User login
Timing of initiation of renal-replacement therapy in acute kidney injury
Background: Acute kidney injury (AKI) is a common complication that occurs in seriously ill patients admitted to the ICU, and many of these patients eventually require RRT. When complicated by major metabolic disorders, it is usually clear when therapy should be initiated. However, when these complications are absent, the most appropriate time to initiate RRT is unclear. There are potential advantages to performing early RRT in patients with severe AKI, such as restoring acid-base balance, preventing fluid accumulation, and preventing major electrolyte disturbances.
Study design: Multinational, randomized, controlled trial.
Setting: 168 hospitals in 15 countries.
Synopsis: Eligible patients were adults admitted to an ICU with severe AKI. Patients were randomly assigned to an accelerated strategy of RRT (initiated within 12 hours, 1,465 patients) or a standard strategy of RRT (held until conventional indications developed or AKI lasted more than 72 hours, 1,462 patients). RRT was performed in 1,418 (96.8%) in the accelerated group and 903 (61.8%) in the standard group. At 90 days, 643 deaths (43.9%) occurred in the accelerated group and 639 deaths (43.7%) occurred in the standard group (RR, 1.00; 95% CI, 0.93-1.09; P = .92). Among survivors at 90 days, 85 out of 814 accelerated patients (10.4%) and 49 of 815 standard patients (6.0%) continued to require RRT (RR, 1.75; 95% CI, 1.24-2.43), suggesting the possibility of increased dependence on long-term RRT if introduced early. Limitations include use of clinical equipoise to confirm full eligibility, introducing possible patient heterogeneity into the trial. In addition, broad discretion was given to clinicians on when to start RRT in the standard group resulting in variable initiation times.
Bottom line: In critically ill patients with severe AKI, earlier RRT did not result in lower mortality at 90 days compared with standard therapy and increased the risk of requiring RRT at 90 days.
Citation: Bagshaw SM et al. Timing of initiation of renal-replacement therapy in acute kidney injury. N Engl J Med. 2020;383:240-51. doi: 10.1056/NEJMoa2000741.
Dr. Kim is a hospitalist in the Division of Hospital Medicine, Mount Sinai Health System, New York.
Background: Acute kidney injury (AKI) is a common complication that occurs in seriously ill patients admitted to the ICU, and many of these patients eventually require RRT. When complicated by major metabolic disorders, it is usually clear when therapy should be initiated. However, when these complications are absent, the most appropriate time to initiate RRT is unclear. There are potential advantages to performing early RRT in patients with severe AKI, such as restoring acid-base balance, preventing fluid accumulation, and preventing major electrolyte disturbances.
Study design: Multinational, randomized, controlled trial.
Setting: 168 hospitals in 15 countries.
Synopsis: Eligible patients were adults admitted to an ICU with severe AKI. Patients were randomly assigned to an accelerated strategy of RRT (initiated within 12 hours, 1,465 patients) or a standard strategy of RRT (held until conventional indications developed or AKI lasted more than 72 hours, 1,462 patients). RRT was performed in 1,418 (96.8%) in the accelerated group and 903 (61.8%) in the standard group. At 90 days, 643 deaths (43.9%) occurred in the accelerated group and 639 deaths (43.7%) occurred in the standard group (RR, 1.00; 95% CI, 0.93-1.09; P = .92). Among survivors at 90 days, 85 out of 814 accelerated patients (10.4%) and 49 of 815 standard patients (6.0%) continued to require RRT (RR, 1.75; 95% CI, 1.24-2.43), suggesting the possibility of increased dependence on long-term RRT if introduced early. Limitations include use of clinical equipoise to confirm full eligibility, introducing possible patient heterogeneity into the trial. In addition, broad discretion was given to clinicians on when to start RRT in the standard group resulting in variable initiation times.
Bottom line: In critically ill patients with severe AKI, earlier RRT did not result in lower mortality at 90 days compared with standard therapy and increased the risk of requiring RRT at 90 days.
Citation: Bagshaw SM et al. Timing of initiation of renal-replacement therapy in acute kidney injury. N Engl J Med. 2020;383:240-51. doi: 10.1056/NEJMoa2000741.
Dr. Kim is a hospitalist in the Division of Hospital Medicine, Mount Sinai Health System, New York.
Background: Acute kidney injury (AKI) is a common complication that occurs in seriously ill patients admitted to the ICU, and many of these patients eventually require RRT. When complicated by major metabolic disorders, it is usually clear when therapy should be initiated. However, when these complications are absent, the most appropriate time to initiate RRT is unclear. There are potential advantages to performing early RRT in patients with severe AKI, such as restoring acid-base balance, preventing fluid accumulation, and preventing major electrolyte disturbances.
Study design: Multinational, randomized, controlled trial.
Setting: 168 hospitals in 15 countries.
Synopsis: Eligible patients were adults admitted to an ICU with severe AKI. Patients were randomly assigned to an accelerated strategy of RRT (initiated within 12 hours, 1,465 patients) or a standard strategy of RRT (held until conventional indications developed or AKI lasted more than 72 hours, 1,462 patients). RRT was performed in 1,418 (96.8%) in the accelerated group and 903 (61.8%) in the standard group. At 90 days, 643 deaths (43.9%) occurred in the accelerated group and 639 deaths (43.7%) occurred in the standard group (RR, 1.00; 95% CI, 0.93-1.09; P = .92). Among survivors at 90 days, 85 out of 814 accelerated patients (10.4%) and 49 of 815 standard patients (6.0%) continued to require RRT (RR, 1.75; 95% CI, 1.24-2.43), suggesting the possibility of increased dependence on long-term RRT if introduced early. Limitations include use of clinical equipoise to confirm full eligibility, introducing possible patient heterogeneity into the trial. In addition, broad discretion was given to clinicians on when to start RRT in the standard group resulting in variable initiation times.
Bottom line: In critically ill patients with severe AKI, earlier RRT did not result in lower mortality at 90 days compared with standard therapy and increased the risk of requiring RRT at 90 days.
Citation: Bagshaw SM et al. Timing of initiation of renal-replacement therapy in acute kidney injury. N Engl J Med. 2020;383:240-51. doi: 10.1056/NEJMoa2000741.
Dr. Kim is a hospitalist in the Division of Hospital Medicine, Mount Sinai Health System, New York.
Comparing the efficacy and safety of common SIADH treatments
Background: Hyponatremia caused by SIADH is common in hospitalized patients, and most evidence for treatment comes from noncontrolled studies. This study aims to investigate the efficacy and safety of fluid restriction compared with furosemide, with or without NaCl supplementation, for treating SIADH.
Study design: Open-label randomized controlled trial.
Setting: Single center in Thailand.
Synopsis: There were 92 participants randomized to fluid restriction alone, fluid restriction and furosemide, or fluid restriction, furosemide, and NaCl supplementation. The authors assessed the primary outcome, change in sodium, at 4, 7, 14, and 28 days (baseline mean Na 125 mmol/L). By day 4, all groups had a significant increase in sodium (mean delta 5 mmol/L). The time to achieve a safe sodium level (Na less than 130 mmol/L) was not different among groups. Acute kidney injury was most common in patients who received furosemide and NaCl supplementation, compared with the fluid restriction and fluid restriction plus furosemide groups (32%, 10%, 17%, respectively; P = .07). Hypokalemia was also most common in the furosemide and NaCl group (42%, 13%, 23%, respectively; P = .01). Limitations include open-label study design, poor fluid restriction adherence (63% overall), and inflexible treatment regimens that excluded treatment with oral potassium.
Bottom line: In treatment of hyponatremia caused by SIADH, there was no benefit to adding furosemide with or without NaCl supplementation to fluid restriction. However, there was potential associated risk of acute kidney injury and hypokalemia.Citation: Krisanapan P et al. Efficacy of furosemide, oral sodium chloride, and fluid restriction for treatment of syndrome of inappropriate antidiuresis (SIADH): An open-label randomized controlled study (the EFFUSE-FLUID trial). Am J Kidney Dis. 2020 Aug;76(2):203-12. doi: 10.1053/j.ajkd.2019.11.012.
Dr. Welter is a hospitalist at Northwestern Memorial Hospital and instructor of medicine, Feinberg School of Medicine, both in Chicago.
Background: Hyponatremia caused by SIADH is common in hospitalized patients, and most evidence for treatment comes from noncontrolled studies. This study aims to investigate the efficacy and safety of fluid restriction compared with furosemide, with or without NaCl supplementation, for treating SIADH.
Study design: Open-label randomized controlled trial.
Setting: Single center in Thailand.
Synopsis: There were 92 participants randomized to fluid restriction alone, fluid restriction and furosemide, or fluid restriction, furosemide, and NaCl supplementation. The authors assessed the primary outcome, change in sodium, at 4, 7, 14, and 28 days (baseline mean Na 125 mmol/L). By day 4, all groups had a significant increase in sodium (mean delta 5 mmol/L). The time to achieve a safe sodium level (Na less than 130 mmol/L) was not different among groups. Acute kidney injury was most common in patients who received furosemide and NaCl supplementation, compared with the fluid restriction and fluid restriction plus furosemide groups (32%, 10%, 17%, respectively; P = .07). Hypokalemia was also most common in the furosemide and NaCl group (42%, 13%, 23%, respectively; P = .01). Limitations include open-label study design, poor fluid restriction adherence (63% overall), and inflexible treatment regimens that excluded treatment with oral potassium.
Bottom line: In treatment of hyponatremia caused by SIADH, there was no benefit to adding furosemide with or without NaCl supplementation to fluid restriction. However, there was potential associated risk of acute kidney injury and hypokalemia.Citation: Krisanapan P et al. Efficacy of furosemide, oral sodium chloride, and fluid restriction for treatment of syndrome of inappropriate antidiuresis (SIADH): An open-label randomized controlled study (the EFFUSE-FLUID trial). Am J Kidney Dis. 2020 Aug;76(2):203-12. doi: 10.1053/j.ajkd.2019.11.012.
Dr. Welter is a hospitalist at Northwestern Memorial Hospital and instructor of medicine, Feinberg School of Medicine, both in Chicago.
Background: Hyponatremia caused by SIADH is common in hospitalized patients, and most evidence for treatment comes from noncontrolled studies. This study aims to investigate the efficacy and safety of fluid restriction compared with furosemide, with or without NaCl supplementation, for treating SIADH.
Study design: Open-label randomized controlled trial.
Setting: Single center in Thailand.
Synopsis: There were 92 participants randomized to fluid restriction alone, fluid restriction and furosemide, or fluid restriction, furosemide, and NaCl supplementation. The authors assessed the primary outcome, change in sodium, at 4, 7, 14, and 28 days (baseline mean Na 125 mmol/L). By day 4, all groups had a significant increase in sodium (mean delta 5 mmol/L). The time to achieve a safe sodium level (Na less than 130 mmol/L) was not different among groups. Acute kidney injury was most common in patients who received furosemide and NaCl supplementation, compared with the fluid restriction and fluid restriction plus furosemide groups (32%, 10%, 17%, respectively; P = .07). Hypokalemia was also most common in the furosemide and NaCl group (42%, 13%, 23%, respectively; P = .01). Limitations include open-label study design, poor fluid restriction adherence (63% overall), and inflexible treatment regimens that excluded treatment with oral potassium.
Bottom line: In treatment of hyponatremia caused by SIADH, there was no benefit to adding furosemide with or without NaCl supplementation to fluid restriction. However, there was potential associated risk of acute kidney injury and hypokalemia.Citation: Krisanapan P et al. Efficacy of furosemide, oral sodium chloride, and fluid restriction for treatment of syndrome of inappropriate antidiuresis (SIADH): An open-label randomized controlled study (the EFFUSE-FLUID trial). Am J Kidney Dis. 2020 Aug;76(2):203-12. doi: 10.1053/j.ajkd.2019.11.012.
Dr. Welter is a hospitalist at Northwestern Memorial Hospital and instructor of medicine, Feinberg School of Medicine, both in Chicago.
What makes a urinary tract infection complicated?
Consider anatomical and severity risk factors
Case
A 72-year-old woman with type 2 diabetes mellitus presents with acute dysuria, fever, and flank pain. She had a urinary tract infection (UTI) 3 months prior treated with nitrofurantoin. Temperature is 102° F, heart rate 112 beats per minute, and the remainder of vital signs are normal. She has left costovertebral angle tenderness. Urine microscopy shows 70 WBCs per high power field and bacteria. Is this urinary tract infection complicated?
Background
The urinary tract is divided into the upper tract, which includes the kidneys and ureters, and the lower urinary tract, which includes the bladder, urethra, and prostate. Infection of the lower urinary tract is referred to as cystitis while infection of the upper urinary tract is pyelonephritis. A UTI is the colonization of pathogen(s) within the urinary system that causes an inflammatory response resulting in symptoms and requiring treatment. UTIs occur when there is reduced urine flow, an increase in colonization risk, and when there are factors that facilitate ascent such as catheterization or incontinence.
There are an estimated 150 million cases of UTIs worldwide per year, accounting for $6 billion in health care expenditures.1 In the inpatient setting, about 40% of nosocomial infections are associated with urinary catheters. This equates to about 1 million catheter-associated UTIs per year in the United States, and up to 40% of hospital gram-negative bacteremia per year are caused by UTIs.1
UTIs are often classified as either uncomplicated or complicated infections, which can influence the depth of management. UTIs have a wide spectrum of symptoms and can manifest anywhere from mild dysuria treated successfully with outpatient antibiotics to florid sepsis. Uncomplicated simple cystitis is often treated as an outpatient with oral nitrofurantoin or trimethoprim-sulfamethoxazole.2 Complicated UTIs are treated with broader antimicrobial coverage, and depending on severity, could require intravenous antibiotics. Many factors affect how a UTI manifests and determining whether an infection is “uncomplicated” or “complicated” is an important first step in guiding management. Unfortunately, there are differing classifications of “complicated” UTIs, making it a complicated issue itself. We outline two common approaches.
Anatomic approach
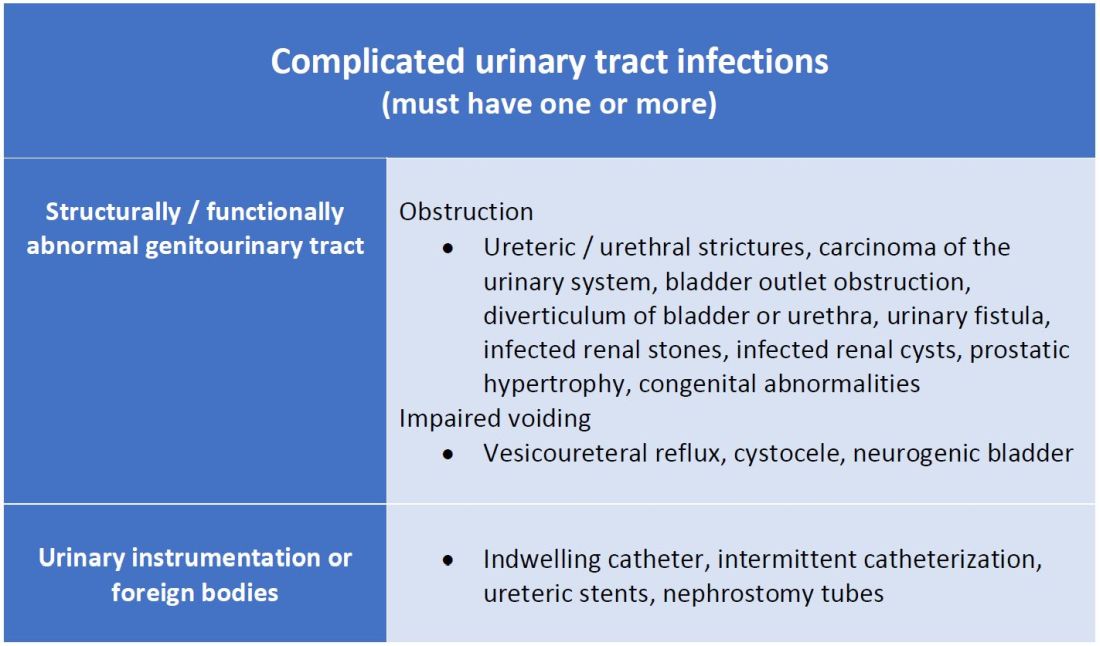
A commonly recognized definition is from the American Urological Association, which states that complicated UTIs are symptomatic cases associated with the presence of “underlying, predisposing conditions and not necessarily clinical severity, invasiveness, or complications.”3 These factors include structural or functional urinary tract abnormalities or urinary instrumentation (see Table 1). These predisposing conditions can increase microbial colonization and decrease therapy efficacy, thus increasing the frequency of infection and relapse.
This population of patients is at high risk of infections with more resistant bacteria such as extended-spectrum beta-lactamase (ESBL) producing Escherichia coli since they often lack the natural genitourinary barriers to infection. In addition, these patients more often undergo multiple antibiotic courses for their frequent infections, which also contributes to their risk of ESBL infections. Genitourinary abnormalities interfere with normal voiding, resulting in impaired flushing of bacteria. For instance, obstruction inhibits complete urinary drainage and increases the persistence of bacteria in biofilms, especially if there are stones or indwelling devices present. Biofilms usually contain a high concentration of organisms including Proteus mirabilis, Morgenella morganii, and Providencia spp.4 Keep in mind that, if there is an obstruction, the urinalysis might be without pyuria or bacteriuria.
Instrumentation increases infection risks through the direct introduction of bacteria into the genitourinary tract. Despite the efforts in maintaining sterility in urinary catheter placement, catheters provide a nidus for infection. Catheter-associated UTI (CAUTI) is defined by the Infectious Disease Society of America as UTIs that occur in patients with an indwelling catheter or who had a catheter removed for less than 48 hours who develop urinary symptoms and cultures positive for uropathogenic bacteria.4 Studies show that in general, patients with indwelling catheters will develop bacteriuria over time, with 10%-25% eventually developing symptoms.
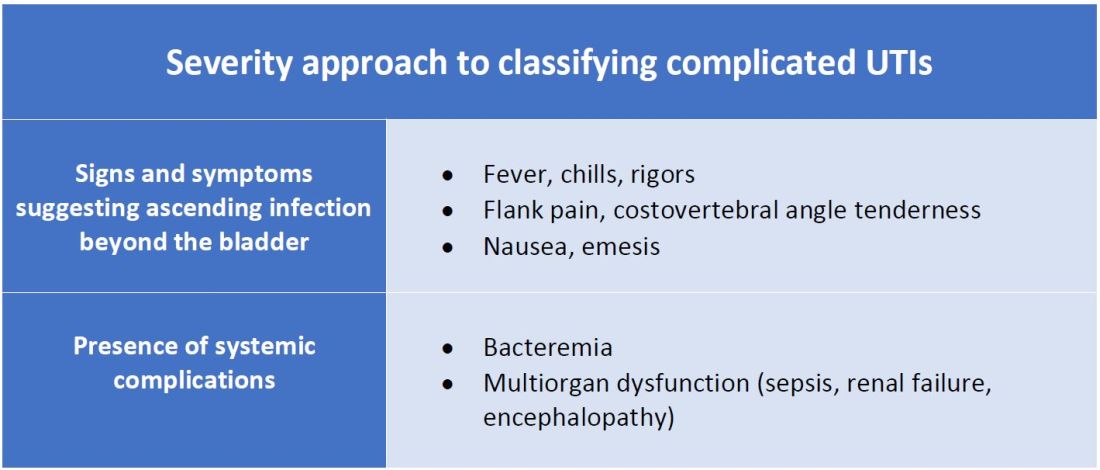
Severity approach
There are other schools of thought that categorize uncomplicated versus complicated UTIs based on the severity of presentation (see Table 2). An uncomplicated UTI would be classified as symptoms and signs of simple cystitis limited to dysuria, frequency, urgency, and suprapubic pain. Using a symptom severity approach, systemic findings such as fever, chills, emesis, flank pain, costovertebral angle tenderness, or other findings of sepsis would be classified as a complicated UTI. These systemic findings would suggest an extension of infection beyond the bladder.
