User login
Vitamin D pearls
Case: A 56-year-old man with a history of type 2 diabetes, hypertension, hyperlipidemia, and obesity calls clinic to discuss concerns about COVID-19, stating: “I want to do everything I can to reduce my risk of infection.” In addition to physical distancing, mask wearing, hand hygiene, and control of chronic conditions, which of the following supplements would you recommend for this patient?
1. Coenzyme Q10 160 mg twice a day
2. Vitamin D 2,000 IU daily
3. Vitamin E 400 IU daily
4. Vitamin B12 1,000 mcg daily
Of these choices, vitamin D supplementation is likely the best option, based on the limited data that is available.
Risk factors for worse COVID-19 outcome, such as older age, obesity, and more pigmented skin are also risk factors for vitamin D deficiency. This makes the study of vitamin D and COVID-19 both challenging and relevant.
In a recent study of 7,807 people living in Israel, Merzon and colleagues found that low plasma vitamin D level was an independent risk factor for COVID-19 infection. Mean plasma vitamin D level was significantly lower among those who tested positive for COVID-19 (19.00 ng/mL) than negative (20.55 ng/ mL). After controlling for demographic variables and several medical conditions, the adjusted odds ratio of COVID-19 infection in those with lower vitamin D was 1.45 (95% confidence interval, 1.08-1.95; P < .001). However, the odds of hospitalization for COVID-19 was not significantly associated with vitamin D level.1
Prior studies have also looked at vitamin D and respiratory infection. Martineau and colleagues analyzed 25 randomized, controlled trials with a pooled number of 11,321 individuals, including healthy ones and those with comorbidities, and found that oral vitamin D supplementation in daily or weekly doses had a protective effect against acute respiratory infection (adjusted odds ratio, 0.88; 95% CI, 0.81-0.96; P < .001). Patients with vitamin D deficiency (less than 25 nmol/L) experienced the most protective benefit. Vitamin D did not influence respiratory infection outcome.2
These studies suggest an adequate vitamin D level may be protective against infection with COVID-19, but who will benefit from vitamin D supplementation, and in what dose? Per U.S. Preventive Services Task Force guidelines, there is insufficient evidence to recommend screening for vitamin D deficiency in asymptomatic adults. Regarding daily dietary intake, the Institute of Medicine recommends 600 IU for persons aged 1-70, and 800 IU for those aged over 70 years. Salmon (447 IU per 3 oz serving), tuna (154 IU), and fortified milk (116 IU) are among the most vitamin D–rich foods.3 The recommended upper level of intake is 4,000 IU/day.
Too much of a good thing?
Extra vitamin D is stored in adipose tissue. If it builds up over time, storage sites may be overwhelmed, causing a rise in serum D level. While one might expect a subsequent rise in calcium levels, studies have shown this happens inconsistently, and at very high vitamin D levels, over 120 ng/mL.4 Most people would have to take at least 50,000 IU daily for several months to see an effect. The main adverse outcome of vitamin D toxicity is kidney stones, mediated by increased calcium in the blood and urine.
Several animal models have demonstrated hypervitaminosis D–induced aortic and coronary artery calcification. Like with kidney stones, the mechanism appears to be through increased calcium and phosphate levels. Shroff and colleagues studied serum vitamin D levels and vascular disease in children with renal disease on dialysis and found a U-shaped distribution: Children with both low and high vitamin D levels had significantly increased carotid artery intima-media thickness and calcification.5 Given the specialized nature of this population, it’s unclear whether these results can be generalized to most people. More studies are warranted on this topic.
Other benefits
Vitamin D is perhaps most famous for helping to build strong bones. Avenell and colleagues performed a Cochrane meta-analysis of vitamin D supplementation in older adults and found that vitamin D alone did not significantly reduce the risk of hip or other new fracture. Vitamin D plus calcium supplementation did reduce the risk of hip fracture (nine trials, pooled number of individuals was 49,853; relative risk, 0.84; P = .01).6
A lesser-known benefit of vitamin D is muscle protection. A prospective study out of the Jewish Hospital of Cincinnati followed 146 adults who were intolerant to two or more statins because of muscle side effects and found to have a vitamin D level below 32 ng per mL. Subjects were given vitamin D replacement (50,000 units weekly) and followed for 2 years. On statin rechallenge, 88-95% tolerated a statin with vitamin D levels 53-55 ng/mL.7
Pearl
Vitamin D supplementation may protect against COVID-19 infection and has very low chance of harm at daily doses at or below 4,000 IU. Other benefits of taking vitamin D include bone protection and reduction in statin-induced myopathy. The main adverse effect is kidney stones.
Ms. Sharninghausen is a medical student at the University of Washington, Seattle. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Merzon E et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID‐19 infection: An Israeli population‐based study. FEBS J. 2020. doi: 10.1111/febs.15495.
2. Martineau AR et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583. doi:10.1136/bmj.i6583
3. “How to Get More Vitamin D From Your Food,” Cleveland Clinic. 2019 Oct 23. https://health.clevelandclinic.org/how-to-get-more-vitamin-d-from-your-food/.
4. Galior K et al. Development of vitamin d toxicity from overcorrection of vitamin D Deficiency: A review of case reports. Nutrients. 2018;10(8):953. doi: 10.3390/nu10080953
5. Shroff R et al. A bimodal association of vitamin D levels and vascular disease in children on dialysis. J Am Soc Nephrol. 2008;19(6):1239-46. doi: 10.1681/ASN.2007090993.
6. Avenell A et al. Vitamin D and vitamin D analogues for preventing fractures in post‐menopausal women and older men. Cochrane Database Syst Rev. 2014 Apr 14;2014(4):CD000227. doi: 10.1002/14651858.CD000227.pub4.
7. Khayznikov M et al. Statin intolerance because of myalgia, myositis, myopathy, or myonecrosis can in most cases be safely resolved by vitamin D supplementation. N Am J Med Sci. 2015;7(3):86-93. doi:10.4103/1947-2714.153919
Case: A 56-year-old man with a history of type 2 diabetes, hypertension, hyperlipidemia, and obesity calls clinic to discuss concerns about COVID-19, stating: “I want to do everything I can to reduce my risk of infection.” In addition to physical distancing, mask wearing, hand hygiene, and control of chronic conditions, which of the following supplements would you recommend for this patient?
1. Coenzyme Q10 160 mg twice a day
2. Vitamin D 2,000 IU daily
3. Vitamin E 400 IU daily
4. Vitamin B12 1,000 mcg daily
Of these choices, vitamin D supplementation is likely the best option, based on the limited data that is available.
Risk factors for worse COVID-19 outcome, such as older age, obesity, and more pigmented skin are also risk factors for vitamin D deficiency. This makes the study of vitamin D and COVID-19 both challenging and relevant.
In a recent study of 7,807 people living in Israel, Merzon and colleagues found that low plasma vitamin D level was an independent risk factor for COVID-19 infection. Mean plasma vitamin D level was significantly lower among those who tested positive for COVID-19 (19.00 ng/mL) than negative (20.55 ng/ mL). After controlling for demographic variables and several medical conditions, the adjusted odds ratio of COVID-19 infection in those with lower vitamin D was 1.45 (95% confidence interval, 1.08-1.95; P < .001). However, the odds of hospitalization for COVID-19 was not significantly associated with vitamin D level.1
Prior studies have also looked at vitamin D and respiratory infection. Martineau and colleagues analyzed 25 randomized, controlled trials with a pooled number of 11,321 individuals, including healthy ones and those with comorbidities, and found that oral vitamin D supplementation in daily or weekly doses had a protective effect against acute respiratory infection (adjusted odds ratio, 0.88; 95% CI, 0.81-0.96; P < .001). Patients with vitamin D deficiency (less than 25 nmol/L) experienced the most protective benefit. Vitamin D did not influence respiratory infection outcome.2
These studies suggest an adequate vitamin D level may be protective against infection with COVID-19, but who will benefit from vitamin D supplementation, and in what dose? Per U.S. Preventive Services Task Force guidelines, there is insufficient evidence to recommend screening for vitamin D deficiency in asymptomatic adults. Regarding daily dietary intake, the Institute of Medicine recommends 600 IU for persons aged 1-70, and 800 IU for those aged over 70 years. Salmon (447 IU per 3 oz serving), tuna (154 IU), and fortified milk (116 IU) are among the most vitamin D–rich foods.3 The recommended upper level of intake is 4,000 IU/day.
Too much of a good thing?
Extra vitamin D is stored in adipose tissue. If it builds up over time, storage sites may be overwhelmed, causing a rise in serum D level. While one might expect a subsequent rise in calcium levels, studies have shown this happens inconsistently, and at very high vitamin D levels, over 120 ng/mL.4 Most people would have to take at least 50,000 IU daily for several months to see an effect. The main adverse outcome of vitamin D toxicity is kidney stones, mediated by increased calcium in the blood and urine.
Several animal models have demonstrated hypervitaminosis D–induced aortic and coronary artery calcification. Like with kidney stones, the mechanism appears to be through increased calcium and phosphate levels. Shroff and colleagues studied serum vitamin D levels and vascular disease in children with renal disease on dialysis and found a U-shaped distribution: Children with both low and high vitamin D levels had significantly increased carotid artery intima-media thickness and calcification.5 Given the specialized nature of this population, it’s unclear whether these results can be generalized to most people. More studies are warranted on this topic.
Other benefits
Vitamin D is perhaps most famous for helping to build strong bones. Avenell and colleagues performed a Cochrane meta-analysis of vitamin D supplementation in older adults and found that vitamin D alone did not significantly reduce the risk of hip or other new fracture. Vitamin D plus calcium supplementation did reduce the risk of hip fracture (nine trials, pooled number of individuals was 49,853; relative risk, 0.84; P = .01).6
A lesser-known benefit of vitamin D is muscle protection. A prospective study out of the Jewish Hospital of Cincinnati followed 146 adults who were intolerant to two or more statins because of muscle side effects and found to have a vitamin D level below 32 ng per mL. Subjects were given vitamin D replacement (50,000 units weekly) and followed for 2 years. On statin rechallenge, 88-95% tolerated a statin with vitamin D levels 53-55 ng/mL.7
Pearl
Vitamin D supplementation may protect against COVID-19 infection and has very low chance of harm at daily doses at or below 4,000 IU. Other benefits of taking vitamin D include bone protection and reduction in statin-induced myopathy. The main adverse effect is kidney stones.
Ms. Sharninghausen is a medical student at the University of Washington, Seattle. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Merzon E et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID‐19 infection: An Israeli population‐based study. FEBS J. 2020. doi: 10.1111/febs.15495.
2. Martineau AR et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583. doi:10.1136/bmj.i6583
3. “How to Get More Vitamin D From Your Food,” Cleveland Clinic. 2019 Oct 23. https://health.clevelandclinic.org/how-to-get-more-vitamin-d-from-your-food/.
4. Galior K et al. Development of vitamin d toxicity from overcorrection of vitamin D Deficiency: A review of case reports. Nutrients. 2018;10(8):953. doi: 10.3390/nu10080953
5. Shroff R et al. A bimodal association of vitamin D levels and vascular disease in children on dialysis. J Am Soc Nephrol. 2008;19(6):1239-46. doi: 10.1681/ASN.2007090993.
6. Avenell A et al. Vitamin D and vitamin D analogues for preventing fractures in post‐menopausal women and older men. Cochrane Database Syst Rev. 2014 Apr 14;2014(4):CD000227. doi: 10.1002/14651858.CD000227.pub4.
7. Khayznikov M et al. Statin intolerance because of myalgia, myositis, myopathy, or myonecrosis can in most cases be safely resolved by vitamin D supplementation. N Am J Med Sci. 2015;7(3):86-93. doi:10.4103/1947-2714.153919
Case: A 56-year-old man with a history of type 2 diabetes, hypertension, hyperlipidemia, and obesity calls clinic to discuss concerns about COVID-19, stating: “I want to do everything I can to reduce my risk of infection.” In addition to physical distancing, mask wearing, hand hygiene, and control of chronic conditions, which of the following supplements would you recommend for this patient?
1. Coenzyme Q10 160 mg twice a day
2. Vitamin D 2,000 IU daily
3. Vitamin E 400 IU daily
4. Vitamin B12 1,000 mcg daily
Of these choices, vitamin D supplementation is likely the best option, based on the limited data that is available.
Risk factors for worse COVID-19 outcome, such as older age, obesity, and more pigmented skin are also risk factors for vitamin D deficiency. This makes the study of vitamin D and COVID-19 both challenging and relevant.
In a recent study of 7,807 people living in Israel, Merzon and colleagues found that low plasma vitamin D level was an independent risk factor for COVID-19 infection. Mean plasma vitamin D level was significantly lower among those who tested positive for COVID-19 (19.00 ng/mL) than negative (20.55 ng/ mL). After controlling for demographic variables and several medical conditions, the adjusted odds ratio of COVID-19 infection in those with lower vitamin D was 1.45 (95% confidence interval, 1.08-1.95; P < .001). However, the odds of hospitalization for COVID-19 was not significantly associated with vitamin D level.1
Prior studies have also looked at vitamin D and respiratory infection. Martineau and colleagues analyzed 25 randomized, controlled trials with a pooled number of 11,321 individuals, including healthy ones and those with comorbidities, and found that oral vitamin D supplementation in daily or weekly doses had a protective effect against acute respiratory infection (adjusted odds ratio, 0.88; 95% CI, 0.81-0.96; P < .001). Patients with vitamin D deficiency (less than 25 nmol/L) experienced the most protective benefit. Vitamin D did not influence respiratory infection outcome.2
These studies suggest an adequate vitamin D level may be protective against infection with COVID-19, but who will benefit from vitamin D supplementation, and in what dose? Per U.S. Preventive Services Task Force guidelines, there is insufficient evidence to recommend screening for vitamin D deficiency in asymptomatic adults. Regarding daily dietary intake, the Institute of Medicine recommends 600 IU for persons aged 1-70, and 800 IU for those aged over 70 years. Salmon (447 IU per 3 oz serving), tuna (154 IU), and fortified milk (116 IU) are among the most vitamin D–rich foods.3 The recommended upper level of intake is 4,000 IU/day.
Too much of a good thing?
Extra vitamin D is stored in adipose tissue. If it builds up over time, storage sites may be overwhelmed, causing a rise in serum D level. While one might expect a subsequent rise in calcium levels, studies have shown this happens inconsistently, and at very high vitamin D levels, over 120 ng/mL.4 Most people would have to take at least 50,000 IU daily for several months to see an effect. The main adverse outcome of vitamin D toxicity is kidney stones, mediated by increased calcium in the blood and urine.
Several animal models have demonstrated hypervitaminosis D–induced aortic and coronary artery calcification. Like with kidney stones, the mechanism appears to be through increased calcium and phosphate levels. Shroff and colleagues studied serum vitamin D levels and vascular disease in children with renal disease on dialysis and found a U-shaped distribution: Children with both low and high vitamin D levels had significantly increased carotid artery intima-media thickness and calcification.5 Given the specialized nature of this population, it’s unclear whether these results can be generalized to most people. More studies are warranted on this topic.
Other benefits
Vitamin D is perhaps most famous for helping to build strong bones. Avenell and colleagues performed a Cochrane meta-analysis of vitamin D supplementation in older adults and found that vitamin D alone did not significantly reduce the risk of hip or other new fracture. Vitamin D plus calcium supplementation did reduce the risk of hip fracture (nine trials, pooled number of individuals was 49,853; relative risk, 0.84; P = .01).6
A lesser-known benefit of vitamin D is muscle protection. A prospective study out of the Jewish Hospital of Cincinnati followed 146 adults who were intolerant to two or more statins because of muscle side effects and found to have a vitamin D level below 32 ng per mL. Subjects were given vitamin D replacement (50,000 units weekly) and followed for 2 years. On statin rechallenge, 88-95% tolerated a statin with vitamin D levels 53-55 ng/mL.7
Pearl
Vitamin D supplementation may protect against COVID-19 infection and has very low chance of harm at daily doses at or below 4,000 IU. Other benefits of taking vitamin D include bone protection and reduction in statin-induced myopathy. The main adverse effect is kidney stones.
Ms. Sharninghausen is a medical student at the University of Washington, Seattle. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Merzon E et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID‐19 infection: An Israeli population‐based study. FEBS J. 2020. doi: 10.1111/febs.15495.
2. Martineau AR et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583. doi:10.1136/bmj.i6583
3. “How to Get More Vitamin D From Your Food,” Cleveland Clinic. 2019 Oct 23. https://health.clevelandclinic.org/how-to-get-more-vitamin-d-from-your-food/.
4. Galior K et al. Development of vitamin d toxicity from overcorrection of vitamin D Deficiency: A review of case reports. Nutrients. 2018;10(8):953. doi: 10.3390/nu10080953
5. Shroff R et al. A bimodal association of vitamin D levels and vascular disease in children on dialysis. J Am Soc Nephrol. 2008;19(6):1239-46. doi: 10.1681/ASN.2007090993.
6. Avenell A et al. Vitamin D and vitamin D analogues for preventing fractures in post‐menopausal women and older men. Cochrane Database Syst Rev. 2014 Apr 14;2014(4):CD000227. doi: 10.1002/14651858.CD000227.pub4.
7. Khayznikov M et al. Statin intolerance because of myalgia, myositis, myopathy, or myonecrosis can in most cases be safely resolved by vitamin D supplementation. N Am J Med Sci. 2015;7(3):86-93. doi:10.4103/1947-2714.153919
First guideline on NGS testing in cancer, from ESMO
Recommendations on the use of next-generation sequencing (NGS) tests for patients with metastatic cancer have been issued by the European Society for Medical Oncology, the first recommendations of their kind to be published by any medical society.
“Until now, there were no recommendations from scientific societies on how to use this technique in daily clinical practice to profile metastatic cancers,” Fernanda Mosele, MD, medical oncologist, Gustave Roussy, Villejuif, France, said in a statement.
NGS testing is already used extensively in oncology, particularly in metastatic cancer, she noted. The technology is used to assess the sequence of DNA in genes from a tumor tissue sample. Numerous genes can be quickly sequenced at the same time at relatively low cost. The results provide information on mutations that are present, which, in turn, helps with deciding which treatments to use, including drugs targeting the identified mutations.
“Our intent is that they [the guidelines] will unify decision-making about how NGS should be used for patients with metastatic cancer,” Dr. Mosele said.
The recommendations were published online August 25 in Annals of Oncology.
Overall, ESMO recommends the use of tumor multigene NGS for non–small cell lung cancer (NSCLC), prostate cancer, ovarian cancer, and cholangiocarcinoma.
For other cancers, the authors said that NGS is not recommended in clinical practice but could be used for research purposes.
However, patients should be informed that it is unlikely that test results would benefit them much personally.
Physicians and patients may decide together to subject the tumor to mutational testing using a large panel of genes, provided testing doesn’t burden the health care system with additional costs.
“This recommendation acknowledges that a small number of patients could benefit from a drug because they have a rare mutation,” Joaquin Mateo, MD, chair of the ESMO working group, said in a statement.
“So beyond the cancers in which everyone should receive NGS, there is room for physicians and patients to discuss the pros and cons of ordering these tests,” he added.
ESMO also does not recommend the use of off-label drugs matched to any genomic alteration detected by NGS unless an access program and a decisional procedure have been developed, either regionally or nationally.
No need for NGS testing of other cancers
In contrast to NSCLC, “there is currently no need to perform tumor multigene NGS for patients with mBC [metastatic breast cancer] in the context of daily practice,” ESMO stated.
