User login
ctDNA predicts early outcomes in DLBCL
Measurement of circulating tumor DNA (ctDNA) could be a new and useful tool for predicting survival outcomes and response to therapy in patients with diffuse large B-cell lymphoma (DLBCL), according to authors of a recent prospective study.
Pretreatment ctDNA levels predicted 24-month event-free survival – an important disease milestone in DLBCL – as well as overall survival in the study, which included more than 200 patients at six institutions in North America and Europe.
Changes in ctDNA during treatment were prognostic for outcomes as early as 21 days into therapy, according to corresponding author Ash A. Alizadeh, MD, PhD, of Stanford (Calif.) University and his coinvestigators.
“Our data suggest that both pretreatment and dynamic assessments of ctDNA are feasible and can add to established risk factors,” Dr. Alizadeh and his coauthors reported in the Journal of Clinical Oncology.
ctDNA was detected in 98% of the 217 patients evaluated, which demonstrated the “potentially universal applicability” of this approach, they wrote in the report.
In an evaluation of pretreatment ctDNA levels, investigators found a 2.5 log haploid genome equivalents per milliliter (hGE/mL) threshold stratified patient outcomes. Event-free survival was significantly inferior at 24 months in patients with ctDNA above that threshold, with hazard ratios of 2.6 (P = .007) for frontline treatment and 2.9 (P = 0.01) for salvage.
On-treatment ctDNA levels were favorably prognostic for outcomes in patients receiving frontline therapy, according to investigators. An early molecular response (EMR), defined as a 2-log decrease in ctDNA levels after one cycle of treatment, was associated with a 24-month event-free survival of 83% versus 50% for no EMR (P = .0015).
Major molecular response (MMR), defined as a 2.5-log drop in ctDNA after two cycles of treatment, was associated with a 24-month event-free survival of 82% versus 46% for no MMR in patients on frontline therapy (P less than .001).
In one cohort of patients receiving salvage therapy, EMR also predicted superior 24-month event-free survival, according to investigators.
The EMR measure was also favorably prognostic for overall survival in both the frontline and salvage settings.
The prognostic value of measuring ctDNA was independent of International Prognostic Index (IPI) and interim PET/CT studies, results of multivariable analysis showed.
Patients had “excellent outcomes” if they had both molecular response and favorable interim PET results, and conversely, patients were at “extremely high risk” for treatment failure if they had no molecular response and a positive PET scan.
“The identification of patients at exceptionally high risk (i.e., interim PET/CT positive and not achieving EMR/MMR) could provide an opportunity for early intervention with alternative treatments, including autologous bone marrow transplantation or chimeric antigen receptor T cells,” the researchers wrote.
Patients in the study were all treated with combination immunochemotherapy according to local standards.
Dr. Alizadeh reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, as well as patent filings on ctDNA detection assigned to Stanford University.
SOURCE: Kurtz DM et al. J Clin Oncol. 2018 Aug 20. doi: 10.1200/JCO.2018.78.5246.
Measurement of circulating tumor DNA (ctDNA) could be a new and useful tool for predicting survival outcomes and response to therapy in patients with diffuse large B-cell lymphoma (DLBCL), according to authors of a recent prospective study.
Pretreatment ctDNA levels predicted 24-month event-free survival – an important disease milestone in DLBCL – as well as overall survival in the study, which included more than 200 patients at six institutions in North America and Europe.
Changes in ctDNA during treatment were prognostic for outcomes as early as 21 days into therapy, according to corresponding author Ash A. Alizadeh, MD, PhD, of Stanford (Calif.) University and his coinvestigators.
“Our data suggest that both pretreatment and dynamic assessments of ctDNA are feasible and can add to established risk factors,” Dr. Alizadeh and his coauthors reported in the Journal of Clinical Oncology.
ctDNA was detected in 98% of the 217 patients evaluated, which demonstrated the “potentially universal applicability” of this approach, they wrote in the report.
In an evaluation of pretreatment ctDNA levels, investigators found a 2.5 log haploid genome equivalents per milliliter (hGE/mL) threshold stratified patient outcomes. Event-free survival was significantly inferior at 24 months in patients with ctDNA above that threshold, with hazard ratios of 2.6 (P = .007) for frontline treatment and 2.9 (P = 0.01) for salvage.
On-treatment ctDNA levels were favorably prognostic for outcomes in patients receiving frontline therapy, according to investigators. An early molecular response (EMR), defined as a 2-log decrease in ctDNA levels after one cycle of treatment, was associated with a 24-month event-free survival of 83% versus 50% for no EMR (P = .0015).
Major molecular response (MMR), defined as a 2.5-log drop in ctDNA after two cycles of treatment, was associated with a 24-month event-free survival of 82% versus 46% for no MMR in patients on frontline therapy (P less than .001).
In one cohort of patients receiving salvage therapy, EMR also predicted superior 24-month event-free survival, according to investigators.
The EMR measure was also favorably prognostic for overall survival in both the frontline and salvage settings.
The prognostic value of measuring ctDNA was independent of International Prognostic Index (IPI) and interim PET/CT studies, results of multivariable analysis showed.
Patients had “excellent outcomes” if they had both molecular response and favorable interim PET results, and conversely, patients were at “extremely high risk” for treatment failure if they had no molecular response and a positive PET scan.
“The identification of patients at exceptionally high risk (i.e., interim PET/CT positive and not achieving EMR/MMR) could provide an opportunity for early intervention with alternative treatments, including autologous bone marrow transplantation or chimeric antigen receptor T cells,” the researchers wrote.
Patients in the study were all treated with combination immunochemotherapy according to local standards.
Dr. Alizadeh reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, as well as patent filings on ctDNA detection assigned to Stanford University.
SOURCE: Kurtz DM et al. J Clin Oncol. 2018 Aug 20. doi: 10.1200/JCO.2018.78.5246.
Measurement of circulating tumor DNA (ctDNA) could be a new and useful tool for predicting survival outcomes and response to therapy in patients with diffuse large B-cell lymphoma (DLBCL), according to authors of a recent prospective study.
Pretreatment ctDNA levels predicted 24-month event-free survival – an important disease milestone in DLBCL – as well as overall survival in the study, which included more than 200 patients at six institutions in North America and Europe.
Changes in ctDNA during treatment were prognostic for outcomes as early as 21 days into therapy, according to corresponding author Ash A. Alizadeh, MD, PhD, of Stanford (Calif.) University and his coinvestigators.
“Our data suggest that both pretreatment and dynamic assessments of ctDNA are feasible and can add to established risk factors,” Dr. Alizadeh and his coauthors reported in the Journal of Clinical Oncology.
ctDNA was detected in 98% of the 217 patients evaluated, which demonstrated the “potentially universal applicability” of this approach, they wrote in the report.
In an evaluation of pretreatment ctDNA levels, investigators found a 2.5 log haploid genome equivalents per milliliter (hGE/mL) threshold stratified patient outcomes. Event-free survival was significantly inferior at 24 months in patients with ctDNA above that threshold, with hazard ratios of 2.6 (P = .007) for frontline treatment and 2.9 (P = 0.01) for salvage.
On-treatment ctDNA levels were favorably prognostic for outcomes in patients receiving frontline therapy, according to investigators. An early molecular response (EMR), defined as a 2-log decrease in ctDNA levels after one cycle of treatment, was associated with a 24-month event-free survival of 83% versus 50% for no EMR (P = .0015).
Major molecular response (MMR), defined as a 2.5-log drop in ctDNA after two cycles of treatment, was associated with a 24-month event-free survival of 82% versus 46% for no MMR in patients on frontline therapy (P less than .001).
In one cohort of patients receiving salvage therapy, EMR also predicted superior 24-month event-free survival, according to investigators.
The EMR measure was also favorably prognostic for overall survival in both the frontline and salvage settings.
The prognostic value of measuring ctDNA was independent of International Prognostic Index (IPI) and interim PET/CT studies, results of multivariable analysis showed.
Patients had “excellent outcomes” if they had both molecular response and favorable interim PET results, and conversely, patients were at “extremely high risk” for treatment failure if they had no molecular response and a positive PET scan.
“The identification of patients at exceptionally high risk (i.e., interim PET/CT positive and not achieving EMR/MMR) could provide an opportunity for early intervention with alternative treatments, including autologous bone marrow transplantation or chimeric antigen receptor T cells,” the researchers wrote.
Patients in the study were all treated with combination immunochemotherapy according to local standards.
Dr. Alizadeh reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, as well as patent filings on ctDNA detection assigned to Stanford University.
SOURCE: Kurtz DM et al. J Clin Oncol. 2018 Aug 20. doi: 10.1200/JCO.2018.78.5246.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: Early molecular response (a 2-log decrease in ctDNA levels after one treatment cycle) was associated with a 24-month event-free survival of 83% versus 50% for no early molecular response (P = .0015).
Study details: Prospective analysis of pretreatment and dynamic on-treatment ctDNA levels in patients with DLBCL who received standard immunochemotherapy.
Disclosures: Study authors reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, among others.
Source: Kurtz DM et al. J Clin Oncol. 2018 Aug 20. doi: 10.1200/JCO.2018.78.5246.
FDA approves ibrutinib with rituximab in Waldenström’s macroglobulinemia
The Food and Drug Administration has approved ibrutinib (Imbruvica) for use in combination with rituximab to treat adults with Waldenström’s macroglobulinemia (WM).
Ibrutinib was approved for use as a single agent in adults with WM in January 2015.
The latest approval was supported by the phase 3 iNNOVATE trial, in which researchers compared ibrutinib plus rituximab to rituximab alone in patients with previously untreated or relapsed/refractory WM.
Results from iNNOVATE were presented at the 2018 annual meeting of the American Society of Clinical Oncology and simultaneously published in the New England Journal of Medicine (2018;378:2399-2410).
The 30-month progression-free survival rates were 82% in the ibrutinib arm and 28% in the placebo arm. The median progression-free survival was not reached in the ibrutinib arm and was 20.3 months in the placebo arm (hazard ratio, 0.20; P less than .0001).
The 30-month overall survival rates were 94% in the ibrutinib arm and 92% in the placebo arm.
Grade 3 or higher treatment-emergent adverse events (AEs) occurred in 60% of patients in the ibrutinib arm and 61% in the placebo arm. Serious AEs occurred in 43% and 33%, respectively. There were no fatal AEs in the ibrutinib arm and three in the rituximab arm.
Ibrutinib is jointly developed and commercialized by Pharmacyclics, an AbbVie company, and Janssen Biotech.
The Food and Drug Administration has approved ibrutinib (Imbruvica) for use in combination with rituximab to treat adults with Waldenström’s macroglobulinemia (WM).
Ibrutinib was approved for use as a single agent in adults with WM in January 2015.
The latest approval was supported by the phase 3 iNNOVATE trial, in which researchers compared ibrutinib plus rituximab to rituximab alone in patients with previously untreated or relapsed/refractory WM.
Results from iNNOVATE were presented at the 2018 annual meeting of the American Society of Clinical Oncology and simultaneously published in the New England Journal of Medicine (2018;378:2399-2410).
The 30-month progression-free survival rates were 82% in the ibrutinib arm and 28% in the placebo arm. The median progression-free survival was not reached in the ibrutinib arm and was 20.3 months in the placebo arm (hazard ratio, 0.20; P less than .0001).
The 30-month overall survival rates were 94% in the ibrutinib arm and 92% in the placebo arm.
Grade 3 or higher treatment-emergent adverse events (AEs) occurred in 60% of patients in the ibrutinib arm and 61% in the placebo arm. Serious AEs occurred in 43% and 33%, respectively. There were no fatal AEs in the ibrutinib arm and three in the rituximab arm.
Ibrutinib is jointly developed and commercialized by Pharmacyclics, an AbbVie company, and Janssen Biotech.
The Food and Drug Administration has approved ibrutinib (Imbruvica) for use in combination with rituximab to treat adults with Waldenström’s macroglobulinemia (WM).
Ibrutinib was approved for use as a single agent in adults with WM in January 2015.
The latest approval was supported by the phase 3 iNNOVATE trial, in which researchers compared ibrutinib plus rituximab to rituximab alone in patients with previously untreated or relapsed/refractory WM.
Results from iNNOVATE were presented at the 2018 annual meeting of the American Society of Clinical Oncology and simultaneously published in the New England Journal of Medicine (2018;378:2399-2410).
The 30-month progression-free survival rates were 82% in the ibrutinib arm and 28% in the placebo arm. The median progression-free survival was not reached in the ibrutinib arm and was 20.3 months in the placebo arm (hazard ratio, 0.20; P less than .0001).
The 30-month overall survival rates were 94% in the ibrutinib arm and 92% in the placebo arm.
Grade 3 or higher treatment-emergent adverse events (AEs) occurred in 60% of patients in the ibrutinib arm and 61% in the placebo arm. Serious AEs occurred in 43% and 33%, respectively. There were no fatal AEs in the ibrutinib arm and three in the rituximab arm.
Ibrutinib is jointly developed and commercialized by Pharmacyclics, an AbbVie company, and Janssen Biotech.
Nivolumab plus ipilimumab effective in melanoma brain metastases
Treatment with nivolumab plus ipilimumab resulted in clinically meaningful efficacy for melanoma patients with asymptomatic, previously untreated brain metastases, results of an open-label, multicenter, phase 2 study have shown.
The combination of these two immune checkpoint inhibitors produced intracranial responses in more than half of the patients treated, and perhaps more importantly, according to the study investigators, the combination treatment prevented intracranial progression for more than 6 months in 64% of the study population.
“These results are relevant in a population in whom progression can quickly result in substantial neurologic symptoms, functional impairment, and the need for glucocorticoid therapy,” the study investigators wrote in the New England Journal of Medicine.
The investigators, led by Hussein A. Tawbi, MD, PhD, of the University of Texas MD Anderson Cancer, Houston, initially enrolled 101 patients with histologically confirmed melanoma and metastases to the brain that were asymptomatic. All patients had an Eastern Cooperative Oncology Group performance status of 0-1 and had not received systemic glucocorticoid therapy within 10 days of study treatment.
The primary endpoint of the study was the rate of intracranial benefit, defined as the percentage of patients with complete response, partial response, or stable disease for at least 6 months after starting treatment.
For 94 patients with at least 6 months of follow-up at the time of analysis (median follow-up, 14 months), the rate of intracranial benefit was 57%, including complete responses in 26%, partial responses in 30%, and stable disease in 2%, the investigators reported. The rate of extracranial benefit was similar, at 56%.
The 6-month rate of progression-free survival was 64.2% for intracranial assessments, while the 6-month overall survival rate was 92.3%, according to results of an initial assessment.
Grade 3 or 4 adverse events thought to be related to treatment occurred in 55% of patients and led to treatment discontinuation in 20%; the most common were increased levels of ALT and AST.
Dr. Tawbi and his colleagues said that, while cross-trial comparisons have inherent limitations, the rate of intracranial response seen in this trial is similar to what was seen in the COMBI-MB study of dabrafenib plus trametinib in patients with BRAF-mutant melanoma and brain metastases. However, in that study, published in 2017 in the Lancet, the combination of a BRAF inhibitor and MEK inhibitor had rates of intracranial response and progression-free survival that were “substantially shorter” than the rates of extracranial response and progression-free survival.
“In our study, the use of immunotherapy seemed capable of inducing intracranial responses that were very similar to extracranial responses in character, depth, and duration,” they wrote.
Dr. Tawbi and his coinvestigators enrolled an additional 20 symptomatic patients with brain metastases following a study protocol amendment; however, results from that cohort are not being reported yet because of inadequate follow-up length, they said.
The study was supported by Bristol-Myers Squibb and a grant from the National Cancer Institute. Dr. Tawbi reported disclosures related to Bristol-Myers Squibb, Merck, Genentech, and Novartis. His coauthors reported additional disclosures related to MedImmune, AstraZeneca, Dynavax Technologies, Genoptix, Exelixis, Acceleron Pharma, and Eisai, among others.
SOURCE: Tawbi HA et al. N Engl J Med. 2018 Aug 23. doi: 10.1056/NEJMoa1805453.
These data show that checkpoint inhibitors can be similarly effective in CNS metastases as they can be in extracranial metastases related to melanoma, according to Samra Turajlic, MD, PhD, and James Larkin, FRCP, PhD, of the Renal and Skin Units at the Royal Marsden National Health Service Foundation Trust in London.
Based on the study results, larger trials are warranted, including patients with CNS metastases from melanoma, kidney, lung, and other cancers where checkpoint inhibitors have demonstrated efficacy, Dr. Turajlic, who is also with the Translational Cancer Therapeutics Laboratory at the Francis Crick Institute in London, and Dr. Larkin wrote in an editorial.