The argument for a symptomatic-based approach of classification is that the severity of symptoms should dictate the degree of management. Not all UTIs in the anatomic approach are severe. In fact, populations that are considered at risk for complicated UTIs by the AUA guidelines in Table 1 often have mild symptomatic cystitis or asymptomatic bacteriuria. Asymptomatic bacteriuria is the colonization of organisms in the urinary tract without active infection. For instance, bacteriuria is present in almost 100% of people with chronic indwelling catheters, 30%-40% of neurogenic bladder requiring intermittent catheterization, and 50% of elderly nursing home residents.4 Not all bacteriuria triggers enough of an inflammatory response to cause symptoms that require treatment.
Ultimate clinical judgment
Although there are multiple different society recommendations in distinguishing uncomplicated versus complicated UTIs, considering both anatomical and severity risk factors can better aid in clinical decision-making rather than abiding by one classification method alone.
Uncomplicated UTIs from the AUA guidelines can cause severe infections that might require longer courses of broad-spectrum antibiotics. On the other hand, people with anatomic abnormalities can present with mild symptoms that can be treated with a narrow-spectrum antibiotic for a standard time course. Recognizing the severity of the infection and using clinical judgment aids in antibiotic stewardship.
Although the existence of algorithmic approaches can help guide clinical judgment, accounting for the spectrum of host and bacterial factors should ultimately determine the complexity of the disease and management.3 Using clinical suspicion to determine when a UTI should be treated as a complicated infection can ensure effective treatment and decrease the likelihood of sepsis, renal scarring, or end-stage disease.5
Back to the case
The case presents an elderly woman with diabetes presenting with sepsis from a UTI. Because of a normal urinary tract and no prior instrumentation, by the AUA definition, she would be classified as an uncomplicated UTI; however, we would classify her as a complicated UTI based on the severity of her presentation. She has a fever, tachycardia, flank pain, and costovertebral angle tenderness that are evidence of infection extending beyond the bladder. She has sepsis warranting inpatient management. Prior urine culture results could aid in determining empiric treatment while waiting for new cultures. In her case, an intravenous antibiotic with broad gram-negative coverage such as ceftriaxone would be appropriate.
Bottom line
There are multiple interpretations of complicated UTIs including both an anatomical and severity approach. Clinical judgment regarding infection severity should determine the depth of management.
Dr. Vu is a hospitalist at the University of Kentucky, Lexington. Dr. Gray is a hospitalist at the University of Kentucky and the Lexington Veterans Affairs Medical Center.
References
1. Folk CS. AUA Core Curriculum: Urinary Tract Infection (Adult). 2021 Mar 1. https://university.auanet.org/core_topic.cfm?coreid=92.
2. Gupta K et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011 Mar 1;52(5):e103-20. doi: 10.1093/cid/ciq257.
3. Johnson JR. Definition of Complicated Urinary Tract Infection. Clin Infect Dis. 2017 February 15;64(4):529. doi: 10.1093/cid/ciw751.
4. Nicolle LE, AMMI Canada Guidelines Committee. Complicated urinary tract infection in adults. Can J Infect Dis Med Microbiol. 2005;16(6):349-60. doi: 10.1155/2005/385768.
5. Melekos MD and Naber KG. Complicated urinary tract infections. Int J Antimicrob Agents. 2000;15(4):247-56. doi: 10.1016/s0924-8579(00)00168-0.
Key points
- The anatomical approach to defining complicated UTIs considers the presence of underlying, predisposing conditions such as structurally or functionally abnormal genitourinary tract or urinary instrumentation or foreign bodies.
- The severity approach to defining complicated UTIs considers the severity of presentation including the presence of systemic manifestations.
- Both approaches should consider populations that are at risk for recurrent or multidrug-resistant infections and infections that can lead to high morbidity.
- Either approach can be used as a guide, but neither should replace clinical suspicion and judgment in determining the depth of treatment.
Additional reading
Choe HS et al. Summary of the UAA‐AAUS guidelines for urinary tract infections. Int J Urol. 2018 Mar;25(3):175-85. doi:10.1111/iju.13493.
Nicolle LE et al. Infectious Diseases Society of America Guidelines for the Diagnosis and Treatment of Asymptomatic Bacteriuria in Adults. Clin Infect Dis. 2005 Mar;40(5):643-54. doi: 10.1086/427507.
Wagenlehner FME et al. Epidemiology, definition and treatment of complicated urinary tract infections. Nat Rev Urol. 2020 Oct;17:586-600. doi:10.1038/s41585-020-0362-4.
Wallace DW et al. Urinalysis: A simple test with complicated interpretation. J Urgent Care Med. 2020 July-Aug;14(10):11-4.
Quiz
A 68-year-old woman with type 2 diabetes mellitus presents to the emergency department with acute fever, chills, dysuria, frequency, and suprapubic pain. She has associated nausea, malaise, and fatigue. She takes metformin and denies recent antibiotic use. Her temperature is 102.8° F, heart rate 118 beats per minute, blood pressure 118/71 mm Hg, and her respiratory rate is 24 breaths per minute. She is ill-appearing and has mild suprapubic tenderness. White blood cell count is 18 k/mcL. Urinalysis is positive for leukocyte esterase, nitrites, and bacteria. Urine microscopy has 120 white blood cells per high power field. What is the most appropriate treatment?
A. Azithromycin
B. Ceftriaxone
C. Cefepime and vancomycin
D. Nitrofurantoin
The answer is B. The patient presents with sepsis secondary to a urinary tract infection. Using the anatomic approach this would be classified as uncomplicated. Using the severity approach, this would be classified as a complicated urinary tract infection. With fever, chills, and signs of sepsis, it’s likely her infection extends beyond the bladder. Given the severity of her presentation, we’d favor treating her as a complicated urinary tract infection with intravenous ceftriaxone. There is no suggestion of resistance or additional MRSA risk factors requiring intravenous vancomycin or cefepime. Nitrofurantoin, although a first-line treatment for uncomplicated cystitis, would not be appropriate if there is suspicion infection extends beyond the bladder. Azithromycin is a first-line option for chlamydia trachomatis, but not a urinary tract infection.
Consider anatomical and severity risk factors
Consider anatomical and severity risk factors
Case
A 72-year-old woman with type 2 diabetes mellitus presents with acute dysuria, fever, and flank pain. She had a urinary tract infection (UTI) 3 months prior treated with nitrofurantoin. Temperature is 102° F, heart rate 112 beats per minute, and the remainder of vital signs are normal. She has left costovertebral angle tenderness. Urine microscopy shows 70 WBCs per high power field and bacteria. Is this urinary tract infection complicated?
Background
The urinary tract is divided into the upper tract, which includes the kidneys and ureters, and the lower urinary tract, which includes the bladder, urethra, and prostate. Infection of the lower urinary tract is referred to as cystitis while infection of the upper urinary tract is pyelonephritis. A UTI is the colonization of pathogen(s) within the urinary system that causes an inflammatory response resulting in symptoms and requiring treatment. UTIs occur when there is reduced urine flow, an increase in colonization risk, and when there are factors that facilitate ascent such as catheterization or incontinence.
There are an estimated 150 million cases of UTIs worldwide per year, accounting for $6 billion in health care expenditures.1 In the inpatient setting, about 40% of nosocomial infections are associated with urinary catheters. This equates to about 1 million catheter-associated UTIs per year in the United States, and up to 40% of hospital gram-negative bacteremia per year are caused by UTIs.1
UTIs are often classified as either uncomplicated or complicated infections, which can influence the depth of management. UTIs have a wide spectrum of symptoms and can manifest anywhere from mild dysuria treated successfully with outpatient antibiotics to florid sepsis. Uncomplicated simple cystitis is often treated as an outpatient with oral nitrofurantoin or trimethoprim-sulfamethoxazole.2 Complicated UTIs are treated with broader antimicrobial coverage, and depending on severity, could require intravenous antibiotics. Many factors affect how a UTI manifests and determining whether an infection is “uncomplicated” or “complicated” is an important first step in guiding management. Unfortunately, there are differing classifications of “complicated” UTIs, making it a complicated issue itself. We outline two common approaches.
Anatomic approach
A commonly recognized definition is from the American Urological Association, which states that complicated UTIs are symptomatic cases associated with the presence of “underlying, predisposing conditions and not necessarily clinical severity, invasiveness, or complications.”3 These factors include structural or functional urinary tract abnormalities or urinary instrumentation (see Table 1). These predisposing conditions can increase microbial colonization and decrease therapy efficacy, thus increasing the frequency of infection and relapse.
This population of patients is at high risk of infections with more resistant bacteria such as extended-spectrum beta-lactamase (ESBL) producing Escherichia coli since they often lack the natural genitourinary barriers to infection. In addition, these patients more often undergo multiple antibiotic courses for their frequent infections, which also contributes to their risk of ESBL infections. Genitourinary abnormalities interfere with normal voiding, resulting in impaired flushing of bacteria. For instance, obstruction inhibits complete urinary drainage and increases the persistence of bacteria in biofilms, especially if there are stones or indwelling devices present. Biofilms usually contain a high concentration of organisms including Proteus mirabilis, Morgenella morganii, and Providencia spp.4 Keep in mind that, if there is an obstruction, the urinalysis might be without pyuria or bacteriuria.
Instrumentation increases infection risks through the direct introduction of bacteria into the genitourinary tract. Despite the efforts in maintaining sterility in urinary catheter placement, catheters provide a nidus for infection. Catheter-associated UTI (CAUTI) is defined by the Infectious Disease Society of America as UTIs that occur in patients with an indwelling catheter or who had a catheter removed for less than 48 hours who develop urinary symptoms and cultures positive for uropathogenic bacteria.4 Studies show that in general, patients with indwelling catheters will develop bacteriuria over time, with 10%-25% eventually developing symptoms.
Severity approach
There are other schools of thought that categorize uncomplicated versus complicated UTIs based on the severity of presentation (see Table 2). An uncomplicated UTI would be classified as symptoms and signs of simple cystitis limited to dysuria, frequency, urgency, and suprapubic pain. Using a symptom severity approach, systemic findings such as fever, chills, emesis, flank pain, costovertebral angle tenderness, or other findings of sepsis would be classified as a complicated UTI. These systemic findings would suggest an extension of infection beyond the bladder.
The argument for a symptomatic-based approach of classification is that the severity of symptoms should dictate the degree of management. Not all UTIs in the anatomic approach are severe. In fact, populations that are considered at risk for complicated UTIs by the AUA guidelines in Table 1 often have mild symptomatic cystitis or asymptomatic bacteriuria. Asymptomatic bacteriuria is the colonization of organisms in the urinary tract without active infection. For instance, bacteriuria is present in almost 100% of people with chronic indwelling catheters, 30%-40% of neurogenic bladder requiring intermittent catheterization, and 50% of elderly nursing home residents.4 Not all bacteriuria triggers enough of an inflammatory response to cause symptoms that require treatment.
Ultimate clinical judgment
Although there are multiple different society recommendations in distinguishing uncomplicated versus complicated UTIs, considering both anatomical and severity risk factors can better aid in clinical decision-making rather than abiding by one classification method alone.
Uncomplicated UTIs from the AUA guidelines can cause severe infections that might require longer courses of broad-spectrum antibiotics. On the other hand, people with anatomic abnormalities can present with mild symptoms that can be treated with a narrow-spectrum antibiotic for a standard time course. Recognizing the severity of the infection and using clinical judgment aids in antibiotic stewardship.
Although the existence of algorithmic approaches can help guide clinical judgment, accounting for the spectrum of host and bacterial factors should ultimately determine the complexity of the disease and management.3 Using clinical suspicion to determine when a UTI should be treated as a complicated infection can ensure effective treatment and decrease the likelihood of sepsis, renal scarring, or end-stage disease.5
Back to the case
The case presents an elderly woman with diabetes presenting with sepsis from a UTI. Because of a normal urinary tract and no prior instrumentation, by the AUA definition, she would be classified as an uncomplicated UTI; however, we would classify her as a complicated UTI based on the severity of her presentation. She has a fever, tachycardia, flank pain, and costovertebral angle tenderness that are evidence of infection extending beyond the bladder. She has sepsis warranting inpatient management. Prior urine culture results could aid in determining empiric treatment while waiting for new cultures. In her case, an intravenous antibiotic with broad gram-negative coverage such as ceftriaxone would be appropriate.
Bottom line
There are multiple interpretations of complicated UTIs including both an anatomical and severity approach. Clinical judgment regarding infection severity should determine the depth of management.
Dr. Vu is a hospitalist at the University of Kentucky, Lexington. Dr. Gray is a hospitalist at the University of Kentucky and the Lexington Veterans Affairs Medical Center.
References
1. Folk CS. AUA Core Curriculum: Urinary Tract Infection (Adult). 2021 Mar 1. https://university.auanet.org/core_topic.cfm?coreid=92.
2. Gupta K et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011 Mar 1;52(5):e103-20. doi: 10.1093/cid/ciq257.
3. Johnson JR. Definition of Complicated Urinary Tract Infection. Clin Infect Dis. 2017 February 15;64(4):529. doi: 10.1093/cid/ciw751.
4. Nicolle LE, AMMI Canada Guidelines Committee. Complicated urinary tract infection in adults. Can J Infect Dis Med Microbiol. 2005;16(6):349-60. doi: 10.1155/2005/385768.
5. Melekos MD and Naber KG. Complicated urinary tract infections. Int J Antimicrob Agents. 2000;15(4):247-56. doi: 10.1016/s0924-8579(00)00168-0.
Key points
- The anatomical approach to defining complicated UTIs considers the presence of underlying, predisposing conditions such as structurally or functionally abnormal genitourinary tract or urinary instrumentation or foreign bodies.
- The severity approach to defining complicated UTIs considers the severity of presentation including the presence of systemic manifestations.
- Both approaches should consider populations that are at risk for recurrent or multidrug-resistant infections and infections that can lead to high morbidity.
- Either approach can be used as a guide, but neither should replace clinical suspicion and judgment in determining the depth of treatment.
Additional reading
Choe HS et al. Summary of the UAA‐AAUS guidelines for urinary tract infections. Int J Urol. 2018 Mar;25(3):175-85. doi:10.1111/iju.13493.
Nicolle LE et al. Infectious Diseases Society of America Guidelines for the Diagnosis and Treatment of Asymptomatic Bacteriuria in Adults. Clin Infect Dis. 2005 Mar;40(5):643-54. doi: 10.1086/427507.
Wagenlehner FME et al. Epidemiology, definition and treatment of complicated urinary tract infections. Nat Rev Urol. 2020 Oct;17:586-600. doi:10.1038/s41585-020-0362-4.
Wallace DW et al. Urinalysis: A simple test with complicated interpretation. J Urgent Care Med. 2020 July-Aug;14(10):11-4.
Quiz
A 68-year-old woman with type 2 diabetes mellitus presents to the emergency department with acute fever, chills, dysuria, frequency, and suprapubic pain. She has associated nausea, malaise, and fatigue. She takes metformin and denies recent antibiotic use. Her temperature is 102.8° F, heart rate 118 beats per minute, blood pressure 118/71 mm Hg, and her respiratory rate is 24 breaths per minute. She is ill-appearing and has mild suprapubic tenderness. White blood cell count is 18 k/mcL. Urinalysis is positive for leukocyte esterase, nitrites, and bacteria. Urine microscopy has 120 white blood cells per high power field. What is the most appropriate treatment?
A. Azithromycin
B. Ceftriaxone
C. Cefepime and vancomycin
D. Nitrofurantoin
The answer is B. The patient presents with sepsis secondary to a urinary tract infection. Using the anatomic approach this would be classified as uncomplicated. Using the severity approach, this would be classified as a complicated urinary tract infection. With fever, chills, and signs of sepsis, it’s likely her infection extends beyond the bladder. Given the severity of her presentation, we’d favor treating her as a complicated urinary tract infection with intravenous ceftriaxone. There is no suggestion of resistance or additional MRSA risk factors requiring intravenous vancomycin or cefepime. Nitrofurantoin, although a first-line treatment for uncomplicated cystitis, would not be appropriate if there is suspicion infection extends beyond the bladder. Azithromycin is a first-line option for chlamydia trachomatis, but not a urinary tract infection.
Case
A 72-year-old woman with type 2 diabetes mellitus presents with acute dysuria, fever, and flank pain. She had a urinary tract infection (UTI) 3 months prior treated with nitrofurantoin. Temperature is 102° F, heart rate 112 beats per minute, and the remainder of vital signs are normal. She has left costovertebral angle tenderness. Urine microscopy shows 70 WBCs per high power field and bacteria. Is this urinary tract infection complicated?
Background
The urinary tract is divided into the upper tract, which includes the kidneys and ureters, and the lower urinary tract, which includes the bladder, urethra, and prostate. Infection of the lower urinary tract is referred to as cystitis while infection of the upper urinary tract is pyelonephritis. A UTI is the colonization of pathogen(s) within the urinary system that causes an inflammatory response resulting in symptoms and requiring treatment. UTIs occur when there is reduced urine flow, an increase in colonization risk, and when there are factors that facilitate ascent such as catheterization or incontinence.
There are an estimated 150 million cases of UTIs worldwide per year, accounting for $6 billion in health care expenditures.1 In the inpatient setting, about 40% of nosocomial infections are associated with urinary catheters. This equates to about 1 million catheter-associated UTIs per year in the United States, and up to 40% of hospital gram-negative bacteremia per year are caused by UTIs.1
UTIs are often classified as either uncomplicated or complicated infections, which can influence the depth of management. UTIs have a wide spectrum of symptoms and can manifest anywhere from mild dysuria treated successfully with outpatient antibiotics to florid sepsis. Uncomplicated simple cystitis is often treated as an outpatient with oral nitrofurantoin or trimethoprim-sulfamethoxazole.2 Complicated UTIs are treated with broader antimicrobial coverage, and depending on severity, could require intravenous antibiotics. Many factors affect how a UTI manifests and determining whether an infection is “uncomplicated” or “complicated” is an important first step in guiding management. Unfortunately, there are differing classifications of “complicated” UTIs, making it a complicated issue itself. We outline two common approaches.
