User login
FDA approves new immunotherapy for endometrial cancer
Use limited to patients with biomarker
Usage of the new checkpoint inhibitor is limited to patients who have progressed on or following prior treatment with a platinum-containing chemotherapy. Eligibility must also be determined by an FDA-approved test for the dMMR biomarker. Approximately 25%-30% of patients with advanced endometrial cancer have dMMR tumors, according to the FDA.
The approval is “evidence of the FDA’s progress in applying precision medicine to expand treatment options for patients with cancer,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Oncologic Diseases in the FDA’s Center for Drug Evaluation and Research.
He explained that the immunotherapy was “specifically studied to target dMMR endometrial cancer and leverages scientific knowledge surrounding the mechanism of immunotherapy response.”
The new drug also addresses an unmet medical need, as there are limited therapeutic options in this setting following frontline standard treatment with a platinum-containing chemotherapy.
The approval is based on safety and efficacy data from a single-arm, multicohort clinical trial. Of the 71 patients with dMMR recurrent or advanced endometrial cancer who received dostarlimab, 42.3% had a response. For 93% of that group, the response lasted 6 months or longer.
The drug’s maker, GlaxoSmithKline, is currently conducting additional, larger trials in more patients with dMMR endometrial tumors to verify and further describe clinical benefits.
Common side effects of dostarlimab include fatigue, nausea, diarrhea, anemia, and constipation. Like other checkpoint inhibitors, the new drug can cause immune-mediated side effects such as pneumonitis, colitis, hepatitis, endocrinopathies, and nephritis.
Dostarlimab is contraindicated in women who are pregnant or breastfeeding because it may cause harm to a developing fetus or newborn baby.
The FDA approval comes a month after the Committee for Medicinal Products for Human Use of the European Medicines Agency recommended granting conditional marketing authorization for dostarlimab for use as monotherapy in this same patient group.
In the United States, dostarlimab received Priority Review designation and Breakthrough Therapy designation for this indication.
A version of this article first appeared on Medscape.com.
Use limited to patients with biomarker
Use limited to patients with biomarker
Usage of the new checkpoint inhibitor is limited to patients who have progressed on or following prior treatment with a platinum-containing chemotherapy. Eligibility must also be determined by an FDA-approved test for the dMMR biomarker. Approximately 25%-30% of patients with advanced endometrial cancer have dMMR tumors, according to the FDA.
The approval is “evidence of the FDA’s progress in applying precision medicine to expand treatment options for patients with cancer,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Oncologic Diseases in the FDA’s Center for Drug Evaluation and Research.
He explained that the immunotherapy was “specifically studied to target dMMR endometrial cancer and leverages scientific knowledge surrounding the mechanism of immunotherapy response.”
The new drug also addresses an unmet medical need, as there are limited therapeutic options in this setting following frontline standard treatment with a platinum-containing chemotherapy.
The approval is based on safety and efficacy data from a single-arm, multicohort clinical trial. Of the 71 patients with dMMR recurrent or advanced endometrial cancer who received dostarlimab, 42.3% had a response. For 93% of that group, the response lasted 6 months or longer.
The drug’s maker, GlaxoSmithKline, is currently conducting additional, larger trials in more patients with dMMR endometrial tumors to verify and further describe clinical benefits.
Common side effects of dostarlimab include fatigue, nausea, diarrhea, anemia, and constipation. Like other checkpoint inhibitors, the new drug can cause immune-mediated side effects such as pneumonitis, colitis, hepatitis, endocrinopathies, and nephritis.
Dostarlimab is contraindicated in women who are pregnant or breastfeeding because it may cause harm to a developing fetus or newborn baby.
The FDA approval comes a month after the Committee for Medicinal Products for Human Use of the European Medicines Agency recommended granting conditional marketing authorization for dostarlimab for use as monotherapy in this same patient group.
In the United States, dostarlimab received Priority Review designation and Breakthrough Therapy designation for this indication.
A version of this article first appeared on Medscape.com.
Usage of the new checkpoint inhibitor is limited to patients who have progressed on or following prior treatment with a platinum-containing chemotherapy. Eligibility must also be determined by an FDA-approved test for the dMMR biomarker. Approximately 25%-30% of patients with advanced endometrial cancer have dMMR tumors, according to the FDA.
The approval is “evidence of the FDA’s progress in applying precision medicine to expand treatment options for patients with cancer,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Oncologic Diseases in the FDA’s Center for Drug Evaluation and Research.
He explained that the immunotherapy was “specifically studied to target dMMR endometrial cancer and leverages scientific knowledge surrounding the mechanism of immunotherapy response.”
The new drug also addresses an unmet medical need, as there are limited therapeutic options in this setting following frontline standard treatment with a platinum-containing chemotherapy.
The approval is based on safety and efficacy data from a single-arm, multicohort clinical trial. Of the 71 patients with dMMR recurrent or advanced endometrial cancer who received dostarlimab, 42.3% had a response. For 93% of that group, the response lasted 6 months or longer.
The drug’s maker, GlaxoSmithKline, is currently conducting additional, larger trials in more patients with dMMR endometrial tumors to verify and further describe clinical benefits.
Common side effects of dostarlimab include fatigue, nausea, diarrhea, anemia, and constipation. Like other checkpoint inhibitors, the new drug can cause immune-mediated side effects such as pneumonitis, colitis, hepatitis, endocrinopathies, and nephritis.
Dostarlimab is contraindicated in women who are pregnant or breastfeeding because it may cause harm to a developing fetus or newborn baby.
The FDA approval comes a month after the Committee for Medicinal Products for Human Use of the European Medicines Agency recommended granting conditional marketing authorization for dostarlimab for use as monotherapy in this same patient group.
In the United States, dostarlimab received Priority Review designation and Breakthrough Therapy designation for this indication.
A version of this article first appeared on Medscape.com.
Vaccinating homebound patients is an uphill battle

There are about 2 million to 4 million homebound patients in the United States, according to a webinar from The Trust for America’s Health, which was broadcast in March. But many of these individuals have not been vaccinated yet because of logistical challenges.
Some homebound COVID-19 immunization programs are administering Moderna and Pfizer vaccines to their patients, but many state, city, and local programs administered the Johnson & Johnson vaccine after it was cleared for use by the Food and Drug Administration in February 2021. The efficacy of the one-shot vaccine, as well as it being easier to store and ship than the Moderna and Pfizer vaccines, makes getting it to homebound patients less challenging.
“With Pfizer and Moderna, transportation is a challenge because the temperature demands and the fragility of [messenger] RNA–based vaccines,” Brent Feorene, executive director of the American Academy of Home Care Medicine, said in an interview. That’s why [the Johnson & Johnson] vaccine held such promise – it’s less fragile, [can be stored in] higher temperatures, and was a one shot.”
Other hurdles to getting homebound patients vaccinated had already been in place prior to the 10-day-pause on using the J&J vaccine that occurred for federal agencies to consider possible serious side effects linked to it.
Many roadblocks to vaccination
Although many homebound patients can’t readily go out into the community and be exposed to the COVID-19 virus themselves, they are dependent on caregivers and family members who do go out into the community.
“Their friends, family, neighbors, home health aides, and other kinds of health care workers come into the home,” said Shawn Amer, clinical program director at Central Ohio Primary Care in Columbus.
Nurses from Ms. Amer’s practice vaccinated approximately ten homebound patients with the J&J vaccine through a pilot program in March. Then on April 24, nurses from Central Ohio Primary Care vaccinated just under 40 homebound patients and about a handful of their caregivers who were not able to get their vaccines elsewhere, according to Ms. Amer. This time they used the Pfizer vaccine and will be returning to these patients’ homes on May 15 to administer the second dose.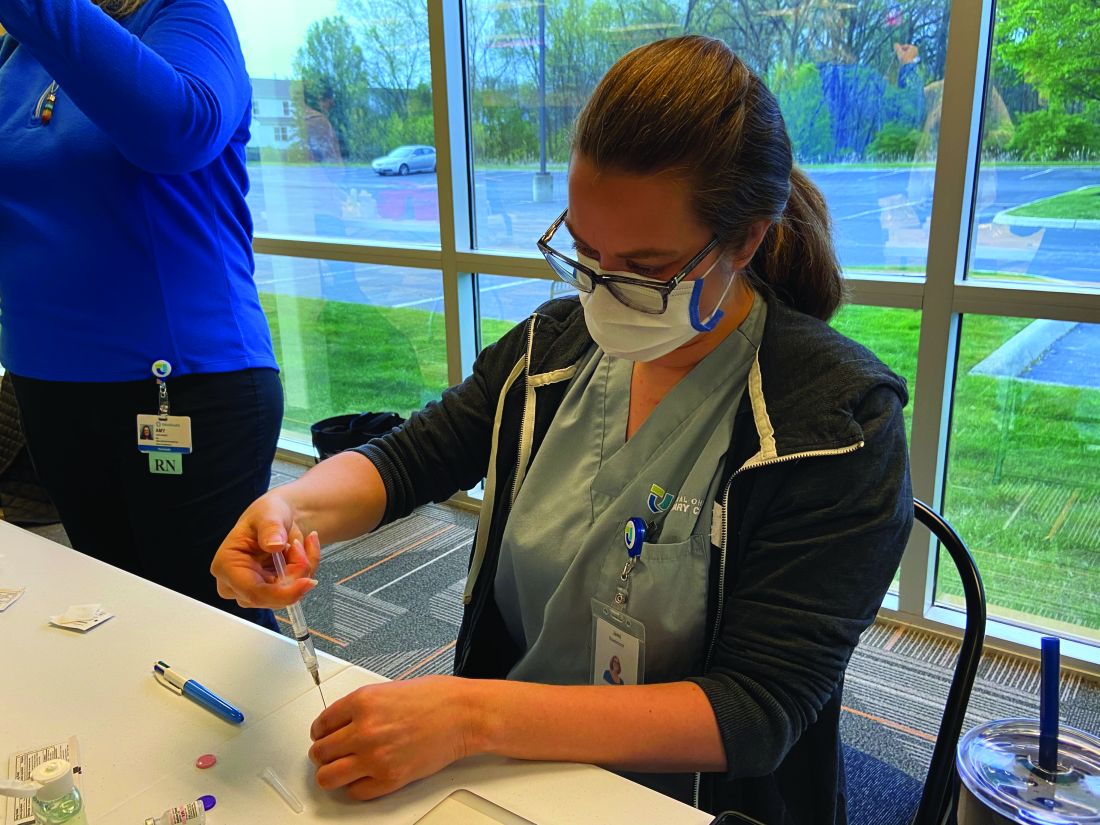
“Any time you are getting in the car and adding miles, it adds complexity,” Ms. Amer said.
“We called patients 24 to 36 hours before coming to their homes to make sure they were ready, but we learned that just because the healthcare power of attorney agrees to a patient getting vaccinated does not mean that patient will be willing to get the vaccine when the nurse shows up," she noted.
Ms. Amer elaborated that three patients with dementia refused the vaccine when nurses arrived at their home on April 24.
“We had to pivot and find other people,” Ms. Amer. Her practice ended up having to waste one shot.
Expenses are greater
The higher costs of getting homebound patients vaccinated is an additional hurdle to getting these vulnerable individuals protected by COVID-19 shots.
Vaccinating patients in their homes “doesn’t require a lot of technology, but it does require a lot of time” and the staffing expense becomes part of the challenge, Ms. Amer noted.
For each of the two days that Central Ohio Primary Care provides the Pfizer vaccine to homebound patients, the practice needs to pay seven nurses to administer the vaccine, Ms. Amer explained.
There have also been reports of organizations that administer the vaccines – which are free for patients because the federal government is paying for them – not being paid enough by Medicare to cover staff time and efforts to vaccinate patients in their homes, Kaiser Health News reported. According to the Centers for Medicare & Medicaid Services, they pay $40 for the administration of a single-dose COVID-19 vaccine and, for COVID-19 vaccines requiring multiple doses, Medicare pays approximately $40 for each dose in the series. These rates were implemented after March 15. Before that date, the rates were even lower, with the Medicare reimbursement rates for initial doses of COVID-19 vaccines being $16.94 and final doses being $28.39.
William Dombi, president of the National Association for Home Care & Hospice, told Kaiser Health News that the actual cost of these homebound visits are closer to $150 or $160.
“The reimbursement for the injection is pretty minimal,” Mr. Feorene said. “So unless you’re a larger organization and able to have staff to deploy some of your smaller practices, just couldn’t afford to do it.”
Many homebound patients have also been unable to get the lifesaving shots because of logistical roadblocks and many practices not being able to do home visits.
“I think that initially when the [Centers for Disease Control and Prevention] came out with vaccine guidance for medical providers, they offered no guidance for in-home medical providers and we had to go back and ask for that, which they did produce,” Mr. Feorene said. “And we’re grateful for that. But I think just this general understanding that there is a population of folks that are [limited to their home], that they do receive medical care and other care in the home, and that we have to remember that the medical providers who provide care in the home are also primary care providers.”
Furthermore, trying to navigate or find programs delivering vaccines to the homebound can be difficult depending on where a patient lives.
While some programs have been launched on the country or city level – the New York Fire Department launched a pilot program to bring the Johnson & Johnson vaccine to homebound seniors – other programs have been spearheaded by hospital networks like Northwell and Mount Sinai. However, many of these hospital networks only reach out to people who already have a relationship with the hospital.
Ms Amer said identifying homebound patients and reaching out to them can be tough and can contribute to the logistics and time involved in setting patients up for the vaccine.
“Reaching some of these patients is difficult,” Ms. Amer noted. “Sometimes the best way to reach them or get a hold of them is through their caregiver. And so do you have the right phone number? Do you have the right name?”
Overcoming the challenges
With the absence of a national plan targeting homebound patients, many local initiatives were launched to help these individuals get vaccinated. Local fire department paramedics have gone door to door to administer the COVID-19 vaccine in cities like Chicago, New York, and Miami. The suspension of the Johnson & Johnson vaccine resulted in the suspension of in-home vaccinations for some people in New York City. However, the program resumed after the FDA and CDC lifted the pause on April 24. 
Health systems like Mount Sinai vaccinated approximately 530 people through the Mount Sinai Visiting Doctors Program, including patients and their caregivers, according to Peter Gliatto, MD, associate director of the Mount Sinai Visiting Doctors Program.
“In different cities, townships, and jurisdictions, different health departments and different provider groups are approaching [the distribution of the COVID-19 vaccine] slightly differently,” Ms. Amer said. So a lot of the decisions surrounding the distribution of shots are local or dependent on local resourcing.
People who live in rural areas present a unique challenge, but Mr. Feorene said reaching out to local emergency medical services or the local health departments can provide some insight on what their town is doing to vaccinate homebound patients.
“I think understanding what a [public health department] is doing would be the very first place to start,” Mr. Feorene said in an interview.
