User login
For MD-IQ use only
Taking a global leap into GI technology
Sharmila Anandasabapathy, MD, knew she wanted to focus on endoscopy when she first started her career.
While leading an endoscopy unit in New York City, Dr. Anandasabapathy began developing endoscopic and imaging technologies for underresourced and underserved areas. These technologies eventually made their way into global clinical trials.
“We’ve gone to clinical trial in over 2,000 patients worldwide. When I made that jump into global GI, I was able to make that jump into global health in general,” said Dr. Anandasabapathy.
As vice president for global programs at Baylor College of Medicine in Houston, Dr. Anandasabapathy currently focuses on clinical and translational research.
“We’re looking at the development of new, low-cost devices for early cancer detection in GI globally. I oversee our global programs across the whole college, so it’s GI, it’s surgery, it’s anesthesia, it’s obstetrics, it’s everything.”
In an interview, Dr. Anandasabapathy discussed what attracted her to gastroenterology and why she always takes the time to smile at her patients.
Q: Why did you choose GI?
A: There’s two questions in there: Why I chose GI and why I chose endoscopy.
I chose GI because when I was in my internal medicine training, they seemed like the happiest people in the hospital. They liked what they did. You could make a meaningful impact even at 3 a.m. if you were coming in for a variceal bleed. Everybody seemed happy with their choice of specialty. I was ready to be an oncologist, and I ended up becoming a gastroenterologist.
I chose endoscopy because it was where I wanted to be when I woke up in the morning. I was happy there. I love the procedures; I love the hand-eye coordination. I liked the fact that these were relatively shorter procedures, that it was technology based, and there was infinite growth.
Q: Was there a time when you really helped a patient by doing that endoscopy, preventing Barrett’s esophagus or even cancer?
A: I can think of several times where we had early cancers and it was a question between endoscopic treatment or surgery. It was always discussed with the surgeons. We made the decision within a multidisciplinary group and with the patient, but we usually went with the endoscopic options and the patients have done great. We’ve given them a greater quality of life, and I think that’s really rewarding.
Q: What gives you the most joy in your day-to-day practice?
A: My patients. I work with Barrett’s esophagus patients, and they tend to be well informed about the research and the science. I’m lucky to have a patient population that is really interested and willing to participate in that. I also like my students, my junior faculty. I like teaching and the global application of teaching.
Q: What fears did you have to push past to get to where you are in your career?
A: That I would never become an independent researcher and do it alone. I was able to, over time. The ability to transition from being independent to teaching others and making them independent is a wonderful one.
Early on when I was doing GI, I remember looking at my division, and there were about 58 gastroenterologists and only 2 women. I thought at the time, “Well, can I do it? Is this a field that is conducive with being a woman and having a family?” It turned out that it is. Today, I’m really gratified to see that there are more women in GI than there ever were before.
Q: Have you ever received advice that you’ve ignored?A: Yes. Early in my training in internal medicine, I was told that I smiled too much and that my personality was such that patients and others would think I was too glib. Medicine was a serious business, and you shouldn’t be smiling. That’s not my personality – I’m not Eeyore. I think it’s served me well to be positive, and it’s served me well with patients to be smiling. Especially when you’re dealing with patients who have precancer or dysplasia and are scared – they want reassurance and they want a level of confidence. I’m glad I ignored that advice.
Q: What would be your advice to medical students?
A: Think about where you want to be when you wake up in the morning. If it’s either in a GI practice or doing GI research or doing endoscopy, then you should absolutely do it.
Lightning round
Cat person or dog person
Dog
Favorite sport
Tennis
What song do you have to sing along with when you hear it?
Dancing Queen
Favorite music genre
1980s pop
Favorite movie, show, or book
Wuthering Heights
Dr. Anandasabapathy is on LinkedIn and on Twitter at @anandasabapathy , @bcmglobalhealth , and @bcm_gihep .
Sharmila Anandasabapathy, MD, knew she wanted to focus on endoscopy when she first started her career.
While leading an endoscopy unit in New York City, Dr. Anandasabapathy began developing endoscopic and imaging technologies for underresourced and underserved areas. These technologies eventually made their way into global clinical trials.
“We’ve gone to clinical trial in over 2,000 patients worldwide. When I made that jump into global GI, I was able to make that jump into global health in general,” said Dr. Anandasabapathy.
As vice president for global programs at Baylor College of Medicine in Houston, Dr. Anandasabapathy currently focuses on clinical and translational research.
“We’re looking at the development of new, low-cost devices for early cancer detection in GI globally. I oversee our global programs across the whole college, so it’s GI, it’s surgery, it’s anesthesia, it’s obstetrics, it’s everything.”
In an interview, Dr. Anandasabapathy discussed what attracted her to gastroenterology and why she always takes the time to smile at her patients.
Q: Why did you choose GI?
A: There’s two questions in there: Why I chose GI and why I chose endoscopy.
I chose GI because when I was in my internal medicine training, they seemed like the happiest people in the hospital. They liked what they did. You could make a meaningful impact even at 3 a.m. if you were coming in for a variceal bleed. Everybody seemed happy with their choice of specialty. I was ready to be an oncologist, and I ended up becoming a gastroenterologist.
I chose endoscopy because it was where I wanted to be when I woke up in the morning. I was happy there. I love the procedures; I love the hand-eye coordination. I liked the fact that these were relatively shorter procedures, that it was technology based, and there was infinite growth.
Q: Was there a time when you really helped a patient by doing that endoscopy, preventing Barrett’s esophagus or even cancer?
A: I can think of several times where we had early cancers and it was a question between endoscopic treatment or surgery. It was always discussed with the surgeons. We made the decision within a multidisciplinary group and with the patient, but we usually went with the endoscopic options and the patients have done great. We’ve given them a greater quality of life, and I think that’s really rewarding.
Q: What gives you the most joy in your day-to-day practice?
A: My patients. I work with Barrett’s esophagus patients, and they tend to be well informed about the research and the science. I’m lucky to have a patient population that is really interested and willing to participate in that. I also like my students, my junior faculty. I like teaching and the global application of teaching.
Q: What fears did you have to push past to get to where you are in your career?
A: That I would never become an independent researcher and do it alone. I was able to, over time. The ability to transition from being independent to teaching others and making them independent is a wonderful one.
Early on when I was doing GI, I remember looking at my division, and there were about 58 gastroenterologists and only 2 women. I thought at the time, “Well, can I do it? Is this a field that is conducive with being a woman and having a family?” It turned out that it is. Today, I’m really gratified to see that there are more women in GI than there ever were before.
Q: Have you ever received advice that you’ve ignored?A: Yes. Early in my training in internal medicine, I was told that I smiled too much and that my personality was such that patients and others would think I was too glib. Medicine was a serious business, and you shouldn’t be smiling. That’s not my personality – I’m not Eeyore. I think it’s served me well to be positive, and it’s served me well with patients to be smiling. Especially when you’re dealing with patients who have precancer or dysplasia and are scared – they want reassurance and they want a level of confidence. I’m glad I ignored that advice.
Q: What would be your advice to medical students?
A: Think about where you want to be when you wake up in the morning. If it’s either in a GI practice or doing GI research or doing endoscopy, then you should absolutely do it.
Lightning round
Cat person or dog person
Dog
Favorite sport
Tennis
What song do you have to sing along with when you hear it?
Dancing Queen
Favorite music genre
1980s pop
Favorite movie, show, or book
Wuthering Heights
Dr. Anandasabapathy is on LinkedIn and on Twitter at @anandasabapathy , @bcmglobalhealth , and @bcm_gihep .
Sharmila Anandasabapathy, MD, knew she wanted to focus on endoscopy when she first started her career.
While leading an endoscopy unit in New York City, Dr. Anandasabapathy began developing endoscopic and imaging technologies for underresourced and underserved areas. These technologies eventually made their way into global clinical trials.
“We’ve gone to clinical trial in over 2,000 patients worldwide. When I made that jump into global GI, I was able to make that jump into global health in general,” said Dr. Anandasabapathy.
As vice president for global programs at Baylor College of Medicine in Houston, Dr. Anandasabapathy currently focuses on clinical and translational research.
“We’re looking at the development of new, low-cost devices for early cancer detection in GI globally. I oversee our global programs across the whole college, so it’s GI, it’s surgery, it’s anesthesia, it’s obstetrics, it’s everything.”
In an interview, Dr. Anandasabapathy discussed what attracted her to gastroenterology and why she always takes the time to smile at her patients.
Q: Why did you choose GI?
A: There’s two questions in there: Why I chose GI and why I chose endoscopy.
I chose GI because when I was in my internal medicine training, they seemed like the happiest people in the hospital. They liked what they did. You could make a meaningful impact even at 3 a.m. if you were coming in for a variceal bleed. Everybody seemed happy with their choice of specialty. I was ready to be an oncologist, and I ended up becoming a gastroenterologist.
I chose endoscopy because it was where I wanted to be when I woke up in the morning. I was happy there. I love the procedures; I love the hand-eye coordination. I liked the fact that these were relatively shorter procedures, that it was technology based, and there was infinite growth.
Q: Was there a time when you really helped a patient by doing that endoscopy, preventing Barrett’s esophagus or even cancer?
A: I can think of several times where we had early cancers and it was a question between endoscopic treatment or surgery. It was always discussed with the surgeons. We made the decision within a multidisciplinary group and with the patient, but we usually went with the endoscopic options and the patients have done great. We’ve given them a greater quality of life, and I think that’s really rewarding.
Q: What gives you the most joy in your day-to-day practice?
A: My patients. I work with Barrett’s esophagus patients, and they tend to be well informed about the research and the science. I’m lucky to have a patient population that is really interested and willing to participate in that. I also like my students, my junior faculty. I like teaching and the global application of teaching.
Q: What fears did you have to push past to get to where you are in your career?
A: That I would never become an independent researcher and do it alone. I was able to, over time. The ability to transition from being independent to teaching others and making them independent is a wonderful one.
Early on when I was doing GI, I remember looking at my division, and there were about 58 gastroenterologists and only 2 women. I thought at the time, “Well, can I do it? Is this a field that is conducive with being a woman and having a family?” It turned out that it is. Today, I’m really gratified to see that there are more women in GI than there ever were before.
Q: Have you ever received advice that you’ve ignored?A: Yes. Early in my training in internal medicine, I was told that I smiled too much and that my personality was such that patients and others would think I was too glib. Medicine was a serious business, and you shouldn’t be smiling. That’s not my personality – I’m not Eeyore. I think it’s served me well to be positive, and it’s served me well with patients to be smiling. Especially when you’re dealing with patients who have precancer or dysplasia and are scared – they want reassurance and they want a level of confidence. I’m glad I ignored that advice.
Q: What would be your advice to medical students?
A: Think about where you want to be when you wake up in the morning. If it’s either in a GI practice or doing GI research or doing endoscopy, then you should absolutely do it.
Lightning round
Cat person or dog person
Dog
Favorite sport
Tennis
What song do you have to sing along with when you hear it?
Dancing Queen
Favorite music genre
1980s pop
Favorite movie, show, or book
Wuthering Heights
Dr. Anandasabapathy is on LinkedIn and on Twitter at @anandasabapathy , @bcmglobalhealth , and @bcm_gihep .
News & Perspectives from Ob.Gyn. News
MASTER CLASS
Prepare for endometriosis excision surgery with a multidisciplinary approach
Iris Kerin Orbuch, MD
Director, Advanced Gynecologic Laparoscopy Center, Los Angeles and New York City.
Series introduction
Charles Miller, MD
Professor, Obstetrics and Gynecology, Department of Clinical Sciences, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois.
As I gained more interest and expertise in the treatment of endometriosis, I became aware of several articles concluding that if a woman sought treatment for chronic pelvic pain with an internist, the diagnosis would be irritable bowel syndrome (IBS); with a urologist, it would be interstitial cystitis; and with a gynecologist, endometriosis. Moreover, there is an increased propensity for IBS and IC in patients with endometriosis. There also is an increased risk of small intestine bacterial overgrowth (SIBO), as noted by our guest author for this latest installment of the Master Class in Gynecologic Surgery, Iris Orbuch, MD.
Like our guest author, I have also noted increased risk of pelvic floor myalgia. Dr. Orbuch clearly outlines why this occurs. In fact, we can now understand why many patients have multiple pelvic pain–inducing issues compounding their pain secondary to endometriosis and leading to remodeling of the central nervous system. Therefore, it certainly makes sense to follow Dr. Orbuch’s recommendation for a multidisciplinary pre- and postsurgical approach “to downregulate the pain generators.”
Dr. Orbuch is a minimally invasive gynecologic surgeon in Los Angeles who specializes in the treatment of patients diagnosed with endometriosis. Dr. Orbuch serves on the Board of Directors of the Foundation of the American Association of Gynecologic Laparoscopists and has served as the chair of the AAGL’s Special Interest Group on Endometriosis and Reproductive Surgery. She is the coauthor of the book “Beating Endo —How to Reclaim Your Life From Endometriosis” (New York: HarperCollins; 2019). The book is written for patients but addresses many issues discussed in this installment of the Master Class in Gynecologic Surgery.
https://www.mdedge.com/obgyn/master-class
GYNECOLOGIC ONCOLOGY CONSULT
The perils of CA-125 as a diagnostic tool in patients with adnexal masses
Katherine Tucker, MD
Assistant Professor of Gynecologic Oncology at the University of North Carolina at Chapel Hill.
CA-125, or cancer antigen 125, is an epitope (antigen) on the transmembrane glycoprotein MUC16, or mucin 16. This protein is expressed on the surface of tissue derived from embryonic coelomic and Müllerian epithelium including the reproductive tract. CA-125 is also expressed in other tissue such as the pleura, lungs, pericardium, intestines, and kidneys. MUC16 plays an important role in tumor proliferation, invasiveness, and cell motility.1 In patients with epithelial ovarian cancer (EOC), CA-125 may be found on the surface of ovarian cancer cells. It is shed in the bloodstream and can be quantified using a serum test.
There are a number of CA-125 assays in commercial use, and although none have been deemed to be clinically superior, there can be some differences between assays. It is important, if possible, to use the same assay when following serial CA-125 values. Most frequently, this will mean getting the test through the same laboratory.
https://www.mdedge.com/obgyn/gynecologic-oncology-consult
LATEST NEWS
Few women identify breast density as a breast cancer risk
Walter Alexander
A qualitative study of breast cancer screening–age women finds that few women identified breast density as a risk factor for breast cancer.
Most women did not feel confident they knew what actions could mitigate breast cancer risk, leading researchers to the conclusion that comprehensive education about breast cancer risks and prevention strategies is needed.
CDC recommends universal hepatitis B screening of adults
Adults should be tested for hepatitis B virus (HBV) at least once in their lifetime, according to updated guidelines from the Centers for Disease Control and Prevention.
This is the first update to HBV screening guidelines since 2008, the agency said.
“Risk-based testing alone has not identified most persons living with chronic HBV infection and is considered inefficient for providers to implement,” the authors write in the new guidance, published in the CDC’s Morbidity and Mortality Weekly Report. “Universal screening of adults for HBV infection is cost-effective, compared with risk-based screening and averts liver disease and death. Although a curative treatment is not yet available, early diagnosis and treatment of chronic HBV infections reduces the risk for cirrhosis, liver cancer, nd death.”
An estimated 580,000 to 2.4 million individuals are living with HBV infection in the United States, and two-thirds may be unaware they are infected, the agency said.
The virus spreads through contact with blood, semen, and other body fluids of an infected person.
The guidance now recommends using the triple panel (HBsAg, anti-HBs, total anti-HBc) for initial screening.
“It can help identify persons who have an active HBV infection and could be linked to care; have [a] resolved infection and might be susceptible to reactivation (for example, immunosuppressed persons); are susceptible and need vaccination; or are vaccinated,” the authors write.
Ectopic pregnancy risk and levonorgestrel-releasing IUD
Diana Swift
Researchers report that use of any levonorgestrel-releasing intrauterine system was associated with a significantly increased risk of ectopic pregnancy, compared with other hormonal contraceptives, in a study published in JAMA.
A national health database analysis headed by Amani Meaidi, MD, PhD, of the Danish Cancer Society Research Center, Cancer Surveillance and Pharmacoepidemiology, in Copenhagen, compared the 13.5-mg with the 19.5-mg and 52-mg dosages of levonorgestrel-releasing intrauterine systems (IUSs).
The hormone content in levonorgestrel-releasing IUSs must be high enough to maintain optimal contraceptive effect but sufficiently low to minimize progestin-related adverse events, Dr. Meaidi and colleagues noted; they advised using the middle dosage of 19.5 mg. All dosages are recommended for contraception, with the highest dosage also recommended for heavy menstrual bleeding.
“If 10,000 women using the hormonal IUD for 1 year were given the 19.5-mg hormonal IUD instead of the 13.5-mg hormonal IUD, around nine ectopic pregnancies would be avoided,” Dr. Meaidi said in an interview.
EPA seeks to limit ‘forever’ chemicals in U.S. drinking water
The Environmental Protection Agency is proposing a new rule that would greatly limit the concentration of endocrine-disrupting “forever” chemicals in drinking water.
The EPA on Tuesday announced the proposed National Primary Drinking Water Regulation (NPDWR) for six polyfluoroalkyl substances, more commonly known as PFAS, which are human-made chemicals used as oil and water repellents and coatings for common products including cookware, carpets, and textiles. Such substances are also widely used in cosmetics and food packaging.
The Endocrine Society, which represents more than 18,000 doctors who treat hormone disorders, says it fully supports the new EPA proposal. It explains that these substances, also known as endocrine-disrupting chemicals, “do not break down when they are released into the environment, and they continue to accumulate over time. They pose health dangers at incredibly low levels and have been linked to endocrine disorders such as cancer, thyroid disruption, and reproductive difficulties.”
https://www.mdedge.com /obgyn/latest-news
MASTER CLASS
Prepare for endometriosis excision surgery with a multidisciplinary approach
Iris Kerin Orbuch, MD
Director, Advanced Gynecologic Laparoscopy Center, Los Angeles and New York City.
Series introduction
Charles Miller, MD
Professor, Obstetrics and Gynecology, Department of Clinical Sciences, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois.
As I gained more interest and expertise in the treatment of endometriosis, I became aware of several articles concluding that if a woman sought treatment for chronic pelvic pain with an internist, the diagnosis would be irritable bowel syndrome (IBS); with a urologist, it would be interstitial cystitis; and with a gynecologist, endometriosis. Moreover, there is an increased propensity for IBS and IC in patients with endometriosis. There also is an increased risk of small intestine bacterial overgrowth (SIBO), as noted by our guest author for this latest installment of the Master Class in Gynecologic Surgery, Iris Orbuch, MD.
Like our guest author, I have also noted increased risk of pelvic floor myalgia. Dr. Orbuch clearly outlines why this occurs. In fact, we can now understand why many patients have multiple pelvic pain–inducing issues compounding their pain secondary to endometriosis and leading to remodeling of the central nervous system. Therefore, it certainly makes sense to follow Dr. Orbuch’s recommendation for a multidisciplinary pre- and postsurgical approach “to downregulate the pain generators.”
Dr. Orbuch is a minimally invasive gynecologic surgeon in Los Angeles who specializes in the treatment of patients diagnosed with endometriosis. Dr. Orbuch serves on the Board of Directors of the Foundation of the American Association of Gynecologic Laparoscopists and has served as the chair of the AAGL’s Special Interest Group on Endometriosis and Reproductive Surgery. She is the coauthor of the book “Beating Endo —How to Reclaim Your Life From Endometriosis” (New York: HarperCollins; 2019). The book is written for patients but addresses many issues discussed in this installment of the Master Class in Gynecologic Surgery.
https://www.mdedge.com/obgyn/master-class
GYNECOLOGIC ONCOLOGY CONSULT
The perils of CA-125 as a diagnostic tool in patients with adnexal masses
Katherine Tucker, MD
Assistant Professor of Gynecologic Oncology at the University of North Carolina at Chapel Hill.
CA-125, or cancer antigen 125, is an epitope (antigen) on the transmembrane glycoprotein MUC16, or mucin 16. This protein is expressed on the surface of tissue derived from embryonic coelomic and Müllerian epithelium including the reproductive tract. CA-125 is also expressed in other tissue such as the pleura, lungs, pericardium, intestines, and kidneys. MUC16 plays an important role in tumor proliferation, invasiveness, and cell motility.1 In patients with epithelial ovarian cancer (EOC), CA-125 may be found on the surface of ovarian cancer cells. It is shed in the bloodstream and can be quantified using a serum test.
There are a number of CA-125 assays in commercial use, and although none have been deemed to be clinically superior, there can be some differences between assays. It is important, if possible, to use the same assay when following serial CA-125 values. Most frequently, this will mean getting the test through the same laboratory.
https://www.mdedge.com/obgyn/gynecologic-oncology-consult
LATEST NEWS
Few women identify breast density as a breast cancer risk
Walter Alexander
A qualitative study of breast cancer screening–age women finds that few women identified breast density as a risk factor for breast cancer.
Most women did not feel confident they knew what actions could mitigate breast cancer risk, leading researchers to the conclusion that comprehensive education about breast cancer risks and prevention strategies is needed.
CDC recommends universal hepatitis B screening of adults
Adults should be tested for hepatitis B virus (HBV) at least once in their lifetime, according to updated guidelines from the Centers for Disease Control and Prevention.
This is the first update to HBV screening guidelines since 2008, the agency said.
“Risk-based testing alone has not identified most persons living with chronic HBV infection and is considered inefficient for providers to implement,” the authors write in the new guidance, published in the CDC’s Morbidity and Mortality Weekly Report. “Universal screening of adults for HBV infection is cost-effective, compared with risk-based screening and averts liver disease and death. Although a curative treatment is not yet available, early diagnosis and treatment of chronic HBV infections reduces the risk for cirrhosis, liver cancer, nd death.”
An estimated 580,000 to 2.4 million individuals are living with HBV infection in the United States, and two-thirds may be unaware they are infected, the agency said.
The virus spreads through contact with blood, semen, and other body fluids of an infected person.
The guidance now recommends using the triple panel (HBsAg, anti-HBs, total anti-HBc) for initial screening.
“It can help identify persons who have an active HBV infection and could be linked to care; have [a] resolved infection and might be susceptible to reactivation (for example, immunosuppressed persons); are susceptible and need vaccination; or are vaccinated,” the authors write.
Ectopic pregnancy risk and levonorgestrel-releasing IUD
Diana Swift
Researchers report that use of any levonorgestrel-releasing intrauterine system was associated with a significantly increased risk of ectopic pregnancy, compared with other hormonal contraceptives, in a study published in JAMA.
A national health database analysis headed by Amani Meaidi, MD, PhD, of the Danish Cancer Society Research Center, Cancer Surveillance and Pharmacoepidemiology, in Copenhagen, compared the 13.5-mg with the 19.5-mg and 52-mg dosages of levonorgestrel-releasing intrauterine systems (IUSs).
The hormone content in levonorgestrel-releasing IUSs must be high enough to maintain optimal contraceptive effect but sufficiently low to minimize progestin-related adverse events, Dr. Meaidi and colleagues noted; they advised using the middle dosage of 19.5 mg. All dosages are recommended for contraception, with the highest dosage also recommended for heavy menstrual bleeding.
“If 10,000 women using the hormonal IUD for 1 year were given the 19.5-mg hormonal IUD instead of the 13.5-mg hormonal IUD, around nine ectopic pregnancies would be avoided,” Dr. Meaidi said in an interview.
EPA seeks to limit ‘forever’ chemicals in U.S. drinking water
The Environmental Protection Agency is proposing a new rule that would greatly limit the concentration of endocrine-disrupting “forever” chemicals in drinking water.
The EPA on Tuesday announced the proposed National Primary Drinking Water Regulation (NPDWR) for six polyfluoroalkyl substances, more commonly known as PFAS, which are human-made chemicals used as oil and water repellents and coatings for common products including cookware, carpets, and textiles. Such substances are also widely used in cosmetics and food packaging.
The Endocrine Society, which represents more than 18,000 doctors who treat hormone disorders, says it fully supports the new EPA proposal. It explains that these substances, also known as endocrine-disrupting chemicals, “do not break down when they are released into the environment, and they continue to accumulate over time. They pose health dangers at incredibly low levels and have been linked to endocrine disorders such as cancer, thyroid disruption, and reproductive difficulties.”
https://www.mdedge.com /obgyn/latest-news
MASTER CLASS
Prepare for endometriosis excision surgery with a multidisciplinary approach
Iris Kerin Orbuch, MD
Director, Advanced Gynecologic Laparoscopy Center, Los Angeles and New York City.
Series introduction
Charles Miller, MD
Professor, Obstetrics and Gynecology, Department of Clinical Sciences, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois.
As I gained more interest and expertise in the treatment of endometriosis, I became aware of several articles concluding that if a woman sought treatment for chronic pelvic pain with an internist, the diagnosis would be irritable bowel syndrome (IBS); with a urologist, it would be interstitial cystitis; and with a gynecologist, endometriosis. Moreover, there is an increased propensity for IBS and IC in patients with endometriosis. There also is an increased risk of small intestine bacterial overgrowth (SIBO), as noted by our guest author for this latest installment of the Master Class in Gynecologic Surgery, Iris Orbuch, MD.
Like our guest author, I have also noted increased risk of pelvic floor myalgia. Dr. Orbuch clearly outlines why this occurs. In fact, we can now understand why many patients have multiple pelvic pain–inducing issues compounding their pain secondary to endometriosis and leading to remodeling of the central nervous system. Therefore, it certainly makes sense to follow Dr. Orbuch’s recommendation for a multidisciplinary pre- and postsurgical approach “to downregulate the pain generators.”
Dr. Orbuch is a minimally invasive gynecologic surgeon in Los Angeles who specializes in the treatment of patients diagnosed with endometriosis. Dr. Orbuch serves on the Board of Directors of the Foundation of the American Association of Gynecologic Laparoscopists and has served as the chair of the AAGL’s Special Interest Group on Endometriosis and Reproductive Surgery. She is the coauthor of the book “Beating Endo —How to Reclaim Your Life From Endometriosis” (New York: HarperCollins; 2019). The book is written for patients but addresses many issues discussed in this installment of the Master Class in Gynecologic Surgery.
https://www.mdedge.com/obgyn/master-class
GYNECOLOGIC ONCOLOGY CONSULT
The perils of CA-125 as a diagnostic tool in patients with adnexal masses
Katherine Tucker, MD
Assistant Professor of Gynecologic Oncology at the University of North Carolina at Chapel Hill.
CA-125, or cancer antigen 125, is an epitope (antigen) on the transmembrane glycoprotein MUC16, or mucin 16. This protein is expressed on the surface of tissue derived from embryonic coelomic and Müllerian epithelium including the reproductive tract. CA-125 is also expressed in other tissue such as the pleura, lungs, pericardium, intestines, and kidneys. MUC16 plays an important role in tumor proliferation, invasiveness, and cell motility.1 In patients with epithelial ovarian cancer (EOC), CA-125 may be found on the surface of ovarian cancer cells. It is shed in the bloodstream and can be quantified using a serum test.
There are a number of CA-125 assays in commercial use, and although none have been deemed to be clinically superior, there can be some differences between assays. It is important, if possible, to use the same assay when following serial CA-125 values. Most frequently, this will mean getting the test through the same laboratory.
https://www.mdedge.com/obgyn/gynecologic-oncology-consult
LATEST NEWS
Few women identify breast density as a breast cancer risk
Walter Alexander
A qualitative study of breast cancer screening–age women finds that few women identified breast density as a risk factor for breast cancer.
