User login
Early results favor combo IL-15/anti-CD20 in indolent NHL
CHICAGO – A combination of an immunostimulatory IL-15-based agent, ALT-803, with a therapeutic monoclonal antibody (mAb) against CD20, was well tolerated and had clinical activity in patients with indolent non-Hodgkin lymphoma (iNHL), according to preliminary findings from a phase 1 study.
“The cancer immunotherapy breakthrough that happened several years ago continues year after year, with a plethora of different modalities of immunotherapy at our disposal,” Todd A. Fehniger, MD, PhD, said at the annual meeting of the American Association for Cancer Research.
Immunotherapy with anti-CD20 mAbs, alone or in combination with chemotherapy, is a standard therapy for iNHL patients. Since iNHL cells express CD20, targeting it with mAbs triggers antitumor responses via cell surface receptors resulting in a potent antibody-dependent cellular toxicity. However, response in patients is highly heterogeneous, with relapse within a few months in a subset of patients. In addition, chemotherapeutic combinations can be toxic and result in serious and long-term complications.
“Relapsed or refractory iNHL is not curable and treatment strategies without long-term complications are needed,” said Dr. Fehniger, associate professor of medicine at Washington University, St. Louis.
In an attempt to address this, Dr. Fehniger and his colleagues combined rituximab, an anti-CD20 antibody, with a relatively new IL-15 agonist immunostimulatory agent called ALT-803.
In the phase 1 trial, the researchers enrolled patients with indolent non-Hodgkin lymphoma who had relapsed after at least 1 prior to CD20 antibody containing therapy. The study was a standard 3+3 dose escalation design with rituximab administered by intravenous infusion, 375 mg/m2 in four weekly doses, followed by a rest and four consolidation doses every 8 weeks for four cycles.
ALT-803 was administered concurrently at dose levels of 1 mcg/kg, 3 mcg/kg, and 6 mcg/kg IV followed by 6 mcg/kg, 10 mcg/kg, 15 mcg/kg, and 20 mcg/kg subcutaneously.
In total, 21 patients were treated: 16 patients had follicular lymphoma, four patients had marginal zone lymphoma, and one patient had small lymphocytic lymphoma. The median prior therapies received was two (range: 1-18) and five patients were treated who were refractory to prior anti-CD20 MAb therapy.
ALT-803 was well tolerated with no dose limiting toxicities or grade 4 or 5 adverse events. No patients discontinued ALT-803 and the recommended phase 2 dose was 20 mcg/kg subcutaneously. Grade 3 adverse events, regardless of attribution to ALT-803, included transient hypertension (14%), anemia (5%), nausea (5%), chills (5%), fever (5%), neutropenia (5%), and hyperglycemia (5%).
“Patients who received [subcutaneous] ALT-803 developed a unique injection site rash reaction that peaked 7-10 days later but resolved typically within 14 days. It was self-limited and resolved on its own,” Dr. Fehniger said.
At the time of the presentation, the best overall response rate was achieved in 11 of 21 patients (52%), with 9 complete responders (43%), and 2 partial responders (10%).
Of the 12 patients treated with ALT-803 subcutaneously, 11 patients had either stable disease, or partial or complete responses. All 11 patients remained on study and were in consolidation or follow-up and have not relapsed, Dr. Fehniger reported.
Among the five rituximab-refractory patients, the researchers observed one complete response, two patients with stable disease (45% and 36% tumor volume decrease), and two patients with partial disease. The durability of the responses can only be understood with longer follow-up, Dr. Fehniger said.
The peripheral blood of the patients was analyzed via flow cytometry and mass cytometry. Over the duration of four weekly doses, there was an increase in percentage (sixfold, P less than .001) and absolute number (10-fold, P less than .001) of natural killer cells at the 15-mcg/kg and 20-mcg/kg subcutaneous dose levels of ALT-803.
These results suggest that further studies of ALT-803 with other therapeutic targeting mAbs, or other immunotherapy modalities, are warranted, the researchers concluded.
Dr. Fehniger reported research funding from Altor BioScience.
SOURCE: Fehniger TA et al. AACR Annual Meeting, Abstract CT146.
CHICAGO – A combination of an immunostimulatory IL-15-based agent, ALT-803, with a therapeutic monoclonal antibody (mAb) against CD20, was well tolerated and had clinical activity in patients with indolent non-Hodgkin lymphoma (iNHL), according to preliminary findings from a phase 1 study.
“The cancer immunotherapy breakthrough that happened several years ago continues year after year, with a plethora of different modalities of immunotherapy at our disposal,” Todd A. Fehniger, MD, PhD, said at the annual meeting of the American Association for Cancer Research.
Immunotherapy with anti-CD20 mAbs, alone or in combination with chemotherapy, is a standard therapy for iNHL patients. Since iNHL cells express CD20, targeting it with mAbs triggers antitumor responses via cell surface receptors resulting in a potent antibody-dependent cellular toxicity. However, response in patients is highly heterogeneous, with relapse within a few months in a subset of patients. In addition, chemotherapeutic combinations can be toxic and result in serious and long-term complications.
“Relapsed or refractory iNHL is not curable and treatment strategies without long-term complications are needed,” said Dr. Fehniger, associate professor of medicine at Washington University, St. Louis.
In an attempt to address this, Dr. Fehniger and his colleagues combined rituximab, an anti-CD20 antibody, with a relatively new IL-15 agonist immunostimulatory agent called ALT-803.
In the phase 1 trial, the researchers enrolled patients with indolent non-Hodgkin lymphoma who had relapsed after at least 1 prior to CD20 antibody containing therapy. The study was a standard 3+3 dose escalation design with rituximab administered by intravenous infusion, 375 mg/m2 in four weekly doses, followed by a rest and four consolidation doses every 8 weeks for four cycles.
ALT-803 was administered concurrently at dose levels of 1 mcg/kg, 3 mcg/kg, and 6 mcg/kg IV followed by 6 mcg/kg, 10 mcg/kg, 15 mcg/kg, and 20 mcg/kg subcutaneously.
In total, 21 patients were treated: 16 patients had follicular lymphoma, four patients had marginal zone lymphoma, and one patient had small lymphocytic lymphoma. The median prior therapies received was two (range: 1-18) and five patients were treated who were refractory to prior anti-CD20 MAb therapy.
ALT-803 was well tolerated with no dose limiting toxicities or grade 4 or 5 adverse events. No patients discontinued ALT-803 and the recommended phase 2 dose was 20 mcg/kg subcutaneously. Grade 3 adverse events, regardless of attribution to ALT-803, included transient hypertension (14%), anemia (5%), nausea (5%), chills (5%), fever (5%), neutropenia (5%), and hyperglycemia (5%).
“Patients who received [subcutaneous] ALT-803 developed a unique injection site rash reaction that peaked 7-10 days later but resolved typically within 14 days. It was self-limited and resolved on its own,” Dr. Fehniger said.
At the time of the presentation, the best overall response rate was achieved in 11 of 21 patients (52%), with 9 complete responders (43%), and 2 partial responders (10%).
Of the 12 patients treated with ALT-803 subcutaneously, 11 patients had either stable disease, or partial or complete responses. All 11 patients remained on study and were in consolidation or follow-up and have not relapsed, Dr. Fehniger reported.
Among the five rituximab-refractory patients, the researchers observed one complete response, two patients with stable disease (45% and 36% tumor volume decrease), and two patients with partial disease. The durability of the responses can only be understood with longer follow-up, Dr. Fehniger said.
The peripheral blood of the patients was analyzed via flow cytometry and mass cytometry. Over the duration of four weekly doses, there was an increase in percentage (sixfold, P less than .001) and absolute number (10-fold, P less than .001) of natural killer cells at the 15-mcg/kg and 20-mcg/kg subcutaneous dose levels of ALT-803.
These results suggest that further studies of ALT-803 with other therapeutic targeting mAbs, or other immunotherapy modalities, are warranted, the researchers concluded.
Dr. Fehniger reported research funding from Altor BioScience.
SOURCE: Fehniger TA et al. AACR Annual Meeting, Abstract CT146.
CHICAGO – A combination of an immunostimulatory IL-15-based agent, ALT-803, with a therapeutic monoclonal antibody (mAb) against CD20, was well tolerated and had clinical activity in patients with indolent non-Hodgkin lymphoma (iNHL), according to preliminary findings from a phase 1 study.
“The cancer immunotherapy breakthrough that happened several years ago continues year after year, with a plethora of different modalities of immunotherapy at our disposal,” Todd A. Fehniger, MD, PhD, said at the annual meeting of the American Association for Cancer Research.
Immunotherapy with anti-CD20 mAbs, alone or in combination with chemotherapy, is a standard therapy for iNHL patients. Since iNHL cells express CD20, targeting it with mAbs triggers antitumor responses via cell surface receptors resulting in a potent antibody-dependent cellular toxicity. However, response in patients is highly heterogeneous, with relapse within a few months in a subset of patients. In addition, chemotherapeutic combinations can be toxic and result in serious and long-term complications.
“Relapsed or refractory iNHL is not curable and treatment strategies without long-term complications are needed,” said Dr. Fehniger, associate professor of medicine at Washington University, St. Louis.
In an attempt to address this, Dr. Fehniger and his colleagues combined rituximab, an anti-CD20 antibody, with a relatively new IL-15 agonist immunostimulatory agent called ALT-803.
In the phase 1 trial, the researchers enrolled patients with indolent non-Hodgkin lymphoma who had relapsed after at least 1 prior to CD20 antibody containing therapy. The study was a standard 3+3 dose escalation design with rituximab administered by intravenous infusion, 375 mg/m2 in four weekly doses, followed by a rest and four consolidation doses every 8 weeks for four cycles.
ALT-803 was administered concurrently at dose levels of 1 mcg/kg, 3 mcg/kg, and 6 mcg/kg IV followed by 6 mcg/kg, 10 mcg/kg, 15 mcg/kg, and 20 mcg/kg subcutaneously.
In total, 21 patients were treated: 16 patients had follicular lymphoma, four patients had marginal zone lymphoma, and one patient had small lymphocytic lymphoma. The median prior therapies received was two (range: 1-18) and five patients were treated who were refractory to prior anti-CD20 MAb therapy.
ALT-803 was well tolerated with no dose limiting toxicities or grade 4 or 5 adverse events. No patients discontinued ALT-803 and the recommended phase 2 dose was 20 mcg/kg subcutaneously. Grade 3 adverse events, regardless of attribution to ALT-803, included transient hypertension (14%), anemia (5%), nausea (5%), chills (5%), fever (5%), neutropenia (5%), and hyperglycemia (5%).
“Patients who received [subcutaneous] ALT-803 developed a unique injection site rash reaction that peaked 7-10 days later but resolved typically within 14 days. It was self-limited and resolved on its own,” Dr. Fehniger said.
At the time of the presentation, the best overall response rate was achieved in 11 of 21 patients (52%), with 9 complete responders (43%), and 2 partial responders (10%).
Of the 12 patients treated with ALT-803 subcutaneously, 11 patients had either stable disease, or partial or complete responses. All 11 patients remained on study and were in consolidation or follow-up and have not relapsed, Dr. Fehniger reported.
Among the five rituximab-refractory patients, the researchers observed one complete response, two patients with stable disease (45% and 36% tumor volume decrease), and two patients with partial disease. The durability of the responses can only be understood with longer follow-up, Dr. Fehniger said.
The peripheral blood of the patients was analyzed via flow cytometry and mass cytometry. Over the duration of four weekly doses, there was an increase in percentage (sixfold, P less than .001) and absolute number (10-fold, P less than .001) of natural killer cells at the 15-mcg/kg and 20-mcg/kg subcutaneous dose levels of ALT-803.
These results suggest that further studies of ALT-803 with other therapeutic targeting mAbs, or other immunotherapy modalities, are warranted, the researchers concluded.
Dr. Fehniger reported research funding from Altor BioScience.
SOURCE: Fehniger TA et al. AACR Annual Meeting, Abstract CT146.
REPORTING FROM THE AACR ANNUAL MEETING
Key clinical point:
Major finding: The ALT-803 plus rituximab combination achieved an overall response rate in 52% of patients, a complete response in 43%, and partial response in 10%.
Study details: A phase 1 study of 21 patients with indolent non-Hodgkin lymphoma.
Disclosures: Dr. Fehniger reported research funding from Altor BioScience LLC.
Source: Fehniger TA et al. AACR Annual Meeting, Abstract CT146.
Mohs Micrographic Surgery for Digital Melanoma and Nonmelanoma Skin Cancers
Mohs micrographic surgery (MMS) is a specialized surgical technique for the treatment of melanoma and nonmelanoma skin cancers (NMSCs).1-3 The procedure involves surgical excision, histopathologic examination, precise mapping of malignant tissue, and wound management. Indications for MMS in skin cancer patients include recurring lesions, lesions in high-risk anatomic locations, aggressive histologic subtypes (ie, morpheaform, micronodular, infiltrative, high-grade, poorly differentiated), perineural invasion, large lesion size (>2 cm in diameter), poorly defined lateral or vertical clinical borders, rapid growth of the lesion, immunocompromised status, and sites of positive margins on prior excision. The therapeutic advantages of MMS include tissue conservation and optimal margin control in cosmetically or functionally sensitive areas, such as acral sites (eg, hands, feet, digits).1,3
The intricacies of the nail apparatus complicate diagnostic biopsy and precise delineation of peripheral margins in digital skin cancers; thus, early diagnosis and intraoperative histologic examination of the margins are essential. Traditionally, the surgical approach to subungual cutaneous tumors such as melanoma has included digital amputation4; however, a study of the treatment of subungual melanoma revealed no difference in survival based on the level of amputation, therefore advocating for less radical treatment.4
Interestingly, MMS for cutaneous tumors localized to the digits is not frequently reviewed in the dermatologic literature. We present a retrospective case series evaluating the clinical outcomes of digital melanoma and NMSCs treated with MMS.
Methods
A retrospective chart review was performed at a private dermatology practice to identify patients who underwent MMS for melanoma or NMSC localized to the digits from January 2009 to December 2014. All patients were treated in the office by 1 Mohs surgeon (A.H.) and were evaluated before and after MMS. Data were collected from the electronic medical record of the practice, including patient demographics, histopathologic diagnosis, tumor status (primary or recurrent lesion), anatomic site of the tumor, preoperative and postoperative size of the lesion, number of MMS stages, surgical repair technique, postoperative complications, and follow-up period.