This is largely because somatic sequencing cannot fully substitute for germline testing for BRCA status, and other mutations, such as HER2, can be detected using immunohistochemistry (IHC).
The same can be said for patients with metastatic gastric cancer, inasmuch as detection of alterations can and should be done using cheaper testing methods, ESMO pointed out.
However, ESMO members still emphasized that it’s important to include patients with metastatic breast cancer in molecular screening programs as well as in clinical trials testing targeted agents.
Similarly, there is no need to test metastatic colorectal cancer (mCRC) using multigene NGS in daily practice, inasmuch as most level 1 alterations in mCRC can be determined by IHC or PCR.
However, NGS can be considered as an alternative to PCR-based tests in mCRC, provided NGS is not associated with additional cost.
ESMO again recommended that research centers include mCRC patients in molecular screening programs in order for them to have access to innovative clinical trial agents.
As for advanced prostate cancer, ESMO does recommend that clinicians perform NGS on tissue samples to assess the tumor’s mutational status, at least for the presence of BRCA1 and BRCA2 mutations, when patients have access to the poly (ADP-ribose) polymerase inhibitors for treatment.
The authors cautioned, however, that this strategy is unlikely to be cost-effective, so larger panels should be used only when there are specific agreements with payers.
Multigene NGS is also not recommended for patients with advanced pancreatic ductal adenocarcinoma (PDAC), although ESMO points out that it is the role of research centers to propose multigene sequencing for these patients in the context of molecular screening programs.
This is again to facilitate access to innovative drugs for these patients.
Similar to recommendations for patients with advanced PDAC, patients with advanced hepatocellular carcinoma (HCC) do not need to have tumor multigene NGS either.
Considering the high unmet needs of HCC patients, ESMO feels that research centers should propose multigene sequencing to patients with advanced HCC in the context of molecular screening programs.
In contrast, ESMO recommended that tumor multigene NGS be used to detect actionable alterations in patients with advanced cholangiocarcinoma.
Again, they predict that this strategy is unlikely to be cost-effective, so larger panels should only be used if a specific agreement is in place with payers.
ESMO also assessed the frequency of level 1 alterations in less frequent tumor types, including ovarian cancers. Because BRCA1 and BRCA2 somatic mutations in ovarian tumors have been associated with increased response to the PARP inhibitors, the use of multigene NGS is justified with this malignancy, ESMO states.
The authors also recommend that tumor mutational burden be determined in cervical cancer, moderately differentiated neuroendocrine tumors, salivary cancers, vulvar cancer, and thyroid cancers.
Dr. Mosele has disclosed no relevant financial relationships. Many coauthors have relationships with the pharmaceutical industry, as listed in the article.
This article first appeared on Medscape.com.
Recommendations on the use of next-generation sequencing (NGS) tests for patients with metastatic cancer have been issued by the European Society for Medical Oncology, the first recommendations of their kind to be published by any medical society.
“Until now, there were no recommendations from scientific societies on how to use this technique in daily clinical practice to profile metastatic cancers,” Fernanda Mosele, MD, medical oncologist, Gustave Roussy, Villejuif, France, said in a statement.
NGS testing is already used extensively in oncology, particularly in metastatic cancer, she noted. The technology is used to assess the sequence of DNA in genes from a tumor tissue sample. Numerous genes can be quickly sequenced at the same time at relatively low cost. The results provide information on mutations that are present, which, in turn, helps with deciding which treatments to use, including drugs targeting the identified mutations.
“Our intent is that they [the guidelines] will unify decision-making about how NGS should be used for patients with metastatic cancer,” Dr. Mosele said.
The recommendations were published online August 25 in Annals of Oncology.
Overall, ESMO recommends the use of tumor multigene NGS for non–small cell lung cancer (NSCLC), prostate cancer, ovarian cancer, and cholangiocarcinoma.
For other cancers, the authors said that NGS is not recommended in clinical practice but could be used for research purposes.
However, patients should be informed that it is unlikely that test results would benefit them much personally.
Physicians and patients may decide together to subject the tumor to mutational testing using a large panel of genes, provided testing doesn’t burden the health care system with additional costs.
“This recommendation acknowledges that a small number of patients could benefit from a drug because they have a rare mutation,” Joaquin Mateo, MD, chair of the ESMO working group, said in a statement.
“So beyond the cancers in which everyone should receive NGS, there is room for physicians and patients to discuss the pros and cons of ordering these tests,” he added.
ESMO also does not recommend the use of off-label drugs matched to any genomic alteration detected by NGS unless an access program and a decisional procedure have been developed, either regionally or nationally.
No need for NGS testing of other cancers
In contrast to NSCLC, “there is currently no need to perform tumor multigene NGS for patients with mBC [metastatic breast cancer] in the context of daily practice,” ESMO stated.
This is largely because somatic sequencing cannot fully substitute for germline testing for BRCA status, and other mutations, such as HER2, can be detected using immunohistochemistry (IHC).
The same can be said for patients with metastatic gastric cancer, inasmuch as detection of alterations can and should be done using cheaper testing methods, ESMO pointed out.
However, ESMO members still emphasized that it’s important to include patients with metastatic breast cancer in molecular screening programs as well as in clinical trials testing targeted agents.
Similarly, there is no need to test metastatic colorectal cancer (mCRC) using multigene NGS in daily practice, inasmuch as most level 1 alterations in mCRC can be determined by IHC or PCR.
However, NGS can be considered as an alternative to PCR-based tests in mCRC, provided NGS is not associated with additional cost.
ESMO again recommended that research centers include mCRC patients in molecular screening programs in order for them to have access to innovative clinical trial agents.
As for advanced prostate cancer, ESMO does recommend that clinicians perform NGS on tissue samples to assess the tumor’s mutational status, at least for the presence of BRCA1 and BRCA2 mutations, when patients have access to the poly (ADP-ribose) polymerase inhibitors for treatment.
The authors cautioned, however, that this strategy is unlikely to be cost-effective, so larger panels should be used only when there are specific agreements with payers.
Multigene NGS is also not recommended for patients with advanced pancreatic ductal adenocarcinoma (PDAC), although ESMO points out that it is the role of research centers to propose multigene sequencing for these patients in the context of molecular screening programs.
This is again to facilitate access to innovative drugs for these patients.
Similar to recommendations for patients with advanced PDAC, patients with advanced hepatocellular carcinoma (HCC) do not need to have tumor multigene NGS either.
Considering the high unmet needs of HCC patients, ESMO feels that research centers should propose multigene sequencing to patients with advanced HCC in the context of molecular screening programs.
In contrast, ESMO recommended that tumor multigene NGS be used to detect actionable alterations in patients with advanced cholangiocarcinoma.
Again, they predict that this strategy is unlikely to be cost-effective, so larger panels should only be used if a specific agreement is in place with payers.
ESMO also assessed the frequency of level 1 alterations in less frequent tumor types, including ovarian cancers. Because BRCA1 and BRCA2 somatic mutations in ovarian tumors have been associated with increased response to the PARP inhibitors, the use of multigene NGS is justified with this malignancy, ESMO states.
The authors also recommend that tumor mutational burden be determined in cervical cancer, moderately differentiated neuroendocrine tumors, salivary cancers, vulvar cancer, and thyroid cancers.
Dr. Mosele has disclosed no relevant financial relationships. Many coauthors have relationships with the pharmaceutical industry, as listed in the article.
This article first appeared on Medscape.com.
Recommendations on the use of next-generation sequencing (NGS) tests for patients with metastatic cancer have been issued by the European Society for Medical Oncology, the first recommendations of their kind to be published by any medical society.
“Until now, there were no recommendations from scientific societies on how to use this technique in daily clinical practice to profile metastatic cancers,” Fernanda Mosele, MD, medical oncologist, Gustave Roussy, Villejuif, France, said in a statement.
NGS testing is already used extensively in oncology, particularly in metastatic cancer, she noted. The technology is used to assess the sequence of DNA in genes from a tumor tissue sample. Numerous genes can be quickly sequenced at the same time at relatively low cost. The results provide information on mutations that are present, which, in turn, helps with deciding which treatments to use, including drugs targeting the identified mutations.
“Our intent is that they [the guidelines] will unify decision-making about how NGS should be used for patients with metastatic cancer,” Dr. Mosele said.
The recommendations were published online August 25 in Annals of Oncology.
Overall, ESMO recommends the use of tumor multigene NGS for non–small cell lung cancer (NSCLC), prostate cancer, ovarian cancer, and cholangiocarcinoma.
For other cancers, the authors said that NGS is not recommended in clinical practice but could be used for research purposes.
However, patients should be informed that it is unlikely that test results would benefit them much personally.
Physicians and patients may decide together to subject the tumor to mutational testing using a large panel of genes, provided testing doesn’t burden the health care system with additional costs.
“This recommendation acknowledges that a small number of patients could benefit from a drug because they have a rare mutation,” Joaquin Mateo, MD, chair of the ESMO working group, said in a statement.
“So beyond the cancers in which everyone should receive NGS, there is room for physicians and patients to discuss the pros and cons of ordering these tests,” he added.
ESMO also does not recommend the use of off-label drugs matched to any genomic alteration detected by NGS unless an access program and a decisional procedure have been developed, either regionally or nationally.
No need for NGS testing of other cancers
In contrast to NSCLC, “there is currently no need to perform tumor multigene NGS for patients with mBC [metastatic breast cancer] in the context of daily practice,” ESMO stated.
This is largely because somatic sequencing cannot fully substitute for germline testing for BRCA status, and other mutations, such as HER2, can be detected using immunohistochemistry (IHC).
The same can be said for patients with metastatic gastric cancer, inasmuch as detection of alterations can and should be done using cheaper testing methods, ESMO pointed out.
However, ESMO members still emphasized that it’s important to include patients with metastatic breast cancer in molecular screening programs as well as in clinical trials testing targeted agents.
Similarly, there is no need to test metastatic colorectal cancer (mCRC) using multigene NGS in daily practice, inasmuch as most level 1 alterations in mCRC can be determined by IHC or PCR.
However, NGS can be considered as an alternative to PCR-based tests in mCRC, provided NGS is not associated with additional cost.
ESMO again recommended that research centers include mCRC patients in molecular screening programs in order for them to have access to innovative clinical trial agents.
As for advanced prostate cancer, ESMO does recommend that clinicians perform NGS on tissue samples to assess the tumor’s mutational status, at least for the presence of BRCA1 and BRCA2 mutations, when patients have access to the poly (ADP-ribose) polymerase inhibitors for treatment.
The authors cautioned, however, that this strategy is unlikely to be cost-effective, so larger panels should be used only when there are specific agreements with payers.
Multigene NGS is also not recommended for patients with advanced pancreatic ductal adenocarcinoma (PDAC), although ESMO points out that it is the role of research centers to propose multigene sequencing for these patients in the context of molecular screening programs.
This is again to facilitate access to innovative drugs for these patients.
Similar to recommendations for patients with advanced PDAC, patients with advanced hepatocellular carcinoma (HCC) do not need to have tumor multigene NGS either.
Considering the high unmet needs of HCC patients, ESMO feels that research centers should propose multigene sequencing to patients with advanced HCC in the context of molecular screening programs.
In contrast, ESMO recommended that tumor multigene NGS be used to detect actionable alterations in patients with advanced cholangiocarcinoma.
Again, they predict that this strategy is unlikely to be cost-effective, so larger panels should only be used if a specific agreement is in place with payers.
ESMO also assessed the frequency of level 1 alterations in less frequent tumor types, including ovarian cancers. Because BRCA1 and BRCA2 somatic mutations in ovarian tumors have been associated with increased response to the PARP inhibitors, the use of multigene NGS is justified with this malignancy, ESMO states.
The authors also recommend that tumor mutational burden be determined in cervical cancer, moderately differentiated neuroendocrine tumors, salivary cancers, vulvar cancer, and thyroid cancers.
Dr. Mosele has disclosed no relevant financial relationships. Many coauthors have relationships with the pharmaceutical industry, as listed in the article.
This article first appeared on Medscape.com.
Kathleen Healey, APRN, PhD, on the Multiple Sclerosis At Home Program
Kathleen Healey, APRN, PhD, is an assistant professor in the Department of Neurological Sciences at the University of Nebraska in Omaha, NE, and a nurse practitioner in the Multiple Sclerosis Program at the University of Nebraska Medical Center. She has worked in the MS area since 1998. Dr. Healey has presented numerous programs on MS to patient and provider groups locally and regionally, has presented her research nationally, and is a consultant for Can-do MS. She has developed and led initiatives to improve care access and delivery of care to individuals with MS and significant disability since 2013.
Dr. Healey discloses that she has received grant funding through the MS Foundation.
What barriers to coordinated comprehensive care do patients with progressive multiple sclerosis (MS) face under current health care delivery models?
KATHLEEN HEALEY, PhD: In spite of the 1990 Americans with Disabilities Act, evidence suggests that disparities in health services for people with disabilities remain. These individuals receive health care less often, receive poorer quality care, have unmet health care needs, lack basic screening for health care maintenance, and are offered fewer treatment options, compared to people without disability.
Health care delivery for individuals with disabling progressive forms of MS presents some unique challenges. This disorder is chronic, medically complex, generally progressive, and heterogenous in its effects on the central nervous system (unlike relatively fixed spinal cord and brain injury), producing varying degrees of immobility and loss of function. As the disease progresses, a significant proportion of patients need assistive devices, including power mobility, urinary catheters, gastric tubes, hospital beds, home modifications, sleep and respiratory aides, and other devices. Family members are also likely to suffer from caregiver burden.
In the early stages of MS, individuals may be successful in careers and raising families, but with advancing disability, the majority will incur severe financial and social consequences. Many will become unemployed and face financial hardship, and, furthermore, many lack social support and appropriate transportation and become socially isolated.
One of the bigger challenges in accessing care is transportation, especially for those in wheelchairs and power mobility. Ironically, beyond that, many of the obstacles to comprehensive care are deeply embedded in the traditional health care system itself. The traditional medical model and clinic structure was not designed to serve individuals with complex disability.
Studies have identified specific obstacles to care individuals with MS and disability encounter before, during, and after clinic appointments.1 For an individual with complex disability, something as simple as trying to contact a clinic can be difficult. Clinicians typically don't think about the time MS patients with disability must spend preparing for a visit. Individuals I work with tell me it takes about 5 hours for them to get ready and to schedule transportation. When they arrive, often there are too few handicapped parking spaces, and equipment adapted for persons with disability, like appropriate exam tables and even wheelchair scales, may not be available. In traditional check-ins to clinic, no additional time is allotted for those with disability. So, check-in generally is rushed and not complete.
The traditional medical fee-for-service volume model is based on time. Clinics typically allot perhaps 20 to at the most 40 minutes for a return visit. When a person gets into the room with a provider, it’s for an abbreviated period of time. And I've had patients tell me that such visits are not really beneficial.
Follow-up instructions and following through with additional referrals are problematic as well. Clinic visits can be very hurried: “Here's your discharge instructions,” or “Here's your after-visit summary.” Because of the heterogenic complexity of disability in MS, education and follow-up require an extremely individualized approach and instructions to accommodate specific disability. Although we have translation services for non-English speaking patients and large fonts for those with visual impairment, integrating follow-up for a person who has profound ataxia, or is blind, and or has some cognitive dysfunction and is in a power wheelchair is challenging. Also, ordering and accessing durable medical equipment needed to preserve independence in the community is becoming increasingly difficult, if not impossible, especially in many managed Medicare and dual-eligible programs.
What is the Multiple Sclerosis at Home Access (MAHA) program and what are its goals?
Kathleen Healey, PhD: The MS Clinic at the University of Nebraska is part of an urban academic medical center in Omaha and serves more than 2500 people with MS. The MAHA program was designed specifically for individuals with progressive MS and significant disability. The individuals we serve are often in wheelchairs, and if ambulatory, able to walk only a few steps (patients with Expanded Disability Scale (Kurtzke) scores of 7.5 or greater). At this time, over 100 individuals are enrolled in our MAHA programs.
The majority of the individuals we serve are low income—at least half are dually eligible beneficiaries under Medicare/Medicaid. A substantial number of those we serve are eligible for Medicaid waiver, with incomes at or below the poverty level. Most of these individuals are still fiercely residing in the community, with assistance, and wish to remain so.
Our objectives are to coordinate and deliver comprehensive medical care, improve patient satisfaction, and prevent or treat common complications related to immobility, with an expected decrease in preventable/avoidable health care utilization. Our long-term goals are to improve quality-of-life, promote wellness, increase independence, and promote community reintegration.
The MAHA initiative derives its name from its city of origin, Omaha, Nebraska. This region was first settled by the Maha Native American tribe, and maha means “against the wind, against the current.” This word and meaning seemed to capture the struggles of patients with MS and their families trying to access comprehensive quality care.
MAHA focuses on the identified common problems, especially access to care and fragmentation in care. Our programs attempt to bridge primary and MS specialty care. Central to the model is productive interactions at each encounter. So, it’s not just checking off boxes, it is integration of an agreed upon plan of care, and that takes time and expertise to develop.
Initially, the program focused on house calls (established in 2013) and has now expanded to a transdisciplinary clinic and extensive use of telehealth across Nebraska, including for many in rural areas and in long-term nursing facilities. Our care delivery model is drastically different from a traditional medical model and includes the following components:
More time: New-patient encounters are templated for 1 to 2 hours, house calls up to 3 hours, and established follow-up “return” visits are at least 1 hour and may exceed 2 to 3 hours.
Continuity and competency in care: Limited core team members have frequent contact with patients. Initially, with house calls we had numerous providers going to the home, including physical therapy (PT), occupational therapy (OT), and, in some cases, speech therapy. Patients and family reported frustration with layers of numerous providers, frequent phone calls, and scheduling them to come into their home. Patients wanted to be able to count on a certain trusted few, familiar with their issues. If another discipline is needed, then the patient and core team make that decision and call that person in.
Designated team leader: The MAHA team is led by a ”MS-comprehensivist,” defined as a practitioner with expertise in MS care as well as a background in chronic illness and primary care. This practitioner bridges the specialist-generalist elements in care and serves as an expert care manager or integrator to coordinate and communicate care among providers.
Enhanced communication and follow-up: The patient and designated support person (family or primary paid caregiver) always know the plan of care and are on the same page. This includes a weekly care conference with the core team community nurse, PT, neurology comprehensivists, and nurse coordinator.
In addition, the MAHA program continually monitors outcomes, with immediate investigation regarding preventable complications; incorporates protocols and guidelines, generally from paralyzed veterans or other spinal cord organizations as well as the National MS Society; and commonly calls upon subspecialty physicians (Best Friends)
Finally, the program incorporates lessons learned from individuals with lived experience. Individuals with MS and severe disability are unique, talented, tenacious, and often fiercely independent. The challenges for these individuals and their families were initially underestimated by our team; the lessons learned from these experts allowed us to tailor our program to become better.
Over the course of 7 years, core team members reported increased knowledge and keen awareness of needs and issues of patients with severe disability, suggesting that a transdisciplinary team with multifaceted expertise was evolving. Transdisciplinary, to us, means relating to more than 1 branch of knowledge; examples included our community physical therapist gaining knowledge of necessary steps to obtain grants for direct assistance for equipment needed to prevent falls/injury, and becoming knowledgeable about MS and all of its complexity. Our care coordinator is a medical assistant who became an expert regarding transportation issues in community, and has gained advanced knowledge of MS and disability and integrated social services needs and connections to obtain needed resources. As a nurse practitioner and comprehensivist, over time I gained knowledge of PT and OT disciplines, and learned more about evaluation of the need for durable medical equipment, the importance of the whole person and environment, and acquisition of equipment, with frequent appeals and justification.