Most women did not feel confident they knew what actions could mitigate breast cancer risk, leading researchers to the conclusion that comprehensive education about breast cancer risks and prevention strategies is needed.
CDC recommends universal hepatitis B screening of adults
Adults should be tested for hepatitis B virus (HBV) at least once in their lifetime, according to updated guidelines from the Centers for Disease Control and Prevention.
This is the first update to HBV screening guidelines since 2008, the agency said.
“Risk-based testing alone has not identified most persons living with chronic HBV infection and is considered inefficient for providers to implement,” the authors write in the new guidance, published in the CDC’s Morbidity and Mortality Weekly Report. “Universal screening of adults for HBV infection is cost-effective, compared with risk-based screening and averts liver disease and death. Although a curative treatment is not yet available, early diagnosis and treatment of chronic HBV infections reduces the risk for cirrhosis, liver cancer, nd death.”
An estimated 580,000 to 2.4 million individuals are living with HBV infection in the United States, and two-thirds may be unaware they are infected, the agency said.
The virus spreads through contact with blood, semen, and other body fluids of an infected person.
The guidance now recommends using the triple panel (HBsAg, anti-HBs, total anti-HBc) for initial screening.
“It can help identify persons who have an active HBV infection and could be linked to care; have [a] resolved infection and might be susceptible to reactivation (for example, immunosuppressed persons); are susceptible and need vaccination; or are vaccinated,” the authors write.
Ectopic pregnancy risk and levonorgestrel-releasing IUD
Diana Swift
Researchers report that use of any levonorgestrel-releasing intrauterine system was associated with a significantly increased risk of ectopic pregnancy, compared with other hormonal contraceptives, in a study published in JAMA.
A national health database analysis headed by Amani Meaidi, MD, PhD, of the Danish Cancer Society Research Center, Cancer Surveillance and Pharmacoepidemiology, in Copenhagen, compared the 13.5-mg with the 19.5-mg and 52-mg dosages of levonorgestrel-releasing intrauterine systems (IUSs).
The hormone content in levonorgestrel-releasing IUSs must be high enough to maintain optimal contraceptive effect but sufficiently low to minimize progestin-related adverse events, Dr. Meaidi and colleagues noted; they advised using the middle dosage of 19.5 mg. All dosages are recommended for contraception, with the highest dosage also recommended for heavy menstrual bleeding.
“If 10,000 women using the hormonal IUD for 1 year were given the 19.5-mg hormonal IUD instead of the 13.5-mg hormonal IUD, around nine ectopic pregnancies would be avoided,” Dr. Meaidi said in an interview.
EPA seeks to limit ‘forever’ chemicals in U.S. drinking water
The Environmental Protection Agency is proposing a new rule that would greatly limit the concentration of endocrine-disrupting “forever” chemicals in drinking water.
The EPA on Tuesday announced the proposed National Primary Drinking Water Regulation (NPDWR) for six polyfluoroalkyl substances, more commonly known as PFAS, which are human-made chemicals used as oil and water repellents and coatings for common products including cookware, carpets, and textiles. Such substances are also widely used in cosmetics and food packaging.
The Endocrine Society, which represents more than 18,000 doctors who treat hormone disorders, says it fully supports the new EPA proposal. It explains that these substances, also known as endocrine-disrupting chemicals, “do not break down when they are released into the environment, and they continue to accumulate over time. They pose health dangers at incredibly low levels and have been linked to endocrine disorders such as cancer, thyroid disruption, and reproductive difficulties.”
https://www.mdedge.com /obgyn/latest-news
ObGyn’s steady progress toward going green in the OR—but gaps persist
Have you ever looked at the operating room (OR) trash bin at the end of a case and wondered if all that waste is necessary? Since I started my residency, not a day goes by that I have not asked myself this question.
In the mid-1990s, John Elkington introduced the concept of the triple bottom line—that is, people, planet, and profit—for implementation and measurement of sustainability in businesses.1 The health care sector is no exception when it comes to the bottom line! However, “people” remain the priority. What is our role, as ObGyns, in protecting the “planet” while keeping the “people” safe?
According to the World Health Organization (WHO), climate change remains the single biggest health threat to humanity.2 The health care system is both the victim and the culprit. Studies suggest that the health care system, second to the food industry, is the biggest contributor to waste production in the United States. This sector generates more than 6,000 metric tons of waste each day and nearly 4 million tons (3.6 million metric tons) of solid waste each year.3 The health care system is responsible for an estimated 8% to 10% of total greenhouse gas emissions in the United States; the US health care system alone contributes to more than one-fourth of the global health care carbon footprint. If it were a country, the US health care system would rank 13th among all countries in emissions.4In turn, pollution produced by the health sector negatively impacts population health, further burdening the health care system. According to 2013 study data, the annual health damage caused by health care pollution was comparable to that of the deaths caused by preventable medical error.4
Aside from the environmental aspects, hospital waste disposal is expensive; reducing this cost is a potential area of interest for institutions.
As ObGyns, what is our role in reducing our waste generation and carbon footprint while keeping patients safe?
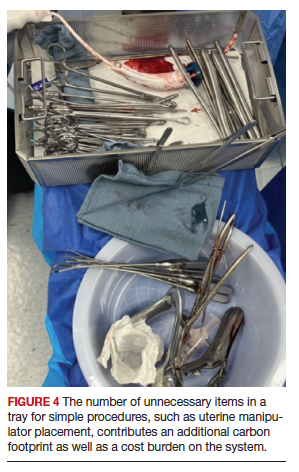
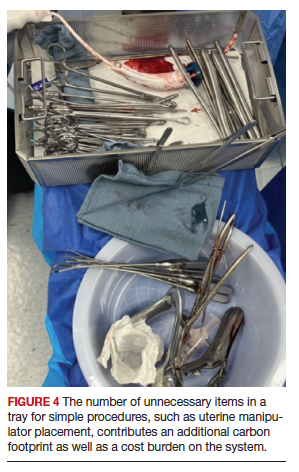
Defining health care waste, and disposal considerations
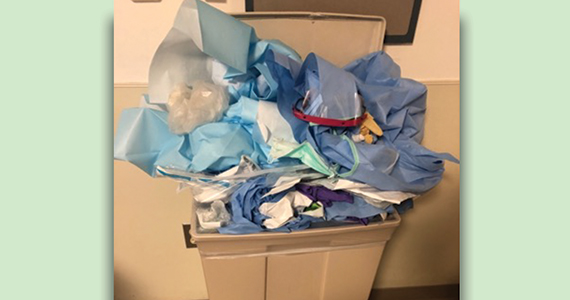
The WHO defines health care waste as including “the waste generated by health-care establishments, research facilities, and laboratories” as well as waste from scattered sources such as home dialysis and insulin injections.5 Despite representing a relatively small physical area of hospitals, labor and delivery units combined with ORs account for approximately 70% of all hospital waste.3 Operating room waste consists of disposable surgical supplies, personal protective equipment, drapes, plastic wrappers, sterile blue wraps, glass, cardboard, packaging material, medications, fluids, and other materials (FIGURE 1).
The WHO also notes that of all the waste generated by health care activities, about 85% is general, nonhazardous waste that is comparable to domestic waste.6 Hazardous waste is any material that poses a health risk, including potentially infectious materials, such as blood-soaked gauze, sharps, pharmaceuticals, or radioactive materials.6
Disposal of hazardous waste is expensiveand energy consuming as it is typically incinerated rather than disposed of in a landfill. This process produces substantial greenhouse gases, about 3 kg of carbon dioxide for every 1 kg of hazardous waste.7
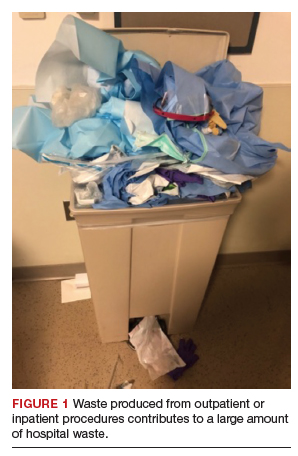
Red bags are used for hazardous waste disposal, while clear bags are used for general waste. Operating rooms produce about two-thirds of the hospital red-bag waste.8 Waste segregation unfortunately is not accurate, and as much as 90% of OR general waste is improperly designated as hazardous waste.3 Drapes and uncontaminated, needleless syringes, for example, should be disposed of in clear bags, but often they are instead directed to the red-bag and sharps container (FIGURE 2).
Obstetrics and gynecology has an important role to play in accurate waste segregation given the specialty’s frequent interaction with bodily fluids. Clinicians and other staff need to recognize and appropriately separate hazardous waste from general waste. For instance, not all fabrics involved in a case should be disposed of in the red bin, only those saturated with blood or body fluids. Educating health care staff and placing instruction posters on the red trash bins potentially could aid in accurate waste segregation and reduce regulated waste while decreasing disposal costs.
Recycling in the OR
Recycling has become an established practice in many health care facilities and ORs. Studies suggest that introducing recycling programs in ORs not only reduces carbon footprints but also reduces costs.3 One study reported that US academic medical centers consume 2 million lb ($15 million) each year of recoverable medical supplies.9
Single-stream recycling, a system in which all recyclable material—including plastics, paper, metal, and glass—are placed in a single bin without segregation at the collection site, has gained in popularity. Recycling can be implemented both in ORs and in other perioperative areas where regular trash bins are located.
In a study done at Oxford University Hospitals in the United Kingdom, introducing recycling bins in every OR, as well as in recovery and staff rest areas, helped improve waste segregation such that approximately 22% of OR waste was recycled.10 Studies show that recycling programs not only decrease the health care carbon footprint but also have a considerable financial impact. Albert and colleagues demonstrated that introducing a single-stream recycling program to a 9-OR day (or ambulatory) surgery center could redirect more than 4 tons of waste each month and saved thousands of dollars.11
Despite continued improvement in recycling programs, the segregation process is still far from optimal. In a survey done at the Mayo Clinic by Azouz and colleagues, more than half of the staff reported being unclear about which OR items are recyclable and nearly half reported that lack of knowledge was the barrier to proper recycling.12 That study also showed that after implementation of a recycling education program, costs decreased 10% relative to the same time period in prior years.12
Blue wraps. One example of recycling optimization is blue wraps, the polypropylene (No. 5 plastic) material used for wrapping surgical instruments. Blue wraps account for approximately 19% of OR waste and 5% of all hospital waste.11 Blue wraps are not biodegradable and also are not widely recycled. In recent years, a resale market has emerged for blue wraps, as they can be used for production of other No. 5 plastic items.9 By reselling blue wraps, revenue can be generated by recycling a necessary packing material that would otherwise require payment for disposal.
Sterility considerations. While recycling in ORs may raise concern due to the absolute sterility required in procedural settings, technologic developments have been promising in advancing safe recycling to reduce carbon footprints and health care costs without compromising patients’ safety. Segregation of waste from recyclable packaging material prior to the case, as well as directing trash to the correct bin (regular vs red bin), is one example. Moreover, because about 80% of all OR waste is generated during the set up before the patient arrives in the OR, it is not contaminated and can be safely recycled.13
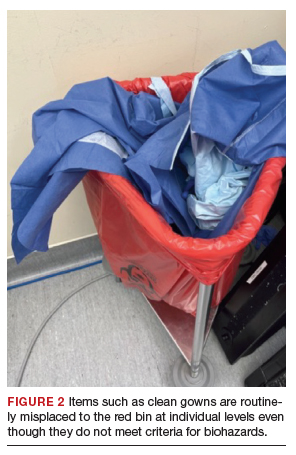
Continue to: Packaging material...
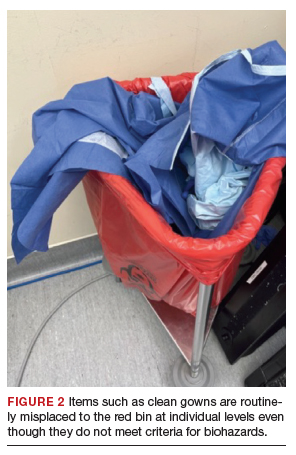
Packaging material
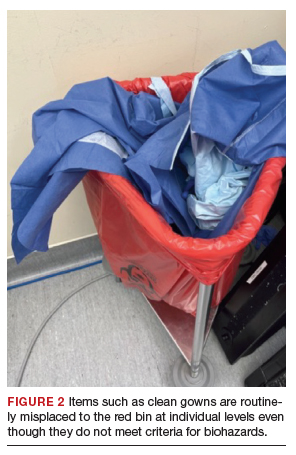
A substantial part of OR waste consists of packaging material; of all OR waste, 26% consists of plastics and 7%, paper and cartons.14 Increasing use of disposable or “single use” medical products in ORs, along with the intention to safeguard sterility, contributes significantly to the generation of medical waste in operating units. Containers, wraps and overwraps, cardboard, and plastic packaging are all composed of materials that when clean, can be recycled; however, these items often end up in the landfill (FIGURE 3).
Although the segregation of packaging material to recycling versus regular trash versus red bin is of paramount importance, packaging design plays a significant role as well. In 2018, Boston Scientific introduced a new packaging design for ureteral stents that reduced plastic use in packaging by 120,000 lb each year.15 Despite the advances in the medical packaging industry to increase sustainability while safeguarding sterility for medical devices, there is still room for innovation in this area.
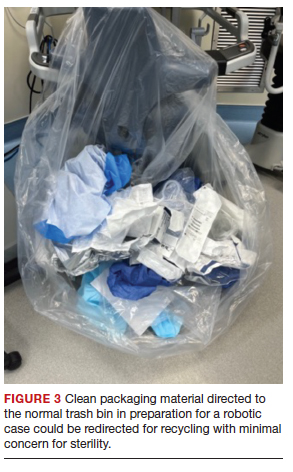
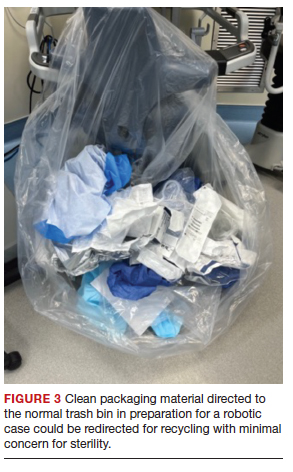
Reducing overage by judicious selection of surgical devices, instruments, and supplies
Overage is the term used to describe surgical inventory that is opened and prepared for surgery but ultimately not used and therefore discarded. Design of surgical carts and instrument and supply selection requires direct input from ObGyns. Opening only the needed instruments while ensuring ready availability of potentially needed supplies can significantly reduce OR waste generation as well as decrease chemical pollution generated by instrument sterilization. Decreasing OR overage reduces overall costs as well (FIGURE 4).
In a pilot study at the University of Massachusetts, Albert and colleagues examined the sets of disposable items and instruments designated for common plastic and hand surgery procedures.11 They identified the supplies and instruments that are routinely opened and wasted, based on surgeons’ interview responses, and redesigned the sets. Fifteen items were removed from disposable plastic surgery packs and 7 items from hand surgery packs. The authors reported saving thousands of dollars per year with these changes alone, as well as reducing waste.11 This same concept easily could be implemented in obstetrics and gynecology. We must ask ourselves: Do we always need, for example, a complete dilation and curettage kit to place the uterine manipulator prior to a minimally invasive hysterectomy?
In another pilot study, Greenberg and colleagues investigated whether cesarean deliveries consistently could be performed in a safe manner with only 20 instruments in the surgical kit.16 Obstetricians rated the 20-instrument kit an 8.7 out of 10 for performing cesarean deliveries safely.16
In addition to instrument selection, surgeons have a role in other supply use and waste generation: for instance, opening multiple pairs of surgical gloves and surgical gowns in advance when most of them will not be used during the case. Furthermore, many ObGyn surgeons routinely change gloves or even gowns during gynecologic procedures when they go back and forth between the vaginal and abdominal fields. Is the perineum “dirty” after application of a surgical prep solution?
In an observational study, Shockley and colleagues investigated the type and quantity of bacteria found intraoperatively on the abdomen, vagina, surgical gloves, instrument tips, and uterus at distinct time points during total laparoscopic hysterectomy.17 They showed that in 98.9% of cultures, the overall bacterial concentrations did not exceed the threshold for infection. There was no bacterial growth from vaginal cultures, and the only samples with some bacterial growth belonged to the surgeon’s gloves after specimen extraction; about one-third of samples showed growth after specimen extraction, but only 1 sample had a bacterial load above the infectious threshold of 5,000 colony-forming units per mL. The authors therefore suggested that if a surgeon changes gloves, doing so after specimen extraction and before turning attention back to the abdomen for vaginal cuff closure may be most effective in reducing bacterial load.17
Surgical site infection contributes to medical cost and likely medical waste as well. For example, surgical site infection may require prolonged treatments, tests, and medical instruments. In severe cases with abscesses, treatment entails hospitalization with prolonged antibiotic therapy with or without procedures to drain the collections. Further research therefore is warranted to investigate safe and environmentally friendly practices.
Myriad products are introduced to the medical system each day, some of which replace conventional tools. For instance, low-density polyethylene, or LDPE, transfer sheet is advertised for lateral patient transfer from the OR table to the bed or stretcher. This No. 4–coded plastic, while recyclable, is routinely discarded as trash in ORs. One ergonomic study found that reusable slide boards are as effective for reducing friction and staff muscle activities and are noninferior to the plastic sheets.18
Steps to making an impact
Operating rooms and labor and delivery units are responsible for a large proportion of hospital waste, and therefore they are of paramount importance in reducing waste and carbon footprint at the individual and institutional level. Reduction of OR waste not only is environmentally conscious but also decreases cost. Steps as small as individual practices to as big as changing infrastructures can make an impact. For instance:
- redesigning surgical carts
- reformulating surgeon-specific supply lists
- raising awareness about surgical overage
- encouraging recycling through education and audit
- optimizing surgical waste segregation through educational posters.
These are all simple steps that could significantly reduce waste and carbon footprint.
Bottom line
Although waste reduction is the responsibility of all health care providers, as leaders in their workplace physicians can serve as role models by implementing “green” practices in procedural units. Raising awareness and using a team approach is critical to succeed in our endeavors to move toward an environmentally friendly future. ●
- Elkington J. Towards the sustainable corporation: win-winwin business strategies for sustainable development. Calif Manage Rev. 1994;36:90-100.
- Climate change and health. October 30, 2021. World Health Organization. Accessed October 10, 2022. https://www.who .int/news-room/fact-sheets/detail/climate-change-and -health
- Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg. 2011;146:131-136.
- Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PloS One. 2016;11:e0157014.
- Pruss A, Giroult E, Rushbrook P. Safe management of wastes from health-care activities. World Health Organization; 1999.
- Health-care waste. February 8, 2018. World Health Organization. Accessed October 4, 2022. https://www.who. int/news-room/fact-sheets/detail/health-care-waste2
- Southorn T, Norrish AR, Gardner K, et al. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J Perioper Pract. 2013;23:144-146.
- Greening the OR. Practice Greenhealth. Accessed October 24, 2022. https://practicegreenhealth.org/topics/greening -operating-room/greening-or
- Babu MA, Dalenberg AK, Goodsell G, et al. Greening the operating room: results of a scalable initiative to reduce waste and recover supply costs. Neurosurgery. 2019;85:432-437.
- Oxford University Hospitals NHS Trust. Introducing recycling into the operating theatres. Mapping Greener Healthcare. Accessed October 14, 2022. https://map .sustainablehealthcare.org.uk/oxford-radcliffe-hospitals -nhs-trust/introducing-recycling-operating-theatres
- Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg. 2015;23:235-238.
- Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg. 2019;217:634-638.
- Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives—the old, the new, and the way forward: a narrative review. Waste Manag Res. 2019;37:3-19.
- Tieszen ME, Gruenberg JC. A quantitative, qualitative, and critical assessment of surgical waste: surgeons venture through the trash can. JAMA. 1992;267:2765-2768.
- Boston Scientific 2018 Performance Report. Boston Scientific. Accessed November 19, 2022. https://www.bostonscientific. com/content/dam/bostonscientific/corporate/citizenship /sustainability/Boston_Scientific_Performance _Report_2018.pdf
- Greenberg JA, Wylie B, Robinson JN. A pilot study to assess the adequacy of the Brigham 20 Kit for cesarean delivery. Int J Gynaecol Obstet. 2012;117:157-159.
- Shockley ME, Beran B, Nutting H, et al. Sterility of selected operative sites during total laparoscopic hysterectomy. J Minim Invasive Gynecol. 2017;24:990-997.
- Al-Qaisi SK, El Tannir A, Younan LA, et al. An ergonomic assessment of using laterally-tilting operating room tables and friction reducing devices for patient lateral transfers. Appl Ergon. 2020;87:103122.
Have you ever looked at the operating room (OR) trash bin at the end of a case and wondered if all that waste is necessary? Since I started my residency, not a day goes by that I have not asked myself this question.
In the mid-1990s, John Elkington introduced the concept of the triple bottom line—that is, people, planet, and profit—for implementation and measurement of sustainability in businesses.1 The health care sector is no exception when it comes to the bottom line! However, “people” remain the priority. What is our role, as ObGyns, in protecting the “planet” while keeping the “people” safe?
According to the World Health Organization (WHO), climate change remains the single biggest health threat to humanity.2 The health care system is both the victim and the culprit. Studies suggest that the health care system, second to the food industry, is the biggest contributor to waste production in the United States. This sector generates more than 6,000 metric tons of waste each day and nearly 4 million tons (3.6 million metric tons) of solid waste each year.3 The health care system is responsible for an estimated 8% to 10% of total greenhouse gas emissions in the United States; the US health care system alone contributes to more than one-fourth of the global health care carbon footprint. If it were a country, the US health care system would rank 13th among all countries in emissions.4In turn, pollution produced by the health sector negatively impacts population health, further burdening the health care system. According to 2013 study data, the annual health damage caused by health care pollution was comparable to that of the deaths caused by preventable medical error.4
Aside from the environmental aspects, hospital waste disposal is expensive; reducing this cost is a potential area of interest for institutions.
As ObGyns, what is our role in reducing our waste generation and carbon footprint while keeping patients safe?
Defining health care waste, and disposal considerations
The WHO defines health care waste as including “the waste generated by health-care establishments, research facilities, and laboratories” as well as waste from scattered sources such as home dialysis and insulin injections.5 Despite representing a relatively small physical area of hospitals, labor and delivery units combined with ORs account for approximately 70% of all hospital waste.3 Operating room waste consists of disposable surgical supplies, personal protective equipment, drapes, plastic wrappers, sterile blue wraps, glass, cardboard, packaging material, medications, fluids, and other materials (FIGURE 1).
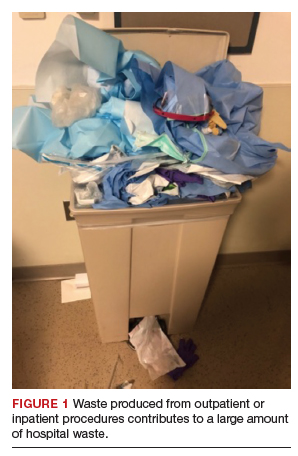
The WHO also notes that of all the waste generated by health care activities, about 85% is general, nonhazardous waste that is comparable to domestic waste.6 Hazardous waste is any material that poses a health risk, including potentially infectious materials, such as blood-soaked gauze, sharps, pharmaceuticals, or radioactive materials.6
Disposal of hazardous waste is expensiveand energy consuming as it is typically incinerated rather than disposed of in a landfill. This process produces substantial greenhouse gases, about 3 kg of carbon dioxide for every 1 kg of hazardous waste.7
Red bags are used for hazardous waste disposal, while clear bags are used for general waste. Operating rooms produce about two-thirds of the hospital red-bag waste.8 Waste segregation unfortunately is not accurate, and as much as 90% of OR general waste is improperly designated as hazardous waste.3 Drapes and uncontaminated, needleless syringes, for example, should be disposed of in clear bags, but often they are instead directed to the red-bag and sharps container (FIGURE 2).
Obstetrics and gynecology has an important role to play in accurate waste segregation given the specialty’s frequent interaction with bodily fluids. Clinicians and other staff need to recognize and appropriately separate hazardous waste from general waste. For instance, not all fabrics involved in a case should be disposed of in the red bin, only those saturated with blood or body fluids. Educating health care staff and placing instruction posters on the red trash bins potentially could aid in accurate waste segregation and reduce regulated waste while decreasing disposal costs.
Recycling in the OR
Recycling has become an established practice in many health care facilities and ORs. Studies suggest that introducing recycling programs in ORs not only reduces carbon footprints but also reduces costs.3 One study reported that US academic medical centers consume 2 million lb ($15 million) each year of recoverable medical supplies.9
Single-stream recycling, a system in which all recyclable material—including plastics, paper, metal, and glass—are placed in a single bin without segregation at the collection site, has gained in popularity. Recycling can be implemented both in ORs and in other perioperative areas where regular trash bins are located.
In a study done at Oxford University Hospitals in the United Kingdom, introducing recycling bins in every OR, as well as in recovery and staff rest areas, helped improve waste segregation such that approximately 22% of OR waste was recycled.10 Studies show that recycling programs not only decrease the health care carbon footprint but also have a considerable financial impact. Albert and colleagues demonstrated that introducing a single-stream recycling program to a 9-OR day (or ambulatory) surgery center could redirect more than 4 tons of waste each month and saved thousands of dollars.11
Despite continued improvement in recycling programs, the segregation process is still far from optimal. In a survey done at the Mayo Clinic by Azouz and colleagues, more than half of the staff reported being unclear about which OR items are recyclable and nearly half reported that lack of knowledge was the barrier to proper recycling.12 That study also showed that after implementation of a recycling education program, costs decreased 10% relative to the same time period in prior years.12
Blue wraps. One example of recycling optimization is blue wraps, the polypropylene (No. 5 plastic) material used for wrapping surgical instruments. Blue wraps account for approximately 19% of OR waste and 5% of all hospital waste.11 Blue wraps are not biodegradable and also are not widely recycled. In recent years, a resale market has emerged for blue wraps, as they can be used for production of other No. 5 plastic items.9 By reselling blue wraps, revenue can be generated by recycling a necessary packing material that would otherwise require payment for disposal.
Sterility considerations. While recycling in ORs may raise concern due to the absolute sterility required in procedural settings, technologic developments have been promising in advancing safe recycling to reduce carbon footprints and health care costs without compromising patients’ safety. Segregation of waste from recyclable packaging material prior to the case, as well as directing trash to the correct bin (regular vs red bin), is one example. Moreover, because about 80% of all OR waste is generated during the set up before the patient arrives in the OR, it is not contaminated and can be safely recycled.13
Continue to: Packaging material...
Packaging material
A substantial part of OR waste consists of packaging material; of all OR waste, 26% consists of plastics and 7%, paper and cartons.14 Increasing use of disposable or “single use” medical products in ORs, along with the intention to safeguard sterility, contributes significantly to the generation of medical waste in operating units. Containers, wraps and overwraps, cardboard, and plastic packaging are all composed of materials that when clean, can be recycled; however, these items often end up in the landfill (FIGURE 3).