Anatomic approach
A commonly recognized definition is from the American Urological Association, which states that complicated UTIs are symptomatic cases associated with the presence of “underlying, predisposing conditions and not necessarily clinical severity, invasiveness, or complications.”3 These factors include structural or functional urinary tract abnormalities or urinary instrumentation (see Table 1). These predisposing conditions can increase microbial colonization and decrease therapy efficacy, thus increasing the frequency of infection and relapse.
This population of patients is at high risk of infections with more resistant bacteria such as extended-spectrum beta-lactamase (ESBL) producing Escherichia coli since they often lack the natural genitourinary barriers to infection. In addition, these patients more often undergo multiple antibiotic courses for their frequent infections, which also contributes to their risk of ESBL infections. Genitourinary abnormalities interfere with normal voiding, resulting in impaired flushing of bacteria. For instance, obstruction inhibits complete urinary drainage and increases the persistence of bacteria in biofilms, especially if there are stones or indwelling devices present. Biofilms usually contain a high concentration of organisms including Proteus mirabilis, Morgenella morganii, and Providencia spp.4 Keep in mind that, if there is an obstruction, the urinalysis might be without pyuria or bacteriuria.
Instrumentation increases infection risks through the direct introduction of bacteria into the genitourinary tract. Despite the efforts in maintaining sterility in urinary catheter placement, catheters provide a nidus for infection. Catheter-associated UTI (CAUTI) is defined by the Infectious Disease Society of America as UTIs that occur in patients with an indwelling catheter or who had a catheter removed for less than 48 hours who develop urinary symptoms and cultures positive for uropathogenic bacteria.4 Studies show that in general, patients with indwelling catheters will develop bacteriuria over time, with 10%-25% eventually developing symptoms.
Severity approach
There are other schools of thought that categorize uncomplicated versus complicated UTIs based on the severity of presentation (see Table 2). An uncomplicated UTI would be classified as symptoms and signs of simple cystitis limited to dysuria, frequency, urgency, and suprapubic pain. Using a symptom severity approach, systemic findings such as fever, chills, emesis, flank pain, costovertebral angle tenderness, or other findings of sepsis would be classified as a complicated UTI. These systemic findings would suggest an extension of infection beyond the bladder.
The argument for a symptomatic-based approach of classification is that the severity of symptoms should dictate the degree of management. Not all UTIs in the anatomic approach are severe. In fact, populations that are considered at risk for complicated UTIs by the AUA guidelines in Table 1 often have mild symptomatic cystitis or asymptomatic bacteriuria. Asymptomatic bacteriuria is the colonization of organisms in the urinary tract without active infection. For instance, bacteriuria is present in almost 100% of people with chronic indwelling catheters, 30%-40% of neurogenic bladder requiring intermittent catheterization, and 50% of elderly nursing home residents.4 Not all bacteriuria triggers enough of an inflammatory response to cause symptoms that require treatment.
Ultimate clinical judgment
Although there are multiple different society recommendations in distinguishing uncomplicated versus complicated UTIs, considering both anatomical and severity risk factors can better aid in clinical decision-making rather than abiding by one classification method alone.
Uncomplicated UTIs from the AUA guidelines can cause severe infections that might require longer courses of broad-spectrum antibiotics. On the other hand, people with anatomic abnormalities can present with mild symptoms that can be treated with a narrow-spectrum antibiotic for a standard time course. Recognizing the severity of the infection and using clinical judgment aids in antibiotic stewardship.
Although the existence of algorithmic approaches can help guide clinical judgment, accounting for the spectrum of host and bacterial factors should ultimately determine the complexity of the disease and management.3 Using clinical suspicion to determine when a UTI should be treated as a complicated infection can ensure effective treatment and decrease the likelihood of sepsis, renal scarring, or end-stage disease.5
Back to the case
The case presents an elderly woman with diabetes presenting with sepsis from a UTI. Because of a normal urinary tract and no prior instrumentation, by the AUA definition, she would be classified as an uncomplicated UTI; however, we would classify her as a complicated UTI based on the severity of her presentation. She has a fever, tachycardia, flank pain, and costovertebral angle tenderness that are evidence of infection extending beyond the bladder. She has sepsis warranting inpatient management. Prior urine culture results could aid in determining empiric treatment while waiting for new cultures. In her case, an intravenous antibiotic with broad gram-negative coverage such as ceftriaxone would be appropriate.
Bottom line
There are multiple interpretations of complicated UTIs including both an anatomical and severity approach. Clinical judgment regarding infection severity should determine the depth of management.
Dr. Vu is a hospitalist at the University of Kentucky, Lexington. Dr. Gray is a hospitalist at the University of Kentucky and the Lexington Veterans Affairs Medical Center.
References
1. Folk CS. AUA Core Curriculum: Urinary Tract Infection (Adult). 2021 Mar 1. https://university.auanet.org/core_topic.cfm?coreid=92.
2. Gupta K et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011 Mar 1;52(5):e103-20. doi: 10.1093/cid/ciq257.
3. Johnson JR. Definition of Complicated Urinary Tract Infection. Clin Infect Dis. 2017 February 15;64(4):529. doi: 10.1093/cid/ciw751.
4. Nicolle LE, AMMI Canada Guidelines Committee. Complicated urinary tract infection in adults. Can J Infect Dis Med Microbiol. 2005;16(6):349-60. doi: 10.1155/2005/385768.
5. Melekos MD and Naber KG. Complicated urinary tract infections. Int J Antimicrob Agents. 2000;15(4):247-56. doi: 10.1016/s0924-8579(00)00168-0.
Key points
- The anatomical approach to defining complicated UTIs considers the presence of underlying, predisposing conditions such as structurally or functionally abnormal genitourinary tract or urinary instrumentation or foreign bodies.
- The severity approach to defining complicated UTIs considers the severity of presentation including the presence of systemic manifestations.
- Both approaches should consider populations that are at risk for recurrent or multidrug-resistant infections and infections that can lead to high morbidity.
- Either approach can be used as a guide, but neither should replace clinical suspicion and judgment in determining the depth of treatment.
Additional reading
Choe HS et al. Summary of the UAA‐AAUS guidelines for urinary tract infections. Int J Urol. 2018 Mar;25(3):175-85. doi:10.1111/iju.13493.
Nicolle LE et al. Infectious Diseases Society of America Guidelines for the Diagnosis and Treatment of Asymptomatic Bacteriuria in Adults. Clin Infect Dis. 2005 Mar;40(5):643-54. doi: 10.1086/427507.
Wagenlehner FME et al. Epidemiology, definition and treatment of complicated urinary tract infections. Nat Rev Urol. 2020 Oct;17:586-600. doi:10.1038/s41585-020-0362-4.
Wallace DW et al. Urinalysis: A simple test with complicated interpretation. J Urgent Care Med. 2020 July-Aug;14(10):11-4.
Quiz
A 68-year-old woman with type 2 diabetes mellitus presents to the emergency department with acute fever, chills, dysuria, frequency, and suprapubic pain. She has associated nausea, malaise, and fatigue. She takes metformin and denies recent antibiotic use. Her temperature is 102.8° F, heart rate 118 beats per minute, blood pressure 118/71 mm Hg, and her respiratory rate is 24 breaths per minute. She is ill-appearing and has mild suprapubic tenderness. White blood cell count is 18 k/mcL. Urinalysis is positive for leukocyte esterase, nitrites, and bacteria. Urine microscopy has 120 white blood cells per high power field. What is the most appropriate treatment?
A. Azithromycin
B. Ceftriaxone
C. Cefepime and vancomycin
D. Nitrofurantoin
The answer is B. The patient presents with sepsis secondary to a urinary tract infection. Using the anatomic approach this would be classified as uncomplicated. Using the severity approach, this would be classified as a complicated urinary tract infection. With fever, chills, and signs of sepsis, it’s likely her infection extends beyond the bladder. Given the severity of her presentation, we’d favor treating her as a complicated urinary tract infection with intravenous ceftriaxone. There is no suggestion of resistance or additional MRSA risk factors requiring intravenous vancomycin or cefepime. Nitrofurantoin, although a first-line treatment for uncomplicated cystitis, would not be appropriate if there is suspicion infection extends beyond the bladder. Azithromycin is a first-line option for chlamydia trachomatis, but not a urinary tract infection.
Timing of renal-replacement therapy for AKI in the ICU
Background: Acute kidney injury (AKI) in the ICU is associated with high mortality. It is hypothesized that earlier initiation of RRT may benefit patients by controlling fluid overload and reducing metabolic stress caused by electrolyte and acid-base imbalances. However, prior studies have been conflicting, with the IDEAL-ICU study (2018) demonstrating no improvement in 90-day mortality with early RRT in septic shock.
Study design: Open-label randomized controlled trial.
Setting: 168 hospitals in 15 countries.
Synopsis: Of ICU patients with severe AKI, 3,019 were randomized to either early or standard initiation of RRT. Early RRT was defined as occurring within 12 hours of eligibility; in the standard-therapy group, RRT was delayed until specifically indicated or if there was no improvement after 72 hours. Those needing immediate renal replacement or deemed likely to recover without need for RRT were excluded in order to study only those in whom ideal timing of dialysis was uncertain. There was no difference in 90-day mortality between the groups (43.9% vs. 43.7%; P = .92). Early initiation did not improve length of ICU stay, ventilator-free days, days out of the hospital, or quality of life. The early-initiation patients experienced more adverse events related to RRT and were more likely to have continued dependence on RRT at 90 days (10.4% vs. 6.0% in standard initiation). Of note, approximately 40% of those randomized to standard initiation never required RRT.
Bottom line: This large, multicenter, well-conducted trial demonstrates no benefit for early initiation of RRT in critically ill patients.
Citation: STARRT-AKI investigators. Timing of initiation of renal-replacement therapy in acute kidney injury. N Engl J Med. 2020;383:240-51. doi: 10.1056/NEJMoa2000741.
Dr. Lee is a hospitalist at Northwestern Memorial Hospital and Lurie Children’s Hospital and assistant professor of medicine, Feinberg School of Medicine, all in Chicago.
Background: Acute kidney injury (AKI) in the ICU is associated with high mortality. It is hypothesized that earlier initiation of RRT may benefit patients by controlling fluid overload and reducing metabolic stress caused by electrolyte and acid-base imbalances. However, prior studies have been conflicting, with the IDEAL-ICU study (2018) demonstrating no improvement in 90-day mortality with early RRT in septic shock.
Study design: Open-label randomized controlled trial.
Setting: 168 hospitals in 15 countries.
Synopsis: Of ICU patients with severe AKI, 3,019 were randomized to either early or standard initiation of RRT. Early RRT was defined as occurring within 12 hours of eligibility; in the standard-therapy group, RRT was delayed until specifically indicated or if there was no improvement after 72 hours. Those needing immediate renal replacement or deemed likely to recover without need for RRT were excluded in order to study only those in whom ideal timing of dialysis was uncertain. There was no difference in 90-day mortality between the groups (43.9% vs. 43.7%; P = .92). Early initiation did not improve length of ICU stay, ventilator-free days, days out of the hospital, or quality of life. The early-initiation patients experienced more adverse events related to RRT and were more likely to have continued dependence on RRT at 90 days (10.4% vs. 6.0% in standard initiation). Of note, approximately 40% of those randomized to standard initiation never required RRT.
Bottom line: This large, multicenter, well-conducted trial demonstrates no benefit for early initiation of RRT in critically ill patients.
Citation: STARRT-AKI investigators. Timing of initiation of renal-replacement therapy in acute kidney injury. N Engl J Med. 2020;383:240-51. doi: 10.1056/NEJMoa2000741.
Dr. Lee is a hospitalist at Northwestern Memorial Hospital and Lurie Children’s Hospital and assistant professor of medicine, Feinberg School of Medicine, all in Chicago.
Background: Acute kidney injury (AKI) in the ICU is associated with high mortality. It is hypothesized that earlier initiation of RRT may benefit patients by controlling fluid overload and reducing metabolic stress caused by electrolyte and acid-base imbalances. However, prior studies have been conflicting, with the IDEAL-ICU study (2018) demonstrating no improvement in 90-day mortality with early RRT in septic shock.
Study design: Open-label randomized controlled trial.
Setting: 168 hospitals in 15 countries.
Synopsis: Of ICU patients with severe AKI, 3,019 were randomized to either early or standard initiation of RRT. Early RRT was defined as occurring within 12 hours of eligibility; in the standard-therapy group, RRT was delayed until specifically indicated or if there was no improvement after 72 hours. Those needing immediate renal replacement or deemed likely to recover without need for RRT were excluded in order to study only those in whom ideal timing of dialysis was uncertain. There was no difference in 90-day mortality between the groups (43.9% vs. 43.7%; P = .92). Early initiation did not improve length of ICU stay, ventilator-free days, days out of the hospital, or quality of life. The early-initiation patients experienced more adverse events related to RRT and were more likely to have continued dependence on RRT at 90 days (10.4% vs. 6.0% in standard initiation). Of note, approximately 40% of those randomized to standard initiation never required RRT.
Bottom line: This large, multicenter, well-conducted trial demonstrates no benefit for early initiation of RRT in critically ill patients.
Citation: STARRT-AKI investigators. Timing of initiation of renal-replacement therapy in acute kidney injury. N Engl J Med. 2020;383:240-51. doi: 10.1056/NEJMoa2000741.
Dr. Lee is a hospitalist at Northwestern Memorial Hospital and Lurie Children’s Hospital and assistant professor of medicine, Feinberg School of Medicine, all in Chicago.
Advanced CKD doesn’t derail empagliflozin in EMPEROR-preserved
More than half of the nearly 6,000 patients with heart failure and HFpEF enrolled in EMPEROR-Preserved had CKD (although renal function was not an enrollment criterion), including 10% with an estimated glomerular filtration rate (eGFR) that fell in the range of 20-29 mL/min/1.73 m2, which categorized them as having stage 4 CKD.
The results showed, in a prespecified analysis, that treatment with empagliflozin led to a consistent, significant relative risk reduction compared with placebo in the primary endpoint of cardiovascular death or hospitalization for heart failure “across the full spectrum of kidney function, down to an eGFR of 20 mL/min/1.73m2,” said Faiez Zannad, MD, PhD, who presented the findings at the annual meeting of the American Society of Nephrology.
Among the 46.5% of enrolled patients without CKD, empagliflozin produced a significant 20% drop in the primary outcome relative to those who received placebo. Among the 53.5% of patients with CKD at time of randomization (defined as an eGFR <60 mL/min/1/73 m2 or a urinary albumin to creatinine ratio >300 mg/g), treatment with empagliflozin was associated with a significant 25% cut in the primary endpoint compared with placebo.
Empagliflozin was also “well tolerated” by patients with HFpEF, whether or not they also had CKD, “including patients with severely impaired kidney function,” said Dr. Zannad, a professor of cardiology therapeutics at the University of Lorraine in Nancy, France, at the virtual meeting.
An end to ‘renalism’
“This is a nail in the coffin for the concept of ‘renalism,’” the erroneous notion held by many clinicians and researchers that various treatments are not as effective and potentially more likely to cause adverse effects in patients with CKD compared with those with better renal function, commented Janani Rangaswami, MD, a nephrologist who is a professor and director of the cardiorenal program at George Washington University, Washington, D.C.
In addition to EMPEROR-Preserved, other large trials of agents from the SGLT2 inhibitor class bucked the premise of renalism and took the “groundbreaking step” of enrolling patients with moderate-severe CKD, noted Dr. Rangaswami in an interview. In particular, two trials took this approach when enrolling patients with heart failure with reduced ejection fraction (HFrEF), EMPEROR-Reduced (which also tested empagliflozin and matched the design of EMPEROR-Preserved) and DAPA-HF (which tested the SGLT2 inhibitor dapagliflozin [Farxiga, AstraZeneca]).
“It was a huge, bold step, especially in EMPEROR-Preserved and in EMPEROR-Reduced, which both enrolled patients with eGFRs as low as 20 mL/min/1.73m2,” Dr. Rangaswami said. DAPA-HF included patients with eGFRs as low as 30 mL/min/1.73m2.
EMPEROR-Reduced and DAPA-HF – published earlier this year – both had similar findings as EMPEROR-Preserved as reported by Dr. Zannad: consistent benefit from empagliflozin or dapagliflozin regardless of eGFR level and no signal of increased adverse events from treatment.
In fact, all three analyses show that patients with worse renal function had the highest risk for cardiovascular death and hospitalization for heart failure; hence, the beneficial impact from SGLT2 inhibitors is greatest in these patients.
These observations “make it easier to focus on the group with moderate-to-severe CKD,” both in the routine care setting as well as in future trials, said Dr. Rangaswami.
“This is a welcome trend that paves the way to test more treatments in patients with stage 4 and even stage 5 CKD, patients ... excluded from trials in the past,” she said.
In addition, the consistent benefit from SGLT2 inhibitors in these three heart failure trials regardless of CKD “means there is simply no room for renalism. There is no room for clinicians to say that because a patient’s eGFR is 30 mL/min/1.73m2 they are worried about starting an SGLT2 inhibitor,” she stressed.
More CKD-independent effects of empagliflozin
Results of other new analyses from EMPEROR-Preserved, also reported by Dr. Zannad, included the finding that empagliflozin was associated with a similar slowing of loss of renal function over time compared with placebo, regardless of CKD status.
In patients with CKD, empagliflozin slowed eGFR loss by 1.4 mL/min/1.73 m2/year, and in those without CKD, by 1.3 mL/min/1.73 m2/year, relative to placebo.
“Even in patients without CKD, there was a relevant eGFR decline in the placebo group that was attenuated by empagliflozin,” Dr. Zannad said.
At the end of the study, when empagliflozin was stopped, patients with or without CKD had their eGFR bounce back by an identical 2.4 mL/min/1.73 m2 relative to placebo.
Empagliflozin slowed progression to macroalbuminuria and significantly reduced the incidence of acute kidney injury by a similar amount regardless of CKD status compared with placebo.
EMPEROR-Preserved enrolled patients with function-limiting HFpEF, a left ventricular ejection fraction >40%, and a minimum level of a reliable serum marker of heart failure, N-terminal pro-B-type natriuretic peptide (NT-proBNP). Compared with placebo, empagliflozin reduced the trial’s primary outcome by an absolute 3.3 percentage points and by a significant relative risk reduction of 21% after a median 26 months of follow-up, according to a report published in October 2021.
EMPEROR-Preserved is the first prospective, randomized trial to unequivocally show the efficacy and safety of a drug for improving outcomes in patients with HFpEF.
EMPEROR-Preserved was sponsored by Boehringer-Ingelheim and Lilly, which market empagliflozin (Jardiance). Dr. Zannad has reported financial relationships with Boehringer Ingelheim as well as other companies. Dr. Rangaswami has reported being a consultant for Boehringer Ingelheim, Lilly, and AstraZeneca.
A version of this article first appeared on Medscape.com.
More than half of the nearly 6,000 patients with heart failure and HFpEF enrolled in EMPEROR-Preserved had CKD (although renal function was not an enrollment criterion), including 10% with an estimated glomerular filtration rate (eGFR) that fell in the range of 20-29 mL/min/1.73 m2, which categorized them as having stage 4 CKD.
