User login
Experiencing DDW as an Early Career GI
Dear Friends,
Like many readers, I just returned from Digestive Disease Week® (DDW) in San Diego, California. For the first time in my early career, my experience was not just overwhelming and exhausting. Before, I wanted to do everything – lectures, posters, meetings with friends, prospective research collaborators, and more! This year, I acknowledged that instead of spreading myself thin and not fully engaging, I made a focused daily schedule mixed with productivity and social events, selecting only what was most important to me at this time in my career. This time, after DDW, instead of giving in to my inner introvert and holing myself in my house for a week to recover, I am invigorated by what I learned and the people I met. I can’t wait to see what’s to come next year!
In this issue’s “In Focus”, Dr. Evan Dellon describes his diagnostic approach, including a clear history, endoscopic evaluation with biopsy, and ruling out other causes of esophageal eosinophilia. He emphasizes that treatment should target both inflammation and fibrostenosis and reviews the guidelines and evidence behind first-line treatments, surveillance, and long-term maintenance.
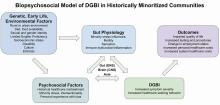
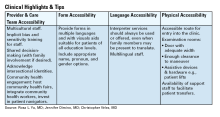
In the second of a two-part series in the “Short Clinical Review” section, Dr. Christopher Vélez, Dr. Rosa L. Yu, and Dr. Jennifer Dimino discuss care for patients with disorders of brain-gut interaction from historically marginalized communities. They highlight ways to improve care for these patients in day-to-day clinical practice.
The transition from trainee to a practicing gastroenterologist may bring with it responsibilities of giving feedback to trainees and/or colleagues to improve. In the “Early Career” section, Dr. Michelle Baliss and Dr. Christine Hachem give practical tips on how best to deliver feedback, with a focus on creating time, building rapport, bidirectional communication, and more.
Lastly, in the “Finance/Legal” section, John S. Gardner, a financial advisor, guides trainees and early career gastroenterologists through estate planning – why it’s important, how to do it effectively, and long-term benefits to starting early.
If you are interested in contributing or have ideas for future TNG topics, please contact me (tjudy@wustl.edu) or Danielle Kiefer (dkiefer@gastro.org), Communications/Managing Editor of TNG.
Until next time, I leave you with a historical fun fact because we would not be where we are now without appreciating where we were: the first case of eosinophilic esophagitis was only first described in 1978 and became a distinct entity in the early 1990s.
Yours truly,
Judy A. Trieu, MD, MPH
Editor-in-Chief
Assistant Professor of Medicine
Interventional Endoscopy, Division of Gastroenterology
Washington University School of Medicine in St. Louis
Dear Friends,
Like many readers, I just returned from Digestive Disease Week® (DDW) in San Diego, California. For the first time in my early career, my experience was not just overwhelming and exhausting. Before, I wanted to do everything – lectures, posters, meetings with friends, prospective research collaborators, and more! This year, I acknowledged that instead of spreading myself thin and not fully engaging, I made a focused daily schedule mixed with productivity and social events, selecting only what was most important to me at this time in my career. This time, after DDW, instead of giving in to my inner introvert and holing myself in my house for a week to recover, I am invigorated by what I learned and the people I met. I can’t wait to see what’s to come next year!
In this issue’s “In Focus”, Dr. Evan Dellon describes his diagnostic approach, including a clear history, endoscopic evaluation with biopsy, and ruling out other causes of esophageal eosinophilia. He emphasizes that treatment should target both inflammation and fibrostenosis and reviews the guidelines and evidence behind first-line treatments, surveillance, and long-term maintenance.
In the second of a two-part series in the “Short Clinical Review” section, Dr. Christopher Vélez, Dr. Rosa L. Yu, and Dr. Jennifer Dimino discuss care for patients with disorders of brain-gut interaction from historically marginalized communities. They highlight ways to improve care for these patients in day-to-day clinical practice.
The transition from trainee to a practicing gastroenterologist may bring with it responsibilities of giving feedback to trainees and/or colleagues to improve. In the “Early Career” section, Dr. Michelle Baliss and Dr. Christine Hachem give practical tips on how best to deliver feedback, with a focus on creating time, building rapport, bidirectional communication, and more.
Lastly, in the “Finance/Legal” section, John S. Gardner, a financial advisor, guides trainees and early career gastroenterologists through estate planning – why it’s important, how to do it effectively, and long-term benefits to starting early.
If you are interested in contributing or have ideas for future TNG topics, please contact me (tjudy@wustl.edu) or Danielle Kiefer (dkiefer@gastro.org), Communications/Managing Editor of TNG.
Until next time, I leave you with a historical fun fact because we would not be where we are now without appreciating where we were: the first case of eosinophilic esophagitis was only first described in 1978 and became a distinct entity in the early 1990s.
Yours truly,
Judy A. Trieu, MD, MPH
Editor-in-Chief
Assistant Professor of Medicine
Interventional Endoscopy, Division of Gastroenterology
Washington University School of Medicine in St. Louis
Dear Friends,
Like many readers, I just returned from Digestive Disease Week® (DDW) in San Diego, California. For the first time in my early career, my experience was not just overwhelming and exhausting. Before, I wanted to do everything – lectures, posters, meetings with friends, prospective research collaborators, and more! This year, I acknowledged that instead of spreading myself thin and not fully engaging, I made a focused daily schedule mixed with productivity and social events, selecting only what was most important to me at this time in my career. This time, after DDW, instead of giving in to my inner introvert and holing myself in my house for a week to recover, I am invigorated by what I learned and the people I met. I can’t wait to see what’s to come next year!
In this issue’s “In Focus”, Dr. Evan Dellon describes his diagnostic approach, including a clear history, endoscopic evaluation with biopsy, and ruling out other causes of esophageal eosinophilia. He emphasizes that treatment should target both inflammation and fibrostenosis and reviews the guidelines and evidence behind first-line treatments, surveillance, and long-term maintenance.
In the second of a two-part series in the “Short Clinical Review” section, Dr. Christopher Vélez, Dr. Rosa L. Yu, and Dr. Jennifer Dimino discuss care for patients with disorders of brain-gut interaction from historically marginalized communities. They highlight ways to improve care for these patients in day-to-day clinical practice.
The transition from trainee to a practicing gastroenterologist may bring with it responsibilities of giving feedback to trainees and/or colleagues to improve. In the “Early Career” section, Dr. Michelle Baliss and Dr. Christine Hachem give practical tips on how best to deliver feedback, with a focus on creating time, building rapport, bidirectional communication, and more.
Lastly, in the “Finance/Legal” section, John S. Gardner, a financial advisor, guides trainees and early career gastroenterologists through estate planning – why it’s important, how to do it effectively, and long-term benefits to starting early.
If you are interested in contributing or have ideas for future TNG topics, please contact me (tjudy@wustl.edu) or Danielle Kiefer (dkiefer@gastro.org), Communications/Managing Editor of TNG.
Until next time, I leave you with a historical fun fact because we would not be where we are now without appreciating where we were: the first case of eosinophilic esophagitis was only first described in 1978 and became a distinct entity in the early 1990s.
Yours truly,
Judy A. Trieu, MD, MPH
Editor-in-Chief
Assistant Professor of Medicine
Interventional Endoscopy, Division of Gastroenterology
Washington University School of Medicine in St. Louis
Practical Tips on Delivering Feedback to Trainees and Colleagues
Feedback is the purposeful practice of offering constructive, goal-directed input rooted in the power of observation and behavioral assessment. Healthcare inherently fosters a broad range of interactions among people with unique insights, and feedback can naturally emerge from this milieu. In medical training, feedback is an indispensable element that personalizes the learning process and drives the professional development of physicians through all career stages.
If delivered effectively, feedback can strengthen the relationship between the evaluator and recipient, promote self-reflection, and enhance motivation. As such, it has the potential to impact us and those we serve for a lifetime. Feedback has been invaluable to our growth as clinicians and has been embedded into our roles as educators. However, Here, we provide some “tried and true” practical tips on delivering feedback to trainees and co-workers and on navigating potential barriers based on lessons learned.
Barriers to Effective Feedback
- Time: Feedback is predicated on observation over time and consideration of repetitive processes rather than isolated events. Perhaps the most challenging factor faced by both parties is that of time constraints, leading to limited ability to engage and build rapport.
- Fear: Hesitancy by evaluators to provide feedback in fear of negative impacts on the recipient’s morale or rapport can lead them to shy away from personalized corrective feedback strategies and choose to rely on written evaluations or generic advice.
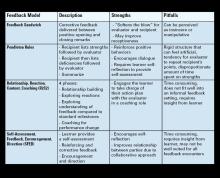
- Varying approaches: Feedback strategies have evolved from unidirectional, critique-based, hierarchical practices that emphasize the evaluator’s skills to models that prioritize the recipient’s goals and participation (see Table 1). Traditionally employed feedback models such as the “Feedback Sandwich” or the “Pendleton Rules” are criticized because of a lack of proven benefit on performance, recipient goal prioritization, and open communication.1,2 Studies showing incongruent perceptions of feedback adequacy between trainees and faculty further support the need for recipient-focused strategies.3 Recognition of the foundational role of the reciprocal learner-teacher alliance in feedback integration inspired newer feedback models, such as the “R2C2” and the “Self-Assessment, Feedback, Encouragement, Direction.”4,5
But which way is best? With increasing abundance and complexity of feedback frameworks, selecting an approach can feel overwhelming and impractical. A generic “one-size-fits-all” strategy or avoidance of feedback altogether can be detrimental. Structured feedback models can also lead to rigid, inauthentic interactions. Below, we suggest a more practical approach through our tips that unifies the common themes of various feedback models and embeds them into daily practice habits while leaving room for personalization.
Our Practical Feedback Tips
Tip 1: Set the scene: Create a positive feedback culture
Proactively creating a culture in which feedback is embedded and encouraged is perhaps the most important step. Priming both parties for feedback clarifies intent, increases receptiveness, and paves the way for growth and open communication. It also prevents the misinterpretation of unexpected feedback as an expression of disapproval. To do this, start by regularly stating your intentions at the start of every experience. Explicitly expressing your vision for mutual learning, bidirectional feedback, and growth in your respective roles attaches a positive intention to feedback. Providing a reminder that we are all works in progress and acknowledging this on a regular basis sets the stage for structured growth opportunities.
Scheduling future feedback encounters from the start maintains accountability and prevents feedback from being perceived as the consequence of a particular behavior. The number and timing of feedback sessions can be customized to the duration of the working relationship, generally allowing enough time for a second interaction (at the end of each week, halfway point, etc.).
Tip 2: Build rapport
Increasing clinical workloads and pressure to teach in time-constrained settings often results in insufficient time to engage in conversation and trust building. However, a foundational relationship is an essential precursor to meaningful feedback. Ramani et al. state that “relationships, not recipes, are more likely to promote feedback that has an impact on learner performance and ultimately patient care.”6 Building this rapport can begin by dedicating a few minutes (before/during rounds, between cases) to exchange information about career interests, hobbies, favorite restaurants, etc. This “small talk” is the beginning of a two-way exchange that ultimately develops into more meaningful exchanges.
In our experience, this simple step is impactful and fulfilling to both parties. This is also a good time for shared vulnerability by talking about what you are currently working on or have worked on at their stage to affirm that feedback is a continuous part of professional development and not a reflection of how far they are from competence at a given point in time.
Tip 3: Consider Timing, assess readiness, and preschedule sessions
Lack of attention to timing can hinder feedback acceptance. We suggest adhering to delivering positive feedback publicly and corrective feedback privately (“Praise in public, perfect in private”). This reinforces positive behaviors, increases motivation, and minimizes demoralization. Prolonged delays between the observed behavior and feedback can decrease its relevance. Conversely, delivering feedback too soon after an emotionally charged experience can be perceived as blame. Pre-designated times for feedback can minimize the guesswork and maintain your accountability for giving feedback without inadvertently linking it to one particular behavior. If the recipient does not appear to be in a state to receive feedback at the predesignated time, you can pivot to a “check-in” session to show support and strengthen rapport.
Tip 4: Customize to the learner and set shared goals
Diversity in backgrounds, perspectives, and personalities can impact how people perceive their own performances and experience feedback. Given the profound impact of sociocultural factors on feedback assimilation, maintaining the recipient and their goals at the core of performance evaluations is key to feedback acceptance.
A. Trainees
We suggest starting by introducing the idea of feedback as a partnership and something you feel privileged to do to help them achieve mutual goals. It helps to ask them to use the first day to get oriented with the experience, general expectations, challenges they expect to encounter, and their feedback goals. Tailoring your feedback to their goals creates a sense of shared purpose which increases motivation. Encouraging them to develop their own strategies allows them to play an active role in their growth. Giving them the opportunity to share their perceived strengths and deficiencies provides you with valuable information regarding their insight and ability to self-evaluate. This can help you predict their readiness for your feedback and to tailor your approach when there is a mismatch.
Examples:
- Medical student: Start with “What do you think you are doing well?” and “What do you think you need to work on?” Build on their response with encouragement and empathy. This helps make them more deliberate with what they work on because being a medical student can be overwhelming and can feel as though they have everything to work on.
- Resident/Fellow: By this point, trainees usually have an increased awareness of their strengths and deficiencies. Your questions can then be more specific, giving them autonomy over their learning, such as “What are some of the things you are working on that you want me to give you feedback on this week?” This makes them more aware, intentional, and receptive to your feedback because it is framed as something that they sought out.
B. Colleagues/Staff
Unlike the training environment in which feedback is built-in, giving feedback to co-workers requires you to establish a feedback-conducive environment and to develop a more in-depth understanding of coworkers’ personalities. Similar strategies can be applied, such as proactively setting the scene for open communication, scheduling check-ins, demonstrating receptiveness to feedback, and investing in trust-building.
Longer working relationships allow for strong foundational connections that make feedback less threatening. Personality assessment testing like Myers-Briggs Type Indicator or DiSC Assessment can aid in tailoring feedback to different individuals.7,8 An analytical thinker may appreciate direct, data-driven feedback. Relationship-oriented individuals might respond better to softer, encouragement-based approaches. Always maintain shared goals at the center of your interactions and consider collaborative opportunities such as quality improvement projects. This can improve your working relationship in a constructive way without casting blame.
Tip 5: Work on delivery: Bidirectional communication and body language
Non-verbal cues can have a profound impact on how your feedback is interpreted and on the recipient’s comfort to engage in conversation. Sitting down, making eye contact, nodding, and avoiding closed-off body posture can project support and feel less judgmental. Creating a safe and non-distracted environment with privacy can make them feel valued. Use motivating, respectful language focused on directly observed behaviors rather than personal attributes or second-hand reports.
Remember that focusing on repetitive patterns is likely more helpful than isolated incidents. Validate their hard work and give them a global idea of where they stand before diving into individual behaviors. Encourage their participation and empower them to suggest changes they plan to implement. Conclude by having them summarize their action plan to give them ownership and to verify that your feedback was interpreted as you intended. Thank them for being a part of the process, as it does take a partnership for feedback to be effective.
Tip 6: Be open to feedback
Demonstrating your willingness to accept and act on feedback reinforces a positive culture where feedback is normalized and valued. After an unintended outcome, initiate a two-way conversation and ask their input on anything they wish you would have done differently. This reaffirms your commitment to maintaining culture that does not revolve around one-sided critiques. Frequently soliciting feedback about your feedback skills can also guide you to adapt your approach and to recognize any ineffective feedback practices.
Tip 7: When things don’t go as planned
Receiving feedback, no matter how thoughtfully it is delivered, can be an emotionally-charged experience ending in hurt feelings. This happens because of misinterpretation of feedback as an indicator of inadequacy, heightened awareness of underlying insecurities, sociocultural or personal circumstances, frustration with oneself, needing additional guidance, or being caught off-guard by the assessment.
The evaluator should always acknowledge the recipient’s feelings, show compassion, and allow time for processing. When they are ready to talk, it is important to help reframe the recipients’ mindsets to recognize that feedback is not personal or defining and is not a “one and done” reflection of whether they have “made it.” Instead, it is a continual process that we benefit from through all career stages. Again, shared vulnerability can help to normalize feedback and maintain open dialogue. Setting an opportunity for a future check-in can reinforce support and lead to a more productive conversation after they have had time to process.
Conclusion
Effective feedback delivery is an invaluable skill that can result in meaningful goal-directed changes while strengthening professional relationships. Given the complexity of feedback interactions and the many factors that influence its acceptance, no single approach is suitable for all recipients and frequent adaptation of the approach is essential.
In our experience, adhering to these general overarching feedback principles (see Figure 1) has allowed us to have more successful interactions with trainees and colleagues.
Dr. Baliss is based in the Division of Gastroenterology, Washington University in St. Louis, Missouri. Dr. Hachem is director of the Division of Gastroenterology and Digestive Health at Intermountain Medical, Sandy, Utah. Both authors declare no conflicts of interest.
References
1. Parkes J, et al. Feedback sandwiches affect perceptions but not performance. Adv Health Sci Educ Theory Pract. 2013 Aug. doi:10.1007/s10459-012-9377-9.
2. van de Ridder JMM and Wijnen-Meijer M. Pendleton’s Rules: A Mini Review of a Feedback Method. Am J Biomed Sci & Res. 2023 May. doi: 10.34297/AJBSR.2023.19.002542.
3. Sender Liberman A, et al. Surgery residents and attending surgeons have different perceptions of feedback. Med Teach. 2005 Aug. doi: 10.1080/0142590500129183.
4. Sargeant J, et al. R2C2 in Action: Testing an Evidence-Based Model to Facilitate Feedback and Coaching in Residency. J Grad Med Educ. 2017 Apr. doi: 10.4300/JGME-D-16-00398.1.
5. Liakos W, et al. Frameworks for Effective Feedback in Health Professions Education. Acad Med. 2023 May. doi: 10.1097/ACM.0000000000004884.
6. Ramani S, et al. Feedback Redefined: Principles and Practice. J Gen Intern Med. 2019 May. doi: 10.1007/s11606-019-04874-2.
7. Woods RA and Hill PB. Myers-Briggs Type Indicator. StatPearls. StatPearls Publishing. 2022 Sept. https://www.ncbi.nlm.nih.gov/books/NBK554596/
8. Slowikowski MK. Using the DISC behavioral instrument to guide leadership and communication. AORN J. 2005 Nov. doi: 10.1016/s0001-2092(06)60276-7.
Feedback is the purposeful practice of offering constructive, goal-directed input rooted in the power of observation and behavioral assessment. Healthcare inherently fosters a broad range of interactions among people with unique insights, and feedback can naturally emerge from this milieu. In medical training, feedback is an indispensable element that personalizes the learning process and drives the professional development of physicians through all career stages.
If delivered effectively, feedback can strengthen the relationship between the evaluator and recipient, promote self-reflection, and enhance motivation. As such, it has the potential to impact us and those we serve for a lifetime. Feedback has been invaluable to our growth as clinicians and has been embedded into our roles as educators. However, Here, we provide some “tried and true” practical tips on delivering feedback to trainees and co-workers and on navigating potential barriers based on lessons learned.
Barriers to Effective Feedback
- Time: Feedback is predicated on observation over time and consideration of repetitive processes rather than isolated events. Perhaps the most challenging factor faced by both parties is that of time constraints, leading to limited ability to engage and build rapport.
- Fear: Hesitancy by evaluators to provide feedback in fear of negative impacts on the recipient’s morale or rapport can lead them to shy away from personalized corrective feedback strategies and choose to rely on written evaluations or generic advice.
- Varying approaches: Feedback strategies have evolved from unidirectional, critique-based, hierarchical practices that emphasize the evaluator’s skills to models that prioritize the recipient’s goals and participation (see Table 1). Traditionally employed feedback models such as the “Feedback Sandwich” or the “Pendleton Rules” are criticized because of a lack of proven benefit on performance, recipient goal prioritization, and open communication.1,2 Studies showing incongruent perceptions of feedback adequacy between trainees and faculty further support the need for recipient-focused strategies.3 Recognition of the foundational role of the reciprocal learner-teacher alliance in feedback integration inspired newer feedback models, such as the “R2C2” and the “Self-Assessment, Feedback, Encouragement, Direction.”4,5
But which way is best? With increasing abundance and complexity of feedback frameworks, selecting an approach can feel overwhelming and impractical. A generic “one-size-fits-all” strategy or avoidance of feedback altogether can be detrimental. Structured feedback models can also lead to rigid, inauthentic interactions. Below, we suggest a more practical approach through our tips that unifies the common themes of various feedback models and embeds them into daily practice habits while leaving room for personalization.
Our Practical Feedback Tips
Tip 1: Set the scene: Create a positive feedback culture
Proactively creating a culture in which feedback is embedded and encouraged is perhaps the most important step. Priming both parties for feedback clarifies intent, increases receptiveness, and paves the way for growth and open communication. It also prevents the misinterpretation of unexpected feedback as an expression of disapproval. To do this, start by regularly stating your intentions at the start of every experience. Explicitly expressing your vision for mutual learning, bidirectional feedback, and growth in your respective roles attaches a positive intention to feedback. Providing a reminder that we are all works in progress and acknowledging this on a regular basis sets the stage for structured growth opportunities.
Scheduling future feedback encounters from the start maintains accountability and prevents feedback from being perceived as the consequence of a particular behavior. The number and timing of feedback sessions can be customized to the duration of the working relationship, generally allowing enough time for a second interaction (at the end of each week, halfway point, etc.).
Tip 2: Build rapport
Increasing clinical workloads and pressure to teach in time-constrained settings often results in insufficient time to engage in conversation and trust building. However, a foundational relationship is an essential precursor to meaningful feedback. Ramani et al. state that “relationships, not recipes, are more likely to promote feedback that has an impact on learner performance and ultimately patient care.”6 Building this rapport can begin by dedicating a few minutes (before/during rounds, between cases) to exchange information about career interests, hobbies, favorite restaurants, etc. This “small talk” is the beginning of a two-way exchange that ultimately develops into more meaningful exchanges.
In our experience, this simple step is impactful and fulfilling to both parties. This is also a good time for shared vulnerability by talking about what you are currently working on or have worked on at their stage to affirm that feedback is a continuous part of professional development and not a reflection of how far they are from competence at a given point in time.
