User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
New year, old you
This column should arrive just in time. By this time in February, eighty percent of us will abort what we resolved to do this year. If this was you, it could be considered a catastrophic failure because not only is it a new year, it is a new decade. That’s right, the opportunity to fix the 10-year-imperfect you won’t come again until 2030!
I’m among you. I intended to read fiction daily (starting with “The Great Gatsby,” not “Moby Dick” – I thought I would give myself a fighting chance, but alas ...), to workout at least 5 days every week (I tore my left triangular fibrocartilage complex, so there’s that), to write at least 500 words daily (I’m typing this one-handed: I’m lucky to get 500 letters a day). So I’m out.
If you resolved to do something this year, chances are it was to make a better you: a self-improvement goal such as losing weight, saving more money, or exercising more. According to a Marist Poll, these were the most popular resolutions for 2020. At the bottom of the most-likely-resolutions list were things like “worry less” or “be kinder to others.” These are important goals we’d agree, but we don’t deem them resolution-worthy. Why?
And why do we have New Year’s resolutions in the first place? When I looked into this further, I was surprised by some of the history I discovered.
As far back as the Babylonians, once a year, we’ve tried our best to get better. At the feast of Akitu, the Babylonian new year festival (about March on our modern calendar), people resolved to do a better job of paying debts and returning favors – spin had not been invented, and yoga hadn’t caught on in the Middle East yet. This fundamental desire to be a better human seems hardwired, and long before Bullet Journals we seem to have loved “fresh start” days on the calendar. Yet, we’re doomed to fail, over and over, at least for the last 5,000 or so attempts.
We know so much more now. Put your Nike Renue Fusion shoes next to your bed so you get up and run first thing. Set SMART goals. Sign up for automatic retirement contribution and for automatic, plant-based meal delivery from Blue Apron. (I’ve no conflict of interest in these products).
Good ideas all, but I’m suggesting a different approach: Resolve to do something else this year.
Rather than try the same things we’ve attempted, how about selecting something from the bottom of the Marist Poll list – such as resolving to be more humble. Admit when you don’t know something or don’t understand what’s being discussed. Recognize and acknowledge when you’ve screwed up. Or resolve to be more selfless. Add on someone else’s patient, an extra call without expecting a favor in return, or do what you can to help a curbside consult, even if there is no reward or even a small risk to you. Repay the debt you owe your friends, family, colleagues, staff, and patients.
These things are a little trickier to track, but you can find a way to keep yourself accountable. Add a box to your weekly planner that says “Be humble and kind” and check it off for the next 42 weeks. Good news, March 1 falls on a Sunday this year – let’s call it the feast of Akitu.
Happy New Year! And good luck!
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
This column should arrive just in time. By this time in February, eighty percent of us will abort what we resolved to do this year. If this was you, it could be considered a catastrophic failure because not only is it a new year, it is a new decade. That’s right, the opportunity to fix the 10-year-imperfect you won’t come again until 2030!
I’m among you. I intended to read fiction daily (starting with “The Great Gatsby,” not “Moby Dick” – I thought I would give myself a fighting chance, but alas ...), to workout at least 5 days every week (I tore my left triangular fibrocartilage complex, so there’s that), to write at least 500 words daily (I’m typing this one-handed: I’m lucky to get 500 letters a day). So I’m out.
If you resolved to do something this year, chances are it was to make a better you: a self-improvement goal such as losing weight, saving more money, or exercising more. According to a Marist Poll, these were the most popular resolutions for 2020. At the bottom of the most-likely-resolutions list were things like “worry less” or “be kinder to others.” These are important goals we’d agree, but we don’t deem them resolution-worthy. Why?
And why do we have New Year’s resolutions in the first place? When I looked into this further, I was surprised by some of the history I discovered.
As far back as the Babylonians, once a year, we’ve tried our best to get better. At the feast of Akitu, the Babylonian new year festival (about March on our modern calendar), people resolved to do a better job of paying debts and returning favors – spin had not been invented, and yoga hadn’t caught on in the Middle East yet. This fundamental desire to be a better human seems hardwired, and long before Bullet Journals we seem to have loved “fresh start” days on the calendar. Yet, we’re doomed to fail, over and over, at least for the last 5,000 or so attempts.
We know so much more now. Put your Nike Renue Fusion shoes next to your bed so you get up and run first thing. Set SMART goals. Sign up for automatic retirement contribution and for automatic, plant-based meal delivery from Blue Apron. (I’ve no conflict of interest in these products).
Good ideas all, but I’m suggesting a different approach: Resolve to do something else this year.
Rather than try the same things we’ve attempted, how about selecting something from the bottom of the Marist Poll list – such as resolving to be more humble. Admit when you don’t know something or don’t understand what’s being discussed. Recognize and acknowledge when you’ve screwed up. Or resolve to be more selfless. Add on someone else’s patient, an extra call without expecting a favor in return, or do what you can to help a curbside consult, even if there is no reward or even a small risk to you. Repay the debt you owe your friends, family, colleagues, staff, and patients.
These things are a little trickier to track, but you can find a way to keep yourself accountable. Add a box to your weekly planner that says “Be humble and kind” and check it off for the next 42 weeks. Good news, March 1 falls on a Sunday this year – let’s call it the feast of Akitu.
Happy New Year! And good luck!
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
This column should arrive just in time. By this time in February, eighty percent of us will abort what we resolved to do this year. If this was you, it could be considered a catastrophic failure because not only is it a new year, it is a new decade. That’s right, the opportunity to fix the 10-year-imperfect you won’t come again until 2030!
I’m among you. I intended to read fiction daily (starting with “The Great Gatsby,” not “Moby Dick” – I thought I would give myself a fighting chance, but alas ...), to workout at least 5 days every week (I tore my left triangular fibrocartilage complex, so there’s that), to write at least 500 words daily (I’m typing this one-handed: I’m lucky to get 500 letters a day). So I’m out.
If you resolved to do something this year, chances are it was to make a better you: a self-improvement goal such as losing weight, saving more money, or exercising more. According to a Marist Poll, these were the most popular resolutions for 2020. At the bottom of the most-likely-resolutions list were things like “worry less” or “be kinder to others.” These are important goals we’d agree, but we don’t deem them resolution-worthy. Why?
And why do we have New Year’s resolutions in the first place? When I looked into this further, I was surprised by some of the history I discovered.
As far back as the Babylonians, once a year, we’ve tried our best to get better. At the feast of Akitu, the Babylonian new year festival (about March on our modern calendar), people resolved to do a better job of paying debts and returning favors – spin had not been invented, and yoga hadn’t caught on in the Middle East yet. This fundamental desire to be a better human seems hardwired, and long before Bullet Journals we seem to have loved “fresh start” days on the calendar. Yet, we’re doomed to fail, over and over, at least for the last 5,000 or so attempts.
We know so much more now. Put your Nike Renue Fusion shoes next to your bed so you get up and run first thing. Set SMART goals. Sign up for automatic retirement contribution and for automatic, plant-based meal delivery from Blue Apron. (I’ve no conflict of interest in these products).
Good ideas all, but I’m suggesting a different approach: Resolve to do something else this year.
Rather than try the same things we’ve attempted, how about selecting something from the bottom of the Marist Poll list – such as resolving to be more humble. Admit when you don’t know something or don’t understand what’s being discussed. Recognize and acknowledge when you’ve screwed up. Or resolve to be more selfless. Add on someone else’s patient, an extra call without expecting a favor in return, or do what you can to help a curbside consult, even if there is no reward or even a small risk to you. Repay the debt you owe your friends, family, colleagues, staff, and patients.
These things are a little trickier to track, but you can find a way to keep yourself accountable. Add a box to your weekly planner that says “Be humble and kind” and check it off for the next 42 weeks. Good news, March 1 falls on a Sunday this year – let’s call it the feast of Akitu.
Happy New Year! And good luck!
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Hippocampal sparing temporal lobectomy recommended for medically refractory epilepsy
BALTIMORE – according to a review from researchers at Thomas Jefferson University in Philadelphia.
Often, the hippocampus and other mesial structures are removed even if they appear normal. The concern is that even normal looking tissue could harbor epileptogenic elements and leaving them in tact could reduce postoperative seizure control, explained senior investigator and neurologist Michael Sperling, MD, director of the Jefferson Comprehensive Epilepsy Center.
He and his colleagues wanted to see if that was really true, so they compared outcomes in 21 patients who had mesial-sparing lobectomies with 19 patients who had the standard approach. Cases and controls were matched for age, preoperative seizure frequency, side of surgery, and other factors. None of the patients had MTS.
There was no significant difference in postoperative seizure recurrence between the two groups (P = .974). The standard procedure had a slight edge early on, but at 2.5 years, just over 60% of patients in both groups were seizure free. At 5 years, about 50% were seizure free, and almost 40% in both arms at 7.5 years.
About two-thirds of patients in each arm had pre- and postoperative verbal memory testing, with similar duration from surgery to postop evaluation. There was no change among the hippocampus-sparing patients, but a roughly one standard deviation drop in delayed recall and logical memory on the California Verbal Learning Test in the standard group.
Even so, it wasn’t enough to affect employment, which the investigators used as a surrogate for disability; postoperative employment was comparable in both groups. People mostly retained their jobs, and there was no difference in job loss. A few people in each arm actually found jobs after surgery.
The investigators concluded that “it is reasonable to recommend mesial temporal sparing procedure in patients with dominant neocortical temporal lobe epilepsy when the hippocampus appears normal in the MRI. However, as resecting the mesial temporal structures was not associated with a greater chance of becoming unemployed following the surgery, there appears to be no major contraindication to performing an [anterior temporal lobectomy] if clinically warranted.”
The results are reassuring. “My bias walking in was that” seizure recurrence would be worse after hippocampal-sparing surgery. “I was pleased to see that it was about the same. If you want to try to preserve verbal memory and the MRI is normal, you can get away with sparing the mesial temporal structures, and still get a good seizure outcome,” Dr. Sperling said at the annual meeting of the American Epilepsy Society, where the study was presented.
“But if you have to take the hippocampus for whatever reason, the functional consequence of a decline in verbal memory is not severe enough as to be disabling,” which is “one of the big concerns” with temporal lobectomy, he said.
The findings “will make us more likely to recommend mesial-sparing surgery, but at the same time” perhaps not be quite as worried about disability with the standard approach.
Temporal lobe epilepsy with normal mesial structures isn’t very common, which explains the small numbers in the series. It’s possible subtle difference in seizure control and employment outcomes would have been found with a larger series, “but obviously there were no major differences. I think the fundamental questions have been answered to my satisfaction,” Dr. Sperling said.
Overall, “it’s better to operate and try to cure people than to worry that you will make their memory worse when the consequences of having uncontrolled epilepsy is a higher death rate,” he said.
There were about equal numbers of men and women in the review; patients were in their early 30s, on average; and most had left-sided surgery. Just over half in each arm had preoperative tonic-clonic seizures. The mean duration of epilepsy was 14.9 years in the mesial-sparing group, and 8.6 years in the standard arm.
There was no funding for the review, and Dr. Sperling didn’t have any relevant disclosures.
SOURCE: Goldstein L et al. AES 2019. Abstract 1.339.
BALTIMORE – according to a review from researchers at Thomas Jefferson University in Philadelphia.
Often, the hippocampus and other mesial structures are removed even if they appear normal. The concern is that even normal looking tissue could harbor epileptogenic elements and leaving them in tact could reduce postoperative seizure control, explained senior investigator and neurologist Michael Sperling, MD, director of the Jefferson Comprehensive Epilepsy Center.
He and his colleagues wanted to see if that was really true, so they compared outcomes in 21 patients who had mesial-sparing lobectomies with 19 patients who had the standard approach. Cases and controls were matched for age, preoperative seizure frequency, side of surgery, and other factors. None of the patients had MTS.
There was no significant difference in postoperative seizure recurrence between the two groups (P = .974). The standard procedure had a slight edge early on, but at 2.5 years, just over 60% of patients in both groups were seizure free. At 5 years, about 50% were seizure free, and almost 40% in both arms at 7.5 years.
About two-thirds of patients in each arm had pre- and postoperative verbal memory testing, with similar duration from surgery to postop evaluation. There was no change among the hippocampus-sparing patients, but a roughly one standard deviation drop in delayed recall and logical memory on the California Verbal Learning Test in the standard group.
Even so, it wasn’t enough to affect employment, which the investigators used as a surrogate for disability; postoperative employment was comparable in both groups. People mostly retained their jobs, and there was no difference in job loss. A few people in each arm actually found jobs after surgery.
The investigators concluded that “it is reasonable to recommend mesial temporal sparing procedure in patients with dominant neocortical temporal lobe epilepsy when the hippocampus appears normal in the MRI. However, as resecting the mesial temporal structures was not associated with a greater chance of becoming unemployed following the surgery, there appears to be no major contraindication to performing an [anterior temporal lobectomy] if clinically warranted.”
The results are reassuring. “My bias walking in was that” seizure recurrence would be worse after hippocampal-sparing surgery. “I was pleased to see that it was about the same. If you want to try to preserve verbal memory and the MRI is normal, you can get away with sparing the mesial temporal structures, and still get a good seizure outcome,” Dr. Sperling said at the annual meeting of the American Epilepsy Society, where the study was presented.
“But if you have to take the hippocampus for whatever reason, the functional consequence of a decline in verbal memory is not severe enough as to be disabling,” which is “one of the big concerns” with temporal lobectomy, he said.
The findings “will make us more likely to recommend mesial-sparing surgery, but at the same time” perhaps not be quite as worried about disability with the standard approach.
Temporal lobe epilepsy with normal mesial structures isn’t very common, which explains the small numbers in the series. It’s possible subtle difference in seizure control and employment outcomes would have been found with a larger series, “but obviously there were no major differences. I think the fundamental questions have been answered to my satisfaction,” Dr. Sperling said.
Overall, “it’s better to operate and try to cure people than to worry that you will make their memory worse when the consequences of having uncontrolled epilepsy is a higher death rate,” he said.
There were about equal numbers of men and women in the review; patients were in their early 30s, on average; and most had left-sided surgery. Just over half in each arm had preoperative tonic-clonic seizures. The mean duration of epilepsy was 14.9 years in the mesial-sparing group, and 8.6 years in the standard arm.
There was no funding for the review, and Dr. Sperling didn’t have any relevant disclosures.
SOURCE: Goldstein L et al. AES 2019. Abstract 1.339.
BALTIMORE – according to a review from researchers at Thomas Jefferson University in Philadelphia.
Often, the hippocampus and other mesial structures are removed even if they appear normal. The concern is that even normal looking tissue could harbor epileptogenic elements and leaving them in tact could reduce postoperative seizure control, explained senior investigator and neurologist Michael Sperling, MD, director of the Jefferson Comprehensive Epilepsy Center.
He and his colleagues wanted to see if that was really true, so they compared outcomes in 21 patients who had mesial-sparing lobectomies with 19 patients who had the standard approach. Cases and controls were matched for age, preoperative seizure frequency, side of surgery, and other factors. None of the patients had MTS.
There was no significant difference in postoperative seizure recurrence between the two groups (P = .974). The standard procedure had a slight edge early on, but at 2.5 years, just over 60% of patients in both groups were seizure free. At 5 years, about 50% were seizure free, and almost 40% in both arms at 7.5 years.
About two-thirds of patients in each arm had pre- and postoperative verbal memory testing, with similar duration from surgery to postop evaluation. There was no change among the hippocampus-sparing patients, but a roughly one standard deviation drop in delayed recall and logical memory on the California Verbal Learning Test in the standard group.
Even so, it wasn’t enough to affect employment, which the investigators used as a surrogate for disability; postoperative employment was comparable in both groups. People mostly retained their jobs, and there was no difference in job loss. A few people in each arm actually found jobs after surgery.
The investigators concluded that “it is reasonable to recommend mesial temporal sparing procedure in patients with dominant neocortical temporal lobe epilepsy when the hippocampus appears normal in the MRI. However, as resecting the mesial temporal structures was not associated with a greater chance of becoming unemployed following the surgery, there appears to be no major contraindication to performing an [anterior temporal lobectomy] if clinically warranted.”
The results are reassuring. “My bias walking in was that” seizure recurrence would be worse after hippocampal-sparing surgery. “I was pleased to see that it was about the same. If you want to try to preserve verbal memory and the MRI is normal, you can get away with sparing the mesial temporal structures, and still get a good seizure outcome,” Dr. Sperling said at the annual meeting of the American Epilepsy Society, where the study was presented.
“But if you have to take the hippocampus for whatever reason, the functional consequence of a decline in verbal memory is not severe enough as to be disabling,” which is “one of the big concerns” with temporal lobectomy, he said.
The findings “will make us more likely to recommend mesial-sparing surgery, but at the same time” perhaps not be quite as worried about disability with the standard approach.
Temporal lobe epilepsy with normal mesial structures isn’t very common, which explains the small numbers in the series. It’s possible subtle difference in seizure control and employment outcomes would have been found with a larger series, “but obviously there were no major differences. I think the fundamental questions have been answered to my satisfaction,” Dr. Sperling said.
