User login
Common parasite now tied to impaired cognitive function
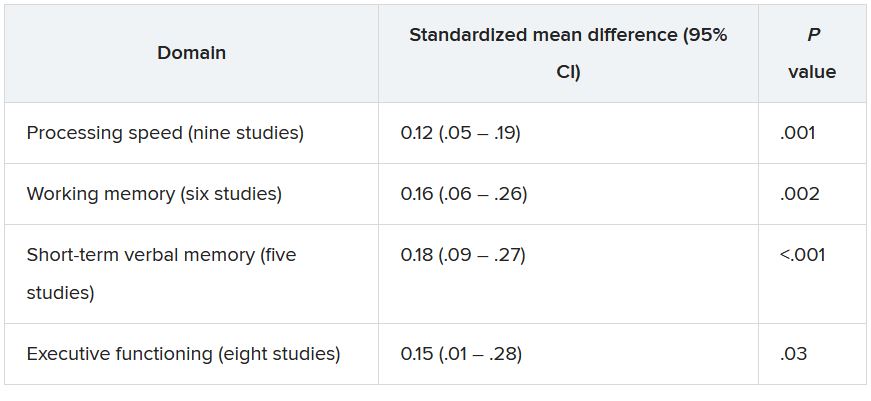
Investigators reviewed and conducted a meta-analysis of 13 studies that encompassed more than 13,000 healthy adults and found a modest but significant association between T. gondii seropositivity and impaired performance on cognitive tests of processing speed, working memory, short-term verbal memory, and executive function. The average age of the persons in the studies was close to 50 years.
“Our findings show that T. gondii could have a negative but small effect on cognition,” study investigator Arjen Sutterland, MD, of the Amsterdam Neuroscience Research Institute and the Amsterdam Institute for Infection and Immunity, University of Amsterdam, said in an interview.
The study was published online July 14, 2021, in JAMA Psychiatry.
Mental illness link
T. gondii is “an intracellular parasite that produces quiescent infection in approximately 30% of humans worldwide,” the authors wrote. The parasite that causes the infection not only settles in muscle and liver tissue but also can cross the blood-brain barrier and settle quiescently in brain tissue. It can be spread through contact with cat feces or by consuming contaminated meat.
Previous research has shown that neurocognitive changes associated with toxoplasmosis can occur in humans, and meta-analyses suggest an association with neuropsychiatric disorders. Some research has also tied T. gondii infection to increased motor vehicle crashes and suicide attempts.
Dr. Sutterland said he had been inspired by the work of E. Fuller Torrey and Bob Yolken, who proposed the connection between T. gondii and schizophrenia.
Some years ago, Dr. Sutterland and his group analyzed the mental health consequences of T. gondii infection and found “several interesting associations,” but they were unable to “rule out reverse causation – i.e., people with mental health disorders more often get these infections – as well as determine the impact on the population of this common infection.”
For the current study, the investigators analyzed studies that examined specifically cognitive functioning in otherwise healthy individuals in relation to T. gondii infection, “because reverse causation would be less likely in this population and a grasp of global impact would become more clear.”
The researchers conducted a literature search of studies conducted through June 7, 2019, that analyzed cognitive function among healthy participants for whom data on T. gondii seropositivity were available.
A total of 13 studies (n = 13,289 participants; mean age, 46.7 years; 49.6% male) were used in the review and meta-analysis. Some of the studies enrolled a healthy population sample; other studies compared participants with and those without psychiatric disorders. From these, the researchers extracted only the data concerning healthy participants.
The studies analyzed four cognitive domains: processing speed, working memory, short-term verbal memory, and executive functioning.
All cognitive domains affected
Of all the participants, 22.6% had antibodies against T. gondii.
Participants who were seropositive for T. gondii had less favorable functioning in all cognitive domains, with “small but significant” differences.
The researchers conducted a meta-regression analysis of mean age in the analysis of executive functioning and found greater effect sizes as age increased (Q = 6.17; R2 = 81%; P = .01).
The studies were of “high quality,” and there was “little suggestion of publication bias was detected,” the authors noted.
“Although the extent of the associations was modest, the ubiquitous prevalence of the quiescent infection worldwide ... suggests that the consequences for cognitive function of the population as a whole may be substantial, although it is difficult to quantify the global impact,” they wrote.
They note that because the studies were cross-sectional in nature, causality cannot be established.
Nevertheless, Dr. Sutterland suggested several possible mechanisms through which T. gondii might affect neurocognition.
“We know the parasite forms cysts in the brain and can influence dopaminergic neurotransmission, which, in turn, affects neurocognition. Alternatively, it is also possible that the immune response to the infection in the brain causes cognitive impairment. This remains an important question to explore further,” he said.
He noted that clinicians can reassure patients who test positive for T. gondii that although the infection can have a negative impact on cognition, the effect is “small.”
Prevention programs warranted
Commenting on the study in an interview, Shawn D. Gale, PhD, associate professor, department of psychology and neuroscience center, Brigham Young University, Provo, Utah, called it a “great meta-analysis.” He noted that his group is researching the subject and has obtained similar findings. A big plus is that the researchers assessed several cognitive domains, not just one.
Although the data showed “mild effects,” the findings could be important on a population level. Because 30% of the world’s population are seropositive for T. gondii, a potentially large number of people are at risk for cognitive impairment, noted Dr. Gale, who was not involved with the study.
“If you look at the United States, perhaps 10%-15% of people might test positive [for T. gondii], but in Germany and France, the number comes closer to 50%, and in other places in the world – especially countries that have a harder time economically – the rates are even higher. So if it can affect cognition, even a small effect is a big deal,” Dr. Gale said.
“I think prevention will be the most important thing, and perhaps down the road, I hope that a vaccine will be considered,” Dr. Gale added.
“These findings indicate that primary prevention of the infection could have substantial global impact on mental health” and that public health programs to prevent T. gondii “are warranted.”
These programs might consist of hygienic measures, especially after human contact with contaminated sources, as well as research into vaccine development.
No source of funding for the study was listed. The authors and Dr. Gale reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators reviewed and conducted a meta-analysis of 13 studies that encompassed more than 13,000 healthy adults and found a modest but significant association between T. gondii seropositivity and impaired performance on cognitive tests of processing speed, working memory, short-term verbal memory, and executive function. The average age of the persons in the studies was close to 50 years.
“Our findings show that T. gondii could have a negative but small effect on cognition,” study investigator Arjen Sutterland, MD, of the Amsterdam Neuroscience Research Institute and the Amsterdam Institute for Infection and Immunity, University of Amsterdam, said in an interview.
The study was published online July 14, 2021, in JAMA Psychiatry.
Mental illness link
T. gondii is “an intracellular parasite that produces quiescent infection in approximately 30% of humans worldwide,” the authors wrote. The parasite that causes the infection not only settles in muscle and liver tissue but also can cross the blood-brain barrier and settle quiescently in brain tissue. It can be spread through contact with cat feces or by consuming contaminated meat.
Previous research has shown that neurocognitive changes associated with toxoplasmosis can occur in humans, and meta-analyses suggest an association with neuropsychiatric disorders. Some research has also tied T. gondii infection to increased motor vehicle crashes and suicide attempts.
Dr. Sutterland said he had been inspired by the work of E. Fuller Torrey and Bob Yolken, who proposed the connection between T. gondii and schizophrenia.
Some years ago, Dr. Sutterland and his group analyzed the mental health consequences of T. gondii infection and found “several interesting associations,” but they were unable to “rule out reverse causation – i.e., people with mental health disorders more often get these infections – as well as determine the impact on the population of this common infection.”
For the current study, the investigators analyzed studies that examined specifically cognitive functioning in otherwise healthy individuals in relation to T. gondii infection, “because reverse causation would be less likely in this population and a grasp of global impact would become more clear.”
The researchers conducted a literature search of studies conducted through June 7, 2019, that analyzed cognitive function among healthy participants for whom data on T. gondii seropositivity were available.
A total of 13 studies (n = 13,289 participants; mean age, 46.7 years; 49.6% male) were used in the review and meta-analysis. Some of the studies enrolled a healthy population sample; other studies compared participants with and those without psychiatric disorders. From these, the researchers extracted only the data concerning healthy participants.
The studies analyzed four cognitive domains: processing speed, working memory, short-term verbal memory, and executive functioning.
All cognitive domains affected
Of all the participants, 22.6% had antibodies against T. gondii.
Participants who were seropositive for T. gondii had less favorable functioning in all cognitive domains, with “small but significant” differences.
The researchers conducted a meta-regression analysis of mean age in the analysis of executive functioning and found greater effect sizes as age increased (Q = 6.17; R2 = 81%; P = .01).
The studies were of “high quality,” and there was “little suggestion of publication bias was detected,” the authors noted.
“Although the extent of the associations was modest, the ubiquitous prevalence of the quiescent infection worldwide ... suggests that the consequences for cognitive function of the population as a whole may be substantial, although it is difficult to quantify the global impact,” they wrote.
They note that because the studies were cross-sectional in nature, causality cannot be established.
Nevertheless, Dr. Sutterland suggested several possible mechanisms through which T. gondii might affect neurocognition.
“We know the parasite forms cysts in the brain and can influence dopaminergic neurotransmission, which, in turn, affects neurocognition. Alternatively, it is also possible that the immune response to the infection in the brain causes cognitive impairment. This remains an important question to explore further,” he said.
He noted that clinicians can reassure patients who test positive for T. gondii that although the infection can have a negative impact on cognition, the effect is “small.”
Prevention programs warranted
Commenting on the study in an interview, Shawn D. Gale, PhD, associate professor, department of psychology and neuroscience center, Brigham Young University, Provo, Utah, called it a “great meta-analysis.” He noted that his group is researching the subject and has obtained similar findings. A big plus is that the researchers assessed several cognitive domains, not just one.
Although the data showed “mild effects,” the findings could be important on a population level. Because 30% of the world’s population are seropositive for T. gondii, a potentially large number of people are at risk for cognitive impairment, noted Dr. Gale, who was not involved with the study.
“If you look at the United States, perhaps 10%-15% of people might test positive [for T. gondii], but in Germany and France, the number comes closer to 50%, and in other places in the world – especially countries that have a harder time economically – the rates are even higher. So if it can affect cognition, even a small effect is a big deal,” Dr. Gale said.
“I think prevention will be the most important thing, and perhaps down the road, I hope that a vaccine will be considered,” Dr. Gale added.
“These findings indicate that primary prevention of the infection could have substantial global impact on mental health” and that public health programs to prevent T. gondii “are warranted.”
These programs might consist of hygienic measures, especially after human contact with contaminated sources, as well as research into vaccine development.
No source of funding for the study was listed. The authors and Dr. Gale reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators reviewed and conducted a meta-analysis of 13 studies that encompassed more than 13,000 healthy adults and found a modest but significant association between T. gondii seropositivity and impaired performance on cognitive tests of processing speed, working memory, short-term verbal memory, and executive function. The average age of the persons in the studies was close to 50 years.
“Our findings show that T. gondii could have a negative but small effect on cognition,” study investigator Arjen Sutterland, MD, of the Amsterdam Neuroscience Research Institute and the Amsterdam Institute for Infection and Immunity, University of Amsterdam, said in an interview.
The study was published online July 14, 2021, in JAMA Psychiatry.
Mental illness link
T. gondii is “an intracellular parasite that produces quiescent infection in approximately 30% of humans worldwide,” the authors wrote. The parasite that causes the infection not only settles in muscle and liver tissue but also can cross the blood-brain barrier and settle quiescently in brain tissue. It can be spread through contact with cat feces or by consuming contaminated meat.
