User login
Improving Dermatologic Care for South Asian Patients: Understanding Religious and Cultural Practices
Traditional garments are particularly important in both Sikhism and Islam. Sikhs began wearing symbolic garments in the 16th century as markers of their identity during periods of religious persecution. Today, many Sikhs continue to maintain this tradition of wearing the Five Ks—kesh (uncut hair, often tied in a turban), kanga (wooden hair comb), kirpan (symbolic dagger), kachha (cotton underwear), and kara (steel bracelet).2 Similarly, Islamic traditions also provide guidance for clothing. Many Muslim women wear the hijab (headscarf), a garment that originated as protective headgear for nomadic desert cultures and has come to symbolize modest dress. Traditionally, the hijab is worn in the presence of all men who are not immediate relatives, although patients may make exceptions for medical care. Some Muslim men also may cover their heads with a skullcap and/or maintain long beards (occasionally dyed with henna pigment) as a way of keeping continuity with the tradition of the Prophet Muhammad and his companions.3
Certain styles of headwear can cause high tension on hair follicles and have been associated with traction alopecia.4 Persistent use of the same turban, hijab, or comb also may lead to seborrheic dermatitis or fungal scalp infections. Dermatologists should advise patients about these potential challenges and suggest modifications in accordance with the patient’s religious beliefs; for example, providers can suggest removing headwear at night, using prophylactic antifungal shampoos, and/or tying the hair in a ponytail or loosening the headgear to reduce traction.
Although Hinduism does not have a unifying garment or hair tradition in the vein of Sikhism or Islam, all 3 religions share a strong emphasis on bodily modesty, which may affect dermatologic examinations. Patients from all 3 religions may seek to expose as little skin as possible during a physical examination, and many patients may be uncomfortable with a physician of the opposite gender. Dermatologists may find the following practices to be helpful5:
• Talk through each aspect of the skin examination while it is being performed and expose the least amount of skin necessary during the process
• Offer the patient a chaperone or a same-gender provider, if possible
• Empower patients to assist in adjusting garments themselves to help the physician visualize all parts of the skin
Some Sikhs also may have specific concerns regarding cutting their hair. One aspect of kesh is that every hair is sacred, and thus, many Sikhs refrain from removing hair on any part of the body. As such, providers should carefully obtain the patient’s informed consent before performing any procedure or physical examination maneuvers (eg, hair pull test) that may result in loss of hair.2
Physicians of all disciplines can help address these challenges through increased outreach and cultural awareness; for example, dermatologists can create skin care pamphlets translated into various South Asian languages and distribute them at houses of worship or other community centers. This may help patients identify their skin needs and seek appropriate care. The onus must be on physicians to make these patients feel comfortable seeking care by creating nonjudgmental, culturally knowledgeable clinical environments. When asking about social history, the physician might consider asking an open-ended question such as, “What role does religion/spirituality play in your life?” They can then proceed to ask specific questions about practices that might affect the patient’s care.5
Given the current coronavirus disease 2019 pandemic, South Asian patients may be even further discouraged from seeking dermatologic care. By understanding religious traditions and taking steps to address biases, dermatologists can help mitigate health care disparities and provide culturally competent care to South Asian patients.
- Nadimpalli SB, Cleland CM, Hutchinson MK, et al. The association between discrimination and the health of Sikh Asian Indians. Health Psychol. 2016;35:351-355.
- The five Ks. BBC website. Updated September 29, 2009. Accessed February 4, 2021. https://www.bbc.co.uk/religion/religions/sikhism/customs/fiveks.shtml
- Islam. BBC website. Accessed February 2, 2021. https://www.bbc.co.uk/religion/religions/islam/
- James J, Saladi RN, Fox JL. Traction alopecia in Sikh male patients. J Am Board Fam Med. 2007;20:497-498.
- Hussain A. Recommendations for culturally competent dermatology care of Muslim patients. J Am Acad Dermatol. 2017;77:388-389.
Traditional garments are particularly important in both Sikhism and Islam. Sikhs began wearing symbolic garments in the 16th century as markers of their identity during periods of religious persecution. Today, many Sikhs continue to maintain this tradition of wearing the Five Ks—kesh (uncut hair, often tied in a turban), kanga (wooden hair comb), kirpan (symbolic dagger), kachha (cotton underwear), and kara (steel bracelet).2 Similarly, Islamic traditions also provide guidance for clothing. Many Muslim women wear the hijab (headscarf), a garment that originated as protective headgear for nomadic desert cultures and has come to symbolize modest dress. Traditionally, the hijab is worn in the presence of all men who are not immediate relatives, although patients may make exceptions for medical care. Some Muslim men also may cover their heads with a skullcap and/or maintain long beards (occasionally dyed with henna pigment) as a way of keeping continuity with the tradition of the Prophet Muhammad and his companions.3
Certain styles of headwear can cause high tension on hair follicles and have been associated with traction alopecia.4 Persistent use of the same turban, hijab, or comb also may lead to seborrheic dermatitis or fungal scalp infections. Dermatologists should advise patients about these potential challenges and suggest modifications in accordance with the patient’s religious beliefs; for example, providers can suggest removing headwear at night, using prophylactic antifungal shampoos, and/or tying the hair in a ponytail or loosening the headgear to reduce traction.
Although Hinduism does not have a unifying garment or hair tradition in the vein of Sikhism or Islam, all 3 religions share a strong emphasis on bodily modesty, which may affect dermatologic examinations. Patients from all 3 religions may seek to expose as little skin as possible during a physical examination, and many patients may be uncomfortable with a physician of the opposite gender. Dermatologists may find the following practices to be helpful5:
• Talk through each aspect of the skin examination while it is being performed and expose the least amount of skin necessary during the process
• Offer the patient a chaperone or a same-gender provider, if possible
• Empower patients to assist in adjusting garments themselves to help the physician visualize all parts of the skin
Some Sikhs also may have specific concerns regarding cutting their hair. One aspect of kesh is that every hair is sacred, and thus, many Sikhs refrain from removing hair on any part of the body. As such, providers should carefully obtain the patient’s informed consent before performing any procedure or physical examination maneuvers (eg, hair pull test) that may result in loss of hair.2
Physicians of all disciplines can help address these challenges through increased outreach and cultural awareness; for example, dermatologists can create skin care pamphlets translated into various South Asian languages and distribute them at houses of worship or other community centers. This may help patients identify their skin needs and seek appropriate care. The onus must be on physicians to make these patients feel comfortable seeking care by creating nonjudgmental, culturally knowledgeable clinical environments. When asking about social history, the physician might consider asking an open-ended question such as, “What role does religion/spirituality play in your life?” They can then proceed to ask specific questions about practices that might affect the patient’s care.5
Given the current coronavirus disease 2019 pandemic, South Asian patients may be even further discouraged from seeking dermatologic care. By understanding religious traditions and taking steps to address biases, dermatologists can help mitigate health care disparities and provide culturally competent care to South Asian patients.
Traditional garments are particularly important in both Sikhism and Islam. Sikhs began wearing symbolic garments in the 16th century as markers of their identity during periods of religious persecution. Today, many Sikhs continue to maintain this tradition of wearing the Five Ks—kesh (uncut hair, often tied in a turban), kanga (wooden hair comb), kirpan (symbolic dagger), kachha (cotton underwear), and kara (steel bracelet).2 Similarly, Islamic traditions also provide guidance for clothing. Many Muslim women wear the hijab (headscarf), a garment that originated as protective headgear for nomadic desert cultures and has come to symbolize modest dress. Traditionally, the hijab is worn in the presence of all men who are not immediate relatives, although patients may make exceptions for medical care. Some Muslim men also may cover their heads with a skullcap and/or maintain long beards (occasionally dyed with henna pigment) as a way of keeping continuity with the tradition of the Prophet Muhammad and his companions.3
Certain styles of headwear can cause high tension on hair follicles and have been associated with traction alopecia.4 Persistent use of the same turban, hijab, or comb also may lead to seborrheic dermatitis or fungal scalp infections. Dermatologists should advise patients about these potential challenges and suggest modifications in accordance with the patient’s religious beliefs; for example, providers can suggest removing headwear at night, using prophylactic antifungal shampoos, and/or tying the hair in a ponytail or loosening the headgear to reduce traction.
Although Hinduism does not have a unifying garment or hair tradition in the vein of Sikhism or Islam, all 3 religions share a strong emphasis on bodily modesty, which may affect dermatologic examinations. Patients from all 3 religions may seek to expose as little skin as possible during a physical examination, and many patients may be uncomfortable with a physician of the opposite gender. Dermatologists may find the following practices to be helpful5:
• Talk through each aspect of the skin examination while it is being performed and expose the least amount of skin necessary during the process
• Offer the patient a chaperone or a same-gender provider, if possible
• Empower patients to assist in adjusting garments themselves to help the physician visualize all parts of the skin
Some Sikhs also may have specific concerns regarding cutting their hair. One aspect of kesh is that every hair is sacred, and thus, many Sikhs refrain from removing hair on any part of the body. As such, providers should carefully obtain the patient’s informed consent before performing any procedure or physical examination maneuvers (eg, hair pull test) that may result in loss of hair.2
Physicians of all disciplines can help address these challenges through increased outreach and cultural awareness; for example, dermatologists can create skin care pamphlets translated into various South Asian languages and distribute them at houses of worship or other community centers. This may help patients identify their skin needs and seek appropriate care. The onus must be on physicians to make these patients feel comfortable seeking care by creating nonjudgmental, culturally knowledgeable clinical environments. When asking about social history, the physician might consider asking an open-ended question such as, “What role does religion/spirituality play in your life?” They can then proceed to ask specific questions about practices that might affect the patient’s care.5
Given the current coronavirus disease 2019 pandemic, South Asian patients may be even further discouraged from seeking dermatologic care. By understanding religious traditions and taking steps to address biases, dermatologists can help mitigate health care disparities and provide culturally competent care to South Asian patients.
- Nadimpalli SB, Cleland CM, Hutchinson MK, et al. The association between discrimination and the health of Sikh Asian Indians. Health Psychol. 2016;35:351-355.
- The five Ks. BBC website. Updated September 29, 2009. Accessed February 4, 2021. https://www.bbc.co.uk/religion/religions/sikhism/customs/fiveks.shtml
- Islam. BBC website. Accessed February 2, 2021. https://www.bbc.co.uk/religion/religions/islam/
- James J, Saladi RN, Fox JL. Traction alopecia in Sikh male patients. J Am Board Fam Med. 2007;20:497-498.
- Hussain A. Recommendations for culturally competent dermatology care of Muslim patients. J Am Acad Dermatol. 2017;77:388-389.
- Nadimpalli SB, Cleland CM, Hutchinson MK, et al. The association between discrimination and the health of Sikh Asian Indians. Health Psychol. 2016;35:351-355.
- The five Ks. BBC website. Updated September 29, 2009. Accessed February 4, 2021. https://www.bbc.co.uk/religion/religions/sikhism/customs/fiveks.shtml
- Islam. BBC website. Accessed February 2, 2021. https://www.bbc.co.uk/religion/religions/islam/
- James J, Saladi RN, Fox JL. Traction alopecia in Sikh male patients. J Am Board Fam Med. 2007;20:497-498.
- Hussain A. Recommendations for culturally competent dermatology care of Muslim patients. J Am Acad Dermatol. 2017;77:388-389.
Practice Points
- Providers should familiarize themselves with traditional garments of Sikhism and Islam, including head coverings and other symbolic items.
- Inform patients about health-conscious methods of wearing traditional headwear, such as removing certain headwear at night and tying hair in methods to avoid causing traction alopecia.
- Talk through each aspect of the skin examination while it is being performed and expose the least amount of skin necessary during the process. Offer the patient a chaperone or a same-gender provider, if possible.
- Empower patients to assist in adjusting garments themselves to help the physician visualize all parts of the skin.
Short sleep predicts incident dementia and all-cause mortality
More evidence has emerged linking sleep deficiency, dementia, and mortality.
“Sleep disturbance and insufficiency have been shown to be associated with both the development and progression of Alzheimer’s disease and with all-cause mortality,” wrote Rebecca S. Robbins, PhD, of Brigham and Women’s Hospital, Boston, and colleagues. However, research on this topic has yielded conflicting results, and “few studies have included a comprehensive set of sleep characteristics in a single examination of incident dementia and all-cause mortality.”
In a study published in Aging, the researchers identified 2,812 adults aged 65 years and older from the National Health and Aging Trends Study (NHATS), a nationally representative longitudinal study of Medicare beneficiaries aged 65 years and older in the United States.
Participants completed surveys about sleep disturbance and duration in 2013 (1,575 individuals) and in 2014 (1,237 individuals), and the researchers examined the relationship between sleep disturbance and deficiency and incident dementia and all-cause mortality over the next 5 years. The average age of the study participants was 76.9 years, 60% were women, and 72% were White.
Overall, approximately 60% of the participants reported never or rarely having problems with alertness, approximately half said that they rarely or never napped, and more than half said they fell asleep in 15 minutes or less. Approximately 70% rated their sleep quality as good or very good, and more than 90% said they rarely or never snored.
The researchers examined the relationships between sleep characteristics and the development of incident dementia over 5 years. In a fully adjusted Cox multivariate analysis, individuals who slept 5 hours or less per night had approximately twice the risk for incident dementia as those who slept longer (hazard ratio, 2.04); risk of dementia also was higher among those who took 30 minutes or longer to fall asleep (HR, 1.45).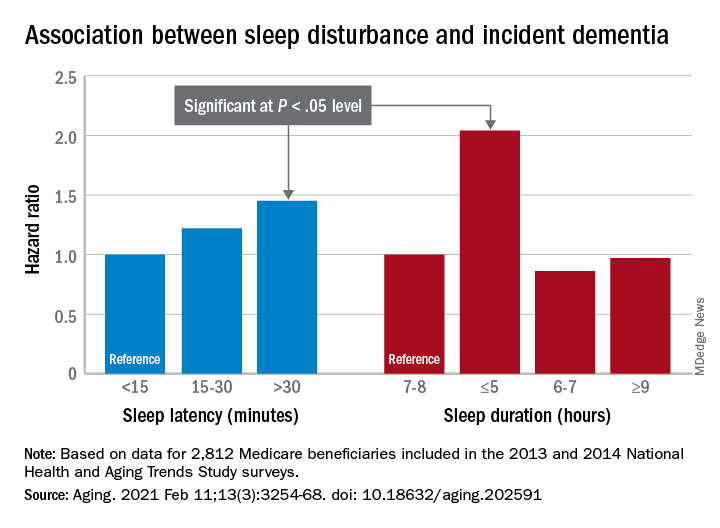
In addition, the risk of all-cause mortality was significantly higher among individuals who reported difficulty maintaining alertness some days or most days/every day (HR, 1.49 and HR, 1.65, respectively), routinely napping some days or most days/every day (HR, 1.38 and HR, 1.73, respectively), poor or very poor sleep quality (HR, 1.75), and sleeping 5 hours or less each night (HR, 2.38).
The study findings were limited by several factors including a population representing only one-quarter of the NHATS cohort, which prevented nationally representative estimates, the availability of only 2 years of sleep data, and small sample size for certain response categories, the researchers noted.
However, “our study offers a contribution to the literature on sleep among aging populations in its assessment of incident dementia and all-cause mortality and a range of sleep characteristics among older adults,” they said. In particular, “short sleep duration was a strong predictor of both incident dementia and all-cause mortality, suggesting this may be a sleep characteristic that is important – over and above the other predictors – of adverse outcomes among older adults,” and future areas for research include the development of novel behavioral interventions to improve sleep in this population.
The study was supported in part by the National Institute for Occupational Safety and Health; the National Heart, Lung, and Blood Institute; the National Institute on Aging; and the Brigham Research Institute Fund to Sustain Research Excellence. Lead author Dr. Robbins disclosed fees from Denihan Hospitality, Rituals Cosmetics, Dagmejan, Asystem, and SleepCycle. Several coauthors disclosed relationships with multiple pharmaceutical companies, and support from various philanthropic organizations.
More evidence has emerged linking sleep deficiency, dementia, and mortality.
