User login
In California, abortion could become a constitutional right. So could birth control.
SACRAMENTO, CALIF. –
If they vote “yes” on Proposition 1, they will also lock in a right that has gotten less attention: The right to birth control.
Should the measure succeed, California would become one of the first states – if not the first – to create explicit constitutional rights to both abortion and contraception.
The lawmakers and activists behind the constitutional amendment said they hope to score a one-two punch: Protect abortion in California after the U.S. Supreme Court ended the federal constitutional right to abortion under Roe v. Wade, and get ahead of what they see as the next front in the reproductive rights fight: Birth control.
“The United States Supreme Court said that the privacy and liberty protections in the United States Constitution did not extend to abortion,” said UCLA law professor Cary Franklin, an expert in constitutional law and reproductive rights who has testified before the California legislature in support of the amendment. “If they said ‘no’ on abortion, they’re probably going to say ‘no’ on birth control because that has a similar history.”
In June, the U.S. Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization ended the federal right to abortion and left states to regulate the service. In his concurring opinion, Justice Clarence Thomas said the court should revisit other cases that have created protections for Americans based on an implicit right to privacy in the U.S. Constitution, such as the 1965 case Griswold v. Connecticut, which established a federal right to contraception for married people, and which was later extended to unmarried people.
Some congressional Democrats are now trying to codify the right to contraception in federal law. In July, the U.S. House of Representatives passed the Right to Contraception Act, which would give patients the right to access and use contraception and providers the right to furnish it. But the bill has little chance of success in the U.S. Senate, where Republicans have already blocked it once.
Protecting access to contraception is popular with voters. A national poll from Morning Consult and Politico conducted in late July found that 75% of registered voters support a federal law that protects a right to birth control access.
California isn’t the only state where voters are considering reproductive rights in their constitutions.
On Aug. 2, Kansas voters decisively rejected a constitutional amendment that would have allowed state lawmakers to ban or dramatically restrict abortion. It failed by nearly 18 percentage points.
Kentucky voters will face a similar decision in November with a proposed constitutional amendment that would declare that the state’s constitutional right to privacy does not cover abortion.
Vermont is going in the opposite direction. Voters there will weigh a ballot measure in November that would add a right to “personal reproductive autonomy” to the state constitution, though it does not explicitly mention abortion or contraception. In Michigan, a proposed constitutional amendment that would guarantee a right to both abortion and contraception is expected to qualify for the November ballot.
In California, Proposition 1 would prevent the state from denying or interfering with “an individual’s reproductive freedom in their most intimate decisions, which includes their fundamental right to choose to have an abortion and their fundamental right to choose or refuse contraceptives.”
The proposed constitutional amendment doesn’t go into detail about what enshrining the right to contraception in the state constitution would mean.
California already has some of the strongest contraceptive-access laws in the country – and lawmakers are considering more proposals this year. For instance, state-regulated health plans must cover all Food and Drug Administration–approved contraception; pharmacists must dispense emergency contraception to anyone with a prescription, regardless of age; and pharmacists can prescribe birth control pills on the spot. State courts have also interpreted California’s constitution to include a right to privacy that covers reproductive health decisions.
The amendment, if adopted, could provide a new legal pathway for people to sue when they’re denied contraceptives, said Michele Goodwin, chancellor’s professor of law at the University of California, Irvine.
If a pharmacist refused to fill a birth control prescription or a cashier declined to ring up condoms, she said, customers could make a case that their rights had been violated.
Making the rights to abortion and contraception explicit in the state constitution – instead of relying on a right to privacy – would also protect against shifting political winds, said state Senate leader Toni Atkins (D–San Diego), who was the director of a women’s health clinic in the 1980s. Although California’s lawmakers and executive officers are solid supporters of abortion rights, she said, the composition of the legislature and courts’ interpretation of laws could change.
“I want to know for sure that that right is protected,” Ms. Atkins said at a legislative hearing in June. “We are protecting ourselves from future courts and future politicians.”
The amendment would solidify California’s role as a reproductive rights sanctuary as much of the country chips away at birth control availability, Ms. Goodwin added.
Experts said two forms of birth control that are vulnerable to restrictions in other states are intrauterine devices, or IUDs, and emergency contraception such as Plan B. These methods are often incorrectly conflated with abortion pills, which end a pregnancy instead of preventing it.
Nine states have laws that restrict emergency contraception – for example, by allowing pharmacies to refuse to dispense it or excluding it from state family planning programs – according to the Guttmacher Institute, a research organization that supports abortion rights. In Alabama and Louisiana this year, abortion opponents introduced legislation that would restrict or ban abortion, and would also apply to emergency contraception.
“We’re seeing an erosion of abortion access that is playing out in statehouses across the country that have and will continue to target contraceptive care as well,” said Audrey Sandusky, senior director of policy and communications for the National Family Planning and Reproductive Health Association.
Susan Arnall, vice president of California’s Right to Life League, said the proposed amendment is symbolic and merely echoes current laws. Ms. Arnall said the campaign is mostly about Democratic politicians trying to score political points.
“It just allows the pro-abort legislators to trumpet and give them talking points about how they’re doing something about the overturn of Roe v. Wade,” she said. “It is political virtue signaling. I don’t think it does much of anything else.”
Ms. Goodwin argues that the measure’s symbolism is significant and overdue. She pointed to the Civil War era, when enslaved people in Southern states could look to free states for spiritual hope and material help. “Symbolically, what that meant is a kind of beacon of hope, that those places did exist, where one’s humanity could be regarded,” Ms. Goodwin said.
But California’s reputation as a haven for contraceptive availability may not be fully warranted, said Dima Qato, PharmD, PhD, an associate professor at the University of Southern California School of Pharmacy. In her 2020 study of contraceptive access in Los Angeles County, which has some of the highest rates of teen and unintended pregnancy in the country, Dr. Qato found that only 10% of pharmacies surveyed offered pharmacist-prescribed birth control. Pharmacies in low-income and minority communities were the least likely to offer the service, Dr. Qato said, worsening disparities instead of solving them.
Dr. Qato supports the constitutional amendment but said California should focus on improving and enforcing the laws it already has.
“We don’t need more laws when we don’t address the root cause of a lack of effectiveness of these laws in these communities,” she said. “Lack of enforcement and accountability disproportionately impacts communities of color.”
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. Rachel Bluth is a correspondent for California Healthline. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
SACRAMENTO, CALIF. –
If they vote “yes” on Proposition 1, they will also lock in a right that has gotten less attention: The right to birth control.
Should the measure succeed, California would become one of the first states – if not the first – to create explicit constitutional rights to both abortion and contraception.
The lawmakers and activists behind the constitutional amendment said they hope to score a one-two punch: Protect abortion in California after the U.S. Supreme Court ended the federal constitutional right to abortion under Roe v. Wade, and get ahead of what they see as the next front in the reproductive rights fight: Birth control.
“The United States Supreme Court said that the privacy and liberty protections in the United States Constitution did not extend to abortion,” said UCLA law professor Cary Franklin, an expert in constitutional law and reproductive rights who has testified before the California legislature in support of the amendment. “If they said ‘no’ on abortion, they’re probably going to say ‘no’ on birth control because that has a similar history.”
In June, the U.S. Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization ended the federal right to abortion and left states to regulate the service. In his concurring opinion, Justice Clarence Thomas said the court should revisit other cases that have created protections for Americans based on an implicit right to privacy in the U.S. Constitution, such as the 1965 case Griswold v. Connecticut, which established a federal right to contraception for married people, and which was later extended to unmarried people.
Some congressional Democrats are now trying to codify the right to contraception in federal law. In July, the U.S. House of Representatives passed the Right to Contraception Act, which would give patients the right to access and use contraception and providers the right to furnish it. But the bill has little chance of success in the U.S. Senate, where Republicans have already blocked it once.
Protecting access to contraception is popular with voters. A national poll from Morning Consult and Politico conducted in late July found that 75% of registered voters support a federal law that protects a right to birth control access.
California isn’t the only state where voters are considering reproductive rights in their constitutions.
On Aug. 2, Kansas voters decisively rejected a constitutional amendment that would have allowed state lawmakers to ban or dramatically restrict abortion. It failed by nearly 18 percentage points.
Kentucky voters will face a similar decision in November with a proposed constitutional amendment that would declare that the state’s constitutional right to privacy does not cover abortion.
Vermont is going in the opposite direction. Voters there will weigh a ballot measure in November that would add a right to “personal reproductive autonomy” to the state constitution, though it does not explicitly mention abortion or contraception. In Michigan, a proposed constitutional amendment that would guarantee a right to both abortion and contraception is expected to qualify for the November ballot.
In California, Proposition 1 would prevent the state from denying or interfering with “an individual’s reproductive freedom in their most intimate decisions, which includes their fundamental right to choose to have an abortion and their fundamental right to choose or refuse contraceptives.”
The proposed constitutional amendment doesn’t go into detail about what enshrining the right to contraception in the state constitution would mean.
California already has some of the strongest contraceptive-access laws in the country – and lawmakers are considering more proposals this year. For instance, state-regulated health plans must cover all Food and Drug Administration–approved contraception; pharmacists must dispense emergency contraception to anyone with a prescription, regardless of age; and pharmacists can prescribe birth control pills on the spot. State courts have also interpreted California’s constitution to include a right to privacy that covers reproductive health decisions.
The amendment, if adopted, could provide a new legal pathway for people to sue when they’re denied contraceptives, said Michele Goodwin, chancellor’s professor of law at the University of California, Irvine.
If a pharmacist refused to fill a birth control prescription or a cashier declined to ring up condoms, she said, customers could make a case that their rights had been violated.
Making the rights to abortion and contraception explicit in the state constitution – instead of relying on a right to privacy – would also protect against shifting political winds, said state Senate leader Toni Atkins (D–San Diego), who was the director of a women’s health clinic in the 1980s. Although California’s lawmakers and executive officers are solid supporters of abortion rights, she said, the composition of the legislature and courts’ interpretation of laws could change.
“I want to know for sure that that right is protected,” Ms. Atkins said at a legislative hearing in June. “We are protecting ourselves from future courts and future politicians.”
The amendment would solidify California’s role as a reproductive rights sanctuary as much of the country chips away at birth control availability, Ms. Goodwin added.
Experts said two forms of birth control that are vulnerable to restrictions in other states are intrauterine devices, or IUDs, and emergency contraception such as Plan B. These methods are often incorrectly conflated with abortion pills, which end a pregnancy instead of preventing it.
Nine states have laws that restrict emergency contraception – for example, by allowing pharmacies to refuse to dispense it or excluding it from state family planning programs – according to the Guttmacher Institute, a research organization that supports abortion rights. In Alabama and Louisiana this year, abortion opponents introduced legislation that would restrict or ban abortion, and would also apply to emergency contraception.
“We’re seeing an erosion of abortion access that is playing out in statehouses across the country that have and will continue to target contraceptive care as well,” said Audrey Sandusky, senior director of policy and communications for the National Family Planning and Reproductive Health Association.
Susan Arnall, vice president of California’s Right to Life League, said the proposed amendment is symbolic and merely echoes current laws. Ms. Arnall said the campaign is mostly about Democratic politicians trying to score political points.
“It just allows the pro-abort legislators to trumpet and give them talking points about how they’re doing something about the overturn of Roe v. Wade,” she said. “It is political virtue signaling. I don’t think it does much of anything else.”
Ms. Goodwin argues that the measure’s symbolism is significant and overdue. She pointed to the Civil War era, when enslaved people in Southern states could look to free states for spiritual hope and material help. “Symbolically, what that meant is a kind of beacon of hope, that those places did exist, where one’s humanity could be regarded,” Ms. Goodwin said.
But California’s reputation as a haven for contraceptive availability may not be fully warranted, said Dima Qato, PharmD, PhD, an associate professor at the University of Southern California School of Pharmacy. In her 2020 study of contraceptive access in Los Angeles County, which has some of the highest rates of teen and unintended pregnancy in the country, Dr. Qato found that only 10% of pharmacies surveyed offered pharmacist-prescribed birth control. Pharmacies in low-income and minority communities were the least likely to offer the service, Dr. Qato said, worsening disparities instead of solving them.
Dr. Qato supports the constitutional amendment but said California should focus on improving and enforcing the laws it already has.
“We don’t need more laws when we don’t address the root cause of a lack of effectiveness of these laws in these communities,” she said. “Lack of enforcement and accountability disproportionately impacts communities of color.”
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. Rachel Bluth is a correspondent for California Healthline. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
SACRAMENTO, CALIF. –
If they vote “yes” on Proposition 1, they will also lock in a right that has gotten less attention: The right to birth control.
Should the measure succeed, California would become one of the first states – if not the first – to create explicit constitutional rights to both abortion and contraception.
The lawmakers and activists behind the constitutional amendment said they hope to score a one-two punch: Protect abortion in California after the U.S. Supreme Court ended the federal constitutional right to abortion under Roe v. Wade, and get ahead of what they see as the next front in the reproductive rights fight: Birth control.
“The United States Supreme Court said that the privacy and liberty protections in the United States Constitution did not extend to abortion,” said UCLA law professor Cary Franklin, an expert in constitutional law and reproductive rights who has testified before the California legislature in support of the amendment. “If they said ‘no’ on abortion, they’re probably going to say ‘no’ on birth control because that has a similar history.”
In June, the U.S. Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization ended the federal right to abortion and left states to regulate the service. In his concurring opinion, Justice Clarence Thomas said the court should revisit other cases that have created protections for Americans based on an implicit right to privacy in the U.S. Constitution, such as the 1965 case Griswold v. Connecticut, which established a federal right to contraception for married people, and which was later extended to unmarried people.
Some congressional Democrats are now trying to codify the right to contraception in federal law. In July, the U.S. House of Representatives passed the Right to Contraception Act, which would give patients the right to access and use contraception and providers the right to furnish it. But the bill has little chance of success in the U.S. Senate, where Republicans have already blocked it once.
Protecting access to contraception is popular with voters. A national poll from Morning Consult and Politico conducted in late July found that 75% of registered voters support a federal law that protects a right to birth control access.
California isn’t the only state where voters are considering reproductive rights in their constitutions.
On Aug. 2, Kansas voters decisively rejected a constitutional amendment that would have allowed state lawmakers to ban or dramatically restrict abortion. It failed by nearly 18 percentage points.
Kentucky voters will face a similar decision in November with a proposed constitutional amendment that would declare that the state’s constitutional right to privacy does not cover abortion.
Vermont is going in the opposite direction. Voters there will weigh a ballot measure in November that would add a right to “personal reproductive autonomy” to the state constitution, though it does not explicitly mention abortion or contraception. In Michigan, a proposed constitutional amendment that would guarantee a right to both abortion and contraception is expected to qualify for the November ballot.