Previous research has shown that neurocognitive changes associated with toxoplasmosis can occur in humans, and meta-analyses suggest an association with neuropsychiatric disorders. Some research has also tied T. gondii infection to increased motor vehicle crashes and suicide attempts.
Dr. Sutterland said he had been inspired by the work of E. Fuller Torrey and Bob Yolken, who proposed the connection between T. gondii and schizophrenia.
Some years ago, Dr. Sutterland and his group analyzed the mental health consequences of T. gondii infection and found “several interesting associations,” but they were unable to “rule out reverse causation – i.e., people with mental health disorders more often get these infections – as well as determine the impact on the population of this common infection.”
For the current study, the investigators analyzed studies that examined specifically cognitive functioning in otherwise healthy individuals in relation to T. gondii infection, “because reverse causation would be less likely in this population and a grasp of global impact would become more clear.”
The researchers conducted a literature search of studies conducted through June 7, 2019, that analyzed cognitive function among healthy participants for whom data on T. gondii seropositivity were available.
A total of 13 studies (n = 13,289 participants; mean age, 46.7 years; 49.6% male) were used in the review and meta-analysis. Some of the studies enrolled a healthy population sample; other studies compared participants with and those without psychiatric disorders. From these, the researchers extracted only the data concerning healthy participants.
The studies analyzed four cognitive domains: processing speed, working memory, short-term verbal memory, and executive functioning.
All cognitive domains affected
Of all the participants, 22.6% had antibodies against T. gondii.
Participants who were seropositive for T. gondii had less favorable functioning in all cognitive domains, with “small but significant” differences.
The researchers conducted a meta-regression analysis of mean age in the analysis of executive functioning and found greater effect sizes as age increased (Q = 6.17; R2 = 81%; P = .01).
The studies were of “high quality,” and there was “little suggestion of publication bias was detected,” the authors noted.
“Although the extent of the associations was modest, the ubiquitous prevalence of the quiescent infection worldwide ... suggests that the consequences for cognitive function of the population as a whole may be substantial, although it is difficult to quantify the global impact,” they wrote.
They note that because the studies were cross-sectional in nature, causality cannot be established.
Nevertheless, Dr. Sutterland suggested several possible mechanisms through which T. gondii might affect neurocognition.
“We know the parasite forms cysts in the brain and can influence dopaminergic neurotransmission, which, in turn, affects neurocognition. Alternatively, it is also possible that the immune response to the infection in the brain causes cognitive impairment. This remains an important question to explore further,” he said.
He noted that clinicians can reassure patients who test positive for T. gondii that although the infection can have a negative impact on cognition, the effect is “small.”
Prevention programs warranted
Commenting on the study in an interview, Shawn D. Gale, PhD, associate professor, department of psychology and neuroscience center, Brigham Young University, Provo, Utah, called it a “great meta-analysis.” He noted that his group is researching the subject and has obtained similar findings. A big plus is that the researchers assessed several cognitive domains, not just one.
Although the data showed “mild effects,” the findings could be important on a population level. Because 30% of the world’s population are seropositive for T. gondii, a potentially large number of people are at risk for cognitive impairment, noted Dr. Gale, who was not involved with the study.
“If you look at the United States, perhaps 10%-15% of people might test positive [for T. gondii], but in Germany and France, the number comes closer to 50%, and in other places in the world – especially countries that have a harder time economically – the rates are even higher. So if it can affect cognition, even a small effect is a big deal,” Dr. Gale said.
“I think prevention will be the most important thing, and perhaps down the road, I hope that a vaccine will be considered,” Dr. Gale added.
“These findings indicate that primary prevention of the infection could have substantial global impact on mental health” and that public health programs to prevent T. gondii “are warranted.”
These programs might consist of hygienic measures, especially after human contact with contaminated sources, as well as research into vaccine development.
No source of funding for the study was listed. The authors and Dr. Gale reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
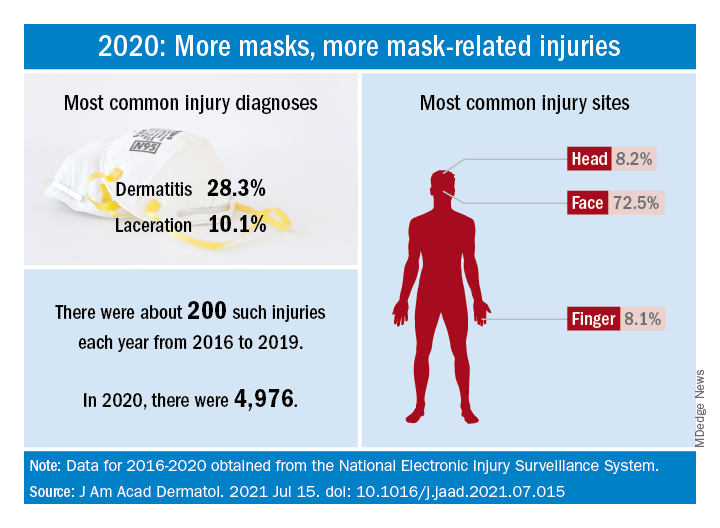
Face mask–related injuries rose dramatically in 2020
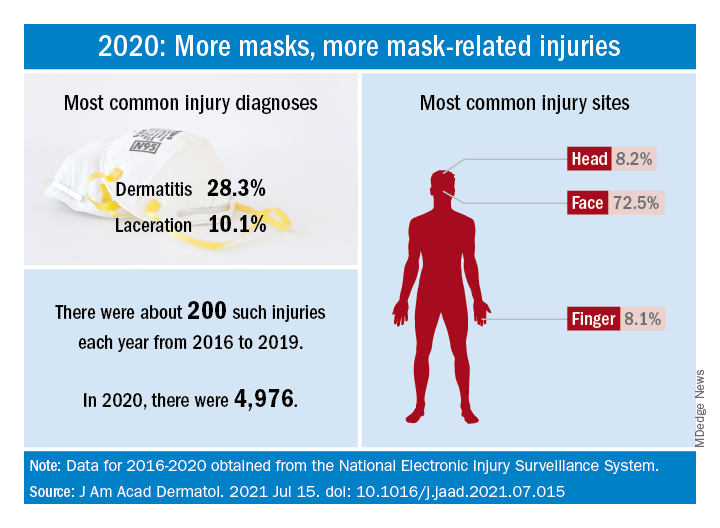
How dramatic? The number of mask-related injuries treated in U.S. emergency departments averaged about 200 per year from 2016 to 2019. In 2020, that figure soared to 4,976 – an increase of almost 2,400%, Gerald McGwin Jr., PhD, and associates said in a research letter published in the Journal to the American Academy of Dermatology.
“Prior to the COVID-19 pandemic the use of respiratory protection equipment was largely limited to healthcare and industrial settings. As [face mask] use by the general population increased, so too have reports of dermatologic reactions,” said Dr. McGwin and associates of the department of epidemiology at the University of Alabama at Birmingham.
Dermatitis was the most common mask-related injury treated last year, affecting 28.3% of those presenting to EDs, followed by lacerations at 10.1%. Injuries were more common in women than men, but while and black patients “were equally represented,” they noted, based on data from the National Electronic Injury Surveillance System, which includes about 100 hospitals and EDs.
Most injuries were caused by rashes/allergic reactions (38%) from prolonged use, poorly fitting masks (19%), and obscured vision (14%). “There was a small (5%) but meaningful number of injuries, all among children, attributable to consuming pieces of a mask or inserting dismantled pieces of a mask into body orifices,” the investigators said.
Guidance from the Centers for Disease Control and Prevention is available “to aid in the choice and proper fit of face masks,” they wrote, and “increased awareness of these resources [could] minimize the future occurrence of mask-related injuries.”
There was no funding source for the study, and the investigators did not declare any conflicts of interest.
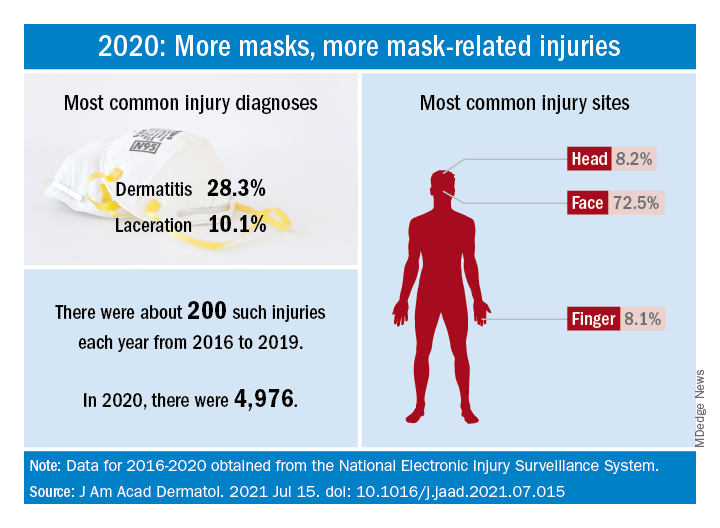
How dramatic? The number of mask-related injuries treated in U.S. emergency departments averaged about 200 per year from 2016 to 2019. In 2020, that figure soared to 4,976 – an increase of almost 2,400%, Gerald McGwin Jr., PhD, and associates said in a research letter published in the Journal to the American Academy of Dermatology.
“Prior to the COVID-19 pandemic the use of respiratory protection equipment was largely limited to healthcare and industrial settings. As [face mask] use by the general population increased, so too have reports of dermatologic reactions,” said Dr. McGwin and associates of the department of epidemiology at the University of Alabama at Birmingham.
Dermatitis was the most common mask-related injury treated last year, affecting 28.3% of those presenting to EDs, followed by lacerations at 10.1%. Injuries were more common in women than men, but while and black patients “were equally represented,” they noted, based on data from the National Electronic Injury Surveillance System, which includes about 100 hospitals and EDs.
Most injuries were caused by rashes/allergic reactions (38%) from prolonged use, poorly fitting masks (19%), and obscured vision (14%). “There was a small (5%) but meaningful number of injuries, all among children, attributable to consuming pieces of a mask or inserting dismantled pieces of a mask into body orifices,” the investigators said.
Guidance from the Centers for Disease Control and Prevention is available “to aid in the choice and proper fit of face masks,” they wrote, and “increased awareness of these resources [could] minimize the future occurrence of mask-related injuries.”
There was no funding source for the study, and the investigators did not declare any conflicts of interest.
How dramatic? The number of mask-related injuries treated in U.S. emergency departments averaged about 200 per year from 2016 to 2019. In 2020, that figure soared to 4,976 – an increase of almost 2,400%, Gerald McGwin Jr., PhD, and associates said in a research letter published in the Journal to the American Academy of Dermatology.
“Prior to the COVID-19 pandemic the use of respiratory protection equipment was largely limited to healthcare and industrial settings. As [face mask] use by the general population increased, so too have reports of dermatologic reactions,” said Dr. McGwin and associates of the department of epidemiology at the University of Alabama at Birmingham.
Dermatitis was the most common mask-related injury treated last year, affecting 28.3% of those presenting to EDs, followed by lacerations at 10.1%. Injuries were more common in women than men, but while and black patients “were equally represented,” they noted, based on data from the National Electronic Injury Surveillance System, which includes about 100 hospitals and EDs.
Most injuries were caused by rashes/allergic reactions (38%) from prolonged use, poorly fitting masks (19%), and obscured vision (14%). “There was a small (5%) but meaningful number of injuries, all among children, attributable to consuming pieces of a mask or inserting dismantled pieces of a mask into body orifices,” the investigators said.
Guidance from the Centers for Disease Control and Prevention is available “to aid in the choice and proper fit of face masks,” they wrote, and “increased awareness of these resources [could] minimize the future occurrence of mask-related injuries.”