“Sleep disturbance and insufficiency have been shown to be associated with both the development and progression of Alzheimer’s disease and with all-cause mortality,” wrote Rebecca S. Robbins, PhD, of Brigham and Women’s Hospital, Boston, and colleagues. However, research on this topic has yielded conflicting results, and “few studies have included a comprehensive set of sleep characteristics in a single examination of incident dementia and all-cause mortality.”
In a study published in Aging, the researchers identified 2,812 adults aged 65 years and older from the National Health and Aging Trends Study (NHATS), a nationally representative longitudinal study of Medicare beneficiaries aged 65 years and older in the United States.
Participants completed surveys about sleep disturbance and duration in 2013 (1,575 individuals) and in 2014 (1,237 individuals), and the researchers examined the relationship between sleep disturbance and deficiency and incident dementia and all-cause mortality over the next 5 years. The average age of the study participants was 76.9 years, 60% were women, and 72% were White.
Overall, approximately 60% of the participants reported never or rarely having problems with alertness, approximately half said that they rarely or never napped, and more than half said they fell asleep in 15 minutes or less. Approximately 70% rated their sleep quality as good or very good, and more than 90% said they rarely or never snored.
The researchers examined the relationships between sleep characteristics and the development of incident dementia over 5 years. In a fully adjusted Cox multivariate analysis, individuals who slept 5 hours or less per night had approximately twice the risk for incident dementia as those who slept longer (hazard ratio, 2.04); risk of dementia also was higher among those who took 30 minutes or longer to fall asleep (HR, 1.45).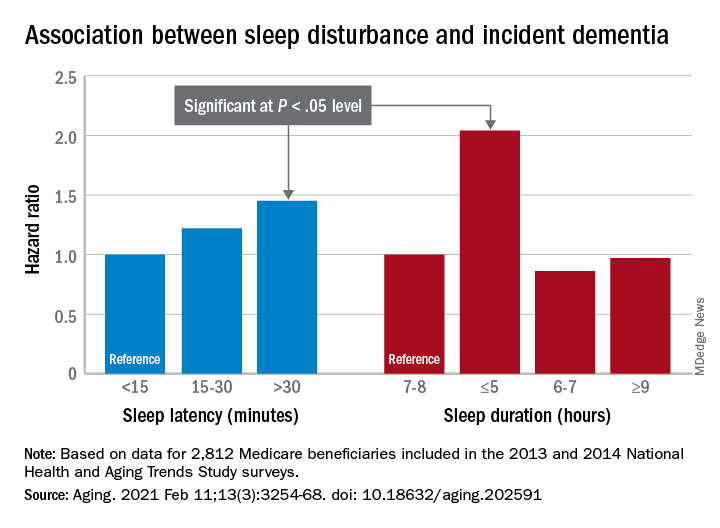
In addition, the risk of all-cause mortality was significantly higher among individuals who reported difficulty maintaining alertness some days or most days/every day (HR, 1.49 and HR, 1.65, respectively), routinely napping some days or most days/every day (HR, 1.38 and HR, 1.73, respectively), poor or very poor sleep quality (HR, 1.75), and sleeping 5 hours or less each night (HR, 2.38).
The study findings were limited by several factors including a population representing only one-quarter of the NHATS cohort, which prevented nationally representative estimates, the availability of only 2 years of sleep data, and small sample size for certain response categories, the researchers noted.
However, “our study offers a contribution to the literature on sleep among aging populations in its assessment of incident dementia and all-cause mortality and a range of sleep characteristics among older adults,” they said. In particular, “short sleep duration was a strong predictor of both incident dementia and all-cause mortality, suggesting this may be a sleep characteristic that is important – over and above the other predictors – of adverse outcomes among older adults,” and future areas for research include the development of novel behavioral interventions to improve sleep in this population.
The study was supported in part by the National Institute for Occupational Safety and Health; the National Heart, Lung, and Blood Institute; the National Institute on Aging; and the Brigham Research Institute Fund to Sustain Research Excellence. Lead author Dr. Robbins disclosed fees from Denihan Hospitality, Rituals Cosmetics, Dagmejan, Asystem, and SleepCycle. Several coauthors disclosed relationships with multiple pharmaceutical companies, and support from various philanthropic organizations.
More evidence has emerged linking sleep deficiency, dementia, and mortality.
“Sleep disturbance and insufficiency have been shown to be associated with both the development and progression of Alzheimer’s disease and with all-cause mortality,” wrote Rebecca S. Robbins, PhD, of Brigham and Women’s Hospital, Boston, and colleagues. However, research on this topic has yielded conflicting results, and “few studies have included a comprehensive set of sleep characteristics in a single examination of incident dementia and all-cause mortality.”
In a study published in Aging, the researchers identified 2,812 adults aged 65 years and older from the National Health and Aging Trends Study (NHATS), a nationally representative longitudinal study of Medicare beneficiaries aged 65 years and older in the United States.
Participants completed surveys about sleep disturbance and duration in 2013 (1,575 individuals) and in 2014 (1,237 individuals), and the researchers examined the relationship between sleep disturbance and deficiency and incident dementia and all-cause mortality over the next 5 years. The average age of the study participants was 76.9 years, 60% were women, and 72% were White.
Overall, approximately 60% of the participants reported never or rarely having problems with alertness, approximately half said that they rarely or never napped, and more than half said they fell asleep in 15 minutes or less. Approximately 70% rated their sleep quality as good or very good, and more than 90% said they rarely or never snored.
The researchers examined the relationships between sleep characteristics and the development of incident dementia over 5 years. In a fully adjusted Cox multivariate analysis, individuals who slept 5 hours or less per night had approximately twice the risk for incident dementia as those who slept longer (hazard ratio, 2.04); risk of dementia also was higher among those who took 30 minutes or longer to fall asleep (HR, 1.45).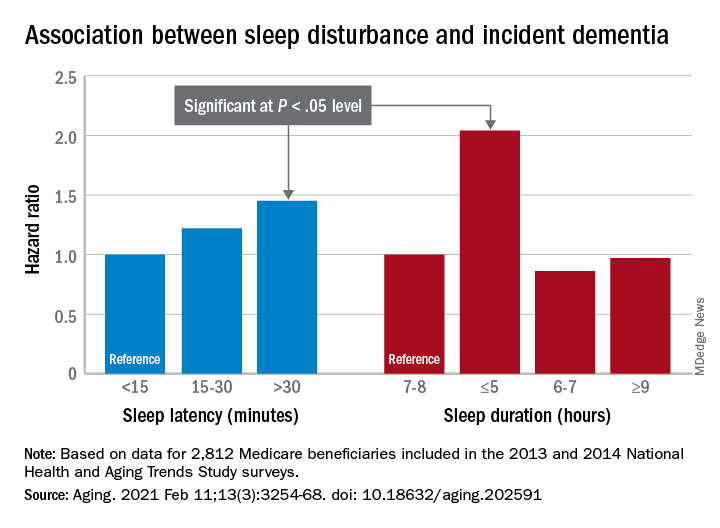
In addition, the risk of all-cause mortality was significantly higher among individuals who reported difficulty maintaining alertness some days or most days/every day (HR, 1.49 and HR, 1.65, respectively), routinely napping some days or most days/every day (HR, 1.38 and HR, 1.73, respectively), poor or very poor sleep quality (HR, 1.75), and sleeping 5 hours or less each night (HR, 2.38).
The study findings were limited by several factors including a population representing only one-quarter of the NHATS cohort, which prevented nationally representative estimates, the availability of only 2 years of sleep data, and small sample size for certain response categories, the researchers noted.
However, “our study offers a contribution to the literature on sleep among aging populations in its assessment of incident dementia and all-cause mortality and a range of sleep characteristics among older adults,” they said. In particular, “short sleep duration was a strong predictor of both incident dementia and all-cause mortality, suggesting this may be a sleep characteristic that is important – over and above the other predictors – of adverse outcomes among older adults,” and future areas for research include the development of novel behavioral interventions to improve sleep in this population.
The study was supported in part by the National Institute for Occupational Safety and Health; the National Heart, Lung, and Blood Institute; the National Institute on Aging; and the Brigham Research Institute Fund to Sustain Research Excellence. Lead author Dr. Robbins disclosed fees from Denihan Hospitality, Rituals Cosmetics, Dagmejan, Asystem, and SleepCycle. Several coauthors disclosed relationships with multiple pharmaceutical companies, and support from various philanthropic organizations.
FROM AGING
COMMENT & CONTROVERSY
9vHPV VACCINE: PREVENTION OF OROPHARYNGEAL CANCER
ROBERT L. BARBIERI, MD (EDITORIAL; NOVEMBER 2020)
HPV vaccine for older ObGyns?
I am 67 years old and recently retired. I breathed in the smoke from laser conizations, LEEPs (loop electrosurgical excision procedures), and cautery of condyloma for 35 years. Am I a good candidate for the HPV vaccine?
Gus Barkett, DO
Muskegon, Michigan
Dr. Barbieri responds
I thank Dr. Barkett for his important question. As you know, the US Food and Drug Administration has approved 9vHPV vaccination for people 27 to 45 years of age. I do not believe there are sufficient data to provide an evidence-based answer for physicians with occupational exposure to HPV who are more than 45 years of age. My recommendation would be to have a consult with an otolaryngologist expert in HPV-induced oral-pharyngeal cancer.
EXAMINING THE EVIDENCE: HOW EFFECTIVE IS SCREENING MAMMOGRAPHY FOR PREVENTING BREAST CANCER MORTALITY?
ANDREW M. KAUNITZ, MD (AUGUST 2020)
Discordant results on screening mammography
In regard to the discussion on screening mammography for preventing breast cancer mortality, I would like to call attention to a more recent study than the ones referenced in the article. The study by Duffy and colleagues was from Sweden and included almost 550,000 women.1 Results of the study showed a statistically significant reduction of 41% in 10-year mortality and a 25% reduction in the incidence of advanced-stage disease at the time of diagnosis in women who underwent routine screening mammograms. In Sweden, routine screening is defined as a mammogram every 18 months for women aged 40 to 54 years and every 24 months after that, up to age 69.
I do not know if we will ever come to a consensus on the utility of mammograms or how often they should be done, but I wanted to illustrate this counterpoint.
Lisa Gennari, MD
Cincinnati, Ohio
Reference
1. Duffy SW, Tabar L, Yen AM, et al. Mammography screening reduces rates of advanced and fatal breast cancers: results in 549,091 women. Cancer. 2020;126:2971-2979.
Dr. Kaunitz responds
I thank Dr. Gennari for her interest in the Examining the Evidence discussion that summarized the findings of an article from Australia published in late summer of last year.1 That article indicated that as screening mammograms became common in the state of Victoria over several decades, the incidence of advanced breast cancer doubled, mirroring findings from the United States, Holland, and Norway. During the same time period, breast cancer mortality declined substantially. The authors concluded that all of the decline in breast cancer mortality that they observed since 1994 could be attributed not to screening mammography but rather to the introduction and uptake of adjuvant therapy (tamoxifen and chemotherapy).
In contrast, in the article Dr. Gennari cites, also published last summer, the authors found that the widespread uptake of screening mammograms among women residing in 9 counties in Sweden was associated with a decline in the incidence of advanced breast cancer. I am not able to explain these discrepant findings. However, as the authors pointed out, they employed a new strategy: measuring the incidence of breast cancer that proved fatal one decade after diagnosis.
Differing findings and interpretations of data that address benefits and risks of screening mammography lead to differing recommendations from professional societies and confusion among clinicians and our patients. Although it can be challenging in the constraints of time allotted for well-woman visits, I try to engage in shared decision making with my patients regarding when to start/stop mammography as well as frequency of screening.
Reference
- Burton R, Stevenson C. Assessment of breast cancer mortality trends associated with mammographic screening and adjuvant therapy from 1986 to 2013 in the state of Victoria, Australia. JAMA Netw Open. 2020:3:e208249.
Continue to: NEW HORMONAL MEDICAL TREATMENT...
NEW HORMONAL MEDICAL TREATMENT IS AN IMPORTANT ADVANCE FOR AUB CAUSED BY UTERINE FIBROIDS
ROBERT L. BARBIERI, MD (EDITORIAL; AUGUST 2020)
New AUB medical treatment
I appreciate Dr. Barbieri’s concise and pertinent review of myomatous disease etiology and treatments. I have a question regarding therapy with Oriahnn (elagolix, estradiol, and norethindrone acetate capsules). Most myomatous-related bleeding occurs in premenopausal women. The elagolix suppresses luteinizing hormone and follicle stimulating hormone, and the norethindrone is added to protect the endometrium from the estradiol. Do the elagolix and norethindrone also provide contraception?
Geoffrey J. Zann, MD, MBA
Boca Raton, Florida
Dr. Barbieri responds
Dr. Zann raises an important clinical question that arises often in practice. The US Food and Drug Administration (FDA) has not approved Oriahnn as a contraceptive. The FDA prescribing information recommends: Advise women to use non-hormonal contraception during treatment and for one week after discontinuing Oriahnn. Oriahnn may delay the ability to recognize the occurrence of a pregnancy because it alters menstrual bleeding. Perform pregnancy testing if pregnancy is suspected and discontinue Oriahnn if pregnancy is confirmed.
In Oriahnn, the elagolix dose is 300 mg twice daily. If a patient reliably takes 600 mg of elagolix daily, it is highly unlikely that she will ovulate. However, in practice, many patients miss doses of their medication, reducing the contraceptive effectiveness. For example, the combined estrogen-progestin contraceptive is highly effective at suppressing ovulation, but the Centers for Disease Control and Prevention (CDC) estimates that 9% of women taking an estrogen-progestin contraceptive will become pregnant each year.1,2
Oriahnn also contains norethindrone acetate at a dose of 0.5 mg daily. The FDA has approved norethindrone at a dose of 0.35 mg daily as a contraceptive. The CDC estimates that 9% of women prescribed a progestin-only pill will become pregnant each year with typical use.1,2
I counsel my patients that if they reliably take their prescribed Oriahnn medication as directed, they are unlikely to become pregnant, and a backup method of contraception will further help to reduce their risk of becoming pregnant.
References
- Centers for Disease Control and Prevention. US selected practice recommendations for contraceptive use, 2013. MMWR Morbid Mortal Weekly Rep. 2013;62(RR-5):1-59.
- Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397-404.
9vHPV VACCINE: PREVENTION OF OROPHARYNGEAL CANCER
ROBERT L. BARBIERI, MD (EDITORIAL; NOVEMBER 2020)
HPV vaccine for older ObGyns?
I am 67 years old and recently retired. I breathed in the smoke from laser conizations, LEEPs (loop electrosurgical excision procedures), and cautery of condyloma for 35 years. Am I a good candidate for the HPV vaccine?
Gus Barkett, DO
Muskegon, Michigan
Dr. Barbieri responds
I thank Dr. Barkett for his important question. As you know, the US Food and Drug Administration has approved 9vHPV vaccination for people 27 to 45 years of age. I do not believe there are sufficient data to provide an evidence-based answer for physicians with occupational exposure to HPV who are more than 45 years of age. My recommendation would be to have a consult with an otolaryngologist expert in HPV-induced oral-pharyngeal cancer.
EXAMINING THE EVIDENCE: HOW EFFECTIVE IS SCREENING MAMMOGRAPHY FOR PREVENTING BREAST CANCER MORTALITY?
ANDREW M. KAUNITZ, MD (AUGUST 2020)
Discordant results on screening mammography
In regard to the discussion on screening mammography for preventing breast cancer mortality, I would like to call attention to a more recent study than the ones referenced in the article. The study by Duffy and colleagues was from Sweden and included almost 550,000 women.1 Results of the study showed a statistically significant reduction of 41% in 10-year mortality and a 25% reduction in the incidence of advanced-stage disease at the time of diagnosis in women who underwent routine screening mammograms. In Sweden, routine screening is defined as a mammogram every 18 months for women aged 40 to 54 years and every 24 months after that, up to age 69.
I do not know if we will ever come to a consensus on the utility of mammograms or how often they should be done, but I wanted to illustrate this counterpoint.
Lisa Gennari, MD
Cincinnati, Ohio
Reference
1. Duffy SW, Tabar L, Yen AM, et al. Mammography screening reduces rates of advanced and fatal breast cancers: results in 549,091 women. Cancer. 2020;126:2971-2979.
