User login
Expanding APRN practice and more
What FPs should know about pharmacogenetic testing
VIDEO: Don’t miss reservoirs when treating recurrent onychomycosis
WAILEA, HAWAII – Patients attribute every nail problem to nail fungus, but part of the problem with nails is concomitant tinea pedis, tinea corporis, and other reservoirs of infection, according to Neal Bhatia, MD, director of clinical dermatology at Therapeutics Clinical Research in San Diego.
Failure to locate and treat these other reservoirs can lead to recurrence of the nail infection, Dr. Bhatia said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
“If we aren’t treating the skin as well as the nails, it is creating a reservoir effect that reaccumulates in the nail itself,” he said. Similarly, the nails can serve as a reservoir of infection for the skin.
“That makes it all the more important” to treat both skin and nails and “treat through the disease state,” he commented in a video interview. Cost can influence treatment decisions, and there is a role for both topical and systemic therapy, he said. However, “if there’s not adequate testing or if there’s not a good proof of the diagnosis, we are just losing out no matter what we use,” he cautioned.
Dr. Bhatia disclosed relationships with companies including Actavis, Aqua, Allergan, Anacor, Bayer, Biofrontera, Biopharmx, Dermira, Dusa, Exceltis, Ferndale, Foamix, Galderma, Intraderm, ISDIN, LaRoche-Posay, Leo, Novartis, Sanofi, and Valeant.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAILEA, HAWAII – Patients attribute every nail problem to nail fungus, but part of the problem with nails is concomitant tinea pedis, tinea corporis, and other reservoirs of infection, according to Neal Bhatia, MD, director of clinical dermatology at Therapeutics Clinical Research in San Diego.
Failure to locate and treat these other reservoirs can lead to recurrence of the nail infection, Dr. Bhatia said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
“If we aren’t treating the skin as well as the nails, it is creating a reservoir effect that reaccumulates in the nail itself,” he said. Similarly, the nails can serve as a reservoir of infection for the skin.
“That makes it all the more important” to treat both skin and nails and “treat through the disease state,” he commented in a video interview. Cost can influence treatment decisions, and there is a role for both topical and systemic therapy, he said. However, “if there’s not adequate testing or if there’s not a good proof of the diagnosis, we are just losing out no matter what we use,” he cautioned.
Dr. Bhatia disclosed relationships with companies including Actavis, Aqua, Allergan, Anacor, Bayer, Biofrontera, Biopharmx, Dermira, Dusa, Exceltis, Ferndale, Foamix, Galderma, Intraderm, ISDIN, LaRoche-Posay, Leo, Novartis, Sanofi, and Valeant.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAILEA, HAWAII – Patients attribute every nail problem to nail fungus, but part of the problem with nails is concomitant tinea pedis, tinea corporis, and other reservoirs of infection, according to Neal Bhatia, MD, director of clinical dermatology at Therapeutics Clinical Research in San Diego.
Failure to locate and treat these other reservoirs can lead to recurrence of the nail infection, Dr. Bhatia said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
“If we aren’t treating the skin as well as the nails, it is creating a reservoir effect that reaccumulates in the nail itself,” he said. Similarly, the nails can serve as a reservoir of infection for the skin.
“That makes it all the more important” to treat both skin and nails and “treat through the disease state,” he commented in a video interview. Cost can influence treatment decisions, and there is a role for both topical and systemic therapy, he said. However, “if there’s not adequate testing or if there’s not a good proof of the diagnosis, we are just losing out no matter what we use,” he cautioned.
Dr. Bhatia disclosed relationships with companies including Actavis, Aqua, Allergan, Anacor, Bayer, Biofrontera, Biopharmx, Dermira, Dusa, Exceltis, Ferndale, Foamix, Galderma, Intraderm, ISDIN, LaRoche-Posay, Leo, Novartis, Sanofi, and Valeant.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF HAWAII DERMATOLOGY SEMINAR
VIDEO: Consider PPIs as a cause of cutaneous reactions
WAILEA, HAWAII – Any proton pump inhibitor (PPI) has the potential to cause skin reactions, so it is important to ask patients about their use, according to J. Mark Jackson, MD, of the University of Louisville (Ky.).
If patients are going to react to a PPI, they usually will do so within 3 or 4 months of starting treatment, rather than in the first week or so of treatment, Dr. Jackson said in a video interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Skin reactions to PPIs are often maculopapular, with a flat and a raised component that can be nonspecific, Dr. Jackson noted.
Interestingly, he added, many times patients can switch to a different PPI and not get a skin reaction. However, there are some patients who develop a lupuslike reaction on the skin, and in these cases, there tends to be cross reactivity, “so they couldn’t switch to a different PPI and be risk-free” of the same reaction, he noted.
