User login
Higher death rate seen in cancer patients with nosocomial COVID-19
, according to researchers.
In an observational study of patients with COVID-19 and cancer, 19% of patients had COVID-19 acquired during a non-COVID-related hospital stay, and 81% had community-acquired COVID-19.
At a median follow-up of 23 days, the overall mortality rate was 28%. However, the all-cause mortality rate in patients with nosocomial COVID-19 was more than double that of patients with community-acquired COVID-19, at 47% and 23%, respectively.
Arielle Elkrief, MD, of the University of Montreal, reported these results during the AACR virtual meeting: COVID-19 and Cancer.
“This is the first report that describes a high rate of hospital-acquired COVID-19 in patients with cancer, at a rate of 19%,” Dr. Elkrief said. “This was associated with high mortality in both univariate and multivariate analyses.”
The study included 250 adults and 3 children with COVID-19 and cancer who were identified between March 3 and May 23, 2020. They ranged in age from 4 to 95 years, but the median age was 73 years.
All patients had either laboratory-confirmed (95%) or presumed COVID-19 (5%) and invasive cancer. The most common cancer types were similar to those seen in the general population. Lung and breast cancer were the most common, followed by lymphoma, prostate cancer, and colorectal cancer. Most patients were on active anticancer therapy, most often chemotherapy.
Most patients (n = 236) were residents of Quebec, but 17 patients were residents of British Columbia.
“It is important to note that Quebec was one of the most heavily affected areas in North America at the time of the study,” Dr. Elkrief said.
Outcomes by group
There were 206 patients (81%) who had community-acquired COVID-19 and 47 (19%) who had nosocomial COVID-19. The two groups were similar with respect to sex, performance status, and cancer stage. A small trend toward more patients on active therapy was seen in the nosocomial group, but the difference did not reach statistical significance.
The median overall survival was 27 days in the nosocomial group and 71 days in the community-acquired group (hazard ratio, 2.2; P = .002).
A multivariate analysis showed that nosocomial infection was “strongly and independently associated with death,” Dr. Elkrief said. “Other risk factors for poor prognosis included age, poor [performance] status, and advanced stage of cancer.”
There were no significant differences between the hospital-acquired and community-acquired groups for other outcomes, including oxygen requirements (43% and 47%, respectively), ICU admission (13% and 11%), need for mechanical ventilation (6% and 5%), or length of stay (median, 9.5 days and 8.5 days).
The low rate of ICU admission, considering the mortality rate of 28%, “could reflect that patients with cancer are less likely to be admitted to the ICU,” Dr. Elkrief noted.
Applying the findings to practice
The findings reinforce the importance of adherence to stringent infection control guidelines to protect vulnerable patients, such as those with cancer, Dr. Elkrief said.
In ambulatory settings, this means decreasing in-person visits through increased use of teleconsultations, and for those who need to be seen in person, screening for symptoms or use of polymerase chain reaction testing should be used when resources are available, she said.
“Similar principles apply to chemotherapy treatment units,” Dr. Elkrief said. She added that staff must avoid cross-contamination between COVID and COVID-free zones, and that “dedicated personnel and equipment should be maintained and separate between these two zones.
“Adequate protective personal equipment and strict hand hygiene protocols are also of utmost importance,” Dr. Elkrief said. “The threat of COVID-19 is not behind us, and so we continue to enforce these strategies to protect our patients.”
Session moderator Gypsyamber D’Souza, PhD, an infectious disease epidemiologist at Johns Hopkins University in Baltimore, raised the question of whether the high nosocomial infection and death rate in this study was related to patients having more severe disease because of underlying comorbidities.
Dr. Elkrief explained that the overall mortality rate was indeed higher than the 13% reported in other studies, and it may reflect an overrepresentation of hospitalized or more severely ill patients in the cohort.
However, the investigators made every effort to include all patients with both cancer and COVID-19 by using systematic screening of inpatient and outpatients lists and registries.
Further, the multivariate analysis included both inpatients and outpatients and adjusted for known negative prognostic factors for COVID-19 outcomes. These included increasing age, poor performance status, and different comorbidities.
The finding that nosocomial infection was an independent predictor of death “pushed us to look at nosocomial infection as a new independent risk factor,” Dr. Elkrief said.
Dr. Elkrief reported grant support from AstraZeneca. Dr. D’Souza did not report any disclosures.
SOURCE: Elkrief A et al. AACR: COVID and Cancer, Abstract S12-01.
, according to researchers.
In an observational study of patients with COVID-19 and cancer, 19% of patients had COVID-19 acquired during a non-COVID-related hospital stay, and 81% had community-acquired COVID-19.
At a median follow-up of 23 days, the overall mortality rate was 28%. However, the all-cause mortality rate in patients with nosocomial COVID-19 was more than double that of patients with community-acquired COVID-19, at 47% and 23%, respectively.
Arielle Elkrief, MD, of the University of Montreal, reported these results during the AACR virtual meeting: COVID-19 and Cancer.
“This is the first report that describes a high rate of hospital-acquired COVID-19 in patients with cancer, at a rate of 19%,” Dr. Elkrief said. “This was associated with high mortality in both univariate and multivariate analyses.”
The study included 250 adults and 3 children with COVID-19 and cancer who were identified between March 3 and May 23, 2020. They ranged in age from 4 to 95 years, but the median age was 73 years.
All patients had either laboratory-confirmed (95%) or presumed COVID-19 (5%) and invasive cancer. The most common cancer types were similar to those seen in the general population. Lung and breast cancer were the most common, followed by lymphoma, prostate cancer, and colorectal cancer. Most patients were on active anticancer therapy, most often chemotherapy.
Most patients (n = 236) were residents of Quebec, but 17 patients were residents of British Columbia.
“It is important to note that Quebec was one of the most heavily affected areas in North America at the time of the study,” Dr. Elkrief said.
Outcomes by group
There were 206 patients (81%) who had community-acquired COVID-19 and 47 (19%) who had nosocomial COVID-19. The two groups were similar with respect to sex, performance status, and cancer stage. A small trend toward more patients on active therapy was seen in the nosocomial group, but the difference did not reach statistical significance.
The median overall survival was 27 days in the nosocomial group and 71 days in the community-acquired group (hazard ratio, 2.2; P = .002).
A multivariate analysis showed that nosocomial infection was “strongly and independently associated with death,” Dr. Elkrief said. “Other risk factors for poor prognosis included age, poor [performance] status, and advanced stage of cancer.”
There were no significant differences between the hospital-acquired and community-acquired groups for other outcomes, including oxygen requirements (43% and 47%, respectively), ICU admission (13% and 11%), need for mechanical ventilation (6% and 5%), or length of stay (median, 9.5 days and 8.5 days).
The low rate of ICU admission, considering the mortality rate of 28%, “could reflect that patients with cancer are less likely to be admitted to the ICU,” Dr. Elkrief noted.
Applying the findings to practice
The findings reinforce the importance of adherence to stringent infection control guidelines to protect vulnerable patients, such as those with cancer, Dr. Elkrief said.
In ambulatory settings, this means decreasing in-person visits through increased use of teleconsultations, and for those who need to be seen in person, screening for symptoms or use of polymerase chain reaction testing should be used when resources are available, she said.
“Similar principles apply to chemotherapy treatment units,” Dr. Elkrief said. She added that staff must avoid cross-contamination between COVID and COVID-free zones, and that “dedicated personnel and equipment should be maintained and separate between these two zones.
“Adequate protective personal equipment and strict hand hygiene protocols are also of utmost importance,” Dr. Elkrief said. “The threat of COVID-19 is not behind us, and so we continue to enforce these strategies to protect our patients.”
Session moderator Gypsyamber D’Souza, PhD, an infectious disease epidemiologist at Johns Hopkins University in Baltimore, raised the question of whether the high nosocomial infection and death rate in this study was related to patients having more severe disease because of underlying comorbidities.
Dr. Elkrief explained that the overall mortality rate was indeed higher than the 13% reported in other studies, and it may reflect an overrepresentation of hospitalized or more severely ill patients in the cohort.
However, the investigators made every effort to include all patients with both cancer and COVID-19 by using systematic screening of inpatient and outpatients lists and registries.
Further, the multivariate analysis included both inpatients and outpatients and adjusted for known negative prognostic factors for COVID-19 outcomes. These included increasing age, poor performance status, and different comorbidities.
The finding that nosocomial infection was an independent predictor of death “pushed us to look at nosocomial infection as a new independent risk factor,” Dr. Elkrief said.
Dr. Elkrief reported grant support from AstraZeneca. Dr. D’Souza did not report any disclosures.
SOURCE: Elkrief A et al. AACR: COVID and Cancer, Abstract S12-01.
, according to researchers.
In an observational study of patients with COVID-19 and cancer, 19% of patients had COVID-19 acquired during a non-COVID-related hospital stay, and 81% had community-acquired COVID-19.
At a median follow-up of 23 days, the overall mortality rate was 28%. However, the all-cause mortality rate in patients with nosocomial COVID-19 was more than double that of patients with community-acquired COVID-19, at 47% and 23%, respectively.
Arielle Elkrief, MD, of the University of Montreal, reported these results during the AACR virtual meeting: COVID-19 and Cancer.
“This is the first report that describes a high rate of hospital-acquired COVID-19 in patients with cancer, at a rate of 19%,” Dr. Elkrief said. “This was associated with high mortality in both univariate and multivariate analyses.”
The study included 250 adults and 3 children with COVID-19 and cancer who were identified between March 3 and May 23, 2020. They ranged in age from 4 to 95 years, but the median age was 73 years.
All patients had either laboratory-confirmed (95%) or presumed COVID-19 (5%) and invasive cancer. The most common cancer types were similar to those seen in the general population. Lung and breast cancer were the most common, followed by lymphoma, prostate cancer, and colorectal cancer. Most patients were on active anticancer therapy, most often chemotherapy.
Most patients (n = 236) were residents of Quebec, but 17 patients were residents of British Columbia.
“It is important to note that Quebec was one of the most heavily affected areas in North America at the time of the study,” Dr. Elkrief said.
Outcomes by group
There were 206 patients (81%) who had community-acquired COVID-19 and 47 (19%) who had nosocomial COVID-19. The two groups were similar with respect to sex, performance status, and cancer stage. A small trend toward more patients on active therapy was seen in the nosocomial group, but the difference did not reach statistical significance.
The median overall survival was 27 days in the nosocomial group and 71 days in the community-acquired group (hazard ratio, 2.2; P = .002).
A multivariate analysis showed that nosocomial infection was “strongly and independently associated with death,” Dr. Elkrief said. “Other risk factors for poor prognosis included age, poor [performance] status, and advanced stage of cancer.”
There were no significant differences between the hospital-acquired and community-acquired groups for other outcomes, including oxygen requirements (43% and 47%, respectively), ICU admission (13% and 11%), need for mechanical ventilation (6% and 5%), or length of stay (median, 9.5 days and 8.5 days).
The low rate of ICU admission, considering the mortality rate of 28%, “could reflect that patients with cancer are less likely to be admitted to the ICU,” Dr. Elkrief noted.
Applying the findings to practice
The findings reinforce the importance of adherence to stringent infection control guidelines to protect vulnerable patients, such as those with cancer, Dr. Elkrief said.
In ambulatory settings, this means decreasing in-person visits through increased use of teleconsultations, and for those who need to be seen in person, screening for symptoms or use of polymerase chain reaction testing should be used when resources are available, she said.
“Similar principles apply to chemotherapy treatment units,” Dr. Elkrief said. She added that staff must avoid cross-contamination between COVID and COVID-free zones, and that “dedicated personnel and equipment should be maintained and separate between these two zones.
“Adequate protective personal equipment and strict hand hygiene protocols are also of utmost importance,” Dr. Elkrief said. “The threat of COVID-19 is not behind us, and so we continue to enforce these strategies to protect our patients.”
Session moderator Gypsyamber D’Souza, PhD, an infectious disease epidemiologist at Johns Hopkins University in Baltimore, raised the question of whether the high nosocomial infection and death rate in this study was related to patients having more severe disease because of underlying comorbidities.
Dr. Elkrief explained that the overall mortality rate was indeed higher than the 13% reported in other studies, and it may reflect an overrepresentation of hospitalized or more severely ill patients in the cohort.
However, the investigators made every effort to include all patients with both cancer and COVID-19 by using systematic screening of inpatient and outpatients lists and registries.
Further, the multivariate analysis included both inpatients and outpatients and adjusted for known negative prognostic factors for COVID-19 outcomes. These included increasing age, poor performance status, and different comorbidities.
The finding that nosocomial infection was an independent predictor of death “pushed us to look at nosocomial infection as a new independent risk factor,” Dr. Elkrief said.
Dr. Elkrief reported grant support from AstraZeneca. Dr. D’Souza did not report any disclosures.
SOURCE: Elkrief A et al. AACR: COVID and Cancer, Abstract S12-01.
FROM AACR: COVID-19 AND CANCER
Low vitamin D linked to increased COVID-19 risk
Low plasma vitamin D levels emerged as an independent risk factor for COVID-19 infection and hospitalization in a large, population-based study.
Participants positive for COVID-19 were 50% more likely to have low vs normal 25(OH)D levels in a multivariate analysis that controlled for other confounders, for example.
The take home message for physicians is to “test patients’ vitamin D levels and keep them optimal for the overall health – as well as for a better immunoresponse to COVID-19,” senior author Milana Frenkel-Morgenstern, PhD, head of the Cancer Genomics and BioComputing of Complex Diseases Lab at Bar-Ilan University in Ramat Gan, Israel, said in an interview.
The study was published online July 23 in The FEBS Journal.
Previous and ongoing studies are evaluating a potential role for vitamin D to prevent or minimize the severity of SARS-CoV-2 infection, building on years of research addressing vitamin D for other viral respiratory infections. The evidence to date regarding COVID-19, primarily observational studies, has yielded mixed results.
Multiple experts weighed in on the controversy in a previous report. Many point out the limitations of observational data, particularly when it comes to ruling out other factors that could affect the severity of COVID-19 infection. In addition, in a video report, JoAnn E. Manson, MD, DrPH, of Harvard Medical School in Boston, cited an observational study from three South Asian hospitals that found more severe COVID-19 patients had lower vitamin D levels, as well as other “compelling evidence” suggesting an association.
Dr. Frenkel-Morgenstern and colleagues studied data for 7,807 people, of whom 10.1% were COVID-19 positive. They assessed electronic health records for demographics, potential confounders, and outcomes between February 1 and April 30.
Participants positive for COVID-19 tended to be younger and were more likely to be men and live in a lower socioeconomic area, compared with the participants who were negative for COVID-19, in a univariate analysis.
Key findings
A higher proportion of COVID-19–positive patients had low plasma 25(OH)D concentrations, about 90% versus 85% of participants who were negative for COVID-19. The difference was statistically significant (P < .001). Furthermore, the increased likelihood for low vitamin D levels among those positive for COVID-19 held in a multivariate analysis that controlled for demographics and psychiatric and somatic disorders (adjusted odds ratio, 1.50). The difference remained statistically significant (P < .001).
The study also was noteworthy for what it did not find among participants with COVID-19. For example, the prevalence of dementia, cardiovascular disease, chronic lung disorders, and hypertension were significantly higher among the COVID-19 negative participants.
“Severe social contacts restrictions that were imposed on all the population and were even more emphasized in this highly vulnerable population” could explain these findings, the researchers noted.
“We assume that following the Israeli Ministry of Health instructions, patients with chronic medical conditions significantly reduced their social contacts” and thereby reduced their infection risk.
In contrast to previous reports, obesity was not a significant factor associated with increased likelihood for COVID-19 infection or hospitalization in the current study.
The researchers also linked low plasma 25(OH)D level to an increased likelihood of hospitalization for COVID-19 infection (crude OR, 2.09; P < .05).
After controlling for demographics and chronic disorders, the aOR decreased to 1.95 (P = .061) in a multivariate analysis. The only factor that remained statistically significant for hospitalization was age over 50 years (aOR, 2.71; P < .001).
Implications and future plans
The large number of participants and the “real world,” population-based design are strengths of the study. Considering potential confounders is another strength, the researchers noted. The retrospective database design was a limitation.
Going forward, Dr. Frenkel-Morgenstern and colleagues will “try to decipher the potential role of vitamin D in prevention and/or treatment of COVID-19” through three additional studies, she said. Also, they would like to conduct a meta-analysis to combine data from different countries to further explore the potential role of vitamin D in COVID-19.
“A compelling case”
“This is a strong study – large, adjusted for confounders, consistent with the biology and other clinical studies of vitamin D, infections, and COVID-19,” Wayne Jonas, MD, a practicing family physician and executive director of Samueli Integrative Health Programs, said in an interview.
Because the research was retrospective and observational, a causative link between vitamin D levels and COVID-19 risk cannot be interpreted from the findings. “That would need a prospective, randomized study,” said Dr. Jonas, who was not involved with the current study.
However, “the study makes a compelling case for possibly screening vitamin D levels for judging risk of COVID infection and hospitalization,” Dr. Jonas said, “and the compelling need for a large, randomized vitamin D supplement study to see if it can help prevent infection.”
“Given that vitamin D is largely safe, such a study could be done quickly and on healthy people with minimal risk for harm,” he added.
More confounders likely?
“I think the study is of interest,” Naveed Sattar, PhD, professor of metabolic medicine at the University of Glasgow, who also was not affiliated with the research, said in an interview.
“Whilst the authors adjusted for some confounders, there is a strong potential for residual confounding,” said Dr. Sattar, a coauthor of a UK Biobank study that did not find an association between vitamin D stages and COVID-19 infection in multivariate models.
For example, Dr. Sattar said, “Robust adjustment for social class is important since both Vitamin D levels and COVID-19 severity are both strongly associated with social class.” Further, it remains unknown when and what time of year the vitamin D concentrations were measured in the current study.
“In the end, only a robust randomized trial can tell us whether vitamin D supplementation helps lessen COVID-19 severity,” Dr. Sattar added. “I am not hopeful we will find this is the case – but I am glad some such trials are [ongoing].”
Dr. Frenkel-Morgenstern received a COVID-19 Data Sciences Institute grant to support this work. Dr. Frenkel-Morgenstern, Dr. Jonas, and Dr. Sattar have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Low plasma vitamin D levels emerged as an independent risk factor for COVID-19 infection and hospitalization in a large, population-based study.
Participants positive for COVID-19 were 50% more likely to have low vs normal 25(OH)D levels in a multivariate analysis that controlled for other confounders, for example.
The take home message for physicians is to “test patients’ vitamin D levels and keep them optimal for the overall health – as well as for a better immunoresponse to COVID-19,” senior author Milana Frenkel-Morgenstern, PhD, head of the Cancer Genomics and BioComputing of Complex Diseases Lab at Bar-Ilan University in Ramat Gan, Israel, said in an interview.
The study was published online July 23 in The FEBS Journal.
Previous and ongoing studies are evaluating a potential role for vitamin D to prevent or minimize the severity of SARS-CoV-2 infection, building on years of research addressing vitamin D for other viral respiratory infections. The evidence to date regarding COVID-19, primarily observational studies, has yielded mixed results.
Multiple experts weighed in on the controversy in a previous report. Many point out the limitations of observational data, particularly when it comes to ruling out other factors that could affect the severity of COVID-19 infection. In addition, in a video report, JoAnn E. Manson, MD, DrPH, of Harvard Medical School in Boston, cited an observational study from three South Asian hospitals that found more severe COVID-19 patients had lower vitamin D levels, as well as other “compelling evidence” suggesting an association.
Dr. Frenkel-Morgenstern and colleagues studied data for 7,807 people, of whom 10.1% were COVID-19 positive. They assessed electronic health records for demographics, potential confounders, and outcomes between February 1 and April 30.
Participants positive for COVID-19 tended to be younger and were more likely to be men and live in a lower socioeconomic area, compared with the participants who were negative for COVID-19, in a univariate analysis.
Key findings
A higher proportion of COVID-19–positive patients had low plasma 25(OH)D concentrations, about 90% versus 85% of participants who were negative for COVID-19. The difference was statistically significant (P < .001). Furthermore, the increased likelihood for low vitamin D levels among those positive for COVID-19 held in a multivariate analysis that controlled for demographics and psychiatric and somatic disorders (adjusted odds ratio, 1.50). The difference remained statistically significant (P < .001).
The study also was noteworthy for what it did not find among participants with COVID-19. For example, the prevalence of dementia, cardiovascular disease, chronic lung disorders, and hypertension were significantly higher among the COVID-19 negative participants.
“Severe social contacts restrictions that were imposed on all the population and were even more emphasized in this highly vulnerable population” could explain these findings, the researchers noted.
“We assume that following the Israeli Ministry of Health instructions, patients with chronic medical conditions significantly reduced their social contacts” and thereby reduced their infection risk.
In contrast to previous reports, obesity was not a significant factor associated with increased likelihood for COVID-19 infection or hospitalization in the current study.
The researchers also linked low plasma 25(OH)D level to an increased likelihood of hospitalization for COVID-19 infection (crude OR, 2.09; P < .05).
After controlling for demographics and chronic disorders, the aOR decreased to 1.95 (P = .061) in a multivariate analysis. The only factor that remained statistically significant for hospitalization was age over 50 years (aOR, 2.71; P < .001).
Implications and future plans
The large number of participants and the “real world,” population-based design are strengths of the study. Considering potential confounders is another strength, the researchers noted. The retrospective database design was a limitation.
Going forward, Dr. Frenkel-Morgenstern and colleagues will “try to decipher the potential role of vitamin D in prevention and/or treatment of COVID-19” through three additional studies, she said. Also, they would like to conduct a meta-analysis to combine data from different countries to further explore the potential role of vitamin D in COVID-19.
“A compelling case”
“This is a strong study – large, adjusted for confounders, consistent with the biology and other clinical studies of vitamin D, infections, and COVID-19,” Wayne Jonas, MD, a practicing family physician and executive director of Samueli Integrative Health Programs, said in an interview.
Because the research was retrospective and observational, a causative link between vitamin D levels and COVID-19 risk cannot be interpreted from the findings. “That would need a prospective, randomized study,” said Dr. Jonas, who was not involved with the current study.
However, “the study makes a compelling case for possibly screening vitamin D levels for judging risk of COVID infection and hospitalization,” Dr. Jonas said, “and the compelling need for a large, randomized vitamin D supplement study to see if it can help prevent infection.”
“Given that vitamin D is largely safe, such a study could be done quickly and on healthy people with minimal risk for harm,” he added.
More confounders likely?
“I think the study is of interest,” Naveed Sattar, PhD, professor of metabolic medicine at the University of Glasgow, who also was not affiliated with the research, said in an interview.
“Whilst the authors adjusted for some confounders, there is a strong potential for residual confounding,” said Dr. Sattar, a coauthor of a UK Biobank study that did not find an association between vitamin D stages and COVID-19 infection in multivariate models.
For example, Dr. Sattar said, “Robust adjustment for social class is important since both Vitamin D levels and COVID-19 severity are both strongly associated with social class.” Further, it remains unknown when and what time of year the vitamin D concentrations were measured in the current study.
“In the end, only a robust randomized trial can tell us whether vitamin D supplementation helps lessen COVID-19 severity,” Dr. Sattar added. “I am not hopeful we will find this is the case – but I am glad some such trials are [ongoing].”