Tip 3: Consider Timing, assess readiness, and preschedule sessions
Lack of attention to timing can hinder feedback acceptance. We suggest adhering to delivering positive feedback publicly and corrective feedback privately (“Praise in public, perfect in private”). This reinforces positive behaviors, increases motivation, and minimizes demoralization. Prolonged delays between the observed behavior and feedback can decrease its relevance. Conversely, delivering feedback too soon after an emotionally charged experience can be perceived as blame. Pre-designated times for feedback can minimize the guesswork and maintain your accountability for giving feedback without inadvertently linking it to one particular behavior. If the recipient does not appear to be in a state to receive feedback at the predesignated time, you can pivot to a “check-in” session to show support and strengthen rapport.
Tip 4: Customize to the learner and set shared goals
Diversity in backgrounds, perspectives, and personalities can impact how people perceive their own performances and experience feedback. Given the profound impact of sociocultural factors on feedback assimilation, maintaining the recipient and their goals at the core of performance evaluations is key to feedback acceptance.
A. Trainees
We suggest starting by introducing the idea of feedback as a partnership and something you feel privileged to do to help them achieve mutual goals. It helps to ask them to use the first day to get oriented with the experience, general expectations, challenges they expect to encounter, and their feedback goals. Tailoring your feedback to their goals creates a sense of shared purpose which increases motivation. Encouraging them to develop their own strategies allows them to play an active role in their growth. Giving them the opportunity to share their perceived strengths and deficiencies provides you with valuable information regarding their insight and ability to self-evaluate. This can help you predict their readiness for your feedback and to tailor your approach when there is a mismatch.
Examples:
- Medical student: Start with “What do you think you are doing well?” and “What do you think you need to work on?” Build on their response with encouragement and empathy. This helps make them more deliberate with what they work on because being a medical student can be overwhelming and can feel as though they have everything to work on.
- Resident/Fellow: By this point, trainees usually have an increased awareness of their strengths and deficiencies. Your questions can then be more specific, giving them autonomy over their learning, such as “What are some of the things you are working on that you want me to give you feedback on this week?” This makes them more aware, intentional, and receptive to your feedback because it is framed as something that they sought out.
B. Colleagues/Staff
Unlike the training environment in which feedback is built-in, giving feedback to co-workers requires you to establish a feedback-conducive environment and to develop a more in-depth understanding of coworkers’ personalities. Similar strategies can be applied, such as proactively setting the scene for open communication, scheduling check-ins, demonstrating receptiveness to feedback, and investing in trust-building.
Longer working relationships allow for strong foundational connections that make feedback less threatening. Personality assessment testing like Myers-Briggs Type Indicator or DiSC Assessment can aid in tailoring feedback to different individuals.7,8 An analytical thinker may appreciate direct, data-driven feedback. Relationship-oriented individuals might respond better to softer, encouragement-based approaches. Always maintain shared goals at the center of your interactions and consider collaborative opportunities such as quality improvement projects. This can improve your working relationship in a constructive way without casting blame.
Tip 5: Work on delivery: Bidirectional communication and body language
Non-verbal cues can have a profound impact on how your feedback is interpreted and on the recipient’s comfort to engage in conversation. Sitting down, making eye contact, nodding, and avoiding closed-off body posture can project support and feel less judgmental. Creating a safe and non-distracted environment with privacy can make them feel valued. Use motivating, respectful language focused on directly observed behaviors rather than personal attributes or second-hand reports.
Remember that focusing on repetitive patterns is likely more helpful than isolated incidents. Validate their hard work and give them a global idea of where they stand before diving into individual behaviors. Encourage their participation and empower them to suggest changes they plan to implement. Conclude by having them summarize their action plan to give them ownership and to verify that your feedback was interpreted as you intended. Thank them for being a part of the process, as it does take a partnership for feedback to be effective.
Tip 6: Be open to feedback
Demonstrating your willingness to accept and act on feedback reinforces a positive culture where feedback is normalized and valued. After an unintended outcome, initiate a two-way conversation and ask their input on anything they wish you would have done differently. This reaffirms your commitment to maintaining culture that does not revolve around one-sided critiques. Frequently soliciting feedback about your feedback skills can also guide you to adapt your approach and to recognize any ineffective feedback practices.
Tip 7: When things don’t go as planned
Receiving feedback, no matter how thoughtfully it is delivered, can be an emotionally-charged experience ending in hurt feelings. This happens because of misinterpretation of feedback as an indicator of inadequacy, heightened awareness of underlying insecurities, sociocultural or personal circumstances, frustration with oneself, needing additional guidance, or being caught off-guard by the assessment.
The evaluator should always acknowledge the recipient’s feelings, show compassion, and allow time for processing. When they are ready to talk, it is important to help reframe the recipients’ mindsets to recognize that feedback is not personal or defining and is not a “one and done” reflection of whether they have “made it.” Instead, it is a continual process that we benefit from through all career stages. Again, shared vulnerability can help to normalize feedback and maintain open dialogue. Setting an opportunity for a future check-in can reinforce support and lead to a more productive conversation after they have had time to process.
Conclusion
Effective feedback delivery is an invaluable skill that can result in meaningful goal-directed changes while strengthening professional relationships. Given the complexity of feedback interactions and the many factors that influence its acceptance, no single approach is suitable for all recipients and frequent adaptation of the approach is essential.
In our experience, adhering to these general overarching feedback principles (see Figure 1) has allowed us to have more successful interactions with trainees and colleagues.
Dr. Baliss is based in the Division of Gastroenterology, Washington University in St. Louis, Missouri. Dr. Hachem is director of the Division of Gastroenterology and Digestive Health at Intermountain Medical, Sandy, Utah. Both authors declare no conflicts of interest.
References
1. Parkes J, et al. Feedback sandwiches affect perceptions but not performance. Adv Health Sci Educ Theory Pract. 2013 Aug. doi:10.1007/s10459-012-9377-9.
2. van de Ridder JMM and Wijnen-Meijer M. Pendleton’s Rules: A Mini Review of a Feedback Method. Am J Biomed Sci & Res. 2023 May. doi: 10.34297/AJBSR.2023.19.002542.
3. Sender Liberman A, et al. Surgery residents and attending surgeons have different perceptions of feedback. Med Teach. 2005 Aug. doi: 10.1080/0142590500129183.
4. Sargeant J, et al. R2C2 in Action: Testing an Evidence-Based Model to Facilitate Feedback and Coaching in Residency. J Grad Med Educ. 2017 Apr. doi: 10.4300/JGME-D-16-00398.1.
5. Liakos W, et al. Frameworks for Effective Feedback in Health Professions Education. Acad Med. 2023 May. doi: 10.1097/ACM.0000000000004884.
6. Ramani S, et al. Feedback Redefined: Principles and Practice. J Gen Intern Med. 2019 May. doi: 10.1007/s11606-019-04874-2.
7. Woods RA and Hill PB. Myers-Briggs Type Indicator. StatPearls. StatPearls Publishing. 2022 Sept. https://www.ncbi.nlm.nih.gov/books/NBK554596/
8. Slowikowski MK. Using the DISC behavioral instrument to guide leadership and communication. AORN J. 2005 Nov. doi: 10.1016/s0001-2092(06)60276-7.
Feedback is the purposeful practice of offering constructive, goal-directed input rooted in the power of observation and behavioral assessment. Healthcare inherently fosters a broad range of interactions among people with unique insights, and feedback can naturally emerge from this milieu. In medical training, feedback is an indispensable element that personalizes the learning process and drives the professional development of physicians through all career stages.
If delivered effectively, feedback can strengthen the relationship between the evaluator and recipient, promote self-reflection, and enhance motivation. As such, it has the potential to impact us and those we serve for a lifetime. Feedback has been invaluable to our growth as clinicians and has been embedded into our roles as educators. However, Here, we provide some “tried and true” practical tips on delivering feedback to trainees and co-workers and on navigating potential barriers based on lessons learned.
Barriers to Effective Feedback
- Time: Feedback is predicated on observation over time and consideration of repetitive processes rather than isolated events. Perhaps the most challenging factor faced by both parties is that of time constraints, leading to limited ability to engage and build rapport.
- Fear: Hesitancy by evaluators to provide feedback in fear of negative impacts on the recipient’s morale or rapport can lead them to shy away from personalized corrective feedback strategies and choose to rely on written evaluations or generic advice.
- Varying approaches: Feedback strategies have evolved from unidirectional, critique-based, hierarchical practices that emphasize the evaluator’s skills to models that prioritize the recipient’s goals and participation (see Table 1). Traditionally employed feedback models such as the “Feedback Sandwich” or the “Pendleton Rules” are criticized because of a lack of proven benefit on performance, recipient goal prioritization, and open communication.1,2 Studies showing incongruent perceptions of feedback adequacy between trainees and faculty further support the need for recipient-focused strategies.3 Recognition of the foundational role of the reciprocal learner-teacher alliance in feedback integration inspired newer feedback models, such as the “R2C2” and the “Self-Assessment, Feedback, Encouragement, Direction.”4,5
But which way is best? With increasing abundance and complexity of feedback frameworks, selecting an approach can feel overwhelming and impractical. A generic “one-size-fits-all” strategy or avoidance of feedback altogether can be detrimental. Structured feedback models can also lead to rigid, inauthentic interactions. Below, we suggest a more practical approach through our tips that unifies the common themes of various feedback models and embeds them into daily practice habits while leaving room for personalization.
Our Practical Feedback Tips
Tip 1: Set the scene: Create a positive feedback culture
Proactively creating a culture in which feedback is embedded and encouraged is perhaps the most important step. Priming both parties for feedback clarifies intent, increases receptiveness, and paves the way for growth and open communication. It also prevents the misinterpretation of unexpected feedback as an expression of disapproval. To do this, start by regularly stating your intentions at the start of every experience. Explicitly expressing your vision for mutual learning, bidirectional feedback, and growth in your respective roles attaches a positive intention to feedback. Providing a reminder that we are all works in progress and acknowledging this on a regular basis sets the stage for structured growth opportunities.
Scheduling future feedback encounters from the start maintains accountability and prevents feedback from being perceived as the consequence of a particular behavior. The number and timing of feedback sessions can be customized to the duration of the working relationship, generally allowing enough time for a second interaction (at the end of each week, halfway point, etc.).
Tip 2: Build rapport
Increasing clinical workloads and pressure to teach in time-constrained settings often results in insufficient time to engage in conversation and trust building. However, a foundational relationship is an essential precursor to meaningful feedback. Ramani et al. state that “relationships, not recipes, are more likely to promote feedback that has an impact on learner performance and ultimately patient care.”6 Building this rapport can begin by dedicating a few minutes (before/during rounds, between cases) to exchange information about career interests, hobbies, favorite restaurants, etc. This “small talk” is the beginning of a two-way exchange that ultimately develops into more meaningful exchanges.
In our experience, this simple step is impactful and fulfilling to both parties. This is also a good time for shared vulnerability by talking about what you are currently working on or have worked on at their stage to affirm that feedback is a continuous part of professional development and not a reflection of how far they are from competence at a given point in time.
Tip 3: Consider Timing, assess readiness, and preschedule sessions
Lack of attention to timing can hinder feedback acceptance. We suggest adhering to delivering positive feedback publicly and corrective feedback privately (“Praise in public, perfect in private”). This reinforces positive behaviors, increases motivation, and minimizes demoralization. Prolonged delays between the observed behavior and feedback can decrease its relevance. Conversely, delivering feedback too soon after an emotionally charged experience can be perceived as blame. Pre-designated times for feedback can minimize the guesswork and maintain your accountability for giving feedback without inadvertently linking it to one particular behavior. If the recipient does not appear to be in a state to receive feedback at the predesignated time, you can pivot to a “check-in” session to show support and strengthen rapport.
Tip 4: Customize to the learner and set shared goals
Diversity in backgrounds, perspectives, and personalities can impact how people perceive their own performances and experience feedback. Given the profound impact of sociocultural factors on feedback assimilation, maintaining the recipient and their goals at the core of performance evaluations is key to feedback acceptance.
A. Trainees
We suggest starting by introducing the idea of feedback as a partnership and something you feel privileged to do to help them achieve mutual goals. It helps to ask them to use the first day to get oriented with the experience, general expectations, challenges they expect to encounter, and their feedback goals. Tailoring your feedback to their goals creates a sense of shared purpose which increases motivation. Encouraging them to develop their own strategies allows them to play an active role in their growth. Giving them the opportunity to share their perceived strengths and deficiencies provides you with valuable information regarding their insight and ability to self-evaluate. This can help you predict their readiness for your feedback and to tailor your approach when there is a mismatch.
Examples:
- Medical student: Start with “What do you think you are doing well?” and “What do you think you need to work on?” Build on their response with encouragement and empathy. This helps make them more deliberate with what they work on because being a medical student can be overwhelming and can feel as though they have everything to work on.
- Resident/Fellow: By this point, trainees usually have an increased awareness of their strengths and deficiencies. Your questions can then be more specific, giving them autonomy over their learning, such as “What are some of the things you are working on that you want me to give you feedback on this week?” This makes them more aware, intentional, and receptive to your feedback because it is framed as something that they sought out.
B. Colleagues/Staff
Unlike the training environment in which feedback is built-in, giving feedback to co-workers requires you to establish a feedback-conducive environment and to develop a more in-depth understanding of coworkers’ personalities. Similar strategies can be applied, such as proactively setting the scene for open communication, scheduling check-ins, demonstrating receptiveness to feedback, and investing in trust-building.
Longer working relationships allow for strong foundational connections that make feedback less threatening. Personality assessment testing like Myers-Briggs Type Indicator or DiSC Assessment can aid in tailoring feedback to different individuals.7,8 An analytical thinker may appreciate direct, data-driven feedback. Relationship-oriented individuals might respond better to softer, encouragement-based approaches. Always maintain shared goals at the center of your interactions and consider collaborative opportunities such as quality improvement projects. This can improve your working relationship in a constructive way without casting blame.
Tip 5: Work on delivery: Bidirectional communication and body language
Non-verbal cues can have a profound impact on how your feedback is interpreted and on the recipient’s comfort to engage in conversation. Sitting down, making eye contact, nodding, and avoiding closed-off body posture can project support and feel less judgmental. Creating a safe and non-distracted environment with privacy can make them feel valued. Use motivating, respectful language focused on directly observed behaviors rather than personal attributes or second-hand reports.
Remember that focusing on repetitive patterns is likely more helpful than isolated incidents. Validate their hard work and give them a global idea of where they stand before diving into individual behaviors. Encourage their participation and empower them to suggest changes they plan to implement. Conclude by having them summarize their action plan to give them ownership and to verify that your feedback was interpreted as you intended. Thank them for being a part of the process, as it does take a partnership for feedback to be effective.
Tip 6: Be open to feedback
Demonstrating your willingness to accept and act on feedback reinforces a positive culture where feedback is normalized and valued. After an unintended outcome, initiate a two-way conversation and ask their input on anything they wish you would have done differently. This reaffirms your commitment to maintaining culture that does not revolve around one-sided critiques. Frequently soliciting feedback about your feedback skills can also guide you to adapt your approach and to recognize any ineffective feedback practices.
Tip 7: When things don’t go as planned
Receiving feedback, no matter how thoughtfully it is delivered, can be an emotionally-charged experience ending in hurt feelings. This happens because of misinterpretation of feedback as an indicator of inadequacy, heightened awareness of underlying insecurities, sociocultural or personal circumstances, frustration with oneself, needing additional guidance, or being caught off-guard by the assessment.
The evaluator should always acknowledge the recipient’s feelings, show compassion, and allow time for processing. When they are ready to talk, it is important to help reframe the recipients’ mindsets to recognize that feedback is not personal or defining and is not a “one and done” reflection of whether they have “made it.” Instead, it is a continual process that we benefit from through all career stages. Again, shared vulnerability can help to normalize feedback and maintain open dialogue. Setting an opportunity for a future check-in can reinforce support and lead to a more productive conversation after they have had time to process.
Conclusion
Effective feedback delivery is an invaluable skill that can result in meaningful goal-directed changes while strengthening professional relationships. Given the complexity of feedback interactions and the many factors that influence its acceptance, no single approach is suitable for all recipients and frequent adaptation of the approach is essential.
In our experience, adhering to these general overarching feedback principles (see Figure 1) has allowed us to have more successful interactions with trainees and colleagues.
Dr. Baliss is based in the Division of Gastroenterology, Washington University in St. Louis, Missouri. Dr. Hachem is director of the Division of Gastroenterology and Digestive Health at Intermountain Medical, Sandy, Utah. Both authors declare no conflicts of interest.
References
1. Parkes J, et al. Feedback sandwiches affect perceptions but not performance. Adv Health Sci Educ Theory Pract. 2013 Aug. doi:10.1007/s10459-012-9377-9.
2. van de Ridder JMM and Wijnen-Meijer M. Pendleton’s Rules: A Mini Review of a Feedback Method. Am J Biomed Sci & Res. 2023 May. doi: 10.34297/AJBSR.2023.19.002542.
3. Sender Liberman A, et al. Surgery residents and attending surgeons have different perceptions of feedback. Med Teach. 2005 Aug. doi: 10.1080/0142590500129183.
4. Sargeant J, et al. R2C2 in Action: Testing an Evidence-Based Model to Facilitate Feedback and Coaching in Residency. J Grad Med Educ. 2017 Apr. doi: 10.4300/JGME-D-16-00398.1.
5. Liakos W, et al. Frameworks for Effective Feedback in Health Professions Education. Acad Med. 2023 May. doi: 10.1097/ACM.0000000000004884.
6. Ramani S, et al. Feedback Redefined: Principles and Practice. J Gen Intern Med. 2019 May. doi: 10.1007/s11606-019-04874-2.
7. Woods RA and Hill PB. Myers-Briggs Type Indicator. StatPearls. StatPearls Publishing. 2022 Sept. https://www.ncbi.nlm.nih.gov/books/NBK554596/
8. Slowikowski MK. Using the DISC behavioral instrument to guide leadership and communication. AORN J. 2005 Nov. doi: 10.1016/s0001-2092(06)60276-7.
Vital Partners in GI Care
Demand for specialized GI care has skyrocketed in recent years, eclipsing the supply of gastroenterologists and impairing patient access to high-quality GI care, particularly in rural and other underserved areas. In this environment,
Across specialties, APPs are estimated to constitute roughly a third of the US clinical workforce, and demand is only growing. A June 2024 MGMA Stat poll found that 63% of medical groups planned to add new APP roles in the next year. As the GI APP workforce grows, so too will demand for advanced training tailored to the APP role.
AGA has invested heavily in professional development opportunities for NPs and PAs, in recognition of their vital role in providing high-quality GI care. The newly formed AGA NPPA Task Force, co-chaired by Abigail Meyers (who we featured in GIHN’s April issue) and Kimberly Kearns, works closely with the Education and Training Committee to develop education programs to meet the specific needs of NPs and PAs, and advocate for more APP involvement in AGA programming. One example of this is AGA’s 2025 Principles of GI for the NP and PA course, which will be held in Chicago in early August – I encourage you to spread the word and support your APP colleagues in getting involved in these important initiatives as our vital partners in GI care delivery.
In this month’s issue of GIHN, we present the exciting results of the BOSS trial, showing no survival difference between regular and at need surveillance for Barrett’s esophagus, suggesting that at need endoscopy may be a safe alternative for low-risk patients. Continuing our coverage of potentially practice-changing research from DDW, we highlight another recent RCT challenging the use of papillary sphincterotomy as a treatment for pancreas divisum.
In our July Member Spotlight, Eric Shah, MD, MBA (University of Michigan), a past AGA Research Scholar Award recipient, highlights how this critical research support aided him in his journey to develop a now FDA-approved point-of care screening tool used to evaluate patients with chronic constipation for pelvic floor dysfunction during a routine clinic visit. In our quarterly Perspectives column, Dr. David Wan (a GI hospitalist) and Dr. Zeyed Metwalli (an interventional radiologist) discuss best practices in management of lower GI bleeding. We hope you have a restful summer!
Megan A. Adams, MD, JD, MSc
Editor in Chief
Demand for specialized GI care has skyrocketed in recent years, eclipsing the supply of gastroenterologists and impairing patient access to high-quality GI care, particularly in rural and other underserved areas. In this environment,
Across specialties, APPs are estimated to constitute roughly a third of the US clinical workforce, and demand is only growing. A June 2024 MGMA Stat poll found that 63% of medical groups planned to add new APP roles in the next year. As the GI APP workforce grows, so too will demand for advanced training tailored to the APP role.
AGA has invested heavily in professional development opportunities for NPs and PAs, in recognition of their vital role in providing high-quality GI care. The newly formed AGA NPPA Task Force, co-chaired by Abigail Meyers (who we featured in GIHN’s April issue) and Kimberly Kearns, works closely with the Education and Training Committee to develop education programs to meet the specific needs of NPs and PAs, and advocate for more APP involvement in AGA programming. One example of this is AGA’s 2025 Principles of GI for the NP and PA course, which will be held in Chicago in early August – I encourage you to spread the word and support your APP colleagues in getting involved in these important initiatives as our vital partners in GI care delivery.
In this month’s issue of GIHN, we present the exciting results of the BOSS trial, showing no survival difference between regular and at need surveillance for Barrett’s esophagus, suggesting that at need endoscopy may be a safe alternative for low-risk patients. Continuing our coverage of potentially practice-changing research from DDW, we highlight another recent RCT challenging the use of papillary sphincterotomy as a treatment for pancreas divisum.
In our July Member Spotlight, Eric Shah, MD, MBA (University of Michigan), a past AGA Research Scholar Award recipient, highlights how this critical research support aided him in his journey to develop a now FDA-approved point-of care screening tool used to evaluate patients with chronic constipation for pelvic floor dysfunction during a routine clinic visit. In our quarterly Perspectives column, Dr. David Wan (a GI hospitalist) and Dr. Zeyed Metwalli (an interventional radiologist) discuss best practices in management of lower GI bleeding. We hope you have a restful summer!