If a patient is bedridden and is mobile enough to sit in a car, Mr. Feorene also recommends finding out if there are vaccine fairs “within a reasonable driving distance.”
Ms. Amer said continuing this mission of getting homebound patients vaccinated is necessary for public health.
“Even if it’s going to take longer to vaccinate these homebound patients, we still have to make an effort. So much of the country’s vaccine efforts have been focused on getting as many shots in as many arms as quickly as possible. And that is definitely super important,” she said.
Ms. Amer is working with her practice’s primary care physicians to try to identify all of those patients who are functionally debilitated or unable to leave their home to get vaccinated and that Central Ohio Primary Care will vaccinate more homebound patients, she added.
The experts interviewed in this article have no conflicts.
Katie Lennon contributed to this report.
This article was updated 4/29/21.

There are about 2 million to 4 million homebound patients in the United States, according to a webinar from The Trust for America’s Health, which was broadcast in March. But many of these individuals have not been vaccinated yet because of logistical challenges.
Some homebound COVID-19 immunization programs are administering Moderna and Pfizer vaccines to their patients, but many state, city, and local programs administered the Johnson & Johnson vaccine after it was cleared for use by the Food and Drug Administration in February 2021. The efficacy of the one-shot vaccine, as well as it being easier to store and ship than the Moderna and Pfizer vaccines, makes getting it to homebound patients less challenging.
“With Pfizer and Moderna, transportation is a challenge because the temperature demands and the fragility of [messenger] RNA–based vaccines,” Brent Feorene, executive director of the American Academy of Home Care Medicine, said in an interview. That’s why [the Johnson & Johnson] vaccine held such promise – it’s less fragile, [can be stored in] higher temperatures, and was a one shot.”
Other hurdles to getting homebound patients vaccinated had already been in place prior to the 10-day-pause on using the J&J vaccine that occurred for federal agencies to consider possible serious side effects linked to it.
Many roadblocks to vaccination
Although many homebound patients can’t readily go out into the community and be exposed to the COVID-19 virus themselves, they are dependent on caregivers and family members who do go out into the community.
“Their friends, family, neighbors, home health aides, and other kinds of health care workers come into the home,” said Shawn Amer, clinical program director at Central Ohio Primary Care in Columbus.
Nurses from Ms. Amer’s practice vaccinated approximately ten homebound patients with the J&J vaccine through a pilot program in March. Then on April 24, nurses from Central Ohio Primary Care vaccinated just under 40 homebound patients and about a handful of their caregivers who were not able to get their vaccines elsewhere, according to Ms. Amer. This time they used the Pfizer vaccine and will be returning to these patients’ homes on May 15 to administer the second dose.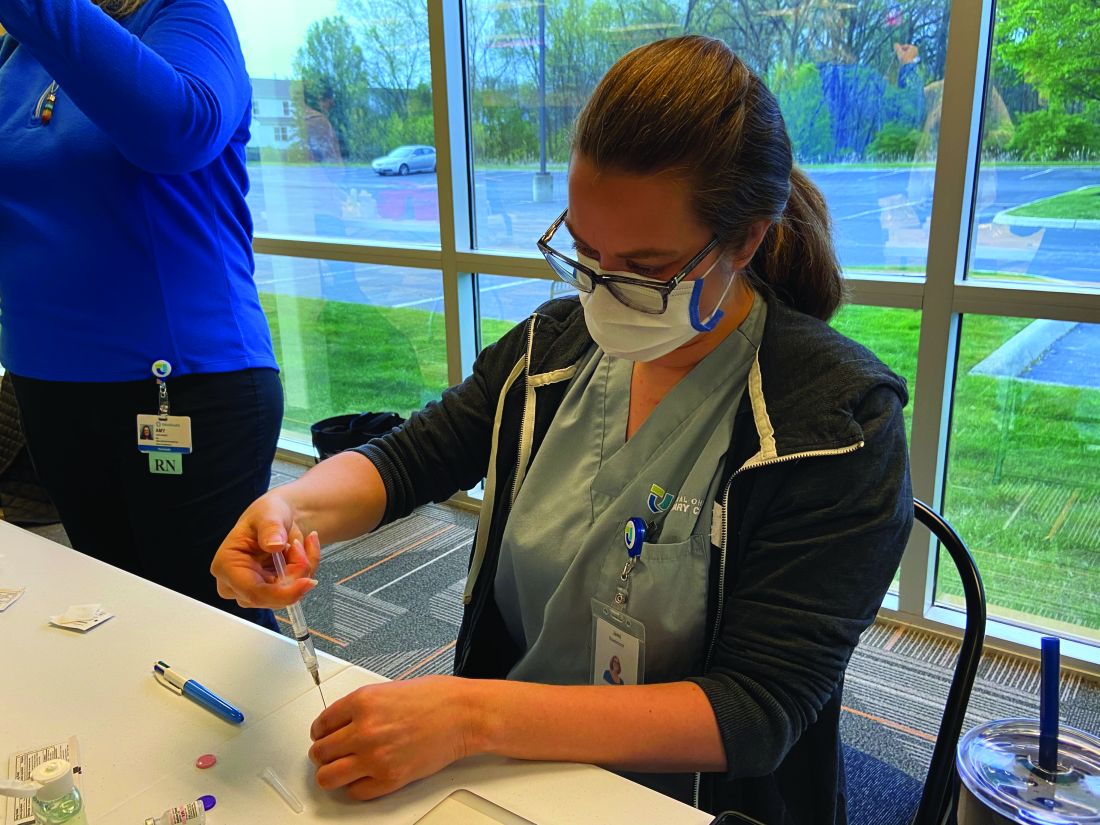
“Any time you are getting in the car and adding miles, it adds complexity,” Ms. Amer said.
“We called patients 24 to 36 hours before coming to their homes to make sure they were ready, but we learned that just because the healthcare power of attorney agrees to a patient getting vaccinated does not mean that patient will be willing to get the vaccine when the nurse shows up," she noted.
Ms. Amer elaborated that three patients with dementia refused the vaccine when nurses arrived at their home on April 24.
“We had to pivot and find other people,” Ms. Amer. Her practice ended up having to waste one shot.
Expenses are greater
The higher costs of getting homebound patients vaccinated is an additional hurdle to getting these vulnerable individuals protected by COVID-19 shots.
Vaccinating patients in their homes “doesn’t require a lot of technology, but it does require a lot of time” and the staffing expense becomes part of the challenge, Ms. Amer noted.
For each of the two days that Central Ohio Primary Care provides the Pfizer vaccine to homebound patients, the practice needs to pay seven nurses to administer the vaccine, Ms. Amer explained.
There have also been reports of organizations that administer the vaccines – which are free for patients because the federal government is paying for them – not being paid enough by Medicare to cover staff time and efforts to vaccinate patients in their homes, Kaiser Health News reported. According to the Centers for Medicare & Medicaid Services, they pay $40 for the administration of a single-dose COVID-19 vaccine and, for COVID-19 vaccines requiring multiple doses, Medicare pays approximately $40 for each dose in the series. These rates were implemented after March 15. Before that date, the rates were even lower, with the Medicare reimbursement rates for initial doses of COVID-19 vaccines being $16.94 and final doses being $28.39.
William Dombi, president of the National Association for Home Care & Hospice, told Kaiser Health News that the actual cost of these homebound visits are closer to $150 or $160.
“The reimbursement for the injection is pretty minimal,” Mr. Feorene said. “So unless you’re a larger organization and able to have staff to deploy some of your smaller practices, just couldn’t afford to do it.”
Many homebound patients have also been unable to get the lifesaving shots because of logistical roadblocks and many practices not being able to do home visits.
“I think that initially when the [Centers for Disease Control and Prevention] came out with vaccine guidance for medical providers, they offered no guidance for in-home medical providers and we had to go back and ask for that, which they did produce,” Mr. Feorene said. “And we’re grateful for that. But I think just this general understanding that there is a population of folks that are [limited to their home], that they do receive medical care and other care in the home, and that we have to remember that the medical providers who provide care in the home are also primary care providers.”
Furthermore, trying to navigate or find programs delivering vaccines to the homebound can be difficult depending on where a patient lives.
While some programs have been launched on the country or city level – the New York Fire Department launched a pilot program to bring the Johnson & Johnson vaccine to homebound seniors – other programs have been spearheaded by hospital networks like Northwell and Mount Sinai. However, many of these hospital networks only reach out to people who already have a relationship with the hospital.
Ms Amer said identifying homebound patients and reaching out to them can be tough and can contribute to the logistics and time involved in setting patients up for the vaccine.
“Reaching some of these patients is difficult,” Ms. Amer noted. “Sometimes the best way to reach them or get a hold of them is through their caregiver. And so do you have the right phone number? Do you have the right name?”
Overcoming the challenges
With the absence of a national plan targeting homebound patients, many local initiatives were launched to help these individuals get vaccinated. Local fire department paramedics have gone door to door to administer the COVID-19 vaccine in cities like Chicago, New York, and Miami. The suspension of the Johnson & Johnson vaccine resulted in the suspension of in-home vaccinations for some people in New York City. However, the program resumed after the FDA and CDC lifted the pause on April 24. 
Health systems like Mount Sinai vaccinated approximately 530 people through the Mount Sinai Visiting Doctors Program, including patients and their caregivers, according to Peter Gliatto, MD, associate director of the Mount Sinai Visiting Doctors Program.
“In different cities, townships, and jurisdictions, different health departments and different provider groups are approaching [the distribution of the COVID-19 vaccine] slightly differently,” Ms. Amer said. So a lot of the decisions surrounding the distribution of shots are local or dependent on local resourcing.
People who live in rural areas present a unique challenge, but Mr. Feorene said reaching out to local emergency medical services or the local health departments can provide some insight on what their town is doing to vaccinate homebound patients.
“I think understanding what a [public health department] is doing would be the very first place to start,” Mr. Feorene said in an interview.
If a patient is bedridden and is mobile enough to sit in a car, Mr. Feorene also recommends finding out if there are vaccine fairs “within a reasonable driving distance.”
Ms. Amer said continuing this mission of getting homebound patients vaccinated is necessary for public health.
“Even if it’s going to take longer to vaccinate these homebound patients, we still have to make an effort. So much of the country’s vaccine efforts have been focused on getting as many shots in as many arms as quickly as possible. And that is definitely super important,” she said.
Ms. Amer is working with her practice’s primary care physicians to try to identify all of those patients who are functionally debilitated or unable to leave their home to get vaccinated and that Central Ohio Primary Care will vaccinate more homebound patients, she added.
The experts interviewed in this article have no conflicts.
Katie Lennon contributed to this report.
This article was updated 4/29/21.

There are about 2 million to 4 million homebound patients in the United States, according to a webinar from The Trust for America’s Health, which was broadcast in March. But many of these individuals have not been vaccinated yet because of logistical challenges.
Some homebound COVID-19 immunization programs are administering Moderna and Pfizer vaccines to their patients, but many state, city, and local programs administered the Johnson & Johnson vaccine after it was cleared for use by the Food and Drug Administration in February 2021. The efficacy of the one-shot vaccine, as well as it being easier to store and ship than the Moderna and Pfizer vaccines, makes getting it to homebound patients less challenging.
“With Pfizer and Moderna, transportation is a challenge because the temperature demands and the fragility of [messenger] RNA–based vaccines,” Brent Feorene, executive director of the American Academy of Home Care Medicine, said in an interview. That’s why [the Johnson & Johnson] vaccine held such promise – it’s less fragile, [can be stored in] higher temperatures, and was a one shot.”
Other hurdles to getting homebound patients vaccinated had already been in place prior to the 10-day-pause on using the J&J vaccine that occurred for federal agencies to consider possible serious side effects linked to it.
Many roadblocks to vaccination
Although many homebound patients can’t readily go out into the community and be exposed to the COVID-19 virus themselves, they are dependent on caregivers and family members who do go out into the community.
“Their friends, family, neighbors, home health aides, and other kinds of health care workers come into the home,” said Shawn Amer, clinical program director at Central Ohio Primary Care in Columbus.
Nurses from Ms. Amer’s practice vaccinated approximately ten homebound patients with the J&J vaccine through a pilot program in March. Then on April 24, nurses from Central Ohio Primary Care vaccinated just under 40 homebound patients and about a handful of their caregivers who were not able to get their vaccines elsewhere, according to Ms. Amer. This time they used the Pfizer vaccine and will be returning to these patients’ homes on May 15 to administer the second dose.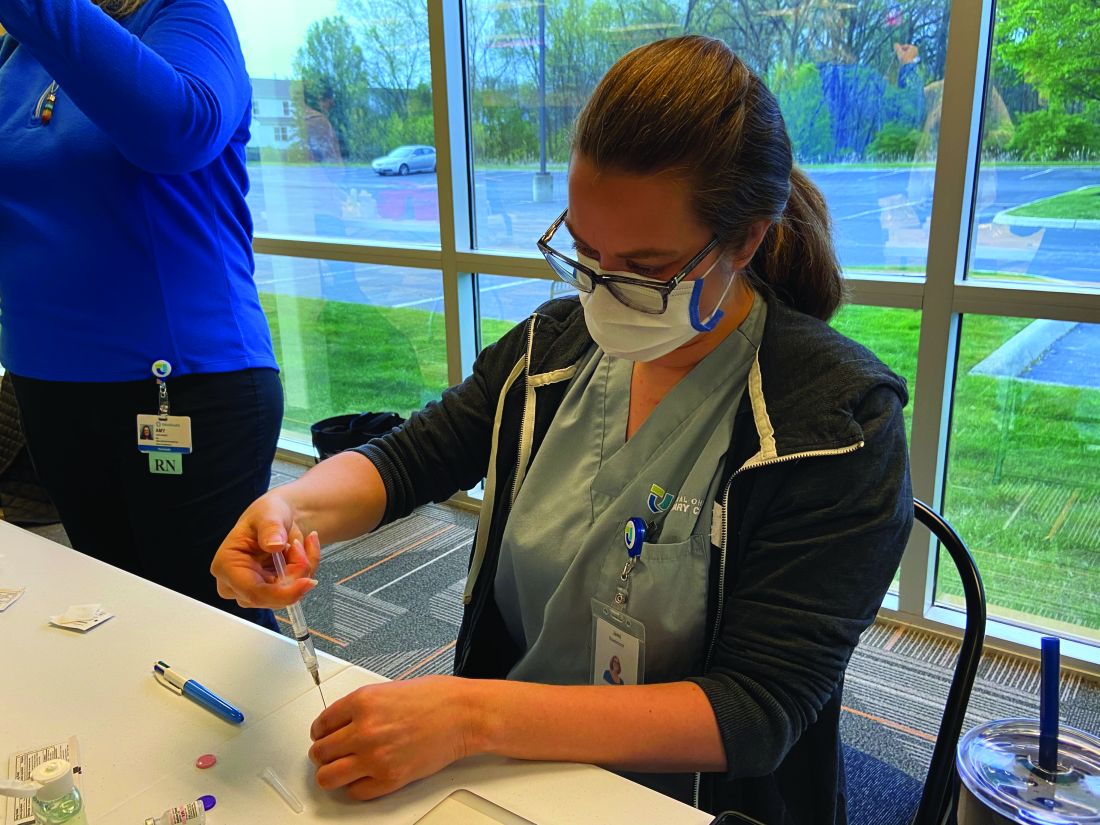
“Any time you are getting in the car and adding miles, it adds complexity,” Ms. Amer said.