In California, Proposition 1 would prevent the state from denying or interfering with “an individual’s reproductive freedom in their most intimate decisions, which includes their fundamental right to choose to have an abortion and their fundamental right to choose or refuse contraceptives.”
The proposed constitutional amendment doesn’t go into detail about what enshrining the right to contraception in the state constitution would mean.
California already has some of the strongest contraceptive-access laws in the country – and lawmakers are considering more proposals this year. For instance, state-regulated health plans must cover all Food and Drug Administration–approved contraception; pharmacists must dispense emergency contraception to anyone with a prescription, regardless of age; and pharmacists can prescribe birth control pills on the spot. State courts have also interpreted California’s constitution to include a right to privacy that covers reproductive health decisions.
The amendment, if adopted, could provide a new legal pathway for people to sue when they’re denied contraceptives, said Michele Goodwin, chancellor’s professor of law at the University of California, Irvine.
If a pharmacist refused to fill a birth control prescription or a cashier declined to ring up condoms, she said, customers could make a case that their rights had been violated.
Making the rights to abortion and contraception explicit in the state constitution – instead of relying on a right to privacy – would also protect against shifting political winds, said state Senate leader Toni Atkins (D–San Diego), who was the director of a women’s health clinic in the 1980s. Although California’s lawmakers and executive officers are solid supporters of abortion rights, she said, the composition of the legislature and courts’ interpretation of laws could change.
“I want to know for sure that that right is protected,” Ms. Atkins said at a legislative hearing in June. “We are protecting ourselves from future courts and future politicians.”
The amendment would solidify California’s role as a reproductive rights sanctuary as much of the country chips away at birth control availability, Ms. Goodwin added.
Experts said two forms of birth control that are vulnerable to restrictions in other states are intrauterine devices, or IUDs, and emergency contraception such as Plan B. These methods are often incorrectly conflated with abortion pills, which end a pregnancy instead of preventing it.
Nine states have laws that restrict emergency contraception – for example, by allowing pharmacies to refuse to dispense it or excluding it from state family planning programs – according to the Guttmacher Institute, a research organization that supports abortion rights. In Alabama and Louisiana this year, abortion opponents introduced legislation that would restrict or ban abortion, and would also apply to emergency contraception.
“We’re seeing an erosion of abortion access that is playing out in statehouses across the country that have and will continue to target contraceptive care as well,” said Audrey Sandusky, senior director of policy and communications for the National Family Planning and Reproductive Health Association.
Susan Arnall, vice president of California’s Right to Life League, said the proposed amendment is symbolic and merely echoes current laws. Ms. Arnall said the campaign is mostly about Democratic politicians trying to score political points.
“It just allows the pro-abort legislators to trumpet and give them talking points about how they’re doing something about the overturn of Roe v. Wade,” she said. “It is political virtue signaling. I don’t think it does much of anything else.”
Ms. Goodwin argues that the measure’s symbolism is significant and overdue. She pointed to the Civil War era, when enslaved people in Southern states could look to free states for spiritual hope and material help. “Symbolically, what that meant is a kind of beacon of hope, that those places did exist, where one’s humanity could be regarded,” Ms. Goodwin said.
But California’s reputation as a haven for contraceptive availability may not be fully warranted, said Dima Qato, PharmD, PhD, an associate professor at the University of Southern California School of Pharmacy. In her 2020 study of contraceptive access in Los Angeles County, which has some of the highest rates of teen and unintended pregnancy in the country, Dr. Qato found that only 10% of pharmacies surveyed offered pharmacist-prescribed birth control. Pharmacies in low-income and minority communities were the least likely to offer the service, Dr. Qato said, worsening disparities instead of solving them.
Dr. Qato supports the constitutional amendment but said California should focus on improving and enforcing the laws it already has.
“We don’t need more laws when we don’t address the root cause of a lack of effectiveness of these laws in these communities,” she said. “Lack of enforcement and accountability disproportionately impacts communities of color.”
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. Rachel Bluth is a correspondent for California Healthline. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Patient CRC screening preferences don’t match what they’re being offered
Patients said they’d prefer fecal immunochemical test (FIT)–fecal DNA tests over any of the other colorectal cancer screening (CRC) modalities currently recommended by the U.S. Multi-Society Task Force, according to a study published in Clinical Gastroenterology and Hepatology.
Just over a third of American adults aged 40 and older who hadn’t yet been screened for CRC preferred the FIT–fecal DNA test every 3 years, whereas just one in seven respondents preferred a colonoscopy – considered the gold standard in colorectal cancer screening – every 10 years.
"When you talk to patients and to your friends and family members, people tend to think colonoscopy is synonymous with colon cancer screening, but we have lots of different tests,” senior author Christopher V. Almario, MD, MSHPM, of the department of medicine at the Karsh division of gastroenterology and hepatology, Cedars-Sinai Medical Center, Los Angeles, said in an interview.
“Most people in general tend to prefer noninvasive stool tests, and when we try to predict who would prefer what, we actually couldn’t, so this is a very personal decision,” Dr. Almario said. “It’s important for clinicians to offer multiple choices to their patients, not to mention just colonoscopy. We have data from observing clinician-patient interactions showing that, a lot of times, colonoscopy is the only test that’s offered, despite there being multiple options.”
At the very least, Dr. Almario said, providers should offer patients a colonoscopy along with a noninvasive test, particularly a stool test, and discuss the two options, getting the patient’s input in terms of what they prefer. “The best test is the test that actually gets done,” he said.
Offering patients options
Reid M. Ness, MD, MPH, an associate professor of medicine in the division of gastroenterology, hepatology and nutrition at Vanderbilt University Medical Center in Nashville, was not involved with the study but wasn’t surprised at the findings since “most people wisely prefer to avoid invasive procedures,” he said in an interview. He agreed that many patients aren’t necessarily informed of all their options for screening.
“Many people who are now being offered colonoscopy as their only screening option may prefer a noninvasive option, such as FIT or multitarget stool DNA testing,” Dr. Ness said. “Also, people now refusing colonoscopy for colorectal cancer screening may instead accept FIT or multitarget stool DNA testing. It is difficult to know how many people now refusing colorectal cancer screening may have accepted screening if it had been offered differently.”
That’s precisely what Dr. Almario and his colleagues wanted to find out. They surveyed 1,000 people aged 40 and older who were at average risk for colorectal cancer to find out their preferences for different screening modalities and what features of different screening types they most valued. The researchers asked about the following screening tests recommended by the U.S. Multi-Society Task Force:
- FIT every year.
- FIT–fecal DNA every 3 years.
- Colon video capsule every 5 years.
- CT colonography every 5 years.
- Colonoscopy every 10 years.
The respondents who completed the online survey were recruited from a sample of more than 20 million people across the United States who have agreed to receive survey invitations. Respondents were excluded if they had a first-degree relative with colorectal cancer, had already undergone colorectal cancer screening or had been diagnosed with colon polyps, Crohn’s disease, or ulcerative colitis.
The respondents were split into those aged 40-49 (61% of the sample) who had not yet discussed colorectal cancer screening with their providers and those aged 50 and older, who might have already discussed it and declined. Eighty percent of the respondents were White, 6% were Black, 6% were Hispanic, 4% were Asian, and 3% reported another race/ethnicity. Just over half (52%) had at least two comorbidities. A quarter (25%) reported one comorbidity, and 22% reported none.
In thinking about the decision to get screened, respondents ranked the test type as the most important consideration, followed by the reduction in their chance of developing colorectal cancer and then frequency of the test. Lower priority on the list of considerations were their chances of a complication, bowel prep before the test, and required diet changes before the test.
The test preferred by the highest proportion of respondents was the FIT–fecal DNA test every 3 years, preferred by 35% of respondents, followed by the colon capsule video test every 5 years (28%). About one in seven respondents (14%) preferred a colonoscopy every 10 years, followed by the annual FIT (12%) and CT colonography every 5 years (11%). When limited only to the two tier 1–option tests – the annual FIT or a colonoscopy every 10 years – a substantial majority of the younger (69%) and older (77%) groups preferred the annual FIT.
”This finding is discordant with current CRC screening utilization in the United States where colonoscopy is the most commonly performed test, and this may partially explain our suboptimal screening rates,” the authors wrote. “Our findings suggest that screening programs should strongly consider a sequential-based strategy where FIT is offered first, and if declined then colonoscopy.”
Underlying factors
Dr. Ness said that many primary care providers might prefer to offer colonoscopies instead of annual FIT tests because it’s easier to track a test given every 10 years instead of every year or every 3 years.
“Providers across most of the U.S. are incentivized to recommend colonoscopy as the primary screening modality because the burden of follow-up on them is less,” Dr. Ness said. “They are able to justify this choice given colonoscopy remains the most accurate screening modality.”
Dr. Ness pointed to the programmatic screening program at Kaiser Permanente of Northern California health care system as a model for a program that utilizes FIT tests more often.
“The only way to accomplish an efficient and equitable colorectal cancer screening program is within the context of a national health service or plan,” Dr. Ness added. “Otherwise, the uninsured and underinsured will remain excluded from the benefits of colorectal cancer screening.”
Preferences did not differ a great deal between the age groups, with 35% of the younger group and 37% of the older group both preferring the FIT–fecal DNA tests every 3 years. Slightly more people in the 50+ age group preferred an annual fit (19% vs. 12%) as opposed to the colon capsule video every 5 years (28% of younger group vs. 23%) or colon CT scan every 5 years (11% of younger group vs. 8%), but the differences were statistically significant (P = .019).
In fact, “sociodemographic, clinical characteristics, and colorectal cancer screening knowledge, attitudes, and beliefs were not predictive of selecting FIT or colonoscopy,” the authors found. ”This demonstrates the individualized nature of decision making on colorectal cancer screening tests. Moreover, as most individuals preferred FIT, it again emphasizes the importance of sequential or choice-based strategies for colorectal cancer screening.”
However, one of the study’s notable limitations was its high proportion of White patients relative to other racial/ethnic groups, so additional research may illuminate whether different sociodemographic groups do have slight preferences for one test over another, Dr. Almario said. The advantage to colonoscopies, he noted, is that they only occur every 10 years and if polyps are discovered, they can be taken care of right away.
”You don’t have to think about it for a decade, which is certainly a pro for the colonoscopy,” Dr. Almario said. “The FIT test is obviously less invasive, but you have to do it every year for it to be an effective screening test.” He noted that some data have shown a drop-off in compliance over multiple years. “We certainly need more systems in place to remind patients and providers to do it annually so that we can see the ultimate screening benefit from doing that test specifically.”
“The most important point from the clinical perspective is, when we’re talking to patients about colon cancer screening, make sure to give them a choice,” Dr. Almario said. “We just can’t look at someone’s chart, their clinical characteristics or demographics, and predict what tests they would prefer. We need to ask them. We need to present them with the options, go over the pros and cons of colonoscopy, the pros and cons of the stool test, and ask the patient what they would prefer to do.”
The research was funded by the National Cancer Institute and the National Institutes of Health. One author served on an advisory panel with Exact Sciences. The other authors and Dr. Ness had no disclosures.
Help your patients understand colorectal cancer prevention and screening options by sharing AGA’s patient education from the GI Patient Center: www.gastro.org/CRC.
This article was updated on Aug. 18, 2022.
Patients said they’d prefer fecal immunochemical test (FIT)–fecal DNA tests over any of the other colorectal cancer screening (CRC) modalities currently recommended by the U.S. Multi-Society Task Force, according to a study published in Clinical Gastroenterology and Hepatology.
Just over a third of American adults aged 40 and older who hadn’t yet been screened for CRC preferred the FIT–fecal DNA test every 3 years, whereas just one in seven respondents preferred a colonoscopy – considered the gold standard in colorectal cancer screening – every 10 years.
"When you talk to patients and to your friends and family members, people tend to think colonoscopy is synonymous with colon cancer screening, but we have lots of different tests,” senior author Christopher V. Almario, MD, MSHPM, of the department of medicine at the Karsh division of gastroenterology and hepatology, Cedars-Sinai Medical Center, Los Angeles, said in an interview.
“Most people in general tend to prefer noninvasive stool tests, and when we try to predict who would prefer what, we actually couldn’t, so this is a very personal decision,” Dr. Almario said. “It’s important for clinicians to offer multiple choices to their patients, not to mention just colonoscopy. We have data from observing clinician-patient interactions showing that, a lot of times, colonoscopy is the only test that’s offered, despite there being multiple options.”
At the very least, Dr. Almario said, providers should offer patients a colonoscopy along with a noninvasive test, particularly a stool test, and discuss the two options, getting the patient’s input in terms of what they prefer. “The best test is the test that actually gets done,” he said.
Offering patients options
Reid M. Ness, MD, MPH, an associate professor of medicine in the division of gastroenterology, hepatology and nutrition at Vanderbilt University Medical Center in Nashville, was not involved with the study but wasn’t surprised at the findings since “most people wisely prefer to avoid invasive procedures,” he said in an interview. He agreed that many patients aren’t necessarily informed of all their options for screening.
“Many people who are now being offered colonoscopy as their only screening option may prefer a noninvasive option, such as FIT or multitarget stool DNA testing,” Dr. Ness said. “Also, people now refusing colonoscopy for colorectal cancer screening may instead accept FIT or multitarget stool DNA testing. It is difficult to know how many people now refusing colorectal cancer screening may have accepted screening if it had been offered differently.”
That’s precisely what Dr. Almario and his colleagues wanted to find out. They surveyed 1,000 people aged 40 and older who were at average risk for colorectal cancer to find out their preferences for different screening modalities and what features of different screening types they most valued. The researchers asked about the following screening tests recommended by the U.S. Multi-Society Task Force:
- FIT every year.
- FIT–fecal DNA every 3 years.
- Colon video capsule every 5 years.
- CT colonography every 5 years.
- Colonoscopy every 10 years.
The respondents who completed the online survey were recruited from a sample of more than 20 million people across the United States who have agreed to receive survey invitations. Respondents were excluded if they had a first-degree relative with colorectal cancer, had already undergone colorectal cancer screening or had been diagnosed with colon polyps, Crohn’s disease, or ulcerative colitis.
The respondents were split into those aged 40-49 (61% of the sample) who had not yet discussed colorectal cancer screening with their providers and those aged 50 and older, who might have already discussed it and declined. Eighty percent of the respondents were White, 6% were Black, 6% were Hispanic, 4% were Asian, and 3% reported another race/ethnicity. Just over half (52%) had at least two comorbidities. A quarter (25%) reported one comorbidity, and 22% reported none.
In thinking about the decision to get screened, respondents ranked the test type as the most important consideration, followed by the reduction in their chance of developing colorectal cancer and then frequency of the test. Lower priority on the list of considerations were their chances of a complication, bowel prep before the test, and required diet changes before the test.