Megan A. Adams, MD, JD, MSc
Editor in Chief
Demand for specialized GI care has skyrocketed in recent years, eclipsing the supply of gastroenterologists and impairing patient access to high-quality GI care, particularly in rural and other underserved areas. In this environment,
Across specialties, APPs are estimated to constitute roughly a third of the US clinical workforce, and demand is only growing. A June 2024 MGMA Stat poll found that 63% of medical groups planned to add new APP roles in the next year. As the GI APP workforce grows, so too will demand for advanced training tailored to the APP role.
AGA has invested heavily in professional development opportunities for NPs and PAs, in recognition of their vital role in providing high-quality GI care. The newly formed AGA NPPA Task Force, co-chaired by Abigail Meyers (who we featured in GIHN’s April issue) and Kimberly Kearns, works closely with the Education and Training Committee to develop education programs to meet the specific needs of NPs and PAs, and advocate for more APP involvement in AGA programming. One example of this is AGA’s 2025 Principles of GI for the NP and PA course, which will be held in Chicago in early August – I encourage you to spread the word and support your APP colleagues in getting involved in these important initiatives as our vital partners in GI care delivery.
In this month’s issue of GIHN, we present the exciting results of the BOSS trial, showing no survival difference between regular and at need surveillance for Barrett’s esophagus, suggesting that at need endoscopy may be a safe alternative for low-risk patients. Continuing our coverage of potentially practice-changing research from DDW, we highlight another recent RCT challenging the use of papillary sphincterotomy as a treatment for pancreas divisum.
In our July Member Spotlight, Eric Shah, MD, MBA (University of Michigan), a past AGA Research Scholar Award recipient, highlights how this critical research support aided him in his journey to develop a now FDA-approved point-of care screening tool used to evaluate patients with chronic constipation for pelvic floor dysfunction during a routine clinic visit. In our quarterly Perspectives column, Dr. David Wan (a GI hospitalist) and Dr. Zeyed Metwalli (an interventional radiologist) discuss best practices in management of lower GI bleeding. We hope you have a restful summer!
Megan A. Adams, MD, JD, MSc
Editor in Chief
The Essential Guide to Estate Planning for Physicians: Securing Your Legacy and Protecting Your Wealth
As a physician, you’ve spent years building a career that not only provides financial security for your family but also allows you to make a meaningful impact in your community. However, without a comprehensive estate plan in place, much of what you’ve worked so hard to build may not be preserved according to your wishes.
Many physicians delay estate planning, assuming it’s something to consider later in life. However, the most successful estate plans are those that are established early and evolve over time. Proper planning ensures that your assets are protected, your loved ones are provided for, and your legacy is preserved in the most tax-efficient and legally-sound manner possible.1
This article explores why estate planning is particularly crucial for physicians, the key elements of a strong estate plan, and how beginning early can create long-term financial advantages.
Why Estate Planning Matters for Physicians
Physicians are in a unique financial position compared to many other professionals. With high earning potential, specialized assets, and significant liability exposure, their estate planning needs differ from those of the average individual. A well-structured estate plan not only facilitates the smooth transfer of wealth but also protects assets from excessive taxation, legal complications, and potential risks such as malpractice claims.
1. High Net-Worth Considerations
Physicians often accumulate substantial wealth over time. Without a clear estate plan, your estate could face excessive taxation, with a large portion of your assets potentially going to the government rather than your heirs. Estate taxes, probate costs, and legal fees can significantly erode your legacy if not properly planned for.
2. Asset Protection from Liability Risks
Unlike most professionals, physicians are at a higher risk of litigation. A comprehensive estate plan can incorporate asset protection strategies, such as irrevocable trusts, family limited partnerships, or liability insurance, to shield your wealth from lawsuits or creditor claims.
3. Family and Generational Wealth Planning
Many physicians prioritize ensuring their family’s financial stability. Whether you want to provide for your spouse, children, or even charitable causes, estate planning allows you to dictate how your wealth is distributed. Establishing trusts for your children or grandchildren can help manage how and when they receive their inheritance, preventing mismanagement and ensuring financial responsibility.
4. Business and Practice Continuity
If you own a medical practice, succession planning should be part of your estate plan. Without clear directives, the future of your practice may be uncertain in the event of your passing or incapacitation. A well-drafted estate plan provides a roadmap for ownership transition, ensuring continuity for patients, employees, and business partners.
Key Elements of an Effective Estate Plan
Every estate plan should be customized based on your financial situation, goals, and family dynamics. However, certain fundamental components apply to nearly all high-net-worth individuals, including physicians.
1. Revocable Living Trusts
A revocable living trust allows you to manage your assets during your lifetime while providing a clear path for distribution after your passing. Unlike a will, a trust helps your estate avoid probate, ensuring a smoother and more private transition of wealth. You maintain control over your assets while also establishing clear rules for distribution, particularly useful if you have minor children or complex family structures.2
2. Irrevocable Trusts for Asset Protection
For physicians concerned about lawsuits or estate tax exposure, irrevocable trusts can offer robust asset protection. Since assets placed in these trusts are no longer legally owned by you, they are shielded from creditors and legal claims while also reducing your taxable estate.2
3. Powers of Attorney and Healthcare Directives
Estate planning isn’t just about what happens after your passing—it’s also about protecting you and your family if you become incapacitated. A durable power of attorney allows a trusted individual to manage your financial affairs, while a healthcare directive ensures your medical decisions align with your wishes.3
4. Life Insurance Planning
Life insurance is an essential estate planning tool for physicians, providing liquidity to cover estate taxes, debts, or income replacement for your family. A properly structured life insurance trust can help ensure that policy proceeds remain outside of your taxable estate while being efficiently distributed according to your wishes.4
5. Business Succession Planning
If you own a medical practice, a well-designed succession plan can ensure that your business continues to operate smoothly in your absence. This may involve buy-sell agreements, key-person insurance, or identifying a successor to take over your role.5
The Long-Term Benefits of Early Estate Planning
Estate planning is not a one-time event—it’s a process that should evolve with your career, financial growth, and family dynamics. The earlier you begin, the more control you have over your financial future. Here’s why starting early is a strategic advantage:
1. Maximizing Tax Efficiency
Many estate planning strategies, such as gifting assets or establishing irrevocable trusts, are most effective when implemented over time. By spreading out wealth transfers and taking advantage of annual gift exclusions, you can significantly reduce estate tax liability while maintaining financial security.
2. Adjusting for Life Changes
Your financial situation and family needs will change over the years. Marriages, births, career advancements, and new investments all impact your estate planning needs. By starting early, you can make gradual adjustments rather than facing an overwhelming restructuring later in life.1
3. Ensuring Asset Protection Strategies Are in Place
Many asset protection strategies require time to be effective. For instance, certain types of trusts must be in place for a number of years before they fully shield assets from legal claims. Delaying planning could leave your wealth unnecessarily exposed.
4. Creating a Legacy Beyond Wealth
Estate planning is not just about finances—it’s about legacy. Whether you want to support a charitable cause, endow a scholarship, or establish a foundation, early planning gives you the ability to shape your long-term impact.
5. Adapt to Ever Changing Legislation
Estate planning needs to be adaptable. The federal government can change the estate tax exemption at any time; this was even a topic of the last election cycle. Early planning allows you to implement necessary changes throughout your life to minimize estate taxes. At present, unless new policy is enacted, the exemption per individual will reduce by half in 2026 (see Figure 1).
Final Thoughts: Taking Action Today
The complexity of physician finances—ranging from high income and significant assets to legal risks—makes individualized estate planning an absolute necessity.
By taking proactive steps today, you can maximize tax efficiency, safeguard your assets, and ensure your wishes are carried out without unnecessary delays or legal battles. Working with a financial advisor and estate planning attorney who understands the unique needs of physicians can help you craft a plan that aligns with your goals and evolves as your career progresses.
Mr. Gardner is a financial advisor at Lifetime Financial Growth, LLC, in Columbus, Ohio, one of the largest privately held wealth management firms in the country. John has had a passion for finance since his early years in college when his tennis coach introduced him. He also has a passion for helping physicians, as his wife is a gastroenterologist at Ohio State University. He reports no relevant disclosures relevant to this article. If you have additional questions, please contact John at 740-403-4891 or john_s_gardner@glic.com.
References
1. The Law Offices of Diron Rutty, LLC. https://www.dironruttyllc.com/reasons-to-start-estate-planning-early/.
2. Physician Side Gigs. https://www.physiciansidegigs.com/estateplanning.
3. Afshar, A & MacBeth, S. https://www.schwabe.com/publication/estate-planning-for-physicians-why-its-important-and-how-to-get-started/. December 2024.
4. Skeeles, JC. https://ohioline.osu.edu/factsheet/ep-1. July 2012.
5. Rosenfeld, J. Physician estate planning guide. Medical Economics. 2022 Nov. https://www.medicaleconomics.com/view/physician-estate-planning-guide.
As a physician, you’ve spent years building a career that not only provides financial security for your family but also allows you to make a meaningful impact in your community. However, without a comprehensive estate plan in place, much of what you’ve worked so hard to build may not be preserved according to your wishes.
Many physicians delay estate planning, assuming it’s something to consider later in life. However, the most successful estate plans are those that are established early and evolve over time. Proper planning ensures that your assets are protected, your loved ones are provided for, and your legacy is preserved in the most tax-efficient and legally-sound manner possible.1
This article explores why estate planning is particularly crucial for physicians, the key elements of a strong estate plan, and how beginning early can create long-term financial advantages.
Why Estate Planning Matters for Physicians
Physicians are in a unique financial position compared to many other professionals. With high earning potential, specialized assets, and significant liability exposure, their estate planning needs differ from those of the average individual. A well-structured estate plan not only facilitates the smooth transfer of wealth but also protects assets from excessive taxation, legal complications, and potential risks such as malpractice claims.
1. High Net-Worth Considerations
Physicians often accumulate substantial wealth over time. Without a clear estate plan, your estate could face excessive taxation, with a large portion of your assets potentially going to the government rather than your heirs. Estate taxes, probate costs, and legal fees can significantly erode your legacy if not properly planned for.
2. Asset Protection from Liability Risks
Unlike most professionals, physicians are at a higher risk of litigation. A comprehensive estate plan can incorporate asset protection strategies, such as irrevocable trusts, family limited partnerships, or liability insurance, to shield your wealth from lawsuits or creditor claims.
3. Family and Generational Wealth Planning
Many physicians prioritize ensuring their family’s financial stability. Whether you want to provide for your spouse, children, or even charitable causes, estate planning allows you to dictate how your wealth is distributed. Establishing trusts for your children or grandchildren can help manage how and when they receive their inheritance, preventing mismanagement and ensuring financial responsibility.
4. Business and Practice Continuity
If you own a medical practice, succession planning should be part of your estate plan. Without clear directives, the future of your practice may be uncertain in the event of your passing or incapacitation. A well-drafted estate plan provides a roadmap for ownership transition, ensuring continuity for patients, employees, and business partners.
Key Elements of an Effective Estate Plan
Every estate plan should be customized based on your financial situation, goals, and family dynamics. However, certain fundamental components apply to nearly all high-net-worth individuals, including physicians.
1. Revocable Living Trusts
A revocable living trust allows you to manage your assets during your lifetime while providing a clear path for distribution after your passing. Unlike a will, a trust helps your estate avoid probate, ensuring a smoother and more private transition of wealth. You maintain control over your assets while also establishing clear rules for distribution, particularly useful if you have minor children or complex family structures.2
2. Irrevocable Trusts for Asset Protection
For physicians concerned about lawsuits or estate tax exposure, irrevocable trusts can offer robust asset protection. Since assets placed in these trusts are no longer legally owned by you, they are shielded from creditors and legal claims while also reducing your taxable estate.2
3. Powers of Attorney and Healthcare Directives
Estate planning isn’t just about what happens after your passing—it’s also about protecting you and your family if you become incapacitated. A durable power of attorney allows a trusted individual to manage your financial affairs, while a healthcare directive ensures your medical decisions align with your wishes.3
4. Life Insurance Planning
Life insurance is an essential estate planning tool for physicians, providing liquidity to cover estate taxes, debts, or income replacement for your family. A properly structured life insurance trust can help ensure that policy proceeds remain outside of your taxable estate while being efficiently distributed according to your wishes.4
5. Business Succession Planning
If you own a medical practice, a well-designed succession plan can ensure that your business continues to operate smoothly in your absence. This may involve buy-sell agreements, key-person insurance, or identifying a successor to take over your role.5
The Long-Term Benefits of Early Estate Planning
Estate planning is not a one-time event—it’s a process that should evolve with your career, financial growth, and family dynamics. The earlier you begin, the more control you have over your financial future. Here’s why starting early is a strategic advantage:
1. Maximizing Tax Efficiency
Many estate planning strategies, such as gifting assets or establishing irrevocable trusts, are most effective when implemented over time. By spreading out wealth transfers and taking advantage of annual gift exclusions, you can significantly reduce estate tax liability while maintaining financial security.
2. Adjusting for Life Changes
Your financial situation and family needs will change over the years. Marriages, births, career advancements, and new investments all impact your estate planning needs. By starting early, you can make gradual adjustments rather than facing an overwhelming restructuring later in life.1
3. Ensuring Asset Protection Strategies Are in Place
Many asset protection strategies require time to be effective. For instance, certain types of trusts must be in place for a number of years before they fully shield assets from legal claims. Delaying planning could leave your wealth unnecessarily exposed.
4. Creating a Legacy Beyond Wealth
Estate planning is not just about finances—it’s about legacy. Whether you want to support a charitable cause, endow a scholarship, or establish a foundation, early planning gives you the ability to shape your long-term impact.
5. Adapt to Ever Changing Legislation
Estate planning needs to be adaptable. The federal government can change the estate tax exemption at any time; this was even a topic of the last election cycle. Early planning allows you to implement necessary changes throughout your life to minimize estate taxes. At present, unless new policy is enacted, the exemption per individual will reduce by half in 2026 (see Figure 1).
Final Thoughts: Taking Action Today
The complexity of physician finances—ranging from high income and significant assets to legal risks—makes individualized estate planning an absolute necessity.
By taking proactive steps today, you can maximize tax efficiency, safeguard your assets, and ensure your wishes are carried out without unnecessary delays or legal battles. Working with a financial advisor and estate planning attorney who understands the unique needs of physicians can help you craft a plan that aligns with your goals and evolves as your career progresses.
Mr. Gardner is a financial advisor at Lifetime Financial Growth, LLC, in Columbus, Ohio, one of the largest privately held wealth management firms in the country. John has had a passion for finance since his early years in college when his tennis coach introduced him. He also has a passion for helping physicians, as his wife is a gastroenterologist at Ohio State University. He reports no relevant disclosures relevant to this article. If you have additional questions, please contact John at 740-403-4891 or john_s_gardner@glic.com.
References
1. The Law Offices of Diron Rutty, LLC. https://www.dironruttyllc.com/reasons-to-start-estate-planning-early/.
2. Physician Side Gigs. https://www.physiciansidegigs.com/estateplanning.
3. Afshar, A & MacBeth, S. https://www.schwabe.com/publication/estate-planning-for-physicians-why-its-important-and-how-to-get-started/. December 2024.
4. Skeeles, JC. https://ohioline.osu.edu/factsheet/ep-1. July 2012.
5. Rosenfeld, J. Physician estate planning guide. Medical Economics. 2022 Nov. https://www.medicaleconomics.com/view/physician-estate-planning-guide.
As a physician, you’ve spent years building a career that not only provides financial security for your family but also allows you to make a meaningful impact in your community. However, without a comprehensive estate plan in place, much of what you’ve worked so hard to build may not be preserved according to your wishes.
Many physicians delay estate planning, assuming it’s something to consider later in life. However, the most successful estate plans are those that are established early and evolve over time. Proper planning ensures that your assets are protected, your loved ones are provided for, and your legacy is preserved in the most tax-efficient and legally-sound manner possible.1
This article explores why estate planning is particularly crucial for physicians, the key elements of a strong estate plan, and how beginning early can create long-term financial advantages.
Why Estate Planning Matters for Physicians
Physicians are in a unique financial position compared to many other professionals. With high earning potential, specialized assets, and significant liability exposure, their estate planning needs differ from those of the average individual. A well-structured estate plan not only facilitates the smooth transfer of wealth but also protects assets from excessive taxation, legal complications, and potential risks such as malpractice claims.
1. High Net-Worth Considerations
Physicians often accumulate substantial wealth over time. Without a clear estate plan, your estate could face excessive taxation, with a large portion of your assets potentially going to the government rather than your heirs. Estate taxes, probate costs, and legal fees can significantly erode your legacy if not properly planned for.
2. Asset Protection from Liability Risks
Unlike most professionals, physicians are at a higher risk of litigation. A comprehensive estate plan can incorporate asset protection strategies, such as irrevocable trusts, family limited partnerships, or liability insurance, to shield your wealth from lawsuits or creditor claims.
3. Family and Generational Wealth Planning
Many physicians prioritize ensuring their family’s financial stability. Whether you want to provide for your spouse, children, or even charitable causes, estate planning allows you to dictate how your wealth is distributed. Establishing trusts for your children or grandchildren can help manage how and when they receive their inheritance, preventing mismanagement and ensuring financial responsibility.
4. Business and Practice Continuity
If you own a medical practice, succession planning should be part of your estate plan. Without clear directives, the future of your practice may be uncertain in the event of your passing or incapacitation. A well-drafted estate plan provides a roadmap for ownership transition, ensuring continuity for patients, employees, and business partners.
Key Elements of an Effective Estate Plan
Every estate plan should be customized based on your financial situation, goals, and family dynamics. However, certain fundamental components apply to nearly all high-net-worth individuals, including physicians.
1. Revocable Living Trusts
A revocable living trust allows you to manage your assets during your lifetime while providing a clear path for distribution after your passing. Unlike a will, a trust helps your estate avoid probate, ensuring a smoother and more private transition of wealth. You maintain control over your assets while also establishing clear rules for distribution, particularly useful if you have minor children or complex family structures.2
2. Irrevocable Trusts for Asset Protection
For physicians concerned about lawsuits or estate tax exposure, irrevocable trusts can offer robust asset protection. Since assets placed in these trusts are no longer legally owned by you, they are shielded from creditors and legal claims while also reducing your taxable estate.2
3. Powers of Attorney and Healthcare Directives
Estate planning isn’t just about what happens after your passing—it’s also about protecting you and your family if you become incapacitated. A durable power of attorney allows a trusted individual to manage your financial affairs, while a healthcare directive ensures your medical decisions align with your wishes.3
4. Life Insurance Planning
Life insurance is an essential estate planning tool for physicians, providing liquidity to cover estate taxes, debts, or income replacement for your family. A properly structured life insurance trust can help ensure that policy proceeds remain outside of your taxable estate while being efficiently distributed according to your wishes.4
5. Business Succession Planning
If you own a medical practice, a well-designed succession plan can ensure that your business continues to operate smoothly in your absence. This may involve buy-sell agreements, key-person insurance, or identifying a successor to take over your role.5
The Long-Term Benefits of Early Estate Planning
Estate planning is not a one-time event—it’s a process that should evolve with your career, financial growth, and family dynamics. The earlier you begin, the more control you have over your financial future. Here’s why starting early is a strategic advantage:
1. Maximizing Tax Efficiency
Many estate planning strategies, such as gifting assets or establishing irrevocable trusts, are most effective when implemented over time. By spreading out wealth transfers and taking advantage of annual gift exclusions, you can significantly reduce estate tax liability while maintaining financial security.
2. Adjusting for Life Changes
Your financial situation and family needs will change over the years. Marriages, births, career advancements, and new investments all impact your estate planning needs. By starting early, you can make gradual adjustments rather than facing an overwhelming restructuring later in life.1
3. Ensuring Asset Protection Strategies Are in Place
Many asset protection strategies require time to be effective. For instance, certain types of trusts must be in place for a number of years before they fully shield assets from legal claims. Delaying planning could leave your wealth unnecessarily exposed.
4. Creating a Legacy Beyond Wealth
Estate planning is not just about finances—it’s about legacy. Whether you want to support a charitable cause, endow a scholarship, or establish a foundation, early planning gives you the ability to shape your long-term impact.
5. Adapt to Ever Changing Legislation
Estate planning needs to be adaptable. The federal government can change the estate tax exemption at any time; this was even a topic of the last election cycle. Early planning allows you to implement necessary changes throughout your life to minimize estate taxes. At present, unless new policy is enacted, the exemption per individual will reduce by half in 2026 (see Figure 1).
Final Thoughts: Taking Action Today
The complexity of physician finances—ranging from high income and significant assets to legal risks—makes individualized estate planning an absolute necessity.
By taking proactive steps today, you can maximize tax efficiency, safeguard your assets, and ensure your wishes are carried out without unnecessary delays or legal battles. Working with a financial advisor and estate planning attorney who understands the unique needs of physicians can help you craft a plan that aligns with your goals and evolves as your career progresses.
Mr. Gardner is a financial advisor at Lifetime Financial Growth, LLC, in Columbus, Ohio, one of the largest privately held wealth management firms in the country. John has had a passion for finance since his early years in college when his tennis coach introduced him. He also has a passion for helping physicians, as his wife is a gastroenterologist at Ohio State University. He reports no relevant disclosures relevant to this article. If you have additional questions, please contact John at 740-403-4891 or john_s_gardner@glic.com.
References
1. The Law Offices of Diron Rutty, LLC. https://www.dironruttyllc.com/reasons-to-start-estate-planning-early/.
2. Physician Side Gigs. https://www.physiciansidegigs.com/estateplanning.
3. Afshar, A & MacBeth, S. https://www.schwabe.com/publication/estate-planning-for-physicians-why-its-important-and-how-to-get-started/. December 2024.
4. Skeeles, JC. https://ohioline.osu.edu/factsheet/ep-1. July 2012.
5. Rosenfeld, J. Physician estate planning guide. Medical Economics. 2022 Nov. https://www.medicaleconomics.com/view/physician-estate-planning-guide.
Lower Gastrointestinal Bleeding: Two Perspectives
Dear colleagues,
: What is the role and optimal timing of colonoscopy? How can we best utilize radiologic studies like CTA or tagged RBC scans? How should we manage patients with recurrent or intermittent bleeding that defies localization?