Overall, “it’s better to operate and try to cure people than to worry that you will make their memory worse when the consequences of having uncontrolled epilepsy is a higher death rate,” he said.
There were about equal numbers of men and women in the review; patients were in their early 30s, on average; and most had left-sided surgery. Just over half in each arm had preoperative tonic-clonic seizures. The mean duration of epilepsy was 14.9 years in the mesial-sparing group, and 8.6 years in the standard arm.
There was no funding for the review, and Dr. Sperling didn’t have any relevant disclosures.
SOURCE: Goldstein L et al. AES 2019. Abstract 1.339.
REPORTING FROM AES 2019
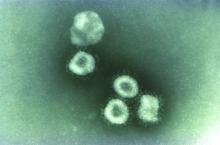
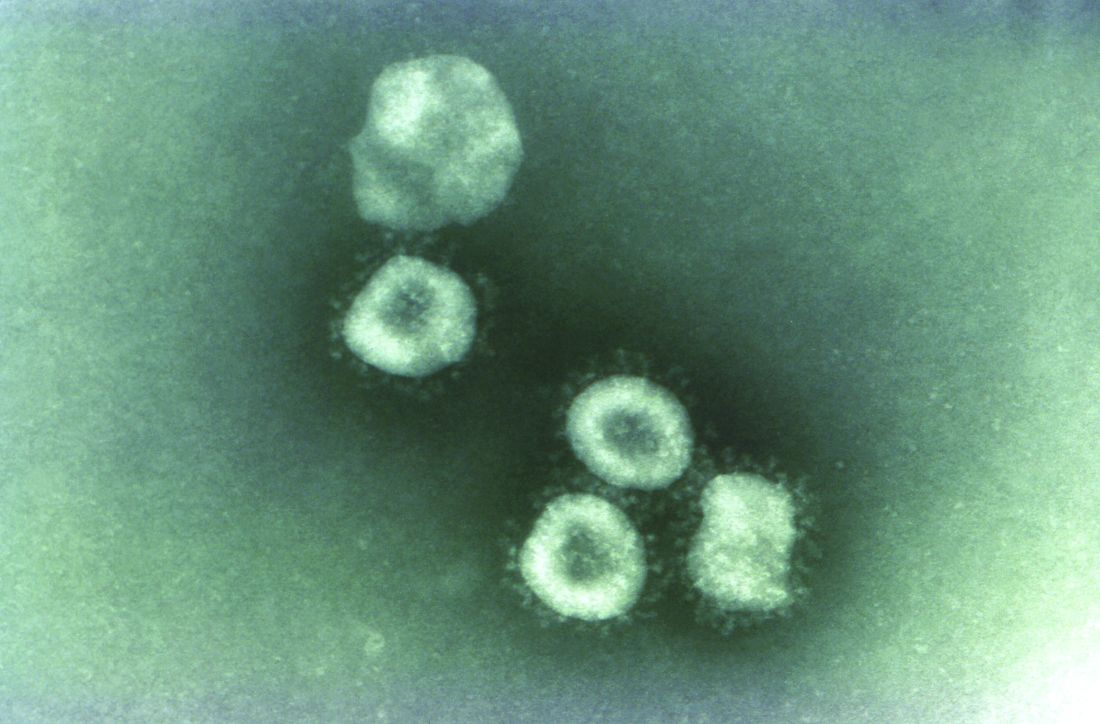
Washington state patient is first U.S. case of novel coronavirus
The first case of the novel coronavirus, named 2019-nCoV, in the United States has been diagnosed in a traveler from China who came through Seattle-Tacoma International Airport on Jan 15, the Centers for Disease Control and Prevention announced today at a press briefing.
The outbreak began at a animal and meat market in China and now has spread to at least three other countries, including Thailand, Japan and South Korea. While originally thought to be spreading from animal to person, it appears that limited person-to-person transmission is occurring, although it is currently unknown how easily this virus spreads between people.
More than 300 cases have been reported and six deaths have occurred. Fourteen health care workers have been infected.
Scott Lindquist, MD, MPH, Washington state epidemiologist, said at the briefing that the patient, a man who had been in Wuhan, arrived at Sea-Tac on Jan. 15, 2 days before airport screening had been initiated. He was symptom free at the time of his arrival and probably would not have been identified as infected with 2019-nCoV. The patient had been aware of the public health and news media coverage of 2019-nCoV and, after developing symptoms, contacted his health care provider on Jan. 19. The patient did not fly directly from Wuhan, but Dr. Lindquist said that he has been fully cooperative and has been helpful to authorities in tracing his route and contacts. The man is being treated at Providence Regional Medical Center, Everett, Wash.
The CDC obtained a specimen from the patient immediately and identified the 2019-nCoV within 24 hours.
Screening at airports is part of a multipart strategy to address this type of infection that includes public health information dissemination, patient education, as well as hospital preparation and training exercises. Currently, a strategy referred to as “funneling” is being implemented wherein travelers from China are rerouted and reticketed to one of the five airports conducting screening. At present, JFK in New York, San Francisco International, Los Angeles International, Hartsfield-Jackson Atlanta International Airport, and Chicago O’Hare International Airport are conducting inbound traveler screening.
The CDC is working in close cooperation with the Department of Homeland Security and the Federal Aviation Administration to coordinate travel screenings and reroutings. In addition, the CDC is working with the World Health Organization and the international global health community to share information about this outbreak. The CDC also has staff on site in Wuhan and is communicating with local health authorities. The CDC has activated its Emergency Operations Center to better provide ongoing support to the 2019-nCoV response. Currently, the focus is on tracing contacts and the means of transmission of this virus.
Updates on the outbreak will be posted on the CDC coronavirus website.
CORRECTION: 1/21/2020: The name of the medical center where the 2019-nCoV patient is being treated was corrected.
The first case of the novel coronavirus, named 2019-nCoV, in the United States has been diagnosed in a traveler from China who came through Seattle-Tacoma International Airport on Jan 15, the Centers for Disease Control and Prevention announced today at a press briefing.
The outbreak began at a animal and meat market in China and now has spread to at least three other countries, including Thailand, Japan and South Korea. While originally thought to be spreading from animal to person, it appears that limited person-to-person transmission is occurring, although it is currently unknown how easily this virus spreads between people.
More than 300 cases have been reported and six deaths have occurred. Fourteen health care workers have been infected.
Scott Lindquist, MD, MPH, Washington state epidemiologist, said at the briefing that the patient, a man who had been in Wuhan, arrived at Sea-Tac on Jan. 15, 2 days before airport screening had been initiated. He was symptom free at the time of his arrival and probably would not have been identified as infected with 2019-nCoV. The patient had been aware of the public health and news media coverage of 2019-nCoV and, after developing symptoms, contacted his health care provider on Jan. 19. The patient did not fly directly from Wuhan, but Dr. Lindquist said that he has been fully cooperative and has been helpful to authorities in tracing his route and contacts. The man is being treated at Providence Regional Medical Center, Everett, Wash.
The CDC obtained a specimen from the patient immediately and identified the 2019-nCoV within 24 hours.
Screening at airports is part of a multipart strategy to address this type of infection that includes public health information dissemination, patient education, as well as hospital preparation and training exercises. Currently, a strategy referred to as “funneling” is being implemented wherein travelers from China are rerouted and reticketed to one of the five airports conducting screening. At present, JFK in New York, San Francisco International, Los Angeles International, Hartsfield-Jackson Atlanta International Airport, and Chicago O’Hare International Airport are conducting inbound traveler screening.
The CDC is working in close cooperation with the Department of Homeland Security and the Federal Aviation Administration to coordinate travel screenings and reroutings. In addition, the CDC is working with the World Health Organization and the international global health community to share information about this outbreak. The CDC also has staff on site in Wuhan and is communicating with local health authorities. The CDC has activated its Emergency Operations Center to better provide ongoing support to the 2019-nCoV response. Currently, the focus is on tracing contacts and the means of transmission of this virus.
Updates on the outbreak will be posted on the CDC coronavirus website.
CORRECTION: 1/21/2020: The name of the medical center where the 2019-nCoV patient is being treated was corrected.
The first case of the novel coronavirus, named 2019-nCoV, in the United States has been diagnosed in a traveler from China who came through Seattle-Tacoma International Airport on Jan 15, the Centers for Disease Control and Prevention announced today at a press briefing.
The outbreak began at a animal and meat market in China and now has spread to at least three other countries, including Thailand, Japan and South Korea. While originally thought to be spreading from animal to person, it appears that limited person-to-person transmission is occurring, although it is currently unknown how easily this virus spreads between people.
More than 300 cases have been reported and six deaths have occurred. Fourteen health care workers have been infected.
Scott Lindquist, MD, MPH, Washington state epidemiologist, said at the briefing that the patient, a man who had been in Wuhan, arrived at Sea-Tac on Jan. 15, 2 days before airport screening had been initiated. He was symptom free at the time of his arrival and probably would not have been identified as infected with 2019-nCoV. The patient had been aware of the public health and news media coverage of 2019-nCoV and, after developing symptoms, contacted his health care provider on Jan. 19. The patient did not fly directly from Wuhan, but Dr. Lindquist said that he has been fully cooperative and has been helpful to authorities in tracing his route and contacts. The man is being treated at Providence Regional Medical Center, Everett, Wash.
The CDC obtained a specimen from the patient immediately and identified the 2019-nCoV within 24 hours.
Screening at airports is part of a multipart strategy to address this type of infection that includes public health information dissemination, patient education, as well as hospital preparation and training exercises. Currently, a strategy referred to as “funneling” is being implemented wherein travelers from China are rerouted and reticketed to one of the five airports conducting screening. At present, JFK in New York, San Francisco International, Los Angeles International, Hartsfield-Jackson Atlanta International Airport, and Chicago O’Hare International Airport are conducting inbound traveler screening.
The CDC is working in close cooperation with the Department of Homeland Security and the Federal Aviation Administration to coordinate travel screenings and reroutings. In addition, the CDC is working with the World Health Organization and the international global health community to share information about this outbreak. The CDC also has staff on site in Wuhan and is communicating with local health authorities. The CDC has activated its Emergency Operations Center to better provide ongoing support to the 2019-nCoV response. Currently, the focus is on tracing contacts and the means of transmission of this virus.
Updates on the outbreak will be posted on the CDC coronavirus website.
CORRECTION: 1/21/2020: The name of the medical center where the 2019-nCoV patient is being treated was corrected.
REPORTING FROM CDC
FDA advisers set high bar for new opioids
During an opioid-addiction epidemic, can any new opioid pain drug meet prevailing safety demands to gain regulatory approval?
On Jan. 14 and 15, a Food and Drug Administration advisory committee voted virtually unanimously against two new opioid formulations and evenly split for and against a third; the 2 days of data and discussion showed how high a bar new opioids face these days for getting onto the U.S. market.
The bar’s height is very understandable given how many Americans have become addicted to opioids over the past decade, more often than not by accident while using pain medications as they believed they had been directed, said experts during the sessions held on the FDA’s campus in White Oak, Md.
Among the many upshots of the opioid crisis, the meetings held to discuss these three contender opioids highlighted the bitter irony confronting attempts to bring new, safer opioids to the U.S. market: While less abusable pain-relief medications that still harness the potent analgesic power of mu opioid receptor agonists are desperately desired, new agents in this space now receive withering scrutiny over their safeguards against misuse and abuse, and over whether they add anything meaningfully new to what’s already available. While these demands seem reasonable, perhaps even essential, it’s unclear whether any new opioid-based pain drugs will ever fully meet the safety that researchers, clinicians, and the public now seek.
A special FDA advisory committee that combined the Anesthetic and Analgesic Drug Products Advisory Committee with members of the Drug Safety and Risk Management Advisory Committee considered the application for three different opioid drugs from three separate companies. None received a clear endorsement. Oxycodegol, a new type of orally delivered opioid molecule engineered to slow brain entry and thereby delay an abuser’s high, got voted down without any votes in favor and 27 votes against agency approval. Aximris XR, an extended-release oxycodone formulation that successfully deterred intravenous abuse but had no deterrence efficacy for intranasal or oral abuse failed by a 2-24 vote against. The third agent, CTC, a novel formulation of the schedule IV opioid tramadol with the NSAID celecoxib designed to be analgesic but with limited opioid-abuse appeal, came the closest to meaningful support with a tied 13-13 vote from advisory committee members for and against agency approval. FDA staff takes advisory committee opinions and votes into account when making their final decisions about drug marketing approvals.
In each case, the committee members, mostly the same roster assembled for each of the three agents, identified specific concerns with the data purported to show each drug’s safety and efficacy. But the gathered experts and consumer representatives also consistently cited holistic challenges to approving new opioids and the stiffer criteria these agents face amid a continuing wave of opioid misuse and abuse.
“In the context of the public health issues, we don’t want to be perceived in any way of taking shortcuts,” said Linda S. Tyler, PharmD,, an advisory committee member and professor of pharmacy and chief pharmacy officer at the University of Utah in Salt Lake City. “There is no question that for a new product to come to market in this space it needs to add to what’s on the market, meet a high bar, and provide advantages compared with what’s already on the market,” she said.
Tramadol plus celecoxib gains some support
The proposed combined formulation of tramadol and celecoxib came closest to meeting that bar, as far as the advisory committee was concerned, coming away with 13 votes favoring approval to match 13 votes against. The premise behind this agent, know as CTC (cocrystal of tramadol and celecoxib), was that it combined a modest dose (44 mg) of the schedule IV opioid tramadol with a 56-mg dose of celecoxib in a twice-daily pill. Eugene R. Viscusi, MD, professor of anesthesiology and director of acute pain management at Thomas Jefferson University in Philadelphia and a speaker at the session on behalf of the applicant company, spelled out the rationale behind CTC: “We are caught in a dilemma. We need to reduce opioid use, but we also need to treat pain. We have an urgent need to have pain treatment options that are effective but have low potential for abuse and dependence. We are looking at multimodal analgesia, that uses combination of agents, recognizing that postoperative pain is a mixed pain syndrome. Multimodal pain treatments are now considered standard care. We want to minimize opioids to the lowest dose possible to produce safe analgesia. Tramadol is the least-preferred opioid for abuse,” and is rated as schedule IV, the U.S. designation for drugs considered to have a low level of potential for causing abuse or dependence. “Opioids used as stand-alone agents have contributed to the current opioid crisis,” Dr. Viscusi told the committee.
In contrast to tramadol’s schedule IV status, the mainstays of recent opioid pain therapy have been hydrocodone and oxycodone, schedule II opioids rated as having a “high potential for abuse.”
Several advisory committee members agreed that CTC minimized patient exposure to an opioid. “This drug isn’t even tramadol; it’s tramadol light. It has about as low a dose [of an opioid] as you can have and still have a drug,” said member Lee A. Hoffer, PhD, a medical anthropologist at Case Western Reserve University, Cleveland, who studies substance use disorders. “All opioids are dangerous, even at a low dose, but there is a linear relationship based on potency, so if we want to have an opioid for acute pain, I’d like it to have the lowest morphine milligram equivalent possible. The ideal is no opioids, but that is not what happens,” he said. The CTC formulation delivers 17.6 morphine milligram equivalents (MME) per pill, the manufacturer’s representatives said. The Centers for Disease Control and Prevention defines a “relatively low” daily opioid dose as 20-50 MME.
Some committee members hailed the CTC formulation as a meaningful step toward cutting opioid consumption.
“We may be very nervous about abuse of scheduled opioids, but a schedule IV opioid in an opioid-sparing formulation is as good as it gets in 2020,” said committee member Kevin L. Zacharoff, MD, a pain medicine specialist at the State University of New York at Stony Brook. “Any opioid has potential for abuse, but this is a safer alternative to the schedule II drugs. There is less public health risk with this,” said committee member Sherif Zaafran, MD, a Houston anesthesiologist. “This represents an incremental but important approach to addressing the opioid crisis, especially if used to replace schedule II opioids,” said Brandon D.L. Marshall, PhD, an epidemiologist and substance abuse researcher at Brown University in Providence, R.I.
But despite agreement that CTC represented a new low in the MME of an opioid given to patients, several committee members still saw the formulation as problematic by introducing any opioid, no matter how small the dose.
“The landscape of tramadol use and prescribing is evolving. There’s been an exponential upturn in tramadol prescribing. It’s perceived [as] safer, but it’s not completely safe. Will this change tramadol abuse and open the door to abuse of other opioids? This is what got us into trouble with opioids in the first place. Patients start with a prescription opioid that they perceive is safe. Patients don’t start with oxycodone or heroin. They start with drugs that are believed to be safe. I feel this combination has less risk for abuse, but I’m worried that it would produce a false sense of security for tolerability and safety,” said committee member Maryann E. Amirshahi, MD, a medical toxicologist at Georgetown University and MedStar Health in Washington.
Several other committee members returned to this point throughout the 2 days of discussions: The majority of Americans who have become hooked on opioids reached that point by taking an opioid pain medication for a legitimate medical reason and using the drug the way they had understood they should.