“Such patients should no longer generally be excluded from clinical trials,” they wrote.
While the study by Dr. Tawbi and his colleagues was small, they added, its results are relevant to clinical practice because of the high rate of response, rapid response time, and side effect profile, which was manageable.
In fact, the nivolumab plus ipilimumab regimen described in this study should be considered first-line therapy for all patients who meet the study’s inclusion criteria, they asserted.
However, the results should “absolutely not” be extrapolated to higher-risk patients, such as those with leptomeningeal disease or with low performance status, which investigators excluded from the present study.
“There are good data showing that patients with cerebral metastases can be stratified into groups that have very different survival and morbidity,” Dr. Turajlic and Dr. Larkin wrote. “Caution is necessary until we have data across all the groups.”
These comment are based on an editorial in the New England Journal of Medicine (doi: 10.1056/NEJMe1807752) . Dr. Turajlic reported patents pending for an indel biomarker (PCT/GB2018/051893) and an indel therapeutic (PCT/GB2018/051892). Dr. Larkin reported disclosures related to Bristol-Myers Squibb, Novartis, Genentech, Pierre-Fabre, Incyte, and AstraZeneca.
These data show that checkpoint inhibitors can be similarly effective in CNS metastases as they can be in extracranial metastases related to melanoma, according to Samra Turajlic, MD, PhD, and James Larkin, FRCP, PhD, of the Renal and Skin Units at the Royal Marsden National Health Service Foundation Trust in London.
Based on the study results, larger trials are warranted, including patients with CNS metastases from melanoma, kidney, lung, and other cancers where checkpoint inhibitors have demonstrated efficacy, Dr. Turajlic, who is also with the Translational Cancer Therapeutics Laboratory at the Francis Crick Institute in London, and Dr. Larkin wrote in an editorial.
“Such patients should no longer generally be excluded from clinical trials,” they wrote.
While the study by Dr. Tawbi and his colleagues was small, they added, its results are relevant to clinical practice because of the high rate of response, rapid response time, and side effect profile, which was manageable.
In fact, the nivolumab plus ipilimumab regimen described in this study should be considered first-line therapy for all patients who meet the study’s inclusion criteria, they asserted.
However, the results should “absolutely not” be extrapolated to higher-risk patients, such as those with leptomeningeal disease or with low performance status, which investigators excluded from the present study.
“There are good data showing that patients with cerebral metastases can be stratified into groups that have very different survival and morbidity,” Dr. Turajlic and Dr. Larkin wrote. “Caution is necessary until we have data across all the groups.”
These comment are based on an editorial in the New England Journal of Medicine (doi: 10.1056/NEJMe1807752) . Dr. Turajlic reported patents pending for an indel biomarker (PCT/GB2018/051893) and an indel therapeutic (PCT/GB2018/051892). Dr. Larkin reported disclosures related to Bristol-Myers Squibb, Novartis, Genentech, Pierre-Fabre, Incyte, and AstraZeneca.
These data show that checkpoint inhibitors can be similarly effective in CNS metastases as they can be in extracranial metastases related to melanoma, according to Samra Turajlic, MD, PhD, and James Larkin, FRCP, PhD, of the Renal and Skin Units at the Royal Marsden National Health Service Foundation Trust in London.
Based on the study results, larger trials are warranted, including patients with CNS metastases from melanoma, kidney, lung, and other cancers where checkpoint inhibitors have demonstrated efficacy, Dr. Turajlic, who is also with the Translational Cancer Therapeutics Laboratory at the Francis Crick Institute in London, and Dr. Larkin wrote in an editorial.
“Such patients should no longer generally be excluded from clinical trials,” they wrote.
While the study by Dr. Tawbi and his colleagues was small, they added, its results are relevant to clinical practice because of the high rate of response, rapid response time, and side effect profile, which was manageable.
In fact, the nivolumab plus ipilimumab regimen described in this study should be considered first-line therapy for all patients who meet the study’s inclusion criteria, they asserted.
However, the results should “absolutely not” be extrapolated to higher-risk patients, such as those with leptomeningeal disease or with low performance status, which investigators excluded from the present study.
“There are good data showing that patients with cerebral metastases can be stratified into groups that have very different survival and morbidity,” Dr. Turajlic and Dr. Larkin wrote. “Caution is necessary until we have data across all the groups.”
These comment are based on an editorial in the New England Journal of Medicine (doi: 10.1056/NEJMe1807752) . Dr. Turajlic reported patents pending for an indel biomarker (PCT/GB2018/051893) and an indel therapeutic (PCT/GB2018/051892). Dr. Larkin reported disclosures related to Bristol-Myers Squibb, Novartis, Genentech, Pierre-Fabre, Incyte, and AstraZeneca.
Treatment with nivolumab plus ipilimumab resulted in clinically meaningful efficacy for melanoma patients with asymptomatic, previously untreated brain metastases, results of an open-label, multicenter, phase 2 study have shown.
The combination of these two immune checkpoint inhibitors produced intracranial responses in more than half of the patients treated, and perhaps more importantly, according to the study investigators, the combination treatment prevented intracranial progression for more than 6 months in 64% of the study population.
“These results are relevant in a population in whom progression can quickly result in substantial neurologic symptoms, functional impairment, and the need for glucocorticoid therapy,” the study investigators wrote in the New England Journal of Medicine.
The investigators, led by Hussein A. Tawbi, MD, PhD, of the University of Texas MD Anderson Cancer, Houston, initially enrolled 101 patients with histologically confirmed melanoma and metastases to the brain that were asymptomatic. All patients had an Eastern Cooperative Oncology Group performance status of 0-1 and had not received systemic glucocorticoid therapy within 10 days of study treatment.
The primary endpoint of the study was the rate of intracranial benefit, defined as the percentage of patients with complete response, partial response, or stable disease for at least 6 months after starting treatment.
For 94 patients with at least 6 months of follow-up at the time of analysis (median follow-up, 14 months), the rate of intracranial benefit was 57%, including complete responses in 26%, partial responses in 30%, and stable disease in 2%, the investigators reported. The rate of extracranial benefit was similar, at 56%.
The 6-month rate of progression-free survival was 64.2% for intracranial assessments, while the 6-month overall survival rate was 92.3%, according to results of an initial assessment.
Grade 3 or 4 adverse events thought to be related to treatment occurred in 55% of patients and led to treatment discontinuation in 20%; the most common were increased levels of ALT and AST.
Dr. Tawbi and his colleagues said that, while cross-trial comparisons have inherent limitations, the rate of intracranial response seen in this trial is similar to what was seen in the COMBI-MB study of dabrafenib plus trametinib in patients with BRAF-mutant melanoma and brain metastases. However, in that study, published in 2017 in the Lancet, the combination of a BRAF inhibitor and MEK inhibitor had rates of intracranial response and progression-free survival that were “substantially shorter” than the rates of extracranial response and progression-free survival.
“In our study, the use of immunotherapy seemed capable of inducing intracranial responses that were very similar to extracranial responses in character, depth, and duration,” they wrote.
Dr. Tawbi and his coinvestigators enrolled an additional 20 symptomatic patients with brain metastases following a study protocol amendment; however, results from that cohort are not being reported yet because of inadequate follow-up length, they said.
The study was supported by Bristol-Myers Squibb and a grant from the National Cancer Institute. Dr. Tawbi reported disclosures related to Bristol-Myers Squibb, Merck, Genentech, and Novartis. His coauthors reported additional disclosures related to MedImmune, AstraZeneca, Dynavax Technologies, Genoptix, Exelixis, Acceleron Pharma, and Eisai, among others.
SOURCE: Tawbi HA et al. N Engl J Med. 2018 Aug 23. doi: 10.1056/NEJMoa1805453.
Treatment with nivolumab plus ipilimumab resulted in clinically meaningful efficacy for melanoma patients with asymptomatic, previously untreated brain metastases, results of an open-label, multicenter, phase 2 study have shown.
The combination of these two immune checkpoint inhibitors produced intracranial responses in more than half of the patients treated, and perhaps more importantly, according to the study investigators, the combination treatment prevented intracranial progression for more than 6 months in 64% of the study population.
“These results are relevant in a population in whom progression can quickly result in substantial neurologic symptoms, functional impairment, and the need for glucocorticoid therapy,” the study investigators wrote in the New England Journal of Medicine.
The investigators, led by Hussein A. Tawbi, MD, PhD, of the University of Texas MD Anderson Cancer, Houston, initially enrolled 101 patients with histologically confirmed melanoma and metastases to the brain that were asymptomatic. All patients had an Eastern Cooperative Oncology Group performance status of 0-1 and had not received systemic glucocorticoid therapy within 10 days of study treatment.
The primary endpoint of the study was the rate of intracranial benefit, defined as the percentage of patients with complete response, partial response, or stable disease for at least 6 months after starting treatment.
For 94 patients with at least 6 months of follow-up at the time of analysis (median follow-up, 14 months), the rate of intracranial benefit was 57%, including complete responses in 26%, partial responses in 30%, and stable disease in 2%, the investigators reported. The rate of extracranial benefit was similar, at 56%.
The 6-month rate of progression-free survival was 64.2% for intracranial assessments, while the 6-month overall survival rate was 92.3%, according to results of an initial assessment.
Grade 3 or 4 adverse events thought to be related to treatment occurred in 55% of patients and led to treatment discontinuation in 20%; the most common were increased levels of ALT and AST.
Dr. Tawbi and his colleagues said that, while cross-trial comparisons have inherent limitations, the rate of intracranial response seen in this trial is similar to what was seen in the COMBI-MB study of dabrafenib plus trametinib in patients with BRAF-mutant melanoma and brain metastases. However, in that study, published in 2017 in the Lancet, the combination of a BRAF inhibitor and MEK inhibitor had rates of intracranial response and progression-free survival that were “substantially shorter” than the rates of extracranial response and progression-free survival.
“In our study, the use of immunotherapy seemed capable of inducing intracranial responses that were very similar to extracranial responses in character, depth, and duration,” they wrote.
Dr. Tawbi and his coinvestigators enrolled an additional 20 symptomatic patients with brain metastases following a study protocol amendment; however, results from that cohort are not being reported yet because of inadequate follow-up length, they said.
The study was supported by Bristol-Myers Squibb and a grant from the National Cancer Institute. Dr. Tawbi reported disclosures related to Bristol-Myers Squibb, Merck, Genentech, and Novartis. His coauthors reported additional disclosures related to MedImmune, AstraZeneca, Dynavax Technologies, Genoptix, Exelixis, Acceleron Pharma, and Eisai, among others.
SOURCE: Tawbi HA et al. N Engl J Med. 2018 Aug 23. doi: 10.1056/NEJMoa1805453.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Nivolumab plus ipilimumab resulted in clinically meaningful responses and progression-free survival for melanoma patients with asymptomatic, previously untreated brain metastases.
Major finding: The reported rate of intracranial benefit was 57% of patients, including complete responses in 26%, partial responses in 30%, and stable disease for at least 6 months in 2%.
Study details: An open-label, multicenter, phase 2 study initially enrolling 101 patients with histologically confirmed melanoma and metastases to the brain.
Disclosures: The study was supported by Bristol-Myers Squibb and a grant from the National Cancer Institute. The study authors reported disclosures related to Bristol-Myers Squibb, Merck, Genentech, Novartis, MedImmune, AstraZeneca, Dynavax Technologies, Genoptix, Exelixis, Acceleron Pharma, Eisai, and others.
Source: Tawbi HA et al. N Engl J Med. 2018 Aug 23. doi: 10.1056/NEJMoa1805453.
Hand, foot, and mouth disease: From self-limited to fatal
Hand, foot, and mouth disease (HFMD) has become a global challenge since its first description in 1957 in New Zealand and Canada. Clinicians readily recognize the characteristic syndrome in young children: fever associated with a papulovesicular rash affecting the palms or soles, or both, usually in spring, summer, or fall. In most cases the disease is self-limited, and brief. However, aseptic meningitis, brainstem encephalitis, acute flaccid paralysis or autonomic nervous system deregulation or cardiorespiratory failure may complicate the clinical course.
HFMD is caused by enterovirus A (formerly called human enterovirus A) which consists of 25 serotypes including multiple coxsackie A viruses, multiple enteroviruses, simian enteroviruses, and baboon enterovirus A13. The clinical spectrum spans from herpangina, characterized by fever and painful mouth ulcers most prominent in the posterior oral cavity (uvula, tonsils, soft plates, and anterior pharyngeal folds), to HFMD with papulovesicular rash on palms and soles with or without mouth ulcers/vesicles.1 In atypical cases, the rash may be maculopapular and may include the buttocks, knees or elbows.
In the United States, the predominant cause is coxsackie A16. However, coxsackie A6 appears to be emerging; often more than one HFMD causing virus is circulating concurrently and clinically indistinguishable. Globally, especially, in Asia, enterovirus 1 is a major cause of HFMD and more often associated with prominent central nervous system involvement. Disease can be sporadic or epidemic. An outbreak is usually defined as two or more cases within a defined geographic area; global epidemics as large as 1.5 million cases (Taiwan, 1998) have been reported, and outbreaks in China involving tens of thousands with multiple deaths have been reported.
In 2015, an outbreak of HFMD occurred during basic military training at Lackland Air Force Base, Bexar County, Texas, due to coxsackie A6.2 The illness was characterized by prodromal symptoms of fever and malaise followed by erosive stomatitis and a rash that began on the palms and soles. The rate of infection among trainees was 4.7% (50 of 1,054 persons).
The differential diagnosis includes aphthous ulcers and herpetic gingivostomatitis.3 Aphthous ulcers are seen more commonly in older children and adolescents, are often recurrent, are not seasonal, and are not associated with rash. Herpes simplex virus gingivostomatitis usually has a febrile prodrome, perioral lesions are frequent in addition to gum and tongue involvement, and gingival bleeding is common. HFMD usually has an incubation period of 3-5 days and fever, malaise, and myalgia prodrome followed by onset of oral and dermatologic manifestations in sequence. The skin rash has features that may overlap with varicella, erythema multiforme (EM) or drug eruption. Varicella usually involves the face before spreading to the extremities, and the lesions are characterized by umbilication and subsequent crusting. EM is characterized by target lesions and drug eruptions are morbilliform or maculopapular. The majority of cases of HFMD are diagnosed clinically; polymerase chain reaction testing is available and best performed on throat or vesicle specimens. Serologic testing for A16 and enterovirus 71 (IgM) is available. Infected patients shed virus for 2-4 weeks and virus is stable in the environment resulting in fecal-oral or oral-oral transmission.
Atypical features of HFMD include occurrence in the winter (outbreak in Alabama in 2011/2012) or an atypical distribution of rash involving the antecubital and popliteal fossae distribution of rash, or “eczema coxsackium” – the accentuation of rash in areas previously affected by atopic dermatitis. Additional features may include nail dystrophies that manifest as Beau lines (deep grooved lines that run from side to side on the fingernail or the toenail) and nail shedding.
A spectrum of neurologic complications has been observed, more frequently with EV71 and more frequently in Asia. The spectrum includes aseptic meningitis and brainstem encephalitis. Progressive cardiopulmonary failure also can be observed in severe cases. The hallmark of severe disease is often presentation with high fever, sweating, mottled skin, and tachycardia. Early signs of CNS involvement include myoclonic jerks, ataxia, and “wandering eyes.”3 Elevated white blood count and/or hyperglycemia may distinguish children with severe disease from benign disease. Anecdotal reports of response to treatment with high-dose methylprednisolone and intravenous immune globulin suggest that the neurologic disease may be an autoimmune phenomenon.
The clinician’s primary role is to accurately diagnose HFMD, provide supportive care for fever and dehydration, and identify those with early signs or laboratory features heralding a more severe course of disease.3 The Centers for Disease Control and Prevention recommends frequent hand washing after toileting and changing diapers, disinfecting surfaces such as toys, avoiding close contact with infected individuals or sharing of personal items for all affected patients. No antiviral treatment is available although improvement following early treatment with acyclovir has been reported anecdotally. Intravenous immunoglobulin has been used in severe cases in Asia with retrospective data analysis suggesting a potential for improvement when administered prior to cardiopulmonary arrest.1
Dr. Pelton is professor of pediatrics and epidemiology at Boston University. Dr. Pelton said he had no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. Cleveland Clinic Journal of Medicine 2014;81(9):537-43.
