User login
Cardiogenic shock teams again tied to lower mortality
A large multicenter study provides further evidence supporting the rationale for multidisciplinary teams for cardiogenic shock, one of the most lethal diseases in cardiovascular medicine.
The analysis of 24 critical care ICUs in the Critical Care Cardiology Trials Network showed that the presence of a shock team was independently associated with a 28% lower risk for CICU mortality (23% vs. 29%; odds ratio, 0.72; P = .016).
Patients treated by a shock team also had significantly shorter CICU stays and less need for mechanical ventilation or renal replacement therapy, as reported in the Journal of the American College of Cardiology.
“It’s observational, but the association that we’re seeing here, just because of our sample size, is the strongest that’s been published yet,” lead author Alexander Papolos, MD, MedStar Washington Hospital Center, said in an interview.
Although a causal relationship cannot be drawn, the authors suggest several factors that could explain the findings, including a shock team’s ability to rapidly diagnose and treat cardiogenic shock before multiorgan dysfunction occurs.
Centers with shock teams also used significantly more pulmonary artery catheters (60% vs. 49%; adjusted OR, 1.86; P < .001) and placed them earlier (0.3 vs. 0.66 days; P = .019).
Pulmonary artery catheter (PAC) use has declined after earlier trials like ESCAPE showed little or no benefit in other acutely ill patient groups, but positive results have been reported recently in cardiogenic shock, where a PAC is needed to determine the severity of the lesion and the phenotype, Dr. Papolos observed.
A 2018 study showed PAC use was tied to increased survival among patients with acute myocardial infarction cardiogenic shock (AMI-CS) supported with the Impella (Abiomed) device. Additionally, a 2021 study by the Cardiogenic Shock Working Group demonstrated a dose-dependent survival response based on the completeness of hemodynamic assessment by PAC prior to initiating mechanical circulatory support (MCS).
A third factor might be that a structured, team-based evaluation can facilitate timely and optimal MCS device selection, deployment, and management, suggested Dr. Papolos.
Centers with shock teams used more advanced types of MCS – defined as Impella, TandemHeart (LivaNova), extracorporeal membrane oxygenation, and temporary or durable surgical ventricular assist devices – than those without a shock team (53% vs. 43%; adjusted OR, 1.73; P = .005) and did so more often as the initial device (42% vs. 28%; P = .002).
Overall MCS use was lower at shock team centers (35% vs. 43%), driven by less frequent use of intra-aortic balloon pumps (58% vs. 72%).
“The standard, basic MCS has always been the balloon pump because it’s something that’s easy to put in at the cath lab or at the bedside,” Dr. Papolos said. “So, if you take away having all of the information and having the right people at the table to discuss what the best level of support is, then you’re going to end up with balloon pumps, and that’s what we saw here.”
The study involved 6,872 consecutive medical admissions at 24 level 1 CICU centers during an annual 2-month period from 2017 to 2019. Of these, 1,242 admissions were for cardiogenic shock and 546 (44%) were treated at one of 10 centers with a shock team.
Shock team centers had higher-acuity patients than centers without a shock team (Sequential Organ Failure Assessment score, 4 vs. 3) but a similar proportion of patients with AMI-CS (27% vs. 28%).
Among all admissions, CICU mortality was not significantly different between centers with and without a shock team.
For cardiogenic shock patients treated at centers with and without a shock team, the median CICU stay was 4.0 and 5.1 days, respectively, mechanical ventilation was used in 41% and 52%, respectively, and new renal replacement therapy in 11% and 19%, respectively (P < .001 for all).
Shock team centers used significantly more PACs for AMI-CS and non–AMI-CS admissions; advanced MCS therapy was also greater in the AMI-CS subgroup.
Lower CICU mortality at shock team centers persisted among patients with non-AMI-CS (adjusted OR, 0.67; P = .017) and AMI-CS (adjusted OR, 0.79; P = .344).
“This analysis supports that all AHA level 1 cardiac ICUs should strongly consider having a shock team,” Dr. Papolos said.
Evidence from single centers and the National Cardiogenic Shock Initiative has shown improved survival with a cardiogenic shock algorithm, but this is the first report specifically comparing no shock teams with shock teams, Perwaiz Meraj, MD, Northwell Health, Manhansett, N.Y., told this news organization.
“People may say that it’s just another paper that’s saying, ‘shock teams, shock teams, rah, rah, rah,’ but it’s important for all of us to really take a close look under the covers and see how are we best managing these patients, what teams are we putting together, and to create systems of care, where if you’re at a center that really doesn’t have the capabilities of doing this, then you should partner up with a center that does,” he said.
Notably, the 10 shock teams were present only in medium or large urban, academic medical centers with more than 500 beds. Although they followed individual protocols, survey results show service-line representation, structure, and operations were similar across centers.
They all had a centralized way to activate the shock team, the service was 24/7, and members came from areas such as critical care cardiology (100%), cardiac surgery (100%), interventional cardiology (90%), advanced heart failure (80%), and extracorporeal membrane oxygenation service (70%).
Limitations of the study include the possibility of residual confounding, the fact that the registry did not capture patients with cardiogenic shock managed outside the CICU or the time of onset of cardiogenic shock, and data were limited on inotropic strategies, sedation practices, and ventilator management, the authors wrote.
“Although many critics will continue to discuss the lack of randomized controlled trials in cardiogenic shock, this paper supports the process previously outlined of a multidisciplinary team-based approach improving survival,” Dr. Meraj and William W. O’Neill, MD, director of the Center for Structural Heart Disease and Henry Ford Health System, Detroit, and the force behind the National Cardiogenic Shock Initiative, wrote in an accompanying editorial.
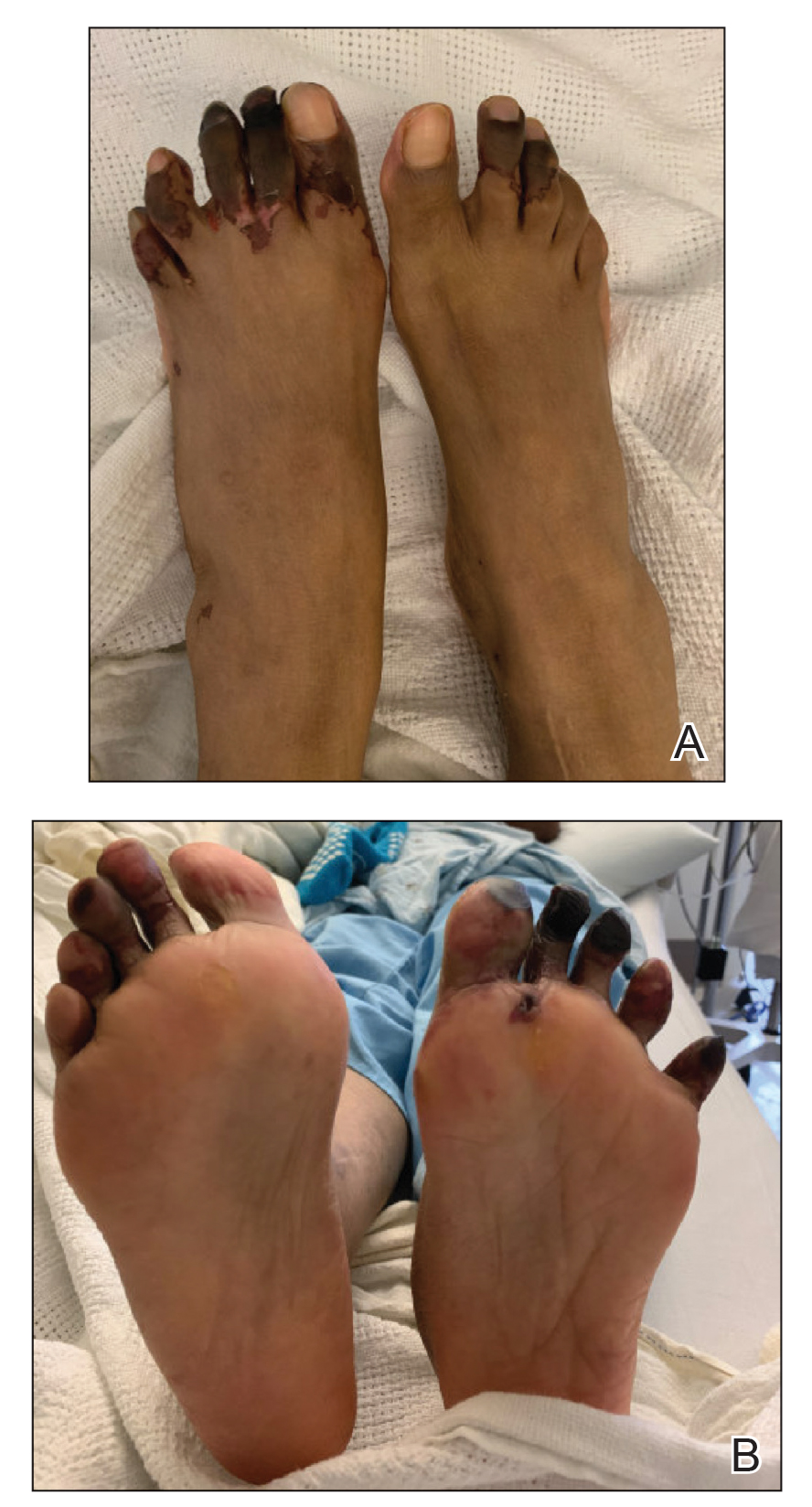
They point out that the report doesn’t address the escalation of care based on invasive hemodynamics in the CICU and the protocols to prevent acute vascular/limb complications (ALI) that can arise from the use of MCS.
“Many procedural techniques and novel CICU models exist to mitigate the risk of ALI in CS patients with MCS,” they wrote. “Finally, escalation of care and support is vital to the continued success of any shock team and center.”
One coauthor has served as a consultant to Abbott. Another has served as a consultant to the Abiomed critical care advisory board. All other authors reported having no relevant financial relationships. Dr. Meraj has received research and grant funding from Abiomed, Medtronic, CSI, and Boston Scientific. Dr. O’Neill has received consulting/speaker honoraria from Abiomed, Boston Scientific, and Abbott.
A version of this article first appeared on Medscape.com.
A large multicenter study provides further evidence supporting the rationale for multidisciplinary teams for cardiogenic shock, one of the most lethal diseases in cardiovascular medicine.
The analysis of 24 critical care ICUs in the Critical Care Cardiology Trials Network showed that the presence of a shock team was independently associated with a 28% lower risk for CICU mortality (23% vs. 29%; odds ratio, 0.72; P = .016).
Patients treated by a shock team also had significantly shorter CICU stays and less need for mechanical ventilation or renal replacement therapy, as reported in the Journal of the American College of Cardiology.
“It’s observational, but the association that we’re seeing here, just because of our sample size, is the strongest that’s been published yet,” lead author Alexander Papolos, MD, MedStar Washington Hospital Center, said in an interview.
Although a causal relationship cannot be drawn, the authors suggest several factors that could explain the findings, including a shock team’s ability to rapidly diagnose and treat cardiogenic shock before multiorgan dysfunction occurs.
Centers with shock teams also used significantly more pulmonary artery catheters (60% vs. 49%; adjusted OR, 1.86; P < .001) and placed them earlier (0.3 vs. 0.66 days; P = .019).
Pulmonary artery catheter (PAC) use has declined after earlier trials like ESCAPE showed little or no benefit in other acutely ill patient groups, but positive results have been reported recently in cardiogenic shock, where a PAC is needed to determine the severity of the lesion and the phenotype, Dr. Papolos observed.
A 2018 study showed PAC use was tied to increased survival among patients with acute myocardial infarction cardiogenic shock (AMI-CS) supported with the Impella (Abiomed) device. Additionally, a 2021 study by the Cardiogenic Shock Working Group demonstrated a dose-dependent survival response based on the completeness of hemodynamic assessment by PAC prior to initiating mechanical circulatory support (MCS).
A third factor might be that a structured, team-based evaluation can facilitate timely and optimal MCS device selection, deployment, and management, suggested Dr. Papolos.
Centers with shock teams used more advanced types of MCS – defined as Impella, TandemHeart (LivaNova), extracorporeal membrane oxygenation, and temporary or durable surgical ventricular assist devices – than those without a shock team (53% vs. 43%; adjusted OR, 1.73; P = .005) and did so more often as the initial device (42% vs. 28%; P = .002).
Overall MCS use was lower at shock team centers (35% vs. 43%), driven by less frequent use of intra-aortic balloon pumps (58% vs. 72%).
“The standard, basic MCS has always been the balloon pump because it’s something that’s easy to put in at the cath lab or at the bedside,” Dr. Papolos said. “So, if you take away having all of the information and having the right people at the table to discuss what the best level of support is, then you’re going to end up with balloon pumps, and that’s what we saw here.”
The study involved 6,872 consecutive medical admissions at 24 level 1 CICU centers during an annual 2-month period from 2017 to 2019. Of these, 1,242 admissions were for cardiogenic shock and 546 (44%) were treated at one of 10 centers with a shock team.
Shock team centers had higher-acuity patients than centers without a shock team (Sequential Organ Failure Assessment score, 4 vs. 3) but a similar proportion of patients with AMI-CS (27% vs. 28%).
Among all admissions, CICU mortality was not significantly different between centers with and without a shock team.
For cardiogenic shock patients treated at centers with and without a shock team, the median CICU stay was 4.0 and 5.1 days, respectively, mechanical ventilation was used in 41% and 52%, respectively, and new renal replacement therapy in 11% and 19%, respectively (P < .001 for all).
Shock team centers used significantly more PACs for AMI-CS and non–AMI-CS admissions; advanced MCS therapy was also greater in the AMI-CS subgroup.
Lower CICU mortality at shock team centers persisted among patients with non-AMI-CS (adjusted OR, 0.67; P = .017) and AMI-CS (adjusted OR, 0.79; P = .344).
“This analysis supports that all AHA level 1 cardiac ICUs should strongly consider having a shock team,” Dr. Papolos said.
Evidence from single centers and the National Cardiogenic Shock Initiative has shown improved survival with a cardiogenic shock algorithm, but this is the first report specifically comparing no shock teams with shock teams, Perwaiz Meraj, MD, Northwell Health, Manhansett, N.Y., told this news organization.
“People may say that it’s just another paper that’s saying, ‘shock teams, shock teams, rah, rah, rah,’ but it’s important for all of us to really take a close look under the covers and see how are we best managing these patients, what teams are we putting together, and to create systems of care, where if you’re at a center that really doesn’t have the capabilities of doing this, then you should partner up with a center that does,” he said.
Notably, the 10 shock teams were present only in medium or large urban, academic medical centers with more than 500 beds. Although they followed individual protocols, survey results show service-line representation, structure, and operations were similar across centers.
They all had a centralized way to activate the shock team, the service was 24/7, and members came from areas such as critical care cardiology (100%), cardiac surgery (100%), interventional cardiology (90%), advanced heart failure (80%), and extracorporeal membrane oxygenation service (70%).
Limitations of the study include the possibility of residual confounding, the fact that the registry did not capture patients with cardiogenic shock managed outside the CICU or the time of onset of cardiogenic shock, and data were limited on inotropic strategies, sedation practices, and ventilator management, the authors wrote.
“Although many critics will continue to discuss the lack of randomized controlled trials in cardiogenic shock, this paper supports the process previously outlined of a multidisciplinary team-based approach improving survival,” Dr. Meraj and William W. O’Neill, MD, director of the Center for Structural Heart Disease and Henry Ford Health System, Detroit, and the force behind the National Cardiogenic Shock Initiative, wrote in an accompanying editorial.
They point out that the report doesn’t address the escalation of care based on invasive hemodynamics in the CICU and the protocols to prevent acute vascular/limb complications (ALI) that can arise from the use of MCS.
“Many procedural techniques and novel CICU models exist to mitigate the risk of ALI in CS patients with MCS,” they wrote. “Finally, escalation of care and support is vital to the continued success of any shock team and center.”
One coauthor has served as a consultant to Abbott. Another has served as a consultant to the Abiomed critical care advisory board. All other authors reported having no relevant financial relationships. Dr. Meraj has received research and grant funding from Abiomed, Medtronic, CSI, and Boston Scientific. Dr. O’Neill has received consulting/speaker honoraria from Abiomed, Boston Scientific, and Abbott.
A version of this article first appeared on Medscape.com.
A large multicenter study provides further evidence supporting the rationale for multidisciplinary teams for cardiogenic shock, one of the most lethal diseases in cardiovascular medicine.
The analysis of 24 critical care ICUs in the Critical Care Cardiology Trials Network showed that the presence of a shock team was independently associated with a 28% lower risk for CICU mortality (23% vs. 29%; odds ratio, 0.72; P = .016).
Patients treated by a shock team also had significantly shorter CICU stays and less need for mechanical ventilation or renal replacement therapy, as reported in the Journal of the American College of Cardiology.
“It’s observational, but the association that we’re seeing here, just because of our sample size, is the strongest that’s been published yet,” lead author Alexander Papolos, MD, MedStar Washington Hospital Center, said in an interview.
Although a causal relationship cannot be drawn, the authors suggest several factors that could explain the findings, including a shock team’s ability to rapidly diagnose and treat cardiogenic shock before multiorgan dysfunction occurs.
Centers with shock teams also used significantly more pulmonary artery catheters (60% vs. 49%; adjusted OR, 1.86; P < .001) and placed them earlier (0.3 vs. 0.66 days; P = .019).
Pulmonary artery catheter (PAC) use has declined after earlier trials like ESCAPE showed little or no benefit in other acutely ill patient groups, but positive results have been reported recently in cardiogenic shock, where a PAC is needed to determine the severity of the lesion and the phenotype, Dr. Papolos observed.
A 2018 study showed PAC use was tied to increased survival among patients with acute myocardial infarction cardiogenic shock (AMI-CS) supported with the Impella (Abiomed) device. Additionally, a 2021 study by the Cardiogenic Shock Working Group demonstrated a dose-dependent survival response based on the completeness of hemodynamic assessment by PAC prior to initiating mechanical circulatory support (MCS).
A third factor might be that a structured, team-based evaluation can facilitate timely and optimal MCS device selection, deployment, and management, suggested Dr. Papolos.
Centers with shock teams used more advanced types of MCS – defined as Impella, TandemHeart (LivaNova), extracorporeal membrane oxygenation, and temporary or durable surgical ventricular assist devices – than those without a shock team (53% vs. 43%; adjusted OR, 1.73; P = .005) and did so more often as the initial device (42% vs. 28%; P = .002).
Overall MCS use was lower at shock team centers (35% vs. 43%), driven by less frequent use of intra-aortic balloon pumps (58% vs. 72%).
“The standard, basic MCS has always been the balloon pump because it’s something that’s easy to put in at the cath lab or at the bedside,” Dr. Papolos said. “So, if you take away having all of the information and having the right people at the table to discuss what the best level of support is, then you’re going to end up with balloon pumps, and that’s what we saw here.”
The study involved 6,872 consecutive medical admissions at 24 level 1 CICU centers during an annual 2-month period from 2017 to 2019. Of these, 1,242 admissions were for cardiogenic shock and 546 (44%) were treated at one of 10 centers with a shock team.
Shock team centers had higher-acuity patients than centers without a shock team (Sequential Organ Failure Assessment score, 4 vs. 3) but a similar proportion of patients with AMI-CS (27% vs. 28%).
Among all admissions, CICU mortality was not significantly different between centers with and without a shock team.
