User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Clown-tox, tattooed immunity, and cingulum-bundle comedy
Quit clowning around
Would you like a balloon giraffe, elephant, or hypodermic needle? A recently published study examined how the use of “medical clowns” eased the anxiety and pain of children during botulinum toxin injections. These injections are used to treat spasticity in children, and researchers hypothesized that a clown might be an effective distraction.
As anyone who has been to a circus can surmise, the clowns did not perform better than the control distractions.
Researchers concluded that the clowns were appreciated by the parents but not particularly effective on the children. Maybe that’s because the parents weren’t the ones being stuck with needles while some crazy person in clown makeup attempted to distract them. Or maybe they were all just big fans of Stephen King’s “It.”
Inked immunity
Starting to feel a bit under the weather? Head to the local tattoo artist for the cure! Research from the University of Alabama at Birmingham found evidence that the immune systems of heavily tattooed people are stronger than those without, proving once and for all that tats = toughness. Hell's Angels were on to something all along.
While your immune system can actually grow temporarily weaker after one tattoo, multiple tattoos create a stronger immunological response. Researchers tested the immunoglobulin A levels in those getting a first tattoo and those with many tattoos. They found that the latter group had higher IgA levels.
Maybe that’s why Adam Levine showed off his ink at the Super Bowl halftime show – he was just signaling his strong immune system to the rest of us.
Brain surgery is a laughing matter
This certainly came as a surprise to us, but as it turns out, undergoing brain surgery while conscious and awake can be extremely stressful and panic inducing to the patient. We’re sure most people (including us) would prefer to be asleep for their surgery, but sometimes when dealing with the brain, the surgeon needs to be able to talk to the patient to accurately assess their faculties in case they damage something important.
So the question is: How do you keep brain surgery patients from panicking? Why, with the power of laughter, of course! Specifically, a group at Emory University, Atlanta, published a case study in the Journal of Clinical Investigation about their treatment of a patient with moderate anxiety. When the patient woke up from initial anesthesia, she began to panic. However, after electrical stimulation of the cingulum bundle, the patient immediately turned her frown upside down and began laughing and joking with the surgeons.
Sadly, while the team did not report on the quality of the jokes being told, we can only assume the phrase “this isn’t brain surgery” was thrown around multiple times.
A male brain is a terrible thing to waste
In the future, comedy may mean pressing a button to stimulate your cingulum bundle, but for now we still have jokes. One old joke goes like this: Some aliens land on earth and want to learn about humans, so they go into a store to buy some brains. “Why does the male brain cost twice as much as the female brain?” one asks the store owner, who replies, “It’s hardly been used.”
There may be another explanation: Womens’ brains appear to age more slowly than mens’, investigators at Washington University, St. Louis, said in the Proceedings of the National Academy of Sciences.
They performed PET scans on 121 women and 84 men aged 20-82 years to determine the fraction of sugar committed to aerobic glycolysis in various regions of the brain, and then a machine-learning algorithm used those data to calculate metabolic ages.
The womens’ brains were younger than the mens’ brains, with various calculations producing average differences of 2.7-5.3 years, they reported.
The male brain, it seems, is used for something, and after one LOTME staffer spent 5 minutes explaining total quarterback rating (QBR) to his wife, we think we’ve figured out what it is: sports trivia.
Quit clowning around
Would you like a balloon giraffe, elephant, or hypodermic needle? A recently published study examined how the use of “medical clowns” eased the anxiety and pain of children during botulinum toxin injections. These injections are used to treat spasticity in children, and researchers hypothesized that a clown might be an effective distraction.
As anyone who has been to a circus can surmise, the clowns did not perform better than the control distractions.
Researchers concluded that the clowns were appreciated by the parents but not particularly effective on the children. Maybe that’s because the parents weren’t the ones being stuck with needles while some crazy person in clown makeup attempted to distract them. Or maybe they were all just big fans of Stephen King’s “It.”
Inked immunity
Starting to feel a bit under the weather? Head to the local tattoo artist for the cure! Research from the University of Alabama at Birmingham found evidence that the immune systems of heavily tattooed people are stronger than those without, proving once and for all that tats = toughness. Hell's Angels were on to something all along.
While your immune system can actually grow temporarily weaker after one tattoo, multiple tattoos create a stronger immunological response. Researchers tested the immunoglobulin A levels in those getting a first tattoo and those with many tattoos. They found that the latter group had higher IgA levels.
Maybe that’s why Adam Levine showed off his ink at the Super Bowl halftime show – he was just signaling his strong immune system to the rest of us.
Brain surgery is a laughing matter
This certainly came as a surprise to us, but as it turns out, undergoing brain surgery while conscious and awake can be extremely stressful and panic inducing to the patient. We’re sure most people (including us) would prefer to be asleep for their surgery, but sometimes when dealing with the brain, the surgeon needs to be able to talk to the patient to accurately assess their faculties in case they damage something important.
So the question is: How do you keep brain surgery patients from panicking? Why, with the power of laughter, of course! Specifically, a group at Emory University, Atlanta, published a case study in the Journal of Clinical Investigation about their treatment of a patient with moderate anxiety. When the patient woke up from initial anesthesia, she began to panic. However, after electrical stimulation of the cingulum bundle, the patient immediately turned her frown upside down and began laughing and joking with the surgeons.
Sadly, while the team did not report on the quality of the jokes being told, we can only assume the phrase “this isn’t brain surgery” was thrown around multiple times.
A male brain is a terrible thing to waste
In the future, comedy may mean pressing a button to stimulate your cingulum bundle, but for now we still have jokes. One old joke goes like this: Some aliens land on earth and want to learn about humans, so they go into a store to buy some brains. “Why does the male brain cost twice as much as the female brain?” one asks the store owner, who replies, “It’s hardly been used.”
There may be another explanation: Womens’ brains appear to age more slowly than mens’, investigators at Washington University, St. Louis, said in the Proceedings of the National Academy of Sciences.
They performed PET scans on 121 women and 84 men aged 20-82 years to determine the fraction of sugar committed to aerobic glycolysis in various regions of the brain, and then a machine-learning algorithm used those data to calculate metabolic ages.
The womens’ brains were younger than the mens’ brains, with various calculations producing average differences of 2.7-5.3 years, they reported.
The male brain, it seems, is used for something, and after one LOTME staffer spent 5 minutes explaining total quarterback rating (QBR) to his wife, we think we’ve figured out what it is: sports trivia.
Quit clowning around
Would you like a balloon giraffe, elephant, or hypodermic needle? A recently published study examined how the use of “medical clowns” eased the anxiety and pain of children during botulinum toxin injections. These injections are used to treat spasticity in children, and researchers hypothesized that a clown might be an effective distraction.
As anyone who has been to a circus can surmise, the clowns did not perform better than the control distractions.
Researchers concluded that the clowns were appreciated by the parents but not particularly effective on the children. Maybe that’s because the parents weren’t the ones being stuck with needles while some crazy person in clown makeup attempted to distract them. Or maybe they were all just big fans of Stephen King’s “It.”
Inked immunity
Starting to feel a bit under the weather? Head to the local tattoo artist for the cure! Research from the University of Alabama at Birmingham found evidence that the immune systems of heavily tattooed people are stronger than those without, proving once and for all that tats = toughness. Hell's Angels were on to something all along.
While your immune system can actually grow temporarily weaker after one tattoo, multiple tattoos create a stronger immunological response. Researchers tested the immunoglobulin A levels in those getting a first tattoo and those with many tattoos. They found that the latter group had higher IgA levels.
Maybe that’s why Adam Levine showed off his ink at the Super Bowl halftime show – he was just signaling his strong immune system to the rest of us.
Brain surgery is a laughing matter
This certainly came as a surprise to us, but as it turns out, undergoing brain surgery while conscious and awake can be extremely stressful and panic inducing to the patient. We’re sure most people (including us) would prefer to be asleep for their surgery, but sometimes when dealing with the brain, the surgeon needs to be able to talk to the patient to accurately assess their faculties in case they damage something important.
So the question is: How do you keep brain surgery patients from panicking? Why, with the power of laughter, of course! Specifically, a group at Emory University, Atlanta, published a case study in the Journal of Clinical Investigation about their treatment of a patient with moderate anxiety. When the patient woke up from initial anesthesia, she began to panic. However, after electrical stimulation of the cingulum bundle, the patient immediately turned her frown upside down and began laughing and joking with the surgeons.
Sadly, while the team did not report on the quality of the jokes being told, we can only assume the phrase “this isn’t brain surgery” was thrown around multiple times.
A male brain is a terrible thing to waste
In the future, comedy may mean pressing a button to stimulate your cingulum bundle, but for now we still have jokes. One old joke goes like this: Some aliens land on earth and want to learn about humans, so they go into a store to buy some brains. “Why does the male brain cost twice as much as the female brain?” one asks the store owner, who replies, “It’s hardly been used.”
There may be another explanation: Womens’ brains appear to age more slowly than mens’, investigators at Washington University, St. Louis, said in the Proceedings of the National Academy of Sciences.
They performed PET scans on 121 women and 84 men aged 20-82 years to determine the fraction of sugar committed to aerobic glycolysis in various regions of the brain, and then a machine-learning algorithm used those data to calculate metabolic ages.
The womens’ brains were younger than the mens’ brains, with various calculations producing average differences of 2.7-5.3 years, they reported.
The male brain, it seems, is used for something, and after one LOTME staffer spent 5 minutes explaining total quarterback rating (QBR) to his wife, we think we’ve figured out what it is: sports trivia.
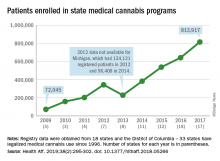
Cloud of inconsistency hangs over cannabis data
More people are using medical cannabis as it becomes legal in more states, but the lack of standardization in states’ data collection hindered investigators’ efforts to track that use.
Legalized medical cannabis is now available in 33 states and the District of Columbia, and the number of users has risen from just over 72,000 in 2009 to almost 814,000 in 2017. That 814,000, however, covers only 16 states and D.C., since 1 state (Connecticut) does not publish reports on medical cannabis use, 12 did not have statistics available, 2 (New York and Vermont) didn’t report data for 2017, and 2 (California and Maine) have voluntary registries that are unlikely to be accurate, according to Kevin F. Boehnke, PhD, of the University of Michigan, Ann Arbor, and his associates.
Michigan had the largest reported number of patients enrolled in its medical cannabis program in 2017, almost 270,000. California – the state with the oldest medical cannabis legislation (passed in 1996) and the largest overall population but a voluntary cannabis registry – reported its highest number of enrollees, 12,659, in 2009-2010, the investigators said. Colorado had more than 116,000 patients in its medical cannabis program in 2010 (Health Aff. 2019;38[2]:295-302).
The “many inconsistencies in data quality across states [suggest] the need for further standardization of data collection. Such standardization would add transparency to understanding how medical cannabis programs are used, which would help guide both research and policy needs,” Dr. Boehnke and his associates wrote.
More consistency was seen in the reasons for using medical cannabis. Chronic pain made up 62.2% of all qualifying conditions reported by patients during 1999-2016, with the annual average varying between 33.3% and 73%. Multiple sclerosis spasticity symptoms had the second-highest number of reports over the study period, followed by chemotherapy-induced nausea and vomiting, posttraumatic stress disorder, and cancer, they reported.
The investigators also looked at the appropriateness of cannabis and determined that its use in 85.5% of patient-reported conditions was “supported by conclusive or substantial evidence of therapeutic effectiveness, according to the 2017 National Academies report” on the health effects of cannabis.
“We believe not only that it is inappropriate for cannabis to remain a Schedule I substance, but also that state and federal policy makers should begin evaluating evidence-based ways for safely integrating cannabis research and products into the health care system,” they concluded.
SOURCE: Boehnke KF et al. Health Aff. 2019;38(2):295-302.
More people are using medical cannabis as it becomes legal in more states, but the lack of standardization in states’ data collection hindered investigators’ efforts to track that use.
Legalized medical cannabis is now available in 33 states and the District of Columbia, and the number of users has risen from just over 72,000 in 2009 to almost 814,000 in 2017. That 814,000, however, covers only 16 states and D.C., since 1 state (Connecticut) does not publish reports on medical cannabis use, 12 did not have statistics available, 2 (New York and Vermont) didn’t report data for 2017, and 2 (California and Maine) have voluntary registries that are unlikely to be accurate, according to Kevin F. Boehnke, PhD, of the University of Michigan, Ann Arbor, and his associates.
Michigan had the largest reported number of patients enrolled in its medical cannabis program in 2017, almost 270,000. California – the state with the oldest medical cannabis legislation (passed in 1996) and the largest overall population but a voluntary cannabis registry – reported its highest number of enrollees, 12,659, in 2009-2010, the investigators said. Colorado had more than 116,000 patients in its medical cannabis program in 2010 (Health Aff. 2019;38[2]:295-302).