The test preferred by the highest proportion of respondents was the FIT–fecal DNA test every 3 years, preferred by 35% of respondents, followed by the colon capsule video test every 5 years (28%). About one in seven respondents (14%) preferred a colonoscopy every 10 years, followed by the annual FIT (12%) and CT colonography every 5 years (11%). When limited only to the two tier 1–option tests – the annual FIT or a colonoscopy every 10 years – a substantial majority of the younger (69%) and older (77%) groups preferred the annual FIT.
”This finding is discordant with current CRC screening utilization in the United States where colonoscopy is the most commonly performed test, and this may partially explain our suboptimal screening rates,” the authors wrote. “Our findings suggest that screening programs should strongly consider a sequential-based strategy where FIT is offered first, and if declined then colonoscopy.”
Underlying factors
Dr. Ness said that many primary care providers might prefer to offer colonoscopies instead of annual FIT tests because it’s easier to track a test given every 10 years instead of every year or every 3 years.
“Providers across most of the U.S. are incentivized to recommend colonoscopy as the primary screening modality because the burden of follow-up on them is less,” Dr. Ness said. “They are able to justify this choice given colonoscopy remains the most accurate screening modality.”
Dr. Ness pointed to the programmatic screening program at Kaiser Permanente of Northern California health care system as a model for a program that utilizes FIT tests more often.
“The only way to accomplish an efficient and equitable colorectal cancer screening program is within the context of a national health service or plan,” Dr. Ness added. “Otherwise, the uninsured and underinsured will remain excluded from the benefits of colorectal cancer screening.”
Preferences did not differ a great deal between the age groups, with 35% of the younger group and 37% of the older group both preferring the FIT–fecal DNA tests every 3 years. Slightly more people in the 50+ age group preferred an annual fit (19% vs. 12%) as opposed to the colon capsule video every 5 years (28% of younger group vs. 23%) or colon CT scan every 5 years (11% of younger group vs. 8%), but the differences were statistically significant (P = .019).
In fact, “sociodemographic, clinical characteristics, and colorectal cancer screening knowledge, attitudes, and beliefs were not predictive of selecting FIT or colonoscopy,” the authors found. ”This demonstrates the individualized nature of decision making on colorectal cancer screening tests. Moreover, as most individuals preferred FIT, it again emphasizes the importance of sequential or choice-based strategies for colorectal cancer screening.”
However, one of the study’s notable limitations was its high proportion of White patients relative to other racial/ethnic groups, so additional research may illuminate whether different sociodemographic groups do have slight preferences for one test over another, Dr. Almario said. The advantage to colonoscopies, he noted, is that they only occur every 10 years and if polyps are discovered, they can be taken care of right away.
”You don’t have to think about it for a decade, which is certainly a pro for the colonoscopy,” Dr. Almario said. “The FIT test is obviously less invasive, but you have to do it every year for it to be an effective screening test.” He noted that some data have shown a drop-off in compliance over multiple years. “We certainly need more systems in place to remind patients and providers to do it annually so that we can see the ultimate screening benefit from doing that test specifically.”
“The most important point from the clinical perspective is, when we’re talking to patients about colon cancer screening, make sure to give them a choice,” Dr. Almario said. “We just can’t look at someone’s chart, their clinical characteristics or demographics, and predict what tests they would prefer. We need to ask them. We need to present them with the options, go over the pros and cons of colonoscopy, the pros and cons of the stool test, and ask the patient what they would prefer to do.”
The research was funded by the National Cancer Institute and the National Institutes of Health. One author served on an advisory panel with Exact Sciences. The other authors and Dr. Ness had no disclosures.
Help your patients understand colorectal cancer prevention and screening options by sharing AGA’s patient education from the GI Patient Center: www.gastro.org/CRC.
This article was updated on Aug. 18, 2022.
Patients said they’d prefer fecal immunochemical test (FIT)–fecal DNA tests over any of the other colorectal cancer screening (CRC) modalities currently recommended by the U.S. Multi-Society Task Force, according to a study published in Clinical Gastroenterology and Hepatology.
Just over a third of American adults aged 40 and older who hadn’t yet been screened for CRC preferred the FIT–fecal DNA test every 3 years, whereas just one in seven respondents preferred a colonoscopy – considered the gold standard in colorectal cancer screening – every 10 years.
"When you talk to patients and to your friends and family members, people tend to think colonoscopy is synonymous with colon cancer screening, but we have lots of different tests,” senior author Christopher V. Almario, MD, MSHPM, of the department of medicine at the Karsh division of gastroenterology and hepatology, Cedars-Sinai Medical Center, Los Angeles, said in an interview.
“Most people in general tend to prefer noninvasive stool tests, and when we try to predict who would prefer what, we actually couldn’t, so this is a very personal decision,” Dr. Almario said. “It’s important for clinicians to offer multiple choices to their patients, not to mention just colonoscopy. We have data from observing clinician-patient interactions showing that, a lot of times, colonoscopy is the only test that’s offered, despite there being multiple options.”
At the very least, Dr. Almario said, providers should offer patients a colonoscopy along with a noninvasive test, particularly a stool test, and discuss the two options, getting the patient’s input in terms of what they prefer. “The best test is the test that actually gets done,” he said.
Offering patients options
Reid M. Ness, MD, MPH, an associate professor of medicine in the division of gastroenterology, hepatology and nutrition at Vanderbilt University Medical Center in Nashville, was not involved with the study but wasn’t surprised at the findings since “most people wisely prefer to avoid invasive procedures,” he said in an interview. He agreed that many patients aren’t necessarily informed of all their options for screening.
“Many people who are now being offered colonoscopy as their only screening option may prefer a noninvasive option, such as FIT or multitarget stool DNA testing,” Dr. Ness said. “Also, people now refusing colonoscopy for colorectal cancer screening may instead accept FIT or multitarget stool DNA testing. It is difficult to know how many people now refusing colorectal cancer screening may have accepted screening if it had been offered differently.”
That’s precisely what Dr. Almario and his colleagues wanted to find out. They surveyed 1,000 people aged 40 and older who were at average risk for colorectal cancer to find out their preferences for different screening modalities and what features of different screening types they most valued. The researchers asked about the following screening tests recommended by the U.S. Multi-Society Task Force:
- FIT every year.
- FIT–fecal DNA every 3 years.
- Colon video capsule every 5 years.
- CT colonography every 5 years.
- Colonoscopy every 10 years.
The respondents who completed the online survey were recruited from a sample of more than 20 million people across the United States who have agreed to receive survey invitations. Respondents were excluded if they had a first-degree relative with colorectal cancer, had already undergone colorectal cancer screening or had been diagnosed with colon polyps, Crohn’s disease, or ulcerative colitis.
The respondents were split into those aged 40-49 (61% of the sample) who had not yet discussed colorectal cancer screening with their providers and those aged 50 and older, who might have already discussed it and declined. Eighty percent of the respondents were White, 6% were Black, 6% were Hispanic, 4% were Asian, and 3% reported another race/ethnicity. Just over half (52%) had at least two comorbidities. A quarter (25%) reported one comorbidity, and 22% reported none.
In thinking about the decision to get screened, respondents ranked the test type as the most important consideration, followed by the reduction in their chance of developing colorectal cancer and then frequency of the test. Lower priority on the list of considerations were their chances of a complication, bowel prep before the test, and required diet changes before the test.
The test preferred by the highest proportion of respondents was the FIT–fecal DNA test every 3 years, preferred by 35% of respondents, followed by the colon capsule video test every 5 years (28%). About one in seven respondents (14%) preferred a colonoscopy every 10 years, followed by the annual FIT (12%) and CT colonography every 5 years (11%). When limited only to the two tier 1–option tests – the annual FIT or a colonoscopy every 10 years – a substantial majority of the younger (69%) and older (77%) groups preferred the annual FIT.
”This finding is discordant with current CRC screening utilization in the United States where colonoscopy is the most commonly performed test, and this may partially explain our suboptimal screening rates,” the authors wrote. “Our findings suggest that screening programs should strongly consider a sequential-based strategy where FIT is offered first, and if declined then colonoscopy.”
Underlying factors
Dr. Ness said that many primary care providers might prefer to offer colonoscopies instead of annual FIT tests because it’s easier to track a test given every 10 years instead of every year or every 3 years.
“Providers across most of the U.S. are incentivized to recommend colonoscopy as the primary screening modality because the burden of follow-up on them is less,” Dr. Ness said. “They are able to justify this choice given colonoscopy remains the most accurate screening modality.”
Dr. Ness pointed to the programmatic screening program at Kaiser Permanente of Northern California health care system as a model for a program that utilizes FIT tests more often.
“The only way to accomplish an efficient and equitable colorectal cancer screening program is within the context of a national health service or plan,” Dr. Ness added. “Otherwise, the uninsured and underinsured will remain excluded from the benefits of colorectal cancer screening.”
Preferences did not differ a great deal between the age groups, with 35% of the younger group and 37% of the older group both preferring the FIT–fecal DNA tests every 3 years. Slightly more people in the 50+ age group preferred an annual fit (19% vs. 12%) as opposed to the colon capsule video every 5 years (28% of younger group vs. 23%) or colon CT scan every 5 years (11% of younger group vs. 8%), but the differences were statistically significant (P = .019).
In fact, “sociodemographic, clinical characteristics, and colorectal cancer screening knowledge, attitudes, and beliefs were not predictive of selecting FIT or colonoscopy,” the authors found. ”This demonstrates the individualized nature of decision making on colorectal cancer screening tests. Moreover, as most individuals preferred FIT, it again emphasizes the importance of sequential or choice-based strategies for colorectal cancer screening.”
However, one of the study’s notable limitations was its high proportion of White patients relative to other racial/ethnic groups, so additional research may illuminate whether different sociodemographic groups do have slight preferences for one test over another, Dr. Almario said. The advantage to colonoscopies, he noted, is that they only occur every 10 years and if polyps are discovered, they can be taken care of right away.
”You don’t have to think about it for a decade, which is certainly a pro for the colonoscopy,” Dr. Almario said. “The FIT test is obviously less invasive, but you have to do it every year for it to be an effective screening test.” He noted that some data have shown a drop-off in compliance over multiple years. “We certainly need more systems in place to remind patients and providers to do it annually so that we can see the ultimate screening benefit from doing that test specifically.”
“The most important point from the clinical perspective is, when we’re talking to patients about colon cancer screening, make sure to give them a choice,” Dr. Almario said. “We just can’t look at someone’s chart, their clinical characteristics or demographics, and predict what tests they would prefer. We need to ask them. We need to present them with the options, go over the pros and cons of colonoscopy, the pros and cons of the stool test, and ask the patient what they would prefer to do.”
The research was funded by the National Cancer Institute and the National Institutes of Health. One author served on an advisory panel with Exact Sciences. The other authors and Dr. Ness had no disclosures.
Help your patients understand colorectal cancer prevention and screening options by sharing AGA’s patient education from the GI Patient Center: www.gastro.org/CRC.
This article was updated on Aug. 18, 2022.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Topical ruxolitinib quickly relieves atopic dermatitis itch in Black patients
“Ruxolitinib cream monotherapy over 8 weeks was associated with rapid and considerable itch relief in Black or African American patients with AD and was well tolerated,” the study authors wrote in a poster presented at the annual meeting of the Society for Investigative Dermatology.
AD can behave differently in different racial groups and can be especially bothersome in Black patients. AD has a prevalence of about 20% in Black children and 5%-10% in Black adults. Black children are roughly twice as likely to be diagnosed with AD, and to have severe AD, than White children, according to the authors.
Lead author Lawrence F. Eichenfield, MD, professor of dermatology and pediatrics at the University of California, San Diego, and colleagues used pooled data from two identically designed phase 3 studies to describe the effects of the cream formulation of the Janus kinase (JAK) 1 and JAK 2 inhibitor ruxolitinib on itch in Black patients.
Topical ruxolitinib (Opzelura), 1.5%, was approved last September for treating AD in non-immunocompromised patients with mild to moderate AD, ages 12 years and older. In July 2022, it was approved for the treatment of nonsegmental vitiligo in the same age group.
FDA approval for AD was based on the results of the TRuE-AD1 and TRuE-AD2 double-blind randomized trials, which enrolled about 1,200 patients over age 12 with AD. These patients included 292 Black teenagers and adults between aged 12-71 years who had AD for 2 years or longer, with an Investigator’s Global Assessment (IGA) score of 2 or 3, with 3%-20% affected body surface area, excluding the scalp.
Of the 292 patients, those in the two treatment groups (n = 231) applied ruxolitinib cream twice a day for 8 weeks (0.75% in 118 patients and 1.5% in 113 patients) and 61 applied the vehicle. They used electronic diaries to record the worst level of itch they had experienced each day, from 0 (no itch) to 10 (worst imaginable itch). The main results were as follows:
- Mean itch numerical rating scale (NRS) scores at baseline were 5.3 and 5.4 for ruxolitinib cream 0.75% and 1.5%, respectively, and 5.7 for vehicle. Within about 12 hours of first application, mean itch NRS scores dropped –0.6 and –0.7 from baseline among those treated with ruxolitinib cream 0.75% and 1.5%, respectively, compared with –0.2 for those on the vehicle. At day 4, the decreases were –1.4 and –1.6 for ruxolitinib cream 0.75% and 1.5%, respectively, versus –0.6 for the vehicle (P = .026 and P = .005, respectively, vs. vehicle).
- At day 2, among the 187 patients with a baseline itch NRS score 4 or higher, more patients achieved 4-point or greater itch NRS improvement: 6.1% and 16.4% for ruxolitinib cream 0.75% and 1.5%, respectively versus 0% for vehicle. At day 7, the differences were 15.9% and 26.6% versus 3%, respectively. And by week 8, they increased to 30.1% and 43.2% versus 17.5% (P = .212 and P = .009), respectively.
- At week 2, 19% of patients in the 0.75% formulation group and 19.4% of patients in the 1.5% formulation group, compared with 5.3% in the vehicle group, reported no days of itch on question 1 of the Patient-Oriented Eczema Measure (POEM) questionnaire that evaluated various aspects of the disease over the previous week. By week 8, the differences grew to 34% and 30.8% versus 12.2%, respectively.
- Adverse events, reported by 14.4% and 22.1% of patients on 0.75% and 1.5% ruxolitinib, respectively, and by 32.8% of patients who received the vehicle, were headaches, upper respiratory tract infection, and application site pain.
Ruxolitinib may be an alternative to systemic immunosuppressives
Asked to comment on the results, Amy J. McMichael, MD, professor of dermatology at Wake Forest University School of Medicine, Winston-Salem, N.C., called itch “one of the major life disruptors in atopic dermatitis.”