2. Morbidity and Mortality Weekly Report MMWR. 2016 Jul 8;65(26);678-80.
3. A Guide to clinical management and public health response for hand, foot and mouth disease (HFMD).
Hand, foot, and mouth disease (HFMD) has become a global challenge since its first description in 1957 in New Zealand and Canada. Clinicians readily recognize the characteristic syndrome in young children: fever associated with a papulovesicular rash affecting the palms or soles, or both, usually in spring, summer, or fall. In most cases the disease is self-limited, and brief. However, aseptic meningitis, brainstem encephalitis, acute flaccid paralysis or autonomic nervous system deregulation or cardiorespiratory failure may complicate the clinical course.
HFMD is caused by enterovirus A (formerly called human enterovirus A) which consists of 25 serotypes including multiple coxsackie A viruses, multiple enteroviruses, simian enteroviruses, and baboon enterovirus A13. The clinical spectrum spans from herpangina, characterized by fever and painful mouth ulcers most prominent in the posterior oral cavity (uvula, tonsils, soft plates, and anterior pharyngeal folds), to HFMD with papulovesicular rash on palms and soles with or without mouth ulcers/vesicles.1 In atypical cases, the rash may be maculopapular and may include the buttocks, knees or elbows.
In the United States, the predominant cause is coxsackie A16. However, coxsackie A6 appears to be emerging; often more than one HFMD causing virus is circulating concurrently and clinically indistinguishable. Globally, especially, in Asia, enterovirus 1 is a major cause of HFMD and more often associated with prominent central nervous system involvement. Disease can be sporadic or epidemic. An outbreak is usually defined as two or more cases within a defined geographic area; global epidemics as large as 1.5 million cases (Taiwan, 1998) have been reported, and outbreaks in China involving tens of thousands with multiple deaths have been reported.
In 2015, an outbreak of HFMD occurred during basic military training at Lackland Air Force Base, Bexar County, Texas, due to coxsackie A6.2 The illness was characterized by prodromal symptoms of fever and malaise followed by erosive stomatitis and a rash that began on the palms and soles. The rate of infection among trainees was 4.7% (50 of 1,054 persons).
The differential diagnosis includes aphthous ulcers and herpetic gingivostomatitis.3 Aphthous ulcers are seen more commonly in older children and adolescents, are often recurrent, are not seasonal, and are not associated with rash. Herpes simplex virus gingivostomatitis usually has a febrile prodrome, perioral lesions are frequent in addition to gum and tongue involvement, and gingival bleeding is common. HFMD usually has an incubation period of 3-5 days and fever, malaise, and myalgia prodrome followed by onset of oral and dermatologic manifestations in sequence. The skin rash has features that may overlap with varicella, erythema multiforme (EM) or drug eruption. Varicella usually involves the face before spreading to the extremities, and the lesions are characterized by umbilication and subsequent crusting. EM is characterized by target lesions and drug eruptions are morbilliform or maculopapular. The majority of cases of HFMD are diagnosed clinically; polymerase chain reaction testing is available and best performed on throat or vesicle specimens. Serologic testing for A16 and enterovirus 71 (IgM) is available. Infected patients shed virus for 2-4 weeks and virus is stable in the environment resulting in fecal-oral or oral-oral transmission.
Atypical features of HFMD include occurrence in the winter (outbreak in Alabama in 2011/2012) or an atypical distribution of rash involving the antecubital and popliteal fossae distribution of rash, or “eczema coxsackium” – the accentuation of rash in areas previously affected by atopic dermatitis. Additional features may include nail dystrophies that manifest as Beau lines (deep grooved lines that run from side to side on the fingernail or the toenail) and nail shedding.
A spectrum of neurologic complications has been observed, more frequently with EV71 and more frequently in Asia. The spectrum includes aseptic meningitis and brainstem encephalitis. Progressive cardiopulmonary failure also can be observed in severe cases. The hallmark of severe disease is often presentation with high fever, sweating, mottled skin, and tachycardia. Early signs of CNS involvement include myoclonic jerks, ataxia, and “wandering eyes.”3 Elevated white blood count and/or hyperglycemia may distinguish children with severe disease from benign disease. Anecdotal reports of response to treatment with high-dose methylprednisolone and intravenous immune globulin suggest that the neurologic disease may be an autoimmune phenomenon.
The clinician’s primary role is to accurately diagnose HFMD, provide supportive care for fever and dehydration, and identify those with early signs or laboratory features heralding a more severe course of disease.3 The Centers for Disease Control and Prevention recommends frequent hand washing after toileting and changing diapers, disinfecting surfaces such as toys, avoiding close contact with infected individuals or sharing of personal items for all affected patients. No antiviral treatment is available although improvement following early treatment with acyclovir has been reported anecdotally. Intravenous immunoglobulin has been used in severe cases in Asia with retrospective data analysis suggesting a potential for improvement when administered prior to cardiopulmonary arrest.1
Dr. Pelton is professor of pediatrics and epidemiology at Boston University. Dr. Pelton said he had no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. Cleveland Clinic Journal of Medicine 2014;81(9):537-43.
2. Morbidity and Mortality Weekly Report MMWR. 2016 Jul 8;65(26);678-80.
3. A Guide to clinical management and public health response for hand, foot and mouth disease (HFMD).
Hand, foot, and mouth disease (HFMD) has become a global challenge since its first description in 1957 in New Zealand and Canada. Clinicians readily recognize the characteristic syndrome in young children: fever associated with a papulovesicular rash affecting the palms or soles, or both, usually in spring, summer, or fall. In most cases the disease is self-limited, and brief. However, aseptic meningitis, brainstem encephalitis, acute flaccid paralysis or autonomic nervous system deregulation or cardiorespiratory failure may complicate the clinical course.
HFMD is caused by enterovirus A (formerly called human enterovirus A) which consists of 25 serotypes including multiple coxsackie A viruses, multiple enteroviruses, simian enteroviruses, and baboon enterovirus A13. The clinical spectrum spans from herpangina, characterized by fever and painful mouth ulcers most prominent in the posterior oral cavity (uvula, tonsils, soft plates, and anterior pharyngeal folds), to HFMD with papulovesicular rash on palms and soles with or without mouth ulcers/vesicles.1 In atypical cases, the rash may be maculopapular and may include the buttocks, knees or elbows.
In the United States, the predominant cause is coxsackie A16. However, coxsackie A6 appears to be emerging; often more than one HFMD causing virus is circulating concurrently and clinically indistinguishable. Globally, especially, in Asia, enterovirus 1 is a major cause of HFMD and more often associated with prominent central nervous system involvement. Disease can be sporadic or epidemic. An outbreak is usually defined as two or more cases within a defined geographic area; global epidemics as large as 1.5 million cases (Taiwan, 1998) have been reported, and outbreaks in China involving tens of thousands with multiple deaths have been reported.
In 2015, an outbreak of HFMD occurred during basic military training at Lackland Air Force Base, Bexar County, Texas, due to coxsackie A6.2 The illness was characterized by prodromal symptoms of fever and malaise followed by erosive stomatitis and a rash that began on the palms and soles. The rate of infection among trainees was 4.7% (50 of 1,054 persons).
The differential diagnosis includes aphthous ulcers and herpetic gingivostomatitis.3 Aphthous ulcers are seen more commonly in older children and adolescents, are often recurrent, are not seasonal, and are not associated with rash. Herpes simplex virus gingivostomatitis usually has a febrile prodrome, perioral lesions are frequent in addition to gum and tongue involvement, and gingival bleeding is common. HFMD usually has an incubation period of 3-5 days and fever, malaise, and myalgia prodrome followed by onset of oral and dermatologic manifestations in sequence. The skin rash has features that may overlap with varicella, erythema multiforme (EM) or drug eruption. Varicella usually involves the face before spreading to the extremities, and the lesions are characterized by umbilication and subsequent crusting. EM is characterized by target lesions and drug eruptions are morbilliform or maculopapular. The majority of cases of HFMD are diagnosed clinically; polymerase chain reaction testing is available and best performed on throat or vesicle specimens. Serologic testing for A16 and enterovirus 71 (IgM) is available. Infected patients shed virus for 2-4 weeks and virus is stable in the environment resulting in fecal-oral or oral-oral transmission.
Atypical features of HFMD include occurrence in the winter (outbreak in Alabama in 2011/2012) or an atypical distribution of rash involving the antecubital and popliteal fossae distribution of rash, or “eczema coxsackium” – the accentuation of rash in areas previously affected by atopic dermatitis. Additional features may include nail dystrophies that manifest as Beau lines (deep grooved lines that run from side to side on the fingernail or the toenail) and nail shedding.
A spectrum of neurologic complications has been observed, more frequently with EV71 and more frequently in Asia. The spectrum includes aseptic meningitis and brainstem encephalitis. Progressive cardiopulmonary failure also can be observed in severe cases. The hallmark of severe disease is often presentation with high fever, sweating, mottled skin, and tachycardia. Early signs of CNS involvement include myoclonic jerks, ataxia, and “wandering eyes.”3 Elevated white blood count and/or hyperglycemia may distinguish children with severe disease from benign disease. Anecdotal reports of response to treatment with high-dose methylprednisolone and intravenous immune globulin suggest that the neurologic disease may be an autoimmune phenomenon.
The clinician’s primary role is to accurately diagnose HFMD, provide supportive care for fever and dehydration, and identify those with early signs or laboratory features heralding a more severe course of disease.3 The Centers for Disease Control and Prevention recommends frequent hand washing after toileting and changing diapers, disinfecting surfaces such as toys, avoiding close contact with infected individuals or sharing of personal items for all affected patients. No antiviral treatment is available although improvement following early treatment with acyclovir has been reported anecdotally. Intravenous immunoglobulin has been used in severe cases in Asia with retrospective data analysis suggesting a potential for improvement when administered prior to cardiopulmonary arrest.1
Dr. Pelton is professor of pediatrics and epidemiology at Boston University. Dr. Pelton said he had no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. Cleveland Clinic Journal of Medicine 2014;81(9):537-43.
2. Morbidity and Mortality Weekly Report MMWR. 2016 Jul 8;65(26);678-80.
3. A Guide to clinical management and public health response for hand, foot and mouth disease (HFMD).
Sunitinib alone not inferior to nephrectomy-sunitinib in metastatic RCC
Sunitinib alone was not inferior to nephrectomy followed by sunitinib in patients with metastatic, clear cell renal cell carcinoma (RCC), according to results of the randomized, phase 3 CARMENA trial.
Overall survival was not inferior in the sunitinib arm of the trial, which comprised 450 patients who were suitable candidates for nephrectomy and had MSKCC intermediate or poor risk disease.
These findings contrast with those of previous retrospective studies suggesting patients undergoing nephrectomy who were treated with targeted therapies had an overall survival benefit, according to Bernard Escudier, MD, of Gustave Roussy Institute, Villejuif, France, and his coauthors.
“Given the many approved options for systemic targeted therapy that are now available, the reassessment of the role of surgery in disease management is important,” Dr. Escudier and his colleagues noted. The report is in the New England Journal of Medicine.
The CARMENA trial enrolled 450 out of a planned 576 patients in 79 European centers between September 2009 and September 2017. A total of 226 were randomized to sunitinib alone and 224 to nephrectomy and sunitinib.
With a median follow-up of 50.9 months and 326 deaths, the hazard ratio for death was 0.89 (95% confidence interval, 0.71-1.10). The upper boundary of the 95% CI for noninferiority was 1.20, according to the report.
Median overall survival was 18.4 months for the sunitinib alone arm, and 13.9 months for the nephrectomy-plus-sunitinib arm. While the study was statistically underpowered because of incomplete enrollment, that “trend in longer overall survival” supports the findings favoring sunitinib alone in this noninferiority trial, the authors noted.
Safety results were as expected based on previous trial results, according to the investigators. Grade 3/4 adverse events occurred in 91 patients (42.7%) in the sunitinib group, and 61 (32.8%) in the nephrectomy-sunitinib group, they reported. Nine patients in the sunitinib group had grade 3/4 renal or urinary tract disorders, versus 1 in the nephrectomy-sunitinib group (P = .051).
These findings confirm current clinical practice guidelines on the use of systemic targeted therapy in patients with poor-risk metastatic RCC, according to the authors.
However, targeted therapy in this setting has evolved considerably since the CARMENA trial was designed.
Sunitinib remains one of the most commonly used treatments in patients with good or intermediate prognosis metastatic RCC; however, recent randomized trials show the superiority of the c-MET inhibitor cabozantinib and the immune checkpoint inhibitor combination of nivolumab plus ipilimumab over sunitinib.
Those newer agents will likely become initial treatment options for intermediate- and poor-risk groups, according to the authors.
Both cabozantinib and nivolumab plus ipilimumab are listed as first-line treatment options for intermediate- and poor-risk patients in the most recent clinical practice guidelines from the National Comprehensive Cancer Network.
Nephrectomy may have a role for symptom control in some patients with metastatic RCC, based on results of previous retrospective studies suggesting benefit.
“There is no ‘one size fits all’ approach,” Dr. Escudier and his coauthors wrote. “The multimodal approach of individualized treatment provides appropriate management of metastatic renal-cell carcinoma.”
Dr. Escudier reported personal fees from Bristol-Myers Squibb, EUSA Pharma, Ipsen, Novartis, Pfizer, and Roche outside the submitted work. Coauthors reported disclosures with Bayer, MSD, Janssen, Astellas, Bouchara, Ferring, and others.
SOURCE: Méjean A et al. N Engl J Med. 2018 Aug 2. doi: 10.1056/NEJMoa1803675.
The finding of the CARMENA trial that sunitinib was not inferior to nephrectomy should not lead to the abandonment of nephrectomy, according to Robert J. Motzer, MD, and Paul Russo, MD.
Instead, the results emphasize the importance of carefully selecting patients for nephrectomy based on published risk models, Dr. Motzer and Dr. Russo wrote in an editorial.
“We think that nephrectomy in properly chosen patients with metastatic renal cell carcinoma remains an essential component of care,” they said.
It is not surprising that the CARMENA study met its noninferiority endpoint, as it was “heavily weighted” toward poor-risk patients, they added.
Over an 8-year period, 79 European centers enrolled 450 patients out of 576 patients planned, or just 0.7 patients per site per year.
“This slow and incomplete enrollment raises the possibility that many centers saw few patients with stage IV disease, or that when surgeons saw patients with intermediate-risk disease who were likely to benefit from combination therapy, they were unwilling for them to undergo randomization and instead treated them outside the trial,” they wrote.
Over the same time frame at Dr. Motzer’s and Dr. Russo’s center, there were 189 patients with stage IV disease, or about 24 patients each year.
“We took care to avoid operating on poor-risk patients with extensive metastatic disease, instead focusing on intermediate-risk patients,” they explained in their editorial.
Dr. Motzer and Dr. Russo are with Memorial Sloan Kettering Cancer Center and Weill Cornell Medical College in New York. These comments come from their editorial in the New England Journal of Medicine. Dr. Russo had nothing to disclose. Dr. Motzer reported disclosures related to Genentech/Roche, Pfizer, Novartis, Exelixis, Eisai, Bristol-Myers Squibb, and Merck outside the submitted work.
The finding of the CARMENA trial that sunitinib was not inferior to nephrectomy should not lead to the abandonment of nephrectomy, according to Robert J. Motzer, MD, and Paul Russo, MD.
Instead, the results emphasize the importance of carefully selecting patients for nephrectomy based on published risk models, Dr. Motzer and Dr. Russo wrote in an editorial.
“We think that nephrectomy in properly chosen patients with metastatic renal cell carcinoma remains an essential component of care,” they said.
It is not surprising that the CARMENA study met its noninferiority endpoint, as it was “heavily weighted” toward poor-risk patients, they added.
Over an 8-year period, 79 European centers enrolled 450 patients out of 576 patients planned, or just 0.7 patients per site per year.
“This slow and incomplete enrollment raises the possibility that many centers saw few patients with stage IV disease, or that when surgeons saw patients with intermediate-risk disease who were likely to benefit from combination therapy, they were unwilling for them to undergo randomization and instead treated them outside the trial,” they wrote.
Over the same time frame at Dr. Motzer’s and Dr. Russo’s center, there were 189 patients with stage IV disease, or about 24 patients each year.
“We took care to avoid operating on poor-risk patients with extensive metastatic disease, instead focusing on intermediate-risk patients,” they explained in their editorial.
Dr. Motzer and Dr. Russo are with Memorial Sloan Kettering Cancer Center and Weill Cornell Medical College in New York. These comments come from their editorial in the New England Journal of Medicine. Dr. Russo had nothing to disclose. Dr. Motzer reported disclosures related to Genentech/Roche, Pfizer, Novartis, Exelixis, Eisai, Bristol-Myers Squibb, and Merck outside the submitted work.