The “many inconsistencies in data quality across states [suggest] the need for further standardization of data collection. Such standardization would add transparency to understanding how medical cannabis programs are used, which would help guide both research and policy needs,” Dr. Boehnke and his associates wrote.
More consistency was seen in the reasons for using medical cannabis. Chronic pain made up 62.2% of all qualifying conditions reported by patients during 1999-2016, with the annual average varying between 33.3% and 73%. Multiple sclerosis spasticity symptoms had the second-highest number of reports over the study period, followed by chemotherapy-induced nausea and vomiting, posttraumatic stress disorder, and cancer, they reported.
The investigators also looked at the appropriateness of cannabis and determined that its use in 85.5% of patient-reported conditions was “supported by conclusive or substantial evidence of therapeutic effectiveness, according to the 2017 National Academies report” on the health effects of cannabis.
“We believe not only that it is inappropriate for cannabis to remain a Schedule I substance, but also that state and federal policy makers should begin evaluating evidence-based ways for safely integrating cannabis research and products into the health care system,” they concluded.
SOURCE: Boehnke KF et al. Health Aff. 2019;38(2):295-302.
More people are using medical cannabis as it becomes legal in more states, but the lack of standardization in states’ data collection hindered investigators’ efforts to track that use.
Legalized medical cannabis is now available in 33 states and the District of Columbia, and the number of users has risen from just over 72,000 in 2009 to almost 814,000 in 2017. That 814,000, however, covers only 16 states and D.C., since 1 state (Connecticut) does not publish reports on medical cannabis use, 12 did not have statistics available, 2 (New York and Vermont) didn’t report data for 2017, and 2 (California and Maine) have voluntary registries that are unlikely to be accurate, according to Kevin F. Boehnke, PhD, of the University of Michigan, Ann Arbor, and his associates.
Michigan had the largest reported number of patients enrolled in its medical cannabis program in 2017, almost 270,000. California – the state with the oldest medical cannabis legislation (passed in 1996) and the largest overall population but a voluntary cannabis registry – reported its highest number of enrollees, 12,659, in 2009-2010, the investigators said. Colorado had more than 116,000 patients in its medical cannabis program in 2010 (Health Aff. 2019;38[2]:295-302).
The “many inconsistencies in data quality across states [suggest] the need for further standardization of data collection. Such standardization would add transparency to understanding how medical cannabis programs are used, which would help guide both research and policy needs,” Dr. Boehnke and his associates wrote.
More consistency was seen in the reasons for using medical cannabis. Chronic pain made up 62.2% of all qualifying conditions reported by patients during 1999-2016, with the annual average varying between 33.3% and 73%. Multiple sclerosis spasticity symptoms had the second-highest number of reports over the study period, followed by chemotherapy-induced nausea and vomiting, posttraumatic stress disorder, and cancer, they reported.
The investigators also looked at the appropriateness of cannabis and determined that its use in 85.5% of patient-reported conditions was “supported by conclusive or substantial evidence of therapeutic effectiveness, according to the 2017 National Academies report” on the health effects of cannabis.
“We believe not only that it is inappropriate for cannabis to remain a Schedule I substance, but also that state and federal policy makers should begin evaluating evidence-based ways for safely integrating cannabis research and products into the health care system,” they concluded.
SOURCE: Boehnke KF et al. Health Aff. 2019;38(2):295-302.
FROM HEALTH AFFAIRS
Novel plasma biomarkers may predict preclinical Alzheimer’s disease
, researchers reported in Science Advances.
“To our knowledge, this is the first time that a multianalyte plasma biomarker panel for an Alzheimer’s disease–related phenotype has been found and independently replicated by a nontargeted mass spectrometry approach,” said Nicholas J. Ashton, PhD, of King’s College London and the University of Gothenburg in Sweden, and his research colleagues.
Blood-based measures that predict amyloid-beta burden in preclinical Alzheimer’s disease have the potential to help investigators conduct clinical trials and aid in diagnostic management. However, this novel approach needs to be validated and translated “to a simpler automated platform suitable for wider utility,” the investigators noted. In addition, it is unclear whether their classifier can track changes in amyloid-beta or differentiate between other diseases with amyloid-beta pathology.
Advances in mass spectrometry technology have renewed interest in the analysis of plasma proteins in patients with various diseases. To assess whether proteomic discovery in plasma can help predict amyloid-beta burden in preclinical Alzheimer’s disease, Dr. Ashton and his colleagues studied 238 cognitively unimpaired individuals from the Australian Imaging, Biomarker and Lifestyle Flagship Study of Ageing (AIBL) and the Kerr Anglican Retirement Village Initiative in Ageing Health (KARVIAH). The participants had undergone PET to determine their amyloid-beta status. In the AIBL cohort (n = 144), 100 participants were amyloid-beta negative, and 44 were amyloid-beta positive. In the KARVIAH cohort (n = 94), 59 participants were amyloid-beta negative, and 35 were amyloid-beta positive. There were significantly more APOE4 carriers in the amyloid-beta–positive groups than in the amyloid-beta–negative groups. In addition, the amyloid-beta–positive groups tended to be older.
A support vector machine analysis created classifiers predicting amyloid-beta positivity in the AIBL cohort using demographics, proteins, or both. The researchers then tested each classifier in the KARVIAH dataset to identify which model best predicted amyloid-beta positivity. The optimal model included 10 protein features (prothrombin, adhesion G protein–coupled receptor, amyloid-beta A4 protein, NGN2, DNAH10, REST, NfL, RPS6KA3, GPSM2, FHAD1) and two demographic features (APOE4 count and age).
The classifier achieved a testing area under the receiver operator characteristic curve of 0.891 in the KARVIAH cohort to predict amyloid-beta positivity in cognitively unimpaired individuals with a sensitivity of 0.78 and specificity of 0.77.
The 10 protein features “represent a diverse array of pathways,” and the highest ranked feature was the serine protease prothrombin, which is a precursor to thrombin, the authors noted. “Multiple lines of evidence support that cerebrovascular disease may play a role in AD and that amyloid-beta may be involved in thrombosis, fibrinolysis, and inflammation via its interaction with the coagulation cascade,” the researchers wrote.
Two of the biomarkers – amyloid-beta A4 protein and NfL – have been examined in prior research and had a greater effect size in a secondary analysis that included participants with mild cognitive impairment and Alzheimer’s disease. This finding confirms “their connection with the more established disease state,” Dr. Ashton and colleagues said. In the secondary analysis, the optimal classifier included one demographic factor (APOE4 count) and nine protein features, eight of which also were used in the cognitively unimpaired classifier.
The study was funded in part by the National Institute for Health Research Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London, and many authors reported additional research support from various institutions. One author is an employee of Johnson & Johnson and a named inventor on unrelated biomarker intellectual property owned by Proteome Science and King’s College London.
SOURCE: Ashton NJ et al. Sci Adv. 2019 Feb 6. doi: 10.1126/sciadv.aau7220.
, researchers reported in Science Advances.
“To our knowledge, this is the first time that a multianalyte plasma biomarker panel for an Alzheimer’s disease–related phenotype has been found and independently replicated by a nontargeted mass spectrometry approach,” said Nicholas J. Ashton, PhD, of King’s College London and the University of Gothenburg in Sweden, and his research colleagues.
Blood-based measures that predict amyloid-beta burden in preclinical Alzheimer’s disease have the potential to help investigators conduct clinical trials and aid in diagnostic management. However, this novel approach needs to be validated and translated “to a simpler automated platform suitable for wider utility,” the investigators noted. In addition, it is unclear whether their classifier can track changes in amyloid-beta or differentiate between other diseases with amyloid-beta pathology.
Advances in mass spectrometry technology have renewed interest in the analysis of plasma proteins in patients with various diseases. To assess whether proteomic discovery in plasma can help predict amyloid-beta burden in preclinical Alzheimer’s disease, Dr. Ashton and his colleagues studied 238 cognitively unimpaired individuals from the Australian Imaging, Biomarker and Lifestyle Flagship Study of Ageing (AIBL) and the Kerr Anglican Retirement Village Initiative in Ageing Health (KARVIAH). The participants had undergone PET to determine their amyloid-beta status. In the AIBL cohort (n = 144), 100 participants were amyloid-beta negative, and 44 were amyloid-beta positive. In the KARVIAH cohort (n = 94), 59 participants were amyloid-beta negative, and 35 were amyloid-beta positive. There were significantly more APOE4 carriers in the amyloid-beta–positive groups than in the amyloid-beta–negative groups. In addition, the amyloid-beta–positive groups tended to be older.
A support vector machine analysis created classifiers predicting amyloid-beta positivity in the AIBL cohort using demographics, proteins, or both. The researchers then tested each classifier in the KARVIAH dataset to identify which model best predicted amyloid-beta positivity. The optimal model included 10 protein features (prothrombin, adhesion G protein–coupled receptor, amyloid-beta A4 protein, NGN2, DNAH10, REST, NfL, RPS6KA3, GPSM2, FHAD1) and two demographic features (APOE4 count and age).
The classifier achieved a testing area under the receiver operator characteristic curve of 0.891 in the KARVIAH cohort to predict amyloid-beta positivity in cognitively unimpaired individuals with a sensitivity of 0.78 and specificity of 0.77.
The 10 protein features “represent a diverse array of pathways,” and the highest ranked feature was the serine protease prothrombin, which is a precursor to thrombin, the authors noted. “Multiple lines of evidence support that cerebrovascular disease may play a role in AD and that amyloid-beta may be involved in thrombosis, fibrinolysis, and inflammation via its interaction with the coagulation cascade,” the researchers wrote.
Two of the biomarkers – amyloid-beta A4 protein and NfL – have been examined in prior research and had a greater effect size in a secondary analysis that included participants with mild cognitive impairment and Alzheimer’s disease. This finding confirms “their connection with the more established disease state,” Dr. Ashton and colleagues said. In the secondary analysis, the optimal classifier included one demographic factor (APOE4 count) and nine protein features, eight of which also were used in the cognitively unimpaired classifier.
The study was funded in part by the National Institute for Health Research Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London, and many authors reported additional research support from various institutions. One author is an employee of Johnson & Johnson and a named inventor on unrelated biomarker intellectual property owned by Proteome Science and King’s College London.
SOURCE: Ashton NJ et al. Sci Adv. 2019 Feb 6. doi: 10.1126/sciadv.aau7220.
, researchers reported in Science Advances.
“To our knowledge, this is the first time that a multianalyte plasma biomarker panel for an Alzheimer’s disease–related phenotype has been found and independently replicated by a nontargeted mass spectrometry approach,” said Nicholas J. Ashton, PhD, of King’s College London and the University of Gothenburg in Sweden, and his research colleagues.
Blood-based measures that predict amyloid-beta burden in preclinical Alzheimer’s disease have the potential to help investigators conduct clinical trials and aid in diagnostic management. However, this novel approach needs to be validated and translated “to a simpler automated platform suitable for wider utility,” the investigators noted. In addition, it is unclear whether their classifier can track changes in amyloid-beta or differentiate between other diseases with amyloid-beta pathology.
Advances in mass spectrometry technology have renewed interest in the analysis of plasma proteins in patients with various diseases. To assess whether proteomic discovery in plasma can help predict amyloid-beta burden in preclinical Alzheimer’s disease, Dr. Ashton and his colleagues studied 238 cognitively unimpaired individuals from the Australian Imaging, Biomarker and Lifestyle Flagship Study of Ageing (AIBL) and the Kerr Anglican Retirement Village Initiative in Ageing Health (KARVIAH). The participants had undergone PET to determine their amyloid-beta status. In the AIBL cohort (n = 144), 100 participants were amyloid-beta negative, and 44 were amyloid-beta positive. In the KARVIAH cohort (n = 94), 59 participants were amyloid-beta negative, and 35 were amyloid-beta positive. There were significantly more APOE4 carriers in the amyloid-beta–positive groups than in the amyloid-beta–negative groups. In addition, the amyloid-beta–positive groups tended to be older.
A support vector machine analysis created classifiers predicting amyloid-beta positivity in the AIBL cohort using demographics, proteins, or both. The researchers then tested each classifier in the KARVIAH dataset to identify which model best predicted amyloid-beta positivity. The optimal model included 10 protein features (prothrombin, adhesion G protein–coupled receptor, amyloid-beta A4 protein, NGN2, DNAH10, REST, NfL, RPS6KA3, GPSM2, FHAD1) and two demographic features (APOE4 count and age).
The classifier achieved a testing area under the receiver operator characteristic curve of 0.891 in the KARVIAH cohort to predict amyloid-beta positivity in cognitively unimpaired individuals with a sensitivity of 0.78 and specificity of 0.77.