For cardiogenic shock patients treated at centers with and without a shock team, the median CICU stay was 4.0 and 5.1 days, respectively, mechanical ventilation was used in 41% and 52%, respectively, and new renal replacement therapy in 11% and 19%, respectively (P < .001 for all).
Shock team centers used significantly more PACs for AMI-CS and non–AMI-CS admissions; advanced MCS therapy was also greater in the AMI-CS subgroup.
Lower CICU mortality at shock team centers persisted among patients with non-AMI-CS (adjusted OR, 0.67; P = .017) and AMI-CS (adjusted OR, 0.79; P = .344).
“This analysis supports that all AHA level 1 cardiac ICUs should strongly consider having a shock team,” Dr. Papolos said.
Evidence from single centers and the National Cardiogenic Shock Initiative has shown improved survival with a cardiogenic shock algorithm, but this is the first report specifically comparing no shock teams with shock teams, Perwaiz Meraj, MD, Northwell Health, Manhansett, N.Y., told this news organization.
“People may say that it’s just another paper that’s saying, ‘shock teams, shock teams, rah, rah, rah,’ but it’s important for all of us to really take a close look under the covers and see how are we best managing these patients, what teams are we putting together, and to create systems of care, where if you’re at a center that really doesn’t have the capabilities of doing this, then you should partner up with a center that does,” he said.
Notably, the 10 shock teams were present only in medium or large urban, academic medical centers with more than 500 beds. Although they followed individual protocols, survey results show service-line representation, structure, and operations were similar across centers.
They all had a centralized way to activate the shock team, the service was 24/7, and members came from areas such as critical care cardiology (100%), cardiac surgery (100%), interventional cardiology (90%), advanced heart failure (80%), and extracorporeal membrane oxygenation service (70%).
Limitations of the study include the possibility of residual confounding, the fact that the registry did not capture patients with cardiogenic shock managed outside the CICU or the time of onset of cardiogenic shock, and data were limited on inotropic strategies, sedation practices, and ventilator management, the authors wrote.
“Although many critics will continue to discuss the lack of randomized controlled trials in cardiogenic shock, this paper supports the process previously outlined of a multidisciplinary team-based approach improving survival,” Dr. Meraj and William W. O’Neill, MD, director of the Center for Structural Heart Disease and Henry Ford Health System, Detroit, and the force behind the National Cardiogenic Shock Initiative, wrote in an accompanying editorial.
They point out that the report doesn’t address the escalation of care based on invasive hemodynamics in the CICU and the protocols to prevent acute vascular/limb complications (ALI) that can arise from the use of MCS.
“Many procedural techniques and novel CICU models exist to mitigate the risk of ALI in CS patients with MCS,” they wrote. “Finally, escalation of care and support is vital to the continued success of any shock team and center.”
One coauthor has served as a consultant to Abbott. Another has served as a consultant to the Abiomed critical care advisory board. All other authors reported having no relevant financial relationships. Dr. Meraj has received research and grant funding from Abiomed, Medtronic, CSI, and Boston Scientific. Dr. O’Neill has received consulting/speaker honoraria from Abiomed, Boston Scientific, and Abbott.
A version of this article first appeared on Medscape.com.
Consensus statement warns against acetaminophen use during pregnancy
Pregnant women should use paracetamol/acetaminophen only with a medical indication and at the lowest effective dose for the shortest possible time, according to an international consensus statement published online Sept. 23 in Nature Reviews Endocrinology.
With global rates of use high and risks considered negligible, the expert panel of 13 U.S. and European authors call for focused research into how this analgesic and febrifuge may impair fetal development and lead to adverse outcomes in children. They outline several precautionary measures to be taken in the meantime.
According to first author and epidemiologist Ann Z. Bauer, ScD, a postdoctoral research fellow at the University of Massachusetts in Lowell, and colleagues, this drug is used by an estimated 65% of pregnant women in the United States, and more than 50% worldwide. It is currently the active ingredient in more than 600 prescription and nonprescription medications, including Tylenol, which historically has been deemed safe in all trimesters of pregnancy.
But a growing body of experimental and epidemiological evidence suggests prenatal exposure to paracetamol (N-acetyl-p-aminophenol, or APAP) might alter fetal development and elevate the risks of neurodevelopmental, reproductive and urogenital disorders in both sexes. Exposure in utero has been linked, for example, to potential behavioral problems in children.
The new recommendations are based on a review of experimental animal and cell-based research as well as human epidemiological data published from January 1995 to October 2020. The authors include clinicians, epidemiologists, and scientists specializing in toxicology, endocrinology, reproductive medicine and neurodevelopment.
Recommendations
Although the new guidance does not differ markedly from current advice, the authors believe stronger communication and greater awareness of risks are needed. In addition to restricting use of this medication to low doses for short periods when medically necessary, expectant mothers should receive counseling before conception or early in pregnancy. If uncertain about its use, they should consult their physicians or pharmacists.
In other recommendations, the panel said:
- The 2015 FDA Drug Safety Communication recommendations should be updated based on evaluation of all available scientific evidence.
- The European Medicines Agency Pharmacovigilance Risk Assessment Committee should review the most recent epidemiologic and experimental research and issue an updated Drug Safety Communication.
- Obstetric and gynecological associations should update their guidance after reviewing all available research.
- The Acetaminophen Awareness Coalition (“Know Your Dose” Campaign) should add standardized warnings and specifically advise pregnant women to forgo APAP unless it’s medically indicated.
- All sales of APAP-containing medications should be accompanied by recommendations specifically for use in pregnancy. This information should include warning labels on packaging, and if possible, APAP should be sold only in pharmacies (as in France).
Mechanism of action
APAP is an endocrine disruptor (Neuroscientist. 2020 Sep 11. doi: 10.1177/1073858420952046). “Chemicals that disrupt the endocrine system are concerning because they can interfere with the activity of endogenous hormones that are essential for healthy neurological, urogenital, and reproductive development,” researchers wrote.
“The precise mechanism is not clear but its toxicity is thought to be due mainly to hormone disruption,” Dr. Bauer said in an interview.
Moreover, APAP readily crosses the placenta and blood–brain barrier, and changes in APAP metabolism during pregnancy might make women and their fetuses more vulnerable to its toxic effects. For instance, the molar dose fraction of APAP converted to the oxidative metabolite N-acetyl-p-benzoquinone imine increases during pregnancy. In addition to its hepatotoxicity, this poisonous byproduct is thought to be a genotoxin that increases DNA cleavage by acting on the enzyme topoisomerase II.
Asked for her perspective on the statement, Kjersti Aagaard, MD, PhD, a professor of obstetrics and gynecology at Baylor College of Medicine and Texas Children’s Hospital in Houston, called the expert panel’s statement thoughtful and comprehensive, but she urged caution in interpreting the role of acetaminophen.
The challenge in linking any commonly used medication to adverse effects and congenital defects, she said, is “teasing out an association from causation. Given the commonality of the use of acetaminophen with the relative rarity of the outcomes, it is clear that not all cases of exposure result in adverse outcomes.”
As for judicious use, she said, one would be to reduce a high fever, which can cause miscarriage, neural tube defects, and potential heart disease in adulthood. Acetaminophen is the drug of choice in this case since nonsteroidal anti-inflammatory drugs such as ibuprofen are not recommended owing to their known risks to the fetal heart.
Dr. Aagaard emphasized that while acetaminophen use is temporally associated with learning and behavioral problems, and urogenital disorders at birth in male infants such as like hypospadias, so is exposure to multiple environmental chemicals and pollutants, as well as climate change. “It would be a real mistake with real life implications if we associated any congenital disease or disorder with a commonly used medication with known benefits if the true causal link lies elsewhere.”
She said the precautionary statements fall into the time-honored therapeutic principle of first do no harm. “However, the call for research action must be undertaken earnestly and sincerely.”
According to Dr. Bauer, the statement’s essential take-home message is that “physicians should educate themselves and educate women about what we’re learning about the risks of acetaminophen in pregnancy.” Risk can be minimized by using the lowest effective dose for the shortest time and only when medically indicated. “Pregnant women should speak to their physicians about acetaminophen. It’s about empowerment and making smart decisions,” she said.
This study received no specific funding. Coauthor Dr. R.T. Mitchell is supported by a UK Research Institute fellowship.
Pregnant women should use paracetamol/acetaminophen only with a medical indication and at the lowest effective dose for the shortest possible time, according to an international consensus statement published online Sept. 23 in Nature Reviews Endocrinology.
With global rates of use high and risks considered negligible, the expert panel of 13 U.S. and European authors call for focused research into how this analgesic and febrifuge may impair fetal development and lead to adverse outcomes in children. They outline several precautionary measures to be taken in the meantime.
According to first author and epidemiologist Ann Z. Bauer, ScD, a postdoctoral research fellow at the University of Massachusetts in Lowell, and colleagues, this drug is used by an estimated 65% of pregnant women in the United States, and more than 50% worldwide. It is currently the active ingredient in more than 600 prescription and nonprescription medications, including Tylenol, which historically has been deemed safe in all trimesters of pregnancy.
But a growing body of experimental and epidemiological evidence suggests prenatal exposure to paracetamol (N-acetyl-p-aminophenol, or APAP) might alter fetal development and elevate the risks of neurodevelopmental, reproductive and urogenital disorders in both sexes. Exposure in utero has been linked, for example, to potential behavioral problems in children.
The new recommendations are based on a review of experimental animal and cell-based research as well as human epidemiological data published from January 1995 to October 2020. The authors include clinicians, epidemiologists, and scientists specializing in toxicology, endocrinology, reproductive medicine and neurodevelopment.
Recommendations
Although the new guidance does not differ markedly from current advice, the authors believe stronger communication and greater awareness of risks are needed. In addition to restricting use of this medication to low doses for short periods when medically necessary, expectant mothers should receive counseling before conception or early in pregnancy. If uncertain about its use, they should consult their physicians or pharmacists.
In other recommendations, the panel said:
- The 2015 FDA Drug Safety Communication recommendations should be updated based on evaluation of all available scientific evidence.
- The European Medicines Agency Pharmacovigilance Risk Assessment Committee should review the most recent epidemiologic and experimental research and issue an updated Drug Safety Communication.
- Obstetric and gynecological associations should update their guidance after reviewing all available research.
- The Acetaminophen Awareness Coalition (“Know Your Dose” Campaign) should add standardized warnings and specifically advise pregnant women to forgo APAP unless it’s medically indicated.
- All sales of APAP-containing medications should be accompanied by recommendations specifically for use in pregnancy. This information should include warning labels on packaging, and if possible, APAP should be sold only in pharmacies (as in France).
Mechanism of action
APAP is an endocrine disruptor (Neuroscientist. 2020 Sep 11. doi: 10.1177/1073858420952046). “Chemicals that disrupt the endocrine system are concerning because they can interfere with the activity of endogenous hormones that are essential for healthy neurological, urogenital, and reproductive development,” researchers wrote.
“The precise mechanism is not clear but its toxicity is thought to be due mainly to hormone disruption,” Dr. Bauer said in an interview.
Moreover, APAP readily crosses the placenta and blood–brain barrier, and changes in APAP metabolism during pregnancy might make women and their fetuses more vulnerable to its toxic effects. For instance, the molar dose fraction of APAP converted to the oxidative metabolite N-acetyl-p-benzoquinone imine increases during pregnancy. In addition to its hepatotoxicity, this poisonous byproduct is thought to be a genotoxin that increases DNA cleavage by acting on the enzyme topoisomerase II.
Asked for her perspective on the statement, Kjersti Aagaard, MD, PhD, a professor of obstetrics and gynecology at Baylor College of Medicine and Texas Children’s Hospital in Houston, called the expert panel’s statement thoughtful and comprehensive, but she urged caution in interpreting the role of acetaminophen.
The challenge in linking any commonly used medication to adverse effects and congenital defects, she said, is “teasing out an association from causation. Given the commonality of the use of acetaminophen with the relative rarity of the outcomes, it is clear that not all cases of exposure result in adverse outcomes.”
As for judicious use, she said, one would be to reduce a high fever, which can cause miscarriage, neural tube defects, and potential heart disease in adulthood. Acetaminophen is the drug of choice in this case since nonsteroidal anti-inflammatory drugs such as ibuprofen are not recommended owing to their known risks to the fetal heart.
Dr. Aagaard emphasized that while acetaminophen use is temporally associated with learning and behavioral problems, and urogenital disorders at birth in male infants such as like hypospadias, so is exposure to multiple environmental chemicals and pollutants, as well as climate change. “It would be a real mistake with real life implications if we associated any congenital disease or disorder with a commonly used medication with known benefits if the true causal link lies elsewhere.”
She said the precautionary statements fall into the time-honored therapeutic principle of first do no harm. “However, the call for research action must be undertaken earnestly and sincerely.”
According to Dr. Bauer, the statement’s essential take-home message is that “physicians should educate themselves and educate women about what we’re learning about the risks of acetaminophen in pregnancy.” Risk can be minimized by using the lowest effective dose for the shortest time and only when medically indicated. “Pregnant women should speak to their physicians about acetaminophen. It’s about empowerment and making smart decisions,” she said.
This study received no specific funding. Coauthor Dr. R.T. Mitchell is supported by a UK Research Institute fellowship.
Pregnant women should use paracetamol/acetaminophen only with a medical indication and at the lowest effective dose for the shortest possible time, according to an international consensus statement published online Sept. 23 in Nature Reviews Endocrinology.
With global rates of use high and risks considered negligible, the expert panel of 13 U.S. and European authors call for focused research into how this analgesic and febrifuge may impair fetal development and lead to adverse outcomes in children. They outline several precautionary measures to be taken in the meantime.
According to first author and epidemiologist Ann Z. Bauer, ScD, a postdoctoral research fellow at the University of Massachusetts in Lowell, and colleagues, this drug is used by an estimated 65% of pregnant women in the United States, and more than 50% worldwide. It is currently the active ingredient in more than 600 prescription and nonprescription medications, including Tylenol, which historically has been deemed safe in all trimesters of pregnancy.
But a growing body of experimental and epidemiological evidence suggests prenatal exposure to paracetamol (N-acetyl-p-aminophenol, or APAP) might alter fetal development and elevate the risks of neurodevelopmental, reproductive and urogenital disorders in both sexes. Exposure in utero has been linked, for example, to potential behavioral problems in children.
The new recommendations are based on a review of experimental animal and cell-based research as well as human epidemiological data published from January 1995 to October 2020. The authors include clinicians, epidemiologists, and scientists specializing in toxicology, endocrinology, reproductive medicine and neurodevelopment.
Recommendations
Although the new guidance does not differ markedly from current advice, the authors believe stronger communication and greater awareness of risks are needed. In addition to restricting use of this medication to low doses for short periods when medically necessary, expectant mothers should receive counseling before conception or early in pregnancy. If uncertain about its use, they should consult their physicians or pharmacists.
In other recommendations, the panel said:
- The 2015 FDA Drug Safety Communication recommendations should be updated based on evaluation of all available scientific evidence.
- The European Medicines Agency Pharmacovigilance Risk Assessment Committee should review the most recent epidemiologic and experimental research and issue an updated Drug Safety Communication.
- Obstetric and gynecological associations should update their guidance after reviewing all available research.
- The Acetaminophen Awareness Coalition (“Know Your Dose” Campaign) should add standardized warnings and specifically advise pregnant women to forgo APAP unless it’s medically indicated.
- All sales of APAP-containing medications should be accompanied by recommendations specifically for use in pregnancy. This information should include warning labels on packaging, and if possible, APAP should be sold only in pharmacies (as in France).
Mechanism of action
APAP is an endocrine disruptor (Neuroscientist. 2020 Sep 11. doi: 10.1177/1073858420952046). “Chemicals that disrupt the endocrine system are concerning because they can interfere with the activity of endogenous hormones that are essential for healthy neurological, urogenital, and reproductive development,” researchers wrote.
“The precise mechanism is not clear but its toxicity is thought to be due mainly to hormone disruption,” Dr. Bauer said in an interview.
Moreover, APAP readily crosses the placenta and blood–brain barrier, and changes in APAP metabolism during pregnancy might make women and their fetuses more vulnerable to its toxic effects. For instance, the molar dose fraction of APAP converted to the oxidative metabolite N-acetyl-p-benzoquinone imine increases during pregnancy. In addition to its hepatotoxicity, this poisonous byproduct is thought to be a genotoxin that increases DNA cleavage by acting on the enzyme topoisomerase II.
Asked for her perspective on the statement, Kjersti Aagaard, MD, PhD, a professor of obstetrics and gynecology at Baylor College of Medicine and Texas Children’s Hospital in Houston, called the expert panel’s statement thoughtful and comprehensive, but she urged caution in interpreting the role of acetaminophen.
The challenge in linking any commonly used medication to adverse effects and congenital defects, she said, is “teasing out an association from causation. Given the commonality of the use of acetaminophen with the relative rarity of the outcomes, it is clear that not all cases of exposure result in adverse outcomes.”
As for judicious use, she said, one would be to reduce a high fever, which can cause miscarriage, neural tube defects, and potential heart disease in adulthood. Acetaminophen is the drug of choice in this case since nonsteroidal anti-inflammatory drugs such as ibuprofen are not recommended owing to their known risks to the fetal heart.
Dr. Aagaard emphasized that while acetaminophen use is temporally associated with learning and behavioral problems, and urogenital disorders at birth in male infants such as like hypospadias, so is exposure to multiple environmental chemicals and pollutants, as well as climate change. “It would be a real mistake with real life implications if we associated any congenital disease or disorder with a commonly used medication with known benefits if the true causal link lies elsewhere.”
She said the precautionary statements fall into the time-honored therapeutic principle of first do no harm. “However, the call for research action must be undertaken earnestly and sincerely.”
According to Dr. Bauer, the statement’s essential take-home message is that “physicians should educate themselves and educate women about what we’re learning about the risks of acetaminophen in pregnancy.” Risk can be minimized by using the lowest effective dose for the shortest time and only when medically indicated. “Pregnant women should speak to their physicians about acetaminophen. It’s about empowerment and making smart decisions,” she said.
This study received no specific funding. Coauthor Dr. R.T. Mitchell is supported by a UK Research Institute fellowship.
Datopotamab deruxtecan for advanced NSCLC encouraging so far
according to Edward B. Garon, MD, of the University of California, Los Angeles. Prior results from TROPION-PanTumor01, have demonstrated similarly encouraging activity and a manageable safety profile for Dato-DXd, Dr. Garon said in a 2021 European Society for Medical Oncology Congress virtual oral presentation on Sept. 19 (abstract LBA49).
Limited benefit from existing treatments
Once tyrosine kinase inhibitors and platinum chemotherapy have failed, patients with advanced/metastatic NSCLC with AGAs (e.g., EGFR or ALK mutations) derive limited benefit from existing treatments, Dr. Garon observed. Datopotamab deruxtecan is an antibody-drug conjugate composed of a humanized anti-TROP2 monoclonal antibody conjugated to a potent topoisomerase I inhibitor payload via a stable tetrapeptide-based cleavable linker. TROP2 is highly expressed in NSCLC, regardless of genomic mutation status and has been associated with poor prognosis. Patients in TROPION-PanTumor01 were not selected based on TROP2 expression or AGA status, Dr. Garon noted.
TROPION-PanTumor01 (NCT03401385), an ongoing multicenter, open-label, dose-expansion study evaluating datopotamab deruxtecan in solid tumors, including NSCLC in 210 patients, is assessing safety, pharmacokinetics, antitumor activity, and biomarkers. All included patients (n = 180; median age, 62 years; 56% female) had progressed after standard treatment or had measurable disease and had no standard treatment available. Stable/treated brain metastases were permitted.