Providers often assume that patients of different races respond similarly to treatment, but that is not always true, she noted in an email.
“This study proves ruxolitinib’s effectiveness in Black patients, who often have more severe atopic dermatitis signs and symptoms,” said Dr. McMichael, who was not involved in the study. “The fact that atopic dermatitis in patients of color has been singled out to examine efficacy is a great way to show that the findings are not just in those who have thinner plaques and potentially less longstanding thickening of the skin from scratching (lichenification),” she added.
Dr. McMichael welcomed the lack of systemic side effects and quick relief of itch with this treatment, noting that the effect on itch “is rare with other treatments and extremely rare with other topical medications.”
The effect of topical ruxolitinib on pruritus “was interesting and surprising because very few available topical medications can control itch,” she explained. “The strongest topical steroids can help with pruritus, but they have the risk for skin thinning (atrophy),” while topical ruxolitinib is not associated with skin atrophy.
“After topical steroids fail as first-line treatment, it is likely that more patients will be given this topical medication rather than be moved to immunosuppressive systemic medications,” she noted.
All study authors report relevant relationships with Incyte Corporation, which manufactures ruxolitinib and funded the study, and several authors report employment and shareholding interests in the company. Dr. McMichael reports no relevant relationship with the study.
A version of this article first appeared on Medscape.com.
“Ruxolitinib cream monotherapy over 8 weeks was associated with rapid and considerable itch relief in Black or African American patients with AD and was well tolerated,” the study authors wrote in a poster presented at the annual meeting of the Society for Investigative Dermatology.
AD can behave differently in different racial groups and can be especially bothersome in Black patients. AD has a prevalence of about 20% in Black children and 5%-10% in Black adults. Black children are roughly twice as likely to be diagnosed with AD, and to have severe AD, than White children, according to the authors.
Lead author Lawrence F. Eichenfield, MD, professor of dermatology and pediatrics at the University of California, San Diego, and colleagues used pooled data from two identically designed phase 3 studies to describe the effects of the cream formulation of the Janus kinase (JAK) 1 and JAK 2 inhibitor ruxolitinib on itch in Black patients.
Topical ruxolitinib (Opzelura), 1.5%, was approved last September for treating AD in non-immunocompromised patients with mild to moderate AD, ages 12 years and older. In July 2022, it was approved for the treatment of nonsegmental vitiligo in the same age group.
FDA approval for AD was based on the results of the TRuE-AD1 and TRuE-AD2 double-blind randomized trials, which enrolled about 1,200 patients over age 12 with AD. These patients included 292 Black teenagers and adults between aged 12-71 years who had AD for 2 years or longer, with an Investigator’s Global Assessment (IGA) score of 2 or 3, with 3%-20% affected body surface area, excluding the scalp.
Of the 292 patients, those in the two treatment groups (n = 231) applied ruxolitinib cream twice a day for 8 weeks (0.75% in 118 patients and 1.5% in 113 patients) and 61 applied the vehicle. They used electronic diaries to record the worst level of itch they had experienced each day, from 0 (no itch) to 10 (worst imaginable itch). The main results were as follows:
- Mean itch numerical rating scale (NRS) scores at baseline were 5.3 and 5.4 for ruxolitinib cream 0.75% and 1.5%, respectively, and 5.7 for vehicle. Within about 12 hours of first application, mean itch NRS scores dropped –0.6 and –0.7 from baseline among those treated with ruxolitinib cream 0.75% and 1.5%, respectively, compared with –0.2 for those on the vehicle. At day 4, the decreases were –1.4 and –1.6 for ruxolitinib cream 0.75% and 1.5%, respectively, versus –0.6 for the vehicle (P = .026 and P = .005, respectively, vs. vehicle).
- At day 2, among the 187 patients with a baseline itch NRS score 4 or higher, more patients achieved 4-point or greater itch NRS improvement: 6.1% and 16.4% for ruxolitinib cream 0.75% and 1.5%, respectively versus 0% for vehicle. At day 7, the differences were 15.9% and 26.6% versus 3%, respectively. And by week 8, they increased to 30.1% and 43.2% versus 17.5% (P = .212 and P = .009), respectively.
- At week 2, 19% of patients in the 0.75% formulation group and 19.4% of patients in the 1.5% formulation group, compared with 5.3% in the vehicle group, reported no days of itch on question 1 of the Patient-Oriented Eczema Measure (POEM) questionnaire that evaluated various aspects of the disease over the previous week. By week 8, the differences grew to 34% and 30.8% versus 12.2%, respectively.
- Adverse events, reported by 14.4% and 22.1% of patients on 0.75% and 1.5% ruxolitinib, respectively, and by 32.8% of patients who received the vehicle, were headaches, upper respiratory tract infection, and application site pain.
Ruxolitinib may be an alternative to systemic immunosuppressives
Asked to comment on the results, Amy J. McMichael, MD, professor of dermatology at Wake Forest University School of Medicine, Winston-Salem, N.C., called itch “one of the major life disruptors in atopic dermatitis.”
Providers often assume that patients of different races respond similarly to treatment, but that is not always true, she noted in an email.
“This study proves ruxolitinib’s effectiveness in Black patients, who often have more severe atopic dermatitis signs and symptoms,” said Dr. McMichael, who was not involved in the study. “The fact that atopic dermatitis in patients of color has been singled out to examine efficacy is a great way to show that the findings are not just in those who have thinner plaques and potentially less longstanding thickening of the skin from scratching (lichenification),” she added.
Dr. McMichael welcomed the lack of systemic side effects and quick relief of itch with this treatment, noting that the effect on itch “is rare with other treatments and extremely rare with other topical medications.”
The effect of topical ruxolitinib on pruritus “was interesting and surprising because very few available topical medications can control itch,” she explained. “The strongest topical steroids can help with pruritus, but they have the risk for skin thinning (atrophy),” while topical ruxolitinib is not associated with skin atrophy.
“After topical steroids fail as first-line treatment, it is likely that more patients will be given this topical medication rather than be moved to immunosuppressive systemic medications,” she noted.
All study authors report relevant relationships with Incyte Corporation, which manufactures ruxolitinib and funded the study, and several authors report employment and shareholding interests in the company. Dr. McMichael reports no relevant relationship with the study.
A version of this article first appeared on Medscape.com.
“Ruxolitinib cream monotherapy over 8 weeks was associated with rapid and considerable itch relief in Black or African American patients with AD and was well tolerated,” the study authors wrote in a poster presented at the annual meeting of the Society for Investigative Dermatology.
AD can behave differently in different racial groups and can be especially bothersome in Black patients. AD has a prevalence of about 20% in Black children and 5%-10% in Black adults. Black children are roughly twice as likely to be diagnosed with AD, and to have severe AD, than White children, according to the authors.
Lead author Lawrence F. Eichenfield, MD, professor of dermatology and pediatrics at the University of California, San Diego, and colleagues used pooled data from two identically designed phase 3 studies to describe the effects of the cream formulation of the Janus kinase (JAK) 1 and JAK 2 inhibitor ruxolitinib on itch in Black patients.
Topical ruxolitinib (Opzelura), 1.5%, was approved last September for treating AD in non-immunocompromised patients with mild to moderate AD, ages 12 years and older. In July 2022, it was approved for the treatment of nonsegmental vitiligo in the same age group.
FDA approval for AD was based on the results of the TRuE-AD1 and TRuE-AD2 double-blind randomized trials, which enrolled about 1,200 patients over age 12 with AD. These patients included 292 Black teenagers and adults between aged 12-71 years who had AD for 2 years or longer, with an Investigator’s Global Assessment (IGA) score of 2 or 3, with 3%-20% affected body surface area, excluding the scalp.
Of the 292 patients, those in the two treatment groups (n = 231) applied ruxolitinib cream twice a day for 8 weeks (0.75% in 118 patients and 1.5% in 113 patients) and 61 applied the vehicle. They used electronic diaries to record the worst level of itch they had experienced each day, from 0 (no itch) to 10 (worst imaginable itch). The main results were as follows:
- Mean itch numerical rating scale (NRS) scores at baseline were 5.3 and 5.4 for ruxolitinib cream 0.75% and 1.5%, respectively, and 5.7 for vehicle. Within about 12 hours of first application, mean itch NRS scores dropped –0.6 and –0.7 from baseline among those treated with ruxolitinib cream 0.75% and 1.5%, respectively, compared with –0.2 for those on the vehicle. At day 4, the decreases were –1.4 and –1.6 for ruxolitinib cream 0.75% and 1.5%, respectively, versus –0.6 for the vehicle (P = .026 and P = .005, respectively, vs. vehicle).
- At day 2, among the 187 patients with a baseline itch NRS score 4 or higher, more patients achieved 4-point or greater itch NRS improvement: 6.1% and 16.4% for ruxolitinib cream 0.75% and 1.5%, respectively versus 0% for vehicle. At day 7, the differences were 15.9% and 26.6% versus 3%, respectively. And by week 8, they increased to 30.1% and 43.2% versus 17.5% (P = .212 and P = .009), respectively.
- At week 2, 19% of patients in the 0.75% formulation group and 19.4% of patients in the 1.5% formulation group, compared with 5.3% in the vehicle group, reported no days of itch on question 1 of the Patient-Oriented Eczema Measure (POEM) questionnaire that evaluated various aspects of the disease over the previous week. By week 8, the differences grew to 34% and 30.8% versus 12.2%, respectively.
- Adverse events, reported by 14.4% and 22.1% of patients on 0.75% and 1.5% ruxolitinib, respectively, and by 32.8% of patients who received the vehicle, were headaches, upper respiratory tract infection, and application site pain.
Ruxolitinib may be an alternative to systemic immunosuppressives
Asked to comment on the results, Amy J. McMichael, MD, professor of dermatology at Wake Forest University School of Medicine, Winston-Salem, N.C., called itch “one of the major life disruptors in atopic dermatitis.”
Providers often assume that patients of different races respond similarly to treatment, but that is not always true, she noted in an email.
“This study proves ruxolitinib’s effectiveness in Black patients, who often have more severe atopic dermatitis signs and symptoms,” said Dr. McMichael, who was not involved in the study. “The fact that atopic dermatitis in patients of color has been singled out to examine efficacy is a great way to show that the findings are not just in those who have thinner plaques and potentially less longstanding thickening of the skin from scratching (lichenification),” she added.
Dr. McMichael welcomed the lack of systemic side effects and quick relief of itch with this treatment, noting that the effect on itch “is rare with other treatments and extremely rare with other topical medications.”
The effect of topical ruxolitinib on pruritus “was interesting and surprising because very few available topical medications can control itch,” she explained. “The strongest topical steroids can help with pruritus, but they have the risk for skin thinning (atrophy),” while topical ruxolitinib is not associated with skin atrophy.
“After topical steroids fail as first-line treatment, it is likely that more patients will be given this topical medication rather than be moved to immunosuppressive systemic medications,” she noted.
All study authors report relevant relationships with Incyte Corporation, which manufactures ruxolitinib and funded the study, and several authors report employment and shareholding interests in the company. Dr. McMichael reports no relevant relationship with the study.
A version of this article first appeared on Medscape.com.
FROM SID 2022
Ontario MD, Charles Godfrey, who worked until 102, dies
He was 104 and died at his home in Madoc, Ont., just weeks shy of his 105th birthday.
“He had been quite vigorous up until that point,” his son, Mark Godfrey, told CTV News.
If it wasn’t for the pandemic, his father would have probably continued practicing for a little while longer, he added. “He was the smartest guy in the room, all my life, any room we were in.”
Charles Morris Godfrey was born Sept. 24, 1917, in Philadelphia, according to Wikipedia, but his family moved to Toronto when he was 7 years old. His father, a physiotherapist, encouraged him to study medicine.
Dr. Godfrey served in the Canadian military for 5½ years during World War II and qualified as a physiotherapist while serving.
After the war, he enrolled in the faculty of medicine at the University of Toronto and earned his degree in 1953. He paid for his tuition by working as a janitor and scrapyard worker.
In 1956, he studied neurology at Oxford (England) University on a McLaughlin fellowship and became a fellow of the Royal College of Physicians in 1958. He also earned a bachelor of arts degree in 1962 and his master of arts degree in 1975. He was studying for his PhD in the late 1980s, when he was in his 70s.
Upon his return from England in the late 1950s, Godfrey became director of the department of physical medicine and rehabilitation at Toronto East General Hospital. He subsequently worked at Toronto General Hospital, Sunnybrook Hospital, and the Toronto Rehab Hospital before joining Wellesley Hospital’s rheumatic disease unit, ultimately becoming head of the hospital’s rehabilitation clinic.
Dr. Godfrey was a professor in the department of rehabilitative medicine at the University of Toronto for over 2 decades. He was working 13-hour days teaching and maintaining his own practice well into his 70s. He would spend weekends at his country home in Madoc.
For over 20 years, he and his wife Margaret, a nurse, would spend 6 weeks each year as volunteers traveling to developing countries, such as Afghanistan and Pakistan, on lecture tours on behalf of CARE. Dr. Godfrey chaired CARE/MEDICO from 1983 to 1985 and subsequently served as chairman of CARE’s International Health Advisory Committee. In 1986, he was awarded the organization’s Distinguished Service Award.
In 1989, Dr. Godfrey was invested as a Member of the Order of Canada. His citation reads as follows:
“Deeply committed to humankind and the elimination of human suffering, and although of retirement age, he continues to be involved in an exhausting round of activity. Professor Emeritus of Rehabilitation Medicine at the University of Toronto, an environmentalist who was instrumental in the ‘People or Planes’ campaign opposing construction of the Pickering airport and a director of CARE/MEDICO, each year he takes his heart-felt concern for the welfare of the global community to Third World countries as a visiting volunteer doctor.”
Dr. Godfrey was also a political activist. When he learned about plans to build an international airport near his home in Uxbridge, Ont., he organized People or Planes, a group that successfully opposed the proposed airport. He was elected to the Ontario legislature as the Ontario New Democratic Party’s candidate for Durham West and served for 2 years as the NDP’s environment critic.
In 2020, grandson Frazey Ford posted a clip of his “immortal grandfather” being interviewed by David Suzuki as part of a CBC documentary on aging well.
Dr. Godfrey shared his secret to a long life: “The main thing is to keep interested in life,” he told Mr. Suzuki.
“That’s the secret, of course. If you stick in front of your television, you lose your interest in life. That’ll kill you next week. Certainly, the quality of stuff that’s being peddled on television these days is enough to make you wanna die pretty soon.”
A spokesperson for the University of Toronto’s department of medicine told CTV News that Dr. Godfrey was still working at four medical clinics in Toronto 4 days a week, even at age 102.
“He possessed a remarkable longevity in his practice, supported by his enduring love for medicine and incredible care for his patients,” the university said.