Dr. Kaunitz responds
I thank Dr. Gennari for her interest in the Examining the Evidence discussion that summarized the findings of an article from Australia published in late summer of last year.1 That article indicated that as screening mammograms became common in the state of Victoria over several decades, the incidence of advanced breast cancer doubled, mirroring findings from the United States, Holland, and Norway. During the same time period, breast cancer mortality declined substantially. The authors concluded that all of the decline in breast cancer mortality that they observed since 1994 could be attributed not to screening mammography but rather to the introduction and uptake of adjuvant therapy (tamoxifen and chemotherapy).
In contrast, in the article Dr. Gennari cites, also published last summer, the authors found that the widespread uptake of screening mammograms among women residing in 9 counties in Sweden was associated with a decline in the incidence of advanced breast cancer. I am not able to explain these discrepant findings. However, as the authors pointed out, they employed a new strategy: measuring the incidence of breast cancer that proved fatal one decade after diagnosis.
Differing findings and interpretations of data that address benefits and risks of screening mammography lead to differing recommendations from professional societies and confusion among clinicians and our patients. Although it can be challenging in the constraints of time allotted for well-woman visits, I try to engage in shared decision making with my patients regarding when to start/stop mammography as well as frequency of screening.
Reference
- Burton R, Stevenson C. Assessment of breast cancer mortality trends associated with mammographic screening and adjuvant therapy from 1986 to 2013 in the state of Victoria, Australia. JAMA Netw Open. 2020:3:e208249.
Continue to: NEW HORMONAL MEDICAL TREATMENT...
NEW HORMONAL MEDICAL TREATMENT IS AN IMPORTANT ADVANCE FOR AUB CAUSED BY UTERINE FIBROIDS
ROBERT L. BARBIERI, MD (EDITORIAL; AUGUST 2020)
New AUB medical treatment
I appreciate Dr. Barbieri’s concise and pertinent review of myomatous disease etiology and treatments. I have a question regarding therapy with Oriahnn (elagolix, estradiol, and norethindrone acetate capsules). Most myomatous-related bleeding occurs in premenopausal women. The elagolix suppresses luteinizing hormone and follicle stimulating hormone, and the norethindrone is added to protect the endometrium from the estradiol. Do the elagolix and norethindrone also provide contraception?
Geoffrey J. Zann, MD, MBA
Boca Raton, Florida
Dr. Barbieri responds
Dr. Zann raises an important clinical question that arises often in practice. The US Food and Drug Administration (FDA) has not approved Oriahnn as a contraceptive. The FDA prescribing information recommends: Advise women to use non-hormonal contraception during treatment and for one week after discontinuing Oriahnn. Oriahnn may delay the ability to recognize the occurrence of a pregnancy because it alters menstrual bleeding. Perform pregnancy testing if pregnancy is suspected and discontinue Oriahnn if pregnancy is confirmed.
In Oriahnn, the elagolix dose is 300 mg twice daily. If a patient reliably takes 600 mg of elagolix daily, it is highly unlikely that she will ovulate. However, in practice, many patients miss doses of their medication, reducing the contraceptive effectiveness. For example, the combined estrogen-progestin contraceptive is highly effective at suppressing ovulation, but the Centers for Disease Control and Prevention (CDC) estimates that 9% of women taking an estrogen-progestin contraceptive will become pregnant each year.1,2
Oriahnn also contains norethindrone acetate at a dose of 0.5 mg daily. The FDA has approved norethindrone at a dose of 0.35 mg daily as a contraceptive. The CDC estimates that 9% of women prescribed a progestin-only pill will become pregnant each year with typical use.1,2
I counsel my patients that if they reliably take their prescribed Oriahnn medication as directed, they are unlikely to become pregnant, and a backup method of contraception will further help to reduce their risk of becoming pregnant.
References
- Centers for Disease Control and Prevention. US selected practice recommendations for contraceptive use, 2013. MMWR Morbid Mortal Weekly Rep. 2013;62(RR-5):1-59.
- Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397-404.
9vHPV VACCINE: PREVENTION OF OROPHARYNGEAL CANCER
ROBERT L. BARBIERI, MD (EDITORIAL; NOVEMBER 2020)
HPV vaccine for older ObGyns?
I am 67 years old and recently retired. I breathed in the smoke from laser conizations, LEEPs (loop electrosurgical excision procedures), and cautery of condyloma for 35 years. Am I a good candidate for the HPV vaccine?
Gus Barkett, DO
Muskegon, Michigan
Dr. Barbieri responds
I thank Dr. Barkett for his important question. As you know, the US Food and Drug Administration has approved 9vHPV vaccination for people 27 to 45 years of age. I do not believe there are sufficient data to provide an evidence-based answer for physicians with occupational exposure to HPV who are more than 45 years of age. My recommendation would be to have a consult with an otolaryngologist expert in HPV-induced oral-pharyngeal cancer.
EXAMINING THE EVIDENCE: HOW EFFECTIVE IS SCREENING MAMMOGRAPHY FOR PREVENTING BREAST CANCER MORTALITY?
ANDREW M. KAUNITZ, MD (AUGUST 2020)
Discordant results on screening mammography
In regard to the discussion on screening mammography for preventing breast cancer mortality, I would like to call attention to a more recent study than the ones referenced in the article. The study by Duffy and colleagues was from Sweden and included almost 550,000 women.1 Results of the study showed a statistically significant reduction of 41% in 10-year mortality and a 25% reduction in the incidence of advanced-stage disease at the time of diagnosis in women who underwent routine screening mammograms. In Sweden, routine screening is defined as a mammogram every 18 months for women aged 40 to 54 years and every 24 months after that, up to age 69.
I do not know if we will ever come to a consensus on the utility of mammograms or how often they should be done, but I wanted to illustrate this counterpoint.
Lisa Gennari, MD
Cincinnati, Ohio
Reference
1. Duffy SW, Tabar L, Yen AM, et al. Mammography screening reduces rates of advanced and fatal breast cancers: results in 549,091 women. Cancer. 2020;126:2971-2979.
Dr. Kaunitz responds
I thank Dr. Gennari for her interest in the Examining the Evidence discussion that summarized the findings of an article from Australia published in late summer of last year.1 That article indicated that as screening mammograms became common in the state of Victoria over several decades, the incidence of advanced breast cancer doubled, mirroring findings from the United States, Holland, and Norway. During the same time period, breast cancer mortality declined substantially. The authors concluded that all of the decline in breast cancer mortality that they observed since 1994 could be attributed not to screening mammography but rather to the introduction and uptake of adjuvant therapy (tamoxifen and chemotherapy).
In contrast, in the article Dr. Gennari cites, also published last summer, the authors found that the widespread uptake of screening mammograms among women residing in 9 counties in Sweden was associated with a decline in the incidence of advanced breast cancer. I am not able to explain these discrepant findings. However, as the authors pointed out, they employed a new strategy: measuring the incidence of breast cancer that proved fatal one decade after diagnosis.
Differing findings and interpretations of data that address benefits and risks of screening mammography lead to differing recommendations from professional societies and confusion among clinicians and our patients. Although it can be challenging in the constraints of time allotted for well-woman visits, I try to engage in shared decision making with my patients regarding when to start/stop mammography as well as frequency of screening.
Reference
- Burton R, Stevenson C. Assessment of breast cancer mortality trends associated with mammographic screening and adjuvant therapy from 1986 to 2013 in the state of Victoria, Australia. JAMA Netw Open. 2020:3:e208249.
Continue to: NEW HORMONAL MEDICAL TREATMENT...
NEW HORMONAL MEDICAL TREATMENT IS AN IMPORTANT ADVANCE FOR AUB CAUSED BY UTERINE FIBROIDS
ROBERT L. BARBIERI, MD (EDITORIAL; AUGUST 2020)
New AUB medical treatment
I appreciate Dr. Barbieri’s concise and pertinent review of myomatous disease etiology and treatments. I have a question regarding therapy with Oriahnn (elagolix, estradiol, and norethindrone acetate capsules). Most myomatous-related bleeding occurs in premenopausal women. The elagolix suppresses luteinizing hormone and follicle stimulating hormone, and the norethindrone is added to protect the endometrium from the estradiol. Do the elagolix and norethindrone also provide contraception?
Geoffrey J. Zann, MD, MBA
Boca Raton, Florida
Dr. Barbieri responds
Dr. Zann raises an important clinical question that arises often in practice. The US Food and Drug Administration (FDA) has not approved Oriahnn as a contraceptive. The FDA prescribing information recommends: Advise women to use non-hormonal contraception during treatment and for one week after discontinuing Oriahnn. Oriahnn may delay the ability to recognize the occurrence of a pregnancy because it alters menstrual bleeding. Perform pregnancy testing if pregnancy is suspected and discontinue Oriahnn if pregnancy is confirmed.
In Oriahnn, the elagolix dose is 300 mg twice daily. If a patient reliably takes 600 mg of elagolix daily, it is highly unlikely that she will ovulate. However, in practice, many patients miss doses of their medication, reducing the contraceptive effectiveness. For example, the combined estrogen-progestin contraceptive is highly effective at suppressing ovulation, but the Centers for Disease Control and Prevention (CDC) estimates that 9% of women taking an estrogen-progestin contraceptive will become pregnant each year.1,2
Oriahnn also contains norethindrone acetate at a dose of 0.5 mg daily. The FDA has approved norethindrone at a dose of 0.35 mg daily as a contraceptive. The CDC estimates that 9% of women prescribed a progestin-only pill will become pregnant each year with typical use.1,2
I counsel my patients that if they reliably take their prescribed Oriahnn medication as directed, they are unlikely to become pregnant, and a backup method of contraception will further help to reduce their risk of becoming pregnant.
References
- Centers for Disease Control and Prevention. US selected practice recommendations for contraceptive use, 2013. MMWR Morbid Mortal Weekly Rep. 2013;62(RR-5):1-59.
- Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397-404.
Goldenseal may interfere with metformin absorption, jeopardizing glucose control
Goldenseal, a natural botanical product, may interfere with intestinal absorption of metformin, potentially compromising blood glucose control in patients with type 2 diabetes, according to investigators.
The study, which tested for interactions between goldenseal and several drugs in healthy volunteers, reveals that current models for predicting transporter-mediated drug-drug interactions may be insufficient to screen commonly used dietary supplements, reported lead investigator James T. Nguyen, PharmD, a PhD candidate at Washington State University, Spokane, and colleagues.
“Supplements containing goldenseal ... a perennial herb native to North America, have consistently ranked among the top 20 highest selling natural products during the last decade,” the investigators wrote in Clinical Pharmacology & Therapeutics . “As more patients continue to seek goldenseal and other natural products to self-treat their medical conditions, there is an increasing need to characterize their safety profiles, especially when co-consumed with prescribed medications, which can lead to adverse natural product-drug interactions.”
Previous clinical studies have shown that goldenseal inhibits cytochrome P450, with one study showing a roughly 40% increase in systemic midazolam exposure via CYP3A inhibition, “suggesting goldenseal could have prolonged inhibitory effects in vivo similar to grapefruit juice,” the investigators wrote.
Clinical and in vitro results for goldenseal-transporter interactions have been mixed, the investigators noted, specifically for P-glycoprotein, while other transporters remain clinically untested.
“Likewise, the effects of [goldenseal alkaloids], all of which are time-dependent inhibitors of CYP3A and/or CYP2D6, have not been tested on transporter function,” the investigators wrote.
To address this knowledge gap, the investigators first performed in vitro transporter inhibition assays and in vitro–in vivo predictions involving goldenseal, plus the alkaloids berberine, (−)-beta-hydrastine, and hydrastinine.
This analysis revealed that a number of transporters were sensitive to inhibition by goldenseal and its alkaloids.
“Using current [Food and Drug Administration]–recommended basic models, the goldenseal product was predicted to inhibit the intestinal efflux transporter BCRP [breast cancer resistance protein] and the hepatic uptake transporters OATP1B1 and OATP1B3,” the investigators wrote, which suggested that goldenseal would increase the area under the plasma concentration-time curve (AUC) of rosuvastatin acid and lactone.
This prediction was clinically tested in 16 healthy volunteers: 8 men and 8 nonpregnant women.
In the baseline portion of the study, each participant received an oral transporter probe cocktail consisting of 10 mg rosuvastatin (OATP1B1/3 and BCRP), 50 mg metformin (OCT1/2 and MATE1/2-K), 1 mg furosemide (OAT1/3), and 2.5 mg midazolam (CYP3A; positive control). Plasma and urine samples were collected before and after the cocktail, with urine collected up to 24 hours later, and plasma collected up to 96 hours later.
Following a minimum 9-day washout period, the same cohort received 1 gram of goldenseal every 8 hours for 5 days. On the day 6, the drug cocktail was given again, followed by two additional doses of goldenseal at 4-hour intervals. At the same time points used in the baseline protocol, urine and plasma samples were collected.
Plasma concentration vs. time profiles revealed that the model-based prediction was false, in that the presence of goldenseal did not alter the pharmacokinetics of rosuvastatin acid and lactone. The investigators suggested that this could be due to incomplete dissolution of goldenseal in the intestinal lumen, and/or low enterocyte concentrations of goldenseal stemming from “low permeability or extensive enterocyte metabolism or efflux.”
In contrast, and unpredicted by the basic model, goldenseal had a significant impact on apical efflux transporters MATE1 and MATE2-K, which mediate renal excretion of metformin. In consequence, AUC from zero to infinity and maximum plasma concentration of metformin were reduced by 23% and 27%, respectively.
“These observations, coupled with no change in half-life, suggested that goldenseal decreased metformin oral bioavailability by altering intestinal permeability, transport, and/or other processes involved in metformin absorption,” the investigators wrote.
According to principal author Mary Paine, PhD, of Washington State University, Spokane, this finding may have clinically significant implications for patients currently taking metformin for type 2 diabetes.
“Our study showed that goldenseal has an effect on the intestinal absorption of metformin, suggesting that the co-use of metformin and goldenseal may compromise blood glucose control in patients with type 2 diabetes and increase their risk of negative health outcomes,” Dr. Paine said. “While this finding warrants a degree of caution to be exercised among patients and their treating physicians, we have more work to do to confirm whether these findings in healthy volunteers in fact have clinical relevance in the management of diabetes. We are in the process of starting a follow-up study that should ultimately answer that question.”
The study was supported by the National Institutes of Health. The investigators reported no conflicts of interest.
Goldenseal, a natural botanical product, may interfere with intestinal absorption of metformin, potentially compromising blood glucose control in patients with type 2 diabetes, according to investigators.
The study, which tested for interactions between goldenseal and several drugs in healthy volunteers, reveals that current models for predicting transporter-mediated drug-drug interactions may be insufficient to screen commonly used dietary supplements, reported lead investigator James T. Nguyen, PharmD, a PhD candidate at Washington State University, Spokane, and colleagues.
“Supplements containing goldenseal ... a perennial herb native to North America, have consistently ranked among the top 20 highest selling natural products during the last decade,” the investigators wrote in Clinical Pharmacology & Therapeutics . “As more patients continue to seek goldenseal and other natural products to self-treat their medical conditions, there is an increasing need to characterize their safety profiles, especially when co-consumed with prescribed medications, which can lead to adverse natural product-drug interactions.”
Previous clinical studies have shown that goldenseal inhibits cytochrome P450, with one study showing a roughly 40% increase in systemic midazolam exposure via CYP3A inhibition, “suggesting goldenseal could have prolonged inhibitory effects in vivo similar to grapefruit juice,” the investigators wrote.
Clinical and in vitro results for goldenseal-transporter interactions have been mixed, the investigators noted, specifically for P-glycoprotein, while other transporters remain clinically untested.
“Likewise, the effects of [goldenseal alkaloids], all of which are time-dependent inhibitors of CYP3A and/or CYP2D6, have not been tested on transporter function,” the investigators wrote.
To address this knowledge gap, the investigators first performed in vitro transporter inhibition assays and in vitro–in vivo predictions involving goldenseal, plus the alkaloids berberine, (−)-beta-hydrastine, and hydrastinine.