Although the segregation of packaging material to recycling versus regular trash versus red bin is of paramount importance, packaging design plays a significant role as well. In 2018, Boston Scientific introduced a new packaging design for ureteral stents that reduced plastic use in packaging by 120,000 lb each year.15 Despite the advances in the medical packaging industry to increase sustainability while safeguarding sterility for medical devices, there is still room for innovation in this area.
Reducing overage by judicious selection of surgical devices, instruments, and supplies
Overage is the term used to describe surgical inventory that is opened and prepared for surgery but ultimately not used and therefore discarded. Design of surgical carts and instrument and supply selection requires direct input from ObGyns. Opening only the needed instruments while ensuring ready availability of potentially needed supplies can significantly reduce OR waste generation as well as decrease chemical pollution generated by instrument sterilization. Decreasing OR overage reduces overall costs as well (FIGURE 4).
In a pilot study at the University of Massachusetts, Albert and colleagues examined the sets of disposable items and instruments designated for common plastic and hand surgery procedures.11 They identified the supplies and instruments that are routinely opened and wasted, based on surgeons’ interview responses, and redesigned the sets. Fifteen items were removed from disposable plastic surgery packs and 7 items from hand surgery packs. The authors reported saving thousands of dollars per year with these changes alone, as well as reducing waste.11 This same concept easily could be implemented in obstetrics and gynecology. We must ask ourselves: Do we always need, for example, a complete dilation and curettage kit to place the uterine manipulator prior to a minimally invasive hysterectomy?
In another pilot study, Greenberg and colleagues investigated whether cesarean deliveries consistently could be performed in a safe manner with only 20 instruments in the surgical kit.16 Obstetricians rated the 20-instrument kit an 8.7 out of 10 for performing cesarean deliveries safely.16
In addition to instrument selection, surgeons have a role in other supply use and waste generation: for instance, opening multiple pairs of surgical gloves and surgical gowns in advance when most of them will not be used during the case. Furthermore, many ObGyn surgeons routinely change gloves or even gowns during gynecologic procedures when they go back and forth between the vaginal and abdominal fields. Is the perineum “dirty” after application of a surgical prep solution?
In an observational study, Shockley and colleagues investigated the type and quantity of bacteria found intraoperatively on the abdomen, vagina, surgical gloves, instrument tips, and uterus at distinct time points during total laparoscopic hysterectomy.17 They showed that in 98.9% of cultures, the overall bacterial concentrations did not exceed the threshold for infection. There was no bacterial growth from vaginal cultures, and the only samples with some bacterial growth belonged to the surgeon’s gloves after specimen extraction; about one-third of samples showed growth after specimen extraction, but only 1 sample had a bacterial load above the infectious threshold of 5,000 colony-forming units per mL. The authors therefore suggested that if a surgeon changes gloves, doing so after specimen extraction and before turning attention back to the abdomen for vaginal cuff closure may be most effective in reducing bacterial load.17
Surgical site infection contributes to medical cost and likely medical waste as well. For example, surgical site infection may require prolonged treatments, tests, and medical instruments. In severe cases with abscesses, treatment entails hospitalization with prolonged antibiotic therapy with or without procedures to drain the collections. Further research therefore is warranted to investigate safe and environmentally friendly practices.
Myriad products are introduced to the medical system each day, some of which replace conventional tools. For instance, low-density polyethylene, or LDPE, transfer sheet is advertised for lateral patient transfer from the OR table to the bed or stretcher. This No. 4–coded plastic, while recyclable, is routinely discarded as trash in ORs. One ergonomic study found that reusable slide boards are as effective for reducing friction and staff muscle activities and are noninferior to the plastic sheets.18
Steps to making an impact
Operating rooms and labor and delivery units are responsible for a large proportion of hospital waste, and therefore they are of paramount importance in reducing waste and carbon footprint at the individual and institutional level. Reduction of OR waste not only is environmentally conscious but also decreases cost. Steps as small as individual practices to as big as changing infrastructures can make an impact. For instance:
- redesigning surgical carts
- reformulating surgeon-specific supply lists
- raising awareness about surgical overage
- encouraging recycling through education and audit
- optimizing surgical waste segregation through educational posters.
These are all simple steps that could significantly reduce waste and carbon footprint.
Bottom line
Although waste reduction is the responsibility of all health care providers, as leaders in their workplace physicians can serve as role models by implementing “green” practices in procedural units. Raising awareness and using a team approach is critical to succeed in our endeavors to move toward an environmentally friendly future. ●
Have you ever looked at the operating room (OR) trash bin at the end of a case and wondered if all that waste is necessary? Since I started my residency, not a day goes by that I have not asked myself this question.
In the mid-1990s, John Elkington introduced the concept of the triple bottom line—that is, people, planet, and profit—for implementation and measurement of sustainability in businesses.1 The health care sector is no exception when it comes to the bottom line! However, “people” remain the priority. What is our role, as ObGyns, in protecting the “planet” while keeping the “people” safe?
According to the World Health Organization (WHO), climate change remains the single biggest health threat to humanity.2 The health care system is both the victim and the culprit. Studies suggest that the health care system, second to the food industry, is the biggest contributor to waste production in the United States. This sector generates more than 6,000 metric tons of waste each day and nearly 4 million tons (3.6 million metric tons) of solid waste each year.3 The health care system is responsible for an estimated 8% to 10% of total greenhouse gas emissions in the United States; the US health care system alone contributes to more than one-fourth of the global health care carbon footprint. If it were a country, the US health care system would rank 13th among all countries in emissions.4In turn, pollution produced by the health sector negatively impacts population health, further burdening the health care system. According to 2013 study data, the annual health damage caused by health care pollution was comparable to that of the deaths caused by preventable medical error.4
Aside from the environmental aspects, hospital waste disposal is expensive; reducing this cost is a potential area of interest for institutions.
As ObGyns, what is our role in reducing our waste generation and carbon footprint while keeping patients safe?
Defining health care waste, and disposal considerations
The WHO defines health care waste as including “the waste generated by health-care establishments, research facilities, and laboratories” as well as waste from scattered sources such as home dialysis and insulin injections.5 Despite representing a relatively small physical area of hospitals, labor and delivery units combined with ORs account for approximately 70% of all hospital waste.3 Operating room waste consists of disposable surgical supplies, personal protective equipment, drapes, plastic wrappers, sterile blue wraps, glass, cardboard, packaging material, medications, fluids, and other materials (FIGURE 1).
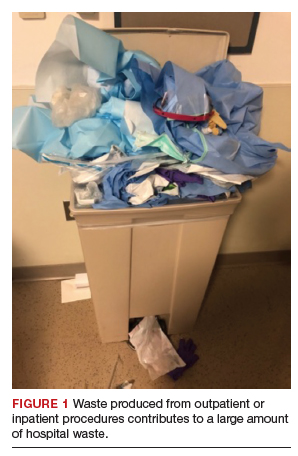
The WHO also notes that of all the waste generated by health care activities, about 85% is general, nonhazardous waste that is comparable to domestic waste.6 Hazardous waste is any material that poses a health risk, including potentially infectious materials, such as blood-soaked gauze, sharps, pharmaceuticals, or radioactive materials.6
Disposal of hazardous waste is expensiveand energy consuming as it is typically incinerated rather than disposed of in a landfill. This process produces substantial greenhouse gases, about 3 kg of carbon dioxide for every 1 kg of hazardous waste.7
Red bags are used for hazardous waste disposal, while clear bags are used for general waste. Operating rooms produce about two-thirds of the hospital red-bag waste.8 Waste segregation unfortunately is not accurate, and as much as 90% of OR general waste is improperly designated as hazardous waste.3 Drapes and uncontaminated, needleless syringes, for example, should be disposed of in clear bags, but often they are instead directed to the red-bag and sharps container (FIGURE 2).
Obstetrics and gynecology has an important role to play in accurate waste segregation given the specialty’s frequent interaction with bodily fluids. Clinicians and other staff need to recognize and appropriately separate hazardous waste from general waste. For instance, not all fabrics involved in a case should be disposed of in the red bin, only those saturated with blood or body fluids. Educating health care staff and placing instruction posters on the red trash bins potentially could aid in accurate waste segregation and reduce regulated waste while decreasing disposal costs.
Recycling in the OR
Recycling has become an established practice in many health care facilities and ORs. Studies suggest that introducing recycling programs in ORs not only reduces carbon footprints but also reduces costs.3 One study reported that US academic medical centers consume 2 million lb ($15 million) each year of recoverable medical supplies.9
Single-stream recycling, a system in which all recyclable material—including plastics, paper, metal, and glass—are placed in a single bin without segregation at the collection site, has gained in popularity. Recycling can be implemented both in ORs and in other perioperative areas where regular trash bins are located.
In a study done at Oxford University Hospitals in the United Kingdom, introducing recycling bins in every OR, as well as in recovery and staff rest areas, helped improve waste segregation such that approximately 22% of OR waste was recycled.10 Studies show that recycling programs not only decrease the health care carbon footprint but also have a considerable financial impact. Albert and colleagues demonstrated that introducing a single-stream recycling program to a 9-OR day (or ambulatory) surgery center could redirect more than 4 tons of waste each month and saved thousands of dollars.11
Despite continued improvement in recycling programs, the segregation process is still far from optimal. In a survey done at the Mayo Clinic by Azouz and colleagues, more than half of the staff reported being unclear about which OR items are recyclable and nearly half reported that lack of knowledge was the barrier to proper recycling.12 That study also showed that after implementation of a recycling education program, costs decreased 10% relative to the same time period in prior years.12
Blue wraps. One example of recycling optimization is blue wraps, the polypropylene (No. 5 plastic) material used for wrapping surgical instruments. Blue wraps account for approximately 19% of OR waste and 5% of all hospital waste.11 Blue wraps are not biodegradable and also are not widely recycled. In recent years, a resale market has emerged for blue wraps, as they can be used for production of other No. 5 plastic items.9 By reselling blue wraps, revenue can be generated by recycling a necessary packing material that would otherwise require payment for disposal.
Sterility considerations. While recycling in ORs may raise concern due to the absolute sterility required in procedural settings, technologic developments have been promising in advancing safe recycling to reduce carbon footprints and health care costs without compromising patients’ safety. Segregation of waste from recyclable packaging material prior to the case, as well as directing trash to the correct bin (regular vs red bin), is one example. Moreover, because about 80% of all OR waste is generated during the set up before the patient arrives in the OR, it is not contaminated and can be safely recycled.13
Continue to: Packaging material...
Packaging material
A substantial part of OR waste consists of packaging material; of all OR waste, 26% consists of plastics and 7%, paper and cartons.14 Increasing use of disposable or “single use” medical products in ORs, along with the intention to safeguard sterility, contributes significantly to the generation of medical waste in operating units. Containers, wraps and overwraps, cardboard, and plastic packaging are all composed of materials that when clean, can be recycled; however, these items often end up in the landfill (FIGURE 3).
Although the segregation of packaging material to recycling versus regular trash versus red bin is of paramount importance, packaging design plays a significant role as well. In 2018, Boston Scientific introduced a new packaging design for ureteral stents that reduced plastic use in packaging by 120,000 lb each year.15 Despite the advances in the medical packaging industry to increase sustainability while safeguarding sterility for medical devices, there is still room for innovation in this area.
Reducing overage by judicious selection of surgical devices, instruments, and supplies
Overage is the term used to describe surgical inventory that is opened and prepared for surgery but ultimately not used and therefore discarded. Design of surgical carts and instrument and supply selection requires direct input from ObGyns. Opening only the needed instruments while ensuring ready availability of potentially needed supplies can significantly reduce OR waste generation as well as decrease chemical pollution generated by instrument sterilization. Decreasing OR overage reduces overall costs as well (FIGURE 4).
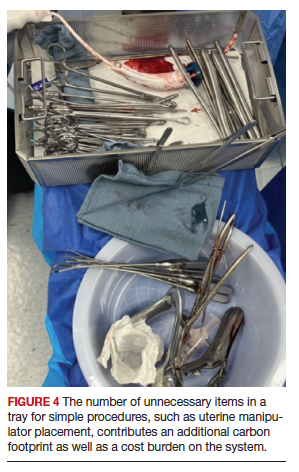
In a pilot study at the University of Massachusetts, Albert and colleagues examined the sets of disposable items and instruments designated for common plastic and hand surgery procedures.11 They identified the supplies and instruments that are routinely opened and wasted, based on surgeons’ interview responses, and redesigned the sets. Fifteen items were removed from disposable plastic surgery packs and 7 items from hand surgery packs. The authors reported saving thousands of dollars per year with these changes alone, as well as reducing waste.11 This same concept easily could be implemented in obstetrics and gynecology. We must ask ourselves: Do we always need, for example, a complete dilation and curettage kit to place the uterine manipulator prior to a minimally invasive hysterectomy?
In another pilot study, Greenberg and colleagues investigated whether cesarean deliveries consistently could be performed in a safe manner with only 20 instruments in the surgical kit.16 Obstetricians rated the 20-instrument kit an 8.7 out of 10 for performing cesarean deliveries safely.16
In addition to instrument selection, surgeons have a role in other supply use and waste generation: for instance, opening multiple pairs of surgical gloves and surgical gowns in advance when most of them will not be used during the case. Furthermore, many ObGyn surgeons routinely change gloves or even gowns during gynecologic procedures when they go back and forth between the vaginal and abdominal fields. Is the perineum “dirty” after application of a surgical prep solution?
In an observational study, Shockley and colleagues investigated the type and quantity of bacteria found intraoperatively on the abdomen, vagina, surgical gloves, instrument tips, and uterus at distinct time points during total laparoscopic hysterectomy.17 They showed that in 98.9% of cultures, the overall bacterial concentrations did not exceed the threshold for infection. There was no bacterial growth from vaginal cultures, and the only samples with some bacterial growth belonged to the surgeon’s gloves after specimen extraction; about one-third of samples showed growth after specimen extraction, but only 1 sample had a bacterial load above the infectious threshold of 5,000 colony-forming units per mL. The authors therefore suggested that if a surgeon changes gloves, doing so after specimen extraction and before turning attention back to the abdomen for vaginal cuff closure may be most effective in reducing bacterial load.17
Surgical site infection contributes to medical cost and likely medical waste as well. For example, surgical site infection may require prolonged treatments, tests, and medical instruments. In severe cases with abscesses, treatment entails hospitalization with prolonged antibiotic therapy with or without procedures to drain the collections. Further research therefore is warranted to investigate safe and environmentally friendly practices.
Myriad products are introduced to the medical system each day, some of which replace conventional tools. For instance, low-density polyethylene, or LDPE, transfer sheet is advertised for lateral patient transfer from the OR table to the bed or stretcher. This No. 4–coded plastic, while recyclable, is routinely discarded as trash in ORs. One ergonomic study found that reusable slide boards are as effective for reducing friction and staff muscle activities and are noninferior to the plastic sheets.18
Steps to making an impact
Operating rooms and labor and delivery units are responsible for a large proportion of hospital waste, and therefore they are of paramount importance in reducing waste and carbon footprint at the individual and institutional level. Reduction of OR waste not only is environmentally conscious but also decreases cost. Steps as small as individual practices to as big as changing infrastructures can make an impact. For instance:
- redesigning surgical carts
- reformulating surgeon-specific supply lists
- raising awareness about surgical overage
- encouraging recycling through education and audit
- optimizing surgical waste segregation through educational posters.
These are all simple steps that could significantly reduce waste and carbon footprint.
Bottom line
Although waste reduction is the responsibility of all health care providers, as leaders in their workplace physicians can serve as role models by implementing “green” practices in procedural units. Raising awareness and using a team approach is critical to succeed in our endeavors to move toward an environmentally friendly future. ●
- Elkington J. Towards the sustainable corporation: win-winwin business strategies for sustainable development. Calif Manage Rev. 1994;36:90-100.
- Climate change and health. October 30, 2021. World Health Organization. Accessed October 10, 2022. https://www.who .int/news-room/fact-sheets/detail/climate-change-and -health
- Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg. 2011;146:131-136.
- Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PloS One. 2016;11:e0157014.
- Pruss A, Giroult E, Rushbrook P. Safe management of wastes from health-care activities. World Health Organization; 1999.
- Health-care waste. February 8, 2018. World Health Organization. Accessed October 4, 2022. https://www.who. int/news-room/fact-sheets/detail/health-care-waste2
- Southorn T, Norrish AR, Gardner K, et al. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J Perioper Pract. 2013;23:144-146.
- Greening the OR. Practice Greenhealth. Accessed October 24, 2022. https://practicegreenhealth.org/topics/greening -operating-room/greening-or
- Babu MA, Dalenberg AK, Goodsell G, et al. Greening the operating room: results of a scalable initiative to reduce waste and recover supply costs. Neurosurgery. 2019;85:432-437.
- Oxford University Hospitals NHS Trust. Introducing recycling into the operating theatres. Mapping Greener Healthcare. Accessed October 14, 2022. https://map .sustainablehealthcare.org.uk/oxford-radcliffe-hospitals -nhs-trust/introducing-recycling-operating-theatres
- Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg. 2015;23:235-238.
- Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg. 2019;217:634-638.
- Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives—the old, the new, and the way forward: a narrative review. Waste Manag Res. 2019;37:3-19.
- Tieszen ME, Gruenberg JC. A quantitative, qualitative, and critical assessment of surgical waste: surgeons venture through the trash can. JAMA. 1992;267:2765-2768.
- Boston Scientific 2018 Performance Report. Boston Scientific. Accessed November 19, 2022. https://www.bostonscientific. com/content/dam/bostonscientific/corporate/citizenship /sustainability/Boston_Scientific_Performance _Report_2018.pdf
- Greenberg JA, Wylie B, Robinson JN. A pilot study to assess the adequacy of the Brigham 20 Kit for cesarean delivery. Int J Gynaecol Obstet. 2012;117:157-159.
- Shockley ME, Beran B, Nutting H, et al. Sterility of selected operative sites during total laparoscopic hysterectomy. J Minim Invasive Gynecol. 2017;24:990-997.
- Al-Qaisi SK, El Tannir A, Younan LA, et al. An ergonomic assessment of using laterally-tilting operating room tables and friction reducing devices for patient lateral transfers. Appl Ergon. 2020;87:103122.
- Elkington J. Towards the sustainable corporation: win-winwin business strategies for sustainable development. Calif Manage Rev. 1994;36:90-100.
- Climate change and health. October 30, 2021. World Health Organization. Accessed October 10, 2022. https://www.who .int/news-room/fact-sheets/detail/climate-change-and -health
- Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg. 2011;146:131-136.
- Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PloS One. 2016;11:e0157014.
- Pruss A, Giroult E, Rushbrook P. Safe management of wastes from health-care activities. World Health Organization; 1999.
- Health-care waste. February 8, 2018. World Health Organization. Accessed October 4, 2022. https://www.who. int/news-room/fact-sheets/detail/health-care-waste2
- Southorn T, Norrish AR, Gardner K, et al. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J Perioper Pract. 2013;23:144-146.
- Greening the OR. Practice Greenhealth. Accessed October 24, 2022. https://practicegreenhealth.org/topics/greening -operating-room/greening-or
- Babu MA, Dalenberg AK, Goodsell G, et al. Greening the operating room: results of a scalable initiative to reduce waste and recover supply costs. Neurosurgery. 2019;85:432-437.
- Oxford University Hospitals NHS Trust. Introducing recycling into the operating theatres. Mapping Greener Healthcare. Accessed October 14, 2022. https://map .sustainablehealthcare.org.uk/oxford-radcliffe-hospitals -nhs-trust/introducing-recycling-operating-theatres
- Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg. 2015;23:235-238.
- Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg. 2019;217:634-638.
- Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives—the old, the new, and the way forward: a narrative review. Waste Manag Res. 2019;37:3-19.
- Tieszen ME, Gruenberg JC. A quantitative, qualitative, and critical assessment of surgical waste: surgeons venture through the trash can. JAMA. 1992;267:2765-2768.
- Boston Scientific 2018 Performance Report. Boston Scientific. Accessed November 19, 2022. https://www.bostonscientific. com/content/dam/bostonscientific/corporate/citizenship /sustainability/Boston_Scientific_Performance _Report_2018.pdf
- Greenberg JA, Wylie B, Robinson JN. A pilot study to assess the adequacy of the Brigham 20 Kit for cesarean delivery. Int J Gynaecol Obstet. 2012;117:157-159.
- Shockley ME, Beran B, Nutting H, et al. Sterility of selected operative sites during total laparoscopic hysterectomy. J Minim Invasive Gynecol. 2017;24:990-997.
- Al-Qaisi SK, El Tannir A, Younan LA, et al. An ergonomic assessment of using laterally-tilting operating room tables and friction reducing devices for patient lateral transfers. Appl Ergon. 2020;87:103122.
Gut microbiome may guide personalized heart failure therapy
Understanding more about the gut microbiome and how it may affect the development and treatment of heart failure could lead to a more personalized approach to managing the condition, a new review article suggests.
the authors note. “Interactions among the gut microbiome, diet, and medications offer potentially innovative modalities for management of patients with heart failure,” they add.
The review was published online in the Journal of the American College of Cardiology.
“Over the past years we have gathered more understanding about how important the gut microbiome is in relation to how our bodies function overall and even though the cardiovascular system and the heart itself may appear to be quite distant from the gut, we know the gut microbiome affects the cardiovascular system and the physiology of heart failure,” lead author Petra Mamic, MD, Stanford (Calif.) University, told this news organization.
“We’ve also learnt that the microbiome is very personalized. It seems to be affected by a lot of intrinsic and as well as extrinsic factors. For cardiovascular diseases in particular, we always knew that diet and lifestyle were part of the environmental risk, and we now believe that the gut microbiome may be one of the factors that mediates that risk,” she said.
“Studies on the gut microbiome are difficult to do and we are right at the beginning of this type of research. But we have learned that the microbiome is altered or dysregulated in many diseases including many cardiovascular diseases, and many of the changes in the microbiome we see in different cardiovascular diseases seem to overlap,” she added.
Dr. Mamic explained that patients with heart failure have a microbiome that appears different and dysregulated, compared with the microbiome in healthy individuals.
“The difficulty is teasing out whether the microbiome changes are causing heart failure or if they are a consequence of the heart failure and all the medications and comorbidities associated with heart failure,” she commented.
Animal studies have shown that many microbial products, small molecules made by the microbiome, seem to affect how the heart recovers from injury, for example after a myocardial infarction, and how much the heart scars and hypertrophies after an injury, Dr. Mamic reported. These microbiome-derived small molecules can also affect blood pressure, which is dysregulated in heart failure.
Other products of the microbiome can be pro-inflammatory or anti-inflammatory, which can again affect the cardiovascular physiology and the heart, she noted.
High-fiber diet may be beneficial
One area of particular interest at present involves the role of short-chain fatty acids, which are a byproduct of microbes in the gut that digest fiber.
“These short chain fatty acids seem to have positive effects on the host physiology. They are anti-inflammatory; they lower blood pressure; and they seem to protect the heart from scarring and hypertrophy after injury. In heart failure, the gut microbes that make these short-chain fatty acids are significantly depleted,” Dr. Mamic explained.
They are an obvious focus of interest because these short-chain fatty acids are produced when gut bacteria break down dietary fiber, raising the possibility of beneficial effects from eating a high-fiber diet.
Another product of the gut microbiome of interest is trimethylamine N-oxide, formed when gut bacteria break down nutrients such as L-carnitine and phosphatidyl choline, nutrients abundant in foods of animal origin, especially red meat. This metabolite has proatherogenic and prothrombotic effects, and negatively affected cardiac remodeling in a mouse heart failure model, the review notes.
However, though it is too early to make specific dietary recommendations based on these findings, Dr. Mamic points out that a high-fiber diet is thought to be beneficial.
“Nutritional research is very hard to do and the data is limited, but as best as we can summarize things, we know that plant-based diets such as the Mediterranean and DASH diets seem to prevent some of the risk factors for the development of heart failure and seem to slow the progression of heart failure,” she added.
One of the major recommendations in these diets is a high intake of fiber, including whole foods, vegetables, fruits, legumes, and nuts, and less intake of processed food and red meat. “In general, I think everyone should eat like that, but I specifically recommend a plant-based diet with a high amount of fiber to my heart failure patients,” Dr. Mamic said.
Large variation in microbiome composition
The review also explores the idea of personalization of diet or specific treatments dependent on an individual’s gut microbiome composition.
Dr. Mamic explains: “When we look at the microbiome composition between individuals, it is very different. There is very little overlap between individuals, even in people who are related. It seems to be more to do with the environment – people who are living together are more likely to have similarities in their microbiome. We are still trying to understand what drives these differences.”
It is thought that these differences may affect the response to a specific diet or medication. Dr. Mamic gives the example of fiber. “Not all bacteria can digest the same types of fiber, so not everyone responds in the same way to a high-fiber diet. That’s probably because of differences in their microbiome.”
Another example is the response to the heart failure drug digoxin, which is metabolized by one particular strain of bacteria in the gut. The toxicity or effectiveness of digoxin seems to be influenced by levels of this bacterial strain, and this again can be influenced by diet, Dr. Mamic says.
Manipulating the microbiome as a therapeutic strategy
Microbiome-targeting therapies may also become part of future treatment strategies for many conditions, including heart failure, the review authors say.
Probiotics (foods and dietary supplements that contain live microbes) interact with the gut microbiota to alter host physiology beneficially. Certain probiotics may specifically modulate processes dysregulated in heart failure, as was suggested in a rodent heart failure model in which supplementation with Lactobacillus-containing and Bifidobacterium-containing probiotics resulted in markedly improved cardiac function, the authors report.
However, a randomized trial (GutHeart) of probiotic yeast Saccharomyces boulardii in patients with heart failure found no improvement in cardiac function, compared with standard care.
Commenting on this, Dr. Mamic suggested that a more specific approach may be needed.
“Some of our preliminary data have shown people who have heart failure have severely depleted Bifidobacteria,” Dr. Mamic said. These bacteria are commercially available as a probiotic, and the researchers are planning a study to give patients with heart failure these specific probiotics. “We are trying to find practical ways forward and to be guided by the data. These people have very little Bifidobacteria, and we know that probiotics seem to be accepted best by the host where there is a specific need for them, so this seems like a sensible approach.”
Dr. Mamic does not recommend that heart failure patients take general probiotic products at present, but she tells her patients about the study she is doing. “Probiotics are quite different from each other. It is a very unregulated market. A general probiotic product may not contain the specific bacteria needed.”
Include microbiome data in biobanks
The review calls for more research on the subject and a more systematic approach to collecting data on the microbiome.
“At present for medical research, blood samples are collected, stored, and analyzed routinely. I think we should also be collecting stool samples in the same way to analyze the microbiome,” Dr. Mamic suggests.
“If we can combine that with data from blood tests on various metabolites/cytokines and look at how the microbiome changes over time or with medication, or with diet, and how the host responds including clinically relevant data, that would be really important. Given how quickly the field is growing I would think there would be biobanks including the microbiome in a few years’ time.”
“We need to gather this data. We would be looking for which bacteria are there, what their functionality is, how it changes over time, with diet or medication, and even whether we can use the microbiome data to predict who will respond to a specific drug.”
Dr. Mamic believes that in the future, analysis of the microbiome could be a routine part of deciding what people eat for good health and to characterize patients for personalized therapies.
“It is clear that the microbiome can influence health, and a dysregulated microbiome negatively affects the host, but there is lot of work to do. We need to learn a lot more about it, but we shouldn’t miss the opportunity to do this,” she concluded.