Dr. Frenkel-Morgenstern received a COVID-19 Data Sciences Institute grant to support this work. Dr. Frenkel-Morgenstern, Dr. Jonas, and Dr. Sattar have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Low plasma vitamin D levels emerged as an independent risk factor for COVID-19 infection and hospitalization in a large, population-based study.
Participants positive for COVID-19 were 50% more likely to have low vs normal 25(OH)D levels in a multivariate analysis that controlled for other confounders, for example.
The take home message for physicians is to “test patients’ vitamin D levels and keep them optimal for the overall health – as well as for a better immunoresponse to COVID-19,” senior author Milana Frenkel-Morgenstern, PhD, head of the Cancer Genomics and BioComputing of Complex Diseases Lab at Bar-Ilan University in Ramat Gan, Israel, said in an interview.
The study was published online July 23 in The FEBS Journal.
Previous and ongoing studies are evaluating a potential role for vitamin D to prevent or minimize the severity of SARS-CoV-2 infection, building on years of research addressing vitamin D for other viral respiratory infections. The evidence to date regarding COVID-19, primarily observational studies, has yielded mixed results.
Multiple experts weighed in on the controversy in a previous report. Many point out the limitations of observational data, particularly when it comes to ruling out other factors that could affect the severity of COVID-19 infection. In addition, in a video report, JoAnn E. Manson, MD, DrPH, of Harvard Medical School in Boston, cited an observational study from three South Asian hospitals that found more severe COVID-19 patients had lower vitamin D levels, as well as other “compelling evidence” suggesting an association.
Dr. Frenkel-Morgenstern and colleagues studied data for 7,807 people, of whom 10.1% were COVID-19 positive. They assessed electronic health records for demographics, potential confounders, and outcomes between February 1 and April 30.
Participants positive for COVID-19 tended to be younger and were more likely to be men and live in a lower socioeconomic area, compared with the participants who were negative for COVID-19, in a univariate analysis.
Key findings
A higher proportion of COVID-19–positive patients had low plasma 25(OH)D concentrations, about 90% versus 85% of participants who were negative for COVID-19. The difference was statistically significant (P < .001). Furthermore, the increased likelihood for low vitamin D levels among those positive for COVID-19 held in a multivariate analysis that controlled for demographics and psychiatric and somatic disorders (adjusted odds ratio, 1.50). The difference remained statistically significant (P < .001).
The study also was noteworthy for what it did not find among participants with COVID-19. For example, the prevalence of dementia, cardiovascular disease, chronic lung disorders, and hypertension were significantly higher among the COVID-19 negative participants.
“Severe social contacts restrictions that were imposed on all the population and were even more emphasized in this highly vulnerable population” could explain these findings, the researchers noted.
“We assume that following the Israeli Ministry of Health instructions, patients with chronic medical conditions significantly reduced their social contacts” and thereby reduced their infection risk.
In contrast to previous reports, obesity was not a significant factor associated with increased likelihood for COVID-19 infection or hospitalization in the current study.
The researchers also linked low plasma 25(OH)D level to an increased likelihood of hospitalization for COVID-19 infection (crude OR, 2.09; P < .05).
After controlling for demographics and chronic disorders, the aOR decreased to 1.95 (P = .061) in a multivariate analysis. The only factor that remained statistically significant for hospitalization was age over 50 years (aOR, 2.71; P < .001).
Implications and future plans
The large number of participants and the “real world,” population-based design are strengths of the study. Considering potential confounders is another strength, the researchers noted. The retrospective database design was a limitation.
Going forward, Dr. Frenkel-Morgenstern and colleagues will “try to decipher the potential role of vitamin D in prevention and/or treatment of COVID-19” through three additional studies, she said. Also, they would like to conduct a meta-analysis to combine data from different countries to further explore the potential role of vitamin D in COVID-19.
“A compelling case”
“This is a strong study – large, adjusted for confounders, consistent with the biology and other clinical studies of vitamin D, infections, and COVID-19,” Wayne Jonas, MD, a practicing family physician and executive director of Samueli Integrative Health Programs, said in an interview.
Because the research was retrospective and observational, a causative link between vitamin D levels and COVID-19 risk cannot be interpreted from the findings. “That would need a prospective, randomized study,” said Dr. Jonas, who was not involved with the current study.
However, “the study makes a compelling case for possibly screening vitamin D levels for judging risk of COVID infection and hospitalization,” Dr. Jonas said, “and the compelling need for a large, randomized vitamin D supplement study to see if it can help prevent infection.”
“Given that vitamin D is largely safe, such a study could be done quickly and on healthy people with minimal risk for harm,” he added.
More confounders likely?
“I think the study is of interest,” Naveed Sattar, PhD, professor of metabolic medicine at the University of Glasgow, who also was not affiliated with the research, said in an interview.
“Whilst the authors adjusted for some confounders, there is a strong potential for residual confounding,” said Dr. Sattar, a coauthor of a UK Biobank study that did not find an association between vitamin D stages and COVID-19 infection in multivariate models.
For example, Dr. Sattar said, “Robust adjustment for social class is important since both Vitamin D levels and COVID-19 severity are both strongly associated with social class.” Further, it remains unknown when and what time of year the vitamin D concentrations were measured in the current study.
“In the end, only a robust randomized trial can tell us whether vitamin D supplementation helps lessen COVID-19 severity,” Dr. Sattar added. “I am not hopeful we will find this is the case – but I am glad some such trials are [ongoing].”
Dr. Frenkel-Morgenstern received a COVID-19 Data Sciences Institute grant to support this work. Dr. Frenkel-Morgenstern, Dr. Jonas, and Dr. Sattar have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Got a short attention span?
Have you every wondered whether you have an attention deficit disorder? I have and I suspect that there are plenty of folks who share my curiosity. Realistically I’m pretty sure I don’t have ADD because while I enjoy being physically active my folks never described me as “bouncing off the walls.” Although I think I am very aware of my surroundings and observant, I wouldn’t say I am unusually distractible. I can multitask reasonably well and have been reasonably successful academically and professionally. But the one characteristic I do share with most ADD patients is a short attention span.
Short, of course, is a relative term. Any academic class longer than 45 minutes pushes me past my limit. The same goes for movies and television documentaries. Reading always has been a challenge for me, and 20 minutes is about as long as I can sit with a book or magazine article – even if it’s about a topic that interests me.
Even when I am painting or wood carving, I need to put down my brushes and knives after 20 minutes and do something else. I am a one-set tennis player and about a seven-hole golfer. I have the physical stamina to go much longer, but by the second set or the 10th hole I would prefer to be moving on to some other activity.
In college, I quickly learned that all-nighters were counterproductive. My usual study pattern evolved into one in which I would spend about 20 minutes on one course, take a trip to the refrigerator and return to studying on another course for 20 minutes, then take a break outside to shoot some hoops and return to work for 20 minutes on a third course. This pattern of relatively short bouts of work punctuated by brief snack or exercise breaks seemed to be my most efficient, productive, and mental health–sparing strategy.
Just last week, I learned that there is a name associated with my system. It’s called the Pomodoro technique and was “invented” by a student in an Italian business school in the 1980s (“This Time-Management Trick Changed My Whole Relationship With Time,”By Dean Kissick, The New York Times, June 23, 2020). At its core is a rigid pattern of 25 minutes of work punctuated by 5-minute breaks. The name comes from the tomato-shaped kitchen timer the inventor used to keep himself on a schedule that kept him at optimal efficiency. Of course I have never needed a timer to prompt me to move to another task. My short attention span always has taken care of that.
It turns out that by stumbling into a career in outpatient general pediatrics I found a perfect fit for my truncated attention span. Visits seldom lasted more than 15 minutes followed by a quick sprint to the next room and a fresh and stimulating set of faces and complaints. You may think I should have been spending a minimum of 20 or 25 minutes, but visits of that length seldom fit the realities of my usual day.
There is a myth floating around that there is always a direct correlation between the length of an office visit and its quality. The patient’s perception of quality is most important, and it is based on multiple factors – not the least of which is the level of engagement the physician exhibits. The problem comes when – for whatever reason – closure can’t be achieved in even a 35- or 40-minute visit. Here is when the provider must fall back on her/his clinical artistry by first acknowledging that neither patient nor provider is content with the current situation, but that a follow-up call that evening or an office visit in a day or two will continue the process.
Of course, there were always days when I wish had more time to devote to certain office visits. But for the most part, the hectic pace of outpatient pediatrics fit with my need for a rapidly changing stream of fresh challenges to keep my attention.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
Have you every wondered whether you have an attention deficit disorder? I have and I suspect that there are plenty of folks who share my curiosity. Realistically I’m pretty sure I don’t have ADD because while I enjoy being physically active my folks never described me as “bouncing off the walls.” Although I think I am very aware of my surroundings and observant, I wouldn’t say I am unusually distractible. I can multitask reasonably well and have been reasonably successful academically and professionally. But the one characteristic I do share with most ADD patients is a short attention span.
Short, of course, is a relative term. Any academic class longer than 45 minutes pushes me past my limit. The same goes for movies and television documentaries. Reading always has been a challenge for me, and 20 minutes is about as long as I can sit with a book or magazine article – even if it’s about a topic that interests me.
Even when I am painting or wood carving, I need to put down my brushes and knives after 20 minutes and do something else. I am a one-set tennis player and about a seven-hole golfer. I have the physical stamina to go much longer, but by the second set or the 10th hole I would prefer to be moving on to some other activity.
In college, I quickly learned that all-nighters were counterproductive. My usual study pattern evolved into one in which I would spend about 20 minutes on one course, take a trip to the refrigerator and return to studying on another course for 20 minutes, then take a break outside to shoot some hoops and return to work for 20 minutes on a third course. This pattern of relatively short bouts of work punctuated by brief snack or exercise breaks seemed to be my most efficient, productive, and mental health–sparing strategy.
Just last week, I learned that there is a name associated with my system. It’s called the Pomodoro technique and was “invented” by a student in an Italian business school in the 1980s (“This Time-Management Trick Changed My Whole Relationship With Time,”By Dean Kissick, The New York Times, June 23, 2020). At its core is a rigid pattern of 25 minutes of work punctuated by 5-minute breaks. The name comes from the tomato-shaped kitchen timer the inventor used to keep himself on a schedule that kept him at optimal efficiency. Of course I have never needed a timer to prompt me to move to another task. My short attention span always has taken care of that.
It turns out that by stumbling into a career in outpatient general pediatrics I found a perfect fit for my truncated attention span. Visits seldom lasted more than 15 minutes followed by a quick sprint to the next room and a fresh and stimulating set of faces and complaints. You may think I should have been spending a minimum of 20 or 25 minutes, but visits of that length seldom fit the realities of my usual day.
There is a myth floating around that there is always a direct correlation between the length of an office visit and its quality. The patient’s perception of quality is most important, and it is based on multiple factors – not the least of which is the level of engagement the physician exhibits. The problem comes when – for whatever reason – closure can’t be achieved in even a 35- or 40-minute visit. Here is when the provider must fall back on her/his clinical artistry by first acknowledging that neither patient nor provider is content with the current situation, but that a follow-up call that evening or an office visit in a day or two will continue the process.
Of course, there were always days when I wish had more time to devote to certain office visits. But for the most part, the hectic pace of outpatient pediatrics fit with my need for a rapidly changing stream of fresh challenges to keep my attention.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
Have you every wondered whether you have an attention deficit disorder? I have and I suspect that there are plenty of folks who share my curiosity. Realistically I’m pretty sure I don’t have ADD because while I enjoy being physically active my folks never described me as “bouncing off the walls.” Although I think I am very aware of my surroundings and observant, I wouldn’t say I am unusually distractible. I can multitask reasonably well and have been reasonably successful academically and professionally. But the one characteristic I do share with most ADD patients is a short attention span.
Short, of course, is a relative term. Any academic class longer than 45 minutes pushes me past my limit. The same goes for movies and television documentaries. Reading always has been a challenge for me, and 20 minutes is about as long as I can sit with a book or magazine article – even if it’s about a topic that interests me.
Even when I am painting or wood carving, I need to put down my brushes and knives after 20 minutes and do something else. I am a one-set tennis player and about a seven-hole golfer. I have the physical stamina to go much longer, but by the second set or the 10th hole I would prefer to be moving on to some other activity.
In college, I quickly learned that all-nighters were counterproductive. My usual study pattern evolved into one in which I would spend about 20 minutes on one course, take a trip to the refrigerator and return to studying on another course for 20 minutes, then take a break outside to shoot some hoops and return to work for 20 minutes on a third course. This pattern of relatively short bouts of work punctuated by brief snack or exercise breaks seemed to be my most efficient, productive, and mental health–sparing strategy.
Just last week, I learned that there is a name associated with my system. It’s called the Pomodoro technique and was “invented” by a student in an Italian business school in the 1980s (“This Time-Management Trick Changed My Whole Relationship With Time,”By Dean Kissick, The New York Times, June 23, 2020). At its core is a rigid pattern of 25 minutes of work punctuated by 5-minute breaks. The name comes from the tomato-shaped kitchen timer the inventor used to keep himself on a schedule that kept him at optimal efficiency. Of course I have never needed a timer to prompt me to move to another task. My short attention span always has taken care of that.
It turns out that by stumbling into a career in outpatient general pediatrics I found a perfect fit for my truncated attention span. Visits seldom lasted more than 15 minutes followed by a quick sprint to the next room and a fresh and stimulating set of faces and complaints. You may think I should have been spending a minimum of 20 or 25 minutes, but visits of that length seldom fit the realities of my usual day.
There is a myth floating around that there is always a direct correlation between the length of an office visit and its quality. The patient’s perception of quality is most important, and it is based on multiple factors – not the least of which is the level of engagement the physician exhibits. The problem comes when – for whatever reason – closure can’t be achieved in even a 35- or 40-minute visit. Here is when the provider must fall back on her/his clinical artistry by first acknowledging that neither patient nor provider is content with the current situation, but that a follow-up call that evening or an office visit in a day or two will continue the process.
Of course, there were always days when I wish had more time to devote to certain office visits. But for the most part, the hectic pace of outpatient pediatrics fit with my need for a rapidly changing stream of fresh challenges to keep my attention.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
Aerobic exercise may up brain-training benefits in schizophrenia
Recent research has shown that social cognition training can benefit patients with schizophrenia, and a new study suggests that adding regular aerobic exercise sessions substantially increases the improvements in a dose-response manner.
In a randomized controlled trial (RCT) in 47 patients with schizophrenia, improvement in cognition tripled after adding an aerobic exercise program to cognitive training (CT) compared with CT alone.
Investigators, led by Keith H. Nuechterlein, PhD, professor of psychology, University of California, Los Angeles, note that there is “increasing evidence” to support the use of aerobic exercise to improve cognition and functioning in schizophrenia.
However, the “extent to which these gains are dependent on the amount of aerobic exercise completed remains unclear, although variability in adherence to intended exercise regiments is evident,” they write.
They also point out that
The findings were scheduled to be presented at the Congress of the Schizophrenia International Research Society (SIRS) 2020, but the meeting was canceled because of the coronavirus pandemic.
Body Circuit Training
In the study, 47 patients with first-episode schizophrenia were randomly assigned to receive 6 months of CT alone or 6 months of CT plus exercise (CT+E).
All participants underwent 4 hours per week of computerized CT with BrainHQ and SocialVille programs (PositScience).
Patients in the CT+E group also took part in total body circuit training. Two aerobic exercise sessions per week were held at the clinic and two were to be completed at home. The goal was 150 minutes of exercise per week in total.
Exercise intensity was titrated to the individual, at a target of 60% to 80% of heart rate reserve.
Both the CT and CT+E groups showed cognitive gains on the MATRICS Consensus Cognitive Battery (MCCB) test, as well as work/school functioning gains on the Global Assessment Scale: Role.
However, results showed that the improvements in the CT+E group were three times greater than those shown in the CT group (P < .02 for the MCCB overall composite score).
Cognitive Gain Predictors
Because there were also substantial differences in the magnitude of cognitive improvement between the CT+E patients, the investigators sought to identify predictors of cognitive gain.
They found that patients in the CT+E group completed, on average, 85% of their in-clinic exercise sessions but only 39% of their home exercise sessions.
Those who completed a higher overall proportion of the exercise sessions had the largest cognitive gains (P = .03). This relationship was even stronger for patients who completed home exercise sessions (P = .02).
“Thus, aerobic exercise showed a dose-response relationship to cognitive improvement,” the researchers report.
To improve completion rates for home sessions, the investigators tried paying the patients $5 for each session completed, which was “helpful” but did not iron out the variability in adherence.
They also tried assigning points for completing the most exercise sessions in the desired heart rate. They awarded a monthly winner and divided the patients into two completion groups. However, there were “mixed” results.
“Development of systematic incentive strategies to encourage regular aerobic exercise will be critical to successful dissemination of exercise programs as part of the treatment of schizophrenia,” the researchers write.
They add that “pilot work with smartphone reminder systems is underway.”
Effective, but Intensity Is Key
Commenting on the study for Medscape Medical News, David Kimhy, PhD, program leader for New Interventions in Schizophrenia, Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York City, said the results are consistent with previous research.
Aerobic exercise is “highly effective in improving neurocognitive functioning” in patients with schizophrenia, said Kimhy, who was not involved in the research.
“Many individuals with schizophrenia tend to have a highly sedentary lifestyle resulting in poor aerobic fitness,” he said. “Thus, aerobic fitness may represent one of the few modifiable risk factors for ameliorating poor neurocognitive functioning.”
He noted that those benefits are in addition to “the many cardiovascular and health benefits aerobic exercise provide, which are nearly nonexistent for cognitive training and pharmacological interventions.”
However, even if patients do take part in exercise sessions, “an important issue is in-session fidelity with training goals, as individuals may attend scheduled sessions but exercise very lightly,” Kimhy noted.
He pointed out that the proportion of time these patients exercise at their designated target training intensity is highly correlated with neurocognitive improvement. Consequently, “exercising with a trainer may increase both attendance and in-session training fidelity.”
Overall, although the current study suggests that in-clinic exercise sessions can be advantageous, “the recent COVID-19 pandemic made such options very challenging,” Kimhy said.
“To address this issue, our research group and others are currently examining employment of aerobic exercise training at home, connected with trainers via live two-way telehealth video calls,” he added.
Plasticity-Based Training
Two recent studies also indicate that remotely administered training programs can improve social cognition.
In the first study, published online July 2 in Schizophrenia Bulletin, 147 outpatients with schizophrenia were randomly assigned to complete 40 sessions of either SocialVille plasticity-based social cognition training or computer-based games such as crossword puzzles and solitaire.
“To develop these social cognition training exercises, we analyzed a tremendous amount of prior research about how the brain processes social information,” lead author Mor Nahum, PhD, School of Occupational Therapy, Hebrew University, Jerusalem, Israel, said in a press release.
“It turns out that social cognition requires fast and accurate brain information processing, so we developed exercises that trained the brain to process social stimuli, like faces and emotions, quickly and accurately,” Nahum added.
The interventions were conducted at home, with 55 participants completing the cognitive training and 53 completing the computer game sessions. (The remaining 39 either dropped out or withdrew.)
An average of 28 hours of social cognition training over 3 months was associated with a significant improvement on social cognitive composite scores compared with computer games (P < .001), but not on the UCSD Performance-Based Skills Assessment.
Further analysis suggested that more time spent on the cognitive training was associated with greater improvements in social cognition and social functioning, as well as on a motivation subscale.
The results “provide support for the efficacy of a remote, plasticity-based social cognitive training program,” the investigators write.
Such programs “may serve as a cost-effective adjunct to existing psychosocial treatments,” they add.
Auditory vs Visual Training
In the other study, published online May 21 in Schizophrenia Research, investigators led by Rogerio Panizzutti, MD, PhD, Instituto de Ciencias Biomedicas, Federal University of Rio de Janeiro, Brazil, randomly assigned 79 patients with schizophrenia to 40 hours of auditory or visual computerized training.
The exercises were dynamically equivalent between the two types of training, and their difficulty increased as the training progressed.
Both groups showed improvements in reasoning, problem-solving, and reported symptoms. However, the group receiving visual training also had greater improvement in global cognition and attention than the group receiving auditory training.
All studies were supported by Posit Science Corporation. The study authors and Kimhy have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Recent research has shown that social cognition training can benefit patients with schizophrenia, and a new study suggests that adding regular aerobic exercise sessions substantially increases the improvements in a dose-response manner.
In a randomized controlled trial (RCT) in 47 patients with schizophrenia, improvement in cognition tripled after adding an aerobic exercise program to cognitive training (CT) compared with CT alone.
Investigators, led by Keith H. Nuechterlein, PhD, professor of psychology, University of California, Los Angeles, note that there is “increasing evidence” to support the use of aerobic exercise to improve cognition and functioning in schizophrenia.
However, the “extent to which these gains are dependent on the amount of aerobic exercise completed remains unclear, although variability in adherence to intended exercise regiments is evident,” they write.
They also point out that
The findings were scheduled to be presented at the Congress of the Schizophrenia International Research Society (SIRS) 2020, but the meeting was canceled because of the coronavirus pandemic.
Body Circuit Training
In the study, 47 patients with first-episode schizophrenia were randomly assigned to receive 6 months of CT alone or 6 months of CT plus exercise (CT+E).
All participants underwent 4 hours per week of computerized CT with BrainHQ and SocialVille programs (PositScience).
Patients in the CT+E group also took part in total body circuit training. Two aerobic exercise sessions per week were held at the clinic and two were to be completed at home. The goal was 150 minutes of exercise per week in total.
Exercise intensity was titrated to the individual, at a target of 60% to 80% of heart rate reserve.
Both the CT and CT+E groups showed cognitive gains on the MATRICS Consensus Cognitive Battery (MCCB) test, as well as work/school functioning gains on the Global Assessment Scale: Role.
However, results showed that the improvements in the CT+E group were three times greater than those shown in the CT group (P < .02 for the MCCB overall composite score).
Cognitive Gain Predictors
Because there were also substantial differences in the magnitude of cognitive improvement between the CT+E patients, the investigators sought to identify predictors of cognitive gain.
They found that patients in the CT+E group completed, on average, 85% of their in-clinic exercise sessions but only 39% of their home exercise sessions.
Those who completed a higher overall proportion of the exercise sessions had the largest cognitive gains (P = .03). This relationship was even stronger for patients who completed home exercise sessions (P = .02).
“Thus, aerobic exercise showed a dose-response relationship to cognitive improvement,” the researchers report.
To improve completion rates for home sessions, the investigators tried paying the patients $5 for each session completed, which was “helpful” but did not iron out the variability in adherence.
They also tried assigning points for completing the most exercise sessions in the desired heart rate. They awarded a monthly winner and divided the patients into two completion groups. However, there were “mixed” results.
“Development of systematic incentive strategies to encourage regular aerobic exercise will be critical to successful dissemination of exercise programs as part of the treatment of schizophrenia,” the researchers write.
They add that “pilot work with smartphone reminder systems is underway.”
Effective, but Intensity Is Key
Commenting on the study for Medscape Medical News, David Kimhy, PhD, program leader for New Interventions in Schizophrenia, Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York City, said the results are consistent with previous research.