“I’m most concerned about unintentional misuse leading to addiction and abuse. Most people with an opioid addiction got it inadvertently, misusing it by mistake,” said committee member Suzanne B. Robotti, a consumer representative and executive director of DES Action USA. “I’m concerned about approving an opioid, even an opioid with a low abuse history, without a clearer picture of the human abuse potential data and what would happen if this drug were abused,” she added, referring to the proposed CTC formulation.
“All the patients I work with started [their opioid addiction] as pain patients,” Dr. Hoffer said.
“The most common use and abuse of opioids is orally. We need to avoid having patients who use the drug as prescribed and still end up addicted,” said committee member Friedhelm Sandbrink, MD, a neurologist and director of pain management at the Veterans Affairs (VA) Medical Center in Washington.
What this means, said several panelists, is functionally clamping down a class-wide lid on new opioids. “The way to reduce deaths from abuse is to reduce addiction, and to have an impact you need to reduce opioid exposure.” said committee member Sonia Hernandez-Diaz, MD, professor of epidemiology at the Harvard School of Public Health in Boston.
“In this opioid crisis, we ask for data that we wouldn’t ordinarily ask for. I feel there are unanswered questions about the abuse potential [of CTC]. We have seen a recent reduction in oxycodone use, which is great, but also an increase in tramadol use. We should not be fooled. Tramadol is an opioid, even if it’s schedule IV,” Dr. Tyler said.
Two other opioids faced greater opposition
The other two agents that the committee considered received much less support and sharper skepticism. The application for Aximris XR, an extended release form of oxycodone with a purported abuse-deterrent formulation (ADF) that relies on being difficult to extract for intravenous use as well as possibly having effective deterrence mechanisms for other forms of abuse. But FDA staffers reported that the only effective deterrence they could document was against manipulation for intravenous use, making Aximris XR the first opioid seeking ADF labeling based on deterrence to a single delivery route. This led several committee members, as well as the FDA, to comment on the clinical meaningfulness of ADF for one route. So far, the FDA approved ADF labeling for seven opioids, most notably OxyContin, an extended-release oxycodone with the biggest share of the U.S. market for opioids with ADF labeling.
“For ADF, we label based on what we expect from the premarket data. We don’t really know how that translates into what happens once the drug is on the market. Every company with an ADF in their label is required to do postmarketing studies on the abuse routes that are supposed to be deterred. We see shifts to other routes. Assessment of ADF is incredibly challenging, both scientifically and logistically, because there has not been a lot of uptake of these products, for a variety of reasons,” said Judy Staffa, PhD, associate director for Public Health Initiatives in the Office of Surveillance & Epidemiology in the FDA’s Center for Drug Evaluation and Research. The company that markets OxyContin has been the first to submit to the FDA all of its required postmarketing data on ADF efficacy, and the agency is now reviewing this filing, Dr. Staffa said.
The data presented for Aximris XR appeared to generally fail to convince committee members that it provided a meaningful addition to the range of opioids with ADF designations already available, which meant that their decision mostly came down to whether they felt it made sense to bring a me-too opioid to the U.S. market. Their answer was mostly no.
“In the end, it’s another opioid, and I’m not sure we need another opioid,” said committee member Lonnie K. Zeltzer, MD, professor of pediatrics, anesthesiology, psychiatry, and biobehavioral sciences and director of pediatric pain at the University of California, Los Angeles “There are so many options for patients and for people who abuse these drug. I don’t see this formulation as having a profound impact, but I’m very concerned about adding more prescription opioids,” said Martin Garcia-Bunuel, MD, deputy chief of staff for the VA Maryland Health Care System in Baltimore. Another concern of some committee members was that ADF remains a designation with an uncertain meaning, pending the FDA’s analysis of the OxyContin data.
“At the end of the day, we don’t know whether any of the [ADF] stuff makes a difference,” noted Steve B. Meisel, PharmD, system director of medication safety for M Health Fairview in Minneapolis and a committee member,
The third agent, oxycodegol, a molecule designed to pass more slowly across the blood-brain barrier because of an attached polyethylene glycol chain that’s supposed to prevent a rapid high after ingestion and hence cut abuse potential. It received unanimous committee rejection, primarily because its safety and efficacy evidence had so many holes, but the shadow of opioid abuse permeated the committee’s discussion.
“One dogma in the abuse world is that slowing entry into the brain reduces abuse potential, but the opioid crisis showed that this is not the only factor. Some people have become addicted to slow-acting drugs. The abuse potential of this drug, oxycodegol, needs to be considered given where we’ve been with the opioid crisis,” said Jane B. Acri, PhD, chief of the Medications Discovery and Toxicology Branch of the National Institute on Drug Abuse.
“During the opioid epidemic, do we want to approve more opioids? If the [pain] efficacy is about the same as oxycodone, is better safety or abuse potential a reason to approve it? We need guidance [from the FDA] about what is ‘better enough.’ No opioid will ever be perfect; there will always be abuse and misuse. But what is good enough to justify bringing another opioid onto the market? What is a good enough improvement? I don’t have an answer,” Dr. Hernandez-Diaz said.
Adviser comments showed that the continued threat of widespread opioid addiction has cooled prospects for new opioid approvals by making FDA advisers skittish over how to properly score the incremental value of a new opioid.
“Do we need to go back to the drawing board on how we make decisions on exposing the American public to these kinds of agents?” Dr. Garcia-Bunuel asked. “I don’t think we have the tools to make these decisions.”
During an opioid-addiction epidemic, can any new opioid pain drug meet prevailing safety demands to gain regulatory approval?
On Jan. 14 and 15, a Food and Drug Administration advisory committee voted virtually unanimously against two new opioid formulations and evenly split for and against a third; the 2 days of data and discussion showed how high a bar new opioids face these days for getting onto the U.S. market.
The bar’s height is very understandable given how many Americans have become addicted to opioids over the past decade, more often than not by accident while using pain medications as they believed they had been directed, said experts during the sessions held on the FDA’s campus in White Oak, Md.
Among the many upshots of the opioid crisis, the meetings held to discuss these three contender opioids highlighted the bitter irony confronting attempts to bring new, safer opioids to the U.S. market: While less abusable pain-relief medications that still harness the potent analgesic power of mu opioid receptor agonists are desperately desired, new agents in this space now receive withering scrutiny over their safeguards against misuse and abuse, and over whether they add anything meaningfully new to what’s already available. While these demands seem reasonable, perhaps even essential, it’s unclear whether any new opioid-based pain drugs will ever fully meet the safety that researchers, clinicians, and the public now seek.
A special FDA advisory committee that combined the Anesthetic and Analgesic Drug Products Advisory Committee with members of the Drug Safety and Risk Management Advisory Committee considered the application for three different opioid drugs from three separate companies. None received a clear endorsement. Oxycodegol, a new type of orally delivered opioid molecule engineered to slow brain entry and thereby delay an abuser’s high, got voted down without any votes in favor and 27 votes against agency approval. Aximris XR, an extended-release oxycodone formulation that successfully deterred intravenous abuse but had no deterrence efficacy for intranasal or oral abuse failed by a 2-24 vote against. The third agent, CTC, a novel formulation of the schedule IV opioid tramadol with the NSAID celecoxib designed to be analgesic but with limited opioid-abuse appeal, came the closest to meaningful support with a tied 13-13 vote from advisory committee members for and against agency approval. FDA staff takes advisory committee opinions and votes into account when making their final decisions about drug marketing approvals.
In each case, the committee members, mostly the same roster assembled for each of the three agents, identified specific concerns with the data purported to show each drug’s safety and efficacy. But the gathered experts and consumer representatives also consistently cited holistic challenges to approving new opioids and the stiffer criteria these agents face amid a continuing wave of opioid misuse and abuse.
“In the context of the public health issues, we don’t want to be perceived in any way of taking shortcuts,” said Linda S. Tyler, PharmD,, an advisory committee member and professor of pharmacy and chief pharmacy officer at the University of Utah in Salt Lake City. “There is no question that for a new product to come to market in this space it needs to add to what’s on the market, meet a high bar, and provide advantages compared with what’s already on the market,” she said.
Tramadol plus celecoxib gains some support
The proposed combined formulation of tramadol and celecoxib came closest to meeting that bar, as far as the advisory committee was concerned, coming away with 13 votes favoring approval to match 13 votes against. The premise behind this agent, know as CTC (cocrystal of tramadol and celecoxib), was that it combined a modest dose (44 mg) of the schedule IV opioid tramadol with a 56-mg dose of celecoxib in a twice-daily pill. Eugene R. Viscusi, MD, professor of anesthesiology and director of acute pain management at Thomas Jefferson University in Philadelphia and a speaker at the session on behalf of the applicant company, spelled out the rationale behind CTC: “We are caught in a dilemma. We need to reduce opioid use, but we also need to treat pain. We have an urgent need to have pain treatment options that are effective but have low potential for abuse and dependence. We are looking at multimodal analgesia, that uses combination of agents, recognizing that postoperative pain is a mixed pain syndrome. Multimodal pain treatments are now considered standard care. We want to minimize opioids to the lowest dose possible to produce safe analgesia. Tramadol is the least-preferred opioid for abuse,” and is rated as schedule IV, the U.S. designation for drugs considered to have a low level of potential for causing abuse or dependence. “Opioids used as stand-alone agents have contributed to the current opioid crisis,” Dr. Viscusi told the committee.
In contrast to tramadol’s schedule IV status, the mainstays of recent opioid pain therapy have been hydrocodone and oxycodone, schedule II opioids rated as having a “high potential for abuse.”
Several advisory committee members agreed that CTC minimized patient exposure to an opioid. “This drug isn’t even tramadol; it’s tramadol light. It has about as low a dose [of an opioid] as you can have and still have a drug,” said member Lee A. Hoffer, PhD, a medical anthropologist at Case Western Reserve University, Cleveland, who studies substance use disorders. “All opioids are dangerous, even at a low dose, but there is a linear relationship based on potency, so if we want to have an opioid for acute pain, I’d like it to have the lowest morphine milligram equivalent possible. The ideal is no opioids, but that is not what happens,” he said. The CTC formulation delivers 17.6 morphine milligram equivalents (MME) per pill, the manufacturer’s representatives said. The Centers for Disease Control and Prevention defines a “relatively low” daily opioid dose as 20-50 MME.
Some committee members hailed the CTC formulation as a meaningful step toward cutting opioid consumption.
“We may be very nervous about abuse of scheduled opioids, but a schedule IV opioid in an opioid-sparing formulation is as good as it gets in 2020,” said committee member Kevin L. Zacharoff, MD, a pain medicine specialist at the State University of New York at Stony Brook. “Any opioid has potential for abuse, but this is a safer alternative to the schedule II drugs. There is less public health risk with this,” said committee member Sherif Zaafran, MD, a Houston anesthesiologist. “This represents an incremental but important approach to addressing the opioid crisis, especially if used to replace schedule II opioids,” said Brandon D.L. Marshall, PhD, an epidemiologist and substance abuse researcher at Brown University in Providence, R.I.
But despite agreement that CTC represented a new low in the MME of an opioid given to patients, several committee members still saw the formulation as problematic by introducing any opioid, no matter how small the dose.
“The landscape of tramadol use and prescribing is evolving. There’s been an exponential upturn in tramadol prescribing. It’s perceived [as] safer, but it’s not completely safe. Will this change tramadol abuse and open the door to abuse of other opioids? This is what got us into trouble with opioids in the first place. Patients start with a prescription opioid that they perceive is safe. Patients don’t start with oxycodone or heroin. They start with drugs that are believed to be safe. I feel this combination has less risk for abuse, but I’m worried that it would produce a false sense of security for tolerability and safety,” said committee member Maryann E. Amirshahi, MD, a medical toxicologist at Georgetown University and MedStar Health in Washington.
Several other committee members returned to this point throughout the 2 days of discussions: The majority of Americans who have become hooked on opioids reached that point by taking an opioid pain medication for a legitimate medical reason and using the drug the way they had understood they should.
“I’m most concerned about unintentional misuse leading to addiction and abuse. Most people with an opioid addiction got it inadvertently, misusing it by mistake,” said committee member Suzanne B. Robotti, a consumer representative and executive director of DES Action USA. “I’m concerned about approving an opioid, even an opioid with a low abuse history, without a clearer picture of the human abuse potential data and what would happen if this drug were abused,” she added, referring to the proposed CTC formulation.
“All the patients I work with started [their opioid addiction] as pain patients,” Dr. Hoffer said.
“The most common use and abuse of opioids is orally. We need to avoid having patients who use the drug as prescribed and still end up addicted,” said committee member Friedhelm Sandbrink, MD, a neurologist and director of pain management at the Veterans Affairs (VA) Medical Center in Washington.
What this means, said several panelists, is functionally clamping down a class-wide lid on new opioids. “The way to reduce deaths from abuse is to reduce addiction, and to have an impact you need to reduce opioid exposure.” said committee member Sonia Hernandez-Diaz, MD, professor of epidemiology at the Harvard School of Public Health in Boston.
“In this opioid crisis, we ask for data that we wouldn’t ordinarily ask for. I feel there are unanswered questions about the abuse potential [of CTC]. We have seen a recent reduction in oxycodone use, which is great, but also an increase in tramadol use. We should not be fooled. Tramadol is an opioid, even if it’s schedule IV,” Dr. Tyler said.
Two other opioids faced greater opposition
The other two agents that the committee considered received much less support and sharper skepticism. The application for Aximris XR, an extended release form of oxycodone with a purported abuse-deterrent formulation (ADF) that relies on being difficult to extract for intravenous use as well as possibly having effective deterrence mechanisms for other forms of abuse. But FDA staffers reported that the only effective deterrence they could document was against manipulation for intravenous use, making Aximris XR the first opioid seeking ADF labeling based on deterrence to a single delivery route. This led several committee members, as well as the FDA, to comment on the clinical meaningfulness of ADF for one route. So far, the FDA approved ADF labeling for seven opioids, most notably OxyContin, an extended-release oxycodone with the biggest share of the U.S. market for opioids with ADF labeling.
“For ADF, we label based on what we expect from the premarket data. We don’t really know how that translates into what happens once the drug is on the market. Every company with an ADF in their label is required to do postmarketing studies on the abuse routes that are supposed to be deterred. We see shifts to other routes. Assessment of ADF is incredibly challenging, both scientifically and logistically, because there has not been a lot of uptake of these products, for a variety of reasons,” said Judy Staffa, PhD, associate director for Public Health Initiatives in the Office of Surveillance & Epidemiology in the FDA’s Center for Drug Evaluation and Research. The company that markets OxyContin has been the first to submit to the FDA all of its required postmarketing data on ADF efficacy, and the agency is now reviewing this filing, Dr. Staffa said.
The data presented for Aximris XR appeared to generally fail to convince committee members that it provided a meaningful addition to the range of opioids with ADF designations already available, which meant that their decision mostly came down to whether they felt it made sense to bring a me-too opioid to the U.S. market. Their answer was mostly no.
“In the end, it’s another opioid, and I’m not sure we need another opioid,” said committee member Lonnie K. Zeltzer, MD, professor of pediatrics, anesthesiology, psychiatry, and biobehavioral sciences and director of pediatric pain at the University of California, Los Angeles “There are so many options for patients and for people who abuse these drug. I don’t see this formulation as having a profound impact, but I’m very concerned about adding more prescription opioids,” said Martin Garcia-Bunuel, MD, deputy chief of staff for the VA Maryland Health Care System in Baltimore. Another concern of some committee members was that ADF remains a designation with an uncertain meaning, pending the FDA’s analysis of the OxyContin data.
“At the end of the day, we don’t know whether any of the [ADF] stuff makes a difference,” noted Steve B. Meisel, PharmD, system director of medication safety for M Health Fairview in Minneapolis and a committee member,
The third agent, oxycodegol, a molecule designed to pass more slowly across the blood-brain barrier because of an attached polyethylene glycol chain that’s supposed to prevent a rapid high after ingestion and hence cut abuse potential. It received unanimous committee rejection, primarily because its safety and efficacy evidence had so many holes, but the shadow of opioid abuse permeated the committee’s discussion.
“One dogma in the abuse world is that slowing entry into the brain reduces abuse potential, but the opioid crisis showed that this is not the only factor. Some people have become addicted to slow-acting drugs. The abuse potential of this drug, oxycodegol, needs to be considered given where we’ve been with the opioid crisis,” said Jane B. Acri, PhD, chief of the Medications Discovery and Toxicology Branch of the National Institute on Drug Abuse.
“During the opioid epidemic, do we want to approve more opioids? If the [pain] efficacy is about the same as oxycodone, is better safety or abuse potential a reason to approve it? We need guidance [from the FDA] about what is ‘better enough.’ No opioid will ever be perfect; there will always be abuse and misuse. But what is good enough to justify bringing another opioid onto the market? What is a good enough improvement? I don’t have an answer,” Dr. Hernandez-Diaz said.