This analysis revealed that a number of transporters were sensitive to inhibition by goldenseal and its alkaloids.
“Using current [Food and Drug Administration]–recommended basic models, the goldenseal product was predicted to inhibit the intestinal efflux transporter BCRP [breast cancer resistance protein] and the hepatic uptake transporters OATP1B1 and OATP1B3,” the investigators wrote, which suggested that goldenseal would increase the area under the plasma concentration-time curve (AUC) of rosuvastatin acid and lactone.
This prediction was clinically tested in 16 healthy volunteers: 8 men and 8 nonpregnant women.
In the baseline portion of the study, each participant received an oral transporter probe cocktail consisting of 10 mg rosuvastatin (OATP1B1/3 and BCRP), 50 mg metformin (OCT1/2 and MATE1/2-K), 1 mg furosemide (OAT1/3), and 2.5 mg midazolam (CYP3A; positive control). Plasma and urine samples were collected before and after the cocktail, with urine collected up to 24 hours later, and plasma collected up to 96 hours later.
Following a minimum 9-day washout period, the same cohort received 1 gram of goldenseal every 8 hours for 5 days. On the day 6, the drug cocktail was given again, followed by two additional doses of goldenseal at 4-hour intervals. At the same time points used in the baseline protocol, urine and plasma samples were collected.
Plasma concentration vs. time profiles revealed that the model-based prediction was false, in that the presence of goldenseal did not alter the pharmacokinetics of rosuvastatin acid and lactone. The investigators suggested that this could be due to incomplete dissolution of goldenseal in the intestinal lumen, and/or low enterocyte concentrations of goldenseal stemming from “low permeability or extensive enterocyte metabolism or efflux.”
In contrast, and unpredicted by the basic model, goldenseal had a significant impact on apical efflux transporters MATE1 and MATE2-K, which mediate renal excretion of metformin. In consequence, AUC from zero to infinity and maximum plasma concentration of metformin were reduced by 23% and 27%, respectively.
“These observations, coupled with no change in half-life, suggested that goldenseal decreased metformin oral bioavailability by altering intestinal permeability, transport, and/or other processes involved in metformin absorption,” the investigators wrote.
According to principal author Mary Paine, PhD, of Washington State University, Spokane, this finding may have clinically significant implications for patients currently taking metformin for type 2 diabetes.
“Our study showed that goldenseal has an effect on the intestinal absorption of metformin, suggesting that the co-use of metformin and goldenseal may compromise blood glucose control in patients with type 2 diabetes and increase their risk of negative health outcomes,” Dr. Paine said. “While this finding warrants a degree of caution to be exercised among patients and their treating physicians, we have more work to do to confirm whether these findings in healthy volunteers in fact have clinical relevance in the management of diabetes. We are in the process of starting a follow-up study that should ultimately answer that question.”
The study was supported by the National Institutes of Health. The investigators reported no conflicts of interest.
Goldenseal, a natural botanical product, may interfere with intestinal absorption of metformin, potentially compromising blood glucose control in patients with type 2 diabetes, according to investigators.
The study, which tested for interactions between goldenseal and several drugs in healthy volunteers, reveals that current models for predicting transporter-mediated drug-drug interactions may be insufficient to screen commonly used dietary supplements, reported lead investigator James T. Nguyen, PharmD, a PhD candidate at Washington State University, Spokane, and colleagues.
“Supplements containing goldenseal ... a perennial herb native to North America, have consistently ranked among the top 20 highest selling natural products during the last decade,” the investigators wrote in Clinical Pharmacology & Therapeutics . “As more patients continue to seek goldenseal and other natural products to self-treat their medical conditions, there is an increasing need to characterize their safety profiles, especially when co-consumed with prescribed medications, which can lead to adverse natural product-drug interactions.”
Previous clinical studies have shown that goldenseal inhibits cytochrome P450, with one study showing a roughly 40% increase in systemic midazolam exposure via CYP3A inhibition, “suggesting goldenseal could have prolonged inhibitory effects in vivo similar to grapefruit juice,” the investigators wrote.
Clinical and in vitro results for goldenseal-transporter interactions have been mixed, the investigators noted, specifically for P-glycoprotein, while other transporters remain clinically untested.
“Likewise, the effects of [goldenseal alkaloids], all of which are time-dependent inhibitors of CYP3A and/or CYP2D6, have not been tested on transporter function,” the investigators wrote.
To address this knowledge gap, the investigators first performed in vitro transporter inhibition assays and in vitro–in vivo predictions involving goldenseal, plus the alkaloids berberine, (−)-beta-hydrastine, and hydrastinine.
This analysis revealed that a number of transporters were sensitive to inhibition by goldenseal and its alkaloids.
“Using current [Food and Drug Administration]–recommended basic models, the goldenseal product was predicted to inhibit the intestinal efflux transporter BCRP [breast cancer resistance protein] and the hepatic uptake transporters OATP1B1 and OATP1B3,” the investigators wrote, which suggested that goldenseal would increase the area under the plasma concentration-time curve (AUC) of rosuvastatin acid and lactone.
This prediction was clinically tested in 16 healthy volunteers: 8 men and 8 nonpregnant women.
In the baseline portion of the study, each participant received an oral transporter probe cocktail consisting of 10 mg rosuvastatin (OATP1B1/3 and BCRP), 50 mg metformin (OCT1/2 and MATE1/2-K), 1 mg furosemide (OAT1/3), and 2.5 mg midazolam (CYP3A; positive control). Plasma and urine samples were collected before and after the cocktail, with urine collected up to 24 hours later, and plasma collected up to 96 hours later.
Following a minimum 9-day washout period, the same cohort received 1 gram of goldenseal every 8 hours for 5 days. On the day 6, the drug cocktail was given again, followed by two additional doses of goldenseal at 4-hour intervals. At the same time points used in the baseline protocol, urine and plasma samples were collected.
Plasma concentration vs. time profiles revealed that the model-based prediction was false, in that the presence of goldenseal did not alter the pharmacokinetics of rosuvastatin acid and lactone. The investigators suggested that this could be due to incomplete dissolution of goldenseal in the intestinal lumen, and/or low enterocyte concentrations of goldenseal stemming from “low permeability or extensive enterocyte metabolism or efflux.”
In contrast, and unpredicted by the basic model, goldenseal had a significant impact on apical efflux transporters MATE1 and MATE2-K, which mediate renal excretion of metformin. In consequence, AUC from zero to infinity and maximum plasma concentration of metformin were reduced by 23% and 27%, respectively.
“These observations, coupled with no change in half-life, suggested that goldenseal decreased metformin oral bioavailability by altering intestinal permeability, transport, and/or other processes involved in metformin absorption,” the investigators wrote.
According to principal author Mary Paine, PhD, of Washington State University, Spokane, this finding may have clinically significant implications for patients currently taking metformin for type 2 diabetes.
“Our study showed that goldenseal has an effect on the intestinal absorption of metformin, suggesting that the co-use of metformin and goldenseal may compromise blood glucose control in patients with type 2 diabetes and increase their risk of negative health outcomes,” Dr. Paine said. “While this finding warrants a degree of caution to be exercised among patients and their treating physicians, we have more work to do to confirm whether these findings in healthy volunteers in fact have clinical relevance in the management of diabetes. We are in the process of starting a follow-up study that should ultimately answer that question.”
The study was supported by the National Institutes of Health. The investigators reported no conflicts of interest.
FROM CLINICAL PHARMACOLOGY & THERAPEUTICS
Roots of physician burnout: It’s the work load
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
FROM THE JOINT COMMISSION JOURNAL ON QUALITY AND PATIENT SAFETY
CDC chief lays out attack plan for COVID variants
earlier this week.
As part of JAMA’s Q&A series with JAMA editor in chief Howard Bauchner, MD, Dr. Walensky referenced the blueprint she coathored with Anthony Fauci, MD, the nation’s top infectious disease expert, and Henry T. Walke, MD, MPH, of the CDC, which was published on Feb. 17 in JAMA.
In the viewpoint article, they explain that the Department of Health & Human Services has established the SARS-CoV-2 Interagency Group to improve coordination among the CDC, the National Institutes of Health, the Food and Drug Administration, the Biomedical Advanced Research and Development Authority, the Department of Agriculture, and the Department of Defense.
Dr. Walensky said the first objective is to reinforce vigilance regarding public health mitigation strategies to decrease the amount of virus that’s circulating.
As part of that strategy, she said, the CDC strongly urges against nonessential travel.
In addition, public health leaders are working on a surveillance system to better understand the SARS-CoV-2 variants. That will take ramping up genome sequencing of the SARS-CoV-2 virus and ensuring that sampling is geographically representative.
She said the CDC is partnering with state health labs to obtain about 750 samples every week and is teaming up with commercial labs and academic centers to obtain an interim target of 6,000 samples per week.
She acknowledged the United States “is not where we need to be” with sequencing but has come a long way since January. At that time, they were sequencing 250 samples every week; they are currently sequencing thousands each week.
Data analysis is another concern: “We need to be able to understand at the basic science level what the information means,” Dr. Walensky said.
Researchers aren’t sure how the variants might affect use of convalescent plasma or monoclonal antibody treatments. It is expected that 5% of persons who are vaccinated against COVID-19 will nevertheless contract the disease. Sequencing will help answer whether such persons who have been vaccinated and who subsequently contract the virus are among those 5% or whether have been infected by a variant that evades the vaccine.
Accelerating vaccine administration globally and in the United States is essential, Dr. Walensky said.
As of Feb. 17, 56 million doses had been administered in the United States.
Top three threats
She updated the numbers on the three biggest variant threats.
Regarding B.1.1.7, which originated in the United Kingdom, she said: “So far, we’ve had over 1,200 cases in 41 states.” She noted that the variant is likely to be about 50% more transmissible and 30% to 50% more virulent.
“So far, it looks like that strain doesn’t have any real decrease in susceptibility to our vaccines,” she said.
The strain from South Africa (B.1.351) has been found in 19 cases in the United States.
The P.1. variant, which originated in Brazil, has been identified in two cases in two states.
Outlook for March and April
Dr. Bauchner asked Dr. Walensky what she envisions for March and April. He noted that public optimism is high in light of the continued reductions in COVID-19 case numbers, hospitalizations, and deaths, as well as the fact that warmer weather is coming and that more vaccinations are on the horizon.
“While I really am hopeful for what could happen in March and April,” Dr. Walensky said, “I really do know that this could go bad so fast. We saw it in November. We saw it in December.”
CDC models have projected that, by March, the more transmissible B.1.1.7 strain is likely to be the dominant strain, she reiterated.
“I worry that it will be spring, and we will all have had enough,” Dr. Walensky said. She noted that some states are already relaxing mask mandates.
“Around that time, life will look and feel a little better, and the motivation for those who might be vaccine hesitant may be diminished,” she said.
Dr. Bauchner also asked her to weigh in on whether a third vaccine, from Johnson & Johnson (J&J), may soon gain FDA emergency-use authorization – and whether its lower expected efficacy rate may result in a tiered system of vaccinations, with higher-risk populations receiving the more efficacious vaccines.
Dr. Walensky said more data are needed before that question can be answered.
“It may very well be that the data point us to the best populations in which to use this vaccine,” she said.
In phase 3 data, the J&J vaccine was shown to be 72% effective in the United States for moderate to severe disease.
Dr. Walensky said it’s important to remember that the projected efficacy for that vaccine is higher than that for the flu shot as well as many other vaccines currently in use for other diseases.
She said it also has several advantages. The vaccine has less-stringent storage requirements, requires just one dose, and protects against hospitalization and death, although it’s less efficacious in protecting against contracting the disease.
“I think many people would opt to get that one if they could get it sooner,” she said.
A version of this article first appeared on Medscape.com.
earlier this week.
As part of JAMA’s Q&A series with JAMA editor in chief Howard Bauchner, MD, Dr. Walensky referenced the blueprint she coathored with Anthony Fauci, MD, the nation’s top infectious disease expert, and Henry T. Walke, MD, MPH, of the CDC, which was published on Feb. 17 in JAMA.
In the viewpoint article, they explain that the Department of Health & Human Services has established the SARS-CoV-2 Interagency Group to improve coordination among the CDC, the National Institutes of Health, the Food and Drug Administration, the Biomedical Advanced Research and Development Authority, the Department of Agriculture, and the Department of Defense.
Dr. Walensky said the first objective is to reinforce vigilance regarding public health mitigation strategies to decrease the amount of virus that’s circulating.
As part of that strategy, she said, the CDC strongly urges against nonessential travel.
In addition, public health leaders are working on a surveillance system to better understand the SARS-CoV-2 variants. That will take ramping up genome sequencing of the SARS-CoV-2 virus and ensuring that sampling is geographically representative.
She said the CDC is partnering with state health labs to obtain about 750 samples every week and is teaming up with commercial labs and academic centers to obtain an interim target of 6,000 samples per week.
She acknowledged the United States “is not where we need to be” with sequencing but has come a long way since January. At that time, they were sequencing 250 samples every week; they are currently sequencing thousands each week.
Data analysis is another concern: “We need to be able to understand at the basic science level what the information means,” Dr. Walensky said.
Researchers aren’t sure how the variants might affect use of convalescent plasma or monoclonal antibody treatments. It is expected that 5% of persons who are vaccinated against COVID-19 will nevertheless contract the disease. Sequencing will help answer whether such persons who have been vaccinated and who subsequently contract the virus are among those 5% or whether have been infected by a variant that evades the vaccine.
Accelerating vaccine administration globally and in the United States is essential, Dr. Walensky said.
As of Feb. 17, 56 million doses had been administered in the United States.
Top three threats
She updated the numbers on the three biggest variant threats.
Regarding B.1.1.7, which originated in the United Kingdom, she said: “So far, we’ve had over 1,200 cases in 41 states.” She noted that the variant is likely to be about 50% more transmissible and 30% to 50% more virulent.
“So far, it looks like that strain doesn’t have any real decrease in susceptibility to our vaccines,” she said.
The strain from South Africa (B.1.351) has been found in 19 cases in the United States.
The P.1. variant, which originated in Brazil, has been identified in two cases in two states.
Outlook for March and April
Dr. Bauchner asked Dr. Walensky what she envisions for March and April. He noted that public optimism is high in light of the continued reductions in COVID-19 case numbers, hospitalizations, and deaths, as well as the fact that warmer weather is coming and that more vaccinations are on the horizon.
“While I really am hopeful for what could happen in March and April,” Dr. Walensky said, “I really do know that this could go bad so fast. We saw it in November. We saw it in December.”
CDC models have projected that, by March, the more transmissible B.1.1.7 strain is likely to be the dominant strain, she reiterated.
“I worry that it will be spring, and we will all have had enough,” Dr. Walensky said. She noted that some states are already relaxing mask mandates.
“Around that time, life will look and feel a little better, and the motivation for those who might be vaccine hesitant may be diminished,” she said.
Dr. Bauchner also asked her to weigh in on whether a third vaccine, from Johnson & Johnson (J&J), may soon gain FDA emergency-use authorization – and whether its lower expected efficacy rate may result in a tiered system of vaccinations, with higher-risk populations receiving the more efficacious vaccines.
Dr. Walensky said more data are needed before that question can be answered.
“It may very well be that the data point us to the best populations in which to use this vaccine,” she said.
In phase 3 data, the J&J vaccine was shown to be 72% effective in the United States for moderate to severe disease.
Dr. Walensky said it’s important to remember that the projected efficacy for that vaccine is higher than that for the flu shot as well as many other vaccines currently in use for other diseases.
She said it also has several advantages. The vaccine has less-stringent storage requirements, requires just one dose, and protects against hospitalization and death, although it’s less efficacious in protecting against contracting the disease.
“I think many people would opt to get that one if they could get it sooner,” she said.
A version of this article first appeared on Medscape.com.
earlier this week.
As part of JAMA’s Q&A series with JAMA editor in chief Howard Bauchner, MD, Dr. Walensky referenced the blueprint she coathored with Anthony Fauci, MD, the nation’s top infectious disease expert, and Henry T. Walke, MD, MPH, of the CDC, which was published on Feb. 17 in JAMA.