The finding of the CARMENA trial that sunitinib was not inferior to nephrectomy should not lead to the abandonment of nephrectomy, according to Robert J. Motzer, MD, and Paul Russo, MD.
Instead, the results emphasize the importance of carefully selecting patients for nephrectomy based on published risk models, Dr. Motzer and Dr. Russo wrote in an editorial.
“We think that nephrectomy in properly chosen patients with metastatic renal cell carcinoma remains an essential component of care,” they said.
It is not surprising that the CARMENA study met its noninferiority endpoint, as it was “heavily weighted” toward poor-risk patients, they added.
Over an 8-year period, 79 European centers enrolled 450 patients out of 576 patients planned, or just 0.7 patients per site per year.
“This slow and incomplete enrollment raises the possibility that many centers saw few patients with stage IV disease, or that when surgeons saw patients with intermediate-risk disease who were likely to benefit from combination therapy, they were unwilling for them to undergo randomization and instead treated them outside the trial,” they wrote.
Over the same time frame at Dr. Motzer’s and Dr. Russo’s center, there were 189 patients with stage IV disease, or about 24 patients each year.
“We took care to avoid operating on poor-risk patients with extensive metastatic disease, instead focusing on intermediate-risk patients,” they explained in their editorial.
Dr. Motzer and Dr. Russo are with Memorial Sloan Kettering Cancer Center and Weill Cornell Medical College in New York. These comments come from their editorial in the New England Journal of Medicine. Dr. Russo had nothing to disclose. Dr. Motzer reported disclosures related to Genentech/Roche, Pfizer, Novartis, Exelixis, Eisai, Bristol-Myers Squibb, and Merck outside the submitted work.
Sunitinib alone was not inferior to nephrectomy followed by sunitinib in patients with metastatic, clear cell renal cell carcinoma (RCC), according to results of the randomized, phase 3 CARMENA trial.
Overall survival was not inferior in the sunitinib arm of the trial, which comprised 450 patients who were suitable candidates for nephrectomy and had MSKCC intermediate or poor risk disease.
These findings contrast with those of previous retrospective studies suggesting patients undergoing nephrectomy who were treated with targeted therapies had an overall survival benefit, according to Bernard Escudier, MD, of Gustave Roussy Institute, Villejuif, France, and his coauthors.
“Given the many approved options for systemic targeted therapy that are now available, the reassessment of the role of surgery in disease management is important,” Dr. Escudier and his colleagues noted. The report is in the New England Journal of Medicine.
The CARMENA trial enrolled 450 out of a planned 576 patients in 79 European centers between September 2009 and September 2017. A total of 226 were randomized to sunitinib alone and 224 to nephrectomy and sunitinib.
With a median follow-up of 50.9 months and 326 deaths, the hazard ratio for death was 0.89 (95% confidence interval, 0.71-1.10). The upper boundary of the 95% CI for noninferiority was 1.20, according to the report.
Median overall survival was 18.4 months for the sunitinib alone arm, and 13.9 months for the nephrectomy-plus-sunitinib arm. While the study was statistically underpowered because of incomplete enrollment, that “trend in longer overall survival” supports the findings favoring sunitinib alone in this noninferiority trial, the authors noted.
Safety results were as expected based on previous trial results, according to the investigators. Grade 3/4 adverse events occurred in 91 patients (42.7%) in the sunitinib group, and 61 (32.8%) in the nephrectomy-sunitinib group, they reported. Nine patients in the sunitinib group had grade 3/4 renal or urinary tract disorders, versus 1 in the nephrectomy-sunitinib group (P = .051).
These findings confirm current clinical practice guidelines on the use of systemic targeted therapy in patients with poor-risk metastatic RCC, according to the authors.
However, targeted therapy in this setting has evolved considerably since the CARMENA trial was designed.
Sunitinib remains one of the most commonly used treatments in patients with good or intermediate prognosis metastatic RCC; however, recent randomized trials show the superiority of the c-MET inhibitor cabozantinib and the immune checkpoint inhibitor combination of nivolumab plus ipilimumab over sunitinib.
Those newer agents will likely become initial treatment options for intermediate- and poor-risk groups, according to the authors.
Both cabozantinib and nivolumab plus ipilimumab are listed as first-line treatment options for intermediate- and poor-risk patients in the most recent clinical practice guidelines from the National Comprehensive Cancer Network.
Nephrectomy may have a role for symptom control in some patients with metastatic RCC, based on results of previous retrospective studies suggesting benefit.
“There is no ‘one size fits all’ approach,” Dr. Escudier and his coauthors wrote. “The multimodal approach of individualized treatment provides appropriate management of metastatic renal-cell carcinoma.”
Dr. Escudier reported personal fees from Bristol-Myers Squibb, EUSA Pharma, Ipsen, Novartis, Pfizer, and Roche outside the submitted work. Coauthors reported disclosures with Bayer, MSD, Janssen, Astellas, Bouchara, Ferring, and others.
SOURCE: Méjean A et al. N Engl J Med. 2018 Aug 2. doi: 10.1056/NEJMoa1803675.
Sunitinib alone was not inferior to nephrectomy followed by sunitinib in patients with metastatic, clear cell renal cell carcinoma (RCC), according to results of the randomized, phase 3 CARMENA trial.
Overall survival was not inferior in the sunitinib arm of the trial, which comprised 450 patients who were suitable candidates for nephrectomy and had MSKCC intermediate or poor risk disease.
These findings contrast with those of previous retrospective studies suggesting patients undergoing nephrectomy who were treated with targeted therapies had an overall survival benefit, according to Bernard Escudier, MD, of Gustave Roussy Institute, Villejuif, France, and his coauthors.
“Given the many approved options for systemic targeted therapy that are now available, the reassessment of the role of surgery in disease management is important,” Dr. Escudier and his colleagues noted. The report is in the New England Journal of Medicine.
The CARMENA trial enrolled 450 out of a planned 576 patients in 79 European centers between September 2009 and September 2017. A total of 226 were randomized to sunitinib alone and 224 to nephrectomy and sunitinib.
With a median follow-up of 50.9 months and 326 deaths, the hazard ratio for death was 0.89 (95% confidence interval, 0.71-1.10). The upper boundary of the 95% CI for noninferiority was 1.20, according to the report.
Median overall survival was 18.4 months for the sunitinib alone arm, and 13.9 months for the nephrectomy-plus-sunitinib arm. While the study was statistically underpowered because of incomplete enrollment, that “trend in longer overall survival” supports the findings favoring sunitinib alone in this noninferiority trial, the authors noted.
Safety results were as expected based on previous trial results, according to the investigators. Grade 3/4 adverse events occurred in 91 patients (42.7%) in the sunitinib group, and 61 (32.8%) in the nephrectomy-sunitinib group, they reported. Nine patients in the sunitinib group had grade 3/4 renal or urinary tract disorders, versus 1 in the nephrectomy-sunitinib group (P = .051).
These findings confirm current clinical practice guidelines on the use of systemic targeted therapy in patients with poor-risk metastatic RCC, according to the authors.
However, targeted therapy in this setting has evolved considerably since the CARMENA trial was designed.
Sunitinib remains one of the most commonly used treatments in patients with good or intermediate prognosis metastatic RCC; however, recent randomized trials show the superiority of the c-MET inhibitor cabozantinib and the immune checkpoint inhibitor combination of nivolumab plus ipilimumab over sunitinib.
Those newer agents will likely become initial treatment options for intermediate- and poor-risk groups, according to the authors.
Both cabozantinib and nivolumab plus ipilimumab are listed as first-line treatment options for intermediate- and poor-risk patients in the most recent clinical practice guidelines from the National Comprehensive Cancer Network.
Nephrectomy may have a role for symptom control in some patients with metastatic RCC, based on results of previous retrospective studies suggesting benefit.
“There is no ‘one size fits all’ approach,” Dr. Escudier and his coauthors wrote. “The multimodal approach of individualized treatment provides appropriate management of metastatic renal-cell carcinoma.”
Dr. Escudier reported personal fees from Bristol-Myers Squibb, EUSA Pharma, Ipsen, Novartis, Pfizer, and Roche outside the submitted work. Coauthors reported disclosures with Bayer, MSD, Janssen, Astellas, Bouchara, Ferring, and others.
SOURCE: Méjean A et al. N Engl J Med. 2018 Aug 2. doi: 10.1056/NEJMoa1803675.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Sunitinib alone was not inferior to nephrectomy plus sunitinib in patients with MSKCC intermediate- or poor-risk metastatic, clear cell renal cell carcinoma (RCC) who were suitable candidates for nephrectomy.
Major finding: Overall survival was not inferior in the sunitinib arm of the trial.
Study details: A randomized phase 3 trial involving 450 patients with metastatic clear-cell RCC who were suitable candidates for nephrectomy.
Disclosures: The authors reported disclosures related to Bristol-Myers Squibb, EUSA Pharma, Ipsen, Novartis, Pfizer, and Roche, among others.
Source: Méjean A et al. N Engl J Med. 2018 Aug 2. doi: 10.1056/NEJMoa1803675.
McCain’s complicated health care legacy: He hated the ACA. He also saved it
There are many lawmakers who made their names in health care, seeking to usher through historic changes to a broken system.
Sen. John McCain was not one of them.
And yet, the six-term senator from Arizona and decorated military veteran leaves behind his own health care legacy, seemingly driven less by his interest in health care policy than his disdain for bullies trampling the “little guy.”
He was not always successful. While Sen. McCain was instrumental in the passage of the Americans with Disabilities Act in 1990, most of the health initiatives he undertook failed after running afoul of traditional Republican priorities. His prescriptions often involved more government regulation and increased taxes.
In 2008, as the Republican nominee for president, he ran on a health care platform that dumbfounded many in his party who worried it would raise taxes on top of overhauling the U.S. tradition of workplace insurance.
Many will remember Sen. McCain as the incidental savior of the Affordable Care Act, whose late-night thumbs-down vote halted his party’s most promising effort to overturn a major Democratic achievement – the signature achievement, in fact, of the Democrat who beat him to become president. It was a vote that earned him regular – and biting – admonishments from President Donald Trump.
Sen. McCain died Aug. 25, following a battle with brain cancer. He was 81. Coincidentally, his Senate colleague and good friend Ted Kennedy died on the same date, Aug. 25, 9 years ago, succumbing to the same type of rare brain tumor.
Whether indulging in conspiracy theories or wishful thinking, some have attributed Sen. McCain’s vote on the ACA in July 2017 to a change of heart shortly after his terminal cancer diagnosis.
But Sen. McCain spent much of his 35 years in Congress fighting a never-ending supply of goliaths, among them health insurance companies, the tobacco industry and, in his estimation, the Affordable Care Act, a law that extended insurance coverage to millions of Americans but did not solve the system’s ballooning costs.
His prey were the sort of boogeymen that made for compelling campaign ads in a career stacked with campaigns. But Sen. McCain was “always for the little guy,” said Douglas Holtz-Eakin, the chief domestic policy adviser on Sen. McCain’s 2008 presidential campaign.
“John’s idea of empathy is saying to you, ‘I’ll punch the bully for you,’ ” he said in an interview before Sen. McCain’s death.
Sen. McCain’s distaste for President Barack Obama’s health care law was no secret. While he agreed that the health care system was broken, he did not think more government involvement would fix it. Like most Republicans, he campaigned in his last Senate race on a promise to repeal and replace the law with something better.
After Republicans spent months bickering amongst themselves about what was better, Sen. McCain was disappointed in the option presented to senators hours before their vote: Hobble the ACA, and trust that a handful of lawmakers would be able to craft an alternative behind closed doors, despite failing to accomplish that very thing after years of trying.
What bothered Sen. McCain more, though, was his party’s strategy to pass their so-called skinny repeal measure, skipping committee consideration and delivering it straight to the floor. They also rejected any input from the opposing party, a tactic for which he had slammed Democrats when the ACA passed in 2010 without a single GOP vote. He lamented that Republican leaders had cast aside compromise-nurturing Senate procedures in pursuit of political victory.
In his 2018 memoirs, “The Restless Wave,” Sen. McCain said even President Obama called to express gratitude for Sen. McCain’s vote against the Republican repeal bill.
“I was thanked for my vote by Democratic friends more profusely than I should have been for helping save Obamacare,” Sen. McCain wrote. “That had not been my goal.”
Better known for his work on campaign finance reform and the military, Sen. McCain did have a hand in one landmark health bill – the Americans with Disabilities Act of 1990, the country’s first comprehensive civil rights law that addressed the needs of those with disabilities. An early cosponsor of the legislation, he championed the rights of the disabled, speaking of the service members and civilians he met in his travels who had become disabled during military conflict.
Sen. McCain himself had limited use of his arms due to injuries inflicted while he was a prisoner of war in Vietnam, though he was quicker to talk about the troubles of others than his own when advocating policy.
Yet two of his biggest bills on health care ended in defeat.
In 1998, Sen. McCain introduced a sweeping bill that would regulate the tobacco industry and increase taxes on cigarettes, hoping to discourage teenagers from smoking and raise money for research and related health care costs. It faltered under opposition from his fellow Republicans.
Sen. McCain also joined an effort with two Democratic senators, Sen. Kennedy of Massachusetts and Sen. John Edwards of North Carolina, to pass a patients’ bill of rights in 2001. He resisted at first, concerned in particular about the right it gave patients to sue health care companies, said Sonya Elling, who served as a health care aide in Sen. McCain’s office for about a decade. But he came around.
“It was the human, the personal aspect of it, basically,” said Ms. Elling, now senior director of federal affairs at Eli Lilly. “It was providing him some of the real stories about how people were being hurt and some of the barriers that existed for people in the current system.”
The legislation would have granted patients with private insurance the right to emergency and specialist care in addition to the right to seek redress for being wrongly denied care. But President George W. Bush threatened to veto the measure, claiming it would fuel frivolous lawsuits. The bill failed.
Sen. McCain’s health care efforts bolstered his reputation as a lawmaker willing to work across the aisle. Sen. Chuck Schumer of New York, now the Senate’s Democratic leader, sought his help on legislation in 2001 to expand access to generic drugs. In 2015, Sen. McCain led a bipartisan coalition to pass a law that would strengthen mental health and suicide prevention programs for veterans, among other veterans’ care measures he undertook.
It was Sen. McCain’s relationship with Sen. Kennedy that stood out, inspiring eerie comparisons when Sen. McCain was diagnosed last year with glioblastoma – a form of brain cancer – shortly before his vote saved the Affordable Care Act.
That same aggressive brain cancer killed Sen. Kennedy in 2009, months before the passage of the law that helped realize his work to secure better access for Americans to health care.
“I had strenuously opposed it, but I was very sorry that Ted had not lived to see his long crusade come to a successful end,” Sen. McCain wrote in his 2018 book.
While some of his biggest health care measures failed, the experiences helped burnish Sen. McCain’s résumé for his 2000 and 2008 presidential campaigns.
In 2007, trailing other favored Republicans, such as former New York City mayor Rudy Giuliani in early polling and fundraising, Sen. McCain asked his advisers to craft a health care proposal, said Mr. Holtz-Eakin. It was an unusual move for a Republican presidential primary.
The result was a remarkable plan that would eliminate the tax break employers get for providing health benefits to workers, known as the employer exclusion, and replace it with refundable tax credits to help people – not just those working in firms that supplied coverage – buy insurance individually. He argued employer-provided plans were driving up costs, as well as keeping salaries lower.
The plan was controversial, triggering “a total freak-out” when Sen. McCain gained more prominence and scrutiny, Mr. Holtz-Eakin said. But Sen. McCain stood by it.
“He might not have been a health guy, but he knew how important that was,” he said. “And he was relentless about getting it done.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
There are many lawmakers who made their names in health care, seeking to usher through historic changes to a broken system.
Sen. John McCain was not one of them.
And yet, the six-term senator from Arizona and decorated military veteran leaves behind his own health care legacy, seemingly driven less by his interest in health care policy than his disdain for bullies trampling the “little guy.”
He was not always successful. While Sen. McCain was instrumental in the passage of the Americans with Disabilities Act in 1990, most of the health initiatives he undertook failed after running afoul of traditional Republican priorities. His prescriptions often involved more government regulation and increased taxes.
In 2008, as the Republican nominee for president, he ran on a health care platform that dumbfounded many in his party who worried it would raise taxes on top of overhauling the U.S. tradition of workplace insurance.