In this issue of Perspectives, Dr. David Wan, Dr. Fredella Lee, and Dr. Zeyad Metwalli offer their expert insights on these difficult questions. Dr. Wan, drawing on over 15 years of experience as a GI hospitalist, shares – along with his coauthor Dr. Lee – a pragmatic approach to LGIB based on clinical patterns, evolving data, and multidisciplinary collaboration. Dr. Metwalli provides the interventional radiologist’s perspective, highlighting how angiographic techniques can complement GI management and introducing novel IR strategies for patients with recurrent or elusive bleeding.
We hope their perspectives will offer valuable guidance for your practice. Join the conversation on X at @AGA_GIHN.
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, and chief of endoscopy at West Haven VA Medical Center, both in Connecticut. He is an associate editor for GI & Hepatology News.
Management of Lower Gastrointestinal Bleeds: GI Perspective
BY FREDELLA LEE, MD; DAVID WAN, MD
Acute lower gastrointestinal bleeding (LGIB) presents unique challenges. Much of this stems from the natural history of diverticular bleeding, the most common etiology of LGIB.
First, while bleeding can be severe, most will spontaneously stop. Second, despite our best efforts with imaging or colonoscopy, finding an intervenable lesion is rare. Third, LGIB has significant rates of rebleeding that are unpredictable.
While serving as a GI hospitalist for 15 years and after managing over 300 cases of LGIB, I often find myself frustrated and colonoscopy feels futile. So how can we rationally approach these patients? We will focus on three clinical questions to develop a framework for LGIB management.
- What is the role and timing for a colonoscopy?
- How do we best utilize radiologic tests?
- How can we prevent recurrent LGIB?
The Role of Colonoscopy
Traditionally, colonoscopy within 24 hours of presentation was recommended. This was based on retrospective cohort data showing higher endoscopic intervention rates and better clinical outcomes. However, this protocol requires patients to drink a significant volume of bowel preparation over a few hours (often requiring an NGT) to achieve clear rectal effluent. Moreover, one needs to mobilize a team (i.e., nurse, technician, anesthesiologist, and gastroenterologist), and find an appropriate location to scope (i.e., ED, ICU, or OR), Understandably, this is challenging, especially overnight. When the therapeutic yield is relatively low, this approach quickly loses enthusiasm.
Importantly, meta-analyses of the randomized controlled trials, have shown that urgent colonoscopies (<24 hours upon presentation), compared to elective colonoscopies (>24 hours upon presentation), do not improve clinical outcomes such as re-bleeding rates, transfusion requirements, mortality, or length of stay. In these studies, the endoscopic intervention rates were 17-34%, however, observational data shows rates of only 8%. In our practice, we will use a clear cap attachment device and water jet irrigation to increase the odds of detecting an active source of bleeding. Colonoscopy has a diagnostic yield of 95% – despite its low therapeutic yield; and while diverticular bleeds constitute up to 64% of cases, one does not want to miss colorectal cancer or other diagnoses. Regardless, there is generally no urgency to perform a colonoscopy. To quote a colleague, Dr. Elizabeth Ross, “there is no such thing as door-to-butt time.”
The Role of Radiology
Given the limits of colonoscopy, can radiographic tests such as computed tomography angiography (CTA) or tagged red blood cell (RBC) scan be helpful? Multiple studies have suggested using CTA as the initial diagnostic test. The advantages of CTAs are:
- Fast, readily available, and does not require a bowel preparation
- If negative, CTAs portend a good prognosis and make it highly unlikely to detect active extravasation on visceral angiography
- If positive, can localize the source of bleed and increase the success of intervention
Whether a positive CTA should be followed with a colonoscopy or visceral angiography remains unclear. Studies show that positive CTAs increase the detection rate of stigmata of recent hemorrhage on colonoscopy. Positive CTAs can also identify a target for embolization by interventional radiology (IR). Though an important caveat is that the success rate of embolization is highest when performed within 90 minutes of a positive CTA. This highlights that if you have IR availability, it is critical to have clear communication, a well-defined protocol, and collaboration among disciplines (i.e., ED, medical team, GI, and IR).
At our institution, we have implemented a CTA-guided protocol for severe LGIB. Those with positive CTAs are referred immediately to IR for embolization. If the embolization is unsuccessful or CTA is negative, the patient will be planned for a non-urgent inpatient colonoscopy. However, our unpublished data and other studies have shown that the overall CTA positivity rates are only between 16-22%. Moreover, one randomized controlled trial comparing CTA versus colonoscopy as an initial test did not show any meaningful difference in clinical outcomes. Thus, the benefit of CTA and the best approach to positive CTAs remains in question.
Lastly, people often ask about the utility of RBC nuclear scans. While they can detect bleeds at a slower rate (as low as 0.1 mL/min) compared to CTA (at least 0.4 mL/min), there are many limitations. RBC scans take time, are not available 24-7, and cannot precisely localize the site of bleeding. Therefore, we rarely recommend them for LGIB.
Approach to Recurrent Diverticular Bleeding
Unfortunately, diverticular bleeding recurs in the hospital 14% of the time and up to 25% at 5 years. When this occurs, is it worthwhile to repeat another colonoscopy or CTA?
Given the lack of clear data, we have adopted a shared decision-making framework with patients. Oftentimes, these patients are older and have significant co-morbidities, and undergoing bowel preparation, anesthesia, and colonoscopy is not trivial. If the patient is stable and prior work-up has excluded pertinent alternative diagnoses other than diverticular bleeding, then we tell patients the chance of finding an intervenable lesion is low and opt for conservative management. Meanwhile, if the patient has persistent, hemodynamically significant bleeding, we recommend a CTA based on the rationale discussed previously.
The most important clinical decision may not be about scoping or obtaining a CTA – it is medication management. If they are taking NSAIDs, they should be discontinued. If antiplatelet or anticoagulation agents were held, they should be restarted promptly in individuals with significant thrombotic risk given studies showing that while rebleeding rates may increase, overall mortality decreases.
In summary, managing LGIB and altering its natural history with either endoscopic or radiographic means is challenging. More studies are needed to guide the optimal approach. Reassuringly, most bleeding self-resolves and patients have good clinical outcomes.
Dr. Lee is a resident physician at New York Presbyterian Weill Cornell Medical Center, New York, NY. Dr. Wan is associate professor of clinical medicine at Weill Cornell Medicine, New York, N.Y. They declare no conflicts of interest.
Lower Gastrointestinal Bleeding: An Interventional Radiologist’s Perspective
BY ZEYAD METWALLI, MD, FSIR
When colonoscopy fails to localize and/or stop lower gastrointestinal bleeding (LGIB), catheter angiography has been commonly employed as a tool for both diagnosis and treatment of bleeding with embolization. Nuclear medicine or CT imaging studies can serve as useful adjuncts for confirming active bleeding and localizing the site of bleeding prior to angiography, particularly if this information is not provided by colonoscopy. Provocative mesenteric angiography has also become increasingly popular as a troubleshooting technique in patients with initially negative angiography.
Localization of Lower Gastrointestinal Bleeding
Radionuclide technetium-99m-lableled red blood cell scintigraphy (RBCS), also known as tagged RBC scintigraphy, has been in use since the early 1980s for investigation of acute gastrointestinal bleeding. RBCS has a high sensitivity for detection of active bleeding with a theoretical ability to detect bleeding at rates as low as 0.04-0.2 mL/minute.
Imaging protocols vary but should include dynamic images, which may aid in localization of bleeding. The relatively long half-life of the tracer used for imaging allows for delayed imaging 12 to 24 hours after injection. This can be useful to confirm active bleeding, particularly when bleeding is intermittent and is not visible on initial images.
With the advent of computed tomography angiography (CTA), which continues to increase in speed, imaging quality and availability, the use of RBCS for evaluation of LGIB has declined. CTA is quicker to perform than RBCS and allows for detection of bleeding as well as accurate anatomic localization, which can guide interventions.
CTA provides a more comprehensive anatomic evaluation, which can aid in the diagnosis of a wide variety of intra-abdominal issues. Conversely, CTA may be less sensitive than RBCS for detection of slower acute bleeding, detecting bleeding at rates of 0.1-1 mL/min. In addition, intermittent bleeding which has temporarily stopped at the time of CTA may evade detection.
Lastly, CTA may not be appropriate in patients with impaired renal function due to risk of contrast-induced nephropathy, particularly in patients with acute kidney injury, which commonly afflicts hospitalized patients with LGIB. Prophylaxis with normal saline hydration should be employed aggressively in patients with impaired renal function, particularly when eGFR is less than 30 mL/minute. Iodinated contrast should be used judiciously in these patients.
In clinical practice, CTA and RBCS have a similar ability to confirm the presence or absence of clinically significant active gastrointestinal bleeding. Given the greater ability to rapidly localize the bleeding site with CTA, this is generally preferred over RBCS unless there is a contraindication to performing CTA, such as severe contrast allergy or high risk for development of contrast-induced nephropathy.
Role of Catheter Angiography and Embolization
Mesenteric angiography is a well-established technique for both detection and treatment of LGIB. Hemodynamic instability and need for packed RBC transfusion increases the likelihood of positive angiography. Limitations include reduced sensitivity for detection of bleeding slower than 0.5-1 mL/minute as well as the intermittent nature of LGIB, which will often resolve spontaneously. Angiography is variably successful in the literature with a diagnostic yield between 40-80%, which encompasses the rate of success in my own practice.
Once bleeding is identified, microcatheter placement within the feeding vessel as close as possible to the site of bleeding is important to ensure treatment efficacy and to limit risk of complications such as non-target embolization and bowel ischemia. Once the feeding vessel is selected with a microcatheter, embolization can be accomplished with a wide variety of tools including metallic coils, liquid embolic agents, and particles. In the treatment of LGIB, liquid embolic agents (e.g., n-butyl cyanoacrylate or NBCA, ethylene vinyl alcohol copolymer, etc.) and particles should be used judiciously as distal penetration increases the risk of bowel ischemia and procedure-related morbidity. For this reason, metallic coils are often preferred in the treatment of LGIB.
Although the source of bleeding is variable and may include diverticulosis, recent polypectomy, ulcer, tumor or angiodysplasia, the techniques employed are similar. Accurate and distal microcatheter selection is a key driver for successful embolization and minimizing the risk of bowel ischemia. Small intestinal bleeds can be challenging to treat due to the redundant supply of the arterial arcades supplying small bowel and may require occlusion of several branches to achieve hemostasis. This approach must be balanced with the risk of developing ischemia after embolization. Angiodysplasia, a less frequently encountered culprit of LGIB, may also be managed with selective embolization with many reports of successful treatment with liquid embolic agents such as NBCA mixed with ethiodized oil.
Provocative Mesenteric Angiography for Occult Bleeding
When initial angiography in a patient with suspected active LGIB is negative, provocative angiography can be considered to uncover an intermittent bleed. This may be particularly helpful in a patient where active bleeding is confirmed on a prior diagnostic test.
The approach to provocative mesenteric angiography varies by center, and a variety of agents have been used to provoke bleeding including heparin, vasodilators (i.e., nitroglycerin, verapamil, etc.) and thrombolytics (i.e., tPA), often in combination. Thrombolytics can be administered directly into the territory of interest (i.e., superior mesenteric or inferior mesenteric artery) while heparin may be administered systemically or directly into the catheterized artery. Reported success rates for provoking angiographically visible bleeding vary, but most larger series report a 40-50% success rate. The newly detected bleeding can then be treated with either embolization or surgery. A surgeon should be involved and available when provocative angiography is planned should bleeding fail to be controlled by embolization.
In summary, when colonoscopy fails to identify or control lower gastrointestinal bleeding (LGIB), imaging techniques such as RBCS and CTA play a crucial role in localizing active bleeding. While RBCS is highly sensitive, especially for intermittent or slow bleeding, CTA offers faster, more detailed anatomical information and is typically preferred unless contraindicated by renal issues or contrast allergies. Catheter-based mesenteric angiography is a well-established method for both diagnosing and treating LGIB, often using metallic coils to minimize complications like bowel ischemia. In cases where initial angiography is negative, provocative angiography – using agents like heparin or thrombolytics – may help unmask intermittent bleeding, allowing for targeted embolization or surgical intervention.
Dr. Metwalli is associate professor in the Department of Interventional Radiology, Division of Diagnostic Imaging, at The University of Texas MD Anderson Cancer Center, Houston, Texas. He declares no conflicts of interest.
Dear colleagues,
: What is the role and optimal timing of colonoscopy? How can we best utilize radiologic studies like CTA or tagged RBC scans? How should we manage patients with recurrent or intermittent bleeding that defies localization?
In this issue of Perspectives, Dr. David Wan, Dr. Fredella Lee, and Dr. Zeyad Metwalli offer their expert insights on these difficult questions. Dr. Wan, drawing on over 15 years of experience as a GI hospitalist, shares – along with his coauthor Dr. Lee – a pragmatic approach to LGIB based on clinical patterns, evolving data, and multidisciplinary collaboration. Dr. Metwalli provides the interventional radiologist’s perspective, highlighting how angiographic techniques can complement GI management and introducing novel IR strategies for patients with recurrent or elusive bleeding.
We hope their perspectives will offer valuable guidance for your practice. Join the conversation on X at @AGA_GIHN.
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, and chief of endoscopy at West Haven VA Medical Center, both in Connecticut. He is an associate editor for GI & Hepatology News.
Management of Lower Gastrointestinal Bleeds: GI Perspective
BY FREDELLA LEE, MD; DAVID WAN, MD
Acute lower gastrointestinal bleeding (LGIB) presents unique challenges. Much of this stems from the natural history of diverticular bleeding, the most common etiology of LGIB.
First, while bleeding can be severe, most will spontaneously stop. Second, despite our best efforts with imaging or colonoscopy, finding an intervenable lesion is rare. Third, LGIB has significant rates of rebleeding that are unpredictable.
While serving as a GI hospitalist for 15 years and after managing over 300 cases of LGIB, I often find myself frustrated and colonoscopy feels futile. So how can we rationally approach these patients? We will focus on three clinical questions to develop a framework for LGIB management.
- What is the role and timing for a colonoscopy?
- How do we best utilize radiologic tests?
- How can we prevent recurrent LGIB?
The Role of Colonoscopy
Traditionally, colonoscopy within 24 hours of presentation was recommended. This was based on retrospective cohort data showing higher endoscopic intervention rates and better clinical outcomes. However, this protocol requires patients to drink a significant volume of bowel preparation over a few hours (often requiring an NGT) to achieve clear rectal effluent. Moreover, one needs to mobilize a team (i.e., nurse, technician, anesthesiologist, and gastroenterologist), and find an appropriate location to scope (i.e., ED, ICU, or OR), Understandably, this is challenging, especially overnight. When the therapeutic yield is relatively low, this approach quickly loses enthusiasm.
Importantly, meta-analyses of the randomized controlled trials, have shown that urgent colonoscopies (<24 hours upon presentation), compared to elective colonoscopies (>24 hours upon presentation), do not improve clinical outcomes such as re-bleeding rates, transfusion requirements, mortality, or length of stay. In these studies, the endoscopic intervention rates were 17-34%, however, observational data shows rates of only 8%. In our practice, we will use a clear cap attachment device and water jet irrigation to increase the odds of detecting an active source of bleeding. Colonoscopy has a diagnostic yield of 95% – despite its low therapeutic yield; and while diverticular bleeds constitute up to 64% of cases, one does not want to miss colorectal cancer or other diagnoses. Regardless, there is generally no urgency to perform a colonoscopy. To quote a colleague, Dr. Elizabeth Ross, “there is no such thing as door-to-butt time.”
The Role of Radiology
Given the limits of colonoscopy, can radiographic tests such as computed tomography angiography (CTA) or tagged red blood cell (RBC) scan be helpful? Multiple studies have suggested using CTA as the initial diagnostic test. The advantages of CTAs are:
- Fast, readily available, and does not require a bowel preparation
- If negative, CTAs portend a good prognosis and make it highly unlikely to detect active extravasation on visceral angiography
- If positive, can localize the source of bleed and increase the success of intervention
Whether a positive CTA should be followed with a colonoscopy or visceral angiography remains unclear. Studies show that positive CTAs increase the detection rate of stigmata of recent hemorrhage on colonoscopy. Positive CTAs can also identify a target for embolization by interventional radiology (IR). Though an important caveat is that the success rate of embolization is highest when performed within 90 minutes of a positive CTA. This highlights that if you have IR availability, it is critical to have clear communication, a well-defined protocol, and collaboration among disciplines (i.e., ED, medical team, GI, and IR).
At our institution, we have implemented a CTA-guided protocol for severe LGIB. Those with positive CTAs are referred immediately to IR for embolization. If the embolization is unsuccessful or CTA is negative, the patient will be planned for a non-urgent inpatient colonoscopy. However, our unpublished data and other studies have shown that the overall CTA positivity rates are only between 16-22%. Moreover, one randomized controlled trial comparing CTA versus colonoscopy as an initial test did not show any meaningful difference in clinical outcomes. Thus, the benefit of CTA and the best approach to positive CTAs remains in question.
Lastly, people often ask about the utility of RBC nuclear scans. While they can detect bleeds at a slower rate (as low as 0.1 mL/min) compared to CTA (at least 0.4 mL/min), there are many limitations. RBC scans take time, are not available 24-7, and cannot precisely localize the site of bleeding. Therefore, we rarely recommend them for LGIB.
Approach to Recurrent Diverticular Bleeding
Unfortunately, diverticular bleeding recurs in the hospital 14% of the time and up to 25% at 5 years. When this occurs, is it worthwhile to repeat another colonoscopy or CTA?
Given the lack of clear data, we have adopted a shared decision-making framework with patients. Oftentimes, these patients are older and have significant co-morbidities, and undergoing bowel preparation, anesthesia, and colonoscopy is not trivial. If the patient is stable and prior work-up has excluded pertinent alternative diagnoses other than diverticular bleeding, then we tell patients the chance of finding an intervenable lesion is low and opt for conservative management. Meanwhile, if the patient has persistent, hemodynamically significant bleeding, we recommend a CTA based on the rationale discussed previously.
The most important clinical decision may not be about scoping or obtaining a CTA – it is medication management. If they are taking NSAIDs, they should be discontinued. If antiplatelet or anticoagulation agents were held, they should be restarted promptly in individuals with significant thrombotic risk given studies showing that while rebleeding rates may increase, overall mortality decreases.
In summary, managing LGIB and altering its natural history with either endoscopic or radiographic means is challenging. More studies are needed to guide the optimal approach. Reassuringly, most bleeding self-resolves and patients have good clinical outcomes.
Dr. Lee is a resident physician at New York Presbyterian Weill Cornell Medical Center, New York, NY. Dr. Wan is associate professor of clinical medicine at Weill Cornell Medicine, New York, N.Y. They declare no conflicts of interest.
Lower Gastrointestinal Bleeding: An Interventional Radiologist’s Perspective
BY ZEYAD METWALLI, MD, FSIR
When colonoscopy fails to localize and/or stop lower gastrointestinal bleeding (LGIB), catheter angiography has been commonly employed as a tool for both diagnosis and treatment of bleeding with embolization. Nuclear medicine or CT imaging studies can serve as useful adjuncts for confirming active bleeding and localizing the site of bleeding prior to angiography, particularly if this information is not provided by colonoscopy. Provocative mesenteric angiography has also become increasingly popular as a troubleshooting technique in patients with initially negative angiography.
Localization of Lower Gastrointestinal Bleeding
Radionuclide technetium-99m-lableled red blood cell scintigraphy (RBCS), also known as tagged RBC scintigraphy, has been in use since the early 1980s for investigation of acute gastrointestinal bleeding. RBCS has a high sensitivity for detection of active bleeding with a theoretical ability to detect bleeding at rates as low as 0.04-0.2 mL/minute.
Imaging protocols vary but should include dynamic images, which may aid in localization of bleeding. The relatively long half-life of the tracer used for imaging allows for delayed imaging 12 to 24 hours after injection. This can be useful to confirm active bleeding, particularly when bleeding is intermittent and is not visible on initial images.
With the advent of computed tomography angiography (CTA), which continues to increase in speed, imaging quality and availability, the use of RBCS for evaluation of LGIB has declined. CTA is quicker to perform than RBCS and allows for detection of bleeding as well as accurate anatomic localization, which can guide interventions.
CTA provides a more comprehensive anatomic evaluation, which can aid in the diagnosis of a wide variety of intra-abdominal issues. Conversely, CTA may be less sensitive than RBCS for detection of slower acute bleeding, detecting bleeding at rates of 0.1-1 mL/min. In addition, intermittent bleeding which has temporarily stopped at the time of CTA may evade detection.
Lastly, CTA may not be appropriate in patients with impaired renal function due to risk of contrast-induced nephropathy, particularly in patients with acute kidney injury, which commonly afflicts hospitalized patients with LGIB. Prophylaxis with normal saline hydration should be employed aggressively in patients with impaired renal function, particularly when eGFR is less than 30 mL/minute. Iodinated contrast should be used judiciously in these patients.
In clinical practice, CTA and RBCS have a similar ability to confirm the presence or absence of clinically significant active gastrointestinal bleeding. Given the greater ability to rapidly localize the bleeding site with CTA, this is generally preferred over RBCS unless there is a contraindication to performing CTA, such as severe contrast allergy or high risk for development of contrast-induced nephropathy.
Role of Catheter Angiography and Embolization
Mesenteric angiography is a well-established technique for both detection and treatment of LGIB. Hemodynamic instability and need for packed RBC transfusion increases the likelihood of positive angiography. Limitations include reduced sensitivity for detection of bleeding slower than 0.5-1 mL/minute as well as the intermittent nature of LGIB, which will often resolve spontaneously. Angiography is variably successful in the literature with a diagnostic yield between 40-80%, which encompasses the rate of success in my own practice.
Once bleeding is identified, microcatheter placement within the feeding vessel as close as possible to the site of bleeding is important to ensure treatment efficacy and to limit risk of complications such as non-target embolization and bowel ischemia. Once the feeding vessel is selected with a microcatheter, embolization can be accomplished with a wide variety of tools including metallic coils, liquid embolic agents, and particles. In the treatment of LGIB, liquid embolic agents (e.g., n-butyl cyanoacrylate or NBCA, ethylene vinyl alcohol copolymer, etc.) and particles should be used judiciously as distal penetration increases the risk of bowel ischemia and procedure-related morbidity. For this reason, metallic coils are often preferred in the treatment of LGIB.
Although the source of bleeding is variable and may include diverticulosis, recent polypectomy, ulcer, tumor or angiodysplasia, the techniques employed are similar. Accurate and distal microcatheter selection is a key driver for successful embolization and minimizing the risk of bowel ischemia. Small intestinal bleeds can be challenging to treat due to the redundant supply of the arterial arcades supplying small bowel and may require occlusion of several branches to achieve hemostasis. This approach must be balanced with the risk of developing ischemia after embolization. Angiodysplasia, a less frequently encountered culprit of LGIB, may also be managed with selective embolization with many reports of successful treatment with liquid embolic agents such as NBCA mixed with ethiodized oil.
Provocative Mesenteric Angiography for Occult Bleeding
When initial angiography in a patient with suspected active LGIB is negative, provocative angiography can be considered to uncover an intermittent bleed. This may be particularly helpful in a patient where active bleeding is confirmed on a prior diagnostic test.
The approach to provocative mesenteric angiography varies by center, and a variety of agents have been used to provoke bleeding including heparin, vasodilators (i.e., nitroglycerin, verapamil, etc.) and thrombolytics (i.e., tPA), often in combination. Thrombolytics can be administered directly into the territory of interest (i.e., superior mesenteric or inferior mesenteric artery) while heparin may be administered systemically or directly into the catheterized artery. Reported success rates for provoking angiographically visible bleeding vary, but most larger series report a 40-50% success rate. The newly detected bleeding can then be treated with either embolization or surgery. A surgeon should be involved and available when provocative angiography is planned should bleeding fail to be controlled by embolization.
In summary, when colonoscopy fails to identify or control lower gastrointestinal bleeding (LGIB), imaging techniques such as RBCS and CTA play a crucial role in localizing active bleeding. While RBCS is highly sensitive, especially for intermittent or slow bleeding, CTA offers faster, more detailed anatomical information and is typically preferred unless contraindicated by renal issues or contrast allergies. Catheter-based mesenteric angiography is a well-established method for both diagnosing and treating LGIB, often using metallic coils to minimize complications like bowel ischemia. In cases where initial angiography is negative, provocative angiography – using agents like heparin or thrombolytics – may help unmask intermittent bleeding, allowing for targeted embolization or surgical intervention.
Dr. Metwalli is associate professor in the Department of Interventional Radiology, Division of Diagnostic Imaging, at The University of Texas MD Anderson Cancer Center, Houston, Texas. He declares no conflicts of interest.
Dear colleagues,
: What is the role and optimal timing of colonoscopy? How can we best utilize radiologic studies like CTA or tagged RBC scans? How should we manage patients with recurrent or intermittent bleeding that defies localization?
In this issue of Perspectives, Dr. David Wan, Dr. Fredella Lee, and Dr. Zeyad Metwalli offer their expert insights on these difficult questions. Dr. Wan, drawing on over 15 years of experience as a GI hospitalist, shares – along with his coauthor Dr. Lee – a pragmatic approach to LGIB based on clinical patterns, evolving data, and multidisciplinary collaboration. Dr. Metwalli provides the interventional radiologist’s perspective, highlighting how angiographic techniques can complement GI management and introducing novel IR strategies for patients with recurrent or elusive bleeding.
We hope their perspectives will offer valuable guidance for your practice. Join the conversation on X at @AGA_GIHN.
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, and chief of endoscopy at West Haven VA Medical Center, both in Connecticut. He is an associate editor for GI & Hepatology News.
Management of Lower Gastrointestinal Bleeds: GI Perspective
BY FREDELLA LEE, MD; DAVID WAN, MD
Acute lower gastrointestinal bleeding (LGIB) presents unique challenges. Much of this stems from the natural history of diverticular bleeding, the most common etiology of LGIB.
First, while bleeding can be severe, most will spontaneously stop. Second, despite our best efforts with imaging or colonoscopy, finding an intervenable lesion is rare. Third, LGIB has significant rates of rebleeding that are unpredictable.
While serving as a GI hospitalist for 15 years and after managing over 300 cases of LGIB, I often find myself frustrated and colonoscopy feels futile. So how can we rationally approach these patients? We will focus on three clinical questions to develop a framework for LGIB management.
- What is the role and timing for a colonoscopy?
- How do we best utilize radiologic tests?
- How can we prevent recurrent LGIB?
The Role of Colonoscopy
Traditionally, colonoscopy within 24 hours of presentation was recommended. This was based on retrospective cohort data showing higher endoscopic intervention rates and better clinical outcomes. However, this protocol requires patients to drink a significant volume of bowel preparation over a few hours (often requiring an NGT) to achieve clear rectal effluent. Moreover, one needs to mobilize a team (i.e., nurse, technician, anesthesiologist, and gastroenterologist), and find an appropriate location to scope (i.e., ED, ICU, or OR), Understandably, this is challenging, especially overnight. When the therapeutic yield is relatively low, this approach quickly loses enthusiasm.
Importantly, meta-analyses of the randomized controlled trials, have shown that urgent colonoscopies (<24 hours upon presentation), compared to elective colonoscopies (>24 hours upon presentation), do not improve clinical outcomes such as re-bleeding rates, transfusion requirements, mortality, or length of stay. In these studies, the endoscopic intervention rates were 17-34%, however, observational data shows rates of only 8%. In our practice, we will use a clear cap attachment device and water jet irrigation to increase the odds of detecting an active source of bleeding. Colonoscopy has a diagnostic yield of 95% – despite its low therapeutic yield; and while diverticular bleeds constitute up to 64% of cases, one does not want to miss colorectal cancer or other diagnoses. Regardless, there is generally no urgency to perform a colonoscopy. To quote a colleague, Dr. Elizabeth Ross, “there is no such thing as door-to-butt time.”
The Role of Radiology
Given the limits of colonoscopy, can radiographic tests such as computed tomography angiography (CTA) or tagged red blood cell (RBC) scan be helpful? Multiple studies have suggested using CTA as the initial diagnostic test. The advantages of CTAs are:
- Fast, readily available, and does not require a bowel preparation
- If negative, CTAs portend a good prognosis and make it highly unlikely to detect active extravasation on visceral angiography
- If positive, can localize the source of bleed and increase the success of intervention
Whether a positive CTA should be followed with a colonoscopy or visceral angiography remains unclear. Studies show that positive CTAs increase the detection rate of stigmata of recent hemorrhage on colonoscopy. Positive CTAs can also identify a target for embolization by interventional radiology (IR). Though an important caveat is that the success rate of embolization is highest when performed within 90 minutes of a positive CTA. This highlights that if you have IR availability, it is critical to have clear communication, a well-defined protocol, and collaboration among disciplines (i.e., ED, medical team, GI, and IR).
At our institution, we have implemented a CTA-guided protocol for severe LGIB. Those with positive CTAs are referred immediately to IR for embolization. If the embolization is unsuccessful or CTA is negative, the patient will be planned for a non-urgent inpatient colonoscopy. However, our unpublished data and other studies have shown that the overall CTA positivity rates are only between 16-22%. Moreover, one randomized controlled trial comparing CTA versus colonoscopy as an initial test did not show any meaningful difference in clinical outcomes. Thus, the benefit of CTA and the best approach to positive CTAs remains in question.
Lastly, people often ask about the utility of RBC nuclear scans. While they can detect bleeds at a slower rate (as low as 0.1 mL/min) compared to CTA (at least 0.4 mL/min), there are many limitations. RBC scans take time, are not available 24-7, and cannot precisely localize the site of bleeding. Therefore, we rarely recommend them for LGIB.
Approach to Recurrent Diverticular Bleeding
Unfortunately, diverticular bleeding recurs in the hospital 14% of the time and up to 25% at 5 years. When this occurs, is it worthwhile to repeat another colonoscopy or CTA?
Given the lack of clear data, we have adopted a shared decision-making framework with patients. Oftentimes, these patients are older and have significant co-morbidities, and undergoing bowel preparation, anesthesia, and colonoscopy is not trivial. If the patient is stable and prior work-up has excluded pertinent alternative diagnoses other than diverticular bleeding, then we tell patients the chance of finding an intervenable lesion is low and opt for conservative management. Meanwhile, if the patient has persistent, hemodynamically significant bleeding, we recommend a CTA based on the rationale discussed previously.
The most important clinical decision may not be about scoping or obtaining a CTA – it is medication management. If they are taking NSAIDs, they should be discontinued. If antiplatelet or anticoagulation agents were held, they should be restarted promptly in individuals with significant thrombotic risk given studies showing that while rebleeding rates may increase, overall mortality decreases.
In summary, managing LGIB and altering its natural history with either endoscopic or radiographic means is challenging. More studies are needed to guide the optimal approach. Reassuringly, most bleeding self-resolves and patients have good clinical outcomes.
Dr. Lee is a resident physician at New York Presbyterian Weill Cornell Medical Center, New York, NY. Dr. Wan is associate professor of clinical medicine at Weill Cornell Medicine, New York, N.Y. They declare no conflicts of interest.
Lower Gastrointestinal Bleeding: An Interventional Radiologist’s Perspective
BY ZEYAD METWALLI, MD, FSIR
When colonoscopy fails to localize and/or stop lower gastrointestinal bleeding (LGIB), catheter angiography has been commonly employed as a tool for both diagnosis and treatment of bleeding with embolization. Nuclear medicine or CT imaging studies can serve as useful adjuncts for confirming active bleeding and localizing the site of bleeding prior to angiography, particularly if this information is not provided by colonoscopy. Provocative mesenteric angiography has also become increasingly popular as a troubleshooting technique in patients with initially negative angiography.
Localization of Lower Gastrointestinal Bleeding
Radionuclide technetium-99m-lableled red blood cell scintigraphy (RBCS), also known as tagged RBC scintigraphy, has been in use since the early 1980s for investigation of acute gastrointestinal bleeding. RBCS has a high sensitivity for detection of active bleeding with a theoretical ability to detect bleeding at rates as low as 0.04-0.2 mL/minute.
Imaging protocols vary but should include dynamic images, which may aid in localization of bleeding. The relatively long half-life of the tracer used for imaging allows for delayed imaging 12 to 24 hours after injection. This can be useful to confirm active bleeding, particularly when bleeding is intermittent and is not visible on initial images.
With the advent of computed tomography angiography (CTA), which continues to increase in speed, imaging quality and availability, the use of RBCS for evaluation of LGIB has declined. CTA is quicker to perform than RBCS and allows for detection of bleeding as well as accurate anatomic localization, which can guide interventions.
CTA provides a more comprehensive anatomic evaluation, which can aid in the diagnosis of a wide variety of intra-abdominal issues. Conversely, CTA may be less sensitive than RBCS for detection of slower acute bleeding, detecting bleeding at rates of 0.1-1 mL/min. In addition, intermittent bleeding which has temporarily stopped at the time of CTA may evade detection.
Lastly, CTA may not be appropriate in patients with impaired renal function due to risk of contrast-induced nephropathy, particularly in patients with acute kidney injury, which commonly afflicts hospitalized patients with LGIB. Prophylaxis with normal saline hydration should be employed aggressively in patients with impaired renal function, particularly when eGFR is less than 30 mL/minute. Iodinated contrast should be used judiciously in these patients.
In clinical practice, CTA and RBCS have a similar ability to confirm the presence or absence of clinically significant active gastrointestinal bleeding. Given the greater ability to rapidly localize the bleeding site with CTA, this is generally preferred over RBCS unless there is a contraindication to performing CTA, such as severe contrast allergy or high risk for development of contrast-induced nephropathy.
Role of Catheter Angiography and Embolization
Mesenteric angiography is a well-established technique for both detection and treatment of LGIB. Hemodynamic instability and need for packed RBC transfusion increases the likelihood of positive angiography. Limitations include reduced sensitivity for detection of bleeding slower than 0.5-1 mL/minute as well as the intermittent nature of LGIB, which will often resolve spontaneously. Angiography is variably successful in the literature with a diagnostic yield between 40-80%, which encompasses the rate of success in my own practice.
Once bleeding is identified, microcatheter placement within the feeding vessel as close as possible to the site of bleeding is important to ensure treatment efficacy and to limit risk of complications such as non-target embolization and bowel ischemia. Once the feeding vessel is selected with a microcatheter, embolization can be accomplished with a wide variety of tools including metallic coils, liquid embolic agents, and particles. In the treatment of LGIB, liquid embolic agents (e.g., n-butyl cyanoacrylate or NBCA, ethylene vinyl alcohol copolymer, etc.) and particles should be used judiciously as distal penetration increases the risk of bowel ischemia and procedure-related morbidity. For this reason, metallic coils are often preferred in the treatment of LGIB.
Although the source of bleeding is variable and may include diverticulosis, recent polypectomy, ulcer, tumor or angiodysplasia, the techniques employed are similar. Accurate and distal microcatheter selection is a key driver for successful embolization and minimizing the risk of bowel ischemia. Small intestinal bleeds can be challenging to treat due to the redundant supply of the arterial arcades supplying small bowel and may require occlusion of several branches to achieve hemostasis. This approach must be balanced with the risk of developing ischemia after embolization. Angiodysplasia, a less frequently encountered culprit of LGIB, may also be managed with selective embolization with many reports of successful treatment with liquid embolic agents such as NBCA mixed with ethiodized oil.
Provocative Mesenteric Angiography for Occult Bleeding
When initial angiography in a patient with suspected active LGIB is negative, provocative angiography can be considered to uncover an intermittent bleed. This may be particularly helpful in a patient where active bleeding is confirmed on a prior diagnostic test.
The approach to provocative mesenteric angiography varies by center, and a variety of agents have been used to provoke bleeding including heparin, vasodilators (i.e., nitroglycerin, verapamil, etc.) and thrombolytics (i.e., tPA), often in combination. Thrombolytics can be administered directly into the territory of interest (i.e., superior mesenteric or inferior mesenteric artery) while heparin may be administered systemically or directly into the catheterized artery. Reported success rates for provoking angiographically visible bleeding vary, but most larger series report a 40-50% success rate. The newly detected bleeding can then be treated with either embolization or surgery. A surgeon should be involved and available when provocative angiography is planned should bleeding fail to be controlled by embolization.
In summary, when colonoscopy fails to identify or control lower gastrointestinal bleeding (LGIB), imaging techniques such as RBCS and CTA play a crucial role in localizing active bleeding. While RBCS is highly sensitive, especially for intermittent or slow bleeding, CTA offers faster, more detailed anatomical information and is typically preferred unless contraindicated by renal issues or contrast allergies. Catheter-based mesenteric angiography is a well-established method for both diagnosing and treating LGIB, often using metallic coils to minimize complications like bowel ischemia. In cases where initial angiography is negative, provocative angiography – using agents like heparin or thrombolytics – may help unmask intermittent bleeding, allowing for targeted embolization or surgical intervention.
Dr. Metwalli is associate professor in the Department of Interventional Radiology, Division of Diagnostic Imaging, at The University of Texas MD Anderson Cancer Center, Houston, Texas. He declares no conflicts of interest.
Improving Care for Patients from Historically Minoritized and Marginalized Communities with Disorders of Gut-Brain Interaction
Introduction: Cases
Patient 1: A 57-year-old man with post-prandial distress variant functional dyspepsia (FD) was recommended to start nortriptyline. He previously established primary care with a physician he met at a barbershop health fair in Harlem, who referred him for specialty evaluation. Today, he presents for follow-up and reports he did not take this medication because he heard it is an antidepressant. How would you counsel him?
Patient 2: A 61-year-old woman was previously diagnosed with mixed variant irritable bowel syndrome (IBS-M). Her symptoms have not significantly changed. Her prior workup has been reassuring and consistent with IBS-M. Despite this, the patient pushes to repeat a colonoscopy, fearful that something is being missed or that she is not being offered care because of her undocumented status. How do you respond?
Patient 3: A 36-year-old man is followed for the management of generalized anxiety disorder and functional heartburn. He was started on low-dose amitriptyline with some benefit, but follow-up has been sporadic. On further discussion, he reports financial stressors, time barriers, and difficulty scheduling a meeting with his union representative for work accommodations as he lives in a more rural community. How do you reply?
Patient 4: A 74-year-old man with Parkinson’s disease who uses a wheelchair has functional constipation that is well controlled on his current regimen. He has never undergone colon cancer screening. He occasionally notices blood in his stool, so a colonoscopy was recommended to confirm that his hematochezia reflects functional constipation complicated by hemorrhoids. He is concerned about the bowel preparation required for a colonoscopy given his limited mobility, as his insurance does not cover assistance at home. He does not have family members to help him. How can you assist him?
Social determinants of health, health disparities, and DGBIs
Social determinants of health affect all aspects of patient care, with an increasing body of published work looking at potential disparities in organ-based and structural diseases.1,2,3,4 However, little has been done to explore their influence on disorders of gut-brain interaction or DGBIs.
. As DGBIs cannot be diagnosed with a single laboratory or endoscopic test, the patient history is of the utmost importance and physician-patient rapport is paramount in their treatment. Such rapport may be more difficult to establish in patients coming from historically marginalized and minoritized communities who may be distrustful of healthcare as an institution of (discriminatory) power.
Potential DGBI management pitfalls in historically marginalized or minoritized communities
For racial and ethnic minorities in the United States, disparities in healthcare take on many forms. People from racial and ethnic minority communities are less likely to receive a gastroenterology consultation and those with IBS are more likely to undergo procedures as compared to White patients with IBS.6 Implicit bias may lead to fewer specialist referrals, and specialty care may be limited or unavailable in some areas. Patients may prefer seeing providers in their own community, with whom they share racial or ethnic identities, which could lead to fewer referrals to specialists outside of the community.
Historical discrimination contributes to a lack of trust in healthcare professionals, which may lead patients to favor more objective diagnostics such as endoscopy or view being counseled against invasive procedures as having necessary care denied. Due to a broader cultural stigma surrounding mental illness, patients may be more hesitant to utilize neuromodulators, which have historically been used for psychiatric diagnoses, as it may lead them to conflate their GI illness with mental illness.7,8
Since DGBIs cannot be diagnosed with a single test or managed with a single treatment modality, providing excellent care for patients with DGBIs requires clear communication. For patients with limited English proficiency (LEP), access to high-quality language assistance is the foundation of comprehensive care. Interpreter use (or lack thereof) may limit the ability to obtain a complete and accurate clinical history, which can lead to fewer referrals to specialists and increased reliance on endoscopic evaluations that may not be clinically indicated.
These language barriers affect patients on many levels – in their ability to understand instructions for medication administration, preparation for procedures, and return precautions – which may ultimately lead to poorer responses to therapy or delays in care. LEP alone is broadly associated with fewer referrals for outpatient follow-up, adverse health outcomes and complications, and longer hospital stays.9 These disparities can be mitigated by investing in high-quality interpreter services, providing instructions and forms in multiple languages, and engaging the patient’s family and social supports according to their preferences.
People experiencing poverty (urban and rural) face challenges across multiple domains including access to healthcare, health insurance, stable housing and employment, and more. Many patients seek care at federally qualified health centers, which may face greater difficulties coordinating care with external gastroenterologists.10
Insurance barriers limit access to essential medications, tests, and procedures, and create delays in establishing care with specialists. Significant psychological stress and higher rates of comorbid anxiety and depression contribute to increased IBS severity.11 Financial limitations may limit dietary choices, which can further exacerbate DGBI symptoms. Long work hours with limited flexibility may prohibit them from presenting for regular follow-ups and establishing advanced DGBI care such as with a dietitian or psychologist.
Patients with disabilities face many of the health inequities previously discussed, as well as additional challenges with physical accessibility, transportation, exclusion from education and employment, discrimination, and stigma. Higher prevalence of comorbid mental illness and higher rates of intimate partner violence and interpersonal violence all contribute to DGBI severity and challenges with access to care.12,13 Patients with disabilities may struggle to arrive at appointments, maneuver through the building or exam room, and ultimately follow recommended care plans.
How to approach DGBIs in historically marginalized and minoritized communities
Returning to the patients from the introduction, how would you counsel each of them?
Patient 1: We can discuss with the patient how nortriptyline and other typical antidepressants can and often are used for indications other than depression. These medications modify centrally-mediated pain signaling and many patients with functional dyspepsia experience a significant benefit. It is critical to build on the rapport that was established at the community health outreach event and to explore the patient’s concerns thoroughly.
Patient 2: We would begin by inquiring about her underlying fears associated with her symptoms and seek to understand her goals for repeat intervention. We can review the risks of endoscopy and shift the focus to improving her symptoms. If we can improve her bowel habits or her pain, her desire for further interventions may lessen.
Patient 3: It will be important to work within the realistic time and monetary constraints in this patient’s life. We can validate him and the challenges he is facing, provide positive reinforcement for the progress he has made so far, and avoid disparaging him for the aspects of the treatment plan he has been unable to follow through with. As he reported a benefit from amitriptyline, we can consider increasing his dose as a feasible next step.
Patient 4: We can encourage the patient to discuss with his primary care physician how they may be able to coordinate an inpatient admission for colonoscopy preparation. Given his co-morbidities, this avenue will provide him dedicated support to help him adequately prep to ensure a higher quality examination and limit the need for repeat procedures.
DGBI care in historically marginalized and minoritized communities: A call to action
Understanding cultural differences and existing disparities in care is essential to improving care for patients from historically minoritized communities with DGBIs. Motivational interviewing and shared decision-making, with acknowledgment of social and cultural differences, allow us to work together with patients and their support systems to set and achieve feasible goals.14
To address known health disparities, offices can take steps to ensure the accessibility of language, forms, physical space, providers, and care teams. Providing culturally sensitive care and lowering barriers to care are the first steps to effecting meaningful change for patients with DGBIs from historically minoritized communities.
Dr. Yu is based at Division of Gastroenterology and Hepatology, Boston Medical Center and Boston University, both in Boston, Massachusetts. Dr. Dimino and Dr. Vélez are based at the Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, both in Boston, Massachusetts. Dr. Yu, Dr. Dimino, and Dr. Vélez do not have any conflicts of interest for this article.