Dr. Mamic reported no disclosures.
A version of this article first appeared on Medscape.com.
Understanding more about the gut microbiome and how it may affect the development and treatment of heart failure could lead to a more personalized approach to managing the condition, a new review article suggests.
the authors note. “Interactions among the gut microbiome, diet, and medications offer potentially innovative modalities for management of patients with heart failure,” they add.
The review was published online in the Journal of the American College of Cardiology.
“Over the past years we have gathered more understanding about how important the gut microbiome is in relation to how our bodies function overall and even though the cardiovascular system and the heart itself may appear to be quite distant from the gut, we know the gut microbiome affects the cardiovascular system and the physiology of heart failure,” lead author Petra Mamic, MD, Stanford (Calif.) University, told this news organization.
“We’ve also learnt that the microbiome is very personalized. It seems to be affected by a lot of intrinsic and as well as extrinsic factors. For cardiovascular diseases in particular, we always knew that diet and lifestyle were part of the environmental risk, and we now believe that the gut microbiome may be one of the factors that mediates that risk,” she said.
“Studies on the gut microbiome are difficult to do and we are right at the beginning of this type of research. But we have learned that the microbiome is altered or dysregulated in many diseases including many cardiovascular diseases, and many of the changes in the microbiome we see in different cardiovascular diseases seem to overlap,” she added.
Dr. Mamic explained that patients with heart failure have a microbiome that appears different and dysregulated, compared with the microbiome in healthy individuals.
“The difficulty is teasing out whether the microbiome changes are causing heart failure or if they are a consequence of the heart failure and all the medications and comorbidities associated with heart failure,” she commented.
Animal studies have shown that many microbial products, small molecules made by the microbiome, seem to affect how the heart recovers from injury, for example after a myocardial infarction, and how much the heart scars and hypertrophies after an injury, Dr. Mamic reported. These microbiome-derived small molecules can also affect blood pressure, which is dysregulated in heart failure.
Other products of the microbiome can be pro-inflammatory or anti-inflammatory, which can again affect the cardiovascular physiology and the heart, she noted.
High-fiber diet may be beneficial
One area of particular interest at present involves the role of short-chain fatty acids, which are a byproduct of microbes in the gut that digest fiber.
“These short chain fatty acids seem to have positive effects on the host physiology. They are anti-inflammatory; they lower blood pressure; and they seem to protect the heart from scarring and hypertrophy after injury. In heart failure, the gut microbes that make these short-chain fatty acids are significantly depleted,” Dr. Mamic explained.
They are an obvious focus of interest because these short-chain fatty acids are produced when gut bacteria break down dietary fiber, raising the possibility of beneficial effects from eating a high-fiber diet.
Another product of the gut microbiome of interest is trimethylamine N-oxide, formed when gut bacteria break down nutrients such as L-carnitine and phosphatidyl choline, nutrients abundant in foods of animal origin, especially red meat. This metabolite has proatherogenic and prothrombotic effects, and negatively affected cardiac remodeling in a mouse heart failure model, the review notes.
However, though it is too early to make specific dietary recommendations based on these findings, Dr. Mamic points out that a high-fiber diet is thought to be beneficial.
“Nutritional research is very hard to do and the data is limited, but as best as we can summarize things, we know that plant-based diets such as the Mediterranean and DASH diets seem to prevent some of the risk factors for the development of heart failure and seem to slow the progression of heart failure,” she added.
One of the major recommendations in these diets is a high intake of fiber, including whole foods, vegetables, fruits, legumes, and nuts, and less intake of processed food and red meat. “In general, I think everyone should eat like that, but I specifically recommend a plant-based diet with a high amount of fiber to my heart failure patients,” Dr. Mamic said.
Large variation in microbiome composition
The review also explores the idea of personalization of diet or specific treatments dependent on an individual’s gut microbiome composition.
Dr. Mamic explains: “When we look at the microbiome composition between individuals, it is very different. There is very little overlap between individuals, even in people who are related. It seems to be more to do with the environment – people who are living together are more likely to have similarities in their microbiome. We are still trying to understand what drives these differences.”
It is thought that these differences may affect the response to a specific diet or medication. Dr. Mamic gives the example of fiber. “Not all bacteria can digest the same types of fiber, so not everyone responds in the same way to a high-fiber diet. That’s probably because of differences in their microbiome.”
Another example is the response to the heart failure drug digoxin, which is metabolized by one particular strain of bacteria in the gut. The toxicity or effectiveness of digoxin seems to be influenced by levels of this bacterial strain, and this again can be influenced by diet, Dr. Mamic says.
Manipulating the microbiome as a therapeutic strategy
Microbiome-targeting therapies may also become part of future treatment strategies for many conditions, including heart failure, the review authors say.
Probiotics (foods and dietary supplements that contain live microbes) interact with the gut microbiota to alter host physiology beneficially. Certain probiotics may specifically modulate processes dysregulated in heart failure, as was suggested in a rodent heart failure model in which supplementation with Lactobacillus-containing and Bifidobacterium-containing probiotics resulted in markedly improved cardiac function, the authors report.
However, a randomized trial (GutHeart) of probiotic yeast Saccharomyces boulardii in patients with heart failure found no improvement in cardiac function, compared with standard care.
Commenting on this, Dr. Mamic suggested that a more specific approach may be needed.
“Some of our preliminary data have shown people who have heart failure have severely depleted Bifidobacteria,” Dr. Mamic said. These bacteria are commercially available as a probiotic, and the researchers are planning a study to give patients with heart failure these specific probiotics. “We are trying to find practical ways forward and to be guided by the data. These people have very little Bifidobacteria, and we know that probiotics seem to be accepted best by the host where there is a specific need for them, so this seems like a sensible approach.”
Dr. Mamic does not recommend that heart failure patients take general probiotic products at present, but she tells her patients about the study she is doing. “Probiotics are quite different from each other. It is a very unregulated market. A general probiotic product may not contain the specific bacteria needed.”
Include microbiome data in biobanks
The review calls for more research on the subject and a more systematic approach to collecting data on the microbiome.
“At present for medical research, blood samples are collected, stored, and analyzed routinely. I think we should also be collecting stool samples in the same way to analyze the microbiome,” Dr. Mamic suggests.
“If we can combine that with data from blood tests on various metabolites/cytokines and look at how the microbiome changes over time or with medication, or with diet, and how the host responds including clinically relevant data, that would be really important. Given how quickly the field is growing I would think there would be biobanks including the microbiome in a few years’ time.”
“We need to gather this data. We would be looking for which bacteria are there, what their functionality is, how it changes over time, with diet or medication, and even whether we can use the microbiome data to predict who will respond to a specific drug.”
Dr. Mamic believes that in the future, analysis of the microbiome could be a routine part of deciding what people eat for good health and to characterize patients for personalized therapies.
“It is clear that the microbiome can influence health, and a dysregulated microbiome negatively affects the host, but there is lot of work to do. We need to learn a lot more about it, but we shouldn’t miss the opportunity to do this,” she concluded.
Dr. Mamic reported no disclosures.
A version of this article first appeared on Medscape.com.
Understanding more about the gut microbiome and how it may affect the development and treatment of heart failure could lead to a more personalized approach to managing the condition, a new review article suggests.
the authors note. “Interactions among the gut microbiome, diet, and medications offer potentially innovative modalities for management of patients with heart failure,” they add.
The review was published online in the Journal of the American College of Cardiology.
“Over the past years we have gathered more understanding about how important the gut microbiome is in relation to how our bodies function overall and even though the cardiovascular system and the heart itself may appear to be quite distant from the gut, we know the gut microbiome affects the cardiovascular system and the physiology of heart failure,” lead author Petra Mamic, MD, Stanford (Calif.) University, told this news organization.
“We’ve also learnt that the microbiome is very personalized. It seems to be affected by a lot of intrinsic and as well as extrinsic factors. For cardiovascular diseases in particular, we always knew that diet and lifestyle were part of the environmental risk, and we now believe that the gut microbiome may be one of the factors that mediates that risk,” she said.
“Studies on the gut microbiome are difficult to do and we are right at the beginning of this type of research. But we have learned that the microbiome is altered or dysregulated in many diseases including many cardiovascular diseases, and many of the changes in the microbiome we see in different cardiovascular diseases seem to overlap,” she added.
Dr. Mamic explained that patients with heart failure have a microbiome that appears different and dysregulated, compared with the microbiome in healthy individuals.
“The difficulty is teasing out whether the microbiome changes are causing heart failure or if they are a consequence of the heart failure and all the medications and comorbidities associated with heart failure,” she commented.
Animal studies have shown that many microbial products, small molecules made by the microbiome, seem to affect how the heart recovers from injury, for example after a myocardial infarction, and how much the heart scars and hypertrophies after an injury, Dr. Mamic reported. These microbiome-derived small molecules can also affect blood pressure, which is dysregulated in heart failure.
Other products of the microbiome can be pro-inflammatory or anti-inflammatory, which can again affect the cardiovascular physiology and the heart, she noted.
High-fiber diet may be beneficial
One area of particular interest at present involves the role of short-chain fatty acids, which are a byproduct of microbes in the gut that digest fiber.
“These short chain fatty acids seem to have positive effects on the host physiology. They are anti-inflammatory; they lower blood pressure; and they seem to protect the heart from scarring and hypertrophy after injury. In heart failure, the gut microbes that make these short-chain fatty acids are significantly depleted,” Dr. Mamic explained.
They are an obvious focus of interest because these short-chain fatty acids are produced when gut bacteria break down dietary fiber, raising the possibility of beneficial effects from eating a high-fiber diet.
Another product of the gut microbiome of interest is trimethylamine N-oxide, formed when gut bacteria break down nutrients such as L-carnitine and phosphatidyl choline, nutrients abundant in foods of animal origin, especially red meat. This metabolite has proatherogenic and prothrombotic effects, and negatively affected cardiac remodeling in a mouse heart failure model, the review notes.
However, though it is too early to make specific dietary recommendations based on these findings, Dr. Mamic points out that a high-fiber diet is thought to be beneficial.
“Nutritional research is very hard to do and the data is limited, but as best as we can summarize things, we know that plant-based diets such as the Mediterranean and DASH diets seem to prevent some of the risk factors for the development of heart failure and seem to slow the progression of heart failure,” she added.
One of the major recommendations in these diets is a high intake of fiber, including whole foods, vegetables, fruits, legumes, and nuts, and less intake of processed food and red meat. “In general, I think everyone should eat like that, but I specifically recommend a plant-based diet with a high amount of fiber to my heart failure patients,” Dr. Mamic said.
Large variation in microbiome composition
The review also explores the idea of personalization of diet or specific treatments dependent on an individual’s gut microbiome composition.
Dr. Mamic explains: “When we look at the microbiome composition between individuals, it is very different. There is very little overlap between individuals, even in people who are related. It seems to be more to do with the environment – people who are living together are more likely to have similarities in their microbiome. We are still trying to understand what drives these differences.”
It is thought that these differences may affect the response to a specific diet or medication. Dr. Mamic gives the example of fiber. “Not all bacteria can digest the same types of fiber, so not everyone responds in the same way to a high-fiber diet. That’s probably because of differences in their microbiome.”
Another example is the response to the heart failure drug digoxin, which is metabolized by one particular strain of bacteria in the gut. The toxicity or effectiveness of digoxin seems to be influenced by levels of this bacterial strain, and this again can be influenced by diet, Dr. Mamic says.
Manipulating the microbiome as a therapeutic strategy
Microbiome-targeting therapies may also become part of future treatment strategies for many conditions, including heart failure, the review authors say.
Probiotics (foods and dietary supplements that contain live microbes) interact with the gut microbiota to alter host physiology beneficially. Certain probiotics may specifically modulate processes dysregulated in heart failure, as was suggested in a rodent heart failure model in which supplementation with Lactobacillus-containing and Bifidobacterium-containing probiotics resulted in markedly improved cardiac function, the authors report.
However, a randomized trial (GutHeart) of probiotic yeast Saccharomyces boulardii in patients with heart failure found no improvement in cardiac function, compared with standard care.
Commenting on this, Dr. Mamic suggested that a more specific approach may be needed.
“Some of our preliminary data have shown people who have heart failure have severely depleted Bifidobacteria,” Dr. Mamic said. These bacteria are commercially available as a probiotic, and the researchers are planning a study to give patients with heart failure these specific probiotics. “We are trying to find practical ways forward and to be guided by the data. These people have very little Bifidobacteria, and we know that probiotics seem to be accepted best by the host where there is a specific need for them, so this seems like a sensible approach.”
Dr. Mamic does not recommend that heart failure patients take general probiotic products at present, but she tells her patients about the study she is doing. “Probiotics are quite different from each other. It is a very unregulated market. A general probiotic product may not contain the specific bacteria needed.”
Include microbiome data in biobanks
The review calls for more research on the subject and a more systematic approach to collecting data on the microbiome.
“At present for medical research, blood samples are collected, stored, and analyzed routinely. I think we should also be collecting stool samples in the same way to analyze the microbiome,” Dr. Mamic suggests.
“If we can combine that with data from blood tests on various metabolites/cytokines and look at how the microbiome changes over time or with medication, or with diet, and how the host responds including clinically relevant data, that would be really important. Given how quickly the field is growing I would think there would be biobanks including the microbiome in a few years’ time.”
“We need to gather this data. We would be looking for which bacteria are there, what their functionality is, how it changes over time, with diet or medication, and even whether we can use the microbiome data to predict who will respond to a specific drug.”
Dr. Mamic believes that in the future, analysis of the microbiome could be a routine part of deciding what people eat for good health and to characterize patients for personalized therapies.
“It is clear that the microbiome can influence health, and a dysregulated microbiome negatively affects the host, but there is lot of work to do. We need to learn a lot more about it, but we shouldn’t miss the opportunity to do this,” she concluded.
Dr. Mamic reported no disclosures.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Drive, chip, and putt your way to osteoarthritis relief
Taking a swing against arthritis
Osteoarthritis is a tough disease to manage. Exercise helps ease the stiffness and pain of the joints, but at the same time, the disease makes it difficult to do that beneficial exercise. Even a relatively simple activity like jogging can hurt more than it helps. If only there were a low-impact exercise that was incredibly popular among the generally older population who are likely to have arthritis.
We love a good golf study here at LOTME, and a group of Australian and U.K. researchers have provided. Osteoarthritis affects 2 million people in the land down under, making it the most common source of disability there. In that population, only 64% reported their physical health to be good, very good, or excellent. Among the 459 golfers with OA that the study authors surveyed, however, the percentage reporting good health rose to more than 90%.
A similar story emerged when they looked at mental health. Nearly a quarter of nongolfers with OA reported high or very high levels of psychological distress, compared with just 8% of golfers. This pattern of improved physical and mental health remained when the researchers looked at the general, non-OA population.
This isn’t the first time golf’s been connected with improved health, and previous studies have shown golf to reduce the risks of cardiovascular disease, diabetes, and obesity, among other things. Just walking one 18-hole round significantly exceeds the CDC’s recommended 150 minutes of physical activity per week. Go out multiple times a week – leaving the cart and beer at home, American golfers – and you’ll be fit for a lifetime.
The golfers on our staff, however, are still waiting for those mental health benefits to kick in. Because when we’re adding up our scorecard after that string of four double bogeys to end the round, we’re most definitely thinking: “Yes, this sport is reducing my psychological distress. I am having fun right now.”
Battle of the sexes’ intestines
There are, we’re sure you’ve noticed, some differences between males and females. Females, for one thing, have longer small intestines than males. Everybody knows that, right? You didn’t know? Really? … Really?
Well, then, we’re guessing you haven’t read “Hidden diversity: Comparative functional morphology of humans and other species” by Erin A. McKenney, PhD, of North Carolina State University, Raleigh, and associates, which just appeared in PeerJ. We couldn’t put it down, even in the shower – a real page-turner/scroller. (It’s a great way to clean a phone, for those who also like to scroll, text, or talk on the toilet.)
The researchers got out their rulers, calipers, and string and took many measurements of the digestive systems of 45 human cadavers (21 female and 24 male), which were compared with data from 10 rats, 10 pigs, and 10 bullfrogs, which had been collected (the measurements, not the animals) by undergraduate students enrolled in a comparative anatomy laboratory course at the university.
There was little intestinal-length variation among the four-legged subjects, but when it comes to humans, females have “consistently and significantly longer small intestines than males,” the investigators noted.
The women’s small intestines, almost 14 feet long on average, were about a foot longer than the men’s, which suggests that women are better able to extract nutrients from food and “supports the canalization hypothesis, which posits that women are better able to survive during periods of stress,” coauthor Amanda Hale said in a written statement from the school. The way to a man’s heart may be through his stomach, but the way to a woman’s heart is through her duodenum, it seems.
Fascinating stuff, to be sure, but the thing that really caught our eye in the PeerJ article was the authors’ suggestion “that organs behave independently of one another, both within and across species.” Organs behaving independently? A somewhat ominous concept, no doubt, but it does explain a lot of the sounds we hear coming from our guts, which can get pretty frightening, especially on chili night.
Dog walking is dangerous business
Yes, you did read that right. A lot of strange things can send you to the emergency department. Go ahead and add dog walking onto that list.
Investigators from Johns Hopkins University estimate that over 422,000 adults presented to U.S. emergency departments with leash-dependent dog walking-related injuries between 2001 and 2020.
With almost 53% of U.S. households owning at least one dog in 2021-2022 in the wake of the COVID pet boom, this kind of occurrence is becoming more common than you think. The annual number of dog-walking injuries more than quadrupled from 7,300 to 32,000 over the course of the study, and the researchers link that spike to the promotion of dog walking for fitness, along with the boost of ownership itself.
The most common injuries listed in the National Electronic Injury Surveillance System database were finger fracture, traumatic brain injury, and shoulder sprain or strain. These mostly involved falls from being pulled, tripped, or tangled up in the leash while walking. For those aged 65 years and older, traumatic brain injury and hip fracture were the most common.
Women were 50% more likely to sustain a fracture than were men, and dog owners aged 65 and older were three times as likely to fall, twice as likely to get a fracture, and 60% more likely to have brain injury than were younger people. Now, that’s not to say younger people don’t also get hurt. After all, dogs aren’t ageists. The researchers have that data but it’s coming out later.
Meanwhile, the pitfalls involved with just trying to get our daily steps in while letting Muffin do her business have us on the lookout for random squirrels.
Taking a swing against arthritis
Osteoarthritis is a tough disease to manage. Exercise helps ease the stiffness and pain of the joints, but at the same time, the disease makes it difficult to do that beneficial exercise. Even a relatively simple activity like jogging can hurt more than it helps. If only there were a low-impact exercise that was incredibly popular among the generally older population who are likely to have arthritis.
We love a good golf study here at LOTME, and a group of Australian and U.K. researchers have provided. Osteoarthritis affects 2 million people in the land down under, making it the most common source of disability there. In that population, only 64% reported their physical health to be good, very good, or excellent. Among the 459 golfers with OA that the study authors surveyed, however, the percentage reporting good health rose to more than 90%.
A similar story emerged when they looked at mental health. Nearly a quarter of nongolfers with OA reported high or very high levels of psychological distress, compared with just 8% of golfers. This pattern of improved physical and mental health remained when the researchers looked at the general, non-OA population.
This isn’t the first time golf’s been connected with improved health, and previous studies have shown golf to reduce the risks of cardiovascular disease, diabetes, and obesity, among other things. Just walking one 18-hole round significantly exceeds the CDC’s recommended 150 minutes of physical activity per week. Go out multiple times a week – leaving the cart and beer at home, American golfers – and you’ll be fit for a lifetime.
The golfers on our staff, however, are still waiting for those mental health benefits to kick in. Because when we’re adding up our scorecard after that string of four double bogeys to end the round, we’re most definitely thinking: “Yes, this sport is reducing my psychological distress. I am having fun right now.”
Battle of the sexes’ intestines
There are, we’re sure you’ve noticed, some differences between males and females. Females, for one thing, have longer small intestines than males. Everybody knows that, right? You didn’t know? Really? … Really?
Well, then, we’re guessing you haven’t read “Hidden diversity: Comparative functional morphology of humans and other species” by Erin A. McKenney, PhD, of North Carolina State University, Raleigh, and associates, which just appeared in PeerJ. We couldn’t put it down, even in the shower – a real page-turner/scroller. (It’s a great way to clean a phone, for those who also like to scroll, text, or talk on the toilet.)
The researchers got out their rulers, calipers, and string and took many measurements of the digestive systems of 45 human cadavers (21 female and 24 male), which were compared with data from 10 rats, 10 pigs, and 10 bullfrogs, which had been collected (the measurements, not the animals) by undergraduate students enrolled in a comparative anatomy laboratory course at the university.
There was little intestinal-length variation among the four-legged subjects, but when it comes to humans, females have “consistently and significantly longer small intestines than males,” the investigators noted.
The women’s small intestines, almost 14 feet long on average, were about a foot longer than the men’s, which suggests that women are better able to extract nutrients from food and “supports the canalization hypothesis, which posits that women are better able to survive during periods of stress,” coauthor Amanda Hale said in a written statement from the school. The way to a man’s heart may be through his stomach, but the way to a woman’s heart is through her duodenum, it seems.
Fascinating stuff, to be sure, but the thing that really caught our eye in the PeerJ article was the authors’ suggestion “that organs behave independently of one another, both within and across species.” Organs behaving independently? A somewhat ominous concept, no doubt, but it does explain a lot of the sounds we hear coming from our guts, which can get pretty frightening, especially on chili night.
Dog walking is dangerous business
Yes, you did read that right. A lot of strange things can send you to the emergency department. Go ahead and add dog walking onto that list.
Investigators from Johns Hopkins University estimate that over 422,000 adults presented to U.S. emergency departments with leash-dependent dog walking-related injuries between 2001 and 2020.
With almost 53% of U.S. households owning at least one dog in 2021-2022 in the wake of the COVID pet boom, this kind of occurrence is becoming more common than you think. The annual number of dog-walking injuries more than quadrupled from 7,300 to 32,000 over the course of the study, and the researchers link that spike to the promotion of dog walking for fitness, along with the boost of ownership itself.
The most common injuries listed in the National Electronic Injury Surveillance System database were finger fracture, traumatic brain injury, and shoulder sprain or strain. These mostly involved falls from being pulled, tripped, or tangled up in the leash while walking. For those aged 65 years and older, traumatic brain injury and hip fracture were the most common.
Women were 50% more likely to sustain a fracture than were men, and dog owners aged 65 and older were three times as likely to fall, twice as likely to get a fracture, and 60% more likely to have brain injury than were younger people. Now, that’s not to say younger people don’t also get hurt. After all, dogs aren’t ageists. The researchers have that data but it’s coming out later.
Meanwhile, the pitfalls involved with just trying to get our daily steps in while letting Muffin do her business have us on the lookout for random squirrels.
Taking a swing against arthritis
Osteoarthritis is a tough disease to manage. Exercise helps ease the stiffness and pain of the joints, but at the same time, the disease makes it difficult to do that beneficial exercise. Even a relatively simple activity like jogging can hurt more than it helps. If only there were a low-impact exercise that was incredibly popular among the generally older population who are likely to have arthritis.
We love a good golf study here at LOTME, and a group of Australian and U.K. researchers have provided. Osteoarthritis affects 2 million people in the land down under, making it the most common source of disability there. In that population, only 64% reported their physical health to be good, very good, or excellent. Among the 459 golfers with OA that the study authors surveyed, however, the percentage reporting good health rose to more than 90%.
A similar story emerged when they looked at mental health. Nearly a quarter of nongolfers with OA reported high or very high levels of psychological distress, compared with just 8% of golfers. This pattern of improved physical and mental health remained when the researchers looked at the general, non-OA population.
This isn’t the first time golf’s been connected with improved health, and previous studies have shown golf to reduce the risks of cardiovascular disease, diabetes, and obesity, among other things. Just walking one 18-hole round significantly exceeds the CDC’s recommended 150 minutes of physical activity per week. Go out multiple times a week – leaving the cart and beer at home, American golfers – and you’ll be fit for a lifetime.
The golfers on our staff, however, are still waiting for those mental health benefits to kick in. Because when we’re adding up our scorecard after that string of four double bogeys to end the round, we’re most definitely thinking: “Yes, this sport is reducing my psychological distress. I am having fun right now.”
Battle of the sexes’ intestines
There are, we’re sure you’ve noticed, some differences between males and females. Females, for one thing, have longer small intestines than males. Everybody knows that, right? You didn’t know? Really? … Really?
Well, then, we’re guessing you haven’t read “Hidden diversity: Comparative functional morphology of humans and other species” by Erin A. McKenney, PhD, of North Carolina State University, Raleigh, and associates, which just appeared in PeerJ. We couldn’t put it down, even in the shower – a real page-turner/scroller. (It’s a great way to clean a phone, for those who also like to scroll, text, or talk on the toilet.)
The researchers got out their rulers, calipers, and string and took many measurements of the digestive systems of 45 human cadavers (21 female and 24 male), which were compared with data from 10 rats, 10 pigs, and 10 bullfrogs, which had been collected (the measurements, not the animals) by undergraduate students enrolled in a comparative anatomy laboratory course at the university.
There was little intestinal-length variation among the four-legged subjects, but when it comes to humans, females have “consistently and significantly longer small intestines than males,” the investigators noted.
The women’s small intestines, almost 14 feet long on average, were about a foot longer than the men’s, which suggests that women are better able to extract nutrients from food and “supports the canalization hypothesis, which posits that women are better able to survive during periods of stress,” coauthor Amanda Hale said in a written statement from the school. The way to a man’s heart may be through his stomach, but the way to a woman’s heart is through her duodenum, it seems.
Fascinating stuff, to be sure, but the thing that really caught our eye in the PeerJ article was the authors’ suggestion “that organs behave independently of one another, both within and across species.” Organs behaving independently? A somewhat ominous concept, no doubt, but it does explain a lot of the sounds we hear coming from our guts, which can get pretty frightening, especially on chili night.
Dog walking is dangerous business
Yes, you did read that right. A lot of strange things can send you to the emergency department. Go ahead and add dog walking onto that list.
Investigators from Johns Hopkins University estimate that over 422,000 adults presented to U.S. emergency departments with leash-dependent dog walking-related injuries between 2001 and 2020.
With almost 53% of U.S. households owning at least one dog in 2021-2022 in the wake of the COVID pet boom, this kind of occurrence is becoming more common than you think. The annual number of dog-walking injuries more than quadrupled from 7,300 to 32,000 over the course of the study, and the researchers link that spike to the promotion of dog walking for fitness, along with the boost of ownership itself.
The most common injuries listed in the National Electronic Injury Surveillance System database were finger fracture, traumatic brain injury, and shoulder sprain or strain. These mostly involved falls from being pulled, tripped, or tangled up in the leash while walking. For those aged 65 years and older, traumatic brain injury and hip fracture were the most common.
Women were 50% more likely to sustain a fracture than were men, and dog owners aged 65 and older were three times as likely to fall, twice as likely to get a fracture, and 60% more likely to have brain injury than were younger people. Now, that’s not to say younger people don’t also get hurt. After all, dogs aren’t ageists. The researchers have that data but it’s coming out later.
Meanwhile, the pitfalls involved with just trying to get our daily steps in while letting Muffin do her business have us on the lookout for random squirrels.