Subgroup with AGAs
The current report includes outcomes from the subgroup of 34 patients with AGAs, who were treated with 4 (n = 8), 6 (n = 10), and 8 mg/kg (n = 16) of datopotamab deruxtecan. AGAs were EGFR in 29 patients, ALK in 3, and ROS1 and RET in 1 each. Most patients (82%) had received three or more prior regimens; 85% had prior TKI, and among EGFR mutation patients, 69% had received osimertinib. Prior systemic treatment consisted of immunotherapy in 41%, platinum-based chemotherapy in 91%, and tyrosine kinase inhibitor in 85%. The primary objectives were to establish the maximum tolerated dose, safety, and tolerability. Efficacy was a secondary outcome.
Treatment-emergent adverse events were reported in all patients, with grade 3 or higher events in 53%. Most common were grade 1-2 nausea, stomatitis, fatigue, and alopecia. Drug-attributed events in 88% were grade 3 or higher in 38%. Treatment-emergent adverse events led to discontinuation in 15%, dose interruption in 27% and dose reductions in 15%. One case of grade 5 interstitial lung disease, in the 8-mg group, was adjudicated as drug related. “The safety profile of Dato-DXd was manageable and consistent with that observed in the overall NSCLC population in TROPION-PanTumor01,” Dr. Garon said, “and were primarily nonhematologic.”
The objective response rate was 35%, all partial responses. The stable disease rate was 41%; the progressive disease rate was 6%. Median duration of response was 9.5 months (95% confidence interval, 3.3-NE). Dr. Garon noted that clinical activity was observed in EGFR (Ex 19del, L858R) including after osimertinib and across other AGAs.
Further evaluation ongoing
Further evaluation of datopotamab deruxtecan is ongoing in the TROPION-Lung05 study among NSCLC patients with AGAs after targeted therapy and platinum-based chemotherapy options have been exhausted. Eligible AGAs include EGFR (including exon 20 insertions), ALK, ROS1, RET, BRAF, NTRK and MET exon 14 skipping.
Session moderator David Gandara, MD, University of California Davis Health, questioned the rationale for targeting oncogene driven cancers with this particular drug: “Is this just because this is felt to be an unmet need, or is there higher expression or some other biologic rationale?”
Dr. Garon responded, “Why are we looking at these driver mutation–positive patients? I think it has less to do with mechanism and more to do with the differences in treatment between these driver mutation positive patients and the rest of the population. This is a group of patients which has TROP2, but TROP2 expression is seen really across non–small cell lung cancer. But, in fact, one of the reasons it has been postulated that TROP2 is not a good biomarker for this class of drugs to date, is that its expression is so ubiquitous in the disease.”
The study was funded by Daiichi Sankyo. Dr. Garon disclosed numerous pharmaceutical-related financial interests.
This article was updated Sept. 24, 2021.
according to Edward B. Garon, MD, of the University of California, Los Angeles. Prior results from TROPION-PanTumor01, have demonstrated similarly encouraging activity and a manageable safety profile for Dato-DXd, Dr. Garon said in a 2021 European Society for Medical Oncology Congress virtual oral presentation on Sept. 19 (abstract LBA49).
Limited benefit from existing treatments
Once tyrosine kinase inhibitors and platinum chemotherapy have failed, patients with advanced/metastatic NSCLC with AGAs (e.g., EGFR or ALK mutations) derive limited benefit from existing treatments, Dr. Garon observed. Datopotamab deruxtecan is an antibody-drug conjugate composed of a humanized anti-TROP2 monoclonal antibody conjugated to a potent topoisomerase I inhibitor payload via a stable tetrapeptide-based cleavable linker. TROP2 is highly expressed in NSCLC, regardless of genomic mutation status and has been associated with poor prognosis. Patients in TROPION-PanTumor01 were not selected based on TROP2 expression or AGA status, Dr. Garon noted.
TROPION-PanTumor01 (NCT03401385), an ongoing multicenter, open-label, dose-expansion study evaluating datopotamab deruxtecan in solid tumors, including NSCLC in 210 patients, is assessing safety, pharmacokinetics, antitumor activity, and biomarkers. All included patients (n = 180; median age, 62 years; 56% female) had progressed after standard treatment or had measurable disease and had no standard treatment available. Stable/treated brain metastases were permitted.
Subgroup with AGAs
The current report includes outcomes from the subgroup of 34 patients with AGAs, who were treated with 4 (n = 8), 6 (n = 10), and 8 mg/kg (n = 16) of datopotamab deruxtecan. AGAs were EGFR in 29 patients, ALK in 3, and ROS1 and RET in 1 each. Most patients (82%) had received three or more prior regimens; 85% had prior TKI, and among EGFR mutation patients, 69% had received osimertinib. Prior systemic treatment consisted of immunotherapy in 41%, platinum-based chemotherapy in 91%, and tyrosine kinase inhibitor in 85%. The primary objectives were to establish the maximum tolerated dose, safety, and tolerability. Efficacy was a secondary outcome.
Treatment-emergent adverse events were reported in all patients, with grade 3 or higher events in 53%. Most common were grade 1-2 nausea, stomatitis, fatigue, and alopecia. Drug-attributed events in 88% were grade 3 or higher in 38%. Treatment-emergent adverse events led to discontinuation in 15%, dose interruption in 27% and dose reductions in 15%. One case of grade 5 interstitial lung disease, in the 8-mg group, was adjudicated as drug related. “The safety profile of Dato-DXd was manageable and consistent with that observed in the overall NSCLC population in TROPION-PanTumor01,” Dr. Garon said, “and were primarily nonhematologic.”
The objective response rate was 35%, all partial responses. The stable disease rate was 41%; the progressive disease rate was 6%. Median duration of response was 9.5 months (95% confidence interval, 3.3-NE). Dr. Garon noted that clinical activity was observed in EGFR (Ex 19del, L858R) including after osimertinib and across other AGAs.
Further evaluation ongoing
Further evaluation of datopotamab deruxtecan is ongoing in the TROPION-Lung05 study among NSCLC patients with AGAs after targeted therapy and platinum-based chemotherapy options have been exhausted. Eligible AGAs include EGFR (including exon 20 insertions), ALK, ROS1, RET, BRAF, NTRK and MET exon 14 skipping.
Session moderator David Gandara, MD, University of California Davis Health, questioned the rationale for targeting oncogene driven cancers with this particular drug: “Is this just because this is felt to be an unmet need, or is there higher expression or some other biologic rationale?”
Dr. Garon responded, “Why are we looking at these driver mutation–positive patients? I think it has less to do with mechanism and more to do with the differences in treatment between these driver mutation positive patients and the rest of the population. This is a group of patients which has TROP2, but TROP2 expression is seen really across non–small cell lung cancer. But, in fact, one of the reasons it has been postulated that TROP2 is not a good biomarker for this class of drugs to date, is that its expression is so ubiquitous in the disease.”
The study was funded by Daiichi Sankyo. Dr. Garon disclosed numerous pharmaceutical-related financial interests.
This article was updated Sept. 24, 2021.
according to Edward B. Garon, MD, of the University of California, Los Angeles. Prior results from TROPION-PanTumor01, have demonstrated similarly encouraging activity and a manageable safety profile for Dato-DXd, Dr. Garon said in a 2021 European Society for Medical Oncology Congress virtual oral presentation on Sept. 19 (abstract LBA49).
Limited benefit from existing treatments
Once tyrosine kinase inhibitors and platinum chemotherapy have failed, patients with advanced/metastatic NSCLC with AGAs (e.g., EGFR or ALK mutations) derive limited benefit from existing treatments, Dr. Garon observed. Datopotamab deruxtecan is an antibody-drug conjugate composed of a humanized anti-TROP2 monoclonal antibody conjugated to a potent topoisomerase I inhibitor payload via a stable tetrapeptide-based cleavable linker. TROP2 is highly expressed in NSCLC, regardless of genomic mutation status and has been associated with poor prognosis. Patients in TROPION-PanTumor01 were not selected based on TROP2 expression or AGA status, Dr. Garon noted.
TROPION-PanTumor01 (NCT03401385), an ongoing multicenter, open-label, dose-expansion study evaluating datopotamab deruxtecan in solid tumors, including NSCLC in 210 patients, is assessing safety, pharmacokinetics, antitumor activity, and biomarkers. All included patients (n = 180; median age, 62 years; 56% female) had progressed after standard treatment or had measurable disease and had no standard treatment available. Stable/treated brain metastases were permitted.
Subgroup with AGAs
The current report includes outcomes from the subgroup of 34 patients with AGAs, who were treated with 4 (n = 8), 6 (n = 10), and 8 mg/kg (n = 16) of datopotamab deruxtecan. AGAs were EGFR in 29 patients, ALK in 3, and ROS1 and RET in 1 each. Most patients (82%) had received three or more prior regimens; 85% had prior TKI, and among EGFR mutation patients, 69% had received osimertinib. Prior systemic treatment consisted of immunotherapy in 41%, platinum-based chemotherapy in 91%, and tyrosine kinase inhibitor in 85%. The primary objectives were to establish the maximum tolerated dose, safety, and tolerability. Efficacy was a secondary outcome.
Treatment-emergent adverse events were reported in all patients, with grade 3 or higher events in 53%. Most common were grade 1-2 nausea, stomatitis, fatigue, and alopecia. Drug-attributed events in 88% were grade 3 or higher in 38%. Treatment-emergent adverse events led to discontinuation in 15%, dose interruption in 27% and dose reductions in 15%. One case of grade 5 interstitial lung disease, in the 8-mg group, was adjudicated as drug related. “The safety profile of Dato-DXd was manageable and consistent with that observed in the overall NSCLC population in TROPION-PanTumor01,” Dr. Garon said, “and were primarily nonhematologic.”
The objective response rate was 35%, all partial responses. The stable disease rate was 41%; the progressive disease rate was 6%. Median duration of response was 9.5 months (95% confidence interval, 3.3-NE). Dr. Garon noted that clinical activity was observed in EGFR (Ex 19del, L858R) including after osimertinib and across other AGAs.
Further evaluation ongoing
Further evaluation of datopotamab deruxtecan is ongoing in the TROPION-Lung05 study among NSCLC patients with AGAs after targeted therapy and platinum-based chemotherapy options have been exhausted. Eligible AGAs include EGFR (including exon 20 insertions), ALK, ROS1, RET, BRAF, NTRK and MET exon 14 skipping.
Session moderator David Gandara, MD, University of California Davis Health, questioned the rationale for targeting oncogene driven cancers with this particular drug: “Is this just because this is felt to be an unmet need, or is there higher expression or some other biologic rationale?”
Dr. Garon responded, “Why are we looking at these driver mutation–positive patients? I think it has less to do with mechanism and more to do with the differences in treatment between these driver mutation positive patients and the rest of the population. This is a group of patients which has TROP2, but TROP2 expression is seen really across non–small cell lung cancer. But, in fact, one of the reasons it has been postulated that TROP2 is not a good biomarker for this class of drugs to date, is that its expression is so ubiquitous in the disease.”
The study was funded by Daiichi Sankyo. Dr. Garon disclosed numerous pharmaceutical-related financial interests.
This article was updated Sept. 24, 2021.
FROM ESMO 2021
TULIP trial shows extended survival in HER2+ metastatic breast cancer
, according to Cristina Saura Manich, MD, Hospital Universitario Valle de Hebrón, Barcelona. In TULIP, trastuzumab duocarmazine (SYD985, Byondis B.V., NL) was compared with physician’s choice of chemotherapy, Dr. Saura said at the virtual European Society for Medical Oncology Congress 2021 on Sept. 18 (abstract LBA15).
Trastuzumab duocarmazine, Dr. Manich noted, is a novel HER2-targeting antibody–drug conjugate based on trastuzumab and a cleavable linker-duocarmycin (vc-seco-DUBA) payload. Its three-way mechanism of action includes uptake of the antibody–drug conjugate by internalization and intracellular release of the payload, and two bystander effects: proteolytic cleavage and subsequent release of payload in the tumor microenvironment and diffusion of active payload to neighboring tumor cells.
Two or more prior therapies for metastatic breast cancer
TULIP investigators enrolled 437 patients from 83 sites in 11 countries with HER2-positive locally advanced or metastatic breast cancer who had received two or more therapies for metastatic disease (treatment for brain metastases allowed). They were randomized 2:1 to SYD985 (1.2 mg/kg IV every 21 days [n = 291]) or physician’s choice (PC) [n = 146] of one of three trastuzumab-containing combinations or lapatinib plus capecitabine. Treatment was continued until progression or unacceptable toxicity. The primary endpoint was centrally assessed PFS.
Longer progression-free survival with SYD985
Median age was 57 years, and the median number of prior metastatic breast cancer regimens was 4.7. Centrally reviewed progression-free survival was significantly longer in the SYD985 group at 7.0 months (5.4-7.2) versus 4.9 months (4.0-5.5) for PC (hazard ratio [HR], 0.64, 95% confidence interval [CI], 0.49-0.84, P = .002). Subgroup analysis, also centrally reviewed, revealed numerical advantage for SYD985 over physician choice across all categories (except for ECOG status 2). Analysis of progression-free survival by investigators showed a similar benefit for SYD985 (6.9 months versus 4.6 months, HR, 0.60, P < .001).
A first look at median overall survival showed a nonsignificant advantage for SYD985 (20.4 months versus 16.3 months (HR, 0.83, 95% CI, 0.62-1.09, P = .153). The overall response rate (partial or complete response) was similar between groups at 27.8% for SYD985 and 29.5% for PC, with reductions in target lesion measurement at 70.2% and 32.2% for SYD985 and physician choice, respectively. The clinical benefit rates were 38.5% for SYD985 and 32.2% for physician choice.
Ocular toxicity
Most patients had at least one treatment-related adverse event (96.5% SD985, 96.4% PC), and grade 3 or higher event rates were similar between groups (52.8% SYD985, 48.2% PC). The most frequently reported adverse events for SYD985 were ocular toxicity, with conjunctivitis reported in 38.2%, and keratitis in 38.2%, with fatigue at 33.3%; for physician’s choice these were diarrhea (35.8%), nausea (31.4%), and fatigue (29.9%). Interstitial lung disease pneumonitis was reported for 7.6% (5.2% grade 1-2) of patients treated with SYD985, including two grade 5 events. Eye toxicity led to discontinuations in 20.8% of SYD985 patients, dose modifications in 22.9%, with dose modifications for interstitial lung disease/pneumonitis in 5.2% of SYD985 patients. Six fatalities (2.1%) were reported in the SYD985 group, with four attributed to treatment. Assessment of health-related quality of life showed no significant difference between groups.
Dr. Manich outlined risk mitigation strategies. Patients with prior keratitis were excluded and patients were given prophylactic lubricating eye drops and regular eye exams by ophthalmologists. Treatment was discontinued if grade 3 or higher keratitis developed, and was delayed if grade 3 conjunctivitis developed until it reduced to grade 2. Also, patients with prior pneumonitis were excluded and CT lung scans were evaluated for lung changes. New or worsening respiratory symptoms triggered a full diagnostic workup. Treatment was discontinued for grade 2 or higher pneumonitis and delayed until resolution for grade 1 pneumonitis.
Another option
“It is encouraging to observe clinically meaningful and potentially practice changing PFS improvements in patients receiving treatment in the third line and beyond,” said Aditya Bardia, MD, of Massachusetts General Hospital and Harvard Medical School, Boston. “Several agents have been approved as treatments for HER2-positive metastatic breast cancer in recent years – including T-DXd, neratinib, tucatinib, and margetuximab – and [vic-]trastuzumab duocarmazine could eventually be another option.”
“At this time, there is only a minor 2-month difference in progression-free survival and a nonsignificant overall survival difference,” said Fatima Cardoso, MD, of Champalimaud Cancer Center, Lisbon, Portugal. “With the high incidence of ocular toxicity and four toxic deaths, we cannot recommend this drug for clinical practice, in my opinion.”
Dr. Manich concluded, “SYD985 can provide a new treatment option for patients with pretreated locally advanced or metastatic HER2-positive metastatic breast cancer.”
The study was funded by Byondis B.V. The authors disclosed numerous pharmaceutical-related financial interests.
This article was updated Sept. 24, 2021.
, according to Cristina Saura Manich, MD, Hospital Universitario Valle de Hebrón, Barcelona. In TULIP, trastuzumab duocarmazine (SYD985, Byondis B.V., NL) was compared with physician’s choice of chemotherapy, Dr. Saura said at the virtual European Society for Medical Oncology Congress 2021 on Sept. 18 (abstract LBA15).
Trastuzumab duocarmazine, Dr. Manich noted, is a novel HER2-targeting antibody–drug conjugate based on trastuzumab and a cleavable linker-duocarmycin (vc-seco-DUBA) payload. Its three-way mechanism of action includes uptake of the antibody–drug conjugate by internalization and intracellular release of the payload, and two bystander effects: proteolytic cleavage and subsequent release of payload in the tumor microenvironment and diffusion of active payload to neighboring tumor cells.
Two or more prior therapies for metastatic breast cancer
TULIP investigators enrolled 437 patients from 83 sites in 11 countries with HER2-positive locally advanced or metastatic breast cancer who had received two or more therapies for metastatic disease (treatment for brain metastases allowed). They were randomized 2:1 to SYD985 (1.2 mg/kg IV every 21 days [n = 291]) or physician’s choice (PC) [n = 146] of one of three trastuzumab-containing combinations or lapatinib plus capecitabine. Treatment was continued until progression or unacceptable toxicity. The primary endpoint was centrally assessed PFS.
Longer progression-free survival with SYD985
Median age was 57 years, and the median number of prior metastatic breast cancer regimens was 4.7. Centrally reviewed progression-free survival was significantly longer in the SYD985 group at 7.0 months (5.4-7.2) versus 4.9 months (4.0-5.5) for PC (hazard ratio [HR], 0.64, 95% confidence interval [CI], 0.49-0.84, P = .002). Subgroup analysis, also centrally reviewed, revealed numerical advantage for SYD985 over physician choice across all categories (except for ECOG status 2). Analysis of progression-free survival by investigators showed a similar benefit for SYD985 (6.9 months versus 4.6 months, HR, 0.60, P < .001).
A first look at median overall survival showed a nonsignificant advantage for SYD985 (20.4 months versus 16.3 months (HR, 0.83, 95% CI, 0.62-1.09, P = .153). The overall response rate (partial or complete response) was similar between groups at 27.8% for SYD985 and 29.5% for PC, with reductions in target lesion measurement at 70.2% and 32.2% for SYD985 and physician choice, respectively. The clinical benefit rates were 38.5% for SYD985 and 32.2% for physician choice.
Ocular toxicity
Most patients had at least one treatment-related adverse event (96.5% SD985, 96.4% PC), and grade 3 or higher event rates were similar between groups (52.8% SYD985, 48.2% PC). The most frequently reported adverse events for SYD985 were ocular toxicity, with conjunctivitis reported in 38.2%, and keratitis in 38.2%, with fatigue at 33.3%; for physician’s choice these were diarrhea (35.8%), nausea (31.4%), and fatigue (29.9%). Interstitial lung disease pneumonitis was reported for 7.6% (5.2% grade 1-2) of patients treated with SYD985, including two grade 5 events. Eye toxicity led to discontinuations in 20.8% of SYD985 patients, dose modifications in 22.9%, with dose modifications for interstitial lung disease/pneumonitis in 5.2% of SYD985 patients. Six fatalities (2.1%) were reported in the SYD985 group, with four attributed to treatment. Assessment of health-related quality of life showed no significant difference between groups.