Many will remember Sen. McCain as the incidental savior of the Affordable Care Act, whose late-night thumbs-down vote halted his party’s most promising effort to overturn a major Democratic achievement – the signature achievement, in fact, of the Democrat who beat him to become president. It was a vote that earned him regular – and biting – admonishments from President Donald Trump.
Sen. McCain died Aug. 25, following a battle with brain cancer. He was 81. Coincidentally, his Senate colleague and good friend Ted Kennedy died on the same date, Aug. 25, 9 years ago, succumbing to the same type of rare brain tumor.
Whether indulging in conspiracy theories or wishful thinking, some have attributed Sen. McCain’s vote on the ACA in July 2017 to a change of heart shortly after his terminal cancer diagnosis.
But Sen. McCain spent much of his 35 years in Congress fighting a never-ending supply of goliaths, among them health insurance companies, the tobacco industry and, in his estimation, the Affordable Care Act, a law that extended insurance coverage to millions of Americans but did not solve the system’s ballooning costs.
His prey were the sort of boogeymen that made for compelling campaign ads in a career stacked with campaigns. But Sen. McCain was “always for the little guy,” said Douglas Holtz-Eakin, the chief domestic policy adviser on Sen. McCain’s 2008 presidential campaign.
“John’s idea of empathy is saying to you, ‘I’ll punch the bully for you,’ ” he said in an interview before Sen. McCain’s death.
Sen. McCain’s distaste for President Barack Obama’s health care law was no secret. While he agreed that the health care system was broken, he did not think more government involvement would fix it. Like most Republicans, he campaigned in his last Senate race on a promise to repeal and replace the law with something better.
After Republicans spent months bickering amongst themselves about what was better, Sen. McCain was disappointed in the option presented to senators hours before their vote: Hobble the ACA, and trust that a handful of lawmakers would be able to craft an alternative behind closed doors, despite failing to accomplish that very thing after years of trying.
What bothered Sen. McCain more, though, was his party’s strategy to pass their so-called skinny repeal measure, skipping committee consideration and delivering it straight to the floor. They also rejected any input from the opposing party, a tactic for which he had slammed Democrats when the ACA passed in 2010 without a single GOP vote. He lamented that Republican leaders had cast aside compromise-nurturing Senate procedures in pursuit of political victory.
In his 2018 memoirs, “The Restless Wave,” Sen. McCain said even President Obama called to express gratitude for Sen. McCain’s vote against the Republican repeal bill.
“I was thanked for my vote by Democratic friends more profusely than I should have been for helping save Obamacare,” Sen. McCain wrote. “That had not been my goal.”
Better known for his work on campaign finance reform and the military, Sen. McCain did have a hand in one landmark health bill – the Americans with Disabilities Act of 1990, the country’s first comprehensive civil rights law that addressed the needs of those with disabilities. An early cosponsor of the legislation, he championed the rights of the disabled, speaking of the service members and civilians he met in his travels who had become disabled during military conflict.
Sen. McCain himself had limited use of his arms due to injuries inflicted while he was a prisoner of war in Vietnam, though he was quicker to talk about the troubles of others than his own when advocating policy.
Yet two of his biggest bills on health care ended in defeat.
In 1998, Sen. McCain introduced a sweeping bill that would regulate the tobacco industry and increase taxes on cigarettes, hoping to discourage teenagers from smoking and raise money for research and related health care costs. It faltered under opposition from his fellow Republicans.
Sen. McCain also joined an effort with two Democratic senators, Sen. Kennedy of Massachusetts and Sen. John Edwards of North Carolina, to pass a patients’ bill of rights in 2001. He resisted at first, concerned in particular about the right it gave patients to sue health care companies, said Sonya Elling, who served as a health care aide in Sen. McCain’s office for about a decade. But he came around.
“It was the human, the personal aspect of it, basically,” said Ms. Elling, now senior director of federal affairs at Eli Lilly. “It was providing him some of the real stories about how people were being hurt and some of the barriers that existed for people in the current system.”
The legislation would have granted patients with private insurance the right to emergency and specialist care in addition to the right to seek redress for being wrongly denied care. But President George W. Bush threatened to veto the measure, claiming it would fuel frivolous lawsuits. The bill failed.
Sen. McCain’s health care efforts bolstered his reputation as a lawmaker willing to work across the aisle. Sen. Chuck Schumer of New York, now the Senate’s Democratic leader, sought his help on legislation in 2001 to expand access to generic drugs. In 2015, Sen. McCain led a bipartisan coalition to pass a law that would strengthen mental health and suicide prevention programs for veterans, among other veterans’ care measures he undertook.
It was Sen. McCain’s relationship with Sen. Kennedy that stood out, inspiring eerie comparisons when Sen. McCain was diagnosed last year with glioblastoma – a form of brain cancer – shortly before his vote saved the Affordable Care Act.
That same aggressive brain cancer killed Sen. Kennedy in 2009, months before the passage of the law that helped realize his work to secure better access for Americans to health care.
“I had strenuously opposed it, but I was very sorry that Ted had not lived to see his long crusade come to a successful end,” Sen. McCain wrote in his 2018 book.
While some of his biggest health care measures failed, the experiences helped burnish Sen. McCain’s résumé for his 2000 and 2008 presidential campaigns.
In 2007, trailing other favored Republicans, such as former New York City mayor Rudy Giuliani in early polling and fundraising, Sen. McCain asked his advisers to craft a health care proposal, said Mr. Holtz-Eakin. It was an unusual move for a Republican presidential primary.
The result was a remarkable plan that would eliminate the tax break employers get for providing health benefits to workers, known as the employer exclusion, and replace it with refundable tax credits to help people – not just those working in firms that supplied coverage – buy insurance individually. He argued employer-provided plans were driving up costs, as well as keeping salaries lower.
The plan was controversial, triggering “a total freak-out” when Sen. McCain gained more prominence and scrutiny, Mr. Holtz-Eakin said. But Sen. McCain stood by it.
“He might not have been a health guy, but he knew how important that was,” he said. “And he was relentless about getting it done.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
There are many lawmakers who made their names in health care, seeking to usher through historic changes to a broken system.
Sen. John McCain was not one of them.
And yet, the six-term senator from Arizona and decorated military veteran leaves behind his own health care legacy, seemingly driven less by his interest in health care policy than his disdain for bullies trampling the “little guy.”
He was not always successful. While Sen. McCain was instrumental in the passage of the Americans with Disabilities Act in 1990, most of the health initiatives he undertook failed after running afoul of traditional Republican priorities. His prescriptions often involved more government regulation and increased taxes.
In 2008, as the Republican nominee for president, he ran on a health care platform that dumbfounded many in his party who worried it would raise taxes on top of overhauling the U.S. tradition of workplace insurance.
Many will remember Sen. McCain as the incidental savior of the Affordable Care Act, whose late-night thumbs-down vote halted his party’s most promising effort to overturn a major Democratic achievement – the signature achievement, in fact, of the Democrat who beat him to become president. It was a vote that earned him regular – and biting – admonishments from President Donald Trump.
Sen. McCain died Aug. 25, following a battle with brain cancer. He was 81. Coincidentally, his Senate colleague and good friend Ted Kennedy died on the same date, Aug. 25, 9 years ago, succumbing to the same type of rare brain tumor.
Whether indulging in conspiracy theories or wishful thinking, some have attributed Sen. McCain’s vote on the ACA in July 2017 to a change of heart shortly after his terminal cancer diagnosis.
But Sen. McCain spent much of his 35 years in Congress fighting a never-ending supply of goliaths, among them health insurance companies, the tobacco industry and, in his estimation, the Affordable Care Act, a law that extended insurance coverage to millions of Americans but did not solve the system’s ballooning costs.
His prey were the sort of boogeymen that made for compelling campaign ads in a career stacked with campaigns. But Sen. McCain was “always for the little guy,” said Douglas Holtz-Eakin, the chief domestic policy adviser on Sen. McCain’s 2008 presidential campaign.
“John’s idea of empathy is saying to you, ‘I’ll punch the bully for you,’ ” he said in an interview before Sen. McCain’s death.
Sen. McCain’s distaste for President Barack Obama’s health care law was no secret. While he agreed that the health care system was broken, he did not think more government involvement would fix it. Like most Republicans, he campaigned in his last Senate race on a promise to repeal and replace the law with something better.
After Republicans spent months bickering amongst themselves about what was better, Sen. McCain was disappointed in the option presented to senators hours before their vote: Hobble the ACA, and trust that a handful of lawmakers would be able to craft an alternative behind closed doors, despite failing to accomplish that very thing after years of trying.
What bothered Sen. McCain more, though, was his party’s strategy to pass their so-called skinny repeal measure, skipping committee consideration and delivering it straight to the floor. They also rejected any input from the opposing party, a tactic for which he had slammed Democrats when the ACA passed in 2010 without a single GOP vote. He lamented that Republican leaders had cast aside compromise-nurturing Senate procedures in pursuit of political victory.
In his 2018 memoirs, “The Restless Wave,” Sen. McCain said even President Obama called to express gratitude for Sen. McCain’s vote against the Republican repeal bill.
“I was thanked for my vote by Democratic friends more profusely than I should have been for helping save Obamacare,” Sen. McCain wrote. “That had not been my goal.”
Better known for his work on campaign finance reform and the military, Sen. McCain did have a hand in one landmark health bill – the Americans with Disabilities Act of 1990, the country’s first comprehensive civil rights law that addressed the needs of those with disabilities. An early cosponsor of the legislation, he championed the rights of the disabled, speaking of the service members and civilians he met in his travels who had become disabled during military conflict.
Sen. McCain himself had limited use of his arms due to injuries inflicted while he was a prisoner of war in Vietnam, though he was quicker to talk about the troubles of others than his own when advocating policy.
Yet two of his biggest bills on health care ended in defeat.
In 1998, Sen. McCain introduced a sweeping bill that would regulate the tobacco industry and increase taxes on cigarettes, hoping to discourage teenagers from smoking and raise money for research and related health care costs. It faltered under opposition from his fellow Republicans.
Sen. McCain also joined an effort with two Democratic senators, Sen. Kennedy of Massachusetts and Sen. John Edwards of North Carolina, to pass a patients’ bill of rights in 2001. He resisted at first, concerned in particular about the right it gave patients to sue health care companies, said Sonya Elling, who served as a health care aide in Sen. McCain’s office for about a decade. But he came around.
“It was the human, the personal aspect of it, basically,” said Ms. Elling, now senior director of federal affairs at Eli Lilly. “It was providing him some of the real stories about how people were being hurt and some of the barriers that existed for people in the current system.”
The legislation would have granted patients with private insurance the right to emergency and specialist care in addition to the right to seek redress for being wrongly denied care. But President George W. Bush threatened to veto the measure, claiming it would fuel frivolous lawsuits. The bill failed.
Sen. McCain’s health care efforts bolstered his reputation as a lawmaker willing to work across the aisle. Sen. Chuck Schumer of New York, now the Senate’s Democratic leader, sought his help on legislation in 2001 to expand access to generic drugs. In 2015, Sen. McCain led a bipartisan coalition to pass a law that would strengthen mental health and suicide prevention programs for veterans, among other veterans’ care measures he undertook.
It was Sen. McCain’s relationship with Sen. Kennedy that stood out, inspiring eerie comparisons when Sen. McCain was diagnosed last year with glioblastoma – a form of brain cancer – shortly before his vote saved the Affordable Care Act.
That same aggressive brain cancer killed Sen. Kennedy in 2009, months before the passage of the law that helped realize his work to secure better access for Americans to health care.
“I had strenuously opposed it, but I was very sorry that Ted had not lived to see his long crusade come to a successful end,” Sen. McCain wrote in his 2018 book.
While some of his biggest health care measures failed, the experiences helped burnish Sen. McCain’s résumé for his 2000 and 2008 presidential campaigns.
In 2007, trailing other favored Republicans, such as former New York City mayor Rudy Giuliani in early polling and fundraising, Sen. McCain asked his advisers to craft a health care proposal, said Mr. Holtz-Eakin. It was an unusual move for a Republican presidential primary.
The result was a remarkable plan that would eliminate the tax break employers get for providing health benefits to workers, known as the employer exclusion, and replace it with refundable tax credits to help people – not just those working in firms that supplied coverage – buy insurance individually. He argued employer-provided plans were driving up costs, as well as keeping salaries lower.
The plan was controversial, triggering “a total freak-out” when Sen. McCain gained more prominence and scrutiny, Mr. Holtz-Eakin said. But Sen. McCain stood by it.
“He might not have been a health guy, but he knew how important that was,” he said. “And he was relentless about getting it done.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Inherited mutations drive 12% of Nigerian breast cancer
About one in eight Nigerian women with breast cancer has an inherited mutation of the BRCA1, BRCA2, PALB2, or TP53 gene.
A new analysis of the Nigerian Breast Cancer Study confirmed that these inherited mutations drive about 12% of the country’s breast cancer cases. The findings could pave the way for the first large-scale national breast cancer gene screening program, wrote Olufunmilayo I. Olopade, MD, and her colleagues. The report is in the Journal of Clinical Oncology.
“We suggest that genomic sequencing to identify women at extremely high risk of breast cancer could be a highly innovative approach to tailored risk management and life-saving interventions,” wrote Dr. Olopade, director of the Center for Clinical Cancer Genetics at the University of Chicago, and her colleagues. “Nigeria now has data to prioritize the integration of genetic testing into its cancer control plan. Women with an extremely high risk of breast cancer because of mutations in these genes can be identified inexpensively and unambiguously and offered interventions to reduce cancer risk.”
And, since about half of the sisters and daughters of affected women will carry the same mutation, such a screening program could reach far beyond every index patient identified, the investigators noted.
“If these women at very high risk can be identified either through their relatives with breast cancer or in the general population, resources can be focused particularly on their behalf. For as-yet unaffected women at high genetic risk, these resources would be intensive surveillance for early detection of breast cancer and, after childbearing is completed, the possibility of preventive salpingo-oophorectomy. Integrated population screening for cancer for all women is the goal, but focused outreach to women at extremely high risk represents an especially efficient use of resources and an attainable evidence-based global health approach.”
The Nigerian Breast Cancer Study enrolled 1,136 women with invasive breast cancer from 1998 to 2014. These were compared with 997 women without cancer, matched from the same communities. Genetic sequencing searched for mutations in both known and breast cancer genes.
Cases and controls were a mean of 47 years old; only 6% of cases reported a family history of breast cancer. Of 577 patients with information on tumor stage, 86% (497) were diagnosed at stage III (241) or IV (256).
Among the cases, 167 (14.7%) carried a mutation in a breast cancer risk gene, compared with 1.8% of controls. BRCA1 was the most common mutation, occurring in 7% of patients; these women were 23 times more likely to develop breast cancer than were those without the gene (odds ratio, 23.4). BRCA2 was the next most common, occurring in 4% of cases and conferring a nearly 11-fold increased risk (OR, 10.76). PALB2 occurred in 11 cases (1%) and no controls, and TP53 in four cases (0.4%).
Women with the BRCA1 mutation were diagnosed at a significantly younger age than were other patients (42.6 vs. 47.9 years), as were carriers of the TP53 mutation (32.8 vs. 47.6 years).
Ten other genes (ATM, BARD1, BRIP1, CHEK1, CHEK2, GEN1, NBN, RAD51C, RAD51D, and XRCC2) carried a mutation in at least one patient each. “When limited to mutations in the four high-risk genes, 11%-12% of cases in this study carried a loss-of-function variant.”
Dr. Olopade had no financial disclosures.
SOURCE: Olopade et al. J Clin Oncol. 2018 Aug 21. doi: 10.1200/JCO.2018.78.3977.
The findings of the Nigerian Breast Cancer Study make a case for large-scale breast cancer gene screening. But even in a wealthy country with good infrastructure, such a program would be dauntingly complex, Ophira Ginsburg, MD, and Paul Brennan, PhD, wrote in an accompanying editorial.
“Given the estimated 40,983 women in Nigeria younger than age 65 years who will be newly diagnosed with breast cancer in 2030, the estimated mutation carrier frequency for a high-risk gene of 11%-12% translates to approximately 5,000 women with breast cancer each year who might benefit directly from tailored risk-reducing strategies. Moreover, 50% of these women’s sisters and daughters would also stand to benefit,” they wrote.
However, 32 million women would need to be screened to find the 220,000 with one of the mutations – a task that is “clearly beyond the scope of most countries.