There was no funding source for the study, and the investigators did not declare any conflicts of interest.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Dyspigmentation common in SOC patients with bullous pemphigoid
Patients of skin of color (SOC) with bullous pemphigoid presented significantly more often with dyspigmentation than did White patients in a retrospective observational study of patients diagnosed with BP at New York University Langone Health and Bellevue Hospital, also in New York.
“Dyspigmentation in the skin-of-color patient population is important to recognize not only for an objective evaluation of the disease process, but also from a quality of life perspective ... to ensure there is timely diagnosis and initiation of treatment in the skin-of-color population,” said medical student Payal Shah, BS, of New York University, in presenting the findings at the annual Skin of Color Society symposium.
Ms. Shah and coresearchers identified 94 cases of BP through retrospective view of electronic health records – 59 in White patients and 35 in SOC patients. The physical examination features most commonly found at initial presentation were bullae or vesicles in both White patients (64.4% ) and SOC patients (80%). Erosions or ulcers were also commonly found in both groups (42.4% of White patients and 60% of SOC patients).
Erythema was more commonly found in White patients at initial presentation: 35.6% vs. 14.3% of SOC patients (P = .032). Dyspigmentation, defined as areas of hyper- or hypopigmentation, was more commonly found in SOC patients: 54.3% versus 10.2% in White patients (P < .001). The difference in erythema of inflammatory bullae in BP may stem from the fact that erythema is more difficult to discern in patients with darker skin types, Ms. Shah said.
SOC patients also were significantly younger at the time of initial presentation; their mean age was 63 years, compared with 77 years in the White population (P < .001).
The time to diagnosis, defined as the time from initial symptoms to dermatologic diagnosis, was greater for the SOC population –7.6 months vs. 6.2 months for white patients –though the difference was not statistically significant, they said in the abstract .
Dyspigmentation has been shown to be among the top dermatologic concerns of Black patients and has important quality of life implications. “Early diagnosis to prevent difficult-to-treat dyspigmentation is therefore of utmost importance,” they said in the abstract.
Prior research has demonstrated that non-White populations are at greater risk for hospitalization secondary to BP and have a greater risk of disease mortality, Ms. Shah noted in her presentation.
Patients of skin of color (SOC) with bullous pemphigoid presented significantly more often with dyspigmentation than did White patients in a retrospective observational study of patients diagnosed with BP at New York University Langone Health and Bellevue Hospital, also in New York.
“Dyspigmentation in the skin-of-color patient population is important to recognize not only for an objective evaluation of the disease process, but also from a quality of life perspective ... to ensure there is timely diagnosis and initiation of treatment in the skin-of-color population,” said medical student Payal Shah, BS, of New York University, in presenting the findings at the annual Skin of Color Society symposium.
Ms. Shah and coresearchers identified 94 cases of BP through retrospective view of electronic health records – 59 in White patients and 35 in SOC patients. The physical examination features most commonly found at initial presentation were bullae or vesicles in both White patients (64.4% ) and SOC patients (80%). Erosions or ulcers were also commonly found in both groups (42.4% of White patients and 60% of SOC patients).
Erythema was more commonly found in White patients at initial presentation: 35.6% vs. 14.3% of SOC patients (P = .032). Dyspigmentation, defined as areas of hyper- or hypopigmentation, was more commonly found in SOC patients: 54.3% versus 10.2% in White patients (P < .001). The difference in erythema of inflammatory bullae in BP may stem from the fact that erythema is more difficult to discern in patients with darker skin types, Ms. Shah said.
SOC patients also were significantly younger at the time of initial presentation; their mean age was 63 years, compared with 77 years in the White population (P < .001).
The time to diagnosis, defined as the time from initial symptoms to dermatologic diagnosis, was greater for the SOC population –7.6 months vs. 6.2 months for white patients –though the difference was not statistically significant, they said in the abstract .
Dyspigmentation has been shown to be among the top dermatologic concerns of Black patients and has important quality of life implications. “Early diagnosis to prevent difficult-to-treat dyspigmentation is therefore of utmost importance,” they said in the abstract.
Prior research has demonstrated that non-White populations are at greater risk for hospitalization secondary to BP and have a greater risk of disease mortality, Ms. Shah noted in her presentation.
Patients of skin of color (SOC) with bullous pemphigoid presented significantly more often with dyspigmentation than did White patients in a retrospective observational study of patients diagnosed with BP at New York University Langone Health and Bellevue Hospital, also in New York.
“Dyspigmentation in the skin-of-color patient population is important to recognize not only for an objective evaluation of the disease process, but also from a quality of life perspective ... to ensure there is timely diagnosis and initiation of treatment in the skin-of-color population,” said medical student Payal Shah, BS, of New York University, in presenting the findings at the annual Skin of Color Society symposium.
Ms. Shah and coresearchers identified 94 cases of BP through retrospective view of electronic health records – 59 in White patients and 35 in SOC patients. The physical examination features most commonly found at initial presentation were bullae or vesicles in both White patients (64.4% ) and SOC patients (80%). Erosions or ulcers were also commonly found in both groups (42.4% of White patients and 60% of SOC patients).
Erythema was more commonly found in White patients at initial presentation: 35.6% vs. 14.3% of SOC patients (P = .032). Dyspigmentation, defined as areas of hyper- or hypopigmentation, was more commonly found in SOC patients: 54.3% versus 10.2% in White patients (P < .001). The difference in erythema of inflammatory bullae in BP may stem from the fact that erythema is more difficult to discern in patients with darker skin types, Ms. Shah said.
SOC patients also were significantly younger at the time of initial presentation; their mean age was 63 years, compared with 77 years in the White population (P < .001).
The time to diagnosis, defined as the time from initial symptoms to dermatologic diagnosis, was greater for the SOC population –7.6 months vs. 6.2 months for white patients –though the difference was not statistically significant, they said in the abstract .
Dyspigmentation has been shown to be among the top dermatologic concerns of Black patients and has important quality of life implications. “Early diagnosis to prevent difficult-to-treat dyspigmentation is therefore of utmost importance,” they said in the abstract.
Prior research has demonstrated that non-White populations are at greater risk for hospitalization secondary to BP and have a greater risk of disease mortality, Ms. Shah noted in her presentation.
FROM SOC 2021
Severe Asthma: Challenges
Dapagliflozin safe, protective in advanced kidney disease
Patients with stage 4 chronic kidney disease (CKD) who were in the DAPA-CKD trial had cardiorenal benefits from dapagliflozin that were similar to those of patients in the overall trial, with no added safety signal.
DAPA-CKD (Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease) was a landmark study of more than 4,000 patients with CKD, with an estimated glomerular filtration rate (eGFR) of 25-75 mL/min per 1.73 m2 and albuminuria with/without type 2 diabetes.
The primary results showed that patients who received the sodium-glucose cotransporter 2 (SGLT2) inhibitor dapagliflozin for a median of 2.4 years were significantly less likely to have worsening kidney disease or die from all causes than were patients who received placebo.
“This prespecified subanalysis of people with an eGFR < 30 mL/min/1.73 m2 [stage 4 CKD] in the DAPA-CKD study shows first, that in this very vulnerable population, use of the SGLT2 inhibitor is safe,” said Chantal Mathieu, MD, PhD.
Furthermore, there was no signal whatsoever of more adverse events and even a trend to fewer events, she said in an email to this news organization.
The analysis also showed that “although now in small numbers (around 300 each in the treated group vs. placebo group), there is no suggestion that the protective effect of dapagliflozin on the renal and cardiovascular front would not happen in this group” with advanced CKD. The efficacy findings just missed statistical significance, noted Dr. Mathieu, of Catholic University, Leuven, Belgium, who was not involved in the study.
Although dapagliflozin is now approved for treating patients with CKD who are at risk of kidney disease progression (on the basis of the DAPA-CKD results), guidelines have not yet been updated to reflect this, lead investigator Glenn M. Chertow, MD, MPH, of Stanford (Calif.) University, told this news organization in an email.
“For clinicians,” Dr. Mathieu said, “this is now the absolute reassurance that we do not have to stop an SGLT2 inhibitor in people with eGFR < 30 mL/min for safety reasons and that we should maintain them at these values for renal and cardiovascular protection!
“I absolutely hope labels will change soon to reflect these observations (and indeed movement on that front is happening),” she continued.
“The American Diabetes Association/European Association for the Study of Diabetes consensus on glucose-lowering therapies in type 2 diabetes already advocated keeping these agents until eGFR 30 mL/min (on the basis of evidence in 2019),” Dr. Mathieu added, “but this study will probably push the statements even further.”
“Of note,” she pointed out, “at these low eGFRs, the glucose-lowering potential of the SGLT2 inhibitor is negligible.”
Dapagliflozin risks and benefits in advanced CKD
Based on the DAPA-CKD study, published in the New England Journal of Medicine Oct. 8, 2020, the Food and Drug Administration expanded the indication for dapagliflozin (Farxiga, AstraZeneca) in April of 2021.
However, relatively little is known about the safety and efficacy of SGLT2 inhibitors in patients with advanced CKD, who are particularly vulnerable to cardiovascular events and progressive kidney failure, Dr. Chertow and colleagues wrote.
The DAPA-CKD trial randomized 4,304 patients with CKD 1:1 to dapagliflozin 10 mg/day or placebo, including 624 patients (14%) who had eGFR < 30 mL/min per 1.73 m2 and albuminuria at baseline.
Patients in the subgroup with advanced CKD had a mean age of 62 years, and 37% were female. About two-thirds had type 2 diabetes and about one-third had cardiovascular disease.
A total of 293 patients received dapagliflozin and 331 patients received placebo.
During a median follow-up of 2.4 years, patients who received dapagliflozin as opposed to placebo had a lower risk of the primary efficacy outcome – a composite of a 50% or greater sustained decline in eGFR, end-stage kidney disease, or death from cardiovascular or renal causes (hazard ratio, 0.73; 95% confidence interval, 0.53-1.02).
In secondary efficacy outcomes, patients who received dapagliflozin as opposed to placebo also had a lower risk of the following:
- A renal composite outcome – a ≥ 50% sustained decline in eGFR, end-stage kidney disease, or death from renal causes (HR, 0.71; 95% CI, 0.49-1.02).
- A cardiovascular composite outcome comprising cardiovascular death or hospitalization for heart failure (HR, 0.83; 95% CI, 0.45-1.53).
- All-cause mortality (HR, 0.68; 95% CI, 0.39 to 1.21).
The eGFR slope declined by 2.15 mL/min per 1.73 m2 per year and by 3.38 mL/min per 1.73 m2 per year in the dapagliflozin and placebo groups, respectively (P = .005).
“The trial was not powered to detect a statistically significant difference in the primary and key secondary endpoints in modest-sized subgroups,” the researchers noted.
The researchers limited their safety analysis to serious adverse events or symptoms of volume depletion, kidney-related events, major hypoglycemia, bone fractures, amputations, and potential diabetic ketoacidosis.
There was no evidence of increased risk of these adverse events in patients who received dapagliflozin.
The subanalysis of the DAPA-CKD trial was published July 16 in the Journal of the American Society of Nephrology.
The study was funded by AstraZeneca. Dr. Chertow has received fees from AstraZeneca for the DAPA-CKD trial steering committee. The disclosures of the other authors are listed in the article. Dr. Mathieu has served on the advisory panel/speakers bureau for AstraZeneca. Dr. Chertow and Dr. Mathieu also have financial relationships with many other pharmaceutical companies.
Patients with stage 4 chronic kidney disease (CKD) who were in the DAPA-CKD trial had cardiorenal benefits from dapagliflozin that were similar to those of patients in the overall trial, with no added safety signal.