Dr. Manich outlined risk mitigation strategies. Patients with prior keratitis were excluded and patients were given prophylactic lubricating eye drops and regular eye exams by ophthalmologists. Treatment was discontinued if grade 3 or higher keratitis developed, and was delayed if grade 3 conjunctivitis developed until it reduced to grade 2. Also, patients with prior pneumonitis were excluded and CT lung scans were evaluated for lung changes. New or worsening respiratory symptoms triggered a full diagnostic workup. Treatment was discontinued for grade 2 or higher pneumonitis and delayed until resolution for grade 1 pneumonitis.
Another option
“It is encouraging to observe clinically meaningful and potentially practice changing PFS improvements in patients receiving treatment in the third line and beyond,” said Aditya Bardia, MD, of Massachusetts General Hospital and Harvard Medical School, Boston. “Several agents have been approved as treatments for HER2-positive metastatic breast cancer in recent years – including T-DXd, neratinib, tucatinib, and margetuximab – and [vic-]trastuzumab duocarmazine could eventually be another option.”
“At this time, there is only a minor 2-month difference in progression-free survival and a nonsignificant overall survival difference,” said Fatima Cardoso, MD, of Champalimaud Cancer Center, Lisbon, Portugal. “With the high incidence of ocular toxicity and four toxic deaths, we cannot recommend this drug for clinical practice, in my opinion.”
Dr. Manich concluded, “SYD985 can provide a new treatment option for patients with pretreated locally advanced or metastatic HER2-positive metastatic breast cancer.”
The study was funded by Byondis B.V. The authors disclosed numerous pharmaceutical-related financial interests.
This article was updated Sept. 24, 2021.
, according to Cristina Saura Manich, MD, Hospital Universitario Valle de Hebrón, Barcelona. In TULIP, trastuzumab duocarmazine (SYD985, Byondis B.V., NL) was compared with physician’s choice of chemotherapy, Dr. Saura said at the virtual European Society for Medical Oncology Congress 2021 on Sept. 18 (abstract LBA15).
Trastuzumab duocarmazine, Dr. Manich noted, is a novel HER2-targeting antibody–drug conjugate based on trastuzumab and a cleavable linker-duocarmycin (vc-seco-DUBA) payload. Its three-way mechanism of action includes uptake of the antibody–drug conjugate by internalization and intracellular release of the payload, and two bystander effects: proteolytic cleavage and subsequent release of payload in the tumor microenvironment and diffusion of active payload to neighboring tumor cells.
Two or more prior therapies for metastatic breast cancer
TULIP investigators enrolled 437 patients from 83 sites in 11 countries with HER2-positive locally advanced or metastatic breast cancer who had received two or more therapies for metastatic disease (treatment for brain metastases allowed). They were randomized 2:1 to SYD985 (1.2 mg/kg IV every 21 days [n = 291]) or physician’s choice (PC) [n = 146] of one of three trastuzumab-containing combinations or lapatinib plus capecitabine. Treatment was continued until progression or unacceptable toxicity. The primary endpoint was centrally assessed PFS.
Longer progression-free survival with SYD985
Median age was 57 years, and the median number of prior metastatic breast cancer regimens was 4.7. Centrally reviewed progression-free survival was significantly longer in the SYD985 group at 7.0 months (5.4-7.2) versus 4.9 months (4.0-5.5) for PC (hazard ratio [HR], 0.64, 95% confidence interval [CI], 0.49-0.84, P = .002). Subgroup analysis, also centrally reviewed, revealed numerical advantage for SYD985 over physician choice across all categories (except for ECOG status 2). Analysis of progression-free survival by investigators showed a similar benefit for SYD985 (6.9 months versus 4.6 months, HR, 0.60, P < .001).
A first look at median overall survival showed a nonsignificant advantage for SYD985 (20.4 months versus 16.3 months (HR, 0.83, 95% CI, 0.62-1.09, P = .153). The overall response rate (partial or complete response) was similar between groups at 27.8% for SYD985 and 29.5% for PC, with reductions in target lesion measurement at 70.2% and 32.2% for SYD985 and physician choice, respectively. The clinical benefit rates were 38.5% for SYD985 and 32.2% for physician choice.
Ocular toxicity
Most patients had at least one treatment-related adverse event (96.5% SD985, 96.4% PC), and grade 3 or higher event rates were similar between groups (52.8% SYD985, 48.2% PC). The most frequently reported adverse events for SYD985 were ocular toxicity, with conjunctivitis reported in 38.2%, and keratitis in 38.2%, with fatigue at 33.3%; for physician’s choice these were diarrhea (35.8%), nausea (31.4%), and fatigue (29.9%). Interstitial lung disease pneumonitis was reported for 7.6% (5.2% grade 1-2) of patients treated with SYD985, including two grade 5 events. Eye toxicity led to discontinuations in 20.8% of SYD985 patients, dose modifications in 22.9%, with dose modifications for interstitial lung disease/pneumonitis in 5.2% of SYD985 patients. Six fatalities (2.1%) were reported in the SYD985 group, with four attributed to treatment. Assessment of health-related quality of life showed no significant difference between groups.
Dr. Manich outlined risk mitigation strategies. Patients with prior keratitis were excluded and patients were given prophylactic lubricating eye drops and regular eye exams by ophthalmologists. Treatment was discontinued if grade 3 or higher keratitis developed, and was delayed if grade 3 conjunctivitis developed until it reduced to grade 2. Also, patients with prior pneumonitis were excluded and CT lung scans were evaluated for lung changes. New or worsening respiratory symptoms triggered a full diagnostic workup. Treatment was discontinued for grade 2 or higher pneumonitis and delayed until resolution for grade 1 pneumonitis.
Another option
“It is encouraging to observe clinically meaningful and potentially practice changing PFS improvements in patients receiving treatment in the third line and beyond,” said Aditya Bardia, MD, of Massachusetts General Hospital and Harvard Medical School, Boston. “Several agents have been approved as treatments for HER2-positive metastatic breast cancer in recent years – including T-DXd, neratinib, tucatinib, and margetuximab – and [vic-]trastuzumab duocarmazine could eventually be another option.”
“At this time, there is only a minor 2-month difference in progression-free survival and a nonsignificant overall survival difference,” said Fatima Cardoso, MD, of Champalimaud Cancer Center, Lisbon, Portugal. “With the high incidence of ocular toxicity and four toxic deaths, we cannot recommend this drug for clinical practice, in my opinion.”
Dr. Manich concluded, “SYD985 can provide a new treatment option for patients with pretreated locally advanced or metastatic HER2-positive metastatic breast cancer.”
The study was funded by Byondis B.V. The authors disclosed numerous pharmaceutical-related financial interests.
This article was updated Sept. 24, 2021.
FROM ESMO 2021
ctDNA may be a better surrogate for survival than RECIST
according to Alexander Noor Shoushtari, MD, Memorial Sloan Kettering Cancer Center, New York.
Tebentafusp is the first therapy to demonstrate an overall survival (OS) benefit in uveal melanoma, Dr. Shoushtari noted in a 2021 European Society of Medical Oncology Congress virtual oral presentation Sept. 17 (abstract 17570). He noted further that, in prior research, OS was improved regardless of RECISTv1.1 best response, suggesting that better surrogate efficacy endpoints are needed.
Uveal melanoma is a rare melanoma type with low mutational burden, but frequent liver metastases. Benefit from immune checkpoint inhibitors is poor, and there is no established standard of care once the disease becomes metastatic. “Immune checkpoint inhibitors are not as good for treating this type of melanoma as they are for treating cutaneous disease, and traditionally preferred treatment is within clinical trials,” Dr. Shoushtari said. In frontline trials, 1-year survival has been in the 50% range. Tebentafusp is an investigational, first-in-class bispecific soluble T-cell receptor (TCR) therapeutic. It is designed to target gp100 (a melanoma-associated antigen) through a high-affinity TCR-binding domain and an anti-CD3 T-cell–engaging domain, which redirects T cells to kill gp100 positive melanocytic expressing tumor cells.
Prior research has demonstrated a disconnect between RECIST response classification and tebentafusp OS benefit. In the IMCgp100-202 study among patients treated first-line for metastatic uveal melanoma with tebentafusp or investigator choice, intent-to-treat analysis showed a survival probability benefit for tebentafusp (hazard ratio, 0.51; 95% CI, 0.37-0.71), with a best response of progressive disease population HR of 0.43 (95% CI, 0.27-0.68). While the RECIST response rate was only 9.1%, the HR for progression-free survival was 0.73 (95% CI, 0.58-0.94). “That suggests that RECIST is not a fantastic way to predict who will benefit from this drug,” Dr. Shoushtari stated.
Similarly in the IMCgp100-102 study of tebentafusp monotherapy in second-line metastatic uveal melanoma (n = 127), the RECIST response rate was 5%. Duration of response was 8.7 months and median OS was 16.8 months. Historical second-line OS has been reported at 7.8 months. The 1- and 2-year survival (62%/37%) compared favorably with historical rates (37%/15%), as well. Dr. Shoushtari noted that 92% of patients had detectable ctDNA with mutations in known uveal melanoma oncogenes. He pointed out that baseline ctDNA levels significantly correlated with tumor burden. Also, 70% of evaluable patients had any ctDNA reduction, with 0.5-3.2 log reduction in 99.9%, a 0.5 log reduction in 68% and 3 log reduction (cleared) in 14% of patients. ctDNA reduction, Dr. Shoushtari said, was associated with greater mean tumor shrinkage and with less tumor growth. Importantly, there was a linear correlation between ctDNA reduction and better OS (R2, 0.88, P < .0001).
Among all evaluable patients, comparing those with less than 0.5 log ctDNA reduction with those with at least a 0.5 log reduction showed a hazard ratio of 0.56 (95% CI, 0.32-0.95; P = .03). Among those whose best response was progressive disease, 35% had at least a 0.5 log reduction in ctDNA with an OS hazard ratio of 0.44 (95% CI, 0.2-0.94; P = .027), compared with less than a 0.5 log reduction. Among those whose best response was stable disease, 28% had at least 1 log reduction with a hazard ratio of 0.48 (95% CI 0.16-1.43; P = .16) for OS, compared with those with less than 1 log reduction. Dr. Shoushtari pointed out that “14% of patients cleared ctDNA, including some (n = 12) with best RECIST responses of stable or progressive disease. All patients with ctDNA clearance were alive beyond 1 year; with a hazard ratio, compared to those who had not cleared ctDNA, of 0.14 (95% CI, 0.03-0.57).
Summing up, Dr. Shoushtari said that ctDNA was detectable in more than 90% of second-line tebentafusp-treated patients with metastatic uveal melanoma and correlated with tumor burden. About 70% had ctDNA reduction versus 39% with tumor shrinkage and 5% RECIST response. The linear correlation between the magnitude of ctDNA reduction and improved OS on tebentafusp, was uncoupled from best RECIST response. “For tebentafusp, ctDNA reduction may be a better surrogate of overall survival than RECIST response.”
The ESMO-appointed discussant for the study, Christian Rolfo, MD, PhD, MBA, Icahan School of Medicine at Mount Sinai, New York, examined the tebentafusp study author’s claim that the radiographic assessment of tumors may underestimate the effect of tebentafusp, compared with ctDNA. The strengths of the study include, he said, that it is a drug- and tumor-specific evaluation of the role of ctDNA as a surrogate of response. “Its strength is that it shows an important correlation between ctDNA levels and overall survival, and that response rate is evaluated better with ctDNA.” A question that remains open, Dr. Rolfo added, is whether RECIST criteria are still a good comparator for biologic response.
The study was funded by Immunocore Dr. Shoushtari disclosed numerous pharmaceutical-related financial interests.
This article was updated Sept. 24, 2021.
according to Alexander Noor Shoushtari, MD, Memorial Sloan Kettering Cancer Center, New York.
Tebentafusp is the first therapy to demonstrate an overall survival (OS) benefit in uveal melanoma, Dr. Shoushtari noted in a 2021 European Society of Medical Oncology Congress virtual oral presentation Sept. 17 (abstract 17570). He noted further that, in prior research, OS was improved regardless of RECISTv1.1 best response, suggesting that better surrogate efficacy endpoints are needed.
Uveal melanoma is a rare melanoma type with low mutational burden, but frequent liver metastases. Benefit from immune checkpoint inhibitors is poor, and there is no established standard of care once the disease becomes metastatic. “Immune checkpoint inhibitors are not as good for treating this type of melanoma as they are for treating cutaneous disease, and traditionally preferred treatment is within clinical trials,” Dr. Shoushtari said. In frontline trials, 1-year survival has been in the 50% range. Tebentafusp is an investigational, first-in-class bispecific soluble T-cell receptor (TCR) therapeutic. It is designed to target gp100 (a melanoma-associated antigen) through a high-affinity TCR-binding domain and an anti-CD3 T-cell–engaging domain, which redirects T cells to kill gp100 positive melanocytic expressing tumor cells.
Prior research has demonstrated a disconnect between RECIST response classification and tebentafusp OS benefit. In the IMCgp100-202 study among patients treated first-line for metastatic uveal melanoma with tebentafusp or investigator choice, intent-to-treat analysis showed a survival probability benefit for tebentafusp (hazard ratio, 0.51; 95% CI, 0.37-0.71), with a best response of progressive disease population HR of 0.43 (95% CI, 0.27-0.68). While the RECIST response rate was only 9.1%, the HR for progression-free survival was 0.73 (95% CI, 0.58-0.94). “That suggests that RECIST is not a fantastic way to predict who will benefit from this drug,” Dr. Shoushtari stated.
Similarly in the IMCgp100-102 study of tebentafusp monotherapy in second-line metastatic uveal melanoma (n = 127), the RECIST response rate was 5%. Duration of response was 8.7 months and median OS was 16.8 months. Historical second-line OS has been reported at 7.8 months. The 1- and 2-year survival (62%/37%) compared favorably with historical rates (37%/15%), as well. Dr. Shoushtari noted that 92% of patients had detectable ctDNA with mutations in known uveal melanoma oncogenes. He pointed out that baseline ctDNA levels significantly correlated with tumor burden. Also, 70% of evaluable patients had any ctDNA reduction, with 0.5-3.2 log reduction in 99.9%, a 0.5 log reduction in 68% and 3 log reduction (cleared) in 14% of patients. ctDNA reduction, Dr. Shoushtari said, was associated with greater mean tumor shrinkage and with less tumor growth. Importantly, there was a linear correlation between ctDNA reduction and better OS (R2, 0.88, P < .0001).
Among all evaluable patients, comparing those with less than 0.5 log ctDNA reduction with those with at least a 0.5 log reduction showed a hazard ratio of 0.56 (95% CI, 0.32-0.95; P = .03). Among those whose best response was progressive disease, 35% had at least a 0.5 log reduction in ctDNA with an OS hazard ratio of 0.44 (95% CI, 0.2-0.94; P = .027), compared with less than a 0.5 log reduction. Among those whose best response was stable disease, 28% had at least 1 log reduction with a hazard ratio of 0.48 (95% CI 0.16-1.43; P = .16) for OS, compared with those with less than 1 log reduction. Dr. Shoushtari pointed out that “14% of patients cleared ctDNA, including some (n = 12) with best RECIST responses of stable or progressive disease. All patients with ctDNA clearance were alive beyond 1 year; with a hazard ratio, compared to those who had not cleared ctDNA, of 0.14 (95% CI, 0.03-0.57).
Summing up, Dr. Shoushtari said that ctDNA was detectable in more than 90% of second-line tebentafusp-treated patients with metastatic uveal melanoma and correlated with tumor burden. About 70% had ctDNA reduction versus 39% with tumor shrinkage and 5% RECIST response. The linear correlation between the magnitude of ctDNA reduction and improved OS on tebentafusp, was uncoupled from best RECIST response. “For tebentafusp, ctDNA reduction may be a better surrogate of overall survival than RECIST response.”
The ESMO-appointed discussant for the study, Christian Rolfo, MD, PhD, MBA, Icahan School of Medicine at Mount Sinai, New York, examined the tebentafusp study author’s claim that the radiographic assessment of tumors may underestimate the effect of tebentafusp, compared with ctDNA. The strengths of the study include, he said, that it is a drug- and tumor-specific evaluation of the role of ctDNA as a surrogate of response. “Its strength is that it shows an important correlation between ctDNA levels and overall survival, and that response rate is evaluated better with ctDNA.” A question that remains open, Dr. Rolfo added, is whether RECIST criteria are still a good comparator for biologic response.
The study was funded by Immunocore Dr. Shoushtari disclosed numerous pharmaceutical-related financial interests.
This article was updated Sept. 24, 2021.
according to Alexander Noor Shoushtari, MD, Memorial Sloan Kettering Cancer Center, New York.
Tebentafusp is the first therapy to demonstrate an overall survival (OS) benefit in uveal melanoma, Dr. Shoushtari noted in a 2021 European Society of Medical Oncology Congress virtual oral presentation Sept. 17 (abstract 17570). He noted further that, in prior research, OS was improved regardless of RECISTv1.1 best response, suggesting that better surrogate efficacy endpoints are needed.
Uveal melanoma is a rare melanoma type with low mutational burden, but frequent liver metastases. Benefit from immune checkpoint inhibitors is poor, and there is no established standard of care once the disease becomes metastatic. “Immune checkpoint inhibitors are not as good for treating this type of melanoma as they are for treating cutaneous disease, and traditionally preferred treatment is within clinical trials,” Dr. Shoushtari said. In frontline trials, 1-year survival has been in the 50% range. Tebentafusp is an investigational, first-in-class bispecific soluble T-cell receptor (TCR) therapeutic. It is designed to target gp100 (a melanoma-associated antigen) through a high-affinity TCR-binding domain and an anti-CD3 T-cell–engaging domain, which redirects T cells to kill gp100 positive melanocytic expressing tumor cells.
Prior research has demonstrated a disconnect between RECIST response classification and tebentafusp OS benefit. In the IMCgp100-202 study among patients treated first-line for metastatic uveal melanoma with tebentafusp or investigator choice, intent-to-treat analysis showed a survival probability benefit for tebentafusp (hazard ratio, 0.51; 95% CI, 0.37-0.71), with a best response of progressive disease population HR of 0.43 (95% CI, 0.27-0.68). While the RECIST response rate was only 9.1%, the HR for progression-free survival was 0.73 (95% CI, 0.58-0.94). “That suggests that RECIST is not a fantastic way to predict who will benefit from this drug,” Dr. Shoushtari stated.
Similarly in the IMCgp100-102 study of tebentafusp monotherapy in second-line metastatic uveal melanoma (n = 127), the RECIST response rate was 5%. Duration of response was 8.7 months and median OS was 16.8 months. Historical second-line OS has been reported at 7.8 months. The 1- and 2-year survival (62%/37%) compared favorably with historical rates (37%/15%), as well. Dr. Shoushtari noted that 92% of patients had detectable ctDNA with mutations in known uveal melanoma oncogenes. He pointed out that baseline ctDNA levels significantly correlated with tumor burden. Also, 70% of evaluable patients had any ctDNA reduction, with 0.5-3.2 log reduction in 99.9%, a 0.5 log reduction in 68% and 3 log reduction (cleared) in 14% of patients. ctDNA reduction, Dr. Shoushtari said, was associated with greater mean tumor shrinkage and with less tumor growth. Importantly, there was a linear correlation between ctDNA reduction and better OS (R2, 0.88, P < .0001).