“We called patients 24 to 36 hours before coming to their homes to make sure they were ready, but we learned that just because the healthcare power of attorney agrees to a patient getting vaccinated does not mean that patient will be willing to get the vaccine when the nurse shows up," she noted.
Ms. Amer elaborated that three patients with dementia refused the vaccine when nurses arrived at their home on April 24.
“We had to pivot and find other people,” Ms. Amer. Her practice ended up having to waste one shot.
Expenses are greater
The higher costs of getting homebound patients vaccinated is an additional hurdle to getting these vulnerable individuals protected by COVID-19 shots.
Vaccinating patients in their homes “doesn’t require a lot of technology, but it does require a lot of time” and the staffing expense becomes part of the challenge, Ms. Amer noted.
For each of the two days that Central Ohio Primary Care provides the Pfizer vaccine to homebound patients, the practice needs to pay seven nurses to administer the vaccine, Ms. Amer explained.
There have also been reports of organizations that administer the vaccines – which are free for patients because the federal government is paying for them – not being paid enough by Medicare to cover staff time and efforts to vaccinate patients in their homes, Kaiser Health News reported. According to the Centers for Medicare & Medicaid Services, they pay $40 for the administration of a single-dose COVID-19 vaccine and, for COVID-19 vaccines requiring multiple doses, Medicare pays approximately $40 for each dose in the series. These rates were implemented after March 15. Before that date, the rates were even lower, with the Medicare reimbursement rates for initial doses of COVID-19 vaccines being $16.94 and final doses being $28.39.
William Dombi, president of the National Association for Home Care & Hospice, told Kaiser Health News that the actual cost of these homebound visits are closer to $150 or $160.
“The reimbursement for the injection is pretty minimal,” Mr. Feorene said. “So unless you’re a larger organization and able to have staff to deploy some of your smaller practices, just couldn’t afford to do it.”
Many homebound patients have also been unable to get the lifesaving shots because of logistical roadblocks and many practices not being able to do home visits.
“I think that initially when the [Centers for Disease Control and Prevention] came out with vaccine guidance for medical providers, they offered no guidance for in-home medical providers and we had to go back and ask for that, which they did produce,” Mr. Feorene said. “And we’re grateful for that. But I think just this general understanding that there is a population of folks that are [limited to their home], that they do receive medical care and other care in the home, and that we have to remember that the medical providers who provide care in the home are also primary care providers.”
Furthermore, trying to navigate or find programs delivering vaccines to the homebound can be difficult depending on where a patient lives.
While some programs have been launched on the country or city level – the New York Fire Department launched a pilot program to bring the Johnson & Johnson vaccine to homebound seniors – other programs have been spearheaded by hospital networks like Northwell and Mount Sinai. However, many of these hospital networks only reach out to people who already have a relationship with the hospital.
Ms Amer said identifying homebound patients and reaching out to them can be tough and can contribute to the logistics and time involved in setting patients up for the vaccine.
“Reaching some of these patients is difficult,” Ms. Amer noted. “Sometimes the best way to reach them or get a hold of them is through their caregiver. And so do you have the right phone number? Do you have the right name?”
Overcoming the challenges
With the absence of a national plan targeting homebound patients, many local initiatives were launched to help these individuals get vaccinated. Local fire department paramedics have gone door to door to administer the COVID-19 vaccine in cities like Chicago, New York, and Miami. The suspension of the Johnson & Johnson vaccine resulted in the suspension of in-home vaccinations for some people in New York City. However, the program resumed after the FDA and CDC lifted the pause on April 24. 
Health systems like Mount Sinai vaccinated approximately 530 people through the Mount Sinai Visiting Doctors Program, including patients and their caregivers, according to Peter Gliatto, MD, associate director of the Mount Sinai Visiting Doctors Program.
“In different cities, townships, and jurisdictions, different health departments and different provider groups are approaching [the distribution of the COVID-19 vaccine] slightly differently,” Ms. Amer said. So a lot of the decisions surrounding the distribution of shots are local or dependent on local resourcing.
People who live in rural areas present a unique challenge, but Mr. Feorene said reaching out to local emergency medical services or the local health departments can provide some insight on what their town is doing to vaccinate homebound patients.
“I think understanding what a [public health department] is doing would be the very first place to start,” Mr. Feorene said in an interview.
If a patient is bedridden and is mobile enough to sit in a car, Mr. Feorene also recommends finding out if there are vaccine fairs “within a reasonable driving distance.”
Ms. Amer said continuing this mission of getting homebound patients vaccinated is necessary for public health.
“Even if it’s going to take longer to vaccinate these homebound patients, we still have to make an effort. So much of the country’s vaccine efforts have been focused on getting as many shots in as many arms as quickly as possible. And that is definitely super important,” she said.
Ms. Amer is working with her practice’s primary care physicians to try to identify all of those patients who are functionally debilitated or unable to leave their home to get vaccinated and that Central Ohio Primary Care will vaccinate more homebound patients, she added.
The experts interviewed in this article have no conflicts.
Katie Lennon contributed to this report.
This article was updated 4/29/21.
U.S. Surgeon General Vivek Murthy to Speak at SHM Converge
U.S. Surgeon General, Vice Admiral Vivek H. Murthy, MD, MBA, will be a keynote speaker at SHM Converge, the Society of Hospital Meidicine’s annual conference.
Dr. Murthy will discuss burnout and well-being in health care, key themes of the conference, during a fireside chat with Danielle Scheurer, MD, MSCR, SFHM, president of SHM’s board of directors. The conversation will be held on Thursday, May 6, 2021 from 1:30 to 2:00 p.m. ET.
“It is an honor to welcome Dr. Murthy back to SHM’s annual conference during a time when his leadership is more important than ever,” said Eric E. Howell, MD, MHM, chief executive officer of SHM. “Dr. Murthy is dedicated to the health of the American people and to the well-being of those who care for them. I know his message will resonate with hospitalists who have been on the front lines of the pandemic since day one. They are key to navigating the future of our nation’s health care system.”
Dr. Murthy has devoted himself to improving public health through service, clinical care, research, education, and entrepreneurship. In addition to clinical practice, Dr. Murthy has two decades of experience in improving health in communities around the world and served as the 19th U.S. Surgeon General from 2014 to 2017, prior to being reappointed with an expanded role earlier in 2021. As “America’s Doctor,” the Surgeon General’s role is to provide clear, consistent guidance and healthcare resources for the public, ensuring to reach the nation’s most vulnerable communities.
“As we guide our nation out of the pandemic, hospitalists can look to Dr. Murthy as a leader and innovator who will do what is best for our hospitalist community and the patients they serve,” Dr. Scheurer said. “Dr. Murthy will provide a unique perspective to help hospitalists care for themselves during a time when they have been hyper-focused on caring for others.”
In addition to Dr. Murthy, SHM Converge will feature three keynote speakers who will address pressing topics in hospital medicine:
- Mark Hertling, DBA: Coming Out of Combat: Post-Pandemic Recovery
- Vineet Arora, MD, MAPP, MHM: Hospitalists Healing: Surviving, Salvaging, Sustaining, and Succeeding for a Pandemic World
- Larry Wellikson, MD, MHM: Out of COVID and Into the Light: Hospitalists More Essential Than Ever
SHM Converge is the premier educational experience for hospital medicine professionals. This year’s virtual conference will be held from May 3-7, 2021 and offers 21 educational tracks, more than 250 speakers, advanced learning courses, networking opportunities, a scientific abstract competition, and more. SHM Converge On Demand is also available until 2024, including the opportunity to earn additional continuing medical education credit.
To register for SHM Converge, visit shmconverge.org. If you are a member of the media who would like to obtain a press pass, email media@hospitalmedicine.org.
U.S. Surgeon General, Vice Admiral Vivek H. Murthy, MD, MBA, will be a keynote speaker at SHM Converge, the Society of Hospital Meidicine’s annual conference.
Dr. Murthy will discuss burnout and well-being in health care, key themes of the conference, during a fireside chat with Danielle Scheurer, MD, MSCR, SFHM, president of SHM’s board of directors. The conversation will be held on Thursday, May 6, 2021 from 1:30 to 2:00 p.m. ET.
“It is an honor to welcome Dr. Murthy back to SHM’s annual conference during a time when his leadership is more important than ever,” said Eric E. Howell, MD, MHM, chief executive officer of SHM. “Dr. Murthy is dedicated to the health of the American people and to the well-being of those who care for them. I know his message will resonate with hospitalists who have been on the front lines of the pandemic since day one. They are key to navigating the future of our nation’s health care system.”
Dr. Murthy has devoted himself to improving public health through service, clinical care, research, education, and entrepreneurship. In addition to clinical practice, Dr. Murthy has two decades of experience in improving health in communities around the world and served as the 19th U.S. Surgeon General from 2014 to 2017, prior to being reappointed with an expanded role earlier in 2021. As “America’s Doctor,” the Surgeon General’s role is to provide clear, consistent guidance and healthcare resources for the public, ensuring to reach the nation’s most vulnerable communities.
“As we guide our nation out of the pandemic, hospitalists can look to Dr. Murthy as a leader and innovator who will do what is best for our hospitalist community and the patients they serve,” Dr. Scheurer said. “Dr. Murthy will provide a unique perspective to help hospitalists care for themselves during a time when they have been hyper-focused on caring for others.”
In addition to Dr. Murthy, SHM Converge will feature three keynote speakers who will address pressing topics in hospital medicine:
- Mark Hertling, DBA: Coming Out of Combat: Post-Pandemic Recovery
- Vineet Arora, MD, MAPP, MHM: Hospitalists Healing: Surviving, Salvaging, Sustaining, and Succeeding for a Pandemic World
- Larry Wellikson, MD, MHM: Out of COVID and Into the Light: Hospitalists More Essential Than Ever
SHM Converge is the premier educational experience for hospital medicine professionals. This year’s virtual conference will be held from May 3-7, 2021 and offers 21 educational tracks, more than 250 speakers, advanced learning courses, networking opportunities, a scientific abstract competition, and more. SHM Converge On Demand is also available until 2024, including the opportunity to earn additional continuing medical education credit.
To register for SHM Converge, visit shmconverge.org. If you are a member of the media who would like to obtain a press pass, email media@hospitalmedicine.org.
U.S. Surgeon General, Vice Admiral Vivek H. Murthy, MD, MBA, will be a keynote speaker at SHM Converge, the Society of Hospital Meidicine’s annual conference.
Dr. Murthy will discuss burnout and well-being in health care, key themes of the conference, during a fireside chat with Danielle Scheurer, MD, MSCR, SFHM, president of SHM’s board of directors. The conversation will be held on Thursday, May 6, 2021 from 1:30 to 2:00 p.m. ET.
“It is an honor to welcome Dr. Murthy back to SHM’s annual conference during a time when his leadership is more important than ever,” said Eric E. Howell, MD, MHM, chief executive officer of SHM. “Dr. Murthy is dedicated to the health of the American people and to the well-being of those who care for them. I know his message will resonate with hospitalists who have been on the front lines of the pandemic since day one. They are key to navigating the future of our nation’s health care system.”
Dr. Murthy has devoted himself to improving public health through service, clinical care, research, education, and entrepreneurship. In addition to clinical practice, Dr. Murthy has two decades of experience in improving health in communities around the world and served as the 19th U.S. Surgeon General from 2014 to 2017, prior to being reappointed with an expanded role earlier in 2021. As “America’s Doctor,” the Surgeon General’s role is to provide clear, consistent guidance and healthcare resources for the public, ensuring to reach the nation’s most vulnerable communities.
“As we guide our nation out of the pandemic, hospitalists can look to Dr. Murthy as a leader and innovator who will do what is best for our hospitalist community and the patients they serve,” Dr. Scheurer said. “Dr. Murthy will provide a unique perspective to help hospitalists care for themselves during a time when they have been hyper-focused on caring for others.”
In addition to Dr. Murthy, SHM Converge will feature three keynote speakers who will address pressing topics in hospital medicine:
- Mark Hertling, DBA: Coming Out of Combat: Post-Pandemic Recovery
- Vineet Arora, MD, MAPP, MHM: Hospitalists Healing: Surviving, Salvaging, Sustaining, and Succeeding for a Pandemic World
- Larry Wellikson, MD, MHM: Out of COVID and Into the Light: Hospitalists More Essential Than Ever
SHM Converge is the premier educational experience for hospital medicine professionals. This year’s virtual conference will be held from May 3-7, 2021 and offers 21 educational tracks, more than 250 speakers, advanced learning courses, networking opportunities, a scientific abstract competition, and more. SHM Converge On Demand is also available until 2024, including the opportunity to earn additional continuing medical education credit.
To register for SHM Converge, visit shmconverge.org. If you are a member of the media who would like to obtain a press pass, email media@hospitalmedicine.org.
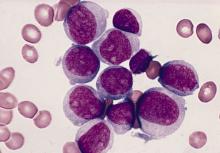
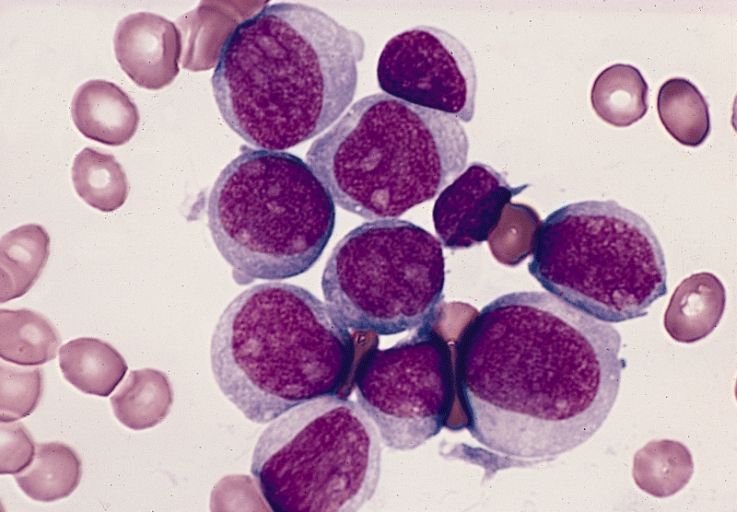
Predicting outcomes in therapy-related AML
Therapy-related acute myeloid leukemia (t-AML) occurs as a complication of chemotherapy and/or radiotherapy for previous cancer or for nonmalignant disorders, with an estimated prevalence of 10%-15% of all AML cases, according to Ram Vasudevan Nampoothiri, MD, and colleagues at the Princess Margaret Cancer Center, University of Toronto.