DAPA-CKD (Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease) was a landmark study of more than 4,000 patients with CKD, with an estimated glomerular filtration rate (eGFR) of 25-75 mL/min per 1.73 m2 and albuminuria with/without type 2 diabetes.
The primary results showed that patients who received the sodium-glucose cotransporter 2 (SGLT2) inhibitor dapagliflozin for a median of 2.4 years were significantly less likely to have worsening kidney disease or die from all causes than were patients who received placebo.
“This prespecified subanalysis of people with an eGFR < 30 mL/min/1.73 m2 [stage 4 CKD] in the DAPA-CKD study shows first, that in this very vulnerable population, use of the SGLT2 inhibitor is safe,” said Chantal Mathieu, MD, PhD.
Furthermore, there was no signal whatsoever of more adverse events and even a trend to fewer events, she said in an email to this news organization.
The analysis also showed that “although now in small numbers (around 300 each in the treated group vs. placebo group), there is no suggestion that the protective effect of dapagliflozin on the renal and cardiovascular front would not happen in this group” with advanced CKD. The efficacy findings just missed statistical significance, noted Dr. Mathieu, of Catholic University, Leuven, Belgium, who was not involved in the study.
Although dapagliflozin is now approved for treating patients with CKD who are at risk of kidney disease progression (on the basis of the DAPA-CKD results), guidelines have not yet been updated to reflect this, lead investigator Glenn M. Chertow, MD, MPH, of Stanford (Calif.) University, told this news organization in an email.
“For clinicians,” Dr. Mathieu said, “this is now the absolute reassurance that we do not have to stop an SGLT2 inhibitor in people with eGFR < 30 mL/min for safety reasons and that we should maintain them at these values for renal and cardiovascular protection!
“I absolutely hope labels will change soon to reflect these observations (and indeed movement on that front is happening),” she continued.
“The American Diabetes Association/European Association for the Study of Diabetes consensus on glucose-lowering therapies in type 2 diabetes already advocated keeping these agents until eGFR 30 mL/min (on the basis of evidence in 2019),” Dr. Mathieu added, “but this study will probably push the statements even further.”
“Of note,” she pointed out, “at these low eGFRs, the glucose-lowering potential of the SGLT2 inhibitor is negligible.”
Dapagliflozin risks and benefits in advanced CKD
Based on the DAPA-CKD study, published in the New England Journal of Medicine Oct. 8, 2020, the Food and Drug Administration expanded the indication for dapagliflozin (Farxiga, AstraZeneca) in April of 2021.
However, relatively little is known about the safety and efficacy of SGLT2 inhibitors in patients with advanced CKD, who are particularly vulnerable to cardiovascular events and progressive kidney failure, Dr. Chertow and colleagues wrote.
The DAPA-CKD trial randomized 4,304 patients with CKD 1:1 to dapagliflozin 10 mg/day or placebo, including 624 patients (14%) who had eGFR < 30 mL/min per 1.73 m2 and albuminuria at baseline.
Patients in the subgroup with advanced CKD had a mean age of 62 years, and 37% were female. About two-thirds had type 2 diabetes and about one-third had cardiovascular disease.
A total of 293 patients received dapagliflozin and 331 patients received placebo.
During a median follow-up of 2.4 years, patients who received dapagliflozin as opposed to placebo had a lower risk of the primary efficacy outcome – a composite of a 50% or greater sustained decline in eGFR, end-stage kidney disease, or death from cardiovascular or renal causes (hazard ratio, 0.73; 95% confidence interval, 0.53-1.02).
In secondary efficacy outcomes, patients who received dapagliflozin as opposed to placebo also had a lower risk of the following:
- A renal composite outcome – a ≥ 50% sustained decline in eGFR, end-stage kidney disease, or death from renal causes (HR, 0.71; 95% CI, 0.49-1.02).
- A cardiovascular composite outcome comprising cardiovascular death or hospitalization for heart failure (HR, 0.83; 95% CI, 0.45-1.53).
- All-cause mortality (HR, 0.68; 95% CI, 0.39 to 1.21).
The eGFR slope declined by 2.15 mL/min per 1.73 m2 per year and by 3.38 mL/min per 1.73 m2 per year in the dapagliflozin and placebo groups, respectively (P = .005).
“The trial was not powered to detect a statistically significant difference in the primary and key secondary endpoints in modest-sized subgroups,” the researchers noted.
The researchers limited their safety analysis to serious adverse events or symptoms of volume depletion, kidney-related events, major hypoglycemia, bone fractures, amputations, and potential diabetic ketoacidosis.
There was no evidence of increased risk of these adverse events in patients who received dapagliflozin.
The subanalysis of the DAPA-CKD trial was published July 16 in the Journal of the American Society of Nephrology.
The study was funded by AstraZeneca. Dr. Chertow has received fees from AstraZeneca for the DAPA-CKD trial steering committee. The disclosures of the other authors are listed in the article. Dr. Mathieu has served on the advisory panel/speakers bureau for AstraZeneca. Dr. Chertow and Dr. Mathieu also have financial relationships with many other pharmaceutical companies.
Patients with stage 4 chronic kidney disease (CKD) who were in the DAPA-CKD trial had cardiorenal benefits from dapagliflozin that were similar to those of patients in the overall trial, with no added safety signal.
DAPA-CKD (Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease) was a landmark study of more than 4,000 patients with CKD, with an estimated glomerular filtration rate (eGFR) of 25-75 mL/min per 1.73 m2 and albuminuria with/without type 2 diabetes.
The primary results showed that patients who received the sodium-glucose cotransporter 2 (SGLT2) inhibitor dapagliflozin for a median of 2.4 years were significantly less likely to have worsening kidney disease or die from all causes than were patients who received placebo.
“This prespecified subanalysis of people with an eGFR < 30 mL/min/1.73 m2 [stage 4 CKD] in the DAPA-CKD study shows first, that in this very vulnerable population, use of the SGLT2 inhibitor is safe,” said Chantal Mathieu, MD, PhD.
Furthermore, there was no signal whatsoever of more adverse events and even a trend to fewer events, she said in an email to this news organization.
The analysis also showed that “although now in small numbers (around 300 each in the treated group vs. placebo group), there is no suggestion that the protective effect of dapagliflozin on the renal and cardiovascular front would not happen in this group” with advanced CKD. The efficacy findings just missed statistical significance, noted Dr. Mathieu, of Catholic University, Leuven, Belgium, who was not involved in the study.
Although dapagliflozin is now approved for treating patients with CKD who are at risk of kidney disease progression (on the basis of the DAPA-CKD results), guidelines have not yet been updated to reflect this, lead investigator Glenn M. Chertow, MD, MPH, of Stanford (Calif.) University, told this news organization in an email.
“For clinicians,” Dr. Mathieu said, “this is now the absolute reassurance that we do not have to stop an SGLT2 inhibitor in people with eGFR < 30 mL/min for safety reasons and that we should maintain them at these values for renal and cardiovascular protection!
“I absolutely hope labels will change soon to reflect these observations (and indeed movement on that front is happening),” she continued.
“The American Diabetes Association/European Association for the Study of Diabetes consensus on glucose-lowering therapies in type 2 diabetes already advocated keeping these agents until eGFR 30 mL/min (on the basis of evidence in 2019),” Dr. Mathieu added, “but this study will probably push the statements even further.”
“Of note,” she pointed out, “at these low eGFRs, the glucose-lowering potential of the SGLT2 inhibitor is negligible.”
Dapagliflozin risks and benefits in advanced CKD
Based on the DAPA-CKD study, published in the New England Journal of Medicine Oct. 8, 2020, the Food and Drug Administration expanded the indication for dapagliflozin (Farxiga, AstraZeneca) in April of 2021.
However, relatively little is known about the safety and efficacy of SGLT2 inhibitors in patients with advanced CKD, who are particularly vulnerable to cardiovascular events and progressive kidney failure, Dr. Chertow and colleagues wrote.
The DAPA-CKD trial randomized 4,304 patients with CKD 1:1 to dapagliflozin 10 mg/day or placebo, including 624 patients (14%) who had eGFR < 30 mL/min per 1.73 m2 and albuminuria at baseline.
Patients in the subgroup with advanced CKD had a mean age of 62 years, and 37% were female. About two-thirds had type 2 diabetes and about one-third had cardiovascular disease.
A total of 293 patients received dapagliflozin and 331 patients received placebo.
During a median follow-up of 2.4 years, patients who received dapagliflozin as opposed to placebo had a lower risk of the primary efficacy outcome – a composite of a 50% or greater sustained decline in eGFR, end-stage kidney disease, or death from cardiovascular or renal causes (hazard ratio, 0.73; 95% confidence interval, 0.53-1.02).
In secondary efficacy outcomes, patients who received dapagliflozin as opposed to placebo also had a lower risk of the following:
- A renal composite outcome – a ≥ 50% sustained decline in eGFR, end-stage kidney disease, or death from renal causes (HR, 0.71; 95% CI, 0.49-1.02).
- A cardiovascular composite outcome comprising cardiovascular death or hospitalization for heart failure (HR, 0.83; 95% CI, 0.45-1.53).
- All-cause mortality (HR, 0.68; 95% CI, 0.39 to 1.21).
The eGFR slope declined by 2.15 mL/min per 1.73 m2 per year and by 3.38 mL/min per 1.73 m2 per year in the dapagliflozin and placebo groups, respectively (P = .005).
“The trial was not powered to detect a statistically significant difference in the primary and key secondary endpoints in modest-sized subgroups,” the researchers noted.
The researchers limited their safety analysis to serious adverse events or symptoms of volume depletion, kidney-related events, major hypoglycemia, bone fractures, amputations, and potential diabetic ketoacidosis.
There was no evidence of increased risk of these adverse events in patients who received dapagliflozin.
The subanalysis of the DAPA-CKD trial was published July 16 in the Journal of the American Society of Nephrology.
The study was funded by AstraZeneca. Dr. Chertow has received fees from AstraZeneca for the DAPA-CKD trial steering committee. The disclosures of the other authors are listed in the article. Dr. Mathieu has served on the advisory panel/speakers bureau for AstraZeneca. Dr. Chertow and Dr. Mathieu also have financial relationships with many other pharmaceutical companies.
FROM THE JOURNAL OF THE AMERICAN SOCIETY OF NEPHROLOGY
Trauma, psychiatric comorbidities tied to functional motor disorders
Most adults with functional motor disorders (FMDs) report a history of psychological or physical trauma 6 months before the onset of symptoms, a retrospective study of 482 individuals suggests. Those challenges prevent more than half of those patients – most of whom are women – from working, the researchers found.
“This finding points to the huge socioeconomical burden of FMD and emphasizes the need for better diagnostic procedure and active management,” wrote Béatrice Garcin, MD, of Sorbonne Université, Paris, and associates.
FMDs are a common presentation of functional neurologic disorders, but clinical characteristics of FMDs are not well understood because large series of consecutive patients are limited, Dr. Garcin and associates said.
In the study, published in the Journal of Psychosomatic Research, the investigators reviewed data from consecutive patients with FMD who were seen at a single hospital in France between 2008 and 2016. Half of the patients had functional motor weakness (241) and half had functional movement disorders (241). All of the patients had been referred for transcranial magnetic stimulation (TMS) as treatment for FMD.
The median age of the patients was 40 years, the median age at the onset of symptoms was 35.5 years, and 74% were women. The most common clinical presentations were tremor and dystonia (83.4%), and no demographic differences were observed between patients with functional motor weakness and functional movement disorders. Symptoms were bilateral in about half of the patients (51.7%), with left- and right-sided symptoms in 28.2% and 20.1%, respectively.