Among all evaluable patients, comparing those with less than 0.5 log ctDNA reduction with those with at least a 0.5 log reduction showed a hazard ratio of 0.56 (95% CI, 0.32-0.95; P = .03). Among those whose best response was progressive disease, 35% had at least a 0.5 log reduction in ctDNA with an OS hazard ratio of 0.44 (95% CI, 0.2-0.94; P = .027), compared with less than a 0.5 log reduction. Among those whose best response was stable disease, 28% had at least 1 log reduction with a hazard ratio of 0.48 (95% CI 0.16-1.43; P = .16) for OS, compared with those with less than 1 log reduction. Dr. Shoushtari pointed out that “14% of patients cleared ctDNA, including some (n = 12) with best RECIST responses of stable or progressive disease. All patients with ctDNA clearance were alive beyond 1 year; with a hazard ratio, compared to those who had not cleared ctDNA, of 0.14 (95% CI, 0.03-0.57).
Summing up, Dr. Shoushtari said that ctDNA was detectable in more than 90% of second-line tebentafusp-treated patients with metastatic uveal melanoma and correlated with tumor burden. About 70% had ctDNA reduction versus 39% with tumor shrinkage and 5% RECIST response. The linear correlation between the magnitude of ctDNA reduction and improved OS on tebentafusp, was uncoupled from best RECIST response. “For tebentafusp, ctDNA reduction may be a better surrogate of overall survival than RECIST response.”
The ESMO-appointed discussant for the study, Christian Rolfo, MD, PhD, MBA, Icahan School of Medicine at Mount Sinai, New York, examined the tebentafusp study author’s claim that the radiographic assessment of tumors may underestimate the effect of tebentafusp, compared with ctDNA. The strengths of the study include, he said, that it is a drug- and tumor-specific evaluation of the role of ctDNA as a surrogate of response. “Its strength is that it shows an important correlation between ctDNA levels and overall survival, and that response rate is evaluated better with ctDNA.” A question that remains open, Dr. Rolfo added, is whether RECIST criteria are still a good comparator for biologic response.
The study was funded by Immunocore Dr. Shoushtari disclosed numerous pharmaceutical-related financial interests.
This article was updated Sept. 24, 2021.
FROM ESMO 2021
Your bathroom towel rack has a dirty little secret
Bacteria get the rack ... the towel rack
Obviously, bathrooms have germs. Some people are cleaner about their bathrooms than others, but in general most people just try not to think about the microscopic critters crawling about.
Now you would probably think that the toilet is the dirtiest part of the bathroom because that’s where ... you know, most of the business takes place. Or maybe you’d guess the floor. Truth be told, though, the dirtiest part of the bathroom is where the towels are hung.
According to research conducted by electric heating company Rointe in the United Kingdom, bathroom radiators and towel racks/bars are the most germy and dirty parts of the bathroom.
Company investigators examined five bathrooms using swabs that changed color on contact with bacteria and found that 60% of towel racks and radiators were “really dirty,” compared with 50% of sink drains and just 10% of toilets.
Most people probably pay more attention to the sink, floors, and toilets while cleaning, the company suggested, and dampness is a factor in bacteria growth, so it’s no surprise that towels that stay wet on a rack are prime spots for dust, mildew, and mold.
The toilet may be busier, but you don’t put your face in it.
Anti-vaxxers would like to be called ‘purebloods’
COVID-19 anti-vaxxers are an interesting bunch, to be kind. And TikTok is a wacky place. So you can just imagine that anti-vaxxer TikTok is a very strange place. The citizens of anti-vax TikTok have decided that the real reason so many people dislike them is branding. They consider anti-vaccination to be a negative word (duh), so they now want to be referred to as “purebloods.”
Harry Potter doesn’t quite occupy the zeitgeist as it once did, so let’s give you a reminder: In the books, purebloods came from old wizarding families and claimed not to have any Muggle, or nonmagic, blood. While having pure wizard blood was no guarantee of being a villain, most of them were. In addition, it is made quite clear throughout the novels that having supposedly pure blood had no relevance on one’s wizarding ability. Pureblood was a meaningless title, and only the characters with small, cruel minds concerned themselves over it.
Perhaps the anti-vaxxers have decided that they want to be called the same thing. Maybe they just like the name. It does sound impressive and vaguely regal: Pureblood. Like something the nobles of medieval Europe might have used.
Critical-thinking skills may be in short supply here, or maybe the anti-vaxxers know exactly what they’re doing.
Hated broccoli? Blame your DNA
Were you that kid who would rather sit at the table for hours than eat your broccoli? Well, as much as your parents might have pushed you, new research suggests that it might be their fault you didn’t like it to begin with.
Investigators at Australia’s national science agency, CSIRO, recently reported that distaste for Brassica vegetables – broccoli, Brussels sprouts, cabbage, and cauliflower – can be traced to the oral microbiome.
These vegetables have a compound called S-methyl-L-cysteine sulfoxide that gives off sulfurous odors ... mmm, sulfurous ... when mixed with an enzyme in the plant, and that enzyme is also produced by bacteria in some people’s oral microbiomes. So why do adults tolerate these Brassica veggies more than children? It’s all about levels.
The researchers tested the idea by asking 98 child/parent pairs to rate the odors and by using gas chromatography-olfactometry-mass spectrometry to identify the odor-active compounds in both raw and steamed cauliflower and broccoli. The children whose saliva produced high levels of sulfur volatiles disliked Brassica vegetables the most, they reported, and the children with high levels of sulfur volatiles usually had parents who produced high levels.
Despite that connection, however, the distaste for raw Brassica seen in children wasn’t seen in adults.
Maybe it’s not that taste buds change as we age, maybe we just learn to tolerate the sulfurousness.
Bacteria get the rack ... the towel rack
Obviously, bathrooms have germs. Some people are cleaner about their bathrooms than others, but in general most people just try not to think about the microscopic critters crawling about.
Now you would probably think that the toilet is the dirtiest part of the bathroom because that’s where ... you know, most of the business takes place. Or maybe you’d guess the floor. Truth be told, though, the dirtiest part of the bathroom is where the towels are hung.
According to research conducted by electric heating company Rointe in the United Kingdom, bathroom radiators and towel racks/bars are the most germy and dirty parts of the bathroom.
Company investigators examined five bathrooms using swabs that changed color on contact with bacteria and found that 60% of towel racks and radiators were “really dirty,” compared with 50% of sink drains and just 10% of toilets.
Most people probably pay more attention to the sink, floors, and toilets while cleaning, the company suggested, and dampness is a factor in bacteria growth, so it’s no surprise that towels that stay wet on a rack are prime spots for dust, mildew, and mold.
The toilet may be busier, but you don’t put your face in it.
Anti-vaxxers would like to be called ‘purebloods’
COVID-19 anti-vaxxers are an interesting bunch, to be kind. And TikTok is a wacky place. So you can just imagine that anti-vaxxer TikTok is a very strange place. The citizens of anti-vax TikTok have decided that the real reason so many people dislike them is branding. They consider anti-vaccination to be a negative word (duh), so they now want to be referred to as “purebloods.”
Harry Potter doesn’t quite occupy the zeitgeist as it once did, so let’s give you a reminder: In the books, purebloods came from old wizarding families and claimed not to have any Muggle, or nonmagic, blood. While having pure wizard blood was no guarantee of being a villain, most of them were. In addition, it is made quite clear throughout the novels that having supposedly pure blood had no relevance on one’s wizarding ability. Pureblood was a meaningless title, and only the characters with small, cruel minds concerned themselves over it.
Perhaps the anti-vaxxers have decided that they want to be called the same thing. Maybe they just like the name. It does sound impressive and vaguely regal: Pureblood. Like something the nobles of medieval Europe might have used.
Critical-thinking skills may be in short supply here, or maybe the anti-vaxxers know exactly what they’re doing.
Hated broccoli? Blame your DNA
Were you that kid who would rather sit at the table for hours than eat your broccoli? Well, as much as your parents might have pushed you, new research suggests that it might be their fault you didn’t like it to begin with.
Investigators at Australia’s national science agency, CSIRO, recently reported that distaste for Brassica vegetables – broccoli, Brussels sprouts, cabbage, and cauliflower – can be traced to the oral microbiome.
These vegetables have a compound called S-methyl-L-cysteine sulfoxide that gives off sulfurous odors ... mmm, sulfurous ... when mixed with an enzyme in the plant, and that enzyme is also produced by bacteria in some people’s oral microbiomes. So why do adults tolerate these Brassica veggies more than children? It’s all about levels.
The researchers tested the idea by asking 98 child/parent pairs to rate the odors and by using gas chromatography-olfactometry-mass spectrometry to identify the odor-active compounds in both raw and steamed cauliflower and broccoli. The children whose saliva produced high levels of sulfur volatiles disliked Brassica vegetables the most, they reported, and the children with high levels of sulfur volatiles usually had parents who produced high levels.
Despite that connection, however, the distaste for raw Brassica seen in children wasn’t seen in adults.
Maybe it’s not that taste buds change as we age, maybe we just learn to tolerate the sulfurousness.
Bacteria get the rack ... the towel rack
Obviously, bathrooms have germs. Some people are cleaner about their bathrooms than others, but in general most people just try not to think about the microscopic critters crawling about.
Now you would probably think that the toilet is the dirtiest part of the bathroom because that’s where ... you know, most of the business takes place. Or maybe you’d guess the floor. Truth be told, though, the dirtiest part of the bathroom is where the towels are hung.
According to research conducted by electric heating company Rointe in the United Kingdom, bathroom radiators and towel racks/bars are the most germy and dirty parts of the bathroom.
Company investigators examined five bathrooms using swabs that changed color on contact with bacteria and found that 60% of towel racks and radiators were “really dirty,” compared with 50% of sink drains and just 10% of toilets.
Most people probably pay more attention to the sink, floors, and toilets while cleaning, the company suggested, and dampness is a factor in bacteria growth, so it’s no surprise that towels that stay wet on a rack are prime spots for dust, mildew, and mold.
The toilet may be busier, but you don’t put your face in it.
Anti-vaxxers would like to be called ‘purebloods’
COVID-19 anti-vaxxers are an interesting bunch, to be kind. And TikTok is a wacky place. So you can just imagine that anti-vaxxer TikTok is a very strange place. The citizens of anti-vax TikTok have decided that the real reason so many people dislike them is branding. They consider anti-vaccination to be a negative word (duh), so they now want to be referred to as “purebloods.”
Harry Potter doesn’t quite occupy the zeitgeist as it once did, so let’s give you a reminder: In the books, purebloods came from old wizarding families and claimed not to have any Muggle, or nonmagic, blood. While having pure wizard blood was no guarantee of being a villain, most of them were. In addition, it is made quite clear throughout the novels that having supposedly pure blood had no relevance on one’s wizarding ability. Pureblood was a meaningless title, and only the characters with small, cruel minds concerned themselves over it.
Perhaps the anti-vaxxers have decided that they want to be called the same thing. Maybe they just like the name. It does sound impressive and vaguely regal: Pureblood. Like something the nobles of medieval Europe might have used.
Critical-thinking skills may be in short supply here, or maybe the anti-vaxxers know exactly what they’re doing.
Hated broccoli? Blame your DNA
Were you that kid who would rather sit at the table for hours than eat your broccoli? Well, as much as your parents might have pushed you, new research suggests that it might be their fault you didn’t like it to begin with.
Investigators at Australia’s national science agency, CSIRO, recently reported that distaste for Brassica vegetables – broccoli, Brussels sprouts, cabbage, and cauliflower – can be traced to the oral microbiome.
These vegetables have a compound called S-methyl-L-cysteine sulfoxide that gives off sulfurous odors ... mmm, sulfurous ... when mixed with an enzyme in the plant, and that enzyme is also produced by bacteria in some people’s oral microbiomes. So why do adults tolerate these Brassica veggies more than children? It’s all about levels.
The researchers tested the idea by asking 98 child/parent pairs to rate the odors and by using gas chromatography-olfactometry-mass spectrometry to identify the odor-active compounds in both raw and steamed cauliflower and broccoli. The children whose saliva produced high levels of sulfur volatiles disliked Brassica vegetables the most, they reported, and the children with high levels of sulfur volatiles usually had parents who produced high levels.
Despite that connection, however, the distaste for raw Brassica seen in children wasn’t seen in adults.
Maybe it’s not that taste buds change as we age, maybe we just learn to tolerate the sulfurousness.
Methylation patterns correlate with prognosis in children with T-ALL
In childhood patients with T-cell acute lymphoblastic leukemia (T-ALL) the hypomethylation status of the arginine synthetase (ASNS) gene was significantly associated with poor therapeutic outcome, according to the results of a Japanese cohort study published online in Blood Advances.
Researchers Koshi Akahane, PHD, of the University of Yamanashi, Kofu, Japan, and colleagues conducted a comprehensive genetic analysis of diagnostic samples of 22 cell lines from childhood patients with T-ALL in Japan.
They also correlated known methylation status with outcomes in two large patient cohorts of Japanese children with T-ALL: the Tokyo Children’s Cancer Study Group (n = 57) and the Japan Association of Childhood Leukemia Study Group (n = 20).
Methylation results
For the 22 cell lines tested, sequencing technology revealed a stepwise allele-specific methylation of the ASNS gene. Mean ASNS gene expression level was significantly upregulated in 14 weakly methylated cell lines (P = .0001), but not significantly upregulated in 3 intermediately methylated cell lines (P = .25) or in 5 highly methylated cell lines (P = .063).
Among the 77 patient cohorts, 20 (26%) samples showed high methylation (> 66.7%), while 15 (19%) samples and 42 (55%) samples showed intermediate (33.3%-66.7%) and weak (< 33.3%) methylation status, respectively.
For the 75 patients where information was provided on outcomes, 25 patients (33%) showed induction failure or disease relapse. A highly methylated status of the ASNS gene was significantly more common in non-refractory/relapse cases (18/50 cases, 36%), while intermediately or weakly methylated status was more common in refractory/relapsed cases (23/25 cases, 92 %; P = .0001). In a log-rank test, the patients with weakly methylated status of the ASNS gene showed significantly shorter event-free survival and overall survival than the patients with an intermediate or highly methylated status (P = .00012 and P = .00016, respectively).
Asparaginase sensitivity
Asparaginase treatment is a key component of chemotherapy for patients with T-ALL, according to the researchers. Asparaginase depletes serum asparagine by deamination into aspartic acid. While normal hematopoietic cells can survive due to ASNS activity, leukemia cells are expected to undergo apoptosis due to silencing of the ASNS gene.
ASNS hypomethylation status was significantly associated with poor therapeutic outcome, and all cases with the poor prognostic SPI1 fusion exclusively showed ASNS hypomethylation status. These observations demonstrate that ASNS hypomethylation status is associated with asparaginase resistance, the researchers stated.
“ASNS methylation status may be a clinically useful biomarker to predict sensitivity to asparaginase therapy in T-ALL patients. Considering the severe complications of asparaginase therapy particularly in adolescents and adults, stratifying prospective asparaginase therapy according to ASNS methylation status may be beneficial for safer and more effective treatment of T-ALL patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
In childhood patients with T-cell acute lymphoblastic leukemia (T-ALL) the hypomethylation status of the arginine synthetase (ASNS) gene was significantly associated with poor therapeutic outcome, according to the results of a Japanese cohort study published online in Blood Advances.
Researchers Koshi Akahane, PHD, of the University of Yamanashi, Kofu, Japan, and colleagues conducted a comprehensive genetic analysis of diagnostic samples of 22 cell lines from childhood patients with T-ALL in Japan.
They also correlated known methylation status with outcomes in two large patient cohorts of Japanese children with T-ALL: the Tokyo Children’s Cancer Study Group (n = 57) and the Japan Association of Childhood Leukemia Study Group (n = 20).
Methylation results
For the 22 cell lines tested, sequencing technology revealed a stepwise allele-specific methylation of the ASNS gene. Mean ASNS gene expression level was significantly upregulated in 14 weakly methylated cell lines (P = .0001), but not significantly upregulated in 3 intermediately methylated cell lines (P = .25) or in 5 highly methylated cell lines (P = .063).
Among the 77 patient cohorts, 20 (26%) samples showed high methylation (> 66.7%), while 15 (19%) samples and 42 (55%) samples showed intermediate (33.3%-66.7%) and weak (< 33.3%) methylation status, respectively.
For the 75 patients where information was provided on outcomes, 25 patients (33%) showed induction failure or disease relapse. A highly methylated status of the ASNS gene was significantly more common in non-refractory/relapse cases (18/50 cases, 36%), while intermediately or weakly methylated status was more common in refractory/relapsed cases (23/25 cases, 92 %; P = .0001). In a log-rank test, the patients with weakly methylated status of the ASNS gene showed significantly shorter event-free survival and overall survival than the patients with an intermediate or highly methylated status (P = .00012 and P = .00016, respectively).
Asparaginase sensitivity
Asparaginase treatment is a key component of chemotherapy for patients with T-ALL, according to the researchers. Asparaginase depletes serum asparagine by deamination into aspartic acid. While normal hematopoietic cells can survive due to ASNS activity, leukemia cells are expected to undergo apoptosis due to silencing of the ASNS gene.
ASNS hypomethylation status was significantly associated with poor therapeutic outcome, and all cases with the poor prognostic SPI1 fusion exclusively showed ASNS hypomethylation status. These observations demonstrate that ASNS hypomethylation status is associated with asparaginase resistance, the researchers stated.
“ASNS methylation status may be a clinically useful biomarker to predict sensitivity to asparaginase therapy in T-ALL patients. Considering the severe complications of asparaginase therapy particularly in adolescents and adults, stratifying prospective asparaginase therapy according to ASNS methylation status may be beneficial for safer and more effective treatment of T-ALL patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
In childhood patients with T-cell acute lymphoblastic leukemia (T-ALL) the hypomethylation status of the arginine synthetase (ASNS) gene was significantly associated with poor therapeutic outcome, according to the results of a Japanese cohort study published online in Blood Advances.
Researchers Koshi Akahane, PHD, of the University of Yamanashi, Kofu, Japan, and colleagues conducted a comprehensive genetic analysis of diagnostic samples of 22 cell lines from childhood patients with T-ALL in Japan.
They also correlated known methylation status with outcomes in two large patient cohorts of Japanese children with T-ALL: the Tokyo Children’s Cancer Study Group (n = 57) and the Japan Association of Childhood Leukemia Study Group (n = 20).
Methylation results
For the 22 cell lines tested, sequencing technology revealed a stepwise allele-specific methylation of the ASNS gene. Mean ASNS gene expression level was significantly upregulated in 14 weakly methylated cell lines (P = .0001), but not significantly upregulated in 3 intermediately methylated cell lines (P = .25) or in 5 highly methylated cell lines (P = .063).
Among the 77 patient cohorts, 20 (26%) samples showed high methylation (> 66.7%), while 15 (19%) samples and 42 (55%) samples showed intermediate (33.3%-66.7%) and weak (< 33.3%) methylation status, respectively.
For the 75 patients where information was provided on outcomes, 25 patients (33%) showed induction failure or disease relapse. A highly methylated status of the ASNS gene was significantly more common in non-refractory/relapse cases (18/50 cases, 36%), while intermediately or weakly methylated status was more common in refractory/relapsed cases (23/25 cases, 92 %; P = .0001). In a log-rank test, the patients with weakly methylated status of the ASNS gene showed significantly shorter event-free survival and overall survival than the patients with an intermediate or highly methylated status (P = .00012 and P = .00016, respectively).