Aerobic exercise is “highly effective in improving neurocognitive functioning” in patients with schizophrenia, said Kimhy, who was not involved in the research.
“Many individuals with schizophrenia tend to have a highly sedentary lifestyle resulting in poor aerobic fitness,” he said. “Thus, aerobic fitness may represent one of the few modifiable risk factors for ameliorating poor neurocognitive functioning.”
He noted that those benefits are in addition to “the many cardiovascular and health benefits aerobic exercise provide, which are nearly nonexistent for cognitive training and pharmacological interventions.”
However, even if patients do take part in exercise sessions, “an important issue is in-session fidelity with training goals, as individuals may attend scheduled sessions but exercise very lightly,” Kimhy noted.
He pointed out that the proportion of time these patients exercise at their designated target training intensity is highly correlated with neurocognitive improvement. Consequently, “exercising with a trainer may increase both attendance and in-session training fidelity.”
Overall, although the current study suggests that in-clinic exercise sessions can be advantageous, “the recent COVID-19 pandemic made such options very challenging,” Kimhy said.
“To address this issue, our research group and others are currently examining employment of aerobic exercise training at home, connected with trainers via live two-way telehealth video calls,” he added.
Plasticity-Based Training
Two recent studies also indicate that remotely administered training programs can improve social cognition.
In the first study, published online July 2 in Schizophrenia Bulletin, 147 outpatients with schizophrenia were randomly assigned to complete 40 sessions of either SocialVille plasticity-based social cognition training or computer-based games such as crossword puzzles and solitaire.
“To develop these social cognition training exercises, we analyzed a tremendous amount of prior research about how the brain processes social information,” lead author Mor Nahum, PhD, School of Occupational Therapy, Hebrew University, Jerusalem, Israel, said in a press release.
“It turns out that social cognition requires fast and accurate brain information processing, so we developed exercises that trained the brain to process social stimuli, like faces and emotions, quickly and accurately,” Nahum added.
The interventions were conducted at home, with 55 participants completing the cognitive training and 53 completing the computer game sessions. (The remaining 39 either dropped out or withdrew.)
An average of 28 hours of social cognition training over 3 months was associated with a significant improvement on social cognitive composite scores compared with computer games (P < .001), but not on the UCSD Performance-Based Skills Assessment.
Further analysis suggested that more time spent on the cognitive training was associated with greater improvements in social cognition and social functioning, as well as on a motivation subscale.
The results “provide support for the efficacy of a remote, plasticity-based social cognitive training program,” the investigators write.
Such programs “may serve as a cost-effective adjunct to existing psychosocial treatments,” they add.
Auditory vs Visual Training
In the other study, published online May 21 in Schizophrenia Research, investigators led by Rogerio Panizzutti, MD, PhD, Instituto de Ciencias Biomedicas, Federal University of Rio de Janeiro, Brazil, randomly assigned 79 patients with schizophrenia to 40 hours of auditory or visual computerized training.
The exercises were dynamically equivalent between the two types of training, and their difficulty increased as the training progressed.
Both groups showed improvements in reasoning, problem-solving, and reported symptoms. However, the group receiving visual training also had greater improvement in global cognition and attention than the group receiving auditory training.
All studies were supported by Posit Science Corporation. The study authors and Kimhy have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Recent research has shown that social cognition training can benefit patients with schizophrenia, and a new study suggests that adding regular aerobic exercise sessions substantially increases the improvements in a dose-response manner.
In a randomized controlled trial (RCT) in 47 patients with schizophrenia, improvement in cognition tripled after adding an aerobic exercise program to cognitive training (CT) compared with CT alone.
Investigators, led by Keith H. Nuechterlein, PhD, professor of psychology, University of California, Los Angeles, note that there is “increasing evidence” to support the use of aerobic exercise to improve cognition and functioning in schizophrenia.
However, the “extent to which these gains are dependent on the amount of aerobic exercise completed remains unclear, although variability in adherence to intended exercise regiments is evident,” they write.
They also point out that
The findings were scheduled to be presented at the Congress of the Schizophrenia International Research Society (SIRS) 2020, but the meeting was canceled because of the coronavirus pandemic.
Body Circuit Training
In the study, 47 patients with first-episode schizophrenia were randomly assigned to receive 6 months of CT alone or 6 months of CT plus exercise (CT+E).
All participants underwent 4 hours per week of computerized CT with BrainHQ and SocialVille programs (PositScience).
Patients in the CT+E group also took part in total body circuit training. Two aerobic exercise sessions per week were held at the clinic and two were to be completed at home. The goal was 150 minutes of exercise per week in total.
Exercise intensity was titrated to the individual, at a target of 60% to 80% of heart rate reserve.
Both the CT and CT+E groups showed cognitive gains on the MATRICS Consensus Cognitive Battery (MCCB) test, as well as work/school functioning gains on the Global Assessment Scale: Role.
However, results showed that the improvements in the CT+E group were three times greater than those shown in the CT group (P < .02 for the MCCB overall composite score).
Cognitive Gain Predictors
Because there were also substantial differences in the magnitude of cognitive improvement between the CT+E patients, the investigators sought to identify predictors of cognitive gain.
They found that patients in the CT+E group completed, on average, 85% of their in-clinic exercise sessions but only 39% of their home exercise sessions.
Those who completed a higher overall proportion of the exercise sessions had the largest cognitive gains (P = .03). This relationship was even stronger for patients who completed home exercise sessions (P = .02).
“Thus, aerobic exercise showed a dose-response relationship to cognitive improvement,” the researchers report.
To improve completion rates for home sessions, the investigators tried paying the patients $5 for each session completed, which was “helpful” but did not iron out the variability in adherence.
They also tried assigning points for completing the most exercise sessions in the desired heart rate. They awarded a monthly winner and divided the patients into two completion groups. However, there were “mixed” results.
“Development of systematic incentive strategies to encourage regular aerobic exercise will be critical to successful dissemination of exercise programs as part of the treatment of schizophrenia,” the researchers write.
They add that “pilot work with smartphone reminder systems is underway.”
Effective, but Intensity Is Key
Commenting on the study for Medscape Medical News, David Kimhy, PhD, program leader for New Interventions in Schizophrenia, Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York City, said the results are consistent with previous research.
Aerobic exercise is “highly effective in improving neurocognitive functioning” in patients with schizophrenia, said Kimhy, who was not involved in the research.
“Many individuals with schizophrenia tend to have a highly sedentary lifestyle resulting in poor aerobic fitness,” he said. “Thus, aerobic fitness may represent one of the few modifiable risk factors for ameliorating poor neurocognitive functioning.”
He noted that those benefits are in addition to “the many cardiovascular and health benefits aerobic exercise provide, which are nearly nonexistent for cognitive training and pharmacological interventions.”
However, even if patients do take part in exercise sessions, “an important issue is in-session fidelity with training goals, as individuals may attend scheduled sessions but exercise very lightly,” Kimhy noted.
He pointed out that the proportion of time these patients exercise at their designated target training intensity is highly correlated with neurocognitive improvement. Consequently, “exercising with a trainer may increase both attendance and in-session training fidelity.”
Overall, although the current study suggests that in-clinic exercise sessions can be advantageous, “the recent COVID-19 pandemic made such options very challenging,” Kimhy said.
“To address this issue, our research group and others are currently examining employment of aerobic exercise training at home, connected with trainers via live two-way telehealth video calls,” he added.
Plasticity-Based Training
Two recent studies also indicate that remotely administered training programs can improve social cognition.
In the first study, published online July 2 in Schizophrenia Bulletin, 147 outpatients with schizophrenia were randomly assigned to complete 40 sessions of either SocialVille plasticity-based social cognition training or computer-based games such as crossword puzzles and solitaire.
“To develop these social cognition training exercises, we analyzed a tremendous amount of prior research about how the brain processes social information,” lead author Mor Nahum, PhD, School of Occupational Therapy, Hebrew University, Jerusalem, Israel, said in a press release.
“It turns out that social cognition requires fast and accurate brain information processing, so we developed exercises that trained the brain to process social stimuli, like faces and emotions, quickly and accurately,” Nahum added.
The interventions were conducted at home, with 55 participants completing the cognitive training and 53 completing the computer game sessions. (The remaining 39 either dropped out or withdrew.)
An average of 28 hours of social cognition training over 3 months was associated with a significant improvement on social cognitive composite scores compared with computer games (P < .001), but not on the UCSD Performance-Based Skills Assessment.
Further analysis suggested that more time spent on the cognitive training was associated with greater improvements in social cognition and social functioning, as well as on a motivation subscale.
The results “provide support for the efficacy of a remote, plasticity-based social cognitive training program,” the investigators write.
Such programs “may serve as a cost-effective adjunct to existing psychosocial treatments,” they add.
Auditory vs Visual Training
In the other study, published online May 21 in Schizophrenia Research, investigators led by Rogerio Panizzutti, MD, PhD, Instituto de Ciencias Biomedicas, Federal University of Rio de Janeiro, Brazil, randomly assigned 79 patients with schizophrenia to 40 hours of auditory or visual computerized training.
The exercises were dynamically equivalent between the two types of training, and their difficulty increased as the training progressed.
Both groups showed improvements in reasoning, problem-solving, and reported symptoms. However, the group receiving visual training also had greater improvement in global cognition and attention than the group receiving auditory training.
All studies were supported by Posit Science Corporation. The study authors and Kimhy have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Memphis clinic created to care for children and adolescents diagnosed with melanoma
Pediatric melanoma remains a rare diagnosis – representing just 1%-4% of all melanomas – and it continues to be poorly understood.
“There are many questions about its biology, histopathology, and clinical behavior,” Teresa S. Wright, MD, said during the virtual annual meeting of the Society for Pediatric Dermatology. “This diagnosis can be very difficult to establish. These lesions can be very unusual and require several different expert opinions to arrive at a diagnosis. Oftentimes, there may be an initial misdiagnosis or disagreement about diagnosis. This frequently results in a delay of treatment.”
Dr. Wright, chief of pediatric dermatology at LeBonheur Children’s Hospital and associate professor of dermatology at the University of Tennessee Health Science Center, Memphis, added that once a diagnosis of pediatric melanoma has been established, things don’t get any easier because of the lack of evidence-based guidelines for management. “There are really no standard recommendations regarding the workup, treatment, or follow-up for these patients,” she said.
Referral Clinic Launched
In 2016, under the direction of Alberto Pappo, MD, director of the solid tumor division at St. Jude Children’s Research Hospital in Memphis, Dr. Wright and several colleagues at “As a group, we address questions surrounding the diagnosis and pathology of the patient’s lesion, as well as therapy and follow-up for each individual patient,” Dr. Wright said.
Members of the clinic team include a pediatric oncologist, an adult oncologist, and a surgical oncologist (all with melanoma expertise); a pediatric surgeon, a pediatric dermatologist, a pediatric radiologist, a pathologist, and a nursing team, which includes a pediatric nurse practitioner, three registered nurses, and other support staff, including those that provide genetic counseling and child life specialists. To be eligible for the clinic, which typically is scheduled in April and November every year, patients must be no older than 21 years, must be referred by a physician, and must have a diagnosis of melanoma or Spitzoid melanoma, not including ocular melanoma. They must be currently undergoing treatment or followed by a physician who requests or supports a consult to optimize clinical management of the patient. St. Jude foots the bill for all travel, housing, and meal expenses. All pertinent materials are collected in advance of the 2-day clinic, including medical records, lab results, histology slides, tissue samples, and radiographic studies. The pathologist performs an initial review of the histology slides and additional genomic studies are performed based on the pathologist’s diagnosis.
Patients typically arrive on a Wednesday evening and have their first clinic visit Thursday morning. First, the oncology team performs a thorough history and physical examination, then Dr. Wright performs a thorough skin examination and a professional photographer captures images of relevant skin lesions. That afternoon, members of the multidisciplinary team meet to review each patient’s entire course, including previous surgeries and any medical therapies.
“We review their pathology, including histology slides and results of any genomic studies,” Dr. Wright said. “We also review all the radiographic studies they’ve had, which may include plain films, CT scans, PET scans, MRIs, and ultrasounds. Then we form a consensus opinion regarding a diagnosis. Sometimes we feel a change in diagnosis is warranted.” For example, she added, “we have had a number of patients referred to us with an initial diagnosis of Spitzoid melanoma where, after review, we felt that a diagnosis of atypical Spitzoid tumor was more appropriate for them. We also talk about any treatment they’ve had in the past and decide if any additional surgical or medical treatment is indicated at this time. Lastly, we make recommendations for follow-up or surveillance.”
On Thursday evening, the clinic sponsors a casual dinner for families, which features an educational presentation by one or more faculty members. Topics covered in the past include sun protection, melanoma in children, and an overview of melanoma research.
The next morning, each family meets with the panel of specialists. “The team members introduce themselves and describe their roles within the team, and family members introduce themselves and tell their child’s story. “Then, each team member describes their findings and gives their overall assessment. The family receives recommendations for any additional testing, therapy, and follow-up, and the patient and family’s questions are answered.”
Families are also offered the opportunity to participate in research. “They can donate samples to a tissue bank, and patients may qualify for future clinical trials at St. Jude Children’s Research Hospital,” Dr. Wright said.
To date, 20 female and 18 male patients have traveled to the Pediatric and Adolescent Melanoma Referral Clinic from 21 states and Puerto Rico for assessment and consultation. They ranged in age from 6 months to 18 years, and their average age is 9 years. Members of the clinic team have seen 13 patients with a diagnosis of Spitzoid melanoma, 10 with malignant melanoma, 8 with atypical melanocytic neoplasm, 3 with congenital melanoma, 3 with atypical Spitz tumor, and 1 with congenital melanocytic nevus.
The median age at diagnosis was 12 years for malignant melanoma and 9 years for Spitzoid melanoma; and the male to female ratio is 7:3 for malignant melanoma and 4:9 for Spitzoid melanoma. These are the patients who have come to the multidisciplinary clinic, these specialists see other patients with a diagnosis of pediatric or adolescent melanoma at other times of the year, Dr. Wright noted.
A common refrain she hears from pediatric melanoma patients and their families is that the initial skin lesion appears to be unremarkable. “Many times, this is a skin-colored or pink papule, which starts out looking very much like a molluscum or a wart or an insect bite, or something else that nobody’s worried about,” Dr. Wright said. “But over time, something happens, and the common factor is rapid growth. Time and again when I ask parents, ‘What changed? What got your attention?’ The answer is nearly always rapid growth.”
She emphasized that patients frequently arrive at the clinic with multiple opinions about their diagnosis. “It’s not unusual for a significant amount of time to pass between the initial biopsy and the final diagnosis,” she said. “Given the lack of evidence-based guidelines for children, a delay in diagnosis can make decisions about management even more difficult. Because pediatric melanoma is so rare, and there are no standard guidelines for management, there’s a major lack of consistency in terms of how patients are evaluated, treated, and followed.”
Dr. Wright said the team’s goals are to continue the biannual clinic and collect more data and tissue samples for further genomic studies on pediatric melanoma. “Ultimately, we would like to hold a consensus summit meeting of experts to develop and publish evidence-based guidelines for the management of pediatric and adolescent melanoma.”
Dr. Wright reported having no relevant disclosures.
Pediatric melanoma remains a rare diagnosis – representing just 1%-4% of all melanomas – and it continues to be poorly understood.
“There are many questions about its biology, histopathology, and clinical behavior,” Teresa S. Wright, MD, said during the virtual annual meeting of the Society for Pediatric Dermatology. “This diagnosis can be very difficult to establish. These lesions can be very unusual and require several different expert opinions to arrive at a diagnosis. Oftentimes, there may be an initial misdiagnosis or disagreement about diagnosis. This frequently results in a delay of treatment.”
Dr. Wright, chief of pediatric dermatology at LeBonheur Children’s Hospital and associate professor of dermatology at the University of Tennessee Health Science Center, Memphis, added that once a diagnosis of pediatric melanoma has been established, things don’t get any easier because of the lack of evidence-based guidelines for management. “There are really no standard recommendations regarding the workup, treatment, or follow-up for these patients,” she said.
Referral Clinic Launched
In 2016, under the direction of Alberto Pappo, MD, director of the solid tumor division at St. Jude Children’s Research Hospital in Memphis, Dr. Wright and several colleagues at “As a group, we address questions surrounding the diagnosis and pathology of the patient’s lesion, as well as therapy and follow-up for each individual patient,” Dr. Wright said.
Members of the clinic team include a pediatric oncologist, an adult oncologist, and a surgical oncologist (all with melanoma expertise); a pediatric surgeon, a pediatric dermatologist, a pediatric radiologist, a pathologist, and a nursing team, which includes a pediatric nurse practitioner, three registered nurses, and other support staff, including those that provide genetic counseling and child life specialists. To be eligible for the clinic, which typically is scheduled in April and November every year, patients must be no older than 21 years, must be referred by a physician, and must have a diagnosis of melanoma or Spitzoid melanoma, not including ocular melanoma. They must be currently undergoing treatment or followed by a physician who requests or supports a consult to optimize clinical management of the patient. St. Jude foots the bill for all travel, housing, and meal expenses. All pertinent materials are collected in advance of the 2-day clinic, including medical records, lab results, histology slides, tissue samples, and radiographic studies. The pathologist performs an initial review of the histology slides and additional genomic studies are performed based on the pathologist’s diagnosis.
Patients typically arrive on a Wednesday evening and have their first clinic visit Thursday morning. First, the oncology team performs a thorough history and physical examination, then Dr. Wright performs a thorough skin examination and a professional photographer captures images of relevant skin lesions. That afternoon, members of the multidisciplinary team meet to review each patient’s entire course, including previous surgeries and any medical therapies.
“We review their pathology, including histology slides and results of any genomic studies,” Dr. Wright said. “We also review all the radiographic studies they’ve had, which may include plain films, CT scans, PET scans, MRIs, and ultrasounds. Then we form a consensus opinion regarding a diagnosis. Sometimes we feel a change in diagnosis is warranted.” For example, she added, “we have had a number of patients referred to us with an initial diagnosis of Spitzoid melanoma where, after review, we felt that a diagnosis of atypical Spitzoid tumor was more appropriate for them. We also talk about any treatment they’ve had in the past and decide if any additional surgical or medical treatment is indicated at this time. Lastly, we make recommendations for follow-up or surveillance.”
On Thursday evening, the clinic sponsors a casual dinner for families, which features an educational presentation by one or more faculty members. Topics covered in the past include sun protection, melanoma in children, and an overview of melanoma research.
The next morning, each family meets with the panel of specialists. “The team members introduce themselves and describe their roles within the team, and family members introduce themselves and tell their child’s story. “Then, each team member describes their findings and gives their overall assessment. The family receives recommendations for any additional testing, therapy, and follow-up, and the patient and family’s questions are answered.”
Families are also offered the opportunity to participate in research. “They can donate samples to a tissue bank, and patients may qualify for future clinical trials at St. Jude Children’s Research Hospital,” Dr. Wright said.
To date, 20 female and 18 male patients have traveled to the Pediatric and Adolescent Melanoma Referral Clinic from 21 states and Puerto Rico for assessment and consultation. They ranged in age from 6 months to 18 years, and their average age is 9 years. Members of the clinic team have seen 13 patients with a diagnosis of Spitzoid melanoma, 10 with malignant melanoma, 8 with atypical melanocytic neoplasm, 3 with congenital melanoma, 3 with atypical Spitz tumor, and 1 with congenital melanocytic nevus.
The median age at diagnosis was 12 years for malignant melanoma and 9 years for Spitzoid melanoma; and the male to female ratio is 7:3 for malignant melanoma and 4:9 for Spitzoid melanoma. These are the patients who have come to the multidisciplinary clinic, these specialists see other patients with a diagnosis of pediatric or adolescent melanoma at other times of the year, Dr. Wright noted.
A common refrain she hears from pediatric melanoma patients and their families is that the initial skin lesion appears to be unremarkable. “Many times, this is a skin-colored or pink papule, which starts out looking very much like a molluscum or a wart or an insect bite, or something else that nobody’s worried about,” Dr. Wright said. “But over time, something happens, and the common factor is rapid growth. Time and again when I ask parents, ‘What changed? What got your attention?’ The answer is nearly always rapid growth.”
She emphasized that patients frequently arrive at the clinic with multiple opinions about their diagnosis. “It’s not unusual for a significant amount of time to pass between the initial biopsy and the final diagnosis,” she said. “Given the lack of evidence-based guidelines for children, a delay in diagnosis can make decisions about management even more difficult. Because pediatric melanoma is so rare, and there are no standard guidelines for management, there’s a major lack of consistency in terms of how patients are evaluated, treated, and followed.”
Dr. Wright said the team’s goals are to continue the biannual clinic and collect more data and tissue samples for further genomic studies on pediatric melanoma. “Ultimately, we would like to hold a consensus summit meeting of experts to develop and publish evidence-based guidelines for the management of pediatric and adolescent melanoma.”
Dr. Wright reported having no relevant disclosures.
Pediatric melanoma remains a rare diagnosis – representing just 1%-4% of all melanomas – and it continues to be poorly understood.
“There are many questions about its biology, histopathology, and clinical behavior,” Teresa S. Wright, MD, said during the virtual annual meeting of the Society for Pediatric Dermatology. “This diagnosis can be very difficult to establish. These lesions can be very unusual and require several different expert opinions to arrive at a diagnosis. Oftentimes, there may be an initial misdiagnosis or disagreement about diagnosis. This frequently results in a delay of treatment.”
Dr. Wright, chief of pediatric dermatology at LeBonheur Children’s Hospital and associate professor of dermatology at the University of Tennessee Health Science Center, Memphis, added that once a diagnosis of pediatric melanoma has been established, things don’t get any easier because of the lack of evidence-based guidelines for management. “There are really no standard recommendations regarding the workup, treatment, or follow-up for these patients,” she said.
Referral Clinic Launched
In 2016, under the direction of Alberto Pappo, MD, director of the solid tumor division at St. Jude Children’s Research Hospital in Memphis, Dr. Wright and several colleagues at “As a group, we address questions surrounding the diagnosis and pathology of the patient’s lesion, as well as therapy and follow-up for each individual patient,” Dr. Wright said.
Members of the clinic team include a pediatric oncologist, an adult oncologist, and a surgical oncologist (all with melanoma expertise); a pediatric surgeon, a pediatric dermatologist, a pediatric radiologist, a pathologist, and a nursing team, which includes a pediatric nurse practitioner, three registered nurses, and other support staff, including those that provide genetic counseling and child life specialists. To be eligible for the clinic, which typically is scheduled in April and November every year, patients must be no older than 21 years, must be referred by a physician, and must have a diagnosis of melanoma or Spitzoid melanoma, not including ocular melanoma. They must be currently undergoing treatment or followed by a physician who requests or supports a consult to optimize clinical management of the patient. St. Jude foots the bill for all travel, housing, and meal expenses. All pertinent materials are collected in advance of the 2-day clinic, including medical records, lab results, histology slides, tissue samples, and radiographic studies. The pathologist performs an initial review of the histology slides and additional genomic studies are performed based on the pathologist’s diagnosis.