All of our persistent team members also unexpectedly became experts in community advocacy for persons with disability, attending city transportation meetings, conferencing with Department of Health and Human Services, and developing public awareness material.
What are the outcomes of the MAHA program in terms of patient response, quality indicators, and financial sustainability?
Kathleen Healey, PhD: We tailored the program to impact the frequency of secondary complications, which are generally preventable, such as urinary and respiratory infection, sepsis, skin pressure and other injury, falls, and fractures. These complications cause suffering and may worsen MS baseline symptoms, especially with severe infections. We know that individuals with significant disability who are hospitalized are at risk for a host of other complications. A recent study published in Neurology showed that 11% of all patients with a neurologic diagnosis admitted to hospitals developed hospital-acquired adverse events or complications.2
In our initial house call program, half of the hospital admissions were related to secondary and generally preventable complications, both during the 2-year preevaluation and postevaluation period. After program implementation, we saw decreases in the number of individuals hospitalized, hospitalizations/skilled facility admissions, and hospital days; the total number of emergency department (ED) visits decreased; and ED-only visits increased (ie, ED visits without hospital admission).3
Patient satisfaction reports and quality indicators were positive. We also measured perceived benefit by asking patients to write their thoughts on the benefits of the program, and we received really robust responses:
“This is the first time somebody actually sat down and listened to me, talked to me.”
“The program was very helpful for me.”
“It was a Godsend. They helped us so much.”
“It helps tremendously, I don’t have to worry so much, I’ve recommended it to others.”
“They get it done; it’s amazing, I have the equipment I need now to be more independent.”
So, you asked about sustainability. Programs like this are difficult to justify in traditional hospital/clinic accounting structures. Initiatives like MAHA may be more sustainable in a value-based structure, but this remains to be seen. Cost avoidance, especially in preventable complications, is likely the best financial indicator at this time.
We have been able to sustain our programs only with the help of grant money through the MS Foundation and through a community donor, to whom we are forever grateful. In addition, our division chair, Dr. Rana Zabad, has been supportive of this innovative initiative because she knows how essential it is for comprehensive care of all individuals with MS.
Importantly, we continue to track our clinical outcome data and have robust longitudinal data, giving us more information about the trajectory of the patients in our program.
Beyond in-home care, what opportunities exist to improve comprehensive care of MS patients via telehealth?
Kathleen Healey, PhD: We have been doing telehealth since 2013, well before the pandemic, but we were receiving variable to no reimbursement. Prior to the pandemic, the Centers for Medicare & Medicaid Services did not reimburse for telehealth unless it was done at a critical access hospital, generally in rural parts of our state.
Since the pandemic and the release of telehealth waivers, we have been able to increase our telemedicine visits to individuals and be appropriately reimbursed. However, about 30% of our patients have limitations regarding telehealth with video due to specific disability, cost, or lack of reliable broadband. Telephone encounters are important if an individual can’t do a telehealth visit, but reimbursement is lower. In my opinion, lack of IT capability may add another dimension to health care disparity.
The benefit of telemedicine, in my opinion, is close to a home visit, because the patient or their caregiver can take their device and show us their environment, show us where the problem areas are. Like when you do a home visit, you get this incredible mosaic of different assessments and develop a deep understanding of the day-to-day challenges facing persons with disability.
Our team agrees that user-friendly adapted devices and reliable broadband are needed, especially for those who are disabled, lack or have inadequate transportation, are low income, or live in rural or underserved urban areas. For these individuals, this is “infrastructure” as important as highways or roads.
Has the coronavirus pandemic presented challenges to delivering in-home care? If so, how have you managed these challenges?
Kathleen Healey, PhD: During the pandemic, we have not been making as many house calls. However, we’ve been able to work around this because all of our home-care patients qualify for skilled home health care. So, with approval of the patient, and with the home health nurse (who is a core team member), we are able coordinate televisits and involve more members of the team, if needed, from remote locations. Importantly, if a family member is working or distant, we can bring them in also, which literally does get everyone on the same page. It must be noted that this takes a significant amount of time to coordinate, but, in our opinion, results in a very productive interaction.
As far as COVID testing, for a 2-month period of time we were unable to test a homebound patient. Some of our patients cannot leave their home—they are disabled in place, and the only way that they can leave their home is generally with an ambulance. Others rely on paratransit systems, which were not operating during the shutdown. Since then, we have worked with a nursing agency to have a nurse visit the homes of our patients with MS to conduct COVID testing.
The pandemic has uncovered significant disparities in health care that persons with disability face. About 15% of those we serve reside in nursing homes, and a substantial proportion of residents with MS and disability have tested positive for COVID-19.
The community-dwelling individuals we serve are younger (in the initial house call program, approximately 50% were between 35 and 54 years of age). To remain independent in the community, individuals require care assistance from family or paid caregivers. At this point, very few have tested positive for COVID-19, but with increased community prevalence, we are expecting that could change. Most of the people we serve are well educated on mitigation and taking extra precautions. Regardless, we field daily calls, many times from family caregivers with questions such as, “What if I get COVID, how will my loved one receive care.”
Paid caregivers assisting persons with disability are key to improving quality of life and health outcomes of people with disability. Unfortunately, these essential workers are poorly paid, generally have no benefits, including health care, and likely are more at risk for COVID-19. However, at this point, persons with MS and disability residing in the community clearly have fared better than those in nursing facilities.
References
1. Chiu C, Bishop M, Pionke JJ, et al. Barriers in the accessibility and continuity of health-care services in people with multiple sclerosis: a literature review. Int J MS Care. 2017;19:313-321.
2.Sauro KM, Quan H, Sikdar KC, et al. Hospital safety among neurologic patients: a population-based cohort study of adverse events. Neurology. 2017;89:284-290.
3. Healey K, Zabad RK, Young L, et al. Multiple Sclerosis at Home Access (MAHA): An Initiative to Improve Care in the Community. Int J MS Care. 2019;21(3):101-112.
1. Chiu C, Bishop M, Pionke JJ, et al. Barriers in the accessibility and continuity of health-care services in people with multiple sclerosis: a literature review. Int J MS Care. 2017;19:313-321.
2.Sauro KM, Quan H, Sikdar KC, et al. Hospital safety among neurologic patients: a population-based cohort study of adverse events. Neurology. 2017;89:284-290.
3. Healey K, Zabad RK, Young L, et al. Multiple Sclerosis at Home Access (MAHA): An Initiative to Improve Care in the Community. Int J MS Care. 2019;21(3):101-112.
Kathleen Healey, APRN, PhD, is an assistant professor in the Department of Neurological Sciences at the University of Nebraska in Omaha, NE, and a nurse practitioner in the Multiple Sclerosis Program at the University of Nebraska Medical Center. She has worked in the MS area since 1998. Dr. Healey has presented numerous programs on MS to patient and provider groups locally and regionally, has presented her research nationally, and is a consultant for Can-do MS. She has developed and led initiatives to improve care access and delivery of care to individuals with MS and significant disability since 2013.
Dr. Healey discloses that she has received grant funding through the MS Foundation.
What barriers to coordinated comprehensive care do patients with progressive multiple sclerosis (MS) face under current health care delivery models?
KATHLEEN HEALEY, PhD: In spite of the 1990 Americans with Disabilities Act, evidence suggests that disparities in health services for people with disabilities remain. These individuals receive health care less often, receive poorer quality care, have unmet health care needs, lack basic screening for health care maintenance, and are offered fewer treatment options, compared to people without disability.
Health care delivery for individuals with disabling progressive forms of MS presents some unique challenges. This disorder is chronic, medically complex, generally progressive, and heterogenous in its effects on the central nervous system (unlike relatively fixed spinal cord and brain injury), producing varying degrees of immobility and loss of function. As the disease progresses, a significant proportion of patients need assistive devices, including power mobility, urinary catheters, gastric tubes, hospital beds, home modifications, sleep and respiratory aides, and other devices. Family members are also likely to suffer from caregiver burden.
In the early stages of MS, individuals may be successful in careers and raising families, but with advancing disability, the majority will incur severe financial and social consequences. Many will become unemployed and face financial hardship, and, furthermore, many lack social support and appropriate transportation and become socially isolated.
One of the bigger challenges in accessing care is transportation, especially for those in wheelchairs and power mobility. Ironically, beyond that, many of the obstacles to comprehensive care are deeply embedded in the traditional health care system itself. The traditional medical model and clinic structure was not designed to serve individuals with complex disability.
Studies have identified specific obstacles to care individuals with MS and disability encounter before, during, and after clinic appointments.1 For an individual with complex disability, something as simple as trying to contact a clinic can be difficult. Clinicians typically don't think about the time MS patients with disability must spend preparing for a visit. Individuals I work with tell me it takes about 5 hours for them to get ready and to schedule transportation. When they arrive, often there are too few handicapped parking spaces, and equipment adapted for persons with disability, like appropriate exam tables and even wheelchair scales, may not be available. In traditional check-ins to clinic, no additional time is allotted for those with disability. So, check-in generally is rushed and not complete.
The traditional medical fee-for-service volume model is based on time. Clinics typically allot perhaps 20 to at the most 40 minutes for a return visit. When a person gets into the room with a provider, it’s for an abbreviated period of time. And I've had patients tell me that such visits are not really beneficial.
Follow-up instructions and following through with additional referrals are problematic as well. Clinic visits can be very hurried: “Here's your discharge instructions,” or “Here's your after-visit summary.” Because of the heterogenic complexity of disability in MS, education and follow-up require an extremely individualized approach and instructions to accommodate specific disability. Although we have translation services for non-English speaking patients and large fonts for those with visual impairment, integrating follow-up for a person who has profound ataxia, or is blind, and or has some cognitive dysfunction and is in a power wheelchair is challenging. Also, ordering and accessing durable medical equipment needed to preserve independence in the community is becoming increasingly difficult, if not impossible, especially in many managed Medicare and dual-eligible programs.
What is the Multiple Sclerosis at Home Access (MAHA) program and what are its goals?
Kathleen Healey, PhD: The MS Clinic at the University of Nebraska is part of an urban academic medical center in Omaha and serves more than 2500 people with MS. The MAHA program was designed specifically for individuals with progressive MS and significant disability. The individuals we serve are often in wheelchairs, and if ambulatory, able to walk only a few steps (patients with Expanded Disability Scale (Kurtzke) scores of 7.5 or greater). At this time, over 100 individuals are enrolled in our MAHA programs.
The majority of the individuals we serve are low income—at least half are dually eligible beneficiaries under Medicare/Medicaid. A substantial number of those we serve are eligible for Medicaid waiver, with incomes at or below the poverty level. Most of these individuals are still fiercely residing in the community, with assistance, and wish to remain so.
Our objectives are to coordinate and deliver comprehensive medical care, improve patient satisfaction, and prevent or treat common complications related to immobility, with an expected decrease in preventable/avoidable health care utilization. Our long-term goals are to improve quality-of-life, promote wellness, increase independence, and promote community reintegration.
The MAHA initiative derives its name from its city of origin, Omaha, Nebraska. This region was first settled by the Maha Native American tribe, and maha means “against the wind, against the current.” This word and meaning seemed to capture the struggles of patients with MS and their families trying to access comprehensive quality care.
MAHA focuses on the identified common problems, especially access to care and fragmentation in care. Our programs attempt to bridge primary and MS specialty care. Central to the model is productive interactions at each encounter. So, it’s not just checking off boxes, it is integration of an agreed upon plan of care, and that takes time and expertise to develop.
Initially, the program focused on house calls (established in 2013) and has now expanded to a transdisciplinary clinic and extensive use of telehealth across Nebraska, including for many in rural areas and in long-term nursing facilities. Our care delivery model is drastically different from a traditional medical model and includes the following components:
More time: New-patient encounters are templated for 1 to 2 hours, house calls up to 3 hours, and established follow-up “return” visits are at least 1 hour and may exceed 2 to 3 hours.
Continuity and competency in care: Limited core team members have frequent contact with patients. Initially, with house calls we had numerous providers going to the home, including physical therapy (PT), occupational therapy (OT), and, in some cases, speech therapy. Patients and family reported frustration with layers of numerous providers, frequent phone calls, and scheduling them to come into their home. Patients wanted to be able to count on a certain trusted few, familiar with their issues. If another discipline is needed, then the patient and core team make that decision and call that person in.
Designated team leader: The MAHA team is led by a ”MS-comprehensivist,” defined as a practitioner with expertise in MS care as well as a background in chronic illness and primary care. This practitioner bridges the specialist-generalist elements in care and serves as an expert care manager or integrator to coordinate and communicate care among providers.
Enhanced communication and follow-up: The patient and designated support person (family or primary paid caregiver) always know the plan of care and are on the same page. This includes a weekly care conference with the core team community nurse, PT, neurology comprehensivists, and nurse coordinator.
In addition, the MAHA program continually monitors outcomes, with immediate investigation regarding preventable complications; incorporates protocols and guidelines, generally from paralyzed veterans or other spinal cord organizations as well as the National MS Society; and commonly calls upon subspecialty physicians (Best Friends)
Finally, the program incorporates lessons learned from individuals with lived experience. Individuals with MS and severe disability are unique, talented, tenacious, and often fiercely independent. The challenges for these individuals and their families were initially underestimated by our team; the lessons learned from these experts allowed us to tailor our program to become better.
Over the course of 7 years, core team members reported increased knowledge and keen awareness of needs and issues of patients with severe disability, suggesting that a transdisciplinary team with multifaceted expertise was evolving. Transdisciplinary, to us, means relating to more than 1 branch of knowledge; examples included our community physical therapist gaining knowledge of necessary steps to obtain grants for direct assistance for equipment needed to prevent falls/injury, and becoming knowledgeable about MS and all of its complexity. Our care coordinator is a medical assistant who became an expert regarding transportation issues in community, and has gained advanced knowledge of MS and disability and integrated social services needs and connections to obtain needed resources. As a nurse practitioner and comprehensivist, over time I gained knowledge of PT and OT disciplines, and learned more about evaluation of the need for durable medical equipment, the importance of the whole person and environment, and acquisition of equipment, with frequent appeals and justification.
All of our persistent team members also unexpectedly became experts in community advocacy for persons with disability, attending city transportation meetings, conferencing with Department of Health and Human Services, and developing public awareness material.
What are the outcomes of the MAHA program in terms of patient response, quality indicators, and financial sustainability?
Kathleen Healey, PhD: We tailored the program to impact the frequency of secondary complications, which are generally preventable, such as urinary and respiratory infection, sepsis, skin pressure and other injury, falls, and fractures. These complications cause suffering and may worsen MS baseline symptoms, especially with severe infections. We know that individuals with significant disability who are hospitalized are at risk for a host of other complications. A recent study published in Neurology showed that 11% of all patients with a neurologic diagnosis admitted to hospitals developed hospital-acquired adverse events or complications.2
In our initial house call program, half of the hospital admissions were related to secondary and generally preventable complications, both during the 2-year preevaluation and postevaluation period. After program implementation, we saw decreases in the number of individuals hospitalized, hospitalizations/skilled facility admissions, and hospital days; the total number of emergency department (ED) visits decreased; and ED-only visits increased (ie, ED visits without hospital admission).3
Patient satisfaction reports and quality indicators were positive. We also measured perceived benefit by asking patients to write their thoughts on the benefits of the program, and we received really robust responses:
“This is the first time somebody actually sat down and listened to me, talked to me.”
“The program was very helpful for me.”
“It was a Godsend. They helped us so much.”
“It helps tremendously, I don’t have to worry so much, I’ve recommended it to others.”
“They get it done; it’s amazing, I have the equipment I need now to be more independent.”
So, you asked about sustainability. Programs like this are difficult to justify in traditional hospital/clinic accounting structures. Initiatives like MAHA may be more sustainable in a value-based structure, but this remains to be seen. Cost avoidance, especially in preventable complications, is likely the best financial indicator at this time.
We have been able to sustain our programs only with the help of grant money through the MS Foundation and through a community donor, to whom we are forever grateful. In addition, our division chair, Dr. Rana Zabad, has been supportive of this innovative initiative because she knows how essential it is for comprehensive care of all individuals with MS.
Importantly, we continue to track our clinical outcome data and have robust longitudinal data, giving us more information about the trajectory of the patients in our program.
Beyond in-home care, what opportunities exist to improve comprehensive care of MS patients via telehealth?
Kathleen Healey, PhD: We have been doing telehealth since 2013, well before the pandemic, but we were receiving variable to no reimbursement. Prior to the pandemic, the Centers for Medicare & Medicaid Services did not reimburse for telehealth unless it was done at a critical access hospital, generally in rural parts of our state.
Since the pandemic and the release of telehealth waivers, we have been able to increase our telemedicine visits to individuals and be appropriately reimbursed. However, about 30% of our patients have limitations regarding telehealth with video due to specific disability, cost, or lack of reliable broadband. Telephone encounters are important if an individual can’t do a telehealth visit, but reimbursement is lower. In my opinion, lack of IT capability may add another dimension to health care disparity.
The benefit of telemedicine, in my opinion, is close to a home visit, because the patient or their caregiver can take their device and show us their environment, show us where the problem areas are. Like when you do a home visit, you get this incredible mosaic of different assessments and develop a deep understanding of the day-to-day challenges facing persons with disability.
Our team agrees that user-friendly adapted devices and reliable broadband are needed, especially for those who are disabled, lack or have inadequate transportation, are low income, or live in rural or underserved urban areas. For these individuals, this is “infrastructure” as important as highways or roads.
Has the coronavirus pandemic presented challenges to delivering in-home care? If so, how have you managed these challenges?
Kathleen Healey, PhD: During the pandemic, we have not been making as many house calls. However, we’ve been able to work around this because all of our home-care patients qualify for skilled home health care. So, with approval of the patient, and with the home health nurse (who is a core team member), we are able coordinate televisits and involve more members of the team, if needed, from remote locations. Importantly, if a family member is working or distant, we can bring them in also, which literally does get everyone on the same page. It must be noted that this takes a significant amount of time to coordinate, but, in our opinion, results in a very productive interaction.
As far as COVID testing, for a 2-month period of time we were unable to test a homebound patient. Some of our patients cannot leave their home—they are disabled in place, and the only way that they can leave their home is generally with an ambulance. Others rely on paratransit systems, which were not operating during the shutdown. Since then, we have worked with a nursing agency to have a nurse visit the homes of our patients with MS to conduct COVID testing.
The pandemic has uncovered significant disparities in health care that persons with disability face. About 15% of those we serve reside in nursing homes, and a substantial proportion of residents with MS and disability have tested positive for COVID-19.
The community-dwelling individuals we serve are younger (in the initial house call program, approximately 50% were between 35 and 54 years of age). To remain independent in the community, individuals require care assistance from family or paid caregivers. At this point, very few have tested positive for COVID-19, but with increased community prevalence, we are expecting that could change. Most of the people we serve are well educated on mitigation and taking extra precautions. Regardless, we field daily calls, many times from family caregivers with questions such as, “What if I get COVID, how will my loved one receive care.”
Paid caregivers assisting persons with disability are key to improving quality of life and health outcomes of people with disability. Unfortunately, these essential workers are poorly paid, generally have no benefits, including health care, and likely are more at risk for COVID-19. However, at this point, persons with MS and disability residing in the community clearly have fared better than those in nursing facilities.