Dr. Jackson disclosed financial relationships with companies including AbbVie, Amgen, Celgene, Dermira, Galderma, Genentech, Janssen, Lilly, Medimetriks, Merck, Novartis, Pfizer, Promius, and Top MD.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAILEA, HAWAII – Any proton pump inhibitor (PPI) has the potential to cause skin reactions, so it is important to ask patients about their use, according to J. Mark Jackson, MD, of the University of Louisville (Ky.).
If patients are going to react to a PPI, they usually will do so within 3 or 4 months of starting treatment, rather than in the first week or so of treatment, Dr. Jackson said in a video interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Skin reactions to PPIs are often maculopapular, with a flat and a raised component that can be nonspecific, Dr. Jackson noted.
Interestingly, he added, many times patients can switch to a different PPI and not get a skin reaction. However, there are some patients who develop a lupuslike reaction on the skin, and in these cases, there tends to be cross reactivity, “so they couldn’t switch to a different PPI and be risk-free” of the same reaction, he noted.
Dr. Jackson disclosed financial relationships with companies including AbbVie, Amgen, Celgene, Dermira, Galderma, Genentech, Janssen, Lilly, Medimetriks, Merck, Novartis, Pfizer, Promius, and Top MD.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAILEA, HAWAII – Any proton pump inhibitor (PPI) has the potential to cause skin reactions, so it is important to ask patients about their use, according to J. Mark Jackson, MD, of the University of Louisville (Ky.).
If patients are going to react to a PPI, they usually will do so within 3 or 4 months of starting treatment, rather than in the first week or so of treatment, Dr. Jackson said in a video interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Skin reactions to PPIs are often maculopapular, with a flat and a raised component that can be nonspecific, Dr. Jackson noted.
Interestingly, he added, many times patients can switch to a different PPI and not get a skin reaction. However, there are some patients who develop a lupuslike reaction on the skin, and in these cases, there tends to be cross reactivity, “so they couldn’t switch to a different PPI and be risk-free” of the same reaction, he noted.
Dr. Jackson disclosed financial relationships with companies including AbbVie, Amgen, Celgene, Dermira, Galderma, Genentech, Janssen, Lilly, Medimetriks, Merck, Novartis, Pfizer, Promius, and Top MD.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF HAWAII DERMATOLOGY SEMINAR
VIDEO: Dermatologists often miss adult onset atopic dermatitis
WAILEA, HAWAII – Evidence from several recent studies suggests that the prevalence of adult onset atopic dermatitis in the United States may be as high as 7%-10%, said Jonathan I. Silverberg, MD, of the department of dermatology, preventive medicine, and medical social sciences, Northwestern University, Chicago.
Many features are similar to atopic dermatitis (AD) seen in childhood, but in adults the eczema is more likely to affect the hands and the eyelids. “We often have a hard time telling that apart from contact dermatitis,” Dr. Silverberg said in a video interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Some adults may have forgotten they had AD as children and don’t recognize it if it reappears in adulthood, but sometimes AD appears with no childhood history, he noted. “There’s a skepticism that if it is adult onset, it must not be atopic dermatitis,” but he has found that is not always the case.
A take-home message for clinicians: “Don’t be surprised when a patient walks in the door as an adult meeting all criteria for atopic dermatitis. It can be, and you can diagnose them comfortably,” said Dr. Silverberg, who is also director of the Northwestern Medicine Multidisciplinary Eczema Center, Northwestern Memorial Hospital, Chicago.
Most of the treatments for adult AD “cover many different arms of the immune system,” and include topical steroids and immunosuppressants, he added.
Dr. Silverberg disclosed relationships with companies including AbbVie, Anacor, Celgene, Chugai, GlaxoSmithKline, Lilly, MedImmune-AstraZeneca, Pfizer, Procter & Gamble, Puricore, and Regeneron-Sanofi. SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAILEA, HAWAII – Evidence from several recent studies suggests that the prevalence of adult onset atopic dermatitis in the United States may be as high as 7%-10%, said Jonathan I. Silverberg, MD, of the department of dermatology, preventive medicine, and medical social sciences, Northwestern University, Chicago.
Many features are similar to atopic dermatitis (AD) seen in childhood, but in adults the eczema is more likely to affect the hands and the eyelids. “We often have a hard time telling that apart from contact dermatitis,” Dr. Silverberg said in a video interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Some adults may have forgotten they had AD as children and don’t recognize it if it reappears in adulthood, but sometimes AD appears with no childhood history, he noted. “There’s a skepticism that if it is adult onset, it must not be atopic dermatitis,” but he has found that is not always the case.
A take-home message for clinicians: “Don’t be surprised when a patient walks in the door as an adult meeting all criteria for atopic dermatitis. It can be, and you can diagnose them comfortably,” said Dr. Silverberg, who is also director of the Northwestern Medicine Multidisciplinary Eczema Center, Northwestern Memorial Hospital, Chicago.
Most of the treatments for adult AD “cover many different arms of the immune system,” and include topical steroids and immunosuppressants, he added.
Dr. Silverberg disclosed relationships with companies including AbbVie, Anacor, Celgene, Chugai, GlaxoSmithKline, Lilly, MedImmune-AstraZeneca, Pfizer, Procter & Gamble, Puricore, and Regeneron-Sanofi. SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAILEA, HAWAII – Evidence from several recent studies suggests that the prevalence of adult onset atopic dermatitis in the United States may be as high as 7%-10%, said Jonathan I. Silverberg, MD, of the department of dermatology, preventive medicine, and medical social sciences, Northwestern University, Chicago.
Many features are similar to atopic dermatitis (AD) seen in childhood, but in adults the eczema is more likely to affect the hands and the eyelids. “We often have a hard time telling that apart from contact dermatitis,” Dr. Silverberg said in a video interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Some adults may have forgotten they had AD as children and don’t recognize it if it reappears in adulthood, but sometimes AD appears with no childhood history, he noted. “There’s a skepticism that if it is adult onset, it must not be atopic dermatitis,” but he has found that is not always the case.
A take-home message for clinicians: “Don’t be surprised when a patient walks in the door as an adult meeting all criteria for atopic dermatitis. It can be, and you can diagnose them comfortably,” said Dr. Silverberg, who is also director of the Northwestern Medicine Multidisciplinary Eczema Center, Northwestern Memorial Hospital, Chicago.
Most of the treatments for adult AD “cover many different arms of the immune system,” and include topical steroids and immunosuppressants, he added.
Dr. Silverberg disclosed relationships with companies including AbbVie, Anacor, Celgene, Chugai, GlaxoSmithKline, Lilly, MedImmune-AstraZeneca, Pfizer, Procter & Gamble, Puricore, and Regeneron-Sanofi. SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF HAWAII DERMATOLOGY SEMINAR
VIDEO: Sofosbuvir with velpatasvir beat other HCV GT3 regimens
Regimens containing sofosbuvir and velpatasvir were most effective for treating both cirrhotic and noncirrhotic genotype 3 hepatitis C virus infection (HCV GT3), according to a meta-analysis reported in the March issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2016.10.03).
“Our analyses indicated that ribavirin significantly increases SVR [sustained viral response] rates and should be considered, if tolerated,” added Floor A.C. Berden, MD, of Radboud University Medical Center, Nijmegen, the Netherlands, and her associates.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Direct-acting antiviral regimens successfully treat chronic HCV infection, but tend to perform suboptimally in HCV GT3, especially when patients are treatment experienced and have cirrhosis. Options for HCV GT3 infection include sofosbuvir combined with ribavirin, daclatasvir, or velpatasvir. But head-to-head trials of these regimens are lacking, and are unlikely to occur, in part because the Food and Drug Administration permits single-arm trials with historical controls as the comparator, the investigators said.
Therefore, they searched PubMed, Embase, and the Web of Science database through March 15, 2016, for randomized trials and real-world studies of at least one direct-acting antiviral agent in adults with chronic HCV GT3 infection. They also manually searched abstracts presented at the 2015 conferences of the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases. This work yielded 27 studies: 16 randomized controlled trials, 6 single-arm studies, and 5 observational cohort studies. The researchers used a Bayesian analysis based on Markov chain Monte Carlo methods.
For patients without cirrhosis, sofosbuvir and velpatasvir with ribavirin yielded the highest estimated likelihood of SVR (99%; 95% confidence interval, 98%-100%), followed by sofosbuvir and velpatasvir without ribavirin (97%; 95% CI, 95%-99%), sofosbuvir and daclatasvir with ribavirin (96%; 95% CI, 92%-98%), and sofosbuvir and peginterferon with ribavirin (95%; 95% CI, 91%-98%), all for 12 weeks, the investigators reported.
For patients with cirrhosis, the most effective regimen was sofosbuvir with velpatasvir for 24 weeks (estimated SVR, 96%; 95% CI, 92%-99%), followed by sofosbuvir and daclatasvir with ribavirin for 24 weeks (94%; 95% CI, 87%-98%), sofosbuvir and velpatasvir and ribavirin for 12 weeks (94%; 95% CI, 86%-98%). The estimated efficacy of sofosbuvir and velpatasvir held up in sensitivity analyses that honed in on studies with a low risk of bias, approved regimens, or those under regulatory evaluation, patients without decompensated cirrhosis, and patients without HIV coinfection.
Adding ribavirin to a direct-acting antiviral regimen improved the odds of SVR about 2.6-fold (95% CI, 1.3-4.7) among noncirrhotic patients and by about 4.5 times in cirrhotic patients (95% CI, 2.5-7.7), the investigators reported. “In clinical practice, choice of treatment may depend on several factors, such as availability and price of direct-acting antivirals, tolerance of ribavirin, risk of adverse events or drug-drug interactions, and the presence of resistance-associated substitutions,” they added. Nonetheless, these findings can help prioritize therapies for HCV GT3 infection in both clinical guidelines and practice, they emphasized.
Dr. Berden and four coinvestigators had no relevant financial disclosures. Senior author Joost Drenth, MD, PhD, disclosed serving on advisory boards and receiving research grants from several pharmaceutical companies.
The rapid development of direct-acting antiviral agents (DAAs) to treat hepatitis C has yielded many surprises and left some gaps in our knowledge.
One of the surprises was that genotype 3, previously considered “easier to treat,” proved quite resistant to the first generation of DAAs. One of the gaps in knowledge was a lack of randomized and head-to-head trials for current medications. One could argue that randomized trials have limited utility in a disease with essentially no spontaneous cures, and that head-to-head trials are pointless in a rapidly evolving field where regimens may be obsolete by the time the study is completed.
On the bright side, a hard endpoint like sustained virologic response (SVR) makes comparison between trials possible. The paper by Bergen et al. offers some guidance in closing the knowledge gap. Their meta-analysis using Bayesian Markov Chain Monte Carlo methods examined the effectiveness of currently available antiviral agents in 27 studies that focused entirely on genotype 3. All studies used antiviral agents that are currently available in the United States, and effectiveness was tested in both noncirrhotic and cirrhotic patients.
The evolution of antiviral therapy has been amazing. After decades of incremental gains, we entered an era of dizzying progress. Genotype 3 went from great news to bad news, and genotype 1 went from a scourge to a piece of cake.
Norman L. Sussman, MD, is associate professor of surgery, Baylor College of Medicine, Houston; director, Project ECHO. He has received speaking and consulting fees for AbbVie, BMS, Gilead, and Merck.
The rapid development of direct-acting antiviral agents (DAAs) to treat hepatitis C has yielded many surprises and left some gaps in our knowledge.
One of the surprises was that genotype 3, previously considered “easier to treat,” proved quite resistant to the first generation of DAAs. One of the gaps in knowledge was a lack of randomized and head-to-head trials for current medications. One could argue that randomized trials have limited utility in a disease with essentially no spontaneous cures, and that head-to-head trials are pointless in a rapidly evolving field where regimens may be obsolete by the time the study is completed.
On the bright side, a hard endpoint like sustained virologic response (SVR) makes comparison between trials possible. The paper by Bergen et al. offers some guidance in closing the knowledge gap. Their meta-analysis using Bayesian Markov Chain Monte Carlo methods examined the effectiveness of currently available antiviral agents in 27 studies that focused entirely on genotype 3. All studies used antiviral agents that are currently available in the United States, and effectiveness was tested in both noncirrhotic and cirrhotic patients.
The evolution of antiviral therapy has been amazing. After decades of incremental gains, we entered an era of dizzying progress. Genotype 3 went from great news to bad news, and genotype 1 went from a scourge to a piece of cake.
Norman L. Sussman, MD, is associate professor of surgery, Baylor College of Medicine, Houston; director, Project ECHO. He has received speaking and consulting fees for AbbVie, BMS, Gilead, and Merck.
The rapid development of direct-acting antiviral agents (DAAs) to treat hepatitis C has yielded many surprises and left some gaps in our knowledge.
One of the surprises was that genotype 3, previously considered “easier to treat,” proved quite resistant to the first generation of DAAs. One of the gaps in knowledge was a lack of randomized and head-to-head trials for current medications. One could argue that randomized trials have limited utility in a disease with essentially no spontaneous cures, and that head-to-head trials are pointless in a rapidly evolving field where regimens may be obsolete by the time the study is completed.
On the bright side, a hard endpoint like sustained virologic response (SVR) makes comparison between trials possible. The paper by Bergen et al. offers some guidance in closing the knowledge gap. Their meta-analysis using Bayesian Markov Chain Monte Carlo methods examined the effectiveness of currently available antiviral agents in 27 studies that focused entirely on genotype 3. All studies used antiviral agents that are currently available in the United States, and effectiveness was tested in both noncirrhotic and cirrhotic patients.
The evolution of antiviral therapy has been amazing. After decades of incremental gains, we entered an era of dizzying progress. Genotype 3 went from great news to bad news, and genotype 1 went from a scourge to a piece of cake.
Norman L. Sussman, MD, is associate professor of surgery, Baylor College of Medicine, Houston; director, Project ECHO. He has received speaking and consulting fees for AbbVie, BMS, Gilead, and Merck.
Regimens containing sofosbuvir and velpatasvir were most effective for treating both cirrhotic and noncirrhotic genotype 3 hepatitis C virus infection (HCV GT3), according to a meta-analysis reported in the March issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2016.10.03).
“Our analyses indicated that ribavirin significantly increases SVR [sustained viral response] rates and should be considered, if tolerated,” added Floor A.C. Berden, MD, of Radboud University Medical Center, Nijmegen, the Netherlands, and her associates.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Direct-acting antiviral regimens successfully treat chronic HCV infection, but tend to perform suboptimally in HCV GT3, especially when patients are treatment experienced and have cirrhosis. Options for HCV GT3 infection include sofosbuvir combined with ribavirin, daclatasvir, or velpatasvir. But head-to-head trials of these regimens are lacking, and are unlikely to occur, in part because the Food and Drug Administration permits single-arm trials with historical controls as the comparator, the investigators said.
Therefore, they searched PubMed, Embase, and the Web of Science database through March 15, 2016, for randomized trials and real-world studies of at least one direct-acting antiviral agent in adults with chronic HCV GT3 infection. They also manually searched abstracts presented at the 2015 conferences of the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases. This work yielded 27 studies: 16 randomized controlled trials, 6 single-arm studies, and 5 observational cohort studies. The researchers used a Bayesian analysis based on Markov chain Monte Carlo methods.
For patients without cirrhosis, sofosbuvir and velpatasvir with ribavirin yielded the highest estimated likelihood of SVR (99%; 95% confidence interval, 98%-100%), followed by sofosbuvir and velpatasvir without ribavirin (97%; 95% CI, 95%-99%), sofosbuvir and daclatasvir with ribavirin (96%; 95% CI, 92%-98%), and sofosbuvir and peginterferon with ribavirin (95%; 95% CI, 91%-98%), all for 12 weeks, the investigators reported.
For patients with cirrhosis, the most effective regimen was sofosbuvir with velpatasvir for 24 weeks (estimated SVR, 96%; 95% CI, 92%-99%), followed by sofosbuvir and daclatasvir with ribavirin for 24 weeks (94%; 95% CI, 87%-98%), sofosbuvir and velpatasvir and ribavirin for 12 weeks (94%; 95% CI, 86%-98%). The estimated efficacy of sofosbuvir and velpatasvir held up in sensitivity analyses that honed in on studies with a low risk of bias, approved regimens, or those under regulatory evaluation, patients without decompensated cirrhosis, and patients without HIV coinfection.
Adding ribavirin to a direct-acting antiviral regimen improved the odds of SVR about 2.6-fold (95% CI, 1.3-4.7) among noncirrhotic patients and by about 4.5 times in cirrhotic patients (95% CI, 2.5-7.7), the investigators reported. “In clinical practice, choice of treatment may depend on several factors, such as availability and price of direct-acting antivirals, tolerance of ribavirin, risk of adverse events or drug-drug interactions, and the presence of resistance-associated substitutions,” they added. Nonetheless, these findings can help prioritize therapies for HCV GT3 infection in both clinical guidelines and practice, they emphasized.
Dr. Berden and four coinvestigators had no relevant financial disclosures. Senior author Joost Drenth, MD, PhD, disclosed serving on advisory boards and receiving research grants from several pharmaceutical companies.
Regimens containing sofosbuvir and velpatasvir were most effective for treating both cirrhotic and noncirrhotic genotype 3 hepatitis C virus infection (HCV GT3), according to a meta-analysis reported in the March issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2016.10.03).
“Our analyses indicated that ribavirin significantly increases SVR [sustained viral response] rates and should be considered, if tolerated,” added Floor A.C. Berden, MD, of Radboud University Medical Center, Nijmegen, the Netherlands, and her associates.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Direct-acting antiviral regimens successfully treat chronic HCV infection, but tend to perform suboptimally in HCV GT3, especially when patients are treatment experienced and have cirrhosis. Options for HCV GT3 infection include sofosbuvir combined with ribavirin, daclatasvir, or velpatasvir. But head-to-head trials of these regimens are lacking, and are unlikely to occur, in part because the Food and Drug Administration permits single-arm trials with historical controls as the comparator, the investigators said.
Therefore, they searched PubMed, Embase, and the Web of Science database through March 15, 2016, for randomized trials and real-world studies of at least one direct-acting antiviral agent in adults with chronic HCV GT3 infection. They also manually searched abstracts presented at the 2015 conferences of the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases. This work yielded 27 studies: 16 randomized controlled trials, 6 single-arm studies, and 5 observational cohort studies. The researchers used a Bayesian analysis based on Markov chain Monte Carlo methods.
For patients without cirrhosis, sofosbuvir and velpatasvir with ribavirin yielded the highest estimated likelihood of SVR (99%; 95% confidence interval, 98%-100%), followed by sofosbuvir and velpatasvir without ribavirin (97%; 95% CI, 95%-99%), sofosbuvir and daclatasvir with ribavirin (96%; 95% CI, 92%-98%), and sofosbuvir and peginterferon with ribavirin (95%; 95% CI, 91%-98%), all for 12 weeks, the investigators reported.