Adviser comments showed that the continued threat of widespread opioid addiction has cooled prospects for new opioid approvals by making FDA advisers skittish over how to properly score the incremental value of a new opioid.
“Do we need to go back to the drawing board on how we make decisions on exposing the American public to these kinds of agents?” Dr. Garcia-Bunuel asked. “I don’t think we have the tools to make these decisions.”
During an opioid-addiction epidemic, can any new opioid pain drug meet prevailing safety demands to gain regulatory approval?
On Jan. 14 and 15, a Food and Drug Administration advisory committee voted virtually unanimously against two new opioid formulations and evenly split for and against a third; the 2 days of data and discussion showed how high a bar new opioids face these days for getting onto the U.S. market.
The bar’s height is very understandable given how many Americans have become addicted to opioids over the past decade, more often than not by accident while using pain medications as they believed they had been directed, said experts during the sessions held on the FDA’s campus in White Oak, Md.
Among the many upshots of the opioid crisis, the meetings held to discuss these three contender opioids highlighted the bitter irony confronting attempts to bring new, safer opioids to the U.S. market: While less abusable pain-relief medications that still harness the potent analgesic power of mu opioid receptor agonists are desperately desired, new agents in this space now receive withering scrutiny over their safeguards against misuse and abuse, and over whether they add anything meaningfully new to what’s already available. While these demands seem reasonable, perhaps even essential, it’s unclear whether any new opioid-based pain drugs will ever fully meet the safety that researchers, clinicians, and the public now seek.
A special FDA advisory committee that combined the Anesthetic and Analgesic Drug Products Advisory Committee with members of the Drug Safety and Risk Management Advisory Committee considered the application for three different opioid drugs from three separate companies. None received a clear endorsement. Oxycodegol, a new type of orally delivered opioid molecule engineered to slow brain entry and thereby delay an abuser’s high, got voted down without any votes in favor and 27 votes against agency approval. Aximris XR, an extended-release oxycodone formulation that successfully deterred intravenous abuse but had no deterrence efficacy for intranasal or oral abuse failed by a 2-24 vote against. The third agent, CTC, a novel formulation of the schedule IV opioid tramadol with the NSAID celecoxib designed to be analgesic but with limited opioid-abuse appeal, came the closest to meaningful support with a tied 13-13 vote from advisory committee members for and against agency approval. FDA staff takes advisory committee opinions and votes into account when making their final decisions about drug marketing approvals.
In each case, the committee members, mostly the same roster assembled for each of the three agents, identified specific concerns with the data purported to show each drug’s safety and efficacy. But the gathered experts and consumer representatives also consistently cited holistic challenges to approving new opioids and the stiffer criteria these agents face amid a continuing wave of opioid misuse and abuse.
“In the context of the public health issues, we don’t want to be perceived in any way of taking shortcuts,” said Linda S. Tyler, PharmD,, an advisory committee member and professor of pharmacy and chief pharmacy officer at the University of Utah in Salt Lake City. “There is no question that for a new product to come to market in this space it needs to add to what’s on the market, meet a high bar, and provide advantages compared with what’s already on the market,” she said.
Tramadol plus celecoxib gains some support
The proposed combined formulation of tramadol and celecoxib came closest to meeting that bar, as far as the advisory committee was concerned, coming away with 13 votes favoring approval to match 13 votes against. The premise behind this agent, know as CTC (cocrystal of tramadol and celecoxib), was that it combined a modest dose (44 mg) of the schedule IV opioid tramadol with a 56-mg dose of celecoxib in a twice-daily pill. Eugene R. Viscusi, MD, professor of anesthesiology and director of acute pain management at Thomas Jefferson University in Philadelphia and a speaker at the session on behalf of the applicant company, spelled out the rationale behind CTC: “We are caught in a dilemma. We need to reduce opioid use, but we also need to treat pain. We have an urgent need to have pain treatment options that are effective but have low potential for abuse and dependence. We are looking at multimodal analgesia, that uses combination of agents, recognizing that postoperative pain is a mixed pain syndrome. Multimodal pain treatments are now considered standard care. We want to minimize opioids to the lowest dose possible to produce safe analgesia. Tramadol is the least-preferred opioid for abuse,” and is rated as schedule IV, the U.S. designation for drugs considered to have a low level of potential for causing abuse or dependence. “Opioids used as stand-alone agents have contributed to the current opioid crisis,” Dr. Viscusi told the committee.
In contrast to tramadol’s schedule IV status, the mainstays of recent opioid pain therapy have been hydrocodone and oxycodone, schedule II opioids rated as having a “high potential for abuse.”
Several advisory committee members agreed that CTC minimized patient exposure to an opioid. “This drug isn’t even tramadol; it’s tramadol light. It has about as low a dose [of an opioid] as you can have and still have a drug,” said member Lee A. Hoffer, PhD, a medical anthropologist at Case Western Reserve University, Cleveland, who studies substance use disorders. “All opioids are dangerous, even at a low dose, but there is a linear relationship based on potency, so if we want to have an opioid for acute pain, I’d like it to have the lowest morphine milligram equivalent possible. The ideal is no opioids, but that is not what happens,” he said. The CTC formulation delivers 17.6 morphine milligram equivalents (MME) per pill, the manufacturer’s representatives said. The Centers for Disease Control and Prevention defines a “relatively low” daily opioid dose as 20-50 MME.
Some committee members hailed the CTC formulation as a meaningful step toward cutting opioid consumption.
“We may be very nervous about abuse of scheduled opioids, but a schedule IV opioid in an opioid-sparing formulation is as good as it gets in 2020,” said committee member Kevin L. Zacharoff, MD, a pain medicine specialist at the State University of New York at Stony Brook. “Any opioid has potential for abuse, but this is a safer alternative to the schedule II drugs. There is less public health risk with this,” said committee member Sherif Zaafran, MD, a Houston anesthesiologist. “This represents an incremental but important approach to addressing the opioid crisis, especially if used to replace schedule II opioids,” said Brandon D.L. Marshall, PhD, an epidemiologist and substance abuse researcher at Brown University in Providence, R.I.
But despite agreement that CTC represented a new low in the MME of an opioid given to patients, several committee members still saw the formulation as problematic by introducing any opioid, no matter how small the dose.
“The landscape of tramadol use and prescribing is evolving. There’s been an exponential upturn in tramadol prescribing. It’s perceived [as] safer, but it’s not completely safe. Will this change tramadol abuse and open the door to abuse of other opioids? This is what got us into trouble with opioids in the first place. Patients start with a prescription opioid that they perceive is safe. Patients don’t start with oxycodone or heroin. They start with drugs that are believed to be safe. I feel this combination has less risk for abuse, but I’m worried that it would produce a false sense of security for tolerability and safety,” said committee member Maryann E. Amirshahi, MD, a medical toxicologist at Georgetown University and MedStar Health in Washington.
Several other committee members returned to this point throughout the 2 days of discussions: The majority of Americans who have become hooked on opioids reached that point by taking an opioid pain medication for a legitimate medical reason and using the drug the way they had understood they should.
“I’m most concerned about unintentional misuse leading to addiction and abuse. Most people with an opioid addiction got it inadvertently, misusing it by mistake,” said committee member Suzanne B. Robotti, a consumer representative and executive director of DES Action USA. “I’m concerned about approving an opioid, even an opioid with a low abuse history, without a clearer picture of the human abuse potential data and what would happen if this drug were abused,” she added, referring to the proposed CTC formulation.
“All the patients I work with started [their opioid addiction] as pain patients,” Dr. Hoffer said.
“The most common use and abuse of opioids is orally. We need to avoid having patients who use the drug as prescribed and still end up addicted,” said committee member Friedhelm Sandbrink, MD, a neurologist and director of pain management at the Veterans Affairs (VA) Medical Center in Washington.
What this means, said several panelists, is functionally clamping down a class-wide lid on new opioids. “The way to reduce deaths from abuse is to reduce addiction, and to have an impact you need to reduce opioid exposure.” said committee member Sonia Hernandez-Diaz, MD, professor of epidemiology at the Harvard School of Public Health in Boston.
“In this opioid crisis, we ask for data that we wouldn’t ordinarily ask for. I feel there are unanswered questions about the abuse potential [of CTC]. We have seen a recent reduction in oxycodone use, which is great, but also an increase in tramadol use. We should not be fooled. Tramadol is an opioid, even if it’s schedule IV,” Dr. Tyler said.
Two other opioids faced greater opposition
The other two agents that the committee considered received much less support and sharper skepticism. The application for Aximris XR, an extended release form of oxycodone with a purported abuse-deterrent formulation (ADF) that relies on being difficult to extract for intravenous use as well as possibly having effective deterrence mechanisms for other forms of abuse. But FDA staffers reported that the only effective deterrence they could document was against manipulation for intravenous use, making Aximris XR the first opioid seeking ADF labeling based on deterrence to a single delivery route. This led several committee members, as well as the FDA, to comment on the clinical meaningfulness of ADF for one route. So far, the FDA approved ADF labeling for seven opioids, most notably OxyContin, an extended-release oxycodone with the biggest share of the U.S. market for opioids with ADF labeling.
“For ADF, we label based on what we expect from the premarket data. We don’t really know how that translates into what happens once the drug is on the market. Every company with an ADF in their label is required to do postmarketing studies on the abuse routes that are supposed to be deterred. We see shifts to other routes. Assessment of ADF is incredibly challenging, both scientifically and logistically, because there has not been a lot of uptake of these products, for a variety of reasons,” said Judy Staffa, PhD, associate director for Public Health Initiatives in the Office of Surveillance & Epidemiology in the FDA’s Center for Drug Evaluation and Research. The company that markets OxyContin has been the first to submit to the FDA all of its required postmarketing data on ADF efficacy, and the agency is now reviewing this filing, Dr. Staffa said.
The data presented for Aximris XR appeared to generally fail to convince committee members that it provided a meaningful addition to the range of opioids with ADF designations already available, which meant that their decision mostly came down to whether they felt it made sense to bring a me-too opioid to the U.S. market. Their answer was mostly no.
“In the end, it’s another opioid, and I’m not sure we need another opioid,” said committee member Lonnie K. Zeltzer, MD, professor of pediatrics, anesthesiology, psychiatry, and biobehavioral sciences and director of pediatric pain at the University of California, Los Angeles “There are so many options for patients and for people who abuse these drug. I don’t see this formulation as having a profound impact, but I’m very concerned about adding more prescription opioids,” said Martin Garcia-Bunuel, MD, deputy chief of staff for the VA Maryland Health Care System in Baltimore. Another concern of some committee members was that ADF remains a designation with an uncertain meaning, pending the FDA’s analysis of the OxyContin data.
“At the end of the day, we don’t know whether any of the [ADF] stuff makes a difference,” noted Steve B. Meisel, PharmD, system director of medication safety for M Health Fairview in Minneapolis and a committee member,
The third agent, oxycodegol, a molecule designed to pass more slowly across the blood-brain barrier because of an attached polyethylene glycol chain that’s supposed to prevent a rapid high after ingestion and hence cut abuse potential. It received unanimous committee rejection, primarily because its safety and efficacy evidence had so many holes, but the shadow of opioid abuse permeated the committee’s discussion.
“One dogma in the abuse world is that slowing entry into the brain reduces abuse potential, but the opioid crisis showed that this is not the only factor. Some people have become addicted to slow-acting drugs. The abuse potential of this drug, oxycodegol, needs to be considered given where we’ve been with the opioid crisis,” said Jane B. Acri, PhD, chief of the Medications Discovery and Toxicology Branch of the National Institute on Drug Abuse.
“During the opioid epidemic, do we want to approve more opioids? If the [pain] efficacy is about the same as oxycodone, is better safety or abuse potential a reason to approve it? We need guidance [from the FDA] about what is ‘better enough.’ No opioid will ever be perfect; there will always be abuse and misuse. But what is good enough to justify bringing another opioid onto the market? What is a good enough improvement? I don’t have an answer,” Dr. Hernandez-Diaz said.
Adviser comments showed that the continued threat of widespread opioid addiction has cooled prospects for new opioid approvals by making FDA advisers skittish over how to properly score the incremental value of a new opioid.
“Do we need to go back to the drawing board on how we make decisions on exposing the American public to these kinds of agents?” Dr. Garcia-Bunuel asked. “I don’t think we have the tools to make these decisions.”
Should a normal-appearing hippocampus be resected in a patient with temporal lobe epilepsy?
BALTIMORE – according to an analysis presented at the annual meeting of the American Epilepsy Society. Long-term seizure outcomes, however, are similar between resected and nonresected patients. In addition, sparing a normal-appearing hippocampus is correlated with a lower risk of verbal deficits, but long-term outcomes are unclear.
Neurologists have not arrived at a consensus about the best surgical management of patients with temporal lobe epilepsy and a hippocampus that appears normal on MRI. Few studies have examined seizure and neuropsychologic outcomes in this population, and this scarcity of data makes counseling patients difficult.
A review of data for surgical patients
To investigate this question, Marcia E. Morita-Sherman, MD, from the Cleveland Clinic, and colleagues retrospectively reviewed data for 152 patients who underwent surgery for temporal lobe epilepsy at the Cleveland Clinic during 2010-2018. Eligible participants were older than 16 years, and the researchers excluded patients with MRI or pathologic signs of hippocampal sclerosis and those with prior surgeries from the analysis.
To examine neuropsychological outcomes, Dr. Morita-Sherman and colleagues compared measures of verbal memory, visual memory, and confrontation naming that had been obtained before surgery and at 6 months after surgery. They measured hippocampal volume using Neuroquant. They categorized resections as dominant or nondominant according to patients’ handedness or language lateralization. The investigators classified 74 patients as having a spared hippocampus and 78 patients as having a resected hippocampus. They classified neuropsychological outcomes as showing decline or no decline using epilepsy-specific reliable change indexes.
Type of surgery affected memory and naming
Approximately 40% of patients had seizure recurrence within 1 year after surgery, and 63% had seizure recurrence within 6 years after surgery. The rate of invasive EEG was similar between patients with a spared hippocampus (50%) and those with a resected hippocampus (47%). In a univariate analysis, male sex, longer epilepsy duration, normal MRI, history of invasive evaluation, and acute postoperative seizures were associated with a higher risk of seizure recurrence. Patients with a spared hippocampus had a higher risk of early seizure recurrence, compared with patients with a resected hippocampus, but the difference was not statistically significant. Long-term seizure outcomes were similar between the two groups.
Neuropsychological outcomes were available for 86 patients. Among 56 patients who underwent surgery on the dominant side, those with spared-hippocampal surgery, compared with those with resected-hippocampal surgery, had lower rates of clinically meaningful declines in verbal memory (39.7% vs. 70.4%) and naming (40.7% vs. 79.2%). The investigators found no significant difference in the 30 patients with nondominant surgeries.
“Sparing the hippocampus in a tailored temporal lobe resection doesn’t necessarily prevent any memory decline. Close to 40% of our patients where the hippocampus was spared had a clinically significant memory loss,” said Lara E. Jehi, MD, an epileptologist at the Cleveland Clinic and one of the investigators. “Including the hippocampus in the resection seems to correlate with better odds of seizure freedom, at least in the short term. We need more research to study the long-term memory and naming implications of hippocampal sparing versus resection.”
The study was funded by a grant from the National Institutes of Health. The investigators reported no conflicts of interest. egreb@mdedge.com
SOURCE: Morita-Sherman ME et al. AES 2019, Abstract 1.336.
BALTIMORE – according to an analysis presented at the annual meeting of the American Epilepsy Society. Long-term seizure outcomes, however, are similar between resected and nonresected patients. In addition, sparing a normal-appearing hippocampus is correlated with a lower risk of verbal deficits, but long-term outcomes are unclear.
Neurologists have not arrived at a consensus about the best surgical management of patients with temporal lobe epilepsy and a hippocampus that appears normal on MRI. Few studies have examined seizure and neuropsychologic outcomes in this population, and this scarcity of data makes counseling patients difficult.
A review of data for surgical patients
To investigate this question, Marcia E. Morita-Sherman, MD, from the Cleveland Clinic, and colleagues retrospectively reviewed data for 152 patients who underwent surgery for temporal lobe epilepsy at the Cleveland Clinic during 2010-2018. Eligible participants were older than 16 years, and the researchers excluded patients with MRI or pathologic signs of hippocampal sclerosis and those with prior surgeries from the analysis.
To examine neuropsychological outcomes, Dr. Morita-Sherman and colleagues compared measures of verbal memory, visual memory, and confrontation naming that had been obtained before surgery and at 6 months after surgery. They measured hippocampal volume using Neuroquant. They categorized resections as dominant or nondominant according to patients’ handedness or language lateralization. The investigators classified 74 patients as having a spared hippocampus and 78 patients as having a resected hippocampus. They classified neuropsychological outcomes as showing decline or no decline using epilepsy-specific reliable change indexes.
Type of surgery affected memory and naming
Approximately 40% of patients had seizure recurrence within 1 year after surgery, and 63% had seizure recurrence within 6 years after surgery. The rate of invasive EEG was similar between patients with a spared hippocampus (50%) and those with a resected hippocampus (47%). In a univariate analysis, male sex, longer epilepsy duration, normal MRI, history of invasive evaluation, and acute postoperative seizures were associated with a higher risk of seizure recurrence. Patients with a spared hippocampus had a higher risk of early seizure recurrence, compared with patients with a resected hippocampus, but the difference was not statistically significant. Long-term seizure outcomes were similar between the two groups.
Neuropsychological outcomes were available for 86 patients. Among 56 patients who underwent surgery on the dominant side, those with spared-hippocampal surgery, compared with those with resected-hippocampal surgery, had lower rates of clinically meaningful declines in verbal memory (39.7% vs. 70.4%) and naming (40.7% vs. 79.2%). The investigators found no significant difference in the 30 patients with nondominant surgeries.
“Sparing the hippocampus in a tailored temporal lobe resection doesn’t necessarily prevent any memory decline. Close to 40% of our patients where the hippocampus was spared had a clinically significant memory loss,” said Lara E. Jehi, MD, an epileptologist at the Cleveland Clinic and one of the investigators. “Including the hippocampus in the resection seems to correlate with better odds of seizure freedom, at least in the short term. We need more research to study the long-term memory and naming implications of hippocampal sparing versus resection.”
The study was funded by a grant from the National Institutes of Health. The investigators reported no conflicts of interest. egreb@mdedge.com
SOURCE: Morita-Sherman ME et al. AES 2019, Abstract 1.336.
BALTIMORE – according to an analysis presented at the annual meeting of the American Epilepsy Society. Long-term seizure outcomes, however, are similar between resected and nonresected patients. In addition, sparing a normal-appearing hippocampus is correlated with a lower risk of verbal deficits, but long-term outcomes are unclear.
Neurologists have not arrived at a consensus about the best surgical management of patients with temporal lobe epilepsy and a hippocampus that appears normal on MRI. Few studies have examined seizure and neuropsychologic outcomes in this population, and this scarcity of data makes counseling patients difficult.
A review of data for surgical patients
To investigate this question, Marcia E. Morita-Sherman, MD, from the Cleveland Clinic, and colleagues retrospectively reviewed data for 152 patients who underwent surgery for temporal lobe epilepsy at the Cleveland Clinic during 2010-2018. Eligible participants were older than 16 years, and the researchers excluded patients with MRI or pathologic signs of hippocampal sclerosis and those with prior surgeries from the analysis.
To examine neuropsychological outcomes, Dr. Morita-Sherman and colleagues compared measures of verbal memory, visual memory, and confrontation naming that had been obtained before surgery and at 6 months after surgery. They measured hippocampal volume using Neuroquant. They categorized resections as dominant or nondominant according to patients’ handedness or language lateralization. The investigators classified 74 patients as having a spared hippocampus and 78 patients as having a resected hippocampus. They classified neuropsychological outcomes as showing decline or no decline using epilepsy-specific reliable change indexes.
Type of surgery affected memory and naming
Approximately 40% of patients had seizure recurrence within 1 year after surgery, and 63% had seizure recurrence within 6 years after surgery. The rate of invasive EEG was similar between patients with a spared hippocampus (50%) and those with a resected hippocampus (47%). In a univariate analysis, male sex, longer epilepsy duration, normal MRI, history of invasive evaluation, and acute postoperative seizures were associated with a higher risk of seizure recurrence. Patients with a spared hippocampus had a higher risk of early seizure recurrence, compared with patients with a resected hippocampus, but the difference was not statistically significant. Long-term seizure outcomes were similar between the two groups.
Neuropsychological outcomes were available for 86 patients. Among 56 patients who underwent surgery on the dominant side, those with spared-hippocampal surgery, compared with those with resected-hippocampal surgery, had lower rates of clinically meaningful declines in verbal memory (39.7% vs. 70.4%) and naming (40.7% vs. 79.2%). The investigators found no significant difference in the 30 patients with nondominant surgeries.
“Sparing the hippocampus in a tailored temporal lobe resection doesn’t necessarily prevent any memory decline. Close to 40% of our patients where the hippocampus was spared had a clinically significant memory loss,” said Lara E. Jehi, MD, an epileptologist at the Cleveland Clinic and one of the investigators. “Including the hippocampus in the resection seems to correlate with better odds of seizure freedom, at least in the short term. We need more research to study the long-term memory and naming implications of hippocampal sparing versus resection.”
The study was funded by a grant from the National Institutes of Health. The investigators reported no conflicts of interest. egreb@mdedge.com
SOURCE: Morita-Sherman ME et al. AES 2019, Abstract 1.336.
REPORTING FROM AES 2019
ACP maps two potential paths to universal health care
The American College of Physicians is recommending either a single-payer system or a public option within a regulated private insurance system to help deliver universal and affordable access to health care for all Americans.
“We came to the conclusion that two directions or approaches could get us to where we need to be,” ACP President Robert McLean, MD, said in an interview. “We need ... a system that provides universal, affordable access to care.”
After examining the evidence, ACP discarded one option: a direct market-based approach.
“Direct market-based approaches won’t work,” Dr. McLean explained. “If you look at where direct marketplace approaches ... have been implemented, they just will not get you to a place where you are going to get universal coverage, portability, essential benefits, and preexisting condition protection and administrative simplification.”
Dr. McLean highlighted two paths that could achieve universal coverage and better access to health care: a single-payer–financed system, or a publicly financed coverage option within a system of regulated private insurance.
It’s the first time ACP has endorsed a single-payer approach. The college supported the public option that wasn’t included as part of the Affordable Care Act. But ACP’s latest publicly financed proposal offers a deeper level of detail on how to make that option work in the context of a private insurance system.
While the health reform conversation may be a political, ACP doesn’t want to make it a partisan one. ACP’s policy recommendations represent a carefully researched series of ideas backed by evidence-based research, Dr. McLean said.
“There is a lot of nuance behind” the two recommendations, he noted, and those nuances are explored in a series of articles and editorials published Jan. 21 in Annals of Internal Medicine.
Sizing up single payer
The ACP acknowledges that for its single-payer system, the transition could be “politically difficult and strain the federal budget,” according to Ryan A. Crowley, senior analyst at ACP, and colleagues in an article outlining the organization’s vision. “Taxes would probably replace premiums, and private insurance would have a reduced role or be eliminated altogether.”
However, the authors note that a single-payer system could be designed to address concerns from a generally skeptical public, such as providing bulk funding or setting minimum standards to guide state operations. It also could include private insurance to provide supplemental coverage.
Even so, “adopting a single-payer system would be highly disruptive and could lead to price controls that would perpetuate flaws in the current Medicare payment system, including the undervaluation of primary care,” Mr. Crowley and colleagues wrote. “If prices are set too low, it could lead to shortages and longer wait times for services. Without sufficient cost controls, however, the cost of a single-payer system could be too high to be feasible.”
Pondering the public option
Given a single-payer plan’s potential challenges, ACP also is endorsing a public option model, which provides the choice of a government-sponsored health insurance plan to compete with existing private insurance options.
“Depending on its structure and implementation, a public choice (or public option) model available to all could help to achieve universal coverage, better access, and improved outcomes without the disruption of a single-payer approach,” the ACP authors noted.
The public option has its own drawbacks, they acknowledge. Those include an inability to achieve better savings on prescription drugs, compared with a single-payer system. The public option approach also doesn’t do away with the current administrative burden, and access issues related to narrow provider networks would persist.
Dr. McLean noted that a more highly regulated insurance market would be needed to help make the public option model work.
“Insurance companies don’t have regulation in a lot of things that they do,” Dr. McLean said. “We see that as quite problematic. They are kind of running amok at this point.”
Expanding the role of primary care
In either reform scenario, primary care would play a much greater role.
“We need to promote primary care,” Dr. McLean said. That includes better incentives to draw physicians to it. “We have to pay them enough,” he added.
The health care models will need to move away from higher pay to specialties for high-cost, high-volume procedural reimbursement. And they’ll need to recognize the need for placing a higher value on the cognitive services provided at the primary care level.
Also in need of change: physicians’ administrative burdens. Reforms need to address the burden created by value-based care and the poor application and misapplication of quality measures.
Migration to a single-payer environment could would make reducing the administrative burden a lot easier, Dr. McLean said. But it also could be done with a public option approach.
That’s where regulators can play a big role in working with insurers to help address administrative burden – streamlining prior authorization of procedures, the types of forms used, and other policies, Dr. McLean explained.
“The number of insurers and their ability to have their own rules and regulations [make it] incredibly complex for patients as well as physicians trying to figure out how to deliver the care that they need,” he noted.
Dr. McLean hopes that the ACP’s papers will spark conversation, particularly among legislators and regulators.
“The bottom line is we cannot afford to not do something bold,” he cautioned. “It is just not working. Our patients deserve better, and we can do better.”
The American College of Physicians is recommending either a single-payer system or a public option within a regulated private insurance system to help deliver universal and affordable access to health care for all Americans.
“We came to the conclusion that two directions or approaches could get us to where we need to be,” ACP President Robert McLean, MD, said in an interview. “We need ... a system that provides universal, affordable access to care.”
After examining the evidence, ACP discarded one option: a direct market-based approach.
“Direct market-based approaches won’t work,” Dr. McLean explained. “If you look at where direct marketplace approaches ... have been implemented, they just will not get you to a place where you are going to get universal coverage, portability, essential benefits, and preexisting condition protection and administrative simplification.”
Dr. McLean highlighted two paths that could achieve universal coverage and better access to health care: a single-payer–financed system, or a publicly financed coverage option within a system of regulated private insurance.
It’s the first time ACP has endorsed a single-payer approach. The college supported the public option that wasn’t included as part of the Affordable Care Act. But ACP’s latest publicly financed proposal offers a deeper level of detail on how to make that option work in the context of a private insurance system.
While the health reform conversation may be a political, ACP doesn’t want to make it a partisan one. ACP’s policy recommendations represent a carefully researched series of ideas backed by evidence-based research, Dr. McLean said.
“There is a lot of nuance behind” the two recommendations, he noted, and those nuances are explored in a series of articles and editorials published Jan. 21 in Annals of Internal Medicine.
Sizing up single payer
The ACP acknowledges that for its single-payer system, the transition could be “politically difficult and strain the federal budget,” according to Ryan A. Crowley, senior analyst at ACP, and colleagues in an article outlining the organization’s vision. “Taxes would probably replace premiums, and private insurance would have a reduced role or be eliminated altogether.”
However, the authors note that a single-payer system could be designed to address concerns from a generally skeptical public, such as providing bulk funding or setting minimum standards to guide state operations. It also could include private insurance to provide supplemental coverage.
Even so, “adopting a single-payer system would be highly disruptive and could lead to price controls that would perpetuate flaws in the current Medicare payment system, including the undervaluation of primary care,” Mr. Crowley and colleagues wrote. “If prices are set too low, it could lead to shortages and longer wait times for services. Without sufficient cost controls, however, the cost of a single-payer system could be too high to be feasible.”
Pondering the public option
Given a single-payer plan’s potential challenges, ACP also is endorsing a public option model, which provides the choice of a government-sponsored health insurance plan to compete with existing private insurance options.
“Depending on its structure and implementation, a public choice (or public option) model available to all could help to achieve universal coverage, better access, and improved outcomes without the disruption of a single-payer approach,” the ACP authors noted.
The public option has its own drawbacks, they acknowledge. Those include an inability to achieve better savings on prescription drugs, compared with a single-payer system. The public option approach also doesn’t do away with the current administrative burden, and access issues related to narrow provider networks would persist.
Dr. McLean noted that a more highly regulated insurance market would be needed to help make the public option model work.
“Insurance companies don’t have regulation in a lot of things that they do,” Dr. McLean said. “We see that as quite problematic. They are kind of running amok at this point.”
Expanding the role of primary care
In either reform scenario, primary care would play a much greater role.
“We need to promote primary care,” Dr. McLean said. That includes better incentives to draw physicians to it. “We have to pay them enough,” he added.
The health care models will need to move away from higher pay to specialties for high-cost, high-volume procedural reimbursement. And they’ll need to recognize the need for placing a higher value on the cognitive services provided at the primary care level.
Also in need of change: physicians’ administrative burdens. Reforms need to address the burden created by value-based care and the poor application and misapplication of quality measures.
Migration to a single-payer environment could would make reducing the administrative burden a lot easier, Dr. McLean said. But it also could be done with a public option approach.
That’s where regulators can play a big role in working with insurers to help address administrative burden – streamlining prior authorization of procedures, the types of forms used, and other policies, Dr. McLean explained.
“The number of insurers and their ability to have their own rules and regulations [make it] incredibly complex for patients as well as physicians trying to figure out how to deliver the care that they need,” he noted.
Dr. McLean hopes that the ACP’s papers will spark conversation, particularly among legislators and regulators.
“The bottom line is we cannot afford to not do something bold,” he cautioned. “It is just not working. Our patients deserve better, and we can do better.”
The American College of Physicians is recommending either a single-payer system or a public option within a regulated private insurance system to help deliver universal and affordable access to health care for all Americans.
“We came to the conclusion that two directions or approaches could get us to where we need to be,” ACP President Robert McLean, MD, said in an interview. “We need ... a system that provides universal, affordable access to care.”
After examining the evidence, ACP discarded one option: a direct market-based approach.
“Direct market-based approaches won’t work,” Dr. McLean explained. “If you look at where direct marketplace approaches ... have been implemented, they just will not get you to a place where you are going to get universal coverage, portability, essential benefits, and preexisting condition protection and administrative simplification.”
Dr. McLean highlighted two paths that could achieve universal coverage and better access to health care: a single-payer–financed system, or a publicly financed coverage option within a system of regulated private insurance.
It’s the first time ACP has endorsed a single-payer approach. The college supported the public option that wasn’t included as part of the Affordable Care Act. But ACP’s latest publicly financed proposal offers a deeper level of detail on how to make that option work in the context of a private insurance system.
While the health reform conversation may be a political, ACP doesn’t want to make it a partisan one. ACP’s policy recommendations represent a carefully researched series of ideas backed by evidence-based research, Dr. McLean said.
“There is a lot of nuance behind” the two recommendations, he noted, and those nuances are explored in a series of articles and editorials published Jan. 21 in Annals of Internal Medicine.
Sizing up single payer
The ACP acknowledges that for its single-payer system, the transition could be “politically difficult and strain the federal budget,” according to Ryan A. Crowley, senior analyst at ACP, and colleagues in an article outlining the organization’s vision. “Taxes would probably replace premiums, and private insurance would have a reduced role or be eliminated altogether.”
However, the authors note that a single-payer system could be designed to address concerns from a generally skeptical public, such as providing bulk funding or setting minimum standards to guide state operations. It also could include private insurance to provide supplemental coverage.
Even so, “adopting a single-payer system would be highly disruptive and could lead to price controls that would perpetuate flaws in the current Medicare payment system, including the undervaluation of primary care,” Mr. Crowley and colleagues wrote. “If prices are set too low, it could lead to shortages and longer wait times for services. Without sufficient cost controls, however, the cost of a single-payer system could be too high to be feasible.”
Pondering the public option
Given a single-payer plan’s potential challenges, ACP also is endorsing a public option model, which provides the choice of a government-sponsored health insurance plan to compete with existing private insurance options.
“Depending on its structure and implementation, a public choice (or public option) model available to all could help to achieve universal coverage, better access, and improved outcomes without the disruption of a single-payer approach,” the ACP authors noted.
The public option has its own drawbacks, they acknowledge. Those include an inability to achieve better savings on prescription drugs, compared with a single-payer system. The public option approach also doesn’t do away with the current administrative burden, and access issues related to narrow provider networks would persist.
Dr. McLean noted that a more highly regulated insurance market would be needed to help make the public option model work.
“Insurance companies don’t have regulation in a lot of things that they do,” Dr. McLean said. “We see that as quite problematic. They are kind of running amok at this point.”
Expanding the role of primary care
In either reform scenario, primary care would play a much greater role.
“We need to promote primary care,” Dr. McLean said. That includes better incentives to draw physicians to it. “We have to pay them enough,” he added.
The health care models will need to move away from higher pay to specialties for high-cost, high-volume procedural reimbursement. And they’ll need to recognize the need for placing a higher value on the cognitive services provided at the primary care level.
Also in need of change: physicians’ administrative burdens. Reforms need to address the burden created by value-based care and the poor application and misapplication of quality measures.
Migration to a single-payer environment could would make reducing the administrative burden a lot easier, Dr. McLean said. But it also could be done with a public option approach.
That’s where regulators can play a big role in working with insurers to help address administrative burden – streamlining prior authorization of procedures, the types of forms used, and other policies, Dr. McLean explained.
“The number of insurers and their ability to have their own rules and regulations [make it] incredibly complex for patients as well as physicians trying to figure out how to deliver the care that they need,” he noted.
Dr. McLean hopes that the ACP’s papers will spark conversation, particularly among legislators and regulators.
“The bottom line is we cannot afford to not do something bold,” he cautioned. “It is just not working. Our patients deserve better, and we can do better.”