The results showed, in a prespecified analysis, that treatment with empagliflozin led to a consistent, significant relative risk reduction compared with placebo in the primary endpoint of cardiovascular death or hospitalization for heart failure “across the full spectrum of kidney function, down to an eGFR of 20 mL/min/1.73m2,” said Faiez Zannad, MD, PhD, who presented the findings at the annual meeting of the American Society of Nephrology.
Among the 46.5% of enrolled patients without CKD, empagliflozin produced a significant 20% drop in the primary outcome relative to those who received placebo. Among the 53.5% of patients with CKD at time of randomization (defined as an eGFR <60 mL/min/1/73 m2 or a urinary albumin to creatinine ratio >300 mg/g), treatment with empagliflozin was associated with a significant 25% cut in the primary endpoint compared with placebo.
Empagliflozin was also “well tolerated” by patients with HFpEF, whether or not they also had CKD, “including patients with severely impaired kidney function,” said Dr. Zannad, a professor of cardiology therapeutics at the University of Lorraine in Nancy, France, at the virtual meeting.
An end to ‘renalism’
“This is a nail in the coffin for the concept of ‘renalism,’” the erroneous notion held by many clinicians and researchers that various treatments are not as effective and potentially more likely to cause adverse effects in patients with CKD compared with those with better renal function, commented Janani Rangaswami, MD, a nephrologist who is a professor and director of the cardiorenal program at George Washington University, Washington, D.C.
In addition to EMPEROR-Preserved, other large trials of agents from the SGLT2 inhibitor class bucked the premise of renalism and took the “groundbreaking step” of enrolling patients with moderate-severe CKD, noted Dr. Rangaswami in an interview. In particular, two trials took this approach when enrolling patients with heart failure with reduced ejection fraction (HFrEF), EMPEROR-Reduced (which also tested empagliflozin and matched the design of EMPEROR-Preserved) and DAPA-HF (which tested the SGLT2 inhibitor dapagliflozin [Farxiga, AstraZeneca]).
“It was a huge, bold step, especially in EMPEROR-Preserved and in EMPEROR-Reduced, which both enrolled patients with eGFRs as low as 20 mL/min/1.73m2,” Dr. Rangaswami said. DAPA-HF included patients with eGFRs as low as 30 mL/min/1.73m2.
EMPEROR-Reduced and DAPA-HF – published earlier this year – both had similar findings as EMPEROR-Preserved as reported by Dr. Zannad: consistent benefit from empagliflozin or dapagliflozin regardless of eGFR level and no signal of increased adverse events from treatment.
In fact, all three analyses show that patients with worse renal function had the highest risk for cardiovascular death and hospitalization for heart failure; hence, the beneficial impact from SGLT2 inhibitors is greatest in these patients.
These observations “make it easier to focus on the group with moderate-to-severe CKD,” both in the routine care setting as well as in future trials, said Dr. Rangaswami.
“This is a welcome trend that paves the way to test more treatments in patients with stage 4 and even stage 5 CKD, patients ... excluded from trials in the past,” she said.
In addition, the consistent benefit from SGLT2 inhibitors in these three heart failure trials regardless of CKD “means there is simply no room for renalism. There is no room for clinicians to say that because a patient’s eGFR is 30 mL/min/1.73m2 they are worried about starting an SGLT2 inhibitor,” she stressed.
More CKD-independent effects of empagliflozin
Results of other new analyses from EMPEROR-Preserved, also reported by Dr. Zannad, included the finding that empagliflozin was associated with a similar slowing of loss of renal function over time compared with placebo, regardless of CKD status.
In patients with CKD, empagliflozin slowed eGFR loss by 1.4 mL/min/1.73 m2/year, and in those without CKD, by 1.3 mL/min/1.73 m2/year, relative to placebo.
“Even in patients without CKD, there was a relevant eGFR decline in the placebo group that was attenuated by empagliflozin,” Dr. Zannad said.
At the end of the study, when empagliflozin was stopped, patients with or without CKD had their eGFR bounce back by an identical 2.4 mL/min/1.73 m2 relative to placebo.
Empagliflozin slowed progression to macroalbuminuria and significantly reduced the incidence of acute kidney injury by a similar amount regardless of CKD status compared with placebo.
EMPEROR-Preserved enrolled patients with function-limiting HFpEF, a left ventricular ejection fraction >40%, and a minimum level of a reliable serum marker of heart failure, N-terminal pro-B-type natriuretic peptide (NT-proBNP). Compared with placebo, empagliflozin reduced the trial’s primary outcome by an absolute 3.3 percentage points and by a significant relative risk reduction of 21% after a median 26 months of follow-up, according to a report published in October 2021.
EMPEROR-Preserved is the first prospective, randomized trial to unequivocally show the efficacy and safety of a drug for improving outcomes in patients with HFpEF.
EMPEROR-Preserved was sponsored by Boehringer-Ingelheim and Lilly, which market empagliflozin (Jardiance). Dr. Zannad has reported financial relationships with Boehringer Ingelheim as well as other companies. Dr. Rangaswami has reported being a consultant for Boehringer Ingelheim, Lilly, and AstraZeneca.
A version of this article first appeared on Medscape.com.
More than half of the nearly 6,000 patients with heart failure and HFpEF enrolled in EMPEROR-Preserved had CKD (although renal function was not an enrollment criterion), including 10% with an estimated glomerular filtration rate (eGFR) that fell in the range of 20-29 mL/min/1.73 m2, which categorized them as having stage 4 CKD.
The results showed, in a prespecified analysis, that treatment with empagliflozin led to a consistent, significant relative risk reduction compared with placebo in the primary endpoint of cardiovascular death or hospitalization for heart failure “across the full spectrum of kidney function, down to an eGFR of 20 mL/min/1.73m2,” said Faiez Zannad, MD, PhD, who presented the findings at the annual meeting of the American Society of Nephrology.
Among the 46.5% of enrolled patients without CKD, empagliflozin produced a significant 20% drop in the primary outcome relative to those who received placebo. Among the 53.5% of patients with CKD at time of randomization (defined as an eGFR <60 mL/min/1/73 m2 or a urinary albumin to creatinine ratio >300 mg/g), treatment with empagliflozin was associated with a significant 25% cut in the primary endpoint compared with placebo.
Empagliflozin was also “well tolerated” by patients with HFpEF, whether or not they also had CKD, “including patients with severely impaired kidney function,” said Dr. Zannad, a professor of cardiology therapeutics at the University of Lorraine in Nancy, France, at the virtual meeting.
An end to ‘renalism’
“This is a nail in the coffin for the concept of ‘renalism,’” the erroneous notion held by many clinicians and researchers that various treatments are not as effective and potentially more likely to cause adverse effects in patients with CKD compared with those with better renal function, commented Janani Rangaswami, MD, a nephrologist who is a professor and director of the cardiorenal program at George Washington University, Washington, D.C.
In addition to EMPEROR-Preserved, other large trials of agents from the SGLT2 inhibitor class bucked the premise of renalism and took the “groundbreaking step” of enrolling patients with moderate-severe CKD, noted Dr. Rangaswami in an interview. In particular, two trials took this approach when enrolling patients with heart failure with reduced ejection fraction (HFrEF), EMPEROR-Reduced (which also tested empagliflozin and matched the design of EMPEROR-Preserved) and DAPA-HF (which tested the SGLT2 inhibitor dapagliflozin [Farxiga, AstraZeneca]).
“It was a huge, bold step, especially in EMPEROR-Preserved and in EMPEROR-Reduced, which both enrolled patients with eGFRs as low as 20 mL/min/1.73m2,” Dr. Rangaswami said. DAPA-HF included patients with eGFRs as low as 30 mL/min/1.73m2.
EMPEROR-Reduced and DAPA-HF – published earlier this year – both had similar findings as EMPEROR-Preserved as reported by Dr. Zannad: consistent benefit from empagliflozin or dapagliflozin regardless of eGFR level and no signal of increased adverse events from treatment.
In fact, all three analyses show that patients with worse renal function had the highest risk for cardiovascular death and hospitalization for heart failure; hence, the beneficial impact from SGLT2 inhibitors is greatest in these patients.
These observations “make it easier to focus on the group with moderate-to-severe CKD,” both in the routine care setting as well as in future trials, said Dr. Rangaswami.
“This is a welcome trend that paves the way to test more treatments in patients with stage 4 and even stage 5 CKD, patients ... excluded from trials in the past,” she said.
In addition, the consistent benefit from SGLT2 inhibitors in these three heart failure trials regardless of CKD “means there is simply no room for renalism. There is no room for clinicians to say that because a patient’s eGFR is 30 mL/min/1.73m2 they are worried about starting an SGLT2 inhibitor,” she stressed.
More CKD-independent effects of empagliflozin
Results of other new analyses from EMPEROR-Preserved, also reported by Dr. Zannad, included the finding that empagliflozin was associated with a similar slowing of loss of renal function over time compared with placebo, regardless of CKD status.
In patients with CKD, empagliflozin slowed eGFR loss by 1.4 mL/min/1.73 m2/year, and in those without CKD, by 1.3 mL/min/1.73 m2/year, relative to placebo.
“Even in patients without CKD, there was a relevant eGFR decline in the placebo group that was attenuated by empagliflozin,” Dr. Zannad said.
At the end of the study, when empagliflozin was stopped, patients with or without CKD had their eGFR bounce back by an identical 2.4 mL/min/1.73 m2 relative to placebo.
Empagliflozin slowed progression to macroalbuminuria and significantly reduced the incidence of acute kidney injury by a similar amount regardless of CKD status compared with placebo.
EMPEROR-Preserved enrolled patients with function-limiting HFpEF, a left ventricular ejection fraction >40%, and a minimum level of a reliable serum marker of heart failure, N-terminal pro-B-type natriuretic peptide (NT-proBNP). Compared with placebo, empagliflozin reduced the trial’s primary outcome by an absolute 3.3 percentage points and by a significant relative risk reduction of 21% after a median 26 months of follow-up, according to a report published in October 2021.
EMPEROR-Preserved is the first prospective, randomized trial to unequivocally show the efficacy and safety of a drug for improving outcomes in patients with HFpEF.
EMPEROR-Preserved was sponsored by Boehringer-Ingelheim and Lilly, which market empagliflozin (Jardiance). Dr. Zannad has reported financial relationships with Boehringer Ingelheim as well as other companies. Dr. Rangaswami has reported being a consultant for Boehringer Ingelheim, Lilly, and AstraZeneca.
A version of this article first appeared on Medscape.com.
FROM KIDNEY WEEK 2021
ADVOCATE: Avacopan shows renal benefits in ANCA vasculitis
Treatment of antineutrophil cytoplasmic autoantibody (ANCA)–associated vasculitis and renal disease with the oral C5a receptor inhibitor avacopan (Tavneos, ChemoCentryx) provides significant recovery of kidney function, compared with prednisone, particularly in patients with severe kidney disease, novel research indicates.
The new analysis underscores that “the real value of avacopan is that we can now expect to get our patients steroid free,” said first author David R.W. Jayne, MD, a professor of clinical autoimmunity at the University of Cambridge (England), when presenting the findings at the American Society of Nephrology’s Kidney Week 2021.
“Whether or not we’re brave enough to initiate treatment without steroids, I think that will perhaps come with some patient experience,” he added.
The findings are from a subanalysis of renal effects in the phase 3 ADVOCATE trial, which was published in February 2021 in the New England Journal of Medicine and included 330 patients with ANCA-associated vasculitis.
The trial in large part led to the U.S. approval of avacopan by the Food and Drug Administration in October as an adjunctive treatment for adults with severe active ANCA-associated vasculitis in combination with standard therapy including glucocorticoids.
The approval was greeted with enthusiasm as suggesting a much-needed option to help reduce, or even potentially eliminate, the need for glucocorticoids and their side effects. Other agents included in treatment regimens for ANCA-associated vasculitis include cyclophosphamide and rituximab.
Dr. Jayne emphasized that, before avacopan, treatment options had been limited.
“There is nothing else new in the clinic apart from rituximab, which we have now been using for almost 20 years,” he said in an interview. “Avacopan is new, the mode of action is different from any drugs in use at the moment, and the speed of action is very quick.”
The need to more closely investigate the trial’s renal outcomes in this new analysis was important because the high mortality rates in ANCA-associated vasculitis – a rare systemic autoimmune disease causing overactivation of complement resulting in inflammation of small blood vessels – is largely driven by those with MPO and PR3 autoantibody renal vasculitis, Dr. Jayne explained.
Commenting on the study, J. Charles Jennette, MD, a professor of pathology and laboratory medicine and professor of medicine at the University of North Carolina at Chapel Hill, said the new findings on renal outcomes, such as proteinuria, may offer key insights on avacopan’s efficacy.
“To me, the most impressive outcome of the ADVOCATE Phase 3 trial was the more rapid reduction in hematuria and proteinuria with avacopan compared to conventional prednisone therapy,” he said in an interview.
Recovery of eGFR with avacopan best in those with severe renal disease
In the trial, patients with ANCA-associated vasculitis were randomized 1:1 to treatment with oral avacopan 30 mg twice daily or oral prednisone on a tapering schedule.
All patients also received background immunosuppression – about two-thirds received rituximab and a third received cyclophosphamide – followed by azathioprine.
The main study results showed similar rates of remission in both groups at week 26 and a superior remission rate with avacopan, in terms of sustained remission, at week 52 (65.7% vs. 54.9%; P < .001).
Approximately 80% of patients in the trial had renal involvement of ANCA vasculitis, the focus of the new analysis, and they had a baseline mean estimated glomerular filtration rate (eGFR) of 45 mL/min per 1.73 m2.
Among those with renal involvement, patients treated with avacopan had a significantly greater eGFR recovery, compared with the prednisone group at week 26 (P = .046) and week 52 (P < .029).
The strongest improvements were observed among patients with moderate to severe kidney damage, who had a mean eGFR of 21 mL/min per 1.73 m2 at baseline. Among those patients, the mean increase in eGFR was 13.7 mL/min per 1.73 m2 in the avacopan-treated group (n = 52) versus 8.2 mL/min per 1.73 m2 in the prednisone group (n = 48; P < .01) by week 52.
Improvements in urinary albumin:creatinine ratios (UACR) of as much as 40% were also observed in the avacopan group within the first 4 weeks of treatment, while no changes were observed in the same period in the prednisone group.
In other findings, the study also showed more rapid declines in proteinuria within 4 weeks in the avacopan group, and fewer patients had hematuria and there were greater reductions in MCP-1 in avacopan-treated patients at week 52, Dr. Jayne reported.
In terms of safety, there were no differences between the groups, with trends of fewer deaths and severe adverse events in the avacopan group.
“We found that the improved recovery of eGFR with avacopan was accentuated among those with more severe renal disease,” Dr. Jayne said.
He noted that, while the study’s aim was for the avacopan group to be steroid free, the patients received brief, reduced doses of about a third of the normal oral steroid dose early in the trial. However, using a Glucocorticoid Toxicity Index, the authors found those in the avacopan group did have fewer glucocorticoid-related adverse events.
Future issues to be examined include what happens when avacopan is discontinued and whether there will be a high relapse rate, Dr. Jayne noted.
Overall, however, “we anticipate that with longer-term follow-up, this better eGFR recovery will have a [favorable] effect on kidney failure and potentially mortality risk in these patients,” he concluded.
Targeted therapy is good for patients and doctors
Expanding upon his comments regarding the new drug, Dr. Jennette said it implies “that the C5a receptor inhibitor was targeting an event that blocks injury more quickly and effectively than prednisone.”
“This may be because prednisone has more complex pharmacodynamics and less targeted effects than a C5a receptor inhibitor,” he said.
Overall, the findings bode well for a potentially beneficial therapy, he added. “We have entered a new era of more targeted therapies, for example, targeted B-cell therapy using an anti-CD20 antibody, and targeted complement-mediated injury therapy using C5a receptor inhibitor.”
“The validation of this targeted therapy to block complement-mediated autoimmune inflammatory injury is another advance toward targeted precision therapy versus empirical therapy. This will be good for the doctors and good for the patients,” Dr. Jennette concluded.
The study was funded by ChemoCentryx. Dr. Jayne has reported receiving grants and/or consulting for AstraZeneca, ChemoCentryx, GlaxoSmithKline, MiroBio, Vifor, and Roche/Genentech. Dr. Jennette has received funding from ChemoCentryx for preclinical validation studies of avacopan in a mouse model of ANCA glomerulonephritis.
A version of this article first appeared on Medscape.com.
Treatment of antineutrophil cytoplasmic autoantibody (ANCA)–associated vasculitis and renal disease with the oral C5a receptor inhibitor avacopan (Tavneos, ChemoCentryx) provides significant recovery of kidney function, compared with prednisone, particularly in patients with severe kidney disease, novel research indicates.
The new analysis underscores that “the real value of avacopan is that we can now expect to get our patients steroid free,” said first author David R.W. Jayne, MD, a professor of clinical autoimmunity at the University of Cambridge (England), when presenting the findings at the American Society of Nephrology’s Kidney Week 2021.
“Whether or not we’re brave enough to initiate treatment without steroids, I think that will perhaps come with some patient experience,” he added.
The findings are from a subanalysis of renal effects in the phase 3 ADVOCATE trial, which was published in February 2021 in the New England Journal of Medicine and included 330 patients with ANCA-associated vasculitis.
The trial in large part led to the U.S. approval of avacopan by the Food and Drug Administration in October as an adjunctive treatment for adults with severe active ANCA-associated vasculitis in combination with standard therapy including glucocorticoids.
The approval was greeted with enthusiasm as suggesting a much-needed option to help reduce, or even potentially eliminate, the need for glucocorticoids and their side effects. Other agents included in treatment regimens for ANCA-associated vasculitis include cyclophosphamide and rituximab.
Dr. Jayne emphasized that, before avacopan, treatment options had been limited.
“There is nothing else new in the clinic apart from rituximab, which we have now been using for almost 20 years,” he said in an interview. “Avacopan is new, the mode of action is different from any drugs in use at the moment, and the speed of action is very quick.”
The need to more closely investigate the trial’s renal outcomes in this new analysis was important because the high mortality rates in ANCA-associated vasculitis – a rare systemic autoimmune disease causing overactivation of complement resulting in inflammation of small blood vessels – is largely driven by those with MPO and PR3 autoantibody renal vasculitis, Dr. Jayne explained.
Commenting on the study, J. Charles Jennette, MD, a professor of pathology and laboratory medicine and professor of medicine at the University of North Carolina at Chapel Hill, said the new findings on renal outcomes, such as proteinuria, may offer key insights on avacopan’s efficacy.
“To me, the most impressive outcome of the ADVOCATE Phase 3 trial was the more rapid reduction in hematuria and proteinuria with avacopan compared to conventional prednisone therapy,” he said in an interview.
Recovery of eGFR with avacopan best in those with severe renal disease
In the trial, patients with ANCA-associated vasculitis were randomized 1:1 to treatment with oral avacopan 30 mg twice daily or oral prednisone on a tapering schedule.
All patients also received background immunosuppression – about two-thirds received rituximab and a third received cyclophosphamide – followed by azathioprine.