Dr. Nampoothiri and colleagues performed a retrospective study of 68 patients with t-AML who underwent hematopoietic stem cell transplantation (HSCT) at their institution. They found significant predictors of reduced overall survival, including chromosomal rearrangements, induction regimens, donor type, patient performance status, and the type of graft-versus-host disease (GVHD) prophylaxis the patients received, as reported in Hematology/Oncology and Stem Cell Therapy.
Some populations benefit
Among the 68 patients studied, a total of 59.9% were women; and the median age was 56.5 years. All patients were analyzed for prior malignancy, therapy, time to diagnosis of t-AML, transplant details, relapse-free survival, overall survival, and predictors of outcomes.
At 2 years, the cumulative incidence of relapse, nonrelapse mortality, relapse-free survival, and overall survival were 17.9%, 34.5%, 47.6%, and 49.3%, respectively. Overall, acute and chronic GVHD occurred in 39 (57.4%) and 23 (33.8%) patients, respectively, according to the researchers.
The significant predictors of reduced overall survival were the presence of the 11q23 chromosomal rearrangement (hazard ratio, 3.24), use of induction regimens other than fludarabine, cytarabine, idarubicin, and granulocyte colony-stimulating factor or 7 + 3 (HR, 3.65), use of haploidentical donors (HR, 3.48), an Eastern Cooperative Oncology Group performance status of 2 or higher (HR, 5.83), and use of cyclosporine A–methotrexate as GVHD prophylaxis (HR, 2.41).
The researchers also found that a significant decrease in survival was seen with an increasing number of any of these prognostic factors.
A growing need
The incidence of t-AML is increasing because of longer life expectancy of the general population and also because of the improved survival of patients treated with chemotherapy and/or radiation for prior malignancies, according to the researchers.
They concluded that, even with this increasing prevalence and normally poor prognosis, “patients of t-AML having good-risk karyotypes, good performance status, and having HLA-matched donors have favorable outcomes after allo-HSCT.”
The authors reported that they had no competing financial interests.
Therapy-related acute myeloid leukemia (t-AML) occurs as a complication of chemotherapy and/or radiotherapy for previous cancer or for nonmalignant disorders, with an estimated prevalence of 10%-15% of all AML cases, according to Ram Vasudevan Nampoothiri, MD, and colleagues at the Princess Margaret Cancer Center, University of Toronto.
Dr. Nampoothiri and colleagues performed a retrospective study of 68 patients with t-AML who underwent hematopoietic stem cell transplantation (HSCT) at their institution. They found significant predictors of reduced overall survival, including chromosomal rearrangements, induction regimens, donor type, patient performance status, and the type of graft-versus-host disease (GVHD) prophylaxis the patients received, as reported in Hematology/Oncology and Stem Cell Therapy.
Some populations benefit
Among the 68 patients studied, a total of 59.9% were women; and the median age was 56.5 years. All patients were analyzed for prior malignancy, therapy, time to diagnosis of t-AML, transplant details, relapse-free survival, overall survival, and predictors of outcomes.
At 2 years, the cumulative incidence of relapse, nonrelapse mortality, relapse-free survival, and overall survival were 17.9%, 34.5%, 47.6%, and 49.3%, respectively. Overall, acute and chronic GVHD occurred in 39 (57.4%) and 23 (33.8%) patients, respectively, according to the researchers.
The significant predictors of reduced overall survival were the presence of the 11q23 chromosomal rearrangement (hazard ratio, 3.24), use of induction regimens other than fludarabine, cytarabine, idarubicin, and granulocyte colony-stimulating factor or 7 + 3 (HR, 3.65), use of haploidentical donors (HR, 3.48), an Eastern Cooperative Oncology Group performance status of 2 or higher (HR, 5.83), and use of cyclosporine A–methotrexate as GVHD prophylaxis (HR, 2.41).
The researchers also found that a significant decrease in survival was seen with an increasing number of any of these prognostic factors.
A growing need
The incidence of t-AML is increasing because of longer life expectancy of the general population and also because of the improved survival of patients treated with chemotherapy and/or radiation for prior malignancies, according to the researchers.
They concluded that, even with this increasing prevalence and normally poor prognosis, “patients of t-AML having good-risk karyotypes, good performance status, and having HLA-matched donors have favorable outcomes after allo-HSCT.”
The authors reported that they had no competing financial interests.
Therapy-related acute myeloid leukemia (t-AML) occurs as a complication of chemotherapy and/or radiotherapy for previous cancer or for nonmalignant disorders, with an estimated prevalence of 10%-15% of all AML cases, according to Ram Vasudevan Nampoothiri, MD, and colleagues at the Princess Margaret Cancer Center, University of Toronto.
Dr. Nampoothiri and colleagues performed a retrospective study of 68 patients with t-AML who underwent hematopoietic stem cell transplantation (HSCT) at their institution. They found significant predictors of reduced overall survival, including chromosomal rearrangements, induction regimens, donor type, patient performance status, and the type of graft-versus-host disease (GVHD) prophylaxis the patients received, as reported in Hematology/Oncology and Stem Cell Therapy.
Some populations benefit
Among the 68 patients studied, a total of 59.9% were women; and the median age was 56.5 years. All patients were analyzed for prior malignancy, therapy, time to diagnosis of t-AML, transplant details, relapse-free survival, overall survival, and predictors of outcomes.
At 2 years, the cumulative incidence of relapse, nonrelapse mortality, relapse-free survival, and overall survival were 17.9%, 34.5%, 47.6%, and 49.3%, respectively. Overall, acute and chronic GVHD occurred in 39 (57.4%) and 23 (33.8%) patients, respectively, according to the researchers.
The significant predictors of reduced overall survival were the presence of the 11q23 chromosomal rearrangement (hazard ratio, 3.24), use of induction regimens other than fludarabine, cytarabine, idarubicin, and granulocyte colony-stimulating factor or 7 + 3 (HR, 3.65), use of haploidentical donors (HR, 3.48), an Eastern Cooperative Oncology Group performance status of 2 or higher (HR, 5.83), and use of cyclosporine A–methotrexate as GVHD prophylaxis (HR, 2.41).
The researchers also found that a significant decrease in survival was seen with an increasing number of any of these prognostic factors.
A growing need
The incidence of t-AML is increasing because of longer life expectancy of the general population and also because of the improved survival of patients treated with chemotherapy and/or radiation for prior malignancies, according to the researchers.
They concluded that, even with this increasing prevalence and normally poor prognosis, “patients of t-AML having good-risk karyotypes, good performance status, and having HLA-matched donors have favorable outcomes after allo-HSCT.”
The authors reported that they had no competing financial interests.
FROM HEMATOLOGY/ONCOLOGY AND STEM CELL THERAPY
Hispanic diabetes patients receive less guideline-based care
based on data from more than 7,000 individuals.
Racial and ethnic disparities in diabetes care remain a pervasive health problem, and minorities including non-Hispanic Blacks and Hispanics experience higher rates of complications, including retinopathy and neuropathy, compared with other groups, Felippe Ottoni Marcondes, MD, of Massachusetts General Hospital, Boston, and colleagues noted in a poster presented at the annual meeting of the Society for General Internal Medicine.
Data from previous studies have shown that diabetes patients who receive guideline-directed preventive care soon after diagnosis can reduce their risk of complications, they said.
To identify disparities in the provision of guideline-directed preventive care, the researchers analyzed data from 7,341 individuals who participated in the National Health Interview Survey from 2011 to 2017. They reviewed associations between race/ethnicity and visits to an eye specialist, a foot specialist, and checks of blood pressure and cholesterol in the past year among individuals diagnosed with diabetes within the past 5 years.
Overall, Hispanics had significantly lower rates of insurance coverage (75.9%), compared with non-Hispanic Whites (93.2%) and non-Hispanic Blacks (88.1%; P < .001).
Hispanics also were significantly less likely than Whites to have had a prior year eye exam (odds ratio, 0.80) and blood pressure check (OR, 0.45), after controlling for variables including age, sex, socioeconomic status, health insurance, general health status, U.S. region, marital status, body mass index, and various comorbidities.
Although insurance coverage mediated 42.8% of the total effect of race/ethnicity on annual eye specialist visits for Hispanics as compared with Whites, there was no significant effect for Blacks, compared with Whites.
COVID concerns impact diabetes disparities
“As the diabetes epidemic continues in the U.S., it is important to bring to the front of the diabetes care conversation racial/ethnic disparities that persisted or have been only partially addressed,” Dr. Marcondes said in an interview. “It is also important to emphasize that patients with diabetes are at higher risk for COVID-19 hospitalizations, complications, and death, and COVID-19 has disproportionately affected racial/ethnic minorities, so racial/ethnic minorities with diabetes have compounded risk of complications not only from diabetes but also from COVID-19.
“Importantly, our study highlights disparities in health care that are likely the product of systemic inequalities in access to care and insurance coverage at a moment when conversations about the race/racism and their health impact are fresh in the minds of public and health policy officials and the general public,” he emphasized.
“Unfortunately, I cannot say that I am surprised by our findings,” Dr. Marcondes said. “We expected to see some differences in the receipt of care for racial/ethnic minorities compared to white individuals for those recently diagnosed with diabetes, and that is exactly what our findings show.”
However, “what was perhaps intriguing is that disparities in the receipt of guideline-directed care were greater for Hispanic compared to White individuals than for Black compared to White individuals,” said Dr. Marcondes. “The causes of these differences are many. Hispanic individuals are less likely than White and Black persons to have insurance coverage.” Other unmeasured factors include language barriers that Hispanic individuals may face, as well as the bias and discrimination experienced by Hispanic and Black individuals alike.
Focus on equitable early intervention
“There is plenty of evidence in the medical literature that Black and Hispanic individuals with diabetes, as well as other minorities, have higher risk of complications of diabetes such as retinopathy, nephropathy, as well as cardiovascular risk factors such as high blood pressure and cholesterol,” Dr. Marcondes said. “Yet, complications in the time that immediately follows the diagnosis of diabetes are likely to be low.”
To reduce the risk of complications in the future, “physicians and health providers need to focus on providing equitable, guideline-directed treatment for their minority patients recently diagnosed with diabetes,” Dr. Marcondes emphasized. “Intervening early in the disease course will hopefully lead to a decrease in the rate of complications for racial/ethnic minorities. Clinicians, especially primary care physicians and providers, need to be aware that they are often the first encounter of many patients with the health care system. Effective communication and unbiased language on the part of clinicians will lead to stronger patient-physician relationships that foster opportunity to discuss disease prevention.
“Additional research is needed to evaluate the attitudes and biases of primary care providers and access the impact of patient navigation resources when treating minority patients with diabetes,” he concluded.
Digging Deeper into Disparities
“In diabetes, there are known racial and ethnic disparities such that minorities receive suboptimal screening and treatment, and have worse outcomes,” said Scott J. Pilla, MD, of The Johns Hopkins University School of Medicine, Baltimore, in an interview.
“This study examines disparities in diabetes preventive measures in the U.S. using a national survey (NHIS) over the past decade. They took the important step of stratifying their analyses by health insurance and socioeconomic status which, in addition to race, may have a large impact,” said Dr. Pilla. However, “One critique of the poster is that it is unclear whether the researchers weighted their analyses to account for the nationally representative sampling of the NHIS survey,” he noted.
Dr. Pilla said the finding that Hispanic patients had fewer diabetes preventive measures lines up with previous research in this area.
“I was surprised that the disparities did not extend to black patients, who have been found to also receive suboptimal care compared to white patients in other studies,” he noted.
The message for clinical practice: “Minorities with diabetes are at a higher risk of adverse diabetes outcomes and may need extra support and resources to achieve their evidence-based diabetes prevention,” Dr. Pilla said.
“More research is needed to understand the root cause of racial and ethnic disparities in diabetes management to tease apart possible contributors including health insurance coverage, socioeconomic factors, cultural and community factors, and systemic racism. This will help inform targeted approaches to reducing disparities in diabetes care,” he emphasized.
The researchers had no relevant financial conflicts to disclose. Dr. Pilla had no financial conflicts to disclose.
based on data from more than 7,000 individuals.
Racial and ethnic disparities in diabetes care remain a pervasive health problem, and minorities including non-Hispanic Blacks and Hispanics experience higher rates of complications, including retinopathy and neuropathy, compared with other groups, Felippe Ottoni Marcondes, MD, of Massachusetts General Hospital, Boston, and colleagues noted in a poster presented at the annual meeting of the Society for General Internal Medicine.
Data from previous studies have shown that diabetes patients who receive guideline-directed preventive care soon after diagnosis can reduce their risk of complications, they said.
To identify disparities in the provision of guideline-directed preventive care, the researchers analyzed data from 7,341 individuals who participated in the National Health Interview Survey from 2011 to 2017. They reviewed associations between race/ethnicity and visits to an eye specialist, a foot specialist, and checks of blood pressure and cholesterol in the past year among individuals diagnosed with diabetes within the past 5 years.
Overall, Hispanics had significantly lower rates of insurance coverage (75.9%), compared with non-Hispanic Whites (93.2%) and non-Hispanic Blacks (88.1%; P < .001).
Hispanics also were significantly less likely than Whites to have had a prior year eye exam (odds ratio, 0.80) and blood pressure check (OR, 0.45), after controlling for variables including age, sex, socioeconomic status, health insurance, general health status, U.S. region, marital status, body mass index, and various comorbidities.
Although insurance coverage mediated 42.8% of the total effect of race/ethnicity on annual eye specialist visits for Hispanics as compared with Whites, there was no significant effect for Blacks, compared with Whites.
COVID concerns impact diabetes disparities
“As the diabetes epidemic continues in the U.S., it is important to bring to the front of the diabetes care conversation racial/ethnic disparities that persisted or have been only partially addressed,” Dr. Marcondes said in an interview. “It is also important to emphasize that patients with diabetes are at higher risk for COVID-19 hospitalizations, complications, and death, and COVID-19 has disproportionately affected racial/ethnic minorities, so racial/ethnic minorities with diabetes have compounded risk of complications not only from diabetes but also from COVID-19.
“Importantly, our study highlights disparities in health care that are likely the product of systemic inequalities in access to care and insurance coverage at a moment when conversations about the race/racism and their health impact are fresh in the minds of public and health policy officials and the general public,” he emphasized.
“Unfortunately, I cannot say that I am surprised by our findings,” Dr. Marcondes said. “We expected to see some differences in the receipt of care for racial/ethnic minorities compared to white individuals for those recently diagnosed with diabetes, and that is exactly what our findings show.”