More than 80% of the patients reported a history of trauma within 6 months of the onset of their symptoms, mainly psychological trauma (50.6%). Another 20.1% reported a physical trauma, and 8.7% reported trauma from surgical procedures.
In addition, about two-thirds (66.4%) had psychiatric comorbidities; 52.7% of these were mood disorders: 49.3% depression and 3.3% bipolar disorder. “However, these results about psychiatric comorbidities should be taken with caution,” the researchers emphasized. “ and psychiatric diagnosis may lack precision because of the absence of systematic psychiatric interviews and psychiatric questionnaires in the present study.”
No significant differences appeared between the motor weakness and movement disorders groups in terms of occupation, level of education, medical somatic history, symptom onset, psychiatric comorbidities, or self-reported history of trauma. Patients in the motor weakness group were significantly younger at the time of TMS treatment and had a shorter disease duration prior to that treatment. No differences were noted between the groups with regard to clinical FMD phenotypes.
The study findings were limited by several factors, including the potential selection bias because of enrollment at a neurology referral center, lack of a control group, and underrepresentation of children and older adults, the researchers noted. Also, symptom severity was not assessed and could not be compared among phenotypes or demographic groups.
However, the results contribute to the characterization of FMD patients. “Future studies are needed to clarify the characteristics of FMD patients and the consequences of their symptoms on disability and work status,” they said.
The study received no outside funding. Lead author Dr. Garcin had no disclosures.
Most adults with functional motor disorders (FMDs) report a history of psychological or physical trauma 6 months before the onset of symptoms, a retrospective study of 482 individuals suggests. Those challenges prevent more than half of those patients – most of whom are women – from working, the researchers found.
“This finding points to the huge socioeconomical burden of FMD and emphasizes the need for better diagnostic procedure and active management,” wrote Béatrice Garcin, MD, of Sorbonne Université, Paris, and associates.
FMDs are a common presentation of functional neurologic disorders, but clinical characteristics of FMDs are not well understood because large series of consecutive patients are limited, Dr. Garcin and associates said.
In the study, published in the Journal of Psychosomatic Research, the investigators reviewed data from consecutive patients with FMD who were seen at a single hospital in France between 2008 and 2016. Half of the patients had functional motor weakness (241) and half had functional movement disorders (241). All of the patients had been referred for transcranial magnetic stimulation (TMS) as treatment for FMD.
The median age of the patients was 40 years, the median age at the onset of symptoms was 35.5 years, and 74% were women. The most common clinical presentations were tremor and dystonia (83.4%), and no demographic differences were observed between patients with functional motor weakness and functional movement disorders. Symptoms were bilateral in about half of the patients (51.7%), with left- and right-sided symptoms in 28.2% and 20.1%, respectively.
More than 80% of the patients reported a history of trauma within 6 months of the onset of their symptoms, mainly psychological trauma (50.6%). Another 20.1% reported a physical trauma, and 8.7% reported trauma from surgical procedures.
In addition, about two-thirds (66.4%) had psychiatric comorbidities; 52.7% of these were mood disorders: 49.3% depression and 3.3% bipolar disorder. “However, these results about psychiatric comorbidities should be taken with caution,” the researchers emphasized. “ and psychiatric diagnosis may lack precision because of the absence of systematic psychiatric interviews and psychiatric questionnaires in the present study.”
No significant differences appeared between the motor weakness and movement disorders groups in terms of occupation, level of education, medical somatic history, symptom onset, psychiatric comorbidities, or self-reported history of trauma. Patients in the motor weakness group were significantly younger at the time of TMS treatment and had a shorter disease duration prior to that treatment. No differences were noted between the groups with regard to clinical FMD phenotypes.
The study findings were limited by several factors, including the potential selection bias because of enrollment at a neurology referral center, lack of a control group, and underrepresentation of children and older adults, the researchers noted. Also, symptom severity was not assessed and could not be compared among phenotypes or demographic groups.
However, the results contribute to the characterization of FMD patients. “Future studies are needed to clarify the characteristics of FMD patients and the consequences of their symptoms on disability and work status,” they said.
The study received no outside funding. Lead author Dr. Garcin had no disclosures.
Most adults with functional motor disorders (FMDs) report a history of psychological or physical trauma 6 months before the onset of symptoms, a retrospective study of 482 individuals suggests. Those challenges prevent more than half of those patients – most of whom are women – from working, the researchers found.
“This finding points to the huge socioeconomical burden of FMD and emphasizes the need for better diagnostic procedure and active management,” wrote Béatrice Garcin, MD, of Sorbonne Université, Paris, and associates.
FMDs are a common presentation of functional neurologic disorders, but clinical characteristics of FMDs are not well understood because large series of consecutive patients are limited, Dr. Garcin and associates said.
In the study, published in the Journal of Psychosomatic Research, the investigators reviewed data from consecutive patients with FMD who were seen at a single hospital in France between 2008 and 2016. Half of the patients had functional motor weakness (241) and half had functional movement disorders (241). All of the patients had been referred for transcranial magnetic stimulation (TMS) as treatment for FMD.
The median age of the patients was 40 years, the median age at the onset of symptoms was 35.5 years, and 74% were women. The most common clinical presentations were tremor and dystonia (83.4%), and no demographic differences were observed between patients with functional motor weakness and functional movement disorders. Symptoms were bilateral in about half of the patients (51.7%), with left- and right-sided symptoms in 28.2% and 20.1%, respectively.
More than 80% of the patients reported a history of trauma within 6 months of the onset of their symptoms, mainly psychological trauma (50.6%). Another 20.1% reported a physical trauma, and 8.7% reported trauma from surgical procedures.
In addition, about two-thirds (66.4%) had psychiatric comorbidities; 52.7% of these were mood disorders: 49.3% depression and 3.3% bipolar disorder. “However, these results about psychiatric comorbidities should be taken with caution,” the researchers emphasized. “ and psychiatric diagnosis may lack precision because of the absence of systematic psychiatric interviews and psychiatric questionnaires in the present study.”
No significant differences appeared between the motor weakness and movement disorders groups in terms of occupation, level of education, medical somatic history, symptom onset, psychiatric comorbidities, or self-reported history of trauma. Patients in the motor weakness group were significantly younger at the time of TMS treatment and had a shorter disease duration prior to that treatment. No differences were noted between the groups with regard to clinical FMD phenotypes.
The study findings were limited by several factors, including the potential selection bias because of enrollment at a neurology referral center, lack of a control group, and underrepresentation of children and older adults, the researchers noted. Also, symptom severity was not assessed and could not be compared among phenotypes or demographic groups.
However, the results contribute to the characterization of FMD patients. “Future studies are needed to clarify the characteristics of FMD patients and the consequences of their symptoms on disability and work status,” they said.
The study received no outside funding. Lead author Dr. Garcin had no disclosures.
FROM THE JOURNAL OF PSYCHOSOMATIC RESEARCH
PHM virtual conference promises practical pearls, plus Dr. Fauci
The Pediatric Hospital Medicine annual conference, though virtual in 2021, promises to retain its role as the premier educational event for pediatric hospitalists and other clinicians involved in treating pediatric patients.
The “can’t-miss” session, on August 5, at 6:30 p.m. ET, is a one-on-one discussion between Anthony S. Fauci, MD, and Lee Savio Beers, MD, president of the American Academic of Pediatrics, according to members of the meeting planning committee.
In addition to the conversation between Dr. Beers and Dr. Fauci, this year’s meeting offers a mix of workshops with pointers and pearls to improve practice, keynote and plenary sessions to inform and inspire, and abstract presentations of new research. Three members of the PHM Planning Committee shared their insights on the hot topics, advice for new clinicians, and tips for making the most of this year’s meeting.
Workshops worth watching
“The keynote plenary sessions by Julie Silver, MD, on ‘Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion,’ and by Ilan Alhadeff, MD, on ‘Leading through Adversity’ should inspire even the least enthusiastic among us,” Mirna Giordano, MD, FHM, of Columbia University Medical Center, New York, said in an interview. A talk by Nathan T. Chomilo, MD, “will likely prompt reflection on how George Floyd’s death changed us, and how we practice medicine forever.” In addition, “PHM Stories are not to be missed, they are voices that speak loud and move mountains.”
The PHM Stories are concise, narrative talks with minimal use of slides; each PHM Stories session includes three distinct talks and a 15-minute question and answer session. PHM Stories sessions are scheduled for each day of the conference, and topics include “Practicing Medicine While Human: The Secrets Physicians Keep,” by Uchenna Ewulonu, MD; “Finding the Power of the Imposter: How I Learned to Be Exactly the Color I Am, Everywhere I Go,” by Alexandra Coria, MD; and “Purple Butterflies: A Reflection on Why I’m a Pediatric Hospitalist,” by Joanne Mendoza, MD.
“The PHM community has been through a lot in the aftermath of the pandemic,” said Dr. Giordano. “The mini-plenary session on the mental health needs of our patients, and clinical quick-hit sessions on verbal deescalation of the agitated patients and cardiac effects of COVID-19 will likely be not only very popular, but also useful in clinical endeavors. The workshop on how to navigate the adult issues in hospitalized patients will provide the Med-Peds pearls we all wish we heard earlier.”
Although a 75-minute workshop session may seem long, “the workshop choices will offer something for everyone’s taste: education, research, clinical topics, diversity, and advocacy,” Dr. Giordano said. “I suggest that attendees check in advance which sessions will be available after the meeting, so that they prioritize highly interactive sessions like workshops, and that they experience, even if virtual, small group/room gatherings and networking.” There will be time for fun, too, she emphasized, with social sessions “that we hope will break the screen monotony and bring smiles to everyone’s faces.”
For younger clinicians relatively new to practice, Dr. Giordano recommended several workshops for a wealth of advice and guidance, including “New Kids on the Block: Thriving in your First Faculty Position,” “Channeling Your Inner Coach: Techniques to Enhance Clinical Teaching & Feedback,” “Palliative Care Pearls for the Pediatric Hospitalist,” “Perioperative Medicine for Medically Complex Children: Case Studies in Programmatic Approaches,” “The Bare Necessities: Social Determinant of Health Screening for the Hospitalist,” and “Mentorship, Autonomy, and Supervising a PHM Fellow.”
Classic topics and new concepts
“We are so excited to be able to offer a full spectrum of offerings at this year’s virtual meeting,” Yemisi Jones, MD, FHM, of Cincinnati Children’s Hospital, said in an interview. “We are covering some classic topics that we can’t do without at PHM, such as clinical updates in the management of sick and well newborns; workshops on best practices for educators; as well as the latest in PHM scholarship.” Sessions include “timely topics such as equity for women in medicine with one of our plenary speakers, Julie Silver, MD, and new febrile infant guidelines,” she added.
In particular, the COVID-19 and mental health session will help address clinicians’ evolving understanding of the COVID-19 pandemic and its effects on hospitalized children, said Dr. Jones. “Attendees can expect practical, timely updates on the current state of the science and ways to improve their practice to provide the best care for our patients.”
Attendees will be able to maximize the virtual conference format by accessing archived recordings, including clinical quick hits, mini-plenaries, and PHM Stories, which can be viewed during the scheduled meeting time or after, Dr. Jones said. “Workshops and abstract presentations will involve real-time interaction with presenters, so would be highest yield to attend during the live meeting. We also encourage all participants to take full advantage of the platform and the various networking opportunities to engage with others in our PHM community.”
For residents and new fellows, Dr. Jones advised making the workshop, “A Whole New World: Tips and Tools to Soar Into Your First Year of Fellowship,” a priority. “For early-career faculty, the ‘New Kids on the Block: Thriving in your First Faculty Position workshop will be a valuable resource.”
Make the meeting content a priority
This year’s conference has an exceptional slate of plenary speakers, Michelle Marks, DO, SFHM, of the Cleveland Clinic said in an interview. In addition to the much-anticipated session on vaccinations, school guidelines, and other topics with Dr. Fauci and Dr. Beers, the sessions on leading through adversity and workforce diversity and inclusion are “important topics to the PHM community and to our greater communities as a whole.”
Dr. Marks also highlighted the value of the COVID-19 and mental health session, as the long-term impact of COVID-19 on mental health of children and adults continues to grab headlines. “From this session specifically, I hope the attendees will gain awareness of the special mental health needs for child during a global disaster like a pandemic, which can be generalized to other situations and gain skills and resources to help meet and advocate for children’s mental health needs.”
For clinicians attending the virtual conference, “The most important strategy is to schedule time off of clinical work for the virtual meeting if you can so you can focus on the content,” said Dr. Marks. “For the longer sessions, it would be very important to block time in your day to fully attend the session, attend in a private space if possible since there will be breakouts with discussion, have your camera on, and engage with the workshop group as much as possible. The virtual format can be challenging because of all the external distractions, so intentional focus is necessary,” to get the most out of the experience.
The mini-plenary session on “The New AAP Clinical Practice Guideline on the Evaluation and Management of Febrile Infants 8-60 Days Old,” is an important session for all attendees, Dr. Marks said. She also recommended the Clinical Quick Hits sessions for anyone seeking “a diverse array of practical knowledge which can be easily applied to everyday practice.” The Clinical Quick Hits are designed as 35-minute, rapid-fire presentations focused on clinical knowledge. Each of these presentations will focus on the latest updates or evolutions in clinical practice in one area. Some key topics include counseling parents when a child has an abnormal exam finding, assessing pelvic pain in adolescent girls, and preventing venous thromboembolism in the inpatient setting.
“I would also recommend that younger clinicians take in at least one or two workshops or sessions on nonclinical topics to see the breath of content at the meeting and to develop a niche interest for themselves outside of clinical work,” Dr. Marks noted.
Nonclinical sessions at PHM 2021 include workshops on a pilot for a comprehensive LGBTQ+ curriculum, using media tools for public health messaging, and practicing health literacy.
To register for the Pediatric Hospital Medicine 2021 virtual conference, visit https://apaevents.regfox.com/phm21-virtual-conference.
Dr. Giordano, Dr. Jones, and Dr. Marks are members of the PHM conference planning committee and had no relevant financial conflicts to disclose.
The Pediatric Hospital Medicine annual conference, though virtual in 2021, promises to retain its role as the premier educational event for pediatric hospitalists and other clinicians involved in treating pediatric patients.
The “can’t-miss” session, on August 5, at 6:30 p.m. ET, is a one-on-one discussion between Anthony S. Fauci, MD, and Lee Savio Beers, MD, president of the American Academic of Pediatrics, according to members of the meeting planning committee.
In addition to the conversation between Dr. Beers and Dr. Fauci, this year’s meeting offers a mix of workshops with pointers and pearls to improve practice, keynote and plenary sessions to inform and inspire, and abstract presentations of new research. Three members of the PHM Planning Committee shared their insights on the hot topics, advice for new clinicians, and tips for making the most of this year’s meeting.
Workshops worth watching
“The keynote plenary sessions by Julie Silver, MD, on ‘Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion,’ and by Ilan Alhadeff, MD, on ‘Leading through Adversity’ should inspire even the least enthusiastic among us,” Mirna Giordano, MD, FHM, of Columbia University Medical Center, New York, said in an interview. A talk by Nathan T. Chomilo, MD, “will likely prompt reflection on how George Floyd’s death changed us, and how we practice medicine forever.” In addition, “PHM Stories are not to be missed, they are voices that speak loud and move mountains.”
The PHM Stories are concise, narrative talks with minimal use of slides; each PHM Stories session includes three distinct talks and a 15-minute question and answer session. PHM Stories sessions are scheduled for each day of the conference, and topics include “Practicing Medicine While Human: The Secrets Physicians Keep,” by Uchenna Ewulonu, MD; “Finding the Power of the Imposter: How I Learned to Be Exactly the Color I Am, Everywhere I Go,” by Alexandra Coria, MD; and “Purple Butterflies: A Reflection on Why I’m a Pediatric Hospitalist,” by Joanne Mendoza, MD.
“The PHM community has been through a lot in the aftermath of the pandemic,” said Dr. Giordano. “The mini-plenary session on the mental health needs of our patients, and clinical quick-hit sessions on verbal deescalation of the agitated patients and cardiac effects of COVID-19 will likely be not only very popular, but also useful in clinical endeavors. The workshop on how to navigate the adult issues in hospitalized patients will provide the Med-Peds pearls we all wish we heard earlier.”
Although a 75-minute workshop session may seem long, “the workshop choices will offer something for everyone’s taste: education, research, clinical topics, diversity, and advocacy,” Dr. Giordano said. “I suggest that attendees check in advance which sessions will be available after the meeting, so that they prioritize highly interactive sessions like workshops, and that they experience, even if virtual, small group/room gatherings and networking.” There will be time for fun, too, she emphasized, with social sessions “that we hope will break the screen monotony and bring smiles to everyone’s faces.”
For younger clinicians relatively new to practice, Dr. Giordano recommended several workshops for a wealth of advice and guidance, including “New Kids on the Block: Thriving in your First Faculty Position,” “Channeling Your Inner Coach: Techniques to Enhance Clinical Teaching & Feedback,” “Palliative Care Pearls for the Pediatric Hospitalist,” “Perioperative Medicine for Medically Complex Children: Case Studies in Programmatic Approaches,” “The Bare Necessities: Social Determinant of Health Screening for the Hospitalist,” and “Mentorship, Autonomy, and Supervising a PHM Fellow.”
Classic topics and new concepts
“We are so excited to be able to offer a full spectrum of offerings at this year’s virtual meeting,” Yemisi Jones, MD, FHM, of Cincinnati Children’s Hospital, said in an interview. “We are covering some classic topics that we can’t do without at PHM, such as clinical updates in the management of sick and well newborns; workshops on best practices for educators; as well as the latest in PHM scholarship.” Sessions include “timely topics such as equity for women in medicine with one of our plenary speakers, Julie Silver, MD, and new febrile infant guidelines,” she added.
In particular, the COVID-19 and mental health session will help address clinicians’ evolving understanding of the COVID-19 pandemic and its effects on hospitalized children, said Dr. Jones. “Attendees can expect practical, timely updates on the current state of the science and ways to improve their practice to provide the best care for our patients.”
Attendees will be able to maximize the virtual conference format by accessing archived recordings, including clinical quick hits, mini-plenaries, and PHM Stories, which can be viewed during the scheduled meeting time or after, Dr. Jones said. “Workshops and abstract presentations will involve real-time interaction with presenters, so would be highest yield to attend during the live meeting. We also encourage all participants to take full advantage of the platform and the various networking opportunities to engage with others in our PHM community.”
For residents and new fellows, Dr. Jones advised making the workshop, “A Whole New World: Tips and Tools to Soar Into Your First Year of Fellowship,” a priority. “For early-career faculty, the ‘New Kids on the Block: Thriving in your First Faculty Position workshop will be a valuable resource.”
Make the meeting content a priority
This year’s conference has an exceptional slate of plenary speakers, Michelle Marks, DO, SFHM, of the Cleveland Clinic said in an interview. In addition to the much-anticipated session on vaccinations, school guidelines, and other topics with Dr. Fauci and Dr. Beers, the sessions on leading through adversity and workforce diversity and inclusion are “important topics to the PHM community and to our greater communities as a whole.”
Dr. Marks also highlighted the value of the COVID-19 and mental health session, as the long-term impact of COVID-19 on mental health of children and adults continues to grab headlines. “From this session specifically, I hope the attendees will gain awareness of the special mental health needs for child during a global disaster like a pandemic, which can be generalized to other situations and gain skills and resources to help meet and advocate for children’s mental health needs.”
For clinicians attending the virtual conference, “The most important strategy is to schedule time off of clinical work for the virtual meeting if you can so you can focus on the content,” said Dr. Marks. “For the longer sessions, it would be very important to block time in your day to fully attend the session, attend in a private space if possible since there will be breakouts with discussion, have your camera on, and engage with the workshop group as much as possible. The virtual format can be challenging because of all the external distractions, so intentional focus is necessary,” to get the most out of the experience.
The mini-plenary session on “The New AAP Clinical Practice Guideline on the Evaluation and Management of Febrile Infants 8-60 Days Old,” is an important session for all attendees, Dr. Marks said. She also recommended the Clinical Quick Hits sessions for anyone seeking “a diverse array of practical knowledge which can be easily applied to everyday practice.” The Clinical Quick Hits are designed as 35-minute, rapid-fire presentations focused on clinical knowledge. Each of these presentations will focus on the latest updates or evolutions in clinical practice in one area. Some key topics include counseling parents when a child has an abnormal exam finding, assessing pelvic pain in adolescent girls, and preventing venous thromboembolism in the inpatient setting.
“I would also recommend that younger clinicians take in at least one or two workshops or sessions on nonclinical topics to see the breath of content at the meeting and to develop a niche interest for themselves outside of clinical work,” Dr. Marks noted.
Nonclinical sessions at PHM 2021 include workshops on a pilot for a comprehensive LGBTQ+ curriculum, using media tools for public health messaging, and practicing health literacy.
To register for the Pediatric Hospital Medicine 2021 virtual conference, visit https://apaevents.regfox.com/phm21-virtual-conference.
Dr. Giordano, Dr. Jones, and Dr. Marks are members of the PHM conference planning committee and had no relevant financial conflicts to disclose.
The Pediatric Hospital Medicine annual conference, though virtual in 2021, promises to retain its role as the premier educational event for pediatric hospitalists and other clinicians involved in treating pediatric patients.
The “can’t-miss” session, on August 5, at 6:30 p.m. ET, is a one-on-one discussion between Anthony S. Fauci, MD, and Lee Savio Beers, MD, president of the American Academic of Pediatrics, according to members of the meeting planning committee.
In addition to the conversation between Dr. Beers and Dr. Fauci, this year’s meeting offers a mix of workshops with pointers and pearls to improve practice, keynote and plenary sessions to inform and inspire, and abstract presentations of new research. Three members of the PHM Planning Committee shared their insights on the hot topics, advice for new clinicians, and tips for making the most of this year’s meeting.
Workshops worth watching
“The keynote plenary sessions by Julie Silver, MD, on ‘Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion,’ and by Ilan Alhadeff, MD, on ‘Leading through Adversity’ should inspire even the least enthusiastic among us,” Mirna Giordano, MD, FHM, of Columbia University Medical Center, New York, said in an interview. A talk by Nathan T. Chomilo, MD, “will likely prompt reflection on how George Floyd’s death changed us, and how we practice medicine forever.” In addition, “PHM Stories are not to be missed, they are voices that speak loud and move mountains.”
The PHM Stories are concise, narrative talks with minimal use of slides; each PHM Stories session includes three distinct talks and a 15-minute question and answer session. PHM Stories sessions are scheduled for each day of the conference, and topics include “Practicing Medicine While Human: The Secrets Physicians Keep,” by Uchenna Ewulonu, MD; “Finding the Power of the Imposter: How I Learned to Be Exactly the Color I Am, Everywhere I Go,” by Alexandra Coria, MD; and “Purple Butterflies: A Reflection on Why I’m a Pediatric Hospitalist,” by Joanne Mendoza, MD.
“The PHM community has been through a lot in the aftermath of the pandemic,” said Dr. Giordano. “The mini-plenary session on the mental health needs of our patients, and clinical quick-hit sessions on verbal deescalation of the agitated patients and cardiac effects of COVID-19 will likely be not only very popular, but also useful in clinical endeavors. The workshop on how to navigate the adult issues in hospitalized patients will provide the Med-Peds pearls we all wish we heard earlier.”
Although a 75-minute workshop session may seem long, “the workshop choices will offer something for everyone’s taste: education, research, clinical topics, diversity, and advocacy,” Dr. Giordano said. “I suggest that attendees check in advance which sessions will be available after the meeting, so that they prioritize highly interactive sessions like workshops, and that they experience, even if virtual, small group/room gatherings and networking.” There will be time for fun, too, she emphasized, with social sessions “that we hope will break the screen monotony and bring smiles to everyone’s faces.”
For younger clinicians relatively new to practice, Dr. Giordano recommended several workshops for a wealth of advice and guidance, including “New Kids on the Block: Thriving in your First Faculty Position,” “Channeling Your Inner Coach: Techniques to Enhance Clinical Teaching & Feedback,” “Palliative Care Pearls for the Pediatric Hospitalist,” “Perioperative Medicine for Medically Complex Children: Case Studies in Programmatic Approaches,” “The Bare Necessities: Social Determinant of Health Screening for the Hospitalist,” and “Mentorship, Autonomy, and Supervising a PHM Fellow.”
Classic topics and new concepts
“We are so excited to be able to offer a full spectrum of offerings at this year’s virtual meeting,” Yemisi Jones, MD, FHM, of Cincinnati Children’s Hospital, said in an interview. “We are covering some classic topics that we can’t do without at PHM, such as clinical updates in the management of sick and well newborns; workshops on best practices for educators; as well as the latest in PHM scholarship.” Sessions include “timely topics such as equity for women in medicine with one of our plenary speakers, Julie Silver, MD, and new febrile infant guidelines,” she added.
In particular, the COVID-19 and mental health session will help address clinicians’ evolving understanding of the COVID-19 pandemic and its effects on hospitalized children, said Dr. Jones. “Attendees can expect practical, timely updates on the current state of the science and ways to improve their practice to provide the best care for our patients.”
Attendees will be able to maximize the virtual conference format by accessing archived recordings, including clinical quick hits, mini-plenaries, and PHM Stories, which can be viewed during the scheduled meeting time or after, Dr. Jones said. “Workshops and abstract presentations will involve real-time interaction with presenters, so would be highest yield to attend during the live meeting. We also encourage all participants to take full advantage of the platform and the various networking opportunities to engage with others in our PHM community.”
For residents and new fellows, Dr. Jones advised making the workshop, “A Whole New World: Tips and Tools to Soar Into Your First Year of Fellowship,” a priority. “For early-career faculty, the ‘New Kids on the Block: Thriving in your First Faculty Position workshop will be a valuable resource.”
Make the meeting content a priority
This year’s conference has an exceptional slate of plenary speakers, Michelle Marks, DO, SFHM, of the Cleveland Clinic said in an interview. In addition to the much-anticipated session on vaccinations, school guidelines, and other topics with Dr. Fauci and Dr. Beers, the sessions on leading through adversity and workforce diversity and inclusion are “important topics to the PHM community and to our greater communities as a whole.”
Dr. Marks also highlighted the value of the COVID-19 and mental health session, as the long-term impact of COVID-19 on mental health of children and adults continues to grab headlines. “From this session specifically, I hope the attendees will gain awareness of the special mental health needs for child during a global disaster like a pandemic, which can be generalized to other situations and gain skills and resources to help meet and advocate for children’s mental health needs.”
For clinicians attending the virtual conference, “The most important strategy is to schedule time off of clinical work for the virtual meeting if you can so you can focus on the content,” said Dr. Marks. “For the longer sessions, it would be very important to block time in your day to fully attend the session, attend in a private space if possible since there will be breakouts with discussion, have your camera on, and engage with the workshop group as much as possible. The virtual format can be challenging because of all the external distractions, so intentional focus is necessary,” to get the most out of the experience.
The mini-plenary session on “The New AAP Clinical Practice Guideline on the Evaluation and Management of Febrile Infants 8-60 Days Old,” is an important session for all attendees, Dr. Marks said. She also recommended the Clinical Quick Hits sessions for anyone seeking “a diverse array of practical knowledge which can be easily applied to everyday practice.” The Clinical Quick Hits are designed as 35-minute, rapid-fire presentations focused on clinical knowledge. Each of these presentations will focus on the latest updates or evolutions in clinical practice in one area. Some key topics include counseling parents when a child has an abnormal exam finding, assessing pelvic pain in adolescent girls, and preventing venous thromboembolism in the inpatient setting.
“I would also recommend that younger clinicians take in at least one or two workshops or sessions on nonclinical topics to see the breath of content at the meeting and to develop a niche interest for themselves outside of clinical work,” Dr. Marks noted.
Nonclinical sessions at PHM 2021 include workshops on a pilot for a comprehensive LGBTQ+ curriculum, using media tools for public health messaging, and practicing health literacy.
To register for the Pediatric Hospital Medicine 2021 virtual conference, visit https://apaevents.regfox.com/phm21-virtual-conference.
Dr. Giordano, Dr. Jones, and Dr. Marks are members of the PHM conference planning committee and had no relevant financial conflicts to disclose.
Advice on biopsies, workups, and referrals
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at obnews@mdedge.com.
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at obnews@mdedge.com.
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at obnews@mdedge.com.
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Combination atezolizumab and bevacizumab succeeds in real-world setting
Key clinical point: In the real-world setting, patients with unresectable HCC who did not meet clinical trial criteria had similar responses to the treatment combination as those who met clinical trial criteria.
Major finding: The objective response rates and disease control rates of 5.2% and 82.8% at 6 weeks and 10.0% and 84.0% at 12 weeks, respectively, were similar between patients who met and did not meet the IMbrave150 clinical trial criteria, as were safety profiles.
Study details: The data come from a multicenter study of 64 adults with unresectable hepatocellular carcinoma, including 46 who did not meet the study criteria. All patients were treated with a combination of atezolizumab plus bevacizumab. Treatment response and safety issues were assessed at 6 weeks and 12 weeks.
Disclosures: The study was supported by the Japan Agency for Medical Research and Development. The researchers had no financial conflicts to disclose.
Source: Sho T et al. Hepatol Res. 2021 Jul 10. doi: 10.1111/hepr.13693.
Key clinical point: In the real-world setting, patients with unresectable HCC who did not meet clinical trial criteria had similar responses to the treatment combination as those who met clinical trial criteria.
Major finding: The objective response rates and disease control rates of 5.2% and 82.8% at 6 weeks and 10.0% and 84.0% at 12 weeks, respectively, were similar between patients who met and did not meet the IMbrave150 clinical trial criteria, as were safety profiles.
Study details: The data come from a multicenter study of 64 adults with unresectable hepatocellular carcinoma, including 46 who did not meet the study criteria. All patients were treated with a combination of atezolizumab plus bevacizumab. Treatment response and safety issues were assessed at 6 weeks and 12 weeks.
Disclosures: The study was supported by the Japan Agency for Medical Research and Development. The researchers had no financial conflicts to disclose.
Source: Sho T et al. Hepatol Res. 2021 Jul 10. doi: 10.1111/hepr.13693.
Key clinical point: In the real-world setting, patients with unresectable HCC who did not meet clinical trial criteria had similar responses to the treatment combination as those who met clinical trial criteria.
Major finding: The objective response rates and disease control rates of 5.2% and 82.8% at 6 weeks and 10.0% and 84.0% at 12 weeks, respectively, were similar between patients who met and did not meet the IMbrave150 clinical trial criteria, as were safety profiles.
Study details: The data come from a multicenter study of 64 adults with unresectable hepatocellular carcinoma, including 46 who did not meet the study criteria. All patients were treated with a combination of atezolizumab plus bevacizumab. Treatment response and safety issues were assessed at 6 weeks and 12 weeks.
Disclosures: The study was supported by the Japan Agency for Medical Research and Development. The researchers had no financial conflicts to disclose.
Source: Sho T et al. Hepatol Res. 2021 Jul 10. doi: 10.1111/hepr.13693.
Can family physicians accurately screen for AAA with point-of-care ultrasound?
EVIDENCE SUMMARY
Meta-analysis demonstrates accuracy of nonradiologist providers with POCUS
A systematic review and meta-analysis (11 studies; 946 exams) compared nonradiologist-performed AAA screening with POCUS vs radiologist-performed aortic imaging as a gold standard. Eight trials involved emergency medicine physicians (718 exams); 1 trial, surgical residents (104 exams); 1 trial, primary care internal medicine physicians (79 exams); and 1 trial, rural family physicians (45 exams). The majority of studies were conducted in Ireland, the United Kingdom, Australia, and Canada, with 4 trials performed in the United States.1
Researchers compared all POCUS exam findings with radiologist-performed imaging (using ultrasound, computed tomography, magnetic resonance imaging, or angiography) and with operative findings or pathology where available. There were 193 true positives, 8 false-positives, 740 true negatives, and 5 false-negatives. Primary care physicians identified 6 patients with AAA, with no false-positives or false-negatives. Overall, POCUS demonstrated a sensitivity of 0.975 (95% CI, 0.942 to 0.992) and a specificity of 0.989 (95% CI, 0.979 to 0.995).1
Nonradiologist providers received POCUS training as follows: emergency medicine residents, 5 hours to 3 days; emergency medicine physicians, 4 to 24 hours of didactics, 50 AAA scans, or American College of Emergency Medicine certification; and primary care physicians, 2.3 hours or 50 AAA scans. Information on training for surgical residents was not supplied. The authors rated the studies for quality (10-14 points on the 14-point QUADA quality score) and heterogeneity (I2 = 0 for sensitivity and I2 = .38 for specificity).1
European studies support FPs’ ability to diagnose AAA with POCUS
Two subsequent prospective diagnostic accuracy studies both found that POCUS performed by family physicians had 100% concordance with radiologist overread. The first study (in Spain) included 106 men (ages 50 and older; mean, 69 years) with chronic hypertension or a history of tobacco use. One family physician underwent training (duration not reported) by a radiologist, including experience measuring standard cross-sections of the aorta. Radiologists reviewed all POCUS images, which identified 6 patients with AAA (confirmed by CT scan). The concordance between the family physician and the radiologists was absolute (kappa = 1.0; sensitivity and specificity, 100%; positive and negative predictive values, both 1.0).2
The second study (in Denmark) compared 29 POCUS screenings for AAA performed by 5 family physicians vs a gold standard of a radiologist-performed abdominal ultrasound blinded to previous ultrasound findings. Four of the family physicians were board certified and 1 was a final-year resident in training. They all underwent a 3-day ultrasonography course that included initial e-learning followed by 2 days of hands-on training; all passed a final certification exam. The family physicians identified 1 patient with AAA. Radiologists overread all the scans and found 100% agreement with the 1 positive AAA and the 28 negative scans.3
Recommendations from others
In 2019, the US Preventive Services Task Force (USPSTF) offered a Grade “B” (moderate net benefit) recommendation for screening with ultrasonography for AAA in men ages 65 to 75 years who have ever smoked, and a Grade “C” recommendation (small net benefit) for screening men ages 65 to 75 years who have never smoked.4 In 2017, the Canadian Task Force on Preventive Health Care recommended screening all men ages 65 to 80 years with 1 ultrasound exam for AAA (weak recommendation; moderate-quality evidence). The Canadian Task Force also noted that, with adequate training, AAA screening could be performed in a family practice setting.5
Editor’s takeaway
While these studies evaluating POCUS performed by nonradiologists included a small number of family physicians, their finding that all participants (attending physicians and residents) demonstrate high sensitivity and specificity for AAA detection with relatively limited training bodes well for more widespread use of the technology. Offering POCUS to detect AAAs in family physician offices has the potential to dramatically improve access to USPSTF-recommended screening.
