User login
CRP levels may augur RCC prognosis
In patients with renal cell carcinoma, high levels of the inflammation marker C-reactive protein may signal the presence of an immunosuppressive tumor microenvironment, a feature associated with poor prognosis, investigators contend.
Among 111 patients with renal cell carcinoma (RCC) treated with either partial or radical nephrectomy, those with high C-reactive protein (CRP) levels had significantly worse cancer-specific survival (CSS) compared with patients with normal CRP levels, and CRP levels were significantly higher among patients whose tumors showed strong infiltration of immune-suppressor cells, reported Takayuki Nakayama, MD, of Tokyo Medical and Dental Graduate University in Japan, and his colleagues.
“We have found that CRP level is positively associated with the infiltration of Treg and M2 macrophage[s] in patients with RCC, indicating that CRP reflects an immunosuppressive microenvironment. However, further studies are required to confirm these findings and provide a better understanding of the association between host systemic inflammation and the immunosuppressive microenvironment,” they wrote in Clinical Genitourinary Cancer.
The investigators had previously proposed CRP as a biomarker for urologic malignancies, including RCC. The current study was designed to look at the association between CRP and the tumor microenvironment, and to determine whether serum CRP levels correlate with prognosis.
To do this, they performed immunohistochemistry studies of immune cells, including immunosuppressive M2 macrophages (CD4, CD8, and CD163 cells) and Foxp4 regulatory T cells (Tregs) on resected renal tissues from 111 patients with RCC treated in their center.
They found that 33 of the 111 patients (30%) had high CRP levels, defined as 0.5 mg/L or greater. These patients had a 5-year CSS rate of 51%, compared with 91% for patients with CRP levels below the 0.5 mg/L cutoff (P less than .001).
They also found that tumors with strong infiltration of M2 macrophages had significantly worse disease and poorer prognoses. For example, patients with strong infiltration of CD163-positive cells had higher tumor and nodal stages, as well as higher rates of distant metastases and higher Fuhrman nuclear grade (respective P values less than .001, = .003, less than .001, and = .008).
CRP levels were significantly higher among patients with strong infiltration of CD8-positive cells (P = .041), Foxp3-positive cells (P = .001), or CD163-positive (P = .035). These patients also had significantly worse CSS compared with patients with weak tumor infiltration of the respective cells (P = .040, P = .026, and P less than .001, respectively).
Independent prognostic factors for CSS in multivariate analysis included strong CD163-positive cell infiltration (P =.001), pathologic stage T3 (P = .036), lymph-node involvement (P = .007), distant metastasis (P less than .001), and Fuhrman nuclear grade 4 (P = .003).
The authors acknowledged that the study was limited by its retrospective design, small sample size, and limited analysis of components of the tumor microenvironment.
The study was supported by the Japan Society for the Promotion of Science. The authors reported having no conflicts of interest to disclose.
SOURCE: Nakayama T et al. Clin Genitourin Cancer. 2018 Aug 11. doi: 10.1016/j.clgc.2018.07.027.
In patients with renal cell carcinoma, high levels of the inflammation marker C-reactive protein may signal the presence of an immunosuppressive tumor microenvironment, a feature associated with poor prognosis, investigators contend.
Among 111 patients with renal cell carcinoma (RCC) treated with either partial or radical nephrectomy, those with high C-reactive protein (CRP) levels had significantly worse cancer-specific survival (CSS) compared with patients with normal CRP levels, and CRP levels were significantly higher among patients whose tumors showed strong infiltration of immune-suppressor cells, reported Takayuki Nakayama, MD, of Tokyo Medical and Dental Graduate University in Japan, and his colleagues.
“We have found that CRP level is positively associated with the infiltration of Treg and M2 macrophage[s] in patients with RCC, indicating that CRP reflects an immunosuppressive microenvironment. However, further studies are required to confirm these findings and provide a better understanding of the association between host systemic inflammation and the immunosuppressive microenvironment,” they wrote in Clinical Genitourinary Cancer.
The investigators had previously proposed CRP as a biomarker for urologic malignancies, including RCC. The current study was designed to look at the association between CRP and the tumor microenvironment, and to determine whether serum CRP levels correlate with prognosis.
To do this, they performed immunohistochemistry studies of immune cells, including immunosuppressive M2 macrophages (CD4, CD8, and CD163 cells) and Foxp4 regulatory T cells (Tregs) on resected renal tissues from 111 patients with RCC treated in their center.
They found that 33 of the 111 patients (30%) had high CRP levels, defined as 0.5 mg/L or greater. These patients had a 5-year CSS rate of 51%, compared with 91% for patients with CRP levels below the 0.5 mg/L cutoff (P less than .001).
They also found that tumors with strong infiltration of M2 macrophages had significantly worse disease and poorer prognoses. For example, patients with strong infiltration of CD163-positive cells had higher tumor and nodal stages, as well as higher rates of distant metastases and higher Fuhrman nuclear grade (respective P values less than .001, = .003, less than .001, and = .008).
CRP levels were significantly higher among patients with strong infiltration of CD8-positive cells (P = .041), Foxp3-positive cells (P = .001), or CD163-positive (P = .035). These patients also had significantly worse CSS compared with patients with weak tumor infiltration of the respective cells (P = .040, P = .026, and P less than .001, respectively).
Independent prognostic factors for CSS in multivariate analysis included strong CD163-positive cell infiltration (P =.001), pathologic stage T3 (P = .036), lymph-node involvement (P = .007), distant metastasis (P less than .001), and Fuhrman nuclear grade 4 (P = .003).
The authors acknowledged that the study was limited by its retrospective design, small sample size, and limited analysis of components of the tumor microenvironment.
The study was supported by the Japan Society for the Promotion of Science. The authors reported having no conflicts of interest to disclose.
SOURCE: Nakayama T et al. Clin Genitourin Cancer. 2018 Aug 11. doi: 10.1016/j.clgc.2018.07.027.
In patients with renal cell carcinoma, high levels of the inflammation marker C-reactive protein may signal the presence of an immunosuppressive tumor microenvironment, a feature associated with poor prognosis, investigators contend.
Among 111 patients with renal cell carcinoma (RCC) treated with either partial or radical nephrectomy, those with high C-reactive protein (CRP) levels had significantly worse cancer-specific survival (CSS) compared with patients with normal CRP levels, and CRP levels were significantly higher among patients whose tumors showed strong infiltration of immune-suppressor cells, reported Takayuki Nakayama, MD, of Tokyo Medical and Dental Graduate University in Japan, and his colleagues.
“We have found that CRP level is positively associated with the infiltration of Treg and M2 macrophage[s] in patients with RCC, indicating that CRP reflects an immunosuppressive microenvironment. However, further studies are required to confirm these findings and provide a better understanding of the association between host systemic inflammation and the immunosuppressive microenvironment,” they wrote in Clinical Genitourinary Cancer.
The investigators had previously proposed CRP as a biomarker for urologic malignancies, including RCC. The current study was designed to look at the association between CRP and the tumor microenvironment, and to determine whether serum CRP levels correlate with prognosis.
To do this, they performed immunohistochemistry studies of immune cells, including immunosuppressive M2 macrophages (CD4, CD8, and CD163 cells) and Foxp4 regulatory T cells (Tregs) on resected renal tissues from 111 patients with RCC treated in their center.
They found that 33 of the 111 patients (30%) had high CRP levels, defined as 0.5 mg/L or greater. These patients had a 5-year CSS rate of 51%, compared with 91% for patients with CRP levels below the 0.5 mg/L cutoff (P less than .001).
They also found that tumors with strong infiltration of M2 macrophages had significantly worse disease and poorer prognoses. For example, patients with strong infiltration of CD163-positive cells had higher tumor and nodal stages, as well as higher rates of distant metastases and higher Fuhrman nuclear grade (respective P values less than .001, = .003, less than .001, and = .008).
CRP levels were significantly higher among patients with strong infiltration of CD8-positive cells (P = .041), Foxp3-positive cells (P = .001), or CD163-positive (P = .035). These patients also had significantly worse CSS compared with patients with weak tumor infiltration of the respective cells (P = .040, P = .026, and P less than .001, respectively).
Independent prognostic factors for CSS in multivariate analysis included strong CD163-positive cell infiltration (P =.001), pathologic stage T3 (P = .036), lymph-node involvement (P = .007), distant metastasis (P less than .001), and Fuhrman nuclear grade 4 (P = .003).
The authors acknowledged that the study was limited by its retrospective design, small sample size, and limited analysis of components of the tumor microenvironment.
The study was supported by the Japan Society for the Promotion of Science. The authors reported having no conflicts of interest to disclose.
SOURCE: Nakayama T et al. Clin Genitourin Cancer. 2018 Aug 11. doi: 10.1016/j.clgc.2018.07.027.
FROM CLINICAL GENITOURINARY CANCER
Key clinical point: The nonspecific inflammatory marker C-reactive protein could be a biomarker for renal cell carcinoma prognosis.
Major finding: 5-year cancer specific survival was 51% for patients with high CRP levels, vs. 91% for patients with normal levels.
Study details: Retrospective analysis of the tumor immune microenvironment in tissue samples from 111 patients with RCC.
Disclosures: The study was supported by the Japan Society for the Promotion of Science. The authors reported having no conflicts of interest to disclose.
Source: Nakayama T et al. Clin Genitourin Cancer. 2018 Aug 11. doi: 10.1016/j.clgc.2018.07.027.
Expert panel updates guidelines on antithrombotic therapy for AF
For patients with , experts said in a comprehensive, updated guideline.
The 113-page guideline, published in the journal CHEST®, provides antithrombotic treatment recommendations for atrial fibrillation based on different levels of risk for stroke and in a variety of clinical presentations.
Altogether, the new guidelines highlight 60 key recommendations from the 12-person expert panel, chaired by Gregory Y.H. Lip, MD, of the Institute of Cardiovascular Sciences, University of Birmingham (England).
To develop the guidelines, the panel conducted a systematic literature review of relevant articles released since the 2012 publication of Thrombolytic Therapy: American College of Chest Physicians (ACCP) Evidence-Based Clinical Practice Guidelines (9th Edition).
Since that time, “there have been substantial developments in atrial fibrillation thromboprophylaxis, whether with regard to risk assessment, antithrombotic drugs, or non-drug approaches,” panelists said in their report.
The panel graded the quality of the new evidence found in the literature review, and then undertook a consensus development process. Each recommendation and statement required at least 80% consensus to pass.
Their treatment recommendations in the report are focused on three topic areas: stroke and bleeding risk assessment, antithrombotic therapy in general, and antithrombotic therapy in special situations, such as acute coronary syndrome and stenting, chronic atrial flutter, pregnancy, and chronic kidney disease.
Stroke prevention is the main priority in a “holistic approach” to management of atrial fibrillation, the panelists said in the report.
“Many of the risk factors leading to incident AF are also risk factors for ischemic stroke, and the promotion of an integrated or holistic approach to AF management is needed, incorporating stroke prevention, addressing symptoms and risk factor management,” they said.
No antithrombotic therapy is needed for patients who have atrial fibrillation without valvular heart disease, the panelists concluded.
For patients with at least one nongender CHA2DS2-VASc stroke risk factor, oral anticoagulation is recommended over aspirin, aspirin and clopidogrel, or no therapy, they said.
In high-risk patients, including males with two or more CHA2DS2-VASc risk factors and females with three or more, novel oral anticoagulants are recommended over adjusted-dose warfarin, they added.
At each patient contact, patients with atrial fibrillation should receive bleeding risk assessment starting with potentially modifiable risk factors such as uncontrolled blood pressure or excessive alcohol intake, according to the expert panel.
High-risk patients, as indicated by a HAS-BLED score of 3 or greater, should have more frequent and regular follow-up, they said.
The expert panel report concludes with a discussion on practical and patient-centered issues.
“Patient education is essential to provide patients with sufficient information to enable them to make an informed decision about whether or not they wish to take oral anticoagulants, and if they do, which oral anticoagulant they would prefer,” Dr. Lip and his colleagues said in their report.
Dr. Lip disclosed a potential conflict of interest with Boehringer Ingelheim. Expert panel members reported disclosures related to Boston Scientific, Medtronic, St. Jude Medical, Biotronik, MSD, Novartis, Pfizer, Bayer, Servier, Gilead, Bristol-Myers Squibb, AstraZeneca, and others.
SOURCE: Lip GYH et al. CHEST. 2018 Aug 21. pii: S0012-3692(18)32244-X.
For patients with , experts said in a comprehensive, updated guideline.
The 113-page guideline, published in the journal CHEST®, provides antithrombotic treatment recommendations for atrial fibrillation based on different levels of risk for stroke and in a variety of clinical presentations.
Altogether, the new guidelines highlight 60 key recommendations from the 12-person expert panel, chaired by Gregory Y.H. Lip, MD, of the Institute of Cardiovascular Sciences, University of Birmingham (England).
To develop the guidelines, the panel conducted a systematic literature review of relevant articles released since the 2012 publication of Thrombolytic Therapy: American College of Chest Physicians (ACCP) Evidence-Based Clinical Practice Guidelines (9th Edition).
Since that time, “there have been substantial developments in atrial fibrillation thromboprophylaxis, whether with regard to risk assessment, antithrombotic drugs, or non-drug approaches,” panelists said in their report.
The panel graded the quality of the new evidence found in the literature review, and then undertook a consensus development process. Each recommendation and statement required at least 80% consensus to pass.
Their treatment recommendations in the report are focused on three topic areas: stroke and bleeding risk assessment, antithrombotic therapy in general, and antithrombotic therapy in special situations, such as acute coronary syndrome and stenting, chronic atrial flutter, pregnancy, and chronic kidney disease.
Stroke prevention is the main priority in a “holistic approach” to management of atrial fibrillation, the panelists said in the report.
“Many of the risk factors leading to incident AF are also risk factors for ischemic stroke, and the promotion of an integrated or holistic approach to AF management is needed, incorporating stroke prevention, addressing symptoms and risk factor management,” they said.
No antithrombotic therapy is needed for patients who have atrial fibrillation without valvular heart disease, the panelists concluded.
For patients with at least one nongender CHA2DS2-VASc stroke risk factor, oral anticoagulation is recommended over aspirin, aspirin and clopidogrel, or no therapy, they said.
In high-risk patients, including males with two or more CHA2DS2-VASc risk factors and females with three or more, novel oral anticoagulants are recommended over adjusted-dose warfarin, they added.
At each patient contact, patients with atrial fibrillation should receive bleeding risk assessment starting with potentially modifiable risk factors such as uncontrolled blood pressure or excessive alcohol intake, according to the expert panel.
High-risk patients, as indicated by a HAS-BLED score of 3 or greater, should have more frequent and regular follow-up, they said.
The expert panel report concludes with a discussion on practical and patient-centered issues.
“Patient education is essential to provide patients with sufficient information to enable them to make an informed decision about whether or not they wish to take oral anticoagulants, and if they do, which oral anticoagulant they would prefer,” Dr. Lip and his colleagues said in their report.
Dr. Lip disclosed a potential conflict of interest with Boehringer Ingelheim. Expert panel members reported disclosures related to Boston Scientific, Medtronic, St. Jude Medical, Biotronik, MSD, Novartis, Pfizer, Bayer, Servier, Gilead, Bristol-Myers Squibb, AstraZeneca, and others.
SOURCE: Lip GYH et al. CHEST. 2018 Aug 21. pii: S0012-3692(18)32244-X.
For patients with , experts said in a comprehensive, updated guideline.
The 113-page guideline, published in the journal CHEST®, provides antithrombotic treatment recommendations for atrial fibrillation based on different levels of risk for stroke and in a variety of clinical presentations.
Altogether, the new guidelines highlight 60 key recommendations from the 12-person expert panel, chaired by Gregory Y.H. Lip, MD, of the Institute of Cardiovascular Sciences, University of Birmingham (England).
To develop the guidelines, the panel conducted a systematic literature review of relevant articles released since the 2012 publication of Thrombolytic Therapy: American College of Chest Physicians (ACCP) Evidence-Based Clinical Practice Guidelines (9th Edition).
Since that time, “there have been substantial developments in atrial fibrillation thromboprophylaxis, whether with regard to risk assessment, antithrombotic drugs, or non-drug approaches,” panelists said in their report.
The panel graded the quality of the new evidence found in the literature review, and then undertook a consensus development process. Each recommendation and statement required at least 80% consensus to pass.
Their treatment recommendations in the report are focused on three topic areas: stroke and bleeding risk assessment, antithrombotic therapy in general, and antithrombotic therapy in special situations, such as acute coronary syndrome and stenting, chronic atrial flutter, pregnancy, and chronic kidney disease.
Stroke prevention is the main priority in a “holistic approach” to management of atrial fibrillation, the panelists said in the report.
“Many of the risk factors leading to incident AF are also risk factors for ischemic stroke, and the promotion of an integrated or holistic approach to AF management is needed, incorporating stroke prevention, addressing symptoms and risk factor management,” they said.
No antithrombotic therapy is needed for patients who have atrial fibrillation without valvular heart disease, the panelists concluded.