Botulinum Toxin and Glycopyrrolate Combination Therapy for Hailey-Hailey Disease
To the Editor:
Hailey-Hailey disease (HHD)(also known as familial benign chronic pemphigus) is an inherited autosomal-dominant condition in the family of chronic bullous diseases. It is characterized by flaccid blisters, erosions, and macerated vegetative plaques with a predilection for intertriginous sites. Lesions often are weeping, painful, pruritic, and malodorous, leading to decreased quality of life for patients. Complications of this chronic disease include an increased risk for secondary infection and malignant transformation to squamous cell carcinoma.1
Treatment of HHD remains difficult. Topical steroids, oral steroids, and ablative techniques such as dermabrasion and ablative lasers are the most widely reported therapies. OnabotulinumtoxinA has been described as a successful treatment for patients with HHD, including for disease recalcitrant to other therapies.2 We describe 2 patients with HHD who responded to treatment with intralesional onabotulinumtoxinA injections with and without adjuvant oral glycopyrrolate.
A 54-year-old woman presented with painful flaccid blisters under the breasts (Figure 1A) and in the axillae and groin of 3 weeks’ duration. Biopsy results from this initial visit were consistent with a diagnosis of HHD. The patient reported that the onset of blisters coincided with episodes of severe hyperhidrosis. Therapy with topical and oral steroids, antifungals, antibiotics, and topical aluminum chloride failed to achieve adequate disease control. After a discussion of the risks and benefits, the patient agreed to treatment with injections of onabotulinumtoxinA. At months 0, 3, and 6, the patient received 50 U of onabotulinumtoxinA under the breasts and in the axillae and the groin, for a total of 250 U each session. Each injection consisted of 2.5 U of onabotulinumtoxinA spaced 1-cm apart. Clinical improvement was noted within 2 weeks of initiating neuromodulator therapy. Follow-up at 9 months demonstrated improvement (Figure 1B); however, complete clearance was not achieved, and the patient required ongoing treatment with onabotulinumtoxinA every 3 months.
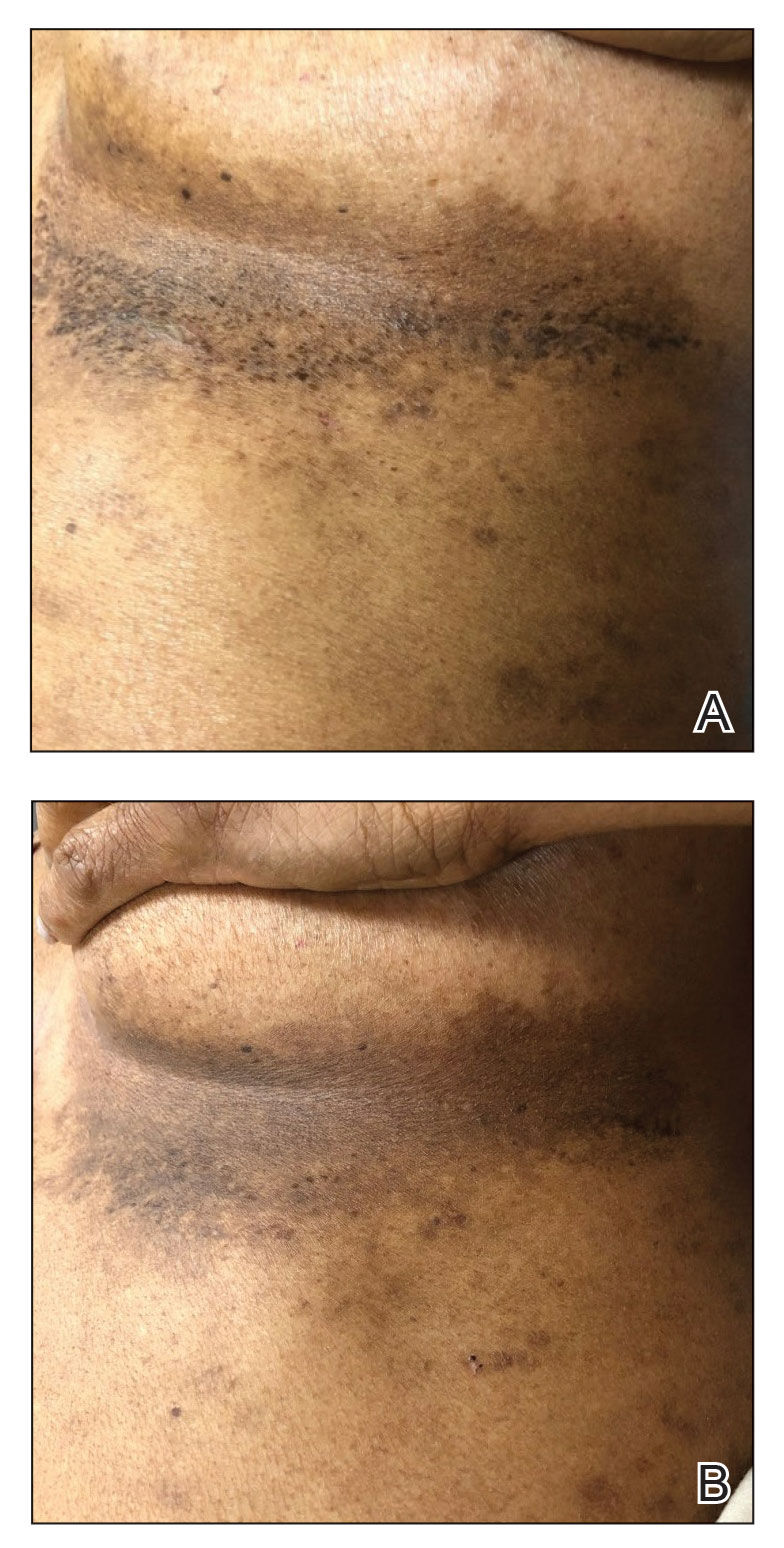
A 43-year-old woman presented with erythematous eroded plaques of the antecubital fossae, axillae, and chest (Figure 2A) of 10 years’ duration. A biopsy from an outside provider demonstrated findings consistent with a diagnosis of HHD. Prior therapies included topical and oral steroids. After a discussion of the risks and benefits, the patient was treated with onabotulinumtoxinA injections in combination with oral glycopyrrolate 5 mg daily. She received 30 U of onabotulinumtoxinA to each axilla, 10 U to each antecubital fossa, and 20 U to the central chest. At 1 month follow-up, the patient reported great improvement in lesion burden and active disease (Figure 2B). Nine months after treatment, her HHD was in complete remission with glycopyrrolate alone and she did not require further therapy with onabotulinumtoxinA.
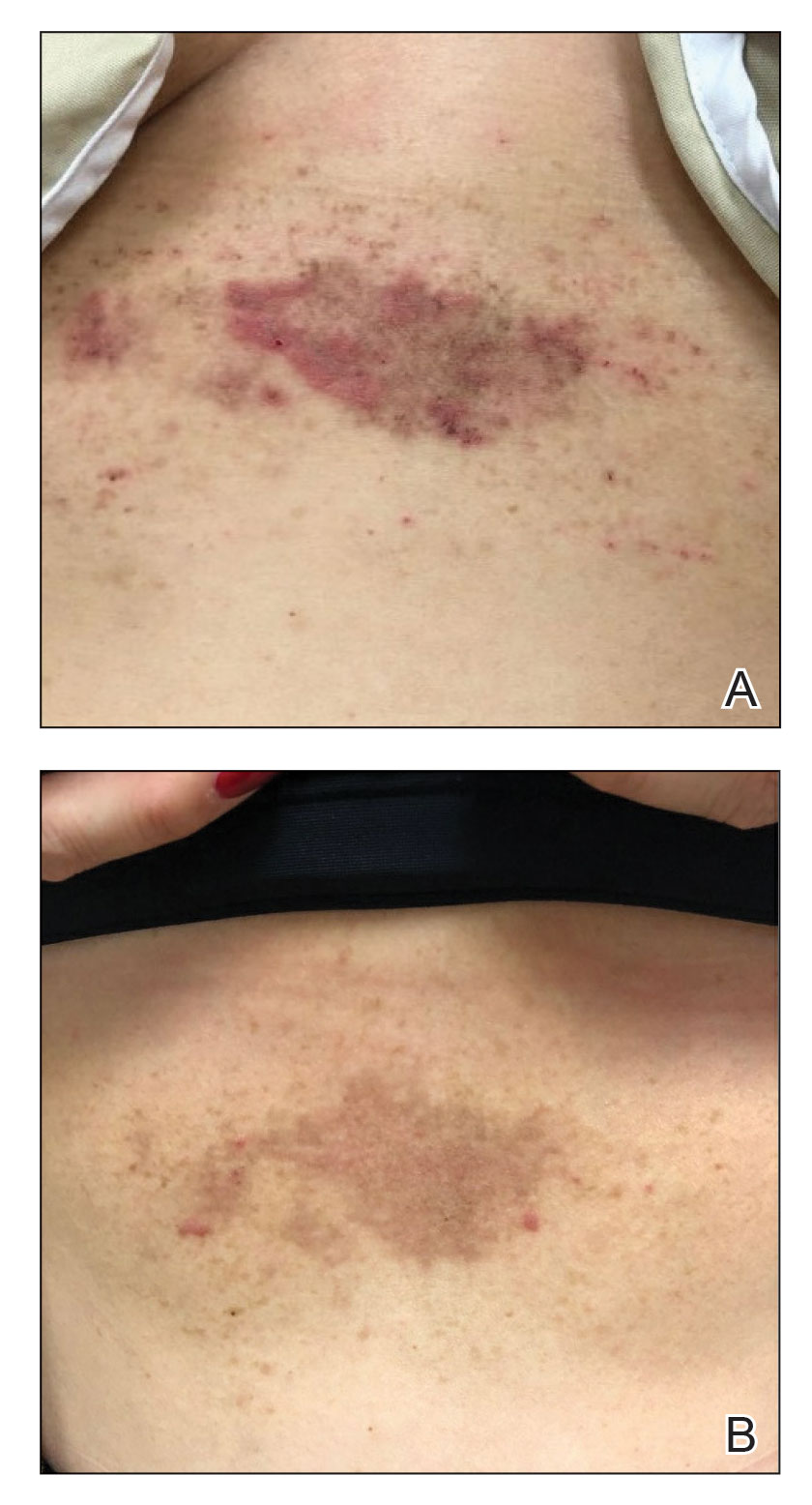
Hailey-Hailey disease has been attributed to mutations of the ATPase secretory pathway Ca2+ transporting 1 gene, ATP2C1, that lead to aberrations in calcium signaling and subsequent impaired adhesion between keratinocytes.2 These compromised cell-cell connections are worsened by the presence of humidity, causing further acantholysis. Chemical denervation of the sweat glands with botulinum toxin has been postulated to improve HHD by reducing moisture in vulnerable areas. Our 2 cases add to the existing literature documenting tangible clinical results that correlate with this hypothesis.3-5
Our second case is unique in that the patient achieved rapid improvement using a combination of onabotulinumtoxinA and glycopyrrolate therapy. Both onabotulinumtoxinA and glycopyrrolate inhibit acetylcholine signaling that is required for sweat production; however, each drug exerts its effect on different zones of the cholinergic pathway, which may partially account for the synergistic effect of onabotulinumtoxinA and glycopyrrolate to improve HHD, as sweating is dually inhibited by the 2 drugs. Additionally, the combined local and systemic administration of these anticholinergic medications may further potentiate the sweat blockade, particularly in areas most prone to disease.
Botulinum toxin for the treatment of HHD is an effective monotherapy. The addition of an oral anticholinergic to local neuromodulator injections may speed symptom resolution and sustain disease remission. Further studies to evaluate this combination are warranted.
- Palmer DD, Perry HO. Benign familial chronic pemphigus. Arch Dermatol. 1962;86:493-502. doi:10.1001/archderm.1962.01590100107020
- Farahnik B, Blattner CM, Mortazie MB, et al. Interventional treatments for Hailey-Hailey disease. J Am Acad Dermatol. 2017;76:551-558.e553. doi:10.1016/j.jaad.2016.08.039
- Bessa GR, Glaziovine TC, Manzoni AP, et al. Hailey-Hailey disease treatment with botulinum toxin type A. An Bras Dermatol. 2010;85:717-722. doi:10.1590/s0365-05962010000500021
- Lapiere JC, Hirsh A, Gordon KB, et al. Botulinum toxin type A for the treatment of axillary Hailey-Hailey disease. Dermatol Surg. 2000;26:371-374. doi:10.1046/j.1524-4725.2000.99278.x
- Koeyers WJ, Van Der Geer S, Krekels G. Botulinum toxin type A as an adjuvant treatment modality for extensive Hailey-Hailey disease. J Dermatolog Treat. 2008;19:251-254. doi:10.1080/09546630801955135
To the Editor:
Hailey-Hailey disease (HHD)(also known as familial benign chronic pemphigus) is an inherited autosomal-dominant condition in the family of chronic bullous diseases. It is characterized by flaccid blisters, erosions, and macerated vegetative plaques with a predilection for intertriginous sites. Lesions often are weeping, painful, pruritic, and malodorous, leading to decreased quality of life for patients. Complications of this chronic disease include an increased risk for secondary infection and malignant transformation to squamous cell carcinoma.1
Treatment of HHD remains difficult. Topical steroids, oral steroids, and ablative techniques such as dermabrasion and ablative lasers are the most widely reported therapies. OnabotulinumtoxinA has been described as a successful treatment for patients with HHD, including for disease recalcitrant to other therapies.2 We describe 2 patients with HHD who responded to treatment with intralesional onabotulinumtoxinA injections with and without adjuvant oral glycopyrrolate.
A 54-year-old woman presented with painful flaccid blisters under the breasts (Figure 1A) and in the axillae and groin of 3 weeks’ duration. Biopsy results from this initial visit were consistent with a diagnosis of HHD. The patient reported that the onset of blisters coincided with episodes of severe hyperhidrosis. Therapy with topical and oral steroids, antifungals, antibiotics, and topical aluminum chloride failed to achieve adequate disease control. After a discussion of the risks and benefits, the patient agreed to treatment with injections of onabotulinumtoxinA. At months 0, 3, and 6, the patient received 50 U of onabotulinumtoxinA under the breasts and in the axillae and the groin, for a total of 250 U each session. Each injection consisted of 2.5 U of onabotulinumtoxinA spaced 1-cm apart. Clinical improvement was noted within 2 weeks of initiating neuromodulator therapy. Follow-up at 9 months demonstrated improvement (Figure 1B); however, complete clearance was not achieved, and the patient required ongoing treatment with onabotulinumtoxinA every 3 months.
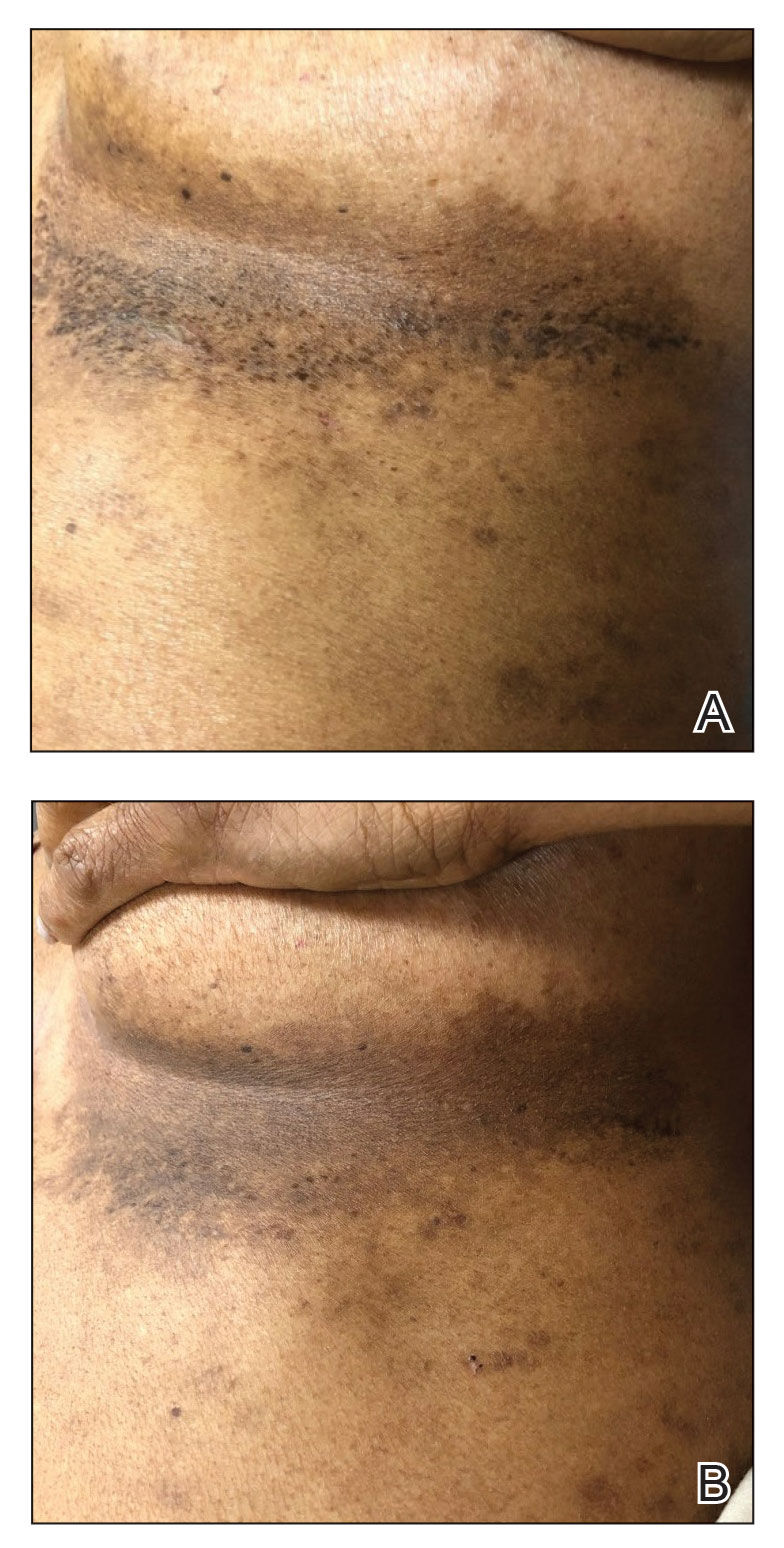
A 43-year-old woman presented with erythematous eroded plaques of the antecubital fossae, axillae, and chest (Figure 2A) of 10 years’ duration. A biopsy from an outside provider demonstrated findings consistent with a diagnosis of HHD. Prior therapies included topical and oral steroids. After a discussion of the risks and benefits, the patient was treated with onabotulinumtoxinA injections in combination with oral glycopyrrolate 5 mg daily. She received 30 U of onabotulinumtoxinA to each axilla, 10 U to each antecubital fossa, and 20 U to the central chest. At 1 month follow-up, the patient reported great improvement in lesion burden and active disease (Figure 2B). Nine months after treatment, her HHD was in complete remission with glycopyrrolate alone and she did not require further therapy with onabotulinumtoxinA.
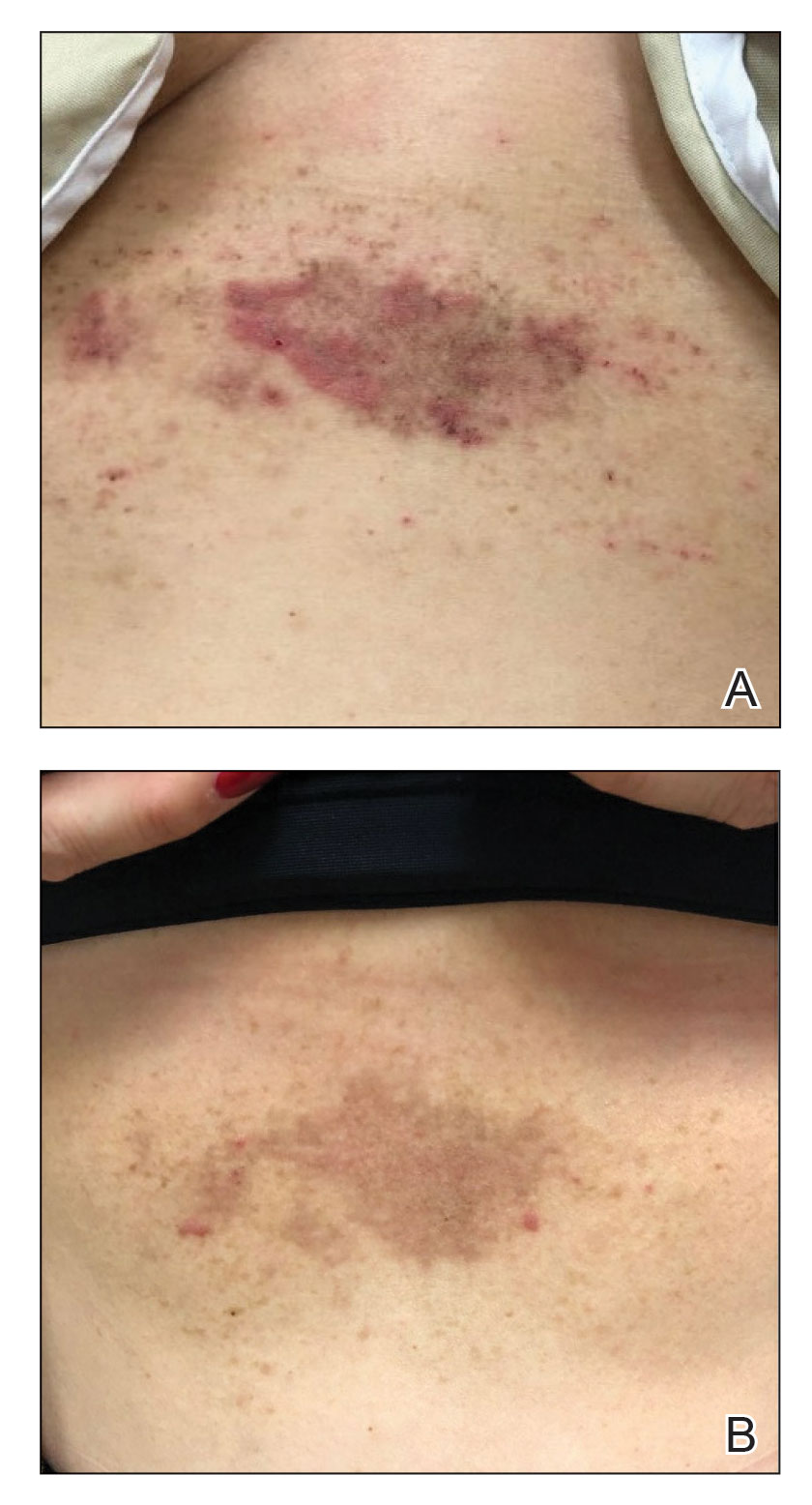
Hailey-Hailey disease has been attributed to mutations of the ATPase secretory pathway Ca2+ transporting 1 gene, ATP2C1, that lead to aberrations in calcium signaling and subsequent impaired adhesion between keratinocytes.2 These compromised cell-cell connections are worsened by the presence of humidity, causing further acantholysis. Chemical denervation of the sweat glands with botulinum toxin has been postulated to improve HHD by reducing moisture in vulnerable areas. Our 2 cases add to the existing literature documenting tangible clinical results that correlate with this hypothesis.3-5
Our second case is unique in that the patient achieved rapid improvement using a combination of onabotulinumtoxinA and glycopyrrolate therapy. Both onabotulinumtoxinA and glycopyrrolate inhibit acetylcholine signaling that is required for sweat production; however, each drug exerts its effect on different zones of the cholinergic pathway, which may partially account for the synergistic effect of onabotulinumtoxinA and glycopyrrolate to improve HHD, as sweating is dually inhibited by the 2 drugs. Additionally, the combined local and systemic administration of these anticholinergic medications may further potentiate the sweat blockade, particularly in areas most prone to disease.
Botulinum toxin for the treatment of HHD is an effective monotherapy. The addition of an oral anticholinergic to local neuromodulator injections may speed symptom resolution and sustain disease remission. Further studies to evaluate this combination are warranted.
To the Editor:
Hailey-Hailey disease (HHD)(also known as familial benign chronic pemphigus) is an inherited autosomal-dominant condition in the family of chronic bullous diseases. It is characterized by flaccid blisters, erosions, and macerated vegetative plaques with a predilection for intertriginous sites. Lesions often are weeping, painful, pruritic, and malodorous, leading to decreased quality of life for patients. Complications of this chronic disease include an increased risk for secondary infection and malignant transformation to squamous cell carcinoma.1
Treatment of HHD remains difficult. Topical steroids, oral steroids, and ablative techniques such as dermabrasion and ablative lasers are the most widely reported therapies. OnabotulinumtoxinA has been described as a successful treatment for patients with HHD, including for disease recalcitrant to other therapies.2 We describe 2 patients with HHD who responded to treatment with intralesional onabotulinumtoxinA injections with and without adjuvant oral glycopyrrolate.
A 54-year-old woman presented with painful flaccid blisters under the breasts (Figure 1A) and in the axillae and groin of 3 weeks’ duration. Biopsy results from this initial visit were consistent with a diagnosis of HHD. The patient reported that the onset of blisters coincided with episodes of severe hyperhidrosis. Therapy with topical and oral steroids, antifungals, antibiotics, and topical aluminum chloride failed to achieve adequate disease control. After a discussion of the risks and benefits, the patient agreed to treatment with injections of onabotulinumtoxinA. At months 0, 3, and 6, the patient received 50 U of onabotulinumtoxinA under the breasts and in the axillae and the groin, for a total of 250 U each session. Each injection consisted of 2.5 U of onabotulinumtoxinA spaced 1-cm apart. Clinical improvement was noted within 2 weeks of initiating neuromodulator therapy. Follow-up at 9 months demonstrated improvement (Figure 1B); however, complete clearance was not achieved, and the patient required ongoing treatment with onabotulinumtoxinA every 3 months.