The main study results showed similar rates of remission in both groups at week 26 and a superior remission rate with avacopan, in terms of sustained remission, at week 52 (65.7% vs. 54.9%; P < .001).
Approximately 80% of patients in the trial had renal involvement of ANCA vasculitis, the focus of the new analysis, and they had a baseline mean estimated glomerular filtration rate (eGFR) of 45 mL/min per 1.73 m2.
Among those with renal involvement, patients treated with avacopan had a significantly greater eGFR recovery, compared with the prednisone group at week 26 (P = .046) and week 52 (P < .029).
The strongest improvements were observed among patients with moderate to severe kidney damage, who had a mean eGFR of 21 mL/min per 1.73 m2 at baseline. Among those patients, the mean increase in eGFR was 13.7 mL/min per 1.73 m2 in the avacopan-treated group (n = 52) versus 8.2 mL/min per 1.73 m2 in the prednisone group (n = 48; P < .01) by week 52.
Improvements in urinary albumin:creatinine ratios (UACR) of as much as 40% were also observed in the avacopan group within the first 4 weeks of treatment, while no changes were observed in the same period in the prednisone group.
In other findings, the study also showed more rapid declines in proteinuria within 4 weeks in the avacopan group, and fewer patients had hematuria and there were greater reductions in MCP-1 in avacopan-treated patients at week 52, Dr. Jayne reported.
In terms of safety, there were no differences between the groups, with trends of fewer deaths and severe adverse events in the avacopan group.
“We found that the improved recovery of eGFR with avacopan was accentuated among those with more severe renal disease,” Dr. Jayne said.
He noted that, while the study’s aim was for the avacopan group to be steroid free, the patients received brief, reduced doses of about a third of the normal oral steroid dose early in the trial. However, using a Glucocorticoid Toxicity Index, the authors found those in the avacopan group did have fewer glucocorticoid-related adverse events.
Future issues to be examined include what happens when avacopan is discontinued and whether there will be a high relapse rate, Dr. Jayne noted.
Overall, however, “we anticipate that with longer-term follow-up, this better eGFR recovery will have a [favorable] effect on kidney failure and potentially mortality risk in these patients,” he concluded.
Targeted therapy is good for patients and doctors
Expanding upon his comments regarding the new drug, Dr. Jennette said it implies “that the C5a receptor inhibitor was targeting an event that blocks injury more quickly and effectively than prednisone.”
“This may be because prednisone has more complex pharmacodynamics and less targeted effects than a C5a receptor inhibitor,” he said.
Overall, the findings bode well for a potentially beneficial therapy, he added. “We have entered a new era of more targeted therapies, for example, targeted B-cell therapy using an anti-CD20 antibody, and targeted complement-mediated injury therapy using C5a receptor inhibitor.”
“The validation of this targeted therapy to block complement-mediated autoimmune inflammatory injury is another advance toward targeted precision therapy versus empirical therapy. This will be good for the doctors and good for the patients,” Dr. Jennette concluded.
The study was funded by ChemoCentryx. Dr. Jayne has reported receiving grants and/or consulting for AstraZeneca, ChemoCentryx, GlaxoSmithKline, MiroBio, Vifor, and Roche/Genentech. Dr. Jennette has received funding from ChemoCentryx for preclinical validation studies of avacopan in a mouse model of ANCA glomerulonephritis.
A version of this article first appeared on Medscape.com.
Treatment of antineutrophil cytoplasmic autoantibody (ANCA)–associated vasculitis and renal disease with the oral C5a receptor inhibitor avacopan (Tavneos, ChemoCentryx) provides significant recovery of kidney function, compared with prednisone, particularly in patients with severe kidney disease, novel research indicates.
The new analysis underscores that “the real value of avacopan is that we can now expect to get our patients steroid free,” said first author David R.W. Jayne, MD, a professor of clinical autoimmunity at the University of Cambridge (England), when presenting the findings at the American Society of Nephrology’s Kidney Week 2021.
“Whether or not we’re brave enough to initiate treatment without steroids, I think that will perhaps come with some patient experience,” he added.
The findings are from a subanalysis of renal effects in the phase 3 ADVOCATE trial, which was published in February 2021 in the New England Journal of Medicine and included 330 patients with ANCA-associated vasculitis.
The trial in large part led to the U.S. approval of avacopan by the Food and Drug Administration in October as an adjunctive treatment for adults with severe active ANCA-associated vasculitis in combination with standard therapy including glucocorticoids.
The approval was greeted with enthusiasm as suggesting a much-needed option to help reduce, or even potentially eliminate, the need for glucocorticoids and their side effects. Other agents included in treatment regimens for ANCA-associated vasculitis include cyclophosphamide and rituximab.
Dr. Jayne emphasized that, before avacopan, treatment options had been limited.
“There is nothing else new in the clinic apart from rituximab, which we have now been using for almost 20 years,” he said in an interview. “Avacopan is new, the mode of action is different from any drugs in use at the moment, and the speed of action is very quick.”
The need to more closely investigate the trial’s renal outcomes in this new analysis was important because the high mortality rates in ANCA-associated vasculitis – a rare systemic autoimmune disease causing overactivation of complement resulting in inflammation of small blood vessels – is largely driven by those with MPO and PR3 autoantibody renal vasculitis, Dr. Jayne explained.
Commenting on the study, J. Charles Jennette, MD, a professor of pathology and laboratory medicine and professor of medicine at the University of North Carolina at Chapel Hill, said the new findings on renal outcomes, such as proteinuria, may offer key insights on avacopan’s efficacy.
“To me, the most impressive outcome of the ADVOCATE Phase 3 trial was the more rapid reduction in hematuria and proteinuria with avacopan compared to conventional prednisone therapy,” he said in an interview.
Recovery of eGFR with avacopan best in those with severe renal disease
In the trial, patients with ANCA-associated vasculitis were randomized 1:1 to treatment with oral avacopan 30 mg twice daily or oral prednisone on a tapering schedule.
All patients also received background immunosuppression – about two-thirds received rituximab and a third received cyclophosphamide – followed by azathioprine.
The main study results showed similar rates of remission in both groups at week 26 and a superior remission rate with avacopan, in terms of sustained remission, at week 52 (65.7% vs. 54.9%; P < .001).
Approximately 80% of patients in the trial had renal involvement of ANCA vasculitis, the focus of the new analysis, and they had a baseline mean estimated glomerular filtration rate (eGFR) of 45 mL/min per 1.73 m2.
Among those with renal involvement, patients treated with avacopan had a significantly greater eGFR recovery, compared with the prednisone group at week 26 (P = .046) and week 52 (P < .029).
The strongest improvements were observed among patients with moderate to severe kidney damage, who had a mean eGFR of 21 mL/min per 1.73 m2 at baseline. Among those patients, the mean increase in eGFR was 13.7 mL/min per 1.73 m2 in the avacopan-treated group (n = 52) versus 8.2 mL/min per 1.73 m2 in the prednisone group (n = 48; P < .01) by week 52.
Improvements in urinary albumin:creatinine ratios (UACR) of as much as 40% were also observed in the avacopan group within the first 4 weeks of treatment, while no changes were observed in the same period in the prednisone group.
In other findings, the study also showed more rapid declines in proteinuria within 4 weeks in the avacopan group, and fewer patients had hematuria and there were greater reductions in MCP-1 in avacopan-treated patients at week 52, Dr. Jayne reported.
In terms of safety, there were no differences between the groups, with trends of fewer deaths and severe adverse events in the avacopan group.
“We found that the improved recovery of eGFR with avacopan was accentuated among those with more severe renal disease,” Dr. Jayne said.
He noted that, while the study’s aim was for the avacopan group to be steroid free, the patients received brief, reduced doses of about a third of the normal oral steroid dose early in the trial. However, using a Glucocorticoid Toxicity Index, the authors found those in the avacopan group did have fewer glucocorticoid-related adverse events.
Future issues to be examined include what happens when avacopan is discontinued and whether there will be a high relapse rate, Dr. Jayne noted.
Overall, however, “we anticipate that with longer-term follow-up, this better eGFR recovery will have a [favorable] effect on kidney failure and potentially mortality risk in these patients,” he concluded.
Targeted therapy is good for patients and doctors
Expanding upon his comments regarding the new drug, Dr. Jennette said it implies “that the C5a receptor inhibitor was targeting an event that blocks injury more quickly and effectively than prednisone.”
“This may be because prednisone has more complex pharmacodynamics and less targeted effects than a C5a receptor inhibitor,” he said.
Overall, the findings bode well for a potentially beneficial therapy, he added. “We have entered a new era of more targeted therapies, for example, targeted B-cell therapy using an anti-CD20 antibody, and targeted complement-mediated injury therapy using C5a receptor inhibitor.”
“The validation of this targeted therapy to block complement-mediated autoimmune inflammatory injury is another advance toward targeted precision therapy versus empirical therapy. This will be good for the doctors and good for the patients,” Dr. Jennette concluded.
The study was funded by ChemoCentryx. Dr. Jayne has reported receiving grants and/or consulting for AstraZeneca, ChemoCentryx, GlaxoSmithKline, MiroBio, Vifor, and Roche/Genentech. Dr. Jennette has received funding from ChemoCentryx for preclinical validation studies of avacopan in a mouse model of ANCA glomerulonephritis.
A version of this article first appeared on Medscape.com.
FROM KIDNEY WEEK 2021
Oral daprodustat safely improves anemia in chronic kidney disease
both in those who are dialysis dependent and those who are not, in a pair of phase 3, randomized trials that together included more than 6,800 patients.
“Daprodustat could represent an oral alternative to ESAs for treating anemia of CKD in both dialysis and nondialysis patients,” said Ajay K. Singh, MBBS, who presented results from both studies at the annual meeting of the American Society of Nephrology.
Concurrently, reports on the trial with dialysis-dependent patients, ASCEND-D, and on the trial with non–dialysis-dependent patients, ASCEND-ND, appeared online in the New England Journal of Medicine.
Singh highlighted that the results prove the noninferiority of oral daprodustat to the injected ESAs – epoetin alfa (Epogen, Procrit) or darbepoetin alfa (Aranesp) – used as the comparator agents in the two trials for the adjudicated safety outcome of major adverse cardiovascular events (MACE). In addition, results from the two studies also showed “no safety signals that pop out, and no new safety signals observed,” he said.
Those were telling assessments, given that two other agents from the same drug class – the hypoxia-inducible factor prolyl hydroxylase inhibitors (HIF-PHIs) roxadustat and vadadustat – have been hobbled by safety concerns that cropped up in their pivotal trials.
A class with a history of safety concerns
The HIF-PHI roxadustat received an overwhelming negative reaction from an advisory committee to the Food and Drug Administration in July 2021 because of safety concerns, although it was approved in the European Union.
And results from a phase 3 trial of the HIF-PHI agent vadadustat reported in April, showed that, in patients with non–dialysis-dependent CKD treated with vadadustat the MACE incidence failed to meet the trial’s criterion for noninferiority, compared with patients treated with the ESA darbepoetin alfa.
In contrast, the safety of daprodustat, based on the results reported so far “is looking really good,” commented Jay B. Wish, MD, a nephrologist and professor at Indiana University in Indianapolis who was not involved with the study.
“You never know what’s behind the curtain, but what’s out there [for daprodustat] seems very encouraging,” Dr. Wish said in an interview.
He cited in particular the data reported by Dr. Singh on thromboembolic events and vascular access thrombosis, adverse effects that were especially problematic for roxadustat. The report by Dr. Singh specifically called out these numbers and showed numerical reductions in these rates, compared with ESA-treated patients among those on dialysis, and small increases among those on daprodustat, compared with ESA treatment among those not on dialysis.
In ASCEND-ND, nonfatal thromboembolic events during median follow-up of 1.9 years occurred 97 times (in 3.0% of patients) among 1,917 patients treated with daprodustat and 65 times (in 2.4% of patients) among 1,935 patients treated with darbepoetin alfa, reported Dr. Singh, a nephrologist at Brigham and Women’s Hospital in Boston. Vascular access thrombosis in ASCEND-ND occurred 69 times in 2.1% of patients on daprodustat and 42 times in 1.5% of patients who received the ESA.
Drugs from the HIF-PHI class for anemia in patients with CKD “have now been evaluated in a number of phase 3, randomized, controlled trials. Initial results in patients with dialysis-dependent CKD are promising, but in patients with non–dialysis-dependent CKD questions about indications and safety warrant further investigations,” Patrick Parfrey, MD, commented in an editorial that accompanied the ASCEND-D and ASCEND-ND reports.
Safety signals seen for cancers and erosions
Dr. Parfrey cited two particular safety findings, both seen in ASCEND-ND. One was a numerically higher rate of cancer-related death, or tumor progression or recurrence, among the daprodustat recipients (3.7%), compared with the controls who received an ESA in the ASCEND-ND trial (2.5%), representing a significant relative risk of 1.47.
In contrast, in ASCEND-D this cancer safety measure showed a reduced relative risk with daprodustat of 0.92 relative to the ESA comparators.
“The safety of HIF-PHIs from the cancer perspective will require longer follow-up, individual patient meta-analysis ... and postmarketing surveillance,” wrote Dr. Parfrey, a nephrologist and professor at Memorial University, St. John’s, Nfld.
Elevated cancer rates are a hypothetical concern with agents from the HIF-PHI class because of their potential for increasing angiogenesis that could support tumor growth, said Dr. Wish.
Dr. Parfrey also cited another safety signal in ASCEND-ND, a higher rate of esophageal or gastric erosions on daprodustat (3.6%), compared with those on darbepoetin alfa (2.1%), with a significant relative risk of 1.7.
Again, this signal was absent in ASCEND-D, where esophageal or gastric erosions were more common in the patients on an ESA, with a relative risk reduction in favor of daprodustat of 0.74.
But even if these cancer and erosion effects in nondialysis patients on daprodustat are real, “these things don’t sink a drug. You deal with them in the drug’s label,” commented Dr. Wish.
During the FDA’s advisory committee meeting on roxadustat, agency staffers especially cited apparent excess rates of thrombosis and seizures associated with the drug. In both ASCEND-D and ASCEND-ND the rate of seizures in both treatment arms was less than 1%.
Dr. Wish speculated that the differences seen between roxadustat and daprodustat are likely more related to the design of their respective studies rather than real drug differences within the class.
Perhaps most importantly, the roxadustat trials in patients with CKD and not requiring dialysis compared the drug against placebo, while in ASCEND-ND the comparator was darbepoetin alfa. He also suggested that patients on dialysis receiving roxadustat may have been “overdosed,” resulting in faster increases in hemoglobin and higher peak levels.
Big potential for oral anemia treatment
In general, having an oral alternative for treating anemia in patients with CKD will be a significant advance, said Dr. Wish, especially for patients not on dialysis as well as for the rapidly growing number of patients who receive dialysis at home.
U.S. patients with CKD who do not require dialysis “often don’t get treated for anemia because it is so cumbersome” to use ESAs on patients not treated at a centralized clinic, said Dr. Wish, medical director of the outpatient dialysis unit at Indiana University Hospital, Indianapolis. “It’s a logistical nightmare.”
On the other hand, Wish did not see nearly as great a need for an oral therapy for anemia in patients treated at a dialysis clinic.
Patients who receive an ESA during their three-times weekly dialysis session usually do very well. “It’s not broken, and does not need to get fixed,” Dr. Wish said.
ASCEND-D and ASCEND-ND were sponsored by GlaxoSmithKline, the company developing daprodustat. Dr. Singh has been a consultant to GlaxoSmithKline and owns stock in Gilead. Dr. Wish has been a consultant to GlaxoSmithKline, as well as an adviser to AstraZeneca, Akebia, Otsuka, Vifor, and Rockwell Medica, and he has been a speaker on behalf of AstraZeneca and Akebia.
A version of this article first appeared on Medscape.com.
both in those who are dialysis dependent and those who are not, in a pair of phase 3, randomized trials that together included more than 6,800 patients.
“Daprodustat could represent an oral alternative to ESAs for treating anemia of CKD in both dialysis and nondialysis patients,” said Ajay K. Singh, MBBS, who presented results from both studies at the annual meeting of the American Society of Nephrology.
Concurrently, reports on the trial with dialysis-dependent patients, ASCEND-D, and on the trial with non–dialysis-dependent patients, ASCEND-ND, appeared online in the New England Journal of Medicine.
Singh highlighted that the results prove the noninferiority of oral daprodustat to the injected ESAs – epoetin alfa (Epogen, Procrit) or darbepoetin alfa (Aranesp) – used as the comparator agents in the two trials for the adjudicated safety outcome of major adverse cardiovascular events (MACE). In addition, results from the two studies also showed “no safety signals that pop out, and no new safety signals observed,” he said.
Those were telling assessments, given that two other agents from the same drug class – the hypoxia-inducible factor prolyl hydroxylase inhibitors (HIF-PHIs) roxadustat and vadadustat – have been hobbled by safety concerns that cropped up in their pivotal trials.
A class with a history of safety concerns
The HIF-PHI roxadustat received an overwhelming negative reaction from an advisory committee to the Food and Drug Administration in July 2021 because of safety concerns, although it was approved in the European Union.
And results from a phase 3 trial of the HIF-PHI agent vadadustat reported in April, showed that, in patients with non–dialysis-dependent CKD treated with vadadustat the MACE incidence failed to meet the trial’s criterion for noninferiority, compared with patients treated with the ESA darbepoetin alfa.
In contrast, the safety of daprodustat, based on the results reported so far “is looking really good,” commented Jay B. Wish, MD, a nephrologist and professor at Indiana University in Indianapolis who was not involved with the study.
“You never know what’s behind the curtain, but what’s out there [for daprodustat] seems very encouraging,” Dr. Wish said in an interview.
He cited in particular the data reported by Dr. Singh on thromboembolic events and vascular access thrombosis, adverse effects that were especially problematic for roxadustat. The report by Dr. Singh specifically called out these numbers and showed numerical reductions in these rates, compared with ESA-treated patients among those on dialysis, and small increases among those on daprodustat, compared with ESA treatment among those not on dialysis.
In ASCEND-ND, nonfatal thromboembolic events during median follow-up of 1.9 years occurred 97 times (in 3.0% of patients) among 1,917 patients treated with daprodustat and 65 times (in 2.4% of patients) among 1,935 patients treated with darbepoetin alfa, reported Dr. Singh, a nephrologist at Brigham and Women’s Hospital in Boston. Vascular access thrombosis in ASCEND-ND occurred 69 times in 2.1% of patients on daprodustat and 42 times in 1.5% of patients who received the ESA.
Drugs from the HIF-PHI class for anemia in patients with CKD “have now been evaluated in a number of phase 3, randomized, controlled trials. Initial results in patients with dialysis-dependent CKD are promising, but in patients with non–dialysis-dependent CKD questions about indications and safety warrant further investigations,” Patrick Parfrey, MD, commented in an editorial that accompanied the ASCEND-D and ASCEND-ND reports.
Safety signals seen for cancers and erosions
Dr. Parfrey cited two particular safety findings, both seen in ASCEND-ND. One was a numerically higher rate of cancer-related death, or tumor progression or recurrence, among the daprodustat recipients (3.7%), compared with the controls who received an ESA in the ASCEND-ND trial (2.5%), representing a significant relative risk of 1.47.