The 10 protein features “represent a diverse array of pathways,” and the highest ranked feature was the serine protease prothrombin, which is a precursor to thrombin, the authors noted. “Multiple lines of evidence support that cerebrovascular disease may play a role in AD and that amyloid-beta may be involved in thrombosis, fibrinolysis, and inflammation via its interaction with the coagulation cascade,” the researchers wrote.
Two of the biomarkers – amyloid-beta A4 protein and NfL – have been examined in prior research and had a greater effect size in a secondary analysis that included participants with mild cognitive impairment and Alzheimer’s disease. This finding confirms “their connection with the more established disease state,” Dr. Ashton and colleagues said. In the secondary analysis, the optimal classifier included one demographic factor (APOE4 count) and nine protein features, eight of which also were used in the cognitively unimpaired classifier.
The study was funded in part by the National Institute for Health Research Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London, and many authors reported additional research support from various institutions. One author is an employee of Johnson & Johnson and a named inventor on unrelated biomarker intellectual property owned by Proteome Science and King’s College London.
SOURCE: Ashton NJ et al. Sci Adv. 2019 Feb 6. doi: 10.1126/sciadv.aau7220.
FROM SCIENCE ADVANCES
Key clinical point: Blood-based measures that predict amyloid-beta burden in preclinical Alzheimer’s disease have the potential to help investigators conduct clinical trials and aid in diagnostic management.
Major finding: A classifier developed using plasma proteomic analysis achieved an area under the receiver operator characteristic curve of 0.891.
Study details: An analysis of data from 238 cognitively unimpaired individuals from the Australian Imaging, Biomarker and Lifestyle Flagship Study of Ageing (AIBL) and the Kerr Anglican Retirement Village Initiative in Ageing Health (KARVIAH).
Disclosures: The study was funded in part by the National Institute for Health Research Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London, and many authors reported additional research support from various institutions. One author is an employee of Johnson & Johnson and a named inventor on unrelated biomarker intellectual property owned by Proteome Science and King’s College London.
Source: Ashton NJ et al. Sci Adv. 2019 Feb 6. doi: 10.1126/sciadv.aau7220.
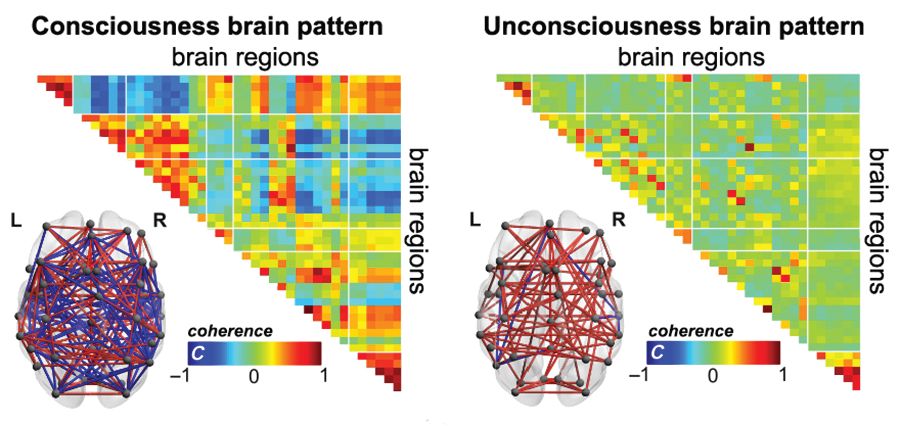
Functional MRI detects consciousness after brain damage
Functional MRI can measure patterns of connectivity to determine levels of consciousness in nonresponsive patients with brain injury, according to results from a multicenter, cross-sectional, observational study.
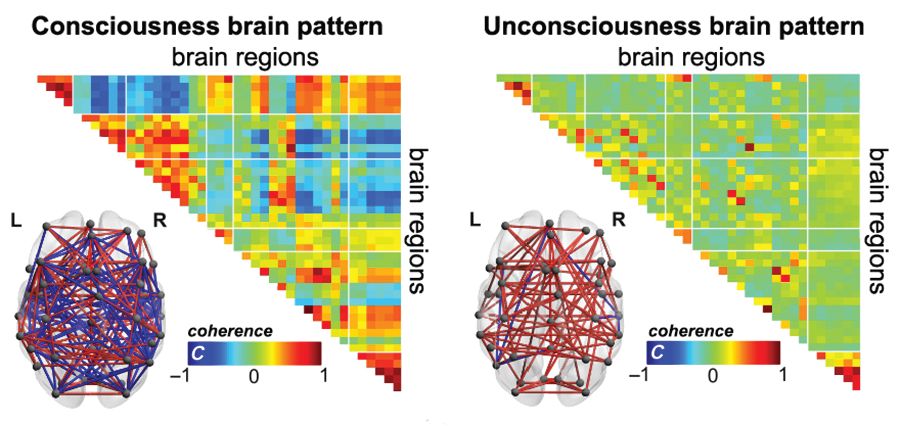
Blood oxygen level–dependent (BOLD) fMRI showed that brain-wide coordination patterns of high complexity became increasingly common moving from unresponsive patients to those with minimal consciousness to healthy individuals, reported lead author Athena Demertzi, PhD, of GIGA Research Institute at the University of Liège in Belgium, and her colleagues.
“Finding reliable markers indicating the presence or absence of consciousness represents an outstanding open problem for science,” the investigators wrote in Science Advances.
In medicine, an fMRI-based measure of consciousness could supplement behavioral assessments of awareness and guide therapeutic strategies; more broadly, image-based markers could help elucidate the nature of consciousness itself.
“We postulate that consciousness has specific characteristics that are based on the temporal dynamics of ongoing brain activity and its coordination over distant cortical regions,” the investigators wrote. “Our hypothesis stems from the common stance of various contemporary theories which propose that consciousness relates to a dynamic process of self-sustained, coordinated brain-scale activity assisting the tuning to a constantly evolving environment, rather than in static descriptions of brain function.”
There is a need for a reliable way of distinguishing consciousness from unconscious states, the investigators said. “Given that nonresponsiveness can be associated with a variety of brain lesions, varying levels of vigilance, and covert cognition, we highlight the need to determine a common set of features capable of accounting for the capacity to sustain conscious experience.”
To search for patterns of brain signal coordination that correlate with consciousness, four independent research centers performed BOLD fMRI scans of participants at rest or under anesthesia with propofol. Of 159 total participants, 47 were healthy individuals and 112 were patients in a vegetative state/with unresponsive wakefulness syndrome (UWS) or in a minimally conscious state (MCS), based on standardized behavioral assessments. The main data analysis, which included 125 participants, assessed BOLD fMRI signal coordination between six brain networks known to have roles in cognitive and functional processes.
The researchers’ analysis revealed four distinct and recurring brain-wide coordination patterns ranging on a scale from highest activity (pattern 1) to lowest activity (pattern 4). Pattern 1, which exhibited most long-distance edges, spatial complexity, efficiency, and community structure, became increasingly common when moving from UWS patients to MCS patients to healthy control individuals (UWS < MCS < HC, rho = 0.7, Spearman rank correlation between rate and group, P less than 1 x 10-16).
In contrast, pattern 4, characterized by low interareal coordination, showed an inverse trend; it became less common when moving from vegetative patients to healthy individuals (UWS > MCS > HC, Spearman rank correlation between rate and group, rho = –0.6, P less than 1 x 10-11). Although patterns 2 and 3 occurred with equal frequency across all groups, the investigators noted that switching between patterns was most common and predictably sequential in healthy individuals, versus patients with UWS, who were least likely to switch patterns. A total of 23 patients who were scanned under propofol anesthesia were equally likely to exhibit pattern 4, regardless of health status, suggesting that pattern 4 depends upon fixed anatomical pathways. Results were not affected by scanning site or other patient characteristics, such as age, gender, etiology, or chronicity.
“We conclude that these patterns of transient brain signal coordination are characteristic of conscious and unconscious brain states,” the investigators wrote, “warranting future research concerning their relationship to ongoing conscious content, and the possibility of modifying their prevalence by external perturbations, both in healthy and pathological individuals, as well as across species.”
The study was funded by a James S. McDonnell Foundation Collaborative Activity Award, INSERM, the Belgian National Funds for Scientific Research, the Canada Excellence Research Chairs program, and others. The authors declared having no conflicts of interest.
SOURCE: Demertzi A et al. Sci Adv. 2019 Feb 6. doi: 10.1126/sciadv.aat7603.
Functional MRI can measure patterns of connectivity to determine levels of consciousness in nonresponsive patients with brain injury, according to results from a multicenter, cross-sectional, observational study.
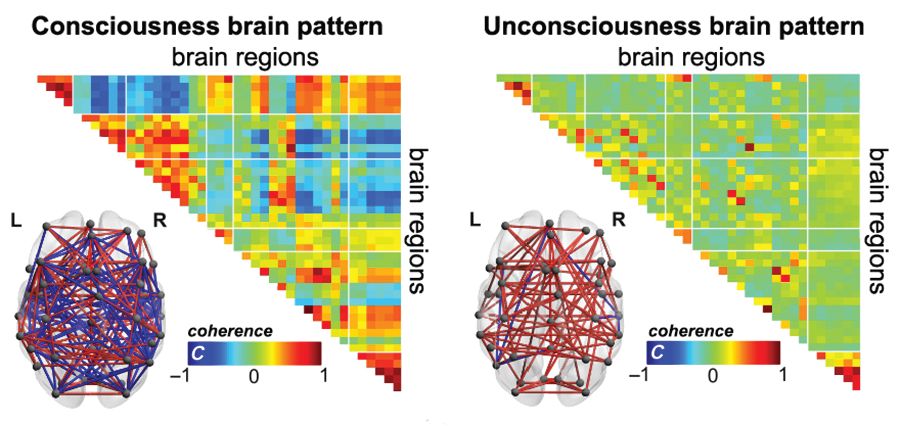
Blood oxygen level–dependent (BOLD) fMRI showed that brain-wide coordination patterns of high complexity became increasingly common moving from unresponsive patients to those with minimal consciousness to healthy individuals, reported lead author Athena Demertzi, PhD, of GIGA Research Institute at the University of Liège in Belgium, and her colleagues.
“Finding reliable markers indicating the presence or absence of consciousness represents an outstanding open problem for science,” the investigators wrote in Science Advances.
In medicine, an fMRI-based measure of consciousness could supplement behavioral assessments of awareness and guide therapeutic strategies; more broadly, image-based markers could help elucidate the nature of consciousness itself.
“We postulate that consciousness has specific characteristics that are based on the temporal dynamics of ongoing brain activity and its coordination over distant cortical regions,” the investigators wrote. “Our hypothesis stems from the common stance of various contemporary theories which propose that consciousness relates to a dynamic process of self-sustained, coordinated brain-scale activity assisting the tuning to a constantly evolving environment, rather than in static descriptions of brain function.”
There is a need for a reliable way of distinguishing consciousness from unconscious states, the investigators said. “Given that nonresponsiveness can be associated with a variety of brain lesions, varying levels of vigilance, and covert cognition, we highlight the need to determine a common set of features capable of accounting for the capacity to sustain conscious experience.”
To search for patterns of brain signal coordination that correlate with consciousness, four independent research centers performed BOLD fMRI scans of participants at rest or under anesthesia with propofol. Of 159 total participants, 47 were healthy individuals and 112 were patients in a vegetative state/with unresponsive wakefulness syndrome (UWS) or in a minimally conscious state (MCS), based on standardized behavioral assessments. The main data analysis, which included 125 participants, assessed BOLD fMRI signal coordination between six brain networks known to have roles in cognitive and functional processes.
The researchers’ analysis revealed four distinct and recurring brain-wide coordination patterns ranging on a scale from highest activity (pattern 1) to lowest activity (pattern 4). Pattern 1, which exhibited most long-distance edges, spatial complexity, efficiency, and community structure, became increasingly common when moving from UWS patients to MCS patients to healthy control individuals (UWS < MCS < HC, rho = 0.7, Spearman rank correlation between rate and group, P less than 1 x 10-16).
In contrast, pattern 4, characterized by low interareal coordination, showed an inverse trend; it became less common when moving from vegetative patients to healthy individuals (UWS > MCS > HC, Spearman rank correlation between rate and group, rho = –0.6, P less than 1 x 10-11). Although patterns 2 and 3 occurred with equal frequency across all groups, the investigators noted that switching between patterns was most common and predictably sequential in healthy individuals, versus patients with UWS, who were least likely to switch patterns. A total of 23 patients who were scanned under propofol anesthesia were equally likely to exhibit pattern 4, regardless of health status, suggesting that pattern 4 depends upon fixed anatomical pathways. Results were not affected by scanning site or other patient characteristics, such as age, gender, etiology, or chronicity.
“We conclude that these patterns of transient brain signal coordination are characteristic of conscious and unconscious brain states,” the investigators wrote, “warranting future research concerning their relationship to ongoing conscious content, and the possibility of modifying their prevalence by external perturbations, both in healthy and pathological individuals, as well as across species.”