Patients typically arrive on a Wednesday evening and have their first clinic visit Thursday morning. First, the oncology team performs a thorough history and physical examination, then Dr. Wright performs a thorough skin examination and a professional photographer captures images of relevant skin lesions. That afternoon, members of the multidisciplinary team meet to review each patient’s entire course, including previous surgeries and any medical therapies.
“We review their pathology, including histology slides and results of any genomic studies,” Dr. Wright said. “We also review all the radiographic studies they’ve had, which may include plain films, CT scans, PET scans, MRIs, and ultrasounds. Then we form a consensus opinion regarding a diagnosis. Sometimes we feel a change in diagnosis is warranted.” For example, she added, “we have had a number of patients referred to us with an initial diagnosis of Spitzoid melanoma where, after review, we felt that a diagnosis of atypical Spitzoid tumor was more appropriate for them. We also talk about any treatment they’ve had in the past and decide if any additional surgical or medical treatment is indicated at this time. Lastly, we make recommendations for follow-up or surveillance.”
On Thursday evening, the clinic sponsors a casual dinner for families, which features an educational presentation by one or more faculty members. Topics covered in the past include sun protection, melanoma in children, and an overview of melanoma research.
The next morning, each family meets with the panel of specialists. “The team members introduce themselves and describe their roles within the team, and family members introduce themselves and tell their child’s story. “Then, each team member describes their findings and gives their overall assessment. The family receives recommendations for any additional testing, therapy, and follow-up, and the patient and family’s questions are answered.”