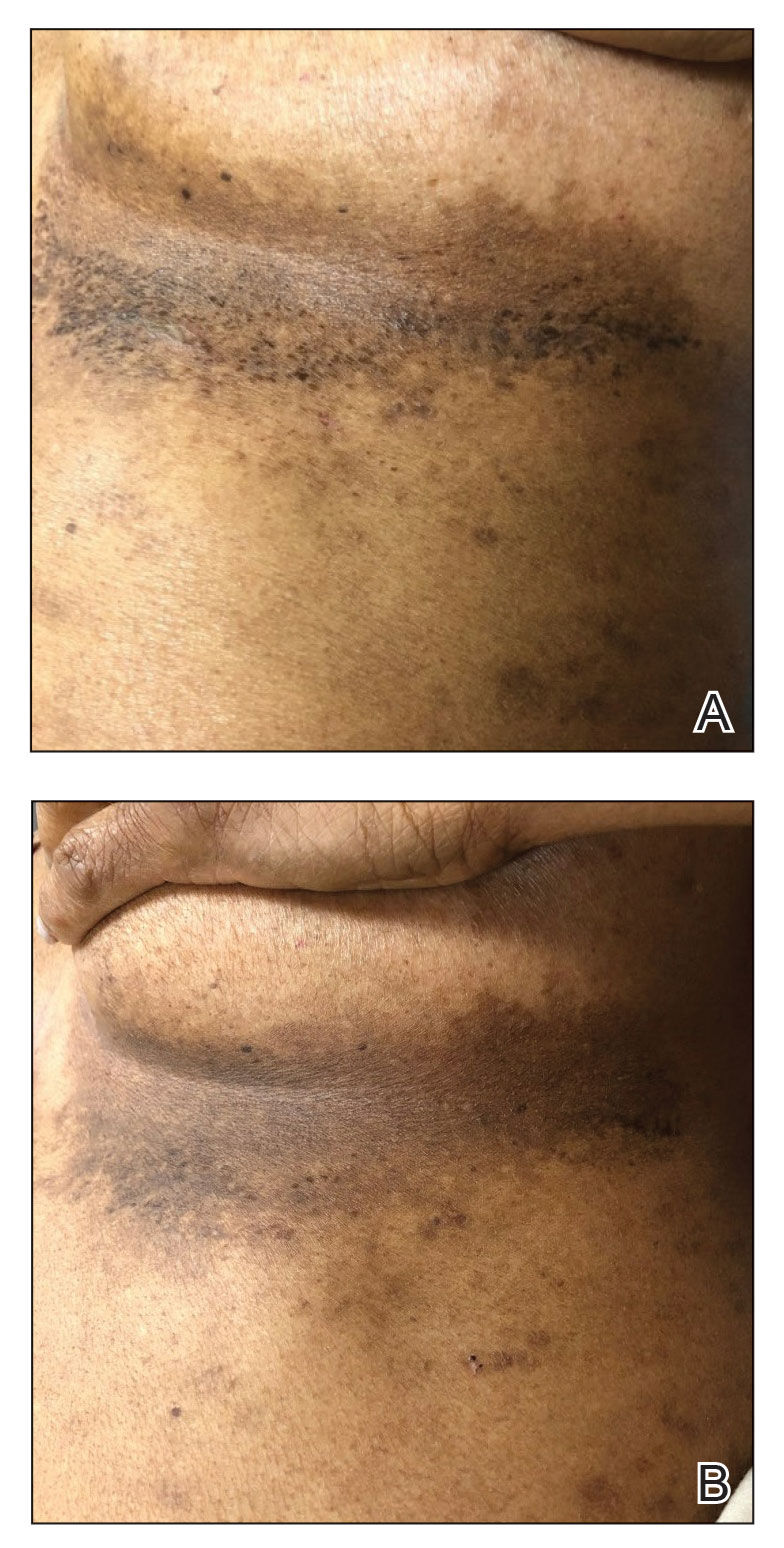
A 43-year-old woman presented with erythematous eroded plaques of the antecubital fossae, axillae, and chest (Figure 2A) of 10 years’ duration. A biopsy from an outside provider demonstrated findings consistent with a diagnosis of HHD. Prior therapies included topical and oral steroids. After a discussion of the risks and benefits, the patient was treated with onabotulinumtoxinA injections in combination with oral glycopyrrolate 5 mg daily. She received 30 U of onabotulinumtoxinA to each axilla, 10 U to each antecubital fossa, and 20 U to the central chest. At 1 month follow-up, the patient reported great improvement in lesion burden and active disease (Figure 2B). Nine months after treatment, her HHD was in complete remission with glycopyrrolate alone and she did not require further therapy with onabotulinumtoxinA.
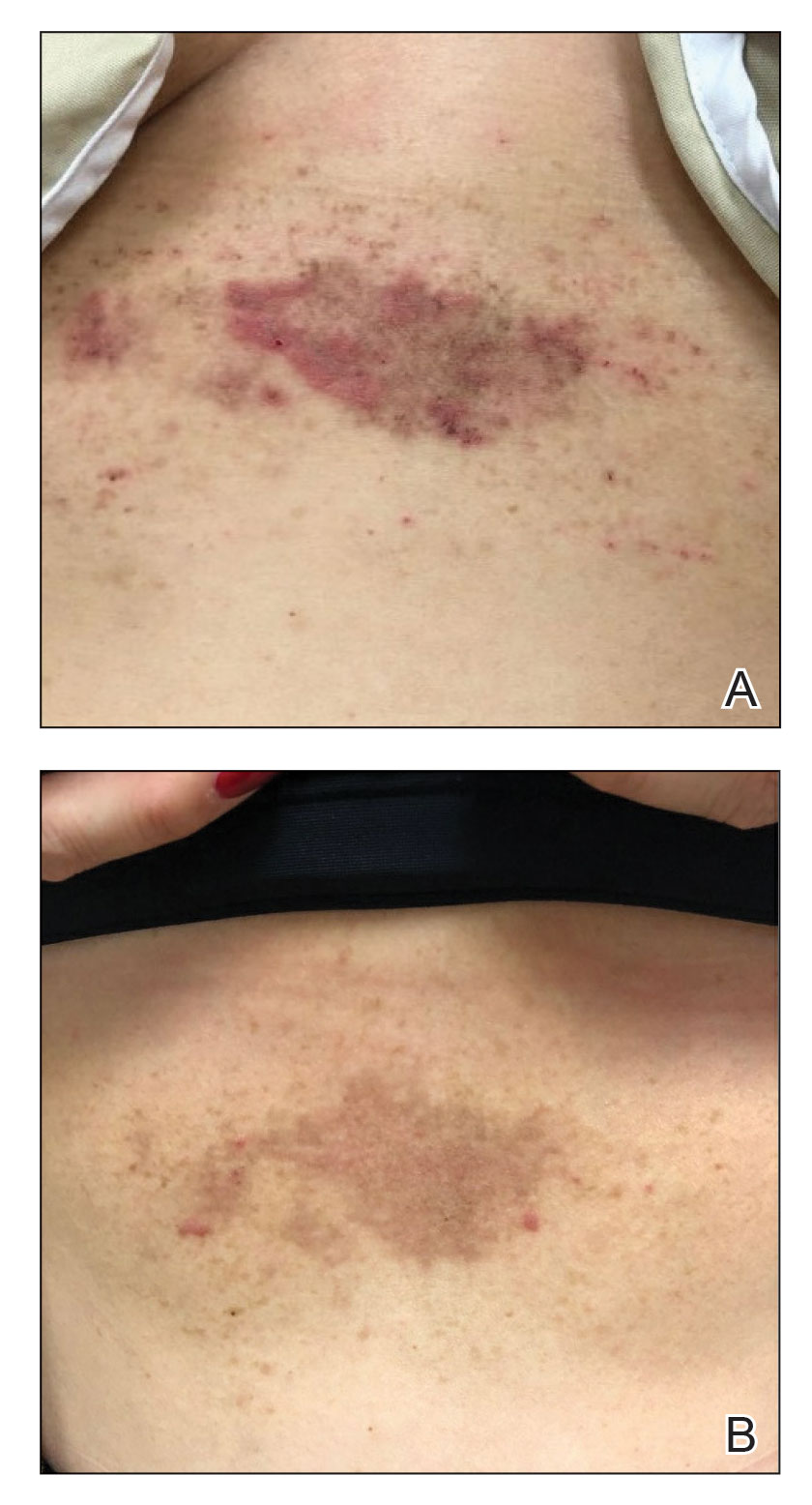
Hailey-Hailey disease has been attributed to mutations of the ATPase secretory pathway Ca2+ transporting 1 gene, ATP2C1, that lead to aberrations in calcium signaling and subsequent impaired adhesion between keratinocytes.2 These compromised cell-cell connections are worsened by the presence of humidity, causing further acantholysis. Chemical denervation of the sweat glands with botulinum toxin has been postulated to improve HHD by reducing moisture in vulnerable areas. Our 2 cases add to the existing literature documenting tangible clinical results that correlate with this hypothesis.3-5
Our second case is unique in that the patient achieved rapid improvement using a combination of onabotulinumtoxinA and glycopyrrolate therapy. Both onabotulinumtoxinA and glycopyrrolate inhibit acetylcholine signaling that is required for sweat production; however, each drug exerts its effect on different zones of the cholinergic pathway, which may partially account for the synergistic effect of onabotulinumtoxinA and glycopyrrolate to improve HHD, as sweating is dually inhibited by the 2 drugs. Additionally, the combined local and systemic administration of these anticholinergic medications may further potentiate the sweat blockade, particularly in areas most prone to disease.
Botulinum toxin for the treatment of HHD is an effective monotherapy. The addition of an oral anticholinergic to local neuromodulator injections may speed symptom resolution and sustain disease remission. Further studies to evaluate this combination are warranted.
- Palmer DD, Perry HO. Benign familial chronic pemphigus. Arch Dermatol. 1962;86:493-502. doi:10.1001/archderm.1962.01590100107020
- Farahnik B, Blattner CM, Mortazie MB, et al. Interventional treatments for Hailey-Hailey disease. J Am Acad Dermatol. 2017;76:551-558.e553. doi:10.1016/j.jaad.2016.08.039
- Bessa GR, Glaziovine TC, Manzoni AP, et al. Hailey-Hailey disease treatment with botulinum toxin type A. An Bras Dermatol. 2010;85:717-722. doi:10.1590/s0365-05962010000500021
- Lapiere JC, Hirsh A, Gordon KB, et al. Botulinum toxin type A for the treatment of axillary Hailey-Hailey disease. Dermatol Surg. 2000;26:371-374. doi:10.1046/j.1524-4725.2000.99278.x
- Koeyers WJ, Van Der Geer S, Krekels G. Botulinum toxin type A as an adjuvant treatment modality for extensive Hailey-Hailey disease. J Dermatolog Treat. 2008;19:251-254. doi:10.1080/09546630801955135
- Palmer DD, Perry HO. Benign familial chronic pemphigus. Arch Dermatol. 1962;86:493-502. doi:10.1001/archderm.1962.01590100107020
- Farahnik B, Blattner CM, Mortazie MB, et al. Interventional treatments for Hailey-Hailey disease. J Am Acad Dermatol. 2017;76:551-558.e553. doi:10.1016/j.jaad.2016.08.039
- Bessa GR, Glaziovine TC, Manzoni AP, et al. Hailey-Hailey disease treatment with botulinum toxin type A. An Bras Dermatol. 2010;85:717-722. doi:10.1590/s0365-05962010000500021
- Lapiere JC, Hirsh A, Gordon KB, et al. Botulinum toxin type A for the treatment of axillary Hailey-Hailey disease. Dermatol Surg. 2000;26:371-374. doi:10.1046/j.1524-4725.2000.99278.x
- Koeyers WJ, Van Der Geer S, Krekels G. Botulinum toxin type A as an adjuvant treatment modality for extensive Hailey-Hailey disease. J Dermatolog Treat. 2008;19:251-254. doi:10.1080/09546630801955135
Practice Points
- Hailey-Hailey disease is associated with decreased quality of life for patients, and current treatment options are limited.
- A combination of local neuromodulator injections and systemic oral anticholinergic therapy may provide sustained disease remission compared to neuromodulator therapy alone.
The newest form of mommy shaming: The 'narcissistic mother'
Narcissists appear to be everywhere. A few minutes on the Internet shows the dangers of narcissistic romantic partners, friends, and employers. Identifying and limiting the reach of their manipulative and self-centered endeavors is cast as both urgent and necessary. The destructive powers of the narcissistic mother are viewed as especially in need of remedy, and any bookstore can reveal the risks they pose: “Will I Ever Be Good Enough? Healing the Daughters of Narcissistic Mothers;” “You’re Not Crazy – It’s Your Mother: Freedom for Daughters of Narcissistic Mothers;” “Healing for Daughters of Narcissistic Mothers: A Practical Guide on How to Recover from the Childhood Trauma of Toxic Relationship with Your Mother and How You Can Handle Her Abuse Now As An Adult” – to name just a few (there are more).
As a psychologist specializing in parental estrangement, I (Dr. Coleman) regularly see letters from adult children explaining their discovery-through-therapy that their mother is a narcissist. The proclamation often comes when the therapist has never met the mother. Typically, the discovery is presented as a justification for ending the relationship with the parent. While these mothers could rightly be accused of being anxious, over-involved, depressed, or hurt by the lack of gratitude or reciprocity, the vast majority are not narcissists.
Which begs the question, why are so many being labeled in this way? Are therapists only now discovering the power of narcissistic mothers? Have they always existed, casting their spells upon unwary children? Are those now-grown children only today able to disentangle themselves from the longstanding, pervasive, and harmful influence of these parents, with the help of therapy? Or is this the newest form of mommy shaming as it engages head-on with our Diagnostic and Statistical Manuals?
We believe it is the latter.
Blaming mothers has a long reach. Mothers have been blamed for causing schizophrenia, autism, homosexuality, and effeminacy in men. While we used to call people selfish and “controlling,” narcissism is a more consequential label as it confers diagnostic validity from the mental health profession. Worse, it suggests an individual beyond reach, where the only answer is distance, containment, or estrangement.
The rise of the narcissistic mother comes during a time when, for the past 4 decades, the average working mother spends more time with her children than stay-at-home moms did in the supposed halcyon days of the 1960s’ middle class, before “parenting” was a common term. A variety of economists and sociologists observed that an increase in parental effort became necessary to launch children into adulthood given the retreat of governmental and corporate support for parents that began in the 1980s.
“The financial and emotional burden on families has grown in ways that were almost unimaginable just a half-century ago,” writes the University of Pennsylvania sociologist Frank Furstenberg in “On a New Schedule: Transitions to Adulthood and Family Change.” In addition, a view of children as vulnerable and in need of intense parental investment gained momentum over the course of the 20th century and has continued unabated into the present. As a result, an environment of intense maternal preoccupation, worry, guilt, and involvement with children’s grades, safety, health, and emotional states – referred to as “helicopter” and “tiger” mothering – grew into the norm across the classes.
While prior generations of parents could, by today’s standards, be viewed as being insufficiently involved, today’s parents have become “over-involved” – aided by the ability of parents to be in constant contact with their adult children through technology. While this shift to a more hands-on, more conscientious parenting has been a boon to parent–adult child relationships in the main, the downside has meant, for some, too much of a good thing. From that perspective, pathologizing a mother’s involvement or her expressions of hurt for that child’s lack of availability provides a shield against the child’s feelings of guilt or obligation.
Diagnoses can serve a social purpose: They can allow individuals to use the authority of our profession to decide who to be close to and who to let go. They can provide insulation against feelings of obligation or guilt. They create a way to label behavior as dysfunctional that in other eras or cultures would be considered normal, even valued. To that extent, diagnoses don’t occur in a cultural void. They are inextricably tied to larger ideals, be they individualistic – as exists in the United States – or collectivist, as exists in many other parts of the world.
While we have decided what parents owe our children, it is unclear what parents might ask in return. To that end, mothers who want more interest, availability, or gratitude today are vulnerable to being cast as selfish, uncaring, needy, and controlling. They can now be viewed as failing in their task of selfless devotion. Their desires for closeness or repair can be regarded as incompatible with the quest for the adult child’s self-fulfillment and identity; her identification with her children too great a barrier to their individuation.
There may well be good reasons to estrange family members for their intolerable behaviors, especially ones who have threatened personal safety. Yet, while there are plenty of problematic parents, few meet the diagnostic criteria of narcissistic personality disorder. More important, such labels can discourage a discussion of boundaries that both the parents and the adult children might find acceptable – which sometimes means asking family members to tolerate behavior or individuals not to their liking.
Diagnoses carry enormous social weight and can facilitate estrangements or negativity to mothers that are far more workable than our patients’ characterization of them might lead them or us to believe. ; it devalues their years of love and dedication, however flawed; and it weakens the fabric of connection that could otherwise exist. Rather than provide a path toward compassion or understanding, “narcissistic mother” just becomes the latest form of mommy shaming.
Dr. Coleman is a clinical psychologist and author of “Rules of Estrangement: Why Adult Children Cut Ties and How to Heal the Conflict” (New York: Penguin Random House, 2021). Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University in Baltimore.
Narcissists appear to be everywhere. A few minutes on the Internet shows the dangers of narcissistic romantic partners, friends, and employers. Identifying and limiting the reach of their manipulative and self-centered endeavors is cast as both urgent and necessary. The destructive powers of the narcissistic mother are viewed as especially in need of remedy, and any bookstore can reveal the risks they pose: “Will I Ever Be Good Enough? Healing the Daughters of Narcissistic Mothers;” “You’re Not Crazy – It’s Your Mother: Freedom for Daughters of Narcissistic Mothers;” “Healing for Daughters of Narcissistic Mothers: A Practical Guide on How to Recover from the Childhood Trauma of Toxic Relationship with Your Mother and How You Can Handle Her Abuse Now As An Adult” – to name just a few (there are more).
As a psychologist specializing in parental estrangement, I (Dr. Coleman) regularly see letters from adult children explaining their discovery-through-therapy that their mother is a narcissist. The proclamation often comes when the therapist has never met the mother. Typically, the discovery is presented as a justification for ending the relationship with the parent. While these mothers could rightly be accused of being anxious, over-involved, depressed, or hurt by the lack of gratitude or reciprocity, the vast majority are not narcissists.
Which begs the question, why are so many being labeled in this way? Are therapists only now discovering the power of narcissistic mothers? Have they always existed, casting their spells upon unwary children? Are those now-grown children only today able to disentangle themselves from the longstanding, pervasive, and harmful influence of these parents, with the help of therapy? Or is this the newest form of mommy shaming as it engages head-on with our Diagnostic and Statistical Manuals?
We believe it is the latter.
Blaming mothers has a long reach. Mothers have been blamed for causing schizophrenia, autism, homosexuality, and effeminacy in men. While we used to call people selfish and “controlling,” narcissism is a more consequential label as it confers diagnostic validity from the mental health profession. Worse, it suggests an individual beyond reach, where the only answer is distance, containment, or estrangement.
The rise of the narcissistic mother comes during a time when, for the past 4 decades, the average working mother spends more time with her children than stay-at-home moms did in the supposed halcyon days of the 1960s’ middle class, before “parenting” was a common term. A variety of economists and sociologists observed that an increase in parental effort became necessary to launch children into adulthood given the retreat of governmental and corporate support for parents that began in the 1980s.
“The financial and emotional burden on families has grown in ways that were almost unimaginable just a half-century ago,” writes the University of Pennsylvania sociologist Frank Furstenberg in “On a New Schedule: Transitions to Adulthood and Family Change.” In addition, a view of children as vulnerable and in need of intense parental investment gained momentum over the course of the 20th century and has continued unabated into the present. As a result, an environment of intense maternal preoccupation, worry, guilt, and involvement with children’s grades, safety, health, and emotional states – referred to as “helicopter” and “tiger” mothering – grew into the norm across the classes.
While prior generations of parents could, by today’s standards, be viewed as being insufficiently involved, today’s parents have become “over-involved” – aided by the ability of parents to be in constant contact with their adult children through technology. While this shift to a more hands-on, more conscientious parenting has been a boon to parent–adult child relationships in the main, the downside has meant, for some, too much of a good thing. From that perspective, pathologizing a mother’s involvement or her expressions of hurt for that child’s lack of availability provides a shield against the child’s feelings of guilt or obligation.
Diagnoses can serve a social purpose: They can allow individuals to use the authority of our profession to decide who to be close to and who to let go. They can provide insulation against feelings of obligation or guilt. They create a way to label behavior as dysfunctional that in other eras or cultures would be considered normal, even valued. To that extent, diagnoses don’t occur in a cultural void. They are inextricably tied to larger ideals, be they individualistic – as exists in the United States – or collectivist, as exists in many other parts of the world.
While we have decided what parents owe our children, it is unclear what parents might ask in return. To that end, mothers who want more interest, availability, or gratitude today are vulnerable to being cast as selfish, uncaring, needy, and controlling. They can now be viewed as failing in their task of selfless devotion. Their desires for closeness or repair can be regarded as incompatible with the quest for the adult child’s self-fulfillment and identity; her identification with her children too great a barrier to their individuation.
There may well be good reasons to estrange family members for their intolerable behaviors, especially ones who have threatened personal safety. Yet, while there are plenty of problematic parents, few meet the diagnostic criteria of narcissistic personality disorder. More important, such labels can discourage a discussion of boundaries that both the parents and the adult children might find acceptable – which sometimes means asking family members to tolerate behavior or individuals not to their liking.
Diagnoses carry enormous social weight and can facilitate estrangements or negativity to mothers that are far more workable than our patients’ characterization of them might lead them or us to believe. ; it devalues their years of love and dedication, however flawed; and it weakens the fabric of connection that could otherwise exist. Rather than provide a path toward compassion or understanding, “narcissistic mother” just becomes the latest form of mommy shaming.
Dr. Coleman is a clinical psychologist and author of “Rules of Estrangement: Why Adult Children Cut Ties and How to Heal the Conflict” (New York: Penguin Random House, 2021). Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University in Baltimore.
Narcissists appear to be everywhere. A few minutes on the Internet shows the dangers of narcissistic romantic partners, friends, and employers. Identifying and limiting the reach of their manipulative and self-centered endeavors is cast as both urgent and necessary. The destructive powers of the narcissistic mother are viewed as especially in need of remedy, and any bookstore can reveal the risks they pose: “Will I Ever Be Good Enough? Healing the Daughters of Narcissistic Mothers;” “You’re Not Crazy – It’s Your Mother: Freedom for Daughters of Narcissistic Mothers;” “Healing for Daughters of Narcissistic Mothers: A Practical Guide on How to Recover from the Childhood Trauma of Toxic Relationship with Your Mother and How You Can Handle Her Abuse Now As An Adult” – to name just a few (there are more).
As a psychologist specializing in parental estrangement, I (Dr. Coleman) regularly see letters from adult children explaining their discovery-through-therapy that their mother is a narcissist. The proclamation often comes when the therapist has never met the mother. Typically, the discovery is presented as a justification for ending the relationship with the parent. While these mothers could rightly be accused of being anxious, over-involved, depressed, or hurt by the lack of gratitude or reciprocity, the vast majority are not narcissists.
Which begs the question, why are so many being labeled in this way? Are therapists only now discovering the power of narcissistic mothers? Have they always existed, casting their spells upon unwary children? Are those now-grown children only today able to disentangle themselves from the longstanding, pervasive, and harmful influence of these parents, with the help of therapy? Or is this the newest form of mommy shaming as it engages head-on with our Diagnostic and Statistical Manuals?
We believe it is the latter.
Blaming mothers has a long reach. Mothers have been blamed for causing schizophrenia, autism, homosexuality, and effeminacy in men. While we used to call people selfish and “controlling,” narcissism is a more consequential label as it confers diagnostic validity from the mental health profession. Worse, it suggests an individual beyond reach, where the only answer is distance, containment, or estrangement.
The rise of the narcissistic mother comes during a time when, for the past 4 decades, the average working mother spends more time with her children than stay-at-home moms did in the supposed halcyon days of the 1960s’ middle class, before “parenting” was a common term. A variety of economists and sociologists observed that an increase in parental effort became necessary to launch children into adulthood given the retreat of governmental and corporate support for parents that began in the 1980s.
“The financial and emotional burden on families has grown in ways that were almost unimaginable just a half-century ago,” writes the University of Pennsylvania sociologist Frank Furstenberg in “On a New Schedule: Transitions to Adulthood and Family Change.” In addition, a view of children as vulnerable and in need of intense parental investment gained momentum over the course of the 20th century and has continued unabated into the present. As a result, an environment of intense maternal preoccupation, worry, guilt, and involvement with children’s grades, safety, health, and emotional states – referred to as “helicopter” and “tiger” mothering – grew into the norm across the classes.
While prior generations of parents could, by today’s standards, be viewed as being insufficiently involved, today’s parents have become “over-involved” – aided by the ability of parents to be in constant contact with their adult children through technology. While this shift to a more hands-on, more conscientious parenting has been a boon to parent–adult child relationships in the main, the downside has meant, for some, too much of a good thing. From that perspective, pathologizing a mother’s involvement or her expressions of hurt for that child’s lack of availability provides a shield against the child’s feelings of guilt or obligation.
Diagnoses can serve a social purpose: They can allow individuals to use the authority of our profession to decide who to be close to and who to let go. They can provide insulation against feelings of obligation or guilt. They create a way to label behavior as dysfunctional that in other eras or cultures would be considered normal, even valued. To that extent, diagnoses don’t occur in a cultural void. They are inextricably tied to larger ideals, be they individualistic – as exists in the United States – or collectivist, as exists in many other parts of the world.
While we have decided what parents owe our children, it is unclear what parents might ask in return. To that end, mothers who want more interest, availability, or gratitude today are vulnerable to being cast as selfish, uncaring, needy, and controlling. They can now be viewed as failing in their task of selfless devotion. Their desires for closeness or repair can be regarded as incompatible with the quest for the adult child’s self-fulfillment and identity; her identification with her children too great a barrier to their individuation.
There may well be good reasons to estrange family members for their intolerable behaviors, especially ones who have threatened personal safety. Yet, while there are plenty of problematic parents, few meet the diagnostic criteria of narcissistic personality disorder. More important, such labels can discourage a discussion of boundaries that both the parents and the adult children might find acceptable – which sometimes means asking family members to tolerate behavior or individuals not to their liking.
Diagnoses carry enormous social weight and can facilitate estrangements or negativity to mothers that are far more workable than our patients’ characterization of them might lead them or us to believe. ; it devalues their years of love and dedication, however flawed; and it weakens the fabric of connection that could otherwise exist. Rather than provide a path toward compassion or understanding, “narcissistic mother” just becomes the latest form of mommy shaming.
Dr. Coleman is a clinical psychologist and author of “Rules of Estrangement: Why Adult Children Cut Ties and How to Heal the Conflict” (New York: Penguin Random House, 2021). Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University in Baltimore.
Small study finds IPL-radiofrequency combination effective for dry eye disease
PHOENIX – and improved meibum quality in both upper and lower eyelids, results from an ongoing, novel study showed.
Dry eye disease affects a large proportion of people in the United States “and the factors that contribute to that are certainly not going away,” lead study author James G. Chelnis MD, said at the annual conference of the American Society for Laser Medicine and Surgery, where he presented the results during an abstract session. “Prepandemic, we used to have meetings in person; now most are on a computer screen,” a common risk factor for worsening dry eyes, he said. Telltale dry eye symptoms include blurry vision, irritation, and corneal damage – mostly caused by meibomian gland dysfunction – which impacts the quality and quantity of meibum secreted. Common treatments include warm compresses, doxycycline, and artificial tears.
While some studies have shown IPL is helpful in treating dry eye disease caused by meibomian gland dysfunction, little information is available on its use alone or in combination with topical RF to preserve and improve the function of meibomian glands, said Dr. Chelnis, an ophthalmic plastic surgeon in New York City. “The theory here is that the radiofrequency would be able to vibrate the water molecules inside the meibomian glands, which would allow you to turn over the meibum faster, as well as improve the blink reflex response by building supporting collagen,” he said. “Our novel study explores the ability of this combined modality treatment to improve upon meibomian gland health.”
Study design, results
Dr. Chelnis and his colleagues enrolled 11 individuals with a previous diagnosis of dry eye disease and meibomian gland dysfunction with Ocular Surface Disease Index (OSDI) survey scores higher than 23, which indicate at least moderate dry eye symptoms. Inclusion criteria were being 22 years of age or older, signs of meibomian gland dysfunction as detected by biomicroscopy, a modified meibomian gland score over 12 in the lower eyelid of at least one eye, and type I-IV skin.