Results
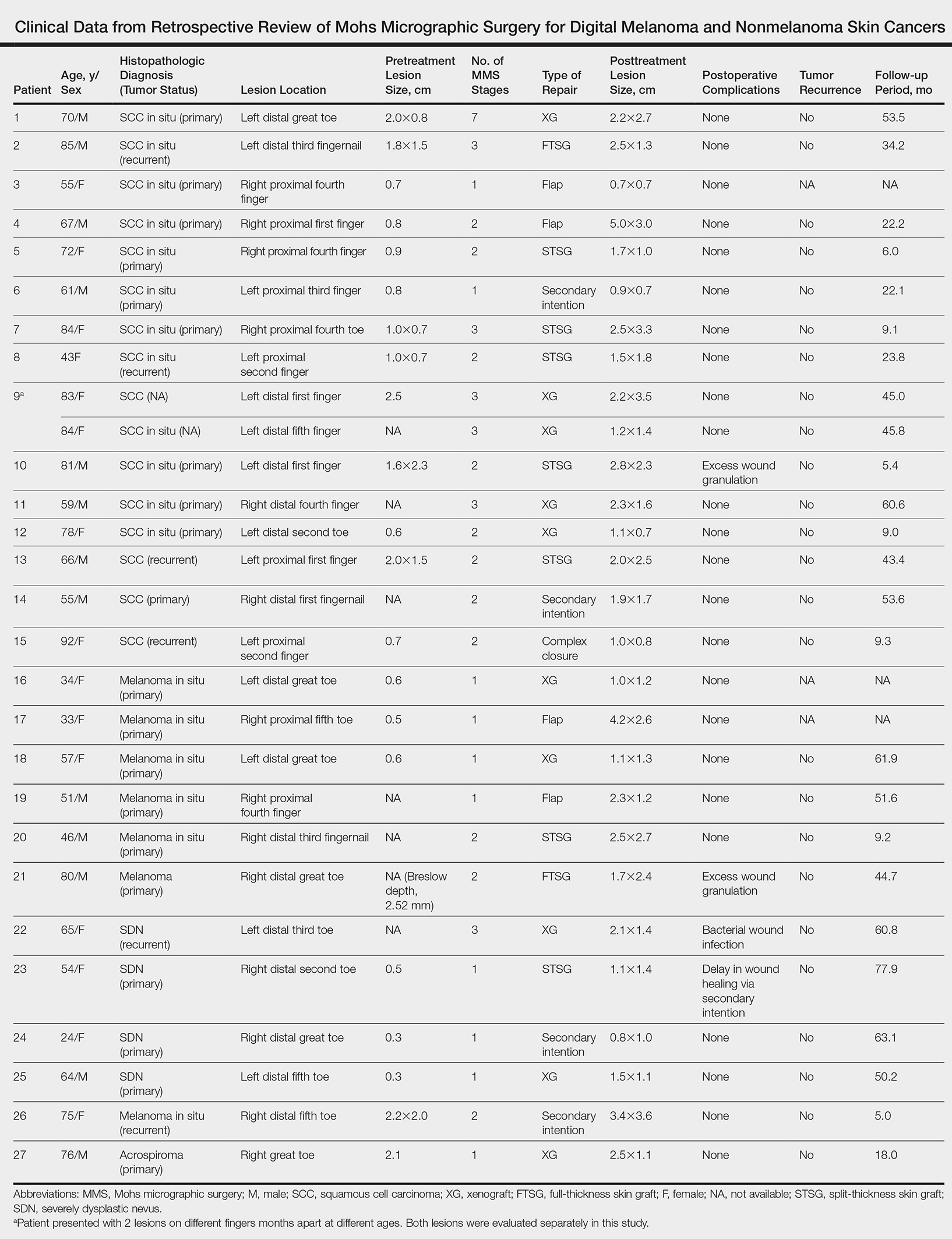
Twenty-seven patients (13 male, 14 female) with a total of 28 lesions (malignant melanoma or NMSC) localized to the digits were identified (Table). The mean age at the time of MMS was 64.07 years.
Surgical techniques used for repair following MMS included xenograft (10/28 [35.71%]); split-thickness skin graft (7/28 [25.0%]); secondary intention (4/28 [14.29%]); flap (4/28 [14.29%]); full-thickness skin graft (2/28 [7.14%]); and complex closure (1/28 [3.57%]). Clinical preoperative, operative, and postoperative photos from Patient 21 in this series are shown here (Figure). Two patients required bony phalanx resection due to invasion of the tumor into the periosteum: 1 had a malignant melanoma (Breslow depth, 2.52 mm); the other had an SCC. In addition, following removal of a severely dysplastic nevus, debulked tissue revealed melanoma in 1 patient.

Postoperative complications were noted in 4 (14.29%) of 28 MMS procedures, including bacterial wound infection (3.57%), excess granulation tissue that required wound debridement (7.14%), and delay in wound healing (3.57%). Follow-up data were available for 25 of the 28 MMS procedures (mean follow-up, 35.4 months), during which no recurrences were observed.
Comment
Mohs micrographic surgery is a specialized technique used in the treatment of cutaneous tumors, including basal cell carcinoma, SCC, melanoma in situ, atypical fibroxanthoma, dermatofibrosarcoma protuberans, sebaceous carcinoma, microcystic adnexal carcinoma, and Merkel cell carcinoma, among other cutaneous tumors.1-3 Mohs micrographic surgery provides the advantage of tissue conservation as well as optimal margin control in cosmetically or functionally sensitive areas while providing a higher cure rate than surgical excision. During the procedure, the surgical margin is examined histologically, thus ensuring definitive removal of the tumor but minimal loss of surrounding normal tissue.1-3 Mohs micrographic surgery is particularly useful for treating lesions on acral sites (eg, hands, feet, and digits).3-5
The treatment of digital skin cancers has evolved over the past 50 years with advancements resulting in more precise, tissue-sparing methods, in contrast to previous treatments such as amputation and wide local excision.6 More specifically, traditional digital amputation for the treatment of subungual melanoma has been reevaluated in multiple studies, which did not demonstrate a statistically significant difference in survival based on the level of amputation, thereby favoring less radical treatment.4,6 Moehrle et al7 found no statistical difference in recurrence rate when comparing patients with digital melanomas treated with partial amputation and those treated with digit-sparing surgery with limited excision and histologic evaluation of margins. Additionally, in a study conducted by Lazar et al,8 no recurrence of 13 subungual malignancies treated with MMS that utilized a full-thickness graft was reported at 4-year follow-up. In a large retrospective series of digital melanomas treated with MMS, Terushkin et al5 reported that 96.5% (55/57) of patients with primary melanomas that were treated with MMS avoided amputation, and the 5- and 10-year melanoma-specific survival rates for all patients treated with MMS were 95.0% and 82.6%, respectively.
In our study, cutaneous malignancies were located most often on the fingers, and the most common skin cancer identified was SCC in situ. The literature has shown that SCC in situ and SCC are the most common cutaneous neoplasms of the digits and nail unit.9 The most common specific anatomic site of cutaneous malignancy in our study was the great toe, followed by the fourth finger. A study conducted by Tan et al9 revealed that the great toe was the most common location of melanoma of the nail bed and subungual region, followed by the thumb. In contrast, primary subungual SCCs occur most frequently on the finger, with rare cases involving the toes.10
The etiology of digital SCC may involve extensive sun exposure, chronic trauma and wounds, and viral infection.9,11 More specifically, the dermatologic literature provides evidence of human papillomavirus (HPV) type 16 involvement in the pathogenesis of digital and periungual SCC. A genital-digital mechanism of spread has been implicated.11,12 An increased recurrence rate of HPV-associated digital SCCs has been reported following MMS, likely secondary to residual postsurgical HPV infection.11,12
Maintaining function and cosmesis of the hands, feet, and digits following MMS can be challenging, sometimes requiring skin grafts and flaps to close the defect. In the 28 MMS procedures evaluated in our study, 19 (67.9%) surgical defects were repaired with a graft (ie, split-thickness skin graft, full-thickness skin graft, xenograft), 4 (14.3%) with a flap (advancement and rotation), 4 (14.3%) by secondary intention, and 1 (3.6%) with primary complex closure.
Surgical grafts can be categorized based on the origin of the graft.2,13 Autografts, derived from the patient’s skin, are the most frequently used dermatologic graft and can be further categorized as full-thickness skin grafts, which include the epidermis and the entire dermis, thus preserving adnexal structures, and split-thickness skin grafts, which include the epidermis and partial dermis.2,13
A cross-sectional survey of fellowship-trained Mohs surgeons revealed that more than two-thirds of repairs for cutaneous acral cancers were performed using a primary closure technique, and one-fourth of closures were performed using secondary intention.15 Of the less frequently utilized skin-graft repairs, more were for acral lesions on the legs than on the arms.14 The type of procedure and graft used is dependent on multiple variables, including the anatomic location of the lesion and final size of the defect following MMS.2 Similarly, the use of specific types of sutures depends on the anatomic location of the lesion, relative thickness of the skin, degree of tension, and desired cosmetic result.15 The expertise of a hand surgeon may be required, particularly in cases in which the extensor tendon of the distal interphalangeal joint is compromised, manifested by a droopy fingertip when the hand is held horizontally. Additionally, special attention should be paid to removing the entire nail matrix before skin grafting for subungual tumors to avoid nail growth under the skin graft.
Evaluation of debulked tissue from digital skin cancers proved to be important in our study. In Patient 21, debulked tissue revealed melanoma following removal of a severely dysplastic nevus. This finding emphasizes the importance of complete excision of such lesions, as remaining underlying portions of the lesion can reveal residual tumor of the same or different histopathology.
In a prospective study, MMS was shown to have a low rate (0.91%; 95% confidence interval, 0.38%-1.45%) of surgical site infection in the absence of prophylactic antibiotics.16 The highest rates of surgical site infection were closely associated with flap closure. In our study, most patients had an uncomplicated and successful postoperative recovery. Only 1 (3.57%) of the 28 MMS procedures (Patient 22) was complicated by a bacterial wound infection postoperatively. The lesion removed in this case was a severely dysplastic melanocytic nevus on the toe. Infection resolved after a course of oral antibiotics, but the underlying cause of the wound infection in the patient was unclear. Other postoperative complications in our study included delayed wound healing and excess granulation tissue requiring wound debridement.
There are limited data in the dermatologic literature regarding outcomes following MMS for the treatment of cutaneous malignancies localized to the digits.
Additional limitations of this case review include its single-center and retrospective design, the small sample size, and 1 Mohs surgeon having performed all surgeries.
Conclusion
This study provides further evidence of the benefit of MMS for the treatment of malignant melanoma and NMSCs of the digits. This procedure provides margin-controlled excision of these malignant neoplasms while preserving maximal normal tissue, thereby providing patients with improved postoperative function and cosmesis. Long-term follow-up data demonstrating a lack of tumor recurrence underscores the assertion that MMS is safe and effective for the treatment of skin cancer of the digits.
- Dim-Jamora KC, Perone JB. Management of cutaneous tumors with mohs micrographic surgery. Semin Plast Surg. 2008;22:247-256.
- McLeod MP, Choudhary S, Alqubaisy YA, et al. Indications for Mohs micrographic surgery. In: Nouri K, ed. Mohs Micrographic Surgery. New York, NY: Springer; 2012:5-13.
- Loosemore MP, Morales-Burgos A, Goldberg LH. Acral lentiginous melanoma of the toe treated using Mohs surgery with sparing of the digit and subsequent reconstruction using split-thickness skin graft. Dermatol Surg. 2013;39:136-138.
- Rayatt SS, Dancey AL, Davison PM. Thumb subungual melanoma: is amputation necessary? J Plast Reconstr Aesthet Surg. 2007;60:635-638.
- Terushkin V, Brodland DG, Sharon DJ, et al. Digit-sparing Mohs surgery for melanoma. Dermatol Surg. 2016;42:83-93.
- Viola KV, Jhaveri MB, Soulos PR, et al. Mohs micrographic surgery and surgical excision for nonmelanoma skin cancer treatment in the Medicare population. Arch Dermatol. 2012;148:473-477.
- Moehrle M, Metzger S, Schippert W. “Functional” surgery in subungual melanoma. Dermatol Surg. 2003;29:366-374.
- Lazar A, Abimelec P, Dumontier C, et al. Full thickness skin graft from nail unit reconstruction. J Hand Surg Br. 2005;30:194-198.
- Tan KB, Moncrieff M, Thompson JF, et al. Subungual melanoma: a study of 124 cases highlighting features of early lesions, potential for histologic reports. Am J Surg Pathol. 2007;31:1902-1912.
- Nasca MR, Innocenzi D, Micali G. Subungual squamous cell carcinoma of the toe: report on three cases. Dermatol Surg. 2004;30:345-348.
- Dika E, Piraccini BM, Balestri RR, et al. Mohs surgery for squamous cell carcinoma of the nail: report of 15 cases. our experience and a long-term follow-up. Br J Dermatol. 2012;167:1310-1314.
- Alam M, Caldwell JB, Eliezri YD. Human papillomavirus-associated digital squamous cell carcinoma: literature review and report of 21 new cases. J Am Acad Dermatol. 2003;48:385-393.
- Filho L, Anselmo J, Dadalti P, et al. Skin grafts in cutaneous oncology. Braz Ann Dermatol. 2006;81:465-472.
- Raimer DW, Group AR, Petitt MS, et al. Porcine xenograft biosynthetic wound dressings for the management of postoperative Mohs wounds. Dermatol Online J. 2011;17:1.
- Alam M, Helenowksi IB, Cohen JL, et al. Association between type of reconstruction after Mohs micrographic surgery and surgeon-, patient-, and tumor-specific features: a cross-sectional study. Dermatol Surg. 2013;39:51-55.
- Rogers HD, Desciak EB, Marcus RP, et al. Prospective study of wound infections in Mohs micrographic surgery using clean surgical technique in the absence of prophylactic antibiotics. J Am Acad Dermatol. 2010;63:842-851.
Mohs micrographic surgery (MMS) is a specialized surgical technique for the treatment of melanoma and nonmelanoma skin cancers (NMSCs).1-3 The procedure involves surgical excision, histopathologic examination, precise mapping of malignant tissue, and wound management. Indications for MMS in skin cancer patients include recurring lesions, lesions in high-risk anatomic locations, aggressive histologic subtypes (ie, morpheaform, micronodular, infiltrative, high-grade, poorly differentiated), perineural invasion, large lesion size (>2 cm in diameter), poorly defined lateral or vertical clinical borders, rapid growth of the lesion, immunocompromised status, and sites of positive margins on prior excision. The therapeutic advantages of MMS include tissue conservation and optimal margin control in cosmetically or functionally sensitive areas, such as acral sites (eg, hands, feet, digits).1,3
The intricacies of the nail apparatus complicate diagnostic biopsy and precise delineation of peripheral margins in digital skin cancers; thus, early diagnosis and intraoperative histologic examination of the margins are essential. Traditionally, the surgical approach to subungual cutaneous tumors such as melanoma has included digital amputation4; however, a study of the treatment of subungual melanoma revealed no difference in survival based on the level of amputation, therefore advocating for less radical treatment.4
Interestingly, MMS for cutaneous tumors localized to the digits is not frequently reviewed in the dermatologic literature. We present a retrospective case series evaluating the clinical outcomes of digital melanoma and NMSCs treated with MMS.
Methods
A retrospective chart review was performed at a private dermatology practice to identify patients who underwent MMS for melanoma or NMSC localized to the digits from January 2009 to December 2014. All patients were treated in the office by 1 Mohs surgeon (A.H.) and were evaluated before and after MMS. Data were collected from the electronic medical record of the practice, including patient demographics, histopathologic diagnosis, tumor status (primary or recurrent lesion), anatomic site of the tumor, preoperative and postoperative size of the lesion, number of MMS stages, surgical repair technique, postoperative complications, and follow-up period.
Results
Twenty-seven patients (13 male, 14 female) with a total of 28 lesions (malignant melanoma or NMSC) localized to the digits were identified (Table). The mean age at the time of MMS was 64.07 years.