In the viewpoint article, they explain that the Department of Health & Human Services has established the SARS-CoV-2 Interagency Group to improve coordination among the CDC, the National Institutes of Health, the Food and Drug Administration, the Biomedical Advanced Research and Development Authority, the Department of Agriculture, and the Department of Defense.
Dr. Walensky said the first objective is to reinforce vigilance regarding public health mitigation strategies to decrease the amount of virus that’s circulating.
As part of that strategy, she said, the CDC strongly urges against nonessential travel.
In addition, public health leaders are working on a surveillance system to better understand the SARS-CoV-2 variants. That will take ramping up genome sequencing of the SARS-CoV-2 virus and ensuring that sampling is geographically representative.
She said the CDC is partnering with state health labs to obtain about 750 samples every week and is teaming up with commercial labs and academic centers to obtain an interim target of 6,000 samples per week.
She acknowledged the United States “is not where we need to be” with sequencing but has come a long way since January. At that time, they were sequencing 250 samples every week; they are currently sequencing thousands each week.
Data analysis is another concern: “We need to be able to understand at the basic science level what the information means,” Dr. Walensky said.
Researchers aren’t sure how the variants might affect use of convalescent plasma or monoclonal antibody treatments. It is expected that 5% of persons who are vaccinated against COVID-19 will nevertheless contract the disease. Sequencing will help answer whether such persons who have been vaccinated and who subsequently contract the virus are among those 5% or whether have been infected by a variant that evades the vaccine.
Accelerating vaccine administration globally and in the United States is essential, Dr. Walensky said.
As of Feb. 17, 56 million doses had been administered in the United States.
Top three threats
She updated the numbers on the three biggest variant threats.
Regarding B.1.1.7, which originated in the United Kingdom, she said: “So far, we’ve had over 1,200 cases in 41 states.” She noted that the variant is likely to be about 50% more transmissible and 30% to 50% more virulent.
“So far, it looks like that strain doesn’t have any real decrease in susceptibility to our vaccines,” she said.
The strain from South Africa (B.1.351) has been found in 19 cases in the United States.
The P.1. variant, which originated in Brazil, has been identified in two cases in two states.
Outlook for March and April
Dr. Bauchner asked Dr. Walensky what she envisions for March and April. He noted that public optimism is high in light of the continued reductions in COVID-19 case numbers, hospitalizations, and deaths, as well as the fact that warmer weather is coming and that more vaccinations are on the horizon.
“While I really am hopeful for what could happen in March and April,” Dr. Walensky said, “I really do know that this could go bad so fast. We saw it in November. We saw it in December.”
CDC models have projected that, by March, the more transmissible B.1.1.7 strain is likely to be the dominant strain, she reiterated.
“I worry that it will be spring, and we will all have had enough,” Dr. Walensky said. She noted that some states are already relaxing mask mandates.
“Around that time, life will look and feel a little better, and the motivation for those who might be vaccine hesitant may be diminished,” she said.
Dr. Bauchner also asked her to weigh in on whether a third vaccine, from Johnson & Johnson (J&J), may soon gain FDA emergency-use authorization – and whether its lower expected efficacy rate may result in a tiered system of vaccinations, with higher-risk populations receiving the more efficacious vaccines.
Dr. Walensky said more data are needed before that question can be answered.
“It may very well be that the data point us to the best populations in which to use this vaccine,” she said.
In phase 3 data, the J&J vaccine was shown to be 72% effective in the United States for moderate to severe disease.
Dr. Walensky said it’s important to remember that the projected efficacy for that vaccine is higher than that for the flu shot as well as many other vaccines currently in use for other diseases.
She said it also has several advantages. The vaccine has less-stringent storage requirements, requires just one dose, and protects against hospitalization and death, although it’s less efficacious in protecting against contracting the disease.
“I think many people would opt to get that one if they could get it sooner,” she said.
A version of this article first appeared on Medscape.com.
CAR T-cell products shine in real-world setting, reveal new insights
Real-world experience with chimeric antigen receptor (CAR) T-cell therapies for large B-cell lymphomas compares favorably with experience in commercial and trial settings and provides new insights for predicting outcomes, according to Paolo Corradini, MD.
The 12-month duration of response (DOR) and progression-free survival (PFS) rates in 152 real-world patients treated with tisagenlecleucel (tisa-cel; Kymriah) for an approved indication were 48.4% and 26.4%, respectively, data reported to the Center for International Blood and Marrow Transplant Research (CIBMTR) and published in November 2020 in Blood Advances showed.
who relapsed or were refractory to at least two prior lines of therapy, Dr. Corradini said at the third European CAR T-cell Meeting, jointly sponsored by the European Society for Blood and Marrow Transplantation and the European Hematology Association.
A clinical update of the JULIET trial, as presented by Dr. Corradini and colleagues in a poster at the 2020 annual conference of the American Society of Hematology, showed a relapse-free probability of 60.4% at 24 and 30 months among 61 patients with an initial response.
The 12- and 36-month PFS rates as of February 2020, with median follow-up of 40.3 months, were 33% and 31%, respectively, and no new safety signals were identified, said Dr. Corradini, chair of hematology at the University of Milan.
Similarly, real-world data from the U.S. Lymphoma CAR T Consortium showing median PFS of 8.3 months at median follow-up of 12.9 months in 275 patients treated with axicabtagene ciloleucel (axi-cel; YESCARTA) were comparable with outcomes in the ZUMA-1 registrational trial, he noted.
An ongoing response was seen at 2 years in 39% of patients in ZUMA-1, and 3-year survival was 47%, according to an update reported at ASH 2019.
Of note, 43% of patients in the real-world study, which was published in the Journal of Clinical Oncology in September 2020, would not have met ZUMA-1 eligibility criteria because of comorbidities at the time of leukapheresis.
Predicting outcomes
The real-world data also demonstrated that performance status and lactate dehydrogenase (LDH) levels can predict outcomes: Patients with poor Eastern Cooperative Oncology Group performance status of 2-4 versus less than 2, and elevated LDH had shorter PFS and overall survival (OS) on both univariate and multivariate analysis, Dr. Corradini noted.
A subsequent multicenter study showed similar response rates of 70% and 68% in ZUMA-1-eligible and noneligible patients, but significantly improved DOR, PFS, and OS outcomes among the ZUMA-1-eligible patients.
The authors also looked for “clinical predictive factors or some easy clinical biomarkers to predict the outcomes in our patients receiving CAR T-cells,” and found that C-reactive protein levels of more than 30 mg at infusion were associated with poorer DOR, PFS, and OS, he said.
In 60 patients in another U.S. study of both tisa-cel- and axi-cel-treated patients at Memorial Sloan Kettering Cancer Center, 1-year event-free survival and OS were 40% and 69%, and Dr. Corradini’s experience with 55 patients at the University of Milan similarly showed 1-year PFS and OS of 40% and 70%, respectively.
“So all these studies support the notion that the results of CAR T-cells in real-world practice are durable for our patients, and are very similar to results obtained in the studies,” he said.
Other factors that have been shown to be associated with poor outcomes after CAR T-cell therapy include systemic bridging therapy, high metabolic tumor volume, and extranodal involvement; patients with these characteristics, along with those who have poor ECOG performance status or elevated LDH or CRP levels, do not comprise “a group to exclude from CAR T-cell therapy, but rather ... a group for whom there is an unmet need with our currently available treatments,” he said, adding: “So, it’s a group for which we have to do clinical trials and studies to improve the outcomes of our patient with large B-cell lymphomas.”
“These are all real-world data with commercially available products, he noted.
Product selection
Tisa-cel received Food and Drug Administration approval in 2017 and is used to treat relapsed or refractory acute lymphoblastic leukemia in those aged up to 25 years, and non-Hodgkin lymphoma that has relapsed or is refractory after at least two prior lines of therapy.
Axi-cel was also approved in 2017 for relapsed/refractory non-Hodgkin lymphoma, and in February 2021, after Dr. Corradini’s meeting presentation, the FDA granted a third approval to lisocabtagene maraleucel (liso-cel; Breyanzi) for this indication.
The information to date from both the trial and real-world settings are limited with respect to showing any differences in outcomes between the CAR T-cell products, but provide “an initial suggestion” that outcomes with tisa-cel and axi-cel are comparable, he said, adding that decisions should be strictly based on product registration data given the absence of reliable data for choosing one product over another.
Dr. Corradini reported honoraria and/or payment for travel and accommodations from Abbvie, Amgen, Bristol-Myers Squibb, Celgene, Daiichi Sankyo, and a number of other pharmaceutical companies.
Real-world experience with chimeric antigen receptor (CAR) T-cell therapies for large B-cell lymphomas compares favorably with experience in commercial and trial settings and provides new insights for predicting outcomes, according to Paolo Corradini, MD.
The 12-month duration of response (DOR) and progression-free survival (PFS) rates in 152 real-world patients treated with tisagenlecleucel (tisa-cel; Kymriah) for an approved indication were 48.4% and 26.4%, respectively, data reported to the Center for International Blood and Marrow Transplant Research (CIBMTR) and published in November 2020 in Blood Advances showed.
who relapsed or were refractory to at least two prior lines of therapy, Dr. Corradini said at the third European CAR T-cell Meeting, jointly sponsored by the European Society for Blood and Marrow Transplantation and the European Hematology Association.
A clinical update of the JULIET trial, as presented by Dr. Corradini and colleagues in a poster at the 2020 annual conference of the American Society of Hematology, showed a relapse-free probability of 60.4% at 24 and 30 months among 61 patients with an initial response.
The 12- and 36-month PFS rates as of February 2020, with median follow-up of 40.3 months, were 33% and 31%, respectively, and no new safety signals were identified, said Dr. Corradini, chair of hematology at the University of Milan.
Similarly, real-world data from the U.S. Lymphoma CAR T Consortium showing median PFS of 8.3 months at median follow-up of 12.9 months in 275 patients treated with axicabtagene ciloleucel (axi-cel; YESCARTA) were comparable with outcomes in the ZUMA-1 registrational trial, he noted.
An ongoing response was seen at 2 years in 39% of patients in ZUMA-1, and 3-year survival was 47%, according to an update reported at ASH 2019.
Of note, 43% of patients in the real-world study, which was published in the Journal of Clinical Oncology in September 2020, would not have met ZUMA-1 eligibility criteria because of comorbidities at the time of leukapheresis.
Predicting outcomes
The real-world data also demonstrated that performance status and lactate dehydrogenase (LDH) levels can predict outcomes: Patients with poor Eastern Cooperative Oncology Group performance status of 2-4 versus less than 2, and elevated LDH had shorter PFS and overall survival (OS) on both univariate and multivariate analysis, Dr. Corradini noted.
A subsequent multicenter study showed similar response rates of 70% and 68% in ZUMA-1-eligible and noneligible patients, but significantly improved DOR, PFS, and OS outcomes among the ZUMA-1-eligible patients.
The authors also looked for “clinical predictive factors or some easy clinical biomarkers to predict the outcomes in our patients receiving CAR T-cells,” and found that C-reactive protein levels of more than 30 mg at infusion were associated with poorer DOR, PFS, and OS, he said.
In 60 patients in another U.S. study of both tisa-cel- and axi-cel-treated patients at Memorial Sloan Kettering Cancer Center, 1-year event-free survival and OS were 40% and 69%, and Dr. Corradini’s experience with 55 patients at the University of Milan similarly showed 1-year PFS and OS of 40% and 70%, respectively.
“So all these studies support the notion that the results of CAR T-cells in real-world practice are durable for our patients, and are very similar to results obtained in the studies,” he said.
Other factors that have been shown to be associated with poor outcomes after CAR T-cell therapy include systemic bridging therapy, high metabolic tumor volume, and extranodal involvement; patients with these characteristics, along with those who have poor ECOG performance status or elevated LDH or CRP levels, do not comprise “a group to exclude from CAR T-cell therapy, but rather ... a group for whom there is an unmet need with our currently available treatments,” he said, adding: “So, it’s a group for which we have to do clinical trials and studies to improve the outcomes of our patient with large B-cell lymphomas.”
“These are all real-world data with commercially available products, he noted.
Product selection
Tisa-cel received Food and Drug Administration approval in 2017 and is used to treat relapsed or refractory acute lymphoblastic leukemia in those aged up to 25 years, and non-Hodgkin lymphoma that has relapsed or is refractory after at least two prior lines of therapy.
Axi-cel was also approved in 2017 for relapsed/refractory non-Hodgkin lymphoma, and in February 2021, after Dr. Corradini’s meeting presentation, the FDA granted a third approval to lisocabtagene maraleucel (liso-cel; Breyanzi) for this indication.
The information to date from both the trial and real-world settings are limited with respect to showing any differences in outcomes between the CAR T-cell products, but provide “an initial suggestion” that outcomes with tisa-cel and axi-cel are comparable, he said, adding that decisions should be strictly based on product registration data given the absence of reliable data for choosing one product over another.
Dr. Corradini reported honoraria and/or payment for travel and accommodations from Abbvie, Amgen, Bristol-Myers Squibb, Celgene, Daiichi Sankyo, and a number of other pharmaceutical companies.
Real-world experience with chimeric antigen receptor (CAR) T-cell therapies for large B-cell lymphomas compares favorably with experience in commercial and trial settings and provides new insights for predicting outcomes, according to Paolo Corradini, MD.
The 12-month duration of response (DOR) and progression-free survival (PFS) rates in 152 real-world patients treated with tisagenlecleucel (tisa-cel; Kymriah) for an approved indication were 48.4% and 26.4%, respectively, data reported to the Center for International Blood and Marrow Transplant Research (CIBMTR) and published in November 2020 in Blood Advances showed.
who relapsed or were refractory to at least two prior lines of therapy, Dr. Corradini said at the third European CAR T-cell Meeting, jointly sponsored by the European Society for Blood and Marrow Transplantation and the European Hematology Association.
A clinical update of the JULIET trial, as presented by Dr. Corradini and colleagues in a poster at the 2020 annual conference of the American Society of Hematology, showed a relapse-free probability of 60.4% at 24 and 30 months among 61 patients with an initial response.
The 12- and 36-month PFS rates as of February 2020, with median follow-up of 40.3 months, were 33% and 31%, respectively, and no new safety signals were identified, said Dr. Corradini, chair of hematology at the University of Milan.
Similarly, real-world data from the U.S. Lymphoma CAR T Consortium showing median PFS of 8.3 months at median follow-up of 12.9 months in 275 patients treated with axicabtagene ciloleucel (axi-cel; YESCARTA) were comparable with outcomes in the ZUMA-1 registrational trial, he noted.
An ongoing response was seen at 2 years in 39% of patients in ZUMA-1, and 3-year survival was 47%, according to an update reported at ASH 2019.
Of note, 43% of patients in the real-world study, which was published in the Journal of Clinical Oncology in September 2020, would not have met ZUMA-1 eligibility criteria because of comorbidities at the time of leukapheresis.
Predicting outcomes
The real-world data also demonstrated that performance status and lactate dehydrogenase (LDH) levels can predict outcomes: Patients with poor Eastern Cooperative Oncology Group performance status of 2-4 versus less than 2, and elevated LDH had shorter PFS and overall survival (OS) on both univariate and multivariate analysis, Dr. Corradini noted.
A subsequent multicenter study showed similar response rates of 70% and 68% in ZUMA-1-eligible and noneligible patients, but significantly improved DOR, PFS, and OS outcomes among the ZUMA-1-eligible patients.
The authors also looked for “clinical predictive factors or some easy clinical biomarkers to predict the outcomes in our patients receiving CAR T-cells,” and found that C-reactive protein levels of more than 30 mg at infusion were associated with poorer DOR, PFS, and OS, he said.
In 60 patients in another U.S. study of both tisa-cel- and axi-cel-treated patients at Memorial Sloan Kettering Cancer Center, 1-year event-free survival and OS were 40% and 69%, and Dr. Corradini’s experience with 55 patients at the University of Milan similarly showed 1-year PFS and OS of 40% and 70%, respectively.
“So all these studies support the notion that the results of CAR T-cells in real-world practice are durable for our patients, and are very similar to results obtained in the studies,” he said.