A version of this article first appeared on Medscape.com.
He was 104 and died at his home in Madoc, Ont., just weeks shy of his 105th birthday.
“He had been quite vigorous up until that point,” his son, Mark Godfrey, told CTV News.
If it wasn’t for the pandemic, his father would have probably continued practicing for a little while longer, he added. “He was the smartest guy in the room, all my life, any room we were in.”
Charles Morris Godfrey was born Sept. 24, 1917, in Philadelphia, according to Wikipedia, but his family moved to Toronto when he was 7 years old. His father, a physiotherapist, encouraged him to study medicine.
Dr. Godfrey served in the Canadian military for 5½ years during World War II and qualified as a physiotherapist while serving.
After the war, he enrolled in the faculty of medicine at the University of Toronto and earned his degree in 1953. He paid for his tuition by working as a janitor and scrapyard worker.
In 1956, he studied neurology at Oxford (England) University on a McLaughlin fellowship and became a fellow of the Royal College of Physicians in 1958. He also earned a bachelor of arts degree in 1962 and his master of arts degree in 1975. He was studying for his PhD in the late 1980s, when he was in his 70s.
Upon his return from England in the late 1950s, Godfrey became director of the department of physical medicine and rehabilitation at Toronto East General Hospital. He subsequently worked at Toronto General Hospital, Sunnybrook Hospital, and the Toronto Rehab Hospital before joining Wellesley Hospital’s rheumatic disease unit, ultimately becoming head of the hospital’s rehabilitation clinic.
Dr. Godfrey was a professor in the department of rehabilitative medicine at the University of Toronto for over 2 decades. He was working 13-hour days teaching and maintaining his own practice well into his 70s. He would spend weekends at his country home in Madoc.
For over 20 years, he and his wife Margaret, a nurse, would spend 6 weeks each year as volunteers traveling to developing countries, such as Afghanistan and Pakistan, on lecture tours on behalf of CARE. Dr. Godfrey chaired CARE/MEDICO from 1983 to 1985 and subsequently served as chairman of CARE’s International Health Advisory Committee. In 1986, he was awarded the organization’s Distinguished Service Award.
In 1989, Dr. Godfrey was invested as a Member of the Order of Canada. His citation reads as follows:
“Deeply committed to humankind and the elimination of human suffering, and although of retirement age, he continues to be involved in an exhausting round of activity. Professor Emeritus of Rehabilitation Medicine at the University of Toronto, an environmentalist who was instrumental in the ‘People or Planes’ campaign opposing construction of the Pickering airport and a director of CARE/MEDICO, each year he takes his heart-felt concern for the welfare of the global community to Third World countries as a visiting volunteer doctor.”
Dr. Godfrey was also a political activist. When he learned about plans to build an international airport near his home in Uxbridge, Ont., he organized People or Planes, a group that successfully opposed the proposed airport. He was elected to the Ontario legislature as the Ontario New Democratic Party’s candidate for Durham West and served for 2 years as the NDP’s environment critic.
In 2020, grandson Frazey Ford posted a clip of his “immortal grandfather” being interviewed by David Suzuki as part of a CBC documentary on aging well.
Dr. Godfrey shared his secret to a long life: “The main thing is to keep interested in life,” he told Mr. Suzuki.
“That’s the secret, of course. If you stick in front of your television, you lose your interest in life. That’ll kill you next week. Certainly, the quality of stuff that’s being peddled on television these days is enough to make you wanna die pretty soon.”
A spokesperson for the University of Toronto’s department of medicine told CTV News that Dr. Godfrey was still working at four medical clinics in Toronto 4 days a week, even at age 102.
“He possessed a remarkable longevity in his practice, supported by his enduring love for medicine and incredible care for his patients,” the university said.
A version of this article first appeared on Medscape.com.
He was 104 and died at his home in Madoc, Ont., just weeks shy of his 105th birthday.
“He had been quite vigorous up until that point,” his son, Mark Godfrey, told CTV News.
If it wasn’t for the pandemic, his father would have probably continued practicing for a little while longer, he added. “He was the smartest guy in the room, all my life, any room we were in.”
Charles Morris Godfrey was born Sept. 24, 1917, in Philadelphia, according to Wikipedia, but his family moved to Toronto when he was 7 years old. His father, a physiotherapist, encouraged him to study medicine.
Dr. Godfrey served in the Canadian military for 5½ years during World War II and qualified as a physiotherapist while serving.
After the war, he enrolled in the faculty of medicine at the University of Toronto and earned his degree in 1953. He paid for his tuition by working as a janitor and scrapyard worker.
In 1956, he studied neurology at Oxford (England) University on a McLaughlin fellowship and became a fellow of the Royal College of Physicians in 1958. He also earned a bachelor of arts degree in 1962 and his master of arts degree in 1975. He was studying for his PhD in the late 1980s, when he was in his 70s.
Upon his return from England in the late 1950s, Godfrey became director of the department of physical medicine and rehabilitation at Toronto East General Hospital. He subsequently worked at Toronto General Hospital, Sunnybrook Hospital, and the Toronto Rehab Hospital before joining Wellesley Hospital’s rheumatic disease unit, ultimately becoming head of the hospital’s rehabilitation clinic.
Dr. Godfrey was a professor in the department of rehabilitative medicine at the University of Toronto for over 2 decades. He was working 13-hour days teaching and maintaining his own practice well into his 70s. He would spend weekends at his country home in Madoc.
For over 20 years, he and his wife Margaret, a nurse, would spend 6 weeks each year as volunteers traveling to developing countries, such as Afghanistan and Pakistan, on lecture tours on behalf of CARE. Dr. Godfrey chaired CARE/MEDICO from 1983 to 1985 and subsequently served as chairman of CARE’s International Health Advisory Committee. In 1986, he was awarded the organization’s Distinguished Service Award.
In 1989, Dr. Godfrey was invested as a Member of the Order of Canada. His citation reads as follows:
“Deeply committed to humankind and the elimination of human suffering, and although of retirement age, he continues to be involved in an exhausting round of activity. Professor Emeritus of Rehabilitation Medicine at the University of Toronto, an environmentalist who was instrumental in the ‘People or Planes’ campaign opposing construction of the Pickering airport and a director of CARE/MEDICO, each year he takes his heart-felt concern for the welfare of the global community to Third World countries as a visiting volunteer doctor.”
Dr. Godfrey was also a political activist. When he learned about plans to build an international airport near his home in Uxbridge, Ont., he organized People or Planes, a group that successfully opposed the proposed airport. He was elected to the Ontario legislature as the Ontario New Democratic Party’s candidate for Durham West and served for 2 years as the NDP’s environment critic.
In 2020, grandson Frazey Ford posted a clip of his “immortal grandfather” being interviewed by David Suzuki as part of a CBC documentary on aging well.
Dr. Godfrey shared his secret to a long life: “The main thing is to keep interested in life,” he told Mr. Suzuki.
“That’s the secret, of course. If you stick in front of your television, you lose your interest in life. That’ll kill you next week. Certainly, the quality of stuff that’s being peddled on television these days is enough to make you wanna die pretty soon.”
A spokesperson for the University of Toronto’s department of medicine told CTV News that Dr. Godfrey was still working at four medical clinics in Toronto 4 days a week, even at age 102.
“He possessed a remarkable longevity in his practice, supported by his enduring love for medicine and incredible care for his patients,” the university said.
A version of this article first appeared on Medscape.com.
Onset and awareness of hypertension varies by race, ethnicity
Black and Hispanic adults are diagnosed with hypertension at a significantly younger age than are white adults, and they also are more likely than Whites to be unaware of undiagnosed high blood pressure, based on national survey data collected from 2011 to 2020.
“Earlier hypertension onset in Black and Hispanic adults may contribute to racial and ethnic CVD disparities,” Xiaoning Huang, PhD, and associates wrote in JAMA Cardiology, also noting that “lower hypertension awareness among racial and ethnic minoritized groups suggests potential for underestimating differences in age at onset.”
Overall mean age at diagnosis was 46 years for the overall study sample of 9,627 participants in the National Health and Nutrition Examination Surveys over the 10 years covered in the analysis. Black adults, with a median age of 42 years, and Hispanic adults (median, 43 years) were significantly younger at diagnosis than White adults, who had a median age of 47 years, the investigators reported.
“Earlier age at hypertension onset may mean greater cumulative exposure to high blood pressure across the life course, which is associated with increased risk of [cardiovascular disease] and may contribute to racial disparities in hypertension-related outcomes,” said Dr. Huang and associates at Northwestern University, Chicago.
The increased cumulative exposure can be seen when age at diagnosis is stratified “across the life course.” Black/Hispanic adults were significantly more likely than White/Asian adults to be diagnosed at or before 30 years of age, and that difference continued to at least age 50 years, the investigators said.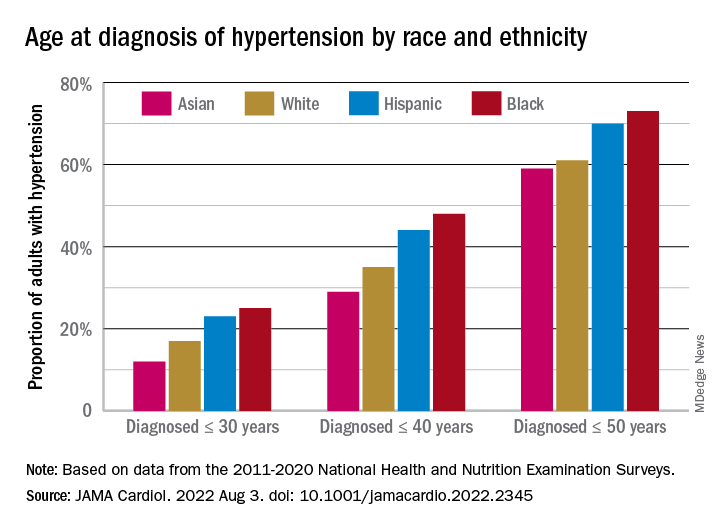
Many adults unaware of their hypertension
There was a somewhat different trend among those in the study population who reported BP at or above 140/90 mm Hg but did not report a hypertension diagnosis. Black, Hispanic, and Asian adults all were significantly more likely than White adults to be unaware of their hypertension, the survey data showed.
Overall, 18% of those who did not report a hypertension diagnosis had a BP of 140/90 mm Hg or higher and 38% had a BP of 130/80 mm Hg or more. Broken down by race and ethnicity, 16% and 36% of Whites reporting no hypertension had BPs of 140/90 and 130/80 mm Hg, respectively; those proportions were 21% and 42% for Hispanics, 24% and 44% for Asians, and 28% and 51% for Blacks, with all of the differences between Whites and the others significant, the research team reported.
One investigator is an associate editor for JAMA Cardiology and reported receiving grants from the American Heart Association and the National Institutes of Health during the conduct of the study. None of the other investigators reported any conflicts.
Black and Hispanic adults are diagnosed with hypertension at a significantly younger age than are white adults, and they also are more likely than Whites to be unaware of undiagnosed high blood pressure, based on national survey data collected from 2011 to 2020.
“Earlier hypertension onset in Black and Hispanic adults may contribute to racial and ethnic CVD disparities,” Xiaoning Huang, PhD, and associates wrote in JAMA Cardiology, also noting that “lower hypertension awareness among racial and ethnic minoritized groups suggests potential for underestimating differences in age at onset.”
Overall mean age at diagnosis was 46 years for the overall study sample of 9,627 participants in the National Health and Nutrition Examination Surveys over the 10 years covered in the analysis. Black adults, with a median age of 42 years, and Hispanic adults (median, 43 years) were significantly younger at diagnosis than White adults, who had a median age of 47 years, the investigators reported.
“Earlier age at hypertension onset may mean greater cumulative exposure to high blood pressure across the life course, which is associated with increased risk of [cardiovascular disease] and may contribute to racial disparities in hypertension-related outcomes,” said Dr. Huang and associates at Northwestern University, Chicago.
The increased cumulative exposure can be seen when age at diagnosis is stratified “across the life course.” Black/Hispanic adults were significantly more likely than White/Asian adults to be diagnosed at or before 30 years of age, and that difference continued to at least age 50 years, the investigators said.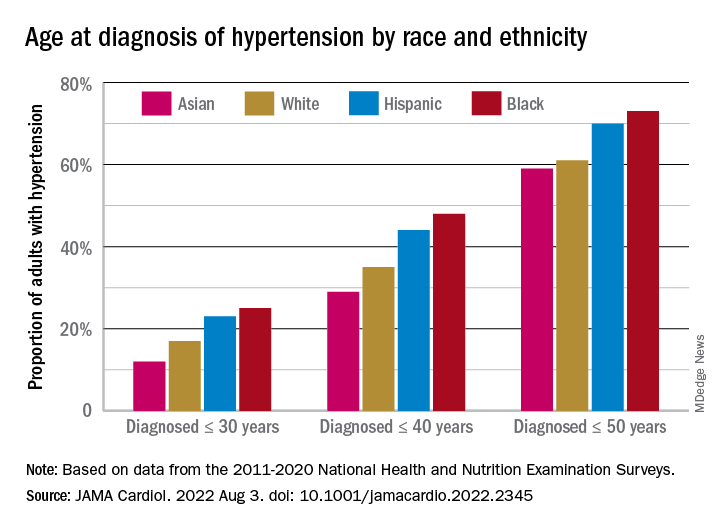
Many adults unaware of their hypertension
There was a somewhat different trend among those in the study population who reported BP at or above 140/90 mm Hg but did not report a hypertension diagnosis. Black, Hispanic, and Asian adults all were significantly more likely than White adults to be unaware of their hypertension, the survey data showed.
Overall, 18% of those who did not report a hypertension diagnosis had a BP of 140/90 mm Hg or higher and 38% had a BP of 130/80 mm Hg or more. Broken down by race and ethnicity, 16% and 36% of Whites reporting no hypertension had BPs of 140/90 and 130/80 mm Hg, respectively; those proportions were 21% and 42% for Hispanics, 24% and 44% for Asians, and 28% and 51% for Blacks, with all of the differences between Whites and the others significant, the research team reported.
One investigator is an associate editor for JAMA Cardiology and reported receiving grants from the American Heart Association and the National Institutes of Health during the conduct of the study. None of the other investigators reported any conflicts.
Black and Hispanic adults are diagnosed with hypertension at a significantly younger age than are white adults, and they also are more likely than Whites to be unaware of undiagnosed high blood pressure, based on national survey data collected from 2011 to 2020.
“Earlier hypertension onset in Black and Hispanic adults may contribute to racial and ethnic CVD disparities,” Xiaoning Huang, PhD, and associates wrote in JAMA Cardiology, also noting that “lower hypertension awareness among racial and ethnic minoritized groups suggests potential for underestimating differences in age at onset.”