For patients with at least one nongender CHA2DS2-VASc stroke risk factor, oral anticoagulation is recommended over aspirin, aspirin and clopidogrel, or no therapy, they said.
In high-risk patients, including males with two or more CHA2DS2-VASc risk factors and females with three or more, novel oral anticoagulants are recommended over adjusted-dose warfarin, they added.
At each patient contact, patients with atrial fibrillation should receive bleeding risk assessment starting with potentially modifiable risk factors such as uncontrolled blood pressure or excessive alcohol intake, according to the expert panel.
High-risk patients, as indicated by a HAS-BLED score of 3 or greater, should have more frequent and regular follow-up, they said.
The expert panel report concludes with a discussion on practical and patient-centered issues.
“Patient education is essential to provide patients with sufficient information to enable them to make an informed decision about whether or not they wish to take oral anticoagulants, and if they do, which oral anticoagulant they would prefer,” Dr. Lip and his colleagues said in their report.
Dr. Lip disclosed a potential conflict of interest with Boehringer Ingelheim. Expert panel members reported disclosures related to Boston Scientific, Medtronic, St. Jude Medical, Biotronik, MSD, Novartis, Pfizer, Bayer, Servier, Gilead, Bristol-Myers Squibb, AstraZeneca, and others.
SOURCE: Lip GYH et al. CHEST. 2018 Aug 21. pii: S0012-3692(18)32244-X.
FROM CHEST
Stop treating gout and start curing it, physician urges
LAS VEGAS – Brian F. Mandell, MD, PhD, of Cleveland Clinic, has a message about one of the most devastating conditions that rheumatologists see: Gout isn’t just a treatable disease. It’s a curable one.
Still, research shows time and time again that physicians manage gout “horrendously,” he told colleagues at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education. “The problem really lies with us,” he said. “We need to do a better job.”
At issue, he believes, is a failure to consider the basic workings of gout when making treatment decisions and advising patients. Lowering serum uric acid (SUA) via medication works, he said, but physicians too frequently don’t go far enough with this approach.
Gout appears to be on the rise in the United States, reflecting increases in related conditions such as obesity and diabetes. A study published this year found that the rate of new-onset gout more than doubled in Olmsted County, Minn., from 1989-1992 to 2009-2010, reaching an adjusted rate of 137/100,000 (J Rheumatol. 2018 Apr;45[4]:574-9).
According to Dr. Mandell, various mysteries regarding gout still need to be cleared up. For one, does resolution of gout also resolve conditions related to hyperuricemia, such as onset of hypertension, progressive chronic kidney disease, and nonalcoholic fatty liver along with higher all-cause mortality?
“We don’t know from interventional studies whether these are as reversible as the gouty arthritis,” he said.
It’s also unknown why so many hyperuricemic patients don’t get flares, with one study estimating that about 50% don’t get them over 15 years (Arthritis Rheumatol. 2017;69[Suppl 10]: Abstract 2843).
One fascinating theory, Dr. Mandell said, suggests “the microbiome is playing a huge [role] in the body’s response to deposits of crystals.”
Fortunately, he said, other mysteries about gout are being solved.
It’s now clear that lowering SUA below 6 mg/dL with medication will reduce flares, Dr. Mandell said. He pointed to a 2017 study of 314 patients with early gout that found 63% of patients who took febuxostat (Uloric) lowered their SUA below 6 mg/dL, compared with just 6% of the placebo group. The overall percentage of patients who had at least one gout flare over 2 years was 29% in the febuxostat group vs. 41% in the placebo group (Arthritis Rheumatol. 2017;69[12]:2386‐95).
It’s also clear that maintenance of lower SUA levels is crucial to prevent recurrence, Dr. Mandell said.
So why is management of hyperuricemia so poor? He ticked off various possible explanations: Maybe it’s the medications. Or perhaps patient compliance is low.
But the drugs are fine, he said, although he cautioned that too-rapid lowering of SUA levels can provoke attacks. He pointed to a 2014 study that suggests allopurinol can help nearly all patients get their SUA below 6 mg/dL, and in the study, the drug was “generally well tolerated” (Semin Arthritis Rheum. 2014 Aug;44[1]:25-30).
As for compliance, Dr. Mandell said, it can be boosted by patient education. The problem, he said, is that physicians are failing patients by not up-titrating allopurinol despite evidence that this approach works.
He added that hyperuricemia can be managed even in patients on diuretic therapy (Arthritis Res Ther. 2018;20:53).
What about patients who are intolerant to allopurinol or don’t fully respond to it on the SUA front? Dr. Mandell said he likes to try febuxostat, although he noted that it’s tremendously more expensive than allopurinol in the United States with a price that could be 10 times higher.
The nonscored design of febuxostat pills makes dose adjustment difficult in patients, he said, and there are concerns about heart-related and all-cause deaths.
Lesinurad (Zurampic) may be helpful for patients with hyperuricemia that doesn’t response to high doses of xanthine oxidase inhibitors (XOI) or if they’re intolerant to lower inadequate doses, he said. Avoid the drug in patients with chronic kidney disease, he cautioned, and be aware that it’s not approved as a monotherapy. Instead, it’s approved by the Food and Drug Administration for use with an XOI.
As for other gout issues, Dr. Mandell said pegloticase (Krystexxa) via infusion can help patients who don’t respond to an XOI but infusion reactions can occur (mainly in nonresponders), and it’s extremely expensive (about $20,000 per month).
He added that anti–IL-1 therapy is effective in hospitalized patients with gout and doesn’t exacerbate other conditions.
Dr. Mandell disclosed various links to drug makers that produce treatments for gout. He has served as clinical investigator for Horizon, has been a consultant to AstraZeneca, Ironwood, and Horizon, and has received honoraria (unrestricted grants) for continuing medical education activities from Takeda and Horizon. He also reported soliciting advertisements for a journal and educational grants for CME activities.
Global Academy for Medical Education and this news organization are owned by the same parent company.
LAS VEGAS – Brian F. Mandell, MD, PhD, of Cleveland Clinic, has a message about one of the most devastating conditions that rheumatologists see: Gout isn’t just a treatable disease. It’s a curable one.
Still, research shows time and time again that physicians manage gout “horrendously,” he told colleagues at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education. “The problem really lies with us,” he said. “We need to do a better job.”
At issue, he believes, is a failure to consider the basic workings of gout when making treatment decisions and advising patients. Lowering serum uric acid (SUA) via medication works, he said, but physicians too frequently don’t go far enough with this approach.
Gout appears to be on the rise in the United States, reflecting increases in related conditions such as obesity and diabetes. A study published this year found that the rate of new-onset gout more than doubled in Olmsted County, Minn., from 1989-1992 to 2009-2010, reaching an adjusted rate of 137/100,000 (J Rheumatol. 2018 Apr;45[4]:574-9).
According to Dr. Mandell, various mysteries regarding gout still need to be cleared up. For one, does resolution of gout also resolve conditions related to hyperuricemia, such as onset of hypertension, progressive chronic kidney disease, and nonalcoholic fatty liver along with higher all-cause mortality?
“We don’t know from interventional studies whether these are as reversible as the gouty arthritis,” he said.
It’s also unknown why so many hyperuricemic patients don’t get flares, with one study estimating that about 50% don’t get them over 15 years (Arthritis Rheumatol. 2017;69[Suppl 10]: Abstract 2843).
One fascinating theory, Dr. Mandell said, suggests “the microbiome is playing a huge [role] in the body’s response to deposits of crystals.”
Fortunately, he said, other mysteries about gout are being solved.
It’s now clear that lowering SUA below 6 mg/dL with medication will reduce flares, Dr. Mandell said. He pointed to a 2017 study of 314 patients with early gout that found 63% of patients who took febuxostat (Uloric) lowered their SUA below 6 mg/dL, compared with just 6% of the placebo group. The overall percentage of patients who had at least one gout flare over 2 years was 29% in the febuxostat group vs. 41% in the placebo group (Arthritis Rheumatol. 2017;69[12]:2386‐95).
It’s also clear that maintenance of lower SUA levels is crucial to prevent recurrence, Dr. Mandell said.
So why is management of hyperuricemia so poor? He ticked off various possible explanations: Maybe it’s the medications. Or perhaps patient compliance is low.
But the drugs are fine, he said, although he cautioned that too-rapid lowering of SUA levels can provoke attacks. He pointed to a 2014 study that suggests allopurinol can help nearly all patients get their SUA below 6 mg/dL, and in the study, the drug was “generally well tolerated” (Semin Arthritis Rheum. 2014 Aug;44[1]:25-30).
As for compliance, Dr. Mandell said, it can be boosted by patient education. The problem, he said, is that physicians are failing patients by not up-titrating allopurinol despite evidence that this approach works.
He added that hyperuricemia can be managed even in patients on diuretic therapy (Arthritis Res Ther. 2018;20:53).
What about patients who are intolerant to allopurinol or don’t fully respond to it on the SUA front? Dr. Mandell said he likes to try febuxostat, although he noted that it’s tremendously more expensive than allopurinol in the United States with a price that could be 10 times higher.
The nonscored design of febuxostat pills makes dose adjustment difficult in patients, he said, and there are concerns about heart-related and all-cause deaths.
Lesinurad (Zurampic) may be helpful for patients with hyperuricemia that doesn’t response to high doses of xanthine oxidase inhibitors (XOI) or if they’re intolerant to lower inadequate doses, he said. Avoid the drug in patients with chronic kidney disease, he cautioned, and be aware that it’s not approved as a monotherapy. Instead, it’s approved by the Food and Drug Administration for use with an XOI.
As for other gout issues, Dr. Mandell said pegloticase (Krystexxa) via infusion can help patients who don’t respond to an XOI but infusion reactions can occur (mainly in nonresponders), and it’s extremely expensive (about $20,000 per month).
He added that anti–IL-1 therapy is effective in hospitalized patients with gout and doesn’t exacerbate other conditions.
Dr. Mandell disclosed various links to drug makers that produce treatments for gout. He has served as clinical investigator for Horizon, has been a consultant to AstraZeneca, Ironwood, and Horizon, and has received honoraria (unrestricted grants) for continuing medical education activities from Takeda and Horizon. He also reported soliciting advertisements for a journal and educational grants for CME activities.
Global Academy for Medical Education and this news organization are owned by the same parent company.
LAS VEGAS – Brian F. Mandell, MD, PhD, of Cleveland Clinic, has a message about one of the most devastating conditions that rheumatologists see: Gout isn’t just a treatable disease. It’s a curable one.
Still, research shows time and time again that physicians manage gout “horrendously,” he told colleagues at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education. “The problem really lies with us,” he said. “We need to do a better job.”
At issue, he believes, is a failure to consider the basic workings of gout when making treatment decisions and advising patients. Lowering serum uric acid (SUA) via medication works, he said, but physicians too frequently don’t go far enough with this approach.
Gout appears to be on the rise in the United States, reflecting increases in related conditions such as obesity and diabetes. A study published this year found that the rate of new-onset gout more than doubled in Olmsted County, Minn., from 1989-1992 to 2009-2010, reaching an adjusted rate of 137/100,000 (J Rheumatol. 2018 Apr;45[4]:574-9).
According to Dr. Mandell, various mysteries regarding gout still need to be cleared up. For one, does resolution of gout also resolve conditions related to hyperuricemia, such as onset of hypertension, progressive chronic kidney disease, and nonalcoholic fatty liver along with higher all-cause mortality?
“We don’t know from interventional studies whether these are as reversible as the gouty arthritis,” he said.
It’s also unknown why so many hyperuricemic patients don’t get flares, with one study estimating that about 50% don’t get them over 15 years (Arthritis Rheumatol. 2017;69[Suppl 10]: Abstract 2843).
One fascinating theory, Dr. Mandell said, suggests “the microbiome is playing a huge [role] in the body’s response to deposits of crystals.”
Fortunately, he said, other mysteries about gout are being solved.
It’s now clear that lowering SUA below 6 mg/dL with medication will reduce flares, Dr. Mandell said. He pointed to a 2017 study of 314 patients with early gout that found 63% of patients who took febuxostat (Uloric) lowered their SUA below 6 mg/dL, compared with just 6% of the placebo group. The overall percentage of patients who had at least one gout flare over 2 years was 29% in the febuxostat group vs. 41% in the placebo group (Arthritis Rheumatol. 2017;69[12]:2386‐95).
It’s also clear that maintenance of lower SUA levels is crucial to prevent recurrence, Dr. Mandell said.
So why is management of hyperuricemia so poor? He ticked off various possible explanations: Maybe it’s the medications. Or perhaps patient compliance is low.
But the drugs are fine, he said, although he cautioned that too-rapid lowering of SUA levels can provoke attacks. He pointed to a 2014 study that suggests allopurinol can help nearly all patients get their SUA below 6 mg/dL, and in the study, the drug was “generally well tolerated” (Semin Arthritis Rheum. 2014 Aug;44[1]:25-30).
As for compliance, Dr. Mandell said, it can be boosted by patient education. The problem, he said, is that physicians are failing patients by not up-titrating allopurinol despite evidence that this approach works.
He added that hyperuricemia can be managed even in patients on diuretic therapy (Arthritis Res Ther. 2018;20:53).
What about patients who are intolerant to allopurinol or don’t fully respond to it on the SUA front? Dr. Mandell said he likes to try febuxostat, although he noted that it’s tremendously more expensive than allopurinol in the United States with a price that could be 10 times higher.
The nonscored design of febuxostat pills makes dose adjustment difficult in patients, he said, and there are concerns about heart-related and all-cause deaths.
Lesinurad (Zurampic) may be helpful for patients with hyperuricemia that doesn’t response to high doses of xanthine oxidase inhibitors (XOI) or if they’re intolerant to lower inadequate doses, he said. Avoid the drug in patients with chronic kidney disease, he cautioned, and be aware that it’s not approved as a monotherapy. Instead, it’s approved by the Food and Drug Administration for use with an XOI.
As for other gout issues, Dr. Mandell said pegloticase (Krystexxa) via infusion can help patients who don’t respond to an XOI but infusion reactions can occur (mainly in nonresponders), and it’s extremely expensive (about $20,000 per month).
He added that anti–IL-1 therapy is effective in hospitalized patients with gout and doesn’t exacerbate other conditions.
Dr. Mandell disclosed various links to drug makers that produce treatments for gout. He has served as clinical investigator for Horizon, has been a consultant to AstraZeneca, Ironwood, and Horizon, and has received honoraria (unrestricted grants) for continuing medical education activities from Takeda and Horizon. He also reported soliciting advertisements for a journal and educational grants for CME activities.
Global Academy for Medical Education and this news organization are owned by the same parent company.
REPORTING FROM THE ANNUAL PERSPECTIVES IN RHEUMATIC DISEASES
Laser treatment tips for pigmented lesions
SAN DIEGO –
Victor Ross, MD, turns to the Q-switched alexandrite laser as his device of choice for most pigmented lesions. “I also use the Q-switched 1,064 nm Nd:YAG and sometimes use the Q-switched 532 nm Nd:YAG, particularly for lighter-skinned patients with lighter lesions,” he said at the annual Masters of Aesthetics Symposium.
Compared with long-pulsed devices, the Q-switched 532 nm neodymium:YAG laser is better for one-time pigment reduction and better for treating lighter pigmented spots, yet it’s associated with a higher risk of postinflammatory hyperpigmentation and short-term crusting. “The Q-switched 532 nm Nd:YAG laser will even treat very tight lentigines, but vascular effects tend to cause an immediate bright red color and more postinflammatory hyperpigmentation,” said Dr. Ross, director of laser and cosmetic dermatology at the Scripps Clinic in San Diego. He cautioned that the Q-switched 532 nm Nd:YAG laser may cause prolonged redness on the legs and arms of some patients. “This laser is best reserved for lighter skinned patients with very light lentigines – the brisk purpura can prove distasteful short term for cosmetic patients,” he said. “For darker lentigines, I prefer the IPL [intense pulse light], KTP [potassium titanyl phosphate] laser, or Q-switched alexandrite lasers.”
Meanwhile, treating pigmented lesions treated with long-pulse IPL, KTP, and pulsed dye lasers show less risk of postinflammatory hyperpigmentation and better coverage rates. However, they are sensitive to background color and are less likely to achieve complete one-time removal. The first treatment works the best because the “low hanging fruit” (darker lesions) will do well, he said.
For clinicians looking to improve their skills in treating pigmented lesions with lasers, Dr. Ross recommended using a skin meter such as Cynosure’s Skintel Melanin Reader, which measures the real-time pigment of skin. “You measure the pigment, and it gives you a reading,” he said. “It gives you a recommended setting based on the hand piece and the pulse duration.”
Melasma remains a difficult condition to treat with laser and light. In fact, Dr. Ross joked that he wouldn’t mind if the words “He cured melasma” graced his tombstone one day. “I have been treating melasma patients for 29 years now, and I’m not closer to a cure than when I started out,” he said. “I’ve tried lots of things. In my defense, I’ve made more people better than worse.”