In contrast, in ASCEND-D this cancer safety measure showed a reduced relative risk with daprodustat of 0.92 relative to the ESA comparators.
“The safety of HIF-PHIs from the cancer perspective will require longer follow-up, individual patient meta-analysis ... and postmarketing surveillance,” wrote Dr. Parfrey, a nephrologist and professor at Memorial University, St. John’s, Nfld.
Elevated cancer rates are a hypothetical concern with agents from the HIF-PHI class because of their potential for increasing angiogenesis that could support tumor growth, said Dr. Wish.
Dr. Parfrey also cited another safety signal in ASCEND-ND, a higher rate of esophageal or gastric erosions on daprodustat (3.6%), compared with those on darbepoetin alfa (2.1%), with a significant relative risk of 1.7.
Again, this signal was absent in ASCEND-D, where esophageal or gastric erosions were more common in the patients on an ESA, with a relative risk reduction in favor of daprodustat of 0.74.
But even if these cancer and erosion effects in nondialysis patients on daprodustat are real, “these things don’t sink a drug. You deal with them in the drug’s label,” commented Dr. Wish.
During the FDA’s advisory committee meeting on roxadustat, agency staffers especially cited apparent excess rates of thrombosis and seizures associated with the drug. In both ASCEND-D and ASCEND-ND the rate of seizures in both treatment arms was less than 1%.
Dr. Wish speculated that the differences seen between roxadustat and daprodustat are likely more related to the design of their respective studies rather than real drug differences within the class.
Perhaps most importantly, the roxadustat trials in patients with CKD and not requiring dialysis compared the drug against placebo, while in ASCEND-ND the comparator was darbepoetin alfa. He also suggested that patients on dialysis receiving roxadustat may have been “overdosed,” resulting in faster increases in hemoglobin and higher peak levels.
Big potential for oral anemia treatment
In general, having an oral alternative for treating anemia in patients with CKD will be a significant advance, said Dr. Wish, especially for patients not on dialysis as well as for the rapidly growing number of patients who receive dialysis at home.
U.S. patients with CKD who do not require dialysis “often don’t get treated for anemia because it is so cumbersome” to use ESAs on patients not treated at a centralized clinic, said Dr. Wish, medical director of the outpatient dialysis unit at Indiana University Hospital, Indianapolis. “It’s a logistical nightmare.”
On the other hand, Wish did not see nearly as great a need for an oral therapy for anemia in patients treated at a dialysis clinic.
Patients who receive an ESA during their three-times weekly dialysis session usually do very well. “It’s not broken, and does not need to get fixed,” Dr. Wish said.
ASCEND-D and ASCEND-ND were sponsored by GlaxoSmithKline, the company developing daprodustat. Dr. Singh has been a consultant to GlaxoSmithKline and owns stock in Gilead. Dr. Wish has been a consultant to GlaxoSmithKline, as well as an adviser to AstraZeneca, Akebia, Otsuka, Vifor, and Rockwell Medica, and he has been a speaker on behalf of AstraZeneca and Akebia.
A version of this article first appeared on Medscape.com.
both in those who are dialysis dependent and those who are not, in a pair of phase 3, randomized trials that together included more than 6,800 patients.
“Daprodustat could represent an oral alternative to ESAs for treating anemia of CKD in both dialysis and nondialysis patients,” said Ajay K. Singh, MBBS, who presented results from both studies at the annual meeting of the American Society of Nephrology.
Concurrently, reports on the trial with dialysis-dependent patients, ASCEND-D, and on the trial with non–dialysis-dependent patients, ASCEND-ND, appeared online in the New England Journal of Medicine.
Singh highlighted that the results prove the noninferiority of oral daprodustat to the injected ESAs – epoetin alfa (Epogen, Procrit) or darbepoetin alfa (Aranesp) – used as the comparator agents in the two trials for the adjudicated safety outcome of major adverse cardiovascular events (MACE). In addition, results from the two studies also showed “no safety signals that pop out, and no new safety signals observed,” he said.
Those were telling assessments, given that two other agents from the same drug class – the hypoxia-inducible factor prolyl hydroxylase inhibitors (HIF-PHIs) roxadustat and vadadustat – have been hobbled by safety concerns that cropped up in their pivotal trials.
A class with a history of safety concerns
The HIF-PHI roxadustat received an overwhelming negative reaction from an advisory committee to the Food and Drug Administration in July 2021 because of safety concerns, although it was approved in the European Union.
And results from a phase 3 trial of the HIF-PHI agent vadadustat reported in April, showed that, in patients with non–dialysis-dependent CKD treated with vadadustat the MACE incidence failed to meet the trial’s criterion for noninferiority, compared with patients treated with the ESA darbepoetin alfa.
In contrast, the safety of daprodustat, based on the results reported so far “is looking really good,” commented Jay B. Wish, MD, a nephrologist and professor at Indiana University in Indianapolis who was not involved with the study.
“You never know what’s behind the curtain, but what’s out there [for daprodustat] seems very encouraging,” Dr. Wish said in an interview.
He cited in particular the data reported by Dr. Singh on thromboembolic events and vascular access thrombosis, adverse effects that were especially problematic for roxadustat. The report by Dr. Singh specifically called out these numbers and showed numerical reductions in these rates, compared with ESA-treated patients among those on dialysis, and small increases among those on daprodustat, compared with ESA treatment among those not on dialysis.
In ASCEND-ND, nonfatal thromboembolic events during median follow-up of 1.9 years occurred 97 times (in 3.0% of patients) among 1,917 patients treated with daprodustat and 65 times (in 2.4% of patients) among 1,935 patients treated with darbepoetin alfa, reported Dr. Singh, a nephrologist at Brigham and Women’s Hospital in Boston. Vascular access thrombosis in ASCEND-ND occurred 69 times in 2.1% of patients on daprodustat and 42 times in 1.5% of patients who received the ESA.
Drugs from the HIF-PHI class for anemia in patients with CKD “have now been evaluated in a number of phase 3, randomized, controlled trials. Initial results in patients with dialysis-dependent CKD are promising, but in patients with non–dialysis-dependent CKD questions about indications and safety warrant further investigations,” Patrick Parfrey, MD, commented in an editorial that accompanied the ASCEND-D and ASCEND-ND reports.
Safety signals seen for cancers and erosions
Dr. Parfrey cited two particular safety findings, both seen in ASCEND-ND. One was a numerically higher rate of cancer-related death, or tumor progression or recurrence, among the daprodustat recipients (3.7%), compared with the controls who received an ESA in the ASCEND-ND trial (2.5%), representing a significant relative risk of 1.47.
In contrast, in ASCEND-D this cancer safety measure showed a reduced relative risk with daprodustat of 0.92 relative to the ESA comparators.
“The safety of HIF-PHIs from the cancer perspective will require longer follow-up, individual patient meta-analysis ... and postmarketing surveillance,” wrote Dr. Parfrey, a nephrologist and professor at Memorial University, St. John’s, Nfld.
Elevated cancer rates are a hypothetical concern with agents from the HIF-PHI class because of their potential for increasing angiogenesis that could support tumor growth, said Dr. Wish.
Dr. Parfrey also cited another safety signal in ASCEND-ND, a higher rate of esophageal or gastric erosions on daprodustat (3.6%), compared with those on darbepoetin alfa (2.1%), with a significant relative risk of 1.7.
Again, this signal was absent in ASCEND-D, where esophageal or gastric erosions were more common in the patients on an ESA, with a relative risk reduction in favor of daprodustat of 0.74.
But even if these cancer and erosion effects in nondialysis patients on daprodustat are real, “these things don’t sink a drug. You deal with them in the drug’s label,” commented Dr. Wish.
During the FDA’s advisory committee meeting on roxadustat, agency staffers especially cited apparent excess rates of thrombosis and seizures associated with the drug. In both ASCEND-D and ASCEND-ND the rate of seizures in both treatment arms was less than 1%.
Dr. Wish speculated that the differences seen between roxadustat and daprodustat are likely more related to the design of their respective studies rather than real drug differences within the class.
Perhaps most importantly, the roxadustat trials in patients with CKD and not requiring dialysis compared the drug against placebo, while in ASCEND-ND the comparator was darbepoetin alfa. He also suggested that patients on dialysis receiving roxadustat may have been “overdosed,” resulting in faster increases in hemoglobin and higher peak levels.
Big potential for oral anemia treatment
In general, having an oral alternative for treating anemia in patients with CKD will be a significant advance, said Dr. Wish, especially for patients not on dialysis as well as for the rapidly growing number of patients who receive dialysis at home.
U.S. patients with CKD who do not require dialysis “often don’t get treated for anemia because it is so cumbersome” to use ESAs on patients not treated at a centralized clinic, said Dr. Wish, medical director of the outpatient dialysis unit at Indiana University Hospital, Indianapolis. “It’s a logistical nightmare.”
On the other hand, Wish did not see nearly as great a need for an oral therapy for anemia in patients treated at a dialysis clinic.
Patients who receive an ESA during their three-times weekly dialysis session usually do very well. “It’s not broken, and does not need to get fixed,” Dr. Wish said.
ASCEND-D and ASCEND-ND were sponsored by GlaxoSmithKline, the company developing daprodustat. Dr. Singh has been a consultant to GlaxoSmithKline and owns stock in Gilead. Dr. Wish has been a consultant to GlaxoSmithKline, as well as an adviser to AstraZeneca, Akebia, Otsuka, Vifor, and Rockwell Medica, and he has been a speaker on behalf of AstraZeneca and Akebia.
A version of this article first appeared on Medscape.com.
FROM KIDNEY WEEK 2021
Finerenone, sotagliflozin exert heart failure benefits despite renal dysfunction
New analyses of trial results for the cardiorenal agents finerenone and sotagliflozin continued the pattern showing that they exert consistent heart failure benefits in patients who span a broad spectrum of renal function, further disproving the notion that more severe stages of chronic kidney disease preclude aggressive medical management.
Analysis of combined data from two pivotal trials of the nonsteroidal mineralocorticoid receptor antagonist (MRA) finerenone (Kerendia), which together enrolled more than 13,000 patients with type 2 diabetes and chronic kidney disease, showed in greater detail that .
That spectrum included patients with estimated glomerular filtration rates (eGFR) as low as 25 mL/min per 1.73m2 and patients with micro- or macroalbuminuria, as well as those with normal urinary albumin levels, Gerasimos Filippatos, MD, reported at the American Heart Association scientific sessions.
And in a separate, unrelated report, combined data from the two pivotal trials, with a total of nearly 12,000 patients with type 2 diabetes, for sotagliflozin (Zynquista), a novel and still unapproved agent that inhibits both the sodium-glucose cotransporter (SGLT) 1 and 2 enzymes, showed a consistent effect significantly reducing cardiovascular death, hospitalization for heart failure, or urgent heart failure outpatient events in patients with eGFR rates as low as 25 mL/min per 1.73m2, Deepak L. Bhatt, MD, reported at the meeting.
These two reports follow a third, presented just a week earlier during Kidney Week, that showed the benefit from the SGLT2 inhibitor empagliflozin (Jardiance) for preventing heart failure hospitalizations or cardiovascular death in patients with heart failure with preserved ejection fraction remained consistent even in patients with an eGFR as low as 20 mL/min/1.73m2 in results from the EMPEROR-Preserved trial. Similar findings for empagliflozin in patients with heart failure with reduced ejection fraction in the EMPEROR-Reduced trial came out nearly a year ago.
A message to clinicians from these reports is, “don’t wait for patients to develop heart failure” to start these drugs, according to Dipti Itchhaporia, MD, director of disease management for the Hoag Heart and Vascular Institute in Newport Beach, Calif. “It’s time to start using these drugs upstream to have fewer patients with heart failure downstream,” she said in an interview.
Finerenone works differently than spironolactone
The new finerenone analysis included 5,734 patients enrolled in the FIDELIO-DKD trial, and 7,437 in the FIGARO-DKD trial, two very similar trials that differed by transposing the primary endpoint of one to the secondary endpoint of the other, and vice versa. The combined analysis is known as FIDELITY.
Expanding on a report that he first gave at the European Society of Cardiology annual congress in August 2021, Dr. Filippatos provided a few additional details on the analysis that showed a consistent effect of finerenone on preventing hospitalizations for heart failure, and on preventing a combined endpoint of hospitalizations for heart failure and cardiovascular death regardless of the severity of chronic kidney disease down to 25 mL/min per 1.73 m2. Statistical analysis showed no hint of an interaction between finerenone’s effect on these outcomes in patients with an eGFR of 60 mL/min per 1.73 m2 or greater and those with reduced renal function. Analyses also showed no interaction based on urinary albumin-to-creatinine ratio, be it more or less than 300 mg/g, reported Dr. Filippatos, professor and director of the heart failure unit at Attikon University Hospital in Athens.
“We use MRAs [such as spironolactone] in heart failure patients, but it’s difficult to use because of the risk of patients developing hyperkalemia,” noted Dr. Itchhaporia, who added that reluctance to use spironolactone is especially high for patients with depressed renal function, which could exacerbate a hyperkalemic effect. Evidence shows that finerenone poses a substantially reduced risk for raising serum potassium levels, making finerenone a more attractive agent to use in patients with CKD who have an elevated risk for heart failure events as well as an increased risk for hyperkalemia, like those enrolled in the two finerenone trials, she said.
Sotagliflozin uniquely inhibits SGLT1 and SGLT2
The new sotagliflozin analyses reported by Dr. Bhatt combined data for more than 11,800 patients randomized into either of two trials, SCORED, which randomized more than 10,000 patients with type 2 diabetes and chronic kidney disease, and SOLOIST, which randomized more than 1,000 patients with type 2 diabetes who were recently hospitalized for worsening heart failure.
A prespecified analysis for the combined data from both studies looked at the impact of sotagliflozin treatment on the combined outcome of cardiovascular death, hospitalization for heart failure, or an urgent outpatient visit because of heart failure based on kidney function at baseline. The analysis showed that sotagliflozin was at least as effective in the 8% of study patients who at baseline had an eGFR of 25-29 mL/min per 1.73 m2 as it was in patients with more preserved renal function.
Benefit from sotagliflozin treatment “was consistent across the full range of eGFR,” said Dr. Bhatt, professor at Harvard Medical School in Boston and executive director of interventional cardiovascular programs at Brigham and Women’s Hospital in Boston.
Results from a second analysis that he reported also showed a consistent effect of sotagliflozin on reducing hemoglobin A1c levels in the enrolled patients, even those with the lowest levels of renal function, an effect not previously seen with the related class of SGLT2 inhibitors (which includes empagliflozin, canagliflozin [Invokana], and dapagliflozin [Farxiga]). Dr. Bhatt suggested that, while SGLT2 inhibitors act entirely in the kidneys and hence their effect on glycemic control is blunted by renal dysfunction, sotagliflozin also inhibits the SGLT1 enzyme, which functions in the gut to transport glucose out of the digestive tract and into the blood, a glycemic control pathway that’s independent of renal function.
FIDELIO-DKD, FIGARO-DKD, and FIDELITY were sponsored by Bayer, the company that markets finerenone (Kerendia). SCORED and SOLOIST were sponsored by Sanofi, and later by Lexicon, the companies developing sotagliflozin (Zynquista). EMPEROR-Preserved and EMPEROR-Reduced were sponsored by Boehringer-Ingelheim and Lilly, the companies that market empagliflozin (Jardiance). Dr. Filippatos has had financial relationships with Bayer and Boehringer-Ingelheim, as well as with Amgen, Medtronic, Novartis, Servier, and Vifor. Dr. Bhatt has received research funding from Sanofi, Lexicon, Bayer, and Boehringer-Ingelheim, Lilly, and numerous other companies, and he has been an adviser to Boehringer-Ingelheim and several other companies.
New analyses of trial results for the cardiorenal agents finerenone and sotagliflozin continued the pattern showing that they exert consistent heart failure benefits in patients who span a broad spectrum of renal function, further disproving the notion that more severe stages of chronic kidney disease preclude aggressive medical management.
Analysis of combined data from two pivotal trials of the nonsteroidal mineralocorticoid receptor antagonist (MRA) finerenone (Kerendia), which together enrolled more than 13,000 patients with type 2 diabetes and chronic kidney disease, showed in greater detail that .
That spectrum included patients with estimated glomerular filtration rates (eGFR) as low as 25 mL/min per 1.73m2 and patients with micro- or macroalbuminuria, as well as those with normal urinary albumin levels, Gerasimos Filippatos, MD, reported at the American Heart Association scientific sessions.
And in a separate, unrelated report, combined data from the two pivotal trials, with a total of nearly 12,000 patients with type 2 diabetes, for sotagliflozin (Zynquista), a novel and still unapproved agent that inhibits both the sodium-glucose cotransporter (SGLT) 1 and 2 enzymes, showed a consistent effect significantly reducing cardiovascular death, hospitalization for heart failure, or urgent heart failure outpatient events in patients with eGFR rates as low as 25 mL/min per 1.73m2, Deepak L. Bhatt, MD, reported at the meeting.
These two reports follow a third, presented just a week earlier during Kidney Week, that showed the benefit from the SGLT2 inhibitor empagliflozin (Jardiance) for preventing heart failure hospitalizations or cardiovascular death in patients with heart failure with preserved ejection fraction remained consistent even in patients with an eGFR as low as 20 mL/min/1.73m2 in results from the EMPEROR-Preserved trial. Similar findings for empagliflozin in patients with heart failure with reduced ejection fraction in the EMPEROR-Reduced trial came out nearly a year ago.
A message to clinicians from these reports is, “don’t wait for patients to develop heart failure” to start these drugs, according to Dipti Itchhaporia, MD, director of disease management for the Hoag Heart and Vascular Institute in Newport Beach, Calif. “It’s time to start using these drugs upstream to have fewer patients with heart failure downstream,” she said in an interview.
Finerenone works differently than spironolactone
The new finerenone analysis included 5,734 patients enrolled in the FIDELIO-DKD trial, and 7,437 in the FIGARO-DKD trial, two very similar trials that differed by transposing the primary endpoint of one to the secondary endpoint of the other, and vice versa. The combined analysis is known as FIDELITY.
Expanding on a report that he first gave at the European Society of Cardiology annual congress in August 2021, Dr. Filippatos provided a few additional details on the analysis that showed a consistent effect of finerenone on preventing hospitalizations for heart failure, and on preventing a combined endpoint of hospitalizations for heart failure and cardiovascular death regardless of the severity of chronic kidney disease down to 25 mL/min per 1.73 m2. Statistical analysis showed no hint of an interaction between finerenone’s effect on these outcomes in patients with an eGFR of 60 mL/min per 1.73 m2 or greater and those with reduced renal function. Analyses also showed no interaction based on urinary albumin-to-creatinine ratio, be it more or less than 300 mg/g, reported Dr. Filippatos, professor and director of the heart failure unit at Attikon University Hospital in Athens.