Surgical techniques used for repair following MMS included xenograft (10/28 [35.71%]); split-thickness skin graft (7/28 [25.0%]); secondary intention (4/28 [14.29%]); flap (4/28 [14.29%]); full-thickness skin graft (2/28 [7.14%]); and complex closure (1/28 [3.57%]). Clinical preoperative, operative, and postoperative photos from Patient 21 in this series are shown here (Figure). Two patients required bony phalanx resection due to invasion of the tumor into the periosteum: 1 had a malignant melanoma (Breslow depth, 2.52 mm); the other had an SCC. In addition, following removal of a severely dysplastic nevus, debulked tissue revealed melanoma in 1 patient.

Postoperative complications were noted in 4 (14.29%) of 28 MMS procedures, including bacterial wound infection (3.57%), excess granulation tissue that required wound debridement (7.14%), and delay in wound healing (3.57%). Follow-up data were available for 25 of the 28 MMS procedures (mean follow-up, 35.4 months), during which no recurrences were observed.
Comment
Mohs micrographic surgery is a specialized technique used in the treatment of cutaneous tumors, including basal cell carcinoma, SCC, melanoma in situ, atypical fibroxanthoma, dermatofibrosarcoma protuberans, sebaceous carcinoma, microcystic adnexal carcinoma, and Merkel cell carcinoma, among other cutaneous tumors.1-3 Mohs micrographic surgery provides the advantage of tissue conservation as well as optimal margin control in cosmetically or functionally sensitive areas while providing a higher cure rate than surgical excision. During the procedure, the surgical margin is examined histologically, thus ensuring definitive removal of the tumor but minimal loss of surrounding normal tissue.1-3 Mohs micrographic surgery is particularly useful for treating lesions on acral sites (eg, hands, feet, and digits).3-5
The treatment of digital skin cancers has evolved over the past 50 years with advancements resulting in more precise, tissue-sparing methods, in contrast to previous treatments such as amputation and wide local excision.6 More specifically, traditional digital amputation for the treatment of subungual melanoma has been reevaluated in multiple studies, which did not demonstrate a statistically significant difference in survival based on the level of amputation, thereby favoring less radical treatment.4,6 Moehrle et al7 found no statistical difference in recurrence rate when comparing patients with digital melanomas treated with partial amputation and those treated with digit-sparing surgery with limited excision and histologic evaluation of margins. Additionally, in a study conducted by Lazar et al,8 no recurrence of 13 subungual malignancies treated with MMS that utilized a full-thickness graft was reported at 4-year follow-up. In a large retrospective series of digital melanomas treated with MMS, Terushkin et al5 reported that 96.5% (55/57) of patients with primary melanomas that were treated with MMS avoided amputation, and the 5- and 10-year melanoma-specific survival rates for all patients treated with MMS were 95.0% and 82.6%, respectively.
In our study, cutaneous malignancies were located most often on the fingers, and the most common skin cancer identified was SCC in situ. The literature has shown that SCC in situ and SCC are the most common cutaneous neoplasms of the digits and nail unit.9 The most common specific anatomic site of cutaneous malignancy in our study was the great toe, followed by the fourth finger. A study conducted by Tan et al9 revealed that the great toe was the most common location of melanoma of the nail bed and subungual region, followed by the thumb. In contrast, primary subungual SCCs occur most frequently on the finger, with rare cases involving the toes.10
The etiology of digital SCC may involve extensive sun exposure, chronic trauma and wounds, and viral infection.9,11 More specifically, the dermatologic literature provides evidence of human papillomavirus (HPV) type 16 involvement in the pathogenesis of digital and periungual SCC. A genital-digital mechanism of spread has been implicated.11,12 An increased recurrence rate of HPV-associated digital SCCs has been reported following MMS, likely secondary to residual postsurgical HPV infection.11,12
Maintaining function and cosmesis of the hands, feet, and digits following MMS can be challenging, sometimes requiring skin grafts and flaps to close the defect. In the 28 MMS procedures evaluated in our study, 19 (67.9%) surgical defects were repaired with a graft (ie, split-thickness skin graft, full-thickness skin graft, xenograft), 4 (14.3%) with a flap (advancement and rotation), 4 (14.3%) by secondary intention, and 1 (3.6%) with primary complex closure.
Surgical grafts can be categorized based on the origin of the graft.2,13 Autografts, derived from the patient’s skin, are the most frequently used dermatologic graft and can be further categorized as full-thickness skin grafts, which include the epidermis and the entire dermis, thus preserving adnexal structures, and split-thickness skin grafts, which include the epidermis and partial dermis.2,13
A cross-sectional survey of fellowship-trained Mohs surgeons revealed that more than two-thirds of repairs for cutaneous acral cancers were performed using a primary closure technique, and one-fourth of closures were performed using secondary intention.15 Of the less frequently utilized skin-graft repairs, more were for acral lesions on the legs than on the arms.14 The type of procedure and graft used is dependent on multiple variables, including the anatomic location of the lesion and final size of the defect following MMS.2 Similarly, the use of specific types of sutures depends on the anatomic location of the lesion, relative thickness of the skin, degree of tension, and desired cosmetic result.15 The expertise of a hand surgeon may be required, particularly in cases in which the extensor tendon of the distal interphalangeal joint is compromised, manifested by a droopy fingertip when the hand is held horizontally. Additionally, special attention should be paid to removing the entire nail matrix before skin grafting for subungual tumors to avoid nail growth under the skin graft.
Evaluation of debulked tissue from digital skin cancers proved to be important in our study. In Patient 21, debulked tissue revealed melanoma following removal of a severely dysplastic nevus. This finding emphasizes the importance of complete excision of such lesions, as remaining underlying portions of the lesion can reveal residual tumor of the same or different histopathology.
In a prospective study, MMS was shown to have a low rate (0.91%; 95% confidence interval, 0.38%-1.45%) of surgical site infection in the absence of prophylactic antibiotics.16 The highest rates of surgical site infection were closely associated with flap closure. In our study, most patients had an uncomplicated and successful postoperative recovery. Only 1 (3.57%) of the 28 MMS procedures (Patient 22) was complicated by a bacterial wound infection postoperatively. The lesion removed in this case was a severely dysplastic melanocytic nevus on the toe. Infection resolved after a course of oral antibiotics, but the underlying cause of the wound infection in the patient was unclear. Other postoperative complications in our study included delayed wound healing and excess granulation tissue requiring wound debridement.
There are limited data in the dermatologic literature regarding outcomes following MMS for the treatment of cutaneous malignancies localized to the digits.
Additional limitations of this case review include its single-center and retrospective design, the small sample size, and 1 Mohs surgeon having performed all surgeries.
Conclusion
This study provides further evidence of the benefit of MMS for the treatment of malignant melanoma and NMSCs of the digits. This procedure provides margin-controlled excision of these malignant neoplasms while preserving maximal normal tissue, thereby providing patients with improved postoperative function and cosmesis. Long-term follow-up data demonstrating a lack of tumor recurrence underscores the assertion that MMS is safe and effective for the treatment of skin cancer of the digits.
Mohs micrographic surgery (MMS) is a specialized surgical technique for the treatment of melanoma and nonmelanoma skin cancers (NMSCs).1-3 The procedure involves surgical excision, histopathologic examination, precise mapping of malignant tissue, and wound management. Indications for MMS in skin cancer patients include recurring lesions, lesions in high-risk anatomic locations, aggressive histologic subtypes (ie, morpheaform, micronodular, infiltrative, high-grade, poorly differentiated), perineural invasion, large lesion size (>2 cm in diameter), poorly defined lateral or vertical clinical borders, rapid growth of the lesion, immunocompromised status, and sites of positive margins on prior excision. The therapeutic advantages of MMS include tissue conservation and optimal margin control in cosmetically or functionally sensitive areas, such as acral sites (eg, hands, feet, digits).1,3
The intricacies of the nail apparatus complicate diagnostic biopsy and precise delineation of peripheral margins in digital skin cancers; thus, early diagnosis and intraoperative histologic examination of the margins are essential. Traditionally, the surgical approach to subungual cutaneous tumors such as melanoma has included digital amputation4; however, a study of the treatment of subungual melanoma revealed no difference in survival based on the level of amputation, therefore advocating for less radical treatment.4
Interestingly, MMS for cutaneous tumors localized to the digits is not frequently reviewed in the dermatologic literature. We present a retrospective case series evaluating the clinical outcomes of digital melanoma and NMSCs treated with MMS.
Methods
A retrospective chart review was performed at a private dermatology practice to identify patients who underwent MMS for melanoma or NMSC localized to the digits from January 2009 to December 2014. All patients were treated in the office by 1 Mohs surgeon (A.H.) and were evaluated before and after MMS. Data were collected from the electronic medical record of the practice, including patient demographics, histopathologic diagnosis, tumor status (primary or recurrent lesion), anatomic site of the tumor, preoperative and postoperative size of the lesion, number of MMS stages, surgical repair technique, postoperative complications, and follow-up period.
Results
Twenty-seven patients (13 male, 14 female) with a total of 28 lesions (malignant melanoma or NMSC) localized to the digits were identified (Table). The mean age at the time of MMS was 64.07 years.
Surgical techniques used for repair following MMS included xenograft (10/28 [35.71%]); split-thickness skin graft (7/28 [25.0%]); secondary intention (4/28 [14.29%]); flap (4/28 [14.29%]); full-thickness skin graft (2/28 [7.14%]); and complex closure (1/28 [3.57%]). Clinical preoperative, operative, and postoperative photos from Patient 21 in this series are shown here (Figure). Two patients required bony phalanx resection due to invasion of the tumor into the periosteum: 1 had a malignant melanoma (Breslow depth, 2.52 mm); the other had an SCC. In addition, following removal of a severely dysplastic nevus, debulked tissue revealed melanoma in 1 patient.

Postoperative complications were noted in 4 (14.29%) of 28 MMS procedures, including bacterial wound infection (3.57%), excess granulation tissue that required wound debridement (7.14%), and delay in wound healing (3.57%). Follow-up data were available for 25 of the 28 MMS procedures (mean follow-up, 35.4 months), during which no recurrences were observed.
Comment
Mohs micrographic surgery is a specialized technique used in the treatment of cutaneous tumors, including basal cell carcinoma, SCC, melanoma in situ, atypical fibroxanthoma, dermatofibrosarcoma protuberans, sebaceous carcinoma, microcystic adnexal carcinoma, and Merkel cell carcinoma, among other cutaneous tumors.1-3 Mohs micrographic surgery provides the advantage of tissue conservation as well as optimal margin control in cosmetically or functionally sensitive areas while providing a higher cure rate than surgical excision. During the procedure, the surgical margin is examined histologically, thus ensuring definitive removal of the tumor but minimal loss of surrounding normal tissue.1-3 Mohs micrographic surgery is particularly useful for treating lesions on acral sites (eg, hands, feet, and digits).3-5
The treatment of digital skin cancers has evolved over the past 50 years with advancements resulting in more precise, tissue-sparing methods, in contrast to previous treatments such as amputation and wide local excision.6 More specifically, traditional digital amputation for the treatment of subungual melanoma has been reevaluated in multiple studies, which did not demonstrate a statistically significant difference in survival based on the level of amputation, thereby favoring less radical treatment.4,6 Moehrle et al7 found no statistical difference in recurrence rate when comparing patients with digital melanomas treated with partial amputation and those treated with digit-sparing surgery with limited excision and histologic evaluation of margins. Additionally, in a study conducted by Lazar et al,8 no recurrence of 13 subungual malignancies treated with MMS that utilized a full-thickness graft was reported at 4-year follow-up. In a large retrospective series of digital melanomas treated with MMS, Terushkin et al5 reported that 96.5% (55/57) of patients with primary melanomas that were treated with MMS avoided amputation, and the 5- and 10-year melanoma-specific survival rates for all patients treated with MMS were 95.0% and 82.6%, respectively.
In our study, cutaneous malignancies were located most often on the fingers, and the most common skin cancer identified was SCC in situ. The literature has shown that SCC in situ and SCC are the most common cutaneous neoplasms of the digits and nail unit.9 The most common specific anatomic site of cutaneous malignancy in our study was the great toe, followed by the fourth finger. A study conducted by Tan et al9 revealed that the great toe was the most common location of melanoma of the nail bed and subungual region, followed by the thumb. In contrast, primary subungual SCCs occur most frequently on the finger, with rare cases involving the toes.10
The etiology of digital SCC may involve extensive sun exposure, chronic trauma and wounds, and viral infection.9,11 More specifically, the dermatologic literature provides evidence of human papillomavirus (HPV) type 16 involvement in the pathogenesis of digital and periungual SCC. A genital-digital mechanism of spread has been implicated.11,12 An increased recurrence rate of HPV-associated digital SCCs has been reported following MMS, likely secondary to residual postsurgical HPV infection.11,12
Maintaining function and cosmesis of the hands, feet, and digits following MMS can be challenging, sometimes requiring skin grafts and flaps to close the defect. In the 28 MMS procedures evaluated in our study, 19 (67.9%) surgical defects were repaired with a graft (ie, split-thickness skin graft, full-thickness skin graft, xenograft), 4 (14.3%) with a flap (advancement and rotation), 4 (14.3%) by secondary intention, and 1 (3.6%) with primary complex closure.
Surgical grafts can be categorized based on the origin of the graft.2,13 Autografts, derived from the patient’s skin, are the most frequently used dermatologic graft and can be further categorized as full-thickness skin grafts, which include the epidermis and the entire dermis, thus preserving adnexal structures, and split-thickness skin grafts, which include the epidermis and partial dermis.2,13
A cross-sectional survey of fellowship-trained Mohs surgeons revealed that more than two-thirds of repairs for cutaneous acral cancers were performed using a primary closure technique, and one-fourth of closures were performed using secondary intention.15 Of the less frequently utilized skin-graft repairs, more were for acral lesions on the legs than on the arms.14 The type of procedure and graft used is dependent on multiple variables, including the anatomic location of the lesion and final size of the defect following MMS.2 Similarly, the use of specific types of sutures depends on the anatomic location of the lesion, relative thickness of the skin, degree of tension, and desired cosmetic result.15 The expertise of a hand surgeon may be required, particularly in cases in which the extensor tendon of the distal interphalangeal joint is compromised, manifested by a droopy fingertip when the hand is held horizontally. Additionally, special attention should be paid to removing the entire nail matrix before skin grafting for subungual tumors to avoid nail growth under the skin graft.
Evaluation of debulked tissue from digital skin cancers proved to be important in our study. In Patient 21, debulked tissue revealed melanoma following removal of a severely dysplastic nevus. This finding emphasizes the importance of complete excision of such lesions, as remaining underlying portions of the lesion can reveal residual tumor of the same or different histopathology.
In a prospective study, MMS was shown to have a low rate (0.91%; 95% confidence interval, 0.38%-1.45%) of surgical site infection in the absence of prophylactic antibiotics.16 The highest rates of surgical site infection were closely associated with flap closure. In our study, most patients had an uncomplicated and successful postoperative recovery. Only 1 (3.57%) of the 28 MMS procedures (Patient 22) was complicated by a bacterial wound infection postoperatively. The lesion removed in this case was a severely dysplastic melanocytic nevus on the toe. Infection resolved after a course of oral antibiotics, but the underlying cause of the wound infection in the patient was unclear. Other postoperative complications in our study included delayed wound healing and excess granulation tissue requiring wound debridement.
There are limited data in the dermatologic literature regarding outcomes following MMS for the treatment of cutaneous malignancies localized to the digits.