References
1. Chiu C, Bishop M, Pionke JJ, et al. Barriers in the accessibility and continuity of health-care services in people with multiple sclerosis: a literature review. Int J MS Care. 2017;19:313-321.
2.Sauro KM, Quan H, Sikdar KC, et al. Hospital safety among neurologic patients: a population-based cohort study of adverse events. Neurology. 2017;89:284-290.
3. Healey K, Zabad RK, Young L, et al. Multiple Sclerosis at Home Access (MAHA): An Initiative to Improve Care in the Community. Int J MS Care. 2019;21(3):101-112.
Kathleen Healey, APRN, PhD, is an assistant professor in the Department of Neurological Sciences at the University of Nebraska in Omaha, NE, and a nurse practitioner in the Multiple Sclerosis Program at the University of Nebraska Medical Center. She has worked in the MS area since 1998. Dr. Healey has presented numerous programs on MS to patient and provider groups locally and regionally, has presented her research nationally, and is a consultant for Can-do MS. She has developed and led initiatives to improve care access and delivery of care to individuals with MS and significant disability since 2013.
Dr. Healey discloses that she has received grant funding through the MS Foundation.
What barriers to coordinated comprehensive care do patients with progressive multiple sclerosis (MS) face under current health care delivery models?
KATHLEEN HEALEY, PhD: In spite of the 1990 Americans with Disabilities Act, evidence suggests that disparities in health services for people with disabilities remain. These individuals receive health care less often, receive poorer quality care, have unmet health care needs, lack basic screening for health care maintenance, and are offered fewer treatment options, compared to people without disability.
Health care delivery for individuals with disabling progressive forms of MS presents some unique challenges. This disorder is chronic, medically complex, generally progressive, and heterogenous in its effects on the central nervous system (unlike relatively fixed spinal cord and brain injury), producing varying degrees of immobility and loss of function. As the disease progresses, a significant proportion of patients need assistive devices, including power mobility, urinary catheters, gastric tubes, hospital beds, home modifications, sleep and respiratory aides, and other devices. Family members are also likely to suffer from caregiver burden.
In the early stages of MS, individuals may be successful in careers and raising families, but with advancing disability, the majority will incur severe financial and social consequences. Many will become unemployed and face financial hardship, and, furthermore, many lack social support and appropriate transportation and become socially isolated.
One of the bigger challenges in accessing care is transportation, especially for those in wheelchairs and power mobility. Ironically, beyond that, many of the obstacles to comprehensive care are deeply embedded in the traditional health care system itself. The traditional medical model and clinic structure was not designed to serve individuals with complex disability.
Studies have identified specific obstacles to care individuals with MS and disability encounter before, during, and after clinic appointments.1 For an individual with complex disability, something as simple as trying to contact a clinic can be difficult. Clinicians typically don't think about the time MS patients with disability must spend preparing for a visit. Individuals I work with tell me it takes about 5 hours for them to get ready and to schedule transportation. When they arrive, often there are too few handicapped parking spaces, and equipment adapted for persons with disability, like appropriate exam tables and even wheelchair scales, may not be available. In traditional check-ins to clinic, no additional time is allotted for those with disability. So, check-in generally is rushed and not complete.
The traditional medical fee-for-service volume model is based on time. Clinics typically allot perhaps 20 to at the most 40 minutes for a return visit. When a person gets into the room with a provider, it’s for an abbreviated period of time. And I've had patients tell me that such visits are not really beneficial.
Follow-up instructions and following through with additional referrals are problematic as well. Clinic visits can be very hurried: “Here's your discharge instructions,” or “Here's your after-visit summary.” Because of the heterogenic complexity of disability in MS, education and follow-up require an extremely individualized approach and instructions to accommodate specific disability. Although we have translation services for non-English speaking patients and large fonts for those with visual impairment, integrating follow-up for a person who has profound ataxia, or is blind, and or has some cognitive dysfunction and is in a power wheelchair is challenging. Also, ordering and accessing durable medical equipment needed to preserve independence in the community is becoming increasingly difficult, if not impossible, especially in many managed Medicare and dual-eligible programs.
What is the Multiple Sclerosis at Home Access (MAHA) program and what are its goals?
Kathleen Healey, PhD: The MS Clinic at the University of Nebraska is part of an urban academic medical center in Omaha and serves more than 2500 people with MS. The MAHA program was designed specifically for individuals with progressive MS and significant disability. The individuals we serve are often in wheelchairs, and if ambulatory, able to walk only a few steps (patients with Expanded Disability Scale (Kurtzke) scores of 7.5 or greater). At this time, over 100 individuals are enrolled in our MAHA programs.
The majority of the individuals we serve are low income—at least half are dually eligible beneficiaries under Medicare/Medicaid. A substantial number of those we serve are eligible for Medicaid waiver, with incomes at or below the poverty level. Most of these individuals are still fiercely residing in the community, with assistance, and wish to remain so.
Our objectives are to coordinate and deliver comprehensive medical care, improve patient satisfaction, and prevent or treat common complications related to immobility, with an expected decrease in preventable/avoidable health care utilization. Our long-term goals are to improve quality-of-life, promote wellness, increase independence, and promote community reintegration.
The MAHA initiative derives its name from its city of origin, Omaha, Nebraska. This region was first settled by the Maha Native American tribe, and maha means “against the wind, against the current.” This word and meaning seemed to capture the struggles of patients with MS and their families trying to access comprehensive quality care.
MAHA focuses on the identified common problems, especially access to care and fragmentation in care. Our programs attempt to bridge primary and MS specialty care. Central to the model is productive interactions at each encounter. So, it’s not just checking off boxes, it is integration of an agreed upon plan of care, and that takes time and expertise to develop.
Initially, the program focused on house calls (established in 2013) and has now expanded to a transdisciplinary clinic and extensive use of telehealth across Nebraska, including for many in rural areas and in long-term nursing facilities. Our care delivery model is drastically different from a traditional medical model and includes the following components:
More time: New-patient encounters are templated for 1 to 2 hours, house calls up to 3 hours, and established follow-up “return” visits are at least 1 hour and may exceed 2 to 3 hours.
Continuity and competency in care: Limited core team members have frequent contact with patients. Initially, with house calls we had numerous providers going to the home, including physical therapy (PT), occupational therapy (OT), and, in some cases, speech therapy. Patients and family reported frustration with layers of numerous providers, frequent phone calls, and scheduling them to come into their home. Patients wanted to be able to count on a certain trusted few, familiar with their issues. If another discipline is needed, then the patient and core team make that decision and call that person in.
Designated team leader: The MAHA team is led by a ”MS-comprehensivist,” defined as a practitioner with expertise in MS care as well as a background in chronic illness and primary care. This practitioner bridges the specialist-generalist elements in care and serves as an expert care manager or integrator to coordinate and communicate care among providers.
Enhanced communication and follow-up: The patient and designated support person (family or primary paid caregiver) always know the plan of care and are on the same page. This includes a weekly care conference with the core team community nurse, PT, neurology comprehensivists, and nurse coordinator.
In addition, the MAHA program continually monitors outcomes, with immediate investigation regarding preventable complications; incorporates protocols and guidelines, generally from paralyzed veterans or other spinal cord organizations as well as the National MS Society; and commonly calls upon subspecialty physicians (Best Friends)
Finally, the program incorporates lessons learned from individuals with lived experience. Individuals with MS and severe disability are unique, talented, tenacious, and often fiercely independent. The challenges for these individuals and their families were initially underestimated by our team; the lessons learned from these experts allowed us to tailor our program to become better.
Over the course of 7 years, core team members reported increased knowledge and keen awareness of needs and issues of patients with severe disability, suggesting that a transdisciplinary team with multifaceted expertise was evolving. Transdisciplinary, to us, means relating to more than 1 branch of knowledge; examples included our community physical therapist gaining knowledge of necessary steps to obtain grants for direct assistance for equipment needed to prevent falls/injury, and becoming knowledgeable about MS and all of its complexity. Our care coordinator is a medical assistant who became an expert regarding transportation issues in community, and has gained advanced knowledge of MS and disability and integrated social services needs and connections to obtain needed resources. As a nurse practitioner and comprehensivist, over time I gained knowledge of PT and OT disciplines, and learned more about evaluation of the need for durable medical equipment, the importance of the whole person and environment, and acquisition of equipment, with frequent appeals and justification.
All of our persistent team members also unexpectedly became experts in community advocacy for persons with disability, attending city transportation meetings, conferencing with Department of Health and Human Services, and developing public awareness material.
What are the outcomes of the MAHA program in terms of patient response, quality indicators, and financial sustainability?
Kathleen Healey, PhD: We tailored the program to impact the frequency of secondary complications, which are generally preventable, such as urinary and respiratory infection, sepsis, skin pressure and other injury, falls, and fractures. These complications cause suffering and may worsen MS baseline symptoms, especially with severe infections. We know that individuals with significant disability who are hospitalized are at risk for a host of other complications. A recent study published in Neurology showed that 11% of all patients with a neurologic diagnosis admitted to hospitals developed hospital-acquired adverse events or complications.2
In our initial house call program, half of the hospital admissions were related to secondary and generally preventable complications, both during the 2-year preevaluation and postevaluation period. After program implementation, we saw decreases in the number of individuals hospitalized, hospitalizations/skilled facility admissions, and hospital days; the total number of emergency department (ED) visits decreased; and ED-only visits increased (ie, ED visits without hospital admission).3
Patient satisfaction reports and quality indicators were positive. We also measured perceived benefit by asking patients to write their thoughts on the benefits of the program, and we received really robust responses:
“This is the first time somebody actually sat down and listened to me, talked to me.”
“The program was very helpful for me.”
“It was a Godsend. They helped us so much.”
“It helps tremendously, I don’t have to worry so much, I’ve recommended it to others.”
“They get it done; it’s amazing, I have the equipment I need now to be more independent.”
So, you asked about sustainability. Programs like this are difficult to justify in traditional hospital/clinic accounting structures. Initiatives like MAHA may be more sustainable in a value-based structure, but this remains to be seen. Cost avoidance, especially in preventable complications, is likely the best financial indicator at this time.
We have been able to sustain our programs only with the help of grant money through the MS Foundation and through a community donor, to whom we are forever grateful. In addition, our division chair, Dr. Rana Zabad, has been supportive of this innovative initiative because she knows how essential it is for comprehensive care of all individuals with MS.
Importantly, we continue to track our clinical outcome data and have robust longitudinal data, giving us more information about the trajectory of the patients in our program.
Beyond in-home care, what opportunities exist to improve comprehensive care of MS patients via telehealth?
Kathleen Healey, PhD: We have been doing telehealth since 2013, well before the pandemic, but we were receiving variable to no reimbursement. Prior to the pandemic, the Centers for Medicare & Medicaid Services did not reimburse for telehealth unless it was done at a critical access hospital, generally in rural parts of our state.
Since the pandemic and the release of telehealth waivers, we have been able to increase our telemedicine visits to individuals and be appropriately reimbursed. However, about 30% of our patients have limitations regarding telehealth with video due to specific disability, cost, or lack of reliable broadband. Telephone encounters are important if an individual can’t do a telehealth visit, but reimbursement is lower. In my opinion, lack of IT capability may add another dimension to health care disparity.
The benefit of telemedicine, in my opinion, is close to a home visit, because the patient or their caregiver can take their device and show us their environment, show us where the problem areas are. Like when you do a home visit, you get this incredible mosaic of different assessments and develop a deep understanding of the day-to-day challenges facing persons with disability.
Our team agrees that user-friendly adapted devices and reliable broadband are needed, especially for those who are disabled, lack or have inadequate transportation, are low income, or live in rural or underserved urban areas. For these individuals, this is “infrastructure” as important as highways or roads.
Has the coronavirus pandemic presented challenges to delivering in-home care? If so, how have you managed these challenges?
Kathleen Healey, PhD: During the pandemic, we have not been making as many house calls. However, we’ve been able to work around this because all of our home-care patients qualify for skilled home health care. So, with approval of the patient, and with the home health nurse (who is a core team member), we are able coordinate televisits and involve more members of the team, if needed, from remote locations. Importantly, if a family member is working or distant, we can bring them in also, which literally does get everyone on the same page. It must be noted that this takes a significant amount of time to coordinate, but, in our opinion, results in a very productive interaction.
As far as COVID testing, for a 2-month period of time we were unable to test a homebound patient. Some of our patients cannot leave their home—they are disabled in place, and the only way that they can leave their home is generally with an ambulance. Others rely on paratransit systems, which were not operating during the shutdown. Since then, we have worked with a nursing agency to have a nurse visit the homes of our patients with MS to conduct COVID testing.
The pandemic has uncovered significant disparities in health care that persons with disability face. About 15% of those we serve reside in nursing homes, and a substantial proportion of residents with MS and disability have tested positive for COVID-19.
The community-dwelling individuals we serve are younger (in the initial house call program, approximately 50% were between 35 and 54 years of age). To remain independent in the community, individuals require care assistance from family or paid caregivers. At this point, very few have tested positive for COVID-19, but with increased community prevalence, we are expecting that could change. Most of the people we serve are well educated on mitigation and taking extra precautions. Regardless, we field daily calls, many times from family caregivers with questions such as, “What if I get COVID, how will my loved one receive care.”
Paid caregivers assisting persons with disability are key to improving quality of life and health outcomes of people with disability. Unfortunately, these essential workers are poorly paid, generally have no benefits, including health care, and likely are more at risk for COVID-19. However, at this point, persons with MS and disability residing in the community clearly have fared better than those in nursing facilities.
References
1. Chiu C, Bishop M, Pionke JJ, et al. Barriers in the accessibility and continuity of health-care services in people with multiple sclerosis: a literature review. Int J MS Care. 2017;19:313-321.
2.Sauro KM, Quan H, Sikdar KC, et al. Hospital safety among neurologic patients: a population-based cohort study of adverse events. Neurology. 2017;89:284-290.
3. Healey K, Zabad RK, Young L, et al. Multiple Sclerosis at Home Access (MAHA): An Initiative to Improve Care in the Community. Int J MS Care. 2019;21(3):101-112.
1. Chiu C, Bishop M, Pionke JJ, et al. Barriers in the accessibility and continuity of health-care services in people with multiple sclerosis: a literature review. Int J MS Care. 2017;19:313-321.
2.Sauro KM, Quan H, Sikdar KC, et al. Hospital safety among neurologic patients: a population-based cohort study of adverse events. Neurology. 2017;89:284-290.
3. Healey K, Zabad RK, Young L, et al. Multiple Sclerosis at Home Access (MAHA): An Initiative to Improve Care in the Community. Int J MS Care. 2019;21(3):101-112.
1. Chiu C, Bishop M, Pionke JJ, et al. Barriers in the accessibility and continuity of health-care services in people with multiple sclerosis: a literature review. Int J MS Care. 2017;19:313-321.
2.Sauro KM, Quan H, Sikdar KC, et al. Hospital safety among neurologic patients: a population-based cohort study of adverse events. Neurology. 2017;89:284-290.
3. Healey K, Zabad RK, Young L, et al. Multiple Sclerosis at Home Access (MAHA): An Initiative to Improve Care in the Community. Int J MS Care. 2019;21(3):101-112.
Batten down the hatches for thyroid storm
Thyroid storm is a life-threatening endocrine emergency for which, remarkably, there are no definitive diagnostic tests, and the management of which is supported by a startlingly weak evidence base.
“What’s tricky is there really are no specific biochemical level cutoffs for thyroid storm, and also no unique laboratory abnormalities. So in the end, it’s a clinical diagnosis and a clinical judgment,” Stephanie B. Mayer, MD, MHSc, observed at HM20 Virtual, hosted by the Society of Hospital Medicine.
Moreover, there are no prospective clinical trials addressing the treatment of thyroid storm, and the 2016 American Thyroid Association clinical practice guidelines on the topic are based upon low-quality evidence from case reports and studies dating back to the 1970s and 1980s. UpToDate reached the same conclusion in 2020, noted Dr. Mayer, an endocrinologist at Virginia Commonwealth University, Richmond.
Thinking that perhaps the guideline writing panel had missed something, she asked a university medical research librarian to custom-build a comprehensive search for studies on thyroid storm management. The search proved unrewarding.
“The evidence is, unfortunately, a little disappointing,” Dr. Mayer said.
Thyroid storm is a rare condition, but one that hospitalists must be ready for. She highlighted current best practices in diagnosis and management.
A high-mortality emergency
Thyroid storm is an extreme manifestation of thyrotoxicosis, which is marked by multiorgan dysfunction and rapid decompensation. In a large, first-of-its-kind, national retrospective U.S. study, the incidence of thyroid storm was 0.57-0.76 cases per 100,000 persons per year. Thyroid storm accounted for 16% of the more than 121,000 hospital discharges featuring a primary diagnosis of thyrotoxicosis. The in-hospital mortality rate for patients with thyroid storm was 1.2%-3.6% during the 10-year study period, a rate 12-fold higher than that among patients with thyrotoxicosis without thyroid storm (Thyroid. 2019 Jan;29[1]:36-43).
Dr. Mayer highlighted a multicenter French study that underscored the current hefty morbidity and mortality associated with thyroid storm. Among 92 patients admitted to the ICU for thyroid storm, the in-ICU mortality rate was 17%, and the mortality rate 6 months after admission was 22%. Independent risk factors for in-ICU mortality were multiorgan failure and the occurrence of cardiogenic shock within the first 48 hours in the ICU (Crit Care Med. 2020 Jan;48[1]:83-90).
How to recognize thyroid storm
The most user-friendly system for assistance in diagnosing thyroid storm is the one put forth by the Japan Thyroid Association and the Japan Endocrine Society, in Dr. Mayer’s view. As a prerequisite to the diagnosis a patient must have thyrotoxicosis as evidenced by elevated free thyroxine (free T4) and free or total triiodothyronine (T3), which in the vast majority of cases, is accompanied by low thyroid stimulating hormone (TSH).
The Japanese diagnostic system for thyroid storm relies on five categories of organ system–based clinical features. This approach places greater weight on disturbances of consciousness – restlessness, delirium, agitation, psychosis, lethargy, coma – than the other four components, which consist of fever of at least 100.4° F, tachycardia of 130 or more beats per minute, heart failure signs and symptoms, and gastrointestinal/hepatic involvement as evidenced by nausea, vomiting, hyperdefecation, and/or a total bilirubin level of 3.0 mg/dL or more.
The Japanese approach offers two paths to a definite diagnosis of thyroid storm. One requires at least one CNS manifestation plus symptoms drawn from any one of the other four categories. The other route, for patients without evident CNS symptoms, requires the presence of symptoms from at least three of the other four categories.
A patient is categorized as having suspected rather than definite thyroid storm if the CNS criterion isn’t met but any two of the others are. A patient also qualifies for suspected thyroid storm when CNS manifestations plus symptoms from at least one other category are present, but thyroid hormone levels aren’t available (Endocr J. 2016 Dec 30;63[12]:1025-64).
Management of thyroid storm
There is usually a precipitating event that drives the transition from smoldering thyrotoxicosis to thyroid storm.
“The big thing is to look for and treat the underlying precipitating event,” the endocrinologist stressed.