Families are also offered the opportunity to participate in research. “They can donate samples to a tissue bank, and patients may qualify for future clinical trials at St. Jude Children’s Research Hospital,” Dr. Wright said.
To date, 20 female and 18 male patients have traveled to the Pediatric and Adolescent Melanoma Referral Clinic from 21 states and Puerto Rico for assessment and consultation. They ranged in age from 6 months to 18 years, and their average age is 9 years. Members of the clinic team have seen 13 patients with a diagnosis of Spitzoid melanoma, 10 with malignant melanoma, 8 with atypical melanocytic neoplasm, 3 with congenital melanoma, 3 with atypical Spitz tumor, and 1 with congenital melanocytic nevus.
The median age at diagnosis was 12 years for malignant melanoma and 9 years for Spitzoid melanoma; and the male to female ratio is 7:3 for malignant melanoma and 4:9 for Spitzoid melanoma. These are the patients who have come to the multidisciplinary clinic, these specialists see other patients with a diagnosis of pediatric or adolescent melanoma at other times of the year, Dr. Wright noted.
A common refrain she hears from pediatric melanoma patients and their families is that the initial skin lesion appears to be unremarkable. “Many times, this is a skin-colored or pink papule, which starts out looking very much like a molluscum or a wart or an insect bite, or something else that nobody’s worried about,” Dr. Wright said. “But over time, something happens, and the common factor is rapid growth. Time and again when I ask parents, ‘What changed? What got your attention?’ The answer is nearly always rapid growth.”