Additional limitations of this case review include its single-center and retrospective design, the small sample size, and 1 Mohs surgeon having performed all surgeries.
Conclusion
This study provides further evidence of the benefit of MMS for the treatment of malignant melanoma and NMSCs of the digits. This procedure provides margin-controlled excision of these malignant neoplasms while preserving maximal normal tissue, thereby providing patients with improved postoperative function and cosmesis. Long-term follow-up data demonstrating a lack of tumor recurrence underscores the assertion that MMS is safe and effective for the treatment of skin cancer of the digits.
- Dim-Jamora KC, Perone JB. Management of cutaneous tumors with mohs micrographic surgery. Semin Plast Surg. 2008;22:247-256.
- McLeod MP, Choudhary S, Alqubaisy YA, et al. Indications for Mohs micrographic surgery. In: Nouri K, ed. Mohs Micrographic Surgery. New York, NY: Springer; 2012:5-13.
- Loosemore MP, Morales-Burgos A, Goldberg LH. Acral lentiginous melanoma of the toe treated using Mohs surgery with sparing of the digit and subsequent reconstruction using split-thickness skin graft. Dermatol Surg. 2013;39:136-138.
- Rayatt SS, Dancey AL, Davison PM. Thumb subungual melanoma: is amputation necessary? J Plast Reconstr Aesthet Surg. 2007;60:635-638.
- Terushkin V, Brodland DG, Sharon DJ, et al. Digit-sparing Mohs surgery for melanoma. Dermatol Surg. 2016;42:83-93.
- Viola KV, Jhaveri MB, Soulos PR, et al. Mohs micrographic surgery and surgical excision for nonmelanoma skin cancer treatment in the Medicare population. Arch Dermatol. 2012;148:473-477.
- Moehrle M, Metzger S, Schippert W. “Functional” surgery in subungual melanoma. Dermatol Surg. 2003;29:366-374.
- Lazar A, Abimelec P, Dumontier C, et al. Full thickness skin graft from nail unit reconstruction. J Hand Surg Br. 2005;30:194-198.
- Tan KB, Moncrieff M, Thompson JF, et al. Subungual melanoma: a study of 124 cases highlighting features of early lesions, potential for histologic reports. Am J Surg Pathol. 2007;31:1902-1912.
- Nasca MR, Innocenzi D, Micali G. Subungual squamous cell carcinoma of the toe: report on three cases. Dermatol Surg. 2004;30:345-348.
- Dika E, Piraccini BM, Balestri RR, et al. Mohs surgery for squamous cell carcinoma of the nail: report of 15 cases. our experience and a long-term follow-up. Br J Dermatol. 2012;167:1310-1314.
- Alam M, Caldwell JB, Eliezri YD. Human papillomavirus-associated digital squamous cell carcinoma: literature review and report of 21 new cases. J Am Acad Dermatol. 2003;48:385-393.
- Filho L, Anselmo J, Dadalti P, et al. Skin grafts in cutaneous oncology. Braz Ann Dermatol. 2006;81:465-472.
- Raimer DW, Group AR, Petitt MS, et al. Porcine xenograft biosynthetic wound dressings for the management of postoperative Mohs wounds. Dermatol Online J. 2011;17:1.
- Alam M, Helenowksi IB, Cohen JL, et al. Association between type of reconstruction after Mohs micrographic surgery and surgeon-, patient-, and tumor-specific features: a cross-sectional study. Dermatol Surg. 2013;39:51-55.
- Rogers HD, Desciak EB, Marcus RP, et al. Prospective study of wound infections in Mohs micrographic surgery using clean surgical technique in the absence of prophylactic antibiotics. J Am Acad Dermatol. 2010;63:842-851.
- Dim-Jamora KC, Perone JB. Management of cutaneous tumors with mohs micrographic surgery. Semin Plast Surg. 2008;22:247-256.
- McLeod MP, Choudhary S, Alqubaisy YA, et al. Indications for Mohs micrographic surgery. In: Nouri K, ed. Mohs Micrographic Surgery. New York, NY: Springer; 2012:5-13.
- Loosemore MP, Morales-Burgos A, Goldberg LH. Acral lentiginous melanoma of the toe treated using Mohs surgery with sparing of the digit and subsequent reconstruction using split-thickness skin graft. Dermatol Surg. 2013;39:136-138.
- Rayatt SS, Dancey AL, Davison PM. Thumb subungual melanoma: is amputation necessary? J Plast Reconstr Aesthet Surg. 2007;60:635-638.
- Terushkin V, Brodland DG, Sharon DJ, et al. Digit-sparing Mohs surgery for melanoma. Dermatol Surg. 2016;42:83-93.
- Viola KV, Jhaveri MB, Soulos PR, et al. Mohs micrographic surgery and surgical excision for nonmelanoma skin cancer treatment in the Medicare population. Arch Dermatol. 2012;148:473-477.
- Moehrle M, Metzger S, Schippert W. “Functional” surgery in subungual melanoma. Dermatol Surg. 2003;29:366-374.
- Lazar A, Abimelec P, Dumontier C, et al. Full thickness skin graft from nail unit reconstruction. J Hand Surg Br. 2005;30:194-198.
- Tan KB, Moncrieff M, Thompson JF, et al. Subungual melanoma: a study of 124 cases highlighting features of early lesions, potential for histologic reports. Am J Surg Pathol. 2007;31:1902-1912.
- Nasca MR, Innocenzi D, Micali G. Subungual squamous cell carcinoma of the toe: report on three cases. Dermatol Surg. 2004;30:345-348.
- Dika E, Piraccini BM, Balestri RR, et al. Mohs surgery for squamous cell carcinoma of the nail: report of 15 cases. our experience and a long-term follow-up. Br J Dermatol. 2012;167:1310-1314.
- Alam M, Caldwell JB, Eliezri YD. Human papillomavirus-associated digital squamous cell carcinoma: literature review and report of 21 new cases. J Am Acad Dermatol. 2003;48:385-393.
- Filho L, Anselmo J, Dadalti P, et al. Skin grafts in cutaneous oncology. Braz Ann Dermatol. 2006;81:465-472.
- Raimer DW, Group AR, Petitt MS, et al. Porcine xenograft biosynthetic wound dressings for the management of postoperative Mohs wounds. Dermatol Online J. 2011;17:1.
- Alam M, Helenowksi IB, Cohen JL, et al. Association between type of reconstruction after Mohs micrographic surgery and surgeon-, patient-, and tumor-specific features: a cross-sectional study. Dermatol Surg. 2013;39:51-55.
- Rogers HD, Desciak EB, Marcus RP, et al. Prospective study of wound infections in Mohs micrographic surgery using clean surgical technique in the absence of prophylactic antibiotics. J Am Acad Dermatol. 2010;63:842-851.
Practice Points
- Melanoma and nonmelanoma skin cancers of the digits traditionally have been treated with wide local surgical excision and even amputation.
- Conservative tissue sparing techniques such as Mohs micrographic surgery can be used to treat digital skin cancers with high cure rates and improved functional and cosmetic results.
Lower glucose target linked to improved mortality in critically ill
compared with patients with a target of 90-140 mg/dL, according to results of a retrospective cohort analysis.
With the computerized intravenous insulin protocol used in the study, the strict target could be achieved with a low rate of hypoglycemia, the authors wrote. The analysis was published in the journal CHEST®.
However, it does raise the possibility that earlier investigations finding an association between intensive insulin therapy and excess mortality “may have been accurate only in the setting of technologies which led to high rates of severe hypoglycemia,” they wrote.
The retrospective cohort analysis by Dr. Hersh and his colleagues included 1,809 adult patients treated at three different ICUs in two hospitals between January 2010 and December 2015. Treatment was delivered with a computerized ICU insulin infusion protocol that allows clinicians to choose between two blood glucose targets: 80-110 mg/dL or 90-140 mg/dL. The lower target was chosen for 951 patients, and the moderate target for 858 patients.
The most common primary admission diagnoses in the cohort included chest pain or acute coronary syndrome in 43.3%, cardiothoracic surgery in 31.9%, heart failure (including cardiogenic shock) in 6.8%, and vascular surgery in 6.0%.
While patients in the low blood glucose target group had a higher rate of moderate hypoglycemia, both groups had a low rate of severe hypoglycemia, at 1.16% in the low target group and 0.35% in the moderate target group (P = .051).
Unadjusted 30-day mortality was significantly lower in the 80-110–mg/dL group compared with the 90-140–mg/dL group (4.3% vs. 9.2%, respectively; P less than .001), according to the investigators.
Furthermore, logistic regression analysis showed that patients treated with a target of 80-110 mg/dL had a lower risk of 30-day mortality compared with patients with a target of 90-140 mg/dL (odds ratio 0.65; 95% confidence interval, 0.43-0.98; P = .04).
These results advance the debate over appropriate blood glucose targets in critically ill patients, as they suggest that the effects of targeting blood glucose and the effects of severe hypoglycemia “can be separated,” the investigators wrote.
Current guidelines on intensive insulin therapy are based in part on findings of the NICE-SUGAR trial, which found that among adults treated in the ICU, intensive glucose control increased mortality. However, a post hoc analysis suggested the mortality increase in NICE-SUGAR was “largely driven by a significant incidence of moderate hypoglycemia, and to a greater degree severe hypoglycemia,” Dr. Hersh and his coauthors noted in their report.
“Given improvements in insulin delivery and glucose monitoring, a reassessment of potential benefits of [intensive insulin therapy] should once again be evaluated in a prospective randomized trial,” they wrote.
Dr. Hersh and his coauthors declared no financial or nonfinancial disclosures related to the study.
SOURCE: Hersh AM et al. CHEST 2018. doi: 10.1016/j.chest.2018.04.025.
compared with patients with a target of 90-140 mg/dL, according to results of a retrospective cohort analysis.
With the computerized intravenous insulin protocol used in the study, the strict target could be achieved with a low rate of hypoglycemia, the authors wrote. The analysis was published in the journal CHEST®.
However, it does raise the possibility that earlier investigations finding an association between intensive insulin therapy and excess mortality “may have been accurate only in the setting of technologies which led to high rates of severe hypoglycemia,” they wrote.
The retrospective cohort analysis by Dr. Hersh and his colleagues included 1,809 adult patients treated at three different ICUs in two hospitals between January 2010 and December 2015. Treatment was delivered with a computerized ICU insulin infusion protocol that allows clinicians to choose between two blood glucose targets: 80-110 mg/dL or 90-140 mg/dL. The lower target was chosen for 951 patients, and the moderate target for 858 patients.
The most common primary admission diagnoses in the cohort included chest pain or acute coronary syndrome in 43.3%, cardiothoracic surgery in 31.9%, heart failure (including cardiogenic shock) in 6.8%, and vascular surgery in 6.0%.
While patients in the low blood glucose target group had a higher rate of moderate hypoglycemia, both groups had a low rate of severe hypoglycemia, at 1.16% in the low target group and 0.35% in the moderate target group (P = .051).
Unadjusted 30-day mortality was significantly lower in the 80-110–mg/dL group compared with the 90-140–mg/dL group (4.3% vs. 9.2%, respectively; P less than .001), according to the investigators.
Furthermore, logistic regression analysis showed that patients treated with a target of 80-110 mg/dL had a lower risk of 30-day mortality compared with patients with a target of 90-140 mg/dL (odds ratio 0.65; 95% confidence interval, 0.43-0.98; P = .04).
These results advance the debate over appropriate blood glucose targets in critically ill patients, as they suggest that the effects of targeting blood glucose and the effects of severe hypoglycemia “can be separated,” the investigators wrote.
Current guidelines on intensive insulin therapy are based in part on findings of the NICE-SUGAR trial, which found that among adults treated in the ICU, intensive glucose control increased mortality. However, a post hoc analysis suggested the mortality increase in NICE-SUGAR was “largely driven by a significant incidence of moderate hypoglycemia, and to a greater degree severe hypoglycemia,” Dr. Hersh and his coauthors noted in their report.
“Given improvements in insulin delivery and glucose monitoring, a reassessment of potential benefits of [intensive insulin therapy] should once again be evaluated in a prospective randomized trial,” they wrote.
Dr. Hersh and his coauthors declared no financial or nonfinancial disclosures related to the study.
SOURCE: Hersh AM et al. CHEST 2018. doi: 10.1016/j.chest.2018.04.025.
compared with patients with a target of 90-140 mg/dL, according to results of a retrospective cohort analysis.
With the computerized intravenous insulin protocol used in the study, the strict target could be achieved with a low rate of hypoglycemia, the authors wrote. The analysis was published in the journal CHEST®.
However, it does raise the possibility that earlier investigations finding an association between intensive insulin therapy and excess mortality “may have been accurate only in the setting of technologies which led to high rates of severe hypoglycemia,” they wrote.
The retrospective cohort analysis by Dr. Hersh and his colleagues included 1,809 adult patients treated at three different ICUs in two hospitals between January 2010 and December 2015. Treatment was delivered with a computerized ICU insulin infusion protocol that allows clinicians to choose between two blood glucose targets: 80-110 mg/dL or 90-140 mg/dL. The lower target was chosen for 951 patients, and the moderate target for 858 patients.
The most common primary admission diagnoses in the cohort included chest pain or acute coronary syndrome in 43.3%, cardiothoracic surgery in 31.9%, heart failure (including cardiogenic shock) in 6.8%, and vascular surgery in 6.0%.
While patients in the low blood glucose target group had a higher rate of moderate hypoglycemia, both groups had a low rate of severe hypoglycemia, at 1.16% in the low target group and 0.35% in the moderate target group (P = .051).
Unadjusted 30-day mortality was significantly lower in the 80-110–mg/dL group compared with the 90-140–mg/dL group (4.3% vs. 9.2%, respectively; P less than .001), according to the investigators.
Furthermore, logistic regression analysis showed that patients treated with a target of 80-110 mg/dL had a lower risk of 30-day mortality compared with patients with a target of 90-140 mg/dL (odds ratio 0.65; 95% confidence interval, 0.43-0.98; P = .04).
These results advance the debate over appropriate blood glucose targets in critically ill patients, as they suggest that the effects of targeting blood glucose and the effects of severe hypoglycemia “can be separated,” the investigators wrote.
Current guidelines on intensive insulin therapy are based in part on findings of the NICE-SUGAR trial, which found that among adults treated in the ICU, intensive glucose control increased mortality. However, a post hoc analysis suggested the mortality increase in NICE-SUGAR was “largely driven by a significant incidence of moderate hypoglycemia, and to a greater degree severe hypoglycemia,” Dr. Hersh and his coauthors noted in their report.
“Given improvements in insulin delivery and glucose monitoring, a reassessment of potential benefits of [intensive insulin therapy] should once again be evaluated in a prospective randomized trial,” they wrote.
Dr. Hersh and his coauthors declared no financial or nonfinancial disclosures related to the study.
SOURCE: Hersh AM et al. CHEST 2018. doi: 10.1016/j.chest.2018.04.025.
FROM THE JOURNAL CHEST®
Key clinical point: Among critically ill cardiac and cardiothoracic patients, a lower glucose target was associated with improved 30-day mortality.
Major finding: Patients treated with a target of 80-110 mg/dL had a lower risk of 30-day mortality compared with patients with a target of 90-140 mg/dL (odds ratio 0.65; 95% confidence interval, 0.43-0.98; P = .04).
Study details: A retrospective cohort analysis of 1,809 adult patients treated at three ICUs from two hospitals between January 2010 and December 2015.
Disclosures: The authors declared no disclosures.
Source: Hersh AM et al. CHEST 2018. doi: 10.1016/j.chest.2018.04.025.
Novel, noninvasive skin cancer detection device shows promise
DALLAS – An investigational device that couples laser spectroscopy with a machine-learning algorithm demonstrated a high sensitivity and specificity for discriminating skin cancers from benign lesions in real time, results from a single-center study showed.
“More than 5.4 million cases of nonmelanoma skin cancer were treated in 2012, but the accuracy of skin cancer screening prior to biopsy is pretty low, about 70%, and is individual dependent,” lead study author Sung Hyun Pyun, PhD, said at the annual conference of the American Society for Laser Medicine and Surgery. “There have been several in vivo skin cancer screening devices based on noninvasive techniques such as multispectral imaging, Raman spectroscopy, and electrical impedance spectroscopy, but their diagnostic accuracies were not sufficient for clinical use and could not be applied in real time.”
For the single-site study, carried out in Australia, the researchers collected 502 emission spectra from skin cancers confirmed with biopsy results. They also collected 1,429 emission spectra from benign lesions. They achieved a sensitivity of 92% and a specificity of 90% out of 1,931 spectral data sets. No adverse events occurred and no microscopic damage of the irradiated skin was observed.
“Pathologic diagnosis-based cancer detection is considered to be time- and labor-consuming, and can sometimes be individual dependent,” Dr. Pyun said. “Our real-time, noninvasive, in vivo skin cancer detection device demonstrated a high sensitivity and specificity for discriminating skin cancers from benign lesions.” He added that the device could be helpful in office-based cancer screening and real-time, on-site cancer detection during skin cancer surgeries.
Larger, multicenter studies of the device are being planned. Dr. Pyun holds ownership interests with Speclipse, and is an employee of the company.
DALLAS – An investigational device that couples laser spectroscopy with a machine-learning algorithm demonstrated a high sensitivity and specificity for discriminating skin cancers from benign lesions in real time, results from a single-center study showed.
“More than 5.4 million cases of nonmelanoma skin cancer were treated in 2012, but the accuracy of skin cancer screening prior to biopsy is pretty low, about 70%, and is individual dependent,” lead study author Sung Hyun Pyun, PhD, said at the annual conference of the American Society for Laser Medicine and Surgery. “There have been several in vivo skin cancer screening devices based on noninvasive techniques such as multispectral imaging, Raman spectroscopy, and electrical impedance spectroscopy, but their diagnostic accuracies were not sufficient for clinical use and could not be applied in real time.”
For the single-site study, carried out in Australia, the researchers collected 502 emission spectra from skin cancers confirmed with biopsy results. They also collected 1,429 emission spectra from benign lesions. They achieved a sensitivity of 92% and a specificity of 90% out of 1,931 spectral data sets. No adverse events occurred and no microscopic damage of the irradiated skin was observed.
“Pathologic diagnosis-based cancer detection is considered to be time- and labor-consuming, and can sometimes be individual dependent,” Dr. Pyun said. “Our real-time, noninvasive, in vivo skin cancer detection device demonstrated a high sensitivity and specificity for discriminating skin cancers from benign lesions.” He added that the device could be helpful in office-based cancer screening and real-time, on-site cancer detection during skin cancer surgeries.
Larger, multicenter studies of the device are being planned. Dr. Pyun holds ownership interests with Speclipse, and is an employee of the company.
DALLAS – An investigational device that couples laser spectroscopy with a machine-learning algorithm demonstrated a high sensitivity and specificity for discriminating skin cancers from benign lesions in real time, results from a single-center study showed.
“More than 5.4 million cases of nonmelanoma skin cancer were treated in 2012, but the accuracy of skin cancer screening prior to biopsy is pretty low, about 70%, and is individual dependent,” lead study author Sung Hyun Pyun, PhD, said at the annual conference of the American Society for Laser Medicine and Surgery. “There have been several in vivo skin cancer screening devices based on noninvasive techniques such as multispectral imaging, Raman spectroscopy, and electrical impedance spectroscopy, but their diagnostic accuracies were not sufficient for clinical use and could not be applied in real time.”
For the single-site study, carried out in Australia, the researchers collected 502 emission spectra from skin cancers confirmed with biopsy results. They also collected 1,429 emission spectra from benign lesions. They achieved a sensitivity of 92% and a specificity of 90% out of 1,931 spectral data sets. No adverse events occurred and no microscopic damage of the irradiated skin was observed.
“Pathologic diagnosis-based cancer detection is considered to be time- and labor-consuming, and can sometimes be individual dependent,” Dr. Pyun said. “Our real-time, noninvasive, in vivo skin cancer detection device demonstrated a high sensitivity and specificity for discriminating skin cancers from benign lesions.” He added that the device could be helpful in office-based cancer screening and real-time, on-site cancer detection during skin cancer surgeries.
Larger, multicenter studies of the device are being planned. Dr. Pyun holds ownership interests with Speclipse, and is an employee of the company.
REPORTING FROM ASLMS 2018
Key clinical point: A novel device that uses spectroscopy and machine-learning algorithms was found to be a promising tool for the detection of skin cancer.
Major finding: Out of 1,931 spectral data sets, the device achieved a sensitivity of 92% and a specificity of 90%.
Study details: A single-center analysis of 502 emission spectra from skin cancers confirmed with biopsy results.
Disclosures: Dr. Pyun holds ownership interests with Speclipse and is an employee of the company.
Physicians voice concern over ibrutinib flat pricing
A group of oncologists is urging the Food and Drug Administration to review a new, flat-pricing strategy for all doses of ibrutinib (Imbruvica), calling the shift potentially dangerous for patients.
Pharmacyclics, an AbbVie company based in Sunnyvale, Calif., recently introduced a new, single-tablet formulation of ibrutinib in varying strengths (140 mg, 280 mg, 420 mg, and 560 mg) and set a flat price across all doses. At the same time, they removed the drug’s original 140-mg capsules – which cost about a third of the new, flat-rate price – from the market. The drug company says the new, single-tablet formulations give patients a convenient, once-a-day dosing regimen that could improve therapy adherence.
Ibrutinib is approved to treat a number of hematologic cancers, including mantle cell lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma, Waldenstrom macroglobulinemia, and marginal zone lymphoma.
But in an April letter published in the Cancer Letter, nine physicians from cancer centers across the country expressed concern that the new dosage and pricing scheme could compromise patient safety and limit doctors’ dosage decisions.
“While the prescribing information is complex, prescribers and patients have had the flexibility of taking anywhere from one to four 140-mg capsules, readily permitting dose reduction to all but the lowest labeled dose [70 mg],” the authors wrote. “However, the new formulation and its associated marketing scheme [YOU&i] greatly impact the ability of the prescriber and patient to follow the prescribing information, resulting in the potential for a greatly enhanced risk of toxicities relative to that observed in the clinical trials which utilized multiples of the 140-mg capsules.”
The problems stem from a cancer drug that often requires dosage adjustments, the authors noted. The specific dosage for an ibrutinib patient depends on the indication, prior toxicities, concomitant medications, occurrence of ibrutinib intolerance, and current hepatic function. Because of such diverse criteria, dosage modifications are made frequently.
The new pricing system makes it harder for physicians to adjust the dose without running afoul of insurers and potentially affecting access for patients.
“In order to ensure that all patients receive a single tablet rather than multiple 140-mg tablets, the manufacturer has priced all tablet strengths at the same price, so that a physician who wished to prescribe 420 mg as three 140-mg tablets would be unlikely to get payer approval to do so, since the cost would be 300% of the single 420-mg tablet,” the letter states. “Furthermore, patients who have been on a daily dose of 140 mg now find that the cost of their 140-mg tablet is more than threefold higher than the cost of their prior 140-mg capsule.”
Pharmacyclics – which jointly markets the drug with Janssen – defended the new pricing regimen, asserting that it was designed to help patients take their medication as prescribed.
“The price is based on the most widely prescribed and lower of the two FDA-approved dosages, which is 420 mg per day. While a patient’s out-of-pocket cost for Imbruvica is ultimately determined by their insurance plan, the vast majority of patients [i.e., patients taking 420-mg and 560-mg doses of Imbruvica] will likely see no increase in out-of-pocket costs when transitioning to the single-tablet formulation,” Pharmacyclics said in a statement. “In fact, current patients on the 560-mg dose will likely see a decrease in their out-of-pocket costs. Out-of-pocket expenses may increase for patients who are taking a lower dose of Imbruvica [140 mg or 280 mg].”
Pharmacyclics stressed that there is “extremely limited data” on the use of lower doses of the drug and said they do not know if lower doses will yield the same clinical outcomes.
The authors of the letter on the other hand, want the FDA to review the safety of the You&i program in the context of the approved drug label.
The FDA should take another look at ibrutinib and make some necessary changes, said letter coauthor Mark J. Ratain, MD, of the University of Chicago.
“The FDA should reconsider whether the drug can be prescribed as labeled,” Dr. Ratain said in an interview. “I would like to see the pricing changed to linear [constant $/mg] pricing, so that prescribers and patients can select the most appropriate strength.”
Brian T. Hill, MD, PhD, director of the Lymphoid Malignancies Program at the Cleveland Clinic’s Taussig Cancer Institute, prescribes ibrutinib fairly regularly. He was not involved in the drafting of the letter but said he supports the intent.
“This is a significant inconvenience and a potential problem for patients taking this medication because patients frequently require dosage modifications, typically dose reductions,” Dr. Hill said in an interview. “Having this new program in which the medication has to be exchanged for a single-tablet dose makes it much more difficult and onerous to make those changes.”
A group of oncologists is urging the Food and Drug Administration to review a new, flat-pricing strategy for all doses of ibrutinib (Imbruvica), calling the shift potentially dangerous for patients.
Pharmacyclics, an AbbVie company based in Sunnyvale, Calif., recently introduced a new, single-tablet formulation of ibrutinib in varying strengths (140 mg, 280 mg, 420 mg, and 560 mg) and set a flat price across all doses. At the same time, they removed the drug’s original 140-mg capsules – which cost about a third of the new, flat-rate price – from the market. The drug company says the new, single-tablet formulations give patients a convenient, once-a-day dosing regimen that could improve therapy adherence.
Ibrutinib is approved to treat a number of hematologic cancers, including mantle cell lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma, Waldenstrom macroglobulinemia, and marginal zone lymphoma.
But in an April letter published in the Cancer Letter, nine physicians from cancer centers across the country expressed concern that the new dosage and pricing scheme could compromise patient safety and limit doctors’ dosage decisions.
“While the prescribing information is complex, prescribers and patients have had the flexibility of taking anywhere from one to four 140-mg capsules, readily permitting dose reduction to all but the lowest labeled dose [70 mg],” the authors wrote. “However, the new formulation and its associated marketing scheme [YOU&i] greatly impact the ability of the prescriber and patient to follow the prescribing information, resulting in the potential for a greatly enhanced risk of toxicities relative to that observed in the clinical trials which utilized multiples of the 140-mg capsules.”
The problems stem from a cancer drug that often requires dosage adjustments, the authors noted. The specific dosage for an ibrutinib patient depends on the indication, prior toxicities, concomitant medications, occurrence of ibrutinib intolerance, and current hepatic function. Because of such diverse criteria, dosage modifications are made frequently.
The new pricing system makes it harder for physicians to adjust the dose without running afoul of insurers and potentially affecting access for patients.
“In order to ensure that all patients receive a single tablet rather than multiple 140-mg tablets, the manufacturer has priced all tablet strengths at the same price, so that a physician who wished to prescribe 420 mg as three 140-mg tablets would be unlikely to get payer approval to do so, since the cost would be 300% of the single 420-mg tablet,” the letter states. “Furthermore, patients who have been on a daily dose of 140 mg now find that the cost of their 140-mg tablet is more than threefold higher than the cost of their prior 140-mg capsule.”
Pharmacyclics – which jointly markets the drug with Janssen – defended the new pricing regimen, asserting that it was designed to help patients take their medication as prescribed.
“The price is based on the most widely prescribed and lower of the two FDA-approved dosages, which is 420 mg per day. While a patient’s out-of-pocket cost for Imbruvica is ultimately determined by their insurance plan, the vast majority of patients [i.e., patients taking 420-mg and 560-mg doses of Imbruvica] will likely see no increase in out-of-pocket costs when transitioning to the single-tablet formulation,” Pharmacyclics said in a statement. “In fact, current patients on the 560-mg dose will likely see a decrease in their out-of-pocket costs. Out-of-pocket expenses may increase for patients who are taking a lower dose of Imbruvica [140 mg or 280 mg].”
Pharmacyclics stressed that there is “extremely limited data” on the use of lower doses of the drug and said they do not know if lower doses will yield the same clinical outcomes.
The authors of the letter on the other hand, want the FDA to review the safety of the You&i program in the context of the approved drug label.
The FDA should take another look at ibrutinib and make some necessary changes, said letter coauthor Mark J. Ratain, MD, of the University of Chicago.
“The FDA should reconsider whether the drug can be prescribed as labeled,” Dr. Ratain said in an interview. “I would like to see the pricing changed to linear [constant $/mg] pricing, so that prescribers and patients can select the most appropriate strength.”
Brian T. Hill, MD, PhD, director of the Lymphoid Malignancies Program at the Cleveland Clinic’s Taussig Cancer Institute, prescribes ibrutinib fairly regularly. He was not involved in the drafting of the letter but said he supports the intent.
“This is a significant inconvenience and a potential problem for patients taking this medication because patients frequently require dosage modifications, typically dose reductions,” Dr. Hill said in an interview. “Having this new program in which the medication has to be exchanged for a single-tablet dose makes it much more difficult and onerous to make those changes.”
A group of oncologists is urging the Food and Drug Administration to review a new, flat-pricing strategy for all doses of ibrutinib (Imbruvica), calling the shift potentially dangerous for patients.
Pharmacyclics, an AbbVie company based in Sunnyvale, Calif., recently introduced a new, single-tablet formulation of ibrutinib in varying strengths (140 mg, 280 mg, 420 mg, and 560 mg) and set a flat price across all doses. At the same time, they removed the drug’s original 140-mg capsules – which cost about a third of the new, flat-rate price – from the market. The drug company says the new, single-tablet formulations give patients a convenient, once-a-day dosing regimen that could improve therapy adherence.
Ibrutinib is approved to treat a number of hematologic cancers, including mantle cell lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma, Waldenstrom macroglobulinemia, and marginal zone lymphoma.
But in an April letter published in the Cancer Letter, nine physicians from cancer centers across the country expressed concern that the new dosage and pricing scheme could compromise patient safety and limit doctors’ dosage decisions.
“While the prescribing information is complex, prescribers and patients have had the flexibility of taking anywhere from one to four 140-mg capsules, readily permitting dose reduction to all but the lowest labeled dose [70 mg],” the authors wrote. “However, the new formulation and its associated marketing scheme [YOU&i] greatly impact the ability of the prescriber and patient to follow the prescribing information, resulting in the potential for a greatly enhanced risk of toxicities relative to that observed in the clinical trials which utilized multiples of the 140-mg capsules.”
The problems stem from a cancer drug that often requires dosage adjustments, the authors noted. The specific dosage for an ibrutinib patient depends on the indication, prior toxicities, concomitant medications, occurrence of ibrutinib intolerance, and current hepatic function. Because of such diverse criteria, dosage modifications are made frequently.