However, “what was perhaps intriguing is that disparities in the receipt of guideline-directed care were greater for Hispanic compared to White individuals than for Black compared to White individuals,” said Dr. Marcondes. “The causes of these differences are many. Hispanic individuals are less likely than White and Black persons to have insurance coverage.” Other unmeasured factors include language barriers that Hispanic individuals may face, as well as the bias and discrimination experienced by Hispanic and Black individuals alike.
Focus on equitable early intervention
“There is plenty of evidence in the medical literature that Black and Hispanic individuals with diabetes, as well as other minorities, have higher risk of complications of diabetes such as retinopathy, nephropathy, as well as cardiovascular risk factors such as high blood pressure and cholesterol,” Dr. Marcondes said. “Yet, complications in the time that immediately follows the diagnosis of diabetes are likely to be low.”
To reduce the risk of complications in the future, “physicians and health providers need to focus on providing equitable, guideline-directed treatment for their minority patients recently diagnosed with diabetes,” Dr. Marcondes emphasized. “Intervening early in the disease course will hopefully lead to a decrease in the rate of complications for racial/ethnic minorities. Clinicians, especially primary care physicians and providers, need to be aware that they are often the first encounter of many patients with the health care system. Effective communication and unbiased language on the part of clinicians will lead to stronger patient-physician relationships that foster opportunity to discuss disease prevention.
“Additional research is needed to evaluate the attitudes and biases of primary care providers and access the impact of patient navigation resources when treating minority patients with diabetes,” he concluded.
Digging Deeper into Disparities
“In diabetes, there are known racial and ethnic disparities such that minorities receive suboptimal screening and treatment, and have worse outcomes,” said Scott J. Pilla, MD, of The Johns Hopkins University School of Medicine, Baltimore, in an interview.
“This study examines disparities in diabetes preventive measures in the U.S. using a national survey (NHIS) over the past decade. They took the important step of stratifying their analyses by health insurance and socioeconomic status which, in addition to race, may have a large impact,” said Dr. Pilla. However, “One critique of the poster is that it is unclear whether the researchers weighted their analyses to account for the nationally representative sampling of the NHIS survey,” he noted.
Dr. Pilla said the finding that Hispanic patients had fewer diabetes preventive measures lines up with previous research in this area.
“I was surprised that the disparities did not extend to black patients, who have been found to also receive suboptimal care compared to white patients in other studies,” he noted.
The message for clinical practice: “Minorities with diabetes are at a higher risk of adverse diabetes outcomes and may need extra support and resources to achieve their evidence-based diabetes prevention,” Dr. Pilla said.
“More research is needed to understand the root cause of racial and ethnic disparities in diabetes management to tease apart possible contributors including health insurance coverage, socioeconomic factors, cultural and community factors, and systemic racism. This will help inform targeted approaches to reducing disparities in diabetes care,” he emphasized.
The researchers had no relevant financial conflicts to disclose. Dr. Pilla had no financial conflicts to disclose.
based on data from more than 7,000 individuals.
Racial and ethnic disparities in diabetes care remain a pervasive health problem, and minorities including non-Hispanic Blacks and Hispanics experience higher rates of complications, including retinopathy and neuropathy, compared with other groups, Felippe Ottoni Marcondes, MD, of Massachusetts General Hospital, Boston, and colleagues noted in a poster presented at the annual meeting of the Society for General Internal Medicine.
Data from previous studies have shown that diabetes patients who receive guideline-directed preventive care soon after diagnosis can reduce their risk of complications, they said.
To identify disparities in the provision of guideline-directed preventive care, the researchers analyzed data from 7,341 individuals who participated in the National Health Interview Survey from 2011 to 2017. They reviewed associations between race/ethnicity and visits to an eye specialist, a foot specialist, and checks of blood pressure and cholesterol in the past year among individuals diagnosed with diabetes within the past 5 years.
Overall, Hispanics had significantly lower rates of insurance coverage (75.9%), compared with non-Hispanic Whites (93.2%) and non-Hispanic Blacks (88.1%; P < .001).
Hispanics also were significantly less likely than Whites to have had a prior year eye exam (odds ratio, 0.80) and blood pressure check (OR, 0.45), after controlling for variables including age, sex, socioeconomic status, health insurance, general health status, U.S. region, marital status, body mass index, and various comorbidities.
Although insurance coverage mediated 42.8% of the total effect of race/ethnicity on annual eye specialist visits for Hispanics as compared with Whites, there was no significant effect for Blacks, compared with Whites.
COVID concerns impact diabetes disparities
“As the diabetes epidemic continues in the U.S., it is important to bring to the front of the diabetes care conversation racial/ethnic disparities that persisted or have been only partially addressed,” Dr. Marcondes said in an interview. “It is also important to emphasize that patients with diabetes are at higher risk for COVID-19 hospitalizations, complications, and death, and COVID-19 has disproportionately affected racial/ethnic minorities, so racial/ethnic minorities with diabetes have compounded risk of complications not only from diabetes but also from COVID-19.
“Importantly, our study highlights disparities in health care that are likely the product of systemic inequalities in access to care and insurance coverage at a moment when conversations about the race/racism and their health impact are fresh in the minds of public and health policy officials and the general public,” he emphasized.
“Unfortunately, I cannot say that I am surprised by our findings,” Dr. Marcondes said. “We expected to see some differences in the receipt of care for racial/ethnic minorities compared to white individuals for those recently diagnosed with diabetes, and that is exactly what our findings show.”
However, “what was perhaps intriguing is that disparities in the receipt of guideline-directed care were greater for Hispanic compared to White individuals than for Black compared to White individuals,” said Dr. Marcondes. “The causes of these differences are many. Hispanic individuals are less likely than White and Black persons to have insurance coverage.” Other unmeasured factors include language barriers that Hispanic individuals may face, as well as the bias and discrimination experienced by Hispanic and Black individuals alike.
Focus on equitable early intervention
“There is plenty of evidence in the medical literature that Black and Hispanic individuals with diabetes, as well as other minorities, have higher risk of complications of diabetes such as retinopathy, nephropathy, as well as cardiovascular risk factors such as high blood pressure and cholesterol,” Dr. Marcondes said. “Yet, complications in the time that immediately follows the diagnosis of diabetes are likely to be low.”
To reduce the risk of complications in the future, “physicians and health providers need to focus on providing equitable, guideline-directed treatment for their minority patients recently diagnosed with diabetes,” Dr. Marcondes emphasized. “Intervening early in the disease course will hopefully lead to a decrease in the rate of complications for racial/ethnic minorities. Clinicians, especially primary care physicians and providers, need to be aware that they are often the first encounter of many patients with the health care system. Effective communication and unbiased language on the part of clinicians will lead to stronger patient-physician relationships that foster opportunity to discuss disease prevention.
“Additional research is needed to evaluate the attitudes and biases of primary care providers and access the impact of patient navigation resources when treating minority patients with diabetes,” he concluded.
Digging Deeper into Disparities
“In diabetes, there are known racial and ethnic disparities such that minorities receive suboptimal screening and treatment, and have worse outcomes,” said Scott J. Pilla, MD, of The Johns Hopkins University School of Medicine, Baltimore, in an interview.
“This study examines disparities in diabetes preventive measures in the U.S. using a national survey (NHIS) over the past decade. They took the important step of stratifying their analyses by health insurance and socioeconomic status which, in addition to race, may have a large impact,” said Dr. Pilla. However, “One critique of the poster is that it is unclear whether the researchers weighted their analyses to account for the nationally representative sampling of the NHIS survey,” he noted.
Dr. Pilla said the finding that Hispanic patients had fewer diabetes preventive measures lines up with previous research in this area.
“I was surprised that the disparities did not extend to black patients, who have been found to also receive suboptimal care compared to white patients in other studies,” he noted.
The message for clinical practice: “Minorities with diabetes are at a higher risk of adverse diabetes outcomes and may need extra support and resources to achieve their evidence-based diabetes prevention,” Dr. Pilla said.
“More research is needed to understand the root cause of racial and ethnic disparities in diabetes management to tease apart possible contributors including health insurance coverage, socioeconomic factors, cultural and community factors, and systemic racism. This will help inform targeted approaches to reducing disparities in diabetes care,” he emphasized.
The researchers had no relevant financial conflicts to disclose. Dr. Pilla had no financial conflicts to disclose.
FROM SGIM 2021
COVID plus MI confers poor prognosis; 1 in 3 die in hospital
COVID-19 patients with ST-segment elevation MI (STEMI) represent a population with unique demographic and clinical features resulting in a high risk for mortality, according to initial findings from the North American Cardiovascular COVID-19 Myocardial Infarction (NACMI) Registry.

“This is the largest registry of COVID-positive patients presenting with STEMI [and] the results clearly illustrate the challenges and uniqueness of this patient population that deserves prompt and special attention,” study cochair Timothy Henry, MD, president-elect of the Society for Cardiovascular Angiography & Interventions, said in a news release.
The NACMI registry is a collaborative effort between the SCAI, the American College of Cardiology Interventional Council, and the Canadian Association of Interventional Cardiology.
“The rapid development of this ongoing, critically important prospective registry reflects the strong and unique collaboration of all three societies. It was gratifying to be part of this process and hopefully the results will improve the care of our patients and stimulate further research,” Dr. Henry said in the news release.
The registry has enrolled 1,185 patients presenting with STEMI at 64 sites across the United States and Canada. Participants include 230 COVID-positive STEMI patients; 495 STEMI patients suspected but ultimately confirmed not to have COVID-19; and 460 age-and sex-matched control STEMI patients treated prior to the pandemic who are part of the Midwest STEMI Consortium.
The initial findings from the registry were published online in the Journal of the American College of Cardiology.
Atypical symptoms may explain high death rate
The primary outcome – a composite of in-hospital death, stroke, recurrent MI, or repeat unplanned revascularization – occurred in 36% of COVID-positive patients, compared with 13% of COVID-negative patients and 5% of control patients (P < .001 relative to controls).
This difference was driven largely by a “very high” in-hospital death rate in COVID-positive patients, lead author Santiago Garcia, MD, Minneapolis Heart Institute Foundation, said in an interview.
The in-hospital death rate was 33% in COVID-positive patients, compared with 11% in COVID-negative patients and 4% in controls. Stroke also occurred more often in COVID-positive patients at 3% versus 2% in COVID-negative and 0% in controls.
These initial findings suggest that the combination of STEMI and COVID-19 infection “confers a poor prognosis, with one in three patients succumbing to the disease, even among patients selected for invasive angiography (28% mortality),” the investigators wrote.
The data also show that STEMI in COVID-positive patients disproportionately affects ethnic minorities (23% Hispanic and 24% Black) with diabetes, which was present in 46% of COVID-positive patients.
COVID-positive patients with STEMI are more likely to present with atypical symptoms such as dyspnea (54%), pulmonary infiltrates on chest x-ray (46%), and high-risk conditions such as cardiogenic shock (18%), “which may explain the high fatality rate,” Dr. Garcia said.
Despite these high-risk features, COVID-positive patients are less apt to undergo invasive angiography when compared with COVID-negative and control STEMI patients (78% vs. 96% vs. 100%).
The majority of patients (71%) who did under angiography received primary percutaneous coronary intervention (PPCI) with very small treatment delays (at 15 minutes) during the pandemic.
Another notable finding is that “many patients (23%) have ‘no culprit’ vessel and may represent different etiologies of ST-segment elevation including microemboli, myocarditis, Takotsubo cardiomyopathy,” Dr. Garcia said in an interview.
“In line with current guidelines, patients with suspected STEMI should be managed with PPCI, without delay while the safety of health care providers is ensured,” Ran Kornowski, MD, and Katia Orvin, MD, both with Rabin Medical Center, Petah Tikva, Israel, and Tel Aviv University, wrote in a linked editorial.
“In this case, PPCI should be performed routinely, even if the patient is presumed to have COVID-19, because PPCI should not be postponed. Confirmation of SARS-CoV-2 infection should not delay urgent decision management concerning reperfusion strategy,” they advised.
Looking ahead, Garcia said plans for the registry include determining predictors of in-hospital mortality and studying demographic and treatment trends as the pandemic continues with more virulent strains of the virus.
Various subgroup analyses are also planned as well as an independent angiographic and electrocardiographic core lab analysis. A comparative analysis of data from the US and Canada is also planned.
This work was supported by an ACC Accreditation Grant, Saskatchewan Health Research Foundation, and grants from Medtronic and Abbott Vascular to SCAI. Dr. Garcia has received institutional research grants from Edwards Lifesciences, BSCI, Medtronic, and Abbott Vascular; has served as a consultant for Medtronic and BSCI; and has served as a proctor for Edwards Lifesciences. Dr. Kornowski and Dr. Orvin disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID-19 patients with ST-segment elevation MI (STEMI) represent a population with unique demographic and clinical features resulting in a high risk for mortality, according to initial findings from the North American Cardiovascular COVID-19 Myocardial Infarction (NACMI) Registry.

“This is the largest registry of COVID-positive patients presenting with STEMI [and] the results clearly illustrate the challenges and uniqueness of this patient population that deserves prompt and special attention,” study cochair Timothy Henry, MD, president-elect of the Society for Cardiovascular Angiography & Interventions, said in a news release.
The NACMI registry is a collaborative effort between the SCAI, the American College of Cardiology Interventional Council, and the Canadian Association of Interventional Cardiology.
“The rapid development of this ongoing, critically important prospective registry reflects the strong and unique collaboration of all three societies. It was gratifying to be part of this process and hopefully the results will improve the care of our patients and stimulate further research,” Dr. Henry said in the news release.
The registry has enrolled 1,185 patients presenting with STEMI at 64 sites across the United States and Canada. Participants include 230 COVID-positive STEMI patients; 495 STEMI patients suspected but ultimately confirmed not to have COVID-19; and 460 age-and sex-matched control STEMI patients treated prior to the pandemic who are part of the Midwest STEMI Consortium.
The initial findings from the registry were published online in the Journal of the American College of Cardiology.
Atypical symptoms may explain high death rate
The primary outcome – a composite of in-hospital death, stroke, recurrent MI, or repeat unplanned revascularization – occurred in 36% of COVID-positive patients, compared with 13% of COVID-negative patients and 5% of control patients (P < .001 relative to controls).
This difference was driven largely by a “very high” in-hospital death rate in COVID-positive patients, lead author Santiago Garcia, MD, Minneapolis Heart Institute Foundation, said in an interview.
The in-hospital death rate was 33% in COVID-positive patients, compared with 11% in COVID-negative patients and 4% in controls. Stroke also occurred more often in COVID-positive patients at 3% versus 2% in COVID-negative and 0% in controls.
These initial findings suggest that the combination of STEMI and COVID-19 infection “confers a poor prognosis, with one in three patients succumbing to the disease, even among patients selected for invasive angiography (28% mortality),” the investigators wrote.
