User login
Ganetespib fails to hit mark in phase III NSCLC trial
VIENNA – The addition of ganetespib to docetaxel for the treatment of advanced non–small cell lung cancer (NSCLC) did not live up to its earlier promise of improved efficacy over docetaxel alone in a phase III study.
Interim results of the GALAXY-2 study, which led to the trial’s termination for futility, showed that there was no difference in the primary endpoint of overall survival (OS). The median OS was a respective 10.9 months and 10.5 months for the combination of ganetespib plus docetaxel versus docetaxel alone (hazard ratio, 1.111, 95% confidence interval, 0.899-1.372, P = .03293).
The combination had looked promising in the phase II GALAXY-1 study (Ann Oncol. 2015;26:1741-8), with a trend towards improved PFS and OS, with patients diagnosed with advanced disease perhaps gaining the most benefit.
“The addition of ganetespib to docetaxel did not result in improved efficacy for the salvage therapy of patients with advanced-stage lung adenocarcinoma,” Rathi Pillai, MD, said at the World Conference on Lung Cancer.
“Based on these findings, further development of Hsp [heat shock protein] 90 inhibitors in lung cancer should be limited to patients with driver mutations with relevant client proteins,” added Dr. Pillai of the Winship Cancer Institute at Emory University in Atlanta.
In GALAXY-2, 672 patients were randomized, 1:1, to receive docetaxel (75 mg/m2 on day 1) with ganetespib (150 mg/m2 on days 1 and 15) or a placebo every 3 weeks. The median number of cycles received was five in the combination arm and four in the docetaxel-only arm. All patients had advanced non–small cell lung adenocarcinoma diagnosed at least 6 months prior to enrollment and had received only one prior treatment regimen.
Response rates were similar between the two groups, with 13.7% and 16% of ganetespib/docetaxel– and docetaxel/placebo–treated patients achieving a partial response (P = .448) and 56.1% and 50.1%, respectively, having stable disease (P = .123).
Almost two-thirds (65%) of patients given ganetespib/docetaxel reported any grade 3-4 adverse event versus 54% of patients given docetaxel/placebo. The most frequent treatment-emergent grade 3-4 adverse event was neutropenia, occurring in 34.6% ad 29.5% of patients in each arm (P = .1807), with only diarrhea (46.2% vs. 14.6%; P less than .0001) and weight loss (11.3% vs. 5.2%; P = .0044) occurring more frequently in the combination than the docetaxel-only arm.
Ganetespib is a second-generation Hsp90 inhibitor and the rationale for using Hsp90 inhibitors as cancer therapy remains sound, Dr. Gandara maintained. One of the issues is finding a biomarker to predict the benefit for these drugs in a clinical setting, he said. In the phase II GALAXY-1 trial it was noted that patients diagnosed with advanced disease more than 6 months prior to study entry fared better than those with more recent diagnosis if they were treated with ganetespib/docetaxel than docetaxel alone. Patients with elevated levels of lactate dehydrogenase (eLDH) also seemed to do better than those with normal LDH levels if they were treated with the combination.
These two subpopulations were specifically looked at the in the phase III study, but again no differences in OS or PFS were observed, nor were differences observed in any of the other subgroups analyzed, which included EGFR- and ALK-negative patients, by response rate or progression because of new metastatic lesions.
“Were these the right surrogates to use as predictive biomarkers for heat shock protein inhibition? Of course, in retrospect, it is easy to say that they were not,” Dr. Gandara said.
“Is there still an opportunity for this class of drugs to make a meaningful impact in NSCLC? In my own opinion I think the answer is yes, but not in this broad page approach and not with these potential surrogates as were used in GALAXY-2,” he said at the meeting sponsored by the International Association for the Study of Lung Cancer.
The study was sponsored by Synta Pharmaceuticals, which became part of Madrigal Pharmaceuticals in June 2016. Dr. Pillai reported having no financial disclosures. Dr. Gandara disclosed that he had received research grants from several pharmaceutical companies.
VIENNA – The addition of ganetespib to docetaxel for the treatment of advanced non–small cell lung cancer (NSCLC) did not live up to its earlier promise of improved efficacy over docetaxel alone in a phase III study.
Interim results of the GALAXY-2 study, which led to the trial’s termination for futility, showed that there was no difference in the primary endpoint of overall survival (OS). The median OS was a respective 10.9 months and 10.5 months for the combination of ganetespib plus docetaxel versus docetaxel alone (hazard ratio, 1.111, 95% confidence interval, 0.899-1.372, P = .03293).
The combination had looked promising in the phase II GALAXY-1 study (Ann Oncol. 2015;26:1741-8), with a trend towards improved PFS and OS, with patients diagnosed with advanced disease perhaps gaining the most benefit.
“The addition of ganetespib to docetaxel did not result in improved efficacy for the salvage therapy of patients with advanced-stage lung adenocarcinoma,” Rathi Pillai, MD, said at the World Conference on Lung Cancer.
“Based on these findings, further development of Hsp [heat shock protein] 90 inhibitors in lung cancer should be limited to patients with driver mutations with relevant client proteins,” added Dr. Pillai of the Winship Cancer Institute at Emory University in Atlanta.
In GALAXY-2, 672 patients were randomized, 1:1, to receive docetaxel (75 mg/m2 on day 1) with ganetespib (150 mg/m2 on days 1 and 15) or a placebo every 3 weeks. The median number of cycles received was five in the combination arm and four in the docetaxel-only arm. All patients had advanced non–small cell lung adenocarcinoma diagnosed at least 6 months prior to enrollment and had received only one prior treatment regimen.
Response rates were similar between the two groups, with 13.7% and 16% of ganetespib/docetaxel– and docetaxel/placebo–treated patients achieving a partial response (P = .448) and 56.1% and 50.1%, respectively, having stable disease (P = .123).
Almost two-thirds (65%) of patients given ganetespib/docetaxel reported any grade 3-4 adverse event versus 54% of patients given docetaxel/placebo. The most frequent treatment-emergent grade 3-4 adverse event was neutropenia, occurring in 34.6% ad 29.5% of patients in each arm (P = .1807), with only diarrhea (46.2% vs. 14.6%; P less than .0001) and weight loss (11.3% vs. 5.2%; P = .0044) occurring more frequently in the combination than the docetaxel-only arm.
Ganetespib is a second-generation Hsp90 inhibitor and the rationale for using Hsp90 inhibitors as cancer therapy remains sound, Dr. Gandara maintained. One of the issues is finding a biomarker to predict the benefit for these drugs in a clinical setting, he said. In the phase II GALAXY-1 trial it was noted that patients diagnosed with advanced disease more than 6 months prior to study entry fared better than those with more recent diagnosis if they were treated with ganetespib/docetaxel than docetaxel alone. Patients with elevated levels of lactate dehydrogenase (eLDH) also seemed to do better than those with normal LDH levels if they were treated with the combination.
These two subpopulations were specifically looked at the in the phase III study, but again no differences in OS or PFS were observed, nor were differences observed in any of the other subgroups analyzed, which included EGFR- and ALK-negative patients, by response rate or progression because of new metastatic lesions.
“Were these the right surrogates to use as predictive biomarkers for heat shock protein inhibition? Of course, in retrospect, it is easy to say that they were not,” Dr. Gandara said.
“Is there still an opportunity for this class of drugs to make a meaningful impact in NSCLC? In my own opinion I think the answer is yes, but not in this broad page approach and not with these potential surrogates as were used in GALAXY-2,” he said at the meeting sponsored by the International Association for the Study of Lung Cancer.
The study was sponsored by Synta Pharmaceuticals, which became part of Madrigal Pharmaceuticals in June 2016. Dr. Pillai reported having no financial disclosures. Dr. Gandara disclosed that he had received research grants from several pharmaceutical companies.
VIENNA – The addition of ganetespib to docetaxel for the treatment of advanced non–small cell lung cancer (NSCLC) did not live up to its earlier promise of improved efficacy over docetaxel alone in a phase III study.
Interim results of the GALAXY-2 study, which led to the trial’s termination for futility, showed that there was no difference in the primary endpoint of overall survival (OS). The median OS was a respective 10.9 months and 10.5 months for the combination of ganetespib plus docetaxel versus docetaxel alone (hazard ratio, 1.111, 95% confidence interval, 0.899-1.372, P = .03293).
The combination had looked promising in the phase II GALAXY-1 study (Ann Oncol. 2015;26:1741-8), with a trend towards improved PFS and OS, with patients diagnosed with advanced disease perhaps gaining the most benefit.
“The addition of ganetespib to docetaxel did not result in improved efficacy for the salvage therapy of patients with advanced-stage lung adenocarcinoma,” Rathi Pillai, MD, said at the World Conference on Lung Cancer.
“Based on these findings, further development of Hsp [heat shock protein] 90 inhibitors in lung cancer should be limited to patients with driver mutations with relevant client proteins,” added Dr. Pillai of the Winship Cancer Institute at Emory University in Atlanta.
In GALAXY-2, 672 patients were randomized, 1:1, to receive docetaxel (75 mg/m2 on day 1) with ganetespib (150 mg/m2 on days 1 and 15) or a placebo every 3 weeks. The median number of cycles received was five in the combination arm and four in the docetaxel-only arm. All patients had advanced non–small cell lung adenocarcinoma diagnosed at least 6 months prior to enrollment and had received only one prior treatment regimen.
Response rates were similar between the two groups, with 13.7% and 16% of ganetespib/docetaxel– and docetaxel/placebo–treated patients achieving a partial response (P = .448) and 56.1% and 50.1%, respectively, having stable disease (P = .123).
Almost two-thirds (65%) of patients given ganetespib/docetaxel reported any grade 3-4 adverse event versus 54% of patients given docetaxel/placebo. The most frequent treatment-emergent grade 3-4 adverse event was neutropenia, occurring in 34.6% ad 29.5% of patients in each arm (P = .1807), with only diarrhea (46.2% vs. 14.6%; P less than .0001) and weight loss (11.3% vs. 5.2%; P = .0044) occurring more frequently in the combination than the docetaxel-only arm.
Ganetespib is a second-generation Hsp90 inhibitor and the rationale for using Hsp90 inhibitors as cancer therapy remains sound, Dr. Gandara maintained. One of the issues is finding a biomarker to predict the benefit for these drugs in a clinical setting, he said. In the phase II GALAXY-1 trial it was noted that patients diagnosed with advanced disease more than 6 months prior to study entry fared better than those with more recent diagnosis if they were treated with ganetespib/docetaxel than docetaxel alone. Patients with elevated levels of lactate dehydrogenase (eLDH) also seemed to do better than those with normal LDH levels if they were treated with the combination.
These two subpopulations were specifically looked at the in the phase III study, but again no differences in OS or PFS were observed, nor were differences observed in any of the other subgroups analyzed, which included EGFR- and ALK-negative patients, by response rate or progression because of new metastatic lesions.
“Were these the right surrogates to use as predictive biomarkers for heat shock protein inhibition? Of course, in retrospect, it is easy to say that they were not,” Dr. Gandara said.
“Is there still an opportunity for this class of drugs to make a meaningful impact in NSCLC? In my own opinion I think the answer is yes, but not in this broad page approach and not with these potential surrogates as were used in GALAXY-2,” he said at the meeting sponsored by the International Association for the Study of Lung Cancer.
The study was sponsored by Synta Pharmaceuticals, which became part of Madrigal Pharmaceuticals in June 2016. Dr. Pillai reported having no financial disclosures. Dr. Gandara disclosed that he had received research grants from several pharmaceutical companies.
AT WCLC 2016
Key clinical point: Adding ganetespib to docetaxel did not improve the survival of the patients studied versus docetaxel alone.
Major finding: Median overall survival was 10.9 months for ganetespib/docetaxel and 10.5 months for docetaxel alone (HR, 1.111; 95% CI, 0.899-1.372; P = .03293).
Data source: International, randomized, phase III, open-label GALAXY-2 study of docetaxel with or without ganetespib in 672 patients with advanced non–small cell lung adenocarcinoma.