His approach to treating melasma is to begin with a KTP laser or a gentle IPL if discrete lesions or telangiectasia are present. Next, he applies hydroquinone followed by a series of treatment sessions with the Q-switched Nd:YAG laser or a conservative fractional laser. “This tends to induce remission, but is associated with a high rate of relapse,” he said.
Dr. Ross disclosed having research and financial ties to numerous pharmaceutical and device companies.
SAN DIEGO –
Victor Ross, MD, turns to the Q-switched alexandrite laser as his device of choice for most pigmented lesions. “I also use the Q-switched 1,064 nm Nd:YAG and sometimes use the Q-switched 532 nm Nd:YAG, particularly for lighter-skinned patients with lighter lesions,” he said at the annual Masters of Aesthetics Symposium.
Compared with long-pulsed devices, the Q-switched 532 nm neodymium:YAG laser is better for one-time pigment reduction and better for treating lighter pigmented spots, yet it’s associated with a higher risk of postinflammatory hyperpigmentation and short-term crusting. “The Q-switched 532 nm Nd:YAG laser will even treat very tight lentigines, but vascular effects tend to cause an immediate bright red color and more postinflammatory hyperpigmentation,” said Dr. Ross, director of laser and cosmetic dermatology at the Scripps Clinic in San Diego. He cautioned that the Q-switched 532 nm Nd:YAG laser may cause prolonged redness on the legs and arms of some patients. “This laser is best reserved for lighter skinned patients with very light lentigines – the brisk purpura can prove distasteful short term for cosmetic patients,” he said. “For darker lentigines, I prefer the IPL [intense pulse light], KTP [potassium titanyl phosphate] laser, or Q-switched alexandrite lasers.”
Meanwhile, treating pigmented lesions treated with long-pulse IPL, KTP, and pulsed dye lasers show less risk of postinflammatory hyperpigmentation and better coverage rates. However, they are sensitive to background color and are less likely to achieve complete one-time removal. The first treatment works the best because the “low hanging fruit” (darker lesions) will do well, he said.
For clinicians looking to improve their skills in treating pigmented lesions with lasers, Dr. Ross recommended using a skin meter such as Cynosure’s Skintel Melanin Reader, which measures the real-time pigment of skin. “You measure the pigment, and it gives you a reading,” he said. “It gives you a recommended setting based on the hand piece and the pulse duration.”
Melasma remains a difficult condition to treat with laser and light. In fact, Dr. Ross joked that he wouldn’t mind if the words “He cured melasma” graced his tombstone one day. “I have been treating melasma patients for 29 years now, and I’m not closer to a cure than when I started out,” he said. “I’ve tried lots of things. In my defense, I’ve made more people better than worse.”
His approach to treating melasma is to begin with a KTP laser or a gentle IPL if discrete lesions or telangiectasia are present. Next, he applies hydroquinone followed by a series of treatment sessions with the Q-switched Nd:YAG laser or a conservative fractional laser. “This tends to induce remission, but is associated with a high rate of relapse,” he said.
Dr. Ross disclosed having research and financial ties to numerous pharmaceutical and device companies.
SAN DIEGO –
Victor Ross, MD, turns to the Q-switched alexandrite laser as his device of choice for most pigmented lesions. “I also use the Q-switched 1,064 nm Nd:YAG and sometimes use the Q-switched 532 nm Nd:YAG, particularly for lighter-skinned patients with lighter lesions,” he said at the annual Masters of Aesthetics Symposium.
Compared with long-pulsed devices, the Q-switched 532 nm neodymium:YAG laser is better for one-time pigment reduction and better for treating lighter pigmented spots, yet it’s associated with a higher risk of postinflammatory hyperpigmentation and short-term crusting. “The Q-switched 532 nm Nd:YAG laser will even treat very tight lentigines, but vascular effects tend to cause an immediate bright red color and more postinflammatory hyperpigmentation,” said Dr. Ross, director of laser and cosmetic dermatology at the Scripps Clinic in San Diego. He cautioned that the Q-switched 532 nm Nd:YAG laser may cause prolonged redness on the legs and arms of some patients. “This laser is best reserved for lighter skinned patients with very light lentigines – the brisk purpura can prove distasteful short term for cosmetic patients,” he said. “For darker lentigines, I prefer the IPL [intense pulse light], KTP [potassium titanyl phosphate] laser, or Q-switched alexandrite lasers.”
Meanwhile, treating pigmented lesions treated with long-pulse IPL, KTP, and pulsed dye lasers show less risk of postinflammatory hyperpigmentation and better coverage rates. However, they are sensitive to background color and are less likely to achieve complete one-time removal. The first treatment works the best because the “low hanging fruit” (darker lesions) will do well, he said.
For clinicians looking to improve their skills in treating pigmented lesions with lasers, Dr. Ross recommended using a skin meter such as Cynosure’s Skintel Melanin Reader, which measures the real-time pigment of skin. “You measure the pigment, and it gives you a reading,” he said. “It gives you a recommended setting based on the hand piece and the pulse duration.”
Melasma remains a difficult condition to treat with laser and light. In fact, Dr. Ross joked that he wouldn’t mind if the words “He cured melasma” graced his tombstone one day. “I have been treating melasma patients for 29 years now, and I’m not closer to a cure than when I started out,” he said. “I’ve tried lots of things. In my defense, I’ve made more people better than worse.”
His approach to treating melasma is to begin with a KTP laser or a gentle IPL if discrete lesions or telangiectasia are present. Next, he applies hydroquinone followed by a series of treatment sessions with the Q-switched Nd:YAG laser or a conservative fractional laser. “This tends to induce remission, but is associated with a high rate of relapse,” he said.
Dr. Ross disclosed having research and financial ties to numerous pharmaceutical and device companies.
EXPERT ANALYSIS FROM MOAS 2018
Task force advises behavioral intervention for obese adults
The U.S. Preventive Services Task Force advises clinicians to refer or offer intensive behavioral weight-loss interventions to obese adults, according to an updated recommendation statement published in JAMA.
Obesity affects more than one-third of U.S. adults, according to federal statistics. It carries increased risk for comorbidities including heart disease, diabetes, and various cancers, as well as increased risk of death among adults younger than 65 years, noted lead author Susan J. Curry, PhD, of the University of Iowa, Iowa City, and members of the Task Force.
The B recommendation applies to obese adults; obesity was defined as a body mass index of 30 kg/m2 or higher. The evidence review focused on interventions for weight loss and weight maintenance that could be provided in primary care or referred from primary care, such as nutrition counseling, exercise strategies, and goal setting.
The Task Force found adequate evidence that behavior-based weight-loss interventions improved weight, reduced incidence of type 2 diabetes, and helped maintain weight loss after interventions ended.
The Task Force found small to no evidence of harm associated with any of the behavioral weight-loss interventions, which included group sessions, personal sessions, print-based interventions, and technology-based interventions (such as text messages). Although interventions that combined drug therapy with behavioral intervention resulted in greater weight loss over 12-18 months, compared with behavioral interventions alone, the attrition rates were high and data on weight-loss maintenance after discontinuation of the drugs were limited, the Task Force noted.
“As a result, the USPSTF encourages clinicians to promote behavioral interventions as the primary focus of effective interventions for weight loss in adults,” they wrote.
The Task Force acknowledged the need for future research in subgroups and to explore whether factors such as genetics and untreated conditions are barriers to behavior-based weight loss interventions.
In the evidence review published in JAMA, Erin S. LeBlanc, MD, of Kaiser Permanente in Portland, Ore., and her colleagues reviewed data from 122 randomized, controlled trials including more than 62,000 persons and 2 observational studies including more than 209,000 persons.
The researchers found behavioral interventions were associated with greater weight loss and less risk of developing diabetes, compared with control interventions.
Intensive behavioral interventions included counseling patients about healthy eating, encouraging physical activity, setting weight and health goals, and assisting with weight monitoring. The interventions ranged from text messaging to in-person sessions for individuals or groups. The average absolute weight loss in the trials included in the review ranged from –0.5 kg to –9.3 kg (–1.1 lb to –20.5 lb) for intervention patients and from +1.4 kg to –5.6 kg (+3.1 lb to –12.3 lb) in controls.
Limitations of the review included a lack of data on population subgroups and a lack of long-term data on weight and health outcomes, the researchers noted. However, the results support the value of behavior-based therapy for obesity treatment.
The final recommendation is consistent with the 2018 draft recommendation and updates the 2012 final recommendation on obesity management.
The researchers and Task Force members had no relevant financial conflicts to disclose.
SOURCE: U.S. Preventive Services Task Force. JAMA. 2018;320(11):1163-71. doi: 10.1001/jama.2018.13022.
For most primary care clinicians, referring obese patients for more advanced behavioral therapy will be the most practical integration of the recommendation, Susan Z. Yanovski, MD, wrote in an accompanying editorial. Clinicians with training in motivational interviewing or counseling may help assess a patient’s readiness for treatment, but even being familiar with weight-management resources in the community can help patients find the right fit.
“Clinicians can do their patients a great service by showing respect for their patients’ struggles with weight management, screening for obesity-related comorbidities, and providing treatment for identified conditions regardless of the patient’s motivation for, or success with, weight-loss treatment,” she said.
Dr. Yanovski noted that pharmacotherapy options have increased since the 2012 recommendations, when orlistat was the only approved drug for long-term treatment of obesity. Five medications are currently available for this indication.
The USPSTF review was limited in scope for both drug and behavior therapy, noted Dr. Yanovski. “Because the recommendations are meant to apply to adults without diseases for which weight loss is part of disease management, some large and long-term clinical trials conducted among patients with type 2 diabetes or cardiovascular disease were not included.”
Another limitation was the exclusion of surgical treatments as being outside the primary care setting, but bariatric surgery remains a viable option for many patients, especially for prevention or resolution of type 2 diabetes. Primary care clinicians are in a position to identify patients who might benefit and to provide referrals to surgeons if appropriate, she wrote.
Dr. Yanovski agreed with the recommendations but concluded that early strategies to prevent obesity should not be neglected. “Research to develop effective prevention strategies throughout the life course, including infancy and early childhood, could ultimately decrease the number of adults who must confront the difficult challenge of losing excess weight.”
Dr. Yanovski is affiliated with the National Institute of Diabetes and Digestive and Kidney Diseases. She disclosed that her spouse has received research funding from Zafgen and Rhythm Pharmaceuticals for studies of investigational products to treat obesity. Her comments are summarized from an editorial accompanying the articles by Curry SJ et al. and LeBlanc ES et al. (JAMA. 2018;320[11]:1111-3).
For most primary care clinicians, referring obese patients for more advanced behavioral therapy will be the most practical integration of the recommendation, Susan Z. Yanovski, MD, wrote in an accompanying editorial. Clinicians with training in motivational interviewing or counseling may help assess a patient’s readiness for treatment, but even being familiar with weight-management resources in the community can help patients find the right fit.
“Clinicians can do their patients a great service by showing respect for their patients’ struggles with weight management, screening for obesity-related comorbidities, and providing treatment for identified conditions regardless of the patient’s motivation for, or success with, weight-loss treatment,” she said.
Dr. Yanovski noted that pharmacotherapy options have increased since the 2012 recommendations, when orlistat was the only approved drug for long-term treatment of obesity. Five medications are currently available for this indication.
The USPSTF review was limited in scope for both drug and behavior therapy, noted Dr. Yanovski. “Because the recommendations are meant to apply to adults without diseases for which weight loss is part of disease management, some large and long-term clinical trials conducted among patients with type 2 diabetes or cardiovascular disease were not included.”
Another limitation was the exclusion of surgical treatments as being outside the primary care setting, but bariatric surgery remains a viable option for many patients, especially for prevention or resolution of type 2 diabetes. Primary care clinicians are in a position to identify patients who might benefit and to provide referrals to surgeons if appropriate, she wrote.
Dr. Yanovski agreed with the recommendations but concluded that early strategies to prevent obesity should not be neglected. “Research to develop effective prevention strategies throughout the life course, including infancy and early childhood, could ultimately decrease the number of adults who must confront the difficult challenge of losing excess weight.”
Dr. Yanovski is affiliated with the National Institute of Diabetes and Digestive and Kidney Diseases. She disclosed that her spouse has received research funding from Zafgen and Rhythm Pharmaceuticals for studies of investigational products to treat obesity. Her comments are summarized from an editorial accompanying the articles by Curry SJ et al. and LeBlanc ES et al. (JAMA. 2018;320[11]:1111-3).
For most primary care clinicians, referring obese patients for more advanced behavioral therapy will be the most practical integration of the recommendation, Susan Z. Yanovski, MD, wrote in an accompanying editorial. Clinicians with training in motivational interviewing or counseling may help assess a patient’s readiness for treatment, but even being familiar with weight-management resources in the community can help patients find the right fit.
“Clinicians can do their patients a great service by showing respect for their patients’ struggles with weight management, screening for obesity-related comorbidities, and providing treatment for identified conditions regardless of the patient’s motivation for, or success with, weight-loss treatment,” she said.
Dr. Yanovski noted that pharmacotherapy options have increased since the 2012 recommendations, when orlistat was the only approved drug for long-term treatment of obesity. Five medications are currently available for this indication.
The USPSTF review was limited in scope for both drug and behavior therapy, noted Dr. Yanovski. “Because the recommendations are meant to apply to adults without diseases for which weight loss is part of disease management, some large and long-term clinical trials conducted among patients with type 2 diabetes or cardiovascular disease were not included.”
Another limitation was the exclusion of surgical treatments as being outside the primary care setting, but bariatric surgery remains a viable option for many patients, especially for prevention or resolution of type 2 diabetes. Primary care clinicians are in a position to identify patients who might benefit and to provide referrals to surgeons if appropriate, she wrote.
Dr. Yanovski agreed with the recommendations but concluded that early strategies to prevent obesity should not be neglected. “Research to develop effective prevention strategies throughout the life course, including infancy and early childhood, could ultimately decrease the number of adults who must confront the difficult challenge of losing excess weight.”
Dr. Yanovski is affiliated with the National Institute of Diabetes and Digestive and Kidney Diseases. She disclosed that her spouse has received research funding from Zafgen and Rhythm Pharmaceuticals for studies of investigational products to treat obesity. Her comments are summarized from an editorial accompanying the articles by Curry SJ et al. and LeBlanc ES et al. (JAMA. 2018;320[11]:1111-3).
The U.S. Preventive Services Task Force advises clinicians to refer or offer intensive behavioral weight-loss interventions to obese adults, according to an updated recommendation statement published in JAMA.
Obesity affects more than one-third of U.S. adults, according to federal statistics. It carries increased risk for comorbidities including heart disease, diabetes, and various cancers, as well as increased risk of death among adults younger than 65 years, noted lead author Susan J. Curry, PhD, of the University of Iowa, Iowa City, and members of the Task Force.
The B recommendation applies to obese adults; obesity was defined as a body mass index of 30 kg/m2 or higher. The evidence review focused on interventions for weight loss and weight maintenance that could be provided in primary care or referred from primary care, such as nutrition counseling, exercise strategies, and goal setting.
The Task Force found adequate evidence that behavior-based weight-loss interventions improved weight, reduced incidence of type 2 diabetes, and helped maintain weight loss after interventions ended.
The Task Force found small to no evidence of harm associated with any of the behavioral weight-loss interventions, which included group sessions, personal sessions, print-based interventions, and technology-based interventions (such as text messages). Although interventions that combined drug therapy with behavioral intervention resulted in greater weight loss over 12-18 months, compared with behavioral interventions alone, the attrition rates were high and data on weight-loss maintenance after discontinuation of the drugs were limited, the Task Force noted.
“As a result, the USPSTF encourages clinicians to promote behavioral interventions as the primary focus of effective interventions for weight loss in adults,” they wrote.
The Task Force acknowledged the need for future research in subgroups and to explore whether factors such as genetics and untreated conditions are barriers to behavior-based weight loss interventions.
In the evidence review published in JAMA, Erin S. LeBlanc, MD, of Kaiser Permanente in Portland, Ore., and her colleagues reviewed data from 122 randomized, controlled trials including more than 62,000 persons and 2 observational studies including more than 209,000 persons.
The researchers found behavioral interventions were associated with greater weight loss and less risk of developing diabetes, compared with control interventions.
Intensive behavioral interventions included counseling patients about healthy eating, encouraging physical activity, setting weight and health goals, and assisting with weight monitoring. The interventions ranged from text messaging to in-person sessions for individuals or groups. The average absolute weight loss in the trials included in the review ranged from –0.5 kg to –9.3 kg (–1.1 lb to –20.5 lb) for intervention patients and from +1.4 kg to –5.6 kg (+3.1 lb to –12.3 lb) in controls.
Limitations of the review included a lack of data on population subgroups and a lack of long-term data on weight and health outcomes, the researchers noted. However, the results support the value of behavior-based therapy for obesity treatment.
The final recommendation is consistent with the 2018 draft recommendation and updates the 2012 final recommendation on obesity management.
The researchers and Task Force members had no relevant financial conflicts to disclose.
SOURCE: U.S. Preventive Services Task Force. JAMA. 2018;320(11):1163-71. doi: 10.1001/jama.2018.13022.