All patients received four treatments (each 2 weeks apart) of IPL to the lower eyelid, surrounding malar region, and nose, followed by 7 minutes of topical RF treatments at 1 MHz and 4 MHz extending to the inferior, lateral, and superior orbital rim. Evaluation of meibomian gland expression and quality of meibum upon expression was conducted following each treatment session, with a final evaluation 4 weeks after the final treatment session.
Meibum quality was evaluated on a scale of 0-3 representing clear (0), cloudy (1), inspissated (2), and blocked (3) meibum, respectively.
Following treatment, meibomian gland expression and meibum quality improved in all eyelids in all 11 patients. Specifically, in the right eye, the number of upper lid expressible glands increased from an average of 13 to 27.9 and the number of lower lid expressible glands increased from an average of 14.6 to 28.2; and in the left eye, the number of upper lid expressible glands increased from an average of 13.3 to 27.3 and the number of lower lid expressible glands increased from an average of 14.8 to 26.8 (P < .001 for all associations).
The overall percentage improvement in meibomian gland expression in the right eye was 82.7% for the upper lids and 136.6% for the lower lids, and in the left eye, 82.9% for the upper lids, and 112.2% for the lower lids.
When comparing upper against lower lids, meibomian gland expression increased 124.4% and 82.8%, respectively. Meibum quality improved in all four eyelids, although upper eyelids displayed a superior improvement compared with lower eyelids.
“We are finding that combining IPL plus RF produces a more complete and comprehensive improvement in the quality of their meibomian gland health, and as such, their dry eyes,” with “a large decrease in their symptom profile,” he concluded.
More patients to be studied
Dr. Chelnis acknowledged certain limitations of the study, including the small number of patients, but he and his colleagues have added an additional clinical site to expand the sample size. “Larger scale studies are needed to evaluate long-term effectiveness of IPL plus RF as well as a comparison with other treatment options.”
During a question-and-answer session Mathew M. Avram, MD, JD, director of laser, cosmetics, and dermatologic surgery at Massachusetts General Hospital, Boston, who served as one of the abstract session moderators, asked Dr. Chelnis to comment on what the mechanism of action of the IPL-RF combination in improving meibomian gland health.
“It’s not fully understood, but part of it is improved vascularity at the lid margin,” said Dr. Chelnis, who holds a faculty position in the department of ophthalmology at Icahn School of Medicine at Mount Sinai, New York. “Your ocular surface is sort of like your screen door; it catches everything that’s in the environment. An increase in vascularity and immunologic cytokines occurs in response to that. If you’re looking at the eye with a slit lamp, you can see a lot of vascularity that occurs at the lid margin and crowds the meibomian glands. When you decrease that crowding and immunogenic response, you move towards a normally functioning lid margin.”
Dr. Chelnis disclosed that he is a consultant to or an adviser for Lumenis, Horizon Therapeutics, and Soniquence.
PHOENIX – and improved meibum quality in both upper and lower eyelids, results from an ongoing, novel study showed.
Dry eye disease affects a large proportion of people in the United States “and the factors that contribute to that are certainly not going away,” lead study author James G. Chelnis MD, said at the annual conference of the American Society for Laser Medicine and Surgery, where he presented the results during an abstract session. “Prepandemic, we used to have meetings in person; now most are on a computer screen,” a common risk factor for worsening dry eyes, he said. Telltale dry eye symptoms include blurry vision, irritation, and corneal damage – mostly caused by meibomian gland dysfunction – which impacts the quality and quantity of meibum secreted. Common treatments include warm compresses, doxycycline, and artificial tears.
While some studies have shown IPL is helpful in treating dry eye disease caused by meibomian gland dysfunction, little information is available on its use alone or in combination with topical RF to preserve and improve the function of meibomian glands, said Dr. Chelnis, an ophthalmic plastic surgeon in New York City. “The theory here is that the radiofrequency would be able to vibrate the water molecules inside the meibomian glands, which would allow you to turn over the meibum faster, as well as improve the blink reflex response by building supporting collagen,” he said. “Our novel study explores the ability of this combined modality treatment to improve upon meibomian gland health.”
Study design, results
Dr. Chelnis and his colleagues enrolled 11 individuals with a previous diagnosis of dry eye disease and meibomian gland dysfunction with Ocular Surface Disease Index (OSDI) survey scores higher than 23, which indicate at least moderate dry eye symptoms. Inclusion criteria were being 22 years of age or older, signs of meibomian gland dysfunction as detected by biomicroscopy, a modified meibomian gland score over 12 in the lower eyelid of at least one eye, and type I-IV skin.
All patients received four treatments (each 2 weeks apart) of IPL to the lower eyelid, surrounding malar region, and nose, followed by 7 minutes of topical RF treatments at 1 MHz and 4 MHz extending to the inferior, lateral, and superior orbital rim. Evaluation of meibomian gland expression and quality of meibum upon expression was conducted following each treatment session, with a final evaluation 4 weeks after the final treatment session.
Meibum quality was evaluated on a scale of 0-3 representing clear (0), cloudy (1), inspissated (2), and blocked (3) meibum, respectively.
Following treatment, meibomian gland expression and meibum quality improved in all eyelids in all 11 patients. Specifically, in the right eye, the number of upper lid expressible glands increased from an average of 13 to 27.9 and the number of lower lid expressible glands increased from an average of 14.6 to 28.2; and in the left eye, the number of upper lid expressible glands increased from an average of 13.3 to 27.3 and the number of lower lid expressible glands increased from an average of 14.8 to 26.8 (P < .001 for all associations).
The overall percentage improvement in meibomian gland expression in the right eye was 82.7% for the upper lids and 136.6% for the lower lids, and in the left eye, 82.9% for the upper lids, and 112.2% for the lower lids.
When comparing upper against lower lids, meibomian gland expression increased 124.4% and 82.8%, respectively. Meibum quality improved in all four eyelids, although upper eyelids displayed a superior improvement compared with lower eyelids.
“We are finding that combining IPL plus RF produces a more complete and comprehensive improvement in the quality of their meibomian gland health, and as such, their dry eyes,” with “a large decrease in their symptom profile,” he concluded.
More patients to be studied
Dr. Chelnis acknowledged certain limitations of the study, including the small number of patients, but he and his colleagues have added an additional clinical site to expand the sample size. “Larger scale studies are needed to evaluate long-term effectiveness of IPL plus RF as well as a comparison with other treatment options.”
During a question-and-answer session Mathew M. Avram, MD, JD, director of laser, cosmetics, and dermatologic surgery at Massachusetts General Hospital, Boston, who served as one of the abstract session moderators, asked Dr. Chelnis to comment on what the mechanism of action of the IPL-RF combination in improving meibomian gland health.
“It’s not fully understood, but part of it is improved vascularity at the lid margin,” said Dr. Chelnis, who holds a faculty position in the department of ophthalmology at Icahn School of Medicine at Mount Sinai, New York. “Your ocular surface is sort of like your screen door; it catches everything that’s in the environment. An increase in vascularity and immunologic cytokines occurs in response to that. If you’re looking at the eye with a slit lamp, you can see a lot of vascularity that occurs at the lid margin and crowds the meibomian glands. When you decrease that crowding and immunogenic response, you move towards a normally functioning lid margin.”
Dr. Chelnis disclosed that he is a consultant to or an adviser for Lumenis, Horizon Therapeutics, and Soniquence.
PHOENIX – and improved meibum quality in both upper and lower eyelids, results from an ongoing, novel study showed.
Dry eye disease affects a large proportion of people in the United States “and the factors that contribute to that are certainly not going away,” lead study author James G. Chelnis MD, said at the annual conference of the American Society for Laser Medicine and Surgery, where he presented the results during an abstract session. “Prepandemic, we used to have meetings in person; now most are on a computer screen,” a common risk factor for worsening dry eyes, he said. Telltale dry eye symptoms include blurry vision, irritation, and corneal damage – mostly caused by meibomian gland dysfunction – which impacts the quality and quantity of meibum secreted. Common treatments include warm compresses, doxycycline, and artificial tears.
While some studies have shown IPL is helpful in treating dry eye disease caused by meibomian gland dysfunction, little information is available on its use alone or in combination with topical RF to preserve and improve the function of meibomian glands, said Dr. Chelnis, an ophthalmic plastic surgeon in New York City. “The theory here is that the radiofrequency would be able to vibrate the water molecules inside the meibomian glands, which would allow you to turn over the meibum faster, as well as improve the blink reflex response by building supporting collagen,” he said. “Our novel study explores the ability of this combined modality treatment to improve upon meibomian gland health.”
Study design, results
Dr. Chelnis and his colleagues enrolled 11 individuals with a previous diagnosis of dry eye disease and meibomian gland dysfunction with Ocular Surface Disease Index (OSDI) survey scores higher than 23, which indicate at least moderate dry eye symptoms. Inclusion criteria were being 22 years of age or older, signs of meibomian gland dysfunction as detected by biomicroscopy, a modified meibomian gland score over 12 in the lower eyelid of at least one eye, and type I-IV skin.
All patients received four treatments (each 2 weeks apart) of IPL to the lower eyelid, surrounding malar region, and nose, followed by 7 minutes of topical RF treatments at 1 MHz and 4 MHz extending to the inferior, lateral, and superior orbital rim. Evaluation of meibomian gland expression and quality of meibum upon expression was conducted following each treatment session, with a final evaluation 4 weeks after the final treatment session.
Meibum quality was evaluated on a scale of 0-3 representing clear (0), cloudy (1), inspissated (2), and blocked (3) meibum, respectively.
Following treatment, meibomian gland expression and meibum quality improved in all eyelids in all 11 patients. Specifically, in the right eye, the number of upper lid expressible glands increased from an average of 13 to 27.9 and the number of lower lid expressible glands increased from an average of 14.6 to 28.2; and in the left eye, the number of upper lid expressible glands increased from an average of 13.3 to 27.3 and the number of lower lid expressible glands increased from an average of 14.8 to 26.8 (P < .001 for all associations).
The overall percentage improvement in meibomian gland expression in the right eye was 82.7% for the upper lids and 136.6% for the lower lids, and in the left eye, 82.9% for the upper lids, and 112.2% for the lower lids.
When comparing upper against lower lids, meibomian gland expression increased 124.4% and 82.8%, respectively. Meibum quality improved in all four eyelids, although upper eyelids displayed a superior improvement compared with lower eyelids.
“We are finding that combining IPL plus RF produces a more complete and comprehensive improvement in the quality of their meibomian gland health, and as such, their dry eyes,” with “a large decrease in their symptom profile,” he concluded.
More patients to be studied
Dr. Chelnis acknowledged certain limitations of the study, including the small number of patients, but he and his colleagues have added an additional clinical site to expand the sample size. “Larger scale studies are needed to evaluate long-term effectiveness of IPL plus RF as well as a comparison with other treatment options.”
During a question-and-answer session Mathew M. Avram, MD, JD, director of laser, cosmetics, and dermatologic surgery at Massachusetts General Hospital, Boston, who served as one of the abstract session moderators, asked Dr. Chelnis to comment on what the mechanism of action of the IPL-RF combination in improving meibomian gland health.
“It’s not fully understood, but part of it is improved vascularity at the lid margin,” said Dr. Chelnis, who holds a faculty position in the department of ophthalmology at Icahn School of Medicine at Mount Sinai, New York. “Your ocular surface is sort of like your screen door; it catches everything that’s in the environment. An increase in vascularity and immunologic cytokines occurs in response to that. If you’re looking at the eye with a slit lamp, you can see a lot of vascularity that occurs at the lid margin and crowds the meibomian glands. When you decrease that crowding and immunogenic response, you move towards a normally functioning lid margin.”
Dr. Chelnis disclosed that he is a consultant to or an adviser for Lumenis, Horizon Therapeutics, and Soniquence.
AT ASLMS 2023
How safe is the blackout rage gallon drinking trend?
This discussion was recorded on April 6, 2023. This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining us today is Dr. Lewis Nelson, professor and chair of emergency medicine at Rutgers New Jersey Medical School and a certified medical toxicologist.
Today, we will be discussing an important and disturbing Gen Z trend circulating on social media, known as blackout rage gallon, or BORG.
Welcome, Lewis.
Lewis S. Nelson, MD: Thanks for having me.
Dr. Glatter: Thanks so much for joining us. This trend that’s been circulating on social media is really disturbing. It has elements that focus on binge drinking: Talking about taking a jug; emptying half of it out; and putting one fifth of vodka and some electrolytes, caffeine, or other things too is just incredibly disturbing. Teens and parents are looking at this. I’ll let you jump into the discussion.
Dr. Nelson: You’re totally right, it is disturbing. Binge drinking is a huge problem in this country in general. It’s a particular problem with young people – teenagers and young adults. I don’t think people appreciate the dangers associated with binge drinking, such as the amount of alcohol they consume and some of the unintended consequences of doing that.
To frame things quickly, we think there are probably around six people a day in the United States who die of alcohol poisoning. Alcohol poisoning basically is binge drinking to such an extent that you die of the alcohol itself. You’re not dying of a car crash or doing something that injures you. You’re dying of the alcohol. You’re drinking so much that your breathing slows, it stops, you have heart rhythm disturbances, and so on. It totals about 2,200 people a year in the United States.
Dr. Glatter: That’s alarming. For this trend, their argument is that half of the gallon is water. Therefore, I’m fine. I can drink it over 8-12 hours and it’s not an issue. How would you respond to that?
Dr. Nelson: Well, alcohol is alcohol. It’s all about how much you take in over what time period. I guess, in concept, it could be safer if you do it right. That’s not the way it’s been, so to speak, marketed on the various social media platforms. It’s meant to be a way to protect yourself from having your drink spiked or eating or ingesting contaminants from other people’s mouths when you share glasses or dip cups into communal pots like jungle juice or something.
Clearly, if you’re going to drink a large amount of alcohol over a short or long period of time, you do run the risk of having significant consequences, including bad decision-making if you’re just a little drunk all the way down to that of the complications you described about alcohol poisoning.
Dr. Glatter: There has been a comment made that this could be a form of harm reduction. The point of harm reduction is that we run trials, we validate it, and we test it. This, certainly in my mind, is no form of true harm reduction. I think you would agree.
Dr. Nelson: Many things that are marketed as harm reduction aren’t. There could be some aspects of this that could be considered harm reduction. You may believe – and there’s no reason not to – that protecting your drink is a good idea. If you’re at a bar and you leave your glass open and somebody put something in it, you can be drugged. Drug-facilitated sexual assault, for example, is a big issue. That means you have to leave your glass unattended. If you tend to your glass, it’s probably fine. One of the ways of harm reduction they mention is that by having a cap and having this bottle with you at all times, that can’t happen.
Now, in fairness, by far the drug most commonly associated with sexual assault is alcohol. It’s not gamma-hydroxybutyrate or ketamine. It’s not the other things that people are concerned about. Those happen, but those are small problems in the big picture. It’s drinking too much.
A form of harm reduction that you can comment on perhaps is that you make this drink concoction yourself, so you know what is in there. You can take that bottle, pour out half the water, and fill up the other half with water and nobody’s going to know. More likely, the way they say you should do it is you take your gallon jug, you pour it out, and you fill it up with one fifth of vodka.
One fifth of vodka is the same amount of volume as a bottle of wine. At 750 mL, that’s a huge amount of alcohol. If you measure the number of shots in that bottle, it’s about 17 shots. Even if you drink that over 6 hours, that’s still several shots an hour. That’s a large amount of alcohol. You might do two or three shots once and then not drink for a few hours. To sit and drink two or three shots an hour for 6 hours, that’s just an exceptional amount of alcohol.
They flavorize it and add caffeine, which only adds to the risk. It doesn’t make it in any way safer. With the volume, 1 gal of water or equivalent over a short period of time in and of itself could be a problem. There’s a large amount of mismessaging here. Whether something’s harm reduction, it could flip around to be easily construed or understood as being harmful.
Not to mention, the idea that when you make something safer, one of the unintended consequences of harm reduction is what we call risk compensation. This is best probably described as what’s called the Peltzman effect. The way that we think about airbags and seatbelts is that they’re going to reduce car crash deaths; and they do, but people drive faster and more recklessly because they know they’re safe.
This is a well-described problem in epidemiology: You expect a certain amount of harm reduction through some implemented process, but you don’t meet that because people take increased risks.
Dr. Glatter: Right. The idea of not developing a hangover is common among many teens and 20-somethings, thinking that because there’s hydration there, because half of it is water, it’s just not going to happen. There’s your “harm reduction,” but your judgment’s impaired. It’s day drinking at its best, all day long. Then someone has the idea to get behind the wheel. These are the disastrous consequences that we all fear.
Dr. Nelson: There is a great example, perhaps of an unintended consequence of harm reduction. By putting caffeine in it, depending on how much caffeine you put in, some of these mixtures can have up to 1,000 mg of caffeine. Remember, a cup of coffee is about 1-200 mg, so you’re talking about several cups of coffee. The idea is that you will not be able to sense, as you normally do, how drunk you are. You’re not going to be a sleepy drunk, you’re going to be an awake drunk.
The idea that you’re going to have to drive so you’re going to drink a strong cup of black coffee before you go driving, you’re not going to drive any better. I can assure you that. You’re going to be more awake, perhaps, and not fall asleep at the wheel, but you’re still going to have psychomotor impairment. Your judgment is going to be impaired. There’s nothing good that comes with adding caffeine except that you’re going to be awake.
From a hangover perspective, there are many things that we’ve guessed at or suggested as either prevention or cures for hangovers. I don’t doubt that you’re going to have some volume depletion if you drink a large amount of alcohol. Alcohol’s a diuretic, so you’re going to lose more volume than you bring in.
Hydrating is probably always a good idea, but there is hydrating and then there’s overhydrating. We don’t need volumes like that. If you drink a cup or two of water, you’re probably fine. You don’t need to drink half a gallon of water. That can lead to problems like delusional hyponatremia, and so forth. There’s not any clear benefit to doing it.
If you want to prevent a hangover, one of the ways you might do it is by using vodka. There are nice data that show that clear alcohols typically, particularly vodka, don’t have many of the congeners that make the specific forms of alcohol what they are. Bourbon smells and tastes like bourbon because of these little molecules, these alkalis and ketones and amino acids and things that make it taste and smell the way it does. That’s true for all the other alcohols.
Vodka has the least amount of that. Even wine and beer have those in them, but vodka is basically alcohol mixed with water. It’s probably the least hangover-prone of all the alcohols; but still, if you drink a lot of vodka, you’re going to have a hangover. It’s just a dose-response curve to how much alcohol you drink, to how drunk you get, and to how much of a hangover you’re going to have.
Dr. Glatter: The hangover is really what it’s about because people want to be functional the next day. There are many companies out there that market hangover remedies, but people are using this as the hangover remedy in a way that’s socially accepted. That’s a good point you make.
The question is how do we get the message out to parents and teens? What’s the best way you feel to really sound the alarm here?
Dr. Nelson: These are challenging issues. We face this all the time with all the sorts of social media in particular. Most parents are not as savvy on social media as their kids are. You have to know what your children are doing. You should know what they’re listening to and watching. You do have to pay attention to the media directed at parents that will inform you a little bit about what your kids are doing. You have to talk with your kids and make sure they understand what it is that they’re doing.
We do this with our kids for some things. Hopefully, we talk about drinking, smoking, sex, and other things with our children (like driving if they get to that stage) and make sure they understand what the risks are and how to mitigate those risks. Being an attentive parent is part of it.
Sometimes you need outside messengers to do it. We’d like to believe that these social media companies are able to police themselves – at least they pay lip service to the fact they do. They have warnings that they’ll take things down that aren’t socially appropriate. Whether they do or not, I don’t know, because you keep seeing things about BORG on these media sites. If they are doing it, they’re not doing it efficiently or quickly enough.
Dr. Glatter: There has to be some censorship. These are young persons who are impressionable, who have developing brains, who are looking at this, thinking that if it’s out there on social media, such as TikTok or Instagram, then it’s okay to do so. That message has to be driven home.
Dr. Nelson: That’s a great point, and it’s tough. We know there’s been debate over the liability of social media or what they post, and whether or not they should be held liable like a more conventional media company or not. That’s politics and philosophy, and we’re probably not going to solve it here.
All these things wind up going viral and there’s probably got to be some filter on things that go viral. Maybe they need to have a bit more attentiveness to that when those things start happening. Now, clearly not every one of these is viral. When you think about some of the challenges we’ve seen in the past, such as the Tide Pod challenge and cinnamon challenge, some of these things could be quickly figured out to be dangerous.
I remember that the ice bucket challenge for amyotrophic lateral sclerosis was pretty benign. You pour a bucket of water over your head, and people aren’t really getting hurt. That’s fun and good, and let people go out and do that. That could pass through the filter. When you start to see people drinking excessive amounts of alcohol, it doesn’t take an emergency physician to know that’s not a good thing. Any parent should know that if my kid drinks half a bottle or a bottle of vodka over a short period of time, that just can’t be okay.
Dr. Glatter: It’s a public health issue. That’s what we need to elevate it to because ultimately that’s what it impacts: welfare and safety.
Speaking of buckets, there’s a new bucket challenge, wherein unsuspecting people have a bucket put on their head, can’t breathe, and then pass out. There’s been a number of these reported and actually filmed on social media. Here’s another example of dangerous types of behavior that essentially are a form of assault. Unsuspecting people suffer injuries from young children and teens trying to play pranks.
Again, had there not been this medium, we wouldn’t necessarily see the extent of the injuries. I guess going forward, the next step would be to send a message to colleges that there should be some form of warning if this trend is seen, at least from a public health standpoint.
Dr. Nelson: Education is a necessary thing to do, but it’s almost never the real solution to a problem. We can educate people as best we can that they need to do things right. At some point, we’re going to need to regulate it or manage it somehow.
Whether it’s through a carrot or a stick approach, or whether you want to give people kudos for doing the right thing or punish them for doing something wrong, that’s a tough decision to make and one that is going to be made by a parent or guardian, a school official, or law enforcement. Somehow, we have to figure out how to make this happen.
There’s not going to be a single size that fits all for this. At some level, we have to do something to educate and regulate. The balance between those two things is going to be political and philosophical in nature.
Dr. Glatter: Right, and the element of peer pressure and conformity in this is really part of the element. If we try to remove that aspect of it, then often these trends would go away. That aspect of conformity and peer pressure is instrumental in fueling these trends. Maybe we can make a full gallon of water be the trend without any alcohol in there.
Dr. Nelson: We say water is only water, but as a medical toxicologist, I can tell you that one of the foundations in medical toxicology is that everything is toxic. It’s just the dose that determines the toxicity. Oxygen is toxic, water is toxic. Everything’s toxic if you take enough of it.
We know that whether it’s psychogenic or intentional, polydipsia by drinking excessive amounts of water, especially without electrolytes, is one of the reasons they say you should add electrolytes. That’s all relative as well, because depending on the electrolyte and how much you put in and things like that, that could also become dangerous. Drinking excessive amounts of water like they’re suggesting, which sounds like a good thing to prevent hangover and so on, can in and of itself be a problem too.
Dr. Glatter: Right, and we know that there’s no magic bullet for a hangover. Obviously, abstinence is the only thing that truly works.
Dr. Nelson: Or moderation.
Dr. Glatter: Until research proves further.
Thank you so much. You’ve made some really important points. Thank you for talking about the BORG phenomenon, how it relates to society in general, and what we can do to try to change people’s perception of alcohol and the bigger picture of binge drinking. I really appreciate it.
Dr. Nelson: Thanks, Rob, for having me. It’s an important topic and hopefully we can get a handle on this. I appreciate your time.
Dr. Glatter is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Hofstra University, Hempstead, N.Y. Dr. Nelson is professor and chair of the department of emergency medicine and chief of the division of medical toxicology at Rutgers New Jersey Medical School, Newark. He is a member of the board of directors of the American Board of Emergency Medicine, the Accreditation Council for Continuing Medical Education, and Association of Academic Chairs in Emergency Medicine and is past-president of the American College of Medical Toxicology. Dr. Glatter and Dr. Nelson disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
This discussion was recorded on April 6, 2023. This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining us today is Dr. Lewis Nelson, professor and chair of emergency medicine at Rutgers New Jersey Medical School and a certified medical toxicologist.
Today, we will be discussing an important and disturbing Gen Z trend circulating on social media, known as blackout rage gallon, or BORG.
Welcome, Lewis.
Lewis S. Nelson, MD: Thanks for having me.
Dr. Glatter: Thanks so much for joining us. This trend that’s been circulating on social media is really disturbing. It has elements that focus on binge drinking: Talking about taking a jug; emptying half of it out; and putting one fifth of vodka and some electrolytes, caffeine, or other things too is just incredibly disturbing. Teens and parents are looking at this. I’ll let you jump into the discussion.
Dr. Nelson: You’re totally right, it is disturbing. Binge drinking is a huge problem in this country in general. It’s a particular problem with young people – teenagers and young adults. I don’t think people appreciate the dangers associated with binge drinking, such as the amount of alcohol they consume and some of the unintended consequences of doing that.
To frame things quickly, we think there are probably around six people a day in the United States who die of alcohol poisoning. Alcohol poisoning basically is binge drinking to such an extent that you die of the alcohol itself. You’re not dying of a car crash or doing something that injures you. You’re dying of the alcohol. You’re drinking so much that your breathing slows, it stops, you have heart rhythm disturbances, and so on. It totals about 2,200 people a year in the United States.
Dr. Glatter: That’s alarming. For this trend, their argument is that half of the gallon is water. Therefore, I’m fine. I can drink it over 8-12 hours and it’s not an issue. How would you respond to that?
Dr. Nelson: Well, alcohol is alcohol. It’s all about how much you take in over what time period. I guess, in concept, it could be safer if you do it right. That’s not the way it’s been, so to speak, marketed on the various social media platforms. It’s meant to be a way to protect yourself from having your drink spiked or eating or ingesting contaminants from other people’s mouths when you share glasses or dip cups into communal pots like jungle juice or something.
Clearly, if you’re going to drink a large amount of alcohol over a short or long period of time, you do run the risk of having significant consequences, including bad decision-making if you’re just a little drunk all the way down to that of the complications you described about alcohol poisoning.
Dr. Glatter: There has been a comment made that this could be a form of harm reduction. The point of harm reduction is that we run trials, we validate it, and we test it. This, certainly in my mind, is no form of true harm reduction. I think you would agree.
Dr. Nelson: Many things that are marketed as harm reduction aren’t. There could be some aspects of this that could be considered harm reduction. You may believe – and there’s no reason not to – that protecting your drink is a good idea. If you’re at a bar and you leave your glass open and somebody put something in it, you can be drugged. Drug-facilitated sexual assault, for example, is a big issue. That means you have to leave your glass unattended. If you tend to your glass, it’s probably fine. One of the ways of harm reduction they mention is that by having a cap and having this bottle with you at all times, that can’t happen.
Now, in fairness, by far the drug most commonly associated with sexual assault is alcohol. It’s not gamma-hydroxybutyrate or ketamine. It’s not the other things that people are concerned about. Those happen, but those are small problems in the big picture. It’s drinking too much.
A form of harm reduction that you can comment on perhaps is that you make this drink concoction yourself, so you know what is in there. You can take that bottle, pour out half the water, and fill up the other half with water and nobody’s going to know. More likely, the way they say you should do it is you take your gallon jug, you pour it out, and you fill it up with one fifth of vodka.