Asparaginase sensitivity
Asparaginase treatment is a key component of chemotherapy for patients with T-ALL, according to the researchers. Asparaginase depletes serum asparagine by deamination into aspartic acid. While normal hematopoietic cells can survive due to ASNS activity, leukemia cells are expected to undergo apoptosis due to silencing of the ASNS gene.
ASNS hypomethylation status was significantly associated with poor therapeutic outcome, and all cases with the poor prognostic SPI1 fusion exclusively showed ASNS hypomethylation status. These observations demonstrate that ASNS hypomethylation status is associated with asparaginase resistance, the researchers stated.
“ASNS methylation status may be a clinically useful biomarker to predict sensitivity to asparaginase therapy in T-ALL patients. Considering the severe complications of asparaginase therapy particularly in adolescents and adults, stratifying prospective asparaginase therapy according to ASNS methylation status may be beneficial for safer and more effective treatment of T-ALL patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
FROM BLOOD ADVANCES
FDA OKs Pfizer COVID booster for 65 and over, those at high risk
The agency’s move comes as a Centers for Disease Control and Prevention (CDC) panel ended the first day of a 2-day meeting. That panel, the Advisory Committee on Immunization Practices (ACIP), is expected to vote Sept. 23 to instruct doctors on how to administer the boosters.
The FDA officially authorized the vaccine not only for individuals 65 and older, but also for people 18 through 64 years of age who are at high risk for severe illness from the coronavirus, including essential workers whose jobs increase their risk for infection.
“After considering the totality of the available scientific evidence and the deliberations of our advisory committee of independent, external experts, the FDA amended the EUA for the Pfizer-BioNTech COVID-19 vaccine to allow for a booster dose in certain populations such as health care workers, teachers and daycare staff, grocery workers and those in homeless shelters or prisons, among others,” Acting FDA Commissioner Janet Woodcock, MD, said in a news release.
The recommendations align with those from an FDA advisory panel Sept. 17.
The agency determined that the benefits of a booster dose outweigh the risks for people now authorized to receive it, according to the news release.
Other questions remain
So, how will this work? That was the main question weighing on the minds of the CDC’s ACIP during their first day of a 2-day meeting where they are expected to make recommendations on booster doses for Americans.
The panel discussed situations the FDA will still need to consider, such as what should be done for Americans who were originally vaccinated with a Moderna or Johnson and Johnson vaccine, but are not covered under the revised EUA, which is only for those people who received Pfizer’s two-dose vaccine regimen.
“That’s going to leave half of the people immunized in this age group having received the vaccine and being told that they’re at risk now for waning immunity and hospitalization unable to get a booster dose,” said committee member Sarah S. Long, MD, a professor of pediatrics at Drexel University College of Medicine in Philadelphia. “So that’s a big public health panic that we would like to avoid.”
Johnson and Johnson recently reported that second doses of its vaccine boosted its efficacy to almost 94% against COVID-19. A new study, published ahead of peer review, suggests that the efficacy of the single-dose Johnson and Johnson shot has fallen to about 78% against symptomatic infection during the Delta surge.
Moderna has applied for permission to market third doses of its vaccine in the United States, but the FDA has given no timeline on when it might make a decision.
Doran Fink, MD, PhD, deputy director of the FDA’s Division of Vaccines and Related Products Applications, a representative advising the committee Sept. 22, said the agency was working as rapidly as possible on Moderna’s submission.
Regarding the question of whether it was OK to mix vaccines, rather than match them, Dr. Fink said there are currently not enough data available to inform that decision.
Those answers are coming, though. John Beigel, MD, associate director of clinical research at the National Institute of Allergy and Infectious Diseases, revealed that the federal government has a study underway to see what happens when the vaccines are mixed with each other.
He said that data from the study would be available later this fall, and would certainly help physicians and other healthcare providers know whether it’s effective or safe to use them interchangeably.
Correlates of immunity
The ACIP left much of its schedule open Sept. 23 to discuss extra Pfizer doses and vote on how they should be used.
Pfizer had originally applied to the FDA for an amendment to its FDA approval, which would have given doctors a freer hand to prescribe third doses as they saw fit, in patients as young as 16.
But the FDA’s Vaccines and Related Biological Products Advisory Committee voted Sept. 17 against granting the amendment. The committee was particularly concerned about the lack of data in teens ages 16 and 17, who have the highest risk for a rare side effect that causes heart inflammation that requires hospital care.
Instead, they recommended — and the FDA agreed per their decision Sept. 22 — that third doses should be given to people at higher risk for severe breakthrough infections because of advanced age or because they work in an occupation that puts them at high risk for exposure.
The CDC panel heard important presentations on new science that is helping to identify the correlates of immunity.
The correlates of immunity are biomarkers that can be measured in blood that help doctors understand how protected a person may be against COVID-19. These markers of immunity are not yet known for the COVID-19 vaccines.
Emerging evidence shows that booster doses of the Pfizer vaccine cause front-line immune defenders — called binding antibodies — to roughly triple soon after a person gets the third shot.
Neutralizing antibodies also jump soon after two vaccine doses, but they fall over time, which is natural. The body doesn’t need these foot soldiers to be on guard all the time, so they go away.
The body retains its memory of how to make them, however, so they can quickly be marshaled again, if needed.
Early studies suggest that antibodies account for about two thirds of a person’s protection against COVID, while the longer-lasting T-cells and B-cells account for about one third.
After the antibody levels fall, it may take a few days to recreate this army. In the meantime, the virus can try to break in. This can cause symptoms, which can make a person feel terrible, but for the most part, vaccinated individuals don’t need hospital care and are nearly always protected from dying — even against the Delta variant.
Those most likely to be at risk for a breakthrough infection are older, because immune function wanes with age.
Essential workers
Essential workers, such as those who work in healthcare, may also benefit from high antibody levels, which can minimize symptoms and help them get back to work more quickly.
Helen Talbot, MD, MPH, an associate professor of medicine at Vanderbilt University Medical Center in Nashville, said that in her area staffing levels are critical right now.
“I’m actually sitting in one of the deepest red [states] with high rates of COVID. We don’t have enough health care workers currently to take care of the unvaccinated,” she said.
“When we have beds, we are often missing staff, and so the idea of vaccinating health care workers is to be a little bit different than our idea of using vaccines in the general population,” Dr. Talbot said.
Oliver Brooks, MD, chief medical officer of the Watts Healthcare Corporation in Los Angeles, said he was in favor of making a public statement about the temporary nature of the potential recommendations Sept. 23, because they probably won’t cover all who might need a third shot.
“We may want to go on record stating what it is that would allow us to broaden our recommendation or restrict our recommendation,” Dr. Brooks said.
The considerations of who should get an extra dose are not always straightforward.
New modeling by the Harvard TH Chan School of Public Health and the CDC to assist the government’s decisions on boosters had a surprise finding: in nursing homes, it’s more effective to vaccinate healthcare workers than it is to give booster doses to these residents. Nursing homes are at the mercy of community transmission.
In regions with high transmission, it’s easy for a caregiver to bring the virus into a facility — so the models found that the transmission from these workers is a more effective strategy than giving third doses to the already highly vaccinated group of seniors who live in them.
A version of this article first appeared on Medscape.com.
The agency’s move comes as a Centers for Disease Control and Prevention (CDC) panel ended the first day of a 2-day meeting. That panel, the Advisory Committee on Immunization Practices (ACIP), is expected to vote Sept. 23 to instruct doctors on how to administer the boosters.
The FDA officially authorized the vaccine not only for individuals 65 and older, but also for people 18 through 64 years of age who are at high risk for severe illness from the coronavirus, including essential workers whose jobs increase their risk for infection.
“After considering the totality of the available scientific evidence and the deliberations of our advisory committee of independent, external experts, the FDA amended the EUA for the Pfizer-BioNTech COVID-19 vaccine to allow for a booster dose in certain populations such as health care workers, teachers and daycare staff, grocery workers and those in homeless shelters or prisons, among others,” Acting FDA Commissioner Janet Woodcock, MD, said in a news release.
The recommendations align with those from an FDA advisory panel Sept. 17.
The agency determined that the benefits of a booster dose outweigh the risks for people now authorized to receive it, according to the news release.
Other questions remain
So, how will this work? That was the main question weighing on the minds of the CDC’s ACIP during their first day of a 2-day meeting where they are expected to make recommendations on booster doses for Americans.
The panel discussed situations the FDA will still need to consider, such as what should be done for Americans who were originally vaccinated with a Moderna or Johnson and Johnson vaccine, but are not covered under the revised EUA, which is only for those people who received Pfizer’s two-dose vaccine regimen.
“That’s going to leave half of the people immunized in this age group having received the vaccine and being told that they’re at risk now for waning immunity and hospitalization unable to get a booster dose,” said committee member Sarah S. Long, MD, a professor of pediatrics at Drexel University College of Medicine in Philadelphia. “So that’s a big public health panic that we would like to avoid.”
Johnson and Johnson recently reported that second doses of its vaccine boosted its efficacy to almost 94% against COVID-19. A new study, published ahead of peer review, suggests that the efficacy of the single-dose Johnson and Johnson shot has fallen to about 78% against symptomatic infection during the Delta surge.
Moderna has applied for permission to market third doses of its vaccine in the United States, but the FDA has given no timeline on when it might make a decision.
Doran Fink, MD, PhD, deputy director of the FDA’s Division of Vaccines and Related Products Applications, a representative advising the committee Sept. 22, said the agency was working as rapidly as possible on Moderna’s submission.
Regarding the question of whether it was OK to mix vaccines, rather than match them, Dr. Fink said there are currently not enough data available to inform that decision.
Those answers are coming, though. John Beigel, MD, associate director of clinical research at the National Institute of Allergy and Infectious Diseases, revealed that the federal government has a study underway to see what happens when the vaccines are mixed with each other.
He said that data from the study would be available later this fall, and would certainly help physicians and other healthcare providers know whether it’s effective or safe to use them interchangeably.
Correlates of immunity
The ACIP left much of its schedule open Sept. 23 to discuss extra Pfizer doses and vote on how they should be used.
Pfizer had originally applied to the FDA for an amendment to its FDA approval, which would have given doctors a freer hand to prescribe third doses as they saw fit, in patients as young as 16.
But the FDA’s Vaccines and Related Biological Products Advisory Committee voted Sept. 17 against granting the amendment. The committee was particularly concerned about the lack of data in teens ages 16 and 17, who have the highest risk for a rare side effect that causes heart inflammation that requires hospital care.
Instead, they recommended — and the FDA agreed per their decision Sept. 22 — that third doses should be given to people at higher risk for severe breakthrough infections because of advanced age or because they work in an occupation that puts them at high risk for exposure.
The CDC panel heard important presentations on new science that is helping to identify the correlates of immunity.
The correlates of immunity are biomarkers that can be measured in blood that help doctors understand how protected a person may be against COVID-19. These markers of immunity are not yet known for the COVID-19 vaccines.
Emerging evidence shows that booster doses of the Pfizer vaccine cause front-line immune defenders — called binding antibodies — to roughly triple soon after a person gets the third shot.
Neutralizing antibodies also jump soon after two vaccine doses, but they fall over time, which is natural. The body doesn’t need these foot soldiers to be on guard all the time, so they go away.
The body retains its memory of how to make them, however, so they can quickly be marshaled again, if needed.
Early studies suggest that antibodies account for about two thirds of a person’s protection against COVID, while the longer-lasting T-cells and B-cells account for about one third.
After the antibody levels fall, it may take a few days to recreate this army. In the meantime, the virus can try to break in. This can cause symptoms, which can make a person feel terrible, but for the most part, vaccinated individuals don’t need hospital care and are nearly always protected from dying — even against the Delta variant.
Those most likely to be at risk for a breakthrough infection are older, because immune function wanes with age.
Essential workers
Essential workers, such as those who work in healthcare, may also benefit from high antibody levels, which can minimize symptoms and help them get back to work more quickly.
Helen Talbot, MD, MPH, an associate professor of medicine at Vanderbilt University Medical Center in Nashville, said that in her area staffing levels are critical right now.
“I’m actually sitting in one of the deepest red [states] with high rates of COVID. We don’t have enough health care workers currently to take care of the unvaccinated,” she said.
“When we have beds, we are often missing staff, and so the idea of vaccinating health care workers is to be a little bit different than our idea of using vaccines in the general population,” Dr. Talbot said.
Oliver Brooks, MD, chief medical officer of the Watts Healthcare Corporation in Los Angeles, said he was in favor of making a public statement about the temporary nature of the potential recommendations Sept. 23, because they probably won’t cover all who might need a third shot.
“We may want to go on record stating what it is that would allow us to broaden our recommendation or restrict our recommendation,” Dr. Brooks said.
The considerations of who should get an extra dose are not always straightforward.
New modeling by the Harvard TH Chan School of Public Health and the CDC to assist the government’s decisions on boosters had a surprise finding: in nursing homes, it’s more effective to vaccinate healthcare workers than it is to give booster doses to these residents. Nursing homes are at the mercy of community transmission.
In regions with high transmission, it’s easy for a caregiver to bring the virus into a facility — so the models found that the transmission from these workers is a more effective strategy than giving third doses to the already highly vaccinated group of seniors who live in them.
A version of this article first appeared on Medscape.com.
The agency’s move comes as a Centers for Disease Control and Prevention (CDC) panel ended the first day of a 2-day meeting. That panel, the Advisory Committee on Immunization Practices (ACIP), is expected to vote Sept. 23 to instruct doctors on how to administer the boosters.
The FDA officially authorized the vaccine not only for individuals 65 and older, but also for people 18 through 64 years of age who are at high risk for severe illness from the coronavirus, including essential workers whose jobs increase their risk for infection.
“After considering the totality of the available scientific evidence and the deliberations of our advisory committee of independent, external experts, the FDA amended the EUA for the Pfizer-BioNTech COVID-19 vaccine to allow for a booster dose in certain populations such as health care workers, teachers and daycare staff, grocery workers and those in homeless shelters or prisons, among others,” Acting FDA Commissioner Janet Woodcock, MD, said in a news release.
The recommendations align with those from an FDA advisory panel Sept. 17.
The agency determined that the benefits of a booster dose outweigh the risks for people now authorized to receive it, according to the news release.
Other questions remain
So, how will this work? That was the main question weighing on the minds of the CDC’s ACIP during their first day of a 2-day meeting where they are expected to make recommendations on booster doses for Americans.
The panel discussed situations the FDA will still need to consider, such as what should be done for Americans who were originally vaccinated with a Moderna or Johnson and Johnson vaccine, but are not covered under the revised EUA, which is only for those people who received Pfizer’s two-dose vaccine regimen.
“That’s going to leave half of the people immunized in this age group having received the vaccine and being told that they’re at risk now for waning immunity and hospitalization unable to get a booster dose,” said committee member Sarah S. Long, MD, a professor of pediatrics at Drexel University College of Medicine in Philadelphia. “So that’s a big public health panic that we would like to avoid.”
Johnson and Johnson recently reported that second doses of its vaccine boosted its efficacy to almost 94% against COVID-19. A new study, published ahead of peer review, suggests that the efficacy of the single-dose Johnson and Johnson shot has fallen to about 78% against symptomatic infection during the Delta surge.
Moderna has applied for permission to market third doses of its vaccine in the United States, but the FDA has given no timeline on when it might make a decision.
Doran Fink, MD, PhD, deputy director of the FDA’s Division of Vaccines and Related Products Applications, a representative advising the committee Sept. 22, said the agency was working as rapidly as possible on Moderna’s submission.
Regarding the question of whether it was OK to mix vaccines, rather than match them, Dr. Fink said there are currently not enough data available to inform that decision.
Those answers are coming, though. John Beigel, MD, associate director of clinical research at the National Institute of Allergy and Infectious Diseases, revealed that the federal government has a study underway to see what happens when the vaccines are mixed with each other.
He said that data from the study would be available later this fall, and would certainly help physicians and other healthcare providers know whether it’s effective or safe to use them interchangeably.
Correlates of immunity
The ACIP left much of its schedule open Sept. 23 to discuss extra Pfizer doses and vote on how they should be used.
Pfizer had originally applied to the FDA for an amendment to its FDA approval, which would have given doctors a freer hand to prescribe third doses as they saw fit, in patients as young as 16.
But the FDA’s Vaccines and Related Biological Products Advisory Committee voted Sept. 17 against granting the amendment. The committee was particularly concerned about the lack of data in teens ages 16 and 17, who have the highest risk for a rare side effect that causes heart inflammation that requires hospital care.
Instead, they recommended — and the FDA agreed per their decision Sept. 22 — that third doses should be given to people at higher risk for severe breakthrough infections because of advanced age or because they work in an occupation that puts them at high risk for exposure.
The CDC panel heard important presentations on new science that is helping to identify the correlates of immunity.
The correlates of immunity are biomarkers that can be measured in blood that help doctors understand how protected a person may be against COVID-19. These markers of immunity are not yet known for the COVID-19 vaccines.
Emerging evidence shows that booster doses of the Pfizer vaccine cause front-line immune defenders — called binding antibodies — to roughly triple soon after a person gets the third shot.
Neutralizing antibodies also jump soon after two vaccine doses, but they fall over time, which is natural. The body doesn’t need these foot soldiers to be on guard all the time, so they go away.
The body retains its memory of how to make them, however, so they can quickly be marshaled again, if needed.
Early studies suggest that antibodies account for about two thirds of a person’s protection against COVID, while the longer-lasting T-cells and B-cells account for about one third.
After the antibody levels fall, it may take a few days to recreate this army. In the meantime, the virus can try to break in. This can cause symptoms, which can make a person feel terrible, but for the most part, vaccinated individuals don’t need hospital care and are nearly always protected from dying — even against the Delta variant.
Those most likely to be at risk for a breakthrough infection are older, because immune function wanes with age.
Essential workers
Essential workers, such as those who work in healthcare, may also benefit from high antibody levels, which can minimize symptoms and help them get back to work more quickly.
Helen Talbot, MD, MPH, an associate professor of medicine at Vanderbilt University Medical Center in Nashville, said that in her area staffing levels are critical right now.
“I’m actually sitting in one of the deepest red [states] with high rates of COVID. We don’t have enough health care workers currently to take care of the unvaccinated,” she said.
“When we have beds, we are often missing staff, and so the idea of vaccinating health care workers is to be a little bit different than our idea of using vaccines in the general population,” Dr. Talbot said.
Oliver Brooks, MD, chief medical officer of the Watts Healthcare Corporation in Los Angeles, said he was in favor of making a public statement about the temporary nature of the potential recommendations Sept. 23, because they probably won’t cover all who might need a third shot.
“We may want to go on record stating what it is that would allow us to broaden our recommendation or restrict our recommendation,” Dr. Brooks said.
The considerations of who should get an extra dose are not always straightforward.
New modeling by the Harvard TH Chan School of Public Health and the CDC to assist the government’s decisions on boosters had a surprise finding: in nursing homes, it’s more effective to vaccinate healthcare workers than it is to give booster doses to these residents. Nursing homes are at the mercy of community transmission.
In regions with high transmission, it’s easy for a caregiver to bring the virus into a facility — so the models found that the transmission from these workers is a more effective strategy than giving third doses to the already highly vaccinated group of seniors who live in them.
A version of this article first appeared on Medscape.com.
Itchy patch on the clavicle
A broad shave biopsy, utilizing dermoscopy to help delineate the edges of the lesion, confirmed the diagnosis of melanoma in situ, superficial spreading type.
From the standpoint of ABCDE criteria (Asymmetry, Border irregularity, Color [varying shades or deep black color], Diameter > 6 mm, or Evolving/changing), this lesion was quite worrisome. Helpful clues on clinical exam included the asymmetry, border irregularity, color variations (brown, pink, and red), size, and history of change. A dermatoscope helped to refine the features of the lesion and highlighted the melanocytic-specific characteristics of its pigment network, streaks, and regression structures (pepper-like gray dots and white streaks).1
A broad shave biopsy allows a very thorough evaluation of such a heterogeneous lesion. A smaller punch biopsy can miss the most worrisome features. That said, a smaller punch biopsy is sometimes necessary in challenging anatomic locations, such as the palm or sole.
Patients given a diagnosis of melanoma in situ should undergo wide local excision with 5-mm margins or 1-cm margins in instances of lentigo maligna, which is a subtype of melanoma in situ with a higher risk of clinically uncertain margins. (A sentinel lymph node biopsy is not recommended for melanoma in situ, as the Breslow depth is 0 mm.)
For this patient, an in-office wide local excision was performed down to the fascia and the skin was repaired in a layered fashion. The plan for this patient was for him to return for skin examinations 3 to 4 times in the first year of diagnosis, followed by twice annually until he was 5 years from his diagnosis. After that, he would undergo annual skin exams.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
Ribero S, Moscarella E, Ferrara G, et al. Regression in cutaneous melanoma: a comprehensive review from diagnosis to prognosis. J Eur Acad Dermatol Venereol. 2016;30:2030-2037. doi: 10.1111/jdv.13815
A broad shave biopsy, utilizing dermoscopy to help delineate the edges of the lesion, confirmed the diagnosis of melanoma in situ, superficial spreading type.
From the standpoint of ABCDE criteria (Asymmetry, Border irregularity, Color [varying shades or deep black color], Diameter > 6 mm, or Evolving/changing), this lesion was quite worrisome. Helpful clues on clinical exam included the asymmetry, border irregularity, color variations (brown, pink, and red), size, and history of change. A dermatoscope helped to refine the features of the lesion and highlighted the melanocytic-specific characteristics of its pigment network, streaks, and regression structures (pepper-like gray dots and white streaks).1
A broad shave biopsy allows a very thorough evaluation of such a heterogeneous lesion. A smaller punch biopsy can miss the most worrisome features. That said, a smaller punch biopsy is sometimes necessary in challenging anatomic locations, such as the palm or sole.
Patients given a diagnosis of melanoma in situ should undergo wide local excision with 5-mm margins or 1-cm margins in instances of lentigo maligna, which is a subtype of melanoma in situ with a higher risk of clinically uncertain margins. (A sentinel lymph node biopsy is not recommended for melanoma in situ, as the Breslow depth is 0 mm.)
For this patient, an in-office wide local excision was performed down to the fascia and the skin was repaired in a layered fashion. The plan for this patient was for him to return for skin examinations 3 to 4 times in the first year of diagnosis, followed by twice annually until he was 5 years from his diagnosis. After that, he would undergo annual skin exams.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
A broad shave biopsy, utilizing dermoscopy to help delineate the edges of the lesion, confirmed the diagnosis of melanoma in situ, superficial spreading type.
From the standpoint of ABCDE criteria (Asymmetry, Border irregularity, Color [varying shades or deep black color], Diameter > 6 mm, or Evolving/changing), this lesion was quite worrisome. Helpful clues on clinical exam included the asymmetry, border irregularity, color variations (brown, pink, and red), size, and history of change. A dermatoscope helped to refine the features of the lesion and highlighted the melanocytic-specific characteristics of its pigment network, streaks, and regression structures (pepper-like gray dots and white streaks).1
A broad shave biopsy allows a very thorough evaluation of such a heterogeneous lesion. A smaller punch biopsy can miss the most worrisome features. That said, a smaller punch biopsy is sometimes necessary in challenging anatomic locations, such as the palm or sole.
Patients given a diagnosis of melanoma in situ should undergo wide local excision with 5-mm margins or 1-cm margins in instances of lentigo maligna, which is a subtype of melanoma in situ with a higher risk of clinically uncertain margins. (A sentinel lymph node biopsy is not recommended for melanoma in situ, as the Breslow depth is 0 mm.)
For this patient, an in-office wide local excision was performed down to the fascia and the skin was repaired in a layered fashion. The plan for this patient was for him to return for skin examinations 3 to 4 times in the first year of diagnosis, followed by twice annually until he was 5 years from his diagnosis. After that, he would undergo annual skin exams.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
Ribero S, Moscarella E, Ferrara G, et al. Regression in cutaneous melanoma: a comprehensive review from diagnosis to prognosis. J Eur Acad Dermatol Venereol. 2016;30:2030-2037. doi: 10.1111/jdv.13815
Ribero S, Moscarella E, Ferrara G, et al. Regression in cutaneous melanoma: a comprehensive review from diagnosis to prognosis. J Eur Acad Dermatol Venereol. 2016;30:2030-2037. doi: 10.1111/jdv.13815
Botulinum Toxin for the Treatment of Intractable Raynaud Phenomenon
To the Editor:
Raynaud phenomenon (RP) is an episodic vasospasm of the digits that can lead to ulceration, gangrene, and autoamputation with prolonged ischemia. OnabotulinumtoxinA has been implemented as a treatment of intractable RP by paralyzing the muscles of the digital arteries. We report a case of a woman with severe RP secondary to systemic lupus erythematosus (SLE) who was treated with onabotulinumtoxinA injections after multiple treatment modalities failed to improve her condition. We describe the dosage and injection technique used to produce clinical improvement in our patient and compare it to prior reports in the literature.
A 33-year-old woman presented to the emergency department for worsening foot pain of 5 days' duration with dusky purple color changes concerning for impending Raynaud crisis related to RP. The patient had a history of antiphospholipid antibody syndrome (APS) and SLE with overlapping symptoms of polymyositis and scleroderma. She had been hospitalized for RP multiple times prior to the current admission. She was medically managed with nifedipine, sildenafil, losartan potassium, aspirin, alprostadil, and prostaglandin infusions, and was surgically managed with a right-hand sympathectomy and right ulnar artery bypass graft that had subsequently thrombosed. At the current presentation, she had painful dusky toes on both feet though more pronounced on the left foot. She endorsed foot pain while walking and tenderness to palpation of the fingers, which were minimally improved with intravenous prostaglandins.
Physical examination revealed blanching of the digits in both hands with pits in the right fourth and left first digits. Dusky patches overlaid all the toes as well as the superior plantar aspects of the feet (Figure 1). Given the history of APS, a punch biopsy was performed on the left medial plantar foot and results showed no histologic evidence of vasculitis or vasculopathy. Necrotic foci were present on the left and right second metatarsal bones, which were not reperfusable (Figure 2). The clinical findings and punch biopsy results favored RP as opposed to vasculopathy from APS.
Several interventions were attempted, and after 4 days with no response, the patient agreed to receive treatment with onabotulinumtoxinA. OnabotulinumtoxinA (5 U) was injected into the subcutaneous tissue of the medial and lateral aspects of each of the first and second toes near the proximal phalanges (40 U total). However, treatment could not be completed due to severe pain caused by the injections despite preprocedure regional nerve blocks to both lower extremities, preinjection icing, and lorazepam. Two days later, the patient tolerated onabotulinumtoxinA injections of all remaining digits of both feet (60 U total). She noted slight clinical improvement soon thereafter. One week after treatment of all 10 toes, she reported decreased pain and reduced duskiness of both feet (Figure 3).
One month later, the patient endorsed recurring pain in the hands and feet. Physical examination revealed reticular cyanosis and increased violaceous patches of the hands; the feet were overall unchanged from the prior hospitalization. At 4-month follow-up, there was gangrene on the left second, third, and fifth toe in addition to areas of induration noted on the fingers. She was repeatedly hospitalized over the next 6 months for pain management and gangrene of the toes, and finally underwent an amputation of the left and right second toe at the proximal and middle phalanx, respectively. She currently is continuing extensive medical management for pain and gangrene of the digits; she has not received additional onabotulinumtoxinA injections.
Raynaud phenomenon is a vascular disorder characterized by intermittent arteriolar vasospasm of the digits, often due to cold temperature or stress. Approximately 90% of RP cases are primarily idiopathic, with the remaining cases secondary to other diseases, typically systemic sclerosis, SLE, or mixed connective tissue disease.1 Symptoms present with characteristic changing of hands from white (ischemia) to blue (hypoxia) to red (reperfusion). Episodic attacks of vasospasm and ischemia can be painful and lead to digital ulcerations and necrosis of the digits or hands. Other complications including digital tuft pits, pterygium inversum unguis, or torturous nail fold capillaries with capillary dropout also may be seen.2
Although the etiology is multifactorial, the pathophysiology primarily is due to an imbalance of vasodilation and vasoconstriction. Perturbed levels of vasodilatory mediators include nitric oxide, prostacyclin, and calcitonin gene-related peptide.3 Meanwhile, abnormal neural sympathetic control of α-adrenergic receptors located on smooth muscle vasculature and subsequent endothelial hyperproliferation may contribute to inappropriate vasoconstriction.4
The first-line therapy for mild to moderate disease refractory to conservative management includes monotherapy with dihydropyridine calcium channel blockers. For severe disease, combination therapy involves addition of other classes of medications including phosphodiesterase 5 inhibitors, topical nitrates, angiotensin receptor blockers, or selective serotonin reuptake inhibitors. Intravenous prostacyclin, endothelin receptor blockers, and onabotulinumtoxinA injections may be added as third-line therapy. Finally, surgical management including sympathectomy with continued pharmacologic therapy may be needed for disease recalcitrant to the aforementioned options.2
OnabotulinumtoxinA is a neurotoxin produced by the bacterium Clostridium botulinum. The toxin’s mechanism of action involves inhibition of the release of presynaptic acetylcholine-containing vesicles at the neuromuscular junction through cleavage of sensory nerve action potential receptor proteins. In addition, it inhibits smooth muscle vasoconstriction and pain by blocking α2-adrenergic receptors on blood vessels and chronic pain-transmitting C fibers in nerves, respectively.3,5
Only recently has onabotulinumtoxinA been used for treatment of RP. Botulinum toxin is approved for the treatment of spastic and dystonic diseases such as blepharospasm, headaches in patients with chronic migraines, upper limb spasticity, cervical dystonia, torticollis, ocular strabismus, and hyperhidrosis.3 However, the versatility of its therapeutic effects is evident in its broad off-label clinical applications, including achalasia; carpal tunnel syndrome; and spasticity relating to stroke, paraplegia, and cerebral palsy, among many others.5
Few studies have analyzed the use of onabotulinumtoxinA for the treatment of RP.3,6 There is no consensus yet regarding dose, dilution, or injection sites. One vial of onabotulinumtoxinA contains 100 U and is reconstituted in 20 mL of normal saline to produce 5 U/mL. The simplest technique involves the injection of 5 U into the medial and lateral aspects of each finger at its base, at the level of or just proximal to the A1 pulley, for a total of 50 U per hand.7 In the foot, injection can be made at the base of each toe near the proximal phalanges. A regimen of 50 to 100 U per hand was used by Neumeister et al5 on 19 patients, who subsequently standardized it to 10 U on each neurovascular bundle in a follow-up study,7 giving a total volume of 2 mL per injection. Associated pain or a burning sensation initially may be experienced, which may be mitigated by a lidocaine hydrochloride wrist block prior to injection.7 This technique produced immediate and lasting pain relief, increased tissue perfusion, and resolved digital ulcers in 28 of 33 patients. Most patients reported immediate relief, and a few noted gradual reduction in pain and resolution of chronic ulcers within 2 months. Of the 33 patients, 7 (21.2%) required repeat injections for recurrent pain, but the majority were pain free up to 6 years later with a single injection schedule.7
Injection into the palmar region, wrists, and/or fingers also may be performed. Effects of using different injection sites (eg, neurovascular bundle, distal palm, proximal hand) have been explored and were not notably different between these locations.8 Lastly, the frequency of injections may be attenuated according to the spectrum and severity of the patient’s symptoms. In a report of 11 patients who received a total of 100 U of onabotulinumtoxinA per hand, 5 required repeat injections within 3 to 8 months.9
Studies have reported onabotulinumtoxinA to be a promising option for the treatment of intractable symptoms. Likewise, our patient had a notable reduction in pain with signs of clinical improvement within 24 to 48 hours after injection. The need for amputation 6 months later likely was because the patient’s toes were already necrosing prior to treatment with onabotulinumtoxinA. Thus, the timing of intervention may play a critical role in response to onabotulinumtoxinA injections, particularly because the severity of our patient’s presentation was comparable to other cases reported in the literature. Even in reports using a smaller dose—2 U injected into each toe as opposed to 10 U per toe, as in our case—follow-up showed favorable results.10 In other reports, response can be perceived within days to a week, with remarkable improvement of numbness, pain, digit color, and wound resolution, in addition to decreased frequency and severity of attacks. Moreover, greater vasodilation and subsequent tissue perfusion have been evidenced by objective measures including digital transcutaneous oxygen saturation and Doppler sonography.7,8 Side effects, which are minimal and temporary, include local pain triggering a vasospastic attack and intrinsic muscle weakness; more rarely, dysesthesia and thenar eminence atrophy have been reported.11
Available studies have shown onabotulinumtoxinA to produce favorable results in the treatment of vasospastic disease. We suspect that an earlier intervention for our patient—before necrosis of the toes developed—would have led to a more positive outcome, consistent with other reports. Treatment with onabotulinumtoxinA is an approach to consider when the standard-of-care treatments for RP have been exhausted, as timely intervention may prevent the need for surgery. The indications and appropriate dosing protocol remain to be defined, in addition to more thorough evaluation of its efficacy relative to other medical and surgical options.
- Neumeister MW. The role of botulinum toxin in vasospastic disorders of the hand. Hand Clin. 2015;31:23-37. doi:10.1016/j.hcl.2014.09.003
- Bakst R, Merola JF, Franks AG, et al. Raynaud’s phenomenon: pathogenesis and management. J Am Acad Dermatol. 2008;59:633-653. doi:10.1016/j.jaad.2008.06.004
- Iorio ML, Masden DL, Higgins JP. Botulinum toxin a treatment of Raynaud’s phenomenon: a review. Semin Arthritis Rheum. 2012;41:599-603. doi:10.1016/j.semarthrit.2011.07.006
- Wigley FM, Flavahan NA. Raynaud’s phenomenon. N Engl J Med. 2016;375:556-565. doi:10.1056/NEJMra1507638
- Neumeister MW, Chambers CB, Herron MS, et al. Botox therapy for ischemic digits. Plast Reconstr Surg. 2009;124:191-200. doi:10.1097/PRS.0b013e3181a80576
- Sycha T, Graninger M, Auff E, et al. Botulinum toxin in the treatment of Raynaud’s phenomenon: a pilot study. Eur J Clin Invest. 2004;34:312-313. doi:10.1016/j.jaad.2013.06.029
- Neumeister MW. Botulinum toxin type A in the treatment of Raynaud’s phenomenon. J Hand Surg Am. 2010;35:2085-2092. doi:10.1016/j.jhsa.2010.09.019
- Fregene A, Ditmars D, Siddiqui A. Botulinum toxin type A: a treatment option for digital ischemia in patients with Raynaud’s phenomenon. J Hand Surg Am. 2009;34:446-452. doi:10.1016/j.jhsa.2008.11.026
- Van Beek AL, Lim PK, Gear AJL, et al. Management of vasospastic disorders with botulinum toxin A. Plast Reconstr Surg. 2007;119:217-226. doi:10.1097/01.prs.0000244860.00674.57
- Dhaliwal K, Griffin M, Denton CP, et al. The novel use of botulinum toxin A for the treatment of Raynaud’s phenomenon in the toes. BMJ Case Rep. 2018;2018:2017-2019. doi:10.1136/bcr-2017-219348
- Eickhoff JC, Smith JK, Landau ME, et al. Iatrogenic thenar eminence atrophy after Botox A injection for secondary Raynaud phenomenon. J Clin Rheumatol. 2016;22:395-396. doi:10.1097/RHU.0000000000000450
To the Editor:
Raynaud phenomenon (RP) is an episodic vasospasm of the digits that can lead to ulceration, gangrene, and autoamputation with prolonged ischemia. OnabotulinumtoxinA has been implemented as a treatment of intractable RP by paralyzing the muscles of the digital arteries. We report a case of a woman with severe RP secondary to systemic lupus erythematosus (SLE) who was treated with onabotulinumtoxinA injections after multiple treatment modalities failed to improve her condition. We describe the dosage and injection technique used to produce clinical improvement in our patient and compare it to prior reports in the literature.
A 33-year-old woman presented to the emergency department for worsening foot pain of 5 days' duration with dusky purple color changes concerning for impending Raynaud crisis related to RP. The patient had a history of antiphospholipid antibody syndrome (APS) and SLE with overlapping symptoms of polymyositis and scleroderma. She had been hospitalized for RP multiple times prior to the current admission. She was medically managed with nifedipine, sildenafil, losartan potassium, aspirin, alprostadil, and prostaglandin infusions, and was surgically managed with a right-hand sympathectomy and right ulnar artery bypass graft that had subsequently thrombosed. At the current presentation, she had painful dusky toes on both feet though more pronounced on the left foot. She endorsed foot pain while walking and tenderness to palpation of the fingers, which were minimally improved with intravenous prostaglandins.
Physical examination revealed blanching of the digits in both hands with pits in the right fourth and left first digits. Dusky patches overlaid all the toes as well as the superior plantar aspects of the feet (Figure 1). Given the history of APS, a punch biopsy was performed on the left medial plantar foot and results showed no histologic evidence of vasculitis or vasculopathy. Necrotic foci were present on the left and right second metatarsal bones, which were not reperfusable (Figure 2). The clinical findings and punch biopsy results favored RP as opposed to vasculopathy from APS.
Several interventions were attempted, and after 4 days with no response, the patient agreed to receive treatment with onabotulinumtoxinA. OnabotulinumtoxinA (5 U) was injected into the subcutaneous tissue of the medial and lateral aspects of each of the first and second toes near the proximal phalanges (40 U total). However, treatment could not be completed due to severe pain caused by the injections despite preprocedure regional nerve blocks to both lower extremities, preinjection icing, and lorazepam. Two days later, the patient tolerated onabotulinumtoxinA injections of all remaining digits of both feet (60 U total). She noted slight clinical improvement soon thereafter. One week after treatment of all 10 toes, she reported decreased pain and reduced duskiness of both feet (Figure 3).
One month later, the patient endorsed recurring pain in the hands and feet. Physical examination revealed reticular cyanosis and increased violaceous patches of the hands; the feet were overall unchanged from the prior hospitalization. At 4-month follow-up, there was gangrene on the left second, third, and fifth toe in addition to areas of induration noted on the fingers. She was repeatedly hospitalized over the next 6 months for pain management and gangrene of the toes, and finally underwent an amputation of the left and right second toe at the proximal and middle phalanx, respectively. She currently is continuing extensive medical management for pain and gangrene of the digits; she has not received additional onabotulinumtoxinA injections.
Raynaud phenomenon is a vascular disorder characterized by intermittent arteriolar vasospasm of the digits, often due to cold temperature or stress. Approximately 90% of RP cases are primarily idiopathic, with the remaining cases secondary to other diseases, typically systemic sclerosis, SLE, or mixed connective tissue disease.1 Symptoms present with characteristic changing of hands from white (ischemia) to blue (hypoxia) to red (reperfusion). Episodic attacks of vasospasm and ischemia can be painful and lead to digital ulcerations and necrosis of the digits or hands. Other complications including digital tuft pits, pterygium inversum unguis, or torturous nail fold capillaries with capillary dropout also may be seen.2
Although the etiology is multifactorial, the pathophysiology primarily is due to an imbalance of vasodilation and vasoconstriction. Perturbed levels of vasodilatory mediators include nitric oxide, prostacyclin, and calcitonin gene-related peptide.3 Meanwhile, abnormal neural sympathetic control of α-adrenergic receptors located on smooth muscle vasculature and subsequent endothelial hyperproliferation may contribute to inappropriate vasoconstriction.4
The first-line therapy for mild to moderate disease refractory to conservative management includes monotherapy with dihydropyridine calcium channel blockers. For severe disease, combination therapy involves addition of other classes of medications including phosphodiesterase 5 inhibitors, topical nitrates, angiotensin receptor blockers, or selective serotonin reuptake inhibitors. Intravenous prostacyclin, endothelin receptor blockers, and onabotulinumtoxinA injections may be added as third-line therapy. Finally, surgical management including sympathectomy with continued pharmacologic therapy may be needed for disease recalcitrant to the aforementioned options.2
OnabotulinumtoxinA is a neurotoxin produced by the bacterium Clostridium botulinum. The toxin’s mechanism of action involves inhibition of the release of presynaptic acetylcholine-containing vesicles at the neuromuscular junction through cleavage of sensory nerve action potential receptor proteins. In addition, it inhibits smooth muscle vasoconstriction and pain by blocking α2-adrenergic receptors on blood vessels and chronic pain-transmitting C fibers in nerves, respectively.3,5
Only recently has onabotulinumtoxinA been used for treatment of RP. Botulinum toxin is approved for the treatment of spastic and dystonic diseases such as blepharospasm, headaches in patients with chronic migraines, upper limb spasticity, cervical dystonia, torticollis, ocular strabismus, and hyperhidrosis.3 However, the versatility of its therapeutic effects is evident in its broad off-label clinical applications, including achalasia; carpal tunnel syndrome; and spasticity relating to stroke, paraplegia, and cerebral palsy, among many others.5
Few studies have analyzed the use of onabotulinumtoxinA for the treatment of RP.3,6 There is no consensus yet regarding dose, dilution, or injection sites. One vial of onabotulinumtoxinA contains 100 U and is reconstituted in 20 mL of normal saline to produce 5 U/mL. The simplest technique involves the injection of 5 U into the medial and lateral aspects of each finger at its base, at the level of or just proximal to the A1 pulley, for a total of 50 U per hand.7 In the foot, injection can be made at the base of each toe near the proximal phalanges. A regimen of 50 to 100 U per hand was used by Neumeister et al5 on 19 patients, who subsequently standardized it to 10 U on each neurovascular bundle in a follow-up study,7 giving a total volume of 2 mL per injection. Associated pain or a burning sensation initially may be experienced, which may be mitigated by a lidocaine hydrochloride wrist block prior to injection.7 This technique produced immediate and lasting pain relief, increased tissue perfusion, and resolved digital ulcers in 28 of 33 patients. Most patients reported immediate relief, and a few noted gradual reduction in pain and resolution of chronic ulcers within 2 months. Of the 33 patients, 7 (21.2%) required repeat injections for recurrent pain, but the majority were pain free up to 6 years later with a single injection schedule.7
Injection into the palmar region, wrists, and/or fingers also may be performed. Effects of using different injection sites (eg, neurovascular bundle, distal palm, proximal hand) have been explored and were not notably different between these locations.8 Lastly, the frequency of injections may be attenuated according to the spectrum and severity of the patient’s symptoms. In a report of 11 patients who received a total of 100 U of onabotulinumtoxinA per hand, 5 required repeat injections within 3 to 8 months.9
Studies have reported onabotulinumtoxinA to be a promising option for the treatment of intractable symptoms. Likewise, our patient had a notable reduction in pain with signs of clinical improvement within 24 to 48 hours after injection. The need for amputation 6 months later likely was because the patient’s toes were already necrosing prior to treatment with onabotulinumtoxinA. Thus, the timing of intervention may play a critical role in response to onabotulinumtoxinA injections, particularly because the severity of our patient’s presentation was comparable to other cases reported in the literature. Even in reports using a smaller dose—2 U injected into each toe as opposed to 10 U per toe, as in our case—follow-up showed favorable results.10 In other reports, response can be perceived within days to a week, with remarkable improvement of numbness, pain, digit color, and wound resolution, in addition to decreased frequency and severity of attacks. Moreover, greater vasodilation and subsequent tissue perfusion have been evidenced by objective measures including digital transcutaneous oxygen saturation and Doppler sonography.7,8 Side effects, which are minimal and temporary, include local pain triggering a vasospastic attack and intrinsic muscle weakness; more rarely, dysesthesia and thenar eminence atrophy have been reported.11
Available studies have shown onabotulinumtoxinA to produce favorable results in the treatment of vasospastic disease. We suspect that an earlier intervention for our patient—before necrosis of the toes developed—would have led to a more positive outcome, consistent with other reports. Treatment with onabotulinumtoxinA is an approach to consider when the standard-of-care treatments for RP have been exhausted, as timely intervention may prevent the need for surgery. The indications and appropriate dosing protocol remain to be defined, in addition to more thorough evaluation of its efficacy relative to other medical and surgical options.
To the Editor:
Raynaud phenomenon (RP) is an episodic vasospasm of the digits that can lead to ulceration, gangrene, and autoamputation with prolonged ischemia. OnabotulinumtoxinA has been implemented as a treatment of intractable RP by paralyzing the muscles of the digital arteries. We report a case of a woman with severe RP secondary to systemic lupus erythematosus (SLE) who was treated with onabotulinumtoxinA injections after multiple treatment modalities failed to improve her condition. We describe the dosage and injection technique used to produce clinical improvement in our patient and compare it to prior reports in the literature.
A 33-year-old woman presented to the emergency department for worsening foot pain of 5 days' duration with dusky purple color changes concerning for impending Raynaud crisis related to RP. The patient had a history of antiphospholipid antibody syndrome (APS) and SLE with overlapping symptoms of polymyositis and scleroderma. She had been hospitalized for RP multiple times prior to the current admission. She was medically managed with nifedipine, sildenafil, losartan potassium, aspirin, alprostadil, and prostaglandin infusions, and was surgically managed with a right-hand sympathectomy and right ulnar artery bypass graft that had subsequently thrombosed. At the current presentation, she had painful dusky toes on both feet though more pronounced on the left foot. She endorsed foot pain while walking and tenderness to palpation of the fingers, which were minimally improved with intravenous prostaglandins.
Physical examination revealed blanching of the digits in both hands with pits in the right fourth and left first digits. Dusky patches overlaid all the toes as well as the superior plantar aspects of the feet (Figure 1). Given the history of APS, a punch biopsy was performed on the left medial plantar foot and results showed no histologic evidence of vasculitis or vasculopathy. Necrotic foci were present on the left and right second metatarsal bones, which were not reperfusable (Figure 2). The clinical findings and punch biopsy results favored RP as opposed to vasculopathy from APS.
Several interventions were attempted, and after 4 days with no response, the patient agreed to receive treatment with onabotulinumtoxinA. OnabotulinumtoxinA (5 U) was injected into the subcutaneous tissue of the medial and lateral aspects of each of the first and second toes near the proximal phalanges (40 U total). However, treatment could not be completed due to severe pain caused by the injections despite preprocedure regional nerve blocks to both lower extremities, preinjection icing, and lorazepam. Two days later, the patient tolerated onabotulinumtoxinA injections of all remaining digits of both feet (60 U total). She noted slight clinical improvement soon thereafter. One week after treatment of all 10 toes, she reported decreased pain and reduced duskiness of both feet (Figure 3).
One month later, the patient endorsed recurring pain in the hands and feet. Physical examination revealed reticular cyanosis and increased violaceous patches of the hands; the feet were overall unchanged from the prior hospitalization. At 4-month follow-up, there was gangrene on the left second, third, and fifth toe in addition to areas of induration noted on the fingers. She was repeatedly hospitalized over the next 6 months for pain management and gangrene of the toes, and finally underwent an amputation of the left and right second toe at the proximal and middle phalanx, respectively. She currently is continuing extensive medical management for pain and gangrene of the digits; she has not received additional onabotulinumtoxinA injections.
Raynaud phenomenon is a vascular disorder characterized by intermittent arteriolar vasospasm of the digits, often due to cold temperature or stress. Approximately 90% of RP cases are primarily idiopathic, with the remaining cases secondary to other diseases, typically systemic sclerosis, SLE, or mixed connective tissue disease.1 Symptoms present with characteristic changing of hands from white (ischemia) to blue (hypoxia) to red (reperfusion). Episodic attacks of vasospasm and ischemia can be painful and lead to digital ulcerations and necrosis of the digits or hands. Other complications including digital tuft pits, pterygium inversum unguis, or torturous nail fold capillaries with capillary dropout also may be seen.2
Although the etiology is multifactorial, the pathophysiology primarily is due to an imbalance of vasodilation and vasoconstriction. Perturbed levels of vasodilatory mediators include nitric oxide, prostacyclin, and calcitonin gene-related peptide.3 Meanwhile, abnormal neural sympathetic control of α-adrenergic receptors located on smooth muscle vasculature and subsequent endothelial hyperproliferation may contribute to inappropriate vasoconstriction.4
The first-line therapy for mild to moderate disease refractory to conservative management includes monotherapy with dihydropyridine calcium channel blockers. For severe disease, combination therapy involves addition of other classes of medications including phosphodiesterase 5 inhibitors, topical nitrates, angiotensin receptor blockers, or selective serotonin reuptake inhibitors. Intravenous prostacyclin, endothelin receptor blockers, and onabotulinumtoxinA injections may be added as third-line therapy. Finally, surgical management including sympathectomy with continued pharmacologic therapy may be needed for disease recalcitrant to the aforementioned options.2
OnabotulinumtoxinA is a neurotoxin produced by the bacterium Clostridium botulinum. The toxin’s mechanism of action involves inhibition of the release of presynaptic acetylcholine-containing vesicles at the neuromuscular junction through cleavage of sensory nerve action potential receptor proteins. In addition, it inhibits smooth muscle vasoconstriction and pain by blocking α2-adrenergic receptors on blood vessels and chronic pain-transmitting C fibers in nerves, respectively.3,5
Only recently has onabotulinumtoxinA been used for treatment of RP. Botulinum toxin is approved for the treatment of spastic and dystonic diseases such as blepharospasm, headaches in patients with chronic migraines, upper limb spasticity, cervical dystonia, torticollis, ocular strabismus, and hyperhidrosis.3 However, the versatility of its therapeutic effects is evident in its broad off-label clinical applications, including achalasia; carpal tunnel syndrome; and spasticity relating to stroke, paraplegia, and cerebral palsy, among many others.5
Few studies have analyzed the use of onabotulinumtoxinA for the treatment of RP.3,6 There is no consensus yet regarding dose, dilution, or injection sites. One vial of onabotulinumtoxinA contains 100 U and is reconstituted in 20 mL of normal saline to produce 5 U/mL. The simplest technique involves the injection of 5 U into the medial and lateral aspects of each finger at its base, at the level of or just proximal to the A1 pulley, for a total of 50 U per hand.7 In the foot, injection can be made at the base of each toe near the proximal phalanges. A regimen of 50 to 100 U per hand was used by Neumeister et al5 on 19 patients, who subsequently standardized it to 10 U on each neurovascular bundle in a follow-up study,7 giving a total volume of 2 mL per injection. Associated pain or a burning sensation initially may be experienced, which may be mitigated by a lidocaine hydrochloride wrist block prior to injection.7 This technique produced immediate and lasting pain relief, increased tissue perfusion, and resolved digital ulcers in 28 of 33 patients. Most patients reported immediate relief, and a few noted gradual reduction in pain and resolution of chronic ulcers within 2 months. Of the 33 patients, 7 (21.2%) required repeat injections for recurrent pain, but the majority were pain free up to 6 years later with a single injection schedule.7
Injection into the palmar region, wrists, and/or fingers also may be performed. Effects of using different injection sites (eg, neurovascular bundle, distal palm, proximal hand) have been explored and were not notably different between these locations.8 Lastly, the frequency of injections may be attenuated according to the spectrum and severity of the patient’s symptoms. In a report of 11 patients who received a total of 100 U of onabotulinumtoxinA per hand, 5 required repeat injections within 3 to 8 months.9
Studies have reported onabotulinumtoxinA to be a promising option for the treatment of intractable symptoms. Likewise, our patient had a notable reduction in pain with signs of clinical improvement within 24 to 48 hours after injection. The need for amputation 6 months later likely was because the patient’s toes were already necrosing prior to treatment with onabotulinumtoxinA. Thus, the timing of intervention may play a critical role in response to onabotulinumtoxinA injections, particularly because the severity of our patient’s presentation was comparable to other cases reported in the literature. Even in reports using a smaller dose—2 U injected into each toe as opposed to 10 U per toe, as in our case—follow-up showed favorable results.10 In other reports, response can be perceived within days to a week, with remarkable improvement of numbness, pain, digit color, and wound resolution, in addition to decreased frequency and severity of attacks. Moreover, greater vasodilation and subsequent tissue perfusion have been evidenced by objective measures including digital transcutaneous oxygen saturation and Doppler sonography.7,8 Side effects, which are minimal and temporary, include local pain triggering a vasospastic attack and intrinsic muscle weakness; more rarely, dysesthesia and thenar eminence atrophy have been reported.11
Available studies have shown onabotulinumtoxinA to produce favorable results in the treatment of vasospastic disease. We suspect that an earlier intervention for our patient—before necrosis of the toes developed—would have led to a more positive outcome, consistent with other reports. Treatment with onabotulinumtoxinA is an approach to consider when the standard-of-care treatments for RP have been exhausted, as timely intervention may prevent the need for surgery. The indications and appropriate dosing protocol remain to be defined, in addition to more thorough evaluation of its efficacy relative to other medical and surgical options.
- Neumeister MW. The role of botulinum toxin in vasospastic disorders of the hand. Hand Clin. 2015;31:23-37. doi:10.1016/j.hcl.2014.09.003
- Bakst R, Merola JF, Franks AG, et al. Raynaud’s phenomenon: pathogenesis and management. J Am Acad Dermatol. 2008;59:633-653. doi:10.1016/j.jaad.2008.06.004
- Iorio ML, Masden DL, Higgins JP. Botulinum toxin a treatment of Raynaud’s phenomenon: a review. Semin Arthritis Rheum. 2012;41:599-603. doi:10.1016/j.semarthrit.2011.07.006
- Wigley FM, Flavahan NA. Raynaud’s phenomenon. N Engl J Med. 2016;375:556-565. doi:10.1056/NEJMra1507638
- Neumeister MW, Chambers CB, Herron MS, et al. Botox therapy for ischemic digits. Plast Reconstr Surg. 2009;124:191-200. doi:10.1097/PRS.0b013e3181a80576
- Sycha T, Graninger M, Auff E, et al. Botulinum toxin in the treatment of Raynaud’s phenomenon: a pilot study. Eur J Clin Invest. 2004;34:312-313. doi:10.1016/j.jaad.2013.06.029
- Neumeister MW. Botulinum toxin type A in the treatment of Raynaud’s phenomenon. J Hand Surg Am. 2010;35:2085-2092. doi:10.1016/j.jhsa.2010.09.019
- Fregene A, Ditmars D, Siddiqui A. Botulinum toxin type A: a treatment option for digital ischemia in patients with Raynaud’s phenomenon. J Hand Surg Am. 2009;34:446-452. doi:10.1016/j.jhsa.2008.11.026
- Van Beek AL, Lim PK, Gear AJL, et al. Management of vasospastic disorders with botulinum toxin A. Plast Reconstr Surg. 2007;119:217-226. doi:10.1097/01.prs.0000244860.00674.57
- Dhaliwal K, Griffin M, Denton CP, et al. The novel use of botulinum toxin A for the treatment of Raynaud’s phenomenon in the toes. BMJ Case Rep. 2018;2018:2017-2019. doi:10.1136/bcr-2017-219348
- Eickhoff JC, Smith JK, Landau ME, et al. Iatrogenic thenar eminence atrophy after Botox A injection for secondary Raynaud phenomenon. J Clin Rheumatol. 2016;22:395-396. doi:10.1097/RHU.0000000000000450
- Neumeister MW. The role of botulinum toxin in vasospastic disorders of the hand. Hand Clin. 2015;31:23-37. doi:10.1016/j.hcl.2014.09.003
- Bakst R, Merola JF, Franks AG, et al. Raynaud’s phenomenon: pathogenesis and management. J Am Acad Dermatol. 2008;59:633-653. doi:10.1016/j.jaad.2008.06.004
- Iorio ML, Masden DL, Higgins JP. Botulinum toxin a treatment of Raynaud’s phenomenon: a review. Semin Arthritis Rheum. 2012;41:599-603. doi:10.1016/j.semarthrit.2011.07.006
- Wigley FM, Flavahan NA. Raynaud’s phenomenon. N Engl J Med. 2016;375:556-565. doi:10.1056/NEJMra1507638
- Neumeister MW, Chambers CB, Herron MS, et al. Botox therapy for ischemic digits. Plast Reconstr Surg. 2009;124:191-200. doi:10.1097/PRS.0b013e3181a80576
- Sycha T, Graninger M, Auff E, et al. Botulinum toxin in the treatment of Raynaud’s phenomenon: a pilot study. Eur J Clin Invest. 2004;34:312-313. doi:10.1016/j.jaad.2013.06.029
- Neumeister MW. Botulinum toxin type A in the treatment of Raynaud’s phenomenon. J Hand Surg Am. 2010;35:2085-2092. doi:10.1016/j.jhsa.2010.09.019
- Fregene A, Ditmars D, Siddiqui A. Botulinum toxin type A: a treatment option for digital ischemia in patients with Raynaud’s phenomenon. J Hand Surg Am. 2009;34:446-452. doi:10.1016/j.jhsa.2008.11.026
- Van Beek AL, Lim PK, Gear AJL, et al. Management of vasospastic disorders with botulinum toxin A. Plast Reconstr Surg. 2007;119:217-226. doi:10.1097/01.prs.0000244860.00674.57
- Dhaliwal K, Griffin M, Denton CP, et al. The novel use of botulinum toxin A for the treatment of Raynaud’s phenomenon in the toes. BMJ Case Rep. 2018;2018:2017-2019. doi:10.1136/bcr-2017-219348
- Eickhoff JC, Smith JK, Landau ME, et al. Iatrogenic thenar eminence atrophy after Botox A injection for secondary Raynaud phenomenon. J Clin Rheumatol. 2016;22:395-396. doi:10.1097/RHU.0000000000000450
Practice Points
- Raynaud phenomenon (RP) is a vascular disorder characterized by episodic vasospasms of the digits often due to cold temperature or stress.
- OnabotulinumtoxinA has been implemented as a treatment of intractable RP after failure with traditional treatments, such as calcium channel blockers, angiotensin receptor blockers, prostaglandins, endothelin receptor blockers, and phosphodiesterase 5 inhibitors.
- A standard technique of delivery of onabotulinumtoxinA involves injection of 5 U/mL into the medial and lateral aspects of each finger at its base (near the metacarpal head) for a total of 50 U per hand or foot.