For patients with cirrhosis, the most effective regimen was sofosbuvir with velpatasvir for 24 weeks (estimated SVR, 96%; 95% CI, 92%-99%), followed by sofosbuvir and daclatasvir with ribavirin for 24 weeks (94%; 95% CI, 87%-98%), sofosbuvir and velpatasvir and ribavirin for 12 weeks (94%; 95% CI, 86%-98%). The estimated efficacy of sofosbuvir and velpatasvir held up in sensitivity analyses that honed in on studies with a low risk of bias, approved regimens, or those under regulatory evaluation, patients without decompensated cirrhosis, and patients without HIV coinfection.
Adding ribavirin to a direct-acting antiviral regimen improved the odds of SVR about 2.6-fold (95% CI, 1.3-4.7) among noncirrhotic patients and by about 4.5 times in cirrhotic patients (95% CI, 2.5-7.7), the investigators reported. “In clinical practice, choice of treatment may depend on several factors, such as availability and price of direct-acting antivirals, tolerance of ribavirin, risk of adverse events or drug-drug interactions, and the presence of resistance-associated substitutions,” they added. Nonetheless, these findings can help prioritize therapies for HCV GT3 infection in both clinical guidelines and practice, they emphasized.
Dr. Berden and four coinvestigators had no relevant financial disclosures. Senior author Joost Drenth, MD, PhD, disclosed serving on advisory boards and receiving research grants from several pharmaceutical companies.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point. Regimens containing sofosbuvir and velpatasvir were more effective than were other direct-acting antiviral combinations for treating genotype 3 hepatitis C virus infection, regardless of cirrhosis status.
Major finding: For patients without cirrhosis, sofosbuvir and velpatasvir with ribavirin for 12 weeks yielded the highest estimated likelihood of sustained viral response (99%). For patients with cirrhosis, the most effective regimen was sofosbuvir with velpatasvir for 24 weeks (estimated SVR, 96%).
Data source: A systematic review and meta-analysis of 27 studies: 16 randomized controlled trials, 6 single-arm studies, and 5 observational cohort studies.
Disclosures: Dr. Berden and four coinvestigators had no relevant financial disclosures. Senior author Joost Drenth, MD, PhD, disclosed serving on advisory boards and receiving research grants from several pharmaceutical companies.
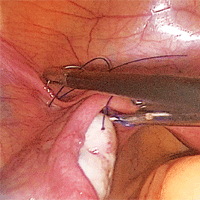
Strategies for prophylactic oophoropexy

Visit the Society of Gynecologic Surgeons online: sgsonline.org
More videos from SGS:
- Tips and tricks for open laparoscopy
- Complete colpectomy & colpocleisis: Model for simulation
- Natural orifice sacral colpopexy
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist

Visit the Society of Gynecologic Surgeons online: sgsonline.org
More videos from SGS:
- Tips and tricks for open laparoscopy
- Complete colpectomy & colpocleisis: Model for simulation
- Natural orifice sacral colpopexy
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist

Visit the Society of Gynecologic Surgeons online: sgsonline.org
More videos from SGS:
- Tips and tricks for open laparoscopy
- Complete colpectomy & colpocleisis: Model for simulation
- Natural orifice sacral colpopexy
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
This video is brought to you by
VIDEO: Health law changes under new administration
WASHINGTON – A new president is taking office along with new staffers to lead the country’s top health care agencies.
In this video, Joyce Hall, chair of the American Bar Association Health Law Section, discusses what changes she foresees in health law issues under the new administration and what to expect from the leadership transition. Ms. Hall also speaks on potential alterations to the Medicare Access and CHIP Reauthorization Act of 2015 and whether the potential appointment of Rep. Tom Price (R-Ga.) as U.S. Department of Health and Human Services Secretary will be positive or negative for health care providers.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
agallegos@frontlinemedcom.com
On Twitter @legal_med
WASHINGTON – A new president is taking office along with new staffers to lead the country’s top health care agencies.
In this video, Joyce Hall, chair of the American Bar Association Health Law Section, discusses what changes she foresees in health law issues under the new administration and what to expect from the leadership transition. Ms. Hall also speaks on potential alterations to the Medicare Access and CHIP Reauthorization Act of 2015 and whether the potential appointment of Rep. Tom Price (R-Ga.) as U.S. Department of Health and Human Services Secretary will be positive or negative for health care providers.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
agallegos@frontlinemedcom.com
On Twitter @legal_med
WASHINGTON – A new president is taking office along with new staffers to lead the country’s top health care agencies.