The U.S. Preventive Services Task Force advises clinicians to refer or offer intensive behavioral weight-loss interventions to obese adults, according to an updated recommendation statement published in JAMA.
Obesity affects more than one-third of U.S. adults, according to federal statistics. It carries increased risk for comorbidities including heart disease, diabetes, and various cancers, as well as increased risk of death among adults younger than 65 years, noted lead author Susan J. Curry, PhD, of the University of Iowa, Iowa City, and members of the Task Force.
The B recommendation applies to obese adults; obesity was defined as a body mass index of 30 kg/m2 or higher. The evidence review focused on interventions for weight loss and weight maintenance that could be provided in primary care or referred from primary care, such as nutrition counseling, exercise strategies, and goal setting.
The Task Force found adequate evidence that behavior-based weight-loss interventions improved weight, reduced incidence of type 2 diabetes, and helped maintain weight loss after interventions ended.
The Task Force found small to no evidence of harm associated with any of the behavioral weight-loss interventions, which included group sessions, personal sessions, print-based interventions, and technology-based interventions (such as text messages). Although interventions that combined drug therapy with behavioral intervention resulted in greater weight loss over 12-18 months, compared with behavioral interventions alone, the attrition rates were high and data on weight-loss maintenance after discontinuation of the drugs were limited, the Task Force noted.
“As a result, the USPSTF encourages clinicians to promote behavioral interventions as the primary focus of effective interventions for weight loss in adults,” they wrote.
The Task Force acknowledged the need for future research in subgroups and to explore whether factors such as genetics and untreated conditions are barriers to behavior-based weight loss interventions.
In the evidence review published in JAMA, Erin S. LeBlanc, MD, of Kaiser Permanente in Portland, Ore., and her colleagues reviewed data from 122 randomized, controlled trials including more than 62,000 persons and 2 observational studies including more than 209,000 persons.
The researchers found behavioral interventions were associated with greater weight loss and less risk of developing diabetes, compared with control interventions.
Intensive behavioral interventions included counseling patients about healthy eating, encouraging physical activity, setting weight and health goals, and assisting with weight monitoring. The interventions ranged from text messaging to in-person sessions for individuals or groups. The average absolute weight loss in the trials included in the review ranged from –0.5 kg to –9.3 kg (–1.1 lb to –20.5 lb) for intervention patients and from +1.4 kg to –5.6 kg (+3.1 lb to –12.3 lb) in controls.
Limitations of the review included a lack of data on population subgroups and a lack of long-term data on weight and health outcomes, the researchers noted. However, the results support the value of behavior-based therapy for obesity treatment.
The final recommendation is consistent with the 2018 draft recommendation and updates the 2012 final recommendation on obesity management.
The researchers and Task Force members had no relevant financial conflicts to disclose.
SOURCE: U.S. Preventive Services Task Force. JAMA. 2018;320(11):1163-71. doi: 10.1001/jama.2018.13022.
FROM JAMA
UN aims to eradicate TB by 2030
A concerted a lethal disease affecting one-quarter of the world’s population by the year 2030.
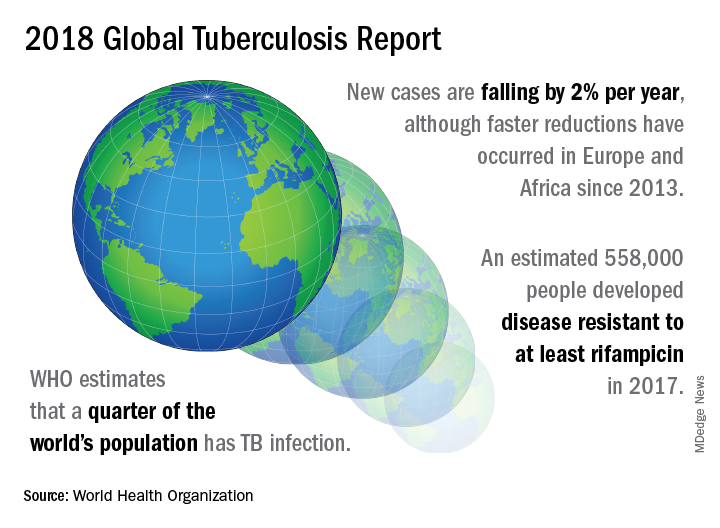
On September 26 the United Nations General Assembly will convene a high-level meeting of global stakeholders to solidify the eradication plan, addressing the global crisis of tuberculosis (TB), the world’s most deadly infectious disease.
“We must seize the moment,” said Tereza Kasaeva, MD, director of the World Health Organization’s global TB program, speaking at a telebriefing and press conference accompanying the release of the World Health Organization’s annual global tuberculosis report. “It’s unacceptable in the 21st century that millions lose their lives to this preventable and curable disease.”
TB caused 1.6 million deaths globally in 2017, and the World Health Organization (WHO) estimates that of the 10 million new cases of TB last year, 558,000 are multi-drug resistant (MDR) infections.
Though death rates and new cases are falling globally each year, significantly more resources are needed to boost access to preventive treatment for latent TB infection; “Most people needing it are not yet accessing care,” according to the press briefing accompanying the report.
A review and commentary on TB incubation and latency published in BMJ (2018;362:k2738 doi: 10.1136/bmj.k2738; e-pub 23 Aug 2018) has called into question the focus preventive treatment of latent cases at the expense of reaching those most likely to die from TB (e.g., HIV patients, children of individuals living with active TB). The authors state that “latent” TB is identified by indirect evidence of present or past infection with Mycobacterium tuberculosis as inferred by a detectable adaptive immune response to M tuberculosis antigens. Active TB infection is overwhelmingly the result of a primary infection and almost always occurs within two years.
In order to meet the ambitious goal of TB eradication by the year 2030, treatment coverage must rise to 90% globally from the current 64%, according to the report.
Progress in southern Africa and in the Russian Federation, where efforts have led to a 30% reduction in TB mortality and a decrease in incidence of 5% per year, show that steep reductions in TB are possible when resources are brought to bear on the problem, said Dr. Kasaeva. “We should acknowledge that actions in some countries and regions show that progress can accelerate,” she said. Still, she noted, “Four thousand lives per day are lost to TB. Tuberculosis is the leading killer of people living with HIV, and the major cause of deaths related to antimicrobial resistance” at a global level.
Two thirds of all TB cases occur in eight countries, with India, China, and Indonesia leading this group. About half of the cases of MDR TB occur in India, China, and Russia, said Dr. Kasaeva, and globally only one in four individuals with MDR TB who need access to treatment have received it. “We need to urgently tackle the multidrug resistant TB public health crisis,” she said.
Major impediments to successful public health efforts against TB are underdiagnosis and underreporting: It is estimated that 3.6 million of 2017’s 10 million new cases were not officially recorded or reported. Countries where these problems are most serious include India, Indonesia, and Nigeria. Fewer than half of the children with TB are reported globally, according to the report.
People living with HIV/AIDS who are also infected with TB number nearly 1,000,000, but only about half of these were officially reported in 2017.
In terms of prevention priorities, WHO has recommended targeting treatment of latent TB in two groups: People living with HIV/AIDS, and children under the age of 5 years who live in households with TB-infected individuals.
“To enable these actions,” said Dr. Kasaeva, “we need strengthened commitments not just for TB care, but for overall health services. So the aim for universal coverage is real.” Underreporting is particularly prevalent in lower income countries with large unregulated private sectors, she said, though India and Indonesia have taken corrective steps to increase reporting.
A meaningful global initiative will not come cheap: The current annual shortfall in funding for TB prevention, diagnosis, and treatment is about $3.5 billion. By the year 2022, the gap between funding and what’s needed to stay on track for the 2030 target will be over $6 billion, said Dr. Kasaeva.
The best use of increased resources for TB eradication will be in locally focused efforts, said Irene Koek, MD, the United States Agency for International Development’s deputy administrator for global health. “It is likely that each region requires a tailored response.” Further, “to improve quality of care we need to ensure that services are patient centered,” she said at the press conference.
To that end, Dr. Koek expects that at the upcoming high-level meeting, the United Nations member states will be called on to develop an open framework, with clear accountability for monitoring and reviewing progress. The road forward should “celebrate accomplishments and acknowledge shortcomings,” she said. Some recent studies have shown that treatment success rates above 80% for patients with MDR TB can be achieved.
“Lessons learned from these experiences should be documented and shared in order to replicate success globally,” said Dr. Koek.
The United States, said Dr. Koek, is the leading global investor in TB research and treatment. “We welcome increased partnerships, especially with countries with the highest burden, to end global suffering from this disease.”
Eric Goosby, MD, the United Nations special envoy on TB, used his speaking time to lend some perspective to the social framework around TB’s longtime lethality.
There are aspects of TB infection that differentiate it from HIV/AIDS, said Dr. Goosby, who has spent most of his clinical and public health career on HIV/AIDS treatment and prevention. In contrast to an infection that at present requires a lifetime of treatment, TB can ordinarily be treated in 6 months, making it an unpleasant episode that an individual may be eager to move past. Additionally, the fact that TB has had a “hold on the world since the time of the ancient Egyptians” may paradoxically have served to lessen urgency in research and treatment efforts, he noted.
Dr. Goosby also spoke of the stigma surrounding TB, whose sufferers are likely to be facing dire poverty, malnutrition, and other infectious disease burdens. Civil society concerned with TB, he said, has spoken up “for those without a voice, for those who have difficulty advocating for themselves.”
Dr. Kasaeva agreed, noting that TB “affects the poorest of the poor, which makes it extraordinarily difficult for activism to come from that population.”
However, others have spoken for those affected, said Dr. Goosby. “The TB civil society has put its heart and soul this last year into gathering political will from leaders around the world…. It’s not a passive effort; it involves a lot of work.” During the past year of concerted effort, he said, “All of us have known the difficulty of pushing a political leader up that learning curve.”
As the upcoming high-level meeting approaches, those who have been working on the effort can feel the momentum, said Dr. Goosby. Still, he noted, “While there’s a significant step forward, this is not the time for a victory dance. This is really the time for a reflection...Do we understand the burden in our respective countries, and has the response been adequate?”
The goal for the meeting is to have leaders “step up to commit, not for one day, or for one meeting, but for the duration of the effort,” said Dr. Goosby. “We must make sure that the words that we hear next week from our leaders translate into action...Next week the world will say, ‘No more. No longer. No one is immune to TB. Tuberculosis is preventable; tuberculosis is treatable; tuberculosis is curable.’”
The BMJ commentary, by Marcel A. Behr, MD, of McGill International TB Centre, Infectious Diseases and Immunity in Global Health Program, McGill University Health Centre Research Institute, and his colleagues, recommend caution when building a prevention strategy around treating many millions of individuals with “latent” TB. They wrote, “Immunoreactivity to TB does not necessarily indicate the presence of live bacteria, as reactivity can persist after infection has been cleared. Classifying two billion people with evidence of immunoreactivity as having latent TB infection may divert fundamental research and public health interventions away from transmissible active TB disease and newly infected people at highest risk of progression to disease.”
This story was updated on 09/24/2018
A concerted a lethal disease affecting one-quarter of the world’s population by the year 2030.
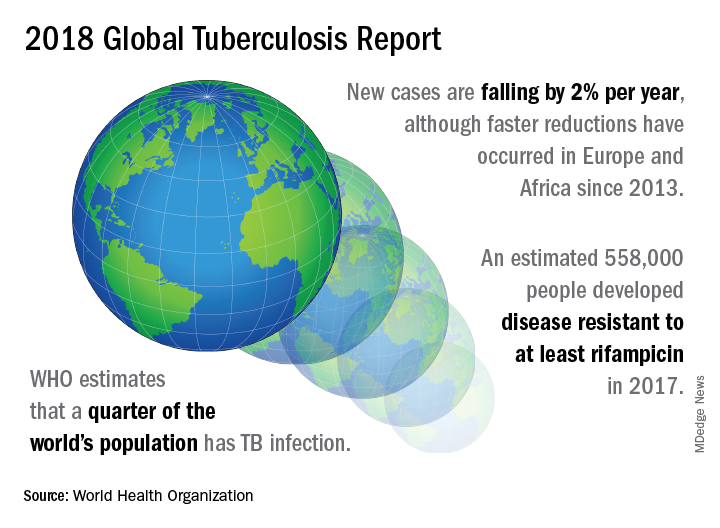
On September 26 the United Nations General Assembly will convene a high-level meeting of global stakeholders to solidify the eradication plan, addressing the global crisis of tuberculosis (TB), the world’s most deadly infectious disease.
“We must seize the moment,” said Tereza Kasaeva, MD, director of the World Health Organization’s global TB program, speaking at a telebriefing and press conference accompanying the release of the World Health Organization’s annual global tuberculosis report. “It’s unacceptable in the 21st century that millions lose their lives to this preventable and curable disease.”
TB caused 1.6 million deaths globally in 2017, and the World Health Organization (WHO) estimates that of the 10 million new cases of TB last year, 558,000 are multi-drug resistant (MDR) infections.
Though death rates and new cases are falling globally each year, significantly more resources are needed to boost access to preventive treatment for latent TB infection; “Most people needing it are not yet accessing care,” according to the press briefing accompanying the report.
A review and commentary on TB incubation and latency published in BMJ (2018;362:k2738 doi: 10.1136/bmj.k2738; e-pub 23 Aug 2018) has called into question the focus preventive treatment of latent cases at the expense of reaching those most likely to die from TB (e.g., HIV patients, children of individuals living with active TB). The authors state that “latent” TB is identified by indirect evidence of present or past infection with Mycobacterium tuberculosis as inferred by a detectable adaptive immune response to M tuberculosis antigens. Active TB infection is overwhelmingly the result of a primary infection and almost always occurs within two years.
In order to meet the ambitious goal of TB eradication by the year 2030, treatment coverage must rise to 90% globally from the current 64%, according to the report.
Progress in southern Africa and in the Russian Federation, where efforts have led to a 30% reduction in TB mortality and a decrease in incidence of 5% per year, show that steep reductions in TB are possible when resources are brought to bear on the problem, said Dr. Kasaeva. “We should acknowledge that actions in some countries and regions show that progress can accelerate,” she said. Still, she noted, “Four thousand lives per day are lost to TB. Tuberculosis is the leading killer of people living with HIV, and the major cause of deaths related to antimicrobial resistance” at a global level.
Two thirds of all TB cases occur in eight countries, with India, China, and Indonesia leading this group. About half of the cases of MDR TB occur in India, China, and Russia, said Dr. Kasaeva, and globally only one in four individuals with MDR TB who need access to treatment have received it. “We need to urgently tackle the multidrug resistant TB public health crisis,” she said.
Major impediments to successful public health efforts against TB are underdiagnosis and underreporting: It is estimated that 3.6 million of 2017’s 10 million new cases were not officially recorded or reported. Countries where these problems are most serious include India, Indonesia, and Nigeria. Fewer than half of the children with TB are reported globally, according to the report.
People living with HIV/AIDS who are also infected with TB number nearly 1,000,000, but only about half of these were officially reported in 2017.
In terms of prevention priorities, WHO has recommended targeting treatment of latent TB in two groups: People living with HIV/AIDS, and children under the age of 5 years who live in households with TB-infected individuals.
“To enable these actions,” said Dr. Kasaeva, “we need strengthened commitments not just for TB care, but for overall health services. So the aim for universal coverage is real.” Underreporting is particularly prevalent in lower income countries with large unregulated private sectors, she said, though India and Indonesia have taken corrective steps to increase reporting.
A meaningful global initiative will not come cheap: The current annual shortfall in funding for TB prevention, diagnosis, and treatment is about $3.5 billion. By the year 2022, the gap between funding and what’s needed to stay on track for the 2030 target will be over $6 billion, said Dr. Kasaeva.
The best use of increased resources for TB eradication will be in locally focused efforts, said Irene Koek, MD, the United States Agency for International Development’s deputy administrator for global health. “It is likely that each region requires a tailored response.” Further, “to improve quality of care we need to ensure that services are patient centered,” she said at the press conference.
To that end, Dr. Koek expects that at the upcoming high-level meeting, the United Nations member states will be called on to develop an open framework, with clear accountability for monitoring and reviewing progress. The road forward should “celebrate accomplishments and acknowledge shortcomings,” she said. Some recent studies have shown that treatment success rates above 80% for patients with MDR TB can be achieved.
“Lessons learned from these experiences should be documented and shared in order to replicate success globally,” said Dr. Koek.
The United States, said Dr. Koek, is the leading global investor in TB research and treatment. “We welcome increased partnerships, especially with countries with the highest burden, to end global suffering from this disease.”
Eric Goosby, MD, the United Nations special envoy on TB, used his speaking time to lend some perspective to the social framework around TB’s longtime lethality.
There are aspects of TB infection that differentiate it from HIV/AIDS, said Dr. Goosby, who has spent most of his clinical and public health career on HIV/AIDS treatment and prevention. In contrast to an infection that at present requires a lifetime of treatment, TB can ordinarily be treated in 6 months, making it an unpleasant episode that an individual may be eager to move past. Additionally, the fact that TB has had a “hold on the world since the time of the ancient Egyptians” may paradoxically have served to lessen urgency in research and treatment efforts, he noted.