The study was funded by a James S. McDonnell Foundation Collaborative Activity Award, INSERM, the Belgian National Funds for Scientific Research, the Canada Excellence Research Chairs program, and others. The authors declared having no conflicts of interest.
SOURCE: Demertzi A et al. Sci Adv. 2019 Feb 6. doi: 10.1126/sciadv.aat7603.
Functional MRI can measure patterns of connectivity to determine levels of consciousness in nonresponsive patients with brain injury, according to results from a multicenter, cross-sectional, observational study.
Blood oxygen level–dependent (BOLD) fMRI showed that brain-wide coordination patterns of high complexity became increasingly common moving from unresponsive patients to those with minimal consciousness to healthy individuals, reported lead author Athena Demertzi, PhD, of GIGA Research Institute at the University of Liège in Belgium, and her colleagues.
“Finding reliable markers indicating the presence or absence of consciousness represents an outstanding open problem for science,” the investigators wrote in Science Advances.
In medicine, an fMRI-based measure of consciousness could supplement behavioral assessments of awareness and guide therapeutic strategies; more broadly, image-based markers could help elucidate the nature of consciousness itself.
“We postulate that consciousness has specific characteristics that are based on the temporal dynamics of ongoing brain activity and its coordination over distant cortical regions,” the investigators wrote. “Our hypothesis stems from the common stance of various contemporary theories which propose that consciousness relates to a dynamic process of self-sustained, coordinated brain-scale activity assisting the tuning to a constantly evolving environment, rather than in static descriptions of brain function.”
There is a need for a reliable way of distinguishing consciousness from unconscious states, the investigators said. “Given that nonresponsiveness can be associated with a variety of brain lesions, varying levels of vigilance, and covert cognition, we highlight the need to determine a common set of features capable of accounting for the capacity to sustain conscious experience.”
To search for patterns of brain signal coordination that correlate with consciousness, four independent research centers performed BOLD fMRI scans of participants at rest or under anesthesia with propofol. Of 159 total participants, 47 were healthy individuals and 112 were patients in a vegetative state/with unresponsive wakefulness syndrome (UWS) or in a minimally conscious state (MCS), based on standardized behavioral assessments. The main data analysis, which included 125 participants, assessed BOLD fMRI signal coordination between six brain networks known to have roles in cognitive and functional processes.
The researchers’ analysis revealed four distinct and recurring brain-wide coordination patterns ranging on a scale from highest activity (pattern 1) to lowest activity (pattern 4). Pattern 1, which exhibited most long-distance edges, spatial complexity, efficiency, and community structure, became increasingly common when moving from UWS patients to MCS patients to healthy control individuals (UWS < MCS < HC, rho = 0.7, Spearman rank correlation between rate and group, P less than 1 x 10-16).
In contrast, pattern 4, characterized by low interareal coordination, showed an inverse trend; it became less common when moving from vegetative patients to healthy individuals (UWS > MCS > HC, Spearman rank correlation between rate and group, rho = –0.6, P less than 1 x 10-11). Although patterns 2 and 3 occurred with equal frequency across all groups, the investigators noted that switching between patterns was most common and predictably sequential in healthy individuals, versus patients with UWS, who were least likely to switch patterns. A total of 23 patients who were scanned under propofol anesthesia were equally likely to exhibit pattern 4, regardless of health status, suggesting that pattern 4 depends upon fixed anatomical pathways. Results were not affected by scanning site or other patient characteristics, such as age, gender, etiology, or chronicity.
“We conclude that these patterns of transient brain signal coordination are characteristic of conscious and unconscious brain states,” the investigators wrote, “warranting future research concerning their relationship to ongoing conscious content, and the possibility of modifying their prevalence by external perturbations, both in healthy and pathological individuals, as well as across species.”
The study was funded by a James S. McDonnell Foundation Collaborative Activity Award, INSERM, the Belgian National Funds for Scientific Research, the Canada Excellence Research Chairs program, and others. The authors declared having no conflicts of interest.
SOURCE: Demertzi A et al. Sci Adv. 2019 Feb 6. doi: 10.1126/sciadv.aat7603.
FROM SCIENCE ADVANCES
Key clinical point:
Major finding: A brain-wide coordination pattern of high complexity became increasingly common when moving from patients with unresponsive wakefulness syndrome (UWS) to patients in a minimally conscious state (MCS) to healthy control individuals.
Study details: A study involving blood oxygen level–dependent (BOLD) fMRI scans at rest or under anesthesia in 159 participants at four independent research facilities.
Disclosures: The study was funded by a James S. McDonnell Foundation Collaborative Activity Award, INSERM, the Belgian National Funds for Scientific Research, the Canada Excellence Research Chairs program, and others. The authors declared having no conflicts of interest.
Source: Demertzi A et al. Sci Adv. 2019 Feb 6. doi: 10.1126/sciadv.aat7603.
Michigan Medicine launches effort to make wellness a cultural norm
CORONADO, CALIF. – Officials at staff, and learners.
“If you look long and hard at your hospitals, health centers, and medical schools, you would find incidences of depression, near-miss suicide, opioid addiction, substance abuse addictions, and suicide,” Carol R. Bradford, MD, said at the Triological Society’s Combined Sections Meeting. “Another component of this is that we all struggle with our work or learning communities where people don’t take care of each other. People don’t treat each other with respect and civility. Promoting a healthy and civil work environment are essential components of a supportive environment.”
According to Dr. Bradford, executive vice dean for academic affairs at the University of Michigan, Ann Arbor, the complexities and stress of the health care environment compromises the well-being of its workforce with a myriad of time-consuming tasks, including navigating electronic records and ever-populating email inboxes. “We are all connected to devices 24/7, and it has become more and more difficult to maintain a healthy work-life balance,” Dr. Bradford said. “The more accepted term now is integration, because it’s almost impossible to achieve balance. Burnout and other physical and health problems are the result of all of these challenges.”
In late 2017, she and her colleagues used two different validated survey questionnaires to assess the health of Michigan Medicine faculty physicians. They found that about 40% of faculty members in both clinical and basic science departments met criteria for burnout. The top 10 stressors based on the survey were email, clerical activity, time worked outside of regular hours, workload time pressure, work expectations, insufficient time for meaningful activities, in-basket messages, lack of decisional transparency, inadequate compensation, and too many work hours. The top 10 coping strategies were finding meaning in work, using all vacation time, paying attention to healthy/balanced eating, engaging in exercise, seek personal/professional balance, protecting time away from work, protecting sleep time, using a social support network, nurturing spiritual aspects, and engaging in recreation or hobbies.
Results of the survey prompted development of a task force to examine wellness and civility at Michigan Medicine, and to devise strategies and tactics to conquer these challenges. “The goal is to help all human beings who are suffering in our work environment,” said Dr. Bradford, who is also chief academic officer for Michigan Medicine. “What we learned initially is that there is a bit of an overlap. Some lack of wellness is due to a lack of civility, but there are wellness issues and civility issues that are independent of one another.”
Members of the task force formulated several recommendations, the first being to create a Michigan Medicine Wellness Office. Dr. Bradford is currently negotiating with a finalist to serve as its faculty director. She characterized the office as a “hub and spoke” model that will partner with existing entities, including human resources, the office of medical student education, the program in biological sciences, graduate medical education, the office of health equality and inclusion, the office of clinical affairs, and the office of counseling and workplace resilience. “The idea is to create a strategic wellness plan,” said Dr. Bradford, who is also a professor of otolaryngology–head and neck surgery. “One key strategy is to endorse the health and well-being of our faculty, staff, and learners as a core value and cultural norm of Michigan Medicine. In other words, the leadership has to make health and well-being a priority and a value.”
Another goal of the office is to improve the overall workplace environment and experience of Michigan Medicine’s faculty, staff, and learners. “You’re not going to have a well workplace if people are not treating each other with respect,” she said at the meeting, jointly sponsored by the Triological Society and the American College of Surgeons. “One of the many challenges is that there is great stigma in our profession for those who are suffering from mental health challenges such as stress, anxiety, depression, and perhaps substance abuse. We need to reduce the stigma, because it’s very dangerous if people who are struggling are unwilling to seek help. We don’t ask people that we supervise or work with how they’re doing, so we have adopted an optional wellness check-in that is incorporated into mid-year and annual evaluations for faculty, staff, and learners to enable leaders to address any challenges that may arise.” In addition, a group of residents is piloting the use of meditation and mindfulness applications such as MoodGym and Headspace to see if they affect resident wellness.
Ultimately, Dr. Bradford and her associates plan to use a standardized benchmark instrument to measure well-being, and include the measure in the institutional performance dashboard. “Administrative burden is a growing problem,” she said. “We’re going to address this for health care professionals, particularly as it relates to the electronic medical record. Our primary care colleagues sometimes spend as many hours outside of clinic documenting as they do in clinic. We want to develop and implement strategies to lessen or remove this burden in order to improve provider efficiency and satisfaction.”
In the course of helping to develop the wellness initiative, Dr. Bradford said that she learned the importance of addressing moral distress in the workplace. “We sort of lose our humanity if we don’t show emotion when tragedies happen. There is really good literature around terminal event debriefings, so if somebody dies unexpectedly in the operating room or in the CT scanner, rather than just walking away and pretending nothing happened, we’re supposed to pause and gather, and reflect on the sadness of the loss. Because if we don’t grieve our losses we become more like machines than human beings. It’s important to provide emotional support for all individuals involved.”
She reported having no relevant financial disclosures.
CORONADO, CALIF. – Officials at staff, and learners.
“If you look long and hard at your hospitals, health centers, and medical schools, you would find incidences of depression, near-miss suicide, opioid addiction, substance abuse addictions, and suicide,” Carol R. Bradford, MD, said at the Triological Society’s Combined Sections Meeting. “Another component of this is that we all struggle with our work or learning communities where people don’t take care of each other. People don’t treat each other with respect and civility. Promoting a healthy and civil work environment are essential components of a supportive environment.”
According to Dr. Bradford, executive vice dean for academic affairs at the University of Michigan, Ann Arbor, the complexities and stress of the health care environment compromises the well-being of its workforce with a myriad of time-consuming tasks, including navigating electronic records and ever-populating email inboxes. “We are all connected to devices 24/7, and it has become more and more difficult to maintain a healthy work-life balance,” Dr. Bradford said. “The more accepted term now is integration, because it’s almost impossible to achieve balance. Burnout and other physical and health problems are the result of all of these challenges.”
In late 2017, she and her colleagues used two different validated survey questionnaires to assess the health of Michigan Medicine faculty physicians. They found that about 40% of faculty members in both clinical and basic science departments met criteria for burnout. The top 10 stressors based on the survey were email, clerical activity, time worked outside of regular hours, workload time pressure, work expectations, insufficient time for meaningful activities, in-basket messages, lack of decisional transparency, inadequate compensation, and too many work hours. The top 10 coping strategies were finding meaning in work, using all vacation time, paying attention to healthy/balanced eating, engaging in exercise, seek personal/professional balance, protecting time away from work, protecting sleep time, using a social support network, nurturing spiritual aspects, and engaging in recreation or hobbies.
Results of the survey prompted development of a task force to examine wellness and civility at Michigan Medicine, and to devise strategies and tactics to conquer these challenges. “The goal is to help all human beings who are suffering in our work environment,” said Dr. Bradford, who is also chief academic officer for Michigan Medicine. “What we learned initially is that there is a bit of an overlap. Some lack of wellness is due to a lack of civility, but there are wellness issues and civility issues that are independent of one another.”
Members of the task force formulated several recommendations, the first being to create a Michigan Medicine Wellness Office. Dr. Bradford is currently negotiating with a finalist to serve as its faculty director. She characterized the office as a “hub and spoke” model that will partner with existing entities, including human resources, the office of medical student education, the program in biological sciences, graduate medical education, the office of health equality and inclusion, the office of clinical affairs, and the office of counseling and workplace resilience. “The idea is to create a strategic wellness plan,” said Dr. Bradford, who is also a professor of otolaryngology–head and neck surgery. “One key strategy is to endorse the health and well-being of our faculty, staff, and learners as a core value and cultural norm of Michigan Medicine. In other words, the leadership has to make health and well-being a priority and a value.”
Another goal of the office is to improve the overall workplace environment and experience of Michigan Medicine’s faculty, staff, and learners. “You’re not going to have a well workplace if people are not treating each other with respect,” she said at the meeting, jointly sponsored by the Triological Society and the American College of Surgeons. “One of the many challenges is that there is great stigma in our profession for those who are suffering from mental health challenges such as stress, anxiety, depression, and perhaps substance abuse. We need to reduce the stigma, because it’s very dangerous if people who are struggling are unwilling to seek help. We don’t ask people that we supervise or work with how they’re doing, so we have adopted an optional wellness check-in that is incorporated into mid-year and annual evaluations for faculty, staff, and learners to enable leaders to address any challenges that may arise.” In addition, a group of residents is piloting the use of meditation and mindfulness applications such as MoodGym and Headspace to see if they affect resident wellness.