“Furthermore, women with pathogenic variants would require intensive follow-up and intervention strategies to reduce their risk of developing breast, ovarian/fallopian tube, and potentially other cancers depending on the gene involved. Importantly, this approach would not address the larger problem of the high breast cancer mortality among the vast majority of women without a pathogenic variant but who make up approximately 85% of the breast cancer burden.”
The World Health Organization recognizes this challenge; the agency doesn’t even recommend mammogram-based population screening unless there is a basic, reliable infrastructure including electricity, quality-assurance measures, referral and recall mechanisms, and monitoring and evaluation frameworks. But WHO does suggest some core elements to guide a country’s comprehensive cancer management strategy, including:
• Considering the whole continuum from prevention to palliation.
• Providing a sustainable strategic plan on the basis of the country’s cancer burden, risk factor prevalence, and the resources available to implement the plan.
• Developing an evidence-based approach generated by population-based cancer registries.
“As many countries improve their cancer systems, investing in human resources, infrastructure, monitoring, and evaluation, it is timely to consider how to evaluate readiness to undertake a population-level cancer genetics intervention and consider the core elements that should be in place to make a substantive effect on cancer mortality.”
Dr. Ginsburg is with the Perlmutter Cancer Center of New York University. Dr. Brennan is with the International Agency for Research on Cancer, Lyon, France.
The findings of the Nigerian Breast Cancer Study make a case for large-scale breast cancer gene screening. But even in a wealthy country with good infrastructure, such a program would be dauntingly complex, Ophira Ginsburg, MD, and Paul Brennan, PhD, wrote in an accompanying editorial.
“Given the estimated 40,983 women in Nigeria younger than age 65 years who will be newly diagnosed with breast cancer in 2030, the estimated mutation carrier frequency for a high-risk gene of 11%-12% translates to approximately 5,000 women with breast cancer each year who might benefit directly from tailored risk-reducing strategies. Moreover, 50% of these women’s sisters and daughters would also stand to benefit,” they wrote.
However, 32 million women would need to be screened to find the 220,000 with one of the mutations – a task that is “clearly beyond the scope of most countries.
“Furthermore, women with pathogenic variants would require intensive follow-up and intervention strategies to reduce their risk of developing breast, ovarian/fallopian tube, and potentially other cancers depending on the gene involved. Importantly, this approach would not address the larger problem of the high breast cancer mortality among the vast majority of women without a pathogenic variant but who make up approximately 85% of the breast cancer burden.”
The World Health Organization recognizes this challenge; the agency doesn’t even recommend mammogram-based population screening unless there is a basic, reliable infrastructure including electricity, quality-assurance measures, referral and recall mechanisms, and monitoring and evaluation frameworks. But WHO does suggest some core elements to guide a country’s comprehensive cancer management strategy, including:
• Considering the whole continuum from prevention to palliation.
• Providing a sustainable strategic plan on the basis of the country’s cancer burden, risk factor prevalence, and the resources available to implement the plan.
• Developing an evidence-based approach generated by population-based cancer registries.
“As many countries improve their cancer systems, investing in human resources, infrastructure, monitoring, and evaluation, it is timely to consider how to evaluate readiness to undertake a population-level cancer genetics intervention and consider the core elements that should be in place to make a substantive effect on cancer mortality.”
Dr. Ginsburg is with the Perlmutter Cancer Center of New York University. Dr. Brennan is with the International Agency for Research on Cancer, Lyon, France.
The findings of the Nigerian Breast Cancer Study make a case for large-scale breast cancer gene screening. But even in a wealthy country with good infrastructure, such a program would be dauntingly complex, Ophira Ginsburg, MD, and Paul Brennan, PhD, wrote in an accompanying editorial.
“Given the estimated 40,983 women in Nigeria younger than age 65 years who will be newly diagnosed with breast cancer in 2030, the estimated mutation carrier frequency for a high-risk gene of 11%-12% translates to approximately 5,000 women with breast cancer each year who might benefit directly from tailored risk-reducing strategies. Moreover, 50% of these women’s sisters and daughters would also stand to benefit,” they wrote.
However, 32 million women would need to be screened to find the 220,000 with one of the mutations – a task that is “clearly beyond the scope of most countries.
“Furthermore, women with pathogenic variants would require intensive follow-up and intervention strategies to reduce their risk of developing breast, ovarian/fallopian tube, and potentially other cancers depending on the gene involved. Importantly, this approach would not address the larger problem of the high breast cancer mortality among the vast majority of women without a pathogenic variant but who make up approximately 85% of the breast cancer burden.”
The World Health Organization recognizes this challenge; the agency doesn’t even recommend mammogram-based population screening unless there is a basic, reliable infrastructure including electricity, quality-assurance measures, referral and recall mechanisms, and monitoring and evaluation frameworks. But WHO does suggest some core elements to guide a country’s comprehensive cancer management strategy, including:
• Considering the whole continuum from prevention to palliation.
• Providing a sustainable strategic plan on the basis of the country’s cancer burden, risk factor prevalence, and the resources available to implement the plan.
• Developing an evidence-based approach generated by population-based cancer registries.
“As many countries improve their cancer systems, investing in human resources, infrastructure, monitoring, and evaluation, it is timely to consider how to evaluate readiness to undertake a population-level cancer genetics intervention and consider the core elements that should be in place to make a substantive effect on cancer mortality.”
Dr. Ginsburg is with the Perlmutter Cancer Center of New York University. Dr. Brennan is with the International Agency for Research on Cancer, Lyon, France.
About one in eight Nigerian women with breast cancer has an inherited mutation of the BRCA1, BRCA2, PALB2, or TP53 gene.
A new analysis of the Nigerian Breast Cancer Study confirmed that these inherited mutations drive about 12% of the country’s breast cancer cases. The findings could pave the way for the first large-scale national breast cancer gene screening program, wrote Olufunmilayo I. Olopade, MD, and her colleagues. The report is in the Journal of Clinical Oncology.
“We suggest that genomic sequencing to identify women at extremely high risk of breast cancer could be a highly innovative approach to tailored risk management and life-saving interventions,” wrote Dr. Olopade, director of the Center for Clinical Cancer Genetics at the University of Chicago, and her colleagues. “Nigeria now has data to prioritize the integration of genetic testing into its cancer control plan. Women with an extremely high risk of breast cancer because of mutations in these genes can be identified inexpensively and unambiguously and offered interventions to reduce cancer risk.”
And, since about half of the sisters and daughters of affected women will carry the same mutation, such a screening program could reach far beyond every index patient identified, the investigators noted.
“If these women at very high risk can be identified either through their relatives with breast cancer or in the general population, resources can be focused particularly on their behalf. For as-yet unaffected women at high genetic risk, these resources would be intensive surveillance for early detection of breast cancer and, after childbearing is completed, the possibility of preventive salpingo-oophorectomy. Integrated population screening for cancer for all women is the goal, but focused outreach to women at extremely high risk represents an especially efficient use of resources and an attainable evidence-based global health approach.”
The Nigerian Breast Cancer Study enrolled 1,136 women with invasive breast cancer from 1998 to 2014. These were compared with 997 women without cancer, matched from the same communities. Genetic sequencing searched for mutations in both known and breast cancer genes.
Cases and controls were a mean of 47 years old; only 6% of cases reported a family history of breast cancer. Of 577 patients with information on tumor stage, 86% (497) were diagnosed at stage III (241) or IV (256).
Among the cases, 167 (14.7%) carried a mutation in a breast cancer risk gene, compared with 1.8% of controls. BRCA1 was the most common mutation, occurring in 7% of patients; these women were 23 times more likely to develop breast cancer than were those without the gene (odds ratio, 23.4). BRCA2 was the next most common, occurring in 4% of cases and conferring a nearly 11-fold increased risk (OR, 10.76). PALB2 occurred in 11 cases (1%) and no controls, and TP53 in four cases (0.4%).
Women with the BRCA1 mutation were diagnosed at a significantly younger age than were other patients (42.6 vs. 47.9 years), as were carriers of the TP53 mutation (32.8 vs. 47.6 years).
Ten other genes (ATM, BARD1, BRIP1, CHEK1, CHEK2, GEN1, NBN, RAD51C, RAD51D, and XRCC2) carried a mutation in at least one patient each. “When limited to mutations in the four high-risk genes, 11%-12% of cases in this study carried a loss-of-function variant.”
Dr. Olopade had no financial disclosures.
SOURCE: Olopade et al. J Clin Oncol. 2018 Aug 21. doi: 10.1200/JCO.2018.78.3977.
About one in eight Nigerian women with breast cancer has an inherited mutation of the BRCA1, BRCA2, PALB2, or TP53 gene.
A new analysis of the Nigerian Breast Cancer Study confirmed that these inherited mutations drive about 12% of the country’s breast cancer cases. The findings could pave the way for the first large-scale national breast cancer gene screening program, wrote Olufunmilayo I. Olopade, MD, and her colleagues. The report is in the Journal of Clinical Oncology.
“We suggest that genomic sequencing to identify women at extremely high risk of breast cancer could be a highly innovative approach to tailored risk management and life-saving interventions,” wrote Dr. Olopade, director of the Center for Clinical Cancer Genetics at the University of Chicago, and her colleagues. “Nigeria now has data to prioritize the integration of genetic testing into its cancer control plan. Women with an extremely high risk of breast cancer because of mutations in these genes can be identified inexpensively and unambiguously and offered interventions to reduce cancer risk.”
And, since about half of the sisters and daughters of affected women will carry the same mutation, such a screening program could reach far beyond every index patient identified, the investigators noted.
“If these women at very high risk can be identified either through their relatives with breast cancer or in the general population, resources can be focused particularly on their behalf. For as-yet unaffected women at high genetic risk, these resources would be intensive surveillance for early detection of breast cancer and, after childbearing is completed, the possibility of preventive salpingo-oophorectomy. Integrated population screening for cancer for all women is the goal, but focused outreach to women at extremely high risk represents an especially efficient use of resources and an attainable evidence-based global health approach.”
The Nigerian Breast Cancer Study enrolled 1,136 women with invasive breast cancer from 1998 to 2014. These were compared with 997 women without cancer, matched from the same communities. Genetic sequencing searched for mutations in both known and breast cancer genes.
Cases and controls were a mean of 47 years old; only 6% of cases reported a family history of breast cancer. Of 577 patients with information on tumor stage, 86% (497) were diagnosed at stage III (241) or IV (256).
Among the cases, 167 (14.7%) carried a mutation in a breast cancer risk gene, compared with 1.8% of controls. BRCA1 was the most common mutation, occurring in 7% of patients; these women were 23 times more likely to develop breast cancer than were those without the gene (odds ratio, 23.4). BRCA2 was the next most common, occurring in 4% of cases and conferring a nearly 11-fold increased risk (OR, 10.76). PALB2 occurred in 11 cases (1%) and no controls, and TP53 in four cases (0.4%).
Women with the BRCA1 mutation were diagnosed at a significantly younger age than were other patients (42.6 vs. 47.9 years), as were carriers of the TP53 mutation (32.8 vs. 47.6 years).
Ten other genes (ATM, BARD1, BRIP1, CHEK1, CHEK2, GEN1, NBN, RAD51C, RAD51D, and XRCC2) carried a mutation in at least one patient each. “When limited to mutations in the four high-risk genes, 11%-12% of cases in this study carried a loss-of-function variant.”
Dr. Olopade had no financial disclosures.
SOURCE: Olopade et al. J Clin Oncol. 2018 Aug 21. doi: 10.1200/JCO.2018.78.3977.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Loss-of-function mutations in four breast cancer risk genes account for much of the disease among Nigerian women with the disease.
Major finding: Inherited mutations of the BRCA1, BRCA2, PALB2, or TP53 gene account for 12% of breast cancer in Nigerian women.
Study details: The Nigerian Breast Cancer Study comprised 1,136 women with invasive breast cancer and 997 controls.
Disclosures: Dr. Olopade had no financial disclosures. The study was largely funded by the National Institutes of Health and the Susan G Komen Foundation.
Source: Olopade et al. J Clin Oncol. 2018 Aug 21. doi: 10.1200/JCO.2018.78.3977.
RA, JIA may raise risk of preterm delivery
according to a study examining autoimmune disease in pregnancy. Corticosteroid use in any trimester increased that risk from 100%-400%, regardless of how active the arthritis was.
The study found that women with RA had more than double the risk for preterm delivery, compared with a cohort without autoimmune disease (relative risk, 2.09; 95% confidence interval, 1.50-2.91). For women with juvenile idiopathic arthritis (JIA), the relative risk was 1.81 for preterm delivery (95% CI, 1.14-2.89).
The prospective cohort study, part of the Organization of Teratology Information Specialists Autoimmune Disease in Pregnancy Project, enrolled 657 women with RA and 170 women with JIA. The study also included a comparison group of 564 women without autoimmune disease. All of those included in the study were enrolled before 19 weeks’ gestation and delivered live-born infants during 2004-2017.
The study adds to a clinically important area of research that has yielded sometimes conflicting results; clarity has also been impeded by a variety of methodologies. Though several analyses have shown higher risk of preterm delivery in women with RA, not all studies have adjusted for medication use and disease activity, Chelsey F. Smith, MD, and her coauthors wrote in Arthritis Care & Research. Further, how women with JIA fare in pregnancy has not been well studied, they said.
Dr. Smith, a rheumatologist at the University of California, San Diego, and her colleagues included many baseline covariates in their analysis of pregnancy outcomes; these included maternal age and race, socioeconomic status, body mass index, previous adverse pregnancy outcomes, and comorbidities, including autoimmune disease. Adverse pregnancy outcomes during the studied pregnancy were also included as covariates, and deliveries were considered preterm if labor began before 37 weeks’ gestation.
For women with RA, a higher active disease score at any point during pregnancy was associated with a significantly higher risk of preterm delivery, even after adjustment for other potential risk factors, including first-trimester corticosteroid use (adjusted risk ratio, 1.52; 95% CI, 1.06-2.18). The persistence of this association, wrote Dr. Smith and her colleagues, implies “that active disease in RA may contribute to [preterm delivery] independent of medications,” perhaps through the action of proinflammatory cytokines that may stimulate prostaglandins and provoke uterine contractions.
The researchers found, though, that this association between disease activity and risk for preterm birth did not hold true for women with JIA, leaving part of the mystery unsolved.
However, women with both RA and JIA who used corticosteroids in any trimester were more likely to have a preterm delivery, as were women with JIA who used NSAIDs in the first trimester of pregnancy. The use of disease-modifying antirheumatic drugs (DMARDs) and biologics in any trimester did not confer increased risk for preterm delivery in women with either disease state.
There were other differences between the groups: Women with JIA were overall younger, but had more prepregnancy hypertension, which “may have contributed to the elevated incidence of preeclampsia seen in this group,” the investigators wrote. Fever was more common in women with JIA, and had an independent association with preterm delivery, as did first trimester NSAID use in this group alone.
Dr. Smith and her colleagues hypothesized that the relative heterogeneity of the JIA group may mean that disease activity still influenced outcomes.
Among other comorbidities, gestational diabetes (GDM) was more common in the RA group than in the JIA group or the comparison cohort, and was associated with a significantly higher risk for preterm delivery in women with RA, even after accounting for preeclampsia and hypertension in a multivariate analysis.
Dr. Smith and her colleagues pointed out that it was difficult to account for physician behavior in managing pregnancy in these high-risk women. “Additionally, given that women with both RA and GDM are at a particularly high risk for perinatal complications, we can speculate that the obstetricians in this group were perhaps more aggressive about inducing at an earlier gestational age than in other groups, but this information was not available in the dataset.”
Through phone interviews, investigators obtained information about prescription and nonprescription medication use during pregnancy; women were also asked about use of other substances and occupational exposures, infections, and prenatal testing and other medical procedures. Another telephone interview conducted soon after delivery asked about birth outcomes. Abstracted medical record data were used to verify and supplement the interview information.
When looking at treatments used, Dr. Smith and her colleagues grouped autoimmune disease medications into DMARDs, non-DMARD biologic medications, corticosteroids, and NSAIDs.
Disease activity assessment, conducted at intake and at 32 weeks’ gestation, used the Health Assessment Questionnaire, pain scores, and patient global disease activity to calculate a Patient Activity Scale score ranging from 0 to 10. Patients with a score over 3.7 were classified as having high disease activity.
Dr. Smith and her colleagues said that the study’s strengths included its prospective design and robust statistical schema. Also, using data about corticosteroid use and disease activity earlier in pregnancy avoided the inclusion of a reverse causation effect, where systemic inflammatory changes associated with preterm delivery might provoke more disease activity and a consequent boost in corticosteroid use.