“We use MRAs [such as spironolactone] in heart failure patients, but it’s difficult to use because of the risk of patients developing hyperkalemia,” noted Dr. Itchhaporia, who added that reluctance to use spironolactone is especially high for patients with depressed renal function, which could exacerbate a hyperkalemic effect. Evidence shows that finerenone poses a substantially reduced risk for raising serum potassium levels, making finerenone a more attractive agent to use in patients with CKD who have an elevated risk for heart failure events as well as an increased risk for hyperkalemia, like those enrolled in the two finerenone trials, she said.
Sotagliflozin uniquely inhibits SGLT1 and SGLT2
The new sotagliflozin analyses reported by Dr. Bhatt combined data for more than 11,800 patients randomized into either of two trials, SCORED, which randomized more than 10,000 patients with type 2 diabetes and chronic kidney disease, and SOLOIST, which randomized more than 1,000 patients with type 2 diabetes who were recently hospitalized for worsening heart failure.
A prespecified analysis for the combined data from both studies looked at the impact of sotagliflozin treatment on the combined outcome of cardiovascular death, hospitalization for heart failure, or an urgent outpatient visit because of heart failure based on kidney function at baseline. The analysis showed that sotagliflozin was at least as effective in the 8% of study patients who at baseline had an eGFR of 25-29 mL/min per 1.73 m2 as it was in patients with more preserved renal function.
Benefit from sotagliflozin treatment “was consistent across the full range of eGFR,” said Dr. Bhatt, professor at Harvard Medical School in Boston and executive director of interventional cardiovascular programs at Brigham and Women’s Hospital in Boston.
Results from a second analysis that he reported also showed a consistent effect of sotagliflozin on reducing hemoglobin A1c levels in the enrolled patients, even those with the lowest levels of renal function, an effect not previously seen with the related class of SGLT2 inhibitors (which includes empagliflozin, canagliflozin [Invokana], and dapagliflozin [Farxiga]). Dr. Bhatt suggested that, while SGLT2 inhibitors act entirely in the kidneys and hence their effect on glycemic control is blunted by renal dysfunction, sotagliflozin also inhibits the SGLT1 enzyme, which functions in the gut to transport glucose out of the digestive tract and into the blood, a glycemic control pathway that’s independent of renal function.
FIDELIO-DKD, FIGARO-DKD, and FIDELITY were sponsored by Bayer, the company that markets finerenone (Kerendia). SCORED and SOLOIST were sponsored by Sanofi, and later by Lexicon, the companies developing sotagliflozin (Zynquista). EMPEROR-Preserved and EMPEROR-Reduced were sponsored by Boehringer-Ingelheim and Lilly, the companies that market empagliflozin (Jardiance). Dr. Filippatos has had financial relationships with Bayer and Boehringer-Ingelheim, as well as with Amgen, Medtronic, Novartis, Servier, and Vifor. Dr. Bhatt has received research funding from Sanofi, Lexicon, Bayer, and Boehringer-Ingelheim, Lilly, and numerous other companies, and he has been an adviser to Boehringer-Ingelheim and several other companies.
New analyses of trial results for the cardiorenal agents finerenone and sotagliflozin continued the pattern showing that they exert consistent heart failure benefits in patients who span a broad spectrum of renal function, further disproving the notion that more severe stages of chronic kidney disease preclude aggressive medical management.
Analysis of combined data from two pivotal trials of the nonsteroidal mineralocorticoid receptor antagonist (MRA) finerenone (Kerendia), which together enrolled more than 13,000 patients with type 2 diabetes and chronic kidney disease, showed in greater detail that .
That spectrum included patients with estimated glomerular filtration rates (eGFR) as low as 25 mL/min per 1.73m2 and patients with micro- or macroalbuminuria, as well as those with normal urinary albumin levels, Gerasimos Filippatos, MD, reported at the American Heart Association scientific sessions.
And in a separate, unrelated report, combined data from the two pivotal trials, with a total of nearly 12,000 patients with type 2 diabetes, for sotagliflozin (Zynquista), a novel and still unapproved agent that inhibits both the sodium-glucose cotransporter (SGLT) 1 and 2 enzymes, showed a consistent effect significantly reducing cardiovascular death, hospitalization for heart failure, or urgent heart failure outpatient events in patients with eGFR rates as low as 25 mL/min per 1.73m2, Deepak L. Bhatt, MD, reported at the meeting.
These two reports follow a third, presented just a week earlier during Kidney Week, that showed the benefit from the SGLT2 inhibitor empagliflozin (Jardiance) for preventing heart failure hospitalizations or cardiovascular death in patients with heart failure with preserved ejection fraction remained consistent even in patients with an eGFR as low as 20 mL/min/1.73m2 in results from the EMPEROR-Preserved trial. Similar findings for empagliflozin in patients with heart failure with reduced ejection fraction in the EMPEROR-Reduced trial came out nearly a year ago.
A message to clinicians from these reports is, “don’t wait for patients to develop heart failure” to start these drugs, according to Dipti Itchhaporia, MD, director of disease management for the Hoag Heart and Vascular Institute in Newport Beach, Calif. “It’s time to start using these drugs upstream to have fewer patients with heart failure downstream,” she said in an interview.
Finerenone works differently than spironolactone
The new finerenone analysis included 5,734 patients enrolled in the FIDELIO-DKD trial, and 7,437 in the FIGARO-DKD trial, two very similar trials that differed by transposing the primary endpoint of one to the secondary endpoint of the other, and vice versa. The combined analysis is known as FIDELITY.
Expanding on a report that he first gave at the European Society of Cardiology annual congress in August 2021, Dr. Filippatos provided a few additional details on the analysis that showed a consistent effect of finerenone on preventing hospitalizations for heart failure, and on preventing a combined endpoint of hospitalizations for heart failure and cardiovascular death regardless of the severity of chronic kidney disease down to 25 mL/min per 1.73 m2. Statistical analysis showed no hint of an interaction between finerenone’s effect on these outcomes in patients with an eGFR of 60 mL/min per 1.73 m2 or greater and those with reduced renal function. Analyses also showed no interaction based on urinary albumin-to-creatinine ratio, be it more or less than 300 mg/g, reported Dr. Filippatos, professor and director of the heart failure unit at Attikon University Hospital in Athens.
“We use MRAs [such as spironolactone] in heart failure patients, but it’s difficult to use because of the risk of patients developing hyperkalemia,” noted Dr. Itchhaporia, who added that reluctance to use spironolactone is especially high for patients with depressed renal function, which could exacerbate a hyperkalemic effect. Evidence shows that finerenone poses a substantially reduced risk for raising serum potassium levels, making finerenone a more attractive agent to use in patients with CKD who have an elevated risk for heart failure events as well as an increased risk for hyperkalemia, like those enrolled in the two finerenone trials, she said.
Sotagliflozin uniquely inhibits SGLT1 and SGLT2
The new sotagliflozin analyses reported by Dr. Bhatt combined data for more than 11,800 patients randomized into either of two trials, SCORED, which randomized more than 10,000 patients with type 2 diabetes and chronic kidney disease, and SOLOIST, which randomized more than 1,000 patients with type 2 diabetes who were recently hospitalized for worsening heart failure.
A prespecified analysis for the combined data from both studies looked at the impact of sotagliflozin treatment on the combined outcome of cardiovascular death, hospitalization for heart failure, or an urgent outpatient visit because of heart failure based on kidney function at baseline. The analysis showed that sotagliflozin was at least as effective in the 8% of study patients who at baseline had an eGFR of 25-29 mL/min per 1.73 m2 as it was in patients with more preserved renal function.
Benefit from sotagliflozin treatment “was consistent across the full range of eGFR,” said Dr. Bhatt, professor at Harvard Medical School in Boston and executive director of interventional cardiovascular programs at Brigham and Women’s Hospital in Boston.
Results from a second analysis that he reported also showed a consistent effect of sotagliflozin on reducing hemoglobin A1c levels in the enrolled patients, even those with the lowest levels of renal function, an effect not previously seen with the related class of SGLT2 inhibitors (which includes empagliflozin, canagliflozin [Invokana], and dapagliflozin [Farxiga]). Dr. Bhatt suggested that, while SGLT2 inhibitors act entirely in the kidneys and hence their effect on glycemic control is blunted by renal dysfunction, sotagliflozin also inhibits the SGLT1 enzyme, which functions in the gut to transport glucose out of the digestive tract and into the blood, a glycemic control pathway that’s independent of renal function.
FIDELIO-DKD, FIGARO-DKD, and FIDELITY were sponsored by Bayer, the company that markets finerenone (Kerendia). SCORED and SOLOIST were sponsored by Sanofi, and later by Lexicon, the companies developing sotagliflozin (Zynquista). EMPEROR-Preserved and EMPEROR-Reduced were sponsored by Boehringer-Ingelheim and Lilly, the companies that market empagliflozin (Jardiance). Dr. Filippatos has had financial relationships with Bayer and Boehringer-Ingelheim, as well as with Amgen, Medtronic, Novartis, Servier, and Vifor. Dr. Bhatt has received research funding from Sanofi, Lexicon, Bayer, and Boehringer-Ingelheim, Lilly, and numerous other companies, and he has been an adviser to Boehringer-Ingelheim and several other companies.
FROM AHA 2021
SGLT2 inhibitors for diabetes: No link to fractures in older adults
Use of sodium-glucose cotransporter-2 (SGLT2) inhibitors does not appear to raise the risk for fractures in older adults, new research suggests.
The data come from a nationwide propensity score-matched study of U.S. Medicare recipients with type 2 diabetes who were new users of either an SGLT2 inhibitor, a dipeptidyl peptidase 4 (DPP-4) inhibitor, or a glucagon-like peptide (GLP-1) receptor agonist.
“The use of SGLT2 inhibitors was not associated with an increased risk of nontraumatic fractures compared with DPP-4 inhibitors or GLP-1 agonists. Results were consistent across categories of sex, frailty, age, and insulin use,” say Min Zhuo, MD, of Harvard Medical School, Boston, and colleagues, who published their work online October 27 in JAMA Network Open.
“Our results add to the evidence base evaluating the safety profile of SGLT2 inhibitors in older adults outside of [randomized controlled trials] and further characterize the risk-benefit balance of SGLT2 inhibitors in clinical practice,” they write.
Asked to comment, Simeon I. Taylor, MD, PhD, told this news organization, “This is a high-quality study that is generally reassuring that relatively short, less than 1 year, treatment with an SGLT2 inhibitor does not appear to significantly increase the risk of bone fractures.”
However, Dr. Taylor, of the Division of Endocrinology, Diabetes, and Nutrition, University of Maryland School of Medicine, Baltimore, also noted: “Notwithstanding these reassuring data, the paper also does a good job of pointing out important limitations.”
“Most importantly, these data do not address questions related to the risk of long-term chronic therapy. It is instructive to refer back to the published data demonstrating an approximately 2-year lag before a significant increase in the risk of fracture was observed in rosiglitazone-treated patients in the ADOPT study. The length of the lag is likely related to the baseline bone mineral density at the time drug therapy is initiated. These considerations may contribute to the observed variation in bone-related outcomes in different studies.”
Concern about SGLT2 inhibitors and fractures first arose in 2017 from the CANVAS study, in which the overall fracture risk with canagliflozin was a significant 26% higher than placebo. However, subsequent larger randomized trials of canagliflozin and other SGLT2 inhibitors did not find the same risk.
In addition, previous observational studies in younger adults have also not found use of SGLT2 inhibitors to be associated with increased fracture risk compared with DPP-4 inhibitors or GLP-1 agonists.
Understanding fracture risk with SGLT2 inhibitors is ‘critical’
Older adults with type 2 diabetes may benefit from reductions in atherosclerotic cardiovascular events, hospitalization for heart failure, end-stage kidney disease, and death associated with SGLT2 inhibitors, but the fact that aging may have negative effects on bone metabolism means “understanding the fracture risk associated with SGLT2 inhibitors in older adults with type 2 diabetes is critical,” say Dr. Zhuo and colleagues.
In the current study, they analyzed claims data for Medicare beneficiaries aged 66 years and older (1 year past Medicare eligibility) who were newly prescribed an SGLT2 inhibitor, DPP-4 inhibitor, or GLP-1 agonist between April 1, 2013 and Dec. 31, 2017.
A total of 45,889 patients from each treatment group were propensity-matched using 58 baseline characteristics, for a total of 137,667 patients.
After matching, there were 501 events of the primary composite outcome (nontraumatic pelvic fracture, hip fracture requiring surgery, or humerus, radius, or ulna fracture requiring intervention) within 30 days. By treatment group, fracture rates per 1,000 person-years were 4.69, 5.26, and 4.71 for SGLT2 inhibitors, DPP-4 inhibitors, and GLP-1 agonists respectively.
The differences between patients taking DPP-4 inhibitors or GLP-1 agonists compared with SGLT2 inhibitors were not significant, with hazard ratios of 0.90 and 1.00, respectively.
Results remained consistent in various sensitivity and subgroup analyses, including limiting the data to just the canagliflozin group. Overall, the fracture rate was greater with female sex, frailty, older age, and insulin use, consistent across drug classes.
The risks for falls and hypoglycemia were lower in the SGLT2 inhibitor versus matched DPP-4 inhibitor groups (hazard ratio, 0.82), and there was no difference in syncope. None of those differences were significant for the SGLT2 inhibitor group compared with the GLP-1 agonist group.
Consistent with previous data, the risk for diabetic ketoacidosis was higher with SGLT2 inhibitors versus DPP-4 inhibitors and GLP-1 agonists (HR, 1.29 and 1.58), and the risk for heart failure hospitalization was lower (HR, 0.42 and 0.69).
The study was funded by the Division of Pharmacoepidemiology and Pharmacoeconomics, department of medicine, Brigham and Women’s Hospital, Harvard Medical School. Dr. Zhuo was supported by the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Taylor is a consultant for Ionis Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Use of sodium-glucose cotransporter-2 (SGLT2) inhibitors does not appear to raise the risk for fractures in older adults, new research suggests.
The data come from a nationwide propensity score-matched study of U.S. Medicare recipients with type 2 diabetes who were new users of either an SGLT2 inhibitor, a dipeptidyl peptidase 4 (DPP-4) inhibitor, or a glucagon-like peptide (GLP-1) receptor agonist.
“The use of SGLT2 inhibitors was not associated with an increased risk of nontraumatic fractures compared with DPP-4 inhibitors or GLP-1 agonists. Results were consistent across categories of sex, frailty, age, and insulin use,” say Min Zhuo, MD, of Harvard Medical School, Boston, and colleagues, who published their work online October 27 in JAMA Network Open.
“Our results add to the evidence base evaluating the safety profile of SGLT2 inhibitors in older adults outside of [randomized controlled trials] and further characterize the risk-benefit balance of SGLT2 inhibitors in clinical practice,” they write.
Asked to comment, Simeon I. Taylor, MD, PhD, told this news organization, “This is a high-quality study that is generally reassuring that relatively short, less than 1 year, treatment with an SGLT2 inhibitor does not appear to significantly increase the risk of bone fractures.”
However, Dr. Taylor, of the Division of Endocrinology, Diabetes, and Nutrition, University of Maryland School of Medicine, Baltimore, also noted: “Notwithstanding these reassuring data, the paper also does a good job of pointing out important limitations.”
“Most importantly, these data do not address questions related to the risk of long-term chronic therapy. It is instructive to refer back to the published data demonstrating an approximately 2-year lag before a significant increase in the risk of fracture was observed in rosiglitazone-treated patients in the ADOPT study. The length of the lag is likely related to the baseline bone mineral density at the time drug therapy is initiated. These considerations may contribute to the observed variation in bone-related outcomes in different studies.”
Concern about SGLT2 inhibitors and fractures first arose in 2017 from the CANVAS study, in which the overall fracture risk with canagliflozin was a significant 26% higher than placebo. However, subsequent larger randomized trials of canagliflozin and other SGLT2 inhibitors did not find the same risk.
In addition, previous observational studies in younger adults have also not found use of SGLT2 inhibitors to be associated with increased fracture risk compared with DPP-4 inhibitors or GLP-1 agonists.
Understanding fracture risk with SGLT2 inhibitors is ‘critical’
Older adults with type 2 diabetes may benefit from reductions in atherosclerotic cardiovascular events, hospitalization for heart failure, end-stage kidney disease, and death associated with SGLT2 inhibitors, but the fact that aging may have negative effects on bone metabolism means “understanding the fracture risk associated with SGLT2 inhibitors in older adults with type 2 diabetes is critical,” say Dr. Zhuo and colleagues.
In the current study, they analyzed claims data for Medicare beneficiaries aged 66 years and older (1 year past Medicare eligibility) who were newly prescribed an SGLT2 inhibitor, DPP-4 inhibitor, or GLP-1 agonist between April 1, 2013 and Dec. 31, 2017.
A total of 45,889 patients from each treatment group were propensity-matched using 58 baseline characteristics, for a total of 137,667 patients.
After matching, there were 501 events of the primary composite outcome (nontraumatic pelvic fracture, hip fracture requiring surgery, or humerus, radius, or ulna fracture requiring intervention) within 30 days. By treatment group, fracture rates per 1,000 person-years were 4.69, 5.26, and 4.71 for SGLT2 inhibitors, DPP-4 inhibitors, and GLP-1 agonists respectively.
The differences between patients taking DPP-4 inhibitors or GLP-1 agonists compared with SGLT2 inhibitors were not significant, with hazard ratios of 0.90 and 1.00, respectively.
Results remained consistent in various sensitivity and subgroup analyses, including limiting the data to just the canagliflozin group. Overall, the fracture rate was greater with female sex, frailty, older age, and insulin use, consistent across drug classes.
The risks for falls and hypoglycemia were lower in the SGLT2 inhibitor versus matched DPP-4 inhibitor groups (hazard ratio, 0.82), and there was no difference in syncope. None of those differences were significant for the SGLT2 inhibitor group compared with the GLP-1 agonist group.
Consistent with previous data, the risk for diabetic ketoacidosis was higher with SGLT2 inhibitors versus DPP-4 inhibitors and GLP-1 agonists (HR, 1.29 and 1.58), and the risk for heart failure hospitalization was lower (HR, 0.42 and 0.69).
The study was funded by the Division of Pharmacoepidemiology and Pharmacoeconomics, department of medicine, Brigham and Women’s Hospital, Harvard Medical School. Dr. Zhuo was supported by the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Taylor is a consultant for Ionis Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Use of sodium-glucose cotransporter-2 (SGLT2) inhibitors does not appear to raise the risk for fractures in older adults, new research suggests.
The data come from a nationwide propensity score-matched study of U.S. Medicare recipients with type 2 diabetes who were new users of either an SGLT2 inhibitor, a dipeptidyl peptidase 4 (DPP-4) inhibitor, or a glucagon-like peptide (GLP-1) receptor agonist.
“The use of SGLT2 inhibitors was not associated with an increased risk of nontraumatic fractures compared with DPP-4 inhibitors or GLP-1 agonists. Results were consistent across categories of sex, frailty, age, and insulin use,” say Min Zhuo, MD, of Harvard Medical School, Boston, and colleagues, who published their work online October 27 in JAMA Network Open.