In this video, Joyce Hall, chair of the American Bar Association Health Law Section, discusses what changes she foresees in health law issues under the new administration and what to expect from the leadership transition. Ms. Hall also speaks on potential alterations to the Medicare Access and CHIP Reauthorization Act of 2015 and whether the potential appointment of Rep. Tom Price (R-Ga.) as U.S. Department of Health and Human Services Secretary will be positive or negative for health care providers.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
agallegos@frontlinemedcom.com
On Twitter @legal_med
AT THE WASHINGTON HEALTH LAW SUMMIT
VIDEO: First multicenter trial of CAR T cells shows response in DLBCL
SAN DIEGO – Aggressive, refractory non-Hodgkin lymphomas responded to anti-CD19 chimeric antigen receptor T cells in ZUMA-1, the first multicenter trial of the cellular immunotherapy, based on early data reported at the annual meeting of the American Society of Hematology.
In an interim analysis of 51 patients with diffuse large B-cell lymphomas, 47% had complete remissions and 29% had partial remissions. But the remission rate declined to 33% complete remissions and 6% partial remissions after 3 months.
There have really been no new treatments in the last 20 years for patients with non-Hodgkin lymphoma that does not respond to chemotherapy or recurs after autologous stem cell transplant. With median overall survival of 6 months, and about 8% complete remissions with existing therapies, CAR T cells might be a solution for these patients, said ZUMA-1 investigator Sattva S. Neelapu, MD, of the University of Texas MD Anderson Cancer Center in Houston.
In our video interview at the meeting, Dr. Neelapu discussed initial results in the real-world setting of 22 participating centers, most of which had no previous experience with CAR T-cell therapy. With an efficient production and logistics plan, 91% of 110 patients were able to receive the investigational product, known as KTE-C19.
ZUMA-1 is funded by Kite, which makes KTE-C19, and the Leukemia & Lymphoma Society Therapy Acceleration Program. Dr. Neelapu receives research support from and is an advisor to Kite.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mdales@frontlinemedcom.com
On Twitter @maryjodales
SAN DIEGO – Aggressive, refractory non-Hodgkin lymphomas responded to anti-CD19 chimeric antigen receptor T cells in ZUMA-1, the first multicenter trial of the cellular immunotherapy, based on early data reported at the annual meeting of the American Society of Hematology.
In an interim analysis of 51 patients with diffuse large B-cell lymphomas, 47% had complete remissions and 29% had partial remissions. But the remission rate declined to 33% complete remissions and 6% partial remissions after 3 months.
There have really been no new treatments in the last 20 years for patients with non-Hodgkin lymphoma that does not respond to chemotherapy or recurs after autologous stem cell transplant. With median overall survival of 6 months, and about 8% complete remissions with existing therapies, CAR T cells might be a solution for these patients, said ZUMA-1 investigator Sattva S. Neelapu, MD, of the University of Texas MD Anderson Cancer Center in Houston.
In our video interview at the meeting, Dr. Neelapu discussed initial results in the real-world setting of 22 participating centers, most of which had no previous experience with CAR T-cell therapy. With an efficient production and logistics plan, 91% of 110 patients were able to receive the investigational product, known as KTE-C19.
ZUMA-1 is funded by Kite, which makes KTE-C19, and the Leukemia & Lymphoma Society Therapy Acceleration Program. Dr. Neelapu receives research support from and is an advisor to Kite.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mdales@frontlinemedcom.com
On Twitter @maryjodales
SAN DIEGO – Aggressive, refractory non-Hodgkin lymphomas responded to anti-CD19 chimeric antigen receptor T cells in ZUMA-1, the first multicenter trial of the cellular immunotherapy, based on early data reported at the annual meeting of the American Society of Hematology.
In an interim analysis of 51 patients with diffuse large B-cell lymphomas, 47% had complete remissions and 29% had partial remissions. But the remission rate declined to 33% complete remissions and 6% partial remissions after 3 months.
There have really been no new treatments in the last 20 years for patients with non-Hodgkin lymphoma that does not respond to chemotherapy or recurs after autologous stem cell transplant. With median overall survival of 6 months, and about 8% complete remissions with existing therapies, CAR T cells might be a solution for these patients, said ZUMA-1 investigator Sattva S. Neelapu, MD, of the University of Texas MD Anderson Cancer Center in Houston.
In our video interview at the meeting, Dr. Neelapu discussed initial results in the real-world setting of 22 participating centers, most of which had no previous experience with CAR T-cell therapy. With an efficient production and logistics plan, 91% of 110 patients were able to receive the investigational product, known as KTE-C19.
ZUMA-1 is funded by Kite, which makes KTE-C19, and the Leukemia & Lymphoma Society Therapy Acceleration Program. Dr. Neelapu receives research support from and is an advisor to Kite.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mdales@frontlinemedcom.com
On Twitter @maryjodales
VIDEO: Despite toxicities, ibrutinib is beneficial for treatment-resistant graft-vs.-host disease
SAN DIEGO – An oral regimen of 420 mg ibrutinib achieved complete response in one-third of allogeneic stem cell recipients with chronic graft-vs.-host disease, David Miklos, MD, reported during a late-breaker session at the annual meeting of the American Society of Hematology.