Overall mean age at diagnosis was 46 years for the overall study sample of 9,627 participants in the National Health and Nutrition Examination Surveys over the 10 years covered in the analysis. Black adults, with a median age of 42 years, and Hispanic adults (median, 43 years) were significantly younger at diagnosis than White adults, who had a median age of 47 years, the investigators reported.
“Earlier age at hypertension onset may mean greater cumulative exposure to high blood pressure across the life course, which is associated with increased risk of [cardiovascular disease] and may contribute to racial disparities in hypertension-related outcomes,” said Dr. Huang and associates at Northwestern University, Chicago.
The increased cumulative exposure can be seen when age at diagnosis is stratified “across the life course.” Black/Hispanic adults were significantly more likely than White/Asian adults to be diagnosed at or before 30 years of age, and that difference continued to at least age 50 years, the investigators said.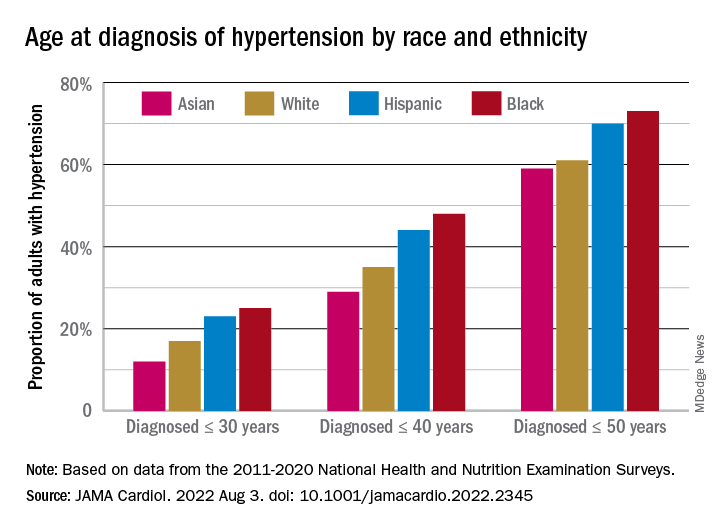
Many adults unaware of their hypertension
There was a somewhat different trend among those in the study population who reported BP at or above 140/90 mm Hg but did not report a hypertension diagnosis. Black, Hispanic, and Asian adults all were significantly more likely than White adults to be unaware of their hypertension, the survey data showed.
Overall, 18% of those who did not report a hypertension diagnosis had a BP of 140/90 mm Hg or higher and 38% had a BP of 130/80 mm Hg or more. Broken down by race and ethnicity, 16% and 36% of Whites reporting no hypertension had BPs of 140/90 and 130/80 mm Hg, respectively; those proportions were 21% and 42% for Hispanics, 24% and 44% for Asians, and 28% and 51% for Blacks, with all of the differences between Whites and the others significant, the research team reported.
One investigator is an associate editor for JAMA Cardiology and reported receiving grants from the American Heart Association and the National Institutes of Health during the conduct of the study. None of the other investigators reported any conflicts.
FROM JAMA CARDIOLOGY
Diffuse Lung Disease & Transplant Network
Interstitial Lung Disease Section
Diagnosis of idiopathic pulmonary fibrosis: Is tissue still an issue?
Per ATS/ERS/JRS/ALAT guidelines, diagnosis of IPF requires exclusion of known causes of interstitial lung disease (ILD) and either the presence of a usual interstitial pneumonia (UIP) or probable UIP pattern on HRCT scan or specific combinations of HRCT scan and histopathologic patterns. Surgical lung biopsy (SLB) is the gold standard for histopathologic diagnosis.
The recent update (Raghu, et al. Am J Respir Crit Care Med. 2022;205[9]:1084-92) made a conditional recommendation for transbronchial lung cryobiopsy (TBLC) as an acceptable alternative to SLB in patients with undetermined ILD. Systematic analysis revealed a diagnostic yield of 79% (85% when ≥ 3 sites were sampled) by TBLC compared with 90% on SLB. With consideration of this diagnostic yield vs the risk of pneumothorax, severe bleeding, and procedural mortality, TBLC is an attractive tool compared with SLB. Overall, the utility of TBLC remains limited to experienced centers due to dependence on proceduralist and pathologist skills for optimal success and more data are awaited.
No recommendation was made for or against the use of genomic classifiers (GC) for the diagnosis of UIP in patients with undetermined ILD undergoing transbronchial biopsy. Although, meta-analysis revealed a specificity of 92%, this may be driven by patient enrichment with a high probability for UIP population. GC has the potential to reduce SLB-associated risks and provide diagnostic information for multidisciplinary discussion in certain scenarios. However, limitations arise from the inability to distinguish specific ILD subtype associated with the UIP pattern; further improvement in sensitivity and understanding of downstream consequences of false-negative results is necessary.
Kevin Dsouza, MD
Fellow-in-Training
Interstitial Lung Disease Section
Diagnosis of idiopathic pulmonary fibrosis: Is tissue still an issue?
Per ATS/ERS/JRS/ALAT guidelines, diagnosis of IPF requires exclusion of known causes of interstitial lung disease (ILD) and either the presence of a usual interstitial pneumonia (UIP) or probable UIP pattern on HRCT scan or specific combinations of HRCT scan and histopathologic patterns. Surgical lung biopsy (SLB) is the gold standard for histopathologic diagnosis.
The recent update (Raghu, et al. Am J Respir Crit Care Med. 2022;205[9]:1084-92) made a conditional recommendation for transbronchial lung cryobiopsy (TBLC) as an acceptable alternative to SLB in patients with undetermined ILD. Systematic analysis revealed a diagnostic yield of 79% (85% when ≥ 3 sites were sampled) by TBLC compared with 90% on SLB. With consideration of this diagnostic yield vs the risk of pneumothorax, severe bleeding, and procedural mortality, TBLC is an attractive tool compared with SLB. Overall, the utility of TBLC remains limited to experienced centers due to dependence on proceduralist and pathologist skills for optimal success and more data are awaited.
No recommendation was made for or against the use of genomic classifiers (GC) for the diagnosis of UIP in patients with undetermined ILD undergoing transbronchial biopsy. Although, meta-analysis revealed a specificity of 92%, this may be driven by patient enrichment with a high probability for UIP population. GC has the potential to reduce SLB-associated risks and provide diagnostic information for multidisciplinary discussion in certain scenarios. However, limitations arise from the inability to distinguish specific ILD subtype associated with the UIP pattern; further improvement in sensitivity and understanding of downstream consequences of false-negative results is necessary.
Kevin Dsouza, MD
Fellow-in-Training
Interstitial Lung Disease Section
Diagnosis of idiopathic pulmonary fibrosis: Is tissue still an issue?
Per ATS/ERS/JRS/ALAT guidelines, diagnosis of IPF requires exclusion of known causes of interstitial lung disease (ILD) and either the presence of a usual interstitial pneumonia (UIP) or probable UIP pattern on HRCT scan or specific combinations of HRCT scan and histopathologic patterns. Surgical lung biopsy (SLB) is the gold standard for histopathologic diagnosis.
The recent update (Raghu, et al. Am J Respir Crit Care Med. 2022;205[9]:1084-92) made a conditional recommendation for transbronchial lung cryobiopsy (TBLC) as an acceptable alternative to SLB in patients with undetermined ILD. Systematic analysis revealed a diagnostic yield of 79% (85% when ≥ 3 sites were sampled) by TBLC compared with 90% on SLB. With consideration of this diagnostic yield vs the risk of pneumothorax, severe bleeding, and procedural mortality, TBLC is an attractive tool compared with SLB. Overall, the utility of TBLC remains limited to experienced centers due to dependence on proceduralist and pathologist skills for optimal success and more data are awaited.
No recommendation was made for or against the use of genomic classifiers (GC) for the diagnosis of UIP in patients with undetermined ILD undergoing transbronchial biopsy. Although, meta-analysis revealed a specificity of 92%, this may be driven by patient enrichment with a high probability for UIP population. GC has the potential to reduce SLB-associated risks and provide diagnostic information for multidisciplinary discussion in certain scenarios. However, limitations arise from the inability to distinguish specific ILD subtype associated with the UIP pattern; further improvement in sensitivity and understanding of downstream consequences of false-negative results is necessary.
Kevin Dsouza, MD
Fellow-in-Training
Antibiotic-resistant bacteria emerging in community settings
A new study from the Centers for Disease Control and Prevention found that
Traditionally, CRE has been thought of as a nosocomial infection, acquired in a hospital or other health care facility (nursing home, long-term acute care hospital, dialysis center, etc.). This is the first population-level study to show otherwise, with fully 10% of the CRE isolates found to be community acquired.
CREs are a group of multidrug-resistant bacteria considered an urgent health threat by the CDC because they can rapidly spread between patients, especially those who are most seriously ill and vulnerable, and because they are so difficult to treat. These patients often require treatment with toxic antibiotics, such as colistin, and carry a high mortality rate – up to 50% in some studies.
Overall, 30% of CREs carry a carbapenemase – an enzyme that can make them resistant to carbapenem antibiotics. The genes for this are readily transferable between bacteria and help account for their spread in hospitals.
But in this study, published in the American Journal of Infection Control, of the 12 isolates that underwent whole-genome sequencing, 42% of the CA-CRE isolates carried the carbapenemase gene. Lead author Sandra Bulens, MPH, a health scientist in the CDC’s division of health care quality promotion, said in an interview, “The findings highlight the potential for CP-CRE to move from health care settings into the community. The fact that 5 of the 12 isolates harbored a carbapenemase gene introduces new challenges for controlling spread of CP-CRE.”
CDC researchers analyzed data from eight U.S. metropolitan areas between 2012 and 2015 as part of the CDC’s Emerging Infections Program (EIP) health care–associated infections – community interface activity, which conducts surveillance for CRE and other drug-resistant gram-negative bacteria. Cases of CA-CRE were compared with HCA-CRE, with 1499 cases in 1,194 case-patients being analyzed. Though Klebsiella pneumoniae was the most common isolate, there were some differences between metropolitan areas.
The incidence of CRE cases per 100,000 population was 2.96 (95% confidence interval, 2.81-3.11) overall and 0.29 (95% CI, 0.25-0.25) for CA-CRE. Most CA-CRE cases were in White persons (73%) and women (84%). Urine cultures were the source of 98% of all CA-CRE cases, compared with 86% of HCA-CRE cases (P < .001). Though small numbers, the numbers of patients with CA-CRE without apparent underlying medical condition (n = 51; 37%) was greater when compared with patients with HCA-CRE (n = 36; 3%; P < .001).
Asked for independent comment, Lance Price, PhD, of George Washington University and the founding director of GW’s Antibiotic Resistance Action Center, Washington, said, “what’s striking about these data is that: ‘Who is the front line, at least in the United States for CRE?’ It’s women, older women. ... At some point, we have to frame drug resistance as a women’s health issue.”
Dr. Price noted that the 10% of patients with CA-CRE acquired it in the community. “I would argue that probably none of them had any idea, because there’s this silent community epidemic,” he said. “It’s asymptomatic carriage and transmission in the community. Somebody can be this walking reservoir of these really dangerous bacteria and have no idea.”
This is an increasingly serious problem for women, Dr. Price said, because, “with a community-acquired bladder infection, you’re going to call your doctor or go to an urgent care, and they’re not going to test you. They’re going to guess what you have, and they’re going to prescribe an antibiotic, and that antibiotic is going to fail. So then your bladder infection continues, and then you wait a few more days, and you start to get flank pain and kidney infection. ... If you start getting a fever, they might admit you. They are going to start treating you immediately, and they might miss it because you’ve got this organism that’s resistant to all the best antibiotics. ... The gateway to the blood is the UTI.”
Because of such empiric treatment and increasing resistance, the risk for treatment failure is quite high, especially for older women. Ms. Bulens, however, said that, “[although] 10% of CRE were in persons without health care risk factors, the proportion of all UTIs in this population that are CRE is going to be very, very small.”
This study involved cultures from 2012 to 2015. Before the pandemic, from 2012 to 2017, U.S. deaths from antibiotic resistance fell by 18% overall and by 30% in hospitals.
But in the first year of the COVID-19 pandemic, there was a 15% increase in infections and deaths from antibiotic-resistant (AMR), hospital-acquired bacteria. In 2020, 29,400 patients died from AMR infections. There was a 78% increase in carbapenem-resistant Acinetobacter baumannii health care–associated infections, a 35% increase in carbapenem-resistant Enterobacterales, and 32% increases in both multidrug-resistant Pseudomonas aeruginosa and extended-spectrum beta-lactamase–producing Enterobacterales. Aside from gram-negative bacteria, methicillin-resistant Staphylococcus aureus rose 13%, and Candida auris rose 60%. But owing to limited surveillance, recent sound figures are lacking.
Ms. Bulens and Dr. Price reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study from the Centers for Disease Control and Prevention found that
Traditionally, CRE has been thought of as a nosocomial infection, acquired in a hospital or other health care facility (nursing home, long-term acute care hospital, dialysis center, etc.). This is the first population-level study to show otherwise, with fully 10% of the CRE isolates found to be community acquired.
CREs are a group of multidrug-resistant bacteria considered an urgent health threat by the CDC because they can rapidly spread between patients, especially those who are most seriously ill and vulnerable, and because they are so difficult to treat. These patients often require treatment with toxic antibiotics, such as colistin, and carry a high mortality rate – up to 50% in some studies.
Overall, 30% of CREs carry a carbapenemase – an enzyme that can make them resistant to carbapenem antibiotics. The genes for this are readily transferable between bacteria and help account for their spread in hospitals.
But in this study, published in the American Journal of Infection Control, of the 12 isolates that underwent whole-genome sequencing, 42% of the CA-CRE isolates carried the carbapenemase gene. Lead author Sandra Bulens, MPH, a health scientist in the CDC’s division of health care quality promotion, said in an interview, “The findings highlight the potential for CP-CRE to move from health care settings into the community. The fact that 5 of the 12 isolates harbored a carbapenemase gene introduces new challenges for controlling spread of CP-CRE.”
CDC researchers analyzed data from eight U.S. metropolitan areas between 2012 and 2015 as part of the CDC’s Emerging Infections Program (EIP) health care–associated infections – community interface activity, which conducts surveillance for CRE and other drug-resistant gram-negative bacteria. Cases of CA-CRE were compared with HCA-CRE, with 1499 cases in 1,194 case-patients being analyzed. Though Klebsiella pneumoniae was the most common isolate, there were some differences between metropolitan areas.
The incidence of CRE cases per 100,000 population was 2.96 (95% confidence interval, 2.81-3.11) overall and 0.29 (95% CI, 0.25-0.25) for CA-CRE. Most CA-CRE cases were in White persons (73%) and women (84%). Urine cultures were the source of 98% of all CA-CRE cases, compared with 86% of HCA-CRE cases (P < .001). Though small numbers, the numbers of patients with CA-CRE without apparent underlying medical condition (n = 51; 37%) was greater when compared with patients with HCA-CRE (n = 36; 3%; P < .001).
Asked for independent comment, Lance Price, PhD, of George Washington University and the founding director of GW’s Antibiotic Resistance Action Center, Washington, said, “what’s striking about these data is that: ‘Who is the front line, at least in the United States for CRE?’ It’s women, older women. ... At some point, we have to frame drug resistance as a women’s health issue.”
Dr. Price noted that the 10% of patients with CA-CRE acquired it in the community. “I would argue that probably none of them had any idea, because there’s this silent community epidemic,” he said. “It’s asymptomatic carriage and transmission in the community. Somebody can be this walking reservoir of these really dangerous bacteria and have no idea.”
This is an increasingly serious problem for women, Dr. Price said, because, “with a community-acquired bladder infection, you’re going to call your doctor or go to an urgent care, and they’re not going to test you. They’re going to guess what you have, and they’re going to prescribe an antibiotic, and that antibiotic is going to fail. So then your bladder infection continues, and then you wait a few more days, and you start to get flank pain and kidney infection. ... If you start getting a fever, they might admit you. They are going to start treating you immediately, and they might miss it because you’ve got this organism that’s resistant to all the best antibiotics. ... The gateway to the blood is the UTI.”
Because of such empiric treatment and increasing resistance, the risk for treatment failure is quite high, especially for older women. Ms. Bulens, however, said that, “[although] 10% of CRE were in persons without health care risk factors, the proportion of all UTIs in this population that are CRE is going to be very, very small.”
This study involved cultures from 2012 to 2015. Before the pandemic, from 2012 to 2017, U.S. deaths from antibiotic resistance fell by 18% overall and by 30% in hospitals.
But in the first year of the COVID-19 pandemic, there was a 15% increase in infections and deaths from antibiotic-resistant (AMR), hospital-acquired bacteria. In 2020, 29,400 patients died from AMR infections. There was a 78% increase in carbapenem-resistant Acinetobacter baumannii health care–associated infections, a 35% increase in carbapenem-resistant Enterobacterales, and 32% increases in both multidrug-resistant Pseudomonas aeruginosa and extended-spectrum beta-lactamase–producing Enterobacterales. Aside from gram-negative bacteria, methicillin-resistant Staphylococcus aureus rose 13%, and Candida auris rose 60%. But owing to limited surveillance, recent sound figures are lacking.
Ms. Bulens and Dr. Price reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study from the Centers for Disease Control and Prevention found that
Traditionally, CRE has been thought of as a nosocomial infection, acquired in a hospital or other health care facility (nursing home, long-term acute care hospital, dialysis center, etc.). This is the first population-level study to show otherwise, with fully 10% of the CRE isolates found to be community acquired.
CREs are a group of multidrug-resistant bacteria considered an urgent health threat by the CDC because they can rapidly spread between patients, especially those who are most seriously ill and vulnerable, and because they are so difficult to treat. These patients often require treatment with toxic antibiotics, such as colistin, and carry a high mortality rate – up to 50% in some studies.
Overall, 30% of CREs carry a carbapenemase – an enzyme that can make them resistant to carbapenem antibiotics. The genes for this are readily transferable between bacteria and help account for their spread in hospitals.
But in this study, published in the American Journal of Infection Control, of the 12 isolates that underwent whole-genome sequencing, 42% of the CA-CRE isolates carried the carbapenemase gene. Lead author Sandra Bulens, MPH, a health scientist in the CDC’s division of health care quality promotion, said in an interview, “The findings highlight the potential for CP-CRE to move from health care settings into the community. The fact that 5 of the 12 isolates harbored a carbapenemase gene introduces new challenges for controlling spread of CP-CRE.”
CDC researchers analyzed data from eight U.S. metropolitan areas between 2012 and 2015 as part of the CDC’s Emerging Infections Program (EIP) health care–associated infections – community interface activity, which conducts surveillance for CRE and other drug-resistant gram-negative bacteria. Cases of CA-CRE were compared with HCA-CRE, with 1499 cases in 1,194 case-patients being analyzed. Though Klebsiella pneumoniae was the most common isolate, there were some differences between metropolitan areas.
The incidence of CRE cases per 100,000 population was 2.96 (95% confidence interval, 2.81-3.11) overall and 0.29 (95% CI, 0.25-0.25) for CA-CRE. Most CA-CRE cases were in White persons (73%) and women (84%). Urine cultures were the source of 98% of all CA-CRE cases, compared with 86% of HCA-CRE cases (P < .001). Though small numbers, the numbers of patients with CA-CRE without apparent underlying medical condition (n = 51; 37%) was greater when compared with patients with HCA-CRE (n = 36; 3%; P < .001).
Asked for independent comment, Lance Price, PhD, of George Washington University and the founding director of GW’s Antibiotic Resistance Action Center, Washington, said, “what’s striking about these data is that: ‘Who is the front line, at least in the United States for CRE?’ It’s women, older women. ... At some point, we have to frame drug resistance as a women’s health issue.”
Dr. Price noted that the 10% of patients with CA-CRE acquired it in the community. “I would argue that probably none of them had any idea, because there’s this silent community epidemic,” he said. “It’s asymptomatic carriage and transmission in the community. Somebody can be this walking reservoir of these really dangerous bacteria and have no idea.”
This is an increasingly serious problem for women, Dr. Price said, because, “with a community-acquired bladder infection, you’re going to call your doctor or go to an urgent care, and they’re not going to test you. They’re going to guess what you have, and they’re going to prescribe an antibiotic, and that antibiotic is going to fail. So then your bladder infection continues, and then you wait a few more days, and you start to get flank pain and kidney infection. ... If you start getting a fever, they might admit you. They are going to start treating you immediately, and they might miss it because you’ve got this organism that’s resistant to all the best antibiotics. ... The gateway to the blood is the UTI.”
Because of such empiric treatment and increasing resistance, the risk for treatment failure is quite high, especially for older women. Ms. Bulens, however, said that, “[although] 10% of CRE were in persons without health care risk factors, the proportion of all UTIs in this population that are CRE is going to be very, very small.”
This study involved cultures from 2012 to 2015. Before the pandemic, from 2012 to 2017, U.S. deaths from antibiotic resistance fell by 18% overall and by 30% in hospitals.
But in the first year of the COVID-19 pandemic, there was a 15% increase in infections and deaths from antibiotic-resistant (AMR), hospital-acquired bacteria. In 2020, 29,400 patients died from AMR infections. There was a 78% increase in carbapenem-resistant Acinetobacter baumannii health care–associated infections, a 35% increase in carbapenem-resistant Enterobacterales, and 32% increases in both multidrug-resistant Pseudomonas aeruginosa and extended-spectrum beta-lactamase–producing Enterobacterales. Aside from gram-negative bacteria, methicillin-resistant Staphylococcus aureus rose 13%, and Candida auris rose 60%. But owing to limited surveillance, recent sound figures are lacking.
Ms. Bulens and Dr. Price reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF INFECTION CONTROL
Thoracic Oncology & Chest Procedures Network
Ultrasound and Chest Imaging Section
Advanced critical care echocardiography: A noninvasive tool for hemodynamic assessment in critically ill patients
Hemodynamic assessments in critically ill patients are important to guide accurate management; however, traditional invasive methods of measuring cardiac output have significant limitations, including risks of infection and bleeding. ACCE can provide a multitude of hemodynamic measurements from cardiac output (CO) to right ventricular systolic pressure (RVSP) and left atrial pressure (LAP). Combinations of left ventricular function parameters, along with estimation of filling pressures, can help distinguish between types of shock. Schmidt and colleagues (Sci Rep. 2022;12[1]:7187) demonstrated that measurement of these indices in the majority of patients helped elucidate the cause for hemodynamic compromise. They found presence of a cardiac index (CI) < 2.5/min.m2 was associated with a doubling of ICU mortality as compared with predictions based on severity of illness scores in otherwise hemodynamically stable patients. Hollenberg and colleagues (Am J Cardiol. 2021;153:135-39) demonstrated the feasibility of a simpler stratification using the left ventricular ejection fraction (LVEF) and CI in coronavirus disease 2019 patients with shock, where low CI despite having a preserved LVEF was associated with worse outcomes.
Quick, reliable data are an intensivist’s friend. Utilizing ACCE at the bedside adds another tool in our arsenal to provide real-time hemodynamic data that can be used to manage patients in the ICU. ACCE also allows repeated measurements to determine changes based on therapeutic interventions initiated.
In recognition of the importance of ACCE as a tool for intensivists, the National Board of Echocardiography (NBE) now offers a pathway toward board certification with the Examination of Special Competence in Critical Care Echocardiography (CCEeXAM). CHEST continues to offer cutting-edge courses in ACCE, as well as a board review course for learners interested in sitting for the CCEeXAM.
Amik Sodhi, MD, FCCP
Gul Zaidi, MD, FCCP
Members-at-Large
Ultrasound and Chest Imaging Section
Advanced critical care echocardiography: A noninvasive tool for hemodynamic assessment in critically ill patients
Hemodynamic assessments in critically ill patients are important to guide accurate management; however, traditional invasive methods of measuring cardiac output have significant limitations, including risks of infection and bleeding. ACCE can provide a multitude of hemodynamic measurements from cardiac output (CO) to right ventricular systolic pressure (RVSP) and left atrial pressure (LAP). Combinations of left ventricular function parameters, along with estimation of filling pressures, can help distinguish between types of shock. Schmidt and colleagues (Sci Rep. 2022;12[1]:7187) demonstrated that measurement of these indices in the majority of patients helped elucidate the cause for hemodynamic compromise. They found presence of a cardiac index (CI) < 2.5/min.m2 was associated with a doubling of ICU mortality as compared with predictions based on severity of illness scores in otherwise hemodynamically stable patients. Hollenberg and colleagues (Am J Cardiol. 2021;153:135-39) demonstrated the feasibility of a simpler stratification using the left ventricular ejection fraction (LVEF) and CI in coronavirus disease 2019 patients with shock, where low CI despite having a preserved LVEF was associated with worse outcomes.
Quick, reliable data are an intensivist’s friend. Utilizing ACCE at the bedside adds another tool in our arsenal to provide real-time hemodynamic data that can be used to manage patients in the ICU. ACCE also allows repeated measurements to determine changes based on therapeutic interventions initiated.
In recognition of the importance of ACCE as a tool for intensivists, the National Board of Echocardiography (NBE) now offers a pathway toward board certification with the Examination of Special Competence in Critical Care Echocardiography (CCEeXAM). CHEST continues to offer cutting-edge courses in ACCE, as well as a board review course for learners interested in sitting for the CCEeXAM.
Amik Sodhi, MD, FCCP
Gul Zaidi, MD, FCCP
Members-at-Large
Ultrasound and Chest Imaging Section
Advanced critical care echocardiography: A noninvasive tool for hemodynamic assessment in critically ill patients
Hemodynamic assessments in critically ill patients are important to guide accurate management; however, traditional invasive methods of measuring cardiac output have significant limitations, including risks of infection and bleeding. ACCE can provide a multitude of hemodynamic measurements from cardiac output (CO) to right ventricular systolic pressure (RVSP) and left atrial pressure (LAP). Combinations of left ventricular function parameters, along with estimation of filling pressures, can help distinguish between types of shock. Schmidt and colleagues (Sci Rep. 2022;12[1]:7187) demonstrated that measurement of these indices in the majority of patients helped elucidate the cause for hemodynamic compromise. They found presence of a cardiac index (CI) < 2.5/min.m2 was associated with a doubling of ICU mortality as compared with predictions based on severity of illness scores in otherwise hemodynamically stable patients. Hollenberg and colleagues (Am J Cardiol. 2021;153:135-39) demonstrated the feasibility of a simpler stratification using the left ventricular ejection fraction (LVEF) and CI in coronavirus disease 2019 patients with shock, where low CI despite having a preserved LVEF was associated with worse outcomes.
Quick, reliable data are an intensivist’s friend. Utilizing ACCE at the bedside adds another tool in our arsenal to provide real-time hemodynamic data that can be used to manage patients in the ICU. ACCE also allows repeated measurements to determine changes based on therapeutic interventions initiated.
In recognition of the importance of ACCE as a tool for intensivists, the National Board of Echocardiography (NBE) now offers a pathway toward board certification with the Examination of Special Competence in Critical Care Echocardiography (CCEeXAM). CHEST continues to offer cutting-edge courses in ACCE, as well as a board review course for learners interested in sitting for the CCEeXAM.
Amik Sodhi, MD, FCCP
Gul Zaidi, MD, FCCP
Members-at-Large
‘Self-boosting’ vaccines could be immunizations of the future
Most vaccines don’t come as one-shot deals. A series of boosters is needed to step up immunity to COVID-19, tetanus, and other infectious threats over time.
But what if you could receive just one shot that boosts itself whenever you need a bump in protection?
Researchers at the Massachusetts Institute of Technology (MIT) have developed microparticles that could be used to create self-boosting vaccines that deliver their contents at carefully set time points. In a new study published in the journal Science Advances, the scientists describe how they tune the particles to release the goods at the right time and offer insights on how they can keep the particles stable until then.
How self-boosting vaccines could work
The team developed tiny particles that look like coffee cups – except instead of your favorite brew, they’re filled with vaccine.
“You can put the lid on, and then inject it into the body, and once the lid breaks, whatever is in there is released,” says study author Ana Jaklenec, PhD, a research scientist at MIT’s Koch Institute for Integrative Cancer Research.
To make the tiny cups, the researchers use various polymers already used in medical applications, such as dissolvable stitches. Then they fill the cups with vaccine material that is dried and combined with sugars and other stabilizers.
The particles can be made in various shapes and fine-tuned using polymers with different properties. Some polymers last longer in the body than others, so their choice helps determine how long everything will stay stable under the skin after the injection and when the particles will release their cargo. It could be days or months after the injection.
One challenge is that as the particles open, the environment around them becomes more acidic. The team is working on ways to curb that acidity to make the vaccine material more stable.
“We have ongoing research that has produced some really, really exciting results about their stability and [shows] that you’re able to maintain really sensitive vaccines, stable for a good period of time,” says study author Morteza Sarmadi, PhD, a research specialist at the Koch Institute.
The potential public health impact
This research, funded by the Bill & Melinda Gates Foundation, started with the developing world in mind.
“The intent was actually helping people in the developing world, because a lot of times, people don’t come back for a second injection,” says study author Robert Langer, ScD, the David H. Koch Institute professor at MIT.
But a one-shot plan could benefit the developed world, too. One reason is that self-boosting vaccines could help those who get one achieve higher antibody responses than they would with just one dose. That could mean more protection for the person and the population, because as people develop stronger immunity, germs may have less of a chance to evolve and spread.
Take the COVID-19 pandemic, for example. Only 67% of Americans are fully vaccinated, and most people eligible for first and second boosters haven’t gotten them. New variants, such as the recent Omicron ones, continue to emerge and infect.
“I think those variants would have had a lot less chance to come about if everybody that had gotten vaccinated the first time got repeat injections, which they didn’t,” says Dr. Langer.
Self-boosting vaccines could also benefit infants, children who fear shots, and older adults who have a hard time getting health care.
Also, because the vaccine material is encapsulated and its release can be staggered, this technology might help people receive multiple vaccines at the same time that must now be given separately.
What comes next
The team is testing self-boosting polio and hepatitis vaccines in non-human primates. A small trial in healthy humans might follow within the next few years.
“We think that there’s really high potential for this technology, and we hope it can be developed and get to the human phase very soon,” says Dr. Jaklenec.
In smaller animal models, they are exploring the potential of self-boosting mRNA vaccines. They’re also working with scientists who are studying HIV vaccines.
“There has been some recent progress where very complex regimens seem to be working, but they’re not practical,” says Dr. Jaklenec. “And so, this is where this particular technology could be useful, because you have to prime and boost with different things, and this allows you to do that.”
This system could also extend beyond vaccines and be used to deliver cancer therapies, hormones, and biologics in a shot.
Through new work with researchers at Georgia Tech University, the team will study the potential of giving self-boosting vaccines through 3D-printed microneedles. These vaccines, which would stick on your skin like a bandage, could be self-administered and deployed globally in response to local outbreaks.
A version of this article first appeared on WebMD.com.
Most vaccines don’t come as one-shot deals. A series of boosters is needed to step up immunity to COVID-19, tetanus, and other infectious threats over time.
But what if you could receive just one shot that boosts itself whenever you need a bump in protection?
Researchers at the Massachusetts Institute of Technology (MIT) have developed microparticles that could be used to create self-boosting vaccines that deliver their contents at carefully set time points. In a new study published in the journal Science Advances, the scientists describe how they tune the particles to release the goods at the right time and offer insights on how they can keep the particles stable until then.
How self-boosting vaccines could work
The team developed tiny particles that look like coffee cups – except instead of your favorite brew, they’re filled with vaccine.
“You can put the lid on, and then inject it into the body, and once the lid breaks, whatever is in there is released,” says study author Ana Jaklenec, PhD, a research scientist at MIT’s Koch Institute for Integrative Cancer Research.
To make the tiny cups, the researchers use various polymers already used in medical applications, such as dissolvable stitches. Then they fill the cups with vaccine material that is dried and combined with sugars and other stabilizers.
The particles can be made in various shapes and fine-tuned using polymers with different properties. Some polymers last longer in the body than others, so their choice helps determine how long everything will stay stable under the skin after the injection and when the particles will release their cargo. It could be days or months after the injection.
One challenge is that as the particles open, the environment around them becomes more acidic. The team is working on ways to curb that acidity to make the vaccine material more stable.
“We have ongoing research that has produced some really, really exciting results about their stability and [shows] that you’re able to maintain really sensitive vaccines, stable for a good period of time,” says study author Morteza Sarmadi, PhD, a research specialist at the Koch Institute.
The potential public health impact
This research, funded by the Bill & Melinda Gates Foundation, started with the developing world in mind.
“The intent was actually helping people in the developing world, because a lot of times, people don’t come back for a second injection,” says study author Robert Langer, ScD, the David H. Koch Institute professor at MIT.
But a one-shot plan could benefit the developed world, too. One reason is that self-boosting vaccines could help those who get one achieve higher antibody responses than they would with just one dose. That could mean more protection for the person and the population, because as people develop stronger immunity, germs may have less of a chance to evolve and spread.
Take the COVID-19 pandemic, for example. Only 67% of Americans are fully vaccinated, and most people eligible for first and second boosters haven’t gotten them. New variants, such as the recent Omicron ones, continue to emerge and infect.
“I think those variants would have had a lot less chance to come about if everybody that had gotten vaccinated the first time got repeat injections, which they didn’t,” says Dr. Langer.
Self-boosting vaccines could also benefit infants, children who fear shots, and older adults who have a hard time getting health care.
Also, because the vaccine material is encapsulated and its release can be staggered, this technology might help people receive multiple vaccines at the same time that must now be given separately.
What comes next
The team is testing self-boosting polio and hepatitis vaccines in non-human primates. A small trial in healthy humans might follow within the next few years.
“We think that there’s really high potential for this technology, and we hope it can be developed and get to the human phase very soon,” says Dr. Jaklenec.
In smaller animal models, they are exploring the potential of self-boosting mRNA vaccines. They’re also working with scientists who are studying HIV vaccines.
“There has been some recent progress where very complex regimens seem to be working, but they’re not practical,” says Dr. Jaklenec. “And so, this is where this particular technology could be useful, because you have to prime and boost with different things, and this allows you to do that.”
This system could also extend beyond vaccines and be used to deliver cancer therapies, hormones, and biologics in a shot.
Through new work with researchers at Georgia Tech University, the team will study the potential of giving self-boosting vaccines through 3D-printed microneedles. These vaccines, which would stick on your skin like a bandage, could be self-administered and deployed globally in response to local outbreaks.
A version of this article first appeared on WebMD.com.
Most vaccines don’t come as one-shot deals. A series of boosters is needed to step up immunity to COVID-19, tetanus, and other infectious threats over time.
But what if you could receive just one shot that boosts itself whenever you need a bump in protection?
Researchers at the Massachusetts Institute of Technology (MIT) have developed microparticles that could be used to create self-boosting vaccines that deliver their contents at carefully set time points. In a new study published in the journal Science Advances, the scientists describe how they tune the particles to release the goods at the right time and offer insights on how they can keep the particles stable until then.
How self-boosting vaccines could work
The team developed tiny particles that look like coffee cups – except instead of your favorite brew, they’re filled with vaccine.
“You can put the lid on, and then inject it into the body, and once the lid breaks, whatever is in there is released,” says study author Ana Jaklenec, PhD, a research scientist at MIT’s Koch Institute for Integrative Cancer Research.
To make the tiny cups, the researchers use various polymers already used in medical applications, such as dissolvable stitches. Then they fill the cups with vaccine material that is dried and combined with sugars and other stabilizers.
The particles can be made in various shapes and fine-tuned using polymers with different properties. Some polymers last longer in the body than others, so their choice helps determine how long everything will stay stable under the skin after the injection and when the particles will release their cargo. It could be days or months after the injection.
One challenge is that as the particles open, the environment around them becomes more acidic. The team is working on ways to curb that acidity to make the vaccine material more stable.
“We have ongoing research that has produced some really, really exciting results about their stability and [shows] that you’re able to maintain really sensitive vaccines, stable for a good period of time,” says study author Morteza Sarmadi, PhD, a research specialist at the Koch Institute.
The potential public health impact
This research, funded by the Bill & Melinda Gates Foundation, started with the developing world in mind.
“The intent was actually helping people in the developing world, because a lot of times, people don’t come back for a second injection,” says study author Robert Langer, ScD, the David H. Koch Institute professor at MIT.
But a one-shot plan could benefit the developed world, too. One reason is that self-boosting vaccines could help those who get one achieve higher antibody responses than they would with just one dose. That could mean more protection for the person and the population, because as people develop stronger immunity, germs may have less of a chance to evolve and spread.
Take the COVID-19 pandemic, for example. Only 67% of Americans are fully vaccinated, and most people eligible for first and second boosters haven’t gotten them. New variants, such as the recent Omicron ones, continue to emerge and infect.
“I think those variants would have had a lot less chance to come about if everybody that had gotten vaccinated the first time got repeat injections, which they didn’t,” says Dr. Langer.
Self-boosting vaccines could also benefit infants, children who fear shots, and older adults who have a hard time getting health care.
Also, because the vaccine material is encapsulated and its release can be staggered, this technology might help people receive multiple vaccines at the same time that must now be given separately.
What comes next
The team is testing self-boosting polio and hepatitis vaccines in non-human primates. A small trial in healthy humans might follow within the next few years.
“We think that there’s really high potential for this technology, and we hope it can be developed and get to the human phase very soon,” says Dr. Jaklenec.
In smaller animal models, they are exploring the potential of self-boosting mRNA vaccines. They’re also working with scientists who are studying HIV vaccines.
“There has been some recent progress where very complex regimens seem to be working, but they’re not practical,” says Dr. Jaklenec. “And so, this is where this particular technology could be useful, because you have to prime and boost with different things, and this allows you to do that.”
This system could also extend beyond vaccines and be used to deliver cancer therapies, hormones, and biologics in a shot.
Through new work with researchers at Georgia Tech University, the team will study the potential of giving self-boosting vaccines through 3D-printed microneedles. These vaccines, which would stick on your skin like a bandage, could be self-administered and deployed globally in response to local outbreaks.
A version of this article first appeared on WebMD.com.
FROM SCIENCE ADVANCES
Thoracic Oncology & Chest Procedures Network
Interventional Procedures Section
Mind the gap: Improving adherence to lung cancer screening follow-up
The gap in adherence rates between a disciplined clinical trial and the heterogenous patchwork of U.S. health care is hardly unusual, but as lung cancer remains the number one cancer killer both worldwide and in the United States, one such disparity bears closer scrutiny.
In 2011, the National Lung Screening Trial (NLST) demonstrated a 20% reduction in lung cancer mortality with the implementation of low dose CT scan screening with 95% adherence to CT scan follow-up within 15 months of initial screening imaging (Aberle, et al. N Engl J Med. 2011;365[5]:395-409). Unfortunately, estimates of real-world adherence to lung cancer screening (LCS) follow-up fall to 51% even within an extended 18-month window (Hirsch, et al. Ann Am Thorac Soc. 2019;16[10]:1329-32).
Recent studies compared adherence to LCS follow-up between centralized and decentralized screening programs. Centralized programs used dedicated program coordinators and a tracking system, while decentralized programs relied on primary care providers.(Sakoda, et al. JAMA Network Open. 2021;4[4]:e218559). A subsequent study demonstrated adherence of 70% vs 41% among patients in centralized vs decentralized programs, respectively (Smith, et al. Chest. 2022;161[3]:818-25).
This gap is even more pronounced in majority-Black populations. Kunitomo and colleagues showed 33% lower odds of adherence to LCS follow-up compared with White patients (Kunitomo, et al. Chest. 2022;161[1]:266-75). Another study in a diverse, majority-Black patient population showed only 31% adherence to LCS follow-up at 1 year (Erkmen, et al. Cancer Causes Control. 2021;32[3]:291-8).
How could we close this gap? Centralized LCS programs show promise of increasing adherence to LCS follow-up. Heightened awareness of and targeted investment to mitigate racial inequities in LCS is imperative.
Jose De Cardenas MD
John Howe, MD
Members-at-Large
Interventional Procedures Section
Mind the gap: Improving adherence to lung cancer screening follow-up
The gap in adherence rates between a disciplined clinical trial and the heterogenous patchwork of U.S. health care is hardly unusual, but as lung cancer remains the number one cancer killer both worldwide and in the United States, one such disparity bears closer scrutiny.
In 2011, the National Lung Screening Trial (NLST) demonstrated a 20% reduction in lung cancer mortality with the implementation of low dose CT scan screening with 95% adherence to CT scan follow-up within 15 months of initial screening imaging (Aberle, et al. N Engl J Med. 2011;365[5]:395-409). Unfortunately, estimates of real-world adherence to lung cancer screening (LCS) follow-up fall to 51% even within an extended 18-month window (Hirsch, et al. Ann Am Thorac Soc. 2019;16[10]:1329-32).
Recent studies compared adherence to LCS follow-up between centralized and decentralized screening programs. Centralized programs used dedicated program coordinators and a tracking system, while decentralized programs relied on primary care providers.(Sakoda, et al. JAMA Network Open. 2021;4[4]:e218559). A subsequent study demonstrated adherence of 70% vs 41% among patients in centralized vs decentralized programs, respectively (Smith, et al. Chest. 2022;161[3]:818-25).
This gap is even more pronounced in majority-Black populations. Kunitomo and colleagues showed 33% lower odds of adherence to LCS follow-up compared with White patients (Kunitomo, et al. Chest. 2022;161[1]:266-75). Another study in a diverse, majority-Black patient population showed only 31% adherence to LCS follow-up at 1 year (Erkmen, et al. Cancer Causes Control. 2021;32[3]:291-8).
How could we close this gap? Centralized LCS programs show promise of increasing adherence to LCS follow-up. Heightened awareness of and targeted investment to mitigate racial inequities in LCS is imperative.
Jose De Cardenas MD
John Howe, MD
Members-at-Large
Interventional Procedures Section
Mind the gap: Improving adherence to lung cancer screening follow-up
The gap in adherence rates between a disciplined clinical trial and the heterogenous patchwork of U.S. health care is hardly unusual, but as lung cancer remains the number one cancer killer both worldwide and in the United States, one such disparity bears closer scrutiny.
In 2011, the National Lung Screening Trial (NLST) demonstrated a 20% reduction in lung cancer mortality with the implementation of low dose CT scan screening with 95% adherence to CT scan follow-up within 15 months of initial screening imaging (Aberle, et al. N Engl J Med. 2011;365[5]:395-409). Unfortunately, estimates of real-world adherence to lung cancer screening (LCS) follow-up fall to 51% even within an extended 18-month window (Hirsch, et al. Ann Am Thorac Soc. 2019;16[10]:1329-32).
Recent studies compared adherence to LCS follow-up between centralized and decentralized screening programs. Centralized programs used dedicated program coordinators and a tracking system, while decentralized programs relied on primary care providers.(Sakoda, et al. JAMA Network Open. 2021;4[4]:e218559). A subsequent study demonstrated adherence of 70% vs 41% among patients in centralized vs decentralized programs, respectively (Smith, et al. Chest. 2022;161[3]:818-25).
This gap is even more pronounced in majority-Black populations. Kunitomo and colleagues showed 33% lower odds of adherence to LCS follow-up compared with White patients (Kunitomo, et al. Chest. 2022;161[1]:266-75). Another study in a diverse, majority-Black patient population showed only 31% adherence to LCS follow-up at 1 year (Erkmen, et al. Cancer Causes Control. 2021;32[3]:291-8).
How could we close this gap? Centralized LCS programs show promise of increasing adherence to LCS follow-up. Heightened awareness of and targeted investment to mitigate racial inequities in LCS is imperative.
Jose De Cardenas MD
John Howe, MD
Members-at-Large





