it? Apparently, even though Alaskans have to fight moose herds on their daily commute, a lot of people wanted to see our moose friend do its thing.
“That’s crazy,” a woman in scrubs said in a video as she snapped a photo with her phone.
“This is the best. Like, what’s the code for this?” asked another bystander.
Despite security’s best efforts to shoo the moose out with barricades and offers of tasty branches, our furry friend left of its own volition, presumably irritated that his breakfast had become a spectator sport. But it didn’t go far. It hung around the front drive for a while, then went around the back of the building for a nap. What has four hooves and still doesn’t give a crap? Bob Moose-o! How you doing?
That click sounded stressed
How can people tell that you’re stressed? Maybe you get irritable and a little snappy. Some people have an inability to concentrate or focus. Eating that muffin when you weren’t really hungry could be a sign you’re not relaxed.
Did you know that your computer can be an indicator of your stress levels?
We tend to be working when we’re using computers, right? That can be a stressor in itself. Well, some researchers at ETH Zürich decided to have a look at the situation. Surprisingly, at least to us, one in three Swiss employees experience workplace stress, which makes us wonder what the percentage is in this country.
The Swiss researchers developed a model that tells how stressed someone is just by the way they use their computer mouse or type. The results of their study showed that those who were stressed clicked and tapped differently than participants who were more relaxed.
Stressed people click “more often and less precisely and cover longer distances on the screen,” while the relaxed take “shorter, more direct routes to reach their destination and take more time doing so,” study author Mara Nägelin explained in a written statement from ETH (Eidgenössische Technische Hochschule, or Swiss Federal Institute of Technology) Zürich.
Ever find when you’re frustrated and in a rush you end up making more mistakes? Same deal. Coauthor Jasmine Kerr noted that “increased levels of stress negatively impact our brain’s ability to process information.” Which totally is going to affect how we move.
Hopefully, these results can give insight to companies on how stressed their employees are and the effect it has on their work performance, eventually leading to, guess what, more research on how to alleviate workplace stress in general, which can benefit us all.
So if you find yourself in the office working on your computer like it’s a game of Perfection and time is running out, take a beat. Maybe try a stress-relieving breathing technique. Nonstressed people, according to the study, take fewer and longer pauses on their computers. Perfection on the job may mean relaxing first.
You and me and baby makes 10,003
If you were a virus hunter, looking for your next big virus discovery, where would you go? The wholesale seafood market in Wuhan? A gathering of unmasked anti-vaxxers in the heartland of America? The frozen snot fields of northwest Siberia?
How about babies? Well, it’s too late now, because that’s what Dennis Sandris Nielsen, PhD, of the University of Copenhagen, and his associates did, and they hit the mother lode. Actually, it was more like the infant load, if we’re being honest here.
“We found an exceptional number of unknown viruses in the faeces of these babies,” Dr. Nielsen said in a written statement from the university. (The study was published in Nature Microbiology, so we get the English spelling of feces.)
The investigators mapped the gut “viromes” of 647 healthy Danish 1-year-old children over the course of 5 years and found 10,000 species of viruses distributed across 248 different viral families, of which only 16 were already known. Incredible stuff, but then things took a turn for the cute. “The researchers named the remaining 232 unknown viral families after the children whose diapers made the study possible. As a result, new viral families include names like Sylvesterviridae, Rigmorviridae and Tristanviridae,” the university said.
About 90% of the viruses found in the feces are bacterial viruses, aka bacteriophages, which have bacteria as their hosts and don’t attack the children’s cells, so they don’t cause disease. The other 10%, however, are eukaryotic: They use human cells as hosts, so they can be either friend or foe. “It is thought-provoking that all children run around with 10-20 of these virus types that infect human cells. So, there is a constant viral infection taking place, which apparently doesn’t make them sick,” Dr. Nielsen said.