However, the researchers said, the overall numbers of participants with preterm delivery was relatively small, and the JIA cohort was small as well.
“Further analyses are necessary to look at other categories of arthritis affecting women of childbearing age, racial disparities in these populations, as well as the influence of disease activity in the later stages of pregnancy on other perinatal factors” that can contribute to preterm delivery, said Dr. Smith and her colleagues.
The collaborative research group that collected data for the study receives research funding from several pharmaceutical companies. None of the authors reported any personal conflicts of interest.
SOURCE: Smith CF et al. Arthritis Care Res. 2018 Aug 21. doi: 10.1002/acr.23730.
according to a study examining autoimmune disease in pregnancy. Corticosteroid use in any trimester increased that risk from 100%-400%, regardless of how active the arthritis was.
The study found that women with RA had more than double the risk for preterm delivery, compared with a cohort without autoimmune disease (relative risk, 2.09; 95% confidence interval, 1.50-2.91). For women with juvenile idiopathic arthritis (JIA), the relative risk was 1.81 for preterm delivery (95% CI, 1.14-2.89).
The prospective cohort study, part of the Organization of Teratology Information Specialists Autoimmune Disease in Pregnancy Project, enrolled 657 women with RA and 170 women with JIA. The study also included a comparison group of 564 women without autoimmune disease. All of those included in the study were enrolled before 19 weeks’ gestation and delivered live-born infants during 2004-2017.
The study adds to a clinically important area of research that has yielded sometimes conflicting results; clarity has also been impeded by a variety of methodologies. Though several analyses have shown higher risk of preterm delivery in women with RA, not all studies have adjusted for medication use and disease activity, Chelsey F. Smith, MD, and her coauthors wrote in Arthritis Care & Research. Further, how women with JIA fare in pregnancy has not been well studied, they said.
Dr. Smith, a rheumatologist at the University of California, San Diego, and her colleagues included many baseline covariates in their analysis of pregnancy outcomes; these included maternal age and race, socioeconomic status, body mass index, previous adverse pregnancy outcomes, and comorbidities, including autoimmune disease. Adverse pregnancy outcomes during the studied pregnancy were also included as covariates, and deliveries were considered preterm if labor began before 37 weeks’ gestation.
For women with RA, a higher active disease score at any point during pregnancy was associated with a significantly higher risk of preterm delivery, even after adjustment for other potential risk factors, including first-trimester corticosteroid use (adjusted risk ratio, 1.52; 95% CI, 1.06-2.18). The persistence of this association, wrote Dr. Smith and her colleagues, implies “that active disease in RA may contribute to [preterm delivery] independent of medications,” perhaps through the action of proinflammatory cytokines that may stimulate prostaglandins and provoke uterine contractions.
The researchers found, though, that this association between disease activity and risk for preterm birth did not hold true for women with JIA, leaving part of the mystery unsolved.
However, women with both RA and JIA who used corticosteroids in any trimester were more likely to have a preterm delivery, as were women with JIA who used NSAIDs in the first trimester of pregnancy. The use of disease-modifying antirheumatic drugs (DMARDs) and biologics in any trimester did not confer increased risk for preterm delivery in women with either disease state.
There were other differences between the groups: Women with JIA were overall younger, but had more prepregnancy hypertension, which “may have contributed to the elevated incidence of preeclampsia seen in this group,” the investigators wrote. Fever was more common in women with JIA, and had an independent association with preterm delivery, as did first trimester NSAID use in this group alone.
Dr. Smith and her colleagues hypothesized that the relative heterogeneity of the JIA group may mean that disease activity still influenced outcomes.
Among other comorbidities, gestational diabetes (GDM) was more common in the RA group than in the JIA group or the comparison cohort, and was associated with a significantly higher risk for preterm delivery in women with RA, even after accounting for preeclampsia and hypertension in a multivariate analysis.
Dr. Smith and her colleagues pointed out that it was difficult to account for physician behavior in managing pregnancy in these high-risk women. “Additionally, given that women with both RA and GDM are at a particularly high risk for perinatal complications, we can speculate that the obstetricians in this group were perhaps more aggressive about inducing at an earlier gestational age than in other groups, but this information was not available in the dataset.”
Through phone interviews, investigators obtained information about prescription and nonprescription medication use during pregnancy; women were also asked about use of other substances and occupational exposures, infections, and prenatal testing and other medical procedures. Another telephone interview conducted soon after delivery asked about birth outcomes. Abstracted medical record data were used to verify and supplement the interview information.
When looking at treatments used, Dr. Smith and her colleagues grouped autoimmune disease medications into DMARDs, non-DMARD biologic medications, corticosteroids, and NSAIDs.
Disease activity assessment, conducted at intake and at 32 weeks’ gestation, used the Health Assessment Questionnaire, pain scores, and patient global disease activity to calculate a Patient Activity Scale score ranging from 0 to 10. Patients with a score over 3.7 were classified as having high disease activity.
Dr. Smith and her colleagues said that the study’s strengths included its prospective design and robust statistical schema. Also, using data about corticosteroid use and disease activity earlier in pregnancy avoided the inclusion of a reverse causation effect, where systemic inflammatory changes associated with preterm delivery might provoke more disease activity and a consequent boost in corticosteroid use.
However, the researchers said, the overall numbers of participants with preterm delivery was relatively small, and the JIA cohort was small as well.
“Further analyses are necessary to look at other categories of arthritis affecting women of childbearing age, racial disparities in these populations, as well as the influence of disease activity in the later stages of pregnancy on other perinatal factors” that can contribute to preterm delivery, said Dr. Smith and her colleagues.
The collaborative research group that collected data for the study receives research funding from several pharmaceutical companies. None of the authors reported any personal conflicts of interest.
SOURCE: Smith CF et al. Arthritis Care Res. 2018 Aug 21. doi: 10.1002/acr.23730.
according to a study examining autoimmune disease in pregnancy. Corticosteroid use in any trimester increased that risk from 100%-400%, regardless of how active the arthritis was.
The study found that women with RA had more than double the risk for preterm delivery, compared with a cohort without autoimmune disease (relative risk, 2.09; 95% confidence interval, 1.50-2.91). For women with juvenile idiopathic arthritis (JIA), the relative risk was 1.81 for preterm delivery (95% CI, 1.14-2.89).
The prospective cohort study, part of the Organization of Teratology Information Specialists Autoimmune Disease in Pregnancy Project, enrolled 657 women with RA and 170 women with JIA. The study also included a comparison group of 564 women without autoimmune disease. All of those included in the study were enrolled before 19 weeks’ gestation and delivered live-born infants during 2004-2017.
The study adds to a clinically important area of research that has yielded sometimes conflicting results; clarity has also been impeded by a variety of methodologies. Though several analyses have shown higher risk of preterm delivery in women with RA, not all studies have adjusted for medication use and disease activity, Chelsey F. Smith, MD, and her coauthors wrote in Arthritis Care & Research. Further, how women with JIA fare in pregnancy has not been well studied, they said.
Dr. Smith, a rheumatologist at the University of California, San Diego, and her colleagues included many baseline covariates in their analysis of pregnancy outcomes; these included maternal age and race, socioeconomic status, body mass index, previous adverse pregnancy outcomes, and comorbidities, including autoimmune disease. Adverse pregnancy outcomes during the studied pregnancy were also included as covariates, and deliveries were considered preterm if labor began before 37 weeks’ gestation.
For women with RA, a higher active disease score at any point during pregnancy was associated with a significantly higher risk of preterm delivery, even after adjustment for other potential risk factors, including first-trimester corticosteroid use (adjusted risk ratio, 1.52; 95% CI, 1.06-2.18). The persistence of this association, wrote Dr. Smith and her colleagues, implies “that active disease in RA may contribute to [preterm delivery] independent of medications,” perhaps through the action of proinflammatory cytokines that may stimulate prostaglandins and provoke uterine contractions.
The researchers found, though, that this association between disease activity and risk for preterm birth did not hold true for women with JIA, leaving part of the mystery unsolved.
However, women with both RA and JIA who used corticosteroids in any trimester were more likely to have a preterm delivery, as were women with JIA who used NSAIDs in the first trimester of pregnancy. The use of disease-modifying antirheumatic drugs (DMARDs) and biologics in any trimester did not confer increased risk for preterm delivery in women with either disease state.
There were other differences between the groups: Women with JIA were overall younger, but had more prepregnancy hypertension, which “may have contributed to the elevated incidence of preeclampsia seen in this group,” the investigators wrote. Fever was more common in women with JIA, and had an independent association with preterm delivery, as did first trimester NSAID use in this group alone.
Dr. Smith and her colleagues hypothesized that the relative heterogeneity of the JIA group may mean that disease activity still influenced outcomes.
Among other comorbidities, gestational diabetes (GDM) was more common in the RA group than in the JIA group or the comparison cohort, and was associated with a significantly higher risk for preterm delivery in women with RA, even after accounting for preeclampsia and hypertension in a multivariate analysis.
Dr. Smith and her colleagues pointed out that it was difficult to account for physician behavior in managing pregnancy in these high-risk women. “Additionally, given that women with both RA and GDM are at a particularly high risk for perinatal complications, we can speculate that the obstetricians in this group were perhaps more aggressive about inducing at an earlier gestational age than in other groups, but this information was not available in the dataset.”
Through phone interviews, investigators obtained information about prescription and nonprescription medication use during pregnancy; women were also asked about use of other substances and occupational exposures, infections, and prenatal testing and other medical procedures. Another telephone interview conducted soon after delivery asked about birth outcomes. Abstracted medical record data were used to verify and supplement the interview information.
When looking at treatments used, Dr. Smith and her colleagues grouped autoimmune disease medications into DMARDs, non-DMARD biologic medications, corticosteroids, and NSAIDs.
Disease activity assessment, conducted at intake and at 32 weeks’ gestation, used the Health Assessment Questionnaire, pain scores, and patient global disease activity to calculate a Patient Activity Scale score ranging from 0 to 10. Patients with a score over 3.7 were classified as having high disease activity.
Dr. Smith and her colleagues said that the study’s strengths included its prospective design and robust statistical schema. Also, using data about corticosteroid use and disease activity earlier in pregnancy avoided the inclusion of a reverse causation effect, where systemic inflammatory changes associated with preterm delivery might provoke more disease activity and a consequent boost in corticosteroid use.
However, the researchers said, the overall numbers of participants with preterm delivery was relatively small, and the JIA cohort was small as well.
“Further analyses are necessary to look at other categories of arthritis affecting women of childbearing age, racial disparities in these populations, as well as the influence of disease activity in the later stages of pregnancy on other perinatal factors” that can contribute to preterm delivery, said Dr. Smith and her colleagues.
The collaborative research group that collected data for the study receives research funding from several pharmaceutical companies. None of the authors reported any personal conflicts of interest.
SOURCE: Smith CF et al. Arthritis Care Res. 2018 Aug 21. doi: 10.1002/acr.23730.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point: The risk of preterm delivery was increased in women with RA and juvenile idiopathic arthritis.
Major finding: The risk ratio for preterm delivery in women with RA was 2.09.
Study details: A prospective cohort study of 657 women with RA, 170 women with juvenile idiopathic arthritis, and 564 women without autoimmune disease.
Disclosures: The study was part of the Organization of Teratology Information Specialists Autoimmune Disease in Pregnancy Project, which receives research funding from several pharmaceutical companies. None of the authors reported any personal conflicts of interest.
Source: Smith CF et al. Arthritis Care Res. 2018 Aug 21. doi: 10.1002/acr.23730.
High-sensitivity cardiac troponin levels linked to cardiovascular outcomes in COPD patients
, according to a post-hoc analysis of a clinical trial.
An increased risk of cardiovascular adverse events and cardiovascular death was seen in COPD patients in the highest quintile of plasma cardiac troponin concentrations at baseline, results of the analysis show.
The findings highlight the potential utility of high-sensitivity cardiac troponin in both clinical trials and clinical practice, according to researcher Nicholas L. Mills, MD, PhD, BHF/University Centre for Cardiovascular Science, The University of Edinburgh, Scotland, and co-investigators.
“Recognizing the risk associated with increased troponin concentrations might encourage clinicians to address cardiovascular risk due to lifestyle choices, and make patients more likely to engage with these recommendations,” Dr. Mills and co-authors wrote in the Journal of the American College of Cardiology.
Improved risk stratification may also help clinicians more appropriately target the use of preventive medications in COPD patients, they added in the report.
The analysis by Dr. Mills and colleagues was based on assessment of cardiac troponin I concentrations for patients in SUMMIT, a randomized trial assessing inhaled corticosteroids and long-acting beta agonists in COPD patients with ele-vated cardiovascular risk.
A total of 1,599 patients in the SUMMIT trial had a baseline cardiac troponin I assessment, and 1,258 had a follow-up assessment at 3 months following randomization.
Compared with those in the lowest quintile, patients in the highest quintile of baseline plasma cardiac troponin concentrations had an increased risk of a cardiovascular composite event, even after adjusting for confounding variables (hazard ratio, 3.67; 95% confidence interval, 1.33-10.13; P = .012)..
Increased risk of cardiovascular death was also seen in the highest quintile as compared with the lowest quintile (HR, 20.06; 95% CI, 2.44-165.15; P = .005), investigators said.
There was no difference in risk of COPD exacerbations between the highest and lowest quintiles, they added.
At 3 months, there were no differences in troponin concentrations related to COPD treatment, consistent with previous observations in the SUMMIT trial that treatment did not impact the cardiovascular composite endpoint, investigators said.
However, patients with a plasma troponin of 5 ng/L or greater recorded at either the baseline or 3-month assessment had an increased rate of the composite cardiovascular endpoint and a “markedly increased” risk of cardiovascular death, they wrote.
The research was supported by GlaxoSmithKline and a Butler British Heart Foundation Senior Clinical Research Fellowship received by Dr. Mills. Disclosures reported by Dr. Mills included consultancy, research grants, and speaker fees from Abbott Diagnostics, Roche, and Singulex. Study co-authors reported disclosures related to GlaxoSmithKline, Veramed Limited, AstraZeneca, Zambon, Bayer, Novartis, and others.
SOURCE: Adamson PD et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1126-37.
The current study data are “robust” and suggest a strong association between high-sensitivity cardiac troponin values and cardiovascular event risk in these COPD patients, according to authors of an editorial.
The study also showed that a change in high-sensitivity cardiac troponin at 3 months is associated with increased risk, noted editorial authors Allan S. Jaffe, MD, and H. Ari Jaffe, MD.
“Most of these events probably represent acceleration of atherosclerosis, given the effects of smoking on atherosclerotic disease and its progression,” the authors said in the Journal of the American College of Cardiology.
However, study authors could have more extensively addressed how to use that information to improve the care of COPD patients at elevated cardiovascular event risk, they added.
A “pilot algorithm” that could be used to apply this biomarker analysis in clinical practice was proposed in an editorial accompanying the research report.
They suggest repeating high-sensitivity cardiac troponin measurements to reduce variability, as well as repeating samples at 3 months to detect changes that could signal increased risk.
“In addition, one should avoid decisions based on small differences,” they wrote.
Allan S. Jaffe, MD, is with the department of cardiovascular medicine and the department of laboratory medicine and pathology at the Mayo Clinic in Rochester, Minn. He reported serving as a consultant for Beckman, Abbott, Siemens, ET Healthcare, Sphingotec, Becton Dickinson, Quindel, and Novartis. H. Ari Jaffe, MD, is with the department of medicine, pulmonary division at University of Illinois at Chicago, Jesse Brown VA Medicine Center, Chicago. He reported he has no relationships to disclose relevant to the contents of the editorial.
The current study data are “robust” and suggest a strong association between high-sensitivity cardiac troponin values and cardiovascular event risk in these COPD patients, according to authors of an editorial.
The study also showed that a change in high-sensitivity cardiac troponin at 3 months is associated with increased risk, noted editorial authors Allan S. Jaffe, MD, and H. Ari Jaffe, MD.
“Most of these events probably represent acceleration of atherosclerosis, given the effects of smoking on atherosclerotic disease and its progression,” the authors said in the Journal of the American College of Cardiology.
However, study authors could have more extensively addressed how to use that information to improve the care of COPD patients at elevated cardiovascular event risk, they added.
A “pilot algorithm” that could be used to apply this biomarker analysis in clinical practice was proposed in an editorial accompanying the research report.
They suggest repeating high-sensitivity cardiac troponin measurements to reduce variability, as well as repeating samples at 3 months to detect changes that could signal increased risk.
“In addition, one should avoid decisions based on small differences,” they wrote.