Ultimately, Dr. Bradford and her associates plan to use a standardized benchmark instrument to measure well-being, and include the measure in the institutional performance dashboard. “Administrative burden is a growing problem,” she said. “We’re going to address this for health care professionals, particularly as it relates to the electronic medical record. Our primary care colleagues sometimes spend as many hours outside of clinic documenting as they do in clinic. We want to develop and implement strategies to lessen or remove this burden in order to improve provider efficiency and satisfaction.”
In the course of helping to develop the wellness initiative, Dr. Bradford said that she learned the importance of addressing moral distress in the workplace. “We sort of lose our humanity if we don’t show emotion when tragedies happen. There is really good literature around terminal event debriefings, so if somebody dies unexpectedly in the operating room or in the CT scanner, rather than just walking away and pretending nothing happened, we’re supposed to pause and gather, and reflect on the sadness of the loss. Because if we don’t grieve our losses we become more like machines than human beings. It’s important to provide emotional support for all individuals involved.”
She reported having no relevant financial disclosures.
CORONADO, CALIF. – Officials at staff, and learners.
“If you look long and hard at your hospitals, health centers, and medical schools, you would find incidences of depression, near-miss suicide, opioid addiction, substance abuse addictions, and suicide,” Carol R. Bradford, MD, said at the Triological Society’s Combined Sections Meeting. “Another component of this is that we all struggle with our work or learning communities where people don’t take care of each other. People don’t treat each other with respect and civility. Promoting a healthy and civil work environment are essential components of a supportive environment.”
According to Dr. Bradford, executive vice dean for academic affairs at the University of Michigan, Ann Arbor, the complexities and stress of the health care environment compromises the well-being of its workforce with a myriad of time-consuming tasks, including navigating electronic records and ever-populating email inboxes. “We are all connected to devices 24/7, and it has become more and more difficult to maintain a healthy work-life balance,” Dr. Bradford said. “The more accepted term now is integration, because it’s almost impossible to achieve balance. Burnout and other physical and health problems are the result of all of these challenges.”
In late 2017, she and her colleagues used two different validated survey questionnaires to assess the health of Michigan Medicine faculty physicians. They found that about 40% of faculty members in both clinical and basic science departments met criteria for burnout. The top 10 stressors based on the survey were email, clerical activity, time worked outside of regular hours, workload time pressure, work expectations, insufficient time for meaningful activities, in-basket messages, lack of decisional transparency, inadequate compensation, and too many work hours. The top 10 coping strategies were finding meaning in work, using all vacation time, paying attention to healthy/balanced eating, engaging in exercise, seek personal/professional balance, protecting time away from work, protecting sleep time, using a social support network, nurturing spiritual aspects, and engaging in recreation or hobbies.
Results of the survey prompted development of a task force to examine wellness and civility at Michigan Medicine, and to devise strategies and tactics to conquer these challenges. “The goal is to help all human beings who are suffering in our work environment,” said Dr. Bradford, who is also chief academic officer for Michigan Medicine. “What we learned initially is that there is a bit of an overlap. Some lack of wellness is due to a lack of civility, but there are wellness issues and civility issues that are independent of one another.”
Members of the task force formulated several recommendations, the first being to create a Michigan Medicine Wellness Office. Dr. Bradford is currently negotiating with a finalist to serve as its faculty director. She characterized the office as a “hub and spoke” model that will partner with existing entities, including human resources, the office of medical student education, the program in biological sciences, graduate medical education, the office of health equality and inclusion, the office of clinical affairs, and the office of counseling and workplace resilience. “The idea is to create a strategic wellness plan,” said Dr. Bradford, who is also a professor of otolaryngology–head and neck surgery. “One key strategy is to endorse the health and well-being of our faculty, staff, and learners as a core value and cultural norm of Michigan Medicine. In other words, the leadership has to make health and well-being a priority and a value.”
Another goal of the office is to improve the overall workplace environment and experience of Michigan Medicine’s faculty, staff, and learners. “You’re not going to have a well workplace if people are not treating each other with respect,” she said at the meeting, jointly sponsored by the Triological Society and the American College of Surgeons. “One of the many challenges is that there is great stigma in our profession for those who are suffering from mental health challenges such as stress, anxiety, depression, and perhaps substance abuse. We need to reduce the stigma, because it’s very dangerous if people who are struggling are unwilling to seek help. We don’t ask people that we supervise or work with how they’re doing, so we have adopted an optional wellness check-in that is incorporated into mid-year and annual evaluations for faculty, staff, and learners to enable leaders to address any challenges that may arise.” In addition, a group of residents is piloting the use of meditation and mindfulness applications such as MoodGym and Headspace to see if they affect resident wellness.
Ultimately, Dr. Bradford and her associates plan to use a standardized benchmark instrument to measure well-being, and include the measure in the institutional performance dashboard. “Administrative burden is a growing problem,” she said. “We’re going to address this for health care professionals, particularly as it relates to the electronic medical record. Our primary care colleagues sometimes spend as many hours outside of clinic documenting as they do in clinic. We want to develop and implement strategies to lessen or remove this burden in order to improve provider efficiency and satisfaction.”
In the course of helping to develop the wellness initiative, Dr. Bradford said that she learned the importance of addressing moral distress in the workplace. “We sort of lose our humanity if we don’t show emotion when tragedies happen. There is really good literature around terminal event debriefings, so if somebody dies unexpectedly in the operating room or in the CT scanner, rather than just walking away and pretending nothing happened, we’re supposed to pause and gather, and reflect on the sadness of the loss. Because if we don’t grieve our losses we become more like machines than human beings. It’s important to provide emotional support for all individuals involved.”
She reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM THE TRIOLOGICAL CSM
President Trump calls for end to HIV/AIDS, pediatric cancer
HIV/AIDS, pediatric cancer research, abortion, prescription drug prices, and preexisting conditions were among the health care highlights of President Donald Trump’s second State of the Union address Feb. 5.

Mr. Trump promised to push for funds to end HIV/AIDS and childhood cancer within in 10 years. “In recent years, we have made remarkable progress in the fight against HIV and AIDS. Scientific breakthroughs have brought a once-distant dream within reach,” he said to assembled members of Congress and leaders of the executive and judicial branches of government. “My budget will ask Democrats and Republicans to make the needed commitment to eliminate the HIV epidemic in the United States within 10 years.”
Following the speech, Alex Azar, secretary of the Department of Health and Human Services, offered more details in a blog post on the agency’s website.
Funding for the initiative, dubbed “Ending the HIV Epidemic: A Plan for America,” will have three components.
The first involves increasing investments in “geographic hotspots” though existing programs like the Ryan White HIV/AIDS Program and a new community health center–based program to provide antiretroviral therapy (ART) and preexposure prophylaxis (PrEP) to those at the highest risk of contracting the disease.
Second is the use of data to track where the disease is spreading most rapidly to help target prevention, care, and treatment at the local level. The third will provide funds for the creation of a local HIV HealthForce in these targeted areas to expand HIV prevention and treatment efforts.
A fact sheet on this initiative called for a 75% reduction in new cases of HIV infection in 5 years and at least a 90% reduction within 10 years.
President Trump called for similar efforts to address pediatric cancer.
“Tonight I am also asking you to join me in another fight that all American can get behind – the fight against childhood cancer,” he said, adding that his budget request will come with a line item of $500 million over 10 years to fund research. “Many childhood cancers have not seen new therapies in decades.”
President Trump also asked Congress to legislate a prohibition of late-term abortion.
“There could be no greater contrast to the beautiful image of a mother holding her infant child than the chilling displays our nation saw in recent days,” he said. “Lawmakers in New York cheered with delight upon the passage of legislation that would allow a baby to be ripped from the mother’s womb moments from birth. These are living, feeling beautiful babies who will never get the chance to share their love and their dreams with the world. ... Let us work together to build a culture that cherishes innocent life.”
He also touched on the recurring themes regarding lowering the cost of health care and prescription drugs, as well as protecting those with preexisting conditions, something he called a major priority.
“It’s unacceptable that Americans pay vastly more than people in other countries for the exact same drugs, often made in the exact same place. This is wrong. This is unfair and together we will stop it, and we will stop it fast,” he said.
He did not offer any specific policy recommendation on how to address prescription drug costs, other than a comment on the need for greater price transparency.
“I am asking Congress to pass legislation that finally takes on the problem of global freeloading and delivers fairness and price transparency for American patients,” he said.
“We should also require drug companies, insurance companies, and hospitals to disclose real prices to foster competition and bring costs way down.”
SOURCE: Trump D. State of the Union Address, Feb. 5, 2019.
HIV/AIDS, pediatric cancer research, abortion, prescription drug prices, and preexisting conditions were among the health care highlights of President Donald Trump’s second State of the Union address Feb. 5.

Mr. Trump promised to push for funds to end HIV/AIDS and childhood cancer within in 10 years. “In recent years, we have made remarkable progress in the fight against HIV and AIDS. Scientific breakthroughs have brought a once-distant dream within reach,” he said to assembled members of Congress and leaders of the executive and judicial branches of government. “My budget will ask Democrats and Republicans to make the needed commitment to eliminate the HIV epidemic in the United States within 10 years.”
Following the speech, Alex Azar, secretary of the Department of Health and Human Services, offered more details in a blog post on the agency’s website.
Funding for the initiative, dubbed “Ending the HIV Epidemic: A Plan for America,” will have three components.
The first involves increasing investments in “geographic hotspots” though existing programs like the Ryan White HIV/AIDS Program and a new community health center–based program to provide antiretroviral therapy (ART) and preexposure prophylaxis (PrEP) to those at the highest risk of contracting the disease.
Second is the use of data to track where the disease is spreading most rapidly to help target prevention, care, and treatment at the local level. The third will provide funds for the creation of a local HIV HealthForce in these targeted areas to expand HIV prevention and treatment efforts.
A fact sheet on this initiative called for a 75% reduction in new cases of HIV infection in 5 years and at least a 90% reduction within 10 years.
President Trump called for similar efforts to address pediatric cancer.
“Tonight I am also asking you to join me in another fight that all American can get behind – the fight against childhood cancer,” he said, adding that his budget request will come with a line item of $500 million over 10 years to fund research. “Many childhood cancers have not seen new therapies in decades.”
President Trump also asked Congress to legislate a prohibition of late-term abortion.
“There could be no greater contrast to the beautiful image of a mother holding her infant child than the chilling displays our nation saw in recent days,” he said. “Lawmakers in New York cheered with delight upon the passage of legislation that would allow a baby to be ripped from the mother’s womb moments from birth. These are living, feeling beautiful babies who will never get the chance to share their love and their dreams with the world. ... Let us work together to build a culture that cherishes innocent life.”
He also touched on the recurring themes regarding lowering the cost of health care and prescription drugs, as well as protecting those with preexisting conditions, something he called a major priority.
“It’s unacceptable that Americans pay vastly more than people in other countries for the exact same drugs, often made in the exact same place. This is wrong. This is unfair and together we will stop it, and we will stop it fast,” he said.
He did not offer any specific policy recommendation on how to address prescription drug costs, other than a comment on the need for greater price transparency.
“I am asking Congress to pass legislation that finally takes on the problem of global freeloading and delivers fairness and price transparency for American patients,” he said.
“We should also require drug companies, insurance companies, and hospitals to disclose real prices to foster competition and bring costs way down.”
SOURCE: Trump D. State of the Union Address, Feb. 5, 2019.
HIV/AIDS, pediatric cancer research, abortion, prescription drug prices, and preexisting conditions were among the health care highlights of President Donald Trump’s second State of the Union address Feb. 5.

Mr. Trump promised to push for funds to end HIV/AIDS and childhood cancer within in 10 years. “In recent years, we have made remarkable progress in the fight against HIV and AIDS. Scientific breakthroughs have brought a once-distant dream within reach,” he said to assembled members of Congress and leaders of the executive and judicial branches of government. “My budget will ask Democrats and Republicans to make the needed commitment to eliminate the HIV epidemic in the United States within 10 years.”
Following the speech, Alex Azar, secretary of the Department of Health and Human Services, offered more details in a blog post on the agency’s website.
Funding for the initiative, dubbed “Ending the HIV Epidemic: A Plan for America,” will have three components.
The first involves increasing investments in “geographic hotspots” though existing programs like the Ryan White HIV/AIDS Program and a new community health center–based program to provide antiretroviral therapy (ART) and preexposure prophylaxis (PrEP) to those at the highest risk of contracting the disease.
Second is the use of data to track where the disease is spreading most rapidly to help target prevention, care, and treatment at the local level. The third will provide funds for the creation of a local HIV HealthForce in these targeted areas to expand HIV prevention and treatment efforts.