Disclosures: The study was sponsored by Synta Pharmaceuticals (Madrigal Pharmaceuticals since June 2016). Dr. Pillai reported having no financial disclosures. Dr. Gandara disclosed that he had received research grants from several pharmaceutical companies.
One in three older adults with epilepsy has poor adherence to antiepileptics
HOUSTON – One in three older Americans with epilepsy had poor adherence to antiepileptic drugs, according to a large retrospective study, and the numbers were even worse for members of minority populations.
In an analysis of Medicare claims, patients who were African American had an odds ratio of 1.56 (95% confidence interval, 1.46-1.68) for being non-adherent to antiepileptic drugs (AEDs). For Hispanic patients, the OR was 1.40 (95% CI, 1.28-1.54), while for Asians, the OR was 1.41 (95% CI, 1.25-1.54).
“Overall, 31.8% were non-adherent to AEDs; range was from 24.1% for whites to 34.3% for African Americans,” wrote Maria Pisu, PhD, and her collaborators in an abstract accompanying the poster presented at the annual meeting of the American Epilepsy Society.
The reasons for poor adherence are unknown, but warrant further investigation, said Dr. Pisu of the division of preventive medicine at the University of Alabama at Birmingham.
The sample included 36,912 patients with epilepsy. In the enhanced sample, 19.2% of patients were white, 62.5% were African American, 11.3% were Hispanic, 5.0% were Asian, and 2.0% were American Indian or Alaskan Native. Of the sample, 61.6% were female; 41.5% of patients were aged 66-74 years; 36.1% were aged 75-84 years; and 22.4% were 85 years or older.
In order to determine whether patients with epilepsy or seizures were adherent, investigators looked at the ratio of days that at least one AED prescription was in the database for a given patient, divided by the total days of follow-up on record (“proportion of days covered”). The primary outcome measure of nonadherence was defined as a proportion of days covered of less than 0.80.
Most patients had one to several comorbidities: only 8.3% had no other comorbidities, while 46.0% had more than four. The remainder fell somewhere in the middle.
A majority of patients (59.2%) had some form of copay or coinsurance for prescriptions. About half of patients (50.2%) lived in the South.
Through multivariable analysis, the investigators explored the relationships between nonadherence and race or ethnicity, demographics, geographic area of residence, comorbidities, and whether the prescribed AEDs were enzyme-inducing. Additionally, socioeconomic status was estimated by factoring in eligibility for Medicare Part D low income subsidies and using zip code–level poverty data.
The differences between ethnic groups, wrote Dr. Pisu, were significant “after accounting for several factors that affect prescription-taking factors, e.g., economic constraints,” so it was not just low socioeconomic status that accounted for the discrepancy.
The retrospective claims-based study was limited by several factors, wrote Dr. Pisu and her colleagues. True adherence is difficult to quantify, and may be overestimated by measuring filled prescriptions; on the other hand, some patients may have had other insurance coverage, and obtained medication through a means not captured in the study. Finally, dose adjustments may mean patients can “stretch” medications, thereby remaining adherent without refilling prescriptions.
Still, the study shows that nonadherence is pervasive among older Americans with epilepsy, with worse adherence among members of minority populations. “Interventions to promote adherence are important. These should account for the impact of drug cost-sharing and socioeconomic status on epilepsy treatment,” wrote Dr. Pisu.
The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Pisu reported no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
HOUSTON – One in three older Americans with epilepsy had poor adherence to antiepileptic drugs, according to a large retrospective study, and the numbers were even worse for members of minority populations.
In an analysis of Medicare claims, patients who were African American had an odds ratio of 1.56 (95% confidence interval, 1.46-1.68) for being non-adherent to antiepileptic drugs (AEDs). For Hispanic patients, the OR was 1.40 (95% CI, 1.28-1.54), while for Asians, the OR was 1.41 (95% CI, 1.25-1.54).
“Overall, 31.8% were non-adherent to AEDs; range was from 24.1% for whites to 34.3% for African Americans,” wrote Maria Pisu, PhD, and her collaborators in an abstract accompanying the poster presented at the annual meeting of the American Epilepsy Society.
The reasons for poor adherence are unknown, but warrant further investigation, said Dr. Pisu of the division of preventive medicine at the University of Alabama at Birmingham.
The sample included 36,912 patients with epilepsy. In the enhanced sample, 19.2% of patients were white, 62.5% were African American, 11.3% were Hispanic, 5.0% were Asian, and 2.0% were American Indian or Alaskan Native. Of the sample, 61.6% were female; 41.5% of patients were aged 66-74 years; 36.1% were aged 75-84 years; and 22.4% were 85 years or older.
In order to determine whether patients with epilepsy or seizures were adherent, investigators looked at the ratio of days that at least one AED prescription was in the database for a given patient, divided by the total days of follow-up on record (“proportion of days covered”). The primary outcome measure of nonadherence was defined as a proportion of days covered of less than 0.80.
Most patients had one to several comorbidities: only 8.3% had no other comorbidities, while 46.0% had more than four. The remainder fell somewhere in the middle.
A majority of patients (59.2%) had some form of copay or coinsurance for prescriptions. About half of patients (50.2%) lived in the South.
Through multivariable analysis, the investigators explored the relationships between nonadherence and race or ethnicity, demographics, geographic area of residence, comorbidities, and whether the prescribed AEDs were enzyme-inducing. Additionally, socioeconomic status was estimated by factoring in eligibility for Medicare Part D low income subsidies and using zip code–level poverty data.
The differences between ethnic groups, wrote Dr. Pisu, were significant “after accounting for several factors that affect prescription-taking factors, e.g., economic constraints,” so it was not just low socioeconomic status that accounted for the discrepancy.
The retrospective claims-based study was limited by several factors, wrote Dr. Pisu and her colleagues. True adherence is difficult to quantify, and may be overestimated by measuring filled prescriptions; on the other hand, some patients may have had other insurance coverage, and obtained medication through a means not captured in the study. Finally, dose adjustments may mean patients can “stretch” medications, thereby remaining adherent without refilling prescriptions.
Still, the study shows that nonadherence is pervasive among older Americans with epilepsy, with worse adherence among members of minority populations. “Interventions to promote adherence are important. These should account for the impact of drug cost-sharing and socioeconomic status on epilepsy treatment,” wrote Dr. Pisu.
The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Pisu reported no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
HOUSTON – One in three older Americans with epilepsy had poor adherence to antiepileptic drugs, according to a large retrospective study, and the numbers were even worse for members of minority populations.
In an analysis of Medicare claims, patients who were African American had an odds ratio of 1.56 (95% confidence interval, 1.46-1.68) for being non-adherent to antiepileptic drugs (AEDs). For Hispanic patients, the OR was 1.40 (95% CI, 1.28-1.54), while for Asians, the OR was 1.41 (95% CI, 1.25-1.54).
“Overall, 31.8% were non-adherent to AEDs; range was from 24.1% for whites to 34.3% for African Americans,” wrote Maria Pisu, PhD, and her collaborators in an abstract accompanying the poster presented at the annual meeting of the American Epilepsy Society.
The reasons for poor adherence are unknown, but warrant further investigation, said Dr. Pisu of the division of preventive medicine at the University of Alabama at Birmingham.
The sample included 36,912 patients with epilepsy. In the enhanced sample, 19.2% of patients were white, 62.5% were African American, 11.3% were Hispanic, 5.0% were Asian, and 2.0% were American Indian or Alaskan Native. Of the sample, 61.6% were female; 41.5% of patients were aged 66-74 years; 36.1% were aged 75-84 years; and 22.4% were 85 years or older.
In order to determine whether patients with epilepsy or seizures were adherent, investigators looked at the ratio of days that at least one AED prescription was in the database for a given patient, divided by the total days of follow-up on record (“proportion of days covered”). The primary outcome measure of nonadherence was defined as a proportion of days covered of less than 0.80.
Most patients had one to several comorbidities: only 8.3% had no other comorbidities, while 46.0% had more than four. The remainder fell somewhere in the middle.
A majority of patients (59.2%) had some form of copay or coinsurance for prescriptions. About half of patients (50.2%) lived in the South.
Through multivariable analysis, the investigators explored the relationships between nonadherence and race or ethnicity, demographics, geographic area of residence, comorbidities, and whether the prescribed AEDs were enzyme-inducing. Additionally, socioeconomic status was estimated by factoring in eligibility for Medicare Part D low income subsidies and using zip code–level poverty data.
The differences between ethnic groups, wrote Dr. Pisu, were significant “after accounting for several factors that affect prescription-taking factors, e.g., economic constraints,” so it was not just low socioeconomic status that accounted for the discrepancy.
The retrospective claims-based study was limited by several factors, wrote Dr. Pisu and her colleagues. True adherence is difficult to quantify, and may be overestimated by measuring filled prescriptions; on the other hand, some patients may have had other insurance coverage, and obtained medication through a means not captured in the study. Finally, dose adjustments may mean patients can “stretch” medications, thereby remaining adherent without refilling prescriptions.
Still, the study shows that nonadherence is pervasive among older Americans with epilepsy, with worse adherence among members of minority populations. “Interventions to promote adherence are important. These should account for the impact of drug cost-sharing and socioeconomic status on epilepsy treatment,” wrote Dr. Pisu.
The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Pisu reported no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT AES 2016
Key clinical point:
Major finding: For African-American patients, the odds ratio was 1.56 for being nonadherent (95% CI, 1.4-1.68).
Data source: Retrospective analysis of Medicare administrative claims data from 2008 to 2010, examining a 5% sample of patients with epilepsy aged 66 and over, and including all members of racial/ethnic minority populations who had claims for diagnoses of seizures or epilepsy.
Disclosures: The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Pisu reported no relevant financial disclosures.
Common Hair Disorders
Review the PDF of the fact sheet on common hair disorders with board-relevant, easy-to-review material. This fact sheet reviews information about the most common hair disorders, including clinical and histopathological features, trichoscopy, and management of these diseases.
Practice Questions
1. A 40-year-old woman presents to the clinic with a burning sensation and tenderness on the scalp. At physical examination you notice erythematous papules and pustules on the vertex scalp. The most likely diagnosis is:
a. alopecia areata
b. CCSA
c. folliculitis decalvans
d. lichen planopilaris
e. traction alopecia
2. A 60-year-old woman presents with receding hair loss on the frontal and bitemporal scalp. She has noticed hair loss on her eyebrows. She has a history of oral ulcers. On physical examination there is mild erythema and perifollicular scales on the frontal hairline. A hair pull test is positive in this area. The most likely diagnosis is:
a. androgenetic alopecia
b. chronic cutaneous lupus erythematosus
c. frontal fibrosing alopecia
d. telogen effluvium
e. trichotillomania
3. A 5-year-old girl with a history of seasonal allergies and eczema presents with recurrent patchy hair loss on the scalp of 6 months’ duration. Her mother has noticed rapidly progressive hair loss affecting the whole scalp. On trichoscopy, you find yellow dots, broken hairs, and tapering hairs. The most likely diagnosis is:
a. alopecia areata
b. androgenetic alopecia
c. telogen effluvium
d. traction alopecia
e. trichotillomania
4. A 30-year-old white woman with history of obsessive-compulsive disorder presents to the clinic with hair loss for the last 3 years. She says she has noticed worsening of the hair loss when she is under stress. She also bites her nails. On physical examination you identify an irregular patch of alopecia with broken hairs on the occipital scalp. The most likely diagnosis is:
a. alopecia areata
b. androgenetic alopecia
c. lichen planopilaris
d. traction alopecia
e. trichotillomania
5. A 45-year-old black woman who has a family history of hair loss in her mother presents with tenderness and burning sensation on the vertex scalp. She reports the hair loss was worse after she got a hair relaxer 6 months prior. She uses braids on her scalp and she has not had a relaxer since then. The most likely diagnosis is:
a. CCSA
b. chronic cutaneous lupus erythematosus
c. folliculitis decalvans
d. lichen planopilaris
e. trichotillomania
Answers to practice questions provided on next page
Practice Question Answers
1. A 40-year-old woman presents to the clinic with a burning sensation and tenderness on the scalp. At physical examination you notice erythematous papules and pustules on the vertex scalp. The most likely diagnosis is:
a. alopecia areata
b. CCSA
c. folliculitis decalvans
d. lichen planopilaris
e. traction alopecia
2. A 60-year-old woman presents with receding hair loss on the frontal and bitemporal scalp. She has noticed hair loss on her eyebrows. She has a history of oral ulcers. On physical examination there is mild erythema and perifollicular scales on the frontal hairline. A hair pull test is positive in this area. The most likely diagnosis is:
a. androgenetic alopecia
b. chronic cutaneous lupus erythematosus
c. frontal fibrosing alopecia
d. telogen effluvium
e. trichotillomania
3. A 5-year-old girl with a history of seasonal allergies and eczema presents with recurrent patchy hair loss on the scalp of 6 months’ duration. Her mother has noticed rapidly progressive hair loss affecting the whole scalp. On trichoscopy, you find yellow dots, broken hairs, and tapering hairs. The most likely diagnosis is:
a. alopecia areata
b. androgenetic alopecia
c. telogen effluvium
d. traction alopecia
e. trichotillomania
4. A 30-year-old white woman with history of obsessive-compulsive disorder presents to the clinic with hair loss for the last 3 years. She says she has noticed worsening of the hair loss when she is under stress. She also bites her nails. On physical examination you identify an irregular patch of alopecia with broken hairs on the occipital scalp. The most likely diagnosis is:
a. alopecia areata
b. androgenetic alopecia
c. lichen planopilaris
d. traction alopecia
e. trichotillomania
5. A 45-year-old black woman who has a family history of hair loss in her mother presents with tenderness and burning sensation on the vertex scalp. She reports the hair loss was worse after she got a hair relaxer 6 months prior. She uses braids on her scalp and she has not had a relaxer since then. The most likely diagnosis is:
a. CCSA
b. chronic cutaneous lupus erythematosus
c. folliculitis decalvans
d. lichen planopilaris
e. trichotillomania
Review the PDF of the fact sheet on common hair disorders with board-relevant, easy-to-review material. This fact sheet reviews information about the most common hair disorders, including clinical and histopathological features, trichoscopy, and management of these diseases.