Additional Online Resources
Form Accessibility
- Intake Form Guidance for Providers
- Making Your Clinic Welcoming to LGBTQ Patients
- Transgender data collection in the electronic health record: Current concepts and issues
Language Accessibility
Physical Accessibility
- Access to Medical Care for Individuals with Mobility Disabilities
- Making your medical office accessible
References
1. Zavala VA, et al. Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer. 2021 Jan. doi: 10.1038/s41416-020-01038-6.
2. Kardashian A, et al. Health disparities in chronic liver disease. Hepatology. 2023 Apr. doi: 10.1002/hep.32743.
3. Nephew LD, Serper M. Racial, Gender, and Socioeconomic Disparities in Liver Transplantation. Liver Transpl. 2021 Jun. doi: 10.1002/lt.25996.
4. Anyane-Yeboa A, et al. The Impact of the Social Determinants of Health on Disparities in Inflammatory Bowel Disease. Clin Gastroenterol Hepatol. 2022 Nov. doi: 10.1016/j.cgh.2022.03.011.
5. Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology. 2016 Feb. doi: 10.1053/j.gastro.2016.02.032.
6. Silvernale C, et al. Racial disparity in healthcare utilization among patients with Irritable Bowel Syndrome: results from a multicenter cohort. Neurogastroenterol Motil. 2021 May. doi: 10.1111/nmo.14039.
7. Hearn M, et al. Stigma and irritable bowel syndrome: a taboo subject? Lancet Gastroenterol Hepatol. 2020 Jun. doi: 10.1016/S2468-1253(19)30348-6.
8. Yan XJ, et al. The impact of stigma on medication adherence in patients with functional dyspepsia. Neurogastroenterol Motil. 2021 Feb. doi: 10.1111/nmo.13956.
9. Twersky SE, et al. The Impact of Limited English Proficiency on Healthcare Access and Outcomes in the U.S.: A Scoping Review. Healthcare (Basel). 2024 Jan. doi: 10.3390/healthcare12030364.
10. Bayly JE, et al. Limited English proficiency and reported receipt of colorectal cancer screening among adults 45-75 in 2019 and 2021. Prev Med Rep. 2024 Feb. doi: 10.1016/j.pmedr.2024.102638.
11. Cheng K, et al. Epidemiology of Irritable Bowel Syndrome in a Large Academic Safety-Net Hospital. J Clin Med. 2024 Feb. doi: 10.3390/jcm13051314.
12. Breiding MJ, Armour BS. The association between disability and intimate partner violence in the United States. Ann Epidemiol. 2015 Jun. doi: 10.1016/j.annepidem.2015.03.017.
13. Mitra M, et al. Prevalence and characteristics of sexual violence against men with disabilities. Am J Prev Med. 2016 Mar. doi: 10.1016/j.amepre.2015.07.030.
14. Bahafzallah L, et al. Motivational Interviewing in Ethnic Populations. J Immigr Minor Health. 2020 Aug. doi: 10.1007/s10903-019-00940-3.
Introduction: Cases
Patient 1: A 57-year-old man with post-prandial distress variant functional dyspepsia (FD) was recommended to start nortriptyline. He previously established primary care with a physician he met at a barbershop health fair in Harlem, who referred him for specialty evaluation. Today, he presents for follow-up and reports he did not take this medication because he heard it is an antidepressant. How would you counsel him?
Patient 2: A 61-year-old woman was previously diagnosed with mixed variant irritable bowel syndrome (IBS-M). Her symptoms have not significantly changed. Her prior workup has been reassuring and consistent with IBS-M. Despite this, the patient pushes to repeat a colonoscopy, fearful that something is being missed or that she is not being offered care because of her undocumented status. How do you respond?
Patient 3: A 36-year-old man is followed for the management of generalized anxiety disorder and functional heartburn. He was started on low-dose amitriptyline with some benefit, but follow-up has been sporadic. On further discussion, he reports financial stressors, time barriers, and difficulty scheduling a meeting with his union representative for work accommodations as he lives in a more rural community. How do you reply?
Patient 4: A 74-year-old man with Parkinson’s disease who uses a wheelchair has functional constipation that is well controlled on his current regimen. He has never undergone colon cancer screening. He occasionally notices blood in his stool, so a colonoscopy was recommended to confirm that his hematochezia reflects functional constipation complicated by hemorrhoids. He is concerned about the bowel preparation required for a colonoscopy given his limited mobility, as his insurance does not cover assistance at home. He does not have family members to help him. How can you assist him?
Social determinants of health, health disparities, and DGBIs
Social determinants of health affect all aspects of patient care, with an increasing body of published work looking at potential disparities in organ-based and structural diseases.1,2,3,4 However, little has been done to explore their influence on disorders of gut-brain interaction or DGBIs.
. As DGBIs cannot be diagnosed with a single laboratory or endoscopic test, the patient history is of the utmost importance and physician-patient rapport is paramount in their treatment. Such rapport may be more difficult to establish in patients coming from historically marginalized and minoritized communities who may be distrustful of healthcare as an institution of (discriminatory) power.
Potential DGBI management pitfalls in historically marginalized or minoritized communities
For racial and ethnic minorities in the United States, disparities in healthcare take on many forms. People from racial and ethnic minority communities are less likely to receive a gastroenterology consultation and those with IBS are more likely to undergo procedures as compared to White patients with IBS.6 Implicit bias may lead to fewer specialist referrals, and specialty care may be limited or unavailable in some areas. Patients may prefer seeing providers in their own community, with whom they share racial or ethnic identities, which could lead to fewer referrals to specialists outside of the community.
Historical discrimination contributes to a lack of trust in healthcare professionals, which may lead patients to favor more objective diagnostics such as endoscopy or view being counseled against invasive procedures as having necessary care denied. Due to a broader cultural stigma surrounding mental illness, patients may be more hesitant to utilize neuromodulators, which have historically been used for psychiatric diagnoses, as it may lead them to conflate their GI illness with mental illness.7,8
Since DGBIs cannot be diagnosed with a single test or managed with a single treatment modality, providing excellent care for patients with DGBIs requires clear communication. For patients with limited English proficiency (LEP), access to high-quality language assistance is the foundation of comprehensive care. Interpreter use (or lack thereof) may limit the ability to obtain a complete and accurate clinical history, which can lead to fewer referrals to specialists and increased reliance on endoscopic evaluations that may not be clinically indicated.
These language barriers affect patients on many levels – in their ability to understand instructions for medication administration, preparation for procedures, and return precautions – which may ultimately lead to poorer responses to therapy or delays in care. LEP alone is broadly associated with fewer referrals for outpatient follow-up, adverse health outcomes and complications, and longer hospital stays.9 These disparities can be mitigated by investing in high-quality interpreter services, providing instructions and forms in multiple languages, and engaging the patient’s family and social supports according to their preferences.
People experiencing poverty (urban and rural) face challenges across multiple domains including access to healthcare, health insurance, stable housing and employment, and more. Many patients seek care at federally qualified health centers, which may face greater difficulties coordinating care with external gastroenterologists.10
Insurance barriers limit access to essential medications, tests, and procedures, and create delays in establishing care with specialists. Significant psychological stress and higher rates of comorbid anxiety and depression contribute to increased IBS severity.11 Financial limitations may limit dietary choices, which can further exacerbate DGBI symptoms. Long work hours with limited flexibility may prohibit them from presenting for regular follow-ups and establishing advanced DGBI care such as with a dietitian or psychologist.
Patients with disabilities face many of the health inequities previously discussed, as well as additional challenges with physical accessibility, transportation, exclusion from education and employment, discrimination, and stigma. Higher prevalence of comorbid mental illness and higher rates of intimate partner violence and interpersonal violence all contribute to DGBI severity and challenges with access to care.12,13 Patients with disabilities may struggle to arrive at appointments, maneuver through the building or exam room, and ultimately follow recommended care plans.
How to approach DGBIs in historically marginalized and minoritized communities
Returning to the patients from the introduction, how would you counsel each of them?
Patient 1: We can discuss with the patient how nortriptyline and other typical antidepressants can and often are used for indications other than depression. These medications modify centrally-mediated pain signaling and many patients with functional dyspepsia experience a significant benefit. It is critical to build on the rapport that was established at the community health outreach event and to explore the patient’s concerns thoroughly.
Patient 2: We would begin by inquiring about her underlying fears associated with her symptoms and seek to understand her goals for repeat intervention. We can review the risks of endoscopy and shift the focus to improving her symptoms. If we can improve her bowel habits or her pain, her desire for further interventions may lessen.
Patient 3: It will be important to work within the realistic time and monetary constraints in this patient’s life. We can validate him and the challenges he is facing, provide positive reinforcement for the progress he has made so far, and avoid disparaging him for the aspects of the treatment plan he has been unable to follow through with. As he reported a benefit from amitriptyline, we can consider increasing his dose as a feasible next step.
Patient 4: We can encourage the patient to discuss with his primary care physician how they may be able to coordinate an inpatient admission for colonoscopy preparation. Given his co-morbidities, this avenue will provide him dedicated support to help him adequately prep to ensure a higher quality examination and limit the need for repeat procedures.
DGBI care in historically marginalized and minoritized communities: A call to action
Understanding cultural differences and existing disparities in care is essential to improving care for patients from historically minoritized communities with DGBIs. Motivational interviewing and shared decision-making, with acknowledgment of social and cultural differences, allow us to work together with patients and their support systems to set and achieve feasible goals.14
To address known health disparities, offices can take steps to ensure the accessibility of language, forms, physical space, providers, and care teams. Providing culturally sensitive care and lowering barriers to care are the first steps to effecting meaningful change for patients with DGBIs from historically minoritized communities.
Dr. Yu is based at Division of Gastroenterology and Hepatology, Boston Medical Center and Boston University, both in Boston, Massachusetts. Dr. Dimino and Dr. Vélez are based at the Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, both in Boston, Massachusetts. Dr. Yu, Dr. Dimino, and Dr. Vélez do not have any conflicts of interest for this article.
Additional Online Resources
Form Accessibility
- Intake Form Guidance for Providers
- Making Your Clinic Welcoming to LGBTQ Patients
- Transgender data collection in the electronic health record: Current concepts and issues
Language Accessibility
Physical Accessibility
- Access to Medical Care for Individuals with Mobility Disabilities
- Making your medical office accessible
References
1. Zavala VA, et al. Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer. 2021 Jan. doi: 10.1038/s41416-020-01038-6.
2. Kardashian A, et al. Health disparities in chronic liver disease. Hepatology. 2023 Apr. doi: 10.1002/hep.32743.
3. Nephew LD, Serper M. Racial, Gender, and Socioeconomic Disparities in Liver Transplantation. Liver Transpl. 2021 Jun. doi: 10.1002/lt.25996.
4. Anyane-Yeboa A, et al. The Impact of the Social Determinants of Health on Disparities in Inflammatory Bowel Disease. Clin Gastroenterol Hepatol. 2022 Nov. doi: 10.1016/j.cgh.2022.03.011.
5. Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology. 2016 Feb. doi: 10.1053/j.gastro.2016.02.032.
6. Silvernale C, et al. Racial disparity in healthcare utilization among patients with Irritable Bowel Syndrome: results from a multicenter cohort. Neurogastroenterol Motil. 2021 May. doi: 10.1111/nmo.14039.
7. Hearn M, et al. Stigma and irritable bowel syndrome: a taboo subject? Lancet Gastroenterol Hepatol. 2020 Jun. doi: 10.1016/S2468-1253(19)30348-6.
8. Yan XJ, et al. The impact of stigma on medication adherence in patients with functional dyspepsia. Neurogastroenterol Motil. 2021 Feb. doi: 10.1111/nmo.13956.
9. Twersky SE, et al. The Impact of Limited English Proficiency on Healthcare Access and Outcomes in the U.S.: A Scoping Review. Healthcare (Basel). 2024 Jan. doi: 10.3390/healthcare12030364.
10. Bayly JE, et al. Limited English proficiency and reported receipt of colorectal cancer screening among adults 45-75 in 2019 and 2021. Prev Med Rep. 2024 Feb. doi: 10.1016/j.pmedr.2024.102638.
11. Cheng K, et al. Epidemiology of Irritable Bowel Syndrome in a Large Academic Safety-Net Hospital. J Clin Med. 2024 Feb. doi: 10.3390/jcm13051314.
12. Breiding MJ, Armour BS. The association between disability and intimate partner violence in the United States. Ann Epidemiol. 2015 Jun. doi: 10.1016/j.annepidem.2015.03.017.
13. Mitra M, et al. Prevalence and characteristics of sexual violence against men with disabilities. Am J Prev Med. 2016 Mar. doi: 10.1016/j.amepre.2015.07.030.
14. Bahafzallah L, et al. Motivational Interviewing in Ethnic Populations. J Immigr Minor Health. 2020 Aug. doi: 10.1007/s10903-019-00940-3.
Introduction: Cases
Patient 1: A 57-year-old man with post-prandial distress variant functional dyspepsia (FD) was recommended to start nortriptyline. He previously established primary care with a physician he met at a barbershop health fair in Harlem, who referred him for specialty evaluation. Today, he presents for follow-up and reports he did not take this medication because he heard it is an antidepressant. How would you counsel him?
Patient 2: A 61-year-old woman was previously diagnosed with mixed variant irritable bowel syndrome (IBS-M). Her symptoms have not significantly changed. Her prior workup has been reassuring and consistent with IBS-M. Despite this, the patient pushes to repeat a colonoscopy, fearful that something is being missed or that she is not being offered care because of her undocumented status. How do you respond?
Patient 3: A 36-year-old man is followed for the management of generalized anxiety disorder and functional heartburn. He was started on low-dose amitriptyline with some benefit, but follow-up has been sporadic. On further discussion, he reports financial stressors, time barriers, and difficulty scheduling a meeting with his union representative for work accommodations as he lives in a more rural community. How do you reply?
Patient 4: A 74-year-old man with Parkinson’s disease who uses a wheelchair has functional constipation that is well controlled on his current regimen. He has never undergone colon cancer screening. He occasionally notices blood in his stool, so a colonoscopy was recommended to confirm that his hematochezia reflects functional constipation complicated by hemorrhoids. He is concerned about the bowel preparation required for a colonoscopy given his limited mobility, as his insurance does not cover assistance at home. He does not have family members to help him. How can you assist him?
Social determinants of health, health disparities, and DGBIs
Social determinants of health affect all aspects of patient care, with an increasing body of published work looking at potential disparities in organ-based and structural diseases.1,2,3,4 However, little has been done to explore their influence on disorders of gut-brain interaction or DGBIs.
. As DGBIs cannot be diagnosed with a single laboratory or endoscopic test, the patient history is of the utmost importance and physician-patient rapport is paramount in their treatment. Such rapport may be more difficult to establish in patients coming from historically marginalized and minoritized communities who may be distrustful of healthcare as an institution of (discriminatory) power.
Potential DGBI management pitfalls in historically marginalized or minoritized communities
For racial and ethnic minorities in the United States, disparities in healthcare take on many forms. People from racial and ethnic minority communities are less likely to receive a gastroenterology consultation and those with IBS are more likely to undergo procedures as compared to White patients with IBS.6 Implicit bias may lead to fewer specialist referrals, and specialty care may be limited or unavailable in some areas. Patients may prefer seeing providers in their own community, with whom they share racial or ethnic identities, which could lead to fewer referrals to specialists outside of the community.
Historical discrimination contributes to a lack of trust in healthcare professionals, which may lead patients to favor more objective diagnostics such as endoscopy or view being counseled against invasive procedures as having necessary care denied. Due to a broader cultural stigma surrounding mental illness, patients may be more hesitant to utilize neuromodulators, which have historically been used for psychiatric diagnoses, as it may lead them to conflate their GI illness with mental illness.7,8
Since DGBIs cannot be diagnosed with a single test or managed with a single treatment modality, providing excellent care for patients with DGBIs requires clear communication. For patients with limited English proficiency (LEP), access to high-quality language assistance is the foundation of comprehensive care. Interpreter use (or lack thereof) may limit the ability to obtain a complete and accurate clinical history, which can lead to fewer referrals to specialists and increased reliance on endoscopic evaluations that may not be clinically indicated.
These language barriers affect patients on many levels – in their ability to understand instructions for medication administration, preparation for procedures, and return precautions – which may ultimately lead to poorer responses to therapy or delays in care. LEP alone is broadly associated with fewer referrals for outpatient follow-up, adverse health outcomes and complications, and longer hospital stays.9 These disparities can be mitigated by investing in high-quality interpreter services, providing instructions and forms in multiple languages, and engaging the patient’s family and social supports according to their preferences.
People experiencing poverty (urban and rural) face challenges across multiple domains including access to healthcare, health insurance, stable housing and employment, and more. Many patients seek care at federally qualified health centers, which may face greater difficulties coordinating care with external gastroenterologists.10
Insurance barriers limit access to essential medications, tests, and procedures, and create delays in establishing care with specialists. Significant psychological stress and higher rates of comorbid anxiety and depression contribute to increased IBS severity.11 Financial limitations may limit dietary choices, which can further exacerbate DGBI symptoms. Long work hours with limited flexibility may prohibit them from presenting for regular follow-ups and establishing advanced DGBI care such as with a dietitian or psychologist.
Patients with disabilities face many of the health inequities previously discussed, as well as additional challenges with physical accessibility, transportation, exclusion from education and employment, discrimination, and stigma. Higher prevalence of comorbid mental illness and higher rates of intimate partner violence and interpersonal violence all contribute to DGBI severity and challenges with access to care.12,13 Patients with disabilities may struggle to arrive at appointments, maneuver through the building or exam room, and ultimately follow recommended care plans.
How to approach DGBIs in historically marginalized and minoritized communities
Returning to the patients from the introduction, how would you counsel each of them?
Patient 1: We can discuss with the patient how nortriptyline and other typical antidepressants can and often are used for indications other than depression. These medications modify centrally-mediated pain signaling and many patients with functional dyspepsia experience a significant benefit. It is critical to build on the rapport that was established at the community health outreach event and to explore the patient’s concerns thoroughly.
Patient 2: We would begin by inquiring about her underlying fears associated with her symptoms and seek to understand her goals for repeat intervention. We can review the risks of endoscopy and shift the focus to improving her symptoms. If we can improve her bowel habits or her pain, her desire for further interventions may lessen.
Patient 3: It will be important to work within the realistic time and monetary constraints in this patient’s life. We can validate him and the challenges he is facing, provide positive reinforcement for the progress he has made so far, and avoid disparaging him for the aspects of the treatment plan he has been unable to follow through with. As he reported a benefit from amitriptyline, we can consider increasing his dose as a feasible next step.
Patient 4: We can encourage the patient to discuss with his primary care physician how they may be able to coordinate an inpatient admission for colonoscopy preparation. Given his co-morbidities, this avenue will provide him dedicated support to help him adequately prep to ensure a higher quality examination and limit the need for repeat procedures.
DGBI care in historically marginalized and minoritized communities: A call to action
Understanding cultural differences and existing disparities in care is essential to improving care for patients from historically minoritized communities with DGBIs. Motivational interviewing and shared decision-making, with acknowledgment of social and cultural differences, allow us to work together with patients and their support systems to set and achieve feasible goals.14
To address known health disparities, offices can take steps to ensure the accessibility of language, forms, physical space, providers, and care teams. Providing culturally sensitive care and lowering barriers to care are the first steps to effecting meaningful change for patients with DGBIs from historically minoritized communities.
Dr. Yu is based at Division of Gastroenterology and Hepatology, Boston Medical Center and Boston University, both in Boston, Massachusetts. Dr. Dimino and Dr. Vélez are based at the Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, both in Boston, Massachusetts. Dr. Yu, Dr. Dimino, and Dr. Vélez do not have any conflicts of interest for this article.
Additional Online Resources
Form Accessibility
- Intake Form Guidance for Providers
- Making Your Clinic Welcoming to LGBTQ Patients
- Transgender data collection in the electronic health record: Current concepts and issues
Language Accessibility
Physical Accessibility
- Access to Medical Care for Individuals with Mobility Disabilities
- Making your medical office accessible
References
1. Zavala VA, et al. Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer. 2021 Jan. doi: 10.1038/s41416-020-01038-6.
2. Kardashian A, et al. Health disparities in chronic liver disease. Hepatology. 2023 Apr. doi: 10.1002/hep.32743.
3. Nephew LD, Serper M. Racial, Gender, and Socioeconomic Disparities in Liver Transplantation. Liver Transpl. 2021 Jun. doi: 10.1002/lt.25996.
4. Anyane-Yeboa A, et al. The Impact of the Social Determinants of Health on Disparities in Inflammatory Bowel Disease. Clin Gastroenterol Hepatol. 2022 Nov. doi: 10.1016/j.cgh.2022.03.011.
5. Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology. 2016 Feb. doi: 10.1053/j.gastro.2016.02.032.
6. Silvernale C, et al. Racial disparity in healthcare utilization among patients with Irritable Bowel Syndrome: results from a multicenter cohort. Neurogastroenterol Motil. 2021 May. doi: 10.1111/nmo.14039.
7. Hearn M, et al. Stigma and irritable bowel syndrome: a taboo subject? Lancet Gastroenterol Hepatol. 2020 Jun. doi: 10.1016/S2468-1253(19)30348-6.
8. Yan XJ, et al. The impact of stigma on medication adherence in patients with functional dyspepsia. Neurogastroenterol Motil. 2021 Feb. doi: 10.1111/nmo.13956.
9. Twersky SE, et al. The Impact of Limited English Proficiency on Healthcare Access and Outcomes in the U.S.: A Scoping Review. Healthcare (Basel). 2024 Jan. doi: 10.3390/healthcare12030364.
10. Bayly JE, et al. Limited English proficiency and reported receipt of colorectal cancer screening among adults 45-75 in 2019 and 2021. Prev Med Rep. 2024 Feb. doi: 10.1016/j.pmedr.2024.102638.
11. Cheng K, et al. Epidemiology of Irritable Bowel Syndrome in a Large Academic Safety-Net Hospital. J Clin Med. 2024 Feb. doi: 10.3390/jcm13051314.
12. Breiding MJ, Armour BS. The association between disability and intimate partner violence in the United States. Ann Epidemiol. 2015 Jun. doi: 10.1016/j.annepidem.2015.03.017.