Dr. Goosby also spoke of the stigma surrounding TB, whose sufferers are likely to be facing dire poverty, malnutrition, and other infectious disease burdens. Civil society concerned with TB, he said, has spoken up “for those without a voice, for those who have difficulty advocating for themselves.”
Dr. Kasaeva agreed, noting that TB “affects the poorest of the poor, which makes it extraordinarily difficult for activism to come from that population.”
However, others have spoken for those affected, said Dr. Goosby. “The TB civil society has put its heart and soul this last year into gathering political will from leaders around the world…. It’s not a passive effort; it involves a lot of work.” During the past year of concerted effort, he said, “All of us have known the difficulty of pushing a political leader up that learning curve.”
As the upcoming high-level meeting approaches, those who have been working on the effort can feel the momentum, said Dr. Goosby. Still, he noted, “While there’s a significant step forward, this is not the time for a victory dance. This is really the time for a reflection...Do we understand the burden in our respective countries, and has the response been adequate?”
The goal for the meeting is to have leaders “step up to commit, not for one day, or for one meeting, but for the duration of the effort,” said Dr. Goosby. “We must make sure that the words that we hear next week from our leaders translate into action...Next week the world will say, ‘No more. No longer. No one is immune to TB. Tuberculosis is preventable; tuberculosis is treatable; tuberculosis is curable.’”
The BMJ commentary, by Marcel A. Behr, MD, of McGill International TB Centre, Infectious Diseases and Immunity in Global Health Program, McGill University Health Centre Research Institute, and his colleagues, recommend caution when building a prevention strategy around treating many millions of individuals with “latent” TB. They wrote, “Immunoreactivity to TB does not necessarily indicate the presence of live bacteria, as reactivity can persist after infection has been cleared. Classifying two billion people with evidence of immunoreactivity as having latent TB infection may divert fundamental research and public health interventions away from transmissible active TB disease and newly infected people at highest risk of progression to disease.”
This story was updated on 09/24/2018
A concerted a lethal disease affecting one-quarter of the world’s population by the year 2030.
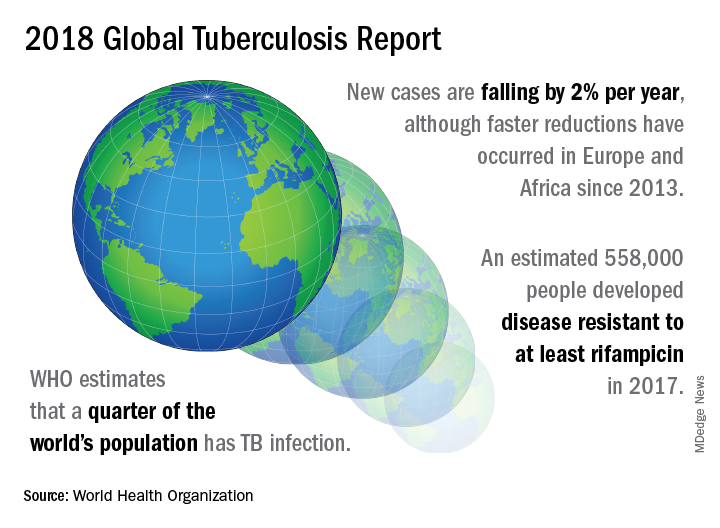
On September 26 the United Nations General Assembly will convene a high-level meeting of global stakeholders to solidify the eradication plan, addressing the global crisis of tuberculosis (TB), the world’s most deadly infectious disease.
“We must seize the moment,” said Tereza Kasaeva, MD, director of the World Health Organization’s global TB program, speaking at a telebriefing and press conference accompanying the release of the World Health Organization’s annual global tuberculosis report. “It’s unacceptable in the 21st century that millions lose their lives to this preventable and curable disease.”
TB caused 1.6 million deaths globally in 2017, and the World Health Organization (WHO) estimates that of the 10 million new cases of TB last year, 558,000 are multi-drug resistant (MDR) infections.
Though death rates and new cases are falling globally each year, significantly more resources are needed to boost access to preventive treatment for latent TB infection; “Most people needing it are not yet accessing care,” according to the press briefing accompanying the report.
A review and commentary on TB incubation and latency published in BMJ (2018;362:k2738 doi: 10.1136/bmj.k2738; e-pub 23 Aug 2018) has called into question the focus preventive treatment of latent cases at the expense of reaching those most likely to die from TB (e.g., HIV patients, children of individuals living with active TB). The authors state that “latent” TB is identified by indirect evidence of present or past infection with Mycobacterium tuberculosis as inferred by a detectable adaptive immune response to M tuberculosis antigens. Active TB infection is overwhelmingly the result of a primary infection and almost always occurs within two years.
In order to meet the ambitious goal of TB eradication by the year 2030, treatment coverage must rise to 90% globally from the current 64%, according to the report.
Progress in southern Africa and in the Russian Federation, where efforts have led to a 30% reduction in TB mortality and a decrease in incidence of 5% per year, show that steep reductions in TB are possible when resources are brought to bear on the problem, said Dr. Kasaeva. “We should acknowledge that actions in some countries and regions show that progress can accelerate,” she said. Still, she noted, “Four thousand lives per day are lost to TB. Tuberculosis is the leading killer of people living with HIV, and the major cause of deaths related to antimicrobial resistance” at a global level.
Two thirds of all TB cases occur in eight countries, with India, China, and Indonesia leading this group. About half of the cases of MDR TB occur in India, China, and Russia, said Dr. Kasaeva, and globally only one in four individuals with MDR TB who need access to treatment have received it. “We need to urgently tackle the multidrug resistant TB public health crisis,” she said.
Major impediments to successful public health efforts against TB are underdiagnosis and underreporting: It is estimated that 3.6 million of 2017’s 10 million new cases were not officially recorded or reported. Countries where these problems are most serious include India, Indonesia, and Nigeria. Fewer than half of the children with TB are reported globally, according to the report.
People living with HIV/AIDS who are also infected with TB number nearly 1,000,000, but only about half of these were officially reported in 2017.
In terms of prevention priorities, WHO has recommended targeting treatment of latent TB in two groups: People living with HIV/AIDS, and children under the age of 5 years who live in households with TB-infected individuals.
“To enable these actions,” said Dr. Kasaeva, “we need strengthened commitments not just for TB care, but for overall health services. So the aim for universal coverage is real.” Underreporting is particularly prevalent in lower income countries with large unregulated private sectors, she said, though India and Indonesia have taken corrective steps to increase reporting.
A meaningful global initiative will not come cheap: The current annual shortfall in funding for TB prevention, diagnosis, and treatment is about $3.5 billion. By the year 2022, the gap between funding and what’s needed to stay on track for the 2030 target will be over $6 billion, said Dr. Kasaeva.
The best use of increased resources for TB eradication will be in locally focused efforts, said Irene Koek, MD, the United States Agency for International Development’s deputy administrator for global health. “It is likely that each region requires a tailored response.” Further, “to improve quality of care we need to ensure that services are patient centered,” she said at the press conference.
To that end, Dr. Koek expects that at the upcoming high-level meeting, the United Nations member states will be called on to develop an open framework, with clear accountability for monitoring and reviewing progress. The road forward should “celebrate accomplishments and acknowledge shortcomings,” she said. Some recent studies have shown that treatment success rates above 80% for patients with MDR TB can be achieved.
“Lessons learned from these experiences should be documented and shared in order to replicate success globally,” said Dr. Koek.
The United States, said Dr. Koek, is the leading global investor in TB research and treatment. “We welcome increased partnerships, especially with countries with the highest burden, to end global suffering from this disease.”
Eric Goosby, MD, the United Nations special envoy on TB, used his speaking time to lend some perspective to the social framework around TB’s longtime lethality.
There are aspects of TB infection that differentiate it from HIV/AIDS, said Dr. Goosby, who has spent most of his clinical and public health career on HIV/AIDS treatment and prevention. In contrast to an infection that at present requires a lifetime of treatment, TB can ordinarily be treated in 6 months, making it an unpleasant episode that an individual may be eager to move past. Additionally, the fact that TB has had a “hold on the world since the time of the ancient Egyptians” may paradoxically have served to lessen urgency in research and treatment efforts, he noted.
Dr. Goosby also spoke of the stigma surrounding TB, whose sufferers are likely to be facing dire poverty, malnutrition, and other infectious disease burdens. Civil society concerned with TB, he said, has spoken up “for those without a voice, for those who have difficulty advocating for themselves.”
Dr. Kasaeva agreed, noting that TB “affects the poorest of the poor, which makes it extraordinarily difficult for activism to come from that population.”
However, others have spoken for those affected, said Dr. Goosby. “The TB civil society has put its heart and soul this last year into gathering political will from leaders around the world…. It’s not a passive effort; it involves a lot of work.” During the past year of concerted effort, he said, “All of us have known the difficulty of pushing a political leader up that learning curve.”
As the upcoming high-level meeting approaches, those who have been working on the effort can feel the momentum, said Dr. Goosby. Still, he noted, “While there’s a significant step forward, this is not the time for a victory dance. This is really the time for a reflection...Do we understand the burden in our respective countries, and has the response been adequate?”
The goal for the meeting is to have leaders “step up to commit, not for one day, or for one meeting, but for the duration of the effort,” said Dr. Goosby. “We must make sure that the words that we hear next week from our leaders translate into action...Next week the world will say, ‘No more. No longer. No one is immune to TB. Tuberculosis is preventable; tuberculosis is treatable; tuberculosis is curable.’”
The BMJ commentary, by Marcel A. Behr, MD, of McGill International TB Centre, Infectious Diseases and Immunity in Global Health Program, McGill University Health Centre Research Institute, and his colleagues, recommend caution when building a prevention strategy around treating many millions of individuals with “latent” TB. They wrote, “Immunoreactivity to TB does not necessarily indicate the presence of live bacteria, as reactivity can persist after infection has been cleared. Classifying two billion people with evidence of immunoreactivity as having latent TB infection may divert fundamental research and public health interventions away from transmissible active TB disease and newly infected people at highest risk of progression to disease.”
This story was updated on 09/24/2018
FROM A WORLD HEALTH ORGANIZATION PRESS CONFERENCE
White coats and provider attire: Does it matter to patients?
What is appropriate “ward garb”?
The question of appropriate ward garb is a problem for the ages. Compared with photo stills and films from the 1960s, the doctors of today appear like vagabonds. No ties, no lab coats, and scrub tops have become the norm for a number (a majority?) of hospital-based docs – and even more so on the surgical wards and in the ER.
Past studies have addressed patient preferences for provider dress, but none like the results of a recent survey.
From the University of Michigan, Ann Arbor, comes a physician attire survey of a convenience sample of 4,000 patients at 10 U.S. academic medical centers. It included both inpatients and outpatients, and used the design of many previous studies, showing patients the same doctor dressed seven different ways. After viewing the photographs, the patients received surveys as to their preference of physician based on attire, as well as being asked to rate the physician in the areas of knowledge, trust, care, approachability, and comfort.
You can see the domains: casual, scrubs, and formal, each with and without a lab coat. The seventh category is business attire (future C-suite wannabes – you know who you are).
Over half of the participants indicated that how a physician dresses was important to them, with more than one in three stating that this influenced how happy they were with care received. Overall, respondents indicated that formal attire with white coats was the most preferred form of physician dress.
I found the discussion in the study worthwhile, along with the strengths and weaknesses of the author’s outline. They went to great lengths to design a nonbiased questionnaire and used a consistent approach to shooting their photos. They also discussed lab coats, long sleeves, and hygiene.
But what to draw from the findings? Does patient satisfaction matter or just clinical outcomes? Is patient happiness a means to an end or an end unto itself? Can I even get you exercised about a score of 6 versus 8 (a 25% difference)? For instance, imagine the worst-dressed doc – say shorts and flip-flops. Is that a 5.8 or a 2.3? The anchor matters, and it helps to put the ratings in context.
Read the full post at hospitalleader.org.
Dr. Flansbaum works for Geisinger Health System in Danville, Pa., in both the divisions of hospital medicine and population health. He is a founding member of the Society of Hospital Medicine and served as a board member and officer.
Also in The Hospital Leader
•Hospitalists Can Improve Patient Trust…in Their Colleagues by Chris Moriates, MD, SFHM
•Treatment of Type II MIs by Brad Flansbaum, MD, MPH, MHM
•The $64,000 Question: How Can Hospitalists Improve Their HCAHPS Scores? by Leslie Flores, MHA, SFHM
What is appropriate “ward garb”?
What is appropriate “ward garb”?
The question of appropriate ward garb is a problem for the ages. Compared with photo stills and films from the 1960s, the doctors of today appear like vagabonds. No ties, no lab coats, and scrub tops have become the norm for a number (a majority?) of hospital-based docs – and even more so on the surgical wards and in the ER.
Past studies have addressed patient preferences for provider dress, but none like the results of a recent survey.
From the University of Michigan, Ann Arbor, comes a physician attire survey of a convenience sample of 4,000 patients at 10 U.S. academic medical centers. It included both inpatients and outpatients, and used the design of many previous studies, showing patients the same doctor dressed seven different ways. After viewing the photographs, the patients received surveys as to their preference of physician based on attire, as well as being asked to rate the physician in the areas of knowledge, trust, care, approachability, and comfort.
You can see the domains: casual, scrubs, and formal, each with and without a lab coat. The seventh category is business attire (future C-suite wannabes – you know who you are).
Over half of the participants indicated that how a physician dresses was important to them, with more than one in three stating that this influenced how happy they were with care received. Overall, respondents indicated that formal attire with white coats was the most preferred form of physician dress.
I found the discussion in the study worthwhile, along with the strengths and weaknesses of the author’s outline. They went to great lengths to design a nonbiased questionnaire and used a consistent approach to shooting their photos. They also discussed lab coats, long sleeves, and hygiene.
But what to draw from the findings? Does patient satisfaction matter or just clinical outcomes? Is patient happiness a means to an end or an end unto itself? Can I even get you exercised about a score of 6 versus 8 (a 25% difference)? For instance, imagine the worst-dressed doc – say shorts and flip-flops. Is that a 5.8 or a 2.3? The anchor matters, and it helps to put the ratings in context.
Read the full post at hospitalleader.org.
Dr. Flansbaum works for Geisinger Health System in Danville, Pa., in both the divisions of hospital medicine and population health. He is a founding member of the Society of Hospital Medicine and served as a board member and officer.
Also in The Hospital Leader
•Hospitalists Can Improve Patient Trust…in Their Colleagues by Chris Moriates, MD, SFHM
•Treatment of Type II MIs by Brad Flansbaum, MD, MPH, MHM
•The $64,000 Question: How Can Hospitalists Improve Their HCAHPS Scores? by Leslie Flores, MHA, SFHM
The question of appropriate ward garb is a problem for the ages. Compared with photo stills and films from the 1960s, the doctors of today appear like vagabonds. No ties, no lab coats, and scrub tops have become the norm for a number (a majority?) of hospital-based docs – and even more so on the surgical wards and in the ER.
Past studies have addressed patient preferences for provider dress, but none like the results of a recent survey.
From the University of Michigan, Ann Arbor, comes a physician attire survey of a convenience sample of 4,000 patients at 10 U.S. academic medical centers. It included both inpatients and outpatients, and used the design of many previous studies, showing patients the same doctor dressed seven different ways. After viewing the photographs, the patients received surveys as to their preference of physician based on attire, as well as being asked to rate the physician in the areas of knowledge, trust, care, approachability, and comfort.
You can see the domains: casual, scrubs, and formal, each with and without a lab coat. The seventh category is business attire (future C-suite wannabes – you know who you are).
Over half of the participants indicated that how a physician dresses was important to them, with more than one in three stating that this influenced how happy they were with care received. Overall, respondents indicated that formal attire with white coats was the most preferred form of physician dress.
I found the discussion in the study worthwhile, along with the strengths and weaknesses of the author’s outline. They went to great lengths to design a nonbiased questionnaire and used a consistent approach to shooting their photos. They also discussed lab coats, long sleeves, and hygiene.
But what to draw from the findings? Does patient satisfaction matter or just clinical outcomes? Is patient happiness a means to an end or an end unto itself? Can I even get you exercised about a score of 6 versus 8 (a 25% difference)? For instance, imagine the worst-dressed doc – say shorts and flip-flops. Is that a 5.8 or a 2.3? The anchor matters, and it helps to put the ratings in context.
Read the full post at hospitalleader.org.
Dr. Flansbaum works for Geisinger Health System in Danville, Pa., in both the divisions of hospital medicine and population health. He is a founding member of the Society of Hospital Medicine and served as a board member and officer.
Also in The Hospital Leader
•Hospitalists Can Improve Patient Trust…in Their Colleagues by Chris Moriates, MD, SFHM
•Treatment of Type II MIs by Brad Flansbaum, MD, MPH, MHM
•The $64,000 Question: How Can Hospitalists Improve Their HCAHPS Scores? by Leslie Flores, MHA, SFHM
PARP inhibitor plus trabectedin shows promise for sarcoma
A combination of trabectedin and the PARP inhibitor olaparib may be a safe and effective therapy for patients with sarcoma, the recent TOMAS trial found.