Doesn’t make them sick? Riiiight. The thought that this gives rise to now? People love babies. Everyone wants to pick up the baby. Now we know why. Because the viruses want us to! Well, those cute little faces aren’t fooling us anymore. No more babies for us. Everyone should stay away from babies and their evil little eukaryotic viruses. STOP THE BABIES!
[Editor’s note: After a short timeout, we explained to the staff that the human species actually needs babies for its survival. They calmed down, picked up their crayons, and quietly went back to work.]
Fooled them. Stop the babies!
At least someone out there appreciates hospital food
Life in Alaska is not for the meek. It’s dark half the year. Summer is 3 weeks in July. And somehow, there’s a moose in line ahead of you at the doctor’s office. To make matters worse, it’s arguing about insurance. “What do you mean, you’ve heard the Moo Cross Moo Shield joke before?”
One might expect that Providence Alaska Health Park, located near downtown Anchorage, the largest city in Alaska by a massive margin, might be safe from ungulate invasion. Nope. In recent days, a young moose has taken to hanging around Providence campus, and it just could not find anything to eat. Remember, it may be early April, but this is Alaska. It’s still winter there. The ground’s still covered in snow.
Eventually, the gears in our young moose friend’s mind turned and it settled on a course of action: “Hey, those are some nice-looking plants behind that door over there. …” And that’s how Providence Alaska Health ended up with a moose munching on decorative potted plants in the hospital lobby.
Funnily enough, the moose didn’t even make a big scene. It just walked through the automatic doors and started chowing down. Security only found out because a tenant called them. Naturally though, once security made the announcement that a massive wild animal had been spotted in the building, the lobby was evacuated. … What do you mean, half the hospital came around to see it? Apparently, even though Alaskans have to fight moose herds on their daily commute, a lot of people wanted to see our moose friend do its thing.
“That’s crazy,” a woman in scrubs said in a video as she snapped a photo with her phone.
“This is the best. Like, what’s the code for this?” asked another bystander.
Despite security’s best efforts to shoo the moose out with barricades and offers of tasty branches, our furry friend left of its own volition, presumably irritated that his breakfast had become a spectator sport. But it didn’t go far. It hung around the front drive for a while, then went around the back of the building for a nap. What has four hooves and still doesn’t give a crap? Bob Moose-o! How you doing?
That click sounded stressed
How can people tell that you’re stressed? Maybe you get irritable and a little snappy. Some people have an inability to concentrate or focus. Eating that muffin when you weren’t really hungry could be a sign you’re not relaxed.
Did you know that your computer can be an indicator of your stress levels?
We tend to be working when we’re using computers, right? That can be a stressor in itself. Well, some researchers at ETH Zürich decided to have a look at the situation. Surprisingly, at least to us, one in three Swiss employees experience workplace stress, which makes us wonder what the percentage is in this country.
The Swiss researchers developed a model that tells how stressed someone is just by the way they use their computer mouse or type. The results of their study showed that those who were stressed clicked and tapped differently than participants who were more relaxed.
Stressed people click “more often and less precisely and cover longer distances on the screen,” while the relaxed take “shorter, more direct routes to reach their destination and take more time doing so,” study author Mara Nägelin explained in a written statement from ETH (Eidgenössische Technische Hochschule, or Swiss Federal Institute of Technology) Zürich.
Ever find when you’re frustrated and in a rush you end up making more mistakes? Same deal. Coauthor Jasmine Kerr noted that “increased levels of stress negatively impact our brain’s ability to process information.” Which totally is going to affect how we move.
Hopefully, these results can give insight to companies on how stressed their employees are and the effect it has on their work performance, eventually leading to, guess what, more research on how to alleviate workplace stress in general, which can benefit us all.
So if you find yourself in the office working on your computer like it’s a game of Perfection and time is running out, take a beat. Maybe try a stress-relieving breathing technique. Nonstressed people, according to the study, take fewer and longer pauses on their computers. Perfection on the job may mean relaxing first.