A fact sheet on this initiative called for a 75% reduction in new cases of HIV infection in 5 years and at least a 90% reduction within 10 years.
President Trump called for similar efforts to address pediatric cancer.
“Tonight I am also asking you to join me in another fight that all American can get behind – the fight against childhood cancer,” he said, adding that his budget request will come with a line item of $500 million over 10 years to fund research. “Many childhood cancers have not seen new therapies in decades.”
President Trump also asked Congress to legislate a prohibition of late-term abortion.
“There could be no greater contrast to the beautiful image of a mother holding her infant child than the chilling displays our nation saw in recent days,” he said. “Lawmakers in New York cheered with delight upon the passage of legislation that would allow a baby to be ripped from the mother’s womb moments from birth. These are living, feeling beautiful babies who will never get the chance to share their love and their dreams with the world. ... Let us work together to build a culture that cherishes innocent life.”
He also touched on the recurring themes regarding lowering the cost of health care and prescription drugs, as well as protecting those with preexisting conditions, something he called a major priority.
“It’s unacceptable that Americans pay vastly more than people in other countries for the exact same drugs, often made in the exact same place. This is wrong. This is unfair and together we will stop it, and we will stop it fast,” he said.
He did not offer any specific policy recommendation on how to address prescription drug costs, other than a comment on the need for greater price transparency.
“I am asking Congress to pass legislation that finally takes on the problem of global freeloading and delivers fairness and price transparency for American patients,” he said.
“We should also require drug companies, insurance companies, and hospitals to disclose real prices to foster competition and bring costs way down.”
SOURCE: Trump D. State of the Union Address, Feb. 5, 2019.
Key clinical point: President Trump calls for an end to HIV/AIDS and pediatric cancer in 10 years.
Major finding: His budget will request $500 million for cancer research and as yet undisclosed amount for HIV/AIDS research.
Study details: More specific details on the proposals will likely come when the president makes his budget submission to Congress in the coming weeks.
Disclosures: There are no disclosures.
Source: Trump D. State of the Union Address, Feb. 5, 2019.
Automated office BP readings
Also today, a positive fecal immunochemical test should prompt colonoscopy, mild aerobic exercise speeds recovery for sports concussions, and phase 2 studies of the antiamyloid Alzheimer’s drug crenezumab are stopped.
Also today, a positive fecal immunochemical test should prompt colonoscopy, mild aerobic exercise speeds recovery for sports concussions, and phase 2 studies of the antiamyloid Alzheimer’s drug crenezumab are stopped.
Also today, a positive fecal immunochemical test should prompt colonoscopy, mild aerobic exercise speeds recovery for sports concussions, and phase 2 studies of the antiamyloid Alzheimer’s drug crenezumab are stopped.
Researchers compare focused ultrasound and DBS for essential tremor
LAS VEGAS – according to two presentations delivered at the annual meeting of the North American Neuromodulation Society. The techniques’ surgical procedures, associated risks, and adverse event profiles may influence neurologists and patients in their choice of treatment.
FUS allows neurosurgeons to apply thermal ablation to create a lesion on the thalamus. MRI guidance enables precise control of the lesion location (within approximately 1 mm) and of the treatment intensity. The surgery can be performed with high-resolution stereotactic framing.
DBS entails the surgical implantation of a neurostimulator and attached leads and electrodes. The neurosurgeon drills a hole of approximately 14 mm in diameter into the skull so that the electrode can be inserted stereotactically while the patient is awake or asleep. The neurostimulator is installed separately.
Both treatments provide functional benefits
In 2016, W. Jeff Elias, MD, director of stereotactic and functional neurosurgery at the University of Virginia in Charlottesville, and his colleagues published the results of a randomized controlled trial that compared FUS with sham treatment in 76 patients with essential tremor. At three months, hand tremor had improved by approximately 50% among treated patients, but controls had no significant benefit(N Engl J Med. 2016 Aug 25;375[8]:730-9). The improvement among treated patients was maintained for 12 months. Disability and quality of life also improved after FUS.
A study by Schuurman et al. published in 2000 (N Engl J Med. 2000 Feb 17;342[7]:461-8) showed that DBS and FUS had similar efficacy at 1 year, said Kathryn L. Holloway, MD, professor of neurosurgery at Virginia Commonwealth University in Richmond. It included 45 patients with Parkinson’s disease, 13 with essential tremor, and 10 with multiple sclerosis who were randomized 1:1 to FUS or DBS. The primary outcome was activities of daily living, and blinded physicians assessed patient videos. Most of the patients who improved had received DBS, and most of the ones who worsened had received FUS, said Dr. Holloway. Among patients with essential tremor, tremor improved by between 94% and 100% with either treatment.
To find more recent data about these treatments, Dr. Holloway searched the literature for studies of FUS or DBS for essential tremor. She analyzed only studies that included unselected populations, blinded evaluations within 1 or 2 years of surgery, and tremor scores for the treated side. She found two studies of FUS, including Dr. Elias’s 2016 trial and a 2018 follow-up (Ann Neurol. 2018 Jan;83[1]:107-14). Dr. Holloway also identified three trials of DBS.
In these studies, reduction of hand tremor was 55% with FUS and between 63% and 69% with DBS. Reduction of postural tremor was approximately 72% with FUS and approximately 67% with DBS. Reduction of action tremor was about 52% with FUS and between 65% and 71% with DBS. Overall, DBS appears to be more effective, said Dr. Holloway.
A 2015 study (Mov Disord. 2015 Dec;30[14]:1937-43) that compared bilateral DBS, unilateral DBS, and unilateral FUS for essential tremor indicated that the treatments provide similar benefits on hand tremor, disability, and quality of life, said Dr. Elias. FUS is inferior to DBS, however, for total tremor and axial tremor.
Furthermore, the efficacy of FUS wanes over time, said Dr. Elias. He and his colleagues conducted a pilot study of 15 patients with essential tremor who received FUS (N Engl J Med. 2013 Aug 15;369[7]:640-8). At 6 years, 6 of 13 patients whose data were available still had a 50% improvement in tremor. “Some went on to [receive] DBS,” said Dr. Elias. “Functional improvements persisted more than the tremor improvement.”
Adverse events
In their 2016 trial of FUS, Dr. Elias and his colleagues observed 210 adverse events, which is approximately “what you would expect with a modern day, FDA-monitored clinical trial.” Sensory effects and gait disturbance accounted for most of the thalamotomy-related adverse events. Sensory problems such as numbness or parestheisa persisted at 1 year in 14% of treated patients, and gait disturbance persisted at 1 year in 9%. The investigators did not observe any hemorrhages, infections, or cavitation-related effects from FUS.
In a 2018 analysis of five clinical trials of FUS for essential tremor, Fishman et al. found that 79% of adverse events were mild and 1% were severe (Mov Disord. 2018 May;33[5]:843-7). The risk of a severe adverse event therefore can be considered low, and it may decrease as neurosurgeons gain experience with the procedure, said Dr. Elias.
In the 2000 Schuurman et al. study, the researchers observed significantly fewer adverse events overall among patients with Parkinson’s disease or essential tremor who received DBS, compared with patients who received FUS. Cognitive deterioration, severe dysarthria, and severe ataxia were more common in the FUS group than in the DBS group. Dr. Holloway’s analysis of adverse events in the five more recent trials that she identified yielded similar results.
Although MRI-guided FUS is a precise way to make lesions, functional areas in the thalamus overlap, which makes it more difficult to target only the intended region, said Dr. Holloway. The functional overlap thus increases the risk of adverse events (e.g., sensory impairments, dysarthria, or ataxia). The adverse events that result from FUS may last as long as a year. “Patients will put up anything for about a month after surgery, and then they start to get annoyed,” said Dr. Holloway.
In addition, Schuurman et al. found that FUS entailed a greater risk of permanent side effects, compared with DBS. “That’s the key point here,” said Dr. Holloway. Most of the adverse effects in the DBS group were resolved by adjusting or turning off the stimulator. Hardware issues resulting from DBS are frustrating, but reversible, but a patient with an adverse event after FUS often is “stuck with it,” said Dr. Holloway. The Schuurman et al. data indicated that, in terms of adverse events, “thalamotomy was inferior to DBS,” she added.
Implantation of DBS entails the risks inherent to surgeries that open the skull (such as seizures, air embolism, and hemorrhage). DBS entails a 2% risk of hemorrhage or infection, said Dr. Elias. Furthermore, as much as 15% of patients who undergo DBS implantation require additional surgery.
“FUS is not going to cause a life-threatening hemorrhage, but DBS certainly can,” said Dr. Holloway.
Managing disease progression
Essential tremor is a progressive disease, and older patients are more likely to have exponential progression than linear progression. Data, such as those published by Zhang et al. (J Neurosurg. 2010 Jun;112[6]:1271-6), indicate that DBS can “keep up with the progression of the disease,” said Dr. Holloway. The authors found that tremor scores did not change significantly over approximately 5 years when patients with essential tremor who had received DBS implantation had periodic assessments and increases in stimulation parameters when appropriate.
If a patient with essential tremor undergoes FUS thalamotomy and has subsequent disease progression, DBS may be considered for reducing tremor, said Dr. Holloway. Most adverse events resulting from DBS implantation are reversible with adjustment of the stimulation parameters. A second thalamotomy, however, could cause severe dysarthria and other irreversible adverse events. “Only DBS can safely address tremor progression,” said Dr. Holloway.
LAS VEGAS – according to two presentations delivered at the annual meeting of the North American Neuromodulation Society. The techniques’ surgical procedures, associated risks, and adverse event profiles may influence neurologists and patients in their choice of treatment.
FUS allows neurosurgeons to apply thermal ablation to create a lesion on the thalamus. MRI guidance enables precise control of the lesion location (within approximately 1 mm) and of the treatment intensity. The surgery can be performed with high-resolution stereotactic framing.
DBS entails the surgical implantation of a neurostimulator and attached leads and electrodes. The neurosurgeon drills a hole of approximately 14 mm in diameter into the skull so that the electrode can be inserted stereotactically while the patient is awake or asleep. The neurostimulator is installed separately.
Both treatments provide functional benefits
In 2016, W. Jeff Elias, MD, director of stereotactic and functional neurosurgery at the University of Virginia in Charlottesville, and his colleagues published the results of a randomized controlled trial that compared FUS with sham treatment in 76 patients with essential tremor. At three months, hand tremor had improved by approximately 50% among treated patients, but controls had no significant benefit(N Engl J Med. 2016 Aug 25;375[8]:730-9). The improvement among treated patients was maintained for 12 months. Disability and quality of life also improved after FUS.
A study by Schuurman et al. published in 2000 (N Engl J Med. 2000 Feb 17;342[7]:461-8) showed that DBS and FUS had similar efficacy at 1 year, said Kathryn L. Holloway, MD, professor of neurosurgery at Virginia Commonwealth University in Richmond. It included 45 patients with Parkinson’s disease, 13 with essential tremor, and 10 with multiple sclerosis who were randomized 1:1 to FUS or DBS. The primary outcome was activities of daily living, and blinded physicians assessed patient videos. Most of the patients who improved had received DBS, and most of the ones who worsened had received FUS, said Dr. Holloway. Among patients with essential tremor, tremor improved by between 94% and 100% with either treatment.
To find more recent data about these treatments, Dr. Holloway searched the literature for studies of FUS or DBS for essential tremor. She analyzed only studies that included unselected populations, blinded evaluations within 1 or 2 years of surgery, and tremor scores for the treated side. She found two studies of FUS, including Dr. Elias’s 2016 trial and a 2018 follow-up (Ann Neurol. 2018 Jan;83[1]:107-14). Dr. Holloway also identified three trials of DBS.
In these studies, reduction of hand tremor was 55% with FUS and between 63% and 69% with DBS. Reduction of postural tremor was approximately 72% with FUS and approximately 67% with DBS. Reduction of action tremor was about 52% with FUS and between 65% and 71% with DBS. Overall, DBS appears to be more effective, said Dr. Holloway.
A 2015 study (Mov Disord. 2015 Dec;30[14]:1937-43) that compared bilateral DBS, unilateral DBS, and unilateral FUS for essential tremor indicated that the treatments provide similar benefits on hand tremor, disability, and quality of life, said Dr. Elias. FUS is inferior to DBS, however, for total tremor and axial tremor.
Furthermore, the efficacy of FUS wanes over time, said Dr. Elias. He and his colleagues conducted a pilot study of 15 patients with essential tremor who received FUS (N Engl J Med. 2013 Aug 15;369[7]:640-8). At 6 years, 6 of 13 patients whose data were available still had a 50% improvement in tremor. “Some went on to [receive] DBS,” said Dr. Elias. “Functional improvements persisted more than the tremor improvement.”
Adverse events
In their 2016 trial of FUS, Dr. Elias and his colleagues observed 210 adverse events, which is approximately “what you would expect with a modern day, FDA-monitored clinical trial.” Sensory effects and gait disturbance accounted for most of the thalamotomy-related adverse events. Sensory problems such as numbness or parestheisa persisted at 1 year in 14% of treated patients, and gait disturbance persisted at 1 year in 9%. The investigators did not observe any hemorrhages, infections, or cavitation-related effects from FUS.
In a 2018 analysis of five clinical trials of FUS for essential tremor, Fishman et al. found that 79% of adverse events were mild and 1% were severe (Mov Disord. 2018 May;33[5]:843-7). The risk of a severe adverse event therefore can be considered low, and it may decrease as neurosurgeons gain experience with the procedure, said Dr. Elias.
In the 2000 Schuurman et al. study, the researchers observed significantly fewer adverse events overall among patients with Parkinson’s disease or essential tremor who received DBS, compared with patients who received FUS. Cognitive deterioration, severe dysarthria, and severe ataxia were more common in the FUS group than in the DBS group. Dr. Holloway’s analysis of adverse events in the five more recent trials that she identified yielded similar results.
Although MRI-guided FUS is a precise way to make lesions, functional areas in the thalamus overlap, which makes it more difficult to target only the intended region, said Dr. Holloway. The functional overlap thus increases the risk of adverse events (e.g., sensory impairments, dysarthria, or ataxia). The adverse events that result from FUS may last as long as a year. “Patients will put up anything for about a month after surgery, and then they start to get annoyed,” said Dr. Holloway.
In addition, Schuurman et al. found that FUS entailed a greater risk of permanent side effects, compared with DBS. “That’s the key point here,” said Dr. Holloway. Most of the adverse effects in the DBS group were resolved by adjusting or turning off the stimulator. Hardware issues resulting from DBS are frustrating, but reversible, but a patient with an adverse event after FUS often is “stuck with it,” said Dr. Holloway. The Schuurman et al. data indicated that, in terms of adverse events, “thalamotomy was inferior to DBS,” she added.
Implantation of DBS entails the risks inherent to surgeries that open the skull (such as seizures, air embolism, and hemorrhage). DBS entails a 2% risk of hemorrhage or infection, said Dr. Elias. Furthermore, as much as 15% of patients who undergo DBS implantation require additional surgery.
“FUS is not going to cause a life-threatening hemorrhage, but DBS certainly can,” said Dr. Holloway.
Managing disease progression
Essential tremor is a progressive disease, and older patients are more likely to have exponential progression than linear progression. Data, such as those published by Zhang et al. (J Neurosurg. 2010 Jun;112[6]:1271-6), indicate that DBS can “keep up with the progression of the disease,” said Dr. Holloway. The authors found that tremor scores did not change significantly over approximately 5 years when patients with essential tremor who had received DBS implantation had periodic assessments and increases in stimulation parameters when appropriate.
If a patient with essential tremor undergoes FUS thalamotomy and has subsequent disease progression, DBS may be considered for reducing tremor, said Dr. Holloway. Most adverse events resulting from DBS implantation are reversible with adjustment of the stimulation parameters. A second thalamotomy, however, could cause severe dysarthria and other irreversible adverse events. “Only DBS can safely address tremor progression,” said Dr. Holloway.
LAS VEGAS – according to two presentations delivered at the annual meeting of the North American Neuromodulation Society. The techniques’ surgical procedures, associated risks, and adverse event profiles may influence neurologists and patients in their choice of treatment.
FUS allows neurosurgeons to apply thermal ablation to create a lesion on the thalamus. MRI guidance enables precise control of the lesion location (within approximately 1 mm) and of the treatment intensity. The surgery can be performed with high-resolution stereotactic framing.
DBS entails the surgical implantation of a neurostimulator and attached leads and electrodes. The neurosurgeon drills a hole of approximately 14 mm in diameter into the skull so that the electrode can be inserted stereotactically while the patient is awake or asleep. The neurostimulator is installed separately.
Both treatments provide functional benefits
In 2016, W. Jeff Elias, MD, director of stereotactic and functional neurosurgery at the University of Virginia in Charlottesville, and his colleagues published the results of a randomized controlled trial that compared FUS with sham treatment in 76 patients with essential tremor. At three months, hand tremor had improved by approximately 50% among treated patients, but controls had no significant benefit(N Engl J Med. 2016 Aug 25;375[8]:730-9). The improvement among treated patients was maintained for 12 months. Disability and quality of life also improved after FUS.
A study by Schuurman et al. published in 2000 (N Engl J Med. 2000 Feb 17;342[7]:461-8) showed that DBS and FUS had similar efficacy at 1 year, said Kathryn L. Holloway, MD, professor of neurosurgery at Virginia Commonwealth University in Richmond. It included 45 patients with Parkinson’s disease, 13 with essential tremor, and 10 with multiple sclerosis who were randomized 1:1 to FUS or DBS. The primary outcome was activities of daily living, and blinded physicians assessed patient videos. Most of the patients who improved had received DBS, and most of the ones who worsened had received FUS, said Dr. Holloway. Among patients with essential tremor, tremor improved by between 94% and 100% with either treatment.
To find more recent data about these treatments, Dr. Holloway searched the literature for studies of FUS or DBS for essential tremor. She analyzed only studies that included unselected populations, blinded evaluations within 1 or 2 years of surgery, and tremor scores for the treated side. She found two studies of FUS, including Dr. Elias’s 2016 trial and a 2018 follow-up (Ann Neurol. 2018 Jan;83[1]:107-14). Dr. Holloway also identified three trials of DBS.
In these studies, reduction of hand tremor was 55% with FUS and between 63% and 69% with DBS. Reduction of postural tremor was approximately 72% with FUS and approximately 67% with DBS. Reduction of action tremor was about 52% with FUS and between 65% and 71% with DBS. Overall, DBS appears to be more effective, said Dr. Holloway.
A 2015 study (Mov Disord. 2015 Dec;30[14]:1937-43) that compared bilateral DBS, unilateral DBS, and unilateral FUS for essential tremor indicated that the treatments provide similar benefits on hand tremor, disability, and quality of life, said Dr. Elias. FUS is inferior to DBS, however, for total tremor and axial tremor.
Furthermore, the efficacy of FUS wanes over time, said Dr. Elias. He and his colleagues conducted a pilot study of 15 patients with essential tremor who received FUS (N Engl J Med. 2013 Aug 15;369[7]:640-8). At 6 years, 6 of 13 patients whose data were available still had a 50% improvement in tremor. “Some went on to [receive] DBS,” said Dr. Elias. “Functional improvements persisted more than the tremor improvement.”
Adverse events
In their 2016 trial of FUS, Dr. Elias and his colleagues observed 210 adverse events, which is approximately “what you would expect with a modern day, FDA-monitored clinical trial.” Sensory effects and gait disturbance accounted for most of the thalamotomy-related adverse events. Sensory problems such as numbness or parestheisa persisted at 1 year in 14% of treated patients, and gait disturbance persisted at 1 year in 9%. The investigators did not observe any hemorrhages, infections, or cavitation-related effects from FUS.
In a 2018 analysis of five clinical trials of FUS for essential tremor, Fishman et al. found that 79% of adverse events were mild and 1% were severe (Mov Disord. 2018 May;33[5]:843-7). The risk of a severe adverse event therefore can be considered low, and it may decrease as neurosurgeons gain experience with the procedure, said Dr. Elias.
In the 2000 Schuurman et al. study, the researchers observed significantly fewer adverse events overall among patients with Parkinson’s disease or essential tremor who received DBS, compared with patients who received FUS. Cognitive deterioration, severe dysarthria, and severe ataxia were more common in the FUS group than in the DBS group. Dr. Holloway’s analysis of adverse events in the five more recent trials that she identified yielded similar results.
Although MRI-guided FUS is a precise way to make lesions, functional areas in the thalamus overlap, which makes it more difficult to target only the intended region, said Dr. Holloway. The functional overlap thus increases the risk of adverse events (e.g., sensory impairments, dysarthria, or ataxia). The adverse events that result from FUS may last as long as a year. “Patients will put up anything for about a month after surgery, and then they start to get annoyed,” said Dr. Holloway.
In addition, Schuurman et al. found that FUS entailed a greater risk of permanent side effects, compared with DBS. “That’s the key point here,” said Dr. Holloway. Most of the adverse effects in the DBS group were resolved by adjusting or turning off the stimulator. Hardware issues resulting from DBS are frustrating, but reversible, but a patient with an adverse event after FUS often is “stuck with it,” said Dr. Holloway. The Schuurman et al. data indicated that, in terms of adverse events, “thalamotomy was inferior to DBS,” she added.
Implantation of DBS entails the risks inherent to surgeries that open the skull (such as seizures, air embolism, and hemorrhage). DBS entails a 2% risk of hemorrhage or infection, said Dr. Elias. Furthermore, as much as 15% of patients who undergo DBS implantation require additional surgery.
“FUS is not going to cause a life-threatening hemorrhage, but DBS certainly can,” said Dr. Holloway.
Managing disease progression
Essential tremor is a progressive disease, and older patients are more likely to have exponential progression than linear progression. Data, such as those published by Zhang et al. (J Neurosurg. 2010 Jun;112[6]:1271-6), indicate that DBS can “keep up with the progression of the disease,” said Dr. Holloway. The authors found that tremor scores did not change significantly over approximately 5 years when patients with essential tremor who had received DBS implantation had periodic assessments and increases in stimulation parameters when appropriate.
If a patient with essential tremor undergoes FUS thalamotomy and has subsequent disease progression, DBS may be considered for reducing tremor, said Dr. Holloway. Most adverse events resulting from DBS implantation are reversible with adjustment of the stimulation parameters. A second thalamotomy, however, could cause severe dysarthria and other irreversible adverse events. “Only DBS can safely address tremor progression,” said Dr. Holloway.
REPORTING FROM NANS 2019
Statins cut vascular events in elderly patients
Statin therapy appears to reduce the risk of major vascular events for patients of all age groups, but there is less evidence that older patients with evidence of occlusive vascular disease benefit from the treatment, according to a recent meta-analysis of 28 trials from the Cholesterol Treatment Trialists’ Collaboration published in The Lancet.
Statins are “useful and affordable drug[s] that reduce heart attacks and strokes in older patients. Until now there has been an evidence gap and we wanted to look at their efficacy and safety in older people,” Jordan Fulcher, BSc (Med), MBBS, from the Cholesterol Treatment Trialists’ (CTT) Collaboration and the University of Sydney stated in a press release. “Our analysis indicates that major cardiovascular events were reduced by about a fifth, per mmol/L lower LDL cholesterol, by statin therapy across all age groups. Despite previous concerns, we found no adverse effect on cancer or nonvascular mortality in any age group.”
The researchers examined 186,854 participants from 28 CTT trials undergoing statin therapy, of whom 14,483 (8%) were older than 75 years. Patients were divided into six groups based on age and examined the risk of major cardiovascular events such as stroke, coronary revascularization and major coronary events, as well as the incidence of cancer and vascular mortality.
Among all age groups, there was a significant reduction in major vascular events, with a 21% proportional per 1.0-mmol/L reduction in LDL cholesterol (risk ratio, 0.79; 95% confidence interval, 0.77-0.81) among patients receiving statin therapy or a more intensive statin regimen, and there was a 24% proportional reduction (RR, 0.76; 95% CI, 0.73-0.79) of major coronary events per 1.0-mmol/L reduction in LDL cholesterol, with older age resulting in a lower proportional reduction of major coronary events (P = .009). The researchers also found a proportional reduction of coronary revascularization procedures by 25% (RR, 0.75; 95% CI, 0.73-0.78) and stroke by 16% (RR, 0.84; 95% CI, 0.80-0.89) among patients of any age group receiving statin therapy or more intensive statin regimen, with no significant differences between age groups.
There was a 12% proportional reduction in vascular mortality per 1.0-mmol/L reduction in LDL cholesterol (RR, 0.88; 95% CI, 0.85-0.91), but this statistic did not remain significant after the researchers excluded four trials that included patients with heart failure or who were receiving renal dialysis. After excluding these trials from the overall analysis, the researchers found the smaller proportional reductions persisted for older patients for major coronary events (P = .01) but was no longer significant for major vascular events.
The researchers noted their study was limited by the highly selected patient population, low percentage of patients older than 75 years, including trials with efficacy endpoints where some nonserious adverse events may not have been recorded, and not including some trials in the meta-analysis if they were not part of the CTT.
This study was funded by Australian National Health and Medical Research Council, National Institute for Health Research Oxford Biomedical Research Centre, UK Medical Research Council, and British Heart Foundation. The authors have reported personal fees, grants, and consulting fees from Abbott, Aegerion, Amgen, Arisaph, AstraZeneca, Bayer, Beckmann, Berlin-Chemie, Boehringer Ingelheim, Daiichi Sankyo, Dalcor, DuPont, Esperion, GlaxoSmithKline, ISIS Pharmaceuticals, Kowa, Mylan, Pfizer, Roche, Sanofi, Singulex, The Medicines Company, and Vatera Capital, as well as the British Heart Foundation, Cancer Research UK, National Institute for Health Research Oxford Biomedical Research Centre, Medical Research Council, Nuffield Department of Population Health, Weill Cornell Medicine, and UK Biobank.