She emphasized that patients frequently arrive at the clinic with multiple opinions about their diagnosis. “It’s not unusual for a significant amount of time to pass between the initial biopsy and the final diagnosis,” she said. “Given the lack of evidence-based guidelines for children, a delay in diagnosis can make decisions about management even more difficult. Because pediatric melanoma is so rare, and there are no standard guidelines for management, there’s a major lack of consistency in terms of how patients are evaluated, treated, and followed.”
Dr. Wright said the team’s goals are to continue the biannual clinic and collect more data and tissue samples for further genomic studies on pediatric melanoma. “Ultimately, we would like to hold a consensus summit meeting of experts to develop and publish evidence-based guidelines for the management of pediatric and adolescent melanoma.”
Dr. Wright reported having no relevant disclosures.
FROM SPD 2020
Federal Health Care Data Trends 2020
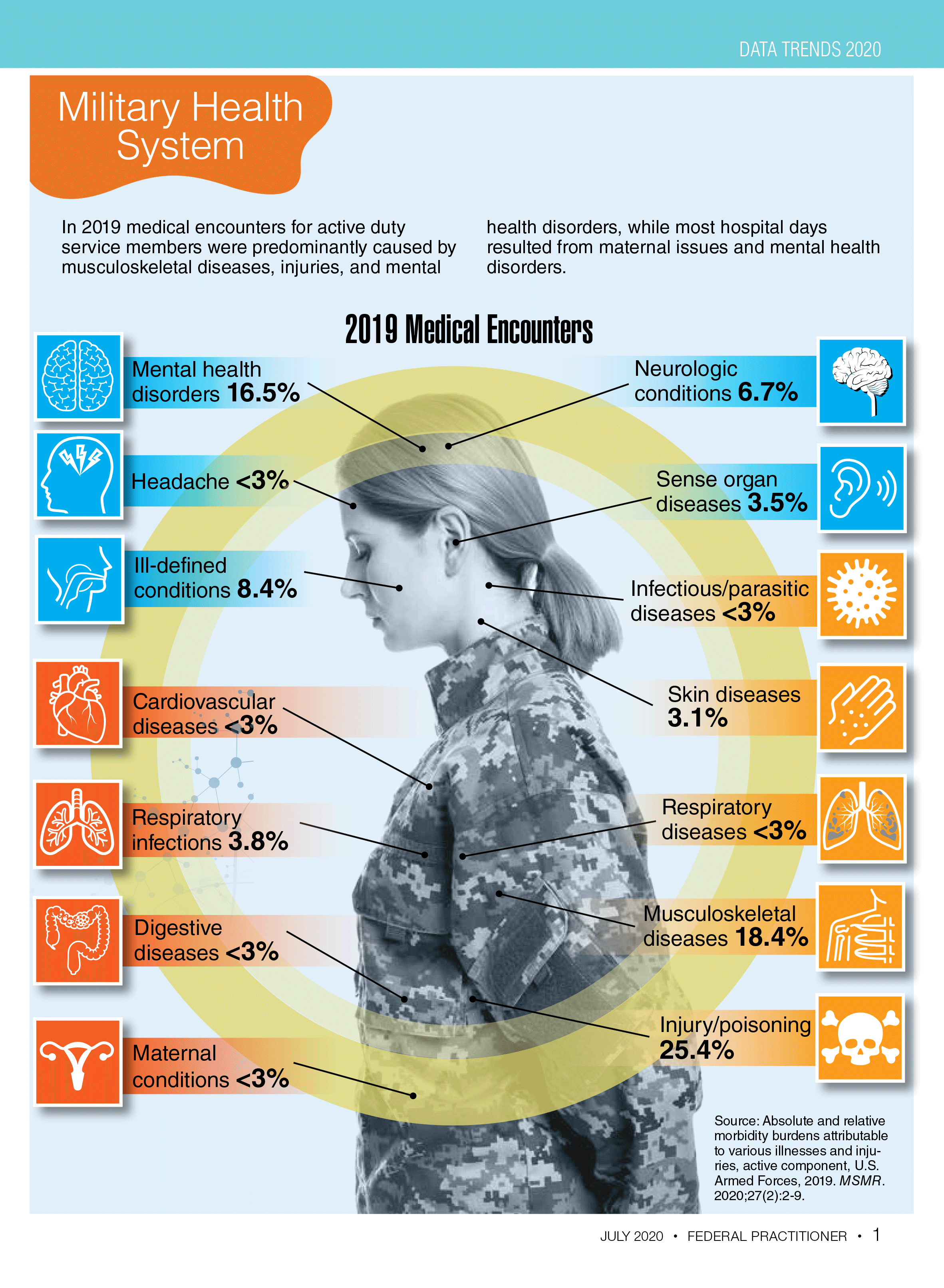
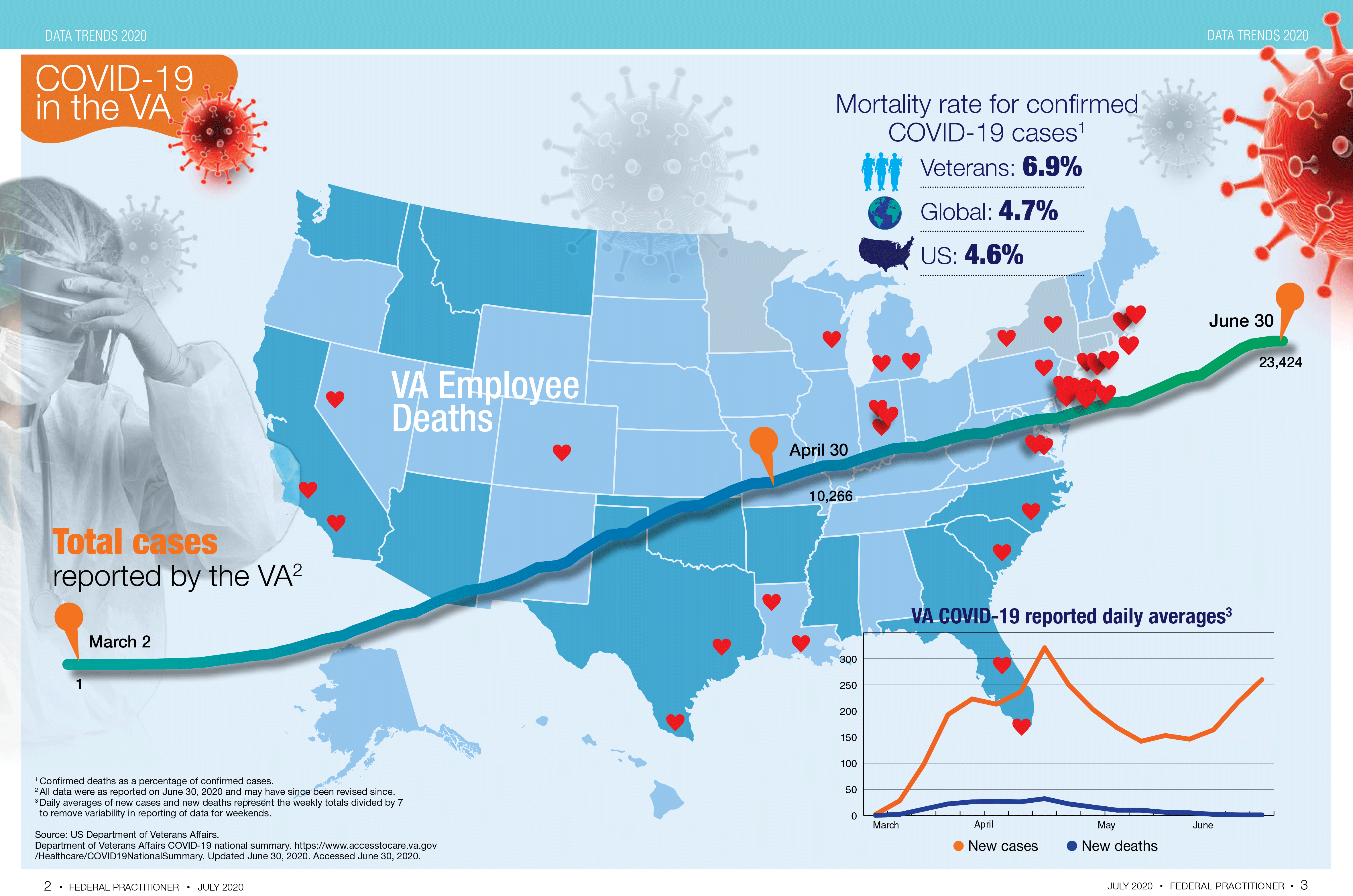

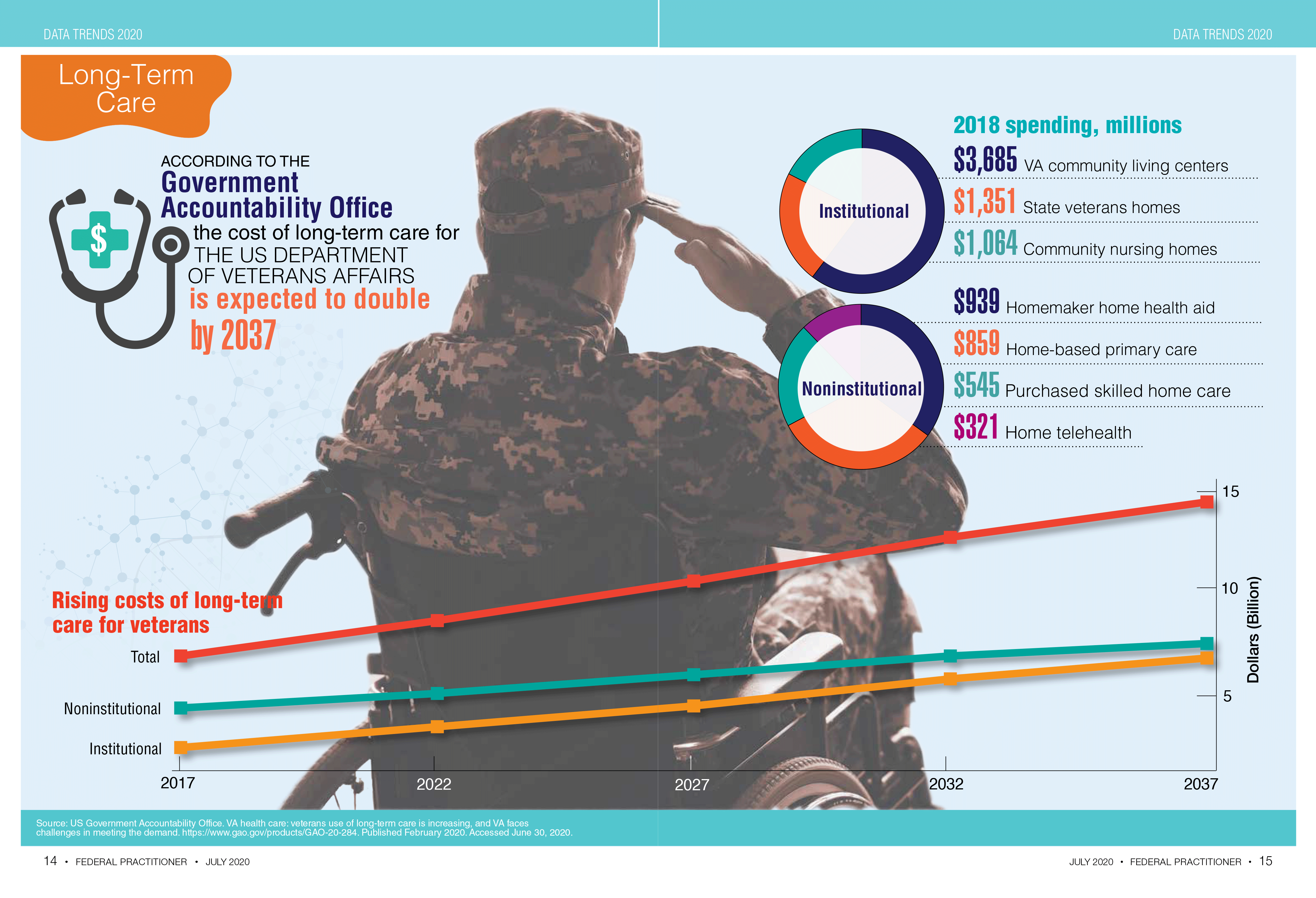
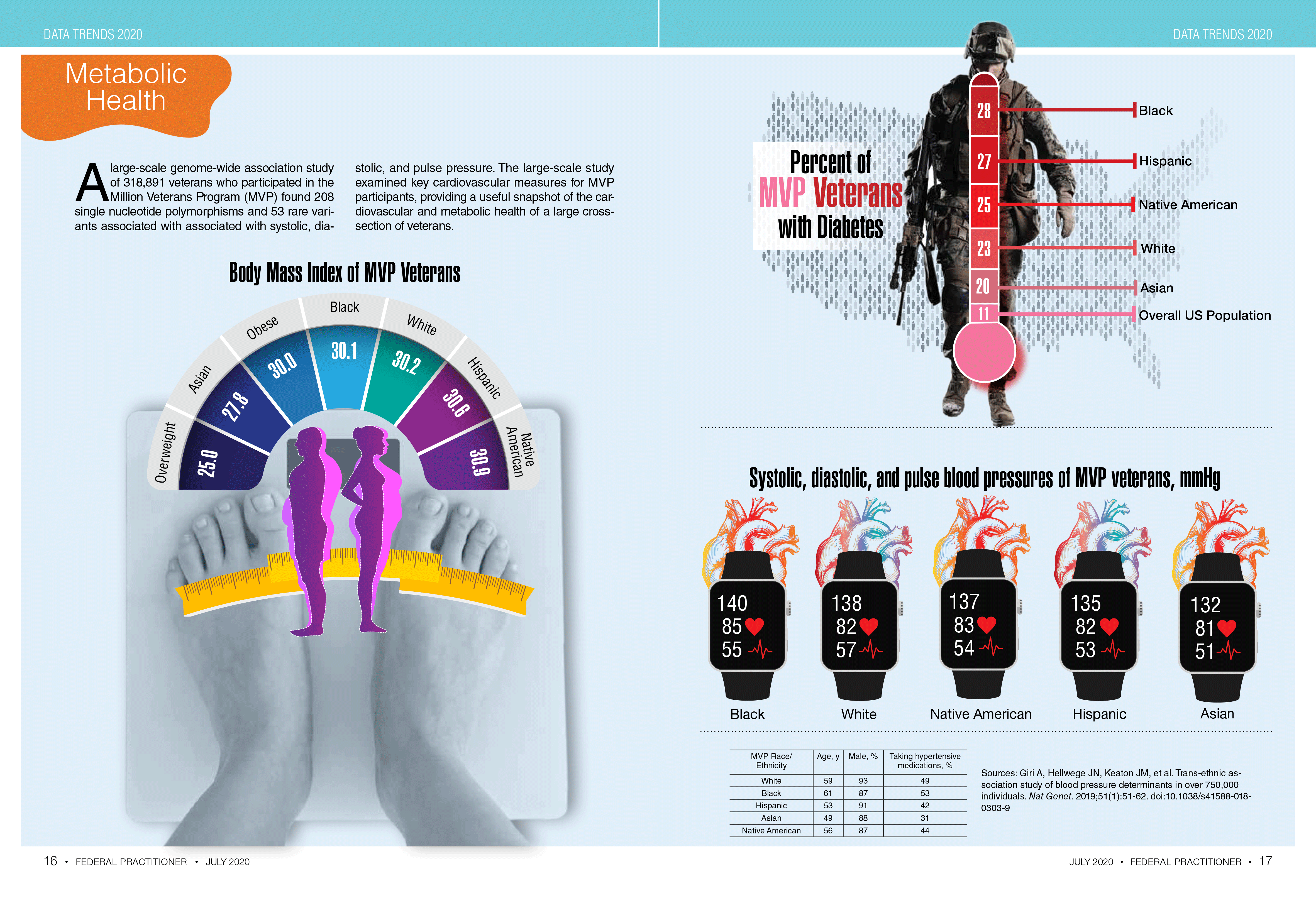
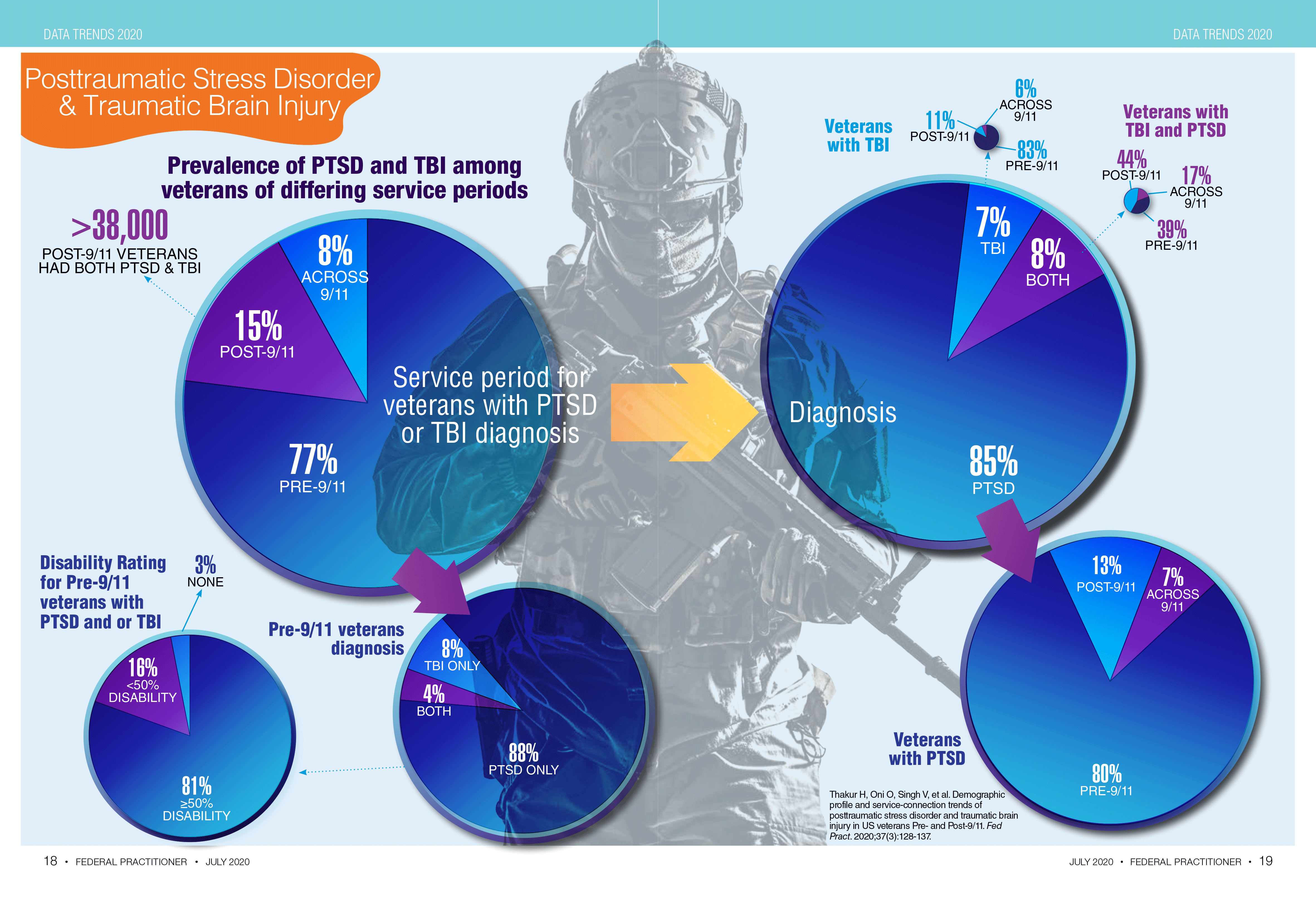
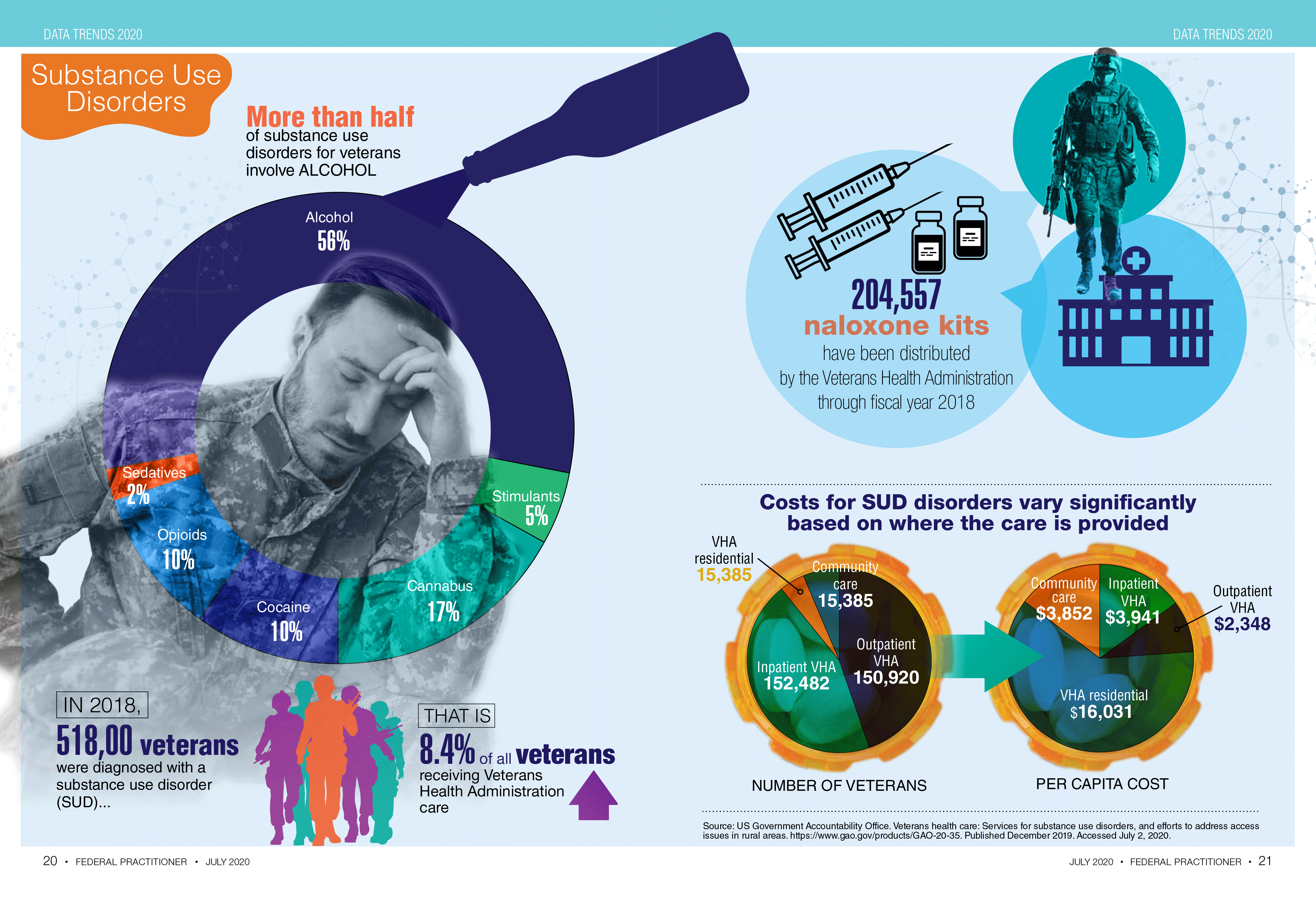
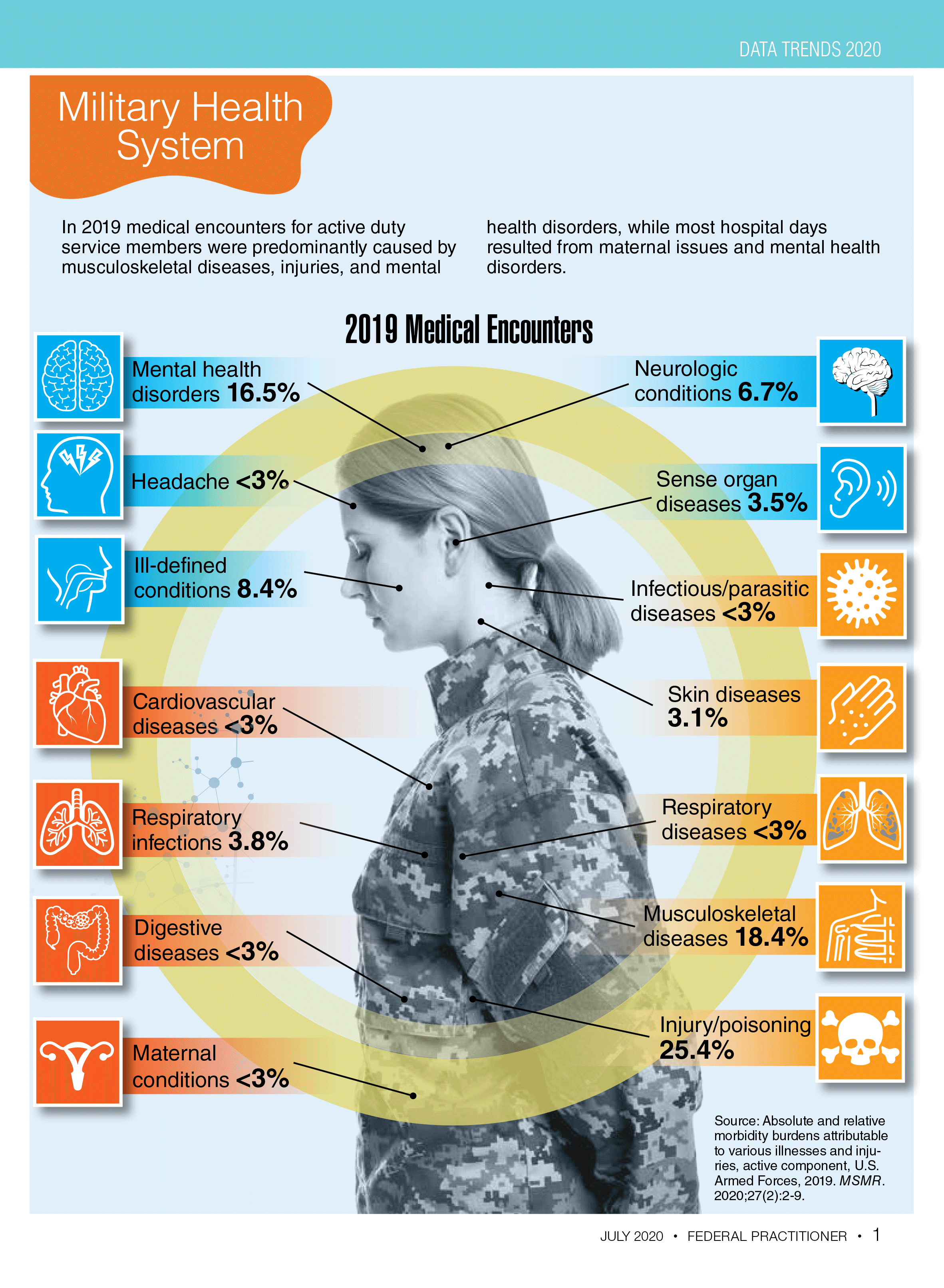
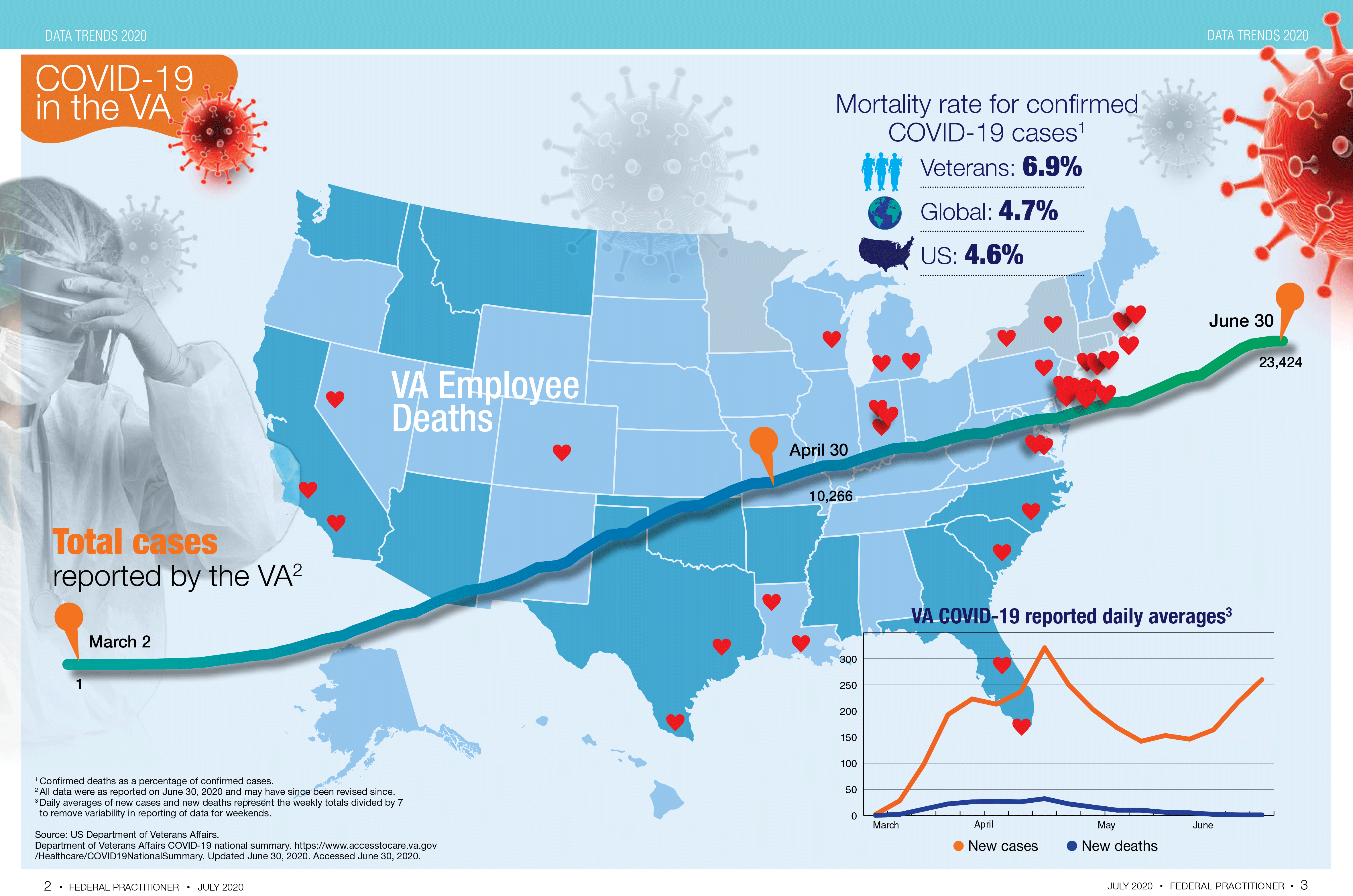

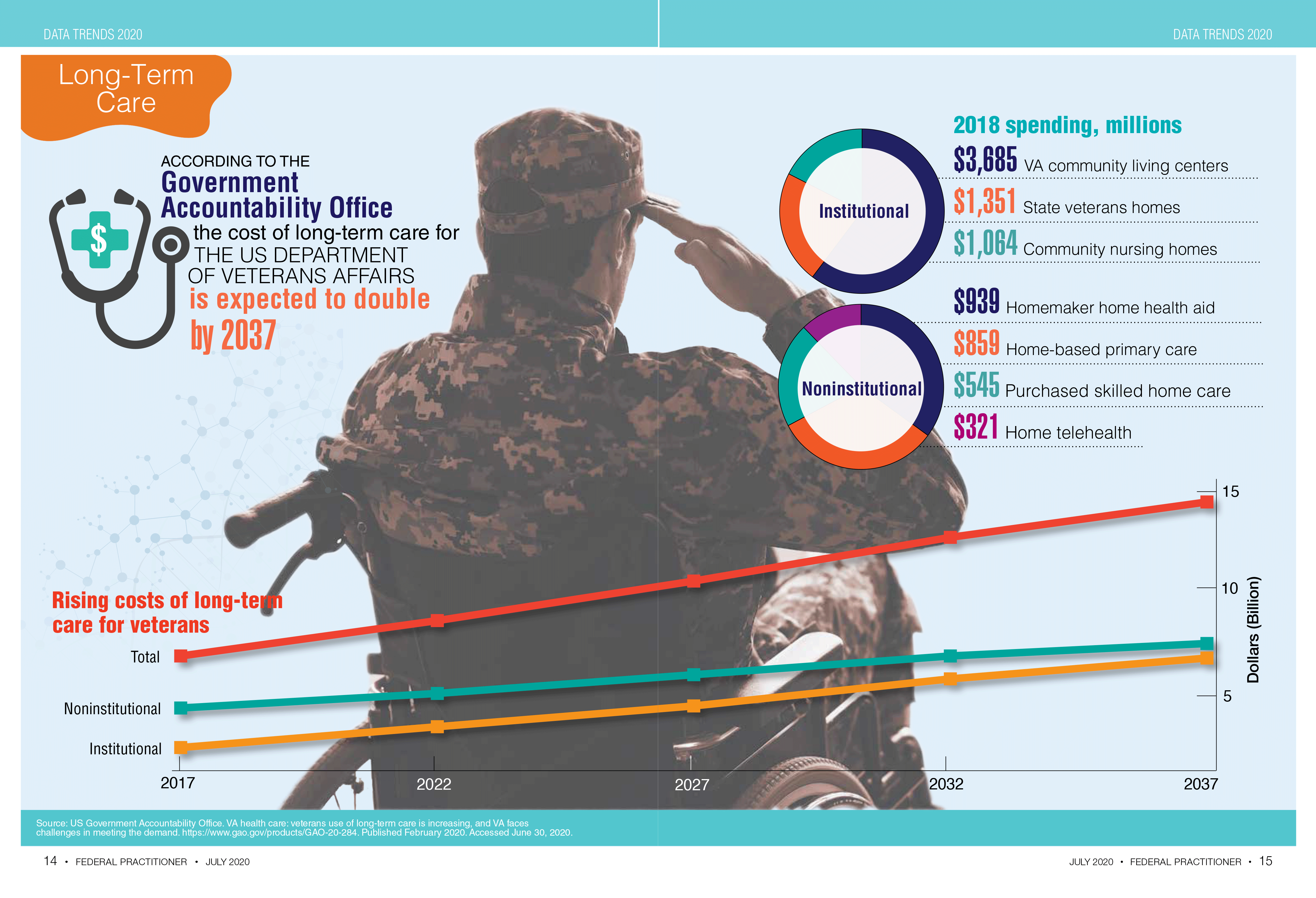
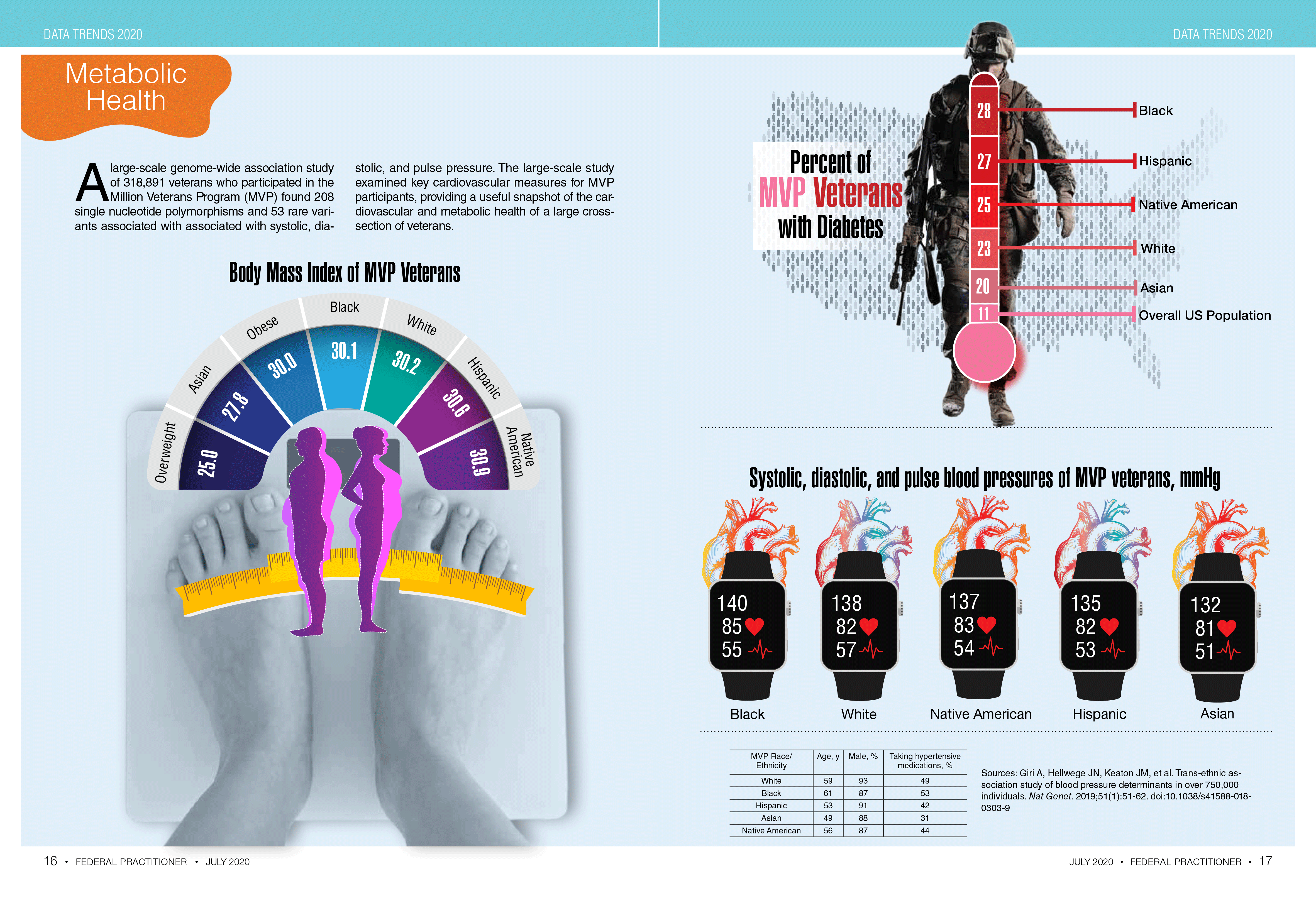
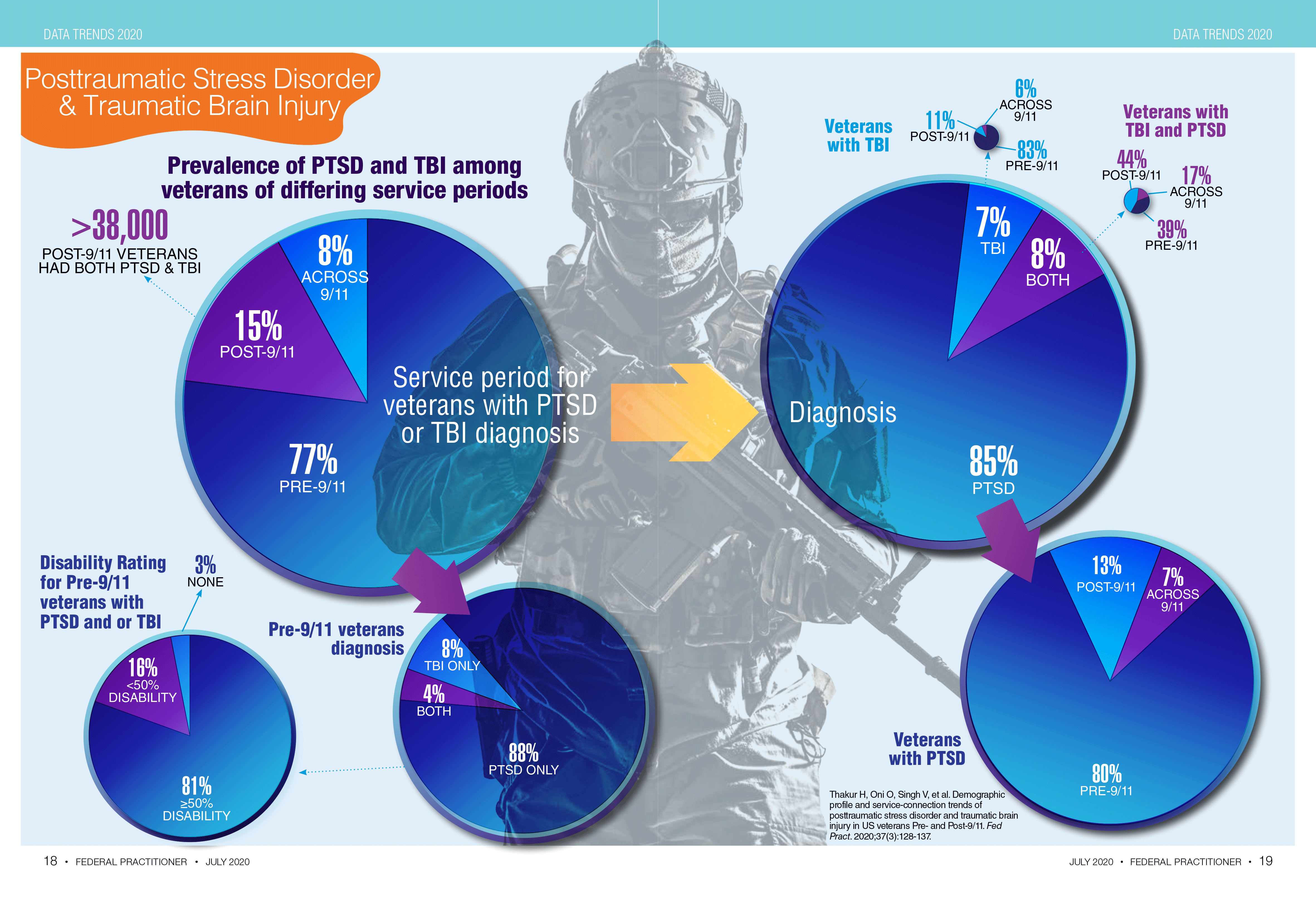
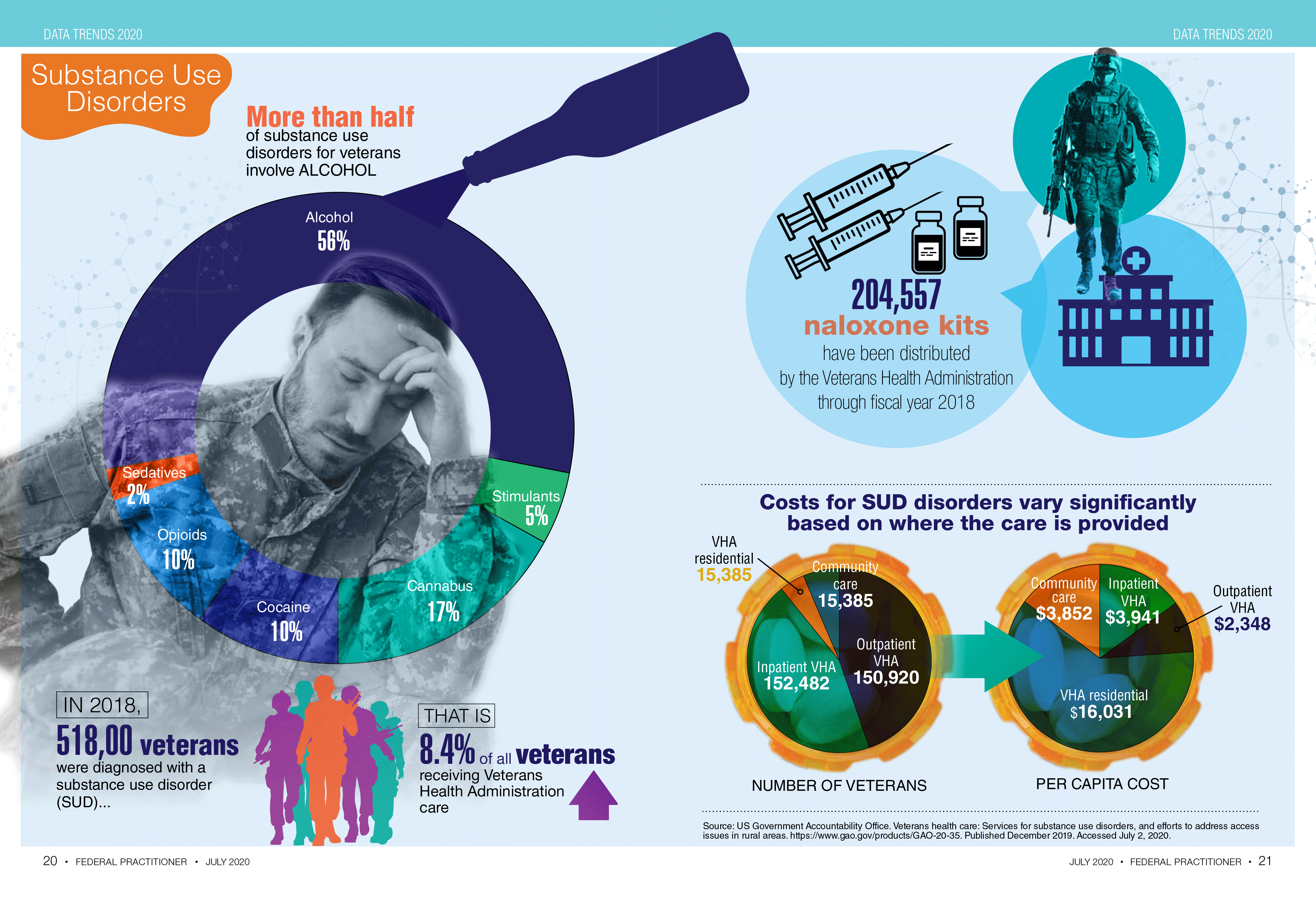
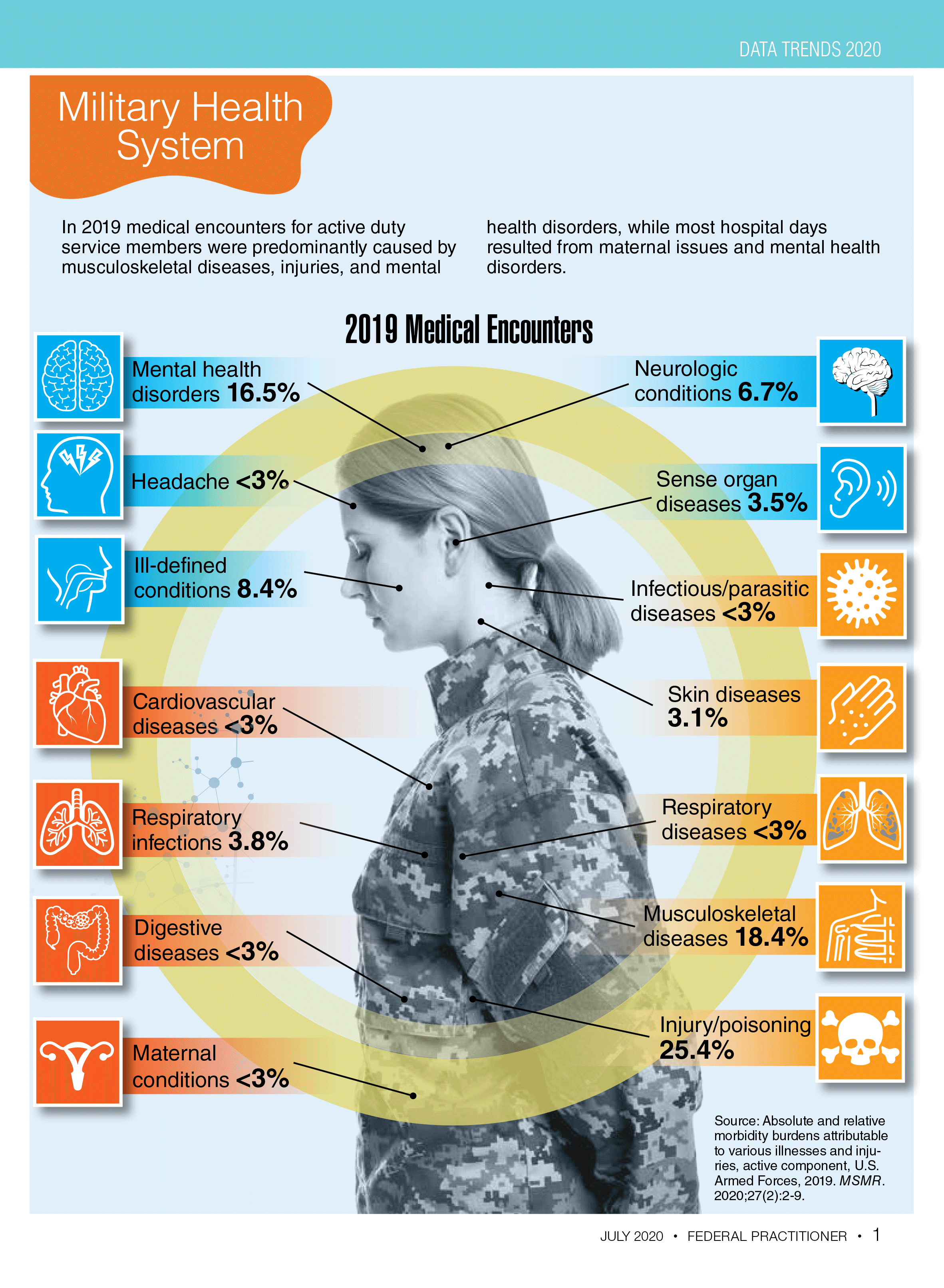
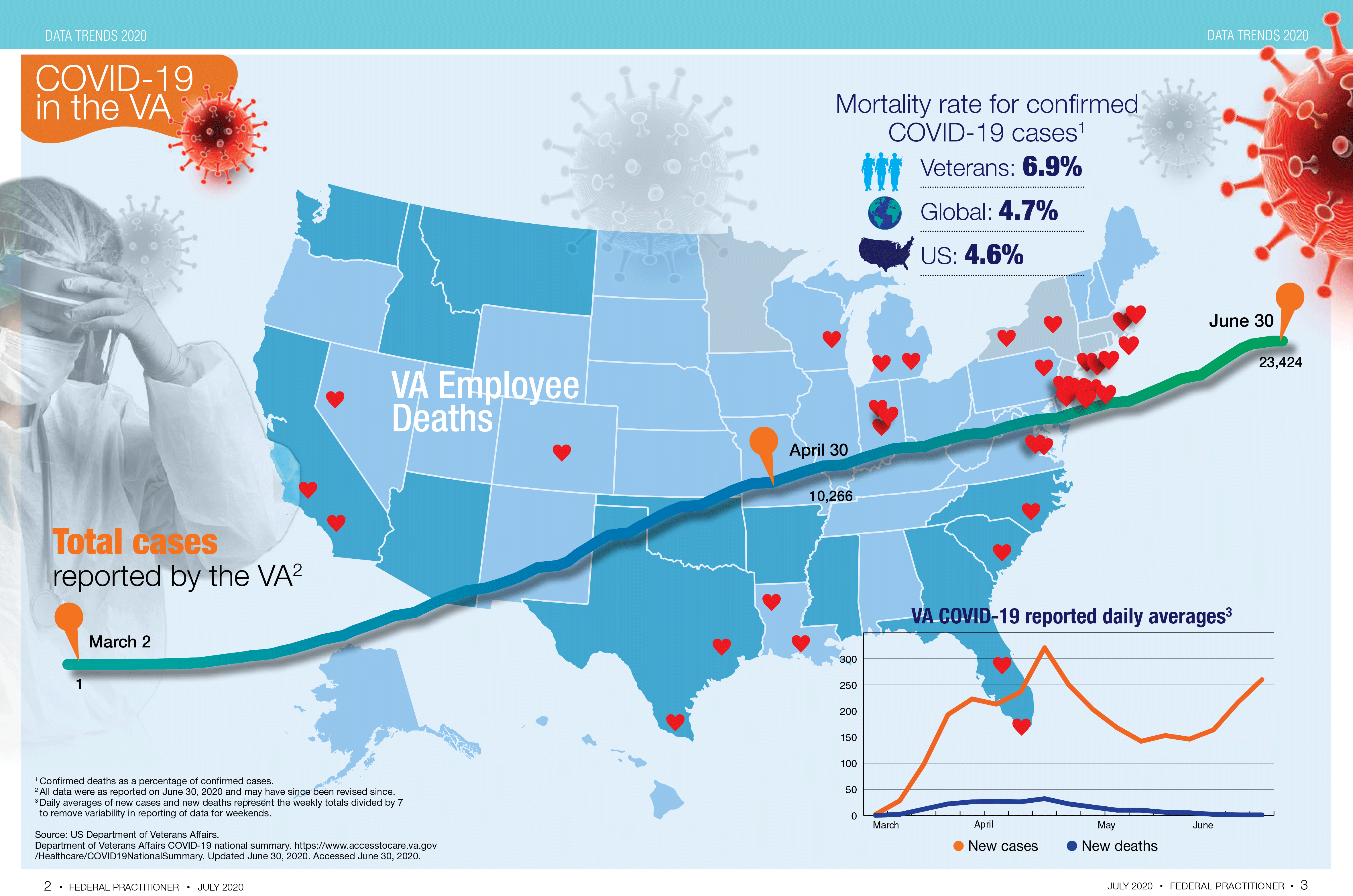

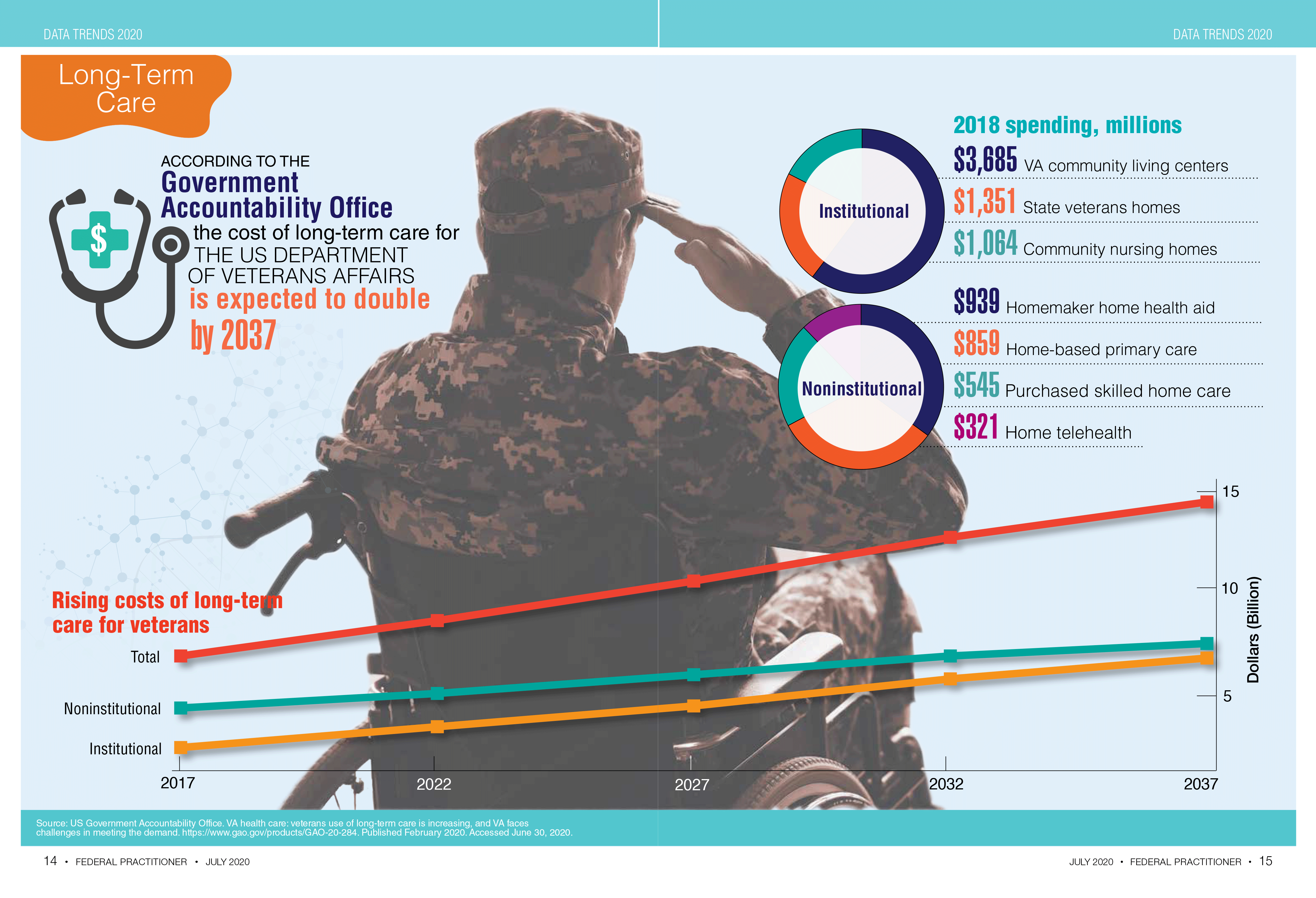
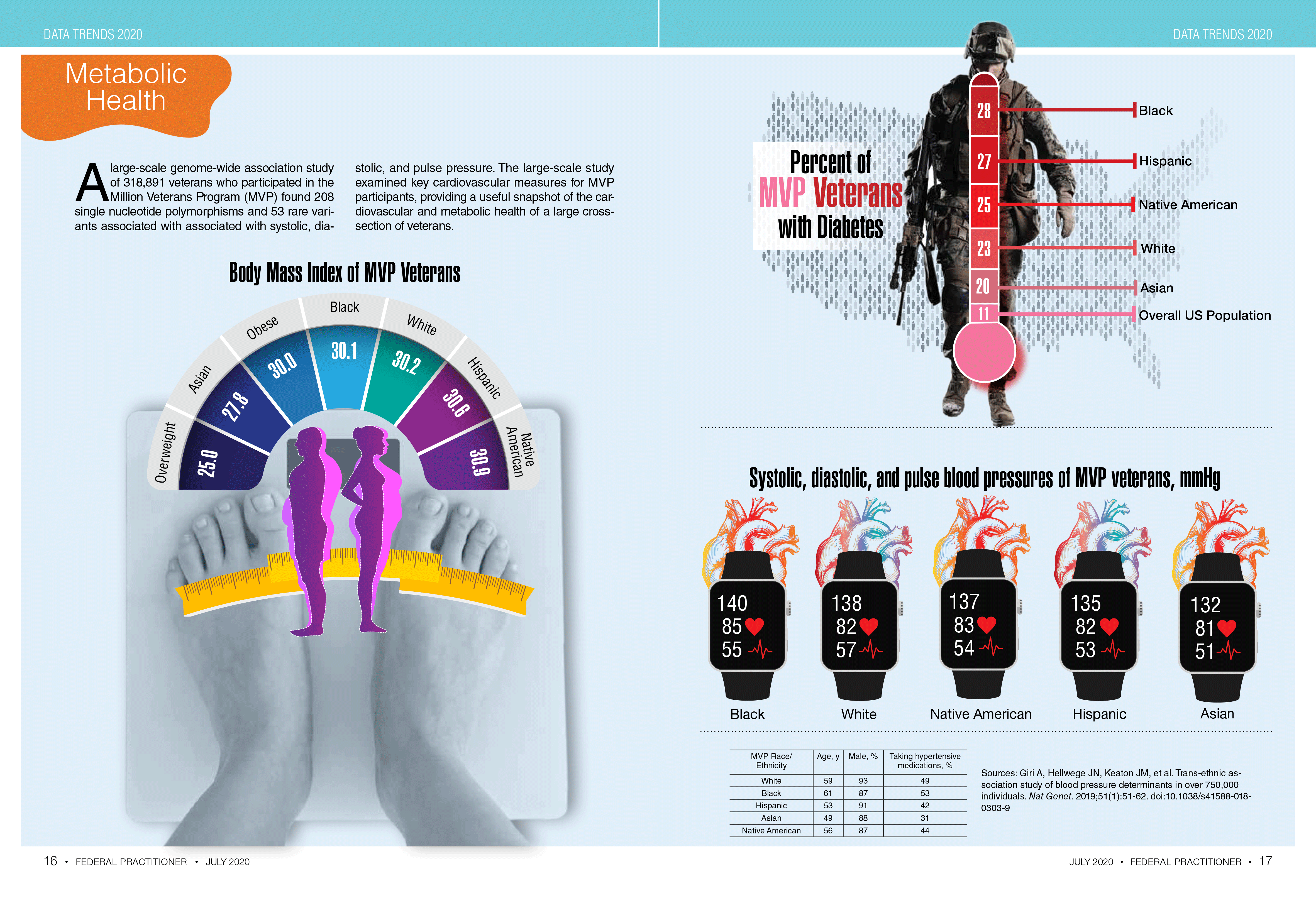
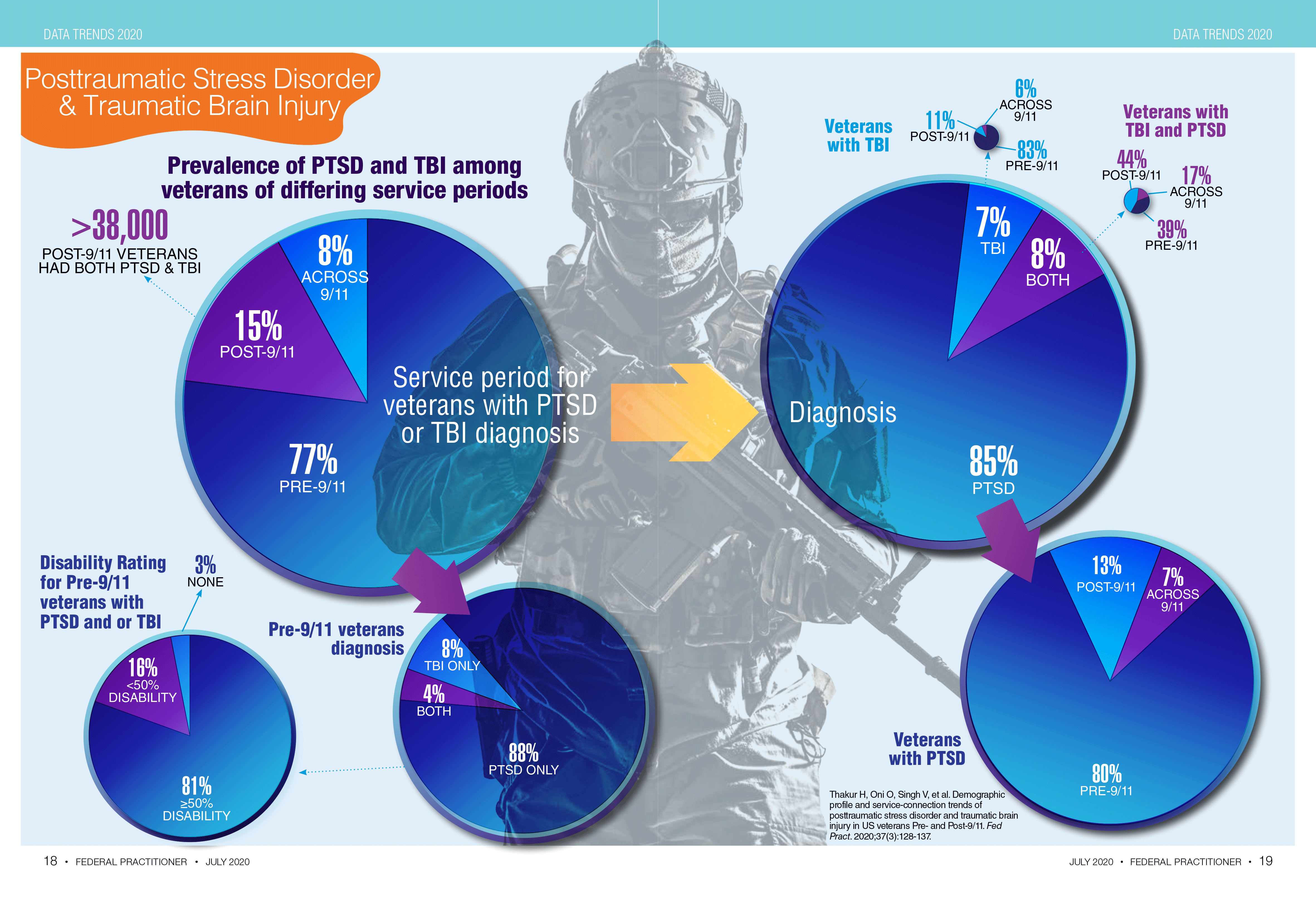
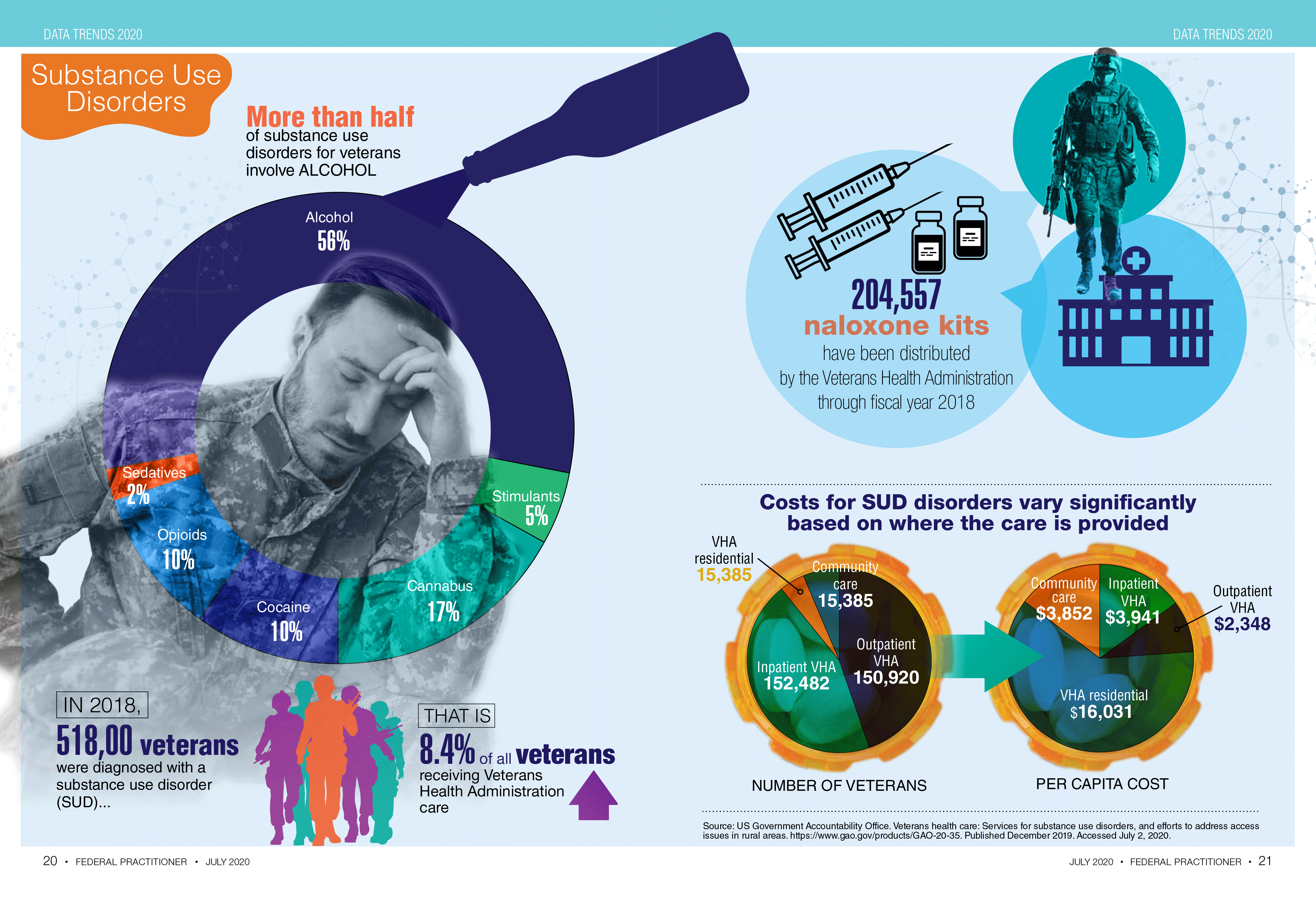
Sleepless in the pandemic
Sleep difficulties during the COVID-19 crisis may be exacerbated by media overexposure and other factors causing fear and stress, according to findings from a large survey of French individuals.