The data also show that STEMI in COVID-positive patients disproportionately affects ethnic minorities (23% Hispanic and 24% Black) with diabetes, which was present in 46% of COVID-positive patients.
COVID-positive patients with STEMI are more likely to present with atypical symptoms such as dyspnea (54%), pulmonary infiltrates on chest x-ray (46%), and high-risk conditions such as cardiogenic shock (18%), “which may explain the high fatality rate,” Dr. Garcia said.
Despite these high-risk features, COVID-positive patients are less apt to undergo invasive angiography when compared with COVID-negative and control STEMI patients (78% vs. 96% vs. 100%).
The majority of patients (71%) who did under angiography received primary percutaneous coronary intervention (PPCI) with very small treatment delays (at 15 minutes) during the pandemic.
Another notable finding is that “many patients (23%) have ‘no culprit’ vessel and may represent different etiologies of ST-segment elevation including microemboli, myocarditis, Takotsubo cardiomyopathy,” Dr. Garcia said in an interview.
“In line with current guidelines, patients with suspected STEMI should be managed with PPCI, without delay while the safety of health care providers is ensured,” Ran Kornowski, MD, and Katia Orvin, MD, both with Rabin Medical Center, Petah Tikva, Israel, and Tel Aviv University, wrote in a linked editorial.
“In this case, PPCI should be performed routinely, even if the patient is presumed to have COVID-19, because PPCI should not be postponed. Confirmation of SARS-CoV-2 infection should not delay urgent decision management concerning reperfusion strategy,” they advised.
Looking ahead, Garcia said plans for the registry include determining predictors of in-hospital mortality and studying demographic and treatment trends as the pandemic continues with more virulent strains of the virus.
Various subgroup analyses are also planned as well as an independent angiographic and electrocardiographic core lab analysis. A comparative analysis of data from the US and Canada is also planned.
This work was supported by an ACC Accreditation Grant, Saskatchewan Health Research Foundation, and grants from Medtronic and Abbott Vascular to SCAI. Dr. Garcia has received institutional research grants from Edwards Lifesciences, BSCI, Medtronic, and Abbott Vascular; has served as a consultant for Medtronic and BSCI; and has served as a proctor for Edwards Lifesciences. Dr. Kornowski and Dr. Orvin disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID-19 patients with ST-segment elevation MI (STEMI) represent a population with unique demographic and clinical features resulting in a high risk for mortality, according to initial findings from the North American Cardiovascular COVID-19 Myocardial Infarction (NACMI) Registry.

“This is the largest registry of COVID-positive patients presenting with STEMI [and] the results clearly illustrate the challenges and uniqueness of this patient population that deserves prompt and special attention,” study cochair Timothy Henry, MD, president-elect of the Society for Cardiovascular Angiography & Interventions, said in a news release.
The NACMI registry is a collaborative effort between the SCAI, the American College of Cardiology Interventional Council, and the Canadian Association of Interventional Cardiology.
“The rapid development of this ongoing, critically important prospective registry reflects the strong and unique collaboration of all three societies. It was gratifying to be part of this process and hopefully the results will improve the care of our patients and stimulate further research,” Dr. Henry said in the news release.
The registry has enrolled 1,185 patients presenting with STEMI at 64 sites across the United States and Canada. Participants include 230 COVID-positive STEMI patients; 495 STEMI patients suspected but ultimately confirmed not to have COVID-19; and 460 age-and sex-matched control STEMI patients treated prior to the pandemic who are part of the Midwest STEMI Consortium.
The initial findings from the registry were published online in the Journal of the American College of Cardiology.
Atypical symptoms may explain high death rate
The primary outcome – a composite of in-hospital death, stroke, recurrent MI, or repeat unplanned revascularization – occurred in 36% of COVID-positive patients, compared with 13% of COVID-negative patients and 5% of control patients (P < .001 relative to controls).
This difference was driven largely by a “very high” in-hospital death rate in COVID-positive patients, lead author Santiago Garcia, MD, Minneapolis Heart Institute Foundation, said in an interview.
The in-hospital death rate was 33% in COVID-positive patients, compared with 11% in COVID-negative patients and 4% in controls. Stroke also occurred more often in COVID-positive patients at 3% versus 2% in COVID-negative and 0% in controls.
These initial findings suggest that the combination of STEMI and COVID-19 infection “confers a poor prognosis, with one in three patients succumbing to the disease, even among patients selected for invasive angiography (28% mortality),” the investigators wrote.
The data also show that STEMI in COVID-positive patients disproportionately affects ethnic minorities (23% Hispanic and 24% Black) with diabetes, which was present in 46% of COVID-positive patients.
COVID-positive patients with STEMI are more likely to present with atypical symptoms such as dyspnea (54%), pulmonary infiltrates on chest x-ray (46%), and high-risk conditions such as cardiogenic shock (18%), “which may explain the high fatality rate,” Dr. Garcia said.
Despite these high-risk features, COVID-positive patients are less apt to undergo invasive angiography when compared with COVID-negative and control STEMI patients (78% vs. 96% vs. 100%).
The majority of patients (71%) who did under angiography received primary percutaneous coronary intervention (PPCI) with very small treatment delays (at 15 minutes) during the pandemic.
Another notable finding is that “many patients (23%) have ‘no culprit’ vessel and may represent different etiologies of ST-segment elevation including microemboli, myocarditis, Takotsubo cardiomyopathy,” Dr. Garcia said in an interview.
“In line with current guidelines, patients with suspected STEMI should be managed with PPCI, without delay while the safety of health care providers is ensured,” Ran Kornowski, MD, and Katia Orvin, MD, both with Rabin Medical Center, Petah Tikva, Israel, and Tel Aviv University, wrote in a linked editorial.
“In this case, PPCI should be performed routinely, even if the patient is presumed to have COVID-19, because PPCI should not be postponed. Confirmation of SARS-CoV-2 infection should not delay urgent decision management concerning reperfusion strategy,” they advised.
Looking ahead, Garcia said plans for the registry include determining predictors of in-hospital mortality and studying demographic and treatment trends as the pandemic continues with more virulent strains of the virus.
Various subgroup analyses are also planned as well as an independent angiographic and electrocardiographic core lab analysis. A comparative analysis of data from the US and Canada is also planned.
This work was supported by an ACC Accreditation Grant, Saskatchewan Health Research Foundation, and grants from Medtronic and Abbott Vascular to SCAI. Dr. Garcia has received institutional research grants from Edwards Lifesciences, BSCI, Medtronic, and Abbott Vascular; has served as a consultant for Medtronic and BSCI; and has served as a proctor for Edwards Lifesciences. Dr. Kornowski and Dr. Orvin disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pros and cons of proposed recommendation for prediabetes and T2D screening
. If accepted as written, the new recommendation will be to “screen all asymptomatic adults ages 35 to 70 years who are overweight or obese.” Upon diagnosis of prediabetes, the recommendation is to offer or refer patients to preventive interventions.
This new recommendation would replace the one from 2015, which recommended screening adults aged 40-70 who are overweight or obese, lowering the age at which screening begins by 5 years. It would also replace the recommendation of referral to intensive behavioral counseling to promote a healthy diet and exercise.1
The American Diabetes Association (ADA) identifies A1c, fasting plasma glucose, or oral glucose tolerance tests as appropriate tests for the diagnosis of prediabetes and type 2 DM, and the new draft recommendation does not provide a preference for method of screening.2
The USPSTF’s draft recommendation could expand screening with the hope of identifying patients with prediabetes, or those with diabetes who are asymptomatic, with the intent of beginning treatment before there are serious complications.
Unknown diabetes or prediabetes diagnosis common
It has been estimated by the Centers for Disease Control and Prevention that 12% of U.S. adults had DM as of 2015, though nearly 24% were not aware that they had it. Also, according to the CDC, the prevalence of DM increases with age and is higher in those with less than a high school education. The same report indicates that more than 30% of U.S. adults have prediabetes, and with less than 12% of those individuals are aware of it.3 A possible explanation for a patient’s being unaware of a diagnosis could be that it has been documented in a chart but the patient does not know such information is in his or her health record. According to the evidence provided for the updated recommendation, earlier diagnosis may have an important benefit in preventing serious complications.
A modeling study compared simulated screening strategies and found that the most optimal screening strategy from a cost-effectiveness perspective begins between the ages of 30 and 45, with rescreening every 3-5 years. Further models have led researchers to conclude that early diagnosis can lead to decreased cardiovascular events as well as an opportunity for multifactorial treatment.1 For this reason, it makes sense to expand the ages of screening for obese and overweight individuals.
Treatment recommendations are more flexible
The change in treatment recommendations for a new diagnosis of prediabetes is potentially more useful. It may not be feasible or reasonable for physicians to always provide or refer their patients for intensive behavior interventions. The updated recommendation would allow for the inclusion of not only behavioral counseling and health education, but also potential medication options that are currently available but not approved, or that may be available in the future. The evidence review seemed to be mixed in outcome in this area, so the increased flexibility will likely allow for future opportunities.
Screening criteria may be too narrow
This recommendation, does not, however, provide any guidance on screening of individuals who have other risk factors besides a body mass index consistent with overweight or obesity. It seems that this may be a missed opportunity.
The draft statement clearly indicates that there are other factors associated with increased risk of developing DM, but does not consider these factors in determining which patients should be screened. Both the ADA and the American Association of Clinical Endocrinology (AACE) have recommendations for universal screening for all adults 45 and older, acknowledging that incidence of DM increases with age. The ADA also recommends screening individuals who are overweight or obese and have an additional risk factor regardless of age. The AACE recommends screening all individuals for risk factors regardless of age.
The current and draft recommendations by the USPSTF do not address other risk factors and indicate only that further research is needed to understand the risk associated with DM and the natural history of pre-DM and who may progress to DM or revert to normoglycemia. Without comment on other risk factors or universal screening with age, the USPSTF recommendation potentially would not be sensitive enough to capture all those who may meet criteria for prediabetes or DM.2,4
In addition to not addressing other risk factors and screening for those of normal and underweight BMI, the USPSTF recommendation does not address frequency of screening. The recommendations from both the ADA and the AACE indicate screening at 3-year intervals for those who are eligible – for any reason. The supporting evidence review did not seem to address this aspect, and so it is understandable that there was no comment. However, I feel this will lead physicians to turn to the other guidelines for guidance where there is disagreement in other aspects.
Ultimately, the draft updated recommendation will provide physicians with the opportunity to identify more patients with prediabetes and DM. This will be wonderful in terms of being able to offer treatments and lifestyle interventions to decrease the morbidity patients would face were these conditions not diagnosed. I hope that future recommendations will also address risk factors in addition to BMI as well as frequency of screening for those who remain at increased risk but initially screen negative.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at fpnews@mdedge.com.
References
1. Screening for prediabetes and type 2 diabetes mellitus. U.S. Preventive Services Task Force. 2021 Mar 16.
2. Classification and diagnosis of diabetes: Standards of medical care in diabetes – 2020. American Diabetes Association. Diabetes Care. 2020 Jan. doi: 10.2337/dc20-S002.
3. National Diabetes Statistics Report, 2020. Centers for Disease Control and Prevention.
4. American Association of Clinical Endocrinologists and American College of Endocrinology – clinical practice guidelines for developing a diabetes mellitus comprehensive care plan. Hadelsman Y et al. Endocr Pract. 2015 Apr. 1-87. doi: 10.4158/EP15672.GL.
. If accepted as written, the new recommendation will be to “screen all asymptomatic adults ages 35 to 70 years who are overweight or obese.” Upon diagnosis of prediabetes, the recommendation is to offer or refer patients to preventive interventions.
This new recommendation would replace the one from 2015, which recommended screening adults aged 40-70 who are overweight or obese, lowering the age at which screening begins by 5 years. It would also replace the recommendation of referral to intensive behavioral counseling to promote a healthy diet and exercise.1
The American Diabetes Association (ADA) identifies A1c, fasting plasma glucose, or oral glucose tolerance tests as appropriate tests for the diagnosis of prediabetes and type 2 DM, and the new draft recommendation does not provide a preference for method of screening.2
The USPSTF’s draft recommendation could expand screening with the hope of identifying patients with prediabetes, or those with diabetes who are asymptomatic, with the intent of beginning treatment before there are serious complications.
Unknown diabetes or prediabetes diagnosis common
It has been estimated by the Centers for Disease Control and Prevention that 12% of U.S. adults had DM as of 2015, though nearly 24% were not aware that they had it. Also, according to the CDC, the prevalence of DM increases with age and is higher in those with less than a high school education. The same report indicates that more than 30% of U.S. adults have prediabetes, and with less than 12% of those individuals are aware of it.3 A possible explanation for a patient’s being unaware of a diagnosis could be that it has been documented in a chart but the patient does not know such information is in his or her health record. According to the evidence provided for the updated recommendation, earlier diagnosis may have an important benefit in preventing serious complications.
A modeling study compared simulated screening strategies and found that the most optimal screening strategy from a cost-effectiveness perspective begins between the ages of 30 and 45, with rescreening every 3-5 years. Further models have led researchers to conclude that early diagnosis can lead to decreased cardiovascular events as well as an opportunity for multifactorial treatment.1 For this reason, it makes sense to expand the ages of screening for obese and overweight individuals.
Treatment recommendations are more flexible
The change in treatment recommendations for a new diagnosis of prediabetes is potentially more useful. It may not be feasible or reasonable for physicians to always provide or refer their patients for intensive behavior interventions. The updated recommendation would allow for the inclusion of not only behavioral counseling and health education, but also potential medication options that are currently available but not approved, or that may be available in the future. The evidence review seemed to be mixed in outcome in this area, so the increased flexibility will likely allow for future opportunities.
Screening criteria may be too narrow
This recommendation, does not, however, provide any guidance on screening of individuals who have other risk factors besides a body mass index consistent with overweight or obesity. It seems that this may be a missed opportunity.
The draft statement clearly indicates that there are other factors associated with increased risk of developing DM, but does not consider these factors in determining which patients should be screened. Both the ADA and the American Association of Clinical Endocrinology (AACE) have recommendations for universal screening for all adults 45 and older, acknowledging that incidence of DM increases with age. The ADA also recommends screening individuals who are overweight or obese and have an additional risk factor regardless of age. The AACE recommends screening all individuals for risk factors regardless of age.
The current and draft recommendations by the USPSTF do not address other risk factors and indicate only that further research is needed to understand the risk associated with DM and the natural history of pre-DM and who may progress to DM or revert to normoglycemia. Without comment on other risk factors or universal screening with age, the USPSTF recommendation potentially would not be sensitive enough to capture all those who may meet criteria for prediabetes or DM.2,4
In addition to not addressing other risk factors and screening for those of normal and underweight BMI, the USPSTF recommendation does not address frequency of screening. The recommendations from both the ADA and the AACE indicate screening at 3-year intervals for those who are eligible – for any reason. The supporting evidence review did not seem to address this aspect, and so it is understandable that there was no comment. However, I feel this will lead physicians to turn to the other guidelines for guidance where there is disagreement in other aspects.