SOURCE: Fulcher J et al. Lancet. 2019;393:407-15.
Statin therapy is often discontinued for older patients who have concomitant disease or other considerations, but it should still be considered in older patients when the benefits outweigh the risks, Bernard M.Y. Cheung, PhD, and Karen S.L. Lam, MD, wrote in a related editorial.
“Even if the relative risk reduction in people older than 75 years is less than expected, statin therapy might still be justified by a high baseline cardiovascular risk, which is usually present in older people,” they said.
One explanation for the decreased relative risk reduction among older patients from the results by Fulcher et al. in the Cholesterol Treatment Trialists’ (CTT) Collaboration trial could have been the inclusion of older patients with cardiac and renal failure, and treating patients with lower cardiac risk or lowering LDL cholesterol in patients at risk of cardiovascular events can help prevent major vascular events later.
Ultimately, no drug is harmless and the risk and benefits must be weighed before making a decision to use statins with older patients just as they would in any other patient population. “The challenge for the health-care profession and the media is to convey risks and benefits in ways that patients can understand, enabling them to make an informed choice,” the authors wrote.
Dr. Cheung and Dr. Lam are from the department of medicine at Queen Mary Hospital, University of Hong Kong in Hong Kong Special Administrative Region, China. They had no relevant disclosures.
Statin therapy is often discontinued for older patients who have concomitant disease or other considerations, but it should still be considered in older patients when the benefits outweigh the risks, Bernard M.Y. Cheung, PhD, and Karen S.L. Lam, MD, wrote in a related editorial.
“Even if the relative risk reduction in people older than 75 years is less than expected, statin therapy might still be justified by a high baseline cardiovascular risk, which is usually present in older people,” they said.
One explanation for the decreased relative risk reduction among older patients from the results by Fulcher et al. in the Cholesterol Treatment Trialists’ (CTT) Collaboration trial could have been the inclusion of older patients with cardiac and renal failure, and treating patients with lower cardiac risk or lowering LDL cholesterol in patients at risk of cardiovascular events can help prevent major vascular events later.
Ultimately, no drug is harmless and the risk and benefits must be weighed before making a decision to use statins with older patients just as they would in any other patient population. “The challenge for the health-care profession and the media is to convey risks and benefits in ways that patients can understand, enabling them to make an informed choice,” the authors wrote.
Dr. Cheung and Dr. Lam are from the department of medicine at Queen Mary Hospital, University of Hong Kong in Hong Kong Special Administrative Region, China. They had no relevant disclosures.
Statin therapy is often discontinued for older patients who have concomitant disease or other considerations, but it should still be considered in older patients when the benefits outweigh the risks, Bernard M.Y. Cheung, PhD, and Karen S.L. Lam, MD, wrote in a related editorial.
“Even if the relative risk reduction in people older than 75 years is less than expected, statin therapy might still be justified by a high baseline cardiovascular risk, which is usually present in older people,” they said.
One explanation for the decreased relative risk reduction among older patients from the results by Fulcher et al. in the Cholesterol Treatment Trialists’ (CTT) Collaboration trial could have been the inclusion of older patients with cardiac and renal failure, and treating patients with lower cardiac risk or lowering LDL cholesterol in patients at risk of cardiovascular events can help prevent major vascular events later.
Ultimately, no drug is harmless and the risk and benefits must be weighed before making a decision to use statins with older patients just as they would in any other patient population. “The challenge for the health-care profession and the media is to convey risks and benefits in ways that patients can understand, enabling them to make an informed choice,” the authors wrote.
Dr. Cheung and Dr. Lam are from the department of medicine at Queen Mary Hospital, University of Hong Kong in Hong Kong Special Administrative Region, China. They had no relevant disclosures.
Statin therapy appears to reduce the risk of major vascular events for patients of all age groups, but there is less evidence that older patients with evidence of occlusive vascular disease benefit from the treatment, according to a recent meta-analysis of 28 trials from the Cholesterol Treatment Trialists’ Collaboration published in The Lancet.
Statins are “useful and affordable drug[s] that reduce heart attacks and strokes in older patients. Until now there has been an evidence gap and we wanted to look at their efficacy and safety in older people,” Jordan Fulcher, BSc (Med), MBBS, from the Cholesterol Treatment Trialists’ (CTT) Collaboration and the University of Sydney stated in a press release. “Our analysis indicates that major cardiovascular events were reduced by about a fifth, per mmol/L lower LDL cholesterol, by statin therapy across all age groups. Despite previous concerns, we found no adverse effect on cancer or nonvascular mortality in any age group.”
The researchers examined 186,854 participants from 28 CTT trials undergoing statin therapy, of whom 14,483 (8%) were older than 75 years. Patients were divided into six groups based on age and examined the risk of major cardiovascular events such as stroke, coronary revascularization and major coronary events, as well as the incidence of cancer and vascular mortality.
Among all age groups, there was a significant reduction in major vascular events, with a 21% proportional per 1.0-mmol/L reduction in LDL cholesterol (risk ratio, 0.79; 95% confidence interval, 0.77-0.81) among patients receiving statin therapy or a more intensive statin regimen, and there was a 24% proportional reduction (RR, 0.76; 95% CI, 0.73-0.79) of major coronary events per 1.0-mmol/L reduction in LDL cholesterol, with older age resulting in a lower proportional reduction of major coronary events (P = .009). The researchers also found a proportional reduction of coronary revascularization procedures by 25% (RR, 0.75; 95% CI, 0.73-0.78) and stroke by 16% (RR, 0.84; 95% CI, 0.80-0.89) among patients of any age group receiving statin therapy or more intensive statin regimen, with no significant differences between age groups.
There was a 12% proportional reduction in vascular mortality per 1.0-mmol/L reduction in LDL cholesterol (RR, 0.88; 95% CI, 0.85-0.91), but this statistic did not remain significant after the researchers excluded four trials that included patients with heart failure or who were receiving renal dialysis. After excluding these trials from the overall analysis, the researchers found the smaller proportional reductions persisted for older patients for major coronary events (P = .01) but was no longer significant for major vascular events.
The researchers noted their study was limited by the highly selected patient population, low percentage of patients older than 75 years, including trials with efficacy endpoints where some nonserious adverse events may not have been recorded, and not including some trials in the meta-analysis if they were not part of the CTT.
This study was funded by Australian National Health and Medical Research Council, National Institute for Health Research Oxford Biomedical Research Centre, UK Medical Research Council, and British Heart Foundation. The authors have reported personal fees, grants, and consulting fees from Abbott, Aegerion, Amgen, Arisaph, AstraZeneca, Bayer, Beckmann, Berlin-Chemie, Boehringer Ingelheim, Daiichi Sankyo, Dalcor, DuPont, Esperion, GlaxoSmithKline, ISIS Pharmaceuticals, Kowa, Mylan, Pfizer, Roche, Sanofi, Singulex, The Medicines Company, and Vatera Capital, as well as the British Heart Foundation, Cancer Research UK, National Institute for Health Research Oxford Biomedical Research Centre, Medical Research Council, Nuffield Department of Population Health, Weill Cornell Medicine, and UK Biobank.
SOURCE: Fulcher J et al. Lancet. 2019;393:407-15.
Statin therapy appears to reduce the risk of major vascular events for patients of all age groups, but there is less evidence that older patients with evidence of occlusive vascular disease benefit from the treatment, according to a recent meta-analysis of 28 trials from the Cholesterol Treatment Trialists’ Collaboration published in The Lancet.
Statins are “useful and affordable drug[s] that reduce heart attacks and strokes in older patients. Until now there has been an evidence gap and we wanted to look at their efficacy and safety in older people,” Jordan Fulcher, BSc (Med), MBBS, from the Cholesterol Treatment Trialists’ (CTT) Collaboration and the University of Sydney stated in a press release. “Our analysis indicates that major cardiovascular events were reduced by about a fifth, per mmol/L lower LDL cholesterol, by statin therapy across all age groups. Despite previous concerns, we found no adverse effect on cancer or nonvascular mortality in any age group.”
The researchers examined 186,854 participants from 28 CTT trials undergoing statin therapy, of whom 14,483 (8%) were older than 75 years. Patients were divided into six groups based on age and examined the risk of major cardiovascular events such as stroke, coronary revascularization and major coronary events, as well as the incidence of cancer and vascular mortality.
Among all age groups, there was a significant reduction in major vascular events, with a 21% proportional per 1.0-mmol/L reduction in LDL cholesterol (risk ratio, 0.79; 95% confidence interval, 0.77-0.81) among patients receiving statin therapy or a more intensive statin regimen, and there was a 24% proportional reduction (RR, 0.76; 95% CI, 0.73-0.79) of major coronary events per 1.0-mmol/L reduction in LDL cholesterol, with older age resulting in a lower proportional reduction of major coronary events (P = .009). The researchers also found a proportional reduction of coronary revascularization procedures by 25% (RR, 0.75; 95% CI, 0.73-0.78) and stroke by 16% (RR, 0.84; 95% CI, 0.80-0.89) among patients of any age group receiving statin therapy or more intensive statin regimen, with no significant differences between age groups.
There was a 12% proportional reduction in vascular mortality per 1.0-mmol/L reduction in LDL cholesterol (RR, 0.88; 95% CI, 0.85-0.91), but this statistic did not remain significant after the researchers excluded four trials that included patients with heart failure or who were receiving renal dialysis. After excluding these trials from the overall analysis, the researchers found the smaller proportional reductions persisted for older patients for major coronary events (P = .01) but was no longer significant for major vascular events.
The researchers noted their study was limited by the highly selected patient population, low percentage of patients older than 75 years, including trials with efficacy endpoints where some nonserious adverse events may not have been recorded, and not including some trials in the meta-analysis if they were not part of the CTT.
This study was funded by Australian National Health and Medical Research Council, National Institute for Health Research Oxford Biomedical Research Centre, UK Medical Research Council, and British Heart Foundation. The authors have reported personal fees, grants, and consulting fees from Abbott, Aegerion, Amgen, Arisaph, AstraZeneca, Bayer, Beckmann, Berlin-Chemie, Boehringer Ingelheim, Daiichi Sankyo, Dalcor, DuPont, Esperion, GlaxoSmithKline, ISIS Pharmaceuticals, Kowa, Mylan, Pfizer, Roche, Sanofi, Singulex, The Medicines Company, and Vatera Capital, as well as the British Heart Foundation, Cancer Research UK, National Institute for Health Research Oxford Biomedical Research Centre, Medical Research Council, Nuffield Department of Population Health, Weill Cornell Medicine, and UK Biobank.
SOURCE: Fulcher J et al. Lancet. 2019;393:407-15.
FROM THE LANCET
Key clinical point: but patients older than 75 years with occlusive vascular disease have a smaller reduction in major coronary events.
Major finding: Major vascular coronary events were reduced by 24% (risk ratio, 0.76; 95% confidence interval, 0.73-0.79) with a decrease in the reduction of coronary events among patients older than 75 years. Study details: A meta-analysis of 28 trials with 186,854 individuals undergoing statin therapy from the Cholesterol Treatment Trialists’ Collaboration.
Disclosures: This study was funded by Australian National Health and Medical Research Council, National Institute for Health Research Oxford Biomedical Research Centre, UK Medical Research Council, and British Heart Foundation. The authors have reported personal fees, grants, and consulting fees from Abbott, Aegerion, Amgen, Arisaph, AstraZeneca, Bayer, Beckmann, Berlin-Chemie, Boehringer Ingelheim, Daiichi Sankyo, Dalcor, DuPont, Esperion, GlaxoSmithKline, ISIS Pharmaceuticals, Kowa, Mylan, Pfizer, Roche, Sanofi, Singulex, The Medicines Company, and Vatera Capital, as well as the British Heart Foundation, Cancer Research UK, National Institute for Health Research Oxford Biomedical Research Centre, Medical Research Council, Nuffield Department of Population Health, Weill Cornell Medicine, and UK Biobank.
Source: Fulcher J et al. Lancet. 2019;393:407-15.
Shifting Part B to D: Who saves?
Also today, there’s no single treatment for fibromyalgia, obesity-related cancers are increasing in younger adults, and pregnancy problems predict cardiovascular future.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, there’s no single treatment for fibromyalgia, obesity-related cancers are increasing in younger adults, and pregnancy problems predict cardiovascular future.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, there’s no single treatment for fibromyalgia, obesity-related cancers are increasing in younger adults, and pregnancy problems predict cardiovascular future.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify