User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
Medicare ‘offers’ cancer patient a choice: Less life or more debt
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
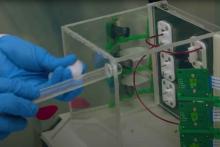
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
COVID-19 shot appears to reduce diabetes risk, even after Omicron
new data suggest.
The findings, from more than 20,000 patients in the Cedars-Sinai Health System in Los Angeles, suggest that “continued efforts to prevent COVID-19 infection may be beneficial to patient health until we develop better understanding of the effects of potential long-term effects of COVID-19,” lead author Alan C. Kwan, MD, of the department of cardiology at Cedars Sinai’s Smidt Heart Institute, said in an interview.
Several studies conducted early in the pandemic suggested increased risks for both new-onset diabetes and cardiometabolic diseases following COVID-19 infection, possibly because of persistent inflammation contributing to insulin resistance.
However, it hasn’t been clear if those risks have persisted with the more recent predominance of the less-virulent Omicron variant or whether the COVID-19 vaccine influences the risk. This new study suggests that both are the case.
“Our results verify that the risk of developing type 2 diabetes after a COVID-19 infection was not just an early observation but, in fact, a real risk that has, unfortunately, persisted through the Omicron era,” Dr. Kwan noted.
“While the level of evidence by our study and others may not reach the degree needed to affect formal guidelines at this time, we believe it is reasonable to have increased clinical suspicion for diabetes after COVID-19 infection and a lower threshold for testing,” he added.
Moreover, “we believe that our study and others suggest the potential role of COVID-19 to affect cardiovascular risk, and so both prevention of COVID-19 infection, through reasonable personal practices and vaccination, and an increased attention to cardiovascular health after COVID-19 infection is warranted.”
The findings were published online in JAMA Network Open.
Dr. Kwan and colleagues analyzed data for a total of 23,709 patients treated (inpatient and outpatient) for at least one COVID-19 infection between March 2020 and June 2022.
Rates of new-onset diabetes (using ICD-10 codes, primarily type 2 diabetes), hypertension, and hyperlipidemia were all elevated in the 90 days following COVID-19 infection compared with the 90 days prior. The same was true of two diagnoses unrelated to COVID-19, urinary tract infection and gastroesophageal reflux, used as benchmarks of health care engagement.
The highest odds for post versus preinfection were for diabetes (odds ratio, 2.35; P < .001), followed by hypertension (OR, 1.54; P < .001), the benchmark diagnoses (OR, 1.42; P < .001), and hyperlipidemia (OR, 1.22; P = .03).
Following adjustments, the risk versus the benchmark conditions for new-onset diabetes before versus after COVID-19 was significantly elevated (OR, 1.58; P < .001), while the risks for hypertension and hyperlipidemia versus benchmark diagnoses were not (OR, 1.06; P = .52 and 0.91, P = .43, respectively).
The diabetes risk after versus before COVID-19 infection was higher among those who had not been vaccinated (OR, 1.78; P < .001), compared with those who had received the vaccine (OR, 1.07; P = .80).
However, there was no significant interaction between vaccination and diabetes diagnosis (P = .08). “For this reason, we believe our data are suggestive of a protective effect in the population who received vaccination prior to infection, but [this is] not definitive,” Dr. Kwan said.
There were no apparent interactions by age, sex, or pre-existing cardiovascular risk factors, including hypertension or hyperlipidemia. Age, sex, and timing of index infection regarding the Omicron variant were not associated with an increased risk of a new cardiometabolic diagnosis before or after COVID-19 infection in any of the models.
Dr. Kwan said in an interview: “We have continued to be surprised by the evolving understanding of the SARS-CoV-2 virus and the effects on human health. In the beginning of the pandemic it was framed as a purely respiratory virus, which we now know to be a severely limited description of all of its potential effects on the human body. We believe that our research and others raise a concern for increased cardiometabolic risk after COVID infection.”
He added that, “while knowledge is incomplete on this topic, we believe that clinical providers may wish to have a higher degree of suspicion for both diabetes and risk of future cardiac events in patients after COVID infection, and that continued efforts to prevent COVID infection may be beneficial to patient health until we develop better understanding of the potential long-term effects of COVID.”
This study was funded by the Erika J. Glazer Family Foundation, the Doris Duke Charitable Foundation, and grants from the National Institutes of Health. Dr. Kwan reported receiving grants from the Doris Duke Charitable Foundation during the conduct of the study.
A version of this article originally appeared on Medscape.com.
new data suggest.
The findings, from more than 20,000 patients in the Cedars-Sinai Health System in Los Angeles, suggest that “continued efforts to prevent COVID-19 infection may be beneficial to patient health until we develop better understanding of the effects of potential long-term effects of COVID-19,” lead author Alan C. Kwan, MD, of the department of cardiology at Cedars Sinai’s Smidt Heart Institute, said in an interview.
Several studies conducted early in the pandemic suggested increased risks for both new-onset diabetes and cardiometabolic diseases following COVID-19 infection, possibly because of persistent inflammation contributing to insulin resistance.
However, it hasn’t been clear if those risks have persisted with the more recent predominance of the less-virulent Omicron variant or whether the COVID-19 vaccine influences the risk. This new study suggests that both are the case.
“Our results verify that the risk of developing type 2 diabetes after a COVID-19 infection was not just an early observation but, in fact, a real risk that has, unfortunately, persisted through the Omicron era,” Dr. Kwan noted.
“While the level of evidence by our study and others may not reach the degree needed to affect formal guidelines at this time, we believe it is reasonable to have increased clinical suspicion for diabetes after COVID-19 infection and a lower threshold for testing,” he added.
Moreover, “we believe that our study and others suggest the potential role of COVID-19 to affect cardiovascular risk, and so both prevention of COVID-19 infection, through reasonable personal practices and vaccination, and an increased attention to cardiovascular health after COVID-19 infection is warranted.”
The findings were published online in JAMA Network Open.
Dr. Kwan and colleagues analyzed data for a total of 23,709 patients treated (inpatient and outpatient) for at least one COVID-19 infection between March 2020 and June 2022.
Rates of new-onset diabetes (using ICD-10 codes, primarily type 2 diabetes), hypertension, and hyperlipidemia were all elevated in the 90 days following COVID-19 infection compared with the 90 days prior. The same was true of two diagnoses unrelated to COVID-19, urinary tract infection and gastroesophageal reflux, used as benchmarks of health care engagement.
The highest odds for post versus preinfection were for diabetes (odds ratio, 2.35; P < .001), followed by hypertension (OR, 1.54; P < .001), the benchmark diagnoses (OR, 1.42; P < .001), and hyperlipidemia (OR, 1.22; P = .03).
Following adjustments, the risk versus the benchmark conditions for new-onset diabetes before versus after COVID-19 was significantly elevated (OR, 1.58; P < .001), while the risks for hypertension and hyperlipidemia versus benchmark diagnoses were not (OR, 1.06; P = .52 and 0.91, P = .43, respectively).
The diabetes risk after versus before COVID-19 infection was higher among those who had not been vaccinated (OR, 1.78; P < .001), compared with those who had received the vaccine (OR, 1.07; P = .80).
However, there was no significant interaction between vaccination and diabetes diagnosis (P = .08). “For this reason, we believe our data are suggestive of a protective effect in the population who received vaccination prior to infection, but [this is] not definitive,” Dr. Kwan said.
There were no apparent interactions by age, sex, or pre-existing cardiovascular risk factors, including hypertension or hyperlipidemia. Age, sex, and timing of index infection regarding the Omicron variant were not associated with an increased risk of a new cardiometabolic diagnosis before or after COVID-19 infection in any of the models.
Dr. Kwan said in an interview: “We have continued to be surprised by the evolving understanding of the SARS-CoV-2 virus and the effects on human health. In the beginning of the pandemic it was framed as a purely respiratory virus, which we now know to be a severely limited description of all of its potential effects on the human body. We believe that our research and others raise a concern for increased cardiometabolic risk after COVID infection.”
He added that, “while knowledge is incomplete on this topic, we believe that clinical providers may wish to have a higher degree of suspicion for both diabetes and risk of future cardiac events in patients after COVID infection, and that continued efforts to prevent COVID infection may be beneficial to patient health until we develop better understanding of the potential long-term effects of COVID.”
This study was funded by the Erika J. Glazer Family Foundation, the Doris Duke Charitable Foundation, and grants from the National Institutes of Health. Dr. Kwan reported receiving grants from the Doris Duke Charitable Foundation during the conduct of the study.
A version of this article originally appeared on Medscape.com.
new data suggest.
The findings, from more than 20,000 patients in the Cedars-Sinai Health System in Los Angeles, suggest that “continued efforts to prevent COVID-19 infection may be beneficial to patient health until we develop better understanding of the effects of potential long-term effects of COVID-19,” lead author Alan C. Kwan, MD, of the department of cardiology at Cedars Sinai’s Smidt Heart Institute, said in an interview.
Several studies conducted early in the pandemic suggested increased risks for both new-onset diabetes and cardiometabolic diseases following COVID-19 infection, possibly because of persistent inflammation contributing to insulin resistance.
However, it hasn’t been clear if those risks have persisted with the more recent predominance of the less-virulent Omicron variant or whether the COVID-19 vaccine influences the risk. This new study suggests that both are the case.
“Our results verify that the risk of developing type 2 diabetes after a COVID-19 infection was not just an early observation but, in fact, a real risk that has, unfortunately, persisted through the Omicron era,” Dr. Kwan noted.
“While the level of evidence by our study and others may not reach the degree needed to affect formal guidelines at this time, we believe it is reasonable to have increased clinical suspicion for diabetes after COVID-19 infection and a lower threshold for testing,” he added.
Moreover, “we believe that our study and others suggest the potential role of COVID-19 to affect cardiovascular risk, and so both prevention of COVID-19 infection, through reasonable personal practices and vaccination, and an increased attention to cardiovascular health after COVID-19 infection is warranted.”
The findings were published online in JAMA Network Open.
Dr. Kwan and colleagues analyzed data for a total of 23,709 patients treated (inpatient and outpatient) for at least one COVID-19 infection between March 2020 and June 2022.
Rates of new-onset diabetes (using ICD-10 codes, primarily type 2 diabetes), hypertension, and hyperlipidemia were all elevated in the 90 days following COVID-19 infection compared with the 90 days prior. The same was true of two diagnoses unrelated to COVID-19, urinary tract infection and gastroesophageal reflux, used as benchmarks of health care engagement.
The highest odds for post versus preinfection were for diabetes (odds ratio, 2.35; P < .001), followed by hypertension (OR, 1.54; P < .001), the benchmark diagnoses (OR, 1.42; P < .001), and hyperlipidemia (OR, 1.22; P = .03).
Following adjustments, the risk versus the benchmark conditions for new-onset diabetes before versus after COVID-19 was significantly elevated (OR, 1.58; P < .001), while the risks for hypertension and hyperlipidemia versus benchmark diagnoses were not (OR, 1.06; P = .52 and 0.91, P = .43, respectively).
The diabetes risk after versus before COVID-19 infection was higher among those who had not been vaccinated (OR, 1.78; P < .001), compared with those who had received the vaccine (OR, 1.07; P = .80).
However, there was no significant interaction between vaccination and diabetes diagnosis (P = .08). “For this reason, we believe our data are suggestive of a protective effect in the population who received vaccination prior to infection, but [this is] not definitive,” Dr. Kwan said.
There were no apparent interactions by age, sex, or pre-existing cardiovascular risk factors, including hypertension or hyperlipidemia. Age, sex, and timing of index infection regarding the Omicron variant were not associated with an increased risk of a new cardiometabolic diagnosis before or after COVID-19 infection in any of the models.
Dr. Kwan said in an interview: “We have continued to be surprised by the evolving understanding of the SARS-CoV-2 virus and the effects on human health. In the beginning of the pandemic it was framed as a purely respiratory virus, which we now know to be a severely limited description of all of its potential effects on the human body. We believe that our research and others raise a concern for increased cardiometabolic risk after COVID infection.”
He added that, “while knowledge is incomplete on this topic, we believe that clinical providers may wish to have a higher degree of suspicion for both diabetes and risk of future cardiac events in patients after COVID infection, and that continued efforts to prevent COVID infection may be beneficial to patient health until we develop better understanding of the potential long-term effects of COVID.”
This study was funded by the Erika J. Glazer Family Foundation, the Doris Duke Charitable Foundation, and grants from the National Institutes of Health. Dr. Kwan reported receiving grants from the Doris Duke Charitable Foundation during the conduct of the study.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Saying goodbye: How to transition teens to adult medical care
However, many clinicians feel insufficiently prepared to provide comprehensive transition services. This can result in the actual handoff or transfer into adult care being abrupt, incomplete, or outright unsuccessful. By following the recommended best practices of transitions, providers of pediatric care can ensure that this challenging goodbye prepares everyone for the next steps ahead.
Using a structured transition process
In 2011, a health care transition clinical report based on expert opinion and practice consensus and endorsed by the American Academy of Pediatrics, American Academy of Family Physicians, and American College of Physicians – Society of Internal Medicine was released. This report provided a decision-making algorithm for “practice-based implementation of transition for all youth beginning in early adolescence.”
The Got Transition organization, funded by the Maternal Child Health Bureau and Health Resources and Services Administration, provides web-based information and materials for health care providers and families to establish a smooth and successful transition. At the center of these recommendations are the Six Core Elements of Health Care Transition – the essential components of a structured transition process: 1) transition policy/guide; 2) tracking and monitoring; 3) readiness; 4) planning; 5) transfer of care, and 6) transition completion.
This transition process should start early in adolescence, preferably by age 12-14 years, to give adequate time to progress successfully through these elements and improve the likelihood of a smooth, final transfer into the care of an adult clinician.
Preparing your patients for transfer
Despite the availability of these recommendations, national surveys show that the overwhelming majority of adolescents with and without special health care needs report not receiving transition services. Lack of time, resources, interest, and patients being lost to care during adolescence all contribute to this deficit in care. Without transition preparation, the actual handoff or transfer to adult care can be difficult for adolescents, caregivers, and clinicians alike. Adolescents and caregivers may feel a sense of abandonment or have inadequate health knowledge/literacy, pediatric clinicians may fear that the patient is not ready for the expected independence, and adult clinicians face numerous challenges integrating these young patients into their practice.
A structured transition process can help the family and clinicians know what to expect during the transfer of care. Pediatric clinicians can gradually move from a pediatric model of care, in which the caregiver is the center of communication, to an adult model, putting the patient at the center. By encouraging the adolescent to be the direct communicator, the pediatric clinician can promote independence and assess health knowledge, allowing for education where gaps exist.
Assisting the patient in identifying and even meeting the adult clinician well ahead of the final transfer date can also make the process less daunting for the adolescent.
Adult clinicians should consider allowing more time for the first visit with a new young adult patient and welcome caregiver input early in the transfer process, particularly for patients with a chronic disease. By engaging patients and families in an intentional, gradual transition process with an expected outcome, all those involved will be more prepared for the final handoff.
Utilizing transition tools and engaging the adolescent
Numerous tools can assist in the preparation for transfer to adult care. These include transition summaries and emergency plans, which contain essential information such as current medical problems, allergies, medications, prior procedures and treatments, and sick day plans. Such tools can also be built into electronic medical records for easy modification and updating. They can be used as methods to engage and teach adolescents about their disease history and current regimen and can contain essential components for information handoff at the time of transfer to adult care. If the patient carries a rare diagnosis, or one that has historically been associated with lower survival to adulthood, these transfer documents can also include summary information about disease states and contact information for pediatric specialty clinicians.
Adolescent engagement in their health care during the time of transition can also be prompted through the use of patient portals within an electronic health record. Such portals put health information directly at the adolescent’s fingertips, provide them with an outlet for communication with their clinicians, and give reminders regarding health maintenance.
Completing the transfer: The final handoff
The best and most recommended means of relaying information at the time of transfer to adult care is a direct, verbal handoff between clinicians. This direct handoff has several goals:
(1) To ensure the patient has scheduled or attended the first appointment with the adult clinician
(2) To ensure record transfer has occurred successfully
(3) To answer any questions the receiving clinician may have about prior or ongoing care.
(4) To offer the adult clinician ongoing access to the pediatric clinician as an “expert” resource for additional questions.
By remaining available as a resource, the pediatric clinician can alleviate concerns for both the patient and caregiver as well as the receiving adult clinician.
As valuable as verbal handoffs can be, they are not always possible due to patients not having selected an adult clinician prior to leaving the pediatric clinician, an inability to reach the receiving clinician, and/or time limitations. Many of these barriers can be alleviated by early discussions of transitions of care as well as utilization of structured documentation tools as noted above.
It is also recommended that the pediatric clinician follows up with the patient and/or caregiver several months after the transfer is complete. This allows for the adolescent and/or the caregiver to reflect on the transition process and provide feedback to the pediatric clinicians and their practice for ongoing process improvement.
Reflection as a pediatrician
Ideally, all transition steps occur for the adolescent; in our opinion, a crucial component is to prepare the adolescent patient for the change from a pediatric to adult model of care, in which they are independent in their health communication and decision-making. By engaging adolescents to understand their health, how to maintain it, and when to seek care, we empower them to advocate for their own health as young adults. With appropriate health knowledge and literacy, adolescents are more likely to actively engage with their health care providers and make healthy lifestyle choices. So though saying goodbye may still be difficult, it can be done with the confidence that the patients will continue to get the care they need as they transition into adulthood.
Dr. Kim is assistant clinical professor, department of pediatrics, University of California, San Diego. Dr. Mennito is associate professor of pediatrics and internal medicine, Medical University of South Carolina, Charleston, S.C. Dr. Kim and Dr. Mennito have disclosed no relevant financial relationships. A version of this article originally appeared on Medscape.com.
However, many clinicians feel insufficiently prepared to provide comprehensive transition services. This can result in the actual handoff or transfer into adult care being abrupt, incomplete, or outright unsuccessful. By following the recommended best practices of transitions, providers of pediatric care can ensure that this challenging goodbye prepares everyone for the next steps ahead.
Using a structured transition process
In 2011, a health care transition clinical report based on expert opinion and practice consensus and endorsed by the American Academy of Pediatrics, American Academy of Family Physicians, and American College of Physicians – Society of Internal Medicine was released. This report provided a decision-making algorithm for “practice-based implementation of transition for all youth beginning in early adolescence.”
The Got Transition organization, funded by the Maternal Child Health Bureau and Health Resources and Services Administration, provides web-based information and materials for health care providers and families to establish a smooth and successful transition. At the center of these recommendations are the Six Core Elements of Health Care Transition – the essential components of a structured transition process: 1) transition policy/guide; 2) tracking and monitoring; 3) readiness; 4) planning; 5) transfer of care, and 6) transition completion.
This transition process should start early in adolescence, preferably by age 12-14 years, to give adequate time to progress successfully through these elements and improve the likelihood of a smooth, final transfer into the care of an adult clinician.
Preparing your patients for transfer
Despite the availability of these recommendations, national surveys show that the overwhelming majority of adolescents with and without special health care needs report not receiving transition services. Lack of time, resources, interest, and patients being lost to care during adolescence all contribute to this deficit in care. Without transition preparation, the actual handoff or transfer to adult care can be difficult for adolescents, caregivers, and clinicians alike. Adolescents and caregivers may feel a sense of abandonment or have inadequate health knowledge/literacy, pediatric clinicians may fear that the patient is not ready for the expected independence, and adult clinicians face numerous challenges integrating these young patients into their practice.
A structured transition process can help the family and clinicians know what to expect during the transfer of care. Pediatric clinicians can gradually move from a pediatric model of care, in which the caregiver is the center of communication, to an adult model, putting the patient at the center. By encouraging the adolescent to be the direct communicator, the pediatric clinician can promote independence and assess health knowledge, allowing for education where gaps exist.
Assisting the patient in identifying and even meeting the adult clinician well ahead of the final transfer date can also make the process less daunting for the adolescent.
Adult clinicians should consider allowing more time for the first visit with a new young adult patient and welcome caregiver input early in the transfer process, particularly for patients with a chronic disease. By engaging patients and families in an intentional, gradual transition process with an expected outcome, all those involved will be more prepared for the final handoff.
Utilizing transition tools and engaging the adolescent
Numerous tools can assist in the preparation for transfer to adult care. These include transition summaries and emergency plans, which contain essential information such as current medical problems, allergies, medications, prior procedures and treatments, and sick day plans. Such tools can also be built into electronic medical records for easy modification and updating. They can be used as methods to engage and teach adolescents about their disease history and current regimen and can contain essential components for information handoff at the time of transfer to adult care. If the patient carries a rare diagnosis, or one that has historically been associated with lower survival to adulthood, these transfer documents can also include summary information about disease states and contact information for pediatric specialty clinicians.
Adolescent engagement in their health care during the time of transition can also be prompted through the use of patient portals within an electronic health record. Such portals put health information directly at the adolescent’s fingertips, provide them with an outlet for communication with their clinicians, and give reminders regarding health maintenance.
Completing the transfer: The final handoff
The best and most recommended means of relaying information at the time of transfer to adult care is a direct, verbal handoff between clinicians. This direct handoff has several goals:
(1) To ensure the patient has scheduled or attended the first appointment with the adult clinician
(2) To ensure record transfer has occurred successfully
(3) To answer any questions the receiving clinician may have about prior or ongoing care.
(4) To offer the adult clinician ongoing access to the pediatric clinician as an “expert” resource for additional questions.
By remaining available as a resource, the pediatric clinician can alleviate concerns for both the patient and caregiver as well as the receiving adult clinician.
As valuable as verbal handoffs can be, they are not always possible due to patients not having selected an adult clinician prior to leaving the pediatric clinician, an inability to reach the receiving clinician, and/or time limitations. Many of these barriers can be alleviated by early discussions of transitions of care as well as utilization of structured documentation tools as noted above.
It is also recommended that the pediatric clinician follows up with the patient and/or caregiver several months after the transfer is complete. This allows for the adolescent and/or the caregiver to reflect on the transition process and provide feedback to the pediatric clinicians and their practice for ongoing process improvement.
Reflection as a pediatrician
Ideally, all transition steps occur for the adolescent; in our opinion, a crucial component is to prepare the adolescent patient for the change from a pediatric to adult model of care, in which they are independent in their health communication and decision-making. By engaging adolescents to understand their health, how to maintain it, and when to seek care, we empower them to advocate for their own health as young adults. With appropriate health knowledge and literacy, adolescents are more likely to actively engage with their health care providers and make healthy lifestyle choices. So though saying goodbye may still be difficult, it can be done with the confidence that the patients will continue to get the care they need as they transition into adulthood.
Dr. Kim is assistant clinical professor, department of pediatrics, University of California, San Diego. Dr. Mennito is associate professor of pediatrics and internal medicine, Medical University of South Carolina, Charleston, S.C. Dr. Kim and Dr. Mennito have disclosed no relevant financial relationships. A version of this article originally appeared on Medscape.com.
However, many clinicians feel insufficiently prepared to provide comprehensive transition services. This can result in the actual handoff or transfer into adult care being abrupt, incomplete, or outright unsuccessful. By following the recommended best practices of transitions, providers of pediatric care can ensure that this challenging goodbye prepares everyone for the next steps ahead.
Using a structured transition process
In 2011, a health care transition clinical report based on expert opinion and practice consensus and endorsed by the American Academy of Pediatrics, American Academy of Family Physicians, and American College of Physicians – Society of Internal Medicine was released. This report provided a decision-making algorithm for “practice-based implementation of transition for all youth beginning in early adolescence.”
The Got Transition organization, funded by the Maternal Child Health Bureau and Health Resources and Services Administration, provides web-based information and materials for health care providers and families to establish a smooth and successful transition. At the center of these recommendations are the Six Core Elements of Health Care Transition – the essential components of a structured transition process: 1) transition policy/guide; 2) tracking and monitoring; 3) readiness; 4) planning; 5) transfer of care, and 6) transition completion.
This transition process should start early in adolescence, preferably by age 12-14 years, to give adequate time to progress successfully through these elements and improve the likelihood of a smooth, final transfer into the care of an adult clinician.
Preparing your patients for transfer
Despite the availability of these recommendations, national surveys show that the overwhelming majority of adolescents with and without special health care needs report not receiving transition services. Lack of time, resources, interest, and patients being lost to care during adolescence all contribute to this deficit in care. Without transition preparation, the actual handoff or transfer to adult care can be difficult for adolescents, caregivers, and clinicians alike. Adolescents and caregivers may feel a sense of abandonment or have inadequate health knowledge/literacy, pediatric clinicians may fear that the patient is not ready for the expected independence, and adult clinicians face numerous challenges integrating these young patients into their practice.
A structured transition process can help the family and clinicians know what to expect during the transfer of care. Pediatric clinicians can gradually move from a pediatric model of care, in which the caregiver is the center of communication, to an adult model, putting the patient at the center. By encouraging the adolescent to be the direct communicator, the pediatric clinician can promote independence and assess health knowledge, allowing for education where gaps exist.
Assisting the patient in identifying and even meeting the adult clinician well ahead of the final transfer date can also make the process less daunting for the adolescent.
Adult clinicians should consider allowing more time for the first visit with a new young adult patient and welcome caregiver input early in the transfer process, particularly for patients with a chronic disease. By engaging patients and families in an intentional, gradual transition process with an expected outcome, all those involved will be more prepared for the final handoff.
Utilizing transition tools and engaging the adolescent
Numerous tools can assist in the preparation for transfer to adult care. These include transition summaries and emergency plans, which contain essential information such as current medical problems, allergies, medications, prior procedures and treatments, and sick day plans. Such tools can also be built into electronic medical records for easy modification and updating. They can be used as methods to engage and teach adolescents about their disease history and current regimen and can contain essential components for information handoff at the time of transfer to adult care. If the patient carries a rare diagnosis, or one that has historically been associated with lower survival to adulthood, these transfer documents can also include summary information about disease states and contact information for pediatric specialty clinicians.
Adolescent engagement in their health care during the time of transition can also be prompted through the use of patient portals within an electronic health record. Such portals put health information directly at the adolescent’s fingertips, provide them with an outlet for communication with their clinicians, and give reminders regarding health maintenance.
Completing the transfer: The final handoff
The best and most recommended means of relaying information at the time of transfer to adult care is a direct, verbal handoff between clinicians. This direct handoff has several goals:
(1) To ensure the patient has scheduled or attended the first appointment with the adult clinician
(2) To ensure record transfer has occurred successfully
(3) To answer any questions the receiving clinician may have about prior or ongoing care.
(4) To offer the adult clinician ongoing access to the pediatric clinician as an “expert” resource for additional questions.
By remaining available as a resource, the pediatric clinician can alleviate concerns for both the patient and caregiver as well as the receiving adult clinician.
As valuable as verbal handoffs can be, they are not always possible due to patients not having selected an adult clinician prior to leaving the pediatric clinician, an inability to reach the receiving clinician, and/or time limitations. Many of these barriers can be alleviated by early discussions of transitions of care as well as utilization of structured documentation tools as noted above.
It is also recommended that the pediatric clinician follows up with the patient and/or caregiver several months after the transfer is complete. This allows for the adolescent and/or the caregiver to reflect on the transition process and provide feedback to the pediatric clinicians and their practice for ongoing process improvement.
Reflection as a pediatrician
Ideally, all transition steps occur for the adolescent; in our opinion, a crucial component is to prepare the adolescent patient for the change from a pediatric to adult model of care, in which they are independent in their health communication and decision-making. By engaging adolescents to understand their health, how to maintain it, and when to seek care, we empower them to advocate for their own health as young adults. With appropriate health knowledge and literacy, adolescents are more likely to actively engage with their health care providers and make healthy lifestyle choices. So though saying goodbye may still be difficult, it can be done with the confidence that the patients will continue to get the care they need as they transition into adulthood.
Dr. Kim is assistant clinical professor, department of pediatrics, University of California, San Diego. Dr. Mennito is associate professor of pediatrics and internal medicine, Medical University of South Carolina, Charleston, S.C. Dr. Kim and Dr. Mennito have disclosed no relevant financial relationships. A version of this article originally appeared on Medscape.com.
Physicians don’t feel safe with some patients: Here’s how to reduce the danger
“I talked to him about whether he was okay seeing me and he said yes,” Dr. Cheng said. “But I remained vigilant and conscious of what the patient was doing the whole time so he couldn’t take advantage of the situation.”
Dr. Cheng never turned his back to the patient and even backed out of the exam room. That encounter passed without incident. However, a urologist Dr. Cheng knew from residency wasn’t so fortunate. Ronald Gilbert, MD, of Newport Beach, Calif., was shot and killed by a patient in his office. The patient blamed him for complications following prostate surgery 25 years earlier.
In 2022, a gunman in Tulsa, Okla., blamed his physician for pain from a recent back surgery and shot and killed him, another physician, and two others in a medical building before taking his own life.
Nearly 9 in 10 physicians reported in a recent Medscape poll that they had experienced one or more violent or potentially violent incidents in the past year. The most common patient behaviors were verbal abuse, getting angry and leaving, and behaving erratically.
About one in three respondents said that the patients threatened to harm them, and about one in five said that the patients became violent.
Experts say that many factors contribute to this potentially lethal situation: Health care services have become more impersonal, patients experience longer wait times, some abuse prescription drugs, mental health services are lacking, and security is poor or nonexistent at some health care facilities.
Violence against hospital workers has become so common that a bill was introduced in 2022 in Congress to better protect them. The Safety From Violence for Healthcare Employees Act includes stiffer penalties for acts involving the use of a dangerous weapon or committed during a public emergency and would also provide $25 million in grants to hospitals for programs aimed at reducing violent incidents in health care settings, including de-escalation training. The American Hospital Association and American College of Emergency Physicians support the bill, which is now before the House Judiciary Subcommittee on Crime, Terrorism, and Homeland Security.
The worst day of their lives
“You have people who already are having the worst day of their lives and feeling on edge. If they already have a short fuse or substance abuse issues, that can translate into agitation, violence, or aggression,” said Scott Zeller, MD, vice president of acute psychiatry at Vituity, a physician-owned multispecialty group that operates in several states.
Health care workers in psychiatric and substance abuse hospitals were 10 times more likely to experience nonfatal injuries by others in 2018 than were health care workers in ambulatory settings, according to an April 2020 Bureau of Labor Statistics report. In addition, health care workers were five times more likely to suffer a workplace violence injury than were workers overall in 2018.
Psychiatrists who responded to the poll were the specialists most likely to report that they encountered violent patients and potentially violent patients. “Historically, inpatient psychiatry, which requires more acute care and monitoring, is considered the most dangerous profession outside of the police,” said Dr. Zeller.
Emergency physicians have reported an uptick in violence from patients; 85% said in a survey by ACEP in 2022 that they believed the rate of violence in emergency departments has increased over the past 5 years, whereas 45% indicated that it has greatly increased.
Some doctors have been threatened with violence or actually killed by family members. Alex Skog, MD, president-elect of ACEP’s Oregon chapter, told HealthCare Dive that “a patient’s family member with a gun holster on his hip threatened to kill me and kill my entire family after I told his father that he needed to be admitted because he had coronavirus.”
“I’ve been scared for my safety as well as the safety of my family,” Dr. Skog said. “That was just not something that we were seeing 3, 4, or 5 years ago.”
Many patients are already upset by the time they see doctors, according to the poll.
“The most common reason patients are upset is that they’re already in a lot of pain, which can be expressed as anger, hostility, or aggression. They’re very anxious and afraid of what’s happening and may be thinking about the worst-case scenario – that a bump or lump is cancer,” Dr. Zeller said.
Patients may also get upset if they disagree with their doctors’ diagnosis or treatment plan or the doctor refuses to prescribe them the drugs or tests they want.
“One doctor commented recently: ‘After over 30 years in this business, I can say patients are worse now than at any point in my career. Entitled, demanding, obnoxious. Any denial is met with outrage and indignity, whether it’s an opioid request or a demand for MRI of something because they ‘want to know.’ ”
An orthopedic surgeon in Indiana lost his life after he refused to prescribe opioids to a patient. Her angry husband shot and killed the doctor in the parking lot only 2 hours after confronting him in his office.
Decreased physician-patient trust
“When doctors experience something frightening, they become more apprehensive in the future. There’s no doubt that after the first violent experience, they think of things differently,” said Dr. Zeller.
More than half of the doctors who reported experiencing at least one violent or potentially violent incident in the poll said they trusted patients less.
This diminished trust can negatively impact the physician-patient relationship, said the authors of a recent Health Affairs article.
“The more patients harm their health care providers, intentionally or unintentionally, the more difficult it will be for those providers to trust them, leading to yet another unfortunate pattern: physicians pulling back on some of the behaviors thought to be most trust-building, for example, talking about their personal lives, building rapport, displaying compassion, or giving out their personal cell phone numbers,” the article stated.
What doctors can do
Most doctors who experienced a violent or potentially violent incident said they had tried to defuse the situation and that they succeeded at least some of the time, the poll results show.
One of the best ways to defuse a situation is to be empathetic and show the person that you’re on their side and not the enemy, said Dr. Cheng,.
“Rather than making general statements like ‘I understand that you’re upset,’ it’s better to be specific about the reason the person is upset. For example: ‘I understand that you’re upset that the pharmacy didn’t fill your prescription’ or ‘I understand how you’re feeling about Doctor So-and-so, who didn’t treat you right,’ ” Dr. Cheng stated.
Dr. Zeller urged physicians to talk to patients about why they’re upset and how they can help them. That approach worked with a patient who was having a psychotic episode.
“I told the staff, who wanted to forcibly restrain him and inject him with medication, that I would talk to him. I asked the patient, who was screaming ‘ya ya ya ya,’ whether he would take his medication if I gave it to him and he said yes. When he was calm, he explained that he was screaming to stop the voices telling him to kill his parents. He then got the help he needed,” said Dr. Zeller.
Dr. Cheng was trained in de-escalation techniques as an Orange County reserve deputy sheriff. He and Dr. Zeller recommended that physicians and staff receive training in how to spot potentially violent behavior and defuse these situations before they escalate.
Dr. Cheng suggests looking at the person’s body language for signs of increasing agitation or tension, such as clenched fists, tense posture, tight jaw, or fidgeting that may be accompanied by shouting and/or verbal abuse.
Physicians also need to consider where they are physically in relation to patients they see. “You don’t want to be too close to the patient or stand in front of them, which can be seen as confrontational. Instead, stand or sit off to the side, and never block the door if the patient’s upset,” said Dr. Cheng.
He recommended that physician practices prepare for violent incidents by developing detailed plans, including how and when to escape, how to protect patients, and how to cooperate with law enforcement.
“If a violent incident is inescapable, physicians and staff must be ready to fight back with whatever tools they have available, which may include fire extinguishers, chairs, or scalpels,” said Dr. Cheng.
A version of this article originally appeared on Medscape.com.
“I talked to him about whether he was okay seeing me and he said yes,” Dr. Cheng said. “But I remained vigilant and conscious of what the patient was doing the whole time so he couldn’t take advantage of the situation.”
Dr. Cheng never turned his back to the patient and even backed out of the exam room. That encounter passed without incident. However, a urologist Dr. Cheng knew from residency wasn’t so fortunate. Ronald Gilbert, MD, of Newport Beach, Calif., was shot and killed by a patient in his office. The patient blamed him for complications following prostate surgery 25 years earlier.
In 2022, a gunman in Tulsa, Okla., blamed his physician for pain from a recent back surgery and shot and killed him, another physician, and two others in a medical building before taking his own life.
Nearly 9 in 10 physicians reported in a recent Medscape poll that they had experienced one or more violent or potentially violent incidents in the past year. The most common patient behaviors were verbal abuse, getting angry and leaving, and behaving erratically.
About one in three respondents said that the patients threatened to harm them, and about one in five said that the patients became violent.
Experts say that many factors contribute to this potentially lethal situation: Health care services have become more impersonal, patients experience longer wait times, some abuse prescription drugs, mental health services are lacking, and security is poor or nonexistent at some health care facilities.
Violence against hospital workers has become so common that a bill was introduced in 2022 in Congress to better protect them. The Safety From Violence for Healthcare Employees Act includes stiffer penalties for acts involving the use of a dangerous weapon or committed during a public emergency and would also provide $25 million in grants to hospitals for programs aimed at reducing violent incidents in health care settings, including de-escalation training. The American Hospital Association and American College of Emergency Physicians support the bill, which is now before the House Judiciary Subcommittee on Crime, Terrorism, and Homeland Security.
The worst day of their lives
“You have people who already are having the worst day of their lives and feeling on edge. If they already have a short fuse or substance abuse issues, that can translate into agitation, violence, or aggression,” said Scott Zeller, MD, vice president of acute psychiatry at Vituity, a physician-owned multispecialty group that operates in several states.
Health care workers in psychiatric and substance abuse hospitals were 10 times more likely to experience nonfatal injuries by others in 2018 than were health care workers in ambulatory settings, according to an April 2020 Bureau of Labor Statistics report. In addition, health care workers were five times more likely to suffer a workplace violence injury than were workers overall in 2018.
Psychiatrists who responded to the poll were the specialists most likely to report that they encountered violent patients and potentially violent patients. “Historically, inpatient psychiatry, which requires more acute care and monitoring, is considered the most dangerous profession outside of the police,” said Dr. Zeller.
Emergency physicians have reported an uptick in violence from patients; 85% said in a survey by ACEP in 2022 that they believed the rate of violence in emergency departments has increased over the past 5 years, whereas 45% indicated that it has greatly increased.
Some doctors have been threatened with violence or actually killed by family members. Alex Skog, MD, president-elect of ACEP’s Oregon chapter, told HealthCare Dive that “a patient’s family member with a gun holster on his hip threatened to kill me and kill my entire family after I told his father that he needed to be admitted because he had coronavirus.”
“I’ve been scared for my safety as well as the safety of my family,” Dr. Skog said. “That was just not something that we were seeing 3, 4, or 5 years ago.”
Many patients are already upset by the time they see doctors, according to the poll.
“The most common reason patients are upset is that they’re already in a lot of pain, which can be expressed as anger, hostility, or aggression. They’re very anxious and afraid of what’s happening and may be thinking about the worst-case scenario – that a bump or lump is cancer,” Dr. Zeller said.
Patients may also get upset if they disagree with their doctors’ diagnosis or treatment plan or the doctor refuses to prescribe them the drugs or tests they want.
“One doctor commented recently: ‘After over 30 years in this business, I can say patients are worse now than at any point in my career. Entitled, demanding, obnoxious. Any denial is met with outrage and indignity, whether it’s an opioid request or a demand for MRI of something because they ‘want to know.’ ”
An orthopedic surgeon in Indiana lost his life after he refused to prescribe opioids to a patient. Her angry husband shot and killed the doctor in the parking lot only 2 hours after confronting him in his office.
Decreased physician-patient trust
“When doctors experience something frightening, they become more apprehensive in the future. There’s no doubt that after the first violent experience, they think of things differently,” said Dr. Zeller.
More than half of the doctors who reported experiencing at least one violent or potentially violent incident in the poll said they trusted patients less.
This diminished trust can negatively impact the physician-patient relationship, said the authors of a recent Health Affairs article.
“The more patients harm their health care providers, intentionally or unintentionally, the more difficult it will be for those providers to trust them, leading to yet another unfortunate pattern: physicians pulling back on some of the behaviors thought to be most trust-building, for example, talking about their personal lives, building rapport, displaying compassion, or giving out their personal cell phone numbers,” the article stated.
What doctors can do
Most doctors who experienced a violent or potentially violent incident said they had tried to defuse the situation and that they succeeded at least some of the time, the poll results show.
One of the best ways to defuse a situation is to be empathetic and show the person that you’re on their side and not the enemy, said Dr. Cheng,.
“Rather than making general statements like ‘I understand that you’re upset,’ it’s better to be specific about the reason the person is upset. For example: ‘I understand that you’re upset that the pharmacy didn’t fill your prescription’ or ‘I understand how you’re feeling about Doctor So-and-so, who didn’t treat you right,’ ” Dr. Cheng stated.
Dr. Zeller urged physicians to talk to patients about why they’re upset and how they can help them. That approach worked with a patient who was having a psychotic episode.
“I told the staff, who wanted to forcibly restrain him and inject him with medication, that I would talk to him. I asked the patient, who was screaming ‘ya ya ya ya,’ whether he would take his medication if I gave it to him and he said yes. When he was calm, he explained that he was screaming to stop the voices telling him to kill his parents. He then got the help he needed,” said Dr. Zeller.
Dr. Cheng was trained in de-escalation techniques as an Orange County reserve deputy sheriff. He and Dr. Zeller recommended that physicians and staff receive training in how to spot potentially violent behavior and defuse these situations before they escalate.
Dr. Cheng suggests looking at the person’s body language for signs of increasing agitation or tension, such as clenched fists, tense posture, tight jaw, or fidgeting that may be accompanied by shouting and/or verbal abuse.
Physicians also need to consider where they are physically in relation to patients they see. “You don’t want to be too close to the patient or stand in front of them, which can be seen as confrontational. Instead, stand or sit off to the side, and never block the door if the patient’s upset,” said Dr. Cheng.
He recommended that physician practices prepare for violent incidents by developing detailed plans, including how and when to escape, how to protect patients, and how to cooperate with law enforcement.
“If a violent incident is inescapable, physicians and staff must be ready to fight back with whatever tools they have available, which may include fire extinguishers, chairs, or scalpels,” said Dr. Cheng.
A version of this article originally appeared on Medscape.com.
“I talked to him about whether he was okay seeing me and he said yes,” Dr. Cheng said. “But I remained vigilant and conscious of what the patient was doing the whole time so he couldn’t take advantage of the situation.”
Dr. Cheng never turned his back to the patient and even backed out of the exam room. That encounter passed without incident. However, a urologist Dr. Cheng knew from residency wasn’t so fortunate. Ronald Gilbert, MD, of Newport Beach, Calif., was shot and killed by a patient in his office. The patient blamed him for complications following prostate surgery 25 years earlier.
In 2022, a gunman in Tulsa, Okla., blamed his physician for pain from a recent back surgery and shot and killed him, another physician, and two others in a medical building before taking his own life.
Nearly 9 in 10 physicians reported in a recent Medscape poll that they had experienced one or more violent or potentially violent incidents in the past year. The most common patient behaviors were verbal abuse, getting angry and leaving, and behaving erratically.
About one in three respondents said that the patients threatened to harm them, and about one in five said that the patients became violent.
Experts say that many factors contribute to this potentially lethal situation: Health care services have become more impersonal, patients experience longer wait times, some abuse prescription drugs, mental health services are lacking, and security is poor or nonexistent at some health care facilities.
Violence against hospital workers has become so common that a bill was introduced in 2022 in Congress to better protect them. The Safety From Violence for Healthcare Employees Act includes stiffer penalties for acts involving the use of a dangerous weapon or committed during a public emergency and would also provide $25 million in grants to hospitals for programs aimed at reducing violent incidents in health care settings, including de-escalation training. The American Hospital Association and American College of Emergency Physicians support the bill, which is now before the House Judiciary Subcommittee on Crime, Terrorism, and Homeland Security.
The worst day of their lives
“You have people who already are having the worst day of their lives and feeling on edge. If they already have a short fuse or substance abuse issues, that can translate into agitation, violence, or aggression,” said Scott Zeller, MD, vice president of acute psychiatry at Vituity, a physician-owned multispecialty group that operates in several states.
Health care workers in psychiatric and substance abuse hospitals were 10 times more likely to experience nonfatal injuries by others in 2018 than were health care workers in ambulatory settings, according to an April 2020 Bureau of Labor Statistics report. In addition, health care workers were five times more likely to suffer a workplace violence injury than were workers overall in 2018.
Psychiatrists who responded to the poll were the specialists most likely to report that they encountered violent patients and potentially violent patients. “Historically, inpatient psychiatry, which requires more acute care and monitoring, is considered the most dangerous profession outside of the police,” said Dr. Zeller.
Emergency physicians have reported an uptick in violence from patients; 85% said in a survey by ACEP in 2022 that they believed the rate of violence in emergency departments has increased over the past 5 years, whereas 45% indicated that it has greatly increased.
Some doctors have been threatened with violence or actually killed by family members. Alex Skog, MD, president-elect of ACEP’s Oregon chapter, told HealthCare Dive that “a patient’s family member with a gun holster on his hip threatened to kill me and kill my entire family after I told his father that he needed to be admitted because he had coronavirus.”
“I’ve been scared for my safety as well as the safety of my family,” Dr. Skog said. “That was just not something that we were seeing 3, 4, or 5 years ago.”
Many patients are already upset by the time they see doctors, according to the poll.
“The most common reason patients are upset is that they’re already in a lot of pain, which can be expressed as anger, hostility, or aggression. They’re very anxious and afraid of what’s happening and may be thinking about the worst-case scenario – that a bump or lump is cancer,” Dr. Zeller said.
Patients may also get upset if they disagree with their doctors’ diagnosis or treatment plan or the doctor refuses to prescribe them the drugs or tests they want.
“One doctor commented recently: ‘After over 30 years in this business, I can say patients are worse now than at any point in my career. Entitled, demanding, obnoxious. Any denial is met with outrage and indignity, whether it’s an opioid request or a demand for MRI of something because they ‘want to know.’ ”
An orthopedic surgeon in Indiana lost his life after he refused to prescribe opioids to a patient. Her angry husband shot and killed the doctor in the parking lot only 2 hours after confronting him in his office.
Decreased physician-patient trust
“When doctors experience something frightening, they become more apprehensive in the future. There’s no doubt that after the first violent experience, they think of things differently,” said Dr. Zeller.
More than half of the doctors who reported experiencing at least one violent or potentially violent incident in the poll said they trusted patients less.
This diminished trust can negatively impact the physician-patient relationship, said the authors of a recent Health Affairs article.
“The more patients harm their health care providers, intentionally or unintentionally, the more difficult it will be for those providers to trust them, leading to yet another unfortunate pattern: physicians pulling back on some of the behaviors thought to be most trust-building, for example, talking about their personal lives, building rapport, displaying compassion, or giving out their personal cell phone numbers,” the article stated.
What doctors can do
Most doctors who experienced a violent or potentially violent incident said they had tried to defuse the situation and that they succeeded at least some of the time, the poll results show.
One of the best ways to defuse a situation is to be empathetic and show the person that you’re on their side and not the enemy, said Dr. Cheng,.
“Rather than making general statements like ‘I understand that you’re upset,’ it’s better to be specific about the reason the person is upset. For example: ‘I understand that you’re upset that the pharmacy didn’t fill your prescription’ or ‘I understand how you’re feeling about Doctor So-and-so, who didn’t treat you right,’ ” Dr. Cheng stated.
Dr. Zeller urged physicians to talk to patients about why they’re upset and how they can help them. That approach worked with a patient who was having a psychotic episode.
“I told the staff, who wanted to forcibly restrain him and inject him with medication, that I would talk to him. I asked the patient, who was screaming ‘ya ya ya ya,’ whether he would take his medication if I gave it to him and he said yes. When he was calm, he explained that he was screaming to stop the voices telling him to kill his parents. He then got the help he needed,” said Dr. Zeller.
Dr. Cheng was trained in de-escalation techniques as an Orange County reserve deputy sheriff. He and Dr. Zeller recommended that physicians and staff receive training in how to spot potentially violent behavior and defuse these situations before they escalate.
Dr. Cheng suggests looking at the person’s body language for signs of increasing agitation or tension, such as clenched fists, tense posture, tight jaw, or fidgeting that may be accompanied by shouting and/or verbal abuse.
Physicians also need to consider where they are physically in relation to patients they see. “You don’t want to be too close to the patient or stand in front of them, which can be seen as confrontational. Instead, stand or sit off to the side, and never block the door if the patient’s upset,” said Dr. Cheng.
He recommended that physician practices prepare for violent incidents by developing detailed plans, including how and when to escape, how to protect patients, and how to cooperate with law enforcement.
“If a violent incident is inescapable, physicians and staff must be ready to fight back with whatever tools they have available, which may include fire extinguishers, chairs, or scalpels,” said Dr. Cheng.
A version of this article originally appeared on Medscape.com.
Meta-analysis throws more shade aspirin’s way
A new meta-analysis has added evidence questioning the utility and efficacy of prophylactic low-dose aspirin for preventing cardiovascular events in people who don’t have atherosclerotic cardiovascular disease (ASCVD), whether or not they’re also taking statins, and finds that at every level of ASCVD risk the aspirin carries a risk of major bleeding that exceeds its potentially protective benefits.
In a study published online in JACC: Advances, the researchers, led by Safi U. Khan, MD, MS, analyzed data from 16 trials with 171,215 individuals, with a median age of 64 years. Of the population analyzed, 35% were taking statins.
“This study focused on patients without ASCVD who are taking aspirin with or without statin therapy to prevent ASCVD events,” Dr. Khan, a cardiovascular disease fellow at Houston Methodist DeBakey Heart and Vascular Institute, told this news organization. “We noted that the absolute risk of major bleeding in this patient population exceeds the absolute reduction in MI by aspirin across different ASCVD risk categories. Furthermore, concomitant statin therapy use further diminishes aspirin’s cardiovascular effects without influencing bleeding risk.”
Across the 16 studies, people taking aspirin had a relative risk reduction of 15% for MI vs. controls (RR .85; 95% confidence interval [CI], .77 to .95; P < .001). However, they had a 48% greater risk of major bleeding (RR, 1.48; 95% CI, 1.31-1.66; P < .001).
The meta-analysis also found that aspirin, either as monotherapy or with a statin, carried a slight to significant benefit depending on the estimated risk of developing ASCVD. The risk of major bleeding exceeded the benefit across all three risk-stratified groups. The greatest benefit, and greatest risk, was in the groups with high to very-high ASCVD risk groups, defined as a 20%-30% and 30% or greater ASCVD risk, respectively: 20-37 fewer MIs per 10,000 with monotherapy and 27-49 fewer with statin, but 78-98 more major bleeding events with monotherapy and 74-95 more with statin.
And aspirin, either as monotherapy or with statin, didn’t reduce the risk of other key endpoints: stroke, all-cause mortality, or cardiovascular mortality. While aspirin was associated with a lower risk of nonfatal MI (RR, .82; 95% CI, .72 to .94; P ≤. 001), it wasn’t associated with reducing the risk of nonfatal stroke. Aspirin patients had a significantly 32% greater risk of intracranial hemorrhage (RR, 1.32; 95% CI, 1.12-1.55; P ≤ .001) and 51% increased risk of gastrointestinal bleeding (RR, 1.51; 95% CI, 1.33-1.72; P ≤ .001).
“We used randomized data from all key primary prevention of aspirin trials and estimated the absolute effects of aspirin therapy with or without concomitant statin across different baseline risks of the patients,” Dr. Khan said. “This approach allowed us to identify aspirin therapy’s risk-benefit equilibrium, which is tilted towards more harm than benefit.”
He acknowledged study limitations included using study-level rather than patient-level meta-analysis, and the inability to calculate effects in younger populations at high absolute risk.
The investigators acknowledged the controversy surrounding aspirin use to prevent ASCVD, noting the three major guidelines: the 2019 American College of Cardiology/American Heart Association and the 2021 European Society of Cardiology guidelines for aspirin only among asymptomatic individuals with high risk of ASCVD events, low bleeding risk, and age 70 years and younger; and the United States Preventive Services Task Force guidelines, updated in 2022, recommending individualized low-dose aspirin only among adults ages 40-59 years with 10-year ASCVD risk of 10% or greater and a low bleeding risk.
The findings are not a clarion call to halt aspirin therapy, Dr. Khan said. “This research focuses only on patients who do not have ASCVD,” he said. “Patients who do have ASCVD should continue with aspirin and statin therapy. However, we noted that aspirin has a limited role for patients who do not have ASCVD beyond lifestyle modifications, smoking cessation, exercise, and preventive statin therapy. Therefore, they should only consider using aspirin if their physicians suggest that the risk of having a cardiovascular event exceeds their bleeding risk. Otherwise, they should discuss with their physicians about omitting aspirin.”
The study confirms the move away from low-dose aspirin to prevent ASCVD, said Tahmid Rahman, MD, cardiologist and associate director of the Center for Advanced Lipid Management at Stony Brook (N.Y.) Heart Institute. “The study really continues to add to essentially what we already know,” he said. “There was a big push that aspirin, initially before the major statin trials, was the way to go to prevent heart disease, but with later studies, and especially now with newer antiplatelet therapies and longer duration of medication for people with both secondary prevention and primary prevention, we are getting away from routine aspirin, especially in primary prevention.”
Lowering LDL cholesterol is the definitive target for lowering risk for MI and stroke, Dr. Rahman said. “Statins don’t lead to a bleeding risk,” he said, “so my recommendation is to be aggressive with lowering your cholesterol and getting the LDL as low possible to really reduce outcomes, especially in secondary prevention, as well as in high-risk patients for primary prevention, especially diabetics.”
He added, however, lifestyle modification also has a key role for preventing ASCVD. “No matter what we have with medication, the most important thing is following a proper diet, especially something like the Mediterranean diet, as well as exercising regularly,” he said.
Dr. Khan and Dr. Rahman have no relevant disclosures.
A new meta-analysis has added evidence questioning the utility and efficacy of prophylactic low-dose aspirin for preventing cardiovascular events in people who don’t have atherosclerotic cardiovascular disease (ASCVD), whether or not they’re also taking statins, and finds that at every level of ASCVD risk the aspirin carries a risk of major bleeding that exceeds its potentially protective benefits.
In a study published online in JACC: Advances, the researchers, led by Safi U. Khan, MD, MS, analyzed data from 16 trials with 171,215 individuals, with a median age of 64 years. Of the population analyzed, 35% were taking statins.
“This study focused on patients without ASCVD who are taking aspirin with or without statin therapy to prevent ASCVD events,” Dr. Khan, a cardiovascular disease fellow at Houston Methodist DeBakey Heart and Vascular Institute, told this news organization. “We noted that the absolute risk of major bleeding in this patient population exceeds the absolute reduction in MI by aspirin across different ASCVD risk categories. Furthermore, concomitant statin therapy use further diminishes aspirin’s cardiovascular effects without influencing bleeding risk.”
Across the 16 studies, people taking aspirin had a relative risk reduction of 15% for MI vs. controls (RR .85; 95% confidence interval [CI], .77 to .95; P < .001). However, they had a 48% greater risk of major bleeding (RR, 1.48; 95% CI, 1.31-1.66; P < .001).
The meta-analysis also found that aspirin, either as monotherapy or with a statin, carried a slight to significant benefit depending on the estimated risk of developing ASCVD. The risk of major bleeding exceeded the benefit across all three risk-stratified groups. The greatest benefit, and greatest risk, was in the groups with high to very-high ASCVD risk groups, defined as a 20%-30% and 30% or greater ASCVD risk, respectively: 20-37 fewer MIs per 10,000 with monotherapy and 27-49 fewer with statin, but 78-98 more major bleeding events with monotherapy and 74-95 more with statin.
And aspirin, either as monotherapy or with statin, didn’t reduce the risk of other key endpoints: stroke, all-cause mortality, or cardiovascular mortality. While aspirin was associated with a lower risk of nonfatal MI (RR, .82; 95% CI, .72 to .94; P ≤. 001), it wasn’t associated with reducing the risk of nonfatal stroke. Aspirin patients had a significantly 32% greater risk of intracranial hemorrhage (RR, 1.32; 95% CI, 1.12-1.55; P ≤ .001) and 51% increased risk of gastrointestinal bleeding (RR, 1.51; 95% CI, 1.33-1.72; P ≤ .001).
“We used randomized data from all key primary prevention of aspirin trials and estimated the absolute effects of aspirin therapy with or without concomitant statin across different baseline risks of the patients,” Dr. Khan said. “This approach allowed us to identify aspirin therapy’s risk-benefit equilibrium, which is tilted towards more harm than benefit.”
He acknowledged study limitations included using study-level rather than patient-level meta-analysis, and the inability to calculate effects in younger populations at high absolute risk.
The investigators acknowledged the controversy surrounding aspirin use to prevent ASCVD, noting the three major guidelines: the 2019 American College of Cardiology/American Heart Association and the 2021 European Society of Cardiology guidelines for aspirin only among asymptomatic individuals with high risk of ASCVD events, low bleeding risk, and age 70 years and younger; and the United States Preventive Services Task Force guidelines, updated in 2022, recommending individualized low-dose aspirin only among adults ages 40-59 years with 10-year ASCVD risk of 10% or greater and a low bleeding risk.
The findings are not a clarion call to halt aspirin therapy, Dr. Khan said. “This research focuses only on patients who do not have ASCVD,” he said. “Patients who do have ASCVD should continue with aspirin and statin therapy. However, we noted that aspirin has a limited role for patients who do not have ASCVD beyond lifestyle modifications, smoking cessation, exercise, and preventive statin therapy. Therefore, they should only consider using aspirin if their physicians suggest that the risk of having a cardiovascular event exceeds their bleeding risk. Otherwise, they should discuss with their physicians about omitting aspirin.”
The study confirms the move away from low-dose aspirin to prevent ASCVD, said Tahmid Rahman, MD, cardiologist and associate director of the Center for Advanced Lipid Management at Stony Brook (N.Y.) Heart Institute. “The study really continues to add to essentially what we already know,” he said. “There was a big push that aspirin, initially before the major statin trials, was the way to go to prevent heart disease, but with later studies, and especially now with newer antiplatelet therapies and longer duration of medication for people with both secondary prevention and primary prevention, we are getting away from routine aspirin, especially in primary prevention.”
Lowering LDL cholesterol is the definitive target for lowering risk for MI and stroke, Dr. Rahman said. “Statins don’t lead to a bleeding risk,” he said, “so my recommendation is to be aggressive with lowering your cholesterol and getting the LDL as low possible to really reduce outcomes, especially in secondary prevention, as well as in high-risk patients for primary prevention, especially diabetics.”
He added, however, lifestyle modification also has a key role for preventing ASCVD. “No matter what we have with medication, the most important thing is following a proper diet, especially something like the Mediterranean diet, as well as exercising regularly,” he said.
Dr. Khan and Dr. Rahman have no relevant disclosures.
A new meta-analysis has added evidence questioning the utility and efficacy of prophylactic low-dose aspirin for preventing cardiovascular events in people who don’t have atherosclerotic cardiovascular disease (ASCVD), whether or not they’re also taking statins, and finds that at every level of ASCVD risk the aspirin carries a risk of major bleeding that exceeds its potentially protective benefits.
In a study published online in JACC: Advances, the researchers, led by Safi U. Khan, MD, MS, analyzed data from 16 trials with 171,215 individuals, with a median age of 64 years. Of the population analyzed, 35% were taking statins.
“This study focused on patients without ASCVD who are taking aspirin with or without statin therapy to prevent ASCVD events,” Dr. Khan, a cardiovascular disease fellow at Houston Methodist DeBakey Heart and Vascular Institute, told this news organization. “We noted that the absolute risk of major bleeding in this patient population exceeds the absolute reduction in MI by aspirin across different ASCVD risk categories. Furthermore, concomitant statin therapy use further diminishes aspirin’s cardiovascular effects without influencing bleeding risk.”
Across the 16 studies, people taking aspirin had a relative risk reduction of 15% for MI vs. controls (RR .85; 95% confidence interval [CI], .77 to .95; P < .001). However, they had a 48% greater risk of major bleeding (RR, 1.48; 95% CI, 1.31-1.66; P < .001).
The meta-analysis also found that aspirin, either as monotherapy or with a statin, carried a slight to significant benefit depending on the estimated risk of developing ASCVD. The risk of major bleeding exceeded the benefit across all three risk-stratified groups. The greatest benefit, and greatest risk, was in the groups with high to very-high ASCVD risk groups, defined as a 20%-30% and 30% or greater ASCVD risk, respectively: 20-37 fewer MIs per 10,000 with monotherapy and 27-49 fewer with statin, but 78-98 more major bleeding events with monotherapy and 74-95 more with statin.
And aspirin, either as monotherapy or with statin, didn’t reduce the risk of other key endpoints: stroke, all-cause mortality, or cardiovascular mortality. While aspirin was associated with a lower risk of nonfatal MI (RR, .82; 95% CI, .72 to .94; P ≤. 001), it wasn’t associated with reducing the risk of nonfatal stroke. Aspirin patients had a significantly 32% greater risk of intracranial hemorrhage (RR, 1.32; 95% CI, 1.12-1.55; P ≤ .001) and 51% increased risk of gastrointestinal bleeding (RR, 1.51; 95% CI, 1.33-1.72; P ≤ .001).
“We used randomized data from all key primary prevention of aspirin trials and estimated the absolute effects of aspirin therapy with or without concomitant statin across different baseline risks of the patients,” Dr. Khan said. “This approach allowed us to identify aspirin therapy’s risk-benefit equilibrium, which is tilted towards more harm than benefit.”
He acknowledged study limitations included using study-level rather than patient-level meta-analysis, and the inability to calculate effects in younger populations at high absolute risk.
The investigators acknowledged the controversy surrounding aspirin use to prevent ASCVD, noting the three major guidelines: the 2019 American College of Cardiology/American Heart Association and the 2021 European Society of Cardiology guidelines for aspirin only among asymptomatic individuals with high risk of ASCVD events, low bleeding risk, and age 70 years and younger; and the United States Preventive Services Task Force guidelines, updated in 2022, recommending individualized low-dose aspirin only among adults ages 40-59 years with 10-year ASCVD risk of 10% or greater and a low bleeding risk.
The findings are not a clarion call to halt aspirin therapy, Dr. Khan said. “This research focuses only on patients who do not have ASCVD,” he said. “Patients who do have ASCVD should continue with aspirin and statin therapy. However, we noted that aspirin has a limited role for patients who do not have ASCVD beyond lifestyle modifications, smoking cessation, exercise, and preventive statin therapy. Therefore, they should only consider using aspirin if their physicians suggest that the risk of having a cardiovascular event exceeds their bleeding risk. Otherwise, they should discuss with their physicians about omitting aspirin.”
The study confirms the move away from low-dose aspirin to prevent ASCVD, said Tahmid Rahman, MD, cardiologist and associate director of the Center for Advanced Lipid Management at Stony Brook (N.Y.) Heart Institute. “The study really continues to add to essentially what we already know,” he said. “There was a big push that aspirin, initially before the major statin trials, was the way to go to prevent heart disease, but with later studies, and especially now with newer antiplatelet therapies and longer duration of medication for people with both secondary prevention and primary prevention, we are getting away from routine aspirin, especially in primary prevention.”
Lowering LDL cholesterol is the definitive target for lowering risk for MI and stroke, Dr. Rahman said. “Statins don’t lead to a bleeding risk,” he said, “so my recommendation is to be aggressive with lowering your cholesterol and getting the LDL as low possible to really reduce outcomes, especially in secondary prevention, as well as in high-risk patients for primary prevention, especially diabetics.”
He added, however, lifestyle modification also has a key role for preventing ASCVD. “No matter what we have with medication, the most important thing is following a proper diet, especially something like the Mediterranean diet, as well as exercising regularly,” he said.
Dr. Khan and Dr. Rahman have no relevant disclosures.
FROM JACC: ADVANCES
Don’t keep your patients waiting
Recently, the results of a survey of consumers regarding their health care experiences were reported by Carta Healthcare. As you might expect, I’ve written about punctuality before, but this is such a ubiquitous problem that it bears repeating. Here are some suggestions:
Start on time. That seems obvious, but I’m always amazed at the number of doctors who admit to running late who also admit that they start late. If you’re in the hole before you even start, you can seldom dig yourself out. Sometimes an on-time start is the solution to the entire problem! If you doubt me, try it.
Book realistically. Everyone works at a different pace. Determine the number of patients you can comfortably see in an hour, and book only that number. If you want to see more patients, the solution is working longer hours or hiring physicians or physician extenders (or both), not overloading your schedule.
Time-stamp each chart. Pay attention to patient arrival times if your EHR records them, and step up your pace if you start to fall behind. If your EHR does not record arrival times or you are still using paper records, buy a time clock and have your receptionist time-stamp the “encounter form” that goes to the back with the patient. One glance at the stamp will tell you exactly how long that patient has been waiting.
Schedule all surgeries. If you haven’t scheduled the time necessary for a surgical procedure, don’t do it. It’s frequently tempting to “squeeze in” an excision, often because you feel guilty that the patient has already had to wait for you. But every unscheduled surgery puts you that much further behind. And hurrying through a procedure increases the risk of mistakes. Tell the patient that surgery requires extra time and it can’t be rushed, so you will have to schedule that time.
Work-ins come last, not first. Patients with urgent problems should be seen after scheduled patients. That may seem counterintuitive; receptionists often assume it’s better to squeeze them in early, while you’re still running on time. But doing that guarantees you will run late, and it isn’t fair to patients who have appointments and expect to be seen promptly.
Work-ins, on the other hand, expect a wait because they have no appointment. We tell them, “Our schedule is full today; but if you come at the end of hours, the doctor will see you. But you may have a wait.” Far from complaining, they invariably thank us for seeing them.
Seize the list. You know the list I mean. “Number 16: My right big toe itches. Number 17: I think I feel something on my back. Number 18: This weird chartreuse thing on my arm ...” One long list can leave an entire half-day schedule in shambles.
When a list is produced, the best option is to take it and read it yourself. Identify the most important two or three problems, and address them. For the rest, I will say, “This group of problems deserves a visit of its own, and we will schedule that visit.”
Ask if you can place the list (or a photocopy) in the patient’s chart. (It is, after all, important clinical information.) All of these problems are important to the patient and should be addressed – but on your schedule, not the patient’s.
Avoid interruptions. Especially phone calls. Unless it’s an emergency or an immediate family member, my receptionists say, “I’m sorry, the doctor is with patients. May I take a message?” Everyone – even other physicians – understands. But be sure to return those calls promptly.
Pharmaceutical reps should not be allowed to interrupt you, either. Have them make an appointment, just like everybody else.
There will be times, of course, when you run late. But these should be the exception rather than the rule. By streamlining your procedures and avoiding the pitfalls mentioned, you can give nearly every patient all the time he or she deserves without keeping the next patient waiting.
Incidentally, other common patient complaints in that survey were the following:
- Couldn’t schedule an appointment within a week.
- Spent too little time with me.
- Didn’t provide test results promptly.
- Didn’t respond to my phone calls promptly.
Now would be an excellent opportunity to identify and address any of those problems as well.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Recently, the results of a survey of consumers regarding their health care experiences were reported by Carta Healthcare. As you might expect, I’ve written about punctuality before, but this is such a ubiquitous problem that it bears repeating. Here are some suggestions:
Start on time. That seems obvious, but I’m always amazed at the number of doctors who admit to running late who also admit that they start late. If you’re in the hole before you even start, you can seldom dig yourself out. Sometimes an on-time start is the solution to the entire problem! If you doubt me, try it.
Book realistically. Everyone works at a different pace. Determine the number of patients you can comfortably see in an hour, and book only that number. If you want to see more patients, the solution is working longer hours or hiring physicians or physician extenders (or both), not overloading your schedule.
Time-stamp each chart. Pay attention to patient arrival times if your EHR records them, and step up your pace if you start to fall behind. If your EHR does not record arrival times or you are still using paper records, buy a time clock and have your receptionist time-stamp the “encounter form” that goes to the back with the patient. One glance at the stamp will tell you exactly how long that patient has been waiting.
Schedule all surgeries. If you haven’t scheduled the time necessary for a surgical procedure, don’t do it. It’s frequently tempting to “squeeze in” an excision, often because you feel guilty that the patient has already had to wait for you. But every unscheduled surgery puts you that much further behind. And hurrying through a procedure increases the risk of mistakes. Tell the patient that surgery requires extra time and it can’t be rushed, so you will have to schedule that time.
Work-ins come last, not first. Patients with urgent problems should be seen after scheduled patients. That may seem counterintuitive; receptionists often assume it’s better to squeeze them in early, while you’re still running on time. But doing that guarantees you will run late, and it isn’t fair to patients who have appointments and expect to be seen promptly.
Work-ins, on the other hand, expect a wait because they have no appointment. We tell them, “Our schedule is full today; but if you come at the end of hours, the doctor will see you. But you may have a wait.” Far from complaining, they invariably thank us for seeing them.
Seize the list. You know the list I mean. “Number 16: My right big toe itches. Number 17: I think I feel something on my back. Number 18: This weird chartreuse thing on my arm ...” One long list can leave an entire half-day schedule in shambles.
When a list is produced, the best option is to take it and read it yourself. Identify the most important two or three problems, and address them. For the rest, I will say, “This group of problems deserves a visit of its own, and we will schedule that visit.”
Ask if you can place the list (or a photocopy) in the patient’s chart. (It is, after all, important clinical information.) All of these problems are important to the patient and should be addressed – but on your schedule, not the patient’s.
Avoid interruptions. Especially phone calls. Unless it’s an emergency or an immediate family member, my receptionists say, “I’m sorry, the doctor is with patients. May I take a message?” Everyone – even other physicians – understands. But be sure to return those calls promptly.
Pharmaceutical reps should not be allowed to interrupt you, either. Have them make an appointment, just like everybody else.
There will be times, of course, when you run late. But these should be the exception rather than the rule. By streamlining your procedures and avoiding the pitfalls mentioned, you can give nearly every patient all the time he or she deserves without keeping the next patient waiting.
Incidentally, other common patient complaints in that survey were the following:
- Couldn’t schedule an appointment within a week.
- Spent too little time with me.
- Didn’t provide test results promptly.
- Didn’t respond to my phone calls promptly.
Now would be an excellent opportunity to identify and address any of those problems as well.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Recently, the results of a survey of consumers regarding their health care experiences were reported by Carta Healthcare. As you might expect, I’ve written about punctuality before, but this is such a ubiquitous problem that it bears repeating. Here are some suggestions:
Start on time. That seems obvious, but I’m always amazed at the number of doctors who admit to running late who also admit that they start late. If you’re in the hole before you even start, you can seldom dig yourself out. Sometimes an on-time start is the solution to the entire problem! If you doubt me, try it.
Book realistically. Everyone works at a different pace. Determine the number of patients you can comfortably see in an hour, and book only that number. If you want to see more patients, the solution is working longer hours or hiring physicians or physician extenders (or both), not overloading your schedule.
Time-stamp each chart. Pay attention to patient arrival times if your EHR records them, and step up your pace if you start to fall behind. If your EHR does not record arrival times or you are still using paper records, buy a time clock and have your receptionist time-stamp the “encounter form” that goes to the back with the patient. One glance at the stamp will tell you exactly how long that patient has been waiting.
Schedule all surgeries. If you haven’t scheduled the time necessary for a surgical procedure, don’t do it. It’s frequently tempting to “squeeze in” an excision, often because you feel guilty that the patient has already had to wait for you. But every unscheduled surgery puts you that much further behind. And hurrying through a procedure increases the risk of mistakes. Tell the patient that surgery requires extra time and it can’t be rushed, so you will have to schedule that time.
Work-ins come last, not first. Patients with urgent problems should be seen after scheduled patients. That may seem counterintuitive; receptionists often assume it’s better to squeeze them in early, while you’re still running on time. But doing that guarantees you will run late, and it isn’t fair to patients who have appointments and expect to be seen promptly.
Work-ins, on the other hand, expect a wait because they have no appointment. We tell them, “Our schedule is full today; but if you come at the end of hours, the doctor will see you. But you may have a wait.” Far from complaining, they invariably thank us for seeing them.
Seize the list. You know the list I mean. “Number 16: My right big toe itches. Number 17: I think I feel something on my back. Number 18: This weird chartreuse thing on my arm ...” One long list can leave an entire half-day schedule in shambles.
When a list is produced, the best option is to take it and read it yourself. Identify the most important two or three problems, and address them. For the rest, I will say, “This group of problems deserves a visit of its own, and we will schedule that visit.”
Ask if you can place the list (or a photocopy) in the patient’s chart. (It is, after all, important clinical information.) All of these problems are important to the patient and should be addressed – but on your schedule, not the patient’s.
Avoid interruptions. Especially phone calls. Unless it’s an emergency or an immediate family member, my receptionists say, “I’m sorry, the doctor is with patients. May I take a message?” Everyone – even other physicians – understands. But be sure to return those calls promptly.
Pharmaceutical reps should not be allowed to interrupt you, either. Have them make an appointment, just like everybody else.
There will be times, of course, when you run late. But these should be the exception rather than the rule. By streamlining your procedures and avoiding the pitfalls mentioned, you can give nearly every patient all the time he or she deserves without keeping the next patient waiting.
Incidentally, other common patient complaints in that survey were the following:
- Couldn’t schedule an appointment within a week.
- Spent too little time with me.
- Didn’t provide test results promptly.
- Didn’t respond to my phone calls promptly.
Now would be an excellent opportunity to identify and address any of those problems as well.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Uptick in natriuretic peptides with long-term serial testing predicts new heart failure
A jump in natriuretic peptide levels over several years in middle-aged adults points to worsened long-term risks for incident heart failure (HF) and death. But their predicted long-term survival improves if serial testing shows a drop in those levels, suggests a new analysis based on a well-known longitudinal study cohort.
The findings support the risk-stratification potential of serial natriuretic peptide testing, which may improve on individual assays for predicting future HF. Such serial assays might also be useful for guiding therapy aimed at preventing, for example, progression to clinical HF, researchers speculate on the basis of the current study,
The analysis of almost 1,000 members of the ARIC (Atherosclerosis Risk in Community) cohort had been free of clinical HF at the first of two NT-proBNP assays, which were performed 6 years apart. Their 20-year clinical risk was linked to the trajectory of NT-proBNP levels across the two earlier assays.
For example, adjusted risk of incident HF more than doubled for participants with NT-proBNP levels exceeding 125 pg/mL on both assays, compared with levels that stayed under the cut point at both assays. Their mortality risk climbed by about two-thirds.
Risk for incident HF and of death climbed 86% and 32%, respectively, if NT-proBNP levels rose over the 6 years from less than to greater than 125 pg/mL. But long-term survival improved if serial assays showed a drop from the higher to the lower level.
Rising NT-proBNP levels over several years probably reflect ongoing exposure to risk factors such as hypertension or diabetes. Conversely, decreasing NT-proBNP levels likely reflect some success at keeping such risk factors under control, propose the authors of the analysis published in JAMA Cardiology. The study was led by Xiaoming Jia, MD, Baylor College of Medicine, Houston.
The findings raise the possibility that reducing NT-proBNP levels through risk-factor modification, tracked by serial assays, may potentially improve long-term risk for death or incident HF.
Such therapy, guided by natriuretic peptides, might prove especially useful in asymptomatic adults with modifiable HF risk factors but without known NT-proBNP elevation or cardiac structural changes, so-called stage A HF, senior author Vijay Nambi, MD, PhD, also of Baylor, observed for this news organization.
The best populations for serial NT-proBNP assays to guide therapy, Dr. Nambi said, should become clear “as more data emerges.” But the threshold for ordering such tests would probably be lower for people in stage A whose rising NT-proBNP levels later reclassify them as stage B, also called pre-HF.
In such cases, he speculated, intensified therapy of HF risk factors such as uncontrolled hypertension or diabetes – prompted by greater NT-proBNP levels at serial testing – might possibly avert progression to clinical HF.
“These investigators have nicely demonstrated that one measurement of the biomarker may not be sufficient, that maybe it undercaptures the true burden of people who eventually will develop heart failure,” Muthiah Vaduganathan, MD, MPH, told this news organization.
The study raises the possibility “that the serial natriuretic peptide strategy may be more efficient and more comprehensive in identifying those who will eventually progress,” said Dr. Vaduganathan, of Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not associated with the ARIC analysis.
An open question, he added, is whether the predicted risk is modifiable. “If you are able to provide the biomarker information to treating clinicians, can they do something to attenuate the risk?”
The outlook is hopeful, given contemporary therapies “that can slow and even prevent heart failure in at-risk populations,” Dr. Vaduganathan said. For example, “The selective allocation of SGLT2 inhibitors to those with elevated natriuretic peptide levels, perhaps as captured in serial measurements, would be of great interest.”
The analysis included 9,776 adults (56.5% women, 21.3% Black) without HF who underwent NT-proBNP testing at the second and – about 6 years later – the fourth scheduled clinical visits in the ARIC study, which had enrolled persons aged 45-64 from four diverse communities from across the United States.
Adjusted hazard ratios for incident HF according to NT-proBNP changes from the first to second assays relative to 125 pg/mL were as follows:
- 1.86 (95% confidence interval, 1.60-2.16) when levels rose to higher than the cut point.
- 2.40 (95% CI, 2.00-2.88) when both levels exceeded the cut point.
The corresponding adjusted HRs for death from any cause were as follows:
- 1.32 (95%CI, 1.19-1.47) when levels rose to higher than 125 mg/mL.
- 1.68 (95% CI, 1.47-1.91) when both levels were above the cut point.
The risks for incident HF and for death rose significantly by 6% and 5%, respectively, per standard deviation NT-proBNP increase from the first to second assay.
Risks for HF and mortality for participants whose NT-proBNP levels declined from greater than to less than 125 pg/mL were similar to those whose levels remained low at both assays.
Cost-effectiveness would be another issue when implementing a strategy that calls for multiple biomarker assays, Dr. Vaduganathan observed.
“Surely, we would want to demonstrate that the laboratory measurement costs are offset by downstream prevention of heart failure events that could be averted by use of effective medical therapy, such SGLT2 inhibitors.”
ARIC has been funded by the National Institutes of Health and Department of Health and Human Services. Dr. Nambi discloses receiving grants from the National Institutes of Health during the conduct of the study; support from Amgen; and stocks from Abbott Laboratories. Disclosures for the other authors are in the report. Dr. Vaduganathan has disclosed receiving grants or serving on advisory boards for American Regent, Amgen, AstraZeneca, Bayer AG, Baxter Healthcare, Boehringer Ingelheim, Cytokinetics, Lexicon Pharmaceuticals, Novartis, Pharmacosmos, Relypsa, Roche Diagnostics, Sanofi, and Tricog Health; speaking for AstraZeneca, Novartis, and Roche Diagnostics; and serving on trial committees for studies sponsored by Galmed, Novartis, Bayer AG, Occlutech, and Impulse Dynamics.
A version of this article originally appeared on Medscape.com.
A jump in natriuretic peptide levels over several years in middle-aged adults points to worsened long-term risks for incident heart failure (HF) and death. But their predicted long-term survival improves if serial testing shows a drop in those levels, suggests a new analysis based on a well-known longitudinal study cohort.
The findings support the risk-stratification potential of serial natriuretic peptide testing, which may improve on individual assays for predicting future HF. Such serial assays might also be useful for guiding therapy aimed at preventing, for example, progression to clinical HF, researchers speculate on the basis of the current study,
The analysis of almost 1,000 members of the ARIC (Atherosclerosis Risk in Community) cohort had been free of clinical HF at the first of two NT-proBNP assays, which were performed 6 years apart. Their 20-year clinical risk was linked to the trajectory of NT-proBNP levels across the two earlier assays.
For example, adjusted risk of incident HF more than doubled for participants with NT-proBNP levels exceeding 125 pg/mL on both assays, compared with levels that stayed under the cut point at both assays. Their mortality risk climbed by about two-thirds.
Risk for incident HF and of death climbed 86% and 32%, respectively, if NT-proBNP levels rose over the 6 years from less than to greater than 125 pg/mL. But long-term survival improved if serial assays showed a drop from the higher to the lower level.
Rising NT-proBNP levels over several years probably reflect ongoing exposure to risk factors such as hypertension or diabetes. Conversely, decreasing NT-proBNP levels likely reflect some success at keeping such risk factors under control, propose the authors of the analysis published in JAMA Cardiology. The study was led by Xiaoming Jia, MD, Baylor College of Medicine, Houston.
The findings raise the possibility that reducing NT-proBNP levels through risk-factor modification, tracked by serial assays, may potentially improve long-term risk for death or incident HF.
Such therapy, guided by natriuretic peptides, might prove especially useful in asymptomatic adults with modifiable HF risk factors but without known NT-proBNP elevation or cardiac structural changes, so-called stage A HF, senior author Vijay Nambi, MD, PhD, also of Baylor, observed for this news organization.
The best populations for serial NT-proBNP assays to guide therapy, Dr. Nambi said, should become clear “as more data emerges.” But the threshold for ordering such tests would probably be lower for people in stage A whose rising NT-proBNP levels later reclassify them as stage B, also called pre-HF.
In such cases, he speculated, intensified therapy of HF risk factors such as uncontrolled hypertension or diabetes – prompted by greater NT-proBNP levels at serial testing – might possibly avert progression to clinical HF.
“These investigators have nicely demonstrated that one measurement of the biomarker may not be sufficient, that maybe it undercaptures the true burden of people who eventually will develop heart failure,” Muthiah Vaduganathan, MD, MPH, told this news organization.
The study raises the possibility “that the serial natriuretic peptide strategy may be more efficient and more comprehensive in identifying those who will eventually progress,” said Dr. Vaduganathan, of Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not associated with the ARIC analysis.
An open question, he added, is whether the predicted risk is modifiable. “If you are able to provide the biomarker information to treating clinicians, can they do something to attenuate the risk?”
The outlook is hopeful, given contemporary therapies “that can slow and even prevent heart failure in at-risk populations,” Dr. Vaduganathan said. For example, “The selective allocation of SGLT2 inhibitors to those with elevated natriuretic peptide levels, perhaps as captured in serial measurements, would be of great interest.”
The analysis included 9,776 adults (56.5% women, 21.3% Black) without HF who underwent NT-proBNP testing at the second and – about 6 years later – the fourth scheduled clinical visits in the ARIC study, which had enrolled persons aged 45-64 from four diverse communities from across the United States.
Adjusted hazard ratios for incident HF according to NT-proBNP changes from the first to second assays relative to 125 pg/mL were as follows:
- 1.86 (95% confidence interval, 1.60-2.16) when levels rose to higher than the cut point.
- 2.40 (95% CI, 2.00-2.88) when both levels exceeded the cut point.
The corresponding adjusted HRs for death from any cause were as follows:
- 1.32 (95%CI, 1.19-1.47) when levels rose to higher than 125 mg/mL.
- 1.68 (95% CI, 1.47-1.91) when both levels were above the cut point.
The risks for incident HF and for death rose significantly by 6% and 5%, respectively, per standard deviation NT-proBNP increase from the first to second assay.
Risks for HF and mortality for participants whose NT-proBNP levels declined from greater than to less than 125 pg/mL were similar to those whose levels remained low at both assays.
Cost-effectiveness would be another issue when implementing a strategy that calls for multiple biomarker assays, Dr. Vaduganathan observed.
“Surely, we would want to demonstrate that the laboratory measurement costs are offset by downstream prevention of heart failure events that could be averted by use of effective medical therapy, such SGLT2 inhibitors.”
ARIC has been funded by the National Institutes of Health and Department of Health and Human Services. Dr. Nambi discloses receiving grants from the National Institutes of Health during the conduct of the study; support from Amgen; and stocks from Abbott Laboratories. Disclosures for the other authors are in the report. Dr. Vaduganathan has disclosed receiving grants or serving on advisory boards for American Regent, Amgen, AstraZeneca, Bayer AG, Baxter Healthcare, Boehringer Ingelheim, Cytokinetics, Lexicon Pharmaceuticals, Novartis, Pharmacosmos, Relypsa, Roche Diagnostics, Sanofi, and Tricog Health; speaking for AstraZeneca, Novartis, and Roche Diagnostics; and serving on trial committees for studies sponsored by Galmed, Novartis, Bayer AG, Occlutech, and Impulse Dynamics.
A version of this article originally appeared on Medscape.com.
A jump in natriuretic peptide levels over several years in middle-aged adults points to worsened long-term risks for incident heart failure (HF) and death. But their predicted long-term survival improves if serial testing shows a drop in those levels, suggests a new analysis based on a well-known longitudinal study cohort.
The findings support the risk-stratification potential of serial natriuretic peptide testing, which may improve on individual assays for predicting future HF. Such serial assays might also be useful for guiding therapy aimed at preventing, for example, progression to clinical HF, researchers speculate on the basis of the current study,
The analysis of almost 1,000 members of the ARIC (Atherosclerosis Risk in Community) cohort had been free of clinical HF at the first of two NT-proBNP assays, which were performed 6 years apart. Their 20-year clinical risk was linked to the trajectory of NT-proBNP levels across the two earlier assays.
For example, adjusted risk of incident HF more than doubled for participants with NT-proBNP levels exceeding 125 pg/mL on both assays, compared with levels that stayed under the cut point at both assays. Their mortality risk climbed by about two-thirds.
Risk for incident HF and of death climbed 86% and 32%, respectively, if NT-proBNP levels rose over the 6 years from less than to greater than 125 pg/mL. But long-term survival improved if serial assays showed a drop from the higher to the lower level.
Rising NT-proBNP levels over several years probably reflect ongoing exposure to risk factors such as hypertension or diabetes. Conversely, decreasing NT-proBNP levels likely reflect some success at keeping such risk factors under control, propose the authors of the analysis published in JAMA Cardiology. The study was led by Xiaoming Jia, MD, Baylor College of Medicine, Houston.
The findings raise the possibility that reducing NT-proBNP levels through risk-factor modification, tracked by serial assays, may potentially improve long-term risk for death or incident HF.
Such therapy, guided by natriuretic peptides, might prove especially useful in asymptomatic adults with modifiable HF risk factors but without known NT-proBNP elevation or cardiac structural changes, so-called stage A HF, senior author Vijay Nambi, MD, PhD, also of Baylor, observed for this news organization.
The best populations for serial NT-proBNP assays to guide therapy, Dr. Nambi said, should become clear “as more data emerges.” But the threshold for ordering such tests would probably be lower for people in stage A whose rising NT-proBNP levels later reclassify them as stage B, also called pre-HF.
In such cases, he speculated, intensified therapy of HF risk factors such as uncontrolled hypertension or diabetes – prompted by greater NT-proBNP levels at serial testing – might possibly avert progression to clinical HF.
“These investigators have nicely demonstrated that one measurement of the biomarker may not be sufficient, that maybe it undercaptures the true burden of people who eventually will develop heart failure,” Muthiah Vaduganathan, MD, MPH, told this news organization.
The study raises the possibility “that the serial natriuretic peptide strategy may be more efficient and more comprehensive in identifying those who will eventually progress,” said Dr. Vaduganathan, of Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not associated with the ARIC analysis.
An open question, he added, is whether the predicted risk is modifiable. “If you are able to provide the biomarker information to treating clinicians, can they do something to attenuate the risk?”
The outlook is hopeful, given contemporary therapies “that can slow and even prevent heart failure in at-risk populations,” Dr. Vaduganathan said. For example, “The selective allocation of SGLT2 inhibitors to those with elevated natriuretic peptide levels, perhaps as captured in serial measurements, would be of great interest.”
The analysis included 9,776 adults (56.5% women, 21.3% Black) without HF who underwent NT-proBNP testing at the second and – about 6 years later – the fourth scheduled clinical visits in the ARIC study, which had enrolled persons aged 45-64 from four diverse communities from across the United States.
Adjusted hazard ratios for incident HF according to NT-proBNP changes from the first to second assays relative to 125 pg/mL were as follows:
- 1.86 (95% confidence interval, 1.60-2.16) when levels rose to higher than the cut point.
- 2.40 (95% CI, 2.00-2.88) when both levels exceeded the cut point.
The corresponding adjusted HRs for death from any cause were as follows:
- 1.32 (95%CI, 1.19-1.47) when levels rose to higher than 125 mg/mL.
- 1.68 (95% CI, 1.47-1.91) when both levels were above the cut point.
The risks for incident HF and for death rose significantly by 6% and 5%, respectively, per standard deviation NT-proBNP increase from the first to second assay.
Risks for HF and mortality for participants whose NT-proBNP levels declined from greater than to less than 125 pg/mL were similar to those whose levels remained low at both assays.
Cost-effectiveness would be another issue when implementing a strategy that calls for multiple biomarker assays, Dr. Vaduganathan observed.
“Surely, we would want to demonstrate that the laboratory measurement costs are offset by downstream prevention of heart failure events that could be averted by use of effective medical therapy, such SGLT2 inhibitors.”
ARIC has been funded by the National Institutes of Health and Department of Health and Human Services. Dr. Nambi discloses receiving grants from the National Institutes of Health during the conduct of the study; support from Amgen; and stocks from Abbott Laboratories. Disclosures for the other authors are in the report. Dr. Vaduganathan has disclosed receiving grants or serving on advisory boards for American Regent, Amgen, AstraZeneca, Bayer AG, Baxter Healthcare, Boehringer Ingelheim, Cytokinetics, Lexicon Pharmaceuticals, Novartis, Pharmacosmos, Relypsa, Roche Diagnostics, Sanofi, and Tricog Health; speaking for AstraZeneca, Novartis, and Roche Diagnostics; and serving on trial committees for studies sponsored by Galmed, Novartis, Bayer AG, Occlutech, and Impulse Dynamics.
A version of this article originally appeared on Medscape.com.
FROM JAMA CARDIOLOGY
Cardiac issues twice as likely with COVID plus high troponin
Hospitalized COVID-19 patients with high troponin levels are twice as likely to have cardiac abnormalities than those with normal troponin, with or without COVID-19, a multicenter U.K. study suggests.
The causes were diverse, myocarditis prevalence was lower than previously reported, and myocardial scar emerged as an independent risk factor for adverse cardiovascular outcomes at 12 months.
“We know that multiorgan involvement in hospitalized patients with COVID-19 is common ... and may result in acute myocardial injury, detected by an increase in cardiac troponin concentrations,” John P. Greenwood, PhD, of the University of Leeds (England), told this news organization. “Elevated cardiac troponin is associated with a worse prognosis.”
“Multiple mechanisms of myocardial injury have been proposed and ... mitigation or prevention strategies likely depend on the underpinning mechanisms,” he said. “The sequelae of scar may predispose to late events.”
The study, published online in Circulation, also identified a new pattern of microinfarction on cardiac magnetic resonance (CMR) imaging, highlighting the pro-thrombotic nature of SARS-CoV-2, Dr. Greenwood said.
Injury patterns different
Three hundred and forty-two patients with COVID-19 and elevated troponin levels (COVID+/troponin+) across 25 centers were enrolled between June 2020 and March 2021 in COVID-HEART, deemed an “urgent public health study” in the United Kingdom. The aim was to characterize myocardial injury and its associations and sequelae in convalescent patients after hospitalization with COVID-19.
Enrollment took place during the Wuhan and Alpha waves of COVID-19: before vaccination and when dexamethasone and anticoagulant protocols were emerging. All participants underwent CMR at a median of 21 days after discharge.
Two prospective control groups also were recruited: 64 patients with COVID-19 and normal troponin levels (COVID+/troponin−) and 113 without COVID-19 or elevated troponin matched by age and cardiovascular comorbidities (COVID−/comorbidity+).
Overall, participants’ median age was 61 years and 69% were men. Common comorbidities included hypertension (47%), obesity (43%), and diabetes (25%).
The frequency of any heart abnormality – for example, left or right ventricular impairment, scar, or pericardial disease – was twice as great (61%) in COVID+/troponin+ cases, compared with controls (36% for COVID+/troponin− patients versus 31% for COVID−/comorbidity+ patients).
Specifically, more cases than controls had ventricular impairment (17.2% vs. 3.1% and 7.1%) or scar (42% vs. 7% and 23%).
The myocardial injury pattern differed between cases and controls, with cases more likely to have infarction (13% vs. 2% and 7%) or microinfarction (9% vs. 0% and 1%).
However, there was no between-group difference in nonischemic scar (13% vs. 5% and 14%).
The prevalence of probable recent myocarditis was 6.7% in cases, compared with 1.7% in controls without COVID-19 – “much lower” than in previous studies, Dr. Greenwood noted.
During follow-up, four COVID+/troponin+ patients (1.2%) died, and 34 (10%) experienced a subsequent major adverse cardiovascular event (MACE; 10.2%), which was similar to controls (6.1%).
Myocardial scar, but not previous COVID-19 infection or troponin level, was an independent predictor of MACE (odds ratio, 2.25).
“These findings suggest that macroangiopathic and microangiopathic thrombosis may be the key pathologic process for myocardial injury in COVID-19 survivors,” the authors conclude.
Dr. Greenwood added, “We are currently analyzing the 6-month follow-up CMR scans, the quality-of-life questionnaires, and the 6-minute walk tests. These will give us great understanding of how the heart repairs after acute myocardial injury associated with COVID-19. It will also allow us to assess the impact on patient quality of life and functional capacity.”
‘Tour de force’
James A. de Lemos, MD, co-chair of the American Heart Association’s COVID-19 CVD Registry Steering Committee and a professor of medicine at the University of Texas Southwestern Medical Center, Dallas, said, “This is a tour de force collaboration – obtaining this many MRIs across multiple centers in the pandemic is quite remarkable. The study highlights the multiple different processes that lead to cardiac injury in COVID patients, complements autopsy studies and prior smaller MRI studies, [and] also provides the best data on the rate of myocarditis to date among the subset of COVID patients with cardiac injury.”
Overall, he said, the findings “do support closer follow-up for patients who had COVID and elevated troponins. We need to see follow-up MRI results in this cohort, as well as longer term outcomes. We also need studies on newer, more benign variants that are likely to have lower rates of cardiac injury and even fewer MRI abnormalities.”
Matthias Stuber, PhD, and Aaron L. Baggish, MD, both of Lausanne University Hospital and University of Lausanne, Switzerland, noted in a related editorial, “We are also reminded that the clinical severity of COVID-19 is most often dictated by the presence of pre-existing comorbidity, with antecedent ischemic scar now added to the long list of bad actors. Although not the primary focus of the COVID-HEART study, the question of whether cardiac troponin levels should be checked routinely and universally during the index admission for COVID-19 remains unresolved,” they noted.
“In general, we are most effective as clinicians when we use tests to confirm or rule out the specific disease processes suspected by careful basic clinical assessment rather than in a shotgun manner among undifferentiated all-comers,” they conclude.
No commercial funding or relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
Hospitalized COVID-19 patients with high troponin levels are twice as likely to have cardiac abnormalities than those with normal troponin, with or without COVID-19, a multicenter U.K. study suggests.
The causes were diverse, myocarditis prevalence was lower than previously reported, and myocardial scar emerged as an independent risk factor for adverse cardiovascular outcomes at 12 months.
“We know that multiorgan involvement in hospitalized patients with COVID-19 is common ... and may result in acute myocardial injury, detected by an increase in cardiac troponin concentrations,” John P. Greenwood, PhD, of the University of Leeds (England), told this news organization. “Elevated cardiac troponin is associated with a worse prognosis.”
“Multiple mechanisms of myocardial injury have been proposed and ... mitigation or prevention strategies likely depend on the underpinning mechanisms,” he said. “The sequelae of scar may predispose to late events.”
The study, published online in Circulation, also identified a new pattern of microinfarction on cardiac magnetic resonance (CMR) imaging, highlighting the pro-thrombotic nature of SARS-CoV-2, Dr. Greenwood said.
Injury patterns different
Three hundred and forty-two patients with COVID-19 and elevated troponin levels (COVID+/troponin+) across 25 centers were enrolled between June 2020 and March 2021 in COVID-HEART, deemed an “urgent public health study” in the United Kingdom. The aim was to characterize myocardial injury and its associations and sequelae in convalescent patients after hospitalization with COVID-19.
Enrollment took place during the Wuhan and Alpha waves of COVID-19: before vaccination and when dexamethasone and anticoagulant protocols were emerging. All participants underwent CMR at a median of 21 days after discharge.
Two prospective control groups also were recruited: 64 patients with COVID-19 and normal troponin levels (COVID+/troponin−) and 113 without COVID-19 or elevated troponin matched by age and cardiovascular comorbidities (COVID−/comorbidity+).
Overall, participants’ median age was 61 years and 69% were men. Common comorbidities included hypertension (47%), obesity (43%), and diabetes (25%).
The frequency of any heart abnormality – for example, left or right ventricular impairment, scar, or pericardial disease – was twice as great (61%) in COVID+/troponin+ cases, compared with controls (36% for COVID+/troponin− patients versus 31% for COVID−/comorbidity+ patients).
Specifically, more cases than controls had ventricular impairment (17.2% vs. 3.1% and 7.1%) or scar (42% vs. 7% and 23%).
The myocardial injury pattern differed between cases and controls, with cases more likely to have infarction (13% vs. 2% and 7%) or microinfarction (9% vs. 0% and 1%).
However, there was no between-group difference in nonischemic scar (13% vs. 5% and 14%).
The prevalence of probable recent myocarditis was 6.7% in cases, compared with 1.7% in controls without COVID-19 – “much lower” than in previous studies, Dr. Greenwood noted.
During follow-up, four COVID+/troponin+ patients (1.2%) died, and 34 (10%) experienced a subsequent major adverse cardiovascular event (MACE; 10.2%), which was similar to controls (6.1%).
Myocardial scar, but not previous COVID-19 infection or troponin level, was an independent predictor of MACE (odds ratio, 2.25).
“These findings suggest that macroangiopathic and microangiopathic thrombosis may be the key pathologic process for myocardial injury in COVID-19 survivors,” the authors conclude.
Dr. Greenwood added, “We are currently analyzing the 6-month follow-up CMR scans, the quality-of-life questionnaires, and the 6-minute walk tests. These will give us great understanding of how the heart repairs after acute myocardial injury associated with COVID-19. It will also allow us to assess the impact on patient quality of life and functional capacity.”
‘Tour de force’
James A. de Lemos, MD, co-chair of the American Heart Association’s COVID-19 CVD Registry Steering Committee and a professor of medicine at the University of Texas Southwestern Medical Center, Dallas, said, “This is a tour de force collaboration – obtaining this many MRIs across multiple centers in the pandemic is quite remarkable. The study highlights the multiple different processes that lead to cardiac injury in COVID patients, complements autopsy studies and prior smaller MRI studies, [and] also provides the best data on the rate of myocarditis to date among the subset of COVID patients with cardiac injury.”
Overall, he said, the findings “do support closer follow-up for patients who had COVID and elevated troponins. We need to see follow-up MRI results in this cohort, as well as longer term outcomes. We also need studies on newer, more benign variants that are likely to have lower rates of cardiac injury and even fewer MRI abnormalities.”
Matthias Stuber, PhD, and Aaron L. Baggish, MD, both of Lausanne University Hospital and University of Lausanne, Switzerland, noted in a related editorial, “We are also reminded that the clinical severity of COVID-19 is most often dictated by the presence of pre-existing comorbidity, with antecedent ischemic scar now added to the long list of bad actors. Although not the primary focus of the COVID-HEART study, the question of whether cardiac troponin levels should be checked routinely and universally during the index admission for COVID-19 remains unresolved,” they noted.
“In general, we are most effective as clinicians when we use tests to confirm or rule out the specific disease processes suspected by careful basic clinical assessment rather than in a shotgun manner among undifferentiated all-comers,” they conclude.
No commercial funding or relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
Hospitalized COVID-19 patients with high troponin levels are twice as likely to have cardiac abnormalities than those with normal troponin, with or without COVID-19, a multicenter U.K. study suggests.
The causes were diverse, myocarditis prevalence was lower than previously reported, and myocardial scar emerged as an independent risk factor for adverse cardiovascular outcomes at 12 months.
“We know that multiorgan involvement in hospitalized patients with COVID-19 is common ... and may result in acute myocardial injury, detected by an increase in cardiac troponin concentrations,” John P. Greenwood, PhD, of the University of Leeds (England), told this news organization. “Elevated cardiac troponin is associated with a worse prognosis.”
“Multiple mechanisms of myocardial injury have been proposed and ... mitigation or prevention strategies likely depend on the underpinning mechanisms,” he said. “The sequelae of scar may predispose to late events.”
The study, published online in Circulation, also identified a new pattern of microinfarction on cardiac magnetic resonance (CMR) imaging, highlighting the pro-thrombotic nature of SARS-CoV-2, Dr. Greenwood said.
Injury patterns different
Three hundred and forty-two patients with COVID-19 and elevated troponin levels (COVID+/troponin+) across 25 centers were enrolled between June 2020 and March 2021 in COVID-HEART, deemed an “urgent public health study” in the United Kingdom. The aim was to characterize myocardial injury and its associations and sequelae in convalescent patients after hospitalization with COVID-19.
Enrollment took place during the Wuhan and Alpha waves of COVID-19: before vaccination and when dexamethasone and anticoagulant protocols were emerging. All participants underwent CMR at a median of 21 days after discharge.
Two prospective control groups also were recruited: 64 patients with COVID-19 and normal troponin levels (COVID+/troponin−) and 113 without COVID-19 or elevated troponin matched by age and cardiovascular comorbidities (COVID−/comorbidity+).
Overall, participants’ median age was 61 years and 69% were men. Common comorbidities included hypertension (47%), obesity (43%), and diabetes (25%).
The frequency of any heart abnormality – for example, left or right ventricular impairment, scar, or pericardial disease – was twice as great (61%) in COVID+/troponin+ cases, compared with controls (36% for COVID+/troponin− patients versus 31% for COVID−/comorbidity+ patients).
Specifically, more cases than controls had ventricular impairment (17.2% vs. 3.1% and 7.1%) or scar (42% vs. 7% and 23%).
The myocardial injury pattern differed between cases and controls, with cases more likely to have infarction (13% vs. 2% and 7%) or microinfarction (9% vs. 0% and 1%).
However, there was no between-group difference in nonischemic scar (13% vs. 5% and 14%).
The prevalence of probable recent myocarditis was 6.7% in cases, compared with 1.7% in controls without COVID-19 – “much lower” than in previous studies, Dr. Greenwood noted.
During follow-up, four COVID+/troponin+ patients (1.2%) died, and 34 (10%) experienced a subsequent major adverse cardiovascular event (MACE; 10.2%), which was similar to controls (6.1%).
Myocardial scar, but not previous COVID-19 infection or troponin level, was an independent predictor of MACE (odds ratio, 2.25).
“These findings suggest that macroangiopathic and microangiopathic thrombosis may be the key pathologic process for myocardial injury in COVID-19 survivors,” the authors conclude.
Dr. Greenwood added, “We are currently analyzing the 6-month follow-up CMR scans, the quality-of-life questionnaires, and the 6-minute walk tests. These will give us great understanding of how the heart repairs after acute myocardial injury associated with COVID-19. It will also allow us to assess the impact on patient quality of life and functional capacity.”
‘Tour de force’
James A. de Lemos, MD, co-chair of the American Heart Association’s COVID-19 CVD Registry Steering Committee and a professor of medicine at the University of Texas Southwestern Medical Center, Dallas, said, “This is a tour de force collaboration – obtaining this many MRIs across multiple centers in the pandemic is quite remarkable. The study highlights the multiple different processes that lead to cardiac injury in COVID patients, complements autopsy studies and prior smaller MRI studies, [and] also provides the best data on the rate of myocarditis to date among the subset of COVID patients with cardiac injury.”
Overall, he said, the findings “do support closer follow-up for patients who had COVID and elevated troponins. We need to see follow-up MRI results in this cohort, as well as longer term outcomes. We also need studies on newer, more benign variants that are likely to have lower rates of cardiac injury and even fewer MRI abnormalities.”
Matthias Stuber, PhD, and Aaron L. Baggish, MD, both of Lausanne University Hospital and University of Lausanne, Switzerland, noted in a related editorial, “We are also reminded that the clinical severity of COVID-19 is most often dictated by the presence of pre-existing comorbidity, with antecedent ischemic scar now added to the long list of bad actors. Although not the primary focus of the COVID-HEART study, the question of whether cardiac troponin levels should be checked routinely and universally during the index admission for COVID-19 remains unresolved,” they noted.
“In general, we are most effective as clinicians when we use tests to confirm or rule out the specific disease processes suspected by careful basic clinical assessment rather than in a shotgun manner among undifferentiated all-comers,” they conclude.
No commercial funding or relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
Type 1 diabetes no longer a disease of the thin: Lifestyle advice needed
About two-thirds of people with type 1 diabetes in the United States have overweight or obesity, nearly the same proportion as Americans without diabetes, new nationwide survey data suggest.
What’s more, among people with overweight or obesity, those with type 1 diabetes are less likely to receive lifestyle recommendations from health care professionals than those with type 2 diabetes, and are less likely to actually engage in lifestyle weight management activities than others with overweight or obesity, with or without type 2 diabetes.
“Among U.S. adults with type 1 diabetes, the burden of overweight and obesity is substantial and remains poorly managed,” write Michael Fang, PhD, of the Johns Hopkins Bloomberg School of Public Health, Baltimore, and colleagues.
Their data, from the National Health Interview Survey (NHIS), were published online in Annals of Internal Medicine.
The need for insulin complicates weight management in people with type 1 diabetes because changes in diet and physical activity typically require adjustments to insulin timing and dosage to prevent hypoglycemia. There is little evidence to guide this for weight management, Dr. Fang and colleagues explain.
Consequently, “the lack of evidence for safe, effective methods of diet- and exercise-based weight control in people with type 1 diabetes may be keeping doctors from recommending such methods,” Dr. Fang said in a statement.
“Large clinical trials have been done in type 2 diabetes patients to establish guidelines for diet- and exercise-based weight management, and we now need something similar for type 1 diabetes patients.”
Asked to comment, M. Sue Kirkman, MD, told this news organization: “The days when we could teach simple concepts about diabetes type like ‘those with type 1 are lean and those with type 2 are overweight’ are long gone. … Of concern, fewer adults with type 1 diabetes and overweight/obesity report that they are engaging in physical activity or caloric restriction than those without diabetes or those with type 2 diabetes.”
There are several likely reasons for the low rates of obesity/overweight lifestyle modification advice and implementation for those with type 1 diabetes, noted Dr. Kirkman, of the University of North Carolina at Chapel Hill, who coauthored joint American/European guidance on type 1 diabetes management.
“Medical visits are often primarily focused on glycemic management and complications screening, and we know that physicians in general are not very knowledgeable about how to counsel people – even those without diabetes – on weight loss. When you add in potential worries, real or not, about hypoglycemia, ketosis with carbohydrate restriction … it’s no wonder that this may not be addressed in busy visits.”
She also observed, “In years of going to diabetes meetings, I’ve noticed occasional sessions on managing ‘elite athletes’ with type 1 diabetes, but rarely are there sessions on how to counsel people about everyday healthy living.”
Many with type 1 diabetes have overweight/obesity
Dr. Fang and colleagues analyzed NHIS data for the years 2016, 2017, 2019, 2020, and 2021, when diabetes subtype data were available, for 128,571 adults. Diabetes type and height/weight data were self-reported. In the 2016, 2017, and 2020 surveys, participants were asked whether their physicians had recommended increasing physical activity and/or reducing calorie or fat consumption, and whether they were currently engaging in those activities.
The study population comprised 733 people with type 1 diabetes, 12,397 with type 2 diabetes, and 115,441 without diabetes. The proportions with overweight (body mass index, 25 to < 30 kg/m2) or obesity (≥ 30 kg/m2) were 62% among those with type 1 diabetes and 64% among those without diabetes, compared with 86% among those with type 2 diabetes.
Among those with overweight or obesity, the proportions who reported having received lifestyle recommendations were greatest among those with type 2 diabetes and least among those without diabetes, with the type 1 diabetes group in the middle.
After adjustment for age, sex, and race/ethnicity, the adjusted prevalence of receiving a provider recommendation to increase physical activity was 60% for those with type 2 diabetes, 54% for type 1 diabetes, and 44% for those without diabetes. Proportions for receiving recommendations for reducing fat/caloric intake were similar, at 60%, 51%, and 41%, respectively.
The proportions who reported actually engaging in lifestyle activities for weight management were lowest among those with type 1 diabetes, with 52% and 56% of them reporting having increased their physical activity and reducing fat/calories, respectively, compared with proportions ranging from 56% to 63% among the other two groups.
Regarding those findings, Dr. Kirkman commented, “In addition to the factors regarding physician interactions, people with type 1 diabetes may see this as a lower-priority health issue after years of being told that glucose control is the main priority.”
“I also wonder if the many, many tasks people with type 1 diabetes must do every day to manage their diabetes – along with other life issues all adults face – mean that there is just too much on the plate to add more lifestyle changes,” she added.
Asked about the potential for off-label use of glucagonlike peptide–1 agonists for weight management for people with type 1 diabetes, Dr. Kirkman said they could probably help some patients. However, she also pointed to two clinical trials in which liraglutide added to insulin therapy helped with glycemic control and weight reduction, but also increased the risk for hypoglycemia and diabetic ketoacidosis.
“It’s really important that researchers engage with adults with type 1 diabetes to better understand the unique priorities and barriers they face in addressing body weight,” Dr. Kirkman said.
Senior study author Elizabeth Selvin, PhD, professor of epidemiology at the Bloomberg School, said in the statement: “Our study busts the myth that people with type 1 diabetes are not being affected by the global obesity epidemic. … These findings should be a wake-up call that we need to be aggressive in addressing the obesity epidemic in persons with type 1 diabetes.”
The study was funded by the U.S. National Institutes of Health. Dr. Fang and Dr. Kirkman have reported no relevant financial relationships. Dr. Selvin has reported receiving royalty payments from Wolters Kluwer for chapters and laboratory monographs in UpToDate. She also reports receiving honoraria for editorial work on journals published by the American Diabetes Association and European Association for the Study of Diabetes.
A version of this article originally appeared on Medscape.com.
About two-thirds of people with type 1 diabetes in the United States have overweight or obesity, nearly the same proportion as Americans without diabetes, new nationwide survey data suggest.
What’s more, among people with overweight or obesity, those with type 1 diabetes are less likely to receive lifestyle recommendations from health care professionals than those with type 2 diabetes, and are less likely to actually engage in lifestyle weight management activities than others with overweight or obesity, with or without type 2 diabetes.
“Among U.S. adults with type 1 diabetes, the burden of overweight and obesity is substantial and remains poorly managed,” write Michael Fang, PhD, of the Johns Hopkins Bloomberg School of Public Health, Baltimore, and colleagues.
Their data, from the National Health Interview Survey (NHIS), were published online in Annals of Internal Medicine.
The need for insulin complicates weight management in people with type 1 diabetes because changes in diet and physical activity typically require adjustments to insulin timing and dosage to prevent hypoglycemia. There is little evidence to guide this for weight management, Dr. Fang and colleagues explain.
Consequently, “the lack of evidence for safe, effective methods of diet- and exercise-based weight control in people with type 1 diabetes may be keeping doctors from recommending such methods,” Dr. Fang said in a statement.
“Large clinical trials have been done in type 2 diabetes patients to establish guidelines for diet- and exercise-based weight management, and we now need something similar for type 1 diabetes patients.”
Asked to comment, M. Sue Kirkman, MD, told this news organization: “The days when we could teach simple concepts about diabetes type like ‘those with type 1 are lean and those with type 2 are overweight’ are long gone. … Of concern, fewer adults with type 1 diabetes and overweight/obesity report that they are engaging in physical activity or caloric restriction than those without diabetes or those with type 2 diabetes.”
There are several likely reasons for the low rates of obesity/overweight lifestyle modification advice and implementation for those with type 1 diabetes, noted Dr. Kirkman, of the University of North Carolina at Chapel Hill, who coauthored joint American/European guidance on type 1 diabetes management.
“Medical visits are often primarily focused on glycemic management and complications screening, and we know that physicians in general are not very knowledgeable about how to counsel people – even those without diabetes – on weight loss. When you add in potential worries, real or not, about hypoglycemia, ketosis with carbohydrate restriction … it’s no wonder that this may not be addressed in busy visits.”
She also observed, “In years of going to diabetes meetings, I’ve noticed occasional sessions on managing ‘elite athletes’ with type 1 diabetes, but rarely are there sessions on how to counsel people about everyday healthy living.”
Many with type 1 diabetes have overweight/obesity
Dr. Fang and colleagues analyzed NHIS data for the years 2016, 2017, 2019, 2020, and 2021, when diabetes subtype data were available, for 128,571 adults. Diabetes type and height/weight data were self-reported. In the 2016, 2017, and 2020 surveys, participants were asked whether their physicians had recommended increasing physical activity and/or reducing calorie or fat consumption, and whether they were currently engaging in those activities.
The study population comprised 733 people with type 1 diabetes, 12,397 with type 2 diabetes, and 115,441 without diabetes. The proportions with overweight (body mass index, 25 to < 30 kg/m2) or obesity (≥ 30 kg/m2) were 62% among those with type 1 diabetes and 64% among those without diabetes, compared with 86% among those with type 2 diabetes.
Among those with overweight or obesity, the proportions who reported having received lifestyle recommendations were greatest among those with type 2 diabetes and least among those without diabetes, with the type 1 diabetes group in the middle.
After adjustment for age, sex, and race/ethnicity, the adjusted prevalence of receiving a provider recommendation to increase physical activity was 60% for those with type 2 diabetes, 54% for type 1 diabetes, and 44% for those without diabetes. Proportions for receiving recommendations for reducing fat/caloric intake were similar, at 60%, 51%, and 41%, respectively.
The proportions who reported actually engaging in lifestyle activities for weight management were lowest among those with type 1 diabetes, with 52% and 56% of them reporting having increased their physical activity and reducing fat/calories, respectively, compared with proportions ranging from 56% to 63% among the other two groups.
Regarding those findings, Dr. Kirkman commented, “In addition to the factors regarding physician interactions, people with type 1 diabetes may see this as a lower-priority health issue after years of being told that glucose control is the main priority.”
“I also wonder if the many, many tasks people with type 1 diabetes must do every day to manage their diabetes – along with other life issues all adults face – mean that there is just too much on the plate to add more lifestyle changes,” she added.
Asked about the potential for off-label use of glucagonlike peptide–1 agonists for weight management for people with type 1 diabetes, Dr. Kirkman said they could probably help some patients. However, she also pointed to two clinical trials in which liraglutide added to insulin therapy helped with glycemic control and weight reduction, but also increased the risk for hypoglycemia and diabetic ketoacidosis.
“It’s really important that researchers engage with adults with type 1 diabetes to better understand the unique priorities and barriers they face in addressing body weight,” Dr. Kirkman said.
Senior study author Elizabeth Selvin, PhD, professor of epidemiology at the Bloomberg School, said in the statement: “Our study busts the myth that people with type 1 diabetes are not being affected by the global obesity epidemic. … These findings should be a wake-up call that we need to be aggressive in addressing the obesity epidemic in persons with type 1 diabetes.”
The study was funded by the U.S. National Institutes of Health. Dr. Fang and Dr. Kirkman have reported no relevant financial relationships. Dr. Selvin has reported receiving royalty payments from Wolters Kluwer for chapters and laboratory monographs in UpToDate. She also reports receiving honoraria for editorial work on journals published by the American Diabetes Association and European Association for the Study of Diabetes.
A version of this article originally appeared on Medscape.com.
About two-thirds of people with type 1 diabetes in the United States have overweight or obesity, nearly the same proportion as Americans without diabetes, new nationwide survey data suggest.
What’s more, among people with overweight or obesity, those with type 1 diabetes are less likely to receive lifestyle recommendations from health care professionals than those with type 2 diabetes, and are less likely to actually engage in lifestyle weight management activities than others with overweight or obesity, with or without type 2 diabetes.
“Among U.S. adults with type 1 diabetes, the burden of overweight and obesity is substantial and remains poorly managed,” write Michael Fang, PhD, of the Johns Hopkins Bloomberg School of Public Health, Baltimore, and colleagues.
Their data, from the National Health Interview Survey (NHIS), were published online in Annals of Internal Medicine.
The need for insulin complicates weight management in people with type 1 diabetes because changes in diet and physical activity typically require adjustments to insulin timing and dosage to prevent hypoglycemia. There is little evidence to guide this for weight management, Dr. Fang and colleagues explain.
Consequently, “the lack of evidence for safe, effective methods of diet- and exercise-based weight control in people with type 1 diabetes may be keeping doctors from recommending such methods,” Dr. Fang said in a statement.
“Large clinical trials have been done in type 2 diabetes patients to establish guidelines for diet- and exercise-based weight management, and we now need something similar for type 1 diabetes patients.”
Asked to comment, M. Sue Kirkman, MD, told this news organization: “The days when we could teach simple concepts about diabetes type like ‘those with type 1 are lean and those with type 2 are overweight’ are long gone. … Of concern, fewer adults with type 1 diabetes and overweight/obesity report that they are engaging in physical activity or caloric restriction than those without diabetes or those with type 2 diabetes.”
There are several likely reasons for the low rates of obesity/overweight lifestyle modification advice and implementation for those with type 1 diabetes, noted Dr. Kirkman, of the University of North Carolina at Chapel Hill, who coauthored joint American/European guidance on type 1 diabetes management.
“Medical visits are often primarily focused on glycemic management and complications screening, and we know that physicians in general are not very knowledgeable about how to counsel people – even those without diabetes – on weight loss. When you add in potential worries, real or not, about hypoglycemia, ketosis with carbohydrate restriction … it’s no wonder that this may not be addressed in busy visits.”
She also observed, “In years of going to diabetes meetings, I’ve noticed occasional sessions on managing ‘elite athletes’ with type 1 diabetes, but rarely are there sessions on how to counsel people about everyday healthy living.”
Many with type 1 diabetes have overweight/obesity
Dr. Fang and colleagues analyzed NHIS data for the years 2016, 2017, 2019, 2020, and 2021, when diabetes subtype data were available, for 128,571 adults. Diabetes type and height/weight data were self-reported. In the 2016, 2017, and 2020 surveys, participants were asked whether their physicians had recommended increasing physical activity and/or reducing calorie or fat consumption, and whether they were currently engaging in those activities.
The study population comprised 733 people with type 1 diabetes, 12,397 with type 2 diabetes, and 115,441 without diabetes. The proportions with overweight (body mass index, 25 to < 30 kg/m2) or obesity (≥ 30 kg/m2) were 62% among those with type 1 diabetes and 64% among those without diabetes, compared with 86% among those with type 2 diabetes.
Among those with overweight or obesity, the proportions who reported having received lifestyle recommendations were greatest among those with type 2 diabetes and least among those without diabetes, with the type 1 diabetes group in the middle.
After adjustment for age, sex, and race/ethnicity, the adjusted prevalence of receiving a provider recommendation to increase physical activity was 60% for those with type 2 diabetes, 54% for type 1 diabetes, and 44% for those without diabetes. Proportions for receiving recommendations for reducing fat/caloric intake were similar, at 60%, 51%, and 41%, respectively.
The proportions who reported actually engaging in lifestyle activities for weight management were lowest among those with type 1 diabetes, with 52% and 56% of them reporting having increased their physical activity and reducing fat/calories, respectively, compared with proportions ranging from 56% to 63% among the other two groups.
Regarding those findings, Dr. Kirkman commented, “In addition to the factors regarding physician interactions, people with type 1 diabetes may see this as a lower-priority health issue after years of being told that glucose control is the main priority.”
“I also wonder if the many, many tasks people with type 1 diabetes must do every day to manage their diabetes – along with other life issues all adults face – mean that there is just too much on the plate to add more lifestyle changes,” she added.
Asked about the potential for off-label use of glucagonlike peptide–1 agonists for weight management for people with type 1 diabetes, Dr. Kirkman said they could probably help some patients. However, she also pointed to two clinical trials in which liraglutide added to insulin therapy helped with glycemic control and weight reduction, but also increased the risk for hypoglycemia and diabetic ketoacidosis.
“It’s really important that researchers engage with adults with type 1 diabetes to better understand the unique priorities and barriers they face in addressing body weight,” Dr. Kirkman said.
Senior study author Elizabeth Selvin, PhD, professor of epidemiology at the Bloomberg School, said in the statement: “Our study busts the myth that people with type 1 diabetes are not being affected by the global obesity epidemic. … These findings should be a wake-up call that we need to be aggressive in addressing the obesity epidemic in persons with type 1 diabetes.”
The study was funded by the U.S. National Institutes of Health. Dr. Fang and Dr. Kirkman have reported no relevant financial relationships. Dr. Selvin has reported receiving royalty payments from Wolters Kluwer for chapters and laboratory monographs in UpToDate. She also reports receiving honoraria for editorial work on journals published by the American Diabetes Association and European Association for the Study of Diabetes.
A version of this article originally appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Could ChatGPT write this column?
, but I am starting to think it is the real deal. Just how powerful is it? Well, ChatGPT might in fact be writing this column right now. It isn’t. No really, it’s me. But if not for the few cues (“super-buzzy”) that you’ll recognize as my writing voice, there might not be any way for you to know if I wrote this or not.
It’s perfectly OK if you’ve no clue what I’m talking about. ChatGPT is an AI chatbot that burst into public view just a couple months ago. Not your parent’s chatbot, this one is capable of answering questions in conversational language. It is jaw-droppingly good. Like Google, you can type in a question and it offers you answers. Rather than giving you a list of websites and a few Wikipedia blurbs, however, ChatGPT answers your question in human-like text. It can also create content on demand. For example, I asked it to write a Valentine poem to a dermatologist, and it gave me five stanzas starting with:
Oh gentle healer of skin so fair,
Not good enough to send to my wife. But not bad.
If you ask it again, it will create a whole new one for you. Amusing, yes? What if you asked ChatGPT to explain psoriasis, or any medical condition for that matter, to a patient? The replies are quite good. Some even better than what I’m currently using for my patients. It can also offer treatment recommendations, vacation advice, and plan, with recipes, a dinner party for six with one vegan and one gluten-free couple. If you are a programmer, it can write code. Ask it for a Wordpress plugin to add to your website and your eyes will widen as you see it magically appear before you. What if you find that you just don’t like your daughter’s new boyfriend? Yep, it will write the text or email for you to help with this discussion. I’ve saved that one.
I tried “What are treatments for bullous pemphigoid that has been refractory to topical steroid, oral prednisone, and oral tetracyclines?” It replied with five ideas, including the standard methotrexate and azathioprine but also IVIG, Rituxan, even other biologics. Write an op note? Appeal a denied prior authorization to a payer? Write a clinic note for a complete skin exam? Check, check, check. Are you starting to think it might be the real deal, too?
Before we sell the farm though, there are significant limitations. Despite how swotty ChatGPT seems, it is not smart. That is, “it” has no idea what “it” is saying. ChatGPT is an incredibly sophisticated algorithm that has learned the probability of what word comes next in a conversation. To do so, it read the Internet. Billions (trillions?) of words make it possible to predict what is the best answer to any question. But – it’s only as good as the Internet, so there’s that. My patient who used ChatGPT has dissecting cellulitis and asked what to do for scarring alopecia. Some of the answers were reasonable, but some, such as transplanting hairs into the scarred areas, would not likely be helpful. That is unless ChatGPT knows something I don’t.
Having wasted hours of time playing with this thing rather than writing my column, I asked ChatGPT to write an article about itself in the style of Christopher Hitchens. It was nothing like his incisive and eloquent prose, but it wrote 500 words in a few seconds ending with:
“The reality is that there is no substitute for human interaction and empathy in the field of dermatology. Dermatologists must be cautious in their adoption of ChatGPT and ensure that they are not sacrificing the quality of patient care in the pursuit of efficiency and convenience.”
I’m not sure I could have said it better myself.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
, but I am starting to think it is the real deal. Just how powerful is it? Well, ChatGPT might in fact be writing this column right now. It isn’t. No really, it’s me. But if not for the few cues (“super-buzzy”) that you’ll recognize as my writing voice, there might not be any way for you to know if I wrote this or not.
It’s perfectly OK if you’ve no clue what I’m talking about. ChatGPT is an AI chatbot that burst into public view just a couple months ago. Not your parent’s chatbot, this one is capable of answering questions in conversational language. It is jaw-droppingly good. Like Google, you can type in a question and it offers you answers. Rather than giving you a list of websites and a few Wikipedia blurbs, however, ChatGPT answers your question in human-like text. It can also create content on demand. For example, I asked it to write a Valentine poem to a dermatologist, and it gave me five stanzas starting with:
Oh gentle healer of skin so fair,
Not good enough to send to my wife. But not bad.
If you ask it again, it will create a whole new one for you. Amusing, yes? What if you asked ChatGPT to explain psoriasis, or any medical condition for that matter, to a patient? The replies are quite good. Some even better than what I’m currently using for my patients. It can also offer treatment recommendations, vacation advice, and plan, with recipes, a dinner party for six with one vegan and one gluten-free couple. If you are a programmer, it can write code. Ask it for a Wordpress plugin to add to your website and your eyes will widen as you see it magically appear before you. What if you find that you just don’t like your daughter’s new boyfriend? Yep, it will write the text or email for you to help with this discussion. I’ve saved that one.
I tried “What are treatments for bullous pemphigoid that has been refractory to topical steroid, oral prednisone, and oral tetracyclines?” It replied with five ideas, including the standard methotrexate and azathioprine but also IVIG, Rituxan, even other biologics. Write an op note? Appeal a denied prior authorization to a payer? Write a clinic note for a complete skin exam? Check, check, check. Are you starting to think it might be the real deal, too?
Before we sell the farm though, there are significant limitations. Despite how swotty ChatGPT seems, it is not smart. That is, “it” has no idea what “it” is saying. ChatGPT is an incredibly sophisticated algorithm that has learned the probability of what word comes next in a conversation. To do so, it read the Internet. Billions (trillions?) of words make it possible to predict what is the best answer to any question. But – it’s only as good as the Internet, so there’s that. My patient who used ChatGPT has dissecting cellulitis and asked what to do for scarring alopecia. Some of the answers were reasonable, but some, such as transplanting hairs into the scarred areas, would not likely be helpful. That is unless ChatGPT knows something I don’t.
Having wasted hours of time playing with this thing rather than writing my column, I asked ChatGPT to write an article about itself in the style of Christopher Hitchens. It was nothing like his incisive and eloquent prose, but it wrote 500 words in a few seconds ending with:
“The reality is that there is no substitute for human interaction and empathy in the field of dermatology. Dermatologists must be cautious in their adoption of ChatGPT and ensure that they are not sacrificing the quality of patient care in the pursuit of efficiency and convenience.”
I’m not sure I could have said it better myself.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
, but I am starting to think it is the real deal. Just how powerful is it? Well, ChatGPT might in fact be writing this column right now. It isn’t. No really, it’s me. But if not for the few cues (“super-buzzy”) that you’ll recognize as my writing voice, there might not be any way for you to know if I wrote this or not.
It’s perfectly OK if you’ve no clue what I’m talking about. ChatGPT is an AI chatbot that burst into public view just a couple months ago. Not your parent’s chatbot, this one is capable of answering questions in conversational language. It is jaw-droppingly good. Like Google, you can type in a question and it offers you answers. Rather than giving you a list of websites and a few Wikipedia blurbs, however, ChatGPT answers your question in human-like text. It can also create content on demand. For example, I asked it to write a Valentine poem to a dermatologist, and it gave me five stanzas starting with:
Oh gentle healer of skin so fair,
Not good enough to send to my wife. But not bad.
If you ask it again, it will create a whole new one for you. Amusing, yes? What if you asked ChatGPT to explain psoriasis, or any medical condition for that matter, to a patient? The replies are quite good. Some even better than what I’m currently using for my patients. It can also offer treatment recommendations, vacation advice, and plan, with recipes, a dinner party for six with one vegan and one gluten-free couple. If you are a programmer, it can write code. Ask it for a Wordpress plugin to add to your website and your eyes will widen as you see it magically appear before you. What if you find that you just don’t like your daughter’s new boyfriend? Yep, it will write the text or email for you to help with this discussion. I’ve saved that one.
I tried “What are treatments for bullous pemphigoid that has been refractory to topical steroid, oral prednisone, and oral tetracyclines?” It replied with five ideas, including the standard methotrexate and azathioprine but also IVIG, Rituxan, even other biologics. Write an op note? Appeal a denied prior authorization to a payer? Write a clinic note for a complete skin exam? Check, check, check. Are you starting to think it might be the real deal, too?
Before we sell the farm though, there are significant limitations. Despite how swotty ChatGPT seems, it is not smart. That is, “it” has no idea what “it” is saying. ChatGPT is an incredibly sophisticated algorithm that has learned the probability of what word comes next in a conversation. To do so, it read the Internet. Billions (trillions?) of words make it possible to predict what is the best answer to any question. But – it’s only as good as the Internet, so there’s that. My patient who used ChatGPT has dissecting cellulitis and asked what to do for scarring alopecia. Some of the answers were reasonable, but some, such as transplanting hairs into the scarred areas, would not likely be helpful. That is unless ChatGPT knows something I don’t.
Having wasted hours of time playing with this thing rather than writing my column, I asked ChatGPT to write an article about itself in the style of Christopher Hitchens. It was nothing like his incisive and eloquent prose, but it wrote 500 words in a few seconds ending with:
“The reality is that there is no substitute for human interaction and empathy in the field of dermatology. Dermatologists must be cautious in their adoption of ChatGPT and ensure that they are not sacrificing the quality of patient care in the pursuit of efficiency and convenience.”
I’m not sure I could have said it better myself.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.