It’s often a systemic insult: severe infection, trauma, surgery, an acute MI, diabetic ketoacidosis, pulmonary embolism, or perhaps having just gone through labor. Iodine exposure in the form of IV contrast or taking amiodarone, which contains 37% iodine by weight, can also fan thyrotoxicosis into thyroid storm. Abrupt discontinuation of antithyroid medication is another common cause.
Fluid and electrolyte replacement, oxygen if appropriate, cooling blankets, and other supportive measures are also important.
Medical management targets multiple steps in thyroid hormone production and action to quell thyroid storm. The first order of business is to inhibit synthesis of new thyroid hormone by prescribing a thioamide. Dr. Mayer favors propylthiouracil over methimazole for this purpose because, not only does it block the thyroid gland from synthesizing new hormone, it also reduces conversion of T4 to T3. Propylthiouracil is usually given orally as a 500- to 1,000-mg loading dose, then 250 mg every 4 hours. The drug can also be given rectally or by nasogastric tube.
One hour or more after starting the thioamide, inorganic iodine is started to inhibit release of preformed hormone from the thyroid gland. Five drops of saturated solution of potassium iodide given every 6 hours is the recommended dose; it provides 764 mg of iodide per day. Lugol’s solution dosed at four to eight drops every 6-8 hours is an effective alternative.
Simultaneous with starting the patient on inorganic iodine, a low-dose beta blocker is introduced to control adrenergic symptoms.
“Propranolol is first line because it also decreases T4 to T3 conversion and it’s noncardioselective, so it’s better than a cardioselective beta blocker at reducing sympathetic tone-related symptoms, such as agitation, fever, and psychosis,” the endocrinologist explained.
At the same time that propranolol at 60-80 mg is given orally every 4 hours and iodine are started, the patient is placed on glucocorticoids as another means of reducing peripheral conversion of T4 to T3. The options are intravenous hydrocortisone at 100-300 mg/day in divided doses or dexamethasone at 2 mg every 6 hours.
Aspirin and NSAIDs should be avoided as antipyretics because they can actually raise T3 and T4 levels. Acetaminophen is the right fever-lowering agent in the setting of thyroid storm.
Dr. Mayer has occasionally had to reach for one of several backup therapies. Prescribing a bile acid sequestrant – 20-30 g/day of cholestyramine or colestipol – will trap thyroid hormone in the intestine, preventing it from recirculating.
“Be careful to dose it away from the other medications,” she cautioned.
Also, therapeutic plasmapheresis is effective at rapidly removing circulating thyroid hormone in patients who don’t show early clinical improvement in response to multipronged medical therapy.
Dr. Mayer offered a couple of final tips to hospitalists regarding thyroid storm: Know who directs plasmapheresis at your hospital, and keep the American Thyroid Association management guidelines handy (Thyroid. 2016 Oct;26[10]:1343-421).
She reported receiving funding from both NovoNordisk and Astra Zeneca.
Thyroid storm is a life-threatening endocrine emergency for which, remarkably, there are no definitive diagnostic tests, and the management of which is supported by a startlingly weak evidence base.
“What’s tricky is there really are no specific biochemical level cutoffs for thyroid storm, and also no unique laboratory abnormalities. So in the end, it’s a clinical diagnosis and a clinical judgment,” Stephanie B. Mayer, MD, MHSc, observed at HM20 Virtual, hosted by the Society of Hospital Medicine.
Moreover, there are no prospective clinical trials addressing the treatment of thyroid storm, and the 2016 American Thyroid Association clinical practice guidelines on the topic are based upon low-quality evidence from case reports and studies dating back to the 1970s and 1980s. UpToDate reached the same conclusion in 2020, noted Dr. Mayer, an endocrinologist at Virginia Commonwealth University, Richmond.
Thinking that perhaps the guideline writing panel had missed something, she asked a university medical research librarian to custom-build a comprehensive search for studies on thyroid storm management. The search proved unrewarding.
“The evidence is, unfortunately, a little disappointing,” Dr. Mayer said.
Thyroid storm is a rare condition, but one that hospitalists must be ready for. She highlighted current best practices in diagnosis and management.
A high-mortality emergency
Thyroid storm is an extreme manifestation of thyrotoxicosis, which is marked by multiorgan dysfunction and rapid decompensation. In a large, first-of-its-kind, national retrospective U.S. study, the incidence of thyroid storm was 0.57-0.76 cases per 100,000 persons per year. Thyroid storm accounted for 16% of the more than 121,000 hospital discharges featuring a primary diagnosis of thyrotoxicosis. The in-hospital mortality rate for patients with thyroid storm was 1.2%-3.6% during the 10-year study period, a rate 12-fold higher than that among patients with thyrotoxicosis without thyroid storm (Thyroid. 2019 Jan;29[1]:36-43).
Dr. Mayer highlighted a multicenter French study that underscored the current hefty morbidity and mortality associated with thyroid storm. Among 92 patients admitted to the ICU for thyroid storm, the in-ICU mortality rate was 17%, and the mortality rate 6 months after admission was 22%. Independent risk factors for in-ICU mortality were multiorgan failure and the occurrence of cardiogenic shock within the first 48 hours in the ICU (Crit Care Med. 2020 Jan;48[1]:83-90).
How to recognize thyroid storm
The most user-friendly system for assistance in diagnosing thyroid storm is the one put forth by the Japan Thyroid Association and the Japan Endocrine Society, in Dr. Mayer’s view. As a prerequisite to the diagnosis a patient must have thyrotoxicosis as evidenced by elevated free thyroxine (free T4) and free or total triiodothyronine (T3), which in the vast majority of cases, is accompanied by low thyroid stimulating hormone (TSH).
The Japanese diagnostic system for thyroid storm relies on five categories of organ system–based clinical features. This approach places greater weight on disturbances of consciousness – restlessness, delirium, agitation, psychosis, lethargy, coma – than the other four components, which consist of fever of at least 100.4° F, tachycardia of 130 or more beats per minute, heart failure signs and symptoms, and gastrointestinal/hepatic involvement as evidenced by nausea, vomiting, hyperdefecation, and/or a total bilirubin level of 3.0 mg/dL or more.
The Japanese approach offers two paths to a definite diagnosis of thyroid storm. One requires at least one CNS manifestation plus symptoms drawn from any one of the other four categories. The other route, for patients without evident CNS symptoms, requires the presence of symptoms from at least three of the other four categories.
A patient is categorized as having suspected rather than definite thyroid storm if the CNS criterion isn’t met but any two of the others are. A patient also qualifies for suspected thyroid storm when CNS manifestations plus symptoms from at least one other category are present, but thyroid hormone levels aren’t available (Endocr J. 2016 Dec 30;63[12]:1025-64).
Management of thyroid storm
There is usually a precipitating event that drives the transition from smoldering thyrotoxicosis to thyroid storm.
“The big thing is to look for and treat the underlying precipitating event,” the endocrinologist stressed.
It’s often a systemic insult: severe infection, trauma, surgery, an acute MI, diabetic ketoacidosis, pulmonary embolism, or perhaps having just gone through labor. Iodine exposure in the form of IV contrast or taking amiodarone, which contains 37% iodine by weight, can also fan thyrotoxicosis into thyroid storm. Abrupt discontinuation of antithyroid medication is another common cause.
Fluid and electrolyte replacement, oxygen if appropriate, cooling blankets, and other supportive measures are also important.
Medical management targets multiple steps in thyroid hormone production and action to quell thyroid storm. The first order of business is to inhibit synthesis of new thyroid hormone by prescribing a thioamide. Dr. Mayer favors propylthiouracil over methimazole for this purpose because, not only does it block the thyroid gland from synthesizing new hormone, it also reduces conversion of T4 to T3. Propylthiouracil is usually given orally as a 500- to 1,000-mg loading dose, then 250 mg every 4 hours. The drug can also be given rectally or by nasogastric tube.
One hour or more after starting the thioamide, inorganic iodine is started to inhibit release of preformed hormone from the thyroid gland. Five drops of saturated solution of potassium iodide given every 6 hours is the recommended dose; it provides 764 mg of iodide per day. Lugol’s solution dosed at four to eight drops every 6-8 hours is an effective alternative.
Simultaneous with starting the patient on inorganic iodine, a low-dose beta blocker is introduced to control adrenergic symptoms.
“Propranolol is first line because it also decreases T4 to T3 conversion and it’s noncardioselective, so it’s better than a cardioselective beta blocker at reducing sympathetic tone-related symptoms, such as agitation, fever, and psychosis,” the endocrinologist explained.
At the same time that propranolol at 60-80 mg is given orally every 4 hours and iodine are started, the patient is placed on glucocorticoids as another means of reducing peripheral conversion of T4 to T3. The options are intravenous hydrocortisone at 100-300 mg/day in divided doses or dexamethasone at 2 mg every 6 hours.
Aspirin and NSAIDs should be avoided as antipyretics because they can actually raise T3 and T4 levels. Acetaminophen is the right fever-lowering agent in the setting of thyroid storm.
Dr. Mayer has occasionally had to reach for one of several backup therapies. Prescribing a bile acid sequestrant – 20-30 g/day of cholestyramine or colestipol – will trap thyroid hormone in the intestine, preventing it from recirculating.
“Be careful to dose it away from the other medications,” she cautioned.
Also, therapeutic plasmapheresis is effective at rapidly removing circulating thyroid hormone in patients who don’t show early clinical improvement in response to multipronged medical therapy.
Dr. Mayer offered a couple of final tips to hospitalists regarding thyroid storm: Know who directs plasmapheresis at your hospital, and keep the American Thyroid Association management guidelines handy (Thyroid. 2016 Oct;26[10]:1343-421).
She reported receiving funding from both NovoNordisk and Astra Zeneca.
Thyroid storm is a life-threatening endocrine emergency for which, remarkably, there are no definitive diagnostic tests, and the management of which is supported by a startlingly weak evidence base.
“What’s tricky is there really are no specific biochemical level cutoffs for thyroid storm, and also no unique laboratory abnormalities. So in the end, it’s a clinical diagnosis and a clinical judgment,” Stephanie B. Mayer, MD, MHSc, observed at HM20 Virtual, hosted by the Society of Hospital Medicine.
Moreover, there are no prospective clinical trials addressing the treatment of thyroid storm, and the 2016 American Thyroid Association clinical practice guidelines on the topic are based upon low-quality evidence from case reports and studies dating back to the 1970s and 1980s. UpToDate reached the same conclusion in 2020, noted Dr. Mayer, an endocrinologist at Virginia Commonwealth University, Richmond.
Thinking that perhaps the guideline writing panel had missed something, she asked a university medical research librarian to custom-build a comprehensive search for studies on thyroid storm management. The search proved unrewarding.
“The evidence is, unfortunately, a little disappointing,” Dr. Mayer said.
Thyroid storm is a rare condition, but one that hospitalists must be ready for. She highlighted current best practices in diagnosis and management.
A high-mortality emergency
Thyroid storm is an extreme manifestation of thyrotoxicosis, which is marked by multiorgan dysfunction and rapid decompensation. In a large, first-of-its-kind, national retrospective U.S. study, the incidence of thyroid storm was 0.57-0.76 cases per 100,000 persons per year. Thyroid storm accounted for 16% of the more than 121,000 hospital discharges featuring a primary diagnosis of thyrotoxicosis. The in-hospital mortality rate for patients with thyroid storm was 1.2%-3.6% during the 10-year study period, a rate 12-fold higher than that among patients with thyrotoxicosis without thyroid storm (Thyroid. 2019 Jan;29[1]:36-43).
Dr. Mayer highlighted a multicenter French study that underscored the current hefty morbidity and mortality associated with thyroid storm. Among 92 patients admitted to the ICU for thyroid storm, the in-ICU mortality rate was 17%, and the mortality rate 6 months after admission was 22%. Independent risk factors for in-ICU mortality were multiorgan failure and the occurrence of cardiogenic shock within the first 48 hours in the ICU (Crit Care Med. 2020 Jan;48[1]:83-90).
How to recognize thyroid storm
The most user-friendly system for assistance in diagnosing thyroid storm is the one put forth by the Japan Thyroid Association and the Japan Endocrine Society, in Dr. Mayer’s view. As a prerequisite to the diagnosis a patient must have thyrotoxicosis as evidenced by elevated free thyroxine (free T4) and free or total triiodothyronine (T3), which in the vast majority of cases, is accompanied by low thyroid stimulating hormone (TSH).
The Japanese diagnostic system for thyroid storm relies on five categories of organ system–based clinical features. This approach places greater weight on disturbances of consciousness – restlessness, delirium, agitation, psychosis, lethargy, coma – than the other four components, which consist of fever of at least 100.4° F, tachycardia of 130 or more beats per minute, heart failure signs and symptoms, and gastrointestinal/hepatic involvement as evidenced by nausea, vomiting, hyperdefecation, and/or a total bilirubin level of 3.0 mg/dL or more.
The Japanese approach offers two paths to a definite diagnosis of thyroid storm. One requires at least one CNS manifestation plus symptoms drawn from any one of the other four categories. The other route, for patients without evident CNS symptoms, requires the presence of symptoms from at least three of the other four categories.
A patient is categorized as having suspected rather than definite thyroid storm if the CNS criterion isn’t met but any two of the others are. A patient also qualifies for suspected thyroid storm when CNS manifestations plus symptoms from at least one other category are present, but thyroid hormone levels aren’t available (Endocr J. 2016 Dec 30;63[12]:1025-64).
Management of thyroid storm
There is usually a precipitating event that drives the transition from smoldering thyrotoxicosis to thyroid storm.
“The big thing is to look for and treat the underlying precipitating event,” the endocrinologist stressed.
It’s often a systemic insult: severe infection, trauma, surgery, an acute MI, diabetic ketoacidosis, pulmonary embolism, or perhaps having just gone through labor. Iodine exposure in the form of IV contrast or taking amiodarone, which contains 37% iodine by weight, can also fan thyrotoxicosis into thyroid storm. Abrupt discontinuation of antithyroid medication is another common cause.
Fluid and electrolyte replacement, oxygen if appropriate, cooling blankets, and other supportive measures are also important.
Medical management targets multiple steps in thyroid hormone production and action to quell thyroid storm. The first order of business is to inhibit synthesis of new thyroid hormone by prescribing a thioamide. Dr. Mayer favors propylthiouracil over methimazole for this purpose because, not only does it block the thyroid gland from synthesizing new hormone, it also reduces conversion of T4 to T3. Propylthiouracil is usually given orally as a 500- to 1,000-mg loading dose, then 250 mg every 4 hours. The drug can also be given rectally or by nasogastric tube.
One hour or more after starting the thioamide, inorganic iodine is started to inhibit release of preformed hormone from the thyroid gland. Five drops of saturated solution of potassium iodide given every 6 hours is the recommended dose; it provides 764 mg of iodide per day. Lugol’s solution dosed at four to eight drops every 6-8 hours is an effective alternative.
Simultaneous with starting the patient on inorganic iodine, a low-dose beta blocker is introduced to control adrenergic symptoms.
“Propranolol is first line because it also decreases T4 to T3 conversion and it’s noncardioselective, so it’s better than a cardioselective beta blocker at reducing sympathetic tone-related symptoms, such as agitation, fever, and psychosis,” the endocrinologist explained.
At the same time that propranolol at 60-80 mg is given orally every 4 hours and iodine are started, the patient is placed on glucocorticoids as another means of reducing peripheral conversion of T4 to T3. The options are intravenous hydrocortisone at 100-300 mg/day in divided doses or dexamethasone at 2 mg every 6 hours.
Aspirin and NSAIDs should be avoided as antipyretics because they can actually raise T3 and T4 levels. Acetaminophen is the right fever-lowering agent in the setting of thyroid storm.
Dr. Mayer has occasionally had to reach for one of several backup therapies. Prescribing a bile acid sequestrant – 20-30 g/day of cholestyramine or colestipol – will trap thyroid hormone in the intestine, preventing it from recirculating.
“Be careful to dose it away from the other medications,” she cautioned.
Also, therapeutic plasmapheresis is effective at rapidly removing circulating thyroid hormone in patients who don’t show early clinical improvement in response to multipronged medical therapy.
Dr. Mayer offered a couple of final tips to hospitalists regarding thyroid storm: Know who directs plasmapheresis at your hospital, and keep the American Thyroid Association management guidelines handy (Thyroid. 2016 Oct;26[10]:1343-421).
She reported receiving funding from both NovoNordisk and Astra Zeneca.
FROM HM20 VIRTUAL
What have we learned? HM20 Virtual edition
The last session of each SHM Annual Conference is traditionally a short presentation titled “What Have We Learned?” that is delivered by next year’s course director (and this year, that is me!).
We’ve learned that by making the heartbreaking decision to cancel the HM20 in-person conference and convert to a virtual platform, SHM leadership is not afraid to do the right thing to protect the health of its members and staff, even when such a decision comes at significant cost to the organization. We’ve learned that the SHM staff are flexible and innovative and are masters of logistics – their ability to pivot so quickly into a virtual format on such short notice is nothing short of amazing. On the Annual Conference Committee (ACC), we already knew that Benji Mathews, the HM20 course director, was an outstanding leader. True to form, despite facing unprecedented uncertainty and tremendous disappointment, Benji continued to lead with the steady, eloquent presence and poise he’s known for, delivering an outstanding HM20 Virtual.
We’ve learned that SHM members can enjoy and engage meaningfully in a virtual format, as evidenced by well-attended sessions, including robust Q&A exchanges that took place during HM20 Virtual’s simulive offerings. Not seeing each other in person this year has reminded us how much the sense of community we enjoy through SHM means to so many of us. I missed catching up with so many colleagues that have become true friends over the years, and I know you did as well.
We also saw how SHM does not hesitate to provide a platform to shine a spotlight on the critical issues of the day. The double pandemic of COVID-19 and structural racism that we face was addressed head-on by expert faculty in sessions such as “Structural Racism and Bias in Hospital Medicine During Two Pandemics,” “The Immigrant Hospitalist: Navigating the Uncertain Terrain During COVID-19,” and “When Grief and Crises Intersect: Perspectives of a Black Physician in the Time of Two Pandemics.” Sessions on different aspects of COVID-19 enabled our members to stay up to date on the continually evolving knowledge base of this new disease.
We are so excited as we look ahead to HM21. There will be content on COVID-19 at HM21 … but not too much COVID. The ACC is mindful that our members come to the Annual Conference to hear experts speak on a broad range of clinical topics, and HM21 will be sure to deliver. An innovative new track on Diagnostic Safety will address this critical aspect of high-quality care. We will also debut a new leadership track. At HM21, the ACC is also proud to introduce a dedicated track that will include sessions that address diversity, disparities, and equity. And if what happens in Vegas cannot stay in Vegas (does that make some of you nervous …?), and a virtual element needs to be part of HM21, we will utilize a sophisticated and highly functional platform that will provide some things that our HM20 Virtual platform didn’t.
Couldn’t make HM20 Virtual? Don’t worry! You can still experience the in-depth, immersive education courtesy of some of the most knowledgeable faculty in the field through HM20 Virtual On Demand.
It has indeed been a year in which we have learned a lot. Most importantly, we have learned that we are resilient and that we are stronger together. That SHM and the Annual Conference – be it virtual or in person – is a place where we value, respect, and support each other. Have a great year. I look forward to welcoming you to HM21 in May 2021!
Dr. Steinberg is associate chair for education and residency program director in the department of medicine at Mount Sinai Beth Israel, New York, and course director of HM21.
The last session of each SHM Annual Conference is traditionally a short presentation titled “What Have We Learned?” that is delivered by next year’s course director (and this year, that is me!).