FROM ANNALS OF INTERNAL MEDICINE
Medscape survey points to generational differences in physician burnout
Burnout among physicians appears to have decreased slightly in the past few years, but remains a significant problem for the medical profession, according to the Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide.
A survey of more than 15,000 physicians revealed that 42% reported being burned out, down from 46% who responded to the survey 5 years ago. However, there are variations in the rates based on certain demographic factors such as specialty, age, and gender.
Urology sits at the top of the list as the specialty that is experiencing the highest rate of burnout, with 54% of urologists responding to the survey reporting burnout. Neurology and nephrology followed with rates of burnout at 50% and 49%, respectively. The next five specialties on the list all reported burnout rates of 46%: diabetes and endocrinology, family medicine, radiology, ob.gyn., and rheumatology. Pulmonology specialists reported a burnout rate of 41%. Gastroenterologists reported burnout rates of 37%.
The survey divided participants into three age categories – Millennial (ages 25-39 years), Generation X (ages 40-54 years), and Baby Boomer (ages 55-73 years). Both Millennials and Baby Boomers reported similar rates of burnout (38% and 39%, respectively) and those in Generation X reported a higher rate of burnout (48%).
This higher rate is not unexpected. The survey results cite Carol Bernstein, MD, of the Albert Einstein College of Medicine, New York, as noting that midcareer “is typically the time of highest burnout, which is where Gen Xers are in their career trajectory, suggesting a number of factors outside of work such as caring for children and elderly parents, planning for retirement, can play a role in contributing to burnout.”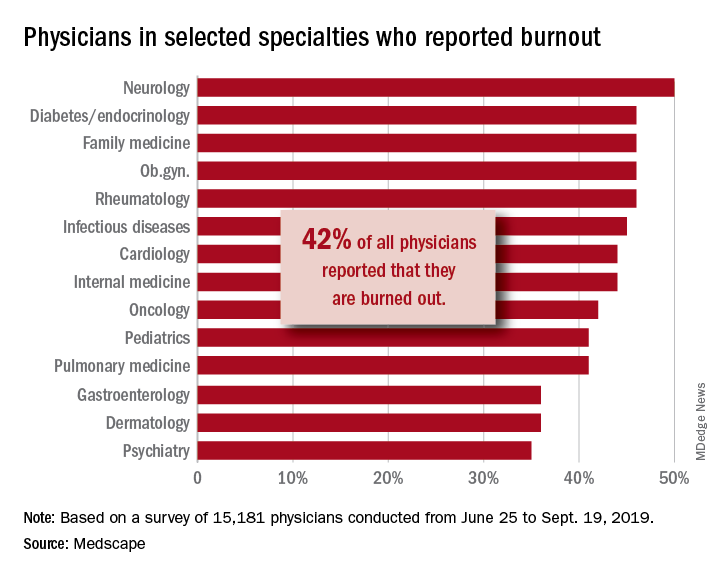
Women also reported a higher rate of burnout, although the rate has dropped from the survey conducted 5 years ago. The rate of burnout among women reported for the 2020 survey was 48%, down from 51% reported 5 years ago. By comparison, the rate of burnout for men was 37% in 2020, down from 43% in 2015.
In terms of what is causing burnout, the biggest contributor is the bureaucratic tasks (charting and paperwork, for example) that physicians must complete, which 55% of respondents to the survey said was the leading cause of burnout. Next was spending too many hours at work (33%); lack of respect from administrators, employers, colleagues, and staff (32%); and the increased computerization of the practice, including the use of electronic health records (30%).
When broken down by age category, the bureaucratic tasks was tops in all three groups (57% for Millennials, 56% for Generation X, and 54% for Baby Boomers), but what ranks next differs slightly by age group. For Millennials, the next two factors were too many hours at work (38%) and lack of respect (35%). Generation X respondents cited the same two factors, both at 33%. Baby Boomers cited computerization as their second-highest factor (41%) and spending too many hours at work as the third-highest factor (31%).
The generations had different approaches to coping with burnout. Millennials (56%) reported sleep as their top-ranked coping strategy, while Gen Xers and Baby Boomers ranked exercise and personal isolation as their top choice. For these two older groups, sleep was ranked last, after other activities such as talking with family and friends.
The survey also asked about depression, and respondents reported a similar rate across all age groups (15%, 18%, and 16%, respectively). Among those who said they were depressed, the three age groups had similar rates of suicidal thoughts (21%, 24%, and 22%).
Perhaps the most striking finding of the survey is the number of physicians who would take a pay cut to achieve a better work-life balance. Among Millennials, 52% would accept a pay cut, compared with 48% of Generation X and 49% of Baby Boomers. A surprising number (36%, 34%, and 31%, respectively, reported that they would accept a $10,000-$20,000 pay cut to have a 20% reduction in work hours. gtwachtman@mdedge.com
*This story was updated on 1/22/2020.
SOURCE: Kane L et al. Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. 2020 Jan 15.
Burnout among physicians appears to have decreased slightly in the past few years, but remains a significant problem for the medical profession, according to the Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide.
A survey of more than 15,000 physicians revealed that 42% reported being burned out, down from 46% who responded to the survey 5 years ago. However, there are variations in the rates based on certain demographic factors such as specialty, age, and gender.
Urology sits at the top of the list as the specialty that is experiencing the highest rate of burnout, with 54% of urologists responding to the survey reporting burnout. Neurology and nephrology followed with rates of burnout at 50% and 49%, respectively. The next five specialties on the list all reported burnout rates of 46%: diabetes and endocrinology, family medicine, radiology, ob.gyn., and rheumatology. Pulmonology specialists reported a burnout rate of 41%. Gastroenterologists reported burnout rates of 37%.
The survey divided participants into three age categories – Millennial (ages 25-39 years), Generation X (ages 40-54 years), and Baby Boomer (ages 55-73 years). Both Millennials and Baby Boomers reported similar rates of burnout (38% and 39%, respectively) and those in Generation X reported a higher rate of burnout (48%).
This higher rate is not unexpected. The survey results cite Carol Bernstein, MD, of the Albert Einstein College of Medicine, New York, as noting that midcareer “is typically the time of highest burnout, which is where Gen Xers are in their career trajectory, suggesting a number of factors outside of work such as caring for children and elderly parents, planning for retirement, can play a role in contributing to burnout.”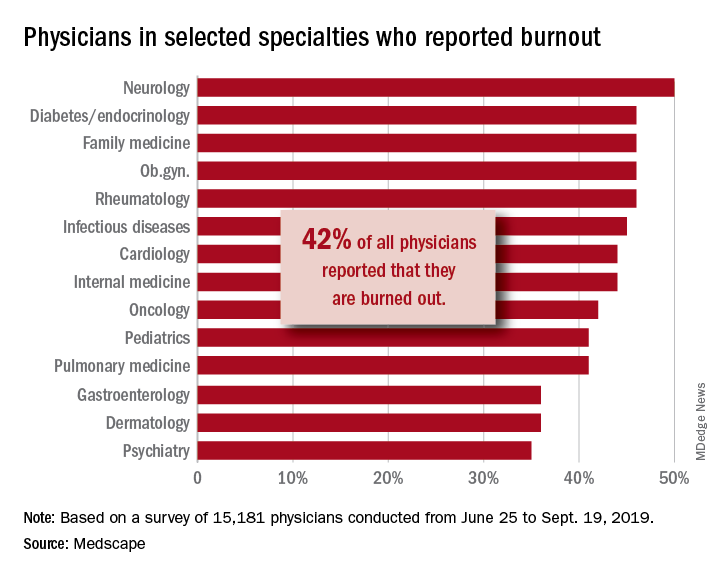
Women also reported a higher rate of burnout, although the rate has dropped from the survey conducted 5 years ago. The rate of burnout among women reported for the 2020 survey was 48%, down from 51% reported 5 years ago. By comparison, the rate of burnout for men was 37% in 2020, down from 43% in 2015.
In terms of what is causing burnout, the biggest contributor is the bureaucratic tasks (charting and paperwork, for example) that physicians must complete, which 55% of respondents to the survey said was the leading cause of burnout. Next was spending too many hours at work (33%); lack of respect from administrators, employers, colleagues, and staff (32%); and the increased computerization of the practice, including the use of electronic health records (30%).
When broken down by age category, the bureaucratic tasks was tops in all three groups (57% for Millennials, 56% for Generation X, and 54% for Baby Boomers), but what ranks next differs slightly by age group. For Millennials, the next two factors were too many hours at work (38%) and lack of respect (35%). Generation X respondents cited the same two factors, both at 33%. Baby Boomers cited computerization as their second-highest factor (41%) and spending too many hours at work as the third-highest factor (31%).
The generations had different approaches to coping with burnout. Millennials (56%) reported sleep as their top-ranked coping strategy, while Gen Xers and Baby Boomers ranked exercise and personal isolation as their top choice. For these two older groups, sleep was ranked last, after other activities such as talking with family and friends.
The survey also asked about depression, and respondents reported a similar rate across all age groups (15%, 18%, and 16%, respectively). Among those who said they were depressed, the three age groups had similar rates of suicidal thoughts (21%, 24%, and 22%).
Perhaps the most striking finding of the survey is the number of physicians who would take a pay cut to achieve a better work-life balance. Among Millennials, 52% would accept a pay cut, compared with 48% of Generation X and 49% of Baby Boomers. A surprising number (36%, 34%, and 31%, respectively, reported that they would accept a $10,000-$20,000 pay cut to have a 20% reduction in work hours. gtwachtman@mdedge.com
*This story was updated on 1/22/2020.
SOURCE: Kane L et al. Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. 2020 Jan 15.
Burnout among physicians appears to have decreased slightly in the past few years, but remains a significant problem for the medical profession, according to the Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide.
A survey of more than 15,000 physicians revealed that 42% reported being burned out, down from 46% who responded to the survey 5 years ago. However, there are variations in the rates based on certain demographic factors such as specialty, age, and gender.
Urology sits at the top of the list as the specialty that is experiencing the highest rate of burnout, with 54% of urologists responding to the survey reporting burnout. Neurology and nephrology followed with rates of burnout at 50% and 49%, respectively. The next five specialties on the list all reported burnout rates of 46%: diabetes and endocrinology, family medicine, radiology, ob.gyn., and rheumatology. Pulmonology specialists reported a burnout rate of 41%. Gastroenterologists reported burnout rates of 37%.
The survey divided participants into three age categories – Millennial (ages 25-39 years), Generation X (ages 40-54 years), and Baby Boomer (ages 55-73 years). Both Millennials and Baby Boomers reported similar rates of burnout (38% and 39%, respectively) and those in Generation X reported a higher rate of burnout (48%).
This higher rate is not unexpected. The survey results cite Carol Bernstein, MD, of the Albert Einstein College of Medicine, New York, as noting that midcareer “is typically the time of highest burnout, which is where Gen Xers are in their career trajectory, suggesting a number of factors outside of work such as caring for children and elderly parents, planning for retirement, can play a role in contributing to burnout.”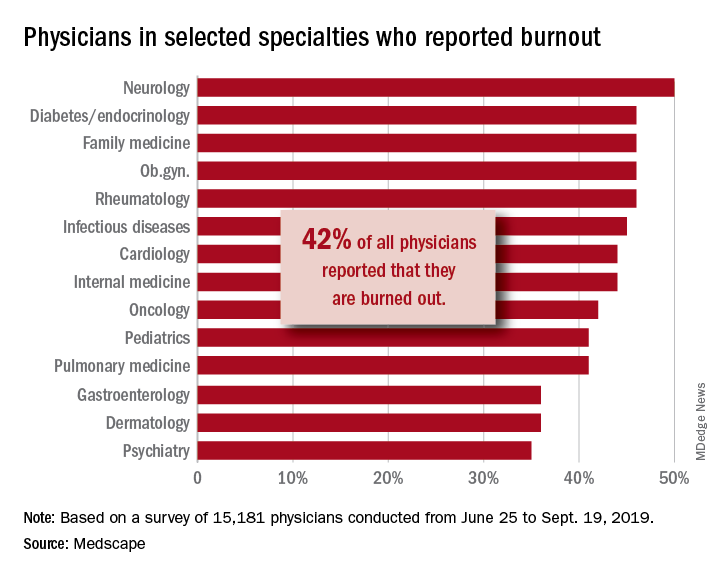
Women also reported a higher rate of burnout, although the rate has dropped from the survey conducted 5 years ago. The rate of burnout among women reported for the 2020 survey was 48%, down from 51% reported 5 years ago. By comparison, the rate of burnout for men was 37% in 2020, down from 43% in 2015.
In terms of what is causing burnout, the biggest contributor is the bureaucratic tasks (charting and paperwork, for example) that physicians must complete, which 55% of respondents to the survey said was the leading cause of burnout. Next was spending too many hours at work (33%); lack of respect from administrators, employers, colleagues, and staff (32%); and the increased computerization of the practice, including the use of electronic health records (30%).
When broken down by age category, the bureaucratic tasks was tops in all three groups (57% for Millennials, 56% for Generation X, and 54% for Baby Boomers), but what ranks next differs slightly by age group. For Millennials, the next two factors were too many hours at work (38%) and lack of respect (35%). Generation X respondents cited the same two factors, both at 33%. Baby Boomers cited computerization as their second-highest factor (41%) and spending too many hours at work as the third-highest factor (31%).
The generations had different approaches to coping with burnout. Millennials (56%) reported sleep as their top-ranked coping strategy, while Gen Xers and Baby Boomers ranked exercise and personal isolation as their top choice. For these two older groups, sleep was ranked last, after other activities such as talking with family and friends.
The survey also asked about depression, and respondents reported a similar rate across all age groups (15%, 18%, and 16%, respectively). Among those who said they were depressed, the three age groups had similar rates of suicidal thoughts (21%, 24%, and 22%).
Perhaps the most striking finding of the survey is the number of physicians who would take a pay cut to achieve a better work-life balance. Among Millennials, 52% would accept a pay cut, compared with 48% of Generation X and 49% of Baby Boomers. A surprising number (36%, 34%, and 31%, respectively, reported that they would accept a $10,000-$20,000 pay cut to have a 20% reduction in work hours. gtwachtman@mdedge.com
*This story was updated on 1/22/2020.
SOURCE: Kane L et al. Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. 2020 Jan 15.
Sleep problems linked to worsening PTSD in veterans
Insomnia is a common problem for veterans with PTSD, and the frequency of sleep problems is associated with increasing severity of PTSD, according to a study published in of the Journal of Traumatic Stress.
Raymond C. Rosen, PhD, of the New England Research Institutes, Watertown, Mass., and coauthors wrote that exploration of the relationship between PTSD and insomnia is complicated by the fact that it can be difficult to separate out disturbed sleep from other elements of PTSD, and because of the presence of other comorbidities in veterans, such as depression and traumatic brain injury.
The cohort study involved 1,643 veterans – roughly equal numbers of women and men – of Iraq and Afghanistan. Around two-thirds of the cohort had a diagnosis of PTSD. The participants completed a self-administered survey online or by mail, and were also assessed in a telephone interview, then followed up within 2-4 years.
While the prevalence of sleep problems was high across the cohort, the study found that 74% of participants with PTSD at baseline said they had experienced sleep difficulties for at least half of the previous 30 days, and one-third had been prescribed for a sedative-hypnotic drug in the past year.
In comparison, veterans without PTSD had fewer sleep problems and were prescribed significantly fewer sedative-hypnotic drugs.
The prevalence of sleep problems was similar in men and women with PTSD, although women had significantly higher rates of sedative-hypnotic prescriptions than men (40.4% vs. 35%, P = .006). A similar gender difference in prescription rates was seen in individuals without PTSD.
The study found that, although there was only a weak association between the severity of PTSD symptoms at baseline and the frequency of sleep problems at follow-up, there was a stronger association in reverse. Veterans with a higher frequency of sleep problems at baseline showed a significant increase in PTSD symptoms at follow-up.
The authors commented that this was in line with previous studies finding a similar effect of sleep disturbance on PTSD severity, both in military personnel and civilians.
“From a neurobiological perspective, it has been proposed that chronic sleep loss can lead to emotional dysregulation or heightened autonomic arousal, which in turn may be a risk factor for PTSD in trauma-exposed individuals,” they wrote. “It has also been proposed that prior sleep disturbance may attenuate the effects of extinction learning, leading to more enduring or severe symptoms in trauma-exposed individuals with concomitant sleep disorders.”
Given this association, the authors called for more attention to be given to identifying, diagnosing, and treating sleep disorders in veterans with and without PTSD.
The authors noted that they did not have access to polysomnographic data for participants, and were also unable to assess the prevalence, frequency, or intensity of nightmares in the cohort.
The study was supported by the Department of Defense. Conflict of interest disclosures were unavailable.
SOURCE: Rosen RC et al. J Trauma Stress. 2020;32:936-45.
Insomnia is a common problem for veterans with PTSD, and the frequency of sleep problems is associated with increasing severity of PTSD, according to a study published in of the Journal of Traumatic Stress.