“Physicians usually recommend coping with sleep disorders by exercising, going outside, avoiding screen time, and having a regular schedule – all recommendations difficult to apply during lockdown. Being forced to stay home and the ensuing boredom and loneliness may have led to increased [media exposure], especially among disadvantaged people and overexposure to media COVID-19 content may have contributed to fright and emotional distress,” Damien Leger of the Centre du Sommeil et de la Vigilance, Hôtel Dieu APHP, Université de Paris, and his colleagues wrote in the journal Sleep.
The investigators analyzed data from survey respondents about their sleep problems since the COVID-19 lockdown and other topics such as employment, daily activities, and sleep medications. The survey was part of a large research project, COCONEL, that has been developed to study the French population on a variety of behaviors and comprises 750,000 permanent panelists who respond to surveys. The survey was sent to random sample of panelists with no topic label to avoid selection bias. Of the 25,800 surveys sent, 1,005 responses were recorded.
Respondents were classified as having severe sleep problems if they reported that their daytime activities were affected or if their sleeping medications had increased since the lockdown. While 73% of respondents reported poor sleep in the 8 previous days, 25% reported severe sleep problems, and 54% reported that their sleep problems had worsened during the COVID-19 lockdown.
A media exposure score was created with a Likert scale (strongly agree, agree, disagree, strongly disagree) about media exposures of different types. The investigators also queried respondents about the degree to which they found media coverage of the pandemic provoked a fear response. Overall, 68% of respondents agreed that media images and stories about COVD-19 were frightening.
The researchers found a strong association between severe sleeping problems and a high media exposure score (risk ratio, 1.49; 95% confidence interval, 1.10-2.01; P < .05).
In addition, trepidation and fear from media exposure to COVID-19 news were also associated with severe sleep problems (RR, 1.27; 95% CI, 0.92-1.75; P < .05). “Suffering from sleep problems may have increased media use at night, and thus increased stress and/or psychological distress and reinforced sleeping problems,” the investigators wrote.
Not surprisingly, respondents with financial difficulties due to the pandemic also reported severe sleeping difficulties (RR, 1.99; 95% CI, 1.49-2.65; P < .05).
For individuals who have been treated for sleep problems, the COVID-19 pandemic may ratchet up their sleep challenges. The strongest association with severe sleep problems was found in those respondents who were already taking sleeping medications before the pandemic (RR, 2.72; 95% CI, 2.04-3.61; P < .05).
The COCONEL survey has been funded by the French and National Agency for Research, the Fondation de France, and the National Research Institute for Sustainable Development.
SOURCE: Leger D et al. Sleep. 2020, Jul 25. doi: 10.1093/sleep/zsaa125.
Sleep difficulties during the COVID-19 crisis may be exacerbated by media overexposure and other factors causing fear and stress, according to findings from a large survey of French individuals.
“Physicians usually recommend coping with sleep disorders by exercising, going outside, avoiding screen time, and having a regular schedule – all recommendations difficult to apply during lockdown. Being forced to stay home and the ensuing boredom and loneliness may have led to increased [media exposure], especially among disadvantaged people and overexposure to media COVID-19 content may have contributed to fright and emotional distress,” Damien Leger of the Centre du Sommeil et de la Vigilance, Hôtel Dieu APHP, Université de Paris, and his colleagues wrote in the journal Sleep.
The investigators analyzed data from survey respondents about their sleep problems since the COVID-19 lockdown and other topics such as employment, daily activities, and sleep medications. The survey was part of a large research project, COCONEL, that has been developed to study the French population on a variety of behaviors and comprises 750,000 permanent panelists who respond to surveys. The survey was sent to random sample of panelists with no topic label to avoid selection bias. Of the 25,800 surveys sent, 1,005 responses were recorded.
Respondents were classified as having severe sleep problems if they reported that their daytime activities were affected or if their sleeping medications had increased since the lockdown. While 73% of respondents reported poor sleep in the 8 previous days, 25% reported severe sleep problems, and 54% reported that their sleep problems had worsened during the COVID-19 lockdown.
A media exposure score was created with a Likert scale (strongly agree, agree, disagree, strongly disagree) about media exposures of different types. The investigators also queried respondents about the degree to which they found media coverage of the pandemic provoked a fear response. Overall, 68% of respondents agreed that media images and stories about COVD-19 were frightening.
The researchers found a strong association between severe sleeping problems and a high media exposure score (risk ratio, 1.49; 95% confidence interval, 1.10-2.01; P < .05).
In addition, trepidation and fear from media exposure to COVID-19 news were also associated with severe sleep problems (RR, 1.27; 95% CI, 0.92-1.75; P < .05). “Suffering from sleep problems may have increased media use at night, and thus increased stress and/or psychological distress and reinforced sleeping problems,” the investigators wrote.
Not surprisingly, respondents with financial difficulties due to the pandemic also reported severe sleeping difficulties (RR, 1.99; 95% CI, 1.49-2.65; P < .05).
For individuals who have been treated for sleep problems, the COVID-19 pandemic may ratchet up their sleep challenges. The strongest association with severe sleep problems was found in those respondents who were already taking sleeping medications before the pandemic (RR, 2.72; 95% CI, 2.04-3.61; P < .05).
The COCONEL survey has been funded by the French and National Agency for Research, the Fondation de France, and the National Research Institute for Sustainable Development.
SOURCE: Leger D et al. Sleep. 2020, Jul 25. doi: 10.1093/sleep/zsaa125.
Sleep difficulties during the COVID-19 crisis may be exacerbated by media overexposure and other factors causing fear and stress, according to findings from a large survey of French individuals.
“Physicians usually recommend coping with sleep disorders by exercising, going outside, avoiding screen time, and having a regular schedule – all recommendations difficult to apply during lockdown. Being forced to stay home and the ensuing boredom and loneliness may have led to increased [media exposure], especially among disadvantaged people and overexposure to media COVID-19 content may have contributed to fright and emotional distress,” Damien Leger of the Centre du Sommeil et de la Vigilance, Hôtel Dieu APHP, Université de Paris, and his colleagues wrote in the journal Sleep.
The investigators analyzed data from survey respondents about their sleep problems since the COVID-19 lockdown and other topics such as employment, daily activities, and sleep medications. The survey was part of a large research project, COCONEL, that has been developed to study the French population on a variety of behaviors and comprises 750,000 permanent panelists who respond to surveys. The survey was sent to random sample of panelists with no topic label to avoid selection bias. Of the 25,800 surveys sent, 1,005 responses were recorded.
Respondents were classified as having severe sleep problems if they reported that their daytime activities were affected or if their sleeping medications had increased since the lockdown. While 73% of respondents reported poor sleep in the 8 previous days, 25% reported severe sleep problems, and 54% reported that their sleep problems had worsened during the COVID-19 lockdown.
A media exposure score was created with a Likert scale (strongly agree, agree, disagree, strongly disagree) about media exposures of different types. The investigators also queried respondents about the degree to which they found media coverage of the pandemic provoked a fear response. Overall, 68% of respondents agreed that media images and stories about COVD-19 were frightening.
The researchers found a strong association between severe sleeping problems and a high media exposure score (risk ratio, 1.49; 95% confidence interval, 1.10-2.01; P < .05).
In addition, trepidation and fear from media exposure to COVID-19 news were also associated with severe sleep problems (RR, 1.27; 95% CI, 0.92-1.75; P < .05). “Suffering from sleep problems may have increased media use at night, and thus increased stress and/or psychological distress and reinforced sleeping problems,” the investigators wrote.
Not surprisingly, respondents with financial difficulties due to the pandemic also reported severe sleeping difficulties (RR, 1.99; 95% CI, 1.49-2.65; P < .05).
For individuals who have been treated for sleep problems, the COVID-19 pandemic may ratchet up their sleep challenges. The strongest association with severe sleep problems was found in those respondents who were already taking sleeping medications before the pandemic (RR, 2.72; 95% CI, 2.04-3.61; P < .05).
The COCONEL survey has been funded by the French and National Agency for Research, the Fondation de France, and the National Research Institute for Sustainable Development.
SOURCE: Leger D et al. Sleep. 2020, Jul 25. doi: 10.1093/sleep/zsaa125.
FROM SLEEP
In a first, proton therapy bests radiotherapy in an RCT
Less toxicity in esophageal cancer
The results, from 107 evaluable patients, were published online July 25 in the Journal of Clinical Oncology.
Proton therapy significantly reduced the total toxicity burden (TTB), a coprimary endpoint, report the study authors, led by Steven Lin, MD, of the University of Texas MD Anderson Cancer Center in Houston.
However, the investigators of the single-center trial acknowledge that the better toxicity outcome is accompanied by a caveat: TTB, which combines 11 adverse effects, was not a previously validated endpoint.
Efficacy was similar. Proton therapy and intensity-modulated radiotherapy (IMRT) had nearly identical 3-year rates of progression-free survival (50.8% vs 51.2%), the other coprimary endpoint, as well as overall survival (44.5% vs 44.5%). Median follow-up was 44.1 months.
Quality of life outcomes were also not significantly different in the phase 2B trial, which was underpowered due to protocol anomalies, including 22 patients who were randomized to proton therapy but then denied insurance coverage, and thus participation in the trial.
Lack of validation of TTB “dampens the enthusiasm of a positive primary endpoint,” writes Charles Simone, MD, of the New York Proton Center and Memorial Sloan Kettering Cancer Center, New York City, in an accompanying editorial.
TTB encompasses seven postoperative complications measured up to 30 days after surgery (such as reintubation) and six toxicities measured up to 12 months from randomization (such as pleural effusion and radiation pneumonitis); two of the adverse events — atrial fibrillation and pneumonia — were included in both categories, depending on the timing of the event.
The posterior mean TTB, which is a synthesis of the cumulative severity of adverse events, was 2.3 times higher for IMRT (39.9) than for proton therapy (17.4), the investigators report.
Simone believes the TTB measure — and associated significant reduction in events with protons compared to IMRT in the current study — has value, especially in “high-stakes malignancies” such as esophageal and lung cancers.
“They are two of only a few cancers where there is an expected mortality rate from treatment,” he told Medscape Medical News. “For proton therapy to reduce those toxicities [measured by TTB in esophageal patients] may be a real benefit.”
Asked for independent comment, Mark Langer, MD, IU Health Simon Cancer Center, Indiana, Indianapolis, said “the novel TTB was well put together and is a credit to the investigators.”
He explained that the esophagus is typically the focus of complications, but that events like atrial fibrillation are important because the esophagus runs down to the stomach and passes by the lungs and heart. “The investigators call attention to morbidities that we may not have previously recognized,” said Langer, a radiation oncologist who does not use protons, as Indiana does not have a unit.
Reduced toxicity is the main claim for superiority for proton therapy over conventional radiotherapy, but to date there has been little clinical evidence.
For example, a randomized trial in inoperable lung cancer published 2 years ago showed that proton therapy was not superior in reducing serious lung toxicity compared with IMRT.
“That trial really disillusioned a lot of people,” Simone commented.
But he points out that protons have been found to be superior compared with photon radiation in terms of toxicity in a variety of observational studies, including multicenter retrospective comparative analyses.
Trial closed early
The RCT conducted by Lin and colleagues, which began in 2012, randomly assigned 145 patients with newly diagnosed locally advanced esophageal cancer to one of the two modalities (72 IMRT and 73 proton therapy). The investigators allowed a wide variety of patients, including those with ECOG performance status 2, differing tumor locations, squamous cell and adenocarcinoma histologies, and unresectable and potentially resectable cases. However, only 107 patients were evaluable (61 IMRT and 46 proton therapy), as the trial did not report on those afore-mentioned patients denied insurance coverage for proton therapy after randomization and those patients in the IMRT group who refused that treatment and wanted proton therapy.
Patients received 50.4 Gy (CGE) with concurrent chemotherapy and 51 patients underwent surgery, generally 8-10 weeks following chemoradiation.
The full list of adverse events for the TTB measure for toxicities was atrial fibrillation, myocardial infarction, pericardial effusion, pleural effusion, pneumonia, and radiation pneumonitis. For post-op complications, the list was acute respiratory distress syndrome, anastomotic leak, atrial fibrillation, pulmonary embolism, reintubation, stroke, and pneumonia.
The most common toxicity was pleural effusion (in 24 patients on IMRT and 13 on proton therapy). The most common post-op complication was atrial fibrillation (in seven patients on IMRT and two on proton therapy).
Simone points out that combining these adverse events in the TTB measure allowed a relatively small number of participants and events to show statistically significant results “without statistically apparent differences for [some] individual events.”
The investigators highlight the fact that 80% of patients in the proton group received passive scattering proton therapy, an older technology that increases normal tissue exposure relative to more modern intensity-modulated proton therapy.
The trial closed early because of the start of the phase 3 NRG-GI006 trial. The stoppage was just before the preplanned third and final interim analysis, which would have exceeded the trial’s stopping boundary (due to a positive result for TTB).
“The now-activated NRG-GI006 phase 3 randomized trial should prove to be the gold standard comparison of protons versus IMRT for esophageal cancer,” writes Simone in his editorial.
The trial was supported by National Cancer Institute. Multiple study authors have financial ties to industry, including radiation therapy manufacturers. Simone has reported financial ties to Varian Medical Systems. Langer has reported no relevant financial relationships.
This article first appeared on Medscape.com.
Less toxicity in esophageal cancer
Less toxicity in esophageal cancer
The results, from 107 evaluable patients, were published online July 25 in the Journal of Clinical Oncology.
Proton therapy significantly reduced the total toxicity burden (TTB), a coprimary endpoint, report the study authors, led by Steven Lin, MD, of the University of Texas MD Anderson Cancer Center in Houston.
However, the investigators of the single-center trial acknowledge that the better toxicity outcome is accompanied by a caveat: TTB, which combines 11 adverse effects, was not a previously validated endpoint.
Efficacy was similar. Proton therapy and intensity-modulated radiotherapy (IMRT) had nearly identical 3-year rates of progression-free survival (50.8% vs 51.2%), the other coprimary endpoint, as well as overall survival (44.5% vs 44.5%). Median follow-up was 44.1 months.
Quality of life outcomes were also not significantly different in the phase 2B trial, which was underpowered due to protocol anomalies, including 22 patients who were randomized to proton therapy but then denied insurance coverage, and thus participation in the trial.
Lack of validation of TTB “dampens the enthusiasm of a positive primary endpoint,” writes Charles Simone, MD, of the New York Proton Center and Memorial Sloan Kettering Cancer Center, New York City, in an accompanying editorial.
TTB encompasses seven postoperative complications measured up to 30 days after surgery (such as reintubation) and six toxicities measured up to 12 months from randomization (such as pleural effusion and radiation pneumonitis); two of the adverse events — atrial fibrillation and pneumonia — were included in both categories, depending on the timing of the event.
The posterior mean TTB, which is a synthesis of the cumulative severity of adverse events, was 2.3 times higher for IMRT (39.9) than for proton therapy (17.4), the investigators report.
Simone believes the TTB measure — and associated significant reduction in events with protons compared to IMRT in the current study — has value, especially in “high-stakes malignancies” such as esophageal and lung cancers.
“They are two of only a few cancers where there is an expected mortality rate from treatment,” he told Medscape Medical News. “For proton therapy to reduce those toxicities [measured by TTB in esophageal patients] may be a real benefit.”
Asked for independent comment, Mark Langer, MD, IU Health Simon Cancer Center, Indiana, Indianapolis, said “the novel TTB was well put together and is a credit to the investigators.”
He explained that the esophagus is typically the focus of complications, but that events like atrial fibrillation are important because the esophagus runs down to the stomach and passes by the lungs and heart. “The investigators call attention to morbidities that we may not have previously recognized,” said Langer, a radiation oncologist who does not use protons, as Indiana does not have a unit.
Reduced toxicity is the main claim for superiority for proton therapy over conventional radiotherapy, but to date there has been little clinical evidence.
For example, a randomized trial in inoperable lung cancer published 2 years ago showed that proton therapy was not superior in reducing serious lung toxicity compared with IMRT.
“That trial really disillusioned a lot of people,” Simone commented.
But he points out that protons have been found to be superior compared with photon radiation in terms of toxicity in a variety of observational studies, including multicenter retrospective comparative analyses.
Trial closed early
The RCT conducted by Lin and colleagues, which began in 2012, randomly assigned 145 patients with newly diagnosed locally advanced esophageal cancer to one of the two modalities (72 IMRT and 73 proton therapy). The investigators allowed a wide variety of patients, including those with ECOG performance status 2, differing tumor locations, squamous cell and adenocarcinoma histologies, and unresectable and potentially resectable cases. However, only 107 patients were evaluable (61 IMRT and 46 proton therapy), as the trial did not report on those afore-mentioned patients denied insurance coverage for proton therapy after randomization and those patients in the IMRT group who refused that treatment and wanted proton therapy.
Patients received 50.4 Gy (CGE) with concurrent chemotherapy and 51 patients underwent surgery, generally 8-10 weeks following chemoradiation.
The full list of adverse events for the TTB measure for toxicities was atrial fibrillation, myocardial infarction, pericardial effusion, pleural effusion, pneumonia, and radiation pneumonitis. For post-op complications, the list was acute respiratory distress syndrome, anastomotic leak, atrial fibrillation, pulmonary embolism, reintubation, stroke, and pneumonia.
The most common toxicity was pleural effusion (in 24 patients on IMRT and 13 on proton therapy). The most common post-op complication was atrial fibrillation (in seven patients on IMRT and two on proton therapy).
Simone points out that combining these adverse events in the TTB measure allowed a relatively small number of participants and events to show statistically significant results “without statistically apparent differences for [some] individual events.”
The investigators highlight the fact that 80% of patients in the proton group received passive scattering proton therapy, an older technology that increases normal tissue exposure relative to more modern intensity-modulated proton therapy.
The trial closed early because of the start of the phase 3 NRG-GI006 trial. The stoppage was just before the preplanned third and final interim analysis, which would have exceeded the trial’s stopping boundary (due to a positive result for TTB).
“The now-activated NRG-GI006 phase 3 randomized trial should prove to be the gold standard comparison of protons versus IMRT for esophageal cancer,” writes Simone in his editorial.
The trial was supported by National Cancer Institute. Multiple study authors have financial ties to industry, including radiation therapy manufacturers. Simone has reported financial ties to Varian Medical Systems. Langer has reported no relevant financial relationships.
This article first appeared on Medscape.com.
The results, from 107 evaluable patients, were published online July 25 in the Journal of Clinical Oncology.
Proton therapy significantly reduced the total toxicity burden (TTB), a coprimary endpoint, report the study authors, led by Steven Lin, MD, of the University of Texas MD Anderson Cancer Center in Houston.
However, the investigators of the single-center trial acknowledge that the better toxicity outcome is accompanied by a caveat: TTB, which combines 11 adverse effects, was not a previously validated endpoint.
Efficacy was similar. Proton therapy and intensity-modulated radiotherapy (IMRT) had nearly identical 3-year rates of progression-free survival (50.8% vs 51.2%), the other coprimary endpoint, as well as overall survival (44.5% vs 44.5%). Median follow-up was 44.1 months.
Quality of life outcomes were also not significantly different in the phase 2B trial, which was underpowered due to protocol anomalies, including 22 patients who were randomized to proton therapy but then denied insurance coverage, and thus participation in the trial.
Lack of validation of TTB “dampens the enthusiasm of a positive primary endpoint,” writes Charles Simone, MD, of the New York Proton Center and Memorial Sloan Kettering Cancer Center, New York City, in an accompanying editorial.
TTB encompasses seven postoperative complications measured up to 30 days after surgery (such as reintubation) and six toxicities measured up to 12 months from randomization (such as pleural effusion and radiation pneumonitis); two of the adverse events — atrial fibrillation and pneumonia — were included in both categories, depending on the timing of the event.
The posterior mean TTB, which is a synthesis of the cumulative severity of adverse events, was 2.3 times higher for IMRT (39.9) than for proton therapy (17.4), the investigators report.
Simone believes the TTB measure — and associated significant reduction in events with protons compared to IMRT in the current study — has value, especially in “high-stakes malignancies” such as esophageal and lung cancers.
“They are two of only a few cancers where there is an expected mortality rate from treatment,” he told Medscape Medical News. “For proton therapy to reduce those toxicities [measured by TTB in esophageal patients] may be a real benefit.”
Asked for independent comment, Mark Langer, MD, IU Health Simon Cancer Center, Indiana, Indianapolis, said “the novel TTB was well put together and is a credit to the investigators.”
He explained that the esophagus is typically the focus of complications, but that events like atrial fibrillation are important because the esophagus runs down to the stomach and passes by the lungs and heart. “The investigators call attention to morbidities that we may not have previously recognized,” said Langer, a radiation oncologist who does not use protons, as Indiana does not have a unit.