We’ve learned that by making the heartbreaking decision to cancel the HM20 in-person conference and convert to a virtual platform, SHM leadership is not afraid to do the right thing to protect the health of its members and staff, even when such a decision comes at significant cost to the organization. We’ve learned that the SHM staff are flexible and innovative and are masters of logistics – their ability to pivot so quickly into a virtual format on such short notice is nothing short of amazing. On the Annual Conference Committee (ACC), we already knew that Benji Mathews, the HM20 course director, was an outstanding leader. True to form, despite facing unprecedented uncertainty and tremendous disappointment, Benji continued to lead with the steady, eloquent presence and poise he’s known for, delivering an outstanding HM20 Virtual.
We’ve learned that SHM members can enjoy and engage meaningfully in a virtual format, as evidenced by well-attended sessions, including robust Q&A exchanges that took place during HM20 Virtual’s simulive offerings. Not seeing each other in person this year has reminded us how much the sense of community we enjoy through SHM means to so many of us. I missed catching up with so many colleagues that have become true friends over the years, and I know you did as well.
We also saw how SHM does not hesitate to provide a platform to shine a spotlight on the critical issues of the day. The double pandemic of COVID-19 and structural racism that we face was addressed head-on by expert faculty in sessions such as “Structural Racism and Bias in Hospital Medicine During Two Pandemics,” “The Immigrant Hospitalist: Navigating the Uncertain Terrain During COVID-19,” and “When Grief and Crises Intersect: Perspectives of a Black Physician in the Time of Two Pandemics.” Sessions on different aspects of COVID-19 enabled our members to stay up to date on the continually evolving knowledge base of this new disease.
We are so excited as we look ahead to HM21. There will be content on COVID-19 at HM21 … but not too much COVID. The ACC is mindful that our members come to the Annual Conference to hear experts speak on a broad range of clinical topics, and HM21 will be sure to deliver. An innovative new track on Diagnostic Safety will address this critical aspect of high-quality care. We will also debut a new leadership track. At HM21, the ACC is also proud to introduce a dedicated track that will include sessions that address diversity, disparities, and equity. And if what happens in Vegas cannot stay in Vegas (does that make some of you nervous …?), and a virtual element needs to be part of HM21, we will utilize a sophisticated and highly functional platform that will provide some things that our HM20 Virtual platform didn’t.
Couldn’t make HM20 Virtual? Don’t worry! You can still experience the in-depth, immersive education courtesy of some of the most knowledgeable faculty in the field through HM20 Virtual On Demand.
It has indeed been a year in which we have learned a lot. Most importantly, we have learned that we are resilient and that we are stronger together. That SHM and the Annual Conference – be it virtual or in person – is a place where we value, respect, and support each other. Have a great year. I look forward to welcoming you to HM21 in May 2021!
Dr. Steinberg is associate chair for education and residency program director in the department of medicine at Mount Sinai Beth Israel, New York, and course director of HM21.
The last session of each SHM Annual Conference is traditionally a short presentation titled “What Have We Learned?” that is delivered by next year’s course director (and this year, that is me!).
We’ve learned that by making the heartbreaking decision to cancel the HM20 in-person conference and convert to a virtual platform, SHM leadership is not afraid to do the right thing to protect the health of its members and staff, even when such a decision comes at significant cost to the organization. We’ve learned that the SHM staff are flexible and innovative and are masters of logistics – their ability to pivot so quickly into a virtual format on such short notice is nothing short of amazing. On the Annual Conference Committee (ACC), we already knew that Benji Mathews, the HM20 course director, was an outstanding leader. True to form, despite facing unprecedented uncertainty and tremendous disappointment, Benji continued to lead with the steady, eloquent presence and poise he’s known for, delivering an outstanding HM20 Virtual.
We’ve learned that SHM members can enjoy and engage meaningfully in a virtual format, as evidenced by well-attended sessions, including robust Q&A exchanges that took place during HM20 Virtual’s simulive offerings. Not seeing each other in person this year has reminded us how much the sense of community we enjoy through SHM means to so many of us. I missed catching up with so many colleagues that have become true friends over the years, and I know you did as well.
We also saw how SHM does not hesitate to provide a platform to shine a spotlight on the critical issues of the day. The double pandemic of COVID-19 and structural racism that we face was addressed head-on by expert faculty in sessions such as “Structural Racism and Bias in Hospital Medicine During Two Pandemics,” “The Immigrant Hospitalist: Navigating the Uncertain Terrain During COVID-19,” and “When Grief and Crises Intersect: Perspectives of a Black Physician in the Time of Two Pandemics.” Sessions on different aspects of COVID-19 enabled our members to stay up to date on the continually evolving knowledge base of this new disease.
We are so excited as we look ahead to HM21. There will be content on COVID-19 at HM21 … but not too much COVID. The ACC is mindful that our members come to the Annual Conference to hear experts speak on a broad range of clinical topics, and HM21 will be sure to deliver. An innovative new track on Diagnostic Safety will address this critical aspect of high-quality care. We will also debut a new leadership track. At HM21, the ACC is also proud to introduce a dedicated track that will include sessions that address diversity, disparities, and equity. And if what happens in Vegas cannot stay in Vegas (does that make some of you nervous …?), and a virtual element needs to be part of HM21, we will utilize a sophisticated and highly functional platform that will provide some things that our HM20 Virtual platform didn’t.
Couldn’t make HM20 Virtual? Don’t worry! You can still experience the in-depth, immersive education courtesy of some of the most knowledgeable faculty in the field through HM20 Virtual On Demand.
It has indeed been a year in which we have learned a lot. Most importantly, we have learned that we are resilient and that we are stronger together. That SHM and the Annual Conference – be it virtual or in person – is a place where we value, respect, and support each other. Have a great year. I look forward to welcoming you to HM21 in May 2021!
Dr. Steinberg is associate chair for education and residency program director in the department of medicine at Mount Sinai Beth Israel, New York, and course director of HM21.
Attempted suicide in high school America, 2019
according to newly released data from the 2019 Youth Risk Behavior Survey.
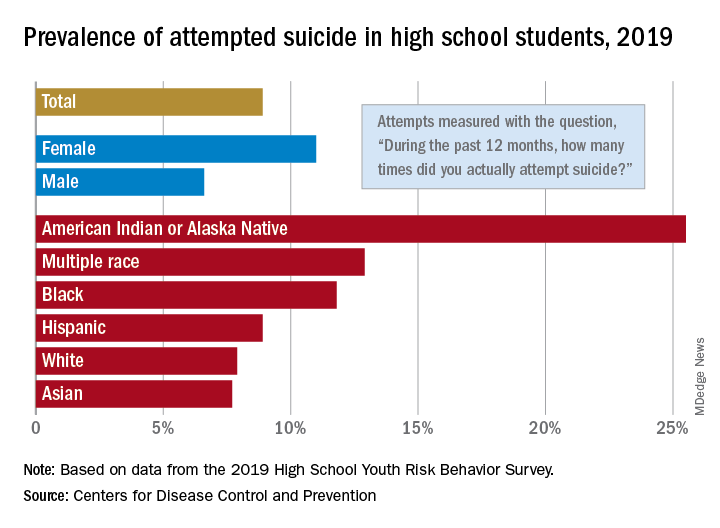
The prevalence of attempted suicide during the previous 12 months was 8.9% among the 13,677 students in grades 9-12 who took the survey last year, but the rate was 25.5% for American Indian/Alaska Native (AI/AN) respondents, almost 2.9 times higher, the YRBS data show.
Respondents with multiple races in their backgrounds, at 12.9%, and African Americans, with a prevalence of 11.8%, also were above the high school average for suicide attempts, while Whites (7.9%) and Asians (7.7%) were under it and Hispanics equaled it, the Centers for Disease Control and Prevention reported.
The number of AI/AN students was insufficient to examine differences by sex, but females in all of the other racial/ethnic groups were more likely than males to have attempted suicide: multiple race (17.8% vs. 7.3%), African American (15.2% vs. 8.5%), Hispanic (11.9% vs. 5.5%), White (9.4% vs. 6.4%), and Asian (8.4% vs. 7.1%), the CDC’s Division of Adolescent and School Health said.
Among all respondents, 11.0% of females had attempted suicide in the 12 months before the survey, a figure that is significantly higher than the 6.6% prevalence in males. Females also were significantly more likely than males to make a plan about how they would attempt suicide (19.9% vs. 11.3%) and to seriously consider an attempt (24.1% vs. 13.3%), CDC investigators said in a separate report.
Significant differences also were seen when looking at sexual identity. Suicide attempts were reported by 6.4% of heterosexuals, 16.1% of those who weren’t sure, and 23.4% of lesbians/gays/bisexuals (LGBs). For serious consideration of suicide, the respective numbers were 14.5%, 30.4%, and 46.8%, they reported (MMWR Supp. 2020 Aug 21;69[1]:47-55).
For nonheterosexuals, however, males were slightly more likely (23.8%) than females (23.6%) to have attempted suicide, but females were more likely to seriously consider it (49.0% vs. 40.4%) and to make a plan (42.4% vs. 33.0%), according to the YRBS data.
“Adolescence … represents a time for expanded identity development, with sexual identity development representing a complex, multidimensional, and often stressful process for youths,” the CDC investigators said in the MMWR. “To address the health differences in suicidal ideation and behaviors observed by student demographics and to decrease these outcomes overall, a comprehensive approach to suicide prevention, including programs, practices, and policies based on the best available evidence, is needed.”
according to newly released data from the 2019 Youth Risk Behavior Survey.
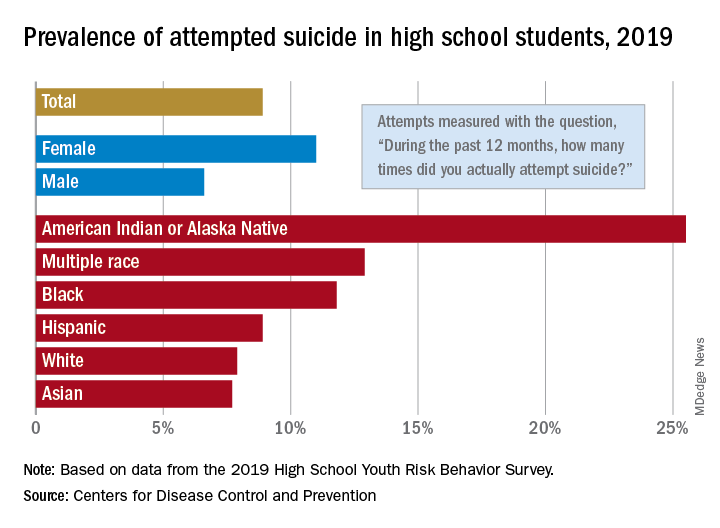
The prevalence of attempted suicide during the previous 12 months was 8.9% among the 13,677 students in grades 9-12 who took the survey last year, but the rate was 25.5% for American Indian/Alaska Native (AI/AN) respondents, almost 2.9 times higher, the YRBS data show.
Respondents with multiple races in their backgrounds, at 12.9%, and African Americans, with a prevalence of 11.8%, also were above the high school average for suicide attempts, while Whites (7.9%) and Asians (7.7%) were under it and Hispanics equaled it, the Centers for Disease Control and Prevention reported.
The number of AI/AN students was insufficient to examine differences by sex, but females in all of the other racial/ethnic groups were more likely than males to have attempted suicide: multiple race (17.8% vs. 7.3%), African American (15.2% vs. 8.5%), Hispanic (11.9% vs. 5.5%), White (9.4% vs. 6.4%), and Asian (8.4% vs. 7.1%), the CDC’s Division of Adolescent and School Health said.
Among all respondents, 11.0% of females had attempted suicide in the 12 months before the survey, a figure that is significantly higher than the 6.6% prevalence in males. Females also were significantly more likely than males to make a plan about how they would attempt suicide (19.9% vs. 11.3%) and to seriously consider an attempt (24.1% vs. 13.3%), CDC investigators said in a separate report.
Significant differences also were seen when looking at sexual identity. Suicide attempts were reported by 6.4% of heterosexuals, 16.1% of those who weren’t sure, and 23.4% of lesbians/gays/bisexuals (LGBs). For serious consideration of suicide, the respective numbers were 14.5%, 30.4%, and 46.8%, they reported (MMWR Supp. 2020 Aug 21;69[1]:47-55).
For nonheterosexuals, however, males were slightly more likely (23.8%) than females (23.6%) to have attempted suicide, but females were more likely to seriously consider it (49.0% vs. 40.4%) and to make a plan (42.4% vs. 33.0%), according to the YRBS data.
“Adolescence … represents a time for expanded identity development, with sexual identity development representing a complex, multidimensional, and often stressful process for youths,” the CDC investigators said in the MMWR. “To address the health differences in suicidal ideation and behaviors observed by student demographics and to decrease these outcomes overall, a comprehensive approach to suicide prevention, including programs, practices, and policies based on the best available evidence, is needed.”
according to newly released data from the 2019 Youth Risk Behavior Survey.
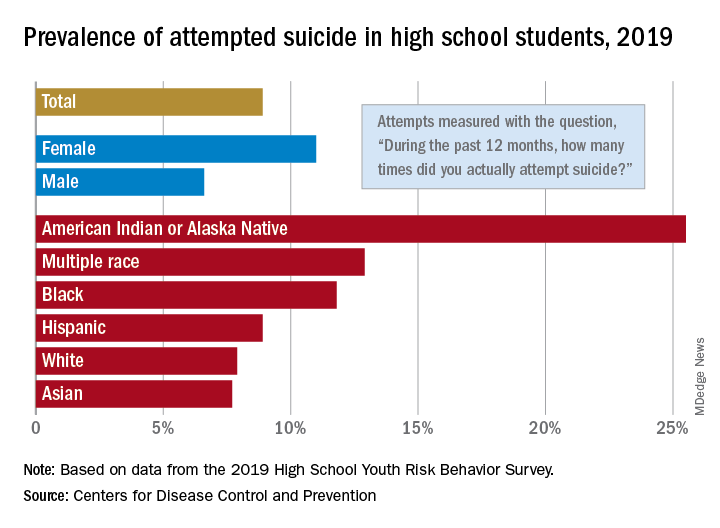
The prevalence of attempted suicide during the previous 12 months was 8.9% among the 13,677 students in grades 9-12 who took the survey last year, but the rate was 25.5% for American Indian/Alaska Native (AI/AN) respondents, almost 2.9 times higher, the YRBS data show.
Respondents with multiple races in their backgrounds, at 12.9%, and African Americans, with a prevalence of 11.8%, also were above the high school average for suicide attempts, while Whites (7.9%) and Asians (7.7%) were under it and Hispanics equaled it, the Centers for Disease Control and Prevention reported.
The number of AI/AN students was insufficient to examine differences by sex, but females in all of the other racial/ethnic groups were more likely than males to have attempted suicide: multiple race (17.8% vs. 7.3%), African American (15.2% vs. 8.5%), Hispanic (11.9% vs. 5.5%), White (9.4% vs. 6.4%), and Asian (8.4% vs. 7.1%), the CDC’s Division of Adolescent and School Health said.
Among all respondents, 11.0% of females had attempted suicide in the 12 months before the survey, a figure that is significantly higher than the 6.6% prevalence in males. Females also were significantly more likely than males to make a plan about how they would attempt suicide (19.9% vs. 11.3%) and to seriously consider an attempt (24.1% vs. 13.3%), CDC investigators said in a separate report.
Significant differences also were seen when looking at sexual identity. Suicide attempts were reported by 6.4% of heterosexuals, 16.1% of those who weren’t sure, and 23.4% of lesbians/gays/bisexuals (LGBs). For serious consideration of suicide, the respective numbers were 14.5%, 30.4%, and 46.8%, they reported (MMWR Supp. 2020 Aug 21;69[1]:47-55).
For nonheterosexuals, however, males were slightly more likely (23.8%) than females (23.6%) to have attempted suicide, but females were more likely to seriously consider it (49.0% vs. 40.4%) and to make a plan (42.4% vs. 33.0%), according to the YRBS data.
“Adolescence … represents a time for expanded identity development, with sexual identity development representing a complex, multidimensional, and often stressful process for youths,” the CDC investigators said in the MMWR. “To address the health differences in suicidal ideation and behaviors observed by student demographics and to decrease these outcomes overall, a comprehensive approach to suicide prevention, including programs, practices, and policies based on the best available evidence, is needed.”
Study links gut microbiome and mRCC treatment outcomes
New research, published in European Urology, has revealed an association between gut microbial diversity and treatment outcomes for patients with metastatic renal cell carcinoma receiving checkpoint inhibitor therapy.
The findings suggest that metastatic renal cell carcinoma (mRCC) patients with a greater abundance of certain bacterial species derive clinical benefit from checkpoint inhibitor (CPI) treatment.
“We conducted a prospective observational study to determine the association between baseline gut microbial diversity and clinical benefit in patients with mRCC receiving CPIs,” study author Nicholas J. Salgia, an MD/PhD student at the State University of New York at Buffalo, and colleagues wrote.
The researchers collected stool samples from 31 mRCC patients within 7 days of them starting nivolumab monotherapy (77%) or nivolumab plus ipilimumab (23%). The microbial composition of each sample was evaluated using whole-metagenome sequencing at baseline, 1 month, and 3 months following treatment initiation.
In all, 58% of patients experienced a clinical benefit of treatment, which was defined as achieving a response or having stable disease for more than 4 months. There were 11 patients (35%) who achieved a complete or partial response and 7 (23%) who had stable disease for more than 4 months.
“Greater microbial diversity was associated with clinical benefit from CPI therapy (P = .001), and multiple species were associated with clinical benefit or lack thereof,” the researchers wrote.
In fact, there were 13 bacterial species with a linear discriminant analysis score of 3 or greater that distinguished between patients who had a clinical benefit (9 species) and those who did not (4 species).
The bacterial species with the greatest significance among patients with a clinical benefit were Bifidobacterium adolescentis (P = .002), Barnesiella intestinihominis (P = .002), Odoribacter splanchnicus (P = .006), and Bacteroides eggerthii (P = .009).
“These results suggest that certain species (e.g., [Prevotella] copri) appear to expand in relative abundance in patients deriving clinical benefit,” the researchers wrote.
The team also found that Akkermansia muciniphila increased in relative abundance in many patients experiencing clinical benefit and decreased in several patients not deriving clinical benefit.
“The patients with the highest benefit from cancer treatment were those with more microbial diversity but also those with a higher abundance of a specific bacterium known as Akkermansia muciniphila,” study author Sarah K. Highlander, PhD, of Translational Genomics Research Institute in Phoenix, said in a statement.
“This organism has been associated with benefit in other immunotherapy studies,” she explained.
The researchers acknowledged that a key limitation of this study was the method of stool collection. Given the use of a small, non–vacuum-sealed container, proliferation of aerobic bacteria could have occurred.
Based on the findings of this study, researchers are conducting a randomized clinical trial to evaluate the role of gut microbial modulation in CPI response. In this phase 1 study, researchers are investigating the use of frontline nivolumab plus ipilimumab, with or without CBM-588, a strain of Clostridium butyricum with both anti-inflammatory and immunomodulatory properties in the intestinal epithelium.
The current study was supported, in part, by a grant from Bristol-Myers Squibb. Several authors disclosed financial affiliations with multiple pharmaceutical companies.
SOURCE: Salgia NJ et al. Eur Urol. 2020 Aug 2. doi: 10.1016/j.eururo.2020.07.011.
New research, published in European Urology, has revealed an association between gut microbial diversity and treatment outcomes for patients with metastatic renal cell carcinoma receiving checkpoint inhibitor therapy.
The findings suggest that metastatic renal cell carcinoma (mRCC) patients with a greater abundance of certain bacterial species derive clinical benefit from checkpoint inhibitor (CPI) treatment.
“We conducted a prospective observational study to determine the association between baseline gut microbial diversity and clinical benefit in patients with mRCC receiving CPIs,” study author Nicholas J. Salgia, an MD/PhD student at the State University of New York at Buffalo, and colleagues wrote.
The researchers collected stool samples from 31 mRCC patients within 7 days of them starting nivolumab monotherapy (77%) or nivolumab plus ipilimumab (23%). The microbial composition of each sample was evaluated using whole-metagenome sequencing at baseline, 1 month, and 3 months following treatment initiation.
In all, 58% of patients experienced a clinical benefit of treatment, which was defined as achieving a response or having stable disease for more than 4 months. There were 11 patients (35%) who achieved a complete or partial response and 7 (23%) who had stable disease for more than 4 months.
“Greater microbial diversity was associated with clinical benefit from CPI therapy (P = .001), and multiple species were associated with clinical benefit or lack thereof,” the researchers wrote.
In fact, there were 13 bacterial species with a linear discriminant analysis score of 3 or greater that distinguished between patients who had a clinical benefit (9 species) and those who did not (4 species).
The bacterial species with the greatest significance among patients with a clinical benefit were Bifidobacterium adolescentis (P = .002), Barnesiella intestinihominis (P = .002), Odoribacter splanchnicus (P = .006), and Bacteroides eggerthii (P = .009).
“These results suggest that certain species (e.g., [Prevotella] copri) appear to expand in relative abundance in patients deriving clinical benefit,” the researchers wrote.
The team also found that Akkermansia muciniphila increased in relative abundance in many patients experiencing clinical benefit and decreased in several patients not deriving clinical benefit.
“The patients with the highest benefit from cancer treatment were those with more microbial diversity but also those with a higher abundance of a specific bacterium known as Akkermansia muciniphila,” study author Sarah K. Highlander, PhD, of Translational Genomics Research Institute in Phoenix, said in a statement.
“This organism has been associated with benefit in other immunotherapy studies,” she explained.
The researchers acknowledged that a key limitation of this study was the method of stool collection. Given the use of a small, non–vacuum-sealed container, proliferation of aerobic bacteria could have occurred.
Based on the findings of this study, researchers are conducting a randomized clinical trial to evaluate the role of gut microbial modulation in CPI response. In this phase 1 study, researchers are investigating the use of frontline nivolumab plus ipilimumab, with or without CBM-588, a strain of Clostridium butyricum with both anti-inflammatory and immunomodulatory properties in the intestinal epithelium.
The current study was supported, in part, by a grant from Bristol-Myers Squibb. Several authors disclosed financial affiliations with multiple pharmaceutical companies.
SOURCE: Salgia NJ et al. Eur Urol. 2020 Aug 2. doi: 10.1016/j.eururo.2020.07.011.
New research, published in European Urology, has revealed an association between gut microbial diversity and treatment outcomes for patients with metastatic renal cell carcinoma receiving checkpoint inhibitor therapy.
The findings suggest that metastatic renal cell carcinoma (mRCC) patients with a greater abundance of certain bacterial species derive clinical benefit from checkpoint inhibitor (CPI) treatment.
“We conducted a prospective observational study to determine the association between baseline gut microbial diversity and clinical benefit in patients with mRCC receiving CPIs,” study author Nicholas J. Salgia, an MD/PhD student at the State University of New York at Buffalo, and colleagues wrote.
The researchers collected stool samples from 31 mRCC patients within 7 days of them starting nivolumab monotherapy (77%) or nivolumab plus ipilimumab (23%). The microbial composition of each sample was evaluated using whole-metagenome sequencing at baseline, 1 month, and 3 months following treatment initiation.
In all, 58% of patients experienced a clinical benefit of treatment, which was defined as achieving a response or having stable disease for more than 4 months. There were 11 patients (35%) who achieved a complete or partial response and 7 (23%) who had stable disease for more than 4 months.
“Greater microbial diversity was associated with clinical benefit from CPI therapy (P = .001), and multiple species were associated with clinical benefit or lack thereof,” the researchers wrote.
In fact, there were 13 bacterial species with a linear discriminant analysis score of 3 or greater that distinguished between patients who had a clinical benefit (9 species) and those who did not (4 species).
The bacterial species with the greatest significance among patients with a clinical benefit were Bifidobacterium adolescentis (P = .002), Barnesiella intestinihominis (P = .002), Odoribacter splanchnicus (P = .006), and Bacteroides eggerthii (P = .009).
“These results suggest that certain species (e.g., [Prevotella] copri) appear to expand in relative abundance in patients deriving clinical benefit,” the researchers wrote.
The team also found that Akkermansia muciniphila increased in relative abundance in many patients experiencing clinical benefit and decreased in several patients not deriving clinical benefit.
“The patients with the highest benefit from cancer treatment were those with more microbial diversity but also those with a higher abundance of a specific bacterium known as Akkermansia muciniphila,” study author Sarah K. Highlander, PhD, of Translational Genomics Research Institute in Phoenix, said in a statement.
“This organism has been associated with benefit in other immunotherapy studies,” she explained.
The researchers acknowledged that a key limitation of this study was the method of stool collection. Given the use of a small, non–vacuum-sealed container, proliferation of aerobic bacteria could have occurred.
Based on the findings of this study, researchers are conducting a randomized clinical trial to evaluate the role of gut microbial modulation in CPI response. In this phase 1 study, researchers are investigating the use of frontline nivolumab plus ipilimumab, with or without CBM-588, a strain of Clostridium butyricum with both anti-inflammatory and immunomodulatory properties in the intestinal epithelium.
The current study was supported, in part, by a grant from Bristol-Myers Squibb. Several authors disclosed financial affiliations with multiple pharmaceutical companies.
SOURCE: Salgia NJ et al. Eur Urol. 2020 Aug 2. doi: 10.1016/j.eururo.2020.07.011.
FROM EUROPEAN UROLOGY
Drug allergy in the chart? Ask patients for specifics
Paige Wickner, MD, MPH, medical director for quality and safety at Brigham and Women’s Hospital and assistant professor at Harvard Medical School, both in Boston, described a scenario that might sound familiar to hospitalists.
A 72-year-old man is admitted to the hospital for a lung transplant, and has a listed allergy to “sulfa,” contained in antibiotics and other medications. His medical records say his reaction was “rash.”
What do you do?
The answer, Dr. Wickner said, speaking at HM20 Virtual, sponsored by the Society of Hospital Medicine, is to first ask more questions for clarification. How bad was the rash? Was it blistering? To what type of sulfa did the patient have a reaction?
These questions can help determine the next steps. For sulfa-based antibiotics, hospitalists can often desensitize patients with certain reaction characteristics using widely studied protocols to allow the patient to temporarily take a sulfa-containing medication.
The dominant message of Dr. Wickner’s talk on drug allergies was to get clear details on the allergic reaction –
“Please, for all of your patients, take an allergy history on every listed medication; often you will be able to remove or clarify the medical record and the changes can be life saving,” she said.
For instance, desensitization to sulfa for patients who’ve had a morbilliform rash without a fever can be done on an outpatient basis. But if the patient had hives, or became short of breath or anaphylactic, it needs to be done as an inpatient by an allergist, she said.
The question of drug allergies is substantial. About 35% of patients have at least one listed drug allergy, with penicillin, NSAIDs, and CT contrast agents topping the list, Dr. Wickner said. Although 10% of the general population and 15% of inpatients have a listed penicillin allergy, more than 90% of listed penicillin allergies turn out not to actually be allergic, in part because penicillin allergies are often diagnosed in childhood and are frequently outgrown over time. Having a listed allergy can impact treatment, Dr. Wickner said, with alternatives not always clear-cut.
She described one patient she saw who had 62 listed drug allergies, prompting her clinicians to wonder, “what can I safely give this patient?” Physicians, she said, subject to drug allergy “alert fatigue,” tend to override about 80% of allergy alerts, but this can sometimes have serious consequences.
“The best time to clarify is when a patient is healthy and well,” said Dr. Wickner, not when they are an inpatient and sick. It is much more difficult to test for an allergy, and to treat an allergic reaction, than when someone’s health is quickly declining.
She urged physicians to ask patients to be specific about the name of a drug they suspect they’re allergic to, about the indications, the symptoms, and the timing – an immediate reaction is much different than a symptom that showed up days later.
“Sometimes they’ll say they’re allergic to penicillin, but will tell you they’ve taken Augmentin or amoxicillin, so you can take that allergy off the list,” Dr. Wickner said.
At Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, physicians have developed protocols for assessing and managing suspected allergies to penicillin, aspirin and NSAIDs, and trimethoprim/sulfamethoxazole – helpful tools, she said, because the nature and context of the reaction can matter a great deal in how to respond to the listed allergy.
If someone has a reaction, and you think it might be anaphylaxis, don’t spend time pondering it, Dr. Wickner said. “If that thought crosses your mind, treat it like anaphylaxis, then analyze after the fact.” Most patients with anaphylaxis have some cutaneous sign, even if it’s just flushing.
Dr. Wickner said that, if an allergist is available, take advantage of that. “If allergy is available in-house, utilize them. Often, skin testing and/or challenge can help patients receive first-line therapy.”
In a question-and-answer session after her presentation, Dr. Wickner said that hospitalists “have a huge role to play” in drug allergy delabeling.
“We would love to have a more standard practice of allergy reconciliation, just like we do with medication reconciliation,” she said. Asking questions to get more specifics is essential – and simply asking directly about each listed allergen is “step one, and you’ll really find it’s going to broaden the things that you can do for your patients.”
Asked about whether reactions listed as allergies are frequently just adverse effects, Dr. Wickner said that patients who say they are frequently nauseous – rather than breaking out into a rash, for example – might not be having a true allergic reaction. After careful consideration, they might be better managed with antinausea medication than avoidance of the drug.
Dr. Wickner reported no relevant financial disclosures.
Paige Wickner, MD, MPH, medical director for quality and safety at Brigham and Women’s Hospital and assistant professor at Harvard Medical School, both in Boston, described a scenario that might sound familiar to hospitalists.
A 72-year-old man is admitted to the hospital for a lung transplant, and has a listed allergy to “sulfa,” contained in antibiotics and other medications. His medical records say his reaction was “rash.”
What do you do?
The answer, Dr. Wickner said, speaking at HM20 Virtual, sponsored by the Society of Hospital Medicine, is to first ask more questions for clarification. How bad was the rash? Was it blistering? To what type of sulfa did the patient have a reaction?
These questions can help determine the next steps. For sulfa-based antibiotics, hospitalists can often desensitize patients with certain reaction characteristics using widely studied protocols to allow the patient to temporarily take a sulfa-containing medication.
The dominant message of Dr. Wickner’s talk on drug allergies was to get clear details on the allergic reaction –
“Please, for all of your patients, take an allergy history on every listed medication; often you will be able to remove or clarify the medical record and the changes can be life saving,” she said.
For instance, desensitization to sulfa for patients who’ve had a morbilliform rash without a fever can be done on an outpatient basis. But if the patient had hives, or became short of breath or anaphylactic, it needs to be done as an inpatient by an allergist, she said.
The question of drug allergies is substantial. About 35% of patients have at least one listed drug allergy, with penicillin, NSAIDs, and CT contrast agents topping the list, Dr. Wickner said. Although 10% of the general population and 15% of inpatients have a listed penicillin allergy, more than 90% of listed penicillin allergies turn out not to actually be allergic, in part because penicillin allergies are often diagnosed in childhood and are frequently outgrown over time. Having a listed allergy can impact treatment, Dr. Wickner said, with alternatives not always clear-cut.
She described one patient she saw who had 62 listed drug allergies, prompting her clinicians to wonder, “what can I safely give this patient?” Physicians, she said, subject to drug allergy “alert fatigue,” tend to override about 80% of allergy alerts, but this can sometimes have serious consequences.
“The best time to clarify is when a patient is healthy and well,” said Dr. Wickner, not when they are an inpatient and sick. It is much more difficult to test for an allergy, and to treat an allergic reaction, than when someone’s health is quickly declining.
She urged physicians to ask patients to be specific about the name of a drug they suspect they’re allergic to, about the indications, the symptoms, and the timing – an immediate reaction is much different than a symptom that showed up days later.
“Sometimes they’ll say they’re allergic to penicillin, but will tell you they’ve taken Augmentin or amoxicillin, so you can take that allergy off the list,” Dr. Wickner said.
At Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, physicians have developed protocols for assessing and managing suspected allergies to penicillin, aspirin and NSAIDs, and trimethoprim/sulfamethoxazole – helpful tools, she said, because the nature and context of the reaction can matter a great deal in how to respond to the listed allergy.
If someone has a reaction, and you think it might be anaphylaxis, don’t spend time pondering it, Dr. Wickner said. “If that thought crosses your mind, treat it like anaphylaxis, then analyze after the fact.” Most patients with anaphylaxis have some cutaneous sign, even if it’s just flushing.
Dr. Wickner said that, if an allergist is available, take advantage of that. “If allergy is available in-house, utilize them. Often, skin testing and/or challenge can help patients receive first-line therapy.”
In a question-and-answer session after her presentation, Dr. Wickner said that hospitalists “have a huge role to play” in drug allergy delabeling.
“We would love to have a more standard practice of allergy reconciliation, just like we do with medication reconciliation,” she said. Asking questions to get more specifics is essential – and simply asking directly about each listed allergen is “step one, and you’ll really find it’s going to broaden the things that you can do for your patients.”
Asked about whether reactions listed as allergies are frequently just adverse effects, Dr. Wickner said that patients who say they are frequently nauseous – rather than breaking out into a rash, for example – might not be having a true allergic reaction. After careful consideration, they might be better managed with antinausea medication than avoidance of the drug.
Dr. Wickner reported no relevant financial disclosures.
Paige Wickner, MD, MPH, medical director for quality and safety at Brigham and Women’s Hospital and assistant professor at Harvard Medical School, both in Boston, described a scenario that might sound familiar to hospitalists.
A 72-year-old man is admitted to the hospital for a lung transplant, and has a listed allergy to “sulfa,” contained in antibiotics and other medications. His medical records say his reaction was “rash.”
What do you do?
The answer, Dr. Wickner said, speaking at HM20 Virtual, sponsored by the Society of Hospital Medicine, is to first ask more questions for clarification. How bad was the rash? Was it blistering? To what type of sulfa did the patient have a reaction?
These questions can help determine the next steps. For sulfa-based antibiotics, hospitalists can often desensitize patients with certain reaction characteristics using widely studied protocols to allow the patient to temporarily take a sulfa-containing medication.
The dominant message of Dr. Wickner’s talk on drug allergies was to get clear details on the allergic reaction –
“Please, for all of your patients, take an allergy history on every listed medication; often you will be able to remove or clarify the medical record and the changes can be life saving,” she said.
For instance, desensitization to sulfa for patients who’ve had a morbilliform rash without a fever can be done on an outpatient basis. But if the patient had hives, or became short of breath or anaphylactic, it needs to be done as an inpatient by an allergist, she said.
The question of drug allergies is substantial. About 35% of patients have at least one listed drug allergy, with penicillin, NSAIDs, and CT contrast agents topping the list, Dr. Wickner said. Although 10% of the general population and 15% of inpatients have a listed penicillin allergy, more than 90% of listed penicillin allergies turn out not to actually be allergic, in part because penicillin allergies are often diagnosed in childhood and are frequently outgrown over time. Having a listed allergy can impact treatment, Dr. Wickner said, with alternatives not always clear-cut.
She described one patient she saw who had 62 listed drug allergies, prompting her clinicians to wonder, “what can I safely give this patient?” Physicians, she said, subject to drug allergy “alert fatigue,” tend to override about 80% of allergy alerts, but this can sometimes have serious consequences.
“The best time to clarify is when a patient is healthy and well,” said Dr. Wickner, not when they are an inpatient and sick. It is much more difficult to test for an allergy, and to treat an allergic reaction, than when someone’s health is quickly declining.
She urged physicians to ask patients to be specific about the name of a drug they suspect they’re allergic to, about the indications, the symptoms, and the timing – an immediate reaction is much different than a symptom that showed up days later.
“Sometimes they’ll say they’re allergic to penicillin, but will tell you they’ve taken Augmentin or amoxicillin, so you can take that allergy off the list,” Dr. Wickner said.
At Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, physicians have developed protocols for assessing and managing suspected allergies to penicillin, aspirin and NSAIDs, and trimethoprim/sulfamethoxazole – helpful tools, she said, because the nature and context of the reaction can matter a great deal in how to respond to the listed allergy.
If someone has a reaction, and you think it might be anaphylaxis, don’t spend time pondering it, Dr. Wickner said. “If that thought crosses your mind, treat it like anaphylaxis, then analyze after the fact.” Most patients with anaphylaxis have some cutaneous sign, even if it’s just flushing.
Dr. Wickner said that, if an allergist is available, take advantage of that. “If allergy is available in-house, utilize them. Often, skin testing and/or challenge can help patients receive first-line therapy.”
In a question-and-answer session after her presentation, Dr. Wickner said that hospitalists “have a huge role to play” in drug allergy delabeling.
“We would love to have a more standard practice of allergy reconciliation, just like we do with medication reconciliation,” she said. Asking questions to get more specifics is essential – and simply asking directly about each listed allergen is “step one, and you’ll really find it’s going to broaden the things that you can do for your patients.”
Asked about whether reactions listed as allergies are frequently just adverse effects, Dr. Wickner said that patients who say they are frequently nauseous – rather than breaking out into a rash, for example – might not be having a true allergic reaction. After careful consideration, they might be better managed with antinausea medication than avoidance of the drug.
Dr. Wickner reported no relevant financial disclosures.
FROM HM20 VIRTUAL
Mitigating psychiatric disorder relapse in pregnancy during pandemic
In a previous column, I addressed some of the issues that quickly arose in the context of the COVID-19 pandemic and their implications for reproductive psychiatry. These issues ranged from the importance of sustaining well-being in pregnant and postpartum women during the pandemic, to temporary restrictions that were in place during the early part of the pandemic with respect to performing infertility procedures, to the practical issues of limiting the number of people who could attend to women during labor and delivery in the hospital.
Five months later, we’ve learned a great deal about trying to sustain emotional well-being among pregnant women during COVID-19. There is a high rate of anxiety among women who are pregnant and women who have particularly young children around the various issues of juggling activities of daily living during the pandemic, including switching to remote work and homeschooling children. There is fear of contracting COVID-19 during pregnancy, the exact effects of which are still somewhat unknown. We have seen a shift to telemedicine for prenatal and postpartum obstetrics visits, and a change with respect to visitors and even in-home nurses that would help during the first weeks of life for some couples.
We wondered whether we would see a falloff in the numbers of women presenting to our clinic with questions about the reproductive safety of taking psychiatric medications during pregnancy. We were unclear as to whether women would defer plans to get pregnant given some of the uncertainties that have come with COVID-19. What we’ve seen, at least early on in the pandemic in Massachusetts, has been the opposite. More women during the first 4 months of the pandemic have been seen in our center compared with the same corresponding period over the last 5 years. The precise reasons for this are unclear, but one reason may be that shifting the practice of reproductive psychiatry and pregnancy planning for reproductive-age women to full virtual care has dropped the number of missed appointments to essentially zero. Women perhaps feel an urgency to have a plan for using psychiatric medication during pregnancy. They may also see the benefit of being able to have extended telemedicine consultations that frequently involve their partners, a practice we have always supported, but posed logistical challenges for some.
As our colleagues learned that we had shifted our clinical rounds at the Center for Women’s Mental Health, which we’ve been doing for 25 years, to a virtual format, we began offering a free 1-hour forum to discuss relevant issues around caring for psychiatrically ill women, with a focus on some of the issues that were particularly relevant during the pandemic. The most common reasons for consultation on our service are the appropriate, safest use of antidepressants and mood stabilizers during pregnancy, and that continues to be the case.
If there has been one guiding principle in treating perinatal depression during pregnancy, it has been our long-standing, laser-like focus on keeping women emotionally well during pregnancy, and to highlight the importance of this with women during consultations prior to and during pregnancy. Relapse of psychiatric disorder during pregnancy is one the strongest predictors of postpartum depression, and the impact of untreated depression during pregnancy has been described in the literature and over the years in this column. However, where we want to minimize, if possible, severe onset of illness requiring hospitalization or emergent attention considering it may make social distancing and some of the other mitigating factors vis-à-vis COVID-19 more challenging.
Despite the accumulated data over the last 2 decades on the reproductive safety of antidepressants, women continue to have questions about the safety of these medications during pregnancy. Studies show now that many women would prefer, if at all possible, to defer treatment with antidepressants, and so they come to us with questions about their reproductive safety, the potential of switching to nonpharmacologic interventions, and the use of alternative interventions that might be used to treat their underlying mood disorder.
Investigators at the University of British Columbia recently have tried to inform the field with still another look, not at reproductive safety per se, but at risk of relapse of depression if women discontinue those medicines during pregnancy.1 There is a timeliness to this investigation, which was a systematic review and meta-analysis of studies that met a priori criteria for inclusion. Since some of our own group’s early work over 15 years ago on relapse of psychiatric disorder during pregnancy,2 which indicated a substantial difference in risk of relapse between women who continued versus who discontinued antidepressants, other investigators have showed the difference in risk for relapse is not as substantial, and that continuation of medication did not appear to mitigate risk for relapse. In fact, in the systematic review, the investigators demonstrated that as a group, maintaining medicine did not appear to confer particular benefit to patients relative to risk for relapse compared to discontinuation of antidepressants.
However, looking more closely, Bayrampour and colleagues note for women with histories of more severe recurrent, major depression, relapse did in fact appear to be greater in women who discontinued compared with those with cases of mild to moderate depression. It is noteworthy that in both our early and later work, and certainly dovetailing with our clinical practice, we have noted severity of illness does not appear to correlate with the actual decisions women ultimately make regarding what they will do with antidepressants. Specifically, some women with very severe illness histories will discontinue antidepressants regardless of their risk for relapse. Alternatively, women with mild to moderate illness will sometimes elect to stay on antidepressant therapy. With all the information that we have about fetal exposure to antidepressants on one hand, the “unknown unknowns” are an understandable concern to both patients and clinicians. Clinicians are faced with the dilemma of how to best counsel women on continuing or discontinuing antidepressants as they plan to conceive or during pregnancy and in the postpartum period.
The literature cited and clinical experience over the last 3 decades suggests rather strongly that there is a relatively low likelihood women with histories of severe recurrent disease will be able to successfully discontinue antidepressants in the absence of relapse. A greater question is, what is the best way to proceed for women who have been on maintenance therapy and had more moderate symptoms?
I am inspired by some of the more recent literature that has tried to elucidate the role of nonpharmacologic interventions such as mindfulness-based cognitive therapy (MBCT) in an effort to mitigate risk for depressive relapse in pregnant women who are well with histories of depression. To date, data do not inform the question as to whether MBCT can be used to mitigate risk of depressive relapse in pregnant women who continue or discontinue antidepressants. That research question is actively being studied by several investigators, including ourselves.
Of particular interest is whether the addition of mindfulness practices such as MBCT in treatment could mitigate risk for depressive relapse in pregnant women who continue or discontinue antidepressant treatment, as that would certainly be a no-harm intervention that could mitigate risk even in a lower risk sample of patients. The question of how to “thread the needle” during the pandemic and best approach woman with a history of recurrent major depression on antidepressants is particularly timely and critical.
Regardless, we make clinical decisions collaboratively with patients based on their histories and individual wishes, and perhaps what we have learned over the last 5 months is the use of telemedicine does afford us the opportunity, regardless of the decisions that patients make, to more closely follow the clinical trajectory of women during pregnancy and the postpartum period so that regardless of treatment, we have an opportunity to intervene early when needed and to ascertain changes in clinical status early to mitigate the risk of frank relapse. From a reproductive psychiatric point of view, that is a silver lining with respect to the associated challenges that have come along with the pandemic.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at obnews@mdedge.com.
References
1. J Clin Psychiatry 2020;81(4):19r13134.
2. JAMA. 2006 Feb 1;295(5):499-507.
In a previous column, I addressed some of the issues that quickly arose in the context of the COVID-19 pandemic and their implications for reproductive psychiatry. These issues ranged from the importance of sustaining well-being in pregnant and postpartum women during the pandemic, to temporary restrictions that were in place during the early part of the pandemic with respect to performing infertility procedures, to the practical issues of limiting the number of people who could attend to women during labor and delivery in the hospital.
Five months later, we’ve learned a great deal about trying to sustain emotional well-being among pregnant women during COVID-19. There is a high rate of anxiety among women who are pregnant and women who have particularly young children around the various issues of juggling activities of daily living during the pandemic, including switching to remote work and homeschooling children. There is fear of contracting COVID-19 during pregnancy, the exact effects of which are still somewhat unknown. We have seen a shift to telemedicine for prenatal and postpartum obstetrics visits, and a change with respect to visitors and even in-home nurses that would help during the first weeks of life for some couples.
We wondered whether we would see a falloff in the numbers of women presenting to our clinic with questions about the reproductive safety of taking psychiatric medications during pregnancy. We were unclear as to whether women would defer plans to get pregnant given some of the uncertainties that have come with COVID-19. What we’ve seen, at least early on in the pandemic in Massachusetts, has been the opposite. More women during the first 4 months of the pandemic have been seen in our center compared with the same corresponding period over the last 5 years. The precise reasons for this are unclear, but one reason may be that shifting the practice of reproductive psychiatry and pregnancy planning for reproductive-age women to full virtual care has dropped the number of missed appointments to essentially zero. Women perhaps feel an urgency to have a plan for using psychiatric medication during pregnancy. They may also see the benefit of being able to have extended telemedicine consultations that frequently involve their partners, a practice we have always supported, but posed logistical challenges for some.
As our colleagues learned that we had shifted our clinical rounds at the Center for Women’s Mental Health, which we’ve been doing for 25 years, to a virtual format, we began offering a free 1-hour forum to discuss relevant issues around caring for psychiatrically ill women, with a focus on some of the issues that were particularly relevant during the pandemic. The most common reasons for consultation on our service are the appropriate, safest use of antidepressants and mood stabilizers during pregnancy, and that continues to be the case.
If there has been one guiding principle in treating perinatal depression during pregnancy, it has been our long-standing, laser-like focus on keeping women emotionally well during pregnancy, and to highlight the importance of this with women during consultations prior to and during pregnancy. Relapse of psychiatric disorder during pregnancy is one the strongest predictors of postpartum depression, and the impact of untreated depression during pregnancy has been described in the literature and over the years in this column. However, where we want to minimize, if possible, severe onset of illness requiring hospitalization or emergent attention considering it may make social distancing and some of the other mitigating factors vis-à-vis COVID-19 more challenging.
Despite the accumulated data over the last 2 decades on the reproductive safety of antidepressants, women continue to have questions about the safety of these medications during pregnancy. Studies show now that many women would prefer, if at all possible, to defer treatment with antidepressants, and so they come to us with questions about their reproductive safety, the potential of switching to nonpharmacologic interventions, and the use of alternative interventions that might be used to treat their underlying mood disorder.
Investigators at the University of British Columbia recently have tried to inform the field with still another look, not at reproductive safety per se, but at risk of relapse of depression if women discontinue those medicines during pregnancy.1 There is a timeliness to this investigation, which was a systematic review and meta-analysis of studies that met a priori criteria for inclusion. Since some of our own group’s early work over 15 years ago on relapse of psychiatric disorder during pregnancy,2 which indicated a substantial difference in risk of relapse between women who continued versus who discontinued antidepressants, other investigators have showed the difference in risk for relapse is not as substantial, and that continuation of medication did not appear to mitigate risk for relapse. In fact, in the systematic review, the investigators demonstrated that as a group, maintaining medicine did not appear to confer particular benefit to patients relative to risk for relapse compared to discontinuation of antidepressants.
However, looking more closely, Bayrampour and colleagues note for women with histories of more severe recurrent, major depression, relapse did in fact appear to be greater in women who discontinued compared with those with cases of mild to moderate depression. It is noteworthy that in both our early and later work, and certainly dovetailing with our clinical practice, we have noted severity of illness does not appear to correlate with the actual decisions women ultimately make regarding what they will do with antidepressants. Specifically, some women with very severe illness histories will discontinue antidepressants regardless of their risk for relapse. Alternatively, women with mild to moderate illness will sometimes elect to stay on antidepressant therapy. With all the information that we have about fetal exposure to antidepressants on one hand, the “unknown unknowns” are an understandable concern to both patients and clinicians. Clinicians are faced with the dilemma of how to best counsel women on continuing or discontinuing antidepressants as they plan to conceive or during pregnancy and in the postpartum period.
The literature cited and clinical experience over the last 3 decades suggests rather strongly that there is a relatively low likelihood women with histories of severe recurrent disease will be able to successfully discontinue antidepressants in the absence of relapse. A greater question is, what is the best way to proceed for women who have been on maintenance therapy and had more moderate symptoms?
I am inspired by some of the more recent literature that has tried to elucidate the role of nonpharmacologic interventions such as mindfulness-based cognitive therapy (MBCT) in an effort to mitigate risk for depressive relapse in pregnant women who are well with histories of depression. To date, data do not inform the question as to whether MBCT can be used to mitigate risk of depressive relapse in pregnant women who continue or discontinue antidepressants. That research question is actively being studied by several investigators, including ourselves.
Of particular interest is whether the addition of mindfulness practices such as MBCT in treatment could mitigate risk for depressive relapse in pregnant women who continue or discontinue antidepressant treatment, as that would certainly be a no-harm intervention that could mitigate risk even in a lower risk sample of patients. The question of how to “thread the needle” during the pandemic and best approach woman with a history of recurrent major depression on antidepressants is particularly timely and critical.
Regardless, we make clinical decisions collaboratively with patients based on their histories and individual wishes, and perhaps what we have learned over the last 5 months is the use of telemedicine does afford us the opportunity, regardless of the decisions that patients make, to more closely follow the clinical trajectory of women during pregnancy and the postpartum period so that regardless of treatment, we have an opportunity to intervene early when needed and to ascertain changes in clinical status early to mitigate the risk of frank relapse. From a reproductive psychiatric point of view, that is a silver lining with respect to the associated challenges that have come along with the pandemic.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at obnews@mdedge.com.
References
1. J Clin Psychiatry 2020;81(4):19r13134.
2. JAMA. 2006 Feb 1;295(5):499-507.
In a previous column, I addressed some of the issues that quickly arose in the context of the COVID-19 pandemic and their implications for reproductive psychiatry. These issues ranged from the importance of sustaining well-being in pregnant and postpartum women during the pandemic, to temporary restrictions that were in place during the early part of the pandemic with respect to performing infertility procedures, to the practical issues of limiting the number of people who could attend to women during labor and delivery in the hospital.
Five months later, we’ve learned a great deal about trying to sustain emotional well-being among pregnant women during COVID-19. There is a high rate of anxiety among women who are pregnant and women who have particularly young children around the various issues of juggling activities of daily living during the pandemic, including switching to remote work and homeschooling children. There is fear of contracting COVID-19 during pregnancy, the exact effects of which are still somewhat unknown. We have seen a shift to telemedicine for prenatal and postpartum obstetrics visits, and a change with respect to visitors and even in-home nurses that would help during the first weeks of life for some couples.
We wondered whether we would see a falloff in the numbers of women presenting to our clinic with questions about the reproductive safety of taking psychiatric medications during pregnancy. We were unclear as to whether women would defer plans to get pregnant given some of the uncertainties that have come with COVID-19. What we’ve seen, at least early on in the pandemic in Massachusetts, has been the opposite. More women during the first 4 months of the pandemic have been seen in our center compared with the same corresponding period over the last 5 years. The precise reasons for this are unclear, but one reason may be that shifting the practice of reproductive psychiatry and pregnancy planning for reproductive-age women to full virtual care has dropped the number of missed appointments to essentially zero. Women perhaps feel an urgency to have a plan for using psychiatric medication during pregnancy. They may also see the benefit of being able to have extended telemedicine consultations that frequently involve their partners, a practice we have always supported, but posed logistical challenges for some.
As our colleagues learned that we had shifted our clinical rounds at the Center for Women’s Mental Health, which we’ve been doing for 25 years, to a virtual format, we began offering a free 1-hour forum to discuss relevant issues around caring for psychiatrically ill women, with a focus on some of the issues that were particularly relevant during the pandemic. The most common reasons for consultation on our service are the appropriate, safest use of antidepressants and mood stabilizers during pregnancy, and that continues to be the case.
If there has been one guiding principle in treating perinatal depression during pregnancy, it has been our long-standing, laser-like focus on keeping women emotionally well during pregnancy, and to highlight the importance of this with women during consultations prior to and during pregnancy. Relapse of psychiatric disorder during pregnancy is one the strongest predictors of postpartum depression, and the impact of untreated depression during pregnancy has been described in the literature and over the years in this column. However, where we want to minimize, if possible, severe onset of illness requiring hospitalization or emergent attention considering it may make social distancing and some of the other mitigating factors vis-à-vis COVID-19 more challenging.
Despite the accumulated data over the last 2 decades on the reproductive safety of antidepressants, women continue to have questions about the safety of these medications during pregnancy. Studies show now that many women would prefer, if at all possible, to defer treatment with antidepressants, and so they come to us with questions about their reproductive safety, the potential of switching to nonpharmacologic interventions, and the use of alternative interventions that might be used to treat their underlying mood disorder.
Investigators at the University of British Columbia recently have tried to inform the field with still another look, not at reproductive safety per se, but at risk of relapse of depression if women discontinue those medicines during pregnancy.1 There is a timeliness to this investigation, which was a systematic review and meta-analysis of studies that met a priori criteria for inclusion. Since some of our own group’s early work over 15 years ago on relapse of psychiatric disorder during pregnancy,2 which indicated a substantial difference in risk of relapse between women who continued versus who discontinued antidepressants, other investigators have showed the difference in risk for relapse is not as substantial, and that continuation of medication did not appear to mitigate risk for relapse. In fact, in the systematic review, the investigators demonstrated that as a group, maintaining medicine did not appear to confer particular benefit to patients relative to risk for relapse compared to discontinuation of antidepressants.
However, looking more closely, Bayrampour and colleagues note for women with histories of more severe recurrent, major depression, relapse did in fact appear to be greater in women who discontinued compared with those with cases of mild to moderate depression. It is noteworthy that in both our early and later work, and certainly dovetailing with our clinical practice, we have noted severity of illness does not appear to correlate with the actual decisions women ultimately make regarding what they will do with antidepressants. Specifically, some women with very severe illness histories will discontinue antidepressants regardless of their risk for relapse. Alternatively, women with mild to moderate illness will sometimes elect to stay on antidepressant therapy. With all the information that we have about fetal exposure to antidepressants on one hand, the “unknown unknowns” are an understandable concern to both patients and clinicians. Clinicians are faced with the dilemma of how to best counsel women on continuing or discontinuing antidepressants as they plan to conceive or during pregnancy and in the postpartum period.
The literature cited and clinical experience over the last 3 decades suggests rather strongly that there is a relatively low likelihood women with histories of severe recurrent disease will be able to successfully discontinue antidepressants in the absence of relapse. A greater question is, what is the best way to proceed for women who have been on maintenance therapy and had more moderate symptoms?
I am inspired by some of the more recent literature that has tried to elucidate the role of nonpharmacologic interventions such as mindfulness-based cognitive therapy (MBCT) in an effort to mitigate risk for depressive relapse in pregnant women who are well with histories of depression. To date, data do not inform the question as to whether MBCT can be used to mitigate risk of depressive relapse in pregnant women who continue or discontinue antidepressants. That research question is actively being studied by several investigators, including ourselves.
Of particular interest is whether the addition of mindfulness practices such as MBCT in treatment could mitigate risk for depressive relapse in pregnant women who continue or discontinue antidepressant treatment, as that would certainly be a no-harm intervention that could mitigate risk even in a lower risk sample of patients. The question of how to “thread the needle” during the pandemic and best approach woman with a history of recurrent major depression on antidepressants is particularly timely and critical.
Regardless, we make clinical decisions collaboratively with patients based on their histories and individual wishes, and perhaps what we have learned over the last 5 months is the use of telemedicine does afford us the opportunity, regardless of the decisions that patients make, to more closely follow the clinical trajectory of women during pregnancy and the postpartum period so that regardless of treatment, we have an opportunity to intervene early when needed and to ascertain changes in clinical status early to mitigate the risk of frank relapse. From a reproductive psychiatric point of view, that is a silver lining with respect to the associated challenges that have come along with the pandemic.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at obnews@mdedge.com.
References
1. J Clin Psychiatry 2020;81(4):19r13134.
2. JAMA. 2006 Feb 1;295(5):499-507.
When to screen for pancreas cancer
AGA has released a new Clinical Practice Update providing best practice advice for clinicians screening and diagnosing pancreatic cancer in high-risk individuals. Screening to detect pancreas cancers and their precursor lesions in high-risk patients can improve survival if it facilitates surgical resection for early-stage disease.
In the AGA Clinical Practice Update on Pancreas Cancer Screening in High-Risk Individuals: Expert Review, published in Gastroenterology’s July issue, the authors provide 13 best practice advice statements to address key issues in clinical management of these patients.
For more information, visit www.gastro.org/PancreasCPU.
AGA has released a new Clinical Practice Update providing best practice advice for clinicians screening and diagnosing pancreatic cancer in high-risk individuals. Screening to detect pancreas cancers and their precursor lesions in high-risk patients can improve survival if it facilitates surgical resection for early-stage disease.
In the AGA Clinical Practice Update on Pancreas Cancer Screening in High-Risk Individuals: Expert Review, published in Gastroenterology’s July issue, the authors provide 13 best practice advice statements to address key issues in clinical management of these patients.
For more information, visit www.gastro.org/PancreasCPU.
AGA has released a new Clinical Practice Update providing best practice advice for clinicians screening and diagnosing pancreatic cancer in high-risk individuals. Screening to detect pancreas cancers and their precursor lesions in high-risk patients can improve survival if it facilitates surgical resection for early-stage disease.
In the AGA Clinical Practice Update on Pancreas Cancer Screening in High-Risk Individuals: Expert Review, published in Gastroenterology’s July issue, the authors provide 13 best practice advice statements to address key issues in clinical management of these patients.
For more information, visit www.gastro.org/PancreasCPU.