The new pricing system makes it harder for physicians to adjust the dose without running afoul of insurers and potentially affecting access for patients.
“In order to ensure that all patients receive a single tablet rather than multiple 140-mg tablets, the manufacturer has priced all tablet strengths at the same price, so that a physician who wished to prescribe 420 mg as three 140-mg tablets would be unlikely to get payer approval to do so, since the cost would be 300% of the single 420-mg tablet,” the letter states. “Furthermore, patients who have been on a daily dose of 140 mg now find that the cost of their 140-mg tablet is more than threefold higher than the cost of their prior 140-mg capsule.”
Pharmacyclics – which jointly markets the drug with Janssen – defended the new pricing regimen, asserting that it was designed to help patients take their medication as prescribed.
“The price is based on the most widely prescribed and lower of the two FDA-approved dosages, which is 420 mg per day. While a patient’s out-of-pocket cost for Imbruvica is ultimately determined by their insurance plan, the vast majority of patients [i.e., patients taking 420-mg and 560-mg doses of Imbruvica] will likely see no increase in out-of-pocket costs when transitioning to the single-tablet formulation,” Pharmacyclics said in a statement. “In fact, current patients on the 560-mg dose will likely see a decrease in their out-of-pocket costs. Out-of-pocket expenses may increase for patients who are taking a lower dose of Imbruvica [140 mg or 280 mg].”
Pharmacyclics stressed that there is “extremely limited data” on the use of lower doses of the drug and said they do not know if lower doses will yield the same clinical outcomes.
The authors of the letter on the other hand, want the FDA to review the safety of the You&i program in the context of the approved drug label.
The FDA should take another look at ibrutinib and make some necessary changes, said letter coauthor Mark J. Ratain, MD, of the University of Chicago.
“The FDA should reconsider whether the drug can be prescribed as labeled,” Dr. Ratain said in an interview. “I would like to see the pricing changed to linear [constant $/mg] pricing, so that prescribers and patients can select the most appropriate strength.”
Brian T. Hill, MD, PhD, director of the Lymphoid Malignancies Program at the Cleveland Clinic’s Taussig Cancer Institute, prescribes ibrutinib fairly regularly. He was not involved in the drafting of the letter but said he supports the intent.
“This is a significant inconvenience and a potential problem for patients taking this medication because patients frequently require dosage modifications, typically dose reductions,” Dr. Hill said in an interview. “Having this new program in which the medication has to be exchanged for a single-tablet dose makes it much more difficult and onerous to make those changes.”
U.S. youth suicide prevention saved nearly 900 lives
WASHINGTON – A U.S. grant program that was started in 2004 to fund youth suicide prevention efforts throughout the country was linked with nearly 900 youth suicide deaths prevented by 2015, according to a matched, case-control analysis.
U.S. counties with a youth suicide prevention effort funded by a grant from the federal Garrett Lee Smith (GLS) Memorial Suicide Prevention program had an average 1.09 fewer youth suicide deaths per 100,000 youths (10-24 years old) 2 years after ongoing funding began, when compared with matched U.S. counties without a GLS-funded program, said Mr. Garraza, an analyst with ICF International in New York. Counties that had GLS-funded programs operating for 3 years showed an average reduction in youth suicide death of roughly 2 fewer deaths per 100,000 population, compared with control counties, and counties with programs in operation for 4 years showed a reduction of roughly 3 fewer deaths per 100,000 population.
“These extremely important data show convincingly that if we want to save lives, suicide prevention can’t be a one-and-done. said Richard McKeon, PhD, chief of the Suicide Prevention Branch of the Substance Abuse and Mental Health Services Administration, the U.S. agency that administers the GLS grant program and commissioned ICF International to analyze the grant program’s effects.
As of October 2017, the GLS grant initiative had made nearly 200 awards to youth suicide prevention programs that operated in all 50 states, the District of Columbia, one territory, and among 49 Native American tribes, Mr. Garraza said.
To assess the effects of the GLS grants on suicide death rates in people aged 10-24 years, Mr. Garraza and his associates used U.S. suicide data collected in 2,095 counties throughout the country that each had more than 3,000 resident youths, including 1,126 counties that had, as of 2015, been exposed to at least 1 year of a program sponsored by a GLS grant that began before 2010 and 969 counties without any GLS-grant exposure. After the counties in each subgroup were propensity-score matched using several criteria, including numbers of youth by specific age, race, household income, employment rates, health insurance status, and urbanization, the researchers analyzed suicide death rates in 481 counties with 1-4 years of exposure of a GLS-funded prevention program and in 851 counties with no exposure.
Their analysis estimated that 882 fewer suicide deaths occurred among youths in counties with GLS-funded programs, compared with the expected suicide mortality based on the unexposed counties.
In addition to showing statistically significant mortality reductions among youths in the counties with GLS-funded programs, compared with the counties with no such programs, the analysis showed, as expected, no difference between the intervention and control counties in rates of suicide deaths among adults and no difference in youth-mortality from causes other than suicide, which indicated that the observed differences linked with GLS funding were specific for youth suicides.
The current analysis looking at the effects of GLS funding on youth suicide deaths rates follows a prior report from the same researchers with similar findings using data collected through 2010 (Am J Public Health. 2015 May;105[5]:986-93). They also published two prior reports that used a similar analysis to assess the effects of GLS-funded suicide prevention programs on suicide attempt rates. One of those reports showed that GLS-funded programs linked with a cut in suicide attempts of nearly 5 per 1,000 population (JAMA Psychiatry. 2015 Nov;72[11]:1143-9), and the second showed that this effect on suicide attempts was cost effective when the cost of the grants was compared with the money saved from avoided emergency department visits and hospitalizations (Suicide Life Threat Behav. 2018 Feb;48[1]:3-11).
WASHINGTON – A U.S. grant program that was started in 2004 to fund youth suicide prevention efforts throughout the country was linked with nearly 900 youth suicide deaths prevented by 2015, according to a matched, case-control analysis.
U.S. counties with a youth suicide prevention effort funded by a grant from the federal Garrett Lee Smith (GLS) Memorial Suicide Prevention program had an average 1.09 fewer youth suicide deaths per 100,000 youths (10-24 years old) 2 years after ongoing funding began, when compared with matched U.S. counties without a GLS-funded program, said Mr. Garraza, an analyst with ICF International in New York. Counties that had GLS-funded programs operating for 3 years showed an average reduction in youth suicide death of roughly 2 fewer deaths per 100,000 population, compared with control counties, and counties with programs in operation for 4 years showed a reduction of roughly 3 fewer deaths per 100,000 population.
“These extremely important data show convincingly that if we want to save lives, suicide prevention can’t be a one-and-done. said Richard McKeon, PhD, chief of the Suicide Prevention Branch of the Substance Abuse and Mental Health Services Administration, the U.S. agency that administers the GLS grant program and commissioned ICF International to analyze the grant program’s effects.
As of October 2017, the GLS grant initiative had made nearly 200 awards to youth suicide prevention programs that operated in all 50 states, the District of Columbia, one territory, and among 49 Native American tribes, Mr. Garraza said.
To assess the effects of the GLS grants on suicide death rates in people aged 10-24 years, Mr. Garraza and his associates used U.S. suicide data collected in 2,095 counties throughout the country that each had more than 3,000 resident youths, including 1,126 counties that had, as of 2015, been exposed to at least 1 year of a program sponsored by a GLS grant that began before 2010 and 969 counties without any GLS-grant exposure. After the counties in each subgroup were propensity-score matched using several criteria, including numbers of youth by specific age, race, household income, employment rates, health insurance status, and urbanization, the researchers analyzed suicide death rates in 481 counties with 1-4 years of exposure of a GLS-funded prevention program and in 851 counties with no exposure.
Their analysis estimated that 882 fewer suicide deaths occurred among youths in counties with GLS-funded programs, compared with the expected suicide mortality based on the unexposed counties.
In addition to showing statistically significant mortality reductions among youths in the counties with GLS-funded programs, compared with the counties with no such programs, the analysis showed, as expected, no difference between the intervention and control counties in rates of suicide deaths among adults and no difference in youth-mortality from causes other than suicide, which indicated that the observed differences linked with GLS funding were specific for youth suicides.
The current analysis looking at the effects of GLS funding on youth suicide deaths rates follows a prior report from the same researchers with similar findings using data collected through 2010 (Am J Public Health. 2015 May;105[5]:986-93). They also published two prior reports that used a similar analysis to assess the effects of GLS-funded suicide prevention programs on suicide attempt rates. One of those reports showed that GLS-funded programs linked with a cut in suicide attempts of nearly 5 per 1,000 population (JAMA Psychiatry. 2015 Nov;72[11]:1143-9), and the second showed that this effect on suicide attempts was cost effective when the cost of the grants was compared with the money saved from avoided emergency department visits and hospitalizations (Suicide Life Threat Behav. 2018 Feb;48[1]:3-11).
WASHINGTON – A U.S. grant program that was started in 2004 to fund youth suicide prevention efforts throughout the country was linked with nearly 900 youth suicide deaths prevented by 2015, according to a matched, case-control analysis.
U.S. counties with a youth suicide prevention effort funded by a grant from the federal Garrett Lee Smith (GLS) Memorial Suicide Prevention program had an average 1.09 fewer youth suicide deaths per 100,000 youths (10-24 years old) 2 years after ongoing funding began, when compared with matched U.S. counties without a GLS-funded program, said Mr. Garraza, an analyst with ICF International in New York. Counties that had GLS-funded programs operating for 3 years showed an average reduction in youth suicide death of roughly 2 fewer deaths per 100,000 population, compared with control counties, and counties with programs in operation for 4 years showed a reduction of roughly 3 fewer deaths per 100,000 population.
“These extremely important data show convincingly that if we want to save lives, suicide prevention can’t be a one-and-done. said Richard McKeon, PhD, chief of the Suicide Prevention Branch of the Substance Abuse and Mental Health Services Administration, the U.S. agency that administers the GLS grant program and commissioned ICF International to analyze the grant program’s effects.
As of October 2017, the GLS grant initiative had made nearly 200 awards to youth suicide prevention programs that operated in all 50 states, the District of Columbia, one territory, and among 49 Native American tribes, Mr. Garraza said.
To assess the effects of the GLS grants on suicide death rates in people aged 10-24 years, Mr. Garraza and his associates used U.S. suicide data collected in 2,095 counties throughout the country that each had more than 3,000 resident youths, including 1,126 counties that had, as of 2015, been exposed to at least 1 year of a program sponsored by a GLS grant that began before 2010 and 969 counties without any GLS-grant exposure. After the counties in each subgroup were propensity-score matched using several criteria, including numbers of youth by specific age, race, household income, employment rates, health insurance status, and urbanization, the researchers analyzed suicide death rates in 481 counties with 1-4 years of exposure of a GLS-funded prevention program and in 851 counties with no exposure.
Their analysis estimated that 882 fewer suicide deaths occurred among youths in counties with GLS-funded programs, compared with the expected suicide mortality based on the unexposed counties.
In addition to showing statistically significant mortality reductions among youths in the counties with GLS-funded programs, compared with the counties with no such programs, the analysis showed, as expected, no difference between the intervention and control counties in rates of suicide deaths among adults and no difference in youth-mortality from causes other than suicide, which indicated that the observed differences linked with GLS funding were specific for youth suicides.
The current analysis looking at the effects of GLS funding on youth suicide deaths rates follows a prior report from the same researchers with similar findings using data collected through 2010 (Am J Public Health. 2015 May;105[5]:986-93). They also published two prior reports that used a similar analysis to assess the effects of GLS-funded suicide prevention programs on suicide attempt rates. One of those reports showed that GLS-funded programs linked with a cut in suicide attempts of nearly 5 per 1,000 population (JAMA Psychiatry. 2015 Nov;72[11]:1143-9), and the second showed that this effect on suicide attempts was cost effective when the cost of the grants was compared with the money saved from avoided emergency department visits and hospitalizations (Suicide Life Threat Behav. 2018 Feb;48[1]:3-11).
REPORTING FROM THE AAS ANNUAL CONFERENCE
Key clinical point: A U.S. youth suicide prevention grant program seems to be making a difference.
Major finding: During 2007-2015, U.S. counties with youth suicide prevention funding had 882 fewer deaths than expected.
Study details: A case-control analysis of U.S. counties that received federal funding for youth-suicide prevention.
Disclosures: Mr. Garraza and Dr. McKeon had no disclosures.
Novartis CAR T-cell therapy adds a lymphoma indication
Novartis’s after failure of two or more lines of systemic therapy.
The Food and Drug Administration approved the expanded indication on May 1. The chimeric antigen receptor (CAR) T-cell therapy was initially approved in Aug. 2017 for refractory or relapsed B-cell precursor acute lymphoblastic leukemia (ALL) in patients up to 25 years old. The new approval brings tisagenlecleucel into direct competition with Gilead Science’s CAR T-cell therapy axicabtagene ciloleucel (Yescarta), which was approved in Oct. 2017 for B-cell lymphoma.
Besides matching the competition, she said the lower price is because tisagenlecleucel takes longer to work for lymphoma, and the response isn’t as potent as for childhood ALL. Novartis is looking into chronic lymphocytic leukemia, multiple myeloma, and solid tumor indications for tisagenlecleucel and other CAR T-cell agents, she added.
The Centers for Medicare & Medicaid Services recently committed to covering outpatient administration of both agents for their initial indications; Novartis is working with CMS for coverage of the new lymphoma indication.
With both products, T cells are collected then shipped off to a company facility where a CAR gene is spliced into their DNA, essentially programming the T cells to attack the targeted cancer. The cells are then infused back into the patient.
In the phase 2 JULIET trial, tisagenlecleucel showed an overall response rate of 50% among 68 B-cell lymphoma patients, with 32% achieving complete response (CR) and 18% achieving partial response (PR). The median duration of response was not reached.
Axicabtagene ciloleucel’s label reports an objective response rate of 72% among 101 patients, with CR in 51% and PR in 21%. Median duration of response was 9.2 months but was also not reached among complete responders.
“Different trials. Different CARTs. Different levels of disease. Our drug is cryopreserved and theirs is not. No way to compare them,” the Novartis spokeswoman said when asked about the response differences.
T-cell reprogramming isn’t clean at this point in medical history; both agents carry black box warnings of potentially fatal cytokine release syndrome and neurologic toxicity, and both are subject to Risk Evaluation and Mitigation Strategy programs.
The B-cell lymphoma indication for both therapies includes diffuse large B-cell lymphoma (DLBCL), high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. The Gilead product carries an additional indication for primary mediastinal large B-cell lymphoma. Neither agent is indicated for primary central nervous system lymphoma. Both labels say that patients should not donate blood, organs, or tissues after treatment. Tisagenlecleucel labeling also notes that some commercial HIV nucleic acid tests may yield false positives after treatment.
Novartis said in a press release that T cells are treated at the company’s Morris Plains, N.J., facility with a turnaround time of about 22 days. Cryopreservation of the harvested cells gives providers some flexibility in treatment timing.
Novartis’s after failure of two or more lines of systemic therapy.