Fully 79% of patients in this open-label phase II study were considered responders when first assessed, 71% of responses lasted at least 5 months, and patients whose disease involved multiple organs generally showed responses in at least two organs, said Dr. Miklos of Stanford (Calif.) University.
Ibrutinib is a first-in-class Bruton’s tyrosine kinase (BTK) inhibitor. Cardiotoxicities have been a concern with ibrutinib, but were not observed in this cohort of 42 patients whose graft-vs.-host disease had not benefited from frontline therapy, Dr. Miklos said during a video interview. However, 52% of patients in this study developed other serious adverse events that are typical with ibrutinib, including pneumonia, septic shock, and fever, he said.
Chronic graft-vs.-host disease is the most common morbidity after allogeneic transplant. This is an “orphan disease” – there are no approved therapies for patients for whom corticosteroids are ineffective, Dr. Miklos noted. Based on these results, investigators are planning a randomized, placebo-controlled, phase III study, he added.
Ibrutinib is jointly commercialized and developed by Janssen Biotech and by Pharmacyclics LLC, an Abbvie company. Dr. Miklos disclosed a consulting relationship, travel and expenses reimbursements, and research funding from Pharmacyclics.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – An oral regimen of 420 mg ibrutinib achieved complete response in one-third of allogeneic stem cell recipients with chronic graft-vs.-host disease, David Miklos, MD, reported during a late-breaker session at the annual meeting of the American Society of Hematology.
Fully 79% of patients in this open-label phase II study were considered responders when first assessed, 71% of responses lasted at least 5 months, and patients whose disease involved multiple organs generally showed responses in at least two organs, said Dr. Miklos of Stanford (Calif.) University.
Ibrutinib is a first-in-class Bruton’s tyrosine kinase (BTK) inhibitor. Cardiotoxicities have been a concern with ibrutinib, but were not observed in this cohort of 42 patients whose graft-vs.-host disease had not benefited from frontline therapy, Dr. Miklos said during a video interview. However, 52% of patients in this study developed other serious adverse events that are typical with ibrutinib, including pneumonia, septic shock, and fever, he said.
Chronic graft-vs.-host disease is the most common morbidity after allogeneic transplant. This is an “orphan disease” – there are no approved therapies for patients for whom corticosteroids are ineffective, Dr. Miklos noted. Based on these results, investigators are planning a randomized, placebo-controlled, phase III study, he added.
Ibrutinib is jointly commercialized and developed by Janssen Biotech and by Pharmacyclics LLC, an Abbvie company. Dr. Miklos disclosed a consulting relationship, travel and expenses reimbursements, and research funding from Pharmacyclics.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – An oral regimen of 420 mg ibrutinib achieved complete response in one-third of allogeneic stem cell recipients with chronic graft-vs.-host disease, David Miklos, MD, reported during a late-breaker session at the annual meeting of the American Society of Hematology.
Fully 79% of patients in this open-label phase II study were considered responders when first assessed, 71% of responses lasted at least 5 months, and patients whose disease involved multiple organs generally showed responses in at least two organs, said Dr. Miklos of Stanford (Calif.) University.
Ibrutinib is a first-in-class Bruton’s tyrosine kinase (BTK) inhibitor. Cardiotoxicities have been a concern with ibrutinib, but were not observed in this cohort of 42 patients whose graft-vs.-host disease had not benefited from frontline therapy, Dr. Miklos said during a video interview. However, 52% of patients in this study developed other serious adverse events that are typical with ibrutinib, including pneumonia, septic shock, and fever, he said.
Chronic graft-vs.-host disease is the most common morbidity after allogeneic transplant. This is an “orphan disease” – there are no approved therapies for patients for whom corticosteroids are ineffective, Dr. Miklos noted. Based on these results, investigators are planning a randomized, placebo-controlled, phase III study, he added.
Ibrutinib is jointly commercialized and developed by Janssen Biotech and by Pharmacyclics LLC, an Abbvie company. Dr. Miklos disclosed a consulting relationship, travel and expenses reimbursements, and research funding from Pharmacyclics.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASH 2016
Key clinical point: Ibrutinib (420 mg) led to complete responses in one-third of patients with chronic, treatment-resistant graft-vs-host disease.
Major finding: No cardiotoxicities were observed, but 52% of patients had other serious adverse effects, such as sepsis, pyrexia, and pneumonia.
Data source: An open-label phase II study of 42 patients who developed chronic, treatment-resistant graft-vs.-host disease after undergoing allogeneic stem cell transplantation.
Disclosures: Ibrutinib is jointly commercialized and developed by Janssen Biotech and by Pharmacyclics LLC, an Abbvie company. Dr. Miklos disclosed a consulting relationship, reimbursement for travel and expenses, and research funding from Pharmacyclics.