Practice Questions
1. A 40-year-old woman presents to the clinic with a burning sensation and tenderness on the scalp. At physical examination you notice erythematous papules and pustules on the vertex scalp. The most likely diagnosis is:
a. alopecia areata
b. CCSA
c. folliculitis decalvans
d. lichen planopilaris
e. traction alopecia
2. A 60-year-old woman presents with receding hair loss on the frontal and bitemporal scalp. She has noticed hair loss on her eyebrows. She has a history of oral ulcers. On physical examination there is mild erythema and perifollicular scales on the frontal hairline. A hair pull test is positive in this area. The most likely diagnosis is:
a. androgenetic alopecia
b. chronic cutaneous lupus erythematosus
c. frontal fibrosing alopecia
d. telogen effluvium
e. trichotillomania
3. A 5-year-old girl with a history of seasonal allergies and eczema presents with recurrent patchy hair loss on the scalp of 6 months’ duration. Her mother has noticed rapidly progressive hair loss affecting the whole scalp. On trichoscopy, you find yellow dots, broken hairs, and tapering hairs. The most likely diagnosis is:
a. alopecia areata
b. androgenetic alopecia
c. telogen effluvium
d. traction alopecia
e. trichotillomania
4. A 30-year-old white woman with history of obsessive-compulsive disorder presents to the clinic with hair loss for the last 3 years. She says she has noticed worsening of the hair loss when she is under stress. She also bites her nails. On physical examination you identify an irregular patch of alopecia with broken hairs on the occipital scalp. The most likely diagnosis is:
a. alopecia areata
b. androgenetic alopecia
c. lichen planopilaris
d. traction alopecia
e. trichotillomania
5. A 45-year-old black woman who has a family history of hair loss in her mother presents with tenderness and burning sensation on the vertex scalp. She reports the hair loss was worse after she got a hair relaxer 6 months prior. She uses braids on her scalp and she has not had a relaxer since then. The most likely diagnosis is:
a. CCSA
b. chronic cutaneous lupus erythematosus
c. folliculitis decalvans
d. lichen planopilaris
e. trichotillomania
Answers to practice questions provided on next page
Practice Question Answers
1. A 40-year-old woman presents to the clinic with a burning sensation and tenderness on the scalp. At physical examination you notice erythematous papules and pustules on the vertex scalp. The most likely diagnosis is:
a. alopecia areata
b. CCSA
c. folliculitis decalvans
d. lichen planopilaris
e. traction alopecia
2. A 60-year-old woman presents with receding hair loss on the frontal and bitemporal scalp. She has noticed hair loss on her eyebrows. She has a history of oral ulcers. On physical examination there is mild erythema and perifollicular scales on the frontal hairline. A hair pull test is positive in this area. The most likely diagnosis is:
a. androgenetic alopecia
b. chronic cutaneous lupus erythematosus
c. frontal fibrosing alopecia
d. telogen effluvium
e. trichotillomania
3. A 5-year-old girl with a history of seasonal allergies and eczema presents with recurrent patchy hair loss on the scalp of 6 months’ duration. Her mother has noticed rapidly progressive hair loss affecting the whole scalp. On trichoscopy, you find yellow dots, broken hairs, and tapering hairs. The most likely diagnosis is:
a. alopecia areata
b. androgenetic alopecia
c. telogen effluvium
d. traction alopecia
e. trichotillomania
4. A 30-year-old white woman with history of obsessive-compulsive disorder presents to the clinic with hair loss for the last 3 years. She says she has noticed worsening of the hair loss when she is under stress. She also bites her nails. On physical examination you identify an irregular patch of alopecia with broken hairs on the occipital scalp. The most likely diagnosis is:
a. alopecia areata
b. androgenetic alopecia
c. lichen planopilaris
d. traction alopecia
e. trichotillomania
5. A 45-year-old black woman who has a family history of hair loss in her mother presents with tenderness and burning sensation on the vertex scalp. She reports the hair loss was worse after she got a hair relaxer 6 months prior. She uses braids on her scalp and she has not had a relaxer since then. The most likely diagnosis is:
a. CCSA
b. chronic cutaneous lupus erythematosus
c. folliculitis decalvans
d. lichen planopilaris
e. trichotillomania
Review the PDF of the fact sheet on common hair disorders with board-relevant, easy-to-review material. This fact sheet reviews information about the most common hair disorders, including clinical and histopathological features, trichoscopy, and management of these diseases.
Practice Questions
1. A 40-year-old woman presents to the clinic with a burning sensation and tenderness on the scalp. At physical examination you notice erythematous papules and pustules on the vertex scalp. The most likely diagnosis is:
a. alopecia areata
b. CCSA
c. folliculitis decalvans
d. lichen planopilaris
e. traction alopecia
2. A 60-year-old woman presents with receding hair loss on the frontal and bitemporal scalp. She has noticed hair loss on her eyebrows. She has a history of oral ulcers. On physical examination there is mild erythema and perifollicular scales on the frontal hairline. A hair pull test is positive in this area. The most likely diagnosis is:
a. androgenetic alopecia
b. chronic cutaneous lupus erythematosus
c. frontal fibrosing alopecia
d. telogen effluvium
e. trichotillomania
3. A 5-year-old girl with a history of seasonal allergies and eczema presents with recurrent patchy hair loss on the scalp of 6 months’ duration. Her mother has noticed rapidly progressive hair loss affecting the whole scalp. On trichoscopy, you find yellow dots, broken hairs, and tapering hairs. The most likely diagnosis is:
a. alopecia areata
b. androgenetic alopecia
c. telogen effluvium
d. traction alopecia
e. trichotillomania
4. A 30-year-old white woman with history of obsessive-compulsive disorder presents to the clinic with hair loss for the last 3 years. She says she has noticed worsening of the hair loss when she is under stress. She also bites her nails. On physical examination you identify an irregular patch of alopecia with broken hairs on the occipital scalp. The most likely diagnosis is:
a. alopecia areata
b. androgenetic alopecia
c. lichen planopilaris
d. traction alopecia
e. trichotillomania
5. A 45-year-old black woman who has a family history of hair loss in her mother presents with tenderness and burning sensation on the vertex scalp. She reports the hair loss was worse after she got a hair relaxer 6 months prior. She uses braids on her scalp and she has not had a relaxer since then. The most likely diagnosis is:
a. CCSA
b. chronic cutaneous lupus erythematosus
c. folliculitis decalvans
d. lichen planopilaris
e. trichotillomania
Answers to practice questions provided on next page
Practice Question Answers
1. A 40-year-old woman presents to the clinic with a burning sensation and tenderness on the scalp. At physical examination you notice erythematous papules and pustules on the vertex scalp. The most likely diagnosis is:
a. alopecia areata
b. CCSA
c. folliculitis decalvans
d. lichen planopilaris
e. traction alopecia
2. A 60-year-old woman presents with receding hair loss on the frontal and bitemporal scalp. She has noticed hair loss on her eyebrows. She has a history of oral ulcers. On physical examination there is mild erythema and perifollicular scales on the frontal hairline. A hair pull test is positive in this area. The most likely diagnosis is:
a. androgenetic alopecia
b. chronic cutaneous lupus erythematosus
c. frontal fibrosing alopecia
d. telogen effluvium
e. trichotillomania
3. A 5-year-old girl with a history of seasonal allergies and eczema presents with recurrent patchy hair loss on the scalp of 6 months’ duration. Her mother has noticed rapidly progressive hair loss affecting the whole scalp. On trichoscopy, you find yellow dots, broken hairs, and tapering hairs. The most likely diagnosis is:
a. alopecia areata
b. androgenetic alopecia
c. telogen effluvium
d. traction alopecia
e. trichotillomania
4. A 30-year-old white woman with history of obsessive-compulsive disorder presents to the clinic with hair loss for the last 3 years. She says she has noticed worsening of the hair loss when she is under stress. She also bites her nails. On physical examination you identify an irregular patch of alopecia with broken hairs on the occipital scalp. The most likely diagnosis is:
a. alopecia areata
b. androgenetic alopecia
c. lichen planopilaris
d. traction alopecia
e. trichotillomania
5. A 45-year-old black woman who has a family history of hair loss in her mother presents with tenderness and burning sensation on the vertex scalp. She reports the hair loss was worse after she got a hair relaxer 6 months prior. She uses braids on her scalp and she has not had a relaxer since then. The most likely diagnosis is:
a. CCSA
b. chronic cutaneous lupus erythematosus
c. folliculitis decalvans
d. lichen planopilaris
e. trichotillomania
Dermoscopy Update and Noninvasive Imaging Devices for Skin Cancer: Report From the Mount Sinai Winter Symposium
At the 19th Annual Mount Sinai Winter Symposium, Dr. Orit Markowitz provided an update on dermoscopy as a first-line noninvasive imaging modality for skin cancer screening and diagnosis along with reflectance confocal microscopy and dynamic optical coherence tomography. She explained how noninvasive imaging offers a more complete picture of lesions along with what is seen clinically and on pathology and discussed how it can help catch aggressive melanomas and other skin cancers at earlier stages. For these reasons, she emphasized that increased use of dermoscopy can be used to justify the need for regular skin cancer screenings. Finally, she discussed how noninvasive imaging can be used to guide dermatologists in performing optimal biposies of suspicious lesions.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At the 19th Annual Mount Sinai Winter Symposium, Dr. Orit Markowitz provided an update on dermoscopy as a first-line noninvasive imaging modality for skin cancer screening and diagnosis along with reflectance confocal microscopy and dynamic optical coherence tomography. She explained how noninvasive imaging offers a more complete picture of lesions along with what is seen clinically and on pathology and discussed how it can help catch aggressive melanomas and other skin cancers at earlier stages. For these reasons, she emphasized that increased use of dermoscopy can be used to justify the need for regular skin cancer screenings. Finally, she discussed how noninvasive imaging can be used to guide dermatologists in performing optimal biposies of suspicious lesions.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At the 19th Annual Mount Sinai Winter Symposium, Dr. Orit Markowitz provided an update on dermoscopy as a first-line noninvasive imaging modality for skin cancer screening and diagnosis along with reflectance confocal microscopy and dynamic optical coherence tomography. She explained how noninvasive imaging offers a more complete picture of lesions along with what is seen clinically and on pathology and discussed how it can help catch aggressive melanomas and other skin cancers at earlier stages. For these reasons, she emphasized that increased use of dermoscopy can be used to justify the need for regular skin cancer screenings. Finally, she discussed how noninvasive imaging can be used to guide dermatologists in performing optimal biposies of suspicious lesions.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
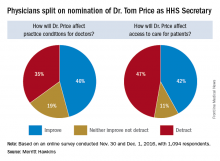
Trump HHS nominee could curb regulations, reshape health insurance
Opinions are mixed on what the nominations of Rep. Tom Price (R-Ga.) as Secretary of Health & Human Services will mean for medicine and health care.