Raymond C. Rosen, PhD, of the New England Research Institutes, Watertown, Mass., and coauthors wrote that exploration of the relationship between PTSD and insomnia is complicated by the fact that it can be difficult to separate out disturbed sleep from other elements of PTSD, and because of the presence of other comorbidities in veterans, such as depression and traumatic brain injury.
The cohort study involved 1,643 veterans – roughly equal numbers of women and men – of Iraq and Afghanistan. Around two-thirds of the cohort had a diagnosis of PTSD. The participants completed a self-administered survey online or by mail, and were also assessed in a telephone interview, then followed up within 2-4 years.
While the prevalence of sleep problems was high across the cohort, the study found that 74% of participants with PTSD at baseline said they had experienced sleep difficulties for at least half of the previous 30 days, and one-third had been prescribed for a sedative-hypnotic drug in the past year.
In comparison, veterans without PTSD had fewer sleep problems and were prescribed significantly fewer sedative-hypnotic drugs.
The prevalence of sleep problems was similar in men and women with PTSD, although women had significantly higher rates of sedative-hypnotic prescriptions than men (40.4% vs. 35%, P = .006). A similar gender difference in prescription rates was seen in individuals without PTSD.
The study found that, although there was only a weak association between the severity of PTSD symptoms at baseline and the frequency of sleep problems at follow-up, there was a stronger association in reverse. Veterans with a higher frequency of sleep problems at baseline showed a significant increase in PTSD symptoms at follow-up.
The authors commented that this was in line with previous studies finding a similar effect of sleep disturbance on PTSD severity, both in military personnel and civilians.
“From a neurobiological perspective, it has been proposed that chronic sleep loss can lead to emotional dysregulation or heightened autonomic arousal, which in turn may be a risk factor for PTSD in trauma-exposed individuals,” they wrote. “It has also been proposed that prior sleep disturbance may attenuate the effects of extinction learning, leading to more enduring or severe symptoms in trauma-exposed individuals with concomitant sleep disorders.”
Given this association, the authors called for more attention to be given to identifying, diagnosing, and treating sleep disorders in veterans with and without PTSD.
The authors noted that they did not have access to polysomnographic data for participants, and were also unable to assess the prevalence, frequency, or intensity of nightmares in the cohort.
The study was supported by the Department of Defense. Conflict of interest disclosures were unavailable.
SOURCE: Rosen RC et al. J Trauma Stress. 2020;32:936-45.
Insomnia is a common problem for veterans with PTSD, and the frequency of sleep problems is associated with increasing severity of PTSD, according to a study published in of the Journal of Traumatic Stress.
Raymond C. Rosen, PhD, of the New England Research Institutes, Watertown, Mass., and coauthors wrote that exploration of the relationship between PTSD and insomnia is complicated by the fact that it can be difficult to separate out disturbed sleep from other elements of PTSD, and because of the presence of other comorbidities in veterans, such as depression and traumatic brain injury.
The cohort study involved 1,643 veterans – roughly equal numbers of women and men – of Iraq and Afghanistan. Around two-thirds of the cohort had a diagnosis of PTSD. The participants completed a self-administered survey online or by mail, and were also assessed in a telephone interview, then followed up within 2-4 years.
While the prevalence of sleep problems was high across the cohort, the study found that 74% of participants with PTSD at baseline said they had experienced sleep difficulties for at least half of the previous 30 days, and one-third had been prescribed for a sedative-hypnotic drug in the past year.
In comparison, veterans without PTSD had fewer sleep problems and were prescribed significantly fewer sedative-hypnotic drugs.
The prevalence of sleep problems was similar in men and women with PTSD, although women had significantly higher rates of sedative-hypnotic prescriptions than men (40.4% vs. 35%, P = .006). A similar gender difference in prescription rates was seen in individuals without PTSD.
The study found that, although there was only a weak association between the severity of PTSD symptoms at baseline and the frequency of sleep problems at follow-up, there was a stronger association in reverse. Veterans with a higher frequency of sleep problems at baseline showed a significant increase in PTSD symptoms at follow-up.
The authors commented that this was in line with previous studies finding a similar effect of sleep disturbance on PTSD severity, both in military personnel and civilians.
“From a neurobiological perspective, it has been proposed that chronic sleep loss can lead to emotional dysregulation or heightened autonomic arousal, which in turn may be a risk factor for PTSD in trauma-exposed individuals,” they wrote. “It has also been proposed that prior sleep disturbance may attenuate the effects of extinction learning, leading to more enduring or severe symptoms in trauma-exposed individuals with concomitant sleep disorders.”
Given this association, the authors called for more attention to be given to identifying, diagnosing, and treating sleep disorders in veterans with and without PTSD.
The authors noted that they did not have access to polysomnographic data for participants, and were also unable to assess the prevalence, frequency, or intensity of nightmares in the cohort.
The study was supported by the Department of Defense. Conflict of interest disclosures were unavailable.
SOURCE: Rosen RC et al. J Trauma Stress. 2020;32:936-45.
FROM THE JOURNAL OF TRAUMATIC STRESS
Alan Alda, Scripps Research join forces to improve science communication
LA JOLLA, CALIF. – The first time that legendary actor Alan Alda conducted an interview for “Scientific American Frontiers” on PBS, an award-winning series that ran for more than a decade, he remembers learning a lesson in humility.
“I wasn’t as smart as I thought I was,” he told a crowd of largely scientists and medical professionals who gathered in a small auditorium on the campus of Scripps Research on Jan. 16, 2020. “I didn’t realize the value of ignorance. I have a natural supply of it. I began to use it and say [to interviewees]: ‘I don’t understand what that means.’ Sometimes it would be basic physics and they’d look at me like I was a school child. I am a very curious person. What I discovered was, I was bringing out their humanity by my own curiosity, by the way I related to them, which I developed through studying improvisation as an actor, and relating as an actor to other actors.”
Mr. Alda, 83, appeared on the research campus to announce that Scripps Research is the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at the State University of New York at Stony Brook, a nonprofit organization that Mr. Alda helped found in 2009.
Immersive training experience
“This will be a center where people can come to get training in effective communication,” said Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards. “It’s an experiential kind of training. We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
To date, the Alan Alda Center for Communicating Science has trained more than 15,000 scientific leaders in the United States and other countries. The location at Scripps Research makes it more convenient for West Coast–based researchers and industry leaders to participate. “One of the things we wished, for years, we had was a place where we could train scientists and researchers and medical professionals all up and down the West Coast,” he said.
Recently, more than 30 of Scripps Research scientists participated in Mr. Alda’s training program, an immersive and engaging experience that helps participants learn to empathize with an audience and present their work in a way that connects with different stakeholders. The skills and strategies can help participants relate to prospective investors and philanthropists, government officials, members of the media, peers across scientific disciplines, and the general public.
Earlier in the day that he spoke on the Scripps campus, Mr. Alda encountered some of the Scripps researchers who had participated in that training. “One group of scientists came in and we shook hands,” he said. “They introduced themselves and said: ‘We’re working on infectious diseases.’ I said: ‘Oh my God; I just shook hands with you!’ No matter what I asked them, they had a clear way to express what they did. Then I realized they had studied with Alda Communications.”
Why communication matters
During the early stages of forming what became the Alan Alda Center for Communicating Science, one Nobel Prize winner at a major university dismissed the importance of improving the communication skills of young scientists. “He said to me: ‘We don’t have time for that; we have too much science to teach,’ ” said Mr. Alda, who played Army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H”. “But communication is the essence of science. How can you do science unless you communicate with other scientists? There’s a stereotype that scientists are not as good at communicating as other people are. It’s true that they often speak a language that a lot of us don’t understand, but we all speak a language that is hard for other people to understand if we know something in great depth. We want to tell all the details; we want to speak in our special language because it makes us feel good.”
He underscored the importance of scientists being able to effectively communicate with the general public, “because the public needs to understand how important science is to their lives. It matters because at a place like [Scripps Research], understanding how nature works is put to work to keep our health secure.” Members of the public, he continued, “are busy living their lives; they’re busy working and bringing up their children. They haven’t spent 20, 30, 40 years devoted to a single aspect of nature the way scientists have. We can’t expect them to know as much as professional scientists, so we have to help them understand it. I hope we find ways to increase curiosity. I don’t know how to do that. I wish somebody would do a study on it, how you can take someone with a modicum of curiosity and help them enlarge it so it gives them the pleasure of discovering things about nature or understanding things about nature that other people don’t discover. Curiosity is the key to staying alive. That would bring us to a point of more people understanding science.”
Cultivating a sense of responsibility is another key to effective communication. “It’s the job of the person leading the discussion to make clear to the person listening,” Mr. Alda said. “You get the impression that ‘this person is my responsibility. I have to take care of them, so they understand what’s going on.’ ”
Parkinson’s disease diagnosis
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that when you get a diagnosis, your life is over,” said Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016. “Under the burden of that belief, some people won’t tell their family or workplace colleagues. There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
He added: “I’ve gone 5 years and I’m almost busier than I’ve ever been. I’m getting a lot accomplished and I look forward to I don’t know how many years. As long as I have them, I’m going to be grateful. It’s amazing how great it feels not to keep the diagnosis a secret.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – The first time that legendary actor Alan Alda conducted an interview for “Scientific American Frontiers” on PBS, an award-winning series that ran for more than a decade, he remembers learning a lesson in humility.
“I wasn’t as smart as I thought I was,” he told a crowd of largely scientists and medical professionals who gathered in a small auditorium on the campus of Scripps Research on Jan. 16, 2020. “I didn’t realize the value of ignorance. I have a natural supply of it. I began to use it and say [to interviewees]: ‘I don’t understand what that means.’ Sometimes it would be basic physics and they’d look at me like I was a school child. I am a very curious person. What I discovered was, I was bringing out their humanity by my own curiosity, by the way I related to them, which I developed through studying improvisation as an actor, and relating as an actor to other actors.”
Mr. Alda, 83, appeared on the research campus to announce that Scripps Research is the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at the State University of New York at Stony Brook, a nonprofit organization that Mr. Alda helped found in 2009.
Immersive training experience
“This will be a center where people can come to get training in effective communication,” said Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards. “It’s an experiential kind of training. We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
To date, the Alan Alda Center for Communicating Science has trained more than 15,000 scientific leaders in the United States and other countries. The location at Scripps Research makes it more convenient for West Coast–based researchers and industry leaders to participate. “One of the things we wished, for years, we had was a place where we could train scientists and researchers and medical professionals all up and down the West Coast,” he said.
Recently, more than 30 of Scripps Research scientists participated in Mr. Alda’s training program, an immersive and engaging experience that helps participants learn to empathize with an audience and present their work in a way that connects with different stakeholders. The skills and strategies can help participants relate to prospective investors and philanthropists, government officials, members of the media, peers across scientific disciplines, and the general public.
Earlier in the day that he spoke on the Scripps campus, Mr. Alda encountered some of the Scripps researchers who had participated in that training. “One group of scientists came in and we shook hands,” he said. “They introduced themselves and said: ‘We’re working on infectious diseases.’ I said: ‘Oh my God; I just shook hands with you!’ No matter what I asked them, they had a clear way to express what they did. Then I realized they had studied with Alda Communications.”
Why communication matters
During the early stages of forming what became the Alan Alda Center for Communicating Science, one Nobel Prize winner at a major university dismissed the importance of improving the communication skills of young scientists. “He said to me: ‘We don’t have time for that; we have too much science to teach,’ ” said Mr. Alda, who played Army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H”. “But communication is the essence of science. How can you do science unless you communicate with other scientists? There’s a stereotype that scientists are not as good at communicating as other people are. It’s true that they often speak a language that a lot of us don’t understand, but we all speak a language that is hard for other people to understand if we know something in great depth. We want to tell all the details; we want to speak in our special language because it makes us feel good.”
He underscored the importance of scientists being able to effectively communicate with the general public, “because the public needs to understand how important science is to their lives. It matters because at a place like [Scripps Research], understanding how nature works is put to work to keep our health secure.” Members of the public, he continued, “are busy living their lives; they’re busy working and bringing up their children. They haven’t spent 20, 30, 40 years devoted to a single aspect of nature the way scientists have. We can’t expect them to know as much as professional scientists, so we have to help them understand it. I hope we find ways to increase curiosity. I don’t know how to do that. I wish somebody would do a study on it, how you can take someone with a modicum of curiosity and help them enlarge it so it gives them the pleasure of discovering things about nature or understanding things about nature that other people don’t discover. Curiosity is the key to staying alive. That would bring us to a point of more people understanding science.”
Cultivating a sense of responsibility is another key to effective communication. “It’s the job of the person leading the discussion to make clear to the person listening,” Mr. Alda said. “You get the impression that ‘this person is my responsibility. I have to take care of them, so they understand what’s going on.’ ”
Parkinson’s disease diagnosis
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that when you get a diagnosis, your life is over,” said Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016. “Under the burden of that belief, some people won’t tell their family or workplace colleagues. There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
He added: “I’ve gone 5 years and I’m almost busier than I’ve ever been. I’m getting a lot accomplished and I look forward to I don’t know how many years. As long as I have them, I’m going to be grateful. It’s amazing how great it feels not to keep the diagnosis a secret.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – The first time that legendary actor Alan Alda conducted an interview for “Scientific American Frontiers” on PBS, an award-winning series that ran for more than a decade, he remembers learning a lesson in humility.
“I wasn’t as smart as I thought I was,” he told a crowd of largely scientists and medical professionals who gathered in a small auditorium on the campus of Scripps Research on Jan. 16, 2020. “I didn’t realize the value of ignorance. I have a natural supply of it. I began to use it and say [to interviewees]: ‘I don’t understand what that means.’ Sometimes it would be basic physics and they’d look at me like I was a school child. I am a very curious person. What I discovered was, I was bringing out their humanity by my own curiosity, by the way I related to them, which I developed through studying improvisation as an actor, and relating as an actor to other actors.”
Mr. Alda, 83, appeared on the research campus to announce that Scripps Research is the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at the State University of New York at Stony Brook, a nonprofit organization that Mr. Alda helped found in 2009.
Immersive training experience
“This will be a center where people can come to get training in effective communication,” said Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards. “It’s an experiential kind of training. We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
To date, the Alan Alda Center for Communicating Science has trained more than 15,000 scientific leaders in the United States and other countries. The location at Scripps Research makes it more convenient for West Coast–based researchers and industry leaders to participate. “One of the things we wished, for years, we had was a place where we could train scientists and researchers and medical professionals all up and down the West Coast,” he said.
Recently, more than 30 of Scripps Research scientists participated in Mr. Alda’s training program, an immersive and engaging experience that helps participants learn to empathize with an audience and present their work in a way that connects with different stakeholders. The skills and strategies can help participants relate to prospective investors and philanthropists, government officials, members of the media, peers across scientific disciplines, and the general public.
Earlier in the day that he spoke on the Scripps campus, Mr. Alda encountered some of the Scripps researchers who had participated in that training. “One group of scientists came in and we shook hands,” he said. “They introduced themselves and said: ‘We’re working on infectious diseases.’ I said: ‘Oh my God; I just shook hands with you!’ No matter what I asked them, they had a clear way to express what they did. Then I realized they had studied with Alda Communications.”
Why communication matters
During the early stages of forming what became the Alan Alda Center for Communicating Science, one Nobel Prize winner at a major university dismissed the importance of improving the communication skills of young scientists. “He said to me: ‘We don’t have time for that; we have too much science to teach,’ ” said Mr. Alda, who played Army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H”. “But communication is the essence of science. How can you do science unless you communicate with other scientists? There’s a stereotype that scientists are not as good at communicating as other people are. It’s true that they often speak a language that a lot of us don’t understand, but we all speak a language that is hard for other people to understand if we know something in great depth. We want to tell all the details; we want to speak in our special language because it makes us feel good.”
He underscored the importance of scientists being able to effectively communicate with the general public, “because the public needs to understand how important science is to their lives. It matters because at a place like [Scripps Research], understanding how nature works is put to work to keep our health secure.” Members of the public, he continued, “are busy living their lives; they’re busy working and bringing up their children. They haven’t spent 20, 30, 40 years devoted to a single aspect of nature the way scientists have. We can’t expect them to know as much as professional scientists, so we have to help them understand it. I hope we find ways to increase curiosity. I don’t know how to do that. I wish somebody would do a study on it, how you can take someone with a modicum of curiosity and help them enlarge it so it gives them the pleasure of discovering things about nature or understanding things about nature that other people don’t discover. Curiosity is the key to staying alive. That would bring us to a point of more people understanding science.”
Cultivating a sense of responsibility is another key to effective communication. “It’s the job of the person leading the discussion to make clear to the person listening,” Mr. Alda said. “You get the impression that ‘this person is my responsibility. I have to take care of them, so they understand what’s going on.’ ”
Parkinson’s disease diagnosis
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that when you get a diagnosis, your life is over,” said Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016. “Under the burden of that belief, some people won’t tell their family or workplace colleagues. There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
He added: “I’ve gone 5 years and I’m almost busier than I’ve ever been. I’m getting a lot accomplished and I look forward to I don’t know how many years. As long as I have them, I’m going to be grateful. It’s amazing how great it feels not to keep the diagnosis a secret.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
Cognitive screening of older physicians: What’s fair?