The Food and Drug Administration approved the expanded indication on May 1. The chimeric antigen receptor (CAR) T-cell therapy was initially approved in Aug. 2017 for refractory or relapsed B-cell precursor acute lymphoblastic leukemia (ALL) in patients up to 25 years old. The new approval brings tisagenlecleucel into direct competition with Gilead Science’s CAR T-cell therapy axicabtagene ciloleucel (Yescarta), which was approved in Oct. 2017 for B-cell lymphoma.
Besides matching the competition, she said the lower price is because tisagenlecleucel takes longer to work for lymphoma, and the response isn’t as potent as for childhood ALL. Novartis is looking into chronic lymphocytic leukemia, multiple myeloma, and solid tumor indications for tisagenlecleucel and other CAR T-cell agents, she added.
The Centers for Medicare & Medicaid Services recently committed to covering outpatient administration of both agents for their initial indications; Novartis is working with CMS for coverage of the new lymphoma indication.
With both products, T cells are collected then shipped off to a company facility where a CAR gene is spliced into their DNA, essentially programming the T cells to attack the targeted cancer. The cells are then infused back into the patient.
In the phase 2 JULIET trial, tisagenlecleucel showed an overall response rate of 50% among 68 B-cell lymphoma patients, with 32% achieving complete response (CR) and 18% achieving partial response (PR). The median duration of response was not reached.
Axicabtagene ciloleucel’s label reports an objective response rate of 72% among 101 patients, with CR in 51% and PR in 21%. Median duration of response was 9.2 months but was also not reached among complete responders.
“Different trials. Different CARTs. Different levels of disease. Our drug is cryopreserved and theirs is not. No way to compare them,” the Novartis spokeswoman said when asked about the response differences.
T-cell reprogramming isn’t clean at this point in medical history; both agents carry black box warnings of potentially fatal cytokine release syndrome and neurologic toxicity, and both are subject to Risk Evaluation and Mitigation Strategy programs.
The B-cell lymphoma indication for both therapies includes diffuse large B-cell lymphoma (DLBCL), high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. The Gilead product carries an additional indication for primary mediastinal large B-cell lymphoma. Neither agent is indicated for primary central nervous system lymphoma. Both labels say that patients should not donate blood, organs, or tissues after treatment. Tisagenlecleucel labeling also notes that some commercial HIV nucleic acid tests may yield false positives after treatment.
Novartis said in a press release that T cells are treated at the company’s Morris Plains, N.J., facility with a turnaround time of about 22 days. Cryopreservation of the harvested cells gives providers some flexibility in treatment timing.
Novartis’s after failure of two or more lines of systemic therapy.
The Food and Drug Administration approved the expanded indication on May 1. The chimeric antigen receptor (CAR) T-cell therapy was initially approved in Aug. 2017 for refractory or relapsed B-cell precursor acute lymphoblastic leukemia (ALL) in patients up to 25 years old. The new approval brings tisagenlecleucel into direct competition with Gilead Science’s CAR T-cell therapy axicabtagene ciloleucel (Yescarta), which was approved in Oct. 2017 for B-cell lymphoma.
Besides matching the competition, she said the lower price is because tisagenlecleucel takes longer to work for lymphoma, and the response isn’t as potent as for childhood ALL. Novartis is looking into chronic lymphocytic leukemia, multiple myeloma, and solid tumor indications for tisagenlecleucel and other CAR T-cell agents, she added.
The Centers for Medicare & Medicaid Services recently committed to covering outpatient administration of both agents for their initial indications; Novartis is working with CMS for coverage of the new lymphoma indication.
With both products, T cells are collected then shipped off to a company facility where a CAR gene is spliced into their DNA, essentially programming the T cells to attack the targeted cancer. The cells are then infused back into the patient.
In the phase 2 JULIET trial, tisagenlecleucel showed an overall response rate of 50% among 68 B-cell lymphoma patients, with 32% achieving complete response (CR) and 18% achieving partial response (PR). The median duration of response was not reached.
Axicabtagene ciloleucel’s label reports an objective response rate of 72% among 101 patients, with CR in 51% and PR in 21%. Median duration of response was 9.2 months but was also not reached among complete responders.
“Different trials. Different CARTs. Different levels of disease. Our drug is cryopreserved and theirs is not. No way to compare them,” the Novartis spokeswoman said when asked about the response differences.
T-cell reprogramming isn’t clean at this point in medical history; both agents carry black box warnings of potentially fatal cytokine release syndrome and neurologic toxicity, and both are subject to Risk Evaluation and Mitigation Strategy programs.
The B-cell lymphoma indication for both therapies includes diffuse large B-cell lymphoma (DLBCL), high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. The Gilead product carries an additional indication for primary mediastinal large B-cell lymphoma. Neither agent is indicated for primary central nervous system lymphoma. Both labels say that patients should not donate blood, organs, or tissues after treatment. Tisagenlecleucel labeling also notes that some commercial HIV nucleic acid tests may yield false positives after treatment.
Novartis said in a press release that T cells are treated at the company’s Morris Plains, N.J., facility with a turnaround time of about 22 days. Cryopreservation of the harvested cells gives providers some flexibility in treatment timing.
Deep Gray Matter Volume Loss May Drive Disability Worsening in MS
Deep gray matter volume loss drives disability accumulation in multiple sclerosis (MS), according to a multicenter, longitudinal study published in the February issue of Annals of Neurology.
The results “suggest that the development of deep gray matter atrophy may drive disability accumulation irrespective of clinical phenotypes, thereby becoming a useful outcome measure in neuroprotective clinical trials,” said Arman Eshaghi, MD, of the Queen Square MS Centre at the University College London Institute of Neurology, and colleagues.
Gray matter atrophy occurs in all MS phenotypes. To investigate whether a spatiotemporal pattern of gray matter atrophy is associated with faster disability accumulation in MS, the investigators analyzed 3,604 high-resolution T1-weighted MRI brain scans from 1,417 participants. The investigators retrospectively collected the scans from seven European centers in the MRI in MS (MAGNIMS) network.
The study included 253 patients with clinically isolated syndrome (CIS), 708 patients with relapsing-remitting MS, 128 patients with secondary progressive MS and 125 patients with primary progressive MS with an average follow-up of 2.41 years, as well as 203 healthy controls with an average follow-up of 1.83 years. The researchers assessed disability using the Expanded Disability Status Scale (EDSS). They obtained volumes of deep gray matter; temporal, frontal, parietal, occipital, and cerebellar gray matter; brainstem; and cerebral white matter. Hierarchical mixed models assessed annual percentage rate of regional tissue loss and identified regional volumes associated with time to EDSS progression.
Of all baseline regional volumes, only deep gray matter predicted time to EDSS progression. For every standard deviation decrease in baseline deep gray matter volume, the risk of having a shorter time to EDSS worsening during follow-up increased by 27%. Of all longitudinal measures, deep gray matter had the fastest annual rate of atrophy. This rate
—Jake Remaly
Suggested Reading
Eshaghi A, Prados F, Brownlee WJ, et al. Deep gray matter volume loss drives disability worsening in multiple sclerosis. Ann Neurol. 2018;83(2):210-222.
Deep gray matter volume loss drives disability accumulation in multiple sclerosis (MS), according to a multicenter, longitudinal study published in the February issue of Annals of Neurology.
The results “suggest that the development of deep gray matter atrophy may drive disability accumulation irrespective of clinical phenotypes, thereby becoming a useful outcome measure in neuroprotective clinical trials,” said Arman Eshaghi, MD, of the Queen Square MS Centre at the University College London Institute of Neurology, and colleagues.
Gray matter atrophy occurs in all MS phenotypes. To investigate whether a spatiotemporal pattern of gray matter atrophy is associated with faster disability accumulation in MS, the investigators analyzed 3,604 high-resolution T1-weighted MRI brain scans from 1,417 participants. The investigators retrospectively collected the scans from seven European centers in the MRI in MS (MAGNIMS) network.
The study included 253 patients with clinically isolated syndrome (CIS), 708 patients with relapsing-remitting MS, 128 patients with secondary progressive MS and 125 patients with primary progressive MS with an average follow-up of 2.41 years, as well as 203 healthy controls with an average follow-up of 1.83 years. The researchers assessed disability using the Expanded Disability Status Scale (EDSS). They obtained volumes of deep gray matter; temporal, frontal, parietal, occipital, and cerebellar gray matter; brainstem; and cerebral white matter. Hierarchical mixed models assessed annual percentage rate of regional tissue loss and identified regional volumes associated with time to EDSS progression.
Of all baseline regional volumes, only deep gray matter predicted time to EDSS progression. For every standard deviation decrease in baseline deep gray matter volume, the risk of having a shorter time to EDSS worsening during follow-up increased by 27%. Of all longitudinal measures, deep gray matter had the fastest annual rate of atrophy. This rate
—Jake Remaly
Suggested Reading
Eshaghi A, Prados F, Brownlee WJ, et al. Deep gray matter volume loss drives disability worsening in multiple sclerosis. Ann Neurol. 2018;83(2):210-222.
Deep gray matter volume loss drives disability accumulation in multiple sclerosis (MS), according to a multicenter, longitudinal study published in the February issue of Annals of Neurology.
The results “suggest that the development of deep gray matter atrophy may drive disability accumulation irrespective of clinical phenotypes, thereby becoming a useful outcome measure in neuroprotective clinical trials,” said Arman Eshaghi, MD, of the Queen Square MS Centre at the University College London Institute of Neurology, and colleagues.
Gray matter atrophy occurs in all MS phenotypes. To investigate whether a spatiotemporal pattern of gray matter atrophy is associated with faster disability accumulation in MS, the investigators analyzed 3,604 high-resolution T1-weighted MRI brain scans from 1,417 participants. The investigators retrospectively collected the scans from seven European centers in the MRI in MS (MAGNIMS) network.
The study included 253 patients with clinically isolated syndrome (CIS), 708 patients with relapsing-remitting MS, 128 patients with secondary progressive MS and 125 patients with primary progressive MS with an average follow-up of 2.41 years, as well as 203 healthy controls with an average follow-up of 1.83 years. The researchers assessed disability using the Expanded Disability Status Scale (EDSS). They obtained volumes of deep gray matter; temporal, frontal, parietal, occipital, and cerebellar gray matter; brainstem; and cerebral white matter. Hierarchical mixed models assessed annual percentage rate of regional tissue loss and identified regional volumes associated with time to EDSS progression.
Of all baseline regional volumes, only deep gray matter predicted time to EDSS progression. For every standard deviation decrease in baseline deep gray matter volume, the risk of having a shorter time to EDSS worsening during follow-up increased by 27%. Of all longitudinal measures, deep gray matter had the fastest annual rate of atrophy. This rate
—Jake Remaly
Suggested Reading
Eshaghi A, Prados F, Brownlee WJ, et al. Deep gray matter volume loss drives disability worsening in multiple sclerosis. Ann Neurol. 2018;83(2):210-222.
Heart disease in GPA exacts high toll in year 2 and beyond
LIVERPOOL, ENGLAND – Cardiovascular disease was the predominant cause of death of patients with granulomatosis with polyangiitis 1-5 years after a diagnosis in a study by U.K. researchers, suggesting that this could be a target for future intervention.
While active disease was the No. 1 cause of death within the first year of diagnosis in 40% of patients with granulomatosis with polyangiitis (GPA), it was overtaken by cardiovascular disease (CVD) as the main cause of death in 37.5% of patients in the next 4 years from diagnosis.
“The idea for this study came from patients with vasculitis who were polled by Vasculitis UK,” Fiona A. Pearce, MBBS, explained at the British Society for Rheumatology annual conference.
“Further research into mortality was one of their top priorities as patients want to know the honest truth about what is going to happen to them,” added Dr. Pearce, of the division of epidemiology and public health at the University of Nottingham (England).
GPA is a rare type of vasculitis that is estimated to occur in around 1,350 people every year in the United Kingdom. Mortality is known to be high, with around 11%-14% of patients dying in the first year of diagnosis, but there are few data on what happens over a longer term.
The aim of the study was therefore to examine patient survival in the long term – what were the mortality rates several years post diagnosis? Did the risk of death remain high throughout this time and did the causes of death change?
“Of course, the important clinical question was, “Can we then improve things?’ ” Dr. Pearce said.
Two U.K. databases – Clinical Practice Research Datalink and Hospital Episode Statistics – were used to identify patients with GPA diagnosed between 1998 and 2014 and match each case to 10 controls based on age, gender, and family practice. Data on the cause and date of any deaths were then obtained from the Office of National Statistics.
Overall, 465 cases of GPA were matched to 4,610 controls. The median age of participants was 61 years and 57% were male. There were 50 cases with more than 10 years of follow-up data available and data on 139 deaths could be analyzed.
A survival analysis showed that there was a significant reduction in cases versus controls, “but it’s not a constant,” Dr. Pearce noted.
“In the time immediately after diagnosis, the risk of death in people with GPA is very high, and over the first 6 months it tails off.” Then the mortalities are very similar, albeit much lower, to those of controls, but with another dip around 8 years.
The number at risk of death in the second year was 310 for GPA vs. 3,543 for controls and 230 vs. 2,622 at 4 years, 138 vs. 1,704 at 6 years, 93 vs. 1,136 at 8 years, and 49 vs. 658 at 10 years.
Looking at the data another way, the hazard ratios for death comparing GPA cases to controls was 24.5 in the first month, 14.6 in months 1-2, 7.5 by 2-3 months, 4.3 at 3-6 months, 1.6 at 6 months to 8 years, and 3.2 at 8-10 years.
Mortality seems to have improved with time. Splitting the cohort into two time periods based on their diagnosis, those diagnosed between 2008 and 2014 had a lower risk of death than did those diagnosed between 1998 and 2007, although it was still more than four times higher than the background population.
The leading cause of death in patients with GPA 5-10 years after diagnosis was cancer (30.3% of cases), but when this was compared against the general population, the risk was no greater (hazard ratio, 1.0).
GPA cases were also 2.9 times more likely than controls to die as a result of an infection, suggesting that this together with CVD could be a target for mortality reduction strategies.
“We can’t get away from the fact that although this is a large study, there are still small numbers of patients because this is rare disease,” Dr. Pearce observed. “We also don’t have detailed clinical information on each patient, so we can’t look for associations or clinical phenotypes at diagnosis, and there are no biomarkers.”
From a clinical perspective, she noted, it is important to remember that deaths in the first year are mainly from active disease and to continue to try to diagnose and treat the condition as early as possible.
Arthritis Research UK funded the trial. Dr. Pearce had nothing to disclose.
SOURCE: Pearce F et al. Rheumatology. 2018;57(Suppl. 3):key075.204.
LIVERPOOL, ENGLAND – Cardiovascular disease was the predominant cause of death of patients with granulomatosis with polyangiitis 1-5 years after a diagnosis in a study by U.K. researchers, suggesting that this could be a target for future intervention.
While active disease was the No. 1 cause of death within the first year of diagnosis in 40% of patients with granulomatosis with polyangiitis (GPA), it was overtaken by cardiovascular disease (CVD) as the main cause of death in 37.5% of patients in the next 4 years from diagnosis.
“The idea for this study came from patients with vasculitis who were polled by Vasculitis UK,” Fiona A. Pearce, MBBS, explained at the British Society for Rheumatology annual conference.
“Further research into mortality was one of their top priorities as patients want to know the honest truth about what is going to happen to them,” added Dr. Pearce, of the division of epidemiology and public health at the University of Nottingham (England).