Ultimately, the draft updated recommendation will provide physicians with the opportunity to identify more patients with prediabetes and DM. This will be wonderful in terms of being able to offer treatments and lifestyle interventions to decrease the morbidity patients would face were these conditions not diagnosed. I hope that future recommendations will also address risk factors in addition to BMI as well as frequency of screening for those who remain at increased risk but initially screen negative.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at fpnews@mdedge.com.
References
1. Screening for prediabetes and type 2 diabetes mellitus. U.S. Preventive Services Task Force. 2021 Mar 16.
2. Classification and diagnosis of diabetes: Standards of medical care in diabetes – 2020. American Diabetes Association. Diabetes Care. 2020 Jan. doi: 10.2337/dc20-S002.
3. National Diabetes Statistics Report, 2020. Centers for Disease Control and Prevention.
4. American Association of Clinical Endocrinologists and American College of Endocrinology – clinical practice guidelines for developing a diabetes mellitus comprehensive care plan. Hadelsman Y et al. Endocr Pract. 2015 Apr. 1-87. doi: 10.4158/EP15672.GL.
. If accepted as written, the new recommendation will be to “screen all asymptomatic adults ages 35 to 70 years who are overweight or obese.” Upon diagnosis of prediabetes, the recommendation is to offer or refer patients to preventive interventions.
This new recommendation would replace the one from 2015, which recommended screening adults aged 40-70 who are overweight or obese, lowering the age at which screening begins by 5 years. It would also replace the recommendation of referral to intensive behavioral counseling to promote a healthy diet and exercise.1
The American Diabetes Association (ADA) identifies A1c, fasting plasma glucose, or oral glucose tolerance tests as appropriate tests for the diagnosis of prediabetes and type 2 DM, and the new draft recommendation does not provide a preference for method of screening.2
The USPSTF’s draft recommendation could expand screening with the hope of identifying patients with prediabetes, or those with diabetes who are asymptomatic, with the intent of beginning treatment before there are serious complications.
Unknown diabetes or prediabetes diagnosis common
It has been estimated by the Centers for Disease Control and Prevention that 12% of U.S. adults had DM as of 2015, though nearly 24% were not aware that they had it. Also, according to the CDC, the prevalence of DM increases with age and is higher in those with less than a high school education. The same report indicates that more than 30% of U.S. adults have prediabetes, and with less than 12% of those individuals are aware of it.3 A possible explanation for a patient’s being unaware of a diagnosis could be that it has been documented in a chart but the patient does not know such information is in his or her health record. According to the evidence provided for the updated recommendation, earlier diagnosis may have an important benefit in preventing serious complications.
A modeling study compared simulated screening strategies and found that the most optimal screening strategy from a cost-effectiveness perspective begins between the ages of 30 and 45, with rescreening every 3-5 years. Further models have led researchers to conclude that early diagnosis can lead to decreased cardiovascular events as well as an opportunity for multifactorial treatment.1 For this reason, it makes sense to expand the ages of screening for obese and overweight individuals.
Treatment recommendations are more flexible
The change in treatment recommendations for a new diagnosis of prediabetes is potentially more useful. It may not be feasible or reasonable for physicians to always provide or refer their patients for intensive behavior interventions. The updated recommendation would allow for the inclusion of not only behavioral counseling and health education, but also potential medication options that are currently available but not approved, or that may be available in the future. The evidence review seemed to be mixed in outcome in this area, so the increased flexibility will likely allow for future opportunities.
Screening criteria may be too narrow
This recommendation, does not, however, provide any guidance on screening of individuals who have other risk factors besides a body mass index consistent with overweight or obesity. It seems that this may be a missed opportunity.
The draft statement clearly indicates that there are other factors associated with increased risk of developing DM, but does not consider these factors in determining which patients should be screened. Both the ADA and the American Association of Clinical Endocrinology (AACE) have recommendations for universal screening for all adults 45 and older, acknowledging that incidence of DM increases with age. The ADA also recommends screening individuals who are overweight or obese and have an additional risk factor regardless of age. The AACE recommends screening all individuals for risk factors regardless of age.
The current and draft recommendations by the USPSTF do not address other risk factors and indicate only that further research is needed to understand the risk associated with DM and the natural history of pre-DM and who may progress to DM or revert to normoglycemia. Without comment on other risk factors or universal screening with age, the USPSTF recommendation potentially would not be sensitive enough to capture all those who may meet criteria for prediabetes or DM.2,4
In addition to not addressing other risk factors and screening for those of normal and underweight BMI, the USPSTF recommendation does not address frequency of screening. The recommendations from both the ADA and the AACE indicate screening at 3-year intervals for those who are eligible – for any reason. The supporting evidence review did not seem to address this aspect, and so it is understandable that there was no comment. However, I feel this will lead physicians to turn to the other guidelines for guidance where there is disagreement in other aspects.
Ultimately, the draft updated recommendation will provide physicians with the opportunity to identify more patients with prediabetes and DM. This will be wonderful in terms of being able to offer treatments and lifestyle interventions to decrease the morbidity patients would face were these conditions not diagnosed. I hope that future recommendations will also address risk factors in addition to BMI as well as frequency of screening for those who remain at increased risk but initially screen negative.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at fpnews@mdedge.com.
References
1. Screening for prediabetes and type 2 diabetes mellitus. U.S. Preventive Services Task Force. 2021 Mar 16.
2. Classification and diagnosis of diabetes: Standards of medical care in diabetes – 2020. American Diabetes Association. Diabetes Care. 2020 Jan. doi: 10.2337/dc20-S002.
3. National Diabetes Statistics Report, 2020. Centers for Disease Control and Prevention.
4. American Association of Clinical Endocrinologists and American College of Endocrinology – clinical practice guidelines for developing a diabetes mellitus comprehensive care plan. Hadelsman Y et al. Endocr Pract. 2015 Apr. 1-87. doi: 10.4158/EP15672.GL.
Assessing the efficacy and safety of dapagliflozin in patients with HFrEF
Background: Guideline-directed medical therapy (use of beta-blockers, ACE inhibitor/angiotensin receptor blockers, and mineralocorticoid antagonists) provides clear benefits on mortality and morbidity in patients with HFrEF. Dapagliflozin (Farxiga) belongs to a class of sodium-glucose transporter 2 (SGLT2) inhibitors that inhibits reabsorption of sodium and glucose in the kidney and treats type 2 diabetes. This new class of drugs is emerging as an effective tool in the management of HFrEF based on the recent publication of the primary results of the DAPA-HF trial (Study to Evaluate the Effect of Dapagliflozin on the Incidence of Worsening Heart Failure or Cardiovascular Death in Patients with Chronic Heart Failure). It demonstrated substantial benefits in terms of heart failure symptoms, hospitalizations, and mortality when added to triple therapy for patients with chronic HFrEF regardless of the presence of diabetes.
Study design: Randomized, controlled double-blind trials.
Setting: 410 participating institutions in 20 countries.
Synopsis: Men and women aged 18 years and older with HFrEF who had New York Heart Association (NYHA) functional class II or higher, and optimally treated with pharmacologic and device therapy for HF were randomized to receive dapagliflozin or placebo. A total of 4,744 patients, aged 22-94 years were enrolled in the study.
- Dapagliflozin showed a clinically significant benefit on health status (symptoms, physical function, and quality of life). Improved health-related quality of life (as measured by the well-validated Kansas City Cardiomyopathy Questionnaire score) with dapagliflozin in comparison with placebo was sustained for more than 8 months.
- Dapagliflozin reduced the risk of death and worsening heart failure and improved symptoms across the broad spectrum of ages studied in DAPA-HF. There was no significant imbalance in tolerability or safety events between dapagliflozin and placebo, even in elderly individuals.
Bottom line: Follow-up DAPA-HF studies further support the role of SGLT2 inhibitor dapagliflozin in improving mortality, reducing hospitalization, and improving the quality of life in patients with HFrEF and is considered a safe option across all age groups.
Citations: Kosiborod MN et al. Effects of dapagliflozin on symptoms, function, and quality of life in patients with heart failure and reduced ejection fraction: Results from the DAPA-HF trial. Circulation. 2020 Jan 14;141(2):90-9. Martinez FA et al. Efficacy and safety of dapagliflozin in heart failure with reduced ejection fraction according to age. Insights from DAPA-HF. Circulation. 2020 Jan 14;141:100-11.
Dr. Garg is assistant professor in the division of hospital medicine, Loyola University Medical Center, Maywood, Ill.
Background: Guideline-directed medical therapy (use of beta-blockers, ACE inhibitor/angiotensin receptor blockers, and mineralocorticoid antagonists) provides clear benefits on mortality and morbidity in patients with HFrEF. Dapagliflozin (Farxiga) belongs to a class of sodium-glucose transporter 2 (SGLT2) inhibitors that inhibits reabsorption of sodium and glucose in the kidney and treats type 2 diabetes. This new class of drugs is emerging as an effective tool in the management of HFrEF based on the recent publication of the primary results of the DAPA-HF trial (Study to Evaluate the Effect of Dapagliflozin on the Incidence of Worsening Heart Failure or Cardiovascular Death in Patients with Chronic Heart Failure). It demonstrated substantial benefits in terms of heart failure symptoms, hospitalizations, and mortality when added to triple therapy for patients with chronic HFrEF regardless of the presence of diabetes.
Study design: Randomized, controlled double-blind trials.
Setting: 410 participating institutions in 20 countries.
Synopsis: Men and women aged 18 years and older with HFrEF who had New York Heart Association (NYHA) functional class II or higher, and optimally treated with pharmacologic and device therapy for HF were randomized to receive dapagliflozin or placebo. A total of 4,744 patients, aged 22-94 years were enrolled in the study.
- Dapagliflozin showed a clinically significant benefit on health status (symptoms, physical function, and quality of life). Improved health-related quality of life (as measured by the well-validated Kansas City Cardiomyopathy Questionnaire score) with dapagliflozin in comparison with placebo was sustained for more than 8 months.
- Dapagliflozin reduced the risk of death and worsening heart failure and improved symptoms across the broad spectrum of ages studied in DAPA-HF. There was no significant imbalance in tolerability or safety events between dapagliflozin and placebo, even in elderly individuals.
Bottom line: Follow-up DAPA-HF studies further support the role of SGLT2 inhibitor dapagliflozin in improving mortality, reducing hospitalization, and improving the quality of life in patients with HFrEF and is considered a safe option across all age groups.
Citations: Kosiborod MN et al. Effects of dapagliflozin on symptoms, function, and quality of life in patients with heart failure and reduced ejection fraction: Results from the DAPA-HF trial. Circulation. 2020 Jan 14;141(2):90-9. Martinez FA et al. Efficacy and safety of dapagliflozin in heart failure with reduced ejection fraction according to age. Insights from DAPA-HF. Circulation. 2020 Jan 14;141:100-11.
Dr. Garg is assistant professor in the division of hospital medicine, Loyola University Medical Center, Maywood, Ill.
Background: Guideline-directed medical therapy (use of beta-blockers, ACE inhibitor/angiotensin receptor blockers, and mineralocorticoid antagonists) provides clear benefits on mortality and morbidity in patients with HFrEF. Dapagliflozin (Farxiga) belongs to a class of sodium-glucose transporter 2 (SGLT2) inhibitors that inhibits reabsorption of sodium and glucose in the kidney and treats type 2 diabetes. This new class of drugs is emerging as an effective tool in the management of HFrEF based on the recent publication of the primary results of the DAPA-HF trial (Study to Evaluate the Effect of Dapagliflozin on the Incidence of Worsening Heart Failure or Cardiovascular Death in Patients with Chronic Heart Failure). It demonstrated substantial benefits in terms of heart failure symptoms, hospitalizations, and mortality when added to triple therapy for patients with chronic HFrEF regardless of the presence of diabetes.
Study design: Randomized, controlled double-blind trials.
Setting: 410 participating institutions in 20 countries.
Synopsis: Men and women aged 18 years and older with HFrEF who had New York Heart Association (NYHA) functional class II or higher, and optimally treated with pharmacologic and device therapy for HF were randomized to receive dapagliflozin or placebo. A total of 4,744 patients, aged 22-94 years were enrolled in the study.
- Dapagliflozin showed a clinically significant benefit on health status (symptoms, physical function, and quality of life). Improved health-related quality of life (as measured by the well-validated Kansas City Cardiomyopathy Questionnaire score) with dapagliflozin in comparison with placebo was sustained for more than 8 months.
- Dapagliflozin reduced the risk of death and worsening heart failure and improved symptoms across the broad spectrum of ages studied in DAPA-HF. There was no significant imbalance in tolerability or safety events between dapagliflozin and placebo, even in elderly individuals.
Bottom line: Follow-up DAPA-HF studies further support the role of SGLT2 inhibitor dapagliflozin in improving mortality, reducing hospitalization, and improving the quality of life in patients with HFrEF and is considered a safe option across all age groups.
Citations: Kosiborod MN et al. Effects of dapagliflozin on symptoms, function, and quality of life in patients with heart failure and reduced ejection fraction: Results from the DAPA-HF trial. Circulation. 2020 Jan 14;141(2):90-9. Martinez FA et al. Efficacy and safety of dapagliflozin in heart failure with reduced ejection fraction according to age. Insights from DAPA-HF. Circulation. 2020 Jan 14;141:100-11.
Dr. Garg is assistant professor in the division of hospital medicine, Loyola University Medical Center, Maywood, Ill.
Malaria resistant to artemisinin emerging in Africa
A new study shows disturbing evidence that malaria is becoming resistant to artemisinin, a drug critical for treatment in Africa. Although artemisinin resistance has long plagued the Mekong Delta, it is relatively new to Africa.
In a study published online April 14 in The Lancet Infectious Diseases, researchers found that the typical 3-day course of treatment did not totally eradicate Plasmodium falciparum, the parasite that causes malaria. A delayed clearance of the parasite was shown and found to be associated with a genetic mutation called Pfkelch13 R561H.
P. falciparum isolates with this mutation were found in 7.5% of infected children in one area of Rwanda. Further genomic studies showed that this mutation was locally acquired and did not emerge from Southeast Asia. This is well illustrated in a genomic tree published in Nature Medicine in August, 2020. That study reported data collected from adults from 2013 to 2015.
The delay in reporting the mutation was due, in part, to the burdensome process of whole-genome sequencing and transfection studies, Pascal Ringwald, MD, PhD, coordinator of the Global Malaria Programme at WHO, and coauthor of the Nature Medicine study, said in an interview. In transfection studies, the mutation is inserted into parasites and the resultant effect is observed.