13. Mitra M, et al. Prevalence and characteristics of sexual violence against men with disabilities. Am J Prev Med. 2016 Mar. doi: 10.1016/j.amepre.2015.07.030.
14. Bahafzallah L, et al. Motivational Interviewing in Ethnic Populations. J Immigr Minor Health. 2020 Aug. doi: 10.1007/s10903-019-00940-3.
An Uncertain Future for No-Cost Preventive Care
Later this month, the U.S. Supreme Court is anticipated to announce its decision in Kennedy vs. Braidwood Management, a case that could significantly impact the no-cost coverage of preventive healthcare services under the Patient Protection and Affordable Care Act (ACA). At the center of the case is whether the structure of the U.S. Preventive Services Task Force (USPSTF) – an independent body convened by the federal government that makes recommendations for preventive services that nearly all private insurances must cover without cost sharing under provisions of the ACA (specifically, Grade A and B recommendations) – violates the Appointments Clause of the U.S. Constitution. This clause states that “officers of the United States” may only be appointed by the president with the Senate’s approval.
The case, initiated in 2022 by a self-insured, Christian-owned business, specifically targeted the coverage of pre-exposure prophylaxis (PrEP) for preventing HIV in high-risk individuals. However, the decision could broadly affect the coverage of other preventive services, including colorectal cancer screening tests. In June 2024, the 5th Circuit Court of Appeals upheld a district court’s ruling that the ACA’s requirement to cover without cost-sharing services recommended by USPSTF is unconstitutional, paving the way for the current Supreme Court showdown.
The consequences of this ruling could be significant. This would likely reverse the progress we have made in increasing colorectal cancer screening rates by reducing financial barriers to care. Interestingly, despite a new administration, the federal government continues to advocate for upholding the law, asserting that USPSTF members are “inferior officers” such that the Secretary of Health and Human Services can dismiss individual members and oversee or veto the Task Force’s recommendations at will, potentially threatening scientific independence. Though it’s often challenging to predict the Supreme Court’s final decision, the tone of questioning during oral arguments in April hinted at a possible win for the ACA and preventive care. Stay tuned, as the decision to be released later this month has seismic clinical implications.
Megan A. Adams, MD, JD, MSc
Editor in Chief
Later this month, the U.S. Supreme Court is anticipated to announce its decision in Kennedy vs. Braidwood Management, a case that could significantly impact the no-cost coverage of preventive healthcare services under the Patient Protection and Affordable Care Act (ACA). At the center of the case is whether the structure of the U.S. Preventive Services Task Force (USPSTF) – an independent body convened by the federal government that makes recommendations for preventive services that nearly all private insurances must cover without cost sharing under provisions of the ACA (specifically, Grade A and B recommendations) – violates the Appointments Clause of the U.S. Constitution. This clause states that “officers of the United States” may only be appointed by the president with the Senate’s approval.
The case, initiated in 2022 by a self-insured, Christian-owned business, specifically targeted the coverage of pre-exposure prophylaxis (PrEP) for preventing HIV in high-risk individuals. However, the decision could broadly affect the coverage of other preventive services, including colorectal cancer screening tests. In June 2024, the 5th Circuit Court of Appeals upheld a district court’s ruling that the ACA’s requirement to cover without cost-sharing services recommended by USPSTF is unconstitutional, paving the way for the current Supreme Court showdown.
The consequences of this ruling could be significant. This would likely reverse the progress we have made in increasing colorectal cancer screening rates by reducing financial barriers to care. Interestingly, despite a new administration, the federal government continues to advocate for upholding the law, asserting that USPSTF members are “inferior officers” such that the Secretary of Health and Human Services can dismiss individual members and oversee or veto the Task Force’s recommendations at will, potentially threatening scientific independence. Though it’s often challenging to predict the Supreme Court’s final decision, the tone of questioning during oral arguments in April hinted at a possible win for the ACA and preventive care. Stay tuned, as the decision to be released later this month has seismic clinical implications.
Megan A. Adams, MD, JD, MSc
Editor in Chief
Later this month, the U.S. Supreme Court is anticipated to announce its decision in Kennedy vs. Braidwood Management, a case that could significantly impact the no-cost coverage of preventive healthcare services under the Patient Protection and Affordable Care Act (ACA). At the center of the case is whether the structure of the U.S. Preventive Services Task Force (USPSTF) – an independent body convened by the federal government that makes recommendations for preventive services that nearly all private insurances must cover without cost sharing under provisions of the ACA (specifically, Grade A and B recommendations) – violates the Appointments Clause of the U.S. Constitution. This clause states that “officers of the United States” may only be appointed by the president with the Senate’s approval.
The case, initiated in 2022 by a self-insured, Christian-owned business, specifically targeted the coverage of pre-exposure prophylaxis (PrEP) for preventing HIV in high-risk individuals. However, the decision could broadly affect the coverage of other preventive services, including colorectal cancer screening tests. In June 2024, the 5th Circuit Court of Appeals upheld a district court’s ruling that the ACA’s requirement to cover without cost-sharing services recommended by USPSTF is unconstitutional, paving the way for the current Supreme Court showdown.
The consequences of this ruling could be significant. This would likely reverse the progress we have made in increasing colorectal cancer screening rates by reducing financial barriers to care. Interestingly, despite a new administration, the federal government continues to advocate for upholding the law, asserting that USPSTF members are “inferior officers” such that the Secretary of Health and Human Services can dismiss individual members and oversee or veto the Task Force’s recommendations at will, potentially threatening scientific independence. Though it’s often challenging to predict the Supreme Court’s final decision, the tone of questioning during oral arguments in April hinted at a possible win for the ACA and preventive care. Stay tuned, as the decision to be released later this month has seismic clinical implications.
Megan A. Adams, MD, JD, MSc
Editor in Chief
Treating Barrett’s Esophagus: Comparing EMR and ESD
Dear colleagues,
Many of us diagnose and treat patients with Barrett’s esophagus, estimated to affect up to 5.6% of the US adult population. There has been an expanding array of tools to help diagnose and effectively treat Barrett’s esophagus with dysplasia and malignancy. In particular, endoscopic submucosal dissection (ESD) has emerged as an important method for treating early cancer in the gastrointestinal tract.
But how do we incorporate ESD into our algorithm for management, especially with the popularity and effectiveness of endoscopic mucosal resection (EMR)? In this issue of Perspectives we aim to provide context for the use of ESD, as compared with EMR. Dr. Silvio de Melo discusses his preferred EMR technique and its many advantages in the management of BE, including for residual or refractory areas. In contrast, Dr. Mohamed Othman reviews the power of ESD and when we should consider this approach over EMR. We hope these discussions will facilitate your care for patients with Barrett’s esophagus.
We also welcome your thoughts on this topic — join the conversation on X at @AGA_GIHN.
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, and chief of endoscopy at West Haven VA Medical Center, both in Connecticut. He is an associate editor for GI & Hepatology News.
Endoscopic Mucosal Resection: The ‘Workhorse’ for Patient Care
BY SILVIO W. DE MELO JR, MD, AGAF
Barrett’s esophagus (BE) remains an important clinical problem, being one of the modifiable risk factors for esophageal adenocarcinoma. The care for BE is complex and requires several steps to correctly formulate a therapeutic plan. It starts with a proper endoscopic examination. It is recommended to spend at least 1 minute inspecting and evaluating every centimeter of the salmon-colored epithelium, looking for change in vascular pattern, erosions/ulcers, nodules, and/or masses. After the inspection, random biopsies every 1-2 cm plus targeted biopsies will guide you. It is still controversial if the addition of other sampling strategies, such as brushings or confocal endomicroscopy, is needed.
The introduction of radiofrequency ablation (RFA) was paramount in popularizing the treatment options for BE and sunsetting the previous dominant modality, photodynamic therapy (PDT). RFA proved to have a superior clinical efficacy in replacing the intestinal metaplasia/BE with neosquamous epithelium while boosting a much better safety profile, compared with PDT. However, RFA is most efficacious for “flat BE” and it is not an effective, nor recommended, method to treat nodular BE or early cancer, such as carcinoma in situ or nodular high-grade dysplasia. Endoscopic mucosal resection (EMR) is utilized to overcome those limitations.
There are several techniques utilized for EMR:
- The lift and snare technique.
- The snare-in-cap technique.
- The Band-snare technique.
The free-hand submucosal lift and snare is not frequently used in the esophagus. It is difficult to maintain visualization while being confident that one has the whole lesion inside the snare and that the distal (anal side) part of the lesion is free of any unwanted tissue (to minimize complications such as perforations or unwelcomed gastric resections). It is difficult after the first resection to lift an adjacent area, as the fluid easily leaks from the first resected spot, thus removing larger lesions in piece-meal fashion is challenging. This technique can be used in small (in my personal experience, less than 5 mm) lesions, but, given that there are better and safer alternatives, I almost never use this technique for my esophageal EMR cases. I prefer to use the band-snare technique even for lesions under 5 mm.
The snare-in-cap technique has been utilized in the esophagus. In this technique, a cap is attached to the distal end of the scope and the size of the resection is determined by the size of the cap, usually under 1.5 cm. Because of the risk of perforation without previous lifting, it is required that the lesion is lifted with a submucosal fluid, saline or any Food and Drug Administration–approved EMR solution. The lesion is then suctioned inside the cap where the snare had been previously opened inside the cap, the snare is closed, and the tissue is resected. The same limitations regarding the inability to remove larger lesions (greater than 1.5 cm) because of the challenge in lifting the adjacent area applies here. However, the perforation risk for this technique is higher than the traditional lift and the band and snare techniques. Thus, this technique has fallen out of favor for most endoscopists.
The third technique (band-snare EMR) is the one that most endoscopists use for endoscopic mucosal resection. It is a small variation of the already time-tested and very familiar procedure of esophageal variceal band ligation (EVL). There are multiple commercially available kits for esophageal EMR. The kit contains the chamber with the bands and a proprietary hexagonal snare used to resect the specimen.
The advantages of this technique are:
- It is widely commercially available.
- It builds on a familiar procedure, EVL, therefore the learning curve is short.
- The set-up is quick and the procedure can be completed safely and effectively.
- There is no need for injecting the submucosal with a lifting solution.
- Despite the band having a size limitation of 1 cm, one can remove larger lesions by repeating the band and resect process, using the rosette technique.
Band-snare EMR also has limitations:
- There are only six bands on each chamber. Depending on the size of the lesion, one may need to use multiple kits.
- It is not suitable for en bloc resection of lesions greater than 1 cm.
My experience with band EMR is that we can complete the procedure in under 1 hour. The dreaded complication of perforation occurs in under 1% of cases, most bleeding episodes can easily be controlled endoscopically, and the risk of post-EMR stricture is minimal. Therefore, band EMR is the most used technique for esophageal endoscopic resections.
Esophageal EMR is also effective for other indications in BE therapy, such as residual and recurrent BE. Band-snare EMR can be used for an en bloc resection or rosette technique for the areas resistant to ablation therapies with great success and safety.
From a financial standpoint, comparing EMR with endoscopic submucosal dissection (ESD), EMR is the superior strategy given that EMR is widely available, has a much shorter learning curve, has a greater safety profile, is applicable to a wider variety of indications, and has a more favorable return on investment. EMR should be the workhorse for the care of patients with BE, reserving ESD for specific indications.
In summary, there is no “one-size-fits-all” endoscopic therapy in the care of BE. Most Barrett’s patients can be successfully treated with a combination of ablation plus EMR, reserving ESD for select cases.
Dr. de Melo is section chief of gastroenterology at the Orlando VA Healthcare System, Orlando, Florida. He declares no conflicts of interest.
ESD Over EMR for Resecting Esophageal Lesions
BY MOHAMED O. OTHMAN, MD, AGAF
Although endoscopic submucosal dissection (ESD) is the preferred endoscopic resection method in the East, the adoption of this technique in the West, particularly in the United States, has faced many hurdles. Many endoscopists who routinely perform piecemeal endoscopic mucosal resection (EMR) question the utility of ESD, arguing that EMR is just as effective. While this may hold true in certain situations, the global trend in the endoscopic treatment of early esophageal squamous cell carcinoma, nodular Barrett’s esophagus (BE), and early esophageal adenocarcinoma (EAC) has clearly shifted toward ESD. In this perspective, I will summarize why ESD is preferred over EMR for these indications and explore why ESD has yet to gain widespread adoption in the United States.
The superiority of ESD over EMR has been well established in multiple publications from both Eastern and Western literature. Mejia-Perez et al, in a multicenter cohort study from eight centers in North America, compared outcomes of ESD vs EMR for BE with high-grade dysplasia (HGD) or T1a adenocarcinoma in 243 patients. ESD achieved significantly higher en bloc resection rates (89% vs 43%) and R0 resection rates (73% vs 56%), compared with EMR, along with a substantially lower recurrence/residual disease rate on follow-up (3.5% in the ESD group vs 31.4% in EMR group). Additionally, more patients required repeat endoscopic resection after EMR to treat residual or recurrent disease (EMR, 24.2% vs ESD, 3.5%; P < .001).
Han et al conducted a meta-analysis of 22 studies comparing ESD and EMR for early esophageal neoplasia, including both squamous cell carcinoma (SCC) and BE-associated lesions. ESD was associated with significantly higher curative resection rates than EMR (OR, 9.74; 95% CI, 4.83-19.62; P < .0001). Of note, lesion size was a critical factor in determining the advantage of ESD. For lesions ≤ 10 mm, curative resection rates were comparable between ESD and EMR. However, for lesions > 10 mm, ESD achieved significantly higher curative resection rates. This size-based recommendation has been adopted by the American Society of Gastrointestinal Endoscopy (ASGE) in their recent guidelines on ESD indications for esophageal lesions. ASGE guidelines favors ESD over EMR for SCC lesions > 15 mm and for nodular BE with dysplasia or early EAC > 20 mm.
ESD is particularly beneficial in patients who develop early adenocarcinoma after RFA or EMR. Mesureur et al evaluated the efficacy of salvage ESD for Barrett’s recurrence or residual BE following RFA. In their multicenter retrospective study of 56 patients, salvage ESD achieved an en bloc resection rate of 89.3%, despite significant fibrosis, with an R0 resection rate of 66%. At a median follow-up of 14 months, most patients remained in endoscopic remission without the need for esophagectomy.
Combining ESD with RFA has also been shown to accelerate the eradication of BE with dysplasia while reducing the number of required sessions. Our group demonstrated the high efficacy of ESD followed by RFA in 18 patients, most of whom had long-segment BE with HGD or EAC. On average, patients required only one to two RFA sessions after ESD to achieve complete eradication of intestinal metaplasia (CE-IM). Over a median follow-up of 42.5 months (IQR, 28-59.25), complete eradication of early esophageal cancer was achieved in 13 patients (100%), eradication of dysplasia in 15 patients (100%), and CE-IM in 14 patients (77.8%).
Despite the overwhelming evidence supporting ESD and the strong endorsement from professional societies, adoption in the West continues to lag. Several factors contribute to this gap. First, ESD has a steep learning curve. Our data showed that, on average, an untutored practitioner achieved competency after 150-250 procedures, a finding corroborated by other US groups.
Second, there is no specific CPT code for ESD in the United States. Physicians are forced to bill the procedure as EMR or use an unlisted code, resulting in reimbursement that does not reflect the time and complexity of the procedure. Our group showed that physician reimbursement for ESD is highly variable, ranging from $50 to $800 per case, depending on insurance type.
Third, the increasing emphasis on productivity and RVU generation in academic settings has hindered the growth of ESD training in many institutions. Still, the outlook for ESD in the United States remains encouraging. Multiple industry-sponsored training courses are held annually, and professional societies are investing heavily in expanding access to structured education in ESD. Industry is also innovating devices that improve procedural efficiency and safety. Adopting novel approaches, such as traction-assisted ESD, has made the technique more appealing to endoscopists concerned about long procedure times. For example, our group proposed a standardized esophageal ESD technique that incorporates specimen self-retraction. This method improves both safety and speed and has helped address several procedural challenges. We’ve demonstrated that consistency in technique can substantially expedite esophageal ESD.
Fast forward 5 years: We anticipate a dedicated CPT code for ESD, broader access to advanced resection tools, and an expanding number of fellowships offering structured ESD training. These developments are poised to eliminate many of the current barriers. In summary, with robust data supporting the efficacy of ESD in early esophageal cancer, the focus in the United States should shift toward mastering and integrating the technique, rather than dismissing it in favor of piecemeal EMR.
Dr. Othman is chief of the gastroenterology and hepatology section at Baylor College of Medicine and Medicine Subspecialities Service Line Chief at Baylor St Luke’s Medical Center, both in Houston. He declares no conflicts of interest.
Dear colleagues,
Many of us diagnose and treat patients with Barrett’s esophagus, estimated to affect up to 5.6% of the US adult population. There has been an expanding array of tools to help diagnose and effectively treat Barrett’s esophagus with dysplasia and malignancy. In particular, endoscopic submucosal dissection (ESD) has emerged as an important method for treating early cancer in the gastrointestinal tract.
But how do we incorporate ESD into our algorithm for management, especially with the popularity and effectiveness of endoscopic mucosal resection (EMR)? In this issue of Perspectives we aim to provide context for the use of ESD, as compared with EMR. Dr. Silvio de Melo discusses his preferred EMR technique and its many advantages in the management of BE, including for residual or refractory areas. In contrast, Dr. Mohamed Othman reviews the power of ESD and when we should consider this approach over EMR. We hope these discussions will facilitate your care for patients with Barrett’s esophagus.
We also welcome your thoughts on this topic — join the conversation on X at @AGA_GIHN.
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, and chief of endoscopy at West Haven VA Medical Center, both in Connecticut. He is an associate editor for GI & Hepatology News.
Endoscopic Mucosal Resection: The ‘Workhorse’ for Patient Care
BY SILVIO W. DE MELO JR, MD, AGAF
Barrett’s esophagus (BE) remains an important clinical problem, being one of the modifiable risk factors for esophageal adenocarcinoma. The care for BE is complex and requires several steps to correctly formulate a therapeutic plan. It starts with a proper endoscopic examination. It is recommended to spend at least 1 minute inspecting and evaluating every centimeter of the salmon-colored epithelium, looking for change in vascular pattern, erosions/ulcers, nodules, and/or masses. After the inspection, random biopsies every 1-2 cm plus targeted biopsies will guide you. It is still controversial if the addition of other sampling strategies, such as brushings or confocal endomicroscopy, is needed.
The introduction of radiofrequency ablation (RFA) was paramount in popularizing the treatment options for BE and sunsetting the previous dominant modality, photodynamic therapy (PDT). RFA proved to have a superior clinical efficacy in replacing the intestinal metaplasia/BE with neosquamous epithelium while boosting a much better safety profile, compared with PDT. However, RFA is most efficacious for “flat BE” and it is not an effective, nor recommended, method to treat nodular BE or early cancer, such as carcinoma in situ or nodular high-grade dysplasia. Endoscopic mucosal resection (EMR) is utilized to overcome those limitations.
There are several techniques utilized for EMR:
- The lift and snare technique.
- The snare-in-cap technique.
- The Band-snare technique.
The free-hand submucosal lift and snare is not frequently used in the esophagus. It is difficult to maintain visualization while being confident that one has the whole lesion inside the snare and that the distal (anal side) part of the lesion is free of any unwanted tissue (to minimize complications such as perforations or unwelcomed gastric resections). It is difficult after the first resection to lift an adjacent area, as the fluid easily leaks from the first resected spot, thus removing larger lesions in piece-meal fashion is challenging. This technique can be used in small (in my personal experience, less than 5 mm) lesions, but, given that there are better and safer alternatives, I almost never use this technique for my esophageal EMR cases. I prefer to use the band-snare technique even for lesions under 5 mm.
The snare-in-cap technique has been utilized in the esophagus. In this technique, a cap is attached to the distal end of the scope and the size of the resection is determined by the size of the cap, usually under 1.5 cm. Because of the risk of perforation without previous lifting, it is required that the lesion is lifted with a submucosal fluid, saline or any Food and Drug Administration–approved EMR solution. The lesion is then suctioned inside the cap where the snare had been previously opened inside the cap, the snare is closed, and the tissue is resected. The same limitations regarding the inability to remove larger lesions (greater than 1.5 cm) because of the challenge in lifting the adjacent area applies here. However, the perforation risk for this technique is higher than the traditional lift and the band and snare techniques. Thus, this technique has fallen out of favor for most endoscopists.
The third technique (band-snare EMR) is the one that most endoscopists use for endoscopic mucosal resection. It is a small variation of the already time-tested and very familiar procedure of esophageal variceal band ligation (EVL). There are multiple commercially available kits for esophageal EMR. The kit contains the chamber with the bands and a proprietary hexagonal snare used to resect the specimen.
The advantages of this technique are:
- It is widely commercially available.
- It builds on a familiar procedure, EVL, therefore the learning curve is short.
- The set-up is quick and the procedure can be completed safely and effectively.
- There is no need for injecting the submucosal with a lifting solution.
- Despite the band having a size limitation of 1 cm, one can remove larger lesions by repeating the band and resect process, using the rosette technique.
Band-snare EMR also has limitations:
- There are only six bands on each chamber. Depending on the size of the lesion, one may need to use multiple kits.
- It is not suitable for en bloc resection of lesions greater than 1 cm.
My experience with band EMR is that we can complete the procedure in under 1 hour. The dreaded complication of perforation occurs in under 1% of cases, most bleeding episodes can easily be controlled endoscopically, and the risk of post-EMR stricture is minimal. Therefore, band EMR is the most used technique for esophageal endoscopic resections.
Esophageal EMR is also effective for other indications in BE therapy, such as residual and recurrent BE. Band-snare EMR can be used for an en bloc resection or rosette technique for the areas resistant to ablation therapies with great success and safety.
From a financial standpoint, comparing EMR with endoscopic submucosal dissection (ESD), EMR is the superior strategy given that EMR is widely available, has a much shorter learning curve, has a greater safety profile, is applicable to a wider variety of indications, and has a more favorable return on investment. EMR should be the workhorse for the care of patients with BE, reserving ESD for specific indications.