Reduced toxicity is the main claim for superiority for proton therapy over conventional radiotherapy, but to date there has been little clinical evidence.
For example, a randomized trial in inoperable lung cancer published 2 years ago showed that proton therapy was not superior in reducing serious lung toxicity compared with IMRT.
“That trial really disillusioned a lot of people,” Simone commented.
But he points out that protons have been found to be superior compared with photon radiation in terms of toxicity in a variety of observational studies, including multicenter retrospective comparative analyses.
Trial closed early
The RCT conducted by Lin and colleagues, which began in 2012, randomly assigned 145 patients with newly diagnosed locally advanced esophageal cancer to one of the two modalities (72 IMRT and 73 proton therapy). The investigators allowed a wide variety of patients, including those with ECOG performance status 2, differing tumor locations, squamous cell and adenocarcinoma histologies, and unresectable and potentially resectable cases. However, only 107 patients were evaluable (61 IMRT and 46 proton therapy), as the trial did not report on those afore-mentioned patients denied insurance coverage for proton therapy after randomization and those patients in the IMRT group who refused that treatment and wanted proton therapy.
Patients received 50.4 Gy (CGE) with concurrent chemotherapy and 51 patients underwent surgery, generally 8-10 weeks following chemoradiation.
The full list of adverse events for the TTB measure for toxicities was atrial fibrillation, myocardial infarction, pericardial effusion, pleural effusion, pneumonia, and radiation pneumonitis. For post-op complications, the list was acute respiratory distress syndrome, anastomotic leak, atrial fibrillation, pulmonary embolism, reintubation, stroke, and pneumonia.
The most common toxicity was pleural effusion (in 24 patients on IMRT and 13 on proton therapy). The most common post-op complication was atrial fibrillation (in seven patients on IMRT and two on proton therapy).
Simone points out that combining these adverse events in the TTB measure allowed a relatively small number of participants and events to show statistically significant results “without statistically apparent differences for [some] individual events.”
The investigators highlight the fact that 80% of patients in the proton group received passive scattering proton therapy, an older technology that increases normal tissue exposure relative to more modern intensity-modulated proton therapy.
The trial closed early because of the start of the phase 3 NRG-GI006 trial. The stoppage was just before the preplanned third and final interim analysis, which would have exceeded the trial’s stopping boundary (due to a positive result for TTB).
“The now-activated NRG-GI006 phase 3 randomized trial should prove to be the gold standard comparison of protons versus IMRT for esophageal cancer,” writes Simone in his editorial.
The trial was supported by National Cancer Institute. Multiple study authors have financial ties to industry, including radiation therapy manufacturers. Simone has reported financial ties to Varian Medical Systems. Langer has reported no relevant financial relationships.
This article first appeared on Medscape.com.
Diagnosing and Managing Tardive Dyskinesia

Click here to read the supplement and earn free CME/CE credits by learning about TD and evidence based treatments.
Educational Objectives
- Discuss the diagnosis, differential diagnosis and risk factors for TD
- Identify the prevalence of TD with antipsychotics
- Use the AIMS examination
- Review the evidence and non-evidence based treatments for TD
- Individualize treatment choices, giving consideration to efficacy, safety, long-term data, and unique patient characteristics
- Formulate appropriate treatment regimens considering
the emergence of new FDA approved treatments for TD
Click here to read the supplement.

Click here to read the supplement and earn free CME/CE credits by learning about TD and evidence based treatments.
Educational Objectives
- Discuss the diagnosis, differential diagnosis and risk factors for TD
- Identify the prevalence of TD with antipsychotics
- Use the AIMS examination
- Review the evidence and non-evidence based treatments for TD
- Individualize treatment choices, giving consideration to efficacy, safety, long-term data, and unique patient characteristics
- Formulate appropriate treatment regimens considering
the emergence of new FDA approved treatments for TD
Click here to read the supplement.

Click here to read the supplement and earn free CME/CE credits by learning about TD and evidence based treatments.
Educational Objectives
- Discuss the diagnosis, differential diagnosis and risk factors for TD
- Identify the prevalence of TD with antipsychotics
- Use the AIMS examination
- Review the evidence and non-evidence based treatments for TD
- Individualize treatment choices, giving consideration to efficacy, safety, long-term data, and unique patient characteristics
- Formulate appropriate treatment regimens considering
the emergence of new FDA approved treatments for TD
Click here to read the supplement.
Experimental blood test detects cancer years before symptoms
A blood test that may be able to detect cancer years before any symptoms appear is under development. The PanSeer assay, which detects methylation markers in blood, was used in healthy individuals and successfully detected five cancer types in 91% of samples from individuals who were diagnosed with cancer 1 to 4 years later.
“We can’t say for sure that the patients didn’t have any symptoms, but we detected the cancer years before they ever walked into the hospital,” said study author Kun Zhang, PhD, a professor of bioengineering at the University of California, San Diego. “We were also able to follow up with patients, so we actually knew that they had cancer.”
Zhang noted that they also followed the individuals whose tests indicated they were cancer free. “They were healthy at the time the samples were obtained, and they remained healthy,” he said. “Follow-up was key to validating these data.”
The PanSeer test is being developed by Singlera Genomics. Zhang is a cofounder and a paid consultant of the company.
The study was published online July 21 in Nature Communications.
Unique among tests
Several blood tests for the detection of cancer have been reported in recent years. A test developed by Grail was able to detect more than 50 types of cancer and also identified the tissues where the cancer originated. The CancerSEEK test identified eight common cancers by measuring circulating tumor DNA from 16 genes, as well as eight protein biomarkers.
Findings regarding the CellMax Life FirstSight blood test were released last month. The test detected all 11 cases of colorectal cancer in a cohort of 354 patients and detected 40 of 53 advanced adenomas.
The latest study with the PanSeer assay is unique, say the investigators, because they had access to blood samples from patients who may have been completely asymptomatic and had not yet been diagnosed with cancer. Other blood tests have typically involved the use of specimens from people with a known diagnosis.
The specimens were collected as part of a 10-year longitudinal study that began in 2007 in China. Zhang and his team were able to test blood samples before individuals had experienced any signs or symptoms of cancer, and they were able to conduct long-term follow-up of the cohort.
Study details
The PanSeer assay uses DNA methylation analysis and screens for a DNA signature called CpG methylation. The results of an early-stage proof-of-concept study were published 3 years ago (Nat Genet. 2017;49:635–642).
For the current study, data were drawn from the Taizhou Longitudinal Study, which included 123,115 individuals aged 25 to 90 years who provided blood samples for long-term storage from 2007 to 2014. Participants were monitored indefinitely for cancer occurrence using local cancer registries and health insurance databases.
The team identified 575 individuals who were initially asymptomatic and healthy but were subsequently diagnosed with one of five common cancer types (stomach, esophagus, colorectum, lung, or liver cancer) within 4 years of their initial blood sampling. The authors selected these five cancer types to study because the incidence rates of these cancers in this population are high and, taken together, account for the highest mortality.
The study design allowed the authors to evaluate specimens both from patients with cancer and from those who were healthy within the same cohort. Using 191 prediagnosis samples, 223 postdiagnosis samples, and 414 healthy samples, they created a training set and validation model.
A machine learning method was created to classify samples as being either from healthy individuals or from those with cancer, using blood samples from the training set. The final classifier achieved 88% sensitivity for postdiagnosis samples and 91% sensitivity for prediagnosis samples at a specificity of 95%.
Zhang feels that initially it would be more appropriate to use the test for high-risk patients and to then evaluate the clinical benefit. “For any test, it is always more prudent to begin with a high-risk population,” he said. “You want to see some benefit with the high-risk population first, and then it can slowly be extended to others at lower risk.”
He emphasized that more rigorous testing is needing before the PanSeer assay is ready for clinical use. The logistics of designing and conducting a clinical trial that would include more than one cancer type would be very complicated. “The option was to break it down to five different studies,” he said. “We decided to begin with colon cancer, and we are currently in the process of talking with the FDA and designing the study.”
High bar to reach
Approached for comment, Benjamin Weinberg, MD, assistant professor of medicine, Division of Hematology and Oncology, the Lombardi Comprehensive Cancer Center, Georgetown University, Washington, DC, noted that there is “quite a ways to go before this can be clinically actionable.
“A lot of us are looking at combining methylation with circulating tumor DNA and throw the kitchen sink at it, but as the paper nicely describes, there are pros and cons to all of these,” he said.
Many tests of this type are in development. Weinberg explained that a circulating tumor DNA test for colon cancer may hit the market soon, pending FDA approval, although that test will be used in a different setting. “This is something that’s used to assess for minimal residual disease in patients who have undergone surgery and appear to be ‘cured’ of the disease,” he said. “The test is looking to see if there is any circulating tumor DNA being shed from whatever tumor is left behind.”
The type of test that has piqued the most interest is one that is “tumor informed,” meaning that the company receives tumor tissue and develops a personalized test of that tumor on the basis of tumor genetics. “That is a very targeted way of surveillance,” said Weinberg, “But it would be very difficult to use a tumor-informed test on the population described in this study because you don’t know if there is going to be a tumor or not.”
The PanSeer test may also prove difficult to use in the clinic because it detects multiple cancers, Weinberg said. “If there is a positive finding, then which cancer do you look for?” he commented. “It has an issue in that regard, and that’s the problem with this type of test, as it is easier if there is one site of origin.”
Overall, the test was fairly sensitive and specific, with a very low false negative rate. Going forward, he noted, there is a very high bar for tests used as screening tools, although the authors do say that their focus is for use in a high-risk population.
“There would have to be a randomized trial, and the test will have to show a survival benefit,” Weinberg said. He noted that it can sometimes be challenging to do so.
“Colonoscopy has been shown to be beneficial, but early mammography has become controversial, and prostate cancer is a whole different animal,” he added. “And these are established tests, and they show how difficult this can be.”
The Taizhou Longitudinal Study study was supported by the National Key Research and Development Program of China, the National Natural Science Foundation of China, the Key Basic Research grants from the Science and Technology Commission of Shanghai Municipality, the International S&T Cooperation Program of China, the Municipal Science and Technology Major Project program, the International Science and Technology Cooperation Program of China, and the 111 Project (B13016). Funding for the DNA methylation assays was provided by Singlera Genomics. Zhang is a cofounder, equity holder, and paid consultant of Singlera Genomics, a company that is developing early cancer detection tests, including the PanSeer test. Weinberg is a speaker or a member of a speakers bureau for Taiho Pharmaceutical Co Ltd, Bayer HealthCare Pharmaceuticals, and Eli Lilly and Company; has received research grant from Novartis Pharmaceuticals Corporation; and has received travel reimbursement from Caris Life Sciences.
This article first appeared on Medscape.com.
A blood test that may be able to detect cancer years before any symptoms appear is under development. The PanSeer assay, which detects methylation markers in blood, was used in healthy individuals and successfully detected five cancer types in 91% of samples from individuals who were diagnosed with cancer 1 to 4 years later.
“We can’t say for sure that the patients didn’t have any symptoms, but we detected the cancer years before they ever walked into the hospital,” said study author Kun Zhang, PhD, a professor of bioengineering at the University of California, San Diego. “We were also able to follow up with patients, so we actually knew that they had cancer.”
Zhang noted that they also followed the individuals whose tests indicated they were cancer free. “They were healthy at the time the samples were obtained, and they remained healthy,” he said. “Follow-up was key to validating these data.”
The PanSeer test is being developed by Singlera Genomics. Zhang is a cofounder and a paid consultant of the company.
The study was published online July 21 in Nature Communications.
Unique among tests
Several blood tests for the detection of cancer have been reported in recent years. A test developed by Grail was able to detect more than 50 types of cancer and also identified the tissues where the cancer originated. The CancerSEEK test identified eight common cancers by measuring circulating tumor DNA from 16 genes, as well as eight protein biomarkers.
Findings regarding the CellMax Life FirstSight blood test were released last month. The test detected all 11 cases of colorectal cancer in a cohort of 354 patients and detected 40 of 53 advanced adenomas.
The latest study with the PanSeer assay is unique, say the investigators, because they had access to blood samples from patients who may have been completely asymptomatic and had not yet been diagnosed with cancer. Other blood tests have typically involved the use of specimens from people with a known diagnosis.
The specimens were collected as part of a 10-year longitudinal study that began in 2007 in China. Zhang and his team were able to test blood samples before individuals had experienced any signs or symptoms of cancer, and they were able to conduct long-term follow-up of the cohort.
Study details
The PanSeer assay uses DNA methylation analysis and screens for a DNA signature called CpG methylation. The results of an early-stage proof-of-concept study were published 3 years ago (Nat Genet. 2017;49:635–642).
For the current study, data were drawn from the Taizhou Longitudinal Study, which included 123,115 individuals aged 25 to 90 years who provided blood samples for long-term storage from 2007 to 2014. Participants were monitored indefinitely for cancer occurrence using local cancer registries and health insurance databases.
The team identified 575 individuals who were initially asymptomatic and healthy but were subsequently diagnosed with one of five common cancer types (stomach, esophagus, colorectum, lung, or liver cancer) within 4 years of their initial blood sampling. The authors selected these five cancer types to study because the incidence rates of these cancers in this population are high and, taken together, account for the highest mortality.
The study design allowed the authors to evaluate specimens both from patients with cancer and from those who were healthy within the same cohort. Using 191 prediagnosis samples, 223 postdiagnosis samples, and 414 healthy samples, they created a training set and validation model.
A machine learning method was created to classify samples as being either from healthy individuals or from those with cancer, using blood samples from the training set. The final classifier achieved 88% sensitivity for postdiagnosis samples and 91% sensitivity for prediagnosis samples at a specificity of 95%.
Zhang feels that initially it would be more appropriate to use the test for high-risk patients and to then evaluate the clinical benefit. “For any test, it is always more prudent to begin with a high-risk population,” he said. “You want to see some benefit with the high-risk population first, and then it can slowly be extended to others at lower risk.”
He emphasized that more rigorous testing is needing before the PanSeer assay is ready for clinical use. The logistics of designing and conducting a clinical trial that would include more than one cancer type would be very complicated. “The option was to break it down to five different studies,” he said. “We decided to begin with colon cancer, and we are currently in the process of talking with the FDA and designing the study.”
High bar to reach
Approached for comment, Benjamin Weinberg, MD, assistant professor of medicine, Division of Hematology and Oncology, the Lombardi Comprehensive Cancer Center, Georgetown University, Washington, DC, noted that there is “quite a ways to go before this can be clinically actionable.
“A lot of us are looking at combining methylation with circulating tumor DNA and throw the kitchen sink at it, but as the paper nicely describes, there are pros and cons to all of these,” he said.
Many tests of this type are in development. Weinberg explained that a circulating tumor DNA test for colon cancer may hit the market soon, pending FDA approval, although that test will be used in a different setting. “This is something that’s used to assess for minimal residual disease in patients who have undergone surgery and appear to be ‘cured’ of the disease,” he said. “The test is looking to see if there is any circulating tumor DNA being shed from whatever tumor is left behind.”
The type of test that has piqued the most interest is one that is “tumor informed,” meaning that the company receives tumor tissue and develops a personalized test of that tumor on the basis of tumor genetics. “That is a very targeted way of surveillance,” said Weinberg, “But it would be very difficult to use a tumor-informed test on the population described in this study because you don’t know if there is going to be a tumor or not.”
The PanSeer test may also prove difficult to use in the clinic because it detects multiple cancers, Weinberg said. “If there is a positive finding, then which cancer do you look for?” he commented. “It has an issue in that regard, and that’s the problem with this type of test, as it is easier if there is one site of origin.”
Overall, the test was fairly sensitive and specific, with a very low false negative rate. Going forward, he noted, there is a very high bar for tests used as screening tools, although the authors do say that their focus is for use in a high-risk population.
“There would have to be a randomized trial, and the test will have to show a survival benefit,” Weinberg said. He noted that it can sometimes be challenging to do so.
“Colonoscopy has been shown to be beneficial, but early mammography has become controversial, and prostate cancer is a whole different animal,” he added. “And these are established tests, and they show how difficult this can be.”
The Taizhou Longitudinal Study study was supported by the National Key Research and Development Program of China, the National Natural Science Foundation of China, the Key Basic Research grants from the Science and Technology Commission of Shanghai Municipality, the International S&T Cooperation Program of China, the Municipal Science and Technology Major Project program, the International Science and Technology Cooperation Program of China, and the 111 Project (B13016). Funding for the DNA methylation assays was provided by Singlera Genomics. Zhang is a cofounder, equity holder, and paid consultant of Singlera Genomics, a company that is developing early cancer detection tests, including the PanSeer test. Weinberg is a speaker or a member of a speakers bureau for Taiho Pharmaceutical Co Ltd, Bayer HealthCare Pharmaceuticals, and Eli Lilly and Company; has received research grant from Novartis Pharmaceuticals Corporation; and has received travel reimbursement from Caris Life Sciences.
This article first appeared on Medscape.com.
A blood test that may be able to detect cancer years before any symptoms appear is under development. The PanSeer assay, which detects methylation markers in blood, was used in healthy individuals and successfully detected five cancer types in 91% of samples from individuals who were diagnosed with cancer 1 to 4 years later.
“We can’t say for sure that the patients didn’t have any symptoms, but we detected the cancer years before they ever walked into the hospital,” said study author Kun Zhang, PhD, a professor of bioengineering at the University of California, San Diego. “We were also able to follow up with patients, so we actually knew that they had cancer.”
Zhang noted that they also followed the individuals whose tests indicated they were cancer free. “They were healthy at the time the samples were obtained, and they remained healthy,” he said. “Follow-up was key to validating these data.”
The PanSeer test is being developed by Singlera Genomics. Zhang is a cofounder and a paid consultant of the company.
The study was published online July 21 in Nature Communications.
Unique among tests
Several blood tests for the detection of cancer have been reported in recent years. A test developed by Grail was able to detect more than 50 types of cancer and also identified the tissues where the cancer originated. The CancerSEEK test identified eight common cancers by measuring circulating tumor DNA from 16 genes, as well as eight protein biomarkers.
Findings regarding the CellMax Life FirstSight blood test were released last month. The test detected all 11 cases of colorectal cancer in a cohort of 354 patients and detected 40 of 53 advanced adenomas.
The latest study with the PanSeer assay is unique, say the investigators, because they had access to blood samples from patients who may have been completely asymptomatic and had not yet been diagnosed with cancer. Other blood tests have typically involved the use of specimens from people with a known diagnosis.
The specimens were collected as part of a 10-year longitudinal study that began in 2007 in China. Zhang and his team were able to test blood samples before individuals had experienced any signs or symptoms of cancer, and they were able to conduct long-term follow-up of the cohort.
Study details
The PanSeer assay uses DNA methylation analysis and screens for a DNA signature called CpG methylation. The results of an early-stage proof-of-concept study were published 3 years ago (Nat Genet. 2017;49:635–642).
For the current study, data were drawn from the Taizhou Longitudinal Study, which included 123,115 individuals aged 25 to 90 years who provided blood samples for long-term storage from 2007 to 2014. Participants were monitored indefinitely for cancer occurrence using local cancer registries and health insurance databases.
The team identified 575 individuals who were initially asymptomatic and healthy but were subsequently diagnosed with one of five common cancer types (stomach, esophagus, colorectum, lung, or liver cancer) within 4 years of their initial blood sampling. The authors selected these five cancer types to study because the incidence rates of these cancers in this population are high and, taken together, account for the highest mortality.
The study design allowed the authors to evaluate specimens both from patients with cancer and from those who were healthy within the same cohort. Using 191 prediagnosis samples, 223 postdiagnosis samples, and 414 healthy samples, they created a training set and validation model.
A machine learning method was created to classify samples as being either from healthy individuals or from those with cancer, using blood samples from the training set. The final classifier achieved 88% sensitivity for postdiagnosis samples and 91% sensitivity for prediagnosis samples at a specificity of 95%.
Zhang feels that initially it would be more appropriate to use the test for high-risk patients and to then evaluate the clinical benefit. “For any test, it is always more prudent to begin with a high-risk population,” he said. “You want to see some benefit with the high-risk population first, and then it can slowly be extended to others at lower risk.”
He emphasized that more rigorous testing is needing before the PanSeer assay is ready for clinical use. The logistics of designing and conducting a clinical trial that would include more than one cancer type would be very complicated. “The option was to break it down to five different studies,” he said. “We decided to begin with colon cancer, and we are currently in the process of talking with the FDA and designing the study.”
High bar to reach
Approached for comment, Benjamin Weinberg, MD, assistant professor of medicine, Division of Hematology and Oncology, the Lombardi Comprehensive Cancer Center, Georgetown University, Washington, DC, noted that there is “quite a ways to go before this can be clinically actionable.
“A lot of us are looking at combining methylation with circulating tumor DNA and throw the kitchen sink at it, but as the paper nicely describes, there are pros and cons to all of these,” he said.
Many tests of this type are in development. Weinberg explained that a circulating tumor DNA test for colon cancer may hit the market soon, pending FDA approval, although that test will be used in a different setting. “This is something that’s used to assess for minimal residual disease in patients who have undergone surgery and appear to be ‘cured’ of the disease,” he said. “The test is looking to see if there is any circulating tumor DNA being shed from whatever tumor is left behind.”
The type of test that has piqued the most interest is one that is “tumor informed,” meaning that the company receives tumor tissue and develops a personalized test of that tumor on the basis of tumor genetics. “That is a very targeted way of surveillance,” said Weinberg, “But it would be very difficult to use a tumor-informed test on the population described in this study because you don’t know if there is going to be a tumor or not.”
The PanSeer test may also prove difficult to use in the clinic because it detects multiple cancers, Weinberg said. “If there is a positive finding, then which cancer do you look for?” he commented. “It has an issue in that regard, and that’s the problem with this type of test, as it is easier if there is one site of origin.”
Overall, the test was fairly sensitive and specific, with a very low false negative rate. Going forward, he noted, there is a very high bar for tests used as screening tools, although the authors do say that their focus is for use in a high-risk population.
“There would have to be a randomized trial, and the test will have to show a survival benefit,” Weinberg said. He noted that it can sometimes be challenging to do so.
“Colonoscopy has been shown to be beneficial, but early mammography has become controversial, and prostate cancer is a whole different animal,” he added. “And these are established tests, and they show how difficult this can be.”
The Taizhou Longitudinal Study study was supported by the National Key Research and Development Program of China, the National Natural Science Foundation of China, the Key Basic Research grants from the Science and Technology Commission of Shanghai Municipality, the International S&T Cooperation Program of China, the Municipal Science and Technology Major Project program, the International Science and Technology Cooperation Program of China, and the 111 Project (B13016). Funding for the DNA methylation assays was provided by Singlera Genomics. Zhang is a cofounder, equity holder, and paid consultant of Singlera Genomics, a company that is developing early cancer detection tests, including the PanSeer test. Weinberg is a speaker or a member of a speakers bureau for Taiho Pharmaceutical Co Ltd, Bayer HealthCare Pharmaceuticals, and Eli Lilly and Company; has received research grant from Novartis Pharmaceuticals Corporation; and has received travel reimbursement from Caris Life Sciences.
This article first appeared on Medscape.com.









