User login
NAMDRC Update Collaboration: Now More Than Ever
Ongoing hospital mergers, acquisitions, and closings demonstrate that reimbursement maximization and cost reduction are the twin sisters of health-care system reform. This focus is not going to change in the foreseeable future, as most experts now view “health system reform” as “health financing reform.”
Reports document that more than 50% of acute care hospitals in the United States experienced negative operating margins for the federal fiscal year ending September 30, 2017. Equally alarming is the increasing number of organizations either reducing or eliminating the roles of medical directors for clinical departments. Hospital and health system executives are increasingly engaging external consultants to find ways to decrease operating costs, with the caveat of maintaining or improving quality, safety, and patient satisfaction and engagement.
Given these cost reduction pressures, what can respiratory therapy medical directors and administrative directors do to ensure that quality and safety are ensured?
We believe that quality and safety can be maintained and improved in this bottom-line-focused environment if we collaborate with stakeholders and communicate the value of respiratory care services. Following are some examples of how to reinvigorate this collaboration. The list is far from complete, but we believe it is a good starting point for making a significant difference.
Science
We recognize that much of our practice is based on levels of evidence, and we must use this evidence as a basis for our services.
In talking and working with RT administrative directors across the country, we continue to see non-value-added “treatments” being provided, such as incentive spirometry and aerosolized acetylcysteine. Not only is this a waste of resources, but, because of it, our clinical RTs are not providing therapy.
One of the best opportunities to decrease cost is to eliminate waste. These services must be eliminated. For those patients who require secretion clearance/lung expansion, we can provide evidence-based services such as oscillating positive expiratory pressure.
Protocols
Respiratory care protocols have been around for decades, but surveys indicate that only half of all RT departments utilize them. Under the guidance of NAMDRC, the AARC has been educating RTs to transition from “treatments” to evidence-based protocols. Various barriers remain, and our challenge remains to implement proven care plans in every department.
Quality Assurance
The health-care industry made the transition from “Quality Control” to “Quality Assurance” several decades ago. However, many RT administrative directors lack the knowledge and/or resources necessary to create a comprehensive QA program, much less participate in clinical research. We suggest creating a standardized model to be adopted by RT departments across the country that would measure and communicate the value of respiratory care services.
Productivity/Staffing
An area where consultants and executives often focus their cost-saving efforts is staffing. Given that 50% to 60% of operating costs are personnel, this is to be expected.
Many organizations, however, are using the wrong metrics—such as procedures, CPT codes , and billables—to project staffing FTEs. Physicians and RTs understand that these metrics are not useful and must convince consultants and executives of this. The AARC Uniform Reporting Manual, which is currently being updated, is the best guide for determining appropriate staffing.
Education
Another common step in cost control has been the significant reduction or total elimination of education budgets.
During the past 5 years, RT leaders attending the AARC Summer Forum have been polled regarding whether they received financial assistance to attend the Management Section program. Sadly, the number attending on their own dime far surpasses those receiving financial assistance.
Additionally, the RT profession is witnessing more department-based education, which, in some cases, is not education at all, but marketing, cleverly packaged in the form of CEUs.
We fully understand these changes and recognize why they have occurred. However, we suggest the need to work together to differentiate marketing from education and ensure that clinical staff receive what is needed to ensure quality care.
It is vital for us to educate our physician leaders and pulmonary and critical care fellows on the science of respiratory care. There is a significant knowledge gap, and we have a great opportunity to improve the training of fellows. It is difficult to attract active medical directors if they don’t understand the science. We believe NAMDRC can play an important role by addressing these knowledge deficits.
Ongoing hospital mergers, acquisitions, and closings demonstrate that reimbursement maximization and cost reduction are the twin sisters of health-care system reform. This focus is not going to change in the foreseeable future, as most experts now view “health system reform” as “health financing reform.”
Reports document that more than 50% of acute care hospitals in the United States experienced negative operating margins for the federal fiscal year ending September 30, 2017. Equally alarming is the increasing number of organizations either reducing or eliminating the roles of medical directors for clinical departments. Hospital and health system executives are increasingly engaging external consultants to find ways to decrease operating costs, with the caveat of maintaining or improving quality, safety, and patient satisfaction and engagement.
Given these cost reduction pressures, what can respiratory therapy medical directors and administrative directors do to ensure that quality and safety are ensured?
We believe that quality and safety can be maintained and improved in this bottom-line-focused environment if we collaborate with stakeholders and communicate the value of respiratory care services. Following are some examples of how to reinvigorate this collaboration. The list is far from complete, but we believe it is a good starting point for making a significant difference.
Science
We recognize that much of our practice is based on levels of evidence, and we must use this evidence as a basis for our services.
In talking and working with RT administrative directors across the country, we continue to see non-value-added “treatments” being provided, such as incentive spirometry and aerosolized acetylcysteine. Not only is this a waste of resources, but, because of it, our clinical RTs are not providing therapy.
One of the best opportunities to decrease cost is to eliminate waste. These services must be eliminated. For those patients who require secretion clearance/lung expansion, we can provide evidence-based services such as oscillating positive expiratory pressure.
Protocols
Respiratory care protocols have been around for decades, but surveys indicate that only half of all RT departments utilize them. Under the guidance of NAMDRC, the AARC has been educating RTs to transition from “treatments” to evidence-based protocols. Various barriers remain, and our challenge remains to implement proven care plans in every department.
Quality Assurance
The health-care industry made the transition from “Quality Control” to “Quality Assurance” several decades ago. However, many RT administrative directors lack the knowledge and/or resources necessary to create a comprehensive QA program, much less participate in clinical research. We suggest creating a standardized model to be adopted by RT departments across the country that would measure and communicate the value of respiratory care services.
Productivity/Staffing
An area where consultants and executives often focus their cost-saving efforts is staffing. Given that 50% to 60% of operating costs are personnel, this is to be expected.
Many organizations, however, are using the wrong metrics—such as procedures, CPT codes , and billables—to project staffing FTEs. Physicians and RTs understand that these metrics are not useful and must convince consultants and executives of this. The AARC Uniform Reporting Manual, which is currently being updated, is the best guide for determining appropriate staffing.
Education
Another common step in cost control has been the significant reduction or total elimination of education budgets.
During the past 5 years, RT leaders attending the AARC Summer Forum have been polled regarding whether they received financial assistance to attend the Management Section program. Sadly, the number attending on their own dime far surpasses those receiving financial assistance.
Additionally, the RT profession is witnessing more department-based education, which, in some cases, is not education at all, but marketing, cleverly packaged in the form of CEUs.
We fully understand these changes and recognize why they have occurred. However, we suggest the need to work together to differentiate marketing from education and ensure that clinical staff receive what is needed to ensure quality care.
It is vital for us to educate our physician leaders and pulmonary and critical care fellows on the science of respiratory care. There is a significant knowledge gap, and we have a great opportunity to improve the training of fellows. It is difficult to attract active medical directors if they don’t understand the science. We believe NAMDRC can play an important role by addressing these knowledge deficits.
Ongoing hospital mergers, acquisitions, and closings demonstrate that reimbursement maximization and cost reduction are the twin sisters of health-care system reform. This focus is not going to change in the foreseeable future, as most experts now view “health system reform” as “health financing reform.”
Reports document that more than 50% of acute care hospitals in the United States experienced negative operating margins for the federal fiscal year ending September 30, 2017. Equally alarming is the increasing number of organizations either reducing or eliminating the roles of medical directors for clinical departments. Hospital and health system executives are increasingly engaging external consultants to find ways to decrease operating costs, with the caveat of maintaining or improving quality, safety, and patient satisfaction and engagement.
Given these cost reduction pressures, what can respiratory therapy medical directors and administrative directors do to ensure that quality and safety are ensured?
We believe that quality and safety can be maintained and improved in this bottom-line-focused environment if we collaborate with stakeholders and communicate the value of respiratory care services. Following are some examples of how to reinvigorate this collaboration. The list is far from complete, but we believe it is a good starting point for making a significant difference.
Science
We recognize that much of our practice is based on levels of evidence, and we must use this evidence as a basis for our services.
In talking and working with RT administrative directors across the country, we continue to see non-value-added “treatments” being provided, such as incentive spirometry and aerosolized acetylcysteine. Not only is this a waste of resources, but, because of it, our clinical RTs are not providing therapy.
One of the best opportunities to decrease cost is to eliminate waste. These services must be eliminated. For those patients who require secretion clearance/lung expansion, we can provide evidence-based services such as oscillating positive expiratory pressure.
Protocols
Respiratory care protocols have been around for decades, but surveys indicate that only half of all RT departments utilize them. Under the guidance of NAMDRC, the AARC has been educating RTs to transition from “treatments” to evidence-based protocols. Various barriers remain, and our challenge remains to implement proven care plans in every department.
Quality Assurance
The health-care industry made the transition from “Quality Control” to “Quality Assurance” several decades ago. However, many RT administrative directors lack the knowledge and/or resources necessary to create a comprehensive QA program, much less participate in clinical research. We suggest creating a standardized model to be adopted by RT departments across the country that would measure and communicate the value of respiratory care services.
Productivity/Staffing
An area where consultants and executives often focus their cost-saving efforts is staffing. Given that 50% to 60% of operating costs are personnel, this is to be expected.
Many organizations, however, are using the wrong metrics—such as procedures, CPT codes , and billables—to project staffing FTEs. Physicians and RTs understand that these metrics are not useful and must convince consultants and executives of this. The AARC Uniform Reporting Manual, which is currently being updated, is the best guide for determining appropriate staffing.
Education
Another common step in cost control has been the significant reduction or total elimination of education budgets.
During the past 5 years, RT leaders attending the AARC Summer Forum have been polled regarding whether they received financial assistance to attend the Management Section program. Sadly, the number attending on their own dime far surpasses those receiving financial assistance.
Additionally, the RT profession is witnessing more department-based education, which, in some cases, is not education at all, but marketing, cleverly packaged in the form of CEUs.
We fully understand these changes and recognize why they have occurred. However, we suggest the need to work together to differentiate marketing from education and ensure that clinical staff receive what is needed to ensure quality care.
It is vital for us to educate our physician leaders and pulmonary and critical care fellows on the science of respiratory care. There is a significant knowledge gap, and we have a great opportunity to improve the training of fellows. It is difficult to attract active medical directors if they don’t understand the science. We believe NAMDRC can play an important role by addressing these knowledge deficits.
Office staff cohesiveness remains important
Recently, a lawyer and I were on the phone about a case, and he mentioned how lucky he was to have had the same staff over the course of a 25-year career, and he was afraid they’d retire before he did.
I feel the same way. My medical assistant has been with me since day one 18 years ago, my secretary since 2004. I hope they keep putting up with me until I hang up my reflex hammer.
It’s impossible to put a great team together just by talent alone. The chemistry and ability to work together are as critical as talent, if not more so, and are far more intangible and unpredictable.
I’ve been lucky that way. The three of us are cohesive. We try to keep some degree of fun in our work routine as each day goes on. My secretary’s 2-year-old daughter, who comes with her every day, adds to the family atmosphere that many patients notice. It’s not uncommon to be asked if the group of us are related. (We’re not.)
Back when I started out, it was with a large group that saw its people as replaceable, and treated them as such. As a result there was a high turnover rate of medical assistants and front office and clerical staff. This led to problems with work-flow and patient care, as there was always someone new being trained.
I can’t imagine having a better team than I have now, and will share this advice with anyone starting a practice: When you get the right people, count yourself lucky and do what you have to do to keep them. They’re worth it.
It’s a lot nicer to work with friends than strangers. It makes the drudgery of the job more interesting, the low points better, and the highs fun.
I wouldn’t have it any other way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, a lawyer and I were on the phone about a case, and he mentioned how lucky he was to have had the same staff over the course of a 25-year career, and he was afraid they’d retire before he did.
I feel the same way. My medical assistant has been with me since day one 18 years ago, my secretary since 2004. I hope they keep putting up with me until I hang up my reflex hammer.
It’s impossible to put a great team together just by talent alone. The chemistry and ability to work together are as critical as talent, if not more so, and are far more intangible and unpredictable.
I’ve been lucky that way. The three of us are cohesive. We try to keep some degree of fun in our work routine as each day goes on. My secretary’s 2-year-old daughter, who comes with her every day, adds to the family atmosphere that many patients notice. It’s not uncommon to be asked if the group of us are related. (We’re not.)
Back when I started out, it was with a large group that saw its people as replaceable, and treated them as such. As a result there was a high turnover rate of medical assistants and front office and clerical staff. This led to problems with work-flow and patient care, as there was always someone new being trained.
I can’t imagine having a better team than I have now, and will share this advice with anyone starting a practice: When you get the right people, count yourself lucky and do what you have to do to keep them. They’re worth it.
It’s a lot nicer to work with friends than strangers. It makes the drudgery of the job more interesting, the low points better, and the highs fun.
I wouldn’t have it any other way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, a lawyer and I were on the phone about a case, and he mentioned how lucky he was to have had the same staff over the course of a 25-year career, and he was afraid they’d retire before he did.
I feel the same way. My medical assistant has been with me since day one 18 years ago, my secretary since 2004. I hope they keep putting up with me until I hang up my reflex hammer.
It’s impossible to put a great team together just by talent alone. The chemistry and ability to work together are as critical as talent, if not more so, and are far more intangible and unpredictable.
I’ve been lucky that way. The three of us are cohesive. We try to keep some degree of fun in our work routine as each day goes on. My secretary’s 2-year-old daughter, who comes with her every day, adds to the family atmosphere that many patients notice. It’s not uncommon to be asked if the group of us are related. (We’re not.)
Back when I started out, it was with a large group that saw its people as replaceable, and treated them as such. As a result there was a high turnover rate of medical assistants and front office and clerical staff. This led to problems with work-flow and patient care, as there was always someone new being trained.
I can’t imagine having a better team than I have now, and will share this advice with anyone starting a practice: When you get the right people, count yourself lucky and do what you have to do to keep them. They’re worth it.
It’s a lot nicer to work with friends than strangers. It makes the drudgery of the job more interesting, the low points better, and the highs fun.
I wouldn’t have it any other way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Radial access PCI best for acute coronary syndrome patients
WASHINGTON – Radial access should be the preferred approach to percutaneous interventions in acute coronary syndromes in the United States as it is now in Europe, according to an investigator whose data from a randomized trial substudy was the topic of a late-breaker presentation at CRT 2018 sponsored by the Cardiovascular Research Institute at Washington Hospital Center..
It was not just these data, but “the totality of the evidence supports radial access as the first choice in PCI [percutaneous intervention] for acute coronary events,” asserted Elmir Omerovic, MD, professor of cardiology at Sahlgrenska University Hospital, Gothenburg, Sweden.
The data for the prespecified substudy was drawn from the VALIDATE-SWEDEHEART trial, published 6 months ago (N Engl J Med 2017;377:1132-42). In that trial, which randomized patients with ACS undergoing PCI to heparin or bivalirudin, there was no difference between anticoagulation strategies for the primary composite endpoint of death from any cause, myocardial infarction or bleeding from any cause.
Of the 6,006 randomized patients in that study, of which about half had an ST-elevation MI and half had a non–ST-elevation MI event, 5,424 (90%) underwent PCI by the radial route and the remainder by the femoral route. The goal of the prespecified subgroup analysis presented by Dr. Omerovic was to evaluate whether choice of access site had an impact on the primary endpoint or its components.
There was a 34% relative risk reduction (P less than .001) in the primary composite endpoint at the end of 180 days of follow-up “after adjusting basically for all of the important differences that might affect risk,” Dr. Omerovic reported. The long list included type of acute coronary syndrome, age, hypertension, diabetes, and history of vascular events or prior procedures.
Radial access was also linked with a 59% lower risk of mortality and a 43% lower risk of major bleeding (both P less than .001) when compared with femoral access, according to Dr. Omerovic. He attributed most of the difference in bleeding to bleeding events at the access site.
Baseline differences between the two groups indicated that patients undergoing PCI with femoral access were a higher-risk group. Femoral patients had higher rates of diabetes, hyperlipidemia, and hypertension (all P less than .001). They were also older, more likely to be in Killip class II or above, and more likely to have history of prior MI, prior stroke, and prior coronary artery bypass grafting (also all P less than .001).
Dr. Omerovic maintained that proper adjustment was made for these confounders. He also defended his conclusion that radial access should be preferred over femoral access by stressing that the data regarding this question, including those from other studies and from registries, are uniformly consistent. “They all go in the same direction,” he said.
Dr. Omerovic claimed that the key message is that “there should be more radial access performed in the United States.” The 90% radial access in this study is reflective of current practice in Sweden and most other European countries, according to Dr. Omerovic. In contrast, the U.S. rate is closer to 60% by some estimates.
“I would always be concerned that if you are performing radial access 90% of the time, you are going to lose your femoral skills,” Dr. Grines said. Like other U.S. interventionalists who commented during an animated discussion, she insisted that a prospective randomized trial, not a subgroup analysis, is needed before declaring radial access preferred.
Dr. Omerovic reports financial relationships with AstraZeneca, Bayer, and Boston Scientific.
SOURCE: Omerovic E. CRT 2018.
WASHINGTON – Radial access should be the preferred approach to percutaneous interventions in acute coronary syndromes in the United States as it is now in Europe, according to an investigator whose data from a randomized trial substudy was the topic of a late-breaker presentation at CRT 2018 sponsored by the Cardiovascular Research Institute at Washington Hospital Center..
It was not just these data, but “the totality of the evidence supports radial access as the first choice in PCI [percutaneous intervention] for acute coronary events,” asserted Elmir Omerovic, MD, professor of cardiology at Sahlgrenska University Hospital, Gothenburg, Sweden.
The data for the prespecified substudy was drawn from the VALIDATE-SWEDEHEART trial, published 6 months ago (N Engl J Med 2017;377:1132-42). In that trial, which randomized patients with ACS undergoing PCI to heparin or bivalirudin, there was no difference between anticoagulation strategies for the primary composite endpoint of death from any cause, myocardial infarction or bleeding from any cause.
Of the 6,006 randomized patients in that study, of which about half had an ST-elevation MI and half had a non–ST-elevation MI event, 5,424 (90%) underwent PCI by the radial route and the remainder by the femoral route. The goal of the prespecified subgroup analysis presented by Dr. Omerovic was to evaluate whether choice of access site had an impact on the primary endpoint or its components.
There was a 34% relative risk reduction (P less than .001) in the primary composite endpoint at the end of 180 days of follow-up “after adjusting basically for all of the important differences that might affect risk,” Dr. Omerovic reported. The long list included type of acute coronary syndrome, age, hypertension, diabetes, and history of vascular events or prior procedures.
Radial access was also linked with a 59% lower risk of mortality and a 43% lower risk of major bleeding (both P less than .001) when compared with femoral access, according to Dr. Omerovic. He attributed most of the difference in bleeding to bleeding events at the access site.
Baseline differences between the two groups indicated that patients undergoing PCI with femoral access were a higher-risk group. Femoral patients had higher rates of diabetes, hyperlipidemia, and hypertension (all P less than .001). They were also older, more likely to be in Killip class II or above, and more likely to have history of prior MI, prior stroke, and prior coronary artery bypass grafting (also all P less than .001).
Dr. Omerovic maintained that proper adjustment was made for these confounders. He also defended his conclusion that radial access should be preferred over femoral access by stressing that the data regarding this question, including those from other studies and from registries, are uniformly consistent. “They all go in the same direction,” he said.
Dr. Omerovic claimed that the key message is that “there should be more radial access performed in the United States.” The 90% radial access in this study is reflective of current practice in Sweden and most other European countries, according to Dr. Omerovic. In contrast, the U.S. rate is closer to 60% by some estimates.
“I would always be concerned that if you are performing radial access 90% of the time, you are going to lose your femoral skills,” Dr. Grines said. Like other U.S. interventionalists who commented during an animated discussion, she insisted that a prospective randomized trial, not a subgroup analysis, is needed before declaring radial access preferred.
Dr. Omerovic reports financial relationships with AstraZeneca, Bayer, and Boston Scientific.
SOURCE: Omerovic E. CRT 2018.
WASHINGTON – Radial access should be the preferred approach to percutaneous interventions in acute coronary syndromes in the United States as it is now in Europe, according to an investigator whose data from a randomized trial substudy was the topic of a late-breaker presentation at CRT 2018 sponsored by the Cardiovascular Research Institute at Washington Hospital Center..
It was not just these data, but “the totality of the evidence supports radial access as the first choice in PCI [percutaneous intervention] for acute coronary events,” asserted Elmir Omerovic, MD, professor of cardiology at Sahlgrenska University Hospital, Gothenburg, Sweden.
The data for the prespecified substudy was drawn from the VALIDATE-SWEDEHEART trial, published 6 months ago (N Engl J Med 2017;377:1132-42). In that trial, which randomized patients with ACS undergoing PCI to heparin or bivalirudin, there was no difference between anticoagulation strategies for the primary composite endpoint of death from any cause, myocardial infarction or bleeding from any cause.
Of the 6,006 randomized patients in that study, of which about half had an ST-elevation MI and half had a non–ST-elevation MI event, 5,424 (90%) underwent PCI by the radial route and the remainder by the femoral route. The goal of the prespecified subgroup analysis presented by Dr. Omerovic was to evaluate whether choice of access site had an impact on the primary endpoint or its components.
There was a 34% relative risk reduction (P less than .001) in the primary composite endpoint at the end of 180 days of follow-up “after adjusting basically for all of the important differences that might affect risk,” Dr. Omerovic reported. The long list included type of acute coronary syndrome, age, hypertension, diabetes, and history of vascular events or prior procedures.
Radial access was also linked with a 59% lower risk of mortality and a 43% lower risk of major bleeding (both P less than .001) when compared with femoral access, according to Dr. Omerovic. He attributed most of the difference in bleeding to bleeding events at the access site.
Baseline differences between the two groups indicated that patients undergoing PCI with femoral access were a higher-risk group. Femoral patients had higher rates of diabetes, hyperlipidemia, and hypertension (all P less than .001). They were also older, more likely to be in Killip class II or above, and more likely to have history of prior MI, prior stroke, and prior coronary artery bypass grafting (also all P less than .001).
Dr. Omerovic maintained that proper adjustment was made for these confounders. He also defended his conclusion that radial access should be preferred over femoral access by stressing that the data regarding this question, including those from other studies and from registries, are uniformly consistent. “They all go in the same direction,” he said.
Dr. Omerovic claimed that the key message is that “there should be more radial access performed in the United States.” The 90% radial access in this study is reflective of current practice in Sweden and most other European countries, according to Dr. Omerovic. In contrast, the U.S. rate is closer to 60% by some estimates.
“I would always be concerned that if you are performing radial access 90% of the time, you are going to lose your femoral skills,” Dr. Grines said. Like other U.S. interventionalists who commented during an animated discussion, she insisted that a prospective randomized trial, not a subgroup analysis, is needed before declaring radial access preferred.
Dr. Omerovic reports financial relationships with AstraZeneca, Bayer, and Boston Scientific.
SOURCE: Omerovic E. CRT 2018.
REPORTING FROM THE 2018 CRT MEETING
Key clinical point:
Major finding: At 180 days, the risk of major cardiac events was 34% lower for PCI performed with radial than with femoral access after risk adjustment.
Data source: Prespecified subgroup analysis of a randomized trial.
Disclosures: Dr. Omerovic reports financial relationships with AstraZeneca, Bayer, and Boston Scientific.
Source: Omerovic E. CRT 2018.
Ultrasound study supports deep Koebner mechanism in PsA pathology
An ultrasonographic study describing the greater presence of thicker digital accessory pulleys in patients with psoriatic arthritis (PsA) than in those with only psoriatic skin disease, rheumatoid arthritis, or no pathology has lent more evidence for a “deep Koebner” response mechanism in the development of joint disease in people with psoriasis.
“The thicker pulleys in RA compared with HCs [healthy controls] might point towards a nonspecific effect of a chronic autoimmune tenosynovitis on the adjacent pulleys,” Ilaria Tinazzi, PhD, of the Sacro Cuore-Don Calabria Hospital, Verona, Italy, and her colleagues wrote in Annals of the Rheumatic Diseases. “However, the greater magnitude of pulley thickening in PsA, especially in the setting of dactylitis, suggests an intrinsic pathology in the pulley contributing to PsA-related tenosynovitis.”
Dr. Tinazzi and her research team found that the pulleys in patients with PsA were thicker in every digit than they were in patients with RA and healthy controls, but pulley thickness also differed for each group of patients when compared with one another. Patients with RA had thicker pulleys than did healthy controls, particularly in the A1 pulley, but showed no differences in the A2 and A4 pulleys of the second and fourth digit. Even patients with only psoriasis had thicker pulleys than did the healthy controls. Patients with PsA exhibited thicker A1 and A4 pulleys, compared with patients with only psoriasis, while A2 pulleys displayed no statistical difference. Among PsA patients, 165 of 243 (68%) pulleys were thickened, whereas only 41 of 243 (17%) were thickened among RA patients (P less than .001). A multiple-regression analysis revealed that only PsA was associated with the number of thickened pulleys (odds ratio, 4.8; 95% confidence interval, 3.3-6.3; P = .001).
The size of the study population and the method for defining pulley thickness limited the study. Measurements were taken only in three digits of the dominant hand of each patient. Among PsA patients, only those with hand involvement participated in the study, which may limit the translation of the results to all PsA patients. Additionally, whether pulley changes trigger PsA tenosynovitis or whether it is a reactive process needs additional investigation.
The results of the study suggest that accessory pulleys are subjected to high physical stress and that they exhibit deep Koebner effects and thicken in response, Dr. Tinazzi and her associates wrote.
“Indeed, these findings suggest that such a mechanism is possible given the frequency of thickening of these structures in PsA” wrote Dr. Tinazzi and her associates. “It will be important to show that such changes are present in early PsA where their presence would support the idea of early biomechanical alterations in tendon function that could contribute to dactylitic tenosynovitis.”
This study received no external funding. Several of the researchers have received grants or honoraria from pharmaceutical companies.
SOURCE: Tinazzi I et al. Ann Rheum Dis. 2018 Mar 6. doi: 10.1136/annrheumdis-2017-212681.
An ultrasonographic study describing the greater presence of thicker digital accessory pulleys in patients with psoriatic arthritis (PsA) than in those with only psoriatic skin disease, rheumatoid arthritis, or no pathology has lent more evidence for a “deep Koebner” response mechanism in the development of joint disease in people with psoriasis.
“The thicker pulleys in RA compared with HCs [healthy controls] might point towards a nonspecific effect of a chronic autoimmune tenosynovitis on the adjacent pulleys,” Ilaria Tinazzi, PhD, of the Sacro Cuore-Don Calabria Hospital, Verona, Italy, and her colleagues wrote in Annals of the Rheumatic Diseases. “However, the greater magnitude of pulley thickening in PsA, especially in the setting of dactylitis, suggests an intrinsic pathology in the pulley contributing to PsA-related tenosynovitis.”
Dr. Tinazzi and her research team found that the pulleys in patients with PsA were thicker in every digit than they were in patients with RA and healthy controls, but pulley thickness also differed for each group of patients when compared with one another. Patients with RA had thicker pulleys than did healthy controls, particularly in the A1 pulley, but showed no differences in the A2 and A4 pulleys of the second and fourth digit. Even patients with only psoriasis had thicker pulleys than did the healthy controls. Patients with PsA exhibited thicker A1 and A4 pulleys, compared with patients with only psoriasis, while A2 pulleys displayed no statistical difference. Among PsA patients, 165 of 243 (68%) pulleys were thickened, whereas only 41 of 243 (17%) were thickened among RA patients (P less than .001). A multiple-regression analysis revealed that only PsA was associated with the number of thickened pulleys (odds ratio, 4.8; 95% confidence interval, 3.3-6.3; P = .001).
The size of the study population and the method for defining pulley thickness limited the study. Measurements were taken only in three digits of the dominant hand of each patient. Among PsA patients, only those with hand involvement participated in the study, which may limit the translation of the results to all PsA patients. Additionally, whether pulley changes trigger PsA tenosynovitis or whether it is a reactive process needs additional investigation.
The results of the study suggest that accessory pulleys are subjected to high physical stress and that they exhibit deep Koebner effects and thicken in response, Dr. Tinazzi and her associates wrote.
“Indeed, these findings suggest that such a mechanism is possible given the frequency of thickening of these structures in PsA” wrote Dr. Tinazzi and her associates. “It will be important to show that such changes are present in early PsA where their presence would support the idea of early biomechanical alterations in tendon function that could contribute to dactylitic tenosynovitis.”
This study received no external funding. Several of the researchers have received grants or honoraria from pharmaceutical companies.
SOURCE: Tinazzi I et al. Ann Rheum Dis. 2018 Mar 6. doi: 10.1136/annrheumdis-2017-212681.
An ultrasonographic study describing the greater presence of thicker digital accessory pulleys in patients with psoriatic arthritis (PsA) than in those with only psoriatic skin disease, rheumatoid arthritis, or no pathology has lent more evidence for a “deep Koebner” response mechanism in the development of joint disease in people with psoriasis.
“The thicker pulleys in RA compared with HCs [healthy controls] might point towards a nonspecific effect of a chronic autoimmune tenosynovitis on the adjacent pulleys,” Ilaria Tinazzi, PhD, of the Sacro Cuore-Don Calabria Hospital, Verona, Italy, and her colleagues wrote in Annals of the Rheumatic Diseases. “However, the greater magnitude of pulley thickening in PsA, especially in the setting of dactylitis, suggests an intrinsic pathology in the pulley contributing to PsA-related tenosynovitis.”
Dr. Tinazzi and her research team found that the pulleys in patients with PsA were thicker in every digit than they were in patients with RA and healthy controls, but pulley thickness also differed for each group of patients when compared with one another. Patients with RA had thicker pulleys than did healthy controls, particularly in the A1 pulley, but showed no differences in the A2 and A4 pulleys of the second and fourth digit. Even patients with only psoriasis had thicker pulleys than did the healthy controls. Patients with PsA exhibited thicker A1 and A4 pulleys, compared with patients with only psoriasis, while A2 pulleys displayed no statistical difference. Among PsA patients, 165 of 243 (68%) pulleys were thickened, whereas only 41 of 243 (17%) were thickened among RA patients (P less than .001). A multiple-regression analysis revealed that only PsA was associated with the number of thickened pulleys (odds ratio, 4.8; 95% confidence interval, 3.3-6.3; P = .001).
The size of the study population and the method for defining pulley thickness limited the study. Measurements were taken only in three digits of the dominant hand of each patient. Among PsA patients, only those with hand involvement participated in the study, which may limit the translation of the results to all PsA patients. Additionally, whether pulley changes trigger PsA tenosynovitis or whether it is a reactive process needs additional investigation.
The results of the study suggest that accessory pulleys are subjected to high physical stress and that they exhibit deep Koebner effects and thicken in response, Dr. Tinazzi and her associates wrote.
“Indeed, these findings suggest that such a mechanism is possible given the frequency of thickening of these structures in PsA” wrote Dr. Tinazzi and her associates. “It will be important to show that such changes are present in early PsA where their presence would support the idea of early biomechanical alterations in tendon function that could contribute to dactylitic tenosynovitis.”
This study received no external funding. Several of the researchers have received grants or honoraria from pharmaceutical companies.
SOURCE: Tinazzi I et al. Ann Rheum Dis. 2018 Mar 6. doi: 10.1136/annrheumdis-2017-212681.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: Patients with psoriatic arthritis have thicker accessory pulleys in their digits than do those with rheumatoid arthritis, psoriasis only, or no inflammatory rheumatologic disease.
Major finding: More accessory pulleys were thickened in the PsA group than in the rheumatoid arthritis group (68% vs. 17%; P less than .001).
Study details: An ultrasonographic study of digital pulley thickness in 96 patients with PsA, RA, psoriasis only, or no inflammatory rheumatologic disease.
Disclosures: This study received no external funding. Several of the researchers have received grants or honoraria from pharmaceutical companies.
Source: Tinazzi I et al. Ann Rheum Dis. 2018 Mar 6. doi: 10.1136/annrheumdis-2017-212681.
Turning Up the Heat on ICU Burnout
The work of critical care clinicians can create a perfect storm for emotional exhaustion, depersonalization, and reduced self-efficacy – widely known as burnout. Burnout is occurring in record numbers among physicians in general – more than twice as frequently as for non-health-care workers – and intensivists top the chart. Clinicians from all specialties in medicine today experience the frustrations of workplace chaos and loss of control, displacement of meaningful work with menial work, and ever increasing documentation requirements and electronic health record challenges – all contributing to burnout. Intensivists and other ICU professionals, such as advanced practice providers and nurses, however, experience the added challenge of working in a highly stressful environment characterized by fast-paced high-stakes decision making, long and irregular hours, and end-of-life scenarios often clouded by moral distress. These and other drivers contribute to high rates of burnout.
Being burned out takes its toll on health-care workers, contributing to psychological and physical manifestations, alcohol or substance abuse, posttraumatic stress disorder, and even suicidal ideation. Additionally, burnout carries important negative consequences for the organization and directly to the patient, including higher rates of employee turnover, lower quality of work, more medical errors, and reduced patient satisfaction. Unfortunately, burnout rates continue to rise with alarming speed.
Fortunately, there is increasing attention paid to the magnitude and potential impact of burnout, compelling important organizations to highlight the problem and assist clinicians in combating burnout and its consequences. For example, the National Academy of Medicine (NAM) has convened an Action Collaborative on Clinician Well-Being and Resilience and invited more than 100 organizations to publish their statement of commitment to improve clinician well-being and reduce clinician burnout (https://nam.edu/initiatives/clinician-resilience-and-well-being/). The American Medical Association (AMA) has developed modules and tools to assist clinicians and administrators in taking important steps to prevent burnout (https://www.stepsforward.org/modules/physician-burnout).
CHEST has been an active participant in addressing burnout in ICU professionals, including in an important partnership with the American Association of Critical-Care Nurses (AACN), the American Thoracic Society (ATS), and the Society of Critical Care Medicine (SCCM) - the Critical Care Societies Collaborative (CCSC). The CCSC, whose members include greater than 150,000 critical care professionals in the United States, has established a principle goal of mitigating ICU burnout (#StopICUBurnout). One of the first CCSC efforts was to publish a white paper simultaneously in all four journals of the CCSC professional societies that provides the rationale and direction for a “call for action” to tackle ICU burnout (Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. Burnout syndrome in critical care health care professionals: A call for action. Chest. 2016;150[1]:17). Recently, the CCSC sponsored a National Summit on the Prevention and Management of Burnout in the ICU (http://ccsconline.org/optimizing-the-workforce/burnout). Fifty-five invited participants brought wide ranging expertise and substantial enthusiasm to the task of deconstructing ICU burnout and identifying knowledge gaps and future directions. Areas of focused discussion included factors influencing burnout, identifying individuals with burnout, the value of organizational and individual interventions to prevent and manage burnout, and translation of these discussions into a research agenda. CHEST and the CCSC are committed to the goals of enhancing clinician well-being and eliminating burnout in the ICU.
The work of critical care clinicians can create a perfect storm for emotional exhaustion, depersonalization, and reduced self-efficacy – widely known as burnout. Burnout is occurring in record numbers among physicians in general – more than twice as frequently as for non-health-care workers – and intensivists top the chart. Clinicians from all specialties in medicine today experience the frustrations of workplace chaos and loss of control, displacement of meaningful work with menial work, and ever increasing documentation requirements and electronic health record challenges – all contributing to burnout. Intensivists and other ICU professionals, such as advanced practice providers and nurses, however, experience the added challenge of working in a highly stressful environment characterized by fast-paced high-stakes decision making, long and irregular hours, and end-of-life scenarios often clouded by moral distress. These and other drivers contribute to high rates of burnout.
Being burned out takes its toll on health-care workers, contributing to psychological and physical manifestations, alcohol or substance abuse, posttraumatic stress disorder, and even suicidal ideation. Additionally, burnout carries important negative consequences for the organization and directly to the patient, including higher rates of employee turnover, lower quality of work, more medical errors, and reduced patient satisfaction. Unfortunately, burnout rates continue to rise with alarming speed.
Fortunately, there is increasing attention paid to the magnitude and potential impact of burnout, compelling important organizations to highlight the problem and assist clinicians in combating burnout and its consequences. For example, the National Academy of Medicine (NAM) has convened an Action Collaborative on Clinician Well-Being and Resilience and invited more than 100 organizations to publish their statement of commitment to improve clinician well-being and reduce clinician burnout (https://nam.edu/initiatives/clinician-resilience-and-well-being/). The American Medical Association (AMA) has developed modules and tools to assist clinicians and administrators in taking important steps to prevent burnout (https://www.stepsforward.org/modules/physician-burnout).
CHEST has been an active participant in addressing burnout in ICU professionals, including in an important partnership with the American Association of Critical-Care Nurses (AACN), the American Thoracic Society (ATS), and the Society of Critical Care Medicine (SCCM) - the Critical Care Societies Collaborative (CCSC). The CCSC, whose members include greater than 150,000 critical care professionals in the United States, has established a principle goal of mitigating ICU burnout (#StopICUBurnout). One of the first CCSC efforts was to publish a white paper simultaneously in all four journals of the CCSC professional societies that provides the rationale and direction for a “call for action” to tackle ICU burnout (Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. Burnout syndrome in critical care health care professionals: A call for action. Chest. 2016;150[1]:17). Recently, the CCSC sponsored a National Summit on the Prevention and Management of Burnout in the ICU (http://ccsconline.org/optimizing-the-workforce/burnout). Fifty-five invited participants brought wide ranging expertise and substantial enthusiasm to the task of deconstructing ICU burnout and identifying knowledge gaps and future directions. Areas of focused discussion included factors influencing burnout, identifying individuals with burnout, the value of organizational and individual interventions to prevent and manage burnout, and translation of these discussions into a research agenda. CHEST and the CCSC are committed to the goals of enhancing clinician well-being and eliminating burnout in the ICU.
The work of critical care clinicians can create a perfect storm for emotional exhaustion, depersonalization, and reduced self-efficacy – widely known as burnout. Burnout is occurring in record numbers among physicians in general – more than twice as frequently as for non-health-care workers – and intensivists top the chart. Clinicians from all specialties in medicine today experience the frustrations of workplace chaos and loss of control, displacement of meaningful work with menial work, and ever increasing documentation requirements and electronic health record challenges – all contributing to burnout. Intensivists and other ICU professionals, such as advanced practice providers and nurses, however, experience the added challenge of working in a highly stressful environment characterized by fast-paced high-stakes decision making, long and irregular hours, and end-of-life scenarios often clouded by moral distress. These and other drivers contribute to high rates of burnout.
Being burned out takes its toll on health-care workers, contributing to psychological and physical manifestations, alcohol or substance abuse, posttraumatic stress disorder, and even suicidal ideation. Additionally, burnout carries important negative consequences for the organization and directly to the patient, including higher rates of employee turnover, lower quality of work, more medical errors, and reduced patient satisfaction. Unfortunately, burnout rates continue to rise with alarming speed.
Fortunately, there is increasing attention paid to the magnitude and potential impact of burnout, compelling important organizations to highlight the problem and assist clinicians in combating burnout and its consequences. For example, the National Academy of Medicine (NAM) has convened an Action Collaborative on Clinician Well-Being and Resilience and invited more than 100 organizations to publish their statement of commitment to improve clinician well-being and reduce clinician burnout (https://nam.edu/initiatives/clinician-resilience-and-well-being/). The American Medical Association (AMA) has developed modules and tools to assist clinicians and administrators in taking important steps to prevent burnout (https://www.stepsforward.org/modules/physician-burnout).
CHEST has been an active participant in addressing burnout in ICU professionals, including in an important partnership with the American Association of Critical-Care Nurses (AACN), the American Thoracic Society (ATS), and the Society of Critical Care Medicine (SCCM) - the Critical Care Societies Collaborative (CCSC). The CCSC, whose members include greater than 150,000 critical care professionals in the United States, has established a principle goal of mitigating ICU burnout (#StopICUBurnout). One of the first CCSC efforts was to publish a white paper simultaneously in all four journals of the CCSC professional societies that provides the rationale and direction for a “call for action” to tackle ICU burnout (Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. Burnout syndrome in critical care health care professionals: A call for action. Chest. 2016;150[1]:17). Recently, the CCSC sponsored a National Summit on the Prevention and Management of Burnout in the ICU (http://ccsconline.org/optimizing-the-workforce/burnout). Fifty-five invited participants brought wide ranging expertise and substantial enthusiasm to the task of deconstructing ICU burnout and identifying knowledge gaps and future directions. Areas of focused discussion included factors influencing burnout, identifying individuals with burnout, the value of organizational and individual interventions to prevent and manage burnout, and translation of these discussions into a research agenda. CHEST and the CCSC are committed to the goals of enhancing clinician well-being and eliminating burnout in the ICU.
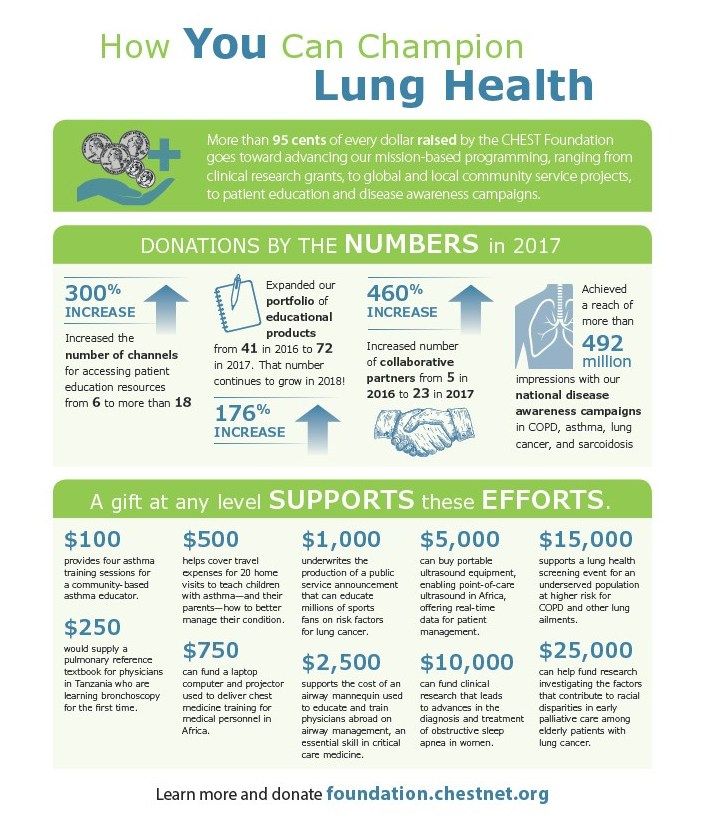
How You Can Champion Lung Health
More than 95 cents of every dollar raised by the CHEST Foundation goes toward advancing our mission-based programming, ranging from clinical research grants, to global and local community service projects, to patient education and disease awareness campaigns.
DONATIONS BY THE NUMBERS in 2017
300% INCREASE
176% INCREASE
Expanded our portfolio of educational products from 41 in 2016 to 72 in 2017. That number continues to grow in 2018!
460% INCREASE
Increased number of collaborative partners from 5 in 2016 to 23 in 2017.
Achieved a reach of more than 492 million impressions with our national disease awareness campaigns in COPD, asthma, lung cancer, and sarcoidosis
A gift at any level SUPPORTS these EFFORTS.
$100
provides four asthma training sessions for a community-based asthma educator.
$250
would supply a pulmonary referencer textbook for physicians in Tanzania who are learning bronchoscopy for the first time.
$500
helps cover travel expenses for 20 home visits to teach children with asthma—and their parents—how to better manage their condition.
$750
can fund a laptop computer and projector used to deliver chest medicine training for medical personnel in Africa.
$1,000
underwrites the production of a public service announcement that can educate millions of sports fans on risk factors for lung cancer.
$2,500
supports the cost of an airway mannequin used to educate and train physicians abroad on airway management, an essential skill in critical care medicine.
$5,000
can buy portable ultrasound equipment, enabling point-of-care ultrasound in Africa, offering real-time data for patient management.
$10,000
can fund clinical research that leads to advances in the diagnosis and treatment of obstructive sleep apnea in women.
$15,000
supports a lung health screening event for an underserved population at higher risk for COPD and other lung ailments.
$25,000
can help fund research investigating the factors that contribute to racial disparities in early palliative care among elderly patients with lung cancer.
Learn more and donate foundation.chestnet.org.
More than 95 cents of every dollar raised by the CHEST Foundation goes toward advancing our mission-based programming, ranging from clinical research grants, to global and local community service projects, to patient education and disease awareness campaigns.
DONATIONS BY THE NUMBERS in 2017
300% INCREASE
176% INCREASE
Expanded our portfolio of educational products from 41 in 2016 to 72 in 2017. That number continues to grow in 2018!
460% INCREASE
Increased number of collaborative partners from 5 in 2016 to 23 in 2017.
Achieved a reach of more than 492 million impressions with our national disease awareness campaigns in COPD, asthma, lung cancer, and sarcoidosis
A gift at any level SUPPORTS these EFFORTS.
$100
provides four asthma training sessions for a community-based asthma educator.
$250
would supply a pulmonary referencer textbook for physicians in Tanzania who are learning bronchoscopy for the first time.
$500
helps cover travel expenses for 20 home visits to teach children with asthma—and their parents—how to better manage their condition.
$750
can fund a laptop computer and projector used to deliver chest medicine training for medical personnel in Africa.
$1,000
underwrites the production of a public service announcement that can educate millions of sports fans on risk factors for lung cancer.
$2,500
supports the cost of an airway mannequin used to educate and train physicians abroad on airway management, an essential skill in critical care medicine.
$5,000
can buy portable ultrasound equipment, enabling point-of-care ultrasound in Africa, offering real-time data for patient management.
$10,000
can fund clinical research that leads to advances in the diagnosis and treatment of obstructive sleep apnea in women.
$15,000
supports a lung health screening event for an underserved population at higher risk for COPD and other lung ailments.
$25,000
can help fund research investigating the factors that contribute to racial disparities in early palliative care among elderly patients with lung cancer.
Learn more and donate foundation.chestnet.org.
More than 95 cents of every dollar raised by the CHEST Foundation goes toward advancing our mission-based programming, ranging from clinical research grants, to global and local community service projects, to patient education and disease awareness campaigns.
DONATIONS BY THE NUMBERS in 2017
300% INCREASE
176% INCREASE
Expanded our portfolio of educational products from 41 in 2016 to 72 in 2017. That number continues to grow in 2018!
460% INCREASE
Increased number of collaborative partners from 5 in 2016 to 23 in 2017.
Achieved a reach of more than 492 million impressions with our national disease awareness campaigns in COPD, asthma, lung cancer, and sarcoidosis
A gift at any level SUPPORTS these EFFORTS.
$100
provides four asthma training sessions for a community-based asthma educator.
$250
would supply a pulmonary referencer textbook for physicians in Tanzania who are learning bronchoscopy for the first time.
$500
helps cover travel expenses for 20 home visits to teach children with asthma—and their parents—how to better manage their condition.
$750
can fund a laptop computer and projector used to deliver chest medicine training for medical personnel in Africa.
$1,000
underwrites the production of a public service announcement that can educate millions of sports fans on risk factors for lung cancer.
$2,500
supports the cost of an airway mannequin used to educate and train physicians abroad on airway management, an essential skill in critical care medicine.
$5,000
can buy portable ultrasound equipment, enabling point-of-care ultrasound in Africa, offering real-time data for patient management.
$10,000
can fund clinical research that leads to advances in the diagnosis and treatment of obstructive sleep apnea in women.
$15,000
supports a lung health screening event for an underserved population at higher risk for COPD and other lung ailments.
$25,000
can help fund research investigating the factors that contribute to racial disparities in early palliative care among elderly patients with lung cancer.
Learn more and donate foundation.chestnet.org.
In Memoriam
W. Gerald Rainer, MD, FCCP, died November 14, 2017, one day after his 90th birthday Dr. Rainer was President of the American College of Chest Physicians in 1982-1983. He practiced thoracic and cardiovascular surgery for 50 years with St. Joseph Hospital in Denver as his professional home. He was a respected leader, researcher, and educator, helping and mentoring countless residents, fellows, and many other health-care professionals. Dr. Rainer was a distinguished clinical professor of surgery at the University of Colorado School of Medicine and served on many University boards and committees. He published prolifically in many respected surgical journals and was able to masterfully blend his private practice with strong academic involvement. As President of the American College of Chest Physicians and many other respected medical and surgical organizations, he was also actively involved in international professional societies. CHEST extends its condolences to Dr. Rainer’s wife of 67 years, Lois, and to his family and friends.
W. Gerald Rainer, MD, FCCP, died November 14, 2017, one day after his 90th birthday Dr. Rainer was President of the American College of Chest Physicians in 1982-1983. He practiced thoracic and cardiovascular surgery for 50 years with St. Joseph Hospital in Denver as his professional home. He was a respected leader, researcher, and educator, helping and mentoring countless residents, fellows, and many other health-care professionals. Dr. Rainer was a distinguished clinical professor of surgery at the University of Colorado School of Medicine and served on many University boards and committees. He published prolifically in many respected surgical journals and was able to masterfully blend his private practice with strong academic involvement. As President of the American College of Chest Physicians and many other respected medical and surgical organizations, he was also actively involved in international professional societies. CHEST extends its condolences to Dr. Rainer’s wife of 67 years, Lois, and to his family and friends.
W. Gerald Rainer, MD, FCCP, died November 14, 2017, one day after his 90th birthday Dr. Rainer was President of the American College of Chest Physicians in 1982-1983. He practiced thoracic and cardiovascular surgery for 50 years with St. Joseph Hospital in Denver as his professional home. He was a respected leader, researcher, and educator, helping and mentoring countless residents, fellows, and many other health-care professionals. Dr. Rainer was a distinguished clinical professor of surgery at the University of Colorado School of Medicine and served on many University boards and committees. He published prolifically in many respected surgical journals and was able to masterfully blend his private practice with strong academic involvement. As President of the American College of Chest Physicians and many other respected medical and surgical organizations, he was also actively involved in international professional societies. CHEST extends its condolences to Dr. Rainer’s wife of 67 years, Lois, and to his family and friends.
This Month in the Journal CHEST®
Original Research
Community-Acquired Pneumonia Visualized on CT Scans but Not Chest Radiographs: Pathogens, Severity, and Clinical Outcomes. By Dr. C. P. Upchurch, et al.
Commentary
CHEST: Home of the Clinician-Educator. By Dr. W. F. Kelly and Dr. A. S. Niven, on behalf of the CHEST Education Committee.
Original Research
Community-Acquired Pneumonia Visualized on CT Scans but Not Chest Radiographs: Pathogens, Severity, and Clinical Outcomes. By Dr. C. P. Upchurch, et al.
Commentary
CHEST: Home of the Clinician-Educator. By Dr. W. F. Kelly and Dr. A. S. Niven, on behalf of the CHEST Education Committee.
Original Research
Community-Acquired Pneumonia Visualized on CT Scans but Not Chest Radiographs: Pathogens, Severity, and Clinical Outcomes. By Dr. C. P. Upchurch, et al.
Commentary
CHEST: Home of the Clinician-Educator. By Dr. W. F. Kelly and Dr. A. S. Niven, on behalf of the CHEST Education Committee.
FDA proposes lower nicotine levels in cigarettes
Nicotine levels in cigarettes could see a significant reduction under regulatory options being considered by the Food and Drug Administration.
Cigarettes “are the only legal consumer product that, when used as intended, will kill half all long-term users,” FDA Commissioner Scott Gottlieb, MD, said in a statement announcing the effort.
The agency is seeking comment on a proposed regulation regarding “a potential maximum nicotine level that would be appropriate for the protection of public health, in light of scientific evidence about the addictive properties of nicotine in cigarettes.” An advance notice of proposed rule making was posted online March 15 and is scheduled for publication in the Federal Register on March 16.
The FDA also is seeking comments on a number of other areas to help inform potential regulatory action down the road, including whether a new standard for lower nicotine levels should be implemented at once or whether a phased-in approach should be taken; whether FDA should specify a method for manufacturers to use in order to detect nicotine levels in their products; and whether the proposed lower level is technically achievable.
The agency also is seeking comment on potential unintended effects of lowering the amount of nicotine in cigarettes, such as turning to other combustible tobacco products such as cigars in conjunction with or as a replacement for cigarette use; increasing the number of cigarettes smoked, or seeking comparable nicotine from noncombustible tobacco sources.
At this time, FDA is not suggesting what the target might be on a specific nicotine level. While the advanced notice asks specifically about the “merits of nicotine levels like 0.3, 0.4, and 0.5 mg nicotine/g of tobacco filler,” it is not suggesting that this is the range being considered.
[polldaddy:9960560]
“Not to prejudge any possible proposed rule that we would do or any possible level, that is the purpose of an advanced proposed rule making, but we share all the science that we are aware of, and we characterize the studies that have been done to date in trying to find out what that right level is,” Mitch Zeller, director of the FDA Center for Tobacco Products, said during a March 15 press call.
He said that the FDA aiming to make sure the level is low enough that it cannot be compensated for by smoking more or inhaling deeper and holding the breath in longer, much like how smokers compensated when they smoked “light” cigarettes in the unregulated market.
Mr. Zeller said that seeking comments on those levels is based on the scientific evidence that is laid out in the advanced notice, but it is not necessarily foreshadowing where the standard will be set.
Drastically reducing the amount of nicotine in cigarettes is expected to significantly lower not only the number of people addicted to cigarettes but also as the negative health effects of nicotine addiction, FDA experts wrote in a perspective piece published March 15 in the New England Journal of Medicine (doi: 10.1065/NEJMsr1714617).
“Our findings show that reducing the nicotine level in cigarettes has the potential to substantially reduce the enormous burden of smoking-related death and disease,” Benjamin J. Apelberg, PhD, director of the Division of Population Health Science, Office of Science, within the FDA Center for Tobacco Products, and his colleagues, wrote in the report.
Modeling for the implementation of a lower nicotine level policy suggests that smoking prevalence will decline from a median of 12.8% in baseline scenario to a median of 10.8% within a year of implementation, with the increase related to smoking cessation.
“We estimate that approximately 5 million additional smokers would quit smoking within a year after implementation of the hypothetical policy,” Dr. Apelberg and his colleagues wrote. “By 2060, smoking prevalence drops from 7.9% in the baseline scenario to 1.4% in the policy scenario.”
Their analysis is based on a nicotine level that is “so low that there would not be enough nicotine available in cigarette tobacco for smokers to sustain addiction,” they noted.
The FDA plans to release two more advanced notices of proposed rule making related to using regulatory levers to reduce cigarette smoking, including one that addresses flavoring in tobacco and one related to the regulation of premium cigars. Other than the 90-day comment period related to the advanced notices, the agency has not set any deadlines on when it will act.
“Legally, we are not going to prejudge how long this will take or what will happen,” Mr. Zeller said. “This is an early step in what could be a potential rule-making process using the product standard authority. We will take a long and hard look at all the comments that come in over the next 90 days and based upon our review of all the information, all the comments that come in, all the feedback that we have, we will then make a decision about taking the next step in the rule-making process.”
Nicotine levels in cigarettes could see a significant reduction under regulatory options being considered by the Food and Drug Administration.
Cigarettes “are the only legal consumer product that, when used as intended, will kill half all long-term users,” FDA Commissioner Scott Gottlieb, MD, said in a statement announcing the effort.
The agency is seeking comment on a proposed regulation regarding “a potential maximum nicotine level that would be appropriate for the protection of public health, in light of scientific evidence about the addictive properties of nicotine in cigarettes.” An advance notice of proposed rule making was posted online March 15 and is scheduled for publication in the Federal Register on March 16.
The FDA also is seeking comments on a number of other areas to help inform potential regulatory action down the road, including whether a new standard for lower nicotine levels should be implemented at once or whether a phased-in approach should be taken; whether FDA should specify a method for manufacturers to use in order to detect nicotine levels in their products; and whether the proposed lower level is technically achievable.
The agency also is seeking comment on potential unintended effects of lowering the amount of nicotine in cigarettes, such as turning to other combustible tobacco products such as cigars in conjunction with or as a replacement for cigarette use; increasing the number of cigarettes smoked, or seeking comparable nicotine from noncombustible tobacco sources.
At this time, FDA is not suggesting what the target might be on a specific nicotine level. While the advanced notice asks specifically about the “merits of nicotine levels like 0.3, 0.4, and 0.5 mg nicotine/g of tobacco filler,” it is not suggesting that this is the range being considered.
[polldaddy:9960560]
“Not to prejudge any possible proposed rule that we would do or any possible level, that is the purpose of an advanced proposed rule making, but we share all the science that we are aware of, and we characterize the studies that have been done to date in trying to find out what that right level is,” Mitch Zeller, director of the FDA Center for Tobacco Products, said during a March 15 press call.
He said that the FDA aiming to make sure the level is low enough that it cannot be compensated for by smoking more or inhaling deeper and holding the breath in longer, much like how smokers compensated when they smoked “light” cigarettes in the unregulated market.
Mr. Zeller said that seeking comments on those levels is based on the scientific evidence that is laid out in the advanced notice, but it is not necessarily foreshadowing where the standard will be set.
Drastically reducing the amount of nicotine in cigarettes is expected to significantly lower not only the number of people addicted to cigarettes but also as the negative health effects of nicotine addiction, FDA experts wrote in a perspective piece published March 15 in the New England Journal of Medicine (doi: 10.1065/NEJMsr1714617).
“Our findings show that reducing the nicotine level in cigarettes has the potential to substantially reduce the enormous burden of smoking-related death and disease,” Benjamin J. Apelberg, PhD, director of the Division of Population Health Science, Office of Science, within the FDA Center for Tobacco Products, and his colleagues, wrote in the report.
Modeling for the implementation of a lower nicotine level policy suggests that smoking prevalence will decline from a median of 12.8% in baseline scenario to a median of 10.8% within a year of implementation, with the increase related to smoking cessation.
“We estimate that approximately 5 million additional smokers would quit smoking within a year after implementation of the hypothetical policy,” Dr. Apelberg and his colleagues wrote. “By 2060, smoking prevalence drops from 7.9% in the baseline scenario to 1.4% in the policy scenario.”
Their analysis is based on a nicotine level that is “so low that there would not be enough nicotine available in cigarette tobacco for smokers to sustain addiction,” they noted.
The FDA plans to release two more advanced notices of proposed rule making related to using regulatory levers to reduce cigarette smoking, including one that addresses flavoring in tobacco and one related to the regulation of premium cigars. Other than the 90-day comment period related to the advanced notices, the agency has not set any deadlines on when it will act.
“Legally, we are not going to prejudge how long this will take or what will happen,” Mr. Zeller said. “This is an early step in what could be a potential rule-making process using the product standard authority. We will take a long and hard look at all the comments that come in over the next 90 days and based upon our review of all the information, all the comments that come in, all the feedback that we have, we will then make a decision about taking the next step in the rule-making process.”
Nicotine levels in cigarettes could see a significant reduction under regulatory options being considered by the Food and Drug Administration.
Cigarettes “are the only legal consumer product that, when used as intended, will kill half all long-term users,” FDA Commissioner Scott Gottlieb, MD, said in a statement announcing the effort.
The agency is seeking comment on a proposed regulation regarding “a potential maximum nicotine level that would be appropriate for the protection of public health, in light of scientific evidence about the addictive properties of nicotine in cigarettes.” An advance notice of proposed rule making was posted online March 15 and is scheduled for publication in the Federal Register on March 16.
The FDA also is seeking comments on a number of other areas to help inform potential regulatory action down the road, including whether a new standard for lower nicotine levels should be implemented at once or whether a phased-in approach should be taken; whether FDA should specify a method for manufacturers to use in order to detect nicotine levels in their products; and whether the proposed lower level is technically achievable.
The agency also is seeking comment on potential unintended effects of lowering the amount of nicotine in cigarettes, such as turning to other combustible tobacco products such as cigars in conjunction with or as a replacement for cigarette use; increasing the number of cigarettes smoked, or seeking comparable nicotine from noncombustible tobacco sources.
At this time, FDA is not suggesting what the target might be on a specific nicotine level. While the advanced notice asks specifically about the “merits of nicotine levels like 0.3, 0.4, and 0.5 mg nicotine/g of tobacco filler,” it is not suggesting that this is the range being considered.
[polldaddy:9960560]
“Not to prejudge any possible proposed rule that we would do or any possible level, that is the purpose of an advanced proposed rule making, but we share all the science that we are aware of, and we characterize the studies that have been done to date in trying to find out what that right level is,” Mitch Zeller, director of the FDA Center for Tobacco Products, said during a March 15 press call.
He said that the FDA aiming to make sure the level is low enough that it cannot be compensated for by smoking more or inhaling deeper and holding the breath in longer, much like how smokers compensated when they smoked “light” cigarettes in the unregulated market.
Mr. Zeller said that seeking comments on those levels is based on the scientific evidence that is laid out in the advanced notice, but it is not necessarily foreshadowing where the standard will be set.
Drastically reducing the amount of nicotine in cigarettes is expected to significantly lower not only the number of people addicted to cigarettes but also as the negative health effects of nicotine addiction, FDA experts wrote in a perspective piece published March 15 in the New England Journal of Medicine (doi: 10.1065/NEJMsr1714617).
“Our findings show that reducing the nicotine level in cigarettes has the potential to substantially reduce the enormous burden of smoking-related death and disease,” Benjamin J. Apelberg, PhD, director of the Division of Population Health Science, Office of Science, within the FDA Center for Tobacco Products, and his colleagues, wrote in the report.
Modeling for the implementation of a lower nicotine level policy suggests that smoking prevalence will decline from a median of 12.8% in baseline scenario to a median of 10.8% within a year of implementation, with the increase related to smoking cessation.
“We estimate that approximately 5 million additional smokers would quit smoking within a year after implementation of the hypothetical policy,” Dr. Apelberg and his colleagues wrote. “By 2060, smoking prevalence drops from 7.9% in the baseline scenario to 1.4% in the policy scenario.”
Their analysis is based on a nicotine level that is “so low that there would not be enough nicotine available in cigarette tobacco for smokers to sustain addiction,” they noted.
The FDA plans to release two more advanced notices of proposed rule making related to using regulatory levers to reduce cigarette smoking, including one that addresses flavoring in tobacco and one related to the regulation of premium cigars. Other than the 90-day comment period related to the advanced notices, the agency has not set any deadlines on when it will act.
“Legally, we are not going to prejudge how long this will take or what will happen,” Mr. Zeller said. “This is an early step in what could be a potential rule-making process using the product standard authority. We will take a long and hard look at all the comments that come in over the next 90 days and based upon our review of all the information, all the comments that come in, all the feedback that we have, we will then make a decision about taking the next step in the rule-making process.”
A Message from the Executive Director: ACS continues to take on the issues of concern to surgeons and their patients
I am pleased to once again submit an annual report for publication in ACS Surgery News. The American College of Surgeons (ACS) had a productive year in 2017 and looks forward to seeing a range of new programs evolve in 2018.
Physician payment
A health policy issue of considerable concern to ACS Fellows is the Centers for Medicare & Medicaid Services’ efforts to implement the payment reforms in the Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act (MACRA) of 2015. Specifically, 2017 was the transition year for implementation of the Quality Payment Program’s (QPP’s) Merit-based Incentive Payment System (MIPS), and MIPS data collected in 2017 will be used to determine annual payment updates in 2019.
In 2018, the second year of MIPS, the penalty for nonparticipation has increased to 5 percent from 4 percent. Over time, the penalty for nonparticpation or poor performance will continue to rise. The College has created a variety of resources to assist Fellows in their efforts to comply with MIPS, which explain the purpose and structure of the MIPS program and help guide surgeons in choosing and achieving the goal that is right for their individual practice. These tools can be found on the ACS website at facs.org/qpp.
In addition to MIPS, the QPP calls for the establishment of Alternative Payment Models (APMs). The College has worked with thought leaders at Brandeis University, Waltham, MA, to develop the ACS-Brandeis Advanced APM. In 2017, the Secretary of the Department of Health and Human Services reviewed the proposal and made recommendations for improvement. Efforts to develop the model continue, and the ACS is working with private insurers and entities that may implement the APM model once available.
Education
The College is leading a significant effort to address the needs of surgeons who are looking to update their skills. The Steering Committee for Retraining and Retooling of Practicing Surgeons is working to define standards and establish a national infrastructure to achieve optimal outcomes. The ACS Accredited Education Institutes are at the core of this infrastructure.
At Clinical Congress 2017, we launched the ACS Academy of Master Surgeon Educators. The goals of the academy are to recognize master surgeon educators, advance the science and practice of leading-edge surgical education and training, foster innovation and collaboration, support faculty development and recognition, and underscore the importance of surgical education and training.
Also at Clinical Congress, the ACS Committee on Ethics unveiled Ethical Issues in Surgical Care, a landmark resource that defines a framework for the field of surgical ethics as it has evolved over the last decade. The book is organized into four sections that address the broad areas of general consideration, the surgeon-patient relationship, the surgeon and the surgical profession, and the surgeon and society.
Quality
The College released Optimal Resources for Surgical Quality and Safety, also known as the “red book,” in July 2017.This manual provides a guide for surgical quality leaders seeking to improve quality and safety in their institutions, departments, and practices. Efforts are under way to develop adjunctive or integrated resources/standards and to potentially establish a Surgical Quality Verification Program.
The red book was released at the 2017 ACS Quality and Safety Conference, formerly the ACS National Surgical Quality Improvement Program (ACS NSQIP®) Annual Conference, in New York, NY. The conference, which focused on a broad range of ACS Quality Programs, boasted a record-breaking attendance of more than 1,800 attendees.
The new Surgeon Specific Registry was the first ACS database to launch as part of the College’s integrated registry of the future, which ultimately will allow users to share relevant quality data across individual ACS Quality Programs, such as ACS NSQIP and the Trauma Quality Improvement Program (TQIP®).
Other new quality initiatives include the Agency for Healthcare Research and Quality Safety Program for Improving Surgical Care and Recovery (ISCR), which the ACS is conducting in collaboration with Johns Hopkins Medicine Armstrong Institute for Patient Safety and Quality, Baltimore, MD. This program supports hospitals in implementing perioperative evidence-based pathways to improve clinical outcomes, reduce hospital length of stay, and improve the patient experience.
The ACS also has become the new home of Strong for Surgery, originally developed by surgeons in Washington State. This program empowers hospitals and clinics to integrate checklists into the preoperative phase of care.
In addition, the ACS was awarded a three-year, multimillion dollar R01 grant from the National Institute on Minority Health and Health Disparities. ACS Past-President L.D. Britt, MD, MPH, DSc(Hon), FACS, FCCM, FRCSEng(Hon), FRCSEd(Hon), FWACS(Hon), FRCSI(Hon), FCS(SA)(Hon), FRCSGlasg(Hon), is the principal investigator on this award, which is aimed at eliminating variances in access to surgical care.
Trauma
The Committee on Trauma (COT), in collaboration with military partners and the National Highway Traffic Safety Administration (NHTSA), hosted a conference in April 2017 to advance the recommendations in the National Academies on Science, Engineering, and Medicine report, A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths after Injury. The meeting brought together approximately 170 trauma care professionals with the goal of creating the framework for a National Trauma Care System Action Plan.
In light of recent tragedies and the ongoing public debate over how to stop the continuing violence at our nation’s schools, churches, and other public places, the COT Injury Prevention and Control Committee (IPCC) is advocating for a consensus-based, public health/trauma system approach to firearm injury prevention. Furthermore, at its February 2018 meeting the ACS Board of Regents unanimously approved a plan to expand the College’s focus from the successful Stop the Bleed® program to a broader prevention initiative focused on strategies that include research, advocacy, and strategic collaborations. An action plan was in development at press time.
ACS leadership
The ACS Board of Governors (B/G) continues to implement initiatives through its Pillars and Workgroups. Specific examples from this past year include the release of a white paper on out-of-network billing; production of the biannual e-newsletter, The Cutting Edge; conduct of the 2017 Board of Governors Annual Survey, which focuses on the Stop the Bleed campaign, the opioid crisis, work-related injuries/surgical ergonomics, and advanced practice providers in surgery; and development of a standardized letter of recommendation for applicants to surgery training programs.
The ACS Board of Regents approved and updated a number of statements in the last 12 months. New statements cover several topics of concern to the Fellowship, including gender salary equity, the use of anesthetics and sedation drugs in children and pregnant women, the opioid abuse epidemic, lithium batteries, opioids and motor vehicle crash prevention, maintaining surgical access with a locum tenens surgeon, social media, the Uniform Emergency Volunteer Health Practitioners Act, credentialing and privileging, and medical students and the electronic health record.
As these few examples demonstrate, the ACS is constantly moving forward to offer surgeons and the other members of the patient care team the tools, resources, and educational opportunities they need to succeed in practice and to provide optimal patient care. As always, you are encouraged to contact the ACS leadership, and let us know how we can best serve you.
Dr. Hoyt is the Executive Director of the ACS, Chicago, IL.
I am pleased to once again submit an annual report for publication in ACS Surgery News. The American College of Surgeons (ACS) had a productive year in 2017 and looks forward to seeing a range of new programs evolve in 2018.
Physician payment
A health policy issue of considerable concern to ACS Fellows is the Centers for Medicare & Medicaid Services’ efforts to implement the payment reforms in the Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act (MACRA) of 2015. Specifically, 2017 was the transition year for implementation of the Quality Payment Program’s (QPP’s) Merit-based Incentive Payment System (MIPS), and MIPS data collected in 2017 will be used to determine annual payment updates in 2019.
In 2018, the second year of MIPS, the penalty for nonparticipation has increased to 5 percent from 4 percent. Over time, the penalty for nonparticpation or poor performance will continue to rise. The College has created a variety of resources to assist Fellows in their efforts to comply with MIPS, which explain the purpose and structure of the MIPS program and help guide surgeons in choosing and achieving the goal that is right for their individual practice. These tools can be found on the ACS website at facs.org/qpp.
In addition to MIPS, the QPP calls for the establishment of Alternative Payment Models (APMs). The College has worked with thought leaders at Brandeis University, Waltham, MA, to develop the ACS-Brandeis Advanced APM. In 2017, the Secretary of the Department of Health and Human Services reviewed the proposal and made recommendations for improvement. Efforts to develop the model continue, and the ACS is working with private insurers and entities that may implement the APM model once available.
Education
The College is leading a significant effort to address the needs of surgeons who are looking to update their skills. The Steering Committee for Retraining and Retooling of Practicing Surgeons is working to define standards and establish a national infrastructure to achieve optimal outcomes. The ACS Accredited Education Institutes are at the core of this infrastructure.
At Clinical Congress 2017, we launched the ACS Academy of Master Surgeon Educators. The goals of the academy are to recognize master surgeon educators, advance the science and practice of leading-edge surgical education and training, foster innovation and collaboration, support faculty development and recognition, and underscore the importance of surgical education and training.
Also at Clinical Congress, the ACS Committee on Ethics unveiled Ethical Issues in Surgical Care, a landmark resource that defines a framework for the field of surgical ethics as it has evolved over the last decade. The book is organized into four sections that address the broad areas of general consideration, the surgeon-patient relationship, the surgeon and the surgical profession, and the surgeon and society.
Quality
The College released Optimal Resources for Surgical Quality and Safety, also known as the “red book,” in July 2017.This manual provides a guide for surgical quality leaders seeking to improve quality and safety in their institutions, departments, and practices. Efforts are under way to develop adjunctive or integrated resources/standards and to potentially establish a Surgical Quality Verification Program.
The red book was released at the 2017 ACS Quality and Safety Conference, formerly the ACS National Surgical Quality Improvement Program (ACS NSQIP®) Annual Conference, in New York, NY. The conference, which focused on a broad range of ACS Quality Programs, boasted a record-breaking attendance of more than 1,800 attendees.
The new Surgeon Specific Registry was the first ACS database to launch as part of the College’s integrated registry of the future, which ultimately will allow users to share relevant quality data across individual ACS Quality Programs, such as ACS NSQIP and the Trauma Quality Improvement Program (TQIP®).
Other new quality initiatives include the Agency for Healthcare Research and Quality Safety Program for Improving Surgical Care and Recovery (ISCR), which the ACS is conducting in collaboration with Johns Hopkins Medicine Armstrong Institute for Patient Safety and Quality, Baltimore, MD. This program supports hospitals in implementing perioperative evidence-based pathways to improve clinical outcomes, reduce hospital length of stay, and improve the patient experience.
The ACS also has become the new home of Strong for Surgery, originally developed by surgeons in Washington State. This program empowers hospitals and clinics to integrate checklists into the preoperative phase of care.
In addition, the ACS was awarded a three-year, multimillion dollar R01 grant from the National Institute on Minority Health and Health Disparities. ACS Past-President L.D. Britt, MD, MPH, DSc(Hon), FACS, FCCM, FRCSEng(Hon), FRCSEd(Hon), FWACS(Hon), FRCSI(Hon), FCS(SA)(Hon), FRCSGlasg(Hon), is the principal investigator on this award, which is aimed at eliminating variances in access to surgical care.
Trauma
The Committee on Trauma (COT), in collaboration with military partners and the National Highway Traffic Safety Administration (NHTSA), hosted a conference in April 2017 to advance the recommendations in the National Academies on Science, Engineering, and Medicine report, A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths after Injury. The meeting brought together approximately 170 trauma care professionals with the goal of creating the framework for a National Trauma Care System Action Plan.
In light of recent tragedies and the ongoing public debate over how to stop the continuing violence at our nation’s schools, churches, and other public places, the COT Injury Prevention and Control Committee (IPCC) is advocating for a consensus-based, public health/trauma system approach to firearm injury prevention. Furthermore, at its February 2018 meeting the ACS Board of Regents unanimously approved a plan to expand the College’s focus from the successful Stop the Bleed® program to a broader prevention initiative focused on strategies that include research, advocacy, and strategic collaborations. An action plan was in development at press time.
ACS leadership
The ACS Board of Governors (B/G) continues to implement initiatives through its Pillars and Workgroups. Specific examples from this past year include the release of a white paper on out-of-network billing; production of the biannual e-newsletter, The Cutting Edge; conduct of the 2017 Board of Governors Annual Survey, which focuses on the Stop the Bleed campaign, the opioid crisis, work-related injuries/surgical ergonomics, and advanced practice providers in surgery; and development of a standardized letter of recommendation for applicants to surgery training programs.
The ACS Board of Regents approved and updated a number of statements in the last 12 months. New statements cover several topics of concern to the Fellowship, including gender salary equity, the use of anesthetics and sedation drugs in children and pregnant women, the opioid abuse epidemic, lithium batteries, opioids and motor vehicle crash prevention, maintaining surgical access with a locum tenens surgeon, social media, the Uniform Emergency Volunteer Health Practitioners Act, credentialing and privileging, and medical students and the electronic health record.
As these few examples demonstrate, the ACS is constantly moving forward to offer surgeons and the other members of the patient care team the tools, resources, and educational opportunities they need to succeed in practice and to provide optimal patient care. As always, you are encouraged to contact the ACS leadership, and let us know how we can best serve you.
Dr. Hoyt is the Executive Director of the ACS, Chicago, IL.
I am pleased to once again submit an annual report for publication in ACS Surgery News. The American College of Surgeons (ACS) had a productive year in 2017 and looks forward to seeing a range of new programs evolve in 2018.
Physician payment
A health policy issue of considerable concern to ACS Fellows is the Centers for Medicare & Medicaid Services’ efforts to implement the payment reforms in the Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act (MACRA) of 2015. Specifically, 2017 was the transition year for implementation of the Quality Payment Program’s (QPP’s) Merit-based Incentive Payment System (MIPS), and MIPS data collected in 2017 will be used to determine annual payment updates in 2019.
In 2018, the second year of MIPS, the penalty for nonparticipation has increased to 5 percent from 4 percent. Over time, the penalty for nonparticpation or poor performance will continue to rise. The College has created a variety of resources to assist Fellows in their efforts to comply with MIPS, which explain the purpose and structure of the MIPS program and help guide surgeons in choosing and achieving the goal that is right for their individual practice. These tools can be found on the ACS website at facs.org/qpp.
In addition to MIPS, the QPP calls for the establishment of Alternative Payment Models (APMs). The College has worked with thought leaders at Brandeis University, Waltham, MA, to develop the ACS-Brandeis Advanced APM. In 2017, the Secretary of the Department of Health and Human Services reviewed the proposal and made recommendations for improvement. Efforts to develop the model continue, and the ACS is working with private insurers and entities that may implement the APM model once available.
Education
The College is leading a significant effort to address the needs of surgeons who are looking to update their skills. The Steering Committee for Retraining and Retooling of Practicing Surgeons is working to define standards and establish a national infrastructure to achieve optimal outcomes. The ACS Accredited Education Institutes are at the core of this infrastructure.
At Clinical Congress 2017, we launched the ACS Academy of Master Surgeon Educators. The goals of the academy are to recognize master surgeon educators, advance the science and practice of leading-edge surgical education and training, foster innovation and collaboration, support faculty development and recognition, and underscore the importance of surgical education and training.
Also at Clinical Congress, the ACS Committee on Ethics unveiled Ethical Issues in Surgical Care, a landmark resource that defines a framework for the field of surgical ethics as it has evolved over the last decade. The book is organized into four sections that address the broad areas of general consideration, the surgeon-patient relationship, the surgeon and the surgical profession, and the surgeon and society.
Quality
The College released Optimal Resources for Surgical Quality and Safety, also known as the “red book,” in July 2017.This manual provides a guide for surgical quality leaders seeking to improve quality and safety in their institutions, departments, and practices. Efforts are under way to develop adjunctive or integrated resources/standards and to potentially establish a Surgical Quality Verification Program.
The red book was released at the 2017 ACS Quality and Safety Conference, formerly the ACS National Surgical Quality Improvement Program (ACS NSQIP®) Annual Conference, in New York, NY. The conference, which focused on a broad range of ACS Quality Programs, boasted a record-breaking attendance of more than 1,800 attendees.
The new Surgeon Specific Registry was the first ACS database to launch as part of the College’s integrated registry of the future, which ultimately will allow users to share relevant quality data across individual ACS Quality Programs, such as ACS NSQIP and the Trauma Quality Improvement Program (TQIP®).
Other new quality initiatives include the Agency for Healthcare Research and Quality Safety Program for Improving Surgical Care and Recovery (ISCR), which the ACS is conducting in collaboration with Johns Hopkins Medicine Armstrong Institute for Patient Safety and Quality, Baltimore, MD. This program supports hospitals in implementing perioperative evidence-based pathways to improve clinical outcomes, reduce hospital length of stay, and improve the patient experience.
The ACS also has become the new home of Strong for Surgery, originally developed by surgeons in Washington State. This program empowers hospitals and clinics to integrate checklists into the preoperative phase of care.
In addition, the ACS was awarded a three-year, multimillion dollar R01 grant from the National Institute on Minority Health and Health Disparities. ACS Past-President L.D. Britt, MD, MPH, DSc(Hon), FACS, FCCM, FRCSEng(Hon), FRCSEd(Hon), FWACS(Hon), FRCSI(Hon), FCS(SA)(Hon), FRCSGlasg(Hon), is the principal investigator on this award, which is aimed at eliminating variances in access to surgical care.
Trauma
The Committee on Trauma (COT), in collaboration with military partners and the National Highway Traffic Safety Administration (NHTSA), hosted a conference in April 2017 to advance the recommendations in the National Academies on Science, Engineering, and Medicine report, A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths after Injury. The meeting brought together approximately 170 trauma care professionals with the goal of creating the framework for a National Trauma Care System Action Plan.
In light of recent tragedies and the ongoing public debate over how to stop the continuing violence at our nation’s schools, churches, and other public places, the COT Injury Prevention and Control Committee (IPCC) is advocating for a consensus-based, public health/trauma system approach to firearm injury prevention. Furthermore, at its February 2018 meeting the ACS Board of Regents unanimously approved a plan to expand the College’s focus from the successful Stop the Bleed® program to a broader prevention initiative focused on strategies that include research, advocacy, and strategic collaborations. An action plan was in development at press time.
ACS leadership
The ACS Board of Governors (B/G) continues to implement initiatives through its Pillars and Workgroups. Specific examples from this past year include the release of a white paper on out-of-network billing; production of the biannual e-newsletter, The Cutting Edge; conduct of the 2017 Board of Governors Annual Survey, which focuses on the Stop the Bleed campaign, the opioid crisis, work-related injuries/surgical ergonomics, and advanced practice providers in surgery; and development of a standardized letter of recommendation for applicants to surgery training programs.
The ACS Board of Regents approved and updated a number of statements in the last 12 months. New statements cover several topics of concern to the Fellowship, including gender salary equity, the use of anesthetics and sedation drugs in children and pregnant women, the opioid abuse epidemic, lithium batteries, opioids and motor vehicle crash prevention, maintaining surgical access with a locum tenens surgeon, social media, the Uniform Emergency Volunteer Health Practitioners Act, credentialing and privileging, and medical students and the electronic health record.
As these few examples demonstrate, the ACS is constantly moving forward to offer surgeons and the other members of the patient care team the tools, resources, and educational opportunities they need to succeed in practice and to provide optimal patient care. As always, you are encouraged to contact the ACS leadership, and let us know how we can best serve you.
Dr. Hoyt is the Executive Director of the ACS, Chicago, IL.