GPA is a rare type of vasculitis that is estimated to occur in around 1,350 people every year in the United Kingdom. Mortality is known to be high, with around 11%-14% of patients dying in the first year of diagnosis, but there are few data on what happens over a longer term.
The aim of the study was therefore to examine patient survival in the long term – what were the mortality rates several years post diagnosis? Did the risk of death remain high throughout this time and did the causes of death change?
“Of course, the important clinical question was, “Can we then improve things?’ ” Dr. Pearce said.
Two U.K. databases – Clinical Practice Research Datalink and Hospital Episode Statistics – were used to identify patients with GPA diagnosed between 1998 and 2014 and match each case to 10 controls based on age, gender, and family practice. Data on the cause and date of any deaths were then obtained from the Office of National Statistics.
Overall, 465 cases of GPA were matched to 4,610 controls. The median age of participants was 61 years and 57% were male. There were 50 cases with more than 10 years of follow-up data available and data on 139 deaths could be analyzed.
A survival analysis showed that there was a significant reduction in cases versus controls, “but it’s not a constant,” Dr. Pearce noted.
“In the time immediately after diagnosis, the risk of death in people with GPA is very high, and over the first 6 months it tails off.” Then the mortalities are very similar, albeit much lower, to those of controls, but with another dip around 8 years.
The number at risk of death in the second year was 310 for GPA vs. 3,543 for controls and 230 vs. 2,622 at 4 years, 138 vs. 1,704 at 6 years, 93 vs. 1,136 at 8 years, and 49 vs. 658 at 10 years.
Looking at the data another way, the hazard ratios for death comparing GPA cases to controls was 24.5 in the first month, 14.6 in months 1-2, 7.5 by 2-3 months, 4.3 at 3-6 months, 1.6 at 6 months to 8 years, and 3.2 at 8-10 years.
Mortality seems to have improved with time. Splitting the cohort into two time periods based on their diagnosis, those diagnosed between 2008 and 2014 had a lower risk of death than did those diagnosed between 1998 and 2007, although it was still more than four times higher than the background population.
The leading cause of death in patients with GPA 5-10 years after diagnosis was cancer (30.3% of cases), but when this was compared against the general population, the risk was no greater (hazard ratio, 1.0).
GPA cases were also 2.9 times more likely than controls to die as a result of an infection, suggesting that this together with CVD could be a target for mortality reduction strategies.
“We can’t get away from the fact that although this is a large study, there are still small numbers of patients because this is rare disease,” Dr. Pearce observed. “We also don’t have detailed clinical information on each patient, so we can’t look for associations or clinical phenotypes at diagnosis, and there are no biomarkers.”
From a clinical perspective, she noted, it is important to remember that deaths in the first year are mainly from active disease and to continue to try to diagnose and treat the condition as early as possible.
Arthritis Research UK funded the trial. Dr. Pearce had nothing to disclose.
SOURCE: Pearce F et al. Rheumatology. 2018;57(Suppl. 3):key075.204.
LIVERPOOL, ENGLAND – Cardiovascular disease was the predominant cause of death of patients with granulomatosis with polyangiitis 1-5 years after a diagnosis in a study by U.K. researchers, suggesting that this could be a target for future intervention.
While active disease was the No. 1 cause of death within the first year of diagnosis in 40% of patients with granulomatosis with polyangiitis (GPA), it was overtaken by cardiovascular disease (CVD) as the main cause of death in 37.5% of patients in the next 4 years from diagnosis.
“The idea for this study came from patients with vasculitis who were polled by Vasculitis UK,” Fiona A. Pearce, MBBS, explained at the British Society for Rheumatology annual conference.
“Further research into mortality was one of their top priorities as patients want to know the honest truth about what is going to happen to them,” added Dr. Pearce, of the division of epidemiology and public health at the University of Nottingham (England).
GPA is a rare type of vasculitis that is estimated to occur in around 1,350 people every year in the United Kingdom. Mortality is known to be high, with around 11%-14% of patients dying in the first year of diagnosis, but there are few data on what happens over a longer term.
The aim of the study was therefore to examine patient survival in the long term – what were the mortality rates several years post diagnosis? Did the risk of death remain high throughout this time and did the causes of death change?
“Of course, the important clinical question was, “Can we then improve things?’ ” Dr. Pearce said.
Two U.K. databases – Clinical Practice Research Datalink and Hospital Episode Statistics – were used to identify patients with GPA diagnosed between 1998 and 2014 and match each case to 10 controls based on age, gender, and family practice. Data on the cause and date of any deaths were then obtained from the Office of National Statistics.
Overall, 465 cases of GPA were matched to 4,610 controls. The median age of participants was 61 years and 57% were male. There were 50 cases with more than 10 years of follow-up data available and data on 139 deaths could be analyzed.
A survival analysis showed that there was a significant reduction in cases versus controls, “but it’s not a constant,” Dr. Pearce noted.
“In the time immediately after diagnosis, the risk of death in people with GPA is very high, and over the first 6 months it tails off.” Then the mortalities are very similar, albeit much lower, to those of controls, but with another dip around 8 years.
The number at risk of death in the second year was 310 for GPA vs. 3,543 for controls and 230 vs. 2,622 at 4 years, 138 vs. 1,704 at 6 years, 93 vs. 1,136 at 8 years, and 49 vs. 658 at 10 years.
Looking at the data another way, the hazard ratios for death comparing GPA cases to controls was 24.5 in the first month, 14.6 in months 1-2, 7.5 by 2-3 months, 4.3 at 3-6 months, 1.6 at 6 months to 8 years, and 3.2 at 8-10 years.
Mortality seems to have improved with time. Splitting the cohort into two time periods based on their diagnosis, those diagnosed between 2008 and 2014 had a lower risk of death than did those diagnosed between 1998 and 2007, although it was still more than four times higher than the background population.
The leading cause of death in patients with GPA 5-10 years after diagnosis was cancer (30.3% of cases), but when this was compared against the general population, the risk was no greater (hazard ratio, 1.0).
GPA cases were also 2.9 times more likely than controls to die as a result of an infection, suggesting that this together with CVD could be a target for mortality reduction strategies.
“We can’t get away from the fact that although this is a large study, there are still small numbers of patients because this is rare disease,” Dr. Pearce observed. “We also don’t have detailed clinical information on each patient, so we can’t look for associations or clinical phenotypes at diagnosis, and there are no biomarkers.”
From a clinical perspective, she noted, it is important to remember that deaths in the first year are mainly from active disease and to continue to try to diagnose and treat the condition as early as possible.
Arthritis Research UK funded the trial. Dr. Pearce had nothing to disclose.
SOURCE: Pearce F et al. Rheumatology. 2018;57(Suppl. 3):key075.204.
REPORTING FROM RHEUMATOLOGY 2018
Key clinical point:
Major finding: The main cause of death changed from active disease (40% of all cases) within the first year to cardiovascular disease at years 1-5 (37.5%).
Study details: Retrospective cohort study of 465 individuals newly diagnosed with granulomatosis with polyangiitis matched to 4,610 controls from the general U.K. primary care population.
Disclosures: Arthritis Research UK funded the trial. Dr. Pearce had nothing to disclose.
Source: Pearce F et al. Rheumatology. 2018;57(Suppl. 3):key075.204.
Hospitalist movers and shakers – May 2018
Dr. Lenchus serves as the Society of Hospital Medicine’s Public Policy Committee chair. He is noted for his work as a clinician, hospital administrator, educator, and researcher.
J. Kevin Shushtari, MD, FHM, recently was named chief medical officer at the New Britain (Conn.) Hospital for Special Care, where he will focus on managing the medical staff, admissions, credentials, infection prevention, and clinical affiliations.
Tianzhong Yang, MD, has been selected as the new long-term care medical director for Van Dyk Healthcare in Montclair, N.J. Dr. Yang began his career 3 decades ago in China and has been a hospitalist at Hackensack University Medical Center Mountainside, also in Montclair, since 2013.
Dr. Yang has been an instructor at Brigham and Women’s Hospital in Boston, specializing in anesthesiology. At Van Dyk, he will work with the nursing staff to help patients recover their independence outside of the hospital setting.
Brent W. Burkey, MD, SFHM, a longtime hospitalist at the Cleveland Clinic, has been named the president of Fisher-Titus Medical Center in Norwalk, Ohio. Dr. Burkey has been the chief medical officer at the Cleveland Clinic’s Avon, Ohio, location the past 2 years. He helped the clinic open the Avon hospital in 2016 when he served as vice president of medical affairs.
Dr. Burkey has been a clinical hospitalist since 2004, and he has a master’s degree in business administration from Cleveland State University. He will run all hospital and medical center operations at Fisher-Titus, including quality and safety.
Dr. Maiona has extensive experience as a practicing hospital physician and as an executive. Most recently, he served as national medical director for TeamHealth of Knoxville, Tenn. He also has been an instructor at Tufts University and Harvard Medical School, both in Boston.
Tom Cummins, MD, has been appointed chief medical officer at Bon Secours St. Francis Health System in Greenville, S.C. Dr. Cummins comes to Bon Secours from Catholic Health Initiatives St. Vincent, Arkansas, where he was senior vice president and CMO; he also first served as a hospitalist within that system.
At Bon Secours, Dr. Cummins will oversee the regional health system’s 11 facilities, including St. Francis Downtown in Judson, S.C., and St. Francis Eastside in Greenville.
BUSINESS MOVES
The South Korean government recently announced that it has given permission for all general hospitals that use integrated nursing care to take part in a hospitalist system.
The Korean hospitalist program is a pilot in which those physicians provide all medical care for inpatients. It was adopted in September 2016, and 15 hospitals take part in the program. Prior to the recent ruling, those facilities with integrated nursing services were not eligible for the hospitalist program.
Surgical Affiliates (Sacramento, Calif.), a provider of surgical hospitalist services, has announced a partnership with Regional Medical Center in San Jose, Calif. The surgical hospitalists will assist and support local providers, providing 24/7 access to RMC of San Jose, a Level II trauma center.
Dr. Lenchus serves as the Society of Hospital Medicine’s Public Policy Committee chair. He is noted for his work as a clinician, hospital administrator, educator, and researcher.
J. Kevin Shushtari, MD, FHM, recently was named chief medical officer at the New Britain (Conn.) Hospital for Special Care, where he will focus on managing the medical staff, admissions, credentials, infection prevention, and clinical affiliations.
Tianzhong Yang, MD, has been selected as the new long-term care medical director for Van Dyk Healthcare in Montclair, N.J. Dr. Yang began his career 3 decades ago in China and has been a hospitalist at Hackensack University Medical Center Mountainside, also in Montclair, since 2013.
Dr. Yang has been an instructor at Brigham and Women’s Hospital in Boston, specializing in anesthesiology. At Van Dyk, he will work with the nursing staff to help patients recover their independence outside of the hospital setting.
Brent W. Burkey, MD, SFHM, a longtime hospitalist at the Cleveland Clinic, has been named the president of Fisher-Titus Medical Center in Norwalk, Ohio. Dr. Burkey has been the chief medical officer at the Cleveland Clinic’s Avon, Ohio, location the past 2 years. He helped the clinic open the Avon hospital in 2016 when he served as vice president of medical affairs.
Dr. Burkey has been a clinical hospitalist since 2004, and he has a master’s degree in business administration from Cleveland State University. He will run all hospital and medical center operations at Fisher-Titus, including quality and safety.
Dr. Maiona has extensive experience as a practicing hospital physician and as an executive. Most recently, he served as national medical director for TeamHealth of Knoxville, Tenn. He also has been an instructor at Tufts University and Harvard Medical School, both in Boston.
Tom Cummins, MD, has been appointed chief medical officer at Bon Secours St. Francis Health System in Greenville, S.C. Dr. Cummins comes to Bon Secours from Catholic Health Initiatives St. Vincent, Arkansas, where he was senior vice president and CMO; he also first served as a hospitalist within that system.
At Bon Secours, Dr. Cummins will oversee the regional health system’s 11 facilities, including St. Francis Downtown in Judson, S.C., and St. Francis Eastside in Greenville.
BUSINESS MOVES
The South Korean government recently announced that it has given permission for all general hospitals that use integrated nursing care to take part in a hospitalist system.
The Korean hospitalist program is a pilot in which those physicians provide all medical care for inpatients. It was adopted in September 2016, and 15 hospitals take part in the program. Prior to the recent ruling, those facilities with integrated nursing services were not eligible for the hospitalist program.
Surgical Affiliates (Sacramento, Calif.), a provider of surgical hospitalist services, has announced a partnership with Regional Medical Center in San Jose, Calif. The surgical hospitalists will assist and support local providers, providing 24/7 access to RMC of San Jose, a Level II trauma center.
Dr. Lenchus serves as the Society of Hospital Medicine’s Public Policy Committee chair. He is noted for his work as a clinician, hospital administrator, educator, and researcher.
J. Kevin Shushtari, MD, FHM, recently was named chief medical officer at the New Britain (Conn.) Hospital for Special Care, where he will focus on managing the medical staff, admissions, credentials, infection prevention, and clinical affiliations.
Tianzhong Yang, MD, has been selected as the new long-term care medical director for Van Dyk Healthcare in Montclair, N.J. Dr. Yang began his career 3 decades ago in China and has been a hospitalist at Hackensack University Medical Center Mountainside, also in Montclair, since 2013.
Dr. Yang has been an instructor at Brigham and Women’s Hospital in Boston, specializing in anesthesiology. At Van Dyk, he will work with the nursing staff to help patients recover their independence outside of the hospital setting.
Brent W. Burkey, MD, SFHM, a longtime hospitalist at the Cleveland Clinic, has been named the president of Fisher-Titus Medical Center in Norwalk, Ohio. Dr. Burkey has been the chief medical officer at the Cleveland Clinic’s Avon, Ohio, location the past 2 years. He helped the clinic open the Avon hospital in 2016 when he served as vice president of medical affairs.
Dr. Burkey has been a clinical hospitalist since 2004, and he has a master’s degree in business administration from Cleveland State University. He will run all hospital and medical center operations at Fisher-Titus, including quality and safety.
Dr. Maiona has extensive experience as a practicing hospital physician and as an executive. Most recently, he served as national medical director for TeamHealth of Knoxville, Tenn. He also has been an instructor at Tufts University and Harvard Medical School, both in Boston.
Tom Cummins, MD, has been appointed chief medical officer at Bon Secours St. Francis Health System in Greenville, S.C. Dr. Cummins comes to Bon Secours from Catholic Health Initiatives St. Vincent, Arkansas, where he was senior vice president and CMO; he also first served as a hospitalist within that system.
At Bon Secours, Dr. Cummins will oversee the regional health system’s 11 facilities, including St. Francis Downtown in Judson, S.C., and St. Francis Eastside in Greenville.
BUSINESS MOVES
The South Korean government recently announced that it has given permission for all general hospitals that use integrated nursing care to take part in a hospitalist system.
The Korean hospitalist program is a pilot in which those physicians provide all medical care for inpatients. It was adopted in September 2016, and 15 hospitals take part in the program. Prior to the recent ruling, those facilities with integrated nursing services were not eligible for the hospitalist program.
Surgical Affiliates (Sacramento, Calif.), a provider of surgical hospitalist services, has announced a partnership with Regional Medical Center in San Jose, Calif. The surgical hospitalists will assist and support local providers, providing 24/7 access to RMC of San Jose, a Level II trauma center.