Aline Uwimana, MD, of Rwanda Biomedical Centre. is the lead author on both studies.
Meera Venkatesan, PhD, chief of the Case Management, Monitoring and Evaluation Branch, President’s Malaria Initiative, USAID, noted that the Lancet Infectious Diseases study was a therapeutic efficacy study (TES) on samples from children from 2018. In an interview, Dr. Venkatesan explained that the study is noteworthy because it demonstrated the clinical significance of this mutation with delayed parasite clearance. She did note that although there was a lag in publication of the initial reports of artemisinin resistance mutations, that information – and its implications – was promptly shared with the global malaria research community, as are other findings of public health importance.
Although most of the children got better, this “partial resistance” emerged while patients were taking artemether–lumefantrine. This is a type of artemisinin-based combination therapy (ACT) with two drugs intended to stall the emergence of resistance.
The delayed clearance will be a problem because it can contribute to the selection and spread of the partially resistant malaria parasite.
To slow the spread of artemisinin resistance, Dr. Ringwald emphasized the need to add a gametocidal drug to block the transmission to humans. “You give a single dose of primaquine, which will help stop the spread,” he said in an interview. “Continuing surveillance and mapping. These are priorities.”
So are following national guidelines and banning the use of artemisinin monotherapy. Dr. Ringwald stressed two additional priorities: the need for accurate diagnosis of malaria, and the need to use “good-quality drugs and to avoid substandard or fake medicines” by not purchasing drugs on the street.
Unscrupulous individuals are also selling artemisia preparations to treat or prevent COVID-19, when it has no such activity. Similarly, artemisia teas are sold as herbal remedies and nutraceuticals.
Philippe Guérin, MD, director of the Worldwide Antimalarial Resistance Network (WWARN), listed the same recommendations, focusing a bit more on accurate detection of malaria and treatment with a multidrug regimen plus primaquine. You need “to have different first-line treatment (different ACTs) to avoid drug pressure” and resistance to the partner drug emerging, he said in an interview.
Such multiple first-line treatments rely on artemisinin in combination with various drugs, but this can cause some logistical challenges. Resistance is so problematic that the MORU (Mahidol Oxford Tropical Medicine Research Unit) Tropical Health Network in Bangkok is studying triple drug combinations, adding amodiaquine or mefloquine to an artemisinin-based combination.
Dr. Guérin emphasized two other problems regarding the monitoring of malaria resistance in Africa (although not specifically Rwanda). One is the inability to do adequate surveillance in active conflict zones and areas of instability. The other is that COVID-19 is causing resources to be taken away from malaria and redirected to the more immediate crisis. By having to focus on the immediate viral pandemic, public-health authorities are missing the chance to address other critically important infectious diseases with large burdens – specifically malaria, TB, and HIV – which might have greater impacts on future generations.
Dr. Guérin noted that although we now have solid evidence of artemisinin resistance in Rwanda, and isolated cases in other African countries, we have little idea of the magnitude of the problem because testing is not widespread throughout parts of the continent.
What would widespread P. falciparum malaria resistance in Africa mean? Children are the most vulnerable to malaria, and account for two-thirds of the deaths. One study suggests there could be 78 million more cases over a 5-year period, along with far more deaths. Hence, there is a heightened urgency to implement the outlined strategies to prevent a looming catastrophe.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study shows disturbing evidence that malaria is becoming resistant to artemisinin, a drug critical for treatment in Africa. Although artemisinin resistance has long plagued the Mekong Delta, it is relatively new to Africa.
In a study published online April 14 in The Lancet Infectious Diseases, researchers found that the typical 3-day course of treatment did not totally eradicate Plasmodium falciparum, the parasite that causes malaria. A delayed clearance of the parasite was shown and found to be associated with a genetic mutation called Pfkelch13 R561H.
P. falciparum isolates with this mutation were found in 7.5% of infected children in one area of Rwanda. Further genomic studies showed that this mutation was locally acquired and did not emerge from Southeast Asia. This is well illustrated in a genomic tree published in Nature Medicine in August, 2020. That study reported data collected from adults from 2013 to 2015.
The delay in reporting the mutation was due, in part, to the burdensome process of whole-genome sequencing and transfection studies, Pascal Ringwald, MD, PhD, coordinator of the Global Malaria Programme at WHO, and coauthor of the Nature Medicine study, said in an interview. In transfection studies, the mutation is inserted into parasites and the resultant effect is observed.
Aline Uwimana, MD, of Rwanda Biomedical Centre. is the lead author on both studies.
Meera Venkatesan, PhD, chief of the Case Management, Monitoring and Evaluation Branch, President’s Malaria Initiative, USAID, noted that the Lancet Infectious Diseases study was a therapeutic efficacy study (TES) on samples from children from 2018. In an interview, Dr. Venkatesan explained that the study is noteworthy because it demonstrated the clinical significance of this mutation with delayed parasite clearance. She did note that although there was a lag in publication of the initial reports of artemisinin resistance mutations, that information – and its implications – was promptly shared with the global malaria research community, as are other findings of public health importance.
Although most of the children got better, this “partial resistance” emerged while patients were taking artemether–lumefantrine. This is a type of artemisinin-based combination therapy (ACT) with two drugs intended to stall the emergence of resistance.
The delayed clearance will be a problem because it can contribute to the selection and spread of the partially resistant malaria parasite.
To slow the spread of artemisinin resistance, Dr. Ringwald emphasized the need to add a gametocidal drug to block the transmission to humans. “You give a single dose of primaquine, which will help stop the spread,” he said in an interview. “Continuing surveillance and mapping. These are priorities.”
So are following national guidelines and banning the use of artemisinin monotherapy. Dr. Ringwald stressed two additional priorities: the need for accurate diagnosis of malaria, and the need to use “good-quality drugs and to avoid substandard or fake medicines” by not purchasing drugs on the street.
Unscrupulous individuals are also selling artemisia preparations to treat or prevent COVID-19, when it has no such activity. Similarly, artemisia teas are sold as herbal remedies and nutraceuticals.
Philippe Guérin, MD, director of the Worldwide Antimalarial Resistance Network (WWARN), listed the same recommendations, focusing a bit more on accurate detection of malaria and treatment with a multidrug regimen plus primaquine. You need “to have different first-line treatment (different ACTs) to avoid drug pressure” and resistance to the partner drug emerging, he said in an interview.
Such multiple first-line treatments rely on artemisinin in combination with various drugs, but this can cause some logistical challenges. Resistance is so problematic that the MORU (Mahidol Oxford Tropical Medicine Research Unit) Tropical Health Network in Bangkok is studying triple drug combinations, adding amodiaquine or mefloquine to an artemisinin-based combination.
Dr. Guérin emphasized two other problems regarding the monitoring of malaria resistance in Africa (although not specifically Rwanda). One is the inability to do adequate surveillance in active conflict zones and areas of instability. The other is that COVID-19 is causing resources to be taken away from malaria and redirected to the more immediate crisis. By having to focus on the immediate viral pandemic, public-health authorities are missing the chance to address other critically important infectious diseases with large burdens – specifically malaria, TB, and HIV – which might have greater impacts on future generations.
Dr. Guérin noted that although we now have solid evidence of artemisinin resistance in Rwanda, and isolated cases in other African countries, we have little idea of the magnitude of the problem because testing is not widespread throughout parts of the continent.
What would widespread P. falciparum malaria resistance in Africa mean? Children are the most vulnerable to malaria, and account for two-thirds of the deaths. One study suggests there could be 78 million more cases over a 5-year period, along with far more deaths. Hence, there is a heightened urgency to implement the outlined strategies to prevent a looming catastrophe.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study shows disturbing evidence that malaria is becoming resistant to artemisinin, a drug critical for treatment in Africa. Although artemisinin resistance has long plagued the Mekong Delta, it is relatively new to Africa.
In a study published online April 14 in The Lancet Infectious Diseases, researchers found that the typical 3-day course of treatment did not totally eradicate Plasmodium falciparum, the parasite that causes malaria. A delayed clearance of the parasite was shown and found to be associated with a genetic mutation called Pfkelch13 R561H.
P. falciparum isolates with this mutation were found in 7.5% of infected children in one area of Rwanda. Further genomic studies showed that this mutation was locally acquired and did not emerge from Southeast Asia. This is well illustrated in a genomic tree published in Nature Medicine in August, 2020. That study reported data collected from adults from 2013 to 2015.
The delay in reporting the mutation was due, in part, to the burdensome process of whole-genome sequencing and transfection studies, Pascal Ringwald, MD, PhD, coordinator of the Global Malaria Programme at WHO, and coauthor of the Nature Medicine study, said in an interview. In transfection studies, the mutation is inserted into parasites and the resultant effect is observed.
Aline Uwimana, MD, of Rwanda Biomedical Centre. is the lead author on both studies.
Meera Venkatesan, PhD, chief of the Case Management, Monitoring and Evaluation Branch, President’s Malaria Initiative, USAID, noted that the Lancet Infectious Diseases study was a therapeutic efficacy study (TES) on samples from children from 2018. In an interview, Dr. Venkatesan explained that the study is noteworthy because it demonstrated the clinical significance of this mutation with delayed parasite clearance. She did note that although there was a lag in publication of the initial reports of artemisinin resistance mutations, that information – and its implications – was promptly shared with the global malaria research community, as are other findings of public health importance.
Although most of the children got better, this “partial resistance” emerged while patients were taking artemether–lumefantrine. This is a type of artemisinin-based combination therapy (ACT) with two drugs intended to stall the emergence of resistance.
The delayed clearance will be a problem because it can contribute to the selection and spread of the partially resistant malaria parasite.
To slow the spread of artemisinin resistance, Dr. Ringwald emphasized the need to add a gametocidal drug to block the transmission to humans. “You give a single dose of primaquine, which will help stop the spread,” he said in an interview. “Continuing surveillance and mapping. These are priorities.”
So are following national guidelines and banning the use of artemisinin monotherapy. Dr. Ringwald stressed two additional priorities: the need for accurate diagnosis of malaria, and the need to use “good-quality drugs and to avoid substandard or fake medicines” by not purchasing drugs on the street.
Unscrupulous individuals are also selling artemisia preparations to treat or prevent COVID-19, when it has no such activity. Similarly, artemisia teas are sold as herbal remedies and nutraceuticals.
Philippe Guérin, MD, director of the Worldwide Antimalarial Resistance Network (WWARN), listed the same recommendations, focusing a bit more on accurate detection of malaria and treatment with a multidrug regimen plus primaquine. You need “to have different first-line treatment (different ACTs) to avoid drug pressure” and resistance to the partner drug emerging, he said in an interview.
Such multiple first-line treatments rely on artemisinin in combination with various drugs, but this can cause some logistical challenges. Resistance is so problematic that the MORU (Mahidol Oxford Tropical Medicine Research Unit) Tropical Health Network in Bangkok is studying triple drug combinations, adding amodiaquine or mefloquine to an artemisinin-based combination.
Dr. Guérin emphasized two other problems regarding the monitoring of malaria resistance in Africa (although not specifically Rwanda). One is the inability to do adequate surveillance in active conflict zones and areas of instability. The other is that COVID-19 is causing resources to be taken away from malaria and redirected to the more immediate crisis. By having to focus on the immediate viral pandemic, public-health authorities are missing the chance to address other critically important infectious diseases with large burdens – specifically malaria, TB, and HIV – which might have greater impacts on future generations.
Dr. Guérin noted that although we now have solid evidence of artemisinin resistance in Rwanda, and isolated cases in other African countries, we have little idea of the magnitude of the problem because testing is not widespread throughout parts of the continent.
What would widespread P. falciparum malaria resistance in Africa mean? Children are the most vulnerable to malaria, and account for two-thirds of the deaths. One study suggests there could be 78 million more cases over a 5-year period, along with far more deaths. Hence, there is a heightened urgency to implement the outlined strategies to prevent a looming catastrophe.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Educational intervention increased use of immediate postpartum long-acting reversible contraception
Key clinical point: Three countries that implemented an immediate postpartum family planning (IPPFP) intervention that focused on long-acting reversible contraception (LARC) showed a significant increase in the number of girls and women who opted for an IUD or implant within 48 hours of delivery.
Major finding: The mean percentage of IPP LARC adoption among all deliveries in the countries that implemented the intervention programs was 10.01%, compared to 0.77% in countries providing standard postpartum care without the intervention.
Study details: The data come from a review of immediate postpartum long-acting reversible contraception (IPP LARC) from 2016 to 2019 in three countries that focused on LARC intervention (Democratic Republic of Congo, Somalia, and Pakistan) including training delivery-room providers on counseling and provision of IPPFP; and three countries the did not implement this intervention (Rwanda, Syria, and Yemen).
Disclosures: The study was supported by an anonymous foundation. The researchers had no financial conflicts to disclose.
Source: Gallagher MC et al. Front Glob Womens Health. 2021 Apr 6. doi: 10.3389/fgwh.2021.613338.
Key clinical point: Three countries that implemented an immediate postpartum family planning (IPPFP) intervention that focused on long-acting reversible contraception (LARC) showed a significant increase in the number of girls and women who opted for an IUD or implant within 48 hours of delivery.
Major finding: The mean percentage of IPP LARC adoption among all deliveries in the countries that implemented the intervention programs was 10.01%, compared to 0.77% in countries providing standard postpartum care without the intervention.
Study details: The data come from a review of immediate postpartum long-acting reversible contraception (IPP LARC) from 2016 to 2019 in three countries that focused on LARC intervention (Democratic Republic of Congo, Somalia, and Pakistan) including training delivery-room providers on counseling and provision of IPPFP; and three countries the did not implement this intervention (Rwanda, Syria, and Yemen).
Disclosures: The study was supported by an anonymous foundation. The researchers had no financial conflicts to disclose.
Source: Gallagher MC et al. Front Glob Womens Health. 2021 Apr 6. doi: 10.3389/fgwh.2021.613338.
Key clinical point: Three countries that implemented an immediate postpartum family planning (IPPFP) intervention that focused on long-acting reversible contraception (LARC) showed a significant increase in the number of girls and women who opted for an IUD or implant within 48 hours of delivery.
Major finding: The mean percentage of IPP LARC adoption among all deliveries in the countries that implemented the intervention programs was 10.01%, compared to 0.77% in countries providing standard postpartum care without the intervention.
Study details: The data come from a review of immediate postpartum long-acting reversible contraception (IPP LARC) from 2016 to 2019 in three countries that focused on LARC intervention (Democratic Republic of Congo, Somalia, and Pakistan) including training delivery-room providers on counseling and provision of IPPFP; and three countries the did not implement this intervention (Rwanda, Syria, and Yemen).
Disclosures: The study was supported by an anonymous foundation. The researchers had no financial conflicts to disclose.
Source: Gallagher MC et al. Front Glob Womens Health. 2021 Apr 6. doi: 10.3389/fgwh.2021.613338.