High PARP1 expression was associated with treatment response, reported Giovanni Grignani, MD, of the Medical Oncology_Sarcoma Unit at Istituto di Ricovero e Cura a Carattere Scientifico in Candiolo, Italy, and his colleagues.
PARP inhibitors prevent repair of DNA damage, suggesting potential synergisms with DNA-damaging anticancer agents. Preclinical models support this strategy; however, clinical trials have found that toxicities restrict doses below antitumor activity levels.
“In view of these findings, trabectedin could be an ideal drug to use in combination with PARP1/2 inhibitors for two reasons: its favourable haemopoietic toxicity profile and its unique mechanisms of action,” the authors wrote in The Lancet Oncology. Trabectedin bends the minor groove of DNA toward the major groove, which activates PARP1 in an attempt to repair the damage. Preclinical trials showed that a PARP inhibitor such as olaparib would block this PARP1 activation, ultimately resulting in a more robust response than with either drug alone.
The phase 1b, open-label TOMAS trial involved 50 patients with sarcoma who had experienced disease progression after standard therapy. The study was divided into two cohorts: dose-escalation and dose-expansion. Patients received a median of four cycles of therapy with a median follow-up of 10 months (some patients are still undergoing treatment). The primary endpoint was maximum tolerated dose. The investigators also evaluated pharmacokinetics, pharmacodynamics, and various response measures.
Although adverse events occurred, these were manageable, and the authors concluded that the combination is safe for further investigation. The most common grade 3 or higher adverse events were lymphopenia (64%), neutropenia (62%), thrombocytopenia (28%), anemia (26%), hypophosphatemia (40%), and alanine aminotransferase elevation (18%). The maximum tolerated dose (recommended phase 2 dose) was olaparib 150 mg twice daily and trabectedin 1.1 mg/m2 every 3 weeks.
“These doses allowed us to minimize the need for dose reductions and continue treatment for as long as tumour control was maintained,” the authors wrote. Previous treatments impacted tolerability. The researchers noted that “patients who had received more than two lines of therapy had a higher risk of developing dose-limiting toxicities than those patients who had been treated with only one line of therapy.”
Overall, 14% of patients responded to therapy. Six-month progression-free survival was more common in patients with soft tissue sarcoma (38%) than other tumor types. More patients with high PARP1 expression achieved 6-month PFS compared with patients who had low PARP1 expression (59% vs. 8%; P = .01).
“The combination of olaparib and trabectedin exploits the potential of two different first-in-class drugs and shows tolerability and activity in homologous repair-proficient tumors,” the authors concluded.
They are planning two phase 2 studies in the future; one “comparing trabectedin alone versus the combination of trabectedin and olaparib, stratifying patients according to PARP1 expression,” and an “after-platinum-failure study of patients with ovarian cancer regardless of patients’ BRCA1/2 and BRCAness status.”
The TOMAS trial was funded by the Italian Association for Cancer Research, the Foundation for Research on Musculoskeletal and Rare Tumors, the Italian Ministry of Health, and PharmaMar. The authors reported compensation from Lilly, Novartis, Bayer, Eisai, Amgen, and others.
SOURCE: Grignani et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30438-8.
The phase 1b TOMAS trial by Grignani et al. showed that PARP inhibitor combination therapy may be a safe and effective option for patients with sarcoma, and a phase 2 study is warranted, according to Benjamin A. Nacev, MD, and William D. Tap, MD.
PARP inhibitors mitigate DNA damage repair, suggesting potential for synergistic combinations with DNA-damaging anticancer agents. Unfortunately, previous combinations have revealed toxicity issues.
“The first clinical example of this approach was the combination of the alkylating drug temozolomide and the PARP inhibitor rucaparib, which was hampered by dose-limiting myelosuppression,” Dr. Nacev and Dr. Tap wrote in an editorial in The Lancet Oncology.
In the TOMAS trial, Grignani et al. assessed a combination of trabectedin and the PARP inhibitor olaparib. Preclinical data showed synergistic activity in sarcoma cell lines, and the authors predicted tolerable myelosuppression with trabectedin.
Their predictions yielded promising results: Approximately one-third of patients with soft-tissue sarcoma were progression free at 6 months. Although myelosuppression did occur, the adverse event profile was tolerable.
As drug synergisms are biologically complex, “a key success of the TOMAS trial is the effective use of exploratory pharmacodynamic endpoints including PARP1 expression, PARylation, and mutational status of the DNA damage repair pathway.”
“For example, efficacy in the TOMAS trial correlated with PARP1 expression, with greater 6-month progression-free survival in the high PARP1 expression group than the low expression group.”
“The TOMAS investigators should be commended for doing the important bench-to-bedside approach of rationally designing and testing a drug combination to leverage available active drugs. We agree with the authors’ call for further investigation of trabectedin and olaparib in a randomised phase 2 trial in soft tissue sarcoma.”
William D. Tap, MD is chief of the Sarcoma Medical Oncology Service and Benjamin A. Nacev, MD is a third-year medical oncology/hematology fellow at Memorial Sloan Kettering Cancer Center in New York. Dr. Tap reported personal fees from Eli Lilly, Novartis, Eisai, and others. These comments are adapted from their accompanying editorial .
The phase 1b TOMAS trial by Grignani et al. showed that PARP inhibitor combination therapy may be a safe and effective option for patients with sarcoma, and a phase 2 study is warranted, according to Benjamin A. Nacev, MD, and William D. Tap, MD.
PARP inhibitors mitigate DNA damage repair, suggesting potential for synergistic combinations with DNA-damaging anticancer agents. Unfortunately, previous combinations have revealed toxicity issues.
“The first clinical example of this approach was the combination of the alkylating drug temozolomide and the PARP inhibitor rucaparib, which was hampered by dose-limiting myelosuppression,” Dr. Nacev and Dr. Tap wrote in an editorial in The Lancet Oncology.
In the TOMAS trial, Grignani et al. assessed a combination of trabectedin and the PARP inhibitor olaparib. Preclinical data showed synergistic activity in sarcoma cell lines, and the authors predicted tolerable myelosuppression with trabectedin.
Their predictions yielded promising results: Approximately one-third of patients with soft-tissue sarcoma were progression free at 6 months. Although myelosuppression did occur, the adverse event profile was tolerable.
As drug synergisms are biologically complex, “a key success of the TOMAS trial is the effective use of exploratory pharmacodynamic endpoints including PARP1 expression, PARylation, and mutational status of the DNA damage repair pathway.”
“For example, efficacy in the TOMAS trial correlated with PARP1 expression, with greater 6-month progression-free survival in the high PARP1 expression group than the low expression group.”
“The TOMAS investigators should be commended for doing the important bench-to-bedside approach of rationally designing and testing a drug combination to leverage available active drugs. We agree with the authors’ call for further investigation of trabectedin and olaparib in a randomised phase 2 trial in soft tissue sarcoma.”
William D. Tap, MD is chief of the Sarcoma Medical Oncology Service and Benjamin A. Nacev, MD is a third-year medical oncology/hematology fellow at Memorial Sloan Kettering Cancer Center in New York. Dr. Tap reported personal fees from Eli Lilly, Novartis, Eisai, and others. These comments are adapted from their accompanying editorial .
The phase 1b TOMAS trial by Grignani et al. showed that PARP inhibitor combination therapy may be a safe and effective option for patients with sarcoma, and a phase 2 study is warranted, according to Benjamin A. Nacev, MD, and William D. Tap, MD.
PARP inhibitors mitigate DNA damage repair, suggesting potential for synergistic combinations with DNA-damaging anticancer agents. Unfortunately, previous combinations have revealed toxicity issues.
“The first clinical example of this approach was the combination of the alkylating drug temozolomide and the PARP inhibitor rucaparib, which was hampered by dose-limiting myelosuppression,” Dr. Nacev and Dr. Tap wrote in an editorial in The Lancet Oncology.
In the TOMAS trial, Grignani et al. assessed a combination of trabectedin and the PARP inhibitor olaparib. Preclinical data showed synergistic activity in sarcoma cell lines, and the authors predicted tolerable myelosuppression with trabectedin.
Their predictions yielded promising results: Approximately one-third of patients with soft-tissue sarcoma were progression free at 6 months. Although myelosuppression did occur, the adverse event profile was tolerable.
As drug synergisms are biologically complex, “a key success of the TOMAS trial is the effective use of exploratory pharmacodynamic endpoints including PARP1 expression, PARylation, and mutational status of the DNA damage repair pathway.”
“For example, efficacy in the TOMAS trial correlated with PARP1 expression, with greater 6-month progression-free survival in the high PARP1 expression group than the low expression group.”
“The TOMAS investigators should be commended for doing the important bench-to-bedside approach of rationally designing and testing a drug combination to leverage available active drugs. We agree with the authors’ call for further investigation of trabectedin and olaparib in a randomised phase 2 trial in soft tissue sarcoma.”
William D. Tap, MD is chief of the Sarcoma Medical Oncology Service and Benjamin A. Nacev, MD is a third-year medical oncology/hematology fellow at Memorial Sloan Kettering Cancer Center in New York. Dr. Tap reported personal fees from Eli Lilly, Novartis, Eisai, and others. These comments are adapted from their accompanying editorial .
A combination of trabectedin and the PARP inhibitor olaparib may be a safe and effective therapy for patients with sarcoma, the recent TOMAS trial found.
High PARP1 expression was associated with treatment response, reported Giovanni Grignani, MD, of the Medical Oncology_Sarcoma Unit at Istituto di Ricovero e Cura a Carattere Scientifico in Candiolo, Italy, and his colleagues.
PARP inhibitors prevent repair of DNA damage, suggesting potential synergisms with DNA-damaging anticancer agents. Preclinical models support this strategy; however, clinical trials have found that toxicities restrict doses below antitumor activity levels.
“In view of these findings, trabectedin could be an ideal drug to use in combination with PARP1/2 inhibitors for two reasons: its favourable haemopoietic toxicity profile and its unique mechanisms of action,” the authors wrote in The Lancet Oncology. Trabectedin bends the minor groove of DNA toward the major groove, which activates PARP1 in an attempt to repair the damage. Preclinical trials showed that a PARP inhibitor such as olaparib would block this PARP1 activation, ultimately resulting in a more robust response than with either drug alone.
The phase 1b, open-label TOMAS trial involved 50 patients with sarcoma who had experienced disease progression after standard therapy. The study was divided into two cohorts: dose-escalation and dose-expansion. Patients received a median of four cycles of therapy with a median follow-up of 10 months (some patients are still undergoing treatment). The primary endpoint was maximum tolerated dose. The investigators also evaluated pharmacokinetics, pharmacodynamics, and various response measures.
Although adverse events occurred, these were manageable, and the authors concluded that the combination is safe for further investigation. The most common grade 3 or higher adverse events were lymphopenia (64%), neutropenia (62%), thrombocytopenia (28%), anemia (26%), hypophosphatemia (40%), and alanine aminotransferase elevation (18%). The maximum tolerated dose (recommended phase 2 dose) was olaparib 150 mg twice daily and trabectedin 1.1 mg/m2 every 3 weeks.
“These doses allowed us to minimize the need for dose reductions and continue treatment for as long as tumour control was maintained,” the authors wrote. Previous treatments impacted tolerability. The researchers noted that “patients who had received more than two lines of therapy had a higher risk of developing dose-limiting toxicities than those patients who had been treated with only one line of therapy.”
Overall, 14% of patients responded to therapy. Six-month progression-free survival was more common in patients with soft tissue sarcoma (38%) than other tumor types. More patients with high PARP1 expression achieved 6-month PFS compared with patients who had low PARP1 expression (59% vs. 8%; P = .01).
“The combination of olaparib and trabectedin exploits the potential of two different first-in-class drugs and shows tolerability and activity in homologous repair-proficient tumors,” the authors concluded.
They are planning two phase 2 studies in the future; one “comparing trabectedin alone versus the combination of trabectedin and olaparib, stratifying patients according to PARP1 expression,” and an “after-platinum-failure study of patients with ovarian cancer regardless of patients’ BRCA1/2 and BRCAness status.”
The TOMAS trial was funded by the Italian Association for Cancer Research, the Foundation for Research on Musculoskeletal and Rare Tumors, the Italian Ministry of Health, and PharmaMar. The authors reported compensation from Lilly, Novartis, Bayer, Eisai, Amgen, and others.
SOURCE: Grignani et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30438-8.
A combination of trabectedin and the PARP inhibitor olaparib may be a safe and effective therapy for patients with sarcoma, the recent TOMAS trial found.
High PARP1 expression was associated with treatment response, reported Giovanni Grignani, MD, of the Medical Oncology_Sarcoma Unit at Istituto di Ricovero e Cura a Carattere Scientifico in Candiolo, Italy, and his colleagues.
PARP inhibitors prevent repair of DNA damage, suggesting potential synergisms with DNA-damaging anticancer agents. Preclinical models support this strategy; however, clinical trials have found that toxicities restrict doses below antitumor activity levels.
“In view of these findings, trabectedin could be an ideal drug to use in combination with PARP1/2 inhibitors for two reasons: its favourable haemopoietic toxicity profile and its unique mechanisms of action,” the authors wrote in The Lancet Oncology. Trabectedin bends the minor groove of DNA toward the major groove, which activates PARP1 in an attempt to repair the damage. Preclinical trials showed that a PARP inhibitor such as olaparib would block this PARP1 activation, ultimately resulting in a more robust response than with either drug alone.
The phase 1b, open-label TOMAS trial involved 50 patients with sarcoma who had experienced disease progression after standard therapy. The study was divided into two cohorts: dose-escalation and dose-expansion. Patients received a median of four cycles of therapy with a median follow-up of 10 months (some patients are still undergoing treatment). The primary endpoint was maximum tolerated dose. The investigators also evaluated pharmacokinetics, pharmacodynamics, and various response measures.
Although adverse events occurred, these were manageable, and the authors concluded that the combination is safe for further investigation. The most common grade 3 or higher adverse events were lymphopenia (64%), neutropenia (62%), thrombocytopenia (28%), anemia (26%), hypophosphatemia (40%), and alanine aminotransferase elevation (18%). The maximum tolerated dose (recommended phase 2 dose) was olaparib 150 mg twice daily and trabectedin 1.1 mg/m2 every 3 weeks.
“These doses allowed us to minimize the need for dose reductions and continue treatment for as long as tumour control was maintained,” the authors wrote. Previous treatments impacted tolerability. The researchers noted that “patients who had received more than two lines of therapy had a higher risk of developing dose-limiting toxicities than those patients who had been treated with only one line of therapy.”
Overall, 14% of patients responded to therapy. Six-month progression-free survival was more common in patients with soft tissue sarcoma (38%) than other tumor types. More patients with high PARP1 expression achieved 6-month PFS compared with patients who had low PARP1 expression (59% vs. 8%; P = .01).
“The combination of olaparib and trabectedin exploits the potential of two different first-in-class drugs and shows tolerability and activity in homologous repair-proficient tumors,” the authors concluded.
They are planning two phase 2 studies in the future; one “comparing trabectedin alone versus the combination of trabectedin and olaparib, stratifying patients according to PARP1 expression,” and an “after-platinum-failure study of patients with ovarian cancer regardless of patients’ BRCA1/2 and BRCAness status.”
The TOMAS trial was funded by the Italian Association for Cancer Research, the Foundation for Research on Musculoskeletal and Rare Tumors, the Italian Ministry of Health, and PharmaMar. The authors reported compensation from Lilly, Novartis, Bayer, Eisai, Amgen, and others.
SOURCE: Grignani et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30438-8.
FROM THE LANCET ONCOLOGY
Key clinical point: A combination of trabectedin and the PARP inhibitor olaparib may be a safe and effective therapy for patients with sarcoma.
Major finding: Of those with high PARP1 expression, 59% were progression free 6 months after treatment.
Study details: TOMAS was an open-label phase 1b trial involving 50 patients with sarcoma who had disease progression after standard therapy.
Disclosures: The study was funded by the Italian Association for Cancer Research, the Foundation for Research on Musculoskeletal and Rare Tumors, the Italian Ministry of Health, and PharmaMar. The authors reported compensation from Lilly, Novartis, Bayer, Eisai, Amgen, and others.
Source: Grignani et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30438-8.
Researchers propose new acute leukemia subtypes
An extensive analysis of mixed phenotype acute leukemia (MPAL) has led to new insights that may have implications for disease classification and treatment.
Researchers believe they have identified new subtypes of MPAL that should be included in the World Health Organization classification for acute leukemia.
Each of these subtypes share genomic characteristics with other acute leukemias, which suggests they might respond to treatments that are already in use.
This research also has shed light on how MPAL evolves and appears to provide an explanation for why MPAL displays characteristics of both acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL).
“ALL and AML have very different treatments, but MPAL has features of both, so the question of how best to treat patients with MPAL has been challenging the leukemia community worldwide, and long-term survival of patients has been poor,” said study author Charles G. Mullighan, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn.