An orthopedic surgeon and six-term congressman, Dr. Price is an outspoken critic of the Affordable Care Act and has sponsored or cosponsored numerous bills to replace it. President-elect Trump called Rep. Price “a renowned physician” who has “earned a reputation for being a tireless problem solver and the go-to expert on health care policy,” according to a statement.
Not everyone agrees.
But Adam Gaffney, MD, a pulmonologist at the Cambridge (Mass.) Health Alliance, said physicians’ ability to care for their patients would be compromised if Rep. Price succeeds with many of his proposals, such as the privatization of Medicare and block grants for Medicaid.
“If these reforms go through, we’re going to see the insurance protections of our patients get worse,” said Dr. Gaffney, a board member for Physicians for a National Health Program, which advocates for a single-payer health care system. “If [his] agenda is successful, I think it’s going to have a detrimental impact on our ability to provide the care that our patients need.”
ACA repeal, malpractice reform
In the House, Rep. Price has introduced the Empowering Patients First Act, legislation, which would allow doctors to opt out of Medicare and enter into private contracts with Medicare patients. The bill is seen by many as a potential blueprint for Trump administration health reform. Rep. Price is also a proponent of malpractice reform that would make it tougher for patients to sue doctors and would lower liability insurance premiums.
The Empowering Patients First Act would repeal the ACA and offer tax credits for the purchase of individual and family health insurance policies. It would also create incentives for patients to contribute to health savings accounts, offer state grants to subsidize coverage for high-risk patients, and authorize businesses to cover members through association health plans.
The American Medical Association praised Rep. Price’s nomination, expressing support for ability to lead HHS.
“Dr. Price has been a leader in the development of health policies to advance patient choice and market-based solutions as well as reduce excessive regulatory burdens that diminish time devoted to patient care and increase costs,” AMA Board of Trustees Chair Patrice A. Harris, MD, said in a statement.
The American College of Surgeons' Executive Director, David B. Hoyt, MD, FACS, issued a supportive statement about the nomination of Dr. Price. "“Dr. Price is a stalwart champion for patients and their surgeons, and the ACS looks forward to working with him on key issues, such as the implementation of the Medicare Access and CHIP Reauthorization Act,” said Dr. Hoyt in a statement. “The ACS encourages the Senate to swiftly confirm Dr. Price’s nomination as Secretary of HHS."
But thousands of physicians disagree. Rep. Price’s proposals on Medicaid and Medicare threaten to harm vulnerable patients and limit access to healthcare, according to an open letter to the AMA published on Medium and credited to Clinician Action Network, a nonpartisan group that supports evidence-based policies. The group was started in opposition to the nomination of Rep. Price.
“We cannot support the dismantling of Medicaid, which has helped 15 million Americans gain health coverage since 2014,” the letter states. “We oppose Dr. Price’s proposals to reduce funding for the Children’s Health Insurance Program, a critical mechanism by which poor children access preventative care.”
Value-based payment or fee for service?
Rep. Price’s experience as a physician fuels his efforts to reduce burdensome regulations for doctors and enhance care efficiency, according to one of his predecessors, Louis W. Sullivan, MD. If confirmed, Rep. Price will become the third physician to be HHS secretary; Dr. Sullivan served in the George H.W. Bush administration and Otis R. Bowen, MD, served in the Reagan administration.
“He is very much aware of the challenges that physicians face in trying to delivery care,” said Dr. Sullivan. “I know that he’ll be working to reduce regulation when feasible so that the cost and delays that some regulatory issues present will hopefully be relieved,”
Some of those regulatory modifications could affect value-based care programs, Dr. Rodriguez said. Rep. Price has been critical of the move from fee for service to quality-based care and has opposed some corresponding programs, such as bundled payment initiatives. Rep. Price and members of the GOP Doctors Caucus wrote to Centers for Medicare & Medicaid Services in October to protest the regulations to implement the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) as too burdensome for smaller practices and calling for flexibility in quality reporting.
Rep. Price voted for passage of MACRA.
“He has been cautious about some of the changes that are being promoted in health care,” Dr. Rodriguez said. “He could slow that down – the processes being put in place. That might delay the impact those systems have in bringing about the improved quality that we want. [This would be] enormous, given the amount of work that we’ve been doing.”
A fair medical liability system also is a priority for Rep. Price, Dr. Sullivan said. His Empowering Patients First bill would require collaboration between HHS and physician associations to develop best practice guidelines that would provide a litigation safe harbor to physicians who practiced in accordance with the standards.
“I know that he will be working to develop strategies to reduce litigation in the health space,” Dr. Sullivan said in an interview. “That is one of the challenges that adds to health care costs, adds tension, and enhances an adversarial relationship between physicians and patients.”
But Dr. Gaffney said that he believes Rep. Price’s views on reproductive rights and gay marriage are regressive and that his agenda regarding health policy issues is bad for medicine.
“The overall [theme] of that agenda can be summed up as ‘take from the poor and sick and give to the rich,’ ” Dr. Gaffney said in an interview. “I think the financing of this [new health reform] system will be much more aggressive, and the result will be greater health care inequity.”
Rep. Price also has supported a ban on federal funding for Planned Parenthood, calling some of their practices barbaric. He has also voted to prohibit the importation of prescription drugs by nonsanctioned importers and has voted to repeal the medical device excise tax.
agallegos@frontlinemedcom.com
On Twitter @legal_med
Opinions are mixed on what the nominations of Rep. Tom Price (R-Ga.) as Secretary of Health & Human Services will mean for medicine and health care.
An orthopedic surgeon and six-term congressman, Dr. Price is an outspoken critic of the Affordable Care Act and has sponsored or cosponsored numerous bills to replace it. President-elect Trump called Rep. Price “a renowned physician” who has “earned a reputation for being a tireless problem solver and the go-to expert on health care policy,” according to a statement.
Not everyone agrees.
But Adam Gaffney, MD, a pulmonologist at the Cambridge (Mass.) Health Alliance, said physicians’ ability to care for their patients would be compromised if Rep. Price succeeds with many of his proposals, such as the privatization of Medicare and block grants for Medicaid.
“If these reforms go through, we’re going to see the insurance protections of our patients get worse,” said Dr. Gaffney, a board member for Physicians for a National Health Program, which advocates for a single-payer health care system. “If [his] agenda is successful, I think it’s going to have a detrimental impact on our ability to provide the care that our patients need.”
ACA repeal, malpractice reform
In the House, Rep. Price has introduced the Empowering Patients First Act, legislation, which would allow doctors to opt out of Medicare and enter into private contracts with Medicare patients. The bill is seen by many as a potential blueprint for Trump administration health reform. Rep. Price is also a proponent of malpractice reform that would make it tougher for patients to sue doctors and would lower liability insurance premiums.
The Empowering Patients First Act would repeal the ACA and offer tax credits for the purchase of individual and family health insurance policies. It would also create incentives for patients to contribute to health savings accounts, offer state grants to subsidize coverage for high-risk patients, and authorize businesses to cover members through association health plans.
The American Medical Association praised Rep. Price’s nomination, expressing support for ability to lead HHS.
“Dr. Price has been a leader in the development of health policies to advance patient choice and market-based solutions as well as reduce excessive regulatory burdens that diminish time devoted to patient care and increase costs,” AMA Board of Trustees Chair Patrice A. Harris, MD, said in a statement.
The American College of Surgeons' Executive Director, David B. Hoyt, MD, FACS, issued a supportive statement about the nomination of Dr. Price. "“Dr. Price is a stalwart champion for patients and their surgeons, and the ACS looks forward to working with him on key issues, such as the implementation of the Medicare Access and CHIP Reauthorization Act,” said Dr. Hoyt in a statement. “The ACS encourages the Senate to swiftly confirm Dr. Price’s nomination as Secretary of HHS."
But thousands of physicians disagree. Rep. Price’s proposals on Medicaid and Medicare threaten to harm vulnerable patients and limit access to healthcare, according to an open letter to the AMA published on Medium and credited to Clinician Action Network, a nonpartisan group that supports evidence-based policies. The group was started in opposition to the nomination of Rep. Price.
“We cannot support the dismantling of Medicaid, which has helped 15 million Americans gain health coverage since 2014,” the letter states. “We oppose Dr. Price’s proposals to reduce funding for the Children’s Health Insurance Program, a critical mechanism by which poor children access preventative care.”
Value-based payment or fee for service?
Rep. Price’s experience as a physician fuels his efforts to reduce burdensome regulations for doctors and enhance care efficiency, according to one of his predecessors, Louis W. Sullivan, MD. If confirmed, Rep. Price will become the third physician to be HHS secretary; Dr. Sullivan served in the George H.W. Bush administration and Otis R. Bowen, MD, served in the Reagan administration.
“He is very much aware of the challenges that physicians face in trying to delivery care,” said Dr. Sullivan. “I know that he’ll be working to reduce regulation when feasible so that the cost and delays that some regulatory issues present will hopefully be relieved,”
Some of those regulatory modifications could affect value-based care programs, Dr. Rodriguez said. Rep. Price has been critical of the move from fee for service to quality-based care and has opposed some corresponding programs, such as bundled payment initiatives. Rep. Price and members of the GOP Doctors Caucus wrote to Centers for Medicare & Medicaid Services in October to protest the regulations to implement the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) as too burdensome for smaller practices and calling for flexibility in quality reporting.
Rep. Price voted for passage of MACRA.
“He has been cautious about some of the changes that are being promoted in health care,” Dr. Rodriguez said. “He could slow that down – the processes being put in place. That might delay the impact those systems have in bringing about the improved quality that we want. [This would be] enormous, given the amount of work that we’ve been doing.”
A fair medical liability system also is a priority for Rep. Price, Dr. Sullivan said. His Empowering Patients First bill would require collaboration between HHS and physician associations to develop best practice guidelines that would provide a litigation safe harbor to physicians who practiced in accordance with the standards.
“I know that he will be working to develop strategies to reduce litigation in the health space,” Dr. Sullivan said in an interview. “That is one of the challenges that adds to health care costs, adds tension, and enhances an adversarial relationship between physicians and patients.”
But Dr. Gaffney said that he believes Rep. Price’s views on reproductive rights and gay marriage are regressive and that his agenda regarding health policy issues is bad for medicine.
“The overall [theme] of that agenda can be summed up as ‘take from the poor and sick and give to the rich,’ ” Dr. Gaffney said in an interview. “I think the financing of this [new health reform] system will be much more aggressive, and the result will be greater health care inequity.”
Rep. Price also has supported a ban on federal funding for Planned Parenthood, calling some of their practices barbaric. He has also voted to prohibit the importation of prescription drugs by nonsanctioned importers and has voted to repeal the medical device excise tax.
agallegos@frontlinemedcom.com
On Twitter @legal_med
Opinions are mixed on what the nominations of Rep. Tom Price (R-Ga.) as Secretary of Health & Human Services will mean for medicine and health care.
An orthopedic surgeon and six-term congressman, Dr. Price is an outspoken critic of the Affordable Care Act and has sponsored or cosponsored numerous bills to replace it. President-elect Trump called Rep. Price “a renowned physician” who has “earned a reputation for being a tireless problem solver and the go-to expert on health care policy,” according to a statement.
Not everyone agrees.
But Adam Gaffney, MD, a pulmonologist at the Cambridge (Mass.) Health Alliance, said physicians’ ability to care for their patients would be compromised if Rep. Price succeeds with many of his proposals, such as the privatization of Medicare and block grants for Medicaid.
“If these reforms go through, we’re going to see the insurance protections of our patients get worse,” said Dr. Gaffney, a board member for Physicians for a National Health Program, which advocates for a single-payer health care system. “If [his] agenda is successful, I think it’s going to have a detrimental impact on our ability to provide the care that our patients need.”
ACA repeal, malpractice reform
In the House, Rep. Price has introduced the Empowering Patients First Act, legislation, which would allow doctors to opt out of Medicare and enter into private contracts with Medicare patients. The bill is seen by many as a potential blueprint for Trump administration health reform. Rep. Price is also a proponent of malpractice reform that would make it tougher for patients to sue doctors and would lower liability insurance premiums.
The Empowering Patients First Act would repeal the ACA and offer tax credits for the purchase of individual and family health insurance policies. It would also create incentives for patients to contribute to health savings accounts, offer state grants to subsidize coverage for high-risk patients, and authorize businesses to cover members through association health plans.
The American Medical Association praised Rep. Price’s nomination, expressing support for ability to lead HHS.
“Dr. Price has been a leader in the development of health policies to advance patient choice and market-based solutions as well as reduce excessive regulatory burdens that diminish time devoted to patient care and increase costs,” AMA Board of Trustees Chair Patrice A. Harris, MD, said in a statement.
The American College of Surgeons' Executive Director, David B. Hoyt, MD, FACS, issued a supportive statement about the nomination of Dr. Price. "“Dr. Price is a stalwart champion for patients and their surgeons, and the ACS looks forward to working with him on key issues, such as the implementation of the Medicare Access and CHIP Reauthorization Act,” said Dr. Hoyt in a statement. “The ACS encourages the Senate to swiftly confirm Dr. Price’s nomination as Secretary of HHS."
But thousands of physicians disagree. Rep. Price’s proposals on Medicaid and Medicare threaten to harm vulnerable patients and limit access to healthcare, according to an open letter to the AMA published on Medium and credited to Clinician Action Network, a nonpartisan group that supports evidence-based policies. The group was started in opposition to the nomination of Rep. Price.
“We cannot support the dismantling of Medicaid, which has helped 15 million Americans gain health coverage since 2014,” the letter states. “We oppose Dr. Price’s proposals to reduce funding for the Children’s Health Insurance Program, a critical mechanism by which poor children access preventative care.”
Value-based payment or fee for service?
Rep. Price’s experience as a physician fuels his efforts to reduce burdensome regulations for doctors and enhance care efficiency, according to one of his predecessors, Louis W. Sullivan, MD. If confirmed, Rep. Price will become the third physician to be HHS secretary; Dr. Sullivan served in the George H.W. Bush administration and Otis R. Bowen, MD, served in the Reagan administration.
“He is very much aware of the challenges that physicians face in trying to delivery care,” said Dr. Sullivan. “I know that he’ll be working to reduce regulation when feasible so that the cost and delays that some regulatory issues present will hopefully be relieved,”
Some of those regulatory modifications could affect value-based care programs, Dr. Rodriguez said. Rep. Price has been critical of the move from fee for service to quality-based care and has opposed some corresponding programs, such as bundled payment initiatives. Rep. Price and members of the GOP Doctors Caucus wrote to Centers for Medicare & Medicaid Services in October to protest the regulations to implement the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) as too burdensome for smaller practices and calling for flexibility in quality reporting.
Rep. Price voted for passage of MACRA.
“He has been cautious about some of the changes that are being promoted in health care,” Dr. Rodriguez said. “He could slow that down – the processes being put in place. That might delay the impact those systems have in bringing about the improved quality that we want. [This would be] enormous, given the amount of work that we’ve been doing.”
A fair medical liability system also is a priority for Rep. Price, Dr. Sullivan said. His Empowering Patients First bill would require collaboration between HHS and physician associations to develop best practice guidelines that would provide a litigation safe harbor to physicians who practiced in accordance with the standards.
“I know that he will be working to develop strategies to reduce litigation in the health space,” Dr. Sullivan said in an interview. “That is one of the challenges that adds to health care costs, adds tension, and enhances an adversarial relationship between physicians and patients.”
But Dr. Gaffney said that he believes Rep. Price’s views on reproductive rights and gay marriage are regressive and that his agenda regarding health policy issues is bad for medicine.
“The overall [theme] of that agenda can be summed up as ‘take from the poor and sick and give to the rich,’ ” Dr. Gaffney said in an interview. “I think the financing of this [new health reform] system will be much more aggressive, and the result will be greater health care inequity.”
Rep. Price also has supported a ban on federal funding for Planned Parenthood, calling some of their practices barbaric. He has also voted to prohibit the importation of prescription drugs by nonsanctioned importers and has voted to repeal the medical device excise tax.
agallegos@frontlinemedcom.com
On Twitter @legal_med
Dermoscopy Pearls: Report From the Mount Sinai Winter Symposium
At the 19th Annual Mount Sinai Winter Symposium, Dr. Orit Markowitz addressed some common questions physicians have about dermoscopy, including what kind of dermatoscope to buy, how to incorporate dermoscopy into a dermatology practice, and how to efficiently perform skin examinations using a dermatoscope. She also emphasized the importance of attending courses and workshops to learn how to utilize dermoscopy and other noninvasive imaging devices effectively.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At the 19th Annual Mount Sinai Winter Symposium, Dr. Orit Markowitz addressed some common questions physicians have about dermoscopy, including what kind of dermatoscope to buy, how to incorporate dermoscopy into a dermatology practice, and how to efficiently perform skin examinations using a dermatoscope. She also emphasized the importance of attending courses and workshops to learn how to utilize dermoscopy and other noninvasive imaging devices effectively.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At the 19th Annual Mount Sinai Winter Symposium, Dr. Orit Markowitz addressed some common questions physicians have about dermoscopy, including what kind of dermatoscope to buy, how to incorporate dermoscopy into a dermatology practice, and how to efficiently perform skin examinations using a dermatoscope. She also emphasized the importance of attending courses and workshops to learn how to utilize dermoscopy and other noninvasive imaging devices effectively.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Aspirin use linked to increased ICH in trauma patients
WAIKOLOA, HAWAII – Among a group of anticoagulated trauma patients, those on aspirin had the highest rate and risk of intracranial hemorrhage (ICH), while those on novel oral anticoagulants were not at higher risk for ICH, ICH progression, or death, a multicenter study found.
“The number of patients on warfarin and antiplatelet agents has significantly increased over time,” Leslie Kobayashi, MD, said at the annual meeting of the American Association for the Surgery of Trauma. “These oral antithrombotic agents have been associated with poor outcomes following traumatic injury, including increased rates of intracranial hemorrhage, increased progression of intracranial hemorrhage, and increased mortality.”
In a prospective, multicenter observational study conducted by the AAST’s Multi-institutional Trials Committee, Dr. Kobayashi and her associates set out identify injury patterns and outcomes in trauma patients taking the NOAs, and to test their hypothesis that patients taking NOAs would have higher rates of ICH, ICH progression, and death, compared with patients taking traditional oral anticoagulant therapies (OATs). Patients were included if they were admitted to the trauma service on warfarin, aspirin, clopidogrel, dabigatran, apixaban, or rivaroxaban. Pregnant patients, prisoners, and minors were excluded from the study. Data collected included demographics, mechanism of injury, vitals on admission, injuries/injury severity scores, labs, interventions, and reversal agents used such as vitamin K, prothrombin complexes, dialysis, and transfusion of fresh frozen plasma (FFP). Outcomes studied included ICH, ICH progression, and death.
In all, 16 Level 1 trauma centers enrolled 1,847 patients over a 2-year period. Their average age was 75 years, 46% were female, 77% were white, their median Injury Severity Score (ISS) was 9, and 99% sustained a blunt mechanism of trauma. The top two causes of injury were falls (71%) and motor vehicle crashes (15%). One-third of patients (33%) were on warfarin, while the remainder were on aspirin (26%), clopidogrel (24%), NOAs (10%), and 7% took multiple or other agents.
The mechanism of injury pattern was similar between patients taking NOAs and those taking OATs, with the exception of patients on aspirin being significantly less likely to have sustained a fall. Patients on aspirin also had a significantly higher median ISS. “Patients on NOAs presented more frequently in shock as defined by a systolic blood pressure of less than 90 mmHg, but this was not associated with increased need for packed red blood cell transfusion, bleeding requiring an intervention, need for surgical procedure, hospital LOS, complications, or death,” Dr. Kobayashi said.
About 30% of all patients studied underwent an attempt at reversal. The types of agents used to reverse the patients differed depending on drug agent, with antiplatelet patients more frequently getting platelets, and patients on warfarin more frequently receiving FFP, vitamin K, and prothrombin complex. “Interestingly, patients on the anti-Xa inhibitors more frequently received prothrombin complex as well,” she said. “This likely reflects some of the recent literature which suggests that there may be a therapeutic benefit to using prothrombin complex in patients taking the oral anti-Xa inhibitors but not in patients on dabigatran.”
Overall, bleeding, need for surgical procedure, need for neurosurgical procedure, complications, length of stay, and death were similar between those on NOAs and those on OATs. However, the rate of ICH was significantly higher in patients on aspirin. “What is even more surprising is that 89% of the patients in the aspirin-only group were on an 81-mg baby aspirin rather than the larger 325-mg dose,” Dr. Kobayashi said. This difference was significant on univariate analysis and was retained after multivariate logistic regression adjusted for differences between populations, with an OR for aspirin of 1.7 and a P value of .024. “This is not to suggest that patients on aspirin are doing markedly worse, compared to their counterparts, but I think most of us would have assumed that aspirin patients would have done better,” she commented. “I think we’ve definitively shown that is not the case.” Other independent predictors of ICH were advanced age (OR, 1.02), Asian race (OR, 3.1), ISS of 10 or greater (OR, 2.2), and a Glasgow coma score (GCS) of 8 or less (OR, 5.6).
Despite their increased risk for ICH, patients on aspirin were significantly less likely to undergo an attempt at reversal with any type of agent, at 16% with a P value of less than .001, on univariate analysis. “This was significantly lower than all other medications and was retained after multivariate logistic regression, with an OR of 0.3 and a P value of less than .001,” she said.
Progression of ICH did not differ by medication group. Other independent predictors included intraparenchymal location of hemorrhage (OR, 2.2), need for a neurosurgical procedure (OR, 5.1), an attempt at reversal (OR, 2.3) and a GCS of 8 or lower at admission (OR, 4.3). Similarly, multivariate analysis of death showed no significant differences between the different medication groups. Independent predictors included advanced age (OR, 1.06), GCS of 8 or less (OR, 13), progression of head injury (OR, 10), bleeding (OR, 2.3), and complications (OR, 2.1).
Dr. Kobayashi acknowledged that the study’s observational design is a limitation, as well as the fact that it lacked a control group of age-matched patients who were not taking anticoagulants. “Additionally, we had a relatively low number of patients on NOAs, at only 10% of the study population,” she said. “Lastly, there is potential for enrollment bias as all sites involved in this study were level one trauma centers.” She reported having no financial disclosures.
WAIKOLOA, HAWAII – Among a group of anticoagulated trauma patients, those on aspirin had the highest rate and risk of intracranial hemorrhage (ICH), while those on novel oral anticoagulants were not at higher risk for ICH, ICH progression, or death, a multicenter study found.
“The number of patients on warfarin and antiplatelet agents has significantly increased over time,” Leslie Kobayashi, MD, said at the annual meeting of the American Association for the Surgery of Trauma. “These oral antithrombotic agents have been associated with poor outcomes following traumatic injury, including increased rates of intracranial hemorrhage, increased progression of intracranial hemorrhage, and increased mortality.”
In a prospective, multicenter observational study conducted by the AAST’s Multi-institutional Trials Committee, Dr. Kobayashi and her associates set out identify injury patterns and outcomes in trauma patients taking the NOAs, and to test their hypothesis that patients taking NOAs would have higher rates of ICH, ICH progression, and death, compared with patients taking traditional oral anticoagulant therapies (OATs). Patients were included if they were admitted to the trauma service on warfarin, aspirin, clopidogrel, dabigatran, apixaban, or rivaroxaban. Pregnant patients, prisoners, and minors were excluded from the study. Data collected included demographics, mechanism of injury, vitals on admission, injuries/injury severity scores, labs, interventions, and reversal agents used such as vitamin K, prothrombin complexes, dialysis, and transfusion of fresh frozen plasma (FFP). Outcomes studied included ICH, ICH progression, and death.
In all, 16 Level 1 trauma centers enrolled 1,847 patients over a 2-year period. Their average age was 75 years, 46% were female, 77% were white, their median Injury Severity Score (ISS) was 9, and 99% sustained a blunt mechanism of trauma. The top two causes of injury were falls (71%) and motor vehicle crashes (15%). One-third of patients (33%) were on warfarin, while the remainder were on aspirin (26%), clopidogrel (24%), NOAs (10%), and 7% took multiple or other agents.
The mechanism of injury pattern was similar between patients taking NOAs and those taking OATs, with the exception of patients on aspirin being significantly less likely to have sustained a fall. Patients on aspirin also had a significantly higher median ISS. “Patients on NOAs presented more frequently in shock as defined by a systolic blood pressure of less than 90 mmHg, but this was not associated with increased need for packed red blood cell transfusion, bleeding requiring an intervention, need for surgical procedure, hospital LOS, complications, or death,” Dr. Kobayashi said.
About 30% of all patients studied underwent an attempt at reversal. The types of agents used to reverse the patients differed depending on drug agent, with antiplatelet patients more frequently getting platelets, and patients on warfarin more frequently receiving FFP, vitamin K, and prothrombin complex. “Interestingly, patients on the anti-Xa inhibitors more frequently received prothrombin complex as well,” she said. “This likely reflects some of the recent literature which suggests that there may be a therapeutic benefit to using prothrombin complex in patients taking the oral anti-Xa inhibitors but not in patients on dabigatran.”
Overall, bleeding, need for surgical procedure, need for neurosurgical procedure, complications, length of stay, and death were similar between those on NOAs and those on OATs. However, the rate of ICH was significantly higher in patients on aspirin. “What is even more surprising is that 89% of the patients in the aspirin-only group were on an 81-mg baby aspirin rather than the larger 325-mg dose,” Dr. Kobayashi said. This difference was significant on univariate analysis and was retained after multivariate logistic regression adjusted for differences between populations, with an OR for aspirin of 1.7 and a P value of .024. “This is not to suggest that patients on aspirin are doing markedly worse, compared to their counterparts, but I think most of us would have assumed that aspirin patients would have done better,” she commented. “I think we’ve definitively shown that is not the case.” Other independent predictors of ICH were advanced age (OR, 1.02), Asian race (OR, 3.1), ISS of 10 or greater (OR, 2.2), and a Glasgow coma score (GCS) of 8 or less (OR, 5.6).
Despite their increased risk for ICH, patients on aspirin were significantly less likely to undergo an attempt at reversal with any type of agent, at 16% with a P value of less than .001, on univariate analysis. “This was significantly lower than all other medications and was retained after multivariate logistic regression, with an OR of 0.3 and a P value of less than .001,” she said.
Progression of ICH did not differ by medication group. Other independent predictors included intraparenchymal location of hemorrhage (OR, 2.2), need for a neurosurgical procedure (OR, 5.1), an attempt at reversal (OR, 2.3) and a GCS of 8 or lower at admission (OR, 4.3). Similarly, multivariate analysis of death showed no significant differences between the different medication groups. Independent predictors included advanced age (OR, 1.06), GCS of 8 or less (OR, 13), progression of head injury (OR, 10), bleeding (OR, 2.3), and complications (OR, 2.1).
Dr. Kobayashi acknowledged that the study’s observational design is a limitation, as well as the fact that it lacked a control group of age-matched patients who were not taking anticoagulants. “Additionally, we had a relatively low number of patients on NOAs, at only 10% of the study population,” she said. “Lastly, there is potential for enrollment bias as all sites involved in this study were level one trauma centers.” She reported having no financial disclosures.
WAIKOLOA, HAWAII – Among a group of anticoagulated trauma patients, those on aspirin had the highest rate and risk of intracranial hemorrhage (ICH), while those on novel oral anticoagulants were not at higher risk for ICH, ICH progression, or death, a multicenter study found.
“The number of patients on warfarin and antiplatelet agents has significantly increased over time,” Leslie Kobayashi, MD, said at the annual meeting of the American Association for the Surgery of Trauma. “These oral antithrombotic agents have been associated with poor outcomes following traumatic injury, including increased rates of intracranial hemorrhage, increased progression of intracranial hemorrhage, and increased mortality.”
In a prospective, multicenter observational study conducted by the AAST’s Multi-institutional Trials Committee, Dr. Kobayashi and her associates set out identify injury patterns and outcomes in trauma patients taking the NOAs, and to test their hypothesis that patients taking NOAs would have higher rates of ICH, ICH progression, and death, compared with patients taking traditional oral anticoagulant therapies (OATs). Patients were included if they were admitted to the trauma service on warfarin, aspirin, clopidogrel, dabigatran, apixaban, or rivaroxaban. Pregnant patients, prisoners, and minors were excluded from the study. Data collected included demographics, mechanism of injury, vitals on admission, injuries/injury severity scores, labs, interventions, and reversal agents used such as vitamin K, prothrombin complexes, dialysis, and transfusion of fresh frozen plasma (FFP). Outcomes studied included ICH, ICH progression, and death.
In all, 16 Level 1 trauma centers enrolled 1,847 patients over a 2-year period. Their average age was 75 years, 46% were female, 77% were white, their median Injury Severity Score (ISS) was 9, and 99% sustained a blunt mechanism of trauma. The top two causes of injury were falls (71%) and motor vehicle crashes (15%). One-third of patients (33%) were on warfarin, while the remainder were on aspirin (26%), clopidogrel (24%), NOAs (10%), and 7% took multiple or other agents.
The mechanism of injury pattern was similar between patients taking NOAs and those taking OATs, with the exception of patients on aspirin being significantly less likely to have sustained a fall. Patients on aspirin also had a significantly higher median ISS. “Patients on NOAs presented more frequently in shock as defined by a systolic blood pressure of less than 90 mmHg, but this was not associated with increased need for packed red blood cell transfusion, bleeding requiring an intervention, need for surgical procedure, hospital LOS, complications, or death,” Dr. Kobayashi said.
About 30% of all patients studied underwent an attempt at reversal. The types of agents used to reverse the patients differed depending on drug agent, with antiplatelet patients more frequently getting platelets, and patients on warfarin more frequently receiving FFP, vitamin K, and prothrombin complex. “Interestingly, patients on the anti-Xa inhibitors more frequently received prothrombin complex as well,” she said. “This likely reflects some of the recent literature which suggests that there may be a therapeutic benefit to using prothrombin complex in patients taking the oral anti-Xa inhibitors but not in patients on dabigatran.”
Overall, bleeding, need for surgical procedure, need for neurosurgical procedure, complications, length of stay, and death were similar between those on NOAs and those on OATs. However, the rate of ICH was significantly higher in patients on aspirin. “What is even more surprising is that 89% of the patients in the aspirin-only group were on an 81-mg baby aspirin rather than the larger 325-mg dose,” Dr. Kobayashi said. This difference was significant on univariate analysis and was retained after multivariate logistic regression adjusted for differences between populations, with an OR for aspirin of 1.7 and a P value of .024. “This is not to suggest that patients on aspirin are doing markedly worse, compared to their counterparts, but I think most of us would have assumed that aspirin patients would have done better,” she commented. “I think we’ve definitively shown that is not the case.” Other independent predictors of ICH were advanced age (OR, 1.02), Asian race (OR, 3.1), ISS of 10 or greater (OR, 2.2), and a Glasgow coma score (GCS) of 8 or less (OR, 5.6).
Despite their increased risk for ICH, patients on aspirin were significantly less likely to undergo an attempt at reversal with any type of agent, at 16% with a P value of less than .001, on univariate analysis. “This was significantly lower than all other medications and was retained after multivariate logistic regression, with an OR of 0.3 and a P value of less than .001,” she said.
Progression of ICH did not differ by medication group. Other independent predictors included intraparenchymal location of hemorrhage (OR, 2.2), need for a neurosurgical procedure (OR, 5.1), an attempt at reversal (OR, 2.3) and a GCS of 8 or lower at admission (OR, 4.3). Similarly, multivariate analysis of death showed no significant differences between the different medication groups. Independent predictors included advanced age (OR, 1.06), GCS of 8 or less (OR, 13), progression of head injury (OR, 10), bleeding (OR, 2.3), and complications (OR, 2.1).
Dr. Kobayashi acknowledged that the study’s observational design is a limitation, as well as the fact that it lacked a control group of age-matched patients who were not taking anticoagulants. “Additionally, we had a relatively low number of patients on NOAs, at only 10% of the study population,” she said. “Lastly, there is potential for enrollment bias as all sites involved in this study were level one trauma centers.” She reported having no financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point:
Major finding: The rate of ICH was significantly higher in patients on aspirin, compared with those on novel oral anticoagulant therapies (OR, 1.7; P = .024).
Data source: A prospective evaluation of 1,847 patients treated at 16 level one trauma centers over a 2-year period.
Disclosures: Dr. Kobayashi reported having no financial disclosures.
HIV research update: Early November 2016
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
HIV-infected U.S. smokers aged 40 years lose more than 6 years of life expectancy from smoking, according to a computer simulation study, possibly outweighing the loss from HIV infection itself.
A study published in JAIDS provides insight into a novel mechanism of ritonavir-induced insulin resistance involving proinflammatory properties of heme oxygenase-1 (HO-1).
Antiretroviral therapy with efavirenz, emtricitabine, and tenofovir disoproxil fumarate (TDF) appeared to have a more favorable renal safety profile than did TDF administered with a protease inhibitor or cobicistat, according to a study in HIV Clinical Trials.
Researchers said the first study to describe the dynamics of the biomarker of cerebrospinal fluid YKL-40 in two groups of HIV-infected individuals, before and after combination antiretroviral therapy, has demonstrated the value of the marker in understanding HIV neuropathogenesis.
A study of HIV testing among ethnic minority adolescents in New Jersey underscored the importance of developing multifaceted HIV/AIDS prevention protocols that provide direct education and skill-building activities, leverage peer education as a means to disseminate health-related information, and deliver broad-based prevention messaging that is culturally tailored and gender specific.
HIV-infected adults in a contemporary, high-resource setting have poor dietary patterns, a recent study found, and alcohol use was associated with worse gut integrity and increased inflammation, while other aspects of diet were not.
A study in BMC Infectious Diseases found immune recovery comparable in primary and chronic HIV infection, whereas differences in absolute counts and proportions of CD4+ T cell subpopulations were found between primary HIV infection and late presenters supporting early initiation of combination antiretroviral therapy.
HIV/HCV coinfection leads to a significant increase in plasma HCV RNA, according to a study in Pathogens and Global Health.
A Canadian study identified elevated rates of intentional and unintentional injury among people living with HIV.
Partner services for persons with acute and early HIV infection (AEH) within 30 days of diagnosis represents an effective tool to find HIV unaware persons, a recent study found, including those with AEH who are at greatest risk of HIV transmission.
Maternal tenofovir use was not associated with lower length or head circumference of HIV-exposed uninfected infants at 2 years of age, a recent study revealed, but may be related to greater weight among those exposed to combination antiretroviral therapy early in pregnancy.
Cryptococcal meningitis may be considered one of the causes of acute vision loss in pregnant/postpartum HIV-positive females, according to a study in BMC Infectious Diseases.
According to a study in JAIDS, red cell distribution width remains a powerful marker of cardiovascular disease in the context of the inflammatory milieu that accompanies HIV infection.
HIV infection moderates the association between vascular remodeling and neurocognitive function but not the association between pulse pressure and neurocognitive function, a recent study revealed.
HIV viral blips on therapy are associated with subsequent viral rebound on stopping antiretroviral therapy among individuals treated in primary HIV infection, according to a new study.
Adipocytokine dysregulation seems to be related to metabolic syndrome in HIV-infected children, according to a study in the Pediatric Infectious Disease Journal.
rpizzi@frontlinemedcom.com
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
HIV-infected U.S. smokers aged 40 years lose more than 6 years of life expectancy from smoking, according to a computer simulation study, possibly outweighing the loss from HIV infection itself.
A study published in JAIDS provides insight into a novel mechanism of ritonavir-induced insulin resistance involving proinflammatory properties of heme oxygenase-1 (HO-1).
Antiretroviral therapy with efavirenz, emtricitabine, and tenofovir disoproxil fumarate (TDF) appeared to have a more favorable renal safety profile than did TDF administered with a protease inhibitor or cobicistat, according to a study in HIV Clinical Trials.
Researchers said the first study to describe the dynamics of the biomarker of cerebrospinal fluid YKL-40 in two groups of HIV-infected individuals, before and after combination antiretroviral therapy, has demonstrated the value of the marker in understanding HIV neuropathogenesis.
A study of HIV testing among ethnic minority adolescents in New Jersey underscored the importance of developing multifaceted HIV/AIDS prevention protocols that provide direct education and skill-building activities, leverage peer education as a means to disseminate health-related information, and deliver broad-based prevention messaging that is culturally tailored and gender specific.
HIV-infected adults in a contemporary, high-resource setting have poor dietary patterns, a recent study found, and alcohol use was associated with worse gut integrity and increased inflammation, while other aspects of diet were not.
A study in BMC Infectious Diseases found immune recovery comparable in primary and chronic HIV infection, whereas differences in absolute counts and proportions of CD4+ T cell subpopulations were found between primary HIV infection and late presenters supporting early initiation of combination antiretroviral therapy.
HIV/HCV coinfection leads to a significant increase in plasma HCV RNA, according to a study in Pathogens and Global Health.
A Canadian study identified elevated rates of intentional and unintentional injury among people living with HIV.
Partner services for persons with acute and early HIV infection (AEH) within 30 days of diagnosis represents an effective tool to find HIV unaware persons, a recent study found, including those with AEH who are at greatest risk of HIV transmission.
Maternal tenofovir use was not associated with lower length or head circumference of HIV-exposed uninfected infants at 2 years of age, a recent study revealed, but may be related to greater weight among those exposed to combination antiretroviral therapy early in pregnancy.
Cryptococcal meningitis may be considered one of the causes of acute vision loss in pregnant/postpartum HIV-positive females, according to a study in BMC Infectious Diseases.
According to a study in JAIDS, red cell distribution width remains a powerful marker of cardiovascular disease in the context of the inflammatory milieu that accompanies HIV infection.
HIV infection moderates the association between vascular remodeling and neurocognitive function but not the association between pulse pressure and neurocognitive function, a recent study revealed.
HIV viral blips on therapy are associated with subsequent viral rebound on stopping antiretroviral therapy among individuals treated in primary HIV infection, according to a new study.
Adipocytokine dysregulation seems to be related to metabolic syndrome in HIV-infected children, according to a study in the Pediatric Infectious Disease Journal.
rpizzi@frontlinemedcom.com
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
HIV-infected U.S. smokers aged 40 years lose more than 6 years of life expectancy from smoking, according to a computer simulation study, possibly outweighing the loss from HIV infection itself.
A study published in JAIDS provides insight into a novel mechanism of ritonavir-induced insulin resistance involving proinflammatory properties of heme oxygenase-1 (HO-1).
Antiretroviral therapy with efavirenz, emtricitabine, and tenofovir disoproxil fumarate (TDF) appeared to have a more favorable renal safety profile than did TDF administered with a protease inhibitor or cobicistat, according to a study in HIV Clinical Trials.
Researchers said the first study to describe the dynamics of the biomarker of cerebrospinal fluid YKL-40 in two groups of HIV-infected individuals, before and after combination antiretroviral therapy, has demonstrated the value of the marker in understanding HIV neuropathogenesis.
A study of HIV testing among ethnic minority adolescents in New Jersey underscored the importance of developing multifaceted HIV/AIDS prevention protocols that provide direct education and skill-building activities, leverage peer education as a means to disseminate health-related information, and deliver broad-based prevention messaging that is culturally tailored and gender specific.
HIV-infected adults in a contemporary, high-resource setting have poor dietary patterns, a recent study found, and alcohol use was associated with worse gut integrity and increased inflammation, while other aspects of diet were not.
A study in BMC Infectious Diseases found immune recovery comparable in primary and chronic HIV infection, whereas differences in absolute counts and proportions of CD4+ T cell subpopulations were found between primary HIV infection and late presenters supporting early initiation of combination antiretroviral therapy.
HIV/HCV coinfection leads to a significant increase in plasma HCV RNA, according to a study in Pathogens and Global Health.
A Canadian study identified elevated rates of intentional and unintentional injury among people living with HIV.
Partner services for persons with acute and early HIV infection (AEH) within 30 days of diagnosis represents an effective tool to find HIV unaware persons, a recent study found, including those with AEH who are at greatest risk of HIV transmission.
Maternal tenofovir use was not associated with lower length or head circumference of HIV-exposed uninfected infants at 2 years of age, a recent study revealed, but may be related to greater weight among those exposed to combination antiretroviral therapy early in pregnancy.
Cryptococcal meningitis may be considered one of the causes of acute vision loss in pregnant/postpartum HIV-positive females, according to a study in BMC Infectious Diseases.
According to a study in JAIDS, red cell distribution width remains a powerful marker of cardiovascular disease in the context of the inflammatory milieu that accompanies HIV infection.
HIV infection moderates the association between vascular remodeling and neurocognitive function but not the association between pulse pressure and neurocognitive function, a recent study revealed.
HIV viral blips on therapy are associated with subsequent viral rebound on stopping antiretroviral therapy among individuals treated in primary HIV infection, according to a new study.
Adipocytokine dysregulation seems to be related to metabolic syndrome in HIV-infected children, according to a study in the Pediatric Infectious Disease Journal.
rpizzi@frontlinemedcom.com
On Twitter @richpizzi
Preventing weight gain after smoking cessation
About three-quarters of current cigarette smokers want to quit, 40% will attempt to quit annually, and 90% of self-initiated attempts will be unsuccessful. Mean weight gain after smoking cessation may be as much as 13 pounds at 1 year, and 21 pounds over 5 years.
Population data suggest that more than one-half of women and one-third of men with a previous attempt to quit smoking report that weight gain was one of the primary reasons for relapse back to smoking.
Lorcaserin is a 5-HT2c (serotonin) receptor agonist FDA-approved for weight loss. Varenicline is the most effective monotherapy for smoking cessation and targets the alpha-4 beta-2 nicotinic acetylcholine receptor.
Ryan Hurt, MD, and his colleagues recently completed a pilot clinical trial evaluating the potential efficacy of combining varenicline and lorcaserin for the prevention of PCWG in obese and overweight smokers (Nicotine Tob Res. 2016 Nov 16. doi: 10.1093/ntr/ntw304).
In this study, 20 smokers with a body mass index of 27-40 kg/m2 received varenicline and lorcaserin for 12 weeks.
Fifty percent of subjects were abstinent from smoking at 12 weeks, among whom weight gain was only +1.1 ± 3.9 kg (90% confidence interval, –0.9 to +3.1). The most-common side effect of the combination was sleep disturbance, reported by five patients.
The study was limited by the small sample size and the absence of a control group or placebo.
As clinicians, we frequently employ combination therapy in chronic diseases such as diabetes and hypertension when single-agent therapy is ineffective. By combining drugs with different therapeutic targets, we can achieve our treatment goals.
In tobacco dependence treatment, we use combination pharmacotherapy for heavier smokers or for those who have tried and failed to quit previously. Interestingly, lorcaserin has been demonstrated in another pilot study to increase smoking cessation rates by itself.
The combination of lorcaserin and varenicline holds promise for the treatment of tobacco dependence by attacking tobacco dependence through two different mechanisms and preventing PCWG, which may prevent relapse back to smoking.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition, nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
About three-quarters of current cigarette smokers want to quit, 40% will attempt to quit annually, and 90% of self-initiated attempts will be unsuccessful. Mean weight gain after smoking cessation may be as much as 13 pounds at 1 year, and 21 pounds over 5 years.
Population data suggest that more than one-half of women and one-third of men with a previous attempt to quit smoking report that weight gain was one of the primary reasons for relapse back to smoking.
Lorcaserin is a 5-HT2c (serotonin) receptor agonist FDA-approved for weight loss. Varenicline is the most effective monotherapy for smoking cessation and targets the alpha-4 beta-2 nicotinic acetylcholine receptor.
Ryan Hurt, MD, and his colleagues recently completed a pilot clinical trial evaluating the potential efficacy of combining varenicline and lorcaserin for the prevention of PCWG in obese and overweight smokers (Nicotine Tob Res. 2016 Nov 16. doi: 10.1093/ntr/ntw304).
In this study, 20 smokers with a body mass index of 27-40 kg/m2 received varenicline and lorcaserin for 12 weeks.
Fifty percent of subjects were abstinent from smoking at 12 weeks, among whom weight gain was only +1.1 ± 3.9 kg (90% confidence interval, –0.9 to +3.1). The most-common side effect of the combination was sleep disturbance, reported by five patients.
The study was limited by the small sample size and the absence of a control group or placebo.
As clinicians, we frequently employ combination therapy in chronic diseases such as diabetes and hypertension when single-agent therapy is ineffective. By combining drugs with different therapeutic targets, we can achieve our treatment goals.
In tobacco dependence treatment, we use combination pharmacotherapy for heavier smokers or for those who have tried and failed to quit previously. Interestingly, lorcaserin has been demonstrated in another pilot study to increase smoking cessation rates by itself.
The combination of lorcaserin and varenicline holds promise for the treatment of tobacco dependence by attacking tobacco dependence through two different mechanisms and preventing PCWG, which may prevent relapse back to smoking.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition, nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
About three-quarters of current cigarette smokers want to quit, 40% will attempt to quit annually, and 90% of self-initiated attempts will be unsuccessful. Mean weight gain after smoking cessation may be as much as 13 pounds at 1 year, and 21 pounds over 5 years.
Population data suggest that more than one-half of women and one-third of men with a previous attempt to quit smoking report that weight gain was one of the primary reasons for relapse back to smoking.
Lorcaserin is a 5-HT2c (serotonin) receptor agonist FDA-approved for weight loss. Varenicline is the most effective monotherapy for smoking cessation and targets the alpha-4 beta-2 nicotinic acetylcholine receptor.
Ryan Hurt, MD, and his colleagues recently completed a pilot clinical trial evaluating the potential efficacy of combining varenicline and lorcaserin for the prevention of PCWG in obese and overweight smokers (Nicotine Tob Res. 2016 Nov 16. doi: 10.1093/ntr/ntw304).
In this study, 20 smokers with a body mass index of 27-40 kg/m2 received varenicline and lorcaserin for 12 weeks.
Fifty percent of subjects were abstinent from smoking at 12 weeks, among whom weight gain was only +1.1 ± 3.9 kg (90% confidence interval, –0.9 to +3.1). The most-common side effect of the combination was sleep disturbance, reported by five patients.
The study was limited by the small sample size and the absence of a control group or placebo.
As clinicians, we frequently employ combination therapy in chronic diseases such as diabetes and hypertension when single-agent therapy is ineffective. By combining drugs with different therapeutic targets, we can achieve our treatment goals.