Allan S. Jaffe, MD, is with the department of cardiovascular medicine and the department of laboratory medicine and pathology at the Mayo Clinic in Rochester, Minn. He reported serving as a consultant for Beckman, Abbott, Siemens, ET Healthcare, Sphingotec, Becton Dickinson, Quindel, and Novartis. H. Ari Jaffe, MD, is with the department of medicine, pulmonary division at University of Illinois at Chicago, Jesse Brown VA Medicine Center, Chicago. He reported he has no relationships to disclose relevant to the contents of the editorial.
The current study data are “robust” and suggest a strong association between high-sensitivity cardiac troponin values and cardiovascular event risk in these COPD patients, according to authors of an editorial.
The study also showed that a change in high-sensitivity cardiac troponin at 3 months is associated with increased risk, noted editorial authors Allan S. Jaffe, MD, and H. Ari Jaffe, MD.
“Most of these events probably represent acceleration of atherosclerosis, given the effects of smoking on atherosclerotic disease and its progression,” the authors said in the Journal of the American College of Cardiology.
However, study authors could have more extensively addressed how to use that information to improve the care of COPD patients at elevated cardiovascular event risk, they added.
A “pilot algorithm” that could be used to apply this biomarker analysis in clinical practice was proposed in an editorial accompanying the research report.
They suggest repeating high-sensitivity cardiac troponin measurements to reduce variability, as well as repeating samples at 3 months to detect changes that could signal increased risk.
“In addition, one should avoid decisions based on small differences,” they wrote.
Allan S. Jaffe, MD, is with the department of cardiovascular medicine and the department of laboratory medicine and pathology at the Mayo Clinic in Rochester, Minn. He reported serving as a consultant for Beckman, Abbott, Siemens, ET Healthcare, Sphingotec, Becton Dickinson, Quindel, and Novartis. H. Ari Jaffe, MD, is with the department of medicine, pulmonary division at University of Illinois at Chicago, Jesse Brown VA Medicine Center, Chicago. He reported he has no relationships to disclose relevant to the contents of the editorial.
, according to a post-hoc analysis of a clinical trial.
An increased risk of cardiovascular adverse events and cardiovascular death was seen in COPD patients in the highest quintile of plasma cardiac troponin concentrations at baseline, results of the analysis show.
The findings highlight the potential utility of high-sensitivity cardiac troponin in both clinical trials and clinical practice, according to researcher Nicholas L. Mills, MD, PhD, BHF/University Centre for Cardiovascular Science, The University of Edinburgh, Scotland, and co-investigators.
“Recognizing the risk associated with increased troponin concentrations might encourage clinicians to address cardiovascular risk due to lifestyle choices, and make patients more likely to engage with these recommendations,” Dr. Mills and co-authors wrote in the Journal of the American College of Cardiology.
Improved risk stratification may also help clinicians more appropriately target the use of preventive medications in COPD patients, they added in the report.
The analysis by Dr. Mills and colleagues was based on assessment of cardiac troponin I concentrations for patients in SUMMIT, a randomized trial assessing inhaled corticosteroids and long-acting beta agonists in COPD patients with ele-vated cardiovascular risk.
A total of 1,599 patients in the SUMMIT trial had a baseline cardiac troponin I assessment, and 1,258 had a follow-up assessment at 3 months following randomization.
Compared with those in the lowest quintile, patients in the highest quintile of baseline plasma cardiac troponin concentrations had an increased risk of a cardiovascular composite event, even after adjusting for confounding variables (hazard ratio, 3.67; 95% confidence interval, 1.33-10.13; P = .012)..
Increased risk of cardiovascular death was also seen in the highest quintile as compared with the lowest quintile (HR, 20.06; 95% CI, 2.44-165.15; P = .005), investigators said.
There was no difference in risk of COPD exacerbations between the highest and lowest quintiles, they added.
At 3 months, there were no differences in troponin concentrations related to COPD treatment, consistent with previous observations in the SUMMIT trial that treatment did not impact the cardiovascular composite endpoint, investigators said.
However, patients with a plasma troponin of 5 ng/L or greater recorded at either the baseline or 3-month assessment had an increased rate of the composite cardiovascular endpoint and a “markedly increased” risk of cardiovascular death, they wrote.
The research was supported by GlaxoSmithKline and a Butler British Heart Foundation Senior Clinical Research Fellowship received by Dr. Mills. Disclosures reported by Dr. Mills included consultancy, research grants, and speaker fees from Abbott Diagnostics, Roche, and Singulex. Study co-authors reported disclosures related to GlaxoSmithKline, Veramed Limited, AstraZeneca, Zambon, Bayer, Novartis, and others.
SOURCE: Adamson PD et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1126-37.
, according to a post-hoc analysis of a clinical trial.
An increased risk of cardiovascular adverse events and cardiovascular death was seen in COPD patients in the highest quintile of plasma cardiac troponin concentrations at baseline, results of the analysis show.
The findings highlight the potential utility of high-sensitivity cardiac troponin in both clinical trials and clinical practice, according to researcher Nicholas L. Mills, MD, PhD, BHF/University Centre for Cardiovascular Science, The University of Edinburgh, Scotland, and co-investigators.
“Recognizing the risk associated with increased troponin concentrations might encourage clinicians to address cardiovascular risk due to lifestyle choices, and make patients more likely to engage with these recommendations,” Dr. Mills and co-authors wrote in the Journal of the American College of Cardiology.
Improved risk stratification may also help clinicians more appropriately target the use of preventive medications in COPD patients, they added in the report.
The analysis by Dr. Mills and colleagues was based on assessment of cardiac troponin I concentrations for patients in SUMMIT, a randomized trial assessing inhaled corticosteroids and long-acting beta agonists in COPD patients with ele-vated cardiovascular risk.
A total of 1,599 patients in the SUMMIT trial had a baseline cardiac troponin I assessment, and 1,258 had a follow-up assessment at 3 months following randomization.
Compared with those in the lowest quintile, patients in the highest quintile of baseline plasma cardiac troponin concentrations had an increased risk of a cardiovascular composite event, even after adjusting for confounding variables (hazard ratio, 3.67; 95% confidence interval, 1.33-10.13; P = .012)..
Increased risk of cardiovascular death was also seen in the highest quintile as compared with the lowest quintile (HR, 20.06; 95% CI, 2.44-165.15; P = .005), investigators said.
There was no difference in risk of COPD exacerbations between the highest and lowest quintiles, they added.
At 3 months, there were no differences in troponin concentrations related to COPD treatment, consistent with previous observations in the SUMMIT trial that treatment did not impact the cardiovascular composite endpoint, investigators said.
However, patients with a plasma troponin of 5 ng/L or greater recorded at either the baseline or 3-month assessment had an increased rate of the composite cardiovascular endpoint and a “markedly increased” risk of cardiovascular death, they wrote.
The research was supported by GlaxoSmithKline and a Butler British Heart Foundation Senior Clinical Research Fellowship received by Dr. Mills. Disclosures reported by Dr. Mills included consultancy, research grants, and speaker fees from Abbott Diagnostics, Roche, and Singulex. Study co-authors reported disclosures related to GlaxoSmithKline, Veramed Limited, AstraZeneca, Zambon, Bayer, Novartis, and others.
SOURCE: Adamson PD et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1126-37.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: In patients with COPD and heightened cardiovascular risk, high levels of high-sensitivity cardiac troponin were strongly associated with risk of cardiovascular outcomes.
Major finding: Compared to those in the lowest quintile, patients in the highest quintile of baseline plasma cardiac troponin concentrations had an increased risk of a cardiovascular composite event (hazard ratio, 3.67; 95% CI, 1.33-10.13; P = 0.012).
Study details: Post-hoc analysis of 1,599 patients in the SUMMIT trial who had a baseline cardiac troponin I assessment and 1,258 who had a 3-month follow-up assessment.
Disclosures: The study was supported by GlaxoSmithKline and a Butler British Heart Foundation Senior Clinical Research Fellowship. Authors reported disclosures related to GlaxoSmithKline, Veramed Limited, Abbott Diagnostics, Roche, Singulex, AstraZeneca, Zambon, Bayer, Novartis, and others.
Source: Adamson PD et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1126-37.
Earnings gap seen among Maryland physicians
Male physicians in Maryland reported higher earnings than did female physicians, even when they all worked 41 or more hours a week, according to a 2018 survey of physicians in the state.
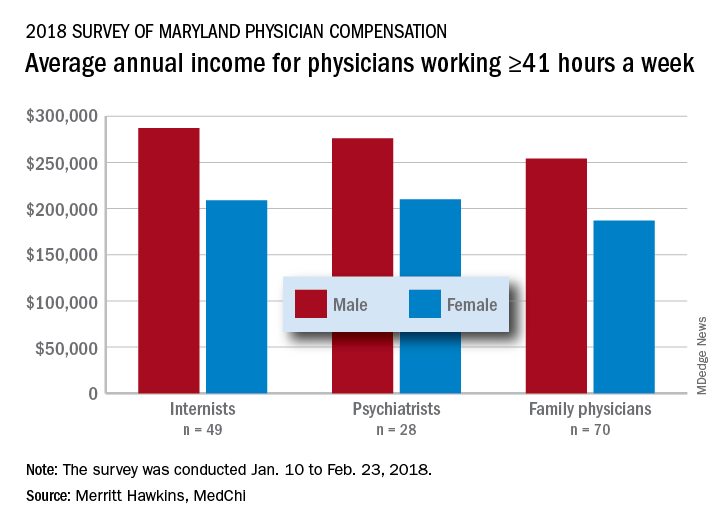
The average pretax income for all 508 respondents was $299,000 in 2016: Male physicians (66.6% of the sample) had an average of $335,000 and women averaged 33% lower at $224,000, MedChi (the Maryland State Medical Society) and Merritt Hawkins reported on July 31. Men did report working a longer week: Their average of 50.5 hours was 11% more than the 45.4-hour average for women.
“The biggest disparities we see in compensation are between male and female physicians in Maryland,” Gene Ransom, MedChi’s chief executive officer, said in a written statement. “Though such disparities have been noted in other research, it is still surprising to see the extent to which they persist.”
Of the respondents who worked an average of 41 or more hours per week – an analysis conducted only for the three largest specialties in the survey – female internists earned 27% less than their male counterparts, female psychiatrists earned 24% less, and female family physicians earned 26% less, the survey results showed.
Earnings were structured somewhat differently for Maryland’s male and female physicians. Women were more likely to be compensated in the form of a straight salary than men (35.0% vs. 30.3%), and men were more likely to paid based on production (22.7% vs. 16.9%) or in the form of an income guarantee (0.9% vs. 0.0%). Proportions receiving a salary with a production bonus were 42.7% for men and 42.5% for women, according to the survey.
Data included in the survey may be of interest to policymakers and media members who track physician compensation trends in Maryland and nationwide.
The survey was commissioned by MedChi and conducted by Merritt Hawkins from Jan. 10 to Feb. 23, 2018. The margin of error was plus or minus 4.4%.
Male physicians in Maryland reported higher earnings than did female physicians, even when they all worked 41 or more hours a week, according to a 2018 survey of physicians in the state.
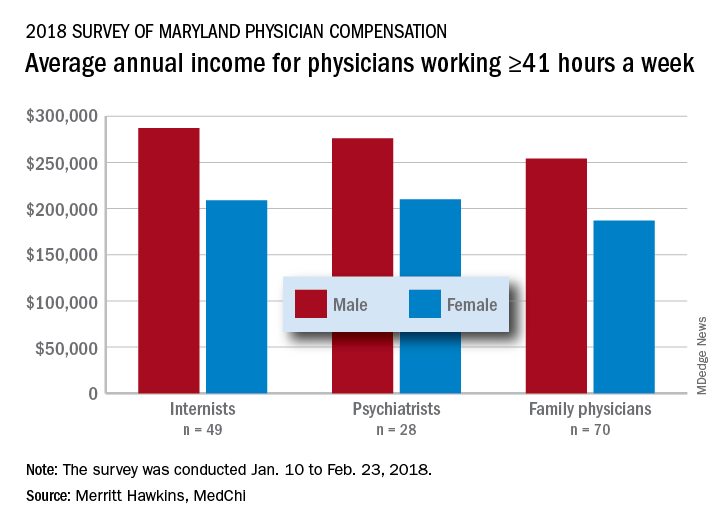
The average pretax income for all 508 respondents was $299,000 in 2016: Male physicians (66.6% of the sample) had an average of $335,000 and women averaged 33% lower at $224,000, MedChi (the Maryland State Medical Society) and Merritt Hawkins reported on July 31. Men did report working a longer week: Their average of 50.5 hours was 11% more than the 45.4-hour average for women.
“The biggest disparities we see in compensation are between male and female physicians in Maryland,” Gene Ransom, MedChi’s chief executive officer, said in a written statement. “Though such disparities have been noted in other research, it is still surprising to see the extent to which they persist.”
Of the respondents who worked an average of 41 or more hours per week – an analysis conducted only for the three largest specialties in the survey – female internists earned 27% less than their male counterparts, female psychiatrists earned 24% less, and female family physicians earned 26% less, the survey results showed.
Earnings were structured somewhat differently for Maryland’s male and female physicians. Women were more likely to be compensated in the form of a straight salary than men (35.0% vs. 30.3%), and men were more likely to paid based on production (22.7% vs. 16.9%) or in the form of an income guarantee (0.9% vs. 0.0%). Proportions receiving a salary with a production bonus were 42.7% for men and 42.5% for women, according to the survey.
Data included in the survey may be of interest to policymakers and media members who track physician compensation trends in Maryland and nationwide.
The survey was commissioned by MedChi and conducted by Merritt Hawkins from Jan. 10 to Feb. 23, 2018. The margin of error was plus or minus 4.4%.
Male physicians in Maryland reported higher earnings than did female physicians, even when they all worked 41 or more hours a week, according to a 2018 survey of physicians in the state.
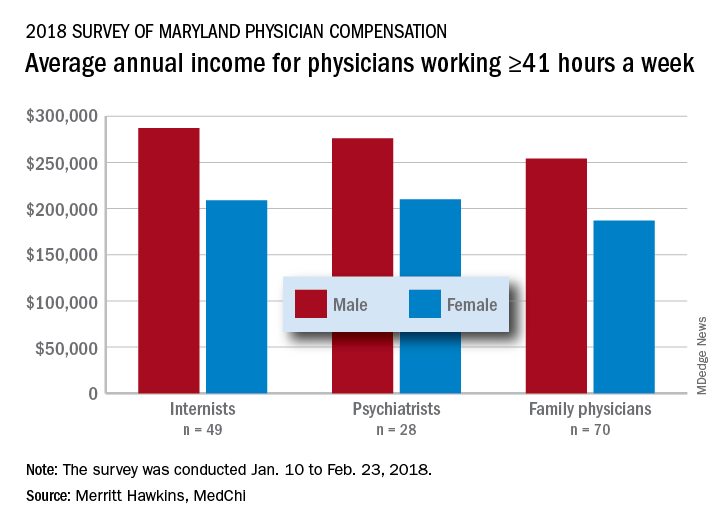
The average pretax income for all 508 respondents was $299,000 in 2016: Male physicians (66.6% of the sample) had an average of $335,000 and women averaged 33% lower at $224,000, MedChi (the Maryland State Medical Society) and Merritt Hawkins reported on July 31. Men did report working a longer week: Their average of 50.5 hours was 11% more than the 45.4-hour average for women.
“The biggest disparities we see in compensation are between male and female physicians in Maryland,” Gene Ransom, MedChi’s chief executive officer, said in a written statement. “Though such disparities have been noted in other research, it is still surprising to see the extent to which they persist.”
Of the respondents who worked an average of 41 or more hours per week – an analysis conducted only for the three largest specialties in the survey – female internists earned 27% less than their male counterparts, female psychiatrists earned 24% less, and female family physicians earned 26% less, the survey results showed.
Earnings were structured somewhat differently for Maryland’s male and female physicians. Women were more likely to be compensated in the form of a straight salary than men (35.0% vs. 30.3%), and men were more likely to paid based on production (22.7% vs. 16.9%) or in the form of an income guarantee (0.9% vs. 0.0%). Proportions receiving a salary with a production bonus were 42.7% for men and 42.5% for women, according to the survey.
Data included in the survey may be of interest to policymakers and media members who track physician compensation trends in Maryland and nationwide.
The survey was commissioned by MedChi and conducted by Merritt Hawkins from Jan. 10 to Feb. 23, 2018. The margin of error was plus or minus 4.4%.