1. Concannon E, McHugh S, Healy DA, et al. Diagnostic accuracy of non-radiologist performed ultrasound for abdominal aortic aneurysm: systematic review and meta-analysis. Int J Clin Pract. 2014;9:1122-1129. doi: 10.1111/ijcp.12453
2. Sisó-Almirall A, Gilabert Solé R, Bru Saumell C, et al. Feasibility of hand-held-ultrasonography in the screening of abdominal aortic aneurysms and abdominal aortic atherosclerosis [article in Spanish]. Med Clin (Barc). 2013;141:417-422. doi: 10.1016/j.medcli.2013.02.038
3. Lindgaard K, Riisgaard L. ‘Validation of ultrasound examinations performed by general practitioners’. Scand J Prim Health Care. 2017;3:256-261. doi: 10.1080/02813432.2017.1358437
4. US Preventive Task Force. Screening for abdominal aortic aneurysm: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;322:2211-2218. doi:10.1001/jama.2019.18928
5. Canadian Task Force on Preventive Health Care. Recommendations on screening for abdominal aortic aneurysm in primary care. CMAJ. 2017;189:E1137-E1145. doi: 10.1503/cmaj.170118
EVIDENCE SUMMARY
Meta-analysis demonstrates accuracy of nonradiologist providers with POCUS
A systematic review and meta-analysis (11 studies; 946 exams) compared nonradiologist-performed AAA screening with POCUS vs radiologist-performed aortic imaging as a gold standard. Eight trials involved emergency medicine physicians (718 exams); 1 trial, surgical residents (104 exams); 1 trial, primary care internal medicine physicians (79 exams); and 1 trial, rural family physicians (45 exams). The majority of studies were conducted in Ireland, the United Kingdom, Australia, and Canada, with 4 trials performed in the United States.1
Researchers compared all POCUS exam findings with radiologist-performed imaging (using ultrasound, computed tomography, magnetic resonance imaging, or angiography) and with operative findings or pathology where available. There were 193 true positives, 8 false-positives, 740 true negatives, and 5 false-negatives. Primary care physicians identified 6 patients with AAA, with no false-positives or false-negatives. Overall, POCUS demonstrated a sensitivity of 0.975 (95% CI, 0.942 to 0.992) and a specificity of 0.989 (95% CI, 0.979 to 0.995).1
Nonradiologist providers received POCUS training as follows: emergency medicine residents, 5 hours to 3 days; emergency medicine physicians, 4 to 24 hours of didactics, 50 AAA scans, or American College of Emergency Medicine certification; and primary care physicians, 2.3 hours or 50 AAA scans. Information on training for surgical residents was not supplied. The authors rated the studies for quality (10-14 points on the 14-point QUADA quality score) and heterogeneity (I2 = 0 for sensitivity and I2 = .38 for specificity).1
European studies support FPs’ ability to diagnose AAA with POCUS
Two subsequent prospective diagnostic accuracy studies both found that POCUS performed by family physicians had 100% concordance with radiologist overread. The first study (in Spain) included 106 men (ages 50 and older; mean, 69 years) with chronic hypertension or a history of tobacco use. One family physician underwent training (duration not reported) by a radiologist, including experience measuring standard cross-sections of the aorta. Radiologists reviewed all POCUS images, which identified 6 patients with AAA (confirmed by CT scan). The concordance between the family physician and the radiologists was absolute (kappa = 1.0; sensitivity and specificity, 100%; positive and negative predictive values, both 1.0).2
The second study (in Denmark) compared 29 POCUS screenings for AAA performed by 5 family physicians vs a gold standard of a radiologist-performed abdominal ultrasound blinded to previous ultrasound findings. Four of the family physicians were board certified and 1 was a final-year resident in training. They all underwent a 3-day ultrasonography course that included initial e-learning followed by 2 days of hands-on training; all passed a final certification exam. The family physicians identified 1 patient with AAA. Radiologists overread all the scans and found 100% agreement with the 1 positive AAA and the 28 negative scans.3
Recommendations from others
In 2019, the US Preventive Services Task Force (USPSTF) offered a Grade “B” (moderate net benefit) recommendation for screening with ultrasonography for AAA in men ages 65 to 75 years who have ever smoked, and a Grade “C” recommendation (small net benefit) for screening men ages 65 to 75 years who have never smoked.4 In 2017, the Canadian Task Force on Preventive Health Care recommended screening all men ages 65 to 80 years with 1 ultrasound exam for AAA (weak recommendation; moderate-quality evidence). The Canadian Task Force also noted that, with adequate training, AAA screening could be performed in a family practice setting.5
Editor’s takeaway
While these studies evaluating POCUS performed by nonradiologists included a small number of family physicians, their finding that all participants (attending physicians and residents) demonstrate high sensitivity and specificity for AAA detection with relatively limited training bodes well for more widespread use of the technology. Offering POCUS to detect AAAs in family physician offices has the potential to dramatically improve access to USPSTF-recommended screening.
EVIDENCE SUMMARY
Meta-analysis demonstrates accuracy of nonradiologist providers with POCUS
A systematic review and meta-analysis (11 studies; 946 exams) compared nonradiologist-performed AAA screening with POCUS vs radiologist-performed aortic imaging as a gold standard. Eight trials involved emergency medicine physicians (718 exams); 1 trial, surgical residents (104 exams); 1 trial, primary care internal medicine physicians (79 exams); and 1 trial, rural family physicians (45 exams). The majority of studies were conducted in Ireland, the United Kingdom, Australia, and Canada, with 4 trials performed in the United States.1
Researchers compared all POCUS exam findings with radiologist-performed imaging (using ultrasound, computed tomography, magnetic resonance imaging, or angiography) and with operative findings or pathology where available. There were 193 true positives, 8 false-positives, 740 true negatives, and 5 false-negatives. Primary care physicians identified 6 patients with AAA, with no false-positives or false-negatives. Overall, POCUS demonstrated a sensitivity of 0.975 (95% CI, 0.942 to 0.992) and a specificity of 0.989 (95% CI, 0.979 to 0.995).1
Nonradiologist providers received POCUS training as follows: emergency medicine residents, 5 hours to 3 days; emergency medicine physicians, 4 to 24 hours of didactics, 50 AAA scans, or American College of Emergency Medicine certification; and primary care physicians, 2.3 hours or 50 AAA scans. Information on training for surgical residents was not supplied. The authors rated the studies for quality (10-14 points on the 14-point QUADA quality score) and heterogeneity (I2 = 0 for sensitivity and I2 = .38 for specificity).1
European studies support FPs’ ability to diagnose AAA with POCUS
Two subsequent prospective diagnostic accuracy studies both found that POCUS performed by family physicians had 100% concordance with radiologist overread. The first study (in Spain) included 106 men (ages 50 and older; mean, 69 years) with chronic hypertension or a history of tobacco use. One family physician underwent training (duration not reported) by a radiologist, including experience measuring standard cross-sections of the aorta. Radiologists reviewed all POCUS images, which identified 6 patients with AAA (confirmed by CT scan). The concordance between the family physician and the radiologists was absolute (kappa = 1.0; sensitivity and specificity, 100%; positive and negative predictive values, both 1.0).2
The second study (in Denmark) compared 29 POCUS screenings for AAA performed by 5 family physicians vs a gold standard of a radiologist-performed abdominal ultrasound blinded to previous ultrasound findings. Four of the family physicians were board certified and 1 was a final-year resident in training. They all underwent a 3-day ultrasonography course that included initial e-learning followed by 2 days of hands-on training; all passed a final certification exam. The family physicians identified 1 patient with AAA. Radiologists overread all the scans and found 100% agreement with the 1 positive AAA and the 28 negative scans.3
Recommendations from others
In 2019, the US Preventive Services Task Force (USPSTF) offered a Grade “B” (moderate net benefit) recommendation for screening with ultrasonography for AAA in men ages 65 to 75 years who have ever smoked, and a Grade “C” recommendation (small net benefit) for screening men ages 65 to 75 years who have never smoked.4 In 2017, the Canadian Task Force on Preventive Health Care recommended screening all men ages 65 to 80 years with 1 ultrasound exam for AAA (weak recommendation; moderate-quality evidence). The Canadian Task Force also noted that, with adequate training, AAA screening could be performed in a family practice setting.5
Editor’s takeaway
While these studies evaluating POCUS performed by nonradiologists included a small number of family physicians, their finding that all participants (attending physicians and residents) demonstrate high sensitivity and specificity for AAA detection with relatively limited training bodes well for more widespread use of the technology. Offering POCUS to detect AAAs in family physician offices has the potential to dramatically improve access to USPSTF-recommended screening.
1. Concannon E, McHugh S, Healy DA, et al. Diagnostic accuracy of non-radiologist performed ultrasound for abdominal aortic aneurysm: systematic review and meta-analysis. Int J Clin Pract. 2014;9:1122-1129. doi: 10.1111/ijcp.12453
2. Sisó-Almirall A, Gilabert Solé R, Bru Saumell C, et al. Feasibility of hand-held-ultrasonography in the screening of abdominal aortic aneurysms and abdominal aortic atherosclerosis [article in Spanish]. Med Clin (Barc). 2013;141:417-422. doi: 10.1016/j.medcli.2013.02.038
3. Lindgaard K, Riisgaard L. ‘Validation of ultrasound examinations performed by general practitioners’. Scand J Prim Health Care. 2017;3:256-261. doi: 10.1080/02813432.2017.1358437
4. US Preventive Task Force. Screening for abdominal aortic aneurysm: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;322:2211-2218. doi:10.1001/jama.2019.18928
5. Canadian Task Force on Preventive Health Care. Recommendations on screening for abdominal aortic aneurysm in primary care. CMAJ. 2017;189:E1137-E1145. doi: 10.1503/cmaj.170118
1. Concannon E, McHugh S, Healy DA, et al. Diagnostic accuracy of non-radiologist performed ultrasound for abdominal aortic aneurysm: systematic review and meta-analysis. Int J Clin Pract. 2014;9:1122-1129. doi: 10.1111/ijcp.12453
2. Sisó-Almirall A, Gilabert Solé R, Bru Saumell C, et al. Feasibility of hand-held-ultrasonography in the screening of abdominal aortic aneurysms and abdominal aortic atherosclerosis [article in Spanish]. Med Clin (Barc). 2013;141:417-422. doi: 10.1016/j.medcli.2013.02.038
3. Lindgaard K, Riisgaard L. ‘Validation of ultrasound examinations performed by general practitioners’. Scand J Prim Health Care. 2017;3:256-261. doi: 10.1080/02813432.2017.1358437
4. US Preventive Task Force. Screening for abdominal aortic aneurysm: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;322:2211-2218. doi:10.1001/jama.2019.18928
5. Canadian Task Force on Preventive Health Care. Recommendations on screening for abdominal aortic aneurysm in primary care. CMAJ. 2017;189:E1137-E1145. doi: 10.1503/cmaj.170118
EVIDENCE-BASED ANSWER:
Likely yes. Point-of-care ultrasound (POCUS) screening for abdominal aortic aneurysm (AAA) by nonradiologist physicians is 98% sensitive and 99% specific, compared with imaging performed by radiologists (strength of recommendation [SOR]: B, meta-analysis of diagnostic accuracy studies mostly involving emergency medicine physicians). European family physicians demonstrated 100% concordance with radiologist readings (SOR: C, very small subsequent diagnostic accuracy studies).