Cognitive screening of 141 clinicians 70 years or older at Yale New Haven (Conn.) Hospital identified 18 with cognitive deficits likely to impair their ability to practice medicine. Six retired and 12 agreed to limit their practice to closely proctored environments, according to a report in JAMA.
It was part of a program to screen all practitioners 70 years or older who apply for reappointment to the medical staff, and every 2 years thereafter, due to “concerns about the potentially compromised ability of older clinicians,” said the authors, Yale rheumatologist and geriatrician Leo M. Cooney Jr., MD, and Thomas Balcezak, MD, Yale New Haven’s chief medical officer.
Yale is not alone. Intermountain Healthcare, Stanford Hospitals and Clinics, Scripps Health Care, Penn Medicine, and the University of California, San Diego, are among the institutions with similar programs.
The move is being driven by the aging of the medical community. About 15% of U.S. physicians are over 65 years old, a tripling from 23,000 in 1980 to 73,000 in 2012-2016, and the number is growing, according to an editorial by Jeffrey L. Saver, MD, professor of neurology and senior associate vice president of neurology at the University of California, Los Angeles.
Given the trend, “it is not surprising that the issue of screening aging physicians for cognitive deficits has gained attention over the last decade,” Katrina Armstrong, MD, chair of the department of medicine at Massachusetts General Hospital, Boston, and Eileen E. Reynolds, MD, associate professor of medicine at Beth Israel Deaconess Medical Center, Boston, noted in a second editorial.
“Cognitive decline often accompanies aging, and the prevalence of dementia increases rapidly after age 70 years,” they said.
The data on whether older clinicians pose a risk to patients is limited and somewhat mixed. An analysis of 736,537 Medicare hospitalizations found no association between physician age and 30-day patient mortality among physicians 60 years or older with more than 201 admissions per year, but higher mortality among older physicians with lower volumes.
A meta-analysis of 62 studies showed that “older physicians have less factual knowledge, are less likely to adhere to appropriate standards of care, and may also have poorer patient outcomes.”
The new Yale data, meanwhile, suggests that “approximately 13% [18 of 141] of physicians and other clinicians older than 70 years should not be practicing independently,” Dr. Armstrong and Dr. Reynolds said in their editorial.
There is support for screening efforts. “As a profession that deals with human life, medical practitioners must obviously have the cognitive capacity to safely practice medicine. I applaud the approach taken by Yale New Haven Hospital in that cognitive abilities themselves, and not simply funds of knowledge, are assessed,” said Richard J. Caselli, MD, professor of neurology at the Mayo Clinic Arizona, Scottsdale, and a leader of the Alzheimer’s disease program there.
However, it’s not hard to imagine highly competent but older physicians taking umbrage at cognitive screening, and there’s been pushback. Stanford was considering a Yale-like approach but opted instead for peer review after opposition. Objections from the Utah Medical Association led Utah to enact a law banning age-based physician screening. In 2015, the American Medical Association issued a report calling for the development of guidelines and standards for assessing competency in aging physicians, but the AMA House of Delegates shelved it pending further study.
There are concerns about age discrimination, discounting the accumulated wisdom of long-practicing physicians, and misclassifying competent physicians, particularly those who provide quality care in rural and other underserved areas. Indeed, 8 of 14 clinicians who screened positive at Yale and underwent more extensive testing were allowed to recredential, “suggesting that the false-positive screening rate could be as high as 57%,” Dr. Armstrong and Dr. Reynolds noted.
The consensus seems to be that there probably is a need for some sort of screening, but it must be both sound and fair. Rather than a piecemeal institutional approach, perhaps there is “an important opportunity for other groups, including specialty boards and state licensing boards” to standardize the process, they said.
Among other things, assessments could focus less on test scores and more on the practice of medicine. For instance, fine motor skill/motor planning assessments for surgeons, and intermediate results could trigger a more extensive assessment of actual clinical performance, perhaps even direct observation, Dr. Saver said in his editorial.
As far as clinical performance goes, none of the 18 clinicians at Yale had previous performance problems. “Was this a failure of the system to report impaired physicians or were these physicians compensating sufficiently to avoid detection?” In either case, “cognitive testing should be a red flag that triggers other clinical assessments,” said Carl I. Cohen, MD, professor and director of the division of geriatric psychiatry at the State University of New York, Brooklyn.
The original plan at Yale was for neurologic and ophthalmologic examinations beginning at age 70, but ultimately it was decided to go with a battery of 16 tests to assess visual scanning and psychomotor efficiency, processing speed under pressure, concentration, and working memory, among other things. Testing takes about 50-90 minutes, and is graded by single neuropsychologist to ensure consistency. Results were compared with normative scores from both older and younger clinicians.
To prevent clinicians from preparing for it, Yale isn’t releasing its test battery.
Suboptimal performance triggered additional evaluations, including in-depth assessment of intellectual, memory, and executive function. Final reviews and recommendations were made by a committee that included a geriatrician, the clinician’s section or department chair, and current and past chief medical officers.
Among the 18 providers who demonstrated deficits impairing their ability to practice medicine, 5 were 70-74 years old; 4 were 75-79; and 9 were 80 years or older. Minor abnormalities were found in 34 other candidates (24.1%); they were allowed to recredential but were scheduled for rescreening at 1-year intervals, instead of every 2 years.
The mean age among the 141 screened clinicians was 74.3 years and ranged from 69 to 92 years; 86% were men. Applicants included 125 physicians (88.7%) as well as 5 advanced practice registered nurses; 4 dentists; 3 psychologists; 2 podiatrists; 1 physician associate; and 1 midwife.
The authors had no relevant disclosures.
SOURCE: Cooney L et al. JAMA. 2020 Jan 14;323(2):179-80.
Cognitive screening of 141 clinicians 70 years or older at Yale New Haven (Conn.) Hospital identified 18 with cognitive deficits likely to impair their ability to practice medicine. Six retired and 12 agreed to limit their practice to closely proctored environments, according to a report in JAMA.
It was part of a program to screen all practitioners 70 years or older who apply for reappointment to the medical staff, and every 2 years thereafter, due to “concerns about the potentially compromised ability of older clinicians,” said the authors, Yale rheumatologist and geriatrician Leo M. Cooney Jr., MD, and Thomas Balcezak, MD, Yale New Haven’s chief medical officer.
Yale is not alone. Intermountain Healthcare, Stanford Hospitals and Clinics, Scripps Health Care, Penn Medicine, and the University of California, San Diego, are among the institutions with similar programs.
The move is being driven by the aging of the medical community. About 15% of U.S. physicians are over 65 years old, a tripling from 23,000 in 1980 to 73,000 in 2012-2016, and the number is growing, according to an editorial by Jeffrey L. Saver, MD, professor of neurology and senior associate vice president of neurology at the University of California, Los Angeles.
Given the trend, “it is not surprising that the issue of screening aging physicians for cognitive deficits has gained attention over the last decade,” Katrina Armstrong, MD, chair of the department of medicine at Massachusetts General Hospital, Boston, and Eileen E. Reynolds, MD, associate professor of medicine at Beth Israel Deaconess Medical Center, Boston, noted in a second editorial.
“Cognitive decline often accompanies aging, and the prevalence of dementia increases rapidly after age 70 years,” they said.
The data on whether older clinicians pose a risk to patients is limited and somewhat mixed. An analysis of 736,537 Medicare hospitalizations found no association between physician age and 30-day patient mortality among physicians 60 years or older with more than 201 admissions per year, but higher mortality among older physicians with lower volumes.
A meta-analysis of 62 studies showed that “older physicians have less factual knowledge, are less likely to adhere to appropriate standards of care, and may also have poorer patient outcomes.”
The new Yale data, meanwhile, suggests that “approximately 13% [18 of 141] of physicians and other clinicians older than 70 years should not be practicing independently,” Dr. Armstrong and Dr. Reynolds said in their editorial.
There is support for screening efforts. “As a profession that deals with human life, medical practitioners must obviously have the cognitive capacity to safely practice medicine. I applaud the approach taken by Yale New Haven Hospital in that cognitive abilities themselves, and not simply funds of knowledge, are assessed,” said Richard J. Caselli, MD, professor of neurology at the Mayo Clinic Arizona, Scottsdale, and a leader of the Alzheimer’s disease program there.
However, it’s not hard to imagine highly competent but older physicians taking umbrage at cognitive screening, and there’s been pushback. Stanford was considering a Yale-like approach but opted instead for peer review after opposition. Objections from the Utah Medical Association led Utah to enact a law banning age-based physician screening. In 2015, the American Medical Association issued a report calling for the development of guidelines and standards for assessing competency in aging physicians, but the AMA House of Delegates shelved it pending further study.
There are concerns about age discrimination, discounting the accumulated wisdom of long-practicing physicians, and misclassifying competent physicians, particularly those who provide quality care in rural and other underserved areas. Indeed, 8 of 14 clinicians who screened positive at Yale and underwent more extensive testing were allowed to recredential, “suggesting that the false-positive screening rate could be as high as 57%,” Dr. Armstrong and Dr. Reynolds noted.
The consensus seems to be that there probably is a need for some sort of screening, but it must be both sound and fair. Rather than a piecemeal institutional approach, perhaps there is “an important opportunity for other groups, including specialty boards and state licensing boards” to standardize the process, they said.
Among other things, assessments could focus less on test scores and more on the practice of medicine. For instance, fine motor skill/motor planning assessments for surgeons, and intermediate results could trigger a more extensive assessment of actual clinical performance, perhaps even direct observation, Dr. Saver said in his editorial.
As far as clinical performance goes, none of the 18 clinicians at Yale had previous performance problems. “Was this a failure of the system to report impaired physicians or were these physicians compensating sufficiently to avoid detection?” In either case, “cognitive testing should be a red flag that triggers other clinical assessments,” said Carl I. Cohen, MD, professor and director of the division of geriatric psychiatry at the State University of New York, Brooklyn.
The original plan at Yale was for neurologic and ophthalmologic examinations beginning at age 70, but ultimately it was decided to go with a battery of 16 tests to assess visual scanning and psychomotor efficiency, processing speed under pressure, concentration, and working memory, among other things. Testing takes about 50-90 minutes, and is graded by single neuropsychologist to ensure consistency. Results were compared with normative scores from both older and younger clinicians.
To prevent clinicians from preparing for it, Yale isn’t releasing its test battery.
Suboptimal performance triggered additional evaluations, including in-depth assessment of intellectual, memory, and executive function. Final reviews and recommendations were made by a committee that included a geriatrician, the clinician’s section or department chair, and current and past chief medical officers.
Among the 18 providers who demonstrated deficits impairing their ability to practice medicine, 5 were 70-74 years old; 4 were 75-79; and 9 were 80 years or older. Minor abnormalities were found in 34 other candidates (24.1%); they were allowed to recredential but were scheduled for rescreening at 1-year intervals, instead of every 2 years.
The mean age among the 141 screened clinicians was 74.3 years and ranged from 69 to 92 years; 86% were men. Applicants included 125 physicians (88.7%) as well as 5 advanced practice registered nurses; 4 dentists; 3 psychologists; 2 podiatrists; 1 physician associate; and 1 midwife.
The authors had no relevant disclosures.
SOURCE: Cooney L et al. JAMA. 2020 Jan 14;323(2):179-80.
Cognitive screening of 141 clinicians 70 years or older at Yale New Haven (Conn.) Hospital identified 18 with cognitive deficits likely to impair their ability to practice medicine. Six retired and 12 agreed to limit their practice to closely proctored environments, according to a report in JAMA.
It was part of a program to screen all practitioners 70 years or older who apply for reappointment to the medical staff, and every 2 years thereafter, due to “concerns about the potentially compromised ability of older clinicians,” said the authors, Yale rheumatologist and geriatrician Leo M. Cooney Jr., MD, and Thomas Balcezak, MD, Yale New Haven’s chief medical officer.
Yale is not alone. Intermountain Healthcare, Stanford Hospitals and Clinics, Scripps Health Care, Penn Medicine, and the University of California, San Diego, are among the institutions with similar programs.
The move is being driven by the aging of the medical community. About 15% of U.S. physicians are over 65 years old, a tripling from 23,000 in 1980 to 73,000 in 2012-2016, and the number is growing, according to an editorial by Jeffrey L. Saver, MD, professor of neurology and senior associate vice president of neurology at the University of California, Los Angeles.
Given the trend, “it is not surprising that the issue of screening aging physicians for cognitive deficits has gained attention over the last decade,” Katrina Armstrong, MD, chair of the department of medicine at Massachusetts General Hospital, Boston, and Eileen E. Reynolds, MD, associate professor of medicine at Beth Israel Deaconess Medical Center, Boston, noted in a second editorial.
“Cognitive decline often accompanies aging, and the prevalence of dementia increases rapidly after age 70 years,” they said.
The data on whether older clinicians pose a risk to patients is limited and somewhat mixed. An analysis of 736,537 Medicare hospitalizations found no association between physician age and 30-day patient mortality among physicians 60 years or older with more than 201 admissions per year, but higher mortality among older physicians with lower volumes.
A meta-analysis of 62 studies showed that “older physicians have less factual knowledge, are less likely to adhere to appropriate standards of care, and may also have poorer patient outcomes.”
The new Yale data, meanwhile, suggests that “approximately 13% [18 of 141] of physicians and other clinicians older than 70 years should not be practicing independently,” Dr. Armstrong and Dr. Reynolds said in their editorial.
There is support for screening efforts. “As a profession that deals with human life, medical practitioners must obviously have the cognitive capacity to safely practice medicine. I applaud the approach taken by Yale New Haven Hospital in that cognitive abilities themselves, and not simply funds of knowledge, are assessed,” said Richard J. Caselli, MD, professor of neurology at the Mayo Clinic Arizona, Scottsdale, and a leader of the Alzheimer’s disease program there.
However, it’s not hard to imagine highly competent but older physicians taking umbrage at cognitive screening, and there’s been pushback. Stanford was considering a Yale-like approach but opted instead for peer review after opposition. Objections from the Utah Medical Association led Utah to enact a law banning age-based physician screening. In 2015, the American Medical Association issued a report calling for the development of guidelines and standards for assessing competency in aging physicians, but the AMA House of Delegates shelved it pending further study.
There are concerns about age discrimination, discounting the accumulated wisdom of long-practicing physicians, and misclassifying competent physicians, particularly those who provide quality care in rural and other underserved areas. Indeed, 8 of 14 clinicians who screened positive at Yale and underwent more extensive testing were allowed to recredential, “suggesting that the false-positive screening rate could be as high as 57%,” Dr. Armstrong and Dr. Reynolds noted.
The consensus seems to be that there probably is a need for some sort of screening, but it must be both sound and fair. Rather than a piecemeal institutional approach, perhaps there is “an important opportunity for other groups, including specialty boards and state licensing boards” to standardize the process, they said.
Among other things, assessments could focus less on test scores and more on the practice of medicine. For instance, fine motor skill/motor planning assessments for surgeons, and intermediate results could trigger a more extensive assessment of actual clinical performance, perhaps even direct observation, Dr. Saver said in his editorial.
As far as clinical performance goes, none of the 18 clinicians at Yale had previous performance problems. “Was this a failure of the system to report impaired physicians or were these physicians compensating sufficiently to avoid detection?” In either case, “cognitive testing should be a red flag that triggers other clinical assessments,” said Carl I. Cohen, MD, professor and director of the division of geriatric psychiatry at the State University of New York, Brooklyn.
The original plan at Yale was for neurologic and ophthalmologic examinations beginning at age 70, but ultimately it was decided to go with a battery of 16 tests to assess visual scanning and psychomotor efficiency, processing speed under pressure, concentration, and working memory, among other things. Testing takes about 50-90 minutes, and is graded by single neuropsychologist to ensure consistency. Results were compared with normative scores from both older and younger clinicians.
To prevent clinicians from preparing for it, Yale isn’t releasing its test battery.
Suboptimal performance triggered additional evaluations, including in-depth assessment of intellectual, memory, and executive function. Final reviews and recommendations were made by a committee that included a geriatrician, the clinician’s section or department chair, and current and past chief medical officers.
Among the 18 providers who demonstrated deficits impairing their ability to practice medicine, 5 were 70-74 years old; 4 were 75-79; and 9 were 80 years or older. Minor abnormalities were found in 34 other candidates (24.1%); they were allowed to recredential but were scheduled for rescreening at 1-year intervals, instead of every 2 years.
The mean age among the 141 screened clinicians was 74.3 years and ranged from 69 to 92 years; 86% were men. Applicants included 125 physicians (88.7%) as well as 5 advanced practice registered nurses; 4 dentists; 3 psychologists; 2 podiatrists; 1 physician associate; and 1 midwife.
The authors had no relevant disclosures.
SOURCE: Cooney L et al. JAMA. 2020 Jan 14;323(2):179-80.
FROM JAMA