Other factors that have been shown to be associated with poor outcomes after CAR T-cell therapy include systemic bridging therapy, high metabolic tumor volume, and extranodal involvement; patients with these characteristics, along with those who have poor ECOG performance status or elevated LDH or CRP levels, do not comprise “a group to exclude from CAR T-cell therapy, but rather ... a group for whom there is an unmet need with our currently available treatments,” he said, adding: “So, it’s a group for which we have to do clinical trials and studies to improve the outcomes of our patient with large B-cell lymphomas.”
“These are all real-world data with commercially available products, he noted.
Product selection
Tisa-cel received Food and Drug Administration approval in 2017 and is used to treat relapsed or refractory acute lymphoblastic leukemia in those aged up to 25 years, and non-Hodgkin lymphoma that has relapsed or is refractory after at least two prior lines of therapy.
Axi-cel was also approved in 2017 for relapsed/refractory non-Hodgkin lymphoma, and in February 2021, after Dr. Corradini’s meeting presentation, the FDA granted a third approval to lisocabtagene maraleucel (liso-cel; Breyanzi) for this indication.
The information to date from both the trial and real-world settings are limited with respect to showing any differences in outcomes between the CAR T-cell products, but provide “an initial suggestion” that outcomes with tisa-cel and axi-cel are comparable, he said, adding that decisions should be strictly based on product registration data given the absence of reliable data for choosing one product over another.
Dr. Corradini reported honoraria and/or payment for travel and accommodations from Abbvie, Amgen, Bristol-Myers Squibb, Celgene, Daiichi Sankyo, and a number of other pharmaceutical companies.
FROM CART21
Breast cancer surgeries deemed ‘low value’ continue, increase
“This is the first study to [evaluate] all four of the low-value breast cancer procedures at the same time and try to draw some conclusions on practice patterns across facilities,” said senior author Lesly A. Dossett, MD, MPH, Center for Health Outcomes and Policy, the University of Michigan, Ann Arbor.
The two low-value procedures that have increased in use are contralateral prophylactic mastectomy for average-risk women with unilateral cancer and sentinel lymph node biopsy for clinically node-negative women aged 70 years and older with hormone receptor–positive (HR+) cancer.
“This suggests that formal efforts to reduce low value care through dissemination of guidelines, education of patients or providers, or alignment of incentives will be necessary to achieve full deimplementation,” she told this news organization.
The researchers emphasize that the providing of services that have no clinically meaningful benefit is a national epidemic, costing the United States more than $100 billion dollars annually.
These trends are notable and likely reflect a broad range of factors, commented Katharine Yao, MD, chief of the division of surgical oncology at the NorthShore University HealthSystem, Evanston, Ill.
“I think the better message here is not so much that facilities are doing too many low-value procedures but more that these procedures are still being performed, and the trends show increased rates over the years – why is that?”
“Perhaps there are other factors here we need to explore: why do these procedures persist, and why, despite the Choosing Wisely campaign, [do] they continue to increase?” she said in an interview. “Maybe there is something we can learn here about patient and physician preferences that perhaps we should be paying more attention to.”
The study was published on Feb. 3 in JAMA Surgery.
For the analysis, Dr. Dossett and her colleagues evaluated surgical data from the National Cancer Database. They examined data from more than 1,500 surgical facilities and from surgeries involving 920,256 women in the United States who were diagnosed with breast cancer between 2004 and 2016.
The team focused on four procedures that have been determined to be of low value by Choosing Wisely, a campaign of the American Board of Internal Medicine Foundation, on the basis of recommendations of the American College of Surgeons, the Society for Surgical Oncology, and the American Society for Breast Surgeons.
The results show that, for two of the four low-value procedures, use declined significantly over the study period. These two procedures were axillary lymph node dissection for limited nodal disease, for patients undergoing lumpectomy and radiotherapy, and lumpectomy re-excision for patients whose surgical margins were close but were negative for invasive cancer.
Axillary lymph node dissection declined from 63% in 2004 to 14% in 2016. The steepest reduction was seen soon after data from the Z0011 study were published in 2010. The rates for this procedure halved in the following year, from 62% in 2010 to 31% in 2011 (P < .001).
Likewise, reoperation rates after lumpectomy dropped from 19% in 2004 to 15% in 2016. The sharpest decline, from 18% in 2013 to 16% in 2014, corresponded to the publishing of the SSO/ASTRO consensus statement, which designated a negative margin as having “no tumor on ink.”
Two of the four low-value procedures increased in use during the study period.
Rates of contralateral prophylactic mastectomy increased nearly 2.5-fold among women with unilateral breast cancer undergoing mastectomy, from 11% in 2004 to 26% in 2016, despite SSO guidelines issued in 2007 recommending that the procedure not be used for women at average risk.
In addition, rates of sentinel lymph node biopsy among women aged 70 years and older with clinically node-negative HR+ breast cancer increased from 78% in 2004 to 87% in 2012. There was no significant decline in the use of this procedure, even after the CALGB 9343 trial from the Cancer and Leukemia Group B showed no survival benefit in 2013.
Patterns at hospitals vary
The authors of the study also examined hospital factors, which can heavily influence choice of procedure.
These results showed that the greatest reductions of the low-value breast cancer procedures occurred at academic research programs and high-volume surgical facilities. Elsewhere, the rates varied widely.
Interfacility rates of axillary lymph node dissection ranged from 7% to 47%; lumpectomy reoperation rates ranged from 3% to 62%; contralateral prophylactic mastectomy rates ranged from 9% to 67%; and sentinel lymph node biopsy rates ranged from 25% to 97%.
Being an outlier for use of one procedure did not necessarily translate to nonconformity for others. Factors such as a hospital’s volume of breast cancer cases or the type of facility did not appear to influence rates of axillary lymph node dissection or lumpectomy reoperation.
However, the rates of contralateral prophylactic mastectomy were significantly higher in high-volume centers and integrated network cancer programs, compared with community cancer programs (23% vs. 2%; P < .001).
Dr. Dossett said the lack of consistency was somewhat unexpected.
“We expected we would find some facilities were constantly good or bad at deimplementation or that there would be stronger associations between certain facility characteristics and performance,” she said. “That really wasn’t the case, and most facilities had mixed performance.”
Evidence may or may not influence trends
The authors speculate on why the low-value designation is in some cases being ignored.
The evidence regarding the risk for lymphedema related to axillary lymph node dissection procedure appears to have helped reduce its use, they note.
However, surgeons have been much less convinced of benefits in omitting sentinel lymph node biopsy, either because they are unfamiliar with the recommendations to avoid the procedure, or they may feel the procedure adds only minimal time and risk to a patient’s operation, the authors explain.
Patients may be convinced to opt to omit sentinel lymph node biopsy if they are properly counseled regarding the risks and benefits of the procedure, Dr. Dossett commented.
Dr. Yao added that, for elderly patients, age can play an important role in sentinel node biopsy.
“Patients’ life expectancy has increased over the years, and node status may impact adjuvant therapy decisions for these patients, even chemotherapy decisions,” she said.
Pressure to continue to perform contralateral prophylactic mastectomy is believed to be significantly patient driven, Dr. Dossett noted.
“I ultimately think the best way to reduce contralateral prophylactic mastectomy is to encourage women with small cancers to undergo breast-conserving surgery, i.e., lumpectomy, instead of mastectomy,” she explained.
“Once the decision for mastectomy is made, there is often a great deal of momentum towards a contralateral prophylactic mastectomy.”
“Contralateral prophylactic mastectomy is a personal preference that many surgeons are willing to do for their patients,” Dr. Yao explained.
“Although no survival benefit has been demonstrated for this procedure, patients find many other benefits that have nothing to do with survival.”
The authors and Dr. Yao have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“This is the first study to [evaluate] all four of the low-value breast cancer procedures at the same time and try to draw some conclusions on practice patterns across facilities,” said senior author Lesly A. Dossett, MD, MPH, Center for Health Outcomes and Policy, the University of Michigan, Ann Arbor.
The two low-value procedures that have increased in use are contralateral prophylactic mastectomy for average-risk women with unilateral cancer and sentinel lymph node biopsy for clinically node-negative women aged 70 years and older with hormone receptor–positive (HR+) cancer.
“This suggests that formal efforts to reduce low value care through dissemination of guidelines, education of patients or providers, or alignment of incentives will be necessary to achieve full deimplementation,” she told this news organization.
The researchers emphasize that the providing of services that have no clinically meaningful benefit is a national epidemic, costing the United States more than $100 billion dollars annually.
These trends are notable and likely reflect a broad range of factors, commented Katharine Yao, MD, chief of the division of surgical oncology at the NorthShore University HealthSystem, Evanston, Ill.
“I think the better message here is not so much that facilities are doing too many low-value procedures but more that these procedures are still being performed, and the trends show increased rates over the years – why is that?”
“Perhaps there are other factors here we need to explore: why do these procedures persist, and why, despite the Choosing Wisely campaign, [do] they continue to increase?” she said in an interview. “Maybe there is something we can learn here about patient and physician preferences that perhaps we should be paying more attention to.”
The study was published on Feb. 3 in JAMA Surgery.
For the analysis, Dr. Dossett and her colleagues evaluated surgical data from the National Cancer Database. They examined data from more than 1,500 surgical facilities and from surgeries involving 920,256 women in the United States who were diagnosed with breast cancer between 2004 and 2016.
The team focused on four procedures that have been determined to be of low value by Choosing Wisely, a campaign of the American Board of Internal Medicine Foundation, on the basis of recommendations of the American College of Surgeons, the Society for Surgical Oncology, and the American Society for Breast Surgeons.
The results show that, for two of the four low-value procedures, use declined significantly over the study period. These two procedures were axillary lymph node dissection for limited nodal disease, for patients undergoing lumpectomy and radiotherapy, and lumpectomy re-excision for patients whose surgical margins were close but were negative for invasive cancer.
Axillary lymph node dissection declined from 63% in 2004 to 14% in 2016. The steepest reduction was seen soon after data from the Z0011 study were published in 2010. The rates for this procedure halved in the following year, from 62% in 2010 to 31% in 2011 (P < .001).
Likewise, reoperation rates after lumpectomy dropped from 19% in 2004 to 15% in 2016. The sharpest decline, from 18% in 2013 to 16% in 2014, corresponded to the publishing of the SSO/ASTRO consensus statement, which designated a negative margin as having “no tumor on ink.”
Two of the four low-value procedures increased in use during the study period.
Rates of contralateral prophylactic mastectomy increased nearly 2.5-fold among women with unilateral breast cancer undergoing mastectomy, from 11% in 2004 to 26% in 2016, despite SSO guidelines issued in 2007 recommending that the procedure not be used for women at average risk.
In addition, rates of sentinel lymph node biopsy among women aged 70 years and older with clinically node-negative HR+ breast cancer increased from 78% in 2004 to 87% in 2012. There was no significant decline in the use of this procedure, even after the CALGB 9343 trial from the Cancer and Leukemia Group B showed no survival benefit in 2013.
Patterns at hospitals vary
The authors of the study also examined hospital factors, which can heavily influence choice of procedure.
These results showed that the greatest reductions of the low-value breast cancer procedures occurred at academic research programs and high-volume surgical facilities. Elsewhere, the rates varied widely.
Interfacility rates of axillary lymph node dissection ranged from 7% to 47%; lumpectomy reoperation rates ranged from 3% to 62%; contralateral prophylactic mastectomy rates ranged from 9% to 67%; and sentinel lymph node biopsy rates ranged from 25% to 97%.
Being an outlier for use of one procedure did not necessarily translate to nonconformity for others. Factors such as a hospital’s volume of breast cancer cases or the type of facility did not appear to influence rates of axillary lymph node dissection or lumpectomy reoperation.
However, the rates of contralateral prophylactic mastectomy were significantly higher in high-volume centers and integrated network cancer programs, compared with community cancer programs (23% vs. 2%; P < .001).
Dr. Dossett said the lack of consistency was somewhat unexpected.
“We expected we would find some facilities were constantly good or bad at deimplementation or that there would be stronger associations between certain facility characteristics and performance,” she said. “That really wasn’t the case, and most facilities had mixed performance.”
Evidence may or may not influence trends
The authors speculate on why the low-value designation is in some cases being ignored.
The evidence regarding the risk for lymphedema related to axillary lymph node dissection procedure appears to have helped reduce its use, they note.
However, surgeons have been much less convinced of benefits in omitting sentinel lymph node biopsy, either because they are unfamiliar with the recommendations to avoid the procedure, or they may feel the procedure adds only minimal time and risk to a patient’s operation, the authors explain.
Patients may be convinced to opt to omit sentinel lymph node biopsy if they are properly counseled regarding the risks and benefits of the procedure, Dr. Dossett commented.
Dr. Yao added that, for elderly patients, age can play an important role in sentinel node biopsy.
“Patients’ life expectancy has increased over the years, and node status may impact adjuvant therapy decisions for these patients, even chemotherapy decisions,” she said.
Pressure to continue to perform contralateral prophylactic mastectomy is believed to be significantly patient driven, Dr. Dossett noted.
“I ultimately think the best way to reduce contralateral prophylactic mastectomy is to encourage women with small cancers to undergo breast-conserving surgery, i.e., lumpectomy, instead of mastectomy,” she explained.
“Once the decision for mastectomy is made, there is often a great deal of momentum towards a contralateral prophylactic mastectomy.”
“Contralateral prophylactic mastectomy is a personal preference that many surgeons are willing to do for their patients,” Dr. Yao explained.
“Although no survival benefit has been demonstrated for this procedure, patients find many other benefits that have nothing to do with survival.”
The authors and Dr. Yao have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“This is the first study to [evaluate] all four of the low-value breast cancer procedures at the same time and try to draw some conclusions on practice patterns across facilities,” said senior author Lesly A. Dossett, MD, MPH, Center for Health Outcomes and Policy, the University of Michigan, Ann Arbor.
The two low-value procedures that have increased in use are contralateral prophylactic mastectomy for average-risk women with unilateral cancer and sentinel lymph node biopsy for clinically node-negative women aged 70 years and older with hormone receptor–positive (HR+) cancer.
“This suggests that formal efforts to reduce low value care through dissemination of guidelines, education of patients or providers, or alignment of incentives will be necessary to achieve full deimplementation,” she told this news organization.
The researchers emphasize that the providing of services that have no clinically meaningful benefit is a national epidemic, costing the United States more than $100 billion dollars annually.
These trends are notable and likely reflect a broad range of factors, commented Katharine Yao, MD, chief of the division of surgical oncology at the NorthShore University HealthSystem, Evanston, Ill.
“I think the better message here is not so much that facilities are doing too many low-value procedures but more that these procedures are still being performed, and the trends show increased rates over the years – why is that?”
“Perhaps there are other factors here we need to explore: why do these procedures persist, and why, despite the Choosing Wisely campaign, [do] they continue to increase?” she said in an interview. “Maybe there is something we can learn here about patient and physician preferences that perhaps we should be paying more attention to.”
The study was published on Feb. 3 in JAMA Surgery.
For the analysis, Dr. Dossett and her colleagues evaluated surgical data from the National Cancer Database. They examined data from more than 1,500 surgical facilities and from surgeries involving 920,256 women in the United States who were diagnosed with breast cancer between 2004 and 2016.
The team focused on four procedures that have been determined to be of low value by Choosing Wisely, a campaign of the American Board of Internal Medicine Foundation, on the basis of recommendations of the American College of Surgeons, the Society for Surgical Oncology, and the American Society for Breast Surgeons.
The results show that, for two of the four low-value procedures, use declined significantly over the study period. These two procedures were axillary lymph node dissection for limited nodal disease, for patients undergoing lumpectomy and radiotherapy, and lumpectomy re-excision for patients whose surgical margins were close but were negative for invasive cancer.
Axillary lymph node dissection declined from 63% in 2004 to 14% in 2016. The steepest reduction was seen soon after data from the Z0011 study were published in 2010. The rates for this procedure halved in the following year, from 62% in 2010 to 31% in 2011 (P < .001).
Likewise, reoperation rates after lumpectomy dropped from 19% in 2004 to 15% in 2016. The sharpest decline, from 18% in 2013 to 16% in 2014, corresponded to the publishing of the SSO/ASTRO consensus statement, which designated a negative margin as having “no tumor on ink.”
Two of the four low-value procedures increased in use during the study period.
Rates of contralateral prophylactic mastectomy increased nearly 2.5-fold among women with unilateral breast cancer undergoing mastectomy, from 11% in 2004 to 26% in 2016, despite SSO guidelines issued in 2007 recommending that the procedure not be used for women at average risk.
In addition, rates of sentinel lymph node biopsy among women aged 70 years and older with clinically node-negative HR+ breast cancer increased from 78% in 2004 to 87% in 2012. There was no significant decline in the use of this procedure, even after the CALGB 9343 trial from the Cancer and Leukemia Group B showed no survival benefit in 2013.
Patterns at hospitals vary
The authors of the study also examined hospital factors, which can heavily influence choice of procedure.
These results showed that the greatest reductions of the low-value breast cancer procedures occurred at academic research programs and high-volume surgical facilities. Elsewhere, the rates varied widely.
Interfacility rates of axillary lymph node dissection ranged from 7% to 47%; lumpectomy reoperation rates ranged from 3% to 62%; contralateral prophylactic mastectomy rates ranged from 9% to 67%; and sentinel lymph node biopsy rates ranged from 25% to 97%.
Being an outlier for use of one procedure did not necessarily translate to nonconformity for others. Factors such as a hospital’s volume of breast cancer cases or the type of facility did not appear to influence rates of axillary lymph node dissection or lumpectomy reoperation.
However, the rates of contralateral prophylactic mastectomy were significantly higher in high-volume centers and integrated network cancer programs, compared with community cancer programs (23% vs. 2%; P < .001).
Dr. Dossett said the lack of consistency was somewhat unexpected.
“We expected we would find some facilities were constantly good or bad at deimplementation or that there would be stronger associations between certain facility characteristics and performance,” she said. “That really wasn’t the case, and most facilities had mixed performance.”
Evidence may or may not influence trends
The authors speculate on why the low-value designation is in some cases being ignored.
The evidence regarding the risk for lymphedema related to axillary lymph node dissection procedure appears to have helped reduce its use, they note.
However, surgeons have been much less convinced of benefits in omitting sentinel lymph node biopsy, either because they are unfamiliar with the recommendations to avoid the procedure, or they may feel the procedure adds only minimal time and risk to a patient’s operation, the authors explain.
Patients may be convinced to opt to omit sentinel lymph node biopsy if they are properly counseled regarding the risks and benefits of the procedure, Dr. Dossett commented.
Dr. Yao added that, for elderly patients, age can play an important role in sentinel node biopsy.
“Patients’ life expectancy has increased over the years, and node status may impact adjuvant therapy decisions for these patients, even chemotherapy decisions,” she said.
Pressure to continue to perform contralateral prophylactic mastectomy is believed to be significantly patient driven, Dr. Dossett noted.
“I ultimately think the best way to reduce contralateral prophylactic mastectomy is to encourage women with small cancers to undergo breast-conserving surgery, i.e., lumpectomy, instead of mastectomy,” she explained.
“Once the decision for mastectomy is made, there is often a great deal of momentum towards a contralateral prophylactic mastectomy.”
“Contralateral prophylactic mastectomy is a personal preference that many surgeons are willing to do for their patients,” Dr. Yao explained.
“Although no survival benefit has been demonstrated for this procedure, patients find many other benefits that have nothing to do with survival.”
The authors and Dr. Yao have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Racial/ethnic disparities in cesarean rates increase with greater maternal education
While the likelihood of a cesarean delivery usually drops as maternal education level increases, the disparities seen in cesarean rates between White and Black or Hispanic women actually increase with more maternal education, according to findings from a new study presented at the Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Typically, higher maternal education is associated with a lower likelihood of cesarean delivery, but this protective effect is much smaller for Black women and nonexistent for Hispanic women, leading to bigger gaps between these groups and White women, found Yael Eliner, MD, an ob.gyn. residency applicant at Boston University who conducted this research with her colleagues in the ob.gyn. department at Lenox Hill Hospital, New York, and Hofstra University, Hempstead, N.Y..
Researchers have previously identified racial and ethnic disparities in a wide range of maternal outcomes, including mortality, overall morbidity, preterm birth, low birth weight, fetal growth restriction, hypertensive disorders of pregnancy, diabetes, and cesarean deliveries. But the researchers wanted to know if the usual protective effects seen for cesarean deliveries existed in the racial and ethnic groups with these disparities. Past studies have already found that the protective effect of maternal education is greater for White women than Black women with infant mortality and overall self-rated health.
The researchers conducted a retrospective analysis of all low-risk nulliparous, term, singleton, vertex live births to U.S. residents from 2016 to 2019 by using the natality database of the Centers for Disease Control and Prevention. They looked only at women who were non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic women. They excluded women with pregestational and gestational diabetes, chronic hypertension, and hypertensive disorders of pregnancy.
Maternal education levels were stratified into those without a high school diploma, high school graduates (including those with some college credit), college graduates, and those with advanced degrees. The total population included 2,969,207 mothers with a 23.4% cesarean delivery rate.
Before considering education or other potential confounders, the cesarean delivery rate was 27.4% in Black women and 25.6% in Asian women, compared with 22.4% in White women and 23% in Hispanic women (P < .001).
Among those with less than a high school education, Black (20.9%), Asian (23.1%), and Hispanic (17.9% cesarean delivery prevalence was greater than that among White women (17.2%) (P < .001). The same was true among those with a high school education (with or without some college): 22% of White women in this group had cesarean deliveries compared with 26.3% of Black women, 26.3% of Asian women, and 22.5% of Hispanic women (P < .001).
At higher levels of education, the disparities not only persisted but actually increased.
The prevalence of cesarean deliveries was 23% in White college graduates, compared with 32.5% of Black college graduates, 26.3% of Asian college graduates, and 27.7% of Hispanic college graduates (P < .001). Similarly, in those with an advanced degree, the prevalence of cesarean deliveries in their population set was 23.6% of Whites, 36.3% of Blacks, 26.1% of Asians, and 30.1% of Hispanics (P < .001).
After adjusting for maternal education as well as age, prepregnancy body mass index, weight gain during pregnancy, insurance type, and neonatal birth weight, the researchers still found substantial disparities in cesarean delivery rates. Black women had 1.54 times greater odds of cesarean delivery than White women (P < .001). Similarly, the odds were 1.45 times greater for Asian women and 1.24 times greater for Hispanic women (P < .001).
Controlling for race, ethnicity, and the other confounders, women with less than a high school education or a high school diploma had similar likelihoods of cesarean delivery. The likelihood of a cesarean delivery was slightly reduced for women with a college degree (odds ratio, 0.93) or advanced degree (OR, 0.88). But this protective effect did not dampen racial/ethnic disparities. In fact, even greater disparities were seen at higher levels of education.
“At each level of education, all the racial/ethnic groups had significantly higher odds of a cesarean delivery than White women,” Dr. Eliner said. “Additionally, the racial/ethnic disparity in cesarean delivery rates increased with increasing level of education, and we specifically see a meaningful jump in the odds ratio at the college graduate level.”
She pointed out that the OR for cesarean delivery in Black women was 1.4 times greater than White women in the group with less than a high school education and 1.44 times greater in those with high school diplomas. Then it jumped to 1.69 in the college graduates group and 1.7 in the advanced degree group.
Higher maternal education was associated with a lower likelihood of cesarean delivery in White women and Asian women. White women with advanced degrees were 17% less likely to have a cesarean than White women with less than a high school education, and the respective reduction in risk was 19% for Asian women.
In Black women, however, education has a much smaller protective effect: An advanced degree reduced the odds of a cesarean delivery by only 7% and no significant difference showed up between high school graduates and college graduates, Dr. Eliner reported.
In Hispanic women, no protective effect showed up, and the odds of a cesarean delivery actually increased slightly in high school and college graduates above those with less than a high school education.
Dr. Eliner discussed a couple possible reasons for a less protective effect from maternal education in Black and Hispanic groups, including higher levels of chronic stress found in past research among racial/ethnic minorities with higher levels of education.
“The impact of racism as a chronic stressor and its association with adverse obstetric and prenatal outcomes is an emerging theme in health disparity research and is yet to be fully understood,” Dr. Eliner said in an interview. “Nonetheless, there is some evidence suggesting that racial/ethnic minorities with higher levels of education suffer from higher levels of stress.”
Implicit and explicit interpersonal bias and institutional racism may also play a role in the disparities, she said, and these factors may disproportionately affect the quality of care for more educated women. She also suggested that White women may be more comfortable advocating for their care.
“While less educated women from all racial/ethnic groups may lack the self-advocacy skills to discuss their labor course, educated White women may be more confident than women from educated minority groups,” Dr. Eliner told attendees. “They may therefore be better equipped to discuss the need for a cesarean delivery with their provider.”
Dr. Eliner elaborated on this: “Given the historical and current disparities of the health care system, women in racial/ethnic minorities may potentially be guarded in their interaction with medical professionals, with a reduced trust in the health care system, and may thus not feel empowered to advocate for themselves in this setting,” she said.
Allison Bryant Mantha, MD, MPH, vice chair for quality, equity, and safety in the ob.gyn. department at Massachusetts General Hospital, Boston, suggested that bias and racism may play a role in this self-advocacy as well.
“I’m wondering if it might not be equally plausible that the advocacy might be met differently by who’s delivering the message,” Dr. Bryant Mantha said. “I think from the story of Dr. Susan Moore and patients who advocate for themselves, I think that we know there is probably some differential by who’s delivering the message.”
Finally, even though education is usually highly correlated with income and frequently used as a proxy for it, but the effect of education on income varies by race/ethnicity.
Since education alone is not sufficient to reduce these disparities, potential interventions should focus on increasing awareness of the disparities and the role of implicit bias, improving patients’ trust in the medical system, and training more doctors from underrepresented groups, Dr. Eliner said.
“I was also wondering about the overall patient choice,” said Sarahn M. Wheeler, MD, an assistant professor of ob.gyn. at Duke University Medical Center in Durham, N.C., who comoderated the session with Dr. Bryant Mantha. “Did we have any understanding of differences in patient values systems that might go into some of these differences in findings as well? There are lots of interesting concepts to explore and that this abstract brings up.”
Dr. Eliner, Dr. Wheeler, and Dr. Bryant Mantha had no disclosures.
While the likelihood of a cesarean delivery usually drops as maternal education level increases, the disparities seen in cesarean rates between White and Black or Hispanic women actually increase with more maternal education, according to findings from a new study presented at the Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Typically, higher maternal education is associated with a lower likelihood of cesarean delivery, but this protective effect is much smaller for Black women and nonexistent for Hispanic women, leading to bigger gaps between these groups and White women, found Yael Eliner, MD, an ob.gyn. residency applicant at Boston University who conducted this research with her colleagues in the ob.gyn. department at Lenox Hill Hospital, New York, and Hofstra University, Hempstead, N.Y..
Researchers have previously identified racial and ethnic disparities in a wide range of maternal outcomes, including mortality, overall morbidity, preterm birth, low birth weight, fetal growth restriction, hypertensive disorders of pregnancy, diabetes, and cesarean deliveries. But the researchers wanted to know if the usual protective effects seen for cesarean deliveries existed in the racial and ethnic groups with these disparities. Past studies have already found that the protective effect of maternal education is greater for White women than Black women with infant mortality and overall self-rated health.
The researchers conducted a retrospective analysis of all low-risk nulliparous, term, singleton, vertex live births to U.S. residents from 2016 to 2019 by using the natality database of the Centers for Disease Control and Prevention. They looked only at women who were non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic women. They excluded women with pregestational and gestational diabetes, chronic hypertension, and hypertensive disorders of pregnancy.
Maternal education levels were stratified into those without a high school diploma, high school graduates (including those with some college credit), college graduates, and those with advanced degrees. The total population included 2,969,207 mothers with a 23.4% cesarean delivery rate.
Before considering education or other potential confounders, the cesarean delivery rate was 27.4% in Black women and 25.6% in Asian women, compared with 22.4% in White women and 23% in Hispanic women (P < .001).
Among those with less than a high school education, Black (20.9%), Asian (23.1%), and Hispanic (17.9% cesarean delivery prevalence was greater than that among White women (17.2%) (P < .001). The same was true among those with a high school education (with or without some college): 22% of White women in this group had cesarean deliveries compared with 26.3% of Black women, 26.3% of Asian women, and 22.5% of Hispanic women (P < .001).
At higher levels of education, the disparities not only persisted but actually increased.
The prevalence of cesarean deliveries was 23% in White college graduates, compared with 32.5% of Black college graduates, 26.3% of Asian college graduates, and 27.7% of Hispanic college graduates (P < .001). Similarly, in those with an advanced degree, the prevalence of cesarean deliveries in their population set was 23.6% of Whites, 36.3% of Blacks, 26.1% of Asians, and 30.1% of Hispanics (P < .001).
After adjusting for maternal education as well as age, prepregnancy body mass index, weight gain during pregnancy, insurance type, and neonatal birth weight, the researchers still found substantial disparities in cesarean delivery rates. Black women had 1.54 times greater odds of cesarean delivery than White women (P < .001). Similarly, the odds were 1.45 times greater for Asian women and 1.24 times greater for Hispanic women (P < .001).
Controlling for race, ethnicity, and the other confounders, women with less than a high school education or a high school diploma had similar likelihoods of cesarean delivery. The likelihood of a cesarean delivery was slightly reduced for women with a college degree (odds ratio, 0.93) or advanced degree (OR, 0.88). But this protective effect did not dampen racial/ethnic disparities. In fact, even greater disparities were seen at higher levels of education.
“At each level of education, all the racial/ethnic groups had significantly higher odds of a cesarean delivery than White women,” Dr. Eliner said. “Additionally, the racial/ethnic disparity in cesarean delivery rates increased with increasing level of education, and we specifically see a meaningful jump in the odds ratio at the college graduate level.”
She pointed out that the OR for cesarean delivery in Black women was 1.4 times greater than White women in the group with less than a high school education and 1.44 times greater in those with high school diplomas. Then it jumped to 1.69 in the college graduates group and 1.7 in the advanced degree group.
Higher maternal education was associated with a lower likelihood of cesarean delivery in White women and Asian women. White women with advanced degrees were 17% less likely to have a cesarean than White women with less than a high school education, and the respective reduction in risk was 19% for Asian women.
In Black women, however, education has a much smaller protective effect: An advanced degree reduced the odds of a cesarean delivery by only 7% and no significant difference showed up between high school graduates and college graduates, Dr. Eliner reported.
In Hispanic women, no protective effect showed up, and the odds of a cesarean delivery actually increased slightly in high school and college graduates above those with less than a high school education.
Dr. Eliner discussed a couple possible reasons for a less protective effect from maternal education in Black and Hispanic groups, including higher levels of chronic stress found in past research among racial/ethnic minorities with higher levels of education.
“The impact of racism as a chronic stressor and its association with adverse obstetric and prenatal outcomes is an emerging theme in health disparity research and is yet to be fully understood,” Dr. Eliner said in an interview. “Nonetheless, there is some evidence suggesting that racial/ethnic minorities with higher levels of education suffer from higher levels of stress.”
Implicit and explicit interpersonal bias and institutional racism may also play a role in the disparities, she said, and these factors may disproportionately affect the quality of care for more educated women. She also suggested that White women may be more comfortable advocating for their care.
“While less educated women from all racial/ethnic groups may lack the self-advocacy skills to discuss their labor course, educated White women may be more confident than women from educated minority groups,” Dr. Eliner told attendees. “They may therefore be better equipped to discuss the need for a cesarean delivery with their provider.”
Dr. Eliner elaborated on this: “Given the historical and current disparities of the health care system, women in racial/ethnic minorities may potentially be guarded in their interaction with medical professionals, with a reduced trust in the health care system, and may thus not feel empowered to advocate for themselves in this setting,” she said.
Allison Bryant Mantha, MD, MPH, vice chair for quality, equity, and safety in the ob.gyn. department at Massachusetts General Hospital, Boston, suggested that bias and racism may play a role in this self-advocacy as well.