In the current study, published in Nature, Dr. Mullighan and his colleagues used whole-genome, whole-exome, and RNA sequencing to analyze 115 samples from pediatric patients with MPAL.
The analysis revealed mutations that define the two most common subtypes of MPAL – B/myeloid and T/myeloid – and suggested these subtypes share similarities with other leukemia subtypes.
The researchers found that 48% of B/myeloid MPAL cases carried rearrangements in ZNF384, a characteristic that is also found in cases of B-cell ALL. In fact, the team said the gene expression profiles of ZNF384r B-ALL and ZNF384r MPAL were indistinguishable.
“That is biologically and clinically important,” Dr. Mullighan said. “The findings suggest the ZNF384 rearrangement defines a distinct leukemia subtype, and the alteration should be used to guide treatment.”
The researchers noted that patients with ZNF384r exhibited higher FLT3 expression than that of patients with other types of B/myeloid or T/myeloid MPAL, so patients with ZNF384r MPAL might respond well to treatment with a FLT3 inhibitor.
This study also showed that cases of B/myeloid MPAL without ZNF384r shared genomic features with other B-ALL subtypes, such as Ph-like B-ALL.
In addition, the analysis showed that T/myeloid MPAL and early T-cell precursor ALL have similar gene expression profiles.
The team identified several genes that were mutated at similar frequencies in T/myeloid MPAL and early T-cell precursor ALL, including WT1, ETV6, EZH2, and FLT3.
WT1 was the most frequently mutated transcription factor gene in T/myeloid MPAL.
Based on these findings, the researchers said the WHO classification of acute leukemia should be updated to include: ZNF384r acute leukemia (either B-ALL or MPAL), WT1-mutant T/myeloid MPAL, and Ph-like B/myeloid MPAL.
This research was supported by the National Cancer Institute, the National Institutes of Health, Cookies for Kids’ Cancer, and other organizations. The researchers reported having no competing interests.
SOURCE: Alexander TB et al. Nature. 2018 Sep 12. doi: 10.1038/s41586-018-0436-0.
An extensive analysis of mixed phenotype acute leukemia (MPAL) has led to new insights that may have implications for disease classification and treatment.
Researchers believe they have identified new subtypes of MPAL that should be included in the World Health Organization classification for acute leukemia.
Each of these subtypes share genomic characteristics with other acute leukemias, which suggests they might respond to treatments that are already in use.
This research also has shed light on how MPAL evolves and appears to provide an explanation for why MPAL displays characteristics of both acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL).
“ALL and AML have very different treatments, but MPAL has features of both, so the question of how best to treat patients with MPAL has been challenging the leukemia community worldwide, and long-term survival of patients has been poor,” said study author Charles G. Mullighan, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn.
In the current study, published in Nature, Dr. Mullighan and his colleagues used whole-genome, whole-exome, and RNA sequencing to analyze 115 samples from pediatric patients with MPAL.
The analysis revealed mutations that define the two most common subtypes of MPAL – B/myeloid and T/myeloid – and suggested these subtypes share similarities with other leukemia subtypes.
The researchers found that 48% of B/myeloid MPAL cases carried rearrangements in ZNF384, a characteristic that is also found in cases of B-cell ALL. In fact, the team said the gene expression profiles of ZNF384r B-ALL and ZNF384r MPAL were indistinguishable.
“That is biologically and clinically important,” Dr. Mullighan said. “The findings suggest the ZNF384 rearrangement defines a distinct leukemia subtype, and the alteration should be used to guide treatment.”
The researchers noted that patients with ZNF384r exhibited higher FLT3 expression than that of patients with other types of B/myeloid or T/myeloid MPAL, so patients with ZNF384r MPAL might respond well to treatment with a FLT3 inhibitor.
This study also showed that cases of B/myeloid MPAL without ZNF384r shared genomic features with other B-ALL subtypes, such as Ph-like B-ALL.
In addition, the analysis showed that T/myeloid MPAL and early T-cell precursor ALL have similar gene expression profiles.
The team identified several genes that were mutated at similar frequencies in T/myeloid MPAL and early T-cell precursor ALL, including WT1, ETV6, EZH2, and FLT3.
WT1 was the most frequently mutated transcription factor gene in T/myeloid MPAL.
Based on these findings, the researchers said the WHO classification of acute leukemia should be updated to include: ZNF384r acute leukemia (either B-ALL or MPAL), WT1-mutant T/myeloid MPAL, and Ph-like B/myeloid MPAL.
This research was supported by the National Cancer Institute, the National Institutes of Health, Cookies for Kids’ Cancer, and other organizations. The researchers reported having no competing interests.
SOURCE: Alexander TB et al. Nature. 2018 Sep 12. doi: 10.1038/s41586-018-0436-0.
An extensive analysis of mixed phenotype acute leukemia (MPAL) has led to new insights that may have implications for disease classification and treatment.
Researchers believe they have identified new subtypes of MPAL that should be included in the World Health Organization classification for acute leukemia.
Each of these subtypes share genomic characteristics with other acute leukemias, which suggests they might respond to treatments that are already in use.
This research also has shed light on how MPAL evolves and appears to provide an explanation for why MPAL displays characteristics of both acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL).
“ALL and AML have very different treatments, but MPAL has features of both, so the question of how best to treat patients with MPAL has been challenging the leukemia community worldwide, and long-term survival of patients has been poor,” said study author Charles G. Mullighan, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn.
In the current study, published in Nature, Dr. Mullighan and his colleagues used whole-genome, whole-exome, and RNA sequencing to analyze 115 samples from pediatric patients with MPAL.
The analysis revealed mutations that define the two most common subtypes of MPAL – B/myeloid and T/myeloid – and suggested these subtypes share similarities with other leukemia subtypes.
The researchers found that 48% of B/myeloid MPAL cases carried rearrangements in ZNF384, a characteristic that is also found in cases of B-cell ALL. In fact, the team said the gene expression profiles of ZNF384r B-ALL and ZNF384r MPAL were indistinguishable.
“That is biologically and clinically important,” Dr. Mullighan said. “The findings suggest the ZNF384 rearrangement defines a distinct leukemia subtype, and the alteration should be used to guide treatment.”
The researchers noted that patients with ZNF384r exhibited higher FLT3 expression than that of patients with other types of B/myeloid or T/myeloid MPAL, so patients with ZNF384r MPAL might respond well to treatment with a FLT3 inhibitor.
This study also showed that cases of B/myeloid MPAL without ZNF384r shared genomic features with other B-ALL subtypes, such as Ph-like B-ALL.
In addition, the analysis showed that T/myeloid MPAL and early T-cell precursor ALL have similar gene expression profiles.
The team identified several genes that were mutated at similar frequencies in T/myeloid MPAL and early T-cell precursor ALL, including WT1, ETV6, EZH2, and FLT3.
WT1 was the most frequently mutated transcription factor gene in T/myeloid MPAL.
Based on these findings, the researchers said the WHO classification of acute leukemia should be updated to include: ZNF384r acute leukemia (either B-ALL or MPAL), WT1-mutant T/myeloid MPAL, and Ph-like B/myeloid MPAL.
This research was supported by the National Cancer Institute, the National Institutes of Health, Cookies for Kids’ Cancer, and other organizations. The researchers reported having no competing interests.
SOURCE: Alexander TB et al. Nature. 2018 Sep 12. doi: 10.1038/s41586-018-0436-0.
FROM NATURE
Key clinical point:
Major finding: In total, 48% of B/myeloid MPAL cases carried rearrangements in ZNF384, a characteristic that is also found in cases of B-cell ALL.
Study details: Whole-genome, -exome, and RNA sequencing of 115 samples from pediatric patients with MPAL.
Disclosures: This research was supported by the National Cancer Institute and other organizations. The researchers reported having no competing interests.
Source: Alexander TB et al. Nature. 2018 Sep 12. doi: 10.1038/s41586-018-0436-0.
Vaginal intraepithelial neoplasia: What to do when dysplasia persists after hysterectomy
Vaginal intraepithelial neoplasia (VAIN) is a condition that frequently poses therapeutic dilemmas for gynecologists. VAIN represents dysplastic changes to the epithelium of the vaginal mucosa, and like cervical neoplasia, the extent of disease is characterized as levels I, II, or III dependent upon the depth of involvement in the epithelial layer by dysplastic cells. While VAIN itself typically is asymptomatic and not a harmful condition, it carries a 12% risk of progression to invasive vaginal carcinoma, so accurate identification, thorough treatment, and ongoing surveillance are essential.1
VAIN is associated with high-risk human papillomavirus (HPV) infection, tobacco use, and prior cervical dysplasia. Of women with VAIN, 65% have undergone a prior hysterectomy for cervical dysplasia, which emphasizes the nondefinitive nature of such an intervention.2 These women should be very closely followed for at least 20 years with vaginal cytologic and/or HPV surveillance. High-risk HPV infection is present in 85% of women with VAIN, and the presence of high-risk HPV is a predictor for recurrent VAIN. Recurrent and persistent VAIN also is more common in postmenopausal women and those with multifocal disease.
The most common location for VAIN is at the upper third of the vagina (including the vaginal cuff). It commonly arises within the vaginal fornices, which may be difficult to fully visualize because of their puckered appearance, redundant vaginal tissues, and extensive vaginal rogation.
A diagnosis of VAIN is typically obtained from vaginal cytology which reveals atypical or dysplastic cells. Such a result should prompt the physician to perform vaginal colposcopy and directed biopsies. Comprehensive visualization of the vaginal cuff can be limited in cases where the vaginal fornices are tethered, deeply puckered, or when there is significant mucosal rogation.
The application of 4% acetic acid or Lugol’s iodine are techniques that can enhance the detection of dysplastic vaginal mucosa. Lugol’s iodine selectively stains normal, glycogenated cells, and spares dysplastic glycogen-free cells. The sharp contrast between the brown iodine-stained tissues and the white dysplastic tissues aids in detection of dysplastic areas.
If colposcopic biopsy reveals low grade dysplasia (VAIN I) it does not require intervention, and has a very low rate of conversion to invasive vaginal carcinoma. However moderate- and high-grade vaginal dysplastic lesions should be treated because of the potential for malignant transformation.
Options for treatment of VAIN include topical, ablative, and excisional procedures. Observation also is an option but should be reserved for patients who are closely monitored with repeated colposcopic examinations, and probably should best be reserved for patients with VAIN I or II lesions.
Excisional procedures
The most common excisional procedure employed for VAIN is upper vaginectomy. In this procedure, the surgeon grasps and tents up the vaginal mucosa, incises the mucosa without penetrating the subepithelial tissue layers such as bladder and rectum. The vaginal mucosa then is carefully separated from the underlying endopelvic fascial plane. The specimen should be oriented, ideally on a cork board, with pins or sutures to ascribe margins and borders. Excision is best utilized for women with unifocal disease, or those who fail or do not tolerate ablative or topical interventions.
The most significant risks of excision include the potential for damage to underlying pelvic visceral structures, which is particularly concerning in postmenopausal women with thin vaginal epithelium. Vaginectomy is commonly associated with vaginal shortening or narrowing, which can be deleterious for quality of life. Retrospective series have described a 30% incidence of recurrence after vaginectomy, likely secondary to incomplete excision of all affected tissue.3
Ablation
Ablation of dysplastic foci with a carbon dioxide (CO2) laser is a common method for treatment of VAIN. CO2 laser should ablate tissue to a 1.5 mm minimum depth.3 The benefit of using CO2 laser is its ability to treat multifocal disease in situ without an extensive excisional procedure.
It is technically more straightforward than upper vaginectomy with less blood loss and shorter surgical times, and it can be easily accomplished in an outpatient surgical or office setting. However, one of its greatest limitations is the difficulty in visualizing all lesions and therefore adequately treating all sites. The vaginal rogations also make adequate laser ablation challenging because laser only is able to effectively ablate tissue that is oriented perpendicular to the laser beam.
In addition, there is no pathologic confirmation of adequacy of excision or margin status. These features may contribute to the modestly higher rates of recurrence of dysplasia following laser ablation, compared with vaginectomy.3 It also has been associated with more vaginal scarring than vaginectomy, which can have a negative effect on sexual health.
Topical agents
The most commonly utilized topical therapy for VAIN is the antimetabolite chemotherapeutic agent 5-fluorouracil (5FU). A typical schedule for 5FU treatment is to apply vaginally, at night, once a week for 8 weeks.4 Because it can cause extensive irritation to the vulvar and urethral epithelium, patients are recommended to apply barrier creams or ointments before and following the use of 5FU for several days, wash hands thoroughly after application, and to rinse and shower in the morning after rising. Severe irritation occurs in up to 16% of patients, but in general it is very well tolerated.
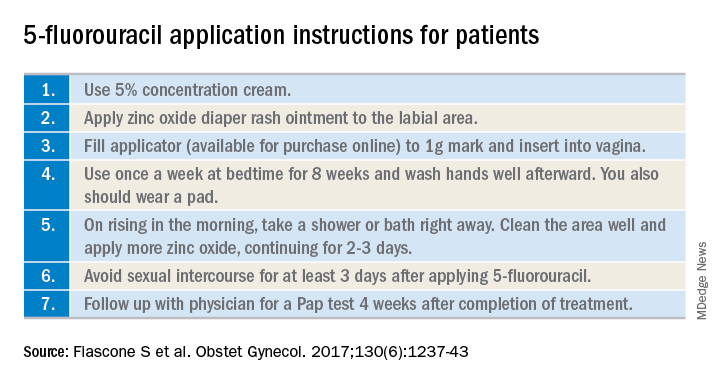
Its virtue is that it is able to conform and travel to all parts of the vaginal mucosa, including those that are poorly visualized within the fornices or vaginal folds. 5FU does not require a hospitalization or surgical procedure, can be applied by the patient at home, and preserves vaginal length and function. In recent reports, 5FU is associated with the lowest rates of recurrence (10%-30%), compared with excision or ablation, and therefore is a very attractive option for primary therapy.3 However, it requires patients to have a degree of comfort with vaginal application of drug and adherence with perineal care strategies to minimize the likelihood of toxicity.
The immune response modifier, imiquimod, that is commonly used in the treatment of vulvar dysplasia also has been described in the treatment of VAIN. It appears to have high rates of clearance (greater than 75%) and be most effective in the treatment of VAIN I.5 It requires application under colposcopic guidance three times a week for 8 weeks, which is a laborious undertaking for both patient and physician. Like 5FU, imiquimod is associated with vulvar and perineal irritation.
Vaginal estrogens are an alternative topical therapy for moderate- and high-grade VAIN and particularly useful for postmenopausal patients. They have been associated with a high rate (up to 90%) of resolution on follow-up vaginal cytology testing and are not associated with toxicities of the above stated therapies.6 Vaginal estrogen can be used alone or in addition to other therapeutic strategies. For example, it can be added to the nontreatment days of 5FU or postoperatively prescribed following laser or excisional procedures.
Radiation
Intracavitary brachytherapy is a technique in which a radiation source is placed within a cylinder or ovoids and placed within the vagina.7 Typically 45 Gy is delivered to a depth 0.5mm below the vaginal mucosal surface (“point z”). Recurrence occurs is approximately 10%-15% of patients, and toxicities can be severe, including vaginal stenosis and ulceration. This aggressive therapy typically is best reserved for cases that are refractory to other therapies. Following radiation, subsequent treatments are more difficult because of radiation-induced changes to the vaginal mucosa that can affect healing.
Vaginal dysplasia is a relatively common sequelae of high-risk HPV, particularly among women who have had a prior hysterectomy for cervical dysplasia. Because of anatomic changes following hysterectomy, adequate visualization and comprehensive vaginal treatment is difficult. Therefore, surgeons should avoid utilization of hysterectomy as a routine strategy to “cure” dysplasia as it may fail to achieve this cure and make subsequent evaluations and treatments of persistent dysplasia more difficult. Women who have had a hysterectomy for dysplasia should be closely followed for several decades, and they should be counseled that they have a persistent risk for vaginal disease. When VAIN develops, clinicians should consider topical therapies as primary treatment options because they may minimize toxicity and have high rates of enduring response.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant conflicts of interest.
References
1. Gynecol Oncol. 2016 Jun;141(3):507-10.
2. Arch Gynecol Obstet. 2016 Feb;293(2):415-9.
3. Anticancer Res. 2013 Jan;33(1):29-38.
4. Obstet Gynecol. 2017 Dec;130(6):1237-43.
5. Eur J Obstet Gynecol Reprod Biol. 2017 Nov;218:129-36.
6. J Low Genit Tract Dis. 2014 Apr;18(2):115-21.
7. Gynecol Oncol. 2007 Jul;106(1):105-11.
Vaginal intraepithelial neoplasia (VAIN) is a condition that frequently poses therapeutic dilemmas for gynecologists. VAIN represents dysplastic changes to the epithelium of the vaginal mucosa, and like cervical neoplasia, the extent of disease is characterized as levels I, II, or III dependent upon the depth of involvement in the epithelial layer by dysplastic cells. While VAIN itself typically is asymptomatic and not a harmful condition, it carries a 12% risk of progression to invasive vaginal carcinoma, so accurate identification, thorough treatment, and ongoing surveillance are essential.1
VAIN is associated with high-risk human papillomavirus (HPV) infection, tobacco use, and prior cervical dysplasia. Of women with VAIN, 65% have undergone a prior hysterectomy for cervical dysplasia, which emphasizes the nondefinitive nature of such an intervention.2 These women should be very closely followed for at least 20 years with vaginal cytologic and/or HPV surveillance. High-risk HPV infection is present in 85% of women with VAIN, and the presence of high-risk HPV is a predictor for recurrent VAIN. Recurrent and persistent VAIN also is more common in postmenopausal women and those with multifocal disease.