“Our results add to the evidence base evaluating the safety profile of SGLT2 inhibitors in older adults outside of [randomized controlled trials] and further characterize the risk-benefit balance of SGLT2 inhibitors in clinical practice,” they write.
Asked to comment, Simeon I. Taylor, MD, PhD, told this news organization, “This is a high-quality study that is generally reassuring that relatively short, less than 1 year, treatment with an SGLT2 inhibitor does not appear to significantly increase the risk of bone fractures.”
However, Dr. Taylor, of the Division of Endocrinology, Diabetes, and Nutrition, University of Maryland School of Medicine, Baltimore, also noted: “Notwithstanding these reassuring data, the paper also does a good job of pointing out important limitations.”
“Most importantly, these data do not address questions related to the risk of long-term chronic therapy. It is instructive to refer back to the published data demonstrating an approximately 2-year lag before a significant increase in the risk of fracture was observed in rosiglitazone-treated patients in the ADOPT study. The length of the lag is likely related to the baseline bone mineral density at the time drug therapy is initiated. These considerations may contribute to the observed variation in bone-related outcomes in different studies.”
Concern about SGLT2 inhibitors and fractures first arose in 2017 from the CANVAS study, in which the overall fracture risk with canagliflozin was a significant 26% higher than placebo. However, subsequent larger randomized trials of canagliflozin and other SGLT2 inhibitors did not find the same risk.
In addition, previous observational studies in younger adults have also not found use of SGLT2 inhibitors to be associated with increased fracture risk compared with DPP-4 inhibitors or GLP-1 agonists.
Understanding fracture risk with SGLT2 inhibitors is ‘critical’
Older adults with type 2 diabetes may benefit from reductions in atherosclerotic cardiovascular events, hospitalization for heart failure, end-stage kidney disease, and death associated with SGLT2 inhibitors, but the fact that aging may have negative effects on bone metabolism means “understanding the fracture risk associated with SGLT2 inhibitors in older adults with type 2 diabetes is critical,” say Dr. Zhuo and colleagues.
In the current study, they analyzed claims data for Medicare beneficiaries aged 66 years and older (1 year past Medicare eligibility) who were newly prescribed an SGLT2 inhibitor, DPP-4 inhibitor, or GLP-1 agonist between April 1, 2013 and Dec. 31, 2017.
A total of 45,889 patients from each treatment group were propensity-matched using 58 baseline characteristics, for a total of 137,667 patients.
After matching, there were 501 events of the primary composite outcome (nontraumatic pelvic fracture, hip fracture requiring surgery, or humerus, radius, or ulna fracture requiring intervention) within 30 days. By treatment group, fracture rates per 1,000 person-years were 4.69, 5.26, and 4.71 for SGLT2 inhibitors, DPP-4 inhibitors, and GLP-1 agonists respectively.
The differences between patients taking DPP-4 inhibitors or GLP-1 agonists compared with SGLT2 inhibitors were not significant, with hazard ratios of 0.90 and 1.00, respectively.
Results remained consistent in various sensitivity and subgroup analyses, including limiting the data to just the canagliflozin group. Overall, the fracture rate was greater with female sex, frailty, older age, and insulin use, consistent across drug classes.
The risks for falls and hypoglycemia were lower in the SGLT2 inhibitor versus matched DPP-4 inhibitor groups (hazard ratio, 0.82), and there was no difference in syncope. None of those differences were significant for the SGLT2 inhibitor group compared with the GLP-1 agonist group.
Consistent with previous data, the risk for diabetic ketoacidosis was higher with SGLT2 inhibitors versus DPP-4 inhibitors and GLP-1 agonists (HR, 1.29 and 1.58), and the risk for heart failure hospitalization was lower (HR, 0.42 and 0.69).
The study was funded by the Division of Pharmacoepidemiology and Pharmacoeconomics, department of medicine, Brigham and Women’s Hospital, Harvard Medical School. Dr. Zhuo was supported by the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Taylor is a consultant for Ionis Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Real-world data favor invasive strategy for NSTEMI with CKD
Most patients with advanced chronic kidney disease (CKD) and non–ST-elevation myocardial infarction (NSTEMI) fare better with coronary angiography with and without revascularization than with medical therapy, a large nationwide study suggests.
“Invasive management was associated with lower mortality, major adverse cardiovascular events (MACE), and need for revascularization, with a minimal increased risk of in-hospital, postprocedural acute kidney injury (AKI) requiring dialysis and major bleeding,” said lead researcher Ankur Kalra, MD, Cleveland Clinic.
Also, similar post-discharge safety outcomes were seen at 6 months, he said in an online presentation of “key abstracts” released in advance of next month’s Transcatheter Cardiovascular Therapeutics (TCT) 2021 hybrid meeting.
Advanced CKD is an independent predictor of mortality and morbidity in patients with NSTEMI. In CKD, however, current guidelines lack evidence on the efficacy and safety of invasive versus medical management, he noted.
A rare randomized clinical trial in this high-risk population, ISCHEMIA-CKD, recently found no benefit and an increase in stroke with initial invasive management compared with optimal medical therapy.
Session co-moderator Ziad A. Ali, MD, DPhil, St. Francis Hospital & Heart Center, New York, said the current study is “incredibly clinically impactful and answers a question that’s very difficult to answer because these patients aren’t randomized in randomized controlled trials, and there’s a general avoidance, which we’ve now coined ‘renalism,’ like racism, where people don’t really want to touch these patients.”
He questioned, however, how the authors reconcile the results of ISCHEMIA-CKD, a “small but meaningful randomized controlled trial,” with their findings from a large dataset. “Perhaps this is all selection bias, even though the numbers are very large.”
Dr. Kalra replied that ISCHEMIA-CKD examined stable ischemic heart disease, whereas they looked at NSTEMI. “Even though it may fall under the same rubric, I truly believe it is a different set of patients – they are at a heightened risk for future cardiovascular events and have had an acute coronary event.”
For the study, ICD-10 coding data from 2016-2018 in the Nationwide Readmission Database was used to identify NSTEMI patients with CKD stages 3, 4, 5, and end-stage renal disease (ESRD). A total of 141,052 patients were available for in-hospital outcomes and 133,642 patients for post-discharge outcomes.
In-hospital and 6-month mortality – the study’s primary outcome – favored invasive management across all CKD stages and ESRD but did not achieve statistical significance for CKD stage 5. The number needed to treat (NNT) for CKD stages 3, 4, 5, and ESRD were 26, 56, 48, and 18, respectively.
Six-month MACE, including mortality, MI, stroke, and heart failure readmission, was significantly better in all groups with invasive management.
Kaplan-Meier curves for mortality showed similar benefits with an invasive strategy across CKD stages, again barring stage 5 disease.
With regard to in-hospital safety, stroke rates were not significantly different between the two treatment strategies across all groups.
Rates of AKI requiring dialysis, however, were lower with medical versus invasive management for CKD stage 3 (0.43% vs. 0.6%; hazard ratio, 1.39; P = .016), stage 4 (1.2% vs. 2.0%; HR 1.87; P < .001), and stage 5 (3.7% vs. 4.3%; HR 1.17; P = .527). The number needed to harm (NNH) was 588 for CKD 3 and 125 for CKD 4.
Major bleeding, defined as requiring transfusion, was lower with medical management for all CKD stages but not for ESRD. The rates are as follows:
- CKD stage 3: 2.5% vs. 2.8% (HR, 1.11; P = .078; NNH = 333)
- CKD stage 4: 2.9% vs. 4.0% (HR, 1.42; P < .001; NNH = 91)
- CKD stage 5: 2.2% vs. 4.7% (HR, 2.17; P = .008; NNH = 40)
- ESRD: 3.4% vs. 3.3% (HR, 0.97; P = .709)
“The risk of AKI requiring dialysis and bleeding, as has been shown previously in other studies, was high, but the number needed to harm was also high,” observed Dr. Kalra.
A separate analysis showed no difference in rates of AKI requiring dialysis among patients with CKD stages 3 and 4 who underwent angiography without revascularization and their peers who were medically managed.
Rates of the composite safety outcome of vascular complications, major bleeding, AKI, or stroke readmission at 6 months were not significantly different for invasive versus medical management for CKD stage 3 (both 3.3%), stage 4 (4.5% and 4.2%), stage 5 (3.9% vs. 4.3%), and ESRD (2.3% vs. 2.1%).
Besides the inherent limitations of observational studies and potential for selection bias, Dr. Kalra pointed out that the analysis relied on coding data for exact glomerular filtration rates and lacked information on contrast use, crystalloids before the procedure, and nephrotoxic medication use before or during admission. Out-of-hospital mortality was also not available in the database.
Co-moderator Allen Jeremias, MD, also with St. Francis Hospital & Heart Center, said one of the study’s strengths was that it included all comers, unlike randomized trials that typically exclude the highest risk patients.
“So, when we do these trials it’s very difficult to find the right balance, whereas this is a real-world analysis including everybody, and I think the benefits are clearly demonstrated,” he said. “So I think I’m bullish on doing complex [percutaneous coronary intervention] PCI in this patient population.”
Dr. Kalra reports having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Most patients with advanced chronic kidney disease (CKD) and non–ST-elevation myocardial infarction (NSTEMI) fare better with coronary angiography with and without revascularization than with medical therapy, a large nationwide study suggests.
“Invasive management was associated with lower mortality, major adverse cardiovascular events (MACE), and need for revascularization, with a minimal increased risk of in-hospital, postprocedural acute kidney injury (AKI) requiring dialysis and major bleeding,” said lead researcher Ankur Kalra, MD, Cleveland Clinic.
Also, similar post-discharge safety outcomes were seen at 6 months, he said in an online presentation of “key abstracts” released in advance of next month’s Transcatheter Cardiovascular Therapeutics (TCT) 2021 hybrid meeting.
Advanced CKD is an independent predictor of mortality and morbidity in patients with NSTEMI. In CKD, however, current guidelines lack evidence on the efficacy and safety of invasive versus medical management, he noted.
A rare randomized clinical trial in this high-risk population, ISCHEMIA-CKD, recently found no benefit and an increase in stroke with initial invasive management compared with optimal medical therapy.
Session co-moderator Ziad A. Ali, MD, DPhil, St. Francis Hospital & Heart Center, New York, said the current study is “incredibly clinically impactful and answers a question that’s very difficult to answer because these patients aren’t randomized in randomized controlled trials, and there’s a general avoidance, which we’ve now coined ‘renalism,’ like racism, where people don’t really want to touch these patients.”
He questioned, however, how the authors reconcile the results of ISCHEMIA-CKD, a “small but meaningful randomized controlled trial,” with their findings from a large dataset. “Perhaps this is all selection bias, even though the numbers are very large.”
Dr. Kalra replied that ISCHEMIA-CKD examined stable ischemic heart disease, whereas they looked at NSTEMI. “Even though it may fall under the same rubric, I truly believe it is a different set of patients – they are at a heightened risk for future cardiovascular events and have had an acute coronary event.”
For the study, ICD-10 coding data from 2016-2018 in the Nationwide Readmission Database was used to identify NSTEMI patients with CKD stages 3, 4, 5, and end-stage renal disease (ESRD). A total of 141,052 patients were available for in-hospital outcomes and 133,642 patients for post-discharge outcomes.
In-hospital and 6-month mortality – the study’s primary outcome – favored invasive management across all CKD stages and ESRD but did not achieve statistical significance for CKD stage 5. The number needed to treat (NNT) for CKD stages 3, 4, 5, and ESRD were 26, 56, 48, and 18, respectively.
Six-month MACE, including mortality, MI, stroke, and heart failure readmission, was significantly better in all groups with invasive management.
Kaplan-Meier curves for mortality showed similar benefits with an invasive strategy across CKD stages, again barring stage 5 disease.
With regard to in-hospital safety, stroke rates were not significantly different between the two treatment strategies across all groups.
Rates of AKI requiring dialysis, however, were lower with medical versus invasive management for CKD stage 3 (0.43% vs. 0.6%; hazard ratio, 1.39; P = .016), stage 4 (1.2% vs. 2.0%; HR 1.87; P < .001), and stage 5 (3.7% vs. 4.3%; HR 1.17; P = .527). The number needed to harm (NNH) was 588 for CKD 3 and 125 for CKD 4.
Major bleeding, defined as requiring transfusion, was lower with medical management for all CKD stages but not for ESRD. The rates are as follows:
- CKD stage 3: 2.5% vs. 2.8% (HR, 1.11; P = .078; NNH = 333)
- CKD stage 4: 2.9% vs. 4.0% (HR, 1.42; P < .001; NNH = 91)
- CKD stage 5: 2.2% vs. 4.7% (HR, 2.17; P = .008; NNH = 40)
- ESRD: 3.4% vs. 3.3% (HR, 0.97; P = .709)
“The risk of AKI requiring dialysis and bleeding, as has been shown previously in other studies, was high, but the number needed to harm was also high,” observed Dr. Kalra.
A separate analysis showed no difference in rates of AKI requiring dialysis among patients with CKD stages 3 and 4 who underwent angiography without revascularization and their peers who were medically managed.
Rates of the composite safety outcome of vascular complications, major bleeding, AKI, or stroke readmission at 6 months were not significantly different for invasive versus medical management for CKD stage 3 (both 3.3%), stage 4 (4.5% and 4.2%), stage 5 (3.9% vs. 4.3%), and ESRD (2.3% vs. 2.1%).
Besides the inherent limitations of observational studies and potential for selection bias, Dr. Kalra pointed out that the analysis relied on coding data for exact glomerular filtration rates and lacked information on contrast use, crystalloids before the procedure, and nephrotoxic medication use before or during admission. Out-of-hospital mortality was also not available in the database.
Co-moderator Allen Jeremias, MD, also with St. Francis Hospital & Heart Center, said one of the study’s strengths was that it included all comers, unlike randomized trials that typically exclude the highest risk patients.
“So, when we do these trials it’s very difficult to find the right balance, whereas this is a real-world analysis including everybody, and I think the benefits are clearly demonstrated,” he said. “So I think I’m bullish on doing complex [percutaneous coronary intervention] PCI in this patient population.”
Dr. Kalra reports having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Most patients with advanced chronic kidney disease (CKD) and non–ST-elevation myocardial infarction (NSTEMI) fare better with coronary angiography with and without revascularization than with medical therapy, a large nationwide study suggests.
“Invasive management was associated with lower mortality, major adverse cardiovascular events (MACE), and need for revascularization, with a minimal increased risk of in-hospital, postprocedural acute kidney injury (AKI) requiring dialysis and major bleeding,” said lead researcher Ankur Kalra, MD, Cleveland Clinic.
Also, similar post-discharge safety outcomes were seen at 6 months, he said in an online presentation of “key abstracts” released in advance of next month’s Transcatheter Cardiovascular Therapeutics (TCT) 2021 hybrid meeting.
Advanced CKD is an independent predictor of mortality and morbidity in patients with NSTEMI. In CKD, however, current guidelines lack evidence on the efficacy and safety of invasive versus medical management, he noted.
A rare randomized clinical trial in this high-risk population, ISCHEMIA-CKD, recently found no benefit and an increase in stroke with initial invasive management compared with optimal medical therapy.
Session co-moderator Ziad A. Ali, MD, DPhil, St. Francis Hospital & Heart Center, New York, said the current study is “incredibly clinically impactful and answers a question that’s very difficult to answer because these patients aren’t randomized in randomized controlled trials, and there’s a general avoidance, which we’ve now coined ‘renalism,’ like racism, where people don’t really want to touch these patients.”
He questioned, however, how the authors reconcile the results of ISCHEMIA-CKD, a “small but meaningful randomized controlled trial,” with their findings from a large dataset. “Perhaps this is all selection bias, even though the numbers are very large.”
Dr. Kalra replied that ISCHEMIA-CKD examined stable ischemic heart disease, whereas they looked at NSTEMI. “Even though it may fall under the same rubric, I truly believe it is a different set of patients – they are at a heightened risk for future cardiovascular events and have had an acute coronary event.”
For the study, ICD-10 coding data from 2016-2018 in the Nationwide Readmission Database was used to identify NSTEMI patients with CKD stages 3, 4, 5, and end-stage renal disease (ESRD). A total of 141,052 patients were available for in-hospital outcomes and 133,642 patients for post-discharge outcomes.
In-hospital and 6-month mortality – the study’s primary outcome – favored invasive management across all CKD stages and ESRD but did not achieve statistical significance for CKD stage 5. The number needed to treat (NNT) for CKD stages 3, 4, 5, and ESRD were 26, 56, 48, and 18, respectively.
Six-month MACE, including mortality, MI, stroke, and heart failure readmission, was significantly better in all groups with invasive management.
Kaplan-Meier curves for mortality showed similar benefits with an invasive strategy across CKD stages, again barring stage 5 disease.
With regard to in-hospital safety, stroke rates were not significantly different between the two treatment strategies across all groups.
Rates of AKI requiring dialysis, however, were lower with medical versus invasive management for CKD stage 3 (0.43% vs. 0.6%; hazard ratio, 1.39; P = .016), stage 4 (1.2% vs. 2.0%; HR 1.87; P < .001), and stage 5 (3.7% vs. 4.3%; HR 1.17; P = .527). The number needed to harm (NNH) was 588 for CKD 3 and 125 for CKD 4.
Major bleeding, defined as requiring transfusion, was lower with medical management for all CKD stages but not for ESRD. The rates are as follows:
- CKD stage 3: 2.5% vs. 2.8% (HR, 1.11; P = .078; NNH = 333)
- CKD stage 4: 2.9% vs. 4.0% (HR, 1.42; P < .001; NNH = 91)
- CKD stage 5: 2.2% vs. 4.7% (HR, 2.17; P = .008; NNH = 40)
- ESRD: 3.4% vs. 3.3% (HR, 0.97; P = .709)
“The risk of AKI requiring dialysis and bleeding, as has been shown previously in other studies, was high, but the number needed to harm was also high,” observed Dr. Kalra.
A separate analysis showed no difference in rates of AKI requiring dialysis among patients with CKD stages 3 and 4 who underwent angiography without revascularization and their peers who were medically managed.
Rates of the composite safety outcome of vascular complications, major bleeding, AKI, or stroke readmission at 6 months were not significantly different for invasive versus medical management for CKD stage 3 (both 3.3%), stage 4 (4.5% and 4.2%), stage 5 (3.9% vs. 4.3%), and ESRD (2.3% vs. 2.1%).
Besides the inherent limitations of observational studies and potential for selection bias, Dr. Kalra pointed out that the analysis relied on coding data for exact glomerular filtration rates and lacked information on contrast use, crystalloids before the procedure, and nephrotoxic medication use before or during admission. Out-of-hospital mortality was also not available in the database.
Co-moderator Allen Jeremias, MD, also with St. Francis Hospital & Heart Center, said one of the study’s strengths was that it included all comers, unlike randomized trials that typically exclude the highest risk patients.
“So, when we do these trials it’s very difficult to find the right balance, whereas this is a real-world analysis including everybody, and I think the benefits are clearly demonstrated,” he said. “So I think I’m bullish on doing complex [percutaneous coronary intervention] PCI in this patient population.”
Dr. Kalra reports having no relevant financial relationships.
A version of this article first appeared on Medscape.com.