“I’m wondering if it might not be equally plausible that the advocacy might be met differently by who’s delivering the message,” Dr. Bryant Mantha said. “I think from the story of Dr. Susan Moore and patients who advocate for themselves, I think that we know there is probably some differential by who’s delivering the message.”
Finally, even though education is usually highly correlated with income and frequently used as a proxy for it, but the effect of education on income varies by race/ethnicity.
Since education alone is not sufficient to reduce these disparities, potential interventions should focus on increasing awareness of the disparities and the role of implicit bias, improving patients’ trust in the medical system, and training more doctors from underrepresented groups, Dr. Eliner said.
“I was also wondering about the overall patient choice,” said Sarahn M. Wheeler, MD, an assistant professor of ob.gyn. at Duke University Medical Center in Durham, N.C., who comoderated the session with Dr. Bryant Mantha. “Did we have any understanding of differences in patient values systems that might go into some of these differences in findings as well? There are lots of interesting concepts to explore and that this abstract brings up.”
Dr. Eliner, Dr. Wheeler, and Dr. Bryant Mantha had no disclosures.
While the likelihood of a cesarean delivery usually drops as maternal education level increases, the disparities seen in cesarean rates between White and Black or Hispanic women actually increase with more maternal education, according to findings from a new study presented at the Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Typically, higher maternal education is associated with a lower likelihood of cesarean delivery, but this protective effect is much smaller for Black women and nonexistent for Hispanic women, leading to bigger gaps between these groups and White women, found Yael Eliner, MD, an ob.gyn. residency applicant at Boston University who conducted this research with her colleagues in the ob.gyn. department at Lenox Hill Hospital, New York, and Hofstra University, Hempstead, N.Y..
Researchers have previously identified racial and ethnic disparities in a wide range of maternal outcomes, including mortality, overall morbidity, preterm birth, low birth weight, fetal growth restriction, hypertensive disorders of pregnancy, diabetes, and cesarean deliveries. But the researchers wanted to know if the usual protective effects seen for cesarean deliveries existed in the racial and ethnic groups with these disparities. Past studies have already found that the protective effect of maternal education is greater for White women than Black women with infant mortality and overall self-rated health.
The researchers conducted a retrospective analysis of all low-risk nulliparous, term, singleton, vertex live births to U.S. residents from 2016 to 2019 by using the natality database of the Centers for Disease Control and Prevention. They looked only at women who were non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic women. They excluded women with pregestational and gestational diabetes, chronic hypertension, and hypertensive disorders of pregnancy.
Maternal education levels were stratified into those without a high school diploma, high school graduates (including those with some college credit), college graduates, and those with advanced degrees. The total population included 2,969,207 mothers with a 23.4% cesarean delivery rate.
Before considering education or other potential confounders, the cesarean delivery rate was 27.4% in Black women and 25.6% in Asian women, compared with 22.4% in White women and 23% in Hispanic women (P < .001).
Among those with less than a high school education, Black (20.9%), Asian (23.1%), and Hispanic (17.9% cesarean delivery prevalence was greater than that among White women (17.2%) (P < .001). The same was true among those with a high school education (with or without some college): 22% of White women in this group had cesarean deliveries compared with 26.3% of Black women, 26.3% of Asian women, and 22.5% of Hispanic women (P < .001).
At higher levels of education, the disparities not only persisted but actually increased.
The prevalence of cesarean deliveries was 23% in White college graduates, compared with 32.5% of Black college graduates, 26.3% of Asian college graduates, and 27.7% of Hispanic college graduates (P < .001). Similarly, in those with an advanced degree, the prevalence of cesarean deliveries in their population set was 23.6% of Whites, 36.3% of Blacks, 26.1% of Asians, and 30.1% of Hispanics (P < .001).
After adjusting for maternal education as well as age, prepregnancy body mass index, weight gain during pregnancy, insurance type, and neonatal birth weight, the researchers still found substantial disparities in cesarean delivery rates. Black women had 1.54 times greater odds of cesarean delivery than White women (P < .001). Similarly, the odds were 1.45 times greater for Asian women and 1.24 times greater for Hispanic women (P < .001).
Controlling for race, ethnicity, and the other confounders, women with less than a high school education or a high school diploma had similar likelihoods of cesarean delivery. The likelihood of a cesarean delivery was slightly reduced for women with a college degree (odds ratio, 0.93) or advanced degree (OR, 0.88). But this protective effect did not dampen racial/ethnic disparities. In fact, even greater disparities were seen at higher levels of education.
“At each level of education, all the racial/ethnic groups had significantly higher odds of a cesarean delivery than White women,” Dr. Eliner said. “Additionally, the racial/ethnic disparity in cesarean delivery rates increased with increasing level of education, and we specifically see a meaningful jump in the odds ratio at the college graduate level.”
She pointed out that the OR for cesarean delivery in Black women was 1.4 times greater than White women in the group with less than a high school education and 1.44 times greater in those with high school diplomas. Then it jumped to 1.69 in the college graduates group and 1.7 in the advanced degree group.
Higher maternal education was associated with a lower likelihood of cesarean delivery in White women and Asian women. White women with advanced degrees were 17% less likely to have a cesarean than White women with less than a high school education, and the respective reduction in risk was 19% for Asian women.
In Black women, however, education has a much smaller protective effect: An advanced degree reduced the odds of a cesarean delivery by only 7% and no significant difference showed up between high school graduates and college graduates, Dr. Eliner reported.
In Hispanic women, no protective effect showed up, and the odds of a cesarean delivery actually increased slightly in high school and college graduates above those with less than a high school education.
Dr. Eliner discussed a couple possible reasons for a less protective effect from maternal education in Black and Hispanic groups, including higher levels of chronic stress found in past research among racial/ethnic minorities with higher levels of education.
“The impact of racism as a chronic stressor and its association with adverse obstetric and prenatal outcomes is an emerging theme in health disparity research and is yet to be fully understood,” Dr. Eliner said in an interview. “Nonetheless, there is some evidence suggesting that racial/ethnic minorities with higher levels of education suffer from higher levels of stress.”
Implicit and explicit interpersonal bias and institutional racism may also play a role in the disparities, she said, and these factors may disproportionately affect the quality of care for more educated women. She also suggested that White women may be more comfortable advocating for their care.
“While less educated women from all racial/ethnic groups may lack the self-advocacy skills to discuss their labor course, educated White women may be more confident than women from educated minority groups,” Dr. Eliner told attendees. “They may therefore be better equipped to discuss the need for a cesarean delivery with their provider.”
Dr. Eliner elaborated on this: “Given the historical and current disparities of the health care system, women in racial/ethnic minorities may potentially be guarded in their interaction with medical professionals, with a reduced trust in the health care system, and may thus not feel empowered to advocate for themselves in this setting,” she said.
Allison Bryant Mantha, MD, MPH, vice chair for quality, equity, and safety in the ob.gyn. department at Massachusetts General Hospital, Boston, suggested that bias and racism may play a role in this self-advocacy as well.
“I’m wondering if it might not be equally plausible that the advocacy might be met differently by who’s delivering the message,” Dr. Bryant Mantha said. “I think from the story of Dr. Susan Moore and patients who advocate for themselves, I think that we know there is probably some differential by who’s delivering the message.”
Finally, even though education is usually highly correlated with income and frequently used as a proxy for it, but the effect of education on income varies by race/ethnicity.
Since education alone is not sufficient to reduce these disparities, potential interventions should focus on increasing awareness of the disparities and the role of implicit bias, improving patients’ trust in the medical system, and training more doctors from underrepresented groups, Dr. Eliner said.
“I was also wondering about the overall patient choice,” said Sarahn M. Wheeler, MD, an assistant professor of ob.gyn. at Duke University Medical Center in Durham, N.C., who comoderated the session with Dr. Bryant Mantha. “Did we have any understanding of differences in patient values systems that might go into some of these differences in findings as well? There are lots of interesting concepts to explore and that this abstract brings up.”
Dr. Eliner, Dr. Wheeler, and Dr. Bryant Mantha had no disclosures.
FROM THE PREGNANCY MEETING
Placenta’s role in schizophrenia ‘bigger than we imagined'
Schizophrenia-related genes in the placenta are predictive of the size of a baby’s brain at birth and the rate of cognitive development. In a complicated pregnancy, such genes could raise the risk of developing schizophrenia later in life, new research suggests.
“This is further evidence that early life matters in schizophrenia, and the placenta plays a bigger role than we imagined,” Daniel R. Weinberger, MD, director and CEO, Lieber Institute for Brain Development, and professor of neurology, psychiatry, and neuroscience, Johns Hopkins University, Baltimore, said in a news release.
“The holy grail would be to identify, based by complicated pregnancies and placental risk scores, who is at maximum risk for schizophrenia from very early in life, and these individuals could be followed more carefully,” Dr. Weinberger said in an interview.
The study was published online Feb. 8 in Proceedings of the National Academy of Sciences.
A therapeutic target?
As reported by this news organization, in 2018, the same group of researchers reported that genes associated with schizophrenia are activated in the placenta during a complicated pregnancy, increasing a child’s risk of developing schizophrenia later in life.
In this latest study, they further explored the biological interplay between placental health and neurodevelopment.
They found that a higher placental genomic risk score for schizophrenia, in conjunction with early-life complications during pregnancy, at labor/delivery, and early in neonatal life, is associated with changes in early brain growth and function, particularly in males.
“, and this was associated with slower cognitive development over the first 2 years of life – particularly in the first year of life,” said Dr. Weinberger.
This research defines a “potentially reversible neurodevelopmental path of risk that may be unique to schizophrenia,” the researchers write.
Although most individuals on this altered neurodevelopmental path likely “canalize” back toward normal development, some may not be rescued and instead “decanalize” toward illness, they add.
To date, prevention of schizophrenia from early life has seemed “unapproachable if not unimaginable, but these new insights offer possibilities to change the paradigm,” Dr. Weinberger said in the news release.
“Measuring schizophrenia genetic scores in the placenta combined with studying the first 2 years of cognitive developmental patterns and early life complications could prove to be an important approach to identify those babies with increased risks,” he added.
Important research
Commenting on the study for this news organization, Christopher A. Ross, MD, PhD, professor of psychiatry and behavioral sciences, Johns Hopkins Medicine, Baltimore, said that this is “an interesting and important paper that replicates and extends previous findings of the relationship of placenta genes to schizophrenia in adults.”
“The hypothesis continues to be – and they are continuing to support it – that events in early development could set a person up for a risk of schizophrenia later in life,” said Dr. Ross.
This research, he added, also supports the concept that there are at least two broad classes of genetic risk for schizophrenia.
“One acts through genes that are expressed in the brain and doesn’t relate to early life events, and the other acts through genes expressed in the placenta in patients with these early life events,” said Dr. Ross.
The study had no specific funding. Dr. Weinberger and Dr. Ross have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Schizophrenia-related genes in the placenta are predictive of the size of a baby’s brain at birth and the rate of cognitive development. In a complicated pregnancy, such genes could raise the risk of developing schizophrenia later in life, new research suggests.
“This is further evidence that early life matters in schizophrenia, and the placenta plays a bigger role than we imagined,” Daniel R. Weinberger, MD, director and CEO, Lieber Institute for Brain Development, and professor of neurology, psychiatry, and neuroscience, Johns Hopkins University, Baltimore, said in a news release.
“The holy grail would be to identify, based by complicated pregnancies and placental risk scores, who is at maximum risk for schizophrenia from very early in life, and these individuals could be followed more carefully,” Dr. Weinberger said in an interview.
The study was published online Feb. 8 in Proceedings of the National Academy of Sciences.
A therapeutic target?
As reported by this news organization, in 2018, the same group of researchers reported that genes associated with schizophrenia are activated in the placenta during a complicated pregnancy, increasing a child’s risk of developing schizophrenia later in life.
In this latest study, they further explored the biological interplay between placental health and neurodevelopment.
They found that a higher placental genomic risk score for schizophrenia, in conjunction with early-life complications during pregnancy, at labor/delivery, and early in neonatal life, is associated with changes in early brain growth and function, particularly in males.
“, and this was associated with slower cognitive development over the first 2 years of life – particularly in the first year of life,” said Dr. Weinberger.
This research defines a “potentially reversible neurodevelopmental path of risk that may be unique to schizophrenia,” the researchers write.
Although most individuals on this altered neurodevelopmental path likely “canalize” back toward normal development, some may not be rescued and instead “decanalize” toward illness, they add.
To date, prevention of schizophrenia from early life has seemed “unapproachable if not unimaginable, but these new insights offer possibilities to change the paradigm,” Dr. Weinberger said in the news release.
“Measuring schizophrenia genetic scores in the placenta combined with studying the first 2 years of cognitive developmental patterns and early life complications could prove to be an important approach to identify those babies with increased risks,” he added.
Important research
Commenting on the study for this news organization, Christopher A. Ross, MD, PhD, professor of psychiatry and behavioral sciences, Johns Hopkins Medicine, Baltimore, said that this is “an interesting and important paper that replicates and extends previous findings of the relationship of placenta genes to schizophrenia in adults.”
“The hypothesis continues to be – and they are continuing to support it – that events in early development could set a person up for a risk of schizophrenia later in life,” said Dr. Ross.
This research, he added, also supports the concept that there are at least two broad classes of genetic risk for schizophrenia.
“One acts through genes that are expressed in the brain and doesn’t relate to early life events, and the other acts through genes expressed in the placenta in patients with these early life events,” said Dr. Ross.
The study had no specific funding. Dr. Weinberger and Dr. Ross have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Schizophrenia-related genes in the placenta are predictive of the size of a baby’s brain at birth and the rate of cognitive development. In a complicated pregnancy, such genes could raise the risk of developing schizophrenia later in life, new research suggests.
“This is further evidence that early life matters in schizophrenia, and the placenta plays a bigger role than we imagined,” Daniel R. Weinberger, MD, director and CEO, Lieber Institute for Brain Development, and professor of neurology, psychiatry, and neuroscience, Johns Hopkins University, Baltimore, said in a news release.
“The holy grail would be to identify, based by complicated pregnancies and placental risk scores, who is at maximum risk for schizophrenia from very early in life, and these individuals could be followed more carefully,” Dr. Weinberger said in an interview.
The study was published online Feb. 8 in Proceedings of the National Academy of Sciences.
A therapeutic target?
As reported by this news organization, in 2018, the same group of researchers reported that genes associated with schizophrenia are activated in the placenta during a complicated pregnancy, increasing a child’s risk of developing schizophrenia later in life.
In this latest study, they further explored the biological interplay between placental health and neurodevelopment.
They found that a higher placental genomic risk score for schizophrenia, in conjunction with early-life complications during pregnancy, at labor/delivery, and early in neonatal life, is associated with changes in early brain growth and function, particularly in males.
“, and this was associated with slower cognitive development over the first 2 years of life – particularly in the first year of life,” said Dr. Weinberger.
This research defines a “potentially reversible neurodevelopmental path of risk that may be unique to schizophrenia,” the researchers write.
Although most individuals on this altered neurodevelopmental path likely “canalize” back toward normal development, some may not be rescued and instead “decanalize” toward illness, they add.
To date, prevention of schizophrenia from early life has seemed “unapproachable if not unimaginable, but these new insights offer possibilities to change the paradigm,” Dr. Weinberger said in the news release.
“Measuring schizophrenia genetic scores in the placenta combined with studying the first 2 years of cognitive developmental patterns and early life complications could prove to be an important approach to identify those babies with increased risks,” he added.
Important research
Commenting on the study for this news organization, Christopher A. Ross, MD, PhD, professor of psychiatry and behavioral sciences, Johns Hopkins Medicine, Baltimore, said that this is “an interesting and important paper that replicates and extends previous findings of the relationship of placenta genes to schizophrenia in adults.”
“The hypothesis continues to be – and they are continuing to support it – that events in early development could set a person up for a risk of schizophrenia later in life,” said Dr. Ross.
This research, he added, also supports the concept that there are at least two broad classes of genetic risk for schizophrenia.
“One acts through genes that are expressed in the brain and doesn’t relate to early life events, and the other acts through genes expressed in the placenta in patients with these early life events,” said Dr. Ross.
The study had no specific funding. Dr. Weinberger and Dr. Ross have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.