The most common location for VAIN is at the upper third of the vagina (including the vaginal cuff). It commonly arises within the vaginal fornices, which may be difficult to fully visualize because of their puckered appearance, redundant vaginal tissues, and extensive vaginal rogation.
A diagnosis of VAIN is typically obtained from vaginal cytology which reveals atypical or dysplastic cells. Such a result should prompt the physician to perform vaginal colposcopy and directed biopsies. Comprehensive visualization of the vaginal cuff can be limited in cases where the vaginal fornices are tethered, deeply puckered, or when there is significant mucosal rogation.
The application of 4% acetic acid or Lugol’s iodine are techniques that can enhance the detection of dysplastic vaginal mucosa. Lugol’s iodine selectively stains normal, glycogenated cells, and spares dysplastic glycogen-free cells. The sharp contrast between the brown iodine-stained tissues and the white dysplastic tissues aids in detection of dysplastic areas.
If colposcopic biopsy reveals low grade dysplasia (VAIN I) it does not require intervention, and has a very low rate of conversion to invasive vaginal carcinoma. However moderate- and high-grade vaginal dysplastic lesions should be treated because of the potential for malignant transformation.
Options for treatment of VAIN include topical, ablative, and excisional procedures. Observation also is an option but should be reserved for patients who are closely monitored with repeated colposcopic examinations, and probably should best be reserved for patients with VAIN I or II lesions.
Excisional procedures
The most common excisional procedure employed for VAIN is upper vaginectomy. In this procedure, the surgeon grasps and tents up the vaginal mucosa, incises the mucosa without penetrating the subepithelial tissue layers such as bladder and rectum. The vaginal mucosa then is carefully separated from the underlying endopelvic fascial plane. The specimen should be oriented, ideally on a cork board, with pins or sutures to ascribe margins and borders. Excision is best utilized for women with unifocal disease, or those who fail or do not tolerate ablative or topical interventions.
The most significant risks of excision include the potential for damage to underlying pelvic visceral structures, which is particularly concerning in postmenopausal women with thin vaginal epithelium. Vaginectomy is commonly associated with vaginal shortening or narrowing, which can be deleterious for quality of life. Retrospective series have described a 30% incidence of recurrence after vaginectomy, likely secondary to incomplete excision of all affected tissue.3
Ablation
Ablation of dysplastic foci with a carbon dioxide (CO2) laser is a common method for treatment of VAIN. CO2 laser should ablate tissue to a 1.5 mm minimum depth.3 The benefit of using CO2 laser is its ability to treat multifocal disease in situ without an extensive excisional procedure.
It is technically more straightforward than upper vaginectomy with less blood loss and shorter surgical times, and it can be easily accomplished in an outpatient surgical or office setting. However, one of its greatest limitations is the difficulty in visualizing all lesions and therefore adequately treating all sites. The vaginal rogations also make adequate laser ablation challenging because laser only is able to effectively ablate tissue that is oriented perpendicular to the laser beam.
In addition, there is no pathologic confirmation of adequacy of excision or margin status. These features may contribute to the modestly higher rates of recurrence of dysplasia following laser ablation, compared with vaginectomy.3 It also has been associated with more vaginal scarring than vaginectomy, which can have a negative effect on sexual health.
Topical agents
The most commonly utilized topical therapy for VAIN is the antimetabolite chemotherapeutic agent 5-fluorouracil (5FU). A typical schedule for 5FU treatment is to apply vaginally, at night, once a week for 8 weeks.4 Because it can cause extensive irritation to the vulvar and urethral epithelium, patients are recommended to apply barrier creams or ointments before and following the use of 5FU for several days, wash hands thoroughly after application, and to rinse and shower in the morning after rising. Severe irritation occurs in up to 16% of patients, but in general it is very well tolerated.
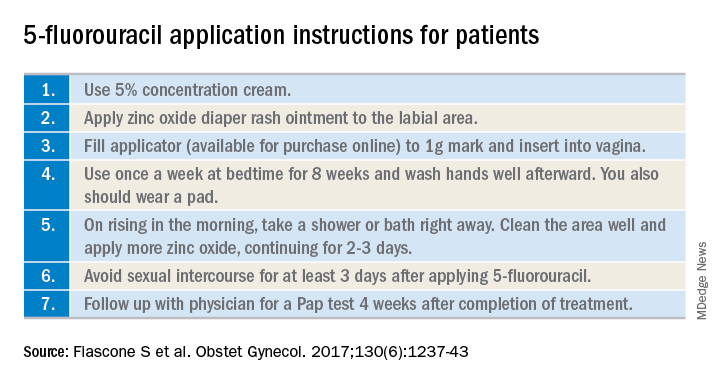
Its virtue is that it is able to conform and travel to all parts of the vaginal mucosa, including those that are poorly visualized within the fornices or vaginal folds. 5FU does not require a hospitalization or surgical procedure, can be applied by the patient at home, and preserves vaginal length and function. In recent reports, 5FU is associated with the lowest rates of recurrence (10%-30%), compared with excision or ablation, and therefore is a very attractive option for primary therapy.3 However, it requires patients to have a degree of comfort with vaginal application of drug and adherence with perineal care strategies to minimize the likelihood of toxicity.
The immune response modifier, imiquimod, that is commonly used in the treatment of vulvar dysplasia also has been described in the treatment of VAIN. It appears to have high rates of clearance (greater than 75%) and be most effective in the treatment of VAIN I.5 It requires application under colposcopic guidance three times a week for 8 weeks, which is a laborious undertaking for both patient and physician. Like 5FU, imiquimod is associated with vulvar and perineal irritation.
Vaginal estrogens are an alternative topical therapy for moderate- and high-grade VAIN and particularly useful for postmenopausal patients. They have been associated with a high rate (up to 90%) of resolution on follow-up vaginal cytology testing and are not associated with toxicities of the above stated therapies.6 Vaginal estrogen can be used alone or in addition to other therapeutic strategies. For example, it can be added to the nontreatment days of 5FU or postoperatively prescribed following laser or excisional procedures.
Radiation
Intracavitary brachytherapy is a technique in which a radiation source is placed within a cylinder or ovoids and placed within the vagina.7 Typically 45 Gy is delivered to a depth 0.5mm below the vaginal mucosal surface (“point z”). Recurrence occurs is approximately 10%-15% of patients, and toxicities can be severe, including vaginal stenosis and ulceration. This aggressive therapy typically is best reserved for cases that are refractory to other therapies. Following radiation, subsequent treatments are more difficult because of radiation-induced changes to the vaginal mucosa that can affect healing.
Vaginal dysplasia is a relatively common sequelae of high-risk HPV, particularly among women who have had a prior hysterectomy for cervical dysplasia. Because of anatomic changes following hysterectomy, adequate visualization and comprehensive vaginal treatment is difficult. Therefore, surgeons should avoid utilization of hysterectomy as a routine strategy to “cure” dysplasia as it may fail to achieve this cure and make subsequent evaluations and treatments of persistent dysplasia more difficult. Women who have had a hysterectomy for dysplasia should be closely followed for several decades, and they should be counseled that they have a persistent risk for vaginal disease. When VAIN develops, clinicians should consider topical therapies as primary treatment options because they may minimize toxicity and have high rates of enduring response.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant conflicts of interest.
References
1. Gynecol Oncol. 2016 Jun;141(3):507-10.
2. Arch Gynecol Obstet. 2016 Feb;293(2):415-9.
3. Anticancer Res. 2013 Jan;33(1):29-38.
4. Obstet Gynecol. 2017 Dec;130(6):1237-43.
5. Eur J Obstet Gynecol Reprod Biol. 2017 Nov;218:129-36.
6. J Low Genit Tract Dis. 2014 Apr;18(2):115-21.
7. Gynecol Oncol. 2007 Jul;106(1):105-11.
Vaginal intraepithelial neoplasia (VAIN) is a condition that frequently poses therapeutic dilemmas for gynecologists. VAIN represents dysplastic changes to the epithelium of the vaginal mucosa, and like cervical neoplasia, the extent of disease is characterized as levels I, II, or III dependent upon the depth of involvement in the epithelial layer by dysplastic cells. While VAIN itself typically is asymptomatic and not a harmful condition, it carries a 12% risk of progression to invasive vaginal carcinoma, so accurate identification, thorough treatment, and ongoing surveillance are essential.1
VAIN is associated with high-risk human papillomavirus (HPV) infection, tobacco use, and prior cervical dysplasia. Of women with VAIN, 65% have undergone a prior hysterectomy for cervical dysplasia, which emphasizes the nondefinitive nature of such an intervention.2 These women should be very closely followed for at least 20 years with vaginal cytologic and/or HPV surveillance. High-risk HPV infection is present in 85% of women with VAIN, and the presence of high-risk HPV is a predictor for recurrent VAIN. Recurrent and persistent VAIN also is more common in postmenopausal women and those with multifocal disease.
The most common location for VAIN is at the upper third of the vagina (including the vaginal cuff). It commonly arises within the vaginal fornices, which may be difficult to fully visualize because of their puckered appearance, redundant vaginal tissues, and extensive vaginal rogation.
A diagnosis of VAIN is typically obtained from vaginal cytology which reveals atypical or dysplastic cells. Such a result should prompt the physician to perform vaginal colposcopy and directed biopsies. Comprehensive visualization of the vaginal cuff can be limited in cases where the vaginal fornices are tethered, deeply puckered, or when there is significant mucosal rogation.
The application of 4% acetic acid or Lugol’s iodine are techniques that can enhance the detection of dysplastic vaginal mucosa. Lugol’s iodine selectively stains normal, glycogenated cells, and spares dysplastic glycogen-free cells. The sharp contrast between the brown iodine-stained tissues and the white dysplastic tissues aids in detection of dysplastic areas.
If colposcopic biopsy reveals low grade dysplasia (VAIN I) it does not require intervention, and has a very low rate of conversion to invasive vaginal carcinoma. However moderate- and high-grade vaginal dysplastic lesions should be treated because of the potential for malignant transformation.
Options for treatment of VAIN include topical, ablative, and excisional procedures. Observation also is an option but should be reserved for patients who are closely monitored with repeated colposcopic examinations, and probably should best be reserved for patients with VAIN I or II lesions.
Excisional procedures
The most common excisional procedure employed for VAIN is upper vaginectomy. In this procedure, the surgeon grasps and tents up the vaginal mucosa, incises the mucosa without penetrating the subepithelial tissue layers such as bladder and rectum. The vaginal mucosa then is carefully separated from the underlying endopelvic fascial plane. The specimen should be oriented, ideally on a cork board, with pins or sutures to ascribe margins and borders. Excision is best utilized for women with unifocal disease, or those who fail or do not tolerate ablative or topical interventions.
The most significant risks of excision include the potential for damage to underlying pelvic visceral structures, which is particularly concerning in postmenopausal women with thin vaginal epithelium. Vaginectomy is commonly associated with vaginal shortening or narrowing, which can be deleterious for quality of life. Retrospective series have described a 30% incidence of recurrence after vaginectomy, likely secondary to incomplete excision of all affected tissue.3
Ablation
Ablation of dysplastic foci with a carbon dioxide (CO2) laser is a common method for treatment of VAIN. CO2 laser should ablate tissue to a 1.5 mm minimum depth.3 The benefit of using CO2 laser is its ability to treat multifocal disease in situ without an extensive excisional procedure.
It is technically more straightforward than upper vaginectomy with less blood loss and shorter surgical times, and it can be easily accomplished in an outpatient surgical or office setting. However, one of its greatest limitations is the difficulty in visualizing all lesions and therefore adequately treating all sites. The vaginal rogations also make adequate laser ablation challenging because laser only is able to effectively ablate tissue that is oriented perpendicular to the laser beam.
In addition, there is no pathologic confirmation of adequacy of excision or margin status. These features may contribute to the modestly higher rates of recurrence of dysplasia following laser ablation, compared with vaginectomy.3 It also has been associated with more vaginal scarring than vaginectomy, which can have a negative effect on sexual health.
Topical agents
The most commonly utilized topical therapy for VAIN is the antimetabolite chemotherapeutic agent 5-fluorouracil (5FU). A typical schedule for 5FU treatment is to apply vaginally, at night, once a week for 8 weeks.4 Because it can cause extensive irritation to the vulvar and urethral epithelium, patients are recommended to apply barrier creams or ointments before and following the use of 5FU for several days, wash hands thoroughly after application, and to rinse and shower in the morning after rising. Severe irritation occurs in up to 16% of patients, but in general it is very well tolerated.
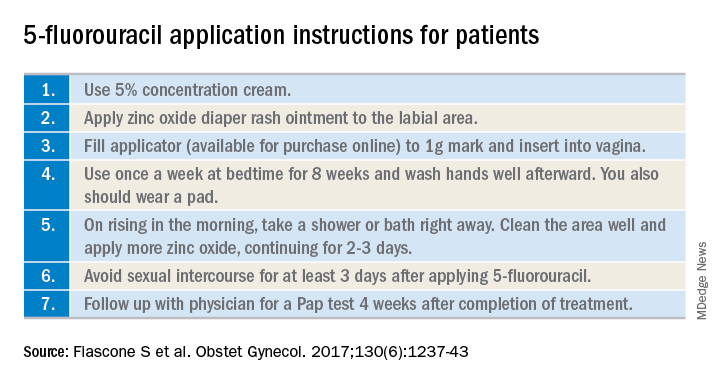
Its virtue is that it is able to conform and travel to all parts of the vaginal mucosa, including those that are poorly visualized within the fornices or vaginal folds. 5FU does not require a hospitalization or surgical procedure, can be applied by the patient at home, and preserves vaginal length and function. In recent reports, 5FU is associated with the lowest rates of recurrence (10%-30%), compared with excision or ablation, and therefore is a very attractive option for primary therapy.3 However, it requires patients to have a degree of comfort with vaginal application of drug and adherence with perineal care strategies to minimize the likelihood of toxicity.
The immune response modifier, imiquimod, that is commonly used in the treatment of vulvar dysplasia also has been described in the treatment of VAIN. It appears to have high rates of clearance (greater than 75%) and be most effective in the treatment of VAIN I.5 It requires application under colposcopic guidance three times a week for 8 weeks, which is a laborious undertaking for both patient and physician. Like 5FU, imiquimod is associated with vulvar and perineal irritation.
Vaginal estrogens are an alternative topical therapy for moderate- and high-grade VAIN and particularly useful for postmenopausal patients. They have been associated with a high rate (up to 90%) of resolution on follow-up vaginal cytology testing and are not associated with toxicities of the above stated therapies.6 Vaginal estrogen can be used alone or in addition to other therapeutic strategies. For example, it can be added to the nontreatment days of 5FU or postoperatively prescribed following laser or excisional procedures.
Radiation
Intracavitary brachytherapy is a technique in which a radiation source is placed within a cylinder or ovoids and placed within the vagina.7 Typically 45 Gy is delivered to a depth 0.5mm below the vaginal mucosal surface (“point z”). Recurrence occurs is approximately 10%-15% of patients, and toxicities can be severe, including vaginal stenosis and ulceration. This aggressive therapy typically is best reserved for cases that are refractory to other therapies. Following radiation, subsequent treatments are more difficult because of radiation-induced changes to the vaginal mucosa that can affect healing.
Vaginal dysplasia is a relatively common sequelae of high-risk HPV, particularly among women who have had a prior hysterectomy for cervical dysplasia. Because of anatomic changes following hysterectomy, adequate visualization and comprehensive vaginal treatment is difficult. Therefore, surgeons should avoid utilization of hysterectomy as a routine strategy to “cure” dysplasia as it may fail to achieve this cure and make subsequent evaluations and treatments of persistent dysplasia more difficult. Women who have had a hysterectomy for dysplasia should be closely followed for several decades, and they should be counseled that they have a persistent risk for vaginal disease. When VAIN develops, clinicians should consider topical therapies as primary treatment options because they may minimize toxicity and have high rates of enduring response.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant conflicts of interest.
References
1. Gynecol Oncol. 2016 Jun;141(3):507-10.
2. Arch Gynecol Obstet. 2016 Feb;293(2):415-9.
3. Anticancer Res. 2013 Jan;33(1):29-38.
4. Obstet Gynecol. 2017 Dec;130(6):1237-43.
5. Eur J Obstet Gynecol Reprod Biol. 2017 Nov;218:129-36.
6. J Low Genit Tract Dis. 2014 Apr;18(2):115-21.
7. Gynecol Oncol. 2007 Jul;106(1):105-11.