In tobacco dependence treatment, we use combination pharmacotherapy for heavier smokers or for those who have tried and failed to quit previously. Interestingly, lorcaserin has been demonstrated in another pilot study to increase smoking cessation rates by itself.
The combination of lorcaserin and varenicline holds promise for the treatment of tobacco dependence by attacking tobacco dependence through two different mechanisms and preventing PCWG, which may prevent relapse back to smoking.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition, nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
Second transplant, consolidation don’t add benefit in upfront multiple myeloma therapy
SAN DIEGO – It took a clinical trial with a byzantine design to prove it, but neither posttransplant consolidation therapy nor second transplant offered any additional survival benefits to patients with multiple myeloma, including patients with high-risk disease who were treated with an upfront thalidomide analogue and a proteasome inhibitor, followed by stem cell transplant and lenalidomide maintenance.
Among 758 patients with multiple myeloma who underwent standard induction therapy, followed by melphalan conditioning and autologous stem cell transplant (ASCT), there were no differences in either progression-free survival (PFS) or overall survival (OS) among patients assigned to follow-on therapy with either lenalidomide (Revlimid) maintenance alone; consolidation therapy with four cycles of lenalidomide (Revlimid), bortezomib (Velcade), and dexamethasone (RVD), followed by lenalidomide maintenance; or second transplant, followed by lenalidomide maintenance, reported Edward A. Stadtmauer, MD, coleader of the hematologic malignancies program at the Abramson Cancer Center, and chief of the section of hematologic malignancies, University of Pennsylvania, Philadelphia.
Investigators in the STAMINA (Stem Cell Transplant With Lenalidomide Maintenance in Patients With Multiple Myeloma) trial (BMT CTN 0702) hypothesized that the use of thalidomide analogues and proteasome inhibitors used in first-line therapy, consolidation, and long-term maintenance after high-dose melphalan and ASCT would improve survival, compared with a second ASCT.
To test this idea, they enrolled 758 patients and randomized them to one of the three aforementioned posttransplant strategies prior to transplant conditioning with high-dose melphalan (200 mg/m2) and ASCT.
Roughly 25% of patients in each treatment arm had high-risk disease, defined as beta2 microglobulin levels greater than 5.5 mg/L, high-risk cytogenetics, and deletion 13 detected by standard cytogenetics only. The remaining patients in each arm had standard-risk disease.
Slightly more than half of patients received RVD upfront; about 13% received cyclophosphamide, bortezomib, and dexamethasone (CyBorD); roughly 10% received lenalidomide dexamethasone; 12% were treated with bortezomib/dexamethasone; and about 8% received other, unspecified combinations.
At a median follow-up time of 37.8 months, the PFS rate, which was the primary endpoint, was 56.5% for the second transplant arm, 56.7% for the RVD arm, and 52.2% for the maintenance-only arm. The differences were not statistically significant.
Similarly, there were no among-arm differences in PFS for patients with standard-risk disease (60.9%, 59.5%, and 55.9%) or for those with high-risk myeloma (42.2%, 48.3%, and 40.2%)
Overall survival, a secondary endpoint, was also not significantly different among the groups, at 82%, 85.7%, and 83.4%, respectively.
Encouragingly, however, despite lower PFS rates, patients with high-risk disease had high OS rates, with 79.6% of patients in the double-transplant arm, 77.5% of those in the RVD consolidation arm, and 79.5% of those in the lenalidomide maintenance-alone arm still alive at 38 months.
Secondary malignancies occurred among 5.1% of patients overall: 14 in the dual-transplant arm, 15 in the consolidation arm, and 10 in the maintenance-only arm. The most frequently reported second malignancies were leukemia, which occurred in 3 of 14 patients with second cancers after second transplant and in 9 of 15 patients with second cancers after consolidation, and solid tumors, which occurred most frequently among second cancers in the maintenance arm.
The investigators are continuing to parse the data by study arm to see whether response assessment correlates with outcomes and with complete remissions. They also plan to examine minimal residual disease via flow cytometry and sequencing, and to obtain long-term data on survival, toxicities, and second primary malignancies.
The trial was funded by the National Institutes of Health with support from Celgene and Millennium/Takeda. Dr. Stadtmauer disclosed consulting for Takeda and travel expenses from Celgene.
SAN DIEGO – It took a clinical trial with a byzantine design to prove it, but neither posttransplant consolidation therapy nor second transplant offered any additional survival benefits to patients with multiple myeloma, including patients with high-risk disease who were treated with an upfront thalidomide analogue and a proteasome inhibitor, followed by stem cell transplant and lenalidomide maintenance.
Among 758 patients with multiple myeloma who underwent standard induction therapy, followed by melphalan conditioning and autologous stem cell transplant (ASCT), there were no differences in either progression-free survival (PFS) or overall survival (OS) among patients assigned to follow-on therapy with either lenalidomide (Revlimid) maintenance alone; consolidation therapy with four cycles of lenalidomide (Revlimid), bortezomib (Velcade), and dexamethasone (RVD), followed by lenalidomide maintenance; or second transplant, followed by lenalidomide maintenance, reported Edward A. Stadtmauer, MD, coleader of the hematologic malignancies program at the Abramson Cancer Center, and chief of the section of hematologic malignancies, University of Pennsylvania, Philadelphia.
Investigators in the STAMINA (Stem Cell Transplant With Lenalidomide Maintenance in Patients With Multiple Myeloma) trial (BMT CTN 0702) hypothesized that the use of thalidomide analogues and proteasome inhibitors used in first-line therapy, consolidation, and long-term maintenance after high-dose melphalan and ASCT would improve survival, compared with a second ASCT.
To test this idea, they enrolled 758 patients and randomized them to one of the three aforementioned posttransplant strategies prior to transplant conditioning with high-dose melphalan (200 mg/m2) and ASCT.
Roughly 25% of patients in each treatment arm had high-risk disease, defined as beta2 microglobulin levels greater than 5.5 mg/L, high-risk cytogenetics, and deletion 13 detected by standard cytogenetics only. The remaining patients in each arm had standard-risk disease.
Slightly more than half of patients received RVD upfront; about 13% received cyclophosphamide, bortezomib, and dexamethasone (CyBorD); roughly 10% received lenalidomide dexamethasone; 12% were treated with bortezomib/dexamethasone; and about 8% received other, unspecified combinations.
At a median follow-up time of 37.8 months, the PFS rate, which was the primary endpoint, was 56.5% for the second transplant arm, 56.7% for the RVD arm, and 52.2% for the maintenance-only arm. The differences were not statistically significant.
Similarly, there were no among-arm differences in PFS for patients with standard-risk disease (60.9%, 59.5%, and 55.9%) or for those with high-risk myeloma (42.2%, 48.3%, and 40.2%)
Overall survival, a secondary endpoint, was also not significantly different among the groups, at 82%, 85.7%, and 83.4%, respectively.
Encouragingly, however, despite lower PFS rates, patients with high-risk disease had high OS rates, with 79.6% of patients in the double-transplant arm, 77.5% of those in the RVD consolidation arm, and 79.5% of those in the lenalidomide maintenance-alone arm still alive at 38 months.
Secondary malignancies occurred among 5.1% of patients overall: 14 in the dual-transplant arm, 15 in the consolidation arm, and 10 in the maintenance-only arm. The most frequently reported second malignancies were leukemia, which occurred in 3 of 14 patients with second cancers after second transplant and in 9 of 15 patients with second cancers after consolidation, and solid tumors, which occurred most frequently among second cancers in the maintenance arm.
The investigators are continuing to parse the data by study arm to see whether response assessment correlates with outcomes and with complete remissions. They also plan to examine minimal residual disease via flow cytometry and sequencing, and to obtain long-term data on survival, toxicities, and second primary malignancies.
The trial was funded by the National Institutes of Health with support from Celgene and Millennium/Takeda. Dr. Stadtmauer disclosed consulting for Takeda and travel expenses from Celgene.
SAN DIEGO – It took a clinical trial with a byzantine design to prove it, but neither posttransplant consolidation therapy nor second transplant offered any additional survival benefits to patients with multiple myeloma, including patients with high-risk disease who were treated with an upfront thalidomide analogue and a proteasome inhibitor, followed by stem cell transplant and lenalidomide maintenance.
Among 758 patients with multiple myeloma who underwent standard induction therapy, followed by melphalan conditioning and autologous stem cell transplant (ASCT), there were no differences in either progression-free survival (PFS) or overall survival (OS) among patients assigned to follow-on therapy with either lenalidomide (Revlimid) maintenance alone; consolidation therapy with four cycles of lenalidomide (Revlimid), bortezomib (Velcade), and dexamethasone (RVD), followed by lenalidomide maintenance; or second transplant, followed by lenalidomide maintenance, reported Edward A. Stadtmauer, MD, coleader of the hematologic malignancies program at the Abramson Cancer Center, and chief of the section of hematologic malignancies, University of Pennsylvania, Philadelphia.
Investigators in the STAMINA (Stem Cell Transplant With Lenalidomide Maintenance in Patients With Multiple Myeloma) trial (BMT CTN 0702) hypothesized that the use of thalidomide analogues and proteasome inhibitors used in first-line therapy, consolidation, and long-term maintenance after high-dose melphalan and ASCT would improve survival, compared with a second ASCT.
To test this idea, they enrolled 758 patients and randomized them to one of the three aforementioned posttransplant strategies prior to transplant conditioning with high-dose melphalan (200 mg/m2) and ASCT.
Roughly 25% of patients in each treatment arm had high-risk disease, defined as beta2 microglobulin levels greater than 5.5 mg/L, high-risk cytogenetics, and deletion 13 detected by standard cytogenetics only. The remaining patients in each arm had standard-risk disease.
Slightly more than half of patients received RVD upfront; about 13% received cyclophosphamide, bortezomib, and dexamethasone (CyBorD); roughly 10% received lenalidomide dexamethasone; 12% were treated with bortezomib/dexamethasone; and about 8% received other, unspecified combinations.
At a median follow-up time of 37.8 months, the PFS rate, which was the primary endpoint, was 56.5% for the second transplant arm, 56.7% for the RVD arm, and 52.2% for the maintenance-only arm. The differences were not statistically significant.
Similarly, there were no among-arm differences in PFS for patients with standard-risk disease (60.9%, 59.5%, and 55.9%) or for those with high-risk myeloma (42.2%, 48.3%, and 40.2%)
Overall survival, a secondary endpoint, was also not significantly different among the groups, at 82%, 85.7%, and 83.4%, respectively.
Encouragingly, however, despite lower PFS rates, patients with high-risk disease had high OS rates, with 79.6% of patients in the double-transplant arm, 77.5% of those in the RVD consolidation arm, and 79.5% of those in the lenalidomide maintenance-alone arm still alive at 38 months.
Secondary malignancies occurred among 5.1% of patients overall: 14 in the dual-transplant arm, 15 in the consolidation arm, and 10 in the maintenance-only arm. The most frequently reported second malignancies were leukemia, which occurred in 3 of 14 patients with second cancers after second transplant and in 9 of 15 patients with second cancers after consolidation, and solid tumors, which occurred most frequently among second cancers in the maintenance arm.
The investigators are continuing to parse the data by study arm to see whether response assessment correlates with outcomes and with complete remissions. They also plan to examine minimal residual disease via flow cytometry and sequencing, and to obtain long-term data on survival, toxicities, and second primary malignancies.
The trial was funded by the National Institutes of Health with support from Celgene and Millennium/Takeda. Dr. Stadtmauer disclosed consulting for Takeda and travel expenses from Celgene.
AT ASH 2016
Key clinical point: Three posttransplant strategies for patients with previously untreated myeloma were comparably effective.
Major finding: There were no differences in PFS or OS among patients treated with upfront therapy and transplant followed by either second transplant, consolidation, or lenalidomide maintenance alone.
Data source: Randomized prospective trial of 758 patients with multiple myeloma treated with a thalidomide analogue, proteasome inhibitor, and autologous stem cell transplant.
Disclosures: The trial was funded by the National Institutes of Health with support from Celgene and Millennium/Takeda. Dr. Stadtmauer disclosed consulting for Takeda and travel expenses from Celgene.