In summary, there is no “one-size-fits-all” endoscopic therapy in the care of BE. Most Barrett’s patients can be successfully treated with a combination of ablation plus EMR, reserving ESD for select cases.
Dr. de Melo is section chief of gastroenterology at the Orlando VA Healthcare System, Orlando, Florida. He declares no conflicts of interest.
ESD Over EMR for Resecting Esophageal Lesions
BY MOHAMED O. OTHMAN, MD, AGAF
Although endoscopic submucosal dissection (ESD) is the preferred endoscopic resection method in the East, the adoption of this technique in the West, particularly in the United States, has faced many hurdles. Many endoscopists who routinely perform piecemeal endoscopic mucosal resection (EMR) question the utility of ESD, arguing that EMR is just as effective. While this may hold true in certain situations, the global trend in the endoscopic treatment of early esophageal squamous cell carcinoma, nodular Barrett’s esophagus (BE), and early esophageal adenocarcinoma (EAC) has clearly shifted toward ESD. In this perspective, I will summarize why ESD is preferred over EMR for these indications and explore why ESD has yet to gain widespread adoption in the United States.
The superiority of ESD over EMR has been well established in multiple publications from both Eastern and Western literature. Mejia-Perez et al, in a multicenter cohort study from eight centers in North America, compared outcomes of ESD vs EMR for BE with high-grade dysplasia (HGD) or T1a adenocarcinoma in 243 patients. ESD achieved significantly higher en bloc resection rates (89% vs 43%) and R0 resection rates (73% vs 56%), compared with EMR, along with a substantially lower recurrence/residual disease rate on follow-up (3.5% in the ESD group vs 31.4% in EMR group). Additionally, more patients required repeat endoscopic resection after EMR to treat residual or recurrent disease (EMR, 24.2% vs ESD, 3.5%; P < .001).
Han et al conducted a meta-analysis of 22 studies comparing ESD and EMR for early esophageal neoplasia, including both squamous cell carcinoma (SCC) and BE-associated lesions. ESD was associated with significantly higher curative resection rates than EMR (OR, 9.74; 95% CI, 4.83-19.62; P < .0001). Of note, lesion size was a critical factor in determining the advantage of ESD. For lesions ≤ 10 mm, curative resection rates were comparable between ESD and EMR. However, for lesions > 10 mm, ESD achieved significantly higher curative resection rates. This size-based recommendation has been adopted by the American Society of Gastrointestinal Endoscopy (ASGE) in their recent guidelines on ESD indications for esophageal lesions. ASGE guidelines favors ESD over EMR for SCC lesions > 15 mm and for nodular BE with dysplasia or early EAC > 20 mm.
ESD is particularly beneficial in patients who develop early adenocarcinoma after RFA or EMR. Mesureur et al evaluated the efficacy of salvage ESD for Barrett’s recurrence or residual BE following RFA. In their multicenter retrospective study of 56 patients, salvage ESD achieved an en bloc resection rate of 89.3%, despite significant fibrosis, with an R0 resection rate of 66%. At a median follow-up of 14 months, most patients remained in endoscopic remission without the need for esophagectomy.
Combining ESD with RFA has also been shown to accelerate the eradication of BE with dysplasia while reducing the number of required sessions. Our group demonstrated the high efficacy of ESD followed by RFA in 18 patients, most of whom had long-segment BE with HGD or EAC. On average, patients required only one to two RFA sessions after ESD to achieve complete eradication of intestinal metaplasia (CE-IM). Over a median follow-up of 42.5 months (IQR, 28-59.25), complete eradication of early esophageal cancer was achieved in 13 patients (100%), eradication of dysplasia in 15 patients (100%), and CE-IM in 14 patients (77.8%).
Despite the overwhelming evidence supporting ESD and the strong endorsement from professional societies, adoption in the West continues to lag. Several factors contribute to this gap. First, ESD has a steep learning curve. Our data showed that, on average, an untutored practitioner achieved competency after 150-250 procedures, a finding corroborated by other US groups.
Second, there is no specific CPT code for ESD in the United States. Physicians are forced to bill the procedure as EMR or use an unlisted code, resulting in reimbursement that does not reflect the time and complexity of the procedure. Our group showed that physician reimbursement for ESD is highly variable, ranging from $50 to $800 per case, depending on insurance type.
Third, the increasing emphasis on productivity and RVU generation in academic settings has hindered the growth of ESD training in many institutions. Still, the outlook for ESD in the United States remains encouraging. Multiple industry-sponsored training courses are held annually, and professional societies are investing heavily in expanding access to structured education in ESD. Industry is also innovating devices that improve procedural efficiency and safety. Adopting novel approaches, such as traction-assisted ESD, has made the technique more appealing to endoscopists concerned about long procedure times. For example, our group proposed a standardized esophageal ESD technique that incorporates specimen self-retraction. This method improves both safety and speed and has helped address several procedural challenges. We’ve demonstrated that consistency in technique can substantially expedite esophageal ESD.
Fast forward 5 years: We anticipate a dedicated CPT code for ESD, broader access to advanced resection tools, and an expanding number of fellowships offering structured ESD training. These developments are poised to eliminate many of the current barriers. In summary, with robust data supporting the efficacy of ESD in early esophageal cancer, the focus in the United States should shift toward mastering and integrating the technique, rather than dismissing it in favor of piecemeal EMR.
Dr. Othman is chief of the gastroenterology and hepatology section at Baylor College of Medicine and Medicine Subspecialities Service Line Chief at Baylor St Luke’s Medical Center, both in Houston. He declares no conflicts of interest.
Dear colleagues,
Many of us diagnose and treat patients with Barrett’s esophagus, estimated to affect up to 5.6% of the US adult population. There has been an expanding array of tools to help diagnose and effectively treat Barrett’s esophagus with dysplasia and malignancy. In particular, endoscopic submucosal dissection (ESD) has emerged as an important method for treating early cancer in the gastrointestinal tract.
But how do we incorporate ESD into our algorithm for management, especially with the popularity and effectiveness of endoscopic mucosal resection (EMR)? In this issue of Perspectives we aim to provide context for the use of ESD, as compared with EMR. Dr. Silvio de Melo discusses his preferred EMR technique and its many advantages in the management of BE, including for residual or refractory areas. In contrast, Dr. Mohamed Othman reviews the power of ESD and when we should consider this approach over EMR. We hope these discussions will facilitate your care for patients with Barrett’s esophagus.
We also welcome your thoughts on this topic — join the conversation on X at @AGA_GIHN.
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, and chief of endoscopy at West Haven VA Medical Center, both in Connecticut. He is an associate editor for GI & Hepatology News.
Endoscopic Mucosal Resection: The ‘Workhorse’ for Patient Care
BY SILVIO W. DE MELO JR, MD, AGAF
Barrett’s esophagus (BE) remains an important clinical problem, being one of the modifiable risk factors for esophageal adenocarcinoma. The care for BE is complex and requires several steps to correctly formulate a therapeutic plan. It starts with a proper endoscopic examination. It is recommended to spend at least 1 minute inspecting and evaluating every centimeter of the salmon-colored epithelium, looking for change in vascular pattern, erosions/ulcers, nodules, and/or masses. After the inspection, random biopsies every 1-2 cm plus targeted biopsies will guide you. It is still controversial if the addition of other sampling strategies, such as brushings or confocal endomicroscopy, is needed.
The introduction of radiofrequency ablation (RFA) was paramount in popularizing the treatment options for BE and sunsetting the previous dominant modality, photodynamic therapy (PDT). RFA proved to have a superior clinical efficacy in replacing the intestinal metaplasia/BE with neosquamous epithelium while boosting a much better safety profile, compared with PDT. However, RFA is most efficacious for “flat BE” and it is not an effective, nor recommended, method to treat nodular BE or early cancer, such as carcinoma in situ or nodular high-grade dysplasia. Endoscopic mucosal resection (EMR) is utilized to overcome those limitations.
There are several techniques utilized for EMR:
- The lift and snare technique.
- The snare-in-cap technique.
- The Band-snare technique.
The free-hand submucosal lift and snare is not frequently used in the esophagus. It is difficult to maintain visualization while being confident that one has the whole lesion inside the snare and that the distal (anal side) part of the lesion is free of any unwanted tissue (to minimize complications such as perforations or unwelcomed gastric resections). It is difficult after the first resection to lift an adjacent area, as the fluid easily leaks from the first resected spot, thus removing larger lesions in piece-meal fashion is challenging. This technique can be used in small (in my personal experience, less than 5 mm) lesions, but, given that there are better and safer alternatives, I almost never use this technique for my esophageal EMR cases. I prefer to use the band-snare technique even for lesions under 5 mm.
The snare-in-cap technique has been utilized in the esophagus. In this technique, a cap is attached to the distal end of the scope and the size of the resection is determined by the size of the cap, usually under 1.5 cm. Because of the risk of perforation without previous lifting, it is required that the lesion is lifted with a submucosal fluid, saline or any Food and Drug Administration–approved EMR solution. The lesion is then suctioned inside the cap where the snare had been previously opened inside the cap, the snare is closed, and the tissue is resected. The same limitations regarding the inability to remove larger lesions (greater than 1.5 cm) because of the challenge in lifting the adjacent area applies here. However, the perforation risk for this technique is higher than the traditional lift and the band and snare techniques. Thus, this technique has fallen out of favor for most endoscopists.
The third technique (band-snare EMR) is the one that most endoscopists use for endoscopic mucosal resection. It is a small variation of the already time-tested and very familiar procedure of esophageal variceal band ligation (EVL). There are multiple commercially available kits for esophageal EMR. The kit contains the chamber with the bands and a proprietary hexagonal snare used to resect the specimen.
The advantages of this technique are:
- It is widely commercially available.
- It builds on a familiar procedure, EVL, therefore the learning curve is short.
- The set-up is quick and the procedure can be completed safely and effectively.
- There is no need for injecting the submucosal with a lifting solution.
- Despite the band having a size limitation of 1 cm, one can remove larger lesions by repeating the band and resect process, using the rosette technique.
Band-snare EMR also has limitations:
- There are only six bands on each chamber. Depending on the size of the lesion, one may need to use multiple kits.
- It is not suitable for en bloc resection of lesions greater than 1 cm.
My experience with band EMR is that we can complete the procedure in under 1 hour. The dreaded complication of perforation occurs in under 1% of cases, most bleeding episodes can easily be controlled endoscopically, and the risk of post-EMR stricture is minimal. Therefore, band EMR is the most used technique for esophageal endoscopic resections.
Esophageal EMR is also effective for other indications in BE therapy, such as residual and recurrent BE. Band-snare EMR can be used for an en bloc resection or rosette technique for the areas resistant to ablation therapies with great success and safety.
From a financial standpoint, comparing EMR with endoscopic submucosal dissection (ESD), EMR is the superior strategy given that EMR is widely available, has a much shorter learning curve, has a greater safety profile, is applicable to a wider variety of indications, and has a more favorable return on investment. EMR should be the workhorse for the care of patients with BE, reserving ESD for specific indications.
In summary, there is no “one-size-fits-all” endoscopic therapy in the care of BE. Most Barrett’s patients can be successfully treated with a combination of ablation plus EMR, reserving ESD for select cases.
Dr. de Melo is section chief of gastroenterology at the Orlando VA Healthcare System, Orlando, Florida. He declares no conflicts of interest.
ESD Over EMR for Resecting Esophageal Lesions
BY MOHAMED O. OTHMAN, MD, AGAF
Although endoscopic submucosal dissection (ESD) is the preferred endoscopic resection method in the East, the adoption of this technique in the West, particularly in the United States, has faced many hurdles. Many endoscopists who routinely perform piecemeal endoscopic mucosal resection (EMR) question the utility of ESD, arguing that EMR is just as effective. While this may hold true in certain situations, the global trend in the endoscopic treatment of early esophageal squamous cell carcinoma, nodular Barrett’s esophagus (BE), and early esophageal adenocarcinoma (EAC) has clearly shifted toward ESD. In this perspective, I will summarize why ESD is preferred over EMR for these indications and explore why ESD has yet to gain widespread adoption in the United States.
The superiority of ESD over EMR has been well established in multiple publications from both Eastern and Western literature. Mejia-Perez et al, in a multicenter cohort study from eight centers in North America, compared outcomes of ESD vs EMR for BE with high-grade dysplasia (HGD) or T1a adenocarcinoma in 243 patients. ESD achieved significantly higher en bloc resection rates (89% vs 43%) and R0 resection rates (73% vs 56%), compared with EMR, along with a substantially lower recurrence/residual disease rate on follow-up (3.5% in the ESD group vs 31.4% in EMR group). Additionally, more patients required repeat endoscopic resection after EMR to treat residual or recurrent disease (EMR, 24.2% vs ESD, 3.5%; P < .001).
Han et al conducted a meta-analysis of 22 studies comparing ESD and EMR for early esophageal neoplasia, including both squamous cell carcinoma (SCC) and BE-associated lesions. ESD was associated with significantly higher curative resection rates than EMR (OR, 9.74; 95% CI, 4.83-19.62; P < .0001). Of note, lesion size was a critical factor in determining the advantage of ESD. For lesions ≤ 10 mm, curative resection rates were comparable between ESD and EMR. However, for lesions > 10 mm, ESD achieved significantly higher curative resection rates. This size-based recommendation has been adopted by the American Society of Gastrointestinal Endoscopy (ASGE) in their recent guidelines on ESD indications for esophageal lesions. ASGE guidelines favors ESD over EMR for SCC lesions > 15 mm and for nodular BE with dysplasia or early EAC > 20 mm.
ESD is particularly beneficial in patients who develop early adenocarcinoma after RFA or EMR. Mesureur et al evaluated the efficacy of salvage ESD for Barrett’s recurrence or residual BE following RFA. In their multicenter retrospective study of 56 patients, salvage ESD achieved an en bloc resection rate of 89.3%, despite significant fibrosis, with an R0 resection rate of 66%. At a median follow-up of 14 months, most patients remained in endoscopic remission without the need for esophagectomy.
Combining ESD with RFA has also been shown to accelerate the eradication of BE with dysplasia while reducing the number of required sessions. Our group demonstrated the high efficacy of ESD followed by RFA in 18 patients, most of whom had long-segment BE with HGD or EAC. On average, patients required only one to two RFA sessions after ESD to achieve complete eradication of intestinal metaplasia (CE-IM). Over a median follow-up of 42.5 months (IQR, 28-59.25), complete eradication of early esophageal cancer was achieved in 13 patients (100%), eradication of dysplasia in 15 patients (100%), and CE-IM in 14 patients (77.8%).
Despite the overwhelming evidence supporting ESD and the strong endorsement from professional societies, adoption in the West continues to lag. Several factors contribute to this gap. First, ESD has a steep learning curve. Our data showed that, on average, an untutored practitioner achieved competency after 150-250 procedures, a finding corroborated by other US groups.
Second, there is no specific CPT code for ESD in the United States. Physicians are forced to bill the procedure as EMR or use an unlisted code, resulting in reimbursement that does not reflect the time and complexity of the procedure. Our group showed that physician reimbursement for ESD is highly variable, ranging from $50 to $800 per case, depending on insurance type.
Third, the increasing emphasis on productivity and RVU generation in academic settings has hindered the growth of ESD training in many institutions. Still, the outlook for ESD in the United States remains encouraging. Multiple industry-sponsored training courses are held annually, and professional societies are investing heavily in expanding access to structured education in ESD. Industry is also innovating devices that improve procedural efficiency and safety. Adopting novel approaches, such as traction-assisted ESD, has made the technique more appealing to endoscopists concerned about long procedure times. For example, our group proposed a standardized esophageal ESD technique that incorporates specimen self-retraction. This method improves both safety and speed and has helped address several procedural challenges. We’ve demonstrated that consistency in technique can substantially expedite esophageal ESD.
Fast forward 5 years: We anticipate a dedicated CPT code for ESD, broader access to advanced resection tools, and an expanding number of fellowships offering structured ESD training. These developments are poised to eliminate many of the current barriers. In summary, with robust data supporting the efficacy of ESD in early esophageal cancer, the focus in the United States should shift toward mastering and integrating the technique, rather than dismissing it in favor of piecemeal EMR.
Dr. Othman is chief of the gastroenterology and hepatology section at Baylor College of Medicine and Medicine Subspecialities Service Line Chief at Baylor St Luke’s Medical Center, both in Houston. He declares no conflicts of interest.
Building Your Referral Base

In this video, Lisa Mathew, MD, of South Denver Gastroenterology in Denver, Colorado, and Raja Taunk, MD, of Anne Arundel Gastroenterology Associates, in Annapolis, Maryland, share insights on private practice gastroenterology and offer tips on building your practice – specifically improving your referral base.

In this video, Lisa Mathew, MD, of South Denver Gastroenterology in Denver, Colorado, and Raja Taunk, MD, of Anne Arundel Gastroenterology Associates, in Annapolis, Maryland, share insights on private practice gastroenterology and offer tips on building your practice – specifically improving your referral base.

In this video, Lisa Mathew, MD, of South Denver Gastroenterology in Denver, Colorado, and Raja Taunk, MD, of Anne Arundel Gastroenterology Associates, in Annapolis, Maryland, share insights on private practice gastroenterology and offer tips on building your practice – specifically improving your referral base.
A Threat to Scientific Progress
The United States has long been recognized as a global leader in biomedical research and scientific discovery, with federal research and development (R&D) funding serving as the bedrock of national innovation. Substantial federal investment in biomedical research has stemmed from a recognition of its importance in fueling critical discoveries that improve patient care and the health of our communities.
In the United States, academic institutions play a key role in conducting research in the national interest and collaborating with industry, with most of the federal research funding distributed by the National Institutes of Health, National Science Foundation, and other agencies awarded to university-based academic investigators. In a 2014 report, the National Academies of Sciences, Engineering and Medicine identified three pillars of a highly productive research system: a talented and interconnected workforce, adequate and dependable resources, and world-class basic research in all major areas of science.
A series of recent, short-sighted federal policy decisions threaten the future of scientific discovery by eroding these pillars. Decisions to freeze previously awarded federal grant funding, delay grant review panels, fire federal scientists, and propose crippling cuts to indirect cost rates (among others) have sent shock waves through the research community and already have led some prominent research institutions to cut staff and divert resources away from groundbreaking research. While the acute effects of these changes are just beginning to be felt, it is the long-term effects of these decisions on future medical and scientific discovery that will be most devastating to society.
In our April issue, we highlight important research advancements in inflammatory bowel disease presented at February’s Congress of the European Crohn’s and Colitis Organisation (ECCO) in Berlin. In this month’s Member Spotlight, Abigail Meyers, MPAS, PA-C, outlines her impactful work as a member of AGA’s newly formed Nurse Practitioner and Physician Assistant Task Force and shares how her personal journey as a patient with inflammatory bowel disease allows her to be a more powerful advocate for important issues impacting other patients with this condition.
Megan A. Adams, MD, JD, MSc
Editor in Chief
The United States has long been recognized as a global leader in biomedical research and scientific discovery, with federal research and development (R&D) funding serving as the bedrock of national innovation. Substantial federal investment in biomedical research has stemmed from a recognition of its importance in fueling critical discoveries that improve patient care and the health of our communities.
In the United States, academic institutions play a key role in conducting research in the national interest and collaborating with industry, with most of the federal research funding distributed by the National Institutes of Health, National Science Foundation, and other agencies awarded to university-based academic investigators. In a 2014 report, the National Academies of Sciences, Engineering and Medicine identified three pillars of a highly productive research system: a talented and interconnected workforce, adequate and dependable resources, and world-class basic research in all major areas of science.
A series of recent, short-sighted federal policy decisions threaten the future of scientific discovery by eroding these pillars. Decisions to freeze previously awarded federal grant funding, delay grant review panels, fire federal scientists, and propose crippling cuts to indirect cost rates (among others) have sent shock waves through the research community and already have led some prominent research institutions to cut staff and divert resources away from groundbreaking research. While the acute effects of these changes are just beginning to be felt, it is the long-term effects of these decisions on future medical and scientific discovery that will be most devastating to society.
In our April issue, we highlight important research advancements in inflammatory bowel disease presented at February’s Congress of the European Crohn’s and Colitis Organisation (ECCO) in Berlin. In this month’s Member Spotlight, Abigail Meyers, MPAS, PA-C, outlines her impactful work as a member of AGA’s newly formed Nurse Practitioner and Physician Assistant Task Force and shares how her personal journey as a patient with inflammatory bowel disease allows her to be a more powerful advocate for important issues impacting other patients with this condition.
Megan A. Adams, MD, JD, MSc
Editor in Chief
The United States has long been recognized as a global leader in biomedical research and scientific discovery, with federal research and development (R&D) funding serving as the bedrock of national innovation. Substantial federal investment in biomedical research has stemmed from a recognition of its importance in fueling critical discoveries that improve patient care and the health of our communities.
In the United States, academic institutions play a key role in conducting research in the national interest and collaborating with industry, with most of the federal research funding distributed by the National Institutes of Health, National Science Foundation, and other agencies awarded to university-based academic investigators. In a 2014 report, the National Academies of Sciences, Engineering and Medicine identified three pillars of a highly productive research system: a talented and interconnected workforce, adequate and dependable resources, and world-class basic research in all major areas of science.
A series of recent, short-sighted federal policy decisions threaten the future of scientific discovery by eroding these pillars. Decisions to freeze previously awarded federal grant funding, delay grant review panels, fire federal scientists, and propose crippling cuts to indirect cost rates (among others) have sent shock waves through the research community and already have led some prominent research institutions to cut staff and divert resources away from groundbreaking research. While the acute effects of these changes are just beginning to be felt, it is the long-term effects of these decisions on future medical and scientific discovery that will be most devastating to society.
In our April issue, we highlight important research advancements in inflammatory bowel disease presented at February’s Congress of the European Crohn’s and Colitis Organisation (ECCO) in Berlin. In this month’s Member Spotlight, Abigail Meyers, MPAS, PA-C, outlines her impactful work as a member of AGA’s newly formed Nurse Practitioner and Physician Assistant Task Force and shares how her personal journey as a patient with inflammatory bowel disease allows her to be a more powerful advocate for important issues impacting other patients with this condition.
Megan A. Adams, MD, JD, MSc
Editor in Chief