One fifth of vodka is the same amount of volume as a bottle of wine. At 750 mL, that’s a huge amount of alcohol. If you measure the number of shots in that bottle, it’s about 17 shots. Even if you drink that over 6 hours, that’s still several shots an hour. That’s a large amount of alcohol. You might do two or three shots once and then not drink for a few hours. To sit and drink two or three shots an hour for 6 hours, that’s just an exceptional amount of alcohol.
They flavorize it and add caffeine, which only adds to the risk. It doesn’t make it in any way safer. With the volume, 1 gal of water or equivalent over a short period of time in and of itself could be a problem. There’s a large amount of mismessaging here. Whether something’s harm reduction, it could flip around to be easily construed or understood as being harmful.
Not to mention, the idea that when you make something safer, one of the unintended consequences of harm reduction is what we call risk compensation. This is best probably described as what’s called the Peltzman effect. The way that we think about airbags and seatbelts is that they’re going to reduce car crash deaths; and they do, but people drive faster and more recklessly because they know they’re safe.
This is a well-described problem in epidemiology: You expect a certain amount of harm reduction through some implemented process, but you don’t meet that because people take increased risks.
Dr. Glatter: Right. The idea of not developing a hangover is common among many teens and 20-somethings, thinking that because there’s hydration there, because half of it is water, it’s just not going to happen. There’s your “harm reduction,” but your judgment’s impaired. It’s day drinking at its best, all day long. Then someone has the idea to get behind the wheel. These are the disastrous consequences that we all fear.
Dr. Nelson: There is a great example, perhaps of an unintended consequence of harm reduction. By putting caffeine in it, depending on how much caffeine you put in, some of these mixtures can have up to 1,000 mg of caffeine. Remember, a cup of coffee is about 1-200 mg, so you’re talking about several cups of coffee. The idea is that you will not be able to sense, as you normally do, how drunk you are. You’re not going to be a sleepy drunk, you’re going to be an awake drunk.
The idea that you’re going to have to drive so you’re going to drink a strong cup of black coffee before you go driving, you’re not going to drive any better. I can assure you that. You’re going to be more awake, perhaps, and not fall asleep at the wheel, but you’re still going to have psychomotor impairment. Your judgment is going to be impaired. There’s nothing good that comes with adding caffeine except that you’re going to be awake.
From a hangover perspective, there are many things that we’ve guessed at or suggested as either prevention or cures for hangovers. I don’t doubt that you’re going to have some volume depletion if you drink a large amount of alcohol. Alcohol’s a diuretic, so you’re going to lose more volume than you bring in.
Hydrating is probably always a good idea, but there is hydrating and then there’s overhydrating. We don’t need volumes like that. If you drink a cup or two of water, you’re probably fine. You don’t need to drink half a gallon of water. That can lead to problems like delusional hyponatremia, and so forth. There’s not any clear benefit to doing it.
If you want to prevent a hangover, one of the ways you might do it is by using vodka. There are nice data that show that clear alcohols typically, particularly vodka, don’t have many of the congeners that make the specific forms of alcohol what they are. Bourbon smells and tastes like bourbon because of these little molecules, these alkalis and ketones and amino acids and things that make it taste and smell the way it does. That’s true for all the other alcohols.
Vodka has the least amount of that. Even wine and beer have those in them, but vodka is basically alcohol mixed with water. It’s probably the least hangover-prone of all the alcohols; but still, if you drink a lot of vodka, you’re going to have a hangover. It’s just a dose-response curve to how much alcohol you drink, to how drunk you get, and to how much of a hangover you’re going to have.
Dr. Glatter: The hangover is really what it’s about because people want to be functional the next day. There are many companies out there that market hangover remedies, but people are using this as the hangover remedy in a way that’s socially accepted. That’s a good point you make.
The question is how do we get the message out to parents and teens? What’s the best way you feel to really sound the alarm here?
Dr. Nelson: These are challenging issues. We face this all the time with all the sorts of social media in particular. Most parents are not as savvy on social media as their kids are. You have to know what your children are doing. You should know what they’re listening to and watching. You do have to pay attention to the media directed at parents that will inform you a little bit about what your kids are doing. You have to talk with your kids and make sure they understand what it is that they’re doing.
We do this with our kids for some things. Hopefully, we talk about drinking, smoking, sex, and other things with our children (like driving if they get to that stage) and make sure they understand what the risks are and how to mitigate those risks. Being an attentive parent is part of it.
Sometimes you need outside messengers to do it. We’d like to believe that these social media companies are able to police themselves – at least they pay lip service to the fact they do. They have warnings that they’ll take things down that aren’t socially appropriate. Whether they do or not, I don’t know, because you keep seeing things about BORG on these media sites. If they are doing it, they’re not doing it efficiently or quickly enough.
Dr. Glatter: There has to be some censorship. These are young persons who are impressionable, who have developing brains, who are looking at this, thinking that if it’s out there on social media, such as TikTok or Instagram, then it’s okay to do so. That message has to be driven home.
Dr. Nelson: That’s a great point, and it’s tough. We know there’s been debate over the liability of social media or what they post, and whether or not they should be held liable like a more conventional media company or not. That’s politics and philosophy, and we’re probably not going to solve it here.
All these things wind up going viral and there’s probably got to be some filter on things that go viral. Maybe they need to have a bit more attentiveness to that when those things start happening. Now, clearly not every one of these is viral. When you think about some of the challenges we’ve seen in the past, such as the Tide Pod challenge and cinnamon challenge, some of these things could be quickly figured out to be dangerous.
I remember that the ice bucket challenge for amyotrophic lateral sclerosis was pretty benign. You pour a bucket of water over your head, and people aren’t really getting hurt. That’s fun and good, and let people go out and do that. That could pass through the filter. When you start to see people drinking excessive amounts of alcohol, it doesn’t take an emergency physician to know that’s not a good thing. Any parent should know that if my kid drinks half a bottle or a bottle of vodka over a short period of time, that just can’t be okay.
Dr. Glatter: It’s a public health issue. That’s what we need to elevate it to because ultimately that’s what it impacts: welfare and safety.
Speaking of buckets, there’s a new bucket challenge, wherein unsuspecting people have a bucket put on their head, can’t breathe, and then pass out. There’s been a number of these reported and actually filmed on social media. Here’s another example of dangerous types of behavior that essentially are a form of assault. Unsuspecting people suffer injuries from young children and teens trying to play pranks.
Again, had there not been this medium, we wouldn’t necessarily see the extent of the injuries. I guess going forward, the next step would be to send a message to colleges that there should be some form of warning if this trend is seen, at least from a public health standpoint.
Dr. Nelson: Education is a necessary thing to do, but it’s almost never the real solution to a problem. We can educate people as best we can that they need to do things right. At some point, we’re going to need to regulate it or manage it somehow.
Whether it’s through a carrot or a stick approach, or whether you want to give people kudos for doing the right thing or punish them for doing something wrong, that’s a tough decision to make and one that is going to be made by a parent or guardian, a school official, or law enforcement. Somehow, we have to figure out how to make this happen.
There’s not going to be a single size that fits all for this. At some level, we have to do something to educate and regulate. The balance between those two things is going to be political and philosophical in nature.
Dr. Glatter: Right, and the element of peer pressure and conformity in this is really part of the element. If we try to remove that aspect of it, then often these trends would go away. That aspect of conformity and peer pressure is instrumental in fueling these trends. Maybe we can make a full gallon of water be the trend without any alcohol in there.
Dr. Nelson: We say water is only water, but as a medical toxicologist, I can tell you that one of the foundations in medical toxicology is that everything is toxic. It’s just the dose that determines the toxicity. Oxygen is toxic, water is toxic. Everything’s toxic if you take enough of it.
We know that whether it’s psychogenic or intentional, polydipsia by drinking excessive amounts of water, especially without electrolytes, is one of the reasons they say you should add electrolytes. That’s all relative as well, because depending on the electrolyte and how much you put in and things like that, that could also become dangerous. Drinking excessive amounts of water like they’re suggesting, which sounds like a good thing to prevent hangover and so on, can in and of itself be a problem too.
Dr. Glatter: Right, and we know that there’s no magic bullet for a hangover. Obviously, abstinence is the only thing that truly works.
Dr. Nelson: Or moderation.
Dr. Glatter: Until research proves further.
Thank you so much. You’ve made some really important points. Thank you for talking about the BORG phenomenon, how it relates to society in general, and what we can do to try to change people’s perception of alcohol and the bigger picture of binge drinking. I really appreciate it.
Dr. Nelson: Thanks, Rob, for having me. It’s an important topic and hopefully we can get a handle on this. I appreciate your time.
Dr. Glatter is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Hofstra University, Hempstead, N.Y. Dr. Nelson is professor and chair of the department of emergency medicine and chief of the division of medical toxicology at Rutgers New Jersey Medical School, Newark. He is a member of the board of directors of the American Board of Emergency Medicine, the Accreditation Council for Continuing Medical Education, and Association of Academic Chairs in Emergency Medicine and is past-president of the American College of Medical Toxicology. Dr. Glatter and Dr. Nelson disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
This discussion was recorded on April 6, 2023. This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining us today is Dr. Lewis Nelson, professor and chair of emergency medicine at Rutgers New Jersey Medical School and a certified medical toxicologist.
Today, we will be discussing an important and disturbing Gen Z trend circulating on social media, known as blackout rage gallon, or BORG.
Welcome, Lewis.
Lewis S. Nelson, MD: Thanks for having me.
Dr. Glatter: Thanks so much for joining us. This trend that’s been circulating on social media is really disturbing. It has elements that focus on binge drinking: Talking about taking a jug; emptying half of it out; and putting one fifth of vodka and some electrolytes, caffeine, or other things too is just incredibly disturbing. Teens and parents are looking at this. I’ll let you jump into the discussion.
Dr. Nelson: You’re totally right, it is disturbing. Binge drinking is a huge problem in this country in general. It’s a particular problem with young people – teenagers and young adults. I don’t think people appreciate the dangers associated with binge drinking, such as the amount of alcohol they consume and some of the unintended consequences of doing that.
To frame things quickly, we think there are probably around six people a day in the United States who die of alcohol poisoning. Alcohol poisoning basically is binge drinking to such an extent that you die of the alcohol itself. You’re not dying of a car crash or doing something that injures you. You’re dying of the alcohol. You’re drinking so much that your breathing slows, it stops, you have heart rhythm disturbances, and so on. It totals about 2,200 people a year in the United States.
Dr. Glatter: That’s alarming. For this trend, their argument is that half of the gallon is water. Therefore, I’m fine. I can drink it over 8-12 hours and it’s not an issue. How would you respond to that?
Dr. Nelson: Well, alcohol is alcohol. It’s all about how much you take in over what time period. I guess, in concept, it could be safer if you do it right. That’s not the way it’s been, so to speak, marketed on the various social media platforms. It’s meant to be a way to protect yourself from having your drink spiked or eating or ingesting contaminants from other people’s mouths when you share glasses or dip cups into communal pots like jungle juice or something.
Clearly, if you’re going to drink a large amount of alcohol over a short or long period of time, you do run the risk of having significant consequences, including bad decision-making if you’re just a little drunk all the way down to that of the complications you described about alcohol poisoning.
Dr. Glatter: There has been a comment made that this could be a form of harm reduction. The point of harm reduction is that we run trials, we validate it, and we test it. This, certainly in my mind, is no form of true harm reduction. I think you would agree.
Dr. Nelson: Many things that are marketed as harm reduction aren’t. There could be some aspects of this that could be considered harm reduction. You may believe – and there’s no reason not to – that protecting your drink is a good idea. If you’re at a bar and you leave your glass open and somebody put something in it, you can be drugged. Drug-facilitated sexual assault, for example, is a big issue. That means you have to leave your glass unattended. If you tend to your glass, it’s probably fine. One of the ways of harm reduction they mention is that by having a cap and having this bottle with you at all times, that can’t happen.
Now, in fairness, by far the drug most commonly associated with sexual assault is alcohol. It’s not gamma-hydroxybutyrate or ketamine. It’s not the other things that people are concerned about. Those happen, but those are small problems in the big picture. It’s drinking too much.
A form of harm reduction that you can comment on perhaps is that you make this drink concoction yourself, so you know what is in there. You can take that bottle, pour out half the water, and fill up the other half with water and nobody’s going to know. More likely, the way they say you should do it is you take your gallon jug, you pour it out, and you fill it up with one fifth of vodka.
One fifth of vodka is the same amount of volume as a bottle of wine. At 750 mL, that’s a huge amount of alcohol. If you measure the number of shots in that bottle, it’s about 17 shots. Even if you drink that over 6 hours, that’s still several shots an hour. That’s a large amount of alcohol. You might do two or three shots once and then not drink for a few hours. To sit and drink two or three shots an hour for 6 hours, that’s just an exceptional amount of alcohol.
They flavorize it and add caffeine, which only adds to the risk. It doesn’t make it in any way safer. With the volume, 1 gal of water or equivalent over a short period of time in and of itself could be a problem. There’s a large amount of mismessaging here. Whether something’s harm reduction, it could flip around to be easily construed or understood as being harmful.
Not to mention, the idea that when you make something safer, one of the unintended consequences of harm reduction is what we call risk compensation. This is best probably described as what’s called the Peltzman effect. The way that we think about airbags and seatbelts is that they’re going to reduce car crash deaths; and they do, but people drive faster and more recklessly because they know they’re safe.
This is a well-described problem in epidemiology: You expect a certain amount of harm reduction through some implemented process, but you don’t meet that because people take increased risks.
Dr. Glatter: Right. The idea of not developing a hangover is common among many teens and 20-somethings, thinking that because there’s hydration there, because half of it is water, it’s just not going to happen. There’s your “harm reduction,” but your judgment’s impaired. It’s day drinking at its best, all day long. Then someone has the idea to get behind the wheel. These are the disastrous consequences that we all fear.
Dr. Nelson: There is a great example, perhaps of an unintended consequence of harm reduction. By putting caffeine in it, depending on how much caffeine you put in, some of these mixtures can have up to 1,000 mg of caffeine. Remember, a cup of coffee is about 1-200 mg, so you’re talking about several cups of coffee. The idea is that you will not be able to sense, as you normally do, how drunk you are. You’re not going to be a sleepy drunk, you’re going to be an awake drunk.
The idea that you’re going to have to drive so you’re going to drink a strong cup of black coffee before you go driving, you’re not going to drive any better. I can assure you that. You’re going to be more awake, perhaps, and not fall asleep at the wheel, but you’re still going to have psychomotor impairment. Your judgment is going to be impaired. There’s nothing good that comes with adding caffeine except that you’re going to be awake.
From a hangover perspective, there are many things that we’ve guessed at or suggested as either prevention or cures for hangovers. I don’t doubt that you’re going to have some volume depletion if you drink a large amount of alcohol. Alcohol’s a diuretic, so you’re going to lose more volume than you bring in.
Hydrating is probably always a good idea, but there is hydrating and then there’s overhydrating. We don’t need volumes like that. If you drink a cup or two of water, you’re probably fine. You don’t need to drink half a gallon of water. That can lead to problems like delusional hyponatremia, and so forth. There’s not any clear benefit to doing it.
If you want to prevent a hangover, one of the ways you might do it is by using vodka. There are nice data that show that clear alcohols typically, particularly vodka, don’t have many of the congeners that make the specific forms of alcohol what they are. Bourbon smells and tastes like bourbon because of these little molecules, these alkalis and ketones and amino acids and things that make it taste and smell the way it does. That’s true for all the other alcohols.
Vodka has the least amount of that. Even wine and beer have those in them, but vodka is basically alcohol mixed with water. It’s probably the least hangover-prone of all the alcohols; but still, if you drink a lot of vodka, you’re going to have a hangover. It’s just a dose-response curve to how much alcohol you drink, to how drunk you get, and to how much of a hangover you’re going to have.
Dr. Glatter: The hangover is really what it’s about because people want to be functional the next day. There are many companies out there that market hangover remedies, but people are using this as the hangover remedy in a way that’s socially accepted. That’s a good point you make.
The question is how do we get the message out to parents and teens? What’s the best way you feel to really sound the alarm here?
Dr. Nelson: These are challenging issues. We face this all the time with all the sorts of social media in particular. Most parents are not as savvy on social media as their kids are. You have to know what your children are doing. You should know what they’re listening to and watching. You do have to pay attention to the media directed at parents that will inform you a little bit about what your kids are doing. You have to talk with your kids and make sure they understand what it is that they’re doing.
We do this with our kids for some things. Hopefully, we talk about drinking, smoking, sex, and other things with our children (like driving if they get to that stage) and make sure they understand what the risks are and how to mitigate those risks. Being an attentive parent is part of it.
Sometimes you need outside messengers to do it. We’d like to believe that these social media companies are able to police themselves – at least they pay lip service to the fact they do. They have warnings that they’ll take things down that aren’t socially appropriate. Whether they do or not, I don’t know, because you keep seeing things about BORG on these media sites. If they are doing it, they’re not doing it efficiently or quickly enough.
Dr. Glatter: There has to be some censorship. These are young persons who are impressionable, who have developing brains, who are looking at this, thinking that if it’s out there on social media, such as TikTok or Instagram, then it’s okay to do so. That message has to be driven home.
Dr. Nelson: That’s a great point, and it’s tough. We know there’s been debate over the liability of social media or what they post, and whether or not they should be held liable like a more conventional media company or not. That’s politics and philosophy, and we’re probably not going to solve it here.
All these things wind up going viral and there’s probably got to be some filter on things that go viral. Maybe they need to have a bit more attentiveness to that when those things start happening. Now, clearly not every one of these is viral. When you think about some of the challenges we’ve seen in the past, such as the Tide Pod challenge and cinnamon challenge, some of these things could be quickly figured out to be dangerous.
I remember that the ice bucket challenge for amyotrophic lateral sclerosis was pretty benign. You pour a bucket of water over your head, and people aren’t really getting hurt. That’s fun and good, and let people go out and do that. That could pass through the filter. When you start to see people drinking excessive amounts of alcohol, it doesn’t take an emergency physician to know that’s not a good thing. Any parent should know that if my kid drinks half a bottle or a bottle of vodka over a short period of time, that just can’t be okay.
Dr. Glatter: It’s a public health issue. That’s what we need to elevate it to because ultimately that’s what it impacts: welfare and safety.
Speaking of buckets, there’s a new bucket challenge, wherein unsuspecting people have a bucket put on their head, can’t breathe, and then pass out. There’s been a number of these reported and actually filmed on social media. Here’s another example of dangerous types of behavior that essentially are a form of assault. Unsuspecting people suffer injuries from young children and teens trying to play pranks.
Again, had there not been this medium, we wouldn’t necessarily see the extent of the injuries. I guess going forward, the next step would be to send a message to colleges that there should be some form of warning if this trend is seen, at least from a public health standpoint.
Dr. Nelson: Education is a necessary thing to do, but it’s almost never the real solution to a problem. We can educate people as best we can that they need to do things right. At some point, we’re going to need to regulate it or manage it somehow.
Whether it’s through a carrot or a stick approach, or whether you want to give people kudos for doing the right thing or punish them for doing something wrong, that’s a tough decision to make and one that is going to be made by a parent or guardian, a school official, or law enforcement. Somehow, we have to figure out how to make this happen.
There’s not going to be a single size that fits all for this. At some level, we have to do something to educate and regulate. The balance between those two things is going to be political and philosophical in nature.
Dr. Glatter: Right, and the element of peer pressure and conformity in this is really part of the element. If we try to remove that aspect of it, then often these trends would go away. That aspect of conformity and peer pressure is instrumental in fueling these trends. Maybe we can make a full gallon of water be the trend without any alcohol in there.
Dr. Nelson: We say water is only water, but as a medical toxicologist, I can tell you that one of the foundations in medical toxicology is that everything is toxic. It’s just the dose that determines the toxicity. Oxygen is toxic, water is toxic. Everything’s toxic if you take enough of it.
We know that whether it’s psychogenic or intentional, polydipsia by drinking excessive amounts of water, especially without electrolytes, is one of the reasons they say you should add electrolytes. That’s all relative as well, because depending on the electrolyte and how much you put in and things like that, that could also become dangerous. Drinking excessive amounts of water like they’re suggesting, which sounds like a good thing to prevent hangover and so on, can in and of itself be a problem too.
Dr. Glatter: Right, and we know that there’s no magic bullet for a hangover. Obviously, abstinence is the only thing that truly works.
Dr. Nelson: Or moderation.
Dr. Glatter: Until research proves further.
Thank you so much. You’ve made some really important points. Thank you for talking about the BORG phenomenon, how it relates to society in general, and what we can do to try to change people’s perception of alcohol and the bigger picture of binge drinking. I really appreciate it.
Dr. Nelson: Thanks, Rob, for having me. It’s an important topic and hopefully we can get a handle on this. I appreciate your time.
Dr. Glatter is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Hofstra University, Hempstead, N.Y. Dr. Nelson is professor and chair of the department of emergency medicine and chief of the division of medical toxicology at Rutgers New Jersey Medical School, Newark. He is a member of the board of directors of the American Board of Emergency Medicine, the Accreditation Council for Continuing Medical Education, and Association of Academic Chairs in Emergency Medicine and is past-president of the American College of Medical Toxicology. Dr. Glatter and Dr. Nelson disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Steep rise in cannabis-related suicide attempts
The increases were notable both during and after the pandemic and were highest among children and female persons.
Investigators examined closed cases of cannabis-related human exposures that were coded as intentional-suspected suicidal.
Of note, there was a statistically significant increase in cannabis poisonings in young children (5-13 years) in 2021, during the pandemic, compared with 2019, a prepandemic year (3.1% vs. 1.3%; P < .001), the researchers report.
“This may speak to both increased access to cannabis as well as poor mental health status during the pandemic period,” study investigator Tracy Klein, PhD, assistant director, Center for Cannabis Policy, Research and Outreach, Washington State University Vancouver, Mount Vista, said in an interview.
The study was published online in JAMA Network Open.
Reports of intentional poisonings with cannabis increased by roughly 17% annually over the study period. Most cases occurred in recent years and involved individuals aged 14-64 years. Nearly all (96.5%) cases involved more than one substance.
“The resemblance of cannabis edibles, implicated in the majority of poisonings to candy, vitamins, and food products, is a risk to patients across the life span who may not fully understand what they are consuming or how potent it is,” Dr. Klein said in an interview.
Overall, nearly 1 in 10 exposures resulted in death or other major outcomes (life-threatening outcomes or outcomes involving major residual disability or disfigurement). For older adults, 19.4% of exposures led to death or other major harm.
“Elderly patients may also have comorbid conditions and polypharmacy, which contributes to their much more serious outcomes from cannabis poisoning,” Dr. Klein said.
The researchers caution that, owing to the cross-sectional nature of the data, they could not identify a causal association between cannabis use and suicide attempt.
With more states legalizing cannabis use by adults, increases in cannabis use will likely persist.
“It is important to further examine the suspected association between cannabis use and suicidal behaviors and how risks can be prevented or mitigated,” the researchers note.
Dr. Klein encourages health care providers to ask patients whether they are using cannabis and how they obtain and store it.
“As with all medications and substances, storage is a key safety issue that is elicited during a careful history,” said Dr. Klein.
Support for the study was provided in part by funds provided for medical and biological research by the State of Washington Initiative Measure No. 171. Dr. Klein has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The increases were notable both during and after the pandemic and were highest among children and female persons.
Investigators examined closed cases of cannabis-related human exposures that were coded as intentional-suspected suicidal.
Of note, there was a statistically significant increase in cannabis poisonings in young children (5-13 years) in 2021, during the pandemic, compared with 2019, a prepandemic year (3.1% vs. 1.3%; P < .001), the researchers report.
“This may speak to both increased access to cannabis as well as poor mental health status during the pandemic period,” study investigator Tracy Klein, PhD, assistant director, Center for Cannabis Policy, Research and Outreach, Washington State University Vancouver, Mount Vista, said in an interview.
The study was published online in JAMA Network Open.
Reports of intentional poisonings with cannabis increased by roughly 17% annually over the study period. Most cases occurred in recent years and involved individuals aged 14-64 years. Nearly all (96.5%) cases involved more than one substance.
“The resemblance of cannabis edibles, implicated in the majority of poisonings to candy, vitamins, and food products, is a risk to patients across the life span who may not fully understand what they are consuming or how potent it is,” Dr. Klein said in an interview.
Overall, nearly 1 in 10 exposures resulted in death or other major outcomes (life-threatening outcomes or outcomes involving major residual disability or disfigurement). For older adults, 19.4% of exposures led to death or other major harm.
“Elderly patients may also have comorbid conditions and polypharmacy, which contributes to their much more serious outcomes from cannabis poisoning,” Dr. Klein said.
The researchers caution that, owing to the cross-sectional nature of the data, they could not identify a causal association between cannabis use and suicide attempt.
With more states legalizing cannabis use by adults, increases in cannabis use will likely persist.
“It is important to further examine the suspected association between cannabis use and suicidal behaviors and how risks can be prevented or mitigated,” the researchers note.
Dr. Klein encourages health care providers to ask patients whether they are using cannabis and how they obtain and store it.
“As with all medications and substances, storage is a key safety issue that is elicited during a careful history,” said Dr. Klein.
Support for the study was provided in part by funds provided for medical and biological research by the State of Washington Initiative Measure No. 171. Dr. Klein has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The increases were notable both during and after the pandemic and were highest among children and female persons.
Investigators examined closed cases of cannabis-related human exposures that were coded as intentional-suspected suicidal.
Of note, there was a statistically significant increase in cannabis poisonings in young children (5-13 years) in 2021, during the pandemic, compared with 2019, a prepandemic year (3.1% vs. 1.3%; P < .001), the researchers report.
“This may speak to both increased access to cannabis as well as poor mental health status during the pandemic period,” study investigator Tracy Klein, PhD, assistant director, Center for Cannabis Policy, Research and Outreach, Washington State University Vancouver, Mount Vista, said in an interview.
The study was published online in JAMA Network Open.
Reports of intentional poisonings with cannabis increased by roughly 17% annually over the study period. Most cases occurred in recent years and involved individuals aged 14-64 years. Nearly all (96.5%) cases involved more than one substance.
“The resemblance of cannabis edibles, implicated in the majority of poisonings to candy, vitamins, and food products, is a risk to patients across the life span who may not fully understand what they are consuming or how potent it is,” Dr. Klein said in an interview.
Overall, nearly 1 in 10 exposures resulted in death or other major outcomes (life-threatening outcomes or outcomes involving major residual disability or disfigurement). For older adults, 19.4% of exposures led to death or other major harm.
“Elderly patients may also have comorbid conditions and polypharmacy, which contributes to their much more serious outcomes from cannabis poisoning,” Dr. Klein said.
The researchers caution that, owing to the cross-sectional nature of the data, they could not identify a causal association between cannabis use and suicide attempt.
With more states legalizing cannabis use by adults, increases in cannabis use will likely persist.
“It is important to further examine the suspected association between cannabis use and suicidal behaviors and how risks can be prevented or mitigated,” the researchers note.
Dr. Klein encourages health care providers to ask patients whether they are using cannabis and how they obtain and store it.
“As with all medications and substances, storage is a key safety issue that is elicited during a careful history,” said Dr. Klein.
Support for the study was provided in part by funds provided for medical and biological research by the State of Washington Initiative Measure No. 171. Dr. Klein has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN